

Cognitive Behavioral Therapy
Solving problems the cognitive-behavioral way, problem solving is another part of behavioral therapy..
Posted February 2, 2022 | Reviewed by Ekua Hagan
- What Is Cognitive Behavioral Therapy?
- Find a therapist who practices CBT
- Problem-solving is one technique used on the behavioral side of cognitive-behavioral therapy.
- The problem-solving technique is an iterative, five-step process that requires one to identify the problem and test different solutions.
- The technique differs from ad-hoc problem-solving in its suspension of judgment and evaluation of each solution.
As I have mentioned in previous posts, cognitive behavioral therapy is more than challenging negative, automatic thoughts. There is a whole behavioral piece of this therapy that focuses on what people do and how to change their actions to support their mental health. In this post, I’ll talk about the problem-solving technique from cognitive behavioral therapy and what makes it unique.
The problem-solving technique
While there are many different variations of this technique, I am going to describe the version I typically use, and which includes the main components of the technique:
The first step is to clearly define the problem. Sometimes, this includes answering a series of questions to make sure the problem is described in detail. Sometimes, the client is able to define the problem pretty clearly on their own. Sometimes, a discussion is needed to clearly outline the problem.
The next step is generating solutions without judgment. The "without judgment" part is crucial: Often when people are solving problems on their own, they will reject each potential solution as soon as they or someone else suggests it. This can lead to feeling helpless and also discarding solutions that would work.
The third step is evaluating the advantages and disadvantages of each solution. This is the step where judgment comes back.
Fourth, the client picks the most feasible solution that is most likely to work and they try it out.
The fifth step is evaluating whether the chosen solution worked, and if not, going back to step two or three to find another option. For step five, enough time has to pass for the solution to have made a difference.
This process is iterative, meaning the client and therapist always go back to the beginning to make sure the problem is resolved and if not, identify what needs to change.

Advantages of the problem-solving technique
The problem-solving technique might differ from ad hoc problem-solving in several ways. The most obvious is the suspension of judgment when coming up with solutions. We sometimes need to withhold judgment and see the solution (or problem) from a different perspective. Deliberately deciding not to judge solutions until later can help trigger that mindset change.
Another difference is the explicit evaluation of whether the solution worked. When people usually try to solve problems, they don’t go back and check whether the solution worked. It’s only if something goes very wrong that they try again. The problem-solving technique specifically includes evaluating the solution.
Lastly, the problem-solving technique starts with a specific definition of the problem instead of just jumping to solutions. To figure out where you are going, you have to know where you are.
One benefit of the cognitive behavioral therapy approach is the behavioral side. The behavioral part of therapy is a wide umbrella that includes problem-solving techniques among other techniques. Accessing multiple techniques means one is more likely to address the client’s main concern.

Salene M. W. Jones, Ph.D., is a clinical psychologist in Washington State.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

The Psychology Square

Affordable Mental Wellness is Possible!
Explore The Psychology Square for Support.
- December 19, 2023
20 Cognitive Behavioral Therapy (CBT) Techniques with Examples
Muhammad Sohail
Table of contents.
Cognitive Behavioral Therapy (CBT) stands as a powerful, evidence-based therapeutic approach for various mental health challenges. At its core lies a repertoire of techniques designed to reframe thoughts, alter behaviors, and alleviate emotional distress. This article explores 20 most commonly used cbt techniques. These therapy techniques are scientifcally valid, diverse in their application and effectiveness, serve as pivotal tools in helping individuals navigate and conquer their mental health obstacles.

Cognitive Restructuring or Reframing:
This is the most talked about of all cbt techniques. CBT employs cognitive restructuring to challenge and alter negative thought patterns. By examining beliefs and questioning their validity, individuals learn to perceive situations from different angles, fostering more adaptive thinking patterns.
John, feeling worthless after a rejected job application, questions his belief that he’s incompetent. He reflects on past achievements and reframes the situation, realizing the rejection doesn’t define his abilities.
Guided Discovery:
In guided discovery, therapists engage individuals in an exploration of their viewpoints. Through strategic questioning, individuals are prompted to examine evidence supporting their beliefs and consider alternate perspectives, fostering a more nuanced understanding and empowering them to choose healthier cognitive pathways.
During therapy, Sarah explores her fear of failure. Her therapist asks, “What evidence supports your belief that you’ll fail? Can we consider alternate outcomes?” Guided by these questions, Sarah acknowledges her exaggerated fears and explores more balanced perspectives.
Journaling and Thought Records:
Writing exercises like journaling and thought records aid in identifying and challenging negative thoughts. Tracking thoughts between sessions and noting positive alternatives enables individuals to monitor progress and recognize cognitive shifts.
James maintains a thought journal. Between sessions, he records negative thoughts about social situations. He then challenges these thoughts, jotting down positive alternatives and notices a shift in his mindset.
Activity Scheduling and Behavior Activation:
By scheduling avoided activities and implementing learned strategies, individuals establish healthier habits and confront avoidance tendencies, fostering behavioral change.
Emily, struggling with social anxiety, schedules coffee outings with friends. By implementing gradual exposure, she confronts her fear and eventually feels more comfortable in social settings.
Relaxation and Stress Reduction Techniques:
CBT incorporates relaxation techniques like deep breathing, muscle relaxation, and imagery to mitigate stress. These methods equip individuals with practical skills to manage phobias, social anxieties, and stressors effectively.
David practices deep breathing exercises when faced with work stress. By incorporating this technique into his routine, he manages work-related anxiety more effectively.
Successive Approximation:
Breaking overwhelming tasks into manageable steps cultivates confidence through incremental progress, enabling individuals to tackle challenges more effectively.
Maria, overwhelmed by academic tasks, breaks down her study sessions into smaller, manageable sections. As she masters each segment, her confidence grows, making the workload seem more manageable.
Interoceptive Exposure:
This technique targets panic and anxiety by exposing individuals to feared bodily sensations, allowing for a recalibration of beliefs around these sensations and reducing avoidance behaviors.
Tom, experiencing panic attacks, deliberately induces shortness of breath in a controlled setting. As he tolerates this discomfort without avoidance, he realizes that the sensation, though distressing, is not harmful.
Play the Script Until the End:
Encouraging individuals to envision worst-case scenarios helps alleviate fear by demonstrating the manageability of potential outcomes, reducing anxiety.
Facing fear of public speaking, Rachel imagines herself stumbling during a presentation. By playing out this scenario mentally, she realizes that even if it happens, it wouldn’t be catastrophic.
Shaping (Successive Approximation):
Shaping involves mastering simpler tasks akin to the challenging ones, aiding individuals in overcoming difficulties through gradual skill development.
Chris, struggling with public speaking, begins by speaking to small groups before gradually addressing larger audiences. Each step builds his confidence for the next challenge.
Contingency Management:
This method utilizes reinforcement and punishment to promote desirable behaviors, leveraging the consequences of actions to shape behavior positively.
To encourage healthier eating habits, Sarah rewards herself with a favorite activity after a week of sticking to a balanced diet.
Acting Out (Role-Playing):
Role-playing scenarios allow individuals to practice new behaviors in a safe environment, facilitating skill development and desensitization to challenging situations.
Alex, preparing for a job interview, engages in role-playing with a friend. They simulate the interview scenario, allowing Alex to practice responses and manage anxiety.
Sleep Hygiene Training:
Addressing the link between depression and sleep problems, this technique provides strategies for improving sleep quality, a critical aspect of mental well-being.
Lisa, struggling with sleep, follows sleep hygiene recommendations. She creates a calming bedtime routine and eliminates screen time before sleep, noticing improvements in her sleep quality.
Mastery and Pleasure Technique:
Encouraging engagement in enjoyable or accomplishment-driven activities serves as a mood enhancer and distraction from depressive thoughts.
After feeling low, Mark engages in gardening (a mastery activity) and then spends time painting (a pleasure activity). He finds joy in these activities, which uplifts his mood.
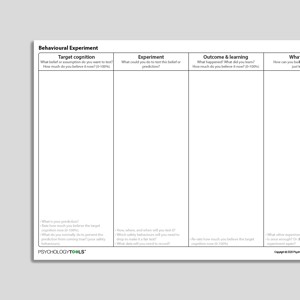
Behavioral Experiments:
This technique involves creating real-life experiments to test the validity of certain beliefs or assumptions. By actively exploring alternative thoughts or behaviors, individuals gather concrete evidence to challenge and modify their existing perspectives.
Laura believes people judge her negatively. She experiments by initiating conversations at social gatherings and observes that most interactions are positive, challenging her belief.
Externalizing:
Externalizing helps individuals separate themselves from their problems by giving those issues an identity or persona. This technique encourages individuals to view their problems as separate entities, facilitating a more objective approach to problem-solving.
Adam, dealing with anger issues, visualizes his anger as a separate entity named “Fury.” This helps him view his emotions objectively and manage them more effectively.
Acceptance and Commitment Therapy (ACT):
ACT combines mindfulness strategies with commitment and behavior-change techniques. It focuses on accepting difficult thoughts and emotions while committing to actions aligned with personal values, promoting psychological flexibility.
Sarah practices mindfulness exercises to accept her anxiety while committing to attend social events aligned with her values of connection and growth.
Imagery-Based Exposure:
This technique involves mentally visualizing feared or distressing situations, allowing individuals to confront and manage their anxieties in a controlled, imaginative setting.
Jack, afraid of flying, visualizes being on a plane, progressively picturing the experience in detail until he feels more comfortable with the idea of flying.
Mindfulness-Based Stress Reduction (MBSR):
MBSR incorporates mindfulness meditation and awareness techniques to help individuals manage stress, improve focus, and enhance overall well-being by staying present in the moment.
Rachel practices mindfulness meditation daily. By focusing on the present moment, she reduces work-related stress and enhances her overall well-being.
Systematic Desensitization:
Similar to exposure therapy, systematic desensitization involves pairing relaxation techniques with gradual exposure to anxiety-inducing stimuli. This process helps individuals associate relaxation with the feared stimuli, reducing anxiety responses over time.
Michael, with a fear of heights, gradually exposes himself to elevators first, then low floors in tall buildings, gradually working up to higher levels, reducing his fear response.
Narrative Therapy:
Narrative therapy focuses on separating individuals from their problems by helping them reconstruct and retell their life stories in a more empowering and positive light, emphasizing strengths and resilience.
Emily reevaluates her life story by focusing on instances where she overcame challenges, emphasizing her resilience and strength rather than her setbacks.
Each of these CBT techniques plays a unique role in helping individuals transform their thoughts, behaviors, and emotions. While some focus on cognitive restructuring, others emphasize behavioral modification or stress reduction. Together, they form a comprehensive toolkit empowering individuals to navigate their mental health challenges and foster positive change in their lives.
more insights

Representativeness Heuristic in Psychology: A Complete Guide
Representativeness heuristic in psychology is a cognitive shortcut influencing decision-making by affecting our judgments about probability.

GARS-3 Gilliam Autism Rating Scale Complete Guide
This is a comprehensive guide on GARS-3 Gilliam Autism Rating Scale, a highly popular assessment scale for autism spectrum disorder

Cognitive Behavioral Therapy (CBT): Types, Techniques, and More
Explore everything you need to know about cognitive behavioral therapy, from types and techniques to theory and modern perspective.
CBT Techniques: 25 Cognitive Behavioral Therapy Worksheets

It’s an extremely common type of talk therapy practiced around the world.
If you’ve ever interacted with a mental health therapist, a counselor, or a psychiatry clinician in a professional setting, it’s likely you’ve participated in CBT.
If you’ve ever heard friends or loved ones talk about how a mental health professional helped them identify unhelpful thoughts and patterns and behavior and alter them to more effectively work towards their goals, you’ve heard about the impacts of CBT.
CBT is one of the most frequently used tools in the psychologist’s toolbox. Though it’s based on simple principles, it can have wildly positive outcomes when put into practice.
In this article, we’ll explore what CBT is, how it works, and how you can apply its principles to improve your own life or the lives of your clients.
Before you read on, we thought you might like to download our three Positive CBT Exercises for free . These science-based exercises will provide you with a comprehensive insight into Positive CBT and will give you the tools to apply it in your therapy or coaching.
This Article Contains:
What is cbt, cognitive distortions, 9 essential cbt techniques and tools.
- Cognitive Behavioral Therapy Worksheets (PDFs) To Print and Use
Some More CBT Interventions and Exercises
A cbt manual and workbook for your own practice and for your client, 5 final cognitive behavioral activities, a take-home message.
“This simple idea is that our unique patterns of thinking, feeling, and behaving are significant factors in our experiences, both good and bad. Since these patterns have such a significant impact on our experiences, it follows that altering these patterns can change our experiences” (Martin, 2016).
Cognitive-behavioral therapy aims to change our thought patterns, our conscious and unconscious beliefs, our attitudes, and, ultimately, our behavior, in order to help us face difficulties and achieve our goals.
Psychiatrist Aaron Beck was the first to practice cognitive behavioral therapy. Like most mental health professionals at the time, Beck was a psychoanalysis practitioner.
While practicing psychoanalysis, Beck noticed the prevalence of internal dialogue in his clients and realized how strong the link between thoughts and feelings can be. He altered the therapy he practiced in order to help his clients identify, understand, and deal with the automatic, emotion-filled thoughts that regularly arose in his clients.
Beck found that a combination of cognitive therapy and behavioral techniques produced the best results for his clients. In describing and honing this new therapy, Beck laid the foundations of the most popular and influential form of therapy of the last 50 years.
This form of therapy is not designed for lifelong participation and aims to help clients meet their goals in the near future. Most CBT treatment regimens last from five to ten months, with clients participating in one 50- to 60-minute session per week.
CBT is a hands-on approach that requires both the therapist and the client to be invested in the process and willing to actively participate. The therapist and client work together as a team to identify the problems the client is facing, come up with strategies for addressing them, and creating positive solutions (Martin, 2016).
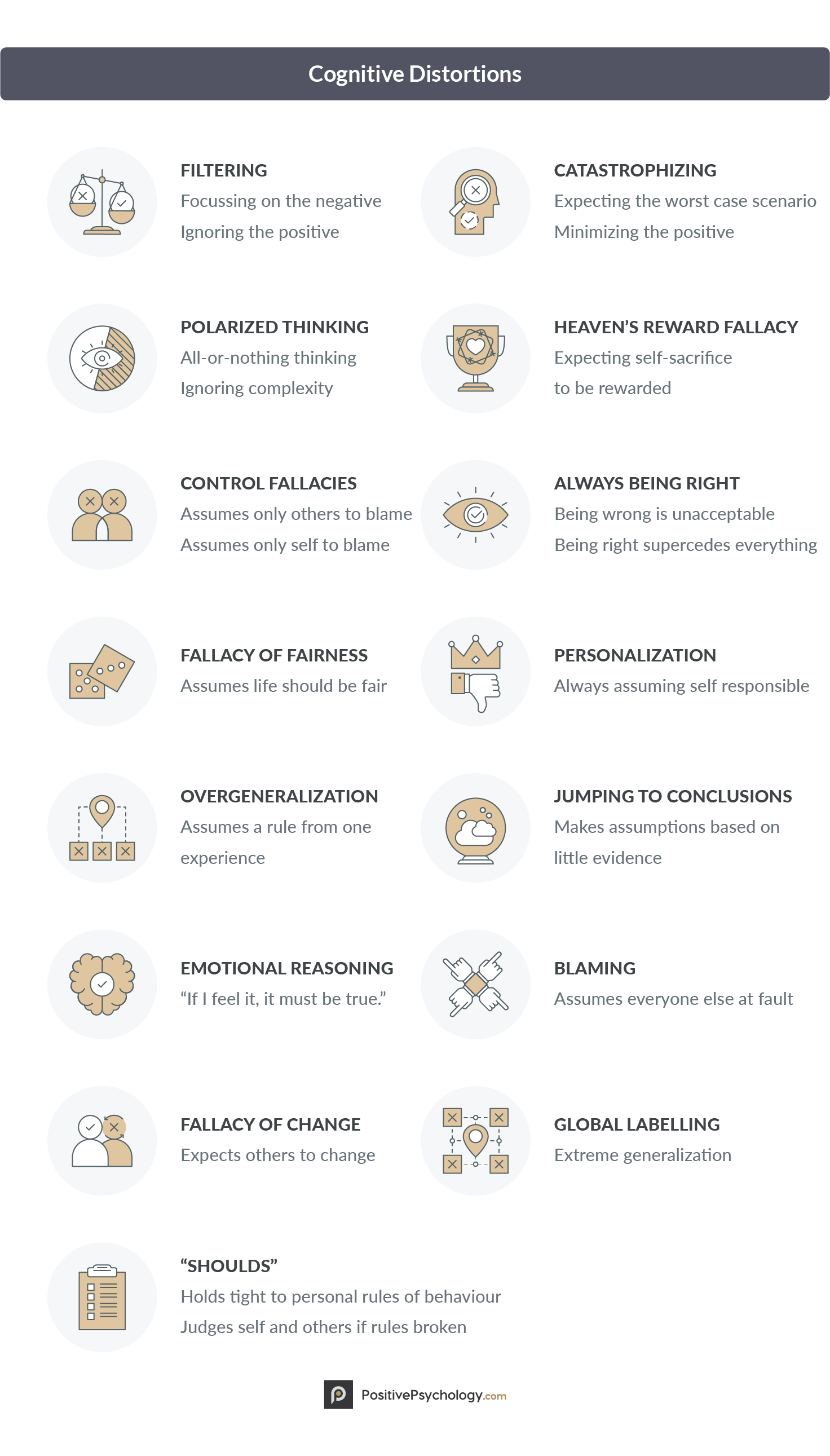
Many of the most popular and effective cognitive-behavioral therapy techniques are applied to what psychologists call “ cognitive distortions ,” inaccurate thoughts that reinforce negative thought patterns or emotions (Grohol, 2016).
There are 15 main cognitive distortions that can plague even the most balanced thinkers.
1. Filtering
Filtering refers to the way a person can ignore all of the positive and good things in life to focus solely on the negative. It’s the trap of dwelling on a single negative aspect of a situation, even when surrounded by an abundance of good things.
2. Polarized thinking / Black-and-white thinking
This cognitive distortion is all-or-nothing thinking, with no room for complexity or nuance—everything’s either black or white, never shades of gray.
If you don’t perform perfectly in some area, then you may see yourself as a total failure instead of simply recognizing that you may be unskilled in one area.
3. Overgeneralization
Overgeneralization is taking a single incident or point in time and using it as the sole piece of evidence for a broad conclusion.
For example, someone who overgeneralizes could bomb an important job interview and instead of brushing it off as one bad experience and trying again, they conclude that they are terrible at interviewing and will never get a job offer.
4. Jumping to conclusions
Similar to overgeneralization, this distortion involves faulty reasoning in how one makes conclusions. Unlike overgeneralizing one incident, jumping to conclusions refers to the tendency to be sure of something without any evidence at all.
For example, we might be convinced that someone dislikes us without having any real evidence, or we might believe that our fears will come true before we have a chance to really find out.
5. Catastrophizing / Magnifying or Minimizing
This distortion involves expecting that the worst will happen or has happened, based on an incident that is nowhere near as catastrophic as it is made out to be. For example, you may make a small mistake at work and be convinced that it will ruin the project you are working on, that your boss will be furious, and that you’ll lose your job.
Alternatively, one might minimize the importance of positive things, such as an accomplishment at work or a desirable personal characteristic.
6. Personalization
This is a distortion where an individual believes that everything they do has an impact on external events or other people, no matter how irrational that may be. A person with this distortion will feel that he or she has an exaggerated role in the bad things that happen around them.
For instance, a person may believe that arriving a few minutes late to a meeting led to it being derailed and that everything would have been fine if they were on time.
7. Control fallacies
This distortion involves feeling like everything that happens to you is either a result of purely external forces or entirely due to your own actions. Sometimes what happens to us is due to forces we can’t control, and sometimes what it’s due to our own actions, but the distortion is assuming that it is always one or the other.
We might assume that difficult coworkers are to blame for our own less-than-stellar work, or alternatively assume that every mistake another person makes is because of something we did.
8. Fallacy of fairness
We are often concerned about fairness, but this concern can be taken to extremes. As we all know, life is not always fair. The person who goes through life looking for fairness in all their experiences will end up resentful and unhappy.
Sometimes things will go our way, and sometimes they will not, regardless of how fair it may seem.
When things don’t go our way, there are many ways we can explain or assign responsibility for the outcome. One method of assigning responsibility is blaming others for what goes wrong.
Sometimes we may blame others for making us feel or act a certain way, but this is a cognitive distortion. Only you are responsible for the way you feel or act.
10. “Shoulds”
“Shoulds” refer to the implicit or explicit rules we have about how we and others should behave. When others break our rules, we are upset. When we break our own rules, we feel guilty. For example, we may have an unofficial rule that customer service representatives should always be accommodating to the customer.
When we interact with a customer service representative that is not immediately accommodating, we might get angry. If we have an implicit rule that we are irresponsible if we spend money on unnecessary things, we may feel exceedingly guilty when we spend even a small amount of money on something we don’t need.
11. Emotional reasoning
This distortion involves thinking that if we feel a certain way, it must be true. For example, if we feel unattractive or uninteresting in the current moment, we think we are unattractive or uninteresting. This cognitive distortion boils down to:
“I feel it, therefore it must be true.”
Clearly, our emotions are not always indicative of the objective truth, but it can be difficult to look past how we feel.
12. Fallacy of change
The fallacy of change lies in expecting other people to change as it suits us. This ties into the feeling that our happiness depends on other people, and their unwillingness or inability to change, even if we demand it, keeps us from being happy.
This is a damaging way to think because no one is responsible for our own happiness except ourselves.
13. Global labeling / mislabeling
This cognitive distortion is an extreme form of generalizing, in which we generalize one or two instances or qualities into a global judgment. For example, if we fail at a specific task, we may conclude that we are a total failure in not only that area but all areas.
Alternatively, when a stranger says something a bit rude, we may conclude that he or she is an unfriendly person in general. Mislabeling is specific to using exaggerated and emotionally loaded language, such as saying a woman has abandoned her children when she leaves her children with a babysitter to enjoy a night out.
14. Always being right
While we all enjoy being right, this distortion makes us think we must be right, that being wrong is unacceptable.
We may believe that being right is more important than the feelings of others, being able to admit when we’ve made a mistake or being fair and objective.
15. Heaven’s Reward Fallacy
This distortion involves expecting that any sacrifice or self-denial will pay off. We may consider this karma, and expect that karma will always immediately reward us for our good deeds. This results in feelings of bitterness when we do not receive our reward (Grohol, 2016).
Many tools and techniques found in cognitive behavioral therapy are intended to address or reverse these cognitive distortions.
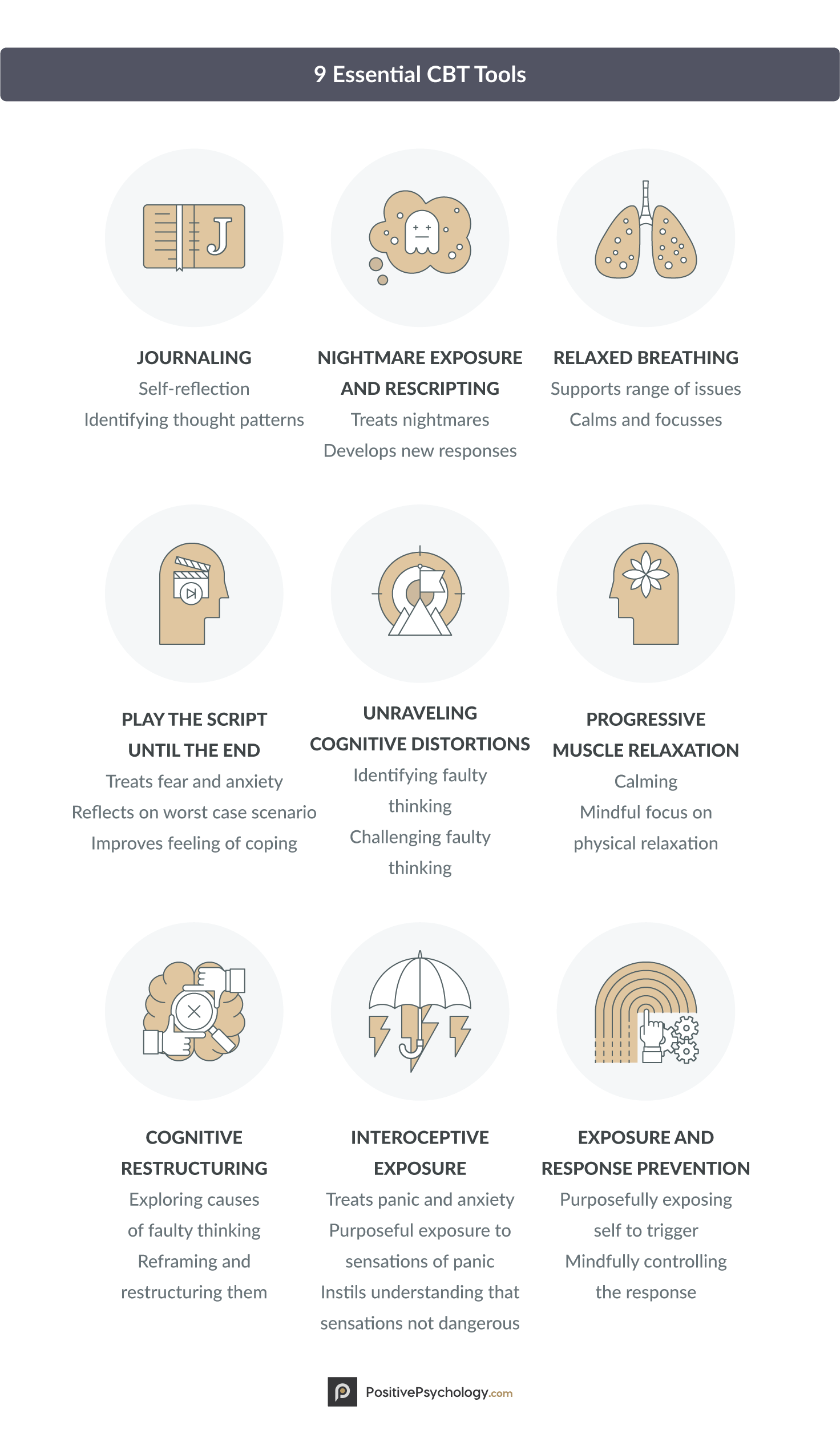
There are many tools and techniques used in cognitive behavioral therapy, many of which can be used in both a therapy context and in everyday life. The nine techniques and tools listed below are some of the most common and effective CBT practices.
1. Journaling
This technique is a way to gather about one’s moods and thoughts. A CBT journal can include the time of the mood or thought, the source of it, the extent or intensity, and how we reacted, among other factors.
This technique can help us to identify our thought patterns and emotional tendencies, describe them, and change, adapt, or cope with them (Utley & Garza, 2011).
Follow the link to find out more about using a thought diary for journaling.
2. Unraveling cognitive distortions
This is a primary goal of CBT and can be practiced with or without the help of a therapist. In order to unravel cognitive distortions, you must first become aware of the distortions from which you commonly suffer (Hamamci, 2002).
Part of this involves identifying and challenging harmful automatic thoughts, which frequently fall into one of the 15 categories listed earlier.
3. Cognitive restructuring
Once you identify the distortions you hold, you can begin to explore how those distortions took root and why you came to believe them. When you discover a belief that is destructive or harmful, you can begin to challenge it (Larsson, Hooper, Osborne, Bennett, & McHugh, 2015).
For example, if you believe that you must have a high-paying job to be a respectable person, but you’re then laid off from your high-paying job, you will begin to feel bad about yourself.
Instead of accepting this faulty belief that leads you to think negative thoughts about yourself, with cognitive restructuring you could take an opportunity to think about what really makes a person “respectable,” a belief you may not have explicitly considered before.
4. Exposure and response prevention
This technique is specifically effective for those who suffer from obsessive-compulsive disorder (OCD; Abramowitz, 1996). You can practice this technique by exposing yourself to whatever it is that normally elicits a compulsive behavior, but doing your best to refrain from the behavior.
You can combine journaling with this technique, or use journaling to understand how this technique makes you feel.
5. Interoceptive exposure
Interoceptive Exposure is intended to treat panic and anxiety. It involves exposure to feared bodily sensations in order to elicit the response (Arntz, 2002). Doing so activates any unhelpful beliefs associated with the sensations, maintains the sensations without distraction or avoidance, and allows new learning about the sensations to take place.
It is intended to help the sufferer see that symptoms of panic are not dangerous, although they may be uncomfortable.
6. Nightmare exposure and rescripting
Nightmare exposure and rescripting are intended specifically for those suffering from nightmares. This technique is similar to interoceptive exposure, in that the nightmare is elicited, which brings up the relevant emotion (Pruiksma, Cranston, Rhudy, Micol, & Davis, 2018).
Once the emotion has arisen, the client and therapist work together to identify the desired emotion and develop a new image to accompany the desired emotion.
7. Play the script until the end
This technique is especially useful for those suffering from fear and anxiety. In this technique, the individual who is vulnerable to crippling fear or anxiety conducts a sort of thought experiment in which they imagine the outcome of the worst-case scenario.
Letting this scenario play out can help the individual to recognize that even if everything he or she fears comes to pass, the outcome will still be manageable (Chankapa, 2018).
8. Progressive muscle relaxation
This is a familiar technique to those who practice mindfulness. Similar to the body scan, progressive muscle relaxation instructs you to relax one muscle group at a time until your whole body is in a state of relaxation (McCallie, Blum, & Hood, 2006).
You can use audio guidance, a YouTube video, or simply your own mind to practice this technique, and it can be especially helpful for calming nerves and soothing a busy and unfocused mind.
9. Relaxed breathing
This is another technique that will be familiar to practitioners of mindfulness . There are many ways to relax and bring regularity to your breath, including guided and unguided imagery, audio recordings, YouTube videos, and scripts. Bringing regularity and calm to your breath will allow you to approach your problems from a place of balance, facilitating more effective and rational decisions (Megan, 2016).
These techniques can help those suffering from a range of mental illnesses and afflictions, including anxiety, depression, OCD, and panic disorder, and they can be practiced with or without the guidance of a therapist. To try some of these techniques without the help of a therapist, see the next section for worksheets and handouts to assist with your practice.
How does cognitive behavioral therapy work – Psych Hub
Cognitive-Behavioral Therapy Worksheets (PDFs) To Print and Use

1. Coping styles worksheet
This PDF Coping Styles Formulation Worksheet instructs you or your client to first list any current perceived problems or difficulties – “The Problem”. You or your client will work backward to list risk factors above (i.e., why you are more likely to experience these problems than someone else) and triggers or events (i.e., the stimulus or source of these problems).
Once you have defined the problems and understand why you are struggling with them, you then list coping strategies. These are not solutions to your problems, but ways to deal with the effects of those problems that can have a temporary impact. Next, you list the effectiveness of the coping strategies, such as how they make you feel in the short- and long-term, and the advantages and disadvantages of each strategy.
Finally, you move on to listing alternative actions. If your coping strategies are not totally effective against the problems and difficulties that are happening, you are instructed to list other strategies that may work better.
This worksheet gets you (or your client) thinking about what you are doing now and whether it is the best way forward.
2. ABC functional analysis
One popular technique in CBT is ABC functional analysis . Functional analysis helps you (or the client) learn about yourself, specifically, what leads to specific behaviors and what consequences result from those behaviors.
In the middle of the worksheet is a box labeled “Behaviors.” In this box, you write down any potentially problematic behaviors you want to analyze.
On the left side of the worksheet is a box labeled “Antecedents,” in which you or the client write down the factors that preceded a particular behavior. These are factors that led up to the behavior under consideration, either directly or indirectly.
On the right side is the final box, labeled “Consequences.” This is where you write down what happened as a result of the behavior under consideration. “Consequences” may sound inherently negative, but that’s not necessarily the case; some positive consequences can arise from many types of behaviors, even if the same behavior also leads to negative consequences.
This ABC Functional Analysis Worksheet can help you or your client to find out whether particular behaviors are adaptive and helpful in striving toward your goals, or destructive and self-defeating.
3. Case formulation worksheet
In CBT, there are 4 “P’s” in Case Formulation:
- Predisposing factors;
- Precipitating factors;
- Perpetuating factors; and
- Protective factors
They help us understand what might be leading a perceived problem to arise, and what might prevent them from being tackled effectively.
In this worksheet, a therapist will work with their client through 4 steps.
First, they identify predisposing factors, which are those external or internal and can add to the likelihood of someone developing a perceived problem (“The Problem”). Examples might include genetics, life events, or their temperament.
Together, they collaborate to identify precipitating factors, which provide insight into precise events or triggers that lead to “The Problem” presenting itself. Then they consider perpetuating factors, to discover what reinforcers may be maintaining the current problem.
Last, they identify protective factors, to understand the client’s strengths, social supports, and adaptive behavioral patterns.
Download 3 Free Positive CBT Exercises (PDF)
These detailed, science-based exercises will equip you or your clients with tools to find new pathways to reduce suffering and more effectively cope with life stressors.
Download 3 Free Positive CBT Tools Pack (PDF)
By filling out your name and email address below.
4. Extended case formulation worksheet
This worksheet builds on the last. It helps you or your client address the “Four P Factors” described just above—predisposing, precipitating, perpetuating, and protective factors. This formulation process can help you or your client connect the dots between core beliefs, thought patterns, and present behavior.
This worksheet presents six boxes on the left of the page (Part A), which should be completed before moving on to the right-hand side of the worksheet (Part B).
- The first box is labeled “The Problem,” and corresponds with the perceived difficulty that your client is experiencing. In this box, you are instructed to write down the events or stimuli that are linked to a certain behavior.
- The next box is labeled “Early Experiences” and corresponds to the predisposing factor. This is where you list the experiences that you had early in life that may have contributed to the behavior.
- The third box is “Core Beliefs,” which is also related to the predisposing factor. This is where you write down some relevant core beliefs you have regarding this behavior. These are beliefs that may not be explicit, but that you believe deep down, such as “I’m bad” or “I’m not good enough.”
- The fourth box is “Conditional assumptions/rules/attitudes,” which is where you list the rules that you adhere to, whether consciously or subconsciously. These implicit or explicit rules can perpetuate the behavior, even if it is not helpful or adaptive. Rules are if-then statements that provide a judgment based on a set of circumstances. For instance, you may have the rule “If I do not do something perfectly, I’m a complete failure.”
- The fifth box is labeled “Maladaptive Coping Strategies” This is where you write down how well these rules are working for you (or not). Are they helping you to be the best you can be? Are they helping you to effectively strive towards your goals?
- Finally, the last box us titled “Positives.” This is where you list the factors that can help you deal with the problematic behavior or thought, and perhaps help you break the perpetuating cycle. These can be things that help you cope once the thought or behavior arises or things that can disrupt the pattern once it is in motion.
On the right, there is a flow chart that you can fill out based on how these behaviors and feelings are perpetuated. You are instructed to think of a situation that produces a negative automatic thought and record the emotion and behavior that this thought provokes, as well as the bodily sensations that can result. Filling out this flow chart can help you see what drives your behavior or thought and what results from it.
Download our PDF Extended Case Formulation Worksheet .
5. Dysfunctional thought record
This worksheet is especially helpful for people who struggle with negative thoughts and need to figure out when and why those thoughts are most likely to pop up. Learning more about what provokes certain automatic thoughts makes them easier to address and reverse.
The worksheet is divided into seven columns:
- On the far left, there is space to write down the date and time a dysfunctional thought arose.
- The second column is where the situation is listed. The user is instructed to describe the event that led up to the dysfunctional thought in detail.
- The third column is for the automatic thought. This is where the dysfunctional automatic thought is recorded, along with a rating of belief in the thought on a scale from 0% to 100%.
- The next column is where the emotion or emotions elicited by this thought are listed, also with a rating of intensity on a scale from 0% to 100%.
- Use this fifth column to note the dysfunctional thought that will be addressed. Example maladaptive thoughts include distortions such as over-inflating the negative while dismissing the positive of a situation, or overgeneralizing.
- The second-to-last column is for the user to write down alternative thoughts that are more positive and functional to replace the negative one.
- Finally, the last column is for the user to write down the outcome of this exercise. Were you able to confront the dysfunctional thought? Did you write down a convincing alternative thought? Did your belief in the thought and/or the intensity of your emotion(s) decrease?
Download this Dysfunctional Thought Record as a PDF.
6. Fact-checking
One of my favorite CBT tools is this Fact Checking Thoughts Worksheet because it can be extremely helpful in recognizing that your thoughts are not necessarily true.
At the top of this worksheet is an important lesson:
Thoughts are not facts.
Of course, it can be hard to accept this, especially when we are in the throes of a dysfunctional thought or intense emotion. Filling out this worksheet can help you come to this realization.
The worksheet includes 16 statements that the user must decide are either fact or opinion. These statements include:
- I’m a bad person.
- I failed the test.
- I’m selfish.
- I didn’t lend my friend money when they asked.
This is not a trick—there is a right answer for each of these statements. (In case you’re wondering, the correct answers for the statements above are as follows: opinion, fact, opinion, fact.)
This simple exercise can help the user to see that while we have lots of emotionally charged thoughts, they are not all objective truths. Recognizing the difference between fact and opinion can assist us in challenging the dysfunctional or harmful opinions we have about ourselves and others.
7. Cognitive restructuring
This worksheet employs the use of Socratic questioning, a technique that can help the user to challenge irrational or illogical thoughts.
The first page of the worksheet has a thought bubble for “What I’m Thinking”. You or your client can use this space to write down a specific thought, usually, one you suspect is destructive or irrational.
Next, you write down the facts supporting and contradicting this thought as a reality. What facts about this thought being accurate? What facts call it into question? Once you have identified the evidence, you can use the last box to make a judgment on this thought, specifically whether it is based on evidence or simply your opinion.
The next page is a mind map of Socratic Questions which can be used to further challenge the thought. You may wish to re-write “What I’m Thinking” in the center so it is easier to challenge the thought against these questions.
- One question asks whether this thought is truly a black-and-white situation, or whether reality leaves room for shades of gray. This is where you think about (and write down) whether you are using all-or-nothing thinking, for example, or making things unreasonably simple when they are complex.
- Another asks whether you could be misinterpreting the evidence or making any unverified assumptions. As with all the other bubbles, writing it down will make this exercise more effective.
- A third bubble instructs you to think about whether other people might have different interpretations of the same situation, and what those interpretations might be.
- Next, ask yourself whether you are looking at all the relevant evidence or just the evidence that backs up the belief you already hold. Try to be as objective as possible.
- It also helps to ask yourself whether your thought may an over-inflation of a truth. Some negative thoughts are based in truth but extend past their logical boundaries.
- You’re also instructed to consider whether you are entertaining this negative thought out of habit or because the facts truly support it.
- Then, think about how this thought came to you. Was it passed on from someone else? If so, is that person a reliable source of truth?
- Finally, you complete the worksheet by identifying how likely the scenario your thought brings up actually is, and whether it is the worst-case scenario.
These Socratic questions encourage a deep dive into the thoughts that plague you and offer opportunities to analyze and evaluate those thoughts. If you are having thoughts that do not come from a place of truth, this Cognitive Restructuring Worksheet can be an excellent tool for identifying and defusing them.
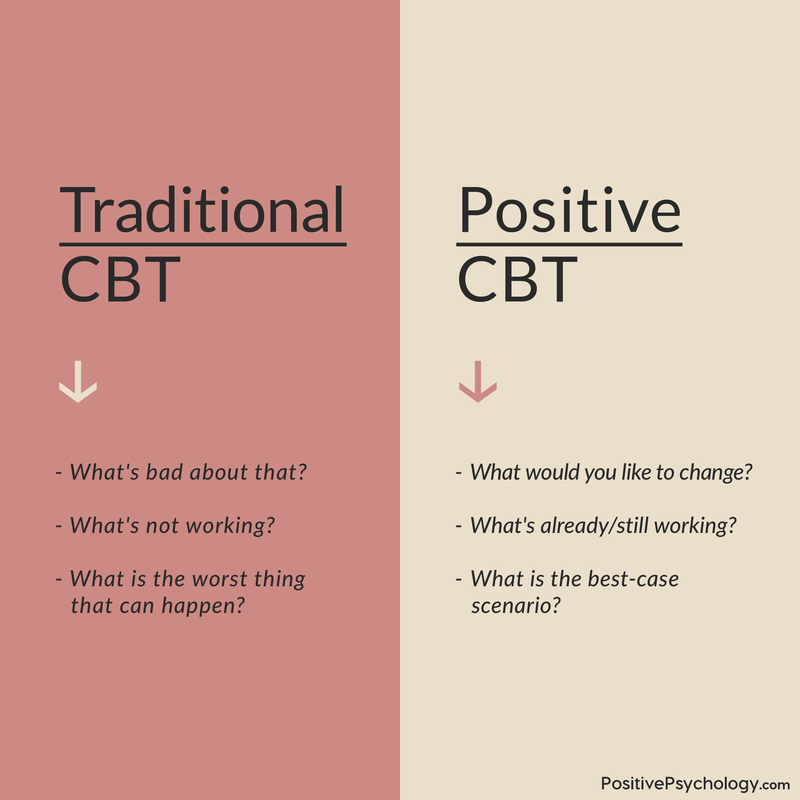
How is positive cognitive-behavioral therapy (CBT) different from traditional CBT?
Although both forms of CBT have the same goal of bringing about positive changes in a client’s life, the pathways used in traditional and positive CBT to actualize this goal differ considerably. Traditional CBT, as initially formulated by Beck (1967), focuses primarily on the following:
- Analyzing problems
- Lessening what causes suffering
- Working on clients’ weaknesses
- Getting away from problems
Instead, positive CBT, as formulated by Bannink (2012), focuses mainly on the following:
- Finding solutions
- Enhancing what causes flourishing
- Working with client’s strengths
- Getting closer to the preferred future
In other words, Positive CBT shifts the focus on what’s right with the person (rather than what’s wrong with them) and on what’s working (rather than what’s not working) to foster a more optimistic process that empowers clients to flourish and thrive.
In an initial study comparing the effects of traditional and Positive CBT in the treatment of depression, positive CBT resulted in a more substantial reduction of depression symptoms, a more significant increase in happiness, and it was associated with less dropout (Geschwind et al., 2019).
Haven’t had enough CBT tools and techniques yet? Read on for additional useful and effective exercises.
1. Behavioral experiments
These are related to thought experiments, in that you engage in a “what if” consideration. Behavioral experiments differ from thought experiments in that you actually test out these “what ifs” outside of your thoughts (Boyes, 2012).
In order to test a thought, you can experiment with the outcomes that different thoughts produce. For example, you can test the thoughts:
“If I criticize myself, I will be motivated to work harder” versus “If I am kind to myself, I will be motivated to work harder.”
First, you would try criticizing yourself when you need the motivation to work harder and record the results. Then you would try being kind to yourself and recording the results. Next, you would compare the results to see which thought was closer to the truth.
These Behavioral Experiments to Test Beliefs can help you learn how to achieve your therapeutic goals and how to be your best self.
2. Thought records
Thought records are useful in testing the validity of your thoughts (Boyes, 2012). They involve gathering and evaluating evidence for and against a particular thought, allowing for an evidence-based conclusion on whether the thought is valid or not.
For example, you may have the belief “My friend thinks I’m a bad friend.” You would think of all the evidence for this belief, such as “She didn’t answer the phone the last time I called,” or “She canceled our plans at the last minute,” and evidence against this belief, like “She called me back after not answering the phone,” and “She invited me to her barbecue next week. If she thought I was a bad friend, she probably wouldn’t have invited me.”
Once you have evidence for and against, the goal is to come up with more balanced thoughts, such as, “My friend is busy and has other friends, so she can’t always answer the phone when I call. If I am understanding of this, I will truly be a good friend.”
Thought records apply the use of logic to ward off unreasonable negative thoughts and replace them with more balanced, rational thoughts (Boyes, 2012).
Here’s a helpful Thought Record Worksheet to download.
3. Pleasant activity scheduling
This technique can be especially helpful for dealing with depression (Boyes, 2012). It involves scheduling activities in the near future that you can look forward to.
For example, you may write down one activity per day that you will engage in over the next week. This can be as simple as watching a movie you are excited to see or calling a friend to chat. It can be anything that is pleasant for you, as long as it is not unhealthy (i.e., eating a whole cake in one sitting or smoking).
You can also try scheduling an activity for each day that provides you with a sense of mastery or accomplishment (Boyes, 2012). It’s great to do something pleasant, but doing something small that can make you feel accomplished may have more long-lasting and far-reaching effects.
This simple technique can introduce more positivity into your life, and our Pleasant Activity Scheduling Worksheet is designed to help.
4. Imagery-based exposure
This exercise involves thinking about a recent memory that produced strong negative emotions and analyzing the situation.
For example, if you recently had a fight with your significant other and they said something hurtful, you can bring that situation to mind and try to remember it in detail. Next, you would try to label the emotions and thoughts you experienced during the situation and identify the urges you felt (e.g., to run away, to yell at your significant other, or to cry).
Visualizing this negative situation, especially for a prolonged period of time, can help you to take away its ability to trigger you and reduce avoidance coping (Boyes, 2012). When you expose yourself to all of the feelings and urges you felt in the situation and survive experiencing the memory, it takes some of its power away.
This Imagery Based Exposure Worksheet is a useful resource for this exercise.
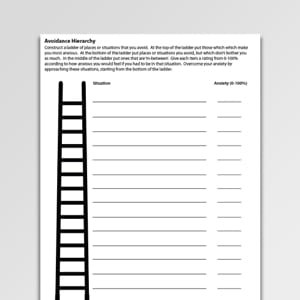
5. Graded exposure worksheet
This technique may sound complicated, but it’s relatively simple.
Making a situation exposure hierarchy involves means listing situations that you would normally avoid (Boyes, 2012). For example, someone with severe social anxiety may typically avoid making a phone call or asking someone on a date.
Next, you rate each item on how distressed you think you would be, on a scale from 0 to 10, if you engaged in it. For the person suffering from severe social anxiety, asking someone on a date may be rated a 10 on the scale, while making a phone call might be rated closer to a 3 or 4.
Once you have rated the situations, you rank them according to their distress rating. This will help you recognize the biggest difficulties you face, which can help you decide which items to address and in what order. It’s often advised to start with the least distressing items and work your way up to the most distressing items.
Download our Graded Exposure Worksheet here.

Some of these books are for the therapist only, and some are to be navigated as a team or with guidance from the therapist.
There are many manuals out there for helping therapists apply cognitive behavioral therapy in their work, but these are some of the most popular:
- A Therapist’s Guide to Brief Cognitive Behavioral Therapy by Jeffrey A. Cully and Andra L. Teten (PDF here );
- Individual Therapy Manual for Cognitive-Behavioral Treatment of Depression by Ricardo F. Munoz and Jeanne Miranda (PDF here );
- Provider’s Guidebook: “Activities and Your Mood” by Community Partners in Care (PDF here );
- Treatment Manual for Cognitive Behavioral Therapy for Depression by Jeannette Rosselló, Guillermo Bernal, and the Institute for Psychological Research (PDF here ).
Here are some of the most popular workbooks and manuals for clients to use alone or with a therapist:
- The CBT Toolbox: A Workbook for Clients and Clinicians by Jeff Riggenbach ( Amazon );
- Client’s Guidebook: “Activities and Your Mood” by Community Partners in Care (PDF here );
- The Cognitive Behavioral Workbook for Anxiety: A Step-by-Step Program by William J. Knaus and Jon Carlson ( Amazon );
- The Cognitive Behavioral Workbook for Depression: A Step-by-Step Program by William J. Knaus and Albert Ellis ( Amazon );
- Cognitive-Behavioral Therapy Skills Workbook by Barry Gregory ( Amazon );
- A Course in CBT Techniques: A Free Online CBT Workbook by Albert Bonfil and Suraji Wagage (online here ).
There are many other manuals and workbooks available that can help get you started with CBT, but the tools above are a good start. Peruse our article: 30 Best CBT Books to Master Cognitive Behavioral Therapy for an excellent list of these books.
1. Mindfulness meditation
Mindfulness can have a wide range of positive impacts, including helping with depression, anxiety, addiction, and many other mental illnesses or difficulties.
The practice can help those suffering from harmful automatic thoughts to disengage from rumination and obsession by helping them stay firmly grounded in the present (Jain et al., 2007).
Mindfulness meditations, in particular, can function as helpful tools for your clients in between therapy sessions, such as to help ground them in the present moment during times of stress.
If you are a therapist who uses mindfulness-based approaches, consider finding or pre-recording some short mindfulness meditation exercises for your clients.
You might then share these with your clients as part of a toolkit they can draw on at their convenience, such as using the blended care platform Quenza (pictured here), which allows clients to access meditations or other psychoeducational activities on-the-go via their portable devices.
2. Successive approximation
This is a fancy name for a simple idea that you have likely already heard of: breaking up large tasks into small steps.
It can be overwhelming to be faced with a huge goal, like opening a business or remodeling a house. This is true in mental health treatment as well, since the goal to overcome depression or anxiety and achieve mental wellness can seem like a monumental task.
By breaking the large goal into small, easy-to-accomplish steps, we can map out the path to success and make the journey seem a little less overwhelming (e.g., Emmelkamp & Ultee, 1974).
3. Writing self-statements to counteract negative thoughts
This technique can be difficult for someone who’s new to CBT treatment or suffering from severe symptoms, but it can also be extremely effective (Anderson, 2014).
When you (or your client) are being plagued by negative thoughts, it can be hard to confront them, especially if your belief in these thoughts is strong. To counteract these negative thoughts, it can be helpful to write down a positive, opposite thought.
For example, if the thought “I am worthless” keeps popping into your head, try writing down a statement like “I am a person with worth,” or “I am a person with potential.” In the beginning, it can be difficult to accept these replacement thoughts, but the more you bring out these positive thoughts to counteract the negative ones, the stronger the association will be.
4. Visualize the best parts of your day
When you are feeling depressed or negative, it is difficult to recognize that there are positive aspects of life. This simple technique of bringing to mind the good parts of your day can be a small step in the direction of recognizing the positive (Anderson, 2014).
All you need to do is write down the things in your life that you are thankful for or the most positive events that happen in a given day. The simple act of writing down these good things can forge new associations in your brain that make it easier to see the positive, even when you are experiencing negative emotions.
5. Reframe your negative thoughts
It can be easy to succumb to negative thoughts as a default setting. If you find yourself immediately thinking a negative thought when you see something new, such as entering an unfamiliar room and thinking “I hate the color of that wall,” give reframing a try (Anderson, 2014).
Reframing involves countering the negative thought(s) by noticing things you feel positive about as quickly as possible. For instance, in the example where you immediately think of how much you hate the color of that wall, you would push yourself to notice five things in the room that you feel positively about (e.g., the carpet looks comfortable, the lampshade is pretty, the windows let in a lot of sunshine).
You can set your phone to remind you throughout the day to stop what you are doing and think of the positive things around you. This can help you to push your thoughts back into the realm of the positive instead of the negative.
17 Science-Based Ways To Apply Positive CBT
These 17 Positive CBT & Cognitive Therapy Exercises [PDF] include our top-rated, ready-made templates for helping others develop more helpful thoughts and behaviors in response to challenges, while broadening the scope of traditional CBT.
Created by Experts. 100% Science-based.
In this post, we offered many techniques, tools, and resources that can be effective in the battle against depression, anxiety, OCD, and a host of other problems or difficulties.
However, as is the case with many treatments, they depend on you (or your client) putting in a lot of effort. We encourage you to give these techniques a real try and allow yourself the luxury of thinking that they could actually work.
When we approach a potential solution with the assumption that it will not work, that assumption often becomes a self-fulfilling prophecy. When we approach a potential solution with an open mind and the belief that it just might work, it has a much better chance of succeeding.
So if you are struggling with negative automatic thoughts , please consider these tips and techniques and give them a shot. Likewise, if your client is struggling, encourage them to make the effort, because the payoff can be better than they can imagine.
If you are struggling with severe symptoms of depression or suicidal thoughts, please call the following number in your respective country:
- USA: National Suicide Prevention Hotline at 988;
- UK: Samaritans hotline at 116 123;
- The Netherlands: Netherlands Suicide Hotline at 09000767;
- France: Suicide écoute at 01 45 39 40 00;
- Germany: Telefonseelsorge at 0800 111 0 111 or 0800 111 0 222
For a list of other suicide prevention websites, phone numbers, and resources, see this website .
Please know that there are people out there who care and that there are treatments that can help.
Please let us know about your experiences with CBT in the comments section. If you’ve tried it, how did it work for you? Are there any other helpful exercises or techniques that we did not touch on in this piece? We’d love to know your thoughts.
We hope you enjoyed this article. For more information, don’t forget to download our three Positive CBT Exercises for free .
- Abramowitz, J. S. (1996). Variants of exposure and response prevention in the treatment of obsessive-compulsive disorder: A meta-analysis. Behavior Therapy , 27 (4), 583-600.
- Anderson, J. (2014, June 12). 5 Get-positive techniques from cognitive behavioral therapy. Retrieved from http://www.everydayhealth.com/hs/major-depression-living-well/cognitive-behavioral-therapy-techniques/
- Arntz, A. (2002). Cognitive therapy versus interoceptive exposure as treatment of panic disorder without agoraphobia. Behaviour Research and Therapy , 40 (3), 325-341.
- Bannink, F. (2012). Practicing positive CBT: From reducing distress to building success . John Wiley & Sons.
- Beck, A. T. (1967). Depression. Hoeber-Harper.
- Boyes, A. (2012, December 6). Cognitive behavioral therapy techniques that work: Mix and match cognitive behavioral therapy techniques to fit your preferences. Retrieved from https://www.psychologytoday.com/blog/in-practice/201212/cognitive-behavioral-therapy-techniques-work
- Chankapa, N. P. (2018). Effectiveness of cognitive behavioral therapy on depression and self-efficacy among out-patient female depressants in Sikkim (Masters dissertation). Retrieved from http://14.139.206.50:8080/jspui/bitstream/1/6059/1/nancy%20chankpa.pdf
- Davis, R. (2019, March 6). The complete list of cognitive behavioral therapy (CBT) techniques. Retrieved from https://www.infocounselling.com/list-of-cbt-techniques/
- Emmelkamp, P. M., & Ultee, K. A. (1974). A comparison of “successive approximation” and “self-observation” in the treatment of agoraphobia. Behavior Therapy, 5 (5), 606–613.
- Geschwind, N., Arntz, A., Bannink, F., & Peeters, F. (2019). Positive cognitive behavior therapy in the treatment of depression: A randomized order within-subject comparison with traditional cognitive behavior therapy. Behaviour research and therapy, 116 , 119-130.
- Grohol, J. (2016). 15 Common cognitive distortions. Retrieved from https://psychcentral.com/lib/15-common-cognitive-distortions/
- Hamamci, Z. (2002). The effect of integrating psychodrama and cognitive behavioral therapy on reducing cognitive distortions in interpersonal relationships. Journal of Group Psychotherapy, Psychodrama & Sociometry , 55 (1), 3–14.
- Jain, S., Shapiro, S. L., Swanick, S., Roesch, S. C., Mills, P. J., Bell, I., & Schwartz, G. E. (2007). A randomized controlled trial of mindfulness meditation versus relaxation training: effects on distress, positive states of mind, rumination, and distraction. Annals of Behavioral Medicine , 33 (1), 11-21.
- Larsson, A., Hooper, N., Osborne, L. A., Bennett, P., & McHugh, L. (2016). Using brief cognitive restructuring and cognitive defusion techniques to cope with negative thoughts. Behavior Modification , 40 (3), 452-482.
- Martin, B. (2016). In-depth: Cognitive behavioral therapy. Retrieved from https://psychcentral.com/lib/in-depth-cognitive-behavioral-therapy/
- McCallie, M. S., Blum, C. M., & Hood, C. J. (2006). Progressive muscle relaxation. Journal of Human Behavior in the Social Environment , 13 (3), 51-66.
- Pathak, N. (Ed.). (2018). Does cognitive behavioral therapy treat depression? Retrieved from https://www.webmd.com/g00/depression/guide/cognitive-behavioral-therapy-for-depression/
- Pruiksma, K. E., Cranston, C. C., Rhudy, J. L., Micol, R. L., & Davis, J. L. (2018). Randomized controlled trial to dismantle exposure, relaxation, and rescripting therapy (ERRT) for trauma-related nightmares. Psychological trauma: theory, research, practice, and policy , 10 (1), 67-75.
- Psychology Tools. (n.d.). Retrieved from https://www.psychologytools.com/
- Therapist Aid. (n.d.). Retrieved from https://www.therapistaid.com/
- Utley, A., & Garza, Y. (2011). The therapeutic use of journaling with adolescents. Journal of Creativity in Mental Health , 6 (1), 29-41.
Share this article:
Article feedback
What our readers think.
Loved the article. This was very useful, and very much appreciate all the free resources you included. Mahalo!
I am a nurse and a holistic life coach and these resources were very helpful to revise and improve my practice!
This is ridiculous. More ad than content. Misleading title.It is not a free website that you flood the viewers with so many ads. And if you are making so much money through ads then make the entire content free , since it is for the betterment of patients with mental health
Dear Prasun, We agree, and we are currently looking for another solution as the site experience is suffering too much from this try-out.
Kind regards, Julia | Community Manager
Thank you for the work put into this amazing article! It encompasses every bit of CBT that is so useful for clients increasing their understanding of how “this” works in a very well-written tone. Well done!
Thank you for the useful material that is free of charge. It will come in handy especially the providers guidebook “activities and your mood” for my client who has been diagnosed with depression.
It is very informative, keep up the good work
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

Sunk Cost Fallacy: Why We Can’t Let Go
If you’ve continued with a decision or an investment of time, money, or resources long after you should have stopped, you’ve succumbed to the ‘sunk [...]

Confirmation Bias: Seeing What We Want to Believe
Believe it or not, we can’t always trust what we see or hear. It seems our memory is influenced by our expectations (Eysenk & Keane, [...]

Behavior Therapy for Kids: 9 Fun Games and Techniques
In its many forms, behavior therapy is a powerful tool for treating a wide range of psychological disorders in children, aiming to increase their skills [...]
Read other articles by their category
- Body & Brain (48)
- Coaching & Application (57)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (45)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (28)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (17)
- Positive Parenting (2)
- Positive Psychology (33)
- Positive Workplace (37)
- Productivity (16)
- Relationships (47)
- Resilience & Coping (35)
- Self Awareness (21)
- Self Esteem (37)
- Strengths & Virtues (30)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)
3 Positive CBT Exercises (PDF)
Cognitive Behavioral Therapy (CBT)
Resource type
Therapy tool.

"Should" Statements
Information handouts
Activity Diary (Hourly Time Intervals)
Activity Diary (No Time Intervals)

Activity Menu
Activity Planning
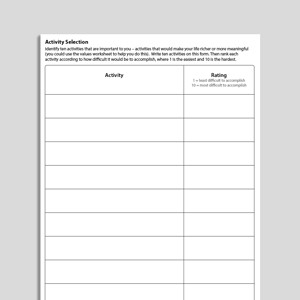
Activity Selection

All-Or-Nothing Thinking
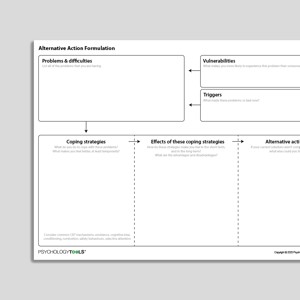
Alternative Action Formulation

An Introduction To CBT (Psychology Tools For Living Well)
Books & Chapters

Anger - Self-Monitoring Record

Anger Decision Sheet
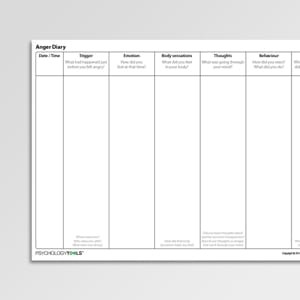
Anger Diary (Archived)

Anger Self-Monitoring Record (Archived)
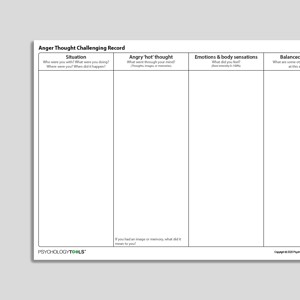
Anger Thought Challenging Record
Anxiety - Self-Monitoring Record
Anxiety Self-Monitoring Record (Archived)

Arbitrary Inference

Assertive Communication

Assertive Responses

Attention - Self-Monitoring Record
Audio Collection: Psychology Tools For Mindfulness
Audio Collection: Psychology Tools For Overcoming PTSD

Autonomic Nervous System
Avoidance Hierarchy (Archived)
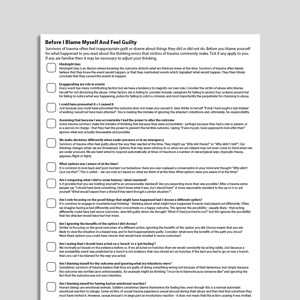
Before I Blame Myself And Feel Guilty

Behavioral Activation Activity Diary

Behavioral Activation Activity Planning Diary
Behavioral Experiment

Behavioral Experiment (Portrait Format)

Belief Driven Formulation

Belief-O-Meter (CYP)

Boundaries - Self-Monitoring Record

Catastrophizing


Catching Your Thoughts (CYP)
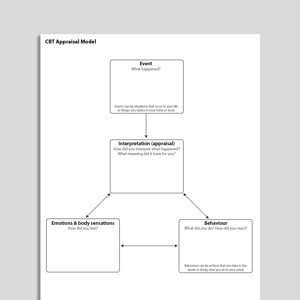
CBT Appraisal Model
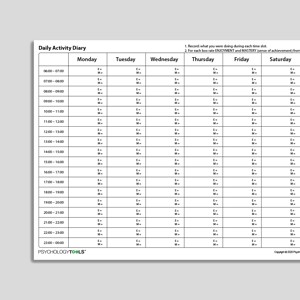
CBT Daily Activity Diary With Enjoyment And Mastery Ratings

CBT Thought Record Portrait

Challenging Your Negative Thinking (Archived)

Changing Avoidance (Behavioral Activation)

Checking Certainty And Doubt

Classical Conditioning
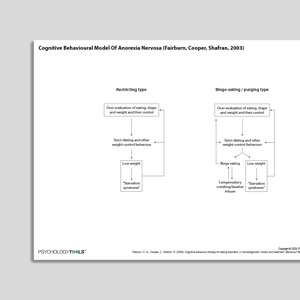
Cognitive Behavioral Model Of Anorexia Nervosa (Fairburn, Cooper, Shafran, 2003)
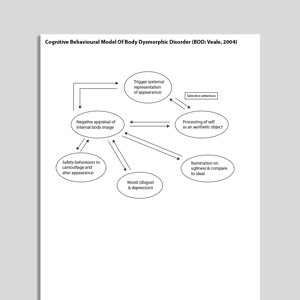
Cognitive Behavioral Model Of Body Dysmorphic Disorder (BDD: Veale, 2004)
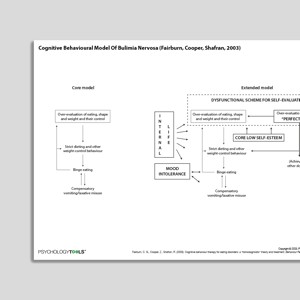
Cognitive Behavioral Model Of Bulimia Nervosa (Fairburn, Cooper, Shafran, 2003)

Cognitive Behavioral Model Of Clinical Perfectionism (Shafran, Cooper, Fairburn, 2002)
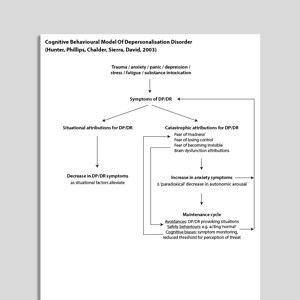
Cognitive Behavioral Model Of Depersonalization (Hunter, Phillips, Chalder, Sierra, David, 2003)
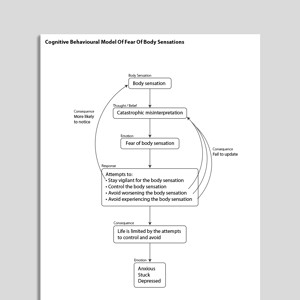
Cognitive Behavioral Model Of Fear Of Body Sensations

Cognitive Behavioral Model Of Generalized Anxiety Disorder (GAD: Dugas, Gagnon, Ladouceur, Freeston, 1998)

Cognitive Behavioral Model Of Health Anxiety (Salkovskis, Warwick, Deale, 2003)
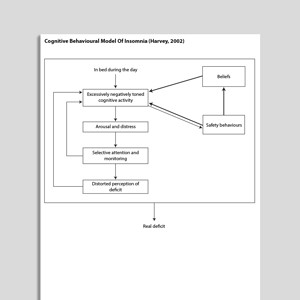
Cognitive Behavioral Model Of Insomnia (Harvey, 2002)

Cognitive Behavioral Model Of Intolerance Of Uncertainty And Generalized Anxiety Disorder Symptoms (Hebert, Dugas, 2019)
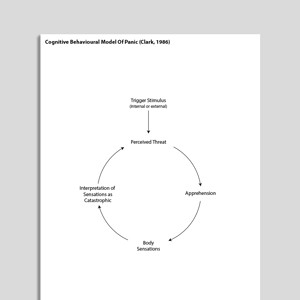
Cognitive Behavioral Model Of Panic (Clark, 1986)

Cognitive Behavioral Model Of Persistent Postural-Perceptual Dizziness (PPPD: Whalley, Cane, 2017)
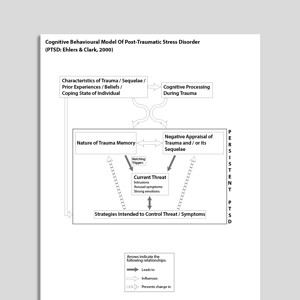
Cognitive Behavioral Model Of Post Traumatic Stress Disorder (PTSD: Ehlers & Clark, 2000)

Cognitive Behavioral Model Of Social Phobia (Clark, Wells, 1995)
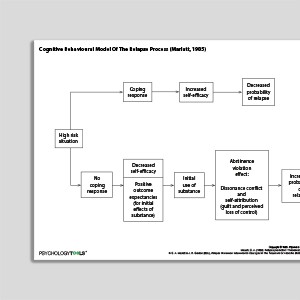
Cognitive Behavioral Model Of The Relapse Process (Marlatt & Gordon, 1985)

Cognitive Behavioral Model Of Tinnitus (McKenna, Handscombe, Hoare, Hall, 2014)

Cognitive Behavioral Treatment Of Childhood OCD: It's Only A False Alarm: Therapist Guide
Treatments That Work™

Cognitive Behavioral Treatment of Childhood OCD: It's Only a False Alarm: Workbook

Cognitive Case Formulation

Cognitive Distortions – Unhelpful Thinking Styles (Common)

Cognitive Distortions – Unhelpful Thinking Styles (Extended)
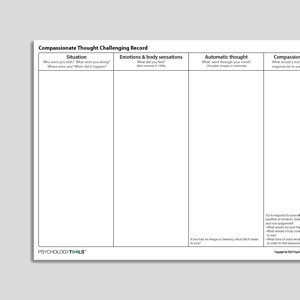
Compassionate Thought Challenging Record

Core Belief Magnet Metaphor

Court Trial Thought Challenging Record (Archived)

Critical Care And PTSD

Critical Illness Intensive Care And Post-Traumatic Stress Disorder (PTSD)

Cross Sectional Formulation

Daily Monitoring Form
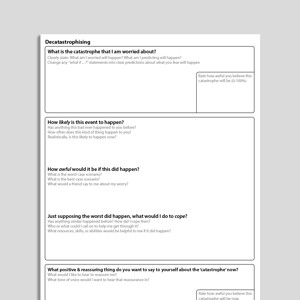
Decatastrophizing
Demanding Standards – Living Well With Your Personal Rules

Depression - Self-Monitoring Record

Discounting In Perfectionism – The Ratchet Effect

Disqualifying Others

Disqualifying The Positive

Dissociation - Self-Monitoring Record

Embracing Uncertainty

Emotional Reasoning
Evaluating Unhelpful Automatic Thoughts

Evaluating Your Demanding Standards

Examining Your Negative Thoughts

Exploring Problems Using A Cross Sectional Model

Exposure And Response (Ritual) Prevention For Obsessive Compulsive Disorder (Second Edition): Therapist Guide

Exposure And Response Prevention

Exposure Practice Form

Exposure Session Record

Exposures For Fear Of Appearing Anxious

Exposures For Fear Of Body Sensations

Exposures For Fear Of Breathlessness

Exposures For Fear Of Death

Exposures For Fear Of Flying

Exposures For Fear Of Heights

Exposures For Fear Of Illness

Exposures For Fear Of Losing Control Of Your Mind

Exposures For Fear Of Uncertainty

Exposures For Fear Of Vomiting

Externalizing

Facing Your Fears (CYP)

Facing Your Fears And Phobias
Links to external resources.
Psychology Tools makes every effort to check external links and review their content. However, we are not responsible for the quality or content of external links and cannot guarantee that these links will work all of the time.
- Scale Download Primary Link Archived Link
- Bern Inventory of Treatment Goals | Grosse, Grawe | 2002 Download Primary Link Archived Link
Cognitive therapy competence / adherence measures
- Manual Download Primary Link Archived Link
- Manual Download Archived Link
- Manual accs-scale.co.uk Download Primary Link
- Feedback form accs-scale.co.uk Download Primary Link
- Website accs-scale.co.uk Download Primary Link
Case Conceptualization / Case Formulation
- Cognitive conceptualisation (excerpt from Basics and Beyond) | J. Beck Download Archived Link
- Dysfunctional assumptions ideas Download Primary Link Archived Link
- Developing a cognitive formulation | Michael Free Download Primary Link Archived Link
- Case formulation in CBT | Caleb Lack Download Primary Link Archived Link
- A case formulation approach to cognitive-behavior therapy | Jacqueline Persons | 2015 Download Primary Link Archived Link
- The case formulation approach to cognitive behavior therapy | Jacqueline Persons | 2014 Download Primary Link Archived Link
Information (Professional)
- Cognitive- behavioural therapy An information guide | Neil Rector | 2010 Download Primary Link Archived Link
- A therapist’s guide to brief cognitive behavioral therapy | Cully, Teten | 2008 Download Primary Link Archived Link
- Problem solving (OCT Practical Guides | Helen Kennerley | 2016 Download Primary Link Archived Link
- Working with Schemas, Core Beliefs, and Assumptions | Frank Wills | 2008 Download Primary Link Archived Link
Presentations
- The role of a case conceptualization model and core tasks of intervention | Donald Miechenbaum | 2014 Download Primary Link Archived Link
- Transdiagnostic treatments for anxiety disorders | Martin Anthony | 2013 Download Primary Link Archived Link
- The unified protocol for the transdiagnostic treatment of emotional disorders | Ellen Frank, Fiona Ritchey | 2015 Download Primary Link Archived Link
- Making CBT Work (Working with your CBT therapist / Making your CBT therapist work with you) | Paul Salkovskis Download Archived Link
Treatment Guide
- A manual of cognitive behavior therapy for people with learning disabilities and common mental disorders | Hassiotis, Serfaty, Azam, Martin, Strydom, King | 2012 Download Primary Link Archived Link
- CBT case formulation | Jacqueline Persons Download Primary Link
Recommended Reading
- Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognitive therapy and research, 36(5), 427-440 Download Primary Link
- Schema change processes in cognitive therapy | Padesky | 1994 Download Primary Link Archived Link
- Wright, B., Williams, C., & Garland, A. (2002). Using the Five Areas cognitive–behavioural therapy model with psychiatric patients. Advances in Psychiatric Treatment, 8(4), 307-315. Download Primary Link
- Williams, C., & Garland, A. (2002). Identifying and challenging unhelpful thinking. Advances in Psychiatric Treatment, 8(5), 377-386. Download Primary Link
- Garland, A., Fox, R., & Williams, C. (2002). Overcoming reduced activity and avoidance: a Five Areas approach. Advances in Psychiatric Treatment, 8(6), 453-462. Download Primary Link
- Williams, C., & Garland, A. (2002). A cognitive–behavioural therapy assessment model for use in everyday clinical practice. Advances in Psychiatric Treatment, 8(3), 172-179. Download Primary Link
- A provider’s guide to brief cognitive behavioral therapy | Cully, Dawson, Hamer, Tharp | 2021 Download Primary Link Archived Link
- Padesky, C. A., Mooney, K. A. (1990). Clinical tip: presenting the cognitive model to clients. International Cognitive Therapy Newsletter, 6, 13-14 Download Primary Link Archived Link
- Arch, J. J., & Craske, M. G. (2009). First-line treatment: a critical appraisal of cognitive behavioral therapy developments and alternatives. Psychiatric Clinics of North America, 32(3), 525-547 Download Archived Link
What Is Cognitive Behavioral Therapy?
Assumptions of cbt.
- people actively process information;
- our appraisals (the way that we think and interpret events) determine how we feel;
- dysfunctional thinking and biases in information processing (cognition/thinking) are responsible for the problems that people experience;
- different problems are associated with different cognitive themes (cognitive specificity theory): depression is associated with loss and defeat; anxiety is associated with danger and threat; obsessive-compulsive disorder is associated with inflated responsibility; substance abuse is associated with permissive beliefs; eating disorders are associated with self-criticism; social anxiety is associated with fear of evaluation; and PTSD is associated with appraisals of immediate threat;
- the thoughts that we have can be ‘distorted’ or biased . Common biases include over-generalization, arbitrary inference, selective abstraction, and catastrophizing;
- changing how we think and act will impact how we feel: cognition, emotion, and behavior interact in a reciprocal manner;
- psychopathology is a result of an interaction between stress and vulnerability;
- cognition happens at multiple levels (Alford & Beck, 1997) and all can influence the way that we feel and behave: preconscious, unintentional, automatic (e.g., negative automatic thoughts); the conscious level (e.g., if a patient is asked to explain the meaning of an automatic thought); and the metacognitive level (beliefs about beliefs);
- experiences, memories, thoughts, attitudes, and beliefs are encapsulated as ‘schemas’ and which may become activated and influence our perceptions and behaviors.
Principles of CBT
Judith Beck (1995) identified 11 principles of the practice of cognitive behavioral therapy, and these were expanded by Wills (2009):
- cognitive behavioral therapists use formulation to focus their therapeutic work
- cognitive behavioral therapists use formulation to tackle interpersonal and alliance issues
- cognitive behavioral therapy requires a sound therapeutic relationship
- cognitive behavioral therapists stress the importance of collaboration in the therapeutic relationship
- cognitive behavioral therapy is brief and time-limited
- cognitive behavioral therapy is structured and directional
- cognitive behavioral therapy is problem- and goal-oriented
- cognitive behavioral therapy initially emphasizes a focus on the present
- cognitive behavioral therapy uses an educational model
- homework and self-practice is a central feature of cognitive behavioral therapy (incorporating the use of CBT worksheets)
- cognitive behavioral therapists teach clients to evaluate and modify their thoughts
- cognitive behavioral therapy uses various methods to change cognitive content including thought records, behavioral experiments, surveys
- cognitive behavior therapy uses a variety of methods to promote behavioral change including exposure, behavioral experiments, role-play.
Procedures and Techniques of CBT
- Data gathering and symptom monitoring are used to understand problems and to measure change. CBT is an evidence-based approach that relies upon accurate data gathering regarding symptoms and experiences.
- Behavioral activation is a set of techniques for encouraging engagement in meaningful activity and is an effective treatment for depression.
- Case formulation is a method for understanding the origin and maintenance of a problem in cognitive and behavioral terms. CBT therapists may use a mixture of cross-sectional formulation to understand difficulties in the here-and-now, longitudinal formulation to understand the origins and precipitants of a problem, and cognitive behavioral models to understand the mechanisms underlying a problem.
- Cognitive restructuring describes techniques for changing what we think. It often involves the use of thought records, behavioral experiments, data gathering, or psychoeducation.
- Exposure is a technique from behavior therapy that is extensively used by CBT therapists, particularly for the treatment of anxiety. ‘Facing your fears’ is an essential behavioral component of CBT.
- Problem solving describes a series of techniques that are often taught as part of a CBT intervention. Effective problem solving helps people to make adaptive choices.
- Socratic methods are used by CBT therapists to help their clients explore what they know, and to form their own opinions on a topic. Aaron Beck encouraged the use of Socratic-like technique in his original treatment manual “use questioning rather than disputation and indoctrination … it is important to try to elicit from the patient what he is thinking rather than telling the patient what the therapist believes he is thinking” (Beck et al, 1979).
- Alford, B. A., & Beck, A. T. (1997). The relation of psychotherapy integration to the established systems of psychotherapy. Journal of psychotherapy integration , 7 (4), 275-289.
- Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression . New York: Guilford.
- Beck, J. S. (1995). Cognitive therapy: Basics and beyond . New York: Guilford.
- Wills, F. (2009). Beck’s cognitive therapy . CBT Distinctive Features Series. New York: Routledge.
- For clinicians
- For students
- Resources at your fingertips
- Designed for effectiveness
- Resources by problem
- Translation Project
- Help center
- Try us for free
- Terms & conditions
- Privacy Policy
- Cookies Policy
Problem solving
Worrying is a natural response to life's problems. But when it takes over and we can start to feel overwhelmed, it can really help to take a step back and break things down.
Learning new ways to work through your problems can make them feel more manageable, and improve your mental and physical wellbeing.
Video: Problem solving
The tips in this video can help you to find strategies and solutions for tackling the problems that can be solved, and learning how to manage and cope with those that cannot.
Steps and strategies to help you solve problems
1. focus on your values.
Feeling like you have lots of problems to solve in different areas of your life can make it difficult to know how and where to start.
A great way to focus is to write down a few areas of your life that are most important to you right now – for example, a relationship, finances or a long-term goal like studying or developing your career.
This can make it easier to prioritise which problems to tackle.
2. Tackle problems with possible solutions first
It's important to work out if your problem can be solved or is a "hypothetical worry" – things that are out of your control even though you might think about them often.
They might be based on something that happened in the past that cannot be changed or a worry about the future that starts with "what if…".
Ask yourself whether a problem can be dealt with by doing something practical. If the answer is no, it's a hypothetical worry.
Make a list of your problems, and work out which are solvable and which are hypothetical.
3. Set aside time to work through solvable problems
Set aside 5 or 10 minutes to think about possible solutions for one of your solvable problems.
Try to be as open-minded as you can, even if some ideas feel silly. Thinking broadly and creatively is often when the best solutions come to mind.
It may feel difficult at first but, over time, this approach can start to feel easier.
Once you have some ideas, think through or write down:
- the pros and cons of each solution
- whether it's likely to work
- if you have everything you need to try it
4. Make a plan
The next step is to choose a solution you want to try and make a plan for putting it into action. Try to be specific:
- What are you going to do?
- Do you need the support of anybody else?
- How much time do you need?
- When will you do it?
5. Try 'worry time'
Not all of our problems can be solved right away, but it can be difficult to switch off and stop ourselves from dwelling on them.
Using the "worry time" technique to stick to a short set time – say 10 to 15 minutes in the evening – for worrying can make this much easier to manage.
You can learn more about the worry time technique on tackling your worries .
6. Find time to relax
Worrying about our problems can make it harder to relax, but there are lots of things you can try to help you clear your mind and feel calmer.
The most important thing is to find what works for you. It might be getting active, spending time on an existing hobby or trying a new one, or techniques like mindfulness, meditation or our progressive muscle relaxation exercise.
Video: Progressive muscle relaxation
This video will guide you through an exercise to help you recognise when you're starting to get tense, and relax your body and mind.
7. Review and reflect
Once you start trying new approaches to solving and managing problems, consider setting aside time to review what went well with your solutions or anything else you noticed.
Make notes of the problems you face and any strategies you use to overcome them. This can come in handy later on and also be a good reminder of what works best for you.
Ticking off on a checklist any problems you manage to solve is a great way to recognise your achievements and boost your confidence.
8. Give journaling a go
Sometimes getting our thoughts out of our head – and down onto paper, our phones or anything else – is a great way to stop our worries and "what ifs" from spiralling out of control.
Expressing ourselves in this way can also make it easier to spot when our thoughts are unhelpful and we may benefit from a more balanced outlook. Give it a go to see if this works for you.
More self-help CBT techniques you can try
Bouncing back from life's challenges.
Taking steps to stay on top of your mental wellbeing and build resilience can really help you deal with problems when times are tougher. Learn more, and see tips and techniques you can use.

Tackling your worries

Facing your fears

Staying on top of things
Find more ideas to try in self-help CBT techniques
- Free Therapy Techniques
- Anxiety Treatment
- Business and Marketing
- CBT Techniques
- Client Motivation
- Dealing With Difficult Clients
- Hypnotherapy Techniques
- Insomnia and Sleep
- Personal Skills
- Practitioner in Focus
- Psychology Research
- Psychotherapy Techniques
- PTSD, Trauma and Phobias
- Relationships
- Self Esteem
- Sensible Psychology Dictionary
- Smoking Cessation and Addiction
- The Dark Side of Your Emotional Needs
- Uncommon Philosophy
15 Core CBT Techniques You Can Use Right Now
My favourite interventions, skills and approaches from cognitive behavioural therapy.
When it comes to cognitive behavioural therapy (CBT), there are many, many techniques, skills, strategies, and interventions at your disposal. Some of these techniques are best used in a therapist-client setting, while others lend themselves quite well to individual or ‘self-help’ situations.
Techniques can also be used in tandem or individually. It depends on the setting, the circumstance or issue, and the individual seeking help. That’s the cool thing about CBT techniques – there is no ‘cookie cutter’, one-size-fits-all way to use them.
What the techniques, skills and strategies I’m going to discuss here all have in common is that they are built upon the foundations of CBT – identifying maladaptive thinking and intentionally making specific, strategic behavioural interventions to achieve a desired outcome. Some are general CBT techniques, while others are more targeted to specific issues or needs.
Let’s start with the basics that form the foundation of CBT.
Behavioural experiments
Behavioural experiments are the cornerstone of CBT. These experiments are designed to test thinking and identify thought patterns that influence behaviour.
By intentionally ‘trying out’ specific ways of thinking and observing the outcome behaviours, clients gain a deeper awareness of the patterns of thinking that may be holding them back from reaching their goals. 1
Thought records
Thought records are also designed to test the validity of our thoughts. Deliberately recording our thoughts provides a way for us to evaluate the evidence for or against a particular way of thinking – essentially, is it true or not true based on the situation? Thought records help the client to establish a more balanced way of thinking based on logic – what is as opposed to what they feel . 1,2
Behavioural activation (aka scheduling pleasant activities)
This strategy is at once so simple yet so powerful. Pleasurable activities are among the first to go when people are faced with adversity. Intentionally taking part in activities that are enjoyable helps to reduce negative thinking and promotes more positive emotions and feelings of wellbeing. Behavioural activation is particularly helpful for clients with depression . 3
Exposure is a powerful intervention used to help clients face their fears or phobias in a controlled way. Basically, you’re asking the client to be exposed to the very thing they fear. It will, of course, be scary for them.
When used properly, exposure has been proven to be effective in the reduction of fears and phobias. Exposure techniques are best utilized as part of a therapeutic intervention with a therapist who is well trained in their use.
There are many exposure techniques, and even more ways to implement them. 4 Here are some of the more common and well known techniques.
- Situation exposure hierarchies
In this technique, the therapist helps the client make a list of feared objects or situations. The client then rates, on a scale of 0 to 10, how distressed they would be by each item. For example, a person who fears dogs might say “Not seeing a dog in the yard” is 0. “A dog licking my hand” might be their 10.
Starting with the least distressing, the therapist helps the client work through each situation in the list. This is a way of gradually increasing exposure and diminishing the distress of exposure.
Flooding also uses exposure hierarchies, but generally begins with the more difficult or distressing scenarios or objects. Caution should be used when choosing this technique, as it can elicit strong responses. This technique is best utilized as part of a therapeutic intervention.
- Systematic desensitization
This technique involves combining exposure with relaxation exercises . The client is taught strategies to remain relaxed in situations that would normally elicit fear. Gradually, they start to associate their feared object or situation with relaxation rather than powerful negative feelings.
However, in general, the approach we favour at Uncommon Knowledge for phobias and PTSD is the Rewind Technique as it is fast, comfortable, effective and non-voyeuristic.
Journaling is a great way to gather information about thoughts and feelings. The journal can be used as a place to identify, describe, and evaluate moods, thoughts, scenarios, and responses. Having a place to ‘unpack’ and explore can lead to tremendous insight.
Cognitive restructuring – unravelling cognitive distortions
Cognitive distortions are patterns of faulty thinking that convince us something is true when it is not. There are several types of cognitive distortions . To unravel them, the client must learn which are present for them and how to challenge those ways of thinking.
There are any number of worksheets on the Internet that can be used to help a client identify and challenge their distortions in thinking. This can also be accomplished through the therapist-client dialogue. The goal, of course, is to help the client learn to do this on their own. 1
Here are five ‘thought challenges’ from the NHS Fife Department of Psychology’s Negative Thinking CBT Tools . 5 You can use these to get your client to take a closer look at their negative thought patterns.
1. What are the chances…?
The things you worry about may be very unlikely to happen. Would you be willing to put money on it happening?
2. What is the worst thing…?
The things you worry about might happen, but you’re making way too much of them. Consider whether it would really be that bad if the worst did happen, and realize that it might not be worth all that anxiety.
3. Am I right to think that…?
You might be missing important information that would help you with decisions. As you gather more information, your worry and stress may abate.
4. The five year rule (‘the history game’)
This challenge has been applied to lots of situations within and outside of CBT to put events that have happened or will happen into perspective. Ask yourself, “Five years from now, will it really matter?”
5. What is this worth?
Consider just how important this thing you’re worrying about is. Life is too short to be spent worrying about things that just don’t deserve that kind of time investment.
Functional assessment (ABCs)
A functional assessment tool allows the client to record the ABCs (antecedents, behaviours, consequences) of a situation. This data allows the therapist and client to begin to identify patterns of behaviour. 3 There are plenty of these forms on the Internet, but it’s also super easy to design your own.
It’s easy to fall into familiar patterns of negative thinking. One way to counteract negative thinking is through reframing . Reframing is the act of changing the meaning attributed to something so that the thought or experience of it no longer causes emotional problems.
Reframing disrupts the negative cycle of perpetuation and resets the focus on something positive. 1 This technique can be used both in sessions and as part of homework, using a thought record or similar tool.
Homework is an essential part of the CBT process. Homework assignments help clients learn new skills and integrate the concepts learned in sessions into daily life, improving treatment compliance and contributing to symptom reduction. 1,3
Relaxation and mindfulness
Four of my favourite relaxation and mindfulness practices are progressive muscle relaxation (PMR), meditation, deep breathing and self hypnosis. Each is a bit different in its implementation and intent.
- PMR involves the systematic tensing and releasing of each muscle group, combined with deep breathing and mental imagery.
- Mindfulness meditation involves clearing the mind and focusing on the sensations and thoughts in the moment, observing them and allowing them to pass.
- Deep breathing is an action that is physiologically incompatible with anxiety.
- Self hypnosis can be easily achieved by listening to audio hypnosis sessions and can calm the mind quickly.
Relaxation and mindfulness skills give the client a new and different way to respond to distressing situations. This change of response can break the cycle of perpetuation. Relaxation also helps the client to quiet their mind so that they can think more rationally and logically. YouTube videos, audio recordings, apps, and even relaxing music can all be good resources here.
The SOLVED technique
This technique is used to teach the client problem-solving skills. 3 While there are many variations on this technique (and lots of other names for it), structured problem solving is a critical skill for clients to learn. The acronym SOLVED gives the client a tangible, memorable tool for working through the problem-solving steps.
S – Select a problem that the client wants to solve.
O – Open your mind to all solutions – brainstorm all the options with your client.
L – List the potential pros and cons of each potential solution.
V – Verify the best solution – decide which choices are practical or desirable.
E – Enact the plan.
D – Decide if the plan worked.
Role play has a significant place in CBT. It can be used to help clients discover automatic thoughts, practise new responses, or modify core beliefs . Role play is also a useful tool for learning new social skills such as assertiveness. 1
The ‘pie’ technique
Based on the simple pie chart, the ‘pie’ technique lets clients see their goals and ideas in graph form. The ‘pie’ technique can help with things like setting goals and determining responsibility for outcomes. 1
Simply have the client place each idea or goal into a pie chart, divided according to importance as they see fit. This process can be done as part of a homework assignment or as part of the ongoing therapist-client dialogue. Beck (2011) has several illustrations and examples of the use of this technique. 1
Credit list technique
This is a simple technique that can yield powerful results. Clients coming to therapy often lack confidence in their ability to change and may not immediately recognize the positive steps they are taking. The credit list is simply a daily list that the client makes of positive things he or she deserves credit for.
Not only does this technique help the client to recognize their progress, it also strengthens their ability to identify underlying positive beliefs and qualities when doing their core beliefs work in therapy. 1
Letting the story play out
This technique is a sort of thought experiment. The therapist asks the client to imagine the outcome of their worst-case scenario, then encourages them to let the scene play out to its conclusion. Allowing the worrisome event to play out allows the client to see that even if their worst fear should come to pass, things can and do pass and get better. 2
So there you have it. A whole set of tools you can add to your CBT toolbox. While you are probably familiar with many of these tools, some might be new to you. As always, be sure you are working within your scope of practice. If you feel unsure about some of these techniques, seek out additional training specifically in CBT.
Watch Mark reduce a client’s stress and increase their exercise motivation in Uncommon Practitioners’ TV
This is this client’s fifth session and although she has lost plenty of weight and got fitter and healthier, she feels she has reached a plateau. She has also been feeling particularly stressed recently due to high work demands, her father, and the need to be supportive to her daughter.
She feels her diet is pretty balanced but that she needs to move more. She feels fine about cycling now but feels she hasn’t been doing enough.
Mark describes the benefits of short but really intense exercise and she agrees she can start with three lots of 30 second sprints on her stationary bike a week.
Mark utilizes the pleasure the client got from a recent holiday with her daughter as the basis for a hypnotic induction and suggests she can feel more motivated to get up to a new level – “find a better plateau” and also feel less stressed day to day.
Members of Uncommon Practitioners TV can watch this session online now. And if you’d like to join, you can sign up to be notified when booking is open here.
FREE Reframing Book! Just subscribe to my therapy techniques newsletter below.
Download my book on reframing, "New Ways of Seeing", when you subscribe for free email updates
Click to subscribe free now
About Mark Tyrrell
Psychology is my passion. I've been a psychotherapist trainer since 1998, specializing in brief, solution focused approaches. I now teach practitioners all over the world via our online courses .
You can get my book FREE when you subscribe to my therapy techniques newsletter. Click here to subscribe free now.
You can also get my articles on YouTube , find me on Instagram , Amazon , Twitter , and Facebook .
(1) Beck, J. (2011). Cognitive behavior therapy: Basics and beyond (2nd ed.). New York, NY: The Guilford Press.
(2) https://positivepsychologyprogram.com/cbt-cognitive-behavioral-therapy-techniques-worksheets/
(3) https://www.mirecc.va.gov/visn16/docs/therapists_guide_to_brief_cbtmanual.pdf
(4) http://www.div12.org/sites/default/files/WhatIsExposureTherapy.pdf
(5) https://www.moodcafe.co.uk/media/19118/Negative%20Thinking.pdf
Related articles:
Read more CBT Techniques therapy techniques »
Search for more therapy techniques:
- Odnoklassniki
- Facebook Messenger
- LiveJournal
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-.

InformedHealth.org [Internet].
Cognitive behavioral therapy.
Created: August 7, 2013 ; Last Update: September 8, 2016 ; Next update: 2022.
Cognitive behavioral therapy (CBT) is one of the most common and best studied forms of psychotherapy. It is a combination of two therapeutic approaches, known as cognitive therapy and behavioral therapy.
Which methods of treatment are applied depends on the illness or problem to be treated. The basic principle behind therapy is however always the same: What we think, how we feel and how we behave are all closely connected – and all of these factors have a decisive influence on our well-being.

- What is cognitive therapy?
The term cognitive comes from the Latin "cognoscere", meaning "to recognize." The point of cognitive therapy is to form a clear idea of your own thoughts, attitudes and expectations. The goal is to reveal and change false and distressing beliefs, because it is often not only the things and situations themselves that cause problems, but the importance that we attach to them too.
For example, a dangerous thought pattern might be when somebody immediately draws negative conclusions from an occurrence, generalizes them and applies them to similar situations. In psychology, this generalized way of thinking is called “over-generalizing.” Another distressing error in reasoning is “catastrophizing”: If something disturbing happens, people immediately draw exaggerated conclusions about the scope of the supposed disaster ahead.
Such thought patterns can sometimes develop into self-fulfilling prophecies and make life difficult for the people affected. Cognitive therapy helps people learn to replace these thought patterns with more realistic and less harmful thoughts. It also helps people to think more clearly and to control their own thoughts better.
- How does behavioral therapy work?
Behavioral therapy has its origins in American “behaviorism.” This theory assumes that human behavior is learned and can therefore be unlearned or learned anew. Behavioral therapy aims to find out whether certain behavioral patterns make your life difficult or intensify your problems. In the second step you work on changing these behavioral habits.
For example, people who have developed depressive thoughts often tend to withdraw and give up their hobbies. As a result, they feel even more unhappy and isolated. Cognitive therapy helps to identify this mechanism and find ways to become more active again.
In anxiety disorders, behavioral therapy often includes learning methods to help you calm down. For example, you can learn to reduce anxiety by consciously breathing in and out deeply so that your body and breathing can relax. When doing this you concentrate on your breathing instead of what is bringing on your anxiety. These kinds of techniques can help you to calm down instead of getting all worked up with anxiety.
By the way, in Germany, most psychotherapists who are trained in cognitive behavioral therapy call themselves behavioral therapists.
- Which thought and behavioral patterns are harmful, which are not?
Harmful thoughts or behavioral habits can make people feel bad about themselves. For example: You see somebody you know on the street and say hello, but they do not say hello back. Your own reaction to that very much depends on how you assess the situation:
View in own window
- How is cognitive behavioral therapy different from other psychotherapies?
Cognitive behavioral therapy is a problem-oriented strategy. It focuses on current problems and finding solutions for them. Unlike psychoanalysis, for example, it does not deal primarily with the past. Cognitive behavioral therapy is much more concerned with dealing with current problems. The most important thing is helping people to help themselves: They should be able to cope with their lives again without therapy as soon as possible. This does not mean that cognitive behavioral therapy completely ignores the influence of past events. But it mainly deals with identifying and changing current distressing thought and behavioral patterns.
Analytic psychotherapy, which has its origin in classic Freudian psychoanalysis, uses different methods. Here the therapist tries to help the patient discover and understand problems and their deeper causes.
- When is cognitive behavioral therapy an option?
Cognitive behavioral therapy is used to treat conditions such as depression , anxiety and obsessive-compulsive disorders, and addictions. But it is also an option for treating physical conditions such as chronic pain, tinnitus and rheumatism. It can help to relieve the symptoms.
Cognitive behavioral therapy requires the patient's commitment and own initiative. Therapy can only be successful if the patient actively takes part in the treatment and also works on their problems between sessions. This can be a considerable challenge, especially with severe conditions such as depression or anxiety disorders. That is why medication is sometimes used at first to quickly relieve the worst symptoms so that psychotherapy can be started.
Choosing a certain kind of psychotherapy also depends on the goals. If you feel the need for deep insight into the causes of your problems, cognitive behavioral therapy is probably not the right choice. It is particularly useful if you are mainly interested in tackling specific problems and are only secondarily concerned with the “why.”
- How does cognitive behavioral therapy work and how long does it take?
It is important that you and your psychotherapist have a close and trusting working relationship. It can sometimes take a while to find the right therapist.
In the first session, you will briefly explain your current problems and outline your expectations. That forms the basis for discussing the goals of therapy and the therapy plan. The plan can be adjusted if your personal goals change over the course of therapy.
Therapy often includes recording your own thoughts in a journal over a certain period of time. The therapist will then check the following things with you: Do I perceive things appropriately and realistically? What happens if I behave differently than I normally do in a certain situation? You will regularly discuss any problems you may have and progress that you have made.
Cognitive behavioral therapy also uses relaxation exercises, stress and pain relief methods, and certain problem-solving strategies.
Compared to analytical psychotherapy approaches, cognitive behavioral therapy is a short-term treatment. But there is also no standard length of cognitive behavioral therapy. Some people already feel much better after a few sessions, while others need treatment for several months. This depends on the kind and severity of the problems, among other things. An individual session lasts about an hour. Sessions usually take place once a week. Cognitive behavioral therapy is offered in psychotherapy practices, hospitals and rehabilitation clinics. It is sometimes also offered as group therapy.
- Can cognitive behavioral therapy also have side effects?
Side effects resulting from psychotherapy cannot be ruled out. Being directly confronted with your problems or anxieties may be very stressful at first, and relationships might also suffer as a result. It is crucial to speak openly with your psychotherapist if any difficulties come up during therapy.
Hardly any research has been done on possible side effects of psychotherapy.
- Who covers the costs?
In Germany, statutory health insurance pays for cognitive behavioral therapy to treat mental illnesses such as depression , anxiety or obsessive-compulsive disorders as well as addictions. The costs of cognitive behavioral therapy can also be covered for the treatment of severe symptoms that result from a chronic illness. It can however sometimes take several weeks or months until you can see a therapist or until the insurance company approves therapy.
In Germany, a psychotherapy practice can bill the statutory health insurance company directly for up to five trial sessions. This way you can get to know the psychotherapist, find out what the problems are and whether therapy is worthwhile. After the trial sessions, you and your psychotherapist have to prepare an application explaining why therapy is needed. You have to submit this application to your health insurance company before therapy can begin. Besides this application, your health insurance company also requires a medical report from your doctor stating that the symptoms are not caused by a physical problem, and that there are no medical reasons against psychotherapy. The statutory health insurance company decides whether to approve therapy based on an evaluation.
- Robert Koch Institute (RKI). Psychotherapeutic healthcare. Berlin: RKI; 2008. ( Federal Health Reporting, Booklet 41 ).
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
- Cite this Page InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Cognitive behavioral therapy. 2013 Aug 7 [Updated 2016 Sep 8].
- Disable Glossary Links
In this Page
Informed health links, recent activity.
- Cognitive behavioral therapy - InformedHealth.org Cognitive behavioral therapy - InformedHealth.org
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
CBT Coping Skills and Strategies
Akeem Marsh, MD, is a board-certified child, adolescent, and adult psychiatrist who has dedicated his career to working with medically underserved communities.
:max_bytes(150000):strip_icc():format(webp)/akeemmarsh_1000-d247c981705a46aba45acff9939ff8b0.jpg)
How CBT Works
Diaphragmatic breathing, progressive muscle relaxation, self-monitoring, behavioral activation, listing pros and cons, cognitive restructuring, setting and managing goals.
CBT coping skills involve dealing with negative emotions in a healthy way. They provide strategies for getting through difficult situations with less tension, anxiety, depression , and stress.
CBT coping skills help you deal with uncomfortable emotions (anxiety, depression, etc.) so you can feel better physically, make better decisions, and more. These cognitive strategies are especially beneficial for individuals with certain mental health conditions, such as by helping reduce symptoms in people with post-traumatic stress disorder (PTSD).
Before discussing specific cognitive coping strategies, it's important to first understand how CBT works. This gives some insight into how the various CBT coping skills can help relieve anxiety, sadness, and other distressing emotions.
Tom M Johnson / Blend Images / Getty Images
Cognitive behavioral therapy (CBT) is based on the idea that psychological problems arise as a result of the way in which we interpret or evaluate situations, thoughts, and feelings. When these interpretations and evaluations are negative, it can lead to unhealthy behaviors.
CBT works by changing unhealthy behavioral patterns by changing the interpretations that lead to them. It also teaches you the skills and cognitive strategies needed to better cope with whatever life throws your way. Here are a few CBT coping skills that have this result.
Diaphragmatic breathing, also called breathing retraining or deep breathing , is a basic cognitive coping strategy for managing anxiety. It is a simple technique but can be very powerful.
Diaphragmatic breathing involves pulling your diaphragm down while taking a deep breath in. You should see your abdominal area rise with each breath, which is why it is sometimes referred to as "belly breathing."
Relaxation exercises can be an effective way to reduce your stress and anxiety. One such exercise is called progressive muscle relaxation (PMR) and involves alternating between tensing and relaxing different muscle groups throughout the body.
With PMR, complete muscle relaxation is obtained by first going to the other extreme (that is, by tensing your muscles). In addition, by tensing your muscles—a common anxiety symptom —and immediately relaxing them, over time, the symptom of muscle tension may become a signal to relax.
Self-monitoring is another basic CBT coping skill. To a large extent, is at the core of all the cognitive-behavioral coping strategies described here.
In order to address a problem or a symptom, we need to first become aware of it. Self-monitoring can help with this. With this awareness, we can then take action to regulate our behaviors so we have more positive outcomes.
When people feel depressed or anxious, they may be less likely to do the things they enjoy. Therefore, it is important to learn how to be more active. Behavioral activation is a CBT coping skill that helps with this.
The goal of behavioral activation is simple. Get more active in areas of your life that you find pleasurable and enjoyable. Being more involved with and engaged in these experiences works by improving your mood.
When faced with a decision, we can sometimes feel paralyzed or trapped. If this occurs, we may not know the best choice.
One way to move forward in situations such as this is to weigh the short- and long-term pros and cons of a situation. This cognitive coping strategy can help us identify the best path to take—that is, a path that is associated with less risk and is consistent with our goals and priorities.
Cognitive restructuring is a common CBT coping skill. How we evaluate and think about ourselves, other people, and events can have a major impact on our mood. This cognitive strategy focuses on identifying negative thoughts or evaluations and modifying them.
Cognitive restructuring involves gathering evidence about certain thoughts, recognizing how they may be misinterpreted or distorted, then replacing them with more positive affirmations. By modifying our thoughts, we can improve mood and make better choices with regard to our behaviors.
Goals (or things that you want to accomplish in the future) can give your life purpose and direction, as well as motivate healthy behaviors focused on improving your life. However, they can also be very overwhelming and a source of stress. Because of this, you want to be careful when setting goals .
This CBT coping skill involves approaching your goals in a way that improves your mood and quality of life as opposed to increasing distress. This could be by setting smaller goals versus bigger ones, for instance, or breaking larger goals down into more manageable chunks.
A Word From Verywell
CBT coping skills can help you better handle and manage difficult emotions and situations. They work by changing how you interpret feelings and events. You can use CBT coping skills for anxiety, stress , depression, and more—providing some much-needed relief.
Frequently Asked Questions
CBT coping skills teach you how to better deal with difficult situations, such as how to relax your body (so your mind can also relax), also changing how you look at circumstances and events so you have more positivity. These processes use the same types of strategies like those used in cognitive behavioral therapy (CBT).
Regularly practicing cognitive coping strategies such as these can help improve your skills. It can also be beneficial to work with a mental health professional as they can focus directly on improving your CBT coping skills in the therapy session. Taking care of your physical health, such as through a healthy diet and exercise, can also help improve your cognitive health.
CBT coping skills such as cognitive restructuring can help change thought patterns that lead to anxiety. Other skills, like diaphragmatic breathing and progressive muscle relaxation, help relax your body when in an anxious state, thereby reducing your feelings of anxiousness.
American Psychological Association. Cognitive behavioral therapy (CBT) .
Fenn K, Byrne M. The key principles of cognitive behavioural therapy . InnovAiT. 2013;6(9):579-585. doi:10.1177/1755738012471029
Ma X, Yue ZQ, Gong ZQ, et al. The effect of diaphragmatic breathing on attention, negative affect and stress in healthy adults . Front Psychol . 2017;8:874. doi:10.3389/fpsyg.2017.00874
Safi SZ. A fresh look at the potential mechanisms of progressive muscle relaxation therapy on depression in female patients with multiple sclerosis . Iran J Psychiatry Behav Sci . 2015;9(1):e340. doi:10.17795/ijpbs340
Hirano M, Ogura K, Kitahara M, Sakamoto D, Shimoyama H. Designing behavioral self-regulation application for preventive personal mental healthcare . Health Psychol Open . 2017;4(1):2055102917707185. doi:10.1177/2055102917707185
Hirayama T, Ogawa Y, Yanai Y, Suzuki SI, Shimizu K. Behavioral activation therapy for depression and anxiety in cancer patients: a case series study . Biopsychosoc Med . 2019;13:9.doi:10.1186/s13030-019-0151-6
National Institute on Aging. Cognitive health and older adults .
By Matthew Tull, PhD Matthew Tull, PhD is a professor of psychology at the University of Toledo, specializing in post-traumatic stress disorder.

Get weekly notifications for new group therapy session times.
Are you interested in joining an online group therapy session? Subscribe and receive weekly updates for new group therapy session times at Grouport.
Thank you for your interest.
We’ll keep you updated on our schedule weekly.
.png)
Learn DBT Skills In A Group
Weekly sessions are available. Grouport offers therapist-led dialectical behavior therapy skills groups online. The first 12 weeks covers fundamental DBT skills.
Cognitive Behavior Therapy (CBT) And Role Play Techniques

Cognitive Behavioral Therapy (CBT) is a psychotherapeutic approach that focuses on changing negative thought patterns and behaviors to improve mental health and well-being. One technique used in CBT is role play, which involves the patient and therapist acting out scenarios to challenge negative thought patterns and behaviors.
What can I expect from a session in role-playing for CBT?
During a role-playing session in Cognitive Behavioral Therapy (CBT), you can expect to work collaboratively with your therapist to identify and address negative thought patterns and behaviors that are causing difficulties in your life. Here is what you can expect from a typical role-playing session:
- Discussion of Goals: Your therapist will likely start the session by discussing your treatment goals and what you hope to achieve through CBT. Creating plans will help them tailor the session to your needs and concerns.
- Scenario Selection: Once your goals have been discussed, your therapist will work with you to select a scenario to role-play. This task may involve discussing situations that have caused you anxiety or distress or techniques you anticipate encountering in the future.
- Role Play: During the role-play, your therapist will act as the other person or situation, and you will act as yourself. You will be encouraged to respond to the situation in a way that challenges negative thought patterns or behaviors that aligns with your treatment goals.
- Feedback and Analysis: After the role-play, your therapist will provide feedback and analysis. They may ask questions to help you better understand your thoughts and behaviors and to identify areas where you can make changes. They will also guide how to develop more positive thought patterns and behaviors.
- Homework: Your therapist may give you homework to practice outside the session to reinforce what you learned during the session. The assignment may involve practicing new skills, journaling, or reflecting on your progress.
- Follow-up: At your next session, your therapist will check your progress and discuss any challenges or successes you may have experienced. They will continue to work with you to develop new skills and strategies to manage your thoughts and behaviors more effectively.
Overall, a role-playing session in CBT is a collaborative process that involves active participation from both you and your therapist. Through this process, you can expect to understand your thoughts and behaviors better and learn new skills to manage them more effectively.
How is role play effective for CBT?
Role-playing is an effective technique in Cognitive Behavioral Therapy (CBT) because it provides a safe and controlled environment for patients to practice new skills and strategies. Here are several ways in which role-play is effective for CBT:
- Provides a safe space: Role-playing delivers a safe and supportive environment for patients to confront their fears, negative thoughts, and maladaptive behaviors. It allows patients to practice new skills in a controlled setting and receive feedback and support from their therapist.
- Helps identify negative thought patterns and behaviors: Role-playing can help patients identify negative thoughts and behaviors that may contribute to their mental health issues. By acting out different scenarios, patients can better understand their reactions and develop strategies to challenge negative thoughts and behaviors.
- Allows for experimentation: Role-playing will enable patients to experiment with new ways of thinking and behaving in a safe and controlled environment. Patients can test different strategies and receive feedback from their therapist to determine what works best for them.
- Increases self-efficacy: Role-playing can help patients build confidence in their ability to handle challenging situations. By practicing new skills and strategies, patients can feel more prepared and confident in coping with difficult real-life situations.
- Provides real-time feedback: Role-playing allows for immediate feedback from the therapist, which can help patients identify areas where they need to improve and make adjustments in real time. The input can lead to more rapid progress in treatment.
Overall, role-playing is an effective technique in CBT because it provides patients with a safe and supportive environment to practice new skills and strategies. Through role-playing, patients can identify negative thought patterns and behaviors, experiment with new ways of thinking and behave, build confidence, and receive real-time feedback from their therapist.
Example of CBT and role play
Let's say that a person struggles with social anxiety and finds it difficult to interact with people in social situations. During a therapy session, the therapist may use CBT techniques to help the person recognize and challenge negative thoughts and beliefs about social situations and replace them with more positive and realistic ones.
The therapist may suggest role-playing scenarios with the person to help reinforce these new ways of thinking and behaving. For example, the therapist could pretend to be a stranger at a party, and the person would practice engaging in conversation with them.
As they engage in the role-play, the therapist would guide them in using their new cognitive and behavioral skills. They might encourage the person to challenge negative thoughts during the interaction and use specific coping strategies, such as deep breathing or positive self-talk, to help them feel calmer and more confident.
After the role-play, the therapist and person would reflect on the experience, identifying what went well and what could be improved. This feedback can help the person continue to develop their social skills and build confidence in real-life social situations outside of therapy.
Combining CBT and role-play can be a powerful tool for helping people overcome social anxiety and other challenges by teaching them new ways of thinking and behaving and giving them a safe space to practice these skills in a supportive and structured environment.
What are some other techniques in CBT other than role-playing?
Cognitive Behavioral Therapy (CBT) is a structured, evidence-based form of psychotherapy that focuses on changing negative thought patterns and behaviors to improve mental health and well-being. In addition to role-playing, here are some other standard techniques used in CBT:
- Cognitive Restructuring: Cognitive restructuring involves identifying and challenging negative thoughts and beliefs contributing to mental health issues. This technique helps patients develop more positive and accurate ways of thinking, leading to improved mood and behavior.
- Behavioral Activation: Behavioral activation involves identifying and engaging in positive and rewarding activities to increase feelings of pleasure and accomplishment. This technique is beneficial for patients with depression, as it helps to counteract feelings of lethargy and lack of motivation.
- Exposure Therapy: Exposure therapy involves gradually exposing patients to feared situations or stimuli in a safe and controlled environment. This technique helps patients overcome anxiety and phobias by reducing the intensity of their emotional response over time.
- Mindfulness-Based Interventions: Mindfulness-based interventions involve developing a non-judgmental awareness of the present moment. These techniques can be helpful for patients with anxiety or stress, as they help patients learn to manage their thoughts and emotions more effectively.
- Problem-Solving Therapy: Problem-solving therapy involves identifying and addressing specific problems or stressors contributing to mental health issues. This technique helps patients develop problem-solving skills and more effective strategies for managing difficult situations.
- Relaxation Training: Relaxation training involves teaching patients relaxation techniques such as deep breathing, progressive muscle relaxation, and guided imagery. These techniques can be helpful for patients with anxiety and stress, as they promote feelings of calm and relaxation.
CBT is a versatile form of therapy that incorporates various techniques to help patients overcome negative thought patterns and behaviors. Patients can improve their mental health and well-being by working collaboratively with a therapist and practicing these techniques.
Grouport offers CBT online group therapy
Grouport Therapy offers a range of online cognitive behavioral therapy (CBT) groups to support individuals struggling with anxiety , depression , PTSD, and trauma . In these sessions, our primary focus is to help members integrate CBT techniques into their daily routines to identify triggers, challenge negative thought patterns, and develop more positive behaviors to manage and recover from their symptoms.
Our licensed therapist conducts weekly group sessions remotely, allowing members to participate from the comfort of their own homes. Participant feedback shows that 70% of them experienced significant improvements within 8 weeks.
Don't face these challenges alone. Join our community and use our resources to begin your journey toward lasting change and renewed hope. Sign up for one of our groups today and start your path toward a brighter future.
Join a Group Support Session for Depression
We infuse cognitive behavioral techniques in our group therapy sessions for depression. Get effective and affordable treatment for depression.
Space is limited, so reserve your seat today.
Share This Post:
Discovering Anxiety Treatment Options in Ocala: The Benefits of Online Group Therapy and Dialectical Behavior Therapy
The power of dbt notebooks: a guide to creating and using your own dialectical behavior therapy journal, self-soothing techniques: finding calm amidst chaos, get started with grouport today.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
Research: How Different Fields Are Using GenAI to Redefine Roles
- Maryam Alavi
Examples from customer support, management consulting, professional writing, legal analysis, and software and technology.
The interactive, conversational, analytical, and generative features of GenAI offer support for creativity, problem-solving, and processing and digestion of large bodies of information. Therefore, these features can act as cognitive resources for knowledge workers. Moreover, the capabilities of GenAI can mitigate various hindrances to effective performance that knowledge workers may encounter in their jobs, including time pressure, gaps in knowledge and skills, and negative feelings (such as boredom stemming from repetitive tasks or frustration arising from interactions with dissatisfied customers). Empirical research and field observations have already begun to reveal the value of GenAI capabilities and their potential for job crafting.
There is an expectation that implementing new and emerging Generative AI (GenAI) tools enhances the effectiveness and competitiveness of organizations. This belief is evidenced by current and planned investments in GenAI tools, especially by firms in knowledge-intensive industries such as finance, healthcare, and entertainment, among others. According to forecasts, enterprise spending on GenAI will increase by two-fold in 2024 and grow to $151.1 billion by 2027 .
- Maryam Alavi is the Elizabeth D. & Thomas M. Holder Chair & Professor of IT Management, Scheller College of Business, Georgia Institute of Technology .
Partner Center

IMAGES
VIDEO
COMMENTS
Problem-solving is one technique used on the behavioral side of cognitive-behavioral therapy. The problem-solving technique is an iterative, five-step process that requires one to identify the ...
A more detailed description and further examples of each worksheet can be found in Beck, J. S. Cognitive Behavior Therapy: Basics and Beyond, 3rd ed. (2020), and Beck, J. S. Cognitive Therapy for Challenging Problems (2005). As noted in these books, the decision to use any given worksheet is based on the
"Problem-solving therapy (PST) is a psychosocial intervention, generally considered to be under a cognitive-behavioral umbrella" (Nezu, Nezu, & D'Zurilla, 2013, p. ix). It aims to encourage the client to cope better with day-to-day problems and traumatic events and reduce their impact on mental and physical wellbeing.
Cognitive Behavioral Therapy (CBT) stands as a powerful, evidence-based therapeutic approach for various mental health challenges. At its core lies a repertoire of techniques designed to reframe thoughts, alter behaviors, and alleviate emotional distress. ... facilitating a more objective approach to problem-solving. Example: Adam, dealing with ...
Problem-solving therapy (PST) is an intervention with cognitive and behavioral influences used to assist individuals in managing life problems. Therapists help clients learn effective skills to address their issues directly and make positive changes. PST is used in various settings to address mental health concerns such as depression, anxiety, and more.
Cognitive-Behavioral Therapy Worksheets (PDFs) To Print and Use. If you're a therapist looking for ways to guide your client through treatment or a hands-on person who loves to learn by doing, there are many cognitive-behavioral therapy worksheets that can help. 1. Coping styles worksheet.
In this manner you are a facilitator who possesses problem -solving skills. Problem solving may be difficult for the following individuals: 1. Persons with serious mental illness (psychotic disorders, bipolar disorder) 2. Persons with severe depression, who might require more focused cognitive work or medications 3.
worksheet. Guide your clients and groups through the problem solving process with the help of the Problem Solving Packet. Each page covers one of five problem solving steps with a rationale, tips, and questions. The steps include defining the problem, generating solutions, choosing one solution, implementing the solution, and reviewing the ...
This self-help guide is intended for people with mild-to-moderate mental health issues. If you're feeling distressed, in a state of despair, suicidal or in need of emotional support you can phone NHS 24 on 111. For an emergency ambulance phone 999. It's easy to feel overwhelmed by problems, particularly if you're experiencing mental health ...
Consider your own behavior, as well as external factors. Define your problem. Be as clear and comprehensive as possible. If there are many parts to your problem, describe each of them. TIP: If you find it difficult to separate your emotions from the problem, try to complete this step from the perspective of an impartial friend.
Problem-solving therapy is a brief intervention that provides people with the tools they need to identify and solve problems that arise from big and small life stressors. It aims to improve your overall quality of life and reduce the negative impact of psychological and physical illness. Problem-solving therapy can be used to treat depression ...
Problem Solving is a helpful intervention whenever clients present with difficulties, dilemmas, and conundrums, or when they experience repetitive thought such as rumination or worry. Effective problem solving is an essential life skill and this Problem Solving worksheet is designed to guide adults through steps which will help them to generate ...
Basically, CBT works by identifying, tackling, and changing unhelpful thinking so that your mindset, behaviors, and overall well-being improve with practice. When you change the way you feel about ...
Research indicates that cognitive behavioral therapy is the leading evidence-based treatment for eating disorders.; CBT has been proven helpful in those with insomnia, as well as those who have a medical condition that interferes with sleep, including those with pain or mood disorders such as depression.; Cognitive behavioral therapy has been scientifically proven to be effective in treating ...
Cognitive behavior therapy (CBT) is a popular form of psychological therapy that works with our thoughts, feelings, and behaviors. CBT is an integration of principles from behavior therapy with theory and methods from the cognitive therapies developed by Aaron Beck and Albert Ellis. The CBT that is practiced today has evolved with new ...
Several mental processes are at work during problem-solving. Among them are: Perceptually recognizing the problem. Representing the problem in memory. Considering relevant information that applies to the problem. Identifying different aspects of the problem. Labeling and describing the problem.
Make a list of your problems, and work out which are solvable and which are hypothetical. 3. Set aside time to work through solvable problems. Set aside 5 or 10 minutes to think about possible solutions for one of your solvable problems. Try to be as open-minded as you can, even if some ideas feel silly. Thinking broadly and creatively is often ...
This technique is used to teach the client problem-solving skills. 3 While there are many variations on this technique (and lots of other names for it), structured problem solving is a critical skill for clients to learn. The acronym SOLVED gives the client a tangible, memorable tool for working through the problem-solving steps.
For worries about a problem that can be solved, use the technique of problem solving: Some worries are about current or future situations that the child has some control over. Kids who perceive they have some control and have a plan worry less. Problem-solving steps: 1. Identify the problem 2. Brainstorm possible solutions 3.
Cognitive behavioral therapy also uses relaxation exercises, stress and pain relief methods, and certain problem-solving strategies. Compared to analytical psychotherapy approaches, cognitive behavioral therapy is a short-term treatment. But there is also no standard length of cognitive behavioral therapy.
CBT coping skills involve dealing with negative emotions in a healthy way. They provide strategies for getting through difficult situations with less tension, anxiety, depression, and stress. CBT coping skills help you deal with uncomfortable emotions (anxiety, depression, etc.) so you can feel better physically, make better decisions, and more.
Cognitive Behavioral Therapy (CBT) is a psychotherapeutic approach that focuses on changing negative thought patterns and behaviors to improve mental health and well-being. ... For example, the therapist could pretend to be a stranger at a party, and the person would practice engaging in conversation with them. ... Problem-Solving Therapy ...
The interactive, conversational, analytical, and generative features of GenAI offer support for creativity, problem-solving, and processing and digestion of large bodies of information. Therefore ...