
- Aims and Objectives – A Guide for Academic Writing
- Doing a PhD
One of the most important aspects of a thesis, dissertation or research paper is the correct formulation of the aims and objectives. This is because your aims and objectives will establish the scope, depth and direction that your research will ultimately take. An effective set of aims and objectives will give your research focus and your reader clarity, with your aims indicating what is to be achieved, and your objectives indicating how it will be achieved.

Introduction
There is no getting away from the importance of the aims and objectives in determining the success of your research project. Unfortunately, however, it is an aspect that many students struggle with, and ultimately end up doing poorly. Given their importance, if you suspect that there is even the smallest possibility that you belong to this group of students, we strongly recommend you read this page in full.
This page describes what research aims and objectives are, how they differ from each other, how to write them correctly, and the common mistakes students make and how to avoid them. An example of a good aim and objectives from a past thesis has also been deconstructed to help your understanding.
What Are Aims and Objectives?
Research aims.
A research aim describes the main goal or the overarching purpose of your research project.
In doing so, it acts as a focal point for your research and provides your readers with clarity as to what your study is all about. Because of this, research aims are almost always located within its own subsection under the introduction section of a research document, regardless of whether it’s a thesis , a dissertation, or a research paper .
A research aim is usually formulated as a broad statement of the main goal of the research and can range in length from a single sentence to a short paragraph. Although the exact format may vary according to preference, they should all describe why your research is needed (i.e. the context), what it sets out to accomplish (the actual aim) and, briefly, how it intends to accomplish it (overview of your objectives).
To give an example, we have extracted the following research aim from a real PhD thesis:
Example of a Research Aim
The role of diametrical cup deformation as a factor to unsatisfactory implant performance has not been widely reported. The aim of this thesis was to gain an understanding of the diametrical deformation behaviour of acetabular cups and shells following impaction into the reamed acetabulum. The influence of a range of factors on deformation was investigated to ascertain if cup and shell deformation may be high enough to potentially contribute to early failure and high wear rates in metal-on-metal implants.
Note: Extracted with permission from thesis titled “T he Impact And Deformation Of Press-Fit Metal Acetabular Components ” produced by Dr H Hothi of previously Queen Mary University of London.
Research Objectives
Where a research aim specifies what your study will answer, research objectives specify how your study will answer it.
They divide your research aim into several smaller parts, each of which represents a key section of your research project. As a result, almost all research objectives take the form of a numbered list, with each item usually receiving its own chapter in a dissertation or thesis.
Following the example of the research aim shared above, here are it’s real research objectives as an example:
Example of a Research Objective
- Develop finite element models using explicit dynamics to mimic mallet blows during cup/shell insertion, initially using simplified experimentally validated foam models to represent the acetabulum.
- Investigate the number, velocity and position of impacts needed to insert a cup.
- Determine the relationship between the size of interference between the cup and cavity and deformation for different cup types.
- Investigate the influence of non-uniform cup support and varying the orientation of the component in the cavity on deformation.
- Examine the influence of errors during reaming of the acetabulum which introduce ovality to the cavity.
- Determine the relationship between changes in the geometry of the component and deformation for different cup designs.
- Develop three dimensional pelvis models with non-uniform bone material properties from a range of patients with varying bone quality.
- Use the key parameters that influence deformation, as identified in the foam models to determine the range of deformations that may occur clinically using the anatomic models and if these deformations are clinically significant.
It’s worth noting that researchers sometimes use research questions instead of research objectives, or in other cases both. From a high-level perspective, research questions and research objectives make the same statements, but just in different formats.
Taking the first three research objectives as an example, they can be restructured into research questions as follows:
Restructuring Research Objectives as Research Questions
- Can finite element models using simplified experimentally validated foam models to represent the acetabulum together with explicit dynamics be used to mimic mallet blows during cup/shell insertion?
- What is the number, velocity and position of impacts needed to insert a cup?
- What is the relationship between the size of interference between the cup and cavity and deformation for different cup types?
Difference Between Aims and Objectives
Hopefully the above explanations make clear the differences between aims and objectives, but to clarify:
- The research aim focus on what the research project is intended to achieve; research objectives focus on how the aim will be achieved.
- Research aims are relatively broad; research objectives are specific.
- Research aims focus on a project’s long-term outcomes; research objectives focus on its immediate, short-term outcomes.
- A research aim can be written in a single sentence or short paragraph; research objectives should be written as a numbered list.
How to Write Aims and Objectives
Before we discuss how to write a clear set of research aims and objectives, we should make it clear that there is no single way they must be written. Each researcher will approach their aims and objectives slightly differently, and often your supervisor will influence the formulation of yours on the basis of their own preferences.
Regardless, there are some basic principles that you should observe for good practice; these principles are described below.
Your aim should be made up of three parts that answer the below questions:
- Why is this research required?
- What is this research about?
- How are you going to do it?
The easiest way to achieve this would be to address each question in its own sentence, although it does not matter whether you combine them or write multiple sentences for each, the key is to address each one.
The first question, why , provides context to your research project, the second question, what , describes the aim of your research, and the last question, how , acts as an introduction to your objectives which will immediately follow.
Scroll through the image set below to see the ‘why, what and how’ associated with our research aim example.
Note: Your research aims need not be limited to one. Some individuals per to define one broad ‘overarching aim’ of a project and then adopt two or three specific research aims for their thesis or dissertation. Remember, however, that in order for your assessors to consider your research project complete, you will need to prove you have fulfilled all of the aims you set out to achieve. Therefore, while having more than one research aim is not necessarily disadvantageous, consider whether a single overarching one will do.
Research Objectives
Each of your research objectives should be SMART :
- Specific – is there any ambiguity in the action you are going to undertake, or is it focused and well-defined?
- Measurable – how will you measure progress and determine when you have achieved the action?
- Achievable – do you have the support, resources and facilities required to carry out the action?
- Relevant – is the action essential to the achievement of your research aim?
- Timebound – can you realistically complete the action in the available time alongside your other research tasks?
In addition to being SMART, your research objectives should start with a verb that helps communicate your intent. Common research verbs include:
Table of Research Verbs to Use in Aims and Objectives
Last, format your objectives into a numbered list. This is because when you write your thesis or dissertation, you will at times need to make reference to a specific research objective; structuring your research objectives in a numbered list will provide a clear way of doing this.
To bring all this together, let’s compare the first research objective in the previous example with the above guidance:
Checking Research Objective Example Against Recommended Approach
Research Objective:
1. Develop finite element models using explicit dynamics to mimic mallet blows during cup/shell insertion, initially using simplified experimentally validated foam models to represent the acetabulum.
Checking Against Recommended Approach:
Q: Is it specific? A: Yes, it is clear what the student intends to do (produce a finite element model), why they intend to do it (mimic cup/shell blows) and their parameters have been well-defined ( using simplified experimentally validated foam models to represent the acetabulum ).
Q: Is it measurable? A: Yes, it is clear that the research objective will be achieved once the finite element model is complete.
Q: Is it achievable? A: Yes, provided the student has access to a computer lab, modelling software and laboratory data.
Q: Is it relevant? A: Yes, mimicking impacts to a cup/shell is fundamental to the overall aim of understanding how they deform when impacted upon.
Q: Is it timebound? A: Yes, it is possible to create a limited-scope finite element model in a relatively short time, especially if you already have experience in modelling.
Q: Does it start with a verb? A: Yes, it starts with ‘develop’, which makes the intent of the objective immediately clear.
Q: Is it a numbered list? A: Yes, it is the first research objective in a list of eight.
Mistakes in Writing Research Aims and Objectives
1. making your research aim too broad.
Having a research aim too broad becomes very difficult to achieve. Normally, this occurs when a student develops their research aim before they have a good understanding of what they want to research. Remember that at the end of your project and during your viva defence , you will have to prove that you have achieved your research aims; if they are too broad, this will be an almost impossible task. In the early stages of your research project, your priority should be to narrow your study to a specific area. A good way to do this is to take the time to study existing literature, question their current approaches, findings and limitations, and consider whether there are any recurring gaps that could be investigated .
Note: Achieving a set of aims does not necessarily mean proving or disproving a theory or hypothesis, even if your research aim was to, but having done enough work to provide a useful and original insight into the principles that underlie your research aim.
2. Making Your Research Objectives Too Ambitious
Be realistic about what you can achieve in the time you have available. It is natural to want to set ambitious research objectives that require sophisticated data collection and analysis, but only completing this with six months before the end of your PhD registration period is not a worthwhile trade-off.
3. Formulating Repetitive Research Objectives
Each research objective should have its own purpose and distinct measurable outcome. To this effect, a common mistake is to form research objectives which have large amounts of overlap. This makes it difficult to determine when an objective is truly complete, and also presents challenges in estimating the duration of objectives when creating your project timeline. It also makes it difficult to structure your thesis into unique chapters, making it more challenging for you to write and for your audience to read.
Fortunately, this oversight can be easily avoided by using SMART objectives.
Hopefully, you now have a good idea of how to create an effective set of aims and objectives for your research project, whether it be a thesis, dissertation or research paper. While it may be tempting to dive directly into your research, spending time on getting your aims and objectives right will give your research clear direction. This won’t only reduce the likelihood of problems arising later down the line, but will also lead to a more thorough and coherent research project.
Finding a PhD has never been this easy – search for a PhD by keyword, location or academic area of interest.
Browse PhDs Now
Join thousands of students.
Join thousands of other students and stay up to date with the latest PhD programmes, funding opportunities and advice.

Formulating Research Aims and Objectives
Formulating research aim and objectives in an appropriate manner is one of the most important aspects of your thesis. This is because research aim and objectives determine the scope, depth and the overall direction of the research. Research question is the central question of the study that has to be answered on the basis of research findings.
Research aim emphasizes what needs to be achieved within the scope of the research, by the end of the research process. Achievement of research aim provides answer to the research question.
Research objectives divide research aim into several parts and address each part separately. Research aim specifies WHAT needs to be studied and research objectives comprise a number of steps that address HOW research aim will be achieved.
As a rule of dumb, there would be one research aim and several research objectives. Achievement of each research objective will lead to the achievement of the research aim.
Consider the following as an example:
Research title: Effects of organizational culture on business profitability: a case study of Virgin Atlantic
Research aim: To assess the effects of Virgin Atlantic organizational culture on business profitability
Following research objectives would facilitate the achievement of this aim:
- Analyzing the nature of organizational culture at Virgin Atlantic by September 1, 2022
- Identifying factors impacting Virgin Atlantic organizational culture by September 16, 2022
- Analyzing impacts of Virgin Atlantic organizational culture on employee performances by September 30, 2022
- Providing recommendations to Virgin Atlantic strategic level management in terms of increasing the level of effectiveness of organizational culture by October 5, 2022
Figure below illustrates additional examples in formulating research aims and objectives:

Formulation of research question, aim and objectives
Common mistakes in the formulation of research aim relate to the following:
1. Choosing the topic too broadly . This is the most common mistake. For example, a research title of “an analysis of leadership practices” can be classified as too broad because the title fails to answer the following questions:
a) Which aspects of leadership practices? Leadership has many aspects such as employee motivation, ethical behaviour, strategic planning, change management etc. An attempt to cover all of these aspects of organizational leadership within a single research will result in an unfocused and poor work.
b) An analysis of leadership practices in which country? Leadership practices tend to be different in various countries due to cross-cultural differences, legislations and a range of other region-specific factors. Therefore, a study of leadership practices needs to be country-specific.
c) Analysis of leadership practices in which company or industry? Similar to the point above, analysis of leadership practices needs to take into account industry-specific and/or company-specific differences, and there is no way to conduct a leadership research that relates to all industries and organizations in an equal manner.
Accordingly, as an example “a study into the impacts of ethical behaviour of a leader on the level of employee motivation in US healthcare sector” would be a more appropriate title than simply “An analysis of leadership practices”.
2. Setting an unrealistic aim . Formulation of a research aim that involves in-depth interviews with Apple strategic level management by an undergraduate level student can be specified as a bit over-ambitious. This is because securing an interview with Apple CEO Tim Cook or members of Apple Board of Directors might not be easy. This is an extreme example of course, but you got the idea. Instead, you may aim to interview the manager of your local Apple store and adopt a more feasible strategy to get your dissertation completed.
3. Choosing research methods incompatible with the timeframe available . Conducting interviews with 20 sample group members and collecting primary data through 2 focus groups when only three months left until submission of your dissertation can be very difficult, if not impossible. Accordingly, timeframe available need to be taken into account when formulating research aims and objectives and selecting research methods.
Moreover, research objectives need to be formulated according to SMART principle,
where the abbreviation stands for specific, measurable, achievable, realistic, and time-bound.
Examples of SMART research objectives
At the conclusion part of your research project you will need to reflect on the level of achievement of research aims and objectives. In case your research aims and objectives are not fully achieved by the end of the study, you will need to discuss the reasons. These may include initial inappropriate formulation of research aims and objectives, effects of other variables that were not considered at the beginning of the research or changes in some circumstances during the research process.
John Dudovskiy
Research Question 101 📖
Everything you need to know to write a high-quality research question
By: Derek Jansen (MBA) | Reviewed By: Dr. Eunice Rautenbach | October 2023
If you’ve landed on this page, you’re probably asking yourself, “ What is a research question? ”. Well, you’ve come to the right place. In this post, we’ll explain what a research question is , how it’s differen t from a research aim, and how to craft a high-quality research question that sets you up for success.
Research Question 101
What is a research question.
- Research questions vs research aims
- The 4 types of research questions
- How to write a research question
- Frequently asked questions
- Examples of research questions
As the name suggests, the research question is the core question (or set of questions) that your study will (attempt to) answer .
In many ways, a research question is akin to a target in archery . Without a clear target, you won’t know where to concentrate your efforts and focus. Essentially, your research question acts as the guiding light throughout your project and informs every choice you make along the way.
Let’s look at some examples:
What impact does social media usage have on the mental health of teenagers in New York?
How does the introduction of a minimum wage affect employment levels in small businesses in outer London?
How does the portrayal of women in 19th-century American literature reflect the societal attitudes of the time?
What are the long-term effects of intermittent fasting on heart health in adults?
As you can see in these examples, research questions are clear, specific questions that can be feasibly answered within a study. These are important attributes and we’ll discuss each of them in more detail a little later . If you’d like to see more examples of research questions, you can find our RQ mega-list here .
Research Questions vs Research Aims
At this point, you might be asking yourself, “ How is a research question different from a research aim? ”. Within any given study, the research aim and research question (or questions) are tightly intertwined , but they are separate things . Let’s unpack that a little.
A research aim is typically broader in nature and outlines what you hope to achieve with your research. It doesn’t ask a specific question but rather gives a summary of what you intend to explore.
The research question, on the other hand, is much more focused . It’s the specific query you’re setting out to answer. It narrows down the research aim into a detailed, researchable question that will guide your study’s methods and analysis.
Let’s look at an example:
Research Aim: To explore the effects of climate change on marine life in Southern Africa.
Research Question: How does ocean acidification caused by climate change affect the reproduction rates of coral reefs?
As you can see, the research aim gives you a general focus , while the research question details exactly what you want to find out.
Need a helping hand?
Types of research questions
Now that we’ve defined what a research question is, let’s look at the different types of research questions that you might come across. Broadly speaking, there are (at least) four different types of research questions – descriptive , comparative , relational , and explanatory .
Descriptive questions ask what is happening. In other words, they seek to describe a phenomena or situation . An example of a descriptive research question could be something like “What types of exercise do high-performing UK executives engage in?”. This would likely be a bit too basic to form an interesting study, but as you can see, the research question is just focused on the what – in other words, it just describes the situation.
Comparative research questions , on the other hand, look to understand the way in which two or more things differ , or how they’re similar. An example of a comparative research question might be something like “How do exercise preferences vary between middle-aged men across three American cities?”. As you can see, this question seeks to compare the differences (or similarities) in behaviour between different groups.
Next up, we’ve got exploratory research questions , which ask why or how is something happening. While the other types of questions we looked at focused on the what, exploratory research questions are interested in the why and how . As an example, an exploratory research question might ask something like “Why have bee populations declined in Germany over the last 5 years?”. As you can, this question is aimed squarely at the why, rather than the what.
Last but not least, we have relational research questions . As the name suggests, these types of research questions seek to explore the relationships between variables . Here, an example could be something like “What is the relationship between X and Y” or “Does A have an impact on B”. As you can see, these types of research questions are interested in understanding how constructs or variables are connected , and perhaps, whether one thing causes another.
Of course, depending on how fine-grained you want to get, you can argue that there are many more types of research questions , but these four categories give you a broad idea of the different flavours that exist out there. It’s also worth pointing out that a research question doesn’t need to fit perfectly into one category – in many cases, a research question might overlap into more than just one category and that’s okay.
The key takeaway here is that research questions can take many different forms , and it’s useful to understand the nature of your research question so that you can align your research methodology accordingly.
How To Write A Research Question
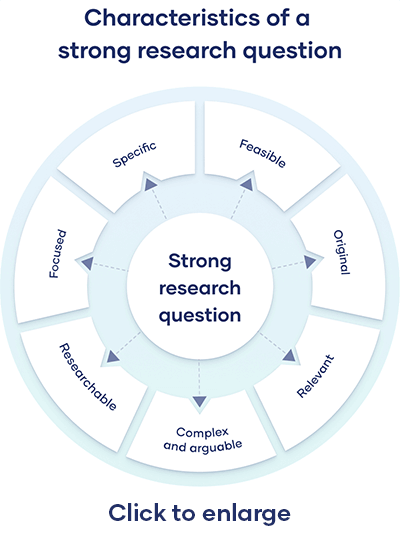
As we alluded earlier, a well-crafted research question needs to possess very specific attributes, including focus , clarity and feasibility . But that’s not all – a rock-solid research question also needs to be rooted and aligned . Let’s look at each of these.
A strong research question typically has a single focus. So, don’t try to cram multiple questions into one research question; rather split them up into separate questions (or even subquestions), each with their own specific focus. As a rule of thumb, narrow beats broad when it comes to research questions.
Clear and specific
A good research question is clear and specific, not vague and broad. State clearly exactly what you want to find out so that any reader can quickly understand what you’re looking to achieve with your study. Along the same vein, try to avoid using bulky language and jargon – aim for clarity.
Unfortunately, even a super tantalising and thought-provoking research question has little value if you cannot feasibly answer it. So, think about the methodological implications of your research question while you’re crafting it. Most importantly, make sure that you know exactly what data you’ll need (primary or secondary) and how you’ll analyse that data.
A good research question (and a research topic, more broadly) should be rooted in a clear research gap and research problem . Without a well-defined research gap, you risk wasting your effort pursuing a question that’s already been adequately answered (and agreed upon) by the research community. A well-argued research gap lays at the heart of a valuable study, so make sure you have your gap clearly articulated and that your research question directly links to it.
As we mentioned earlier, your research aim and research question are (or at least, should be) tightly linked. So, make sure that your research question (or set of questions) aligns with your research aim . If not, you’ll need to revise one of the two to achieve this.
FAQ: Research Questions
Research question faqs, how many research questions should i have, what should i avoid when writing a research question, can a research question be a statement.
Typically, a research question is phrased as a question, not a statement. A question clearly indicates what you’re setting out to discover.
Can a research question be too broad or too narrow?
Yes. A question that’s too broad makes your research unfocused, while a question that’s too narrow limits the scope of your study.
Here’s an example of a research question that’s too broad:
“Why is mental health important?”
Conversely, here’s an example of a research question that’s likely too narrow:
“What is the impact of sleep deprivation on the exam scores of 19-year-old males in London studying maths at The Open University?”
Can I change my research question during the research process?
How do i know if my research question is good.
A good research question is focused, specific, practical, rooted in a research gap, and aligned with the research aim. If your question meets these criteria, it’s likely a strong question.
Is a research question similar to a hypothesis?
Not quite. A hypothesis is a testable statement that predicts an outcome, while a research question is a query that you’re trying to answer through your study. Naturally, there can be linkages between a study’s research questions and hypothesis, but they serve different functions.
How are research questions and research objectives related?
The research question is a focused and specific query that your study aims to answer. It’s the central issue you’re investigating. The research objective, on the other hand, outlines the steps you’ll take to answer your research question. Research objectives are often more action-oriented and can be broken down into smaller tasks that guide your research process. In a sense, they’re something of a roadmap that helps you answer your research question.
Need some inspiration?
If you’d like to see more examples of research questions, check out our research question mega list here . Alternatively, if you’d like 1-on-1 help developing a high-quality research question, consider our private coaching service .
Psst… there’s more (for free)
This post is part of our dissertation mini-course, which covers everything you need to get started with your dissertation, thesis or research project.
You Might Also Like:

Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly

Research Aims and Objectives: The dynamic duo for successful research
Picture yourself on a road trip without a destination in mind — driving aimlessly, not knowing where you’re headed or how to get there. Similarly, your research is navigated by well-defined research aims and objectives. Research aims and objectives are the foundation of any research project. They provide a clear direction and purpose for the study, ensuring that you stay focused and on track throughout the process. They are your trusted navigational tools, leading you to success.
Understanding the relationship between research objectives and aims is crucial to any research project’s success, and we’re here to break it down for you in this article. Here, we’ll explore the importance of research aims and objectives, understand their differences, and delve into the impact they have on the quality of research.
Understanding the Difference between Research Aims and Objectives
In research, aims and objectives are two important components but are often used interchangeably. Though they may sound similar, they are distinct and serve different purposes.
Research Aims:
Research aims are broad statements that describe the overall purpose of your study. They provide a general direction for your study and indicate the intended achievements of your research. Aims are usually written in a general and abstract manner describing the ultimate goal of the research.
Research Objectives:
Research objectives are specific, measurable, and achievable goals that you aim to accomplish within a specified timeframe. They break down the research aims into smaller, more manageable components and provide a clear picture of what you want to achieve and how you plan to achieve it.

In the example, the objectives provide specific targets that must be achieved to reach the aim. Essentially, aims provide the overall direction for the research while objectives provide specific targets that must be achieved to accomplish the aims. Aims provide a broad context for the research, while the objectives provide smaller steps that the researcher must take to accomplish the overall research goals. To illustrate, when planning a road trip, your research aim is the destination you want to reach, and your research objectives are the specific routes you need to take to get there.
Aims and objectives are interconnected. Objectives play a key role in defining the research methodology, providing a roadmap for how you’ll collect and analyze data, while aim is the final destination, which represents the ultimate goal of your research. By setting specific goals, you’ll be able to design a research plan that helps you achieve your objectives and, ultimately, your research aim.
Importance of Well-defined Aims and Objectives
The impact of clear research aims and objectives on the quality of research cannot be understated. But it’s not enough to simply have aims and objectives. Well-defined research aims and objectives are important for several reasons:
- Provides direction: Clear aims and well-defined objectives provide a specific direction for your research study, ensuring that the research stays focused on a specific topic or problem. This helps to prevent the research from becoming too broad or unfocused, and ensures that the study remains relevant and meaningful.
- Guides research design: The research aim and objectives help guide the research design and methodology, ensuring that your study is designed in a way that will answer the research questions and achieve the research objectives.
- Helps with resource allocation: Clear research aims and objectives helps you to allocate resources effectively , including time, financial resources, human resources, and other required materials. With a well-defined aim and objectives, you can identify the resources required to conduct the research, and allocate them in a way that maximizes efficiency and productivity.
- Assists in evaluation: Clearly specified research aims and objectives allow for effective evaluation of your research project’s success. You can assess whether the research has achieved its objectives, and whether the aim has been met. This evaluation process can help to identify areas of the research project that may require further attention or modification.
- Enhances communication: Well-defined research aims and objectives help to enhance communication among the research team, stakeholders, funding agencies, and other interested parties. Clear aims and objectives ensure that everyone involved in your research project understands the purpose and goals of the study. This can help to foster collaboration and ensure that everyone is working towards the same end goal.
How to Formulate Research Aims and Objectives
Formulating effective research aims and objectives involves a systematic process to ensure that they are clear, specific, achievable, and relevant. Start by asking yourself what you want to achieve through your research. What impact do you want your research to have? Once you have a clear understanding of your aims, you can then break them down into specific, achievable objectives. Here are some steps you can follow when developing research aims and objectives:
- Identify the research question : Clearly identify the questions you want to answer through your research. This will help you define the scope of your research. Understanding the characteristics of a good research question will help you generate clearer aims and objectives.
- Conduct literature review : When defining your research aim and objectives, it’s important to conduct a literature review to identify key concepts, theories, and methods related to your research problem or question. Conducting a thorough literature review can help you understand what research has been done in the area and what gaps exist in the literature.
- Identify the research aim: Develop a research aim that summarizes the overarching goal of your research. The research aim should be broad and concise.
- Develop research objectives: Based on your research questions and research aim, develop specific research objectives that outline what you intend to achieve through your research. These objectives should be specific, measurable, achievable, relevant, and time-bound (SMART).
- Use action verbs: Use action verbs such as “investigate,” “examine,” “analyze,” and “compare” to describe your research aims and objectives. This makes them more specific and measurable.
- Ensure alignment with research question: Ensure that the research aim and objectives are aligned with the research question. This helps to ensure that the research remains focused and that the objectives are specific enough to answer your research question.
- Refine and revise: Once the research aim and objectives have been developed, refine and revise them as needed. Seek feedback from your colleagues, mentors, or supervisors to ensure that they are clear, concise, and achievable within the given resources and timeframe.
- Communicate: After finalizing the research aim and objectives, they should be communicated to the research team, stakeholders, and other interested parties. This helps to ensure that everyone is working towards the same end goal and understands the purpose of the study.
Common Pitfalls to Avoid While Formulating Aims and Objectives
There are several common mistakes that researchers can make when writing research aims and objectives. These include:
- Being too broad or vague: Aims and objectives that are too general or unclear can lead to confusion and lack of focus. It is important to ensure that the aims and objectives are concise and clear.
- Being too narrow or specific: On the other hand, aims and objectives that are too narrow or specific may limit the scope of the research and make it difficult to draw meaningful conclusions or implications.
- Being too ambitious: While it is important to aim high, being too ambitious with the aims and objectives can lead to unrealistic expectations and can be difficult to achieve within the constraints of the research project.
- Lack of alignment: The aims and objectives should be directly linked to the research questions being investigated. Otherwise, this will lead to a lack of coherence in the research project.
- Lack of feasibility: The aims and objectives should be achievable within the constraints of the research project, including time, budget, and resources. Failing to consider feasibility may cause compromise of the research quality.
- Failing to consider ethical considerations: The aims and objectives should take into account any ethical considerations, such as ensuring the safety and well-being of study participants.
- Failing to involve all stakeholders: It’s important to involve all relevant stakeholders, such as participants, supervisors, and funding agencies, in the development of the aims and objectives to ensure they are appropriate and relevant.
To avoid these common pitfalls, it is important to be specific, clear, relevant, and realistic when writing research aims and objectives. Seek feedback from colleagues or supervisors to ensure that the aims and objectives are aligned with the research problem , questions, and methodology, and are achievable within the constraints of the research project. It’s important to continually refine your aims and objectives as you go. As you progress in your research, it’s not uncommon for research aims and objectives to evolve slightly, but it’s important that they remain consistent with the study conducted and the research topic.
In summary, research aims and objectives are the backbone of any successful research project. They give you the ability to cut through the noise and hone in on what really matters. By setting clear goals and aligning them with your research questions and methodology, you can ensure that your research is relevant, impactful, and of the highest quality. So, before you hit the road on your research journey, make sure you have a clear destination and steps to get there. Let us know in the comments section below the challenges you faced and the strategies you followed while fomulating research aims and objectives! Also, feel free to reach out to us at any stage of your research or publication by using #AskEnago and tagging @EnagoAcademy on Twitter , Facebook , and Quora . Happy researching!
This particular material has added important but overlooked concepts regarding my experiences in explaining research aims and objectives. Thank you
Rate this article Cancel Reply
Your email address will not be published.

Enago Academy's Most Popular Articles

- AI in Academia
- Trending Now
Simplifying the Literature Review Journey — A comparative analysis of 6 AI summarization tools
Imagine having to skim through and read mountains of research papers and books, only to…

- Reporting Research
Choosing the Right Analytical Approach: Thematic analysis vs. content analysis for data interpretation
In research, choosing the right approach to understand data is crucial for deriving meaningful insights.…

Comparing Cross Sectional and Longitudinal Studies: 5 steps for choosing the right approach
The process of choosing the right research design can put ourselves at the crossroads of…

- Career Corner
Unlocking the Power of Networking in Academic Conferences
Embarking on your first academic conference experience? Fear not, we got you covered! Academic conferences…

Research Recommendations – Guiding policy-makers for evidence-based decision making
Research recommendations play a crucial role in guiding scholars and researchers toward fruitful avenues of…
Choosing the Right Analytical Approach: Thematic analysis vs. content analysis for…
Comparing Cross Sectional and Longitudinal Studies: 5 steps for choosing the right…
8 Effective Strategies to Write Argumentative Essays

Sign-up to read more
Subscribe for free to get unrestricted access to all our resources on research writing and academic publishing including:
- 2000+ blog articles
- 50+ Webinars
- 10+ Expert podcasts
- 50+ Infographics
- 10+ Checklists
- Research Guides
We hate spam too. We promise to protect your privacy and never spam you.
I am looking for Editing/ Proofreading services for my manuscript Tentative date of next journal submission:

What should universities' stance be on AI tools in research and academic writing?
404 Not found
Frequently asked questions
What’s the difference between research aims and objectives.
A research aim is a broad statement indicating the general purpose of your research project. It should appear in your introduction at the end of your problem statement , before your research objectives.
Research objectives are more specific than your research aim. They indicate the specific ways you’ll address the overarching aim.
Frequently asked questions: Writing a research paper
A research project is an academic, scientific, or professional undertaking to answer a research question . Research projects can take many forms, such as qualitative or quantitative , descriptive , longitudinal , experimental , or correlational . What kind of research approach you choose will depend on your topic.
The best way to remember the difference between a research plan and a research proposal is that they have fundamentally different audiences. A research plan helps you, the researcher, organize your thoughts. On the other hand, a dissertation proposal or research proposal aims to convince others (e.g., a supervisor, a funding body, or a dissertation committee) that your research topic is relevant and worthy of being conducted.
Formulating a main research question can be a difficult task. Overall, your question should contribute to solving the problem that you have defined in your problem statement .
However, it should also fulfill criteria in three main areas:
- Researchability
- Feasibility and specificity
- Relevance and originality
Research questions anchor your whole project, so it’s important to spend some time refining them.
In general, they should be:
- Focused and researchable
- Answerable using credible sources
- Complex and arguable
- Feasible and specific
- Relevant and original
All research questions should be:
- Focused on a single problem or issue
- Researchable using primary and/or secondary sources
- Feasible to answer within the timeframe and practical constraints
- Specific enough to answer thoroughly
- Complex enough to develop the answer over the space of a paper or thesis
- Relevant to your field of study and/or society more broadly
Once you’ve decided on your research objectives , you need to explain them in your paper, at the end of your problem statement .
Keep your research objectives clear and concise, and use appropriate verbs to accurately convey the work that you will carry out for each one.
I will compare …
Your research objectives indicate how you’ll try to address your research problem and should be specific:
Research objectives describe what you intend your research project to accomplish.
They summarize the approach and purpose of the project and help to focus your research.
Your objectives should appear in the introduction of your research paper , at the end of your problem statement .
The main guidelines for formatting a paper in Chicago style are to:
- Use a standard font like 12 pt Times New Roman
- Use 1 inch margins or larger
- Apply double line spacing
- Indent every new paragraph ½ inch
- Include a title page
- Place page numbers in the top right or bottom center
- Cite your sources with author-date citations or Chicago footnotes
- Include a bibliography or reference list
To automatically generate accurate Chicago references, you can use Scribbr’s free Chicago reference generator .
The main guidelines for formatting a paper in MLA style are as follows:
- Use an easily readable font like 12 pt Times New Roman
- Set 1 inch page margins
- Include a four-line MLA heading on the first page
- Center the paper’s title
- Use title case capitalization for headings
- Cite your sources with MLA in-text citations
- List all sources cited on a Works Cited page at the end
To format a paper in APA Style , follow these guidelines:
- Use a standard font like 12 pt Times New Roman or 11 pt Arial
- If submitting for publication, insert a running head on every page
- Apply APA heading styles
- Cite your sources with APA in-text citations
- List all sources cited on a reference page at the end
No, it’s not appropriate to present new arguments or evidence in the conclusion . While you might be tempted to save a striking argument for last, research papers follow a more formal structure than this.
All your findings and arguments should be presented in the body of the text (more specifically in the results and discussion sections if you are following a scientific structure). The conclusion is meant to summarize and reflect on the evidence and arguments you have already presented, not introduce new ones.
The conclusion of a research paper has several key elements you should make sure to include:
- A restatement of the research problem
- A summary of your key arguments and/or findings
- A short discussion of the implications of your research
Don’t feel that you have to write the introduction first. The introduction is often one of the last parts of the research paper you’ll write, along with the conclusion.
This is because it can be easier to introduce your paper once you’ve already written the body ; you may not have the clearest idea of your arguments until you’ve written them, and things can change during the writing process .
The way you present your research problem in your introduction varies depending on the nature of your research paper . A research paper that presents a sustained argument will usually encapsulate this argument in a thesis statement .
A research paper designed to present the results of empirical research tends to present a research question that it seeks to answer. It may also include a hypothesis —a prediction that will be confirmed or disproved by your research.
The introduction of a research paper includes several key elements:
- A hook to catch the reader’s interest
- Relevant background on the topic
- Details of your research problem
and your problem statement
- A thesis statement or research question
- Sometimes an overview of the paper
Ask our team
Want to contact us directly? No problem. We are always here for you.
- Email [email protected]
- Start live chat
- Call +1 (510) 822-8066
- WhatsApp +31 20 261 6040

Our team helps students graduate by offering:
- A world-class citation generator
- Plagiarism Checker software powered by Turnitin
- Innovative Citation Checker software
- Professional proofreading services
- Over 300 helpful articles about academic writing, citing sources, plagiarism, and more
Scribbr specializes in editing study-related documents . We proofread:
- PhD dissertations
- Research proposals
- Personal statements
- Admission essays
- Motivation letters
- Reflection papers
- Journal articles
- Capstone projects
Scribbr’s Plagiarism Checker is powered by elements of Turnitin’s Similarity Checker , namely the plagiarism detection software and the Internet Archive and Premium Scholarly Publications content databases .
The add-on AI detector is powered by Scribbr’s proprietary software.
The Scribbr Citation Generator is developed using the open-source Citation Style Language (CSL) project and Frank Bennett’s citeproc-js . It’s the same technology used by dozens of other popular citation tools, including Mendeley and Zotero.
You can find all the citation styles and locales used in the Scribbr Citation Generator in our publicly accessible repository on Github .
- Privacy Policy
Buy Me a Coffee

Home » Research Objectives – Types, Examples and Writing Guide
Research Objectives – Types, Examples and Writing Guide
Table of Contents

Research Objectives
Research objectives refer to the specific goals or aims of a research study. They provide a clear and concise description of what the researcher hopes to achieve by conducting the research . The objectives are typically based on the research questions and hypotheses formulated at the beginning of the study and are used to guide the research process.
Types of Research Objectives
Here are the different types of research objectives in research:
- Exploratory Objectives: These objectives are used to explore a topic, issue, or phenomenon that has not been studied in-depth before. The aim of exploratory research is to gain a better understanding of the subject matter and generate new ideas and hypotheses .
- Descriptive Objectives: These objectives aim to describe the characteristics, features, or attributes of a particular population, group, or phenomenon. Descriptive research answers the “what” questions and provides a snapshot of the subject matter.
- Explanatory Objectives : These objectives aim to explain the relationships between variables or factors. Explanatory research seeks to identify the cause-and-effect relationships between different phenomena.
- Predictive Objectives: These objectives aim to predict future events or outcomes based on existing data or trends. Predictive research uses statistical models to forecast future trends or outcomes.
- Evaluative Objectives : These objectives aim to evaluate the effectiveness or impact of a program, intervention, or policy. Evaluative research seeks to assess the outcomes or results of a particular intervention or program.
- Prescriptive Objectives: These objectives aim to provide recommendations or solutions to a particular problem or issue. Prescriptive research identifies the best course of action based on the results of the study.
- Diagnostic Objectives : These objectives aim to identify the causes or factors contributing to a particular problem or issue. Diagnostic research seeks to uncover the underlying reasons for a particular phenomenon.
- Comparative Objectives: These objectives aim to compare two or more groups, populations, or phenomena to identify similarities and differences. Comparative research is used to determine which group or approach is more effective or has better outcomes.
- Historical Objectives: These objectives aim to examine past events, trends, or phenomena to gain a better understanding of their significance and impact. Historical research uses archival data, documents, and records to study past events.
- Ethnographic Objectives : These objectives aim to understand the culture, beliefs, and practices of a particular group or community. Ethnographic research involves immersive fieldwork and observation to gain an insider’s perspective of the group being studied.
- Action-oriented Objectives: These objectives aim to bring about social or organizational change. Action-oriented research seeks to identify practical solutions to social problems and to promote positive change in society.
- Conceptual Objectives: These objectives aim to develop new theories, models, or frameworks to explain a particular phenomenon or set of phenomena. Conceptual research seeks to provide a deeper understanding of the subject matter by developing new theoretical perspectives.
- Methodological Objectives: These objectives aim to develop and improve research methods and techniques. Methodological research seeks to advance the field of research by improving the validity, reliability, and accuracy of research methods and tools.
- Theoretical Objectives : These objectives aim to test and refine existing theories or to develop new theoretical perspectives. Theoretical research seeks to advance the field of knowledge by testing and refining existing theories or by developing new theoretical frameworks.
- Measurement Objectives : These objectives aim to develop and validate measurement instruments, such as surveys, questionnaires, and tests. Measurement research seeks to improve the quality and reliability of data collection and analysis by developing and testing new measurement tools.
- Design Objectives : These objectives aim to develop and refine research designs, such as experimental, quasi-experimental, and observational designs. Design research seeks to improve the quality and validity of research by developing and testing new research designs.
- Sampling Objectives: These objectives aim to develop and refine sampling techniques, such as probability and non-probability sampling methods. Sampling research seeks to improve the representativeness and generalizability of research findings by developing and testing new sampling techniques.
How to Write Research Objectives
Writing clear and concise research objectives is an important part of any research project, as it helps to guide the study and ensure that it is focused and relevant. Here are some steps to follow when writing research objectives:
- Identify the research problem : Before you can write research objectives, you need to identify the research problem you are trying to address. This should be a clear and specific problem that can be addressed through research.
- Define the research questions : Based on the research problem, define the research questions you want to answer. These questions should be specific and should guide the research process.
- Identify the variables : Identify the key variables that you will be studying in your research. These are the factors that you will be measuring, manipulating, or analyzing to answer your research questions.
- Write specific objectives: Write specific, measurable objectives that will help you answer your research questions. These objectives should be clear and concise and should indicate what you hope to achieve through your research.
- Use the SMART criteria: To ensure that your research objectives are well-defined and achievable, use the SMART criteria. This means that your objectives should be Specific, Measurable, Achievable, Relevant, and Time-bound.
- Revise and refine: Once you have written your research objectives, revise and refine them to ensure that they are clear, concise, and achievable. Make sure that they align with your research questions and variables, and that they will help you answer your research problem.
Example of Research Objectives
Examples of research objectives Could be:
Research Objectives for the topic of “The Impact of Artificial Intelligence on Employment”:
- To investigate the effects of the adoption of AI on employment trends across various industries and occupations.
- To explore the potential for AI to create new job opportunities and transform existing roles in the workforce.
- To examine the social and economic implications of the widespread use of AI for employment, including issues such as income inequality and access to education and training.
- To identify the skills and competencies that will be required for individuals to thrive in an AI-driven workplace, and to explore the role of education and training in developing these skills.
- To evaluate the ethical and legal considerations surrounding the use of AI for employment, including issues such as bias, privacy, and the responsibility of employers and policymakers to protect workers’ rights.
When to Write Research Objectives
- At the beginning of a research project : Research objectives should be identified and written down before starting a research project. This helps to ensure that the project is focused and that data collection and analysis efforts are aligned with the intended purpose of the research.
- When refining research questions: Writing research objectives can help to clarify and refine research questions. Objectives provide a more concrete and specific framework for addressing research questions, which can improve the overall quality and direction of a research project.
- After conducting a literature review : Conducting a literature review can help to identify gaps in knowledge and areas that require further research. Writing research objectives can help to define and focus the research effort in these areas.
- When developing a research proposal: Research objectives are an important component of a research proposal. They help to articulate the purpose and scope of the research, and provide a clear and concise summary of the expected outcomes and contributions of the research.
- When seeking funding for research: Funding agencies often require a detailed description of research objectives as part of a funding proposal. Writing clear and specific research objectives can help to demonstrate the significance and potential impact of a research project, and increase the chances of securing funding.
- When designing a research study : Research objectives guide the design and implementation of a research study. They help to identify the appropriate research methods, sampling strategies, data collection and analysis techniques, and other relevant aspects of the study design.
- When communicating research findings: Research objectives provide a clear and concise summary of the main research questions and outcomes. They are often included in research reports and publications, and can help to ensure that the research findings are communicated effectively and accurately to a wide range of audiences.
- When evaluating research outcomes : Research objectives provide a basis for evaluating the success of a research project. They help to measure the degree to which research questions have been answered and the extent to which research outcomes have been achieved.
- When conducting research in a team : Writing research objectives can facilitate communication and collaboration within a research team. Objectives provide a shared understanding of the research purpose and goals, and can help to ensure that team members are working towards a common objective.
Purpose of Research Objectives
Some of the main purposes of research objectives include:
- To clarify the research question or problem : Research objectives help to define the specific aspects of the research question or problem that the study aims to address. This makes it easier to design a study that is focused and relevant.
- To guide the research design: Research objectives help to determine the research design, including the research methods, data collection techniques, and sampling strategy. This ensures that the study is structured and efficient.
- To measure progress : Research objectives provide a way to measure progress throughout the research process. They help the researcher to evaluate whether they are on track and meeting their goals.
- To communicate the research goals : Research objectives provide a clear and concise description of the research goals. This helps to communicate the purpose of the study to other researchers, stakeholders, and the general public.
Advantages of Research Objectives
Here are some advantages of having well-defined research objectives:
- Focus : Research objectives help to focus the research effort on specific areas of inquiry. By identifying clear research questions, the researcher can narrow down the scope of the study and avoid getting sidetracked by irrelevant information.
- Clarity : Clearly stated research objectives provide a roadmap for the research study. They provide a clear direction for the research, making it easier for the researcher to stay on track and achieve their goals.
- Measurability : Well-defined research objectives provide measurable outcomes that can be used to evaluate the success of the research project. This helps to ensure that the research is effective and that the research goals are achieved.
- Feasibility : Research objectives help to ensure that the research project is feasible. By clearly defining the research goals, the researcher can identify the resources required to achieve those goals and determine whether those resources are available.
- Relevance : Research objectives help to ensure that the research study is relevant and meaningful. By identifying specific research questions, the researcher can ensure that the study addresses important issues and contributes to the existing body of knowledge.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

How to Cite Research Paper – All Formats and...

Data Collection – Methods Types and Examples

Delimitations in Research – Types, Examples and...

Research Paper Format – Types, Examples and...

Research Process – Steps, Examples and Tips

Research Design – Types, Methods and Examples
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.53(4); 2010 Aug

Research questions, hypotheses and objectives
Patricia farrugia.
* Michael G. DeGroote School of Medicine, the
Bradley A. Petrisor
† Division of Orthopaedic Surgery and the
Forough Farrokhyar
‡ Departments of Surgery and
§ Clinical Epidemiology and Biostatistics, McMaster University, Hamilton, Ont
Mohit Bhandari
There is an increasing familiarity with the principles of evidence-based medicine in the surgical community. As surgeons become more aware of the hierarchy of evidence, grades of recommendations and the principles of critical appraisal, they develop an increasing familiarity with research design. Surgeons and clinicians are looking more and more to the literature and clinical trials to guide their practice; as such, it is becoming a responsibility of the clinical research community to attempt to answer questions that are not only well thought out but also clinically relevant. The development of the research question, including a supportive hypothesis and objectives, is a necessary key step in producing clinically relevant results to be used in evidence-based practice. A well-defined and specific research question is more likely to help guide us in making decisions about study design and population and subsequently what data will be collected and analyzed. 1
Objectives of this article
In this article, we discuss important considerations in the development of a research question and hypothesis and in defining objectives for research. By the end of this article, the reader will be able to appreciate the significance of constructing a good research question and developing hypotheses and research objectives for the successful design of a research study. The following article is divided into 3 sections: research question, research hypothesis and research objectives.

Research question
Interest in a particular topic usually begins the research process, but it is the familiarity with the subject that helps define an appropriate research question for a study. 1 Questions then arise out of a perceived knowledge deficit within a subject area or field of study. 2 Indeed, Haynes suggests that it is important to know “where the boundary between current knowledge and ignorance lies.” 1 The challenge in developing an appropriate research question is in determining which clinical uncertainties could or should be studied and also rationalizing the need for their investigation.
Increasing one’s knowledge about the subject of interest can be accomplished in many ways. Appropriate methods include systematically searching the literature, in-depth interviews and focus groups with patients (and proxies) and interviews with experts in the field. In addition, awareness of current trends and technological advances can assist with the development of research questions. 2 It is imperative to understand what has been studied about a topic to date in order to further the knowledge that has been previously gathered on a topic. Indeed, some granting institutions (e.g., Canadian Institute for Health Research) encourage applicants to conduct a systematic review of the available evidence if a recent review does not already exist and preferably a pilot or feasibility study before applying for a grant for a full trial.
In-depth knowledge about a subject may generate a number of questions. It then becomes necessary to ask whether these questions can be answered through one study or if more than one study needed. 1 Additional research questions can be developed, but several basic principles should be taken into consideration. 1 All questions, primary and secondary, should be developed at the beginning and planning stages of a study. Any additional questions should never compromise the primary question because it is the primary research question that forms the basis of the hypothesis and study objectives. It must be kept in mind that within the scope of one study, the presence of a number of research questions will affect and potentially increase the complexity of both the study design and subsequent statistical analyses, not to mention the actual feasibility of answering every question. 1 A sensible strategy is to establish a single primary research question around which to focus the study plan. 3 In a study, the primary research question should be clearly stated at the end of the introduction of the grant proposal, and it usually specifies the population to be studied, the intervention to be implemented and other circumstantial factors. 4
Hulley and colleagues 2 have suggested the use of the FINER criteria in the development of a good research question ( Box 1 ). The FINER criteria highlight useful points that may increase the chances of developing a successful research project. A good research question should specify the population of interest, be of interest to the scientific community and potentially to the public, have clinical relevance and further current knowledge in the field (and of course be compliant with the standards of ethical boards and national research standards).
FINER criteria for a good research question
Adapted with permission from Wolters Kluwer Health. 2
Whereas the FINER criteria outline the important aspects of the question in general, a useful format to use in the development of a specific research question is the PICO format — consider the population (P) of interest, the intervention (I) being studied, the comparison (C) group (or to what is the intervention being compared) and the outcome of interest (O). 3 , 5 , 6 Often timing (T) is added to PICO ( Box 2 ) — that is, “Over what time frame will the study take place?” 1 The PICOT approach helps generate a question that aids in constructing the framework of the study and subsequently in protocol development by alluding to the inclusion and exclusion criteria and identifying the groups of patients to be included. Knowing the specific population of interest, intervention (and comparator) and outcome of interest may also help the researcher identify an appropriate outcome measurement tool. 7 The more defined the population of interest, and thus the more stringent the inclusion and exclusion criteria, the greater the effect on the interpretation and subsequent applicability and generalizability of the research findings. 1 , 2 A restricted study population (and exclusion criteria) may limit bias and increase the internal validity of the study; however, this approach will limit external validity of the study and, thus, the generalizability of the findings to the practical clinical setting. Conversely, a broadly defined study population and inclusion criteria may be representative of practical clinical practice but may increase bias and reduce the internal validity of the study.
PICOT criteria 1
A poorly devised research question may affect the choice of study design, potentially lead to futile situations and, thus, hamper the chance of determining anything of clinical significance, which will then affect the potential for publication. Without devoting appropriate resources to developing the research question, the quality of the study and subsequent results may be compromised. During the initial stages of any research study, it is therefore imperative to formulate a research question that is both clinically relevant and answerable.
Research hypothesis
The primary research question should be driven by the hypothesis rather than the data. 1 , 2 That is, the research question and hypothesis should be developed before the start of the study. This sounds intuitive; however, if we take, for example, a database of information, it is potentially possible to perform multiple statistical comparisons of groups within the database to find a statistically significant association. This could then lead one to work backward from the data and develop the “question.” This is counterintuitive to the process because the question is asked specifically to then find the answer, thus collecting data along the way (i.e., in a prospective manner). Multiple statistical testing of associations from data previously collected could potentially lead to spuriously positive findings of association through chance alone. 2 Therefore, a good hypothesis must be based on a good research question at the start of a trial and, indeed, drive data collection for the study.
The research or clinical hypothesis is developed from the research question and then the main elements of the study — sampling strategy, intervention (if applicable), comparison and outcome variables — are summarized in a form that establishes the basis for testing, statistical and ultimately clinical significance. 3 For example, in a research study comparing computer-assisted acetabular component insertion versus freehand acetabular component placement in patients in need of total hip arthroplasty, the experimental group would be computer-assisted insertion and the control/conventional group would be free-hand placement. The investigative team would first state a research hypothesis. This could be expressed as a single outcome (e.g., computer-assisted acetabular component placement leads to improved functional outcome) or potentially as a complex/composite outcome; that is, more than one outcome (e.g., computer-assisted acetabular component placement leads to both improved radiographic cup placement and improved functional outcome).
However, when formally testing statistical significance, the hypothesis should be stated as a “null” hypothesis. 2 The purpose of hypothesis testing is to make an inference about the population of interest on the basis of a random sample taken from that population. The null hypothesis for the preceding research hypothesis then would be that there is no difference in mean functional outcome between the computer-assisted insertion and free-hand placement techniques. After forming the null hypothesis, the researchers would form an alternate hypothesis stating the nature of the difference, if it should appear. The alternate hypothesis would be that there is a difference in mean functional outcome between these techniques. At the end of the study, the null hypothesis is then tested statistically. If the findings of the study are not statistically significant (i.e., there is no difference in functional outcome between the groups in a statistical sense), we cannot reject the null hypothesis, whereas if the findings were significant, we can reject the null hypothesis and accept the alternate hypothesis (i.e., there is a difference in mean functional outcome between the study groups), errors in testing notwithstanding. In other words, hypothesis testing confirms or refutes the statement that the observed findings did not occur by chance alone but rather occurred because there was a true difference in outcomes between these surgical procedures. The concept of statistical hypothesis testing is complex, and the details are beyond the scope of this article.
Another important concept inherent in hypothesis testing is whether the hypotheses will be 1-sided or 2-sided. A 2-sided hypothesis states that there is a difference between the experimental group and the control group, but it does not specify in advance the expected direction of the difference. For example, we asked whether there is there an improvement in outcomes with computer-assisted surgery or whether the outcomes worse with computer-assisted surgery. We presented a 2-sided test in the above example because we did not specify the direction of the difference. A 1-sided hypothesis states a specific direction (e.g., there is an improvement in outcomes with computer-assisted surgery). A 2-sided hypothesis should be used unless there is a good justification for using a 1-sided hypothesis. As Bland and Atlman 8 stated, “One-sided hypothesis testing should never be used as a device to make a conventionally nonsignificant difference significant.”
The research hypothesis should be stated at the beginning of the study to guide the objectives for research. Whereas the investigators may state the hypothesis as being 1-sided (there is an improvement with treatment), the study and investigators must adhere to the concept of clinical equipoise. According to this principle, a clinical (or surgical) trial is ethical only if the expert community is uncertain about the relative therapeutic merits of the experimental and control groups being evaluated. 9 It means there must exist an honest and professional disagreement among expert clinicians about the preferred treatment. 9
Designing a research hypothesis is supported by a good research question and will influence the type of research design for the study. Acting on the principles of appropriate hypothesis development, the study can then confidently proceed to the development of the research objective.
Research objective
The primary objective should be coupled with the hypothesis of the study. Study objectives define the specific aims of the study and should be clearly stated in the introduction of the research protocol. 7 From our previous example and using the investigative hypothesis that there is a difference in functional outcomes between computer-assisted acetabular component placement and free-hand placement, the primary objective can be stated as follows: this study will compare the functional outcomes of computer-assisted acetabular component insertion versus free-hand placement in patients undergoing total hip arthroplasty. Note that the study objective is an active statement about how the study is going to answer the specific research question. Objectives can (and often do) state exactly which outcome measures are going to be used within their statements. They are important because they not only help guide the development of the protocol and design of study but also play a role in sample size calculations and determining the power of the study. 7 These concepts will be discussed in other articles in this series.
From the surgeon’s point of view, it is important for the study objectives to be focused on outcomes that are important to patients and clinically relevant. For example, the most methodologically sound randomized controlled trial comparing 2 techniques of distal radial fixation would have little or no clinical impact if the primary objective was to determine the effect of treatment A as compared to treatment B on intraoperative fluoroscopy time. However, if the objective was to determine the effect of treatment A as compared to treatment B on patient functional outcome at 1 year, this would have a much more significant impact on clinical decision-making. Second, more meaningful surgeon–patient discussions could ensue, incorporating patient values and preferences with the results from this study. 6 , 7 It is the precise objective and what the investigator is trying to measure that is of clinical relevance in the practical setting.
The following is an example from the literature about the relation between the research question, hypothesis and study objectives:
Study: Warden SJ, Metcalf BR, Kiss ZS, et al. Low-intensity pulsed ultrasound for chronic patellar tendinopathy: a randomized, double-blind, placebo-controlled trial. Rheumatology 2008;47:467–71.
Research question: How does low-intensity pulsed ultrasound (LIPUS) compare with a placebo device in managing the symptoms of skeletally mature patients with patellar tendinopathy?
Research hypothesis: Pain levels are reduced in patients who receive daily active-LIPUS (treatment) for 12 weeks compared with individuals who receive inactive-LIPUS (placebo).
Objective: To investigate the clinical efficacy of LIPUS in the management of patellar tendinopathy symptoms.
The development of the research question is the most important aspect of a research project. A research project can fail if the objectives and hypothesis are poorly focused and underdeveloped. Useful tips for surgical researchers are provided in Box 3 . Designing and developing an appropriate and relevant research question, hypothesis and objectives can be a difficult task. The critical appraisal of the research question used in a study is vital to the application of the findings to clinical practice. Focusing resources, time and dedication to these 3 very important tasks will help to guide a successful research project, influence interpretation of the results and affect future publication efforts.
Tips for developing research questions, hypotheses and objectives for research studies
- Perform a systematic literature review (if one has not been done) to increase knowledge and familiarity with the topic and to assist with research development.
- Learn about current trends and technological advances on the topic.
- Seek careful input from experts, mentors, colleagues and collaborators to refine your research question as this will aid in developing the research question and guide the research study.
- Use the FINER criteria in the development of the research question.
- Ensure that the research question follows PICOT format.
- Develop a research hypothesis from the research question.
- Develop clear and well-defined primary and secondary (if needed) objectives.
- Ensure that the research question and objectives are answerable, feasible and clinically relevant.
FINER = feasible, interesting, novel, ethical, relevant; PICOT = population (patients), intervention (for intervention studies only), comparison group, outcome of interest, time.
Competing interests: No funding was received in preparation of this paper. Dr. Bhandari was funded, in part, by a Canada Research Chair, McMaster University.
404 Not found
- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->

- Clinical articles
- Expert advice
- Career advice
- Revalidation
Question development Previous Next
Setting a research question, aim and objective, owen doody lecturer, department of nursing and midwifery, university of limerick, limerick, republic of ireland, maria e bailey lecturer, department of nursing and midwifery, university of limerick, republic of ireland.
Aim To describe the development of a research question, aim and objective.
Background The first steps of any study are developing the research question, aim and objective. Subsequent steps develop from these and they govern the researchers’ choice of population, setting, data to be collected and time period for the study. Clear, succinctly posed research questions, aims and objectives are essential if studies are to be successful.
Discussion Researchers developing their research questions, aims and objectives generally experience difficulties. They are often overwhelmed trying to convert what they see as a relevant issue from practice into research. This necessitates engaging with the relevant published literature and knowledgeable people.
Conclusion This paper identifies the issues to be considered when developing a research question, aim and objective. Understanding these considerations will enable researchers to effectively present their research question, aim and objective.
Implications for practice To conduct successful studies, researchers should develop clear research questions, aims and objectives.
Nurse Researcher . 23, 4, 19-23. doi: 10.7748/nr.23.4.19.s5
This article has been subject to double-blind review and has been checked using antiplagiarism software
None declared
Received: 04 November 2014
Accepted: 27 May 2015
research question - research aim - research objective - study development - nursing research - novice researchers
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

21 March 2016 / Vol 23 issue 4
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: Setting a research question, aim and objective
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
- How it works
How to Write the Dissertation Aims and Objectives – Guide & Examples
Published by Grace Graffin at January 27th, 2023 , Revised On October 9, 2023
Aims and objectives are among the essential aspects of a dissertation. If you write aims and objectives effectively, they can act as a foundation to give your research clarity and focus.
This article will provide you with all the necessary information regarding aims and objectives, their differences, writing tips , and the common mistakes you should avoid while writing them.
The aim is often a single sentence or a short paragraph that describes your dissertation’s main goal and intent. It tells what you hope to achieve at the end. You should write the aim so that it becomes identifiable when it is achieved with the completion of your dissertation .
The aim is written in a subsection of the introduction to clarify the overall purpose of the dissertation .
Example: It is often observed that employees in culturally diverse workplaces struggle to work effectively in a team. A probable cause of this issue is bullying at the workplace. This research investigates the impact of bullying on employee job satisfaction at culturally diverse workplaces and the resulting loss of employee productivity. This research will use surveys and case study analysis to analyze the impact of bullying on employees.
The objectives in a dissertation describe the ways through which you intend to achieve the research aim. They are specific statements that break down the aim into several smaller key sections of the overall research. Suitable objectives can help you stay focused and conduct research in the direction of your aim.
The number of objectives should be realistic; usually, between three to six, and each one should be possible to achieve. The following example shows the objectives for the previously-mentioned dissertation aim.
1. identification of the behaviors that are considered as bullying 2. exploring the factors that cause bullying at a culturally diverse workplace 3. analyzing the relationship between bullying and job satisfaction of employees 4. providing suitable recommendations on minimizing the bullying at the workplace
The objectives of a dissertation should be SMART.
- Specific: should be precise, focused, and well-defined
- Measurable: the progress should be measurable, and you should be able to determine when you have achieved an objective.
- Achievable: you should be able to carry out the required action within your available resources
- Relevant: should be related to the dissertation aim
- Time-bound: should be possible within the available time
Differences between aims and objectives
Aims and objectives are often mixed, but there are clear differences between them.
Hire an Expert Writer
Orders completed by our expert writers are
- Formally drafted in an academic style
- Free Amendments and 100% Plagiarism Free – or your money back!
- 100% Confidential and Timely Delivery!
- Free anti-plagiarism report
- Appreciated by thousands of clients. Check client reviews
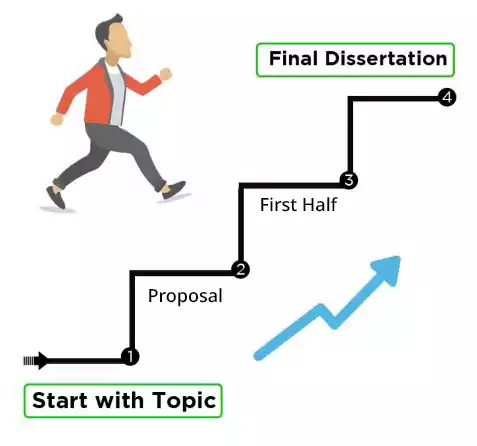
How to write aims and objectives?
There is no particular way or standard to write the aims and objectives. Different researchers have different writing styles, and often it can be influenced by your research supervisor. However, you should follow certain basic principles while writing aims and objectives in a dissertation.
Writing the aim statement
The aim statement should cover the following essential elements.
- Why is the research necessary? (covers the underlying problem on which the study is to be conducted)
- What is the research about? (description of the research title)
- How are you going to conduct it? (a brief statement of intended research methods)
An appropriate aim clearly defines the research purpose without confusing the reader. If you struggle to explain your research and its importance in simpler terms, you should consider refining your research to clarify it further.
Writing objectives
The objectives describe how you would achieve your research aim. You can do this through the following steps,
- The first one to two objectives can be applied to the literature review . (Verbs to be used: investigate, examine, study)
- One objective can be applied to the methodology portion. (Verbs to be used: collect, select, demonstrate, estimate)
- Two to three objectives can cover the critical evaluation or discussion chapters (Verbs to be used: analyze, compare, evaluate)
- The final objective will cover the conclusion or recommendation portion. (Verbs to be used: conclude, recommend)
Instead of writing like a paragraph, the objectives should be written as a numbered list to give them more clarity.
How many aims and objectives should be there?
It depends upon the topic of your research and mainly upon your supervisor’s requirements. Generally, a dissertation has a single broad statement as the research aim. However, it is acceptable to include a main aim along with two to three subsidiary aims.
Similarly, the number of objectives should be realistic and sufficient to measure the progress regarding the achievement of the research aim. Their number can generally vary from three to six depending upon the aim.
Common mistakes to avoid while writing research aims and objectives
- Writing a broad research aim
Writing a broad research aim is a common mistake, and it often becomes difficult to achieve. It may create a problem when you are asked to prove how you have achieved your aims during your viva defense . It would be best to narrow your study to a specific area in the early stages of the dissertation.
- Formulating overlapping research objectives
The objectives should be written such that they are measurable and distinct from each other. If they overlap, it makes it difficult to structure your dissertation properly in specific chapters.
- Setting unrealistic aims
Students often get over-ambitious while describing the research aim and face problems afterward in achieving those aims. You should avoid this mistake and be realistic about what you can achieve in the available time and resources.
Aims and objectives are the sections that require significant time and attention to avoid future hassles while conducting research and writing your dissertation.
Frequently Asked Questions
How to set dissertation aims and objectives.
To set dissertation aims and objectives, define your research goals clearly. Aims state what you want to achieve, while objectives outline specific, measurable steps to reach those goals. Ensure they align with your research question and contribute to your study’s significance.
You May Also Like
What are the key factors influencing language development and what can do to accelerate the process of language acquisition? Here is all you need to know!
If you’ve got kids, writing a dissertation is even harder, because kids do tend to take up a fair amount of time. That said, it’s not impossible.
Are you about to shift to a university housing accommodation? Consider these three things before shifting to have a comfortable time.
USEFUL LINKS
LEARNING RESOURCES

COMPANY DETAILS

- How It Works
Setting a research question, aim and objective
Affiliations.
- 1 Department of Nursing and Midwifery, University of Limerick, Limerick, Republic of Ireland.
- 2 Department of Nursing and Midwifery, University of Limerick, Republic of Ireland.
- PMID: 26997231
- DOI: 10.7748/nr.23.4.19.s5
Aim: To describe the development of a research question, aim and objective.
Background: The first steps of any study are developing the research question, aim and objective. Subsequent steps develop from these and they govern the researchers' choice of population, setting, data to be collected and time period for the study. Clear, succinctly posed research questions, aims and objectives are essential if studies are to be successful.
Discussion: Researchers developing their research questions, aims and objectives generally experience difficulties. They are often overwhelmed trying to convert what they see as a relevant issue from practice into research. This necessitates engaging with the relevant published literature and knowledgeable people.
Conclusion: This paper identifies the issues to be considered when developing a research question, aim and objective. Understanding these considerations will enable researchers to effectively present their research question, aim and objective.
Implications for practice: To conduct successful studies, researchers should develop clear research questions, aims and objectives.
Keywords: novice researchers; nursing research; research aim; research objective; research question; study development.
- Nursing Research / methods
- Nursing Research / organization & administration*
- Organizational Objectives
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Setting a research question, aim and objective

2016, Nurse researcher
To describe the development of a research question, aim and objective. The first steps of any study are developing the research question, aim and objective. Subsequent steps develop from these and they govern the researchers' choice of population, setting, data to be collected and time period for the study. Clear, succinctly posed research questions, aims and objectives are essential if studies are to be successful. Researchers developing their research questions, aims and objectives generally experience difficulties. They are often overwhelmed trying to convert what they see as a relevant issue from practice into research. This necessitates engaging with the relevant published literature and knowledgeable people. This paper identifies the issues to be considered when developing a research question, aim and objective. Understanding these considerations will enable researchers to effectively present their research question, aim and objective. To conduct successful studies, resear...
Related Papers
The Cyprus Journal of Sciences
Kakia Avgousti
Carrying out a research paper is concerned to be a simple task. However, in practice it is far more complicated. The most important factor is for the researcher to know the main principles of the research process. It is vital to identify the research methods progression, the meaning and purpose of the research to be carried out, by the formulation of hypothesis, aims and questions, the use of methodology-both quantitative and qualitative-their characteristics and suitability when utilized, and the need of sampling and ethical considerations. By the use of theoretical framework, the current research paper firstly discusses and analyses the principles of bringing about a research paper, and most importantly it emphasizes the advantages and disadvantages of research methodology.
British journal of community nursing
Keith Meadows
The development of the research question for a study can be where a lot of research fails. Without a well-defined and specific research question or hypothesis, findings from the research are unlikely to tell us very much. Developing a tightly focused research question or hypothesis defines how and what data is collected and analysed and provides a context for the results. This article, the second in a series of six, focuses on the process of developing a research question or hypothesis from the initial idea through to the final research question, using examples to illustrate the key principles. Approaches to reviewing the literature, including hand searching and the use of electronic sources, are described together with their different strengths and weaknesses. An overview of the deductive and inductive approaches to research are described, as well as the underlying rationale of the null hypothesis and one and two-tailed tests. Finally, issues around the feasibility of the study, in...
Ponsian P R O T Ntui
rhoda taller
Janet Gilbertson
mabuta mustafa
lecture notes
Palwasha Jalal
Tinashe Paul
Jackie Campbell
RELATED PAPERS
Physical Review B
Andreas Honecker
Bibliodoc Anuari De Biblioteconomia Documentacio I Informacio
Rafael Peris-bonet
Journal of the Korean Institute of Electrical and Electronic Material Engineers
Woon Ik Park
Hüseyin Dönmez
Geophysics and Geophysical Exploration
ChangSoo Cho
Mutiara Harapan
Riyadhoh : Jurnal Pendidikan Olahraga
Rahmat Iqbal
Historia Da Ciencia E Ensino Construindo Interfaces Issn 2178 2911
EDIANA BARP
Journal of Crystal Growth
zohreh ebrahimi
Canadian Journal of Sociology
Tanya Titchkosky
Juliette Kennedy
FEBS Letters
thao nguyen
Environmental Earth Sciences
Broder Merkel
Maderas. Ciencia y tecnología
Aysenur Kilic
Revista Acadêmica: Ciência Animal
Marcelo Molento
Gabriel Mauro
Santiago Villanueva
Eastern Mediterranean Health Journal
Remote Sensing
Bernard Lyan
University of Chicago Law Review
Andrew Deiss
Antiquité Tardive
Andreas Hartmann-Virnich
Rami Grossberg
22CSEAIML053 SOURAV MAHAPATRA
Applied and Environmental Microbiology
Pallavi Singh
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

QUALITATIVE RESEARCH PLANNING
A strong foundation for a research study is based on careful planning, including defining what, where, when, why, and how. Research planning comes before collecting and analyzing data. You need to identify what you are trying to understand, the reasons why you want to undertake the project, and the resources needed for it.
Research Questions, Aims, and Goals
What is it? Research questions, aims, and goals provide a starting point for your research, as well as boundaries by which to focus your study. A project that begins with sound research questions, aims, and goals is more likely to be successful and yield results that address a specific problem, need, or objective.
Your research questions guide your research, as well as clarify the specific directions your study will take, such as research design, data collection, and analysis approach. They should always be filling a knowledge “gap” — regardless of your field of work. They should be clear, focused, appropriately complex, and worded in a way that aligns properly with the nature of your inquiry.
It is invaluable to discuss your ideas with those who understand the data collection and analysis needs of your study, as well as the end goal. Our consultants can help you craft your FINER (feasible, interesting, novel, ethical, and relevant) research questions, with the end goal in mind.
Depending on your research interest, you may be required to create research aims and/or goals . In some instances, aims or goals fill the place of your research questions. A research aim or goal is also referred to as a research objective. It is a statement about the specific actions that will be taken in a research study, or a statement giving details on actions taken to answer a research question. Our consultants can help you define your research questions, aims, and goals so that the steps required to move forward are clear.
How can we help you?
- Soundboard and hone compelling questions, ideas, and concepts
- Assist in crafting the language of your questions with analysis in mind
- Develop aims and overall goals for your research project
- Identify potential directions from potential research findings
Share this with...

Qualitative Research Planning
Coaching & training, cultural context, feasibility, international collaborations and logistics, research proposals, research questions, aims, goals.
Thank you for your interest in Elite Research, LLC. A consultant will respond to your inquiry within one business day. Please check your email settings to ensure that our response does not end up in your spam folder. If you do not receive an email from us within 24 hours, please feel free to call us directly at 1-800-806-5661 or (972)538-1374
All fields with * are required!
By submitting this form, you accept and agree our privacy policy in terms of conditions.

- Research Group
- Job Seekers

Research Tips
Understanding the Difference between Research Questions and Objectives
January 13, 2023
When conducting research, clearly understanding the difference between research questions and objectives is important. While these terms are often used interchangeably, they refer to two distinct aspects of the research process.
Research questions are broad statements that guide the overall direction of the research. They identify the main problem or area of inquiry that the research will address. For example, a research question might be, "What is the impact of social media on teenage mental health?" This question sets the stage for the research and helps to define the scope of the study.

- Research questions are more general and open-ended, while objectives are specific and measurable.
- Research questions identify the main problem or area of inquiry, while objectives define the specific outcomes that the researcher is looking to achieve.
- Research questions help define the study's scope, while objectives help guide the research process.
- Research questions are often used to generate hypotheses or identify gaps in existing knowledge, while objectives are used to establish clear and achievable targets for the research.
- Research questions and objectives are not mutually exclusive, but well-defined research questions should lead to specific objectives necessary to answer the question.
On the other hand, research objectives are specific, measurable goals that the research aims to achieve. They are used to guide the research process and help to define the specific outcomes that the researcher is looking to achieve. For example, an objective for the above research question might be "To determine the correlation between social media usage and rates of depression in teenagers." This objective is more specific and measurable than the research question and helps define the specific outcomes that the researcher is looking to achieve.
It is important to note that research questions and objectives are not mutually exclusive; a study can have one or several questions and objectives. A well-defined research question should lead to specific objectives necessary to answer the question.
In summary, research questions and objectives are two distinct aspects of the research process. Research questions are broad statements that guide the overall direction of the research, while research objectives are specific, measurable goals that the research aims to achieve. Understanding these two terms' differences is essential for conducting effective and meaningful research.
- Research article
- Open access
- Published: 15 April 2024
What is quality in long covid care? Lessons from a national quality improvement collaborative and multi-site ethnography
- Trisha Greenhalgh ORCID: orcid.org/0000-0003-2369-8088 1 ,
- Julie L. Darbyshire 1 ,
- Cassie Lee 2 ,
- Emma Ladds 1 &
- Jenny Ceolta-Smith 3
BMC Medicine volume 22 , Article number: 159 ( 2024 ) Cite this article
51 Altmetric
Metrics details
Long covid (post covid-19 condition) is a complex condition with diverse manifestations, uncertain prognosis and wide variation in current approaches to management. There have been calls for formal quality standards to reduce a so-called “postcode lottery” of care. The original aim of this study—to examine the nature of quality in long covid care and reduce unwarranted variation in services—evolved to focus on examining the reasons why standardizing care was so challenging in this condition.
In 2021–2023, we ran a quality improvement collaborative across 10 UK sites. The dataset reported here was mostly but not entirely qualitative. It included data on the origins and current context of each clinic, interviews with staff and patients, and ethnographic observations at 13 clinics (50 consultations) and 45 multidisciplinary team (MDT) meetings (244 patient cases). Data collection and analysis were informed by relevant lenses from clinical care (e.g. evidence-based guidelines), improvement science (e.g. quality improvement cycles) and philosophy of knowledge.
Participating clinics made progress towards standardizing assessment and management in some topics; some variation remained but this could usually be explained. Clinics had different histories and path dependencies, occupied a different place in their healthcare ecosystem and served a varied caseload including a high proportion of patients with comorbidities. A key mechanism for achieving high-quality long covid care was when local MDTs deliberated on unusual, complex or challenging cases for which evidence-based guidelines provided no easy answers. In such cases, collective learning occurred through idiographic (case-based) reasoning , in which practitioners build lessons from the particular to the general. This contrasts with the nomothetic reasoning implicit in evidence-based guidelines, in which reasoning is assumed to go from the general (e.g. findings of clinical trials) to the particular (management of individual patients).
Not all variation in long covid services is unwarranted. Largely because long covid’s manifestations are so varied and comorbidities common, generic “evidence-based” standards require much individual adaptation. In this complex condition, quality improvement resources may be productively spent supporting MDTs to optimise their case-based learning through interdisciplinary discussion. Quality assessment of a long covid service should include review of a sample of individual cases to assess how guidelines have been interpreted and personalized to meet patients’ unique needs.
Study registration
NCT05057260, ISRCTN15022307.
Peer Review reports
The term “long covid” [ 1 ] means prolonged symptoms following SARS-CoV-2 infection not explained by an alternative diagnosis [ 2 ]. It embraces the US term “post-covid conditions” (symptoms beyond 4 weeks) [ 3 ], the UK terms “ongoing symptomatic covid-19” (symptoms lasting 4–12 weeks) and “post covid-19 syndrome” (symptoms beyond 12 weeks) [ 4 ] and the World Health Organization’s “post covid-19 condition” (symptoms occurring beyond 3 months and persisting for at least 2 months) [ 5 ]. Long covid thus defined is extremely common. In UK, for example, 1.8 million of a population of 67 million met the criteria for long covid in early 2023 and 41% of these had been unwell for more than 2 years [ 6 ].
Long covid is characterized by a constellation of symptoms which may include breathlessness, fatigue, muscle and joint pain, chest pain, memory loss and impaired concentration (“brain fog”), sleep disturbance, depression, anxiety, palpitations, dizziness, gastrointestinal problems such as diarrhea, skin rashes and allergy to food or drugs [ 2 ]. These lead to difficulties with essential daily activities such as washing and dressing, impaired exercise tolerance and ability to work, and reduced quality of life [ 2 , 7 , 8 ]. Symptoms typically cluster (e.g. in different patients, long covid may be dominated by fatigue, by breathlessness or by palpitations and dizziness) [ 9 , 10 ]. Long covid may follow a fairly constant course or a relapsing and remitting one, perhaps with specific triggers [ 11 ]. Overlaps between fatigue-dominant subtypes of long covid, myalgic encephalomyelitis and chronic fatigue syndrome have been hypothesized [ 12 ] but at the time of writing remain unproven.
Long covid has been a contested condition from the outset. Whilst long-term sequelae following other coronavirus (SARS and MERS) infections were already well-documented [ 13 ], SARS-CoV-2 was originally thought to cause a short-lived respiratory illness from which the patient either died or recovered [ 14 ]. Some clinicians dismissed protracted or relapsing symptoms as due to anxiety or deconditioning, especially if the patient had not had laboratory-confirmed covid-19. People with long covid got together in online groups and shared accounts of their symptoms and experiences of such “gaslighting” in their healthcare encounters [ 15 , 16 ]. Some groups conducted surveys on their members, documenting the wide range of symptoms listed in the previous paragraph and showing that whilst long covid is more commonly a sequel to severe acute covid-19, it can (rarely) follow a mild or even asymptomatic acute infection [ 17 ].
Early publications on long covid depicted a post-pneumonia syndrome which primarily affected patients who had been hospitalized (and sometimes ventilated) [ 18 , 19 ]. Later, covid-19 was recognized to be a multi-organ inflammatory condition (the pneumonia, for example, was reclassified as pneumonitis ) and its long-term sequelae attributed to a combination of viral persistence, dysregulated immune response (including auto-immunity), endothelial dysfunction and immuno-thrombosis, leading to damage to the lining of small blood vessels and (thence) interference with transfer of oxygen and nutrients to vital organs [ 20 , 21 , 22 , 23 , 24 ]. But most such studies were highly specialized, laboratory-based and written primarily for an audience of fellow laboratory researchers. Despite demonstrating mean differences in a number of metabolic variables, they failed to identify a reliable biomarker that could be used routinely in the clinic to rule a diagnosis of long covid in or out. Whilst the evidence base from laboratory studies grew rapidly, it had little influence on clinical management—partly because most long covid clinics had been set up with impressive speed by front-line clinical teams to address an immediate crisis, with little or no input from immunologists, virologists or metabolic specialists [ 25 ].
Studies of the patient experience revealed wide geographical variation in whether any long covid services were provided and (if they were) which patients were eligible for these and what tests and treatments were available [ 26 ]. An interim UK clinical guideline for long covid had been produced at speed and published in December 2020 [ 27 ], but it was uncertain about diagnostic criteria, investigations, treatments and prognosis. Early policy recommendations for long covid services in England, based on wide consultation across UK, had proposed a tiered service with “tier 1” being supported self-management, “tier 2” generalist assessment and management in primary care, “tier 3” specialist rehabilitation or respiratory follow-up with oversight from a consultant physician and “tier 4” tertiary care for patients with complications or complex needs [ 28 ]. In 2021, ring-fenced funding was allocated to establish 90 multidisciplinary long covid clinics in England [ 29 ]; some clinics were also set up with local funding in Scotland and Wales. These clinics varied widely in eligibility criteria, referral pathways, staffing mix (some had no doctors at all) and investigations and treatments offered. A further policy document on improving long covid services was published in 2022 [ 30 ]; it recommended that specialist long covid clinics should continue, though the long-term funding of these services remains uncertain [ 31 ]. To build the evidence base for delivering long covid services, major programs of publicly funded research were commenced in both UK [ 32 ] and USA [ 33 ].
In short, at the time this study began (late 2021), there appeared to be much scope for a program of quality improvement which would capture fast-emerging research findings, establish evidence-based standards and ensure these were rapidly disseminated and consistently adopted across both specialist long covid services and in primary care.
Quality improvement collaboratives
The quality improvement movement in healthcare was born in the early 1980s when clinicians and policymakers US and UK [ 34 , 35 , 36 , 37 ] began to draw on insights from outside the sector [ 38 , 39 , 40 ]. Adapting a total quality management approach that had previously transformed the Japanese car industry, they sought to improve efficiency, reduce waste, shift to treating the upstream causes of problems (hence preventing disease) and help all services approach the standards of excellence achieved by the best. They developed an approach based on (a) understanding healthcare as a complex system (especially its key interdependencies and workflows), (b) analysing and addressing variation within the system, (c) learning continuously from real-world data and (d) developing leaders who could motivate people and help them change structures and processes [ 41 , 42 , 43 , 44 ].
Quality improvement collaboratives (originally termed “breakthrough collaboratives” [ 45 ]), in which representatives from different healthcare organizations come together to address a common problem, identify best practice, set goals, share data and initiate and evaluate improvement efforts [ 46 ], are one model used to deliver system-wide quality improvement. It is widely assumed that these collaboratives work because—and to the extent that—they identify, interpret and implement high-quality evidence (e.g. from randomized controlled trials).
Research on why quality improvement collaboratives succeed or fail has produced the following list of critical success factors: taking a whole-system approach, selecting a topic and goal that fits with organizations’ priorities, fostering a culture of quality improvement (e.g. that quality is everyone’s job), engagement of everyone (including the multidisciplinary clinical team, managers, patients and families) in the improvement effort, clearly defining people’s roles and contribution, engaging people in preliminary groundwork, providing organizational-level support (e.g. chief executive endorsement, protected staff time, training and support for teams, resources, quality-focused human resource practices, external facilitation if needed), training in specific quality improvement techniques (e.g. plan-do-study-act cycle), attending to the human dimension (including cultivating trust and working to ensure shared vision and buy-in), continuously generating reliable data on both processes (e.g. current practice) and outcomes (clinical, satisfaction) and a “learning system” infrastructure in which knowledge that is generated feeds into individual, team and organizational learning [ 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 ].
The quality improvement collaborative approach has delivered many successes but it has been criticized at a theoretical level for over-simplifying the social science of human motivation and behaviour and for adopting a somewhat mechanical approach to the study of complex systems [ 55 , 56 ]. Adaptations of the original quality improvement methodology (e.g. from Sweden [ 57 , 58 ]) have placed greater emphasis on human values and meaning-making, on the grounds that reducing the complexities of a system-wide quality improvement effort to a set of abstract and generic “success factors” will miss unique aspects of the case such as historical path dependencies, personalities, framing and meaning-making and micropolitics [ 59 ].
Perhaps this explains why, when the abovementioned factors are met, a quality improvement collaborative’s success is more likely but is not guaranteed, as a systematic review demonstrated [ 60 ]. Some well-designed and well-resourced collaboratives addressing clear knowledge gaps produced few or no sustained changes in key outcome measures [ 49 , 53 , 60 , 61 , 62 ]. To identify why this might be, a detailed understanding of a service’s history, current challenges and contextual constraints is needed. This explains our decision, part-way through the study reported here, to collect rich contextual data on participating sites so as to better explain success or failure of our own collaborative.
Warranted and unwarranted variation in clinical practice
A generation ago, Wennberg described most variation in clinical practice as “unwarranted” (which he defined as variation in the utilization of health care services that cannot be explained by variation in patient illness or patient preferences) [ 63 ]. Others coined the term “postcode lottery” to depict how such variation allegedly impacted on health outcomes [ 64 ]. Wennberg and colleagues’ Atlas of Variation , introduced in 1999 [ 65 ], and its UK equivalent, introduced in 2010 [ 66 ], described wide regional differences in the rates of procedures from arthroscopy to hysterectomy, and were used to prompt services to identify and address examples of under-treatment, mis-treatment and over-treatment. Numerous similar initiatives, mostly based on hospital activity statistics, have been introduced around the world [ 66 , 67 , 68 , 69 ]. Sutherland and Levesque’s proposed framework for analysing variation, for example, has three domains: capacity (broadly, whether sufficient resources are allocated at organizational level and whether individuals have the time and headspace to get involved), evidence (the extent to which evidence-based guidelines exist and are followed), and agency (e.g. whether clinicians are engaged with the issue and the effect of patient choice) [ 70 ].
Whilst it is clearly a good idea to identify unwarranted variation in practice, it is also important to acknowledge that variation can be warranted . The very act of measuring and describing variation carries great rhetorical power, since revealing geographical variation in any chosen metric effectively frames this as a problem with a conceptually simple solution (reducing variation) that will appeal to both politicians and the public [ 71 ]. The temptation to expose variation (e.g. via visualizations such as maps) and address it in mechanistic ways should be resisted until we have fully understood the reasons why it exists, which may include perverse incentives, insufficient opportunities to discuss cases with colleagues, weak or absent feedback on practice, unclear decision processes, contested definitions of appropriate care and professional challenges to guidelines [ 72 ].
Research question, aims and objectives
Research question.
What is quality in long covid care and how can it best be achieved?
To identify best practice and reduce unwarranted variation in UK long covid services.
To explain aspects of variation in long covid services that are or may be warranted.
Our original objectives were to:
Establish a quality improvement collaborative for 10 long covid clinics across UK.
Use quality improvement methods in collaboration with patients and clinic staff to prioritize aspects of care to improve. For each priority topic, identify best (evidence-informed) clinical practice, measure performance in each clinic, compare performance with a best practice benchmark and improve performance.
Produce organizational case studies of participating long covid clinics to explain their origins, evolution, leadership, ethos, population served, patient pathways and place in the wider healthcare ecosystem.
Examine these case studies to explain variation in practice, especially in topics where the quality improvement cycle proves difficult to follow or has limited impact.
The LOCOMOTION study
LOCOMOTION (LOng COvid Multidisciplinary consortium Optimising Treatments and services across the NHS) was a 30-month multi-site case study of 10 long covid clinics (8 in England, 1 in Wales and 1 in Scotland), beginning in 2021, which sought to optimise long covid care. Each clinic offered multidisciplinary care to patients referred from primary or secondary care (and, in some cases, self-referred), and held regular multidisciplinary team (MDT) meetings, mostly online via Microsoft Teams, to discuss cases. A study protocol for LOCOMOTION, with details of ethical approvals, management, governance and patient involvement has been published [ 25 ]. The three main work packages addressed quality improvement, technology-supported patient self-management and phenotyping and symptom clustering. This paper reports on the first work package, focusing mainly on qualitative findings.
Setting up the quality improvement collaborative
We broadly followed standard methodology for “breakthrough” quality improvement collaboratives [ 44 , 45 ], with two exceptions. First, because of geographical distance, continuing pandemic precautions and developments in videoconferencing technology, meetings were held online. Second, unlike in the original breakthrough model, patients were included in the collaborative, reflecting the cultural change towards patient partnerships since the model was originally proposed 40 years ago.
Each site appointed a clinical research fellow (doctor, nurse or allied health professional) funded partly by the LOCOMOTION study and partly with clinical sessions; some were existing staff who were backfilled to take on a research role whilst others were new appointments. The quality improvement meetings were held approximately every 8 weeks on Microsoft Teams and lasted about 2 h; there was an agenda and a chair, and meetings were recorded with consent. The clinical research fellow from each clinic attended, sometimes joined by the clinical lead for that site. In the initial meeting, the group proposed and prioritized topics before merging their consensus with the list of priority topics generated separately by patients (there was much overlap but also some differences).
In subsequent meetings, participants attempted to reach consensus on how to define, measure and achieve quality for each priority topic in turn, implement this approach in their own clinic and monitor its impact. Clinical leads prepared illustrative clinical cases and summaries of the research evidence, which they presented using Microsoft Powerpoint; the group then worked towards consensus on the implications for practice through general discussion. Clinical research fellows assisted with literature searches, collected baseline data from their own clinic, prepared and presented anonymized case examples, and contributed to collaborative goal-setting for improvement. Progress on each topic was reviewed at a later meeting after an agreed interval.
An additional element of this work package was semi-structured interviews with 29 patients, recruited from 9 of the 10 participating sites, about their clinic experiences with a view to feeding into service improvement (in the other site, no patient volunteered).
Our patient advisory group initially met separately from the quality improvement collaborative. They designed a short survey of current practice and sent it to each clinic; the results of this informed a prioritization exercise for topics where they considered change was needed. The patient-generated list was tabled at the quality improvement collaborative discussions, but patients were understandably keen to join these discussions directly. After about 9 months, some patient advisory group members joined the regular collaborative meetings. This dynamic was not without its tensions, since sharing performance data requires trust and there were some concerns about confidentiality when real patient cases were discussed with other patients present.
How evidence-informed quality targets were set
At the time the study began, there were no published large-scale randomized controlled trials of any interventions for long covid. We therefore followed a model used successfully in other quality improvement efforts where research evidence was limited or absent or it did not translate unambiguously into models for current services. In such circumstances, the best evidence may be custom and practice in the best-performing units. The quality improvement effort becomes oriented to what one group of researchers called “potentially better practices”—that is, practices that are “developed through analysis of the processes of care, literature review, and site visits” (page 14) [ 73 ]. The idea was that facilitated discussion among clinical teams, drawing on published research where available but also incorporating clinical experience, established practice and systematic analysis of performance data across participating clinics would surface these “potentially better practices”—an approach which, though not formally tested in controlled trials, appears to be associated with improved outcomes [ 46 , 73 ].
Adding an ethnographic component
Following limited progress made on some topics that had been designated high priority, we interviewed all 10 clinical research fellows (either individually or, in two cases, with a senior clinician present) and 18 other clinic staff (five individually plus two groups of 5 and 8), along with additional informal discussions, to explore the challenges of implementing the changes that had been agreed. These interviews were not audiotaped but detailed notes were made and typed up immediately afterwards. It became evident that some aspects of what the collaborative had deemed “evidence-informed” care were contested by front-line clinic staff, perceived as irrelevant to the service they were delivering, or considered impossible to implement. To unpack these issues further, the research protocol was amended to include an ethnographic component.
TG and EL (academic general practitioners) and JLD (a qualitative researcher with a PhD in the patient experience) attended a total of 45 MDT meetings in participating clinics (mostly online or hybrid). Staff were informed in advance that there would be an observer present; nobody objected. We noted brief demographic and clinical details of cases discussed (but no identifying data), dilemmas and uncertainties on which discussions focused, and how different staff members contributed.
TG made 13 in-person visits to participating long covid clinics. Staff were notified in advance; all were happy to be observed. Visits lasted between 5 and 8 h (54 h in total). We observed support staff booking patients in and processing requests and referrals, and shadowed different clinical staff in turn as they saw patients. Patients were informed of our presence and its purpose beforehand and given the opportunity to decline (three of 53 patients approached did). We discussed aspects of each case with the clinician after the patient left. When invited, we took breaks with staff and used these as an opportunity to ask them informally what it was like working in the clinic.
Ethnographic observation, analysis and reporting was geared to generating a rich interpretive account of the clinical, operational and interpersonal features of each clinic—what Van Maanen calls an “impressionist tales” [ 74 ]. Our work was also guided by the principles set out by Golden-Biddle and Locke, namely authenticity (spending time in the field and basing interpretations on these direct observations), plausibility (creating a plausible account through rich persuasive description) and criticality (e.g. reflexively examining our own assumptions) [ 75 ]. Our collection and analysis of qualitative data was informed by our own professional backgrounds (two general practitioners, one physical therapist, two non-clinicians).
In both MDTs and clinics, we took contemporaneous notes by hand and typed these up immediately afterwards.
Data management and analysis
Typed interview notes and field notes from clinics were collated in a set of Word documents, one for each clinic attended. They were analysed thematically [ 76 ] with attention to the literature on quality improvement and variation (see “ Background ”). Interim summaries were prepared on each clinic, setting out the narrative of how it had been established, its ethos and leadership, setting and staffing, population served and key links with other parts of the local healthcare ecosystem.
Minutes and field notes from the quality improvement collaborative meetings were summarized topic by topic, including initial data collected by the researchers-in-residence, improvement actions taken (or attempted) in that clinic, and any follow-up data shared. Progress or lack of it was interpreted in relation to the contextual case summary for that clinic.
Patient cases seen in clinic, and those discussed by MDTs, were summarized as brief case narratives in Word documents. Using the constant comparative method [ 77 ], we produced an initial synthesis of the clinical picture and principles of management based on the first 10 patient cases seen, and refined this as each additional case was added. Demographic and brief clinical and social details were also logged on Excel spreadsheets. When writing up clinical cases, we used the technique of composite case construction (in which we drew on several actual cases to generate a fictitious one, thereby protecting anonymity whilst preserving key empirical findings [ 78 ]); any names reported in this paper are pseudonyms.
Member checking
A summary was prepared for each clinic, including a narrative of the clinic’s own history and a summary of key quality issues raised across the ten clinics. These summaries included examples from real cases in our dataset. These were shared with the clinical research fellow and a senior clinician from the clinic, and amended in response to feedback. We also shared these summaries with representatives from the patient advisory group.
Overview of dataset
This study generated three complementary datasets. First, the video recordings, minutes, and field notes of 12 quality improvement collaborative meetings, along with the evidence summaries prepared for these meetings and clinic summaries (e.g. descriptions of current practice, audits) submitted by the clinical research fellows. This dataset illustrated wide variation in practice, and (in many topics) gaps or ambiguities in the evidence base.
Second, interviews with staff ( n = 30) and patients ( n = 29) from the clinics, along with ethnographic field notes (approximately 100 pages) from 13 in-person clinic visits (54 h), including notes on 50 patient consultations (40 face-to-face, 6 telephone, 4 video). This dataset illustrated the heterogeneity among the ten participating clinics.
Third, field notes (approximately 100 pages), including discussions on 244 clinical cases from the 45 MDT meetings (49 h) that we observed. This dataset revealed further similarities and contrasts among clinics in how patients were managed. In particular, it illustrated how, for the complex patients whose cases were presented at these meetings, teams made sense of, and planned for, each case through multidisciplinary dialogue. This dialogue typically began with one staff member presenting a detailed clinical history along with a narrative of how it had affected the patient’s life and what was at stake for them (e.g. job loss), after which professionals from various backgrounds (nursing, physical therapy, occupational therapy, psychology, dietetics, and different medical specialties) joined in a discussion about what to do.
The ten participating sites are summarized in Table 1 .
In the next two sections, we explore two issues—difficulty defining best practice and the heterogeneous nature of the clinics—that were key to explaining why quality, when pursued in a 10-site collaborative, proved elusive. We then briefly summarize patients’ accounts of their experience in the clinics and give three illustrative examples of the elusiveness of quality improvement using selected topics that were prioritized in our collaborative: outcome measures, investigation of palpitations and management of fatigue. In the final section of the results, we describe how MDT deliberations proved crucial for local quality improvement. Further detail on clinical priority topics will be presented in a separate paper.
“Best practice” in long covid: uncertainty and conflict
The study period (September 2021 to December 2023) corresponded with an exponential increase in published research on long covid. Despite this, the quality improvement collaborative found few unambiguous recommendations for practice. This gap between what the research literature offered and what clinical practice needed was partly ontological (relating what long covid is ). One major bone of contention between patients and clinicians (also evident in discussions with our patient advisory group), for example, was how far (and in whom) clinicians should look for and attempt to treat the various metabolic abnormalities that had been documented in laboratory research studies. The literature on this topic was extensive but conflicting [ 20 , 21 , 22 , 23 , 24 , 79 , 80 , 81 , 82 ]; it was heavy on biological detail but light on clinical application.
Patients were often aware of particular studies that appeared to offer plausible molecular or cellular explanations for symptom clusters along with a drug (often repurposed and off-label) whose mechanism of action appeared to be a good fit with the metabolic chain of causation. In one clinic, for example, we were shown an email exchange between a patient (not medically qualified) and a consultant, in which the patient asked them to reconsider their decision not to prescribe low-dose naltrexone, an opioid receptor antagonist with anti-inflammatory properties. The request included a copy of a peer-reviewed academic paper describing a small, uncontrolled pre-post study (i.e. a weak study design) in which this drug appeared to improve symptoms and functional performance in patients with long covid, as well as a mechanistic argument explaining why the patient felt this drug was a plausible choice in their own case.
This patient’s clinician, in common with most clinicians delivering front-line long covid services, considered that the evidence for such mechanism-based therapies was weak. Clinicians generally felt that this evidence, whilst promising, did not yet support routine measurement of clotting factors, antibodies, immune cells or other biomarkers or the prescription of mechanism-based therapies such as antivirals, anti-inflammatories or anticoagulants. Low-dose naltroxone, for example, is currently being tested in at least one randomized controlled trial (see National Clinical Trials Registry NCT05430152), which had not reported at the time of our observations.
Another challenge to defining best practice was the oft-repeated phrase that long covid is a “diagnosis by exclusion”, but the high prevalence of comorbidities meant that the “pure” long covid patient untainted by other potential explanations for their symptoms was a textbook ideal. In one MDT, for example, we observed a discussion about a patient who had had both swab-positive covid-19 and erythema migrans (a sign of Lyme disease) in the weeks before developing fatigue, yet local diagnostic criteria for each condition required the other to be excluded.
The logic of management in most participating clinics was pragmatic: prompt multidisciplinary assessment and treatment with an emphasis on obtaining a detailed clinical history (including premorbid health status), excluding serious complications (“red flags”), managing specific symptom clusters (for example, physical therapy for breathing pattern disorder), treating comorbidities (for example, anaemia, diabetes or menopause) and supporting whole-person rehabilitation [ 7 , 83 ]. The evidentiary questions raised in MDT discussions (which did not include patients) addressed the practicalities of the rehabilitation model (for example, whether cognitive therapy for neurocognitive complications is as effective when delivered online as it is when delivered in-person) rather than the molecular or cellular mechanisms of disease. For example, the question of whether patients with neurocognitive impairment should be tested for micro-clots or treated with anticoagulants never came up in the MDTs we observed, though we did visit a tertiary referral clinic (the tier 4 clinic in site H), whose lead clinician had a research interest in inflammatory coagulopathies and offered such tests to selected patients.
Because long covid typically produces dozens of symptoms that tend to be uniquely patterned in each patient, the uncertainties on which MDT discussions turned were rarely about general evidence of the kind that might be found in a guideline (e.g. how should fatigue be managed?). Rather they concerned particular case-based clinical decisions (e.g. how should this patient’s fatigue be managed, given the specifics of this case?). An example from our field notes illustrates this:
Physical therapist presents the case of a 39-year-old woman who works as a cleaner on an overnight ferry. Has had long covid for 2 years. Main symptoms are shortness of breath and possible anxiety attacks, especially when at work. She has had a course of physical therapy to teach diaphragmatic breathing but has found that focusing on her breathing makes her more anxious. Patient has to do a lot of bending in her job (e.g. cleaning toilets and under seats), which makes her dizzy, but Active Stand Test was normal. She also has very mild tricuspid incompetence [someone reads out a cardiology report—not hemodynamically significant].
Rehabilitation guidelines (e.g. WHO) recommend phased return to work (e.g. with reduced hours) and frequent breaks. “Tricky!” says someone. The job is intense and busy, and the patient can’t afford not to work. Discussion on whether all her symptoms can be attributed to tension and anxiety. Physical therapist who runs the breathing group says, “No, it’s long covid”, and describes severe initial covid-19 episode and results of serial chest X-rays which showed gradual clearing of ground glass shadows. Team discussion centers on how to negotiate reduced working hours in this particular job, given the overnight ferry shifts. --MDT discussion, Site D
This example raises important considerations about the nature of clinical knowledge in long covid. We return to it in the final section of the “ Results ” and in the “ Discussion ”.
Long covid clinics: a heterogeneous context for quality improvement
Most participating clinics had been established in mid-2020 to follow up patients who had been hospitalized (and perhaps ventilated) for severe acute covid-19. As mass vaccination reduced the severity of acute covid-19 for most people, the patient population in all clinics progressively shifted to include fewer “post-ICU [intensive care unit]” patients (in whom respiratory symptoms almost always dominated), and more people referred by their general practitioners or other secondary care specialties who had not been hospitalized for their acute covid-19 infection, and in whom fatigue, brain fog and palpitations were often the most troubling symptoms. Despite these similarities, the ten clinics had very different histories, geographical and material settings, staffing structures, patient pathways and case mix, as Table 1 illustrates. Below, we give more detail on three example sites.
Site C was established as a generalist “assessment-only” service by a general practitioner with an interest in infectious diseases. It is led jointly by that general practitioner and an occupational therapist, assisted by a wide range of other professionals including speech and language therapy, dietetics, clinical psychology and community-based physical therapy and occupational therapy. It has close links with a chronic fatigue service and a pain clinic that have been running in the locality for over 20 years. The clinic, which is entirely virtual (staff consult either from home or from a small side office in the community trust building), is physically located in a low-rise building on the industrial outskirts of a large town, sharing office space with various community-based health and social care services. Following a 1-h telephone consultation by one of the clinical leads, each patient is discussed at the MDT and then either discharged back to their general practitioner with a detailed management plan or referred on to one of the specialist services. This arrangement evolved to address a particular problem in this locality—that many patients with long covid were being referred by their general practitioner to multiple specialties (e.g. respiratory, neurology, fatigue), leading to a fragmented patient experience, unnecessary specialist assessments and wasteful duplication. The generalist assessment by telephone is oriented to documenting what is often a complex illness narrative (including pre-existing physical and mental comorbidities) and working with the patient to prioritize which symptoms or problems to pursue in which order.
Site E, in a well-regarded inner-city teaching hospital, had been set up in 2020 by a respiratory physician. Its initial ethos and rationale had been “respiratory follow-up”, with strong emphasis on monitoring lung damage via repeated imaging and lung function tests and in ensuring that patients received specialist physical therapy to “re-learn” efficient breathing techniques. Over time, this site has tried to accommodate a more multi-system assessment, with the introduction of a consultant-led infectious disease clinic for patients without a dominant respiratory component, reflecting the shift towards a more fatigue-predominant case mix. At the time of our fieldwork, each patient was seen in turn by a physician, psychologist, occupational therapist and respiratory physical therapist (half an hour each) before all four staff reconvened in a face-to-face MDT meeting to form a plan for each patient. But whilst a wide range of patients with diverse symptoms were discussed at these meetings, there remained a strong focus on respiratory pathology (e.g. tracking improvements in lung function and ensuring that coexisting asthma was optimally controlled).
Site F, one of the first long covid clinics in UK, was set up by a rehabilitation consultant who had been drafted to work on the ICU during the first wave of covid-19 in early 2020. He had a longstanding research interest in whole-patient rehabilitation, especially the assessment and management of chronic fatigue and pain. From the outset, clinic F was more oriented to rehabilitation, including vocational rehabilitation to help patients return to work. There was less emphasis on monitoring lung function or pursuing respiratory comorbidities. At the time of our fieldwork, clinic F offered both a community-based service (“tier 2”) led by an occupational therapist, supported by a respiratory physical therapist and psychologist, and a hospital-based service (“tier 3”) led by the rehabilitation consultant, supported by a wider MDT. Staff in both tiers emphasized that each patient needs a full physical and mental assessment and help to set and work towards achievable goals, whilst staying within safe limits so as to avoid post-exertional symptom exacerbation. Because of the research interest of the lead physician, clinic F adapted well to the growing numbers of patients with fatigue and quickly set up research studies on this cohort [ 84 ].
Details of the other seven sites are shown in Table 1 . Broadly speaking, sites B, E, G and H aligned with the “respiratory follow-up” model and sites F and I aligned with the “rehabilitation” model. Sites A and J had a high-volume, multi-tiered service whose community tier aligned with the “holistic GP assessment” model (site C above) and which also offered a hospital-based, rehabilitation-focused tier. The small service in Scotland (site D) had evolved from an initial respiratory focus to become part of the infectious diseases (ME/CFS) service; Lyme disease (another infectious disease whose sequelae include chronic fatigue) was also prevalent in this region.
The patient experience
Whilst the 10 participating clinics were very diverse in staffing, ethos and patient flows, the 29 patient interviews described remarkably consistent clinic experiences. Almost all identified the biggest problem to be the extended wait of several months before they were seen and the limited awareness (when initially referred) of what long covid clinics could provide. Some talked of how they cried with relief when they finally received an appointment. When the quality improvement collaborative was initially established, waiting times and bottlenecks were patients’ the top priority for quality improvement, and this ranking was shared by clinic staff, who were very aware of how much delays and uncertainties in assessment and treatment compounded patients’ suffering. This issue resolved to a large extent over the study period in all clinics as the referral backlog cleared and the incidence of new cases of long covid fell [ 85 ]; it will be covered in more detail in a separate publication.
Most patients in our sample were satisfied with the care they received when they were finally seen in clinic, especially how they finally felt “heard” after a clinician took a full history. They were relieved to receive affirmation of their experience, a diagnosis of what was wrong and reassurance that they were believed. They were grateful for the input of different members of the multidisciplinary teams and commented on the attentiveness, compassion and skill of allied professionals in particular (“she was wonderful, she got me breathing again”—patient BIR145 talking about a physical therapist). One or two patient participants expressed confusion about who exactly they had seen and what advice they had been given, and some did not realize that a telephone assessment had been an actual clinical consultation. A minority expressed disappointment that an expected investigation had not been ordered (one commented that they had not had any blood tests at all). Several had assumed that the help and advice from the long covid clinic would continue to be offered until they were better and were disappointed that they had been discharged after completing the various courses on offer (since their clinic had been set up as an “assessment only” service).
In the next sections, we give examples of topics raised in the quality improvement collaborative and how they were addressed.
Example quality topic 1: Outcome measures
The first topic considered by the quality improvement collaborative was how (that is, using which measures and metrics) to assess and monitor patients with long covid. In the absence of a validated biomarker, various symptom scores and quality of life scales—both generic and disease-specific—were mooted. Site F had already developed and validated a patient-reported outcome measure (PROM), the C19-YRS (Covid-19 Yorkshire Rehabilitation Scale) and used it for both research and clinical purposes [ 86 ]. It was quickly agreed that, for the purposes of generating comparative research findings across the ten clinics, the C19-YRS should be used at all sites and completed by patients three-monthly. A commercial partner produced an electronic version of this instrument and an app for patient smartphones. The quality improvement collaborative also agreed that patients should be asked to complete the EUROQOL EQ5D, a widely used generic health-related quality of life scale [ 87 ], in order to facilitate comparisons between long covid and other chronic conditions.
In retrospect, the discussions which led to the unopposed adoption of these two measures as a “quality” initiative in clinical care were somewhat aspirational. A review of progress at a subsequent quality improvement meeting revealed considerable variation among clinics, with a wide variety of measures used in different clinics to different degrees. Reasons for this variation were multiple. First, although our patient advisory group were keen that we should gather as much data as possible on the patient experience of this new condition, many clinic patients found the long questionnaires exhausting to complete due to cognitive impairment and fatigue. In addition, whilst patients were keen to answer questions on symptoms that troubled them, many had limited patience to fill out repeated surveys on symptoms that did not trouble them (“it almost felt as if I’ve not got long covid because I didn’t feel like I fit the criteria as they were laying it out”—patient SAL001). Staff assisted patients in completing the measures when needed, but this was time-consuming (up to 45 min per instrument) and burdensome for both staff and patients. In clinics where a high proportion of patients required assistance, staff time was the rate-limiting factor for how many instruments got completed. For some patients, one short instrument was the most that could be asked of them, and the clinician made a judgement on which one would be in their best interests on the day.
The second reason for variation was that the clinical diagnosis and management of particular features, complications and comorbidities of long covid required more nuance than was provided by these relatively generic instruments, and the level of detail sought varied with the specialist interest of the clinic (and the clinician). The modified C19-YRS [ 88 ], for example, contained 19 items, of which one asked about sleep quality. But if a patient had sleep difficulties, many clinicians felt that these needed to be documented in more detail—for example using the 8-item Epworth Sleepiness Scale, originally developed for conditions such as narcolepsy and obstructive sleep apnea [ 89 ]. The “Epworth score” was essential currency for referrals to some but not all specialist sleep services. Similarly, the C19-YRS had three items relating to anxiety, depression and post-traumatic stress disorder, but in clinics where there was a strong focus on mental health (e.g. when there was a resident psychologist), patients were usually invited to complete more specific tools (e.g. the Patient Health Questionnaire 9 [ 90 ], a 9-item questionnaire originally designed to assess severity of depression).
The third reason for variation was custom and practice. Ethnographic visits revealed that paper copies of certain instruments were routinely stacked on clinicians’ desks in outpatient departments and also (in some cases) handed out by administrative staff in waiting areas so that patients could complete them before seeing the clinician. These familiar clinic artefacts tended to be short (one-page) instruments that had a long tradition of use in clinical practice. They were not always fit for purpose. For example, the Nijmegen questionnaire was developed in the 1980s to assess hyperventilation; it was validated against a longer, “gold standard” instrument for that condition [ 91 ]. It subsequently became popular in respiratory clinics to diagnose or exclude breathing pattern disorder (a condition in which the normal physiological pattern of breathing becomes replaced with less efficient, shallower breathing [ 92 ]), so much so that the researchers who developed the instrument published a paper to warn fellow researchers that it had not been validated for this purpose [ 93 ]. Whilst a validated 17-item instrument for breathing pattern disorder (the Self-Evaluation of Breathing Questionnaire [ 94 ]) does exist, it is not in widespread clinical use. Most clinics in LOCOMOTION used Nijmegen either on all patients (e.g. as part of a comprehensive initial assessment, especially if the service had begun as a respiratory follow-up clinic) or when breathing pattern disorder was suspected.
In sum, the use of outcome measures in long covid clinics was a compromise between standardization and contingency. On the one hand, all clinics accepted the need to use “validated” instruments consistently. On the other hand, there were sometimes good reasons why they deviated from agreed practice, including mismatch between the clinic’s priorities as a research site, its priorities as a clinical service, and the particular clinical needs of a patient; the clinic’s—and the clinician’s—specialist focus; and long-held traditions of using particular instruments with which staff and patients were familiar.
Example quality topic 2: Postural orthostatic tachycardia syndrome (POTS)
Palpitations (common in long covid) and postural orthostatic tachycardia syndrome (POTS, a disproportionate acceleration in heart rate on standing, the assumed cause of palpitations in many long covid patients) was the top priority for quality improvement identified by our patient advisory group. Reflecting discussions and evidence (of various kinds) shared in online patient communities, the group were confident that POTS is common in long covid patients and that many cases remain undetected (perhaps misdiagnosed as anxiety). Their request that all long covid patients should be “screened” for POTS prompted a search for, and synthesis of, evidence (which we published in the BMJ [ 95 ]). In sum, that evidence was sparse and contested, but, combined with standard practice in specialist clinics, broadly supported the judicious use of the NASA Lean Test [ 96 ]. This test involves repeated measurements of pulse and blood pressure with the patient first lying and then standing (with shoulders resting against a wall).
The patient advisory group’s request that the NASA Lean Test should be conducted on all patients met with mixed responses from the clinics. In site F, the lead physician had an interest in autonomic dysfunction in chronic fatigue and was keen; he had already published a paper on how to adapt the NASA Lean Test for self-assessment at home [ 97 ]. Several other sites were initially opposed. Staff at site E, for example, offered various arguments:
The test is time-consuming, labor-intensive, and takes up space in the clinic which has an opportunity cost in terms of other potential uses;
The test is unvalidated and potentially misleading (there is a high incidence of both false negative and false positive results);
There is no proven treatment for POTS, so there is no point in testing for it;
It is a specialist test for a specialist condition, so it should be done in a specialist clinic where its benefits and limitations are better understood;
Objective testing does not change clinical management since what we treat is the patient’s symptoms (e.g. by a pragmatic trial of lifestyle measures and medication);
People with symptoms suggestive of dysautonomia have already been “triaged out” of this clinic (that is, identified in the initial telephone consultation and referred directly to neurology or cardiology);
POTS is a manifestation of the systemic nature of long covid; it does not need specific treatment but will improve spontaneously as the patient goes through standard interventions such as active pacing, respiratory physical therapy and sleep hygiene;
Testing everyone, even when asymptomatic, runs counter to the ethos of rehabilitation, which is to “de-medicalize” patients so as to better orient them to their recovery journey.
When clinics were invited to implement the NASA Lean Test on a consecutive sample of patients to resolve a dispute about the incidence of POTS (from “we’ve only seen a handful of people with it since the clinic began” to “POTS is common and often missed”), all but one site agreed to participate. The tertiary POTS centre linked to site H was already running the NASA Lean Test as standard on all patients. Site C, which operated entirely virtually, passed the work to the referring general practitioner by making this test a precondition for seeing the patient; site D, which was largely virtual, sent instructions for patients to self-administer the test at home.
The NASA Lean Test study has been published separately [ 98 ]. In sum, of 277 consecutive patients tested across the eight clinics, 20 (7%) had a positive NASA Lean Test for POTS and a further 28 (10%) a borderline result. Six of 20 patients who met the criteria for POTS on testing had no prior history of orthostatic intolerance. The question of whether this test should be used to “screen” all patients was not answered definitively. But the experience of participating in the study persuaded some sceptics that postural changes in heart rate could be severe in some long covid patients, did not appear to be fully explained by their previously held theories (e.g. “functional”, anxiety, deconditioning), and had likely been missed in some patients. The outcome of this particular quality improvement cycle was thus not a wholescale change in practice (for which the evidence base was weak) but a more subtle increase in clinical awareness, a greater willingness to consider testing for POTS and a greater commitment to contribute to research into this contested condition.
More generally, the POTS audit prompted some clinicians to recognize the value of quality improvement in novel clinical areas. One physician who had initially commented that POTS was not seen in their clinic, for example, reflected:
“ Our clinic population is changing. […] Overall there’s far fewer post-ICU patients with ECMO [extra-corporeal membrane oxygenation] issues and far more long covid from the community, and this is the bit our clinic isn’t doing so well on. We’re doing great on breathing pattern disorder; neuro[logists] are helping us with the brain fogs; our fatigue and occupational advice is ok but some of the dysautonomia symptoms that are more prevalent in the people who were not hospitalized – that’s where we need to improve .” -Respiratory physician, site G (from field visit 6.6.23)
Example quality topic 3: Management of fatigue
Fatigue was the commonest symptom overall and a high priority among both patients and clinicians for quality improvement. It often coexisted with the cluster of neurocognitive symptoms known as brain fog, with both conditions relapsing and remitting in step. Clinicians were keen to systematize fatigue management using a familiar clinical framework oriented around documenting a full clinical history, identifying associated symptoms, excluding or exploring comorbidities and alternative explanations (e.g. poor sleep patterns, depression, menopause, deconditioning), assessing how fatigue affects physical and mental function, implementing a program of physical and cognitive therapy that was sensitive to the patient’s condition and confidence level, and monitoring progress using validated patient-reported outcome measures and symptom diaries.
The underpinning logic of this approach, which broadly reflected World Health Organization guidance [ 99 ], was that fatigue and linked cognitive impairment could be a manifestation of many—perhaps interacting—conditions but that a whole-patient (body and mind) rehabilitation program was the cornerstone of management in most cases. Discussion in the quality improvement collaborative focused on issues such as whether fatigue was so severe that it produced safety concerns (e.g. in a person’s job or with childcare), the pros and cons of particular online courses such as yoga, relaxation and mindfulness (many were viewed positively, though the evidence base was considered weak), and the extent to which respiratory physical therapy had a crossover impact on fatigue (systematic reviews suggested that it may do, but these reviews also cautioned that primary studies were sparse, methodologically flawed, and heterogeneous [ 100 , 101 ]). They also debated the strengths and limitations of different fatigue-specific outcome measures, each of which had been developed and validated in a different condition, with varying emphasis on cognitive fatigue, physical fatigue, effect on daily life, and motivation. These instruments included the Modified Fatigue Impact Scale; Fatigue Severity Scale [ 102 ]; Fatigue Assessment Scale; Functional Assessment Chronic Illness Therapy—Fatigue (FACIT-F) [ 103 ]; Work and Social Adjustment Scale [ 104 ]; Chalder Fatigue Scale [ 105 ]; Visual Analogue Scale—Fatigue [ 106 ]; and the EQ5D [ 87 ]. In one clinic (site F), three of these scales were used in combination for reasons discussed below.
Some clinicians advocated melatonin or nutritional supplements (such as vitamin D or folic acid) for fatigue on the grounds that many patients found them helpful and formal placebo-controlled trials were unlikely ever to be conducted. But neurostimulants used in other fatigue-predominant conditions (e.g. brain injury, stroke), which also lacked clinical trial evidence in long covid, were viewed as inappropriate in most patients because of lack of evidence of clear benefit and hypothetical risk of harm (e.g. adverse drug reactions, polypharmacy).
Whilst the patient advisory group were broadly supportive of a whole-patient rehabilitative approach to fatigue, their primary concern was fatiguability , especially post-exertional symptom exacerbation (PESE, also known as “crashes”). In these, the patient becomes profoundly fatigued some hours or days after physical or mental exertion, and this state can last for days or even weeks [ 107 ]. Patients viewed PESE as a “red flag” symptom which they felt clinicians often missed and sometimes caused. They wanted the quality improvement effort to focus on ensuring that all clinicians were aware of the risks of PESE and acted accordingly. A discussion among patients and clinicians at a quality improvement collaborative meeting raised a new research hypothesis—that reducing the number of repeated episodes of PESE may improve the natural history of long covid.
These tensions around fatigue management played out differently in different clinics. In site C (the GP-led virtual clinic run from a community hub), fatigue was viewed as one manifestation of a whole-patient condition. The lead general practitioner used the metaphor of untangling a skein of wool: “you have to find the end and then gently pull it”. The underlying problem in a fatigued patient, for example, might be an undiagnosed physical condition such as anaemia, disturbed sleep, or inadequate pacing. These required (respectively) the chronic fatigue service (comprising an occupational therapist and specialist psychologist and oriented mainly to teaching the techniques of goal-setting and pacing), a “tiredness” work-up (e.g. to exclude anaemia or menopause), investigation of poor sleep (which, not uncommonly, was due to obstructive sleep apnea), and exploration of mental health issues.
In site G (a hospital clinic which had evolved from a respiratory service), patients with fatigue went through a fatigue management program led by the occupational therapist with emphasis on pacing, energy conservation, avoidance of PESE and sleep hygiene. Those without ongoing respiratory symptoms were often discharged back to their general practitioner once they had completed this; there was no consultant follow-up of unresolved fatigue.
In site F (a rehabilitation clinic which had a longstanding interest in chronic fatigue even before the pandemic), active interdisciplinary management of fatigue was commenced at or near the patient’s first visit, on the grounds that the earlier this began, the more successful it would be. In this clinic, patients were offered a more intensive package: a similar occupational therapy-led fatigue course as those in site G, plus input from a dietician to advise on regular balanced meals and caffeine avoidance and a group-based facilitated peer support program which centred on fatigue management. The dietician spoke enthusiastically about how improving diet in longstanding long covid patients often improved fatigue (e.g. because they had often lost muscle mass and tended to snack on convenience food rather than make meals from scratch), though she agreed there was no evidence base from trials to support this approach.
Pursuing local quality improvement through MDTs
Whilst some long covid patients had “textbook” symptoms and clinical findings, many cases were unique and some were fiendishly complex. One clinician commented that, somewhat paradoxically, “easy cases” were often the post-ICU follow-ups who had resolving chest complications; they tended to do well with a course of respiratory physical therapy and a return-to-work program. Such cases were rarely brought to MDT meetings. “Difficult cases” were patients who had not been hospitalized for their acute illness but presented with a months- or years-long history of multiple symptoms with fatigue typically predominant. Each one was different, as the following example (some details of which have been fictionalized to protect anonymity) illustrates.
The MDT is discussing Mrs Fermah, a 65-year-old homemaker who had covid-19 a year ago. She has had multiple symptoms since, including fluctuating fatigue, brain fog, breathlessness, retrosternal chest pain of burning character, dry cough, croaky voice, intermittent rashes (sometimes on eating), lips going blue, ankle swelling, orthopnoea, dizziness with the room spinning which can be triggered by stress, low back pain, aches and pains in the arms and legs and pins and needles in the fingertips, loss of taste and smell, palpitations and dizziness (unclear if postural, but clear association with nausea), headaches on waking, and dry mouth. She is somewhat overweight (body mass index 29) and admits to low mood. Functionally, she is mostly confined to the house and can no longer manage the stairs so has begun to sleep downstairs. She has stumbled once or twice but not fallen. Her social life has ceased and she rarely has the energy to see her grandchildren. Her 70-year-old husband is retired and generally supportive, though he spends most evenings at his club. Comorbidities include glaucoma which is well controlled and overseen by an ophthalmologist, mild club foot (congenital) and stage 1 breast cancer 20 years ago. Various tests, including a chest X-ray, resting and exercise oximetry and a blood panel, were normal except for borderline vitamin D level. Her breathing questionnaire score suggests she does not have breathing pattern disorder. ECG showed first-degree atrioventricular block and left axis deviation. No clinician has witnessed the blue lips. Her current treatment is online group respiratory physical therapy; a home visit is being arranged to assess her climbing stairs. She has declined a psychologist assessment. The consultant asks the nurse who assessed her: “Did you get a feel if this is a POTS-type dizziness or an ENT-type?” She sighs. “Honestly it was hard to tell, bless her.”—Site A MDT
This patient’s debilitating symptoms and functional impairments could all be due to long covid, yet “evidence-based” guidance for how to manage her complex suffering does not exist and likely never will exist. The question of which (if any) additional blood or imaging tests to do, in what order of priority, and what interventions to offer the patient will not be definitively answered by consulting clinical trials involving hundreds of patients, since (even if these existed) the decision involves weighing this patient’s history and the multiple factors and uncertainties that are relevant in her case. The knowledge that will help the MDT provide quality care to Mrs Fermah is case-based knowledge—accumulated clinical experience and wisdom from managing and deliberating on multiple similar cases. We consider case-based knowledge further in the “ Discussion ”.
Summary of key findings
This study has shown that a quality improvement collaborative of UK long covid clinics made some progress towards standardizing assessment and management in some topics, but some variation remained. This could be explained in part by the fact that different clinics had different histories and path dependencies, occupied a different place in the local healthcare ecosystem, served different populations, were differently staffed, and had different clinical interests. Our patient advisory group and clinicians in the quality improvement collaborative broadly prioritized the same topics for improvement but interpreted them somewhat differently. “Quality” long covid care had multiple dimensions, relating to (among other things) service set-up and accessibility, clinical provision appropriate to the patient’s need (including options for referral to other services locally), the human qualities of clinical and support staff, how knowledge was distributed across (and accessible within) the system, and the accumulated collective wisdom of local MDTs in dealing with complex cases (including multiple kinds of specialist expertise as well as relational knowledge of what was at stake for the patient). Whilst both staff and patients were keen to contribute to the quality improvement effort, the burden of measurement was evident: multiple outcome measures, used repeatedly, were resource-intensive for staff and exhausting for patients.
Strengths and limitations of this study
To our knowledge, we are the first to report both a quality improvement collaborative and an in-depth qualitative study of clinical work in long covid. Key strengths of this work include the diverse sampling frame (with sites from three UK jurisdictions and serving widely differing geographies and demographics); the use of documents, interviews and reflexive interpretive ethnography to produce meaningful accounts of how clinics emerged and how they were currently organized; the use of philosophical concepts to analyse data on how MDTs produced quality care on a patient-by-patient basis; and the close involvement of patient co-researchers and coauthors during the research and writing up.
Limitations of the study include its exclusive UK focus (the external validity of findings to other healthcare systems is unknown); the self-selecting nature of participants in a quality improvement collaborative (our patient advisory group suggested that the MDTs observed in this study may have represented the higher end of a quality spectrum, hence would be more likely than other MDTs to adhere to guidelines); and the particular perspective brought by the researchers (two GPs, a physical therapist and one non-clinical person) in ethnographic observations. Hospital specialists or organizational scholars, for example, may have noticed different things or framed what they observed differently.
Explaining variation in long covid care
Sutherland and Levesque’s framework mentioned in the “ Background ” section does not explain much of the variation found in our study [ 70 ]. In terms of capacity, at the time of this study most participating clinics benefited from ring-fenced resources. In terms of evidence, guidelines existed and were not greatly contested, but as illustrated by the case of Mrs Fermah above, many patients were exceptions to the guideline because of complex symptomatology and relevant comorbidities. In terms of agency, clinicians in most clinics were passionately engaged with long covid (they were pioneers who had set up their local clinic and successfully bid for national ring-fenced resources) and were generally keen to support patient choice (though not if the patient requested tests which were unavailable or deemed not indicated).
Astma et al.’s list of factors that may explain variation in practice (see “ Background ”) includes several that may be relevant to long covid, especially that the definition of appropriate care in this condition remains somewhat contested. But lack of opportunity to discuss cases was not a problem in the clinics in our sample. On the contrary, MDT meetings in each locality gave clinicians multiple opportunities to discuss cases with colleagues and reflect collectively on whether and how to apply particular guidelines.
The key problem was not that clinicians disputed the guidelines for managing long covid or were unaware of them; it was that the guidelines were not self-interpreting . Rather, MDTs had to deliberate on the balance of benefits and harms in different aspects of individual cases. In patients whose symptoms suggested a possible diagnosis of POTS (or who suspected themselves of having POTS), for example, these deliberations were sometimes lengthy and nuanced. Should a test result that is not technically in the abnormal range but close to it be treated as diagnostic, given that symptoms point to this diagnosis? If not, should the patient be told that the test excludes POTS or that it is equivocal? If a cardiology opinion has stated firmly that the patient does not have POTS but the cardiologist is not known for their interest in this condition, should a second specialist opinion be sought? If the gold standard “tilt test” [ 108 ] for POTS (usually available only in tertiary centres) is not available locally, does this patient merit a costly out-of-locality referral? Should the patient’s request for a trial of off-label medication, reflecting discussions in an online support group, be honoured? These are the kinds of questions on which MDTs deliberated at length.
The fact that many cases required extensive deliberation does not necessarily justify variation in practice among clinics. But taking into account the clinics’ very different histories, set-up, and local referral pathways, the variation begins to make sense. A patient who is being assessed in a clinic that functions as a specialist chronic fatigue centre and attracts referrals which reflect this interest (e.g. site F in our sample) will receive different management advice from one that functions as a telephone-only generalist assessment centre and refers on to other specialties (site C in our sample). The wide variation in case mix, coupled with the fact that a different proportion of these cases were highly complex in each clinic (and in different ways), suggests that variation in practice may reflect appropriate rather than inappropriate care.
Our patient advisory group affirmed that many of the findings reported here resonated with their own experience, but they raised several concerns. These included questions about patient groups who may have been missed in our sample because they were rarely discussed in MDTs. The decision to take a case to MDT discussion is taken largely by a clinician, and there was evidence from online support groups that some patients’ requests for their case to be taken to an MDT had been declined (though not, to our knowledge, in the clinics participating in the LOCOMOTION study).
We began this study by asking “what is quality in long covid care?”. We initially assumed that this question referred to a generalizable evidence base, which we felt we could identify, and we believed that we could then determine whether long covid clinics were following the evidence base through conventional audits of structure, process, and outcome. In retrospect, these assumptions were somewhat naïve. On the basis of our findings, we suggest that a better (and more individualized) research question might be “to what extent does each patient with long covid receive evidence-based care appropriate to their needs?”. This question would require individual case review on a sample of cases, tracking each patient longitudinally including cross-referrals, and also interviewing the patient.
Nomothetic versus idiographic knowledge
In a series of lectures first delivered in the 1950s and recently republished [ 109 ], psychiatrist Dr Maurice O’Connor Drury drew on the later philosophy of his friend and mentor Ludwig Wittgenstein to challenge what he felt was a concerning trend: that the nomothetic (generalizable, abstract) knowledge from randomized controlled trials (RCTs) was coming to over-ride the idiographic (personal, situated) knowledge about particular patients. Based on Wittgenstein’s writings on the importance of the particular, Drury predicted—presciently—that if implemented uncritically, RCTs would result in worse, not better, care for patients, since it would go hand-in-hand with a downgrading of experience, intuition, subjective judgement, personal reflection, and collective deliberation.
Much conventional quality improvement methodology is built on an assumption that nomothetic knowledge (for example, findings from RCTs and systematic reviews) is a higher form of knowing than idiographic knowledge. But idiographic, case-based reasoning—despite its position at the very bottom of evidence-based medicine’s hierarchy of evidence [ 110 ]—is a legitimate and important element of medical practice. Bioethicist Kathryn Montgomery, drawing on Aristotle’s notion of praxis , considers clinical practice to be an example of case-based reasoning [ 111 ]. Medicine is governed not by hard and fast laws but by competing maxims or rules of thumb ; the essence of judgement is deciding which (if any) rule should be applied in a particular circumstance. Clinical judgement incorporates science (especially the results of well-conducted research) and makes use of available tools and technologies (including guidelines and decision-support algorithms that incorporate research findings). But rather than being determined solely by these elements, clinical judgement is guided both by the scientific evidence and by the practical and ethical question “what is it best to do, for this individual, given these circumstances?”.
In this study, we observed clinical management of, and MDT deliberations on, hundreds of clinical cases. In the more straightforward ones (for example, recovering pneumonitis), guideline-driven care was not difficult to implement and such cases were rarely brought to the MDT. But cases like Mrs Fermah (see last section of “ Results ”) required much discussion on which aspects of which guideline were in the patient’s best interests to bring into play at any particular stage in their illness journey.
Conclusions
One systematic review on quality improvement collaboratives concluded that “ [those] reporting success generally addressed relatively straightforward aspects of care, had a strong evidence base and noted a clear evidence-practice gap in an accepted clinical pathway or guideline” (page 226) [ 60 ]. The findings from this study suggest that to the extent that such collaboratives address clinical cases that are not straightforward, conventional quality improvement methods may be less useful and even counterproductive.
The question “what is quality in long covid care?” is partly a philosophical one. Our findings support an approach that recognizes and values idiographic knowledge —including establishing and protecting a safe and supportive space for deliberation on individual cases to occur and to value and draw upon the collective learning that occurs in these spaces. It is through such deliberation that evidence-based guidelines can be appropriately interpreted and applied to the unique needs and circumstances of individual patients. We suggest that Drury’s warning about the limitations of nomothetic knowledge should prompt a reassessment of policies that rely too heavily on such knowledge, resulting in one-size-fits-all protocols. We also cautiously hypothesize that the need to centre the quality improvement effort on idiographic rather than nomothetic knowledge is unlikely to be unique to long covid. Indeed, such an approach may be particularly important in any condition that is complex, unpredictable, variable in presentation and clinical course, and associated with comorbidities.
Availability of data and materials
Selected qualitative data (ensuring no identifiable information) will be made available to formal research teams on reasonable request to Professor Greenhalgh at the University of Oxford, on condition that they have research ethics approval and relevant expertise. The quantitative data on NASA Lean Test have been published in full in a separate paper [ 98 ].
Abbreviations
Chronic fatigue syndrome
Intensive care unit
Jenny Ceolta-Smith
Julie Darbyshire
LOng COvid Multidisciplinary consortium Optimising Treatments and services across the NHS
Multidisciplinary team
Myalgic encephalomyelitis
Middle East Respiratory Syndrome
National Aeronautics and Space Association
Occupational therapy/ist
Post-exertional symptom exacerbation
Postural orthostatic tachycardia syndrome
Speech and language therapy
Severe Acute Respiratory Syndrome
Trisha Greenhalgh
United Kingdom
United States
World Health Organization
Perego E, Callard F, Stras L, Melville-JÛhannesson B, Pope R, Alwan N. Why the Patient-Made Term “Long Covid” is needed. Wellcome Open Res. 2020;5:224.
Article Google Scholar
Greenhalgh T, Sivan M, Delaney B, Evans R, Milne R: Long covid—an update for primary care. bmj 2022;378:e072117.
Centers for Disease Control and Prevention (US): Long COVID or Post-COVID Conditions (updated 16th December 2022). Atlanta: CDC. Accessed 2nd June 2023 at https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html ; 2022.
National Institute for Health and Care Excellence (NICE) Scottish Intercollegiate Guidelines Network (SIGN) and Royal College of General Practitioners (RCGP): COVID-19 rapid guideline: managing the long-term effects of COVID-19, vol. Accessed 30th January 2022 at https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-effects-of-covid19-pdf-51035515742 . London: NICE; 2022.
Organization WH: Post Covid-19 Condition (updated 7th December 2022), vol. Accessed 2nd June 2023 at https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition#:~:text=It%20is%20defined%20as%20the,months%20with%20no%20other%20explanation . Geneva: WHO; 2022.
Office for National Statistics: Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 31st March 2023. London: ONS. Accessed 30th May 2023 at https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/datasets/alldatarelatingtoprevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk ; 2023.
Crook H, Raza S, Nowell J, Young M, Edison P: Long covid—mechanisms, risk factors, and management. bmj 2021;374.
Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, Pujol JC, Klaser K, Antonelli M, Canas LS. Attributes and predictors of long COVID. Nat Med. 2021;27(4):626–31.
Article CAS PubMed PubMed Central Google Scholar
Reese JT, Blau H, Casiraghi E, Bergquist T, Loomba JJ, Callahan TJ, Laraway B, Antonescu C, Coleman B, Gargano M: Generalisable long COVID subtypes: findings from the NIH N3C and RECOVER programmes. EBioMedicine 2023;87.
Thaweethai T, Jolley SE, Karlson EW, Levitan EB, Levy B, McComsey GA, McCorkell L, Nadkarni GN, Parthasarathy S, Singh U. Development of a definition of postacute sequelae of SARS-CoV-2 infection. JAMA. 2023;329(22):1934–46.
Brown DA, O’Brien KK. Conceptualising Long COVID as an episodic health condition. BMJ Glob Health. 2021;6(9): e007004.
Article PubMed Google Scholar
Tate WP, Walker MO, Peppercorn K, Blair AL, Edgar CD. Towards a Better Understanding of the Complexities of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Long COVID. Int J Mol Sci. 2023;24(6):5124.
Ahmed H, Patel K, Greenwood DC, Halpin S, Lewthwaite P, Salawu A, Eyre L, Breen A, Connor RO, Jones A. Long-term clinical outcomes in survivors of severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome coronavirus (MERS) outbreaks after hospitalisation or ICU admission: a systematic review and meta-analysis. J Rehabil Med. 2020;52(5):1–11.
Google Scholar
World Health Organisation: Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: Interim guidance (13th March 2020). Geneva: WHO. Accessed 3rd January 2023 at https://t.co/JpNdP8LcV8?amp=1 ; 2020.
Rushforth A, Ladds E, Wieringa S, Taylor S, Husain L, Greenhalgh T: Long Covid – the illness narratives. Under review for Sociology of Health and Illness 2021.
Russell D, Spence NJ. Chase J-AD, Schwartz T, Tumminello CM, Bouldin E: Support amid uncertainty: Long COVID illness experiences and the role of online communities. SSM-Qual Res Health. 2022;2: 100177.
Article PubMed PubMed Central Google Scholar
Ziauddeen N, Gurdasani D, O’Hara ME, Hastie C, Roderick P, Yao G, Alwan NA. Characteristics and impact of Long Covid: Findings from an online survey. PLoS ONE. 2022;17(3): e0264331.
Evans RA, McAuley H, Harrison EM, Shikotra A, Singapuri A, Sereno M, Elneima O, Docherty AB, Lone NI, Leavy OC. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir Med. 2021;9(11):1275–87.
Sykes DL, Holdsworth L, Jawad N, Gunasekera P, Morice AH, Crooks MG. Post-COVID-19 symptom burden: what is long-COVID and how should we manage it? Lung. 2021;199(2):113–9.
Altmann DM, Whettlock EM, Liu S, Arachchillage DJ, Boyton RJ: The immunology of long COVID. Nat Rev Immunol 2023:1–17.
Klein J, Wood J, Jaycox J, Dhodapkar RM, Lu P, Gehlhausen JR, Tabachnikova A, Greene K, Tabacof L, Malik AA et al : Distinguishing features of Long COVID identified through immune profiling. Nature 2023.
Chen B, Julg B, Mohandas S, Bradfute SB. Viral persistence, reactivation, and mechanisms of long COVID. Elife. 2023;12: e86015.
Wang C, Ramasamy A, Verduzco-Gutierrez M, Brode WM, Melamed E. Acute and post-acute sequelae of SARS-CoV-2 infection: a review of risk factors and social determinants. Virol J. 2023;20(1):124.
Cervia-Hasler C, Brüningk SC, Hoch T, Fan B, Muzio G, Thompson RC, Ceglarek L, Meledin R, Westermann P, Emmenegger M et al Persistent complement dysregulation with signs of thromboinflammation in active Long Covid Science 2024;383(6680):eadg7942.
Sivan M, Greenhalgh T, Darbyshire JL, Mir G, O’Connor RJ, Dawes H, Greenwood D, O’Connor D, Horton M, Petrou S. LOng COvid Multidisciplinary consortium Optimising Treatments and servIces acrOss the NHS (LOCOMOTION): protocol for a mixed-methods study in the UK. BMJ Open. 2022;12(5): e063505.
Rushforth A, Ladds E, Wieringa S, Taylor S, Husain L, Greenhalgh T. Long covid–the illness narratives. Soc Sci Med. 2021;286: 114326.
National Institute for Health and Care Excellence: COVID-19 rapid guideline: managing the long-term effects of COVID-19, vol. Accessed 4th October 2023 at https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-effects-of-covid19-pdf-51035515742 . London: NICE 2020.
NHS England: Long COVID: the NHS plan for 2021/22. London: NHS England. Accessed 2nd August 2022 at https://www.england.nhs.uk/coronavirus/documents/long-covid-the-nhs-plan-for-2021-22/ ; 2021.
NHS England: NHS to offer ‘long covid’ sufferers help at specialist centres. London: NHS England. Accessed 10th October 2020 at https://www.england.nhs.uk/2020/10/nhs-to-offer-long-covid-help/ ; 2020 (7th October).
NHS England: The NHS plan for improving long COVID services, vol. Acessed 4th February 2024 at https://www.england.nhs.uk/publication/the-nhs-plan-for-improving-long-covid-services/ .London: Gov.uk; 2022.
NHS England: Commissioning guidance for post-COVID services for adults, children and young people, vol. Accessed 6th February 2024 at https://www.england.nhs.uk/long-read/commissioning-guidance-for-post-covid-services-for-adults-children-and-young-people/ . London: gov.uk; 2023.
National Institute for Health Research: Researching Long Covid: Adressing a new global health challenge, vol. Accessed 9.8.23 at https://evidence.nihr.ac.uk/collection/researching-long-covid-addressing-a-new-global-health-challenge/ . London: NIHR; 2022.
Subbaraman N. NIH will invest $1 billion to study long COVID. Nature. 2021;591(7850):356–356.
Article CAS PubMed Google Scholar
Donabedian A. The definition of quality and approaches to its assessment and monitoring. Ann Arbor: Michigan; 1980.
Laffel G, Blumenthal D. The case for using industrial quality management science in health care organizations. JAMA. 1989;262(20):2869–73.
Maxwell RJ. Quality assessment in health. BMJ. 1984;288(6428):1470.
Berwick DM, Godfrey BA, Roessner J. Curing health care: New strategies for quality improvement. The Journal for Healthcare Quality (JHQ). 1991;13(5):65–6.
Deming WE. Out of the Crisis. Cambridge, MA: MIT Press; 1986.
Argyris C: Increasing leadership effectiveness: New York: J. Wiley; 1976.
Juran JM: A history of managing for quality: The evolution, trends, and future directions of managing for quality: Asq Press; 1995.
Institute of Medicine (US): Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
McNab D, McKay J, Shorrock S, Luty S, Bowie P. Development and application of ‘systems thinking’ principles for quality improvement. BMJ Open Qual. 2020;9(1): e000714.
Sampath B, Rakover J, Baldoza K, Mate K, Lenoci-Edwards J, Barker P. Whole-System Quality: A Unified Approach to Building Responsive, Resilient Health Care Systems. Boston: Institute for Healthcare Immprovement; 2021.
Batalden PB, Davidoff F: What is “quality improvement” and how can it transform healthcare? In . , vol. 16: BMJ Publishing Group Ltd; 2007: 2–3.
Baker G. Collaborating for improvement: the Institute for Healthcare Improvement’s breakthrough series. New Med. 1997;1:5–8.
Plsek PE. Collaborating across organizational boundaries to improve the quality of care. Am J Infect Control. 1997;25(2):85–95.
Ayers LR, Beyea SC, Godfrey MM, Harper DC, Nelson EC, Batalden PB. Quality improvement learning collaboratives. Qual Manage Healthcare. 2005;14(4):234–47.
Brandrud AS, Schreiner A, Hjortdahl P, Helljesen GS, Nyen B, Nelson EC. Three success factors for continual improvement in healthcare: an analysis of the reports of improvement team members. BMJ Qual Saf. 2011;20(3):251–9.
Dückers ML, Spreeuwenberg P, Wagner C, Groenewegen PP. Exploring the black box of quality improvement collaboratives: modelling relations between conditions, applied changes and outcomes. Implement Sci. 2009;4(1):1–12.
Nadeem E, Olin SS, Hill LC, Hoagwood KE, Horwitz SM. Understanding the components of quality improvement collaboratives: a systematic literature review. Milbank Q. 2013;91(2):354–94.
Shortell SM, Marsteller JA, Lin M, Pearson ML, Wu S-Y, Mendel P, Cretin S, Rosen M: The role of perceived team effectiveness in improving chronic illness care. Medical Care 2004:1040–1048.
Wilson T, Berwick DM, Cleary PD. What do collaborative improvement projects do? Experience from seven countries. Joint Commission J Qual Safety. 2004;30:25–33.
Schouten LM, Hulscher ME, van Everdingen JJ, Huijsman R, Grol RP. Evidence for the impact of quality improvement collaboratives: systematic review. BMJ. 2008;336(7659):1491–4.
Hulscher ME, Schouten LM, Grol RP, Buchan H. Determinants of success of quality improvement collaboratives: what does the literature show? BMJ Qual Saf. 2013;22(1):19–31.
Dixon-Woods M, Bosk CL, Aveling EL, Goeschel CA, Pronovost PJ. Explaining Michigan: developing an ex post theory of a quality improvement program. Milbank Q. 2011;89(2):167–205.
Bate P, Mendel P, Robert G: Organizing for quality: the improvement journeys of leading hospitals in Europe and the United States: CRC Press; 2007.
Andersson-Gäre B, Neuhauser D. The health care quality journey of Jönköping County Council. Sweden Qual Manag Health Care. 2007;16(1):2–9.
Törnblom O, Stålne K, Kjellström S. Analyzing roles and leadership in organizations from cognitive complexity and meaning-making perspectives. Behav Dev. 2018;23(1):63.
Greenhalgh T, Russell J. Why Do Evaluations of eHealth Programs Fail? An Alternative Set of Guiding Principles. PLoS Med. 2010;7(11): e1000360.
Wells S, Tamir O, Gray J, Naidoo D, Bekhit M, Goldmann D. Are quality improvement collaboratives effective? A systematic review. BMJ Qual Saf. 2018;27(3):226–40.
Landon BE, Wilson IB, McInnes K, Landrum MB, Hirschhorn L, Marsden PV, Gustafson D, Cleary PD. Effects of a quality improvement collaborative on the outcome of care of patients with HIV infection: the EQHIV study. Ann Intern Med. 2004;140(11):887–96.
Mittman BS. Creating the evidence base for quality improvement collaboratives. Ann Intern Med. 2004;140(11):897–901.
Wennberg JE. Unwarranted variations in healthcare delivery: implications for academic medical centres. BMJ. 2002;325(7370):961–4.
Bungay H. Cancer and health policy: the postcode lottery of care. Soc Policy Admin. 2005;39(1):35–48.
Wennberg JE, Cooper MM: The Quality of Medical Care in the United States: A Report on the Medicare Program: The Dartmouth Atlas of Health Care 1999: The Center for the Evaluative Clinical Sciences [Internet]. 1999.
DaSilva P, Gray JM. English lessons: can publishing an atlas of variation stimulate the discussion on appropriateness of care? Med J Aust. 2016;205(S10):S5–7.
Gray WK, Day J, Briggs TW, Harrison S. Identifying unwarranted variation in clinical practice between healthcare providers in England: Analysis of administrative data over time for the Getting It Right First Time programme. J Eval Clin Pract. 2021;27(4):743–50.
Wabe N, Thomas J, Scowen C, Eigenstetter A, Lindeman R, Georgiou A. The NSW Pathology Atlas of Variation: Part I—Identifying Emergency Departments With Outlying Laboratory Test-Ordering Practices. Ann Emerg Med. 2021;78(1):150–62.
Jamal A, Babazono A, Li Y, Fujita T, Yoshida S, Kim SA. Elucidating variations in outcomes among older end-stage renal disease patients on hemodialysis in Fukuoka Prefecture, Japan. PLoS ONE. 2021;16(5): e0252196.
Sutherland K, Levesque JF. Unwarranted clinical variation in health care: definitions and proposal of an analytic framework. J Eval Clin Pract. 2020;26(3):687–96.
Tanenbaum SJ. Reducing variation in health care: The rhetorical politics of a policy idea. J Health Polit Policy Law. 2013;38(1):5–26.
Atsma F, Elwyn G, Westert G. Understanding unwarranted variation in clinical practice: a focus on network effects, reflective medicine and learning health systems. Int J Qual Health Care. 2020;32(4):271–4.
Horbar JD, Rogowski J, Plsek PE, Delmore P, Edwards WH, Hocker J, Kantak AD, Lewallen P, Lewis W, Lewit E. Collaborative quality improvement for neonatal intensive care. Pediatrics. 2001;107(1):14–22.
Van Maanen J: Tales of the field: On writing ethnography: University of Chicago Press; 2011.
Golden-Biddle K, Locke K. Appealing work: An investigation of how ethnographic texts convince. Organ Sci. 1993;4(4):595–616.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Glaser BG. The constant comparative method of qualitative analysis. Soc Probl. 1965;12:436–45.
Willis R. The use of composite narratives to present interview findings. Qual Res. 2019;19(4):471–80.
Vojdani A, Vojdani E, Saidara E, Maes M. Persistent SARS-CoV-2 Infection, EBV, HHV-6 and other factors may contribute to inflammation and autoimmunity in long COVID. Viruses. 2023;15(2):400.
Choutka J, Jansari V, Hornig M, Iwasaki A. Unexplained post-acute infection syndromes. Nat Med. 2022;28(5):911–23.
Connors JM, Ariëns RAS. Uncertainties about the roles of anticoagulation and microclots in postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection. J Thromb Haemost. 2023;21(10):2697–701.
Patel MA, Knauer MJ, Nicholson M, Daley M, Van Nynatten LR, Martin C, Patterson EK, Cepinskas G, Seney SL, Dobretzberger V. Elevated vascular transformation blood biomarkers in Long-COVID indicate angiogenesis as a key pathophysiological mechanism. Mol Med. 2022;28(1):122.
Greenhalgh T, Sivan M, Delaney B, Evans R, Milne R: Long covid—an update for primary care. bmj 2022, 378.
Parkin A, Davison J, Tarrant R, Ross D, Halpin S, Simms A, Salman R, Sivan M. A multidisciplinary NHS COVID-19 service to manage post-COVID-19 syndrome in the community. J Prim Care Commun Health. 2021;12:21501327211010990.
NHS England: COVID-19 Post-Covid Assessment Service, vol. Accessed 5th March 2024 at https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-post-covid-assessment-service/ . London: NHS England; 2024.
Sivan M, Halpin S, Gee J, Makower S, Parkin A, Ross D, Horton M, O'Connor R: The self-report version and digital format of the COVID-19 Yorkshire Rehabilitation Scale (C19-YRS) for Long Covid or Post-COVID syndrome assessment and monitoring. Adv Clin Neurosci Rehabil 2021;20(3).
The EuroQol Group. EuroQol-a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208.
Sivan M, Preston NJ, Parkin A, Makower S, Gee J, Ross D, Tarrant R, Davison J, Halpin S, O’Connor RJ, et al. The modified COVID-19 Yorkshire Rehabilitation Scale (C19-YRSm) patient-reported outcome measure for Long Covid or Post-COVID syndrome. J Med Virol. 2022;94(9):4253–64.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Van Dixhoorn J, Duivenvoorden H. Efficacy of Nijmegen Questionnaire in recognition of the hyperventilation syndrome. J Psychosom Res. 1985;29(2):199–206.
Evans R, Pick A, Lardner R, Masey V, Smith N, Greenhalgh T: Breathing difficulties after covid-19: a guide for primary care. BMJ 2023;381.
Van Dixhoorn J, Folgering H: The Nijmegen Questionnaire and dysfunctional breathing. In . , vol. 1: Eur Respiratory Soc; 2015.
Courtney R, Greenwood KM. Preliminary investigation of a measure of dysfunctional breathing symptoms: The Self Evaluation of Breathing Questionnaire (SEBQ). Int J Osteopathic Med. 2009;12(4):121–7.
Espinosa-Gonzalez A, Master H, Gall N, Halpin S, Rogers N, Greenhalgh T. Orthostatic tachycardia after covid-19. BMJ (Clinical Research ed). 2023;380:e073488–e073488.
PubMed Google Scholar
Bungo M, Charles J, Johnson P Jr. Cardiovascular deconditioning during space flight and the use of saline as a countermeasure to orthostatic intolerance. Aviat Space Environ Med. 1985;56(10):985–90.
CAS PubMed Google Scholar
Sivan M, Corrado J, Mathias C. The Adapted Autonomic Profile (Aap) Home-Based Test for the Evaluation of Neuro-Cardiovascular Autonomic Dysfunction. Adv Clin Neurosci Rehabil. 2022;3:10–13. https://doi.org/10.47795/QKBU46715 .
Lee C, Greenwood DC, Master H, Balasundaram K, Williams P, Scott JT, Wood C, Cooper R, Darbyshire JL, Gonzalez AE. Prevalence of orthostatic intolerance in long covid clinic patients and healthy volunteers: A multicenter study. J Med Virol. 2024;96(3): e29486.
World Health Organization: Clinical management of covid-19 - living guideline. Geneva: WHO. Accessed 4th October 2023 at https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2 ; 2023.
Ahmed I, Mustafaoglu R, Yeldan I, Yasaci Z, Erhan B: Effect of pulmonary rehabilitation approaches on dyspnea, exercise capacity, fatigue, lung functions and quality of life in patients with COVID-19: A Systematic Review and Meta-Analysis. Arch Phys Med Rehabil 2022.
Dillen H, Bekkering G, Gijsbers S, Vande Weygaerde Y, Van Herck M, Haesevoets S, Bos DAG, Li A, Janssens W, Gosselink R, et al. Clinical effectiveness of rehabilitation in ambulatory care for patients with persisting symptoms after COVID-19: a systematic review. BMC Infect Dis. 2023;23(1):419.
Learmonth Y, Dlugonski D, Pilutti L, Sandroff B, Klaren R, Motl R. Psychometric properties of the fatigue severity scale and the modified fatigue impact scale. J Neurol Sci. 2013;331(1–2):102–7.
Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness T herapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1(1):1–7.
Mundt JC, Marks IM, Shear MK, Greist JM. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry. 2002;180(5):461–4.
Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, Wallace E. Development of a fatigue scale. J Psychosom Res. 1993;37(2):147–53.
Shahid A, Wilkinson K, Marcu S, Shapiro CM: Visual analogue scale to evaluate fatigue severity (VAS-F). In: STOP, THAT and one hundred other sleep scales . edn.: Springer; 2011:399–402.
Parker M, Sawant HB, Flannery T, Tarrant R, Shardha J, Bannister R, Ross D, Halpin S, Greenwood DC, Sivan M. Effect of using a structured pacing protocol on post-exertional symptom exacerbation and health status in a longitudinal cohort with the post-COVID-19 syndrome. J Med Virol. 2023;95(1): e28373.
Kenny RA, Bayliss J, Ingram A, Sutton R. Head-up tilt: a useful test for investigating unexplained syncope. The Lancet. 1986;327(8494):1352–5.
Drury MOC: Science and Psychology. In: The selected writings of Maurice O’Connor Drury: On Wittgenstein, philosophy, religion and psychiatry. edn.: Bloomsbury Publishing; 2017.
Concato J, Shah N, Horwitz RI. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med. 2000;342(25):1887–92.
Mongtomery K: How doctors think: Clinical judgment and the practice of medicine: Oxford University Press; 2005.
Download references
Acknowledgements
We are grateful to clinic staff for allowing us to study their work and to patients for allowing us to sit in on their consultations. We also thank the funder of LOCOMOTION (National Institute for Health Research) and the patient advisory group for lived experience input.
This research is supported by National Institute for Health Research (NIHR) Long Covid Research Scheme grant (Ref COV-LT-0016).
Author information
Authors and affiliations.
Nuffield Department of Primary Care Health Sciences, University of Oxford, Woodstock Rd, Oxford, OX2 6GG, UK
Trisha Greenhalgh, Julie L. Darbyshire & Emma Ladds
Imperial College Healthcare NHS Trust, London, UK
LOCOMOTION Patient Advisory Group and Lived Experience Representative, London, UK
You can also search for this author in PubMed Google Scholar
Contributions
TG conceptualized the overall study, led the empirical work, supported the quality improvement meetings, conducted the ethnographic visits, led the data analysis, developed the theorization and wrote the first draft of the paper. JLD organized and led the quality improvement meetings, supported site-based researchers to collect and analyse data on their clinic, collated and summarized data on quality topics, and liaised with the patient advisory group. CL conceptualized and led the quality topic on POTS, including exploring reasons for some clinics’ reluctance to conduct testing and collating and analysing the NASA Lean Test data across all sites. EL assisted with ethnographic visits, data analysis, and theorization. JCS contributed lived experience of long covid and also clinical experience as an occupational therapist; she liaised with the wider patient advisory group, whose independent (patient-led) audit of long covid clinics informed the quality improvement prioritization exercise. All authors provided extensive feedback on drafts and contributed to discussions and refinements. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Trisha Greenhalgh .
Ethics declarations
Ethics approval and consent to participate.
LOng COvid Multidisciplinary consortium Optimising Treatments and servIces acrOss the NHS study is sponsored by the University of Leeds and approved by Yorkshire & The Humber—Bradford Leeds Research Ethics Committee (ref: 21/YH/0276) and subsequent amendments.
Patient participants in clinic were approached by the clinician (without the researcher present) and gave verbal informed consent for a clinically qualified researcher to observe the consultation. If they consented, the researcher was then invited to sit in. A written record was made in field notes of this verbal consent. It was impractical to seek consent from patients whose cases were discussed (usually with very brief clinical details) in online MDTs. Therefore, clinical case examples from MDTs presented in the paper are fictionalized cases constructed from multiple real cases and with key clinical details changed (for example, comorbidities were replaced with different conditions which would produce similar symptoms). All fictionalized cases were checked by our patient advisory group to check that they were plausible to lived experience experts.
Consent for publication
No direct patient cases are reported in this manuscript. For details of how the fictionalized cases were constructed and validated, see “Consent to participate” above.
Competing interests
TG was a member of the UK National Long Covid Task Force 2021–2023 and on the Oversight Group for the NICE Guideline on Long Covid 2021–2022. She is a member of Independent SAGE.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Greenhalgh, T., Darbyshire, J.L., Lee, C. et al. What is quality in long covid care? Lessons from a national quality improvement collaborative and multi-site ethnography. BMC Med 22 , 159 (2024). https://doi.org/10.1186/s12916-024-03371-6
Download citation
Received : 04 December 2023
Accepted : 26 March 2024
Published : 15 April 2024
DOI : https://doi.org/10.1186/s12916-024-03371-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Post-covid-19 syndrome
- Quality improvement
- Breakthrough collaboratives
- Warranted variation
- Unwarranted variation
- Improvement science
- Ethnography
- Idiographic reasoning
- Nomothetic reasoning
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Summary. One of the most important aspects of a thesis, dissertation or research paper is the correct formulation of the aims and objectives. This is because your aims and objectives will establish the scope, depth and direction that your research will ultimately take. An effective set of aims and objectives will give your research focus and ...
Formulating research aim and objectives in an appropriate manner is one of the most important aspects of your thesis. This is because research aim and objectives determine the scope, depth and the overall direction of the research. Research question is the central question of the study that has to be answered on the basis of research findings.
questions, aims and objectives. Developing a research question is an interactive and inductive endeavour that takes place over time. A clear research question is vital and sets the scene for development of a clear research aim and objective that are inextricably linked (Martindale and Taylor 2014). Abstract Aim To describe the development of a ...
How to write research aims and objectives. Once you've established a research problem you want to address, you need to decide how you will address it. This is where your research aim and objectives come in. Step 1: Decide on a general aim. Your research aim should reflect your research problem and should be relatively broad.
Among the many sections that constitute a research paper, the introduction plays a key role in providing a background and setting the context. 1 Research objectives, which define the aims of the study, are usually stated in the introduction. Every study has a research question that the authors are trying to answer, and the objective is an ...
Research Questions vs Research Aims. ... The research objective, on the other hand, outlines the steps you'll take to answer your research question. Research objectives are often more action-oriented and can be broken down into smaller tasks that guide your research process. In a sense, they're something of a roadmap that helps you answer ...
A good research question is essential to guide your research paper, dissertation, or thesis. All research questions should be: Focused on a single problem or issue. Researchable using primary and/or secondary sources. Feasible to answer within the timeframe and practical constraints. Specific enough to answer thoroughly.
The research aim should be broad and concise. Develop research objectives: Based on your research questions and research aim, develop specific research objectives that outline what you intend to achieve through your research. These objectives should be specific, measurable, achievable, relevant, and time-bound (SMART).
The search aims, objectives and research questions (collectively called the "golden thread") are arguably the of important point you need to get right at you're crafting a research propose, dissertation or thesis.We receive questions almost every days about all "holy trinity" of find and there's certainly a lot of confusion out there, so we've designed the post to help your ...
A research aim is a broad statement indicating the general purpose of your research project. It should appear in your introduction at the end of your problem statement, before your research objectives. Research objectives are more specific than your research aim. They indicate the specific ways you'll address the overarching aim.
Research Objectives. Research objectives refer to the specific goals or aims of a research study. They provide a clear and concise description of what the researcher hopes to achieve by conducting the research.The objectives are typically based on the research questions and hypotheses formulated at the beginning of the study and are used to guide the research process.
The development of the research question, including a supportive hypothesis and objectives, is a necessary key step in producing clinically relevant results to be used in evidence-based practice. A well-defined and specific research question is more likely to help guide us in making decisions about study design and population and subsequently ...
The research aims, objectives and research questions (collectively called which "golden thread") represent arguably the most important thing you need to get right available you're crafting a research proposal, theses or thesis.We accept questions almost ever day with diese "holy trinity" are research and there's certainly a plot of bewilderment out on, so we've crafted is send to ...
Background The first steps of any study are developing the research question, aim and objective. Subsequent steps develop from these and they govern the researchers' choice of population, setting, data to be collected and time period for the study. Clear, succinctly posed research questions, aims and objectives are essential if studies are to ...
Once a topic of interest develops into a research question, the next step is to ponder the closely linked aims and objectives. A study's aim is its overall purpose-its planned long-term accomplishments and goals. According to Newman et al. 14, there are nine types (Table 18.1).Research objectives are slightly more specific than aims and may be subdivided into primary (must be achieved) and ...
Writing objectives. The objectives describe how you would achieve your research aim. You can do this through the following steps, The first one to two objectives can be applied to the literature review. (Verbs to be used: investigate, examine, study) One objective can be applied to the methodology portion.
Learn about the research aims, research objectives and research questions, also known as the Golden Thread. Dr David Phair and Dr Alexandra Shaeffer unpack e...
Background: The first steps of any study are developing the research question, aim and objective. Subsequent steps develop from these and they govern the researchers' choice of population, setting, data to be collected and time period for the study. Clear, succinctly posed research questions, aims and objectives are essential if studies are to ...
The first steps of any study are developing the research question, aim and objective. Subsequent steps develop from these and they govern the researchers' choice of population, setting, data to be collected and time period for the study. Clear, succinctly posed research questions, aims and objectives are essential if studies are to be successful.
A project that begins with sound research questions, aims, and goals is more likely to be successful and yield results that address a specific problem, need, or objective. Your research questions guide your research, as well as clarify the specific directions your study will take, such as research design, data collection, and analysis approach ...
It trains by enabling participants critique examples aims and objectives and research questions so they can understand what the shortcomings are. Discover the world's research 25+ million members
In summary, research questions and objectives are two distinct aspects of the research process. Research questions are broad statements that guide the overall direction of the research, while research objectives are specific, measurable goals that the research aims to achieve. Understanding these two terms' differences is essential for ...
In every research, the terms 'research aim', 'research objectives', 'research questions' and 'research hypotheses' tend to have precise meaning, therefore defining the core objectives is the ...
Research question. What is quality in long covid care and how can it best be achieved? Aims (1) To identify best practice and reduce unwarranted variation in UK long covid services. (2) To explain aspects of variation in long covid services that are or may be warranted. Objectives. Our original objectives were to: (1)