

Nursing Case Study Analysis [10 Examples & How-To Guides]
- Wilson Logan
- August 6, 2022
- blog , Nursing Topics and Ideas
What is a case study analysis?
A case study analysis is a detailed examination of a specific real-world situation or event. It is typically used in business or nursing school to help students learn how to analyze complex problems and make decisions based on limited information.
Preparing a good case study analysis is not an easy task and requires a lot of time and effort. This article provides some tips on how to write a case study analysis that will help you get the most out of your research and provide a solid foundation for your writing.(Nursing Case Study Analysis)
Nursing Case Study Analysis
Nurses are constantly faced with decisions that have to be made in a timely and effective manner. Often, these decisions are based on the available information, which may be limited.
In order to make the best possible decisions, nurses need to be able to analyze and interpret data. Nursing case studies are an important tool that can help nurses improve their decision-making skills.
10 Nursing Case Study Analysis Examples
How to write case study analysis in nursing.
A case study analysis requires you to investigate a nursing scenario, examine the alternative solutions, and propose the most effective solution using supporting evidence.(Nursing Case Study Analysis)
Nurses have to constantly make decisions that affect the lives of their patients. In order to ensure that these decisions are made correctly, nurses need to have strong problem-solving and critical-thinking skills. Case studies are an excellent way for nurses to hone these skills.
Writing a nursing case study analysis is not as difficult as it may first seem. Follow these steps and you will be well on your way to writing a successful case study analysis.(Nursing Case Study Analysis)
- Read the case study carefully. As you read, take note of any key facts or information that could be important for your analysis.
- Once you have finished reading the case study, identify the main problem or issue that needs to be addressed.
- Brainstorm possible solutions to the problem or issue . Try to come up with a few different options.
- Choose the best solution based on the information in the case study and your own clinical experience.
- Write up your analysis in a clear and concise manner. Be sure to support your chosen solution with evidence from the case study and your own professional experience .
Here’s How To Write A Nursing Case Study
How do you analyze a case study in nursing?
A nursing case study is an in-depth examination of a single individual. It is usually used to identify new areas of knowledge or to validate existing knowledge.
When analyzing a nursing case study, it is important to consider the following elements:
- The patient’s medical history. This includes any prior illnesses, treatments, and medications.
- The patient’s current condition. This includes symptoms, vital signs, and laboratory results.
- The nurse’s observations. This includes the nurse’s notes on the patient’s condition and behavior.
- The patient’s family and social history. This includes information on the patient’s family, friends, and social support network.(Nursing Case Study Analysis)
- The patient’s response to treatment. This includes any changes in the patient’s condition or symptoms after receiving treatment.
How nursing practitioners can analyze Patient’s Cases
As a nurse practitioner, you will often be asked to provide a case analysis for your patients. This can be a daunting task, but there are some key elements that you should always include in your analysis.
- The first element is the patient history. This should include any relevant medical history, as well as any personal information that may be pertinent to the case.
- The second element is the physical examination. This should include a thorough examination of the patient, including any relevant test results.(Nursing Case Study Analysis)
- The third element is the diagnosis. This is where you will provide your assessment of the patient’s condition and identify any potential problems.
- The fourth element is the treatment plan. This is where you will outline the course of treatment that you recommend for the patient.
- The fifth and final element is the prognosis. This is where you will provide your assessment of the likely outcome of the case, based on the information that you have gathered.
Steps of writing nursing case study analysis
Furthermore; there are different ways to approach writing a nursing case study analysis, but there are generally three main steps that need to be followed.
- First, you will need to perform a thorough analysis of the case study. This means looking at all aspects of the case and trying to identify any key issues or problems.(Nursing Case Study Analysis)
- Once you have done this, you will need to develop a hypothesis or research question that you can test.
- Finally, you will need to write up your findings in a clear and concise manner.
Assuming that you have been given the task of writing a case study analysis, there are a few key steps that you will need to take in order to ensure that your document is well-written and informative.
- Make sure that you understand all of the information presented in the case study , and take note of any key points or details that you think may be important.
- What points do you want to make in your analysis?
- What evidence will you use to support these points?
- Once you have a good idea of what you want to say in your analysis, start organizing your thoughts and putting them into a coherent structure.(Nursing Case Study Analysis)
- Once you have a rough outline of your case study analysis , start filling in the details. Flesh out your arguments and provide evidence to support them. In addition, make sure to address any counterarguments that could be made against your points.
- Finally, conclude your analysis by summarizing your main points and providing any recommendations or suggestions for further action .
Nursing Case study Analysis Format and Structure
When it comes to writing a case study analysis, there is no one-size-fits-all approach. However, there is a general format and structure that you can follow to ensure your analysis is well-organized and flows smoothly. Here are the basics:
A nursing case study is a detailed study of a patient that is encountered by a nurse. The purpose of the case study is to provide a comprehensive view of the patient’s health condition and history. Nurse practitioners use case studies to enhance their ability to care for patients by providing them with a more complete picture of the patient’s health . Nurse practitioners may use different formats for their nursing case studies. However, all case studies should include certain key elements. These key elements include:
- Patient information – This section should include basic demographic information about the patient, such as age, gender, race/ethnicity, and chief complaint
- Medical history – This section should detail the patient’s past medical history, including any chronic conditions, medications, allergies, and surgeries.(Nursing Case Study Analysis)
- Family history – This section should detail the patient’s family medical history, including any chronic conditions or genetic diseases that may be relevant to the patient’s current condition.
- Social history – This section should detail the patient’s social circumstances, such as employment status, living situation, and alcohol/drug use.
- Review of symptoms –A physical examination will help you to identify any physical abnormalities that may be causing or contributing to the patient’s condition.
- Diagnostic testing – Diagnostic testing may be necessary in order to confirm or rule out a diagnosis . Common tests used in case analysis include blood work, imaging tests, and biopsies.
- Treatment options – Once a diagnosis has been made, you will need to consider treatment options. Treatment options will vary depending on the diagnosis and the severity of the condition.(Nursing Case Study Analysis)
- The prognosis (Evaluation and outcomes) – After considering all of the above factors, you will be able to give the patient a prognosis. The prognosis is an educated guess as to how the condition will progress.
When writing a nursing case study, nurse practitioners should use a clear and concise format. The format should be easy to follow and understand. Nurse practitioners should also include all of the key elements in their nursing case studies.
As a nurse practitioner, you will be required to conduct case analyses on patients in order to make treatment decisions. There are key elements that you will need to take into consideration when conducting a case analysis. These elements include the patient’s history, physical examination, laboratory data, and imaging studies.(Nursing Case Study Analysis)
By taking into consideration all of these elements, you will be able to develop a comprehensive picture of the patient’s condition. This will allow you to make an informed decision about the best course of treatment.

Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Have a subject expert Write for You Now
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, what you'll learn.
Working On A Paper On This Topic?
Use our nursing writing service and save your time. We guarantee high quality, on-time delivery, and 100% confidentiality.
- Nursing Careers
- Nursing Paper Solutions
- Nursing Theories
- Nursing Topics and Ideas
- Nursing Writing Guides
Related Posts
- How to become a Hospice Nurse
- How to Become a Labor and Delivery Nurse
- Role of an Intensive Care Unit Nurse: How to Become, Role and Requirements
Important Links
Knowledge base, paper examples, nursing writing services.
Nursingstudy.org helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Phone: +1 628 261 0844
Mail: [email protected]

We Accept:

@2015-2024, Nursingstudy.org

How to Write a Nursing Case Study Paper (A Guide)

Most nursing students dread writing a nursing case study analysis paper, yet it is a mandatory assignment; call it a rite of passage in nursing school. This is because it is a somewhat tricky process that is often overwhelming for nursing students. Nevertheless, by reading this guide prepared by our best nursing students, you should be able to easily and quickly write a nursing case study that can get you an excellent grade.
How different is this guide from similar guides all over the internet? Very different!
This guide provides all the pieces of information that one would need to write an A-grade nursing case study. These include the format for a nursing case study, a step-by-step guide on how to write a nursing case study, and all the important tips to follow when writing a nursing case study.
This comprehensive guide was developed by the top nursing essay writers at NurseMyGrade, so you can trust that the information herein is a gem that will catapult your grades to the next level. Expect updates as we unravel further information about writing a nursing case study.
Now that you know you’ve discovered a gold mine , let’s get right into it.
What Is a Nursing Case Study?
A nursing case study is a natural or imagined patient scenario designed to test the knowledge and skills of student nurses. Nursing case study assignments usually focus on testing knowledge and skills in areas of nursing study related to daily nursing practice.
As a nursing student, you must expect a nursing case study assignment at some point in your academic life. The fact that you are reading this post means that point is now.
While there is no standard structure for writing a nursing case study assignment, some things or elements must be present in your nursing assignment for your professor to consider it complete.
In the next section, you will discover what your instructor n expects in your nursing case study analysis. Remember, these are assignments where you are given a case study and are expected to write a case analysis report explaining how to handle such scenarios in real-life settings.
The Nursing Case Study Template
The typical nursing case study has nine sections. These are:
- Introduction
- Case presentation (Patient info, history, and medical condition)
- Diagnosis/Nursing assessment
- Intervention/Nursing care plan
- Discussion and recommendations
The Structure of a Nursing Case Study Analysis
You now know what nursing professors expect in a nursing case study analysis. In this section, we will explain what to include in each section of your nursing case study analysis to make it an excellent one.
1. Title page
The title page is essential in all types of academic writing. You must include it in your nursing case study analysis or any other essay or paper. And you must include it in the format recommended by your college.
If your college has no specific title page format, use the title page format of the style requested in the assignment prompt. In nursing college, virtually all assignments should be written in Harvard or APA format .
So, check your assignment prompt and create your title page correctly. The typical title page should include the topic of your paper, your name, the name of your professor, the course name, the date you are submitting the paper, and the name of your college.
2. Abstract
Most nursing professors require you to include an abstract in your nursing case study analysis. And even when you are not explicitly required to write one, it is good to do so. Of course, you should consult with your professor before doing so.
When writing an abstract for your paper, make sure it is about 200 words long. The abstract should include a brief summary of the case study, including all the essential information in the patient presentation, such as the history, age, and current diagnosis.
The summary should also include the nursing assessment, the current interventions, and recommendations.
3. Introduction
After writing the title page and the abstract, start writing the introduction. The introduction of a nursing case study analysis must briefly include the patient’s presentation, current diagnosis and medication, and recommendations. It must also include a strong thesis statement that shows what the paper is all about.
You shouldn’t just write an introduction for the sake of it. If you do so, your introduction will be bland. You need to put in good effort when writing your introduction. The best way to do this is to use your introduction to show you understand the case study perfectly and that you will analyze it right.
You can always write your introduction last. Many students do this because they believe writing an introduction last makes it more precise and accurate.
4. Case Presentation (Status of the Patient)
After introducing your nursing case study analysis, you should present the case where you outline the patient's status. It is usually straightforward to present a case.
You must paraphrase the patient scenario in the assignment prompt or brief. Focus on the demographic data of the patient (who they are, age, race, height, skin tone, occupation, relationships, marital status, appearance, etc.), why they are in the case study or scenario, reasons they sought medical attention, chief complaint, and current diagnosis and treatment. You should also discuss the actions performed on the patient, such as admission to the ICU, taking vital signs, recommending tests, etc.
In short, everything necessary in the patient scenario should be in your case presentation. You only need to avoid copying the patient scenario or case study word-for-word when writing your case presentation.
5. Diagnosis and Assessment
After the case presentation, you should explain the diagnosis. In other words, you should explain the condition, disease, or medical situation highlighted in the case presentation. For example, if the patient is a heavy smoker and he has COPD, it is at this point that you explain how COPD is linked to heavy smoking.
This is the section where you thoroughly discuss the disease process (pathophysiology) by highlighting the causes, symptoms, observations, and treatment methods. You should relate these to the patient’s status and give concrete evidence. You should describe the progression of the disease from when the client was admitted to a few hours or days after they were stabilized. Consider the first indication of the disease that prompted the patient to seek further medical assistance.
Your paper should also elucidate the diagnostic tests that should be conducted and the differential diagnosis. Ensure that each is given a well-founded rationale.
When explaining the condition, go deep into the pathophysiology. Focus specifically on the patient’s risk factors. Ensure you get your explanation from recent nursing literature (peer-reviewed scholarly journals published in the last 5 years). And do not forget to cite all the literature you get your facts from.
In short, this section should explain the patient’s condition or suffering.
6. Nursing Intervention
After the diagnosis and nursing assessment section, your nursing case study analysis should have an intervention section. This section is also known as the nursing care planning section. What you are supposed to do in this section is to present a nursing care plan for the patient presented in the patient scenario. You should describe the nursing care plan and goals for the patient. Record all the anticipated positive changes and assess whether the care plan addresses the patient's condition.
A good nursing care plan details the patient’s chief complaints or critical problems. It then describes the causes of these problems using evidence from recent medical or nursing literature. It then details the potential intervention for each problem. Lastly, it includes goals and evaluation strategies for the measures. Most professors, predominantly Australian and UK professors, prefer if this section is in table format.
Some nursing professors regard the intervention section (or nursing care plan section) as the most critical part of a nursing case study. This is because this part details precisely how the student nurse will react to the patient scenario (which is what the nursing professors want to know). So, ensure you make a reasonable effort when developing this section to get an excellent grade.
7. Discussion and Recommendations
The intervention section in a nursing case study is followed by a discussion and recommendations section. In this section, you are supposed to expound on the patient scenario, the diagnosis, and the nursing care plan. You should also expound on the potential outcomes if the care plan is followed correctly. The discussion should also explain the rationale for the care plan or its significant bits.
Recommendations should follow the discussion. Recommendations usually involve everything necessary that can be done or changed to manage a patient’s condition or prevent its reoccurrence. Anything that enhances the patient’s well-being can be a recommendation. Just make sure your key recommendations are supported by evidence.
8. Conclusion
This is the second last section of a typical nursing case study. What you need here is to summarize the entire case study. Ensure your summary has at least the case presentation, the nursing assessment/diagnosis, the intervention, and the key recommendations.
At the very end of your conclusion, add a closing statement. The statement should wrap up the whole thing nicely. Try to make it as impressive as possible.
9. References
This is the last section of a nursing case study. No nursing case study is complete without a references section. You should ensure your case study has in-text citations and a references page.
And you should make sure both are written as recommended in the assignment. The style section is usually Harvard or APA. Follow the recommended style to get a good grade on your essay.
Step-By-Step Guide to Writing a Nursing Case Study
You know all the key sections you must include in a nursing case study. You also know what exactly you need to do in each section. It is time to learn how to write a nursing case study. The process detailed below should be easy to follow because you know the typical nursing case study structure.
1. Understand the Assignment
When given a nursing case study assignment, the first thing you need to do is to read. You need to read two pieces of information slowly and carefully.
First, you need to read the prompt itself slowly and carefully. This is important because the prompt will have essential bits of information you need to know, including the style, the format, the word count, and the number of references needed. All these bits of information are essential to ensure your writing is correct.
Second, you need to read the patient scenario slowly and carefully. You should do this to understand it clearly so that you do not make any mistakes in your analysis.
2. Create a Rough Outline
Failure to plan is a plan to fail. That is not what you are in it for anyway! In other words, do not fail to create an outline for your case study analysis. Use the template provided in this essay to create a rough outline for your nursing case study analysis.
Ensure your outline is as detailed as it can be at this stage. You can do light research to achieve this aim. However, this is not exactly necessary because this is just a rough outline.
3. Conduct thorough research
After creating a rough outline, you should conduct thorough research. Your research should especially focus on providing a credible and evidence-based nursing assessment of the patient problem(s). You should only use evidence from recent nursing or medical literature.
You must also conduct thorough research to develop an effective intervention or nursing care plan. So when researching the patient’s problem and its diagnosis, you should also research the most suitable intervention or do it right after.
When conducting research, you should always note down your sources. So for every piece of information you find, and what to use, you should have its reference.
After conducting thorough research, you should enhance your rough outline using the new information you have discovered. Make sure it is as comprehensive as possible.
4. Write your nursing case study
You must follow your comprehensive outline to write your case study analysis at this stage. If you created a good outline, you should find it very easy to write your nursing case study analysis.
If you did not, writing your nursing case study will be challenging. Whenever you are stuck writing your case study analysis paper, you should re-read the part where we explain what to include in every section of your analysis. Doing so will help you know what to write to continue your essay. Writing a nursing case study analysis usually takes only a few hours.
5. Reference your case study
After writing your case study, ensure you add all in-text citations if you have not already. And when adding them, you should follow the style/format recommended in the assignment prompt (usually APA or Harvard style).
After adding in-text citations exactly where they need to be and in the correct format, add all the references you have used in a references page. And you should add them correctly as per the rules of the style you were asked to use.
Do not forget to organize your references alphabetically after creating your references page.
6. Thoroughly edit your case study
After STEP 5 above, you need to edit your case study. You should edit it slowly and carefully. Do this by proofreading it twice. Proofread it slowly each time to discover all the grammar, style, and punctuation errors. Remove all the errors you find.
After proofreading your essay twice, recheck it to ensure every sentence is straightforward. This will transform your ordinary case study into an A-grade one. Of course, it must also have all the standard sections expected in a case study.
Recheck your case study using a grammarly.com or a similar computer grammar checker to ensure it is perfect. Doing this will help you catch and eliminate all the remaining errors in your work.
7. Submit your case study analysis
After proofreading and editing your case study analysis, it will be 100% ready for submission. Just convert it into the format it is required in and submit it.
Nursing Case Study Tips and Tricks
The guide above and other information in this article should help you develop a good nursing case study analysis. Note that this guide focuses entirely on nursing case scenario-based papers, not research study-based nursing case studies. The tips and tricks in this section should help you ensure that the nursing case study analysis you create is excellent.
1. Begin early
The moment you see a nursing case study assignment prompt, identify a date to start writing it and create your own deadline to beat before the deadline stated in the prompt.
Do this and start writing your case study analysis early before your deadline. You will have plenty of time to do excellent research, develop an excellent paper, and edit your final paper as thoroughly as you want.
Most student nurses combine work and study. Therefore, if you decide to leave a nursing case study assignment until late to complete it, something could come up, and you could end up failing to submit it or submitting a rushed case study analysis.
2. Use the proper terminology
When writing an essay or any other academic paper, you are always encouraged to use the most straightforward language to make your work easy to understand. However, this is not true when writing a nursing case study analysis. While your work should certainly be easy to understand, you must use the right nursing terminology at every point where it is necessary. Failure to do this could damage your work or make it look less professional or convincing.
3. Avoid copying and pasting
If you are a serious nursing student, you know that copying and pasting are prohibited in assignments. However, sometimes copying and pasting can seem okay in nursing case studies. For example, it can seem okay to copy-paste the patient presentation. However, this is not okay. You are supposed to paraphrase the verbatim when presenting the patient presentation in your essay. You should also avoid copy-pasting information or texts directly. Every fact or evidence you research and find should be paraphrased to appear in your work. And it should be cited correctly.
4. Always ask for help if stuck
This is very important. Students are usually overwhelmed with academic work, especially a month or two to the end of the semester. If you are overwhelmed and think you will not have the time to complete your nursing case study analysis or submit a quality one, ask for help. Ask for help from a nursing assignment-help website like ours, and you will soon have a paper ready that you can use as you please. If you choose to get help from us, you will get a well-researched, well-planned, well-developed, and fully edited nursing case study.
5. Format your paper correctly
Many students forget to do proper formatting after writing their nursing case study analyses. Before you submit your paper, make sure you format it correctly. If you do not format your paper correctly, you will lose marks because of poor formatting. If you feel you are not very confident with your APA or Harvard formatting skills, send your paper to us to get it correctly formatted and ready for submission.
Now that you are all set up …
Our company has been among the best-rated nursing homework help companies in the last few years. Thousands of students have benefitted from our many academic writing guides. Many more have benefitted from direct help given by our experts.
- How to write a nursing philosophy statement.
- Writing an abstract poster presentation.
We have experienced nursing experts available every day of the week to provide nursing assignment help. They can easily research and write virtually any nursing assignment, including a nursing case study. So, if the information provided in this article isn’t making you feel any optimistic about writing an excellent nursing case study, get help from us.
Get help by ordering a custom nursing case study through this very website. If you do so, you will get a 100% original paper that is well-researched, well-written, well-formatted, and adequately referenced. Since the paper is original, you can use it anywhere without problems.
Thousands of students trust our company every week, month, and year. Be like them! Trust us for 100% confidentiality and speedy delivery.
Struggling with
Related Articles

Tips for Going Back to Nursing School after a Hiatus
How to Ace Online Nursing Classes: Tips & Tricks
Applying Carper’s Ways of Knowing in Essays & Practice
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
The Nursing Process: A Comprehensive Guide

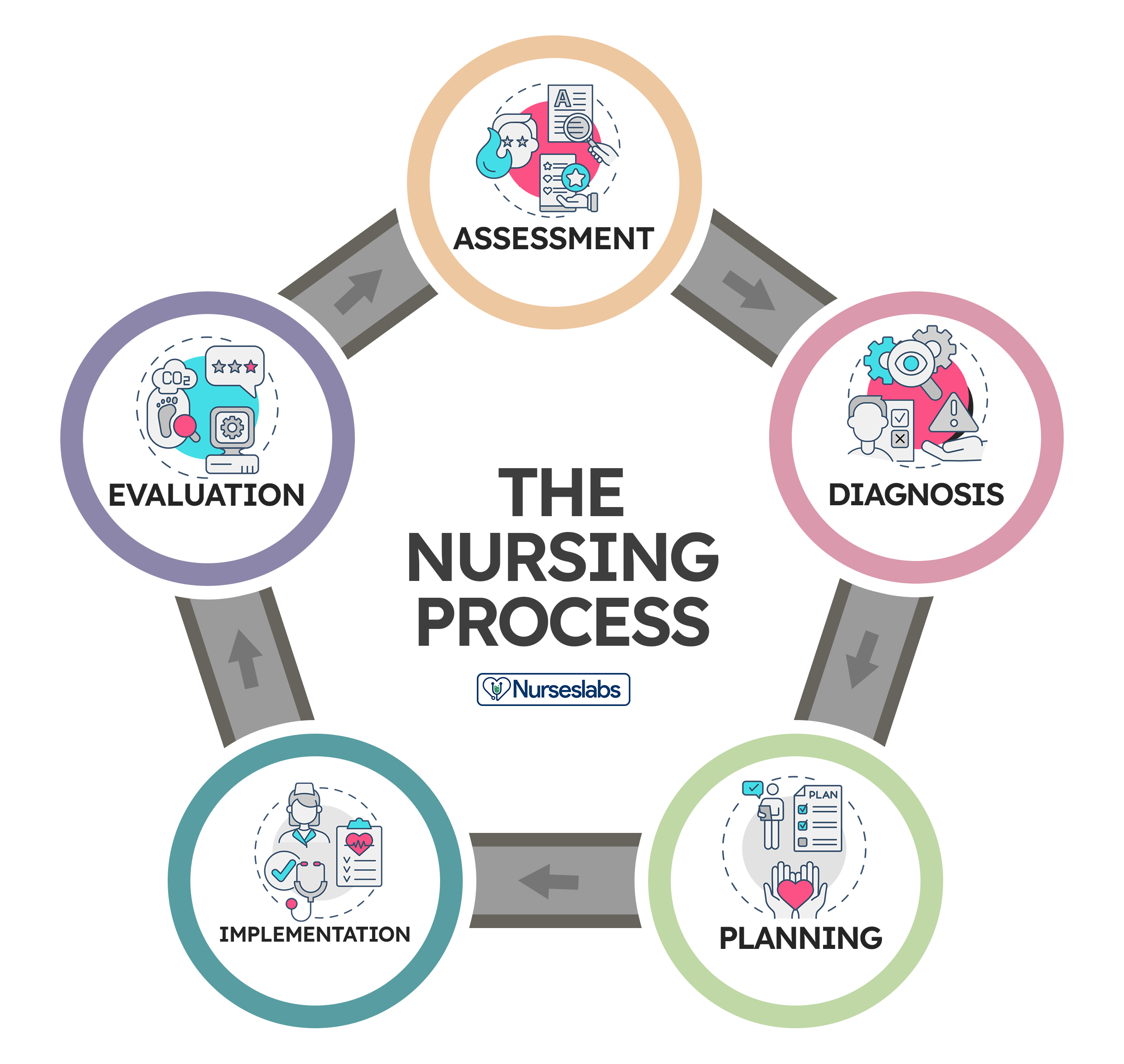
In 1958, Ida Jean Orlando began developing the nursing process still evident in nursing care today. According to Orlando’s theory, the patient’s behavior sets the nursing process in motion. Through the nurse’s knowledge to analyze and diagnose the behavior to determine the patient’s needs.
Application of the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EBP) recommendations, and nursing intuition, the nursing process functions as a systematic guide to client-centered care with five subsequent steps. These are assessment , diagnosis, planning, implementation, and evaluation ( ADPIE ).
Table of Contents
What is the nursing process.
- What is the purpose of the nursing process?
Characteristics of the nursing process
Nursing process steps, collecting data, objective data or signs, subjective data or symptoms, verbal data, nonverbal data, primary source, secondary source, tertiary source, health interview, physical examination, observation, validating data, documenting data.
- 2. Diagnosis: “What is the problem?”
Initial Planning
Ongoing planning, discharge planning, developing a nursing care plan, behavioral nursing interventions, community nursing interventions, family nursing interventions, health system nursing interventions, physiological nursing interventions, safety nursing interventions, skills used in implementing nursing care, 1. reassessing the client, 2. determining the nurse’s need for assistance, nursing intervention categories, independent nursing interventions, dependent nursing interventions, interdependent nursing interventions, 4. supervising the delegated care, 5. documenting nursing activities, 1. collecting data, 2. comparing data with desired outcomes, 3. analyzing client’s response relating to nursing activities, 4. identifying factors contributing to success or failure, 5. continuing, modifying, or terminating the nursing care plan, 6. discharge planning.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse’s critical thinking to provide the best care possible to the client.
What is the purpose of the nursing process?
The following are the purposes of the nursing process:
- To identify the client’s health status and actual or potential health care problems or needs (through assessment).
- To establish plans to meet the identified needs.
- To deliver specific nursing interventions to meet those needs.
- To apply the best available caregiving evidence and promote human functions and responses to health and illness (ANA, 2010).
- To protect nurses against legal problems related to nursing care when the standards of the nursing process are followed correctly.
- To help the nurse perform in a systematically organized way their practice.
- To establish a database about the client’s health status, health concerns, response to illness, and the ability to manage health care needs.
The following are the unique characteristics of the nursing process:
- Patient-centered . The unique approach of the nursing process requires care respectful of and responsive to the individual patient’s needs, preferences, and values. The nurse functions as a patient advocate by keeping the patient’s right to practice informed decision-making and maintaining patient-centered engagement in the health care setting.
- Interpersonal . The nursing process provides the basis for the therapeutic process in which the nurse and patient respect each other as individuals, both of them learning and growing due to the interaction. It involves the interaction between the nurse and the patient with a common goal.
- Collaborative . The nursing process functions effectively in nursing and inter-professional teams, promoting open communication, mutual respect, and shared decision-making to achieve quality patient care.
- Dynamic and cyclical .The nursing process is a dynamic, cyclical process in which each phase interacts with and is influenced by the other phases.
- Requires critical thinking . The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes.
The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation. The acronym ADPIE is an easy way to remember the components of the nursing process. Nurses need to learn how to apply the process step-by-step. However, as critical thinking develops through experience, they learn how to move back and forth among the steps of the nursing process.
The steps of the nursing process are not separate entities but overlapping, continuing subprocesses. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps of the nursing process are detailed below:
1. Assessment: “What data is collected?”
The first phase of the nursing process is assessment . It involves collecting, organizing, validating, and documenting the clients’ health status. This data can be obtained in a variety of ways. Usually, when the nurse first encounters a patient, the nurse is expected to assess to identify the patient’s health problems as well as the physiological, psychological, and emotional state and to establish a database about the client’s response to health concerns or illness and the ability to manage health care needs. Critical thinking skills are essential to the assessment, thus requiring concept-based curriculum changes.
Data collection is the process of gathering information regarding a client’s health status. The process must be systematic and continuous in collecting data to prevent the omission of important information concerning the client.
The best way to collect data is through head-to-toe assessment. Learn more about it at our guide: Head to Toe Assessment: Complete Physical Assessment Guide
Types of Data
Data collected about a client generally falls into objective or subjective categories, but data can also be verbal and nonverbal.
Objective data are overt, measurable, tangible data collected via the senses, such as sight, touch, smell, or hearing, and compared to an accepted standard, such as vital signs, intake and output , height and weight, body temperature, pulse, and respiratory rates, blood pressure, vomiting , distended abdomen, presence of edema , lung sounds, crying, skin color, and presence of diaphoresis.
Subjective data involve covert information, such as feelings, perceptions, thoughts, sensations, or concerns that are shared by the patient and can be verified only by the patient, such as nausea , pain , numbness, pruritus, attitudes, beliefs, values, and perceptions of the health concern and life events.
Verbal data are spoken or written data such as statements made by the client or by a secondary source. Verbal data requires the listening skills of the nurse to assess difficulties such as slurring, tone of voice, assertiveness, anxiety , difficulty in finding the desired word, and flight of ideas.
Nonverbal data are observable behavior transmitting a message without words, such as the patient’s body language, general appearance, facial expressions, gestures, eye contact, proxemics (distance), body language, touch, posture, clothing. Nonverbal data obtained can sometimes be more powerful than verbal data, as the client’s body language may not be congruent with what they really think or feel. Obtaining and analyzing nonverbal data can help reinforce other forms of data and understand what the patient really feels.
Sources of Data
Sources of data can be primary, secondary, and tertiary . The client is the primary source of data, while family members, support persons, records and reports, other health professionals, laboratory and diagnostics fall under secondary sources.
The client is the only primary source of data and the only one who can provide subjective data. Anything the client says or reports to the members of the healthcare team is considered primary.
A source is considered secondary data if it is provided from someone else other than the client but within the client’s frame of reference. Information provided by the client’s family or significant others are considered secondary sources of data if the client cannot speak for themselves, is lacking facts and understanding, or is a child. Additionally, the client’s records and assessment data from other nurses or other members of the healthcare team are considered secondary sources of data.
Sources from outside the client’s frame of reference are considered tertiary sources of data . Examples of tertiary data include information from textbooks, medical and nursing journals, drug handbooks, surveys, and policy and procedural manuals.
Methods of Data Collection
The main methods used to collect data are health interviews, physical examination, and observation.
The most common approach to gathering important information is through an interview. An interview is an intended communication or a conversation with a purpose, for example, to obtain or provide information, identify problems of mutual concern, evaluate change, teach, provide support, or provide counseling or therapy. One example of the interview is the nursing health history, which is a part of the nursing admission assessment. Patient interaction is generally the heaviest during the assessment phase of the nursing process so rapport must be established during this step.
Aside from conducting interviews, nurses will perform physical examinations, referencing a patient’s health history, obtaining a patient’s family history, and general observation can also be used to gather assessment data. Establishing a good physical assessment would, later on, provide a more accurate diagnosis, planning, and better interventions and evaluation.
Observation is an assessment tool that depends on the use of the five senses (sight, touch, hearing, smell, and taste) to learn information about the client. This information relates to characteristics of the client’s appearance, functioning, primary relationships, and environment. Although nurses observe mainly through sight, most of the senses are engaged during careful observations such as smelling foul odors, hearing or auscultating lung and heart sounds and feeling the pulse rate and other palpable skin deformations.
Validation is the process of verifying the data to ensure that it is accurate and factual. One way to validate observations is through “double-checking,” and it allows the nurse to complete the following tasks:
- Ensures that assessment information is double-checked, verified, and complete. For example, during routine assessment, the nurse obtains a reading of 210/96 mm Hg of a client with no history of hypertension . To validate the data, the nurse should retake the blood pressure and if necessary, use another equipment to confirm the measurement or ask someone else to perform the assessment.
- Ensure that objective and related subjective data are valid and accurate. For example, the client’s perceptions of “feeling hot” need to be compared with the measurement of the body temperature.
- Ensure that the nurse does not come to a conclusion without adequate data to support the conclusion. A nurse assumes tiny purple or bluish-black swollen areas under the tongue of an older adult client to be abnormal until reading about physical changes of aging.
- Ensure that any ambiguous or vague statements are clarified. For example, a 86-year-old female client who is not a native English speaker says that “I am in pain on and off for 4 weeks,” would require verification for clarity from the nurse by asking “Can you describe what your pain is like? What do you mean by on and off?”
- Acquire additional details that may have been overlooked. For example, the nurse is asking a 32-year-old client if he is allergic to any prescription or non-prescription medications. And what would happen if he takes these medications.
- Distinguish between cues and inferences. Cues are subjective or objective data that can be directly observed by the nurse; that is, what the client says or what the nurse can see, hear, feel, smell, or measure. On the other hand, inferences are the nurse’s interpretation or conclusions made based on the cues. For example, the nurse observes the cues that the incision is red, hot, and swollen and makes an inference that the incision is infected.
Once all the information has been collected, data can be recorded and sorted. Excellent record-keeping is fundamental so that all the data gathered is documented and explained in a way that is accessible to the whole health care team and can be referenced during evaluation.
2. Diagnosis: “What is the problem?”
The second step of the nursing process is the nursing diagnosis . The nurse will analyze all the gathered information and diagnose the client’s condition and needs. Diagnosing involves analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements about a patient’s potential or actual health problem. More than one diagnosis is sometimes made for a single patient. Formulating a nursing diagnosis by employing clinical judgment assists in the planning and implementation of patient care.
The types, components, processes, examples, and writing nursing diagnosis are discussed more in detail here “ Nursing Diagnosis Guide: All You Need To Know To Master Diagnosing ”
3. Planning: “How to manage the problem?”
Planning is the third step of the nursing process. It provides direction for nursing interventions. When the nurse, any supervising medical staff, and the patient agree on the diagnosis, the nurse will plan a course of treatment that takes into account short and long-term goals. Each problem is committed to a clear, measurable goal for the expected beneficial outcome.
The planning phase is where goals and outcomes are formulated that directly impact patient care based on evidence-based practice (EBP) guidelines. These patient-specific goals and the attainment of such assist in ensuring a positive outcome. Nursing care plans are essential in this phase of goal setting. Care plans provide a course of direction for personalized care tailored to an individual’s unique needs. Overall condition and comorbid conditions play a role in the construction of a care plan. Care plans enhance communication, documentation, reimbursement, and continuity of care across the healthcare continuum.
Types of Planning
Planning starts with the first client contact and resumes until the nurse-client relationship ends, preferably when the client is discharged from the health care facility.
Initial planning is done by the nurse who conducts the admission assessment. Usually, the same nurse would be the one to create the initial comprehensive plan of care.
Ongoing planning is done by all the nurses who work with the client. As a nurse obtain new information and evaluate the client’s responses to care, they can individualize the initial care plan further. An ongoing care plan also occurs at the beginning of a shift. Ongoing planning allows the nurse to:
- determine if the client’s health status has changed
- set priorities for the client during the shift
- decide which problem to focus on during the shift
- coordinate with nurses to ensure that more than one problem can be addressed at each client contact
Discharge planning is the process of anticipating and planning for needs after discharge. To provide continuity of care, nurses need to accomplish the following:
- Start discharge planning for all clients when they are admitted to any health care setting.
- Involve the client and the client’s family or support persons in the planning process.
- Collaborate with other health care professionals as needed to ensure that biopsychosocial, cultural, and spiritual needs are met.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes potential needs or risks. Care plans provide communication among nurses, their patients, and other healthcare providers to achieve health care outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
The planning step of the nursing process is discussed in detail in Nursing Care Plans (NCP): Ultimate Guide and Database .
4. Implementation : “Putting the plan into action!”
The implementation phase of the nursing process is when the nurse puts the treatment plan into effect. It involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care. This typically begins with the medical staff conducting any needed medical interventions.
Interventions should be specific to each patient and focus on achievable outcomes. Actions associated with a nursing care plan include monitoring the patient for signs of change or improvement, directly caring for the patient or conducting important medical tasks such as medication administration , educating and guiding the patient about further health management, and referring or contacting the patient for a follow-up.
A taxonomy of nursing interventions referred to as the Nursing Interventions Classification (NIC) taxonomy, was developed by the Iowa Intervention Project. The nurse can look up a client’s nursing diagnosis to see which nursing interventions are recommended.
Nursing Interventions Classification (NIC) System
There are more than 550 nursing intervention labels that nurses can use to provide the proper care to their patients. These interventions are categorized into seven fields or classes of interventions according to the Nursing Interventions Classification system.
These are interventions designed to help a patient change their behavior. With behavioral interventions, in contrast, patient behavior is the key and the goal is to modify it. The following measures are examples of behavioral nursing interventions:
- Encouraging stress and relaxation techniques
- Providing support to quit smoking
- Engaging the patient in some form of physical activity , like walking, to reduce the patient’s anxiety, anger, and hostility
These are interventions that refer to the community-wide approach to health behavior change. Instead of focusing mainly on the individual as a change agent, community interventionists recognize a host of other factors that contribute to an individual’s capacity to achieve optimal health, such as:
- Implementing an education program for first-time mothers
- Promoting diet and physical activities
- Initiating HIV awareness and violence-prevention programs
- Organizing a fun run to raise money for breast cancer research
These are interventions that influence a patient’s entire family.
- Implementing a family-centered approach in reducing the threat of illness spreading when one family member is diagnosed with a communicable disease
- Providing a nursing woman support in breastfeeding her new baby
- Educating family members about caring for the patient
These are interventions that designed to maintain a safe medical facility for all patients and staff, such as:
- Following procedures to reduce the risk of infection for patients during hospital stays.
- Ensuring that the patient’s environment is safe and comfortable, such as repositioning them to avoid pressure ulcers in bed
These are interventions related to a patient’s physical health to make sure that any physical needs are being met and that the patient is in a healthy condition. These nursing interventions are classified into two types: basic and complex.
- Basic. Basic interventions regarding the patient’s physical health include hands-on procedures ranging from feeding to hygiene assistance.
- Complex. Some physiological nursing interventions are more complex, such as the insertion of an IV line to administer fluids to a dehydrated patient.
These are interventions that maintain a patient’s safety and prevent injuries, such as:
- Educating a patient about how to call for assistance if they are not able to safely move around on their own
- Providing instructions for using assistive devices such as walkers or canes, or how to take a shower safely.
When implementing care, nurses need cognitive, interpersonal, and technical skills to perform the care plan successfully.
- Cognitive Skills are also known as Intellectual Skills are skills involve learning and understanding fundamental knowledge including basic sciences, nursing procedures, and their underlying rationale before caring for clients. Cognitive skills also include problem-solving, decision-making, critical thinking, clinical reasoning, and creativity.
- Interpersonal Skills are skills that involve believing, behaving, and relating to others. The effectiveness of a nursing action usually leans mainly on the nurse’s ability to communicate with the patient and the members of the health care team.
- Technical Skills are purposeful “hands-on” skills such as changing a sterile dressing, administering an injection, manipulating equipment, bandaging, moving, lifting, and repositioning clients. All of these activities require safe and competent performance.
Process of Implementing
The process of implementing typically includes the following:
Prior to implementing an intervention, the nurse must reassess the client to make sure the intervention is still needed. Even if an order is written on the care plan, the client’s condition may have changed.
Other nursing tasks or activities may also be performed by non-RN members of the healthcare team. Members of this team may include unlicensed assistive personnel (UAP) and caregivers , as well as other licensed healthcare workers, such as licensed practical nurses/licensed vocational nurses (LPNs/LVNs). The nurse may need assistance when implementing some nursing intervention, such as ambulating an unsteady obese client, repositioning a client, or when a nurse is not familiar with a particular model of traction equipment needs assistance the first time it is applied.
3. Implementing the nursing interventions
Nurses must not only have a substantial knowledge base of the sciences, nursing theory , nursing practice, and legal parameters of nursing interventions but also must have the psychomotor skills to implement procedures safely. It is necessary for nurses to describe, explain, and clarify to the client what interventions will be done, what sensations to anticipate, what the client is expected to do, and what the expected outcome is. When implementing care, nurses perform activities that may be independent, dependent, or interdependent.
Nursing interventions are grouped into three categories according to the role of the healthcare professional involved in the patient’s care:
A registered nurse can perform independent interventions on their own without the help or assistance from other medical personnel, such as:
- routine nursing tasks such as checking vital signs
- educating a patient on the importance of their medication so they can administer it as prescribed
A nurse cannot initiate dependent interventions alone. Some actions require guidance or supervision from a physician or other medical professional, such as:
- prescribing new medication
- inserting and removing a urinary catheter
- providing diet
- Implementing wound or bladder irrigations
A nurse performs as part of collaborative or interdependent interventions that involve team members across disciplines.
- In some cases, such as post- surgery , the patient’s recovery plan may require prescription medication from a physician, feeding assistance from a nurse, and treatment by a physical therapist or occupational therapist.
- The physician may prescribe a specific diet to a patient. The nurse includes diet counseling in the patient care plan. To aid the patient, even more, the nurse enlists the help of the dietician that is available in the facility.
Delegate specific nursing interventions to other members of the nursing team as appropriate. Consider the capabilities and limitations of the members of the nursing team and supervise the performance of the nursing interventions. Deciding whether delegation is indicated is another activity that arises during the nursing process.
The American Nurses Association and the National Council of State Boards of Nursing (2006) define delegation as “the process for a nurse to direct another person to perform nursing tasks and activities.” It generally concerns the appointment of the performance of activities or tasks associated with patient care to unlicensed assistive personnel while retaining accountability for the outcome.
Nevertheless, registered nurses cannot delegate responsibilities related to making nursing judgments. Examples of nursing activities that cannot be delegated to unlicensed assistive personnel include assessment and evaluation of the impact of interventions on care provided to the patient.
Record what has been done as well as the patient’s responses to nursing interventions precisely and concisely.
5. Evaluation : “Did the plan work?”
Evaluating is the fifth step of the nursing process. This final phase of the nursing process is vital to a positive patient outcome. Once all nursing intervention actions have taken place, the team now learns what works and what doesn’t by evaluating what was done beforehand. Whenever a healthcare provider intervenes or implements care, they must reassess or evaluate to ensure the desired outcome has been met. The possible patient outcomes are generally explained under three terms: the patient’s condition improved, the patient’s condition stabilized, and the patient’s condition worsened.
Steps in Evaluation
Nursing evaluation includes (1) collecting data, (2) comparing collected data with desired outcomes, (3) analyzing client’s response relating to nursing activities, (4) identifying factors that contributed to the success or failure of the care plan, (5) continuing, modifying, or terminating the nursing care plan, and (6) planning for future nursing care.
The nurse recollects data so that conclusions can be drawn about whether goals have been fulfilled. It is usually vital to collect both objective and subjective data. Data must be documented concisely and accurately to facilitate the next part of the evaluating process.
The documented goals and objectives of the nursing care plan become the standards or criteria by which to measure the client’s progress whether the desired outcome has been met, partially met, or not met.
- The goal was met , when the client response is the same as the desired outcome.
- The goal was partially met , when either a short-term outcome was achieved but the long-term goal was not, or the desired goal was incompletely attained.
- The goal was not met.
It is also very important to determine whether the nursing activities had any relation to the outcomes whether it was successfully accomplished or not.
It is required to collect more data to confirm if the plan was successful or a failure. Different factors may contribute to the achievement of goals. For example, the client’s family may or may not be supportive, or the client may be uncooperative to perform such activities.
The nursing process is dynamic and cyclical. If goals were not sufficed, the nursing process begins again from the first step. Reassessment and modification may continually be needed to keep them current and relevant depending upon general patient condition. The plan of care may be adjusted based on new assessment data. Problems may arise or change accordingly. As clients complete their goals, new goals are set. If goals remain unmet, nurses must evaluate the reasons these goals are not being achieved and recommend revisions to the nursing care plan.
Discharge planning is the process of transitioning a patient from one level of care to the next. Discharge plans are individualized instructions provided as the client is prepared for continued care outside the healthcare facility or for independent living at home. The main purpose of a discharge plan is to improve the client’s quality of life by ensuring continuity of care together with the client’s family or other healthcare workers providing continuing care.
The following are the key elements of IDEAL discharge planning according to the Agency for Healthcare Research and Quality:
- I nclude the patient and family as full partners in the discharge planning process.
- Describe what life at home will be like
- Review medications
- Highlight warning signs and problems
- Explain test results
- Schedule follow-up appointments
- E ducate the patient and family in plain language about the patient’s condition, the discharge process, and next steps throughout the hospital stay.
- A ssess how well doctors and nurses explain the diagnosis, condition, and next steps in the patient’s care to the patient and family and use teach back.
- L isten to and honor the patient’s and family’s goals, preferences, observations, and concerns.
A discharge plan includes specific components of client teaching with documentation such as:
- Equipment needed at home. Coordinate home-based care and special equipment needed.
- Dietary needs or special diet . Discuss what the patient can or cannot eat at home.
- Medications to be taken at home. List the patient’s medications and discuss the purpose of each medicine, how much to take, how to take it, and potential side effects.
- Resources such as contact numbers and addresses of important people. Write down the name and contact information of someone to call if there is a problem.
- Emergency response: Danger signs. Identify and educate patients and families about warning signs or potential problems.
- Home care activities. Educate patient on what activities to do or avoid at home.
- Summary. Discuss with the patient and family about the patient’s condition, the discharge process, and follow-up checkups.
38 thoughts on “The Nursing Process: A Comprehensive Guide”
This article is helpful
So helpful And easy to understand A very good guide for nurses
I’m a clinical instructor teaching Fundamentals this semester. The article will be very helpful to give an in-depth explanation of “The Nursing Process” to students. Thank you.
Very detailed and easy to understand. Thx
Am a student I find it very educative
This is so helpful
Excellent information that is clearly outlined and user friendly.
This is so wonderful thank you
So helpful thank you
this is very helpful thank you
Helpful. So grateful
Is the nursing process the same as “critical thinking”?
Great information! Thanks!
This is very helpful. Thank you
Great explanation, in the understanding of Nursing process
Very Helpful to students, thank you for sharing
Excellent job. A great help to all nursing students. Thank you for sharing. God bless you.
Hi Joycelyn, Thank you so much for your kind words! It’s really rewarding to hear that it’s helping nursing students out there. We’re all about sharing knowledge and making things a bit easier. 😊 If there’s anything else you’d like to see or know, just let me know. And blessings right back at you!
Thank you so much…It’s a very comprehensive reference.
You’re very welcome, A.C! I’m glad you found the nursing process reference comprehensive and useful. Just out of curiosity, is there a particular step in the nursing process you’d like to explore more deeply, or do you have any specific areas where you’d like more detailed information?
I am a nursing student and I see this as a helpful tool, very detailed and easy to understand thanks for sharing
Hi Mawuli, I’m delighted to know that you’re finding our resources helpful! If you have any specific questions or if there’s a particular topic you’d like more information on, please feel free to ask. I’m here to assist you with any nursing-related inquiries you may have. Keep up the great work in your studies! 🩺📚🌟
Keep updating me about Nursing pdfs. You guys are really good at your work!!
Hey Mokete, Thank you so much for the kind words! We’re thrilled to hear that you’re finding our nursing resources helpful. We’ll do our best to keep you updated with more valuable nursing PDFs and information. If there’s anything specific you’d like to see or if you have any questions, feel free to let us know. Keep up the great work in your nursing journey! 👩⚕️📚🌟
Thanks it really helps alot
Glad to be of help! Thank you!
This guideline very useful for Nurses building their competency and practice quality of care of Nursing to use as reference please allow to download free especially to Nurses who live in developing countries since it is not affordable to buy it
You can download the articles by printing them as PDF :) You can use a service called printfriendly (google it) to make PDFs of our webpages.
Excellent work done I’m very happy to see this stuffs
Thank you so much…It’s a very comprehensive reference. God bless you
Hello Theophilus, You’re very welcome, and thank you for the blessings! 😊 I’m glad you found the reference on the nursing process comprehensive. Just out of curiosity, is there a particular part of the nursing process you’re most interested in, or any aspect you’d like to explore more deeply?
God bless you too, and if you have any more questions, feel free to ask!
Very helpful information. Thank you.
Thank you so much, Alisa. If you need more information or help regarding this, let us know.
You’re doing a great job here. Please can you do it in such a way for us to download it as a pdf?
Hi Millicent, Thank you so much for the kind words! 😊 I’m really glad you’re finding the site useful.
Regarding your request to download content as a PDF, a neat trick you can use is the “print” function in your web browser. Here’s how you can do it:
Open the page you want to save as a PDF. -Go to the “File” menu in your browser and select “Print,” or simply press Ctrl+P (Cmd+P on Mac). -In the print window, look for a destination option and select “Save as PDF” or something similar. -Adjust any settings as needed, then click “Save” or “Print,” and choose where you want to save the file on your computer.
This way, you can turn any page into a PDF for your personal use. If you have any more questions or need further assistance, feel free to ask. Always here to help!
Leave a Comment Cancel reply

Mastering Nursing Case Study Assignments: A Comprehensive Guide
Introduction: Nursing case study assignments are an integral part of nursing education, allowing students to apply their theoretical knowledge to real-world patient scenarios. Mastering these assignments requires a deep understanding of the process and techniques involved. At Nurse Homework s, we are dedicated to helping nursing students excel in their case study assignments. In this comprehensive guide, we will explore the importance of nursing case study assignments, provide step-by-step approaches, offer tips for effective research and analysis, and highlight common mistakes to avoid. Additionally, we will showcase examples of successful nursing case study assignments to inspire and guide your own work.
Understanding Nursing Case Study Assignments
Table of Contents
Get Your Custom Essay Written From Scratch Mastering Nursing Case Study Assignments: A Comprehensive Guide
Just from $13/Page
Gain a solid understanding of what nursing case study assignments entail. Learn about the purpose of these assignments, their relevance to nursing education, and the skills they help develop. Explore the different components typically included in nursing case study assignments and how they contribute to a holistic understanding of patient care.
Importance of Nursing Case Study Assignments
Discover the significance of nursing case study assignments in your academic and professional journey. Understand how these assignments help you develop critical thinking, clinical reasoning, and decision-making skills essential for nursing practice. Learn how nursing case studies bridge the gap between theory and practice, preparing you to provide high-quality, evidence-based care to patients.
Steps to Approach a Nursing Case Study Assignment
Follow a systematic approach to effectively tackle nursing case study assignments. Learn how to carefully analyze the case study, conduct comprehensive research, and organize your thoughts. Understand the importance of data collection, patient assessment, nursing diagnoses, interventions, and evaluation. These step-by-step guidelines will help you navigate through the assignment with confidence.
Tips for Effective Research in Nursing Case Studies
Research is a crucial aspect of nursing case study assignments. Explore tips and strategies for conducting effective research, including utilizing reputable sources, incorporating evidence-based practice, and staying up-to-date with current literature. Learn how to critically evaluate research findings and apply them to your case study analysis.
Analyzing and Interpreting Data in Nursing Case Studies
Master the art of analyzing and interpreting data in nursing case studies. Discover techniques for identifying key information, recognizing patterns, and formulating nursing diagnoses. Understand how to critically analyze patient data to develop a comprehensive understanding of the case and make informed decisions in your nursing interventions.
Developing a Clear and Concise Nursing Case Study Report
Learn how to effectively communicate your findings in a clear and concise manner. Understand the importance of structuring your report, using appropriate nursing terminology, and presenting your analysis in a logical flow. Explore strategies for creating a well-organized and professional nursing case study report that effectively conveys your knowledge and insights.
Common Mistakes to Avoid in Nursing Case Study Assignments
Identify common pitfalls and errors that students often encounter in nursing case study assignments. Learn how to avoid these mistakes, such as inaccuracies in data interpretation, lack of evidence-based practice, or insufficient analysis. By recognizing these pitfalls, you can ensure the quality and credibility of your work.
Examples of Successful Nursing Case Study Assignments
Gain inspiration from real-life examples of successful nursing case study assignments. Explore exemplary case studies that showcase effective approaches, insightful analysis, and evidence-based interventions. These examples serve as valuable references to guide and inspire your own work.
Resources for Further Learning and Practice in Nursing Case Studies
Access additional resources to enhance your understanding and practice of nursing case studies. Discover recommended textbooks, online databases, research journals, and professional organizations that provide valuable insights, research articles, and educational materials to support your learning journey.
Conclusion: Mastering Nursing Case Study Assignments
In conclusion, mastering nursing case study assignments is essential
Needs help with nursing assignment?
We are available 24x7 to deliver the best services and assignment ready within 3-4 hours? Order a custom-written, plagiarism-free paper

7 steps to successful nursing case study writing.
A nursing case study is a detailed study of a patient that is encountered during a nurse’s daily practice. They are usually written by nurses in training as part of their coursework, but they can also be written by experienced nurses as a way of sharing best practice.
Case studies are an important part of the nursing curriculum as they provide students with a real-life insight into the complexities of patient care. They also allow nurses to reflect on their own practice and identify areas where they could make improvements.
When writing a nursing case study, it is important to follow the instructions provided by your tutor. This will ensure that your case study is relevant and meets the required academic standards. It is also important to be clear and concise in your writing, and to use evidence-based sources to support your claims.
If you are struggling to write a nursing case study, there are a number of resources that can help you. The following books are all recommended reading for anyone wanting to write a case study:
- The Complete Guide to Case Study Research by Elaine M. Hubbell
- Nursing Case Studies: A Guide to Understanding and Writing Them by Jennifer R. Gray
- Writing Nursing Case Studies by Sally G. Reed
Once you have a good understanding of how to write a nursing case study, you will be able to produce high-quality studies that will be of benefit to both yourself and your patients.
Importance of nursing case study writing.
Nursing case studies are an important part of your nursing education. They provide you with the opportunity to apply the knowledge and skills you have learned in the classroom to real-world scenarios. Nursing case studies also allow you to develop critical thinking and problem-solving skills.
The nursing case study should be a detailed and accurate account of the care that was provided to the patient. It should be used to evaluate the outcome of that care and to identify any areas where improvements can be made.
Steps when writing a nursing case study paper.
There are various steps you should keep in mind in order to help you write a successful nursing case study.
These important steps include:
- Define the problem.
- Gathering information.
- Developing alternatives.
- Analyzing the alternatives.
- Selecting the best alternative.
- Implementing the solution.
- Evaluating the outcome.
Defining the Problem
When writing a nursing case study, it is important to first define the problem. The problem should be something that can be solved through nursing interventions. Once the problem is defined, the nursing case study can be written to discuss the interventions that were used to solve the problem.
Nursing case studies are a great way to learn about different nursing interventions and how they can be used to solve problems. By reading nursing case studies, nurses can learn about different diseases and conditions and how to treat them. Nursing case studies can also be used to teach other nurses about different interventions.
Gathering Information
When it comes to writing a nursing case study, the first and most important step is gathering information. This is where you will need to do your research and collect data from a variety of sources. Once you have all of the information you need, you can begin to write your case study.
It is crucial to gather information before starting to write your nursing case study. This ensures that you include all of the relevant information. This means including details about the patient’s medical history, symptoms, and treatment.
Developing Alternatives
Once you have all of the necessary information, you can begin developing alternatives for the patient’s treatment. This will involve looking at the different options and deciding which is best based on the specific case. You will need to consider the risks and benefits of each option before making a recommendation.
Once you have developed a few different options, you can then start writing the case study. This should include an overview of the patient’s history, their current condition, and the different treatment options that were considered. Be sure to explain why you ultimately recommended the chosen course of treatment.
Analyzing the Alternatives
When you are given a nursing case study to write, the first step is to read the case thoroughly. Make sure you understand the situation and the patient’s history. Once you have a good understanding of the case, you can start to analyze the alternatives.
There are usually three alternatives in a nursing case study: nursing intervention, medical intervention, and no intervention. You will need to evaluate each alternative and decide which is best for the patient.
Nursing intervention is usually the first choice because it is the least invasive and has the least risk. Medical intervention is usually the next choice because it is more invasive but has a higher chance of success. No intervention is usually the last choice because it means doing nothing and letting the patient’s condition worsen.
Once you have evaluated the alternatives, you can start to write your case study. Remember to include all of the important information, such as the patient’s history, the alternatives you considered, and your recommendation.
Selecting the Best Alternative
When you are presented with a nursing case study, the first thing you need to do is identify the problem. Once you have identified the problem, you need to gather information about the patient. This information will help you to develop a plan of care. Once you have developed a plan of care, you need to select the best alternative.
The best alternative is the one that will best meet the needs of the patient. When selecting the best alternative, you need to consider the patient’s preferences, the severity of the problem, the risks and benefits of each alternative, and the resources available.
Implementing the Solution
Once you have selected the best alternative, you need to implement the plan of care. After you have implemented the plan of care, you need to evaluate the patient’s response. If the patient’s condition improves, you need to continue the plan of care. If the patient’s condition does not improve, you need to reevaluate the plan of care and select a different alternative.
Evaluating the Outcome
A nursing case study is a detailed account of a patient’s medical history and treatment. It is used to evaluate the outcome of a patient’s care and to identify any areas where improvements can be made.
When writing a nursing case study, it is important to include a detailed description of the patient’s symptoms and medical history. The case study should also include a discussion of the treatment that was provided and the outcome of that treatment.
It is also important to discuss any areas where improvements could be made in the care that was provided. This could include changes to the treatment plan, changes to the way that the patient was monitored, or changes to the way that the patient’s symptoms were managed.
Conclusion.
Writing a successful nursing case study can be a challenging task. However, by following the steps provided in this blog that is, first defining the problem, gathering information, developing alternatives., analyzing the alternatives, selecting the best alternative, implementing the solution and evaluating the outcome. You will be able to write a top-notch nursing case study that meets your requirements.
If you need professional assistance, place your order right here to get help from expert nursing paper writers.

Work with professional online writers

- Affordable Nursing Papers
- Nursing Coursework Writing
- Nursing Essay Writing Service
- Nursing Essay Assignments
- Nursing Assignment Writing
- Nursing Case Study Writing
- Nursing Process Essay Writing
- Nursing Capstone Project
- BSN Capstone Project
- Reliable Nursing Writers
- PICO Question Examples
- Nursing Speeches
- Nursing PowerPoint Presentations
- Online Nursing Essay Writers
- Nursing Thesis
- Nursing Coursework
- Nursing Term Papers
- Legit Nursing Writers
- Best Nursing Writing Company
- Nursing Students Writing Help
- Cheap Nursing Term Paper

- Refund Guarantee
- On time delivery
- Plagiarism-free papers
- Safe and Confidential
- Trained Writers
- Nursing Essay Writing
- Nursing Coursework Help
- Nursing Dissertations
- Nursing Case Studies
- Nursing Assignment Help
Contact Info
- 123 Fifth Ave, New York, NY 12004, United States.
- +1(413) 798-7210
- [email protected]

How to Write a Case Study Paper for Nursing
A well-written case study paper for a nursing program requires some planning and consideration. All too often, students begin writing before they complete appropriate, preliminary steps. Ideally, before you start a paper, you should already have determined the focus and format of it. You will then follow this up with a fact-gathering step in which you will gather and collate the content of your paper. Finally, there is the construction/execution step in which you will write the paper in a standard format (such as the APA style) and edit it.
A nursing case study paper contains several sections that fall into three categories:
1. The status of the patient
- Demographic data
- Medical History
- Current diagnosis and treatment
2. The nursing assessment of the patient
- Vital signs and test results
- Nursing observations (i.e., range of motion, mental state)
3. Current Care Plan and Recommendations
- Details of the nursing care plan (including nursing goals and interventions)
- Evaluation of the current care plan
- Recommendations for changes in the current care plan
Patient Status
The first portion of the case study paper will talk about the patient — who they are, why they are being included in the study, their demographic data (i.e., age, race), the reason(s) they sought medical attention and the subsequent diagnosis. It will also discuss the role that nursing plays in the care of this patient.
Next, thoroughly discuss any disease process. Make sure you outline causes, symptoms, observations, and how preferred treatments can affect nursing care. Also, describe the history and progression of the disease. Some important questions for you to answer are: 1) What were the first indications that there was something wrong, and 2) What symptoms convinced the patient to seek help?
Nursing Assessment
When you are discussing the nursing assessment of the patient, describe the patientΓÇÖs problems in terms of nursing diagnoses. Be specific as to why you have identified a particular diagnosis. For example, is frequent urination causing an alteration in the patientΓÇÖs sleep patterns? The nursing diagnoses you identify in your assessment will help form the nursing care plan.
Current Care Plan and Recommendations for Improvement
Describe the nursing care plan and goals, and explain how the nursing care plan improves the quality of the patientΓÇÖs life. What positive changes does the nursing care plan hope to achieve in the patientΓÇÖs life? How will the care plan be executed? Who will be responsible for the delivery of the care plan? What measurable goals will they track to determine the success of the plan?
The final discussion should be your personal recommendations. Based on the current status of the patient, the diagnosis, prognosis, and the nursing care plan, what other actions do you recommend can be taken to improve the patientΓÇÖs chances of recovery? You must support your recommendations with authoritative sources and cite appropriately per APA style guidelines.
Creating a well-written nursing case study paper doesnΓÇÖt need to be a grueling challenge. It can be gratifying, and itΓÇÖs good practice for assessing patients while out in the field, too. Keep in mind that your instructor will not only grade you on the quality of the content of your paper but by how you apply the APA style, as well. If you find that you are spending too much time formatting your paper, consider using formatting software as a helpful tool to ensure accuracy, so you donΓÇÖt lose points on a well-written paper because of some formatting errors.
For more information about APA or MLA formats, contact us today.
David Plaut
David Plaut is the founder of Reference Point Software (RPS). RPS offers a complete suite of easy-to-use formatting template products featuring MLA and APA style templates, freeing up time to focus on substance while ensuring formatting accuracy. 
Reference Point Software is not associated with, endorsed by, or affiliated with the American Psychological Association (APA) or with the Modern Language Association (MLA).
Tags: medical writing tips , nurse writing tips , reference point software
Comments are closed.

A Guide on How To Write a Nursing Case Study Assignment
Many students who don’t have nursing as a major subject mistakenly believe nursing students do not complete research assignments. After all, they spend most of their time in biology and chemistry labs, conducting field experiments. However, a patient’s nursing case study is a tough assignment and will likely freak you out. Many students have claimed they get overwhelmed by writing a nursing case study with patient scenarios.
What is a Nursing Case Study?
A nursing case study assignment brings up a specific patient’s health condition to test a nursing student’s skills, aptitude, and knowledge in their research area. The case study nursing students work on are most likely the practicum or procedures they will be encountering in their daily routine. These projects are assigned to student nurses as a part of their study course. The research paper helps students integrate the theoretical learning from lectures into a real world scenario.
A well-written research paper for a nursing program requires extensive reading, critical thinking, proper application, and consideration of recent scholarly literature.
Nursing Case Study Structure
Have a look at the patient’s condition and the details mentioned by your instructor before starting the case study. Once you have sufficient know-how of the case, you can write about it in the following steps:
Abstract of the Report
An abstract can be written in a narrative or organised form. A description is a condensed version of an entire document summarising everything into a coherent, flowing plot but lacks headers. Structured abstracts include subheadings to aid with online searches. A structured abstract is divided into categories of a nursing case study, including the introduction, case presentation, management and outcome, and conclusion.
How to Write an Introduction for a Case Study
Your report’s intro should briefly present the patient, covering medical history, current medicine and diagnosis, prospective therapies, and suggestions.
You may always write the introduction last to ensure you’ve covered everything in your research work. The first paragraph aims to display you can decipher the patient’s message. It also enhances your arguments on care planning later in the paper.
• Practice Pathophysiology
You can discuss how the patient illness have occurred after studying the patient’s raw data. For example, if it is sepsis-induced cardiomyopathy, use the necessary facts to explain how it may have happened. A patient working in an unsanitary environment is one example. If a patient has the chronic obstructive pulmonary disease (COPD) and has been a long-time smoker, explain how smoking causes COPD. Focus on the patient’s aetiology and risk factors as you discuss pathophysiology. Use nursing literature released within the previous five years to back up your writing.
• Nursing Care Plan
With the diagnosis done and the source of the patient’s suffering understood, it is now time to plan the patient’s care. With this following written guide on nursing care plans, you can write a care plan yourself in no time. However, suppose you are not sure how to write your case study. In that case, for quality work, you can always ask for assignment help UK from expert and professional writers who are always available to provide relief to struggling students.
The nurse care plan details the topmost complaints or the critical problems that a patient has, comprising at least three top-priority issues. You can help define the reasons for these problems while drawing facts and evidence from the literature.
You also need to detail the possible intervention plans, including pharmacological and non-pharmacological interferences, develop objectives and measures, and come up with evaluation approaches for your project.
• Recommend and Discuss Your Paper
While writing a case study, you can always discuss the predictable outcomes and pen down your recommendations. The discussion covers your assignment, giving you an area to expound on the research, relate your patient’s care plan to the case, and offer a rationale.
You can then make recommendations based on the care plan. Your recommendations on the diagnosis, prognosis, and nursing care plan should be sound. For example, if it is time to release the patient who had fall injuries, recommend some homework and management strategies that can work in the home setting. Emphasis on all and everything that can be done to improve the well-being of a patient.
• Conclude Your Case Study Assignment
As you introduce every detail of your study, you must concisely conclude all of it. Then, end your nursing care study by recapping the argument. Include the critical facts such as patient performance throughout the analysis, nursing assessment, care plan, rationale, evaluation, and recommendations.
• Acknowledge the Peer's Who Helped
Write a brief thank-you paragraph to everyone who helped with the case study preparation. It is not conventional to acknowledge the patients, as they are already at medical centres to receive treatment. Furthermore, it is excessive to express gratitude for all the assignment help you have received and thank the individuals who did not directly contribute to preparing the nursing case study assignment, such as peers and lecturers.
• Give References
List all the writers whose study helped and supported your case study argument. However, make sure not to go over fifteen sources. Also, avoid referencing a personal statement or information while giving references. In your paper, provide all the facts and figures, photographs, tables, and other non-textual material. A nursing case study assignment is a healthcare academic paper. Therefore, you should use authentic sources to support recommendations and cite your case study appropriately as per style guidelines to make your research stronger than the other candidates.
Types of Nursing Assignment
Five different methods in which you can write best nursing case study assignments are: • Case Study • Group Study • Functional Study • Team Nursing Study • Primary Nursing Study
In this study method, a researcher can work one-on-one with the patient, hence providing all the functions for the patient. This result in individual work satisfaction and extra patient care
Group Study
A single nurse is assigned a group of patients, and that one nurse is responsible for taking care of all the provided patients.
Functional Study
Nurses are assigned tasks like TPR, medicine, maintenance, responsibility, and so forth. In this study, nursing care becomes fragmented and impersonal due to many nurses. (However, for practical purposes, a few activities are fictionally assigned to nurses such as providing meals and accompanying while dressing) This strategy has various advantages, so instructors are usually unwilling to abandon it. The biggest benefit of the functional study is it allows more to be accomplished in a shorter period.
However, this study gives the patient inadequate attention as the strategy is more divided and inconsistent.
Team Nursing Study
In this study, a team of nurses (2 or more – headed by staff nurse) are assigned a group of patients. This study is given to students to see how they handle the shortage of staff situation to maintain patients’ well-being.
Additional nurses incorporate into the team to take care of the load. This tactic is possible because most parts of patient care do not require any technical skills.
The assignment is based upon analysis of tasks to be performed, skills available, and supervision required. This study method is an effective strategy if properly organised and supervised.
Primary Nursing Study
The primary nursing study is similar to the case study. In this study, the nurse assumes 24-hour responsibility for the care, evaluation and planning. When the nurses are on their duty, they undertake accountability for providing total maintenance.
Another task of this study is the coordination of nursing activities with doctors and surgeons other health experts.
Example of Case Study Report Format
You can find many nursing case study examples if you google with your particular subject. In addition, a few people had researched similar topics and have posted their case studies online for new students trying to excel at their case studies. For example, the Canadian journal of nursing research archive has described how several social servants are directly connected to the nursing assignment patterns practised at the unit level. This case study describes the characteristic components of a nursing unit’s currently practised assignment pattern.
Also, the Goronlogist report on “Consistent Assignment of Nursing Staff to Residents in Nursing Homes: A Critical Review of Conceptual and Methodological Issues” talks about nursing staff being promoted to residency. In addition, this report discusses the strategies planned to improve nursing home quality and shows varying effects of consistent assignment on quality conclusions.
Similarly, nursing case study reports published by different writers are available on many platforms. So, to get good grades and improve your assignment statement, you can always take the help of these examples, and if you find a similar topic, you can always give references and use those examples in your paper.
Tricks to Remember!
A nursing case study paper is a methodological paper in essence. Therefore, it should display expertise, professionalism, and understanding of nursing concepts.
Being a nurse isn’t easy; they are sometimes given case studies, such as implementing healthcare systems or an ethical dilemma. This guide helps write a decent case study on a patient. However, if you are analysing a nursing case study on a given area of interest, here are tips and tricks to use. • Read the instructions carefully • Begin writing early • Paraphrase and Cite • Write Accordingly to the Format • Revise, Check, and Edit carefully
Finally, writing an assignment for the final exam can be overwhelming for many students. And sometimes you wonder “if I can pay someone to write my essay “. Well, yes! You can always ask people and experts for help. Not everyone is meant for writing and academic excellence, and there is no shame to admit you need help. So, you can ask your seniors, professors and even expert writers of the UK Writing Experts for assignment help whenever you see yourself struggling. At UK Writing Experts, customer support is everything – a little help and assistance never harmed anyone.
Can you write 'I' or 'in my opinion' in an assignment?
Yes, you can write I or in my opinion while doing your assignment. The significant point is to use these types of terminologies when they suit your purpose, such as when you want to distance yourself from a certain view. But beware, don’t confuse giving your personal opinion with writing about your personal experience!
Can an assignment have bullet points?
There is no rule you cannot have bullets in your assignment. That being said, if you are writing a formal assignment, be careful with the formatting of your paper. For instance, a few instructors consider too many bullet points informal for an assignment.
How can I get nursing assignment help?
Educational pressure affects your mental health, and it gets overwhelming to write or work on the research or nursing assignment. However, you can contact academic writing websites like the UK Writing Experts and hire them for nursing assignment help. Medical students often face such academic trouble, and these expert writers make student life a bit easier. Also, they maintain the privacy of every individual who seeks them for assignment help.
Administrator - AUTHOR
Recent post.

May 6, 2022
How To Write an Informative Essay Like Expert Essay Writers?

March 2, 2022 March 15, 2022
How to Write An A-Level History Essay Structure

February 22, 2022 March 15, 2022
How to Write Your Dissertation the Right Way: Do’s and Don’ts
Save my name, email, and website in this browser for the next time I comment.
How to Write a Nursing Case Study [Examples, Format, & Tips]
✒️ case study topics for nursing students.
- 🩺️ The Basics
- 💉 Nursing Case Study: Writing Rules
📑 Nursing Case Study Format
📝 nursing case study examples.
- ⏱️ Tips on Quick Writing
🔗 References
A nursing case study is an in-depth analysis of the health situation of an individual patient.
The analysis is based on:
- medical history,
- other relevant criteria.
In most cases, you will be asked to diagnose to suggest the first aid measures. Alternatively, nurses can be asked to describe a patient in their practice and analyze the correctness of their actions. The purpose is to recreate a realistic hospital setting in the classroom and make students reflect on the treatment process from diagnosis to treatment.
- Anaphylactic shock in a teenager with peanut allergy.
- Non-compliant patient with diabetes: ways to improve adherence.
- Telehealth intervention for managing chronic disease.
- Communication strategies to address vaccine hesitancy in a rural community.
- Postpartum hemorrhage in a new mother: risk factors and interventions.
- Ways to improve recognition of dehydration in aging adults.
- The effective ways of maintaining work-life balance for nurses.
- Cultural competency in providing care to migrants and refugees.
- Why should every patient’s medical history remain confidential?
- The use of massage therapy in relieving pain.
- The challenges facing medicine in 2024.
- How does modern technology impact nursing?
- The significance of regular follow-up appointments with the healthcare provider.
- What are the primary treatments for postpartum depression?
- The use of steroids in cancer treatment.
🩺️ Nursing Case Study: What Is It About?
As a nursing student, you should understand that no two patients are the same. Each has a unique clinical record and condition. And although most nursing case study tasks will ask you to suggest a diagnosis or treatment, your focus should rest on the patient.
Busy nurses can sometimes see their patients in the framework of an illness to be treated or a procedure to be fulfilled. But you should do your best to remember that each patient is a living person with a complex set of needs, emotions, and preferences. A ready-made textbook answer is rarely the best solution for them. Moreover, it rarely helps to analyze a condition in isolation from the patient.
In a nursing case study, your task is to analyze a disorder or illness as a part of a specific medical situation. If you don’t do that, your case study becomes an essay (theoretical and generalized). It is the difference between the two assignment types.
Once again:
A case study in nursing emphasizes the particular patient’s condition. Meanwhile, a nursing essay will explore the disease, prevention methods, treatment, or possible consequences of the disease.
Even if the case is hypothetical, it should focus on the suggested reality. On the other hand, essays are usually literature-based. You are expected to do some reading for a case study too, but you should research and present the information within the context of the patient. In simple terms, a case study uses information in the actual application, and an essay uses it for the sake of generalized suggestions.
💉 How to Write a Nursing Case Study: 3 Key Rules
- Do the fieldwork. Before setting your hands to writing, you should collect all of the available materials: clinical notes, results of medical tests, x-rays, sickness records, etc. Use this information to draw a clear picture of the story. It is always helpful to ask yourself, “What is interesting or unusual about this patient’s condition?” In the course of writing, recall your answer from time to time not to get lost in words. It will help you to convey a definite and appropriate message.
- Stick to the facts. A nursing case study should be an accurate description of the actual situation. Restrain from speculating about the inherent mechanisms of the illness or the general treatment methodology. In fact, students are rarely prepared enough to discuss pathology and physiology. Leave this to reputable experts. The best result you can provide in a case study is an honest account of clinical events.
- Concentrate on the patients and their progress. Remember that a nursing case study is a story of a patient’s progress and not a narrative about their nurse. No matter how efficiently the medical specialist acted, it would be incorrect to add any praiseful remarks. The optimal way is to tell the story in its logical and time order and outline the result of treatment. In this case, the outcome will speak for itself.
Introduction
It is where you should tell the reader why this case is interesting . Place your study in a social or historical context. If, during your preliminary research, you found some similar cases, describe them briefly. If you had a hard time diagnosing the patient or your proposed treatment is complicated, mention it here. Don’t forget to cite the references to each of them!
The introduction should not exceed several paragraphs. The purpose is to explain why the reader will benefit from reading about the case.
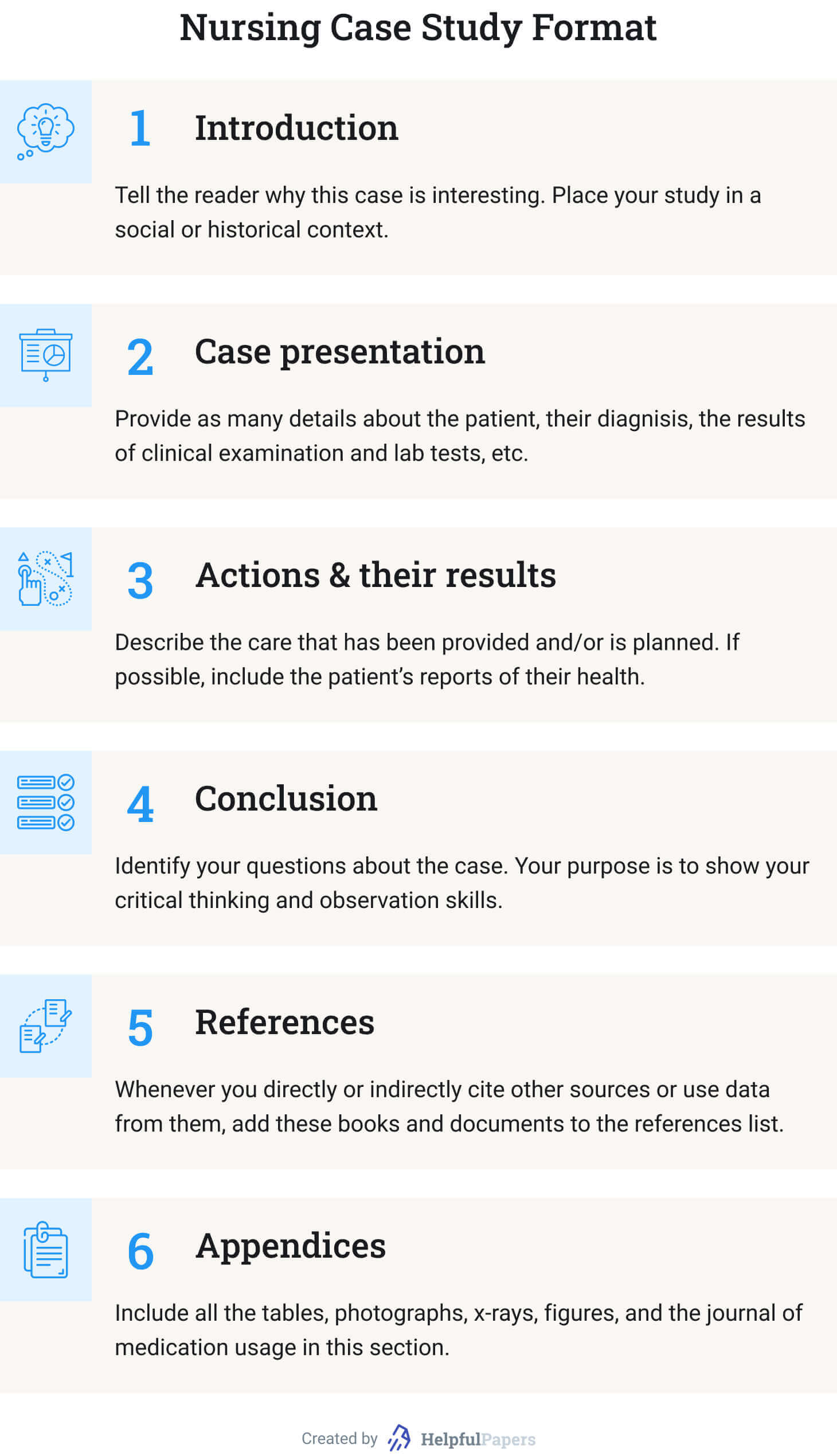
Case Presentation
- Why did the patient seek medical help? (Describe the symptoms.)
- What is known about the patient? (Mention only the information that influenced your diagnosis. Otherwise, explain why some information is irrelevant to the diagnosis.)
- Stick to the narrative form. (Make it a story!)
- What are the variants for diagnosis? (Make a shortlist of possible disorders that fall under the patient’s symptoms. But make it specific: not just “pneumonia” but “bilateral pneumonia,” for example. Besides, this point is optional.)
- What were the results of your clinical examination? (If you saw the patient in person.)
- Explain the results of lab tests. (The words “positive” or “negative” are not always clear.)
Actions and Their Results
This section describes the care that has been provided and/or is planned. You can answer the following questions in narrative form . If some information is missing, skip the point:
- What preliminary actions have been taken? (Be specific: not just “wound care,” but “wound cleaning and dressing.”)
- How long has the patient been under care?
- Has the previous treatment given any visible result?
- Why was it suspended or finished?
- Why did the patient withdraw from treatment (if applicable)?
- How could you improve the patient’s condition if the result was negative?
- If the disease is incurable (like in the case of diabetes), which activities would stabilize the patient’s condition?
- If possible, include the patient’s reports of their own physical and mental health.
In this section, you should identify your questions about the case. It is impossible to answer all of them in one case study. Likewise, it is unreal to suggest all the relevant hypotheses explaining the patient’s condition. Your purpose is to show your critical thinking and observation skills. Finalize your conclusion by summarizing the lessons you learned from the nursing case study.
Whenever you directly or indirectly cite other sources or use data from them, add these books and documents to the references list. Follow the citation style assigned by your professor. Besides, 15 items are already too much. Try to make a list of up to 10. Using textbooks as references can be viewed as bad manners.
Include all the tables, photographs, x-rays, figures, and the journal of medication usage in this section. Unless required otherwise in the assignment, start each item from a new page, naming them “Appendix A,” “Appendix B…”.
Below you will find case study samples for various topics. Using them as a reference will improve your writing. If you need more ideas, you are welcome to use our free title-generating tool .
- Case study: healing and autonomy.
- Sara’s case study: maternal and child nursing.
- COPD medical diagnostics: case study.
- Care standards in healthcare institutions: case study.
- Acute bacterial prostatitis: case study analysis.
- Alzheimer disease: the patient case study.
- The treatment of foot ulcers in diabetic patients: case study.
- Hypertension: C.D’s case study.
- Myocardial infarction: cardiovascular case study.
- Major depressive disorder case.
- Case study of the patient with metabolic syndrome .
- Pulmonary analysis case study .
- Older adults isolation: Case study .
- The holistic care: Case study .
- Medical ethics: Case study .
- Patient diagnoses and treatment: Case study .
- Obesity case study: Mr. C .
- Nurse Joserine: Case study problems .
- Chronic stable angina: Case study .
- Fetal abnormality: Case study .
- Researching SOAP: Case study .
- Case study for a patient with hormonal disorders .
- Obesity in the elderly: The case study .
- “Walking the Tightrope”: A case study analysis .
- ARNP approach: Case study analysis .
- Case study on biomedical ethics in the Christian narrative .
- Thermal injury: Case study .
- Ethical dilemma in nursing: Case study .
- Asthma: A case study of the patient .
- Asthma discharge plan: Mini case study .
- Case study: An ethics of euthanasia .
- Case study: Head-to-toe assessment steps .
- Pain management strategies: Case study .
- Case study: Inflammatory bowel disease .
- Sleep deprivation and insomnia: The case study .
- The case study of a heart failure .
- Porphyria cutanea tarda: Disease case study .
- Case study: Hardy Hospital case summary .
- Obesity and its complications: Case study .
- Angina disease case study .
- Nursing ethics case study .
- Case study of a patient: Assessment and treatment plan .
- Cecile case study: Mrs. J .
- Nursing power in the emergency department: Case study .
- Heart failure case study: Mrs. J .
- Application of ethics in nursing: Case study .
- Sudden visual impairment: Case study .
- Epidemiology case study: Outbreak at Watersedge — Public health discovery game .
- Wellness of senior citizens: Case study .
- Healthcare organization evaluation: Case study of Banner Health .
⏱️ Bonus: Tips on Writing a Case Study in Record Time
Need to prepare a case study on nursing or in another field? Below you’ll find a collection fo tips that will help you do it as quickly as possible!
3 Shortcuts for a Quick Start
If you’re about to start writing a case study, you should check yourself if you’re not doing any of the following:
- spending too much time on selecting a topic;
- reading too much before selecting a topic;
- making conclusions too early – creating bias.
Instead of killing time doing the three useless things discussed above, consider these:
- Choose approach. Note that there are 2 major approaches to case studies: the analytical approach (investigating possible reasons without making any conclusions) and problem-oriented approach (focusing on a particular problem and investigating it).
- Skim some sources (DON’T READ THEM). Select several sources. Simply skim abstracts and conclusions.
- Start making notes early. Simply reading is ineffective unless you’re lucky to have a phenomenal memory. Always make notes of any useful arguments.
4 Shortcuts Not to Get Stuck in the Middle
Even if you kick started your case study, it’s too early to celebrate it. Consider the following traps in the middle of the project:
- Watch the structure. The classic logical structure is your formula of success. It will help you move from one point to another without the unnecessary procrastination:
- Respect the logic. Make your case study flow – make logical transitions between the different parts and make it consistent. Avoid changing your position throughout the paper.
- Be detail-oriented. Any trifle deserves attention when you write a case study.
- Avoid bias. Be sure that all your opinions are based on the specific arguments form the case study. Avoid pouring your biased views into the project.
3 Shortcuts for a Happy Ending
- Offer a realistic solution. College case study is a rehearsal of real-life situations. Take the responsibility for your suggestions.
- Keep your conclusion short. Avoid repeating the details and don’t include any new information.
- Consider creating a Power Point. If your task is not only writing a case study, but also presenting it – why not create PowerPoint slides to help you?
As the last step on your way to a perfect nursing case study, prepare the title page. Its format usually depends on the professor’s requirements. But if you know the citation style, our Title Page Maker is a perfect tool to apply the right formatting and accelerate the process. And if you have any know-how on how to write a medical case study, you are very welcome to share it with other students in the comments below.
❓ Nursing Case Study: FAQ
What is a case study in nursing.
A nursing case study explores the condition of a patient. It is based on previous clinical records, lab reports, and other medical and personal information. A case study focuses on the patient and describes the treatment that was (or should be) applied and its (expected) outcome.
How to Write a Nursing Case Study?
- Collect the bulk of data available about the patient.
- Read literature about the diagnosed condition.
- Focus on the individual patient and their symptoms.
- Describe the situation and outline its development in time.
- Analyze the actions of the medical personnel that have been done.
- Plan further treatment of the patient.
Why Are Case Studies Good for Nursing Students?
Nursing case studies offer you a priceless opportunity to gain experience of different patient conditions and cure methods without visiting the clinic. You can think about whether the proposed treatment was appropriate or wrong and suggest a better solution. And the best thing, your teacher will indicate your mistakes (and no patient will be hurt in the process).
Why Are Case Studies Important in Nursing?
- You learn to distinguish the relevant data and analyze it.
- You learn to ask the right questions.
- You learn to evaluate the severity of symptoms.
- You learn to make better diagnoses.
- You train your critical thinking in terms of treatment methods
- Case studies are in-class simulators of authentic atmosphere in a clinical ward.
- What is a case study? | Evidence-Based Nursing
- Case Studies – Johns Hopkins Medicine
- Case Study Research Design in Nursing
- Case study report for Nursing | Learning Lab – RMIT University
- Case Study or Nursing Care Study? – jstor
Research Paper Analysis: How to Analyze a Research Article + Example
Film analysis: example, format, and outline + topics & prompts.

Nursing Case Study
ScienceDirect posted a nursing ethics case study where an end-stage prostate cancer patient, Mr. Green, confided to nursing staff about his plan to commit suicide. The patient asked the nurse to keep it a secret. The ethical problem is whether the nurse should tell the health care team members about the patient’s thought without his permission. The best ethical decision for this nursing case study was to share this critical information with other health care professionals, which was the action the nurse took. The team adhered to the proper self-harm and suicide protocol. The appropriate team performed a palliative therapy. As a result, the patient didn’t harm himself and died peacefully a few months after he was discharged.
What Is a Nursing Case Study? A nursing case study is a detailed study of an individual patient. Through this type of research, you can gain more information about the symptoms and the medical history of a patient. It will also allow you to provide the proper diagnoses of the patient’s illness based on the symptoms he or she experienced and other affecting factors. Nursing students usually perform this study as part of their practicum, making it an essential experience because, through this research methodology , they can apply the lessons they have learned from school. The situation mentioned above was an excellent example of a nursing case study.
Nursing Case Study Format
1. introduction.
Purpose: Briefly introduces the case study, including the main health issue or condition being explored. Background: Provides context for the patient scenario, outlining the significance of the case in nursing practice. Objectives: Lists the learning objectives or goals that the case study aims to achieve.
2. Patient Information
Demographics: Age, gender, ethnicity, and relevant personal information. Medical History: Past medical history, including any chronic conditions, surgeries, or significant health events. Current Health Assessment: Presents the patient’s current health status, including symptoms, vital signs, and results from initial examinations.
3. Case Description
Clinical Presentation: Detailed description of the patient’s presentation, including physical examination findings and patient-reported symptoms. Diagnostic Findings: Summarizes diagnostic tests that were performed, including lab tests, imaging studies, and other diagnostic procedures, along with their results. Treatment Plan: Outlines the initial treatment provided to the patient, including medications, therapies, surgeries, or other interventions.
4. Nursing Care Plan
Nursing Diagnoses: Identifies the nursing diagnoses based on the assessment data. Goals and Outcomes: Establishes short-term and long-term goals for the patient’s care, including expected outcomes. Interventions: Describes specific nursing interventions planned or implemented to address each nursing diagnosis and achieve the stated goals. Evaluation: Discusses the effectiveness of the nursing interventions, including patient progress and any adjustments made to the care plan.
5. Analysis
Critical Analysis: Analyzes the case in depth, considering different aspects of patient care, decision-making processes, and the application of nursing theories and principles. Reflection: Reflects on the nursing practice, lessons learned, and how the case study has impacted the understanding and application of nursing knowledge.

6. Conclusion
Summary: Provides a concise summary of the key points from the case study, including the patient outcome and the nursing care impact. Implications for Practice: Discusses the implications of the case for nursing practice, including any changes to practice or policy that could improve patient care. Recommendations: Offers recommendations for future care or areas for further study based on the case study findings.
Examples of Nursing Case Study
Management of Acute Myocardial Infarction (AMI) Introduction: A 58-year-old male with a history of hypertension and smoking presents to the emergency department with chest pain. This case study explores the nursing management for patients with AMI. Patient Information: Demographics: 58-year-old male, smoker. Medical History: Hypertension, no previous diagnosis of heart disease. Current Health Assessment: Reports severe chest pain radiating to his left arm, sweating, and nausea. Case Description: Clinical Presentation: Patient appeared in distress, clutching his chest. Diagnostic Findings: ECG showed ST-elevation in anterior leads. Troponin levels were elevated. Treatment Plan: Immediate administration of aspirin, nitroglycerin, and morphine for pain. Referred for emergency coronary angiography. Nursing Care Plan: Nursing Diagnoses: Acute pain related to myocardial ischemia. Goals: Relieve pain and prevent further myocardial damage. Interventions: Monitoring vital signs, administering prescribed medications, and providing emotional support. Evaluation: Pain was managed effectively, and the patient was stabilized for angiography. Analysis: The timely nursing interventions contributed to stabilizing the patient’s condition, showcasing the critical role nurses play in acute care settings. Conclusion: This case highlights the importance of quick assessment and intervention in patients with AMI, emphasizing the nurse’s role in pain management and support.
Managing Type 1 Diabetes in a Pediatric Patient Introduction: A 10-year-old female diagnosed with type 1 diabetes presents for a routine check-up. This case study focuses on the nursing care plan for managing diabetes in pediatric patients. Patient Information: Demographics: 10-year-old female. Medical History: Diagnosed with type 1 diabetes six months ago. Current Health Assessment: Well-controlled blood glucose levels, but expresses difficulty with frequent insulin injections. Case Description: Clinical Presentation: Patient is active, engaging in school activities but struggles with diabetes management. Diagnostic Findings: HbA1c is 7.2%, indicating good control. Treatment Plan: Insulin therapy, carbohydrate counting, and regular blood glucose monitoring. Nursing Care Plan: Nursing Diagnoses: Risk for unstable blood glucose levels. Goals: Maintain blood glucose within target range and increase patient comfort with diabetes management. Interventions: Education on insulin pump use, dietary advice, and coping strategies. Evaluation: Patient showed interest in using an insulin pump and understood dietary recommendations. Analysis: This case emphasizes the importance of education and emotional support in managing chronic conditions in pediatric patients. Conclusion: Effective management of type 1 diabetes in children requires a comprehensive approach that includes education, technological aids, and psychological support.
Elderly Care for Alzheimer’s Disease Introduction: An 82-year-old female with Alzheimer’s disease presents with increased confusion and agitation. This case study examines the complexities of caring for elderly patients with Alzheimer’s. Patient Information: Demographics: 82-year-old female. Medical History: Alzheimer’s disease, osteoarthritis. Current Health Assessment: Increased confusion, agitation, and occasional aggression. Case Description: Clinical Presentation: Patient exhibits signs of advanced Alzheimer’s with memory loss and disorientation. Diagnostic Findings: Cognitive tests confirm the progression of Alzheimer’s. Treatment Plan: Non-pharmacological interventions for agitation, memory aids, and safety measures in the home. Nursing Care Plan: Nursing Diagnoses: Impaired memory related to Alzheimer’s disease. Goals: Reduce agitation and prevent harm. Interventions: Use of calming techniques, establishing a routine, and environmental modifications. Evaluation: Agitation was reduced, and the patient’s safety was improved through environmental adjustments. Analysis: The case underscores the need for tailored interventions to manage Alzheimer’s symptoms and improve the quality of life for the elderly. Conclusion: Nursing care for Alzheimer’s patients requires a multifaceted approach focusing on safety, symptom management, and patient dignity.
Nursing Case Study Topics with Samples to Edit & Download
- Telehealth Nursing
- Mental Health and Psychiatric Nursing
- Geriatric Nursing Care
- Palliative and End-of-Life Care
- Pediatric Nursing
- Emergency and Critical Care Nursing
- Chronic Disease Management
- Nursing Ethics and Patient Rights
- Infection Control and Prevention
- Oncology Nursing
- Nursing Leadership and Management
- Cultural Competence in Nursing
- Substance Abuse and Addiction Nursing
- Technological Innovations in Nursing
- Nursing Education and Training
Nursing Case Study Examples & Templates
1. nursing case study template.
2. Free Nursing Student Care Plan Template
3. Nursing Action Case Study Example
4. Hospital Nursing Care Case Study Example
5. Printable Nursing Health Case Study Example
professays.com
6. Fundamentals of Nursing Case Study Example
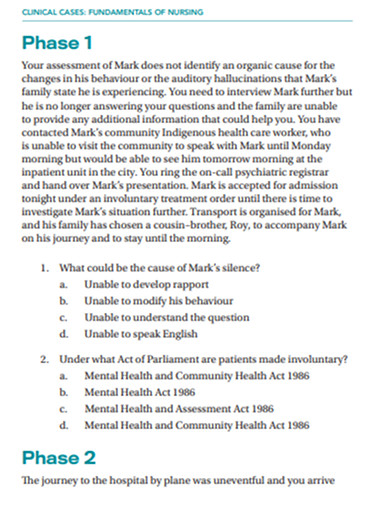
secure-ecsd.elsevier.com
7. Sample Nursing Case Study Example
caresearch.com.au
8. Nursing Research Case Study Example
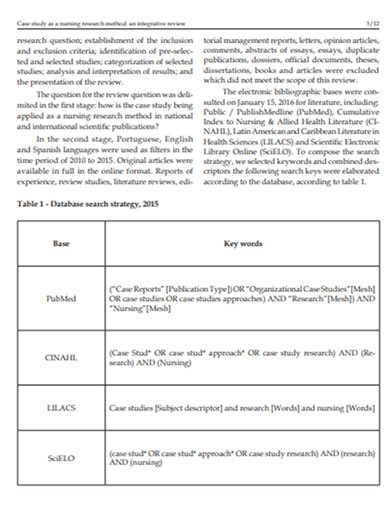
9. Standard Nursing Case Study Example
resourcecenter.ovid.com
10. Nursing Disability Case Study Example
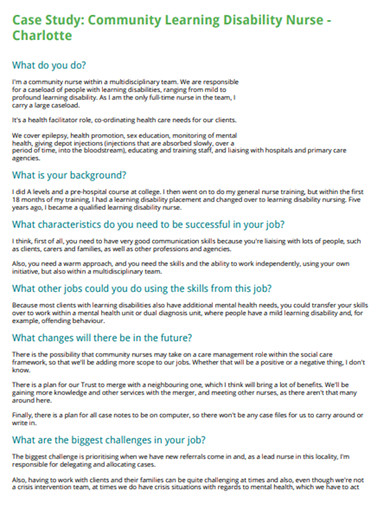
careerswales.com
11. Nursing care Patients Case Study Example

12. School of Nursing Case Study Example

ebn.bmj.com
13. Evaluation of Nursing Care Case Study Example
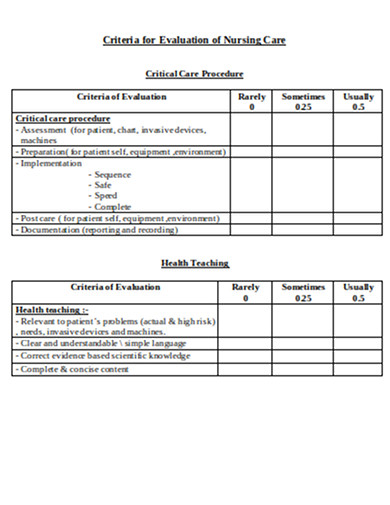
philadelphia.edu
Nursing Case Study Segments
Typically, a nursing case study contains three main categories, such as the items below.
1. The Status of a Patient
In this section, you will provide the patient’s information, such as medical history, and give the current patient’s diagnosis, condition, and treatment. Always remember to write down all the relevant information about the patient. Other items that you can collect in this stage are the reasons for the patient to seek medical care and the initial symptoms that he or she is experiencing. After that, based on the gathered information, you will explain the nature and cause of the illness of the patient.
2. The Nursing Assessment of the Patient
In this stage, you will need to prepare your evaluation of the patient’s condition. You should explain each observation that you have collected based on the vital signs and test results. You will also explain each nursing diagnosis that you have identified and determine the proper nursing care plan for the patient.
3. The Current Care Plan and Recommendations
Describe the appropriate care plan that you can recommend to the patient based on the diagnosis, current status, and prognosis in detail, including how the care plan will affect his or her life quality. If needed, you can also evaluate the patient’s existing care plan and give recommendations to enhance it. It is also crucial to cite relevant authoritative sources that will support your recommendations .
Objectives of Nursing Case Study
Nursing case studies are integral educational tools that bridge theoretical knowledge with practical application in patient care. They serve several key objectives essential for the development of nursing students and professionals. Here are the primary objectives of nursing case studies:
1. Enhance Critical Thinking and Clinical Reasoning
Case studies encourage nurses to analyze complex patient scenarios, make informed decisions, and apply critical thinking skills to solve problems. They simulate real-life situations, requiring nurses to evaluate data, consider multiple outcomes, and choose the best course of action.
2. Improve Diagnostic Skills
Through the detailed analysis of patient information, symptoms, and diagnostic results, nursing case studies help improve diagnostic skills. They allow nurses to practice interpreting clinical data to identify patient conditions and understand the underlying causes of symptoms.
3. Facilitate Application of Theoretical Knowledge
Nursing case studies provide a direct bridge between classroom learning and clinical practice. They offer a practical venue for applying theoretical knowledge about anatomy, physiology, pharmacology, and nursing theories to real-world patient care situations.
4. Promote Understanding of Comprehensive Patient Care
These studies emphasize the importance of holistic care, considering the physical, emotional, social, and psychological aspects of patient well-being. Nurses learn to develop comprehensive care plans that address all facets of a patient’s health.
5. Encourage Reflective Practice and Self-Assessment
Reflecting on case study outcomes enables nurses to evaluate their own decision-making processes, clinical judgments, and actions. This self-assessment promotes continuous learning and professional growth by identifying areas for improvement.
6. Foster Interdisciplinary Collaboration
Case studies often involve scenarios that require collaboration among healthcare professionals from various disciplines. They teach nurses the value of teamwork, communication, and the integration of different expertise to achieve optimal patient outcomes.
7. Enhance Patient Education and Advocacy Skills
By working through case studies, nurses improve their ability to educate patients and families about health conditions, treatment plans, and preventive measures. They also learn to advocate for their patients’ needs and preferences within the healthcare system.
8. Prepare for Real-Life Challenges
Nursing case studies prepare students and new nurses for the unpredictability and challenges of real-life clinical settings. They provide safe, controlled environments to practice responses to emergencies, ethical dilemmas, and complex patient needs without the risk of actual harm.
Steps in Nursing Process
Whether you are handling a patient with schizophrenia, pneumonia, diabetes, appendicitis, hypertension, COPD, etc, you will need to follow specific steps to ensure that you are executing the critical nursing process.
1. Assess the Patient
The first step of the nursing process requires critical thinking skills as it involves gathering both subjective and objective data. Subjective data includes verbal statements that you can collect from the patient or caregiver. In contrast, objective information refers to measurable and tangible data, such as vital signs, height, weight, etc. You can also use other sources of information, such as electronic health records, and friends that are in direct contact with the patient.
2. Diagnose the Patient
This critical step will help you in the next steps, such as planning and implementation of patient care. In this step, you will formulate a nursing diagnosis by applying clinical judgment. As a nurse, the North American Nursing Diagnosis Association (NANDA) will give you an up-to-date nursing diagnosis list, which will allow you to form a diagnosis based on the actual health problem.
3. Plan for a Proper Patient Care Plan
This part is where you will plan out the appropriate care plan for the patient. You will set this goal following the evidence-based practice (EDP) guidelines. The goal you will set should be specific, measurable, attainable, realistic, and timely ( SMART ).
4. Implement the Plan
In this stage, you can execute the plan that you have developed in the previous step. The implementation may need interventions such as a cardiac monitor, medication administration, etc.
5. Evaluate the Results
It is crucial to remember that every time the team does an intervention, you must do a reassessment to ensure that the process will lead to a positive result. You may need to reassess the patient depending on his progress, and the care plan may be modified based on the reassessment result.
Where to find nursing case studies?
Nursing case studies can be found in a variety of academic, professional, and medical resources. Here are some key places to look for nursing case studies:
- Academic Journals : Many academic journals focus on nursing and healthcare and publish case studies regularly. Examples include the “Journal of Clinical Nursing,” “Nursing Case Studies,” and “American Journal of Nursing.”
- University and College Libraries : Many academic institutions provide access to databases and journals that contain nursing case studies. Libraries often have subscriptions to these resources.
- Online Medical Libraries : Websites like PubMed, ScienceDirect, and Wiley Online Library offer a vast collection of nursing and medical case studies.
- Professional Nursing Organizations : Organizations such as the American Nurses Association (ANA) and the National League for Nursing (NLN) often provide resources, including case studies, for their members.
- Nursing Education Websites : Websites dedicated to nursing education, such as Lippincott NursingCenter and Nurse.com, often feature case studies for educational purposes.
- Government Health Websites : The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) sometimes publish case studies related to public health nursing and disease outbreaks.
- Nursing Textbooks and eBooks : Many nursing textbooks and eBooks include case studies to illustrate key concepts and scenarios encountered in practice.
- Online Nursing Forums and Communities : Forums and online communities for nursing professionals may share or discuss case studies as part of their content.
- Conference Proceedings : Nursing and healthcare conferences often include presentations of case studies. Many of these are published in the conference proceedings, which may be accessible online.
Carrying out a nursing case study can be a delicate task since it puts the life of a person at stake. Thus, it requires a thorough investigation. With that said, it is essential to gain intensive knowledge about this type of study. Today, we have discussed an overview of how to conduct a nursing case study. However, if you think that you are having problems with your writing skills , we recommend you to consider looking for an essay writing service from the experts in the nursing department to ensure that the output follows the appropriate writing style and terminology.

AI Generator
Text prompt
- Instructive
- Professional
10 Examples of Public speaking
20 Examples of Gas lighting
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Fundamentals [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021.

Nursing Fundamentals [Internet].
- About Open RN
Chapter 4 Nursing Process
4.1. nursing process introduction, learning objectives.
- Use the nursing process to provide patient care
- Identify nursing diagnoses from evidence-based sources
- Describe the development of a care plan
- Prioritize patient care
- Describe documentation for each step of the nursing process
- Differentiate between the role of the PN and RN
Have you ever wondered how a nurse can receive a quick handoff report from another nurse and immediately begin providing care for a patient they previously knew nothing about? How do they know what to do? How do they prioritize and make a plan?
Nurses do this activity every shift. They know how to find pertinent information and use the nursing process as a critical thinking model to guide patient care. The nursing process becomes a road map for the actions and interventions that nurses implement to optimize their patients’ well-being and health. This chapter will explain how to use the nursing process as standards of professional nursing practice to provide safe, patient-centered care.
4.2. BASIC CONCEPTS
Before learning how to use the nursing process, it is important to understand some basic concepts related to critical thinking and nursing practice. Let’s take a deeper look at how nurses think.
Critical Thinking and Clinical Reasoning
Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.” [ 1 ] Using critical thinking means that nurses take extra steps to maintain patient safety and don’t just “follow orders.” It also means the accuracy of patient information is validated and plans for caring for patients are based on their needs, current clinical practice, and research.
“Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentricity: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentricity)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.” [ 2 ] To make sound judgments about patient care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action. The ability to clinically reason develops over time and is based on knowledge and experience. [ 3 ]
Inductive and Deductive Reasoning and Clinical Judgment
Inductive and deductive reasoning are important critical thinking skills. They help the nurse use clinical judgment when implementing the nursing process.
Inductive reasoning involves noticing cues, making generalizations, and creating hypotheses. Cues are data that fall outside of expected findings that give the nurse a hint or indication of a patient’s potential problem or condition. The nurse organizes these cues into patterns and creates a generalization. A generalization is a judgment formed from a set of facts, cues, and observations and is similar to gathering pieces of a jigsaw puzzle into patterns until the whole picture becomes more clear. Based on generalizations created from patterns of data, the nurse creates a hypothesis regarding a patient problem. A hypothesis is a proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring. If a “why” is identified, then a solution can begin to be explored.
No one can draw conclusions without first noticing cues. Paying close attention to a patient, the environment, and interactions with family members is critical for inductive reasoning. As you work to improve your inductive reasoning, begin by first noticing details about the things around you. A nurse is similar to the detective looking for cues in Figure 4.1 . [ 4 ] Be mindful of your five primary senses: the things that you hear, feel, smell, taste, and see. Nurses need strong inductive reasoning patterns and be able to take action quickly, especially in emergency situations. They can see how certain objects or events form a pattern (i.e., generalization) that indicates a common problem (i.e., hypothesis).
Inductive Reasoning Includes Looking for Cues
Example: A nurse assesses a patient and finds the surgical incision site is red, warm, and tender to the touch. The nurse recognizes these cues form a pattern of signs of infection and creates a hypothesis that the incision has become infected. The provider is notified of the patient’s change in condition, and a new prescription is received for an antibiotic. This is an example of the use of inductive reasoning in nursing practice.
Deductive reasoning is another type of critical thinking that is referred to as “top-down thinking.” Deductive reasoning relies on using a general standard or rule to create a strategy. Nurses use standards set by their state’s Nurse Practice Act, federal regulations, the American Nursing Association, professional organizations, and their employer to make decisions about patient care and solve problems.
Example: Based on research findings, hospital leaders determine patients recover more quickly if they receive adequate rest. The hospital creates a policy for quiet zones at night by initiating no overhead paging, promoting low-speaking voices by staff, and reducing lighting in the hallways. (See Figure 4.2 ). [ 5 ] The nurse further implements this policy by organizing care for patients that promotes periods of uninterrupted rest at night. This is an example of deductive thinking because the intervention is applied to all patients regardless if they have difficulty sleeping or not.
Deductive Reasoning Example: Implementing Interventions for a Quiet Zone Policy
Clinical judgment is the result of critical thinking and clinical reasoning using inductive and deductive reasoning. Clinical judgment is defined by the National Council of State Boards of Nursing (NCSBN) as, “The observed outcome of critical thinking and decision-making. It uses nursing knowledge to observe and assess presenting situations, identify a prioritized patient concern, and generate the best possible evidence-based solutions in order to deliver safe patient care.” [ 6 ] The NCSBN administers the national licensure exam (NCLEX) that measures nursing clinical judgment and decision-making ability of prospective entry-level nurses to assure safe and competent nursing care by licensed nurses.
Evidence-based practice (EBP) is defined by the American Nurses Association (ANA) as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values.” [ 7 ]
Nursing Process
The nursing process is a critical thinking model based on a systematic approach to patient-centered care. Nurses use the nursing process to perform clinical reasoning and make clinical judgments when providing patient care. The nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses Association (ANA). These standards are authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently. [ 8 ] The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: A ssessment, D iagnosis, O utcomes Identification, P lanning, I mplementation, and E valuation.
The nursing process is a continuous, cyclic process that is constantly adapting to the patient’s current health status. See Figure 4.3 [ 9 ] for an illustration of the nursing process.
The Nursing Process
Review Scenario A in the following box for an example of a nurse using the nursing process while providing patient care.
Patient Scenario A: Using the Nursing Process [ 10 ]

A hospitalized patient has a prescription to receive Lasix 80mg IV every morning for a medical diagnosis of heart failure. During the morning assessment, the nurse notes that the patient has a blood pressure of 98/60, heart rate of 100, respirations of 18, and a temperature of 98.7F. The nurse reviews the medical record for the patient’s vital signs baseline and observes the blood pressure trend is around 110/70 and the heart rate in the 80s. The nurse recognizes these cues form a pattern related to fluid imbalance and hypothesizes that the patient may be dehydrated. The nurse gathers additional information and notes the patient’s weight has decreased 4 pounds since yesterday. The nurse talks with the patient and validates the hypothesis when the patient reports that their mouth feels like cotton and they feel light-headed. By using critical thinking and clinical judgment, the nurse diagnoses the patient with the nursing diagnosis Fluid Volume Deficit and establishes outcomes for reestablishing fluid balance. The nurse withholds the administration of IV Lasix and contacts the health care provider to discuss the patient’s current fluid status. After contacting the provider, the nurse initiates additional nursing interventions to promote oral intake and closely monitor hydration status. By the end of the shift, the nurse evaluates the patient status and determines that fluid balance has been restored.
In Scenario A, the nurse is using clinical judgment and not just “following orders” to administer the Lasix as scheduled. The nurse assesses the patient, recognizes cues, creates a generalization and hypothesis regarding the fluid status, plans and implements nursing interventions, and evaluates the outcome. Additionally, the nurse promotes patient safety by contacting the provider before administering a medication that could cause harm to the patient at this time.
The ANA’s Standards of Professional Nursing Practice associated with each component of the nursing process are described below.
The “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.” [ 11 ] A registered nurse uses a systematic method to collect and analyze patient data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, a nurse’s assessment of a hospitalized patient in pain includes the patient’s response to pain, such as the inability to get out of bed, refusal to eat, withdrawal from family members, or anger directed at hospital staff. [ 12 ]
The “Assessment” component of the nursing process is further described in the “ Assessment ” section of this chapter.
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.” [ 13 ] A nursing diagnosis is the nurse’s clinical judgment about the client's response to actual or potential health conditions or needs. Nursing diagnoses are the bases for the nurse’s care plan and are different than medical diagnoses. [ 14 ]
The “Diagnosis” component of the nursing process is further described in the “ Diagnosis ” section of this chapter.
Outcomes Identification
The “Outcomes Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” [ 15 ] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the patient based on their assessment data and nursing diagnoses.
The “Outcomes Identification” component of the nursing process is further described in the “ Outcomes Identification ” section of this chapter.
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” [ 16 ] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each patient’s needs and concerns. Goals, expected outcomes, and nursing interventions are documented in the patient’s nursing care plan so that nurses, as well as other health professionals, have access to it for continuity of care. [ 17 ]
The “Planning” component of the nursing process is further described in the “ Planning ” section of this chapter.
NURSING CARE PLANS
Creating nursing care plans is a part of the “Planning” step of the nursing process. A nursing care plan is a type of documentation that demonstrates the individualized planning and delivery of nursing care for each specific patient using the nursing process. Registered nurses (RNs) create nursing care plans so that the care provided to the patient across shifts is consistent among health care personnel. Some interventions can be delegated to Licensed Practical Nurses (LPNs) or trained Unlicensed Assistive Personnel (UAPs) with the RN’s supervision. Developing nursing care plans and implementing appropriate delegation are further discussed under the “ Planning ” and “ Implementing ” sections of this chapter.
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.” [ 18 ] Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the patient. Interventions are also documented in the patient’s electronic medical record as they are completed. [ 19 ]
The “Implementation” Standard of Professional Practice also includes the subcategories “Coordination of Care” and “Health Teaching and Health Promotion” to promote health and a safe environment. [ 20 ]
The “Implementation” component of the nursing process is further described in the “ Implementation ” section of this chapter.
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.” [ 21 ] During evaluation, nurses assess the patient and compare the findings against the initial assessment to determine the effectiveness of the interventions and overall nursing care plan. Both the patient’s status and the effectiveness of the nursing care must be continuously evaluated and modified as needed. [ 22 ]
The “Evaluation” component of the nursing process is further described in the “ Evaluation ” section of this chapter.
Benefits of Using the Nursing Process
Using the nursing process has many benefits for nurses, patients, and other members of the health care team. The benefits of using the nursing process include the following:
- Promotes quality patient care
- Decreases omissions and duplications
- Provides a guide for all staff involved to provide consistent and responsive care
- Encourages collaborative management of a patient’s health care problems
- Improves patient safety
- Improves patient satisfaction
- Identifies a patient’s goals and strategies to attain them
- Increases the likelihood of achieving positive patient outcomes
- Saves time, energy, and frustration by creating a care plan or path to follow
By using these components of the nursing process as a critical thinking model, nurses plan interventions customized to the patient’s needs, plan outcomes and interventions, and determine whether those actions are effective in meeting the patient’s needs. In the remaining sections of this chapter, we will take an in-depth look at each of these components of the nursing process. Using the nursing process and implementing evidence-based practices are referred to as the “science of nursing.” Let’s review concepts related to the “art of nursing” while providing holistic care in a caring manner using the nursing process.
Holistic Nursing Care
The American Nurses Association (ANA) recently updated the definition of nursing as, “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.” [ 23 ]
The ANA further describes nursing is a learned profession built on a core body of knowledge that integrates both the art and science of nursing. The art of nursing is defined as, “Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.” [ 24 ]
Nurses care for individuals holistically, including their emotional, spiritual, psychosocial, cultural, and physical needs. They consider problems, issues, and needs that the person experiences as a part of a family and a community as they use the nursing process. Review a scenario illustrating holistic nursing care provided to a patient and their family in the following box.
Holistic Nursing Care Scenario
A single mother brings her child to the emergency room for ear pain and a fever. The physician diagnoses the child with an ear infection and prescribes an antibiotic. The mother is advised to make a follow-up appointment with their primary provider in two weeks. While providing discharge teaching, the nurse discovers that the family is unable to afford the expensive antibiotic prescribed and cannot find a primary care provider in their community they can reach by a bus route. The nurse asks a social worker to speak with the mother about affordable health insurance options and available providers in her community and follows up with the prescribing physician to obtain a prescription for a less expensive generic antibiotic. In this manner, the nurse provides holistic care and advocates for improved health for the child and their family.
Review how to provide culturally responsive care and reduce health disparities in the “ Diverse Patients ” chapter.
Caring and the nursing process.
The American Nurses Association (ANA) states, “The act of caring is foundational to the practice of nursing.” [ 25 ] Successful use of the nursing process requires the development of a care relationship with the patient. A care relationship is a mutual relationship that requires the development of trust between both parties. This trust is often referred to as the development of rapport and underlies the art of nursing. While establishing a caring relationship, the whole person is assessed, including the individual’s beliefs, values, and attitudes, while also acknowledging the vulnerability and dignity of the patient and family. Assessing and caring for the whole person takes into account the physical, mental, emotional, and spiritual aspects of being a human being. [ 26 ] Caring interventions can be demonstrated in simple gestures such as active listening, making eye contact, touching, and verbal reassurances while also respecting and being sensitive to the care recipient’s cultural beliefs and meanings associated with caring behaviors. [ 27 ] See Figure 4.4 [ 28 ] for an image of a nurse using touch as a therapeutic communication technique to communicate caring.
Touch as a Therapeutic Communication Technique
Review how to communicate with patients using therapeutic communication techniques like active listening in the “ Communication ” chapter.
Dr. Jean Watson is a nurse theorist who has published many works on the art and science of caring in the nursing profession. Her theory of human caring sought to balance the cure orientation of medicine, giving nursing its unique disciplinary, scientific, and professional standing with itself and the public. Dr. Watson’s caring philosophy encourages nurses to be authentically present with their patients while creating a healing environment. [ 29 ]
Read more about Dr. Watson’s theory of caring at the Watson Caring Science Institute .
Now that we have discussed basic concepts related to the nursing process, let’s look more deeply at each component of the nursing process in the following sections.
4.3. ASSESSMENT
Assessment is the first step of the nursing process (and the first Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.” This includes collecting “pertinent data related to the health and quality of life in a systematic, ongoing manner, with compassion and respect for the wholeness, inherent dignity, worth, and unique attributes of every person, including but not limited to, demographics, environmental and occupational exposures, social determinants of health, health disparities, physical, functional, psychosocial, emotional, cognitive, spiritual/transpersonal, sexual, sociocultural, age-related, environmental, and lifestyle/economic assessments.” [ 1 ]
Nurses assess patients to gather clues, make generalizations, and diagnose human responses to health conditions and life processes. Patient data is considered either subjective or objective, and it can be collected from multiple sources.
Subjective Assessment Data
Subjective data is information obtained from the patient and/or family members and offers important cues from their perspectives. When documenting subjective data stated by a patient, it should be in quotation marks and start with verbiage such as, The patient reports. It is vital for the nurse to establish rapport with a patient to obtain accurate, valuable subjective data regarding the mental, emotional, and spiritual aspects of their condition.
There are two types of subjective information, primary and secondary. Primary data is information provided directly by the patient. Patients are the best source of information about their bodies and feelings, and the nurse who actively listens to a patient will often learn valuable information while also promoting a sense of well-being. Information collected from a family member, chart, or other sources is known as secondary data . Family members can provide important information, especially for individuals with memory impairments, infants, children, or when patients are unable to speak for themselves.
See Figure 4.5 [ 2 ] for an illustration of a nurse obtaining subjective data and establishing rapport after obtaining permission from the patient to sit on the bed.
Example. An example of documented subjective data obtained from a patient assessment is, “The patient reports, ‘My pain is a level 2 on a 1-10 scale.’”
Objective Assessment Data
Objective data is anything that you can observe through your sense of hearing, sight, smell, and touch while assessing the patient. Objective data is reproducible, meaning another person can easily obtain the same data. Examples of objective data are vital signs, physical examination findings, and laboratory results. See Figure 4.6 [ 3 ] for an image of a nurse performing a physical examination.
Physical Examination
Example. An example of documented objective data is, “The patient’s radial pulse is 58 and regular, and their skin feels warm and dry.”
Sources of Assessment Data
There are three sources of assessment data: interview, physical examination, and review of laboratory or diagnostic test results.
Interviewing
Interviewing includes asking the patient questions, listening, and observing verbal and nonverbal communication. Reviewing the chart prior to interviewing the patient may eliminate redundancy in the interview process and allows the nurse to hone in on the most significant areas of concern or need for clarification. However, if information in the chart does not make sense or is incomplete, the nurse should use the interview process to verify data with the patient.
After performing patient identification, the best way to initiate a caring relationship is to introduce yourself to the patient and explain your role. Share the purpose of your interview and the approximate time it will take. When beginning an interview, it may be helpful to start with questions related to the patient’s medical diagnoses to gather information about how they have affected the patient’s functioning, relationships, and lifestyle. Listen carefully and ask for clarification when something isn’t clear to you. Patients may not volunteer important information because they don’t realize it is important for their care. By using critical thinking and active listening, you may discover valuable cues that are important to provide safe, quality nursing care. Sometimes nursing students can feel uncomfortable having difficult conversations or asking personal questions due to generational or other cultural differences. Don’t shy away from asking about information that is important to know for safe patient care. Most patients will be grateful that you cared enough to ask and listen.
Be alert and attentive to how the patient answers questions, as well as when they do not answer a question. Nonverbal communication and body language can be cues to important information that requires further investigation. A keen sense of observation is important. To avoid making inappropriate inferences , the nurse should validate any cues. For example, a nurse may make an inference that a patient is depressed when the patient avoids making eye contact during an interview. However, upon further questioning, the nurse may discover that the patient’s cultural background believes direct eye contact to be disrespectful and this is why they are avoiding eye contact. To read more information about communicating with patients, review the “ Communication ” chapter of this book.
A physical examination is a systematic data collection method of the body that uses the techniques of inspection, auscultation, palpation, and percussion. Inspection is the observation of a patient’s anatomical structures. Auscultation is listening to sounds, such as heart, lung, and bowel sounds, created by organs using a stethoscope. Palpation is the use of touch to evaluate organs for size, location, or tenderness. Percussion is an advanced physical examination technique typically performed by providers where body parts are tapped with fingers to determine their size and if fluid is present. Detailed physical examination procedures of various body systems can be found in the Open RN Nursing Skills textbook with a head-to-toe checklist in Appendix C . Physical examination also includes the collection and analysis of vital signs.
Registered Nurses (RNs) complete the initial physical examination and analyze the findings as part of the nursing process. Collection of follow-up physical examination data can be delegated to Licensed Practical Nurses/Licensed Vocational Nurses (LPNs/LVNs) , or measurements such as vital signs and weight may be delegated to trained Unlicensed Assistive Personnel (UAP) when appropriate to do so. However, the RN remains responsible for supervising these tasks, analyzing the findings, and ensuring they are documented .
A physical examination can be performed as a comprehensive, head-to-toe assessment or as a focused assessment related to a particular condition or problem. Assessment data is documented in the patient’s Electronic Medical Record (EMR) , an electronic version of the patient’s medical chart.
Reviewing Laboratory and Diagnostic Test Results
Reviewing laboratory and diagnostic test results provides relevant and useful information related to the needs of the patient. Understanding how normal and abnormal results affect patient care is important when implementing the nursing care plan and administering provider prescriptions. If results cause concern, it is the nurse’s responsibility to notify the provider and verify the appropriateness of prescriptions based on the patient’s current status before implementing them.
Types of Assessments
Several types of nursing assessment are used in clinical practice:
- Primary Survey: Used during every patient encounter to briefly evaluate level of consciousness, airway, breathing, and circulation and implement emergency care if needed.
- Admission Assessment: A comprehensive assessment completed when a patient is admitted to a facility that involves assessing a large amount of information using an organized approach.
- Ongoing Assessment: In acute care agencies such as hospitals, a head-to-toe assessment is completed and documented at least once every shift. Any changes in patient condition are reported to the health care provider.
- Focused Assessment: Focused assessments are used to reevaluate the status of a previously diagnosed problem.
- Time-lapsed Reassessment: Time-lapsed reassessments are used in long-term care facilities when three or more months have elapsed since the previous assessment to evaluate progress on previously identified outcomes. [ 4 ]
Putting It Together
Review Scenario C in the following box to apply concepts of assessment to a patient scenario.
Scenario C [5]

Ms. J. is a 74-year-old woman who is admitted directly to the medical unit after visiting her physician because of shortness of breath, increased swelling in her ankles and calves, and fatigue. Her medical history includes hypertension (30 years), coronary artery disease (18 years), heart failure (2 years), and type 2 diabetes (14 years). She takes 81 mg of aspirin every day, metoprolol 50 mg twice a day, furosemide 40 mg every day, and metformin 2,000 mg every day.
Ms. J.’s vital sign values on admission were as follows:
- Blood Pressure: 162/96 mm Hg
- Heart Rate: 88 beats/min
- Oxygen Saturation: 91% on room air
- Respiratory Rate: 28 breaths/minute
- Temperature: 97.8 degrees F orally
Her weight is up 10 pounds since the last office visit three weeks prior. The patient states, “I am so short of breath” and “My ankles are so swollen I have to wear my house slippers.” Ms. J. also shares, “I am so tired and weak that I can’t get out of the house to shop for groceries,” and “Sometimes I’m afraid to get out of bed because I get so dizzy.” She confides, “I would like to learn more about my health so I can take better care of myself.”
The physical assessment findings of Ms. J. are bilateral basilar crackles in the lungs and bilateral 2+ pitting edema of the ankles and feet. Laboratory results indicate a decreased serum potassium level of 3.4 mEq/L.
As the nurse completes the physical assessment, the patient’s daughter enters the room. She confides, “We are so worried about mom living at home by herself when she is so tired all the time!”
Critical Thinking Questions
Identify subjective data.
Identify objective data.
Provide an example of secondary data.
Answers are located in the Answer Key at the end of the book.
4.4. DIAGNOSIS
Diagnosis is the second step of the nursing process (and the second Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse analyzes assessment data to determine actual or potential diagnoses, problems, and issues.” The RN “prioritizes diagnoses, problems, and issues based on mutually established goals to meet the needs of the health care consumer across the health–illness continuum and the care continuum.” Diagnoses, problems, strengths, and issues are documented in a manner that facilitates the development of expected outcomes and a collaborative plan. [ 1 ]
Analyzing Assessment Data
After collection of assessment data, the registered nurse analyzes the data to form generalizations and create hypotheses for nursing diagnoses. Steps for analyzing assessment data include performing data analysis, clustering of information, identifying hypotheses for potential nursing diagnosis, performing additional in-depth assessment as needed, and establishing nursing diagnosis statements. The nursing diagnoses are then prioritized and drive the nursing care plan. [ 2 ]
Performing Data Analysis
After nurses collect assessment data from a patient, they use their nursing knowledge to analyze that data to determine if it is “expected” or “unexpected” or “normal” or “abnormal” for that patient according to their age, development, and baseline status. From there, nurses determine what data are “clinically relevant” as they prioritize their nursing care. [ 3 ]
Example. In Scenario C in the “Assessment” section of this chapter, the nurse analyzes the vital signs data and determines the blood pressure, heart rate, and respiratory rate are elevated, and the oxygen saturation is decreased for this patient. These findings are considered “relevant cues.”
Clustering Information/Seeing Patterns/Making Hypotheses
After analyzing the data and determining relevant cues, the nurse clusters data into patterns. Assessment frameworks such as Gordon’s Functional Health Patterns assist nurses in clustering information according to evidence-based patterns of human responses. See the box below for an outline of Gordon’s Functional Health Patterns. [ 4 ] Concepts related to many of these patterns will be discussed in chapters later in this book.
Example. Refer to Scenario C of the “Assessment” section of this chapter. The nurse clusters the following relevant cues: elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, shortness of breath, a medical history of heart failure, and currently prescribed a diuretic medication. These cues are clustered into a generalization/pattern of fluid balance, which can be classified under Gordon’s Nutritional-Metabolic Functional Health Pattern. The nurse makes a hypothesis that the patient has excess fluid volume present.
Gordon’s Functional Health Patterns [ 5 ]
Health Perception-Health Management: A patient’s perception of their health and well-being and how it is managed
Nutritional-Metabolic: Food and fluid consumption relative to metabolic need
Elimination: Excretory function, including bowel, bladder, and skin
Activity-Exercise: Exercise and daily activities
Sleep-Rest: Sleep, rest, and daily activities
Cognitive-Perceptual: Perception and cognition
Self-perception and Self-concept: Self-concept and perception of self-worth, self-competency, body image, and mood state
Role-Relationship: Role engagements and relationships
Sexuality-Reproductive: Reproduction and satisfaction or dissatisfaction with sexuality
Coping-Stress Tolerance: Coping and effectiveness in terms of stress tolerance
Value-Belief: Values, beliefs (including spiritual beliefs), and goals that guide choices and decisions
Identifying Nursing Diagnoses
After the nurse has analyzed and clustered the data from the patient assessment, the next step is to begin to answer the question, “What are my patient’s human responses (i.e., nursing diagnoses)?” A nursing diagnosis is defined as, “A clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group, or community.” [ 6 ] Nursing diagnoses are customized to each patient and drive the development of the nursing care plan. The nurse should refer to a care planning resource and review the definitions and defining characteristics of the hypothesized nursing diagnoses to determine if additional in-depth assessment is needed before selecting the most accurate nursing diagnosis.
Nursing diagnoses are developed by nurses, for use by nurses. For example, NANDA International (NANDA-I) is a global professional nursing organization that develops nursing terminology that names actual or potential human responses to health problems and life processes based on research findings. [ 7 ] Currently, there are over 220 NANDA-I nursing diagnoses developed by nurses around the world. This list is continuously updated, with new nursing diagnoses added and old nursing diagnoses retired that no longer have supporting evidence. A list of commonly used NANDA-I diagnoses are listed in Appendix A . For a full list of NANDA-I nursing diagnoses, refer to a current nursing care plan reference.
NANDA-I nursing diagnoses are grouped into 13 domains that assist the nurse in selecting diagnoses based on the patterns of clustered data. These domains are similar to Gordon’s Functional Health Patterns and include health promotion, nutrition, elimination and exchange, activity/rest, perception/cognition, self-perception, role relationship, sexuality, coping/stress tolerance, life principles, safety/protection, comfort, and growth/development.
Knowledge regarding specific NANDA-I nursing diagnoses is not assessed on the NCLEX. However, analyzing cues and creating hypotheses are part of the measurement model used to assess a candidate’s clinical judgment. Read more about the NCLEX and Next Generation NCLEX in the “ Scope of Practice ” chapter.
Nursing diagnoses vs. medical diagnoses.
You may be asking yourself, “How are nursing diagnoses different from medical diagnoses?” Medical diagnoses focus on diseases or other medical problems that have been identified by the physician, physician’s assistant, or advanced nurse practitioner. Nursing diagnoses focus on the human response to health conditions and life processes and are made independently by RNs. Patients with the same medical diagnosis will often respond differently to that diagnosis and thus have different nursing diagnoses. For example, two patients have the same medical diagnosis of heart failure. However, one patient may be interested in learning more information about the condition and the medications used to treat it, whereas another patient may be experiencing anxiety when thinking about the effects this medical diagnosis will have on their family. The nurse must consider these different responses when creating the nursing care plan. Nursing diagnoses consider the patient’s and family’s needs, attitudes, strengths, challenges, and resources as a customized nursing care plan is created to provide holistic and individualized care for each patient.
Example. A medical diagnosis identified for Ms. J. in Scenario C in the “Assessment” section is heart failure. This cannot be used as a nursing diagnosis, but it can be considered as an “associated condition” when creating hypotheses for nursing diagnoses. Associated conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents that are not independently modifiable by the nurse, but support accuracy in nursing diagnosis. The nursing diagnosis in Scenario C will be related to the patient’s response to heart failure.
Additional Definitions Used in NANDA-I Nursing Diagnoses
The following definitions of patient, age, and time are used in association with NANDA-I nursing diagnoses:
The NANDA-I definition of a “patient” includes:
- Individual: a single human being distinct from others (i.e., a person).
- Caregiver: a family member or helper who regularly looks after a child or a sick, elderly, or disabled person.
- Family: two or more people having continuous or sustained relationships, perceiving reciprocal obligations, sensing common meaning, and sharing certain obligations toward others; related by blood and/or choice.
- Group: a number of people with shared characteristics generally referred to as an ethnic group.
- Community: a group of people living in the same locale under the same governance. Examples include neighborhoods and cities. [ 8 ]
The age of the person who is the subject of the diagnosis is defined by the following terms: [ 9 ]
- Fetus: an unborn human more than eight weeks after conception, until birth.
- Neonate: a person less than 28 days of age.
- Infant: a person greater than 28 days and less than 1 year of age.
- Child: a person aged 1 to 9 years
- Adolescent: a person aged 10 to 19 years
- Adult: a person older than 19 years of age unless national law defines a person as being an adult at an earlier age.
- Older adult: a person greater than 65 years of age.
The duration of the diagnosis is defined by the following terms: [ 10 ]
- Acute: lasting less than 3 months.
- Chronic: lasting greater than 3 months.
- Intermittent: stopping or starting again at intervals
- Continuous: uninterrupted, going on without stop.
New Terms Used in 2018-2020 NANDA-I Diagnoses
The 2018-2020 edition of Nursing Diagnoses includes two new terms to assist in creating nursing diagnoses: at-risk populations and associated conditions. [ 11 ]
At-Risk Populations are groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences.
Associated Conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis [ 12 ]
Types of Nursing Diagnoses
There are four types of NANDA-I nursing diagnoses: [ 13 ]
- Problem-Focused
- Health Promotion – Wellness
A problem-focused nursing diagnosis is a “clinical judgment concerning an undesirable human response to health condition/life processes that exist in an individual, family, group, or community.” [ 14 ] To make an accurate problem-focused diagnosis, related factors and defining characteristics must be present. Related factors (also called etiology) are causes that contribute to the diagnosis. Defining characteristics are cues, signs, and symptoms that cluster into patterns. [ 15 ]
A health promotion-wellness nursing diagnosis is “a clinical judgment concerning motivation and desire to increase well-being and to actualize human health potential.” These responses are expressed by the patient’s readiness to enhance specific health behaviors. [ 16 ] A health promotion-wellness diagnosis is used when the patient is willing to improve a lack of knowledge, coping, or other identified need.
A risk nursing diagnosis is “a clinical judgment concerning the vulnerability of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes.” [ 17 ] A risk nursing diagnosis must be supported by risk factors that contribute to the increased vulnerability. A risk nursing diagnosis is different from the problem-focused diagnosis in that the problem has not yet actually occurred. Problem diagnoses should not be automatically viewed as more important than risk diagnoses because sometimes a risk diagnosis can have the highest priority for a patient. [ 18 ]
A syndrome diagnosis is a “clinical judgment concerning a specific cluster of nursing diagnoses that occur together, and are best addressed together and through similar interventions.” [ 19 ]
Establishing Nursing Diagnosis Statements
When using NANDA-I nursing diagnoses, NANDA-I recommends the structure of a nursing diagnosis should be a statement that includes the nursing diagnosis and related factors as exhibited by defining characteristics . The accuracy of the nursing diagnosis is validated when a nurse is able to clearly link the defining characteristics, related factors, and/or risk factors found during the patient’s assessment. [ 20 ]
To create a nursing diagnosis statement, the registered nurse completes the following steps. After analyzing the patient’s subjective and objective data and clustering the data into patterns, the nurse generates hypotheses for nursing diagnoses based on how the patterns meet defining characteristics of a nursing diagnosis. Defining characteristics is the terminology used for observable signs and symptoms related to a nursing diagnosis. [ 21 ] Defining characteristics are included in care planning resources for each nursing diagnosis, along with a definition of that diagnosis, so the nurse can select the most accurate diagnosis. For example, objective and subjective data such as weight, height, and dietary intake can be clustered together as defining characteristics for the nursing diagnosis of nutritional status.
When creating a nursing diagnosis statement, the nurse also identifies the cause of the problem for that specific patient. Related factors is the terminology used for the underlying causes (etiology) of a patient’s problem or situation. Related factors should not be a medical diagnosis, but instead should be attributed to the underlying pathophysiology that the nurse can treat. When possible, the nursing interventions planned for each nursing diagnosis should attempt to modify or remove these related factors that are the underlying cause of the nursing diagnosis. [ 22 ]
Creating nursing diagnosis statements has traditionally been referred to as “using PES format.” The PES mnemonic no longer applies to the current terminology used by NANDA-I, but the components of a nursing diagnosis statement remain the same. A nursing diagnosis statement should contain the problem, related factors, and defining characteristics. These terms fit under the former PES format in this manner:
Problem (P) – the patient p roblem (i.e., the nursing diagnosis)
Etiology (E) – related factors (i.e., the e tiology/cause) of the nursing diagnosis; phrased as “related to” or “R/T”
Signs and Symptoms (S) – defining characteristics manifested by the patient (i.e., the s igns and s ymptoms/subjective and objective data) that led to the identification of that nursing diagnosis for the patient; phrased with “as manifested by” or “as evidenced by.”
Examples of different types of nursing diagnoses are further explained below.
Problem-Focused Nursing Diagnosis
A problem-focused nursing diagnosis contains all three components of the PES format :
Problem (P) – statement of the patient response (nursing diagnosis)
Etiology (E) – related factors contributing to the nursing diagnosis
Signs and Symptoms (S) – defining characteristics manifested by that patient
SAMPLE PROBLEM-FOCUSED NURSING DIAGNOSIS STATEMENT
Refer to Scenario C of the “Assessment” section of this chapter. The cluster of data for Ms. J. (elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, and shortness of breath) are defining characteristics for the NANDA-I Nursing Diagnosis Excess Fluid Volume . The NANDA-I definition of Excess Fluid Volume is “surplus intake and/or retention of fluid.” The related factor (etiology) of the problem is that the patient has excessive fluid intake. [ 23 ]
The components of a problem-focused nursing diagnosis statement for Ms. J. would be:
Fluid Volume Excess
Related to excessive fluid intake
As manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, increased weight of 10 pounds, and the patient reports, “ My ankles are so swollen .”
A correctly written problem-focused nursing diagnosis statement for Ms. J. would look like this:
Fluid Volume Excess related to excessive fluid intake as manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, an increase weight of 10 pounds, and the patient reports, “My ankles are so swollen.”
Health-Promotion Nursing Diagnosis
A health-promotion nursing diagnosis statement contains the problem (P) and the defining characteristics (S). The defining characteristics component of a health-promotion nursing diagnosis statement should begin with the phrase “expresses desire to enhance”: [ 24 ]
Signs and Symptoms (S) – the patient’s expressed desire to enhance
SAMPLE HEALTH-PROMOTION NURSING DIAGNOSIS STATEMENT
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. demonstrates a readiness to improve her health status when she told the nurse that she would like to “learn more about my health so I can take better care of myself.” This statement is a defining characteristic of the NANDA-I nursing diagnosis Readiness for Enhanced Health Management , which is defined as “a pattern of regulating and integrating into daily living a therapeutic regimen for the treatment of illness and its sequelae, which can be strengthened.” [ 25 ]
The components of a health-promotion nursing diagnosis for Ms. J. would be:
Problem (P): Readiness for Enhanced Health Management
Symptoms (S): Expressed desire to “learn more about my health so I can take better care of myself.”
A correctly written health-promotion nursing diagnosis statement for Ms. J. would look like this:
Enhanced Readiness for Health Promotion as manifested by expressed desire to “learn more about my health so I can take better care of myself.”
Risk Nursing Diagnosis
A risk nursing diagnosis should be supported by evidence of the patient’s risk factors for developing that problem. Different experts recommend different phrasing. NANDA-I 2018-2020 recommends using the phrase “as evidenced by” to refer to the risk factors for developing that problem. [ 26 ]
A risk diagnosis consists of the following:
As Evidenced By – Risk factors for developing the problem
SAMPLE RISK DIAGNOSIS STATEMENT
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. has an increased risk of falling due to vulnerability from the dizziness and weakness she is experiencing. The NANDA-I definition of Risk for Falls is “increased susceptibility to falling, which may cause physical harm and compromise health.” [ 27 ]
The components of a risk diagnosis statement for Ms. J. would be:
Problem (P) – Risk for Falls
As Evidenced By – Dizziness and decreased lower extremity strength
A correctly written risk nursing diagnosis statement for Ms. J. would look like this:
Risk for Falls as evidenced by dizziness and decreased lower extremity strength.
Syndrome Diagnosis
A syndrome is a cluster of nursing diagnoses that occur together and are best addressed together and through similar interventions. To create a syndrome diagnosis, two or more nursing diagnoses must be used as defining characteristics (S) that create a syndrome. Related factors may be used if they add clarity to the definition, but are not required. [ 28 ]
A syndrome statement consists of these items:
Problem (P) – the syndrome
Signs and Symptoms (S) – the defining characteristics are two or more similar nursing diagnoses
SAMPLE SYNDROME DIAGNOSIS STATEMENT
Refer to Scenario C in the “Assessment” section of this chapter. Clustering the data for Ms. J. identifies several similar NANDA-I nursing diagnoses that can be categorized as a syndrome . For example, Activity Intolerance is defined as “insufficient physiological or psychological energy to endure or complete required or desired daily activities.” Social Isolation is defined as “aloneness experienced by the individual and perceived as imposed by others and as a negative or threatening state.” These diagnoses can be included under the the NANDA-I syndrome named Risk for Frail Elderly Syndrome. This syndrome is defined as a “dynamic state of unstable equilibrium that affects the older individual experiencing deterioration in one or more domains of health (physical, functional, psychological, or social) and leads to increased susceptibility to adverse health effects, in particular disability.” [ 29 ]
The components of a syndrome nursing diagnosis for Ms. J. would be:
– Risk for Frail Elderly Syndrome
– The nursing diagnoses of Activity Intolerance and Social Isolation
Additional related factor: Fear of falling
A correctly written syndrome diagnosis statement for Ms. J. would look like this:
Risk for Frail Elderly Syndrome related to activity intolerance, social isolation, and fear of falling
Prioritization
After identifying nursing diagnoses, the next step is prioritization according to the specific needs of the patient. Nurses prioritize their actions while providing patient care multiple times every day. Prioritization is the process that identifies the most significant nursing problems, as well as the most important interventions, in the nursing care plan.
It is essential that life-threatening concerns and crises are identified immediately and addressed quickly. Depending on the severity of a problem, the steps of the nursing process may be performed in a matter of seconds for life-threatening concerns. In critical situations, the steps of the nursing process are performed through rapid clinical judgment. Nurses must recognize cues signaling a change in patient condition, apply evidence-based practices in a crisis, and communicate effectively with interprofessional team members. Most patient situations fall somewhere between a crisis and routine care.
There are several concepts used to prioritize, including Maslow’s Hierarchy of Needs, the “ABCs” (Airway, Breathing and Circulation), and acute, uncompensated conditions. See the infographic in Figure 4.7 [30] on The How To of Prioritization .
The How To of Prioritization
Maslow’s Hierarchy of Needs is used to categorize the most urgent patient needs. The bottom levels of the pyramid represent the top priority needs of physiological needs intertwined with safety. See Figure 4.8 [31] for an image of Maslow’s Hierarchy of Needs. You may be asking yourself, “What about the ABCs – isn’t airway the most important?” The answer to that question is “it depends on the situation and the associated safety considerations.” Consider this scenario – you are driving home after a lovely picnic in the country and come across a fiery car crash. As you approach the car, you see that the passenger is not breathing. Using Maslow’s Hierarchy of Needs to prioritize your actions, you remove the passenger from the car first due to safety even though he is not breathing. After ensuring safety and calling for help, you follow the steps to perform cardiopulmonary resuscitation (CPR) to establish circulation, airway, and breathing until help arrives.
Maslow’s Hierarchy of Needs
In addition to using Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation, the nurse also considers if the patient’s condition is an acute or chronic problem. Acute, uncompensated conditions generally require priority interventions over chronic conditions. Additionally, actual problems generally receive priority over potential problems, but risk problems sometimes receive priority depending on the patient vulnerability and risk factors.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Four types of nursing diagnoses were identified for Ms. J.: Fluid Volume Excess, Enhanced Readiness for Health Promotion, Risk for Falls , and Risk for Frail Elderly Syndrome . The top priority diagnosis is Fluid Volume Excess because it affects the physiological needs of breathing, homeostasis, and excretion. However, the Risk for Falls diagnosis comes in a close second because of safety implications and potential injury that could occur if the patient fell.
American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020 . Thieme Publishers New York. ↵
Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
Gordon, M. (2008). Assess notes: Nursing assessment and diagnostic reasoning. F.A. Davis Company. ↵
NANDA International. (n.d.). Glossary of terms . https://nanda .org/nanda-i-resources /glossary-of-terms / ↵
NANDA International. (n.d.). Glossary of terms . https://nanda .org/nanda-i-resources /glossary-of-terms/ ↵
NANDA International. (n.d.). Glossary of terms. https://nanda .org/nanda-i-resources /glossary-of-terms/ ↵
“The How To of Prioritization” by Valerie Palarski for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
“ Maslow's hierarchy of needs.svg ” by J. Finkelstein is licensed under CC BY-SA 3.0 ↵
4.5. OUTCOME IDENTIFICATION
Outcome Identification is the third step of the nursing process (and the third Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” The RN collaborates with the health care consumer, interprofessional team, and others to identify expected outcomes integrating the health care consumer’s culture, values, and ethical considerations. Expected outcomes are documented as measurable goals with a time frame for attainment. [ 1 ]
An outcome is a “measurable behavior demonstrated by the patient responsive to nursing interventions.” [ 2 ] Outcomes should be identified before nursing interventions are planned. After nursing interventions are implemented, the nurse will evaluate if the outcomes were met in the time frame indicated for that patient.
Outcome identification includes setting short- and long-term goals and then creating specific expected outcome statements for each nursing diagnosis.
Short-Term and Long-Term Goals
Nursing care should always be individualized and patient-centered. No two people are the same, and neither should nursing care plans be the same for two people. Goals and outcomes should be tailored specifically to each patient’s needs, values, and cultural beliefs. Patients and family members should be included in the goal-setting process when feasible. Involving patients and family members promotes awareness of identified needs, ensures realistic goals, and motivates their participation in the treatment plan to achieve the mutually agreed upon goals and live life to the fullest with their current condition.
The nursing care plan is a road map used to guide patient care so that all health care providers are moving toward the same patient goals. Goals are broad statements of purpose that describe the overall aim of care. Goals can be short- or long-term. The time frame for short- and long-term goals is dependent on the setting in which the care is provided. For example, in a critical care area, a short-term goal might be set to be achieved within an 8-hour nursing shift, and a long-term goal might be in 24 hours. In contrast, in an outpatient setting, a short-term goal might be set to be achieved within one month and a long-term goal might be within six months.
A nursing goal is the overall direction in which the patient must progress to improve the problem/nursing diagnosis and is often the opposite of the problem.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. had a priority nursing diagnosis of Fluid Volume Excess. A broad goal would be, “ Ms. J. will achieve a state of fluid balance. ”
Expected Outcomes
Goals are broad, general statements, but outcomes are specific and measurable. Expected outcomes are statements of measurable action for the patient within a specific time frame that are responsive to nursing interventions. Nurses may create expected outcomes independently or refer to classification systems for assistance. Just as NANDA-I creates and revises standardized nursing diagnoses, a similar classification and standardization process exists for expected nursing outcomes. The Nursing Outcomes Classification (NOC) is a list of over 330 nursing outcomes designed to coordinate with established NANDA-I diagnoses. [ 3 ]
Patient-Centered
Outcome statements are always patient-centered. They should be developed in collaboration with the patient and individualized to meet a patient’s unique needs, values, and cultural beliefs. They should start with the phrase “The patient will…” Outcome statements should be directed at resolving the defining characteristics for that nursing diagnosis. Additionally, the outcome must be something the patient is willing to cooperate in achieving.
Outcome statements should contain five components easily remembered using the “SMART” mnemonic: [ 4 ]
- M easurable
- A ttainable/Action oriented
- R elevant/Realistic
See Figure 4.9 [ 5 ] for an image of the SMART components of outcome statements. Each of these components is further described in the following subsections.
SMART Components of Outcome Statements
Outcome statements should state precisely what is to be accomplished. See the following examples:
- Not specific: “The patient will increase the amount of exercise.”
- Specific: “The patient will participate in a bicycling exercise session daily for 30 minutes.”
Additionally, only one action should be included in each expected outcome. See the following examples:
- “The patient will walk 50 feet three times a day with standby assistance of one and will shower in the morning until discharge” is actually two goals written as one. The outcome of ambulation should be separate from showering for precise evaluation. For instance, the patient could shower but not ambulate, which would make this outcome statement very difficult to effectively evaluate.
- Suggested revision is to create two outcomes statements so each can be measured: The patient will walk 50 feet three times a day with standby assistance of one until discharge. The patient will shower every morning until discharge.
Measurable outcomes have numeric parameters or other concrete methods of judging whether the outcome was met. It is important to use objective data to measure outcomes. If terms like “acceptable” or “normal” are used in an outcome statement, it is difficult to determine whether the outcome is attained. Refer to Figure 4.10 [ 6 ] for examples of verbs that are measurable and not measurable in outcome statements.
Figure 4.10
Measurable Outcomes
See the following examples:
- Not measurable: “The patient will drink adequate fluid amounts every shift.”
- Measurable: “The patient will drink 24 ounces of fluids during every day shift (0600-1400).”
Action-Oriented and Attainable
Outcome statements should be written so that there is a clear action to be taken by the patient or significant others. This means that the outcome statement should include a verb. Refer to Figure 4.11 [ 7 ] for examples of action verbs.
Figure 4.11
Action Verbs
- Not action-oriented: “The patient will get increased physical activity.”
- Action-oriented: “The patient will list three types of aerobic activity that he would enjoy completing every week.”
Realistic and Relevant
Realistic outcomes consider the patient’s physical and mental condition; their cultural and spiritual values, beliefs, and preferences; and their socioeconomic status in terms of their ability to attain these outcomes. Consideration should be also given to disease processes and the effects of conditions such as pain and decreased mobility on the patient’s ability to reach expected outcomes. Other barriers to outcome attainment may be related to health literacy or lack of available resources. Outcomes should always be reevaluated and revised for attainability as needed. If an outcome is not attained, it is commonly because the original time frame was too ambitious or the outcome was not realistic for the patient.
- Not realistic: “The patient will jog one mile every day when starting the exercise program.”
- Realistic: “The patient will walk ½ mile three times a week for two weeks.”
Time Limited
Outcome statements should include a time frame for evaluation. The time frame depends on the intervention and the patient’s current condition. Some outcomes may need to be evaluated every shift, whereas other outcomes may be evaluated daily, weekly, or monthly. During the evaluation phase of the nursing process, the outcomes will be assessed according to the time frame specified for evaluation. If it has not been met, the nursing care plan should be revised.
- Not time limited: “The patient will stop smoking cigarettes.”
- Time limited: “The patient will complete the smoking cessation plan by December 12, 2021.”
In Scenario C in Box 4.3, Ms. J.’s priority nursing diagnosis statement was Fluid Volume Excess related to excess fluid intake as manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, an increase weight of 10 pounds, and the patient reports, “My ankles are so swollen.” An example of an expected outcome meeting SMART criteria for Ms. J. is, “The patient will have clear bilateral lung sounds within the next 24 hours.”
4.6. PLANNING
Planning is the fourth step of the nursing process (and the fourth Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” The RN develops an individualized, holistic, evidence-based plan in partnership with the health care consumer, family, significant others, and interprofessional team. Elements of the plan are prioritized. The plan is modified according to the ongoing assessment of the health care consumer’s response and other indicators. The plan is documented using standardized language or terminology. [ 1 ]
After expected outcomes are identified, the nurse begins planning nursing interventions to implement. Nursing interventions are evidence-based actions that the nurse performs to achieve patient outcomes. Just as a provider makes medical diagnoses and writes prescriptions to improve the patient’s medical condition, a nurse formulates nursing diagnoses and plans nursing interventions to resolve patient problems. Nursing interventions should focus on eliminating or reducing the related factors (etiology) of the nursing diagnoses when possible. [ 2 ] Nursing interventions, goals, and expected outcomes are written in the nursing care plan for continuity of care across shifts, nurses, and health professionals.
Planning Nursing Interventions
You might be asking yourself, “How do I know what evidence-based nursing interventions to include in the nursing care plan?” There are several sources that nurses and nursing students can use to select nursing interventions. Many agencies have care planning tools and references included in the electronic health record that are easily documented in the patient chart. Nurses can also refer to other care planning books our sources such as the Nursing Interventions Classification (NIC) system. Based on research and input from the nursing profession, NIC categorizes and describes nursing interventions that are constantly evaluated and updated. Interventions included in NIC are considered evidence-based nursing practices. The nurse is responsible for using clinical judgment to make decisions about which interventions are best suited to meet an individualized patient’s needs. [ 3 ]
Direct and Indirect Care
Nursing interventions are considered direct care or indirect care. Direct care refers to interventions that are carried out by having personal contact with patients. Examples of direct care interventions are wound care, repositioning, and ambulation. Indirect care interventions are performed when the nurse provides assistance in a setting other than with the patient. Examples of indirect care interventions are attending care conferences, documenting, and communicating about patient care with other providers.
Classification of Nursing Interventions
There are three types of nursing interventions: independent, dependent, and collaborative. (See Figure 4.12 [ 4 ] for an image of a nurse collaborating with the health care team when planning interventions.)
Figure 4.12
Collaborative nursing interventions, independent nursing interventions.
Any intervention that the nurse can independently provide without obtaining a prescription is considered an independent nursing intervention . An example of an independent nursing intervention is when the nurses monitor the patient’s 24-hour intake/output record for trends because of a risk for imbalanced fluid volume. Another example of independent nursing interventions is the therapeutic communication that a nurse uses to assist patients to cope with a new medical diagnosis.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Fluid Volume Excess . An example of an evidence-based independent nursing intervention is, “The nurse will reposition the patient with dependent edema frequently, as appropriate.” [ 5 ] The nurse would individualize this evidence-based intervention to the patient and agency policy by stating, “The nurse will reposition the patient every 2 hours.”
Dependent Nursing Interventions
Dependent nursing interventions require a prescription before they can be performed. Prescriptions are orders, interventions, remedies, or treatments ordered or directed by an authorized primary health care provider. [ 6 ] A primary health care provider is a member of the health care team (usually a physician, advanced practice nurse, or physician’s assistant) who is licensed and authorized to formulate prescriptions on behalf of the client. For example, administering medication is a dependent nursing intervention. The nurse incorporates dependent interventions into the patient’s overall care plan by associating each intervention with the appropriate nursing diagnosis.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Fluid Volume Excess . An example of a dependent nursing intervention is, “The nurse will administer scheduled diuretics as prescribed.”
Collaborative nursing interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, respiratory therapists, physical therapists, and occupational therapists. These actions are developed in consultation with other health care professionals and incorporate their professional viewpoint. [ 7 ]
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Fluid Volume Excess . An example of a collaborative nursing intervention is consulting with a respiratory therapist when the patient has deteriorating oxygen saturation levels. The respiratory therapist plans oxygen therapy and obtains a prescription from the provider. The nurse would document “ The nurse will manage oxygen therapy in collaboration with the respiratory therapist ” in the care plan.
Individualization of Interventions
It is vital for the planned interventions to be individualized to the patient to be successful. For example, adding prune juice to the breakfast meal of a patient with constipation will only work if the patient likes to drink the prune juice. If the patient does not like prune juice, then this intervention should not be included in the care plan. Collaboration with the patient, family members, significant others, and the interprofessional team is essential for selecting effective interventions. The number of interventions included in a nursing care plan is not a hard and fast rule, but enough quality, individualized interventions should be planned to meet the identified outcomes for that patient.
Creating Nursing Care Plans
Nursing care plans are created by registered nurses (RNs). Documentation of individualized nursing care plans are legally required in long-term care facilities by the Centers for Medicare and Medicaid Services (CMS) and in hospitals by The Joint Commission. CMS guidelines state, “Residents and their representative(s) must be afforded the opportunity to participate in their care planning process and to be included in decisions and changes in care, treatment, and/or interventions. This applies both to initial decisions about care and treatment, as well as the refusal of care or treatment. Facility staff must support and encourage participation in the care planning process. This may include ensuring that residents, families, or representatives understand the comprehensive care planning process, holding care planning meetings at the time of day when a resident is functioning best and patient representatives can be present, providing sufficient notice in advance of the meeting, scheduling these meetings to accommodate a resident’s representative (such as conducting the meeting in-person, via a conference call, or video conferencing), and planning enough time for information exchange and decision-making. A resident has the right to select or refuse specific treatment options before the care plan is instituted.” [ 8 ] The Joint Commission conceptualizes the care planning process as the structuring framework for coordinating communication that will result in safe and effective care. [ 9 ]
Many facilities have established standardized nursing care plans with lists of possible interventions that can be customized for each specific patient. Other facilities require the nurse to develop each care plan independently. Whatever the format, nursing care plans should be individualized to meet the specific and unique needs of each patient. See Figure 4.13 [ 10 ] for an image of a standardized care plan.
Figure 4.13
Standardized Care Plan
Nursing care plans created in nursing school can also be in various formats such as concept maps or tables. Some are fun and creative, while others are more formal. Appendix B contains a template that can be used for creating nursing care plans.
4.7. IMPLEMENTATION OF INTERVENTIONS
Implementation is the fifth step of the nursing process (and the fifth Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse implements the identified plan.” The RN may delegate planned interventions after considering the circumstance, person, task, communication, supervision, and evaluation, as well as the state Nurse Practice Act, federal regulation, and agency policy. [ 1 ]
Implementation of interventions requires the RN to use critical thinking and clinical judgment. After the initial plan of care is developed, continual reassessment of the patient is necessary to detect any changes in the patient’s condition requiring modification of the plan. The need for continual patient reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
During the implementation phase of the nursing process, the nurse prioritizes planned interventions, assesses patient safety while implementing interventions, delegates interventions as appropriate, and documents interventions performed.
Prioritizing Implementation of Interventions
Prioritizing implementation of interventions follows a similar method as to prioritizing nursing diagnoses. Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation are used to establish top priority interventions. When possible, least invasive actions are usually preferred due to the risk of injury from invasive options. Read more about methods for prioritization under the “ Diagnosis ” subsection of this chapter.
The potential impact on future events, especially if a task is not completed at a certain time, is also included when prioritizing nursing interventions. For example, if a patient is scheduled to undergo a surgical procedure later in the day, the nurse prioritizes initiating a NPO (nothing by mouth) prescription prior to completing pre-op patient education about the procedure. The rationale for this decision is that if the patient ate food or drank water, the surgery time would be delayed. Knowing and understanding the patient’s purpose for care, current situation, and expected outcomes are necessary to accurately prioritize interventions.
Patient Safety
It is essential to consider patient safety when implementing interventions. At times, patients may experience a change in condition that makes a planned nursing intervention or provider prescription no longer safe to implement. For example, an established nursing care plan for a patient states, “The nurse will ambulate the patient 100 feet three times daily.” However, during assessment this morning, the patient reports feeling dizzy today, and their blood pressure is 90/60. Using critical thinking and clinical judgment, the nurse decides to not implement the planned intervention of ambulating the patient. This decision and supporting assessment findings should be documented in the patient’s chart and also communicated during the shift handoff report, along with appropriate notification of the provider of the patient’s change in condition.
Implementing interventions goes far beyond implementing provider prescriptions and completing tasks identified on the nursing care plan and must focus on patient safety. As front-line providers, nurses are in the position to stop errors before they reach the patient. [ 2 ]
In 2000 the Institute of Medicine (IOM) issued a groundbreaking report titled To Err Is Human: Building a Safer Health System . The report stated that as many as 98,000 people die in U.S. hospitals each year as a result of preventable medical errors. To Err Is Human broke the silence that previously surrounded the consequences of medical errors and set a national agenda for reducing medical errors and improving patient safety through the design of a safer health system. [ 3 ] In 2007 the IOM published a follow-up report titled Preventing Medication Errors and reported that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized patient experiences at least one medication error each day. This report emphasized actions that health care systems could take to improve medication safety. [ 4 ]
Read additional information about specific actions that nurses can take to prevent medication errors; go to the “Preventing Medication Errors” section of the “ Legal/Ethical” chapter of the Open RN Nursing Pharmacology textbook.
In an article released by the Robert Wood Johnson Foundation, errors involving nurses that endanger patient safety cover broad territory. This territory spans “wrong site, wrong patient, wrong procedure” errors, medication mistakes, failures to follow procedures that prevent central line bloodstream and other infections, errors that allow unsupervised patients to fall, and more. Some errors can be traced to shifts that are too long that leave nurses fatigued, some result from flawed systems that do not allow for adequate safety checks, and others are caused by interruptions to nurses while they are trying to administer medications or provide other care. [ 5 ]
The Quality and Safety Education for Nurses (QSEN) project began in 2005 to assist in preparing future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.” [ 6 ] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and assisting in implementing initiatives to resolve these gaps. Quality improvement is defined as, “The combined and unceasing efforts of everyone – health care professionals, patients and their families, researchers, payers, planners and educators – to make the changes that will lead to better patient outcomes (health), better system performance (care), and better professional development (learning).” [ 7 ]
Delegation of Interventions
While implementing interventions, RNs may elect to delegate nursing tasks. Delegation is defined by the American Nurses Association as, “The assignment of the performance of activities or tasks related to patient care to unlicensed assistive personnel or licensed practical nurses (LPNs) while retaining accountability for the outcome.” [ 8 ] RNs are accountable for determining the appropriateness of the delegated task according to condition of the patient and the circumstance; the communication provided to an appropriately trained LPN or UAP; the level of supervision provided; and the evaluation and documentation of the task completed. The RN must also be aware of the state Nurse Practice Act, federal regulations, and agency policy before delegating. The RN cannot delegate responsibilities requiring clinical judgment. [ 9 ] See the following box for information regarding legal requirements associated with delegation according to the Wisconsin Nurse Practice Act.
Delegation According to the Wisconsin Nurse Practice Act
During the supervision and direction of delegated acts a Registered Nurse shall do all of the following:
Delegate tasks commensurate with educational preparation and demonstrated abilities of the person supervised.
Provide direction and assistance to those supervised.
Observe and monitor the activities of those supervised.
Evaluate the effectiveness of acts performed under supervision. [ 10 ]
The standard of practice for Licensed Practical Nurses in Wisconsin states, “In the performance of acts in basic patient situations, the LPN. shall, under the general supervision of an RN or the direction of a provider:
Accept only patient care assignments which the LPN is competent to perform.
Provide basic nursing care. Basic nursing care is defined as care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable.
Record nursing care given and report to the appropriate person changes in the condition of a patient.
Consult with a provider in cases where an LPN knows or should know a delegated act may harm a patient.
Perform the following other acts when applicable:
Assist with the collection of data.
Assist with the development and revision of a nursing care plan.
Reinforce the teaching provided by an RN provider and provide basic health care instruction.
Participate with other health team members in meeting basic patient needs.” [ 11 ]
Read additional details about the scope of practice of registered nurses (RNs) and licensed practical nurses (LPNs) in Wisconsin’s Nurse Practice Act in Chapter N 6 Standards of Practice .
Read more about the American Nurses Association’s Principles of Delegation.
Table 4.7 outlines general guidelines for delegating nursing tasks in the state of Wisconsin according to the role of the health care team member.
General Guidelines for Delegating Nursing Tasks
Documentation of Interventions
As interventions are performed, they must be documented in the patient’s record in a timely manner. As previously discussed in the “Ethical and Legal Issues” subsection of the “ Basic Concepts ” section, lack of documentation is considered a failure to communicate and a basis for legal action. A basic rule of thumb is if an intervention is not documented, it is considered not done in a court of law. It is also important to document administration of medication and other interventions in a timely manner to prevent errors that can occur due to delayed documentation time.
Coordination of Care and Health Teaching/Health Promotion
ANA’s Standard of Professional Practice for Implementation also includes the standards 5A Coordination of Care and 5B Health Teaching and Health Promotion . [ 12 ] Coordination of Care includes competencies such as organizing the components of the plan, engaging the patient in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team. Health Teaching and Health Promotion is defined as, “Employing strategies to teach and promote health and wellness.” [ 13 ] Patient education is an important component of nursing care and should be included during every patient encounter. For example, patient education may include teaching about side effects while administering medications or teaching patients how to self-manage their conditions at home.
Refer to Scenario C in the “Assessment” section of this chapter. The nurse implemented the nursing care plan documented in Appendix C. Interventions related to breathing were prioritized. Administration of the diuretic medication was completed first, and lung sounds were monitored frequently for the remainder of the shift. Weighing the patient before breakfast was delegated to the CNA. The patient was educated about her medications and methods to use to reduce peripheral edema at home. All interventions were documented in the electronic medical record (EMR).
4.8. EVALUATION
Evaluation is the sixth step of the nursing process (and the sixth Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.” [ 1 ] Both the patient status and the effectiveness of the nursing care must be continuously evaluated and the care plan modified as needed. [ 2 ]
Evaluation focuses on the effectiveness of the nursing interventions by reviewing the expected outcomes to determine if they were met by the time frames indicated. During the evaluation phase, nurses use critical thinking to analyze reassessment data and determine if a patient’s expected outcomes have been met, partially met, or not met by the time frames established. If outcomes are not met or only partially met by the time frame indicated, the care plan should be revised. Reassessment should occur every time the nurse interacts with a patient, discusses the care plan with others on the interprofessional team, or reviews updated laboratory or diagnostic test results. Nursing care plans should be updated as higher priority goals emerge. The results of the evaluation must be documented in the patient’s medical record.
Ideally, when the planned interventions are implemented, the patient will respond positively and the expected outcomes are achieved. However, when interventions do not assist in progressing the patient toward the expected outcomes, the nursing care plan must be revised to more effectively address the needs of the patient. These questions can be used as a guide when revising the nursing care plan:
- Did anything unanticipated occur?
- Has the patient’s condition changed?
- Were the expected outcomes and their time frames realistic?
- Are the nursing diagnoses accurate for this patient at this time?
- Are the planned interventions appropriately focused on supporting outcome attainment?
- What barriers were experienced as interventions were implemented?
- Does ongoing assessment data indicate the need to revise diagnoses, outcome criteria, planned interventions, or implementation strategies?
- Are different interventions required?
Refer to Scenario C in the “Assessment” section of this chapter and Appendix C . The nurse evaluates the patient’s progress toward achieving the expected outcomes.
For the nursing diagnosis Fluid Volume Excess , the nurse evaluated the four expected outcomes to determine if they were met during the time frames indicated:
The patient will report decreased dyspnea within the next 8 hours.
The patient will have clear lung sounds within the next 24 hours.
The patient will have decreased edema within the next 24 hours.
The patient’s weight will return to baseline by discharge.
Evaluation of the patient condition on Day 1 included the following data: “ The patient reported decreased shortness of breath, and there were no longer crackles in the lower bases of the lungs. Weight decreased by 1 kg, but 2+ edema continued in ankles and calves .” Based on this data, the nurse evaluated the expected outcomes as “ Partially Met ” and revised the care plan with two new interventions:
Request prescription for TED hose from provider.
Elevate patient’s legs when sitting in chair.
For the second nursing diagnosis, Risk for Falls , the nurse evaluated the outcome criteria as “ Met ” based on the evaluation, “ The patient verbalizes understanding and is appropriately calling for assistance when getting out of bed. No falls have occurred. ”
The nurse will continue to reassess the patient’s progress according to the care plan during hospitalization and make revisions to the care plan as needed. Evaluation of the care plan is documented in the patient’s medical record.
4.9. SUMMARY OF THE NURSING PROCESS
You have now learned how to perform each step of the nursing process according to the ANA Standards of Professional Nursing Practice. Critical thinking, clinical reasoning, and clinical judgment are used when assessing the patient, creating a nursing care plan, and implementing interventions. Frequent reassessment, with revisions to the care plan as needed, is important to help the patient achieve expected outcomes. Throughout the entire nursing process, the patient always remains the cornerstone of nursing care. Providing individualized, patient-centered care and evaluating whether that care has been successful in achieving patient outcomes are essential for providing safe, professional nursing practice.
Video Review of Creating a Sample Care Plan [ 1 ]
4.10. LEARNING ACTIVITIES
Learning activities.
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Instructions: Apply what you’ve learned in this chapter by creating a nursing care plan using the following scenario. Use the template in Appendix B as a guide.
The client, Mark S., is a 57-year-old male who was admitted to the hospital with “severe” abdominal pain that was unable to be managed in the Emergency Department. The physician has informed Mark that he will need to undergo some diagnostic tests. The tests are scheduled for the morning.
After receiving the news about his condition and the need for diagnostic tests, Mark begins to pace the floor. He continues to pace constantly. He keeps asking the nurse the same question (“How long will the tests take?”) about his tests over and over again. The patient also remarked, “I’m so uptight I will never be able to sleep tonight.” The nurse observes that the client avoids eye contact during their interactions and that he continually fidgets with the call light. His eyes keep darting around the room. He appears tense and has a strained expression on his face. He states, “My mouth is so dry.” The nurse observes his vital signs to be: T 98, P 104, R 30, BP 180/96. The nurse notes that his skin feels sweaty (diaphoretic) and cool to the touch.
Critical Thinking Activity:
Group (cluster) the subjective and objective data.
Create a problem-focused nursing diagnosis (hypothesis).
Develop a broad goal and then identify an expected outcome in “SMART” format.
Outline three interventions for the nursing diagnosis to meet the goal. Cite an evidence-based source.
Imagine that you implemented the interventions that you identified. Evaluate the degree to which the expected outcome was achieved: Met – Partially Met – Not Met.

- IV GLOSSARY
The act or process of pleading for, supporting, or recommending a cause or course of action. [ 1 ]
Unconditionally acceptance of the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care. [ 2 ]
Groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences. [ 3 ]
Medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis. [ 4 ]
Care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable. [ 5 ]
A relationship described as one in which the whole person is assessed while balancing the vulnerability and dignity of the patient and family. [ 6 ]
Individual, family, or group, which includes significant others and populations. [ 7 ]
The observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care. [ 8 ]
A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions. [ 9 ]
Grouping data into similar domains or patterns.
Nursing interventions that require cooperation among health care professionals and unlicensed assistive personnel (UAP).
While implementing interventions during the nursing process, includes components such as organizing the components of the plan with input from the health care consumer, engaging the patient in self-care to achieve goals, and advocating for the delivery of dignified and person-centered care by the interprofessional team. [ 10 ]
Reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow. [ 11 ]
Subjective or objective data that gives the nurse a hint or indication of a potential problem, process, or disorder.
“Top-down thinking” or moving from the general to the specific. Deductive reasoning relies on a general statement or hypothesis—sometimes called a premise or standard—that is held to be true. The premise is used to reach a specific, logical conclusion.
Observable cues/inferences that cluster as manifestations of a problem-focused, health-promotion diagnosis, or syndrome. This does not only imply those things that the nurse can see, but also things that are seen, heard (e.g., the patient/family tells us), touched, or smelled. [ 12 ]
The assignment of the performance of activities or tasks related to patient care to unlicensed assistive personnel while retaining accountability for the outcome. [ 13 ]
Interventions that require a prescription from a physician, advanced practice nurse, or physician’s assistant.
Interventions that are carried out by having personal contact with a patient.
An electronic version of the patient’s medical record.
A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values. [ 14 ]
Statements of measurable action for the patient within a specific time frame and in response to nursing interventions. “SMART” outcome statements are specific, measurable, action-oriented, realistic, and include a time frame.
An evidence-based assessment framework for identifying patient problems and risks during the assessment phase of the nursing process.
A judgment formed from a set of facts, cues, and observations.
Broad statements of purpose that describe the aim of nursing care.
Employing strategies to teach and promote health and wellness. [ 15 ]
Any intervention that the nurse can provide without obtaining a prescription or consulting anyone else.
Interventions performed by the nurse in a setting other than directly with the patient. An example of indirect care is creating a nursing care plan.
A type of reasoning that involves forming generalizations based on specific incidents.
Interpretations or conclusions based on cues, personal experiences, preferences, or generalizations.
Nurses who have had specific training and passed a licensing exam. The training is generally less than that of a Registered Nurse. The scope of practice of an LPN/LVN is determined by the facility and the state’s Nurse Practice Act.
A disease or illness diagnosed by a physician or advanced health care provider such as a nurse practitioner or physician’s assistant. Medical diagnoses are a result of clustering signs and symptoms to determine what is medically affecting an individual.
Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity. [ 16 ]
Specific documentation of the planning and delivery of nursing care that is required by The Joint Commission.
A systematic approach to patient-centered care with steps including assessment, diagnosis, outcome identification, planning, implementation, and evaluation; otherwise known by the mnemonic “ADOPIE.”
Data that the nurse can see, touch, smell, or hear or is reproducible such as vital signs. Laboratory and diagnostic results are also considered objective data.
A measurable behavior demonstrated by the patient that is responsive to nursing interventions. [ 17 ]
The format of a nursing diagnosis statement that includes:
Problem (P) – statement of the patient problem (i.e., the nursing diagnosis)
Etiology (E) – related factors (etiology) contributing to the cause of the nursing diagnosis
Signs and Symptoms (S) – defining characteristics manifested by the patient of that nursing diagnosis
Orders, interventions, remedies, or treatments ordered or directed by an authorized primary health care provider. [ 18 ]
Information collected from the patient.
Member of the health care team (usually a medical physician, nurse practitioner, etc.) licensed and authorized to formulate prescriptions on behalf of the client. [ 19 ]
The skillful process of deciding which actions to complete first, second, or third for optimal patient outcomes and to improve patient safety.
The “combined and unceasing efforts of everyone — health care professionals, patients and their families, researchers, payers, planners, and educators — to make the changes that will lead to better patient outcomes (health), better system performance (care), and better professional development (learning).” [ 20 ]
Developing a relationship of mutual trust and understanding.
A nurse who has had a designated amount of education and training in nursing and is licensed by a state Board of Nursing.
The underlying cause (etiology) of a nursing diagnosis when creating a PES statement.
Patients have the right to determine what will be done with and to their own person.
Principles and procedures in the discovery of knowledge involving the recognition and formulation of a problem, the collection of data, and the formulation and testing of a hypothesis.
Information collected from sources other than the patient.
Data that the patient or family reports or data that the nurse makes as an inference, conclusion, or assumption, such as “The patient appears anxious.”
Any unlicensed personnel trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. [ 21 ]
Obtaining Subjective Data in a Care Relationship
Licensed under a Creative Commons Attribution 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/ .
- Cite this Page Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Fundamentals [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021. Chapter 4 Nursing Process.
- PDF version of this title (216M)
In this Page
- NURSING PROCESS INTRODUCTION
- BASIC CONCEPTS
- OUTCOME IDENTIFICATION
- IMPLEMENTATION OF INTERVENTIONS
- SUMMARY OF THE NURSING PROCESS
- LEARNING ACTIVITIES
Other titles in this collection
- Open RN OER Textbooks
Related Items in Bookshelf
- All Textbooks
Bulk Download
- Bulk download content from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Chapter 4 Nursing Process - Nursing Fundamentals Chapter 4 Nursing Process - Nursing Fundamentals
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Effects of a simulation-based nursing process educational program: A mixed-methods study
Affiliations.
- 1 Department of Nursing and the Clinical Competency Center at Chang Gung University of Science and Technology, No.261, Wenhua 1st Rd., Guishan District, Taoyuan 33303, Republic of China (Taiwan); Department of Rehabilitation at Taoyuan Chang Gung Memorial Hospital, No. 5, Fuxing Street, Guishan District, Taoyuan City 33305, Republic of China (Taiwan). Electronic address: [email protected].
- 2 Department of Nursing and the Clinical Competency Center at Chang Gung University of Science and Technology, No.261, Wenhua 1st Rd., Guishan District, Taoyuan 33303, Republic of China (Taiwan); Department of Emergency Medicine at Chang Gung Memorial Hospital Linkou, No. 5, Fuxing Street, Guishan Dist., Taoyuan City 33305, Republic of China (Taiwan). Electronic address: [email protected].
- 3 Clinical Competency Center at Chang Gung University of Science and Technology, No.261, Wenhua 1st Rd., Guishan District, Taoyuan 33303, Republic of China (Taiwan). Electronic address: [email protected].
- 4 Department of Nursing at Chang Gung University of Science and Technology, No. 261, Wenhua 1st Rd., Guishan District, Taoyuan 33303, Republic of China (Taiwan). Electronic address: [email protected].
- PMID: 34544010
- DOI: 10.1016/j.nepr.2021.103188
Aims: To examine the effects of a simulation-based nursing process educational program on nursing students' confidence in communication and foundational understanding of the nursing process.
Background: The nursing process is a core component of patient-centered nursing care that is underpinned by effective communication. However, learning how to engage patients and carry out the distinct steps of the nursing process can be challenging if students are not able to apply knowledge to practice. Simulation-based learning programs can provide an immersive opportunity for students to enhance their understanding of the nursing process as well as improve their communication skills.
Design: A mixed methods randomized controlled trial METHODS: Two Fundamentals of Nursing classes were recruited from a university in northern Taiwan. The experimental group (n = 58) engaged with the simulation-based nursing process educational program, which consisted of an online interactive animation and a standardized patient simulation. The control group (n = 49) was assigned a case-study. Confidence in Communication surveys, assignment and examination scores, satisfaction questionnaires and post-simulation reflection logs were used for data collection. Data were analyzed using SPSS 22.0 and qualitative content analysis.
Results: Both groups showed statistically significant improvement in Confidence in Communication (p < .001). The experimental group performed better on the assignment than the control group (p < .001). No significant difference was seen between either groups' examination performances. The animation's high usage rate (mean 5.91 interactions per-user) and the results of the satisfaction questionnaires indicate the program's positive reception from the experimental group. The following themes emerged: effective communication skills, problem solving, confidence, feeling prepared and novel learning experience.
Conclusion: The results demonstrate that the simulation-based nursing process educational program increased students' self-confidence in communication and non-verbal communication skills as well as foundational understanding of how to carry out the nursing process. The use of interactive simulation-based learning experiences is recommended to improve nursing students' understanding of how to apply abstract concepts into practice.
Keywords: Communication skills; Interactive animation; Nursing process; Simulation-based learning.
Copyright © 2021 Elsevier Ltd. All rights reserved.
Publication types
- Randomized Controlled Trial
- Clinical Competence
- Education, Nursing*
- Education, Nursing, Baccalaureate*
- Nursing Process*
- Patient Simulation
- Students, Nursing*

Nursing Process Assignment
Emotional: Subjective: Mr. Smith advised that he often feels mood is very low, this is related to his COOP and coping skills. He can no longer participate in activities that he did previously due to SOB and feeling fatigued. Has no appetite and states he does not feel hungry. Advises he often feels anxious due to threat of death, purposes that are not being met. Coping skills reduced caused by anxiety, lack of solicitation, depression, low activity levels and an inability to work. Objective: Facial expressions are often observed being sad. Spends a lot of time in bed with no solicitation with nursing staff or other patients.
Appears withdrawn and quiet. Does not eat food at mealtimes unless encouraged by his wife. Subjective: Mr. Smith enjoys a daily walk around the lake close to his home and helps his wife around the house. He is retired and receives a government pension to insane his needs. Does not want to eat at meal times as states he has no appetite. He states he would like to participate in social activities and help his wife with daily chores but is unable due to lack of energy and this causes anxiety. Objective: His wife visits him on the ward every day, offering him support and encouragement at his bedside.
Don’t waste your time! Order your assignment!
She is often present at meal times and encourages her husband to eat. Spiritual: Subjective: Mr. Smith denies being involved in any religious beliefs but attends Church with his wife on Christmas Eve as a tradition. Objective: Mood and effect appears to be low. Diagnostic Phase: From the assessment information, abnormal data highlighted includes: pneumonia, ineffective breathing pattern related to SOB. Ineffective airway clearance caused by increased sputum production, ineffective cough, fatigue / lack of energy. Impaired Gas Exchange related to ventilation perfusion inequality.
Imbalanced Nutrition – less than body requirements. Activity Intolerance related to imbalance between oxygen supply with demand. Anxiety related to threat of death, purposes that are not being met. Ineffective individual coping related to anxiety, lack of solicitation, depression, owe activity levels and an inability to take part in social activities and help wife with dally snores. Preventing RAFF In Mr.. Smelt Is ten enlist nursing poorly Tort ten next 24 hours as it affects his airway and breathing, is life threatening and can increase mortality significantly (Drills, 2008; ,Lines & Kelly, 2013).
Mr.. Smith is at risk of RAFF, as evidenced by his is mildly hypersonic state with compensated respiratory acidosis and 82% oxygen saturation levels on Room Air (RA). His COOP may cause inadequate gas exchange, resulting in hyperemia and hyperplasia (Lines & Kelly 2013; Moore, 2013). Mr.. Smith’s symptoms of COOP deteriorated once he was admitted to emergency. He become confused, agitated, was saturating at 84% via a Hudson marks and his arterial blood gases showed respiratory acidosis and hyperplasia, all of which are signs of RAFF (Lines and Kelly, 2013).
This suggests that Mr.. Smith is oxygen sensitive, and was retaining CO as a result of the TO. Because of this Mr.. Smith requires close monitoring and risk management while on the respiratory ward, especially while receiving TO to avoid hyperemia and hyperplasia leading to RAFF. Oxygen Therapy (TO) increases oxygen in the luminary capillary bed and promotes the exchange of gases in the lungs, increasing oxygen levels in the blood, while removing carbon dioxide (CO) from the body’s tissues (Health Quality Ontario, 2012; Simmons and Simmons, 2004).
If uncontrolled high concentration of oxygen is given inappropriately in COOP patients, some may retain CO, which puts them at risk of hyperplasia and respiratory acidosis (Moore, 2013; Stroller, Panics, Churchman & Moore, 2013). It is a fine line between optimal and excessive TO, therefore risk management should always be a nursing priority (Simmons and Simmons, 2004). Lines and Kelly (2013) encourage the use of pulse geometry to establish the needs of a patient with COOP before administering TO.
However they emphasis its limitations, including that false readings can occur due to poor perfusion or patient movement and its inability to detect CO in the blood. Because of this close monitoring of the patient is required for signs of Hyperplasia (Simmons and Simmons, 2004; Lines & Kelly, 2013). Moore (2013) recommends allocating those patients identified as CO retainers or those at risk of hyperplasia, an oxygen alert card to ensure all medical staff are aware that only titrated Oxygen would be administered.
The risk of rebound hypothermia is also present, where due to the sudden cessation of TO, the remaining oxygen is absorbed into the bloodstream resulting in tattletales (Lines & Kelly, 2013; Drilldown, Howard & Davison, 2008,’). Planning Phase: Goals: Mr. Smith is at high risk of developing acute hyperplasia respiratory failure. Immediate: Mr.. Smith’s oxygen saturation levels will be maintained between 88-92% at all times during the next 24 hours to avoid oxygen induced hyperplasia and hyperemia leading to RAFF. Intermediate: Mr.. Smith maintains optimal gas exchange as evidenced by normal
Abs, appears alert and responsive with no reduction in mental status. Long- term: Rater Mr. Smelt to none Neal services Tort nursing care, oxygen management and COOP rehabilitation. Abed and Hunks (2012) found that oxygen saturation levels need to be maintained between 88-92% to reduce the risk of oxygen induced hyperplasia and to avoid hyperemia. Moore (2013) agrees and adds that either 28% or 24% oxygen delivered via TO is ideal to achieve this. Although Lines and Kelly (2013) explain that it is important to realize that individuals will respond to TO differently.
Their declaration hat this is particularly important for those patients over 70 is especially relevant considering Mr.. Smith’s age of 74. For this reason, an TO assessment will be performed on Mr.. Smith, using a pulse geometry device, to detect the appropriate oxygen concentration range to maintain his oxygen saturation between 88-92%. Once the assessment is complete, and in conjunction with Mr.. Smith’s multidisciplinary medical team, titrating oxygen between 24-28% will be administrated via a Ventura mask. Lines and Kelly (2013), emphasis the importance of selecting the correct delivery device to administer titrated oxygen to COOP patients.
Moore agrees, explaining that a COOP patient at risk of RAFF should only be administrated oxygen via a Ventura mask, which helps to ensure the correct dose of oxygen is administered and prevents the patient rebating CO, reducing the risk of RAFF. Mr.. Smith’s will be monitored closely for signs hyperplasia and hyperemia. His respiratory rate, rhythm and depth will be taken along with observations of My Smith’s respiratory effort and his color noted. His oxygen saturation levels will be measured and recorded every 30 minutes using a pulse geometry device to ensure they stay teen 88-92% over the 24-hour period.
These measurements will also be used to determine the success of these interventions in meeting the nursing goal. Planned nursing care to meet these goal include monitoring Mr.. Smith’s vital signs and cardiac rhythm. Initial signs of hypoxia and hyperplasia indicate an increase in Blood Pressure (BP), respiratory and heart rate. If either of these conditions progress in severity, BP might drop, a rapid heart rate with arrhythmias endures and respiratory failure may result in Mr.. Smith being incapable of sustaining the rapid respiratory rate.
Tachycardia, BP changes and dysphasia can reflect systemic hyperemia on cardiac function. Maintain Mr.. Smith’s airway potency by teaching “huff” coughing techniques to effectively loosen mucus and secretions, reducing fatigue and conserving energy (Brown et al. , 2012). A fluid intake of 2-AL per day will be maintained to keep secretions thin and easy to expectorate. Position Mr.. Smith with proper body alignment elevating head of bed to at least 45 degrees. Oxygen delivery and work of breathing may be improved by upright position decreasing the risk of airway collapse, and dyspepsia. Mr..
Smith will be assessed for any change in behavior or orientation. Early indications of hypoxia include restlessness and anxiety, worsening Arterial Blood Gases (Abs) accompanied by confusion are signs of cerebral dysfunction. Monitor and investigate changes and assess color of skin and mucous membranes. Indications of cyanogens can be observed peripherally (in nail beds) or centrally (around lips/or earlobes). Signs of advanced hyperemia include darkness Ana central cyanogens. I en respiratory status Ana level AT consciousness AT Mr.. Smith will be assessed every 1 to 2 hours until stable, then at least every 4 hours.
Hyperplasia is caused by low oxygen saturation, symptoms of this include confusion and anxiety and decreased respiratory rate (Brown et al. , 2012). Worsening Abs accompanied by confusion are indicative of cerebral dysfunction due to hyperemia. Mr.. Smith’s response to oxygen therapy will be monitored closely oxygen including saturation, sputum consistency, and respiratory rate. Monitor Abs and note any changes, signs of respiratory failure are increasing Apace and decreasing Papa. If this occurs the respiratory rate will decrease and Apace will begin to rise (Kananga, Ninja, Sahara, 2009).
Patients with COOP have a substantial decrease in pulmonary reserves, and any physiological stress may result in acute respiratory failure. Maintain oxygen administration device as ordered, attempting to preserve oxygen saturation at 90% or greater provides adequate oxygenation (Mckenzie & Firth, 2003). Close monitoring is crucial to prevent dangerous increases in the patient’s Papa. Administering a high concentration of oxygen to COOP patients should be avoided, as hypoxia stimulates the drive to breathe in chronic CO retainer patients.
Close monitoring is essential to prevent unsafe increases in the patient’s Papa, as apneas may occur. Mr.. Smith will be assisted with ambulation, to promote lung expansion, stimulate deep breathing and assist with clearance of mucus and secretions (Hurst, Headache, 2009). Scheduled rest periods and paced activities following treatments and procedures will prevent fatigue. Simple activities during bed rest such as coughing exercises and bathing can cause fatigue and increase oxygen consumption. Deep breathing should be encouraged, reducing alveolar collapse.
Administer medications as ordered and provide mouth care after inhalers. An evaluation of the goals set out should involve observations of Mr.. Smith’s ability to cough and deep breathe effectively. Calculate the lungs for adventitious sounds and assess respiratory rate and hydration. Observe color and consistency of sputum and note on the Fluid Balance Chart (Crisp & Taylor, 2008). Implementation Phase: Please put the information in these sections under the ‘planning’ title where they belong and write a small paragraph indicating that the planned care was actually carried out for Mr. Smith.
In addition, please provide a clear indication of who did what to fulfill the need to address the importance of teamwork and I will be happy to ass this section of your assignment. There is no evidence to demonstrate that these beautiful plans were carried out by the multi-professional health care team with the exception of the paragraph entitled ‘expected outcomes’ which is a perfect example of implementation of care – (that can stay in this section). The implementation phase usually has a focus on side effects of medication provided and your extensive considerations related to administration of oxygen certainly achieves that.
Expect EAI outcomes: At the duration of 24 hours Mr.. Smith should demonstrate improved ventilation and adequate oxygenation of tissues with Abs within normal range and symptoms of respiratory distress should have diminished. He will participate in a nursing care plan within his level of ability and demonstrate the use of deep breathing and coughing techniques to clear expectorate and increase lung expansion and be referred to home health services for nursing care or oxygen management. Collaborative Problem: Mr. Smith is at risk of malnutrition due to complications of COOP.
Goals: Immediate: Prevent fluid volume insufficiency and electrolyte imbalance. Intermediate: Consume a high-energy diet and encourage regular eating and rest tatters. Long- term: Consult with dietician in order to plan and implement dietary regime upon discharge. Mr. Smith will be weighed each day to assess nutritional status and determine caloric needs, set weight goal, and evaluate an adequate nutritional plan. Evaluate Body Mass Index (IBM) to assess dietary habits and monitor amount of fluid and food ingested to determine efficiency of intake.
Medications can interfere with the body’s absorption of nutrients and loss of appetite can be attributed to lack of taste, or being too fatigued to chew, swallow and/or breathe (Mckenzie & Firth, 2003). Calculate Mr.. Smith for bowel sounds. Hypoactive or diminished bowel sounds may indicate a decrease in gastric motility and constipation related to reduced fluid intake, decreased activity, poor food choices, and hyperemia. Remove expectorated secretions promptly and provide oral care prior to meals to moisten and clean the mount AT sputum taste.
Noxious tastes, slants, Ana smells are major deterrents to appetite and can provide a stimulus for nausea and vomiting causing respiratory exertion (Brown et al. , 2012). Select nutritional supplements to provide nutritional between-meal snacks. Provide Mr.. Smith with high protein, high-energy nutritious knacks and drinks that contain adequate energy and protein, and that require minimal effort to consume. Mr.. Smith will be encouraged to rest for a period of 1 hour before and after meals to reduce fatigue during mealtime, and create an opportunity to increase his total calorie intake (Epidermal, 2013).
Eating requires energy and more oxygen will be consumed than at rest. Administer supplemental oxygen during meals as indicated. Oxygen must be administered via a different method during mealtime (e. G. , changing mask to a nasal canals) decreasing the risk of dyspepsia and increasing energy for eating, enhancing intake. Immediately after eels the original oxygen delivery system should be resumed. Carbonated beverages and gas-producing foods should be avoided; abdominal distension may result, which hinders abdominal breathing and diaphragmatic movement increasing the risk of dyspepsia.
Mr.. Smith will not be given very cold or very hot foods as coughing spasms may be aggravated by extremes in temperature (Brown et al. , 2012). Refer a dietician to provide Mr.. Smith with appropriate information regarding nutritional needs and how to meet them, ensuring nutritional adequacy after discharge. Evaluation Phase: Evaluation of the 19 actions you planned for Mr. Smith is not valuated here. Provision of such clarity ensures that no aspect of patient care gets overlooked which really improves efficiency and the effectiveness of care provision.
The planning and implementation of these nursing interventions was deemed a success due to all goals being achieved. Over a period of 24 hrs Mr. Smith’s oxygen saturation levels were measured and recorded every 30 minutes at a level of 88-92%. Over the next day he appeared to remain alert and responsive which indicated optimal gas exchange via oxygen therapy. At the end of 72 hours Mr.. Smith’s condition was stable and he was discharged and referred to home health services for urging care and oxygen management for further education and COOP rehabilitation.
His fluid volume and electrolytes were increased and he consumed a high-energy diet and met with a dietician to plan and implement a dietary regime upon discharge. Due to his responsiveness to the planning and implementation of this nursing process, it proves that this was effective as his condition improved. Upon discharge from hospital, Mr.. Smith is at risk of readmission due to the chronic of his COOP. One area identified to reduce this risk is health promotion and education through access to comprehensive pulmonary rehabilitation (Assignations, Workman, 010).
Pulmonary rehabilitation is one of the most successful interventions in COOP, enhancing health-related quality of life and self-efficacy, and reducing depression and anxiety, dispensed and the possibility of future hospitalizing (Engel, 2012). Rehabilitation incorporating exercise programs, education and psychosocial support can provide the greatest benefits firstly by improving cardiovascular fitness, muscle strength Ana exercise endurance leaning to Improved Tunnel Ana reach symptoms of COOP; enhancing Mr..
Smith’s self-confidence and coping strategies, and improving medication adherence and use of respiratory treatment devices; and lastly by enlightening mood by controlling anxiety and panic, diminishing depression, and reducing social barriers (Squadron, Mandarin, 2009). Mr.. Smith and his family will be advised of support groups providing emotional support, social outlets and interaction, new knowledge and coping strategies. These strategies have been administered upon discharge to enhance Mr..
Smith’s quality of life and reduce the risk of any further complications resulting from COOP and future hospital admissions. In conclusion, the first priority for Mr.. Smith is to maintain adequate oxygen levels via the administration of 02 therapy and close monitoring of his vital signs and other interventions to maintain optimal breathing and airway clearance. The second priority is to enhance his nutritional intake to encourage increased energy levels needed for function and to restore energy levels diminished by factors relating to his COOP.
Thirdly a plan for post discharge care and support is required for Mr.. Smith and his family, to enhance his quality of life and reduce the risk of COOP exacerbation and re-admission to hospital. In relation to your reticence ten Dates Tort Bases Ana Burt & cordage onto tally between the body of the assignment and reference list. Brown et al; (2012), Discoid; (2008) and Stroller, Panics, Karachi & Moor, (2013) don’t appear in your reference list. Stroller, Pens, Churchman, Doherty & Make (2010) don’ appear in the body of your assignment.
How to cite this assignment
Related assignments:.
- Nursing Process Paper Assignment
- Nursing Process Workbook Part a Assignment
- The Process Of Promotion – Assignment
Haven't Found The Paper You Want?
For Only $13.90/page

Provide details on what you need help with along with a budget and time limit. Questions are posted anonymously and can be made 100% private.

Studypool matches you to the best tutor to help you with your question. Our tutors are highly qualified and vetted.

Your matched tutor provides personalized help according to your question details. Payment is made only after you have completed your 1-on-1 session and are satisfied with your session.
Written Assignment Nursing Process - Case Study
User Generated
lbhatbe1977
Health Medical
Description
Module 04 Written Assignment Nursing Process - Case Study
Please read the following case study and complete the questions below.
Daniel is a 16 year old boy who is an identical twin. He and his brother Jeff are very close and do most things together. While Daniel excels at sports he believe his brother is much better at most everything. Daniel, his brother, and their two sisters live with their parents in the Midwest. Recently Daniel has been feeling more tired than usual. He thought it was because of his schedule and school work, which he is fairly good at. He gets mostly Bs, but his grades have been slipping of late. One day he fainted while getting ready for a game. His coach called his parents to let them know Daniel was taken to the Emergency Room. While there the doctor decided to admit Daniel to the hospital for observation. At the time he was running a slight fever, his breathing was shallow, and he was sweating. He was also very sleepy and his blood pressure was high. He did have some abnormal laboratory work, but his doctor was not too concerned at present. Daniel also stated that he felt achy.
You are assigned to take care of Daniel today and when you walk into his room, his mother and brother Jeff are there. Daniel appears to be sleeping. In your written assignment, respond to the following questions applying the nursing process:
Assessment : What type of objective and subjective data can you collect with what you know? How will you collect these data? What further evidence do you need?
Analysis and Identification of the Problem : What do you believe Daniel's problem(s) are? What might be the nursing diagnoses? Use the following for identification.
Planning : Identify two goals and one nursing intervention for each, based on your nursing diagnoses.
While you will not be able to implement or evaluate , how well do you think your nursing interventions might help with Daniel's care.

Explanation & Answer

Hello, I'm done, all areas are well answered as instructed. looking forward to help you in the future assignments. Running Head: NURSING PROCESS CASE STUDY Nursing Process Case Study Institution Name Date 1 NURSING PROCESS CASE STUDY 2 Assessment According to Daniel’s medical condition, the subjective data will be collected based on the client’s point of view symptoms. Therefore, the subjective data to be collected will comprise of: sweating, breathing difficulties, weaknesses and tiredness. Secondly, the objective...

24/7 Homework Help
Stuck on a homework question? Our verified tutors can answer all questions, from basic math to advanced rocket science !

Similar Content
Related tags.
teaching plan personal training health and medical prevention articles nursing theories project health Thyroid disorders poison, GLOMERULONEPHRITIS united states
Animal Farm
by George Orwell
Cry the Beloved Country
by Alan Paton
by Wiliam Shakespeare
The Turn of the Screw
by Henry James
We Were Eight Years in Power
by Ta-Nehisi Coates
by Cormac McCarthy
Alice in Wonderland
by Lewis Carroll
Good Kids Bad City
by Kyle Swenson
The Scarlet Letter
by Nathaniel Hawthorne
working on a homework question?
Studypool is powered by Microtutoring TM
Copyright © 2024. Studypool Inc.
Studypool is not sponsored or endorsed by any college or university.
Ongoing Conversations
Access over 20 million homework documents through the notebank
Get on-demand Q&A homework help from verified tutors
Read 1000s of rich book guides covering popular titles

Sign up with Google
Sign up with Facebook
Already have an account? Login
Login with Google
Login with Facebook
Don't have an account? Sign Up

IMAGES
VIDEO
COMMENTS
Formulating client goals for prioritized problems is a component of planning, which is the third step in the nursing process. Study with Quizlet and memorize flashcards containing terms like A nurse is caring for a group of clients. Which of the following actions by the nurse demonstrates the use of critical thinking skills?, A nurse is ...
Explore our extensive category of nursing case study examples and solutions to gain valuable insights, improve your critical thinking abilities, and enhance your overall clinical knowledge. Services. ... NUR 403 Week 2 Individual Assignment Case Study comprises: Resources: The case study found on p. 131 in Nursing Theory and the Case Study Grid ...
1. Nursing Case Study Example - Meadowvale University School Of Nursing -. The case analysis explores some of the ways in which the curriculum development leader can adopt measures that enhance faculty support and development in the task of curriculum development (Nursing Case Study Analysis) Problem-solving case analysis. 2.
Conclusion: Summarize the key takeaways from the case study and reflect on the overall experience. Conclusion. Completing a nursing assignment or case study with a real patient scenario is a significant educational opportunity, enabling nurses to cultivate vital skills for their clinical practice. This multifaceted process encompasses ...
6 Steps to Replace Clinical Using Case Studies. 1. Watch the intro video as a group. Gather the entire class together and view the intro video. This video lays out the scenario for the given case study and helps them begin to consider the disease process. 2.
You also know what exactly you need to do in each section. It is time to learn how to write a nursing case study. The process detailed below should be easy to follow because you know the typical nursing case study structure. 1. Understand the Assignment. When given a nursing case study assignment, the first thing you need to do is to read.
The nursing process functions effectively in nursing and inter-professional teams, promoting open communication, mutual respect, and shared decision-making to achieve quality patient care. Dynamic and cyclical .The nursing process is a dynamic, cyclical process in which each phase interacts with and is influenced by the other phases.
Introduction: Nursing case study assignments are an integral part of nursing education, allowing students to apply their theoretical knowledge to real-world patient scenarios. Mastering these assignments requires a deep understanding of the process and techniques involved.
Writing a successful nursing case study can be a challenging task. However, by following the steps provided in this blog that is, first defining the problem, gathering information, developing alternatives., analyzing the alternatives, selecting the best alternative, implementing the solution and evaluating the outcome.
Running head: NURSING. Nursing Process Case Study. Samuel Kollmorgen. MCPHS University. Assessment. Subjective Data Shortness of Breath Fatigue Productive Cough Chills Sharp, 7/10 pain upon inspiration and coughing Symptoms have persisted for five days Patient feels symptoms are getting worse New onset insomnia Has used Robitussin and Nyquil Retired construction worker No prior hospitalizations
Module 4 Assignment Nursing Process Case Study (see page 2 for scenario) 1. What is the objective data? What other data will you gather? Fever, hypertensive, sweating, breathing shallow, abnormal labs Unless we wake him, I can take is respirations without touching him. 2. What is the subjective data? What other data will you gather?
A nursing case study paper contains several sections that fall into three categories: 1. The status of the patient. Demographic data. Medical History. Current diagnosis and treatment. 2. The nursing assessment of the patient. Vital signs and test results.
The nurse can promote adherence to Mich's asthma treatment regimen by providing education and resources, such as written instructions and referrals to support groups. The nurse can also encourage open communication with Mich and his family and address any barriers to adherence, such as cost or access to medications. 5.
While writing a case study, you can always discuss the predictable outcomes and pen down your recommendations. The discussion covers your assignment, giving you an area to expound on the research, relate your patient's care plan to the case, and offer a rationale. You can then make recommendations based on the care plan.
In a nursing case study, your task is to analyze a disorder or illness as a part of a specific medical situation. If you don't do that, your case study becomes an essay (theoretical and generalized). It is the difference between the two assignment types. Once again: A case study in nursing emphasizes the particular patient's condition.
ScienceDirect posted a nursing ethics case study where an end-stage prostate cancer patient, Mr. Green, confided to nursing staff about his plan to commit suicide. The patient asked the nurse to keep it a secret. The ethical problem is whether the nurse should tell the health care team members about the patient's thought without his permission.
Case Study during One Shift. This case study will focus on the implementation and evaluation stages of the nursing process while doing one shift in Theatres. I will highlight the involvement of physiological, pharmacological and psycho-sociological aspects of my given care. The patient's history and current situation will be examined ...
The nursing process becomes a road map for the actions and interventions that nurses implement to optimize their patients' well-being and health. This chapter will explain how to use the nursing process as standards of professional nursing practice to provide safe, patient-centered care. Go to: 4.2. BASIC CONCEPTS.
ScholarWorks@UMass Amherst
Aims: To examine the effects of a simulation-based nursing process educational program on nursing students' confidence in communication and foundational understanding of the nursing process. Background: The nursing process is a core component of patient-centered nursing care that is underpinned by effective communication. However, learning how to engage patients and carry out the distinct ...
ATI Video Case Studies - Fundamentals Nursing Process - Clinical Judgment. Nursing Process Video Challenge Question. The nurse in the video is using the nursing process to care for the client. What are the steps of the nursing process? The nursing process consists of ADPIE: Assessment, Diagnosis, Planning, Implementation, and Evaluation.
Nursing Process Assignment. Emotional: Subjective: Mr. Smith advised that he often feels mood is very low, this is related to his COOP and coping skills. He can no longer participate in activities that he did previously due to SOB and feeling fatigued. Has no appetite and states he does not feel hungry. Advises he often feels anxious due to ...
Module 04 Written Assignment Nursing Process - Case StudyPlease read the following case study and complete the questions below.Daniel is a 16 year old boy who is an identical twin. He and his brother Jeff are very close and do most things together. While Daniel excels at sports he believe his brother is much better at most everything. Daniel, his brother, and their two sisters live with their ...