Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries
Affiliations.
- 1 Surveillance and Health Equity Science, American Cancer Society, Atlanta, Georgia.
- 2 Section of Cancer Surveillance, International Agency for Research on Cancer, Lyon, France.
- PMID: 33538338
- DOI: 10.3322/caac.21660
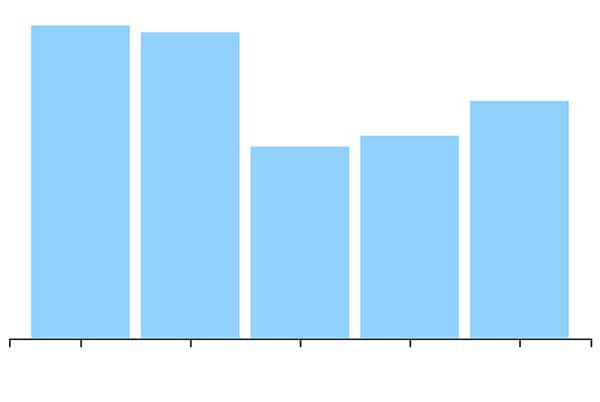
This article provides an update on the global cancer burden using the GLOBOCAN 2020 estimates of cancer incidence and mortality produced by the International Agency for Research on Cancer. Worldwide, an estimated 19.3 million new cancer cases (18.1 million excluding nonmelanoma skin cancer) and almost 10.0 million cancer deaths (9.9 million excluding nonmelanoma skin cancer) occurred in 2020. Female breast cancer has surpassed lung cancer as the most commonly diagnosed cancer, with an estimated 2.3 million new cases (11.7%), followed by lung (11.4%), colorectal (10.0 %), prostate (7.3%), and stomach (5.6%) cancers. Lung cancer remained the leading cause of cancer death, with an estimated 1.8 million deaths (18%), followed by colorectal (9.4%), liver (8.3%), stomach (7.7%), and female breast (6.9%) cancers. Overall incidence was from 2-fold to 3-fold higher in transitioned versus transitioning countries for both sexes, whereas mortality varied <2-fold for men and little for women. Death rates for female breast and cervical cancers, however, were considerably higher in transitioning versus transitioned countries (15.0 vs 12.8 per 100,000 and 12.4 vs 5.2 per 100,000, respectively). The global cancer burden is expected to be 28.4 million cases in 2040, a 47% rise from 2020, with a larger increase in transitioning (64% to 95%) versus transitioned (32% to 56%) countries due to demographic changes, although this may be further exacerbated by increasing risk factors associated with globalization and a growing economy. Efforts to build a sustainable infrastructure for the dissemination of cancer prevention measures and provision of cancer care in transitioning countries is critical for global cancer control.
Keywords: burden; cancer; epidemiology; incidence; mortality.
© 2021 American Cancer Society.
- Africa / epidemiology
- Americas / epidemiology
- Asia / epidemiology
- Databases, Factual
- Developed Countries / statistics & numerical data*
- Developing Countries / statistics & numerical data*
- Global Health / statistics & numerical data*
- Internationality
- Neoplasms / epidemiology*
- Neoplasms / mortality
- Oceania / epidemiology
- Population Dynamics*
- Risk Factors
- Sex Distribution

Grants and funding
- 001/WHO_/World Health Organization/International
Cancer Epidemiology Research
Current projections indicate that the burden of cancer will increase from 10 million new cases globally in 2000, to 15 million in 2020. This public health burden will necessitate further research into the etiology and prevention of cancer. The primary goal of the Cancer Epidemiology Program is to develop new knowledge relevant to cancer etiology, diagnosis, prognosis, and prevention using interdisciplinary and epidemiologic approaches. The cancer epidemiology faculty have developed a rich research program including diverse cancers (breast, prostate, colon, head and neck, childhood, melanoma, esophageal, and bladder) and exposures (lifestyle, diet, genes, tumor biology, occupational and environmental, health care, screening, socioeconomic factors). Research spans etiology, survivorship, comparative effectiveness, and access to health care, with many studies emphasizing health disparities, especially among African-Americans. Several population-based studies in North Carolina have yielded high impact findings and contribute to large international consortia. Students in the cancer epidemiology program receive training in epidemiologic methods, biostatistics, related substantive areas, and cancer biology. Outside the classroom, students obtain an appreciation for interdisciplinary, collaborative research by working with diverse and strong faculty in the department, school, and Lineberger Comprehensive Cancer Center .
Learning Objectives
- Understand cancer statistics and the descriptive epidemiology of cancer;
- Understand known risk factors and gaps in knowledge for the major cancers;
- Understand the pathobiology of cancer;
- Apply epidemiologic methods in the design, conduct, and analysis of cancer research studies;
- Apply critical thinking in the review of projects and publications in cancer epidemiology;
- Appreciate the interdisciplinary aspect of cancer including the contributions of basic sciences, clinical medicine, health services research, and the social sciences to the understanding of cancer etiology and progression;
- Appreciate methods for cancer risk assessment and screening;
- Appreciate the role and interdisciplinary methods of cancer control and prevention.
- Appreciate the practical aspects of conducting research in cancer epidemiology
Program Courses
- EPID 770: Cancer Epidemiology and Pathogenesis ( Dr. Eboneé Butler )
- EPID 771: Cancer Epidemiology Methods ( Hazel Nichols )
- EPID 775: Advanced Cancer Epidemiology ( Andy Olshan )
Related Courses
- EPID 772: Cancer Prevention and Control
- PATH 225: Cancer Pathology
- EPID 742: Integrating Biomarkers into Population-Based Research
- EPID 743: Genetic Epidemiology
- EPID 745: Molecular Techniques for Public Health Research
- EPID 785: Environmental Epidemiology
- EPID 815: Diet and Cancer
- EPID 826 Introduction to Social Epidemiology
Core Faculty – Research Projects
Dr. Jeannette Bensen : North Carolina-Louisiana Prostate Cancer Study (PCaP), Carolina Breast Cancer Study, and UNC Cancer Survivorship Cohort.-->
Dr. Kathleen Conway-Dorsey : Genes, Environment and Melanoma (GEM) study, Carolina Breast Cancer Study (CBCS), I-SPY InterSPORE Breast Cancer Neoadjuvant Chemotherapy Trial, Mayo Clinic Benign Breast Disease study, and Carolina Head and Neck Cancer CHANCE) Study.-->
Dr. Eboneé Butler : North Carolina-Louisiana Prostate Cancer Study (PCaP), Carolina Breast Cancer Study.
Dr. Marc Emerson : Carolina Breast Cancer Study, Carolina Head and Neck Cancer Study.
Dr. Lawrence S. Engel : GuLF STUDY, and an international study examining blood levels of organochlorines and aflatoxin adducts in relation to risk of primary liver cancer.
Dr. Marilie D. Gammon : Long Island Breast Cancer Study Project, Barrett's and Esophageal Adenocarcinoma Consortium (BEACON). -->
Dr. Jennifer Lund : SEER-Medicare, UNC Integrated Cancer Information and Surveillance System (ICISS), and other health care claims databases.
Dr. Hazel Nichols : Carolina Endometrial Cancer Study, UNC Cancer Survivorship Cohort, Adolescent and Young Adult (AYA) Cancer Horizon Study, AYA Valuing Opinions and Insight from Cancer Experiences (VOICE) Study, SEER-linked data.
Dr. Andrew Olshan : Carolina Head and Neck Cancer Study (CHANCE), Carolina Breast Cancer Study (CBCS), and NENA childhood neuroblastoma study.
Dr. Charles Poole : Epidemiologic methods in cancer epidemiology.
Dr. David B. Richardson : Studies of cancer among nuclear workers at several U.S. Department of Energy facilities, cancer among the Japanese survivors of the atomic bombings of Hiroshima and Nagasaki. (Not taking students for Fall 2022) -->
Dr. Whitney Robinson : Carolina Breast Cancer Study. (Not taking students for Fall 2022) -->
Dr. Jennifer Smith : Cervical Cancer-Free Coalition, international studies of HPV and cervical disease.
Dr. Til Stürmer : SEER-Medicare, UNC Integrated Cancer Information and Surveillance System (ICISS), and other health care claims databases.
Dr. Caroline Thompson : SEER-Medicare, UNC Cancer Information & Population Health Resource (CIPHR), UNC Carolina Data Warehouse for Health (CDW-H), California Teachers Study.
Dr. Melissa Troester : Carolina Breast Cancer Study, Normal Breast Study.
Selected Collaborative Groups at UNC
- Lineberger Comprehensive Cancer Center
- Carolina Population Center
- Center for Environmental Health and Susceptibility
- UNC Center for Gastrointestinal Biology and Disease
- Carolina Center for Genome Sciences
- Biostatistics
- City and Regional Planning
Selected Research Projects
- Carolina Breast Cancer Study
- North Carolina Colon Cancer Study
- Genetic Epidemiology of Melanoma Study
- Carolina Mammography Study
- Carolina Head and Neck Cancer Study
- UNC Health Registry
- Neuroblastoma Epidemiology in North America (NENA) study
- North Carolina-Louisiana Prostate Cancer Study
- Long Island Breast Cancer Study
- The AMBER Consortium
- UNC Breast Cancer SPORE
The UNC Lineberger Comprehensive Cancer Center is a cancer research and treatment center at the University of North Carolina at Chapel Hill. Serving patients at the N.C. Basnight Cancer Hospital, UNC Lineberger is the only public comprehensive cancer center in the state of North Carolina.
The Carolina Population Center brings together a remarkable group of faculty fellows who address pressing research questions about population dynamics, fertility, health, mortality, migration, and the environment.
The UNC Center for Environmental Health and Susceptibility (CEHS) facilitates collaborations by funding university infrastructure to support scientific equipment, facilities, and other resources that can be shared among environmental health researchers.
The Institute for Global Health and Infectious Diseases is a research engine for global health innovation and pan-university collaboration, transforming health in North Carolina and around the world through research, training and service.
For more than 30 years, the Injury Prevention Research Center has been combining innovative science in injury and violence prevention with collaborative evidence-based action in the form of programs, practices, and policies.
The Center for Pharmacoepidemiology provides a unique forum to generate innovative, evidence-based solutions to challenges related to comparative effectiveness research and evaluation of the safety of drugs and devices in real-world clinical settings.
Radon-associated cardiovascular risks highlight need for household testing
Information for:.
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Cancer Epidemiology
- Initiatives
- Statement Denouncing Racism
- Job Openings
- Goal of the Track
- Curriculum and Faculty
- Social Epidemiology Courses
- Social Epidemiology Faculty
- Guidelines for Writing Statement of Objectives
- Comorbid Patterns with Alcohol Use Disorders
- Guaranteed Income and Health Consortium
- Stylish Man/Stylish Living Study
- The Chennai HIV, Hepatitis C and EERal Study (CHHEERS)
- Translational Epidemiology Initiative
- Internalizing Symptoms and Alcohol Involvement
- Pediatric Antiretroviral Therapy (PART) Study in Rural Zambia
- Department Leadership
- News Releases By Year
- Make a Gift
Our vision is to reduce cancer incidence, mortality and morbidity in the U.S. and globally, by conducting cutting edge epidemiological research and training the next generation of population-based scientists.

This is an exciting time in the field of Cancer Epidemiology as technological advancements have led to more precise measurements of exposures, the creation of large more complex databases, and the development of new analytic methods. The Cancer Epidemiology faculty at Johns Hopkins conduct a wide range of public health research that covers the entire cancer continuum including cancer etiology, early detection, cancer prevention, control, surveillance, survivorship and disparities of a number of cancers. There is a strong emphasis on translational epidemiology and team science, both within Johns Hopkins (including collaboration with investigators at the Sidney Kimmel Comprehensive Cancer Center ) and other institutes as well as nationally and internationally. Many of the faculty are also involved in large international consortia efforts and have access to a variety of data.

The Cancer Epidemiology track offers a rich, vibrant and dynamic environment for masters and doctoral students, and post-doctoral fellows to actively participate, learn, explore, and conduct cancer related population-based and clinical research. The track has a long and successful history of training masters and doctoral students and post-doctoral fellows. Past students continue to conduct population-based cancer research and have made successful transitions to positions in academia, government and private sector organizations . Funding opportunities are available and students are strongly encouraged to apply. The Cancer Epidemiology track also has a T32 fellowship sponsored by the National Cancer Institute.
We hope you will consider applying to our program!
- Current Research
- Curriculum and Faculty

Discovering the causes of cancer and informing the means for prevention
Featured news & research.
NIH Intramural Research Program highlights Dr. Sinha's research on the health effects and cancer risk associated with red meat.

New study investigates the role of common inherited genetic factors in the development of subsequent cancers.
Dr. McGee-Avila led this study using data from the HIV/AIDS Cancer Match Study.
Our Research

Our scientists (epidemiologists, geneticists, biostatisticians, and clinicians) form interdisciplinary teams to study complex questions often in collaboration with scientists around the world.
- What We Study
- Who We Study
- How We Study
- Active Clinical Studies
- Interdisciplinary Working Groups
- Public Health Impact of DCEG Research
Join the DCEG Team

Browse a range of opportunities for every career stage: tenure-eligible senior investigator, staff scientist, postdoctoral fellow, and more.
- Careers at DCEG
- Commitment to Equity & Inclusion
- Apply to Be a Fellow
- Advantages of a DCEG Fellowship
- Meet Current Fellows
- Clinical Investigator Development Program
Research Tools

We have created many tools for study design and planning, analysis, and risk assessment.

Exposure assessment tools and methods developed by DCEG experts to measure exposures for diet and activity, occupation and environment, radiation, and more.
NCIDose is a collection of medical radiation dosimetry tools developed by medical physicists.
Connect with Us
Subscribe to our newsletter, Linkage, published March, July, and November with longer-format articles and summaries of research and staff news from DCEG.

Follow us on LinkedIn for research stories, career and fellowship opportunities, and more.

DCEG sponsors seminars by in-house experts, lectures by visiting scholars, and informal meetings—all on a wide range of scientific topics.

Diversity and Inclusion
DCEG is committed to the recruitment, retention, and development of a diverse group of investigators and trainees.

DCEG Publications
Search a complete library of our published research, including papers in journals not indexed in PubMed and books.
DCEG's Commitment to Training

The Cancer Epidemiology and Prevention program at the Harvard T.H. Chan School of Public Health is one of the first comprehensive academic programs in the world dedicated to the training of cancer epidemiologists.

Prospective and Current Students
News from the school.

Bethany Kotlar, PhD '24, studies how children fare when they're born to incarcerated mothers

Soccer, truffles, and exclamation points: Dean Baccarelli shares his story

Health care transformation in Africa highlighted at conference

COVID, four years in
Research Resources for Cancer Epidemiology and Genomics
The Epidemiology and Genomics Research Program (EGRP) has compiled collections of research tools and resources that are freely available through NCI, other institutes and centers at NIH, as well as NIH-funded research projects and partnering organizations.
Featured Resources
Cancer epidemiology descriptive cohort database.
The Cancer Epidemiology Descriptive Cohort Database (CEDCD) contains information about cohort studies that follow groups of persons over time for cancer incidence, mortality, and other health outcomes.
Automated Self-Administered 24-hour (ASA24®) Dietary Assessment Tool
The Automated Self-Administered 24-hour (ASA24®) Dietary Assessment Tool is a free, web-based tool that enables multiple, automatically coded, self-administered 24-hour diet recalls and/or single or multi-day food records for epidemiologic, intervention, behavioral, or clinical research.
Human Health Exposure Analysis Resource (HHEAR)
HHEAR provides researchers access to high-quality, exposure-assessment services including, state of the art laboratory analysis of biological and environmental samples, statistical analysis, and expert consultation on exposure analysis, study design, and data analysis and interpretation.
Healthy Eating Index (HEI)
The HEI is a scoring metric that can be used to determine overall diet quality, as well as the quality of several dietary components. HEI–2020 is the most recent version of the index for the American population age 2 years and older, and new in 2023 is the HEI-Toddlers-2020, which was created to align with new dietary recommendations for infants and toddlers in the 2020-2025 Dietary Guidelines for Americans .
DNA Sequencing and Genotyping Services
Thirteen institutes at the NIH, including NCI, support a contract with the Center for Inherited Disease Research at The Johns Hopkins University that offers investigators access to next generation sequencing, genotyping, and statistical genetics services at a reduced cost.
Biospecimen Resources for Population Scientists
Biospecimen sharing policies and request forms from population-based studies and potential sources of biospecimens.
Cancer Epidemiology Cohorts
EGRP-supported cancer epidemiology cohorts (CECs), relevant funding opportunities, research resources, and publications.
NCI Cohort Consortium
Details about the NCI Cohort Consortium, a collaborative network of investigators representing cohort studies from around the world.
Cancer Registry Resources
Compilation of resources provides links to information on cancer statistics, such as incidence, mortality, and the prevalence of certain risk factors.
Consortia to Advance Collaboration in Epidemiologic and Cancer Research
National and international research consortia focusing on interdisciplinary and translational research to understand determinants of health in human populations which may influence cancer risk.
Dietary Assessment Resources
Data collection resources and tools, food composition databases, diet analysis tools, surveys and resources for dietary monitoring.
Genomic Summary Results for Cancer Research Studies
Resources for investigators to find and make publicly available genomic summary results data from cancer research studies.
Geospatial Approaches
Resources for interactive mapping, exploring, and downloading, geographically based cancer related information
Physical Activity Research Resources
National surveys, databases, and methodological reviews related to measures of physical activity for use in human research.
Surveillance, Epidemiology and End Results Program, SEER-Medicare datasets, cancer survivor prevalence data, and Cancer Trends Progress Report.
Surveys containing information which may be useful for cancer epidemiology and genomics studies, including behavioral risk factors, health information, medical care, and more.
Video Library
A library of videos created by NCI and featured by the Epidemiology and Genomics Research Program.
Please read our guidelines before visiting Rutgers Cancer Institute. | COVID-19: What Cancer Patients Should Know
Cancer Epidemiology and Health Outcomes
Administration.
LaTasha Maloney (732) 507-3987 [email protected]
Susan Fenker [email protected]
Vanessa Johnson [email protected]
Research Coordinator / Research Teaching Specialists

Graduate Fellows

Post-doctoral Fellow

Carola Sanchez Diaz, PhD [email protected]
Graduate Students
Tina Dharamdasani [email protected]

Medical Students
Internal Medicine Resident
Advertisement
Circulating microRNA signature predicts cancer incidence in Lynch syndrome – a pilot study
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
- Accepted Manuscript March 29 2024
Tero Sievänen , Tiina Jokela , Matti Hyvärinen , Tia-Marje Korhonen , Kirsi Pylvänäinen , Jukka-Pekka Mecklin , Juha Karvanen , Elina Sillanpää , Toni T. Seppälä , Eija K. Laakkonen; Circulating microRNA signature predicts cancer incidence in Lynch syndrome – a pilot study. Cancer Prev Res (Phila) 2024; https://doi.org/10.1158/1940-6207.CAPR-23-0368
Download citation file:
- Ris (Zotero)
- Reference Manager
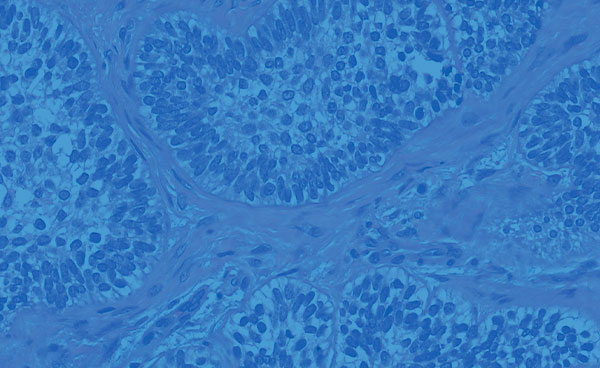
Lynch syndrome (LS) is the most common autosomal dominant cancer syndrome and is characterized by high genetic cancer risk modified by lifestyle factors. This study explored whether a circulating microRNA (c-miR) signature predicts LS cancer incidence within a 4-year prospective surveillance period. To gain insight how lifestyle behavior could affect LS cancer risk, we investigated whether the cancer-predicting c-miR signature correlates with known risk-reducing factors such as physical activity, body mass index (BMI), dietary fiber or non-steroidal anti-inflammatory drug usage. The study included 110 c-miR samples from LS carriers, 18 of whom were diagnosed with cancer during a 4-year prospective surveillance period. Lasso regression was utilized to find c-miRs associated with cancer risk. Individual risk sum derived from the chosen c-miRs was used to develop a model to predict LS cancer incidence. This model was validated using 5-fold cross-validation. Correlation and pathway analyses were applied to inspect biological functions of c-miRs. Pearson correlation was used to examine the associations of c-miR risk sum and lifestyle factors. Hsa-miR-10b-5p, hsa-miR-125b-5p, hsa-miR-200a-3p, hsa-miR-3613-5p and hsa-miR-3615 were identified as cancer predictors by Lasso, and their risk sum score associated with higher likelihood of cancer incidence (HR 2.72, 95% CI 1.64-4.52, C-index=0.72). In cross-validation, the model indicated good concordance with the average C-index of 0.75 (0.6-1.0). Co-regulated hsa-miR-10b-5p, hsa-miR-125b-5p and hsa-miR-200a-3p targeted genes involved in cancer-associated biological pathways. The c-miR risk sum score correlated with BMI (r=0.23, p<0.01). In summary, BMI-associated c-miRs predict LS cancer incidence within four years, although further validation is required.
Article PDF first page preview
Supplementary data.
Figure S1: Schoenfeld residuals of the c-miR risk prediction models. A, Unadjusted c-miR risk sum score prediction model. B, Sex and MMR-variant adjusted c-miR risk sum score prediction model.
Figure S2: STRING database complete gene node map. Edges represent gene-gene associations. Thickness of edges indicates association confidence (www.string-db.org).
Table S1: Missing values for cancer and cancer-free groups.
Table S2: Cancer characteristics.
Table S3: Differentially expressed c-miRs between cancer-free LS carriers and healthy non-carrier controls. Lasso-selected c- miRs used for computing c-miR risk sum score are bolded. SE = standard error, Wald = Wald-test statistic, FDR = False discovery rate.
Table S4: C-miR full model. HR = hazard ratio, 95% CI = 95% confidence interval, b= regression coefficient, SE = standard error, df = degrees of freedom. P significant at 0.05 level.
Table S5: 5-fold cross-validation of c-miR risk sum score models.
Table S6: Model fits in the full MLH1 sample. b = regression coefficient; HR = hazard ratio; 95% CI = 95% confidence interval; P-value = P-value significant at <0.05 level; Full model C-index = Harrel’s concordance (C) index. N = 74 of whom 14 developed cancers during the surveillance.
Table S7: C-miR risk sum score of hsa-let-7e-5p, hsa-miR-10b-5p and hsa-miR-3613-5p in MLH1 sample. Unadjusted and sex- adjusted models. b = regression coefficient; HR = hazard ratio; 95% CI = 95% confidence interval; P-value = P-value significant at <0.05 level; Full model C-index = Harrel’s concordance (C) index. N = 74 of whom 14 developed cancers during the surveillance
Table S8: 5-fold cross-validated MLH1 c-miR risk sum score model.
Table S9: Model fits in the full CRC sample. b = regression coefficient; HR = hazard ratio; 95% CI = 95% confidence interval; P- value = P-value significant at <0.05 level; Full model C-index = Harrel’s concordance (C) index. N = 101 of whom 9 developed CRC during the surveillance.
Table S10: C-miR risk sum score in CRC samples. Unadjusted and sex and MMR-variant adjusted models. b = regression coefficient; HR = hazard ratio; 95% CI = 95% confidence interval; P-value = P-value significant at <0.05 level; Full model C- index = Harrel’s concordance (C) index. N = 74 of whom 14 developed cancers during the surveillance.
Table S11: 5-fold cross-validated CRC c-miR risk sum score model.
Table S12: The experimentally verified c-miR risk sum target genes from miRTarBase.
Table S13: The significantly enriched Reactome pathways. FDR = False discovery rate.
Table S14: Pearson correlations of c-miR risk sum score and physical activity, BMI, dietary fiber consumption, NSAID usage and age in the complete-case analysis. Lifestyle data was collected in 2017 or 2020 with a questionnaire. Blood sample was taken at regular colonoscopy visit between 2018 and 2020. The average time-period between lifestyle data collection and blood sample was 2.0 (0.3-3.9) years.
Methods S1: This code supplementary file was used to perform the differential expression analysis as well as to develop the c-miR cancer risk prediction model described in the manuscript.
Citing articles via
Email alerts.
- Online First
- Online ISSN 1940-6215
- Print ISSN 1940-6207
AACR Journals
- Blood Cancer Discovery
- Cancer Discovery
- Cancer Epidemiology, Biomarkers & Prevention
- Cancer Immunology Research
- Cancer Prevention Research
- Cancer Research
- Cancer Research Communications
- Clinical Cancer Research
- Molecular Cancer Research
- Molecular Cancer Therapeutics
- Info for Advertisers
- Information for Institutions/Librarians
- Privacy Policy
- Copyright © 2023 by the American Association for Cancer Research.
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 28 March 2024
Global epidemiology of epithelial ovarian cancer
- Penelope M. Webb ORCID: orcid.org/0000-0003-0733-5930 1 , 2 &
- Susan J. Jordan ORCID: orcid.org/0000-0002-4566-1414 2
Nature Reviews Clinical Oncology ( 2024 ) Cite this article
3 Altmetric
Metrics details
- Epidemiology
- Ovarian cancer
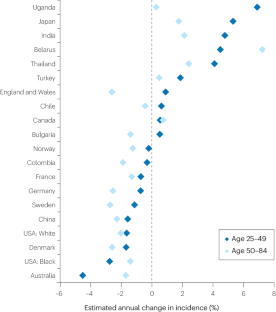
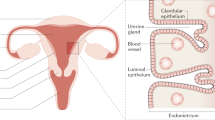
- Risk factors
Globally, ovarian cancer is the eighth most common cancer in women, accounting for an estimated 3.7% of cases and 4.7% of cancer deaths in 2020. Until the early 2000s, age-standardized incidence was highest in northern Europe and North America, but this trend has changed; incidence is now declining in these regions and increasing in parts of eastern Europe and Asia. Ovarian cancer is a very heterogeneous disease and, even among the most common type, namely epithelial ovarian cancer, five major clinically and genetically distinct histotypes exist. Most high-grade serous ovarian carcinomas are now recognized to originate in the fimbrial ends of the fallopian tube. This knowledge has led to more cancers being coded as fallopian tube in origin, which probably explains some of the apparent declines in ovarian cancer incidence, particularly in high-income countries; however, it also suggests that opportunistic salpingectomy offers an important opportunity for prevention. The five histotypes share several reproductive and hormonal risk factors, although differences also exist. In this Review, we summarize the epidemiology of this complex disease, comparing the different histotypes, and consider the potential for prevention. We also discuss how changes in the prevalence of risk and protective factors might have contributed to the observed changes in incidence and what this might mean for incidence in the future.
The disease we call ‘ovarian’ cancer encompasses a wide range of tumour types, including cancers that arise in the fallopian tube; changes in coding and reporting make incidence trends over the past decade difficult to interpret.
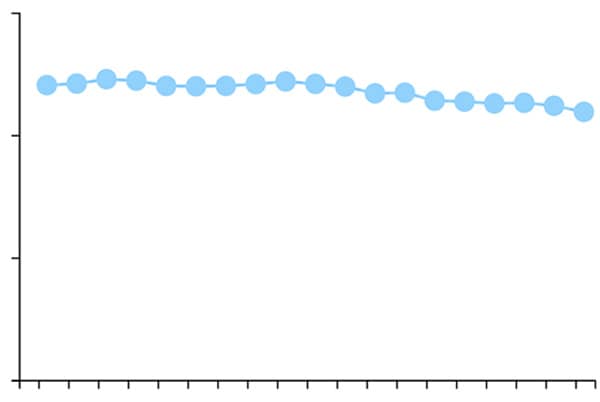
Between 1920 and 1960, successive birth cohorts had lower risk of developing ovarian cancer, although incidence might be increasing again in women born after about 1970.
With the recognition that high-grade serous cancers originate in the fallopian tube, salpingectomy (opportunistic or targeted) offers the opportunity for prevention and could delay the need for oophorectomy among women with a high genetic risk.
Hormonally related factors, including pregnancy, oral contraceptive use and breastfeeding, reduce the risk of ovarian cancer, particularly the endometrioid and clear cell histotypes; the benefits of newer contraceptive formulations are less clear.
Lifestyle exposures, including smoking, obesity and, potentially, sedentary behaviour or inactivity, all increase the risk of a woman developing the less common histotypes but do not appear to affect the risk of developing the most common high-grade serous cancers.
If current trends continue, the incidence of ovarian cancer might start to increase, although widespread uptake of salpingectomy and expanded identification and interventions targeting BRCA mutation carriers have the potential to reduce incidence.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Natural history of ovarian high-grade serous carcinoma from time effects of ovulation inhibition and progesterone clearance of p53-defective lesions
Na-Yi Yuan Wu, Chao Fang, … Tang-Yuan Chu
Endometrial cancer
Vicky Makker, Helen MacKay, … Ana Oaknin

The molecular origin and taxonomy of mucinous ovarian carcinoma
Dane Cheasley, Matthew J. Wakefield, … Kylie L. Gorringe
McCluggage, W. G., Singh, N. & Gilks, C. B. Key changes to the World Health Organization (WHO) classification of female genital tumours introduced in the 5th edition (2020). Histopathology 80 , 762–778 (2022).
Article PubMed Google Scholar
Shih, I. M., Wang, Y. & Wang, T. L. The origin of ovarian cancer species and precancerous landscape. Am. J. Pathol. 191 , 26–39 (2021).
Article CAS PubMed PubMed Central Google Scholar
Cheasley, D. et al. The molecular origin and taxonomy of mucinous ovarian carcinoma. Nat. Commun. 10 , 3935 (2019).
Article PubMed PubMed Central Google Scholar
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71 , 209–249 (2021).
Webb, P. M., Green, A. C. & Jordan, S. J. Trends in hormone use and ovarian cancer incidence in US white and Australian women: implications for the future. Cancer Causes Control. 28 , 365–370 (2017).
Cabasag, C. J. et al. The influence of birth cohort and calendar period on global trends in ovarian cancer incidence. Int. J. Cancer 146 , 749–758 (2020).
Article CAS PubMed Google Scholar
Ervik, M., Lam, F., Laversanne, M., Ferlay, J. & Bray, F. Global Cancer Observatory: Cancer Over Time https://gco.iarc.fr/overtime (2021).
GBD 2019 Cancer Risk Factors Collaborators. The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 400 , 563–591 (2022).
Article Google Scholar
Long Roche, K. C., Abu-Rustum, N. R., Nourmoussavi, M. & Zivanovic, O. Risk-reducing salpingectomy: let us be opportunistic. Cancer 123 , 1714–1720 (2017).
Nitschke, A. S., do Valle, H. A., Dawson, L., Kwon, J. S. & Hanley, G. E. Long-term non-cancer risks in people with BRCA mutations following risk-reducing bilateral salpingo-oophorectomy and the role of hormone replacement therapy: a review. Cancers 15 , 711 (2023).
Yoon, S. H., Kim, S. N., Shim, S. H., Kang, S. B. & Lee, S. J. Bilateral salpingectomy can reduce the risk of ovarian cancer in the general population: a meta-analysis. Eur. J. Cancer 55 , 38–46 (2016).
Chen, Y., Du, H., Bao, L. & Liu, W. Opportunistic salpingectomy at benign gynecological surgery for reducing ovarian cancer risk: a 10-year single centre experience from China and a literature review. J. Cancer 9 , 141–147 (2018).
Hanley, G. E. et al. Outcomes from opportunistic salpingectomy for ovarian cancer prevention. JAMA Netw. Open 5 , e2147343 (2022).
Darelius, A., Kristjansdottir, B., Dahm-Kahler, P. & Strandell, A. Risk of epithelial ovarian cancer type I and II after hysterectomy, salpingectomy and tubal ligation — a nationwide case-control study. Int. J. Cancer 149 , 1544–1552 (2021).
Duus, A. H., Zheng, G., Baandrup, L., Faber, M. T. & Kjaer, S. K. Risk of ovarian cancer after salpingectomy and tubal ligation: prospects on histology and time since the procedure. Gynecol. Oncol. 177 , 125–131 (2023).
Leblanc, E. et al. Prophylactic radical fimbriectomy with delayed oophorectomy in women with a high risk of developing an ovarian carcinoma: results of a prospective national pilot study. Cancers 15 , 1141 (2023).
Webb, P. M. & Jordan, S. J. Epidemiology of epithelial ovarian cancer. Best Pract. Res. Clin. Obstet. Gynaecol. 41 , 3–14 (2017).
Peres, L. C. et al. Racial/ethnic differences in the epidemiology of ovarian cancer: a pooled analysis of 12 case-control studies. Int. J. Epidemiol. 47 , 460–472 (2018).
Jervis, S. et al. Ovarian cancer familial relative risks by tumour subtypes and by known ovarian cancer genetic susceptibility variants. J. Med. Genet. 51 , 108–113 (2014).
Flaum, N., Crosbie, E. J., Edmondson, R. J., Smith, M. J. & Evans, D. G. Epithelial ovarian cancer risk: a review of the current genetic landscape. Clin. Genet. 97 , 54–63 (2020).
Norquist, B. M. et al. Inherited mutations in women with ovarian carcinoma. JAMA Oncol. 2 , 482–490 (2016).
Phelan, C. M. et al. Identification of 12 new susceptibility loci for different histotypes of epithelial ovarian cancer. Nat. Genet. 49 , 680–691 (2017).
Setiawan, V. W. et al. Type I and II endometrial cancers: have they different risk factors? J. Clin. Oncol. 31 , 2607–2618 (2013).
Gong, T. T., Wu, Q. J., Vogtmann, E., Lin, B. & Wang, Y. L. Age at menarche and risk of ovarian cancer: a meta-analysis of epidemiological studies. Int. J. Cancer 132 , 2894–2900 (2013).
Wentzensen, N. et al. Ovarian cancer risk factors by histologic subtype: an analysis from the ovarian cancer cohort consortium. J. Clin. Oncol. 34 , 2888–2898 (2016).
Yarmolinsky, J. et al. Appraising the role of previously reported risk factors in epithelial ovarian cancer risk: a Mendelian randomization analysis. PLoS Med. 16 , e1002893 (2019).
Yang, H. et al. Age at menarche and epithelial ovarian cancer risk: a meta-analysis and Mendelian randomization study. Cancer Med. 8 , 4012–4022 (2019).
Fu, Z. et al. Lifetime ovulatory years and risk of epithelial ovarian cancer: a multinational pooled analysis. J. Natl Cancer Inst. 115 , 539–551 (2023).
Husby, A., Wohlfahrt, J. & Melbye, M. Pregnancy duration and ovarian cancer risk: a 50-year nationwide cohort study. Int. J. Cancer 151 , 1717–1725 (2022).
Wu, Y., Sun, W., Xin, X., Wang, W. & Zhang, D. Age at last birth and risk of developing epithelial ovarian cancer: a meta-analysis. Biosci. Rep. 39 , BSR20182035 (2019).
Lee, A. W. et al. Expanding our understanding of ovarian cancer risk: the role of incomplete pregnancies. J. Natl Cancer Inst. 113 , 301–308 (2021).
World Cancer Research Fund/American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective (World Cancer Research Fund International, 2018).
Gaitskell, K. et al. Histological subtypes of ovarian cancer associated with parity and breastfeeding in the prospective Million Women Study. Int. J. Cancer 142 , 281–289 (2018).
Babic, A. et al. Association between breastfeeding and ovarian cancer risk. JAMA Oncol. 6 , e200421 (2020).
Kotsopoulos, J. et al. Breastfeeding and the risk of epithelial ovarian cancer among women with a BRCA1 or BRCA2 mutation. Gynecol. Oncol. 159 , 820–826 (2020).
Barcroft, J. F. et al. Fertility treatment and cancers-the eternal conundrum: a systematic review and meta-analysis. Hum. Reprod. 36 , 1093–1107 (2021).
Lerner-Geva, L. et al. Subfertility, use of fertility treatments and BRCA mutation status and the risk of ovarian cancer. Arch. Gynecol. Obstet. 306 , 209–217 (2022).
Dixon-Suen, S. C. et al. The association between hysterectomy and ovarian cancer risk: a population-based record-linkage study. J. Natl Cancer Inst. 111 , 1097–1103 (2019).
Khoja, L. et al. Endometriosis and menopausal hormone therapy impact the hysterectomy-ovarian cancer association. Gynecol. Oncol. 164 , 195–201 (2022).
Ring, L. L. et al. Hysterectomy and risk of epithelial ovarian cancer by histologic type, endometriosis, and menopausal hormone therapy. Cancer Epidemiol. 84 , 102359 (2023).
Taylor, J. A. et al. Association of hysterectomy and invasive epithelial ovarian and tubal cancer: a cohort study within UKCTOCS. Br. J. Obstet. Gynecol. 129 , 110–118 (2022).
Article CAS Google Scholar
Sieh, W. et al. Tubal ligation and risk of ovarian cancer subtypes: a pooled analysis of case-control studies. Int. J. Epidemiol. 42 , 579–589 (2013).
Collaborative Group on Epidemiological Studies of Ovarian Cancer et al. Ovarian cancer and oral contraceptives: collaborative reanalysis of data from 45 epidemiological studies including 23,257 women with ovarian cancer and 87,303 controls. Lancet 371 , 303–314 (2008).
Moorman, P. G. et al. Reproductive factors and ovarian cancer risk in African-American women. Ann. Epidemiol. 26 , 654–662 (2016).
Sarink, D. et al. Racial/ethnic differences in ovarian cancer risk: results from the multiethnic cohort study. Cancer Epidemiol. Biomark. Prev. 29 , 2019–2025 (2020).
Schrijver, L. H. et al. Oral contraceptive use and ovarian cancer risk for BRCA1/2 mutation carriers: an international cohort study. Am. J. Obstet. Gynecol. 225 , 51.e1–51.e17 (2021).
Xia, Y. Y. et al. Contraceptive use and the risk of ovarian cancer among women with a BRCA1 or BRCA2 mutation. Gynecol. Oncol. 164 , 514–521 (2022).
van Bommel, M. H. D. et al. Contraceptives and cancer risks in BRCA1/2 pathogenic variant carriers: a systematic review and meta-analysis. Hum. Reprod. Update 29 , 197–217 (2023).
Shafrir, A. L. et al. A prospective cohort study of oral contraceptive use and ovarian cancer among women in the United States born from 1947 to 1964. Cancer Causes Control. 28 , 371–383 (2017).
Iversen, L. et al. Association between contemporary hormonal contraception and ovarian cancer in women of reproductive age in Denmark: prospective, nationwide cohort study. Br. Med. J. 362 , k3609 (2018).
Haakenstad, A. et al. Measuring contraceptive method mix, prevalence, and demand satisfied by age and marital status in 204 countries and territories, 1970-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 400 , 295–327 (2022).
Balayla, J., Gil, Y., Lasry, A. & Mitric, C. Ever-use of the intra-uterine device and the risk of ovarian cancer. J. Obstet. Gynaecol. 41 , 848–853 (2021).
Phung, M. T. et al. Depot-medroxyprogesterone acetate use is associated with decreased risk of ovarian cancer: the mounting evidence of a protective role of progestins. Cancer Epidemiol. Biomark. Prev. 30 , 927–935 (2021).
Faber, M. T. et al. Oral contraceptive use and impact of cumulative intake of estrogen and progestin on risk of ovarian cancer. Cancer Causes Control. 24 , 2197–2206 (2013).
Collaborative Group on Epidemiological Studies of Ovarian Cancer et al. Menopausal hormone use and ovarian cancer risk: individual participant meta-analysis of 52 epidemiological studies. Lancet 385 , 1835–1842 (2015).
Article PubMed Central Google Scholar
Pearce, C. L., Chung, K., Pike, M. C. & Wu, A. H. Increased ovarian cancer risk associated with menopausal estrogen therapy is reduced by adding a progestin. Cancer 115 , 531–539 (2009).
Lee, A. W. et al. Estrogen plus progestin hormone therapy and ovarian cancer: a complicated relationship explored. Epidemiology 31 , 402–408 (2020).
Fournier, A. et al. Use of menopausal hormone therapy and ovarian cancer risk in a French cohort study. J. Natl Cancer Inst. 115 , 671–679 (2023).
Phung, M. T. et al. Effects of risk factors for ovarian cancer in women with and without endometriosis. Fertil. Steril. 118 , 960–969 (2022).
Tsilidis, K. K. et al. Menopausal hormone therapy and risk of ovarian cancer in the European prospective investigation into cancer and nutrition. Cancer Causes Control. 22 , 1075–1084 (2011).
Lokkegaard, E. C. L. & Morch, L. S. Tibolone and risk of gynecological hormone sensitive cancer. Int. J. Cancer 142 , 2435–2440 (2018).
Yuk, J. S. & Kim, M. Effects of menopausal hormone therapy on the risk of ovarian cancer: health insurance database in South Korea-based cohort study. Menopause 30 , 490–496 (2023).
Neven, P. et al. The effect of raloxifene on the incidence of ovarian cancer in postmenopausal women. Gynecol. Oncol. 85 , 388–390 (2002).
Tuesley, K. M. et al. Nitrogen-based bisphosphonate use and ovarian cancer risk in women aged 50 years and older. J. Natl Cancer Inst. 114 , 878–884 (2022).
Kvaskoff, M. et al. Endometriosis and cancer: a systematic review and meta-analysis. Hum. Reprod. Update 27 , 393–420 (2020).
Harris, H. R. et al. Racial differences in the association of endometriosis and uterine leiomyomas with the risk of ovarian cancer. Obstet. Gynecol. 141 , 1124–1138 (2023).
Gersekowski, K. et al. Folate intake and ovarian cancer risk among women with endometriosis: a case-control study from the Ovarian Cancer Association Consortium. Cancer Epidemiol. Biomark. Prev. 32 , 1087–1096 (2023).
Harris, H. R. et al. Polycystic ovary syndrome, oligomenorrhea, and risk of ovarian cancer histotypes: evidence from the Ovarian Cancer Association Consortium. Cancer Epidemiol. Biomark. 27 , 174–182 (2018).
Harris, H. R. et al. Association between genetically predicted polycystic ovary syndrome and ovarian cancer: a Mendelian randomization study. Int. J. Epidemiol. 48 , 822–830 (2019).
Frandsen, C. L. B. et al. Risk of epithelial ovarian tumors among women with polycystic ovary syndrome: a nationwide population-based cohort study. Int. J. Cancer 153 , 958–968 (2023).
Yin, W., Falconer, H., Yin, L., Xu, L. & Ye, W. Association between polycystic ovary syndrome and cancer risk. JAMA Oncol. 5 , 106–107 (2019).
Rasmussen, C. B. et al. Pelvic inflammatory disease and the risk of ovarian cancer and borderline ovarian tumors: a pooled analysis of 13 case-control studies. Am. J. Epidemiol. 185 , 8–20 (2017).
Stewart, L. M. et al. Risk of high-grade serous ovarian cancer associated with pelvic inflammatory disease, parity and breast cancer. Cancer Epidemiol. 55 , 110–116 (2018).
Falconer, H., Yin, L., Salehi, S. & Altman, D. Association between pelvic inflammatory disease and subsequent salpingectomy on the risk for ovarian cancer. Eur. J. Cancer 145 , 38–43 (2021).
Jonsson, S., Jonsson, H., Lundin, E., Haggstrom, C. & Idahl, A. Pelvic inflammatory disease and risk of epithelial ovarian cancer. A national population-based case-control study in Sweden. Am. J. Obstet. Gynecol. 230 , 75.e1–75.e15 (2023).
Trabert, B. et al. Antibodies against Chlamydia trachomatis and ovarian cancer risk in two independent populations. J. Natl Cancer Inst. 111 , 129–136 (2019).
Fortner, R. T. et al. Sexually transmitted infections and risk of epithelial ovarian cancer: results from the Nurses’ Health Studies. Br. J. Cancer 120 , 855–860 (2019).
Idahl, A. et al. Serologic markers of Chlamydia trachomatis and other sexually transmitted infections and subsequent ovarian cancer risk: results from the EPIC cohort. Int. J. Cancer 147 , 2042–2052 (2020).
Wang, L. H., Zhong, L., Xu, B., Chen, M. & Huang, H. X. Diabetes mellitus and the risk of ovarian cancer: a systematic review and meta-analysis of cohort and case-control studies. BMJ Open 10 , e040137 (2020).
Saarela, K., Tuomilehto, J., Sund, R., Keskimäki, I. & Hartikainen, S. Cancer incidence among Finnish people with type 2 diabetes during 1989–2014. Eur. J. Epidemiol. 34 , 259–265 (2019).
Yuan, S. et al. Is type 2 diabetes causally associated with cancer risk? evidence from a two-sample mendelian randomization study. Diabetes 69 , 1588–1596 (2020).
Pearson-Stuttard, J. et al. Type 2 diabetes and cancer: an umbrella review of observational and mendelian randomization studies. Cancer Epidemiol. Biomark. Prev. 30 , 1218–1228 (2021).
Urpilainen, E., Puistola, U., Boussios, S. & Karihtala, P. Metformin and ovarian cancer: the evidence. Ann. Transl. Med. 8 , 1711 (2020).
Hurwitz, L. M. et al. Association of frequent aspirin use with ovarian cancer risk according to genetic susceptibility. JAMA Netw. Open 6 , e230666 (2023).
Baandrup, L., Kjaer, S. K., Olsen, J. H., Dehlendorff, C. & Friis, S. Low-dose aspirin use and the risk of ovarian cancer in Denmark. Ann. Oncol. 26 , 787–792 (2015).
Hurwitz, L. M. et al. Modification of the association between frequent aspirin use and ovarian cancer risk: a meta-analysis using individual-level data from two ovarian cancer consortia. J. Clin. Oncol. 40 , 4207–4217 (2022).
Trabert, B. et al. Analgesic use and ovarian cancer risk: an analysis in the ovarian cancer cohort consortium. J. Natl Cancer Inst. 111 , 137–145 (2019).
Zeleznik, O. A., Irvin, S. R., Samimi, G. & Trabert, B. The role of statins in the prevention of ovarian and endometrial cancers. Cancer Prev. Res. 16 , 191–197 (2023).
Yarmolinsky, J. et al. Association between genetically proxied inhibition of HMG-CoA reductase and epithelial ovarian cancer. J. Am. Med. Assoc. 323 , 646–655 (2020).
Tuesley, K. M. et al. Association between antihypertensive medicine use and risk of ovarian cancer in women aged 50 years and older. Cancer Epidemiol. 86 , 102444 (2023).
Zhuang, Y. J. et al. The incidence risk of breast and gynecological cancer by antidepressant use: a systematic review and dose-response meta-analysis of epidemiological studies involving 160,727 patients. Front. Oncol. 12 , 939636 (2022).
Lauby-Secretan, B. et al. Body fatness and cancer — viewpoint of the IARC Working Group. N. Engl. J. Med. 375 , 794–798 (2016).
Dixon, S. C. et al. Adult body mass index and risk of ovarian cancer by subtype: a Mendelian randomization study. Int. J. Epidemiol. 45 , 884–895 (2016).
Friedenreich, C. M., Ryder-Burbidge, C. & McNeil, J. Physical activity, obesity and sedentary behavior in cancer etiology: epidemiologic evidence and biologic mechanisms. Mol. Oncol. 15 , 790–800 (2021).
Vithayathil, M. et al. Body size and composition and risk of site-specific cancers in the UK Biobank and large international consortia: a Mendelian randomisation study. PLoS Med. 18 , e1003706 (2021).
Olsen, C. M. et al. Obesity and risk of ovarian cancer subtypes: evidence from the Ovarian Cancer Association Consortium. Endocr. Relat. Cancer 20 , 251–262 (2013).
Aarestrup, J. et al. Childhood overweight, tallness, and growth increase risks of ovarian cancer. Cancer Epidemiol. Biomark. Prev. 28 , 183–188 (2019).
Schauer, D. P. et al. Bariatric surgery and the risk of cancer in a large multisite cohort. Ann. Surg. 269 , 95–101 (2019).
Cannioto, R. et al. Chronic recreational physical inactivity and epithelial ovarian cancer risk: evidence from the Ovarian Cancer Association Consortium. Cancer Epidemiol. Biomark. Prev. 25 , 1114–1124 (2016).
McTiernan, A. et al. Physical activity in cancer prevention and survival: a systematic review. Med. Sci. Sports Exerc. 51 , 1252–1261 (2019).
Biller, V. S. et al. Sedentary behaviour in relation to ovarian cancer risk: a systematic review and meta-analysis. Eur. J. Epidemiol. 36 , 769–780 (2021).
Chen, J. W. et al. Genetic associations of leisure sedentary behaviors and the risk of 15 site-specific cancers: a Mendelian randomization study. Cancer Med. 12 , 13623–13636 (2023).
Collaborative Group on Epidemiological Studies of Ovarian Cancer. Ovarian cancer and body size: individual participant meta-analysis including 25157 women with ovarian cancer from 47 epidemiological studies. PLoS Med. 9 , e1001200 (2012).
Faber, M. T. et al. Cigarette smoking and risk of ovarian cancer: a pooled analysis of 21 case-control studies. Cancer Causes Control. 24 , 989–1004 (2013).
Baron, J. A., Nichols, H. B., Anderson, C. & Safe, S. Cigarette smoking and estrogen-related cancer. Cancer Epidemiol. Biomark. Prev. 30 , 1462–1471 (2021).
Ko, K. P. et al. The association between smoking and cancer incidence in BRCA1 and BRCA2 mutation carriers. Int. J. Cancer 142 , 2263–2272 (2018).
Gersekowski, K. et al. Risk factors for ovarian cancer by BRCA status: a collaborative case-only analysis. Cancer Epidemiol. Biomark. Prev. https://doi.org/10.1158/1055-9965.EPI-23-0984 (2024).
Endogenous Hormones Breast Cancer Collaborative Group et al. Circulating sex hormones and breast cancer risk factors in postmenopausal women: reanalysis of 13 studies. Br. J. Cancer 105 , 709–722 (2011).
Larsson, S. C. et al. Smoking, alcohol consumption, and cancer: a mendelian randomisation study in UK Biobank and international genetic consortia participants. PLoS Med. 17 , e1003178 (2020).
Ong, J. S. et al. Association between coffee consumption and overall risk of being diagnosed with or dying from cancer among >300 000 UK Biobank participants in a large-scale Mendelian randomization study. Int. J. Epidemiol. 48 , 1447–1456 (2019).
Yang, C. S., Wang, X., Lu, G. & Picinich, S. C. Cancer prevention by tea: animal studies, molecular mechanisms and human relevance. Nat. Rev. Cancer 9 , 429–439 (2009).
Byrd, D. A. et al. Development and validation of novel dietary and lifestyle inflammation scores. J. Nutr. 149 , 2206–2218 (2019).
Yang, J. et al. Dietary inflammatory index and ovarian cancer risk: a meta-analysis. Nutr. Cancer 74 , 796–805 (2022).
Vojdeman, F. J. et al. Vitamin D levels and cancer incidence in 217,244 individuals from primary health care in Denmark. Int. J. Cancer 145 , 338–346 (2019).
Keum, N., Lee, D. H., Greenwood, D. C., Manson, J. E. & Giovannucci, E. Vitamin D supplementation and total cancer incidence and mortality: a meta-analysis of randomized controlled trials. Ann. Oncol. 30 , 733–743 (2019).
Ong, J. S. et al. A comprehensive re-assessment of the association between vitamin D and cancer susceptibility using Mendelian randomization. Nat. Commun. 12 , 246 (2021).
Wentzensen, N. & O’Brien, K. M. Talc, body powder, and ovarian cancer: a summary of the epidemiologic evidence. Gynecol. Oncol. 163 , 199–208 (2021).
O’Brien, K. M. et al. Association of powder use in the genital area with risk of ovarian cancer. J. Am. Med. Assoc. 323 , 49–59 (2020).
Utada, M. et al. Radiation risk of ovarian cancer in atomic bomb survivors: 1958-2009. Radiat. Res. 195 , 60–65 (2021).
CAS PubMed PubMed Central Google Scholar
Leung, L. et al. Shift work patterns, chronotype, and epithelial ovarian cancer risk. Cancer Epidemiol. Biomark. Prev. 28 , 987–995 (2019).
Liang, X. et al. Sleep characteristics and risk of ovarian cancer among postmenopausal women. Cancer Prev. Res. 14 , 55–64 (2021).
Nash, Z. & Menon, U. Ovarian cancer screening: current status and future directions. Best Pract. Res. Clin. Obstet. Gynaecol. 65 , 32–45 (2020).
Naumann, R. W., Hughes, B. N., Brown, J., Drury, L. K. & Herzog, T. J. The impact of opportunistic salpingectomy on ovarian cancer mortality and healthcare costs: a call for universal insurance coverage. Am. J. Obstet. Gynecol. 225 , 397.e391–397.e6 (2021).
Idahl, A., Darelius, A., Sundfeldt, K., Palsson, M. & Strandell, A. Hysterectomy and opportunistic salpingectomy (HOPPSA): study protocol for a register-based randomized controlled trial. Trials 20 , 10 (2019).
Steenbeek, M. P. et al. TUBectomy with delayed oophorectomy as an alternative to risk-reducing salpingo-oophorectomy in high-risk women to assess the safety of prevention: the TUBA-WISP II study protocol. Int. J. Gynecol. Cancer 33 , 982–987 (2023).
Huh, W. et al. NRG-CC008: a nonrandomized prospective clinical trial comparing the non-inferiority of salpingectomy to salpingo-oophorectomy to reduce the risk of ovarian cancer among BRCA1 carriers [SOROCk]. J. Clin. Oncol. 60 , https://doi.org/10.1200/JCO.2022.40.16_suppl.TPS106 (2022).
Evans, O., Gaba, F. & Manchanda, R. Population-based genetic testing for women’s cancer prevention. Best Pract. Res. Clin. Obstet. Gynaecol. 65 , 139–153 (2020).
Alsop, K. et al. BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: a report from the Australian Ovarian Cancer Study Group. J. Clin. Oncol. 30 , 2654–2663 (2012).
Konstantinopoulos, P. A. et al. Germline and somatic tumor testing in epithelial ovarian cancer: ASCO guideline. J. Clin. Oncol. 38 , 1222–1245 (2020).
Samimi, G. et al. Traceback: a proposed framework to increase identification and genetic counseling of BRCA1 and BRCA2 mutation carriers through family-based outreach. J. Clin. Oncol. 35 , 2329–2337 (2017).
Brown, K. F. et al. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br. J. Cancer 118 , 1130–1141 (2018).
Jordan, S. J. et al. Cancers in Australia in 2010 attributable to total breastfeeding durations of 12 months or less by parous women. Aust. N. Z. J. Public Health 39 , 418–421 (2015).
ClinicalTrials.gov. US National Library of Medicine https://clinicaltrials.gov/study/NCT03480776 (2023).
Appiah, D., Nwabuo, C. C., Ebong, I. A., Wellons, M. F. & Winters, S. J. Trends in age at natural menopause and reproductive life span among US women, 1959-2018. J. Am. Med. Assoc. 325 , 1328–1330 (2021).
Cheng, H. et al. Global trends in total fertility rate and its relation to national wealth, life expectancy and female education. BMC Public Health 22 , 1346 (2022).
Boutari, C. & Mantzoros, C. S. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism 133 , 155217 (2022).
Kurman, R., Carcangiu, M., Herrington, C. & Young, R. WHO Classification of Tumours. Female Reproductive Organs (IARC, 2014).
Surveillance Epidemiology and End Results (SEER) Program ( www.seer.cancer.gov ) SEER*Stat Database: Incidence — SEER Research Plus Data with Delay-Adjustment, 17 Registries, Malignant Only, Nov 2022 Sub (2000-2020) — Linked To County Attributes — Total U.S., 1969-2021 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2023, based on the November 2022 submission (accessed 2023).
Australian Institute of Health and Welfare (AIHW). Cancer Data in Australia https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/ (2023).
Larønningen, S. et al. NORDCAN: Cancer Incidence, Mortality, Prevalence and Survival in the Nordic Countries, Version 9.3 (02.10.2023). Association of the Nordic Cancer Registries. Cancer Registry of Norway. Available from : https://nordcan.iarc.fr/ , (accessed 22 October 2023).
Rosenberg, P. S., Check, D. P. & Anderson, W. F. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol. Biomark. Prev. 23 , 2296–2302 (2014).
The US National Cancer Institute. Site Recode ICD-O-3 2023 Revision Expanded Definition https://seer.cancer.gov/siterecode/icdo3_2023_expanded/ (2024).
WHO Classification of Tumours Editorial Board. World Health Organization Classification of Female Genital Tumours . 5 th Edition (IARC Press, 2020).
McCluggage, W. G., Hirschowitz, L., Gilks, C. B., Wilkinson, N. & Singh, N. The fallopian tube origin and primary site assignment in extrauterine high-grade serous carcinoma: findings of a survey of pathologists and clinicians. Int. J. Gynecol. Pathol. 36 , 230–239 (2017).
McCluggage, W. G. Progress in the pathological arena of gynecological cancers. Int. J. Gynaecol. Obstet. 155 , 107–114 (2021).
Cancer Research UK. Ovarian Cancer Incidence Statistics https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/ovarian-cancer/incidence#collapseTwo (2024).
National Cancer Institute (NCI). Cancer Stat Facts: Ovarian Cancer . https://seer.cancer.gov/statfacts/html/ovary.html (accessed 31 January 2024).
Global Burden of Disease Cancer Collaboration et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 8 , 420–444 (2022).
Download references
Author information
Authors and affiliations.
Population Health Program, QIMR Berghofer Medical Research Institute, Brisbane, Queensland, Australia
Penelope M. Webb
School of Public Health, The University of Queensland, Herston, Queensland, Australia
Penelope M. Webb & Susan J. Jordan
You can also search for this author in PubMed Google Scholar
Contributions
Both authors made a substantial contribution to all aspects of the preparation of this manuscript.
Corresponding author
Correspondence to Penelope M. Webb .
Ethics declarations
Competing interests.
P.M.W. has received speaker’s fees and research funding from AstraZeneca. S.J.J. declares no competing interests.
Peer review
Peer review information.
Nature Reviews Clinical Oncology thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Webb, P.M., Jordan, S.J. Global epidemiology of epithelial ovarian cancer. Nat Rev Clin Oncol (2024). https://doi.org/10.1038/s41571-024-00881-3
Download citation
Accepted : 04 March 2024
Published : 28 March 2024
DOI : https://doi.org/10.1038/s41571-024-00881-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Cancer Data and Statistics
This video highlights the features of U.S. Cancer Statistics, the official federal cancer statistics.
In the United States in 2020, 1,603,844 new cancer cases were reported and 602,347 people died of cancer. For every 100,000 people, 403 new cancer cases were reported and 144 people died of cancer. 2020 is the latest year for which incidence data are available.
The United States Cancer Statistics (USCS) are the official federal cancer statistics. They come from combined cancer registry data collected by CDC’s National Program of Cancer Registries and the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program. These data are used to understand cancer burden and trends, support cancer research, measure progress in cancer control and prevention efforts, target action on eliminating disparities, and improve cancer outcomes for all.
Data Visualizations Tool
The Data Visualizations tool makes it easy for anyone to explore and use the latest official federal government cancer data from USCS. It includes the latest cancer data covering the U.S. population.
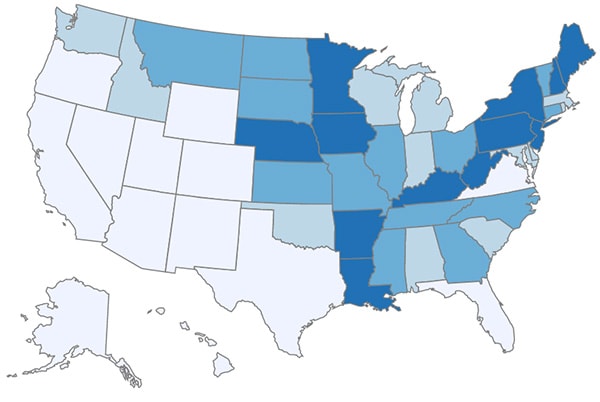
See rates of new cancers or cancer deaths for the entire United States and individual states for common cancers. Also, see the top 10 cancers for men and women.
See rates or numbers of new cancers or cancer deaths by race/ethnicity, sex, and age group for all cancers combined or for common cancers.
See how the rates of new cancers or cancer deaths changed over time for the entire United States and individual states, for all cancers combined or for common cancers.
USCS Public Use Databases
Researchers can access and analyze high-quality population-based cancer incidence data on the entire United States population. De-identified cancer incidence data are available to researchers for free in public use databases.

Tools that provide various statistics about cancer, as well as databases available to researchers.

Other sources of cancer data for the United States and worldwide.
Stay Informed
Exit notification / disclaimer policy.
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Cancer Topics
- Research Branches
- Research Teams
- Knowledge Transfer
- Research Project Websites
- International Research Collaborations
- Useful Links
- Press Releases
- Featured News
- Videos and Podcasts
- Infographics and Photos
- Questions and Answers
- Publications
- Scientific Meetings and Lectures
- IARC Seminar Series
- IARC/NCI Tumour Seminars
- Medals of Honour
- Professional Staff
- General service Staff
- Talent Pools
- Visiting Scientist and Postdoctoral Opportunities
- Postdoctoral Fellowships
- Call for Tenders
- Office of the Director
- Organization and Management
- Supporters and Friends
- IARC Newsletter
- Visitor Information
- Terms of use
- Privacy Policy
- iarc newsletter
IARC Publications – Cancer Epidemiology: Principles and Methods
Published in section: IARC News
Publication date: 18 May, 2009, 0:00
Direct link: https://www.iarc.who.int/news-events/iarc-publications-cancer-epidemiology-principles-and-methods/
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- 25 year trends in...

25 year trends in cancer incidence and mortality among adults aged 35-69 years in the UK, 1993-2018: retrospective secondary analysis
Linked editorial.
Cancer trends in the UK
- Related content
- Peer review
- Jon Shelton , head of cancer intelligence 1 ,
- Ewa Zotow , visiting lecturer (statistics) 2 ,
- Lesley Smith , senior research fellow 3 ,
- Shane A Johnson , senior data and research analyst 1 ,
- Catherine S Thomson , service manager (cancer and adult screening) 4 ,
- Amar Ahmad , principal statistician 1 ,
- Lars Murdock , data analysis and research manager 1 ,
- Diana Nagarwalla , data analysis and research manager 1 ,
- David Forman , visiting professor of epidemiology 5
- 1 Cancer Research UK, London, UK
- 2 University College London, London, UK
- 3 Leeds Institute of Clinical Trials Research, University of Leeds, Leeds, UK
- 4 Public Health Scotland, Edinburgh, UK
- 5 Faculty of Medicine and Health, University of Leeds, Leeds, UK
- Correspondence to: J Shelton jon.shelton{at}cancer.org.uk
- Accepted 19 January 2024
Objective To examine and interpret trends in UK cancer incidence and mortality for all cancers combined and for the most common cancer sites in adults aged 35-69 years.
Design Retrospective secondary data analysis.
Data sources Cancer registration data, cancer mortality and national population data from the Office for National Statistics, Public Health Wales, Public Health Scotland, Northern Ireland Cancer Registry, NHS England, and the General Register Office for Northern Ireland.
Setting 23 cancer sites were included in the analysis in the UK.
Participants Men and women aged 35-69 years diagnosed with or who died from cancer between 1993 to 2018.
Main outcome measures Change in cancer incidence and mortality age standardised rates over time.
Results The number of cancer cases in this age range rose by 57% for men (from 55 014 cases registered in 1993 to 86 297 in 2018) and by 48% for women (60 187 to 88 970) with age standardised rates showing average annual increases of 0.8% in both sexes. The increase in incidence was predominantly driven by increases in prostate (male) and breast (female) cancers. Without these two sites, all cancer trends in age standardised incidence rates were relatively stable. Trends for a small number of less common cancers showed concerning increases in incidence rates, for example, in melanoma skin, liver, oral, and kidney cancers. The number of cancer deaths decreased over the 25 year period, by 20% in men (from 32 878 to 26 322) and 17% in women (28 516 to 23 719); age standardised mortality rates reduced for all cancers combined by 37% in men (−2.0% per year) and 33% in women (−1.6% per year). The largest decreases in mortality were noted for stomach, mesothelioma, and bladder cancers in men and stomach and cervical cancers and non-Hodgkin lymphoma in women. Most incidence and mortality changes were statistically significant even when the size of change was relatively small.
Conclusions Cancer mortality had a substantial reduction during the past 25 years in both men and women aged 35-69 years. This decline is likely a reflection of the successes in cancer prevention (eg, smoking prevention policies and cessation programmes), earlier detection (eg, screening programmes) and improved diagnostic tests, and more effective treatment. By contrast, increased prevalence of non-smoking risk factors are the likely cause of the observed increased incidence for a small number of specific cancers. This analysis also provides a benchmark for the following decade, which will include the impact of covid-19 on cancer incidence and outcomes.
Introduction
The availability of comprehensive cancer registration data across the UK since 1993 makes comparison of cancer incidence and mortality trends over 25 years possible. We examined UK trends in cancer incidence and mortality for men and women, aged 35-69 years, for all cancers combined and for the most common sites (or site groups) of cancer between 1993 and 2018.
This study focuses on the 35-69 years age group because cancer trend data are more reliable and easier to interpret in this age range. 1 Diagnostic accuracy is better in this age range than in older patients who have a greater proportion of clinical and uncertain diagnoses, as evidenced by the relatively low proportion of microscopically verified tumours, 2 especially in the earlier part of the period analysed. By the age of 35 years, the pattern of cancer broadly represents the usual adult profiles because specific cancers that are observed in childhood, adolescence, and young people would not impact on the overall pattern. Trends in the 35-69 years age group are also reflective of causal factors in the more recent and medium term past rather than in the longer term and, therefore, will be more indicative of future patterns of cancer in the older populations.
This time period has also seen the introduction of three population screening programmes across the UK, which have affected trends by diagnosing some cancers at an earlier stage, preventing cancers, but also had the potential for diagnosing some cancers that would not have otherwise caused harm to the individual, particularly breast cancer. 3 4 Cervical smear tests have been used since the 1960s and the national screening programme was introduced in 1988, with over 85% coverage of the target population (women and people with a cervix aged 25-64 years) in the UK by 1994. 5 The breast screening programme was introduced in 1988 and covered all UK countries by the mid-1990s, with women aged 50-70 years being invited. 6 The bowel screening programme was introduced from 2006 and took a number of years to reach full roll-out. Currently, people aged 60-74 across England, Wales, and Northern Ireland, and 50-74 for Scotland are eligible. Prostate specific antigen testing is not part of the national screening programme. Anyone older than 50 years with a prostate can request a prostate specific antigen test from their family doctor (general practitioner).
The past 25 years have seen differing trends in cancer risk factors, with the two most important risk factors displaying trends in opposing directions. In one direction, smoking prevalence is reducing due to introductions of tax rises on tobacco products, further advertising bans, and smokefree policies, including education and encouraging quitting, and, in the other direction, the proportion of the population classified as overweight or obese is increasing, of which diet and exercise contribute to, as well as being independent risk factors for cancer. 7
Cancer registration data are currently collected by four national registries in the UK. These organisations collect detailed information on newly diagnosed primary tumours, referred to as registrations. Prior to 2013, cancer registrations in England were collected by eight regional registries and compiled by the Office for National Statistics, 8 with these regional registries producing complete population coverage for England since 1971. 9 Cancer Research UK aggregate these data from the UK registries, with incidence, mortality, and corresponding national population data provided by the Office for National Statistics, Public Health Wales, 10 Public Health Scotland, 11 the Northern Ireland Cancer Registry, 12 NHS England, 13 and the General Register Office for Northern Ireland. 14 Coding of cancer registrations is consistent between countries of the UK, using internationally accepted codes from the International Classification of Diseases 10th revision (ICD-10) and collaboration through the UK and Ireland Association of Cancer Registries. 15
Cancer sites (for single sites) or site groups (with multiple sites, such as oral) included in these analyses were selected as the most common causes of cancer incidence or death. These cancer sites are: all cancers combined (excluding non-melanoma skin cancer for incidence) (C00-C97, excluding C44); bladder (C67); bowel (C18-C20); brain and central nervous system (C70-C72, C75.1-C75.3, D32-D33, D35.2-D35.4, D42-D43, D44.3-D44.5); breast (women only) (C50); cervix (C53); Hodgkin lymphoma (C81); kidney (C64-C66, C68); larynx (C32); leukaemia (C91-C95); liver (C22); lung (C33-C34); melanoma skin(C43); mesothelioma (C45); myeloma (C90); non-Hodgkin lymphoma (C82-C86); oesophagus (C15); lip, oral cavity, and pharynx (oral) (C00-C06, C09-C10, C12-C14); ovary (C56-C57.4); pancreas (C25); prostate (C61); stomach (C16); testis (C62); and uterus (C54-C55). In addition, sex specific all cancer groups are also presented without breast and prostate cancers to inspect the overall trends in the absence of the most common cancer site for each sex. Sex is reported as recorded by the cancer registries at the time of registration. Mesothelioma was a new specific code introduced in ICD-10 and no reliable mortality data are available for this site before 2001, hence, we have not included this type of cancer prior to then. Non-malignant brain and central nervous system codes (ICD-10 D codes) are included despite their benign nature because they can cause mortality due to their location in the cranial cavity. The codes included for the brain and central nervous system have been chosen following clinical engagement and discussion with cancer registries across the UK. Non-melanoma skin cancer is excluded for incidence data because of the lack of completeness in the recording of these cancers and therefore unreliability of the data; this process is standard practice among UK cancer registries. 16 A proportion of non-melanoma skin cancer cases can be diagnosed and treated within primary care and have not consistently been captured within cancer registration data. 17
To overcome yearly variation for sites with low numbers of cases, we calculated three-year rolling average age standardised rates per 100 000 population. 18 These rates were based on the European standard population 2013 for men and women separately for each cancer site or site group for both incidence and mortality, restricted to the 35-69 years age group. 19
The estimated annual percentage change is commonly computed using a generalised linear regression model with Gaussian or Poisson link function. 18 20 In this analysis, a generalised linear model was performed with quasi-Poisson link function as overdispersion is very common when modelling rates and count data. 21 The outcome was the age standardised cancer (incidence or mortality) rate per 100 000 and the independent variable was the period variable, which was defined as the three year period for each data point, starting from 1993-95 and ending with 2016-18. Estimated annual percentage change was estimated as (exp (β^−1)' 100, where β^ is the estimated slope of the period variable, with corresponding 95% confidence interval, which is derived from the fitted quasi-Poisson regression model. 22 The determination of trends was based on the following criteria: firstly, an increasing trend was identified when the estimated annual percentage change value and its 95% confidence interval were greater than zero. This value suggests a statistically significant increase in the age standardised rate over time. Secondly, a decreasing trend was indicated when both the estimated annual percentage change value and its 95% confidence interval were less than zero, signifying a statistically significant decline in the age standardised rate over the period considered. Finally, in cases where these conditions were not met, the age standardised rate was concluded to have remained relatively stable. This designation means that no significant change in the age standardised rate over the period examined was noted. These criteria ensure a thorough and precise interpretation of the estimated annual percentage change values and their corresponding trends. These analyses were carried out for each sex and site or site group separately. Statistical analysis was performed using R version 4.0.2. 23
Patient and public involvement
This work uses aggregated and non-identifiable routine data that have been provided by patients and collected by the health services of the UK as part of their care and support. Given the aggregated nature of the data, attempts to identify or involve any of the patients whose data are included is not possible nor permitted. Although patients and the public were not involved in the design and conduct of this research, the aim of this research is to provide an assessment of trends in cancer incidence and mortality and the impacts of treatment and policy changes to improve outcomes for cancer patients across the UK. Dissemination to the public will include a press release and a summary published online, written using layman’s terms, and a webinar to discuss the results.
Table 1 and table 2 show the percentage of all newly diagnosed cancer cases and deaths by age group in 1993 and 2018. For male registrations, around 43% of all registrations were in the 35-69 years age group in 1993 and 2018, while for female registrations, between 47% and 48% of all registrations were in this age group in 1993 and 2018, respectively. For mortality, around 40% of male cancer deaths occurred in the 35-69 years age group in 1993 and this value was lower at 30% in 2018. For female cancer deaths, a slightly smaller reduction was noted, from 38% in the 35-69 years age group in 1993 to 31% in 2018.
Number of newly diagnosed cancer cases (% of total) in the UK for all cancers, excluding non-melanoma skin cancer, (ICD-10 C00-C97 excluding C44) by sex and age group in 1993 and 2018
- View inline
Number of deaths (% of total) in the UK for all cancers, (ICD-10 C00-C97) by sex and age group in 1993 and 2018
Figure 1 shows the number of newly diagnosed cancer cases and deaths in the 35-69 years age group between 1993 and 2018 by sex. Across the UK, of cancer registrations in 2018, 83% were from England, and 5.1% from Wales, 9.2% from Scotland, and 2.7% from Northern Ireland; for deaths in 2018, 81.4%, 5.3%, 10.4%, and 2.9% were from England, Wales, Scotland, and Northern Ireland, respectively. These proportions remained relatively stable over the study period. For men, the number of cancer registrations increased by 57% from 55 014 cases registered in 1993 to 86 297 cases registered in 2018, while for women, cases increased by 48% from 60 187 in 1993 to 88 970 in 2018. The rate of increase in the number of cases of cancer was more marked between 2003 and 2013 for both sexes than in other time periods in the study.

Number of newly diagnosed cancer cases and deaths in the UK for all cancers, excluding non-melanoma skin cancer for incidence (International Classification of Diseases (10th revision) codes C00-C97 (excluding C44 for incidence)), men and women, 35-69 years, 1993 to 2018. An interactive version of this graphic is available at https://bit.ly/4acPDjP
- Download figure
- Open in new tab
- Download powerpoint
The number of cancer deaths in men and women aged 35-69 years decreased: by 20% in men from 32 878 in 1993 to 26 322 deaths in 2018 and by 17% in women from 28 516 in 1993 to 23 719 deaths in 2018. The main decrease in the number of deaths per year occurred before the year 2000 ( fig 1 ) with a decrease of 14% in males and 11% in females between 1993 and 2000. Since 2000, the number of deaths each year in both men and women has remained fairly constant ( fig 1 ).
Table 3 , table 4 , figure 2 and figure 3 , and figure 4 and figure 5 show the trends over time in both incidence and mortality rates by sex and cancer site or site group. The tables only include specific age standardised incidence and mortality rates for the first (1993-95) and last (2016-18) period to give an indication of the change over the 25 year period. The trends in incidence and mortality age standardised rates for all years are shown in the figures. Figure 6 and figure 7 show the age adjusted average annual percentage change in the rates. Between 1993-95 and 2016-18, the age standardised incidence rate for all cancers (excluding non-melanoma skin cancer) increased slightly in men and women with age adjusted annual increases of 0.8% for both sexes. The trends in prostate and breast cancer, as the two largest cancer sites in men and women, respectively, substantially contribute to the overall all sites trends for cancer incidence. Figure 3 shows the trends for each sex without the largest cancer site. In contrast to the male age standardised incidence rate for all cancers, which showed a general increase, the incidence trend for men for all cancers excluding non-melanoma skin and prostate cancer, showed a decrease before 2000, but very little change in the following period. For women, an increase in age standardised incidence rates for all cancers excluding non-melanoma skin and breast cancer is still observed but the rate of increase is lower, at 0.7% per annum on average, over the 25 year period. Over the same period reductions in age standardised mortality for all cancers, including non-melanoma skin cancer, were −2.0% per year in men and −1.6% in women. Exclusion of prostate cancer from the mortality trends for men had a negligible effect on the average annual percentage change. For women, the exclusion of breast cancer from mortality trends led to a smaller decrease in mortality of −1.3% per annum.
Age standardised* incidence and mortality rates in 1993-95 and 2016-18 and percentage change by cancer type, men aged 35-69 years, UK
Age standardised* incidence and mortality rates in 1993-95 and 2016-18 and percentage change by cancer type, women aged 35-69 years, UK

European 2013 population age standardised incidence and mortality rates in the UK for all cancers, 19 excluding non-melanoma skin cancer for incidence (International Classification of Diseases (10th revision) codes C00-C97 excluding C44 for incidence), men and women, 35-69 years, 1993-95 to 2016-18. An interactive version of this graphic is available at https://bit.ly/4a484aE

European 2013 population age standardised incidence and mortality rates in the UK for all cancers in men and women aged 35-69 years during 1993-95 to 2016-18, 19 excluding non-melanoma skin cancer for incidence, and breast cancer in women and prostate cancer in men were excluded for incidence and mortality (International Classification of Diseases (10th revision) codes C00-C97 excluding C44 for incidence, C50, C61). An interactive version of this graphic is available at https://bit.ly/3vakQoX

European 2013 age standardised incidence and mortality rates by year, 19 in the UK, for men and women aged 35-69 years from 1993-95 to 2016-18, by cancer site. An interactive version of this graphic is available at https://bit.ly/49a6ovn

Relative European 2013 age standardised incidence and mortality rates by year, 19 in the UK, for men and women aged 35-69 years from 1993-95 to 2016-18 (the reference year is 1993-95=100), by cancer site. CNS=central nervous system. An interactive version of this graphic is available at https://bit.ly/3PiKGOk

Average annual percentage change in incidence and mortality rates, in the UK, for men aged 35-69 years from 1993-95 to 2016-18 by cancer site. An interactive version of this graphic is available at https://bit.ly/3wMR6yU

Average annual percentage change in incidence and mortality rates, in the UK, for women aged 35-69 years, from 1993-95 to 2016-18, by cancer site. An interactive version of this graphic is available at https://bit.ly/3v0QdT7
Incidence rates varied over time across the different cancer sites and site groups. The largest average annual percentage increases over time for cancer incidence rates for men aged 35-69 years were for cancers of the liver (4.7%), prostate (4.2%), and melanoma skin cancer (4.2%). Increases of 1% or more per annum were also seen for oral cancer (3.4%), kidney cancer (2.7%), myeloma (1.6%), Hodgkin lymphoma (1.5%), testicular cancer (1.3%), non-Hodgkin lymphoma (1.0%), and leukaemia (1.0%). The largest annual decreases over the two decades were seen for stomach (−4.2%), bladder (−4.1%), and lung cancers (−2.1%), with decreases of more than 1% per annum also observed for mesothelioma (−1.9% from 2001 onwards) and laryngeal cancer (−1.5%).
For women, the largest average annual percentage increases in incidence rates were noted for liver (3.9%), melanoma skin (3.5%), and oral (3.3%) cancers with increases in incidence of more than 1% per annum also observed for kidney (2.9%), uterus (1.9%), brain and central nervous system cancers (1.8%), Hodgkin lymphoma (1.6%), myeloma (1.1%), and non-Hodgkin lymphoma (1.0%). The largest annual decreases were reported for bladder (−3.6%) and stomach (−3.1%) cancers while the only other site showing a decrease of more than 1% per annum was cervical cancer (−1.3%). Although breast cancer represents the largest individual cancer site for women and therefore plays a large part in all cancer trends, the average annual increase was only 0.9%. All the incidence changes mentioned, for both men and women, and most incidence changes shown in table 3 and table 4 and in figure 6 and figure 7 were statistically significant (P<0.05) even when the size of change was relatively small.
Mortality rates mainly decreased over time in both sexes. For men, the cancer sites that showed average annual percentage reductions in mortality rates of more than 1% per annum were stomach (−5.1%), mesothelioma (–4.2% from 2001), bladder (–3.2%), lung (–3.1%), non-Hodgkin lymphoma (–2.9%), testis (–2.8%), Hodgkin lymphoma (–2.6%), bowel (–2.5%), larynx (–2.5%), prostate (–1.8%), myeloma (–1.7%), and leukaemia (–1.6%). Only liver (3.0%) and oral (1.1%) cancers showed an average annual increase in mortality of 1% or more with melanoma skin cancer (0.3%) the only other site showing an increase. For women, the cancer sites with average annual decreases in mortality per year of 1% or more were stomach (–4.2%), cervix (–3.6%), non-Hodgkin lymphoma (–3.2%), breast (–2.8%), Hodgkin lymphoma (–2.8%), ovary (–2.8%), myeloma (–2.3%), bowel (–2.2%), leukaemia (–2.1%), larynx (–2.0%), mesothelioma (–2.0% since 2001), bladder (–1.6%), oesophagus (–1.2%), and kidney (1.0%). As with men, liver (2.7%) and oral (1.2%) cancers showed average annual increases of more than 1%, in addition to uterine cancer (1.1%). For both men and women, the mortality changes mentioned previously and most mortality changes shown in table 3 and table 4 and in figure 6 and figure 7 were statistically significant (P<0.05), even when the size of change was relatively small.
Principal findings
The most striking finding in this analysis of UK cancer trends among the 35-69 years age group is the substantial decline in cancer mortality rates observed in both sexes (37% decline in men and 33% decline in women) across the period examined. A decrease in mortality was reported across nearly all the specific types of cancer examined (23 in total), with only liver, oral, and uterine cancers showing an increase together with melanoma skin cancer in men and pancreatic cancer in women, both showing small increases. By contrast, the incidence trends in this age group showed varying patterns with some sites increasing, some decreasing and some remaining relatively constant. Over all sites, a modest increase was noted in cancer incidence rates of around 0.8% per annum in both sexes, amounting to an increase of 15% in men and 16% in women over the 25 year time frame.
The increase in prostate cancer incidence over this period, especially in the 35-69 years age group considered here, is very likely to be a direct result of the uptake of prostate specific antigen testing, which results in the detection of early stage disease and, to an unknown extent, indolent disease that may otherwise never have been regarded as clinically significant. 24 25 The results do, however, affect people diagnosed and represent a large increase in workload for clinical staff. The fact that the overall mortality trends for men show no difference whether prostate cancer is included or excluded in the analysis indicates that the incidence increase for this cancer has largely been of non-fatal disease. That the specific mortality rates for prostate cancer showed an appreciable rate of decline during this time (–1.8% per annum) also indicates improved clinical treatment of the disease or an increase in the proportion of men diagnosed with a favourable prognosis, or both. 24 26 However, the increase in prostate cancer incidence still results in thousands of men each year dealing with the concerns of a cancer diagnosis and the impact this may have on their lives.
Breast cancer comprehensively dominated incidence and mortality trends in female cancer. Even though the average annual incidence increase of breast cancer over this period (0.9%) was modest in comparison to the prostate cancer increase in men (4.2%), breast cancer incidence rates remained substantially higher than those for any other cancer site in either sex. Inspection of figure 4 shows that breast cancer incidence rates (age standardised) increased at a faster rate until around 2003-05 (from 194.7 in 1993-95 to 229.9 in 2003-05), a slower rate from then until 2013-15 (240.8) but have levelled off in the most recent years analysed (238.0 in 2016-18). These changes in the incidence trend likely reflect a reduced effect of the initial incidence increases brought about by mammography screening in the UK introduced from the late 1980s or a possible effect of a decline in usage of hormone replacement treatment. 27 28 However, the effect of hormone replacement treatment on breast cancer risk is small in comparison to other risk factors, 7 and trends in this treatment has varied over time, such as changes in preferred formulations, doses, and treatment durations, 29 30 31 which may impact breast cancer risk levels. 32 33 As has been reported elsewhere, 34 35 36 mortality for breast cancer has declined substantially despite the incidence increase, which is indicative of improvements in early detection (including through screening 37 ) and improved treatment.
The other two major sites of cancer in men apart from prostate cancer, namely lung and bowel cancers, showed substantial reductions in mortality. These results are likely from primary prevention (historical reduction in smoking rates) 38 39 40 41 for lung cancer and earlier detection (including screening) and improved treatment for bowel cancer. 42 43 44 While lung cancer incidence substantially decreased, the incidence rates of bowel cancer remained unchanged. However, closer inspection of the bowel cancer incidence trends over the full period shows an increase from the point the bowel screening programme was first introduced from 2006 in the UK. This rate, however, has now decreased back to the observed level prior to the introduction of the screening programme. As others have shown, the introduction of bowel screening leads to an initial short-term increase in cancer incidence due to detection of as-yet undiagnosed cancer cases, followed by a decrease because of removal of adenomas. 42 45 46 Therefore, bowel cancer incidence trends can reasonably be assumed to decrease further over the coming years, unless other preventable risk factors for bowel cancer affect the trend.
Similarly, lung and bowel were the other two major cancer sites for women (alongside breast cancer), and both showed reductions in mortality. The decline in lung cancer mortality was, however, not as extensive as that for men (–0.5% compared with –3.1% per annum) likely reflecting the different demographic pattern in smoking rates that led to peak smoking prevalence in women occurring around 30 years later than men, albeit at around half the peak prevalence observed in men. 40 47 Smoking prevalence in women has always been lower than in men. 39 48 The lung cancer incidence trends showed a significant increase in women of 0.8% per annum as opposed to the –2.1% per annum decrease in men. That the incidence rate in 2016-18 was still higher in men than in women again is almost certainly a reflection of historical differences in smoking patterns. 39 49 50 Bowel cancer incidence in women followed a similar pattern to men and is equally reflective of the introduction of the bowel screening programme. Bowel cancer mortality in women has declined at a similar rate to men (–2.2% compared with –2.5% per annum), indicative of the same improvements in early detection and improved treatment.
These reductions in mortality across the most common cancers in both sexes are likely a representation of considerable success in cancer prevention, diagnosis, and treatment. Further improvements are likely to be realised from the continued reduction in smoking prevalence, of which smoking prevention policies continue to contribute, 51 alongside the recent move to faecal immunochemical testing in the bowel screening programme adopted throughout the UK during 2019. 52 The recommended rollout of targeted lung screening is expected to further help with the earlier diagnosis of lung cancer where surgery is a viable treatment option and outcomes are vastly improved. 53 54
Although four major sites influenced the overall pattern of cancer incidence and mortality, increases in rates among some of the less common sites do raise concerns. Four cancers showed substantial increases in incidence (more than 2% per annum) in both sexes: liver, melanoma skin, oral, and kidney cancers. All have strong associations with established risk factors: alcohol consumption, smoking, and HPV for oral cancer; 7 55 56 overweight and obesity, smoking, alcohol, and hepatitis B and C for liver cancer; 7 57 58 ultraviolet light for melanoma; 59 60 and obesity and smoking for kidney cancer. 61 62 63 Increases in liver cancer incidence and mortality for both men and women are very concerning, with nearly one in two attributable to modifiable risk factors. 7 With high prevalence of overweight and obesity and diabetes in the general population, other studies expect the rates to remain high. 64 For oral and kidney cancer, despite the association with smoking, incidence rates have not followed the decrease seen for lung cancer incidence in men. This is likely to be due to the smaller proportion of cases attributable to smoking in these two sites. Whilst smoking accounts for around 17% of oral cancers, over one in three are attributed to alcohol consumption. 7 For kidney cancer, smoking is attributable to 13% of cases whereas obesity causes around 25%, however, increasing trends in kidney mortality are shown for this age group and period. 7 Therefore, the increasing incidence trends could potentially have been worse, especially in men, if the reduction in smoking prevalence had not occurred. The increased incidence of melanoma skin cancer is likely to be caused by the increased sunlight and ultraviolet exposure caused by the availability of cheaper air travel to countries with a warmer climate and insufficient regulation of tanning beds until 2010. 65 66
In women, uterine cancer incidence increased by 1.9% per annum; although, this increase was predominantly seen over the period 1993-2007 and since then incidence trends have increased at a slower rate. One of the main risk factors for uterine cancer is the use of oestrogen-based hormone replacement therapy, 67 68 and since around 2000, use has substantially declined. 27 Around a third of uterine cancers in the UK are also attributed to overweight and obesity, but the increase in incidence is also likely to be caused by a decrease in the number of women undergoing hysterectomies for menorrhagia, in favour of endometrial ablation. 69
Other cancers that showed increases in incidence were cancers of the pancreas, brain, and central nervous system, together with Hodgkin and non-Hodgkin lymphoma, myeloma, and leukaemia in both sexes, and oesophageal and testicular cancers in men. With the exception of pancreatic cancer, which only decreased in women, all these cancers also showed a reduction in mortality in both sexes, indicating improving treatment or earlier detection, or both. Generally, the causes of these cancers are not well understood although obesity is associated with the adenocarcinoma histological subtype of oesophageal cancer, 70 especially in men, 7 while a combination of smoking and alcohol is implicated in the squamous cell carcinoma subtype. 71 The considerable male excess in oesophageal adenocarcinoma in comparison with squamous cell carcinoma rates, 72 possibly underlined by the higher incidence of gastroesophageal reflux disease in men 73 and the protective effect of oestrogen, 74 75 may explain the differing trends now observed between men and women.
Several cancer sites showed decreases in both incidence and mortality rates over the time period, notably stomach, larynx, and bladder cancer in both sexes, as well as cervical and ovarian cancers in women and mesothelioma in men. The changes in stomach cancer rates were of a similar magnitude and represented the largest percentage mortality decline in both sexes. This decline can probably be attributed to a combination of a reduction in the prevalence of Helicobacter pylori infection and an increase over time in fruit and vegetable consumption reducing the dependency on preserved foods. 76 77 Challenges in coding of stomach and oesophageal cancer before 2000 may also have had a role in shaping these trends. Laryngeal cancer is associated with tobacco use and alcohol consumption as well as occupational exposures, 56 78 79 and the decline in rates is most likely to be related to the decrease in smoking prevalence as well as decreases in occupational exposure. 80 The refinement of understanding pathology for bladder cancer during this period, in which previously diagnosed malignant disease is now categorised as benign, 81 is likely to have resulted in an artificial decline in incidence rates. 82 83 This artefact should not, however, have affected the decline in mortality rates given the benign nature of these tumours that do not cause death. 81 This decline in mortality, although not as marked as that for incidence, remained appreciable. The changes in cervical cancer rates, which showed the largest percentage mortality decline amongst gynaecological cancers, are almost certainly attributed to the success of the cytological screening programme during the whole of the time period considered. 84 85 With the introduction of the HPV vaccination programme for girls in 2008 86 and the subsequent expansion to boys in 2019, 87 rates of cervical cancer are expected to fall substantially over the following decades as the first cohort of vaccinated women reaches the peak age for cervical cancer incidence (aged 30-34 years). A reduction has already been shown for women aged 20-24. 88 The absolute incidence rates of mesothelioma in women were small in magnitude in 1993-95 (0.8 per 100 000 per annum) and remained similar over time (0.7 per 100 000 per annum in 2016-18). The incidence rates of mesothelioma in men were considerably greater, especially in 1993-95 (around 6.3 per 100 000 per annum), due largely to occupational asbestos exposure, 89 but a significant decrease was noted over time (to 3.6 per 100 000 per annum in 2016-18) resulting from both the decline in asbestos exposure and the decline in heavy industries, such as coal mining. Mortality decreased substantially in both sexes over the period for which data are available (2001-03 to 2016-18).
The conclusions that can be drawn from this analysis are, overall, positive and reassuring. Within the 35-69 year age group, cancer mortality rates have shown a substantial overall decline during the last quarter of a century in both men and women. The most probable causes are a combination of changes in the underlying risk of disease for some cancers (notably lung and stomach), in increased levels of early detection (notably breast 37 and cervix 90 ) and improved treatment (notably breast and bowel) for others. The specific circumstances leading to the increased incidence of breast cancer, of which risk factors are complex, need to be better understood and controlled. Similar results have been shown for incidence within Great Britain and mortality in the UK for some cancer sites. 91 Speculated overdiagnosis, where tumours are detected that would not have caused the patient any harm during their lifetimes, has been thought to increase rates for breast and prostate cancers in particular, of which prostate is especially affected by the widespread use of prostate specific antigen testing. 4 92 However, given the decreases in mortality across the wide set of cancer sites analysed here, improvements in early diagnosis, treatment, or both are having a positive effect for most cancer patients, although cancer mortality in this age group still needs reducing.
After accounting for the major two sites in men and women, the increase in overall incidence rates disappeared in men while it remained significant in women. This difference between sexes is due to a decrease in cancers with substantially higher initial incidence rates in men, such as lung, stomach, and bladder, resulting in a higher overall impact on male incidence, combined with an increase in incidence in uterine cancer, one of the most common cancers in women.
Strengths and limitations
This study benefits from high quality cancer registry data collected by all four cancer registries in each country across the UK, which allows for the inspection of a wide range of cancer sites over 25 years. ICD-10 coding changes have been minimal, only affecting trends in cancer incidence for bladder and ovarian cancers and cancer mortality for mesothelioma, whereas challenges in coding stomach and oesophageal cancer may have affected trends for these sites. Changes in registration practice may well have had a small effect on certain cancer sites. By focusing only on the 35-69 age range, we present a clear and reliable comparative picture of cancer incidence across 25 years within the UK, which provides a reliable indicator regarding future cancer incidence trends. Understanding cancer in older people and changes in the trends of different cancers is also of interest, but subject to a different study given the increasing life expectancy over this period, impact of comorbidities, and differing interaction with health services in this age group.
Limitations include the absence of staging data to substantiate any improvements in earlier diagnosis. Due to the number of sites analysed, we also have not broken down sites by histological type, which could be beneficial in certain sites to understand the trends within cancer sites—eg, small cell and non-small cell lung cancer or oestrogen receptor-positive and oestrogen receptor-negative breast cancer. In focusing on the age group selected, we are excluding older ages where rates of cancer are higher. Although this exclusion reduces the number of cases included, providing a smaller cohort for each year, the age group selected provides a more reliable comparator for future trends given the accuracy of incidence recording and also focuses on the cancers that lead to a larger number of years of life lost. The age range included in this study has been well defined; however, other studies are indicating potentially different trends worldwide in young adults with potential increases in risk factors such as dietary risk factors playing a role. 93 94 The data captured across the UK registries provides a basis for further understanding to see whether different trends are observed across younger age groups and whether the causes of this can be determined. Additionally, although we have included a broad range of cancer sites, cancers that have not been included in this study could well be showing different trends, such as a more recent increase in thyroid cancer in the UK. 95
This study also provides a baseline covering a 25 year period uninterrupted by covid-19. Trends in cancer incidence and mortality beyond these years will be affected and therefore understanding the causes of trends will be more complicated. Having a 25 year baseline provides the observed trend for which expected cases can be assessed against observed. This benchmark will present a comparison for the following decade as the presentation, diagnosis, and treatment of cancer have been hugely affected by rules and regulations affecting public and health service staff. Mortality trends will also be impacted with decision making regarding coding of deaths with covid-19 likely to be the underlying cause of death for people with cancer if that has directly led to the patient dying, rather than their cancer.
This study focuses on the overall sex specific trends for cancer incidence and mortality in the specified age group to observe and understand trends over the 25 year period across the entire UK. Further breakdowns have not been possible. Paucity of numbers for less common cancers precluded separate analyses for the individual UK nations while data limitations precluded analyses by other demographic characteristics, for example, ethnic group and deprivation. The main obstacle to analysing data by ethnic group is the completeness of recordings in hospitals. In England, completeness improved substantially in 2012, but prior to this, the proportion of cases with unknown ethnic group renders results over time to be incomparable. In other UK countries, completeness of ethnic group recording is still not good enough to conduct country-wide cancer incidence or mortality analyses by ethnicity. For deprivation, the measures currently available are derived within each UK nation, and a specific validated UK-wide deprivation measure does not yet exist. Given the obvious importance of looking at variation in UK trends within ethnic groups and deprivation categories, such analyses represent a priority for further research and highlights the importance of data collection across all UK nations.
Conclusions
Overall, these results substantiate the view that in this age group there is no generalised increase in cancer incidence, while there is a substantial decrease in cancer mortality in the UK over the 25 year study period. Specific concerns about individual cancer sites identified were raised, of which the most important numerically, apart from the increases in breast and prostate cancer incidence, was the need to accelerate the decrease in female lung cancer. After which, concerns about oral cancer, liver cancer, kidney cancer, uterine cancer, and melanoma skin cancer present the most pressing issues. There are also several cancer sites that showed decreases in both incidence and mortality, notably, stomach, larynx, bladder, and cervical.
What is already known on this topic
No recent studies have investigated cancer incidence and mortality rates over such a long time frame within the 35-69 year age group in the UK
Short term trends for specific cancer sites are related to known risk factors, screening programmes, and improved treatment
Trends in the 35-69 years age group can be indicative of future patterns of cancer in older people
What this study adds
Decreased rates of many cancers, including lung and laryngeal, is positive, and likely to be driven by the decrease in smoking prevalence across the UK
An increase in rates of other cancer sites, including uterine and kidney, was noted, which may be a result of the increasing prevalence of overweight/obesity and other risk factors
Organised population screening programmes have led to an increase in cancer incidence but also look to have contributed to a reduction in cancer mortality across the UK
Ethics statements
Ethical approval.
Ethics approval for this work was not required as the study used publicly available data.
Data availability statement
Data sharing may be possible for additional analyses. All code used for analyses in this paper are also available from the Cancer Research UK website and GitHub. Information on how to access the data used in this analysis are available from the Cancer Research UK website.
Acknowledgments
This work uses data that has been provided by patients and collected by the health services as part of their care and support. The data is collated, maintained, and quality assured by NHS England, Public Health Wales, Public Health Scotland, and the Northern Ireland Cancer Registry.
Contributors: All authors participated in study conception and design, and/or the analysis and interpretation of results. Conception and design: DF, LS, and CT. Analysis and interpretation: all authors. Writing manuscript: all authors. Supervision and guarantor: JS and DF. All authors critically reviewed drafts of the manuscript, read and approved the final manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
The manuscript’s guarantor (DF) affirms that this manuscript is an honest, accurate, and transparent account of the study being reported, that no important aspects of the study have been omitted and that any discrepancies from the study as planned have been explained.
Dissemination to participants and related and public communities: study results will be disseminated to the public and health professionals by a press release written using layman’s terms; findings will also be shared through mass media communications and social media postings. A webinar produced alongside a patient advocacy group is also planned to accompany the publication of this study, a recording of which will be made available on the Cancer Research UK website. Since the study analyses cancer registry data collected during routine care, and provided in aggregated form, we are unable to specifically disseminate results to study participants beyond the usual channels of publication.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Queen’s University Belfast, Northern Ireland Cancer Registry
- van Seijen M ,
- Thompson AM ,
- PRECISION team
- Independent UK Panel on Breast Cancer Screening
- Kitchener H ,
- ↵ Cancer Research UK. Screening for cancer. https://www.cancerresearchuk.org/about-cancer/screening
- Office for National Statistics
- Public Health Wales
- Public Health Scotland
- NHS Digital
- NI Direct Government Services
- United Kingdom and Ireland Association of Cancer Registries
- UK Health Security Agency
- National Cancer Intelligence Network
- Benhamou E ,
- Laversanne M ,
- Gardner W ,
- Mulvey EP ,
- Hankey BF ,
- Kosary CL ,
- R Core Team
- Pashayan N ,
- Pharoah P ,
- Martin RM ,
- Donovan JL ,
- Turner EL ,
- CAP Trial Group
- Neuberger MM ,
- Djulbegovic M ,
- Johnson A ,
- Bromley SE ,
- de Vries CS ,
- Burkard T ,
- Alsugeir D ,
- Adesuyan M ,
- Vinogradova Y ,
- Coupland C ,
- Hippisley-Cox J
- Collaborative Group on Hormonal Factors in Breast Cancer
- Early Breast Cancer Trialists’ Collaborative Group (EBCTCG)
- Coleman DA ,
- Swerdlow AJ ,
- Youlden DR ,
- Cancer Research UK
- ↵ International Agency for Research on Cancer, World Health Organization. Tobacco Smoke and Involuntary Smoking. 2004. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans; vol. 83. https://publications.iarc.fr/Book-And-Report-Series/Iarc-Monographs-On-The-Identification-Of-Carcinogenic-Hazards-To-Humans/Tobacco-Smoke-And-Involuntary-Smoking-2004
- McClements PL ,
- Madurasinghe V ,
- Thomson CS ,
- Ait Ouakrim D ,
- Niikura R ,
- Brenner H ,
- Schrotz-King P ,
- Holleczek B ,
- Katalinic A ,
- Hoffmeister M
- Lieberman DA ,
- McFarland B ,
- American Cancer Society Colorectal Cancer Advisory Group ,
- US Multi-Society Task Force ,
- American College of Radiology Colon Cancer Committee
- Silcocks P ,
- Whitley E ,
- Malvezzi M ,
- Bertuccio P ,
- Lortet-Tieulent J ,
- Renteria E ,
- UK National Screening Committee
- Royal College of Physicians
- McLaughlin JK ,
- Hashibe M ,
- Brennan P ,
- Chuang SC ,
- Armstrong GL ,
- Farrington LA ,
- Hutin YJF ,
- Miyamura T ,
- Gilchrest BA ,
- Geller AC ,
- Berwick M ,
- van der Hel OL ,
- McMillan GP ,
- Boffetta P ,
- Zeegers MPA ,
- van Den Brandt PA
- Driver RJ ,
- HCC-UK/BASL/NCRAS Partnership Steering Group
- Doherty VR ,
- Brewster DH ,
- UK government
- Gebretsadik T ,
- Kerlikowske K ,
- Ernster V ,
- Million Women Study Collaborators
- Mukhopadhaya N ,
- Manyonda IT
- Lagergren J
- Rubenstein JH
- Czanner G ,
- Chandanos E ,
- Roberts SE ,
- Morrison-Rees S ,
- Samuel DG ,
- Williams JG
- Rothenbacher D ,
- Talamini R ,
- Bosetti C ,
- La Vecchia C ,
- Menvielle G ,
- Goldberg P ,
- National Institute for Health and Care Excellence
- Vaccarella S ,
- Plummer M ,
- Franceschi S ,
- University of Oxford
- Castanon A ,
- Windridge P ,
- Hodgson JT ,
- Matthews FE ,
- Castañón A ,
- O’Sullivan JW ,
- Nicholson BD
- Bjurlin MA ,
- Nicholson J ,
- Sasamoto N ,
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Chin J Cancer Res
- v.32(6); 2020 Dec 31
Cervical cancer: Epidemiology, risk factors and screening
Shaokai zhang.
1 Department of Cancer Epidemiology, Affiliated Cancer Hospital of Zhengzhou University/Henan Cancer Hospital, Henan Engineering Research Center of Cancer Prevention and Control, Henan International Joint Laboratory of Cancer Prevention, Zhengzhou 450008, China
Luyao Zhang
Youlin qiao.
2 Department of Epidemiology, National Cancer Center, Chinese Academy of Medical Sciences, School of Population Medicine and Public Health, Peking Union Medical College, Beijing 100021, China
Cervical cancer is one of the leading causes of cancer death among females worldwide and its behavior epidemiologically likes a venereal disease of low infectiousness. Early age at first intercourse and multiple sexual partners have been shown to exert strong effects on risk. The wide differences in the incidence among different countries also influenced by the introduction of screening. Although the general picture remains one of decreasing incidence and mortality, there are signs of an increasing cervical cancer risk probably due to changes in sexual behavior. Smoking and human papillomavirus (HPV) 16/18 are currently important issues in a concept of multifactorial, stepwise carcinogenesis at the cervix uteri. Therefore, society-based preventive and control measures, screening activities and HPV vaccination are recommended. Cervical cancer screening methods have evolved from cell morphology observation to molecular testing. High-risk HPV genotyping and liquid-based cytology are common methods which have been widely recommended and used worldwide. In future, accurate, cheap, fast and easy-to-use methods would be more popular. Artificial intelligence also shows to be promising in cervical cancer screening by integrating image recognition with big data technology. Meanwhile, China has achieved numerous breakthroughs in cervical cancer prevention and control which could be a great demonstration for other developing and resource-limited areas. In conclusion, although cervical cancer threatens female health, it could be the first cancer that would be eliminated by human beings with comprehensive preventive and control strategy.
Introduction
Cervical cancer is the second common female malignant tumor globally which seriously threatens female’s health. Persistent infection of high-risk human papillomavirus (HPV) has been clarified to be the necessary cause of cervical cancer ( 1 , 2 ). The clear etiology accelerated the establishment and implementation of comprehensive prevention and control system of cervical cancer. In May 2018, the World Health Organization (WHO) issued a call for the elimination of cervical cancer globally, and more than 70 countries and international academic societies acted positively immediately ( 3 - 6 ). Thereafter, in November 17, 2020, WHO released the global strategy to accelerate the elimination of cervical cancer as a public health problem to light the road of cervical cancer prevention and control in future which mean that 194 countries promise together to eliminate cervical cancer for the first time ( 7 ). At this milestone time point, we reviewed the update progress of cervical cancer prevention and control in epidemiology, risk factors and screening, in order to pave the way of cervical cancer elimination.
Epidemiology for cervical cancer
Cervical cancer is one of the leading causes of cancer death among women ( 8 ). Over the past 30 years, the increasing proportion of young women affected by cervical cancer has ranged from 10% to 40% ( 9 ). According to the WHO and International Agency for Research on Cancer (IARC) estimates, the year 2008 saw 529,000 new cases of cervical cancer globally. In developing countries, the number of new cases of cervical cancer was 452,000 and ranked second among malignancies in female patients ( 10 ). Conversely, the number of new cases of cervical cancer was 77,000 in developed countries and ranked tenth among female malignancies.
In 2018 worldwide with an estimated 570,000 cases and 311,000 deaths, cervical cancer ranks as the fourth most frequently diagnosed cancer and the fourth leading cause of cancer death in women ( 11 ). However, approximately 85% of the worldwide deaths from cervical cancer occur in underdeveloped or developing countries, and the death rate is 18 times higher in low-income and middle-income countries compared with wealthier countries ( 12 ). Cervical cancer ranks second in incidence and mortality behind breast cancer in lower Human Development Index (HDI) settings; however, it is the most commonly diagnosed cancer in 28 countries and the leading cause of cancer death in 42 countries, the vast majority of which are in Sub-Saharan Africa and South Eastern Asia ( 13 ). The highest regional incidence and mortality rates are seen in Africa ( 14 ). In relative terms, the rates are 7−10 times lower in North America, Australia/New Zealand, and Western Asia (Saudi Arabia and Iraq) ( 15 ).
In China, cervical cancer is the second largest female malignant tumor ( 11 ). According to the data from National Cancer Center in 2015, there were 98,900 new cases and 30,500 deaths of cervical cancer ( 16 ). In the past 20 years, the incidence and mortality of cervical cancer have been increasing gradually in China ( 17 ).
Between 2004 and 2007, the Chinese scientific research team, cooperated with WHO/IARC and the Cleveland Medical Center in the United States in 8 rural and urban areas (Xiangyuan county of Shanxi Province, Yangcheng county of Shanxi Province, Xinmi county of Henan Province, Hotan Prefecture of Xinjiang Uygur Autonomous Region, Shanghai City, Beijing City, Shenzhen City of Guangdong Province, and Shenyang City of Liaoning Province), carried out a population-based multicenter HPV type distribution study among females aged 15−59 years old, clarifying the dominant HPV types of rural and urban populations in China, as well as female HPV infection status and age distribution ( 18 ). Studies have confirmed that persistent infection of high-risk HPV is closely related to the occurrence of cervical cancer. There are 14 types of high-risk HPV, namely HPV16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68 and 73. A multi-center cross-sectional survey study showed that the infection rate of high-risk HPV in China is about 14.3%, and the dominant types are HPV16 (2.9%), HPV52 (1.7%), HPV58 (1.5%), HPV33 (1%) and HPV18 (0.8%), and showed double peaks during adolescence and perimenopause ( 19 ). Globally, HPV16 has the highest infection rate, HPV18 is the second most common type, while HPV 33 is common in Asia, and HPV52 and HPV58 have relatively low infection rates. This shows that compared with the global HPV epidemiology, HPV epidemiology in China has both similarities and differences.
Subsequently, the Chinese scientific research team conducted a cross-sectional multi-center cervical cancer and precancerous HPV genotyping study based on 19 hospitals in 7 geographic regions (Northeast China, North China, Northwest China, Central China, East China, Southwest, and South China). Through the pathological laboratory procedures of strict quality control, it was found that the dominant HPV types in cervical cancer tissue were HPV16, 18, 31, 52 and 58, respectively, and that HPV16 and 18 were the most carcinogenic, which could cause more than 84.5% of cervical cancer ( 20 ). The above research on HPV dominant types from different perspectives provides solid scientific evidence and support for the future research and application of preventive HPV vaccine and in vitro diagnostic technology, epidemiological research and health economics research in the Chinese population.
Risk factors for cervical cancer
A number of risk factors for cervical cancer are linked to exposure to the HPV ( 21 , 22 ). Invasive cancer development process could prolong up to 20 years from the precursor lesion caused by sexually transmitted HPV ( 23 ). However, there are also other numerous risk factors (such as reproductive and sexual factors, behavioral factors, etc) for cervical cancers which include sexual intercourse at a young age (<16 years old), multiple sexual partners, smoking, high parity and low socio-economic level ( 24 , 25 ).
Sexually transmitted infections (STI)
The primary cause of pre-cancerous and cancerous cervical lesions is infection with a high-risk or oncogenic HPV types. Most cases of cervical cancer occur as a result of infection with HPV16 and 18. High-risk types, especially HPV16, are found to be highly prevalent in human populations ( 22 ). The infection is usually transmitted by sexual contact, causing squamous intraepithelial lesions. Most lesions disappear after 6−12 months due to immunological intervention. However, a small percentage of these lesions remain and can cause cancer.
The results of a meta-analysis showed that the highest prevalence of HPV occurs at the age of 25 years, which could be related to changes in sexual behavior ( 26 ). In a meta-analysis study, the bimodal distribution of cervical cancer in some regions has been studied. In this distribution, immediately after sexual intercourse, an outbreak of HPV can be observed, which is followed by a plateau at adult age; the second peak again is observed after 45 years old ( 27 ). Permanent infection with one of the high-risk types of HPV over time leads to the development of cervical intraepithelial neoplasia (CIN). The major mechanisms through which HPV contributes to carcinogenesis involve the activity of two viral oncoproteins, E6 and E7, which interfere with major tumor suppressor genes, P53 and retinoblastoma. In addition, E6 and E7 are associated with changes in host DNA and virus DNA methylation. Interactions of E6 and E7 with cellular proteins and DNA methylation modifications are associated with changes in key cellular pathways that regulate genetic integrity, cell adhesion, immune response, apoptosis, and cellular control ( 28 ).
Human immunodeficiency virus (HIV)
The risk of developing infection from high-risk HPV types is higher in women with HIV ( 29 ). The results of the studies on the relationship between HIV and cervical cancer suggested a higher rate of persistent HPV infection with multiple oncogene viruses, more abnormal Papanicolau (Pap) smears, and higher incidence of CIN and invasive cervix carcinoma among people with HIV ( 23 ). Women infected with HIV are at increased risk of HPV infection at an early age (13−18 years) and are at high risk of cervical cancer. Compared with non-infected women, HIV positive patients with cervical cancer are diagnosed at an earlier age (15−49 years old) ( 30 ).
Reproductive and sexual factors
Sexual partners.
Factors relating to sexual behavior have also been linked to cervical cancer. One study found that an increased risk of cervical cancer is observed in people with multiple sexual partners ( 31 ). Moreover, many studies have also suggested that women with multiple sexual partners are at high risk for HPV acquisition and cervical cancer ( 32 , 33 ). From the meta-analysis, a significant increased risk of cervical diseases was observed in individuals with multiple sexual partners compared to individuals with few partners, both in non-malignant cervical disease and in cervical cancer ( 34 ). The association remained exist even after controlling for the status of HPV infection, which is a major cause of cervical cancer. Also, early age at first intercourse is a risk factor for cervical cancer ( 35 ).
Oral contraceptive (OC) pills
OC pills are known to be a risk factor for cervical cancer. In an international collaborative epidemiological study of cervical cancer, the relative risk in current users increased with an increase in the duration of OC use. It has been reported that the use of OC for 5 years or more can double the risk of cancer ( 36 ). And in a multi-center case-control study, among women who tested positive for HPV DNA, the risk of cervical cancer increased by 3 times if they have used OC pills for 5 years or more ( 37 ). In addition, a recent systematic review & meta-analysis also suggested that OC pills use had a definite associated risk for developing cervical cancer especially for adenocarcinoma. This study concluded that use of OC pills is an independent risk factor in causing cervical cancer ( 38 ).
Cervical cancer screening
With the background of cervical cancer elimination worldwide, cervical cancer screening plays an increased role in the comprehensive prevention and control besides HPV vaccination, especially those methods that demonstrated excellent clinical performance.
Overview of cervical cancer screening methods
The screening methods for cervical cancer are mainly as following: traditional Pap smear, visual inspection with acetic acid & Lugol’s iodine (VIA/VILI), liquid-based cytology (LBC) and HPV testing. The disease burden of cervical cancer has been significantly reduced in developed countries by Pap smear, mainly in the United States, since 1950s. However, the accuracy of traditional Pap smear could be easily affected by following factors: the level of cytological room, professional technicians, sampling method, slide quality, dyeing skills, and cytological personnel experience. In developed countries with high standard experimental conditions and technical level, the sensitivity of cytology is as high as 80%−90%, in contrast, in resource-limited regions, it could be as low as 30%−40%. To overcome the limitations of traditional Pap smear in cervical cancer screening, LBC was developed and approved by Food and Drug Administration (FDA) in 1996 for clinical-use purpose. Compared with the traditional Pap smear, the sensitivity of LBC was significantly improved. Meanwhile, organized and practicable LBC screening program has also been established in developed countries which could ensure cervical cancer screening strategy is carried out continuously and effectively.
Cervical cancer screening has been facilitated since the cause clarified. HPV-based testing is a pivotal part for cervical cancer screening besides cytology-based tests.
The detection of high-risk HPV in cervical lesion biopsies and exfoliated cells has evolved from restriction endonuclease cleavage patterns and hybridization techniques to polymerase chain reaction (PCR)-based system ( 39 ) and most recently next-generation sequencing (NGS) assays ( 40 ). Currently, HPV genotyping is primarily based on the detection of individual types by various methods that utilizing the highly conserved L1 gene and PCR-based methods. These PCR methods employed consensus primers that could target and amplify different sized fragments such as 455 bp with the MY09/11|PGMY system ( 41 ), 150 bp with the GP5+/6+ system ( 42 ), or <100 bp with SPF10 ( 43 ). And another point that is worth noting is that all these techniques remained the most validated methodology to identify and characterize clinically relevant HPV ( 44 - 46 ).
Additionally, the type-specific probes are always to be used to achieve HPV genotyping, besides DNA sequencing ( 46 , 47 ). Other types of assays may be type-specific with immediate discrimination and quantitation of specific HPV types in an “onetube” assay. These methods employ real-time (RT)-PCR techniques, coupled with beta-globin detection for internal quality control utilizing specialized detection systems ( 48 ).
Cervical cancer malignant pathways are tightly correlated to the viral E6 and E7 oncoprotein activities which could also contribute to the accumulation of cellular genomic mutations and viral integration ( 47 ). Therefore, identification of HPV E6/E7 mRNA has been shown to be promising in cervical cancer screening. And most of the assays utilized reverse transcriptase PCR or nucleic acid sequence-based amplification to identify E6/E7 genome fragments ( 49 ).
Recently, the correlation between increased HPV CpG site methylation levels and high-grade cervical lesions has also been demonstrated in numerous studies and has facilitated the development of quantitative assays targeted CpG methylation ( 50 , 51 ). . Studies indicate that NGS assays can provide single-molecule CpG methylation levels to help unravel the mechanism of methylation in cervical cancer development ( 39 , 50 ).
The application of HPV detection has accelerated the transition of cervical cancer screening from morphology to molecular biology. HPV testing was initially used as a triage method for the reflex triage of population with atypical squamous cells of undetermined significance (ASC-US). In 2014, FDA approved HPV detection for the use in cervical screening. Thereafter, HPV detection plays an increasingly important role in the practice of cervical cancer screening. At present, more than 425 HPV testing has been developed worldwide, of which more than 150 is from China. To restrict and standardize HPV testing market, China released guidelines for the clinical performance evaluation for HPV testing against clinical endpoints in 2015. In other countries, it is also necessary to set similar regulations in consideration that 59.7% of HPV tests on the global market without a single peer-reviewed publication ( 49 ). To improve the coverage of cervical cancer screening, HPV testing that is rapid, simple, inexpensive could be more popular and can further promote the application in practice. In 2008, care HPV was developed in China, which demonstrated excellent performance in screening, although it was easy to use, cheap, fast and friendly to the laboratory requirements ( 52 , 53 ). In 2018, the care HPV achieved the pre-qualification certification issued by WHO, which was expected to benefit more people in developing countries and resource-poor areas such as Africa and Southeast Asia ( 54 ). In addition, the cost-effective reflex triage, referral of women, and management strategies appropriate to various resource level areas were also in evaluation ( 55 - 58 ).
In recent years, with the rapid development of science and technology, the application of artificial intelligence (AI) based products is booming. In cervical cancer prevention and control, AI also showed to be promising in cytology-based screening and colposcopy examination based on the image pattern recognition ( 59 , 60 ). These AI-based technology or system can intelligently identify lesions and assist medical staff in clinical examination and diagnosis which could alleviate difficulties in diagnosis in primary clinics.
Screening practice in China
In China, cervical cancer screening started since 1990s, although late compared with Western countries, China still achieved great breakthroughs. Common screening methods were introduced into China for the first time after clinical performance evaluation in high-risk areas which included HPV DNA detection (Hybrid Capture II, HC2), LBC and visual inspection with VIA/VILI ( 61 - 63 ). At the same time, these studies also further made it clear that “one or more HPV tests in a lifetime for cervical cancer screening could be feasible in developing countries” which had important impact on the clinical practice of cervical cancer screening in China and even in the world.
In July 2019, the State Council issued the “Healthy China Action (2019−2030)” plan, emphasizing the need to move forward the diagnosis and treatment and optimize the allocation of medical resources, from the treatment-centered to the health-centered, and to improve health level of the whole people. The program also clearly points out that cervical cancer screening coverage rate needs to reach more than 80% by 2030 ( 64 ), indicating the importance and severity of cervical cancer prevention and control.
Finally, the achievements of scientific research should be able to be developed into products and applied in practice. Based on the experience and study findings, two “National Demonstration Base for Early Diagnosis and Treatment of Cervical Cancer” were set up in Shenzhen Maternal and Child Health Hospital (City type) and Xiangyuan Maternal and Child Health Hospital (Rural type) in Shanxi Province in February 2005 ( 65 ). Thereafter, National Health and Family Planning Commission of China and China Women’s Federation launched cervical cancer and breast cancer screening program for women aged 35−64 years old in rural areas in 2009 ( 66 ), which was also one of the major public health service projects in China organized by national government. Different screening and management strategies have been set up for various resource-level regions. Up to 2017, the project has offered cervical cancer screening for 73.99 million women. Currently, the project has covered 1,501 counties ( 67 ). Meanwhile, China has developed effective cervical cancer prevention and control network which covered screening, diagnosis to treatment, follow-up and rehabilitation step by integrating government support and leadership, multi-sectors’ cooperation, professional personnel support and whole society participation. In 2017, Chinese Preventive Medicine Association released the “Guideline for Comprehensive Prevention and Control of Cervical Cancer” to further promote the standardized and development of cervical cancer prevention and control in China ( 68 ).
The priority of public health measures for cancer prevention and control reflects the government and society’s attention to public’s health, especially in resource-limited areas, and also reflects the civilization and progress of a country and society.
A large number of studies around the world have confirmed that cervical cancer could be prevented and controlled well by screening and early treatment. And it has been widely recognized if only considering the effect of cancer screening. However, the screening methods or solutions with the best effect may be not the best one. In the case of limited health resources, it is necessary to analyze and compare the input and output of different programs from the perspective of health economics which included how to scientifically determine the initial age of screening and time interval, select appropriate screening programs according to local health resources, and focus on cancer intervention in order to maximize the use of limited health resources. And then, we could determine the screening solution that not only has a good effect of disease prevention and control, but also is in line with the principle of cost-effectiveness.
Conclusions
The disease burden of cervical cancer has decreased significantly in developed countries and regions in last decades, however it is still serious in less developed countries and regions, and effective preventive measures in these areas still face serious challenges. At present, there are various available prevention and control measures that are cost-effective and scientific evidence-based to meet the needs of areas with different economic levels. It is gratifying to note that the globe has achieved a strategic consensus on the elimination of cervical cancer and also has developed and released the global strategy to accelerate the elimination of cervical cancer. Although the global elimination of cervical cancer has a long way to go, it is believed that through large-scale continuous promotion and widely use of existing effective prevention and control measures, cervical cancer will become the first cancer eliminated by human beings.
Acknowledgements
This study was supported by grants from the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (No. 2017-I2M-B&R-03 and No. 2016-I2M-1-019).
Conflicts of Interest : The authors have no conflicts of interest to declare.
Together we are beating cancer
- Cancer types
- Breast cancer
- Bowel cancer
- Lung cancer
- Prostate cancer
- Cancers in general
- Clinical trials
- Causes of cancer
- Coping with cancer
- Managing symptoms and side effects
- Mental health and cancer
- Money and travel
- Death and dying
- Cancer Chat forum
- Health Professionals
- Cancer Statistics
- Cancer Screening
- Learning and Support
- NICE suspected cancer referral guidelines
- Make a donation
- By cancer type
- Leave a legacy gift
- Donate in Memory
- Find an event
- Race for Life
- Charity runs
- Charity walks
- Search events
- Relay for Life
- Volunteer in our shops
- Help at an event
- Help us raise money
- Campaign for us
- Do your own fundraising
- Fundraising ideas
- Get a fundraising pack
- Return fundraising money
- Fundraise by cancer type
- Set up a Cancer Research UK Giving Page
- Find a shop or superstore
- Become a partner
- Cancer Research UK for Children & Young People
- Our Play Your Part campaign
- Brain tumours
- Skin cancer
- All cancer types
- By cancer topic
- New treatments
- Cancer biology
- Cancer drugs
- All cancer subjects
- All locations
- By Researcher
- Professor Duncan Baird
- Professor Fran Balkwill
- Professor Andrew Biankin
- See all researchers
- Our achievements timeline
- Our research strategy
- Involving animals in research
- Research opportunities
- For discovery researchers
- For clinical researchers
- For population researchers
- In drug discovery & development
- In early detection & diagnosis
- For students & postdocs
- Our funding schemes
- Career Development Fellowship
- Discovery Programme Awards
- Clinical Trial Award
- Biology to Prevention Award
- View all schemes and deadlines
- Applying for funding
- Start your application online
- How to make a successful applicant
- Funding committees
- Successful applicant case studies
- How we deliver research
- Our research infrastructure
- Events and conferences
- Our research partnerships
- Facts & figures about our funding
- Develop your research career
- Recently funded awards
- Manage your research grant
- Notify us of new publications
- Find a shop
- Volunteer in a shop
- Donate goods to a shop
- Our superstores
- Shop online
- Wedding favours
- Cancer Care
- Flower Shop
- Our eBay store
- Shoes and boots
- Bags and purses
- We beat cancer
- We fundraise
- We develop policy
- Our global role
- Our organisation
- Our strategy
- Our Trustees
- CEO and Executive Board
- How we spend your money
- Early careers
- Your development
Cancer News
- For Researchers
- For Supporters
- Press office
- Publications
- Update your contact preferences
- About cancer
- Get involved
- Our research
- Funding for researchers
The latest news, analysis and opinion from Cancer Research UK
- Science & Technology
- Health & Medicine
- Personal Stories
- Charity News
- Health & Medicine
Cancer deaths plummet in middle-aged people

14 March 2024

Fewer middle-aged people are dying from cancer in the UK than at any point over the last 25 years, a new study from Cancer Research UK has revealed. *
Published today in the British Medical Journal , this is the first major study to examine trends in cancer incidence and mortality amongst middle-aged adults (35-69 yrs.) in the UK between 1993 to 2018.
Researchers said that analysing trends in this age group helps to understand the impact of different risk factors on the population as well as the likely future patterns of cancer in older patients.
“This study helps us to see the progress we’ve made in beating cancer and where challenges clearly remain,” said Jon Shelton, Cancer Research UK’s head of cancer intelligence and lead author of the study.
“This research is a useful benchmarking tool for the next 25 years and beyond so that we can take action to save more lives from cancer. We must continue to prevent as many cancer cases as possible, diagnose cancers sooner and develop kinder treatments.”
The good news
The study showed that overall, mortality rates had dropped by 37% in men and by 33% in women.
In examining data for 23 cancer groups or types, it also found that cervical cancer mortality rates decreased by 54.3%, showing how cervical screening has already helped to prevent cancer and stop the disease in its tracks, with HPV vaccination set to make a further huge impact on reducing the disease.
The study also revealed that lung cancer mortality rates decreased by 53.2% in men and by 20.7% in women, linked to reduced smoking rates in recent decades.
Deaths in breast and bowel cancers have also dropped, showing how screening programme s help to save lives by preventing bowel cancers and by diagnosing both cancers earlier leading to more treatment options.
Despite progress, challenges remain
Although rates in premature cancer deaths fell by over a third in this period, the data also exposed challenges across the UK’s health system.
T he charity warned that cancer cases are on the rise overall . The data highlights that cancer cases rose by 57% in men and 48% in women over the 25 years, largely due to a growing and ageing population as well as some lifestyle factors impacting people’s cancer risk.
Researchers also found concerning increases in rates of melanoma, liver, oral and kidney cancers.
In addition, death rates for liver, oral and uterine cancers – all linked to risk factors including UV exposure, alcohol, overweight and obesity, and smoking – were all increasing, following the increase in rates for these cancers.
Cancer Research UK said there is an immense challenge ahead to maintain progress, with all UK nations failing to meet their cancer waiting times targets and NHS staff under extreme pressure.
“With cancer cases and mortality for some sites on the rise and improvements in survival slowing, it’s vital that the UK Government takes bold action to keep momentum up,” added Shelton. “Now is the time to go further and faster, building on the successes of decades of research and improvements in healthcare.”
We need to take action
The findings of this research highlight where the UK Government can focus its efforts to help to save more lives from cancer, as well as the steps people can take to reduce their risk of the disease.
Cancer Research UK is urging political leaders to deliver long-term cancer strategies in all UK nations, including a National Cancer Council in England to drive cross-government action on cancer.
If bold action is taken against smoking, overweight and obesity and alcohol, nearly 37,000 cancer cases could be prevented by 2040 in the UK and tens of thousands more in future years. ** Preventing ill health not only benefits cancer patients and their families, it also leads to huge gains for the economy and the NHS.
Cancer Research UK is also calling on the Government to diagnose more cancers earlier. Bowel cancer screening should be optimised to reduce inequalities in access and reach as many eligible people as possible.
Targeted lung screening, which is being rolled out across England, will help to save more lives from a cancer type that takes more lives than any other. It is vital that other UK nations follow suit to reach more at-risk people.

Anne’s story
Anne Parmenter, 68-years-old from Suffolk, was diagnosed with bowel cancer in 2015. Anne’s cancer was caught after receiving a bowel cancer testing kit in the post on her 60th birthday. She said it was screening that saved her life.
Anne explained: “I had no symptoms before receiving the kit. I didn’t feel unwell, so I don’t think my cancer would have been caught if I didn’t take up the NHS screening offer.
“Weeks after doing the test I was invited into hospital to have part of my bowel removed, and this was followed by chemotherapy. My story shows how early diagnosis can save lives.”
Nine years have passed since Anne’s diagnosis. Reflecting on her experience, Anne said: “Getting diagnosed with cancer has changed how I look at life. None of us know what is around the corner, which is why it’s so important that cancer is found as soon as it can be, and that the NHS is ready to help everyone who needs treatment.”
A defining health issue
“This major study brings to life improvements that have been made to tackle cancer in recent decades,” said Michelle Mitchell, Cancer Research UK’s chief executive.
“If we take lung cancer, for example, we can clearly see that reducing smoking prevalence saves lives. The UK Government can build on this success by raising the age of sale of tobacco and continuing to fund a world-leading programme of measures to help people who smoke quit.
“But c ancer is still a defining health issue in the UK that impacts nearly one in two people. P eople face long waits for vital tests and treatment and cancer cases are on the rise.
“Cancer patients won’t feel the full benefits of advances in research breakthroughs and innovation, including new cancer treatments, without long-term plan and funding from the UK Government.”
* Age-standardised mortality rate for males and females aged 35-69 years, between 1993-2018 in the UK
** Longer, better lives: A manifesto for cancer research and care (cancerresearchuk.org) p.13
this is a really poor article – there’s no link to the study and the link to the BMJ site is an internal link to cervical cancer ?
You’ve had a lot of press on this today (the reason I wanted to find out more) and tbh I would have expected a bit more diligence on this article :( really disappointed
Thanks for pointing out that the wrong link was embedded in the article, that’s now been updated to the correct one. Or, you can read the paper here
Jacob, Cancer Research UK
Tell us what you think
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Read our comment policy .
Highlighted content

£1.7 million for the world’s first vaccine to prevent lung cancer

Can vaping cause changes in our cells?

A message to MPs: Don’t miss the opportunity to make smoking history
From lemonade stand to grand challenge: changing how we treat cancer in children and young people

Cancer Grand Challenges gives a record £100m to five cancer research teams
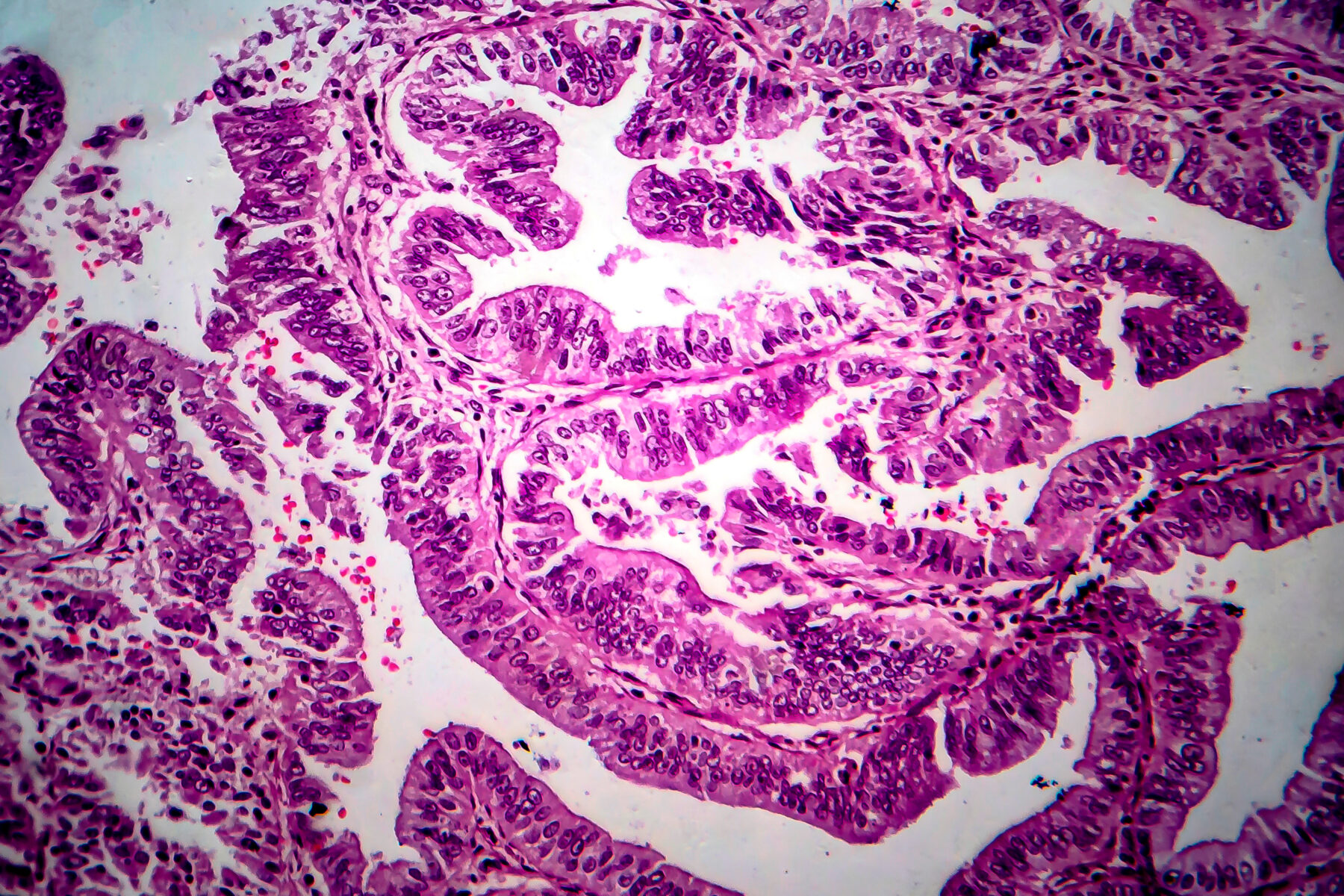
New treatment option made available for advanced womb cancers

Related topics
- Manifesto for Cancer Research and Care
- Screening and early diagnosis
- Preventing cancer
- Jobs & Internships
- Micro-Internships and Mentoring Program
- Calendar of Upcoming Events
- Students: Preparing for Career Fairs
- Employers: Just In Time Fair Details
- Employers: Agriculture & Food Systems Career Expo Details
- Employers: University Career and Internship Pre-Fair Details
- Employers: Education Pre-Fair Details
- Agriculture and Food Systems
- Architecture, Engineering & Construction
- Arts, Entertainment, Media & Design
- Computing, Software, & Data Analytics
- Economics, Banking & Finance
- Government, Policy, International Affairs & Law
- Health & Wellness
- Hospitality, Sports & Recreation
- Human Services, Teaching & Training
- Management, Marketing & Sales
- Science, Research & Development
- The Environment, Sustainability & Natural Resources
- University Career Services
- College of Agricultural Sciences & Natural Resources
- College of Architecture
- College of Arts & Sciences
- College of Business
- College of Education & Human Sciences
- College of Engineering
- College of Fine and Performing Arts
- College of Journalism & Mass Communications
- School of Criminology and Criminal Justice
- Alumni Association
- Explore Center
- Graduate Studies
- International & National Fellowships
- Military & Veteran Success Center
- Undergraduate Research
- DIY Resources
- Career Coaching
- Diversity, Equity, & Inclusion Resources
- DACA and Undocumented Students
- First Generation
- International Students
- Military & Veteran
- Black, Indigenous, and People of Color
- Students with Disabilities
- Women’s Career Resources
- Recruiting at UNL
- Internship & Early Talent Toolkit
- Connect With Campus
- Fairs & Events
- Husker Circle
- Micro-Internship Program
- UNL HuskerWork
Moffitt Cancer Center
Applied research scientist_cancer epidemiology.
- Share This: Share Applied Research Scientist_Cancer Epidemiology on Facebook Share Applied Research Scientist_Cancer Epidemiology on LinkedIn Share Applied Research Scientist_Cancer Epidemiology on X
At Moffitt Cancer Center, we come face-to-face with cancer every day, but we also see courage. And it inspires us to be the safest and best place for cancer care – to bring greater hope to every patient we serve. It’s why we’ve been continually named One of the Top Places to Work in the Tampa Bay Area. As the only National Cancer Institute-designated Comprehensive Cancer Center based in Florida, Moffitt employs some of the best and brightest minds from around the world. Moffitt is the leading cancer hospital in both Florida and the Southeast and has been nationally ranked by U.S. News & World Report since 1999. Because working at Moffitt is both a career and a mission: to contribute to the prevention and cure of cancer. Join a dedicated, diverse and inclusive team of over 7,000 to be a part of the Courageous future we envision.
Applied Research Scientist
The Applied Research Scientist position will support the research and research team activities of Dr. Anna Giuliano , an epidemiologist with ongoing investigations to understand infection-related cancers, particularly to develop improved methods for their prevention through screening and improved treatments. Dr. Giuliano leads multiple domestic and multinational studies, including development of early detection cancer biomarkers, clinical trials for the prevention of HPV-related cancers among people living with HIV in Latin America and the Caribbean, and research of understudied virally-associated cancers among men and women living with HIV in sub-Saharan Africa.
This position is comparable to a staff scientist role: an essential contributor to analysis, writing, and grant preparation for ongoing and future research projects under the general direction of Dr. Giuliano. This position will have ample opportunities for authorship and other documentable career-enhancing activities.
Position Highlights:
- Writes and prepares manuscripts for peer-reviewed publication of a variety of research studies
- Independently works with biostatisticians to complete statistical analyses
- Generates scientific sections of grant applications with appropriate guidance
- Develops and initiates protocols for and high-level coordination of multiple studies
- Potential to network in large international research consortia
The Ideal Candidate:
- PhD in epidemiology, with a focus in infectious disease and/or cancer epidemiology, or a closely aligned quantitative field
- Has research experience in the academic and/or clinical setting, preferably in oncology
- Strong writing skills and enthusiasm for writing as demonstrated by first author publications
- Statistical programming experience, including demonstrated proficiency in SAS and R
- Experience collaborating in a multidisciplinary environment
- A critical, independent, and creative thinker
- A professional, personable, and organized individual
- Excellent oral and written communication skills. Grant writing experience is highly desired
Responsibilities:
- Under appropriate direction and guidance, performs research and related support activities including, (a) development, implementation, and management of research projects; (b) preparation of drafts of regulatory protocols and reports, manuscripts, and grants and (c) presentation of research at scientific meetings
- Interacts closely with Investigators and their collaborators in the consortium setting.
- Maintains membership and regularly attends appropriate professional associations, conferences, workshops, lectures, and seminars as supported by the overseeing Investigators.
Credentials and Qualifications:
- Minimum of an M.D. or Ph.D. in a discipline relevant to epidemiology or related field is required
- 2 years post-doctoral experience is preferred
- Experience working on research related to HPV and/or HIV is preferred
Equal Employment Opportunity
Moffitt Cancer Center is an Equal Opportunity/Affirmative Action Employer. All qualified applicants will receive consideration for employment without regard to race, color, religion, sex, sexual orientation, gender identity, national origin, age, or protected veteran or disabled status. We seek candidates whose skills, and personal and professional experience, have prepared them to contribute to our commitment to diversity and excellence.
Reasonable Accommodation
Federal law requires employers to provide reasonable accommodation to qualified individuals with disabilities. Please tell us if you require a reasonable accommodation to apply for a job or to perform your job. Examples of reasonable accommodation include making a change to the application process or work procedures, providing documents in an alternate format, using a sign language interpreter, or using specialized equipment. Moffitt endeavors to make moffitt.org/careers accessible to any and all users. If you would like to contact us regarding the accessibility of our website or need assistance completing the application process, please contact one of the Human Resources receptionists by phone at 813-745-7899 or by email at [email protected]. This contact information is for accommodation requests only and cannot be used to inquire about the status of applications. If you’d like more information on your EEO rights under the law, please click here.
Career Services
225 Nebraska Union Lincoln, NE 68588-0451 402-472-3145 [email protected]
Related Links
- Counseling and Psychological Services (CAPS)
- Office of the Registrar
- Office of Scholarships and Financial Aid
- Student Affairs
- Undergraduate Admissions
Campus Links
- Office of the Chancellor
- Report an Incident
Policies & Reports
- Emergency Planning and Preparedness
- Institutional Equity and Compliance
- Notice of Nondiscrimination
- Security and Fire Safety Report
- Student Information Disclosures
- Privacy Policy
- Terms of Service
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
March 29, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Researchers demonstrate technique for identifying single cancer cells in blood for the first time
by Keele University
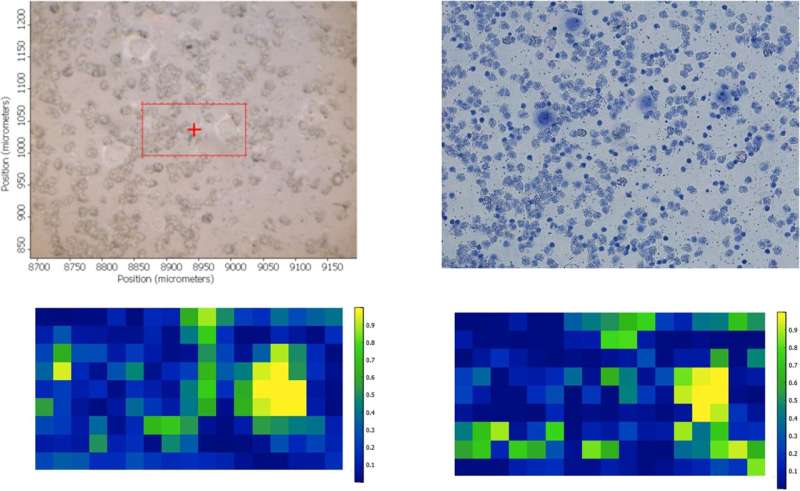
A pioneering study led by a Keele scientist has demonstrated how a single cancer cell can be identified in a sample of blood, paving the way for more personalized and targeted treatments for cancer patients.
Led by Professor of Oncology Josep Sulé-Suso, the team of academics from Keele University, the Cancer center at University Hospitals North Midlands NHS Trust, and Loughborough University (Professor Paul Roach), used a technique called Fourier Transform Infrared (FTIR) microspectroscopy, which can separate cells based on their biochemical composition using an infrared light.
Publishing their findings in the journal PLOS One , the team has shown for the first time that FTIR microspectroscopy, used together with a machine learning algorithm, is able to identify a single lung cancer cell in a sample of blood.
The advent of personalized medicine has greatly improved the treatment and management of patients with cancer, by tailoring therapies to individuals based on their specific needs and the type of cancer they have.
Professor Sulé-Suso and his colleagues believe that by identifying individual tumor cells circulating in blood using this technique, patients can be assessed more effectively during the initial tumor screening, staging, response to treatment, and follow up stages of cancer treatment.
These findings could therefore lead to improving the personalized medicine approach even further by making screening for cancer cells more robust than current processes.
Professor Sule-Suso said, "Identifying cancer cells in blood using this technique could be a game-changer in the management of patients with cancer."
The team has now had approval to expand their research with a further study, looking at blood samples from patients with different types of cancer, not just lung, to see if this technique can be replicated successfully with other cancer types.
Professor Kamaraj Karunanithi, Director of Research and Innovation at University Hospitals of North Midlands NHS Trust (UHNM), said, "The UHNM Research and Innovation Department is thrilled to back research targeting the early detection of cancer cells in the bloodstream. Detecting cancer spread early is vital for improving patient care.
"This research has the potential to establish new standards in treating cancer at various stages. The UHNM research strategy not only backs delivery of national and international research but also concentrates on identifying and developing local research in collaboration with our local universities."
Explore further
Feedback to editors

An infamous 'inflammasome'—a rogue protein complex—appears to underlie a rare and disabling autoimmune disorder
6 hours ago

Researchers discover skin biomarkers in infants that predict early development of food allergies

Veterans help provide greater insight into Klinefelter and Jacobs syndromes

High-resolution images reveal similarities in protein structures between Alzheimer's disease and Down syndrome

How blocking a neural receptor responsible for addiction could reduce alcohol use

Study finds few hospitals promoting potentially predatory medical payment products
7 hours ago

COVID-19 research: Study reveals new details about potentially deadly inflammation

Enhanced melanoma vaccine offers improved survival for men

How music choices can affect productivity

Prescribing alcohol use disorder medications upon discharge from alcohol-related hospitalizations works
Related stories.

Targeted immunotherapy could lead to pioneering treatment for breast cancer
Feb 29, 2024

Is lung cancer treatment working? This chip can tell from a blood draw
Jan 29, 2024

Era of hope for patients with lung cancer
Nov 21, 2022

Glass filters developed to separate tumor cells from blood may increase efficiency of blood tests for cancer
May 2, 2023

Scientists develop liquid biopsy technique to help detect cancer in blood
Jul 20, 2022

New gene target for aggressive lung cancer discovered
Oct 5, 2022
Recommended for you

Researchers develop AI-based tool paving the way for personalized cancer treatments
9 hours ago

Private and secure generative AI tool supports operations and research in a cancer center

New research highlights combining prostate MRI with a blood test to avoid unnecessary prostate biopsies

Discovery suggests new strategy against follicular lymphoma
Mar 28, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
COMMENTS
Cancer Epidemiology publishes original research, prioritizing studies that contribute new information about cancer causes, prevention and control. As such, the journal's scope covers all aspects of cancer epidemiology including studies of: • Risk factors for cancer initiation, development, and prognosis. • Early detection, prevention, and ...
The Biology of Cancer. Cancer is a disease that begins with genetic and epigenetic alterations occurring in specific cells, some of which can spread and migrate to other tissues. 4 Although the biological processes affected in carcinogenesis and the evolution of neoplasms are many and widely different, we will focus on 4 aspects that are particularly relevant in tumor biology: genomic and ...
Cancer epidemiology is the study of the causes of cancer and the evaluation of outcomes in defined population groups. As a population science, epidemiology plays an important role in cancer prevention and control with discoveries leading to improved guidelines, practices, and policies with wide-reaching public health impact.
Cancer epidemiology is the study of the distribution and determinants of the likelihood of cancer development. Cancer epidemiology can be used to identify events that increase or decrease cancer ...
Cancer epidemiology. Cancer is one of leading causes of mortality worldwide. Therefore, understanding incidence and mortality trends for each cancer is a public health priority in many countries ...
The incidence of early-onset colorectal cancer (CRC) is increasing worldwide for reasons that are currently unclear. Herein, the authors review the current epidemiological, clinical, pathological ...
Cancer Epidemiology, Biomarkers & Prevention publishes articles featuring population-based research on cancer etiology, prevention, surveillance, survivorship, and cancer health disparities—with a particular focus on articles with a transdisciplinary approach. Read More About the Journal.
This article provides an update on the global cancer burden using the GLOBOCAN 2020 estimates of cancer incidence and mortality produced by the International Agency for Research on Cancer. Worldwide, an estimated 19.3 million new cancer cases (18.1 million excluding nonmelanoma skin cancer) and almo …
Real-world data are necessitated to counsel patients about the risk for recurrent disease after curative treatment of colorectal cancer. This study provided a population-based overview of the epidemiology of recurrent disease in patients with surgically resected stage II/III colorectal cancer. February 07 2024.
The overall 0-74 years risk of developing cancer is 20.2% (22.4% in men and 18.2% in women, respectively). A total number of 18 million new cases have been diagnosed in 2018, the most frequent of which are lung (2.09 million cases), breast (2.09 million cases), and prostate (1.28 million cases) cancers. Beside sex-specific malignancies, the ...
The cancer epidemiology faculty have developed a rich research program including diverse cancers (breast, prostate, colon, head and neck, childhood, melanoma, esophageal, and bladder) and exposures (lifestyle, diet, genes, tumor biology, occupational and environmental, health care, screening, socioeconomic factors).
The Cancer Epidemiology faculty at Johns Hopkins conduct a wide range of public health research that covers the entire cancer continuum including cancer etiology, early detection, cancer prevention, control, surveillance, survivorship and disparities of a number of cancers. There is a strong emphasis on translational epidemiology and team ...
Research Tools. We have created many tools for study design and planning, analysis, and risk assessment. Exposure assessment tools and methods developed by DCEG experts to measure exposures for diet and activity, occupation and environment, radiation, and more. NCIDose is a collection of medical radiation dosimetry tools developed by medical ...
The Cancer Epidemiology and Prevention program at the Harvard T.H. Chan School of Public Health is one of the first comprehensive academic programs in the world ... The program's curriculum includes a breadth of courses on cancer research methodology, substantive courses on cancer epidemiology and prevention, as well as courses on genetic ...
INTRODUCTION. Epidemiology provides information on the distribution of cancer in a population and on cancer determinants and then applies this knowledge to disease control 1.Cancer surveillance, a key attribute of epidemiology and public health practice, provides intelligence data on the burden of different types of cancer in a specified population and, through evidence-based health programs ...
Research Resources for Cancer Epidemiology and Genomics. The Epidemiology and Genomics Research Program (EGRP) has compiled collections of research tools and resources that are freely available through NCI, other institutes and centers at NIH, as well as NIH-funded research projects and partnering organizations.
The Global Cancer Observatory (GCO) is an interactive web-based platform presenting global cancer statistics to inform cancer control and research. This website uses cookies to enhance your user experience. By using the website, you consent to our use of cookies.
Stroup Research Program. Bo (Bonnie) Qin, PhD. Assistant Professor. Division of Medical Oncology and Section of Cancer Epidemiology and Health Outcomes. Dr. Qin is an epidemiologist with research interests in multilevel modifiable risk factors that influence cancer health disparities, especially breast and ovarian cancers. Qin Research Program.
Abstract. Lynch syndrome (LS) is the most common autosomal dominant cancer syndrome and is characterized by high genetic cancer risk modified by lifestyle factors. This study explored whether a circulating microRNA (c-miR) signature predicts LS cancer incidence within a 4-year prospective surveillance period. To gain insight how lifestyle behavior could affect LS cancer risk, we investigated ...
Globally, ovarian cancer is the eighth most common cancer in women, accounting for an estimated 3.7% of cases and 4.7% of cancer deaths in 2020. Until the early 2000s, age-standardized incidence ...
Colorectal cancer (CRC) is the second most common cause of cancer death in the United States. Every 3 years, the American Cancer Society provides an update of CRC statistics based on incidence from population-based cancer registries and mortality from the National Center for Health Statistics.
This video highlights the features of U.S. Cancer Statistics, the official federal cancer statistics. In the United States in 2020, 1,603,844 new cancer cases were reported and 602,347 people died of cancer. For every 100,000 people, 403 new cancer cases were reported and 144 people died of cancer. 2020 is the latest year for which incidence ...
Professor Jürgen Wahrendorf (23 April 1948-15 March 2024) The International Agency for Research on Cancer (IARC) is saddened by the passing of Professor J ... 19.03.2024. IARC hosts the Advisory Group to Recommend Priorities for the IARC Monographs during 2025-2029. The International Agency for Research on Cancer (IARC) is hosting the ...
Objective To examine and interpret trends in UK cancer incidence and mortality for all cancers combined and for the most common cancer sites in adults aged 35-69 years. Design Retrospective secondary data analysis. Data sources Cancer registration data, cancer mortality and national population data from the Office for National Statistics, Public Health Wales, Public Health Scotland, Northern ...
Epidemiology for cervical cancer. Cervical cancer is one of the leading causes of cancer death among women ().Over the past 30 years, the increasing proportion of young women affected by cervical cancer has ranged from 10% to 40% ().According to the WHO and International Agency for Research on Cancer (IARC) estimates, the year 2008 saw 529,000 new cases of cervical cancer globally.
Fewer middle-aged people are dying from cancer in the UK than at any point over the last 25 years, a new study from Cancer Research UK has revealed. * Published today in the British Medical Journal, this is the first major study to examine trends in cancer incidence and mortality amongst middle-aged adults (35-69 yrs.) in the UK between 1993 to ...
Potential to network in large international research consortia; The Ideal Candidate: PhD in epidemiology, with a focus in infectious disease and/or cancer epidemiology, or a closely aligned quantitative field; Has research experience in the academic and/or clinical setting, preferably in oncology
New research from Memorial Sloan Kettering Cancer Center (MSK) shows the effectiveness of cryoablation for large breast cancer tumors; helps win the approval of a drug to treat one type of metastatic non-small cell lung cancer; identifies a gene essential for the formation of a common childhood brain tumor; and unlocks the secrets of natural killer cell metabolism.
St. Jude Children's Research Hospital scientists reversed an aggressive cancer, reverting malignant cells towards a more normal state. Rhabdoid tumors are an aggressive cancer which is missing a key tumor suppressor protein. Findings showed that with the missing tumor suppressor, deleting or degrading the quality control protein DCAF5 reversed the cancer cell state.
Brightfield image of a cytospun sample containing PBMC and individual CALU-1 cancer cells. Credit: PLOS ONE (2023). DOI: 10.1371/journal.pone.0289824