Using the Medical Research Council framework for the development and evaluation of complex interventions in a theory-based infant feeding intervention to prevent childhood obesity: the baby milk intervention and trial
Affiliations.
- 1 MRC Epidemiology Unit, University of Cambridge, Addenbrooke's Hospital, P.O. Box 285, Cambridge CB2 0QQ, UK ; UKCRC Centre for Diet and Activity Research, University of Cambridge, Cambridge CB2 0QQ, UK.
- 2 MRC Epidemiology Unit, University of Cambridge, Addenbrooke's Hospital, P.O. Box 285, Cambridge CB2 0QQ, UK ; UKCRC Centre for Diet and Activity Research, University of Cambridge, Cambridge CB2 0QQ, UK ; The Primary Care Unit, Department of Public Health and Primary Care, University of Cambridge, Cambridge CB2 0SR, UK.
- 3 The Primary Care Unit, Department of Public Health and Primary Care, University of Cambridge, Cambridge CB2 0SR, UK.
- 4 UKCRC Centre for Diet and Activity Research, University of Cambridge, Cambridge CB2 0QQ, UK.
- 5 MRC Epidemiology Unit, University of Cambridge, Addenbrooke's Hospital, P.O. Box 285, Cambridge CB2 0QQ, UK ; Department of Paediatrics, University of Cambridge, Cambridge CB2 0QQ, UK.
- PMID: 25143830
- PMCID: PMC4131118
- DOI: 10.1155/2014/646504
Introduction: We describe our experience of using the Medical Research Council framework on complex interventions to guide the development and evaluation of an intervention to prevent obesity by modifying infant feeding behaviours.
Methods: We reviewed the epidemiological evidence on early life risk factors for obesity and interventions to prevent obesity in this age group. The review suggested prevention of excess weight gain in bottle-fed babies and appropriate weaning as intervention targets; hence we undertook systematic reviews to further our understanding of these behaviours. We chose theory and behaviour change techniques that demonstrated evidence of effectiveness in altering dietary behaviours. We subsequently developed intervention materials and evaluation tools and conducted qualitative studies with mothers (intervention recipients) and healthcare professionals (intervention deliverers) to refine them. We developed a questionnaire to assess maternal attitudes and feeding practices to understand the mechanism of any intervention effects.
Conclusions: In addition to informing development of our specific intervention and evaluation materials, use of the Medical Research Council framework has helped to build a generalisable evidence base for early life nutritional interventions. However, the process is resource intensive and prolonged, and this should be taken into account by public health research funders. This trial is registered with ISRTCN: 20814693 Baby Milk Trial.

Publication types
- Clinical Trial
- Research Support, Non-U.S. Gov't
- Biomedical Research
- Feasibility Studies
- Feeding Behavior / psychology*
- Health Behavior*
- Health Knowledge, Attitudes, Practice
- Infant Nutritional Physiological Phenomena*
- Infant, Newborn
- Mothers* / psychology
- Pediatric Obesity / prevention & control*
- Pediatric Obesity / psychology
- Socioeconomic Factors
- Surveys and Questionnaires
- Weight Gain
Grants and funding
- MC_EX_G0701655/MRC_/Medical Research Council/United Kingdom
- MC_U106179474/MRC_/Medical Research Council/United Kingdom
- MR/K023187/1/MRC_/Medical Research Council/United Kingdom
- BHF_/British Heart Foundation/United Kingdom
- MC_EX_MR/J000361/1/MRC_/Medical Research Council/United Kingdom
- MR/J000361/1/MRC_/Medical Research Council/United Kingdom
- MC_UU_12015/2/MRC_/Medical Research Council/United Kingdom
- MC_U106179472/MRC_/Medical Research Council/United Kingdom
- MC_EX_UU_MR/J000361/1/MRC_/Medical Research Council/United Kingdom
- WT_/Wellcome Trust/United Kingdom
- CRUK_/Cancer Research UK/United Kingdom
- DH_/Department of Health/United Kingdom
- BB_/Biotechnology and Biological Sciences Research Council/United Kingdom
- MC_UU_12015/4/MRC_/Medical Research Council/United Kingdom
- G070165/MRC_/Medical Research Council/United Kingdom
- CSO_/Chief Scientist Office/United Kingdom
- G0200391/MRC_/Medical Research Council/United Kingdom
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
February 11, 2022
Reusable plastic bottles shown to release hundreds of chemicals
by University of Copenhagen

Researchers at the University of Copenhagen have found several hundred different chemical substances in tap water stored in reusable plastic bottles. Several of these substances are potentially harmful to human health. There is a need for better regulation and manufacturing standards for manufacturers, according to the chemists behind the study.
Have you ever experienced the strange taste of water after it has been in a reusable plastic bottle for a while? It appears that there is a solid, yet worrying reason for this.
Two chemists from the University of Copenhagen have studied which chemical substances are released into liquids by popular types of soft plastic reusable bottles. The results were quite a surprise.
"We were taken aback by the large amount of chemical substances we found in water after 24 hours in the bottles. There were hundreds of substances in the water—including substances never before found in plastic, as well as substances that are potentially harmful to health. After a dishwasher cycle, there were several thousand," says Jan H. Christensen, Professor of Environmental Analytical Chemistry at the University of Copenhagen's Department of Plant and Environmental Sciences.
Endocrine disruptors and insecticide
Professor Christensen and fellow researcher Selina Tisler detected more than 400 different substances from the bottle plastic and over 3,500 substances derived from dishwasher soap. A large portion of these are unknown substances that the researchers have yet to identify. But even of the identified chemicals, the toxicity of at least 70 % remains unknown.
Photo-initiators are among the toxic substances in the water which worry the researchers. These are known to have potentially harmful effects on health in organisms, such as being endocrine disruptors and carcinogens. Furthermore, the researchers found a variety of plastic softeners, antioxidants and release agents used in the manufacture of the plastic, as well as Diethyltoluamide (DEET), commonly known as the active substance in mosquito spray.
Machine washing adds more substances into the bottled water
In their experiments, the researchers mimicked the ways in which many people typically use plastic drinks bottles. People often drink water that has been kept in bottles for several hours. The researchers left ordinary tap water in both new and used drinking bottles for 24 hours, both before and after machine washing, as well as after the bottles had been in the dishwasher and rinsed thoroughly in tap water.
"What is released most after machine washing are the soap substances from the surface. Most of the chemicals that come from the water bottle itself remain after machine washing and extra rinsing. The most toxic substances that we identified actually came after the bottle had been in the dishwasher—presumably because washing wears down the plastic and thereby increases leaching," explains postdoctoral researcher and first author Selina Tisler of the Department of Plant and Environmental Sciences.
In new reusable bottles, close to 500 different substances remained in the water after an additional rinse. Over 100 of these substances came from the plastic itself.
She emphasizes that they have yet to conclude whether the water in the bottles is harmful to health, as they currently have only an estimate of the concentrations of the substances and toxicological assessments have yet to be completed.
"Just because these substances are in the water, doesn't mean that the water is toxic and affects us humans. But the problem is, is that we just don't know. And in principle, it isn't all that great to be drinking soap residues or other chemicals," says Selina Tisler.
Using chromatography the researchers screened the drinking water in the bottles for all substances present. Credit: Selina Tisler "From now on, I'll use a glass bottle"
"We care so much about low levels of pesticides in our drinking water. But when we pour water into a container to drink from, we unflinchingly add hundreds or thousands of substances to the water ourselves. Although we cannot yet say whether the substances in the reusable bottles affect our health, I'll be using a glass or quality stainless steel bottle in the future," says Jan H. Christensen.
The researchers suspect that bottle manufacturers only add a small proportion of the substances found intentionally. The majority have inadvertently occurred either during the production process or during use, where substances may have been converted from other substances. This includes the presence of the mosquito repellent DEET, where the researchers hypothesize that as one of the plastic softeners degrades, it is converted into DEET.
"But even of the known substances that manufacturers deliberately add, only a tiny fraction of the toxicity has been studied. So, as a consumer, you don't know if any of the others have a detrimental effect on your health," says Selina Tisler.
Too little knowledge, too leniently regulated
According to the researchers, the results reflect a lack of both knowledge and regulation:
"The study exemplifies how little knowledge there is about the chemicals emitted from the products that our food and drink come in contact with. And, it is a general problem that measurement regulations during production are very lenient. Fortunately, both in Denmark and internationally, we are looking into how to better regulate this area," says Jan H. Christensen.
In the meantime, Selina Tisler hopes that companies take responsibility on their own accord:
"Hopefully, companies that put their names on reusable plastic bottles will be more careful about the products they purchase from suppliers and perhaps place greater demands on suppliers to investigate the substances found in what they manufacture," Tisler concludes.
The study results are published in the Journal of Hazardous Materials.
How they did it
Three different types of drinking bottles were tested, all of which are found in Danish stores. Two of the bottles are made of biodegradable plastic , according to the manufacturer. Both new and heavily used bottles were used. The bottles were tested both before and after machine washing, and after five extra rinses in tap water .
The researchers carried out a so-called non-target screening (NTS) using a liquid chromatograph and a mass spectrometer, where, as with traditional methods, it is not limited to analyzing the substances that are suspected to be present, but instead screen for all substances present.
Explore further
Feedback to editors

Research shows 'profound' link between dietary choices and brain health
18 hours ago

Component of keto diet plus immunotherapy may reduce prostate cancer
22 hours ago

Study finds big jump in addiction treatment at community health clinics

Positive childhood experiences can boost mental health and reduce depression and anxiety in teens

Gene linked to epilepsy and autism decoded in new study
Apr 26, 2024

Blood test finds knee osteoarthritis up to eight years before it appears on X-rays

Researchers find pregnancy cytokine levels impact fetal brain development and offspring behavior

Study finds biomarkers for psychiatric symptoms in patients with rare genetic condition 22q

Clinical trial evaluates azithromycin for preventing chronic lung disease in premature babies

Scientists report that new gene therapy slows down amyotrophic lateral sclerosis disease progression
Related stories.

Chemicals in plastic may contribute to weight gain
Jan 26, 2022

Pop those 'BPA-free' drinking bottles into the dishwasher before using them
Apr 29, 2021

Bioplastics contain substances that are as toxic as those in ordinary plastics
Oct 23, 2020

Students seek to ban plastic water bottles from campus
May 1, 2017

New measuring method reveals there may be more plastic on than in your salad
Jan 20, 2022

Consumer protection: Novel method for detecting hormonally active substances
Oct 7, 2021
Recommended for you

How buildings influence the microbiome and human health

Study identifies driver of liver cancer that could be target for treatment

Homelessness found to be a major issue for many patients in the emergency department

Creatine found to improve cognitive performance during sleep deprivation
Apr 25, 2024

Living at higher altitudes in India linked to increased risk of childhood stunting
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- A new framework for...
A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance
- Related content
- Peer review
- Kathryn Skivington , research fellow 1 ,
- Lynsay Matthews , research fellow 1 ,
- Sharon Anne Simpson , professor of behavioural sciences and health 1 ,
- Peter Craig , professor of public health evaluation 1 ,
- Janis Baird , professor of public health and epidemiology 2 ,
- Jane M Blazeby , professor of surgery 3 ,
- Kathleen Anne Boyd , reader in health economics 4 ,
- Neil Craig , acting head of evaluation within Public Health Scotland 5 ,
- David P French , professor of health psychology 6 ,
- Emma McIntosh , professor of health economics 4 ,
- Mark Petticrew , professor of public health evaluation 7 ,
- Jo Rycroft-Malone , faculty dean 8 ,
- Martin White , professor of population health research 9 ,
- Laurence Moore , unit director 1
- 1 MRC/CSO Social and Public Health Sciences Unit, Institute of Health and Wellbeing, University of Glasgow, Glasgow, UK
- 2 Medical Research Council Lifecourse Epidemiology Unit, University of Southampton, Southampton, UK
- 3 Medical Research Council ConDuCT-II Hub for Trials Methodology Research and Bristol Biomedical Research Centre, Bristol, UK
- 4 Health Economics and Health Technology Assessment Unit, Institute of Health and Wellbeing, University of Glasgow, Glasgow, UK
- 5 Public Health Scotland, Glasgow, UK
- 6 Manchester Centre for Health Psychology, University of Manchester, Manchester, UK
- 7 London School of Hygiene and Tropical Medicine, London, UK
- 8 Faculty of Health and Medicine, Lancaster University, Lancaster, UK
- 9 Medical Research Council Epidemiology Unit, University of Cambridge, Cambridge, UK
- Correspondence to: K Skivington Kathryn.skivington{at}glasgow.ac.uk
- Accepted 9 August 2021
The UK Medical Research Council’s widely used guidance for developing and evaluating complex interventions has been replaced by a new framework, commissioned jointly by the Medical Research Council and the National Institute for Health Research, which takes account of recent developments in theory and methods and the need to maximise the efficiency, use, and impact of research.
Complex interventions are commonly used in the health and social care services, public health practice, and other areas of social and economic policy that have consequences for health. Such interventions are delivered and evaluated at different levels, from individual to societal levels. Examples include a new surgical procedure, the redesign of a healthcare programme, and a change in welfare policy. The UK Medical Research Council (MRC) published a framework for researchers and research funders on developing and evaluating complex interventions in 2000 and revised guidance in 2006. 1 2 3 Although these documents continue to be widely used and are now accompanied by a range of more detailed guidance on specific aspects of the research process, 4 5 6 7 8 several important conceptual, methodological and theoretical developments have taken place since 2006. These developments have been included in a new framework commissioned by the National Institute of Health Research (NIHR) and the MRC. 9 The framework aims to help researchers work with other stakeholders to identify the key questions about complex interventions, and to design and conduct research with a diversity of perspectives and appropriate choice of methods.
Summary points
Complex intervention research can take an efficacy, effectiveness, theory based, and/or systems perspective, the choice of which is based on what is known already and what further evidence would add most to knowledge
Complex intervention research goes beyond asking whether an intervention works in the sense of achieving its intended outcome—to asking a broader range of questions (eg, identifying what other impact it has, assessing its value relative to the resources required to deliver it, theorising how it works, taking account of how it interacts with the context in which it is implemented, how it contributes to system change, and how the evidence can be used to support real world decision making)
A trade-off exists between precise unbiased answers to narrow questions and more uncertain answers to broader, more complex questions; researchers should answer the questions that are most useful to decision makers rather than those that can be answered with greater certainty
Complex intervention research can be considered in terms of phases, although these phases are not necessarily sequential: development or identification of an intervention, assessment of feasibility of the intervention and evaluation design, evaluation of the intervention, and impactful implementation
At each phase, six core elements should be considered to answer the following questions:
How does the intervention interact with its context?
What is the underpinning programme theory?
How can diverse stakeholder perspectives be included in the research?
What are the key uncertainties?
How can the intervention be refined?
What are the comparative resource and outcome consequences of the intervention?
The answers to these questions should be used to decide whether the research should proceed to the next phase, return to a previous phase, repeat a phase, or stop
Development of the Framework for Developing and Evaluating Complex Interventions
The updated Framework for Developing and Evaluating Complex Interventions is the culmination of a process that included four stages:
A gap analysis to identify developments in the methods and practice since the previous framework was published
A full day expert workshop, in May 2018, of 36 participants to discuss the topics identified in the gap analysis
An open consultation on a draft of the framework in April 2019, whereby we sought stakeholder opinion by advertising via social media, email lists and other networks for written feedback (52 detailed responses were received from stakeholders internationally)
Redraft using findings from the previous stages, followed by a final expert review.
We also sought stakeholder views at various interactive workshops throughout the development of the framework: at the annual meetings of the Society for Social Medicine and Population Health (2018), the UK Society for Behavioural Medicine (2017, 2018), and internationally at the International Congress of Behavioural Medicine (2018). The entire process was overseen by a scientific advisory group representing the range of relevant NIHR programmes and MRC population health investments. The framework was reviewed by the MRC-NIHR Methodology Research Programme Advisory Group and then approved by the MRC Population Health Sciences Group in March 2020 before undergoing further external peer and editorial review through the NIHR Journals Library peer review process. More detailed information and the methods used to develop this new framework are described elsewhere. 9 This article introduces the framework and summarises the main messages for producers and users of evidence.
What are complex interventions?
An intervention might be considered complex because of properties of the intervention itself, such as the number of components involved; the range of behaviours targeted; expertise and skills required by those delivering and receiving the intervention; the number of groups, settings, or levels targeted; or the permitted level of flexibility of the intervention or its components. For example, the Links Worker Programme was an intervention in primary care in Glasgow, Scotland, that aimed to link people with community resources to help them “live well” in their communities. It targeted individual, primary care (general practitioner (GP) surgery), and community levels. The intervention was flexible in that it could differ between primary care GP surgeries. In addition, the Link Workers did not support just one specific health or wellbeing issue: bereavement, substance use, employment, and learning difficulties were all included. 10 11 The complexity of this intervention had implications for many aspects of its evaluation, such as the choice of appropriate outcomes and processes to assess.
Flexibility in intervention delivery and adherence might be permitted to allow for variation in how, where, and by whom interventions are delivered and received. Standardisation of interventions could relate more to the underlying process and functions of the intervention than on the specific form of components delivered. 12 For example, in surgical trials, protocols can be designed with flexibility for intervention delivery. 13 Interventions require a theoretical deconstruction into components and then agreement about permissible and prohibited variation in the delivery of those components. This approach allows implementation of a complex intervention to vary across different contexts yet maintain the integrity of the core intervention components. Drawing on this approach in the ROMIO pilot trial, core components of minimally invasive oesophagectomy were agreed and subsequently monitored during main trial delivery using photography. 14
Complexity might also arise through interactions between the intervention and its context, by which we mean “any feature of the circumstances in which an intervention is conceived, developed, implemented and evaluated.” 6 15 16 17 Much of the criticism of and extensions to the existing framework and guidance have focused on the need for greater attention on understanding how and under what circumstances interventions bring about change. 7 15 18 The importance of interactions between the intervention and its context emphasises the value of identifying mechanisms of change, where mechanisms are the causal links between intervention components and outcomes; and contextual factors, which determine and shape whether and how outcomes are generated. 19
Thus, attention is given not only to the design of the intervention itself but also to the conditions needed to realise its mechanisms of change and/or the resources required to support intervention reach and impact in real world implementation. For example, in a cluster randomised trial of ASSIST (a peer led, smoking prevention intervention), researchers found that the intervention worked particularly well in cohesive communities that were served by one secondary school where peer supporters were in regular contact with their peers—a key contextual factor consistent with diffusion of innovation theory, which underpinned the intervention design. 20 A process evaluation conducted alongside a trial of robot assisted surgery identified key contextual factors to support effective implementation of this procedure, including engaging staff at different levels and surgeons who would not be using robot assisted surgery, whole team training, and an operating theatre of suitable size. 21
With this framing, complex interventions can helpfully be considered as events in systems. 16 Thinking about systems helps us understand the interaction between an intervention and the context in which it is implemented in a dynamic way. 22 Systems can be thought of as complex and adaptive, 23 characterised by properties such as emergence, feedback, adaptation, and self-organisation ( table 1 ).
Properties and examples of complex adaptive systems
- View inline
For complex intervention research to be most useful to decision makers, it should take into account the complexity that arises both from the intervention’s components and from its interaction with the context in which it is being implemented.
Research perspectives
The previous framework and guidance were based on a paradigm in which the salient question was to identify whether an intervention was effective. Complex intervention research driven primarily by this question could fail to deliver interventions that are implementable, cost effective, transferable, and scalable in real world conditions. To deliver solutions for real world practice, complex intervention research requires strong and early engagement with patients, practitioners, and policy makers, shifting the focus from the “binary question of effectiveness” 26 to whether and how the intervention will be acceptable, implementable, cost effective, scalable, and transferable across contexts. In line with a broader conception of complexity, the scope of complex intervention research needs to include the development, identification, and evaluation of whole system interventions and the assessment of how interventions contribute to system change. 22 27 The new framework therefore takes a pluralistic approach and identifies four perspectives that can be used to guide the design and conduct of complex intervention research: efficacy, effectiveness, theory based, and systems ( table 2 ).
Although each research perspective prompts different types of research question, they should be thought of as overlapping rather than mutually exclusive. For example, theory based and systems perspectives to evaluation can be used in conjunction, 33 while an effectiveness evaluation can draw on a theory based or systems perspective through an embedded process evaluation to explore how and under what circumstances outcomes are achieved. 34 35 36
Most complex health intervention research so far has taken an efficacy or effectiveness perspective and for some research questions these perspectives will continue to be the most appropriate. However, some questions equally relevant to the needs of decision makers cannot be answered by research restricted to an efficacy or effectiveness perspective. A wider range and combination of research perspectives and methods, which answer questions beyond efficacy and effectiveness, need to be used by researchers and supported by funders. Doing so will help to improve the extent to which key questions for decision makers can be answered by complex intervention research. Example questions include:
Will this effective intervention reproduce the effects found in the trial when implemented here?
Is the intervention cost effective?
What are the most important things we need to do that will collectively improve health outcomes?
In the absence of evidence from randomised trials and the infeasibility of conducting such a trial, what does the existing evidence suggest is the best option now and how can this be evaluated?
What wider changes will occur as a result of this intervention?
How are the intervention effects mediated by different settings and contexts?
Phases and core elements of complex intervention research
The framework divides complex intervention research into four phases: development or identification of the intervention, feasibility, evaluation, and implementation ( fig 1 ). A research programme might begin at any phase, depending on the key uncertainties about the intervention in question. Repeating phases is preferable to automatic progression if uncertainties remain unresolved. Each phase has a common set of core elements—considering context, developing and refining programme theory, engaging stakeholders, identifying key uncertainties, refining the intervention, and economic considerations. These elements should be considered early and continually revisited throughout the research process, and especially before moving between phases (for example, between feasibility testing and evaluation).

Framework for developing and evaluating complex interventions. Context=any feature of the circumstances in which an intervention is conceived, developed, evaluated, and implemented; programme theory=describes how an intervention is expected to lead to its effects and under what conditions—the programme theory should be tested and refined at all stages and used to guide the identification of uncertainties and research questions; stakeholders=those who are targeted by the intervention or policy, involved in its development or delivery, or more broadly those whose personal or professional interests are affected (that is, who have a stake in the topic)—this includes patients and members of the public as well as those linked in a professional capacity; uncertainties=identifying the key uncertainties that exist, given what is already known and what the programme theory, research team, and stakeholders identify as being most important to discover—these judgments inform the framing of research questions, which in turn govern the choice of research perspective; refinement=the process of fine tuning or making changes to the intervention once a preliminary version (prototype) has been developed; economic considerations=determining the comparative resource and outcome consequences of the interventions for those people and organisations affected
- Download figure
- Open in new tab
- Download powerpoint
Core elements
The effects of a complex intervention might often be highly dependent on context, such that an intervention that is effective in some settings could be ineffective or even harmful elsewhere. 6 As the examples in table 1 show, interventions can modify the contexts in which they are implemented, by eliciting responses from other agents, or by changing behavioural norms or exposure to risk, so that their effects will also vary over time. Context can be considered as both dynamic and multi-dimensional. Key dimensions include physical, spatial, organisational, social, cultural, political, or economic features of the healthcare, health system, or public health contexts in which interventions are implemented. For example, the evaluation of the Breastfeeding In Groups intervention found that the context of the different localities (eg, staff morale and suitable premises) influenced policy implementation and was an explanatory factor in why breastfeeding rates increased in some intervention localities and declined in others. 37
Programme theory
Programme theory describes how an intervention is expected to lead to its effects and under what conditions. It articulates the key components of the intervention and how they interact, the mechanisms of the intervention, the features of the context that are expected to influence those mechanisms, and how those mechanisms might influence the context. 38 Programme theory can be used to promote shared understanding of the intervention among diverse stakeholders, and to identify key uncertainties and research questions. Where an intervention (such as a policy) is developed by others, researchers still need to theorise the intervention before attempting to evaluate it. 39 Best practice is to develop programme theory at the beginning of the research project with involvement of diverse stakeholders, based on evidence and theory from relevant fields, and to refine it during successive phases. The EPOCH trial tested a large scale quality improvement programme aimed at improving 90 day survival rates for patients undergoing emergency abdominal surgery; it included a well articulated programme theory at the outset, which supported the tailoring of programme delivery to local contexts. 40 The development, implementation, and post-study reflection of the programme theory resulted in suggested improvements for future implementation of the quality improvement programme.
A refined programme theory is an important evaluation outcome and is the principal aim where a theory based perspective is taken. Improved programme theory will help inform transferability of interventions across settings and help produce evidence and understanding that is useful to decision makers. In addition to full articulation of programme theory, it can help provide visual representations—for example, using a logic model, 41 42 43 realist matrix, 44 or a system map, 45 with the choice depending on which is most appropriate for the research perspective and research questions. Although useful, any single visual representation is unlikely to sufficiently articulate the programme theory—it should always be articulated well within the text of publications, reports, and funding applications.
Stakeholders
Stakeholders include those individuals who are targeted by the intervention or policy, those involved in its development or delivery, or those whose personal or professional interests are affected (that is, all those who have a stake in the topic). Patients and the public are key stakeholders. Meaningful engagement with appropriate stakeholders at each phase of the research is needed to maximise the potential of developing or identifying an intervention that is likely to have positive impacts on health and to enhance prospects of achieving changes in policy or practice. For example, patient and public involvement 46 activities in the PARADES programme, which evaluated approaches to reduce harm and improve outcomes for people with bipolar disorder, were wide ranging and central to the project. 47 Involving service users with lived experiences of bipolar disorder had many benefits, for example, it enhanced the intervention but also improved the evaluation and dissemination methods. Service users involved in the study also had positive outcomes, including more settled employment and progression to further education. Broad thinking and consultation is needed to identify a diverse range of appropriate stakeholders.
The purpose of stakeholder engagement will differ depending on the context and phase of the research, but is essential for prioritising research questions, the co-development of programme theory, choosing the most useful research perspective, and overcoming practical obstacles to evaluation and implementation. Researchers should nevertheless be mindful of conflicts of interest among stakeholders and use transparent methods to record potential conflicts of interest. Research should not only elicit stakeholder priorities, but also consider why they are priorities. Careful consideration of the appropriateness and methods of identification and engagement of stakeholders is needed. 46 48
Key uncertainties
Many questions could be answered at each phase of the research process. The design and conduct of research need to engage pragmatically with the multiple uncertainties involved and offer a flexible and emergent approach to exploring them. 15 Therefore, researchers should spend time developing the programme theory, clearly identifying the remaining uncertainties, given what is already known and what the research team and stakeholders identify as being most important to determine. Judgments about the key uncertainties inform the framing of research questions, which in turn govern the choice of research perspective.
Efficacy trials of relatively uncomplicated interventions in tightly controlled conditions, where research questions are answered with great certainty, will always be important, but translation of the evidence into the diverse settings of everyday practice is often highly problematic. 27 For intervention research in healthcare and public health settings to take on more challenging evaluation questions, greater priority should be given to mixed methods, theory based, or systems evaluation that is sensitive to complexity and that emphasises implementation, context, and system fit. This approach could help improve understanding and identify important implications for decision makers, albeit with caveats, assumptions, and limitations. 22 Rather than maintaining the established tendency to prioritise strong research designs that answer some questions with certainty but are unsuited to resolving many important evaluation questions, this more inclusive, deliberative process could place greater value on equivocal findings that nevertheless inform important decisions where evidence is sparse.
Intervention refinement
Within each phase of complex intervention research and on transition from one phase to another, the intervention might need to be refined, on the basis of data collected or development of programme theory. 4 The feasibility and acceptability of interventions can be improved by engaging potential intervention users to inform refinements. For example, an online physical activity planner for people with diabetes mellitus was found to be difficult to use, resulting in the tool providing incorrect personalised advice. To improve usability and the advice given, several iterations of the planner were developed on the basis of interviews and observations. This iterative process led to the refined planner demonstrating greater feasibility and accuracy. 49
Refinements should be guided by the programme theory, with acceptable boundaries agreed and specified at the beginning of each research phase, and with transparent reporting of the rationale for change. Scope for refinement might also be limited by the policy or practice context. Refinement will be rare in the evaluation phase of efficacy and effectiveness research, where interventions will ideally not change or evolve within the course of the study. However, between the phases of research and within systems and theory based evaluation studies, refinement of interventions in response to accumulated data or as an adaptive and variable response to context and system change are likely to be desirable features of the intervention and a key focus of the research.
Economic considerations
Economic evaluation—the comparative analysis of alternative courses of action in terms of both costs (resource use) and consequences (outcomes, effects)—should be a core component of all phases of intervention research. Early engagement of economic expertise will help identify the scope of costs and benefits to assess in order to answer questions that matter most to decision makers. 50 Broad ranging approaches such as cost benefit analysis or cost consequence analysis, which seek to capture the full range of health and non-health costs and benefits across different sectors, 51 will often be more suitable for an economic evaluation of a complex intervention than narrower approaches such as cost effectiveness or cost utility analysis. For example, evaluation of the New Orleans Intervention Model for infants entering foster care in Glasgow included short and long term economic analysis from multiple perspectives (the UK’s health service and personal social services, public sector, and wider societal perspectives); and used a range of frameworks, including cost utility and cost consequence analysis, to capture changes in the intersectoral costs and outcomes associated with child maltreatment. 52 53 The use of multiple economic evaluation frameworks provides decision makers with a comprehensive, multi-perspective guide to the cost effectiveness of the New Orleans Intervention Model.
Developing or identifying a complex intervention
Development refers to the whole process of designing and planning an intervention, from initial conception through to feasibility, pilot, or evaluation study. Guidance on intervention development has recently been developed through the INDEX study 4 ; although here we highlight that complex intervention research does not always begin with new or researcher led interventions. For example:
A key source of intervention development might be an intervention that has been developed elsewhere and has the possibility of being adapted to a new context. Adaptation of existing interventions could include adapting to a new population, to a new setting, 54 55 or to target other outcomes (eg, a smoking prevention intervention being adapted to tackle substance misuse and sexual health). 20 56 57 A well developed programme theory can help identify what features of the antecedent intervention(s) need to be adapted for different applications, and the key mechanisms that should be retained even if delivered slightly differently. 54 58
Policy or practice led interventions are an important focus of evaluation research. Again, uncovering the implicit theoretical basis of an intervention and developing a programme theory is essential to identifying key uncertainties and working out how the intervention might be evaluated. This step is important, even if rollout has begun, because it supports the identification of mechanisms of change, important contextual factors, and relevant outcome measures. For example, researchers evaluating the UK soft drinks industry levy developed a bounded conceptual system map to articulate their understanding (drawing on stakeholder views and document review) of how the intervention was expected to work. This system map guided the evaluation design and helped identify data sources to support evaluation. 45 Another example is a recent analysis of the implicit theory of the NHS diabetes prevention programme, involving analysis of documentation by NHS England and four providers, showing that there was no explicit theoretical basis for the programme, and no logic model showing how the intervention was expected to work. This meant that the justification for the inclusion of intervention components was unclear. 59
Intervention identification and intervention development represent two distinct pathways of evidence generation, 60 but in both cases, the key considerations in this phase relate to the core elements described above.
Feasibility
A feasibility study should be designed to assess predefined progression criteria that relate to the evaluation design (eg, reducing uncertainty around recruitment, data collection, retention, outcomes, and analysis) or the intervention itself (eg, around optimal content and delivery, acceptability, adherence, likelihood of cost effectiveness, or capacity of providers to deliver the intervention). If the programme theory suggests that contextual or implementation factors might influence the acceptability, effectiveness, or cost effectiveness of the intervention, these questions should be considered.
Despite being overlooked or rushed in the past, the value of feasibility testing is now widely accepted with key terms and concepts well defined. 61 62 Before initiating a feasibility study, researchers should consider conducting an evaluability assessment to determine whether and how an intervention can usefully be evaluated. Evaluability assessment involves collaboration with stakeholders to reach agreement on the expected outcomes of the intervention, the data that could be collected to assess processes and outcomes, and the options for designing the evaluation. 63 The end result is a recommendation on whether an evaluation is feasible, whether it can be carried out at a reasonable cost, and by which methods. 64
Economic modelling can be undertaken at the feasibility stage to assess the likelihood that the expected benefits of the intervention justify the costs (including the cost of further research), and to help decision makers decide whether proceeding to a full scale evaluation is worthwhile. 65 Depending on the results of the feasibility study, further work might be required to progressively refine the intervention before embarking on a full scale evaluation.
The new framework defines evaluation as going beyond asking whether an intervention works (in the sense of achieving its intended outcome), to a broader range of questions including identifying what other impact it has, theorising how it works, taking account of how it interacts with the context in which it is implemented, how it contributes to system change, and how the evidence can be used to support decision making in the real world. This implies a shift from an exclusive focus on obtaining unbiased estimates of effectiveness 66 towards prioritising the usefulness of information for decision making in selecting the optimal research perspective and in prioritising answerable research questions.
A crucial aspect of evaluation design is the choice of outcome measures or evidence of change. Evaluators should work with stakeholders to assess which outcomes are most important, and how to deal with multiple outcomes in the analysis with due consideration of statistical power and transparent reporting. A sharp distinction between one primary outcome and several secondary outcomes is not necessarily appropriate, particularly where the programme theory identifies impacts across a range of domains. Where needed to support the research questions, prespecified subgroup analyses should be carried out and reported. Even where such analyses are underpowered, they should be included in the protocol because they might be useful for subsequent meta-analyses, or for developing hypotheses for testing in further research. Outcome measures could capture changes to a system rather than changes in individuals. Examples include changes in relationships within an organisation, the introduction of policies, changes in social norms, or normalisation of practice. Such system level outcomes include how changing the dynamics of one part of a system alters behaviours in other parts, such as the potential for displacement of smoking into the home after a public smoking ban.
A helpful illustration of the use of system level outcomes is the evaluation of the Delaware Young Health Program—an initiative to improve the health and wellbeing of young people in Delaware, USA. The intervention aimed to change underlying system dynamics, structures, and conditions, so the evaluation identified systems oriented research questions and methods. Three systems science methods were used: group model building and viable systems model assessment to identify underlying patterns and structures; and social network analysis to evaluate change in relationships over time. 67
Researchers have many study designs to choose from, and different designs are optimally suited to consider different research questions and different circumstances. 68 Extensions to standard designs of randomised controlled trials (including adaptive designs, SMART trials (sequential multiple assignment randomised trials), n-of-1 trials, and hybrid effectiveness-implementation designs) are important areas of methods development to improve the efficiency of complex intervention research. 69 70 71 72 Non-randomised designs and modelling approaches might work best if a randomised design is not practical, for example, in natural experiments or systems evaluations. 5 73 74 A purely quantitative approach, using an experimental design with no additional elements such as a process evaluation, is rarely adequate for complex intervention research, where qualitative and mixed methods designs might be necessary to answer questions beyond effectiveness. In many evaluations, the nature of the intervention, the programme theory, or the priorities of stakeholders could lead to a greater focus on improving theories about how to intervene. In this view, effect estimates are inherently context bound, so that average effects are not a useful guide to decision makers working in different contexts. Contextualised understandings of how an intervention induces change might be more useful, as well as details on the most important enablers and constraints on its delivery across a range of settings. 7
Process evaluation can answer questions around fidelity and quality of implementation (eg, what is implemented and how?), mechanisms of change (eg, how does the delivered intervention produce change?), and context (eg, how does context affect implementation and outcomes?). 7 Process evaluation can help determine why an intervention fails unexpectedly or has unanticipated consequences, or why it works and how it can be optimised. Such findings can facilitate further development of the intervention programme theory. 75 In a theory based or systems evaluation, there is not necessarily such a clear distinction between process and outcome evaluation as there is in an effectiveness study. 76 These perspectives could prioritise theory building over evidence production and use case study or simulation methods to understand how outcomes or system behaviour are generated through intervention. 74 77
Implementation
Early consideration of implementation increases the potential of developing an intervention that can be widely adopted and maintained in real world settings. Implementation questions should be anticipated in the intervention programme theory, and considered throughout the phases of intervention development, feasibility testing, process, and outcome evaluation. Alongside implementation specific outcomes (such as reach or uptake of services), attention to the components of the implementation strategy, and contextual factors that support or hinder the achievement of impacts, are key. Some flexibility in intervention implementation might support intervention transferability into different contexts (an important aspect of long term implementation 78 ), provided that the key functions of the programme are maintained, and that the adaptations made are clearly understood. 8
In the ASSIST study, 20 a school based, peer led intervention for smoking prevention, researchers considered implementation at each phase. The intervention was developed to have minimal disruption on school resources; the feasibility study resulted in intervention refinements to improve acceptability and improve reach to male students; and in the evaluation (cluster randomised controlled trial), the intervention was delivered as closely as possible to real world implementation. Drawing on the process evaluation, the implementation included an intervention manual that identified critical components and other components that could be adapted or dropped to allow flexible implementation while achieving delivery of the key mechanisms of change; and a training manual for the trainers and ongoing quality assurance built into rollout for the longer term.
In a natural experimental study, evaluation takes place during or after the implementation of the intervention in a real world context. Highly pragmatic effectiveness trials or specific hybrid effectiveness-implementation designs also combine effectiveness and implementation outcomes in one study, with the aim of reducing time for translation of research on effectiveness into routine practice. 72 79 80
Implementation questions should be included in economic considerations during the early stages of intervention and study development. How the results of economic analyses are reported and presented to decision makers can affect whether and how they act on the results. 81 A key consideration is how to deal with interventions across different sectors, where those paying for interventions and those receiving the benefits of them could differ, reducing the incentive to implement an intervention, even if shown to be beneficial and cost effective. Early engagement with appropriate stakeholders will help frame appropriate research questions and could anticipate any implementation challenges that might arise. 82
Conclusions
One of the motivations for developing this new framework was to answer calls for a change in research priorities, towards allocating greater effort and funding to research that can have the optimum impact on healthcare or population health outcomes. The framework challenges the view that unbiased estimates of effectiveness are the cardinal goal of evaluation. It asserts that improving theories and understanding how interventions contribute to change, including how they interact with their context and wider dynamic systems, is an equally important goal. For some complex intervention research problems, an efficacy or effectiveness perspective will be the optimal approach, and a randomised controlled trial will provide the best design to achieve an unbiased estimate. For others, alternative perspectives and designs might work better, or might be the only way to generate new knowledge to reduce decision maker uncertainty.
What is important for the future is that the scope of intervention research is not constrained by an unduly limited set of perspectives and approaches that might be less risky to commission and more likely to produce a clear and unbiased answer to a specific question. A bolder approach is needed—to include methods and perspectives where experience is still quite limited, but where we, supported by our workshop participants and respondents to our consultations, believe there is an urgent need to make progress. This endeavour will involve mainstreaming new methods that are not yet widely used, as well as undertaking methodological innovation and development. The deliberative and flexible approach that we encourage is intended to reduce research waste, 83 maximise usefulness for decision makers, and increase the efficiency with which complex intervention research generates knowledge that contributes to health improvement.
Monitoring the use of the framework and evaluating its acceptability and impact is important but has been lacking in the past. We encourage research funders and journal editors to support the diversity of research perspectives and methods that are advocated here and to seek evidence that the core elements are attended to in research design and conduct. We have developed a checklist to support the preparation of funding applications, research protocols, and journal publications. 9 This checklist offers one way to monitor impact of the guidance on researchers, funders, and journal editors.
We recommend that the guidance is continually updated, and future updates continue to adopt a broad, pluralist perspective. Given its wider scope, and the range of detailed guidance that is now available on specific methods and topics, we believe that the framework is best seen as meta-guidance. Further editions should be published in a fluid, web based format, and more frequently updated to incorporate new material, further case studies, and additional links to other new resources.
Acknowledgments
We thank the experts who provided input at the workshop, those who responded to the consultation, and those who provided advice and review throughout the process. The many people involved are acknowledged in the full framework document. 9 Parts of this manuscript have been reproduced (some with edits and formatting changes), with permission, from that longer framework document.
Contributors: All authors made a substantial contribution to all stages of the development of the framework—they contributed to its development, drafting, and final approval. KS and LMa led the writing of the framework, and KS wrote the first draft of this paper. PC, SAS, and LMo provided critical insights to the development of the framework and contributed to writing both the framework and this paper. KS, LMa, SAS, PC, and LMo facilitated the expert workshop, KS and LMa developed the gap analysis and led the analysis of the consultation. KAB, NC, and EM contributed the economic components to the framework. The scientific advisory group (JB, JMB, DPF, MP, JR-M, and MW) provided feedback and edits on drafts of the framework, with particular attention to process evaluation (JB), clinical research (JMB), implementation (JR-M, DPF), systems perspective (MP), theory based perspective (JR-M), and population health (MW). LMo is senior author. KS and LMo are the guarantors of this work and accept the full responsibility for the finished article. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting authorship criteria have been omitted.
Funding: The work was funded by the National Institute for Health Research (Department of Health and Social Care 73514) and Medical Research Council (MRC). Additional time on the study was funded by grants from the MRC for KS (MC_UU_12017/11, MC_UU_00022/3), LMa, SAS, and LMo (MC_UU_12017/14, MC_UU_00022/1); PC (MC_UU_12017/15, MC_UU_00022/2); and MW (MC_UU_12015/6 and MC_UU_00006/7). Additional time on the study was also funded by grants from the Chief Scientist Office of the Scottish Government Health Directorates for KS (SPHSU11 and SPHSU18); LMa, SAS, and LMo (SPHSU14 and SPHSU16); and PC (SPHSU13 and SPHSU15). KS and SAS were also supported by an MRC Strategic Award (MC_PC_13027). JMB received funding from the NIHR Biomedical Research Centre at University Hospitals Bristol NHS Foundation Trust and the University of Bristol and by the MRC ConDuCT-II Hub (Collaboration and innovation for Difficult and Complex randomised controlled Trials In Invasive procedures - MR/K025643/1). DF is funded in part by the NIHR Manchester Biomedical Research Centre (IS-BRC-1215-20007) and NIHR Applied Research Collaboration - Greater Manchester (NIHR200174). MP is funded in part as director of the NIHR’s Public Health Policy Research Unit. This project was overseen by a scientific advisory group that comprised representatives of NIHR research programmes, of the MRC/NIHR Methodology Research Programme Panel, of key MRC population health research investments, and authors of the 2006 guidance. A prospectively agreed protocol, outlining the workplan, was agreed with MRC and NIHR, and signed off by the scientific advisory group. The framework was reviewed and approved by the MRC/NIHR Methodology Research Programme Advisory Group and MRC Population Health Sciences Group and completed NIHR HTA Monograph editorial and peer review processes.
Competing interests: All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/coi_disclosure.pdf and declare: support from the NIHR, MRC, and the funders listed above for the submitted work; KS has project grant funding from the Scottish Government Chief Scientist Office; SAS is a former member of the NIHR Health Technology Assessment Clinical Evaluation and Trials Programme Panel (November 2016 - November 2020) and member of the Chief Scientist Office Health HIPS Committee (since 2018) and NIHR Policy Research Programme (since November 2019), and has project grant funding from the Economic and Social Research Council, MRC, and NIHR; LMo is a former member of the MRC-NIHR Methodology Research Programme Panel (2015-19) and MRC Population Health Sciences Group (2015-20); JB is a member of the NIHR Public Health Research Funding Committee (since May 2019), and a core member (since 2016) and vice chairperson (since 2018) of a public health advisory committee of the National Institute for Health and Care Excellence; JMB is a former member of the NIHR Clinical Trials Unit Standing Advisory Committee (2015-19); DPF is a former member of the NIHR Public Health Research programme research funding board (2015-2019), the MRC-NIHR Methodology Research Programme panel member (2014-2018), and is a panel member of the Research Excellence Framework 2021, subpanel 2 (public health, health services, and primary care; November 2020 - February 2022), and has grant funding from the European Commission, NIHR, MRC, Natural Environment Research Council, Prevent Breast Cancer, Breast Cancer Now, Greater Sport, Manchester University NHS Foundation Trust, Christie Hospital NHS Trust, and BXS GP; EM is a member of the NIHR Public Health Research funding board; MP has grant funding from the MRC, UK Prevention Research Partnership, and NIHR; JR-M is programme director and chairperson of the NIHR’s Health Services Delivery Research Programme (since 2014) and member of the NIHR Strategy Board (since 2014); MW received a salary as director of the NIHR PHR Programme (2014-20), has grant funding from NIHR, and is a former member of the MRC’s Population Health Sciences Strategic Committee (July 2014 to June 2020). There are no other relationships or activities that could appear to have influenced the submitted work.
Patient and public involvement: This project was methodological; views of patients and the public were included at the open consultation stage of the update. The open consultation, involving access to an initial draft, was promoted to our networks via email and digital channels, such as our unit Twitter account ( @theSPHSU ). We received five responses from people who identified as service users (rather than researchers or professionals in a relevant capacity). Their input included helpful feedback on the main complexity diagram, the different research perspectives, the challenge of moving interventions between different contexts and overall readability and accessibility of the document. Several respondents also highlighted useful signposts to include for readers. Various dissemination events are planned, but as this project is methodological we will not specifically disseminate to patients and the public beyond the planned dissemination activities.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/ .
- Macintyre S ,
- Nazareth I ,
- Petticrew M ,
- Medical Research Council Guidance
- Campbell M ,
- Fitzpatrick R ,
- O’Cathain A ,
- Gunnell D ,
- Ruggiero ED ,
- Frohlich KL ,
- Copeland L ,
- Skivington K ,
- Matthews L ,
- Simpson SA ,
- Hawkins K ,
- Fitzpatrick B ,
- Mercer SW ,
- Blencowe NS ,
- Skilton A ,
- ROMIO Study team
- Greenhalgh T ,
- Petticrew M
- Campbell R ,
- Starkey F ,
- Holliday J ,
- ↵ Randell R, Honey S, Hindmarsh J, et al. A realist process evaluation of robot-assisted surgery: integration into routine practice and impacts on communication, collaboration and decision-making . NIHR Journals Library, 2017. https://www.ncbi.nlm.nih.gov/books/NBK447438/ .
- ↵ The Health Foundation. Evidence Scan. Complex adaptive systems. Health Foundation 2010. https://www.health.org.uk/publications/complex-adaptive-systems .
- Wiggins M ,
- Sawtell M ,
- Robinson M ,
- Kessler R ,
- Folegatti PM ,
- Oxford COVID Vaccine Trial Group
- Clemens SAC ,
- Shearer JC ,
- Burgess RA ,
- Osborne RH ,
- Yongabi KA ,
- Paltiel AD ,
- Schwartz JL ,
- Walensky RP
- Lhussier M ,
- Williams L ,
- Guthrie B ,
- Pinnock H ,
- ↵ Penney T, Adams J, Briggs A, et al. Evaluation of the impacts on health of the proposed UK industry levy on sugar sweetened beverages: developing a systems map and data platform, and collection of baseline and early impact data. National Institute for Health Research, 2018. https://www.journalslibrary.nihr.ac.uk/programmes/phr/164901/#/ .
- Hoddinott P ,
- Britten J ,
- Funnell SC ,
- Lawless A ,
- Delany-Crowe T ,
- Stephens TJ ,
- Pearse RM ,
- EPOCH trial group
- Melendez-Torres GJ ,
- Mounier-Jack S ,
- Hargreaves SC ,
- Manzano A ,
- Uzochukwu B ,
- ↵ White M, Cummins S, Raynor M, et al. Evaluation of the health impacts of the UK Treasury Soft Drinks Industry Levy (SDIL) Project Protocol. NIHR Journals Library, 2018. https://www.journalslibrary.nihr.ac.uk/programmes/phr/1613001/#/summary-of-research .
- ↵ National Institute for Health and Care Excellence. What is public involvement in research? – INVOLVE. https://www.invo.org.uk/find-out-more/what-is-public-involvement-in-research-2/ .
- Barrowclough C ,
- Stuckler D ,
- Monteiro C ,
- Lancet NCD Action Group
- Yardley L ,
- Ainsworth B ,
- Arden-Close E ,
- Barnett ML ,
- Ettner SL ,
- Powell BJ ,
- ↵ National Institute for Health and Care Excellence. Developing NICE guidelines: the manual. NICE, 2014. https://www.nice.org.uk/process/pmg20/resources/developing-nice-guidelines-the-manual-pdf-72286708700869 .
- Balogun MO ,
- BeST study team
- Escoffery C ,
- Lebow-Skelley E ,
- Haardoerfer R ,
- Stirman SW ,
- Miller CJ ,
- Forsyth R ,
- Purcell C ,
- Hawkins J ,
- Movsisyan A ,
- Rehfuess E ,
- ADAPT Panel ,
- ADAPT Panel comprises of Laura Arnold
- Hawkes RE ,
- Ogilvie D ,
- Eldridge SM ,
- Campbell MJ ,
- PAFS consensus group
- Thabane L ,
- Hopewell S ,
- Lancaster GA ,
- ↵ Craig P, Campbell M. Evaluability Assessment: a systematic approach to deciding whether and how to evaluate programmes and policies. Evaluability Assessment working paper. 2015. http://whatworksscotland.ac.uk/wp-content/uploads/2015/07/WWS-Evaluability-Assessment-Working-paper-final-June-2015.pdf
- Cummins S ,
- ↵ Expected Value of Perfect Information (EVPI). YHEC - York Health Econ. Consort. https://yhec.co.uk/glossary/expected-value-of-perfect-information-evpi/ .
- Cartwright N
- Britton A ,
- McPherson K ,
- Sanderson C ,
- Burnett T ,
- Mozgunov P ,
- Pallmann P ,
- Villar SS ,
- Wheeler GM ,
- Collins LM ,
- Murphy SA ,
- McDonald S ,
- Coronado GD ,
- Schwartz M ,
- Tugwell P ,
- Knottnerus JA ,
- McGowan J ,
- ↵ Egan M, McGill E, Penney T, et al. NIHR SPHR Guidance on Systems Approaches to Local Public Health Evaluation. Part 1: Introducing systems thinking. NIHR School for Public Health Research, 2019. https://sphr.nihr.ac.uk/wp-content/uploads/2018/08/NIHR-SPHR-SYSTEM-GUIDANCE-PART-1-FINAL_SBnavy.pdf .
- Fletcher A ,
- ↵ Bicket M, Christie I, Gilbert N, et al. Magenta Book 2020 Supplementary Guide: Handling Complexity in Policy Evaluation. Lond HM Treas 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/879437/Magenta_Book_supplementary_guide._Handling_Complexity_in_policy_evaluation.pdf
- Pfadenhauer LM ,
- Gerhardus A ,
- Mozygemba K ,
- Curran GM ,
- Mittman B ,
- Landes SJ ,
- McBain SA ,
- ↵ Imison C, Curry N, Holder H, et al. Shifting the balance of care: great expectations. Research report. Nuffield Trust. https://www.nuffieldtrust.org.uk/research/shifting-the-balance-of-care-great-expectations
- Martinez-Alvarez M ,
- Chalmers I ,
IU researchers receive $4.8 million grant to study the role of misfolded protein TDP-43 in neurodegenerative diseases
IU School of Medicine Apr 23, 2024

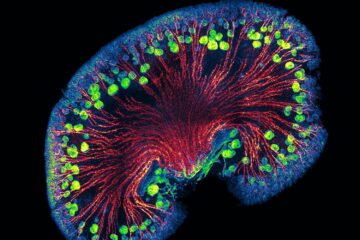
INDIANAPOLIS—A new $4.8 million grant will support researchers from Indiana University School of Medicine and the Medical Research Council Laboratory of Molecular Biology to study how human neurodegenerative diseases are affected by the misfolding of the protein TDP-43. Misfolding occurs when a protein adopts a conformation which differs from the native one.
The researchers, funded by the National Institute of Neurological Disorders and Stroke, have developed an innovative approach to deciphering the role of TDP-43 misfolding in the pathology of frontotemporal dementias, limbic predominant age-related TDP-43 encephalopathy and Alzheimer’s disease.

“The presence of misfolded proteins in the central nervous system is the hallmark of neurodegenerative diseases,” said Kathy Newell, MD , Jay C. and Lucile L. Kahn Professor of Alzheimer's Disease Research and Education at IU School of Medicine and a principal investigator of the project. “The argument for the pathogenic significance of various misfolded proteins results from the fact that mutations in the various genes encoding those proteins cause distinct genetically determined neurodegenerative diseases. Furthermore, misfolding of those proteins also occurs in sporadic neurodegenerative diseases.”

An international, multidisciplinary team has been assembled with expertise in neuropathology, digital pathology, molecular genetics, biochemistry, protein misfolding, proteomics, structural biology and cryogenic electron microscopy. The team is supported by experts in clinical neurology, protein misfolding and biostatistics, as well as by the Dementia Laboratory’s Brain Library.
“The protein TDP-43 is central to the pathogenesis of half of all frontotemporal lobar degeneration cases. Finding out how TDP-43, when misfolded, gives rise to multiple proteinopathies is extremely important for the design of diagnostic and therapeutic compounds that will target pathologic TDP-43,” Newell said.
The project is called “Investigating the role of TDP-43 mislocalization, structure, and post-translational modifications in the neuropathologically heterogeneous TDP-43 proteinopathies.”

In addition to Newell, the other principal investigators are Laura Cracco, PhD, MS , assistant research professor of pathology and laboratory medicine at IU School of Medicine and Benjamin Ryskeldi-Falcon, PhD , group leader at the Medical Research Council Laboratory of Molecular Biology in the United Kingdom. This project is the first National Institutes of Health funded research for all three investigators as principal investigators.
About IU School of Medicine
The IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability. According to the Blue Ridge Institute for Medical Research, the IU School of Medicine ranks No. 13 in 2023 National Institutes of Health funding among all public medical schools in the country.
SEARCH THE NEWSROOM
Subscribe to the news.
We've added you to our mailing list!
Sorry, there was a problem
Media Contacts
Related news.

Medical Research Council (MRC)
MRC funds research at the forefront of science to prevent illness, develop therapies and improve human health.

MRC content
- Funding, assessment and award management
- Strategy, remit and programmes
- People, skills and fellowships
- Investments, impacts and engagement
- Institutes, facilities and resources
MRC impact showcase
MRC funded discovery science underpins gene therapy cures

18 April 2024
Potential new treatment strategy for aggressive leukaemia

Trial finds first potential drug for gut damage in malnutrition

15 April 2024
Specific nasal cells protect against COVID-19 in children
View all MRC news

3 April 2024
Extreme pregnancy sickness: the quest for a cause

15 March 2024
Five things we learned from watching a funding board meeting
View all MRC blog posts
Funding opportunities
Small molecule high throughput screen using astrazeneca facilities.
Apply for funding to run a High Throughput Screen (HTS) using AstraZeneca’s compound library and screening robots.
Two funding opportunities per year with changing themes. This funding opportunity will have a focus on new targets related to Fibrosis or Extracellular Matrix.
Collaborate with the functional genomics screening laboratory
Apply to collaborate with the functional genomics screening laboratory on projects using complex human in vitro models for CRISPR screening to better understand model biology.
You must be a researcher eligible for MRC funding.
Applications from UK based industry parties may also be considered.
View all MRC opportunities
Medical Research Council (MRC) Polaris House, North Star Avenue, Swindon, SN2 1FL
Connect with MRC
Subscribe to ukri emails.
Sign up for news, views, events and funding alerts.
Conference on outputs from sustainable healthcare research
29 April 2024
Online and at The Francis Crick Institute, 1 Midland Road, London NW1 1AT
View all MRC events
This is the website for UKRI: our seven research councils, Research England and Innovate UK. Let us know if you have feedback or would like to help improve our online products and services .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J R Soc Med
- v.104(8); 2011 Aug
The Medical Research Council and clinical trial methodologies before the 1940s: the failure to develop a ‘scientific’ approach
In 1989 Joan Austoker and I set out our goal in Historical Perspectives of the Role of the MRC ‘to discuss the role of the Medical Research Council in shaping a national system of medical research in Britain’. 1 We noted that the only general history of the Medical Research Council (MRC) at that time was authored by an MRC staff member, A Landsborough Thomson, who had produced two volumes in 1973 and 1975. 2 , 3 Our book remains the only attempt apart from Landsborough Thomson's to construct a general overview of the work of the MRC, but over the past two decades, there has been considerable interest in the history of the MRC, particularly in relation to the lead-up to its world-famous streptomycin trial for pulmonary tuberculosis, which it reported in 1948. 4 This commentary provides a review of the information that has accumulated since 1989 – which is scattered in monographs, articles and unpublished theses – relating to the pre-history of this important trial.

Walter Morley Fletcher and ‘pure science’
The Medical Research Committee was set up in 1913 under the 1911 National Insurance Act. In 1914, Walter Morley Fletcher (1873–1933) was appointed Secretary of the Committee and from 1920, the Medical Research Council (MRC), a post he held until his death in 1933. Our 1989 history argued that Fletcher played a crucial role in determining the direction of medical research in Britain. Joan Austoker stated in her chapter on Fletcher that ‘The development and expansion of the medical sciences in Britain was, to a considerable extent, dominated by a single individual [Fletcher]’. 5 Specifically, Fletcher prioritized basic biomedical science and laboratory-based research over clinical research. In his chapter in our volume, David Cantor also pointed out that Fletcher tended to differentiate ‘science’ from ‘clinical practice’ and believed that medical research should not be in the hands of clinicians. Cantor cited Lord Moynihan, President of the Royal College of Surgeons, who lamented that only one of the 12 members of the MRC ‘possesses any adequate knowledge of scientific clinical surgery; one only practises medicine, and his very able mind sways rather to the laboratory than to the wards’. 6 In his chapter on clinical medicine, Christopher Booth, too, wrote that Moynihan attacked the MRC ‘for its concern with mice rather than men’ 7 and that the latter complained that the MRC was ‘too aloof from the day-to-day practice of medicine’. Booth acknowledged that under Fletcher the MRC did set up a Clinical Committee in 1932 to oversee and provide grants for research projects carried out at medical schools around the country. 7 The Clinical Committee included the MRC's clinical members (Lord Dawson, President of the Royal College of Physicians, Edward Mellanby and Wilfred Trotter) with Thomas Lewis, who was based at University College Hospital London, as secretary. Trotter and Lewis were also members of the Therapeutic Trials Committee, which had been established the previous year specifically to test therapeutics, and is further discussed below. Nevertheless, Booth pointed to Fletcher's continued distrust of clinicians, claiming ‘Fletcher … had little sympathy for fashionable practitioners, who to their financial advantage “hoodwinked” the public with such transient crazes as ultra-violet treatment, opsonic indices and superstitions such as “status lymphaticus”’. 7
Subsequent researchers have endorsed the view that Fletcher thought medical research should be laboratory-based rather than ward-based. In his 2007 monograph, Martin Edwards wrote that Fletcher ‘repeatedly affirmed his conviction that medicine and therapeutics could only progress through fundamental scientific research, frequently performed by non-clinical scientists rather than clinicians’. 8 , 9 Edwards noted that this trend was reinforced in 1920 when the Medical Research Committee was separated from the Ministry of Health, and became the Medical Research Council , which was responsible to the Privy Council. The way in which the new Council distinguished itself from the Ministry of Health was through its laboratory-based research, with the National Institute of Medical Research at the centre of its operations. The two bodies reached an agreement in 1924: the Ministry of Health was to be concerned with ‘applied research’ relating to clinical problems; the MRC would initiate and organize all new research in the basic biomedical sciences. Fletcher argued that ‘progress in physiology, biochemistry, and pathology was essential to the development of clinical practice’. 8 , 9
The National Institute of Medical Research
In 1914 the Medical Research Committee had acquired premises for its research on the site of the Mount Vernon Hospital, in Hampstead, London. In 1920, this became the National Institute for Medical Research, which remained there until it moved to Mill Hill in 1950. While there was some discussion initially about establishing hospital beds for research purposes, this was quickly rejected in favour of the alternative of giving financial support to hospital units already in existence. As Booth has pointed out, the MRC supported the research of the Department of Clinical Research and Experimental Medicine at University College Hospital in London, and provided grants to other hospitals for research purposes. 7 The National Institute for Medical Research absorbed about one-third of the MRC budget. Those based at the new research centre included Henry Dale (biochemistry and pharmacology, and director of the new Institute), Almroth Wright (bacteriology), Leonard Hill (applied physiology) and John Brownlee (medical statistics).
Under Sir Henry Dale's leadership from 1924, the National Institute for Medical Research became a centre for international biological standardization of therapeutic drugs, under the auspices of the League of Nations. The work of the centre enabled new therapies to be seen to be based on physiological principles. As Benjamin Toth noted in his 1998 PhD thesis, ‘The proof of newer therapies did not rely on empirical clinical testing, but on the demonstration that they behaved according to scientific laws and principles, which could be established under a microscope, in a test-tube, or in a laboratory animal. Clinical trials on patients were therefore of secondary importance, as well as being difficult to organise.’ 10 Drugs were tested in animals and their effects and dosages calibrated. This began during World War I, when German supplies of salvarsan for syphilis were disrupted owing to war conditions. 11 , 12 The MRC was responsible for testing the quality of British-manufactured salvarsan and neosalvarsan, as well as other sera and anti-toxins which had been imported before the war. The National Institute for Medical Research went on to play a key role in the biological standardization of insulin from 1922, as discussed by Jonathan Liebenau in our 1989 volume. 13 The Therapeutic Substances Act of 1925 gave the MRC statutory responsibility for the preparation and custody of British national standards for certain therapeutic drugs. Internationally, the task of establishing standards was shared by the State Serum Institute in Copenhagen and the National Institute for Medical Research, and both entered into a formal contract with the League of Nations for this purpose.
The National Institute for Medical Research included a Statistical Unit, set up in 1914 under John Brownlee. As Keith Williams concluded in his 2005 PhD thesis, the MRC ‘did invoke the use of statistics to a degree, but mostly for their public health, epidemiology and vaccination studies’. 11 In 1920 the Industrial Health Statistics Committee was established under the MRC's Industrial Fatigue Research Board (set up in 1918). Austin Bradford Hill, Leonard Hill's son, received a grant from this Committee in 1923 to collect information on mortality related to migration from rural to industrial areas. In 1925 the Industrial Health Statistics Committee was renamed the Statistics Committee, and Major Greenwood was appointed chairman. When Brownlee died in 1927, the MRC amalgamated Brownlee's former Statistical Unit and the Statistics Committee chaired by Greenwood, who was now Professor of Epidemiology and Vital Statistics at the London School of Hygiene and Tropical Medicine. In 1945, Austin Bradford Hill succeeded Greenwood as chair at the London School of Hygiene and as head of the MRC Statistical Unit. Like Williams, Martin Edwards maintained that the Statistical Unit had little to do with clinical trials before the 1940s, pointing out that, ‘The designs of the therapeutic trials conducted by MRC prior to the 1940s appear to have been influenced very little by statistical considerations’. 8 , 9 Bradford Hill himself later reflected that he and Greenwood had worked on correcting and improving reports the MRC planned to publish, implying that they had had little involvement at the planning stage. Edwards further pointed out that ‘Greenwood's published output prior to the 1940s reveals more interest in epidemiology and statistical experiments on mouse populations than in any application of statistical methodology on therapeutic innovation’. 8 , 9
The origins of the MRC Therapeutic Trials Committee
In 1926 the MRC and the Department of Scientific and Industrial Research set up an ad hoc committee to report on the scope of work required for chemotherapy. In their joint report, they recommended more permanent facilities for conducting clinical trials of proposed new remedies. As a result, the MRC set up the Chemotherapy Committee in 1927, headed by Henry Dale. The Chemotherapy Committee was tasked with organizing the biological study or clinical testing of new drugs prepared at the National Institute for Medical Research. This was intended to promote co-operation between chemists, biologists, pathologists and clinicians in the production of new compounds, and their evaluation in preclinical and clinical research. 14 In 1929, for instance, the Chemotherapy Committee agreed to promote clinical trials of a concentrated pneumococcal serum that had been first described in America. With supplies from America and from Burroughs Wellcome in the UK, these trials were to take place at the Royal Infirmary in Edinburgh, at University College Hospital in London and in Glasgow (and later in Aberdeen).
This Chemotherapy Committee does not appear to have been particularly effectual, however. Two years later, following consultation with the Association of British Chemical Manufacturers, the MRC decided to establish more formal machinery for clinical trials; this was the Therapeutic Trials Committee. The impetus for its establishment appears to have come partly from the pharmaceutical industry itself, which had approached the MRC several times in the decade prior to the Committee's establishment, particularly through Francis Carr, who developed synthetic drugs at Burroughs Wellcome, Boots and British Drug Houses. 11 The industry was keen to secure an authoritative system of clinical testing and ‘approval’ of new drugs, including synthetics. The Therapeutic Trials Committee also seems to have resulted from nationalistic concerns, namely the desire to test British-made drugs, particularly in the wake of the economic crisis in the early 1930s. 11 , 12 Finally, the new Committee must be seen in the light of the growing public demand for the regulation of drugs, which had led to the passage of the Therapeutic Substances Act in 1925. The Times reported in 1931 that the MRC had announced a new Therapeutic Trials Committee, ‘to advise and assist them in arranging for properly controlled trials of new products that seem likely on experimental grounds to have value in the treatment of diseases’. 11
The new Committee looked impressive. The chairman was Professor Thomas Renton Elliott, of University College Hospital, whose department at the hospital had long been supported by the MRC. 7 Henry Dale, director of the National Institute for Medical Research, represented the Chemotherapy Committee and provided a link between the MRC and the pharmaceutical industry, having worked at Burroughs Wellcome and on the standardization of salvarsan and other drugs. Also appointed to the new committee was Sir Thomas Lewis, an eminent cardiologist at University College Hospital who had enjoyed a long association with the MRC. Lewis was first appointed to its staff in 1916 and became secretary to the MRC's Clinical Committee in 1932. 7 Other members included Professor Francis Fraser (later Sir Francis) of the Clinical Laboratories at St Bartholomew's Hospital, London, Professor Arthur Ellis of the London Hospital, Dr John Ryle (later Sir John), Regius Professor of Physic at Cambridge and subsequently Professor of Social Medicine at Oxford, Sir John Thomson-Walker, senior urologist at Kings College Hospital and surgeon at St Peters Hospital, London, Sir Edward Farquhar Buzzard, a neurologist and successor to William Osler as Regius Professor of Medicine at Oxford, Professor David Wilkie (later Sir David), a general surgeon and urologist in Edinburgh, Sir John Parsons CBE, a senior ophthalmologist, and Wilfred Trotter, a distinguished thyroid surgeon at University College Hospital (and also a member of the MRC's 1932 Clinical Committee). Edward Mellanby, who was to become secretary of the MRC in 1933, also joined the Therapeutic Trials Committee, as did Thomas Watts Eden, one of the foremost gynaecologists in London who had helped to found the British College of Obstetricians and Gynaecologists in 1929, and was President of the Royal Society in 1930. 11 The British Medical Journal declared that the new Therapeutic Trials Committee was a strong one, ‘including individuals of the highest reputes, and both medicine and pharmacy ought to benefit by its existence’. 11
The Therapeutic Trials Committee and the trial of serum treatment of pneumonia
The Therapeutic Trials Committee inherited from the Chemotherapy Committee a study of the use of serum for lobar pneumonia which had been initiated in 1931. 15 Discussion about the design of this study had existed since at least 1929, when Francis Green, who was appointed secretary of the new Committee, had written to Professor Murray Lyon in Edinburgh, who had proposed that serum be given ‘to every alternate case’. 8 , 9 There had already been a remarkable series of alternate allocation trials of serum for pneumonia during the previous two decades in the United States. 16 Furthermore, another such trial was done during the winter of 1931–1932 at St Bartholomew's Hospital and a number of London County Council hospitals. 17 However, the Committee paid little attention to these methodologically important precedents in overseeing its own trial.
The MRC study had commenced in four centres around the country – London, Edinburgh, Aberdeen and Glasgow (though the Glasgow element remained independent of the MRC). The Committee called a meeting to ‘draw up a standardised scheme of investigation’. In his history of therapeutic trials, Edwards analysed how the Committee envisaged controlling the trial and concluded that it ‘rendered the serum trial “controlled” by regulating the activities of individual clinicians, co-ordinating their activities and unifying the means of public presentation of their results’. 8 , 9
The Committee did specify that future researchers should use adequate controls in trials and that they should alternate patients to treatment and control groups wherever possible. 18 But, as Edwards showed, the investigators at each centre used different criteria for deciding which patients to recruit to the study and for allocating patients to control or treatment groups. Moreover, they adopted different treatment regimens and different measures of treatment outcome. 8 , 9 Edwards maintained that the results of the Edinburgh study were worthless: ‘patients had not been allocated to receive serum, or to function as controls, alternately. Instead, patients with a poorer prognosis – those aged over sixty, and those moribund on admission to hospital – had frequently been allocated to the control group for fear of wasting precious serum on them. The control and treatment groups were therefore not comparable, and the results impossible to interpret.’ 8 , 9
Toth argued that when the Therapeutic Trials Committee sent instructions to the groups experimenting with serum for lobar pneumonia, the aim was primarily to assert some form of central control over researchers, to make the trials appear more scientific and reliable. 10 Edwards came to a similar conclusion, noting that, upon inheriting the study and its attendant embarrassments, the Committee tried to bring idiosyncratic or maverick investigators into line, and hence contain them within the rhetoric of its own ‘properly controlled clinical tests’. 8 , 9 But the Committee's attempts to enforce some sort of uniformity apparently failed.
What did the MRC Therapeutic Trials Committee achieve?
The Therapeutic Trials Committee met only 10 times between 1931 and 1939. During that time it considered 67 applications for clinical trials, of which it supported 51. 10 , 11 In his 500-page, two-volume history of the MRC, Landsborough Thomson devoted a mere five pages to ‘Clinical evaluation of remedies’, 3 yet declared that the Therapeutic Trials Committee had ‘set a standard for the methods of trial’. 3 Similarly, Joan Austoker and I wrote of this Committee: ‘The success of its ventures had made the clinical trial of new products respectable in the eyes of the pharmaceutical industry’. 14 More recent researchers are not so convinced, and a more detailed study of the operations of the Committee and the clinical trials it oversaw supports their assessment.
The process followed by the Committee was that it sent drugs to doctors for simultaneous ‘trials’ at different centres around the country, where, as Desirée Cox-Maksimov noted in her 1997 PhD thesis, ‘each physician tested the therapy in his own idiosyncratic way’. 18 Cox-Maksimov cited the views of one of the Committee's members, John Ryle, ‘who explained that whether the experiment was controlled or not depended on the physician who could compare cases and judge therapeutic efficacy … by control he meant that they should conduct a close study of the case. It was not cases that made a controlled experiment, but the care and scrutiny with which those cases were examined.’ 18
In his PhD on the history of clinical trials in British medicine, Benjamin Toth provided the following assessment of the Therapeutic Trials Committee:
During its existence [the Therapeutic Trials Committee] did not organise one rigorous comparative clinical trial, despite prima facie evidence of the problems of not doing so. None of the factors that were later to be recognised as vital to producing meaningful evaluations of therapies were advocated by the TTC. By standards soon to be regarded as the norm, there was little attempt to frame research questions, little attempt to select patients, no random allocation, little systematic recording of results, and almost no attempt to measure results. In the case of multi-centre studies, it was usual for Green [the Committee's secretary] to ask the clinicians to work to a standard schedule, but there was no enforcement of a schedule. 10
Toth attempted to explain why this was the case. He believed that the MRC saw the laboratory as the more important site for experimentation, with clinical trials of secondary importance. He thought the Committee members conceptualized the clinical trial primarily as a test on a series of cases, selected because they were likely to benefit from the drug. Furthermore, Toth thought that an overriding goal of the Committee was to compare British drugs with foreign products.
Similarly, Martin Edwards argued that:
Examination of the trials published by the TTC until its winding-up at the start of the Second World War rather belies any suggestion that a unified methodology was in place. A minority of studies employed untreated or placebo-treated comparison subjects, sometimes referred to as ‘controls’. Subjects in these studies were allocated to receive active or inactive therapy either by alternation or at the discretion of the investigator, who frequently allotted most of his patients to receive the new drug, reserving just a few as ‘controls’. Many more trials were simply as reports, describing the effects of drug therapy on any number of patients from one, to a handful, or as series of a hundred or more. Most authors simply described these case reports in some narrative detail; others presented additional animal experiments or employed detailed quantification and tabulation of findings such as blood pressure, blood chemistry, weight, temperature, signs and symptoms. 8 , 9
Edwards went on to explain that many of the investigators cherished their autonomy and disliked being dictated to. As the Therapeutic Trials Committee had no clinical facilities of its own, it relied on the goodwill of individual investigators to test products. He maintained that, as a result, the Committee failed to introduce any methodological innovation during its existence, in spite of the claim by the MRC that the Committee was efficient, and uniquely British. This, Edwards argued, was a rhetorical device to help establish the authority of the MRC in the arena of therapeutic evaluation. Thus, he concluded, ‘the MRC's attempts to present the output of the TTC as representative of a unified therapeutic trial methodology were essentially rhetorical’. 8 , 9
Keith Williams, likewise, found little evidence of planning for the trials done under the auspices of the Therapeutic Trials Committee. Rather, he concluded, ‘the TTC arranged for as many patients to be treated as could be mustered’. 11 He also concluded that, ‘Apart from vaccine and toxoid studies, the TTC studies were generally small and often inconclusive, except where even a small study showed some safety problems’. 11
The Committee fulfilled its nationalistic goal, prioritizing British drugs over foreign drugs for evaluation, until it undertook research into prontosil, the first of the new sulphonamides, which had been developed at the Bayer Laboratories in Germany. In 1936, research supported by the Committee and carried out by Leonard Colebrook at Queen Charlotte's Hospital used historical controls to demonstrate a dramatic effect of sulphonamides on puerperal sepsis, 19 – 22 and a later study showed beneficial effects on meningococcal meningitis. 23 Less dramatic effects of these new drugs were investigated under the aegis of the Committee in four alternate allocation trials done by Snodgrass and Anderson at Ruchill Hospital in Glasgow. 24 – 27 However, the reports of a number of other studies which had used alternate allocation during the life of the Committee make no mention of MRC support (see, for example, Ellison, 28 Sutherland, 29 Moir, 30 Peters and Cullum, 31 Theobald, 32 Evans and Gaisford, 33 Johnstone, 34 Peters, 35 Benn, 36 and Price 37 ), although one did. 38
The initiation of well-designed, multicentre controlled trials under the aegis of the MRC
Despite my and Joan Austoker's claim in 1989 that the MRC's Therapeutic Trials Committee frequently sought expert opinion from the Statistical Committee, and in particular from Greenwood and Bradford Hill, 14 subsequent researchers have found little evidence of such interaction. It is true that Bradford Hill had been invited by the Therapeutic Trials Committee to comment on a draft report of the 1934 trial of serum for the treatment of lobar pneumonia, 15 and probably contributed the part of the text of the paper discussing methods. 39 In a critical unpublished internal memorandum before the report of the trial was published Bradford Hill argued that greater effort should be taken ‘that the division of cases really did ensure a random selection’. 12 Unfortunately that memo, viewed by Joan Austoker at the MRC archives in the 1980s, has been lost. However, Edwards reports that Green deemed Bradford Hill's memo so damning that it was ‘to be kept, not only from public scrutiny, but even from the investigators themselves’. 8 , 9 Iain Chalmers has concluded, ‘The limitations of this study – with its relatively small numbers and mixture of ways of generating control groups – are likely to have been very important in leading Bradford Hill to go on to design large trials using concealed allocation schedules’. 39
In 1937, Austin Bradford Hill accepted an invitation from the editor of The Lancet to write a series of articles on principles of medical statistics, including the principles of clinical trial design. The articles were a great success, and were published as a book later that year. 40 In the book Bradford Hill stated that alternate allocation was ‘often satisfactory’, but Chalmers suspects that he did not really believe that it provided adequate assurance against allocation bias. Chalmers noted that ‘in spite of his insistence that alternate allocation must be strictly applied, from the first edition of his book onwards, Bradford Hill did not comment on the fact that the trials of 159 and 163 patients in the serum and control groups [in the 1934 trial] are clearly incompatible with strict alternate allocation’. 39
Bradford Hill was eventually appointed to the Therapeutic Trials Committee the year after the publication of his book, and he attended his first and only meeting in 1939. But he does not appear to have been involved in the first strictly controlled multicentre clinical trial done by the MRC. This was organized by Philip D'Arcy Hart, the medical director of the MRC Tuberculosis Research Unit, 41 who was asked in 1943 to evaluate ‘patulin’, a proposed treatment for the common cold. D'Arcy Hart devised a system of ‘strict rotation’, allocating volunteers suffering from a cold into two groups receiving patulin and another two given a placebo, arguing that this method ensured ‘an effectively random allocation of the subjects’. In the event, the trial failed to detect any benefit of patulin, 42 and Hart considered that this was why the study has tended to be overlooked in histories of the development of controlled trials. For example, Landsborough Thomson did not even mention the trial, nor did Austoker and I in our 1989 history. Chalmers and Clarke concluded, by contrast, that the ‘1944 patulin trial deserves wider recognition as the first well controlled multi-centre clinical trial to have been conducted under the aegis of the MRC’. 43 , 44
Bradford Hill only became involved in MRC controlled trials after World War II, first, in an evaluation of different whooping cough vaccines, 45 , 46 and then, with D'Arcy Hart and Marc Daniels, in an assessment of the effects of the anti-tuberculous drug, streptomycin, which had been developed in the United States. Indeed, the successful organization of the patulin trial appears to have been one of the reasons that the American producers of streptomycin invited the MRC to evaluate it. 43 The MRC Streptomycin Committee was established in 1947 to oversee a ‘rigorously planned investigation with concurrent controls’, and the results of this study were published in the British Medical Journal in 1948. 4 , 47
The details of the allocation schedule for the streptomycin trial were unknown to any of the investigators: they were contained in a set of sealed envelopes, each bearing on the outside only the name of the hospital and a number. Bradford Hill and D'Arcy Hart were both aware of the importance of this precaution to prevent practitioner allocation bias. Chalmers argued, and Bradford Hill himself confirmed, that the decision to use random allocation based on random number tables (not for the first time – see Chalmers 48 ) had nothing to do with the statistical models expounded by Ronald Fisher, for example, in his 1935 book Design of Experiments . Rather, it was as a precaution against allocation bias. Chalmers points out that ‘Nowhere does Bradford Hill allude to randomisation as a way of ensuring the validity of tests of statistical significance. His concern continued to be the control of bias, hence his detailed references to ways of concealing allocation schedules from those involved in recruiting patients for clinical trials.’ 49 ‘The streptomycin trial deserves a place in the history of clinical trials because of this and other exceptionally clear statements about precautions to minimise allocation bias.’ 49 , 50 Other historians have also questioned whether the MRC introduced random allocation as a result of an adoption of mathematical models. Toth, for instance, saw randomization as a continuation of the MRC's attempts to present itself as scientifically valid, to ensure its own centrality in clinical research, and as a means of controlling distribution of streptomycin in Britain. 10
Conclusions
From the start, the MRC prioritized research in ‘pure’ sciences and in the laboratory over clinical research, probably as a result of the preferences of its very powerful secretary, Walter Morley Fletcher. It became internationally renowned for its work on the biological standardization of therapeutic drugs, carried out at its research centre, the National Institute of Medical Research. Although the MRC funded clinical research, for instance, at the Department of Clinical Research and Experimental Medicine at University College Hospital London – and set up a Chemotherapy Committee (1927), a Therapeutic Trials Committee (1931) and a Clinical Committee (1932) – it did not view this research as central to its operations, and failed to introduce rigorous methodology into clinical research prior to World War II.
Although the MRC had its own Statistical Unit and Committee, statisticians played little part, if any, in designing clinical MRC clinical research prior to the mid-1940s. However, the poor performance of the research overseen by the Therapeutic Trials Committee in the 1930s, and specifically the 1934 trial of serum treatment for pneumonia, which medical statistician Bradford Hill was asked to comment on, probably played an important role in Hill's subsequent decision to introduce concealment of an allocation based on random numbers in the 1948 streptomycin trial. By 1950, clinical research had begun to accrue the same scientific status as research in the laboratory.
DECLARATIONS
Competing interests.
None declared
Ethical approval
Not applicable
Contributorship
LB is the sole contributor
Acknowledgements
Additional material for this article is available from the James Lind Library website ( www.jameslindlibrary.org ), where it was originally published

Turn Your Curiosity Into Discovery
Latest facts.
12 Facts About Beer Pong Day May 4th
15 Facts About National Gummi Bear Day April 27th
40 facts about elektrostal.
Written by Lanette Mayes
Modified & Updated: 02 Mar 2024
Reviewed by Jessica Corbett

Elektrostal is a vibrant city located in the Moscow Oblast region of Russia. With a rich history, stunning architecture, and a thriving community, Elektrostal is a city that has much to offer. Whether you are a history buff, nature enthusiast, or simply curious about different cultures, Elektrostal is sure to captivate you.
This article will provide you with 40 fascinating facts about Elektrostal, giving you a better understanding of why this city is worth exploring. From its origins as an industrial hub to its modern-day charm, we will delve into the various aspects that make Elektrostal a unique and must-visit destination.
So, join us as we uncover the hidden treasures of Elektrostal and discover what makes this city a true gem in the heart of Russia.
Key Takeaways:
- Elektrostal, known as the “Motor City of Russia,” is a vibrant and growing city with a rich industrial history, offering diverse cultural experiences and a strong commitment to environmental sustainability.
- With its convenient location near Moscow, Elektrostal provides a picturesque landscape, vibrant nightlife, and a range of recreational activities, making it an ideal destination for residents and visitors alike.
Known as the “Motor City of Russia.”
Elektrostal, a city located in the Moscow Oblast region of Russia, earned the nickname “Motor City” due to its significant involvement in the automotive industry.
Home to the Elektrostal Metallurgical Plant.
Elektrostal is renowned for its metallurgical plant, which has been producing high-quality steel and alloys since its establishment in 1916.
Boasts a rich industrial heritage.
Elektrostal has a long history of industrial development, contributing to the growth and progress of the region.
Founded in 1916.
The city of Elektrostal was founded in 1916 as a result of the construction of the Elektrostal Metallurgical Plant.
Located approximately 50 kilometers east of Moscow.
Elektrostal is situated in close proximity to the Russian capital, making it easily accessible for both residents and visitors.
Known for its vibrant cultural scene.
Elektrostal is home to several cultural institutions, including museums, theaters, and art galleries that showcase the city’s rich artistic heritage.
A popular destination for nature lovers.
Surrounded by picturesque landscapes and forests, Elektrostal offers ample opportunities for outdoor activities such as hiking, camping, and birdwatching.
Hosts the annual Elektrostal City Day celebrations.
Every year, Elektrostal organizes festive events and activities to celebrate its founding, bringing together residents and visitors in a spirit of unity and joy.
Has a population of approximately 160,000 people.
Elektrostal is home to a diverse and vibrant community of around 160,000 residents, contributing to its dynamic atmosphere.
Boasts excellent education facilities.
The city is known for its well-established educational institutions, providing quality education to students of all ages.
A center for scientific research and innovation.
Elektrostal serves as an important hub for scientific research, particularly in the fields of metallurgy, materials science, and engineering.
Surrounded by picturesque lakes.
The city is blessed with numerous beautiful lakes, offering scenic views and recreational opportunities for locals and visitors alike.
Well-connected transportation system.
Elektrostal benefits from an efficient transportation network, including highways, railways, and public transportation options, ensuring convenient travel within and beyond the city.
Famous for its traditional Russian cuisine.
Food enthusiasts can indulge in authentic Russian dishes at numerous restaurants and cafes scattered throughout Elektrostal.
Home to notable architectural landmarks.
Elektrostal boasts impressive architecture, including the Church of the Transfiguration of the Lord and the Elektrostal Palace of Culture.
Offers a wide range of recreational facilities.
Residents and visitors can enjoy various recreational activities, such as sports complexes, swimming pools, and fitness centers, enhancing the overall quality of life.
Provides a high standard of healthcare.
Elektrostal is equipped with modern medical facilities, ensuring residents have access to quality healthcare services.
Home to the Elektrostal History Museum.
The Elektrostal History Museum showcases the city’s fascinating past through exhibitions and displays.
A hub for sports enthusiasts.
Elektrostal is passionate about sports, with numerous stadiums, arenas, and sports clubs offering opportunities for athletes and spectators.
Celebrates diverse cultural festivals.
Throughout the year, Elektrostal hosts a variety of cultural festivals, celebrating different ethnicities, traditions, and art forms.
Electric power played a significant role in its early development.
Elektrostal owes its name and initial growth to the establishment of electric power stations and the utilization of electricity in the industrial sector.
Boasts a thriving economy.
The city’s strong industrial base, coupled with its strategic location near Moscow, has contributed to Elektrostal’s prosperous economic status.
Houses the Elektrostal Drama Theater.
The Elektrostal Drama Theater is a cultural centerpiece, attracting theater enthusiasts from far and wide.
Popular destination for winter sports.
Elektrostal’s proximity to ski resorts and winter sport facilities makes it a favorite destination for skiing, snowboarding, and other winter activities.
Promotes environmental sustainability.
Elektrostal prioritizes environmental protection and sustainability, implementing initiatives to reduce pollution and preserve natural resources.
Home to renowned educational institutions.
Elektrostal is known for its prestigious schools and universities, offering a wide range of academic programs to students.
Committed to cultural preservation.
The city values its cultural heritage and takes active steps to preserve and promote traditional customs, crafts, and arts.
Hosts an annual International Film Festival.
The Elektrostal International Film Festival attracts filmmakers and cinema enthusiasts from around the world, showcasing a diverse range of films.
Encourages entrepreneurship and innovation.
Elektrostal supports aspiring entrepreneurs and fosters a culture of innovation, providing opportunities for startups and business development.
Offers a range of housing options.
Elektrostal provides diverse housing options, including apartments, houses, and residential complexes, catering to different lifestyles and budgets.
Home to notable sports teams.
Elektrostal is proud of its sports legacy, with several successful sports teams competing at regional and national levels.
Boasts a vibrant nightlife scene.
Residents and visitors can enjoy a lively nightlife in Elektrostal, with numerous bars, clubs, and entertainment venues.
Promotes cultural exchange and international relations.
Elektrostal actively engages in international partnerships, cultural exchanges, and diplomatic collaborations to foster global connections.
Surrounded by beautiful nature reserves.
Nearby nature reserves, such as the Barybino Forest and Luchinskoye Lake, offer opportunities for nature enthusiasts to explore and appreciate the region’s biodiversity.
Commemorates historical events.
The city pays tribute to significant historical events through memorials, monuments, and exhibitions, ensuring the preservation of collective memory.
Promotes sports and youth development.
Elektrostal invests in sports infrastructure and programs to encourage youth participation, health, and physical fitness.
Hosts annual cultural and artistic festivals.
Throughout the year, Elektrostal celebrates its cultural diversity through festivals dedicated to music, dance, art, and theater.
Provides a picturesque landscape for photography enthusiasts.
The city’s scenic beauty, architectural landmarks, and natural surroundings make it a paradise for photographers.
Connects to Moscow via a direct train line.
The convenient train connection between Elektrostal and Moscow makes commuting between the two cities effortless.
A city with a bright future.
Elektrostal continues to grow and develop, aiming to become a model city in terms of infrastructure, sustainability, and quality of life for its residents.
In conclusion, Elektrostal is a fascinating city with a rich history and a vibrant present. From its origins as a center of steel production to its modern-day status as a hub for education and industry, Elektrostal has plenty to offer both residents and visitors. With its beautiful parks, cultural attractions, and proximity to Moscow, there is no shortage of things to see and do in this dynamic city. Whether you’re interested in exploring its historical landmarks, enjoying outdoor activities, or immersing yourself in the local culture, Elektrostal has something for everyone. So, next time you find yourself in the Moscow region, don’t miss the opportunity to discover the hidden gems of Elektrostal.
Q: What is the population of Elektrostal?
A: As of the latest data, the population of Elektrostal is approximately XXXX.
Q: How far is Elektrostal from Moscow?
A: Elektrostal is located approximately XX kilometers away from Moscow.
Q: Are there any famous landmarks in Elektrostal?
A: Yes, Elektrostal is home to several notable landmarks, including XXXX and XXXX.
Q: What industries are prominent in Elektrostal?
A: Elektrostal is known for its steel production industry and is also a center for engineering and manufacturing.
Q: Are there any universities or educational institutions in Elektrostal?
A: Yes, Elektrostal is home to XXXX University and several other educational institutions.
Q: What are some popular outdoor activities in Elektrostal?
A: Elektrostal offers several outdoor activities, such as hiking, cycling, and picnicking in its beautiful parks.
Q: Is Elektrostal well-connected in terms of transportation?
A: Yes, Elektrostal has good transportation links, including trains and buses, making it easily accessible from nearby cities.
Q: Are there any annual events or festivals in Elektrostal?
A: Yes, Elektrostal hosts various events and festivals throughout the year, including XXXX and XXXX.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
Share this Fact:
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- Organisations
Medical Research Council
The Medical Research Council (MRC) is a national funding agency dedicated to improving human health by supporting research across the entire spectrum of medical sciences, in universities and hospitals, in MRC units, centres and institutes in the UK, and in MRC units in Africa.
MRC works with the UK Research and Innovation .
News and communications
- 12 September 2023
- Press release
- 21 June 2023
Transparency and freedom of information releases
- 10 November 2021
- Corporate report
- 3 February 2021
Is this page useful?
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. We’ll send you a link to a feedback form. It will take only 2 minutes to fill in. Don’t worry we won’t send you spam or share your email address with anyone.

IMAGES
VIDEO
COMMENTS
Bottle‐feeding guidelines and recommendations, however, tend to focus on aspects of health and safety (National Health & Medical Research Council, 2012; WHO, 1981). Bottle‐feeding advice concentrates on more procedural recommendations: cleaning and sterilizing of feeding equipment, correct preparation of formula, and the storage and ...
The Guidelines are a revision of the 2003 edition (and incorporate evidence based information). They were prepared by experts in paediatric nutrition, nutrition research, nutrition communication, public health and primary health.The Guidelines provide advice and recommendations on breastfeeding, supporting mothers and parents, the introduction of solids, preparing infant formula and other ...
We would like to thank Isla Kuhn, Reader Services Librarian at the University of Cambridge Medical Library, for her help in developing the search strategy and the first authors whom we contacted for their assistance. Funding This work was supported by the Medical Research Council. RL is funded by a MRC health services and health of the public ...
The Australian dietary guidelines have been slated for update in 2024 (National Health and Medical Research Council, 2021); accordingly, the infant feeding guidelines should be concomitantly updated to include responsive feeding practices (UNICEF United Kingdom & First Steps Nutrition Trust, 2019). Uptake of best-practice formula-feeding ...
National Health and Medical Research Council. iv. Acknowledgements. Infant Feeding Sub Committee of the Dietary Guidelines Working Committee. The production of a document such as this requires a considerable effort over a long period. Special thanks and . acknowledgment are due to the Infant Feeding Sub Committee members for their generous ...
rights are to be sent to Strategic Communications, National Health and Medical Research Council, GPO Box 1421, Canberra ACT 2600 or via email to [email protected]. ISBN Print: 1864965541 ... Preparing bottles 58 Storing bottles 58 Heating bottles 59 3.5.4 Children's cooking classes 59. VII CONTENTS Staying Healthy 5th Edition
The Medical Research Council (MRC) is dedicated to improving human health through excellent medical research, and expects the research it supports to be conducted according to the highest achievable ethical standards. Samples of human biological material are used for many purposes and are of increasing importance as the MRC and other research ...
rights are to be sent to Strategic Communications, National Health and Medical Research Council, GPO Box 1421, Canberra ACT 2600 or via email to [email protected]. ISBN Online: 1864965827 NHMRC (National Health and Medical Research Council) (2013). Infant Feeding Guidelines: Summary. Canberra: National Health and Medical Research ...
The freezing of human serum and plasma in Medical Research Council transfusion bottles, before drying by sublimation from the frozen state
Details. Annual report and accounts for the period 1 April 2020 to 31 March 2021 presented to Parliament pursuant to paragraphs 2 (2) and 3 (3) of schedule 1 to the Science and Technology Act 1965. Following the transfer of operations to UK Research and Innovation (UKRI) on 1 April 2018 under the Higher Education and Research Act 2017, MRC only ...
Introduction: We describe our experience of using the Medical Research Council framework on complex interventions to guide the development and evaluation of an intervention to prevent obesity by modifying infant feeding behaviours. Methods: We reviewed the epidemiological evidence on early life risk factors for obesity and interventions to prevent obesity in this age group.
IN MEDICAL RESEARCH COUNCIL TRANSFUSION BOTTLES, BEFORE DRYING BY SUBLIMATION FROM THE FROZEN STATE BY E. I. N. GEEAVfiS, M.B. From the Medical Research Council Serum Drying Unit, Department of Pathology, University of Cambridge (With Plates V-VII and 1 Figure in the Text) INTRODUCTION
The Medical Research Council (MRC) is responsible for co-coordinating and funding medical research in the United Kingdom.It is part of United Kingdom Research and Innovation (UKRI), which came into operation 1 April 2018, and brings together the UK's seven research councils, Innovate UK and Research England. UK Research and Innovation is answerable to, although politically independent from ...
The Medical Research Council (MRC) Ethics Series are guides that address specific regulatory and ethical considerations relating to research. Using information about people in health research (2018) Human tissue and biological samples for use in research (2014) Medical research involving adults who cannot consent (2007)
national Health and medical Research council . vii . contents national Health and medical Research council. 5 Expressing and storing breast milk 55. 5.1 Expressing breast milk 55. 5.1.1 Indications for mothers to express breast milk 55 5.1.2 Hand expression 56 5.1.3 Hand pumps 57 5.1.4 electric pumps 57. 5.2 Feeding with expressed breast milk 58
The researchers left ordinary tap water in both new and used drinking bottles for 24 hours, both before and after machine washing, as well as after the bottles had been in the dishwasher and ...
About us. The Medical Research Council (MRC) is a national funding agency dedicated to improving human health by supporting research across the entire spectrum of medical sciences, in universities ...
The UK Medical Research Council's widely used guidance for developing and evaluating complex interventions has been replaced by a new framework, commissioned jointly by the Medical Research Council and the National Institute for Health Research, which takes account of recent developments in theory and methods and the need to maximise the efficiency, use, and impact of research.
INDIANAPOLIS—A new $4.8 million grant will support researchers from Indiana University School of Medicine and the Medical Research Council Laboratory of Molecular Biology to study how human neurodegenerative diseases are affected by the misfolding of the protein TDP-43. Misfolding occurs when a protein adopts a conformation which differs from ...
Medical Research Council (MRC) Funding type: Grant. Total fund: £1,000,000. Maximum award: £270,000. Publication date: 24 April 2024. Opening date: 9 May 2024 9:00am UK time. Closing date: 4 July 2024 4:00pm UK time. Collaborate with the functional genomics screening laboratory.
See other industries within the Health Care and Social Assistance sector: Child Care Services , Community Food and Housing, and Emergency and Other Relief Services , Continuing Care Retirement Communities and Assisted Living Facilities for the Elderly , General Medical and Surgical Hospitals , Home Health Care Services , Individual and Family Services , Medical and Diagnostic Laboratories ...
In 1989 Joan Austoker and I set out our goal in Historical Perspectives of the Role of the MRC 'to discuss the role of the Medical Research Council in shaping a national system of medical research in Britain'. 1 We noted that the only general history of the Medical Research Council (MRC) at that time was authored by an MRC staff member, A Landsborough Thomson, who had produced two volumes ...
Today, Elemash is one of the largest TVEL nuclear fuel production companies in Russia, specializing in fuel assemblies for nuclear power plants, research reactors, and naval nuclear reactors. Its fuel assemblies for RBMK, VVER, and fast reactors are used in 67 reactors worldwide. 2 It also produced MOX fuel assemblies for the BN-800 and the ...
40 Facts About Elektrostal. Elektrostal is a vibrant city located in the Moscow Oblast region of Russia. With a rich history, stunning architecture, and a thriving community, Elektrostal is a city that has much to offer. Whether you are a history buff, nature enthusiast, or simply curious about different cultures, Elektrostal is sure to ...
The Medical Research Council (MRC) is a national funding agency dedicated to improving human health by supporting research across the entire spectrum of medical sciences, in universities and ...