An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.14(9); 2022 Sep


An Atypical Presentation of Crohn's Disease: A Case Report
Asfand yar cheema.
1 Medicine, Services Hospital Lahore, Lahore, PAK
2 Internal Medicine, Lahore Medical & Dental College, Lahore, PAK
Mishaal Munir
3 Medicine, Ghurki Trust & Teaching Hospital, Lahore, PAK
Kaneez Zainab
4 Internal Medicine, Mayo Hospital, Lahore, PAK
Oboseh J Ogedegbe
5 Internal Medicine, Lifeway Medical Center, Abuja, NGA
Crohn’s disease (CD) is an inflammatory bowel disease affecting any portion of the gastrointestinal tract, usually the terminal ileum and the colon, with clinical manifestations such as diarrhea, fever, and weight loss. Clinical presentation of CD may include complications such as enterovesical fistulas, abscesses, strictures, and perianal disease. CD also classically presents with “skipping lesions,” unlike ulcerative colitis (UC), which presents with continuous lesions. It can manifest with a wide range of extra-intestinal symptoms such as pyoderma gangrenosum, aphthous stomatitis, episcleritis, uveitis, and arthritic disease. Such a wide range of presentations leads to diagnostic difficulties, as seen in this case. Treatment modalities include steroids, antibiotics, and surgical removal of affected parts, depending on the extent of the disease. Here, we present a case of a young male who presented with manifestations of mesenteric lymphadenitis and had an intraluminal cecal mass causing obstructive symptoms, and was subsequently diagnosed with CD.
Introduction
Crohn's disease (CD) is one of the two major inflammatory bowel diseases (IBD), more prevalent in developed countries. The incidence of CD is 0.1-0.6 cases per 100,000 patients per year, seen equally amongst males and females [ 1 , 2 ]. The disease typically presents in early adulthood, with frequent abdominal pain, diarrhea, hematochezia, and weight loss. However, symptoms vary from person to person and can range from mild to severe, depending on the severity and location of the inflammation. Several genes have been studied as etiological factors implicated in CD and, thus far, strong and replicated associations have been identified with NOD2 , IL23R , and ATG16L1 genes [ 3 ]. Numerous etiologies of the disease have been proposed, including various environmental factors, autoimmunity, genetics, and gut microbiome derangement. CD can frequently aggravate and cause multiple complications, including fistulas, abscesses, obstruction, and internal bleeding. Prognostic factors for complications and a thorough series of investigations done for diagnosing CD hold significant importance in guiding therapeutic decisions. Being a chronic inflammatory condition with granulomatous inflammation, diffuse mesenteric lymphadenopathy with an intraluminal mass remains a rare initial presentation of CD.
Case presentation
We present a case of a 25-year-old male with no significant past medical history, who presented to the emergency department (ED) with severe diffuse abdominal pain, which was colicky in nature, sudden in onset, 7/10 in intensity. He had nausea, vomiting, and loss of appetite as well. Specific investigations, including complete blood count and serum electrolytes, were carried out, and the results were normal. The patient was an avid smoker for nine years with a history of smoking one cigarette pack per day. Gastroenteritis was suspected. Thus, he was given intravenous normal saline stat, intravenous omeprazole, and intravenous baclofen in the ED and was discharged on oral medication, which included ciprofloxacin 500 mg once daily, metronidazole 400 mg thrice daily, and omeprazole 40 mg once daily for a week. One month later, he presented again to the ED with right iliac fossa pain, nausea, vomiting, loss of weight, loss of appetite, and constipation for two days. On physical examination, there was pain on deep palpation while rebound tenderness, rigidity, and guarding were absent. Investigations including complete blood count (CBC), liver function test (LFT), serum amylase, and lipase levels were ordered, and apart from mild leukocytosis and slightly elevated erythrocyte sedimentary rate (ESR), results came back normal. After reviewing labs and imaging results, a stool sample was sent for calprotectin level, which was >1000.0 ug/g, while the fecal occult blood test was negative. Computed tomography (CT) scan, as shown in Figure Figure1, 1 , showed diffuse long-segment mucosal thickening in the distal ileum, extending over 12cm, as well as enlarged lymph nodes in the right side of the bowel (depicted by the arrow in the figure).

Arrow shows several enlarged lymph nodes on the right side of the bowel.
At this time, differential diagnoses included CD, intestinal lymphoma, Castleman disease, and intestinal tuberculosis. A colonoscopy done for further evaluation showed a friable, nodular ulcerated ileocecal region with complete occlusion of the ileocecal valve and surrounding mucosal edema, as shown in Figure Figure2 2 (A, B). However, the scope could not be passed beyond the ileocecal valve.

(A) and (B) show the cecum and ileocecal valve, with mucosal edema and ulceration, and a completely occluded ileocecal junction. The scope could not be passed beyond this point.
(C) shows the rectum and (D) shows the anorectal junction. Both are normal.
Biopsy reports did not show any specific findings. Due to the deteriorating condition of the patient, a laparoscopic modified right-sided hemicolectomy was performed. Surprisingly, a hard stony nodular mass measuring 2 cm was present at 11 cm from the proximal ileal resection margin, 7 cm from the distal colonic resection margin, and 5.3 cm from the mesenteric resection margin. The mass was predominantly located on the mesenteric border. The specimen was sent for histopathology evaluation and showed acute and chronic transmural inflammation at the cecum along with focal mucosal ulceration and rare non-caseating granulomas (Figure 3 ).

Yellow arrow indicates an area of dense plasma cell and lymphocytic infiltrate; Black arrow indicates intraepithelial lymphocytes.
Twenty-one reactive mesenteric lymph nodes were noted, along with a few lymph nodes showing non-caseating granulomas. IgG and IL-6 levels were normal, and lymph node biopsy ruled out Castleman disease and lymphoma. The patient was subsequently discharged to continue outpatient follow-up for CD.
CD is one of the two main types of intestinal inflammatory disorders, the other one being ulcerative colitis (UC). Transmural inflammation of the intestine is the hallmark of CD, with granulomatous features seen on biopsy [ 3 ]. This report aims to emphasize atypical symptoms and endoscopic and histopathological findings. It is important to stress that reviewing atypical presentations will be helpful in the diagnosis of such cases in the future. The colonoscopy findings of a friable, nodular ulcerated ileocecal region with complete occlusion of the ileocecal valve are not those normally seen in CD. Moreover, it is unusual for colonoscopy biopsies to be inconclusive in this disease, as ileocolonoscopy with biopsy is the gold standard for evaluating the extent and severity [ 4 ].
This atypical presentation of CD deviates from the most common pattern found at the time of diagnosis, where the earliest endoscopic manifestations consist of small aphthous ulcers [ 5 ], followed later by characteristic findings of skip lesions, ulcerations, and strictures [ 6 ]. The essential feature to be noted in this case is the lack of conclusive findings in all investigations conducted, including CT scan, followed by the discovery of a hard mass during laparoscopic surgery. This finding is not very common in early CD. Patients with long-standing CD can present with a large abdominal mass, and the majority of the histopathologic evaluation revealed a neoplasm [ 7 ]. An abdominal mass has also been mentioned as a possible site-specific manifestation of CD [ 8 ]. Furthermore, in cases where suspicion of both CD and UC is present, the finding of an abdominal mass in addition to nausea and colicky abdominal pain favors a diagnosis of CD [ 9 ]. The prolonged and non-self-limiting course of the disease rules out the possibility of other infectious colitis [ 10 ].
Considering CD as the final diagnosis, the patient was started on a six-month course of medications, which included sulfasalazine and corticosteroids. The patient presented in the outpatient department after six months for a follow-up and reported complete remission of symptoms with no acute flare-ups. In addition to the medication, cessation of smoking immensely helped in improving the prognosis.
Conclusions
Analyzing the journey that concluded with the diagnosis of CD in our patient, it is crucial to note that evidence is not always found on colonoscopy biopsies, and it is essential to investigate further by other findings. Though the mesenteric adenitis visible on ultrasonography, along with the symptoms of vomiting, anorexia, and weight loss, raised concerns for possible intestinal tuberculosis, with similar nonspecific manifestations in earlier stages, the histological picture of the mass ultimately overruled any such diagnosis. The diagnostic clue lies in a combined assessment of symptoms, radiology, and histological evidence. However, early aggressive treatment results in a better prognosis, especially in patients with risk factors for complications of CD.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study

- Earn HPCSA and SACNASP CPD Points
- I have spots and my skin burns
- A case of a 10 year old boy with a 3 week history of diarrhoea, vomiting and cough
- A case of fever and general malaise
- A case of persistant hectic fever
- A case of sudden rapid neurological deterioration in an HIV positive 27 year old female
- A case of swollen hands
- An unusual cause of fulminant hepatitis
- Case of a right axillary swelling
- Case of giant wart
- Case of recurrent meningitis
- Case of repeated apnoea and infections in a premature infant
- Case of sudden onset of fever, rash and neck pain
- Doctor, my sister is confused
- Eight month old boy with recurrent infections
- Enlarged Testicles
- Failure to thrive despite appropriate treatment
- Right Axillary Swelling
- Severe anaemia in HIV positive child
- The case of a floppy infant
- Two year old with spiking fevers and depressed level of consciousness
- 17 year old male with fever and decreased level of consciousness
- 3 TB Vignettes
- A 10 year old girl with a hard palate defect
- A case of decreased joint function, fever and rash
- Keep up while the storm is raging
- Fireworks of autoimmunity from birth
- My eyes cross at twilight
- A case of a 3 month old infant with bloody urine and stools
- A case of scaly annular plaques
- Case of eye injury and decreased vision
- My head hurts and I cannot speak?
- TB or not TB: a confusing case
- A 7 year old with severe muscle weakness and difficulty walking
- Why can I not walk today?
- 14 year old with severe hip pain
- A 9 year old girl presents with body swelling, shortness of breath and backache
- A sudden turn of events after successful therapy
- Declining CD4 count, despite viral suppression?
- Defaulted treatment
- 25 year old female presents with persistent flu-like symptoms
- A case of persistent bloody diarrhoea
- I’ve been coughing for so long
- A case of acute fever, rash and vomiting
- Adverse event following routine vaccination
- A case of cough, wasting and lymphadenopathy
- A case of lymphadenopathy and night sweats
- Case of enlarged hard tongue
- A high risk pregnancy
- A four year old with immunodeficiency
- Young girl with recurrent history of mycobacterial disease
- Immunodeficiency and failure to thrive
- Case of recurrent infections
- An 8 year old boy with recurrent respiratory infections
- 4 year old boy with recurrent bacterial infections
- Is this treatment failure or malnutrition
- 1. A Snapshot of the Immune System
- 2. Ontogeny of the Immune System
- 3. The Innate Immune System
- 4. MHC & Antigen Presentation
- 5. Overview of T Cell Subsets
- 6. Thymic T Cell Development
- 7. gamma/delta T Cells
- 8. B Cell Activation and Plasma Cell Differentiation
- 9. Antibody Structure and Classes
- 10. Central and Peripheral Tolerance
- Immuno-Mexico 2024 Introduction
- Modulation of Peripheral Tolerance
- Metabolic Adaptation to Pathologic Milieu
- T Cell Exhaustion
- Suppression in the Context of Disease
- Redirecting Cytotoxicity
- Novel Therapeutic Strategies
- ImmunoInformatics
- Grant Writing
- Introduction to Immuno-Chile 2023
- Core Modules
- Gut Mucosal Immunity
- The Microbiome
- Gut Inflammation
- Viral Infections and Mucosal Immunity
- Colorectal Cancer
- Inflammatory Bowel Disease
- Equity, Diversity, Inclusion in Academia
- Immuno-India 2023 Introduction
- Principles of Epigenetic Regulation
- Epigenetics Research in Systems Immunology
- Epigenetic (De)regulation in Non-Malignant Diseases
- Epigenetic (De)regulation in Immunodeficiency and Malignant Diseases
- Immunometabolism and Therapeutic Applications of Epigenetic Modifiers
- Immuno-Morocco 2023 Introduction
- Cancer Cellular Therapies
- Cancer Antibody Therapies
- Cancer Vaccines
- Immunobiology of Leukemia & Therapies
- Immune Landscape of the Tumour
- Targeting the Tumour Microenvironment
- Flow Cytometry
- Immuno-Zambia 2022 Introduction
- Immunity to Viral Infections
- Immunity to SARS-CoV2
- Basic Immunology of HIV
- Immunity to Tuberculosis
- Immunity to Malaria
- Immunity to Schistosomiasis
- Immunity to Helminths
- Equity, Diversity and Inclusion in Academia
- Immuno-Argentina 2022 Introduction
- Dendritic Cells
- Trained Innate Immunity
- Gamma-Delta T cells
- Natural Killer Cell Memory
- Innate Immunity in Viral Infections
- Lectures – Innate Immunity
- T cells and Beyond
- Lectures – Cellular Immunity
- Strategies for Vaccine Design
- Lectures – Humoral Immunity
- Lectures – Vaccine development
- Lectures – Panel and Posters
- Immuno-Cuba 2022 Introduction
- Poster and Abstract Examples
- Immuno-Tunisia 2021 Introduction
- Basics of Anti-infectious Immunity
- Inborn Errors of Immunity and Infections
- Infection and Auto-Immunity
- Pathogen-Induced Immune Dysregulation & Cancer
- Understanding of Host-Pathogen Interaction & Applications (SARS-CoV-2)
- Day 1 – Basics of Anti-infectious Immunity
- Day 2 – Inborn Errors of Immunity and Infections
- Day 3 – Infection and Auto-immunity
- Day 4 – Pathogen-induced Immune Dysregulation and Cancer
- Day 5 – Understanding of Host-Pathogen Interaction and Applications
- Student Presentations
- Roundtable Discussions
- Orientation Meeting
- Poster Information
- Immuno-Colombia Introduction
- Core Modules Meeting
- Overview of Immunotherapy
- Check-Points Blockade Based Therapies
- Cancer Immunotherapy with γδ T cells
- CAR-T, armored CARs and CAR-NK therapies
- Anti-cytokines Therapies
- Tumor-infiltrating Lymphocytes (TIL)
- MDSC Promote Tumor Growth and Escape
- Immunological lab methods for patient’s follow-up
- Student Orientation Meeting
- Lectures – Week 1
- Lectures – Week 2
- Research Project
- Closing and Social
- Introduction to Immuno-Algeria 2020
- Hypersensitivity Reactions
- Immuno-Algeria Programme
- Online Lectures – Week 1
- Online Lectures – Week 2
- Student Presentations – Week 1
- Student Presentations – Week 2
- Introduction to Immuno-Ethiopia 2020
- Neutrophils
- Leishmaniasis – Transmission and Epidemiology
- Leishmaniasis – Immune Responses
- Leishmaniasis – Treatment and Vaccines
- Immunity to Helminth Infections
- Helminth immunomodulation on co-infections
- Malaria Vaccine Progress
- Immunity to Fungal Infections
- How to be successful scientist
- How to prepare a good academic CV
- Introduction to Immuno-Benin
- Immune Regulation in Pregnancy
- Immunity in infants and consequence of preeclampsia
- Schistosome infections and impact on Pregnancy
- Infant Immunity and Vaccines
- Regulation of Immunity & the Microbiome
- TGF-beta superfamily in infections and diseases
- Infectious Diseases in the Global Health era
- Immunity to Toxoplasma gondii
- A. melegueta inhibits inflammatory responses during Helminth Infections
- Host immune modulation by Helminth-induced products
- Immunity to HIV
- Immunity to Ebola
- Immunity to TB
- Genetic susceptibility in Tuberculosis
- Plant Extract Treatment for Diabetes
- Introduction to Immuno-South Africa 2019
- Models for Testing Vaccines
- Immune Responses to Vaccination
- IDA 2019 Quiz
- Introduction to Immuno-Jaipur
- Inflammation and autoinflammation
- Central and Peripheral Tolerance
- Autoimmunity and Chronic Inflammatory Diseases
- Autoimmunity & Dysregulation
- Novel Therapeutic strategies for Autoimmune Diseases
- Strategies to apply gamma/delta T cells for Immunotherapy
- Immune Responses to Cancer
- Tumour Microenvironment
- Cancer Immunotherapy
- Origin and perspectives of CAR T cells
- Metabolic checkpoints regulating immune responses
- Transplantation
- Primary Immunodeficiencies
- Growing up with Herpes virus
- Introduction to IUIS-ALAI-Mexico-ImmunoInformatics
- Introduction to Immunization Strategies
- Introduction to Immunoinformatics
- Omics Technologies
- Computational Modeling
- Machine Learning Methods
- Introduction to Immuno-Kenya
- Viruses hijacking host immune responses
- IFNs as 1st responders to virus infections
- HBV/HCV & Hepatocellular Carcinoma
- Cytokines as biomarkers for HCV
- HTLV & T cell Leukemia
- HCMV and Cancers
- HPV and Cancers
- EBV-induced Oncogenesis
- Adenoviruses
- KSHV and HIV
- Ethics in Cancer Research
- Sex and gender in Immunity
- Introduction to Immuno-Iran
- Immunity to Leishmaniasis
- Breaking Tolerance: Autoimmunity & Dysregulation
- Introduction to Immuno-Morocco
- Cancer Epidemiology and Aetiology
- Pathogens and Cancer
- Immunodeficiency and Cancer
- Introduction to Immuno-Brazil
- 1. Systems Vaccinology
- 2. Vaccine Development
- 3. Adjuvants
- 4. DNA Vaccines
- 5. Mucosal Vaccines
- 6. Vaccines for Neurodegenerative Diseases
- Introduction to Immuno-Gambia
- Immuno-Gambia Photos
- 1. Infant Immunity and Vaccines
- 2. Dendritic Cells
- 3. Conventional T Cells
- 4. gamma/delta T Cells
- 5. Immunity to Viral Infections
- 6. Immunity to Helminth Infections
- 7. Immunity to TB
- 8. Immunity to Malaria
- 9. Flow Cytometry
- Introduction to Immuno-South Africa
- 1. Introduction to Immunization Strategies
- 2. Immune Responses to Vaccination
- 3. Models for Testing Vaccines
- 4. Immune Escape
- 5. Grant Writing
- Introduction to Immuno-Ethiopia
- 1. Neutrophils
- 3. Exosomes
- 5. Immunity to Leishmania
- 6. Immunity to HIV
- 7. Immunity to Helminth Infections
- 8. Immunity to TB
- 9. Grant Writing
- Introduction to ONCOIMMUNOLOGY-MEXICO
- ONCOIMMUNOLOGY-MEXICO Photos
- 1. Cancer Epidemiology and Etiology
- 2. T lymphocyte mediated immunity
- 3. Immune Responses to Cancer
- 4. Cancer Stem Cells and Tumor-initiating cells.
- 5. Tumor Microenvironment
- 6. Pathogens and Cancer
- 7. Cancer Immunotherapy
- 8. Flow cytometry approaches in cancer
- Introduction to the Immunology Course
- Immuno-Tunisia Photo
- 1. Overview of the Immune System
- 2. Role of cytokines in Immunity
- 3. Tolerance and autoimmunity
- 4. Genetics, Epigenetics and immunoregulation
- 5. Microbes and immunoregulation
- 6. Inflammation and autoinflammation
- 7. T cell mediated autoimmune diseases
- 8. Antibody-mediated autoimmune diseases
- Introduction to the Immunology Symposium
- Immuno-South Africa Photo
- 1. Antibody Generation by B cells
- 2. Mucosal Immunity
- 3. Immunity to TB
- 4. Immunity to Malaria
- 5. Immunity to HIV
- 6. Defining a Biomarker
- 7. Grant Writing Exercise
- Immuno-Colombia Photo
- 1. Overview of Complement
- 2. Transplantation
- 3. Immune Regulation in Pregnancy
- 4. Breaking Tolerance: Autoimmunity & Dysregulation
- 5. Mucosal Immunity & Immunopathology
- 6. Regulation of Immunity & the Microbiome
- 7. Epigenetics & Modulation of Immunity
- 8. Primary Immunodeficiencies
- 9. Anti-tumour Immunity
- 10. Cancer Immunotherapy
- Introduction
- Immune Cells
- NCDs and Multimorbidity
- Mosquito Vector Biology
- Vaccines and Other Interventions
- Autoimmunity
- Career Development
- SUN Honours Introduction
- A Snapshot of the Immune System
- Ontogeny of the Immune System
- The Innate Immune System
- MHC & Antigen Presentation
- Overview of T Cell Subsets
- B Cell Activation and Plasma Cell Differentiation
- Antibody Structure and Classes
- Cellular Immunity and Immunological Memory
- Infectious Diseases Immunology
- Vaccinology
- Mucosal Immunity & Immunopathology
- Central & Peripheral Tolerance
- Epigenetics & Modulation of Immunity
- T cell and Ab-mediated autoimmune diseases
- Immunology of COVID-19 Vaccines
- 11th IDA 2022 Introduction
- Immunity to COVID-19
- Fundamentals of Immunology
- Fundamentals of Infection
- Integrating Immunology & Infection
- Infectious Diseases Symposium
- EULAR Symposium
- Thymic T Cell Development
- Immune Escape
- Genetics, Epigenetics and immunoregulation
- AfriBop 2021 Introduction
- Adaptive Immunity
- Fundamentals of Infection 2
- Fundamentals of Infection 3
- Host pathogen Interaction 1
- Host pathogen Interaction 2
- Student 3 minute Presentations
- 10th IDA 2021 Introduction
- Day 1 – Lectures
- Day 2 – Lectures
- Day 3 – Lectures
- Day 4 – Lectures
- Afribop 2020 Introduction
- WT PhD School Lectures 1
- EULAR symposium
- WT PhD School Lectures 2
- Host pathogen interaction 1
- Host pathogen interaction 2
- Bioinformatics
- Introduction to VACFA Vaccinology 2020
- Overview of Vaccinology
- Basic Principles of Immunity
- Adverse Events Following Immunization
- Targeted Immunization
- Challenges Facing Vaccination
- Vaccine Stakeholders
- Vaccination Questions Answered
- Malaria Vaccines
- IDA 2018 Introduction
- Vaccine Development
- Immune Escape by Pathogens
- Immunity to Viral Infections Introduction
- Flu, Ebola & SARS
- Antiretroviral Drug Treatments
- Responsible Conduct in Research
- Methods for Enhancing Reproducibility
- 6. B Cell Activation and Plasma Cell Differentiation
- 7. Antibody Structure and Classes
- CD Nomenclature
- 1. Transplantation
- 2. Central & Peripheral Tolerance
- 8. Inflammation and autoinflammation
- 9. T cell mediated autoimmune diseases
- 10. Antibody-mediated autoimmune diseases
- 1. Primary Immunodeficiencies
- Cancer Stem Cells and Tumour-initiating Cells
- 6. Tolerance and Autoimmunity
- Discovery of the Thymus as a central immunological organ
- History of Immune Response
- History of Immunoglobulin molecules
- History of MHC – 1901 – 1970
- History of MHC – 1971 – 2011
- SAIS/Immunopaedia Webinars 2022
- Metabolic control of T cell differentiation during immune responses to cancer
- Microbiome control of host immunity
- Shaping of anti-tumor immunity in the tumor microenvironment
- The unusual COVID-19 pandemic: the African story
- Immune responses to SARS-CoV-2
- Adaptive Immunity and Immune Memory to SARS-CoV-2 after COVID-19
- HIV prevention- antibodies and vaccine development (part 2)
- HIV prevention- antibodies and vaccine development (part 1)
- Immunopathology of COVID 19 lessons from pregnancy and from ageing
- Clinical representation of hyperinflammation
- In-depth characterisation of immune cells in Ebola virus
- Getting to the “bottom” of arthritis
- Immunoregulation and the tumor microenvironment
- Harnessing innate immunity from cancer therapy to COVID-19
- Flynn Webinar: Immune features associated natural infection
- Flynn Webinar: What immune cells play a role in protection against M.tb re-infection?
- JoAnne Flynn: BCG IV vaccination induces sterilising M.tb immunity
- IUIS-Immunopaedia-Frontiers Webinar on Immunology taught by P. falciparum
- COVID-19 Cytokine Storm & Paediatric COVID-19
- Immunothrombosis & COVID-19
- Severe vs mild COVID-19 immunity and Nicotinamide pathway
- BCG & COVID-19
- COVID-19 Vaccines
- Antibody responses and serology testing
- Flow Cytometry Part 1
- Flow Cytometry Part 2
- Flow Cytometry Part 3
- Lateral Flow
- Diagnostic Tools
- Diagnostic Tests
- HIV Life Cycle
- ARV Drug Information
- ARV Mode of Action
- ARV Drug Resistance
- Declining CD4 count
- Ambassador of the Month – 2024
- North America
- South America
- Ambassador of the Month – 2023
- Ambassador of the Month – 2022
- The Day of Immunology 2022
- AMBASSADOR SCI-TALKS
- The Day of Immunology 2021
- Ambassador of the Month – 2021
- Ambassador of the Month-2020
- Ambassador of the Month – 2019
- Ambassador of the Month – 2018
- Ambassador of the Month – 2017
- Course Applications
- COLLABORATIONS
We will not share your details
Infectious Diseases

Please choose a Case Study below

© 2004 - 2024 Immunopaedia.org.za Sitemap - Privacy Policy - Cookie Policy - PAIA - Terms & Conditions
Website designed by Personalised Promotions in association with SA Medical Specialists .
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License .

- CLINICAL CASES
- ONLINE COURSES
- AMBASSADORS
- TREATMENT & DIAGNOSTICS
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to present patient...
How to present patient cases
- Related content
- Peer review
- Mary Ni Lochlainn , foundation year 2 doctor 1 ,
- Ibrahim Balogun , healthcare of older people/stroke medicine consultant 1
- 1 East Kent Foundation Trust, UK
A guide on how to structure a case presentation
This article contains...
-History of presenting problem
-Medical and surgical history
-Drugs, including allergies to drugs
-Family history
-Social history
-Review of systems
-Findings on examination, including vital signs and observations
-Differential diagnosis/impression
-Investigations
-Management
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1
The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the patient’s condition and further management can be planned accordingly. 2 To give a high quality presentation you need to take a thorough history. Consultants make decisions about patient care based on information presented to them by junior members of the team, so the importance of accurately presenting your patient cannot be overemphasised.
As a medical student, you are likely to be asked to present in numerous settings. A formal case presentation may take place at a teaching session or even at a conference or scientific meeting. These presentations are usually thorough and have an accompanying PowerPoint presentation or poster. More often, case presentations take place on the wards or over the phone and tend to be brief, using only memory or short, handwritten notes as an aid.
Everyone has their own presenting style, and the context of the presentation will determine how much detail you need to put in. You should anticipate what information your senior colleagues will need to know about the patient’s history and the care he or she has received since admission, to enable them to make further management decisions. In this article, I use a fictitious case to show how you can structure case presentations, which can be adapted to different clinical and teaching settings (box 1).
Box 1: Structure for presenting patient cases
Presenting problem, history of presenting problem, medical and surgical history.
Drugs, including allergies to drugs
Family history
Social history, review of systems.
Findings on examination, including vital signs and observations
Differential diagnosis/impression
Investigations
Case: tom murphy.
You should start with a sentence that includes the patient’s name, sex (Mr/Ms), age, and presenting symptoms. In your presentation, you may want to include the patient’s main diagnosis if known—for example, “admitted with shortness of breath on a background of COPD [chronic obstructive pulmonary disease].” You should include any additional information that might give the presentation of symptoms further context, such as the patient’s profession, ethnic origin, recent travel, or chronic conditions.
“ Mr Tom Murphy is a 56 year old ex-smoker admitted with sudden onset central crushing chest pain that radiated down his left arm.”
In this section you should expand on the presenting problem. Use the SOCRATES mnemonic to help describe the pain (see box 2). If the patient has multiple problems, describe each in turn, covering one system at a time.
Box 2: SOCRATES—mnemonic for pain
Associations
Time course
Exacerbating/relieving factors
“ The pain started suddenly at 1 pm, when Mr Murphy was at his desk. The pain was dull in nature, and radiated down his left arm. He experienced shortness of breath and felt sweaty and clammy. His colleague phoned an ambulance. He rated the pain 9/10 in severity. In the ambulance he was given GTN [glyceryl trinitrate] spray under the tongue, which relieved the pain to 5/10. The pain lasted 30 minutes in total. No exacerbating factors were noted. Of note: Mr Murphy is an ex-smoker with a 20 pack year history”
Some patients have multiple comorbidities, and the most life threatening conditions should be mentioned first. They can also be categorised by organ system—for example, “has a long history of cardiovascular disease, having had a stroke, two TIAs [transient ischaemic attacks], and previous ACS [acute coronary syndrome].” For some conditions it can be worth stating whether a general practitioner or a specialist manages it, as this gives an indication of its severity.
In a surgical case, colleagues will be interested in exercise tolerance and any comorbidity that could affect the patient’s fitness for surgery and anaesthesia. If the patient has had any previous surgical procedures, mention whether there were any complications or reactions to anaesthesia.
“Mr Murphy has a history of type 2 diabetes, well controlled on metformin. He also has hypertension, managed with ramipril, and gout. Of note: he has no history of ischaemic heart disease (relevant negative) (see box 3).”
Box 3: Relevant negatives
Mention any relevant negatives that will help narrow down the differential diagnosis or could be important in the management of the patient, 3 such as any risk factors you know for the condition and any associations that you are aware of. For example, if the differential diagnosis includes a condition that you know can be hereditary, a relevant negative could be the lack of a family history. If the differential diagnosis includes cardiovascular disease, mention the cardiovascular risk factors such as body mass index, smoking, and high cholesterol.
Highlight any recent changes to the patient’s drugs because these could be a factor in the presenting problem. Mention any allergies to drugs or the patient’s non-compliance to a previously prescribed drug regimen.
To link the medical history and the drugs you might comment on them together, either here or in the medical history. “Mrs Walsh’s drugs include regular azathioprine for her rheumatoid arthritis.”Or, “His regular drugs are ramipril 5 mg once a day, metformin 1g three times a day, and allopurinol 200 mg once a day. He has no known drug allergies.”
If the family history is unrelated to the presenting problem, it is sufficient to say “no relevant family history noted.” For hereditary conditions more detail is needed.
“ Mr Murphy’s father experienced a fatal myocardial infarction aged 50.”
Social history should include the patient’s occupation; their smoking, alcohol, and illicit drug status; who they live with; their relationship status; and their sexual history, baseline mobility, and travel history. In an older patient, more detail is usually required, including whether or not they have carers, how often the carers help, and if they need to use walking aids.
“He works as an accountant and is an ex-smoker since five years ago with a 20 pack year history. He drinks about 14 units of alcohol a week. He denies any illicit drug use. He lives with his wife in a two storey house and is independent in all activities of daily living.”
Do not dwell on this section. If something comes up that is relevant to the presenting problem, it should be mentioned in the history of the presenting problem rather than here.
“Systems review showed long standing occasional lower back pain, responsive to paracetamol.”
Findings on examination
Initially, it can be useful to practise presenting the full examination to make sure you don’t leave anything out, but it is rare that you would need to present all the normal findings. Instead, focus on the most important main findings and any abnormalities.
“On examination the patient was comfortable at rest, heart sounds one and two were heard with no additional murmurs, heaves, or thrills. Jugular venous pressure was not raised. No peripheral oedema was noted and calves were soft and non-tender. Chest was clear on auscultation. Abdomen was soft and non-tender and normal bowel sounds were heard. GCS [Glasgow coma scale] was 15, pupils were equal and reactive to light [PEARL], cranial nerves 1-12 were intact, and he was moving all four limbs. Observations showed an early warning score of 1 for a tachycardia of 105 beats/ min. Blood pressure was 150/90 mm Hg, respiratory rate 18 breaths/min, saturations were 98% on room air, and he was apyrexial with a temperature of 36.8 ºC.”
Differential diagnoses
Mentioning one or two of the most likely diagnoses is sufficient. A useful phrase you can use is, “I would like to rule out,” especially when you suspect a more serious cause is in the differential diagnosis. “History and examination were in keeping with diverticular disease; however, I would like to rule out colorectal cancer in this patient.”
Remember common things are common, so try not to mention rare conditions first. Sometimes it is acceptable to report investigations you would do first, and then base your differential diagnosis on what the history and investigation findings tell you.
“My impression is acute coronary syndrome. The differential diagnosis includes other cardiovascular causes such as acute pericarditis, myocarditis, aortic stenosis, aortic dissection, and pulmonary embolism. Possible respiratory causes include pneumonia or pneumothorax. Gastrointestinal causes include oesophageal spasm, oesophagitis, gastro-oesophageal reflux disease, gastritis, cholecystitis, and acute pancreatitis. I would also consider a musculoskeletal cause for the pain.”
This section can include a summary of the investigations already performed and further investigations that you would like to request. “On the basis of these differentials, I would like to carry out the following investigations: 12 lead electrocardiography and blood tests, including full blood count, urea and electrolytes, clotting screen, troponin levels, lipid profile, and glycated haemoglobin levels. I would also book a chest radiograph and check the patient’s point of care blood glucose level.”
You should consider recommending investigations in a structured way, prioritising them by how long they take to perform and how easy it is to get them done and how long it takes for the results to come back. Put the quickest and easiest first: so bedside tests, electrocardiography, followed by blood tests, plain radiology, then special tests. You should always be able to explain why you would like to request a test. Mention the patient’s baseline test values if they are available, especially if the patient has a chronic condition—for example, give the patient’s creatinine levels if he or she has chronic kidney disease This shows the change over time and indicates the severity of the patient’s current condition.
“To further investigate these differentials, 12 lead electrocardiography was carried out, which showed ST segment depression in the anterior leads. Results of laboratory tests showed an initial troponin level of 85 µg/L, which increased to 1250 µg/L when repeated at six hours. Blood test results showed raised total cholesterol at 7.6 mmol /L and nil else. A chest radiograph showed clear lung fields. Blood glucose level was 6.3 mmol/L; a glycated haemoglobin test result is pending.”
Dependent on the case, you may need to describe the management plan so far or what further management you would recommend.“My management plan for this patient includes ACS [acute coronary syndrome] protocol, echocardiography, cardiology review, and treatment with high dose statins. If you are unsure what the management should be, you should say that you would discuss further with senior colleagues and the patient. At this point, check to see if there is a treatment escalation plan or a “do not attempt to resuscitate” order in place.
“Mr Murphy was given ACS protocol in the emergency department. An echocardiogram has been requested and he has been discussed with cardiology, who are going to come and see him. He has also been started on atorvastatin 80 mg nightly. Mr Murphy and his family are happy with this plan.”
The summary can be a concise recap of what you have presented beforehand or it can sometimes form a standalone presentation. Pick out salient points, such as positive findings—but also draw conclusions from what you highlight. Finish with a brief synopsis of the current situation (“currently pain free”) and next step (“awaiting cardiology review”). Do not trail off at the end, and state the diagnosis if you are confident you know what it is. If you are not sure what the diagnosis is then communicate this uncertainty and do not pretend to be more confident than you are. When possible, you should include the patient’s thoughts about the diagnosis, how they are feeling generally, and if they are happy with the management plan.
“In summary, Mr Murphy is a 56 year old man admitted with central crushing chest pain, radiating down his left arm, of 30 minutes’ duration. His cardiac risk factors include 20 pack year smoking history, positive family history, type 2 diabetes, and hypertension. Examination was normal other than tachycardia. However, 12 lead electrocardiography showed ST segment depression in the anterior leads and troponin rise from 85 to 250 µg/L. Acute coronary syndrome protocol was initiated and a diagnosis of NSTEMI [non-ST elevation myocardial infarction] was made. Mr Murphy is currently pain free and awaiting cardiology review.”
Originally published as: Student BMJ 2017;25:i4406
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed
- ↵ Green EH, Durning SJ, DeCherrie L, Fagan MJ, Sharpe B, Hershman W. Expectations for oral case presentations for clinical clerks: opinions of internal medicine clerkship directors. J Gen Intern Med 2009 ; 24 : 370 - 3 . doi:10.1007/s11606-008-0900-x pmid:19139965 . OpenUrl CrossRef PubMed Web of Science
- ↵ Olaitan A, Okunade O, Corne J. How to present clinical cases. Student BMJ 2010;18:c1539.
- ↵ Gaillard F. The secret art of relevant negatives, Radiopedia 2016; http://radiopaedia.org/blog/the-secret-art-of-relevant-negatives .
- Biomarker-Driven Lung Cancer
- HER2-Positive Breast Cancer
- Chronic Lymphocytic Leukemia
- Small Cell Lung Cancer
- Renal Cell Carcinoma

- CONFERENCES
- PUBLICATIONS
Case Presentation: A 67-Year-Old Man with Chronic Lymphocytic Leukemia
John Allan, MD, presents and reviews the case of a 67-year-old man with chronic lymphocytic leukemia.

EP: 1 . Case Presentation: A 67-Year-Old Man with Chronic Lymphocytic Leukemia
Ep: 2 . testing and risk stratification in cll, ep: 3 . first-line therapy options in cll, ep: 4 . chronic lymphocytic leukemia: resonate-2 trial, ep: 5 . comparing btk inhibitors in cll treatment, ep: 6 . treatment approaches for high-risk chronic lymphocytic leukemia, ep: 7 . the future of chronic lymphocytic leukemia treatment.
John Allan, MD: Welcome, everyone. Thank you for joining, I’m John Allan. I'm an assistant professor of medicine here at Weill Cornell Medicine, in New York City.
I'm a lymphoma physician. I have a specialization in CLL [chronic lymphocytic leukemia], and treating patients with CLL, and we'll be going through a case and I’ll be giving you my insights on my thoughts about the case and how I might manage the patient potentially differently or the same. I would like to start out by presenting the case so everyone is on the same page here. This is a 67-year-old male with a diagnosis of chronic lymphocytic leukemia. He's presenting to his primary care physician with complaints of fatigue and night sweats. In terms of past medical history, he's relatively healthy, except that he takes an over-the-counter antacid every few days, a couple times a week, for a sensitive stomach.
On a physical exam, he has a large mobile lymph node, these are bilaterally, in the cervical chain. No palpable spleen or liver, palpable liver is noted. Laboratory findings are consistent with a white blood cell count of a 102,000, lymphocytes are 79,000 of those 102. Hemoglobin is slightly low but relatively OK, and preserved at 11.4 grams per deciliter. His platelets are normal at 180,000. His neutrophil count is normal at 1.9. His LDH [lactate dehydrogenase] is actually very elevated, at 1470. And cytogenetics are showing a chromosome 11q deletion and IgHV [immunoglobulin heavy chain] unmutated status.
I presume this was sent off not by the primary care, but by his hematologist. And a beta-2 macroglobulin was also obtained and that's 3.0, right on the threshold of being abnormal. He's staged as a Rai Stage I, and the patient initiated treatment, and was started on ibrutinib once daily.
John Allan, MD: So, this case is a somewhat common presentation that we see, especially with a patient with these molecular abnormalities. Average age diagnosis of patients as a reminder is about 70 to 71 years of age, so the patient is well within that nice bell-shaped curve. He was relatively healthy, feeling well, up until very recently when these symptoms started.
The disease has been progressive relatively quickly, and associated with these B symptoms with a very elevated white blood cell count, along with the fevers and night sweats. Also note is that the LDH is rather elevated. The high end of normal, at least in my lab, is around 230 or 220. This patient is at 1470.
Additionally, the cytogenetics are identifying relatively high-risk features with the deletion 11q and IgHV unmutated status. This is somebody that I am concerned about. I do agree with the treatment decision to initiate therapy. A few things to note, deletion 11q, it's considered high risk feature, and patients do present a little bit differently with an 11q than some of the other patients with CLL.
Many times, the 11q patients have rather proliferative disease at diagnosis and they can present with a lot of bulky adenopathy. While this patient doesn't have technically bulky adenopathy, and really what's palpable is only about a centimeter and a half, it's very possible that with deep within the abdomen something that we're not palpating he can have a very large lymph node, 6 to 8 centimeters or larger.
Typically, that's associated with signs and symptoms, but given the fact that these fevers, night sweats and rather proliferative disease with an elevated LDH together with these high-risk features, this is someone I might be concerned about even with a transformation as an initial presentation of their CLL and would need to work up and rule that out appropriately.
With that said, the patient was started on ibrutinib, and overall is a good therapy. And so, those are the big, noteworthy aspects of this case, and can be a rather typical presentation for a patient with deletion 11q molecular features like this patient.
John Allan, MD: One other aspect of this case that's unique is that the patient is on over-the-counter antacids, and this is a relatively common thing. Many patients are takig either over-the-counter antacids like Pepcid [famotidine], Prilosec [omeprazole], etc.
I'm sorry, those are more PPIs [proton pump inhibitors] but acid suppressing medications either H2 [histamine2] blockers calcium absorbing, calcium carbonate like medications and or proton pump inhibitors.
And so, this is not just unique to CLL patients, this is just unique to older patients and patient population in general, where in the US specifically there is a lot of PPI use, whether it's over-the-counter or prescribed.
Ultimately, in clinical trials with BTK [Bruton’s tyrosine kinase] inhibitors and targeted agents we do see about 40% to 45% of patients on some type of acid suppressive medication. This is a very common scenario and it may have some relevance based on differentiating between BTKi's at this point in time.
Transcript Edited for Clarity
Initial Presentation
- A 67-year-old man presented to PCP with complaints of fatigue and night sweats
- PMH: patient takes OTC antiacid tablets a few times a week for a “sensitive” stomach
- PE: Enlarged mobile lymph nodes bilaterally (~1.5 cm), no palpable spleen or liver
- Laboratory findings:
- WBC; 102 X 109/L
- Lymphocytes; 79 X 109/L
- Hb; 11.4 g/dL
- Platelets; 180 X 109/L
- ANC; 1,900/mm3
- LDH 1470 U/L
- Cytogenetics; del(11q), IgVH-unmutated
- beta2M, 3.0 mg/L
- Rai Stage I
Treatment Plan
- Patient was started on ibrutinib

Exciting Activity in Chronic Lymphocytic Leukemia
In season 4, episode 7 of Targeted Talks, Cyrus M. Khan, MD, discusses the latest FDA activity in the chronic lymphocytic leukemia space.

Lachowiez Considers the Use of Tagraxofusp in BPDCN as Bridge to SCT With Peers
During a Targeted Oncology™ Case-Based Roundtable™ event, Curtis Lachowiez, MD, discussed targeted therapy for blastic plasmacytoid dendritic cell neoplasm and its role in patients who could receive allogeneic stem cell transplant.

Better Strategies for the Treatment of High-Risk Chronic Lymphocytic Leukemia
In season 3, episode 4 of Targeted Talks, Alexey Danilov, MD, PhD, discusses the shift toward utilizing cellular therapy to treat high-risk patients with chronic lymphocytic leukemia.

Hoffmann Discusses Deciding Factors for Treating Patients With CLL
In the first article of a 2-part series, Marc S. Hoffmann, MD, looks at the factors to take into consideration before initiating another line of treatment in patients with chronic lymphocytic leukemia.

Behind the FDA Approval of Liso-cel for Relapsed/Refractory CLL/SLL
In an interview with Targeted Oncology, Tanya Siddiqi, MD, discussed the rationale behind the TRANSCEND CLL 004 study supporting the FDA approval of lisocabtagene maraleucel in chronic lymphocytic leukemia or small lymphocytic lymphoma.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777


- Previous Article
- Next Article
CASE PRESENTATION
Exercise implications, peripheral arterial disease: a case report from the henry ford hospital.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Guest Access
- Get Permissions
- Cite Icon Cite
- Search Site
Shel D. Levine; Peripheral Arterial Disease: A Case Report From the Henry Ford Hospital. Journal of Clinical Exercise Physiology 1 March 2018; 7 (1): 15–21. doi: https://doi.org/10.31189/2165-6193-7.1.15
Download citation file:
- Ris (Zotero)
- Reference Manager
A.T. is a 65-year-old black female with claudication secondary to peripheral arterial disease (PAD). She has a history of coronary artery disease, myocardial infarction, heart failure, endarterectomy, hypertension, hyperlipidemia, type 1 diabetes mellitus, and asthma.
She was referred to the Division of Vascular Surgery at Henry Ford Hospital complaining of fatigue and heaviness in her lower thighs and calves during walking. Resting ankle-brachial index (ABI) was 0.50 and 0.70 at the right and left dorsalis pedis, respectively. She was prescribed cilostazol and encouraged to “…walk through the pain as much as possible.”
Due to worsening claudication, A.T. underwent an abdominal aortogram with arteriogram of the lower extremities. Results showed aortoiliac disease with multiple stenoses of varying degrees. Areas of calcification were noted from the lower aorta and iliac artery to the anterior tibial artery affecting both the left and right limbs.
Results from a stress echocardiogram showed cardiac wall motion abnormalities consistent with exercise-induced ischemia. She exercised for 5.8 minutes on the Bruce protocol, limited by general fatigue. The electrocardiogram displayed left bundle branch block, resting ejection fraction was 40%, peak blood pressure was 160/80 mmHg, and peak heart rate was 120 b·min −1 . No symptoms were reported. Her medications are cilostazol, carvedilol, amlodipine, isosorbide dinitrate, clopidogrel, simvastatin, potassium, triamcinolone, ipratropium, and pirbuterol.
She began supervised exercise training in cardiac rehabilitation following a hospitalization for angina. At rest her blood pressure was 120/50 mmHg, heart rate was 79 b·min −1 , blood glucose was 6.89 mmol·L −1 (266 mg·dL −1 ) and her HbA1c was 8.0%. Her initial exercise sessions were limited by bilateral claudication of her thighs and calves. Moderate pain occurred after 9 minutes of walking on day 1. A pain-rest walking program was initiated and followed for 12 weeks. She then joined the Henry Ford PREVENT program, which provides patients with a low-cost, long-term supervised exercise environment.
She now exercises at least 3 d·wk −1 for 60 minutes each session. She splits her exercise time between a seated stepper and a treadmill. On most days she is now able to walk 30 continuous minutes without limiting claudication pain.
The natural history of arteriosclerosis involves an intimal plaque that progressively develops until it eventually causes a significant flow limiting occlusion of the vessel and reduction of blood supply relative to demand. Arteriosclerosis is a systemic disorder affecting the major circulations, with the intimal plaque occurring segmentally in multiple locations. When the plaque occurs in the distal aorta or in the arteries of the lower extremities, it is referred to as PAD.
Epidemiology
More than 8 million individuals in the United States above the age of 40 are estimated to have PAD ( 1 ). The prevalence of PAD per ABI is 4.3% in persons older than 40 years and up ( 2 ) and 29% in those 70 years and older ( 3 ). Thus PAD afflicts more than 4 million Americans and more than 200 million people worldwide. The age-adjusted prevalence of PAD increases to approximately 12% when more sensitive vascular imaging studies are used. Unlike coronary artery disease, the incidence of PAD is similar in men and women. Coronary artery disease occurs in 60% to 90% of patients with PAD. The incidence of cerebral vascular disease is increased in patients with PAD as well.
Natural History
Peripheral arterial disease is part of the spectrum of atherosclerosis. It is associated with coronary and carotid artery disease. PAD increases mortality by 6-fold, due mostly to myocardial infarction and stroke. The 5-year mortality rate in patients with PAD is ≈ 30%, with a major lower extremity amputation rate near 1% to 2%. If the patient continues to smoke, the mortality rate doubles and the risk for amputation increases 10-fold. Aortoiliac disease has a higher mortality than femoral artery disease due to a greater prevalence of coronary artery disease in patients with the former.
Ten percent of patients with intermittent claudication will go on to have ischemic pain at rest (aka, critical limb ischemia), often leading to ulceration or amputation. The presence of diabetes mellitus also affects morbidity and mortality in patients with PAD. Sixty percent of leg amputations are the result of diabetic peripheral vascular disease. In fact, among patients with diabetes for 25 years or more, the risk of below the knee amputation is increased 12-fold.
The risk factors for coronary artery disease are also risk factors for the development of PAD (i.e., age greater than 65 years, cigarette smoking, and diabetes mellitus). Patients with type 2 diabetes mellitus have a 4-fold increased risk for PAD, while their risk for myocardial infarction or stroke is increased only 2-fold. The severity of PAD is not related to glycemic control but rather to the number of coexisting risk factors. Therefore, hypertension, hyperlipidemia and hyperhomocysteinemia are also important risk factors for PAD. For each 0.03 mmol·L −1 (1 mg·dL −1 ) increase in total cholesterol, there is a 1% increased incidence of PAD. A reduced high-density lipoprotein cholesterol and increased triglyceride are also closely associated with PAD. In the presence of these risk factors and given the systemic nature of atherosclerosis and its poor prognosis, patients with PAD should be thought of as already having coronary and carotid artery disease.
Clinical Features
Unless there is acute occlusion by thrombosis, the symptoms of PAD occur gradually and progressively. Intermittent claudication is the major symptom of PAD. Claudication is derived from the Latin word claudicato , meaning to limp , which describes the gait of a patient with intermittent claudication. Intermittent claudication is most often described as an aching, cramping, or tightness in the muscles of the leg (usually the calf) that occurs with exercise and is relieved with rest. The pain usually disappears within several minutes after stopping exercise. The discomfort reoccurs at a constant distance. The distance is shorter if the patient is walking uphill or climbing stairs, and this pain does not occur at rest.
Despite claudication being the hallmark symptom of PAD, it is estimated that approximately 60% to 70% of individuals with disease do not have this symptom ( 4 ). The reason for this disparity is not entirely clear, but often patients with PAD may have diabetic neuropathy, which could mask symptoms, or they may simply not report discomfort because of the false assumption that it is simply pain associated with the aging process (e.g., arthritis). Another possibility could be because of avoidance of activities that may cause leg pain (e.g. exercise, yard work, walking long distances).
Some areas of the vascular tree are more likely to develop atherosclerotic plaque than others. In the abdomen, the stenosis usually occurs in the distal aorta or common iliac arteries. Distal to the inguinal ligament, the most common occlusions occur in the adductor canal, the posterior tibial artery at the ankle, and the anterior tibial artery at its origin. Stenosis of the external iliac and popliteal arteries occurs less frequently.
The location of the claudication is useful in predicting the most proximal level of occlusion. Intermittent claudication of the calf muscles does not occur with occlusions in the anterior tibial, posterior tibial, or peroneal arteries. It requires a more proximal lesion. Calf and thigh claudication suggests that the area of stenosis is proximal to the origin of the vascular supply to the thigh muscles (i.e. the profunda femoris artery). Thigh and buttock claudication with impotence in a middle-aged male is called Leriche Syndrome and signifies terminal aortic disease.
Pseudoclaudication must be differentiated from true claudication. Pseudoclaudication occurs from nonvascular causes of leg pain such as spinal stenosis, herniated nucleus pulposus, spinal cord tumors, and degenerative joint disease. It is usually described as a paresthetic discomfort (i.e., numbness, tingling, and/or weakness). The exercise-pain-rest cycle is not consistent in that standing does not relieve the pain. Sitting down may relieve it, and the time required for the pain to disappear is usually several minutes or more.
Physical Examination
Patients with isolated nonobstructive lesions frequently have normal-appearing extremities. Paresthesia, numbness, ulceration, and gangrene are also symptoms of PAD but represent an advanced stage with multiple lesions. Loss of hair, trophic nail changes, and dependent rubor (redness caused by swelling) can also be seen. Loss of the peripheral pulse distal to the occlusion occurs in chronic disease. The pulses that should be checked include the femoral, popliteal, dorsalis pedis, and posterior tibial. Pulses should be described as: 0, absent; 1, diminished; 2, normal; or 3, bounding. Auscultation for bruits should also be performed over the abdomen and femoral arteries.
The resting ABI is considered the first-line test for PAD with a sensitivity ranging from 68% to 84% and a specificity of 84% to 99% compared to the gold standard of vascular imaging ( 1 ). ABI is measured by taking systolic blood pressure in the arm (i.e., brachial artery) and dividing it by pressure in the ipsilateral ankle (greater value between the dorsalis pedis or posterior tibial arteries). A normal value is 1.0 or greater ( Table 1 ). Values less than 0.5 are usually seen in patients with diffuse disease. A study of over 2,000 patients with PAD showed an abnormal ABI (< 0.91) to be an independent predictor of cardiovascular events and total mortality, with an annual mortality of 25% for the lowest ABI values ( 5 ). Values over 1.4 are likely due to noncompressible vessels from extensive disease and calcification.
Interpretation of ABI values.

The ABI can also be measured immediately after exercise. It should be the same or higher than the resting value. A drop in the ABI after exercise in someone who was normal or borderline at rest also suggests significant disease. As the arterioles within the exercising muscles dilate, the stenosis in the artery proximal to the muscle limits augmentation of blood flow and pressure drops. The postexercise ABI is often used to follow disease progression, as well as adequacy of medical and surgical therapy.
Ultrasonic duplex scanning, computed tomography angiography, or magnetic resonance angiography can be used to evaluate the severity of the disease and determining a treatment plan. Ultimately, angiography is necessary to localize the lesion and determine the extent of disease prior to surgery or percutaneous transluminal angioplasty.
The goals of treatment include reducing the symptom of intermittent claudication, improving mobility and quality of life, and halting the progression of atherosclerosis. Aggressive risk factor modification should be the cornerstone of any treatment plan. Due to the poor appreciation that PAD represents systemic atherosclerosis and is associated with a poor prognosis, many patients with PAD are undertreated. Smoking cessation through educational programs, nicotine-replacement therapy, and antidepressant drugs should be strongly considered. In those patients with hyperlipidemia, low density lipoprotein cholesterol should be at least less than 2.59 mmol·L −1 (100 mg·dL −1 ) and triglyceride should be less than 3.89 mmol·L −1 (150 mg·dL −1 ). Statin agents, in addition to lowering cholesterol, also may improve endothelial function. The treatment of hypertension and diabetes mellitus does not alter the natural history of PAD. Similarly, hyperhomocysteinemia is easily measured and treated, but there are no clinical trials assessing efficacy, and thus the current guidelines state that homocysteine lowering is of no benefit. At present there is no role for the use of hormone replacement therapy. Antiplatelet agents (i.e., aspirin and clopidogrel) reduce the risk of fatal and nonfatal cardiovascular events and are approved by the Food & Drug Administration for secondary prevention in patients with atherosclerosis. Probably due to a long history of use and few side effects, aspirin remains the drug of choice ( 1 ). Aspirin may also be administered with clopidogrel, which may reduce the risk of myocardial infarction, stroke, and vascular death in those with symptoms ( 1 ).
Meticulous foot care is extremely important, with special attention to properly fitting shoes and immediate attention to cuts and blisters. This is especially true for patients with diabetes mellitus, because with a peripheral neuropathy they might not experience pain as a warning sign of developing foot problems.
Medical treatment has met with mixed results. Vasodilators are not effective and are not used in the treatment of PAD. Pentoxifylline is no longer recommended as treatment for claudication pain. Cilostazol inhibits platelet aggregation and smooth-muscle proliferation and causes vasodilatation. In 4 randomized placebo-controlled trials, cilostazol improved both pain-free walking and maximal treadmill walking distance, but it did not improve the incidence of cardiovascular death ( 6 , 7 ).
For patients with lifestyle-limiting symptoms and hemodynamically significant aortoiliac disease, percutaneous transluminal angioplasty is an excellent alternative to surgery, giving results comparable to surgery without the morbidity. The ideal lesion for percutaneous transluminal angioplasty is an iliac stenosis less than 5 cm in length or a femoropopliteal stenosis less than 10 cm in length. Long-term results are best when the lesion is above the groin area. The majority of patients with PAD will not require surgical therapy, and a class I recommendation is to offer all patients exercise training therapy initially versus revascularization ( 1 ). Patients who do develop ischemic pain at rest, ulcers, or gangrene may be helped by surgery.
Exercise Testing
Since atherosclerosis represents the most common cause of death in patients with PAD, screening for coronary artery disease is important. Exercise testing guidelines outlined by the American College of Sports Medicine are appropriate for patients with PAD ( 8 ). A common treadmill protocol used in this patient population is the Gardner protocol ( 9 ) (Box 1). In patients with PAD, a symptom-limited exercise test can help identify exercise-induced myocardial ischemia, quantify aerobic capacity, evaluate postexercise ABI, identify time to initial claudication pain, and develop an exercise prescription.
Constant speed of 2.0 mph (3.2 kph)
Increments of elevation every 2 min
○ Start at 0%
○ Increase by 2%
Record pain-free and maximal walking time
Patients with PAD have 6 times the mortality as their age- and gender-matched peers.
Intermittent claudication is the defining symptom of PAD, traditionally affecting the calves but possibly including the thighs or buttocks.
Patients with diabetes mellitus and peripheral neuropathy may not experience claudication in spite of severe PAD.
In addition to detecting PAD, the ankle-brachial index test is an important non-invasive predictor of cardiovascular events and total mortality.
Smoking cessation, exercise, and modification of other risk factors are the foundation for treating PAD.
Reported peak oxygen consumption values in patients with PAD is 13 to 14 mL·kg −1 ·min −1 ( 10 , 11 ). Tests utilizing treadmill exercise will likely be limited by claudication. Although the time to onset of pain and maximal walking time during treadmill exercise are important markers of the severity of PAD and used for outcome comparisons, tests limited by claudication may not provide sufficient myocardial stress for proper assessment of cardiovascular disease risk. Submaximal stress may be avoided by using leg or arm ergometry while still providing information useful for developing an exercise prescription.
Submaximal functional evaluations, such as the 6-minute walk test, may better reflect the impact of claudication on daily physical activities. Among patients with PAD, Montgomery et al. ( 12 ) found the 6-minute walk test to be reliable and correlated with the time to claudication pain during treadmill testing and ABI.
Exercise Training
Exercise training has been recommended to patients with intermittent claudication for many years, with several randomized controlled trials of exercise training reported. And importantly in May 2017 the Centers for Medicare and Medicaid Services (CMS) approved supervised exercise training as a reimbursable intervention for patients with symptomatic PAD who are referred by their physician. The impetus for this approval is an ever-growing amount of research demonstrating functional and quality of life improvements in those with symptomatic PAD who undergo an exercise training program. Virtually all trials that have evaluated the importance of exercise training in patients with PAD have exhibited an increase in exercise tolerance. And the evidence for exercise training benefits has resulted in the higher recommendation by the American Heart Association and American College of Cardiology for supervised exercise training ( 1 ).
Patients with PAD are at increased risk of cardiovascular disease and should be appropriately evaluated for exercise-induced myocardial ischemia.
PAD results in reduced exercise tolerance due to metabolic dysfunction, skeletal muscle abnormalities, diminished cardiorespiratory reserve, and exercise-induced inflammation. Exercise training improves pain-free and peak walking ability. Compared to stenting, improvement with walking is similar for pain-free walking and superior for peak walking time. Both are better than optimal medical therapy.
Optimal exercise training benefits are derived from programs that include walking to moderate pain with intermittent rest, accumulating 30 to 45 minutes, 3 d·wk −1 (or more), for at least 6 months.
The Claudication: Exercise Vs. Endoluminal Revascularization (CLEVER) study was the defining study to convince the CMS to cover supervised exercise training for PAD ( 13 ). CLEVER randomized revascularization-eligible patients to either medical care alone (i.e., advice and cilostazol), medical care plus revascularization, or medical care plus exercise training. The exercise training group had equivalent pain-free walking time as compared to the revascularization group (with both better than medical care alone) at 6 and 18 months. And the exercise group improved more than both other groups in peak walking time, which improved by 4.6 minutes (95% CI, P = 0.001) versus only 2.1 (95% CI, P = 0.04) minutes, respectively for the supervised exercise and control groups. The authors stated that supervised exercise is a reasonable strategy, as compared to stenting, and programs should be developed that are available and affordable to patients ( 13 ).
A meta-analysis from the Cochrane database ( 14 ) involving 32 critically evaluated randomized controlled trials of exercise therapy that randomized a total of 1,835 patients reported an overall improvement in peak walking distance of 120 meters (95% CI 50.79 to 189.92, P < 0.0007, high-quality evidence). Pain-free walking distance was also improved, as compared to a control group, by an average of 82 meters (95% CI 71.73 to 92.48, P < 0.00001, high-quality evidence). These findings are consistent with an earlier meta-analysis that reported improvements of 179% and 122% for walking distance to the onset of pain and to maximal pain, respectively ( 15 ). It is noted that exercise training has not been shown to affect the ABI ( 14 ).
In addition to the reduction in blood flow due to PAD, several factors have been associated with the reduced exercise capacity observed among these patients ( Figure 1 ). These include metabolic dysfunction, skeletal muscle abnormalities, reduced cardiorespiratory reserve, and exercise-induced inflammation. With exercise training there is increased skeletal muscle fiber area and improved oxidative capacity, blood flow, gait biomechanics, and blood rheology (e.g., viscosity, filterability and aggregation) ( 16 ). Due to chronic ischemia and reperfusion, multiple episodes of local and systemic inflammation occur in patients with PAD and is exacerbated by acute exercise, yet its contribution to disease progression is unknown. Also unknown is the role exercise training may have on modifying this inflammatory response.

Factors associated with reduced exercise capacity in patients with PAD.
The majority of exercise training trials in patients with claudication have used walking as the exercise training mode, as well as the primary outcome measured. As a result, walking predominates in the exercise prescription even though the mechanisms by which these patients improve remain unclear. Other exercise modes have also shown benefit. Sanderson et al. ( 17 ) evaluated the training response of 42 patients with symptomatic claudication randomized to 6 weeks of leg cycling, treadmill walking, or non-exercise control. The leg cycling group improved both pain-free and peak walking time versus control. However, this improvement was not as great as the treadmill walking group. Treat-Jacobson et al. ( 18 ) assessed 12 weeks of upper-body ergometry training versus treadmill walking and reported significant improvements in both groups for pain-free and peak walking time. These data suggest a systemic effect with exercise training.
The effects of progressive resistance exercise in patients with claudication are not well investigated. Hiatt et al. ( 19 ) found lesser improvements in walking time following 12 weeks of strength training (36%), compared to treadmill exercise (74%). In addition, strength training combined with treadmill exercise did not provide additional benefits. Similarly, McDermott et al. ( 20 ) compared treadmill walking with progressive resistance training in a group of 156 patients with PAD. They noted improvements in both groups in peak walking time versus control, but the treadmill group improved more than the resistance training group (3.4 vs. 1.9 minutes).
Exercise Prescription
Exercise prescription guidelines outlined by the American College of Sports Medicine are appropriate for patients with PAD ( 8 ). The exercise prescription for maximal walking improvements in patients with claudication secondary to PAD should be walking-focused. Ideally a patient should perform intermittent walking to the point of moderately tolerable claudication pain, alternated with rest ( Figure 2 ). Rest periods should last until pain is completely (or nearly) relieved enough to continue walking. Patients should accumulate at least 30 minutes, but preferably 45 to 60 minutes, of this type of training at least 3 d·wk −1 . Exercise intensity should be slowly increased when a patient can walk more than 8 minutes without at least moderate pain. As exercise tolerance improves, some PAD patients may increase their total continuous walking time, or potentially introduce intermittent bouts throughout the day. Maximal benefits have been reported after 6 months of training, thus it is important to encourage patients to continue exercising beyond a typical 12-week supervised exercise training program. In addition to this standard recommendation, some patients may further improve cardiorespiratory function by performing additional aerobic exercise via exercise modes that are not limited by claudication (e.g., leg cycling, seated stepping, elliptical). This might be useful for select patients who either have a low functional capacity or who are not able to tolerate more than 30 minutes of the walking to moderate claudication pain protocol. Additionally, there are long-term health benefits of performing continuous exercise at an intensity that provides a cardiorespiratory stimulus (i.e., > 50% peak). And it is interesting to note that PAD patients who performed any amount of physical activity beyond light intensity showed a lower mortality rate than similar patients who were effectively sedentary ( 14 ). This reduced risk of mortality remained evident even when the findings were adjusted for age, ABI, and body mass index ( 21 ).

Claudication Training Pain Scale.
“Stop smoking and keep walking” has long been the recommendation for people with claudication. Although significant improvements in pain-free and peak walking distance are well documented by those who perform regular exercise, the mechanisms and their relative contribution remain unclear. In addition, their impact, if any, on disease progression and mortality requires further investigation. In spite of various medical therapies (e.g,, medications, revascularization), exercise training continues to produce the most favorable outcomes and should be routinely incorporated into the treatment plan for patients with PAD.
Author notes
1 School of Health Promotion & Human Performance, Department of Exercise Science, Eastern Michigan University, Ypsilanti, Michigan
Conflicts of Interest and Source of Funding: None.
Recipient(s) will receive an email with a link to 'Peripheral Arterial Disease: A Case Report From the Henry Ford Hospital' and will not need an account to access the content.
Subject: Peripheral Arterial Disease: A Case Report From the Henry Ford Hospital
(Optional message may have a maximum of 1000 characters.)
Citing articles via
Get email alerts.
- Submit an Article
- Subscribe to the Journal
Affiliations

- eISSN 2165-7629
- ISSN 2165-6193
- Privacy Policy
- Get Adobe Acrobat Reader
This Feature Is Available To Subscribers Only
Sign In or Create an Account
We use essential cookies to make Venngage work. By clicking “Accept All Cookies”, you agree to the storing of cookies on your device to enhance site navigation, analyze site usage, and assist in our marketing efforts.
Manage Cookies
Cookies and similar technologies collect certain information about how you’re using our website. Some of them are essential, and without them you wouldn’t be able to use Venngage. But others are optional, and you get to choose whether we use them or not.
Strictly Necessary Cookies
These cookies are always on, as they’re essential for making Venngage work, and making it safe. Without these cookies, services you’ve asked for can’t be provided.
Show cookie providers
- Google Login
Functionality Cookies
These cookies help us provide enhanced functionality and personalisation, and remember your settings. They may be set by us or by third party providers.
Performance Cookies
These cookies help us analyze how many people are using Venngage, where they come from and how they're using it. If you opt out of these cookies, we can’t get feedback to make Venngage better for you and all our users.
- Google Analytics
Targeting Cookies
These cookies are set by our advertising partners to track your activity and show you relevant Venngage ads on other sites as you browse the internet.
- Google Tag Manager
- Infographics
- Daily Infographics
- Graphic Design
- Graphs and Charts
- Data Visualization
- Human Resources
- Training and Development
- Beginner Guides
Blog Case Study
How to Present a Case Study like a Pro (With Examples)
By Danesh Ramuthi , Sep 07, 2023

Okay, let’s get real: case studies can be kinda snooze-worthy. But guess what? They don’t have to be!
In this article, I will cover every element that transforms a mere report into a compelling case study, from selecting the right metrics to using persuasive narrative techniques.
And if you’re feeling a little lost, don’t worry! There are cool tools like Venngage’s Case Study Creator to help you whip up something awesome, even if you’re short on time. Plus, the pre-designed case study templates are like instant polish because let’s be honest, everyone loves a shortcut.
Click to jump ahead:
What is a case study presentation?
What is the purpose of presenting a case study, how to structure a case study presentation, how long should a case study presentation be, 5 case study presentation examples with templates, 6 tips for delivering an effective case study presentation, 5 common mistakes to avoid in a case study presentation, how to present a case study faqs.
A case study presentation involves a comprehensive examination of a specific subject, which could range from an individual, group, location, event, organization or phenomenon.
They’re like puzzles you get to solve with the audience, all while making you think outside the box.
Unlike a basic report or whitepaper, the purpose of a case study presentation is to stimulate critical thinking among the viewers.
The primary objective of a case study is to provide an extensive and profound comprehension of the chosen topic. You don’t just throw numbers at your audience. You use examples and real-life cases to make you think and see things from different angles.

The primary purpose of presenting a case study is to offer a comprehensive, evidence-based argument that informs, persuades and engages your audience.
Here’s the juicy part: presenting that case study can be your secret weapon. Whether you’re pitching a groundbreaking idea to a room full of suits or trying to impress your professor with your A-game, a well-crafted case study can be the magic dust that sprinkles brilliance over your words.
Think of it like digging into a puzzle you can’t quite crack . A case study lets you explore every piece, turn it over and see how it fits together. This close-up look helps you understand the whole picture, not just a blurry snapshot.
It’s also your chance to showcase how you analyze things, step by step, until you reach a conclusion. It’s all about being open and honest about how you got there.
Besides, presenting a case study gives you an opportunity to connect data and real-world scenarios in a compelling narrative. It helps to make your argument more relatable and accessible, increasing its impact on your audience.
One of the contexts where case studies can be very helpful is during the job interview. In some job interviews, you as candidates may be asked to present a case study as part of the selection process.
Having a case study presentation prepared allows the candidate to demonstrate their ability to understand complex issues, formulate strategies and communicate their ideas effectively.
The way you present a case study can make all the difference in how it’s received. A well-structured presentation not only holds the attention of your audience but also ensures that your key points are communicated clearly and effectively.
In this section, let’s go through the key steps that’ll help you structure your case study presentation for maximum impact.
Let’s get into it.
Open with an introductory overview
Start by introducing the subject of your case study and its relevance. Explain why this case study is important and who would benefit from the insights gained. This is your opportunity to grab your audience’s attention.

Explain the problem in question
Dive into the problem or challenge that the case study focuses on. Provide enough background information for the audience to understand the issue. If possible, quantify the problem using data or metrics to show the magnitude or severity.
Detail the solutions to solve the problem
After outlining the problem, describe the steps taken to find a solution. This could include the methodology, any experiments or tests performed and the options that were considered. Make sure to elaborate on why the final solution was chosen over the others.
Key stakeholders Involved
Talk about the individuals, groups or organizations that were directly impacted by or involved in the problem and its solution.
Stakeholders may experience a range of outcomes—some may benefit, while others could face setbacks.
For example, in a business transformation case study, employees could face job relocations or changes in work culture, while shareholders might be looking at potential gains or losses.
Discuss the key results & outcomes
Discuss the results of implementing the solution. Use data and metrics to back up your statements. Did the solution meet its objectives? What impact did it have on the stakeholders? Be honest about any setbacks or areas for improvement as well.
Include visuals to support your analysis
Visual aids can be incredibly effective in helping your audience grasp complex issues. Utilize charts, graphs, images or video clips to supplement your points. Make sure to explain each visual and how it contributes to your overall argument.
Pie charts illustrate the proportion of different components within a whole, useful for visualizing market share, budget allocation or user demographics.
This is particularly useful especially if you’re displaying survey results in your case study presentation.
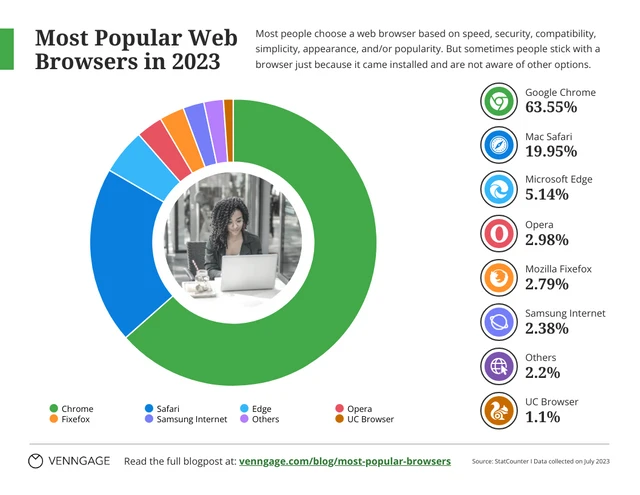
Stacked charts on the other hand are perfect for visualizing composition and trends. This is great for analyzing things like customer demographics, product breakdowns or budget allocation in your case study.
Consider this example of a stacked bar chart template. It provides a straightforward summary of the top-selling cake flavors across various locations, offering a quick and comprehensive view of the data.
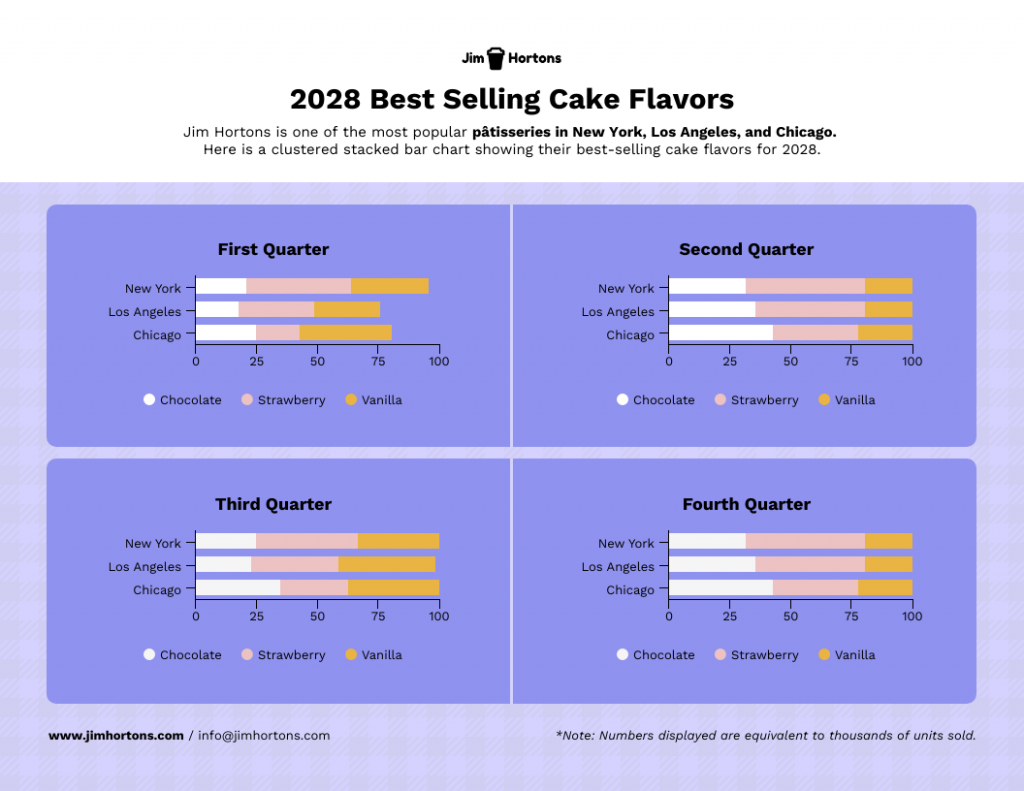
Not the chart you’re looking for? Browse Venngage’s gallery of chart templates to find the perfect one that’ll captivate your audience and level up your data storytelling.
Recommendations and next steps
Wrap up by providing recommendations based on the case study findings. Outline the next steps that stakeholders should take to either expand on the success of the project or address any remaining challenges.
Acknowledgments and references
Thank the people who contributed to the case study and helped in the problem-solving process. Cite any external resources, reports or data sets that contributed to your analysis.
Feedback & Q&A session
Open the floor for questions and feedback from your audience. This allows for further discussion and can provide additional insights that may not have been considered previously.
Closing remarks
Conclude the presentation by summarizing the key points and emphasizing the takeaways. Thank your audience for their time and participation and express your willingness to engage in further discussions or collaborations on the subject.

Well, the length of a case study presentation can vary depending on the complexity of the topic and the needs of your audience. However, a typical business or academic presentation often lasts between 15 to 30 minutes.
This time frame usually allows for a thorough explanation of the case while maintaining audience engagement. However, always consider leaving a few minutes at the end for a Q&A session to address any questions or clarify points made during the presentation.
When it comes to presenting a compelling case study, having a well-structured template can be a game-changer.
It helps you organize your thoughts, data and findings in a coherent and visually pleasing manner.
Not all case studies are created equal and different scenarios require distinct approaches for maximum impact.
To save you time and effort, I have curated a list of 5 versatile case study presentation templates, each designed for specific needs and audiences.
Here are some best case study presentation examples that showcase effective strategies for engaging your audience and conveying complex information clearly.
1 . Lab report case study template
Ever feel like your research gets lost in a world of endless numbers and jargon? Lab case studies are your way out!
Think of it as building a bridge between your cool experiment and everyone else. It’s more than just reporting results – it’s explaining the “why” and “how” in a way that grabs attention and makes sense.
This lap report template acts as a blueprint for your report, guiding you through each essential section (introduction, methods, results, etc.) in a logical order.
Want to present your research like a pro? Browse our research presentation template gallery for creative inspiration!
2. Product case study template
It’s time you ditch those boring slideshows and bullet points because I’ve got a better way to win over clients: product case study templates.
Instead of just listing features and benefits, you get to create a clear and concise story that shows potential clients exactly what your product can do for them. It’s like painting a picture they can easily visualize, helping them understand the value your product brings to the table.
Grab the template below, fill in the details, and watch as your product’s impact comes to life!
3. Content marketing case study template
In digital marketing, showcasing your accomplishments is as vital as achieving them.
A well-crafted case study not only acts as a testament to your successes but can also serve as an instructional tool for others.
With this coral content marketing case study template—a perfect blend of vibrant design and structured documentation, you can narrate your marketing triumphs effectively.

4. Case study psychology template
Understanding how people tick is one of psychology’s biggest quests and case studies are like magnifying glasses for the mind. They offer in-depth looks at real-life behaviors, emotions and thought processes, revealing fascinating insights into what makes us human.
Writing a top-notch case study, though, can be a challenge. It requires careful organization, clear presentation and meticulous attention to detail. That’s where a good case study psychology template comes in handy.
Think of it as a helpful guide, taking care of formatting and structure while you focus on the juicy content. No more wrestling with layouts or margins – just pour your research magic into crafting a compelling narrative.
5. Lead generation case study template
Lead generation can be a real head-scratcher. But here’s a little help: a lead generation case study.
Think of it like a friendly handshake and a confident resume all rolled into one. It’s your chance to showcase your expertise, share real-world successes and offer valuable insights. Potential clients get to see your track record, understand your approach and decide if you’re the right fit.
No need to start from scratch, though. This lead generation case study template guides you step-by-step through crafting a clear, compelling narrative that highlights your wins and offers actionable tips for others. Fill in the gaps with your specific data and strategies, and voilà! You’ve got a powerful tool to attract new customers.
Related: 15+ Professional Case Study Examples [Design Tips + Templates]
So, you’ve spent hours crafting the perfect case study and are now tasked with presenting it. Crafting the case study is only half the battle; delivering it effectively is equally important.
Whether you’re facing a room of executives, academics or potential clients, how you present your findings can make a significant difference in how your work is received.
Forget boring reports and snooze-inducing presentations! Let’s make your case study sing. Here are some key pointers to turn information into an engaging and persuasive performance:
- Know your audience : Tailor your presentation to the knowledge level and interests of your audience. Remember to use language and examples that resonate with them.
- Rehearse : Rehearsing your case study presentation is the key to a smooth delivery and for ensuring that you stay within the allotted time. Practice helps you fine-tune your pacing, hone your speaking skills with good word pronunciations and become comfortable with the material, leading to a more confident, conversational and effective presentation.
- Start strong : Open with a compelling introduction that grabs your audience’s attention. You might want to use an interesting statistic, a provocative question or a brief story that sets the stage for your case study.
- Be clear and concise : Avoid jargon and overly complex sentences. Get to the point quickly and stay focused on your objectives.
- Use visual aids : Incorporate slides with graphics, charts or videos to supplement your verbal presentation. Make sure they are easy to read and understand.
- Tell a story : Use storytelling techniques to make the case study more engaging. A well-told narrative can help you make complex data more relatable and easier to digest.

Ditching the dry reports and slide decks? Venngage’s case study templates let you wow customers with your solutions and gain insights to improve your business plan. Pre-built templates, visual magic and customer captivation – all just a click away. Go tell your story and watch them say “wow!”
Nailed your case study, but want to make your presentation even stronger? Avoid these common mistakes to ensure your audience gets the most out of it:
Overloading with information
A case study is not an encyclopedia. Overloading your presentation with excessive data, text or jargon can make it cumbersome and difficult for the audience to digest the key points. Stick to what’s essential and impactful. Need help making your data clear and impactful? Our data presentation templates can help! Find clear and engaging visuals to showcase your findings.
Lack of structure
Jumping haphazardly between points or topics can confuse your audience. A well-structured presentation, with a logical flow from introduction to conclusion, is crucial for effective communication.
Ignoring the audience
Different audiences have different needs and levels of understanding. Failing to adapt your presentation to your audience can result in a disconnect and a less impactful presentation.
Poor visual elements
While content is king, poor design or lack of visual elements can make your case study dull or hard to follow. Make sure you use high-quality images, graphs and other visual aids to support your narrative.
Not focusing on results
A case study aims to showcase a problem and its solution, but what most people care about are the results. Failing to highlight or adequately explain the outcomes can make your presentation fall flat.
How to start a case study presentation?
Starting a case study presentation effectively involves a few key steps:
- Grab attention : Open with a hook—an intriguing statistic, a provocative question or a compelling visual—to engage your audience from the get-go.
- Set the stage : Briefly introduce the subject, context and relevance of the case study to give your audience an idea of what to expect.
- Outline objectives : Clearly state what the case study aims to achieve. Are you solving a problem, proving a point or showcasing a success?
- Agenda : Give a quick outline of the key sections or topics you’ll cover to help the audience follow along.
- Set expectations : Let your audience know what you want them to take away from the presentation, whether it’s knowledge, inspiration or a call to action.
How to present a case study on PowerPoint and on Google Slides?
Presenting a case study on PowerPoint and Google Slides involves a structured approach for clarity and impact using presentation slides :
- Title slide : Start with a title slide that includes the name of the case study, your name and any relevant institutional affiliations.
- Introduction : Follow with a slide that outlines the problem or situation your case study addresses. Include a hook to engage the audience.
- Objectives : Clearly state the goals of the case study in a dedicated slide.
- Findings : Use charts, graphs and bullet points to present your findings succinctly.
- Analysis : Discuss what the findings mean, drawing on supporting data or secondary research as necessary.
- Conclusion : Summarize key takeaways and results.
- Q&A : End with a slide inviting questions from the audience.
What’s the role of analysis in a case study presentation?
The role of analysis in a case study presentation is to interpret the data and findings, providing context and meaning to them.
It helps your audience understand the implications of the case study, connects the dots between the problem and the solution and may offer recommendations for future action.
Is it important to include real data and results in the presentation?
Yes, including real data and results in a case study presentation is crucial to show experience, credibility and impact. Authentic data lends weight to your findings and conclusions, enabling the audience to trust your analysis and take your recommendations more seriously
How do I conclude a case study presentation effectively?
To conclude a case study presentation effectively, summarize the key findings, insights and recommendations in a clear and concise manner.
End with a strong call-to-action or a thought-provoking question to leave a lasting impression on your audience.
What’s the best way to showcase data in a case study presentation ?
The best way to showcase data in a case study presentation is through visual aids like charts, graphs and infographics which make complex information easily digestible, engaging and creative.
Don’t just report results, visualize them! This template for example lets you transform your social media case study into a captivating infographic that sparks conversation.

Choose the type of visual that best represents the data you’re showing; for example, use bar charts for comparisons or pie charts for parts of a whole.
Ensure that the visuals are high-quality and clearly labeled, so the audience can quickly grasp the key points.
Keep the design consistent and simple, avoiding clutter or overly complex visuals that could distract from the message.
Choose a template that perfectly suits your case study where you can utilize different visual aids for maximum impact.
Need more inspiration on how to turn numbers into impact with the help of infographics? Our ready-to-use infographic templates take the guesswork out of creating visual impact for your case studies with just a few clicks.
Related: 10+ Case Study Infographic Templates That Convert
Congrats on mastering the art of compelling case study presentations! This guide has equipped you with all the essentials, from structure and nuances to avoiding common pitfalls. You’re ready to impress any audience, whether in the boardroom, the classroom or beyond.
And remember, you’re not alone in this journey. Venngage’s Case Study Creator is your trusty companion, ready to elevate your presentations from ordinary to extraordinary. So, let your confidence shine, leverage your newly acquired skills and prepare to deliver presentations that truly resonate.
Go forth and make a lasting impact!
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation
Biographical information.
Svetlana is a 16 year old cisgender girl presenting to your primary care clinic with chief complaints of fatigue and abdominal pain. She has no significant surgical or medical history, and her last menstrual period was three months ago. Svetlana is of Ashkenazi Jewish descent and has a father with Ulcerative Colitis and a maternal grandmother with psoriasis.
Review of Systems
WNL: Neurological, Respiratory, Endocrine, Genitourinary, Cardiovascular, and Musculoskeletal
General: Fatigue
Integumentary: No symptoms reported; thin, fine body hair and inelastic skin turgor observed by provider during assessment
HEENT: Ulcerations in mouth and vision changes reported
GI: Painful diarrhea with extreme urgency accompanied by pain in RLQ
Reproductive: Amenorrhea for the last 3 months (menarche 4 years ago, regular cycle before now)
Lab Results
- WBC count of 20,000
- Ferritin 10 NG/dL
- RBC morphology: Macrocytic and hypochromic (Possibly indicative of Vitamin B12 and iron deficiency)
Stool Sample
- Negative for parasites and ova
- Positive for occult blood
Scope Results
- Skip lesions throughout intestines, with worst disease found in terminal ileum
- Transmural inflammation with characteristic cobblestone mucosa
- Case report
- Open access
- Published: 07 April 2024
Graves’ disease thyroid dermopathy: a case report
- Loay Tashkandi 1 ,
- Afaf Alsagheir ORCID: orcid.org/0000-0002-1844-4377 2 ,
- Saud Alobaida 3 &
- Raghad Alhuthil 2
Journal of Medical Case Reports volume 18 , Article number: 164 ( 2024 ) Cite this article
56 Accesses
1 Altmetric
Metrics details
Graves’ disease is the autoimmune activation of the thyroid gland causing diffuse enlargement and hyperfunction of the gland. Manifestations of Graves’ disease are multisystemic and include thyroid orbitopathy; pretibial myxedema, also referred to as thyroid dermopathy; and thyroid acropachy, described as a severe form of thyroid dermopathy. Our paper focuses on an atypical case of thyroid dermopathy.
Case presentation
An 11-year-old Saudi male presented with a prominent diffuse goiter and exophthalmos. Investigations were consistent with a diagnosis of Graves’ disease. The physical exam showed diffuse, non-pitting swelling of the ankle and penis, mimicking a lymphatic malformation. Further, multiple nodules were found on the hands and feet. Treatment of the nodules with cautery resulted in more severe nodules.
This report describes rare presentations of thyroid dermopathy mimicking lymphatic malformation. The Koebner phenomenon can explain this patient’s atypical presentations. Intralesional injections of triamcinolone and total thyroidectomy showed clear improvement.
Peer Review reports
Introduction
Graves’ disease (GD) is the most common cause of hyperthyroidism in childhood. It is defined as the autoimmune activation of the thyroid gland causing diffuse enlargement and hyperfunction of the gland. The autoantibodies implicated in the pathogenesis of the disease interact with the thyroid-stimulating hormone (TSH) receptor in the thyroid follicles; these include anti-thyroid peroxidase antibodies (anti-TPO), thyroglobulin antibodies (anti-thyroglobulin), and TSH-binding inhibitory immunoglobulins. The autoantibodies block the interaction of TSH with its receptor and mimic its function [ 1 ].
The manifestations of GD are multisystemic, including thyroid orbitopathy (TO); pretibial myxedema, also referred to as thyroid dermopathy (TD); and thyroid acropachy (TA), described as a severe form of TD [ 2 , 3 ].
Thyroid dermopathy is an uncommon manifestation of GD; the onset usually ranges from 12 to 24 months after diagnosis. Its incidence in patients with GD ranged between 0.5% and 4.4% [ 4 ]. Furthermore, an association between the severity of TO and the prevalence of TD was made clear; among severe TO patients requiring aggressive intervention, 13% also had TD [ 1 ].
Thyroid dermopathy is described as bilateral, asymmetric, non-pitting thickening of the skin that may present in different forms. A retrospective study of 178 patients described the incidence of each form: isolated nonpitting edema (43.3%), well-demarcated nodules or plaques (27.0%), and more severe cases presented with elephantiasis (2.8%). The nodules may be hyperpigmented or violaceous. The lesions may have an orange-peel appearance. Furthermore, the lesions can be asymptomatic, pruritic, or painful [ 5 ].
This highlights the need for increased reporting of such extra-thyroid manifestations in the pediatric population, as discussed in this case report.
An 11-year-old Saudi male was referred to our hospital from a local hospital in Haʼil (north-western Saudi Arabia) with thyrotoxicosis and post-trauma penile swelling for further management. He presented to our hospital in July 2018 with a history of hyperthyroidism and thyroid goiter with diffuse toxic goiter for 1 month.
A pediatric multidisciplinary team managed the patient, including endocrinologists, urologists, dermatologists, ophthalmologists, and otolaryngologists. At presentation, he had prominent diffuse goiter, exophthalmos with no tremors, and pretibial myxedema for 1.5 months. History showed an increase in appetite and weight loss. However, no palpitation, excessive sweating, or tremors were present. Patient was already started on oral methimazole 5 mg, twice daily, for 2 months, with good compliance, and no other past medical history. Family history noted that the parents are third-degree consanguineous; he is enrolled in school and progressing as expected for his age.
Physical examination noted the patient looking well, with a heart rate of 100 beats/minute, a regular rhythm, a weight of 29 kg (10th percentile), and a height of 140 cm (50th percentile). Respiratory examination showed equal bilateral air entry, with no added sounds. Cardiovascular examination was normal: S1 and S2 heart sounds heard with no added sounds. Abdomen was soft and not distended, there was no tenderness, and no masses were palpated. Neurological examination was unremarkable.
Initial investigations were consistent with a diagnosis of Graves’ disease; white blood cell count (WBC) was 5.63/L \(\times {10}^{9}\) (4.5–13.0 \(\times {10}^{9}\) /L), hemoglobin was 11.3 g/dL (12.0–15.2 g/dL), hematocrit was 38.8% (36–47%), mean corpuscular volume (MCV) was 74.9 fL (78–96 fL), and mean corpuscular hemoglobin (MCH) was 21.8 pg (25–35 pg). Sodium was 139 mEq/L (136–145 mEq/L), chloride was 104 mEq/L (95–105 mEq/L), and calcium was 2.46 mmol/L (2.2–2.7 mmol/L). Regarding liver function tests, total bilirubin was 8.5 μmol/L (5–17 μmol/L), direct bilirubin was 2.3 μmol/L (1.7–5 μmol/L), AST was 20.9 units/L (15–46 units/L), ALT was 14.4 units/L (8–36 units/L), ALP was 359 units/L (85–400 units/L), and albumin was 40.8 g/L (34–54 g/L). Renal function tests found creatinine of 33 units/L (10–90 units/L), and urea was 2.6 mg/dL (5–20 mg/dL). Thyroid-stimulating hormone (TSH) was 0.005 mU/L (0.27–4.2 mU/L), total triiodothyronine (T3) was 8.9 nmol/L (1.3–3.1 nmol/L), and free thyroxine (FT4) was 62.11 pmol/L (12–22 pmol/L). The thyroid ultrasound noted mild diffuse enlargement of both lobes and isthmus, heterogeneous echo pattern, and no focal lesions—diffuse mild goiter. The diagnostic iodine uptake scan showed a mildly enlarged thyroid gland with homogeneous increased radiotracer uptake. The 4-hour I-123 thyroid scan uptake was 73.5%, and 24-hour was 63%. The thyroid antibodies were tested. Anti-thyroglobulin was 144 U/mL (< 115 U/mL), while anti-TPO was 413 U/mL (< 34 U/L); thyroid-stimulating hormone (TSAB) was 575% (< 140%). Thus, the patient was continued on methimazole and was seen regularly at a follow-up clinic.
In June 2019, the patient was referred to the ophthalmology clinic owing to progressive exophthalmos, and the visual screening showed 20/30 vision for both the left and right eye. Ophthalmology management was conservative with regular follow-up.
Furthermore, the patient noticed bilateral soft tissue swelling of the feet and penile region, with nodules on the hands and feet, and was referred to dermatology in August 2019. On physical examination of the ankle and penis, the swelling was diffuse, tense, and non-pitting (Figs. 1 and 2 ). The swelling on both ankles and in the penile region raised the possibility of an associated vascular malformation.

Anterior and lateral views showing diffuse penile swelling

Lateral view showing diffuse ankle swelling
Detailed physical examination noted deep swelling imitating lymphatic malformation with multiple nodules; right lateral foot near lateral malleolus (9 × 7.5 cm), fifth suitable toe base (3 × 1 × 5 cm), right foot medial aspect (1 × 1 cm), left lateral foot near lateral malleolus (8 × 7 cm), dorsum of left foot (3 × 2 cm), left fifth toe base (3 × 2 cm), and a solitary lesion on both the right and left hands were observed. On both hands and feet, lesions were treated with cautery initially. Upon follow-up in November 2020, new, more severe, brownish nodules appeared on the areas treated (Fig. 3 ).

Multiple nodules on sites of cautery
Workup for the patient started with magnetic resonance imaging (MRI) of the penile region and showed subcutaneous soft tissue swelling around the penis, with no focal nodules or masses, no loculated fluid collections, and no vascular malformations (Fig. 4 ). Furthermore, ultrasound imaging of the feet was done, which reported left foot edema and bilateral, multiple, well-defined, heterogeneously hypoechoic cutaneous and subcutaneous nodules (Fig. 5 ). A 4 mm skin biopsy was taken from the right foot and showed mucin accumulation in the dermis, consistent with pretibial myxedema (Figs. 3 , 6 ). Management of the lesions with multiple rounds of intralesional injection of triamcinolone showed clinical improvement.
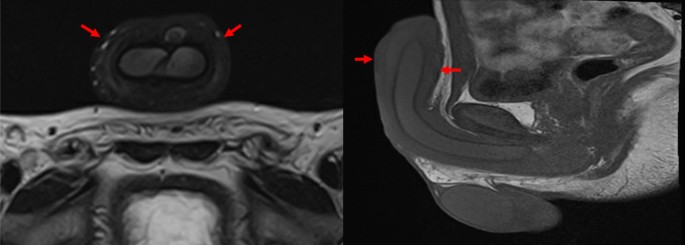
Pelvis magnetic resonance imaging showed non-specific subcutaneous soft tissue thickening surrounding the penis (see the red arrows). No evidence of collections/lymphatic malformation within the pelvic region
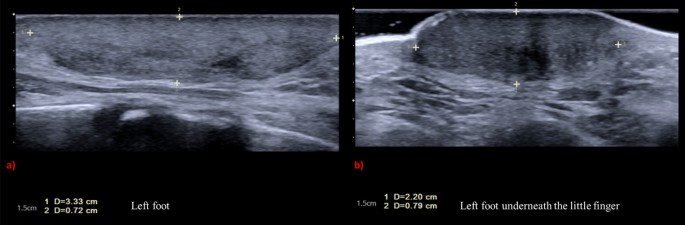
Standard ultrasound scan of the feet showed bilateral multiple fairly well-defined heterogeneously hypoechoic cutaneous/subcutaneous nodules. The largest nodule is seen around the left ankle joint, which measures 3.33 × 0.72 cm ( a ). The similar smaller lesion seen in the dorsum of the left measures 2.20 × 0.79 cm, with no evidence of extension to deep structures and no internal vascularity or calcifications ( b ). These nodules are of non-specific sonographic appearance
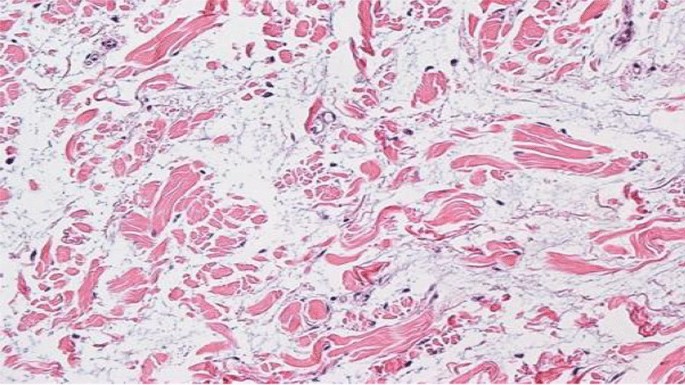
Mucin accumulation in the dermis
The patient had blepharospasm and severe thyroid orbitopathy that required orbital decompression and bilateral lateral tarsorrhaphy in March 2021 owing to progressive worsening despite medical management. Eventually, the patient underwent total thyroidectomy in June 2021; he showed further clear improvement in TD, and was prescribed daily oral levothyroxine 100 mcg.
The patient’s last follow-up was in the endocrine clinic (May 2023). He was compliant with the levothyroxine, his TD and TO had improved, and he was considered clinically euthyroid. His FT4 was normal (14.1 pmol/L), and TSH was high (16.200 mU/L). He had no active complaints, and his parents were satisfied with his overall improvement.
The patient, an 11-year-old Saudi male, was referred to the hospital with thyrotoxicosis and penile swelling post-trauma. Investigations were consistent with a diagnosis of Graves’ disease. A multidisciplinary team managed his condition, which included prominent diffuse goiter, progressive exophthalmos, and pretibial myxedema. The patient had a unique presentation with soft tissue swelling of the feet and penile region, and nodules on the hands and feet that became more severe with cautery treatment, but he improved with intralesional injections of triamcinolone. Eventually, the patient underwent orbital decompression, blepharospasm, and finally total thyroidectomy showing clear clinical improvement.
The Koebner phenomenon was first described in 1878; it is the appearance of new skin lesions subsequent to trauma on areas previously unaffected. In that regard, the patient is described as Koebner-positive [ 6 ]. This phenomenon explains the atypical presentation of the patient’s thyroid dermopathy, which was seen as a lymphatic malformation imitator present on the lower limbs bilaterally and the penile shaft, with development of new lesions following trauma to the sites. This position is further strengthened upon the resolution of the lesions only after total thyroidectomy.
A substantial amount of research has been directed at TO compared with TD. It has been speculated that both presentations share similar pathogenesis where cellular, immunologic, molecular, and mechanical factors result in glycosaminoglycan accumulation, causing expansion of the connective tissue and leading to lymphedema through obstruction of the lymphatic microcirculation [ 1 ].
Research into the prevention of TD needs to be improved. However, with the assumption of shared pathogenesis between TD and TO, one may be able to prevent TD in the same manner as TO. Normalization of thyroid function is essential in the management and prevention of TO [ 1 ].
As for the treatment of TD, standard therapy has been topical corticosteroids. Furthermore, intralesional injections would be the preferred treatment for plaques and nodules. It has been reported that surgical excision can improve short-term outcomes of severe cases if used in conjunction with octreotide. Lastly, possible directed therapy options include plasmapheresis, octreotide, tumor necrosis factor (TNF) inhibitors, tyrosine kinase inhibitors, rituximab, tocilizumab, TSH-receptor‐blocking antibodies, and IGF‐1-receptor‐blocking agents [ 1 ].
In this case, the presentation is unique and resembles a lymphatic malformation involving both feet and the penile region; to our knowledge, a similar presentation has not been described in the past. Given that an intralesional form was not injected in the penile region owing to the safety profile, no improvement was seen.
This case shows pretibial myxedema that developed Koebner’s phenomenon on the sites of cautery, where more severe nodules developed.
The long-term outcomes of these rare presentations need to be followed. Thus, monitoring and publishing long-term outcomes of the proposed management options should be a topic for future studies.
In summary, we present a case with a rare presentation of thyroid dermopathy mimicking lymphatic malformation. The Koebner phenomenon can explain this patient’s atypical presentation. The rarity of the presentations has been emphasized by the lack of studies on the topic, specifically in the pediatric population. The severe manifestation of thyroid dermopathy responded well after intralesional triamcinolone and total thyroidectomy. Therefore, we recommend that management of such atypical cases of TD should consist of normalization of the thyroid function and intralesional injections.
Availability of data and materials
The datasets used in the current study are available from the corresponding author upon reasonable request.
Fatourechi V. Thyroid dermopathy and acropachy. Best Pract Res Clin Endocrinol Metab. 2012;26(4):553–65.
Article CAS PubMed Google Scholar
Kraus CN, Sodha P, Vaidyanathan P, Kirkorian AY. Thyroid dermopathy and acropachy in pediatric patients. Pediatric Dermatol. 2018;35(6): e371.
Article Google Scholar
Sanchez DP, Sonthalia S. Koebner phenomenon. U.S. National Library of Medicine; 2023. https://pubmed.ncbi.nlm.nih.gov/31971748/#:~:text=The%20Koebner%20phenomenon%20(KP)%2C,unaffected%20skin%20secondary%20to%20trauma . Accessed 10 May 2023.
Fatourechi V. Pretibial myxedema. Am J Clin Dermatol. 2005;6(5):295–309.
Article PubMed Google Scholar
Malabu UH, Alfadda A, Sulimani RA, Al-Rubeaan KA, Al-Ruhaily AD, Fouda MA, Al-Maatouq MA, El-Desouki MI. Graves’ disease in Saudi Arabia: a ten-year hospital study. J Pak Med Assoc. 2008;58(6):302–4.
PubMed Google Scholar
LaFranchi S. Clinical manifestations and diagnosis of Graves disease in children and adolescents. In: UptoDate. UptoDate; 2021.
Download references
Acknowledgements
Not applicable.
No funding was received during the preparation of this study.

Author information
Authors and affiliations.
King Faisal Specialist Hospital and Research Centre, 11211, Riyadh, Saudi Arabia
Loay Tashkandi
Department of Pediatrics, King Faisal Specialist Hospital and Research Centre, Al Takhassousi & 12713, 11211, Riyadh, Saudi Arabia
Afaf Alsagheir & Raghad Alhuthil
Department of Dermatology, King Faisal Specialist Hospital and Research Centre, 11211, Riyadh, Saudi Arabia
Saud Alobaida
You can also search for this author in PubMed Google Scholar
Contributions
LT drafted the manuscript and designed the figures. SA and AA aided in interpreting the results and worked on the manuscript. RA critically edited and drafted the final version of the manuscript. All authors discussed the results and commented on the final version.
Corresponding author
Correspondence to Afaf Alsagheir .
Ethics declarations
Ethics approval and consent to participate.
The study was cleared for publication by the institutional review board in King Faisal Specialist Hospital and Research Centre (KFSHRC; reference: 2235180). Informed consent was obtained from the patient’s legal guardian in this study.
Consent for publication
Written informed consent was obtained from the patient’s legal guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors state that they do not have any competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tashkandi, L., Alsagheir, A., Alobaida, S. et al. Graves’ disease thyroid dermopathy: a case report. J Med Case Reports 18 , 164 (2024). https://doi.org/10.1186/s13256-024-04462-x
Download citation
Received : 27 May 2023
Accepted : 13 February 2024
Published : 07 April 2024
DOI : https://doi.org/10.1186/s13256-024-04462-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Graves’ disease
- Koebner phenomenon
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- International edition
- Australia edition
- Europe edition

Prostate cancer cases worldwide likely to double by 2040, analysis finds
Largest study of its kind predicts 85% increase in deaths from the disease in same period as more men live longer
The number of men diagnosed with prostate cancer worldwide is projected to double to 2.9 million a year by 2040, with annual deaths predicted to rise by 85%, according to the largest study of its kind.
Prostate cancer is already a major cause of death and disability, and the most common form of male cancer in more than 100 countries. But with populations ageing and life expectancy rising globally, a new analysis forecasts a dramatic surge in cases and deaths over the next 15 years.
Diagnoses are projected to increase from 1.4m a year in 2020 to 2.9m by 2040, which will mean about 330 men being told they have the disease every hour.
The number of deaths worldwide is predicted to rise by 85% over the 20-year period, from 375,000 in 2020 to almost 700,000 by 2040. The true death toll will probably be higher, experts say, because of underdiagnosis and missing data in low- and middle-income countries.
The findings were published in the Lancet as part of its landmark commission on prostate cancer, and will be presented at the European Association of Urology’s annual congress in Paris on Saturday.
Ageing populations and increasing life expectancy mean the number of older men worldwide who are living for longer is rising. As the main risk factors for prostate cancer – such as being 50 or older and having a family history of the disease – are unavoidable, experts say it will be impossible to prevent the surge in cases simply via lifestyle changes or public health interventions.
However, wider awareness of the symptoms of the disease, access to testing initiatives, earlier diagnosis, and advances in treatments could still help reduce the burden and save lives, according to the authors of the 40-page report.
“As more and more men around the world live to middle and old age, there will be an inevitable rise in the number of prostate cancer cases,” said Prof Nick James, the lead author of the study. “We know this surge in cases is coming, so we need to start planning and take action now.”
“Evidence-based interventions, such as improved early detection and education programmes, will help to save lives and prevent ill health from prostate cancer in the years to come,” added James, a professor of prostate cancer research at the Institute of Cancer Research, London, and a consultant clinical oncologist at the Royal Marsden NHS foundation trust.
James said there was a global need for new and improved ways to test for the disease, to reduce overdiagnosis and overtreatment while detecting potentially lethal tumours earlier.
Boosting knowledge among men and their families of signs to look for was also key, according to the report.
Symptoms of prostate cancer can include needing to urinate more frequently, often during the night; needing to rush to the toilet; difficulty in starting to pee; feeling that your bladder has not emptied fully, and blood in your urine or semen.
These symptoms do not always mean you have prostate cancer. Many men’s prostates become larger as they get older because of a condition called benign prostate enlargement. Signs that prostate cancer may have spread include testicle, back or bone pain, a loss of appetite, and unintentional weight loss.

The study also highlighted the need for more research to better understand prostate cancer in black men, as most research has focused on white men.
Alfred Samuels was 54 when he learned he had advanced prostate cancer in 2012. He had worked in the entertainment industry for three decades, providing security for celebrities including Beyoncé and Bob Dylan – but the shock diagnosis ended his career overnight. Doctors ruled out surgery when tests showed his cancer had spread, and the father of six started to lose hope.
However, he then joined a clinical trial and began treatment with a drug that is now extending the lives of thousands of men worldwide. Twelve years later, Samuels, from Harrow in north-west London, has welcomed six grandchildren to the world and pivoted to a second career raising awareness of cancer research.
“Due to the late stage that my prostate cancer was diagnosed, I wouldn’t be here today if I hadn’t been able to access a clinical trial. It was my lifeline,” said Samuels, now 66. “This report has been a long time coming. Now it needs to be mandatory to record ethnicity in clinical trials, and trials must reflect the ethnic diversity of the population, so that we can find better treatments for people like me.”
Amy Rylance, the head of improving care at the charity Prostate Cancer UK, said the Lancet report was a “a timely call to action”. She added that healthcare systems must do better at recognising those at highest risk: black men and men with a family history of prostate cancer or genetic risk factors such as BRCA variations .
- Prostate cancer
- Cancer research
- Medical research
- Men's health

Study offers hope in identifying high-risk prostate cancer patients

Getting fitter can reduce prostate cancer risk by 35%, study finds

New prostate cancer treatment may be ‘on the horizon’, say scientists

Lock, Stock and Two Smoking Barrels actor Jake Abraham dies aged 56

Radiotherapy doses for prostate cancer could be cut by three-quarters, trial finds

BBC presenter Nick Owen announces prostate cancer diagnosis

UK prostate cancer screening programme ‘could be running in three years’

Thousands of UK men to benefit after NHS approves prostate cancer drug

Scientists launch search for genetic test to spot killer prostate cancer
Most viewed.

Case study: infectious disease
Aug 09, 2012
100 likes | 673 Views
Case study: infectious disease. Professor Anne Johnson FMedSci Head, Department of Primary Care and Population Sciences, Royal Free and University College Medical School, London. Background. Globally: infections cause over a fifth of all deaths
Share Presentation
- professor anne johnson fmedscihead
- population surveillance
- public health measures
- infectious diseases
- university college medical school

Presentation Transcript
Case study: infectious disease Professor Anne Johnson FMedSciHead, Department of Primary Care and Population Sciences, Royal Free and University College Medical School, London
Background Globally: • infections cause over a fifth of all deaths • a million children die each year from diseases preventable through vaccination In the UK, infectious diseases account for: • over 10% of deaths • one in three GP consultations New infectious diseases: one per year
Public health measures relating to infectious disease • Prevention through vaccination • Surveillance • Control strategies
Prevention through vaccination • Aims of vaccination: • to protect individuals • to protect vulnerable or at-risk individuals • to achieve ‘population immunity’ • Concerns about safety of vaccines • ‘Free riders’
Prevention through vaccination • Three broad approaches to vaccination policy: • voluntary • incentivised • quasi-mandatory Conclusions: • No justification for moving beyond voluntary system in UK for childhood vaccination
Surveillance • Population surveillance using anonymised data • Conclusion: acceptable for predicting trends • Notifiable disease surveillance using identifying data • Conclusion: acceptable for avoiding harm to others if invasion of privacy is minimised
Surveillance • Global surveillance of infectious diseases is vital • Problems if countries do not have capacity or do not cooperate • Conclusions: • UK should enhance surveillance capacities of developing countries • WHO should explore virus isolates as ‘public good’ • WHO should impress social responsibilities on pharmaceutical companies
Control • Quarantine and isolation are at the top of the intervention ladder • Conclusion: ethical justification involves weighing the harm principle with consent and avoiding intrusive interventions
Information and communication • Effective communication is crucial • Risks should not be downplayed or overstated • Conclusions: • Government should ensure the timely provision of information about outbreaks • Those who report research have a duty to communicate findings in a responsible manner
- More by User
The Epidemiology of Infectious Disease
The Epidemiology of Infectious Disease. Chapter 37 Todd Kitten, Ph.D. Epidemiology. The science that evaluates occurrence, determinants, distribution, and control of health and disease in a defined human population
3.49k views • 55 slides
Imported Diseases and Infectious Disease Surveillance
Imported Diseases and Infectious Disease Surveillance. George Turabelidze, MD, PhD Missouri Department of Health and Senior Services. International Tourism. Popularity of international tourism continues to grow Growth of travel to developing countries exceeds travel growth to developed world
1.26k views • 57 slides
StudentAffairs Virtual Case Study February 19, 2006
StudentAffairs.com Virtual Case Study February 19, 2006. Image ©2006, www.Facebook.com. Building Online Communities: A Case Study of Facebook.com. Karen Eilers Scott Graves David Merry The University of Iowa. Presentation Overview: Slide Colors.
1.09k views • 83 slides
Water and Infectious Disease - Waterborne Disease
Water and Infectious Disease - Waterborne Disease. Global distribution of infectious disease Transmission cycles Water and infectious disease Enteric disease in children Case studies E.coli Cholera ( Vibrio cholerae ) Cryptosporidium parvum. What is needed to control water-borne disease?.
1.41k views • 55 slides
A Guide for Shipping Infectious Substances
A Guide for Shipping Infectious Substances. Click here to continue. Introduction. Infectious substances are shipped around the world by air, road, rail, sea every day. Some of these infectious substances are very hazardous, and direct exposure to them should be avoided.
1.36k views • 100 slides
Module 2 (of 3): Antibiotic Review *
Module 2 (of 3): Antibiotic Review *. Review of selected antimicrobials By Keith Teelucksingh , PharmD Infectious Disease Pharmacist, Kaiser Permanente Vallejo With contributions by Linh Van , PharmD Infectious Disease Pharmacist, Kaiser Permanente Oakland. See Notes. Goals.
2.54k views • 90 slides

Transmission of Infectious Disease: Role of Virulence Factors in Bacterial Invasiveness
Transmission of Infectious Disease: Role of Virulence Factors in Bacterial Invasiveness. General Definitions. Normal Flora. Microorganisms that are associated with a host, established at a particular anatomical location and don’t harm their host Important part of innate immunity
1.45k views • 75 slides
Noninfectious Diseases
Chapter 18. Noninfectious Diseases. Chapter 18. Lesson 1 Disease and Disease Prevention. Bellringer. Explain the difference between infectious diseases and noninfectious diseases. Chapter 18. Lesson 1 Disease and Disease Prevention. Objectives.
1.1k views • 92 slides
COMMUNICABLE DISEASE
COMMUNICABLE DISEASE . HEAD START Joyce M. Smith M.D., MPH. CHILD CARE / EARLY EDUCATION SETTING. Group Setting Increased risk of infectious disease spread Among children Younger than 2 years Rates of Infection tend to Increase for first 6 months
1.16k views • 80 slides

Moonlight Medicine
Moonlight Medicine. Adrian Paul J Rabe, MD. 8 Targets of Moonlight Medicine. Infectious Disease Cardiovascular Medicine Pulmonary Medicine Endocrinology Gastroenterology Poisons and Snakebites Pain Medication Electrolyte Correction. Infectious Disease. Infectious Disease. URTI
3.28k views • 307 slides

Alzheimer’s Disease
Alzheimer’s Disease. By Sarah Chorn. Why Alzheimer’s? . Topics to be Covered. History of Alzheimer’s Alzheimer’s Basics Dementia vs. Alzheimer's How Alzheimer’s Spreads Stages of the Disease Risk Factors Diagnosing Common Medical Tests Treating the Disease. The Framingham Heart Study
2.68k views • 23 slides

Bioterrorism
Bioterrorism. Preparation Recognition And Response. Bioterrorism is defined by the Centers For Disease Control as the deliberate release of infectious agents with the intent to cause disease or Death in animals people or plants. 1. First Reference to Bioterrorism?.
1.37k views • 66 slides
H.M.S PINAFORE – Case Study Analysis
H.M.S PINAFORE – Case Study Analysis. Bajtosova Katarina Ratkelyte Milda. Presentation Overview. Main objectives and deliverables Main activities based on the case study analysis Network diagram & Critical Path Finance Options to shorten the time Revision of the activities’ table
6.87k views • 12 slides
Infectious Disease Clinical Case Presentation
Infectious Disease Clinical Case Presentation. Samina Syed, MS IV Kees Van Dam, MD September 12, 2007. CC: Acute mental status changes “I feel like I’m going crazy”. History of Present Illness
1.02k views • 83 slides
Infectious and Rheumatic Disease in Children
Infectious and Rheumatic Disease in Children. 박 수 성 울산대학교 의과대학 서울아산병원 정형외과. Infectious disease in children Acute hematogenous osteomyelitis (AHO) Acute septic arthritis Special conditions Rheumatic disease in children Juvenile Idiopathic Arthritis (JIA). Introduction.
1.29k views • 96 slides
Case Study Hepatic Encephalopathy
Case Study Hepatic Encephalopathy. By: Cynthia Topley, MS Meredith College Dietetic Intern February 17, 2013. Overview. Introduction to Hepatic Encephalopathy (HE) Literature Reviews (3): Branched Chain Amino Acids (BCAAs), Lactulose, and Rifaximin Case Study Discussion Questions.
3.96k views • 62 slides
Atherosclerotic Heart Disease Part I: Angina Pectoris
Atherosclerotic Heart Disease Part I: Angina Pectoris. Humayun J. Chaudhry, D.O., M.S., S.M., FACP, FACOI Chairman, Department of Medicine and Assistant Dean for Health Policy New York College of Osteopathic Medicine of NYIT September 20, 2005. Case Study.
1.98k views • 82 slides
Goals of the course
ECOL/MCB/CPH/VSC 409/509 Evolution of Infectious Disease Dr. Michael Worobey BSW 324 [email protected] 626-3456. Goals of the course. Learn some fundamental evolutionary theory as it relates to infectious disease
1.01k views • 92 slides
STUDY DESIGNS: case control, cohort and qualitative
STUDY DESIGNS: case control, cohort and qualitative. Dr TAMSIN Newlove-delgado DOCTORAL RESEARCH FELLOW UNIVERSITY OF EXETER. Aims and objectives. To outline and revise: Causation Case control study design, advantages and disadvantages The odds ratio
1.14k views • 66 slides
CASE STUDY. Research. Case Study Defined. Yin (1994). Merriam (1988). A qualitative case study is an intensive, holistic description and analysis of a single instance, phenonomenon, or social unit (p. 21).
2k views • 52 slides
描述性研究. Descriptive Study. 哈尔滨医科大学流行病学教研室 Department of epidemiology , Harbin Medical University. Methods of study. three types of basic methods. Observational. Cross-sectional study Ecological study. Descriptive study. Case-control study Cohort study. Analytic study. Clinical trial
1.63k views • 78 slides
- Open access
- Published: 03 April 2024
Heavy metal association with chronic kidney disease of unknown cause in central India-results from a case-control study
- Mahendra Atlani 1 na1 ,
- Ashok Kumar 2 na1 ,
- Rajesh Ahirwar 3 ,
- M. N. Meenu 1 ,
- Sudhir K. Goel 2 ,
- Ravita Kumari 2 ,
- Athira Anirudhan 1 ,
- Saikrishna Vallamshetla 4 &
- G. Sai Tharun Reddy 4
BMC Nephrology volume 25 , Article number: 120 ( 2024 ) Cite this article
130 Accesses
2 Altmetric
Metrics details
Chronic Kidney Disease of unknown cause (CKDu) a disease of exclusion, and remains unexplained in various parts of the world, including India. Previous studies have reported mixed findings about the role of heavy metals or agrochemicals in CKDu. These studies compared CKDu with healthy controls but lacked subjects with CKD as controls. The purpose of this study was to test the hypothesis whether heavy metals, i.e. Arsenic (As), Cadmium (Cd), Lead (Pb), and Chromium (Cr) are associated with CKDu, in central India.
The study was conducted in a case-control manner at a tertiary care hospital. CKDu cases ( n = 60) were compared with CKD ( n = 62) and healthy subjects ( n = 54). Blood and urine levels of As, Cd, Pb, and Cr were measured by Inductively Coupled Plasma- Optical Emission Spectrometry. Pesticide use, painkillers, smoking, and alcohol addiction were also evaluated. The median blood and urine metal levels were compared among the groups by the Kruskal-Wallis rank sum test.
CKDu had significantly higher pesticide and surface water usage as a source of drinking water. Blood As levels (median, IQR) were significantly higher in CKDu 91.97 (1.3–132.7) µg/L compared to CKD 4.5 (0.0–58.8) µg/L and healthy subjects 39.01 (4.8–67.4) µg/L ( p < 0.001) On multinominal regression age and sex adjusted blood As was independently associated with CKDu[ OR 1.013 (95%CI 1.003–1.024) P < .05].Blood and urinary Cd, Pb, and Cr were higher in CKD compared to CKDu ( p > .05). Urinary Cd, Pb and Cr were undetectable in healthy subjects and were significantly higher in CKDu and CKD compared to healthy subjects ( P = < 0.001). There was a significant correlation of Cd, Pb and Cr in blood and urine with each other in CKDu and CKD subjects as compared to healthy subjects. Surface water use also associated with CKDu [OR 3.178 (95%CI 1.029–9.818) p < .05).
The study showed an independent association of age and sex adjusted blood As with CKDu in this Indian cohort. Subjects with renal dysfunction (CKDu and CKD) were found to have significantly higher metal burden of Pb, Cd, As, and Cr as compared to healthy controls. CKDu subjects had significantly higher pesticide and surface water usage, which may be the source of differential As exposure in these subjects.
Peer Review reports
Chronic kidney disease of unknown cause (CKDu) has been reported in various parts of the world (i.e., Nicaragua, El Salvador, Sri Lanka), including India, as an endemic disease. The disease is a diagnosis of exclusion, made when a patient fulfils the Kidney Disease Improving Global Outcomes (KDIGO) CKD criteria but without the evidence of a recognized cause such as diabetes, hypertension, or glomerulonephritis [ 1 ]. No uniform and definite cause has yet been identified, though various environmental factors have been associated with and suggested to play a role in the pathogenesis. For example, heat stress, strenuous exercise, agrochemicals, and heavy metals have been held responsible for Mesoamerican nephropathy [ 2 ]. Mixed evidence has been reported for association with agrochemicals, heavy metals, and genetic variability for CKDu in Sri Lanka [ 3 , 4 , 5 ]. In India, one small study reported an association of heavy metals with CKD [ 6 ]. A study done on groundwater samples from the Uddanam region of Andhra Pradesh (India), which has a high prevalence of CKDu reported water as acidic (pH < 6.5) and to contain higher silica and lead in wet and dry seasons, respectively. Phthalates were also detected in the groundwater [ 7 ]. Previous studies have attempted to find a correlation between heavy metals and CKDu by comparing cases and endemic and nonendemic controls [ 4 ]. No study has yet tried to find the association of heavy metals comparing CKDu with CKD. Furthermore, previous studies have used urinary metal levels as a biomarker of metal exposure. There is an inherent issue of reverse causality i.e., reduced excretion of metals in urine with a reduction in glomerular filtration rate (GFR) [ 8 ]. Measurement of metals in blood has also been reported to be a promising biomarker of metal exposure [ 9 , 10 ]. Some studies have employed urine to blood ratio for deciding whether urine or blood levels should be used for a particular metal. For metals with urine/blood ratio more than one blood metal levels, whereas for metals with urine/blood ratio less than one, urine metal levels were used in estimation analysis [ 11 ]. The purpose of this study was to test hypothesis whether heavy metals i.e. Arsenic (As), Cadmium (Cd), Lead (Pb) and Chromium (Cr) are associated with CKDu, in central India using blood and urine levels as biomarker of metal exposure.
Materials and methods
Study setting and population.
Study was conducted in a tertiary care hospital setting in the Department of Nephrology in India in a case-control design between December 2019 to June 2022. Participants were enrolled between December 2019 -December 2021. The data collection was done simultaneously. The sample analysis was carried out between January to June-2022. The study was performed according to the guidelines of the Declaration of Helsinki. The study objective was to compare CKDu cases with CKD and healthy controls with regard to biomarkers of exposure of heavy metals [blood and urine levels of cadmium (Cd), lead (Pb), arsenic (As) and chromium (Cr)]. The study included adults aged 18–70 years with CKDu and two groups of the control population, one with CKD and another group of healthy controls without evidence of CKD.
The CKDu and CKD cases were inducted among the patients visiting the nephrology outpatient department and based on pre-defined criteria. At the same time, healthy controls were inducted among the healthy relatives accompanying the patients visiting other departments of the institute for treatment. Written informed consent was obtained from all the participants.
The case definition of CKDu was based on criteria proposed by the Indian Society of Nephrology for the diagnosis of CKDu [ 12 ]. The inclusion criteria included- eGFR < 60 mL/min/1.73m2 (CKD-EPI) [ 13 ] and albumin-to-creatinine ratio (ACR) > 30 mg/g for more than 3 months with:
Urine protein creatinine ratio(PCR) less than 2g/g.
No history of glomerulonephritis, pyelonephritis, renal calculi, polycystic kidneys or obstruction on renal ultrasound.
Not on treatment for diabetes and HbA1c less than 6.5%.
Blood pressure less than 140/90 if CKD stage 1 and 2; and less than 160/100 if CKD stage 3,4, and 5 and on a single drug for blood pressure control.
Case definition of CKD was based on: eGFR < 60 mL/min/1.73m2 (CKD-EPI) and albumin-to-creatinine ratio > 30 mg/g for more than 3 months. Patients were included in the CKD group only if PCR > 2g/g. Hypertension with BP > 140/90 in stages 1–2 and > 160/100 in stages 3–5 or on two or more drugs for BP control.
CKD staging was based on the KDIGO-2008 classification [ 1 ]. The same stages were applied to categorize the renal functions of subjects with CKDu.
Inclusion criteria for healthy controls included: Absence of CKD as evidenced by eGFR more than 90 ml/min/1.73m2, ACR < 30mg/g and lack of anatomical renal disease, obstruction or stone on renal ultrasound, no history of diabetes, HbA1C less than 6.5 and BP less than 140/90.
Biases were kept a minimum by adhering to the case definition described above, and study exposures are mainly objectively assessed with very less dependency on recall i.e. for pesticide or painkiller use. The urine metal levels were adjusted for urine dilution by estimating metals per gram of creatinine in urine.
Sample size
Assuming a difference of moderate effect size (0.25), between three groups (CKDu cases, CKD Controls, Normal Controls) with a confidence level of 95% and power of 80%, the calculated sample size was 159. The final sample size estimated, including a 10% non-response rate, was 180 (60 per group).
Specimen collection and analysis
For the analysis of heavy metals, venous blood (2 ml) was collected in trace element free Trace Element K2-EDTA Vacutainer (Cat# BD 368381). Whole blood was stored at -40 °C until analysis. Ten millilitres (10 ml) of first-morning urine was collected in 50 ml polypropylene tubes. Urine was stored at -40 °C in aliquots until analysis. Serum and urine creatinine was measured using a modified kinetic Jaffe’s method using a Random Access Fully Automated Chemistry Analyzer (Beckman Coulter). Urinary protein and urine albumin were estimated using a colorimetric and immune-turbidimetric methods, respectively, using a Random Access Fully Automated Chemistry Analyzer (Beckman Coulter). HbA1c was analyzed by ion-exchange high pressure liquid chromatography method using a D10 Haemoglobin testing system (BioRad Laboratories). eGFR was calculated from serum creatinine and CKD -EPI equation (Ref). A kidney ultrasound was performed in standard B Mode grey scale in 3.5–5 MHz, the longitudinal length was measured along with the width and thickness of the kidney, renal stones, and any other anatomical abnormality.
Estimation of heavy metals in blood and urine
Levels of Cd, Pb, Cr and As were measured in whole blood and urine. Urinary spot sample results of metal analysis were adjusted for dilution by urine creatinine. Metal analysis was carried out at NIREH, Bhopal (India).
Levels of various heavy metals, viz. Cd, Pb, Cr, As in the collected blood and urine samples were analyzed through inductively coupled plasma optical emission spectroscopy (iCAP® 7400 Duo ICP-OES, ThermoFisher Scientific® Pvt. Ltd). Blood and urine samples were acid-digested in a microwave oven prior to metal detection on ICP-OES. For blood digestion, 1 mL of whole blood sample was mixed with 6 ml of a freshly prepared mixture of concentrated trace metal grade nitric acid (HNO3) and hydrogen peroxide (H2O2) in a ratio 2:1 (v/v) in high-purity polytetrafluoroethylene (PTFE-TFM) vessels. For urine digestion, 5 mL of urine sample was mixed with 6 ml of a freshly prepared mixture of HNO3 and H2O2 in a ratio of 2:1. After gentle mixing of these reactants with blood, the PTFE-TFM vessels were arranged in the rotor (24HVT80, Anton PAAR) and digestion was carried out in the Anton Paar, multi microwave PRO Reaction System at 200 C for 15 min. Digested samples were cooled to 40°C and diluted to 30 ml with distilled water. Blank was prepared for each cycle of digestion using distilled water, nitric acid, and hydrogen peroxide mixture. All the chemicals were trace-element free.
Before the analysis of metal ions in processed blood and urine samples, calibration standards for each element were prepared from multi-element stock solutions (1000 mg L − 1) in triple distilled water. Detection of Cd, Pb, and Cr was performed using a standard sample introduction setup, whereas for As, the hydride generation sample introduction system was utilized. Online hydride generation for As was achieved with an Enhanced Vapor System sample introduction kit using 0.5% m/v sodium tetrahydroborate (NaBH4) stabilized in 0.5% m/v NaOH and 50% v/v HCl solution. Emission data acquisition was performed using the Qtegra ISDS Software at interference-free wavelengths.
Statistical analysis
Statistical analyses were performed with R version 4.2 (R Foundation for Statistical Computing, Vienna, Austria) and IBM SPSS 26 version. The distribution of data in groups was evaluated with Shapiro-Wilk, kurtosis, skewness, and histograms. Skewed data for three groups was compared with the Kruskal-Wallis test. Subgroup analysis in three groups was performed with pairwise comparisons by Dunn test. Parameters with homogeneous distribution were compared with the chi-square test. Data are presented as %, for categorical variables or as median (Q1-Q3) for continuous variables.
Detection rates for blood and urinary metal levels were calculated. For urine metal levels, all statistical analyses were performed with creatinine-adjusted metal concentrations.
Urine to blood ratio was calculated for all metal levels. Spearman correlation coefficient was used to find the association between blood and urine metal levels of individual metals as well as for the association between different metals both in blood and urine. Correlation of blood and urine As with GFR was also performed.
We performed multinominal regression analysis for significantly different metal level in CKDu cases with respect to CKD and healthy controls. We included age and gender (confounding factors) in the model to see the y independence of association and effect estimate of the factor associated with CKDu. Regression model matrices and goodness-of-fit were also determined by the pseudo R 2 coefficient and Hosmer-Lemeshow goodness-of-fit test.
For all analyses, we have considered a p -value less than 0.05 as statistically significant.
A total of 568 patients who visited Nephrology OPD during the study period were screened for inclusion in the study. Out of these, 66 CKDu and 70 CKD cases were found eligible to enroll in the study. Eight patients withdrew consent in the CKD group, whereas four patients in the CKDu group had uncontrolled blood pressure with a single drug, and two withdrew consent. Finally, 60 CKDu and 62 CKD cases were included in the study for outcome analysis. We have approached 120 relatives of patients attending other OPDs and screened them for eligibility criteria of the healthy control group. Out of these, 60 were eligible, and 54 provided consent for participation in the study.
Demography and lab parameters
The CKD and CKDu subjects were similar in demographics for age and sex. However, healthy subjects were younger (Table 1 ). There was no significant difference between CKDu and CKD with reference to stage V (32 vs. 44, P-0.107).There were 05 diabetic kidney disease 04 CKD due to secondary glomerular disease patients (3-lupus nephritis, 1-FSGS), 12 hypertension-associated renal disease, 01 ADPKD, 36 Chronic glomerulonephritis patients, and 04 Chronic pyelonephritis patients in the CKD group. Use of smoking, Alcohol, and painkillers was similar across the three groups (Table 1 ). A significant difference was found between the three study groups with respect to the source of drinking water (ground or surface water). A significantly higher number of CKDu subjects used surface water as a source of drinking water (Table 1 and Table-S 1 and Fig-S 1 ) and a higher number of CKDu subjects reported pesticide usage. As shown in Table 1 , blood pressures were significantly higher in CKD subjects compared to CKDu and healthy subjects and reflect the inclusion criteria with appropriate patient inclusion in three groups. Both ACR and PCR were also significantly different between CKD and CKDu. The eGFR was calculated based on the CKD-EPI formula and was not significantly different between the CKD and CKDu subjects, however, CKD subjects had lower median eGFR compared to CKDu subjects. The healthy subjects had significantly higher eGFR compared to both groups. HbA1c, were similar across the three groups (Table 1 ).
Analytical results
The urinary and blood levels of As, Cd, Pb, and Cr (Table 2 ) were measured in ppb (micrograms per litre), and median with interquartile ranges were reported. Urinary metal levels were also measured in ppb (micrograms per liter) and then adjusted for urinary dilution by urine creatinine value and were finally expressed as micrograms/grams of urine creatinine (Table 2 ).
Detection limits
The lowest detectable concentrations of various heavy metals analyzed on ICP OES with a signal-to-noise ratio of 1 were as follows: As (193.759 nm) - 0.191 ppb; Cd (214.438 nm) - 0 ppb; Pb (220.353 nm) - 0.822 ppb; Cr (283.563 nm) - 3.156 ppb (Table 2 , Figs-S 2 -S 5 ).
Detection percentage
The number of subjects with blood and urine metal levels above the respective detection limits in each study group is reported in Table 2 .
Urine to blood ratio
A urine/blood ratio for each metal in all study groups was calculated for patients with metal levels above the detection limit. The distribution of urine/blood ratios for all metals is presented in Table 2 . Ratios were different between healthy and subjects with deranged kidney functions i.e. low GFR (CKD and CKDu). Median urine/blood Ratio for As was > 1 in healthy subjects and < 1 in CKD and CKDu, reflecting higher urinary levels compared to blood in healthy and reverse in CKD and CKDu subjects. For Pb, it was < 1 in healthy subjects and > 1 in subjects with CKD and CKDu, reflecting higher blood levels compared to urine in healthy and reverse in CKD and CKDu subjects. For Cd and Cr the ratio were < 1 across all three groups suggesting higher urine levels compared to blood levels.
Correlation
A spearman correlation (ρ) was also performed to see the association between each urine and blood metal and among the metals with each other as well. In CKDu, UAs were negatively associated with BAs (ρ-0.260, p -0.11) and in CKD positively (0.138, p -0.37). There was a positive association between urine and blood levels of As,Pb, and Cr and negative association of urine and blood Cd in CKD. In CKDu, a positive association was found in blood and urine Cd,Pb and Cr. In addition, there was a strong correlation of blood Cd, Pb, and Cr ( p < 0.01) [ρ = 0.68 (BCd and BPb), 0.88 (BCd and BCr), 0.71 (BPb and BCr) in CKDu and [ρ = 0.55 (BCd and BPb), 0.82 (BCd and BCr), 0.65 (BPb and BCr) in CKD. The Urine Cd, Pb, and Cr also had strong correlations [ρ = 0.33 (UCd and UPb), and 0.48(UPb and UCr)] in CKD and [ρ = 0.19(UCd and UPb), 0.67 (UCd and UCr), and 0.69 (UPb and UCr)] in CKDu < 0.05 (Table-S 2 -S 4 and Fig-S 6 ). Association of Blood and urine As with GFR was also evaluated, and BAs were found to be negatively associated with GFR (ρ = -0.097, p = 0.56), whereas UAs were positively associated (ρ = 0.14, p = 0.25) with GFR (Table-S 5 ). Metal levels: Blood As: was significantly higher in CKDu ( n = 37) subjects compared to CKD ( n = 41) and healthy ( n = 53) subjects (Table 2 ). On the other hand, the urinary As (UAs) was significantly low in CKD ( n = 50) and CKDu ( n = 48) subjects compared to healthy subjects ( n = 38) and was non significantly higher in CKD subjects compared to CKDu subjects (Fig. 1 , Table 2 ).The blood and urine As values were below detection limits in 21.6%, 35.7%, and 18.8% and in 6%, 16.6%, and 0% of subjects in CKDu, CKD, and healthy groups, respectively.
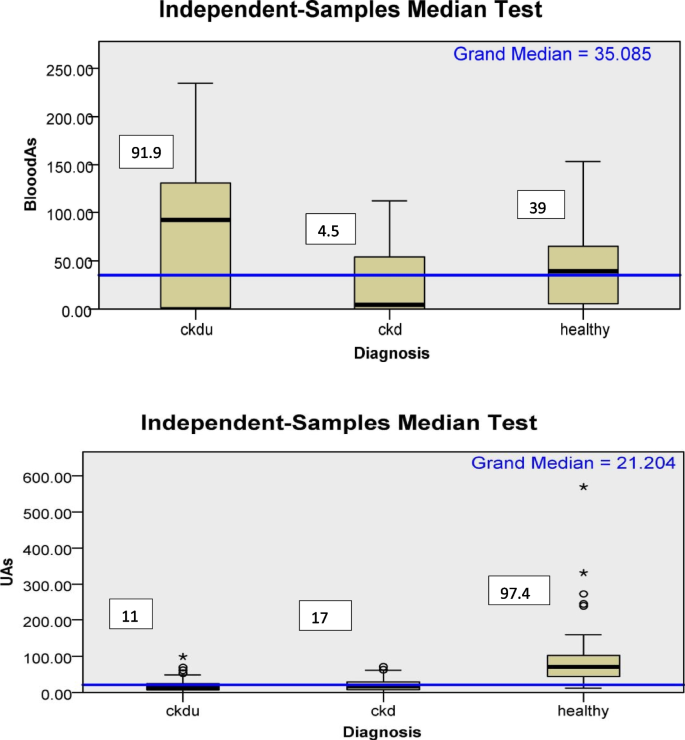
Box plot for distribution of blood and urine arsenic according to diagnosis categories. Median; microgram/Lt (blood); microgram/gm(urine); UAs- Urine arsenic;CKDu-Chronic kidney disease of unknown cause; CKD-Chronic kidney disease
Blood Cd also was significantly higher in CKD and CKDu subjects compared to healthy subjects. Urinary Cd (UCd) levels were significantly higher in CKD and CKDu subjects compared to healthy subjects,. There was a weak association of ( p = 0.06) UCd with CKD subjects compared to CKDu subjects.UCd was higher in CKD subjects compared to CKDu (Fig. 2 , Table 2 ). The blood and urine Cd values were below detection limits in 8.3%, 8.1%, and 0% and 37.2%, 19.3%, and 75.9% of subjects in CKDu, CKD, and healthy groups, respectively.
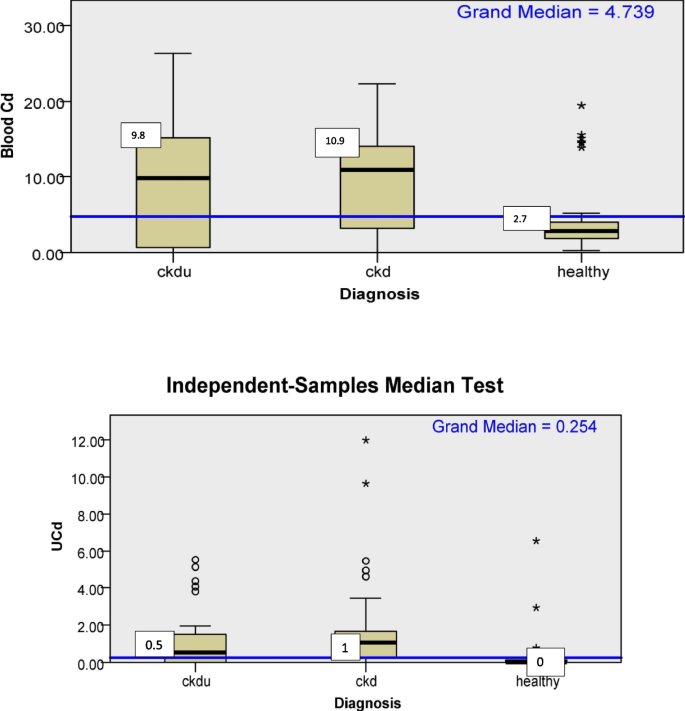
Box plot for distribution of blood and urine cadmium according to diagnosis categories. Median, microgram/Lt (blood); micrograms/gm (urine); UCd- Urine cadmium;CKDu-Chronic kidney disease of unknown cause; CKD-Chronic kidney disease
Pb levels in the blood of CKD and CKDu as well as in urine of CKD and CKDu subjects were significantly higher compared to healthy subjects. The Pb levels were higher in CKD subjects compared to CKDu subjects, but it was not statistically significant (Fig. 3 , Table 2 ). The blood and urine Pb values were below detection limits in 15%, 20%, and 25.9% and 23.3%, 19.4% and 70.4% of subjects in CKDu, CKD, and healthy groups, respectively.
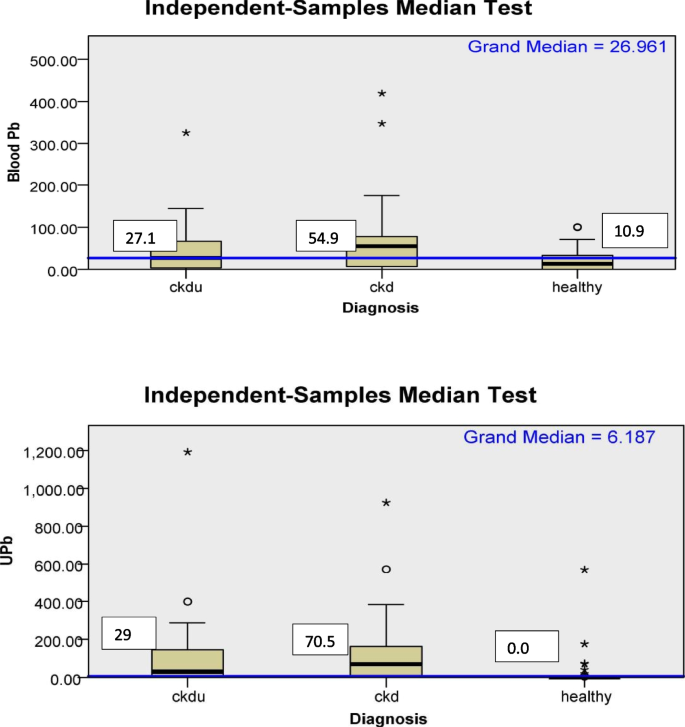
Box plot for distribution of blood and urine lead according to diagnosis categories. microgram/Lt (blood); microgram/gm(urine); UPb- Urine lead;CKDu-Chronic kidney disease of unknown cause; CKD-Chronic kidney disease
As shown in Table 2 and Fig. 4 , urinary and blood Cr was significantly higher in CKD, and CKDu patients than healthy subjects. The blood and urine Cr values were below detection limits in 13%, 0%, and 0% and 13.3%, 14.5% and 85.2% of subjects in CKDu, CKD, and healthy groups, respectively.
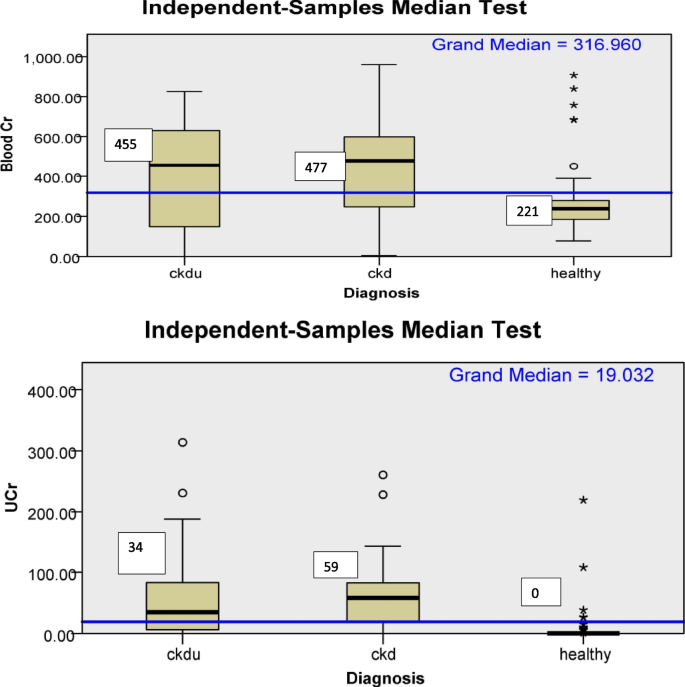
Box plot for distribution of blood and urine chromium according to diagnosis categories. Median; microgram/Lt(blood); microgram/gm(urine); UCr-urine chromium, CKDu-Chronic kidney disease of unknown cause; CKD-Chronic kidney disease
Multinominal regression
Though age, gender, were not significantly different between CKDu and CKD, on univariate analysis, we included these In the multinominal regression analysis between CKDu and CKD in reference to healthy subjects in addition to factors found significantly different ( p < 0.01 on univariate analysis) i.e. blood As and source of drinking water.After the final model, gender had no association with CKDu. Blood As, surface water as drinking water source and age were independently associated with CKDu. Age was associated independently with CKD also (Table 3 ).
To the best of our knowledge, this is the first study wherein an attempt has been made to analyze the association of heavy metals with CKDu in central India, using blood and urine levels as biomarkers of metal exposure. In addition, CKD and healthy subjects have been used as control groups.
The current study showed that blood and urine creatinine-adjusted urinary levels of heavy metals Cd, Pb and Cr were significantly higher in patients with CKD and CKDu as compared to healthy subjects. The urinary levels of the above metals were undetectable in healthy subjects. The study also showed a weak association of ( p = < 0.06) higher urinary Cd in CKD subjects compared to CKDu subjects of this Indian cohort.
The study also showed that Blood As was significantly higher in CKDu subjects compared to CKD and healthy subjects. On multinominalregression, blood As was independently ( p < 0.05) associated with CKDu after age adjustment.
In our study, median GFR was rather high in CKDu subjects [14.5 (7.0, 34.2)] compared to GFR in CKD subjects [9.0 (6.0, 17.0)ml/min/1.73m 2 )] and it was non significantly different between the two groups. On correlation analysis, there was a negative correlation between Blood As and GFR and a positive correlation of urine As with GFR. Based on this, the higher blood As in CKDu with higher GFR appears to be truly elevated.
Previously a study from Sri Lanka has also reported an association of CKDu with chronic As toxicity. In that study, 48% of CKDu patients and 17.4% of the control subjects fulfilled the criteria to be diagnosed with chronic arsenical toxicity(CAT), indicating the potential link between CAT and CKDu and suggesting agrochemicals could be the possible source [ 14 ]. Later, it was reported that glyphosate was the most widely used pesticide in Sri Lanka, which contains an average of 1.9 mg/kg arsenic. Findings suggest that agrochemicals, especially phosphate fertilizers, are a major source of inorganic arsenic in CKDu endemic areas [ 15 ]. However, another study from Sri Lanka did not find any difference in UAs levels in patients of CKDu in endemic areas and controls from endemic and nonendemic areas [ 4 ].
Some other studies have reported associations of As with CKD. A study from Taiwan found total UAs to be associated with a four-fold risk of CKD [ 6 ]. Another study reported an association of MMA V (mono methyl arsenate pentavalent) and DMA V (dimethyl arsenate pentavalent) in urine with prevalence of CKD [ 16 ]. However, in both studies, the type of CKD was not reported.
The higher blood As in CKDu compared to CKD may be associated with exposures in our study; a significantly higher number of subjects in CKDu group reported use of pesticides, surface water as a source of drinking water in CKDu subjects.On regression analysis also, surface water was independently associated with CKDu.
A study from north India reported increased levels of OCPs, namely α-HCH, aldrin, and β-endosulfan, in CKDu patients as compared to healthy control and CKD patients of known etiology [ 17 ] and it is also known that arsenic is an important component of pesticides [ 18 ]. The contamination of surface water with various pollutants i.e. pesticides, is common [ 19 ]. Arsenic is a known nephrotoxin, and one of the case reports where kidney histopathology was evaluated reported As causes tubulointerstitial disease (TID) [ 20 ]. The difference in methylation processes of As has also been found responsible for various diseases associated with As i.e. for example, high proportions of urinary MMAs (%U-MMAs) have been associated with a higher risk of cancers and skin lesions [ 21 ]. In contrast, high %U-DMAs has been associated with diabetes risk [ 22 ]. We have measured only iAs in our study. Whether methylation resulting in various metabolite species has different associations with CKDu or CKD should be explored further. We recently found a significant association of single nucleotide polymorphism in a gene coding for sodium-dependent dicarboxylate transporter (SLC13A3) with the susceptibility to CKDu [ 23 ].
In the current study, the UAs results suggest that As levels of 97 µg/gm of creatinine in healthy subjects were not associated with decreased GFR or proteinuria. Similar results were reported by a study from China where researchers found a lower confidence limit on the benchmark dose (LBMD) of 102 and 0.88 µg/gm creatinine for As and Cd, respectively, in order to prevent renal damage in the general population co-exposed to arsenic and cadmium [ 24 ]. The UAs in healthy subjects in our study were nearly similar to the LBMD reference and, not surprisingly, not to be associated with CKD or proteinuria.
Some studies have reported lead to be associated with CKDu. An Indian study reported high levels of lead and silicon concentrations in Indian groundwater in the endemic Uddanam area [ 7 ]. Jaysuman et al. also reported higher levels of Pb (26.5 µg/gm) in the urine of patients with Sri Lankan agricultural nephropathy compared to endemic and nonendemic control [ 25 ].
In the current study, although the median level of blood Pb was almost double in CKD patients compared to CKDu, the result was not statistically significant.
Our study showed that Cd was significantly associated with renal disease. Blood Cd and urine Cd (UCd) levels were significantly higher in patients with renal disease (CKD and CKDu) as compared to healthy subjects. The findings of UCd also showed a weak association (p-0.06) of Cd with CKD compared to CKDu among patients with renal diseases. There are some concerns that UCd may not be truly reflective of metal burden in patients with advanced CKD [ 26 ], because initially, in the course of Cd toxicity with early tubular damage, the normal reabsorption of cadmium-metallothionein decreases, and the UCd concentration increases. However, in the long run, cadmium-induced kidney damage gives rise to low Cd concentrations in both the kidney and urine, while the tubular damage remains [ 27 ]. The U/B ratio of < 1 for Cd in our study supports the above findings.
The mean eGFR in our CKD cohort was lower compared to CKDu; despite this, higher UCd values in patients with CKD compared to CKDu in our study indicate a potential association of Cd with CKD.
Studies have reported variable association of Cd with CKDu when compared to healthy subjects. Nanayakkara et al. [ 28 ] did not find an association of UCd with CKDu in stages 1–4 compared to healthy controls. Whereas another Sri Lankan [ 4 ] study found significantly high UCd in patients with CKDu against the endemic and nonendemic controls. We also observed significantly higher UCd in CKDu vs. healthy controls.
In the current study, urinary Cr (UCr) was not detected in healthy subjects, whereas it was significantly higher in patients with CKD and CKDu as compared to healthy subjects. UCr levels were higher in CKD compared to CKDu. Epidemiologically, Cr exposure has been reported to be associated with kidney damage in occupational populations [ 26 ]. Recently, a study from Taiwan reported that a significant and independent association between Cr exposure and decreased renal function in the general population, and co-exposure to Cr with Pb and Cd is potentially associated with an additional decline in the GFR in Taiwanese adults [ 27 ]. A study from Bangladesh reported outcomes similar to our study; however, the study included only CKD ( n = 30) patients and compared them with healthy subjects ( n = 20). In that study, compared to the controls, CKD patients exhibited significantly higher levels of Pb, Cd, and Cr levels in their urine samples. This signifies a potential association between heavy metal co-exposure and CKD [ 29 ]. In the current study a significant correlation between blood Cd, Pb, and Cr and urine Cd, Pb, and Cr were found in CKDu and CKD subjects compared to healthy subjects. The levels of UCd, UPb, and UCr in CKD and CKDu patients were significantly higher compared to healthy controls; The possibility of the combined effect of Cd, Pb, and Cr in the causation of renal diseases could be evaluated further in future studies. As CKDu is an endemic disease, the results of our study suggest an association of arsenic with CKDu in the Indian population, and so the generalizability of the result should be used with caution.
Strengths and limitations
This is the first study which has included two controls (CKD and healthy) and compared metal levels in patients with CKDu. In addition, the comparison of metals in both blood and urine is another advantage, as falling GFR levels and urine levels of several metals do not reflect true metal burden in patients. Inclusion of CKDu patients, as per the suggested definition by the Indian society of Nephrology, is another strength of our study.
The small sample size of our study may be a limitation of our study though it was calculated scientifically. The study involved Indian patients and controls only so the generalization of the results should be with caution. Healthy controls were of younger age is also a limitation of the study.
Also the study included patients from central India, comparatively a larger area and does not points out endemicity.
The study finds an association of environmental toxins with CKDu and CKD. The age and sex-adjusted As were observed to have an independent association with CKDu. A weak association of Cd with CKD was also observed in this Indian cohort. Subjects with renal dysfunction (CKDu and CKD) were observed to have a significantly higher metal burden of Pb, Cd, As, and Cr as compared to healthy controls. CKDu patients may have higher exposure to As via pesticides, surface water usage, or both.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Chronic Kidney Disease of unknown cause
Chronic Kidney Disease
Kidney Disease Improving Global Outcomes
Glomerular filteration rate
Institutional Human Ethics committee
Concentrated trace metal grade nitric acid
Hydrogen peroxide
High-purity polytetrafluoroethylene
Inorganic As
Tubulo-interstitial disease
Pentavalent monomethylarsonic acid
Pentavalent dimethylarsinic acid
Methylarsenous acid
Sodium-dependent dicarboxylate transporter
Limit on the benchmark dose
Arsenobetaine
Urinary MMAs
Urinary DMAs
Blood lead levels
End-stage kidney disease
Chapter 1: definition and classification of CKD. Kidney Int Suppl (2011). 2013;3(1):19–62. https://doi.org/10.1038/kisup.2012.64 .
Gifford FJ, Gifford RM, Eddleston M, Dhaun N. Endemic nephropathy around the world. Kidney Int Rep. 2017;2(2):282–92. https://doi.org/10.1016/j.ekir.2016.11.003 .
Article PubMed Google Scholar
Nanayakkara S, Senevirathna S, Parahitiyawa NB, et al. Whole-exome sequencing reveals genetic variants associated with chronic kidney disease characterized by tubulointerstitial damages in North Central Region, Sri Lanka. Environ Health Prev Med. 2015;20(5):354–9. https://doi.org/10.1007/s12199-015-0475-1 .
Article CAS PubMed PubMed Central Google Scholar
Jayatilake N, Mendis S, Maheepala P, Mehta FR. Chronic kidney disease of uncertain aetiology: prevalence and causative factors in a developing country. BMC Nephrol. 2013;14(1):180. https://doi.org/10.1186/1471-2369-14-180 .
Article PubMed PubMed Central Google Scholar
Jayasumana C, Gunatilake S, Senanayake P. Glyphosate, hard water and nephrotoxic metals: are they the culprits behind the epidemic of chronic kidney disease of unknown etiology in Sri Lanka? Int J Environ Res Public Health. 2014;11(2):2125–47. https://doi.org/10.3390/ijerph110202125 .
Bawaskar HS, HimmatraoBawaskar P, Himmatrao BP. Chronic renal failure associated with heavy metal contamination of drinking water: a clinical report from a small village in Maharashtra. Clin Toxicol. 2010;48(7):768–768. https://doi.org/10.3109/15563650.2010.497763 .
Article Google Scholar
Lal K, Sehgal M, Gupta V, et al. Assessment of groundwater quality of CKDu affected Uddanam region in Srikakulam district and across Andhra Pradesh, India. Groundw Sustain Dev. 2020;11:100432. https://doi.org/10.1016/j.gsd.2020.100432 .
Zhang X, Cornelis R, de Kimpe J, et al. Accumulation of arsenic species in serum of patients with chronic renal disease. Clin Chem. 1996;42(8):1231–7. https://doi.org/10.1093/clinchem/42.8.1231 .
Article CAS PubMed Google Scholar
Bommarito PA, Beck R, Douillet C, et al. Evaluation of plasma arsenicals as potential biomarkers of exposure to inorganic arsenic. J Expo Sci Environ Epidemiol. 2019;29(5):718–29. https://doi.org/10.1038/s41370-019-0121-x .
Environmental Health Criteria 165. Joint sponsorship of The United Nations Environment Programme, The International Labour Organization, and The World Health Organization. 1995. https://apps.who.int/iris/bitstream/handle/10665/37241/9241571659-eng.pdf?sequence=1 . Accessed 10 Nov 2022.
Ashrap P, Watkins DJ, Mukherjee B, et al. Predictors of urinary and blood Metal(loid) concentrations among pregnant women in Northern Puerto Rico. Environ Res. 2020;183:109178. https://doi.org/10.1016/j.envres.2020.109178 .
Anupama Y, Sankarasubbaiyan S, Taduri G. Chronic kidney disease of unknown etiology: case definition for India – a perspective. Indian J Nephrol. 2019. https://doi.org/10.4103/ijn.IJN_327_18 .
Levey AS, Stevens LA, Schmid CH, et al. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12. https://doi.org/10.7326/0003-4819-150-9-200905050-00006 .
Jayasumana MACS, Paranagama PA, Amarasinghe KMRC, et al. Possible link of chronic arsenic toxicity with chronic kidney disease of unknown etiology in Sri Lanka. J Nat Sci Res. 2013;3(1). www.iiste.org ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online).
Jayasumana C, Fonseka S, Fernando A, et al. Phosphate fertilizer is a main source of arsenic in areas affected with chronic kidney disease of unknown etiology in Sri Lanka. Springerplus. 2015;4:90. https://doi.org/10.1186/s40064-015-0868-z .
Zheng LY, Umans JG, Yeh F, et al. The association of urine arsenic with prevalent and incident chronic kidney disease. Epidemiology. 2015;26(4):601–12. https://doi.org/10.1097/EDE.0000000000000313 .
Ghosh R, Siddarth M, Singh N, et al. Organochlorine pesticide level in patients with chronic kidney disease of unknown etiology and its association with renal function. Environ Health Prev Med. 2017;22(1):49. https://doi.org/10.1186/s12199-017-0660-5 . Published 2017 May 26.
Li Y, Ye F, Wang A, et al. Chronic arsenic poisoning probably caused by arsenic-based pesticides: findings from an investigation study of a household. Int J Environ Res Public Health. 2016;13(1):133. https://doi.org/10.3390/ijerph13010133 .
Agrawal A, Pandey R, Sharma B. Water pollution with special reference to pesticide contamination in India. J Water Resource Prot. 2010;2(5):432–48. https://doi.org/10.4236/jwarp.2010.25050 .
Prasad GVR, Rossi NF. Arsenic intoxication associated with tubulointerstitial nephritis. Am J Kidney Dis. 1995;26(2):373–6. https://doi.org/10.1016/0272-6386(95)90660-6 .
Kuo CC, Moon KA, Wang SL, Silbergeld E, Navas-Acien A. The association of arsenic metabolism with cancer, cardiovascular disease, and diabetes: a systematic review of the epidemiological evidence. Environ Health Perspect. 2017;125(8):087001. https://doi.org/10.1289/EHP577 .
del Razo LM, García-Vargas GG, Valenzuela OL, et al. Exposure to arsenic in drinking water is associated with increased prevalence of diabetes: a cross-sectional study in the Zimapán and Lagunera regions in Mexico. Environ Health. 2011;10(1):73. https://doi.org/10.1186/1476-069X-10-73 .
Kumari R, Tiwari S, Atlani M, et al. Association of single nucleotide polymorphisms in KCNA10 and SLC13A3 genes with the susceptibility to chronic kidney disease of unknown etiology in central Indian patients [published online ahead of print, 2023 Jan 25]. Biochem Genet. 2023. https://doi.org/10.1007/s10528-023-10335-7 .
Hong F, Jin T, Zhang A. Risk assessment on renal dysfunction caused by co-exposure to arsenic and cadmium using benchmark dose calculation in a Chinese population. Biometals. 2004;17(5):573–80. https://doi.org/10.1023/B:BIOM.0000045741.22924.d .
Jayasumana C, Gunatilake S, Siribaddana S. Simultaneous exposure to multiple heavy metals and glyphosate may contribute to Sri Lankan agricultural nephropathy. BMC Nephrol. 2015;16(1):103. https://doi.org/10.1186/s12882-015-0109-2 .
Wilbur S, Abadin H, Fay M, et al. Toxicological profile for chromium. Atlanta: Agency for Toxic Substances and Disease Registry (US); 2012.
Google Scholar
Tsai TL, Kuo CC, Pan WH, et al. The decline in kidney function with chromium exposure is exacerbated with co-exposure to lead and cadmium. Kidney Int. 2017;92(3):710–20. https://doi.org/10.1016/j.kint.2017.03.013 .
Nanayakkara S, Senevirathna STMLD, Karunaratne U, et al. evidence of tubular damage in the very early stage of chronic kidney disease of uncertain etiology in the North Central Province of Sri Lanka: a cross-sectional study. Environ Health Prev Med. 2012;17(2):109–17. https://doi.org/10.1007/s12199-011-0224-z .
Choudhury TR, Zaman SKZ, Chowdhury TI, Begum BA, Islam MDA, Rahman MDM. Status of metals in serum and urine samples of chronic kidney disease patients in a rural area of Bangladesh: an observational study. Heliyon. 2021;7(11):e08382. https://doi.org/10.1016/j.heliyon.2021.e08382 .
Download references
Acknowledgements
Not applicable.
The Study was funded by Indian council of Medical Research (ICMR),New Delhi, India. Sanction no.:5/4/7-14/2019-NCD-II.
Author information
Mahendra Atlani and Ashok Kumar contributed equally to this work.
Authors and Affiliations
Department of Nephrology, All India Institute of Medical Sciences (AIIMS), Room No-3022, Academic Block, 3rd Floor, Saket Nagar, Bhopal, Madhya Pradesh, 462020, India
Mahendra Atlani, M. N. Meenu & Athira Anirudhan
Department of Biochemistry, All India Institute of Medical Sciences (AIIMS), Saket Nagar, Bhopal, Madhya Pradesh, 462020, India
Ashok Kumar, Sudhir K. Goel & Ravita Kumari
Department of Environmental Biochemistry, ICMR-National Institute for Research in Environmental Health (NIREH), Bhopal, Madhya Pradesh, India
Rajesh Ahirwar
All India Institute of Medical Sciences (AIIMS), Bhopal, Madhya Pradesh, India
Saikrishna Vallamshetla & G. Sai Tharun Reddy
You can also search for this author in PubMed Google Scholar
Contributions
MA and AK were equally involved in conceptualising the study, winning the grant, analyzing the results, monitoring the progress of study. MA prepared the manuscript. AK and SKG did the editing. RA supervised analysis of metal levels, sample collection done by MMN, RK. Metal analysis done by AA. Data entry and file preparation for results done by MMN, AA, SKV and STR.
Corresponding authors
Correspondence to Mahendra Atlani or Ashok Kumar .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Institutional Human Ethics Committee (IHEC) approval No- EF0125. The study was performed according to the guidelines of the Declaration of Helsinki. All participants gave informed consent for participation before enrolment.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Atlani, M., Kumar, A., Ahirwar, R. et al. Heavy metal association with chronic kidney disease of unknown cause in central India-results from a case-control study. BMC Nephrol 25 , 120 (2024). https://doi.org/10.1186/s12882-024-03564-4
Download citation
Received : 28 April 2023
Accepted : 26 March 2024
Published : 03 April 2024
DOI : https://doi.org/10.1186/s12882-024-03564-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Chronic kidney disease of unknown cause
- Heavy metals
- Environmental toxins
BMC Nephrology
ISSN: 1471-2369
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Watermelon and Chronic Kidney Disease: Understanding the Risks of High Potassium Intake from Case Studies
A s the mercury rises, many envision the joy of biting into a crisp, juicy slice of watermelon. Yet, this summertime staple may pose unexpected health risks for the 14% of American adults suffering from chronic kidney disease (CKD). A collection of three case studies recently published in the Annals of Internal Medicine, watermelon’s high potassium content can have potentially life-threatening consequences for individuals with CKD.
The dangers of hyperkalemia, a condition characterized by elevated levels of potassium in the blood, are particularly acute for CKD patients. Their impaired kidneys struggle to filter and excrete potassium efficiently, a situation that can escalate when consuming potassium-rich foods such as watermelon. The case studies reveal three CKD patients who developed hyperkalemia after eating large quantities of watermelon over several weeks to months.
One case involved a 56-year-old man with severe CKD and insulin-dependent type 2 diabetes who experienced a syncope episode and was found to have a potassium level of 7 mmol/L – significantly higher than the normal range. His regular consumption of “large amounts” of watermelon was identified as a key factor in his hyperkalemia, alongside his CKD and medication. Another patient, a 72-year-old man with a history of ischemic cardiomyopathy, developed ventricular tachycardia and fibrillation, serious heart rhythm disturbances, after drinking watermelon juice daily. In both cases, reducing intake of high-potassium foods, including watermelon, brought their potassium levels back to normal.
These findings underscore the importance of potassium regulation in CKD patients. While the general population is encouraged by the World Health Organization to increase potassium intake for cardiovascular benefits, those with kidney disease must tread more cautiously. Potassium plays a crucial role in cellular function, regulating heartbeat and muscle contractions, but balance is key.
Relevant articles:
– 14% of American adults are affected by chronic kidney disease – and anyone in that category should be very careful about how much watermelon they eat | A new series of case studies examines how a favorite fruit can cause life-threatening issues.
– Potassium: Uses, Benefits, Side Effects, Dosage , Verywell Health, Fri, 01 Mar 2024 08:00:00 GMT
– 10 Potential Side Effects of Eating Veggies: What You Need to Know , Everyday Health, Fri, 05 Jan 2024 08:00:00 GMT
![As the mercury rises, many envision the joy of biting into a crisp, juicy slice of watermelon. Yet, this summertime staple may pose unexpected health risks for the 14% of American adults suffering from chronic kidney disease (CKD). A collection of three case studies recently published in the Annals of Internal Medicine, watermelon’s high potassium […] As the mercury rises, many envision the joy of biting into a crisp, juicy slice of watermelon. Yet, this summertime staple may pose unexpected health risks for the 14% of American adults suffering from chronic kidney disease (CKD). A collection of three case studies recently published in the Annals of Internal Medicine, watermelon’s high potassium […]](https://img-s-msn-com.akamaized.net/tenant/amp/entityid/BB1lcHz1.img?w=768&h=512&m=6)
Darier disease: Histopathology revisited
Affiliations.
- 1 Department of Pathology, St. John's Medical College, Bengaluru, Karnataka, India.
- 2 Department of Dermatology, St. John's Medical College, Bengaluru, Karnataka, India.
- PMID: 38563701
- DOI: 10.4103/ijpm.ijpm_610_23
Darier disease (DD) is a rare genodermatosis. Literature on this topic is overwhelmingly dominated by case reports with rare clinical presentations, which have mentioned the histopathologic features briefly. The aim of this study was to document the histopathology of DD. Skin biopsies diagnosed as Darier disease based on clinicopathologic correlation over 12 years were reviewed for various epidermal and dermal features. There were 16 patients included, who most commonly presented in the third decade, with slight female predilection. The most common clinical presentation was hyperpigmented, hyperkeratotic, papules and plaques (91%), with 69% affecting the trunk. In addition to the classic suprabasal acantholytic clefts, we noted some unusual features: absence of parakeratosis (19%), a cornoid lamella-like pattern (62%), follicular acantholysis (13%) and multiple foci of involvement within a single biopsy (63%). Features such as the presence of dyskeratotic cells and minimal dermal lymphocytic infiltrates were concordant with previous literature. The limitation of this study was the small sample size. To conclude, pathologists must be aware of the variations in histopathology of Darier's disease, especially when challenged with atypical clinical presentations. The Darier-like pattern is met within several acantholytic diseases, and clinicopathologic correlation has the last word in arriving at a diagnosis.
Copyright © 2024 Copyright: © 2024 Indian Journal of Pathology and Microbiology.

IMAGES
VIDEO
COMMENTS
A 44-year-old woman presented with cough, dyspnea, and chest pain. On examination, she had tachycardia and hypotension. Evaluation revealed SARS-CoV-2 RNA in a nasopharyngeal swab, as well as eleva...
Case Presentation. History of Present Illness: A 33-year-old white female presents after admission to the general medical/surgical hospital ward with a chief complaint of shortness of breath on exertion. She reports that she was seen for similar symptoms previously at her primary care physician's office six months ago.
Case Presentation. The patient is a 60-year-old white female presenting to the emergency department with acute onset shortness of breath. Symptoms began approximately 2 days before and had progressively worsened with no associated, aggravating, or relieving factors noted. She had similar symptoms approximately 1 year ago with an acute, chronic ...
Below are a few examples of the fantastic cases and case presentations our first-year fellows are engaged with: October 3, 2023. Case 1: An 8-year old boy with fever and maculopapular rash ... Case 1: A 37-year-old man with painful neck swelling Case 2: A 44-year-old woman with Crohn's disease and acute-onset fever, headache, and myalgia ...
Abstract. Crohn's disease (CD) is an inflammatory bowel disease affecting any portion of the gastrointestinal tract, usually the terminal ileum and the colon, with clinical manifestations such as diarrhea, fever, and weight loss. Clinical presentation of CD may include complications such as enterovesical fistulas, abscesses, strictures, and ...
Introduction. Hashimoto's thyroiditis was first discovered in 1912 by Japanese physician Hakaru Hashimoto (1881−1934). Hashimoto's thyroiditis or chronic lymphocytic thyroiditis is an organ specific autoimmune disease in which the thyroid gland is attacked by cell and antibody mediated responses [1]. Hashimoto's is the most common cause ...
Please choose a Case Study below. I have spots and my skin burns. A case of a 10 year old boy with a 3 week history of diarrhoea, vomiting and cough. A case of fever and general malaise. A case of persistant hectic fever. A case of sudden rapid neurological deterioration in an HIV positive 27 year old female. A case of swollen hands.
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
Patient Case Presentation. A 61-year-old American woman was referred to a Gastroenterology Clinic from primary care provider due to consistent discomfort and significant weight loss. She looked for a PCP's advice as she had a tarry stool in the early morning which she had never experienced before. She presented with a 2-month history of ...
And so, those are the big, noteworthy aspects of this case, and can be a rather typical presentation for a patient with deletion 11q molecular features like this patient. John Allan, MD: One other aspect of this case that's unique is that the patient is on over-the-counter antacids, and this is a relatively common thing. Many patients are takig ...
This case study highlights the importance of early diagnosis and personalized treatment plans for patients with Parkinson's disease. ... Overall, the unique clinical presentation, disease course .
A.T. is a 65-year-old black female with claudication secondary to peripheral arterial disease (PAD). She has a history of coronary artery disease, myocardial infarction, heart failure, endarterectomy, hypertension, hyperlipidemia, type 1 diabetes mellitus, and asthma.She was referred to the Division of Vascular Surgery at Henry Ford Hospital complaining of fatigue and heaviness in her lower ...
CASE PRESENTATION. A 27-year-old African American woman presented to the emergency department, with complaints of shortness of breath, fever, and upper abdominal pain for 4 days. The shortness of breath was progressive, worse with supine position, and improved by leaning forward. The patient described the abdominal pain as sharp and ...
To save you time and effort, I have curated a list of 5 versatile case study presentation templates, each designed for specific needs and audiences. Here are some best case study presentation examples that showcase effective strategies for engaging your audience and conveying complex information clearly. 1. Lab report case study template.
Integumentary: No symptoms reported; thin, fine body hair and inelastic skin turgor observed by provider during assessment. HEENT: Ulcerations in mouth and vision changes reported. GI: Painful diarrhea with extreme urgency accompanied by pain in RLQ. Reproductive: Amenorrhea for the last 3 months (menarche 4 years ago, regular cycle before now)
In summary, we present a case with a rare presentation of thyroid dermopathy mimicking lymphatic malformation. The Koebner phenomenon can explain this patient's atypical presentation. The rarity of the presentations has been emphasized by the lack of studies on the topic, specifically in the pediatric population.
Symptoms of a heart attack can include chest pain or discomfort, shortness of breath, nausea, vomiting, and pain or discomfort in other parts of the body, such as the neck, jaw, back, or arms. However, these symptoms can be mistaken for other conditions, such as indigestion or muscle strain, leading to delays in seeking medical treatment.
A CASE STUDY: CHRONIC KIDNEY DISEASE. A Case Study Report Presented to. The Faculty of the School of Nursing. Saint Louis University. Submitted by: BSN IV-A. ... CASE PRESENTATION: In the case of the patient, a transudate (filtrate of plasma that move across intact capillary walls) occurs because there is altered formation and reabsorption of ...
Largest study of its kind predicts 85% increase in deaths from the disease in same period as more men live longer The number of men diagnosed with prostate cancer worldwide is projected to double ...
May 12, 2022 •. 7 likes • 12,163 views. DR. METI.BHARATH KUMAR. A CASE PRESENTATION ON CHRONIC KIDNEY DISEASE (CKD) STAGE V. Healthcare. 1 of 23. A CASE PRESENTATION ON CHRONIC KIDNEY DISEASE (CKD)- (1).pptx - Download as a PDF or view online for free.
Presentation Transcript. Case study: infectious disease Professor Anne Johnson FMedSciHead, Department of Primary Care and Population Sciences, Royal Free and University College Medical School, London. Background Globally: • infections cause over a fifth of all deaths • a million children die each year from diseases preventable through ...
Case discussion of a patient of Alzheimer's disease. Healthcare. 1 of 36. Download Now. Download to read offline. Case discussion of Alzheimer's Dementia - Download as a PDF or view online for free.
Chronic Kidney Disease of unknown cause (CKDu) a disease of exclusion, and remains unexplained in various parts of the world, including India. Previous studies have reported mixed findings about the role of heavy metals or agrochemicals in CKDu. These studies compared CKDu with healthy controls but lacked subjects with CKD as controls. The purpose of this study was to test the hypothesis ...
Yet, this summertime staple may pose unexpected health risks for the 14% of American adults suffering from chronic kidney disease (CKD). A collection of three case studies recently published in ...
Darier disease (DD) is a rare genodermatosis. Literature on this topic is overwhelmingly dominated by case reports with rare clinical presentations, which have mentioned the histopathologic features briefly. The aim of this study was to document the histopathology of DD. Skin biopsies diagnosed as Darier disease based on clinicopathologic ...
Getty Images. The syndrome was first reported by diplomats at the US embassy in Cuba in 2016. A mysterious illness that has affected US diplomats in recent years has been linked to a Russian ...