- About the Hub
- Announcements
- Faculty Experts Guide
- Subscribe to the newsletter

Explore by Topic
- Arts+Culture
- Politics+Society
- Science+Technology
- Student Life
- University News
- Voices+Opinion
- About Hub at Work
- Gazette Archive
- Benefits+Perks
- Health+Well-Being
- Current Issue
- About the Magazine
- Past Issues
- Support Johns Hopkins Magazine
- Subscribe to the Magazine
You are using an outdated browser. Please upgrade your browser to improve your experience.

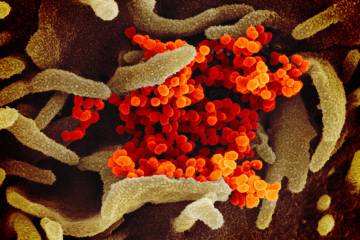
Credit: Getty Images
What is social distancing and how can it slow the spread of COVID-19?
Read the latest guidance from cdc and johns hopkins experts on measures to curtail the coronavirus outbreak.
By Katie Pearce
To slow the spread of COVID-19 through U.S. communities, the U.S. Centers for Disease Control and Prevention has encouraged Americans to practice "social distancing" measures. But what is social distancing, and how is it practiced?
For more information on the latest guidance, the Hub compiled information from the CDC and from Johns Hopkins experts Caitlin Rivers , an epidemiologist from the Johns Hopkins Center for Health Security, and Tom Inglesby , the center's director. Here's what they had to say.
What is social distancing?
Social distancing is a public health practice that aims to prevent sick people from coming in close contact with healthy people in order to reduce opportunities for disease transmission. It can include large-scale measures like canceling group events or closing public spaces, as well as individual decisions such as avoiding crowds.
With COVID-19, the goal of social distancing right now is to slow down the outbreak in order to reduce the chance of infection among high-risk populations and to reduce the burden on health care systems and workers. Experts describe this as "flattening the curve," which generally refers to the potential success of social distancing measures to prevent surges in illness that could overwhelm health care systems.
Image credit : Siouxsie Wiles and Toby Morris / Wikimedia Commons
"The goal of social distancing in the U.S. should be to lower the pace and extent of spread of COVID-19 in any given city or community," Inglesby wrote recently on Twitter . "If that can happen, then there will be less people with disease, and less people needing hospitalization and ventilators at any one time."
How do I practice social distancing?
The CDC defines social distancing as it applies to COVID-19 as "remaining out of congregrate settings, avoiding mass gatherings, and maintaining distance (approximately 6 feet or 2 meters) from others when possible."
This means, says Rivers, "no hugs, no handshakes."
It's particularly important—and perhaps obvious—to maintain that same 6-foot distance from anyone who is demonstrating signs of illness, including coughing, sneezing, or fever.
Along with physical distance, proper hand-washing is important for protecting not only yourself but others around you—because the virus can be spread even without symptoms.
"Don't wait for evidence that there's circulation [of COVID-19] in your community," says Rivers. "Go ahead and step up that hand-washing right now because it really does help to reduce transmission."
She recommends washing hands any time you enter from outdoors to indoors, before you eat, and before you spend time with people who are more vulnerable to the effects of COVID-19, including older adults and those with serious chronic medical conditions. ( See full CDC guidance on hand-washing techniques here .)
On the broader scale, a number of actions taken in recent days are designed to encourage social distancing, including:
- Schools, colleges, and universities suspending in-person classes and converting to remote online instruction
- Cities canceling events, including sporting events, festivals, and parades
- Workplaces encouraging or mandating flexible work options, including telecommuting
- Organizations and businesses canceling large gatherings, including conferences
- Houses of worship suspending services
"Community interventions like event closures play an important role," Rivers says, "but individual behavior changes are even more important. Individual actions are humble but powerful."
Does social distancing work?
Experts point to lessons from history that indicate these measures work, including those from the 1918 Spanish influenza pandemic. A 2007 PNAS study found that cities that deployed multiple interventions at an early phase of the pandemic—such as closing schools and banning public gatherings—had significantly lower death rates.
The do's and don'ts of 'social distancing'
A chart of the 1918 spanish flu shows why social distancing works.
Although Inglesby says the concept has little modern precedent at a large scale, he points to an early study, not yet peer reviewed, showing the different experience of peak coronavirus rates for two Chinese cities. The city of Guangzhou, which implemented disease control measures early into the outbreak, had significantly lower numbers of hospitalizations from COVID-19 on its peak day than the city of Wuhan, which put measures in place a month into the outbreak.
Inglesby says people shouldn't fret about a "perfect" approach to social distancing: "It's a big country and we will need partial solutions that fit into different communities. A 75% solution to a social distancing measure may be all that is possible … [which] is a lot better than 0%, or forcing a 100% solution that will fail."
What are other ways to limit the spread of disease?
Other public health measures could include isolation and quarantine. According to the CDC's latest guidance:
Isolation refers to the separation of a person or people known or reasonably believed to be infected or contagious from those who are not infected in order to prevent spread of the disease. Isolation may be voluntary, or compelled by governmental or public health authorities.
Quarantine in general means the separation of a person or people reasonably believed to have been exposed to a communicable disease but not yet symptomatic from others who have not been so exposed in order to prevent the possible spread of the disease. With COVID-19, the CDC has recommended a 14-day period to monitor for symptoms.
The CDC offers more details on which populations face greater risks, and specific cautionary measures they should take.
Posted in Health
Tagged public health , global health , coronavirus
Related Content

Serum stopgap could slow COVID-19 spread
Study: COVID-19 symptoms start about five days after exposure

Hopkins experts present latest coronavirus information on Capitol Hill

Map tracks coronavirus outbreak
You might also like, news network.
- Johns Hopkins Magazine
- Get Email Updates
- Submit an Announcement
- Submit an Event
- Privacy Statement
- Accessibility
Discover JHU
- About the University
- Schools & Divisions
- Academic Programs
- Plan a Visit
- my.JohnsHopkins.edu
- © 2024 Johns Hopkins University . All rights reserved.
- University Communications
- 3910 Keswick Rd., Suite N2600, Baltimore, MD
- X Facebook LinkedIn YouTube Instagram
Social distancing: What it is and why it’s the best tool we have to fight the coronavirus
Professor of Medicine, Boston University
Disclosure statement
Thomas Perls does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Boston University provides funding as a founding partner of The Conversation US.
View all partners
- Bahasa Indonesia
As the coronavirus spreads into more and more communities, public health officials are placing responsibility on individuals to help slow the pandemic. Social distancing is the way to do it. Geriatrician Thomas Perls explains how this crucial tool works.
What is social distancing?
Social distancing is a tool public health officials recommend to slow the spread of a disease that is being passed from person to person. Simply put, it means that people stay far enough away from each other so that the coronavirus – or any pathogen – cannot spread from one person to another.
The Centers for Disease Control and Prevention describes social distancing as staying away from mass gatherings and keeping a distance of 6 feet or 2 meters – about one body length – away from other people. In New York City, for example, theaters have closed temporarily , many conventions around the world are being canceled and schools are closing all across the U.S. I’ve stopped taking the train during rush hour. Now I either work from home or drive in with my wife, or I take the train during off-hours so I can maintain the 6-foot distance.
Social distancing also means not touching other people, and that includes handshakes. Physical touch is the most likely way a person will catch the coronavirus and the easiest way to spread it. Remember, keep that 6-foot distance and don’t touch.
Social distancing can never prevent 100% of transmissions, but by following these simple rules, individuals can play a critical role in slowing the spread of the coronavirus. If the number of cases isn’t kept below what the health care system can handle at any one time – called flattening the curve – hospitals could become overwhelmed, leading to unnecessary deaths and suffering.
There are a few other terms besides social distancing that you are likely to hear. One is “self-quarantine.” This means staying put, isolating yourself from others because there is a reasonable possibility you have been exposed to someone with the virus.
Another is “mandatory quarantine.” A mandatory quarantine occurs when government authorities indicate that a person must stay in one place, for instance their home or a facility, for 14 days. Mandatory quarantines can be ordered for people who test negative for the virus, but have likely been exposed . Officials have imposed mandatory quarantines in the U.S. for people on cruise ships and those traveling from Hubei province, China .
Why does social distancing work?
If done correctly and on a large scale, social distancing breaks or slows the chain of transmission from person to person. People can spread the coronavirus for at least five days before they show symptoms . Social distancing limits the number of people an infected person comes into contact with – and potentially spreads the virus to – before they even realize they have the coronavirus.
It’s very important to take a possibility of exposure seriously and quarantine yourself. According to recently published research, self-quarantine should last 14 days to cover the period of time during which a person could reasonably present with symptoms of COVID-19, the disease caused by the coronavirus. If after two weeks they still don’t have symptoms, then it’s reasonable to end the quarantine. Shorter quarantine periods could happen for asymptomatic people as tests to rule out the virus become widely available.

Why is social distancing so crucial?
At the moment, it’s the only tool available to fight the spread of the coronavirus.
Experts estimate that a vaccine is 12 to 18 months away . For now, there are no drugs available that can slow down a coronavirus infection.
Without a way to make people better once they fall sick or make them less contiguous, the only effective tactic is making sure hospital-level care is available to those who need it. The way to do that is to slow or stop the spread of the virus and decrease the number of cases at any one time.
Who should do it?
Everyone must practice social distancing in order to prevent a tidal wave of cases. I am a geriatrician who cares for the most vulnerable people: frail older adults . Certainly, such individuals should be doing all they can to protect themselves, diligently practicing social distancing and significantly changing their public ways until this pandemic blows over. People who are not frail need to do all they can to protect those who are, by helping to minimize their exposure to COVID-19.
If the public as a whole takes social distancing seriously, overwhelming the medical system could be avoided. Much of how the coronavirus pandemic unfolds in the U.S. will come down to individuals’ choices.
[ Deep knowledge, daily. Sign up for The Conversation’s newsletter .]
- Public health
- Coronavirus
- Coronavirus transmission
- Social distancing

Project Offier - Diversity & Inclusion

Senior Lecturer - Earth System Science

Sydney Horizon Educators (Identified)

Deputy Social Media Producer

Associate Professor, Occupational Therapy

The Ethics of Social Distancing
Nicholas G. Evans thinks through the tangle of rights and wrongs
If you’re reading this piece as it comes out, there’s a good chance you are reading it at home. That’s because you’re engaged, like so many of us, in social distancing as part of the broader response to coronavirus disease 2019, or COVID-19. As of the 8 th of May, 2020, 3.8 million people have been confirmed with the disease, and more than 261,000 have died. Of those deaths, more than a quarter have occurred in the United States.
Social distancing is an integral part of our response to this pandemic. Nonetheless, particular instances of social distancing, of which they are many, require some kind of ethical justification. That’s because like most public health measures, social distancing measures can interfere with individual freedoms, and cause harm. In this short essay I’ll ask what social distancing entails, why it raises ethical issues, and then finally what kind of social distancing measures are justified.
What is Social Distancing?
We’re all probably at the stage of knowing social distancing when we see it, because we’re living it day to day. But unlike quarantine -- the confinement of persons who are suspected to have been exposed to the disease -- social distancing isn’t well defined as a practice. That’s because social distancing isn’t a single thing. In fact, the use of “social distancing” as a catch all is fairly recent: in their 2004 planning for a return of SARS or a similar disease, for example, the US Centers for Disease Control and Prevention refer to “ measures to increase social distance ,” rather than “social distancing,” and those measures are extremely varied. The term social distancing seems to appear a few years later in the context of pandemic influenza , which gives you an idea of how recent the term is. That’s not to say that social distancing practices themselves are new. Jason Schwartz’s account of the turn to biomedical responses in public health shows us that until relatively recently, social distancing measures -- and “nonpharmaceutical interventions” in general -- were more or less all of public health.
Social distancing then, describes a wide range of practices. It includes stay-at-home orders by governments, which may be more or less enforced through curfews and travel restrictions; the shuttering of businesses, schools, and government offices; banning or restricting public gatherings; the use of masks in public; and the 6-foot separation recommendation many of you are familiar with in the case of COVID-19. These measures are merely physically distancing us. They are intended to remove points of interaction between us, and in particular between different subgroups of our community, to prevent a communicable disease from spreading between groups. Stopping people within families, for example, getting sick off each other is very labour intensive. But stopping transmission between families either through shared workspaces or schools can be effective at breaking chains of transmission in society.
Social distancing practices arguably include the design of social institutions, or even our environments. Mandated sick leave policies , among other employment rights, are effective forms of social distancing, and have been found to reduce flu infection rates. Urban architecture may also provide social distance: Bogotá is opening new bike lanes to further reduce the number on commuters on public transit, allowing individuals who can to use bicycles stay apart rather than use transit where they can be infected or transmit COVID-19 -- which also makes transit safer for those who can’t ride. People have been planning the physical shape of communities around infectious disease even before the advent of germ theory, such as Frank Olmstead’s design of Central Park.
Why Does Social Distancing Raise Ethical Issues?
Before dealing with the current controversy and its distinctive political elements, it’s worth asking why social distancing might raise ethical issues. The main reason it that social distancing can entail what the public health ethics literature sometimes refers to as a <href="#LibLimConCenTasPubHeaEth">liberty-limiting or liberty-restricting measures. That is, enacting public health measures that constitute social distancing can harm people, or infringe upon their freedoms in important ways.
Public health ethics hasn’t paid a lot of attention to social distancing measures, however. I think this is because social distancing differs from other public health measures in terms of the kinds of liberties it infringes upon. Quarantine is the paradigm of a liberty-limiting measure, because it directly and obviously restricts an individual’s freedom of movement in the name of public health. Rights to freedom of movement are recognised as fundamental human rights , though they aren’t unlimited in their scope. Moreover, insofar as our rights to freedom of movement constitutes a right to be free from interference in our movement, quarantine clearly infringes upon our freedom in some important way. So it requires a compelling justification.
On its face, social distancing doesn’t seem quite so bad. After all, social distancing need not require anyone to force you to stay at home. It might in some cases, but it’s definitely not an essential feature of social distancing measures. In some cases, social distancing might be effective without directly interfering with your movement at all. I’m sure a lot of you are currently familiar with the feeling that no one needs to force you to stay home, because there’s not really anywhere to go right now.
But I think that feeling points to a way social distancing impacts us in an important way, albeit one that is a little less obvious than quarantine (which involves locking someone or even many someones up). Applied broadly enough, and for enough time, social distancing can damage our ability to form communities, and limit our opportunities. It reveals that freedom of movement and freedom of association are, in small but deeply important ways, positive or welfare rights. That is, we have a right to community, and to travel, because doing so is deeply important for humans. We obviously don’t have absolute latitude in the kinds of community we can form (especially if others don’t want to form community with us!), but we have some minimal claim that is currently being infringed upon.
Moreover, the way these liberties were infringed upon -- particularly for people whose communities didn’t take the problem seriously at first, and then suddenly “ Cancelled Everything ”, this may seem like a form of domination . That is, the way some social distancing measures have been enacted has revealed the degree to which our employers, government, and other powerful actors in our lives have the arbitrary ability to close off our options, and potentially leave us without any recourse.
Social Distancing Kills
Social distancing can also hurt you. Again, not every measure we can use to increase social distance, and not every way of implementing the same measure, hurts us to the same degree. But social distancing can and does harm individuals. Those harms can be direct or indirect; proximate or long-term.
Direct and proximate harms of social distancing arise because social distancing itself is hurting them right now. These are the people who can’t get seen because acute care centres are closed, physicians aren’t taking new places, and getting care over the phone is hard. They are the folks who are having cardiac events and can’t get help. They might also be people form whom home is not safe, and now have nowhere else to go, including victims of domestic abuse. These are the people for whom the infringements and potential domination above is harming them in clear-cut ways.
Some are being indirectly harmed by social distancing arrangements right now. These are the “essential personnel” who are still expected to be on the job, but may lack the support that allows them to stay home if they are sick without losing their job, or who aren’t given appropriate protective gear. These are the people who we can’t afford to lose, and sometimes don’t permit to be socially distanced because they fulfil important roles in society. But they can be harmed just in case they’re expected to shoulder risk on our behalf in a way that isn’t a fair or proportionate form of sharing risk in society. Many of the ways they are put at risk, moreover -- access to paid leave, hazard pay, and protective gear -- are failures of our social institutions that predate COVID-19, often by decades.
People may be directly harmed by social distancing, but experience it as a slow burn. These are folks who won’t get screening fast enough to catch that cancer in its earliest stages, or who will live with chronic pain because they couldn’t get access to a physical therapist. Shutting down elective medical procedures will -- has -- harm people. It just won’t do it today, or tomorrow, but sometime in the future.
Finally, there are the people who are indirectly harmed by social distancing, over a long period of time. Some will struggle to make ends meet for years, even decades, because of the aggregate toll of social distancing and a slow recovery -- the folks caught up in the projected 15% unemployment in the USA for April 2020 who, even if only temporary, will be harmed. We know that income disparities and injustices kill; those who suffer the most deprivation under social distancing might weather this storm, but in doing so may borrow against the end of their life to get by.
The Ethics of Social Distancing: More Than a Binary
This is, then, where the rubber hits the road. Social distancing has clear benefits, and COVID-19 is an incredibly dangerous global pandemic. These measures slow the progress of the disease which takes pressure off the medical system, and reduces the overall number of infections. It could save millions of lives in the long run. It also has indirect benefits just as it has indirect harms: in the US, for example, road deaths are down.
On the other hand, it infringes on our liberties and imposes harms. It, moreover, arguably imposes harms, directly or indirectly, on some of the most vulnerable groups in society. The folks who benefit most from social distancing are people like me, and my colleagues in public health who have stable jobs that allow us to work from home. Folks who can’t work from home are the most at risk , and benefit the least from these measures.
Social distancing measures thus need to be necessary and effective in responding to the threat we face, proportionate, and minimally invasive and harmful relative to other options. What does that look like?
To start, the ongoing debate between social distancing and “reopening the economy” is false choice. That’s because social distancing isn’t one thing, and so we can layer measures, or not, as the need arises and as evidence dictates. But it’s also false choice because simply arguing based on the restrictiveness of social distancing measures -- between “Cancel Everything” and rescinding all measures that increase social distance -- ignores that in many cases the harms of social distancing can be ameliorated with appropriate policies. Not all, but many of the potential harms of social distancing measures are not endogenous to the measures themselves. People can, and should be supported during this time.
Finding ethically justified social distancing measures necessarily entails those supports. The reasons for this are broad. For the consequentialists, and particularly maximisers, the reasons are easy. Presented with a series of options, we ought to take the one that maximises expected global value (whatever we take that to be). Neither simply shutting down everything without support for those who might be harmed by social distancing, nor shutting down nothing/reopening, are going to top a maximiser’s list. Piecewise choices between two terrible options are false choices. Moreover, failing to maximise expected value, for those who subscribe to this, is unethical no matter how you slice it. It may be less unethical to shut everything down without these support measures, but it is still not maximising expected value and thus still fails to meet the demands of ethics.
For the deontologists among us, things can be a bit more varied. With the exception of the most devoted libertarians, however, it seems like most would subscribe to theories that mean that if it doesn’t cost us much (or anything), we ought to take on small risks to prevent others from coming to serious harm -- call this a limited “no means to harm” principle. This same principle, however, means that we should take on some costs (say, through the government) to prevent the most serious harms of social distancing.
Moreover, respecting others means understanding that for some, going to work might not be instrumentally irrational. It’s so easy for me to say, as an academic who can work from home (from anywhere, really), that all things considered I should stay home. But if I was faced with a set of choices that entailed either a nonzero, but potentially low chance of getting sick, and -- given at my age, the chances of dying from COVID-19 are quite low -- a nonzero but potentially low chance of progressing to serious disease and dying from COVID-19 if I am infected; or almost certainly losing my housing (and my family losing their housing) and other basic needs. There are lots of people in that situation, and if we’re committed to respecting the agency of others it seems like we should respect those people by giving them a reason to stay home that they can endorse.
It’s thus likely that most people would be committed to social distancing measures that support not just the most vulnerable, but everyone as they aid in defeating COVID-19 by staying home and staying apart. That mechanism has been achieved to greater or lesser degrees by different countries. But its clear there are basics that need to be in place as we go forward.
Ethical Social Distancing
The most obvious measures are those that reduce the time social distancing measures must be in force. This means comprehensive, accurate testing; ongoing contact tracing and monitoring; increased hospital capacities to pull the threshold of disaster back; and accurate seroprevalence studies to work out who has had the virus, so we have a better picture of where we are globally.
Less obvious, at least if you read the rapidly proliferating “roadmaps to reopening”, is attending to the most vulnerable in society. It is well understood that marginalised populations can become reservoirs for a disease because they are insufficiently protected. Sterling Johnson and Leo Beletsky have outlined how supporting harm reduction facilities can protect individuals suffering from substance abuse disorder and other diseases of despair, and support the pandemic response effort by preventing those marginalised communities from contracting and transmitting COVID-19. This is not only to the considerable benefit of those populations, but will also deprive the disease of places to lurk in our communities -- which, if we allow it, will only increase the time we live under comprehensive social distancing.
The next is to expand our concept of “frontline workers”, and support all those on all the front lines through hazard pay, more protective equipment and infection control, and better testing. I am referring to healthcare workers, yes, but also grocery store clerks, take out delivery drivers, food service workers, agricultural workers, workers on critical infrastructure, and major industries that we cannot or should not close. It is fashionable to refer to this outbreak as if it were a war. If that is true than the person at the grocery store or on a farm is as much on the front lines as a nurse, and -- assuming you enjoy eating as much as you enjoy hospitals -- deserves the same protection.
Next, propping up individuals and families whose economic futures hang in the balance should be done with minimal burden. In the USA, the $1200 individual pay-out has been slow to arrive , and is almost certainly insufficient given the length social distancing measures may last. In Australia, the JobKeeper program has been hampered by confusion and delays , some of which are part of the decades-long tradition of administrative hurdles introduced by conservative approaches to welfare. It is true that crisis demands we cut red tape, but we need to be cutting the right red tape, such as protecting people from entering into poverty, and ideally lifting people out of poverty to avoid the attendant and severe public health costs.
This goes the same for local businesses are threatened by the shutdown. The administrative hurdles presented by small business loans, globally, should be cut. The overall savings, if any, those hurdles imposed are almost certainly less than the benefits of preventing local economies from collapsing before the end of the ongoing shutdown.
Social distancing is absolutely necessary to stem the tide of COVID-19, and if some models are to be believed it could be years before those restrictions can be lifted indefinitely. Lots of people will suffer and die without it, but lots of people will suffer and die through it as well. There is no reason to choose one of those groups over the other, and ethical public health response requires attending to both. We don’t lack the skill or resources to accomplish this, only the political will. As such, we have an obligation to provide the most comprehensive support we can during this crisis.
Nicholas G. Evans is Assistant Professor of Philosophy at the University of Massachusetts Lowell. He maintains an active research program on the ethics of infectious disease, with a focus on clinical and public health decision making during disease pandemics. His edited volume, Ebola’s Message: Public Health and Medicine in the 21st Century focuses on the clinical, political, and bioethical impact of EVD.
You might also like...

The Transgender-Rights Issue

Of Our Great Propensity to the Absurd and Marvellous
The Art and Style of Crosswords

Woman as Resource: A Reply to Catharine MacKinnon

Women, Men and Criminal Justice

Philosophia

What Is the Philosophy of Madness?

Who Is Feminism For?
Subscribe to The Philosophers' Magazine for exclusive content and access to 20 years of back issues.
Most popular.

The Fact/Opinion Distinction

The Meaning of "Asshole"
Want to Be Good at Philosophy? Study Maths and Science

Do Animals Have Free Will?

Can Psychologists Tell Us Anything About Morality?
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 18 January 2021
Effects of social distancing on the spreading of COVID-19 inferred from mobile phone data
- Hamid Khataee 1 ,
- Istvan Scheuring 2 , 3 ,
- Andras Czirok 4 , 5 &
- Zoltan Neufeld 1
Scientific Reports volume 11 , Article number: 1661 ( 2021 ) Cite this article
13k Accesses
37 Citations
130 Altmetric
Metrics details
- Applied mathematics
- Infectious diseases
A better understanding of how the COVID-19 pandemic responds to social distancing efforts is required for the control of future outbreaks and to calibrate partial lock-downs. We present quantitative relationships between key parameters characterizing the COVID-19 epidemiology and social distancing efforts of nine selected European countries. Epidemiological parameters were extracted from the number of daily deaths data, while mitigation efforts are estimated from mobile phone tracking data. The decrease of the basic reproductive number ( \(R_0\) ) as well as the duration of the initial exponential expansion phase of the epidemic strongly correlates with the magnitude of mobility reduction. Utilizing these relationships we decipher the relative impact of the timing and the extent of social distancing on the total death burden of the pandemic.
Similar content being viewed by others
Non-compulsory measures sufficiently reduced human mobility in Tokyo during the COVID-19 epidemic
Fine-grained data reveal segregated mobility networks and opportunities for local containment of COVID-19
Impacts of social distancing policies on mobility and COVID-19 case growth in the US
Introduction.
The COVID-19 pandemic started in late 2019 and within a few months it spread around the World infecting 9 million people, out of which half a million succumbed to the disease. As of June 2020, the transmission of the disease is still progressing in many countries, especially in the American continent. While there have been big regional differences in the extent of the pandemic, in most countries of Europe and Asia the initial exponential growth has gradually transitioned into a decaying phase 8 . An epidemic outbreak can recede either due to reduction of the transmission probability across contacts, or due to a gradual build up of immunity within the population. According to currently available immunological data 1 , 2 at most locations only a relatively small fraction of the population was infected, typically well below 10%, thus the receding disease mostly reflects changes in social behavior and the associated reduction in disease transmission. Changes in social behavior can include state-mandated control measures as well as voluntary reduction of social interactions. However, especially with the view of potential future outbreaks, it is important to better understand how the timing and extent of social distancing impacted the dynamics of the COVID-19 pandemic.
Previous studies estimated the effect of social distancing on the dynamics of COVID-19 pandemic either by direct data analysis or by modeling methods 7 , 15 , 16 , 17 . A statistical analysis of the number of diagnosed cases, deaths and patients in intensive care units (ICU) in Italy and Spain have indicated that the epidemic started to decrease only after the introduction of strict lock-down action 3 . This was especially visible in Italy, where the final strict social distancing has been reached in a number of consecutive steps. A statistically more comprehensive analysis of hospitalized and ICU patients in France identified a 77% decrease in the growth rate of these numbers after the introduction of the lock-down 4 . The comparison of social distancing efforts in China, South Korea, Italy, France, Iran and USA 5 revealed that the initial doubling time of identified cases was about 2 days which was prolonged substantially by the various restrictions introduced in these countries. Epidemic models are widely used to estimate how various intervention strategies affect the transmission rate, however, the quantitative relationship between social interventions and epidemic parameters are hardly known 6 , 7 .
In this paper, we quantitatively characterise the time course of the COVID-19 pandemic using daily death data from nine selected European countries 8 . Statistical data on COVID-19-related deaths are considered to be more robust than that of daily cases of new infections. The latter is affected by the number of tests performed as well as by the testing strategy – e.g. its restriction to symptomatic patients – which may be highly variable across countries and often changes during the course of the epidemic. The time course of daily deaths can be considered as a more reliable indirect delayed indicator of daily infections. We thus do not address apparent differences in the case fatality ratio, and restrict our focus to the recorded COVID-19-associated death toll.
Our choice of countries was motivated by the requirements that each of these countries (i) had a relatively large disease-associated death toll (i.e. typically above 10/day and more than 2000 overall) so we can assume that the deterministic component of the epidemic dynamics dominates over random fluctuations. (ii) The selected countries spent a suitably long time in the decaying phase of the epidemic, thus allowing its precise characterisation. Based on these two criteria, we analysed data from the following, socio-economically similar countries, each implementing a somewhat distinct social distancing response: Italy, Spain, France, UK, Germany, Switzerland, Netherlands, Belgium and Sweden.
To characterise social distancing responses we used mobile phone mobility trend data from Apple Inc. 9 . Our aim is to quantitatively determine the characteristic features of the progression of the epidemic, such as initial growth rate, timing of the peak, and final decay rate and investigate how these parameters are determined by the timing and strictness of social distancing measures. We demonstrate that the overall death burden of the epidemic can be well explained by both the timing and extent of social distancing, often organized voluntarily well in advance of the state-mandated lock-down, and present quantitative relationships between changes in epidemiological parameters and mobile phone mobility data.
Characterization of the epidemic
Daily COVID-19 death data, D ( t ), is presented in Fig. 1 for the nine countries analysed. We selected the t = 0 reference time point as the date when the daily death rate first exceeded 5 deaths. In each country D ( t ) indicates the presence of a well defined exponential growth phase, followed by a crossover region and later an exponential decay stage. The initial growth and final decay regions are characterized by fitting the exponential \({\tilde{D}}(t)\) as
where the fitted functions are distinguished from the actual time series using a tilde. \(R_0\) is the basic reproductive number (i.e. number of new secondary infections caused by a single infected in a fully susceptible population) based on a simple SIR dynamics 10 and \(\gamma \) is the inverse average duration of the infectious period. For calculating the basic reproductive number we use \(\gamma = 0.1\; \text{day}^{-1}\) . The exact value of \(\gamma \) is somewhat uncertain at present 11 , 12 , however our analysis and results do not rely on the value of this parameter or on any modelling assumption regarding the disease dynamics.
To characterize the growth and decay phases, the values of \(R_{0_1}\) and \(R_{0_2}\) are approximated, respectively, by fitting Eq. ( 1 ) to the death data points (see Fig. 1 ). Least-squares fitting of Eq. ( 1 ) was performed using Mathematica (version 11, Wolfram Research, Inc.) routine NonlinearModelFit; see Supplementary Tables 1 and 2. The initial growth rate \(R_{0_1}\) is similar in the selected countries except in Sweden where it is substantially lower. This difference may reflect weaker social mixing, different cultural habits or a somewhat lower population density – an interesting problem outside of the scope of this report. The reproductive number in the decaying phase \(R_{0_2}\) is more variable across the different countries: in particular the decay is significantly slower in Sweden and somewhat slower in the UK.
A third parameter characterizes the transition from the growth to decay phases, i.e., the peak of the epidemic in terms of deaths. We define \((t_c,{\tilde{D}}_c)\) as the intersection point of the two fitted exponential functions. This is a more robust estimator than the actual maximum in daily deaths \(D_c\) as at the time of transition daily deaths can exhibit a plateau, hence the value and location of the maximum is sensitive to stochastic fluctuations. The gradual transition from exponential growth to decay in the actual data D ( t ) can be due to gradual implementation of social distancing as well as to the case-to-case variability of the time elapsed from infection to death.
The total death toll of the disease can be estimated analytically using the three parameters \(\alpha _1=(R_{0_1}-1)\gamma \) , \(\alpha _2=(1-R_{0_2})\gamma \) and \({\tilde{D}}_c\) as
Approximations by Eq. ( 2 ) are compared with the actual total death toll, \(D_{\text{tot}}\) , calculated as the area under death data points added to the area under the decaying curve (blue curve in Fig. 1 ) approaching zero. As Fig. 2 demonstrates, despite the substantial variation in death toll among the nine countries, it can be fairly well estimated by the expression ( 2 ). Specifically, details of the cross-over region, which do not fit well to the two exponential functions, contribute only around 10% to the overall death toll, while variations in the three epidemiological parameters ( \(R_{0_1}, R_{0_2}, t_c\) ) can change the death burden by an order of magnitude.
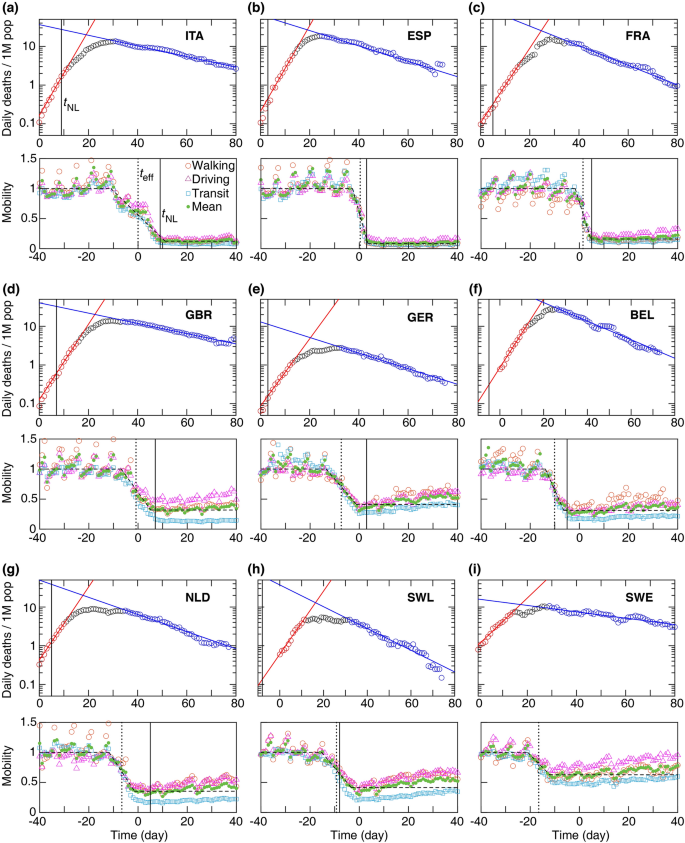
Daily death and mobility data for 9 European countries ( a – i ). Time 0 corresponds to the day when a country first reported \(\ge \) 5 daily deaths. Top: Growth and decay phases (red and blue lines) were fitted using Eq. ( 1 ) to the data points visually highlighted by red and blue, respectively. Vertical line: national lock-down date \(t_{\text{NL}}\) . Bottom: Mobile phone tracking data, normalized by the average values before the epidemic ( \(M_1\) ). Quantitative parameters were extracted by a fit (dashed line) to the mean mobility data (green circles, average of walking, driving, and transit data) calculated using Eq. ( 3 ). Dotted vertical line indicates the effective lock-down date \(t_{\text{eff}}\) calculated using Eq. ( 4 ). Fit parameters are summarised in Supplementary Tables 1 and 2 .

Analytical estimate of the total number of COVID-19 deaths \({\tilde{D}}_{\text{tot}}\) versus \(D_{\text{tot}}\) , the actual total death toll ( a ). ( b ) The same data are presented as per million (1M) population. The dashed and solid lines represent the identity and a linear regression, respectively. The slope of the linear regression is \(0.85 \pm 0.01\) ( a ) and \(0.84 \pm 0.02\) ( b ). Pearson coefficients of determination are ( a ) \(r^2 = 0.99\) \((p < 0.001)\) and ( b ) \(r^2 = 0.98\) \((p < 0.001)\) . Statistical data analysis was performed using MATLAB (version 2017b, The MathWorks, Inc.).
Characterization of social distancing
The timing and strictness of the often voluntary social distancing is quantified from the average mobility data (green circles in Fig. 1 ), by fitting the following piece-wise linear function:
where \(M_1\) and \(M_2\) are the average mobility levels before and after social distancing (i.e., before \(t_1\) and after \(t_2\) ), respectively. To fit Eq. ( 3 ) to the mobility data, we used the data recorded over 90 days starting from 13-January-2020. The mobility data show a relative daily volume of requests made to Apple Maps for directions by transportation type per country compared to a baseline volume on 13-January-2020. Data is sent from users’ devices to the Apple Maps service and is associated with randomised rotating identifiers so that Apple does not have a profile of individual movements and searches. The availability of data in a particular country is subject to a number of factors, including minimum thresholds for direction requests made per day. A day is defined as midnight-to-midnight, US Pacific time 9 . Although the mobility data may have bias in the mobility signal, it may have relatively little direct effect on data reported for the countries studied here. In the 90-day period considered in this study, the data indicates the mobility levels before and after implementing the social distancing. For clarity, to set a unique time-scale for the mobility data for all the countries, we added more data points after \(t_2\) in Fig. 1 . These additional data points were not used in the fitting. The walking, driving and transit data are first averaged, then Eq. ( 3 ) was fitted to the average mobility level using Mathematica routine NonlinearModelFit. The fitted values of \(t_1, M_1, t_2\) , and \(M_2\) are listed in Supplementary Table 3. The mobility data with average pre-pandemic value scaled to unity, \(M(t)/M_1\) , is shown in Fig. 1 . We characterize the extent of social distancing by the ratio \(\mu =M_2/M_1<1\) . A strict restriction of social interaction is expected to be reflected as \(\mu \approx 0\) .
Using the fitted parameters \(t_1\) and \(t_2\) obtained from Eq. ( 3 ), an effective social distancing date is approximated. The mobility data shows a transition period in dropping the mobility level due to the social distancing. We define the midpoint of this transition period as an approximation for the average date when the social distancing becomes effective, given by:
The Supplementary Table 3 summaries the approximated \(t_{\text{eff}}\) . It is noteworthy that \(t_{\text{eff}}\) often preceded the official national lock-down \(t_{\text{NL}}\) .
The effect of social distancing on epidemic parameters
Next, we investigate how the timing and extent of the social distancing changes the epidemic parameters, and as a consequence, the total death toll. First, we note that surprisingly neither the date of the official national lock-down \(t_{\text{NL}}\) nor the effective date of social distancing predicts well – in itself – the time of the epidemic peak \(t_c\) (Fig. 3 ). As the average time between infection and succumbing to COVID-19 is 18 days 13 , a delay of approximately 18 days is expected (dashed line in Fig. 3 ) between the introduction of social distancing and the change in the trend of the daily death count. Instead, we find that the time to the peak from the official national lock-down \(t_c-t_{\text{NL}}\) varies in a range from 10 days in Italy to more than 3 weeks in case of Switzerland, and the time from the change in mobility to the peak, \(t_c-t_{\text{eff}}\) , ranges from 19 days (Italy and Spain) up to 34 days (Sweden) as shown in Table. 1 .
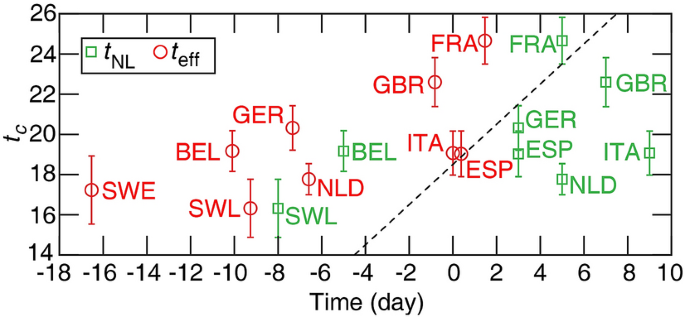
The time of the peak in daily deaths \(t_c\) versus the official national lock-down date \(t_{\text{NL}}\) and the effective social distancing date \(t_{\text{eff}}\) . The correlation is weak with \(r^2= 0.45\) ( \(p = 0.06\) ) for \(t_{\text{eff}}\) , and \(r^2=0.12\) ( \(p = 0.37\) ) for \(t_{\text{NL}}\) . Neither correlations are statistically significant. Dashed line: time (identity line) with a delay of 18.5 days. Error bars indicate standard error (SE).
Furthermore, neither the time of the peak \(t_c\) nor the parameters characterising the time and strength of social distancing \(t_{\text{eff}}, t_{\text{NL}}\) , \(\mu \) correlates—as a single parameter—well with the total number of deaths (Fig. 4 ). For example, Belgium registers a very high per capita death toll despite an early official lock-down, 5 days before the reference time \(t=0\) , and even earlier change is observed in mobility data ( \(t_{\text{eff}} = -10\) days). On the other hand, a moderate social distancing in Germany, indicated by the mobility ratio \(\mu = 0.4\) , led to the lowest death toll within this group of countries. Thus, we decided to investigate more carefully how social distancing affects the three epidemic parameters \(R_{0_1}\) , \(R_{0_2}\) and \({\tilde{D}}_c\) —with the hypothesis that the non-linear, multi-factor relationship ( 2 ) effectively masks correlations between the death toll and any single control parameter.

Actual total number of deaths per million (1M) population versus mean \(t_{\text{c}}\) , the peak time of daily deaths ( a ), \(t_{\text{NL}}\) national lock-down date ( b ), \(t_{\text{eff}}\) effective lock-down date ( c ), and \(1 - \mu \) , the relative mobility drop ( d ). Pearson correlation coefficients are ( a ) \(r^2 = 0.01\) ( \(p = 0.77\) ), ( b ) \(r^2 = 0.06\) ( \(p = 0.52\) ), ( c ) \(r^2 = 0.002\) ( \(p = 0.92\) ), and ( d ) \(r^2 = 0.04\) \((p = 0.62)\) indicating that there is no statistically significant correlation among these epidemic characteristics.
As Fig. 5 indicates, we found two strong relationships between the epidemiological parameters and measures of social distancing. Figure 5 a indicates a strong positive correlation between the drop in basic reproductive number, \(R_{0_1}-R_{0_2}\) and the restriction of mobility \(\mu \) . The relationship can be well approximated by the quantitative formula:
with \(\rho =0.56 \pm 0.09\) and \(\zeta = 3.18 \pm 0.11\) . Furthermore, the time elapsed between the peak and the social distancing, \(t_c-t_{\text{eff}}\) , correlates negatively with the severity of the mobility restrictions (Fig. 5 b) as
where \(\tau _0 = 17.04 \pm 1.62\) days is comparable with the mean value of the time from infection to death in fatal COVID-19 disease 13 , and \(\eta =1.50 \pm 0.40\) is the factor characterizing the lengthening of the delay for less severe reduction of mobility. Thus, the peak follows strict lock-downs (small \(\mu \) as in Italy and Spain) by around 18 days. For less restrictive social distancing ( \(\mu \approx 0.6\) as in Sweden), however, the peak can be delayed by as much as 5 weeks. This delay is of crucial importance, as the peak of the daily death toll \({\tilde{D}}_c\) is determined as
where \({\tilde{D}}(t_{\text{eff}})\) is a natural measure of how early the social distancing took place relative to the dynamics of the epidemic. As \({\tilde{D}}(t)\) is the exponential fit equation ( 1 ) instead of the actual daily death count D ( t ), unfortunately it is difficult to know in real-time. The country-specific values of \({\tilde{D}}(t_{\text{eff}})\) are listed in Table 2 .
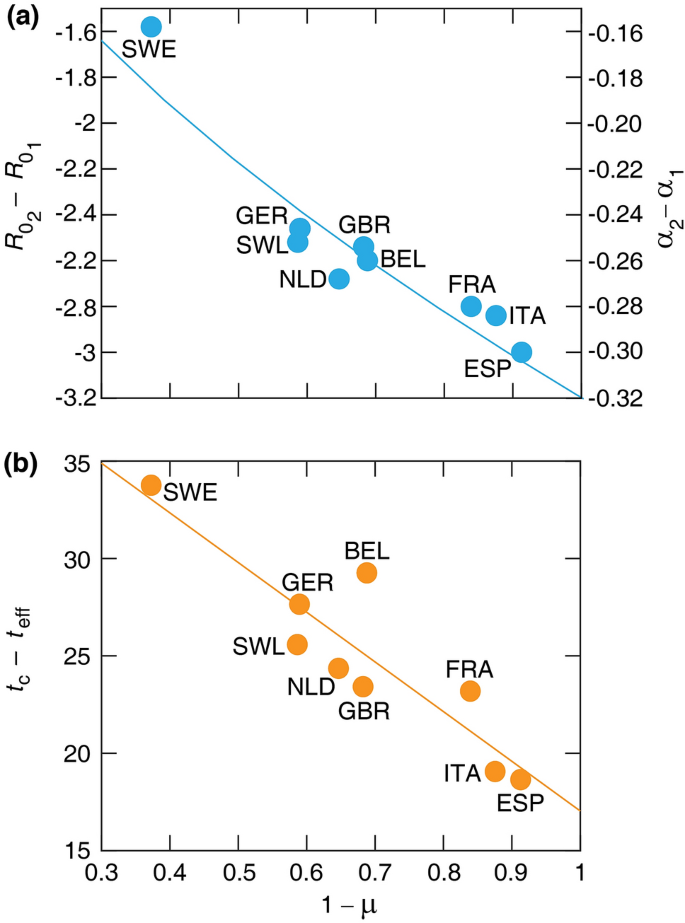
Relationships between key parameters of the COVID-19 pandemics and mobility data. ( a ) Change of basic reproductive number \(R_{0_2} - R_{0_1}\) (left axis) and \(\alpha _2 - \alpha _1\) (right axis) versus the mobility drop \(1 - \mu \) . Solid line indicates a power-law fit \(-\zeta (1- \mu )^\rho \) , where \(\zeta = 3.18 \pm 0.11\) and \(\rho =0.56\pm 0.09\) . \(r^2=0.85\) , \((p = 0.0005)\) . ( b ) Elapsed time between the epidemic peak and the effective lock-down, \(t_c - t_{\text{eff}}\) , versus the mobility drop \(1 - \mu \) . Solid line indicates the linear fit Eq. ( 6 ), where \(\tau _0 = 17.04 \pm 1.62\) and \(\eta = 1.50 \pm 0.40\) .
Our analysis thus indicates that social distancing has two effects: it reduces the basic reproduction number of the infection as expected, and shortens the time required for the epidemic to peak. This latter effect is unexpected, as changes in behavior should reduce transmission immediately, which, after a fixed delay – involving manifestation of symptoms and in a fraction of the patients death – should also appear in the daily death toll D ( t ). We propose that the increased time between the peak and the time of the social distancing may indicate the presence of subpopulations in which the disease continues to propagate with the initial reproduction number \(R_{0_1}\) . In these populations the transmission is eventually blocked, not by the overall social distancing efforts within the society, but by some other means. As a potential mechanism, we suggest that the local outbreak can reach such a magnitude that it either triggers an intervention or allows the establishment of herd immunity. Prominent examples of such events that collectively expand the duration of the initial growth phase are outbreaks in nursing homes, meat processing plants, warehouses and prisons – which become more likely when the overall social distancing is weak. Furthermore, weak overall social distancing could also fail to protect and segregate these vulnerable subpopulations specifically, thus increase the effective size of such subpopulations.
In this paper we analysed the interdependence of epidemic and mobility data and identified a quantitative relation between parameters of social distancing and key characteristics of the COVID-19 pandemic. Our sample consisted of 9 European countries where suitable data was available at current time. We found that the total death toll does not correlate well with any single parameter such as the timing of the official lock-down or the strictness of social distancing extracted from mobile phone location data. The total death toll, however, could be well estimated by a non-linear combination of three parameters: exponents characterising (i) the initial exponential growth rate (or reproductive number, \(R_{0_1}\) ) and (ii) the final decay rate of the epidemic, \(R_{0_2}\) , and (iii) the peak death rate \({\tilde{D}}_c\) which separates the two stages. The initial growth rate is an intrinsic parameter which may vary somewhat across different countries, but is not affected by control measures or social responses to the pandemic. Based on our data analysis we find that the two remaining parameters, \(R_{0_2}\) and \({\tilde{D}}_c\) can be related to the timing ( \(t_{\text{eff}}\) ) and strength ( \(\mu \) ) of social distancing.
Since the estimated daily death toll at the peak increases exponentially with the difference between the effective lock-down time ( \(t_{\text{eff}}\) ) and time of the peak ( \(t_c\) ), small changes in \(t_c-t_{\text{eff}}\) can yield substantial differences in the total death toll. The per capita values of \({{\tilde{D}}}(t_{\text{eff}})\) are fairly similar: within the range 0.1-0.16 for 7 of the countries analysed, suggesting that social distancing started at similar stages of the epidemic. The important exception is Germany, where a much smaller value of 0.02 corresponds to roughly a week earlier response. According to the analysis presented here, this explains the substantially lower German death toll, in spite of the relatively moderate social distancing. The slightly higher value of \({{\tilde{D}}}(t_{\text{eff}})\) /population in Spain (0.23) was compensated by a strict lock-down (lower \(\mu \) ).
The higher death toll in Belgium cannot be explained by the proposed set of parameters ( \(R_{0_1}, D(t_{\text{eff}}), \mu \) ) as all three values are close to the average of the sample. This anomaly can be traced to Fig. 5 (b), where the deviation of the Belgian data point from the fitted curve indicates that the peak of the epidemic was delayed by approximately 4 days compared to what could be expected based on the proxy measure for social distancing \(\mu \) . While the high Belgian death toll is often attributed to the different methodology of recording COVID-19 related fatalities, including suspected deaths which were not confirmed by lab analysis, such a difference in methodology cannot explain the markedly high time distance between the effective date of social distancing ( \(t_{\text{eff}}\) ) and the epidemic peak ( \(t_{c}\) ); see Fig. 5 (b). As we propose that \(t_c-t_{\text{eff}}\) reflects the presence of subpopulations in which the disease can spread unmitigated by social distancing efforts, we suggest that such groups were relatively larger in Belgium than in the other countries within our sample.
While in the case of Sweden the initial growth rate was the slowest and even the timing ( \(D(t_{\text{eff}})\) ) was similar to other countries the weakness of the mobility restriction (i.e. large \(\mu \) ) led to high death toll resulting from a strongly delayed peak. We would like to emphasize, that this delay was unexpected at the time of social distancing efforts, and still unaccounted by the typical SIR-based epidemiological models 10 .
In the case of the UK the timing of the social distancing ( \(D(t_{\text{eff}})\) ) is similar to other countries, however the mobility restriction appears to be weaker (i.e. higher \(\mu \) ) compared to similar countries (Spain, Italy and France) which results in a slower decay of the epidemic.
The phone mobility data is an indirect measure of the social distancing and disease transmission probabilities. However, it can be compared to more traditional measures in the Netherlands, where a study directly determined the number of daily personal interactions before and after the lock-down. Using questionnaires, the study identified a 71% decrease in interactions on average, which is fairly close to the 65% drop estimated from the phone mobility data 14 . While mobile phone tracking data thus can characterize the relatively early stages of social distancing efforts, it may be less useful to detect more subtle efforts like wearing masks or staggered working shifts at later stages of the pandemic.
In conclusion, we demonstrated a quantitative relation between social distancing efforts and statistical parameters describing the current COVID-19 pandemic. We identified an unexpected extension of the exponential growth phase when social distancing efforts are weak, which can substantially increase the death toll of the disease. Future studies are required to extend this analysis to countries with a markedly different socio-economical arrangements.
Data availability
The datasets analysed in the manuscript are publicly available, see References 8 , 9 .
Brotons, C., Serrano, J., Fernandez, D., Garcia-Ramos, C., Ichazo, B., Lemaire, J., Montenegro, P. et al . Seroprevalence against COVID-19 and follow-up of suspected cases in primary health care in Spain. medRxiv (2020).
Jacqui, W. Covid-19: surveys indicate low infection level in community. BMJ 369 , m1992 (2020).
Google Scholar
Tobías, A. Evaluation of the lockdowns for the SARS-CoV-2 epidemic in Italy and Spain after one month follow up. Sci. Total Environ. 725 , 138539. https://doi.org/10.1016/j.scitotenv.2020.138539 (2020).
Article ADS CAS PubMed PubMed Central Google Scholar
Salje, H., Kiem, C. T., Lefrancq, N., et al . Estimating the burden of SARS-CoV-2 in France [published online ahead of print, 2020 May 13]. Science . https://doi.org/10.1126/science.abc3517 (2020).
Article PubMed PubMed Central Google Scholar
Hsiang, S. et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature . https://doi.org/10.1038/s41586-020-2404-8 (2020).
Article PubMed Google Scholar
Flaxman, S. et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature . https://doi.org/10.1038/s41586-020-2405-7 (2020).
Giordano, G. et al. Modelling the COVID-19 epidemic and implementation of population-wide interventions in Italy. Nat. Med. 26 , 855–860. https://doi.org/10.1038/s41591-020-0883-7 (2020).
Article CAS PubMed Google Scholar
Ritchie, H., Ortiz-Ospina, E., Beltekian, D., Mathieu, E., Hasell, J., Macdonald, B., Giattino, C., \& Roser, M. Coronavirus Pandemic (COVID-19). Published online at OurWorldInData.org. https://ourworldindata.org/coronavirus (2020).
https://www.apple.com/covid19/mobility .
Anderson, R. M. & May, R. M. Infectious Diseases of Humans: Dynamics and Control (Oxford University Press, Oxford, 1992).
Bi, Q., Wu, Y, Mei, S., et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect. Dis. . https://doi.org/10.1016/S1473-3099(20)30287-5 (2020).
He, X., Lau, E. H. Y., Wu, P., et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 26 , 672–675. https://doi.org/10.1038/s41591-020-0869-5 (2020).
Zhou, F., Yu, T., Du, R., et al . Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears in Lancet. 2020 Mar 28;395(10229):1038]. Lancet 395 (10229):1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3 (2020).
Article CAS PubMed PubMed Central Google Scholar
Backer, J. A., Mollema, L., Klinkenberg, D., van der Klis, F. R., de Melker, H. E., van den Hof, S. & Wallinga, J. The impact of physical distancing measures against COVID-19 transmission on contacts and mixing patterns in the Netherlands: repeated cross-sectional surveys. medRxiv . https://doi.org/10.1101/2020.05.18.20101501 (2020).
Article Google Scholar
Kucharski, A. J. et al. Early dynamics of transmission and control of COVID-19: a mathematical modelling study. Lancet Infect. Dis. 20 (5), 553–558 (2020).
Neufeld, Z., Khataee, H., & Czirok, A. Targeted adaptive isolation strategy for COVID-19 pandemic. Infect. Dis. Model. 5 , 357–361 (2020).
PubMed PubMed Central Google Scholar
Dandekar, R. A., Henderson, S.G., Jansen, M., Moka, S., Nazarathy, Y., Rackauckas, C., Taylor, P. G., & Vuorinen, A. Safe blues: a method for estimation and control in the fight against COVID-19. medRxiv . https://doi.org/10.1101/2020.05.04.20090258. (2020).
Download references
Acknowledgements
IS was supported by GINOP 2.3.2-15-2016-00057 and the Hungarian Scientific Research Fund (OTKA, K128289). AC was supported by the Hungarian Scientific Research Fund (OTKA, ANN 132225).
Author information
Authors and affiliations.
School of Mathematics and Physics, The University of Queensland, St. Lucia, Brisbane, QLD 4072, Australia
Hamid Khataee & Zoltan Neufeld
Evolutionary Systems Research Group, Centre for Ecological Research, Tihany, 8237, Hungary
Istvan Scheuring
MTA-ELTE Theoretical Biology and Evolutionary Ecology Research Group, Eotvos University, Budapest, 1117, Hungary
Department of Biological Physics, Eotvos University, Budapest, 1053, Hungary
Andras Czirok
Department of Anatomy and Cell Biology, University of Kansas Medical Center, Kansas City, KS, 66160, USA
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the data analysis and to the writing of the manuscript.
Corresponding author
Correspondence to Zoltan Neufeld .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Khataee, H., Scheuring, I., Czirok, A. et al. Effects of social distancing on the spreading of COVID-19 inferred from mobile phone data. Sci Rep 11 , 1661 (2021). https://doi.org/10.1038/s41598-021-81308-2
Download citation
Received : 02 September 2020
Accepted : 21 December 2020
Published : 18 January 2021
DOI : https://doi.org/10.1038/s41598-021-81308-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Impact of national culture on the severity of the covid-19 pandemic.
- Yasheng Chen
- Mohammad Islam Biswas
Current Psychology (2023)
Effect of the COVID-19 pandemic on the pediatric infectious disease landscape
- Moshe Shmueli
- Idan Lendner
- Shalom Ben-Shimol
European Journal of Pediatrics (2023)
Human behaviour, NPI and mobility reduction effects on COVID-19 transmission in different countries of the world
- Zahra Mohammadi
- Monica Gabriela Cojocaru
- Edward Wolfgang Thommes
BMC Public Health (2022)
Novel mobility index tracks COVID-19 transmission following stay-at-home orders
- Peter Hyunwuk Her
- Sahar Saeed
- Sahir R Bhatnagar
Scientific Reports (2022)
Scheduling Diagnostic Testing Kit Deliveries with the Mothership and Drone Routing Problem
- Hyung Jin Park
- Reza Mirjalili
- Gino J. Lim
Journal of Intelligent & Robotic Systems (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: AI and Robotics newsletter — what matters in AI and robotics research, free to your inbox weekly.
- Share full article
Advertisement
Supported by
We Need Social Solidarity, Not Just Social Distancing
To combat the coronavirus, Americans need to do more than secure their own safety.

By Eric Klinenberg
Dr. Klinenberg is a sociologist.
Social distancing — canceling large gatherings, closing schools and offices, quarantining individuals and even sequestering entire cities or neighborhoods — seems to be the best way to slow the spread of the coronavirus. But it’s a crude and costly public health strategy. Shuttering shared spaces and institutions means families lose child care, wages and social support. What’s more, it’s insufficient to protect the older, sick, homeless and isolated people who are most vulnerable to the virus. They need extra care and attention to survive, not society’s back.
I learned this firsthand while studying another recent health crisis , the great Chicago heat wave of 1995. In that event, as in so many other American disasters, social isolation was a leading risk factor and social connections made the difference between life and death.
In Chicago, social isolation among older people in poor, segregated and abandoned neighborhoods made the heat wave far more lethal than it should have been. Some 739 people died during one deadly week in July, even though saving them required little more than a cold bath or exposure to air-conditioning. There was plenty of water and artificial cooling available in the city that week. For the truly disadvantaged, however, social contact was in short supply.
Good governments can mitigate damage during health crises by communicating clearly and honestly with the public and providing extra service and support to those in need. But as the heat settled into Chicago, the mayor focused more on public relations than public health. He neglected to issue an official emergency or call in additional paramedics until it was too late. He publicly challenged the medical examiner’s reports that hundreds were dying from heat. In news conferences, he insisted that his administration was doing everything possible. His health service commissioner blamed those who died for neglecting to take care of themselves.
It’s chilling, how familiar this seems. And it’s disturbing, how little we’ve heard about helping the people and places most threatened by the coronavirus, about the ways in which, amid so much isolation, we can offer a hand.
In addition to social distancing, societies have often drawn on another resource to survive disasters and pandemics: social solidarity, or the interdependence between individuals and across groups. This an essential tool for combating infectious diseases and other collective threats. Solidarity motivates us to promote public health, not just our own personal security. It keeps us from hoarding medicine, toughing out a cold in the workplace or sending a sick child to school. It compels us to let a ship of stranded people dock in our safe harbors, to knock on our older neighbor’s door.
Social solidarity leads to policies that benefit public well-being, even if it costs some individuals more. Consider paid sick leave. When governments guarantee it (as most developed democracies do), it can be a burden for employers and businesses. The United States does not guarantee it, and as a consequence many low-wage American workers, even in the food service industry , are on the job when they’re contagiously ill.
It’s an open question whether Americans have enough social solidarity to stave off the worst possibilities of the coronavirus pandemic. There’s ample reason to be skeptical. We’re politically divided, socially fragmented, skeptical of one another’s basic facts and news sources. The federal government has failed to prepare for the crisis. The president and his staff have repeatedly dissembled about the mounting dangers to our health and security. Distrust and confusion are rampant. In this context, people take extreme measures to protect themselves and their families. Concern for the common good diminishes. We put ourselves, not America, first.
But crises can be switching points for states and societies, and the coronavirus pandemic could well be the moment when the United States rediscovers its better, collective self. Ordinary Americans, regardless of age or party, already have abundant will to promote public health and protect the most vulnerable. Although only a fraction of us are old, sick or fragile, nearly all of us love and care for someone who is.
Today Americans everywhere are worried about the fate of friends and family members. Without stronger solidarity and better leadership, though, millions of our neighbors may not get the support they need.
We’re not likely to get better leadership from the Trump administration, but there’s a lot we can do to build social solidarity. Develop lists of local volunteers who can contact vulnerable neighbors. Provide them companionship. Help them order food and medications. Recruit teenagers and college students to teach digital communications skills to older people with distant relatives and to deliver groceries to those too weak or anxious to shop. Call the nearest homeless shelter or food pantry and ask if it needs anything.
Why not begin right now?
Eric Klinenberg ( @EricKlinenberg ) is a professor in the social sciences at New York University and the author of “Palaces for the People: How Social Infrastructure Can Help Us Fight Inequality, Polarization, and the Decline of Civic Life.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow The New York Times Opinion section on Facebook , Twitter (@NYTopinion) and Instagram .
To revisit this article, visit My Profile, then View saved stories .
- Backchannel
- Newsletters
- WIRED Insider
- WIRED Consulting
Hilda Bastian
Social Distancing Has Become the Norm. What Have We Learned?

United States federal guidelines for social distancing expired last week, though there’s no indication of consensus over when and to what extent policies should be relaxed around the nation. White House coronavirus coordinator Deborah Birx had said just the previous weekend that social distancing measures would “ be with us through the summer .” Though the current advice from the White House is that there should be a “ downward trajectory ” for 14 days before easing up, about half the nation’s governors have moved toward rollbacks of their interventions—while rates of infection and death in their states are often stable or increasing.
In an ideal world, science would show us how to avoid further chaos, or at least how to minimize it. But the total impact of social distancing measures, in terms of their benefits and harms to public health, remains uncertain. So what, exactly, should be done? I’m a meta-scientist, which means I do research on research; and my expertise is in evaluating evidence behind health claims. I believe it can be helpful to take a step back from these debates, from time to time, and consider what is actually known, unknown, and becoming-known on important questions. Let’s do just that for social distancing.
“Social distancing” is, in fact, an umbrella term that comprises several very complex interventions for keeping healthy people spaced apart from anyone who could be infectious. Measures range from telling people to avoid crowds to issuing wholesale stay-at-home orders, with just about endless variations and possible combinations. Each of these may work to differing degrees, and they come with varying social and economic costs. When we ask whether social distancing “works,” we’re collapsing all these boundaries.
In general, once it’s clear the spread of a new virus as dangerous as this one has not been contained by testing and contact tracing, and for which there isn’t any treatment or vaccine, more drastic forms of social distancing are the only options left to slow it down. But the body of knowledge about social distancing in all its forms is changing rapidly in real time, as the pandemic brings a blizzard of new data, research, and analysis. Say anything on some subjects, and there’s quite a good chance it could be out of date in hours, if not minutes.
Here’s what I think we know right now.
First, on the question of large gatherings, and the degree to which their prohibition slows viral spread. Covid-19 outbreaks appear to have spiraled out from large religious meetings both in South Korea and in France , each resulting in thousands of infections. A soccer match was at the epicenter of Italy’s devastating wave. When even one large event draws in people from far and wide, with SARS-CoV-2 circulating, the virus can break out of containment in a region. Indeed, shutting down such gatherings may have saved some parts of the US from the worst during the catastrophic 1918–1920 influenza pandemic. Cities deploying multiple distancing interventions a century ago had lower death rates , though few of them maintained these restrictions for longer than 6 weeks in 1918. Avoiding crowded living conditions , though, isn’t always feasible.
Got a coronavirus-related news tip? Send it to us at [email protected] .
What about travel restrictions? A systematic review of research on their deployment to prevent the spread of influenza looked at 20 studies conducted through May 2014. The link between travel and contagion appeared to be significant: When there was more travel, for example around Thanksgiving, more people got influenza; in contrast, when air travel decreased after 9/11, the rate of influenza decreased. Taken together, the studies suggest that domestic travel restrictions can delay influenza outbreaks for about a week; while international border closures may extend that window to 2 months.
Data from the Covid-19 pandemic might change the balance of evidence here. Restricting travel from Wuhan around Chinese Lunar New Year was seen as a success in helping to stop the spread of the coronavirus across China. A modeling study based on Wuhan data concluded that if international travel restrictions were combined with contact tracing and quarantine, it might be possible to keep the disease under control. Several countries may try to last the distance to a vaccine this way. Australia and New Zealand, for example, may allow cross-border travel only within their shared bubble of well-controlled infection rates; and perhaps to other countries in the region, too, if they become and stay Covid-19-free.

By Meghan Herbst
The question of school closures has been especially contentious, given the major social costs of the intervention. In New York City , where more than 173,000 people have now been diagnosed with Covid-19, and there have been more than 18,000 confirmed or probably associated deaths, local politicians resisted taking this step until mid-March . Do we know for sure that shutting schools can help? In fact, this is the element of social distancing that has been studied the most: A systematic review just undertaken for the World Health Organization analyzed 101 studies on the matter. In aggregate, these showed that closing schools may not do much to slow down an epidemic, while it can create a childcare crisis, among other added harms. This absence of clear benefit comes despite the fact that the studies in question looked at influenza outbreaks, where children are a major source of spread and can be affected significantly by illness. The role of children in the spread of Covid-19 is much less clear: They don’t appear to get as sick as adults do, though there are reports of their being contagious even without symptoms. On the other hand, influenza outbreaks don’t threaten health systems in the same way Covid-19 has.
There are lots of different ways to implement school closures. A class or whole school can be shut when children or teachers are diagnosed with Covid-19, as happens in Taiwan. Or all schools could be closed completely. Two modeling studies of influenza-like illnesses, in France and the UK , found that Taiwan-style targeting for school closures could have the same health benefits as total closures, with less harm to education and parents’ lives. When parents work in essential services, school disruption can hamper pandemic response. Although closing all schools might be able to reduce the transmission of influenza, it wasn’t decisive for the SARS outbreak in 2003. Closing schools may have been one of the social distancing measures most responsible for reducing people’s mobility and social contact in the US, although it’s hard to be certain. And as with every aspect of pandemic response, understanding the impact on social disparities is going to be vital: School is critical to mitigating the effects of poverty in many ways. The American Academy of Pediatrics has issued considerations for local decisions on safe opening of schools that basically boil down to, it’s complicated and it depends .

Mark Andrews

Andy Greenberg

Morgan Meaker
Matt Burgess
Shutting workplaces, and having people telecommute if possible, may also help. However, the privileges of flexible work arrangements and the impact of shutting workplaces are tied to steep social and race inequalities. Such measures have been substantially effective at mitigating influenza epidemics—but only if the proportion of workplaces shut down is substantial, too. According to one study , you need to close one-third of workplaces in order to reduce an influenza infection rate from 19 percent to 5 percent; but that calculation assumes that schools would also be closed. Because the SARS-CoV-2 virus is so much more threatening than influenza, a lot more than one-third of workplaces have been closed down in many locations. A closely related issue to workplace and school closure is public transit. Aside from the occupational hazards for transit workers, the potential risks for passengers in this pandemic are the subject of heated debate around the world . We’re seeing conflicting conclusions on this question for New York City , too.
Read all of our coronavirus coverage here .
In addition to the known benefits to social distancing, there are devastating costs. Confined living, unemployment, and other pandemic pressures can increase the already high burden of family abuse and violence , for example. Reports from several countries already suggest that an epidemic of interpersonal violence could be traveling alongside the virus. Studies confirm that being quarantined or in isolation takes a heavy psychological toll, sometimes even long after it’s over. Economic crises also harm health : The global financial crisis of 2008 has been linked to higher suicide rates among men in many countries, especially where it brought significant unemployment.
That doesn’t mean we face a trade-off between protection from Covid-19 and protection of the economy: Both are necessary. A 2005 analysis of the potential economic impact of a pandemic stressed that mass deaths damage the economy, too. Large-scale, severe illness from Covid-19 would decimate the workforce: As May began, most of those people who had been hospitalized with Covid-19 in New York City’s outbreak were under 65, along with just over one-fourth of those who died with confirmed Covid-19. It’s vital to support both those who are most vulnerable to the disease and those at greatest risk of the hardships associated with social distancing. Monitoring and acting on what happens to vulnerable groups is critical.
We don’t know at what scale, and for how long, social distancing measures will be needed or can be sustained. According to an Australian modeling study , we need at least 70 percent of the population to stick to social distancing rules to make a serious difference. Meanwhile, researchers from the University of Hong Kong found promising signs that social distancing, among other measures, had been quite successful at reducing viral spread in early February; but they worried whether social distancing would be sustainable in the long term. Studies on this topic have mixed results , with quarantine times only up to 2 weeks. When people aren’t committed to the measures, cannot comply, or don’t understand critical aspects of what they are supposed to do, then it can be a struggle to maintain community-wide social distancing. When solidarity and trust have been high, though, and enough people believed it was essential, it has been sustained. This time, people have been exposed to harrowing images and personal stories through social media from northern Italy and New York, and that is new territory. We may be about to find out how long communities can maintain social distancing. Italians are now emerging from more than two months of severe lockdown, desperately keen to not go back.
The risk of backpedaling among some communities in the US seems awfully high . While policymakers can do their level best to determine what happens, it’s not entirely up to them: Social distancing interventions and social distancing behavior aren’t the same thing. Stay-at-home orders may have had less impact on people’s actual staying-at-home than news of deaths and declarations of a state of emergency. People in areas that had stay-at-home orders may not have acted dramatically differently from those in other places. That adds complexity to the task of working out the impact of social distancing in all its many forms. The major doubts that still remain about which interventions are most effective could be reduced by rigorous studies, though. We are benefiting from past studies, but there were nowhere near enough really good ones. One thing policymakers can definitely influence is the level of support for research that can test the impact of different policies. We need better science to guide us in our further bouts with Covid-19—and with whichever pandemic infection comes next.
Photographs: Anthony Kwan/Getty Images; Oli Scarff/Getty Images
- How Argentina’s strict lockdown saved lives
- An oral history of the day everything changed
- In one hospital, finding humanity in an inhuman crisis
- How is the coronavirus pandemic affecting climate change ?
- FAQs: All your Covid-19 questions, answered
- Read all of our coronavirus coverage here
To Beat COVID-19, Social Distancing is a Must
Posted on March 19th, 2020 by Dr. Francis Collins

Even in less challenging times, many of us try to avoid close contact with someone who is sneezing, coughing, or running a fever to avoid getting sick ourselves. Our attention to such issues has now been dramatically heightened by the emergence of a novel coronavirus causing a pandemic of an illness known as COVID-19.
Many have wondered if we couldn’t simply protect ourselves by avoiding people with symptoms of respiratory illness. Unfortunately, the answer is no. A new study shows that simply avoiding symptomatic people will not go far enough to curb the COVID-19 pandemic. That’s because researchers have discovered that many individuals can carry the novel coronavirus without showing any of the typical symptoms of COVID-19: fever, dry cough, and shortness of breath. But these asymptomatic or only mildly ill individuals can still shed virus and infect others.
This conclusion adds further weight to the recent guidance from U.S. public health experts: what we need most right now to slow the stealthy spread of this new coronavirus is a full implementation of social distancing. What exactly does social distancing mean? Well, for starters, it is recommended that people stay at home as much as possible, going out only for critical needs like groceries and medicines, or to exercise and enjoy the outdoors in wide open spaces. Other recommendations include avoiding gatherings of more than 10 people, no handshakes, regular handwashing, and, when encountering someone outside of your immediate household, trying to remain at least 6 feet apart.
These may sound like extreme measures. But the new study by NIH-funded researchers, published in the journal Science , documents why social distancing may be our best hope to slow the spread of COVID-19 [1]. Here are a few highlights of the paper, which looks back to January 2020 and mathematically models the spread of the coronavirus within China:
• For every confirmed case of COVID-19, there are likely another five to 10 people with undetected infections. • Although they are thought to be only about half as infectious as individuals with confirmed COVID-19, individuals with undetected infections were so prevalent in China that they apparently were the infection source for 86 percent of confirmed cases. • After China established travel restrictions and social distancing, the spread of COVID-19 slowed considerably.
The findings come from a small international research team that included NIH grantee Jeffrey Shaman, Columbia University Mailman School of Public Health, New York. The team developed a computer model that enabled researchers to simulate the time and place of infections in a grid of 375 Chinese cities. The researchers did so by combining existing data on the spread of COVID-19 in China with mobility information collected by a location-based service during the country’s popular 40-day Spring Festival, when travel is widespread.
As these new findings clearly demonstrate, each of us must take social distancing seriously in our daily lives. Social distancing helped blunt the pandemic in China, and it will work in other nations, including the United States. While many Americans will likely spend weeks working and studying from home and practicing other social distancing measures, the stakes remain high. If this pandemic isn’t contained, this novel coronavirus could well circulate around the globe for years to come, at great peril to us and our loved ones.
As we commit ourselves to spending more time at home, progress continues to be made in using the power of biomedical research to combat this novel coronavirus. A notable step this week was the launch of an early-stage human clinical trial of an investigational vaccine, called mRNA-1273, to protect against COVID-19 [2]. The vaccine candidate was developed by researchers at NIH’s National Institute of Allergy and Infectious Diseases (NIAID) and their collaborators at the biotechnology company Moderna, Inc., Cambridge, MA.
This Phase 1 NIAID-supported trial will look at the safety of the vaccine—which cannot cause infection because it is made of RNA, not the whole coronavirus—in 45 healthy adults. The first volunteer was injected this past Monday at Kaiser Permanente Washington Health Research Institute, Seattle. If all goes well and larger follow-up clinical studies establish the vaccine’s safety and efficacy, it will then be necessary to scale up production to make millions of doses. While initiating this trial in record time is reason for hope, it is important to be realistic about all of the steps that still remain. If the vaccine candidate proves safe and effective, it will likely take at least 12–18 months before it would be widely available.
In the meantime, social distancing remains one of the best weapons we have to slow the silent spread of this virus and flatten the curve of the COVID-19 pandemic. This will give our health-care professionals, hospitals, and other institutions more valuable time to prepare, protect themselves, and aid the many people whose lives may be on the line from this coronavirus.
Importantly, saving lives from COVID-19 requires all of us—young, old and in-between—to take part. Healthy young people, whose risk of dying from coronavirus is not zero but quite low, might argue that they shouldn’t be constrained by social distancing. However, the research highlighted here demonstrates that such individuals are often the unwitting vector for a dangerous virus that can do great harm—and even take the lives of older and more vulnerable people. Think about your grandparents. Then skip the big gathering. We are all in this together
Reference s:
[1] Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) . Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, Shaman J. Science. 16 March 2020. [Preprint ahead of publication]
[2] NIH clinical trial of investigational vaccine for COVID-19 begins . NIH News Release, March 16, 2020.
Coronavirus (COVID-19) (NIH)
COVID-19, MERS & SARS (National Institute of Allergy and Infectious Diseases/NIH)
Coronavirus (COVID-19) (Centers for Disease Control and Prevention, Atlanta)
NIH Support: National Institute of Allergy and Infectious Diseases; National Institute of General Medical Sciences
Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)
Posted In: News
Tags: China , coronavirus , COVID-19 , infectious disease , Kaiser Permanente , Moderna , mRNA-1273 , novel coronavirus , pandemic , respiratory infections , SARS , social distancing , travel restrictions , undetected infections , vaccine , viral transmission , virus

60 Comments
great blog . . .
Really nice article.
really nice article and great blog.
Nice blog author. Thank you. Keep it up.
Your article is so good and helpful for us. Thanks for your share. Keep it up.
Nice blog author. Thank you. keep it up.
Leave a Comment Cancel reply
@nihdirector on twitter, nih on facebook.
Kendall Morgan, Ph.D.
Comments and Questions
If you have comments or questions not related to the current discussions, please direct them to Ask NIH .
You are encouraged to share your thoughts and ideas. Please review the NIH Comments Policy

- Visitor Information
- Privacy Notice
- Accessibility
- No Fear Act
- HHS Vulnerability Disclosure
- U.S. Department of Health and Human Services
- USA.gov – Government Made Easy
Discover more from NIH Director's Blog
Subscribe now to keep reading and get access to the full archive.
Type your email…
Continue reading
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
How effective are social distancing policies? Evidence on the fight against COVID-19
Contributed equally to this work with: Ulrich Glogowsky, Emanuel Hansen, Simeon Schächtele
Roles Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Economics, Johannes Kepler University Linz, Linz, Austria
Roles Data curation, Methodology, Visualization, Writing – original draft, Writing – review & editing
Affiliation Center for Macroeconomic Research, University of Cologne, Cologne, Germany
Roles Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing
Affiliation Inter-American Development Bank, Washington, D.C., United States of America
- Ulrich Glogowsky,
- Emanuel Hansen,
- Simeon Schächtele

- Published: September 22, 2021
- https://doi.org/10.1371/journal.pone.0257363
- Reader Comments
To fight the spread of COVID-19, many countries implemented social distancing policies. This is the first paper that examines the effects of the German social distancing policies on behavior and the epidemic’s spread. Exploiting the staggered timing of COVID-19 outbreaks in extended event-study models, we find that the policies heavily reduced mobility and contagion. In comparison to a no-social-distancing benchmark, within three weeks, the policies avoided 84% of the potential COVID-19 cases (point estimate: 499.3K) and 66% of the potential fatalities (5.4K). The policies’ relative effects were smaller for individuals above 60 and in rural areas.
Citation: Glogowsky U, Hansen E, Schächtele S (2021) How effective are social distancing policies? Evidence on the fight against COVID-19. PLoS ONE 16(9): e0257363. https://doi.org/10.1371/journal.pone.0257363
Editor: Ming Tang, East China Normal University, CHINA
Received: April 21, 2021; Accepted: August 24, 2021; Published: September 22, 2021
Copyright: © 2021 Glogowsky et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: We rely on administrative health data that are freely available. We also use purchasable mobility data from Teralytics. For data access, contact Laura Galamb ( [email protected] ). Replication files are available on http://www.glogowsky.com/research.html .
Funding: Ulrich Glogowsky (UG) received financial support by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation): CRC TRR 190, Rationality and Competition. Emanuel Hansen (EH) received financial support by Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) under Germany’s Excellence Strategy – EXC2126/1 – 390838866. The funder provided support in the form of salaries for author SS, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist. Part of this research was conducted while Simeon Schächtele was employed by the Inter-American Development Bank, a multilateral international organization with the mandate to foster economic and social development in Latin America and the Caribbean. This does not alter our adherence to PLOS ONE policies on sharing data and materials.
1 Introduction
Since its outbreak in Wuhan, the SARS-CoV-2 virus causing the respiratory disease COVID-19 has spread across the globe [ 1 – 3 ]. To prevent human-to-human transmission of the virus, many governments have adopted social distancing (SD) policies. For example, more than 190 countries have implemented nationwide school closures [ 4 ]. These and similar policies aimed at reducing interpersonal contacts to dissipate the epidemic and, ultimately, save lives.
In this paper, we evaluate the effectiveness of the German social distancing policies in the fight against COVID-19. We offer two contributions. First, we provide a comprehensive analysis of the policies. We do not only estimate their impact on confirmed COVID-19 cases but also on fatalities. Additionally, we investigate if the policies affected certain socio-demographic groups more than others, and we use cell phone data to link the policies to changes in mobility behavior. Second, we propose a flexible quasi-experimental strategy that can be applied to many settings. At the core, it exploits variation in the spread of COVID-19 at the subnational level.
As for the policy variation, we focus on nationwide SD policies that the German federal and state governments jointly enacted in mid-March 2020. The most significant pieces of this policy response were Chancellor Merkel’s televised appeal for voluntary social distancing (March 12), the closure of schools, childcare facilities, and retail stores (March 16), and the implementation of a national contact ban (March 23). Our paper identifies the combined effect of all these policies. As the entire set of policies were simultaneously introduced in all German districts and within a short period of time, it is impossible to estimate their effects separately.
It is challenging to identify the effects of nationwide SD policies. The impact of such policies is the difference in an outcome of interest (e.g., confirmed cases) between states of the world with and without them. After the policy interventions, however, we cannot observe how the outcome would have developed without the policies. We tackle this problem with an extended event-study approach that exploits variation at the level of German districts (NUTS-3 regions; comparable to US counties). Some districts experienced a COVID-19 outbreak several weeks before the policies took effect; others were not yet affected. Hence, we can compare how the outcomes developed after a local outbreak without SD policies (former districts) and with SD policies (latter districts). This comparison identifies the policies’ effects if, in the counterfactual state without policy interventions, the outcome would have evolved similarly in both types of districts. We cannot test this assumption directly, but we verify its plausibility.
Three features render our approach and setting especially suited to estimate the policies’ effects. First, focusing on within-country variation lowers the potential for bias from heterogeneity in institutions, measurement, and populations. Particularly, in the first phase of the epidemic, all German districts faced the same policies and identical testing and reporting rules. Second, the German data are sufficiently granular for quantitative impact analysis: 401 districts with varying local outbreak dates report cases and fatalities to one federal agency. Third, the data quality is arguably high, and the expected share of undetected cases is lower than in most other countries [ 5 ]. The main reasons why epidemiologists expect a low share of undetected cases in Germany are low case fatality rates and extensive testing. As of April 22, Germany conducted 2.07 million tests (2.6% of the population).
Fig 1 gives a graphical account of our key results. It shows how the SD policies affected the number of cases ( Fig 1A ) and fatalities (Sub Fig 1B ) within three weeks of implementation. According to our estimates, the policies avoided 499.3 thousand cases (95% CI: 389.4K-634.1K) and 5.4 thousand fatalities (95% CI: 3.0K-8.7K) until April 2. Put differently, the policies prevented around 84% of the confirmed cases and 66% of the fatalities that would have occurred without policy interventions by that time. The heterogeneity analysis shows that the policies’ relative effects were smaller for (a) the oldest age group (60+) and (b) in rural areas.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Notes : Fig 1A and 1B summarize the main takeaway message of the paper. Fig 1A depicts our estimates on the number of cases avoided due to social distancing policies. Fig 1B depicts our estimates on the number of fatalities avoided due to these policies. The three vertical lines mark the Chancellor’s appeal for social distancing (March 12), the nationwide school closures (March 16), and the nationwide contact bans (March 23). The dashed lines represent 95% confidence intervals based on district-levelclustered standard errors.
https://doi.org/10.1371/journal.pone.0257363.g001
Furthermore, our analysis of cell phone data implies that, without SD policies, citizens would not have limited their social contacts to the same extent: According to our estimates, individuals reduced their mobility by about 30.7% with SD policies. Without them, they only would have lowered it by 3.9%. This suggests that the citizens limited their social contacts as intended by the German authorities.
By providing the first comprehensive evaluation of the German SD policies, we add to an ongoing public and scientific debate on whether SD policies contained the virus. In Germany, for example, many citizens consider the lockdown measures appropriate to fight the pandemic [ 6 ]. Other individuals, including German or US citizens, stage large-scale protests against them and question their effectiveness. The scientific debate on the policies’ effectiveness is not settled, either. Particularly, researchers have argued that the prevalent model-based evaluations of SD policies [ 7 – 15 ] suffer from methodological issues [ 16 ]. In particular, it has been argued that epidemiological models (a) are frequently weakly identified as they fit many parameters to a single time series [ 17 , 18 ], (b) rely on too restrictive assumptions [ 19 ], and (c) often have limited predictive ability [ 20 ].
A recent suggestion to evaluate SD policies while avoiding these issues is to use quasi-experimental (instead of model-based) methods [ 21 ]. In this spirit, we propose a flexible and widely-applicable quasi-experimental approach that exploits district-level variation in the spread of COVID-19. We then apply this method to provide a broad analysis of SD policies, including their effects on individual behavior, confirmed cases, and fatalities. Hereby, we contribute to a small but growing literature that exploits quasi-experimental techniques to evaluate the effectiveness of non-pharmaceutical interventions [ 22 – 24 ]. Compared to our study, the corresponding papers have different focuses: They study fewer or other outcomes, employ different identification approaches, and investigate other policies. For example, one study investigates the effectiveness of travel restrictions [ 22 ], a second one studies the effect of SD policies on hospitalizations and cases [ 23 ], and a third paper examines the impacts of shelter-in-place orders on cases in the US [ 24 ]. Methodologically, these papers exploit policy variation across countries or regions in difference-in-difference models. Another study employs a similar empirical strategy to examine the role of social capital in the spread of COVID-19 [ 25 ]. In contrast to us, they do not focus on the impact of policies.
The paper’s structure is as follows: Section 2 describes the institutional background and Section 3 our estimation approach. Section 4 contains the results for mobility (Subsection 4.1), cases and deaths (Subsection 4.2), each with a description of the relevant data. The results section also features our heterogeneity analyses (Subsection 4.3) and robustness checks (Subsection 4.4). Section 5 concludes.
2 COVID-19 and social distancing in Germany
2.1 covid-19 outbreak.
In Germany, COVID-19 spread after the detection of two cases on February 25, 2020 (an earlier outbreak detected on January 27 had been completely contained). In the following weeks, the infection propagated to the entire country. On March 20, there were confirmed infections in all but one of the 401 German districts. S7 Fig in S1 File shows the distribution of district-specific outbreak dates. We define the local outbreak date as the first day when ten cases had occurred within two weeks. S8 and S9 Figs in S1 File consider other outbreak definitions.
2.2 Social distancing policies
We classify the policy response during the first month of the epidemic into three phases (see Fig 2 ). In the first phase, starting with the detection of the first COVID-19 cases, the German authorities only took limited actions: They put infected persons under quarantine, recommended intensified hygiene practices to the public, and canceled large events with more than thousand participants around March 9.
https://doi.org/10.1371/journal.pone.0257363.g002
In the second phase, the German federal and state governments agreed on additional simultaneous, nationwide containment policies to fight the epidemic. This phase began on March 12, when Chancellor Merkel appealed to all citizens to avoid social contacts whenever possible. Between March 13–15, the state governments announced the closure of schools, childcare facilities, and most retail stores starting on March 16. On March 22, they declared a strict contact ban: From March 23, meeting more than one person from outside the household was prohibited and keeping a minimum distance of 1.5 meters was required. As apparent, these policies’ goal was to limit the social contacts of German citizens. Henceforth, we refer to them as “social distancing policies.” Notably, our analysis identifies the combined effect of all these nationwide social distancing policies. In a different vein, data on internet search behavior suggests that citizens did not anticipate these interventions (see S16–S19 Figs in S1 File ).
The third phase started on April 20, when the authorities gradually relaxed the policies.
2.3 COVID-19 testing
Official guidelines determine who qualifies for a COVID-19 test. During the study period, patients with flu-like symptoms were tested if they had been in contact with a person diagnosed with COVID-19 or in a high-risk area. This general rule applied in all federal states and remained almost unchanged during the sample period. After the virus had spread all over Europe, the authorities dropped the high-risk criterion on March 24.
3 Estimation method
Because it is impossible to observe the scenarios with and without SD policies simultaneously, one cannot estimate the policies’ effects by directly comparing outcomes between both states. Instead, we need to find a way to approximate the latter, counterfactual scenario. To that end, we present an extended event-study model [ 26 – 28 ]. While this section briefly introduces the event-study model, the S.1 Section in S1 File discuss in more detail how this model identifies the effects of SD policies.
3.2 Interpretation of estimated parameters
3.3 Further aspects
Notes : Fig 3A and 3B show how social distancing policies affect mobility behavior. Fig 3A demonstrates how individuals’ behave in the realized world with social distancing policies (red line) and in the counterfactual world without SD policies (blue line). The spike on March 29 reflects very bad weather conditions at this particular day. Fig 3B shows the implied social distancing effect, measured in percentage points. The three vertical lines mark the Chancellor’s appeal for social distancing (March 12), the nationwide school closures (March 16), and the nationwide contact bans (March 23). The dashed lines represent 95% confidence intervals based on district-level-clustered standard errors.
https://doi.org/10.1371/journal.pone.0257363.g003
Until April 2, there is, on average, at least one no-SD control observation per district i . Therefore, our analysis focuses on the policy effects up to this date. For interested readers, we nevertheless provide estimates from an extended analysis until the policies’ relaxation on April 19 (see S1 File ).
4.1 Mobility
Did citizens limit their human-to-human interactions due to the SD policies? One approach to studying this question is to examine if the policies changed mobility [ 15 ]. The rationale is simple: Individuals who travel less or stay at home cut back the personal contacts outside their household.
4.1.1 Measuring mobility.
4.1.2 Results.
To study the effects of the SD policies on mobility, we use measure (2) as the outcome of model (1) . Fig 3 presents our results graphically. Fig 3A plots the estimated mobility behavior without policies (blue line) and the actually realized behavior with SD policies (red line). For each date t , the SD effect corresponds to the vertical difference between these two lines. Fig 3B shows this effect measured in percentage points. In both figures (and all following figures), the dashed lines represent 95% confidence intervals based on district-level clustered standard errors.
Three observations stand out. First, before the start of the second phase on March 12, individuals hardly changed their behavior relative to the baseline year 2019 (see red line in Fig 3A ). This suggests that the cancellation of large events around March 9 did not affect mobility. Second, from March 12 on, citizens became less and less mobile. Shortly after Merkel’s appeal, they traveled slightly less. Mobility decreased more sharply and persistently, however, after the school and business closures on March 16. From March 16 to April 2, individuals traveled, on average, 30% less than in 2019. This reduction is six times larger than the estimated change without SD policies (-3.9%). Third, the effects of SD policies on mobility are large over the entire second phase, although they decrease over time (see Fig 3B ). In sum, Fig 3 suggests that the SD policies reduced mobility considerably and, presumably, also social contacts.
4.1.3 Further evidence.
In the S1 File , we provide additional descriptive evidence that Germans became less mobile after the implementation of SD policies. For example, they reduced their trips to workplaces by more than 30% and used public transportation by about 50% less (see S14 Fig in S1 File ).
4.2 Cases and fatalities
Next, we explore if SD policies effectively constrained the spread of COVID-19. Again, we focus on the period until April 2. S1 and S2 Figs in S1 File provide our estimates for the extended period until April 19.
4.2.1 Measuring COVID-19 cases and fatalities.
The district-level health offices are legally obliged to report confirmed COVID-19 cases and fatalities to the federal Robert Koch Institute, which collates and publishes these data daily [ 30 , 31 ]. We use the data set provided on April 30, 2020. S5 and S6 Figs in S1 File show descriptive statistics. The data quality is comparatively high. First, the share of undetected cases is expected to be lower than in many other countries [ 5 ]. Second, all COVID-19 cases and fatalities are laboratory-confirmed. Third, all health offices apply the same testing and reporting criteria. Fourth, the data contain information on the day of the first symptoms for most cases and fatalities. For asymptomatic cases, the day of the first symptoms is set equal to the registration date. Additionally, we gathered state-level data on the numbers of conducted COVID-19 tests for robustness checks.
4.2.2 Results for confirmed COVID-19 cases.
To study the SD effects on COVID-19 cases, we use the inverse hyperbolic sine (IHS) of the cumulative number of confirmed cases in each district as the outcome in model (1) . To simplify the interpretation, Fig 4 presents our estimation results re-transformed to cases (rather than IHS-values). Fig 4A displays how the confirmed cases per district truly evolved with SD policies (red line) and, according to our estimations, would have evolved without SD policies (blue line). We present the results on a log scale.
Notes : Fig 4A and 4B show how social distancing policies affect confirmed COVID-19 cases; Fig 4C and 4D show how the policies affected fatalities related to COVID-19. More specifically, Fig 4A demonstrates the development of cases in the realized world with SD policies (red line) and in the counterfactual world without SD policies (blue line). It shows average cases per district, using a logarithmic scale. Fig 4B presents the implied social distancing effect on cases using a linear scale. Fig 4C presents the development of fatalities in the realized world with (red line) and in the counterfactual world without (blue line) SD policies. Fig 4D presents the social distancing effect on fatalities. The three vertical lines mark the Chancellor’s appeal for social distancing (March 12), the nationwide school closures (March 16), and the nationwide contact bans (March 23). The dashed lines represent 95% confidence intervals based on district-level-clustered standard errors.
https://doi.org/10.1371/journal.pone.0257363.g004
Importantly, our analysis is based on the day of the first symptoms. Therefore, if the blue line lies above the red one, our estimates imply that the number of individuals suffering from first symptoms at date t would have been higher without SD policies. Fig 4B depicts the corresponding effects of the SD policies on a linear scale. To make the timing of the policy effects more easily visible, the figure zooms in on the period until April 2. As the mean incubation period is 5–6 days [ 32 ], we do not expect to find significant policy effects before March 16.
The key insights from the Fig 4A and 4B are as follows: First, before the closure of schools, the case numbers with and without SD policies match closely (see Fig 4A ). This finding suggests that our identifying assumption holds. Second, the growth rate of actual cases (red line) starts to diminish a few days after the start of the nationwide policy response, while counterfactual cases (blue line) continue to grow at a similar rate as before. Specifically, the first significant (yet small) SD effects appear on March 18, six days after Merkel’s appeal (see Fig 4B ). Given the mean incubation period, the timing of the effects is hence in line with the policies’ implementation dates. Third, on April 2, our point estimate indicates that the SD policies reduced COVID-19 cases by about 84% or 846 cases per district. Converted to the national level, this estimate indicates that the SD policies prevented 499.3 thousand cases (95% CI: 389.4K-634.1K). The extended analysis suggests that the effects would have continued to grow strongly over time. Fourth, we can also interpret our results in terms of the reproduction number R , calculated according to the official methodology of the Robert Koch Institute [ 33 ]. After the policies’ introduction, R quickly decreased from above 2 to below 1 (see S12 Fig in S1 File ). Our estimates suggest that, without SD policies, it would have stayed above 2 until April 2. In summary, the analysis implies that the SD policies effectively contained COVID-19.
4.2.3 Results for fatalities.
Next, we estimate model (1) with the IHS of the cumulative number of fatalities as our outcome. Recall that each fatality is reported together with the day of the patient’s disease onset. Hence, we study the effects of the SD policies on the number of (eventually) lethal infections that started on date t . Fig 4C and 4D present our estimation results for fatalities. The abscissa starts with February 26, the first day with ten or more eventually lethal infections.
The results are in line with those for confirmed cases: The fatalities in the SD and no-SD scenarios initially follow the same growth path (see blue and red lines in Fig 4C ). A few days after the implementation of the policies, however, the scenarios diverge: While actual growth in fatalities slows down sharply (red line), the number of counterfactual fatalities continues to grow at a similar rate (blue line). Specifically, the SD effects are significant from March 21 on and increase strongly over time. We estimate that during the period March 11 to April 2, the SD policies decreased fatalities by 66% or 8.8 per district. Transformed to the national level, this estimate suggests that the policies reduced lethal cases with first symptoms until April 2 by 5.4 thousand (95% CI: 3.0K-8.7K). Again, the extended analysis hints at steadily growing effects over time.
4.3 Heterogeneity analyses
Some groups are at higher risk to suffer from severe COVID-19 progressions [ 32 , 34 ]. International data show that hospitalization rates increase above 60 years of age. Furthermore, men seem to be at higher risk than women. Therefore, in the next step, we investigate how the SD effects differ (a) across age groups, (b) by gender, and (c) between urban and rural districts.
Fig 5 shows the subgroup-specific SD effects on confirmed cases. The estimates rely on sample splits and indicate the percentages of cases avoided due to the policies until April 2. Three results emerge. First and foremost, we find large effects in all groups. The point estimates range from 76% to 88%. Second, Fig 5 presents evidence for age-group heterogeneity. The policies prevented 88% (182.5K) of the cases among individuals below 35 that would have otherwise occurred, 86% (257.5k) of the cases in the medium-age group, and 76% (76.9k) of the cases among persons of age 60 and above. The difference between the relative effects in the last and the two former groups is significant at the 5% level. The finding is in line with the observation that, after the policy intervention, the share of persons above 60 among all infected persons increased from about 20% (March 11) to 27% (April 2). This age heterogeneity seems plausible: Policies such as school and business closures likely have stronger implications for the working-age population and for children and their parents than for retirees. Third, we also find somewhat larger relative effects for urban districts than for rural districts and for men than for women. While the former difference is significant at the 10% level, the gender difference is not.
Notes : The three panels of Fig 5 show how the effect of the nationwide social distancing policies on April 2 differed across age groups (Fig 5A), by gender (Fig 5B), and between urban and rural districts (Fig 5C). The estimates rely on sample splits and show the percentage of confirmed COVID-19 cases avoided by the nationwide policies. The vertical lines represent 95% confidence intervals based on district-level-clustered standard errors.
https://doi.org/10.1371/journal.pone.0257363.g005
S3 Fig in S1 File shows the same pattern of subgroup-specific SD effects on fatalities. However, due to lower numbers, we cannot study some groups and the estimation uncertainty is higher. S4 Fig in S1 File extends the analysis until April 19. Again, the patterns are similar.
4.4 Robustness analyses
We probe the robustness of our results in various dimensions. First, we explore different definitions of a local outbreak. Second, we run additional regressions in which we control for the number of conducted COVID-19 tests per day. Third, we repeat our analysis using alternative outcome definitions. For example, we drop districts with zero cases or fatalities and estimate models in logarithms. We also apply the ln(1+ x ) transformation to our outcomes. Fourth, we cluster the standard errors at the state level. S10 and S11 Figs in S1 File report the corresponding results. All conclusions remain substantially unchanged.
5 Conclusion
This paper provides evidence on the effects of the German social distancing (SD) policies on (a) individual behavior, (b) confirmed COVID-19 cases, and (c) fatalities. We show that, first, the SD policies affected individuals’ mobility. Second, we find that the policies sharply slowed down the spread of the epidemic: According to our estimates, they precluded about 84% (499.3K) of the COVID-19 cases and about 66% (5.4K) of the related fatalities that would have occurred without SD policies within three weeks (until April 2). While large effects emerged across the entire population, the relative effects were smaller for the oldest age group.
From a broader perspective, we have made a step towards quantifying the effects of SD policies. At the same time, we believe that we still need a more comprehensive evaluation of such policies. First, the evidence on confirmed cases may not capture the entire impact of the policies on the epidemic spread. One reason is that, although we use high-quality data, not all infections are detected. If the data improve over time, our analysis can be repeated. Second, we estimate the number of confirmed COVID-19 cases and fatalities avoided within three weeks after the policies’ introduction. In the medium or long run, the picture might change in many ways. On the one hand, some of the avoided infections may have only been shifted to a later time. On the other hand, medical capacities may have been exceeded without SD policies, resulting in even higher numbers of fatalities. Third, our analysis identifies the joint effects of all elements of the policy response. Ideally, future studies find ways to disentangle the effects of appeals for voluntary SD, school closures, and contact bans. To shed light on these and other issues, researchers could adapt the event-study approach to new data and settings, including the policies’ removals.
Supporting information
https://doi.org/10.1371/journal.pone.0257363.s001
Acknowledgments
We have benefited from comments by and discussions with Felix Bierbrauer, Tobias Hauck, Erik Hornung, Andreas Peichl, Johannes Rincke, Dominik Sachs, Paul Schempp, Sebastian Siegloch, Marc Stoeckli, and Anthony Strittmatter. David Gstrein, Marvin Immesberger, and Vincent Weber provided excellent research assistance. We also thank Ute Rexroth and Muna Abu Sin from the Robert Koch Institut for providing the data on conducted COVID-19 tests. The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the Inter-American Development Bank (IDB), its Board of Directors, or the countries they represent.
- View Article
- Google Scholar
- 4. UNESCO. Education: From disruption to recovery; 2021. Available from: https://en.unesco.org/covid19/educationresponse .
- 6. Wagschal U, Jäckle S, Hildebrandt A, Trüdinger EM. Politikpanel Deutschland: Ausgewählte Ergebnisse einer Bevölkerungsumfrage zu den Auswirkungen des Corona-Virus; 2020. Available from: https://www.politikpanel.uni-freiburg.de/docs/Auswertung_PPD_Corona_Umfrage_Mai2020.pdf .
- 12. Greenstone M, Nigam V. Does social distancing matter? Working Paper 2020-26, Becker Friedman Institute, University of Chicago; 2020. Available from: https://bfi.uchicago.edu/working-paper/2020-26/ .
- 16. Fernández-Villaverde J, Jones CI. Estimating and simulating a SIRD model of COVID-19 for many countries, states, and cities. NBER Working Paper 27128; 2020. Available from: https://www.nber.org/papers/w27128 .
- 17. Atkeson A. How deadly is COVID-19? Understanding the difficulties with estimation of its fatality rate. NBER Working Paper 26965; 2020. Available from: https://www.nber.org/papers/w26965 .
- 19. Kuhbandner C, Homburg S, Hockertz S, Walach H. Comment on Dehning et al. (Science, 15 May 2020, eabb9789). SageSubmissions. 2020;.
- 25. Bartscher AK, Seitz S, Siegloch S, Michaela S, Werhöfer N. Social capital and the spread of COVID-19: insights from European Countries. IZA Discussion Paper 13310; 2020. Available from: https://covid-19.iza.org/publications/dp13310/ .
- 26. Borusyak K, Jaravel X. Revisiting event study designs. SSRN Working Paper; 2017. Available from: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2826228 .
- 28. Schmidheiny K, Siegloch S. On event study designs and distributed-lag models: equivalence, generalization and practical implications. CESifo Working Paper 7481; 2019. Available from: https://www.cesifo.org/DocDL/cesifo1_wp7481.pdf .
- 30. Robert Koch-Institut. Fallzahlen in Deutschland; 2020. Available from: https://services7.arcgis.com/mOBPykOjAyBO2ZKk/arcgis/rest/services/RKI_COVID19/FeatureServer/0/query?where=1%3D1&outFields=*&outSR=4326&f=json .
- 31. Robert Koch-Institut. COVID-19 Datenhub; 2020. Available from: https://npgeo-corona-npgeo-de.hub.arcgis.com/datasets .
- 32. WHO-China Joint Mission. Report of the WHO-China Joint Mission on coronavirus disease 2019 (COVID-19); 2020.
- 33. Robert Koch-Institut. Erläuterung der Schätzung der zeitlich variierenden Reproduktionszahl R; 2020.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Oxford University Press - PMC COVID-19 Collection

COVID-19 pandemic: health impact of staying at home, social distancing and ‘lockdown’ measures—a systematic review of systematic reviews
Valentina chiesa.
Local Health Unit of Reggio Emilia, Via Giovanni Amendola, 2, 42122, Reggio Emilia, Italy
London School of Hygiene & Tropical Medicine London, WC1H 9SH, 15-17 Tavistock Place, United Kingdom
Gabriele Antony
Austrian National Public Health Institute (Gesundheit Österreich GmbH, GÖG)
Matthias Wismar
European Observatory on Health Systems and Policies Place Victor Horta 40/10, 1060 Brussels, Belgium
Bernd Rechel
European Observatory on Health Systems and Policies, London School of Hygiene & Tropical Medicine, London, WC1H 9SH, 15-17 Tavistock Place, United Kingdom
Associated Data
To systematically review the evidence published in systematic reviews (SR) on the health impact of staying at home, social distancing and lockdown measures. We followed a systematic review approach, in line with PRISMA guidelines.
In October 2020, we searched the databases Cochrane Database of Systematic Reviews, Ovid Medline, Ovid Embase and Web of Science, using a pre-defined search strategy.
The literature search yielded an initial list of 2172 records. After screening of titles and abstracts, followed by full-text screening, 51 articles were retained and included in the analysis. All of them referred to the first wave of the coronavirus disease 2019 pandemic. The direct health impact that was covered in the greatest number (25) of SR related to mental health, followed by 13 SR on healthcare delivery and 12 on infection control. The predominant areas of indirect health impacts covered by the included studies relate to the economic and social impacts. Only three articles mentioned the negative impact on education.
Conclusions
The focus of SR so far has been uneven, with mental health receiving the most attention. The impact of measures to contain the spread of the virus can be direct and indirect, having both intended and unintended consequences.
- This article provides a snapshot of systematic reviews published by October 2020.
- Most of the emphasis has been on the mental health impact of policy measures.
- The impact on health care delivery and infection control was explored in fewer studies.
- Other policy areas and social determinants of health had hardly been studied in systematic reviews.
- The impact of policy measures on health can be direct and indirect.
Introduction
In response to the coronavirus disease 2019 (COVID-19) pandemic, governments worldwide adopted policies that aimed to reduce transmission, culminating in March and April 2020 in many countries in staying at home and physical (or ‘social’) distancing measures, often referred to as ‘lockdown’. While these measures helped to bring down the number of new infections, gaining valuable time for the health sector to shore up its capacity and expertise for dealing with infected patients, it has become clear that the policy response had wide-ranging impacts on the health and well-being of populations across all sectors of society and affecting all health determinants.
Faced with new waves of infections in autumn 2020 and winter 2020/2021 and the imposition of new lockdowns in many countries, it is important to understand the positive and negative impacts of lockdowns on the health and well-being of populations to inform future policy responses.
A Health Impact Assessment conducted by Public Health Wales April–May 2020 found that there was a scarcity of academic peer-reviewed research literature regarding the impacts of prolonged quarantine periods and social distancing on health and well-being. 14 However, the academic literature on COVID-19 is evolving rapidly and so a renewed assessment of the academic literature was appropriate.
The overarching aim of this study was to systematically review the evidence published in systematic reviews on the health impact of staying at home, social distancing and lockdown measures.
A systematic review of systematic reviews was conducted following the Prepared Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. 15 Relevant publications were identified by systematically searching the scientific literature, with the search undertaken on 20 October 2020. We searched the scientific databases Cochrane Database of Systematic Reviews, Ovid Medline, Ovid Embase and Web of Science, using a pre-defined search strategy (detailed search strategies are provided in the Supplementary material ).
Inclusion and exclusion criteria for study selection were defined a priori, after piloting them on a sample of 70 articles. Articles were included if they were published in English, were systematic reviews and focused on the health impact of staying at home, social distancing and lockdown measures related to the COVID-19 pandemic or other pandemics. There was no limitation set on the date of publication or the country of study implementation.
Articles published in languages other than English, not concerned with humans, not following a systematic review study design, or not concerned with the health impact of measures were excluded.
Identified studies were reviewed independently for eligibility in a two-step process: a first screen was performed on title and abstract, followed by the screening of full texts. Data were extracted using a standardized data extraction spreadsheet. In cases of doubt, studies were discussed within the research group and consensus reached. Because of the heterogeneity of included studies, no meta-analysis could be undertaken, and the results of our systematic review are presented in the form of a narrative synthesis.
The literature search yielded an initial list of 2172 records that provided 450 relevant articles after the first screening of title and abstract. Papers were screened and selected, as illustrated in Fig. 1 . After the second screening based on full texts, 51 articles were retained. 1–13 , 16–53

PRISMA diagram of systematic article selection.
General description of included articles
The overall characteristics of the articles included in the systematic review are shown in Table 1 . All of them referred to the first wave of the COVID-19 pandemic. April and March 2020 represent the time limits for almost half of the systematic reviews included ( n = 25). Overall, eight systematic reviews were performed with a meta-analysis. 3 , 5 , 6 , 24 , 29 , 33 , 38 , 44 Almost one third of articles inclu-ded ( n = 16) describes other outbreaks or pandemics in addition to the COVID-19 pandemic, including Severe acute respiratory syndrome (SARS), Middle East Respiratory Syndrome (MERS), Influenza A (H1N1), Ebola, Chikungunya, Zika, Multiple drug resistance (MDR) bacteria, Methicillin-resistant Staphylococcus aureus (MRSA), and human immunodeficiency virus (HIV). 17 , 21–23 , 25 , 26 , 29–31 , 34 , 37 , 41 , 42 , 49–51
Main characteristics of the studies included
Characteristics of included articles
The majority of systematic reviews included focused on the impact of lockdown measures, with only nine articles focussing mostly on the impact of the pandemic.
Concerning the type of lockdown restrictions, the majority of the systematic reviews was focused on isolation, quarantine and social isolation, with many articles discussing multiple restrictive measures.
As regards other lockdown measures, four articles described the impact of school closures, 41–43 , 50 seven systematic reviews explored the impact of travel restrictions, 23 , 32 , 41–43 , 47 , 49 two examined the impact of workplace distancing, 42 , 43 and one explored the impact of restrictions of funeral practices. 24
With regard to the impact on health services, two systematic reviews 1 , 4 explored the rescheduling of non-urgent outpatient visits, non-urgent surgery interventions, the putting on hold of ‘non-essential’ activities and the limitations in accessing hospitals. The indirect effect of restrictions of health services, and lockdown more generally, is represented by telemedicine, which is described by the 10 systematic reviews. 1 , 3 , 5–11 , 13
The health impact of lockdown measures can be direct or indirect ( Table 2 ). The direct health impact that has been covered in the greatest number of included articles relates to mental health, 16–19 , 21 , 22 , 24–26 , 28–34 , 36–38 , 40 , 44 , 45 , 48 , 49 , 52 followed by systematic reviews on healthcare delivery, 1–13 and those on infection control. 23 , 27 , 35 , 36 , 41–43 , 46 , 48 , 50 , 51 The predominant areas of indirect health impacts covered by the included studies relate to the economic 9 , 21 , 23 , 27 , 28 , 31 , 33 , 43 , 44 , 47–52 and social impacts. 9 , 23 , 31 , 43 , 44 , 50 , 52 Only 3 articles mentioned the negative impact on education. 17 , 33 , 50
Health impact areas of the studies included
a The same articles can be included in more than one area of impact
Direct health impact
Mental health.
Overall, almost half of the studies explore the impact of lockdown measures on mental health. 16–19 , 21 , 22 , 24–26 , 28–34 , 36–38 , 40 , 44 , 45 , 48 , 49 , 52 While the rapid implementation of quarantine, isolation and social distancing measures seems to be the most effective strategy to contain the spread of the virus, these measures, when implemented at short notice, can produce alarm and anxiety. 49
The studies reported a high burden of mental health problems among several groups of the population who experienced quarantine or isolation: patients, the general population and health workers. Prevalent mental health issues include anxiety, 17 , 18 , 21 , 29–31 , 33 , 37 , 44 , 49 , 52 depression, 17 , 18 , 29 , 30 , 37 , 44 , 52 post-traumatic stress disorder (PTSD), stress, 17 , 19 , 21 , 22 , 25 , 26 , 29–31 , 37 , 49 , 52 and stigmatization. In particular among children, older people and health workers the evidence suggests a link between PTSD and quarantine or isolation. 21 , 25 , 30 , 31 , 37 , 52 Stigma is linked both to quarantine and isolation 30 and particularly experienced by health workers 21 and children 31 , 48 ; the two groups experienced stigma due to quarantine even if they had been confirmed to be negative. 31 , 48
Health care delivery
The pandemic and the subsequent lockdown measures had a negative impact on health care delivery, resulting in limitations to available health care services. These restrictions included: the postponement of non-urgent outpatient visits and of non-urgent surgical interventions, the reduction of non-essential services, and restrictions in accessing hospitals for both patients and their caregivers. 1
The included studies find that restrictions of health care services posed enormous challenges to patients and health care providers, and telemedicine has been proposed by several authors as a potential solution to overcoming the barrier in accessing health care services, especially for outpatient care. 3 , 5–11 , 13
Tele-psychotherapy 8 , 11 has been evaluated in treating common mental-health disorders such as anxiety, depression and PTSD. The use of telemedicine has also been investigated in orthopaedic care. 3 , 7 The resulting reduction in inpatient and outpatient orthopaedic care and the increase in remote orthopaedic care was associated with high patient satisfaction related to convenience and reduced waiting and travelling times. Evidence suggests that telemedicine in orthopaedic care can be safe and cost-effective, with high patient and clinician satisfaction. 7
The restrictions of rehabilitation services due to lockdown measures increased, especially among older people, the risk of frailty, sarcopenia, dementia, cognitive decline and depression, in particular among those quarantined at home or with restricted mobility. 1 Yet, a systematic review on tele-rehabilitation identified 53 challenges in the literature (e.g.: on sustainability and privacy) that could affect the development of tele-rehabilitation. 9
Finally, a systematic review on the delivery of urogynaecology care using telemedicine 6 identified the clinical situations that would allow virtual settings and those that should be managed with an in-person visit despite the risks of COVID-19 transmission.
Infection control
The effect of lockdown measures on infection control was investigated in 12 systematic reviews. 23 , 27 , 35 , 36 , 41–43 , 46 , 48 , 50 , 51 According to Chandana et al ., 27 quarantine is one ‘of the most misunderstood and feared methods of controlling COVID-19, because it may affect both infected and non-infected individuals with psychological, economical and emotional complications such as post-traumatic stress disorder, depression, insomnia, mood swings’. They continue that the lockdown of a city ‘was proved to be effective when a study reported 72% drop in the number of infected people’. 27 A systematic review conducted in China 35 emphasises that the lockdown of a city reduced the reproduction number (R0) from 3.77 to a controlled reproduction number (Rc) of 1.88 after lockdown. Other public health measures implemented, apart from citywide lockdowns and, encompassing contact tracing, intensification of screening, quarantine and mask utilisation, may also be contributing to containing the spread of the virus. 35 In fact, some systematic reviews suggest that combinations of different control measures are the most effective way to reduce transmission of the disease, prevent the collapse of health care services and reduce mortality. 41 , 43
Concerning travel restrictions, a systematic review on COVID-19, SARS and MERS suggested that travel restrictions leading to reduced transmissibility can be highly effective in containing the spread. 42 In line with these results are those retrieved by the Cochrane Systematic Reviews developed by Burns et al ., 23 which found that travel-related control measures during the COVID-19 pandemic may have a positive impact on infectious disease outcomes. In particular, travel restrictions may limit the spread of disease across national borders, while entry and exit symptom screening measures on their own are not likely to be effective. The evidence is scant on the effectiveness of travel-related quarantine 23 and there is very low-certainty evidence on the effect of quarantine of travellers from a country with a declared outbreak on reducing incidence and death. 41
Finally, systematic reviews on the impact of school closures found that they do not seem to be effective 42 and do not contribute to the control of the epidemic. 50
Children, child development and desire for parenthood
Six systematic reviews on children and their development 17 , 20 , 28 , 37 , 42 , 50 have been included in our study. The focus on the limited effect of school closures on pandemic control, 42 , 50 as discussed above, and on adverse effects of school closures on issues including: increased risk of transmission from children to grandparents, harms to child welfare particularly among the most vulnerable pupils, nutritional issues and the loss of teaching/learning and socialization processes. Importantly, children miss out on public policies taking place in schools, such as balanced and free food programs, guidance about personal hygiene, physical activity and citizenship initiatives. 50
Social isolation in children may increase the risk for cardiovascular disease, reduce physical activity and have negative effects on mental health, 20 , 50 such as an increased likelihood of high rates of depression and anxiety during and after enforced isolation. 37
Quarantine in children is linked to anxiety, stress and depression and can become a risk factor for child growth and development. 17
Isolation and quarantine together are related to an increased risk of requiring mental health services and to higher levels of post-traumatic stress. 37
A systematic review found that during quarantine, despite a reduction in the quality of life, there was an increased desire for parenthood, although it is unknown if these changes are associated with an increase in terms of birth rates. 39
Older people
Despite quarantine and isolation being the most effective strategies for prevention of the secondary transmission of disease, the evidence suggests a greater vulnerability of older people for secondary transmission than other household members. 46 Other negative consequences were also experienced, particularly if quarantine and isolation were in place for an extended period, and the loneliness caused by social isolation has been associated with impaired cognitive function in older adults. 36
Lockdown in older people with a subsequent reduction in social participation and physical activity during home confinement was identified as a serious concern, as they are typically more inactive and more disposed to chronic disease. 18 , 20 Finally, a systematic review on older people in nursing homes emphasized that older people suffer from social distancing due to isolation and confinement. The evidence on this however was limited because only few studies with a small sample size and using unreliable methods were included in this systematic review. 40
Well-being and quality of life
Only five systematic reviews were retrieved on well-being and quality of life (QOL). 18 , 19 , 21 , 39 , 44 Importantly, four systematic reviews explored the impact of lockdown measures on health workers in terms of well-being and QOL. 18 , 19 , 21 , 44 According to the evidence summarised in these studies, healthcare professionals who had been quarantined had more severe symptoms of post-traumatic stress than the general population, felt stigmatised, presented more avoidance behaviours, reported huger lost income and were more affected at the psychological level. 21
Quarantine in the general population was linked to a reduction of the mean wellbeing scores, 39 work-related stress, burnout, 19 frustration, fears of infection, boredom, inadequate supplies and inadequate information. 21
Finally, lockdown and social distancing were linked in the general population to a negative psychosocial impact, an increased prevalence of depression, anxiety, sleep, alcohol use disorders and the fear of being infected. People were also worried about their loved ones. 18 , 19 , 44
Substance abuse
The four systematic reviews 16 , 18 , 28 , 52 focussed on the correlation of infection control measures and substance abuse found that lockdown was associated with increased alcohol use disorders in the general population, 18 and social isolation and quarantine were identified as potential contributors to the aggravation of substance abuse. 16 , 52
Violence and abuse
A link between lockdown and domestic violence and abuse was identified in four systematic reviews, 16 , 28 , 45 , 52 with three of them 16 , 28 , 52 also exploring substance abuse (see previous section).
Social isolation was linked to domestic abuse and violence-related behaviour in the home. 52 A systematic review identified that some factors increasing women’s vulnerabilities to violence were exacerbated during the social distancing and lockdown period. 45 Even quarantine can increase the power and control abusers hold over victims and trigger violence. 16 , 45 To overcome this issue with regard to children, South Africa’s strict lockdown offered protective pathways, including a policy to protect children at risk of abuse. 28
Lifestyle and dietary habits
Among the 51 systematic reviews included in our study, only two 20 , 53 focussed on lifestyle and dietary habits. Lockdown and quarantine were found to be associated with an increase of carbohydrate consumption, as well as more frequent consumption of snacks, although together with a high consumption of fruits and vegetables, and protein sources. 20 , 53
Social isolation was found to cause a decrease in physical activity and, for children, a decrease in the time devoted to sports, and an increase in time sleeping and spent in front of screens, potentially increasing overweight and obesity among children. 20 , 53
Indirect health impact
The areas of indirect health impact 9 , 17 , 21 , 23 , 27 , 28 , 31 , 33 , 43 , 44 , 47–52 identified in the included studies concern the economic and social impact, the impact on education and the lack of supplies and food ( Table 2 ).
Overall, the non-pharmaceutical interventions implemented to contain the virus, such as quarantine, isolation, social distancing and community containment, were noted to have important economic 21 , 27 , 28 , 31 , 43 , 48 , 49 , 51 , 52 and social consequences. 27 , 31 , 43 , 44 , 52 In particular, quarantine was associated with the necessity to work, the fear of loss of income, the lost income itself and a reduction in overall productivity resulting in a decline of economic growth. 21 , 27 Moreover, some systematic reviews 21 , 28 , 31 , 49 identified other fundamental issues, such as the lack or insecurity of supplies and food, and inadequate information, particularly linked to quarantine.
School closures were associated with a loss in teaching/learning and education, as well as with wider social impact and economic harm on working parents, health workers and other key workers being forced from work to care for children at home. 17 , 50 Moreover, a systematic review 33 on the prevalence of anxiety in medical students during the pandemic identified concerns on economic impact, academic delay, curricular factors and impact on their daily life.
Travel-related control measures related to quarantine had far-reaching economic, social, legal, ethical and political implications. 23
Some populations, such as in west Africa, 47 had difficulties complying with certain measures, such as travel limitations and the closure of markets and places of worship, as the majority of people work in the informal sector, including trading, other businesses, transport and restoration and these jobs are not subject to social protection.
This systematic review set out to systematically review the evidence published in systematic reviews on the health impact of staying at home, social distancing and lockdown measures. A number of important findings emerged.
The first relates to the areas that have been studies so far. We intentionally kept a broad focus on all policy areas that are associated with the social determinants of health. Surprisingly, almost half of the studies (25 of 51) explore the impact of lockdown measures on mental health, with the common finding that these measures put a strain on the mental health of patients, the health workers and the general population. The second most commonly studied area, explored in 14 of the 51 included studies, was concerned with health care delivery. Many of these 14 systematic reviews explore the issue of telemedicine, with only indirect references to the Coronavirus pandemic. The impact of lockdown measures on containing the spread of the virus was explored in 12 studies, with the overall finding that these measures are successful and most promising when used in combination. In general, lockdown measures are enacted to contain the virus, but often discontinued for economic or political rather than purely epidemiological reasons. Other areas of the health impact of lockdown measures have received far less attention so far and warrant further research.
A second key finding of our study highlights that the complex and multifactorial nature of the health impact of lockdown measures, which can be both direct and indirect. While the closure of schools, for example, will have a direct impact on the education, mental and physical health of children, an indirect impact is that parents will have to stay at home to look after young children, preventing them from going to work. While our primary interest was on the impact of lockdown measures, it was sometimes difficult to ascertain whether the impact was due to these measures or the pandemic itself. We found that many studies were struggling with the same challenge. Causal pathways are often blurred, as mental health, for example, can be affected by both, policy measures and the pandemic itself. Policy measures aimed at containing the spread of the virus will have to mindful of direct and indirect impacts and intended and unintended consequences.
A third key finding relates to the strength of evidence gathered by October 2020. Unsurprisingly, the evidence on the topic was still mainly focused on the first wave of the COVID-19 pandemic that occurred in spring 2020 and a renewed search of the literature is needed to capture more up-to-date evidence. We also identified methodological and terminological challenges. With regard to the methods used, some narrative reviews are defined by the authors as systematic reviews and vice versa. Furthermore, in many systematic reviews, conclusions are drawn based on a very limited number of papers with often low quality. In addition, in some systematic reviews, the impact of lockdown measures is mainly described in the introduction and the conclusions, rather than in the results section. There is also a need for more terminological clarity. Some authors misuse the terms ‘isolation’ and ‘quarantine’ and confuse ‘social isolation’ with ‘isolation’.
Supplementary Material
Supplementary_material_fdab102, acknowledgements and funding.
This work was funded by the European Observatory on Health Systems and Policies in support of a request by the Austrian Ministry of Social Affairs, Health, Care and Comsumer Protection. The funder had no involvement in the conduct of the research. The authors would like to express their gratitude to Anja Laschkolnig (Austrian National Public Health Institute) for her input into the search strategy.
Valentina Chiesa, MD, Local Helath Unit of Reggio Emilia
Gabriele Antony, Health Expert, Austrian National Public Health Institute
Matthias Wismar, Programme Manager, Health Systems and Policies Place
Bernd Rechel, Researcher at European Observatory on Health Systems and Policies
Contributor Information
Valentina Chiesa, Local Health Unit of Reggio Emilia, Via Giovanni Amendola, 2, 42122, Reggio Emilia, Italy. London School of Hygiene & Tropical Medicine London, WC1H 9SH, 15-17 Tavistock Place, United Kingdom.
Gabriele Antony, Austrian National Public Health Institute (Gesundheit Österreich GmbH, GÖG)
Matthias Wismar, European Observatory on Health Systems and Policies Place Victor Horta 40/10, 1060 Brussels, Belgium.
Bernd Rechel, European Observatory on Health Systems and Policies, London School of Hygiene & Tropical Medicine, London, WC1H 9SH, 15-17 Tavistock Place, United Kingdom.
Competing interests
The authors have no conflicts of interest to declare.
Ethical approval
Not required.
All data are incorporated into the article and its online supplementary material .
Social Distancing as Prevention
Introduction.
Social distancing or physical distancing is a complex of non-pharmacological sanitary and epidemiological measures aimed at stopping or declining the spread of an infectious disease. Social distancing means limiting close contacts between people, even if they are not sick, not being in any of the risk groups. It is a voluntary measure to help stop the spread of COVID-19. Concerning quarantine or self-isolation, a person stays at home and avoids contact with other people, since there is an exposure that this person became infected with COVID-19 due to possible contact with the source of the virus. Meanwhile, quarantine can be declared by the government; the authorities have already introduced restrictive measures.
During self-isolation, there are some issues related to the flow of time. I have been chronicling and documenting my social distancing period for two months to understand the time changing and the differences between the passing days. It is necessary to stay current and not to lose a sense of the present. Moreover, describing emotions occurring during the period of self-isolation is a therapeutic practice. It reduces stress levels opening the reasons and effects on mental health. Besides, it can be useful for writing an article and doing research about what socially significant processes the pandemic has provoked. For example, the stories of people allowed historians to reconstruct the picture of events during the Spanish flu in 1918. These stories of social distancing and the healthcare system are still in the library archives.
Humans are social beings; throughout history, humanity has been living in communities, and interaction with relatives has become a vital necessity. As soon as people had lost the opportunity to interact with each other, they started enduring the negative impact of social distancing (Anderson, 2020). For those who have already experienced a feeling of loneliness, social distancing reinforced the sense of isolation. Lockdown concerns not only the inconvenience associated with distance working and the inability to go to the cinema, bar, or restaurant, but also affects mental health. In some cases, it takes only a few days to feel the adverse effects. According to Kumar (2020), self-isolation can cause anxiety or depression within a few days. Due to the situation with COVID-19, people with issues that are psychologically and emotionally troubling turned out to be in a hazardous condition. Instability, negative information flow, and lack of support contribute to suicidal thoughts, regardless of age, social status, and residence.
Lonely life and the short of full social interaction have many adverse effects on mental and cognitive health. Among the most common consequences, there are depression, poor sleep, and cognitive decline (Hotopf et al., 2020). The matter is complicated by the fact that people were cut off from each other against the backdrop of a severe epidemiological threat, global difficulties in the economy, and border closure. Depending on the psychological state and specific circumstances, isolation can provoke both depressive moods and increased aggression (Hotopf et al., 2020). According to Kumar (2020), isolation stimulates aggressive behavior at the chemical level. For preventing outbursts of rage, a person needs both discipline and consciousness.
As people were forced to stay at home, it has become essential to conduct some rules. The measures, including paying attention to each family member’s personal space and avoiding sharing household items, were not crucial for me, as I was alone during my self-isolation period. Meanwhile, I limited the number of guests, friends, and relatives. I stayed at home whenever possible, refraining from visiting public places, such as shopping malls, gyms, cinemas, and restaurants. I have reduced the usage of public transport, preferring to walk rather than take a bus. I tried to keep surfaces that are often touched clean, primarily frequently used phones and keyboards. I left home only to buy food, choosing a period when there were fewer people on the streets. Any crisis reveals people’s weaknesses, so it was essential to adhere to a strict daily routine. Besides, a person needs to watch less TV, social networks, and other sources of information. In my free time, I could occupy my mind with an urgent matter and engage myself in self-education.
My social distancing period has taken almost two months, and as I have been living by myself for a long time, I decided to self-isolate alone in my apartment. During self-isolation, when it was allowed to go outside only to go for grocery shopping, pharmacy, or dog walking, the presence of an ample yard space near the accommodation has become an essential reason for me.
The main factors that can provoke the negative consequences for the mental health of social distancing during the COVID-19 pandemic are the unknown duration of quarantine, fear of infection, boredom, demanding access to medical and domestic services, and the dissemination of inadequate information through social media. As part of a WHO, the group of scientists analyzed the medical work related to this topic (Brooks et al., 2020). Most respondents reported negative psychological effects, including symptoms of depression, stress, anger, confusion, irritability, and lack of sleep (Brooks et al., 2020). Studies have shown that emotional deterioration occurs when quarantine lasts more than ten days (Brooks et al., 2020). After quarantine, a specific effect called avoidance behavior may persist. When I was chronicling social distancing, I noticed that this phenomenon occurred to me as well. For instance, I minimized contact with other people or peers and stopped working for a while.
Those people accustomed to a large number of social contacts try to maintain them through the Internet. The phone remains one of the best communication tools because people can talk directly with others (Allington et al., 2020). On the other hand, there is a significant drawback when people absorb a large number of fake news overwhelming social media. Users experience the effect of echo chambers when any information can lead to panic reactions and changes in the perception of the situation (Allington et al., 2020). Nevertheless, social networks make it possible to stay connected. Living in the age of digital communications, during the quarantine period, a person can also use technologies to overcome the social distance while preserving the physical one.
With regard to the virus, COVID-19 may be easily transmitted with microscopic drops when sneezing and coughing. The infection can spread through everyday contacts: by shaking hands or touching the same surfaces. Some people have an asymptomatic course of the disease, but they can be the virus conductor. Even when the patient’s well-being improves, he or she can be a disease carrier for some time. The purpose of social distancing is to diminish the spread of the virus, which is called to flatten the curve (Roberts, 2020). When people keep indoors and avoid contact with each other, the virus does not spread as fast.
At the same time, fewer people will get sick. Although the number of patients continues to grow, the curve on the graph of reported virus cases is more gentle (Roberts, 2020). This tendency allows doctors and hospitals to provide the necessary assistance to all patients with COVID-19. As long as I was not infected, there was a positive side to my social distancing. According to the doctors’ observations, children and young people easily tolerate coronavirus infection. However, I did not bring the virus to my grandparents or relatives who are in a high-risk group. This was the most prominent effect that my social distancing on preventing transmission of COVID-19.
Any situation of crisis serves as a good base for useful change adoption: developing desired habits, restructuring schedule for a more convenient one, and solving other personal problems. Meanwhile, concerning families that are bound to self-isolate together, quarantine noticeably affects the relations among members. Difficulties of isolation in the family may be associated with excessive communication and a lack of privacy. Not every household has a separate room and workspace. During this period, family time management, the distribution of duties, and their fulfillment, the difference in communication needs, and privacy can become big problems.
Being alone for the first time in a long time, people cannot always get used to a new lifestyle, which helps to explore difficulties in relationships and solve them. People are less interested in some petty issues related to everyday life, fuss, there are more questions about themselves, about interaction, about the quality of intimacy. Nevertheless, after social distancing, reuniting with other people has restored good mental and physical health. This experience helped me to realize a sense of affection with family and friends, to grow emotionally, or to gain a positive outlook on life despite the difficulties I have been through.
The reaction to staying at home depends on a person’s habits. If people used to work remotely, nothing has changed dramatically for them with the introduction of quarantine. Therefore those who were interested in face-to-face contact, social distancing looks like a torment. The human psyche prefers constancy; the more new is around, the higher the anxiety level, which might transform into a panic. A reaction may occur after some time if a person experiencing an acute response to stress does not receive timely help. This happens if a person experiences a severe situational reaction alone or in an inconspicuous way for others. Social distancing has not become a period of panic and anxiety for everyone. For example, when employees are exhausted and tired of a non-stop work process, this might be a valuable time to take a break, rest, rethink, and understand hidden needs and wishes. The quarantine can also benefit freelancers working online as these days it is a profiting area of business.
With regard to the future and scientists’ forecasts, they are not entirely positive. They show the tendencies that prove the necessity to do more research related to the mental health of people practicing social distancing. According to a study published by Harvard University (2020), social distancing measures will have to be followed for another two years. Experts made this conclusion based on the computer simulation of a pandemic. Researchers note that the situation can develop in multiple ways (Kissler et al., 2020). Firstly, adherence to restrictive measures with enhanced epidemiological control can eradicate coronavirus. The same situation happened in 2003 with the SARS-CoV-1 virus, which provoked an outbreak of SARS (Kissler et al., 2020). Another model is as follows: after 20 weeks of self-isolation, another explosion occurs. Scientists explain this phenomenon by saying that quarantine measures may be useful, but the population does not obtain proper immunity. It is considered the first scenario less likely in the current circumstances, given the number of cases of COVID-19 (Kissler et al., 2020). The coronavirus infection will remain for a long time and will become a seasonal disease.
The rich can either work from home or go to their summer cottages. The poor remain in large cities and violate quarantine to survive. So, in New York, the residents of poor neighborhoods – Quinx and Bronx – were most affected by a coronavirus (Cook & Goldbaum, 2020). After analyzing the data from smartphones, experts found out that the citizens temporarily stopped the movement, but after a pause, they resumed it (Cook & Goldbaum, 2020). The infection has revealed widespread social stratification and polarization. Due to the circumstances, anomie growth can be expected as a result of the socio-economic crisis. Social distancing, especially the possible stress resulting, can exacerbate chronic somatic and psychosomatic diseases and provoke anxiety, panic, and depression. The easiest way of coping with issues is to self-isolate in appropriate circumstances. It would be more useful to endure restrictions if there were resources: money, health, stable work, a supportive environment, friends, relatives.
However, social distancing aggravates the serious problem of the isolation of older people. They are at higher risk of poverty and social exclusion, which directly affect their health. They need more support than ever before in this crisis, the measures applied to combat this pandemic must take this need into account. Quarantine as an extreme measure of isolation can lead to mental disturbance, including people without any psychiatric disorders. After a long time after quarantine, the likelihood of distress associated with fears, sleep disorders, or post-traumatic stress remains increased. Moreover, the gender and age of the patients, in this case, do not matter. Such measures should be resorted to only when they are inevitable and should always be limited in time.
Allington, D., Duffy, B., Wessely, S., Dhavan, N., & Rubin, J. (2020). Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychological Medicine , 1-7.
Anderson, J. (2020) Social distancing isn’t the right language for what Covid-19 asks of us. Quartz. Web.
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet . 395 (10227), 912-920.
Cook,L.R., & Goldbaum C. (2020). They can’t afford to quarantine. So they brave the subway. The New York Times. Web.
Hotopf, M., Bullmore, E., O’Connor, R. C., & Holmes, E. A. (2020). The scope of mental health research in the COVID-19 Pandemic and its aftermath. The British Journal of Psychiatry , 1-7.
Kissler, S. M., Tedijanto, C., Goldstein, E., Grad, Y. H., & Lipsitch, M. (2020). Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science , 368 (6493), 860-868.
Kumar, V. (2020). Psychological impact of lockdown period of COVID-19 on human behaviour. Tathapi with ISSN 2320-0693 is an UGC CARE Journal , 19 (23), 65-71.
Roberts, R. (2020) Flattening the Coronavirus curve. The New York Times. Web.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, January 30). Social Distancing as Prevention. https://studycorgi.com/social-distancing-as-prevention/
"Social Distancing as Prevention." StudyCorgi , 30 Jan. 2022, studycorgi.com/social-distancing-as-prevention/.
StudyCorgi . (2022) 'Social Distancing as Prevention'. 30 January.
1. StudyCorgi . "Social Distancing as Prevention." January 30, 2022. https://studycorgi.com/social-distancing-as-prevention/.
Bibliography
StudyCorgi . "Social Distancing as Prevention." January 30, 2022. https://studycorgi.com/social-distancing-as-prevention/.
StudyCorgi . 2022. "Social Distancing as Prevention." January 30, 2022. https://studycorgi.com/social-distancing-as-prevention/.
This paper, “Social Distancing as Prevention”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: March 27, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
Staying Active While Social Distancing: Questions and Answers
Why is it important for me to be active?
Physical activity can provide immediate benefits. Physical activity can help to boost your mood, reduce stress, improve sleep, and sharpen your focus — benefits that can be especially important during stressful times. Physical activity can also help you live a longer, healthier life by reducing the risk of many common chronic diseases, like type 2 diabetes and some cancers.
How much activity do adults need?
According to the Physical Activity Guidelines for Americans, adults need a mix of activities to stay healthy , including at least:
- 150 minutes of moderate-intensity aerobic activity a week
- 2 days of muscle-strengthening activity a week
During stressful times, it’s important to remember that some physical activity is better than none! Adults should move more and sit less throughout the day. If you’re working from home, try taking activity breaks throughout the day or walking around your house during conference calls.

How much activity do kids need?
With many children home from school, parents and caregivers might be wondering how to get kids moving. The Physical Activity Guidelines for Americans recommends that kids and teens ages 6 to 17 get 60 minutes of activity every day . Kids younger than 6 need physical activity too — it helps support their growth and development. Preschool-aged children are active naturally, so aim to help them be active throughout the day and avoid time just sitting around.
Remember, lots of things count as physical activity — and it all adds up! Ask your kids to teach you their favorite game from physical education class or recess, have a family dance party, or challenge each other to learn a new yoga pose or do another push-up.
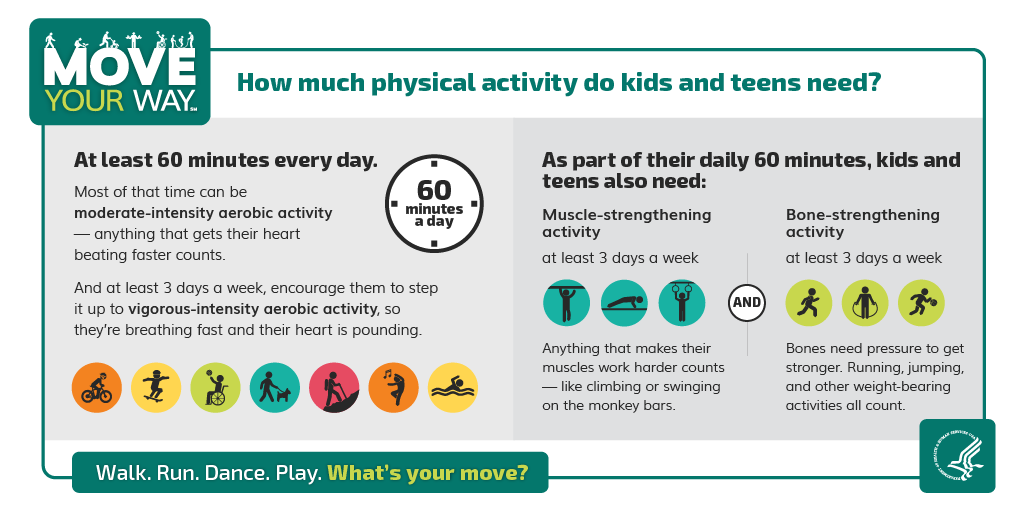
Is it safe for me to be active outside?
Before making a decision about whether or not to be active outside, be sure to check the latest guidance from your local health department and community or state leaders. In most places across the United States, residents can go for a walk or run as long as they practice social distancing and good hygiene.
Going for a walk, run, or bike ride in your neighborhood can be a good way to get active, as long as you can safely maintain distance between yourself and other active neighbors. If you decide to go to a nearby park or community space, first check for closures or restrictions. Then consider the number of other people who might be there and if you’d be able to ensure enough space — at least 6 feet —between yourself and other people.
If you can’t practice safe social distancing outdoors, stay home and find ways to get active indoors. If you have to go outside near other people — like to walk your dog — wear a cloth face covering .
If you have a yard, gardening and yardwork are also great ways to stay active and count toward meeting the Physical Activity Guidelines.
Can I be active outside with people who aren’t in my household?
It’s important that we all do our part to slow the spread of the coronavirus. That means following local, state, and national guidance. Try to limit social interactions when possible and always stay home if you’re feeling sick.
The safest way to be active outdoors is to stick with members of your household or go solo. When you’re deciding where to go outside, avoid busy areas that might make it hard for you to keep your distance from others.
If you’re meeting up with someone who isn’t in your household, make sure to avoid all physical contact and keep at least 6 feet of space between you at all times. And remember, you don’t have to meet in person to get active together! Consider others ways to stay connected like talking on the phone while walking.
Is it safe for me to go to a park or a playground?
Be sure to follow local guidance so you know if it’s safe to use parks and playgrounds in your community.
Playgrounds
Lots of people use and touch playground equipment, so an empty playground can still be full of germs. CDC recommends that visitors do not use playgrounds, including water playgrounds, within public spaces and parks. There are lots of ways to get active with your kids away from the playground. Consider playing hopscotch or four-square in an open space.
Parks can help make it easier to keep your distance from others, but not if they’re too crowded. Make sure you look for outdoor spaces that make it easy for you to keep your distance from others. Focus on parks that are close to your home, and avoid traveling long distances to visit a park. It's best to prepare in advance, because facilities — like concessions or bathrooms — may be closed to visitors.
Are there physical activities I need to avoid?
You can continue to do many of the activities you love, but you might have to make some adjustments to be safe.
- Do you love group fitness classes? Try streaming a group workout online in your home.
- Are you used to lifting weights at a gym and don’t have any at home? Get creative! Try lifting canned goods or laundry detergent. Or try some bodyweight exercises — they can help you build strength, just like lifting weights.
- Are team sports your thing? Find an open space to practice your individual skills.
Just be sure to avoid social gatherings, keep your distance from others, and practice good hygiene.
How can I be active without a gym?
There are all kinds of ways to get active at home. Workout videos, dancing, and even active video games are great ways to get moving. Many gyms and organizations across the country are offering free streaming or on-demand fitness options. This might be the perfect opportunity to try something new!
Household chores and gardening are also good ways to get moving, and a great way to multitask. If you can distance yourself from others outside — and it’s allowed under local guidance — take a walk, run, or bike ride in a quiet neighborhood, or hike on a trail away from others.
Where can I find free resources to help me stay active at home?
Without the ability to go to a gym or playground, getting active might feel tougher than normal. Many organizations and agencies on the local, state, and national levels are working hard to support activity in the home during this time.
The Move Your Way Activity Planner is a great way to identify activities you can do at home! Your local parks department or recreation center website might also have guidance. And you can find plenty of free streaming or on-demand videos to help you maintain or improve your physical and mental health online.
Here are a few resources to jump-start your new physical activity routine:
Resources for all ages:
- American College of Sports Medicine provides suggested aerobic and strength-training activities
- Cooper Institute has free videos with tips to help you get active on their YouTube channel
- National Center for Health, Physical Activity and Disability features inclusive videos that people with disabilities can do at home
- National Academy of Sports Medicine shares 9 bodyweight exercises you can do without equipment
- YMCA features Your Y at Home resources for kids and families, adults, and older adults
Resources for youth:
- ACE Fitness gives instructions for creating a simple obstacle course for kids
- American Heart Association shares 25 Ways to Get Moving at Home for kids
- Fit Kids is providing access to a curriculum that kids and adults can use to get active at home
- SHAPE America has instructions for creating a Multi-Game Fitness Card Deck with games for kids of all ages
Is it safe for my sports team to practice?
For now, it’s best to be active solo or only with members of your household. Virtual training options are on the rise, with many offering their services free of charge during the pandemic. Check with your coach or sports organization for guidance on how to maintain fitness and training while following social distancing recommendations.
How do I stay connected to others while being active?
Practicing social distancing doesn’t mean disconnecting with others in your life. Here are some ideas to stay connected and active while apart:
- Call a friend or loved one while taking a walk.
- Post your physical activity plans to social media and invite your network to move along with you.
- Get moving with friends via video chat or virtual streaming service. Motivate each other through a virtual meetup while doing an at-home workout.
- Get creative with your neighbors! Use a neighborhood listserv or phone tree to organize fun things to see in yards, windows, or apartment balconies, like a social distance scavenger hunt or art show , or a fun challenge like wearing your Halloween costumes on a walk.
For more information about coronavirus and COVID-19, visit covid.gov and cdc.gov/coronavirus . For more information on all U.S. government activities related to coronavirus and COVID-19, visit usa.gov/coronavirus .
The Office of Disease Prevention and Health Promotion (ODPHP) cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
Disclaimer: This translation was last updated on August 2, 2022. For up-to-date content, please visit the English version of this page.
Disclaimer: The Spanish COVID-19 site is currently undergoing significant updates which may lead to a delay in translated content. We apologize for any inconvenience.
How to Protect Yourself and Others
CDC’s Respiratory Virus Guidance provides strategies you can use to help protect yourself and others from health risks caused by COVID-19 and other respiratory viruses. These actions can help you lower the risk of COVID-19 transmission (spreading or catching COVID-19) and lower the risk of severe illness if you get sick.
Core Prevention Strategies

CDC recommends that all people use core prevention strategies to protect themselves and others from COVID-19:
- Although vaccinated people sometimes get infected with the virus that causes COVID-19, staying up to date on COVID-19 vaccines significantly lowers the risk of getting very sick, being hospitalized, or dying from COVID-19.
- Practice good hygiene (practices that improve cleanliness)
- Take steps for cleaner air
When you are sick:
- Learn when you can go back to your normal activities .
- Seek health care promptly for testing and/or treatment if you have risk factors for severe illness . Treatment may help lower your risk of severe illness, but it needs to be started within a few days of when your symptoms begin.
Additional Prevention Strategies
In addition, there are other prevention strategies that you can choose to further protect yourself and others.
- Wearing a mask and putting distance between yourself and others can help lower the risk of COVID-19 transmission.
- Testing for COVID-19 can help you decide what to do next, like getting treatment to reduce your risk of severe illness and taking steps to lower your chances of spreading COVID-19 to others.
Key Times for Prevention
Using these prevention strategies can be especially helpful when:
- Respiratory viruses, such as COVID-19, flu, and RSV, are causing a lot of illness in your community
- You or those around you have risk factors for severe illness
- You or those around you were recently exposed to a respiratory virus, are sick, or are recovering
Check Your Community
Find out if respiratory viruses are causing a lot of illness in your community. Data updated weekly.
Learn more about all three of these respiratory viruses, who is most at risk, and how they are affecting your state right now. You can use some of the same strategies to protect yourself from all three viruses.
Get the Latest on COVID-19, Flu, and RSV
- COVID-19 Testing
- COVID-19 Vaccines
- COVID-19 Treatments and Medications
- Preventing Respiratory Viruses
- Protect Yourself from COVID-19, Flu, and RSV
Additional Resources
- Respirators and Masks
- Improving Ventilation in Your Home
- Improving Ventilation In Buildings
Search for and find historical COVID-19 pages and files. Please note the content on these pages and files is no longer being updated and may be out of date.
- Visit archive.cdc.gov for a historical snapshot of the COVID-19 website, capturing the end of the Federal Public Health Emergency on June 28, 2023.
- Visit the dynamic COVID-19 collection to search the COVID-19 website as far back as July 30, 2021.
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
COVID-19: Why is social distancing so important?
Medically reviewed by Leigh Ann Anderson, PharmD . Last updated on Sep 14, 2023.
Official answer
What is social distancing.
Social or physical distancing is just that -- keep a minimum space between yourself and others. To effectively implement social distancing for COVID-19, you should:
- Keep at least 6 feet (~2 meters) between yourself and other people outside your household at all times.
- Stay out of crowded places and avoid mass gatherings: this includes mass transit, large church groups, conferences, festivals, parades, concerts, sporting events, weddings, and other types of assemblies.
COVID-19 is highly contagious. Even those who exhibit few or no symptoms can spread the disease. In other words, you cannot identify those who have COVID-19 and are contagious just by taking their temperature or looking for a cough. This also applies to children who often have no symptoms and could easily infect older adults and seniors.
The virus spreads primarily from person-to-person. It spreads
- between people who are within about 6 feet) of each other.
- through respiratory droplets produced when an infected person coughs, sneezes or talks. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs.
Why should I practice social distancing?
Besides protecting yourself and those in your family, social distancing and wearing a mask when you test positive for COVID-19 can have wide-reaching outcomes.
Symptoms of COVID-19 usually result in mild or moderate illness, such as a fever, dry cough, body aches, and fatigue that resolves over a week in most people. In older adults and people with existing health problems, it can cause a more severe outcome, which can include pneumonia, acute respiratory distress syndrome and death.
Adhering to social distancing norms can help protect groups at higher risk, for example:
- older people 65 years and over
- people with chronic conditions, like lung disease, heart disease, high blood pressure, diabetes or obesity, among others
- people with weak immune systems
Related Questions
- Can you have Covid without a fever?
- Which breathing techniques help with COVID-19?
- Is Omicron worse than Delta?
Bottom Line
When needed, social distancing for COVID-19 disease can protect you and your family, health care workers, and help limit overcrowding of hospitals and ICUs.
As many people are asymptomatic or pre-symptomatic when they contract COVID-19, social distancing can protect the high-risk groups, such as the elderly, and those with diabetes, obesity, heart and lung disease and weak immune systems.
- Social Distancing, Quarantine, and Isolation. US Centers for Disease Control and Prevention (CDC). Accessed April 9, 2020 at https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
Can you become immune to COVID-19?
Patients who recover from COVID-19 make antibodies to the virus that may impart immunity for at least 6 months; however, breakthrough infections do occur and may be more likely with newly circulating variants of the virus. Immunizing with the latest recommended COVID-19 vaccine can help to extend your immunity and prevent disease. Continue reading
Is obesity a major risk factor for Covid-19?
Obesity is a major risk factor for covid-19 and people who are obese are more likely than those who are not obese to contract Covid-19 at a younger age, develop severe Covid-19, require hospitalization, oxygen, mechanical ventilation, intubation, or admission into ICU, end up in hospital sooner, or die from Covid-19. Continue reading
COVID-19 vaccines and variants: What you should know
The top 3 SARS-CoV-2 variants in the U.S. in early December 2023 are all of Omicron lineage and include: HV.1 (30%), JN.1 (21%) and EG.5 (9%). Currently the JN.1 variant is increasing, while HV.1 seems to be decreasing. These percentages are based on modeled predictions of variant proportions. Continue reading
Related medical questions
- How effective is Lagevrio (molnupiravir) for COVID-19?
- Should I wear a face mask to protect myself from COVID-19?
- Why do more men die from coronavirus?
- Can Ivermectin be used to treat COVID-19?
- Can you take Ibuprofen if you have COVID-19 (coronavirus)?
- What antibiotics kill Covid-19 (coronavirus)?
- COVID-19: What are the Stages and Causes of Death?
- What's the difference between Bacteria and Viruses?
- Does Zinc protect you from Covid-19 or boost your immune system?
- Does Losartan block the receptor used by the Coronavirus?
- An Update: Is hydroxychloroquine effective for COVID-19?
- How do I Treat Nasal Congestion with COVID-19?
- Where can I buy an at-home test kit for COVID-19 (coronavirus)?
- Does Mucinex help with Covid?
- Can you take Paxlovid twice if COVID rebounds?
- Does Tamiflu (oseltamivir) work on COVID-19?
- Can vitamin C prevent or treat COVID-19 (coronavirus)?
- Should I take Paxlovid after a Positive COVID-19 Test?
- How long does COVID-19 last? and other COVID-19 FAQ
- Can I take NyQuil with COVID or after the COVID vaccine?
- How effective is Paxlovid for COVID-19?
- Can you take Ibuprofen after the COVID booster vaccine?
- Do ACE inhibitors make COVID-19 worse?
- Does Paxlovid prevent Long COVID?
- Does methylprednisolone help with COVID?
- Can NSAIDs be used to treat a COVID-19 fever?
- What are JAK inhibitors and how do they work?
- Can Colchicine be used to treat COVID-19 (coronavirus)?
- Does the BCG vaccine for TB help with COVID-19 (coronavirus)?
- Do statins help treat COVID-19?
Related support groups
- COVID-19 (103 questions, 87 members)
- Viral Infection (32 questions, 12 members)
Medical Disclaimer
Our approach
- Responsibility
- Infrastructure
- Try Meta AI
RECOMMENDED READS
- 5 Steps to Getting Started with Llama 2
- The Llama Ecosystem: Past, Present, and Future
- Introducing Code Llama, a state-of-the-art large language model for coding
- Meta and Microsoft Introduce the Next Generation of Llama
- Today, we’re introducing Meta Llama 3, the next generation of our state-of-the-art open source large language model.
- Llama 3 models will soon be available on AWS, Databricks, Google Cloud, Hugging Face, Kaggle, IBM WatsonX, Microsoft Azure, NVIDIA NIM, and Snowflake, and with support from hardware platforms offered by AMD, AWS, Dell, Intel, NVIDIA, and Qualcomm.
- We’re dedicated to developing Llama 3 in a responsible way, and we’re offering various resources to help others use it responsibly as well. This includes introducing new trust and safety tools with Llama Guard 2, Code Shield, and CyberSec Eval 2.
- In the coming months, we expect to introduce new capabilities, longer context windows, additional model sizes, and enhanced performance, and we’ll share the Llama 3 research paper.
- Meta AI, built with Llama 3 technology, is now one of the world’s leading AI assistants that can boost your intelligence and lighten your load—helping you learn, get things done, create content, and connect to make the most out of every moment. You can try Meta AI here .
Today, we’re excited to share the first two models of the next generation of Llama, Meta Llama 3, available for broad use. This release features pretrained and instruction-fine-tuned language models with 8B and 70B parameters that can support a broad range of use cases. This next generation of Llama demonstrates state-of-the-art performance on a wide range of industry benchmarks and offers new capabilities, including improved reasoning. We believe these are the best open source models of their class, period. In support of our longstanding open approach, we’re putting Llama 3 in the hands of the community. We want to kickstart the next wave of innovation in AI across the stack—from applications to developer tools to evals to inference optimizations and more. We can’t wait to see what you build and look forward to your feedback.
Our goals for Llama 3
With Llama 3, we set out to build the best open models that are on par with the best proprietary models available today. We wanted to address developer feedback to increase the overall helpfulness of Llama 3 and are doing so while continuing to play a leading role on responsible use and deployment of LLMs. We are embracing the open source ethos of releasing early and often to enable the community to get access to these models while they are still in development. The text-based models we are releasing today are the first in the Llama 3 collection of models. Our goal in the near future is to make Llama 3 multilingual and multimodal, have longer context, and continue to improve overall performance across core LLM capabilities such as reasoning and coding.
State-of-the-art performance
Our new 8B and 70B parameter Llama 3 models are a major leap over Llama 2 and establish a new state-of-the-art for LLM models at those scales. Thanks to improvements in pretraining and post-training, our pretrained and instruction-fine-tuned models are the best models existing today at the 8B and 70B parameter scale. Improvements in our post-training procedures substantially reduced false refusal rates, improved alignment, and increased diversity in model responses. We also saw greatly improved capabilities like reasoning, code generation, and instruction following making Llama 3 more steerable.

*Please see evaluation details for setting and parameters with which these evaluations are calculated.
In the development of Llama 3, we looked at model performance on standard benchmarks and also sought to optimize for performance for real-world scenarios. To this end, we developed a new high-quality human evaluation set. This evaluation set contains 1,800 prompts that cover 12 key use cases: asking for advice, brainstorming, classification, closed question answering, coding, creative writing, extraction, inhabiting a character/persona, open question answering, reasoning, rewriting, and summarization. To prevent accidental overfitting of our models on this evaluation set, even our own modeling teams do not have access to it. The chart below shows aggregated results of our human evaluations across of these categories and prompts against Claude Sonnet, Mistral Medium, and GPT-3.5.

Preference rankings by human annotators based on this evaluation set highlight the strong performance of our 70B instruction-following model compared to competing models of comparable size in real-world scenarios.
Our pretrained model also establishes a new state-of-the-art for LLM models at those scales.

To develop a great language model, we believe it’s important to innovate, scale, and optimize for simplicity. We adopted this design philosophy throughout the Llama 3 project with a focus on four key ingredients: the model architecture, the pretraining data, scaling up pretraining, and instruction fine-tuning.
Model architecture
In line with our design philosophy, we opted for a relatively standard decoder-only transformer architecture in Llama 3. Compared to Llama 2, we made several key improvements. Llama 3 uses a tokenizer with a vocabulary of 128K tokens that encodes language much more efficiently, which leads to substantially improved model performance. To improve the inference efficiency of Llama 3 models, we’ve adopted grouped query attention (GQA) across both the 8B and 70B sizes. We trained the models on sequences of 8,192 tokens, using a mask to ensure self-attention does not cross document boundaries.
Training data
To train the best language model, the curation of a large, high-quality training dataset is paramount. In line with our design principles, we invested heavily in pretraining data. Llama 3 is pretrained on over 15T tokens that were all collected from publicly available sources. Our training dataset is seven times larger than that used for Llama 2, and it includes four times more code. To prepare for upcoming multilingual use cases, over 5% of the Llama 3 pretraining dataset consists of high-quality non-English data that covers over 30 languages. However, we do not expect the same level of performance in these languages as in English.
To ensure Llama 3 is trained on data of the highest quality, we developed a series of data-filtering pipelines. These pipelines include using heuristic filters, NSFW filters, semantic deduplication approaches, and text classifiers to predict data quality. We found that previous generations of Llama are surprisingly good at identifying high-quality data, hence we used Llama 2 to generate the training data for the text-quality classifiers that are powering Llama 3.
We also performed extensive experiments to evaluate the best ways of mixing data from different sources in our final pretraining dataset. These experiments enabled us to select a data mix that ensures that Llama 3 performs well across use cases including trivia questions, STEM, coding, historical knowledge, etc.
Scaling up pretraining
To effectively leverage our pretraining data in Llama 3 models, we put substantial effort into scaling up pretraining. Specifically, we have developed a series of detailed scaling laws for downstream benchmark evaluations. These scaling laws enable us to select an optimal data mix and to make informed decisions on how to best use our training compute. Importantly, scaling laws allow us to predict the performance of our largest models on key tasks (for example, code generation as evaluated on the HumanEval benchmark—see above) before we actually train the models. This helps us ensure strong performance of our final models across a variety of use cases and capabilities.
We made several new observations on scaling behavior during the development of Llama 3. For example, while the Chinchilla-optimal amount of training compute for an 8B parameter model corresponds to ~200B tokens, we found that model performance continues to improve even after the model is trained on two orders of magnitude more data. Both our 8B and 70B parameter models continued to improve log-linearly after we trained them on up to 15T tokens. Larger models can match the performance of these smaller models with less training compute, but smaller models are generally preferred because they are much more efficient during inference.
To train our largest Llama 3 models, we combined three types of parallelization: data parallelization, model parallelization, and pipeline parallelization. Our most efficient implementation achieves a compute utilization of over 400 TFLOPS per GPU when trained on 16K GPUs simultaneously. We performed training runs on two custom-built 24K GPU clusters . To maximize GPU uptime, we developed an advanced new training stack that automates error detection, handling, and maintenance. We also greatly improved our hardware reliability and detection mechanisms for silent data corruption, and we developed new scalable storage systems that reduce overheads of checkpointing and rollback. Those improvements resulted in an overall effective training time of more than 95%. Combined, these improvements increased the efficiency of Llama 3 training by ~three times compared to Llama 2.
Instruction fine-tuning
To fully unlock the potential of our pretrained models in chat use cases, we innovated on our approach to instruction-tuning as well. Our approach to post-training is a combination of supervised fine-tuning (SFT), rejection sampling, proximal policy optimization (PPO), and direct preference optimization (DPO). The quality of the prompts that are used in SFT and the preference rankings that are used in PPO and DPO has an outsized influence on the performance of aligned models. Some of our biggest improvements in model quality came from carefully curating this data and performing multiple rounds of quality assurance on annotations provided by human annotators.
Learning from preference rankings via PPO and DPO also greatly improved the performance of Llama 3 on reasoning and coding tasks. We found that if you ask a model a reasoning question that it struggles to answer, the model will sometimes produce the right reasoning trace: The model knows how to produce the right answer, but it does not know how to select it. Training on preference rankings enables the model to learn how to select it.
Building with Llama 3
Our vision is to enable developers to customize Llama 3 to support relevant use cases and to make it easier to adopt best practices and improve the open ecosystem. With this release, we’re providing new trust and safety tools including updated components with both Llama Guard 2 and Cybersec Eval 2, and the introduction of Code Shield—an inference time guardrail for filtering insecure code produced by LLMs.
We’ve also co-developed Llama 3 with torchtune , the new PyTorch-native library for easily authoring, fine-tuning, and experimenting with LLMs. torchtune provides memory efficient and hackable training recipes written entirely in PyTorch. The library is integrated with popular platforms such as Hugging Face, Weights & Biases, and EleutherAI and even supports Executorch for enabling efficient inference to be run on a wide variety of mobile and edge devices. For everything from prompt engineering to using Llama 3 with LangChain we have a comprehensive getting started guide and takes you from downloading Llama 3 all the way to deployment at scale within your generative AI application.
A system-level approach to responsibility
We have designed Llama 3 models to be maximally helpful while ensuring an industry leading approach to responsibly deploying them. To achieve this, we have adopted a new, system-level approach to the responsible development and deployment of Llama. We envision Llama models as part of a broader system that puts the developer in the driver’s seat. Llama models will serve as a foundational piece of a system that developers design with their unique end goals in mind.

Instruction fine-tuning also plays a major role in ensuring the safety of our models. Our instruction-fine-tuned models have been red-teamed (tested) for safety through internal and external efforts. Our red teaming approach leverages human experts and automation methods to generate adversarial prompts that try to elicit problematic responses. For instance, we apply comprehensive testing to assess risks of misuse related to Chemical, Biological, Cyber Security, and other risk areas. All of these efforts are iterative and used to inform safety fine-tuning of the models being released. You can read more about our efforts in the model card .
Llama Guard models are meant to be a foundation for prompt and response safety and can easily be fine-tuned to create a new taxonomy depending on application needs. As a starting point, the new Llama Guard 2 uses the recently announced MLCommons taxonomy, in an effort to support the emergence of industry standards in this important area. Additionally, CyberSecEval 2 expands on its predecessor by adding measures of an LLM’s propensity to allow for abuse of its code interpreter, offensive cybersecurity capabilities, and susceptibility to prompt injection attacks (learn more in our technical paper ). Finally, we’re introducing Code Shield which adds support for inference-time filtering of insecure code produced by LLMs. This offers mitigation of risks around insecure code suggestions, code interpreter abuse prevention, and secure command execution.
With the speed at which the generative AI space is moving, we believe an open approach is an important way to bring the ecosystem together and mitigate these potential harms. As part of that, we’re updating our Responsible Use Guide (RUG) that provides a comprehensive guide to responsible development with LLMs. As we outlined in the RUG, we recommend that all inputs and outputs be checked and filtered in accordance with content guidelines appropriate to the application. Additionally, many cloud service providers offer content moderation APIs and other tools for responsible deployment, and we encourage developers to also consider using these options.
Deploying Llama 3 at scale
Llama 3 will soon be available on all major platforms including cloud providers, model API providers, and much more. Llama 3 will be everywhere .
Our benchmarks show the tokenizer offers improved token efficiency, yielding up to 15% fewer tokens compared to Llama 2. Also, Group Query Attention (GQA) now has been added to Llama 3 8B as well. As a result, we observed that despite the model having 1B more parameters compared to Llama 2 7B, the improved tokenizer efficiency and GQA contribute to maintaining the inference efficiency on par with Llama 2 7B.
For examples of how to leverage all of these capabilities, check out Llama Recipes which contains all of our open source code that can be leveraged for everything from fine-tuning to deployment to model evaluation.
What’s next for Llama 3?
The Llama 3 8B and 70B models mark the beginning of what we plan to release for Llama 3. And there’s a lot more to come.
Our largest models are over 400B parameters and, while these models are still training, our team is excited about how they’re trending. Over the coming months, we’ll release multiple models with new capabilities including multimodality, the ability to converse in multiple languages, a much longer context window, and stronger overall capabilities. We will also publish a detailed research paper once we are done training Llama 3.
To give you a sneak preview for where these models are today as they continue training, we thought we could share some snapshots of how our largest LLM model is trending. Please note that this data is based on an early checkpoint of Llama 3 that is still training and these capabilities are not supported as part of the models released today.

We’re committed to the continued growth and development of an open AI ecosystem for releasing our models responsibly. We have long believed that openness leads to better, safer products, faster innovation, and a healthier overall market. This is good for Meta, and it is good for society. We’re taking a community-first approach with Llama 3, and starting today, these models are available on the leading cloud, hosting, and hardware platforms with many more to come.
Try Meta Llama 3 today
We’ve integrated our latest models into Meta AI, which we believe is the world’s leading AI assistant. It’s now built with Llama 3 technology and it’s available in more countries across our apps.
You can use Meta AI on Facebook, Instagram, WhatsApp, Messenger, and the web to get things done, learn, create, and connect with the things that matter to you. You can read more about the Meta AI experience here .
Visit the Llama 3 website to download the models and reference the Getting Started Guide for the latest list of all available platforms.
You’ll also soon be able to test multimodal Meta AI on our Ray-Ban Meta smart glasses.
As always, we look forward to seeing all the amazing products and experiences you will build with Meta Llama 3.
Our latest updates delivered to your inbox
Subscribe to our newsletter to keep up with Meta AI news, events, research breakthroughs, and more.
Join us in the pursuit of what’s possible with AI.

Product experiences
Foundational models
Latest news
Meta © 2024

IMAGES
VIDEO
COMMENTS
Social distancing is a public health practice that aims to prevent sick people from coming in close contact with healthy people in order to reduce opportunities for disease transmission. It can include large-scale measures like canceling group events or closing public spaces, as well as individual decisions such as avoiding crowds. With COVID ...
To society, social distancing presents the dangers of increasing social rejection, growing impersonality and individualism, and the loss of a sense of community. It negatively affects learning and growth, and it prevents people from effectively socializing, which is a fundamental human need. First and foremost, the measures carried a strong ...
Social distancing is a tool public health officials recommend to slow the spread of a disease that is being passed from person to person. Simply put, it means that people stay far enough away from ...
Physical distancing is the practice of staying at least 6 feet away from others to avoid catching a disease such as COVID-19. As noted above, "social distancing" is a term that was used earlier in the pandemic as many people stayed home to help prevent spread of the virus. Now as communities are reopening and people are in public more often ...
Social distancing involved keeping a distance of 1.5 m between people, which can prevent the spread of most respiratory infectious diseases. Social distancing is one of the most effective measures to reduce the spread of the virus, which is transmitted by air droplets. The droplets produced by coughing, sneezing or forced speaking have a ...
The Ethics of Social Distancing: More Than a Binary. This is, then, where the rubber hits the road. Social distancing has clear benefits, and COVID-19 is an incredibly dangerous global pandemic. These measures slow the progress of the disease which takes pressure off the medical system, and reduces the overall number of infections.
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery.
Here, the social distancing level was increased to 60%, 80%, and 100%, respectively, which led to reducing the spread of COVID-19 dramatically. The results show that applying 80% or higher of social distancing results in the lowest levels of infected cases and the highest survival rate and the lowest rate of death. These results suggest that ...
A better understanding of how the COVID-19 pandemic responds to social distancing efforts is required for the control of future outbreaks and to calibrate partial lock-downs. We present ...
Dr. Klinenberg is a sociologist. Social distancing — canceling large gatherings, closing schools and offices, quarantining individuals and even sequestering entire cities or neighborhoods ...
"Social distancing" is, in fact, an umbrella term that comprises several very complex interventions for keeping healthy people spaced apart from anyone who could be infectious. Measures range ...
Adoption of government-imposed social distancing measures reduced the daily growth rate of confirmed COVID-19 cases by 5.4 percentage points after one to five days, 6.8 percentage points after six ...
But the new study by NIH-funded researchers, published in the journal Science, documents why social distancing may be our best hope to slow the spread of COVID-19 [1]. Here are a few highlights of the paper, which looks back to January 2020 and mathematically models the spread of the coronavirus within China: • For every confirmed case of ...
To fight the spread of COVID-19, many countries implemented social distancing policies. This is the first paper that examines the effects of the German social distancing policies on behavior and the epidemic's spread. Exploiting the staggered timing of COVID-19 outbreaks in extended event-study models, we find that the policies heavily reduced mobility and contagion. In comparison to a no ...
that the benefits from social distancing also remain substantial in less aggressive COVID-19 scenarios; for example, the benefits of social distancing are $3.6 trillion even in a scenario where the peak of daily death rates is 60% lower than in the Imperial College model (Ferguson et al. 2020) of COVID-19 spread that we rely on in this paper.
Papers were screened and selected, as illustrated in Fig. 1. After the second screening based on full texts, ... Social distancing: during the pandemic it could increase PFD-related suffering and other morbidities affecting women's quality of life because of multiple factors such as increased obesity, physical inactivity, stress and problems ...
Keep physical distance of at least 1 metre from others, even if they don't appear to be sick. Avoid crowds and close contact. Wear a properly fitted mask when physical distancing is not possible and in poorly ventilated settings. Clean your hands frequently with alcohol-based hand rub or soap and water.
Introduction. Social distancing or physical distancing is a complex of non-pharmacological sanitary and epidemiological measures aimed at stopping or declining the spread of an infectious disease. Social distancing means limiting close contacts between people, even if they are not sick, not being in any of the risk groups.
Here are some ideas to stay connected and active while apart: Call a friend or loved one while taking a walk. Post your physical activity plans to social media and invite your network to move along with you. Get moving with friends via video chat or virtual streaming service.
In addition, there are other prevention strategies that you can choose to further protect yourself and others. Wearing a mask and putting distance between yourself and others can help lower the risk of COVID-19 transmission. Testing for COVID-19 can help you decide what to do next, like getting treatment to reduce your risk of severe illness ...
Bottom Line. When needed, social distancing for COVID-19 disease can protect you and your family, health care workers, and help limit overcrowding of hospitals and ICUs. As many people are asymptomatic or pre-symptomatic when they contract COVID-19, social distancing can protect the high-risk groups, such as the elderly, and those with diabetes ...
Today, we're introducing Meta Llama 3, the next generation of our state-of-the-art open source large language model. Llama 3 models will soon be available on AWS, Databricks, Google Cloud, Hugging Face, Kaggle, IBM WatsonX, Microsoft Azure, NVIDIA NIM, and Snowflake, and with support from hardware platforms offered by AMD, AWS, Dell, Intel ...