Evaluation of the plaque removal efficacy of a water flosser compared to string floss in adults after a single use
Affiliation.
- 1 BioSci Research Canada Ltd., Mississauga, Ontario, Canada.
- PMID: 24282867
Objective: To compare the plaque removal efficacy of a water flosser to string floss combined with a manual toothbrush after a single use.
Methods: Seventy adult subjects participated in this randomized, single-use, single-blind, parallel clinical study. Subjects were assigned to one of two groups; Waterpik Water Flosser plus a manual toothbrush (WF) or waxed string floss plus a manual toothbrush (SF). Each participant brushed for two minutes using the Bass technique. The WF group added 500 ml of warm water to the reservoir and followed the manufacturer's instructions, and the SF group used waxed string floss between each tooth, cleaning the mesial and distal surfaces as instructed. Subjects were observed to ensure they covered all areas and followed instructions. Scores were recorded for whole mouth, marginal, approximal, facial, and lingual regions for each subject using the Rustogi Modification of the Navy Plaque Index.
Results: The WF group had a 74.4% reduction in whole mouth plaque and 81.6% for approximal plaque compared to 57.7% and 63.4% for the SF group, respectively (p < 0.001). The differences between the groups showed the water flosser was 29% more effective than string floss for overall plaque removal and approximal surfaces specifically (p < 0.001). The WF group was more effective in removing plaque from the marginal, lingual, and facial regions; 33%, 39%, and 24%, respectively (p < 0.001).
Conclusion: The Waterpik Water Flosser and manual toothbrush is significantly more effective than a manual brush and string floss in removing plaque from tooth surfaces.

Publication types
- Comparative Study
- Randomized Controlled Trial
- Research Support, Non-U.S. Gov't
- Dental Devices, Home Care*
- Dental Plaque / pathology
- Dental Plaque / therapy*
- Dental Plaque Index
- Equipment Design
- Erythrosine
- Fluorescent Dyes
- Middle Aged
- Single-Blind Method
- Time Factors
- Tooth / pathology
- Toothbrushing / instrumentation
- Toothbrushing / methods
- Toothpastes / therapeutic use
- Toothpastes
- Online Only
- Special Issues
- Inside Dentistry
- Inside Dental Technology
- Inside Dental Hygiene
- The Dental Genius
- View Current Issue
- Clinical Categories
- General Dentistry
- Restorative
- Endodontics
- Implantology
- Oral Surgery
Orthodontics
- Pediatric Dentistry
- Periodontics
- Prosthodontics
- Specialty Care
- Additional Categories
- Business of Dentistry
- Infection Control
- Pain Management
Compendium, April 2024
, March 2024

Relevance of the Water Flosser: 50 Years of Data
Deborah M. Lyle, RDH, BS, MS
A review of the literature answers many questions related to the use of water flossers, the first of which was introduced in 1962. Numerous studies suggest that water flossers remove biofilm from tooth surfaces and bacteria from periodontal pockets better than string flossing and manual toothbrushing—together or alone. Clinicians should review these findings and consider recommending water flossers for appropriate patients to improve their oral health. As different irrigation or water-flossing devices now on the market offer different features, designs, and combinations of pulsation and pressure, clinicians must consider the needs of individual patients and supporting research in selecting a model that the patient will like and use, and that will provide improved oral health.
The first oral irrigator was introduced to the dental profession in 1962. It was developed by a Colorado dentist who, in an effort to improve his patients’ oral hygiene, enlisted the help of a patient, a hydraulic engineer. The oral irrigator—also called a dental water jet—is known today as a water flosser. While it is one of the most studied self-care devices on the market, questions remain regarding its efficacy, safety, and outcomes. This literature review will provide answers to many of these questions based on clinical research findings.
Does a Water Flosser Remove Plaque (Biofilm)?
A 1971 study by Hoover and Robinson 1 reported a significant reduction in the accumulation of plaque and formation of calculus in the group that used the oral irrigator. Likewise, Lobene 2 reported a 50% reduction in calculus in the water flosser group, and Phelps-Sandall 3 reported a significant reduction in plaque for individuals in intermaxillary fixation. Reductions in plaque have been demonstrated in studies with patients who had gingivitis, 4 periodontitis, 5 orthodontic appliances, 6 and diabetes. 7
In 2009, Costerton and his team evaluated the removal of biofilm from the tooth surface using a water flosser.8 In this ex-vivo study, periodontally involved teeth were extracted and new biofilm was grown over the existing deposits. The teeth were then treated with a water flosser for 3 seconds on medium pressure. The results were viewed under scanning electron microscopy (SEM) and showed the removal of 99.9% of the biofilm from the treated area.
A recent study measured the plaque removal of a water flosser after a single use and then evaluated the results after 4 weeks. 4 When used with a manual toothbrush, the water flosser removed 75% of whole-mouth plaque after a one-time use. When isolating specific areas, the results were: 84% for facial surfaces, 66% for lingual surfaces, 59% for marginal area, and 92% for approximal area. Four-week results showed 51% whole-mouth reduction in plaque, with specific areas showing 53% for facial, 49% for lingual, 25% for marginal, and 77% for approximal.
Does a Water Flosser Push Bacteria into the Pocket?
Research shows that the water flosser does not push bacteria into the periodontal pocket; in fact, the reverse is true. The water flosser removes bacteria from the pocket. Several studies have shown the reduction of bacteria from the periodontal pocket following irrigation with a water flosser. An early study to measure the ability of a water flosser to reduce bacteria was conducted on subjects with fixed orthodontic appliances. At the end of the 63-day study, results from the group of patients who used a manual toothbrush and water flosser device showed that this method was 80% more effective than toothbrushing and rinsing in reducing total aerobic flora and 60% more effective in reducing the lactobacillus count. 9
Cobb and colleagues 10 examined 32 teeth with 6-mm pockets that were scheduled for extraction. Half the teeth were treated with water irrigation using a pulsating water flosser device set on medium pressure, and the other half (control group) received no treatment. The experimental teeth were treated for 8 seconds prior to extraction. All teeth were extracted, keeping the epithelial tissue intact. SEM and transmission electron microscopy (TEM) were used to evaluate epithelial cavitation or ulceration. The investigators found that the water flosser group had reduced the numbers of microorganisms by up to 6 mm compared to the untreated areas, which had thick mattes of microbes. Importantly, they reported no differences in the epithelial lining of the pocket or evidence of penetration into the tissue.
The removal of bacteria is accomplished by the pulsating action of the device. This results in an impact and flushing zone, which produces a compression and decompression phase ( Figure 1 ) and allows for clearing of the bacteria and debris from the pocket. Drisko et al11 demonstrated a reduction in the number of spirochetes from pretreatment levels in 3-mm and 6-mm pockets. Chaves and colleagues 12 compared water irrigation, chlorhexidine (CHX) irrigation, CHX rinsing, and brushing alone, and found only the irrigation groups showed a reduction in subgingival bacteria.
Is a Water Flosser as Effective as String Flossing?
To date, only one device, the Waterpik ® Water Flosser (Water Pik, Inc., www.waterpik.com ), has been compared to dental floss in three different studies. 13-15 The first study, published in 2005, compared a water flosser plus either a power toothbrush or a manual toothbrush to a manual toothbrush and string floss. 13 The 4-week study showed that regardless of the toothbrush used, the water flosser was significantly better at reducing bleeding and gingivitis than a manual toothbrush and string floss.
In 2008, a study was conducted with adolescents in fixed orthodontic appliances. 14 In this study, there were three groups: Group 1 used a water flosser plus a manual toothbrush; Group 2 used string floss with a floss threader plus a manual toothbrush; and Group 3 used only a manual toothbrush (control). The water flosser group was shown to be more effective than the methods used by the other groups, with a 26% greater reduction in bleeding compared to string floss and 53% greater reduction in bleeding compared to toothbrushing alone. The differences for plaque removal were also significant, with the water flosser group showing three times greater reduction than the string floss group and five times greater reduction than the group that used brushing alone.
The most recent study was published in 2011. 15 Over a 4-week period, subjects used either a water flosser with a traditional jet tip ( Figure 2 ), a water flosser plus a jet tip with three tufts of bristles ( Figure 3 ), or string floss. All subjects brushed using a manual toothbrush twice a day. In both water flosser groups, bleeding was significantly reduced compared with the string floss group. At 2 weeks, the traditional tip was shown to be twice as effective as string floss. At the end of the study, the differences were even greater.
How Can a Water Flosser Perform Better Than String Floss?
The recommendation of dental floss may be more academic than research-based. This was brought to light when a systematic review reported on the results of comparing brushing alone to brushing and flossing. A meta-analysis was performed for the plaque and gingival indices and showed no differences between the groups. 16 The authors concluded that the regular recommendation of flossing is not supported by research. Add this to poor compliance, 17,18 patient preference for alternatives, 19 and poor technique, 20 and the need for alternatives is evident. Regarding the question of whether string floss prevents interdental caries, this was addressed by Hujoel et al, 21 who found that string flossing was only effective in reducing interproximal caries risk when it was performed by dental professionals on children with a low exposure to fluoride. Self-flossing by adolescents failed to show a benefit, and there were no studies found either for adults or under unsupervised conditions.
How Does a Water Flosser Work?
There are two basic types of irrigation or water-flossing devices. The first is a mechanized device powered by an electrical outlet or batteries. It typically delivers a pulsating stream of water, although not all mechanized units pulsate. Its pressure can be changed, and the pulsations are controlled by the motor. The other is a non-mechanized device that is attached to a water source such as a faucet or shower and delivers a constant stream of water. Devices on the market have different features, designs, and, most importantly, different combinations of pulsation and pressure.
Early studies evaluated the safety and mechanism of action—specifically the combination of pulsation and pressure. It was reported that the combination of 1,200 to 1,400 pulsations per minute is a key component to effectiveness, as this produces a compression and decompression phase. 22,23 This hydrokinetic activity creates an impact and flushing zone ( Figure 1 ) that allows for debris and bacteria to be expelled from the sulcus or pocket and is reported to be three times more effective than a continuous-stream device. 24 Likewise, a medium-to-high pressure setting—in the range of 50 to 90 pounds per square inch (psi)—was shown to be safe and more effective than lower settings. 22-24
Who Should Use a Water Flosser?
Recommendation of self-care devices by dental professionals is based on individual needs, values, preferences, and desired outcomes. Studies have shown that a water flosser can benefit many patient types and oral conditions.
Orthodontic appliances present oral hygiene challenges regardless of age. A study of 105 adolescents between the ages of 11 and 17 who used a water flosser with an orthodontic tip ( Figure 4 ) showed significant reductions in plaque and bleeding over 4 weeks. 6 These results are similar to a previous study that paired a water flosser with either a manual or power toothbrush and compared it to toothbrushing alone in adult orthodontic patients. Regardless of the toothbrush used, the water flosser groups showed significantly greater reduction in bleeding and inflammation compared to subjects who only brushed. 25
Periodontal Maintenance
Patients undergoing periodontal maintenance therapy have an increased risk of future loss of attachment, requiring excellent oral hygiene. Patients may have to clean the concavity of the proximal surfaces of the teeth and may be left with 4-mm to 6-mm pockets to maintain. Interdental devices such as floss, wood sticks, and interdental brushes cannot clean into these pockets and may not reach the concavity or furcation.
Several studies have evaluated the subgingival penetration of an oral irrigator. Eakle et al 26 tested a standard or classic jet tip placed at 90-degree and 45-degree angles to the long axis of the tooth at the gingival margin ( Figure 2 ). With both angles, depth of penetration varied with pocket depth, with an average of 50%. When placing the tip at a 90-degree angle, a mean percentage of 71% for shallow pockets (0 mm to 3 mm), 44% for moderate pockets (4 mm to 7 mm), and 67% for deep pockets (> 7 mm) was obtained. Placing the tip at a 45-degree angle did not increase penetration, and in some cases penetration was less than when using a 90-degree angle. Notably, 75% or more penetration was seen in 60% of pockets > 7 mm. Larner et al27 reported 42% penetration in 4-mm to 6-mm pockets and 39% for 7-mm to 10-mm pockets. A specialized subgingivally placed tip with reduced flow and pressure ( Figure 5 ) was reported to reach 90% of a 6-mm pocket and 67% in pockets ≥ 7 mm. 28
Implants require daily care similar to natural teeth. A water flosser was tested on implants by comparing rinsing with 0.12% CHX to irrigating using a specialized subgingival tip with 0.06% CHX. The researchers found that using a dilute of CHX with a water flosser was more effective than rinsing with CHX—29% versus 9% for plaque, and 45% versus 10% for gingivitis. The difference in bleeding between groups was 62% for irrigation and 33% for rinsing, but this did not reach significance. 29
Diabetic Patients
People living with diabetes have an increased risk for periodontal disease that can present earlier and be more severe. Finding ways to keep the inflammation in check is important and may require a more focused or rigorous homecare program. In a 3-month clinical trial, the water flosser was shown to be beneficial to this population. Fifty-two type 1 and type 2 diabetics were randomly assigned to one of two groups. Group 1 used a water flosser plus subgingival tip twice a day with manual brushing. Those in the control group continued with their current oral hygiene routine. At the end of 3 months, the irrigation group had significantly better improvements in gingivitis, plaque, and bleeding on probing compared to controls. 30
Multiple studies show a benefit for patients with varying degrees of gingivitis. 2,4,6,13-15 Others who may benefit are those with an increased risk of infection or inflammation, and even those who have relatively good homecare. 12 It is important to monitor risk, as situations and medical histories may change.
The research supports the recommendation and use of a water flosser for patients who present with different needs and concerns. There are multiple studies to help practitioners make informed decisions, and they should discuss these with their patients to help them improve their oral health. Clinicians should remind patients that it is never too early or too late to begin a good oral hygiene regimen. Rather than wait for a problem to arise, practitioners should prescribe devices and methods that their patients will like and use. It is especially helpful to instruct patients when they are young.
When evaluating an oral irrigator, dental water jet, or water flosser, clinicians should be aware that research on one device is not transferable to other devices. Each product should be reviewed based on the body of evidence specific to that particular product.
1. Hoover DR, Robinson HB. The comparative effectiveness of a pulsating oral irrigator as an adjunct in maintaining oral health. J Periodontol . 1971;42(1):37-39.
2. Lobene RR. The effect of a pulsed water pressure device on oral health. J Periodontol . 1969;40(11):667-670.
3. Phelps-Sandall BA, Oxford SJ. Effectiveness of oral hygiene techniques on plaque and gingivitis in patients placed in intermaxillary fixation. Oral Surg Oral Med Oral Pathol . 1983;56(5):487-490.
4. Sharma NC, Lyle DM, Qaqish JG, Schuller R. Comparison of two interdental cleaning devices on plaque removal. J Clin Dent . 2012;23(1):17-21.
5. Cutler CW, Stanford TW, Abraham C, et al. Clinical benefits of oral irrigation for periodontitis are related to reduction of pro-inflammatory cytokine levels and plaque. J Clin Periodontol . 2000;27(2):134-143.
6. Sharma NC, Lyle DM, Qaqish JG, et al. Effect of a dental water jet with orthodontic tip on plaque and bleeding in adolescent patients with fixed orthodontic appliances. Am J Ortho Dentofacial Orthop . 2008;133(4):565-571.
7. Al-Mubarak S, Ciancio S, Aljada A, et al. Comparative evaluation of adjunctive oral irrigation in diabetics. J Clin Periodontol . 2002;29(4):295-300.
8. Gorur A, Lyle DM, Schaudinn C, Costerton JW. Biofilm removal with a dental water jet. Compend Contin Educ Dent . 2009;30 Spec No 1:1-6.
9. Hurst JE, Madonia JV. The effect of an oral irrigating device on the oral hygiene of orthodontic patients. J Am Dent Assoc . 1970;81(3):678-682.
10. Cobb CM, Rodgers RL, Killoy WJ. Ultrastructural examination of human periodontal pockets following the use of an oral irrigation device in vivo. J Periodontol . 1988;59(3):155-163.
11. Drisko CL, White CL, Killoy WJ, Mayberry WE. Comparison of dark-field microscopy and a flagella stain for monitoring the effect of a Water Pik on bacterial motility. J Periodontol . 1987;58(6):381-386.
12. Chaves ES, Kornman KS, Manwell MA, et al. Mechanism of irrigation effects on gingivitis. J Periodontol . 1994;65(11):1016-1021.
13. Barnes CM, Russell CM, Reinhardt RA, et al. Comparison of irrigation to floss as an adjunct to tooth brushing: effect on bleeding, gingivitis, and supragingival plaque. J Clin Dent . 2005;16(3):71-77.
14. Sharma NC, Lyle DM, Qaqish JG, et al. Effect of a dental water jet with orthodontic tip on plaque and bleeding in adolescent patients with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop . 2008;133(4):565-571.
15. Rosema NA, Hennequin-Hoenderdos NL, Berchier CE, et al. The effect of different interdental cleaning devices on gingival bleeding. J Int Acad Periodontol . 2011;13(1):2-10.
16. Berchier CE, Slot DE, Haps S, van der Weijden GA. The efficacy of dental floss in addition to a toothbrush on plaque and parameters of gingival inflammation: a systematic review. Int J Dent Hyg . 2008;6(4):265-279.
17. Claydon NC. Current concepts in toothbrushing and interdental cleaning. Periodontol 2000 . 2008;48:10-22.
18. Kleber CJ, Putt MS. Formation of flossing habit using a floss-holding device. J Dent Hyg . 1990;64(3):140-143.
19. Christou V, Timmerman MF, van der Velden U, van der Weijden FA. Comparison of different approaches of interdental oral hygiene: interdental brushes versus dental floss. J Periodontol . 1998;69(7):759-764.
20. Lang WP, Farghaly MM, Ronis DL. The relation of preventive dental behaviors to periodontal health status. J Clin Periodontol . 1994;21(3):194-198.
21. Hujoel PP, Cunha-Cruz J, Banting DW, Loesche WJ. Dental flossing and interproximal caries: a systematic review. J Dent Res . 2006;85(4):298-305.
22. Bashkar S, Cutright DE, Gross A, et al. Water jet devices in dental practice. J Periodontol . 1971;42(10):658-664.
23. Selting WJ, Bhaskar SN, Mueller RP. Water jet direction and periodontal pocket debridement. J Periodontol . 1972;43(9):569-572.
24. Bhaskar SN, Cutright DE, Frisch J. Effect of high pressure water jet on oral mucosa of varied density. J Periodontol . 1969;40(10):593-598.
25. Burch JG, Lanese R, Ngan P. A two-month study of the effects of oral irrigation and automatic toothbrush use in an adult orthodontic population with fixed appliances. Am J Orthod Dentofacial Orthop . 1994;106(2):121-126.
26. Eakle WS, Ford C, Boyd RL. Depth of penetration in periodontal pockets with oral irrigation. J Clin Periodontol . 1986;13(1):39-44.
27. Larner JR, Greenstein G. Effect of calculus and irrigation tip design on depth of subgingival irrigation. Int J Periodontics Restorative Dent . 1993;13(3):289-297.
28. Braun RD, Ciancio SG. Subgingival delivery by an oral irrigation device. J Periodontol . 1992;63(5):469-472.
29. Felo A, Shibly O, Ciancio SG, et al. Effects of subgingival chlorhexidine irrigation on peri-implant maintenance. Am J Dent . 1997;10(2):107-110.
30. Al-Mubarak S, Ciancio S, Aljada A, et al. Comparative evaluation of adjunctive oral irrigation in diabetics. J Clin Periodontol . 2002;29(4):295-300.
About the Author
Deborah M. Lyle, RDH, BS, MS Director of Professional and Clinical Affairs Water Pik, Inc. Fort Collins, Colorado

- View All of Our Brands
- Advertisers
- Creative Services

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10212231

Effects of water flossing on gingival inflammation and supragingival plaque microbiota: a 12-week randomized controlled trial
1 The State Key Laboratory of Oral Diseases & National Clinical Research Center for Oral Diseases, West China Hospital of Stomatology, Sichuan University, Chengdu, Sichuan China
2 Department of Cariology and Endodontics, West China Hospital of Stomatology, Sichuan University, Chengdu, Sichuan China
Yishan Zhou
Chengcheng liu.
3 Department of Periodontology, West China Hospital of Stomatology, Sichuan University, Chengdu, Sichuan China
4 State Institute of Drug/Medical Device Clinical Trial, West China Hospital of Stomatology, Sichuan University, Chengdu, Sichuan China
5 Bixdo (SH) Healthcare Technology Co., Ltd., Shanghai, China
Xingqun Cheng
6 Department of Geriatric Dentistry, West China Hospital of Stomatology, Sichuan University, No. 14, 3rd section of Renmin South Road, Chengdu, 610041 Sichuan China
Associated Data
The data are available upon request from the corresponding author. The 16S rRNA sequencing raw data were deposited in the public database Sequence Read Archive ( http://www.ncbi.nlm.nih.gov/Traces/sra ) under accession number PRJNA861384.
The effects of water flossing on dental plaque removal have been suggested, but its ecological impact on dental plaque microbiota needs further investigation. In addition, whether this plaque control measure by water flossing promotes the control of halitosis still needs clinical validation. The aim of this study was to evaluate the effects of water flossing on gingival inflammation and supragingival plaque microbiota.
Materials and methods
Seventy participants with gingivitis were randomly assigned to control (toothbrushing) and experimental (toothbrushing + water flossing) groups ( n = 35). Participants were recalled at 4, 8, and 12 weeks, and their gingival index, sulcus bleeding index, bleeding on probing, dental plaque index, and oral malodor values were measured. The microbiota of supragingival plaque was further investigated using 16S rRNA sequencing and qPCR.
Sixty-three participants completed all revisits (control: n = 33; experimental: n = 30). The experimental and control groups exhibited similar clinical characteristics and dental plaque microbiota at baseline. Adjunctive water flossing effectively reduced the gingival index and sulcus bleeding index as compared to the toothbrushing control group. The water-flossing group showed reduced oral malodor at week 12 as compared to the baseline. Consistently, the water-flossing group exhibited altered dental plaque microbiota at week 12, characterized by a depletion of Prevotella at genus level and Prevotella intermedia at species level as compared to the toothbrushing control. In addition, the plaque microbiota of water-flossing group exhibited a more aerobic phenotype, while the control group was more anaerobic.
Conclusions
Daily water flossing can effectively alleviate gingival inflammation and reduce oral malodor, possibly by depleting oral anaerobes and altering the oral microbiota to a more aerobic phenotype.
Clinical relevance
Water flossing adjunctive to toothbrushing effectively alleviated gingival inflammation, representing a promising oral hygiene practice to promote oral health.
Clinical trial registration
The trial was registered in the Chinese Clinical Trial Registry ( http://www.chictr.org.cn/showprojen.aspx?proj=61797 , #ChiCTR2000038508) on September 23, 2020.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00784-023-05081-4.
Introduction
The periodontal diseases are highly prevalent and can affect up to 90% of the worldwide population [ 1 ]. Gingivitis is the most prevalent form of periodontal disease. According to the released data from the fourth national oral health epidemiology survey of China, the prevalence of gingival bleeding is over 87.4% in middle-aged and elderly people in China [ 2 ]. Gingivitis is typically caused by dental plaque accumulation. Streptococcus , Fusobacterium , Actinomyces , Veillonella , and Treponema , and possibly Bacteroides , Capnocytophaga , and Eikenella , are etiologically involved [ 3 ]. Microbial colonization and participation is sequential, with the complexity of the associated flora increasing with time [ 3 ]. Other local or systemic etiologic factors such as defective prosthesis, smoking, and hormones may also promote plaque deposition and/or predispose the host to microbial attack [ 4 ]. The ecological balance via both inter-microbial and host-microbial interactions plays a critical role in maintaining the gingival tissue health [ 5 ]. Disruption of this homeostatic balance leads to selective outgrowth of species with potential for destructive inflammation, and increases in the bacterial burden promote gingival inflammation in this condition [ 5 , 6 ]. Gingivitis is a key risk factor of periodontitis, and control of gingival inflammation is crucial for the primary prevention of periodontitis [ 7 ]. In addition, halitosis, which shares risk factors with periodontal diseases, is also common among patients with gingivitis or periodontitis [ 8 ].
Dental plaque control, typically by toothbrushing, is the most effective measure for preventing and treating gingivitis [ 9 ]. However, toothbrushing leaves approximately 40% of the dental plaque on the tooth surface [ 10 ]. A toothbrush combined with interdental cleaning device can achieve sufficient oral hygiene [ 10 , 11 ]. Regular flossing can remove up to 80% of the interproximal plaques as reported by American Dental Association [ 12 ]. Daily use of dental floss can effectively reduce the gingival inflammation and halitosis [ 13 , 14 ]. However, regular flossing requires time and skill, limiting its daily use [ 15 ]. Interdental brushes can effectively reduce the dental plaque between the teeth, and alleviate the gingival inflammation [ 16 , 17 ]. However, interdental brushes can only be used if there is sufficient space between the teeth, and we should choose the appropriate diameters; otherwise, the cleaning efficiency will be influenced and the periodontal tissue may be destroyed [ 17 , 18 ].
The power-driven water flosser, with claims of easy home use, has become a widely recommended oral hygiene product. Through pulsation and pressure, it disrupts plaque and removes loosely lodged debris, and can deliver antimicrobial solutions into the sulcus and interproximal regions [ 19 ]. The effects of water flossing on dental plaque removal and gingivitis management were better than those of regular floss and interdental brushes [ 20 , 21 ]. Water flossing adjunctive to manual toothbrushing can inhibit dental plaque formation and reduce the levels of pro-inflammatory factors, alleviating gingivitis and reducing periodontitis recurrence as compared to solely toothbrushing [ 22 - 24 ]. In addition, water flossing can alleviate gingivitis in orthodontic patients and manage peri-implant mucositis [ 25 , 26 ]. With the widespread acceptance and application of water flossing, the safety regarding its daily use has drawn increasing attention. Studies have demonstrated that daily use of water flosser for 3 months did not increase the risk of bacteremia during periodontal maintenance therapy [ 27 , 28 ]. In addition, water flossing was safe to be used on composite restorations with no influence on their surface roughness and color stability [ 29 ].
However, water flossing cannot completely eradicate dental plaque due to microbial recolonization on the tooth surface shortly after cleaning [ 30 ]. Long-term disturbance of oral microbiota by measures such as antimicrobial mouthwash (chlorhexidine) may have the risk of microbial dysbiosis and bacterial resistance [ 31 , 32 ]. Therefore, the long-term effect of water flossing on oral microbial ecology still needs clinical validation. In addition, whether this plaque control measure by water flossing promotes the control of halitosis, which is a common complaint among patients with gingivitis, still needs investigation. Here, we conducted a 12-week prospective clinical trial to investigate the effect of water flossing on gingival inflammation and bleeding, plaque accumulation, and halitosis in individuals with gingivitis, and the ecological impact of water flossing on oral microbiota was further evaluated.
Study participants
This article is reported according to CONSORT guidelines for reporting randomized clinical trials. This study was approved by the Research Ethics Committee of West China Hospital of Stomatology (WCHSIRB-D-2020-309) and was in agreement with the Declaration of Helsinki and complied with Chinese Good Clinical Practice (GCP) regulations. All participants were recruited at the West China Hospital of Stomatology, Sichuan University, and signed informed consent. The trial was registered in the Chinese Clinical Trial Registry ( http://www.chictr.org.cn/showprojen.aspx?proj=61797 , #ChiCTR2000038508) on September 23, 2020.
The participants were aged 18–65 years with no systemic diseases. All participants had intact Ramfjord teeth (16, 21, 24, 36, 41, 44) in the oral cavity. Participants had gingivitis, with a modified gingival index ≥ 1, dental plaque index ≥ 1.5, and gingival sulcus depth < 3 mm [ 33 ]. Participants were excluded if they had periodontitis, had undergone surgical/non-surgical periodontal therapy or antibacterial/hormonal drug therapy in the last 6 weeks, had participated in other clinical trials within the last 3 months, had an allergic constitution, or were pregnant [ 34 ].
Experimental design
This was a single-center, randomized controlled clinical trial with a duration of 14 weeks (2-week washout and 12-week treatment phase) (Fig. 1 ). The washout phase was introduced to normalize the oral hygiene habits of participants as also suggested by Sreenivasan et al. [ 35 ]. Participants who met the inclusion and exclusion criteria were recruited in the 2-week washout phase, and were instructed to brush their teeth with Bass brushing technique twice daily for 3 min using Crest herbal crystal toothpaste and a Crest triple care toothbrush (P&G Technology Co., Ltd., Beijing, China). Participants were asked not to use antibiotics/hormonal drug and have periodontal therapy during the washout phase. These participants were re-screened according to the inclusion and exclusion criteria at baseline, and then were enrolled in the 12-week treatment phase.

Schematic of study design
The sample size was calculated using G*Power 3.1 software and was based on the primary data of gingival bleeding. Based on inequality and two independent groups (Fisher’s exact test), the sample size was determined to be 60, with an 0.05 alpha level (type II error) and 90% power (type I error). Considering a 15% dropout rate, 70 participants were eventually enrolled in this study.
The participants were randomly allocated to two groups ( n = 35/group) using a computer-generated randomization list. The control group only brushed their teeth with Bass brushing technique twice daily for 3 min using abovementioned toothbrush and toothpaste, but the experimental group was additionally instructed to use a Bixdo P50 water flosser (Bixdo SH Healthcare Technology Co., Ltd., Shanghai, China) to irrigate all the teeth in the oral cavity with water for 3 min immediately after toothbrushing. Participants were recalled at 4, 8, and 12 weeks, and their modified gingival index, sulcus bleeding index, bleeding on probing (BOP), dental plaque index, and oral malodor values were determined. Supragingival plaque samples were also collected. Participants were asked to refrain from brushing, flossing, eating, and drinking anything other than water for 4 h prior to sample collection visits. The names and groups of the participants were covered for blinding to those collecting samples or clinical assessments. Over the experimental period, participants received weekly oral hygiene instruction and supervised plaque removal using the devices assigned for each group.
Periodontal examination and supragingival plaque collection
Periodontal examination was performed by an operator, previously trained until reaching a low intra-operator variability, using an UNC-15 periodontal probe with a controlled (ca. 0.25 N) force. The gingival sulcus depth (distance from the gingival margin to the bottom of the gingival sulcus, evaluated at each tooth surface, for all teeth), modified Loe–Silness gingival index (assessment of gingival color, texture, and bleeding tendency, evaluated at four specific sites of each tooth), sulcus bleeding index (assessment of gingival bleeding, with a score of 0–5 per site), BOP (recorded based on the presence or absence of bleeding up to 20 s after probing at the experimental sites), and dental plaque index (evaluation of the presence of plaque, with a score of 0–5 per site) were measured [ 36 ]. After drying saliva off the collection site, supragingival plaque samples were collected from facial and lingual sites of all six Ramfjord teeth of each subject, by using a sterile curette. Scraped plaque was immediately transferred to and dispersed in 1 × phosphate-buffered saline in a sterile microcentrifuge tube. The plaque sample was divided into three parts after vibration and stored at − 80 °C until analysis.
Oral malodor measurement using a halimeter
Oral malodor values were measured using a halimeter (RH-17 K; Interscan Co., Chatsworth, CA). Subjects refrained from any oral activity, such as food intake, for at least 2 h pre-measurement. The subjects were instructed to close their mouths for 3 min (using only nasal breathing) before every measurement, followed by placing a straw, connected to the halimeter, 4-cm deep into their mouth. The measurement was performed automatically, and the mean value of three consecutive measurements was used for analysis [ 37 ].
16S rRNA sequencing
Barcoded 16S rRNA amplicon (V3–V4 regions) sequencing was performed using Illumina MiSeq technology (Personalbio, Shanghai, China) and primers F (5′-ACTCCTACGGGAGGCAGCA-3′) and R (5′-TCGGACTACHVGGGTWTCTAAT-3′). A unique 12-mer tag for each DNA sample was added to the 5′-end of both primers to allow pooling of multiple samples in one run. The PCR products were visualized on a 3% agarose gel, gel purified, quantified with a Pico-Green kit, pooled in an equimolar ratio, assessed using an Agilent BioAnalyzer 2100 (Invitrogen, Carlsbad, CA), and sequenced. Sequences were trimmed using Trimmomatic 2 based on a quality score of 20, and pair-end reads were merged into longer reads using FLASH 3. Unqualified sequences were removed if they were too short or if they contained ambiguous residues. Operational taxonomic units (OTUs) were clustered using Usearch (version 7.1, http://drive5.com/uparse/ ) at a 97% similarity level. The final OTUs were generated based on clustering results. The raw sequencing data were deposited in the public database Sequence Read Archive ( http://www.ncbi.nlm.nih.gov/Traces/sra ) with accession no. PRJNA861384.
Before bioinformatic analysis, sequencing reads of all samples were standardized by rarefying OTU tables to the minimum read number. Analyses were performed using the online Majorbio Cloud Platform ( www.majorbio.com ) [ 38 ]. The Kruskal–Wallis H and Wilcoxon rank-sum tests were used to compare differences in taxa. Alpha diversity was calculated in terms of Chao, Shannon, and Simpson indices and was compared using the Wilcoxon rank-sum test. Beta diversity was assessed by principal coordinate analysis (PCoA) or non-metric multidimensional scaling (NMDS) analysis using weighted-unifrac distance and Adonis with 999 permutations. Analysis of similarity values and heatmaps were constructed using R (version 3.3.1; https://www.r-project.org/ ) “vegan” (version 2.4–3) package. Linear discriminant analysis (LDA) of the effect size (LEfSe) was performed to identify the significant taxa that most likely explained the differences between groups, with a threshold LDA score of 2. Bugbase was used for the predictions of the functional profile of a microbial community based on 16S rDNA sequence data. BugBase is able to predict seven phenotype types, including gram-positive, gram-negative, biofilm forming, pathogenic, mobile element containing, oxygen utilizing, and oxidative stress tolerant. A p value of < 0.05 was considered statistically significant in the current study.
Bacterial quantification
Quantitative polymerase chain reaction (qPCR) was used to quantify dental plaque bacteria. qPCR amplification was performed using the CFX96 system (Bio-Rad, Hercules, CA). The 25-μl reaction mixture contained the SYBR reaction mix (TaKaRa, Kusatsu, Japan), template DNA (100 ng), and forward and reverse primers (500 nM each). Thermal cycling conditions were as follows: initial denaturation at 95 °C for 30 s, followed by 40 cycles each consisting of 95 °C for 15 s, and 60 °C for 30 s. Threshold cycle (CT) values were determined, and the relative abundance was calculated based on the 2 −ΔΔCT method. Porphyromonas gingivalis , Fusobacterium nucleatum , Actinobacillus actinomycetemcomitans , and Prevotella intermedia were quantified using primers listed in Table S1 . Each sample was examined in triplicate.

Statistical analysis
Statistical analysis of data other than 16S rRNA sequencing was performed using SPSS software (version 16.0; SPSS Inc., Chicago, IL) and GraphPad Prism 8 (GraphPad Software Inc., La Jolla, CA). Categorical variables are presented as natural frequencies, and continuous variables as mean ± standard deviation. The clinical characteristics of the participants were analyzed using Kruskal–Wallis (with Dunn–Bonferroni post hoc) or chi-squared tests. Within-group and between-group differences in gingival, sulcus bleeding, and dental plaque indices, BOP%, and oral malodor values were analyzed by repeated measure (RM) ANOVA, followed by Bonferroni post hoc tests and Student’s t tests, respectively. Other data were analyzed using one-way ANOVA, followed by Tukey’s test or the Student–Newman–Keuls test to compare all pairs of groups. Data were considered significantly different if the two-tailed p value was < 0.05.
Clinical characteristics of the study participants
This study enrolled 70 gingivitis participants, of which seven dropped out, who missed the recall time due to closed management amid COVID-19 outbreak. Thirty-three control and 30 experimental participants attended all recall visits. The baseline clinical characteristics are shown in Table Table1. 1 . Demographics, gingival, and halitosis parameters were similar between the groups ( p > 0.05). No adverse reaction including gingival recession reported during the 12-week experimental period in terms of water flossing.
Clinical characteristics of the participants at baseline
Continuous variables are presented as mean ± standard deviation. Categorical variables are presented as natural frequencies
M male, F female, BMI body mass index
Effects of water flossing on clinical parameters
The effects of water flossing on periodontal parameters, dental plaque index, and oral malodor were assessed. Two-way RM-ANOVA identified time and group as statistically significant factors ( p < 0.05) in the gingival index, sulcus bleeding index, and BOP% (Table (Table2). 2 ). These indices improved significantly in both groups at all observation time points (weeks 4, 8, 12) compared with baseline ( p < 0.05). However, the improvement in the control group slowed after 4 weeks. Gingival index and sulcus bleeding index at weeks 8 and 12 were significantly better in the experimental than in the control group, and BOP% improved significantly in the experimental group at weeks 8 as compared with the control group (Table (Table2). 2 ). These results suggest that water flossing had a good clinical effect on managing gingival bleeding and inflammation.
Two-way repeated-measure ANOVA analysis results of the clinical parameters
W week, RM-ANOVA analysis repeated-measure ANOVA analysis
# Significant differences compared with the baseline in the control group
$ Significant differences compared with the baseline in the experimental group
* Between-group differences at the same time point
* p < 0.05, ** p < 0.01
Two-way RM-ANOVA of the dental plaque index identified time as a statistically significant factor ( p < 0.05), with significant differences among time points (Table (Table2). 2 ). However, the control and experimental groups did not differ at any time point (Table (Table2). 2 ). There was no significant difference in the oral malodor values between groups after the use of the respective oral hygiene regimens (Table (Table2). 2 ). However, the value was significantly decreased after 12-week water flossing as compared with that at baseline in the experimental group (Table (Table2 2 ).
Effects of water flossing on dental plaque microbiota
The 16S rRNA sequencing data are detailed in the supplementary information (Fig. S1 ). In total, 20.71 million high-quality 16S rRNA sequences were generated from the supragingival plaque samples of 33 control and 30 experimental participants at 0, 4, 8, and 12 weeks (length range 408–480 bp, average length 464.36 bp). After subsampling each sample to equal sequencing depth and clustering, 6442 OTUs with 97% identity were obtained. Good’s coverage for the observed OTUs was 99.72 ± 0.09%, and the rarefaction curves showed clear asymptotes, which together indicated a near-complete sampling of the community.
The α and β diversity of the baseline dental plaque samples showed no significant difference between the two groups, suggesting that the baseline dental plaque microbiota structure of the two groups was comparable (Fig. S2 A and B). Although the PCoA analysis showed no significant difference in the microbiota community structure between the groups, the p value approximated 0.05 ( p = 0.056). NMDS analysis revealed a significant difference between the groups ( p = 0.012) (Fig. S2 C). PCoA and NMDS analyses demonstrated significant differences between the control and experimental groups at week 12 (PCoA: p = 0.038, NMDS: p = 0.029), and samples could be clearly distinguished and clustered into two groups (Fig. 2 A). These results indicate that, after 12 weeks, the dental plaque microbiota of the two groups were distinct, suggesting that water flossing changed the microbial structure.

Comparison of the microbiota community structure and composition between the control and water flossing group. A Principal coordinate analysis (PCoA) and non-metric multidimensional scaling (NMDS) analysis of the dental plaque samples from control and experimental groups at week 12. B Heatmap analysis of the top 30 abundant bacterial taxa at genus level. C Linear discriminant analysis of the effect size (LEfSe) analysis at week 12. D Intergroup difference analysis of the top 15 abundant bacterial taxa at genus level at baseline. E Intergroup difference analysis of the top 15 abundant bacterial taxa at genus level at week 12. F Relative quantification of Porphyromonas gingivalis , Fusobacterium nucleatum , Actinobacillus actinomycetemcomitans , and Prevotella intermedia at weeks 4 and 12 as compared to baseline. * p < 0.05, ** p < 0.01
Further analysis of the top 30 abundant bacterial taxa revealed genus-level differences between the control and water-flossing groups (Fig. 2 B). The abundance of Aggregatibacter , Porphyromonas , Prevotella , and Fusobacterium increased over time in the control, but not in the experimental group (Fig. 2 B). There was no significant difference in the top 15 most abundant bacterial taxa between groups at baseline (Fig. 2 D). However, after 12 weeks, the water-flossing group exhibited significantly lower Prevotella and higher Corynebacterium genus as compared with the control group (Fig. 2 C, E). qPCR showed no difference in the relative abundance of Porphyromonas gingivalis , F. nucleatum , and A. actinomycetemcomitans between the groups at weeks 4 or 12, as compared to baseline, but the abundance of Prevotella intermedia in the experimental group was significantly lower at week 12 than week 4 or that in the control group at week 12 (Fig. 2 F).
The BugBase phenotype prediction showed no significant difference in the seven metabolic phenotypes between the control and experimental groups at baseline (Fig. 3 A). At week 4, the water-flossing group exhibited significantly higher aerobic phenotype, while the control group exhibited significantly higher anaerobic and gram-negative phenotypes (Fig. 3 B). At week 12, the water-flossing group still exhibited significantly higher aerobic phenotype, while the control group exhibited significantly higher anaerobic phenotype (Fig. 3 C). These data further suggest that water flossing may benefit periodontal health by altering the microbial composition and reducing the virulence of the dental plaque.

Phenotype prediction of the dental plaque community. A . BugBase phenotype prediction of the control and experimental groups at baseline. B . BugBase phenotype prediction of the control and experimental groups at week 4. C . BugBase phenotype prediction of the control and experimental group at week 12. * p < 0.05, ** p < 0.01
Gingivitis is a typical plaque-related oral diseases, and plaque control has been proved to be an effective way to prevent and treat this disease. Accumulating evidence has demonstrated that water flossing can ameliorate gingival inflammation by removing dental plaque [ 25 , 39 , 40 ]. Although relatively easy and safe to apply as a daily oral hygiene instruction, the ecological impact of water flossing on oral microbiota after long-term use has yet to be investigated. In addition, as oral malodor is usually accompanied with periodontal diseases including gingivitis and periodontitis, whether or not water flossing can benefit oral malodor control still needs clinical validation. Here, we performed a prospective clinical trial to investigate the effects of water flossing on plaque accumulation, gingival inflammation, and halitosis, as well as the ecological impact on supragingival plaque microbiota in a duration of 12-week application. We demonstrate that water flossing is an effective adjuvant to control gingival inflammation.
Water flossing promotes gingival health by facilitating removal of dental plaque. Here, we found that both water-flossing and toothbrushing groups exhibited ameliorated gingival inflammation as reflected by gingival index, sulcus bleeding index, and BOP%. More importantly, the gingival and sulcus bleeding indices in the water-flossing group were lower than those in toothbrushing control at 8 and 12 weeks, indicating that adjunctive application of water flossing to toothbrushing can better promote periodontal health. Consistently, several randomized controlled trials found that the addition of a water flosser to toothbrush could significantly reduce the BOP, gingival index, and plaque index at 4-week compared with the toothbrush alone [ 39 , 41 ]. Of note, although both groups exhibited significantly reduced plaque accumulating as reflected by dental plaque index, no significant between-group difference in dental plaque index was observed in this study. Studies also demonstrated that although use of water flosser plus manual toothbrushing significantly reduced the plaque index at 8-week compared with that at baseline, no between-group difference was achieved [ 42 , 43 ]. The possible explanation is that dental plaque may have reformed overnight as the participants were instructed not to brush, floss, or eat for 4 h prior to sample collection. Moreover, the participants received good oral hygiene instruction and supervision during the study, and this may overwhelm the differences in dental plaque accumulation between the adjunctive water-flossing group and toothbrushing control group.
As water flossing is a well-recognized oral hygiene technique via active agitation and removal of supragingival dental plaque, whether its daily use may pose long-term disturbance on oral microecology is worth clinical validation. Here, we observed an altered microbial structure and composition after 12-week use of the respective oral hygiene regimens. More importantly, we also observed that periodontal anaerobes, such as P. intermedia , was depleted in the water-flossing group, while this anaerobe increased in toothbrushing control during the 12-week study. P. intermedia , known as “orange complex” species, is associated with gingivitis and periodontitis [ 44 ]. P. intermedia can stimulate the release of proteinases, matrix metalloproteinases, and proinflammatory cytokines, and favors the colonization of red complex species (i.e., P. gingivalis , Treponema denticola , Tannerella forsythia ), triggering dental plaque dysbiosis and contributing to gingival inflammation, and eventually periodontitis [ 35 , 44 ]. Consistently, we found that the oral microbiota of individuals using water flossing was prone to an aerobic phenotype, while the oral microbiota of the toothbrushing control was characterized with anaerobic and gram-negative phenotypes. Periodontal pathogens are mostly gram-negative anaerobes, enrichment of which can shift the composition and structure of the microbial community, leading to a breakdown of the normal homeostatic state [ 45 ]. It is speculated that water flossing may increase the presence of oxygen in the dental plaque, and thus favor the outgrowth of aerobes over anaerobic species. In addition, we also found that Corynebacterium genus was increased after 12-week use of water flosser. Corynebacterium genus is an important bridge organism in dental plaque, which is usually enriched in the periodontal healthy group, and is negatively associated with probe depth in patients with chronic periodontitis [ 46 , 47 ]. Our findings indicate that water flossing may benefit gingival health by altering microbial composition, preventing overgrowth of oral pathobionts, and promoting anerobic phenotype of the dental plaque.
In addition to gingival inflammation, oral malodor, which is mainly derived from the metabolic production of volatile sulfur compounds (VSCs) by periodontal anaerobes, is usually accompanied with periodontal conditions such as periodontitis and gingivitis [ 48 , 49 ]. Although there still lacks clinical evidence, it is conceivable that water flossing may help reduce oral malodor by alleviating gingival inflammation and reducing oral anaerobes. The current study measured the halimeter score of participants during the 12-week use of water flosser. We found that participants in the water flossing group had significantly lower oral malodor values at week 12 as compared to its baseline. This may be accredited to the reduced anaerobes and relative aerobic phenotype of dental plaque in the water flossing group.
In conclusion, the current study demonstrates that water flossing can effectively alleviate gingival inflammation and reduce oral malodor, possibly by depleting oral anaerobes and altering the oral microbiota to a more aerobic phenotype.
Below is the link to the electronic supplementary material.
Acknowledgements
This project was supported by clinical research projects of the State Institute of Drug/Medical Device Clinical Trial, West China Hospital of Stomatology, Sichuan University (QX2020-02-01, QX2020-02-02), the Technology Innovation Research and Development project of Chengdu (2021-YF05-01866-SN), and the research fund from the West China School/Hospital of Stomatology, Sichuan University (LCYJ2019-4, RCDWJS2021-16).
Author contribution
XX contributed to the conception, design, data interpretation, and drafted and critically revised the manuscript; YZ contributed to data acquisition and analysis; CL, LZ, LZ, HL, and YL contributed to conception, design, data analysis, and critically revised the manuscript; XC contributed to the conception, design, data acquisition, analysis, and interpretation, and drafted and critically revised the manuscript. All authors critically revised and approved the final manuscript for submission.
Data availability
Declarations.
XX reports grants from Bixdo SH Healthcare Technology Co., Ltd., Shanghai, China, during the conduct of the study. XC reports grants from Science and Technology Bureau of Chengdu, China, during the conduct of the study. YL reports three patents licensed. The authors YZ, CL, LZ, LZ, and HL declare no conflict of interest regarding this work.
This study was approved by the Research Ethics Committee of West China Hospital of Stomatology (WCHSIRB-D-2020-309). The study procedures were conducted in accordance with the principles outlined in the Declaration of Helsinki and complied with the laws and regulations covering Good Clinical Practice (GCP) in China. All participants provided written informed consent.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Advertisement
- Health and fitness
- Personal care
The Best Water Flossers

By Nancy Redd
Nancy Redd is a writer who covers health and grooming. She has tested dozens of hair dryers, toothbrushes, and pairs of period underwear.
Water flossers, also known as oral irrigators, cost a lot more up-front than string floss. And they can still be pretty uncomfortable to use—get ready to drool. Also, there’s no clear evidence that they’re superior to traditional floss. Yet some people really like the way the water jets feel between their teeth, and some find it’s easier to work with a wand than a piece of string. Of the 14 models we’ve tested, we recommend the Waterpik Ion , a compact traditional water flosser with a cordless charging base. It cleans mouths thoroughly and takes up less counter space than most of its competitors.
Everything we recommend

Waterpik Ion
Customizable, cordless charging.
This countertop flosser made our mouths feel the cleanest, and it can operate cordlessly (between the unit and the wall), which saves a ton of counter space.
Buying Options
Waterpik Aquarius Professional
Just as effective, but bulkier.
This model cleans just as well as our pick, and it has the same warranty and 10 pressure settings. But it’s slightly larger, and it requires an outlet and more counter space.

Philips Sonicare Power Flosser 3000 Cordless
Powerful and portable.
This handheld, battery-operated cordless model is powerful and more portable than our countertop picks.
Budget pick
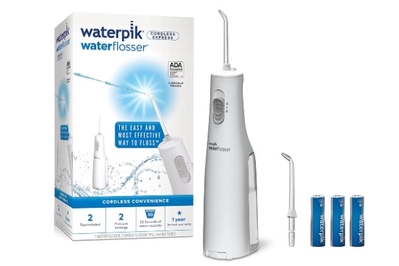
Waterpik Cordless Express
Smaller tank, non-rechargeable batteries.
Another portable, handheld model, this flosser requires AA batteries and more-frequent refilling when compared with our other cordless pick.
How we picked
A larger tank allows you to floss longer without having to refill.
Some models are bulkier than others, which can make a difference on already crowded countertops.
Models that run on batteries (either rechargeable or replaceable) can be helpful when there’s no convenient outlet near your sink.
Customizing the pressure of your water stream can make your flossing experience more enjoyable and comfortable.
Testers unanimously chose the Waterpik Ion as the best countertop water flosser both in terms of cleaning and saving counter space. It tied with our runner-up pick, the Waterpik Aquarius Professional , for being the “most likely to deliver that ‘just left the dentist’ feeling.” But the Ion’s unique cordless charging base is a significant upgrade because it successfully mitigates one of the biggest hurdles we’ve had with traditional water flossers: needing an outlet near your countertop. (A cord connects the flossing device to the countertop water tank.)
The Ion has 10 pressure settings and comes with multiple tips of different stream widths. So you should be able to dial in a setting with the mix of comfort and effectiveness you prefer. This model also comes with a three-year warranty, which is as long as we’ve seen.
The Waterpik Aquarius Professional cleans mouths just as well as the Ion, and it has the same 10 pressure settings and three-year warranty. This model does, however, require more counter space than most flossers, and it needs to be plugged in while you use it. Even so, we found it easy to use and clean, like the Ion. The Aquarius Professional is the only one of our picks that comes with a “massage” setting, which emits pulses of water.
If you’d like to use a water flosser in places other than at the sink (such as in the shower), consider the Philips Sonicare Power Flosser 3000 Cordless . It’s a portable, cordless flosser that’s as powerful as our other picks. Unlike its countertop counterparts (which feature large water reservoirs and handheld sprayers), this battery-operated flosser combines the sprayer with a single-use reservoir, for an all-in-one, handheld experience. Plus, this model fits in a bathroom drawer (or a suitcase) between uses.
The Waterpik Cordless Express is the best cordless water flosser under $50 we’ve tested. Its reservoir is a lot smaller than that on the Power Flosser 3000 Cordless (5 ounces versus 8), and it produces a less powerful stream, but it gets the job done—for half the price of the Power Flosser 3000 Cordless.
The research
Why you should trust us, who this is for, how we picked and tested, our pick: waterpik ion, runner-up: waterpik aquarius professional, also great: philips sonicare power flosser 3000 cordless, budget pick: waterpik cordless express, other good water flossers, the competition.
We spoke with Jessica Hilburg , then associate dean for clinical affairs at NYU College of Dentistry and now a clinical associate at the University of Pennsylvania School of Dental Medicine, and Ruchi Sahota , a dentist in Fremont, California, who serves as a media spokesperson for the American Dental Association (ADA). We also spoke with Chhaju Ram Goyal, co-founder and director of All Sum Research Center (an independent research lab in Canada that tests oral-health-care products), whose name is on much of the scientific research related to water flossers (though, that research was paid for and designed by none other than Waterpik).
If you won’t or can’t use dental floss , and you don’t mind spending some cash on a device that might break or get disastrously moldy, consider a water flosser.
Water flossers are an alternative (or an addition) to string floss. They don’t require the same dexterity that string floss does (though you still need fine-motor skills). They can make it easier to clean around braces . And they are arguably more fun to use than string floss.
But they’re also pricier, bulkier, and fussier. Even using a generous 18 inches of string per floss —which allows you to use a new section of string for each tooth—you’ll go through under $10 worth of floss per year. By contrast, the least expensive water flossers cost about $40. Plus, you’ll need to clean your water flosser from time to time, but string floss is maintenance-free.
Only your own dentist can tell you whether a water flosser is the best choice for your oral hygiene, according to the dentists we spoke with. “Everyone’s teeth are different, everyone’s gums are different,” Ruchi Sahota , a dentist in Fremont, California, said. If you embark on a water-flosser experiment, get feedback from your dentist about how well it’s working.
By and large, it’s unclear how water flossers compare to regular string floss in terms of cleaning. Water flossers that bear a seal from the American Dental Association (ADA) have been evaluated by the organization and are shown to clean teeth better than a toothbrush alone. However, the ADA doesn’t compare water flossing to string flossing. (The ADA isn’t entirely independent of companies that sell dental goods: Member companies pay the organization a fee to evaluate their products. The ADA designs and controls the evaluations itself, though.) There’s a paper arguing that water flossers are superior to string floss . But the research was funded and overseen by Waterpik. Thus, we’re skeptical of the results, even though the journal the paper appeared in is peer reviewed by an editorial board of dentists.
Actually, the evidence that even string flossing improves overall oral health isn’t of great quality . But the ADA recommends some sort of daily flossing, and the experts we spoke with likened interdental cleaning to any other routine hygiene step. “There might not be a study, but most people would agree that taking a shower is a good thing,” said Jessica Hilburg, who at the time of our interview was associate dean for clinical affairs at NYU College of Dentistry. Sahota likened it to cleaning out any of the little crevices on your body, like your belly button.

There are dozens upon dozens of water flossers available. Over five years of testing these devices, we’ve considered a mix of countertop and portable, corded and cordless models in a variety of sizes, favoring those with the most favorable customer reviews and/or the ADA Seal of Acceptance .
We pinpointed the features that will have the biggest impact on what it’s like to use a particular water flosser:
- Tank size: Many flossers don’t hold enough water to work through your whole mouth. Having a larger tank can be nice because it allows you to focus on any trouble spots (like a stubborn fleck of popcorn) or do a touch-up without having to refill.
- Power source: Some flossers need to be plugged into the wall during use, and some are cordless. Some cordless models have a built-in rechargeable battery; others run on replaceable batteries.
- Counter space: Some models take up a bit more space than an electric toothbrush, whereas others need as much room as a couple of rolls of toilet paper.
- Settings: The more you can adjust the water stream, the better you can adjust the flosser’s feel to your exact preferences.
- Tips: All water flossers shoot water out of a removable tip, allowing multiple people in a household to use the same device without sharing germs. Some models have holsters for multiple tips, while others have no storage. Some come with a range of tips that vary the stream width, though not all of these are useful.
No matter which model you pick, buy a water flosser only if it’s under warranty. Across the category, water flossers tend to fail easily: They can leak, wane in strength, or simply give up the ghost. Our picks have earned fewer customer complaints than the competition. But your best option is to buy something with a long warranty (two or three years is typical), and be prepared to file a claim if needed.
We rotated through our selection of finalist flossers for several weeks (the experience of using them was so satisfying and novel that one tester water-flossed upwards of four times a day). We are continuing to test them over the long term.

The Waterpik Ion is the best countertop water flosser. It cleans mouths thoroughly, and it is highly adjustable. And, thanks to its cordless charging base, the Ion can be used in all types of bathrooms—regardless of whether there’s an outlet nearby. The removable charging cord can be stored anywhere and brought out every few weeks to recharge the flosser. The Ion features a strong, steady water stream. And it has a larger-than-average, 26-ounce water tank (with a wide, easy-to-refill mouth), which holds enough water to floss between each tooth and then some.
Like many Waterpik countertop flossers, the Ion has 10 pressure settings, so you can find the perfect water-stream strength. This model also comes with six tips that offer different stream widths. But unlike other flossers, the Ion has a magnetized handle cradle, which makes it easier to store the handle and the cord that connects it to the reservoir compactly.
The Ion takes up less counter space than other countertop flossers we’ve considered, including our runner-up pick, the Waterpik Aquarius Professional . Because with the Ion you’re not tied to an outlet, you can move the device wherever on the counter you prefer.
As with most flossers that produce a constant flow of water, you’ll have to learn how to artfully drool while using the Ion.

The Ion is one of the easiest water flossers to refill after each use or so (a requirement of all flossers) and to wipe out regularly: It has a wide, dishwasher-safe reservoir that is easily removed and that doesn’t have any hard-to-reach nooks and crannies. The tank lid attaches to the unit and flips up, so there’s nothing to set aside while you fill and clean the tank. It holds around 90 seconds’ worth of water, which gives you plenty of time (and then some) to floss your entire mouth. One tester found they could do a quick floss in about 30 seconds; if they spent more than a minute, their teeth felt fantastically clean.
The Ion comes in two colors (black and white) and is warrantied for three years.
Flaws but not dealbreakers
Although Waterpik claims the Ion can last for a month between charges, we needed to recharge the device every three weeks or so when water flossing every day. Even so, we found this model to be a worthwhile upgrade over having to keep a countertop flosser plugged in at all times in order to run it.
There’s no place to store the included extra tips, so if that is more important to you than cordless charging, consider our runner-up pick, the Aquarius Professional .
Like most water flossers, the Ion is slightly noisy (similar to electric razors and many bathroom electronics), but not terribly so.
Because of its continuous stream, the Ion (like all of our picks) involves a learning curve. That stream means your mouth fills up with water pretty quickly. You’ll either have to pause to spit several times during a flossing session or learn to let it dribble out (even the official Waterpik literature features an image of a person straight-up drooling ). And if you pull the nozzle out of your mouth too quickly, you’ll send water spraying across the bathroom.

If plugging in is not an issue, the Waterpik Aquarius Professional is a solid water flosser that offers a similar experience to that of our pick, the Ion . The Aquarius made our mouths feel totally clean, thanks to its strong, continuous stream (which is similar to the Ion’s). This model also ties with the Ion for having the most stream pressure settings and tips of all the flossers we tested. So the Aquarius Professional gives you the best chance of finding the pressure, pulse, and stream size that feels good to you.
With the Aquarius Professional, there’s no charging system or batteries to contend with because it plugs into the wall via a 4-foot electrical cord. (Though, unlike the Ion, this model must remain plugged in to operate.) Although there are more reports of it breaking down or becoming caked with mold than we’d like , in five years of research and long-term testing, we’ve found the Aquarius Professional to be a reliable device.
Though the Aquarius Professional is not quite as easy to clean as the Ion, it does have a wide, dishwasher-safe reservoir that holds plenty of water for at least a single flossing session. This model, in part due to the bulky cord, takes up more counter space than our other picks. As with all of our picks, with the Aquarius Professional you’ll be drooling a lot because of the constant water flow. Unlike our other picks, this model has two modes (for a regular “floss” stream or a “massage” mode, which shoots pulses of water), and it comes with seven different tips (same as the Ion).
The floss mode delivers a continuous stream of water, which we found to be the most effective for cleaning. On the strongest setting, it actually made one of our tester’s gums bleed, possibly because they were not used to flossing. Some water-flosser manuals acknowledge a week or two of bleeding as part of the “training period,” when your gums get used to being power-washed.
The massage mode is a pulsing stream. This mode also felt like it cleaned well, and it filled our mouths with water at a slower rate, which in turn made for less awkward drooling. The massage mode could be helpful for folks who prefer a gentler stream.
The Aquarius Professional comes with seven basic tips offering five different types of water streams (though you probably wouldn’t use most of them on a regular basis). Unlike the Ion, this model has a spot next to the tank to store tips; this is handy if you want to share the flosser with family members or switch between a couple of tips yourself. The curly cord that connects the handle to the tank is about 33 inches long, an inch shorter than the Ion’s.

Like the Ion, the Aquarius Professional comes with a three-year warranty. It is available in four colors: black, white, blue, and gray.

A cordless water flosser can be a useful tool for both portability and space-saving purposes. The best one we’ve tested is the Philips Sonicare Power Flosser 3000 Cordless . It is, as one reviewer called it, “like a power washer for your teeth .”
Because it’s an all-in-one device, with the water reservoir attached to the handheld sprayer, this model is much wider and heavier to hold than our other picks. When they are filled with water, cordless water flossers, including this one, can weigh more than a pound—versus the single ounce of most countertop flosser handles. (If you have hand-grip issues, a cordless water flosser may not be right for you.)
However, the Power Flosser 3000 Cordless has an impressively strong water stream to rival those of countertop flossers, and it offers an extremely pleasant and versatile flossing experience. And unlike our countertop picks, this one is fully waterproof—you can use it in the shower. We found this extremely helpful both for remembering to floss and for limiting cleanup (what better place to drool on oneself than in the shower?).
The Power Flosser 3000 has a rechargeable battery (and comes with a USB-C charging cord). And it can hold a lot more water than most cordless flossers (over 8 ounces), so most people won’t have to refill during a single flossing session. It holds enough water or mouthwash (or other antibacterial solutions) for almost an entire minute of spray (give or take 10 seconds, depending upon your settings); this is usually enough to complete a single floss.
The Power Flosser 3000 comes with two nozzles, has two flossing modes (“clean” and “deep clean”), and has three stream intensities, which our testers enjoyed tooling with. It comes in three colors (white, black, mint green).
As with those of our other picks, this model’s water reservoir can go in the dishwasher; weekly cleaning is recommended.
The Power Flosser 3000 Cordless comes with a two-year warranty (our two countertop picks have three-year warranties).

The Waterpik Cordless Express is a great flosser under $50. But, unlike our other cordless flosser pick, the water tank on this model requires refilling mid-floss.
With just two settings and a single stream intensity, the Cordless Express is much simpler than our other picks. It holds enough water or mouthwash (or other antibacterial solutions) for 30 seconds of spray, which is generally not enough to complete a full floss. It’s easy to fill, however, so you can be back to drooling in mere seconds (especially when flossing in the shower ).
The Cordless Express uses three AA batteries, instead of plugging into the wall with a charging cord, so you’ll want to have extra batteries on hand (or use rechargeable ones ). Removing and replacing the batteries is an easy process, as is cleaning the device. And, as with our other picks, this model’s water reservoir can go in the dishwasher; weekly cleaning is recommended.
This model comes with two tips—like our cordless pick from Philips Sonicare. But the Cordless Express is compatible with all other Waterpik tips.
This flosser’s body has a useful grip pattern, to help you avoid dropping the device. But people with smaller hands may have difficulty holding its 5-inch circumference, which is much more unwieldy than the comparatively slim Power Flosser 3000 Cordless.
The Cordless Express has a one-year warranty (much shorter than that of our other picks), and it comes in white or black.
If you can’t find the regular Waterpik Ion in stock: Consider the rechargeable Waterpik Ion Professional . This model has the same 5.5-inch footprint and 34-inch flosser cord as our pick , the Ion, but it holds 20 ounces of water (instead of 22 ounces).
If you’re looking for a traditional corded water flosser for a child, or for an adult with smaller hands or dexterity issues: Waterpik’s Water Flosser For Kids may be a worthy compact option. Its neon green coloring isn’t exactly subtle, but this flosser has the same per-minute pulses and flow rate as our picks. However, its highest pressure option is lower than that of our picks (80 psi versus 100 psi). And this model also offers only 60 seconds of flossing capacity (our picks offer 90 seconds) and a shorter warranty (two years versus three). We found this flosser’s smaller, thinner handle easy to grip, but it does not have a rotating tip option or an on/off switch. Since this one is meant to be refilled after every use, it does not come with a lid.
Countertop water flossers
The reservoir of the Philips Sonicare Power Flosser 5000 holds less water than that of our top pick, and it’s more expensive.
In our experience, the Waterpik Ultra cleans just as well as the Ion and the Aquarius Professional. But its lid isn’t attached to the tank (which is less preferable for regular maintenance).
We found combination water flossers and electric toothbrushes like Waterpik’s Complete Care 5.0 to be less appealing than using our water flosser pick and electric toothbrush pick separately.
We didn’t test the Waterpik Sidekick Water Flosser , despite its pluses. We like that this corded model is smaller than other countertop Waterpiks, can fit in a small travel case, and looks quite nice (especially the black-and-copper model ). But, unfortunately, it comes with only one tip, which cannot be changed (making it a little gross for use by multiple people). Also, it has just five pressure settings, and, at the time of publication, the Sidekick was nearly double the price of the Aquarius.
The Waterpik Classic Professional Water Flosser , which we also did not test, is similar in function and size to our top pick and costs a bit less. But it has only six pressure settings and comes with just two styles of tips. There’s also no cover on the tank lid.
Cordless water flossers
The cordless Oral-B Water Flosser Advanced ’s reservoir holds less water than we needed for a single test flossing session. Because this model produces a lower pressure water stream than our pick, in our experience it felt less effective when compared with the Philips Sonicare Power Flosser 3000 Cordless and the Waterpik Cordless Express.
The Panasonic EW-DJ10-W Oral Irrigator is a well-reviewed water flosser. But due to its collapsible design, it tends to stay damp for a while, which, well, dampens the overall experience. It also looks and feels a little cheaper than the Cordless Express, despite being the same price. It has a two-year warranty.
We found two other cordless offerings from Waterpik, the Waterpik Cordless Freedom and the Waterpik Cordless Advanced Water Flosser , that are bulkier and less enjoyable to use than the Power Flosser 3000 Cordless and the Cordless Express.
The Burst Water Flosser has an especially strong water stream, but it holds less water than our budget pick.
Quip’s Rechargeable Cordless Water Flosser has the same capacity and number of settings as our budget pick, but is more expensive.
The Aquasonic Aqua Flosser is overall more cumbersome to use when compared with our picks.
Shannon Palus contributed reporting in 2018.
This article was edited by Tracy Vence and Kalee Thompson.
Jessica Hilburg, associate dean for clinical affairs at NYU College of Dentistry , phone interview , September 25, 2018
Ruchi Sahota, dentist and media spokesperson for the American Dental Association , phone interview , October 15, 2018
Chhaju Ram Goyal, BDS, director at All Sum Research Center , phone interview , October 16, 2018
Federal Government, ADA Emphasize Importance of Flossing and Interdental Cleaners , American Dental Association , August 4, 2016
Meet your guide

Nancy Redd is a senior staff writer covering health and grooming at Wirecutter. She is a GLAAD Award–nominated on-air host and a New York Times best-selling author. Her latest nonfiction book, The Real Body Manual , is a visual health and wellness guide for young adults of all genders. Her other books include Bedtime Bonnet and Pregnancy, OMG!
Further reading

The Best Electric Toothbrush
by Nancy Redd
After more than 100 hours of research and considering nearly every model available, we think the Oral-B Pro 1000 is the best rechargeable electric toothbrush.

Quip Review: What to Know Before You Buy an AAA-Battery–Powered Electric Toothbrush
We compared the ultra-popular Quip with four similarly priced competitors—plus three drugstore electric toothbrushes, for good measure.

Small Bathroom Ideas
by Alex Arpaia and Dorie Chevlen
After 20 hours researching dozens of organizing solutions, we recommend these items to maximize storage and keep small bathrooms clutter-free.

Most People Don’t Need This Fancy Toothbrush Feature. But I Do.
by Phillip Zminda
My dentist told me I’m brushing so hard that my gums are receding. My toothbrush’s pressure sensor is teaching me to brush right and keeping my gums healthy.

COMMENTS
Abstract. Since their introduction more than 50 years ago, water flossers (also known as oral irrigators) have been subject to numerous studies on their safety, efficacy, and delivery of antimicrobial agents, particularly in relation to their ability to impact clinical parameters such as plaque, bleeding, gingivitis, pocket depth, and calculus.
This literature review includes published studies that focus on the safety findings in microscopic and clinical trials. Histological Findings. In a pilot study by Krajewski et al, 11 treatment of 10 subjects with periodontitis who were scheduled for surgery added twice-daily irrigation with water on the left side of the mouth only. Tissue ...
Request PDF | Safety of a Water Flosser: A Literature Review. | Since their introduction more than 50 years ago, water flossers (also known as oral irrigators) have been subject to numerous ...
Out of all participants who used the dental water flosser, 99 (86.84%) described their experience as Amazing and very effective, 5 (4.39%) described it as Not effective . 97 (85.09%) of all ...
Objective: To compare the plaque removal efficacy of a water flosser to string floss combined with a manual toothbrush after a single use. Methods: Seventy adult subjects participated in this randomized, single-use, single-blind, parallel clinical study. Subjects were assigned to one of two groups; Waterpik Water Flosser plus a manual toothbrush (WF) or waxed string floss plus a manual ...
Evidence based on studies and decades of use by the public continues to support their safety and efficacy and disproves suggestions of possible detrimental effects on the attachment, junctional epithelium, or pocket depth. Since their introduction more than 50 years ago, water flossers (also known as oral irrigators) have been subject to numerous studies on their safety, efficacy, and delivery ...
Abstract. Since their introduction more than 50 years ago, water flossers (also known as oral irrigators) have been subject to numerous studies on their safety, efficacy, and delivery of antimicrobial agents, particularly in relation to their ability to impact clinical parameters such as plaque, bleeding, gingivitis, pocket depth, and calculus.
Waterpik® Water Flosser: Unequivocally Proven Safe in Clinical Studies Safety of a Water Flosser: A Literature Review Jolkovsky DL, Lyle DM. Compendium of Continuing Education in Dentistry 2015; 36(2):2-5. Objective Since the introduction of the first Waterpik® Water Flosser in 1962, over 60 clinical trials have been published.
Group 1 (experimental): patients were provided with water flosser (Waterpik Water Flosser WP-600, Water Pik, Inc, Fort Collins, CO, USA) and were asked to refill it with tap water. The recommended tip was the standard JTR tip set in floss mode with the power button set at 5. Patients were also asked to change the water daily and to clean each ...
A review of the literature answers many questions related to the use of water flossers, the first of which was introduced in 1962. ... Implants require daily care similar to natural teeth. A water flosser was tested on implants by comparing rinsing with 0.12% CHX to irrigating using a specialized subgingival tip with 0.06% CHX. The researchers ...
Four studies showed that there was a significant plaque reduction with water flosser as compared to dental floss.[23,27,28,31] In the study conducted by Goyal et al., there was a 57.7% reduction in whole mouth plaque after using dental floss while there was a 74.4% reduction in whole mouth plaque after using water flosser.
Safety of a water flosser: A literature review. Compend Contin Educ Dent. 2015;36(2):146-149. 9. Al-Mubarak S, Ciancio S, Aljada A, et al. Comparative evaluation of adjunctive oral irrigation in diabetics. J Clin Periodontol. 2009;29(4):295-300. 10. Genovesi AM, Lorenzi C, Lyle DM, et al. Periodontal maintenance following scaling and root ...
Safety of a water flosser: a literature review. David L Jolkovsky Lecturer, UCLA School of Dentistry; Private Practice, Davis, California; Diplomate, American Board of Periodontology.
Literature review confirms safety profile of Waterpik Water Flosser. Feb. 25, 2015. Five Decades of research show there is an abundance of evidence demonstrating the safety of a Waterpik Water Flosser. DentistryIQ Editors. If you work with a dentist, hygienist, or specialist who is still on the fence about the safety of a Waterpik Water Flosser ...
Safety of a Water Flosser: A Literature Review. Jolkovsky DL et al. Compendium of Continuing Education in Dentistry 2015; 36(2):2-5. Objective. Since the introduction of the first Waterpik TM water flosser in 1962, over sixty clinical trials have been published. Collectively, the studies demonstrate significant plaque removal, reduction of ...
Studies also demonstrated that although use of water flosser plus manual toothbrushing significantly reduced the plaque index at 8-week compared with that at baseline, ... Jolkovsky DL, Lyle DM. Safety of a water flosser: a literature review. Compend Contin Educ Dent. 2015; 36 (2):146-9. [Google Scholar] 29.
This study investigated the efficacy of water flossers (WFs), devices used to irrigate the interdental and subgingival areas, compared to other interdental care methods, in the management of periodontal disease. A computerized PubMed search was conducted by the author, encompassing the years 1962 to 2023. The year 1962 was selected due to it being the introduction of the first WF. Keywords ...
The Waterpik Cordless Express is the best cordless water flosser under $50 we've tested. Its reservoir is a lot smaller than that on the Power Flosser 3000 Cordless (5 ounces versus 8), and it ...
The inclusion criteria for selecting articles were precise. The literature had to be published in English and needed to be available in full-text format. This review encompassed a diverse range of study types, including prospective or retrospective studies, randomized controlled trials, case series, case reports, and review papers.
Search life-sciences literature (43,442,925 articles, preprints and more) (43,442,925 articles, preprints and more)