- Research article
- Open access
- Published: 27 August 2020

The top 100 most cited articles on bronchoscopy: a bibliometric analysis
- Boxue He 1 , 2 na1 ,
- Pengfei Zhang 1 , 2 na1 ,
- Qidong Cai 1 , 2 ,
- Shuai Shi 1 , 2 ,
- Hui Xie 1 , 2 ,
- Yuqian Zhang 1 , 2 ,
- Xiong Peng 1 , 2 ,
- Zhenyu Zhao 1 , 2 ,
- Wei Yin 1 , 2 &
- Xiang Wang ORCID: orcid.org/0000-0002-5211-7206 1 , 2
BMC Pulmonary Medicine volume 20 , Article number: 229 ( 2020 ) Cite this article
3399 Accesses
5 Citations
Metrics details
Bronchoscopy is applied broadly in the diagnosis and treatment of pulmonary diseases. Over the past few decades, an increasing number of studies about bronchoscopy have been published. However, little is known about their qualities and characteristics.
All of the databases in Web of Science (including the Web of Science Core Collection, BIOSIS Citation Index, KCI-Korean Journal Database, MEDLINE, Russian Science Citation Index, and SciELO Citation Index) were utilized to identify articles published from 1990 to 2020. The top 100 most cited articles about bronchoscopy were selected for degree centrality analysis and analyses regarding publication time, total citation number, the citation density, time-related flux, first author, published journal, geographic origin, and research theme.
The selected articles were published mainly in the 2000s and 1990s. Citations per article ranged from 731 to 196. The leading country was the USA, followed by the United Kingdom. The most frequently studied themes were bronchoalveolar lavage (BAL) fluid and biopsy. The degree centrality analysis connoted that “BAL, inflammation, diagnosis” had a high degree of centrality in the 1990s, while “diagnosis, BAL, biopsy, prospective” took centre stage in the 2000s.
Conclusions
The time, area, and theme distribution of the 100 most cited articles on bronchoscopy have been thoroughly analyzed. It is noticeable that researches based on BAL and endobronchial or transbronchial biopsies currently plays a major role.
Peer Review reports
Introduction
German laryngologist Gustav Killian performed the first bronchoscopy by using rigid bronchoscopy to remove a pork bone from a patient’s airway in 1897 [ 1 ]. The procedure was performed while the patient was awake and cocaine was utilized as a local anesthetic. Nowadays, endoscopy techniques have developed into an approach which can effectively detect and localize critical early pathological changes occurring in the bronchial epithelium and subepithelial regions of human bodies [ 2 ]. Bronchoscopies including autofluorescence bronchoscopy, optical fluorescence and reflectance spectroscopy, high-magnification bronchoscopy, high-frequency endobronchial ultrasound, optical coherence tomography, etc. remain a cornerstone in helping identify the etiology of radiographic abnormalities in human bronchial and lung [ 3 ]. Under the assistance of bronchoscopies, diseases which can be diagnosed cover chronic lung diseases such as asthma, chronic obstructive pulmonary disease, interstitial lung disease, some lung cancer, and even pulmonary infectious diseases [ 4 , 5 , 6 ]. It has aroused our interest that what are the common laws of the complex literature surrounding bronchoscopy these years, and how will it guide future research. Therefore, we hope to carry out a literature-based analysis of bronchoscopy.
There is a unique tool called bibliometrics for analyzing the quality and characteristics of published articles. It was first published in JAMA in 1987 and has been widely used in various fields to assess the importance of published articles or research trends [ 7 ]. Through a literature search, we found that there were quite a few highly cited literature (citation time > 150) on bronchoscopy or utilizing bronchoscopy as the main research method, but no literature on bibliometrics analysis yet. The purpose of this study was to investigate the 100 most cited publications in the field of bronchoscopy, to highlight knowledge milestones in the field, and to analyze the quality and characteristics of the most cited original papers of the past 30 years. We also look forward to finding out the most promising research direction about bronchoscopy.
Search strategy and criteria
Web of Science (Thomson Reuters, New York, USA) allows access to more than 12,000 peer-reviewed journals published since 1945, along with their collected citation data [ 8 ]. On February 10, 2020, we searched online via all of the databases in Web of Science (including the Web of Science Core Collection, BIOSIS Citation Index, KCI-Korean Journal Database, MEDLINE, Russian Science Citation Index, and SciELO Citation Index). To enhance the sensitivity, two independent researchers used the same search terms (“bronchoscopy” OR “bronchoscopies” OR “bronchoscopic”) with the determined period of 1990 to 2020 and without any language restrictions to search simultaneously. A total of 35,637 results were gathered, and after filtering by Literature type as “articles” and/or “clinical trial”, 29,030 pieces of literature was listed. Thus, only typical original articles were included, and literature such as reviews, meta-analyses, and guidelines was excluded.
To reduce the number of articles that need to be screened and improve the gold content of selected documents, we then exported articles that have been cited at least 150 times to EndNote. These 423 articles included were all reviewed by two independent researchers based on the title and the abstract of each. Articles which met the following criteria were included to our study group: (1) The article mainly focuses on bronchoscopy (including rigid bronchoscopy, fiber bronchoscopy, fluorescent bronchoscopy, and so on) with the topic of technical improvement or evaluation; (2) The article compares the advantages or disadvantages of bronchoscopy and other examination or sampling methods; (3) The article mentions bronchial thermoplasty, bronchial valve surgery or other bronchoscope-based operation to solve clinical problems; (4) The article is mainly based on bronchoalveolar lavage (BAL) fluid or bronchoscopy biopsies to get samples for later research. The disagreement between the two researchers was discussed in sequence to reach an agreement. Finally, there remained 185 articles for the following research. These articles were ranked by the number of citations and the top 100 articles were included in this analysis (Fig. 1 ).
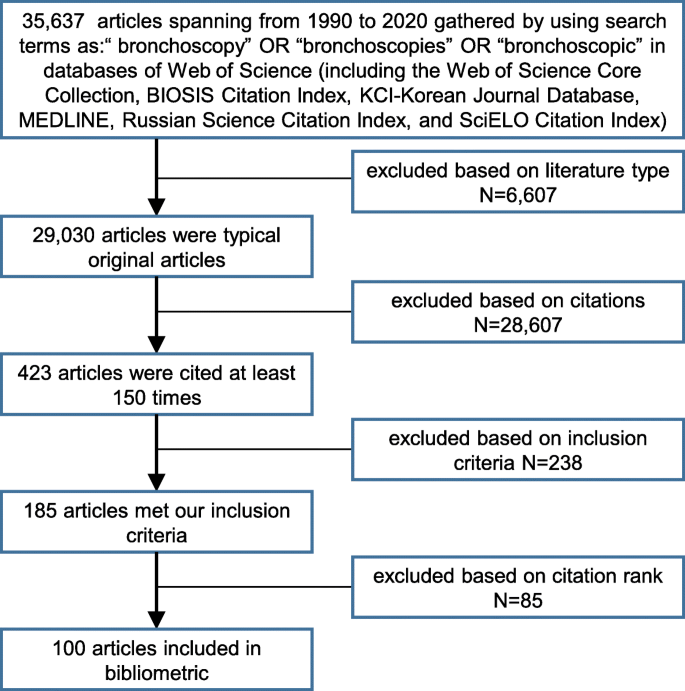
Flowchart illustrating the article allocation process
All articles were reviewed by two independent experienced investigators. The following information was listed for all articles: the journal name, year of publication, article age (2020 minus the year of publication), first author, geographic origin, total citation number, the citation density (total citation number/article age), and research theme (introduced later).
Statistical analysis
The distribution of individual variables for normality was tested using the Shapiro-Wilk test and the Kolmogorov-Smirnov test. Normally distributed data were presented as mean ± standard deviation. A comparison between means was performed using a one-way analysis of variance (ANOVA). Time-dependent trends were tested by the Mann-Kendall trend test. Correlation between variables was performed by the Spearman rank test. P < 0.05 was considered to be statistically significant. The analysis was performed using IBM SPSS Statistics, Version 24.0. The Ucinet for windows, version 6.212 was used for the degree of centrality analysis. At last, we used the same search strategy to search 1000 most cited articles in the core data set of Web of Science, and then used HistCite Pro 2.1 software to re-analyze and compare with the former-mentioned 100 articles.
We gathered the 100 most cited articles on bronchoscopy (Table 1 , Additional file 1 ). The number of citations ranged from 731 to 196, and a majority of articles presented in the 2000s (50%) and 1990s (42%), while articles published in 2010s only accounted for 8% (Fig. 2 ). The year with the highest number of articles was 2006 ( n = 9), followed by 2007 ( n = 8), 1995 ( n = 7), and 1997 ( n = 7). The mean number of citations was 290 overall, 293 in the 1990s, 276 in the 2000s, and 368 in the 2010s. The mean number of citation density was 17.5 overall, 12.0 in the 1990s, 18.0 in the 2000s, and 42.2 in the 2010s. The Mann-Kendall trend test showed an increasing trend between the top-cited articles’ citation density and their published time ( P < 0.0001) (Fig. 3 ). The Spearman rank showed a positive correlation between year of publication and citation density ( r = 0.764, P < 0.01). Both the Shapiro-Wilk test and the Kolmogorov-Smirnov test indicated an abnormal distribution in total citation number as well as the citation density.
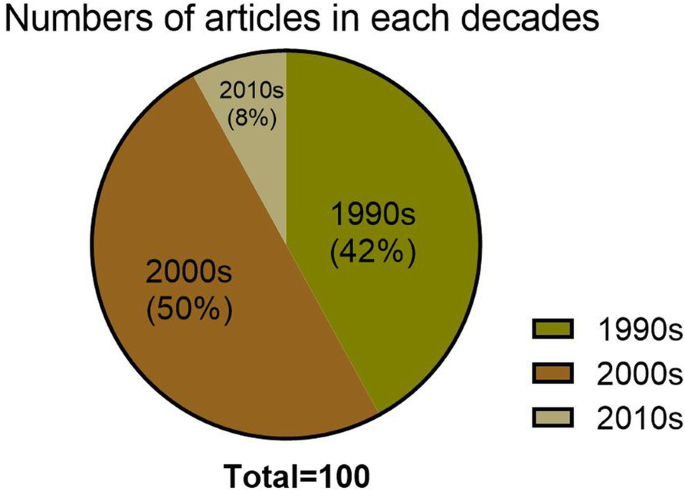
Time distribution of 100 top-cited articles in bronchoscopy. A majority of articles were published in the 1990s (42%, n = 42) and 2000s (50%, n = 50)
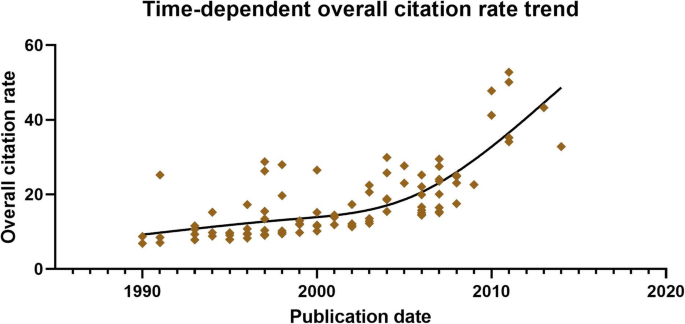
Time-dependent citation density trend. Mann-Kendall trend test showed an increasing trend between the citation density and the time ( p < 0.0001)
All of the articles were distributed in 16 countries, led by the USA ( n = 35), followed by the United Kingdom ( n = 14), France ( n = 10), and so on. The distribution was illustrated on the world map (Fig. 4 ). The map showed that two regions, North America and Western Europe, kept most of the articles. Besides, Japan had 6 articles, Australia had 4, Argentina and Israel both had 2, while Korea had 1.
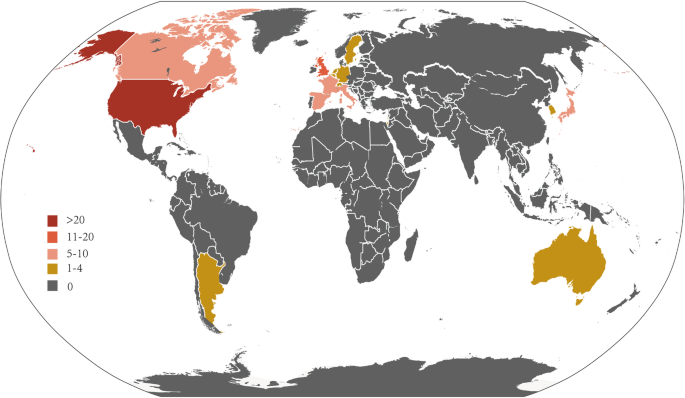
Geographical distribution of all articles. The map showed that most articles came from two regions: North America and Western Europe
(Due to limited space, the national borders are not completely accurate. This figure was modified based on an original image downloaded from Wikimedia Commons https://upload.wikimedia.org/wikipedia/commons/e/e7/GDP_per_capita-worldmap-2006.svg )
These articles were published in 25 kinds of journals. Thirty-nine articles were published in American journal of respiratory and critical care medicine , followed by Chest ( n = 20), The American review of respiratory disease ( n = 5), Thorax ( n = 5), New England Journal of Medicine ( n = 4), Annals of Internal Medicine ( n = 3), Pediatric Pulmonology ( n = 3), and other three journals ( n = 2) (Table 2 ).
The first authors with the most occurrences and their basic research institutions were listed in Table 3 . Yasufuku K, from Japan, had acted as the first authorship in four articles out of our list, in which two written in Chiba University, one in Department Hospital de Sabadell, and one in University of Toronto. The total citations of his four selected articles were 1484.
We collected the research institutions of first authors in these top-cited articles. Eight institutions had 3 articles included, and they were Hospital Bichat, University of Barcelona, Royal Brompton Hospital, University of London, University of Southampton, Mayo Clinic, National Jewish Medical and Research Center, and University of California at San Francisco. Besides, 10 research institutions were involved by two articles listed, and 56 institutions with one article, respectively (Supplementary Table 1 ).
We divided these top 100 most cited articles into eight categories based on the main content. In particular, some articles cover two or three types of topics at the same time, and we also recorded them repeatedly. Three professional researchers discussed each article and reached consensus. List these theme categories in descending order according to the number of relevant literature as: BAL fluid ( n = 50), bronchoscopy and biopsy ( n = 29), comparison of different examinations ( n = 19), evaluation of new technologies ( n = 12), bronchial thermoplasty ( n = 4), new technique of bronchoscopy ( n = 4), bronchoscope-based operation ( n = 3), and bronchoscopy assisted valve implantation ( n = 2) (Fig. 5 ). One-way ANOVA showed no significant difference between citations and these themes ( P = 0.486) (Fig. 6 ).
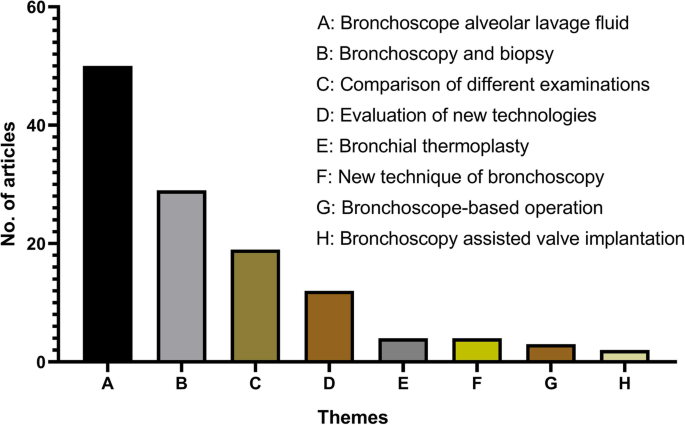
The themes distribution of all the articles. The most mentioned theme was bronchoalveolar lavage fluid ( n = 50), followed by bronchoscopy and biopsy ( n = 29)
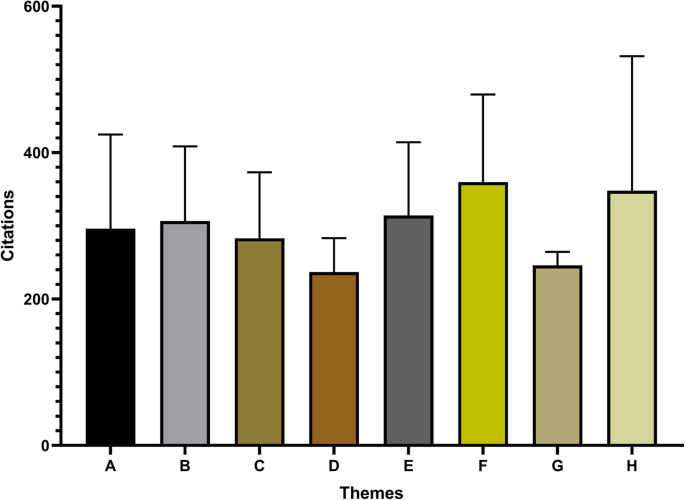
Mean citation per article based on the theme. One-way ANOVA showed no significant difference in citations per article among the various themes ( P = 0.486). A: bronchoalveolar lavage fluid, B: bronchoscopy and biopsy, C: comparison of different examinations, D: evaluation of new technologies, E: bronchial thermoplasty, F: new technique of bronchoscopy, G: bronchoscope-based operation, H: bronchoscopy assisted valve implantation
These article’s keywords and subject terms were checked one by one by two researchers, and then degree centrality analysis has been done in two periods of article published time: in the 1990s (42 articles) and the 2000s (50 articles). The result indicated that “BAL, inflammation, diagnosis, biopsy” had a high degree of centrality in the 1990s (Fig. 7 ), while “diagnosis, BAL, biopsy, prospective, outcome, EBUS, evaluation” had a high degree of centrality in the 2000s (Fig. 8 ).
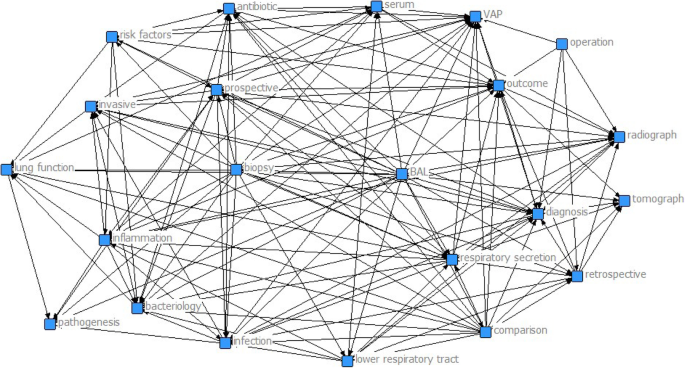
Degree centrality analysis in the 1990s (42 articles). It showed that “BAL, inflammation, diagnosis, biopsy” had a high degree of centrality in the 1990s
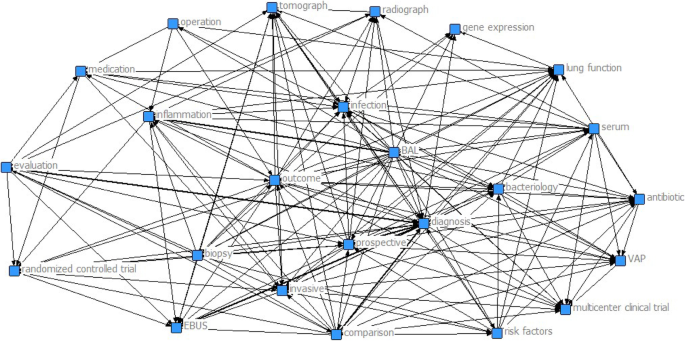
Degree centrality analysis in the 2000s (50 articles). It showed that “diagnosis, BAL, biopsy, prospective, outcome, EBUS, evaluation” had a high degree of centrality in the 2000s
By ranking the Local Citation Score (LCS) index from high to low, we got the top 30 articles with the LCS of 46 to 13 in HistCite Pro 2.1(Table 4 ). We compared them with the top 100 articles selected by the former method and found that 12 of them appeared again.
As far as we can know, this is the first bibliometric analysis of papers on bronchoscopy. From the analysis of the top 100 most cited articles published on the theme of bronchoscopy, we can get several significant findings. The maximum number of citations in these articles reached 731, and this was a paper based on a bacteriologic analysis of BAL fluid for the diagnosis of ventilator-associated pneumonia [ 9 ]. When it comes to such relatively limited citation numbers, one explanation is that our analysis only focuses on articles published in the last 30 years, so there may not be enough time for them to be fully cited. Half of the top-cited articles were published in the 2000s, seconded by the 1990s with the article number of 42 in the top 100 most cited. The phenomenon of “obliteration by incorporation”, which refers to articles no longer be cited when their substance has been treated as current knowledge [ 7 ], maybe exists in this analysis. Besides, there is an increasing trend between top-cited articles’ citation density and their published time, showing that more and more high-quality articles are published in this field. Interestingly, there are eight articles published since 2010 making the top 100 most cited. The most recent literature in them was published in 2014, with the citation of 197 now [ 10 ]; followed by an article in 2013, with the citation of 303 here [ 11 ]. These results above also suggest that quite a few highly cited articles about bronchoscopy have appeared in the past 10 years.
We also have demonstrated the regional distribution of these articles. On the one hand, the majority of them originated from two regions, North America and Western Europe. Many research institutions there also performed well. For example, eight institutions each contributed three articles in the top 100 most cited, three of them (Mayo Clinic, National Jewish Medical and Research Center, and the University of California at San Francisco) from the USA, three of them (University of Southampton, University of London, and Royal Brompton Hospital) from the United Kingdom, along with Hospital Bichat and University of Barcelona from France and Spain individually. The reason for this phenomenon may be countries such as the USA and the United Kingdom have a fairly developed economy for supporting medical research. And it has previously been illustrated that a weak correlation exists between a country’s gross domestic product per capita and its research achievements [ 12 ]. On the other hand, we can see that some papers are from Japan and Korea in Asia, the Republic of Argentina in South America, and Australia in Oceania, suggesting that the application of bronchoscopy is universal and proving that this inspection technique has always been of research value once again. It means a lot that the research achievements from all these countries are shared in public so that more people can benefit from their studies.
We noticed that two journals contributed more than a half articles in the top 100 most cited, demonstrating strong professional attributes. They are American journal of respiratory and critical care medicine ( AJRCCM ) with the Impact Factor of 17.452 now and Chest Journal, whose Impact Factor in 2019 is 8.308. In our analysis, there are 39 articles from AJRCCM with 6 kinds of theme categories, and 20 articles from Chest also got involved in almost all of the themes we cared about. Among them, 9 articles of Chest and 3 articles of AJRCCM talked about the evaluation of new technologies, making up all articles in such category. Unlike the phenomenon in a similar bibliometric analysis of respiratory articles [ 13 ], it seems several core journals here gleaned a lot of citations. Apart from those specific journals in this field, some general medical journals such as The New England Journal of Medicine and Annals of Internal Medicine take an important part in this analysis, too. As for the authors, Yasufuku K, with the H-index of 47 when we searched, had four studies published between 2004 and 2011 imported in our study, performing the best. These studies were mainly based on endobronchial ultrasound-guided transbronchial needle aspiration for lymph node staging of lung cancer, and compared different examinations such as positron emission tomography and computed tomography (CT) [ 14 , 15 , 16 , 17 ].
From the perspective of published design, we also study the topic distribution characteristics of the most cited articles. Two themes, BAL fluid along with Bronchoscopy and biopsy, occupy the primary part. Since the application of bronchoscopy in clinical practice, the two have been the focus of researches in human bronchial and lung diseases as an important means of bronchoscopy sampling and testing.
BAL is widely used to sample the lower respiratory tract from the perspective of clinical bronchoscopy, and materials obtained in this way are mainly alveolar contents such as respiratory mucous secretions [ 18 ]. BAL is a technique for sampling respiratory epithelial fluid, and analysis of the cellular and non-cellular components of the reflow may provide valuable information about airway inflammation [ 19 ]. BAL fluid collected through bronchoscopy can be used for bacteriological analysis to diagnose related diseases, such as ventilator-associated pneumonia [ 9 , 20 ]. The keyword centrality analysis also shows that BAL had a high centrality in the 1990s and 2000s, showing such research direction is the absolute core, which is consistent with the research on subject words. These results suggest that BAL is still a bronchoscopy procedure that needs to be addressed in the future and that it is necessary to explore the drawbacks of this area, such as mucosal damage to the respiratory tract and invasive infections. Because of the invasive property, clinical workers should also be concerned about the possible damage to patients when using bronchoscopy for BAL fluid sampling in the future. Research and development of BAL sampling technology with more safety and comfort is also a possible direction in the prospective technology field.
In addition to BAL, bronchoscopy and biopsy are other keywords with high involvement. As an important method of respiratory tract sampling, bronchoscopy biopsy plays an important role in the diagnosis of lung cancer and other bronchial-related diseases, the fibreoptic bronchoscopy has been routinely used for the diagnosis of suspected lung cancer [ 21 ]. It is reported that bronchoscopy can be considered as the safest and most accurate tool for assessing the mucous membranes of the central and distal airways [ 22 ]. We also found in some studies that both bronchoscopies with or without a narrow range and radial endobronchial ultrasound (R-EBUS) were poorly diagnosed by the investigators for pulmonary lesions [ 23 ]. Thus, from a technical point of view, future work should focus on cutting edge technology to improve diagnostic accuracy.
As for the degree centrality analysis, there are differences between the 1990s and the 2000s. The hot words of the 1990s were those like BAL, inflammation, diagnosis, and biopsy. It is also consistent with the fact that there was a lot of attention paid to diagnosis in the 1990s. As for the 2000s, keywords with high-frequency became BAL, outcome, infection, and so on. Among them, it can be seen that researchers still pay high attention to the highest-frequency BAL. In addition, the focus of the 1990s on the diagnostic and technical aspects of treatment has shifted, with researchers focusing more on the evaluation of prognosis, infection control, and other aspects of treatment with bronchoscopy. Research on a number of treatments such as bronchial thermoplasty [ 24 , 25 , 26 ], bronchial valve implantation [ 27 , 28 , 29 ], and bronchoscopic removal of the tracheal foreign body [ 30 ] began to expand. Gradually, the study of bronchoscopy began to blossom.
The LCS represents the number of citations that a document has in the local data set. If a document has a high LCS value, we’d say it’s an important document in the special field and may even be a groundbreaking article [ 31 ]. Chronologically, we can notice these 30 articles obtained by using the LCS method in the 1000 most cited articles published from 1990 to 2020 actually ranged from 1999 to 2007, and even one-fifth of them presented in one single year, 2004. In connection with the previous analysis that the 2000s made the most articles in three decades, this interesting phenomenon may suggest that the research on bronchoscopy has been further expanded and deepened in these years. There is a consistency between the two methods because of 12 overlapping articles obtained. Throughout these 12 articles on the topic of research, more than half linked with E-BUS. This reflects a high research interest in this technology in the 2000s. For example, Yasufuku et al. pointed out in 2004 that lymph node sampling of hilum and mediastinum by EBUS-guided transbronchial needle aspiration (TBNA) technique was accurate and safe in diagnosing pulmonary diseases [ 14 ]. This research, in our analysis, has a citation number of 479 (Ranked 6th) and the LCS of 19. Electromagnetic navigation bronchoscopy (ENB) is another hot theme in 12 articles. It was concluded that ENB is a safe and effective diagnostic technique in the years around 2006 [ 32 , 33 ], which has led to broad studies. These new techniques have undoubtedly received more and more attention, suggesting important directions for bronchoscopy research in the future.
We also took note of the progress of bronchoscopy-related research in recent years. Some researchers pointed out that bronchoscopic lung volume reduction using an endobronchial valve (EBV) is safe and effective in the treatment of chronic respiratory diseases such as emphysema. And with advances in one-way valve therapy, this is now a routine treatment option [ 34 ]; Bronchoscopic lung cryobiopsy, a novel biopsy method, was thought to have a meaningful effect on the multidisciplinary diagnosis of idiopathic pulmonary fibrosis [ 35 ]; Endoscopic ultrasound with bronchoscope fine needle aspiration (EUS-B-FNA) is a new technique which can be performed by interventional pulmonologists/thoracic surgeons with an echo-bronchoscope. With the help of EBUS, doctors can explore all the mediastinal lymph node stations in one endoscopic session, improving the accuracy in the diagnosis and staging of lung cancer [ 36 ]; Newer navigational modalities, such as robotic bronchoscopy and CT-guided cone beam bronchoscopy, might foreshadow the future in the bronchoscopic management of peripheral pulmonary lesions [ 37 , 38 ]; Besides, a recent study illustrated the role of bronchoscopy in the management of hemoptysis, which still represents a frequent diagnostic challenge in routine clinical practice [ 39 ]. Those novel developments are so fantastic and instructive, while whether they are high-quality researches or not need more time to test. We will continue to monitor the progress of the discipline.
Admittedly, although our results produce some valuable information, which may play a certain role in suggesting the topic selection and research direction of intending researchers, there are also some limitations. First, as articles are filtered according to the number of citations, new publications that are significant in the field but have not yet reached high citation levels are ignored. Therefore, it tends to be a kind of retrospective study of historical articles. Second, this analysis included only published articles and excluded other papers like clinical guidelines, meeting notes, textbooks, meta-analyses, and reviews, which may lead to omission bias. Thirdly, although we did search without any language restrictions on Web of Science, some famous articles in languages other than English may have been omitted because of database limits. Last but not least, although we use bronchoscopy as the keyword to search for articles, we may miss some famous articles retrieved by other keywords.
This article highlights the top 100 most cited articles in bronchoscopy over the past 30 years (1990–2020), including their time and geographical distribution, research topics, authors, research institutions, and research keywords. From the aspect of the research theme, we found that BAL and bronchial biopsies currently plays a major role. At the same time, they mostly focus on clinical trials, whereas basic laboratory research is inadequate, so more research on the subject is needed. In addition, because of the inherent limitation of our analysis, novel and instructive researches such as fluorescent bronchoscopy and advanced electromagnetic guided bronchoscopy may fail to enter our horizons. In summary, the field of bronchoscopy looks promising. With the advent of modern technology and easy access to different data, we can look forward to getting deeper researches in this area during the next 5–10 years.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information file.
Abbreviations
Bronchoalveolar lavage
Analysis of variance
Local citation score
American journal of respiratory and critical care medicine
Computed tomography
Radial endobronchial ultrasound
Transbronchial needle aspiration
Electromagnetic navigation bronchoscopy
Endobronchial valve
Endoscopic ultrasound with bronchoscope fine needle aspiration
Ninan N, Wahidi MM. Basic bronchoscopy: technology, techniques, and professional fees. Chest. 2019;155(5):1067–74.
Article Google Scholar
Rano A, Agusti C, Benito N, Rovira M, Angrill J, Pumarola T, Torres A. Prognostic factors of non-HIV immunocompromised patients with pulmonary infiltrates. Chest. 2002;122(1):253–61.
Thiberville L, Moreno-Swirc S, Vercauteren T, Peltier E, Cave C, Bourg Heckly G. In vivo imaging of the bronchial wall microstructure using fibered confocal fluorescence microscopy. Am J Respir Crit Care Med. 2007;175(1):22–31.
Busse WW, Wanner A, Adams K, Reynolds HY, Castro M, Chowdhury B, Kraft M, Levine RJ, Peters SP, Sullivan EJ. Investigative bronchoprovocation and bronchoscopy in airway diseases. Am J Respir Crit Care Med. 2005;172(7):807–16.
Denning DW, Cadranel J, Beigelman-Aubry C, Ader F, Chakrabarti A, Blot S, Ullmann AJ, Dimopoulos G, Lange C. Chronic pulmonary aspergillosis: rationale and clinical guidelines for diagnosis and management. Eur Respir J. 2016;47(1):45–68.
Article CAS Google Scholar
Ashraf SF, Lau KKW. Navigation bronchoscopy: A new tool for pulmonary infections. Med Mycol. 2019;57(Supplement_3):S287–s293.
Garfield E. 100 citation classics from the journal of the American Medical Association. Jama. 1987;257(1):52–9.
Jin K, Hu Q, Xu J, Wu C, Hsin MK, Zirafa CC, Novoa NM, Bongiolatti S, Cerfolio RJ, Shen J, et al. The 100 most cited articles on thoracic surgery management of lung cancer. J Thorac Dis. 2019;11(11):4886–903.
Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic "blind" bronchoalveolar lavage fluid. Am Rev Respir Dis. 1991;143(5 Pt 1):1121–9.
Molyneaux PL, Cox MJ, Willis-Owen SA, Mallia P, Russell KE, Russell AM, Murphy E, Johnston SL, Schwartz DA, Wells AU, et al. The role of bacteria in the pathogenesis and progression of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2014;190(8):906–13.
Morris A, Beck JM, Schloss PD, Campbell TB, Crothers K, Curtis JL, Flores SC, Fontenot AP, Ghedin E, Huang L, et al. Comparison of the respiratory microbiome in healthy nonsmokers and smokers. Am J Respir Crit Care Med. 2013;187(10):1067–75.
Zhang W, Tang N, Li X, George DM, He G, Huang T. The top 100 most cited articles on total hip arthroplasty: a bibliometric analysis. J Orthop Surg Res. 2019;14(1):412.
Seriwala HM, Khan MS, Shuaib W, Shah SR. Bibliometric analysis of the top 50 cited respiratory articles. Expert Rev Respir Med. 2015;9(6):817–24.
Yasufuku K, Chiyo M, Sekine Y, Chhajed PN, Shibuya K, Iizasa T, Fujisawa T. Real-time endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. Chest. 2004;126(1):122–8.
Yasufuku K, Chiyo M, Koh E, Moriya Y, Iyoda A, Sekine Y, Shibuya K, Iizasa T, Fujisawa T. Endobronchial ultrasound guided transbronchial needle aspiration for staging of lung cancer. Lung Cancer. 2005;50(3):347–54.
Yasufuku K, Pierre A, Darling G, de Perrot M, Waddell T, Johnston M, da Cunha SG, Geddie W, Boerner S, Le LW, et al. A prospective controlled trial of endobronchial ultrasound-guided transbronchial needle aspiration compared with mediastinoscopy for mediastinal lymph node staging of lung cancer. J Thorac Cardiovasc Surg. 2011;142(6):1393–400 e1391.
Yasufuku K, Nakajima T, Motoori K, Sekine Y, Shibuya K, Hiroshima K, Fujisawa T. Comparison of endobronchial ultrasound, positron emission tomography, and CT for lymph node staging of lung cancer. Chest. 2006;130(3):710–8.
Rennard SI, Ghafouri M, Thompson AB, Linder J, Vaughan W, Jones K, Ertl RF, Christensen K, Prince A, Stahl MG. Fractional processing of sequential bronchoalveolar lavage to separate bronchial and alveolar samples. Am Rev Respir Dis. 1990;141(1):208–17.
Connett GJ. Bronchoalveolar lavage. Paediatr Respir Rev. 2000;1(1):52–6.
CAS PubMed Google Scholar
Armstrong DS, Grimwood K, Carlin JB, Carzino R, Olinsky A, Phelan PD. Bronchoalveolar lavage or oropharyngeal cultures to identify lower respiratory pathogens in infants with cystic fibrosis. Pediatr Pulmonol. 1996;21(5):267–75.
Kawaraya M, Gemba K, Ueoka H, Nishii K, Kiura K, Kodani T, Tabata M, Shibayama T, Kitajima T, Tanimoto M. Evaluation of various cytological examinations by bronchoscopy in the diagnosis of peripheral lung cancer. Br J Cancer. 2003;89(10):1885–8.
Andolfi M, Potenza R, Capozzi R, Liparulo V, Puma F, Yasufuku K. The role of bronchoscopy in the diagnosis of early lung cancer: a review. J Thorac Dis. 2016;8(11):3329–37.
Tanner NT, Yarmus L, Chen A, Wang Memoli J, Mehta HJ, Pastis NJ, Lee H, Jantz MA, Nietert PJ, Silvestri GA. Standard bronchoscopy with fluoroscopy vs thin bronchoscopy and radial Endobronchial ultrasound for biopsy of pulmonary lesions: a multicenter, prospective, radomized trial. Chest. 2018;154(5):1035–43.
Cox G, Miller JD, McWilliams A, FitzGerald JM, Lam S. Bronchial thermoplasty for asthma. Am J Respir Crit Care Med. 2006;173(9):965–9.
Cox G, Thomson NC, Rubin AS, Niven RM, Corris PA, Siersted HC, Olivenstein R, Pavord ID, McCormack D, Chaudhuri R, et al. Asthma control during the year after bronchial thermoplasty. N Engl J Med. 2007;356(13):1327–37.
Pavord ID, Cox G, Thomson NC, Rubin AS, Corris PA, Niven RM, Chung KF, Laviolette M, Grp RTS. Safety and efficacy of bronchial thermoplasty in symptomatic, severe asthma. Am J Respir Crit Care Med. 2007;176(12):1185–91.
Snell GI, Holsworth L, Borrill ZL, Thomson KR, Kalff V, Smith JA, Williams TJ. The potential for bronchoscopic lung volume reduction using bronchial prostheses - a pilot study. Chest. 2003;124(3):1073–80.
Toma TP, Hopkinson NS, Hillier J, Hansell DM, Morgan C, Goldstraw PG, Polkey MI, Geddes DM. Bronchoscopic volume reduction with valve implants in patients with severe emphysema. Lancet. 2003;361(9361):931–3.
Hopkinson NS, Toma TP, Hansell DM, Goldstraw P, Moxharn J, Geddes DM, Polkey MI. Effect of Bronchoscopic lung volume reduction on dynamic hyperinflation and exercise in emphysema. Am J Respir Crit Care Med. 2005;171(5):453–60.
Tan HKK, Brown K, McGill T, Kenna MA, Lund DP, Healy GB. Airway foreign bodies (FB): a 10-year review. Int J Pediatr Otorhinolaryngol. 2000;56(2):91–9.
Hao X, Liu Y, Li X, Zheng J. Visualizing the history and perspectives of disaster medicine: a Bibliometric analysis. Disaster Med Public Health Prep. 2019;13(5–6):966–73.
Gildea TR, Mazzone PJ, Karnak D, Meziane M, Mehta AC. Electromagnetic navigation diagnostic bronchoscopy - a prospective study. Am J Respir Crit Care Med. 2006;174(9):982–9.
Eberhardt R, Anantham D, Herth F, Feller-Kopman D, Ernst A. Electromagnetic navigation diagnostic bronchoscopy in peripheral lung lesions. Chest. 2007;131(6):1800–5.
Hartman JE, Vanfleteren LEGW, van Rikxoort EM, Klooster K, Slebos DJ. Endobronchial valves for severe emphysema. Eur Respir Rev. 2019;28(152):180121.
Tomassetti S, Wells AU, Costabel U, Cavazza A, Colby TV, Rossi G, Sverzellati N, Carloni A, Carretta E, Buccioli M, et al. Bronchoscopic lung Cryobiopsy increases diagnostic confidence in the multidisciplinary diagnosis of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2016;193(7):745–52.
Vilmann P, Clementsen PF, Colella S, Siemsen M, De Leyn P, Dumonceau JM, Herth FJ, Larghi A, Vazquez-Sequeiros E, Hassan C, et al. Combined endobronchial and oesophageal endosonography for the diagnosis and staging of lung cancer. European Society of Gastrointestinal Endoscopy (ESGE) guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Eur Respir J. 2015;46(1):40–60.
Chaddha U, Kovacs SP, Manley C, Hogarth DK, Cumbo-Nacheli G, Bhavani SV, Kumar R, Shende M, Egan JP 3rd, Murgu S. Robot-assisted bronchoscopy for pulmonary lesion diagnosis: results from the initial multicenter experience. BMC Pulm Med. 2019;19(1):243.
Cheng GZ, Liu L, Nobari M, Miller R, Wahidi M. Cone beam navigation bronchoscopy: the next frontier. J Thorac Dis. 2020;12(6):3272–8.
Mondoni M, Carlucci P, Cipolla G, Fois A, Gasparini S, Marani S, Centanni S, Sotgiu G. Bronchoscopy to assess patients with hemoptysis: which is the optimal timing? BMC Pulm Med. 2019;19(1):36.
Download references
Acknowledgements
Not applicable.
This work was supported by the National Natural Science Foundation of China (81672308, X. Wang) and the Hunan Provincial Key Area R&D Programmes (2019SK2253, X. Wang). The funders had no role in the design of the study, the collection, analysis or interpretation of data, or the writing of the manuscript.
Author information
Boxue He and Pengfei Zhang contributed equally to this work.
Authors and Affiliations
Department of Thoracic Surgery, The Second Xiangya Hospital, Central South University, Changsha, 410011, Hunan, China
Boxue He, Pengfei Zhang, Qidong Cai, Shuai Shi, Hui Xie, Yuqian Zhang, Xiong Peng, Zhenyu Zhao, Wei Yin & Xiang Wang
Hunan Key Laboratory of Early Diagnosis and Precision Therapy, Department of Thoracic Surgery, The Second Xiangya Hospital, Central South University, Changsha, 410011, Hunan, China
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. XW conceived and designed the work. Material preparation and data collection and analysis were performed by BH, PZ, QC, SS, HX, YZ XP, ZZ, and WY. The first draft of the manuscript was written by BH and PZ, and all authors commented on previous versions of the manuscript. Then, QC revised the manuscript and all authors read and approved the final manuscript.
Corresponding author
Correspondence to Xiang Wang .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they do not have any competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
He, B., Zhang, P., Cai, Q. et al. The top 100 most cited articles on bronchoscopy: a bibliometric analysis. BMC Pulm Med 20 , 229 (2020). https://doi.org/10.1186/s12890-020-01266-9
Download citation
Received : 20 July 2020
Accepted : 17 August 2020
Published : 27 August 2020
DOI : https://doi.org/10.1186/s12890-020-01266-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Most-cited papers
- Bronchoscopy
BMC Pulmonary Medicine
ISSN: 1471-2466
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 17 November 2020
Risk factors for post-bronchoscopy pneumonia: a case–control study
- Yu Sato 1 ,
- Kengo Murata 1 , 3 ,
- Miake Yamamoto 1 ,
- Tsukasa Ishiwata 2 ,
- Miyako Kitazono-Saitoh 1 ,
- Akihiko Wada 1 &
- Mikio Takamori 1
Scientific Reports volume 10 , Article number: 19983 ( 2020 ) Cite this article
5320 Accesses
4 Citations
1 Altmetric
Metrics details
- Bacterial infection
- Respiratory tract diseases
The bronchoscopy, though usually safe, is occasionally associated with complications, such as pneumonia. However, the use of prophylactic antibiotics is not recommended by the guidelines of the British Thoracic Society. Thus far there are few reports of the risk factors for post-bronchoscopy pneumonia; the purpose of this study was to evaluate these risk factors. We retrospectively collected data on patients in whom post-bronchoscopy pneumonia developed from the medical records of 2,265 patients who received 2666 diagnostic bronchoscopies at our institution between April 2006 and November 2011. Twice as many patients were enrolled in the control group as in the pneumonia group. The patients were matched for age and sex. In total, 37 patients (1.4%) had post-bronchoscopy pneumonia. Univariate analysis showed that a significantly larger proportion of patients in the pneumonia group had tracheobronchial stenosis (75.7% vs 18.9%, p < 0.01) and a final diagnosis of primary lung cancer (75.7% vs 43.2%, p < 0.01) than in the control group. The pneumonia group tended to have more patients with a history of smoking (83.8% vs 67.1%, p = 0.06) or bronchoalveolar lavage (BAL) (4.3% vs 14.9%, p = 0.14) than the control group. In multivariate analysis, we found that tracheobronchial stenosis remained an independent risk factor for post-bronchoscopy pneumonia (odds ratio: 7.8, 95%CI: 2.5–24.2). In conclusion, tracheobronchial stenosis was identified as an independent risk factor for post-bronchoscopy pneumonia by multivariate analysis in this age- and sex- matched case control study.
Similar content being viewed by others
Impact of non-cystic fibrosis bronchiectasis on critically ill patients in Korea: a retrospective observational study
Clinical characteristics, radiological features, and disease severity of bronchiectasis according to the spirometric pattern
Increased hospitalizations and economic burden in COPD with bronchiectasis: a nationwide representative study
Introduction.
Bronchoscopy is one of the standard methods for diagnosing respiratory diseases including malignant tumors and diffuse lung diseases 1 . Bronchoscopy is usually a safe procedure but is sometimes associated with complications such as pneumonia 2 , 3 , 4 , 5 , 6 . The incidence of post-bronchoscopy pneumonia ranges from 0.02% to 6.3% and differs according to the reports 2 , 3 , 5 , 6 . Post-bronchoscopy pneumonia is not only a dangerous condition in itself but also delays treatment of the primary disease 2 . A small number of studies have examined the risk factors for post-bronchoscopy pneumonia. Aging, abnormal findings in the bronchial lumen, lung cancer, central location of the tumor, and current smoking have been reported as risk factors for post-bronchoscopy pneumonia, but the reports are inconsistent 2 , 3 , 6 . In the current study, we evaluated the risk factors for post-bronchoscopy pneumonia development.
Materials and methods
Our study was a retrospective, single-center case–control study and was performed in accordance with the Declaration of Helsinki and the guidelines and regulations of the ethics committee of Tokyo Metropolitan Tama Medical Center, which approved the study, including a waiver of informed consent for retrospective data collection and deidentified analysis. All patients 20 years old or older who underwent a diagnostic flexible bronchoscopy for abnormal pulmonary lesions in our bronchoscopy unit were eligible for enrollment. The sampling methods included bronchial washing, bronchoalveolar lavage (BAL), endobronchial brushing, needle aspiration, and forceps biopsy as well as transbronchial needle aspiration (TBNA) with or without endobronchial ultrasound (EBUS) assistance. During the study period, radial EBUS, biopsy via guide sheath, and cryobiopsy were not performed. Patients who received therapeutic bronchoscopy, such as laser resection, argon plasma coagulation, stenting, airway foreign body removal, bronchial occlusion, and balloon dilation, were excluded. Data from the medical records of patients who underwent a bronchoscopy at Tokyo Metropolitan Tama Medical Center, a tertiary teaching hospital in Tokyo, between April 2006 and November 2011, were retrospectively collected, and patients in whom post-bronchoscopy pneumonia developed were extracted for allocation to the pneumonia group.
In the present study, post-bronchoscopy pneumonia was defined as pneumonia or a lung abscess diagnosed by the attending physician, the presence of new pulmonary lesions on a chest radiograph or the development or exacerbation of purulent sputum, and was treated with antibiotics within 30 days after the bronchoscopy. Twice as many patients were randomly selected for the control group as for the pneumonia group and were matched for age and sex, with the latter based on a random number table 7 , 8 . Patients who received antimicrobial agents were excluded (Fig. 1 ). Only the initial procedures were included if a patient underwent two or more bronchoscopies.
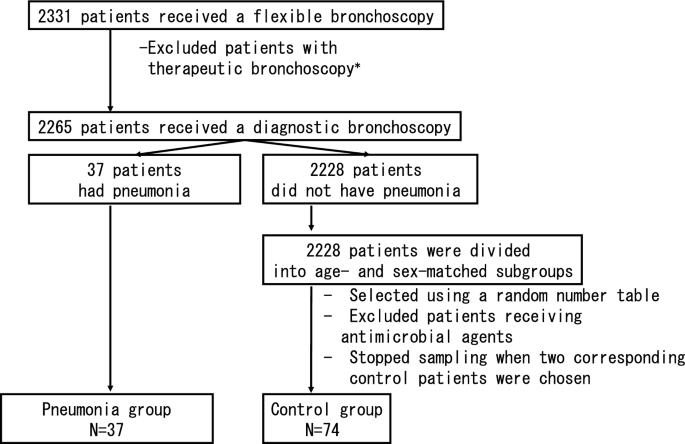
Flowchart of patient selection. Patients without pneumonia were divided into groups by sex and age (by decade). Patients who received antimicrobial agents on the day before their bronchoscopy were excluded from the control group. *Therapeutic bronchoscopy is defined as laser resection, argon plasma coagulation, stenting, airway foreign body removal, bronchial occlusion or balloon dilation.
The factors evaluated were: history of smoking, immunocompromised state, findings of tracheobronchial stenosis, final diagnosis, and bronchoscopic sampling methods. Patients with a history of smoking one year or longer were defined as smokers. An immunocompromised patient was defined as an individual who received corticosteroids, immunosuppressants or chemotherapy or had diabetes, renal failure, liver failure, an hematologic malignancy or asplenia. Tracheobronchial stenosis was defined as the finding of stenosis in any area between the trachea and the subsegmental bronchi by bronchoscopy that was diagnosed by a certified bronchoscopist. The final diagnosis was defined as a diagnosis based on an analysis of the lesions for which bronchoscopy was indicated.
The bronchoscopies were performed under local anesthesia using lidocaine, intramuscular injections of hydroxyzine pamoate or intravenous injections of pethidine without intubation. The bronchoscopes used were 1T200, 1T240, 1T260, F260 (Olympus, Japan). The procedure was performed by two or more experienced respiratory physicians, including one or more bronchoscopists certified by the Japan Society for Respiratory Endoscopy.
The patients’ age was analyzed using Student's t-test while the physician’s experience was analyzed using Mann–Whitney’s U-test. The other univariate analyses were performed using the chi-square test. Multivariate analysis was performed using logistic regression analysis for factors with p < 0.2 on univariate analysis. P < 0.05 indicated statistical significance. SPSS® (version 19) was used for the statistical analysis.
In 68 months, 2331 patients received 2773 bronchoscopies. Sixty-six patients who received therapeutic bronchoscopies, such as laser resection, argon plasma coagulation, stenting, airway foreign body removal, bronchial occlusion or balloon dilation, were excluded. The median (+ /− SD) age was 65 (+ /− 14) years, and 1393 (61.5%) patients were male. In total, 37 patients (1.4%) had pneumonia. No lung abscess was found. The median duration to pneumonia development after a bronchoscopy was three days (range: 0–20 days). Seventy-four patients who received a bronchoscopy and did not have pneumonia were randomly chosen to be the age- and sex-matched controls (Table 1 ). Although TBNA with or without EBUS was not excluded, none of the patients in the present study underwent this procedure.
Univariate analysis showed that the pneumonia group had a significantly larger proportion of patients with tracheobronchial stenosis (75.7% vs 18.9%, p < 0.01) and a final diagnosis of primary lung cancer (75.7% vs 43.2%, p < 0.01) than the control group. The pneumonia group tended to have more patients with a smoking history (83.8% vs 67.1%, p = 0.06) than the control group. With respect to the sampling measures, the pneumonia group had slightly more patients who received BAL than the control group (4.3% vs 14.9%, p = 0.14). There was no significant difference in the physicians’ experience between the two groups (p = 0.26) (Table 2 ). Of the 28 patients who had tracheobronchial stenosis in the pneumonia group, most (24/28, 86%) had lung cancer. Other diagnoses included esophageal cancer (2/28), nontuberculous mycobacterial infection (1/28), and bronchial asthma (1/28). In contrast, of the 14 patients who had tracheobronchial stenosis in the control group, most (8/14, 57%) also had lung cancer. Other diagnoses included diffuse large B cell lymphoma (1/14), metastatic breast cancer (1/14), obstructive pneumonia (1/14), bronchial asthma, and tuberculosis (1/14). Two patients did not receive a diagnosis.
Multivariate analysis performed to identify factors with p < 0.20 found that tracheobronchial stenosis was an independent factor in post-bronchoscopy pneumonia (OR: 15.1, 95%CI: 4.8–48.1) (Table 3 ).
Although previous studies identified variables, such as aging, abnormal findings in the bronchial lumen, lung cancer, central location of the tumor, and current smoking as risk factors 2 , 3 , 5 , 6 (Table 4 ), this age- and sex-matched controlled study demonstrated that tracheobronchial stenosis was the only independent risk factor for post-bronchoscopy pneumonia.
The mechanism of post-bronchoscopy pneumonia in patients with tracheobronchial stenosis can be adequately explained based on that of obstructive pneumonia: first, intramural or extramural stenosis of the normal bronchi occurs due to primary lung cancer, metastatic lung tumor, benign tumor, hematoma, edema, foreign body, pleural effusion or fibrosis. Second, progression to endogenous lipoid pneumonia occurs due to the accumulation of foamy macrophages and mucus and cell invasion caused by disorders of the mucociliary transport system distal to the stenosis. Finally, development of obstructive pneumonia occurs via colonization of bacteria flowing into the lesion 9 , 10 . Bronchoscopy can aggravate this condition by carrying the oropharyngeal flora attached to the bronchoscope into the lesion, thereby leading to obstructive pneumonia.
Although several previous studies suggested that lung cancer was associated with post-bronchoscopy pneumonia based on univariate analysis 2 , 3 (Table 4 ), lung cancer itself was not identified as an independent risk factor on multivariate analysis in our study. Pneumonia developed in four patients in the pneumonia group with bronchial stenosis who did not have lung cancer while pneumonia did not develop in any of the patients in the control group with lung cancer. Indeed, some reports showed that a predisposition for pneumonia was caused by tracheobronchial stenosis due to diseases other than lung cancer. Pneumonia developed in 4.2% of the patients with endobronchial valves for advanced emphysema, and most of the cases were resolved by antibiotic treatment and valve removal 11 . Obstructive pneumonia also developed due to occlusion by endobronchial Watanabe spigots for refractory pneumothorax and resolved through antibiotic treatment and spigot removal 12 . A recent study suggested that the central tumor location was one of the risk factors for post-bronchoscopy pneumonia. However, the study did not analyze the bronchoscopic findings and only included patients with lung cancer, which was difficult to diagnose during the bronchoscopy 2 . Another study suggested that patients with lung cancer with necrosis and/or cavity or large tumor diameter tend to develop a lung abscess 13 . In the article, the authors suggested that radial EBUS using the guide-sheath (EBUS-GS) technique might contribute to the incidence of lung abscess in patients with lung cancer. However, patients with non-neoplastic lung diseases who do not receive EBUS-GS also acquired pneumonia after bronchoscopy. While the previous study only included patients with lung cancer, the present study included patients with any pulmonary lesions. Notably, there were no patients with a lung abscess in our study. This clear distinction might be due to differences in the patients’ background, sampling methods or the developmental mechanisms of post-bronchoscopy respiratory infection. Thus, our study suggested that it was not lung cancer itself, but the bronchial stenosis caused by any of a number of diseases (including lung cancer), that directly induced post-bronchoscopy pneumonia.
Multivariate analysis did not demonstrate that smoking history was a risk factor for post-bronchoscopy pneumonia despite the promising results of the univariate analysis. Smoking, which is well-known as a risk factor for numerous lung diseases, such as lung cancer, chronic bronchitis, and chronic obstructive pulmonary diseases, can also disturb mucociliary transportation, increase sputum production, and depress the cough reflex 14 , 15 . Indeed, a retrospective study of 237 patients with lung cancer who underwent a bronchoscopy reported that current smoking was a risk factor 2 . However, a previous prospective study of 100 patients who underwent a bronchoscopy suggested that smoking history was not associated with post-bronchoscopy pulmonary complications including pneumonia 6 , and a study that compared obstructive pneumonia and bacterial, community-acquired pneumonia suggested that smoking was not a risk factor for obstructive pneumonia 9 . While smoking might directly or indirectly exacerbate post-bronchoscopy pneumonia, its exact role is still unknown.
There are no widely accepted criteria for diagnosing post-bronchoscopy pneumonia, and the definition and observation period for this condition vary 2 , 3 , 5 , 6 . We defined pneumonia occurring within 30 days after the procedure as a bronchoscopy-related infection in accordance with the surgical-site infection guidelines issued by the Centers for Disease Control and Prevention, which state that an organ infection occurring within 30 days after an operation is likely to be related to the operation if no implant has been left in place 16 . Our study did not require radiographic confirmation because chest X-rays may fail to detect pneumonia 17 .
Our study concluded that tracheobronchial stenosis is the only independent risk factor for post-bronchoscopy pneumonia. Tracheobronchial stenosis can be judged promptly during bronchoscopy, and there is no need to wait for the diagnosis. Also, whether tracheobronchial stenosis is caused by lung cancer or not is irrelevant. Our study enrolled the largest number of patients to date for the purpose of determining the risk factors for post-bronchoscopy pneumonia. However, it has some limitations. First, since the study was retrospective and a definitive diagnosis of post-bronchoscopy pneumonia is difficult to establish, the condition might have been underdiagnosed. However, since our criteria for pneumonia included antibiotic administration, few cases of pneumonia were likely to have been overlooked. Second, immune status and bronchoscopic sampling methods varied. A carefully stratified evaluation is needed to address these issues. Third, the role of age and sex was not able to be examined because our study was designed as an age- and sex-matched control study. Finally, since patients who received EBUS-GS, endobronchial cryobiopsy or therapeutic bronchoscopy were not included, the issue of whether tracheobronchial stenosis contributed to post-bronchoscopy pneumonia development in these patients was unable to be addressed.
The present case–control study matching patient age and sex was the first to demonstrate by multivariate analysis that stenosis of the trachea or bronchi is an independent risk factor for the development of post-bronchoscopy pneumonia. This finding will help to identify patients at risk of post-bronchoscopy pneumonia development without the need to wait for a pathological diagnosis.
British Thoracic Society BTS Flexible Bronchoscopy Guideline Group. BTS Guideline for diagnostic flexible bronchoscopy in adults. Thorax 68 , i10-11 (2013).
Google Scholar
Takiguchi, H. et al. Post-bronchoscopy pneumonia in patients suffering from lung cancer: development and validation of a risk prediction score. Respir. Investig. 55 , 212–218 (2017).
Article Google Scholar
Kanazawa, H. Efficacy of azithromycin administration in prevention of respiratory tract infection after bronchoscopic biopsy: a randomized, controlled trial. Respirology 12 , 70–75 (2007).
Park, J. S. et al. Impact of antibiotic prophylaxis on post-bronchoscopy fever: a randomized controlled study. Int. J. Tuberc. Lung Dis. 15 , 528–535 (2011).
Article CAS Google Scholar
Kanemoto, K. et al. Prospective study of fever and pneumonia after flexible fiberoptic bronchoscopy in older people. J. Am. Geriatr. Soc. 54 , 827–830 (2006).
Pereira, W. et al. Fever and pneumonia after flexible fiberoptic bronchoscopy. Am. Rev. Respir. Dis. 112 , 59–64 (1975).
CAS PubMed Google Scholar
Lewallen, S. & Coutright, P. Epidemiology in practice: case-control studies. Community Eye Health 11 , 57–58 (1998).
CAS PubMed PubMed Central Google Scholar
D’Souza, G. et al. Case-control study of human papillomavirus and oropharyngeal cancer. N. Engl. J. Med. 356 , 1944–1956 (2007).
Abers, M. S. et al. Postobstructive pneumonia: an underdescribed syndrome. Clin. Infect. Dis. 62 , 957–961 (2016).
Burke, M. & Fraser, R. Obstructive pneumonitis: a pathologic and pathogenetic reappraisal. Radiology 166 , 699–704 (1988).
Sciurba, F. C. et al. A randomized study of endobronchial valves for advanced emphysema. N. Engl. J. Med. 363 , 1233–1244 (2010).
Morikawa, S. et al. A simple method of bronchial occlusion with silicone spigots (Endobronchial Watanabe Spigot; EWS®) using a curette. Ther. Adv. Respir. Dis. 10 , 518–524 (2016).
Shimoda, M., Yamana, K., Yano, R., et al . Analysis of risk factors for the development of a post-bronchoscopy respiratory infection in lung cancer patients. J. Infecti. Chemotherapy (2020).
Nakagawa, M., Tanaka, H., Tsukuma, H. & Kishi, Y. Relationship between the duration of the preoperative smoke-free period and the incidence of postoperative pulmonary complications after pulmonary surgery. Chest 120 , 705–710 (2001).
McGowan, N. Surgery and smoking. Semin. Perioper. Nurs. 8 , 146–154 (1999).
Mangram, A. J. et al. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am. J. Infect. Control. 27 (97–132), 1999 (1999).
Upchurch, C. P. et al. Community-acquired pneumonia visualized on CT scans but not chest radiographs: pathogens, severity, and clinical outcomes. Chest 153 , 601–610 (2018).
Download references
Acknowledgements
We thank the Department of Clinical Research at the study institution, which has a qualified statistician on staff, for their excellent support and statistical advice throughout this study. We are also indebted to James R. Valera for his assistance with editing the manuscript.
Author information
Authors and affiliations.
Department of Respiratory Medicine, Tokyo Metropolitan Tama Medical Center, Tokyo, Japan
Yu Sato, Kengo Murata, Miake Yamamoto, Miyako Kitazono-Saitoh, Akihiko Wada & Mikio Takamori
Division of Thoracic Surgery, Toronto General Hospital, University Health Network, Toronto, ON, Canada
Tsukasa Ishiwata
Department of Pulmonology, Tokyo Metropolitan Tama Medical Center, 2-8-29 Musashidai, Fuchu, Tokyo, 183-8524, Japan
Kengo Murata
You can also search for this author in PubMed Google Scholar
Contributions
Y.S., M.Y., T.I. and K.M. designed the study. Y.S., M.Y. and T.I. have contributed to data collection. K.M. conceived the presented idea and contributed to analysis and interpretation of data. Y.S. and K.M. wrote the main manuscript text and prepared tables. Y.S., M.Y., T.I., K.M., M. K.S., A.W., and M.T. have critically reviewed the manuscript. M.Y, T.I, M. K.S., A.W., and M.T. commented on the manuscript. All the authors approved the final version of the manuscript.
Corresponding author
Correspondence to Kengo Murata .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Sato, Y., Murata, K., Yamamoto, M. et al. Risk factors for post-bronchoscopy pneumonia: a case–control study. Sci Rep 10 , 19983 (2020). https://doi.org/10.1038/s41598-020-76998-z
Download citation
Received : 12 May 2020
Accepted : 05 November 2020
Published : 17 November 2020
DOI : https://doi.org/10.1038/s41598-020-76998-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Pulmonary actinomycosis mimicking lung cancer on 18f-fluorodeoxyglucose positron emission tomography: a case report.
- Shinichi Miyazaki
- Takeo Fujito
- Takuya Ikeda
Journal of Medical Case Reports (2022)
Association between oxygen saturation level during bronchoscopy and post-bronchoscopy adverse events: a retrospective cohort study
- So Yeon Kim
- Hyo Jin Lee
- Hyun Woo Lee
Respiratory Research (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 25 September 2021
Oxygenation strategies during flexible bronchoscopy: a review of the literature
- Corrado Pelaia 1 ,
- Andrea Bruni 2 ,
- Eugenio Garofalo 2 ,
- Serena Rovida 3 ,
- Eugenio Arrighi 1 ,
- Gianmaria Cammarota 4 ,
- Paolo Navalesi 5 ,
- Girolamo Pelaia 1 &
- Federico Longhini ORCID: orcid.org/0000-0002-6970-7202 2
Respiratory Research volume 22 , Article number: 253 ( 2021 ) Cite this article
5554 Accesses
20 Citations
2 Altmetric
Metrics details
During flexible fiberoptic bronchoscopy (FOB) the arterial partial pressure of oxygen can drop, increasing the risk for respiratory failure. To avoid desaturation episodes during the procedure several oxygenation strategies have been proposed, including conventional oxygen therapy (COT), high flow nasal cannula (HFNC), continuous positive airway pressure (CPAP) and non-invasive ventilation (NIV). By a review of the current literature, we merely describe the clinical practice of oxygen therapies during FOB. We also conducted a pooled data analysis with respect to oxygenation outcomes, comparing HFNC with COT and NIV, separately. COT showed its benefits in patients undergoing FOB for broncho-alveolar lavage (BAL) or brushing for cytology, in those with peripheral arterial oxyhemoglobin saturation < 93% prior to the procedure or affected by obstructive disorder. HFNC is preferable over COT in patients with mild to moderate acute respiratory failure (ARF) undergoing FOB, by improving oxygen saturation and decreasing the episodes of desaturation. On the opposite, CPAP and NIV guarantee improved oxygenation outcomes as compared to HFNC, and they should be preferred in patients with more severe hypoxemic ARF during FOB.
Introduction
Flexible fiberoptic bronchoscopy (FOB) is a diagnostic and sometimes therapeutic procedure, commonly performed in patients affected by airway or lung parenchyma disorders. FOB has several applications, including plug removal in presence of abundant secretions or ineffective cough, bronchoalveolar lavage (BAL), biopsy, or endoscopic management of bleeding.
The majority of patients undergoing FOB suffer from conditions that impair gas exchange such as pneumonia, interstitial lung diseases, as well as lung and bronchial neoplasms. During the procedure arterial partial pressure of oxygen can drop even more than 10–20 mmHg, with an increased risk for respiratory failure [ 1 , 2 ]. In order to avoid desaturation episodes, oxygen support provided by conventional therapy or non-invasive ventilation is usually required during and after FOB.
Through a review of the literature, we discuss the rationale and all the alternative oxygenation strategies adopted during FOB. In addition, in the attempt to provide some clinical evidences, we have also conducted a quantitative synthesis of findings comparing high flow oxygen through nasal cannula (HFNC) with conventional oxygen therapy (COT) and non-invasive ventilation (NIV), separately, with respect to the lowest saturation during procedures and the number of episodes of desaturation.
Evidence acquisition
This review was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement. The review protocol has been registered in Prospero (CRD42020153343).
Study selection and inclusion criteria
All cited articles include adult patients, receiving one or more modalities of oxygen support administered during flexible bronchoscopy for any reason (diagnostic or interventional), without restrictions related to the type of bronchoscopy procedure and to the anesthetic risk.
We included all randomized, quasi-randomized, prospective and retrospective studies, published in indexed scientific journals from inception to May 1st, 2021. We excluded papers published in languages other than English, Italian, French or Spanish as well as case reports or series, review, systematic reviews or meta-analysis and studies published in abstract form. Papers including patients undergoing rigid bronchoscopy were also excluded. References of included papers, reviews, systematic reviews and meta-analysis were also examined to identify potential studies of interest missed during the primary search.
All oxygen therapy modalities utilized during flexible bronchoscopy were evaluated. Specifically, we considered: (1) COT, consisting of low oxygen flow administration through nasal prongs, oxygen mask with or without reservoir, and Venturi mask [ 3 ]; (2) HFNC, consisting of administration of high flows (up to 60 L/min) of air/oxygen admixtures, heated (at temperatures ranging from 31 to 37 °C) and fully humidified (up to 44 mg H 2 O/L) [ 4 ], providing an inspired oxygen fraction ranging from 21 to 100%; (3) continuous positive airway pressure (CPAP), based on the application of a positive end-expiratory pressure (PEEP) throughout the whole respiratory cycle by means of interfaces such as mask or helmet [ 5 , 6 ], and (4) NIV, based on the application of a PEEP by means of a mask or helmet, with an inspiratory pressure support triggered by the patient and delivered by a ventilator [ 7 , 8 ].
Search strategy
Two authors (A.B. and C.P.) independently searched MEDLINE, EMBASE, and Scopus Database of Systematic Reviews using the following keywords and their related MeSH terms: "bronchoscopy", "conventional oxygen therapy", "continuous positive airway pressure", "bilevel continuous positive airway pressure", "airway pressure release ventilation", "noninvasive ventilation", and "high flow nasal oxygen". The search strategy is detailed in the Electronic Supplemental Material (ESM). Controlled vocabulary terms, text words, and keywords were variably combined. Blocks of terms per concept were created. These authors also independently checked all the articles, and selected those enrolling adult patients undergoing bronchoscopy which required oxygen therapy or other modalities of respiratory support. In case of disagreement, the opinion of a third examiner (F.L.) was requested for a conclusive decision.
Definition of clinical outcomes
A quantitative synthesis of findings has been conducted for the lowest saturation during procedures and the number of episodes of desaturation. The lowest saturation was defined as the lowest value reported by the included studies of the arterial (SaO 2 ) or peripheral (SpO 2 ) oxygen saturation during the FOB procedure. The number of episodes of desaturation was intended as the number of patients with one or more episodes of desaturations during the procedure, as defined by SaO 2 or SpO 2 < 90% for a minimum time defined by every single study.
Statistical analysis
Dichotomous outcomes are presented as risk ratios (RR) with 95% confidence intervals (CIs). For normally distributed continuous data, we have calculated the mean difference (MD) with corresponding 95% CIs. We use medians and interquartile ranges for continuous data that were not normally distributed. Meta‐analyses have been performed using random‐effects models. We have assessed heterogeneity by visually inspecting the forest plots to determine closeness of point estimates with each other and overlap of CIs. We used the χ 2 test with a P value of 0.10 to indicate statistical significance, and the I 2 statistic to measure heterogeneity. We have also considered the magnitude and direction of effects, and the strength of evidence for heterogeneity (e.g. P value from the χ 2 test), when determining the importance of the observed I 2 value. P values < 0.05 were considered statistically significant.
The electronic search identified 5157 potentially relevant studies. Detailed description of the selection process flow is provided in Fig. 1 . We selected 32 full-text manuscripts (Table 1 ), referring to 3 multi-centered and 29 single-centered studies, respectively [ 1 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ]. With the exception of 7 studies, all trials were performed in University Hospitals. Among all studies, 18 were conducted in European countries. Overall, the 32 selected studies enrolled 2517 patients with a median of 40 [ 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ] patients per study, and a median patient age of 60 [53–64] years.
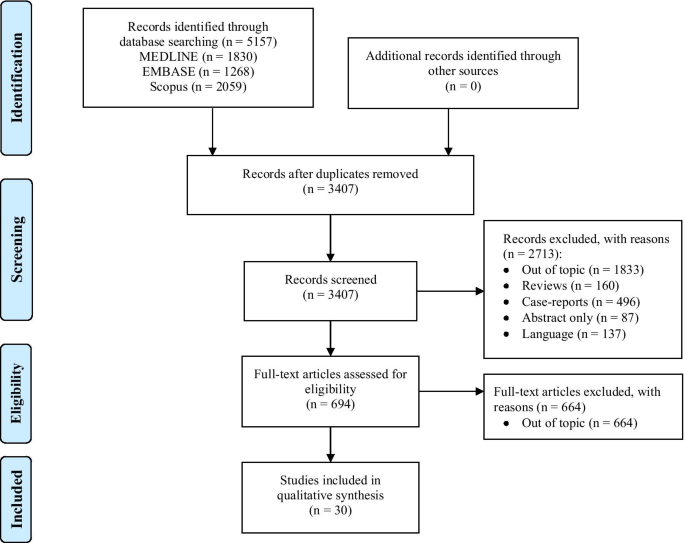
Flow chart of reviewed studies
Different forms of oxygen therapies and ventilatory support: the choice rationale
Alteration of respiratory mechanics during FOB occurs physiologically. In non-intubated patients, the fiberscope occupies about 10% of the cross-sectional area of the trachea, and 15% of the cricoid ring. As a consequence, in patient's airways an increase in air flow resistance develops, and the work of breathing thus enhances [ 40 ]. When suction is applied, end-expiratory lung volume is reduced, leading to alveolar de-recruitment, increased shunt and venous admixture [ 40 , 41 , 42 ]. As mentioned, these respiratory changes revert after FOB, but their reversal may take from 15 min up to several hours in severe parenchymal lung diseases [ 40 ].
In addition, FOB indirectly causes also significant haemodynamic changes. The increase of airway resistance and work of breathing theoretically leads to changes in intra-thoracic pressure, that may also affect venous return and afterload, while reducing cardiac output. However, it has been reported that cardiac output increases by 50% secondary to sympathetic stimulation during FOB, and it returns to baseline in 15 min after its completion [ 40 , 43 , 44 ]. In fragile or cardiopathic patients, FOB may cause a dangerous cardiopulmonary distress, associated with electrocardiographic alteration in up to 21% of awake patients over 60 years old [ 44 ]. This aspect should also drive the clinician to choose the more appropriate oxygenation strategy from a physiological point of view.
COT through nasal prongs is appropriate to reduce transitory hypoxemia [ 42 ]. However, the inspired oxygen fraction (FiO 2 ) cannot be predicted, and might not be enough in severe cases.
When lung parenchyma is already compromised by an underlying pathologic condition, uncomplicated FOB may worsen gas exchange, leading to development of respiratory failure [ 1 , 2 , 41 , 45 ]. HFNC has been introduced in clinical practice as a valuable alternative for oxygen support during FOB [ 4 , 46 , 47 , 48 ]. Four main reasons support its use during and after the procedure: (1) the flow up to 60 L/min ensures a more stable FiO 2 , as it is able to match the increased patient’s inspiratory flow [ 49 ]; (2) the high flow generates a small positive expiratory airway pressure depending on the flow rate, the upper airway anatomy, the breathing through the nose or mouth, and the size of the cannula in relation to the nostrils [ 49 ]; (3) the high flow reduces the dead space in the upper airways up to 70 ml, and increases the alveolar ventilation [ 49 ]; and (4) the HFNC decreases the resistive breathing effort, reducing the upper airway resistance [ 49 ].
The application of CPAP has also been adopted during FOB. CPAP releases a positive pressure throughout the entire breathing cycle, thereby recruiting lung atelectatic regions [ 50 ], reducing venous admixture [ 51 ], and decreasing the patient’s inspiratory effort [ 5 ].
The use of NIV can also ameliorate gas exchange, thus diminishing the respiratory effort. However, despite these benefits NIV is negatively affected by poor patient-ventilator interaction, which impairs its effectiveness [ 7 , 8 , 52 , 53 , 54 ].
COT during FOB
The use of COT during FOB has been investigated in several studies. Although not always required [ 9 ], COT showed its benefits in patients with higher risk of desaturation, including those with baseline (before procedure) peripheral arterial oxyhemoglobin saturation (SpO 2 ) < 93% [ 10 ], an obstructive ventilatory defect [ 11 ], or a forced expiratory volume in the first second (FEV 1 ) lower than 1 L [ 9 , 12 ]. COT is also indicated in those patients suffering from chronic obstructive pulmonary disease and immunosuppression, due to their higher risk of intubation in the 24 h following FOB [ 13 ].
When FOB is carried out for BAL [ 14 ] or brushing performed for cytological examination [ 10 ], COT is needed as well. Oxygen can be delivered by a cannula placed either in the nose or in the mouth, as the average SpO 2 within the procedure is similar between the two modalities, and no sinus symptoms or nasal congestion have been reported [ 15 ].
HFNC during FOB
HFNC consists of a mixture of air and oxygen, delivered through a maximally heated and humidified flow up to 60 L/min.
HFNC has been successfully used to prevent acute respiratory failure (ARF) from worsening during FOB. A small study conducted on 5 patients found that oxygenation was well maintained for 30 min after FOB for BAL, and only one patient required non-invasive positive pressure ventilation 16 h after FOB [ 16 ]. Similar results were reported in regard to a larger observational trial, with 30 critically ill patients affected by ARF during nasal FOB performed with non-open mouth [ 17 ] and 60 patients requiring FOB for BAL [ 18 ]. Improvement of post-FOB SpO 2 was also described, as well as prevention of mucosal injury and patient discomfort, thanks to the humidified and heated gas flow [ 19 ]. In a prospective study carried out using HFNC during FOB for endobronchial ultrasound (EBUS) with deep sedation, no difference in desaturation events was detected between procedures lasting less or more than 40 min [ 20 ]. In several studies, HFNC has also been compared with other oxygen support modalities, as shown below. In a randomized controlled trial on post-lung transplant patients undergoing FOB for transbronchial lung biopsy, the procedure was interrupted when low-flow nasal oxygen was applied, whereas no similar episodes occurred with HFNC [ 21 ]. When compared to Venturi mask, HFNC at 60 L/min provided better oxygenation outcomes, whereas no difference was observed between HFNC 40 L/min and Venturi mask 40 L/min [ 22 ]. A very recent randomized controlled trial showed that the use of HFNC instead of COT, during FOB for EBUS, was associated with a statistically significant lower drop in SpO 2 [ 23 ].
When compared with COT in patients without ARF undergoing EBUS with conscious sedation, HFNC did not significantly reduce the rate of intraprocedural desaturation episodes [ 24 ]. During FOB for BAL, effectiveness and safety of HFNC versus COT was tested in patients with ARF [ 25 ]. No relevant events, such as endotracheal intubation, were reported within the 24 h following FOB for BAL. No statistically significant differences between patients undergoing or not HFNC with regard to transient hypoxemia, fever, hypotensive events, and endotracheal intubation rate were observed [ 25 ].
CPAP during FOB
The use of CPAP through full-face mask during FOB has been investigated in patients with hypoxemic ARF (PaO 2 /FiO 2 < 300 mmHg) by Maitre et al. [ 26 ]. As compared to COT, CPAP guaranteed higher SpO 2 during and after the procedure, and lower numbers of patients required ventilatory assistance within the 6 h following the endoscopic procedure [ 26 ].
NIV during FOB
NIV via face mask was for the first time applied during FOB for BAL in 1996 [ 1 ]. In a cohort of immunosuppressed patients with suspected pneumonia and severe hypoxemia (PaO 2 /FiO 2 < 100 mmHg), Antonelli et al. reported that NIV, applied 10 min before and discontinued 90 min after FOB, was well tolerated by all patients, improved gas exchange, and prevented the need for intubation [ 1 ].
Later on, the application of NIV via face mask was also evaluated in immunocompetent patients with hypoxemic ARF of different severity. NIV provided optimal gas exchange during and after FOB [ 27 , 28 , 29 ], without causing hemodynamic impairments [ 27 ], and was also associated with a low incidence of minor complications [ 29 ], and with a small percentage of patients requiring intubation during the first 8 h after the procedure [ 28 , 29 ].
At that time, facial masks were adapted with swivel connectors [ 28 ] or sealed ports [ 27 ] for the passage of the bronchoscope into the interface and patients’ airways. Nasal masks have been proposed as a valid alternative to facial masks for NIV during FOB [ 30 ]. In addition, new masks for NIV specifically designed for FOB were also tested [ 29 , 30 , 31 ]. Lastly, helmet NIV represents another feasible and safe alternative to NIV via mask during FOB for BAL in patients with hypoxemic ARF [ 32 ].
The use of NIV during FOB has been also extended to more complicated procedures, such as transbronchial lung biopsy [ 33 ] and interventional procedures, including balloon dilation, electrocautery and argon plasma coagulation [ 34 ]. In keeping with the above-mentioned studies, NIV guaranteed a stable oxygenation [ 33 , 34 ] and good patients’ tolerance [ 33 ], whereas minor complications [ 34 ], as well as the number of patients requiring intubation after the procedure [ 33 ], were quite low. Similar findings have been also reported for patients with chronic [ 35 ] and acute-on-chronic [ 36 , 37 ] respiratory failure.
The growing evidence in favor of both HFNC and NIV has yielded some studies comparing the two modalities in patients with mild-to-moderate hypoxemic ARF. Compared to HFNC, NIV improved oxygenation before, during and after FOB [ 38 , 39 ], as well as decreased the number of desaturations < 90% [ 39 ], without any difference in mortality or in the rate of patients requiring intubation and invasive mechanical ventilation [ 38 , 39 ].
Quantitative synthesis of study findings
Figures 2 and 3 depict the quantitative synthesis of HFNC versus COT with respect to the lowest saturation and the episodes of desaturation during the FOB, respectively. Funnel plots for visual inspection of heterogeneity are included in the Additional file 1: Figures S1 and S2, respectively. In comparison with COT, HFNC significantly improves the lowest saturation (MD 7.04 [95%CI: 5.14 to 8.95]%; p < 0.001; I 2 = 50%) and it significantly reduces the number of episodes of desaturation (RR 0.25 [95%CI: 0.14 to 0.42]; p < 0.001; I 2 = 0%).
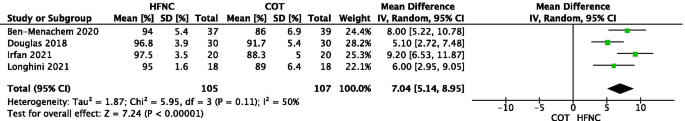
Quantitative synthesis of HFNC versus COT with respect to the lowest saturation
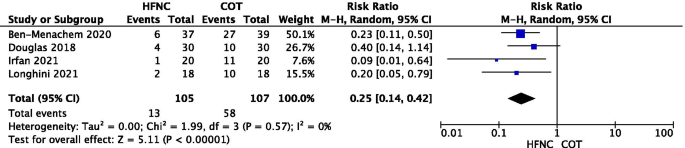
Quantitative synthesis of HFNC versus COT with respect to the episodes of desaturation during the FOB
In addition, Figs. 4 and 5 depict the quantitative synthesis of HFNC versus NIV with respect to the lowest saturation and the episodes of desaturation during the FOB, respectively. Funnel plots for visual inspection of heterogeneity are also included in the Additional file 1: Figures S3 and S4, respectively. As opposed to NIV, HFNC is characterized by a reduced lowest saturation (MD − 2.63 [95%CI: − 4.99 to − 0.28]%; p = 0.03; I 2 = 0%). On the opposite, HFNC and NIV do not differ with respect to the number of episodes of desaturation (RR 2.88 [95%CI: 0.88 to 9.44]; p = 0.08; I 2 = not applicable). Noteworthy, these data are reported only in the study by Simon et al. [ 38 ].
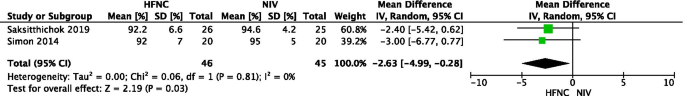
Quantitative synthesis of HFNC versus NIV with respect to the lowest saturation
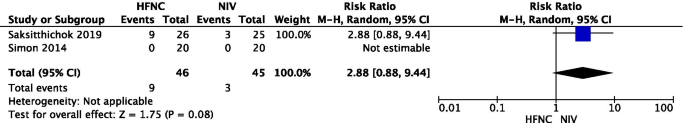
Quantitative synthesis of HFNC versus NIV with respect to the episodes of desaturation during the FOB
Although several studies showed benefits from different oxygenation strategies during FOB, no clear guidelines are yet available in literature. Overall, the worst is the patient's baseline lung function prior to the procedure, the highest is the oxygen requirement within the procedure and the risk of worsening ARF afterwards.
HFNC was shown to be safe in the majority of patients affected by mild-to-moderate ARF undergoing FOB for either diagnosis or treatment, and in those with lung transplant, while NIV ensured stable oxygenation when FOB was carried out for extended procedures or in patients with more severe ARF. However, information is still very scarce about the eventual better advantages of one strategy compared to another. All patients’ categories mentioned in the reviewed studies, as well as the oxygenation modalities which resulted more successful, have been summarized in Table 2 . Generally speaking, by the pooled data analysis, HFNC outperforms COT with respect to oxygenation outcomes in patients with lower oxygen requirement, whereas data suggest the superiority of NIV in patients with more severe ARF, as compared to HFNC. Although the lack of sufficient evidence prevents the possibility to provide a clear or definitive recommendation on the use of an oxygenation strategy over another one, the oxygenation improvement during the procedure still remains an important safety issue for patients undergoing FOB. In addition, it potentially may improve major clinical outcomes (such as the need for hospital or ICU admission for post-procedural respiratory failure); however, such benefits require to be addressed.
In such a heterogeneous scenario of lung conditions, and with FOB implicated in a variety of diagnostic and therapeutic procedures, a score able to predict the occurrence of adverse events could support the clinician when deciding the best oxygenation modality. In order to develop such a score, a relevant scientific effort based on a multicenter research study would be useful.
The choice of oxygenation strategy may interfere with the route of access of the FOB. For example, during HFNC the presence of large bore nasal prongs prevents the possibility to use the nasal route, leading the physician to insert the FOB through the mouth. Noteworthy, the small positive expiratory airway pressure generated by HFNC would be significantly reduced during open mouth breathing, loosing theoretically its benefit on alveolar distending pressure and lung de-recruitment prevention [ 49 ]. However, we have recently demonstrated that in outpatients undergoing FOB with BAL, when compared to COT, HFNC prevents oxygenation worsening by avoiding end-expiratory loss of lung volume and preserves the same tidal volume with a lower diaphragm activation [ 18 ]. Therefore, based on our experience and recent data [ 18 ], we suggest the use of HFNC, rather than COT, in out-patients undergoing FOB with BAL.
On the opposite, some interfaces (helmet and face masks) for CPAP o NIV have been specifically designed to be used during FOB, which allow both oral and nasal route for bronchoscope insertion. For example, Korkmaz Ekren et al. have used a dedicated full-face mask with an interchangeable connector between the ventilator tubing and the mask that allows the insertion of the bronchoscope through a sealed-hole [ 29 ]. In another study by Heunks et al. [ 31 ], the investigators used a total face mask with a dedicated sealed hole below the connector between ventilator tubing and interface allowing the performance of the FOB through the mouth during NIV. However, air-leaks may occur around the interface or through the dedicated hole for FOB insertion, leading to patient-ventilator asynchronies which may be difficult to be managed [ 8 , 55 ]. As a suggestion based on our experience and previous data [ 26 ], CPAP may be preferable over NIV for some reasons: first of all, CPAP is more user-friendly to be applied, as compared to NIV. In fact, the need of a simple flow generator, rather than a ventilator, makes CPAP easy to be applied. Moreover, although both CPAP and NIV guarantee the application of positive airway pressure throughout the whole respiratory cycle, the latter requires to adjust ventilator settings in order to improve the patient-ventilator synchrony during the inspiratory phase [ 8 , 55 ].
The oxygenation strategy should also be chosen according to the procedure. Although some procedures (i.e. FOB with BAL) may be performed with an extensive topical anesthesia, others (i.e. EBUS) may require deeper sedation with different pharmacological strategies including both sedatives (i.e. midazolam, propofol or dexmedetomidine) and analgesics (i.e. remifentanil). However, it must be recognized that these drugs can modify the critical closing pressure of the upper airways, inducing their collapse [ 56 , 57 ], and they can affect the breathing pattern and/or the respiratory drive. In particular, the deeper is the sedation, the higher is the modification [ 58 , 59 ]. Therefore, in case of deep sedation, NIV (or even the placement of a laryngeal mask) may be required and preferred over other oxygenation strategies to ensure breathing and gas-exchange. A literature review and, eventually, trials focused on this topic are advisable.
Finally, in the era of the ongoing epidemic, a careful choice of oxygenation strategy should also be done in case of patients with suspected or confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. FOB is considered as aerosol generating procedure generating a significant number of droplets that can be contagious for other patients and the healthcare personnel [ 60 ]. Operators should firstly check the infection by SARS-CoV-2 through molecular test with naso-pharyngeal swabs; in case of positivity, full personal protective equipment (i.e. FFP-2 masks, gloves, goggles, face shields and gowns) are required. Furthermore, when exhaled air is released into the room, the dispersion of the virus may increase the risk of infection of other patients and the healthcare personnel [ 61 ]. It is well known that different interfaces are characterized by dissimilar air dispersion distances during their application [ 62 , 63 ]. In principle, the use of a helmet for CPAP or NIV with a good seal around the neck is preferable, and, as abovementioned, the appropriate use of personal protective equipment is mandatory. In addition, simple practical measurements like reducing the number of assisting personnel and cough restriction with the administration of oropharyngeal lignocaine can minimize the contamination risk [ 60 ]. Of note, masks with vent holes should be avoided and a filter between the mask and the vent or PEEP valve is advisable to reduce viral transmission [ 61 ].
To our knowledge, this is the first review outlining the oxygenation strategies during FOB, and data are updated to the last available literature sources. Despite the consistent number of cited studies, the majority of them assessed the oxygenation effects on physiological, rather than major clinical outcomes. The quality of reviewed studies is also questionable, due to the small sample size and the high population heterogeneity preventing a further meta-analysis. Moreover, most of included studies are single-centered. Finally, studies enroll patients which are not exclusively chronic or acute, but sometimes are mixed or not clear populations, preventing us to the possibility to separate the findings on different oxygenation strategies according to the clinical status of the patients. Hence, finding generalization is limited, as supported by weak evidence. Noteworthy, this review highlights the need for future research and robust data, in order to draw specific recommendations in a field where clinical practice nowadays is left to single-center experience, rather than scientific evidence.
In conclusion, the oxygenation strategy during FOB should be chosen according to the procedure, lung and heart function, oxygen requirement within the procedure and the risk of worsening ARF afterwards. In patients with mild-to-moderate oxygen requirement, HFNC would be preferable over COT, while the use of CPAP or NIV is encourageable in patients with more severe hypoxemia.
Availability of data and materials
Not applicable.

Abbreviations
Acute respiratory failure
Broncho-alveolar lavage
Conventional oxygen therapy
- Continuous positive airway pressure
Endobronchial ultrasound
Electronic supplemental material
Forced expiratory volume in the first second
Inspired oxygen fraction
Fiberoptic bronchoscopy
- High flow nasal cannula
- Non-invasive ventilation
Arterial partial pressure to inspired oxygen fraction ratio
Positive end-expiratory pressure
Severe acute respiratory syndrome coronavirus 2
Peripheral arterial oxyhemoglobin saturation
Antonelli M, Conti G, Riccioni L, Meduri GU. Noninvasive positive-pressure ventilation via face mask during bronchoscopy with BAL in high-risk hypoxemic patients. Chest. 1996;110(3):724–8.
Article CAS PubMed Google Scholar
Goldstein RA, Rohatgi PK, Bergofsky EH, Block ER, Daniele RP, Dantzker DR, et al. Clinical role of bronchoalveolar lavage in adults with pulmonary disease. Am Rev Respir Dis. 1990;142(2):481–6.
O’Driscoll BR, Howard LS, Davison AG, British Thoracic Society. BTS guideline for emergency oxygen use in adult patients. Thorax. 2008;63(Suppl 6):vi1-68.
PubMed Google Scholar
Bruni A, Garofalo E, Cammarota G, Murabito P, Astuto M, Navalesi P, et al. High flow through nasal cannula in stable and exacerbated chronic obstructive pulmonary disease patients. Rev Recent Clin Trials. 2019;14(4):247–60.
Article PubMed Google Scholar
Lenique F, Habis M, Lofaso F, Dubois-Randé JL, Harf A, Brochard L. Ventilatory and hemodynamic effects of continuous positive airway pressure in left heart failure. Am J Respir Crit Care Med. 1997;155(2):500–5.
Bellani G, Patroniti N, Greco M, Foti G, Pesenti A. The use of helmets to deliver non-invasive continuous positive airway pressure in hypoxemic acute respiratory failure. Minerva Anestesiol. 2008;74(11):651–6.
CAS PubMed Google Scholar
Nava S, Navalesi P, Carlucci A. Non-invasive ventilation. Minerva Anestesiol. 2009;75(1–2):31–6.
Garofalo E, Bruni A, Pelaia C, Liparota L, Lombardo N, Longhini F, et al. Recognizing, quantifying and managing patient-ventilator asynchrony in invasive and noninvasive ventilation. Expert Rev Respir Med. 2018;12(7):557–67.
Jones AM, O’Driscoll R. Do all patients require supplemental oxygen during flexible bronchoscopy? Chest. 2001;119(6):1906–9.
Onakpoya UU, Adewole O, Ogunrombi AB, Adenekan AT. Oxygen supplementation during awake fibreoptic bronchoscopy in a Nigerian tertiary hospital. West Afr J Med. 2012;31(4):238–42.
Golpe R, Mateos A. Supplemental oxygen during flexible bronchoscopy. Chest. 2002;121(2):663–4.
Alijanpour E, Nikbakhsh N, Bijani A, Baleghi M. Evaluation of oxygen requirement in patients during fiberoptic bronchoscopy. Caspian J Intern Med. 2010;1:141–4.
Google Scholar
Cracco C, Fartoukh M, Prodanovic H, Azoulay E, Chenivesse C, Lorut C, et al. Safety of performing fiberoptic bronchoscopy in critically ill hypoxemic patients with acute respiratory failure. Intensive Care Med. 2013;39(1):45–52.
Ghio A, Bassett MA, Levin D, Montilla T. Oxygen supplementation is required in healthy volunteers during bronchoscopy with lavage. J Bronchol. 2007;14(1):19–21.
Article Google Scholar
McCain TW, Dunagan DP, Adair NE, Chin R. Prospective randomized trial comparing oxygen administration during nasal flexible bronchoscopy: oral vs nasal delivery. Chest. 2001;120(5):1671–4.
Miyagi K, Haranaga S, Higa F, Tateyama M, Fujita J. Implementation of bronchoalveolar lavage using a high-flow nasal cannula in five cases of acute respiratory failure. Respir Investig. 2014;52(5):310–4.
La Combe B, Messika J, Labbé V, Razazi K, Maitre B, Sztrymf B, et al. High-flow nasal oxygen for bronchoalveolar lavage in acute respiratory failure patients. Eur Respir J. 2016;47(4):1283–6.
Article PubMed CAS Google Scholar
Longhini F, Pelaia C, Garofalo E, Bruni A, Placida R, Iaquinta C, et al. High-flow nasal cannula oxygen therapy for outpatients undergoing flexible bronchoscopy: a randomised controlled trial. Thorax. 2021. https://doi.org/10.1136/thoraxjnl-2021-217116 .
Chung SM, Choi JW, Lee YS, Choi JH, Oh JY, Min KH, et al. Clinical effectiveness of high-flow nasal cannula in hypoxaemic patients during bronchoscopic procedures. Tuberc Respir Dis. 2019;82(1):81–5.
Service JA, Bain JS, Gardner CP, McNarry AF. Prospective experience of high-flow nasal oxygen during bronchoscopy in 182 patients: a feasibility study. J Bronchol Interv Pulmonol. 2019;26(1):66–70.
Ben-Menachem E, McKenzie J, O’Sullivan C, Havryk AP. High-flow nasal oxygen versus standard oxygen during flexible bronchoscopy in lung transplant patients: a randomized controlled trial. J Bronchol Interv Pulmonol. 2020;27(4):259–65.
Lucangelo U, Vassallo FG, Marras E, Ferluga M, Beziza E, Comuzzi L, et al. High-flow nasal interface improves oxygenation in patients undergoing bronchoscopy. Crit Care Res Pract. 2012;2012: 506382.
PubMed PubMed Central Google Scholar
Irfan M, Ahmed M, Breen D. Assessment of high flow nasal cannula oxygenation in endobronchial ultrasound bronchoscopy: a randomized controlled trial. J Bronchol Interv Pulmonol. 2021;28(2):130–7.
Douglas N, Ng I, Nazeem F, Lee K, Mezzavia P, Krieser R, et al. A randomised controlled trial comparing high-flow nasal oxygen with standard management for conscious sedation during bronchoscopy. Anaesthesia. 2018;73(2):169–76.
Kim EJ, Jung CY, Kim KC. Effectiveness and safety of high-flow nasal cannula oxygen delivery during bronchoalveolar lavage in acute respiratory failure patients. Tuberc Respir Dis. 2018;81(4):319–29.
Maitre B, Jaber S, Maggiore SM, Bergot E, Richard JC, Bakthiari H, et al. Continuous positive airway pressure during fiberoptic bronchoscopy in hypoxemic patients. A randomized double-blind study using a new device. Am J Respir Crit Care Med. 2000;162(3 Pt 1):1063–7.
Antonelli M, Conti G, Rocco M, Arcangeli A, Cavaliere F, Proietti R, et al. Noninvasive positive-pressure ventilation vs conventional oxygen supplementation in hypoxemic patients undergoing diagnostic bronchoscopy. Chest. 2002;121(4):1149–54.
Baumann HJ, Klose H, Simon M, Ghadban T, Braune SA, Hennigs JK, et al. Fiber optic bronchoscopy in patients with acute hypoxemic respiratory failure requiring noninvasive ventilation—a feasibility study. Crit Care. 2011;15(4):R179.
Article PubMed PubMed Central Google Scholar
Korkmaz Ekren P, Basarik Aydogan B, Gurgun A, Tasbakan MS, Bacakoglu F, Nava S. Can fiberoptic bronchoscopy be applied to critically ill patients treated with noninvasive ventilation for acute respiratory distress syndrome? Prospective observational study. BMC Pulm Med. 2016;16(1):89.
Chiner E, Sancho-Chust JN, Llombart M, Senent C, Camarasa A, Signes-Costa J. Fiberoptic bronchoscopy during nasal non-invasive ventilation in acute respiratory failure. Respir Int Rev Thorac Dis. 2010;80(4):321–6.
CAS Google Scholar
Heunks LMA, de Bruin CJR, van der Hoeven JG, van der Heijden HFM. Non-invasive mechanical ventilation for diagnostic bronchoscopy using a new face mask: an observational feasibility study. Intensive Care Med. 2010;36(1):143–7.
Antonelli M, Pennisi MA, Conti G, Bello G, Maggiore SM, Michetti V, et al. Fiberoptic bronchoscopy during noninvasive positive pressure ventilation delivered by helmet. Intensive Care Med. 2003S;29(1):126–9.
Agarwal R, Khan A, Aggarwal AN, Gupta D. Bronchoscopic lung biopsy using noninvasive ventilatory support: case series and review of literature of NIV-assisted bronchoscopy. Respir Care. 2012;57(11):1927–36.
Chen X, Zhou Y, Yu H, Peng Y, Xia L, Liu N, et al. Feasibility analysis of flexible bronchoscopy in conjunction with noninvasive ventilation for therapy of hypoxemic patients with Central Airway Obstruction: a retrospective study. PeerJ. 2020;8: e8687.
Da Conceiçao M, Genco G, Favier JC, Bidallier I, Pitti R. Fiberoptic bronchoscopy during noninvasive positive-pressure ventilation in patients with chronic obstructive lung disease with hypoxemia and hypercapnia. Ann Francaises D’anesthesie Et De Reanimation. 2000;19(4):231–6.
Mohamed AS, El-Sharawy DE. Noninvasive ventilation with add-on fiberoptic bronchoscopy in patients with chronic obstructive pulmonary disease. Egypt J Chest Dis Tuberc. 2018;67(1):26.
Scala R, Naldi M, Maccari U. Early fiberoptic bronchoscopy during non-invasive ventilation in patients with decompensated chronic obstructive pulmonary disease due to community-acquired-pneumonia. Crit Care. 2010;14(2):R80.
Simon M, Braune S, Frings D, Wiontzek A-K, Klose H, Kluge S. High-flow nasal cannula oxygen versus non-invasive ventilation in patients with acute hypoxaemic respiratory failure undergoing flexible bronchoscopy-a prospective randomised trial. Crit Care. 2014;18(6):712.
Saksitthichok B, Petnak T, So-Ngern A, Boonsarngsuk V. A prospective randomized comparative study of high-flow nasal cannula oxygen and non-invasive ventilation in hypoxemic patients undergoing diagnostic flexible bronchoscopy. J Thorac Dis. 2019;11(5):1929–39.
Lindholm CE, Ollman B, Snyder JV, Millen EG, Grenvik A. Cardiorespiratory effects of flexible fiberoptic bronchoscopy in critically ill patients. Chest. 1978;74(4):362–8.
Matsushima Y, Jones RL, King EG, Moysa G, Alton JD. Alterations in pulmonary mechanics and gas exchange during routine fiberoptic bronchoscopy. Chest. 1984;86(2):184–8.
Miller EJ. Hypoxemia during fiberoptic bronchoscopy. Chest. 1979;75(1):103.
Lundgren R, Häggmark S, Reiz S. Hemodynamic effects of flexible fiberoptic bronchoscopy performed under topical anesthesia. Chest. 1982;82(3):295–9.
Davies L, Mister R, Spence DP, Calverley PM, Earis JE, Pearson MG. Cardiovascular consequences of fibreoptic bronchoscopy. Eur Respir J. 1997;10(3):695–8.
Albertini R, Harrel JH, Moser KM. Letter: hypoxemia during fiberoptic bronchoscopy. Chest. 1974;65(1):117–8.
Pisani L, Astuto M, Prediletto I, Longhini F. High flow through nasal cannula in exacerbated COPD patients: a systematic review. Pulmonology. 2019;25(6):348–54.
Cortegiani A, Longhini F, Carlucci A, Scala R, Groff P, Bruni A, et al. High-flow nasal therapy versus noninvasive ventilation in COPD patients with mild-to-moderate hypercapnic acute respiratory failure: study protocol for a noninferiority randomized clinical trial. Trials. 2019;20(1):450.
Article PubMed PubMed Central CAS Google Scholar
Garofalo E, Bruni A, Pelaia C, Cammarota G, Murabito P, Biamonte E, et al. Evaluation of a new interface combining high-flow nasal cannula and CPAP. Respir Care. 2019;64(10):1231–9.
Renda T, Corrado A, Iskandar G, Pelaia G, Abdalla K, Navalesi P. High-flow nasal oxygen therapy in intensive care and anaesthesia. Br J Anaesth. 2018;120(1):18–27.
Cammarota G, Vaschetto R, Turucz E, Dellapiazza F, Colombo D, Blando C, et al. Influence of lung collapse distribution on the physiologic response to recruitment maneuvers during noninvasive continuous positive airway pressure. Intensive Care Med. 2011;37(7):1095–102.
Lindner KH, Lotz P, Ahnefeld FW. Continuous positive airway pressure effect on functional residual capacity, vital capacity and its subdivisions. Chest. 1987;92(1):66–70.
Longhini F, Colombo D, Pisani L, Idone F, Chun P, Doorduin J, et al. Efficacy of ventilator waveform observation for detection of patient-ventilator asynchrony during NIV: a multicentre study. ERJ Open Res. 2017;3(4):00075–2017.
Cammarota G, Olivieri C, Costa R, Vaschetto R, Colombo D, Turucz E, et al. Noninvasive ventilation through a helmet in postextubation hypoxemic patients: physiologic comparison between neurally adjusted ventilatory assist and pressure support ventilation. Intensive Care Med. 2011;37(12):1943–50.
Longhini F, Pan C, Xie J, Cammarota G, Bruni A, Garofalo E, et al. New setting of neurally adjusted ventilatory assist for noninvasive ventilation by facial mask: a physiologic study. Crit Care. 2017;21(1):170.
Bruni A, Garofalo E, Pelaia C, Messina A, Cammarota G, Murabito P, et al. Patient-ventilator asynchrony in adult critically ill patients. Minerva Anestesiol. 2019;85(6):676–88.
Eastwood PR, Platt PR, Shepherd K, Maddison K, Hillman DR. Collapsibility of the upper airway at different concentrations of propofol anesthesia. Anesthesiology. 2005;103(3):470–7.
Shteamer JW, Dedhia RC. Sedative choice in drug-induced sleep endoscopy: a neuropharmacology-based review. Laryngoscope. 2017;127(1):273–9.
Costa R, Navalesi P, Cammarota G, Longhini F, Spinazzola G, Cipriani F, et al. Remifentanil effects on respiratory drive and timing during pressure support ventilation and neurally adjusted ventilatory assist. Respir Physiol Neurobiol. 2017;244:10–6.
Vaschetto R, Cammarota G, Colombo D, Longhini F, Grossi F, Giovanniello A, et al. Effects of propofol on patient-ventilator synchrony and interaction during pressure support ventilation and neurally adjusted ventilatory assist. Crit Care Med. 2014;42(1):74–82.
Sampsonas F, Kakoullis L, Karampitsakos T, Papaioannou O, Katsaras M, Papachristodoulou E, et al. Bronchoscopy during the COVID-19 pandemic: effect on current practices and strategies to reduce procedure-associated transmission. Expert Rev Respir Med. 2021. https://doi.org/10.1080/17476348.2021.1913058 .
Guan L, Zhou L, Zhang J, Peng W, Chen R. More awareness is needed for severe acute respiratory syndrome coronavirus 2019 transmission through exhaled air during non-invasive respiratory support: experience from China. Eur Respir J. 2020;55(3):2000352.
Article CAS PubMed PubMed Central Google Scholar
Hui DS, Chow BK, Lo T, Ng SS, Ko FW, Gin T, et al. Exhaled air dispersion during noninvasive ventilation via helmets and a total facemask. Chest. 2015;147(5):1336–43.
Hui DS, Chow BK, Lo T, Tsang OTY, Ko FW, Ng SS, et al. Exhaled air dispersion during high-flow nasal cannula therapy versus CPAP via different masks. Eur Respir J. 2019;53(4):1802339.
Download references
Acknowledgements
Author information, authors and affiliations.
Pulmonary Medicine Unit, Department of Health Sciences, “Magna Graecia” University, Catanzaro, Italy
Corrado Pelaia, Eugenio Arrighi & Girolamo Pelaia
Anesthesia and Intensive Care Unit, Department of Medical and Surgical Sciences, “Mater Domini” University Hospital, “Magna Graecia” University, Viale Europa, 88100, Catanzaro, Italy
Andrea Bruni, Eugenio Garofalo & Federico Longhini
Department of Emergency Medicine, Royal London Hospital, Barts Health NHS Trust, London, UK
Serena Rovida
Anesthesia and General Intensive Care, “Maggiore Della Carità” University Hospital, Novara, Italy
Gianmaria Cammarota
Department of Medicine-DIMED, Anesthesia and Intensive Care, Padua Hospital, University of Padua, Padua, Italy
Paolo Navalesi
You can also search for this author in PubMed Google Scholar
Contributions
CP conceived the content and collected data, drafted the manuscript. AB conceived the content and collected data, drafted the manuscript. EG conceived the content and participated in the data interpretation, drafted the manuscript. SR participated in the data interpretation, drafted the manuscript. EA conceived the study, drafted the manuscript. GC participated in the data interpretation, revised it critically for important intellectual content. PN conceived the study, participated in the data interpretation, revised it critically for important intellectual content. GP conceived the study, participated in the data interpretation, revised it critically for important intellectual content. FL conceived the content, participated in the data analysis and interpretation, drafted the manuscript, revised it critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Federico Longhini .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
Dr. Navalesi’s research laboratory has received equipment and grants from Draeger and Intersurgical S.p.A. He also received honoraria/speaking fees from Philips, Resmed, MSD and Novartis. Dr. Navalesi contributed to the development of the helmet Next, whose license for patent belongs to Intersurgical S.P.A. and receives royalties for that invention. Dr. Longhini and Dr. Navalesi contributed to the development of a new device (not discussed in the present study), whose patent is in progress (European Patent application number EP20170199831). The remaining authors have no conflict of interest to disclose.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: figure s1..
Funnel plot for HFNC versus COT with respect to the lowest saturation during FOB. Figure S2. Funnel plot for HFNC versus COT with respect to the episodes of desaturation. Figure S3. Funnel plot for HFNC versus NIV with respect to the lowest saturation during FOB. Figure S4. Funnel plot for HFNC versus NIV with respect to the episodes of desaturation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pelaia, C., Bruni, A., Garofalo, E. et al. Oxygenation strategies during flexible bronchoscopy: a review of the literature. Respir Res 22 , 253 (2021). https://doi.org/10.1186/s12931-021-01846-1
Download citation
Received : 24 May 2021
Accepted : 18 September 2021
Published : 25 September 2021
DOI : https://doi.org/10.1186/s12931-021-01846-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Bronchoscopy
Respiratory Research
ISSN: 1465-993X
- General enquiries: [email protected]
Bronchoscopy
Affiliations.
- 1 Louisiana State University/Shreveport
- 2 Mayo Clinic
- 3 Louisiana State University HSC
- PMID: 28846283
- Bookshelf ID: NBK448152
A bronchoscopy is an essential tool for clinicians and health care providers treating patients with lung diseases. Since its introduction to clinical practice by Shigeto Ikeda in 1966, flexible bronchoscopy has become an essential tool in diagnosis and management of patients with lung diseases. Rigid bronchoscopy can be particularly helpful in therapeutic cases.
Copyright © 2024, StatPearls Publishing LLC.
- Continuing Education Activity
- Introduction
- Anatomy and Physiology
- Indications
- Contraindications
- Preparation
- Technique or Treatment
- Complications
- Clinical Significance
- Enhancing Healthcare Team Outcomes
- Review Questions
Publication types
- Study Guide
Advertisement
Role of Bronchoscopy in the Diagnosis and Treatment of Severe Asthma
- Published: 29 May 2023
- Volume 10 , pages 106–119, ( 2023 )
Cite this article

- Miki Ueoka MD ORCID: orcid.org/0000-0002-0162-657X 1 &
- Scott Oh DO 1
72 Accesses
Explore all metrics
Purpose of Review
Severe asthma can be difficult to manage. While not always indicated, bronchoscopy has a role in the diagnosis and management of asthma, particularly in ruling out other differential diagnoses. Additionally, the emergence of biologic therapies has changed the landscape for treating severe asthma, but bronchoscopic techniques such as bronchial thermoplasty (BT) may also play a role.
Recent Findings
More data has emerged regarding the longevity and efficacy of BT as well as in identifying ideal candidates. Other bronchoscopic techniques may also be useful in treating patients with severe asthma but more studies are needed.
This review focuses on the use of bronchoscopy to aid in diagnosis and treatment of asthma with a focus on bronchial thermoplasty.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Bronchial thermoplasty in severe asthma.
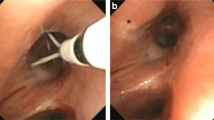
Evidence-Based Assessment of Bronchial Thermoplasty in Asthma: Mechanisms and Outcomes

Bronchial Thermoplasty
Papers of particular interest, published recently, have been highlighted as: • of importance •• of major importance.
Most Recent National Asthma Data | CDC. Published May 26, 2022. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm Accessed October 8 2022.
Global Initiative for Asthma. Global strategy for asthma management and prevention, 2022. Available from: www.ginaasthma.org. https://ginasthma.org/wp-content/uploads/2022/07/GINA-Main-Report-2022-FINAL-22-07-01-WMS.pdf . Accessed October 8 2022. This article reviews the current Asthma guidelines .
Brusselle GG, Koppelman GH. Biologic therapies for severe asthma. Taichman DB, ed. N Engl J Med . 2022;386(2):157–171. https://doi.org/10.1056/NEJMra2032506
Hashmi MD, Khan A, Shafiq M. Bronchial thermoplasty: state of the art. Respirology. 2022;27(9):720–9. https://doi.org/10.1111/resp.14312 . This is a comprehensive,up-to-date review of bronchial thermoplasty.
Article PubMed Google Scholar
Slebos DJ, Klooster K, Koegelenberg CFN, et al. Targeted lung denervation for moderate to severe COPD: a pilot study. Thorax. 2015;70(5):411–9. https://doi.org/10.1136/thoraxjnl-2014-206146 .
Gibeon D, Zhu J, Sogbesan A, et al. Lipid-laden bronchoalveolar macrophages in asthma and chronic cough. Respir Med. 2014;108(1):71–7. https://doi.org/10.1016/j.rmed.2013.10.005 .
Article CAS PubMed Google Scholar
Good JT, Kolakowski CA, Groshong SD, Murphy JR, Martin RJ. Refractory asthma. Chest. 2012;141(3):599–606. https://doi.org/10.1378/chest.11-0741 .
Ichikawa T, Panariti A, Audusseau S, et al. Effect of bronchial thermoplasty on structural changes and inflammatory mediators in the airways of subjects with severe asthma. Respir Med. 2019;150:165–72. https://doi.org/10.1016/j.rmed.2019.03.005 .
Miller JD, Cox G, Vincic L, Lombard CM, Loomas BE, Danek CJ. A prospective feasibility study of bronchial thermoplasty in the human airway. Chest. 2005;127(6):1999–2006. https://doi.org/10.1378/chest.127.6.1999 .
Cox G, Thomson NC, Rubin AS, et al. Asthma control during the year after bronchial thermoplasty. N Engl J Med. 2007;356(13):1327–37. https://doi.org/10.1056/NEJMoa064707 .
Pavord ID, Cox G, Thomson NC, et al. Safety and efficacy of bronchial thermoplasty in symptomatic, severe asthma. Am J Respir Crit Care Med. 2007;176(12):1185–91. https://doi.org/10.1164/rccm.200704-571OC .
Castro M, Rubin AS, Laviolette M, et al. Effectiveness and safety of bronchial thermoplasty in the treatment of severe asthma: a multicenter, randomized, double-blind, sham-controlled clinical trial. Am J Respir Crit Care Med. 2010;181(2):116–24. https://doi.org/10.1164/rccm.200903-0354OC .
Article PubMed PubMed Central Google Scholar
Wechsler ME, Laviolette M, Rubin AS, et al. Bronchial thermoplasty: long-term safety and effectiveness in patients with severe persistent asthma. J Allergy Clin Immunol. 2013;132(6):1295-1302.e3. https://doi.org/10.1016/j.jaci.2013.08.009 .
Chupp G, Laviolette M, Cohn L, et al. Long-term outcomes of bronchial thermoplasty in subjects with severe asthma: a comparison of 3-year follow-up results from two prospective multicentre studies. Eur Respir J. 2017;50(2):1700017. https://doi.org/10.1183/13993003.00017-2017 .
Article CAS PubMed PubMed Central Google Scholar
Chupp G, Kline JN, Khatri SB, et al. Bronchial thermoplasty in patients with severe asthma at 5 years. Chest. 2022;161(3):614–28. https://doi.org/10.1016/j.chest.2021.10.044 .
Chaudhuri R, Rubin A, Sumino K, et al. Safety and effectiveness of bronchial thermoplasty after 10 years in patients with persistent asthma (BT10+): a follow-up of three randomised controlled trials. Lancet Respir Med. 2021;9(5):457–66. https://doi.org/10.1016/S2213-2600(20)30408-2 . This the first study to followup patients>5 years after bronchial thermoplasty.
Goorsenberg AWM, d’Hooghe JNS, Srikanthan K, et al. Bronchial thermoplasty induced airway smooth muscle reduction and clinical response in severe asthma The TASMA Randomized Trial. Am J Respir Crit Care Med. 2021;203(2):175–84. https://doi.org/10.1164/rccm.201911-2298OC .
Ladjemi MZ, Di Candia L, Heddebaut N, et al. Clinical and histopathologic predictors of therapeutic response to bronchial thermoplasty in severe refractory asthma. J Allergy Clin Immunol. 2021;148(5):1227-1235.e6. https://doi.org/10.1016/j.jaci.2020.12.642 .
Langton D, Wang W, Thien F, Plummer V. The acute effects of bronchial thermoplasty on FEV1. Respir Med. 2018;137:147–51. https://doi.org/10.1016/j.rmed.2018.03.003 .
Langton D, Ing A, Fielding D, et al. Safety and effectiveness of bronchial thermoplasty when FEV1 is less than 50%. Chest. 2020;157(3):509–15. https://doi.org/10.1016/j.chest.2019.08.2193 .
Cangelosi MJ, Ortendahl JD, Meckley LM, et al. Cost–effectiveness of bronchial thermoplasty in commercially-insured patients with poorly controlled, severe, persistent asthma. Expert Rev Pharmacoecon Outcomes Res. 2015;15(2):357–64. https://doi.org/10.1586/14737167.2015.978292 .
Nguyen HV, Bose S, Mital S, et al. Is bronchial thermoplasty cost-effective as treatment for problematic asthma patients? Singapore’s perspective on a global model: is bronchial thermoplasty cost-effective. Respirology. 2017;22(6):1102–9. https://doi.org/10.1111/resp.13027 .
Zafari Z, Sadatsafavi M, Marra CA, Chen W, FitzGerald JM. Cost-effectiveness of bronchial thermoplasty, omalizumab, and standard therapy for moderate-to-severe allergic asthma. Feenstra TL, ed. PLOS ONE . 2016;11(1):e0146003. https://doi.org/10.1371/journal.pone.0146003
Perotin JM, Dewolf M, Launois C, Dormoy V, Deslee G. Bronchoscopic management of asthma. COPD and emphysema Eur Respir Rev. 2021;30(159):200029. https://doi.org/10.1183/16000617.0029-2020 .
Valipour A, Shah PL, Pison C, et al. Safety and dose study of targeted lung denervation in moderate/severe COPD patients. Respiration. 2019;98(4):329–39. https://doi.org/10.1159/000500463 .
Pison C, Shah PL, Slebos DJ, et al. Safety of denervation following targeted lung denervation therapy for COPD: AIRFLOW-1 3-year outcomes. Respir Res. 2021;22(1):62. https://doi.org/10.1186/s12931-021-01664-5 .
Slebos DJ, Shah PL, Herth FJF, et al. Safety and adverse events after targeted lung denervation for symptomatic moderate to severe chronic obstructive pulmonary disease (AIRFLOW) A multicenter randomized controlled clinical trial. Am J Respir Crit Care Med. 2019;200(12):1477–86. https://doi.org/10.1164/rccm.201903-0624OC .
Valipour A, Shah PL, Herth FJ, et al. Two-year outcomes for the double-blind, randomized, sham-controlled study of targeted lung denervation in patients with moderate to severe COPD: AIRFLOW-2. Int J Chron Obstruct Pulmon Dis. 2020;15:2807–16. https://doi.org/10.2147/COPD.S267409 .
on behalf of the AIRFLOW-3 Trial Study Group, Slebos DJ, Degano B, et al. Design for a multicenter, randomized, sham-controlled study to evaluate safety and efficacy after treatment with the Nuvaira® lung denervation system in subjects with chronic obstructive pulmonary disease AIRFLOW-3. BMC Pulm Med. 2020;20(1):41. https://doi.org/10.1186/s12890-020-1058-5 .
Article CAS PubMed Central Google Scholar
Hartman JE, Srikanthan K, Caneja C, et al. Bronchoscopic targeted lung denervation in patients with severe asthma: preliminary findings. Respiration. 2022;101(2):184–9. https://doi.org/10.1159/000518515 .
Li X, Xie SS, Li GS, Zeng J, Duan HX, Wang CH. Effects of bronchial thermoplasty and cryoablation on airway smooth muscle. Chin Med J (Engl). 2021;134(18):2166–74. https://doi.org/10.1097/CM9.0000000000001681 .
Valipour A, Fernandez-Bussy S, Ing AJ, et al. Bronchial rheoplasty for treatment of chronic bronchitis Twelve-month results from a multicenter clinical trial. Am J Respir Crit Care Med. 2020;202(5):681–9. https://doi.org/10.1164/rccm.201908-1546OC .
Cramer N, Jabbour N, Tavarez MM, Taylor RS. Foreign body aspiration. In: StatPearls . StatPearls Publishing; 2022. http://www.ncbi.nlm.nih.gov/books/NBK531480/ Accessed October 9, 2022.
Piccione J, Hysinger EB, Vicencio AG. Pediatric advanced diagnostic and interventional bronchoscopy. Semin Pediatr Surg. 2021;30(3):151065. https://doi.org/10.1016/j.sempedsurg.2021.151065 .
Download references
Author information
Authors and affiliations.
University of California, Los Angeles, CA, USA
Miki Ueoka MD & Scott Oh DO
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Miki Ueoka MD .
Ethics declarations
Human and animal rights and informed consent.
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Dermatology and Allergy .
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Ueoka, M., Oh, S. Role of Bronchoscopy in the Diagnosis and Treatment of Severe Asthma. Curr Treat Options Allergy 10 , 106–119 (2023). https://doi.org/10.1007/s40521-023-00341-w
Download citation
Accepted : 26 April 2023
Published : 29 May 2023
Issue Date : June 2023
DOI : https://doi.org/10.1007/s40521-023-00341-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Severe asthma
- Bronchoscopy
- Bronchial thermoplasty
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Evaluation of patients’ satisfaction with bronchoscopy procedure
Aleksandra karewicz.
1 Students’ Research Group”Alveolus”, Medical University of Warsaw, Warsaw, Poland
Katarzyna Faber
2 Department of Internal Medicine, Pulmonary Diseases and Allergy, Medical University of Warsaw, Warsaw, Poland
Katarzyna Karon
Katarzyna januszewska, piotr korczynski, katarzyna gorska, marta dabrowska, rafal krenke, associated data.
The shared database in is an anonymized version - it doesn't have patients' names, surnames, and PESEL Numbers [Polish acronym for "Universal Electronic System for Registration of the Population”]. All other data is available in the shared database. For a full database please contact the Science Department of Medical University of Warsaw: the person responsible for our department is Ewa Hieronimczuk, email: [email protected] ; phone number: (+48 22) 57 20 190.
The bronchoscopy (BS) experience provokes anxiety amongst some patients. It can have a negative impact on the course of the procedure and on the willingness of patients to undergo the next BS in the future.
We aimed to identify factors influencing patients’ satisfaction with BS.
The prospective study had been conducted between January and June 2019. It included patients hospitalized in our Department, who underwent elective BS. Patients assessed their anxiety and satisfaction level before and after BS using the Visual Analogue Scale (VAS). Data concerning the course of the bronchoscopy was collected.
The median level of anxiety prior to the procedure was moderate, higher in women (p<0.0001). The majority of patients (116/125, 93%) were satisfied with appropriate information before the procedure. Almost one-third of the interviewees (39/125, 31%) declared complete satisfaction (VAS = 0) with their procedure, 17 patients (14%) were dissatisfied (VAS >5/10). Overall 113 (90%) patients declared unconditional consent for future bronchoscopy. Multivariate linear regression analysis revealed two factors affecting patients’ satisfaction with bronchoscopy: anxiety prior to BS (standardized regression coefficient β = 0.264, p = 0.003) and discomfort (β = 0.205, p = 0.018). Neither age, degree of amnesia, duration of the procedure nor its type added any significant value as factors affecting patient satisfaction. The most common factors inducing patients’ discomfort during BS were local anesthesia of the throat (56/125, 45%) and cough (47/125, 38%).
Conclusions
Low anxiety level before bronchoscopy and reduced discomfort during the procedure are associated with better patient satisfaction. Thus, it is important to reduce patient anxiety and discomfort during the procedure.
Introduction
Bronchoscopy (BS) is a common medical procedure used to diagnose or treat patients with a variety of respiratory diseases. Although it is considered safe and severe complications are rare [ 1 ], BS may be associated with significant distress and anxiety among patients [ 2 – 4 ]. Anxiety causes increased cortisol levels, blood pressure, heart rate and respiration rate [ 5 , 6 ], which could influence the course of the procedure and cause an increased number of complications. In addition, discomfort produced by bronchoscopy is mostly related to cough, dyspnea, chest pain or nausea [ 3 , 7 ]. The level of anxiety experienced by the patients before and during bronchoscopy is determined by numerous factors, including age, gender [ 8 ], insufficient information about the aim of the procedure, its course and possible complications [ 9 ].
Premedication plays a crucial role in reducing stress-related to any invasive procedures. It is an important issue as stress caused by the fear of bronchoscopy may negatively affect patients’ compliance during the procedure and their willingness to undergo potential re-examination in the future [ 10 ]. Due to the immense progress in interventional bronchoscopy used for advanced diagnostic and therapeutic purposes, the importance of premedication or anesthesia-related to BS is also growing [ 11 ].
Patients’ satisfaction with BS is a subjective feeling that depends on patients’ expectations and may be influenced by various factors. The level of patient satisfaction is increasingly emphasized as a significant outcome measure for bronchoscopy, along with its diagnostic and therapeutic efficacy. Hence, the knowledge of the factors which affect patients’ satisfaction is important in terms of an optimal preparation and conducting the procedure. Therefore, the aim of this study was to identify factors that influence patients’ satisfaction with bronchoscopy.
Material and methods
General study design.
This was a prospective, single-center, observational, cross-sectional study performed in the Department of Internal Medicine, Pulmonary Diseases and Allergy of the Medical University of Warsaw, Poland between January and June 2019. Patients scheduled for an elective bronchoscopy understood as a non-emergency bronchoscopy procedure (diagnostic and therapeutic), scheduled in advance, were included. A written informed consent was obtained from all enrolled patients. The study was approved by the Ethics Committee of the Medical University of Warsaw (AKB/ 234/2018).
Patients with different malignant and nonmalignant pulmonary diseases who were admitted for elective diagnostic bronchoscopy were informed about the aim of the study and asked for their consent to participate. Patients were reassured that their disagreement would not change the course of the procedure. The inclusion criteria were: 1) age above 18 years, 2) indication for an elective bronchoscopy (scheduled non-emergency bronchoscopy procedures) performed on a hospital basis, 3) written informed and voluntary consent to participate in the study. The exclusion criteria were as follows: 1) age under 18 years, 2) urgent interventional bronchoscopy, 3) lack of agreement to participate in the study 4) inability to read, understand, complete surveys, or collaborate with the medical staff; 5) bronchoscopy under general anesthesia, 6) bronchoscopy on the out-patient basis.
All patients included in the study were asked to complete two original questionnaires:
- Questionnaire B (= before) completed the day before the scheduled bronchoscopy.
- Questionnaire P (= post) completed 24 hours after the procedure.
Questionnaire B included basic demographic data, data on the adequacy of information about the procedure provided by the attending physician and the nursing staff, patient’s expectations and the level of fear related to bronchoscopy (see S1 Table ). Questionnaire P included questions aimed at assessing patient satisfaction with bronchoscopy (see S2 Table ). Both questionnaires were originally created for the purpose of the current project and based on the British Thoracic Society (BTS) guideline for diagnostic flexible bronchoscopy in adults [ 12 ]. Satisfaction with bronchoscopy was defined as an overall subjective assessment of impressions and experiences, including complaints related to the procedure. It was measured using a 10 cm Visual Analogue Scale (VAS). Complete satisfaction was rated as 0, while complete dissatisfaction as 10 cm. Both questionnaires included patient identification data (ID) in order to link this data with factors possibly affecting the satisfaction from the procedure.
Outcome points
Primary outcome.
The correlation between patient satisfaction with bronchoscopy and anxiety before the procedure both measured by VAS
Secondary outcome
Identification of factors affecting patient satisfaction with BS
Bronchoscopy
All patients scheduled for bronchoscopy received routine information on the procedure, including its aim, course, and possible complications, from the attending physician and the nursing staff. Importantly, in order to avoid changes in standards of informing the patients about the procedure, the staff was not informed, which patients were included in the study. Patients who had bronchoscopy performed under general anesthesia were excluded from analysis as general anesthesia may influence patients’ satisfaction related to the procedure. Thus, patients who had rigid bronchoscopy were not included in this study. All other types of fiberoptic bronchoscopic procedures were accepted in the study protocol. The oral route was used to introduce all types of bronchoscopes to the lower airways, which is the standard way of bronchoscope insertion in our Department.
The procedures performed during bronchoscopy were as follows: endobronchial secretion removal, bronchoalveolar lavage (BAL), endobronchial forceps biopsy, endobronchial brush biopsy, transbronchial lung biopsy, endobronchial ultrasound and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), endobronchial ultrasound with radial probe and transbronchial biopsy (rEBUS-TBB), and foreign body removal. All bronchoscopies were performed under local anesthesia and conscious sedation (midazolam orally or midazolam and fentanyl intravenously). Sprayed lidocaine (2% and 10%) was applied as a local anesthetic to the throat. Additional doses of 2% lidocaine were applied to the trachea and bronchi via the working channel of the bronchoscope.
In all patients, bronchoscopy was performed by a pulmonologist with 10–15 years of experience in performing bronchoscopy. In the vast majority of procedures, one or more of the following bronchoscopes was used: video bronchoscope BS-1TH190, EBUS scope BS-UC180F (Olympus, Tokyo, Japan). Patients were monitored closely during the procedure, as well as after the bronchoscopy with the use of a dedicated report form (see S3 Table ). All adverse events up to 24 hours after the completion of the procedure were noted by the attending physician in a separate report form (see S4 Table ). Criteria of serious adverse events related to BS were adopted from the BTS guideline for diagnostic flexible bronchoscopy in adults [ 12 ].
Statistical analysis and sample size calculation
Power analysis and sample size calculations for correlation analysis showed that a sample size of 85 patients would provide 80% statistical power to detect weak (r = 0.3) correlation (alpha = 0.05, beta = 0.20) [ 13 ]. The number of enrolled patients was increased by 15 to allow for a 15% drop-out. Thus, a total number of 100 patients was a minimum required to conduct this study.
As data did not have a normal distribution, non-parametric tests were used. Data are presented as the median and interquartile range (IQR) unless otherwise specified. Differences between satisfied (VAS rating < 1 cm) and unsatisfied patients (VAS rating >5 cm), between different types of bronchoscopy and different types of anesthesia were compared using a chi-square test for categorical variables and Mann Whitney U test for continuous variables. Spearman coefficient was used for correlation analysis. The factors affecting patients’ satisfaction with BS were evaluated using correlation analysis, univariate and multivariate linear regression analysis. All parameters (expressed in interval scale) were screened in univariate analysis and selected to build a multivariate linear regression model with backward stepwise analysis. The optimal model was chosen based on the highest adjusted R square value. All analyses were performed using Statistica 13.0 (StatSoft Inc., Tulsa, OK, USA) and MedCalc 13.2.2 (MedCalc Software bvba, Ostend, Belgium). A p-value lower than 0.05 was regarded as significant.
From 200 patients admitted to our Department for elective bronchoscopy, 157 met the inclusion criteria and agreed to participate in the study. All questionnaires were completed by 125 patients and those patients were included in the final analysis ( Fig 1 ).

There were 67 male (54%) and 58 female patients. The median age was 66 years (IQR 58–73); 32 (26%) patients were never smokers, while 39 (31%) and 54 (43%) were active smokers and ex-smokers, respectively. The median smoking history was 29 pack-years (IQR 10–40). Indications for bronchoscopy and comorbidities are stated in S1 and S2 Figs.
The median level of anxiety prior to bronchoscopy was moderate, i.e. 5/10 cm (IQR 2.5–6) according to VAS. Women were significantly more anxious before the procedure than men [5 (IQR 4.6–8) cm vs 3.5 (IQR 0.8–5) cm, respectively, p<0.0001]. As many as 116 patients (93%) were satisfied with the level of information received before bronchoscopy.
Midazolam was given orally as premedication in 125 patients (100%) (in 123–7.5 mg, in 2 patients -3.25 mg) and in 39 patients (31%) intravenous fentanyl was added (median dose 50 mg, IQR 50–87.5).
Seventy-four patients (59%) had flexible (fiberoptic) bronchoscopy (including 3 procedures via tracheostomy), while EBUS had 51 subjects (41%)–linear, radial or both (linear and radial) EBUS was performed 33, 10 and 8 patients, respectively ( Table 1 ).
Data is presented as rank/ median and IQR (in parenthesis) or the number of patients and percentage (in parenthesis). Both groups were compared using the chi-squared test for categorical variables and the Mann-Whitney U test by rank for continuous variables.
n = number of patients, VBS—videobronchocopy, EBUS—endobronchial ultrasound, BS–bronchoscopy, VAS- Visual Analogue Scale, F—Female, M-Male
Subjective satisfaction with bronchoscopy was estimated as good by most patients ( Fig 2 ). The median VAS satisfaction rating was 1 cm (IQR 0–4). Thirty-nine patients (31%) declared absolute satisfaction with their procedure (VAS 0/10), while 17 patients (14%) were unsatisfied (VAS > 5/10). The vast majority of patients (n = 113, 90%) declared unconditional consent for future bronchoscopy. There was a positive correlation between satisfaction and willingness for future bronchoscopy (rho = 0.404, p<0.0001). We did not find a difference in satisfaction after BS between younger and older patients (≤ 65 and >65 years of age, respectively) or those who had the first or a repeated BS. There were no differences in either anxiety level before the procedure or satisfaction with it between patients who had video bronchoscopy and those who had EBUS ( Table 1 ). Similarly, no differences were found between patients who were sedated with midazolam alone or both with midazolam and fentanyl ( Table 2 ).

Data are presented as median and IQR (in parenthesis) or the number of patients and percentage (in parenthesis). Both groups were compared using the chi-squared test for categorical variables and the Mann-Whitney U test by rank for continuous variables.
n = number of patients, BS–bronchoscopy, VAS- Visual Analogue Scale
The primary outcome of the study was a weak positive correlation between dissatisfaction with bronchoscopy and the level of anxiety before the procedure (Spearman coefficient rho = 0.276, p = 0.0014) or patients’ discomfort during the procedure (rho = 0.309, p = 0.0005). The most common factors inducing patient discomfort during BS were local anesthesia of the upper airways (56/125, 45%) and cough (47/125, 38%), the remaining factors are shown in Fig 3 . No other significant correlations between dissatisfaction with BS and other factors were found.

Univariate regression analysis revealed that anxiety prior to bronchoscopy and discomfort during the procedure were the only significant factors affecting patient satisfaction with bronchoscopy ( Table 3 ). Then, multivariate linear regression analysis revealed only two factors affecting patients’ satisfaction with bronchoscopy: anxiety prior to BS (standardized regression coefficient β = 0.264, standard error 0.086, p = 0.003) and discomfort (β = 0.205, standard error 0.086, p = 0.018). Neither age, satisfaction with information about the bronchoscopy, its duration nor the degree of amnesia added any significant value as factors affecting patient satisfaction.
Abbreviations: NI, not included in the best multivariate linear regression model.
In 107 patients (86%) no complications during BS were noted. There was one serious adverse event during BS (1/125, 0.8%). The patient presented acute bradypnoea related to the administration of midazolam (<8 breaths/minute) during bronchoscopy and reversal dose of flumazenil was given with immediate positive effect. Other complications during bronchoscopy occurred rarely (17, 14%) and included: moderate bleeding associated with biopsy procedures (8 patients, 6%), fever (5 patients, 4%) transient oxygen desaturation < 85% (2 persons, 3%), COPD exacerbation (1 patient, 0.8%) and transient bradypnoea with spontaneous reversal (1 patient, 0.8%).
Comparison of satisfied and unsatisfied patients showed differences in the level of anxiety prior to bronchoscopy (p = 0.0009), patient discomfort during the procedure (p = 0.046) and not remembering the procedure due to premedication (p = 0.014) ( Table 4 ).
Data are presented as median and IQR (in parenthesis) or the number of patients and percentage (in parenthesis). Both groups were compared using the chi-squared test for categorical variables and the Mann Whitney U test for continuous variables.
n = number of patients, VAS- Visual Analogue Scale, F—female, M-Male, NS—never smoker, S—smoker, Ex—ex-smoker, VBS- videobronchocopy, sEBUS -linear endobronchial ultrasound, rEBUS- radial endobronchial ultrasound, BS -bronchoscopy, EBUS-TBNA- endobronchial ultrasound-guided transbronchial needle aspiration, rEBUS-TBB—radial probe endobronchial ultrasound-guided transbronchial biopsy.
Our study showed that a lower level of anxiety before bronchoscopy and during the procedure is associated with higher patient satisfaction after BS. It emphasizes that an adequate and comprehensive information on the procedure as well as premedication and sufficient anesthesia are important to reduce patient anxiety and discomfort during bronchoscopy. As the level of patient satisfaction is an important outcome measure for BS, the knowledge of the factors affecting bronchoscopy related patient discomfort is crucial to improve the level of patient tolerance of the procedure.
Our results are consistent with the results of previous studies [ 14 – 16 ]. Lechtzin et al. [ 15 ] reported that dissatisfaction after bronchoscopy was associated with anxiety prior to the procedure or its complications. The pre-bronchoscopy level of anxiety was identified as an important factor predicting patient satisfaction during and after the procedure by other authors as well [ 14 , 16 ]. The results of the study by Yildirim et al. [ 14 ] suggested that the operator should adjust the course of BS to the patient’s anxiety level, i.e. by choosing the oral route or by shortening the procedure time with fewer interventions if the patient is very anxious. In addition, the operator’s experience may also influence the patient’s discomfort during BS [ 15 , 16 ]. Mitsumune et al. [ 16 ] suggested that the more the patient is anxious, the more experienced bronchoscopist should perform the bronchoscopy. On the other hand, there have also been studies that found no correlation between the operator’s experience and patient satisfaction [ 17 ]. This aspect was not addressed in our study, as our aim was to evaluate other factors related to pre-bronchoscopy anxiety level and post-bronchoscopy satisfaction. Thus, all the bronchoscopists participating in the study had a comparable level of expertise.
Similarly to other authors [ 18 ], we have found that the female sex was associated with a higher level of anxiety before bronchoscopy. Albeit other authors [ 10 , 14 , 17 ] also reported a lower level of post-bronchoscopy satisfaction in women, this was not the case in our study. Gender differences in anxiety before and dissatisfaction after BS may be associated with gender differences in the perception of pain. Previous studies demonstrated that postoperative or procedural pain may be more severe in females than males [ 19 ].
Sun et al. [ 20 ] suggested that communication with patients and their education are critical for experiencing satisfaction with BS and readiness to undergo a repeated BS in the future. In our study, 93% of patients were satisfied with the adequate information about upcoming bronchoscopy. Such a high level of satisfaction with the provided information to the patients was certainly related to the elective nature of bronchoscopy applied in an in-patient setting. Some studies showed that the amount of information provided to the patient prior to BS may decrease the level of patient anxiety [ 2 , 10 , 15 ]. However, other studies showed no correlation between the quantity and quality of information given to patients and their satisfaction with the procedure [ 18 , 21 ] or even demonstrated that patients who were provided with a greater amount of information on possible post-BS complications experienced significantly more anxiety compared with the patients who were less informed [ 22 ]. Nonetheless, bronchoscopy guidelines recommend giving patients both verbal and written precise information prior to the procedure [ 12 ]. Additionally, it is reasonable to evaluate patient satisfaction after the procedure and address the areas of dissatisfaction and discomfort to improve the quality of the service [ 12 ].
Although it is crucial to minimize discomfort during bronchoscopy, it cannot be completely eliminated. In this study, discomfort during bronchoscopy obviously affected patient satisfaction with BS. Furthermore, a correlation between dissatisfaction and discomfort was weak, but higher than with anxiety before the procedure. Among our patients, local anesthesia of the upper airways and cough were the most common factors that caused the discomfort. These results correspond to those reported by Fujimoto et al. [ 10 ] who also pointed out throat anesthesia as the most frequent cause of BS-related patient discomfort. Hence, it is crucial to inform patients about this unpleasant but important part of the procedure, which allows the insertion of the bronchoscope to the lower airways, decreases the severity of cough and throat pain. Warning of the patient beforehand is critical, as the unexpected discomfort was shown to enhance patient reluctance to undergo a re-examination [ 10 ]. Other factors related to patient discomfort in our study were cough, postnasal drip and shortness of breath. The better the control of cough, pain and shortness of breath, the more eager the patient is to return for a repeated BS [ 15 ].
Conscious sedation is regarded as an important factor that may reduce anxiety and improve the level of patient satisfaction with the procedure [ 23 , 24 ]. In our study, conscious sedation was used in all patients. We found that satisfied patients declared amnesia more frequently than unsatisfied subjects, however, we did not document any significant correlation between the level of amnesia and patients’ satisfaction with bronchoscopy. Irrespective of the type of sedation, it is important to monitor the sedation effects and titrate the dose of sedatives to avoid respiratory depression [ 12 ].
Another factor that may influence patient satisfaction with bronchoscopy are complications related to the procedure. However, we did not observe such a relationship in our study, which may have resulted from a relatively low percentage of complications, noted in solely 18/125 patients (14%). Only one severe adverse event was noted in our group. Severe complications during bronchoscopy are very rare, and, in some cases cannot be prevented [ 1 , 3 ]. However, it is vital to minimize the risk of complications, such as bleeding, oxygen desaturation, arrhythmia or bradypnoea. The experience of the operator performing the bronchoscopy is an important factor for lowering the number of complications [ 25 , 26 ].
Some factors that have been previously reported to affect patient anxiety and satisfaction with bronchoscopy were not confirmed in our study. Those include patient age and previous bronchoscopies. Data on the relationship between patient age and anxiety are ambiguous. Poi et al. [ 18 ] demonstrated that younger patients were more “fearful”, whereas Aljohaney [ 8 ] found that older patients had a significantly higher anxiety score. According to Hehn et al. [ 27 ], elderly patients tolerate bronchoscopy as well as younger ones. Andrychiewicz et al. [ 21 ] showed that patients who had undergone BS in the past had a significantly better understanding of the rationale for performing the procedure and the type of procedure planned and anxiety was reported significantly more often in patients undergoing BS for the first time.
We are aware of several limitations in our study. Firstly, as it was a single-center study, the results may be specific for our facility and the institutional standards for performing bronchoscopy. The results are certainly highly dependent on the methods of sedation during bronchoscopy, throat anesthesia and preceding information of the examination as well as on the profile of patients including their cultural or ethnic backgrounds. Patients who were awaiting an elective bronchoscopy understood as a non-emergency bronchoscopy procedure (diagnostic and/or therapeutic), scheduled in advance, were included. Secondly, the study group was rather small due to single-center study, inclusion criteria and short duration of the study. Thirdly, we included only in-patients treated in our Department, which may have been associated with a selection bias and our results may not necessarily be extrapolated to BF performed in out-patients. Furthermore, although the questionnaires used in the study were checked for their comprehensibility, we did not validate them in advance, which is a limitation of this study. Next, as we did not use sedation score during the study it is difficult to estimate the influence of sedation on satisfaction with BS precisely. Finally, the sample size calculation was based on an assumption of linear Pearson correlation, but finally, we used Spearman correlation due to lack of normal distribution of data. Despite all these limitations, we believe that the results of our study are important as they indicate how essential it is to make an effort to reduce patient anxiety before BS and discomfort during it.
Low patient anxiety before bronchoscopy and reduced discomfort are associated with higher patient satisfaction after the procedure. Adequate and comprehensive information on the aim and course of bronchoscopy, as well as premedication, allow to reduce patient anxiety and discomfort during the procedure and thus increase their post-bronchoscopy satisfaction.
Supporting information
Acknowledgments.
The authors would like to thank Marta Maskey-Warzęchowska MD, PhD and Katarzyna Mycroft MD for their editorial assistance and manuscript review.
Funding Statement
The authors received no specific funding for this work.
Data Availability
- PLoS One. 2022; 17(10): e0274377.
Decision Letter 0
18 Aug 2021
PONE-D-21-03696
Evaluation of patients’ satisfaction with bronchoscopy procedure.
Dear Dr. Faber,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
The reviewers have identified several aspects of your methodological design and statistical analyses that will require further clarification in order to evaluate fulfilment of the journal's publication criteria. Please respond carefully to each of the points they have raised when preparing your revisions.
Please submit your revised manuscript by Oct 02 2021 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols . Additionally, PLOS ONE offers an option for publishing peer-reviewed Lab Protocol articles, which describe protocols hosted on protocols.io. Read more information on sharing protocols at https://plos.org/protocols?utm_medium=editorial-email&utm_source=authorletters&utm_campaign=protocols .
We look forward to receiving your revised manuscript.
Kind regards,
Jamie Males
Staff Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. Please include additional information regarding the survey or questionnaire used in the study and ensure that you have provided sufficient details that others could replicate the analyses. For instance, if you developed a questionnaire as part of this study and it is not under a copyright more restrictive than CC-BY, please include a copy, in both the original language as well as the English version already provided, as Supporting Information.
3. Thank you for stating the following financial disclosure:
"No"
At this time, please address the following queries:
a) Please clarify the sources of funding (financial or material support) for your study. List the grants or organizations that supported your study, including funding received from your institution.
b) State what role the funders took in the study. If the funders had no role in your study, please state: “The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.”
c) If any authors received a salary from any of your funders, please state which authors and which funders.
d) If you did not receive any funding for this study, please state: “The authors received no specific funding for this work.”
Please include your amended statements within your cover letter; we will change the online submission form on your behalf.
4. Thank you for stating the following in your Competing Interests section:
Please complete your Competing Interests on the online submission form to state any Competing Interests. If you have no competing interests, please state "The authors have declared that no competing interests exist.", as detailed online in our guide for authors at http://journals.plos.org/plosone/s/submit-now
This information should be included in your cover letter; we will change the online submission form on your behalf.
5. In your Data Availability statement, you have not specified where the minimal data set underlying the results described in your manuscript can be found. PLOS defines a study's minimal data set as the underlying data used to reach the conclusions drawn in the manuscript and any additional data required to replicate the reported study findings in their entirety. All PLOS journals require that the minimal data set be made fully available. For more information about our data policy, please see http://journals.plos.org/plosone/s/data-availability .
Upon re-submitting your revised manuscript, please upload your study’s minimal underlying data set as either Supporting Information files or to a stable, public repository and include the relevant URLs, DOIs, or accession numbers within your revised cover letter. For a list of acceptable repositories, please see http://journals.plos.org/plosone/s/data-availability#loc-recommended-repositories . Any potentially identifying patient information must be fully anonymized.
Important: If there are ethical or legal restrictions to sharing your data publicly, please explain these restrictions in detail. Please see our guidelines for more information on what we consider unacceptable restrictions to publicly sharing data: http://journals.plos.org/plosone/s/data-availability#loc-unacceptable-data-access-restrictions . Note that it is not acceptable for the authors to be the sole named individuals responsible for ensuring data access.
We will update your Data Availability statement to reflect the information you provide in your cover letter.
6. Please upload a new copy of Figure 2 as the detail is not clear. Please follow the link for more information: https://blogs.plos.org/plos/2019/06/looking-good-tips-for-creating-your-plos-figures-graphics/ " https://blogs.plos.org/plos/2019/06/looking-good-tips-for-creating-your-plos-figures-graphics/ .
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Partly
Reviewer #2: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #1: Yes
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
Reviewer #1: No
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
Reviewer #2: No
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: This study reported patient satisfaction with elective bronchoscopy and factors related to the bronchoscopy-related anxiety and satisfaction after the procedure. Authors found that low patient anxiety before bronchoscopy, less discomfort during the procedure, amnesia due to premedication and less complications are associated with a higher patient satisfaction after bronchoscopy. However, multivariate regression analysis revealed anxiety prior to BS (standardized regression coefficient β=0.243, p=0.003), discomfort (β=0.186, p=0.021) and complications (β=0.239, p=0.003) as the only significant factors affecting patient satisfaction with bronchoscopy.
There are some issues as below.
Major points
1. On primary endpoint
Authors aimed to identify factors influencing patients’ satisfaction with BS. However, they did sample size calculations for correlation analysis to show that a sample size of 85 patients would provide 80% statistical power to detect weak (r=0.3) correlation (alpha = 0.05, beta = 0.20). In general, sample size calculation should be used to clarify the main objective. I wonder why they use correlation analysis to detect weak (r=0.3) correlation. Furthermore, did they do this sample size calculation in order to find out which factors correlated with which factors?
2. Among the results of this manuscript, I think the result of multivariate regression analysis which described in line 246 is most important information. Authors concluded this result in the Conclusions session in line 379. However, they included “amnesia due to premedication” in Discussion session in line 276 to 278. If they included “amnesia due to premedication” from the results of Table 3, I think that “amnesia due to premedication” should be deleted because Table 3 included lots of confounds.
3. I think the result of multivariate regression analysis which described in line 246 should be presented by additional table.
4. In Statistical analysis and sample size calculation, the authors should present more detail on methods of multivariate regression analysis. That is, how they excluded the dependent factors from the selected factors and how they chose the best model among candidate models as final multivariate model.
5. In this study, questionnaire S1and S2 are very important. Questionnaire S1 include only two VAS on anxiety Q7, Q8. Questionnaire S2 include only one VAS on anxiety Q1. Authors used VAS for only anxiety scale. Other items were type of multiple-choice question. In case of multiple-choice question or Likert type question, they should validate them in order to detect the appropriate answers. Therefore, authors should give us the results of validation on these items.
Minor points
1) Line 74; “it is safe and severe complications are rare [1],”→Reference No.1 is too old. Please replace recent reference and recent information.
2) Line 78; “bronchoscopy is most commonly related to related to cough, dyspnea, chest pain or nausea” Is under lined part misprinted or not? Please correct the under lined part.
3) Line 99; Does “elective bronchoscopy” mean “only diagnostic bronchoscopy”? If this is correct it should be defined in the text at first use.
4) Line 108; Authors mentioned “The inclusion to the study was not limited by the type of the procedure”. Considering statistical view, I think they should balance the type of the procedure when they enrolled patients.
5) Line 129; Outcome points had two points. Which is primary endpoint? Which is secondary endpoint?
6) Line 136; “Importantly, the staff had not been informed which patients were included to the study.” Why had the staff not been informed? Please explain this is important.
7) Line 157 and 159; I think Table S3 and S4 are the clinical report form for bronchoscopists and attending physicians not questionnaire.
8) Line 182 to 193; Authors mentioned background characteristics in this part. Please provide the table of “background characteristics” in text or Supporting Information.
9) Line 200 to 204; “Rigid bronchoscopy was performed in 6 patients (4%)”. Therefore, it would better that authors should compare only between flexible (fiberoptic) bronchoscopy without EBUS and that without EBUS.
10) In Table 1 “Satisfaction with BS in VAS”; Please consider the significant digits. “0 – 4.375” means they measured the degree of tens μm.
11) Line 215 to 217 and 337; How many patients achieved the conscious sedation? Depth of anesthesia is very important to evaluation the satisfaction with BS. Please provide depth of sedation by use of sedation score.
12) Line 221; Authors defined VAS > 6/10 as “very unsatisfied”. However, in Table 3 and Figure 2, they defined VAS ≥ 5-10 as “unsatisfied”. I think there is discrepancy. Please explained it. Furthermore, how did they define these cutoff-value?
13) Line 223 and 238 to 240; Was “correlation between satisfaction and willingness for future bronchoscopy” basis for setting for sample size calculations? Or was “correlation between dissatisfaction with bronchoscopy and the level of anxiety before the procedure” basis for setting for sample size calculations? Or was “correlation between dissatisfaction with bronchoscopy and patients discomfort during the procedure” basis for setting for sample size calculations? Which of them were basis for setting for sample size calculations? Was it primary endpoint?
14) Line 371; “Secondly, the study group was rather small due to single-center study, inclusion criteria and short period of study, however the number of included patient was based on sample size calculation.” If authors set the main objective as sample size calculation, sample size of the study group would seem to be more appropriate size. Why did they use correlation analysis to detect weak (r=0.3) correlation?
Reviewer #2: The authors have done a good work in trying to identify the factors that affect patient satisfaction during bronchoscopy in their study titled "Evaluation of patients’ satisfaction with bronchoscopy procedure". The topic and contents have been appropriately dealt with but the authors need to do some minor revisions for the article to be more suitable. First of all, there are many grammatical errors in the text that needs to be corrected. Secondly, the authors in justifying the use of oral route for bronchoscopy, made a statement of the nasal route being causing more discomfort. This justification is not accurate and the authors should just limit their statement to oral route being their preference. Thank you
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #1: Yes: Yuichiro Takeda
Reviewer #2: Yes: Adamu Issaka
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Author response to Decision Letter 0
27 Oct 2021
We have applied the changes requested both by the editorial staff and the reviewers. We shared an updated cover letter covering the requested funding and COI information. We also shared a file with detailed responses to all of the reviewers' questions and remarks - see file Response to Reviewers.
Submitted filename: Response to Reviewers.docx
Decision Letter 1
PONE-D-21-03696R1Evaluation of patients’ satisfaction with bronchoscopy procedure.PLOS ONE
Dear Dr. Katarzyna Faber,
Please submit your revised manuscript by Dec 23 2021 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: https://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols . Additionally, PLOS ONE offers an option for publishing peer-reviewed Lab Protocol articles, which describe protocols hosted on protocols.io. Read more information on sharing protocols at https://plos.org/protocols?utm_medium=editorial-email&utm_source=authorletters&utm_campaign=protocols .
Yuichiro Takeda, M.D., Ph.D.
Academic Editor
Additional Editor Comments:
There are still some issues as below.
1, Primary outcome: The authors set “a relationship (correlation) between patients’ anxiety and satisfaction with bronchoscopy as the primary outcome. They based their sample size calculation on a study by Bujang MA and Baharum N and provided this article to references. In this provided reference, Bujang MA and Baharum N used Pearson coefficient for correlation analysis. Did they check null hypothesis is equal to zero in this study population? Even if null hypothesis is equal to zero, I wonder why they use Mann Whitney U test or Kruskal- Wallis test that are non-parametric test. Why did they delete Kruskal- Wallis test in Statistical analysis of revised manuscript?
2, Primary outcome: I guess the authors described the result of primary outcome in Line 274 of Manuscript - revised manuscript, clean version.
The authors should describe this study met the primary outcome in Results or Discussion part.
3, Author should describe how to perform the multivariate analysis in this study more detail in in Statistical analysis part. what parameters were they screening by univariate analyses, selection criteria of parameters, how to find independent parameters, how to select best model. Please describe this process in Statistical analysis part.
4. In revised manuscript, you mention only regression model in univariate and multivariate. There are lots of regression method. I think you should not delete “logistic”.
5. In general, univariate analyses are only the screening test for model construction. Table 3 should include multivariate model like below table. However, you should check statistical and clinical independency between “Anxiety before BS” and “Discomfort during what”.
Parameters Univariate Analyses Multivariate Analysis
Beta Standard error P-value Beta Standard error P-value
Anxiety before BS 0.306 0.086 0.0006 0.264 0.086, 0.003
Discomfort during ? 0.255 0.087 0.004 0.366, 0.087 0.00017
Age of patient 0.015 0.090 0.864 NI
Duration of BF 0.039 0.092 0.674 NI
Satisfaction with
information about the BF-0.096 0.090 0.288 NI
Not remembering BF -0.136 0.090 0.135 NI
Abbreviations: NI, not included in the best multivariate logistic regression model.
6. Table 4 is “Differences between satisfied and unsatisfied patients” Why did not authors check all parameters in table 4 by univariate analyses? I think authors should be screening all parameters in table 4. And then they construct some models for the multivariate models. After that, they choose best model and analyze this model as the result. How is it?
7. Although author added the limitation, it is serious issue that they did not validate questionnaires used in the study.
8. There are lots of reports that depth of anesthesia is very important to evaluation the satisfaction with BS. It is serious issue that they did not use sedation score during the study. At least, they should add this point to the study Limitations.
Submitted filename: Reviced paper_Commets and decision for author 20211106.docx
Author response to Decision Letter 1
23 Dec 2021
A file 'Response to Reviewers' has been sent to 'Attached Files'. Below I've copied the text from that file:
Warsaw, 22th December 2021
Dear Editor and Reviewers,
Thank you for reviewing our manuscript PONE-D-21-03696, titled Evaluation of patients’ satisfaction with bronchoscopy procedure. We appreciate Your comments which have certainly helped us improve the manuscript’s quality. The revised version of the manuscript re-submitted for reevaluation includes changes made strictly according to Your suggestions. We believe, all the points raised by the reviews were addressed. We would be grateful for re-considering our manuscript for publication.
Below, we include the specific responses to the Reviewers’ comments with the hope that they will find them adequate.
• Primary outcome: The authors set “a relationship (correlation) between patients’ anxiety and satisfaction with bronchoscopy as the primary outcome. They based their sample size calculation on a study by Bujang MA and Baharum N and provided this article to references. In this provided reference, Bujang MA and Baharum N used Pearson coefficient for correlation analysis. Did they check null hypothesis is equal to zero in this study population? Even if null hypothesis is equal to zero, I wonder why they use Mann Whitney U test or Kruskal- Wallis test that are non-parametric test.
Thank you for this comment and suggestion. The manuscript by Bujang MA and Baharum N is a sample size guideline for Pearson correlation coefficient. However, when estimating for sample size, we could not predict whether the assumption for Pearson correlation would be met or not. Thus, our sample size analysis was based on estimation by Bujang et al.
In our study neither the satisfaction from bronchoscopy (BS) nor anxiety before BS have a normal distribution of values (line 203). Thus we changed the correlation coefficient for Spearman (line 209 and 287, 288) and we used non- parametric tests.
• Why did they delete Kruskal- Wallis test in Statistical analysis of revised manuscript?
Thank you for this remark. As we had excluded patients who had BS under general anesthesia, we compared only two groups (satisfied vs unsatisfied; midazolam vs midazolam +fentanyl; VBS vs EBUS) using Mann-Whitney U test ( Table 1,2,4).
• Primary outcome: I guess the authors described the result of primary outcome in Line 274 of Manuscript - revised manuscript, clean version. The authors should describe this study met the primary outcome in Results or Discussion part.
Thank you for this valuable comment. We changed the text (line 285) to emphasized the primary outcome of the study.
• Author should describe how to perform the multivariate analysis in this study more detail in in Statistical analysis part. what parameters were they screening by univariate analyses, selection criteria of parameters, how to find independent parameters, how to select best model. Please describe this process in Statistical analysis part.
Thank you for this comment. We screened all parameters from the table 4 (that were expressed in interval scale) in univariate analysis. Then we build multivariate linear regression model with backward stepwise analysis with all parameters and choose the model with optimal adjusted R square value (line 215-217).
• In revised manuscript, you mention only regression model in univariate and multivariate. There are lots of regression method. I think you should not delete “logistic”.
Thank you for this issue. We corrected the description of statistical methods for multivariate linear regression analysis (line 215-217).
• In general, univariate analyses are only the screening test for model construction. Table 3 should include multivariate model like below table.
Anxiety before BS 0.306 0.086 0.0006 0.264 0.086 0.003
Discomfort during procedure 0.255 0.087 0.004 0.205 0.086 0.018
information about the BF -0.096 0.090 0.288 NI
Thank you for your comment and suggestion, which is very helpful. We changed Table 3 according to your proposal.
• However, you should check statistical and clinical independency between “Anxiety before BS” and “Discomfort during procedure”.
We found very low non-significant correlation between anxiety prior to BS and discomfort during the procedure (r=0.173, p=0.055), so we used both factors in model of multivariate regression analysis.
• Table 4 is “Differences between satisfied and unsatisfied patients” Why did not authors check all parameters in table 4 by univariate analyses? I think authors should be screening all parameters in table 4. And then they construct some models for the multivariate models. After that, they choose best model and analyze this model as the result. How is it?
Thank you for your suggestion. We screened all parameters with univariate analysis finding only two significant parameters (anxiety before BS and discomfort during procedure), which were selected for multivariate logistic regression analysis.
• Although author added the limitation, it is serious issue that they did not validate questionnaires used in the study.
Thank you for your comment. Indeed, it is an important issue. We emphasized it in limitation of the study (line 489)
• . There are lots of reports that depth of anesthesia is very important to evaluation the satisfaction with BS. It is serious issue that they did not use sedation score during the study. At least, they should add this point to the study Limitations.
Thank you for your important remark. We added it to limitations of the study (line 490-491)
Submitted filename: Response to Reviewers - second review.docx
Decision Letter 2
26 Dec 2021
PONE-D-21-03696R2Evaluation of patients’ satisfaction with bronchoscopy procedure.PLOS ONE
Please submit your revised manuscript by February 25, 2022. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please review your reference list to ensure that it is complete and correct. If you have cited papers that have been retracted, please include the rationale for doing so in the manuscript text, or remove these references and replace them with relevant current references. Any changes to the reference list should be mentioned in the rebuttal letter that accompanies your revised manuscript. If you need to cite a retracted article, indicate the article’s retracted status in the References list and also include a citation and full reference for the retraction notice.
I think your manuscript improved now.
1) “In our study neither the satisfaction from bronchoscopy (BS) nor anxiety before BS have a normal distribution of values (line 203). Thus we changed the correlation coefficient for Spearman (line 209 and 287, 288) and we used non-parametric tests.”
Does this mean sample size calculation was incorrect in your study? You should include this information as a limitation. This is very important.
2) “The primary outcome of the study was a week positive correlation between dissatisfaction with bronchoscopy and the level of anxiety before the procedure (Spearman coefficient r=0.276, p=0.0014) or patients’ discomfort during the procedure (r=0.309, p=0.0005)” Although the correlation between dissatisfaction with bronchoscopy and the level of anxiety before the procedure was statistically significant, coefficient rho was 0.276 that was below 0.3. On the other hand, the correlation between dissatisfaction with bronchoscopy and patients’ discomfort during the procedure was statistically significant and its coefficient rho was 0.309 that was beyond 0.3. Is the latter the only one that met the main outcome? You should explain this result in the discussion part.
3) I think the coefficient is generally rho (ρ) in the Spearman rank test.
4) Although PLOS one is an open-access journal, the discussion part is slightly long. Can you summarize it?
5) I have a comment for your future study. There is a book that explained how to use Multivariable Analysis: A Practical Guide for Clinicians and Public Health Researchers Second edition by Mitchell H. Katz. He said as below: Whenever possible, "do not use variable selection technique." This is because there is a danger that any variable selection method will select confounders into the model and remove variables that are causally related to the outcome. Also, in both the forward and the backward selection, each variable is evaluated individually, so there is a possibility that two variables that start out as a set and have an important effect on the outcome will not be selected as a set in the final model. There is also the possibility that a variable that is very important in explaining the outcome may not be selected for the model because it is related to a variable that has already been adopted in the model. My opinion is the same as above.
6) This manuscript still has some grammatical errors in the text that needs to be corrected. Please check English in the text carefully.
Author response to Decision Letter 2
15 Feb 2022
Warsaw, 15th February 2022
Thank you for reviewing our manuscript PONE-D-21-03696, titled Evaluation of patients’ satisfaction with bronchoscopy procedure once again. We truly appreciate Your comments which have helped us improve the manuscript’s quality. We believe that all the points raised by the reviewer were addressed. We would be grateful for re-considering our manuscript for publication.
Thank you for this remark. We added this information in limitations of the study (line 201-223).
Thank you for your suggestion. We emphasized that correlations were weak, but according to your suggestion we drew more attention to the correlation between dissatisfaction and discomfort (line 406-407). We tried to discuss the significance of discomfort as a factor influencing patients satisfaction with bronchoscopy in detail (line 400-421).
Thank you for this remark. We corrected it for rho (line 286-287).
Thank you for this hint. We tried to shorten the discussion.
Thank you for this remark. We appreciate all comments and suggestion concerning the statistical analysis. We will certainly read this book and use this knowledge in future studies.
Thank you for this suggestion. We checked and corrected the manuscript.
Submitted filename: Response to Reviewers.February 2022.docx
Decision Letter 3
21 Feb 2022
PONE-D-21-03696R3Evaluation of patients’ satisfaction with bronchoscopy procedure.PLOS ONE
Dear Dr. Katarzyna,
Please submit your revised manuscript by April 7, 2022. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers.'
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes.'
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript.'
Additional Editor Comments (if provided):
Still, a few issues were raised in your manuscript.
#1; In Manuscript – revised version. February 2022.
Line 260 to 262; “There was a positive correlation between satisfaction and willingness for future bronchoscopy (r=0.487, p<0.0001)”.
I wonder if this “r” is Spearman coefficient rho or not. Please correct or explain it.
#2; And you also need clear and correct Figures and Tables without any misprints (“diabetes; diabetes mellitus,” “arhytmia; arrhythmia,” “asthma; bronchial asthma” in Supplementary Figure 2 and so on) or any additional linear (Q1 in S2 table and so on) to publish. Therefore, you should check all figures and tables and supplementary tables and figures again.
#3; According to Submission Guidelines, manuscripts must be submitted in English. Your supporting information included the Polish version of the S1 Table to S4 Table. Therefore, you should delete them.
Author response to Decision Letter 3
21 Mar 2022
Thank you for reviewing our manuscript PONE-D-21-03696, titled Evaluation of patients’ satisfaction with bronchoscopy procedure once again. We are grateful for Your comments and suggestions which have helped us improve the manuscript’s quality. We hope that all the points raised by the reviewer were addressed. We would be grateful for re-considering our manuscript for publication.
Below, we included the specific responses to the Reviewers’ comments with the hope that they will find them adequate.
Thank you for this apt remark. In line 260-262 Pearson correlation r=0.487, p< 0.0001 was given, but as distribution of data were not normal, we changed it for Spearman correlation rho= 0.404, p<0.0001 (p=0.000003).
Thank you for a thorough review. We have revised the supplementary files and tabels and provided the required changes.
Thank you for this remark. Files in Polish have been deleted.
Thank you for those suggestions.
Yours sincerely
Marta Dąbrowska
Submitted filename: Response to Reviewers.March 2022.docx
Decision Letter 4
28 Aug 2022
PONE-D-21-03696R4
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
Guest Editor
Additional Editor Comments (optional):
Through several revisions, I think your manuscript has improved.
ACADEMIC EDITOR:
congratulations to the authors and thanks to the reviewers for the suggestions provided which really helped improve the quality of the manuscript
Silvia Fiorelli
Acceptance letter
19 Sep 2022
Dear Dr. Faber:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
If we can help with anything else, please email us at gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Silvia Fiorelli

IMAGES
VIDEO
COMMENTS
Throughout these 12 articles on the topic of research, more than half linked with E-BUS. This reflects a high research interest in this technology in the 2000s. ... We also took note of the progress of bronchoscopy-related research in recent years. Some researchers pointed out that bronchoscopic lung volume reduction using an endobronchial ...
The top 100 most cited articles about bronchoscopy were selected for degree centrality analysis and analyses regarding publication time, total citation number, the citation density, time-related flux, first author, published journal, geographic origin, and research theme. The selected articles were published mainly in the 2000s and 1990s.
The top 100 most cited articles about bronchoscopy were selected for degree centrality analysis and analyses regarding publication time, total citation number, the citation density, time-related flux, first author, published journal, geographic origin, and research theme. Results: The selected articles were published mainly in the 2000s and 1990s.
Lung cancer is the leading cause of cancer-related deaths worldwide with an overall 5-year survival rate of 17% after diagnoses. Indeed many patients tend to have a very poor prognosis, due to being diagnosed at an advanced stage. Conversely patients who are diagnosed at an early stage have a 5-year survival >70%, indicating that early ...
Bronchoscopy has evolved over the past few decades and has been used by respiratory physicians to diagnose various airway and lung diseases. With the popularization of medical check-ups and growing interest in health, early diagnosis of lung diseases is essential. With the development of endobronchial ultrasound, ultrathin bronchoscopy, and ...
Aging, abnormal findings in the bronchial lumen, lung cancer, central location of the tumor, and current smoking have been reported as risk factors for post-bronchoscopy pneumonia, but the reports ...
During flexible fiberoptic bronchoscopy (FOB) the arterial partial pressure of oxygen can drop, increasing the risk for respiratory failure. To avoid desaturation episodes during the procedure several oxygenation strategies have been proposed, including conventional oxygen therapy (COT), high flow nasal cannula (HFNC), continuous positive airway pressure (CPAP) and non-invasive ventilation (NIV).
Bronchoscopy is a diagnostic and therapeutic procedure that directly visualizes the normal and pathological structures of the upper and lower respiratory tracts. Bronchoscope allows seeing the tracheobronchial tree and taking samples from the airways of the lung parenchyma for histopathological diagnosis [1]. Bronchoscopy is the most frequently ...
Bronchoscopy is a fundamental tool in the armamentarium of the intensivist.1 Single-use and reusable flexible bronchoscopes are readily available in the United States, and the learning curve is steep for most of the common procedures encountered in the ICU.2,3 Bronchoscopy is useful in the diagnosis and management of acute respiratory failure. It can be rapidly implemented at any time, at the ...
A bronchoscopy is an essential tool for clinicians and health care providers treating patients with lung diseases. Since its introduction to clinical practice by Shigeto Ikeda in 1966, flexible bronchoscopy has become an essential tool in diagnosis and management of patients with lung diseases. Rigid bronchoscopy can be particularly helpful in ...
Flexible bronchoscopy plays a critical role in both diagnostic and therapeutic management of a variety of pulmonary disorders in the bronchoscopy suite and the intensive care unit. In the set-ting of the ongoing viral pandemic, single-use flexible bronchoscopes (SUFB) have garnered attention as various professional pulmonary societies have released guidelines regarding uses for SUFB given the ...
To identify bronchoscopy-related complications and discomfort, meaningful complication rates, and predictors. Method. ... (EBUS), and interventional ultrasound, which should be topics of separate, future reviews. Although bronchoscopy appeared to be a safe procedure in terms of mortality, bleeding, and pneumothoraces, it was difficult to ...
Purpose of Review Bronchoscopy-related infection is recognized as a leading healthcare hazard, and this review delves into its incidence, causes, and prevention. Recent Findings Due to both the recognition of the scale of bronchoscopy-related infection and the COVID-19 pandemic, single-use or disposable bronchoscopy (SUFB) technology has progressed beyond the ICU setting to the bronchoscopy ...
Flexible bronchoscopy (FB) is commonly performed by respiratory physicians for diagnostic as well as therapeutic purposes. However, bronchoscopy practices vary widely across India and worldwide.
Journal of Bronchology & Interventional Pulmonology is the leading source of information on the latest advances and innovations in bronchoscopy and related procedures. It covers topics such as electromagnetic navigation bronchoscopy, transbronchial cryobiopsy, lung cancer diagnosis and treatment, and more. Read the current issue and access the archives online.
The observed increase in exacerbations during the treatment period is thought to be related to bronchoscopy and anesthesia as it was also observed in the sham bronchoscopy group . This transient increased risk may be mitigated by administering a short course of OCS in the peri-procedural period. Long-term safety data was reported in a 5-year ...
Topics covered in the guideline include: Setting up of a bronchoscopy unit; Indications, complications, and contraindications of flexible bronchoscopy ... and space for storing bronchoscopy-related equipment, resuscitation cart, and drugs. Recommendation. A bronchoscopy suite should have dedicated areas for patient preparation, performance of ...
With the option of a rigid (as pictured in Figure 1) or flexible bronchoscope and advancements in specific and precise tools, the science of bronchoscopy has evolved greatly. Tools include cold, heat, balloons, valves, and stents. Bronchoscopy is used in cancer, interstitial lung disease, vascular disease, foreign body removal, and chronic ...
Background With the recent widespread use of endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), there have been occasional reports on complications associated with its use.
review. 1887/2558 patients underwent bronchoscopy for treatment of severe or critical COVID-19 pneumonia. therapeutic bronchoscopy was performed in 1241/1887 (65.8%) patients and interventional bronchoscopy was performed in 831/1887 (44.03%) patients. Overall, complications observed in 200/1887 (10.5%) patients.
Flexible bronchoscopy is a commonly used method for the diagnosis and treatment of chest diseases. However, there have been few reports regarding bronchoscopic findings in non-CF-related chronic lung diseases that cause BE. In a previous study, Chang et al. 4 classified the bronchoscopic findings of 28 patients with non-CF BE into 5 different ...
forms interface. The survey included various questions related to demographics, sedation, analgesia and anesthesia, technical aspects, and infection control related to the procedure of EBUS-TBNA. Results: Data from 134 respondents (mean age: 42.2 years) were analyzed. Most (97.8%) were pulmonologists or physicians, and a majority (94.8%) practicing in either a private multi-specialty setting ...
Introduction. Bronchoscopy (BS) is a common medical procedure used to diagnose or treat patients with a variety of respiratory diseases. Although it is considered safe and severe complications are rare [], BS may be associated with significant distress and anxiety among patients [2-4].Anxiety causes increased cortisol levels, blood pressure, heart rate and respiration rate [5, 6], which ...