Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Creswell, J. W. (2014). Research Design: Qualitative, Quantitative and Mixed Methods Approaches (4th ed.). Thousand Oaks, CA: Sage

The book Research Design: Qualitative, Quantitative and Mixed Methods Approaches by Creswell (2014) covers three approaches-qualitative, quantitative and mixed methods. This educational book is informative and illustrative and is equally beneficial for students, teachers and researchers. Readers should have basic knowledge of research for better understanding of this book. There are two parts of the book. Part 1 (chapter 1-4) consists of steps for developing research proposal and part II (chapter 5-10) explains how to develop a research proposal or write a research report. A summary is given at the end of every chapter that helps the reader to recapitulate the ideas. Moreover, writing exercises and suggested readings at the end of every chapter are useful for the readers. Chapter 1 opens with-definition of research approaches and the author gives his opinion that selection of a research approach is based on the nature of the research problem, researchers' experience and the audience of the study. The author defines qualitative, quantitative and mixed methods research. A distinction is made between quantitative and qualitative research approaches. The author believes that interest in qualitative research increased in the latter half of the 20th century. The worldviews, Fraenkel, Wallen and Hyun (2012) and Onwuegbuzie and Leech (2005) call them paradigms, have been explained. Sometimes, the use of language becomes too philosophical and technical. This is probably because the author had to explain some technical terms.
Related Papers
Daniel Ortiz
Research Design: Qualitative, Quantitative and Mixed Methods
Esra Öztürk Çalık
Conducting a well-established research requires deep knowledge about the research designs. Doing research can be likened to jumping into the sea which may transform into a huge ocean if the researcher is not experienced. As a PhD candidate and a novice researcher, I believe that the book "Research Design: Qualitative, Quantitative and Mixed Methods Approaches" by J.W. Creswell is a true reference guide for novice researchers since it is the most comprehensive and informative source with its reader-friendly structure.
International Journal of Social Sciences Interdisciplinary Research
Prashant Astalin
rhoda taller
Yan-yi Chang
John W. Creswell was previously a professor in educational psychology in the University of Nebraska–Lincoln. He moved to the University of Michigan in 2015 as a professor in the Department of Family Medicine. He has published many articles and close to 27 books on mixed methods. Professor Creswell is also one of the founding members of the Journal of Mixed Methods Research. He was a Fulbright scholar in South Africa in 2008 and Thailand in 2012. In 2011, he served as a visiting professor in the School of Public Health of Harvard University. In 2014, he became the Chairman of the Mixed Methods International Research Association. Professor Creswell has a personal website called “Mixed Methods Research” at http://johnwcreswell.com/. The site contains the information about his background, his own blog, consulting works and published books. He also posted replies questions from academic researchers and practitioners in the blog.
kassu sileyew
There are a number of approaches used in this research method design. The purpose of this chapter is to design the methodology of the research approach through mixed types of research techniques. The research approach also supports the researcher on how to come across the research result findings. In this chapter, the general design of the research and the methods used for data collection are explained in detail. It includes three main parts. The first part gives a highlight about the dissertation design. The second part discusses about qualitative and quantitative data collection methods. The last part illustrates the general research framework. The purpose of this section is to indicate how the research was conducted throughout the study periods.
Chisomo Mgunda
Gloria Thakane Leutle
Richard Baskas, Ed.D. Candidate
RELATED PAPERS
FUAFUNG Johnson YENWOLUA
Rabaska: Revue d'ethnologie de l'Amérique française
Philippe DUBÉ
Pragmatics & Beyond New Series
Ana I. Moreno
The Journal of medical research
HARUN CERİT
International Journal of Molecular Sciences
Claudio Tana
Hassan Azhdari Zarmehri
David Nichols
Manuel Chacón Mateos
Agricultural and Forest Entomology
Sara Montemayor
Vladimir Ivanovici
사당로미로미〚DALPØCHA4닷NET〛사당오피ꗓ사당오피
maine100 pegoku
International Journal of Pathogen Research
Raghad Onsa
Facial Plastic Surgery
burak erden
International Journal of Environmental Research and Public Health
Surasak Chaiyasong
Shahina Nagoo
Muh furkan Ramadhan
Jose Luis Mancilla-Aguilar
Scientific reports
Neuza Domingues
Andrés S . Antón Rivas
2001 Annual Conference Proceedings
Chinese Science Bulletin
Zuosheng Yang
Rivista di Diritto Romano
Pierangelo Buongiorno
IOSR Journal of Humanities and Social Science
FLORA MARWANGA
Turkish Journal of Plastic Surgery / Türk Plastik, Rekonstrüktif ve Estetik Cerrahi Dergisi
Ozlem Gundeslioglu
Prof. Dr. Masood Sadiq
See More Documents Like This
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- Types of Research Designs Compared | Guide & Examples
Types of Research Designs Compared | Guide & Examples
Published on June 20, 2019 by Shona McCombes . Revised on June 22, 2023.
When you start planning a research project, developing research questions and creating a research design , you will have to make various decisions about the type of research you want to do.
There are many ways to categorize different types of research. The words you use to describe your research depend on your discipline and field. In general, though, the form your research design takes will be shaped by:
- The type of knowledge you aim to produce
- The type of data you will collect and analyze
- The sampling methods , timescale and location of the research
This article takes a look at some common distinctions made between different types of research and outlines the key differences between them.
Table of contents
Types of research aims, types of research data, types of sampling, timescale, and location, other interesting articles.
The first thing to consider is what kind of knowledge your research aims to contribute.
Prevent plagiarism. Run a free check.
The next thing to consider is what type of data you will collect. Each kind of data is associated with a range of specific research methods and procedures.
Finally, you have to consider three closely related questions: how will you select the subjects or participants of the research? When and how often will you collect data from your subjects? And where will the research take place?
Keep in mind that the methods that you choose bring with them different risk factors and types of research bias . Biases aren’t completely avoidable, but can heavily impact the validity and reliability of your findings if left unchecked.
Choosing between all these different research types is part of the process of creating your research design , which determines exactly how your research will be conducted. But the type of research is only the first step: next, you have to make more concrete decisions about your research methods and the details of the study.
Read more about creating a research design
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Normal distribution
- Degrees of freedom
- Null hypothesis
- Discourse analysis
- Control groups
- Mixed methods research
- Non-probability sampling
- Quantitative research
- Ecological validity
Research bias
- Rosenthal effect
- Implicit bias
- Cognitive bias
- Selection bias
- Negativity bias
- Status quo bias
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
McCombes, S. (2023, June 22). Types of Research Designs Compared | Guide & Examples. Scribbr. Retrieved April 9, 2024, from https://www.scribbr.com/methodology/types-of-research/
Is this article helpful?
Shona McCombes
Other students also liked, what is a research design | types, guide & examples, qualitative vs. quantitative research | differences, examples & methods, what is a research methodology | steps & tips, what is your plagiarism score.
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Methodology
- Descriptive Research Design | Definition, Methods & Examples
Descriptive Research Design | Definition, Methods & Examples
Published on 5 May 2022 by Shona McCombes . Revised on 10 October 2022.
Descriptive research aims to accurately and systematically describe a population, situation or phenomenon. It can answer what , where , when , and how questions , but not why questions.
A descriptive research design can use a wide variety of research methods to investigate one or more variables . Unlike in experimental research , the researcher does not control or manipulate any of the variables, but only observes and measures them.
Table of contents
When to use a descriptive research design, descriptive research methods.
Descriptive research is an appropriate choice when the research aim is to identify characteristics, frequencies, trends, and categories.
It is useful when not much is known yet about the topic or problem. Before you can research why something happens, you need to understand how, when, and where it happens.
- How has the London housing market changed over the past 20 years?
- Do customers of company X prefer product Y or product Z?
- What are the main genetic, behavioural, and morphological differences between European wildcats and domestic cats?
- What are the most popular online news sources among under-18s?
- How prevalent is disease A in population B?
Prevent plagiarism, run a free check.
Descriptive research is usually defined as a type of quantitative research , though qualitative research can also be used for descriptive purposes. The research design should be carefully developed to ensure that the results are valid and reliable .
Survey research allows you to gather large volumes of data that can be analysed for frequencies, averages, and patterns. Common uses of surveys include:
- Describing the demographics of a country or region
- Gauging public opinion on political and social topics
- Evaluating satisfaction with a company’s products or an organisation’s services
Observations
Observations allow you to gather data on behaviours and phenomena without having to rely on the honesty and accuracy of respondents. This method is often used by psychological, social, and market researchers to understand how people act in real-life situations.
Observation of physical entities and phenomena is also an important part of research in the natural sciences. Before you can develop testable hypotheses , models, or theories, it’s necessary to observe and systematically describe the subject under investigation.
Case studies
A case study can be used to describe the characteristics of a specific subject (such as a person, group, event, or organisation). Instead of gathering a large volume of data to identify patterns across time or location, case studies gather detailed data to identify the characteristics of a narrowly defined subject.
Rather than aiming to describe generalisable facts, case studies often focus on unusual or interesting cases that challenge assumptions, add complexity, or reveal something new about a research problem .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
McCombes, S. (2022, October 10). Descriptive Research Design | Definition, Methods & Examples. Scribbr. Retrieved 8 April 2024, from https://www.scribbr.co.uk/research-methods/descriptive-research-design/
Is this article helpful?
Shona McCombes
Other students also liked, a quick guide to experimental design | 5 steps & examples, correlational research | guide, design & examples, qualitative vs quantitative research | examples & methods.
- Privacy Policy
Buy Me a Coffee

Home » Descriptive Research Design – Types, Methods and Examples
Descriptive Research Design – Types, Methods and Examples
Table of Contents

Descriptive Research Design
Definition:
Descriptive research design is a type of research methodology that aims to describe or document the characteristics, behaviors, attitudes, opinions, or perceptions of a group or population being studied.
Descriptive research design does not attempt to establish cause-and-effect relationships between variables or make predictions about future outcomes. Instead, it focuses on providing a detailed and accurate representation of the data collected, which can be useful for generating hypotheses, exploring trends, and identifying patterns in the data.
Types of Descriptive Research Design
Types of Descriptive Research Design are as follows:
Cross-sectional Study
This involves collecting data at a single point in time from a sample or population to describe their characteristics or behaviors. For example, a researcher may conduct a cross-sectional study to investigate the prevalence of certain health conditions among a population, or to describe the attitudes and beliefs of a particular group.
Longitudinal Study
This involves collecting data over an extended period of time, often through repeated observations or surveys of the same group or population. Longitudinal studies can be used to track changes in attitudes, behaviors, or outcomes over time, or to investigate the effects of interventions or treatments.
This involves an in-depth examination of a single individual, group, or situation to gain a detailed understanding of its characteristics or dynamics. Case studies are often used in psychology, sociology, and business to explore complex phenomena or to generate hypotheses for further research.
Survey Research
This involves collecting data from a sample or population through standardized questionnaires or interviews. Surveys can be used to describe attitudes, opinions, behaviors, or demographic characteristics of a group, and can be conducted in person, by phone, or online.
Observational Research
This involves observing and documenting the behavior or interactions of individuals or groups in a natural or controlled setting. Observational studies can be used to describe social, cultural, or environmental phenomena, or to investigate the effects of interventions or treatments.
Correlational Research
This involves examining the relationships between two or more variables to describe their patterns or associations. Correlational studies can be used to identify potential causal relationships or to explore the strength and direction of relationships between variables.
Data Analysis Methods
Descriptive research design data analysis methods depend on the type of data collected and the research question being addressed. Here are some common methods of data analysis for descriptive research:
Descriptive Statistics
This method involves analyzing data to summarize and describe the key features of a sample or population. Descriptive statistics can include measures of central tendency (e.g., mean, median, mode) and measures of variability (e.g., range, standard deviation).
Cross-tabulation
This method involves analyzing data by creating a table that shows the frequency of two or more variables together. Cross-tabulation can help identify patterns or relationships between variables.
Content Analysis
This method involves analyzing qualitative data (e.g., text, images, audio) to identify themes, patterns, or trends. Content analysis can be used to describe the characteristics of a sample or population, or to identify factors that influence attitudes or behaviors.
Qualitative Coding
This method involves analyzing qualitative data by assigning codes to segments of data based on their meaning or content. Qualitative coding can be used to identify common themes, patterns, or categories within the data.
Visualization
This method involves creating graphs or charts to represent data visually. Visualization can help identify patterns or relationships between variables and make it easier to communicate findings to others.
Comparative Analysis
This method involves comparing data across different groups or time periods to identify similarities and differences. Comparative analysis can help describe changes in attitudes or behaviors over time or differences between subgroups within a population.
Applications of Descriptive Research Design
Descriptive research design has numerous applications in various fields. Some of the common applications of descriptive research design are:
- Market research: Descriptive research design is widely used in market research to understand consumer preferences, behavior, and attitudes. This helps companies to develop new products and services, improve marketing strategies, and increase customer satisfaction.
- Health research: Descriptive research design is used in health research to describe the prevalence and distribution of a disease or health condition in a population. This helps healthcare providers to develop prevention and treatment strategies.
- Educational research: Descriptive research design is used in educational research to describe the performance of students, schools, or educational programs. This helps educators to improve teaching methods and develop effective educational programs.
- Social science research: Descriptive research design is used in social science research to describe social phenomena such as cultural norms, values, and beliefs. This helps researchers to understand social behavior and develop effective policies.
- Public opinion research: Descriptive research design is used in public opinion research to understand the opinions and attitudes of the general public on various issues. This helps policymakers to develop effective policies that are aligned with public opinion.
- Environmental research: Descriptive research design is used in environmental research to describe the environmental conditions of a particular region or ecosystem. This helps policymakers and environmentalists to develop effective conservation and preservation strategies.
Descriptive Research Design Examples
Here are some real-time examples of descriptive research designs:
- A restaurant chain wants to understand the demographics and attitudes of its customers. They conduct a survey asking customers about their age, gender, income, frequency of visits, favorite menu items, and overall satisfaction. The survey data is analyzed using descriptive statistics and cross-tabulation to describe the characteristics of their customer base.
- A medical researcher wants to describe the prevalence and risk factors of a particular disease in a population. They conduct a cross-sectional study in which they collect data from a sample of individuals using a standardized questionnaire. The data is analyzed using descriptive statistics and cross-tabulation to identify patterns in the prevalence and risk factors of the disease.
- An education researcher wants to describe the learning outcomes of students in a particular school district. They collect test scores from a representative sample of students in the district and use descriptive statistics to calculate the mean, median, and standard deviation of the scores. They also create visualizations such as histograms and box plots to show the distribution of scores.
- A marketing team wants to understand the attitudes and behaviors of consumers towards a new product. They conduct a series of focus groups and use qualitative coding to identify common themes and patterns in the data. They also create visualizations such as word clouds to show the most frequently mentioned topics.
- An environmental scientist wants to describe the biodiversity of a particular ecosystem. They conduct an observational study in which they collect data on the species and abundance of plants and animals in the ecosystem. The data is analyzed using descriptive statistics to describe the diversity and richness of the ecosystem.
How to Conduct Descriptive Research Design
To conduct a descriptive research design, you can follow these general steps:
- Define your research question: Clearly define the research question or problem that you want to address. Your research question should be specific and focused to guide your data collection and analysis.
- Choose your research method: Select the most appropriate research method for your research question. As discussed earlier, common research methods for descriptive research include surveys, case studies, observational studies, cross-sectional studies, and longitudinal studies.
- Design your study: Plan the details of your study, including the sampling strategy, data collection methods, and data analysis plan. Determine the sample size and sampling method, decide on the data collection tools (such as questionnaires, interviews, or observations), and outline your data analysis plan.
- Collect data: Collect data from your sample or population using the data collection tools you have chosen. Ensure that you follow ethical guidelines for research and obtain informed consent from participants.
- Analyze data: Use appropriate statistical or qualitative analysis methods to analyze your data. As discussed earlier, common data analysis methods for descriptive research include descriptive statistics, cross-tabulation, content analysis, qualitative coding, visualization, and comparative analysis.
- I nterpret results: Interpret your findings in light of your research question and objectives. Identify patterns, trends, and relationships in the data, and describe the characteristics of your sample or population.
- Draw conclusions and report results: Draw conclusions based on your analysis and interpretation of the data. Report your results in a clear and concise manner, using appropriate tables, graphs, or figures to present your findings. Ensure that your report follows accepted research standards and guidelines.
When to Use Descriptive Research Design
Descriptive research design is used in situations where the researcher wants to describe a population or phenomenon in detail. It is used to gather information about the current status or condition of a group or phenomenon without making any causal inferences. Descriptive research design is useful in the following situations:
- Exploratory research: Descriptive research design is often used in exploratory research to gain an initial understanding of a phenomenon or population.
- Identifying trends: Descriptive research design can be used to identify trends or patterns in a population, such as changes in consumer behavior or attitudes over time.
- Market research: Descriptive research design is commonly used in market research to understand consumer preferences, behavior, and attitudes.
- Health research: Descriptive research design is useful in health research to describe the prevalence and distribution of a disease or health condition in a population.
- Social science research: Descriptive research design is used in social science research to describe social phenomena such as cultural norms, values, and beliefs.
- Educational research: Descriptive research design is used in educational research to describe the performance of students, schools, or educational programs.
Purpose of Descriptive Research Design
The main purpose of descriptive research design is to describe and measure the characteristics of a population or phenomenon in a systematic and objective manner. It involves collecting data that describe the current status or condition of the population or phenomenon of interest, without manipulating or altering any variables.
The purpose of descriptive research design can be summarized as follows:
- To provide an accurate description of a population or phenomenon: Descriptive research design aims to provide a comprehensive and accurate description of a population or phenomenon of interest. This can help researchers to develop a better understanding of the characteristics of the population or phenomenon.
- To identify trends and patterns: Descriptive research design can help researchers to identify trends and patterns in the data, such as changes in behavior or attitudes over time. This can be useful for making predictions and developing strategies.
- To generate hypotheses: Descriptive research design can be used to generate hypotheses or research questions that can be tested in future studies. For example, if a descriptive study finds a correlation between two variables, this could lead to the development of a hypothesis about the causal relationship between the variables.
- To establish a baseline: Descriptive research design can establish a baseline or starting point for future research. This can be useful for comparing data from different time periods or populations.
Characteristics of Descriptive Research Design
Descriptive research design has several key characteristics that distinguish it from other research designs. Some of the main characteristics of descriptive research design are:
- Objective : Descriptive research design is objective in nature, which means that it focuses on collecting factual and accurate data without any personal bias. The researcher aims to report the data objectively without any personal interpretation.
- Non-experimental: Descriptive research design is non-experimental, which means that the researcher does not manipulate any variables. The researcher simply observes and records the behavior or characteristics of the population or phenomenon of interest.
- Quantitative : Descriptive research design is quantitative in nature, which means that it involves collecting numerical data that can be analyzed using statistical techniques. This helps to provide a more precise and accurate description of the population or phenomenon.
- Cross-sectional: Descriptive research design is often cross-sectional, which means that the data is collected at a single point in time. This can be useful for understanding the current state of the population or phenomenon, but it may not provide information about changes over time.
- Large sample size: Descriptive research design typically involves a large sample size, which helps to ensure that the data is representative of the population of interest. A large sample size also helps to increase the reliability and validity of the data.
- Systematic and structured: Descriptive research design involves a systematic and structured approach to data collection, which helps to ensure that the data is accurate and reliable. This involves using standardized procedures for data collection, such as surveys, questionnaires, or observation checklists.
Advantages of Descriptive Research Design
Descriptive research design has several advantages that make it a popular choice for researchers. Some of the main advantages of descriptive research design are:
- Provides an accurate description: Descriptive research design is focused on accurately describing the characteristics of a population or phenomenon. This can help researchers to develop a better understanding of the subject of interest.
- Easy to conduct: Descriptive research design is relatively easy to conduct and requires minimal resources compared to other research designs. It can be conducted quickly and efficiently, and data can be collected through surveys, questionnaires, or observations.
- Useful for generating hypotheses: Descriptive research design can be used to generate hypotheses or research questions that can be tested in future studies. For example, if a descriptive study finds a correlation between two variables, this could lead to the development of a hypothesis about the causal relationship between the variables.
- Large sample size : Descriptive research design typically involves a large sample size, which helps to ensure that the data is representative of the population of interest. A large sample size also helps to increase the reliability and validity of the data.
- Can be used to monitor changes : Descriptive research design can be used to monitor changes over time in a population or phenomenon. This can be useful for identifying trends and patterns, and for making predictions about future behavior or attitudes.
- Can be used in a variety of fields : Descriptive research design can be used in a variety of fields, including social sciences, healthcare, business, and education.
Limitation of Descriptive Research Design
Descriptive research design also has some limitations that researchers should consider before using this design. Some of the main limitations of descriptive research design are:
- Cannot establish cause and effect: Descriptive research design cannot establish cause and effect relationships between variables. It only provides a description of the characteristics of the population or phenomenon of interest.
- Limited generalizability: The results of a descriptive study may not be generalizable to other populations or situations. This is because descriptive research design often involves a specific sample or situation, which may not be representative of the broader population.
- Potential for bias: Descriptive research design can be subject to bias, particularly if the researcher is not objective in their data collection or interpretation. This can lead to inaccurate or incomplete descriptions of the population or phenomenon of interest.
- Limited depth: Descriptive research design may provide a superficial description of the population or phenomenon of interest. It does not delve into the underlying causes or mechanisms behind the observed behavior or characteristics.
- Limited utility for theory development: Descriptive research design may not be useful for developing theories about the relationship between variables. It only provides a description of the variables themselves.
- Relies on self-report data: Descriptive research design often relies on self-report data, such as surveys or questionnaires. This type of data may be subject to biases, such as social desirability bias or recall bias.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

Questionnaire – Definition, Types, and Examples

Case Study – Methods, Examples and Guide

Observational Research – Methods and Guide

Quantitative Research – Methods, Types and...

Qualitative Research Methods

Explanatory Research – Types, Methods, Guide
- Open access
- Published: 02 April 2024
Towards universal health coverage in Vietnam: a mixed-method case study of enrolling people with tuberculosis into social health insurance
- Rachel Forse ORCID: orcid.org/0000-0002-0716-3342 1 , 2 ,
- Clara Akie Yoshino 2 ,
- Thanh Thi Nguyen 1 ,
- Thi Hoang Yen Phan 3 ,
- Luan N. Q. Vo 1 , 2 ,
- Andrew J. Codlin 1 , 2 ,
- Lan Nguyen 4 ,
- Chi Hoang 4 ,
- Lopa Basu 5 ,
- Minh Pham 5 ,
- Hoa Binh Nguyen 6 ,
- Luong Van Dinh 6 ,
- Maxine Caws 7 , 8 ,
- Tom Wingfield 2 , 7 ,
- Knut Lönnroth 2 &
- Kristi Sidney-Annerstedt 2
Health Research Policy and Systems volume 22 , Article number: 40 ( 2024 ) Cite this article
146 Accesses
4 Altmetric
Metrics details
Vietnam’s primary mechanism of achieving sustainable funding for universal health coverage (UHC) and financial protection has been through its social health insurance (SHI) scheme. Steady progress towards access has been made and by 2020, over 90% of the population were enrolled in SHI. In 2022, as part of a larger transition towards the increased domestic financing of healthcare, tuberculosis (TB) services were integrated into SHI. This change required people with TB to use SHI for treatment at district-level facilities or to pay out of pocket for services. This study was conducted in preparation for this transition. It aimed to understand more about uninsured people with TB, assess the feasibility of enrolling them into SHI, and identify the barriers they faced in this process.
A mixed-method case study was conducted using a convergent parallel design between November 2018 and January 2022 in ten districts of Hanoi and Ho Chi Minh City, Vietnam. Quantitative data were collected through a pilot intervention that aimed to facilitate SHI enrollment for uninsured individuals with TB. Descriptive statistics were calculated. Qualitative interviews were conducted with 34 participants, who were purposively sampled for maximum variation. Qualitative data were analyzed through an inductive approach and themes were identified through framework analysis. Quantitative and qualitative data sources were triangulated.
We attempted to enroll 115 uninsured people with TB into SHI; 76.5% were able to enroll. On average, it took 34.5 days to obtain a SHI card and it cost USD 66 per household. The themes indicated that a lack of knowledge, high costs for annual premiums, and the household-based registration requirement were barriers to SHI enrollment. Participants indicated that alternative enrolment mechanisms and greater procedural flexibility, particularly for undocumented people, is required to achieve full population coverage with SHI in urban centers.
Conclusions
Significant addressable barriers to SHI enrolment for people affected by TB were identified. A quarter of individuals remained unable to enroll after receiving enhanced support due to lack of required documentation. The experience gained during this health financing transition is relevant for other middle-income countries as they address the provision of financial protection for the treatment of infectious diseases.
Peer Review reports
Contributing to universal health coverage (UHC) by improving access to fair and sustainable health financing, of which one mechanism is health insurance, has become a priority among low- and middle-income countries [ 1 , 2 ]. Many countries in the Asia Pacific region have made steady progress towards UHC coverage through sustained political commitments and fiscal policy aligned with their commitment [ 3 ]. By 2020, 27 countries had implemented a social health insurance (SHI) financing mechanism, which typically includes open enrollment for the full population along with partial or full subsidization of healthcare costs for vulnerable groups [ 4 ].
Vietnam’s first SHI scheme was piloted in 1989 and grew through successive pilots and expansions. In 2009 the national-level Health Insurance Law (HIL) went into effect, uniting the existing health insurance programs and schemes for the poor [ 5 ]. Amendments to the HIL effective in 2015 made SHI compulsory for all and pooled risk by re-structuring registration around the household unit [ 4 ]. A household in Vietnam is defined by inclusion in the ‘family book ’, the national system of family and address registration [ 6 ].
Access to SHI in Vietnam increased rapidly, principally through subsidization of premiums. Specific groups were enrolled automatically with full subsidy, including vulnerable populations (e.g., households classified as ‘poor’, children aged < 6, people aged > 80), pensioners and meritorious groups (e.g., veterans). Partial premium subsidization was also available for students, households classified as ‘near-poor’ and some farmers [ 7 ]. More than half of SHI members are entitled to 80% coverage with a 20% co-payment for services [ 8 ]. However, co-payments are reduced to 5% or are eliminated for subsidized groups (e.g., households classified as ‘poor’ and ‘near-poor’, children < 6) [ 4 ].
By 2020, Vietnam recorded a 91% national SHI coverage rate [ 7 ]. Those remaining uninsured mainly consisted of informally employed individuals [ 7 ]. Enrollment rates were highest among low- and high-income groups, leaving the so-called “missing middle” of uninsured [ 5 ].
Vietnam continues to transition to domestic financing of healthcare from donor financing by expanding the breadth of the national SHI. The Ministry of Health and Vietnam Social Security (VSS) have begun to close service gaps and integrate vertical health programs (e.g., those with stand-alone budget allocations and/or direct donor financing) into SHI financing [ 7 ]. The costs for antiretroviral therapy (ART) were transitioned from donor funding to SHI in 2019 [ 9 ], COVID-19 treatments were covered by SHI in 2020, and financing for tuberculosis (TB) care was fully transitioned to SHI in 2022 [ 7 ].
Until this financing transition, anti-TB medications and consultations were provided free of charge in the public sector, funded by a mixture of domestic and international funding [ 10 ]. While first-line TB medications were included in the SHI-reimbursable list of essential medicines, the government network of District TB Units (DTUs) were ineligible for registration with VSS, or reimbursement for services provided. Since July 2022, TB health facilities that met certain conditions could register with VSS and receive reimbursements for TB consultations, diagnostics and anti-TB medications [ 11 ]. The financing for drug-resistant (DR-)TB tests and medications remains largely unchanged, co-financed by the Global Fund and domestic budgets [ 12 ].
This transition of the TB financing model in Vietnam is a large undertaking as the country has the world’s 10th highest TB burden and the SHI benefits package is already considered to be generous, and the sustainability of the SHI fund is a concern [ 4 , 13 ] An estimated 169,000 individuals developed TB in 2021, and the disease killed approximately 14,200 [ 14 ]. A national costing survey of TB-affected households showed that 63% experienced catastrophic costs, spending ≥ 20% of their annual income on TB [ 10 ]. Many face food insecurity and cope with TB-related costs by taking loans, dissavings and informally borrowing money [ 10 , 15 , 16 ].
As Vietnam continues to expand SHI financing for the TB program, it is now vital for people with TB to have SHI. Those without SHI coverage will need to finance their care out of pocket (OOP) or purchase SHI and make co-payments for their care to be subsidized. For these reasons, it is important to understand why certain people with TB are uninsured, the feasibility of enrolling them in insurance when they begin treatment, and the challenges they may face with enrolling in SHI.
We conducted a convergent parallel mixed-method case study [ 17 ]. A case study was selected because it is well-suited to describe a complex issue in a real-life setting [ 18 ]. We used a naturalistic design with theoretical sampling of uninsured persons with TB using an interpretivist approach [ 19 ]. Mixed methods were selected to facilitate comparisons between quantitative and qualitative data and interpretation of the findings. An intervention, assisting TB-affected households to enroll in SHI, was conducted between November 2019 and January 2022, prior to the integration of the TB program into the SHI financing scheme. Quantitative data collection sought to answer questions regarding enrollment success rate, time to enrollment and cost of SHI enrollment for uninsured TB-affected households upon TB treatment initiation. The qualitative data explored barriers to SHI enrollment to explain and contextualize the quantitative findings. The quantitative and qualitative data were weighted equally [ 17 ].
Intervention description
A pilot intervention was conducted to facilitate SHI enrollment for people with TB in ten districts of Ha Noi and Ho Chi Minh City (HCMC). The standard process for first-time enrollment into SHI was mapped and costed from a household’s perspective (Additional file 1 ). Uninsured individuals were identified from the TB treatment register when they were enrolled in drug-susceptible (DS-)TB treatment at DTUs [ 20 ]. Study staff then attempted to facilitate enrollment of the person with TB and up to three household members into SHI.
SHI enrollment support included home visits by study staff to provide detailed information and counseling about the process of SHI enrollment, assistance with SHI application preparation including obtaining photocopies of all required documents, follow-up to obtain missing documentation within the household, accompaniment to the SHI office for application submission, and direct payment of the annual SHI premium for the household. For people who did not have the paperwork certifying temporary residence in Hanoi or Ho Chi Minh City, staff visited the local government office to obtain the information about the process for individual cases to obtain residency certificates and support participants with navigation of the bureaucracy. TB-affected people and their household members were also provided with a hotline number to call and receive support during working hours from the social workers who were employed by the study. Study staff attempted to facilitate the SHI enrollment process throughout the entire 6-month duration of DS-TB treatment. After a TB treatment outcome was recorded by the DTU, study staff stopped assisting with SHI enrollment and participants were recorded as ‘not enrolled in SHI’ in the study’s evaluation.
Quantitative methods
Case-level TB treatment notification data and SHI status were exported from VITIMES, the government-implemented electronic TB register for Vietnam, for all individuals who started TB treatment during the intervention period. The pilot intervention recruited participants from two TB treatment support projects (Project 1, n = 59 and Project 2, n = 56) [ 21 , 22 ] and tracked study forms housed in ONA.io. The sample size was determined by the availability of funding provided by the donor for treatment support service delivery, rather than to measure a specific end point of SHI enrollment. Descriptive statistics summarizing the enrollment cascade and turnaround time of enrollment were calculated using Stata v17 (Stata17 Corp, College Station, USA). To obtain the mean costs for household SHI enrollment, total direct costs for purchasing SHI were summed and divided by the total number of participants. Costs were captured in Vietnamese Dong (VND) and converted to United States Dollars (USD) using the exchange rate from the mid-point of the pilot intervention (1 June 2020) from OANDA.com.
Qualitative methods
Individuals were purposively sampled for maximum variation to ensure representation of all implementation areas and provide gender balance [ 23 ].The concept of information power guided the sample size [ 24 ]. Given the well-defined study aim, high quality in-depth responses from the participants and the authors’ expertise in the subject area, the sample size of 19 individual interviews and three focus group discussions was deemed appropriate. These were conducted in Ha Noi and HCMC. A total of 34 individuals participated in the interviews (Table 1 ).
They included 14 people enrolled in the pilot intervention, five community members who were non-beneficiaries of the treatment support intervention, 13 TB program staff from the national-, provincial- and district-levels and two study staff. Interviews were conducted at two time points: June 2019 and 2020. SHI enrollment barriers were collected as part of a qualitative study on the acceptability of providing cash transfers and SHI enrollment to adults with TB [ 25 ]. During the second round of interviews in 2020, study staff were included due to their in-depth knowledge of the challenges faced by TB-affected households when attempting to enroll in SHI and their ability to suggest programmatic-level solutions to these challenges. These interviews were conducted one-on-one, after the other interviews and focus groups had been conducted to reduce bias. The interviews were conducted at the National Lung Hospital, HCMC Provincial Lung Hospital, study office or DTUs. All interviews were conducted and transcribed in Vietnamese, translated into English, checked and finalized by a lead translator.
The interviews were analyzed through an inductive approach and themes were drawn through a framework analysis [ 26 ] to identify barriers to enrolling in SHI using Dedoose Version 7.0.23 (SocioCultural Research Consultants, Los Angeles, USA).
Data triangulation
Quantitative and qualitative data were collected in parallel. Triangulation of quantitative and qualitative data was conducted to synthesize findings and assess the level of agreement, convergence, and divergence from the findings generated by the different methods [ 17 ].
During the study, 5887 individuals were treated for DS-TB across the 10 intervention districts (Table 2 ). TB registers indicated that 2846 (48.3%) individuals were uninsured upon treatment initiation, or their SHI enrollment status was not recorded. Among 115 uninsured study participants, 88 (76.5%) were successfully enrolled in SHI before the end of their TB treatment. Among those, the household had an average of two members, resulting in a total of 206 individuals living in TB-affected households receiving SHI coverage through the pilot intervention.
The median time between DS-TB treatment initiation and SHI card issuance was 34.5 days (IQR 24–68): 11 days (IQR 5–23) between treatment initiation and pilot enrollment, 7 days (IQR 1–19.5) for SHI application preparation and submission, and 12 days (IQR 9–20) for application processing and SHI card provision.
The qualitative data showed that participants across all participant groups broadly understood that SHI is a system designed to prevent catastrophic OOP medical expenditure. As shown in Table 3 , National and provincial-level TB staff described SHI as a human right and spoke about achieving UHC as a nation; no other participant groups discussed SHI in this way. However, district-level doctors and intervention beneficiaries spoke in greater details about coverage and service gaps, and the practicalities of utilizing SHI. These participant groups expressed that when individuals purchase SHI only after a negative health event, such as a TB diagnosis, then the social safety net is unavailable to provide support until SHI coverage begins. Drawn from these views, the first theme indicated that the optimal time to purchase SHI is prior to a TB diagnosis.
One DTU staff member described how the standard processing time, or delays in processing SHI applications led to periods of high OOP expenditure:
“Unfortunately, claims are not immediately paid upon [SHI registration] submission. They may be handled in about 2 or 3 weeks, or even one month. That is why the insurance is not available at the time that they want to go for an examination and treat their condition using insurance.” (Female, District-level TB staff)
A complementary theme was that perceived lack of knowledge about SHI enrollment procedures prevents or delays enrollment. District-level TB doctors and program staff identified a lack of understanding and knowledge of the SHI enrollment process as a main contributor to lack of insurance or delays in obtaining coverage.
“Actually, for some people [with TB] who do not clearly understand the [enrollment] procedures… it will take a lot of time [to obtain SHI]. It also depends on the staff who handle the files at the commune; some staff are very enthusiastic and they help patients complete forms. There are cases [...] where they [people with TB] are required to fill in all information and write specific codes of each insurance card [from other family members] on a form. Meanwhile some people in their family work far from home and cannot send their insurance cards home in a timely manner.” (Female, program staff)
Participants tended to believe that individuals who lacked information about SHI made up the small minority of uninsured people in Vietnamese society. The above quote illustrated that the complicated administrative process prohibits enrollment; however, a factor potentially facilitating SHI enrollment may be the helpfulness of the person processing the SHI application.
The average cost per household to obtain SHI enrollment for one year (Table 2 ) was VND 1,503,313 (USD 65.52). (For detailed information on the costs of SHI enrollment, see Additional file 1 ). A third theme contextualized this finding and showed that SHI enrollment costs were perceived as prohibitively high for some. Cost was a greater challenge for lower income families, who did not meet the government’s criterion of households classified as ‘poor’ or ‘near-poor’, and were therefore ineligible for premium subsidies and SHI registration with lower co-payment rates. One DTU doctor reported that:
“We think that it is simple to buy health insurance cards, but that is only true for those who have sustainable income - when our income is much higher than the fee for buying health insurance. For some people, buying health insurance is a luxury.” (Male, District-level TB staff)
Twenty-seven people with TB (23.5%) were unable to obtain SHI coverage. The primary reason (70.4%) was missing documentation. In four instances (14.8%) a household member other than the person with TB refused to enroll in SHI. One individual (3.7%) died during the enrollment process. Three individuals (11.1%) did not enroll for other reasons.
SHI refusal by household members was not identified as a barrier to SHI enrollment in the qualitative data. However, a fourth theme confirmed the primary reason for non-enrollment by showing that some individuals do not possess the required documentation to obtain SHI, such as their identity card or ‘family book.’ [See Supplementary File] Even with six months of support from study staff, some TB-affected households were unable to gather the required documents for enrollment. The following quotation by an undocumented, elderly woman with TB illustrates the prolonged challenges she faced with obtaining formal employment, access to government services and SHI:
“I have had problems with my personal papers for a few decades and I cannot adjust my papers because I don’t have the money. […] I searched for my Identity Card and found out that I had lost it. Then I came back there [my hometown] to get the family book, to reissue my ID and to get my CV certified so I could join a company. I was very young at that time, just a little bit more than thirty years old, and I learned that I was cut from the family book.” (Female, pilot beneficiary)
To address challenges with documentation, one DTU officer in HCMC suggested that individuals who had never been insured required a change to the SHI registration requirements to ensure that everyone in Vietnam can access SHI:
“I think we should be flexible with these cases or we can find another way. Normally, the people who really need the support and the insurance or cash support, they are the people who have less information. […] We cannot have the same requirements for these people as for other people. Actually, for those who have [met] all conditions, they already have health insurance cards.” (Male, District-level TB staff)
Participants expressed that the uninsured had often not purchased SHI for a reason, and alternative registration procedures were needed to make SHI accessible for all. A fifth theme was identified indicating that current SHI enrollment procedures may prevent full population coverage.
Beyond the undocumented, some participants reported the enrollment mandate for the entire household (made under the Amendment to the HIL) for first-time enrollees was viewed as prohibitive of SHI coverage.
“Because in the old days, health insurance was sold individually for each person, but now it is sold to households, and many households do not have as good economic [situation]… so they can only afford to buy it for 50% or 60% of the household. Unskilled labor or low-income labor cannot afford to buy it for the whole family. That is to say, it is easier to buy it for each individual and it is difficult to buy for the whole family.” (Male, community member)
Though individual registration would make SHI more accessible to individuals with TB due to lower annual costs, household members with high vulnerability to TB would not be covered if policy promoted individual enrollment solely for TB.
This mixed-methods case study showed that by providing full subsidy and registration assistance, most uninsured people with TB could access SHI. However, the median time to insurance coverage meant that approximately 20% of a person’s DS-TB treatment duration remained uncovered by SHI despite successful enrollment. A substantial number of participants were unable to enroll in SHI and are likely to be perpetually locked out of SHI due to lack of personal documentation. Additional barriers to SHI enrollment were found to be lack of knowledge, the cost of obtaining coverage, and the household-based registration requirement.
The pilot intervention had dedicated staff who facilitated SHI application development and submission, yet it still took a median of 34.5 days for SHI coverage to take effect. In a context where this level of support is not available to all people with TB, it is likely that the turnaround time for SHI coverage is longer due to the complicated bureaucracy involved. This poses a major challenge, as TB-affected households incur the highest cost during the first two months of treatment [ 15 ]. One cost avoidance/mitigation strategy that people with a TB diagnosis may employ following the health financing transition is delaying TB treatment initiation until SHI coverage commences. This will likely lead to worse outcomes and sustained community transmission. The time between diagnosis and treatment should be rigorously monitored to ensure that this coping strategy is not employed, and alternative support should be made available to ensure that people diagnosed with TB are able to receive immediate treatment.
With the TB health financing transition, the uninsured will be asked to pay OOP for TB treatment and most insured individuals must co-pay for TB services which were previously provided free of cost. A national patient cost survey in 2018 found that 63% of TB-affected households experienced catastrophic costs under the previous health financing model [ 10 ]. There is a risk that the proportion of TB-affected households experiencing catastrophic costs could increase with the introduction of fees. This was not found to be the case for people living with HIV (PLHIV) when the costs of ART transitioned to SHI in Vietnam, but a new nationally representative TB costing survey is needed to assess this risk [ 9 ]. Several domestic solutions could ameliorate these challenges. As suggested for the Indian context, domestic revenues allocated by the Ministry of Finance to VSS could be increased to better support TB care [ 27 ]. VSS could also reclassify the category of TB disease and thus ensure that SHI paid for all diagnostics and drugs associated with TB treatment, without the need for a co-payment. A mid-term review of the Global Fund program in Vietnam has also called for a SHI package specifically designed to cover the OOP medical costs of TB care [ 28 ]. There are several potential mechanisms to prevent costs from falling on TB-affected households. A deeper investigation is needed to understand the fiscal space available within the Vietnamese government to cover such costs.
This case study showed that 23.5% of the uninsured people with TB were never able to enroll for the duration of their treatment, primarily due to lack of documentation. Specific provisions need to be made for the undocumented to receive free TB diagnosis, consultations, and medications through routine practice of the TB program. Multi- and bi-lateral funding mechanisms can also play a role in filling gaps by paying for TB tests for the uninsured, purchasing SHI for those diagnosed with TB, subsidizing or reimbursing OOP expenditure in the period before SHI coverage takes effect, and fully financing TB care for the undocumented. Furthermore, longer-term health system strengthening initiatives, such as creating a legal mechanism for the undocumented to obtain SHI, are likely needed to address the challenges faced by the 9% of the general population that remain uninsured. The ILO has called for “determining new strategies, which may include extension of state budget-funded subsidies to further support the participation of workers in the informal economy [ 7 ].” These forms of inclusive initiatives would solve the TB-specific challenges identified in this study and have a large positive impact on society.
We found that addressing the cost of SHI premiums and knowledge gaps in the enrollment procedures may improve SHI coverage. These findings mirror those following the transition of HIV financing to SHI in 2017. A study among PLHIV identified burdensome processes, lack of information about SHI registration procedures, and high SHI premium costs for a household as key barriers to SHI coverage [ 29 ]. However, a cluster randomized control trial which provided education, a 25% premium subsidy, or both to uninsured households found that these interventions had limited effects on SHI enrollment. Yet, “less healthy” individuals had higher SHI enrollment rates [ 30 ]. This suggests that people who have just received a TB diagnosis could be more receptive to interventions promoting SHI enrollment through premium subsidization and education. Vietnam’s National TB Program (NTP) has established a fund to subsidize SHI enrollment costs for TB-affected individuals. The size of the fund could be increased with additional support while access to the fund and the procedures for receiving support could be optimized [ 31 ]. Given the SHI transition, the NTP should also consider providing educational materials about the SHI enrollment process through the DTU network to uninsured persons with TB.
TB registers indicated that 52% of people starting TB treatment in the urban intervention districts had recorded SHI coverage. This rate is lower than other recent SHI coverage reports. A 2018–2022 DS-TB costing survey reported a SHI coverage of 70% [ 32 ], while in a DR-TB costing survey (2020–2022) it was 85% [ 16 ]. All available data sources indicate that SHI coverage among people with TB is lower than the general population, which is indicative of their socioeconomic vulnerability [ 33 ]. However, this large SHI coverage rate discrepancy may be explained by people with TB not revealing they had SHI coverage, or DTU staff could have also inconsistently recorded an individual’s SHI status in the paper TB registers since these data did not have much clinical relevance for TB treatment at the time. Now that DTUs receive financial reimbursements for the TB services from VSS, SHI coverage rates in treatment registers are likely to increase. Further research should be conducted to understand the national SHI coverage rate for people receiving TB treatment, along with the risk factors associated with being uninsured.
Limitations
This case study was conducted in the two largest cities of Vietnam and findings may not be representative of the entire country. Quantitative data were collected in a programmatic setting, and SHI coverage data for all individuals initiating TB treatment in the intervention areas appear to be underreported for reasons described above. Lastly, we were unable to collect SHI enrollment data from a control population, either prospectively during the pilot intervention or retrospectively during the pilot evaluation. As a result, we do not have information on the enrollment status or time to obtain SHI coverage among a population that did not receive assistance from the pilot intervention. However, given the substantial additional support provided by study staff for the enrollment process, we believe it is safe to assume that if left alone, TB-affected households would be slower in the enrollment process and likely enroll in lower rates.
Vietnam is viewed as a leader among Southeast Asian nations in its commitment and progress towards UHC. This mixed-methods case study illustrated the progress that Vietnam has made in its path to greater domestic financing of healthcare through SHI. This study is one of the first to examine the integration of TB services into SHI in Vietnam and define the challenges that people with TB face while attempting to gain access to financial protection after receiving a TB diagnosis. In order to make strides towards UHC in Vietnam and to close population coverage gaps, initiatives are required to specifically address the barriers faced by the uninsured. This study found that the majority of the uninsured were able to gain access to SHI through full subsidization of premiums, enrollment assistance and education. However, initiating TB care and SHI enrollment concomitantly left a significant portion of the 6-month TB treatment duration without financial protection. Additionally, a quarter of the uninsured with TB were unable to gain access to SHI during treatment, primarily due to a lack of documentation. There is great need for official mechanisms to be in place that enable those without sufficient state documents to access the TB program and to address the time-sensitive nature of providing effective financial protection during treatment of an infectious disease. These findings are relevant for other high TB burden, middle-income countries who are on a similar pathway for transitioning away from donor-financed TB programs to ones supported with a higher proportion of domestic resources.
Availability of data and materials
The quantitative dataset used and analyzed during the current study are available from the corresponding author on reasonable request. Seven anonymized transcripts of interviews with the people enrolled in the pilot intervention and non-beneficiaries have been uploaded to the following URL: https://doi.org/ https://doi.org/10.5281/zenodo.7736220 .
Abbreviations
Anti antiretroviral therapy
Drug resistant tuberculosis
Drug susceptible tuberculosis
District TB Unit
Ho Chi Minh City
Health Insurance Law
Human immunodeficiency virus
International Labour Organization
Interquartile range
National Tuberculosis Program
Out of pocket
People Living with HIV
Social Health Insurance
- Tuberculosis
Universal Health Coverage
United States Dollar
Vietnamese Dong
Vietnam Social Security
World health statistics 2023: monitoring health for the SDGs, sustainable development goals. https://www.who.int/publications-detail-redirect/9789240074323 . Accessed 31 May 2023.
SDG Target 3.8 | Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all. https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/sdg-target-3.8-achieve-universal-health-coverage-(uhc)-including-financial-risk-protection . Accessed 29 May 2023.
Hondo D, Kim Y. Achieving universal health coverage in developing Asia and the Pacific. Asian Development Bank Institute; 2023. Report No.: 2023-15 (November). https://doi.org/10.56506/VUWA5043 . Accessed 1 Feb 2024.
Le QN, Blizzard L, Si L, Giang LT, Neil AL. The evolution of social health insurance in Vietnam and its role towards achieving universal health coverage. Health Policy OPEN. 2020;100011. http://www.sciencedirect.com/science/article/pii/S2590229620300095 . Accessed 10 Sep 2023.
Somanathan A, Tandon A, Dao HL, Hurt KL, Fuenzalida-Puelma HL. Moving toward universal coverage of social health insurance in Vietnam: assessments and options. Washington, DC: World Bank; 2014, p. 177. (Directions in Development). https://doi.org/10.1596/978-1-4648-0261-4
Hardy A. Rules and resources: negotiating the household registration system in Vietnam under reform. Sojourn J Soc Issues Southeast Asia. 2001;16(2):187–212.
Article CAS Google Scholar
Bales S, Phe Goursat M, Phuong NK. Extending social health protection in Viet Nam: accelerating progress towards universal health coverage. International Labour Organization; 2021, p. 1–14. (Social Protection in action: building social protection floors for all.). https://www.social-protection.org/gimi/gess/ShowRessource.action;jsessionid=iFmxgS-hSrmJjf_1uG90JAnijskVEc8XJD9-4lubAqbFD4-JPYOm!341651707?id=57668 . Accessed 26 Aug 2022.
Bao Hiem Xa Hoi [Vietnam Social Security]. 2019. Phát triển bền vững BHYT toàn dân [Sustainable development of universal health insurance]. https://baohiemxahoi.gov.vn/congkhai/Pages/so-lieu-thong-ke-nganh.aspx?CateID=130&ItemID=12916 . Accessed 26 Aug 2022.
Vu LTH, Johns B, Bui QTT, Duong Thuy A, Nguyen Thi D, Nguyen Thi H, et al. Moving to social health insurance financing and payment for HIV/AIDS treatment in Vietnam. Health Serves Insights. 2021;14:1178632920988843. https://doi.org/10.1177/1178632920988843 .
Article Google Scholar
Nhung NV, Hoa NB, Anh NT, Anh LTN, Siroka A, Lonnroth K, et al. Measuring catastrophic costs due to tuberculosis in Viet Nam. Int J Tuberc Lung Dis. 2018;22(9):983–90.
Article CAS PubMed Google Scholar
Tran VT. Circular No. 36/2021/TT-BYT dated December 31, 2021 on Medical examination and treatment, and payment for medical examination and treatment costs covered by health insurance relating to tuberculosis examination and treatment. 36/2021/TT-BYT Dec 31, 2021. https://hethongphapluat.com/circular-no-36-2021-tt-byt-dated-december-31-2021-on-medical-examination-and-treatment-and-payment-for-medical-examination-and-treatment-costs-covered-by-health-insurance-relating-to-tuberculosis-examination-and-treatment.html .
The Global Fund. Country Profiles Tuberculosis- 2022- Viet Nam. The Global Fund; 2023. https://data.theglobalfund.org/location/VNM/documents . Accessed 30 May 2023.
Nguyen Thi Thu Cúc. Socialist Republic of Viet Nam: strengthening the policy and institutional framework of social health insurance. Hanoi, Vietnam: Asian Development Bank; 2021, p. 1–27. Report No.: 50139–002. https://www.adb.org/projects/documents/vie-50139-002-tacr-4 . Accessed 26 Aug 2022.
Global tuberculosis report 2022. Geneva: World Health Organization; 2022. Licence: CC BY-NC-SA 3.0 IGO. https://www.who.int/publications-detail-redirect/9789240061729 .
Vo LNQ, Forse RJ, Codlin AJ, Dang HM, Van Truong V, Nguyen LH, et al. Socio-protective effects of active case finding on catastrophic costs from tuberculosis in Ho Chi Minh City, Viet Nam: a longitudinal patient cost survey. BMC Health Serv Res. 2021;21(1):1051. https://doi.org/10.1186/s12913-021-06984-2 .
Article PubMed PubMed Central Google Scholar
Pham TAM, Forse R, Codlin AJ, Phan THY, Nguyen TT, Nguyen N, et al. Determinants of catastrophic costs among households affected by multi-drug resistant tuberculosis in Ho Chi Minh City, Viet Nam: a prospective cohort study. BMC Public Health. 2023;23(1):2372. https://doi.org/10.1186/s12889-023-17078-5 .
Creswell JW, Clark Plano VL. Designing and conducting mixed methods research. 3rd ed. Thousand Oaks, California: SAGE Publications; 2017. p. 520.
Google Scholar
George AL, Bennett A. Case studies and theory development in the social sciences. Cambridge, MA: MIT Press; 2005.
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach. BMC Med Res Methodol. 2011;11(1):100. https://doi.org/10.1186/1471-2288-11-100 .
Thai LH, Nhat LM, Shah N, Lyss S, Ackers M. Sensitivity, completeness and agreement of the tuberculosis electronic system in Ho Chi Minh City. Viet Nam Public Health Act. 2017;7(4):294–8.
IMPACT TB Overview | IMPACT TB. https://impacttbproject.org/impact-tb-overview/ . Accessed 2 Jun 2023.
Fact Sheet: USAID Erase TB Project 2020. 2020. https://www.usaid.gov/vietnam/documents/fact-sheet-erase-tb-project . Accessed 24 Sep 2024.
Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42(5):533–44. https://doi.org/10.1007/s10488-013-0528-y .
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–60. https://doi.org/10.1177/1049732315617444 .
Article PubMed Google Scholar
Forse R, Nguyen TT, Dam T, Vo LNQ, Codlin AJ, Caws M, et al. A qualitative assessment on the acceptability of providing cash transfers and social health insurance for tuberculosis-affected families in Ho Chi Minh City, Vietnam. PLOS Glob Public Health. 2023;3(12): e0002439.
Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative research practice: a guide for social science students and researchers. Second edn. SAGE Publications Ltd; 2013. p. 456.
Behera DK, Dash U, Sahu SK. Exploring the possible sources of fiscal space for health in India: insights from political regimes. Health Res Policy Syst. 2022;20(1):32. https://doi.org/10.1186/s12961-022-00831-4 .
Draft Report: Key Messages from the TB National Strategic Plan Mid Term Review (MTR) for Vietnam, between 8th to 18th January 2023. Hanoi, Vietnam: Vietnam’s National TB Program; 2023 Jan p. 1.
Matsumoto S, Nguyen HDT, Nguyen DT, Van Tran G, Tanuma J, Mizushima D, et al. The patient voice: a survey of worries and anxieties during health system transition in HIV services in Vietnam. BMC Int Health Hum Rights. 2020;20:1.
Wagstaff A, Nguyen HTH, Dao H, Bales S. Encouraging health insurance for the informal sector: a cluster randomized experiment in Vietnam. Health Econ. 2016;25(6):663–74. https://doi.org/10.1002/hec.3293 .
Hoa NB, Nhung NV. National tuberculosis patients cost survey: research findings lead to change in policy and practice. Viet Nam Public Health Act. 2019;9(2):50–2.
Wiemers A, Sidney-Annerstedt K, Forse R, Phan THY, Codlin A, Vo LNQ, et al. EP-13-729 COVID-19 lockdowns resulting in household income decline for people with TB in Ho Chi Minh City: interrupted time series analysis of household income changes. In: Proceedings of the union world conference on lung health 2022. Virtual event, 8–11 November 2022: the international journal of tuberculosis and lung disease (IJTLD); 2022. p. 191.
Lönnroth K, Jaramillo E, Williams BG, Dye C, Raviglione M. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc Sci Med. 2009;68(12):2240–6.
Download references
Acknowledgements
The authors would like to acknowledge the contributions of Hoang Thi My Linh, Chu Thi Hoang Anh, Nguyen Khac Cuong, Nham Thi Yen Ngoc and Tran Thai Hiep for conducting qualitative interviews and assisting with SHI enrollment activities. Special thanks to Dr. Kerri Viney for providing insightful comments on an early draft of this manuscript; they greatly strengthened the final version. This work was graciously supported by the staff of Vietnam’s National TB Program, the Hanoi Lung Hospital, Pham Ngoc Thach Provincial TB Hospital and 10 District TB Units. Lastly, we would like to thank the interview participants who shared their time and insights.
Open access funding provided by Karolinska Institute. The European Commission's Horizon 2020 program supported the provision of SHI and all data collection in 2019 through the IMPACT-TB study under grant agreement number 733174. For the period of 2020–2022, support to implement the pilot and conduct the evaluation was made possible by the generous support of the American people through the USAID under award number 72044020FA00001. TW was supported by grants from: the Wellcome Trust, UK ( Seed Award, grant number 209075/Z/17/Z); the Department of Health and Social Care (DHSC), the Foreign, Commonwealth & Development Office (FCDO), the Medical Research Council (MRC) and Wellcome, UK (Joint Global Health Trials, MR/V004832/1); the Medical Research Council (Public Health Intervention Development Award “PHIND”, APP2293); and the Medical Research Foundation (Dorothy Temple Cross International Collaboration Research Grant, MRF-131–0006-RG-KHOS-C0942). KSA was supported by the ASPECT Trial funded the Swedish Research Council (2022-00727). The contents of this study are the responsibility of the listed authors, and do not necessarily reflect the views of USAID or the United States Government.
Author information
Authors and affiliations.
Friends for International TB Relief, Hanoi, Vietnam
Rachel Forse, Thanh Thi Nguyen, Luan N. Q. Vo & Andrew J. Codlin
Department of Global Public Health, WHO Collaboration Centre on Tuberculosis and Social Medicine, Karolinska Institutet, Stockholm, Sweden
Rachel Forse, Clara Akie Yoshino, Luan N. Q. Vo, Andrew J. Codlin, Tom Wingfield, Knut Lönnroth & Kristi Sidney-Annerstedt
Centre for Development of Community Health Initiatives, Hanoi, Vietnam
Thi Hoang Yen Phan
IRD VN, Ho Chi Minh City, Vietnam
Lan Nguyen & Chi Hoang
USAID Vietnam, Hanoi, Vietnam
Lopa Basu & Minh Pham
National Lung Hospital, Hanoi, Vietnam
Hoa Binh Nguyen & Luong Van Dinh
Centre for TB Research, Department of Clinical Sciences, Liverpool School of Tropical Medicine, Liverpool, UK
Maxine Caws & Tom Wingfield
Birat Nepal Medical Trust, Kathmandu, Nepal
Maxine Caws
You can also search for this author in PubMed Google Scholar
Contributions
This study was conceived of by RF, KSA, TTN, THYP, CAY, AJC, LNQV. The study was administered by RF, YP, TTN, AJC. Support from Vietnam’s National TB program was provided by HBN and LVD. The methodology was developed by RJ, CAY, KV, KL, KSA. The analysis was carried out by RF, CAY, TTN, and THYP. LNQV, AJC, TW, LN, CH, LB, MP, HBN, LVD, MC, KV, KL, and KSA supported the interpretation of findings. The first manuscript was written by RF. All co-authors reviewed and commented on the initial manuscript. The final manuscript was approved and reviewed by all authors.
Corresponding author
Correspondence to Rachel Forse .
Ethics declarations
Ethics approval and consent to participate.
All study procedures were conducted in strict adherence to the Declaration of Helsinki. Ethical approvals were granted by the National Lung Hospital Institutional Review Board (114/19/CT-HĐKH-ĐĐ), the Pham Ngoc Thach Hospital Institutional Review Board (1225/PNT-HĐĐĐ) and Ha Noi University of Public Health Institutional Review Board (300/2020/YTCC-HD3). All participants provided written informed consent and individual-level data were pseudonymized prior to analysis.
Consent for publication
Informed written consent was obtained for all individuals who the study attempted to enroll in SHI, as part of the pilot intervention. It was also obtained for all individuals who participated in the qualitative interviews.
Competing interests
Ten of the authors received salary support from one of the funding agencies to implement the pilot interventions and their evaluation. Two of the authors were employed by United States Agency for International Development (USAID), which funded one of the two pilot interventions. They played no role in the design or implementation of the pilot interventions or their evaluation, but during the development of the manuscript, they provided their insights about the context of the results and Vietnam’s health financing transition as experts in the field.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Mapping of procedures and costs for first-time enrollment into Vietnam's social health insurance scheme.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Forse, R., Yoshino, C.A., Nguyen, T.T. et al. Towards universal health coverage in Vietnam: a mixed-method case study of enrolling people with tuberculosis into social health insurance. Health Res Policy Sys 22 , 40 (2024). https://doi.org/10.1186/s12961-024-01132-8
Download citation
Received : 11 August 2023
Accepted : 13 March 2024
Published : 02 April 2024
DOI : https://doi.org/10.1186/s12961-024-01132-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social health insurance
- Universal health coverage
- Health financing transition
- Financial protection
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 05 December 2023
A scoping review to identify and organize literature trends of bias research within medical student and resident education
- Brianne E. Lewis 1 &
- Akshata R. Naik 2
BMC Medical Education volume 23 , Article number: 919 ( 2023 ) Cite this article
816 Accesses
1 Citations
2 Altmetric
Metrics details
Physician bias refers to the unconscious negative perceptions that physicians have of patients or their conditions. Medical schools and residency programs often incorporate training to reduce biases among their trainees. In order to assess trends and organize available literature, we conducted a scoping review with a goal to categorize different biases that are studied within medical student (MS), resident (Res) and mixed populations (MS and Res). We also characterized these studies based on their research goal as either documenting evidence of bias (EOB), bias intervention (BI) or both. These findings will provide data which can be used to identify gaps and inform future work across these criteria.
Online databases (PubMed, PsycINFO, WebofScience) were searched for articles published between 1980 and 2021. All references were imported into Covidence for independent screening against inclusion criteria. Conflicts were resolved by deliberation. Studies were sorted by goal: ‘evidence of bias’ and/or ‘bias intervention’, and by population (MS or Res or mixed) andinto descriptive categories of bias.
Of the initial 806 unique papers identified, a total of 139 articles fit the inclusion criteria for data extraction. The included studies were sorted into 11 categories of bias and showed that bias against race/ethnicity, specific diseases/conditions, and weight were the most researched topics. Of the studies included, there was a higher ratio of EOB:BI studies at the MS level. While at the Res level, a lower ratio of EOB:BI was found.
Conclusions
This study will be of interest to institutions, program directors and medical educators who wish to specifically address a category of bias and identify where there is a dearth of research. This study also underscores the need to introduce bias interventions at the MS level.
Peer Review reports
Physician bias ultimately impacts patient care by eroding the physician–patient relationship [ 1 , 2 , 3 , 4 ]. To overcome this issue, certain states require physicians to report a varying number of hours of implicit bias training as part of their recurring licensing requirement [ 5 , 6 ]. Research efforts on the influence of implicit bias on clinical decision-making gained traction after the “Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care” report published in 2003 [ 7 ]. This report sparked a conversation about the impact of bias against women, people of color, and other marginalized groups within healthcare. Bias from a healthcare provider has been shown to affect provider-patient communication and may also influence treatment decisions [ 8 , 9 ]. Nevertheless, opportunities within medical education curriculum are created to evaluate biases at an earlier stage of physician-training and provide instruction to intervene them [ 10 , 11 , 12 ]. We aimed to identify trends and organize literature on bias training provided during medical school and residency programs since the meaning of ‘bias’ is broad and encompasses several types of attitudes and predispositions [ 13 ].
Several reviews, narrative or systematic in nature, have been published in the field of bias research in medicine and healthcare [ 14 , 15 , 16 ]. Many of these reviews have a broad focus on implicit bias and they often fail to define the patient’s specific attributes- such as age, weight, disease, or condition against which physicians hold their biases. However, two recently published reviews categorized implicit biases into various descriptive characteristics albeit with research goals different than this study [ 17 , 18 ]. The study by Fitzgerald et al. reviewed literature focused on bias among physicians and nurses to highlight its role in healthcare disparities [ 17 ]. While the study by Gonzalez et al. focused on bias curricular interventions across professions related to social determinants of health such as education, law, medicine and social work [ 18 ]. Our research goal was to identify the various bias characteristics that are studied within medical student and/or resident populations and categorize them. Further, we were interested in whether biases were merely identified or if they were intervened. To address these deficits in the field and provide clarity, we utilized a scoping review approach to categorize the literature based on a) the bias addressed and b) the study goal within medical students (MS), residents (Res) and a mixed population (MS and Res).
To date no literature review has organized bias research by specific categories held solely by medical trainees (medical students and/or residents) and quantified intervention studies. We did not perform a quality assessment or outcome evaluation of the bias intervention strategies, as it was not the goal of this work and is standard with a scoping review methodology [ 19 , 20 ]. By generating a comprehensive list of bias categories researched among medical trainee population, we highlight areas of opportunity for future implicit bias research specifically within the undergraduate and graduate medical education curriculum. We anticipate that the results from this scoping review will be useful for educators, administrators, and stakeholders seeking to implement active programs or workshops that intervene specific biases in pre-clinical medical education and prepare physicians-in-training for patient encounters. Additionally, behavioral scientists who seek to support clinicians, and develop debiasing theories [ 21 ] and models may also find our results informative.
We conducted an exhaustive and focused scoping review and followed the methodological framework for scoping reviews as previously described in the literature [ 20 , 22 ]. This study aligned with the four goals of a scoping review [ 20 ]. We followed the first five out of the six steps outlined by Arksey and O’Malley’s to ensure our review’s validity 1) identifying the research question 2) identifying relevant studies 3) selecting the studies 4) charting the data and 5) collating, summarizing and reporting the results [ 22 ]. We did not follow the optional sixth step of undertaking consultation with key stakeholders as it was not needed to address our research question it [ 23 ]. Furthermore, we used Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) that aided in managing steps 2–5 presented above.
Research question, search strategy and inclusion criteria
The purpose of this study was to identify trends in bias research at the medical school and residency level. Prior to conducting our literature search we developed our research question and detailed the inclusion criteria, and generated the search syntax with the assistance from a medical librarian. Search syntax was adjusted to the requirements of the database. We searched PubMed, Web of Science, and PsycINFO using MeSH terms shown below.
Bias* [ti] OR prejudice*[ti] OR racism[ti] OR homophobia[ti] OR mistreatment[ti] OR sexism[ti] OR ageism[ti]) AND (prejudice [mh] OR "Bias"[Mesh:NoExp]) AND (Education, Medical [mh] OR Schools, Medical [mh] OR students, medical [mh] OR Internship and Residency [mh] OR “undergraduate medical education” OR “graduate medical education” OR “medical resident” OR “medical residents” OR “medical residency” OR “medical residencies” OR “medical schools” OR “medical school” OR “medical students” OR “medical student”) AND (curriculum [mh] OR program evaluation [mh] OR program development [mh] OR language* OR teaching OR material* OR instruction* OR train* OR program* OR curricul* OR workshop*
Our inclusion criteria incorporated studies which were either original research articles, or review articles that synthesized new data. We excluded publications that were not peer-reviewed or supported with data such as narrative reviews, opinion pieces, editorials, perspectives and commentaries. We included studies outside of the U.S. since the purpose of this work was to generate a comprehensive list of biases. Physicians, regardless of their country of origin, can hold biases against specific patient attributes [ 17 ]. Furthermore, physicians may practice in a different country than where they trained [ 24 ]. Manuscripts were included if they were published in the English language for which full-texts were available. Since the goal of this scoping review was to assess trends, we accepted studies published from 1980–2021.
Our inclusion criteria also considered the goal and the population of the study. We defined the study goal as either that documented evidence of bias or a program directed bias intervention. Evidence of bias (EOB) had to originate from the medical trainee regarding a patient attribute. Bias intervention (BI) studies involved strategies to counter biases such as activities, workshops, seminars or curricular innovations. The population studied had to include medical students (MS) or residents (Res) or mixed. We defined the study population as ‘mixed’ when it consisted of both MS and Res. Studies conducted on other healthcare professionals were included if MS or Res were also studied. Our search criteria excluded studies that documented bias against medical professionals (students, residents and clinicians) either by patients, medical schools, healthcare administrators or others, and was focused on studies where the biases were solely held by medical trainees (MS and Res).
Data extraction and analysis
Following the initial database search, references were downloaded and bulk uploaded into Covidence and duplicates were removed. After the initial screening of title and abstracts, full-texts were reviewed. Authors independently completed title and abstract screening, and full text reviews. Any conflicts at the stage of abstract screening were moved to full-text screening. Conflicts during full-text screening were resolved by deliberation and referring to the inclusion and exclusion criteria detailed in the research protocol. The level of agreement between the two authors for full text reviews as measured by inter-rater reliability was 0.72 (Cohen’s Kappa).
A data extraction template was created in Covidence to extract data from included full texts. Data extraction template included the following variables; country in which the study was conducted, year of publication, goal of the study (EOB, BI or both), population of the study (MS, Res or mixed) and the type of bias studied. Final data was exported to Microsoft Excel for quantification. For charting our data and categorizing the included studies, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews(PRISMA-ScR) guidelines [ 25 ]. Results from this scoping review study are meant to provide a visual synthesis of existing bias research and identify gaps in knowledge.
Study selection
Our search strategy yielded a total of 892 unique abstracts which were imported into ‘Covidence’ for screening. A total of 86 duplicate references were removed. Then, 806 titles and abstracts were screened for relevance independently by the authors and 519 studies were excluded at this stage. Any conflicts among the reviewers at this stage were resolved by discussion and referring to the inclusion and exclusion criteria. Then a full text review of the remaining 287 papers was completed by the authors against the inclusion criteria for eligibility. Full text review was also conducted independently by the authors and any conflicts were resolved upon discussion. Finally, we included 139 studies which were used for data extraction (Fig. 1 ).
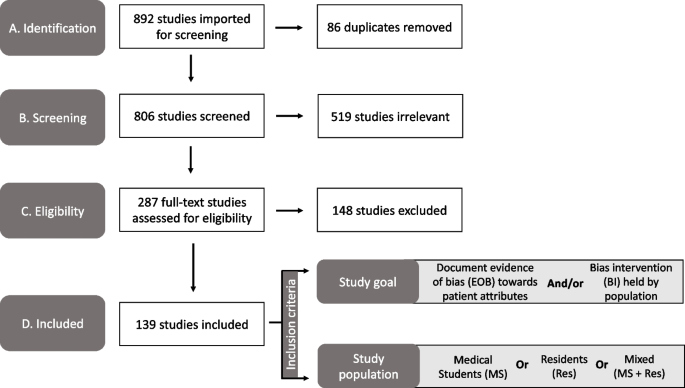
PRISMA diagram of the study selection process used in our scoping review to identify the bias categories that have been reported within medical education literature. Study took place from 2021–2022. Abbreviation: PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Publication trends in bias research
First, we charted the studies to demonstrate the timeline of research focused on bias within the study population of our interest (MS or Res or mixed). Our analysis revealed an increase in publications with respect to time (Fig. 2 ). Of the 139 included studies, fewer studies were published prior to 2001, with a total of only eight papers being published from the years 1985–2000. A substantial increase in publications occurred after 2004, with 2019 being the peak year where most of the studies pertaining to bias were published (Fig. 2 ).
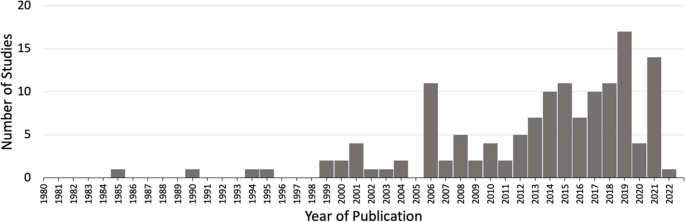
Studies matching inclusion criteria mapped by year of publication. Search criteria included studies addressing bias from 1980–2021 within medical students (MS) or residents (Res) or mixed (MS + Res) populations. * Publication in 2022 was published online ahead of print
Overview of included studies
We present a descriptive analysis of the 139 included studies in Table 1 based on the following parameters: study location, goal of the study, population of the study and the category of bias studied. All of the above parameters except the category of bias included a denominator of 139 studies. Several studies addressed more than one bias characteristic; therefore, we documented 163 biases sorted in 11 categories over the 139 papers. The bias categories that we generated and their respective occurrences are listed in Table 1 . Of the 139 studies that were included, most studies originated in the United States ( n = 89/139, 64%) and Europe ( n = 20/139, 20%).
Sorting of included research by bias category
We grouped the 139 included studies depending on the patient attribute or the descriptive characteristic against which the bias was studied (Table 1 ). By sorting the studies into different bias categories, we aimed to not only quantitate the amount of research addressing a particular topic of bias, but also reveal the biases that are understudied.
Through our analysis, we generated 11 descriptive categories against which bias was studied: Age, physical disability, education level, biological sex, disease or condition, LGBTQ + , non-specified, race/ethnicity, rural/urban, socio-economic status, and weight (Table 1 ). “Age” and “weight” categories included papers that studied bias against older population and higher weight individuals, respectively. The categories “education level” and “socio-economic status” included papers that studied bias against individuals with low education level and individuals belonging to low socioeconomic status, respectively. Within the bias category named ‘biological sex’, we included papers that studied bias against individuals perceived as women/females. Papers that studied bias against gender-identity or sexual orientation were included in its own category named, ‘LGBTQ + ’. The bias category, ‘disease or condition’ was broad and included research on bias against any patient with a specific disease, condition or lifestyle. Studies included in this category researched bias against any physical illnesses, mental illnesses, or sexually transmitted infections. It also included studies that addressed bias against a treatment such as transplant or pain management. It was not significant to report these as individual categories but rather as a whole with a common underlying theme. Rural/urban bias referred to bias that was held against a person based on their place of residence. Studies grouped together in the ‘non-specified bias’ category explored bias without specifying any descriptive characteristic in their methods. These studies did not address any specific bias characteristic in particular but consisted of a study population of our interest (MS or Res or mixed). Based on our analysis, the top five most studied bias categories in our included population within medical education literature were: racial or ethnic bias ( n = 39/163, 24%), disease or condition bias ( n = 29/163, 18%), weight bias ( n = 22/163, 13%), LGBTQ + bias ( n = 21/163, 13%), and age bias ( n = 16/163, 10%) which are presented in Table 1 .
Sorting of included research by population
In order to understand the distribution of bias research based on their populations examined, we sorted the included studies in one of the following: medical students (MS), residents (Res) or mixed (Table 1 ). The following distributions were observed: medical students only ( n = 105/139, 76%), residents only ( n = 19/139, 14%) or mixed which consisted of both medical students and residents ( n = 15/139, 11%). In combination, these results demonstrate that medical educators have focused bias research efforts primarily on medical student populations.
Sorting of included research by goal
A critical component of this scoping review was to quantify the research goal of the included studies within each of the bias categories. We defined the research goal as either to document evidence of bias (EOB) or to evaluate a bias intervention (BI) (see Fig. 1 for inclusion criteria). Some of the included studies focused on both, documenting evidence in addition to intervening biases and those studies were grouped separately. The analysis revealed that 69/139 (50%) of the included studies focused exclusively on documenting evidence of bias (EOB). There were fewer studies ( n = 51/139, 37%) which solely focused on bias interventions such as programs, seminars or curricular innovations. A small minority of the included studies were more comprehensive in that they documented EOB followed by an intervention strategy ( n = 19/139, 11%). These results demonstrate that most bias research is dedicated to documenting evidence of bias among these groups rather than evaluating a bias intervention strategy.
Research goal distribution
Our next objective was to calculate the distribution of studies with respect to the study goal (EOB, BI or both), within the 163 biases studied across the 139 papers as calculated in Table 1 . In general, the goal of the studies favors documenting evidence of bias with the exception of race/ethnic bias which is more focused on bias intervention (Fig. 3 ). Fewer studies were aimed at both, documenting evidence then providing an intervention, across all bias categories.
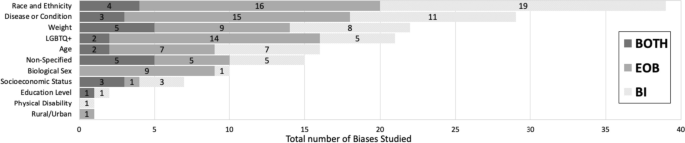
Sorting of total biases ( n = 163) within medical students or residents or a mixed population based on the bias category . Dark grey indicates studies with a dual goal, to document evidence of bias and to intervene bias. Medium grey bars indicate studies which focused on documenting evidence of bias. Light grey bars indicate studies focused on bias intervention within these populations. Numbers inside the bars indicate the total number of biases for the respective study goal. * Non-specified bias includes studies which focused on implicit bias but did not mention the type of bias investigated
Furthermore, we also calculated the ratio of EOB, BI and both (EOB + BI) within each of our population of interest (MS; n = 122, Res; n = 26 and mixed; n = 15) for the 163 biases observed in our included studies. Over half ( n = 64/122, 52%) of the total bias occurrences in MS were focused on documenting EOB (Fig. 4 ). Contrastingly, a shift was observed within resident populations where most biases addressed were aimed at intervention ( n = 12/26, 41%) rather than EOB ( n = 4/26, 14%) (Fig. 4 ). Studies which included both MS and Res (mixed) were primarily focused on documenting EOB ( n = 9/15, 60%), with 33% ( n = 5/15) aimed at bias intervention and 7% ( n = 1/15) which did both (Fig. 4 ). Although far fewer studies were documented in the Res population it is important to highlight that most of these studies were focused on bias intervention when compared to MS population where we documented a majority of studies focused on evidence of bias.
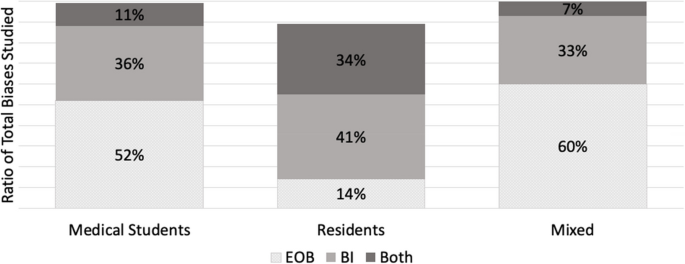
A ratio of the study goal for the total biases ( n = 163) mapped within each of the study population (MS, Res and Mixed). A study goal with a) documenting evidence of bias (EOB) is depicted in dotted grey, b) bias intervention (BI) in medium grey, and c) a dual focus (EOB + BI) is depicted in dark grey. * N = 122 for medical student studies. b N = 26 for residents. c N = 15 for mixed
Addressing biases at an earlier stage of medical career is critical for future physicians engaging with diverse patients, since it is established that bias negatively influences provider-patient interactions [ 171 ], clinical decision-making [ 172 ] and reduces favorable treatment outcomes [ 2 ]. We set out with an intention to explore how bias is addressed within the medical curriculum. Our research question was: how has the trend in bias research changed over time, more specifically a) what is the timeline of papers published? b) what bias characteristics have been studied in the physician-trainee population and c) how are these biases addressed? With the introduction of ‘standards of diversity’ by the Liaison Committee on Medical Education, along with the Association of American Medical Colleges (AAMC) and the American Medical Association (AMA) [ 173 , 174 ], we certainly expected and observed a sustained uptick in research pertaining to bias. As shown here, research addressing bias in the target population (MS and Res) is on the rise, however only 139 papers fit our inclusion criteria. Of these studies, nearly 90% have been published since 2005 after the “Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care” report was published in 2003 [ 7 ]. However, given the well documented effects of physician held bias, we anticipated significantly more number of studies focused on bias at the medical student or resident level.
A key component from this study was that we generated descriptive categories of biases. Sorting the biases into descriptive categories helps to identify a more targeted approach for a specific bias intervention, rather than to broadly intervene bias as a whole. In fact, our analysis found a number of publications (labeled “non-specified bias” in Table 1 ) which studied implicit bias without specifying the patient attribute or the characteristic that the bias was against. In total, we generated 11 descriptive categories of bias from our scoping review which are shown in Table 1 and Fig. 3 . Furthermore, our bias descriptors grouped similar kinds of biases within a single category. For example, the category, “disease or condition” included papers that studied bias against any type of disease (Mental illness, HIV stigma, diabetes), condition (Pain management), or lifestyle. We neither performed a qualitative assessment of the studies nor did we test the efficacy of the bias intervention studies and consider it a future direction of this work.
Evidence suggests that medical educators and healthcare professionals are struggling to find the appropriate approach to intervene biases [ 175 , 176 , 177 ] So far, bias reduction, bias reflection and bias management approaches have been proposed [ 26 , 27 , 178 ]. Previous implicit bias intervention strategies have been shown to be ineffective when biased attitudes of participants were assessed after a lag [ 179 ]. Understanding the descriptive categories of bias and previous existing research efforts, as we present here is only a fraction of the challenge. The theory of “cognitive bias” [ 180 ] and related branches of research [ 13 , 181 , 182 , 183 , 184 ] have been studied in the field of psychology for over three decades. It is only recently that cognitive bias theory has been applied to the field of medical education medicine, to explain its negative influence on clinical decision-making pertaining only to racial minorities [ 1 , 2 , 15 , 16 , 17 , 185 ]. In order to elicit meaningful changes with respect to targeted bias intervention, it is necessary to understand the psychological underpinnings (attitudes) leading to a certain descriptive category of bias (behaviors). The questions which medical educators need to ask are: a) Can these descriptive biases be identified under certain type/s of cognitive errors that elicits the bias and vice versa b) Are we working towards an attitude change which can elicit a sustained positive behavior change among healthcare professionals? And most importantly, c) are we creating a culture where participants voluntarily enroll themselves in bias interventions as opposed to being mandated to participate? Cognitive psychologists and behavioral scientists are well-positioned to help us find answers to these questions as they understand human behavior. Therefore, an interdisciplinary approach, a marriage between cognitive psychologists and medical educators, is key in targeting biases held by medical students, residents, and ultimately future physicians. This review may also be of interest to behavioral psychologists, keen on providing targeted intervening strategies to clinicians depending on the characteristics (age, weight, sex or race) the portrayed bias is against. Further, instead of an individualized approach, we need to strive for systemic changes and evidence-based strategies to intervene biases.
The next element in change is directing intervention strategies at the right stage in clinical education. Our study demonstrated that most of the research collected at the medical student level was focused on documenting evidence of bias. Although the overall number of studies at the resident level were fewer than at the medical student level, the ratio of research in favor of bias intervention was higher at the resident level (see Fig. 3 ). However, it could be helpful to focus on bias intervention earlier in learning, rather than at a later stage [ 186 ]. Additionally, educational resources such as textbooks, preparatory materials, and educators themselves are potential sources of propagating biases and therefore need constant evaluation against best practices [ 187 , 188 ].
This study has limitations. First, the list of the descriptive bias categories that we generated was not grounded in any particular theory so assigning a category was subjective. Additionally, there were studies that were categorized as “nonspecified” bias as the studies themselves did not mention the specific type of bias that they were addressing. Moreover, we had to exclude numerous publications solely because they were not evidence-based and were either perspectives, commentaries or opinion pieces. Finally, there were overall fewer studies focused on the resident population, so the calculated ratio of MS:Res studies did not compare similar sample sizes.
Future directions of our study include working with behavioral scientists to categorize these bias characteristics (Table 1 ) into cognitive error types [ 189 ]. Additionally, we aim to assess the effectiveness of the intervention strategies and categorize the approach of the intervention strategies.
The primary goal of our review was to organize, compare and quantify literature pertaining to bias within medical school curricula and residency programs. We neither performed a qualitative assessment of the studies nor did we test the efficacy of studies that were sorted into “bias intervention” as is typical of scoping reviews [ 22 ]. In summary, our research identified 11 descriptive categories of biases studied within medical students and resident populations with “race and ethnicity”, “disease or condition”, “weight”, “LGBTQ + ” and “age” being the top five most studied biases. Additionally, we found a greater number of studies conducted in medical students (105/139) when compared to residents (19/139). However, most of the studies in the resident population focused on bias intervention. The results from our review highlight the following gaps: a) bias categories where more research is needed, b) biases that are studied within medical school versus in residency programs and c) study focus in terms of demonstrating the presence of bias or working towards bias intervention.
This review provides a visual analysis of the known categories of bias addressed within the medical school curriculum and in residency programs in addition to providing a comparison of studies with respect to the study goal within medical education literature. The results from our review should be of interest to community organizations, institutions, program directors and medical educators interested in knowing and understanding the types of bias existing within healthcare populations. It might be of special interest to researchers who wish to explore other types of biases that have been understudied within medical school and resident populations, thus filling the gaps existing in bias research.
Despite the number of studies designed to provide bias intervention for MS and Res populations, and an overall cultural shift to be aware of one’s own biases, biases held by both medical students and residents still persist. Further, psychologists have recently demonstrated the ineffectiveness of some bias intervention efforts [ 179 , 190 ]. Therefore, it is perhaps unrealistic to expect these biases to be eliminated altogether. However, effective intervention strategies grounded in cognitive psychology should be implemented earlier on in medical training. Our focus should be on providing evidence-based approaches and safe spaces for an attitude and culture change, so as to induce actionable behavioral changes.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- Medical student
Evidence of bias
- Bias intervention
Hagiwara N, Mezuk B, Elston Lafata J, Vrana SR, Fetters MD. Study protocol for investigating physician communication behaviours that link physician implicit racial bias and patient outcomes in Black patients with type 2 diabetes using an exploratory sequential mixed methods design. BMJ Open. 2018;8(10):e022623.
Article Google Scholar
Haider AH, Schneider EB, Sriram N, Dossick DS, Scott VK, Swoboda SM, Losonczy L, Haut ER, Efron DT, Pronovost PJ, et al. Unconscious race and social class bias among acute care surgical clinicians and clinical treatment decisions. JAMA Surg. 2015;150(5):457–64.
Penner LA, Dovidio JF, Gonzalez R, Albrecht TL, Chapman R, Foster T, Harper FW, Hagiwara N, Hamel LM, Shields AF, et al. The effects of oncologist implicit racial bias in racially discordant oncology interactions. J Clin Oncol. 2016;34(24):2874–80.
Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319–26.
Garrett SB, Jones L, Montague A, Fa-Yusuf H, Harris-Taylor J, Powell B, Chan E, Zamarripa S, Hooper S, Chambers Butcher BD. Challenges and opportunities for clinician implicit bias training: insights from perinatal care stakeholders. Health Equity. 2023;7(1):506–19.
Shah HS, Bohlen J. Implicit bias. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Copyright © 2023, StatPearls Publishing LLC.
Google Scholar
Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. In: Smedley BD, Stith AY, Nelson AR, editors. Washington (DC): National Academies Press (US); 2003. PMID: 25032386.
Dehon E, Weiss N, Jones J, Faulconer W, Hinton E, Sterling S. A systematic review of the impact of physician implicit racial bias on clinical decision making. Acad Emerg Med. 2017;24(8):895–904.
Oliver MN, Wells KM, Joy-Gaba JA, Hawkins CB, Nosek BA. Do physicians’ implicit views of African Americans affect clinical decision making? J Am Board Fam Med. 2014;27(2):177–88.
Rincon-Subtirelu M. Education as a tool to modify anti-obesity bias among pediatric residents. Int J Med Educ. 2017;8:77–8.
Gustafsson Sendén M, Renström EA. Gender bias in assessment of future work ability among pain patients - an experimental vignette study of medical students’ assessment. Scand J Pain. 2019;19(2):407–14.
Hardeman RR, Burgess D, Phelan S, Yeazel M, Nelson D, van Ryn M. Medical student socio-demographic characteristics and attitudes toward patient centered care: do race, socioeconomic status and gender matter? A report from the medical student CHANGES study. Patient Educ Couns. 2015;98(3):350–5.
Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102(1):4–27.
Kruse JA, Collins JL, Vugrin M. Educational strategies used to improve the knowledge, skills, and attitudes of health care students and providers regarding implicit bias: an integrative review of the literature. Int J Nurs Stud Adv. 2022;4:100073.
Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit bias in health care: a narrative review. Group Process Intergroup Relat. 2016;19(4):528–42.
Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, Eng E, Day SH, Coyne-Beasley T. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):E60–76.
FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
Gonzalez CM, Onumah CM, Walker SA, Karp E, Schwartz R, Lypson ML. Implicit bias instruction across disciplines related to the social determinants of health: a scoping review. Adv Health Sci Educ. 2023;28(2):541–87.
Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–85.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69.
Pat C, Geeta S, Sílvia M. Cognitive debiasing 1: origins of bias and theory of debiasing. BMJ Qual Saf. 2013;22(Suppl 2):ii58.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Thomas A, Lubarsky S, Durning SJ, Young ME. Knowledge syntheses in medical education: demystifying scoping reviews. Acad Med. 2017;92(2):161–6.
Hagopian A, Thompson MJ, Fordyce M, Johnson KE, Hart LG. The migration of physicians from sub-Saharan Africa to the United States of America: measures of the African brain drain. Hum Resour Health. 2004;2(1):17.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Teal CR, Shada RE, Gill AC, Thompson BM, Frugé E, Villarreal GB, Haidet P. When best intentions aren’t enough: Helping medical students develop strategies for managing bias about patients. J Gen Intern Med. 2010;25(Suppl 2):S115–8.
Gonzalez CM, Walker SA, Rodriguez N, Noah YS, Marantz PR. Implicit bias recognition and management in interpersonal encounters and the learning environment: a skills-based curriculum for medical students. MedEdPORTAL. 2021;17:11168.
Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A. 2016;113(16):4296–301.
Mayfield JJ, Ball EM, Tillery KA, Crandall C, Dexter J, Winer JM, Bosshardt ZM, Welch JH, Dolan E, Fancovic ER, et al. Beyond men, women, or both: a comprehensive, LGBTQ-inclusive, implicit-bias-aware, standardized-patient-based sexual history taking curriculum. MedEdPORTAL. 2017;13:10634.
Morris M, Cooper RL, Ramesh A, Tabatabai M, Arcury TA, Shinn M, Im W, Juarez P, Matthews-Juarez P. Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC Med Educ. 2019;19(1):325.
Perdomo J, Tolliver D, Hsu H, He Y, Nash KA, Donatelli S, Mateo C, Akagbosu C, Alizadeh F, Power-Hays A, et al. Health equity rounds: an interdisciplinary case conference to address implicit bias and structural racism for faculty and trainees. MedEdPORTAL. 2019;15:10858.
Sherman MD, Ricco J, Nelson SC, Nezhad SJ, Prasad S. Implicit bias training in a residency program: aiming for enduring effects. Fam Med. 2019;51(8):677–81.
van Ryn M, Hardeman R, Phelan SM, Burgess DJ, Dovidio JF, Herrin J, Burke SE, Nelson DB, Perry S, Yeazel M, et al. Medical school experiences associated with change in implicit racial bias among 3547 students: a medical student CHANGES study report. J Gen Intern Med. 2015;30(12):1748–56.
Chary AN, Molina MF, Dadabhoy FZ, Manchanda EC. Addressing racism in medicine through a resident-led health equity retreat. West J Emerg Med. 2020;22(1):41–4.
DallaPiazza M, Padilla-Register M, Dwarakanath M, Obamedo E, Hill J, Soto-Greene ML. Exploring racism and health: an intensive interactive session for medical students. MedEdPORTAL. 2018;14:10783.
Dennis SN, Gold RS, Wen FK. Learner reactions to activities exploring racism as a social determinant of health. Fam Med. 2019;51(1):41–7.
Gonzalez CM, Walker SA, Rodriguez N, Karp E, Marantz PR. It can be done! a skills-based elective in implicit bias recognition and management for preclinical medical students. Acad Med. 2020;95(12S Addressing Harmful Bias and Eliminating Discrimination in Health Professions Learning Environments):S150–5.
Motzkus C, Wells RJ, Wang X, Chimienti S, Plummer D, Sabin J, Allison J, Cashman S. Pre-clinical medical student reflections on implicit bias: Implications for learning and teaching. PLoS ONE. 2019;14(11):e0225058.
Phelan SM, Burke SE, Cunningham BA, Perry SP, Hardeman RR, Dovidio JF, Herrin J, Dyrbye LN, White RO, Yeazel MW, et al. The effects of racism in medical education on students’ decisions to practice in underserved or minority communities. Acad Med. 2019;94(8):1178–89.
Zeidan A, Tiballi A, Woodward M, Di Bartolo IM. Targeting implicit bias in medicine: lessons from art and archaeology. West J Emerg Med. 2019;21(1):1–3.
Baker TK, Smith GS, Jacobs NN, Houmanfar R, Tolles R, Kuhls D, Piasecki M. A deeper look at implicit weight bias in medical students. Adv Health Sci Educ Theory Pract. 2017;22(4):889–900.
Eymard AS, Douglas DH. Ageism among health care providers and interventions to improve their attitudes toward older adults: an integrative review. J Gerontol Nurs. 2012;38(5):26–35.
Garrison CB, McKinney-Whitson V, Johnston B, Munroe A. Race matters: addressing racism as a health issue. Int J Psychiatry Med. 2018;53(5–6):436–44.
Geller G, Watkins PA. Addressing medical students’ negative bias toward patients with obesity through ethics education. AMA J Ethics. 2018;20(10):E948-959.
Onyeador IN, Wittlin NM, Burke SE, Dovidio JF, Perry SP, Hardeman RR, Dyrbye LN, Herrin J, Phelan SM, van Ryn M. The value of interracial contact for reducing anti-black bias among non-black physicians: a Cognitive Habits and Growth Evaluation (CHANGE) study report. Psychol Sci. 2020;31(1):18–30.
Poustchi Y, Saks NS, Piasecki AK, Hahn KA, Ferrante JM. Brief intervention effective in reducing weight bias in medical students. Fam Med. 2013;45(5):345–8.
Ruiz JG, Andrade AD, Anam R, Taldone S, Karanam C, Hogue C, Mintzer MJ. Group-based differences in anti-aging bias among medical students. Gerontol Geriatr Educ. 2015;36(1):58–78.
Simpson T, Evans J, Goepfert A, Elopre L. Implementing a graduate medical education anti-racism workshop at an academic university in the Southern USA. Med Educ Online. 2022;27(1):1981803.
Wittlin NM, Dovidio JF, Burke SE, Przedworski JM, Herrin J, Dyrbye L, Onyeador IN, Phelan SM, van Ryn M. Contact and role modeling predict bias against lesbian and gay individuals among early-career physicians: a longitudinal study. Soc Sci Med. 2019;238:112422.
Miller DP Jr, Spangler JG, Vitolins MZ, Davis SW, Ip EH, Marion GS, Crandall SJ. Are medical students aware of their anti-obesity bias? Acad Med. 2013;88(7):978–82.
Gonzalez CM, Deno ML, Kintzer E, Marantz PR, Lypson ML, McKee MD. A qualitative study of New York medical student views on implicit bias instruction: implications for curriculum development. J Gen Intern Med. 2019;34(5):692–8.
Gonzalez CM, Kim MY, Marantz PR. Implicit bias and its relation to health disparities: a teaching program and survey of medical students. Teach Learn Med. 2014;26(1):64–71.
Gonzalez CM, Nava S, List J, Liguori A, Marantz PR. How assumptions and preferences can affect patient care: an introduction to implicit bias for first-year medical students. MedEdPORTAL. 2021;17:11162.
Hernandez RA, Haidet P, Gill AC, Teal CR. Fostering students’ reflection about bias in healthcare: cognitive dissonance and the role of personal and normative standards. Med Teach. 2013;35(4):e1082-1089.
Kushner RF, Zeiss DM, Feinglass JM, Yelen M. An obesity educational intervention for medical students addressing weight bias and communication skills using standardized patients. BMC Med Educ. 2014;14:53.
Nazione S, Silk KJ. Patient race and perceived illness responsibility: effects on provider helping and bias. Med Educ. 2013;47(8):780–9.
Ogunyemi D. Defeating unconscious bias: the role of a structured, reflective, and interactive workshop. J Grad Med Educ. 2021;13(2):189–94.
Phelan SM, Burke SE, Hardeman RR, White RO, Przedworski J, Dovidio JF, Perry SP, Plankey M, A Cunningham B, Finstad D, et al. Medical school factors associated with changes in implicit and explicit bias against gay and lesbian people among 3492 graduating medical students. J Gen Intern Med. 2017;32(11):1193–201.
Phelan SM, Puhl RM, Burke SE, Hardeman R, Dovidio JF, Nelson DB, Przedworski J, Burgess DJ, Perry S, Yeazel MW, et al. The mixed impact of medical school on medical students’ implicit and explicit weight bias. Med Educ. 2015;49(10):983–92.
Barber Doucet H, Ward VL, Johnson TJ, Lee LK. Implicit bias and caring for diverse populations: pediatric trainee attitudes and gaps in training. Clin Pediatr (Phila). 2021;60(9–10):408–17.
Burke SE, Dovidio JF, Przedworski JM, Hardeman RR, Perry SP, Phelan SM, Nelson DB, Burgess DJ, Yeazel MW, van Ryn M. Do contact and empathy mitigate bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. 2015;90(5):645–51.
Johnston B, McKinney-Whitson V, Garrison V. Race matters: addressing racism as a health issue. WMJ. 2021;120(S1):S74–7.
Kost A, Akande T, Jones R, Gabert R, Isaac M, Dettmar NS. Use of patient identifiers at the University of Washington School of Medicine: building institutional consensus to reduce bias and stigma. Fam Med. 2021;53(5):366–71.
Madan AK, Aliabadi-Wahle S, Beech DJ. Ageism in medical students’ treatment recommendations: the example of breast-conserving procedures. Acad Med. 2001;76(3):282–4.
Marbin J, Lewis L, Kuo AK, Schudel C, Gutierrez JR. The power of place: travel to explore structural racism and health disparities. Acad Med. 2021;96(11):1569–73.
Phelan SM, Dovidio JF, Puhl RM, Burgess DJ, Nelson DB, Yeazel MW, Hardeman R, Perry S, van Ryn M. Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student CHANGES study. Obesity (Silver Spring). 2014;22(4):1201–8.
Van J, Aloman C, Reau N. Potential bias and misconceptions in liver transplantation for alcohol- and obesity-related liver disease. Am J Gastroenterol. 2021;116(10):2089–97.
White-Means S, Zhiyong D, Hufstader M, Brown LT. Cultural competency, race, and skin tone bias among pharmacy, nursing, and medical students: implications for addressing health disparities. Med Care Res Rev. 2009;66(4):436–55.
Williams RL, Vasquez CE, Getrich CM, Kano M, Boursaw B, Krabbenhoft C, Sussman AL. Racial/gender biases in student clinical decision-making: a mixed-method study of medical school attributes associated with lower incidence of biases. J Gen Intern Med. 2018;33(12):2056–64.
Cohen RW, Persky S. Influence of weight etiology information and trainee characteristics on physician-trainees’ clinical and interpersonal communication. Patient Educ Couns. 2019;102(9):1644–9.
Haider AH, Sexton J, Sriram N, Cooper LA, Efron DT, Swoboda S, Villegas CV, Haut ER, Bonds M, Pronovost PJ, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA. 2011;306(9):942–51.
Lewis R, Lamdan RM, Wald D, Curtis M. Gender bias in the diagnosis of a geriatric standardized patient: a potential confounding variable. Acad Psychiatry. 2006;30(5):392–6.
Matharu K, Shapiro JF, Hammer RR, Kravitz RL, Wilson MD, Fitzgerald FT. Reducing obesity prejudice in medical education. Educ Health. 2014;27(3):231–7.
McLean ME, McLean LE, McLean-Holden AC, Campbell LF, Horner AM, Kulkarni ML, Melville LD, Fernandez EA. Interphysician weight bias: a cross-sectional observational survey study to guide implicit bias training in the medical workplace. Acad Emerg Med. 2021;28(9):1024–34.
Meadows A, Higgs S, Burke SE, Dovidio JF, van Ryn M, Phelan SM. Social dominance orientation, dispositional empathy, and need for cognitive closure moderate the impact of empathy-skills training, but not patient contact, on medical students’ negative attitudes toward higher-weight patients. Front Psychol. 2017;8:15.
Stone J, Moskowitz GB, Zestcott CA, Wolsiefer KJ. Testing active learning workshops for reducing implicit stereotyping of Hispanics by majority and minority group medical students. Stigma Health. 2020;5(1):94–103.
Symons AB, Morley CP, McGuigan D, Akl EA. A curriculum on care for people with disabilities: effects on medical student self-reported attitudes and comfort level. Disabil Health J. 2014;7(1):88–95.
Ufomata E, Eckstrand KL, Hasley P, Jeong K, Rubio D, Spagnoletti C. Comprehensive internal medicine residency curriculum on primary care of patients who identify as LGBT. LGBT Health. 2018;5(6):375–80.
Aultman JM, Borges NJ. A clinical and ethical investigation of pre-medical and medical students’ attitudes, knowledge, and understanding of HIV. Med Educ Online. 2006;11:1–12.
Bates T, Cohan M, Bragg DS, Bedinghaus J. The Medical College of Wisconsin senior mentor program: experience of a lifetime. Gerontol Geriatr Educ. 2006;27(2):93–103.
Chiaramonte GR, Friend R. Medical students’ and residents’ gender bias in the diagnosis, treatment, and interpretation of coronary heart disease symptoms. Health Psychol. 2006;25(3):255–66.
Friedberg F, Sohl SJ, Halperin PJ. Teaching medical students about medically unexplained illnesses: a preliminary study. Med Teach. 2008;30(6):618–21.
Gonzales E, Morrow-Howell N, Gilbert P. Changing medical students’ attitudes toward older adults. Gerontol Geriatr Educ. 2010;31(3):220–34.
Hinners CK, Potter JF. A partnership between the University of Nebraska College of Medicine and the community: fostering positive attitudes towards the aged. Gerontol Geriatr Educ. 2006;27(2):83–91.
Lee M, Coulehan JL. Medical students’ perceptions of racial diversity and gender equality. Med Educ. 2006;40(7):691–6.
Schmetzer AD, Lafuze JE. Overcoming stigma: involving families in medical student and psychiatric residency education. Acad Psychiatry. 2008;32(2):127–31.
Willen SS, Bullon A, Good MJD. Opening up a huge can of worms: reflections on a “cultural sensitivity” course for psychiatry residents. Harv Rev Psychiatry. 2010;18(4):247–53.
Dogra N, Karnik N. First-year medical students’ attitudes toward diversity and its teaching: an investigation at one U.S. medical school. Acad Med. 2003;78(11):1191–200.
Fitzpatrick C, Musser A, Mosqueda L, Boker J, Prislin M. Student senior partnership program: University of California Irvine School of Medicine. Gerontol Geriatr Educ. 2006;27(2):25–35.
Hoffman KG, Gray P, Hosokawa MC, Zweig SC. Evaluating the effectiveness of a senior mentor program: the University of Missouri-Columbia School of Medicine. Gerontol Geriatr Educ. 2006;27(2):37–47.
Kantor BS, Myers MR. From aging…to saging-the Ohio State Senior Partners Program: longitudinal and experiential geriatrics education. Gerontol Geriatr Educ. 2006;27(2):69–74.
Klamen DL, Grossman LS, Kopacz DR. Medical student homophobia. J Homosex. 1999;37(1):53–63.
Kopacz DR, Grossman LS, Klamen DL. Medical students and AIDS: knowledge, attitudes and implications for education. Health Educ Res. 1999;14(1):1–6.
Leiblum SR. An established medical school human sexuality curriculum: description and evaluation. Sex Relatsh Ther. 2001;16(1):59–70.
Rastegar DA, Fingerhood MI, Jasinski DR. A resident clerkship that combines inpatient and outpatient training in substance abuse and HIV care. Subst Abuse. 2004;25(4):11–5.
Roberts E, Richeson NA, Thornhill JTIV, Corwin SJ, Eleazer GP. The senior mentor program at the University of South Carolina School of Medicine: an innovative geriatric longitudinal curriculum. Gerontol Geriatr Educ. 2006;27(2):11–23.
Burgess DJ, Burke SE, Cunningham BA, Dovidio JF, Hardeman RR, Hou YF, Nelson DB, Perry SP, Phelan SM, Yeazel MW, et al. Medical students’ learning orientation regarding interracial interactions affects preparedness to care for minority patients: a report from medical student CHANGES. BMC Med Educ. 2016;16:254.
Burgess DJ, Hardeman RR, Burke SE, Cunningham BA, Dovidio JF, Nelson DB, Perry SP, Phelan SM, Yeazel MW, Herrin J, et al. Incoming medical students’ political orientation affects outcomes related to care of marginalized groups: results from the medical student CHANGES study. J Health Pol Policy Law. 2019;44(1):113–46.
Kurtz ME, Johnson SM, Tomlinson T, Fiel NJ. Teaching medical students the effects of values and stereotyping on the doctor/patient relationship. Soc Sci Med. 1985;21(9):1043–7.
Matharu K, Kravitz RL, McMahon GT, Wilson MD, Fitzgerald FT. Medical students’ attitudes toward gay men. BMC Med Educ. 2012;12:71.
Pearl RL, Argueso D, Wadden TA. Effects of medical trainees’ weight-loss history on perceptions of patients with obesity. Med Educ. 2017;51(8):802–11.
Perry SP, Dovidio JF, Murphy MC, van Ryn M. The joint effect of bias awareness and self-reported prejudice on intergroup anxiety and intentions for intergroup contact. Cultur Divers Ethnic Minor Psychol. 2015;21(1):89–96.
Phelan SM, Burgess DJ, Burke SE, Przedworski JM, Dovidio JF, Hardeman R, Morris M, van Ryn M. Beliefs about the causes of obesity in a national sample of 4th year medical students. Patient Educ Couns. 2015;98(11):1446–9.
Phelan SM, Puhl RM, Burgess DJ, Natt N, Mundi M, Miller NE, Saha S, Fischer K, van Ryn M. The role of weight bias and role-modeling in medical students’ patient-centered communication with higher weight standardized patients. Patient Educ Couns. 2021;104(8):1962–9.
Polan HJ, Auerbach MI, Viederman M. AIDS as a paradigm of human behavior in disease: impact and implications of a course. Acad Psychiatry. 1990;14(4):197–203.
Reuben DB, Fullerton JT, Tschann JM, Croughan-Minihane M. Attitudes of beginning medical students toward older persons: a five-campus study. J Am Geriatr Soc. 1995;43(12):1430–6.
Tsai J. Building structural empathy to marshal critical education into compassionate practice: evaluation of a medical school critical race theory course. J Law Med Ethics. 2021;49(2):211–21.
Weyant RJ, Bennett ME, Simon M, Palaisa J. Desire to treat HIV-infected patients: similarities and differences across health-care professions. AIDS. 1994;8(1):117–21.
Ross PT, Lypson ML. Using artistic-narrative to stimulate reflection on physician bias. Teach Learn Med. 2014;26(4):344–9.
Calabrese SK, Earnshaw VA, Krakower DS, Underhill K, Vincent W, Magnus M, Hansen NB, Kershaw TS, Mayer KH, Betancourt JR, et al. A closer look at racism and heterosexism in medical students’ clinical decision-making related to HIV Pre-Exposure Prophylaxis (PrEP): implications for PrEP education. AIDS Behav. 2018;22(4):1122–38.
Fitterman-Harris HF, Vander Wal JS. Weight bias reduction among first-year medical students: a quasi-randomized, controlled trial. Clin Obes. 2021;11(6):e12479.
Madan AK, Cooper L, Gratzer A, Beech DJ. Ageism in breast cancer surgical options by medical students. Tenn Med. 2006;99(5):37–8, 41.
Bikmukhametov DA, Anokhin VA, Vinogradova AN, Triner WR, McNutt LA. Bias in medicine: a survey of medical student attitudes towards HIV-positive and marginalized patients in Russia, 2010. J Int AIDS Soc. 2012;15(2):17372.
Dijkstra AF, Verdonk P, Lagro-Janssen AL. Gender bias in medical textbooks: examples from coronary heart disease, depression, alcohol abuse and pharmacology. Med Educ. 2008;42(10):1021–8.
Dobrowolska B, Jędrzejkiewicz B, Pilewska-Kozak A, Zarzycka D, Ślusarska B, Deluga A, Kościołek A, Palese A. Age discrimination in healthcare institutions perceived by seniors and students. Nurs Ethics. 2019;26(2):443–59.
Hamberg K, Risberg G, Johansson EE, Westman G. Gender bias in physicians’ management of neck pain: a study of the answers in a Swedish national examination. J Womens Health Gend Based Med. 2002;11(7):653–66.
Magliano L, Read J, Sagliocchi A, Oliviero N, D’Ambrosio A, Campitiello F, Zaccaro A, Guizzaro L, Patalano M. “Social dangerousness and incurability in schizophrenia”: results of an educational intervention for medical and psychology students. Psychiatry Res. 2014;219(3):457–63.
Reis SP, Wald HS. Contemplating medicine during the Third Reich: scaffolding professional identity formation for medical students. Acad Med. 2015;90(6):770–3.
Schroyen S, Adam S, Marquet M, Jerusalem G, Thiel S, Giraudet AL, Missotten P. Communication of healthcare professionals: Is there ageism? Eur J Cancer Care (Engl). 2018;27(1):e12780.
Swift JA, Hanlon S, El-Redy L, Puhl RM, Glazebrook C. Weight bias among UK trainee dietitians, doctors, nurses and nutritionists. J Hum Nutr Diet. 2013;26(4):395–402.
Swift JA, Tischler V, Markham S, Gunning I, Glazebrook C, Beer C, Puhl R. Are anti-stigma films a useful strategy for reducing weight bias among trainee healthcare professionals? Results of a pilot randomized control trial. Obes Facts. 2013;6(1):91–102.
Yertutanol FDK, Candansayar S, Seydaoğlu G. Homophobia in health professionals in Ankara, Turkey: developing a scale. Transcult Psychiatry. 2019;56(6):1191–217.
Arnold O, Voracek M, Musalek M, Springer-Kremser M. Austrian medical students’ attitudes towards male and female homosexuality: a comparative survey. Wien Klin Wochenschr. 2004;116(21–22):730–6.
Arvaniti A, Samakouri M, Kalamara E, Bochtsou V, Bikos C, Livaditis M. Health service staff’s attitudes towards patients with mental illness. Soc Psychiatry Psychiatr Epidemiol. 2009;44(8):658–65.
Lopes L, Gato J, Esteves M. Portuguese medical students’ knowledge and attitudes towards homosexuality. Acta Med Port. 2016;29(11):684–93.
Papadaki V, Plotnikof K, Gioumidou M, Zisimou V, Papadaki E. A comparison of attitudes toward lesbians and gay men among students of helping professions in Crete, Greece: the cases of social work, psychology, medicine, and nursing. J Homosex. 2015;62(6):735–62.
Papaharitou S, Nakopoulou E, Moraitou M, Tsimtsiou Z, Konstantinidou E, Hatzichristou D. Exploring sexual attitudes of students in health professions. J Sex Med. 2008;5(6):1308–16.
Roberts JH, Sanders T, Mann K, Wass V. Institutional marginalisation and student resistance: barriers to learning about culture, race and ethnicity. Adv Health Sci Educ. 2010;15(4):559–71.
Wilhelmi L, Ingendae F, Steinhaeuser J. What leads to the subjective perception of a ‘rural area’? A qualitative study with undergraduate students and postgraduate trainees in Germany to tailor strategies against physician’s shortage. Rural Remote Health. 2018;18(4):4694.
Herrmann-Werner A, Loda T, Wiesner LM, Erschens RS, Junne F, Zipfel S. Is an obesity simulation suit in an undergraduate medical communication class a valuable teaching tool? A cross-sectional proof of concept study. BMJ Open. 2019;9(8):e029738.
Ahadinezhad B, Khosravizadeh O, Maleki A, Hashtroodi A. Implicit racial bias among medical graduates and students by an IAT measure: a systematic review and meta-analysis. Ir J Med Sci. 2022;191(4):1941–9. https://doi.org/10.1007/s11845-021-02756-3 .
Hsieh JG, Hsu M, Wang YW. An anthropological approach to teach and evaluate cultural competence in medical students - the application of mini-ethnography in medical history taking. Med Educ Online. 2016;21:32561.
Poreddi V, Thimmaiah R, Math SB. Attitudes toward people with mental illness among medical students. J Neurosci Rural Pract. 2015;6(3):349–54.
Mino Y, Yasuda N, Tsuda T, Shimodera S. Effects of a one-hour educational program on medical students’ attitudes to mental illness. Psychiatry Clin Neurosci. 2001;55(5):501–7.
Omori A, Tateno A, Ideno T, Takahashi H, Kawashima Y, Takemura K, Okubo Y. Influence of contact with schizophrenia on implicit attitudes towards schizophrenia patients held by clinical residents. BMC Psychiatry. 2012;12:8.
Banwari G, Mistry K, Soni A, Parikh N, Gandhi H. Medical students and interns’ knowledge about and attitude towards homosexuality. J Postgrad Med. 2015;61(2):95–100.
Lee SY. Obesity education in medical school curricula in Korea. J Obes Metab Syndr. 2018;27(1):35–8.
Aruna G, Mittal S, Yadiyal MB, Acharya C, Acharya S, Uppulari C. Perception, knowledge, and attitude toward mental disorders and psychiatry among medical undergraduates in Karnataka: a cross-sectional study. Indian J Psychiatry. 2016;58(1):70–6.
Wong YL. Review paper: gender competencies in the medical curriculum: addressing gender bias in medicine. Asia Pac J Public Health. 2009;21(4):359–76.
Earnshaw VA, Jin H, Wickersham JA, Kamarulzaman A, John J, Lim SH, Altice FL. Stigma toward men who have sex with men among future healthcare providers in Malaysia: would more interpersonal contact reduce prejudice? AIDS Behav. 2016;20(1):98–106.
Larson B, Herx L, Williamson T, Crowshoe L. Beyond the barriers: family medicine residents’ attitudes towards providing Aboriginal health care. Med Educ. 2011;45(4):400–6.
Wagner AC, Girard T, McShane KE, Margolese S, Hart TA. HIV-related stigma and overlapping stigmas towards people living with HIV among health care trainees in Canada. AIDS Educ Prev. 2017;29(4):364–76.
Tellier P-P, Bélanger E, Rodríguez C, Ware MA, Posel N. Improving undergraduate medical education about pain assessment and management: a qualitative descriptive study of stakeholders’ perceptions. Pain Res Manage. 2013;18(5):259–65.
Loignon C, Boudreault-Fournier A, Truchon K, Labrousse Y, Fortin B. Medical residents reflect on their prejudices toward poverty: a photovoice training project. BMC Med Educ. 2014;14:1050.
Phillips SP, Clarke M. More than an education: the hidden curriculum, professional attitudes and career choice. Med Educ. 2012;46(9):887–93.
Jaworsky D, Gardner S, Thorne JG, Sharma M, McNaughton N, Paddock S, Chew D, Lees R, Makuwaza T, Wagner A, et al. The role of people living with HIV as patient instructors—Reducing stigma and improving interest around HIV care among medical students. AIDS Care. 2017;29(4):524–31.
Sukhera J, Wodzinski M, Teunissen PW, Lingard L, Watling C. Striving while accepting: exploring the relationship between identity and implicit bias recognition and management. Acad Med. 2018;93(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 57th Annual Research in Medical Education Sessions):S82-s88.
Harris R, Cormack D, Curtis E, Jones R, Stanley J, Lacey C. Development and testing of study tools and methods to examine ethnic bias and clinical decision-making among medical students in New Zealand: the Bias and Decision-Making in Medicine (BDMM) study. BMC Med Educ. 2016;16:173.
Cormack D, Harris R, Stanley J, Lacey C, Jones R, Curtis E. Ethnic bias amongst medical students in Aotearoa/New Zealand: findings from the Bias and Decision Making in Medicine (BDMM) study. PLoS ONE. 2018;13(8):e0201168.
Harris R, Cormack D, Stanley J, Curtis E, Jones R, Lacey C. Ethnic bias and clinical decision-making among New Zealand medical students: an observational study. BMC Med Educ. 2018;18(1):18.
Robinson EL, Ball LE, Leveritt MD. Obesity bias among health and non-health students attending an Australian university and their perceived obesity education. J Nutr Educ Behav. 2014;46(5):390–5.
Sopoaga F, Zaharic T, Kokaua J, Covello S. Training a medical workforce to meet the needs of diverse minority communities. BMC Med Educ. 2017;17:19.
Parker R, Larkin T, Cockburn J. A visual analysis of gender bias in contemporary anatomy textbooks. Soc Sci Med. 2017;180:106–13.
Gomes MdM. Doctors’ perspectives and practices regarding epilepsy. Arq Neuropsiquiatr. 2000;58(2):221–6.
Caixeta J, Fernandes PT, Bell GS, Sander JW, Li LM. Epilepsy perception amongst university students - A survey. Arq Neuropsiquiatr. 2007;65:43–8.
Tedrus GMAS, Fonseca LC, da Câmara Vieira AL. Knowledge and attitudes toward epilepsy amongst students in the health area: intervention aimed at enlightenment. Arq Neuropsiquiatr. 2007;65(4-B):1181–5.
Gomez-Moreno C, Verduzco-Aguirre H, Contreras-Garduño S, Perez-de-Acha A, Alcalde-Castro J, Chavarri-Guerra Y, García-Lara JMA, Navarrete-Reyes AP, Avila-Funes JA, Soto-Perez-de-Celis E. Perceptions of aging and ageism among Mexican physicians-in-training. Clin Transl Oncol. 2019;21(12):1730–5.
Campbell MH, Gromer J, Emmanuel MK, Harvey A. Attitudes Toward Transgender People Among Future Caribbean Doctors. Arch Sex Behav. 2022;51(4):1903-11. https://doi.org/10.1007/s10508-021-02205-3 .
Hatala R, Case SM. Examining the influence of gender on medical students’ decision making. J Womens Health Gend Based Med. 2000;9(6):617–23.
Deb T, Lempp H, Bakolis I, et al. Responding to experienced and anticipated discrimination (READ): anti -stigma training for medical students towards patients with mental illness – study protocol for an international multisite non-randomised controlled study. BMC Med Educ. 2019;19:41. https://doi.org/10.1186/s12909-019-1472-7 .
Morgan S, Plaisant O, Lignier B, Moxham BJ. Sexism and anatomy, as discerned in textbooks and as perceived by medical students at Cardiff University and University of Paris Descartes. J Anat. 2014;224(3):352–65.
Alford CL, Miles T, Palmer R, Espino D. An introduction to geriatrics for first-year medical students. J Am Geriatr Soc. 2001;49(6):782–7.
Stone J, Moskowitz GB. Non-conscious bias in medical decision making: what can be done to reduce it? Med Educ. 2011;45(8):768–76.
Nazione S. Slimming down medical provider weight bias in an obese nation. Med Educ. 2015;49(10):954–5.
Dogra N, Connin S, Gill P, Spencer J, Turner M. Teaching of cultural diversity in medical schools in the United Kingdom and Republic of Ireland: cross sectional questionnaire survey. BMJ. 2005;330(7488):403–4.
Aultman JM, Borges NJ. A clinical and ethical investigation of pre-medical and medical students’ attitudes, knowledge, and understanding of HIV. Med Educ Online. 2006;11(1):4596.
Deb T, Lempp H, Bakolis I, Vince T, Waugh W, Henderson C, Thornicroft G, Ando S, Yamaguchi S, Matsunaga A, et al. Responding to experienced and anticipated discrimination (READ): anti -stigma training for medical students towards patients with mental illness – study protocol for an international multisite non-randomised controlled study. BMC Med Educ. 2019;19(1):41.
Gonzalez CM, Grochowalski JH, Garba RJ, Bonner S, Marantz PR. Validity evidence for a novel instrument assessing medical student attitudes toward instruction in implicit bias recognition and management. BMC Med Educ. 2021;21(1):205.
Ogunyemi D. A practical approach to implicit bias training. J Grad Med Educ. 2021;13(4):583–4.
Dennis GC. Racism in medicine: planning for the future. J Natl Med Assoc. 2001;93(3 Suppl):1S-5S.
Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med. 2018;199:219–29.
Blair IV, Steiner JF, Hanratty R, Price DW, Fairclough DL, Daugherty SL, Bronsert M, Magid DJ, Havranek EP. An investigation of associations between clinicians’ ethnic or racial bias and hypertension treatment, medication adherence and blood pressure control. J Gen Intern Med. 2014;29(7):987–95.
Stanford FC. The importance of diversity and inclusion in the healthcare workforce. J Natl Med Assoc. 2020;112(3):247–9.
Education LCoM. Standards on diversity. 2009. https://health.usf.edu/~/media/Files/Medicine/MD%20Program/Diversity/LCMEStandardsonDiversity1.ashx?la=en .
Onyeador IN, Hudson STJ, Lewis NA. Moving beyond implicit bias training: policy insights for increasing organizational diversity. Policy Insights Behav Brain Sci. 2021;8(1):19–26.
Forscher PS, Mitamura C, Dix EL, Cox WTL, Devine PG. Breaking the prejudice habit: mechanisms, timecourse, and longevity. J Exp Soc Psychol. 2017;72:133–46.
Lai CK, Skinner AL, Cooley E, Murrar S, Brauer M, Devos T, Calanchini J, Xiao YJ, Pedram C, Marshburn CK, et al. Reducing implicit racial preferences: II. Intervention effectiveness across time. J Exp Psychol Gen. 2016;145(8):1001–16.
Sukhera J, Watling CJ, Gonzalez CM. Implicit bias in health professions: from recognition to transformation. Acad Med. 2020;95(5):717–23.
Vuletich HA, Payne BK. Stability and change in implicit bias. Psychol Sci. 2019;30(6):854–62.
Tversky A, Kahneman D. Judgment under uncertainty: Heuristics and biases. Science. 1974;185(4157):1124–31.
Miller DT, Ross M. Self-serving biases in the attribution of causality: fact or fiction? Psychol Bull. 1975;82(2):213–25.
Nickerson RS. Confirmation bias: a ubiquitous phenomenon in many guises. Rev Gen Psychol. 1998;2(2):175–220.
Suveren Y. Unconscious bias: definition and significance. Psikiyatride Guncel Yaklasimlar. 2022;14(3):414–26.
Dietrich D, Olson M. A demonstration of hindsight bias using the Thomas confirmation vote. Psychol Rep. 1993;72(2):377–8.
Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–8.
Rushmer R, Davies HT. Unlearning in health care. Qual Saf Health Care. 2004;13 Suppl 2(Suppl 2):ii10-15.
Vu MT, Pham TTT. Gender, critical pedagogy, and textbooks: Understanding teachers’ (lack of) mediation of the hidden curriculum in the EFL classroom. Lang Teach Res. 2022;0(0). https://doi.org/10.1177/13621688221136937 .
Kalantari A, Alvarez A, Battaglioli N, Chung A, Cooney R, Boehmer SJ, Nwabueze A, Gottlieb M. Sex and race visual representation in emergency medicine textbooks and the hidden curriculum. AEM Educ Train. 2022;6(3):e10743.
Satya-Murti S, Lockhart J. Recognizing and reducing cognitive bias in clinical and forensic neurology. Neurol Clin Pract. 2015;5(5):389–96.
Chang EH, Milkman KL, Gromet DM, Rebele RW, Massey C, Duckworth AL, Grant AM. The mixed effects of online diversity training. Proc Natl Acad Sci U S A. 2019;116(16):7778–83.
Download references
Acknowledgements
The authors would like to thank Dr. Misa Mi, Professor and Medical Librarian at the Oakland University William Beaumont School of Medicine (OWUB) for her assistance with selection of databases and construction of literature search strategies for the scoping review. The authors also wish to thank Dr. Changiz Mohiyeddini, Professor in Behavioral Medicine and Psychopathology at Oakland University William Beaumont School of Medicine (OUWB) for his expertise and constructive feedback on our manuscript.
Author information
Authors and affiliations.
Department of Foundational Sciences, Central Michigan University College of Medicine, Mt. Pleasant, MI, 48859, USA
Brianne E. Lewis
Department of Foundational Medical Studies, Oakland University William Beaumont School of Medicine, 586 Pioneer Dr, Rochester, MI, 48309, USA
Akshata R. Naik
You can also search for this author in PubMed Google Scholar

Contributions
A.R.N and B.E.L were equally involved in study conception, design, collecting data and analyzing the data. B.E.L and A.R.N both contributed towards writing the manuscript. A.R.N and B.E.L are both senior authors on this paper. All authors reviewed the manuscript.
Corresponding author
Correspondence to Akshata R. Naik .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lewis, B.E., Naik, A.R. A scoping review to identify and organize literature trends of bias research within medical student and resident education. BMC Med Educ 23 , 919 (2023). https://doi.org/10.1186/s12909-023-04829-6
Download citation
Received : 14 March 2023
Accepted : 01 November 2023
Published : 05 December 2023
DOI : https://doi.org/10.1186/s12909-023-04829-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preclinical curriculum
- Evidence of bis
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Nepal J Epidemiol
- v.12(1); 2022 Mar
The Growing Importance of Mixed-Methods Research in Health
Sharada prasad wasti.
1,2 School of Human and Health Sciences, University of Huddersfield, United Kingdom
Padam Simkhada
3 Centre for Midwifery, Maternal and Perinatal Health, Bournemouth University, Bournemouth, United Kingdom
Edwin R. van Teijlingen
Brijesh sathian.
4 Geriatrics and long term care Department, Rumailah Hospital, Hamad Medical Corporation, Doha, Qatar
Indrajit Banerjee
5 Sir Seewoosagur Ramgoolam Medical College, Belle Rive, Mauritius
All authors have made substantial contributions to all of the following: (1) the conception and design of the study (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted
There is no conflict of interest for any author of this manuscript.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sector.
This paper illustrates the growing importance of mixed-methods research to many health disciplines ranging from nursing to epidemiology. Mixed-methods approaches requires not only the skills of the individual quantitative and qualitative methods but also a skill set to bring two methods/datasets/findings together in the most appropriate way. Health researchers need to pay careful attention to the ‘best’ approach to designing, implementing, analysing, integrating both quantitative (number) and qualitative (word) information and writing this up in a way offers greater insights and enhances its applicability. This paper highlights the strengths and weaknesses of mixed-methods approaches as well as some of the common mistakes made by researchers applying mixed-methods for the first time.
Quantitative and qualitative research methods each address different types of questions, collect different kinds of data and deliver different kinds of answers. Each set of methods has its own inherent strengths and weaknesses, and each offers a particular approach to address specific types of research questions (and agendas). Health disciplines such as dentistry, nursing, speech and language therapy, and physiotherapy often use either quantitative or qualitative research methods on their own. However, there is a steadily growing literature showing the advantages of mixed-methods research is used in the health care and health service field [ 1-2 ]. Although we have advocated the use of mixed-methods in this journal eight years ago [ 3 ], there is still not enough mixed-methods research training in the health research field, particularly for health care practitioners, such as nurses, physiotherapists, midwives, and doctors, wanting to do research. Mixed-methods research has been popular in the social sciences since the twentieth century [ 4 ], and it has been growing in popularity among healthcare professionals [ 5 ], although it is still underdeveloped in disciplines such nursing and midwifery [ 6 , 7 ].
Underpinning philosophies
To help understand that mixed-methods research is not simply employing two different methods in the same study, one needs to consider their underpinning research philosophies (also called paradigms). First, quantitative research is usually underpinned by positivism. This includes most epidemiological studies; such research is typically based on the assumption that there is one single real world out there that can be measured. For example, quantitative research would address the question “What proportion of the population of India drinks coffee?” Secondly, qualitative research is more likely to be based on interpretivism. This includes research based on interviews and focus groups, research which us is typically based on the assumption that we all experience the world differently. Since we all live in a slightly different world in our heads the task of qualitative research is to analyse the interpretations of the people in the sample. For example, qualitative research would address the question “How do people experience drinking coffee in India?”, and “What does drinking coffee mean to them?”
Mixed-methods research brings together questions from two different philosophies in what is being referred to as the third path [ 8 ], third research paradigm [ 9 , 10 ], the third methodology movement [ 11 , 12 ] and pragmatism [ 5 ]. The two paradigms differ in key underlying assumptions that ultimately lead to choices in research methodology and methods and often give a breadth by answering more complicated research questions [ 4 ]. The roles of mixed-methods are clear in an understanding of the situation (the what), meaning, norms, values (the why or how) within a single research question which combine the strength of two different method and offer multiple ways of looking at the research question [ 13 ]. Epidemiology sits strongly in the quantitative research corner, with a strong emphasis on large data sets and sophisticated statistical analysis. Although the use of mixed methods in health research has been discussed widely researchers raised concerns about the explanation of why and how mixed methods are used in a single research question [ 5 ].
The relevance of mixed-methods in health research
The overall goal of the mixed-methods research design is to provide a better and deeper understanding, by providing a fuller picture that can enhance description and understanding of the phenomena [ 4 ]. Mixed-methods research has become popular because it uses quantitative and qualitative data in one single study which provides stronger inference than using either approach on its own [ 4 ]. In other words, a mixed-methods paper helps to understand the holistic picture from meanings obtained from interviews or observation to the prevalence of traits in a population obtained from surveys, which add depth and breadth to the study. For example, a survey questionnaire will include a limited number of structured questions, adding qualitative methods can capture other unanticipated facets of the topic that may be relevant to the research problem and help in the interpretation of the quantitative data. A good example of a mixed-methods study, it one conducted in Australia to understand the nursing care in public hospitals and also explore what factors influence adherence to nursing care [ 14 ]. Another example is a mixed-methods study that explores the relationship between nursing care practices and patient satisfaction. This study started with a quantitative survey to understand the general nursing services followed by qualitative interviews. A logistic regression analysis was performed to quantify the associations between general nursing practice variables supplemented with a thematic analysis of the interviews [ 15 ]. These research questions could not be answered if the researchers had used either qualitative or quantitative alone. Overall, this fits well with the development of evidence-based practice.
Despite the strengths of mixed-methods research but there is not much of it in nursing and other fields [ 7 ]. A recent review paper shows that the prevalence of mixed-methods studies in nursing was only 1.9% [ 7 ]. Similarly, a systematic review synthesised a total of 20 papers [ 16 ], and 16 papers [ 17 ] on nursing-related research paper among these only one mixed-methods paper was identified. Worse, a further two mixed-methods review recently revealed that out of 48 [ 18 , 19 ] synthesised nursing research papers, not one single mixed-methods paper was identified. This clearly depicts that mixed-methods research is still in its infancy stage in nursing but we can say there is huge scope to implement it to understand research questions on both sides of coin [ 4 ]. Therefore, there is a great need for mixed-methods training to enhance the evidence-based decision making in health and nursing practices.
Strengths and weaknesses of mixed-methods
There are several challenges in identifying expertise of both methods and in working with a multidisciplinary, interdisciplinary, or transdisciplinary team [ 20 ]. It increases costs and resources, takes longer to complete as mixed-methods design often involves multiple stages of data collection and separate data analysis [ 4 , 5 ]. Moreover, conducting mixed-methods research does not necessarily guarantee an improvement in the quality of health research. Therefore, mixed-methods research is only appropriate when there are appropriate research questions [ 4 , 6 ].
Identifying an appropriate mixed-methods journal can also be challenging when writing mixed-methods papers [ 21 ]. Mixed-methods papers need considerably more words than single-methods papers as well as sympathetic editors who understand the underlying philosophy of a mixed-methods approach. Such papers, simply require more words. The mixed-methods researcher must be reporting two separate methods with their own characteristics, different samples, and ways of analysing, therefore needs more words to describe both methods as well as both sets of findings. Researcher needs to find a journal that accepts longer articles to help broaden existing evidence-based practice and promote its applicability in the nursing field [ 22 ].
Common mistakes in applying mixed-methods
Not all applied researchers have insight into the underlying philosophy and/or the skills to apply each set of methods appropriately. Younas and colleagues’ review identified that around one-third (29%) of mixed-methods studies did not provide an explicit label of the study design and 95% of studies did not identify the research paradigm [ 7 ]. Whilst several mixed-methods publications did not provide clear research questions covering both quantitative and qualitative approaches. Another common issue is how to collect data either concurrent or sequential and the priority is given to each approach within the study where equal or dominant which are not clearly stated in writing which is important to mention while writing in the methods section. Similarly, a commonly overlooked aspect is how to integrate both findings in a paper. The responsibility lies with the researcher to ensure that findings are sufficiently plausible and credible [ 4 ]. Therefore, intensive mixed-methods research training is required for nursing and other health practitioners to ensure its appropriate.
The way forward
Despite the recognised strengths and benefits of doing mixed-methods research, there is still only a limited number of nursing and related-health research publications using such this approach. Researchers need training in how to design, conduct, analyse, synthesise and disseminate mixed-methods research. Most importantly, they need to consider appropriate research questions that can be addressed using a mixed methods approach to add to our knowledge in evidence-based practice. In short, we need more training on mixed-methods research for a range of health researchers and health professionals.
Acknowledgement
- Open access
- Published: 08 April 2024
The use of positive deviance approach to improve health service delivery and quality of care: a scoping review
- Ayelign Mengesha Kassie ORCID: orcid.org/0000-0003-1505-9390 1 , 2 ,
- Elizabeth Eakin ORCID: orcid.org/0000-0002-8835-9995 1 ,
- Biruk Beletew Abate ORCID: orcid.org/0000-0003-0833-2504 2 ,
- Aklilu Endalamaw ORCID: orcid.org/0000-0002-9121-6549 1 , 3 ,
- Anteneh Zewdie 4 ,
- Eskinder Wolka 4 &
- Yibeltal Assefa ORCID: orcid.org/0000-0002-8636-1282 1
BMC Health Services Research volume 24 , Article number: 438 ( 2024 ) Cite this article
Metrics details
Quality has been a persistent challenge in the healthcare system, particularly in resource-limited settings. As a result, the utilization of innovative approaches is required to help countries in their efforts to enhance the quality of healthcare. The positive deviance (PD) approach is an innovative approach that can be utilized to improve healthcare quality. The approach assumes that solutions to problems are already available within the community and identifying and sharing those solutions can help others to resolve existing issues. Therefore, this scoping review aimed to synthesize the evidence regarding the use of the PD approach in healthcare system service delivery and quality improvement programs.
Articles were retrieved from six international databases. The last date for article search was June 02, 2023, and no date restriction was applied. All articles were assessed for inclusion through a title and/or abstract read. Then, articles that passed the title and abstract review were screened by reading their full texts. In case of duplication, only the full-text published articles were retained. A descriptive mapping and evidence synthesis was done to present data with the guide of the Preferred Reporting Items for Systematic Reviews and Meta-analysis extension for Scoping Reviews checklist and the results are presented in text, table, and figure formats.
A total of 125 articles were included in this scoping review. More than half, 66 (52.8%), of the articles were from the United States, 11(8.8%) from multinational studies, 10 (8%) from Canada, 8 (6.4%) from the United Kingdom and the remaining, 30 (24%) are from other nations around the world. The scoping review indicates that several types of study designs can be applied in utilizing the PD approach for healthcare service and quality improvement programs. However, although validated performance measures are utilized to identify positive deviants (PDs) in many of the articles, some of the selection criteria utilized by authors lack clarity and are subject to potential bias. In addition, several limitations have been mentioned in the articles including issues in operationalizing PD, focus on leaders and senior managers and limited staff involvement, bias, lack of comparison, limited setting, and issues in generalizability/transferability of results from prospects perspective. Nevertheless, the limitations identified are potentially manageable and can be contextually resolved depending on the nature of the study. Furthermore, PD has been successfully employed in healthcare service and quality improvement programs including in increasing surgical care quality, hand hygiene practice, and reducing healthcare-associated infections.
The scoping review findings have indicated that healthcare systems have been able to enhance quality, reduce errors, and improve patient outcomes by identifying lessons from those who exhibit exceptional practices and implementing successful strategies in their practice. All the outcomes of PD-based research, however, are dependent on the first step of identifying true PDs. Hence, it is critical that PDs are identified using objective and validated measures of performance as failure to identify true PDs can subsequently lead to failure in identifying best practices for learning and dissemination to other contextually similar settings.
Peer Review reports
The realization of universal health coverage objectives is an unattainable aspiration without the concurrent provision of healthcare services of the highest quality. For this reason, the sustainable development goal target 3.8 seeks not only financial risk protection, but also to enhance access to safe, and effective essential medications and vaccinations, and high-quality medical services [ 1 ]. To support this, international organizations including the World Health Organization (WHO) and the World Bank have been promoting the idea of universal health coverage for all people to enjoy affordable access to the entire spectrum of high-quality healthcare services they require when and where they need them, and be incorporated into the healthcare system changes in several countries around the world [ 2 , 3 ].
Nevertheless, healthcare systems are grappling with a multitude of challenges when it comes to improving access and providing high-quality healthcare services on a global scale. These challenges encompass deficient data collection and monitoring systems, suboptimal organizational team culture and limited capacity, ineffective leadership, neglect of the incentivization of superior performance [ 4 ], and a dearth of evidence-based health policies to support implementation and augment the proficiency of healthcare professionals [ 5 ]. Furthermore, as highlighted by Darrudi A. et al. (2020), substandard care quality, coupled with inadequately regulated and fragmented healthcare delivery systems, escalating unmet health requirements, and the swift commercialization of healthcare within privatized systems constitute a significant challenge encountered by nations in their pursuit of universal health coverage [ 6 ]. As a result, there is a growing need to explore and use innovative approaches to improve and deliver safe, effective, and high-quality healthcare services in the healthcare system [ 7 , 8 ].
The positive deviance approach represents an innovative strategy aimed at identifying exemplary practices that are present within a given community [ 9 ]. This community in the context of healthcare encompasses various entities, including teams, groups, departments, and organizations [ 10 ]. In this regard, departments and organizations could include regional/provincial, zonal, and district-based administrative health offices, local health facilities, and their respective units. For instance, social service agencies, representatives of health care organizations, and local government bodies have been considered as communities in an article that utilized PD to understand how social service and health care providers collaborate in communities that attain relatively low levels of health care utilization and expenses among senior citizens [ 11 ]. The approach recognizes the value of existing expertise [ 12 ] and operates on the premise that solutions to problems already exist within the community, and the act of identifying and disseminating these solutions can assist others in addressing existing complex and intractable challenges [ 9 , 12 ]. Jason Gordon (2022) further emphasizes that despite having similar resource constraints as everyone else, there are individuals who excel in their performance to rules concerning organizational issues, and when given the opportunity, these PDs are willing to share their experiences as far as leaders facilitate the process [ 13 ]. Positive deviance has been applied in different sectors including social sciences, psychology, and healthcare [ 14 ], and yielded successful results in enhancing the nutritional status of children in multiple countries, such as Haiti, Vietnam, Pakistan, and India [ 15 ] and in preventing and addressing undernutrition and overweight among the adult population [ 15 , 16 , 17 ].
Application of PD is a somewhat lengthy process and involves different stages. The Bradley EH et al.‘s (2009) framework, which articulates a four-stage process, and the 4Ds/6Ds framework are commonly utilized in healthcare service-related articles. According to Bradley et al.‘s framework, the initial phase involves leveraging routinely gathered data to pinpoint organizations exemplifying exceptional performance, which is then subject to qualitative examination to formulate hypotheses regarding their superior outcomes. Subsequent stages involve the empirical validation of these hypotheses through statistical analysis in broader organizational samples and the dissemination of findings in collaboration with pertinent stakeholders to promote the replication of these best practices in comparable contexts [ 18 ]. The 4Ds/6Ds framework similarly starts with defining the issue at hand. In this framework, the first D stands for defining the problem and the next is for determining the presence of PDs or identifying them. The third D stands for discovering the successful but uncommon strategies that PDs apply in their practice and the fourth D represents the designing stage of interventions to allow others to apply these strategies in their practice. The final two Ds focus on evaluating the interventions’ effectiveness and ensuring the diffusion of effective practices to other entities [ 10 , 19 ].
However, the available evidence on PD is mixed and there are controversies on the effectiveness of the approach, particularly in complex and demanding settings including the healthcare system. This is due in large part to methodological limitations of the extant studies including inconsistencies in the quality of strategies employed to identify PDs or positive deviant practices and the challenges related to the approach’s applicability in practical situations. For instance, a systematic review paper has reported that studies that applied the PD approach for quality improvement in complex interventions lack methodological quality and details in their work. The authors further stated that utilizing PD in healthcare settings poses challenges citing engaging staff more broadly in quality enhancement programs as a known difficult aspect [ 20 ]. As such, its potential for future use in the healthcare system is not well documented. Therefore, this scoping review aimed to synthesize the evidence regarding the use of the PD approach in healthcare system service delivery and quality improvement programs.
This scoping review is conducted by using the Preferred Reporting Items for Systematic Reviews and Meta-analysis extension for Scoping Reviews checklist (PRISMA-ScR), as a guide for article screening, extraction, analysis, and presentation of the results [ 21 ]. In addition, the Population, Concept, and Context (PCC) framework was employed to assess the research question’s appropriateness and make amendments. Regarding article search, several international databases including PubMed, Embase, and Scopus were explored to retrieve studies related to PD and its application in the healthcare system. A complete search strategy was developed for the different databases and has been included as a supplementary file in this scoping review (see Additional file 1 ). Details regarding the article search strategy and further clarification of concepts including the PCC framework are available somewhere else [ 22 ].
Research questions
The research questions of this scoping review are: (1) What research designs and methods are utilized in implementing PD in the healthcare system service delivery and quality improvement interventions?; (2) What are the strategies applied to identify PDs or measure positively deviant practices?; (3) What outcomes have been achieved using the PD approach?; and (4) What are the limitations in utilization of the PD approach, and what is its potential for use in the healthcare system service delivery and quality improvement programs?
Eligibility, screening, and data extraction
Articles published only in the English language are included due to feasibility issues, and letters or comments to the editor, commentator, and brief communication articles and literature review studies other than systematic review and meta-analysis articles are excluded due to the nature of the scoping review detailed methodological requirements. In addition, only studies that described the methods used to assess the performance of PDs were included. Furthermore, all articles were assessed independently by two authors for inclusion through a title and, or abstract read, and those that passed the title and abstract review were screened by reading the full texts. Details are available elsewhere [ 22 ].
Data analysis and presentation
A descriptive mapping and synthesis of the literature are employed to present data in text, table, and figure formats by using three major themes: Methodologies employed in using the PD including the strategies researchers utilized to identify PDs; outcomes or achievements reported from the usage of PD approach; and the prospects of PD in future health service research works. In addition, the results of this scoping review are reported based on the PRISMA-ScR guideline, and the entire process of study screening, selection, and inclusion is shown with the support of the PRISMA-ScR flow diagram [ 21 ].
Characteristics of included studies
We identified 2089 articles from different sources: PubMed ( n = 525), Google Scholar ( n = 377), Web of Science ( n = 358), Embase ( n = 339), Scopus ( n = 329), CINAHL ( n = 160), and reference searching ( n = 1). Then, 125 articles were included for the scoping review after the title, abstract, and full-text screening, and removal of duplications (Fig. 1 ). Most of the included articles, 121 (96.8%) are original articles, and the rest, 4 (3.2%) are systematic reviews. Furthermore, more than half, 66 (52.8%) of the articles were from the United States, 11(8.8%) from multinational studies, 10 (8%) from Canada, 8 (6.4%) from the United Kingdom, 4 (3.2%) from Brazil, 4 (3.2%) from Israel, and the remaining, 22 (17.6%) are from other nations around the world (Table 1 ).
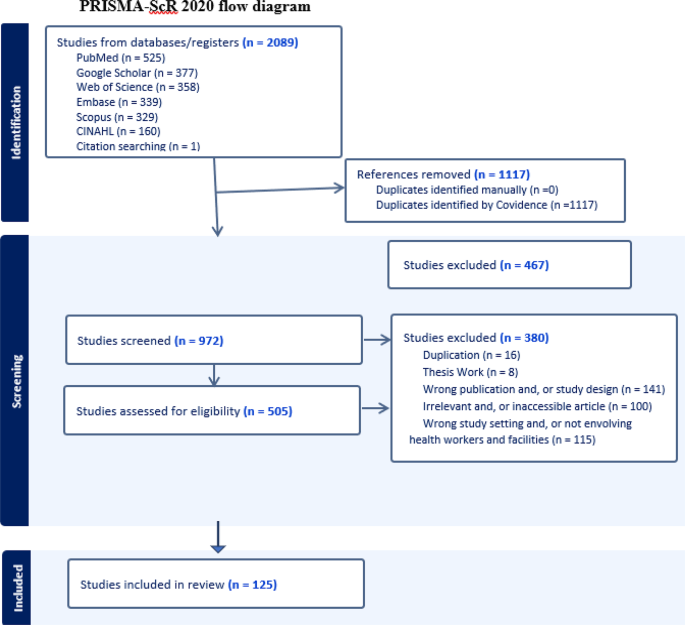
PRISMA-ScR flow diagram for the article selection process
Methods followed in the utilization of PD for the healthcare system
Study design.
Regarding the methodological composition of the research corpus, it was found that qualitative methods predominate, constituting 44.0% of study designs, followed by mixed methods approaches at 20.8%, pre-post intervention studies at 12.8%, and cross-sectional analyses at 12.0%. Notably, the foundational framework employed in most of the scrutinized articles is delineated in Bradley EH et al.‘s (2009) publication, which articulates a four-stage process [ 18 ], and the 4Ds/6Ds framework [ 10 ]. However, the literature exhibits a lack of uniformity in documenting the specific stages of PD examined or employed, and the temporal span of the studies encompasses the period from 2006 to 2023 (Supplementary Table 1 ).
Strategies utilized by researchers to identify PDs
In this scoping review, we found that the selection process of PDs is a difficult job, and no consistent validated criteria are utilized. Recommendation-based criteria have been utilized to identify PDs in twelve papers even though some of the criteria for selection are less clear and subject to potential bias [ 25 , 34 , 49 , 52 , 58 , 79 , 89 , 94 , 98 , 106 , 120 , 123 ]. For instance, Toscos T, et al. (2018) used clinic liaison recommendations to identify positive deviant patients who displayed successful methods or practices for gaining access to healthcare, as well as healthcare workers who had developed successful care-delivery practices [ 94 ]. In addition, a combination of media influence and stakeholder recommendation [ 64 ], implementation-based [ 29 ], and experience-based criteria have also been used [ 31 , 91 ]. In six articles, the criteria for the selection of PDs were unclear or unspecified [ 39 , 47 , 50 , 76 , 143 , 145 ] and in the remaining papers, the selection of PDs does not apply as they are systematic reviews [ 20 , 57 , 59 , 63 ] and adoption program papers that are implemented based on best practices identified from other positive deviant practices [ 28 , 51 , 54 , 67 , 92 , 119 ]. However, performance-based criteria have been used to identify PDs at individual, health facility or health system levels in majority of the articles [ 11 , 23 , 24 , 26 , 27 , 30 , 32 , 33 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 48 , 53 , 55 , 56 , 60 , 61 , 62 , 65 , 66 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 77 , 78 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 90 , 93 , 95 , 96 , 97 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 121 , 122 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 , 141 , 142 , 144 ].
Outcomes reported from the utilization of PD
We found that significant outcomes have been reported in various domains from utilizing the PD approach for healthcare service and quality improvement research and interventions around the world. In some situations, researchers used the PD approach to identify successful strategies of PDs and build conceptual models for best practice. For example, Rakic S, et al. (2021) used the PD approach to identify the strategies top-performing health centers utilized for better financial sustainability in the Republic of Srpska, Bosnia and Herzegovina, and built an organizational-level model for public primary healthcare centers [ 24 ]. Similarly, Assefa Y, et al. (2014) employed the same approach to explore best practices that contributed to patient retention in HIV care and developed a framework for improving patient retention in future implementation programs [ 43 ]. In other cases, most of the included articles are conducted to identify PDs and the strategies that make PDs different from others at the health system, health facility, and, or individual levels. For instance, Klaiman TA, et al. (2014) utilized a PD framework to identify PD local health departments that had exceptional maternal and child health outcomes in the community using uniquely detailed and matched annual maternal and child health-related county-level expenditure data for all local health departments in Florida and Washington, USA [ 83 ].
Effectiveness in reducing medication errors and hospitalizations
Positive deviance is found to be an effective strategy in reducing medication errors and hospitalizations. In this regard, a study has indicated that in a 3-phase PD interventional program, using the approach was effective in reducing medication errors with each intervention resulting in a 0.12% decline rate in reported errors [ 28 ]. In addition, effectiveness in time management and financial expenditure, improved health outcomes, enhanced healthcare service quality, improved hand hygiene practice, reduction of infections, and reductions in adverse events after operation have been reported as indicators of success in utilizing PD in the healthcare system. For example, Tanenbaum J, et al. (2018) reported the evaluation of an adopted PD program in Ohio, USA, from a nationwide primary care–led regional quality improvement collaborative operating with hospitalization rates for ambulatory care sensitive conditions known as “Better Health Partnership” resulted in reductions in age- and sex-adjusted hospitalization rates in targeted ambulatory care sensitive conditions (diabetes, heart failure, and hypertension) in Cuyahoga County more than the rates in the comparator counties in 2009–11 (106 fewer hospitalizations per 100,000 adults) and 2012–14 (91 fewer hospitalizations) [ 143 ].
Effectiveness in time management and financial expenditure
Utilizing the PD approach in healthcare safety and quality programs has led to huge time and cost savings. For instance, Gold R, et al. (2023) revealed that the application of the PD approach has resulted in great improvements in time management in surgical cases across all time intervals of procedures with an overall time of 49.84 min saved per day compared to the baseline values [ 32 ]. Similarly, an improvement in operating room time management after successive value improvement initiatives has also been reported [ 30 ]. In addition, a reduction from 4.0 to 3.0 days in median length of stay after lobectomy in thoracic surgery following local PD seminars and from 4.0 to 3.5 days after multicentre seminars are reported as successes in surgical practice together with trends of decline in multiple adverse event rates [ 34 ]. Furthermore, the Ohio study cited above has also indicated that the decline in hospitalization rates in targeted ambulatory care sensitive cases was estimated to be 5,746 hospitalizations in 2009-14, resulting in nearly $40 million in cost savings [ 143 ]. In other programs, disposable materials cost reduction of $397.53 per lobectomy in thoracic surgery after cost awareness and surgeon engaging PD interventions with futures of sustainability [ 30 ], and an additional estimated $2-2.5 M revenue per year increment from saving time, without affecting quality, safety, and workload, after an introduction of PD strategy-based surgical prepping time protocol had been reported [ 113 ].
Improved hand hygiene practice and infection prevention
Several PD-based interventional studies have indicated that utilizing the approach has resulted in better healthcare service quality practices, including an increase in hand hygiene compliance rates [ 25 , 26 , 36 , 61 , 63 ], and a reduction of infections [ 25 , 26 , 27 , 39 , 61 , 63 , 92 , 98 , 106 , 119 ]. Marra AR. et al. (2013) have revealed that improving hand hygiene practice in multiple inpatient settings has led to a decrease in the incidence of device-related healthcare-associated infections and the median length of stay after a PD intervention [ 61 ]. As an additional example, a monthly time series drop of healthcare-associated infection rates from 4.8 to 2.8 per 1000 patient-days [ 106 ], an increase in hand hygiene compliance, and a decline in Methicillin-resistant staphylococcus infection (MERSA) rates are also reported [ 63 ]. Furthermore, a sustained decreasing trend in the rate of device-related infections as a result of increasing use of alcoholic hand rub in nursing visits over 2 years [ 26 ], and a sharp decline in all access-related bloodstream infections from 2.04 per 100 patient-months preintervention to 0.75 after employing collaborative interventions and to 0.24 after augmenting the interventions with PD are documented in different settings [ 119 ]. Similarly, one program has reported several MRSA-free months in sustained and lasting changes in MERSA reduction rates, in the period after the application of PD without investing additional costs for the intervention [ 39 ].
Improved surgical care quality and reduction of complications
A trend in the reduction of multiple adverse event rates and health facility length of stay after pulmonary resection following best evidence- and best experience-based quality improvement PD seminars has been documented. In addition to the positive outcomes, the generation of universally applicable and successful consensus recommendations is made by the program for surgical safety and quality services [ 34 ]. Similarly, a reduction in post-operation complications after the application of surgeon self-evaluation in combination with a seminar-based PD quality improvement program has been observed in patients following non-cardiac thoracic surgery with a 34% decline in atrial fibrillation rates, a 38% decline in prolonged air leak rates and a 25% drop in anastomotic leak rates [ 34 , 37 ].
Improved performance and care quality
Improvements in the quality of healthcare services and health outcomes have also been reported in different topics. For example, an overall increase in the proportion of controlled blood pressure (< 140/90 mmHg) among adult patients from 67% in 2013 to 74% in 2017) with improvements across all patient demographic and insurance subgroup types has been reported after implementation of a primary care practice regional health improvement collaborative programs in the USA [ 111 ]. In another interventional program, a consistent increase in the use of dual-method contraceptives was found among Ugandan women [ 70 ]. Similarly, PD clinician-owned practices have also been found to be more likely to achieve improvements in cardiovascular quality service outcomes without increasing health workers’ burnout than were practices owned by a hospital or health system [ 114 ]. Related to this, several strategies have also been reported to be significantly associated with lower risk-standardized mortality rates among patients with acute myocardial infarction in hospitals that implemented positive deviant practices in the USA. According to the report, not cross-training nurses from intensive care units for the cardiac catheterization laboratory, having cardiologists always on-site, holding monthly meetings for reviewing acute myocardial infarction cases between hospital clinicians and staff who transported patients to the hospital, fostering an organizational environment in which clinicians are encouraged to solve problems creatively, and having physician and nurse champions rather than nurse champions alone resulted in 0.44, 0.54, 0.70, 0.84 and 0.88% point reductions in a 30-day risk-standardized mortality rate respectively [ 87 ]. Moreover, a mental health support group program facilitated by Women’s Union staff for people with severe mental illness in rural Vietnam has indicated that the use of the PD approach was associated with a substantial improvement in personal functioning and reduction of stigma and discrimination among patients. In addition, the authors have reported that the intervention has resulted in a significant reduction in financial burdens for the families of patients with severe mental illness, and the program was feasible and highly acceptable by the community [ 145 ].
Reported limitations/challenges in using PD
The included articles have mentioned several limitations that can be related to the PD approach even though it is not possible to prove whether it is true or not as many of the limitations can be related to the specific study design of individual articles. Some examples of commonly reported limitations included are thematized and cited below as concerns in operationalizing who positive deviant is or are [ 55 , 57 , 66 , 74 , 95 , 101 , 107 ], the difficulty of confirming true PDs in comparison with others, as a change in time may affect outcomes and PDs are commonly identified with secondary data, and, or stored data in the past [ 83 , 85 , 102 , 107 , 115 , 143 ] a small number of participants [ 31 , 41 , 91 , 107 ], focus on leaders and senior managers and limited staff and patient, or other stakeholder perspective involvement [ 11 , 41 , 64 , 72 , 81 , 82 , 87 , 96 ], response bias including social desirability bias [ 55 , 64 , 81 , 84 , 85 , 86 , 87 , 96 , 101 , 102 ], and issue of not achieving information saturation in qualitative studies as PD is mainly qualitative in its initial stages [ 82 ].
Furthermore, limited study setting/s [ 30 , 31 , 41 , 44 , 80 , 82 , 88 , 90 , 101 ], difficulty of performing statistical tests due to small sample size [ 33 , 65 , 83 ], difficulty of adjusting confounders [ 30 , 34 , 63 , 68 , 114 ], lack of comparison and, or difficulty of doing comparative analysis [ 24 , 71 , 82 ], and issues of generalizability/transferability [ 11 , 30 , 42 , 44 , 64 , 72 , 80 , 82 , 84 , 91 , 96 , 98 , 100 , 102 , 143 ] are also reported as common limitations in several articles. In addition, the none-probability sampling methods used to recruit participants [ 94 ] and the Hawthorne effect, a type of reactivity in which individuals modify an aspect of their behavior in response to their awareness of being observed as positive deviant are included in many articles as limitations in using the approach of PD [ 30 , 32 , 49 , 66 , 71 ]. These limitations highlight the need for careful consideration of a balanced method when using the PD approach [ 146 ].
The overall uptake and publishing of PD studies for health care service and quality of care improvement is quite limited and heavily USA-focused. This distribution is unexpected as the PD approach is primarily believed to have huge significance for resource-limited settings [ 20 ]. The reason for this could be because the PD approach is an emerging science and may not be adequately promoted in many low- and middle-income countries. In addition, from the methodology perspective, the scoping review findings have indicated that diverse types of study designs can be applied in utilizing the PD approach for healthcare service and quality improvement programs. This could be surprising for some people because, during the initial stages of the review protocol development, some of the author’s understanding was that only limited study designs could be applicable in using the PD approach as the method utilized in identifying the strategies of PDs is mainly qualitative [ 18 ]. However, in line with our anticipation, most of the included articles utilized qualitative, mixed, and pre-post interventional designs. These are useful in utilizing PD and identifying the strategies of top performers in comparison with others. This is because, qualitative research is useful to understand the “why” behind the strategies and behaviors of top performers and uncover the motivations, challenges, and contextual factors that contribute to their success, and the mixed cross-sectional and interventional methods research can combine quantitative data to quantify the prevalence and impact of certain strategies, reinforce qualitative findings and offer a more comprehensive picture [ 147 ].
Furthermore, pre-post interventional designs are important to evaluate how the strategies implemented by top performers lead to improvements over time and in comparison with others who do not implement these strategies [ 148 , 149 ]. An example of this is the study conducted by Curry LA, et al. (2018) in 10 hospitals in the USA to enhance improvements in different domains of organizational culture that lead to significant changes in culture between baseline and 24 months, especially with regards to the learning environment and senior management support. The study further added that six hospitals having major cultural transformations reported considerably higher reductions in risk-standardised mortality rates in patients with acute myocardial infarction than four hospitals that did not shift culture citing a 1.07 and 0.23% point changes in the risk-standardised mortality rates between the two groups respectively over the period of 2011–2014 and 2012–2015 [ 150 ]. These findings are supported by studies from other disciplines as well. For instance, a systematic review paper has indicated that 21 randomized controlled trial studies were utilized to improve employee well-being and effectiveness using web-based psychological interventions delivered in the workplace [ 151 ]. In addition, another systematic review paper has indicated that qualitative studies, pre-and post-test design without a control, non-randomized trials, non-randomized cross-sectional studies, and randomized controlled trials were utilized in community-based nutritional programs conducted based on the PD approach to reduce childhood malnutrition across the globe [ 17 ].
Concerning the identification of PDs, the selection process has been reported to be a difficult task in the utilization of PD [ 20 ]. The scoping review findings have supported this statement and depicted that the selection process of PDs appeared to be too complex and dependent on the unique circumstances of each study or project. As a result, different articles and studies have utilized a range of methods and criteria to identify PDs including peer recommendations [ 25 , 49 , 52 , 106 , 120 , 123 ], and performance-based criteria such as lowest risk-adjusted morbidity [ 139 ], mortality [ 82 , 87 , 93 , 102 ], timely service [ 26 , 32 , 33 , 84 , 95 , 99 , 113 , 116 , 134 ], and standardized composite performance measures including high composite quality scores [ 86 , 115 , 137 ], high composite performance/healthcare service scores [ 11 , 23 , 27 , 43 , 44 , 45 , 53 , 62 , 65 , 69 , 75 , 78 , 109 , 110 , 117 , 118 , 122 , 124 , 131 , 138 , 140 , 144 ], and better clinical outcome scores [ 37 , 38 , 111 , 118 , 125 , 130 ]. This justifies the absence of a one-size-fits-all approach to selecting PDs, and the criteria used can vary greatly based on the specific domain and goals of initiatives. However, the use of non-standardized and, or non-validated criteria can lead to bias and this in turn can lead to failure in identifying true PDs [ 55 , 57 , 66 , 74 , 95 , 101 , 107 ]. For instance, recommendation-based criteria can still be used to identify positive deviants in settings where there is no sufficient resource and data to identify positive deviant practices. However, the researchers need to be cautious of possible bias in the process of identifying true positive deviants when using such methods and need to ensure whether the recommenders are genuine or not and use other performance-based rating criteria in other situations when using validated and, or standardized tools are applicable.
In line with the above findings, another scoping review paper has indicated that some researchers have used unstandardized and less clear criteria to select PDs and suggested that objective measures of health outcomes should be used whenever possible to reduce the possibility of bias in examining associations [ 146 ]. Furthermore, it is critical to consider the underlying assumption that the identified PDs are contextually comparable with other groups in terms of access to resources and expertise [ 20 ]. This is because, health workers, health facilities, and/or health systems with better expertise and financial resources could have advantages that can influence their performance and the subsequent outcomes in comparison with their counterparts signifying the need to consider the degree of resources between populations or groups when designing a sampling strategy [ 20 , 146 ]. This challenge can be addressed to some extent in the selection criteria. For instance, in one study, high and low-performing hospitals were purposefully selected from within a random set of top 5% and bottom 5% ranked hospitals to ensure diversity in areas such as volume of patients with acute myocardial infarction, teaching status, and socioeconomic status of patients [ 152 ].
Regarding the reported outcomes, the PD approach has been employed for several aims and objectives. For instance, Klaiman TA, et al. (2014) utilized a PD framework to identify positive deviant local health departments that had exceptional maternal and child health outcomes in the community. The authors used uniquely detailed and matched annual maternal and child health-related county-level expenditure data for all local health departments in Florida and Washington. The data were sourced from the Public Health Activities and Services Tracking database for identifying high-performing local health departments. These data were linked with factors depicting the local context and local health department structures [ 83 ]. In other cases, many of the articles are conducted to identify the strategies of PDs that make them successful and share their experience with the wider community. For example, Borghini A, et al. (2021), employed a mixed-methods study to identify PDs regarding maternal care at the regional level in 10 Italian regions. In the first phase, the researchers used quantitative data including performance metrics and maternity care indicators to identify top-performing regions. In the second phase, they investigated the organizational determinants and the experience of healthcare workers involved in the process qualitatively and identified seven best practices including the existence of trust among healthcare professionals and having shared goals as the reasons for better performance and success in comparison with other regions [ 53 ].
Furthermore, researchers have proved that the utilization of PD has helped them be successful in various healthcare services and quality improvement programs including in the reduction of medication errors [ 28 ], enhancing effectiveness in time management and/or financial expenditure [ 30 , 32 , 143 ], in improving hand hygiene practice and, or reducing infection rates [ 26 , 27 , 36 , 39 , 51 , 61 , 63 , 92 , 98 , 106 , 119 ], in improving surgical care quality and reduction of complications [ 34 , 37 ], and in other reported outcome measures including an increase in the proportion of controlled blood pressure (< 140/90 mmHg) among adult patients in the USA [ 111 ], a consistent increase in the use of dual-method contraceptives among women in Uganda [ 70 ], improvement in cardiovascular quality service outcomes [ 114 ], and improvement in personal functioning’s and reduction of stigma and discriminations among patients with severe mental illnesses after implementation of PD-based programs have indicated the huge potential of utilizing PD in healthcare service quality and other outcome improvement efforts [ 145 ]. These successes from the utilization of the PD approach are supported by other studies from different programs. For instance, a systematic review paper has indicated that the utilization of the PD approach has helped countries to reduce childhood malnutrition across the globe [ 17 ].
Similarly, a 65–80% persistent decline in childhood malnutrition in Vietnam and a substantial reduction in other communities across 41 different nations around the world, in programs that used PD has also been reported [ 8 , 153 ]. In addition, success in the prevention and treatment of undernutrition, overweight, and obesity in socioeconomically vulnerable mothers and the adult population has also been reported [ 15 , 16 ]. Furthermore, a reduction in neonatal mortality has been reported in Pakistan [ 8 , 153 ]. This could be because the strategies of PDs are internally driven and the solutions are generated within the community that can be implemented with minimal expenditures, particularly in settings with financial hardship [ 8 , 57 , 154 ]. However, it is important to note that each healthcare context is unique, and the success of PD interventions may depend on factors such as the specific challenges being addressed, the engagement of stakeholders, and the adaptability of the interventions to the local context [ 18 , 154 ].
From the prospect’s perspective, several limitations have been mentioned in the primary articles including issues in the operationalization of PD, the difficulty of identifying true PDs during selection time because of time-related changes in practice about who positive deviant is or are, bias, and issues in generalizability/transferability of results. Majority of these limitations might be specific to the respective studies design, setting, and contexts [ 155 , 156 ]. However, the cited limitations could have been attributed not only to the nature of specific studies but also to the peculiar nature of the PD approach. This is because the PD approach has assumptions and principles that need to be followed when selecting study participants whether it is at individual, group, or organization level. For instance, Bradley EH, et al.’s (2009) 4-stage framework that is proposed to be followed for healthcare quality research works in using the PD approach suggests using routinely collected data in identifying positive deviant organizations that consistently exhibit exceptionally high performance in the area of interest at stage 1, intensively examine the organizations using qualitative methods to generate hypotheses about practices that help organizations achieve top performance at stage 2; statistically test hypotheses in larger, representative samples of organizations at stage 3 and collaborate with key stakeholders to disseminate the findings, such as the organizations’ customers and suppliers at stage 4 [ 18 ].
As a result, when studies are conducted, following those assumptions can pose a limitation on the research designs selected and procedures followed including selection of PDs and using routinely collected data in measuring performance may affect the results of studies as the practice level is dynamic and progressive over time. For instance, Curry LA, et al. (2011) cited that study sites (hospitals) were visited at a single point in time, and using secondary data might not be good for identifying true PDs as their performance could have been changing (improving or declining) and others, in contrast, could be top performing at the time of applying PD [ 85 ]. The possible reason for this is that the continuous nature of practice improvement over time could affect the selection of positive deviant sites as other comparators may progress as well and top performers might become low-performing at another time [ 85 , 102 ]. This highlights the need to use robust criteria in the selection process of PDs [ 146 ].
Concerning the potentials, utilization of PD not only has been successfully employed in healthcare service and quality improvement programs but also the variables included as limitations or challenges in the articles are potentially manageable. For instance, the issue of operationalization of PD can be reduced or solved by using risk-adjusted and standardized composite measures including utilization of validated performance-based criteria and considering the consistency of top-performing individuals, healthcare organizations, and systems background history as one of the assumptions of PD is the consistency of performance over time [ 20 ]. In addition, combining the evaluation of the current practice level of PDs with their historical data in comparison with other assumed low performers can be a solution for these issues and reduce the effect of the changing and progressive nature of practice between high-performing and low-performing individuals, teams, and, or healthcare facilities. Furthermore, using data that can show consistent performance for several years could be one possible option that can reduce the effect of time change in using such data sources [ 18 ]. For instance, the Curry et al. (2011) study selected hospitals that showed consistency and ranked in either the top or the bottom 5% in risk-standardized mortality rates among patients with acute myocardial infarction over two 2 years. This was seemingly intentionally done to mitigate the effect of time change on the performance level of health facilities and identify the hospitals that are truly positively deviant in comparison to those that are negatively deviant [ 85 ]. In addition, several of the included studies have used validated criteria to identify PDs that can support the above findings including lowest risk-adjusted morbidity [ 139 ], mortality [ 82 , 87 , 93 , 102 ], lowest age-adjusted mortality [ 136 ], and standardized composite performance measures including high composite quality score [ 86 , 115 , 137 ], and high composite performance/healthcare service scores as using row morbidity and mortality rates without confounder adjustment is a non-reliable indicator of high and low performance [ 11 , 23 , 27 , 43 , 44 , 45 , 53 , 62 , 65 , 69 , 75 , 78 , 109 , 110 , 117 , 118 , 122 , 124 , 131 , 138 , 140 , 144 , 157 ].
Limitation of generalizability of results has also been mentioned related to small sample size, limited study setting, study design, and non-probability sampling techniques [ 11 , 30 , 42 , 44 , 64 , 72 , 80 , 82 , 84 , 91 , 96 , 98 , 100 , 102 , 143 ] and, or due to other peculiar nature of included studies as PD approach assumes exceptional performance that is quite different from the norm even with the inclusion of comparators [ 8 , 18 ]. However, it is worth considering that findings from qualitative studies are not intended to be generalized, but rather to provide insights into previously unexplored areas and to generate hypotheses for future quantitative evaluation [ 158 ]. In PD, qualitative studies help researchers to identify best practices from high achievers that can be adopted in other settings with similar contexts. Therefore, the results of PD-related studies may not be generalizable to other settings due to their intentional focus on high-performing teams or organization/s and usage of qualitative research designs as its foundation [ 18 ]. In addition, the issue of not testing statistical relationships [ 33 , 65 , 83 ] might not be an issue as the fundamental principle of qualitative studies is to generate ideas from a small sample of the population; therefore, the results can be tested in a larger and more representative sample of the population. This signifies the need to conduct a quantitative study after developing a testable hypothesis from the qualitative studies depending on the nature of their research questions due to the need for research findings to have a statistically significant relationship if it is to be scientifically accepted as a predictor variable or variable associated with another outcome variable [ 18 ]. Above all, it is paramount to consider that even in qualitative studies, the results can still apply to other contextually similar situations as far as rigorous procedures are followed by authors in conducting their qualitative studies. This is known as theoretical generalizability or transferability [ 159 ].
Moreover, limited study setting [ 30 , 31 , 41 , 44 , 80 , 82 , 88 , 90 , 101 ], and limited staff involvement are also repetitively mentioned as a challenge in utilizing PD [ 11 , 41 , 64 , 72 , 81 , 82 , 87 , 96 ]. This has been reflected in many studies suggesting that the process of recruiting study participants might disproportionately focus on leaders and senior managers, potentially neglecting insights from frontline staff who also contribute to successful practices. Related to this, the issue of possible failure to achieve information saturation has also been included [ 82 ]. This challenge should be addressed via the use of robust qualitative methods that if done well could ensure both a broad sample of respondents (especially the front line) and employ saturation as a criterion for sample size and data collection iteration. This justification has been supported by the fact that several other studies have considered multiple settings and stakeholders including frontline staff in their studies signifying the importance of taking multiple participants from various settings and including different stakeholders if researchers are to get rich sources of information on the performance of health facilities and other responsible bodies within the health system [ 78 , 81 , 84 , 91 , 95 , 110 , 112 ].
Furthermore, although lack of comparison has been mentioned as a limitation in some studies, the inclusion of comparators in the implementation of the PD approach has been mentioned as a strength as well and proved its importance in testing the impact of PD-based interventional studies [ 25 , 26 , 27 , 28 , 32 , 34 , 36 , 37 , 39 , 61 , 70 , 98 , 106 , 113 , 119 , 143 , 145 ]. The reason why it is important to include comparators in the utilization of PD is that it helps researchers to uncover the traits that distinguish high performers from low performers, as well as to shed light on the unproductive practices of low performers. In addition, performing statistical tests by including comparators is also recommended if the later stages are to be implemented after the identification of PDs, as in stage 3 of Bradly EH, et al.’s (2009) framework [ 18 ]. Furthermore, in implementation research, a PD intervention can be applied to one group, and the results can be compared to a control group that was not exposed to the PD intervention, allowing researchers to investigate the true impact of the positive deviant practice/s in other similar settings [ 160 ]. However, this may not be always possible due to various reasons including refusal of low-performing individuals, groups, and, or healthcare settings due to fearing reprisal and other reasons. Moreover, resource constraints may make the inclusion of comparators very challenging in different situations. In such instances, other options can be considered, if comparison is needed including before and after intervention analysis as pre-post interventional designs play a crucial role in assessing the efficacy of strategies employed by high achievers in other similar settings, elucidating their impact over time [ 148 , 149 ].
Different forms of bias including recall, social desirability, interviewer and researcher biases, and the Hawthorne Effect have been also cited as limitations in many articles [ 55 , 64 , 81 , 84 , 85 , 86 , 87 , 96 , 101 , 102 ]. However, even though the approach has a special focus on qualitative studies, these issues are not specific to PD and can be handled contextually. For instance, blinding of study participants, data collectors, and analyzers can be done to reduce the effect of social desirability, interviewer, and researcher biases, respectively. This is because even though the PD approach commands the researchers to identify top-performing individuals, groups, and organizations, and identify their strategies for being successful [ 18 ], the data collectors, study participants, and data analyzers can still be blinded regarding the research design and who positive deviant is and is not. An example of bias in data analysis is a faulty interpretation. This occurs, when authors approach analysis intending to justify their belief or perspective, which can potentially lead to the discovery of facts that support their point of view invariably [ 161 ]. Therefore, having different data analyzers and comparing the results of the outcomes could help in reducing such biases. In addition, blinding study participants about what they are going to be asked may not be applicable, in fact, however, at least they still can be blinded to whether they or their facility is considered as positive deviant or not. Recall and social desirability biases and the Hawthorne Effect would also likely act similarly among participants from positive and negative deviant categories, limiting its impact on the comparisons provided, particularly, if the participants did not know their deviant category, suggesting the importance of blinding high and low performing classifications [ 115 ].
Nevertheless, as with other approaches, different strategies can be employed to minimize the effect of bias in the utilization of PD. For instance, one article used three techniques to minimize the effect of researchers’ preconceived biases from affecting the results. These techniques were (1) enhancing the attention of researchers’ reflexiveness through systematic debriefings with an organizational psychologist; (2) utilizing a multidisciplinary team to analyze transcripts critically with an explicit focus on identifying negative (disconfirming) cases; and (3) training of interviewers on the strategies of data collection including how to encourage participants to get both reliable data during interviews, without interviewer judgment [ 82 ]. In summary, incorporating different strategies can enhance the robustness and applicability of PD-related studies in healthcare and other fields. As a result, careful planning and addressing potential design flaws and methodological limitations are important for deriving meaningful conclusions from such studies [ 10 , 18 ].
Implications
Several articles have proved the successfulness of utilizing the PD approach in multiple areas of the healthcare system including in improving quality of care, increasing hand hygiene compliance rate, infection prevention, prevention of postoperative complications, and medication errors. This indicates the enormous potential of utilizing the PD approach for healthcare service quality improvement programs. Moreover, even though some earlier articles stated that the utility of the PD approach is limited in complex settings including the healthcare system [ 20 ], and various included articles have mentioned several limitations, as highlighted before, these issues are potentially manageable if they are carefully handled [ 10 , 18 ].
Strength and limitations
This scoping review only included articles that are conducted at the health system, health facility, and individual levels within the healthcare systems. In addition, only studies published in the English language were considered. Another limitation is that some articles might be missed due to failing to use the phrase “positive deviance”, despite utilizing the approach in their studies, related to inconsistent use of different terminologies to describe PDs in several situations [ 57 ]. However, comprehensive searches were employed across multiple databases using predefined search strategies.
Positive deviance has been extensively utilized for healthcare service and quality enhancement programs around the world, particularly in developed countries as most of the articles are from three countries (USA, Canada, and the United Kingdom) with the USA contributing to more than half of all the included articles. In addition, several types of study designs including qualitative, mixed-methods, interventional, and randomized controlled trials have been employed by researchers and program implementers depending on the context and specific objectives of their project works. By identifying and learning from those who exhibit exceptional practices, healthcare systems have been able to implement successful strategies, enhance quality, reduce errors, and improve patient outcomes. However, all the outcomes of PD-based research depend on the first step of identifying true PDs. This is because unless studies use objective and validated measures of performance, identification of true PDs is less likely, and this can in turn result in failure to identify best practices for learning. Therefore, researchers need to take different contexts in the initial stages of PD into consideration to avoid the problems reported in the identification processes of PDs including the usage of standardized performance measures. In addition, the use of comparators and exploring the practice of low performers can help to uncover the traits that distinguish good performers from low performers, as well as to shed light on unproductive practices.
Data availability
Data is provided within the manuscript or supplementary information files.
Abbreviations
Population Concept and Context
Preferred Reporting Items for Systematic Reviews and Meta-analysis extension for Scoping Reviews
Positive Deviance
Positive Deviants
Universal Health Coverage
United States of America
World Health Organization
World Health Organization, World Bank. Tracking universal health coverage: 2021 global monitoring report. https://elibrary.worldbank.org/doi/abs/10.1596/36724 . Accessed 05 May 2023.
Giovanella L, Mendoza-Ruiz A, AdCA P, MCd R, Martins GB, Santos IS, et al. Universal health system and universal health coverage: assumptions and strategies. Cien Saude Colet. 2018;23:1763–76.
Article PubMed Google Scholar
Tichenor M, Sridhar D. Universal health coverage, health systems strengthening, and the World Bank. BMJ. 2017;358.
Dixon-Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the Health Foundation’s programme evaluations and relevant literature. BMJ Qual Saf. 2012;21(10):876–84.
Article PubMed PubMed Central Google Scholar
Vogel JP, Moore JE, Timmings C, Khan S, Khan DN, Defar A, et al. Barriers, facilitators and priorities for implementation of WHO maternal and perinatal health guidelines in four lower-income countries: a GREAT network research activity. PLoS One. 2016;11:e0160020.
Darrudi A, Khoonsari MHK, Tajvar M. Challenges to achieving universal health coverage throughout the world: a systematic review. J Preventive Med Public Health. 2022;55(2):125.
Article Google Scholar
Mittelmark MB, Bull T, Bouwman L. Emerging ideas relevant to the salutogenic model of health. In: The handbook of salutogenesis. 2017. pp. 45–56.
Chapter Google Scholar
Pascale R, Monique SJS. The power of positive deviance. Harvard Business Press; 2010.
Google Scholar
Marsh DR, Schroeder DG, Dearden KA, Sternin J, Sternin M. The power of positive deviance. BMJ. 2004;329(7475):1177–79.
Baxter R, Lawton R. The Positive deviance approach. Cambridge: Cambridge University Press; 2022. Available from: https://www.cambridge.org/core/elements/positive-deviance-approach/506CA2D446210E1FE76740B7F835D87C .
Brewster AL, Brault MA, Tan AX, Curry LA, Bradley EH. Patterns of collaboration among health care and social services providers in communities with lower health care utilization and costs. Health Serv Res. 2018;53:2892–909.
Dadich A, Collier A, Hodgins M, Crawford G. Using positive organizational scholarship in healthcare and video reflexive ethnography to examine positive deviance to new public management in healthcare. Qual Health Res. 2018;28(8):1203–16.
Positive deviance model – explained: written by Jason Gordon, Updated on May 11, 2022. https://thebusinessprofessor.com/en_US/management-leadership-organizational-behavior/positive-deviance-model-explained . Accessed 17 May 2023.
Singhal A, Svenkerud PJ. Flipping the diffusion of innovations paradigm: embracing the positive deviance approach to social change. Asia Pacific Media Educator. 2019;29(2):151–63.
Schooley J, Morales L. Learning from the community to improve maternal–child health and nutrition: the positive deviance/hearth approach. J Midwifery Womens Health. 2007;52(4):376–83.
Machado JC, Cotta RMM, da Silva LS. The positive deviance approach to change nutrition behavior: a systematic review/Abordagem do desvio positivo para a mudanca de comportamento alimentar: revisao sistematica. Rev Panam Salud Publica. 2014;36(2):134–41.
PubMed Google Scholar
Bisits Bullen PA. The positive deviance/hearth approach to reducing child malnutrition: systematic review. Trop Med Int Health. 2011;16(11):1354–66.
Bradley EH, Curry LA, Ramanadhan S, Rowe L, Nembhard IM, Krumholz HM. Research in action: using positive deviance to improve quality of health care. Implement Sci. 2009;4(1):1–11.
Singhal A, Dura L. Positive deviance: A non-normative approach to health and risk messaging. Oxford research encyclopedia of communication. 2017.
Baxter R, Taylor N, Kellar I, Lawton R. What methods are used to apply positive deviance within healthcare organisations? A systematic review. BMJ Qual Saf. 2016;25(3):190–201.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Kassie AM, Eakin E, Abate BB, Endalamaw A, Zewdie A, Wolka E, et al. Use of the positive deviance approach for healthcare system service improvement: a scoping review protocol. BMJ Open. 2023;13:e078809.
Ausserhofer D, Rakic S, Novo A, Dropic E, Fisekovic E, Sredic A, et al. Improving the safety and quality of nursing care through standardized operating procedures in Bosnia and Herzegovina. Int Nurs Rev. 2016;63:208–17.
Rakic S, Djudurovic A, Antonic D. Financial sustainability strategies of public primary health care centres in the Republic of Srpska, Bosnia and Herzegovina. Int J Health Plann Manag. 2021;36(5):1772–88.
Marra AR, Reis Guastelli L, Pereira de Araújo CM, Saraiva Dos Santos JL, Filho MAO, Silva CV, et al. Positive deviance: a program for sustained improvement in hand hygiene compliance. Am J Infect Control. 2011;39:1–5.
de Macedo R, Oliveira Jacob EM, da Silva VP, Santana EA, de Souza AF, Gonçalves P, et al. Positive deviance: using a nurse call system to evaluate hand hygiene practices. Am J Infect Control. 2012;40:946–50.
Francimar Tinoco de O, Maria Manuela Frederico F, Silvia Teresa Carvalho de A, Amanda Trindade Teixeira de B, Advi Catarina Barbachan M, Marluci Andrade Conceição S. Positive deviance as a strategy to prevent and control bloodstream infections in intensive care. Rev Esc Enferm USP. 2017;51:1–7.
Ferracini FT, Marra AR, Schvartsman C, Dos Santos OFP, EdS V, Negrini NMM, et al. Using positive deviance to reduce medication errors in a tertiary care hospital. BMC Pharmacol Toxicol. 2016;17(1):1–8.
Green CJ, Fortin P, Maclure M, Macgregor A, Robinson S. Informatics system support as a critical seccess factor for chronic disease management: necessary but not sufficient. Int J Med Inform. 2006;75(12):818–28.
Buduhan G, Chand E, Kidane B, Srinathan S, Tan L, Liu R. Impact of cost-awareness education and surgeon-led positive deviance on intraoperative costs of thoracoscopic lobectomy. J Thorac Cardiovasc Surg. 2023;165(6):1939–46.
Ivanovic J, Anstee C, Ramsay T, Gilbert S, Maziak DE, Shamji FM, et al. Using surgeon-specific outcome reports and positive deviance for continuous quality improvement. Ann Thorac Surg. 2015;100:1188–95.
Gold R, Al Zoubi F, Brillinger J, Kreviazuk C, Garvin D, Schramm D, et al. Use of multidisciplinary positive deviance seminars to improve efficiency in a high-volume arthroplasty practice: a pilot study. Can J Surg. 2023;66:E1–E7.
Derocher M, Davie S, Kiran T. Using positive deviance to improve timely access in primary care. BMJ Open Qual. 2021;10(4).
Seely AJE, Ahmadzai Z, French DG, Gingrich M, Jones D, Anstee C, et al. Multicentre positive deviance to reduce adverse events and length of stay after pulmonary resection. BMJ Open Qual. 2023;12(1).
Létourneau J, Alderson M, Leibing A. Positive deviance and hand hygiene of nurses in a Quebec hospital: what can we learn from the best? Am J Infect Control. 2018;46(5):558–63.
Wong MWH, Xu YZ, Bone J, Srigley JA. Impact of patient and visitor hand hygiene interventions at a pediatric hospital: a stepped wedge cluster randomized controlled trial. Am J Infect Control. 2020;48(5):511–16.
Ivanovic J, Mostofian F, Anstee C, Gilbert S, Maziak DE, Shamji FM, et al. Impact of surgeon self-evaluation and positive deviance on postoperative adverse events after non-cardiac thoracic surgery. J Healthc Qual. 2018;40:e62–e70.
ElChamaa R, Seely AJE, Jeong D, Kitto S. Barriers and facilitators to the implementation and adoption of a continuous quality improvement program in surgery: a case study. J Contin Educ Health Prof. 2022;42(4):227–35.
Escobar NMO, Márquez IAV, Quiroga JA, Trujillo TG, González F, Aguilar MIG, et al. Using positive deviance in the prevention and control of MRSA infections in a Colombian hospital: a time-series analysis. Epidemiol Infect. 2017;145:981–89.
Bourret KM, Larocque S, Hien A, Hogue C, Muray K, Lukusa AT, et al. Midwives’ integration of post abortion manual vacuum aspiration in the Democratic Republic of Congo: a mixed methods case study & positive deviance assessment. BMC Health Serv Res. 2020;20:1–16.
Hølge-Hazelton B, Berthelsen CB. Leading unique cultures in departments with low turnover of nurses. A positive deviance approach study. J Nurs Manag. 2020;28(6):1207–14.
Hølge-Hazelton B, Berthelsen CB. Why nurses stay in departments with low turnover: a constructivist approach. Nord J Nurs Res. 2021;41(3):158–65.
Assefa Y, Lynen L, Wouters E, Rasschaert F, Peeters K, Van Damme W. How to improve patient retention in an antiretroviral treatment program in Ethiopia: a mixed-methods study. BMC Health Serv Res. 2014;14(1):45.
Bradley EH, Byam P, Alpern R, Thompson JW, Zerihun A, Abebe Y, et al. A systems approach to improving rural care in Ethiopia. PloS One. 2012;7:e35042.
Article CAS PubMed PubMed Central Google Scholar
Driesen J, El-Khatib Z, Wulkow N, Joblin M, Vasileva I, Glücker A, et al. Data-powered positive deviance during the SARS-CoV-2 pandemic-an ecological pilot study of German districts. Int J Environ Res Public Health. 2021;18(18).
Waltering I, Schwalbe O, Hempel G. Identification of factors for a successful implementation of medication reviews in community pharmacies: using positive deviance in pharmaceutical care. Int J Clin Pharm. 2022;44(1):79–89.
Maisa EA, Arif Y. The analysis of nurses’ positive deviance behaviours as a measure in preventing the transmission of Healthcare-Associated Infections (HAIs) at M. Djamil Hospital, Padang, West Sumatera. Elevate. 2018;1(1):3–13.
Kim YM, Heerey M, Kols A. Factors that enable nurse-patient communication in a family planning context: a positive deviance study. Int J Nurs Stud. 2008;45(10):1411–21.
Gesser-Edelsburg A, Cohen R, Halavi AM, Zemach M, Van Heerden PV, Sviri S, et al. Beyond the hospital infection control guidelines: a qualitative study using positive deviance to characterize gray areas and to achieve efficacy and clarity in the prevention of healthcare-associated infections. Antimicrob Resist Infect Control. 2018;7(1).
Cohen R, Gesser-Edelsburg A, Singhal A, Benenson S, Moses AE. Translating a theory-based positive deviance approach into an applied tool: mitigating barriers among health professionals (HPs) regarding infection prevention and control (IPC) guidelines. PLoS ONE. 2022;17(6).
Gesser-Edelsburg A, Cohen R, Halavi AM, Zemach M. Motivating healthcare professionals (nurses, nurse assistants, physicians) to integrate new practices for preventing healthcare-associated infections into the care continuum: turning positive deviance into positive norms. BMC Infect Dis. 2021;21(1):1–12.
Cohen R, Gesser-Edelsburg A, Singhal A, Benenson S, Moses AE. Deconstruction of central line insertion guidelines based on the positive deviance approach—reducing gaps between guidelines and implementation: a qualitative ethnographic research. PLoS ONE. 2019;14(9).
Borghini A, Corazza I, Nuti S. Learning from excellence to improve healthcare services: the experience of the maternal and child care pathway. Int J Environ Res Public Health. 2021;18(4):1481.
Crewe S, Girardi A. Nurse managers: being deviant to make a difference. J Manage Organ. 2020;26(3):324–39.
Naimoli JF, Challa S, Schneidman M, Kostermans K. Toward a grounded theory of why some immunization programmes in sub-Saharan Africa are more successful than others: a descriptive and exploratory assessment in six countries. Health Policy Plann. 2008;23(6):379–89.
LaFond A, Kanagat N, Steinglass R, Fields R, Sequeira J, Mookherji S. Drivers of routine immunization coverage improvement in Africa: findings from district-level case studies. Health Policy Plann. 2015;30(3):298–308.
Singh S, Mazor KM, Fisher KA. Positive deviance approaches to improving vaccination coverage rates within healthcare systems: a systematic review. J Comp Eff Res. 2019;8(13):1055–65.
Longhini J, Papastavrou E, Efstathiou G, Andreou P, Stemmer R, Ströhm C, et al. Strategies to prevent missed nursing care: an international qualitative study based upon a positive deviance approach. J Nurs Manag. 2021;29:572–83.
O’Malley R, O’Connor P, Madden C, Lydon S. A systematic review of the use of positive deviance approaches in primary care. Fam Pract. 2022;39(3):493–503.
Rose L, Allum LJ, Istanboulian L, Dale C. Actionable processes of care important to patients and family who experienced a prolonged intensive care unit stay: qualitative interview study. J Adv Nurs (John Wiley & Sons, Inc). 2022;78(4):1089–99.
Marra AR, Noritomi DT, Westheimer Cavalcante AJ, Sampaio Camargo TZ, Bortoleto RP, Durao Junior MS, et al. A multicenter study using positive deviance for improving hand hygiene compliance. Am J Infect Control. 2013;41:984–88.
Lewis TP, McConnell M, Aryal A, Irimu G, Mehata S, Mrisho M, et al. Health service quality in 2929 facilities in six low-income and middle-income countries: a positive deviance analysis. Lancet Glob Health. 2023;11:e862–e70.
Alzunitan MA, Edmond MB, Alsuhaibani MA, Samuelson RJ, Schweizer ML, Marra AR. Positive deviance in infection prevention and control: a systematic literature review. Infect Control Hosp Epidemiol. 2022;43(3):358–65.
Dhital R, Subedi M, Hamal PK, Shrestha C, Bhusal S, Rimal R, et al. How positive deviants helped in fighting the early phase of COVID-19 pandemic? A qualitative study exploring the roles of frontline health workers in Nepal. PLOS Glob Public Health. 2023;3:e0000671.
Lewis TP, Aryal A, Mehata S, Thapa A, Yousafzai AK, Kruk ME. Best and worst performing health facilities: a positive deviance analysis of perceived drivers of primary care performance in Nepal. Soc Sci Med. 2022;309 ((Lewis T.P., [email protected]; Yousafzai A.K., [email protected]; Kruk M.E., [email protected]) Department of Global Health and Population, Harvard T.H. Chan School of Public Health, 677 Huntington Avenue, Boston, MA, United States(A).
Caris MG, Kamphuis PGA, Dekker M, De Bruijne MC, Van Agtmael MA, Cmje V-G.Patient safety culture and the ability to improve: a proof of concept study on hand hygiene. Infect Control Hosp Epidemiol. 2017;38(11):1277–83.
Brandrud AS, Nyen B, Hjortdahl P, Sandvik L, Haldorsen GSH, Bergli M, et al. Domains associated with successful quality improvement in healthcare - a nationwide case study. BMC Health Serv Res. 2017;17.
Włodarczyk D, Ziętalewicz U. Medics as a positive deviant in influenza vaccination: the role of vaccine beliefs, self-efficacy and contextual variables. Vaccines. 2022;10(5).
Alidina S, Chatterjee P, Zanial N, Sanjay Alreja S, Balira R, Barash D, et al. Improving surgical quality in low-income and middle-income countries: why do some health facilities perform better than others? BMJ Qual Saf. 2021;30:937–49.
Kosugi H, Shibanuma A, Kiriya J, Ong KIC, Mucunguzi S, Muzoora C, et al. Positive deviance for promoting dual-method contraceptive use among women in Uganda: a cluster randomised controlled trial. BMJ Open. 2021;11(8).
Altaras R, Nuwa A, Agaba B, Streat E, Tibenderana JK, Strachan CE. Why do health workers give anti-malarials to patients with negative rapid test results? A qualitative study at rural health facilities in western Uganda. Malaria J. 2016;15(1).
Mannion R, Konteh FH, Jacobs R. Organisational drivers of performance in mental health providers. J Health Organiz Manage. 2023;37(2):273–87.
Baxter R, Taylor N, Kellar I, Pye V, Mohammed MA, Lawton R. Identifying positively deviant elderly medical wards using routinely collected NHS safety thermometer data: an observational study. BMJ Open. 2018;8(2).
Baxter R, Shannon R, Murray J, O’Hara JK, Sheard L, Cracknell A, et al. Delivering exceptionally safe transitions of care to older people: a qualitative study of multidisciplinary staff perspectives. BMC Health Serv Res. 2020;20:780.
Newby KV, Parsons J, Brooks J, Leslie R, Inglis N. Identifying strategies to increase influenza vaccination in GP practices: a positive deviance approach. Fam Pract. 2016;33(3):318–23.
Liberati EG, Tarrant C, Willars J, Draycott T, Winter C, Chew S, et al. How to be a very safe maternity unit: an ethnographic study. Soc Sci Med. 2019;223:64–72.
Baxter R, Taylor N, Kellar I, Lawton R. A qualitative positive deviance study to explore exceptionally safe care on medical wards for older people. BMJ Qual Saf. 2019;28(8):618–26.
O’Hara JK, Grasic K, Gutacker N, Street A, Foy R, Thompson C, et al. Identifying positive deviants in healthcare quality and safety: a mixed methods study. J R Soc Med. 2018;111:276–91.
Hughes L, Sheard L, Pinkney L, Lawton RL. Excellence in elective hip and knee surgery: what does it look like? A positive deviance approach. J Health Serv Res Policy. 2020;25(1):5–12.
Mansfield LN, Choi K, Delgado JR, Macias M, Munoz-Plaza C, Lewin B, et al. Decision-making about COVID-19 vaccines among health care workers and their adolescent children. West J Nurs Res. 2023;01939459231170981.
Leyenaar JK, Andrews CB, Tyksinski ER, Biondi E, Parikh K, Ralston S. Facilitators of interdepartmental quality improvement: a mixed-methods analysis of a collaborative to improve pediatric community-acquired pneumonia management. BMJ Qual Saf. 2019;28(3):215–22.
Landman AB, Spatz ES, Cherlin EJ, Krumholz HM, Bradley EH, Curry LA. Hospital collaboration with emergency medical services in the care of patients with acute myocardial infarction: perspectives from key hospital staff. Ann Emerg Med. 2013;61(2):185–95.
Klaiman TA, Pantazis A, Bekemeier B. A method for identifying positive deviant local health departments in maternal and child health. Front Public Health Serv Syst Res. 2014;3(2):5.
Kaiser SV, Lam R, Cabana MD, Bekmezian A, Bardach NS, Auerbach A, et al. Best practices in implementing inpatient pediatric asthma pathways: a qualitative study. J Asthma. 2020;57:744–54.
Curry LA, Spatz E, Cherlin E, Thompson JW, Berg D, Ting HH, et al. What distinguishes top-performing hospitals in acute myocardial infarction mortality rates? A qualitative study. Ann Intern Med. 2011;154:384–90.
Bristol AA, Nibbelink CW, Gephart SM, Carrington JM.Nurses’ use of positive deviance when encountering electronic health records-related unintended consequences. Nurs Adm Q. 2018;42(1):E1–E11.
Bradley EH, Curry LA, Spatz ES, Herrin J, Cherlin EJ, Curtis JP, et al. Hospital strategies for reducing risk-standardized mortality rates in acute myocardial infarction. Ann Intern Med. 2012;156:618–26.
Tseng CL, Soroka O, Maney M, Aron DC, Pogach LM. Assessing potential glycemic overtreatment in persons at hypoglycemic risk. JAMA Intern Med. 2014;174(2):259–68.
Klaiman T, Pracilio V, Kimberly L, Cecil K, Legnini M. Leveraging effective clinical registries to advance medical care quality and transparency. Population Health Manage. 2014;17(2):127–33.
Greene J, Hibbard JH, Alvarez C, Overton V. Supporting patient behavior change: approaches used by primary care clinicians whose patients have an increase in activation levels. Ann Fam Med. 2016;14(2):148–54.
Abrahamson K, Durham M, Norton K, Doebbeling BN, Doebbeling CC, Anderson JG. Provision of psychosocial care for cancer patients: service delivery in urban and rural settings. J Prim Care Community Health. 2011;2(4):220–24.
Bonuel N, Byers P, Gray-Becknell T. Methicillin resistant Staphylococcus aureus (MRSA) prevention through facility-wide culture change. Crit Care Nurs Q. 2009;32(2):144–48.
de Grubb MCM, Levine RS, Kilbourne B, Husaini BA, Skelton T, Gittner L, et al. Rural congestive heart failure mortality among US elderly, 1999-2013: identifying counties with promising outcomes and opportunities for implementation research. Fam Med Comm Health. 2015;3:27–38.
Toscos T, Carpenter M, Flanagan M, Kunjan K, Doebbeling BN. Identifying successful practices to overcome access to care challenges in community health centers: a “Positive Deviance” approach . Health Serv Res Manag Epidemiol. 2018;5:2333392817743406.
PubMed PubMed Central Google Scholar
Spitzer KA, Stefan MS, Priya A, Pack QR, Pekow PS, Lagu T, et al. Promoting participation in pulmonary rehabilitation after hospitalization for chronic obstructive pulmonary disease, strategies of top-performing systems: a qualitative study. Ann Am Thorac Soc. 2023;20:532–38.
Schulson LB, Predmore Z, Sousa JL, McCullough CM, Magit A, Lerner C, et al. Perceptions of pediatric endocrinologists and neurologists on the drivers of telehealth use. Acad Pediatr. 2023;23:271–78.
Plough A, Henrich N, Galvin G, Shah NT. Common challenges managing bed and staff availability on labor and delivery units in the United States: a qualitative analysis. Birth. 2018;45(3):303–10.
Lindberg CM, Lindberg CC, D’Agata EMC, Esposito B, Downham G. Advancing antimicrobial stewardship in outpatient dialysis centers using the positive deviance process. Nephrol Nurs J. 2019;46(5):511–18.
Kotejoshyer R, Eve J, Priya A, Mazor K, Spitzer KA, Pekow PS, et al. Strategies to improve enrollment and participation in pulmonary rehabilitation following a hospitalization for COPD: RESULTS OF A NATIONAL SURVEY. J Cardiopulm Rehabil Prev. 2023;43:192–97.
Gary JC. The wicked question answered: positive deviance delivers patient-centered care. Dimens Crit Care Nurs. 2014;33(3):142–50.
Ellenbogen MI, Wiegand AA, Austin JM, Schoenborn NL, Kodavarti N, Segal JB. Reducing overuse by healthcare systems: a positive deviance analysis. J Gen Intern Med. 2023.
Cherlin EJ, Curry LA, Thompson JW, Greysen SR, Spatz E, Krumholz HM, et al. Features of high quality discharge planning for patients following acute myocardial infarction. J Gen Intern Med. 2013;28:436–43.
Blok AC, May CN, Sadasivam RS, Houston TK. Virtual patient technology: engaging primary care in quality improvement innovations. JMIR Med Educ. 2017;3(1):e3.
Razouki Z, Knighton T, Martinello RA, Hirsch PR, McPhaul KM, Rose AJ, et al. Organizational factors associated with Health Care Provider (HCP) influenza campaigns in the veterans health care system: a qualitative study. BMC Health Serv Res. 2016;16:1–10.
Hendryx M, Guerra-Reyes L, Holland BD, McGinnis MD, Meanwell E, Middlestadt SE, et al. A county-level cross-sectional analysis of positive deviance to assess multiple population health outcomes in Indiana. BMJ Open. 2017;7(10).
Sreeramoju P, Dura L, Fernandez ME, Minhajuddin A, Simacek K, Fomby TB, et al. Using a positive deviance approach to influence the culture of patient safety related to infection prevention. Open Forum Infect Dis. 2018;5(10).
Bates KE, Yu S, Mangeot C, Shea JA, Brown DW, Uzark K. Identifying best practices in interstage care: using a positive deviance approach within the National Pediatric Cardiology Quality Improvement Collaborative. Cardiol Young. 2019;29(3):398–407.
Lyn R, Heath E, Torres A, Andrews C. Investigating improvements in premature death in two rural, majority-minority counties in the south. SSM Popul Health. 2020;11 ((Lyn R., [email protected]; Heath E.; Andrews C.) School of Public Health, Georgia State University, Atlanta, GA, United States(Torres A.) ICF, Fairfax, VA, United States).
Topmiller M, Kieber-Emmons AM, Shaak K, McCann JL. Identifying bright spot counties for appropriate diabetes preventive care: a geospatial, positive deviance approach. J Prim Prev. 2020;41(5):431–43.
Rand CM, Concannon C, Wallace-Brodeur R, Davis W, Albertin CS, Humiston SG, et al. Identifying strategies to reduce missed opportunities for HPV vaccination in primary care: a qualitative study of positive deviants. Clin Pediatr. 2020;59:1058–68.
Bolen SD, Love TE, Einstadter D, Lever J, Lewis S, Persaud H, et al. Improving regional blood pressure control: a positive deviance tiered intensity approach. J Gen Intern Med. 2021;36:1591–97.
Blok AC, Anderson E, Swamy L, Mohr DC. Comparing nurse leader and manager perceptions of and strategies for nurse engagement using a positive deviance approach: a qualitative analysis. J Nurs Manag. 2021;29(6):1476–85.
Fernandez N, Low D, Cain M, Martin L, Merguerian P. Recovering from COVID – improving operating room capacity. J Pediatr Urol. 2022;18(4):411.e1-.e7.
Rotenstein LS, Cohen DJ, Marino M, Bates DW, Edwards ST. Association of clinician practice ownership with ability of primary care practices to improve quality without increasing burnout. JAMA Health Forum. 2023;4(3):e230299.
Gabbay RA, Friedberg MW, Miller-Day M, Cronholm PF, Adelman A, Schneider EC. A positive deviance approach to understanding key features to improving diabetes care in the medical home. Ann Fam Med. 2013;11(Supp 1):S99–S107.
Chang AM, Cohen DJ, Lin A, Augustine J, Handel DA, Howell E, et al. Hospital strategies for reducing emergency department crowding: a mixed-methods study. Ann Emerg Med. 2018;71:497–505.e4.
Kraschnewski JL, Sciamanna CN, Pollak KI, Stuckey HL, Sherwood NE. The epidemiology of weight counseling for adults in the United States: a case of positive deviance. Int J Obesity. 2013;37(5):751–53.
Article CAS Google Scholar
Taliani CA, Bricker PL, Adelman AM, Cronholm PF, Gabbay RA. Implementing effective care management in the patient-centered medical home. Am J Manag Care. 2013;19(12):957–64.
Lindberg C, Downham G, Buscell P, Jones E, Peterson P, Krebs V. Embracing collaboration: a novel strategy for reducing bloodstream infections in outpatient hemodialysis centers. Am J Infect Control. 2013;41(6):513–19.
Klaiman T, O’Connell K, Stoto MA. Learning from successful school-based vaccination clinics during 2009 pH1N1. J Sch Health. 2014;84(1):63–69.
Jadhav ED, Holsinger Jr JW, Mays G, Fardo D. Should they stay or should they go? Leader duration and financial performance in local health departments. J Public Health Manag Pract. 2015;21(2):151–60.
Uscher-Pines L, Sousa J, Zachrison K, Guzik A, Schwamm L, Mehrotra A. What drives greater assimilation of telestroke in emergency departments? J Stroke Cerebrovasc Dis. 2020;29(12):105310.
Klaiman T, O’Connell K, Stoto M. Local health department public vaccination clinic success during 2009 pH1N1. J Public Health Manag Pract. 2013;19(4):E20–E6.
Fisher KA, Mazor KM, Goff S, Stefan MS, Pekow PS, Williams LA, et al. Successful use of noninvasive ventilation in chronic obstructive pulmonary disease. How do high-performing hospitals do it? Ann Am Thoracic Soc. 2017;14:1674–81.
Banerjee ES, Herring SJ, Hurley KE, Puskarz K, Yebernetsky K, LaNoue M. Overcoming obesity: a mixed methods study of the impact of primary care physician counseling on low-income African American women who successfully lost weight. Am J Health Promot. 2018;32(2):374–80.
Pimperl AF, Rodriguez HP, Schmittdiel JA, Shortell SM. A two-step method to identify positive deviant physician organizations of accountable care organizations with robust performance management systems. Health Serv Res. 2018;53(3):1851–69.
Jasuja GK, Engle RL, Skolnik A, Rose AJ, Male A, Reisman JI, et al. Understanding the context of high- and low-testosterone prescribing facilities in the Veterans Health Administration (VHA): a qualitative study. Jgim. 2019;34:2467–74.
Klaiman T, Pantazis A, Chainani A, Bekemeier B. Using a positive deviance framework to identify Local Health Departments in Communities with exceptional maternal and child health outcomes: a cross sectional study. BMC Public Health. 2016;16(1):1–8.
Blayney DW, Simon MK, Podtschaske B, Ramsey S, Shyu M, Lindquist C, et al. Critical lessons from high-value oncology practices. JAMA Oncol. 2018;4:164–71.
Wilson B, Chin-Lin T, Soroka O, Pogach LM, Aron DC, Tseng C-L. Identification of outliers and positive deviants for healthcare improvement: looking for high performers in hypoglycemia safety in patients with diabetes. BMC Health Serv Res. 2017;17:1–10.
Griffith JJ, Fear KM, Lammers E, Banaszak-Holl J, Lemak CH, Zheng K. A positive deviance perspective on hospital knowledge management: analysis of baldrige award recipients 2002-2008. J Healthc Manag. 2013;58(3):187–203.
Klaiman T, Chainani A, Bekemeier B. The importance of partnerships in local health department practice among communities with exceptional maternal and child health outcomes. J Public Health Manag Pract. 2016;22(6):542–49.
Anderson E, Soylemez Wiener R, Resnick K, Elwy AR, Rinne ST. Care coordination for veterans with COPD: a positive deviance study. Am J Manag Care. 2020;26(2):63–68.
Spece LJ, Epler EM, Duan K, Donovan LM, Griffith MF, LaBedz S, et al. Reassessment of home oxygen prescription after hospitalization for chronic obstructive pulmonary disease. a potential target for deimplementation. Ann Am Thoracic Soc. 2021;18:426–32.
Gunn R, Ferrara LK, Dickinson C, Stock I, Griffith-Weprin J, Wiser A, et al. Human Papillomavirus immunization in rural primary care. Am J Prevent Med. 2020;59:377–85.
Scott LC, Bartley S, Dowling NF, Richardson LC. Finding “Bright Spots”: using multiple measures to examine local-area racial equity in cancer mortality outcomes. Am J Epidemiol. 2021;190(4):673–80.
Adeoye-Olatunde OA, Lake LM, Strohmier CA, Gourley AK, Ray AR, Zillich AJ, et al. Positive deviants for medication therapy management: a mixed-methods comparative case study of community pharmacy practices. Res Soc Administrative Pharm. 2021;17:1407–19.
Goff SL, Mazor KM, Priya A, Moran M, Pekow PS, Lindenauer PK. Organizational characteristics associated with high performance on quality measures in pediatric primary care: a positive deviance study. Health Care Manage Rev. 2021;46(3):196–205.
Howell EA, Sofaer S, Balbierz A, Kheyfets A, Glazer KB, Zeitlin J. Distinguishing high-performing from low-performing hospitals for severe maternal morbidity: a focus on quality and equity. Obstetrics Gynecol. 2022;139(6):1061–69.
Goff SL, Mazor KM, Priya A, Pekow PS, Lindenauer PK. Characteristics of high-performing primary care pediatric practices: a qualitative study. Acad Pediatr. 2020;20(2):267–74.
Delgado JR, Mansfield LN, Bruxvoort K, Macias M, Grotts J, Lewin B, et al. Adolescent self-consent for COVID-19 vaccination: views of healthcare workers and their adolescent children on vaccination autonomy. J Adolesc Health. 2023;72:674–81.
Curry L, Cherlin E, Ayedun A, Rubeo C, Straker J, Wilson TL, et al. How do area agencies on aging build partnerships with health care organizations? Gerontologist. 2022;62:1409–19.
Tanenbaum J, Cebul RD, Votruba M, Einstadter D. Association of a regional health improvement collaborative with ambulatory care–sensitive hospitalizations. Health Aff. 2018;37(2):266–74.
Martin N, Frank B, Farrell D, Brady C, Dixon-Hall J, Mueller J, et al. Sharing lessons from successes: long-term care facilities that weathered the storm of COVID-19 and staffing crises. J Nurs Care Qual. 2023;38:19–25.
Nguyen T, Tran T, Green S, Hsueh A, Tran T, Tran H, et al. Proof of concept of participant informed, psycho-educational, community-based intervention for people with severe mental illness in rural Vietnam. Int J Soc Psychiatry. 2020;66:232–39.
Foster BA, Seeley K, Davis M, Boone-Heinonen J. Positive deviance in health and medical research on individual level outcomes–a review of methodology. Ann Epidemiol. 2022;69:48–56.
Rose AJ, McCullough MB. A practical guide to using the positive deviance method in health services research. Health Serv Res. 2017;52(3):1207.
Singhal A. The positive deviance approach to designing and implementing health communication interventions. In: Health communication strategies for developing global health programs. vol. 5. Health Communication; 2014. pp. 176–89.
Young MF, Baik D, Reinsma K, Gosdin L, Rogers HP, Oy S, et al. Evaluation of mobile phone-based Positive Deviance/Hearth child undernutrition program in Cambodia. Matern Child Nutr. 2021;17:e13224.
Curry LA, Brault MA, Linnander EL, McNatt Z, Brewster AL, Cherlin E, et al. Influencing organisational culture to improve hospital performance in care of patients with acute myocardial infarction: a mixed-methods intervention study. BMJ Qual Saf. 2018;27:207–17.
Carolan S, Harris PR, Cavanagh K. Improving employee well-being and effectiveness: systematic review and meta-analysis of web-based psychological interventions delivered in the workplace. J Med Internet Res. 2017;19(7):e271.
Krumholz HM, Curry LA, Bradley EH. Survival after acute myocardial infarction (SAMI) study: the design and implementation of a positive deviance study. Am Heart J. 2011;162(6):981–7. e9.
Marra AR, Pavão Dos Santos OF, Cendoroglo Neto M, Edmond MB. Positive deviance: a new tool for infection prevention and patient safety. Curr Infect Dis Rep. 2013;15:544–48.
Klaiman T. Learning from top performers using a positive deviance approach. Los Angeles, CA: SAGE Publications Sage CA; 2011. p. 422.
Colditz GA. Overview of the epidemiology methods and applications: strengths and limitations of observational study designs. Crit Rev Food Sci Nutr. 2010;50(S1):10–12.
Queirós A, Faria D, Almeida F. Strengths and limitations of qualitative and quantitative research methods. Eur J Educ Stud. 2017.
Goff SL, Mazor KM, Priya A, Moran M, Pekow PS, Lindenauer PK. Organizational characteristics associated with high performance on quality measures in pediatric primary care: a positive deviance study: organizational characteristics and pediatric care quality. Health Care Manage Rev. 2019.
Tenny S, Brannan J, Brannan G. Qualitative study. 2017.
Weise A, Büchter R, Pieper D, Mathes T. Assessing context suitability (generalizability, external validity, applicability or transferability) of findings in evidence syntheses in healthcare—an integrative review of methodological guidance. Res Synth Methods. 2020;11(6):760–79.
Albanna B, Heeks R. Positive deviance, big data, and development: a systematic literature review. Electron J Inf Syst Dev Ctries. 2019;85(1):e12063.
Lawton G. 8 types of bias in data analysis and how to avoid them. https://www.techtarget.com/searchbusinessanalytics/feature/8-types-of-bias-in-data-analysis-and-how-to-avoid-them . Accessed 21 Jan 2024.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
School of Public Health, Faculty of Medicine, The University of Queensland, Brisbane, Australia
Ayelign Mengesha Kassie, Elizabeth Eakin, Aklilu Endalamaw & Yibeltal Assefa
School of Nursing, College of Health Sciences, Woldia University, Woldia, Ethiopia
Ayelign Mengesha Kassie & Biruk Beletew Abate
College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Aklilu Endalamaw
International Institute for Primary Health Care, Ethiopia, Addis Ababa, Ethiopia
Anteneh Zewdie & Eskinder Wolka
You can also search for this author in PubMed Google Scholar
Contributions
AM and YA conceived the idea; AM planned and designed the study protocol and all the other authors participated in reviewing and editing the protocol; AM conducted article searches; AM, YA, and BB planned the data extraction and statistical analysis; AM and BB screened articles, and AM extracted the data from the included articles, performed the analysis and wrote the first draft. YA and EE reviewed the draft and provided critical insights. All authors have reviewed, participated in editions, and approved the submission of the final manuscript.
Corresponding author
Correspondence to Ayelign Mengesha Kassie .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kassie, A.M., Eakin, E., Abate, B.B. et al. The use of positive deviance approach to improve health service delivery and quality of care: a scoping review. BMC Health Serv Res 24 , 438 (2024). https://doi.org/10.1186/s12913-024-10850-2
Download citation
Received : 16 November 2023
Accepted : 11 March 2024
Published : 08 April 2024
DOI : https://doi.org/10.1186/s12913-024-10850-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Healthcare quality
- Healthcare system
- Health service delivery
- Positive deviance
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
This paper is in the following e-collection/theme issue:
Published on 8.4.2024 in Vol 8 (2024)
Mobile Technology Use in Clinical Research Examining Challenges and Implications for Health Promotion in South Africa: Mixed Methods Study
Authors of this article:

Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 14, Issue 4
- Collaborative design of a health research training programme for nurses and midwives in Tshwane district, South Africa: a study protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-8761-2055 Rodwell Gundo ,
- Mavis Fhumulani Mulaudzi
- Department of Nursing Science , University of Pretoria , Pretoria , South Africa
- Correspondence to Dr Rodwell Gundo; rodwell.gundo{at}up.ac.za
Introduction Nurses are essential for implementing evidence-based practices to improve patient outcomes. Unfortunately, nurses lack knowledge about research and do not always understand research terminology. This study aims to develop an in-service training programme for health research for nurses and midwives in the Tshwane district of South Africa.
Methods and analysis This protocol outlines a codesign study guided by the five stages of design thinking proposed by the Hasso-Plattner Institute of Design at Stanford University. The participants will include nurses and midwives at two hospitals in the Tshwane district, Gauteng Province. The five stages will be implemented in three phases: Phase 1: Stage 1—empathise and Stage 2—define. Exploratory sequential mixed methods including focus group discussions with nurses and midwives (n=40), face-to-face interviews (n=6), and surveys (n=330), will be used in this phase. Phase 2: Stage 3—ideate and Stage 4—prototype. A team of research experts (n=5), nurses and midwives (n=20) will develop the training programme based on the identified learning needs. Phase 3: Stage 5—test. The programme will be delivered to clinical nurses and midwives (n=41). The training programme will be evaluated through pretraining and post-training surveys and face-to-face interviews (n=4) following training. SPSS V.29 will be used for quantitative analysis, and content analysis will be used to analyse qualitative data.
Ethics and dissemination The protocol was approved by the Faculty of Health Sciences Research Ethics Committee of the University of Pretoria (reference number 123/2023). The protocol is also registered with the National Health Research Database in South Africa (reference number GP_202305_032). The study findings will be disseminated through conference presentations and publications in peer-reviewed journals.
- Nursing Care
- Patient-Centered Care
- Patient Satisfaction
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2023-076959
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
STRENGTHS AND LIMITATIONS OF THIS STUDY
This study will be strengthened through the use of quantitative and qualitative methods to understand the research problem.
The inclusion of two hospitals and the participation of different nurses and midwives will ensure the credibility of the findings.
Local research experts, nurses and midwives will collaborate to develop a training programme appropriate to the context of the setting.
The findings will be limited to two hospitals; therefore, the findings may not be generalisable to other hospitals.
Introduction
Evidence-based practice (EBP) has gained prominence in health services internationally over the past three decades. 1 EBP integrates individual clinical expertise with clinical evidence generated from systematic research. 2 EBP aims to deliver appropriate, efficient patient care. 3 Consequently, generating evidence that informs care delivery has become increasingly important for improving patient-centred care, patient safety, patient outcomes and the healthcare system. 1 3 In healthcare, nurses are well positioned to implement EBP because they constitute the largest proportion of the health workforce. 1 4 Nurses thus have to be proactive in acquiring, synthesising and using research knowledge and the best evidence to inform their practice and decision-making. 3 4
Recognising the need for EBP, many nursing organisations worldwide have developed best practice guidelines for patient-care decision-making. 4 In South Africa, the roadmap for strengthening nursing and midwifery acknowledges that nurses are vital for providing safe and effective patient care. Strategically, investing in nurse-led research will help develop nurse-led models of care. 5 Similarly, the South African Nursing Council expects nurses to actively participate in research activities, including academic writing, reading and reviewing, as part of continuing professional development. 6 Training nurses and midwives can enhance their research capacity and enable them to use available resources for research, ultimately leading to changes in EBP in clinical settings.
Nurses need to gain research knowledge and become comfortable with research terminology. 7 8 Although undergraduate nursing training includes a research component, this training does not always translate into a strong understanding of research. 7 As such, there needs to be more nurse-led patient-centred research. A recent review of nursing research from 2000 to 2019 showed that most nursing research is conducted by nurses working at higher education institutions. Research output and collaboration are also disproportionately more prominent in high-income countries across North America, Europe, and Oceania than in low-income and middle-income countries. 9 The other challenges that affect health research include limited time, lack of research facilities, research culture, mentors, access to mentors, and workforce capacity. 10
Little is known about the research literacy of nurses and midwives and research training programmes for practicing nurses and midwives in South Africa. Therefore, we developed a protocol to develop a research training programme for nurses and midwives in the Tshwane district of South Africa. This protocol is guided by the following research questions: (a) what are the levels of nurses’ and midwives’ knowledge, attitudes and involvement in research?; (b) what are the learning needs of nurses and midwives regarding research design and implementation?; (c) what content should be included in a research training programme for nurses and midwives?; (d) how does the developed training programme impact nurses’ knowledge about research?
Theoretical framework
The principles of constructivism learning theory will guide this study. This theory is rooted in the work of Piaget and Vygotsky. 11 This paradigm explains how people might acquire and retain knowledge. 12 Through the lens of constructivism learning theory, adult educators acknowledge learners’ previous experiences, appreciate multiple perspectives and embed learning in social contexts. The instructor is a mentor who helps learners understand new information. Constructivism learning theory has three dimensions, namely, individual constructivism, social constructivism and contextualism. In individual constructivism, learners are self-directed and construct knowledge via personal experience. Social constructivism assumes that learning is socially mediated, and that knowledge is constructed through social interaction. In contextualism, learning should be tied to real-life contexts. 13 Some benefits of constructivism theory are that learners enjoy learning because they are actively engaged and have ownership over what they learn. 12 The theory was considered appropriate because the study will be conducted at two research-intensive hospitals. Therefore, nurses and midwives are familiar with the research process.
Methods and analysis
Research design.
We will use a codesign approach guided by the stages of design thinking proposed by the Hasso-Plattner Institute of Design at Stanford University. 14 15 The design originated from participatory research and involves active engagement of the participants to identify needs and collaboratively propose solutions. 14 16 The approach is considered appropriate because it ensures meaningful involvement of end-users, thereby creating meaningful benefits. 17 A codesign approach ensures fewer challenges when implementing the initiative because stakeholders are fully engaged throughout the process. 14 Underpinned by the African philosophy of Ubuntu, the process will promote the culture of working together and collective solidarity. 18
The study will be guided by the five stages of design thinking: empathise, define, ideate, prototype and test. Empathise aims to understand the deeper issues, needs and challenges needed to solve the problem. Define involves data analysis and prioritising the needs of the end users of the training programme. Ideate includes brainstorming for innovative solutions to address the identified needs. In the prototype stage, the idea or innovation is shown to the end users and other stakeholders. Finally, testing involves checking what works in a real-world setting. 14 15
Study setting
The study will be conducted at two public hospitals in the Tshwane district of Gauteng Province in South Africa. The province has the highest population density, the most hospitals and the greatest number of nurses and midwives. 19 According to a 2016 community survey, Gauteng has a population of 13.4 million people. 20 Tshwane is one of the five districts in the province and the third most populous district, accounting for 24% of the population in the province. 21 There are three district hospitals, namely, Tshwane, Pretoria West, Jubilee and ODI; one regional hospital, Mamelodi; and three tertiary hospitals, namely, Steve Biko Academic Hospital, Dr George Mukhari Hospital and Khalafong Hospital. The two hospitals were selected due to their proximity to the University of Pretoria. One of the hospitals is a tertiary hospital with 800 beds. The second hospital is a 240-bed district hospital linked to the University of Pretoria’s Faculty of Health Sciences. 22
Target population
The population will comprise nurses and midwives working at the two hospitals. In South Africa, there are six categories of nurses and midwives based on qualifications as follows: registered auxiliary nurse (higher certificate), registered general nurse (diploma in nursing), registered midwife (advanced diploma), registered professional nurse and midwife (bachelor’s degree), nurse specialist or midwife specialist (postgraduate diploma), advanced specialist nurse (master’s degree) and those with doctorate degrees. 5 Nurses working at academic hospitals are expected to engage in research activities, including academic writing, reading and reviewing, as part of continuing professional development. 6 A preliminary audit revealed 1900 nurses and midwives working at the two hospitals.
Inclusion and exclusion criteria
Participation will be limited to registered auxiliary nurses, registered general nurses, registered midwives, registered professional nurses and midwives older than 18 years, those registered with the South African Nursing Council, and those with more than 3 months of experience. All people older than 18 years are mandated to give legal consent in South Africa. Nurses with less than 3 months of experience or undergoing orientation will be excluded from the study.
As illustrated in table 1 , the study will be implemented in three phases and five stages to address the four objectives. Stage 1 is currently underway. The collection of the qualitative data started in December 2023 at one of the two hospitals. This will proceed at the second hospital until April 2024. The whole study is expected to be completed by September 2024.
- View inline
Illustration of the research process guided by the stages of design thinking
In this phase, we aim to understand the nurses’ and midwives’ perceived knowledge, attitudes and involvement in research and their learning needs. We will base our investigation on empathising and defining. An exploratory sequential mixed methods design will be used. This design begins with collecting and analysing qualitative data. The qualitative findings are used to develop quantitative measures or instruments to test the identified variables. 23 In this study, the qualitative findings will be used to revise a questionnaire for the subsequent quantitative strand.
Strand 1—qualitative study
Qualitative methods are appropriate for investigating the who, what and where of events or experiences of informants of a poorly understood phenomenon. 24 25
Sample size and sampling
Forty-six participants (n=46) will be selected from nurses and midwives working at the two hospitals. The sample size was pragmatically determined according to the mode of data collection and the volume of data to be collected. However, the final sample size will be determined by data saturation.
We will purposively sample nurses and midwives from the following cadres: registered auxiliary nurses, registered general nurses, registered midwives, and registered professional nurses and midwives. As presented in table 2 , two focus group discussions (FGDs) will be held at each hospital and will involve 10 participants each. Due to power differences that can cause a halo effect among the participants, 26 one FGD will include senior professional nurses and midwives. In contrast, the other FDG will include junior nurses and midwives with either diplomas or certificates. For the individual interviews, three participants (one registered auxiliary nurse, one registered general nurse with a diploma and one professional nurse (with either a bachelor’s or postgraduate qualification)) will be invited to participate. The participants will be expected to share their knowledge of the competencies needed for conducting health research.
Sampling plan for the qualitative strand
Data collection
The study information will be communicated through nursing and midwifery managers. Participation will be voluntary. Nurses and midwives willing to participate will be invited for either FGDs or individual interviews. The participants will be given the details of the study and a consent form. The interviews will be conducted in English in hospitals in private settings at times and places that are most convenient for participants. The participants will be requested to use pseudonyms during interviews. A semistructured interview guide will be used for the interviews (refer to online supplemental file 1 ). The interviews will be audiotaped and later transcribed verbatim in English.
Supplemental material
Data analysis.
The data will be analysed manually using conventional content analysis as described by Hsieh and Shannon. 27 The steps of the analysis will be as follows: (a) repeatedly reading the data to achieve immersion and a sense of the whole; (b) deriving and labelling codes by highlighting the words that capture critical thoughts and concepts; (c) sorting the related codes into categories; (d) organising numerous subcategories into fewer categories; (e) defining each category; and (f) identifying the relationship of the categories in terms of their concurrence, antecedents or consequences. To ensure the reliability of the qualitative coding, tHead2he two researchers will code the first transcript independently. The online Coding Analysis Toolkits 28 will be used to calculate intercoder reliability. The two researchers will discuss differences and agree on the coding before proceeding to the next transcript.
Methodological rigour
Trustworthiness will be achieved through credibility, transferability, dependability and confirmability. 24 29 Credibility will be achieved through spatial and personal triangulation. Spatial triangulation refers to collecting data on the same phenomenon from multiple sites, while personal triangulation refers to collecting data from different types and levels of people. 29 This study will collect data from different cadres of nurses and midwives at two hospitals. Transferability will be enhanced by providing sufficient study details. Dependability and confirmability will be achieved by establishing an audit trail describing the procedures and processes. Additionally, reflexivity will be used to ensure the transparency and quality of the study. 29 30 Reflexivity is where researchers critique, appraise and evaluate the influence of subjectivity and context on the research process. 30 In some branches of qualitative inquiries, researchers use reflexive bracketing to prevent subjective influences. However, Olmos-Vega et al 30 observed that this approach is no longer favoured in modern qualitative research because setting aside certain aspects of subjectivity is problematic. In this study, reflexivity will be ensured by keeping memos and field notes to document interpersonal dynamics and critical decisions made throughout the study.
Strand 2—quantitative study
A cross-sectional survey will be used to assess nurses’ and midwives’ perceived knowledge, attitudes and involvement in research.
The sample size was calculated using Yamane’s formula 31 as follows: n=N/(1+N(e2), where n is the sample, N is the population size, and e is the level of precision. Assuming a 95% CI and the estimated proportion of an attribute p=0.5, the calculated sample size for a population N=1900 with ±5% precision is 330. In this study, a convenience sampling technique will be used to select participants.
The researchers will brief nurse managers about the study. Furthermore, posters inviting nurses and midwives to participate in the study will be placed in each department. The poster will include details of the study and relevant contact details. The nurses and midwives willing to participate will be given an information sheet, consent form and questionnaire. They will be requested to leave the completed questionnaire in a designated box in the unit manager’s office.
Data collection instrument
The data will be collected using the Edmonton Research Orientation Survey (EROS). The EROS was developed in Canada and is a valid and reliable self-reported instrument for measuring perceived knowledge, attitudes and involvement in research. The tool has four subscales with 43 items. The four subscales are the value of research, value of innovation, research involvement and research utilisation (EBP). Valuing research is a positive attitude towards research; the value of innovation refers to being on the leading edge or keeping up to date with information; research involvement relates to active participation in research; and research utilisation (EBP) pertains to whether respondents use research to guide their day-to-day practice. Additionally, there is a category for the barriers and support for research. 32–34
The EROS items are measured using a 5-point Likert scale ranging from 1—strongly disagree to 5—strongly agree. The maximum score is 215. Higher overall scores indicate a stronger research orientation. The scores will be categorised into high (between 143 and 215 points), medium (73–142 points) or low (0–72 points). 32 33 The tool has been extensively used to assess the research orientation of health professionals, including physiotherapists, 35 midwives, 36 occupational therapists, 33 academics 32 and undergraduate students. 34 Previous studies reported high internal reliability with Cronbach’s alpha coefficients of 0.95 37 and 0.92. 34
Although the tool has been previously used among South African occupational therapists, 33 the copyright author observed that the tool had been developed at a time when there was no access to information via the internet, hence the need to find ways of incorporating such issues. This study will use qualitative findings to identify items not included in the tool but relevant to the South African context.
The quantitative data will be entered into Microsoft Excel and imported to IBM SPSS statistics V.29. Descriptive statistics will be used to summarise demographic characteristics and questionnaire scores. Mean scores and SD will be calculated for individual items, subgroup scores and overall scores. Independent sample t-tests, Mann-Whitney U tests, and multiple regression will be used to compare the scores of different groups of nurses and midwives. The assumptions for each test will be assessed before analysis. The level of significance will be set at 0.05.
During this phase, we will develop the training programme based on the learning needs identified in Phase 1. Research experts (n=5) will participate in a one-design studio workshop to brainstorm the content to be included in the training programme. Although there is limited literature on the definition and characteristics of an expert, Bruce et al 38 defined an expert as a person who is knowledgeable or informed in a particular discipline. Bruce et al 38 further observed that maximum variation or heterogeneity in sampling experts yields rich information. This study will select experts based on the criteria proposed by Davis 39 and Rubio et al . 40 The characteristics include clinical experience in the setting, professional certification in a related area, research experience, work experience, conference presentation and publication in the topic area.
A design studio workshop is a process in which participants create, and critique proposed interventions. 16 The researcher will share the findings of Phase 1 and explain the workshop’s goal to the participants. Participants will be provided with pens, sticky notes and flip-chart paper. The researcher will facilitate discussion and capture feedback. At the end of the workshop, the researcher will consolidate the ideas, create a more detailed programme design and communicate with the participants.
Next, we will develop a prototype to be discussed in a consultative meeting and validation meeting. An iterative process will be used to validate the developed training programme. The consultative meeting will be held with research experts (n=5). A validation exercise will also be conducted with nurses and midwives (n=20), the programme’s end-users. The nurses and midwives will be identified in consultation with nurse managers at the two hospitals to avoid disruption of services. During the validation exercise, the participants will be grouped into smaller idea groups to review and discuss the developed programme. Each group will be requested to identify a representative to report on behalf of the group. The feedback from the consultative and validation meeting will help to improve the developed programme.
The purpose of this phase is to assess the impact of the developed training programme. The developed training will be delivered to 41 nurses and midwives in the Tshwane district. The sample is based on similar studies that have implemented interventions for health professionals. For example, a study by Gundo et al 41 used G-Power software 42 to calculate the sample size based on a conservative effect size of d=0.5, a power of 80% and an alpha=0.05. The calculated sample size was 34, but 41 participants were invited to participate in training to allow for a dropout rate of at most 20%. The identification and invitation of the participants will be negotiated with nurse managers at the two hospitals to avoid service disruptions. The selection process will ensure the representation of the different cadres of nurses and midwives. We will invite a team of research experts to facilitate the training. The impact of the training will be assessed by comparing pre-survey and post-survey EROS scores, FGDs with participants, and evaluations at the end of the training. A paired-sample t-test will be used to compare the pretest and post-test scores.
This protocol aims to develop a research training programme for nurses and midwives in the Tshwane district of South Africa. Initially, we will investigate the learning needs of nurses and midwives. The learning needs will inform a training programme to improve research capacity. As observed by Hines et al , 7 implementing a training programme will improve nurses’ research knowledge, critical appraisal ability and research efficacy. Building capacity for health research in Africa will enhance the ownership of research activities that target relevant topics.
Furthermore, findings relevant to local populations will be communicated in a culturally acceptable manner. Research recommendations may also resonate better and have a better uptake among African policymakers than research produced by internationally led teams. 43–45 This research training programme could be used in other hospitals with similar contexts and other categories of healthcare professionals. However, this will require a larger, multicentre validation study. Our findings will be limited to the two hospitals; therefore, the findings may not be generalisable to other hospitals.
Ethics and dissemination
The protocol was approved by the Research Ethics Committee, Faculty of Health Sciences at the University of Pretoria (reference number: 123/2023). The protocol is registered with the National Health Research Database in South Africa (reference number GP_202305_032). The two hospitals also provided permission for the study. Permission to use the EROS was obtained from the copyright authors, Dr Kerrie Pain and Dr Paul Hagler.
The participants will receive an information leaflet and be required to provide written informed consent. The researcher will ensure that the participants’ personal information is anonymised. Participants can give the researcher written permission to share their personal information. During the FGDs and individual interviews in Phase 1, the participants will be asked to use pseudonyms of their choice. In Phases 2 and 3, anonymity will not be possible because the meetings will be in person. However, the participants will be requested to maintain confidentiality. The data will be stored in compliance with the research ethics committee’s guidelines. The findings of the study will be disseminated through conference presentations and publications in peer-reviewed journals. The preparation of this manuscript followed the standards for reporting qualitative research 46 and the guidelines for reporting observational studies. 47
Ethics statements
Patient consent for publication.
Not applicable.
Acknowledgments
The manuscript was written during a writing retreat that was funded by the National Research Foundation through the Ubuntu Community Model of Nursing Project at the University of Pretoria in South Africa. We also thank Dr Cheryl Tosh for editing the manuscript.
- Cassidy CE ,
- Sackett DL ,
- Rosenberg WM ,
- Gray JA , et al
- World Health Organization
- Bassendowski S
- Republic of South Africa
- ↵ South African nursing Council . In : Continuing professional development framework for nurses and midwives in South Africa . Pretoria : South African Nursing Council , 2021 .
- Ramsbotham J ,
- Yanbing S ,
- Chao L , et al
- Dempsey O , et al
- Efgivia MG ,
- Adora Rinanda RY , et al
- Baral KP , et al
- Thabrew H ,
- Fleming T ,
- Hetrick S , et al
- Slattery P ,
- Mulaudzi FM ,
- Anokwuru RA ,
- Mogale R , et al
- Coetzee SK ,
- Ellis SM , et al
- Statistics South Africa
- Mutyambizi C ,
- Pavlova M ,
- Hongoro C , et al
- Abdullah F ,
- Basu D , et al
- Shrestha S ,
- Bradshaw C ,
- Atkinson S ,
- Sefcik JS ,
- O.Nyumba T ,
- Derrick CJ , et al
- Hsieh H-F ,
- MacPhail C ,
- Abler L , et al
- Korstjens I ,
- Olmos-Vega FM ,
- Stalmeijer RE ,
- Varpio L , et al
- Sarmah HK ,
- Hazarika BB ,
- Choudhury G
- Fernandez A ,
- Sadownik L ,
- Lisonkova S , et al
- Peachey AA ,
- Janssen J ,
- Mirfin-Veitch B , et al
- Kuliukas L , et al
- Langley GC ,
- Berg-Weger M ,
- Tebb SS , et al
- Chirwa E , et al
- Cunningham JB ,
- McCrum-Gardner E
- Nyirenda T , et al
- Kasprowicz VO ,
- Chopera D ,
- Waddilove KD , et al
- O’Brien BC ,
- Harris IB ,
- Beckman TJ , et al
- von Elm E ,
- Altman DG ,
- Egger M , et al
Contributors RG and MFM conceptualised the study, developed the proposal, drafted and revised the manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Search Cornell
Class Roster
Section menu.
- Toggle Navigation
- Summer 2024
- Spring 2024
- Winter 2024
- Archived Rosters
Last Updated
- Schedule of Classes - April 8, 2024 7:31PM EDT
- Course Catalog - April 8, 2024 7:06PM EDT
PSYCH 2830 Research Methods in Human Development
Course description.
Course information provided by the Courses of Study 2023-2024 . Courses of Study 2024-2025 is scheduled to publish mid-June.
This course will introduce students to the basics of research design and will review several methodologies in the study of human development. The focus of the course will be on descriptive and experimental methods. Students will learn the advantages and challenges to different methodological approaches. The course also places an emphasis on developing students' scientific writing and strengthening their understanding of statistics.
When Offered Fall.
Permission Note Priority given to: HD and PSYCH majors. Prerequisites/Corequisites Prerequisite: HD 1150.
- The goals of the course are to encourage students to think critically, learn how to design basic research studies, and to develop their writing skills.
- Students will demonstrate their knowledge of course content, including theories, in areas of developmental and cognitive psychology in legal contexts.
View Enrollment Information
Regular Academic Session. Combined with: HD 2830
Credits and Grading Basis
3 Credits Stdnt Opt (Letter or S/U grades)
Class Number & Section Details
5566 PSYCH 2830 LEC 001
Meeting Pattern
- TR 10:10am - 11:25am To Be Assigned
- Aug 26 - Dec 9, 2024
Instructors
To be determined. There are currently no textbooks/materials listed, or no textbooks/materials required, for this section. Additional information may be found on the syllabus provided by your professor.
For the most current information about textbooks, including the timing and options for purchase, see the Cornell Store .
Additional Information
Instruction Mode: In Person
Or send this URL:
Available Syllabi
About the class roster.
The schedule of classes is maintained by the Office of the University Registrar . Current and future academic terms are updated daily . Additional detail on Cornell University's diverse academic programs and resources can be found in the Courses of Study . Visit The Cornell Store for textbook information .
Please contact [email protected] with questions or feedback.
If you have a disability and are having trouble accessing information on this website or need materials in an alternate format, contact [email protected] for assistance.
Cornell University ©2024
Methods: Mixed-Methods Research Design
- First Online: 10 November 2019
Cite this chapter

- Ji Yeong I 6 ,
- Hyewon Chang 7 &
- Ji-Won Son 8
Part of the book series: Mathematics Education – An Asian Perspective ((MATHEDUCASPER))
250 Accesses
1 Citations
We employed a convergent design mixed-method research approach that included both qualitative and quantitative data being collected concurrently and analyzed equally. This chapter includes the detailed description of the research design, data collection process, and data analysis method. The Likert scale survey, developed by the research team, was administered online to approximately 100 elementary teachers in South Korea to examine their perspectives of teaching KLLs mathematics based on the five domains of the established framework. Combined with the survey data, we included a case study of two elementary school teachers from the same school, which entailed video recordings of classroom observations, lesson plans, and semi-structured interviews. For this book, we explored one elementary school and two classrooms within this school in great detail. The quantitative data drawn from the survey was analyzed using descriptive statistics, and the qualitative data was analyzed through analytic memos and emerging themes. In sum, the results of the case studies were compared to the results of the survey to help us analyze how teacher perspectives of teaching KLLs mathematics are related to their implementation of culturally responsive teaching strategies.
- Mixed-method
- Likert scale survey
- Descriptive statistics
- Observation
- Semi-structured interview
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Aguirre, J. M., & del Rosario Zavala, M. (2013). Making culturally responsive mathematics teaching explicit: A lesson analysis tool. Pedagogies: An International Journal , 8 (2), 163–190. https://doi.org/10.1080/1554480X.2013.768518 .
Article Google Scholar
Creswell, J. W., & Plano Clark, V. L. (2011). Designing and conducting mixed methods research (2nd ed.). Los Angeles: SAGE Publications.
Google Scholar
Cross, D. I. (2009). Alignment, cohesion, and change: Examining mathematics teachers’ belief structures and their influence on instructional practices. Journal of Mathematics Teacher Education, 12 (5), 325–346. https://doi.org/10.1007/s10857-009-9120-5 .
Ladson-Billings, G. (2009). The dreamkeepers: Successful teachers of African American children (2nd ed.). San Francisco, CA: Jossey-Bass Publishers.
Moschkovich, J. N. (2007). Examining mathematical discourse practices. For the Learning of Mathematics, 27 (1), 24–30.
Pohan, C. A., & Aguilar, T. E. (2001). Measuring educators’ beliefs about diversity in personal and professional contexts. American Educational Research Journal, 38 (1), 159–182. https://doi.org/10.3102/00028312038001159 .
Shulman, L. S. (1986). Those who understand: Knowledge growth in teaching. Educational Researcher, 15, 4–14.
Simic-Muller, K., Fernandes, A., & Felton-Koestler, M. D. (2015). “I just wouldn’t want to get as deep into it”: Preservice teachers’ beliefs about the role of controversial topics in mathematics education. Journal of Urban Mathematics Education, 8 (2), 53–86.
TEACH MATH. (2012). Culturally responsive mathematics teaching lesson analysis tool. Unpublished Instrument.
Villegas, A. M., & Lucas, T. (2002). Preparing culturally responsive teachers rethinking the curriculum. Journal of Teacher Education, 53 (1), 20–32. https://doi.org/10.1177/0022487102053001003 .
Download references
Author information
Authors and affiliations.
Iowa State University, Ames, IA, USA
Seoul National University of Education, Seoul, Korea (Republic of)
Hyewon Chang
Department of Learning and Institution, University at Buffalo - SUNY, Buffalo, NY, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ji Yeong I .
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Singapore
About this chapter
I, J., Chang, H., Son, JW. (2019). Methods: Mixed-Methods Research Design. In: Rethinking the Teaching Mathematics for Emergent Bilinguals. Mathematics Education – An Asian Perspective. Springer, Singapore. https://doi.org/10.1007/978-981-15-0966-7_5
Download citation
DOI : https://doi.org/10.1007/978-981-15-0966-7_5
Published : 10 November 2019
Publisher Name : Springer, Singapore
Print ISBN : 978-981-15-0965-0
Online ISBN : 978-981-15-0966-7
eBook Packages : Education Education (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

IMAGES
VIDEO
COMMENTS
Quantitative dominant [or quantitatively driven] mixed methods research is the type of mixed research in which one relies on a quantitative, postpositivist view of the research process, while concurrently recognizing that the addition of qualitative data and approaches are likely to benefit most research projects. (p.
DOI: 10.1177/1558689812461179. 2013 7: 141 originally published online 4 October 2012 Journal of Mixed Methods Research Greg Guest. Describing Mixed Methods Research : An Alternative to Typologies ...
Mixed methods research designs. There are different types of mixed methods research designs. The differences between them relate to the aim of the research, the timing of the data collection, and the importance given to each data type. As you design your mixed methods study, also keep in mind: Your research approach (inductive vs deductive)
Mixed methods research, then, is more than simply collecting qualitative data from interviews, or collecting multiple forms of qualitative evidence (e.g., observations and interviews) or multiple types of quantitative evidence (e.g., surveys and diagnostic tests). It involves the intentional collection of. both.
Mixed model research ostensibly refers to a research design, which goes beyond mixed methods research in that it combines qualitative and quantitative approaches throughout the research process ...
Mixed‐methods research, or multi‐strategy designs, 1 can be defined as 'the collection, analysis and integration of both qualitative and quantitative data in a single study': 2 semi‐structured interviews and workplace measures (e.g. attendance data) might be undertaken concurrently to gain a multifaceted perspective on a particular ...
Mixed methods research is an approach to inquiry that combines or associates both qualitative and quantitative forms. Mixed methods designs provide researchers, across research disciplines, with a rigorous approach to answering research questions. In the case of holistic analysis of complex systems, such as the mega-project, this is a relevant ...
Introduction. Since the 1990s, mixed methods research as a distinct methodology has seen vigorous institutionalization [1,2] with the launch of a specialized journal (Journal of Mixed Methods Research) in 2007, the establishment of the Mixed Methods International Research Association (MMIRA) in 2013, and the publication of a stream of handbooks, textbooks, and articles on the philosophy and ...
A mixed methods research framework is developed for researchers to gain a comprehensive understanding and implementation of mixed methods research design, according to the nature of their research needs, research problems, and research aims. Quantitative research recognizes the causality of the objective world and believes that the objective ...
As stated b y Creswell and Plano Clark (20 11), a. mixed-methods research design is a research design that has its own philo sophical assumptions and methods of inquiry. As a. methodology, it ...
4.1 Introduction. Efforts to understand the trans-disciplinary search for enhanced urban sustainability through the state-mediated strategy of smart growth within Greater Seattle—the purpose of this book—suggest, I shall argue here, a mixed-methods research design or overall methodological approach. Work in the social sciences remains ...
Descriptive research aims to accurately and systematically describe a population, situation or phenomenon. It can answer what, where, when and how questions, but not why questions. A descriptive research design can use a wide variety of research methods to investigate one or more variables. Unlike in experimental research, the researcher does ...
However, it needs the reader to have some know-how of the qualitative research. Chapter 10 deals with mixed methods approach. Mixed methods approach is described in detail and types of mixed methods research designs are illustrated with figures in brief. More elaborated diagrams might have been more helpful for readers.
You can also create a mixed methods research design that has elements of both. Descriptive research vs experimental research. Descriptive research gathers data without controlling any variables, while experimental research manipulates and controls variables to determine cause and effect.
Descriptive research aims to accurately and systematically describe a population, situation or phenomenon. It can answer what, where, when, and how questions, but not why questions. A descriptive research design can use a wide variety of research methods to investigate one or more variables. Unlike in experimental research, the researcher does ...
A mixed methods research design is a procedure for collecting, analyzing, and "mixing" both quantitative and qualitative research and methods in a single study to understand a research problem. To utilize this design effectively, you must understand both quantitative and qualitative research. Philosophical Approaches.
Mixed Methods Research. Mixed methods research is an approach to research that combines both quantitative and qualitative research methods in a single study or research project. It is a methodological approach that involves collecting and analyzing both numerical (quantitative) and narrative (qualitative) data to gain a more comprehensive understanding of a research problem.
This review examines John W. Creswell and David Creswell's sixth edition, which covers the most popular research methods, offering readers a comprehensive understanding and practical guidance in qualitative, quantitative, and mixed methods. The review includes observations on existing drawbacks, gaps, and ideas on potential areas for improvement in the book. The book is an excellent entry ...
As discussed earlier, common research methods for descriptive research include surveys, case studies, observational studies, cross-sectional studies, and longitudinal studies. Design your study: Plan the details of your study, including the sampling strategy, data collection methods, and data analysis plan.
Mixed methods research can be viewed as an approach which draws upon the strengths and perspectives of each method, ... Qualitative data was analysed by using a process of constant comparison and quantitative data by descriptive and comparative statistical analysis. ... Neri M. Designs for mixed methods research. In: Andrew S., Halcomb E.J ...
Abstract. We employed a convergent design mixed-method research approach that included both qualitative and quantitative data being collected concurrently and analyzed equally. This chapter includes the detailed description of the research design, data collection process, and data analysis method. The Likert scale survey, developed by the ...
A mixed-method case study was conducted using a convergent parallel design between November 2018 and January 2022 in ten districts of Hanoi and Ho Chi Minh City, Vietnam. Quantitative data were collected through a pilot intervention that aimed to facilitate SHI enrollment for uninsured individuals with TB. Descriptive statistics were calculated.
We conducted an exhaustive and focused scoping review and followed the methodological framework for scoping reviews as previously described in the literature [20, 22].This study aligned with the four goals of a scoping review [].We followed the first five out of the six steps outlined by Arksey and O'Malley's to ensure our review's validity 1) identifying the research question 2 ...
Objective The COVID-19 pandemic accelerated changes to clinical research methodology, with clinical studies being carried out via online/remote means. This mixed-methods study aimed to identify which digital tools are currently used across all stages of clinical research by stakeholders in clinical, health and social care research and investigate their experience using digital tools. Design ...
The relevance of mixed-methods in health research. The overall goal of the mixed-methods research design is to provide a better and deeper understanding, by providing a fuller picture that can enhance description and understanding of the phenomena [].Mixed-methods research has become popular because it uses quantitative and qualitative data in one single study which provides stronger inference ...
Methods followed in the utilization of PD for the healthcare system Study design. Regarding the methodological composition of the research corpus, it was found that qualitative methods predominate, constituting 44.0% of study designs, followed by mixed methods approaches at 20.8%, pre-post intervention studies at 12.8%, and cross-sectional analyses at 12.0%.
Methods: A convergent parallel mixed methods research design was used. In the quantitative phase, 363 young women in the age cohorts 18 to 28 years were contacted telephonically between August 2019 and January 2022 to have a session delivered to them or to be booked for a session.
Methods and analysis This protocol outlines a codesign study guided by the five stages of design thinking proposed by the Hasso-Plattner Institute of Design at Stanford University. The participants will include nurses and midwives at two hospitals in the Tshwane district, Gauteng Province. The five stages will be implemented in three phases: Phase 1: Stage 1—empathise and Stage 2—define.
This course will introduce students to the basics of research design and will review several methodologies in the study of human development. The focus of the course will be on descriptive and experimental methods. Students will learn the advantages and challenges to different methodological approaches. The course also places an emphasis on developing students' scientific writing and ...
Design. Abstract We employed a convergent design mixed-method research approach that included both qualitative and quantitative data being collected concurrently and ana-lyzed equally. This chapter includes the detailed description of the research design, data collection process, and data analysis method. The Likert scale survey, devel-oped by ...