- Publications
- Conferences & Events
- Professional Learning
- Science Standards
- Awards & Competitions
- Daily Do Lesson Plans
- Free Resources
- American Rescue Plan
- For Preservice Teachers
- NCCSTS Case Collection
- Partner Jobs in Education
- Interactive eBooks+
- Digital Catalog
- Regional Product Representatives
- e-Newsletters
- Bestselling Books
- Latest Books
- Popular Book Series
- Prospective Authors
- Web Seminars
- Exhibits & Sponsorship
- Conference Reviewers
- National Conference • Denver 24
- Leaders Institute 2024
- National Conference • New Orleans 24
- Submit a Proposal
- Latest Resources
- Professional Learning Units & Courses
- For Districts
- Online Course Providers
- Schools & Districts
- College Professors & Students
- The Standards
- Teachers and Admin
- eCYBERMISSION
- Toshiba/NSTA ExploraVision
- Junior Science & Humanities Symposium
- Teaching Awards
- Climate Change
- Earth & Space Science
- New Science Teachers
- Early Childhood
- Middle School
- High School
- Postsecondary
- Informal Education
- Journal Articles
- Lesson Plans
- e-newsletters
- Science & Children
- Science Scope
- The Science Teacher
- Journal of College Sci. Teaching
- Connected Science Learning
- NSTA Reports
- Next-Gen Navigator
- Science Update
- Teacher Tip Tuesday
- Trans. Sci. Learning

MyNSTA Community
- My Collections
Diabetes and Insulin Signaling
By Kristy J. Wilson
Share Start a Discussion

Cellular signaling, otherwise known as signal transduction, is the mechanism by which cellular context and environmental situation are used to regulate or adjust cellular behavior. Multicellular organisms use cellular signaling to coordinate responses to the environment, facilitate development, and maintain homeostasis. The mechanisms by which a cell receives a message and translates it into short-term or long-term effects are as varied as the responses stimulated by cellular signaling. There are, however, some generalized steps that can be applied to many different signaling situations. This case study uses insulin signaling and the pathological case of diabetes as a lens through which students will learn general signaling mechanisms like kinase cascades and second messenger pathways. The case is designed in the interrupted format and has three parts that could be used either as homework or as an in-class activity. It is written for use in a cell biology class for sophomore or junior undergraduates but could also be utilized in biochemistry, physiology, or genetics courses.
Download Case
Date Posted
- Divide a signaling pathway into generalized parts: signal, receptor, signaling effectors (i.e., signaling cascades or second messengers) and short-term/long-term effects.
- Explain the role of phosphorylation in protein/enzyme activity and how it contributes to signal transduction.
- Apply signal transduction mechanisms to diabetes's physiological symptoms.
- Hypothesize a mechanism to explain how signaling in diabetes might be specific for different tissue types.
- Design a line of inquiry or an experiment that could identify a cause of insulin resistance in type-2 diabetes.
Cellular signaling; signal transduction; insulin; insulin signaling; insulin resistance; diabetes; receptor; kinase; transcription factor; second messenger
Subject Headings
EDUCATIONAL LEVEL
Undergraduate lower division, Undergraduate upper division, Graduate
TOPICAL AREAS
TYPE/METHODS
Teaching Notes & Answer Key
Teaching notes.
Case teaching notes are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Teaching notes are intended to help teachers select and adopt a case. They typically include a summary of the case, teaching objectives, information about the intended audience, details about how the case may be taught, and a list of references and resources.
Download Notes
Answer Keys are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Download Answer Key
Materials & Media
Supplemental materials, you may also like.
Web Seminar
School and district leaders are invited to join us on Thursday, April 11, 2024, from 7:00 PM to 8:00 PM ET, to learn about NSTA’s School and Distric...
Struggling with materials management in your district? Want to learn tips and tricks from the experts at ECA Science Kit Services? Join us on Th...
Insulin signaling in type 2 diabetes: experimental and modeling analyses reveal mechanisms of insulin resistance in human adipocytes
Affiliations.
- 1 Department of Clinical and Experimental Medicine, Linköping University, SE58185 Linköping, Sweden.
- 2 Department of Clinical and Experimental Medicine, Linköping University, SE58185 Linköping, Sweden; Department of Biomedical Engineering, Linköping University, SE58185 Linköping, Sweden.
- 3 Department of Clinical and Experimental Medicine, Linköping University, SE58185 Linköping, Sweden. Electronic address: [email protected].
- PMID: 23400783
- PMCID: PMC3617287
- DOI: 10.1074/jbc.M112.432062
Type 2 diabetes originates in an expanding adipose tissue that for unknown reasons becomes insulin resistant. Insulin resistance reflects impairments in insulin signaling, but mechanisms involved are unclear because current research is fragmented. We report a systems level mechanistic understanding of insulin resistance, using systems wide and internally consistent data from human adipocytes. Based on quantitative steady-state and dynamic time course data on signaling intermediaries, normally and in diabetes, we developed a dynamic mathematical model of insulin signaling. The model structure and parameters are identical in the normal and diabetic states of the model, except for three parameters that change in diabetes: (i) reduced concentration of insulin receptor, (ii) reduced concentration of insulin-regulated glucose transporter GLUT4, and (iii) changed feedback from mammalian target of rapamycin in complex with raptor (mTORC1). Modeling reveals that at the core of insulin resistance in human adipocytes is attenuation of a positive feedback from mTORC1 to the insulin receptor substrate-1, which explains reduced sensitivity and signal strength throughout the signaling network. Model simulations with inhibition of mTORC1 are comparable with experimental data on inhibition of mTORC1 using rapamycin in human adipocytes. We demonstrate the potential of the model for identification of drug targets, e.g. increasing the feedback restores insulin signaling, both at the cellular level and, using a multilevel model, at the whole body level. Our findings suggest that insulin resistance in an expanded adipose tissue results from cell growth restriction to prevent cell necrosis.

Publication types
- Research Support, Non-U.S. Gov't
- Adipocytes / cytology
- Adipocytes / metabolism*
- Diabetes Mellitus, Type 2 / metabolism*
- Glucose / metabolism
- Glucose Transporter Type 4 / metabolism
- Insulin / metabolism*
- Insulin Receptor Substrate Proteins / metabolism*
- Insulin Resistance*
- Mechanistic Target of Rapamycin Complex 1
- Metformin / pharmacology
- Models, Theoretical
- Multiprotein Complexes / metabolism*
- Muscles / metabolism
- Obesity / metabolism
- Receptor, Insulin / metabolism
- Signal Transduction
- Skin / metabolism
- TOR Serine-Threonine Kinases / metabolism*
- Glucose Transporter Type 4
- Insulin Receptor Substrate Proteins
- Multiprotein Complexes
- SLC2A4 protein, human
- Receptor, Insulin
- TOR Serine-Threonine Kinases

Case Study: Insulin Sensitizers as Enhancers in Diabetes Management
- Marina Dykhne PharmD, BCACP, APh, CDCES
The objective of this study is to evaluate the use of low-dose pioglitazone, without relying on high doses of insulin, by enhancing sensitivity as a suitable, cost-effective strategy compared to larger insulin doses in patients with limited access to care.
Thiazolidinediones (TZDs) enhance insulin activity and reverse insulin resistance, a common characteristic of type 2 diabetes. 1 These agents are ligands for peroxisomal proliferator-activated receptor gamma (PPARγ), a nuclear receptor superfamily member and a transcription factor that is expressed at high levels in adipose tissues. 2
PPARγ is involved in modulating the insulin-responsive glucose transporter GLUT 4, which plays a crucial role in glucose uptake and metabolism in insulin target tissues. 3 These insulin sensitizers function on intracellular metabolic pathways.
As a result of this act, there will be an improvement in insulin action and an increase in insulin sensitivity in critical tissues. 4 These agents can facilitate glucose transport activity, enhance glycogen synthesis, and stimulate insulin-mediated glucose uptake and disposal in skeletal muscle tissue. 5 Despite the well-established benefits this class offers in glycemic control, they have fallen out of favor due to concerns over their adverse effects (AEs), such as edema and weight gain.
Studies have shown the AEs of this drug are diminished if low doses of pioglitazone are added to insulin therapy (i.e., 15 mg/day). 4,6 The objective of this study is to evaluate the use of low-dose pioglitazone, without relying on high doses of insulin, by enhancing sensitivity as a suitable, cost-effective strategy compared to larger insulin doses in patients with limited access to care.
The following studies support the benefits of combination therapy of thiazolidinedione and insulin. “Concomitant therapy with pioglitazone and insulin for the treatment of type 2 diabetes” is a study published in 2010 that showed a dramatic lowering effect in plasma glucose when low-dose pioglitazone is used in combination with insulin therapy. 4
Consistent with this observation, a study conducted by Berhanu et al. demonstrated pioglitazone administration in combination with insulin therapy improves glycemic control, reduces insulin dose requirements, and improves lipid profiles. 7 Analysis of another study by Rosenstock et al. demonstrated the addition of pioglitazone to stable insulin regimens significantly improves HbA1c and fasting plasma glucose (FPG) in patients with T2DM. 8
Two large prospective clinical trials have demonstrated that pioglitazone reduces cardiovascular incidents in association with enhanced insulin sensitivity. A decrease in plasma triglyceride and transformation of small dense low-density lipoprotein (LDL) particles to larger and less dense LDL particles are other characteristics of these agents that can lead to the correction of diabetic dyslipidemia and can decrease the risk of cardiovascular complications. 9
Both patients presented in this case report are covered under a formulary that only offers metformin, sulfonylureas, thiazolidinediones, and Neutral Protamine Hagedorn (NPH) insulin to treat diabetes. Due to limited accessible options, increasing insulin doses are, at points, the only feasible option for controlling diabetes in these patients. Addition of pioglitazone 15 mg daily significantly lowered HgA1c by 4% and 6%, respectively, in less than 6 weeks in 2 patients with T2DM and limited access to care who were already receiving insulin.
The first patient was a 52-year-old Hispanic male with uncontrolled diabetes who presented to the clinic to be seen by the primary care provider (PCP) and a clinical pharmacist. His random blood glucose performed by PCP was > 650 mg/dL. His laboratory value showed an HbA1c of 18.4%.
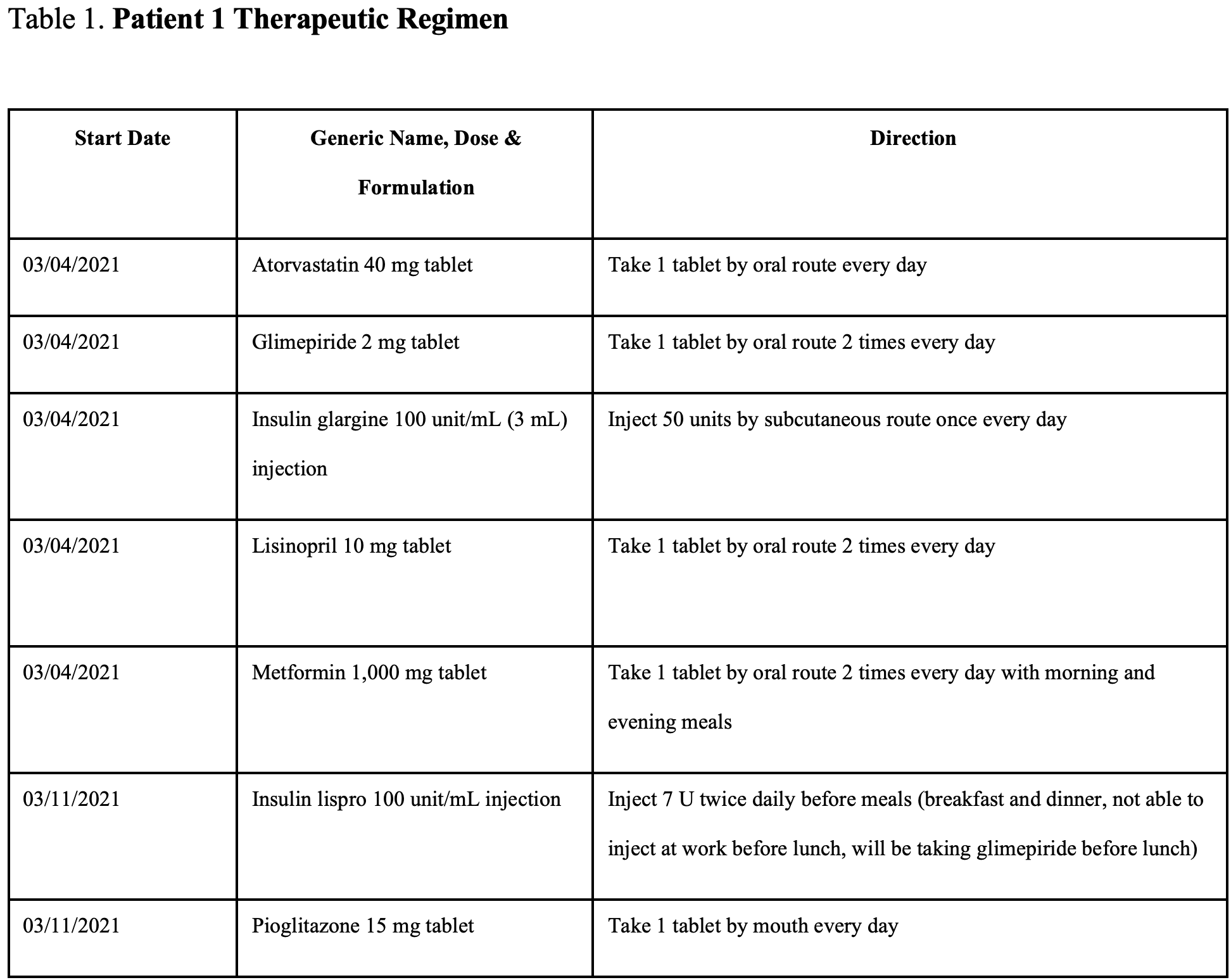
He reported blurry vision, excessive thirst, frequent urination, and tingling in the toes. He was started on short- and long-acting insulin (lispro and glargine), metformin, glimepiride, and pioglitazone. For a complete list of the therapeutic regimen for this patient, please refer to Table 1 .
Public Health Matters: Seacrest Studios’ Impact on Children’s Hospitals and Healing Through Broadcasting
FDA Expands Label for Bempedoic Acid to Reduce Cardiovascular Risk, With or Without Statins

Pharmacy Focus: Limited Series - Celebrity Endorsements in Public Health

V116 Demonstrates Positive Immunogenicity for 21 Pneumococcal Serotypes

AI, Machine Learning Can Bring Significant Benefits to Pharmaceutical Development, Research
2 Commerce Drive Cranbury, NJ 08512
609-716-7777


- Previous Article
- Next Article
Case Study 1
Case study 2, case study 3, case study 4, case study 5, case studies 6 and 7, case studies in insulin therapy: the last arrow in the treatment quiver.
The authors are from the Department of Endocrinology at the Institute of Post Graduate Medical Education & Research in Kolkata, West Bengal, India. Anubhav Thukral, MD, Chitra Selvan, MD, Partha Pratim Chakraborty, MD, Ajitesh Roy, MD, Soumik Goswami, MD, and Rana Bhattacharjee, MD, are postdoctoral trainees. Sujoy Ghosh, DM, is an assistant professor; Satinath Mukherjee, DM, is a professor; and Subhankar Chowdhury, DM, is a professor and head of the department.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Anubhav Thukral , Chitra Selvan , Partha Pratim Chakraborty , Ajitesh Roy , Soumik Goswami , Rana Bhattacharjee , Sujoy Ghosh , Satinath Mukherjee , Subhankar Chowdhury; Case Studies in Insulin Therapy: The Last Arrow in the Treatment Quiver. Clin Diabetes 1 October 2013; 31 (4): 175–178. https://doi.org/10.2337/diaclin.31.4.175
Download citation file:
- Ris (Zotero)
- Reference Manager
B ecause type 2 diabetes is a progressive disease, its natural course requires initiation of insulin in a significant proportion of patients, especially when oral agents fail to achieve glycemic targets. Most practicing physicians and endocrinologists acknowledge that neither the transition to nor the journey with insulin treatment is often as smooth as one would hope. Most have occasionally met with patients who plead for help in controlling their blood glucose levels with oral drugs alone. Often, doctors struggle to persuade such patients to start insulin.
In this article, we share some of our experiences—some common throughout the world and others unique to our country—in caring for patients who are prescribed insulin. It is important to learn from these experiences with insulin because it represents, more often than not, the last arrow in our treatment quiver.
The patient was a 45-year-old man who has had type 2 diabetes for the past 6 years and had been taking insulin for the past 2 years. His body weight was 50 kg (BMI 24 kg/m 2 ). He presented with uncontrolled and recently increased blood glucose levels and a dramatic increase in insulin dose during the past 5 months without any apparent cause. He had no history of fever, infections, or steroid use. He had had multiple hospital visits during the past few months.

Discoloration with hypertrophy on medial aspects of both thighs on the site where the patient described in Case Study 1 was injecting insulin.
The patient appeared to be well educated and concerned about this situation. To our surprise, however, we found he was injecting insulin on the medial aspect of his thighs. Examination showed lipohypertrophy with swelling in that region ( Figure 1 ). The crowded clinic with its lack of trained diabetes educators and nurses was the perfect setting for this gross oversight in checking injection sites.
The patient was a 55-year-old obese (BMI 28 kg/m 2 ) man with known type 2 diabetes for 12 years who had been taking insulin for the past 6 months. He presented with haywire blood glucose levels over several visits, with gradually increasing doses of insulin. There were no documented episodes of hypoglycemia.
The patient was injecting his own insulin, and his injection technique was confirmed to be good. The insulin injection sites were healthy. Insulin was properly stored at his home, and he was using a 40 IU syringe and a compatible vial.
Surprisingly, his A1C level was 7.2%, which was discordant with his venous blood glucose readings. He was not performing self-monitoring of blood glucose at home because of logistical issues. What was perplexing was that, although his dose of premixed insulin before breakfast had increased from 12 to 36 units in the past 6 months, his morning fasting levels were controlled with a predinner dose of 6 units, and although his post-breakfast values crept up from 200 to 340 mg/dl during the past four visits, his fasting blood glucose had decreased from 98 to 66 mg/dl in the same time period.
Through detailed questioning, we learned that dietary irregularities on the days of the test were at the heart of the matter. On a normal day, the patient injected insulin at about 7:40 a.m., ate breakfast at 8:00 a.m., and ate lunch at noon. However, on the days of the test, he had an extended fast, skipping breakfast. He then performed SMBG and took insulin at noon and, instead of a normal lunch, ended up overeating with a large meal essentially comprising both breakfast and lunch. Hence, his insulin dose was always insufficient, and his postprandial glucose values were always high. This would not have happened if the test center had been closer to his house or had opened at 8:00 a.m., which would have allowed him the flexibility to follow his normal dietary routine on test days.
The patient was asked to divide his meals, take voglibose before breakfast and lunch, and perform SMBG at the proper time. We split his doses, with 16 units of regular insulin before breakfast and 16 units before lunch and 6 units of premixed insulin before dinner. His blood glucose was then controlled.
A man with type 2 diabetes who had been taking insulin for the past 4 years with good glycemic control was started on twice-daily premixed insulin with a pen device for the past month. Although he was happy with the convenience and ease of using a pen device, his blood glucose levels became erratic. We decided to confirm his injection technique and asked him to bring his pen device to the clinic. He brought along a pen device with the cartridge in place, but the needle was missing. On questioning, we learned that the patient was injecting insulin without a needle. He thought it normal that he would not feel anything because pen devices were supposed to be painless. In actuality, he was trying to give himself insulin transdermally rather than subcutaneously. This case illustrates that a combination of less-than-adequate education and aggressive marketing by device sales companies can lead to misconceptions on the part of patients.
A woman with type 2 diabetes who had been taking insulin for the past 6 years with reasonable glycemic control presented with high glucose levels and injection site abscesses for the past month ( Figure 2 ). Through thoughtful questioning, we learned that she had been wiping the insulin injection tip with a cotton swab before and after injecting.

Insulin site abscess in patient described in Case Study 4.
A 46-year-old man with type 2 diabetes started noticing nodular swellings and subsequent discharging sinuses from these swellings at the insulin injection site for the past 6 months ( Figure 3 ). These swellings continued to appear when he took insulin from a particular vial. When that vial got finished, new lesions did not appear.

Chronic granulomatous infection at injection site in patient described in Case Study 5.
Patient was treated with multiple courses of different antibiotics with minimal response. Grams stain and multiple bacterial cultures performed on the discharge were negative for any growth. A fine needle aspiration cytology was positive for acid-fast bacilli. The patient refused a biopsy. He was started on anti-tubercular treatment with which the lesions began to regress.
The patient denied having used an insulin syringe that was used earlier for Bacillus Calmette-Guérin vaccination. However, he was sure that a particular vial of insulin was associated with these lesions because no new lesions appeared after he changed vials. Unfortunately, the vial in question could not be retrieved.
The patient was thoroughly evaluated but was not found to have any tubercular foci elsewhere in the body. Although tuberculosis is endemic in our country, tuberculosis at insulin injection sites caught us by surprise. There are no similar case reports or descriptions, although we did find case reports from Columbia of cutaneous tuberculosis after subcutaneous injections for cosmetic mesotherapy. 1
A young woman with diabetes and uncontrolled blood glucose was found to be injecting insulin into her forearm ( Figure 4 ), and yet another man was found to be injecting insulin intradermally on his thigh with residual post-inflammatory hyperpigmentation ( Figure 5 ).
What are some of the causes of insulin therapy failure?
How can clinicians be vigilant in identifying patients with nonadherence to or problems carrying out their insulin regimen?
What are the consequences of nonadherence to insulin therapy?
How can we ensure better adherence to insulin therapy?

Forearm injection sites of the female patient described in Case Study 6.

Post-inflammatory hyperpigmentation in the thighs of the male patient described in Case Study 7.
Incomplete or incorrect initial education and a lack of continuing education are at the root of all of the cases reported above. Apart from the obvious effects they have on glycemic status, incidents such as these leave an indelible trauma in the minds of patients and act as strong deterrents to continuing insulin therapy.
Doctors and patients expend great effort to start insulin, and the manner in which we use this last arrow in our treatment quiver matters. In a busy outpatient department, the easiest thing to do for patients with uncontrolled blood glucose levels is simply to increase the dose of insulin. However, this not only destroys patients' confidence in insulin, but also leads to decreasing self-confidence and depression in patients on insulin. Hence, it would seem prudent and rewarding to devote some time to educating patients and using every visit to reinforce their knowledge and verify their insulin therapy practices. Logistical issues and test conditions need to be factored in when interpreting blood glucose data. This also highlights the importance of the role of diabetes educators and paramedical staff in care of diabetes patients. Unfortunately, these professionals and the services they provide are missing in most diabetes clinics in underdeveloped or developing countries, where the gap between the disease burden and the availability of care providers is widening rapidly.
Recent reviews on insulin adherence in Western countries show adherence rates as low as 62–64%. 2 Estimates of diabetes medication adherence in our country (India) are even worse, especially in populations in which illiteracy and poverty levels are very high. Nonadherence rates as high as 74% (95% CI 69.2–78.3) have been reported from south India. 3
Insulin nonadherence has been shown to be a significant risk factor for increased mortality and increased costs of therapy in the diabetic population. 4 , 5 Many factors determine adherence to insulin. Misinformation and miscommunication between doctors and patients is one of the foremost causes. Illness and treatment perceptions have also been shown to be an important determinant of adherence. 6 Among various suggestions to improve treatment adherence is a participatory model in which patients are made an integral part of decision-making. This has been shown to improve adherence to insulin and antidiabetic drugs and, hence, to improve outcomes. 7
All insulin-requiring patients must learn to position the needle perpendicular to their skin when injecting insulin, rotate injection sites, discard syringes after a single use, inject at appropriate sites, inject subcutaneously into fat, count to 10 after injections, store insulin in a cool and airy place away from direct sunlight, and discard open vials after 1 month or the prescribed shelf life indicated on the vial. 8 Apart from this basic education, they should be taught methods that may reduce the pain of injection, such as allowing the insulin to come to room temperature before injecting, making sure there are no air bubbles in the syringe, and keeping underlying muscles relaxed. This information may help to boost patients' morale. 8
A change in temperature can change the concentration of insulin in the cartridge of a pen device. 9 Hence, it is recommended to remove the needle from the pen immediately after use so the temperature of the insulin is not affected by the leak in thermo insulation caused by the attached needle. 10 Another common mistake is using a 100 IU/ml pen cartridge but injecting insulin through a 40 IU/ml syringe. Patients also should be educated about the color coding of syringes and vials of different insulin concentrations (e.g., a red syringe is 40 IU/ml, whereas an orange syringe is 100 IU/ml).
Although the cases described here expose our shortcomings in diabetes care, highlighting such unusual clinical scenarios might alert other health care providers to recognize similar instances in their practice and enable better outcomes from insulin therapy.
CLINICAL PEARLS
Unexplained deterioration in glycemic control and discrepancies between plasma glucose, SMBG values, and A1C test results should alert physicians to the possibility of patients' nonadherence with or poor practices in carrying out their insulin regimen.
Nonadherence is associated with a significantly higher mortality, higher complication rates, low self-confidence, poor self-image, and adverse disease-related perceptions.
In addition to patient illiteracy and poverty, failure on the part of the health care system to ensure a proper, planned, and staged patient education and confidence-building program before instituting insulin therapy is a major barrier to successful insulin therapy.
A few hours spent by physicians, nurses, or other diabetes educators with patients initiating insulin may save many years of life for these patients.
Email alerts
- Online ISSN 1945-4953
- Print ISSN 0891-8929
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account

IMAGES
VIDEO
COMMENTS
The general purpose of feedback inhibition is to regulate the concentration of compounds in the cell. If feedback inhibition occurs when it isn't supposed to, the concentration of the compound being regulated may decrease to levels that are detrimental to the cell. In this study, elevated levels of glucose stimulate the release of insulin.
Other signaling molecules like the protein insulin are both too hydrophilic and too large to pass through the plasma membrane. The insulin receptor is an integral membrane protein with an extracellular signal-binding domain. 1. by Kristy J. WilsonSchool of Mathematics and SciencesMarian University, Indianapolis, IN Diabetes and Insulin Signaling
Case Study #2 - "Diabetes and Insulin Signaling": Week 1 - February 26 - March 1 Week 2 - March 11 - March 15 Overall Goal: The overall goal of this two-week project is to achieve a number of objectives. First, insulin is a major thread that is woven into this course (e. Humulin - first biologic in 1982, insulin receptor
Study with Quizlet and memorize flashcards containing terms like Notes on the stuff before Part 1, What are the essential parts of a signaling pathway?, how could activating a transcription factor cause long-term cellular changes and more. ... Case Study: Diabetes & Insulin Signaling Questions & Notes. Flashcards; Learn;
Part II - Diabetes and Insulin Signaling 1. How could the study of insulin signaling help people with diabetes? By understanding insulin signaling, better treatment and management of diabetes is possible. In addition to injectable insulins to reduce blood glucose, a number of oral diabetic treatment medications have been developed.
Re-form the groups from Week 1 and begin "Part II - Diabetes and Insulin Signaling." Go over Excerpt 2 and 3, and then answer Questions 1-6 on Page 7. Review the questions as a class and then read "Part III - Insulin Resistance" and Excerpt 4. Answer Questions 1-3 as a group on Page 8, and then go over those questions as a class.
Start studying Case Study: Diabetes & Insulin Signaling Questions & Notes. Learn vocabulary, terms, and more with flashcards, games, and other study tools.
There are, however, some generalized steps that can be applied to many different signaling situations. This case study uses insulin signaling and the pathological case of diabetes as a lens through which students will learn general signaling mechanisms like kinase cascades and second messenger pathways. The case is designed in the interrupted ...
Registered dietitians (RDs) who have earned the Board Certified-Advanced Diabetes Manager (BC-ADM) credential hold a master's or doctorate degree in a clinically relevant area and have at least 500 hours of recent experience helping with the clinical management of people with diabetes.1 They work in both inpatient and outpatient settings, including diabetes or endocrine-based specialty ...
Type 2 diabetes originates in an expanding adipose tissue that for unknown reasons becomes insulin resistant. Insulin resistance reflects impairments in insulin signaling, but mechanisms involved are unclear because current research is fragmented. We report a systems level mechanistic understanding …
Diabetes and Insulin Signaling Case Study - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. m
Page 1 "Diabetes and Insulin Signaling" by Kristy J. Wilson by Kristy J. Wilson School of Mathematics and Sciences Marian University, Indianapolis, IN Diabetes and Insulin Signaling Part I - Research Orientation "Hi, Dr. Kim. My name is Mia. I'm the undergraduate from the Research Experience for Undergraduates program. I've been assigned to work with you this summer." "It's ...
Feedback inhibition acts to shut down a signaling pathway that is no longer required - e.g. often in metabolism, the final product inhibits an enzyme at the beginning of the signaling pathway Specific pathway example - "In the context of insulin signaling, a signaling effector called IRS1 coordinates many different signals. IRS1 binds to the insulin receptor and activates the MAPK kinase cascade.
NATIONAL CENTER FOR CASE STUDY TEACHING IN SCIENCE "Diabetes and Insulin Signaling" by Kristy J. Wilson Page 5 Part II - Diabetes and Insulin Signaling "Mia, now that you understand the basics of signaling and the mechanisms it uses, I want to talk about why this lab studies cellular signaling.
Student Directions for Case Study 2 Case Study #2 - "Diabetes and Insulin Signaling": Week 1 - October 2 - October 6 Week 2 - October 9 - October 13 Overall Goal: The overall goal of this two-week project is to achieve a number of objectives. First, insulin is a major thread that is woven into this course (e.
View diabetes and Insulin Signaling Case STudy Questions.pdf from BIO 123 at Reseda Senior High. Diabetes and Insulin Signaling Case Study Questions (my answers will be in blue font- rumaisa) PART I
Hyperinsulinemia is a marker of insulin resistance, a common feature of type 2 diabetes mellitus (T2DM), and can be associated with metabolic syndrome. 1,10 The main reason for this event can be explained by the impaired transduction of insulin signals as a result of receptor dysfunction. Patients with severe insulin resistance require large doses of insulin, such as >2 units/kg of body weight ...
Diabetes and Insulin Signaling Case Study Read and answer the questions for each part of this case study. Part 1 - Research Orientation 1. What are the essential parts of a signaling pathway? The initial signal, the receptor that binds the signal, the signaling molecules or molecules that transmit the message, and the effect or effectors that result in short-term or lon- term cellular change.
In-Person Answer Sheet for "Diabetes & Insulin Signaling" INSTRUCTIONS: Answer the indicated questions using the PDF "Diabetes & Insulin Signaling." You do not need to use the internet to answer these questions. The information within the case study and the material from week 8 should be sufficient.
The patient was a 45-year-old man who has had type 2 diabetes for the past 6 years and had been taking insulin for the past 2 years. His body weight was 50 kg (BMI 24 kg/m 2).He presented with uncontrolled and recently increased blood glucose levels and a dramatic increase in insulin dose during the past 5 months without any apparent cause.
Project national center for case study teaching in science diabetes and insulin signaling kristy wilson school of mathematics and sciences marian university, Skip to document. University; ... ID#28762251. Case copyright held by the National Center for Case Study Teaching in Science, University at Bufalo, State University of New York. Originally ...
Diabetes of a form that develops especially in adults and most often obese individuals and that is characterized by high blood glucose resulting from impaired insulin utilization coupled with the body's inability to compensate with increased insulin production. 1. the initial signal2.
There is currently no way to prevent type 1 diabetes. But recent studies suggest screening can help avert a life-threatening condition called diabetic ketoacidosis (DKA), which strikes when insulin levels fall perilously low and the body, unable to metabolize sugar, starts to break down fat for energy. Anywhere from 20% to 70% of children have ...
Part 2 - Diabetes and Insulin Signaling 1. How could the study of insulin signaling help people with diabetes? Having a better understanding of the pathway can make it easier to identify what the issue is that is preventing the production of insulin/glucose when needed.