Join thousands of product people at Insight Out Conf on April 11. Register free.
Insights hub solutions

Analyze data
Uncover deep customer insights with fast, powerful features, store insights, curate and manage insights in one searchable platform, scale research, unlock the potential of customer insights at enterprise scale.
Featured reads

Inspiration
Three things to look forward to at Insight Out
Tips and tricks
Make magic with your customer data in Dovetail

Four ways Dovetail helps Product Managers master continuous product discovery
Events and videos
© Dovetail Research Pty. Ltd.
Structured vs. unstructured interviews: A complete guide
Last updated
7 March 2023
Reviewed by
Miroslav Damyanov
Interviews can help you understand the context of a subject, eyewitness accounts of an event, people's perceptions of a product, and more.
In some instances, semi-structured or unstructured interviews can be more helpful; in others, structured interviews are the right choice to obtain the information you seek.
In some cases, structured interviews can save time, making your research more efficient. Let’s dive into everything you need to know about structured interviews.
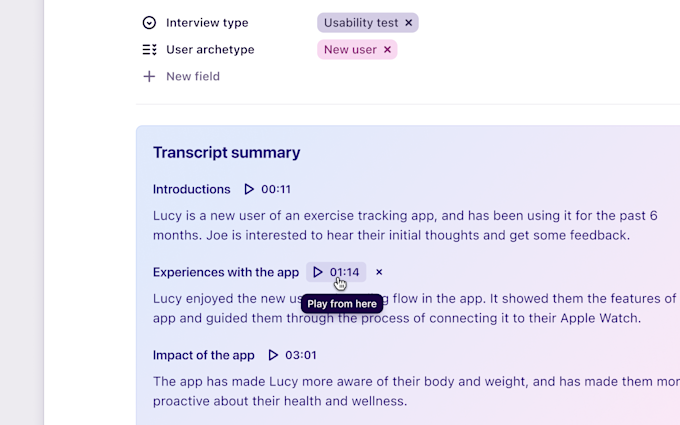
Analyze all kinds of interviews
Bring all your interviews into one place to analyze and understand
- What are structured interviews?
Structured interviews are also known as standardized interviews, patterned interviews, or planned interviews. They’re a research instrument that uses a standard sequence of questions to collect information about the research subject.
Often, you’ll use structured interviews when you need data that’s easy to categorize and quantify for a statistical analysis of responses.
Structured interviews are incredibly effective at helping researchers identify patterns and trends in response data. They’re great at minimizing the time and resources necessary for data collection and analysis.
What types of questions suit structured interviews?
Often, researchers use structured interviews for quantitative research . In these cases, they usually employ close-ended questions.
Close-ended questions have a fixed set of responses from which the interviewer can choose. Because of the limited response selection set, response data from close-ended questions is easy to aggregate and analyze.
Researchers often employ multiple-choice or dichotomous close-ended questions in interviews.
For multiple-choice questions, interviewees may choose between three or more possible answers. The interviewer will often restrict the response to four or five possible options. An interviewee will likely need help recalling more, which can slow down and complicate the interview process.
For dichotomous questions, the interviewee may choose between two possible options. Yes or no and true or false questions are examples of dichotomous questions.
Open-ended questions are common in structured interviews. However, researchers use them when conducting qualitative research and looking for in-depth information about the interviewee's perceptions or experiences.
These questions take longer for the interviewee to answer, and the answers take longer for the researcher to analyze. There's also a higher possibility of the researcher collecting irrelevant data. However, open-ended questions are more effective than close-ended questions in gathering in-depth information.
Sometimes, researchers use structured interviews in qualitative research. In this case, the research instrument contains open-ended questions in the same sequence. This usage is less common because it can be hard to compare feedback, especially with large sample sizes.
- What types of structured interviews are there?
Researchers conduct structured interviews face-to-face, via telephone or videoconference, or through a survey instrument.
Face-to-face interviews help researchers collect data and gather more detailed information. They can collect and analyze facial expressions, body language, tone, and inflection easier than they might through other interview methods .
However, face-to-face interviews are the most resource-intensive to arrange. You'll likely need to assume travel and other related logistical costs for a face-to-face interview.
These interviews also take more time and are more vulnerable to bias than some other formats. For these reasons, face-to-face interviews are best with a small sample size.
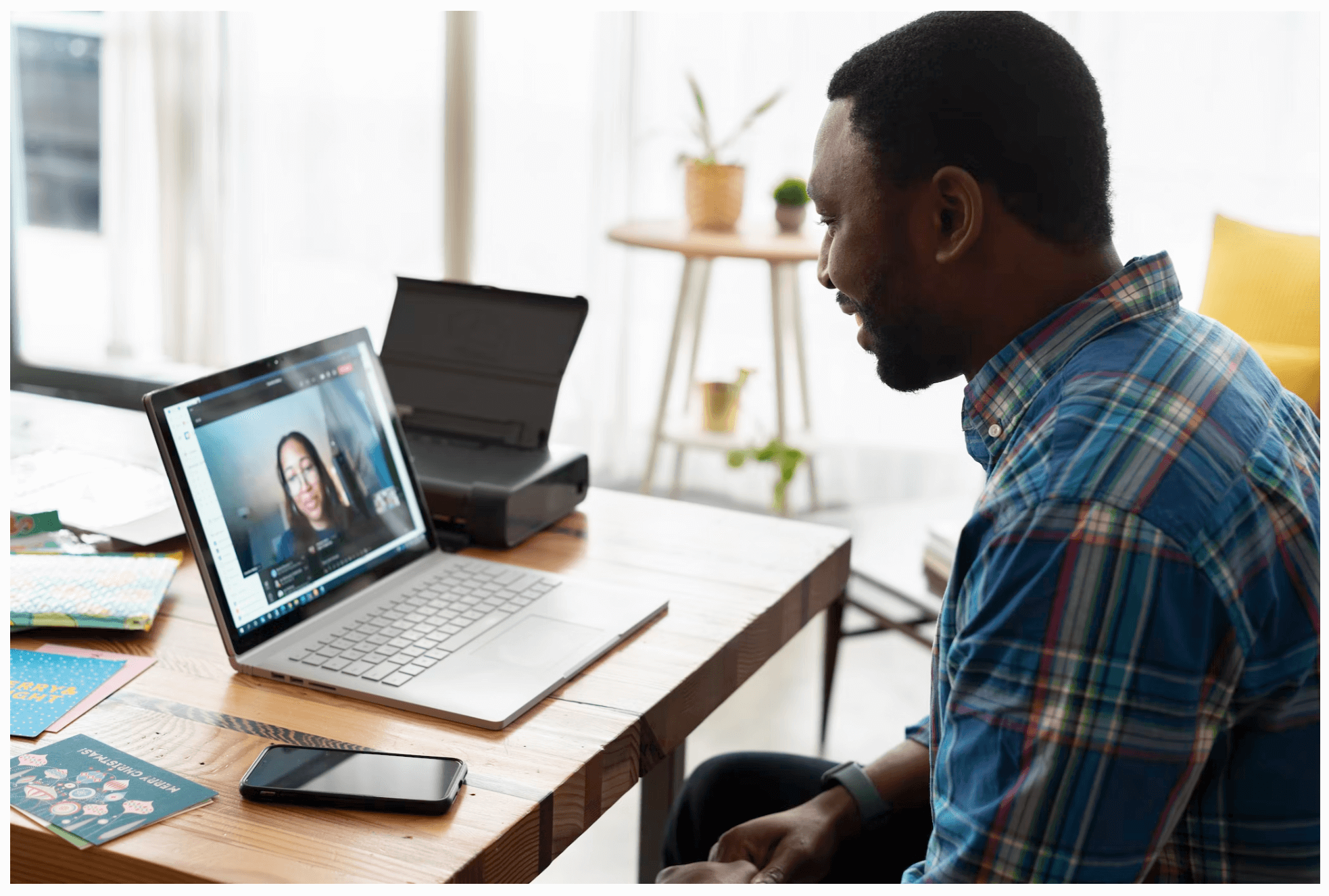
You can conduct interviews via an audio or video call. They are less resource-intensive than face-to-face interviews and can use a larger sample size.
However, it can be difficult for the interviewer to engage effectively with the interviewee within this format, which can inject bias or ambiguity into the responses. This is particularly true for audio calls, especially if the interviewer and interviewee have not met before the interview.
A video call can help the interviewer capture some data from body language and facial expressions, but less so than in a face-to-face interview. Technical issues are another thing to consider. If you’re studying a group of people that live in an area with limited Internet connectivity, this can make a video call challenging.
Survey questionnaires mirror the essential elements of structured interviews by containing a consistent sequence of standard questions. Surveys in quantitative research usually include close-ended questions. This data collection method can be beneficial if you need feedback from a large sample size.
Surveys are resource-efficient from a data administration standpoint but are more limited in the data they can gather. Further, if a survey question is ambiguous, you can’t clear up the ambiguity before someone responds.
By contrast, in a face-to-face or tele-interview, an interviewee may ask clarifying questions or exhibit confusion when asked an unclear question, allowing the interviewer to clarify.
- What are some common examples of structured interviews?
Structured interviews are relevant in many fields. You can find structured interviews in human resources, marketing, political science, psychology, and more.
Academic and applied researchers commonly use them to verify insights from analyzing academic literature or responses from other interview types.
However, one of the most common structured interview applications lies outside the research realm: Human resource professionals and hiring managers commonly use these interviews to hire employees.
A hiring manager can easily compare responses and whittle down the applicant pool by posing a standard set of closed-ended interview questions to multiple applicants.
Further, standard close-ended or open-ended questions can reduce bias and add objectivity and credibility to the hiring process.
Structured interviews are common in political polling. Candidates and political parties may conduct structured interviews with relatively small voter groups to obtain feedback. They ask questions about issues, messaging, and voting intentions to craft policies and campaigns.
- What do you need to conduct a structured interview?
The tools you need to conduct a structured interview vary by format. But fundamentally, you will need:
A participant
An interviewer
A pen and pad (or other note-taking tools)
A recording device
A consent form
A list of interview questions
While some interviewees may express qualms about you recording the interview, it’s challenging to conduct quality interviews while taking detailed notes. Even if you have a note-taker in the room, note-taking may introduce bias and can’t capture body language or facial expressions.
Depending on the nature of your study, others may wish to review your sources. If they call your conclusions into question, audio recordings are additional evidence in your favor.
To record, you should ask the interviewee to sign a consent form. Check with your employer's legal counsel or institutional review board at your academic institution for guidance about obtaining consent legally in your state.
If you're conducting a face-to-face interview, a camcorder, digital camera, or even some smartphones are sufficient for recording.
For a tele-interview, you'll find that today's leading video conferencing software applications feature a convenient recording function for data collection.
If a survey is your method of choice, you'll need the survey and a distribution and collection method. Online survey software applications allow you to create surveys by inputting the questions and distributing your survey via text or email.
In some cases, survey companies even offer packages in which they will call those who do not respond via email or text and conduct the survey over the phone.
- How to conduct a structured interview
If you're planning a face-to-face interview, you'll need to take a few steps to do it efficiently.
First, prepare your questions and double-check that the structured interview format is best for your study. Make sure that they are neutral, unbiased, and close-ended. Ask a friend or colleague to test your questions pre-interview to ensure they are clear and straightforward.
Choose the setting for your interviews. Ideally, you'll select a location that is easy to get to. If you live in a city, consider addresses accessible via public transportation.
The room where your interview takes place should be comfortable, without distraction, and quiet, so your recording device clearly captures your interviewee's audio.
If you're looking to interview people with specific characteristics, you'll need to recruit them. Some companies specialize in interview recruitment. You provide the attributes you need, and they identify a pool of candidates for a fee. Alternatively, you can advertise to participants on social media and other relevant avenues.
If you're looking for college students in a specific region, look at student newspaper ads or affiliated social media pages.
You'll also want to incentivize participation, as recruiting interview respondents without compensation is exceedingly difficult. It’s best to include a line or two about requiring written consent for participation and how you’ll use the interview audio.
When you have an interview participant, discuss the intent of your research and acquire their consent. Ensure your recording tools are working well, and begin your interview.
Don't rely on the recordings alone: Note the most significant insights from your participant, as you could easily forget them when it's time to analyze your data.
You'll want to transcribe your audio at the data analysis stage. Some recording applications use AI to generate transcripts. Remove filler words and other sounds to generate a clear transcript for the best results.
A written transcript will help you analyze data and pull quotes from your audio to include in your final research paper.
- What are other common types of interviews?
Typically, you'll find researchers using at least one of these other common interview types:
Semi-structured interviews
As the name suggests, semi-structured interviews include some elements of a structured interview. You’ll include preplanned questions, but you can deviate from those questions to explore the interviewee's answers in greater depth.
Typically, a researcher will conduct a semi-structured interview with preplanned questions and an interview guide. The guide will include topics and potential questions to ask. Sometimes, the guide may also include areas or questions to avoid asking.
Unstructured interviews
In an unstructured interview , the researchers approach the interview subjects without predetermined questions. Researchers often use this qualitative instrument to probe into personal experiences and testimony, typically toward the beginning of a research study.
Often, you’ll validate the insights you gather during unstructured and semi-structured interviews with structured interviews, surveys, and similar quantitative research tools.
Focus group interviews
Focus group interviews differ from the other three types of interviews as you pose the questions to a small group. Focus groups are typically either structured or semi-structured. When researchers employ structured interview questions, they are typically confident in the areas they wish to explore.
Semi-structured interviews are perfect for a researcher seeking to explore broad issues. However, you must be careful that unplanned questions are unambiguous and neutral. Otherwise, you could wind up with biased results.
What is a structured vs. an unstructured interview?
A structured interview consists of standard preplanned questions for data collection. These questions may be close-ended, open-ended, or a combination.
By contrast, an unstructured interview includes unplanned questions. In these interviews, you’ll usually equip facilitators with an interview guide. This includes guidelines for asking questions and samples that can help them ask relevant questions.
What are the advantages of a structured interview?
Relative to other interview formats, a structured interview is usually more time-efficient. With a preplanned set of questions, your interview is less likely to go into tangents, especially if you use close-ended questions.
The more structure you provide to the interview, the more likely you are to generate responses that are easy to analyze. By contrast, an unstructured interview may involve a freewheeling conversation with off-topic and irrelevant feedback that lasts a long time.
What is an example of a structured question?
A structured question is any question you ask in an interview that you’ve preplanned and standardized.
For example, if you conduct five interviews and the first question you ask each one is, "Do you believe the world is round, yes or no?" you have asked them a structured question. This is also a close-ended dichotomous question.
Get started today
Go from raw data to valuable insights with a flexible research platform
Editor’s picks
Last updated: 21 December 2023
Last updated: 16 December 2023
Last updated: 17 February 2024
Last updated: 19 November 2023
Last updated: 5 March 2024
Last updated: 15 February 2024
Last updated: 11 March 2024
Last updated: 12 December 2023
Last updated: 6 March 2024
Last updated: 10 April 2023
Last updated: 20 December 2023
Latest articles
Related topics, log in or sign up.
Get started for free
Root out friction in every digital experience, super-charge conversion rates, and optimize digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered to teams on the ground
Know how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re are saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Explore the platform powering Experience Management
- Free Account
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Employee Exit Interviews
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
Market Research
- Artificial Intelligence
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results, live in Salt Lake City.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Qualitative Research Interviews
Try Qualtrics for free
How to carry out great interviews in qualitative research.
11 min read An interview is one of the most versatile methods used in qualitative research. Here’s what you need to know about conducting great qualitative interviews.
What is a qualitative research interview?
Qualitative research interviews are a mainstay among q ualitative research techniques, and have been in use for decades either as a primary data collection method or as an adjunct to a wider research process. A qualitative research interview is a one-to-one data collection session between a researcher and a participant. Interviews may be carried out face-to-face, over the phone or via video call using a service like Skype or Zoom.
There are three main types of qualitative research interview – structured, unstructured or semi-structured.
- Structured interviews Structured interviews are based around a schedule of predetermined questions and talking points that the researcher has developed. At their most rigid, structured interviews may have a precise wording and question order, meaning that they can be replicated across many different interviewers and participants with relatively consistent results.
- Unstructured interviews Unstructured interviews have no predetermined format, although that doesn’t mean they’re ad hoc or unplanned. An unstructured interview may outwardly resemble a normal conversation, but the interviewer will in fact be working carefully to make sure the right topics are addressed during the interaction while putting the participant at ease with a natural manner.
- Semi-structured interviews Semi-structured interviews are the most common type of qualitative research interview, combining the informality and rapport of an unstructured interview with the consistency and replicability of a structured interview. The researcher will come prepared with questions and topics, but will not need to stick to precise wording. This blended approach can work well for in-depth interviews.
Free eBook: The qualitative research design handbook
What are the pros and cons of interviews in qualitative research?
As a qualitative research method interviewing is hard to beat, with applications in social research, market research, and even basic and clinical pharmacy. But like any aspect of the research process, it’s not without its limitations. Before choosing qualitative interviewing as your research method, it’s worth weighing up the pros and cons.
Pros of qualitative interviews:
- provide in-depth information and context
- can be used effectively when their are low numbers of participants
- provide an opportunity to discuss and explain questions
- useful for complex topics
- rich in data – in the case of in-person or video interviews , the researcher can observe body language and facial expression as well as the answers to questions
Cons of qualitative interviews:
- can be time-consuming to carry out
- costly when compared to some other research methods
- because of time and cost constraints, they often limit you to a small number of participants
- difficult to standardize your data across different researchers and participants unless the interviews are very tightly structured
- As the Open University of Hong Kong notes, qualitative interviews may take an emotional toll on interviewers
Qualitative interview guides
Semi-structured interviews are based on a qualitative interview guide, which acts as a road map for the researcher. While conducting interviews, the researcher can use the interview guide to help them stay focused on their research questions and make sure they cover all the topics they intend to.
An interview guide may include a list of questions written out in full, or it may be a set of bullet points grouped around particular topics. It can prompt the interviewer to dig deeper and ask probing questions during the interview if appropriate.
Consider writing out the project’s research question at the top of your interview guide, ahead of the interview questions. This may help you steer the interview in the right direction if it threatens to head off on a tangent.
Avoid bias in qualitative research interviews
According to Duke University , bias can create significant problems in your qualitative interview.
- Acquiescence bias is common to many qualitative methods, including focus groups. It occurs when the participant feels obliged to say what they think the researcher wants to hear. This can be especially problematic when there is a perceived power imbalance between participant and interviewer. To counteract this, Duke University’s experts recommend emphasizing the participant’s expertise in the subject being discussed, and the value of their contributions.
- Interviewer bias is when the interviewer’s own feelings about the topic come to light through hand gestures, facial expressions or turns of phrase. Duke’s recommendation is to stick to scripted phrases where this is an issue, and to make sure researchers become very familiar with the interview guide or script before conducting interviews, so that they can hone their delivery.
What kinds of questions should you ask in a qualitative interview?
The interview questions you ask need to be carefully considered both before and during the data collection process. As well as considering the topics you’ll cover, you will need to think carefully about the way you ask questions.
Open-ended interview questions – which cannot be answered with a ‘yes’ ‘no’ or ‘maybe’ – are recommended by many researchers as a way to pursue in depth information.
An example of an open-ended question is “What made you want to move to the East Coast?” This will prompt the participant to consider different factors and select at least one. Having thought about it carefully, they may give you more detailed information about their reasoning.
A closed-ended question , such as “Would you recommend your neighborhood to a friend?” can be answered without too much deliberation, and without giving much information about personal thoughts, opinions and feelings.
Follow-up questions can be used to delve deeper into the research topic and to get more detail from open-ended questions. Examples of follow-up questions include:
- What makes you say that?
- What do you mean by that?
- Can you tell me more about X?
- What did/does that mean to you?
As well as avoiding closed-ended questions, be wary of leading questions. As with other qualitative research techniques such as surveys or focus groups, these can introduce bias in your data. Leading questions presume a certain point of view shared by the interviewer and participant, and may even suggest a foregone conclusion.
An example of a leading question might be: “You moved to New York in 1990, didn’t you?” In answering the question, the participant is much more likely to agree than disagree. This may be down to acquiescence bias or a belief that the interviewer has checked the information and already knows the correct answer.
Other leading questions involve adjectival phrases or other wording that introduces negative or positive connotations about a particular topic. An example of this kind of leading question is: “Many employees dislike wearing masks to work. How do you feel about this?” It presumes a positive opinion and the participant may be swayed by it, or not want to contradict the interviewer.
Harvard University’s guidelines for qualitative interview research add that you shouldn’t be afraid to ask embarrassing questions – “if you don’t ask, they won’t tell.” Bear in mind though that too much probing around sensitive topics may cause the interview participant to withdraw. The Harvard guidelines recommend leaving sensitive questions til the later stages of the interview when a rapport has been established.
More tips for conducting qualitative interviews
Observing a participant’s body language can give you important data about their thoughts and feelings. It can also help you decide when to broach a topic, and whether to use a follow-up question or return to the subject later in the interview.
Be conscious that the participant may regard you as the expert, not themselves. In order to make sure they express their opinions openly, use active listening skills like verbal encouragement and paraphrasing and clarifying their meaning to show how much you value what they are saying.
Remember that part of the goal is to leave the interview participant feeling good about volunteering their time and their thought process to your research. Aim to make them feel empowered , respected and heard.
Unstructured interviews can demand a lot of a researcher, both cognitively and emotionally. Be sure to leave time in between in-depth interviews when scheduling your data collection to make sure you maintain the quality of your data, as well as your own well-being .
Recording and transcribing interviews
Historically, recording qualitative research interviews and then transcribing the conversation manually would have represented a significant part of the cost and time involved in research projects that collect qualitative data.
Fortunately, researchers now have access to digital recording tools, and even speech-to-text technology that can automatically transcribe interview data using AI and machine learning. This type of tool can also be used to capture qualitative data from qualitative research (focus groups,ect.) making this kind of social research or market research much less time consuming.
Data analysis
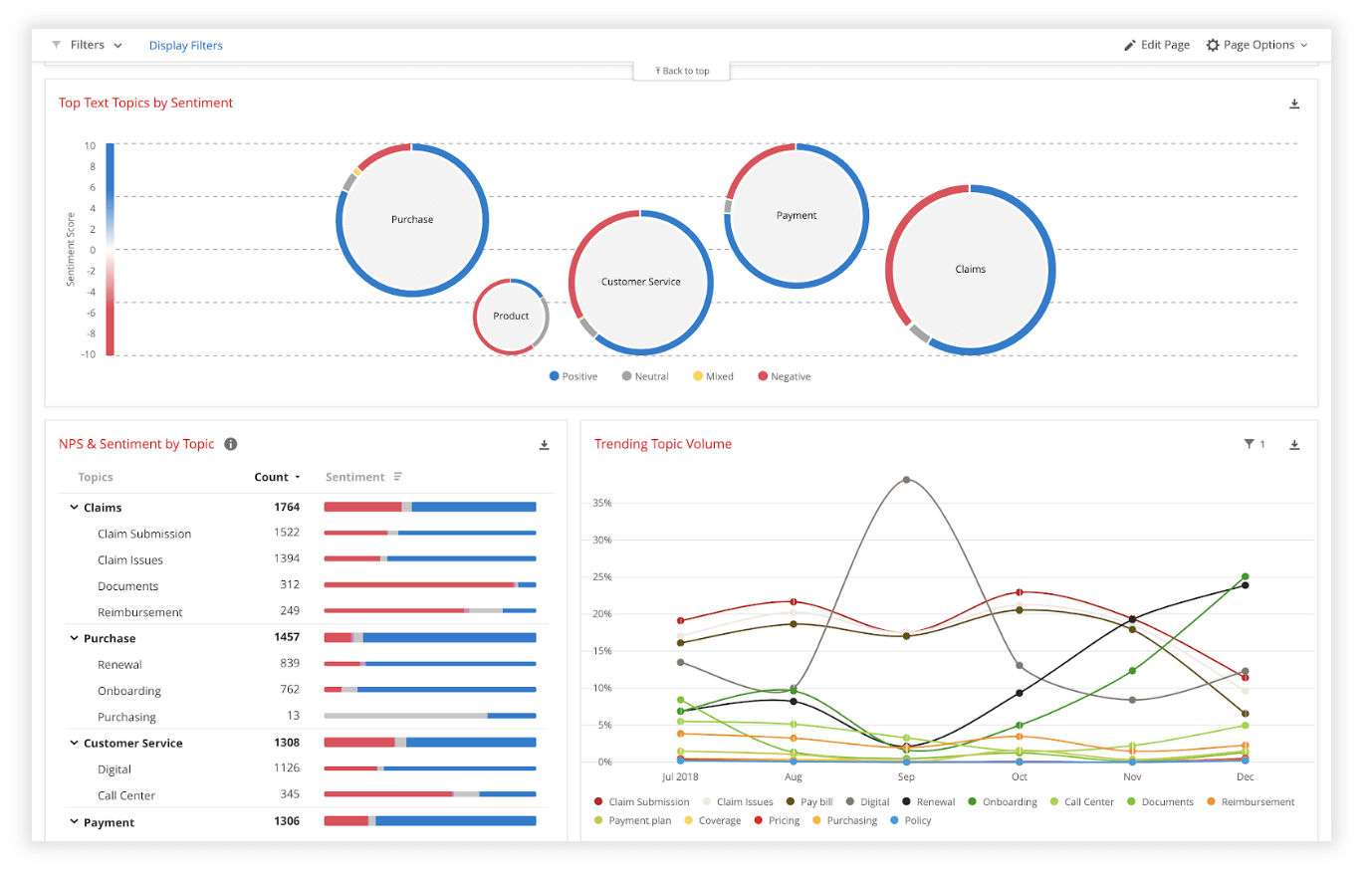
Qualitative interview data is unstructured, rich in content and difficult to analyze without the appropriate tools. Fortunately, machine learning and AI can once again make things faster and easier when you use qualitative methods like the research interview.
Text analysis tools and natural language processing software can ‘read’ your transcripts and voice data and identify patterns and trends across large volumes of text or speech. They can also perform khttps://www.qualtrics.com/experience-management/research/sentiment-analysis/
which assesses overall trends in opinion and provides an unbiased overall summary of how participants are feeling.
Another feature of text analysis tools is their ability to categorize information by topic, sorting it into groupings that help you organize your data according to the topic discussed.
All in all, interviews are a valuable technique for qualitative research in business, yielding rich and detailed unstructured data. Historically, they have only been limited by the human capacity to interpret and communicate results and conclusions, which demands considerable time and skill.
When you combine this data with AI tools that can interpret it quickly and automatically, it becomes easy to analyze and structure, dovetailing perfectly with your other business data. An additional benefit of natural language analysis tools is that they are free of subjective biases, and can replicate the same approach across as much data as you choose. By combining human research skills with machine analysis, qualitative research methods such as interviews are more valuable than ever to your business.
Related resources
Market intelligence 10 min read, marketing insights 11 min read, ethnographic research 11 min read, qualitative vs quantitative research 13 min read, qualitative research questions 11 min read, qualitative research design 12 min read, primary vs secondary research 14 min read, request demo.
Ready to learn more about Qualtrics?

Structured Interviews: Guide to Standardized Questions

Introduction
Types of interviews in qualitative research, what are structured interviews good for, structured interview process.
Qualitative researchers are used to dealing with unstructured data in social settings that are often dynamic and unpredictable. That said, there are research methods that can provide some more control over this unpredictable data while collecting insightful data .
The structured interview is one such method. Researchers can conduct a structured interview when they want to standardize the research process to give all respondents the same questions and analyze differences between answers.
In this article, we'll look at structured interviews, when they are ideal for your research, and how to conduct them.

Interviews are intentionally crafted sources of data in social science research. There are three types of interviews in research that balance research rigor and rich data collection .
To better understand structured interviews, it's important to contrast them with the other types of interviews that also serve useful purposes in research. As always, the best tool for data collection depends on your research inquiry.
Structured interviews
The structured interview format is the most rigid of the three types of interviews conceptualized in qualitative research. Imagine policy makers want to understand the perceptions of dozens or even hundreds of individuals. In this case, it may make it easier to streamline the interview process by simply asking the same questions of all respondents.
The same structured interview questions are posed to each and every respondent, akin to how hiring managers ask the same questions to all applicants during the hiring process. The intention behind this approach is to ensure that the interview is the same no matter who the respondent is, leaving only the differences in responses to be analyzed .
Moreover, the standardized interview format typically involves respondents being asked the same set of questions in the same order. A uniform sequence of questions ensures for an easy analysis when you can line up answers across respondents.
Unstructured interviews
An unstructured interview is the exact opposite of a structured interview, as unstructured interviews have no predetermined set of questions. Instead of a standardized interview, a researcher may opt for a study that remains open to exploring any issues or topics that a participant brings up in their interview. While this can generate unexpected insights, it can also be time-consuming and may not always yield answers that are directly related to the original research question guiding the study.
However, this doesn't make a study that employs unstructured interviews less rigorous . In fact, unstructured interviews are a great tool for inductive inquiry . One typical use for unstructured interviews is to probe not only for answers but for the salient points of a topic to begin with.
When a researcher uses an unstructured interview, they usually have a topic in mind but not a predetermined set of data points to analyze at the outset. This format allows respondents to speak at length on their perspectives and offer the researcher insights that can later form a theoretical framework for future research that could benefit from a structured interview format.
Moreover, this format provides the researcher with the greatest degree of freedom in determining questions depending on how they interact with their respondents. A respondent's body language, for example, may signal discomfort with a particularly controversial question. The interviewer can thus decide to adjust or reword their questions to create a more comfortable environment for the respondent.
Semi-structured interviews
A semi-structured interview lies in the middle ground between the structured and unstructured interview. This type of interview still relies on predetermined questions as a structured interview does. However, unlike structured interviews, a semi-structured interview also allows for follow-up questions to respondents when their answers warrant further probing. The predetermined questions thus serve as a guide for the interviewer, but the wording and ordering of questions can be adjusted, and additional questions can be asked during the course of the interview.
A researcher may conduct semi-structured interviews when they need flexibility in asking questions but can still benefit from advance preparation of key questions. In this case, much of the advice in this article about structured interviews still applies in terms of ensuring some degree of standardization when conducting research.
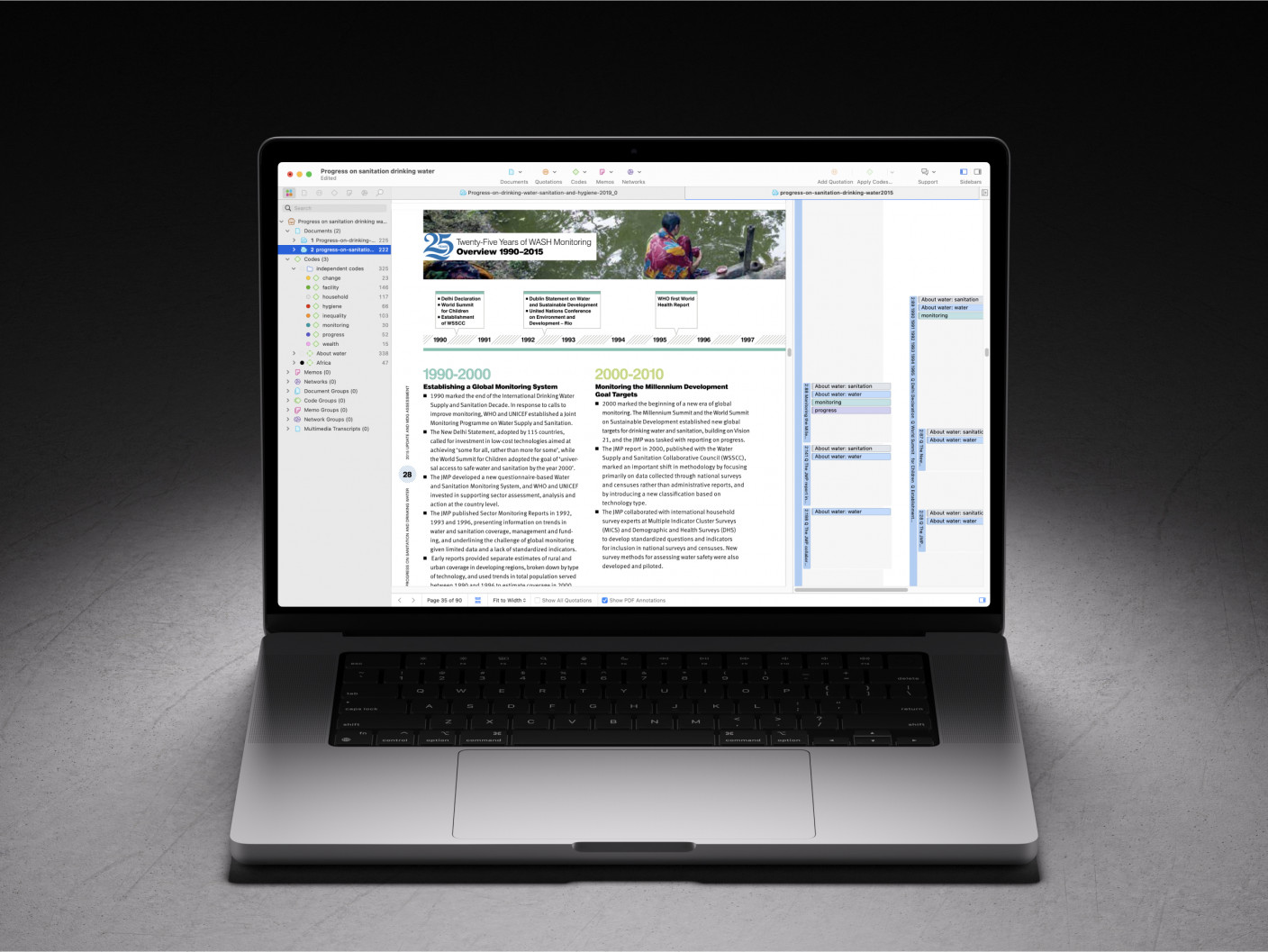
Identify key insights from your data with ATLAS.ti
Analyze interviews, observations, and all qualitative data with ATLAS.ti. Download your free trial here.
Consider that more free-flowing interview formats in qualitative research allow for the interviewer to more freely probe a respondent for deeper, more insightful answers on the topic of inquiry. This approach to research is useful when the researcher needs to develop theoretical coherence surrounding a new topic or research context in which it would be difficult to predict beforehand which questions are worth asking.
In this sense, structured interviews make more sense for research inquiries with a well-defined theoretical framework that guides the data collection and data analysis process . With such a framework in mind, researchers can devise questions that are grounded in existing research so that new insights further develop that scholarship.
Advantages of structured interviews
Formal, structured interviews are ideal for keeping interviewers and interview respondents focused on the topic at hand. A conversation might take unanticipated turns without a set goal or predetermined objective in mind; a structured interview helps keep the dialogue from going down any irrelevant tangents and minimize potentially unnecessary, extended monologues.
Another key advantage of structured interviews is that it makes comparisons across participants easier. Since each person was asked the same questions, the data is produced in a consistent format. Researchers can then focus on analyzing answers to a particular question, and there is minimal data organization work that needs to be done to facilitate the analysis.
There are also benefits in terms of the logistics of conducting structured interviews. Interviewers concerned with time constraints will find this format beneficial to their data collection .
Moreover, ensuring that respondents are asked the same questions in the same order limits the need for training interviewers to conduct interviews in a consistent manner. Unstructured and semi-structured interviews rely on the ability to ask follow-up questions in moments when the responses provide opportunities for deeper elaboration.
Those who conduct a structured interview, on the other hand, need only read from an interview guide with a list of questions to pose to respondents. This allows the researcher more freedom to rely on assistants to conduct interviews with minimal training and resources.
Disadvantages of structured interviews
In structured interviews, there is little room for asking probing questions of respondents, particularly if the researcher believes that follow-up questions might adversely influence how the respondent answers subsequent core questions. Restricting the interview to a predetermined set of questions may mitigate this effect, but it may also prevent a sufficiently clear understanding of respondents' perspectives established from the use of follow-up questions.
Forcing the interviewer to ask the same order of questions in an interview can also have a consequential effect on the data collection . Because every respondent is different, the interview questions may resonate with each person in different ways. A skillful interviewer conducting unstructured or semi-structured interviews has the freedom to make choices about what questions to ask in order to gather the most insightful data.
Ultimately, the biggest disadvantage of structured interviews comes from their biggest advantage: using predetermined questions can be a double-edged sword, providing consistency and systematic organization but also limiting the research to the questions that were decided before conducting the interviews. This makes it crucial that researchers have a clear understanding of which questions they want to ask and why. It can also be helpful to conduct pilot tests of the interview, to test out the structured questions with a handful of people and assess if any changes to the questions need to be made.
Why not just do surveys?
You might think that a structured interview is no different from a survey with open-ended questions. After all, the questions are determined ahead of time and won't change over the course of data collection . In many ways, there are many similarities in both methods.
There are, of course, benefits to either approach. Surveys permit data collection from much larger numbers of respondents than may be feasible for an interview study. Structured interviews, however, allow the interviewer some degree of flexibility, particularly when the respondent has trouble understanding the question or needs further prompting to provide a sufficient response.
Moreover, the interpersonal interaction between the interviewer and respondent offers potential for richer data collection because of the degree of rapport established through face-to-face communication. Where written questions may seem static and impersonal, an in-person interview (or at least one conducted in real time) might make the respondent more comfortable in answering questions.
Individual interviews are also more likely to generate detailed responses to questions in comparison to surveys. Interviews are also well suited for research topics that bear some personal significance for participants, providing ample space for them to express themselves.
When you conduct a structured interview, you are designing a study that is as standardized as possible to mitigate context effects and ensure the ease of data collection and analysis . As with all interviews conducted in qualitative research , there is an intentional process to planning for structured interviews with considerations that researchers should keep in mind.
Research design
As mentioned above, research inquiries with clearly defined theoretical frameworks tend to benefit from structured interviews. Researchers can create a list of questions from such frameworks so that answers speak directly to, affirm, or challenge the existing scholarship surrounding the topic of interest.
A researcher should conduct a literature review to determine the extent of theoretical coherence in the topic they are researching. Are there aspects of a topic or phenomenon that scholars have identified that can serve as key data points around which questions can be crafted? Conversely, is it a topic or phenomenon that lacks sufficient conceptualization?
If your literature review does not allow you to create or use a robust theoretical framework for data collection, consider other types of interviews that allow you to inductively generate that framework in data analysis .
You should also make decisions about the conditions under which you conduct interviews. Some studies go as far as making sure that the interview environment is a uniform context across respondents. Are interviews in a quiet, comfortable environment? What time of day are interviews conducted?
The degree to which you ensure uniform conditions across interviews is up to you. Whatever you decide, however, creating an environment where respondents feel free to volunteer answers will facilitate rich data collection that will make data analysis more meaningful.
Structured interview questions
An interview guide is an essential tool for structured interviews. This guide is little more than a list of required questions to ask, but this list ensures consistency across the interviews in your study.
When you write questions for a structured interview, rely on your literature review to identify salient points around which you can design questions. This approach ensures that you are grounding your data collection in the established research.
When crafting your guide, think about the time constraints and the likely length of answers that your respondents may give. Structured interviews can involve five or 25 questions, but if you are limited to 30-45 minutes per respondent, you will need to consider whether you can ask the required questions and collect sufficient responses within your timeframe.
As a result, it's important to pilot your questions with preliminary respondents or other researchers. A pilot interview allows you to test your interview protocol and make tweaks to your question guide before conducting your study in earnest.
Collecting data from structured interviews
Data collection refers to conducting the interviews , recording what you and your respondents say, and transcribing those recordings for data analysis . While this is a simple enough task, it is important to consider the equipment you use to collect data.
If the verbal utterances of your respondents are your sole concern, then an audio recorder should be sufficient for capturing your respondents' answers. Your choice of equipment can be as simple as a smartphone audio recorder application. Alternatively, you can consider professional equipment to make sure you collect as much audio detail as possible from your interviews.
Communication studies, for example, may be more concerned about the interviewer effect (e.g., studies that ask controversial questions to evoke particular responses) or the context effects (i.e., the effect of the surrounding environment on respondents) in interviews . In such cases, interviewers may capture data with video recordings to analyze body language or facial expressions to certain interview questions. Responses caught on video can be analyzed for any patterns across respondents.
Analyzing structured interviews
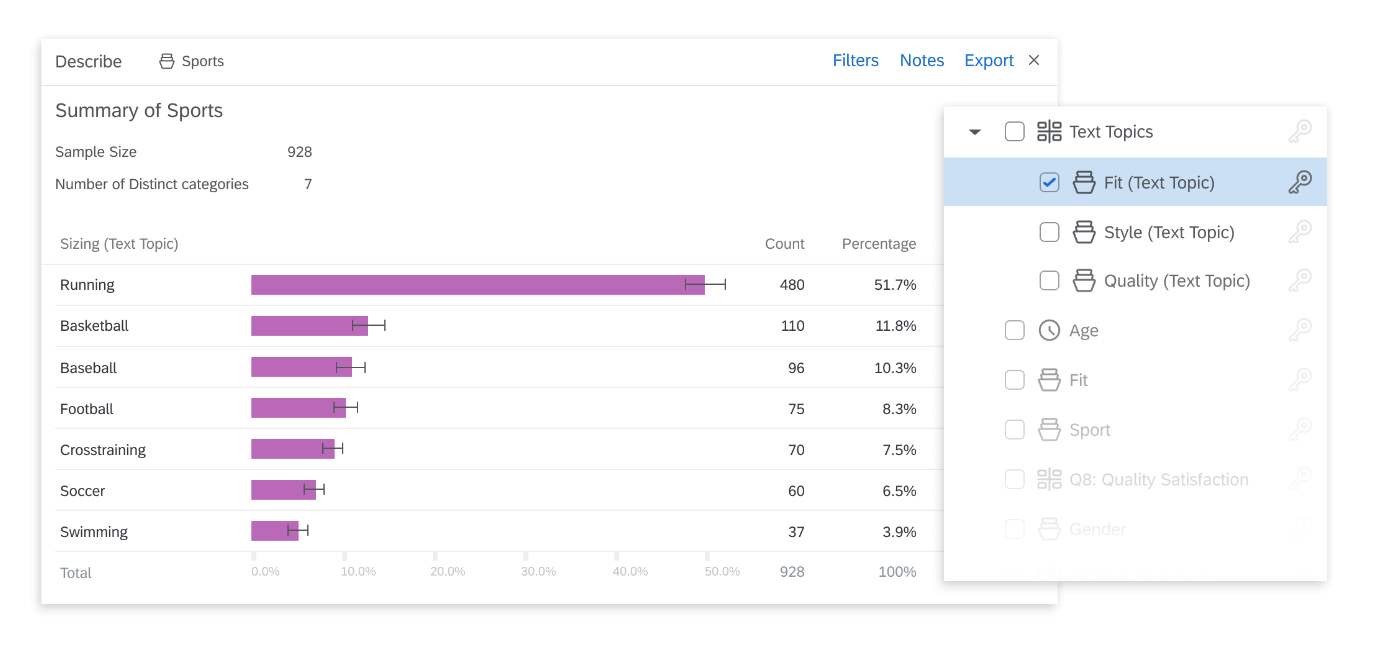
Once you have transcribed your interviews, you can analyze your data. One of the more common means for analyzing qualitative data is thematic analysis , which relies on the identification of commonly recurring themes throughout your research. What codes occur the most often? Are there commonalities across responses that are worth pointing out to your research audience?

It's a good idea to code each response by the question they address. The set order of questions in a structured interview study makes it easy to identify the answers given by each respondent. By coding each answer by the question they respond to and the themes apparent in the response, you will be able to analyze what themes and patterns occur in each set of answers.
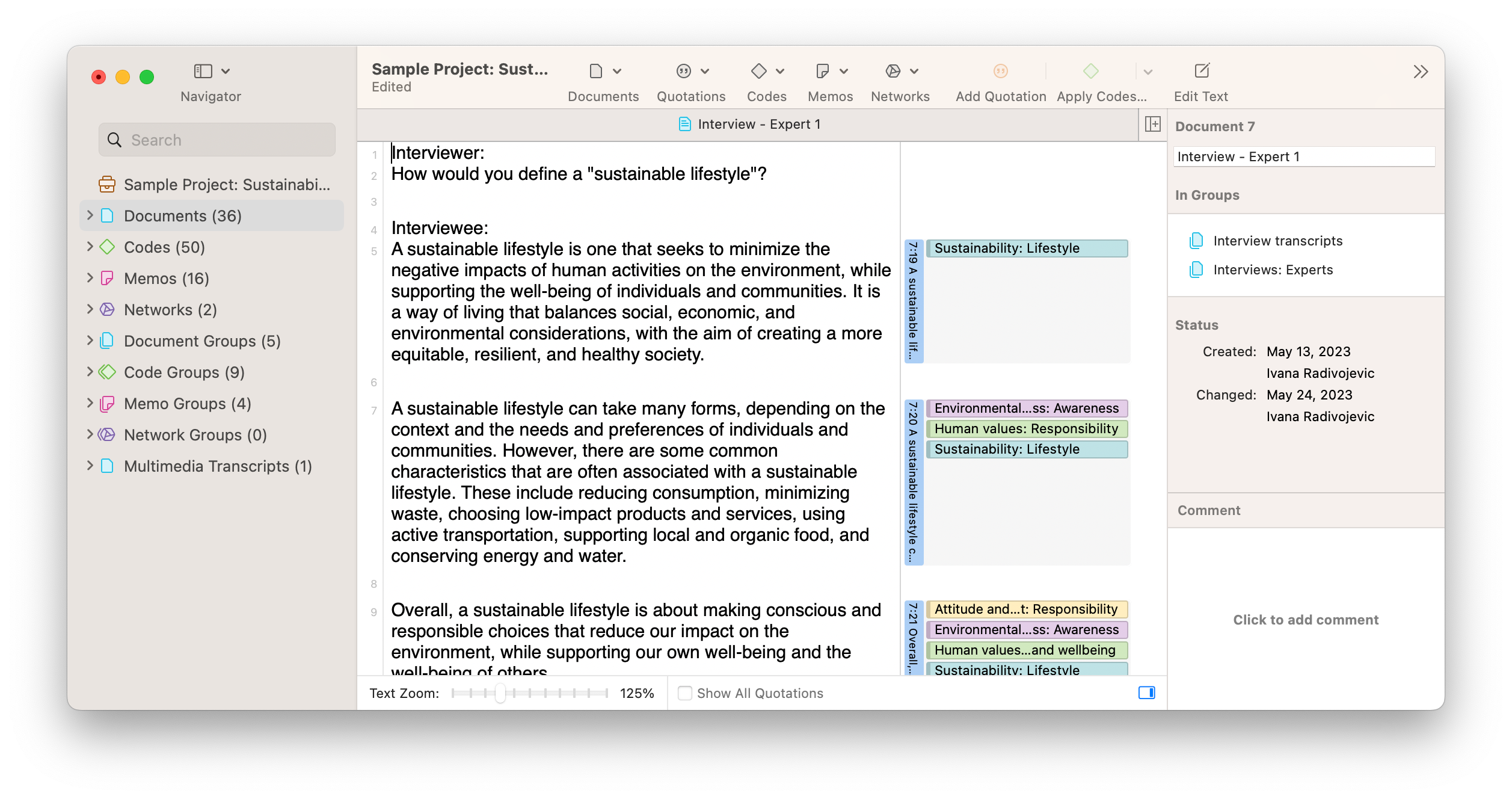
You can also analyze differences between respondents. In ATLAS.ti, you can place interview transcripts into document groups to organize and divide your data along salient categories such as gender, age group, socioeconomic status, and other identifiers you may find useful. In doing so, you will be able to restrict your data analysis to a specific group of interview respondents to see how their answers differ from other groups.
Presenting interview findings
Disseminating qualitative research is often a matter of summarizing the salient points of your data analysis so that it is easy to understand, insightful, and useful to your research audience. For research collecting data from interviews , two of the more common approaches to presenting findings include visualizations and excerpts.
Visualizations are ideal for representing the salient ideas arising from large sets of otherwise unstructured data . Meaningful illustrations such as frequency charts, word clouds, and Sankey diagrams can prove more persuasive than an extended narrative in a research paper or presentation.
Consider the word cloud in the screenshot of ATLAS.ti below. This word cloud was generated from the transcripts of a set of interviews to illustrate what concepts appear the most often in the selected data. Concepts mentioned more often appear closer to the center of the cloud, showing which keywords appear most frequently in the data. Such a visualization can provide a quick illustration to show to your research audience what topics emerged in the data analysis.
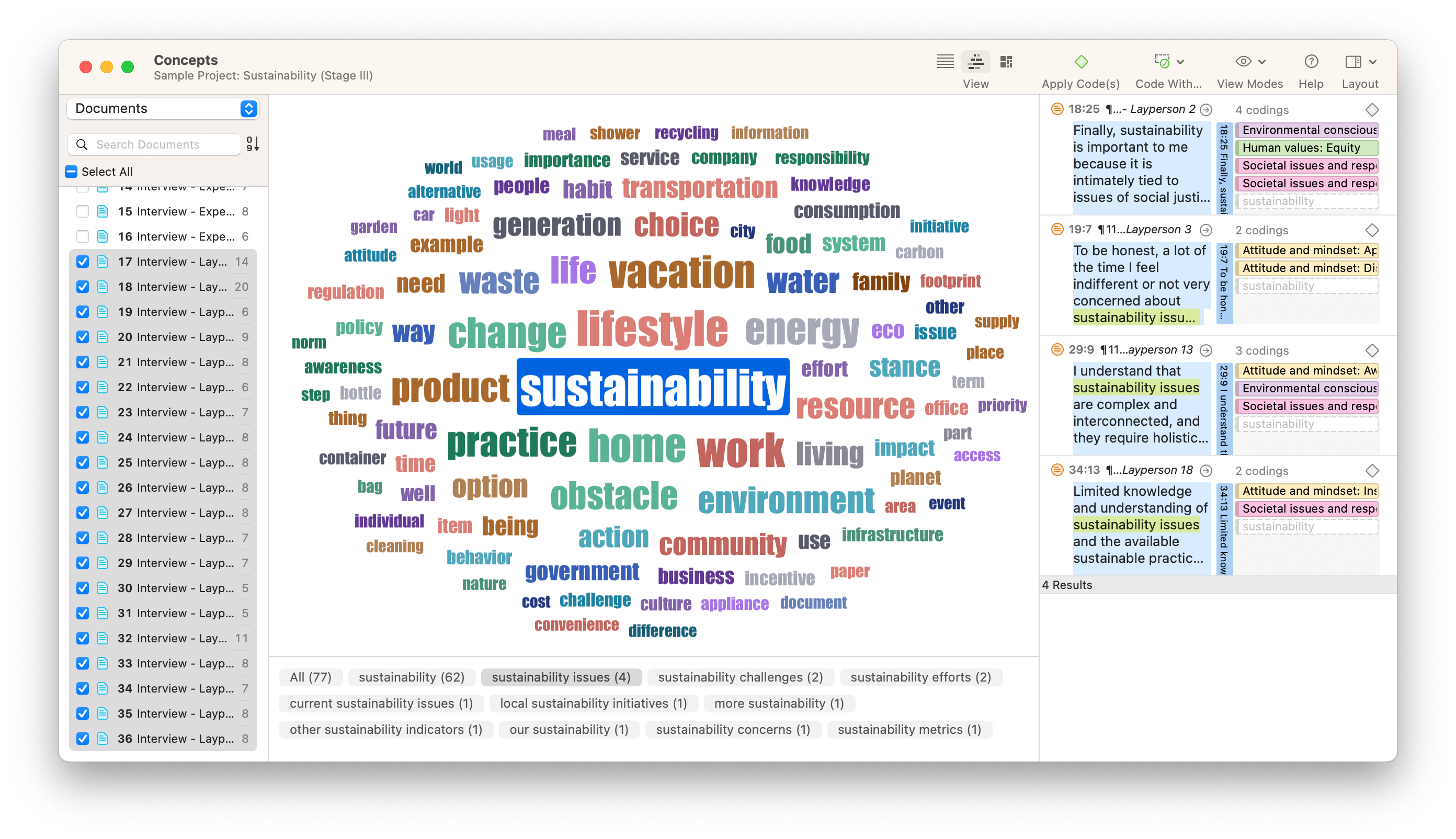
You can also effectively represent each of your themes with an example or two from the responses in your data . Data exemplars are representations that the researcher deems are typical of or significant about the portion of the data under discussion. Often in research that employs interviews or observations , an author will present an exemplar to explain a theme that is significant to theory development or challenges an existing theory.
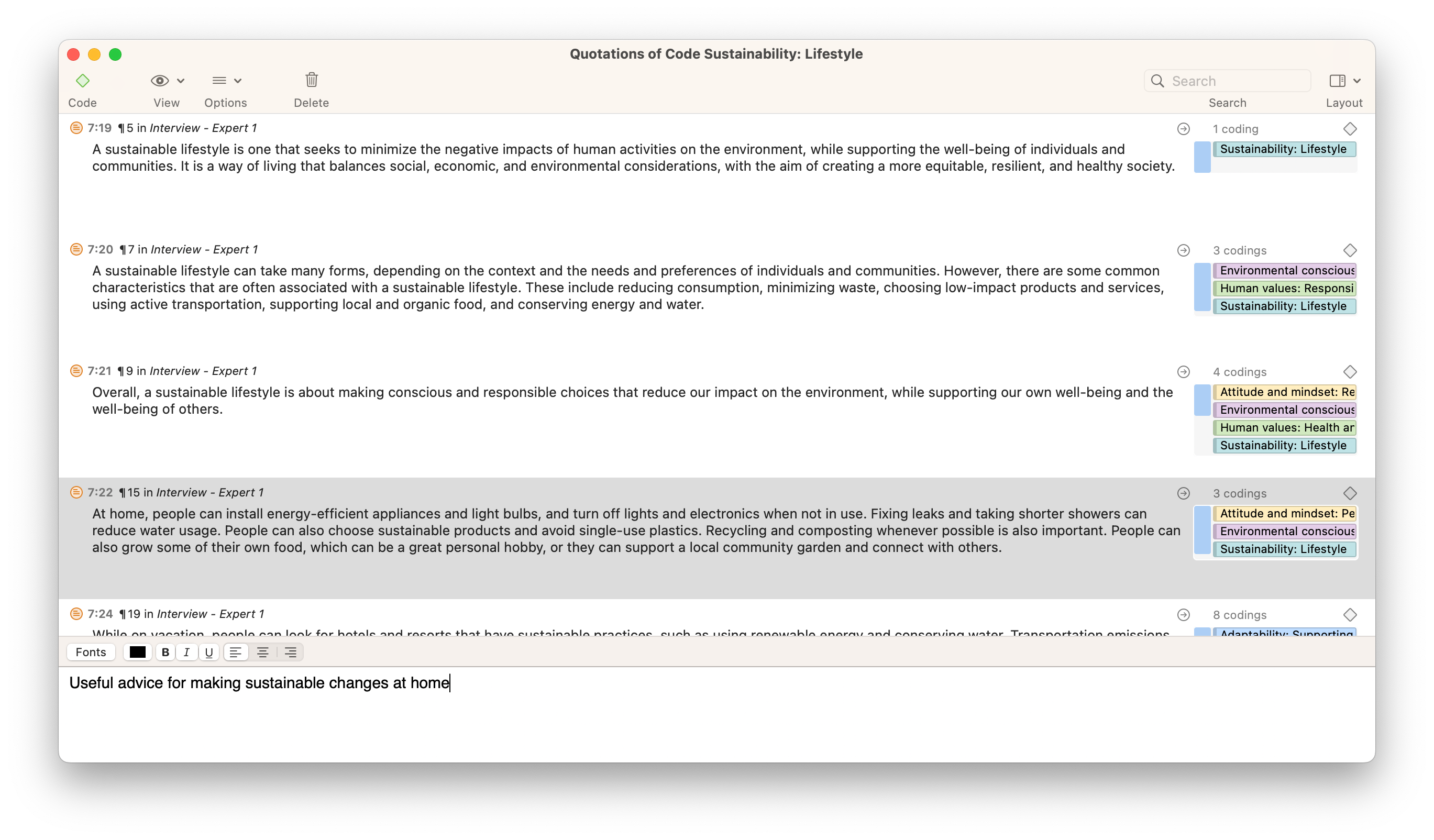
ATLAS.ti provides tools to restrict your view of the data to codes you find significant to your findings. The Code Manager view makes it easy to look not at the entire data set but the specific segments of text that have been coded with a particular code. In similar fashion, ATLAS.ti's Query Tool is ideal for defining a set of criteria based on the codes in the data to see which data segments are most relevant to your research inquiry.
Conduct interview research with ATLAS.ti
Qualitative data analysis made easy with our powerful tools. Try a free trial of ATLAS.ti.

No internet connection.
All search filters on the page have been cleared., your search has been saved..
- All content
- Dictionaries
- Encyclopedias
- Expert Insights
- Foundations
- How-to Guides
- Journal Articles
- Little Blue Books
- Little Green Books
- Project Planner
- Tools Directory
- Sign in to my profile My Profile
- Sign in Signed in
- My profile My Profile
- Offline Playback link

Have you created a personal profile? sign in or create a profile so that you can create alerts, save clips, playlists and searches.
The Structured Interview
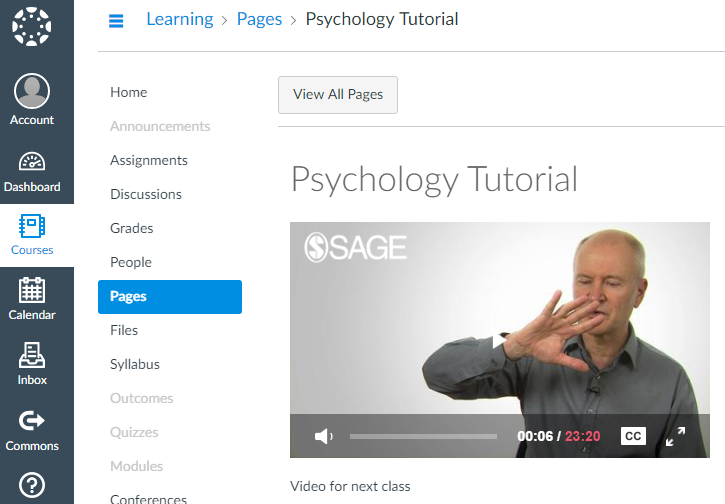
- Watching now: Chapter 1: Overview of the Structured Interview for Qualitative Research Start time: 00:00:00 End time: 00:04:12
Video Type: Tutorial
(2015). The structured interview [Video]. Sage Research Methods. https:// doi. org/10.4135/9781529622171
"The Structured Interview." In Sage Video . : Leigh Hall, 2015. Video, 00:04:12. https:// doi. org/10.4135/9781529622171.
, 2015. The Structured Interview , Sage Video. [Streaming Video] London: Sage Publications Ltd. Available at: <https:// doi. org/10.4135/9781529622171 & gt; [Accessed 30 Mar 2024].
The Structured Interview . Online video clip. SAGE Video. London: SAGE Publications, Ltd., 6 Dec 2022. doi: https:// doi. org/10.4135/9781529622171. 30 Mar 2024.
The Structured Interview [Streaming video]. 2015. doi:10.4135/9781529622171. Accessed 03/30/2024
Please log in from an authenticated institution or log into your member profile to access the email feature.
- Sign in/register
Add this content to your learning management system or webpage by copying the code below into the HTML editor on the page. Look for the words HTML or </>. Learn More about Embedding Video icon link (opens in new window)
Sample View:
- Download PDF opens in new window
- icon/tools/download-video icon/tools/video-downloaded Download video Downloading... Video downloaded
Overview of the structured interview for qualitative research, including defining characteristics, things to know, and reflexive exercises.
Chapter 1: Overview of the Structured Interview for Qualitative Research
- Start time: 00:00:00
- End time: 00:04:12
- Product: Sage Research Methods Video: Qualitative and Mixed Methods
- Type of Content: Tutorial
- Title: The Structured Interview
- Publisher: Leigh Hall
- Series: How To Design & Conduct Interviews for Qualitative Research
- Publication year: 2015
- Online pub date: December 06, 2022
- Discipline: Sociology , History , Education , Criminology and Criminal Justice , Business and Management , Communication and Media Studies , Psychology , Health , Anthropology , Social Policy and Public Policy , Nursing , Political Science and International Relations , Counseling and Psychotherapy , Social Work , Geography , Public Health
- Methods: Qualitative interviewing , Qualitative measures , Structured interviews
- Duration: 00:04:12
- DOI: https:// doi. org/10.4135/9781529622171
- Keywords: interview techniques , qualitative interview , qualitative research , researcher reflexivity , Structured interview Show all Show less
- Online ISBN: 9781529622171 Copyright: Copyright Leigh Hall , 2015 More information Less information
Sign in to access this content
Get a 30 day free trial, more like this, sage recommends.
We found other relevant content for you on other Sage platforms.
Have you created a personal profile? Login or create a profile so that you can save clips, playlists and searches
Navigating away from this page will delete your results
Please save your results to "My Self-Assessments" in your profile before navigating away from this page.
Sign in to my profile
Sign up for a free trial and experience all Sage Learning Resources have to offer.
You must have a valid academic email address to sign up.
Get off-campus access
- View or download all content my institution has access to.
Sign up for a free trial and experience all Sage Research Methods has to offer.
- view my profile
- view my lists
Qualitative Research 101: Interviewing
5 Common Mistakes To Avoid When Undertaking Interviews
By: David Phair (PhD) and Kerryn Warren (PhD) | March 2022
Undertaking interviews is potentially the most important step in the qualitative research process. If you don’t collect useful, useable data in your interviews, you’ll struggle through the rest of your dissertation or thesis. Having helped numerous students with their research over the years, we’ve noticed some common interviewing mistakes that first-time researchers make. In this post, we’ll discuss five costly interview-related mistakes and outline useful strategies to avoid making these.
Overview: 5 Interviewing Mistakes
- Not having a clear interview strategy /plan
- Not having good interview techniques /skills
- Not securing a suitable location and equipment
- Not having a basic risk management plan
- Not keeping your “ golden thread ” front of mind
1. Not having a clear interview strategy
The first common mistake that we’ll look at is that of starting the interviewing process without having first come up with a clear interview strategy or plan of action. While it’s natural to be keen to get started engaging with your interviewees, a lack of planning can result in a mess of data and inconsistency between interviews.
There are several design choices to decide on and plan for before you start interviewing anyone. Some of the most important questions you need to ask yourself before conducting interviews include:
- What are the guiding research aims and research questions of my study?
- Will I use a structured, semi-structured or unstructured interview approach?
- How will I record the interviews (audio or video)?
- Who will be interviewed and by whom ?
- What ethics and data law considerations do I need to adhere to?
- How will I analyze my data?
Let’s take a quick look at some of these.
The core objective of the interviewing process is to generate useful data that will help you address your overall research aims. Therefore, your interviews need to be conducted in a way that directly links to your research aims, objectives and research questions (i.e. your “golden thread”). This means that you need to carefully consider the questions you’ll ask to ensure that they align with and feed into your golden thread. If any question doesn’t align with this, you may want to consider scrapping it.
Another important design choice is whether you’ll use an unstructured, semi-structured or structured interview approach . For semi-structured interviews, you will have a list of questions that you plan to ask and these questions will be open-ended in nature. You’ll also allow the discussion to digress from the core question set if something interesting comes up. This means that the type of information generated might differ a fair amount between interviews.
Contrasted to this, a structured approach to interviews is more rigid, where a specific set of closed questions is developed and asked for each interviewee in exactly the same order. Closed questions have a limited set of answers, that are often single-word answers. Therefore, you need to think about what you’re trying to achieve with your research project (i.e. your research aims) and decided on which approach would be best suited in your case.
It is also important to plan ahead with regards to who will be interviewed and how. You need to think about how you will approach the possible interviewees to get their cooperation, who will conduct the interviews, when to conduct the interviews and how to record the interviews. For each of these decisions, it’s also essential to make sure that all ethical considerations and data protection laws are taken into account.
Finally, you should think through how you plan to analyze the data (i.e., your qualitative analysis method) generated by the interviews. Different types of analysis rely on different types of data, so you need to ensure you’re asking the right types of questions and correctly guiding your respondents.
Simply put, you need to have a plan of action regarding the specifics of your interview approach before you start collecting data. If not, you’ll end up drifting in your approach from interview to interview, which will result in inconsistent, unusable data.

2. Not having good interview technique
While you’re generally not expected to become you to be an expert interviewer for a dissertation or thesis, it is important to practice good interview technique and develop basic interviewing skills .
Let’s go through some basics that will help the process along.
Firstly, before the interview , make sure you know your interview questions well and have a clear idea of what you want from the interview. Naturally, the specificity of your questions will depend on whether you’re taking a structured, semi-structured or unstructured approach, but you still need a consistent starting point . Ideally, you should develop an interview guide beforehand (more on this later) that details your core question and links these to the research aims, objectives and research questions.
Before you undertake any interviews, it’s a good idea to do a few mock interviews with friends or family members. This will help you get comfortable with the interviewer role, prepare for potentially unexpected answers and give you a good idea of how long the interview will take to conduct. In the interviewing process, you’re likely to encounter two kinds of challenging interviewees ; the two-word respondent and the respondent who meanders and babbles. Therefore, you should prepare yourself for both and come up with a plan to respond to each in a way that will allow the interview to continue productively.
To begin the formal interview , provide the person you are interviewing with an overview of your research. This will help to calm their nerves (and yours) and contextualize the interaction. Ultimately, you want the interviewee to feel comfortable and be willing to be open and honest with you, so it’s useful to start in a more casual, relaxed fashion and allow them to ask any questions they may have. From there, you can ease them into the rest of the questions.
As the interview progresses , avoid asking leading questions (i.e., questions that assume something about the interviewee or their response). Make sure that you speak clearly and slowly , using plain language and being ready to paraphrase questions if the person you are interviewing misunderstands. Be particularly careful with interviewing English second language speakers to ensure that you’re both on the same page.
Engage with the interviewee by listening to them carefully and acknowledging that you are listening to them by smiling or nodding. Show them that you’re interested in what they’re saying and thank them for their openness as appropriate. This will also encourage your interviewee to respond openly.
Need a helping hand?
3. Not securing a suitable location and quality equipment
Where you conduct your interviews and the equipment you use to record them both play an important role in how the process unfolds. Therefore, you need to think carefully about each of these variables before you start interviewing.
Poor location: A bad location can result in the quality of your interviews being compromised, interrupted, or cancelled. If you are conducting physical interviews, you’ll need a location that is quiet, safe, and welcoming . It’s very important that your location of choice is not prone to interruptions (the workplace office is generally problematic, for example) and has suitable facilities (such as water, a bathroom, and snacks).
If you are conducting online interviews , you need to consider a few other factors. Importantly, you need to make sure that both you and your respondent have access to a good, stable internet connection and electricity. Always check before the time that both of you know how to use the relevant software and it’s accessible (sometimes meeting platforms are blocked by workplace policies or firewalls). It’s also good to have alternatives in place (such as WhatsApp, Zoom, or Teams) to cater for these types of issues.
Poor equipment: Using poor-quality recording equipment or using equipment incorrectly means that you will have trouble transcribing, coding, and analyzing your interviews. This can be a major issue , as some of your interview data may go completely to waste if not recorded well. So, make sure that you use good-quality recording equipment and that you know how to use it correctly.
To avoid issues, you should always conduct test recordings before every interview to ensure that you can use the relevant equipment properly. It’s also a good idea to spot check each recording afterwards, just to make sure it was recorded as planned. If your equipment uses batteries, be sure to always carry a spare set.

4. Not having a basic risk management plan
Many possible issues can arise during the interview process. Not planning for these issues can mean that you are left with compromised data that might not be useful to you. Therefore, it’s important to map out some sort of risk management plan ahead of time, considering the potential risks, how you’ll minimize their probability and how you’ll manage them if they materialize.
Common potential issues related to the actual interview include cancellations (people pulling out), delays (such as getting stuck in traffic), language and accent differences (especially in the case of poor internet connections), issues with internet connections and power supply. Other issues can also occur in the interview itself. For example, the interviewee could drift off-topic, or you might encounter an interviewee who does not say much at all.
You can prepare for these potential issues by considering possible worst-case scenarios and preparing a response for each scenario. For instance, it is important to plan a backup date just in case your interviewee cannot make it to the first meeting you scheduled with them. It’s also a good idea to factor in a 30-minute gap between your interviews for the instances where someone might be late, or an interview runs overtime for other reasons. Make sure that you also plan backup questions that could be used to bring a respondent back on topic if they start rambling, or questions to encourage those who are saying too little.
In general, it’s best practice to plan to conduct more interviews than you think you need (this is called oversampling ). Doing so will allow you some room for error if there are interviews that don’t go as planned, or if some interviewees withdraw. If you need 10 interviews, it is a good idea to plan for 15. Likely, a few will cancel , delay, or not produce useful data.

5. Not keeping your golden thread front of mind
We touched on this a little earlier, but it is a key point that should be central to your entire research process. You don’t want to end up with pages and pages of data after conducting your interviews and realize that it is not useful to your research aims . Your research aims, objectives and research questions – i.e., your golden thread – should influence every design decision and should guide the interview process at all times.
A useful way to avoid this mistake is by developing an interview guide before you begin interviewing your respondents. An interview guide is a document that contains all of your questions with notes on how each of the interview questions is linked to the research question(s) of your study. You can also include your research aims and objectives here for a more comprehensive linkage.
You can easily create an interview guide by drawing up a table with one column containing your core interview questions . Then add another column with your research questions , another with expectations that you may have in light of the relevant literature and another with backup or follow-up questions . As mentioned, you can also bring in your research aims and objectives to help you connect them all together. If you’d like, you can download a copy of our free interview guide here .
Recap: Qualitative Interview Mistakes
In this post, we’ve discussed 5 common costly mistakes that are easy to make in the process of planning and conducting qualitative interviews.
To recap, these include:
If you have any questions about these interviewing mistakes, drop a comment below. Alternatively, if you’re interested in getting 1-on-1 help with your thesis or dissertation , check out our dissertation coaching service or book a free initial consultation with one of our friendly Grad Coaches.
Psst… there’s more (for free)
This post is part of our dissertation mini-course, which covers everything you need to get started with your dissertation, thesis or research project.
You Might Also Like:

Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
The Interview Method In Psychology
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
Interviews involve a conversation with a purpose, but have some distinct features compared to ordinary conversation, such as being scheduled in advance, having an asymmetry in outcome goals between interviewer and interviewee, and often following a question-answer format.
Interviews are different from questionnaires as they involve social interaction. Unlike questionnaire methods, researchers need training in interviewing (which costs money).

How Do Interviews Work?
Researchers can ask different types of questions, generating different types of data . For example, closed questions provide people with a fixed set of responses, whereas open questions allow people to express what they think in their own words.
The researcher will often record interviews, and the data will be written up as a transcript (a written account of interview questions and answers) which can be analyzed later.
It should be noted that interviews may not be the best method for researching sensitive topics (e.g., truancy in schools, discrimination, etc.) as people may feel more comfortable completing a questionnaire in private.
There are different types of interviews, with a key distinction being the extent of structure. Semi-structured is most common in psychology research. Unstructured interviews have a free-flowing style, while structured interviews involve preset questions asked in a particular order.
Structured Interview
A structured interview is a quantitative research method where the interviewer a set of prepared closed-ended questions in the form of an interview schedule, which he/she reads out exactly as worded.
Interviews schedules have a standardized format, meaning the same questions are asked to each interviewee in the same order (see Fig. 1).

Figure 1. An example of an interview schedule
The interviewer will not deviate from the interview schedule (except to clarify the meaning of the question) or probe beyond the answers received. Replies are recorded on a questionnaire, and the order and wording of questions, and sometimes the range of alternative answers, is preset by the researcher.
A structured interview is also known as a formal interview (like a job interview).
- Structured interviews are easy to replicate as a fixed set of closed questions are used, which are easy to quantify – this means it is easy to test for reliability .
- Structured interviews are fairly quick to conduct which means that many interviews can take place within a short amount of time. This means a large sample can be obtained, resulting in the findings being representative and having the ability to be generalized to a large population.
Limitations
- Structured interviews are not flexible. This means new questions cannot be asked impromptu (i.e., during the interview), as an interview schedule must be followed.
- The answers from structured interviews lack detail as only closed questions are asked, which generates quantitative data . This means a researcher won’t know why a person behaves a certain way.
Unstructured Interview
Unstructured interviews do not use any set questions, instead, the interviewer asks open-ended questions based on a specific research topic, and will try to let the interview flow like a natural conversation. The interviewer modifies his or her questions to suit the candidate’s specific experiences.
Unstructured interviews are sometimes referred to as ‘discovery interviews’ and are more like a ‘guided conservation’ than a strictly structured interview. They are sometimes called informal interviews.
Unstructured interviews are most useful in qualitative research to analyze attitudes and values. Though they rarely provide a valid basis for generalization, their main advantage is that they enable the researcher to probe social actors’ subjective points of view.
Interviewer Self-Disclosure
Interviewer self-disclosure involves the interviewer revealing personal information or opinions during the research interview. This may increase rapport but risks changing dynamics away from a focus on facilitating the interviewee’s account.
In unstructured interviews, the informal conversational style may deliberately include elements of interviewer self-disclosure, mirroring ordinary conversation dynamics.
Interviewer self-disclosure risks changing the dynamics away from facilitation of interviewee accounts. It should not be ruled out entirely but requires skillful handling informed by reflection.
- An informal interviewing style with some interviewer self-disclosure may increase rapport and participant openness. However, it also increases the chance of the participant converging opinions with the interviewer.
- Complete interviewer neutrality is unlikely. However, excessive informality and self-disclosure risk the interview becoming more of an ordinary conversation and producing consensus accounts.
- Overly personal disclosures could also be seen as irrelevant and intrusive by participants. They may invite increased intimacy on uncomfortable topics.
- The safest approach seems to be to avoid interviewer self-disclosures in most cases. Where an informal style is used, disclosures require careful judgment and substantial interviewing experience.
- If asked for personal opinions during an interview, the interviewer could highlight the defined roles and defer that discussion until after the interview.
- Unstructured interviews are more flexible as questions can be adapted and changed depending on the respondents’ answers. The interview can deviate from the interview schedule.
- Unstructured interviews generate qualitative data through the use of open questions. This allows the respondent to talk in some depth, choosing their own words. This helps the researcher develop a real sense of a person’s understanding of a situation.
- They also have increased validity because it gives the interviewer the opportunity to probe for a deeper understanding, ask for clarification & allow the interviewee to steer the direction of the interview, etc. Interviewers have the chance to clarify any questions of participants during the interview.
- It can be time-consuming to conduct an unstructured interview and analyze the qualitative data (using methods such as thematic analysis).
- Employing and training interviewers is expensive and not as cheap as collecting data via questionnaires . For example, certain skills may be needed by the interviewer. These include the ability to establish rapport and knowing when to probe.
- Interviews inevitably co-construct data through researchers’ agenda-setting and question-framing. Techniques like open questions provide only limited remedies.
Focus Group Interview
Focus group interview is a qualitative approach where a group of respondents are interviewed together, used to gain an in‐depth understanding of social issues.
This type of interview is often referred to as a focus group because the job of the interviewer ( or moderator ) is to bring the group to focus on the issue at hand. Initially, the goal was to reach a consensus among the group, but with the development of techniques for analyzing group qualitative data, there is less emphasis on consensus building.
The method aims to obtain data from a purposely selected group of individuals rather than from a statistically representative sample of a broader population.
The role of the interview moderator is to make sure the group interacts with each other and do not drift off-topic. Ideally, the moderator will be similar to the participants in terms of appearance, have adequate knowledge of the topic being discussed, and exercise mild unobtrusive control over dominant talkers and shy participants.
A researcher must be highly skilled to conduct a focus group interview. For example, the moderator may need certain skills, including the ability to establish rapport and know when to probe.
- Group interviews generate qualitative narrative data through the use of open questions. This allows the respondents to talk in some depth, choosing their own words. This helps the researcher develop a real sense of a person’s understanding of a situation. Qualitative data also includes observational data, such as body language and facial expressions.
- Group responses are helpful when you want to elicit perspectives on a collective experience, encourage diversity of thought, reduce researcher bias, and gather a wider range of contextualized views.
- They also have increased validity because some participants may feel more comfortable being with others as they are used to talking in groups in real life (i.e., it’s more natural).
- When participants have common experiences, focus groups allow them to build on each other’s comments to provide richer contextual data representing a wider range of views than individual interviews.
- Focus groups are a type of group interview method used in market research and consumer psychology that are cost – effective for gathering the views of consumers .
- The researcher must ensure that they keep all the interviewees” details confidential and respect their privacy. This is difficult when using a group interview. For example, the researcher cannot guarantee that the other people in the group will keep information private.
- Group interviews are less reliable as they use open questions and may deviate from the interview schedule, making them difficult to repeat.
- It is important to note that there are some potential pitfalls of focus groups, such as conformity, social desirability, and oppositional behavior, that can reduce the usefulness of the data collected.
For example, group interviews may sometimes lack validity as participants may lie to impress the other group members. They may conform to peer pressure and give false answers.
To avoid these pitfalls, the interviewer needs to have a good understanding of how people function in groups as well as how to lead the group in a productive discussion.
Semi-Structured Interview
Semi-structured interviews lie between structured and unstructured interviews. The interviewer prepares a set of same questions to be answered by all interviewees. Additional questions might be asked during the interview to clarify or expand certain issues.
In semi-structured interviews, the interviewer has more freedom to digress and probe beyond the answers. The interview guide contains a list of questions and topics that need to be covered during the conversation, usually in a particular order.
Semi-structured interviews are most useful to address the ‘what’, ‘how’, and ‘why’ research questions. Both qualitative and quantitative analyses can be performed on data collected during semi-structured interviews.
- Semi-structured interviews allow respondents to answer more on their terms in an informal setting yet provide uniform information making them ideal for qualitative analysis.
- The flexible nature of semi-structured interviews allows ideas to be introduced and explored during the interview based on the respondents’ answers.
- Semi-structured interviews can provide reliable and comparable qualitative data. Allows the interviewer to probe answers, where the interviewee is asked to clarify or expand on the answers provided.
- The data generated remain fundamentally shaped by the interview context itself. Analysis rarely acknowledges this endemic co-construction.
- They are more time-consuming (to conduct, transcribe, and analyze) than structured interviews.
- The quality of findings is more dependent on the individual skills of the interviewer than in structured interviews. Skill is required to probe effectively while avoiding biasing responses.
The Interviewer Effect
Face-to-face interviews raise methodological problems. These stem from the fact that interviewers are themselves role players, and their perceived status may influence the replies of the respondents.
Because an interview is a social interaction, the interviewer’s appearance or behavior may influence the respondent’s answers. This is a problem as it can bias the results of the study and make them invalid.
For example, the gender, ethnicity, body language, age, and social status of the interview can all create an interviewer effect. If there is a perceived status disparity between the interviewer and the interviewee, the results of interviews have to be interpreted with care. This is pertinent for sensitive topics such as health.
For example, if a researcher was investigating sexism amongst males, would a female interview be preferable to a male? It is possible that if a female interviewer was used, male participants might lie (i.e., pretend they are not sexist) to impress the interviewer, thus creating an interviewer effect.
Flooding interviews with researcher’s agenda
The interactional nature of interviews means the researcher fundamentally shapes the discourse, rather than just neutrally collecting it. This shapes what is talked about and how participants can respond.
- The interviewer’s assumptions, interests, and categories don’t just shape the specific interview questions asked. They also shape the framing, task instructions, recruitment, and ongoing responses/prompts.
- This flooding of the interview interaction with the researcher’s agenda makes it very difficult to separate out what comes from the participant vs. what is aligned with the interviewer’s concerns.
- So the participant’s talk ends up being fundamentally shaped by the interviewer rather than being a more natural reflection of the participant’s own orientations or practices.
- This effect is hard to avoid because interviews inherently involve the researcher setting an agenda. But it does mean the talk extracted may say more about the interview process than the reality it is supposed to reflect.
Interview Design
First, you must choose whether to use a structured or non-structured interview.
Characteristics of Interviewers
Next, you must consider who will be the interviewer, and this will depend on what type of person is being interviewed. There are several variables to consider:
- Gender and age : This can greatly affect respondents’ answers, particularly on personal issues.
- Personal characteristics : Some people are easier to get on with than others. Also, the interviewer’s accent and appearance (e.g., clothing) can affect the rapport between the interviewer and interviewee.
- Language : The interviewer’s language should be appropriate to the vocabulary of the group of people being studied. For example, the researcher must change the questions’ language to match the respondents’ social background” age / educational level / social class/ethnicity, etc.
- Ethnicity : People may have difficulty interviewing people from different ethnic groups.
- Interviewer expertise should match research sensitivity – inexperienced students should avoid interviewing highly vulnerable groups.
Interview Location
The location of a research interview can influence the way in which the interviewer and interviewee relate and may exaggerate a power dynamic in one direction or another. It is usual to offer interviewees a choice of location as part of facilitating their comfort and encouraging participation.
However, the safety of the interviewer is an overriding consideration and, as mentioned, a minimal requirement should be that a responsible person knows where the interviewer has gone and when they are due back.
Remote Interviews
The COVID-19 pandemic necessitated remote interviewing for research continuity. However online interview platforms provide increased flexibility even under normal conditions.
They enable access to participant groups across geographical distances without travel costs or arrangements. Online interviews can be efficiently scheduled to align with researcher and interviewee availability.
There are practical considerations in setting up remote interviews. Interviewees require access to internet and an online platform such as Zoom, Microsoft Teams or Skype through which to connect.
Certain modifications help build initial rapport in the remote format. Allowing time at the start of the interview for casual conversation while testing audio/video quality helps participants settle in. Minor delays can disrupt turn-taking flow, so alerting participants to speak slightly slower than usual minimizes accidental interruptions.
Keeping remote interviews under an hour avoids fatigue for stare at a screen. Seeking advanced ethical clearance for verbal consent at the interview start saves participant time. Adapting to the remote context shows care for interviewees and aids rich discussion.
However, it remains important to critically reflect on how removing in-person dynamics may shape the co-created data. Perhaps some nuances of trust and disclosure differ over video.
Vulnerable Groups
The interviewer must ensure that they take special care when interviewing vulnerable groups, such as children. For example, children have a limited attention span, so lengthy interviews should be avoided.
Developing an Interview Schedule
An interview schedule is a list of pre-planned, structured questions that have been prepared, to serve as a guide for interviewers, researchers and investigators in collecting information or data about a specific topic or issue.
- List the key themes or topics that must be covered to address your research questions. This will form the basic content.
- Organize the content logically, such as chronologically following the interviewee’s experiences. Place more sensitive topics later in the interview.
- Develop the list of content into actual questions and prompts. Carefully word each question – keep them open-ended, non-leading, and focused on examples.
- Add prompts to remind you to cover areas of interest.
- Pilot test the interview schedule to check it generates useful data and revise as needed.
- Be prepared to refine the schedule throughout data collection as you learn which questions work better.
- Practice skills like asking follow-up questions to get depth and detail. Stay flexible to depart from the schedule when needed.
- Keep questions brief and clear. Avoid multi-part questions that risk confusing interviewees.
- Listen actively during interviews to determine which pre-planned questions can be skipped based on information the participant has already provided.
The key is balancing preparation with the flexibility to adapt questions based on each interview interaction. With practice, you’ll gain skills to conduct productive interviews that obtain rich qualitative data.
The Power of Silence
Strategic use of silence is a key technique to generate interviewee-led data, but it requires judgment about appropriate timing and duration to maintain mutual understanding.
- Unlike ordinary conversation, the interviewer aims to facilitate the interviewee’s contribution without interrupting. This often means resisting the urge to speak at the end of the interviewee’s turn construction units (TCUs).
- Leaving a silence after a TCU encourages the interviewee to provide more material without being led by the interviewer. However, this simple technique requires confidence, as silence can feel socially awkward.
- Allowing longer silences (e.g. 24 seconds) later in interviews can work well, but early on even short silences may disrupt rapport if they cause misalignment between speakers.
- Silence also allows interviewees time to think before answering. Rushing to re-ask or amend questions can limit responses.
- Blunt backchannels like “mm hm” also avoid interrupting flow. Interruptions, especially to finish an interviewee’s turn, are problematic as they make the ownership of perspectives unclear.
- If interviewers incorrectly complete turns, an upside is it can produce extended interviewee narratives correcting the record. However, silence would have been better to let interviewees shape their own accounts.
Recording & Transcription
Design choices.
Design choices around recording and engaging closely with transcripts influence analytic insights, as well as practical feasibility. Weighing up relevant tradeoffs is key.
- Audio recording is standard, but video better captures contextual details, which is useful for some topics/analysis approaches. Participants may find video invasive for sensitive research.
- Digital formats enable the sharing of anonymized clips. Additional microphones reduce audio issues.
- Doing all transcription is time-consuming. Outsourcing can save researcher effort but needs confidentiality assurances. Always carefully check outsourced transcripts.
- Online platform auto-captioning can facilitate rapid analysis, but accuracy limitations mean full transcripts remain ideal. Software cleans up caption file formatting.
- Verbatim transcripts best capture nuanced meaning, but the level of detail needed depends on the analysis approach. Referring back to recordings is still advisable during analysis.
- Transcripts versus recordings highlight different interaction elements. Transcripts make overt disagreements clearer through the wording itself. Recordings better convey tone affiliativeness.
Transcribing Interviews & Focus Groups
Here are the steps for transcribing interviews:
- Play back audio/video files to develop an overall understanding of the interview
- Format the transcription document:
- Add line numbers
- Separate interviewer questions and interviewee responses
- Use formatting like bold, italics, etc. to highlight key passages
- Provide sentence-level clarity in the interviewee’s responses while preserving their authentic voice and word choices
- Break longer passages into smaller paragraphs to help with coding
- If translating the interview to another language, use qualified translators and back-translate where possible
- Select a notation system to indicate pauses, emphasis, laughter, interruptions, etc., and adapt it as needed for your data
- Insert screenshots, photos, or documents discussed in the interview at the relevant point in the transcript
- Read through multiple times, revising formatting and notations
- Double-check the accuracy of transcription against audio/videos
- De-identify transcript by removing identifying participant details
The goal is to produce a formatted written record of the verbal interview exchange that captures the meaning and highlights important passages ready for the coding process. Careful transcription is the vital first step in analysis.
Coding Transcripts
The goal of transcription and coding is to systematically transform interview responses into a set of codes and themes that capture key concepts, experiences and beliefs expressed by participants. Taking care with transcription and coding procedures enhances the validity of qualitative analysis .
- Read through the transcript multiple times to become immersed in the details
- Identify manifest/obvious codes and latent/underlying meaning codes
- Highlight insightful participant quotes that capture key concepts (in vivo codes)
- Create a codebook to organize and define codes with examples
- Use an iterative cycle of inductive (data-driven) coding and deductive (theory-driven) coding
- Refine codebook with clear definitions and examples as you code more transcripts
- Collaborate with other coders to establish the reliability of codes
Ethical Issues
Informed consent.
The participant information sheet must give potential interviewees a good idea of what is involved if taking part in the research.
This will include the general topics covered in the interview, where the interview might take place, how long it is expected to last, how it will be recorded, the ways in which participants’ anonymity will be managed, and incentives offered.
It might be considered good practice to consider true informed consent in interview research to require two distinguishable stages:
- Consent to undertake and record the interview and
- Consent to use the material in research after the interview has been conducted and the content known, or even after the interviewee has seen a copy of the transcript and has had a chance to remove sections, if desired.
Power and Vulnerability
- Early feminist views that sensitivity could equalize power differences are likely naive. The interviewer and interviewee inhabit different knowledge spheres and social categories, indicating structural disparities.
- Power fluctuates within interviews. Researchers rely on participation, yet interviewees control openness and can undermine data collection. Assumptions should be avoided.
- Interviews on sensitive topics may feel like quasi-counseling. Interviewers must refrain from dual roles, instead supplying support service details to all participants.
- Interviewees recruited for trauma experiences may reveal more than anticipated. While generating analytic insights, this risks leaving them feeling exposed.
- Ultimately, power balances resist reconciliation. But reflexively analyzing operations of power serves to qualify rather than nullify situtated qualitative accounts.
Some groups, like those with mental health issues, extreme views, or criminal backgrounds, risk being discredited – treated skeptically by researchers.
This creates tensions with qualitative approaches, often having an empathetic ethos seeking to center subjective perspectives. Analysis should balance openness to offered accounts with critically examining stakes and motivations behind them.
Potter, J., & Hepburn, A. (2005). Qualitative interviews in psychology: Problems and possibilities. Qualitative research in Psychology , 2 (4), 281-307.
Houtkoop-Steenstra, H. (2000). Interaction and the standardized survey interview: The living questionnaire . Cambridge University Press
Madill, A. (2011). Interaction in the semi-structured interview: A comparative analysis of the use of and response to indirect complaints. Qualitative Research in Psychology, 8 (4), 333–353.
Maryudi, A., & Fisher, M. (2020). The power in the interview: A practical guide for identifying the critical role of actor interests in environment research. Forest and Society, 4 (1), 142–150
O’Key, V., Hugh-Jones, S., & Madill, A. (2009). Recruiting and engaging with people in deprived locales: Interviewing families about their eating patterns. Social Psychological Review, 11 (20), 30–35.
Puchta, C., & Potter, J. (2004). Focus group practice . Sage.
Schaeffer, N. C. (1991). Conversation with a purpose— Or conversation? Interaction in the standardized interview. In P. P. Biemer, R. M. Groves, L. E. Lyberg, & N. A. Mathiowetz (Eds.), Measurement errors in surveys (pp. 367–391). Wiley.
Silverman, D. (1973). Interview talk: Bringing off a research instrument. Sociology, 7 (1), 31–48.
- Harvard Library
- Research Guides
- Faculty of Arts & Sciences Libraries
Library Support for Qualitative Research
- Interview Research
- Resources for Methodology
- Remote Research & Virtual Fieldwork
Resources for Research Interviewing
Nih-funded qualitative research.
- Oral History
- Data Management & Repositories
- Campus Access
Types of Interviews
- Engaging Participants
Interview Questions
- Conducting Interviews
- Transcription
- Coding and Analysis
- Managing & Finding Interview Data
- UX & Market Research Interviews
Textbooks, Guidebooks, and Handbooks
- The Ethnographic Interview by James P. Spradley “Spradley wrote this book for the professional and student who have never done ethnographic fieldwork (p. 231) and for the professional ethnographer who is interested in adapting the author’s procedures (p. iv). Part 1 outlines in 3 chapters Spradley’s version of ethnographic research, and it provides the background for Part 2 which consists of 12 guided steps (chapters) ranging from locating and interviewing an informant to writing an ethnography. Most of the examples come from the author’s own fieldwork among U.S. subcultures . . . Steps 6 and 8 explain lucidly how to construct a domain and a taxonomic analysis” (excerpted from book review by James D. Sexton, 1980).
- Fundamentals of Qualitative Research by Johnny Saldana (Series edited by Patricia Leavy) Provides a soup-to-nuts overview of the qualitative data collection process, including interviewing, participant observation, and other methods.
- InterViews by Steinar Kvale Interviewing is an essential tool in qualitative research and this introduction to interviewing outlines both the theoretical underpinnings and the practical aspects of the process. After examining the role of the interview in the research process, Steinar Kvale considers some of the key philosophical issues relating to interviewing: the interview as conversation, hermeneutics, phenomenology, concerns about ethics as well as validity, and postmodernism. Having established this framework, the author then analyzes the seven stages of the interview process - from designing a study to writing it up.
- Practical Evaluation by Michael Quinn Patton Surveys different interviewing strategies, from, a) informal/conversational, to b) interview guide approach, to c) standardized and open-ended, to d) closed/quantitative. Also discusses strategies for wording questions that are open-ended, clear, sensitive, and neutral, while supporting the speaker. Provides suggestions for probing and maintaining control of the interview process, as well as suggestions for recording and transcription.
- The SAGE Handbook of Interview Research by Amir B. Marvasti (Editor); James A. Holstein (Editor); Jaber F. Gubrium (Editor); Karyn D. McKinney (Editor) The new edition of this landmark volume emphasizes the dynamic, interactional, and reflexive dimensions of the research interview. Contributors highlight the myriad dimensions of complexity that are emerging as researchers increasingly frame the interview as a communicative opportunity as much as a data-gathering format. The book begins with the history and conceptual transformations of the interview, which is followed by chapters that discuss the main components of interview practice. Taken together, the contributions to The SAGE Handbook of Interview Research: The Complexity of the Craft encourage readers simultaneously to learn the frameworks and technologies of interviewing and to reflect on the epistemological foundations of the interview craft.
- The SAGE Handbook of Online Research Methods by Nigel G. Fielding, Raymond M. Lee and Grant Blank (Editors) Bringing together the leading names in both qualitative and quantitative online research, this new edition is organised into nine sections: 1. Online Research Methods 2. Designing Online Research 3. Online Data Capture and Data Collection 4. The Online Survey 5. Digital Quantitative Analysis 6. Digital Text Analysis 7. Virtual Ethnography 8. Online Secondary Analysis: Resources and Methods 9. The Future of Online Social Research
ONLINE RESOURCES, COMMUNITIES, AND DATABASES
- Interviews as a Method for Qualitative Research (video) This short video summarizes why interviews can serve as useful data in qualitative research.
- Companion website to Bloomberg and Volpe's Completing Your Qualitative Dissertation: A Road Map from Beginning to End, 4th ed Provides helpful templates and appendices featured in the book, as well as links to other useful dissertation resources.
- International Congress of Qualitative Inquiry Annual conference hosted by the International Center for Qualitative Inquiry at the University of Illinois at Urbana-Champaign, which aims to facilitate the development of qualitative research methods across a wide variety of academic disciplines, among other initiatives.
- METHODSPACE An online home of the research methods community, where practicing researchers share how to make research easier.
- SAGE researchmethods Researchers can explore methods concepts to help them design research projects, understand particular methods or identify a new method, conduct their research, and write up their findings. A "methods map" facilitates finding content on methods.
The decision to conduct interviews, and the type of interviewing to use, should flow from, or align with, the methodological paradigm chosen for your study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these).
Structured:
- Structured Interview. Entry in The SAGE Encyclopedia of Social Science Research Methodsby Floyd J. Fowler Jr., Editors: Michael S. Lewis-Beck; Alan E. Bryman; Tim Futing Liao (Editor) A concise article noting standards, procedures, and recommendations for developing and testing structured interviews. For an example of structured interview questions, you may view the Current Population Survey, May 2008: Public Participation in the Arts Supplement (ICPSR 29641), Apr 15, 2011 at https://doi.org/10.3886/ICPSR29641.v1 (To see the survey questions, preview the user guide, which can be found under the "Data and Documentation" tab. Then, look for page 177 (attachment 8).
Semi-Structured:
- Semi-Structured Interview. Entry in The SAGE Encyclopedia of Qualitative Research Methodsby Lioness Ayres; Editor: Lisa M. Given The semi-structured interview is a qualitative data collection strategy in which the researcher asks informants a series of predetermined but open-ended questions. The researcher has more control over the topics of the interview than in unstructured interviews, but in contrast to structured interviews or questionnaires that use closed questions, there is no fixed range of responses to each question.
Unstructured:
- Unstructured Interview. Entry in The SAGE Encyclopedia of Qualitative Research Methodsby Michael W. Firmin; Editor: Lisa M. Given Unstructured interviews in qualitative research involve asking relatively open-ended questions of research participants in order to discover their percepts on the topic of interest. Interviews, in general, are a foundational means of collecting data when using qualitative research methods. They are designed to draw from the interviewee constructs embedded in his or her thinking and rationale for decision making. The researcher uses an inductive method in data gathering, regardless of whether the interview method is open, structured, or semi-structured. That is, the researcher does not wish to superimpose his or her own viewpoints onto the person being interviewed. Rather, inductively, the researcher wishes to understand the participant's perceptions, helping him or her to articulate percepts such that they will be understood clearly by the journal reader.
Genres and Uses
Focus groups:.
- "Focus Groups." Annual Review of Sociology 22 (1996): 129-1524.by David L. Morgan Discusses the use of focus groups and group interviews as methods for gathering qualitative data used by sociologists and other academic and applied researchers. Focus groups are recommended for giving voice to marginalized groups and revealing the group effect on opinion formation.
- Qualitative Research Methods: A Data Collector's Field Guide (See Module 4: "Focus Groups")by Mack, N., et al. This field guide is based on an approach to doing team-based, collaborative qualitative research that has repeatedly proven successful in research projects sponsored by Family Health International (FHI) throughout the developing world. With its straightforward delivery of information on the main qualitative methods being used in public health research today, the guide speaks to the need for simple yet effective instruction on how to do systematic and ethically sound qualitative research. The aim of the guide is thus practical. In bypassing extensive discussion on the theoretical underpinnings of qualitative research, it distinguishes itself as a how-to guide to be used in the field.
In-Depth (typically One-on-One):
- A Practical Introduction to in-Depth Interviewingby Alan Morris Are you new to qualitative research or a bit rusty and in need of some inspiration? Are you doing a research project involving in-depth interviews? Are you nervous about carrying out your interviews? This book will help you complete your qualitative research project by providing a nuts and bolts introduction to interviewing. With coverage of ethics, preparation strategies and advice for handling the unexpected in the field, this handy guide will help you get to grips with the basics of interviewing before embarking on your research. While recognising that your research question and the context of your research will drive your approach to interviewing, this book provides practical advice often skipped in traditional methods textbooks.
- Qualitative Research Methods: A Data Collector's Field Guide (See Module 3: "In-Depth Interviews")by Mack, N., et al. This field guide is based on an approach to doing team-based, collaborative qualitative research that has repeatedly proven successful in research projects sponsored by Family Health International (FHI) throughout the developing world. With its straightforward delivery of information on the main qualitative methods being used in public health research today, the guide speaks to the need for simple yet effective instruction on how to do systematic and ethically sound qualitative research. The aim of the guide is thus practical. In bypassing extensive discussion on the theoretical underpinnings of qualitative research, it distinguishes itself as a how-to guide to be used in the field.
Folklore Research and Oral Histories:
In addition to the following resource, see the Oral History page of this guide for helpful resources on Oral History interviewing.
American Folklife Center at the Library of Congress. Folklife and Fieldwork: A Layman’s Introduction to Field Techniques Interviews gathered for purposes of folklore research are similar to standard social science interviews in some ways, but also have a good deal in common with oral history approaches to interviewing. The focus in a folklore research interview is on documenting and trying to understand the interviewee's way of life relative to a culture or subculture you are studying. This guide includes helpful advice and tips for conducting fieldwork in folklore, such as tips for planning, conducting, recording, and archiving interviews.
An interdisciplinary scientific program within the Institute for Quantitative Social Science which encourages and facilitates research and instruction in the theory and practice of survey research. The primary mission of PSR is to provide survey research resources to enhance the quality of teaching and research at Harvard.
- Internet, Phone, Mail, and Mixed-Mode Surveysby Don A. Dillman; Jolene D. Smyth; Leah Melani Christian The classic survey design reference, updated for the digital age. The new edition is thoroughly updated and revised, and covers all aspects of survey research. It features expanded coverage of mobile phones, tablets, and the use of do-it-yourself surveys, and Dillman's unique Tailored Design Method is also thoroughly explained. This new edition is complemented by copious examples within the text and accompanying website. It includes: Strategies and tactics for determining the needs of a given survey, how to design it, and how to effectively administer it. How and when to use mail, telephone, and Internet surveys to maximum advantage. Proven techniques to increase response rates. Guidance on how to obtain high-quality feedback from mail, electronic, and other self-administered surveys. Direction on how to construct effective questionnaires, including considerations of layout. The effects of sponsorship on the response rates of surveys. Use of capabilities provided by newly mass-used media: interactivity, presentation of aural and visual stimuli. The Fourth Edition reintroduces the telephone--including coordinating land and mobile.
User Experience (UX) and Marketing:
- See the "UX & Market Research Interviews" tab on this guide, above. May include Focus Groups, above.
Screening for Research Site Selection:
- Research interviews are used not only to furnish research data for theoretical analysis in the social sciences, but also to plan other kinds of studies. For example, interviews may allow researchers to screen appropriate research sites to conduct empirical studies (such as randomized controlled trials) in a variety of fields, from medicine to law. In contrast to interviews conducted in the course of social research, such interviews do not typically serve as the data for final analysis and publication.
ENGAGING PARTICIPANTS
Research ethics .
- Human Subjects (IRB) The Committee on the Use of Human Subjects (CUHS) serves as the Institutional Review Board for the University area which includes the Cambridge and Allston campuses at Harvard. Find your IRB contact person , or learn about required ethics training. You may also find the IRB Lifecycle Guide helpful. This is the preferred IRB portal for Harvard graduate students and other researchers. IRB forms can be downloaded via the ESTR Library (click on the "Templates and Forms" tab, then navigate to pages 2 and 3 to find the documents labelled with “HUA” for the Harvard University Area IRB. Nota bene: You may use these forms only if you submit your study to the Harvard University IRB). The IRB office can be reached through email at [email protected] or by telephone at (617) 496-2847.
- Undergraduate Research Training Program (URTP) Portal The URTP at Harvard University is a comprehensive platform to create better prepared undergraduate researchers. The URTP is comprised of research ethics training sessions, a student-focused curriculum, and an online decision form that will assist students in determining whether their project requires IRB review. Students should examine the URTP's guide for student researchers: Introduction to Human Subjects Research Protection.
- Ethics reports From the Association of Internet Researchers (AoIR)
- Respect, Beneficence, and Justice: QDR General Guidance for Human Participants If you are hoping to share your qualitative interview data in a repository after it has been collected, you will need to plan accordingly via informed consent, careful de-identification procedures, and data access controls. Consider consulting with the Qualitative Research Support Group at Harvard Library and consulting with Harvard's Dataverse contacts to help you think through all of the contingencies and processes.
- "Conducting a Qualitative Child Interview: Methodological Considerations." Journal of Advanced Nursing 42/5 (2003): 434-441 by Kortesluoma, R., et al. The purpose of this article is to illustrate the theoretical premises of child interviewing, as well as to describe some practical methodological solutions used during interviews. Factors that influence data gathered from children and strategies for taking these factors into consideration during the interview are also described.
- "Crossing Cultural Barriers in Research Interviewing." Qualitative Social Work 63/3 (2007): 353-372 by Sands, R., et al. This article critically examines a qualitative research interview in which cultural barriers between a white non-Muslim female interviewer and an African American Muslim interviewee, both from the USA, became evident and were overcome within the same interview.
- Decolonizing Methodologies: Research and Indigenous Peoples by Linda Tuhiwai Smith This essential volume explores intersections of imperialism and research - specifically, the ways in which imperialism is embedded in disciplines of knowledge and tradition as 'regimes of truth.' Concepts such as 'discovery' and 'claiming' are discussed and an argument presented that the decolonization of research methods will help to reclaim control over indigenous ways of knowing and being. The text includes case-studies and examples, and sections on new indigenous literature and the role of research in indigenous struggles for social justice.
This resource, sponsored by University of Oregon Libraries, exemplifies the use of interviewing methodologies in research that foregrounds traditional knowledge. The methodology page summarizes the approach.
- Ethics: The Need to Tread Carefully. Chapter in A Practical Introduction to in-Depth Interviewing by Alan Morris Pay special attention to the sections in chapter 2 on "How to prevent and respond to ethical issues arising in the course of the interview," "Ethics in the writing up of your interviews," and "The Ethics of Care."
- Handbook on Ethical Issues in Anthropology by Joan Cassell (Editor); Sue-Ellen Jacobs (Editor) This publication of the American Anthropological Association presents and discusses issues and sources on ethics in anthropology, as well as realistic case studies of ethical dilemmas. It is meant to help social science faculty introduce discussions of ethics in their courses. Some of the topics are relevant to interviews, or at least to studies of which interviews are a part. See chapters 3 and 4 for cases, with solutions and commentary, respectively.
- Research Ethics from the Chanie Wenjack School for Indigenous Studies, Trent University (Open Access) An overview of Indigenous research ethics and protocols from the across the globe.
- Resources for Equity in Research Consult these resources for guidance on creating and incorporating equitable materials into public health research studies that entail community engagement.
The SAGE Handbook of Qualitative Research Ethics by Ron Iphofen (Editor); Martin Tolich (Editor) This handbook is a much-needed and in-depth review of the distinctive set of ethical considerations which accompanies qualitative research. This is particularly crucial given the emergent, dynamic and interactional nature of most qualitative research, which too often allows little time for reflection on the important ethical responsibilities and obligations. Contributions from leading international researchers have been carefully organized into six key thematic sections: Part One: Thick Descriptions Of Qualitative Research Ethics; Part Two: Qualitative Research Ethics By Technique; Part Three: Ethics As Politics; Part Four: Qualitative Research Ethics With Vulnerable Groups; Part Five: Relational Research Ethics; Part Six: Researching Digitally. This Handbook is a one-stop resource on qualitative research ethics across the social sciences that draws on the lessons learned and the successful methods for surmounting problems - the tried and true, and the new.
RESEARCH COMPLIANCE AND PRIVACY LAWS
Research Compliance Program for FAS/SEAS at Harvard : The Faculty of Arts and Sciences (FAS), including the School of Engineering and Applied Sciences (SEAS), and the Office of the Vice Provost for Research (OVPR) have established a shared Research Compliance Program (RCP). An area of common concern for interview studies is international projects and collaboration . RCP is a resource to provide guidance on which international activities may be impacted by US sanctions on countries, individuals, or entities and whether licenses or other disclosure are required to ship or otherwise share items, technology, or data with foreign collaborators.
- Harvard Global Support Services (GSS) is for students, faculty, staff, and researchers who are studying, researching, or working abroad. Their services span safety and security, health, culture, outbound immigration, employment, financial and legal matters, and research center operations. These include travel briefings and registration, emergency response, guidance on international projects, and managing in-country operations.
Generative AI: Harvard-affiliated researchers should not enter data classified as confidential ( Level 2 and above ), including non-public research data, into publicly-available generative AI tools, in accordance with the University’s Information Security Policy. Information shared with generative AI tools using default settings is not private and could expose proprietary or sensitive information to unauthorized parties.
Privacy Laws: Be mindful of any potential privacy laws that may apply wherever you conduct your interviews. The General Data Protection Regulation is a high-profile example (see below):
- General Data Protection Regulation (GDPR) This Regulation lays down rules relating to the protection of natural persons with regard to the processing of personal data and rules relating to the free movement of personal data. It protects fundamental rights and freedoms of natural persons and in particular their right to the protection of personal data. The free movement of personal data within the Union shall be neither restricted nor prohibited for reasons connected with the protection of natural persons with regard to the processing of personal data. For a nice summary of what the GDPR requires, check out the GDPR "crash course" here .
SEEKING CONSENT
If you would like to see examples of consent forms, ask your local IRB, or take a look at these resources:
- Model consent forms for oral history, suggested by the Centre for Oral History and Digital Storytelling at Concordia University
- For NIH-funded research, see this resource for developing informed consent language in research studies where data and/or biospecimens will be stored and shared for future use.
POPULATION SAMPLING
If you wish to assemble resources to aid in sampling, such as the USPS Delivery Sequence File, telephone books, or directories of organizations and listservs, please contact our data librarian or write to [email protected] .
- Research Randomizer A free web-based service that permits instant random sampling and random assignment. It also contains an interactive tutorial perfect for students taking courses in research methods.
- Practical Tools for Designing and Weighting Survey Samples by Richard Valliant; Jill A. Dever; Frauke Kreuter Survey sampling is fundamentally an applied field. The goal in this book is to put an array of tools at the fingertips of practitioners by explaining approaches long used by survey statisticians, illustrating how existing software can be used to solve survey problems, and developing some specialized software where needed. This book serves at least three audiences: (1) Students seeking a more in-depth understanding of applied sampling either through a second semester-long course or by way of a supplementary reference; (2) Survey statisticians searching for practical guidance on how to apply concepts learned in theoretical or applied sampling courses; and (3) Social scientists and other survey practitioners who desire insight into the statistical thinking and steps taken to design, select, and weight random survey samples. Several survey data sets are used to illustrate how to design samples, to make estimates from complex surveys for use in optimizing the sample allocation, and to calculate weights. Realistic survey projects are used to demonstrate the challenges and provide a context for the solutions. The book covers several topics that either are not included or are dealt with in a limited way in other texts. These areas include: sample size computations for multistage designs; power calculations related to surveys; mathematical programming for sample allocation in a multi-criteria optimization setting; nuts and bolts of area probability sampling; multiphase designs; quality control of survey operations; and statistical software for survey sampling and estimation. An associated R package, PracTools, contains a number of specialized functions for sample size and other calculations. The data sets used in the book are also available in PracTools, so that the reader may replicate the examples or perform further analyses.
- Sampling: Design and Analysis by Sharon L. Lohr Provides a modern introduction to the field of sampling. With a multitude of applications from a variety of disciplines, the book concentrates on the statistical aspects of taking and analyzing a sample. Overall, the book gives guidance on how to tell when a sample is valid or not, and how to design and analyze many different forms of sample surveys.
- Sampling Techniques by William G. Cochran Clearly demonstrates a wide range of sampling methods now in use by governments, in business, market and operations research, social science, medicine, public health, agriculture, and accounting. Gives proofs of all the theoretical results used in modern sampling practice. New topics in this edition include the approximate methods developed for the problem of attaching standard errors or confidence limits to nonlinear estimates made from the results of surveys with complex plans.
- "Understanding the Process of Qualitative Data Collection" in Chapter 13 (pp. 103–1162) of 30 Essential Skills for the Qualitative Researcher by John W. Creswell Provides practical "how-to" information for beginning researchers in the social, behavioral, and health sciences with many applied examples from research design, qualitative inquiry, and mixed methods.The skills presented in this book are crucial for a new qualitative researcher starting a qualitative project.
- Survey Methodology by Robert M. Groves; Floyd J. Fowler; Mick P. Couper; James M. Lepkowski; Eleanor Singer; Roger Tourangeau; Floyd J. Fowler coverage includes sampling frame evaluation, sample design, development of questionnaires, evaluation of questions, alternative modes of data collection, interviewing, nonresponse, post-collection processing of survey data, and practices for maintaining scientific integrity.
The way a qualitative researcher constructs and approaches interview questions should flow from, or align with, the methodological paradigm chosen for the study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these).
Constructing Your Questions
Helpful texts:.
- "Developing Questions" in Chapter 4 (pp. 98–108) of Becoming Qualitative Researchers by Corrine Glesne Ideal for introducing the novice researcher to the theory and practice of qualitative research, this text opens students to the diverse possibilities within this inquiry approach, while helping them understand how to design and implement specific research methods.
- "Learning to Interview in the Social Sciences" Qualitative Inquiry, 9(4) 2003, 643–668 by Roulston, K., deMarrais, K., & Lewis, J. B. See especially the section on "Phrasing and Negotiating Questions" on pages 653-655 and common problems with framing questions noted on pages 659 - 660.
- Qualitative Research Interviewing: Biographic Narrative and Semi-Structured Methods (See sections on “Lightly and Heavily Structured Depth Interviewing: Theory-Questions and Interviewer-Questions” and “Preparing for any Interviewing Sequence") by Tom Wengraf Unique in its conceptual coherence and the level of practical detail, this book provides a comprehensive resource for those concerned with the practice of semi-structured interviewing, the most commonly used interview approach in social research, and in particular for in-depth, biographic narrative interviewing. It covers the full range of practices from the identification of topics through to strategies for writing up research findings in diverse ways.
- "Scripting a Qualitative Purpose Statement and Research Questions" in Chapter 12 (pp. 93–102) of 30 Essential Skills for the Qualitative Researcher by John W. Creswell Provides practical "how-to" information for beginning researchers in the social, behavioral, and health sciences with many applied examples from research design, qualitative inquiry, and mixed methods.The skills presented in this book are crucial for a new qualitative researcher starting a qualitative project.
- Some Strategies for Developing Interview Guides for Qualitative Interviews by Sociology Department, Harvard University Includes general advice for conducting qualitative interviews, pros and cons of recording and transcription, guidelines for success, and tips for developing and phrasing effective interview questions.
- Tip Sheet on Question Wording by Harvard University Program on Survey Research
Let Theory Guide You:
The quality of your questions depends on how you situate them within a wider body of knowledge. Consider the following advice:
A good literature review has many obvious virtues. It enables the investigator to define problems and assess data. It provides the concepts on which percepts depend. But the literature review has a special importance for the qualitative researcher. This consists of its ability to sharpen his or her capacity for surprise (Lazarsfeld, 1972b). The investigator who is well versed in the literature now has a set of expectations the data can defy. Counterexpectational data are conspicuous, readable, and highly provocative data. They signal the existence of unfulfilled theoretical assumptions, and these are, as Kuhn (1962) has noted, the very origins of intellectual innovation. A thorough review of the literature is, to this extent, a way to manufacture distance. It is a way to let the data of one's research project take issue with the theory of one's field.
McCracken, G. (1988), The Long Interview, Sage: Newbury Park, CA, p. 31
When drafting your interview questions, remember that everything follows from your central research question. Also, on the way to writing your "operationalized" interview questions, it's helpful to draft broader, intermediate questions, couched in theory. Nota bene: While it is important to know the literature well before conducting your interview(s), be careful not to present yourself to your research participant(s) as "the expert," which would be presumptuous and could be intimidating. Rather, the purpose of your knowledge is to make you a better, keener listener.
If you'd like to supplement what you learned about relevant theories through your coursework and literature review, try these sources:
- Annual Reviews Review articles sum up the latest research in many fields, including social sciences, biomedicine, life sciences, and physical sciences. These are timely collections of critical reviews written by leading scientists.
- HOLLIS - search for resources on theories in your field Modify this example search by entering the name of your field in place of "your discipline," then hit search.
- Oxford Bibliographies Written and reviewed by academic experts, every article in this database is an authoritative guide to the current scholarship in a variety of fields, containing original commentary and annotations.
- ProQuest Dissertations & Theses (PQDT) Indexes dissertations and masters' theses from most North American graduate schools as well as some European universities. Provides full text for most indexed dissertations from 1990-present.
- Very Short Introductions Launched by Oxford University Press in 1995, Very Short Introductions offer concise introductions to a diverse range of subjects from Climate to Consciousness, Game Theory to Ancient Warfare, Privacy to Islamic History, Economics to Literary Theory.
CONDUCTING INTERVIEWS
Equipment and software: .
- Lamont Library loans microphones and podcast starter kits, which will allow you to capture audio (and you may record with software, such as Garage Band).
- Cabot Library loans digital recording devices, as well as USB microphones.
If you prefer to use your own device, you may purchase a small handheld audio recorder, or use your cell phone.
- Audio Capture Basics (PDF) - Helpful instructions, courtesy of the Lamont Library Multimedia Lab.
- Getting Started with Podcasting/Audio: Guidelines from Harvard Library's Virtual Media Lab for preparing your interviewee for a web-based recording (e.g., podcast, interview)
- Camtasia Screen Recorder and Video Editor
- Zoom: Video Conferencing, Web Conferencing
- Visit the Multimedia Production Resources guide! Consult it to find and learn how to use audiovisual production tools, including: cameras, microphones, studio spaces, and other equipment at Cabot Science Library and Lamont Library.
- Try the virtual office hours offered by the Lamont Multimedia Lab!
TIPS FOR CONDUCTING INTERVIEWS
Quick handout: .
- Research Interviewing Tips (Courtesy of Dr. Suzanne Spreadbury)
Remote Interviews:
- For Online or Distant Interviews, See "Remote Research & Virtual Fieldwork" on this guide .
- Deborah Lupton's Bibliography: Doing Fieldwork in a Pandemic
Seeking Consent:
Books and articles: .
- "App-Based Textual Interviews: Interacting With Younger Generations in a Digitalized Social Reallity."International Journal of Social Research Methodology (12 June 2022). Discusses the use of texting platforms as a means to reach young people. Recommends useful question formulations for this medium.
- "Learning to Interview in the Social Sciences." Qualitative Inquiry, 9(4) 2003, 643–668 by Roulston, K., deMarrais, K., & Lewis, J. B. See especially the section on "Phrasing and Negotiating Questions" on pages 653-655 and common problems with framing questions noted on pages 659-660.
- "Slowing Down and Digging Deep: Teaching Students to Examine Interview Interaction in Depth." LEARNing Landscapes, Spring 2021 14(1) 153-169 by Herron, Brigette A. and Kathryn Roulston. Suggests analysis of videorecorded interviews as a precursor to formulating one's own questions. Includes helpful types of probes.
- Using Interviews in a Research Project by Nigel Joseph Mathers; Nicholas J Fox; Amanda Hunn; Trent Focus Group. A work pack to guide researchers in developing interviews in the healthcare field. Describes interview structures, compares face-to-face and telephone interviews. Outlines the ways in which different types of interview data can be analysed.
- “Working through Challenges in Doing Interview Research.” International Journal of Qualitative Methods, (December 2011), 348–66 by Roulston, Kathryn. The article explores (1) how problematic interactions identified in the analysis of focus group data can lead to modifications in research design, (2) an approach to dealing with reported data in representations of findings, and (3) how data analysis can inform question formulation in successive rounds of data generation. Findings from these types of examinations of interview data generation and analysis are valuable for informing both interview practice as well as research design.
Videos:

The way a qualitative researcher transcribes interviews should flow from, or align with, the methodological paradigm chosen for the study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these).
TRANSCRIPTION
Before embarking on a transcription project, it's worthwhile to invest in the time and effort necessary to capture good audio, which will make the transcription process much easier. If you haven't already done so, check out the audio capture guidelines from Harvard Library's Virtual Media Lab , or contact a media staff member for customized recommendations. First and foremost, be mindful of common pitfalls by watching this short video that identifies the most common errors to avoid!
SOFTWARE:
- Adobe Premiere Pro Speech-To-Text automatically generates transcripts and adds captions to your videos. Harvard affiliates can download Adobe Premiere in the Creative Cloud Suite.
- GoTranscript provides cost-effective human-generated transcriptions.
- pyTranscriber is an app for generating automatic transcription and/or subtitles for audio and video files. It uses the Google Cloud Speech-to-Text service, has a friendly graphical user interface, and is purported to work nicely with Chinese.
- Otter provides a new way to capture, store, search and share voice conversations, lectures, presentations, meetings, and interviews. The startup is based in Silicon Valley with a team of experienced Ph.Ds and engineers from Google, Facebook, Yahoo and Nuance (à la Dragon). Free accounts available. This is the software that Zoom uses to generate automated transcripts, so if you have access to a Zoom subscription, you have access to Otter transcriptions with it (applicable in several languages ). As with any automated approach, be prepared to correct any errors after the fact, by hand.
- Panopto is available to Harvard affiliates and generates ASR (automated speech recognition) captions . You may upload compatible audio files into it. As with any automatically generated transcription, you will need to make manual revisions. ASR captioning is available in several languages . Panopto maintains robust security practices, including strong authentication measures and end-to-end encryption, ensuring your content remains private and protected.
- REV.Com allows you to record and transcribe any calls on the iPhone, both outgoing and incoming. It may be useful for recording phone interviews. Rev lets you choose whether you want an AI- or human-generated transcription, with a fast turnaround. Rev has Service Organization Controls Type II (SOC2) certification (a SOC2 cert looks at and verifies an organization’s processing integrity, privacy practices, and security safeguards).
- Scribie Audio/Video Transcription provides automated or manual transcriptions for a small fee. As with any transcription service, some revisions will be necessary after the fact, particularly for its automated transcripts.
- Sonix automatically transcribes, translates, and helps to organize audio and video files in over 40 languages. It's fast and affordable, with good accuracy. The free trial includes 30 minutes of free transcription.
- TranscriptionWing uses a human touch process to clean up machine-generated transcripts so that the content will far more accurately reflect your audio recording.
- Whisper is a tool from OpenAI that facilitates transcription of sensitive audiovisual recordings (e.g., of research interviews) on your own device. Installation and use depends on your operating system and which version you install. Important Note: The Whisper API, where audio is sent to OpenAI to be processed by them and then sent back (usually through a programming language like Python) is NOT appropriate for sensitive data. The model should be downloaded with tools such as those described in this FAQ , so that audio is kept to your local machine. For assistance, contact James Capobianco .
EQUIPMENT:
- Transcription pedals are in circulation and available to borrow from the Circulation desk at Lamont, or use at Lamont Library's Media Lab on level B. For hand-transcribing your interviews, they work in conjunction with software such as Express Scribe , which is loaded on Media Lab computers, or you may download for free on your own machine (Mac or PC versions; scroll down the downloads page for the latter). The pedals are plug-and-play USB, allow a wide range of playback speeds, and have 3 programmable buttons, which are typically set to rewind/play/fast-forward. Instructions are included in the bag that covers installation and set-up of the software, and basic use of the pedals.
NEED HELP?
- Try the virtual office hours offered by the Lamont Multimedia Lab!
- If you're creating podcasts, login to Canvas and check out the Podcasting/Audio guide .
Helpful Texts:
- "Transcription as a Crucial Step of Data Analysis" in Chapter 5 of The SAGE Handbook of Qualitative Data Analysisby Uwe Flick (Editor) Covers basic terminology for transcription, shares caveats for transcribers, and identifies components of vocal behavior. Provides notation systems for transcription, suggestions for transcribing turn-taking, and discusses new technologies and perspectives. Includes a bibliography for further reading.
- "Transcribing the Oral Interview: Part Art, Part Science " on p. 10 of the Centre for Community Knowledge (CCK) newsletter: TIMESTAMPby Mishika Chauhan and Saransh Srivastav
QUALITATIVE DATA ANALYSIS
Software .
- Free download available for Harvard Faculty of Arts and Sciences (FAS) affiliates
- Desktop access at Lamont Library Media Lab, 3rd floor
- Desktop access at Harvard Kennedy School Library (with HKS ID)
- Remote desktop access for Harvard affiliates from IQSS Computer Labs . Email them at [email protected] and ask for a new lab account and remote desktop access to NVivo.
- Virtual Desktop Infrastructure (VDI) access available to Harvard T.H. Chan School of Public Health affiliates
CODING AND THEMEING YOUR DATA
Data analysis methods should flow from, or align with, the methodological paradigm chosen for your study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these). Some established methods include Content Analysis, Critical Analysis, Discourse Analysis, Gestalt Analysis, Grounded Theory Analysis, Interpretive Analysis, Narrative Analysis, Normative Analysis, Phenomenological Analysis, Rhetorical Analysis, and Semiotic Analysis, among others. The following resources should help you navigate your methodological options and put into practice methods for coding, themeing, interpreting, and presenting your data.
- Users can browse content by topic, discipline, or format type (reference works, book chapters, definitions, etc.). SRM offers several research tools as well: a methods map, user-created reading lists, a project planner, and advice on choosing statistical tests.
- Abductive Coding: Theory Building and Qualitative (Re)Analysis by Vila-Henninger, et al. The authors recommend an abductive approach to guide qualitative researchers who are oriented towards theory-building. They outline a set of tactics for abductive analysis, including the generation of an abductive codebook, abductive data reduction through code equations, and in-depth abductive qualitative analysis.
- Analyzing and Interpreting Qualitative Research: After the Interview by Charles F. Vanover, Paul A. Mihas, and Johnny Saldana (Editors) Providing insight into the wide range of approaches available to the qualitative researcher and covering all steps in the research process, the authors utilize a consistent chapter structure that provides novice and seasoned researchers with pragmatic, "how-to" strategies. Each chapter author introduces the method, uses one of their own research projects as a case study of the method described, shows how the specific analytic method can be used in other types of studies, and concludes with three questions/activities to prompt class discussion or personal study.
- "Analyzing Qualitative Data." Theory Into Practice 39, no. 3 (2000): 146-54 by Margaret D. LeCompte This article walks readers though rules for unbiased data analysis and provides guidance for getting organized, finding items, creating stable sets of items, creating patterns, assembling structures, and conducting data validity checks.
- "Coding is Not a Dirty Word" in Chapter 1 (pp. 1–30) of Enhancing Qualitative and Mixed Methods Research with Technology by Shalin Hai-Jew (Editor) Current discourses in qualitative research, especially those situated in postmodernism, represent coding and the technology that assists with coding as reductive, lacking complexity, and detached from theory. In this chapter, the author presents a counter-narrative to this dominant discourse in qualitative research. The author argues that coding is not necessarily devoid of theory, nor does the use of software for data management and analysis automatically render scholarship theoretically lightweight or barren. A lack of deep analytical insight is a consequence not of software but of epistemology. Using examples informed by interpretive and critical approaches, the author demonstrates how NVivo can provide an effective tool for data management and analysis. The author also highlights ideas for critical and deconstructive approaches in qualitative inquiry while using NVivo. By troubling the positivist discourse of coding, the author seeks to create dialogic spaces that integrate theory with technology-driven data management and analysis, while maintaining the depth and rigor of qualitative research.
- The Coding Manual for Qualitative Researchers by Johnny Saldana An in-depth guide to the multiple approaches available for coding qualitative data. Clear, practical and authoritative, the book profiles 32 coding methods that can be applied to a range of research genres from grounded theory to phenomenology to narrative inquiry. For each approach, Saldaña discusses the methods, origins, a description of the method, practical applications, and a clearly illustrated example with analytic follow-up. Essential reading across the social sciences.
- Flexible Coding of In-depth Interviews: A Twenty-first-century Approach by Nicole M. Deterding and Mary C. Waters The authors suggest steps in data organization and analysis to better utilize qualitative data analysis technologies and support rigorous, transparent, and flexible analysis of in-depth interview data.
- From the Editors: What Grounded Theory is Not by Roy Suddaby Walks readers through common misconceptions that hinder grounded theory studies, reinforcing the two key concepts of the grounded theory approach: (1) constant comparison of data gathered throughout the data collection process and (2) the determination of which kinds of data to sample in succession based on emergent themes (i.e., "theoretical sampling").
- “Good enough” methods for life-story analysis, by Wendy Luttrell. In Quinn N. (Ed.), Finding culture in talk (pp. 243–268). Demonstrates for researchers of culture and consciousness who use narrative how to concretely document reflexive processes in terms of where, how and why particular decisions are made at particular stages of the research process.
- Presentation slides on coding and themeing your data, derived from Saldana, Spradley, and LeCompte Click to request access.
- Qualitative Data Analysis by Matthew B. Miles; A. Michael Huberman A practical sourcebook for researchers who make use of qualitative data, presenting the current state of the craft in the design, testing, and use of qualitative analysis methods. Strong emphasis is placed on data displays matrices and networks that go beyond ordinary narrative text. Each method of data display and analysis is described and illustrated.
- "A Survey of Qualitative Data Analytic Methods" in Chapter 4 (pp. 89–138) of Fundamentals of Qualitative Research by Johnny Saldana Provides an in-depth introduction to coding as a heuristic, particularly focusing on process coding, in vivo coding, descriptive coding, values coding, dramaturgical coding, and versus coding. Includes advice on writing analytic memos, developing categories, and themeing data.
- "Thematic Networks: An Analytic Tool for Qualitative Research." Qualitative Research : QR, 1(3), 385–405 by Jennifer Attride-Stirling Details a technique for conducting thematic analysis of qualitative material, presenting a step-by-step guide of the analytic process, with the aid of an empirical example. The analytic method presented employs established, well-known techniques; the article proposes that thematic analyses can be usefully aided by and presented as thematic networks.
- Using Thematic Analysis in Psychology by Virginia Braun and Victoria Clark Walks readers through the process of reflexive thematic analysis, step by step. The method may be adapted in fields outside of psychology as relevant. Pair this with One Size Fits All? What Counts as Quality Practice in Reflexive Thematic Analysis? by Virginia Braun and Victoria Clark
TESTING OR GENERATING THEORIES
The quality of your data analysis depends on how you situate what you learn within a wider body of knowledge. Consider the following advice:
Once you have coalesced around a theory, realize that a theory should reveal rather than color your discoveries. Allow your data to guide you to what's most suitable. Grounded theory researchers may develop their own theory where current theories fail to provide insight. This guide on Theoretical Models from Alfaisal University Library provides a helpful overview on using theory.
MANAGING & FINDING INTERVIEW DATA
Managing your elicited interview data, general guidance: .
- Research Data Management @ Harvard A reference guide with information and resources to help you manage your research data. See also: Harvard Research Data Security Policy , on the Harvard University Research Data Management website.
- Data Management For Researchers: Organize, Maintain and Share Your Data for Research Success by Kristin Briney. A comprehensive guide for scientific researchers providing everything they need to know about data management and how to organize, document, use and reuse their data.
- Open Science Framework (OSF) An open-source project management tool that makes it easy to collaborate within and beyond Harvard throughout a project's lifecycle. With OSF you can manage, store, and share documents, datasets, and other information with your research team. You can also publish your work to share it with a wider audience. Although data can be stored privately, because this platform is hosted on the Internet and designed with open access in mind, it is not a good choice for highly sensitive data.
- Free cloud storage solutions for Harvard affiliates to consider include: Google Drive , DropBox , or OneDrive ( up to DSL3 )
Data Confidentiality and Secure Handling:
- Data Security Levels at Harvard - Research Data Examples This resource provided by Harvard Data Security helps you determine what level of access is appropriate for your data. Determine whether it should be made available for public use, limited to the Harvard community, or be protected as either "confidential and sensitive," "high risk," or "extremely sensitive." See also: Harvard Data Classification Table
- Harvard's Best Practices for Protecting Privacy and Harvard Information Security Collaboration Tools Matrix Follow the nuts-and-bolts advice for privacy best practices at Harvard. The latter resource reveals the level of security that can be relied upon for a large number of technological tools and platforms used at Harvard to conduct business, such as email, Slack, Accellion Kiteworks, OneDrive/SharePoint, etc.
- “Protecting Participant Privacy While Maintaining Content and Context: Challenges in Qualitative Data De‐identification and Sharing.” Proceedings of the ASIST Annual Meeting 57 (1) (2020): e415-420 by Myers, Long, and Polasek Presents an informed and tested protocol, based on the De-Identification guidelines published by the Qualitative Data Repository (QDR) at Syracuse University. Qualitative researchers may consult it to guide their data de-identification efforts.
- QDS Qualitative Data Sharing Toolkit The Qualitative Data Sharing (QDS) project and its toolkit was funded by the NIH National Human Genome Research Institute (R01HG009351). It provides tools and resources to help researchers, especially those in the health sciences, share qualitative research data while protecting privacy and confidentiality. It offers guidance on preparing data for sharing through de-identification and access control. These health sciences research datasets in ICPSR's Qualitative Data Sharing (QDS) Project Series were de-identified using the QuaDS Software and the project’s QDS guidelines.
- Table of De-Identification Techniques
- Generative AI Harvard-affiliated researchers should not enter data classified as confidential ( Level 2 and above ), including non-public research data, into publicly-available generative AI tools, in accordance with the University’s Information Security Policy. Information shared with generative AI tools using default settings is not private and could expose proprietary or sensitive information to unauthorized parties.
- Harvard Information Security Quick Reference Guide Storage guidelines, based on the data's security classification level (according to its IRB classification) is displayed on page 2, under "handling."
- Email Encryption Harvard Microsoft 365 users can now send encrypted messages and files directly from the Outlook web or desktop apps. Encrypting an email adds an extra layer of security to the message and its attachments (up to 150MB), and means only the intended recipient (and their inbox delegates with full access) can view it. Message encryption in Outlook is approved for sending high risk ( level 4 ) data and below.
Sharing Qualitative Data:
- Repositories for Qualitative Data If you have cleared this intention with your IRB, secured consent from participants, and properly de-identified your data, consider sharing your interviews in one of the data repositories included in the link above. Depending on the nature of your research and the level of risk it may present to participants, sharing your interview data may not be appropriate. If there is any chance that sharing such data will be desirable, you will be much better off if you build this expectation into your plans from the beginning.
- Guide for Sharing Qualitative Data at ICPSR The Inter-university Consortium for Political and Social Research (ICPSR) has created this resource for investigators planning to share qualitative data at ICPSR. This guide provides an overview of elements and considerations for archiving qualitative data, identifies steps for investigators to follow during the research life cycle to ensure that others can share and reuse qualitative data, and provides information about exemplars of qualitative data
International Projects:
- Research Compliance Program for FAS/SEAS at Harvard The Faculty of Arts and Sciences (FAS), including the School of Engineering and Applied Sciences (SEAS), and the Office of the Vice Provost for Research (OVPR) have established a shared Research Compliance Program (RCP). An area of common concern for interview studies is international projects and collaboration . RCP is a resource to provide guidance on which international activities may be impacted by US sanctions on countries, individuals, or entities and whether licenses or other disclosure are required to ship or otherwise share items, technology, or data with foreign collaborators.
Finding Extant Interview Data
Finding journalistic interviews: .
- Academic Search Premier This all-purpose database is great for finding articles from magazines and newspapers. In the Advanced Search, it allows you to specify "Document Type": Interview.
- Guide to Newspapers and Newspaper Indexes Use this guide created to Harvard Librarians to identify newspapers collections you'd like to search. To locate interviews, try adding the term "interview" to your search, or explore a database's search interface for options to limit your search to interviews. Nexis Uni and Factiva are the two main databases for current news.
- Listen Notes Search for podcast episodes at this podcast aggregator, and look for podcasts that include interviews. Make sure to vet the podcaster for accuracy and quality! (Listen Notes does not do much vetting.)
- NPR and ProPublica are two sites that offer high-quality long-form reporting, including journalistic interviews, for free.
Finding Oral History and Social Research Interviews:
- To find oral histories, see the Oral History page of this guide for helpful resources on Oral History interviewing.
- Repositories for Qualitative Data It has not been a customary practice among qualitative researchers in the social sciences to share raw interview data, but some have made this data available in repositories, such as the ones listed on the page linked above. You may find published data from structured interview surveys (e.g., questionnaire-based computer-assisted telephone interview data), as well as some semi-structured and unstructured interviews.
- If you are merely interested in studies interpreting data collected using interviews, rather than finding raw interview data, try databases like PsycInfo , Sociological Abstracts , or Anthropology Plus , among others.
Finding Interviews in Archival Collections at Harvard Library:
In addition to the databases and search strategies mentioned under the "Finding Oral History and Social Research Interviews" category above, you may search for interviews and oral histories (whether in textual or audiovisual formats) held in archival collections at Harvard Library.
- HOLLIS searches all documented collections at Harvard, whereas HOLLIS for Archival Discovery searches only those with finding aids. Although HOLLIS for Archival Discovery covers less material, you may find it easier to parse your search results, especially when you wish to view results at the item level (within collections). Try these approaches:
Search in HOLLIS :
- To retrieve items available online, do an Advanced Search for interview* OR "oral histor*" (in Subject), with Resource Type "Archives/Manuscripts," then refine your search by selecting "Online" under "Show Only" on the right of your initial result list. Revise the search above by adding your topic in the Keywords or Subject field (for example: African Americans ) and resubmitting the search.
- To enlarge your results set, you may also leave out the "Online" refinement; if you'd like to limit your search to a specific repository, try the technique of searching for Code: Library + Collection on the "Advanced Search" page .
Search in HOLLIS for Archival Discovery :
- To retrieve items available online, search for interview* OR "oral histor*" limited to digital materials . Revise the search above by adding your topic (for example: artist* ) in the second search box (if you don't see the box, click +).
- To preview results by collection, search for interview* OR "oral histor*" limited to collections . Revise the search above by adding your topic (for example: artist* ) in the second search box (if you don't see the box, click +). Although this method does not allow you to isolate digitized content, you may find the refinement options on the right side of the screen (refine by repository, subject or names) helpful. Once your select a given collection, you may search within it (e.g., for your topic or the term interview).
UX & MARKET RESEARCH INTERVIEWS
Ux at harvard library .
- User Experience and Market Research interviews can inform the design of tangible products and services through responsive, outcome-driven insights. The User Research Center at Harvard Library specializes in this kind of user-centered design, digital accessibility, and testing. They also offer guidance and resources to members of the Harvard Community who are interested in learning more about UX methods. Contact [email protected] or consult the URC website for more information.
Websites
- User Interviews: The Beginner’s Guide (Chris Mears)
- Interviewing Users (Jakob Nielsen)
Books
- Interviewing Users: How to Uncover Compelling Insights by Steve Portigal; Grant McCracken (Foreword by) Interviewing is a foundational user research tool that people assume they already possess. Everyone can ask questions, right? Unfortunately, that's not the case. Interviewing Users provides invaluable interviewing techniques and tools that enable you to conduct informative interviews with anyone. You'll move from simply gathering data to uncovering powerful insights about people.
- Rapid Contextual Design by Jessamyn Wendell; Karen Holtzblatt; Shelley Wood This handbook introduces Rapid CD, a fast-paced, adaptive form of Contextual Design. Rapid CD is a hands-on guide for anyone who needs practical guidance on how to use the Contextual Design process and adapt it to tactical projects with tight timelines and resources. Rapid Contextual Design provides detailed suggestions on structuring the project and customer interviews, conducting interviews, and running interpretation sessions. The handbook walks you step-by-step through organizing the data so you can see your key issues, along with visioning new solutions, storyboarding to work out the details, and paper prototype interviewing to iterate the design all with as little as a two-person team with only a few weeks to spare *Includes real project examples with actual customer data that illustrate how a CD project actually works.
Videos

Instructional Presentations on Interview Skills
- Interview/Oral History Research for RSRA 298B: Master's Thesis Reading and Research (Spring 2023) Slideshow covers: Why Interviews?, Getting Context, Engaging Participants, Conducting the Interview, The Interview Guide, Note Taking, Transcription, File management, and Data Analysis.
- Interview Skills From an online class on February 13, 2023: Get set up for interview research. You will leave prepared to choose among the three types of interviewing methods, equipped to develop an interview schedule, aware of data management options and their ethical implications, and knowledgeable of technologies you can use to record and transcribe your interviews. This workshop complements Intro to NVivo, a qualitative data analysis tool useful for coding interview data.
NIH Data Management & Sharing Policy (DMSP) This policy, effective January 25, 2023, applies to all research, funded or conducted in whole or in part by NIH, that results in the generation of scientific data , including NIH-funded qualitative research. Click here to see some examples of how the DMSP policy has been applied in qualitative research studies featured in the 2021 Qualitative Data Management Plan (DMP) Competition . As a resource for the community, NIH has developed a resource for developing informed consent language in research studies where data and/or biospecimens will be stored and shared for future use. It is important to note that the DMS Policy does NOT require that informed consent obtained from research participants must allow for broad sharing and the future use of data (either with or without identifiable private information). See the FAQ for more information.
- << Previous: Remote Research & Virtual Fieldwork
- Next: Oral History >>
Except where otherwise noted, this work is subject to a Creative Commons Attribution 4.0 International License , which allows anyone to share and adapt our material as long as proper attribution is given. For details and exceptions, see the Harvard Library Copyright Policy ©2021 Presidents and Fellows of Harvard College.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 05 October 2018
Interviews and focus groups in qualitative research: an update for the digital age
- P. Gill 1 &
- J. Baillie 2
British Dental Journal volume 225 , pages 668–672 ( 2018 ) Cite this article
23k Accesses
47 Citations
20 Altmetric
Metrics details
Highlights that qualitative research is used increasingly in dentistry. Interviews and focus groups remain the most common qualitative methods of data collection.
Suggests the advent of digital technologies has transformed how qualitative research can now be undertaken.
Suggests interviews and focus groups can offer significant, meaningful insight into participants' experiences, beliefs and perspectives, which can help to inform developments in dental practice.
Qualitative research is used increasingly in dentistry, due to its potential to provide meaningful, in-depth insights into participants' experiences, perspectives, beliefs and behaviours. These insights can subsequently help to inform developments in dental practice and further related research. The most common methods of data collection used in qualitative research are interviews and focus groups. While these are primarily conducted face-to-face, the ongoing evolution of digital technologies, such as video chat and online forums, has further transformed these methods of data collection. This paper therefore discusses interviews and focus groups in detail, outlines how they can be used in practice, how digital technologies can further inform the data collection process, and what these methods can offer dentistry.
You have full access to this article via your institution.
Similar content being viewed by others
Persistent interaction patterns across social media platforms and over time
Michele Avalle, Niccolò Di Marco, … Walter Quattrociocchi

Realizing the full potential of behavioural science for climate change mitigation
Kristian S. Nielsen, Viktoria Cologna, … Kimberly S. Wolske

Interviews in the social sciences
Eleanor Knott, Aliya Hamid Rao, … Chana Teeger
Introduction
Traditionally, research in dentistry has primarily been quantitative in nature. 1 However, in recent years, there has been a growing interest in qualitative research within the profession, due to its potential to further inform developments in practice, policy, education and training. Consequently, in 2008, the British Dental Journal (BDJ) published a four paper qualitative research series, 2 , 3 , 4 , 5 to help increase awareness and understanding of this particular methodological approach.
Since the papers were originally published, two scoping reviews have demonstrated the ongoing proliferation in the use of qualitative research within the field of oral healthcare. 1 , 6 To date, the original four paper series continue to be well cited and two of the main papers remain widely accessed among the BDJ readership. 2 , 3 The potential value of well-conducted qualitative research to evidence-based practice is now also widely recognised by service providers, policy makers, funding bodies and those who commission, support and use healthcare research.
Besides increasing standalone use, qualitative methods are now also routinely incorporated into larger mixed method study designs, such as clinical trials, as they can offer additional, meaningful insights into complex problems that simply could not be provided by quantitative methods alone. Qualitative methods can also be used to further facilitate in-depth understanding of important aspects of clinical trial processes, such as recruitment. For example, Ellis et al . investigated why edentulous older patients, dissatisfied with conventional dentures, decline implant treatment, despite its established efficacy, and frequently refuse to participate in related randomised clinical trials, even when financial constraints are removed. 7 Through the use of focus groups in Canada and the UK, the authors found that fears of pain and potential complications, along with perceived embarrassment, exacerbated by age, are common reasons why older patients typically refuse dental implants. 7
The last decade has also seen further developments in qualitative research, due to the ongoing evolution of digital technologies. These developments have transformed how researchers can access and share information, communicate and collaborate, recruit and engage participants, collect and analyse data and disseminate and translate research findings. 8 Where appropriate, such technologies are therefore capable of extending and enhancing how qualitative research is undertaken. 9 For example, it is now possible to collect qualitative data via instant messaging, email or online/video chat, using appropriate online platforms.
These innovative approaches to research are therefore cost-effective, convenient, reduce geographical constraints and are often useful for accessing 'hard to reach' participants (for example, those who are immobile or socially isolated). 8 , 9 However, digital technologies are still relatively new and constantly evolving and therefore present a variety of pragmatic and methodological challenges. Furthermore, given their very nature, their use in many qualitative studies and/or with certain participant groups may be inappropriate and should therefore always be carefully considered. While it is beyond the scope of this paper to provide a detailed explication regarding the use of digital technologies in qualitative research, insight is provided into how such technologies can be used to facilitate the data collection process in interviews and focus groups.
In light of such developments, it is perhaps therefore timely to update the main paper 3 of the original BDJ series. As with the previous publications, this paper has been purposely written in an accessible style, to enhance readability, particularly for those who are new to qualitative research. While the focus remains on the most common qualitative methods of data collection – interviews and focus groups – appropriate revisions have been made to provide a novel perspective, and should therefore be helpful to those who would like to know more about qualitative research. This paper specifically focuses on undertaking qualitative research with adult participants only.
Overview of qualitative research
Qualitative research is an approach that focuses on people and their experiences, behaviours and opinions. 10 , 11 The qualitative researcher seeks to answer questions of 'how' and 'why', providing detailed insight and understanding, 11 which quantitative methods cannot reach. 12 Within qualitative research, there are distinct methodologies influencing how the researcher approaches the research question, data collection and data analysis. 13 For example, phenomenological studies focus on the lived experience of individuals, explored through their description of the phenomenon. Ethnographic studies explore the culture of a group and typically involve the use of multiple methods to uncover the issues. 14
While methodology is the 'thinking tool', the methods are the 'doing tools'; 13 the ways in which data are collected and analysed. There are multiple qualitative data collection methods, including interviews, focus groups, observations, documentary analysis, participant diaries, photography and videography. Two of the most commonly used qualitative methods are interviews and focus groups, which are explored in this article. The data generated through these methods can be analysed in one of many ways, according to the methodological approach chosen. A common approach is thematic data analysis, involving the identification of themes and subthemes across the data set. Further information on approaches to qualitative data analysis has been discussed elsewhere. 1
Qualitative research is an evolving and adaptable approach, used by different disciplines for different purposes. Traditionally, qualitative data, specifically interviews, focus groups and observations, have been collected face-to-face with participants. In more recent years, digital technologies have contributed to the ongoing evolution of qualitative research. Digital technologies offer researchers different ways of recruiting participants and collecting data, and offer participants opportunities to be involved in research that is not necessarily face-to-face.
Research interviews are a fundamental qualitative research method 15 and are utilised across methodological approaches. Interviews enable the researcher to learn in depth about the perspectives, experiences, beliefs and motivations of the participant. 3 , 16 Examples include, exploring patients' perspectives of fear/anxiety triggers in dental treatment, 17 patients' experiences of oral health and diabetes, 18 and dental students' motivations for their choice of career. 19
Interviews may be structured, semi-structured or unstructured, 3 according to the purpose of the study, with less structured interviews facilitating a more in depth and flexible interviewing approach. 20 Structured interviews are similar to verbal questionnaires and are used if the researcher requires clarification on a topic; however they produce less in-depth data about a participant's experience. 3 Unstructured interviews may be used when little is known about a topic and involves the researcher asking an opening question; 3 the participant then leads the discussion. 20 Semi-structured interviews are commonly used in healthcare research, enabling the researcher to ask predetermined questions, 20 while ensuring the participant discusses issues they feel are important.
Interviews can be undertaken face-to-face or using digital methods when the researcher and participant are in different locations. Audio-recording the interview, with the consent of the participant, is essential for all interviews regardless of the medium as it enables accurate transcription; the process of turning the audio file into a word-for-word transcript. This transcript is the data, which the researcher then analyses according to the chosen approach.
Types of interview
Qualitative studies often utilise one-to-one, face-to-face interviews with research participants. This involves arranging a mutually convenient time and place to meet the participant, signing a consent form and audio-recording the interview. However, digital technologies have expanded the potential for interviews in research, enabling individuals to participate in qualitative research regardless of location.
Telephone interviews can be a useful alternative to face-to-face interviews and are commonly used in qualitative research. They enable participants from different geographical areas to participate and may be less onerous for participants than meeting a researcher in person. 15 A qualitative study explored patients' perspectives of dental implants and utilised telephone interviews due to the quality of the data that could be yielded. 21 The researcher needs to consider how they will audio record the interview, which can be facilitated by purchasing a recorder that connects directly to the telephone. One potential disadvantage of telephone interviews is the inability of the interviewer and researcher to see each other. This is resolved using software for audio and video calls online – such as Skype – to conduct interviews with participants in qualitative studies. Advantages of this approach include being able to see the participant if video calls are used, enabling observation of non-verbal communication, and the software can be free to use. However, participants are required to have a device and internet connection, as well as being computer literate, potentially limiting who can participate in the study. One qualitative study explored the role of dental hygienists in reducing oral health disparities in Canada. 22 The researcher conducted interviews using Skype, which enabled dental hygienists from across Canada to be interviewed within the research budget, accommodating the participants' schedules. 22
A less commonly used approach to qualitative interviews is the use of social virtual worlds. A qualitative study accessed a social virtual world – Second Life – to explore the health literacy skills of individuals who use social virtual worlds to access health information. 23 The researcher created an avatar and interview room, and undertook interviews with participants using voice and text methods. 23 This approach to recruitment and data collection enables individuals from diverse geographical locations to participate, while remaining anonymous if they wish. Furthermore, for interviews conducted using text methods, transcription of the interview is not required as the researcher can save the written conversation with the participant, with the participant's consent. However, the researcher and participant need to be familiar with how the social virtual world works to engage in an interview this way.
Conducting an interview
Ensuring informed consent before any interview is a fundamental aspect of the research process. Participants in research must be afforded autonomy and respect; consent should be informed and voluntary. 24 Individuals should have the opportunity to read an information sheet about the study, ask questions, understand how their data will be stored and used, and know that they are free to withdraw at any point without reprisal. The qualitative researcher should take written consent before undertaking the interview. In a face-to-face interview, this is straightforward: the researcher and participant both sign copies of the consent form, keeping one each. However, this approach is less straightforward when the researcher and participant do not meet in person. A recent protocol paper outlined an approach for taking consent for telephone interviews, which involved: audio recording the participant agreeing to each point on the consent form; the researcher signing the consent form and keeping a copy; and posting a copy to the participant. 25 This process could be replicated in other interview studies using digital methods.
There are advantages and disadvantages of using face-to-face and digital methods for research interviews. Ultimately, for both approaches, the quality of the interview is determined by the researcher. 16 Appropriate training and preparation are thus required. Healthcare professionals can use their interpersonal communication skills when undertaking a research interview, particularly questioning, listening and conversing. 3 However, the purpose of an interview is to gain information about the study topic, 26 rather than offering help and advice. 3 The researcher therefore needs to listen attentively to participants, enabling them to describe their experience without interruption. 3 The use of active listening skills also help to facilitate the interview. 14 Spradley outlined elements and strategies for research interviews, 27 which are a useful guide for qualitative researchers:
Greeting and explaining the project/interview
Asking descriptive (broad), structural (explore response to descriptive) and contrast (difference between) questions
Asymmetry between the researcher and participant talking
Expressing interest and cultural ignorance
Repeating, restating and incorporating the participant's words when asking questions
Creating hypothetical situations
Asking friendly questions
Knowing when to leave.
For semi-structured interviews, a topic guide (also called an interview schedule) is used to guide the content of the interview – an example of a topic guide is outlined in Box 1 . The topic guide, usually based on the research questions, existing literature and, for healthcare professionals, their clinical experience, is developed by the research team. The topic guide should include open ended questions that elicit in-depth information, and offer participants the opportunity to talk about issues important to them. This is vital in qualitative research where the researcher is interested in exploring the experiences and perspectives of participants. It can be useful for qualitative researchers to pilot the topic guide with the first participants, 10 to ensure the questions are relevant and understandable, and amending the questions if required.
Regardless of the medium of interview, the researcher must consider the setting of the interview. For face-to-face interviews, this could be in the participant's home, in an office or another mutually convenient location. A quiet location is preferable to promote confidentiality, enable the researcher and participant to concentrate on the conversation, and to facilitate accurate audio-recording of the interview. For interviews using digital methods the same principles apply: a quiet, private space where the researcher and participant feel comfortable and confident to participate in an interview.
Box 1: Example of a topic guide
Study focus: Parents' experiences of brushing their child's (aged 0–5) teeth
1. Can you tell me about your experience of cleaning your child's teeth?
How old was your child when you started cleaning their teeth?
Why did you start cleaning their teeth at that point?
How often do you brush their teeth?
What do you use to brush their teeth and why?
2. Could you explain how you find cleaning your child's teeth?
Do you find anything difficult?
What makes cleaning their teeth easier for you?
3. How has your experience of cleaning your child's teeth changed over time?
Has it become easier or harder?
Have you changed how often and how you clean their teeth? If so, why?
4. Could you describe how your child finds having their teeth cleaned?
What do they enjoy about having their teeth cleaned?
Is there anything they find upsetting about having their teeth cleaned?
5. Where do you look for information/advice about cleaning your child's teeth?
What did your health visitor tell you about cleaning your child's teeth? (If anything)
What has the dentist told you about caring for your child's teeth? (If visited)
Have any family members given you advice about how to clean your child's teeth? If so, what did they tell you? Did you follow their advice?
6. Is there anything else you would like to discuss about this?
Focus groups
A focus group is a moderated group discussion on a pre-defined topic, for research purposes. 28 , 29 While not aligned to a particular qualitative methodology (for example, grounded theory or phenomenology) as such, focus groups are used increasingly in healthcare research, as they are useful for exploring collective perspectives, attitudes, behaviours and experiences. Consequently, they can yield rich, in-depth data and illuminate agreement and inconsistencies 28 within and, where appropriate, between groups. Examples include public perceptions of dental implants and subsequent impact on help-seeking and decision making, 30 and general dental practitioners' views on patient safety in dentistry. 31
Focus groups can be used alone or in conjunction with other methods, such as interviews or observations, and can therefore help to confirm, extend or enrich understanding and provide alternative insights. 28 The social interaction between participants often results in lively discussion and can therefore facilitate the collection of rich, meaningful data. However, they are complex to organise and manage, due to the number of participants, and may also be inappropriate for exploring particularly sensitive issues that many participants may feel uncomfortable about discussing in a group environment.
Focus groups are primarily undertaken face-to-face but can now also be undertaken online, using appropriate technologies such as email, bulletin boards, online research communities, chat rooms, discussion forums, social media and video conferencing. 32 Using such technologies, data collection can also be synchronous (for example, online discussions in 'real time') or, unlike traditional face-to-face focus groups, asynchronous (for example, online/email discussions in 'non-real time'). While many of the fundamental principles of focus group research are the same, regardless of how they are conducted, a number of subtle nuances are associated with the online medium. 32 Some of which are discussed further in the following sections.
Focus group considerations
Some key considerations associated with face-to-face focus groups are: how many participants are required; should participants within each group know each other (or not) and how many focus groups are needed within a single study? These issues are much debated and there is no definitive answer. However, the number of focus groups required will largely depend on the topic area, the depth and breadth of data needed, the desired level of participation required 29 and the necessity (or not) for data saturation.
The optimum group size is around six to eight participants (excluding researchers) but can work effectively with between three and 14 participants. 3 If the group is too small, it may limit discussion, but if it is too large, it may become disorganised and difficult to manage. It is, however, prudent to over-recruit for a focus group by approximately two to three participants, to allow for potential non-attenders. For many researchers, particularly novice researchers, group size may also be informed by pragmatic considerations, such as the type of study, resources available and moderator experience. 28 Similar size and mix considerations exist for online focus groups. Typically, synchronous online focus groups will have around three to eight participants but, as the discussion does not happen simultaneously, asynchronous groups may have as many as 10–30 participants. 33
The topic area and potential group interaction should guide group composition considerations. Pre-existing groups, where participants know each other (for example, work colleagues) may be easier to recruit, have shared experiences and may enjoy a familiarity, which facilitates discussion and/or the ability to challenge each other courteously. 3 However, if there is a potential power imbalance within the group or if existing group norms and hierarchies may adversely affect the ability of participants to speak freely, then 'stranger groups' (that is, where participants do not already know each other) may be more appropriate. 34 , 35
Focus group management
Face-to-face focus groups should normally be conducted by two researchers; a moderator and an observer. 28 The moderator facilitates group discussion, while the observer typically monitors group dynamics, behaviours, non-verbal cues, seating arrangements and speaking order, which is essential for transcription and analysis. The same principles of informed consent, as discussed in the interview section, also apply to focus groups, regardless of medium. However, the consent process for online discussions will probably be managed somewhat differently. For example, while an appropriate participant information leaflet (and consent form) would still be required, the process is likely to be managed electronically (for example, via email) and would need to specifically address issues relating to technology (for example, anonymity and use, storage and access to online data). 32
The venue in which a face to face focus group is conducted should be of a suitable size, private, quiet, free from distractions and in a collectively convenient location. It should also be conducted at a time appropriate for participants, 28 as this is likely to promote attendance. As with interviews, the same ethical considerations apply (as discussed earlier). However, online focus groups may present additional ethical challenges associated with issues such as informed consent, appropriate access and secure data storage. Further guidance can be found elsewhere. 8 , 32
Before the focus group commences, the researchers should establish rapport with participants, as this will help to put them at ease and result in a more meaningful discussion. Consequently, researchers should introduce themselves, provide further clarity about the study and how the process will work in practice and outline the 'ground rules'. Ground rules are designed to assist, not hinder, group discussion and typically include: 3 , 28 , 29
Discussions within the group are confidential to the group
Only one person can speak at a time
All participants should have sufficient opportunity to contribute
There should be no unnecessary interruptions while someone is speaking
Everyone can be expected to be listened to and their views respected
Challenging contrary opinions is appropriate, but ridiculing is not.
Moderating a focus group requires considered management and good interpersonal skills to help guide the discussion and, where appropriate, keep it sufficiently focused. Avoid, therefore, participating, leading, expressing personal opinions or correcting participants' knowledge 3 , 28 as this may bias the process. A relaxed, interested demeanour will also help participants to feel comfortable and promote candid discourse. Moderators should also prevent the discussion being dominated by any one person, ensure differences of opinions are discussed fairly and, if required, encourage reticent participants to contribute. 3 Asking open questions, reflecting on significant issues, inviting further debate, probing responses accordingly, and seeking further clarification, as and where appropriate, will help to obtain sufficient depth and insight into the topic area.
Moderating online focus groups requires comparable skills, particularly if the discussion is synchronous, as the discussion may be dominated by those who can type proficiently. 36 It is therefore important that sufficient time and respect is accorded to those who may not be able to type as quickly. Asynchronous discussions are usually less problematic in this respect, as interactions are less instant. However, moderating an asynchronous discussion presents additional challenges, particularly if participants are geographically dispersed, as they may be online at different times. Consequently, the moderator will not always be present and the discussion may therefore need to occur over several days, which can be difficult to manage and facilitate and invariably requires considerable flexibility. 32 It is also worth recognising that establishing rapport with participants via online medium is often more challenging than via face-to-face and may therefore require additional time, skills, effort and consideration.
As with research interviews, focus groups should be guided by an appropriate interview schedule, as discussed earlier in the paper. For example, the schedule will usually be informed by the review of the literature and study aims, and will merely provide a topic guide to help inform subsequent discussions. To provide a verbatim account of the discussion, focus groups must be recorded, using an audio-recorder with a good quality multi-directional microphone. While videotaping is possible, some participants may find it obtrusive, 3 which may adversely affect group dynamics. The use (or not) of a video recorder, should therefore be carefully considered.
At the end of the focus group, a few minutes should be spent rounding up and reflecting on the discussion. 28 Depending on the topic area, it is possible that some participants may have revealed deeply personal issues and may therefore require further help and support, such as a constructive debrief or possibly even referral on to a relevant third party. It is also possible that some participants may feel that the discussion did not adequately reflect their views and, consequently, may no longer wish to be associated with the study. 28 Such occurrences are likely to be uncommon, but should they arise, it is important to further discuss any concerns and, if appropriate, offer them the opportunity to withdraw (including any data relating to them) from the study. Immediately after the discussion, researchers should compile notes regarding thoughts and ideas about the focus group, which can assist with data analysis and, if appropriate, any further data collection.
Qualitative research is increasingly being utilised within dental research to explore the experiences, perspectives, motivations and beliefs of participants. The contributions of qualitative research to evidence-based practice are increasingly being recognised, both as standalone research and as part of larger mixed-method studies, including clinical trials. Interviews and focus groups remain commonly used data collection methods in qualitative research, and with the advent of digital technologies, their utilisation continues to evolve. However, digital methods of qualitative data collection present additional methodological, ethical and practical considerations, but also potentially offer considerable flexibility to participants and researchers. Consequently, regardless of format, qualitative methods have significant potential to inform important areas of dental practice, policy and further related research.
Gussy M, Dickson-Swift V, Adams J . A scoping review of qualitative research in peer-reviewed dental publications. Int J Dent Hygiene 2013; 11 : 174–179.
Article Google Scholar
Burnard P, Gill P, Stewart K, Treasure E, Chadwick B . Analysing and presenting qualitative data. Br Dent J 2008; 204 : 429–432.
Gill P, Stewart K, Treasure E, Chadwick B . Methods of data collection in qualitative research: interviews and focus groups. Br Dent J 2008; 204 : 291–295.
Gill P, Stewart K, Treasure E, Chadwick B . Conducting qualitative interviews with school children in dental research. Br Dent J 2008; 204 : 371–374.
Stewart K, Gill P, Chadwick B, Treasure E . Qualitative research in dentistry. Br Dent J 2008; 204 : 235–239.
Masood M, Thaliath E, Bower E, Newton J . An appraisal of the quality of published qualitative dental research. Community Dent Oral Epidemiol 2011; 39 : 193–203.
Ellis J, Levine A, Bedos C et al. Refusal of implant supported mandibular overdentures by elderly patients. Gerodontology 2011; 28 : 62–68.
Macfarlane S, Bucknall T . Digital Technologies in Research. In Gerrish K, Lathlean J (editors) The Research Process in Nursing . 7th edition. pp. 71–86. Oxford: Wiley Blackwell; 2015.
Google Scholar
Lee R, Fielding N, Blank G . Online Research Methods in the Social Sciences: An Editorial Introduction. In Fielding N, Lee R, Blank G (editors) The Sage Handbook of Online Research Methods . pp. 3–16. London: Sage Publications; 2016.
Creswell J . Qualitative inquiry and research design: Choosing among five designs . Thousand Oaks, CA: Sage, 1998.
Guest G, Namey E, Mitchell M . Qualitative research: Defining and designing In Guest G, Namey E, Mitchell M (editors) Collecting Qualitative Data: A Field Manual For Applied Research . pp. 1–40. London: Sage Publications, 2013.
Chapter Google Scholar
Pope C, Mays N . Qualitative research: Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ 1995; 311 : 42–45.
Giddings L, Grant B . A Trojan Horse for positivism? A critique of mixed methods research. Adv Nurs Sci 2007; 30 : 52–60.
Hammersley M, Atkinson P . Ethnography: Principles in Practice . London: Routledge, 1995.
Oltmann S . Qualitative interviews: A methodological discussion of the interviewer and respondent contexts Forum Qualitative Sozialforschung/Forum: Qualitative Social Research. 2016; 17 : Art. 15.
Patton M . Qualitative Research and Evaluation Methods . Thousand Oaks, CA: Sage, 2002.
Wang M, Vinall-Collier K, Csikar J, Douglas G . A qualitative study of patients' views of techniques to reduce dental anxiety. J Dent 2017; 66 : 45–51.
Lindenmeyer A, Bowyer V, Roscoe J, Dale J, Sutcliffe P . Oral health awareness and care preferences in patients with diabetes: a qualitative study. Fam Pract 2013; 30 : 113–118.
Gallagher J, Clarke W, Wilson N . Understanding the motivation: a qualitative study of dental students' choice of professional career. Eur J Dent Educ 2008; 12 : 89–98.
Tod A . Interviewing. In Gerrish K, Lacey A (editors) The Research Process in Nursing . Oxford: Blackwell Publishing, 2006.
Grey E, Harcourt D, O'Sullivan D, Buchanan H, Kipatrick N . A qualitative study of patients' motivations and expectations for dental implants. Br Dent J 2013; 214 : 10.1038/sj.bdj.2012.1178.
Farmer J, Peressini S, Lawrence H . Exploring the role of the dental hygienist in reducing oral health disparities in Canada: A qualitative study. Int J Dent Hygiene 2017; 10.1111/idh.12276.
McElhinney E, Cheater F, Kidd L . Undertaking qualitative health research in social virtual worlds. J Adv Nurs 2013; 70 : 1267–1275.
Health Research Authority. UK Policy Framework for Health and Social Care Research. Available at https://www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/uk-policy-framework-health-social-care-research/ (accessed September 2017).
Baillie J, Gill P, Courtenay P . Knowledge, understanding and experiences of peritonitis among patients, and their families, undertaking peritoneal dialysis: A mixed methods study protocol. J Adv Nurs 2017; 10.1111/jan.13400.
Kvale S . Interviews . Thousand Oaks (CA): Sage, 1996.
Spradley J . The Ethnographic Interview . New York: Holt, Rinehart and Winston, 1979.
Goodman C, Evans C . Focus Groups. In Gerrish K, Lathlean J (editors) The Research Process in Nursing . pp. 401–412. Oxford: Wiley Blackwell, 2015.
Shaha M, Wenzell J, Hill E . Planning and conducting focus group research with nurses. Nurse Res 2011; 18 : 77–87.
Wang G, Gao X, Edward C . Public perception of dental implants: a qualitative study. J Dent 2015; 43 : 798–805.
Bailey E . Contemporary views of dental practitioners' on patient safety. Br Dent J 2015; 219 : 535–540.
Abrams K, Gaiser T . Online Focus Groups. In Field N, Lee R, Blank G (editors) The Sage Handbook of Online Research Methods . pp. 435–450. London: Sage Publications, 2016.
Poynter R . The Handbook of Online and Social Media Research . West Sussex: John Wiley & Sons, 2010.
Kevern J, Webb C . Focus groups as a tool for critical social research in nurse education. Nurse Educ Today 2001; 21 : 323–333.
Kitzinger J, Barbour R . Introduction: The Challenge and Promise of Focus Groups. In Barbour R S K J (editor) Developing Focus Group Research . pp. 1–20. London: Sage Publications, 1999.
Krueger R, Casey M . Focus Groups: A Practical Guide for Applied Research. 4th ed. Thousand Oaks, California: SAGE; 2009.
Download references
Author information
Authors and affiliations.
Senior Lecturer (Adult Nursing), School of Healthcare Sciences, Cardiff University,
Lecturer (Adult Nursing) and RCBC Wales Postdoctoral Research Fellow, School of Healthcare Sciences, Cardiff University,
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to P. Gill .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Gill, P., Baillie, J. Interviews and focus groups in qualitative research: an update for the digital age. Br Dent J 225 , 668–672 (2018). https://doi.org/10.1038/sj.bdj.2018.815
Download citation
Accepted : 02 July 2018
Published : 05 October 2018
Issue Date : 12 October 2018
DOI : https://doi.org/10.1038/sj.bdj.2018.815
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Translating brand reputation into equity from the stakeholder’s theory: an approach to value creation based on consumer’s perception & interactions.
- Olukorede Adewole
International Journal of Corporate Social Responsibility (2024)
Perceptions and beliefs of community gatekeepers about genomic risk information in African cleft research
- Abimbola M. Oladayo
- Oluwakemi Odukoya
- Azeez Butali
BMC Public Health (2024)
Assessment of women’s needs, wishes and preferences regarding interprofessional guidance on nutrition in pregnancy – a qualitative study
- Merle Ebinghaus
- Caroline Johanna Agricola
- Birgit-Christiane Zyriax
BMC Pregnancy and Childbirth (2024)
‘Baby mamas’ in Urban Ghana: an exploratory qualitative study on the factors influencing serial fathering among men in Accra, Ghana
- Rosemond Akpene Hiadzi
- Jemima Akweley Agyeman
- Godwin Banafo Akrong
Reproductive Health (2023)
Revolutionising dental technologies: a qualitative study on dental technicians’ perceptions of Artificial intelligence integration
- Galvin Sim Siang Lin
- Yook Shiang Ng
- Kah Hoay Chua
BMC Oral Health (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Neurol Res Pract

How to use and assess qualitative research methods
Loraine busetto.
1 Department of Neurology, Heidelberg University Hospital, Im Neuenheimer Feld 400, 69120 Heidelberg, Germany
Wolfgang Wick
2 Clinical Cooperation Unit Neuro-Oncology, German Cancer Research Center, Heidelberg, Germany
Christoph Gumbinger
Associated data.
Not applicable.
This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions, and focussing on intervention improvement. The most common methods of data collection are document study, (non-) participant observations, semi-structured interviews and focus groups. For data analysis, field-notes and audio-recordings are transcribed into protocols and transcripts, and coded using qualitative data management software. Criteria such as checklists, reflexivity, sampling strategies, piloting, co-coding, member-checking and stakeholder involvement can be used to enhance and assess the quality of the research conducted. Using qualitative in addition to quantitative designs will equip us with better tools to address a greater range of research problems, and to fill in blind spots in current neurological research and practice.
The aim of this paper is to provide an overview of qualitative research methods, including hands-on information on how they can be used, reported and assessed. This article is intended for beginning qualitative researchers in the health sciences as well as experienced quantitative researchers who wish to broaden their understanding of qualitative research.
What is qualitative research?
Qualitative research is defined as “the study of the nature of phenomena”, including “their quality, different manifestations, the context in which they appear or the perspectives from which they can be perceived” , but excluding “their range, frequency and place in an objectively determined chain of cause and effect” [ 1 ]. This formal definition can be complemented with a more pragmatic rule of thumb: qualitative research generally includes data in form of words rather than numbers [ 2 ].
Why conduct qualitative research?
Because some research questions cannot be answered using (only) quantitative methods. For example, one Australian study addressed the issue of why patients from Aboriginal communities often present late or not at all to specialist services offered by tertiary care hospitals. Using qualitative interviews with patients and staff, it found one of the most significant access barriers to be transportation problems, including some towns and communities simply not having a bus service to the hospital [ 3 ]. A quantitative study could have measured the number of patients over time or even looked at possible explanatory factors – but only those previously known or suspected to be of relevance. To discover reasons for observed patterns, especially the invisible or surprising ones, qualitative designs are needed.
While qualitative research is common in other fields, it is still relatively underrepresented in health services research. The latter field is more traditionally rooted in the evidence-based-medicine paradigm, as seen in " research that involves testing the effectiveness of various strategies to achieve changes in clinical practice, preferably applying randomised controlled trial study designs (...) " [ 4 ]. This focus on quantitative research and specifically randomised controlled trials (RCT) is visible in the idea of a hierarchy of research evidence which assumes that some research designs are objectively better than others, and that choosing a "lesser" design is only acceptable when the better ones are not practically or ethically feasible [ 5 , 6 ]. Others, however, argue that an objective hierarchy does not exist, and that, instead, the research design and methods should be chosen to fit the specific research question at hand – "questions before methods" [ 2 , 7 – 9 ]. This means that even when an RCT is possible, some research problems require a different design that is better suited to addressing them. Arguing in JAMA, Berwick uses the example of rapid response teams in hospitals, which he describes as " a complex, multicomponent intervention – essentially a process of social change" susceptible to a range of different context factors including leadership or organisation history. According to him, "[in] such complex terrain, the RCT is an impoverished way to learn. Critics who use it as a truth standard in this context are incorrect" [ 8 ] . Instead of limiting oneself to RCTs, Berwick recommends embracing a wider range of methods , including qualitative ones, which for "these specific applications, (...) are not compromises in learning how to improve; they are superior" [ 8 ].
Research problems that can be approached particularly well using qualitative methods include assessing complex multi-component interventions or systems (of change), addressing questions beyond “what works”, towards “what works for whom when, how and why”, and focussing on intervention improvement rather than accreditation [ 7 , 9 – 12 ]. Using qualitative methods can also help shed light on the “softer” side of medical treatment. For example, while quantitative trials can measure the costs and benefits of neuro-oncological treatment in terms of survival rates or adverse effects, qualitative research can help provide a better understanding of patient or caregiver stress, visibility of illness or out-of-pocket expenses.
How to conduct qualitative research?
Given that qualitative research is characterised by flexibility, openness and responsivity to context, the steps of data collection and analysis are not as separate and consecutive as they tend to be in quantitative research [ 13 , 14 ]. As Fossey puts it : “sampling, data collection, analysis and interpretation are related to each other in a cyclical (iterative) manner, rather than following one after another in a stepwise approach” [ 15 ]. The researcher can make educated decisions with regard to the choice of method, how they are implemented, and to which and how many units they are applied [ 13 ]. As shown in Fig. 1 , this can involve several back-and-forth steps between data collection and analysis where new insights and experiences can lead to adaption and expansion of the original plan. Some insights may also necessitate a revision of the research question and/or the research design as a whole. The process ends when saturation is achieved, i.e. when no relevant new information can be found (see also below: sampling and saturation). For reasons of transparency, it is essential for all decisions as well as the underlying reasoning to be well-documented.

Iterative research process
While it is not always explicitly addressed, qualitative methods reflect a different underlying research paradigm than quantitative research (e.g. constructivism or interpretivism as opposed to positivism). The choice of methods can be based on the respective underlying substantive theory or theoretical framework used by the researcher [ 2 ].
Data collection
The methods of qualitative data collection most commonly used in health research are document study, observations, semi-structured interviews and focus groups [ 1 , 14 , 16 , 17 ].
Document study
Document study (also called document analysis) refers to the review by the researcher of written materials [ 14 ]. These can include personal and non-personal documents such as archives, annual reports, guidelines, policy documents, diaries or letters.
Observations
Observations are particularly useful to gain insights into a certain setting and actual behaviour – as opposed to reported behaviour or opinions [ 13 ]. Qualitative observations can be either participant or non-participant in nature. In participant observations, the observer is part of the observed setting, for example a nurse working in an intensive care unit [ 18 ]. In non-participant observations, the observer is “on the outside looking in”, i.e. present in but not part of the situation, trying not to influence the setting by their presence. Observations can be planned (e.g. for 3 h during the day or night shift) or ad hoc (e.g. as soon as a stroke patient arrives at the emergency room). During the observation, the observer takes notes on everything or certain pre-determined parts of what is happening around them, for example focusing on physician-patient interactions or communication between different professional groups. Written notes can be taken during or after the observations, depending on feasibility (which is usually lower during participant observations) and acceptability (e.g. when the observer is perceived to be judging the observed). Afterwards, these field notes are transcribed into observation protocols. If more than one observer was involved, field notes are taken independently, but notes can be consolidated into one protocol after discussions. Advantages of conducting observations include minimising the distance between the researcher and the researched, the potential discovery of topics that the researcher did not realise were relevant and gaining deeper insights into the real-world dimensions of the research problem at hand [ 18 ].
Semi-structured interviews
Hijmans & Kuyper describe qualitative interviews as “an exchange with an informal character, a conversation with a goal” [ 19 ]. Interviews are used to gain insights into a person’s subjective experiences, opinions and motivations – as opposed to facts or behaviours [ 13 ]. Interviews can be distinguished by the degree to which they are structured (i.e. a questionnaire), open (e.g. free conversation or autobiographical interviews) or semi-structured [ 2 , 13 ]. Semi-structured interviews are characterized by open-ended questions and the use of an interview guide (or topic guide/list) in which the broad areas of interest, sometimes including sub-questions, are defined [ 19 ]. The pre-defined topics in the interview guide can be derived from the literature, previous research or a preliminary method of data collection, e.g. document study or observations. The topic list is usually adapted and improved at the start of the data collection process as the interviewer learns more about the field [ 20 ]. Across interviews the focus on the different (blocks of) questions may differ and some questions may be skipped altogether (e.g. if the interviewee is not able or willing to answer the questions or for concerns about the total length of the interview) [ 20 ]. Qualitative interviews are usually not conducted in written format as it impedes on the interactive component of the method [ 20 ]. In comparison to written surveys, qualitative interviews have the advantage of being interactive and allowing for unexpected topics to emerge and to be taken up by the researcher. This can also help overcome a provider or researcher-centred bias often found in written surveys, which by nature, can only measure what is already known or expected to be of relevance to the researcher. Interviews can be audio- or video-taped; but sometimes it is only feasible or acceptable for the interviewer to take written notes [ 14 , 16 , 20 ].
Focus groups
Focus groups are group interviews to explore participants’ expertise and experiences, including explorations of how and why people behave in certain ways [ 1 ]. Focus groups usually consist of 6–8 people and are led by an experienced moderator following a topic guide or “script” [ 21 ]. They can involve an observer who takes note of the non-verbal aspects of the situation, possibly using an observation guide [ 21 ]. Depending on researchers’ and participants’ preferences, the discussions can be audio- or video-taped and transcribed afterwards [ 21 ]. Focus groups are useful for bringing together homogeneous (to a lesser extent heterogeneous) groups of participants with relevant expertise and experience on a given topic on which they can share detailed information [ 21 ]. Focus groups are a relatively easy, fast and inexpensive method to gain access to information on interactions in a given group, i.e. “the sharing and comparing” among participants [ 21 ]. Disadvantages include less control over the process and a lesser extent to which each individual may participate. Moreover, focus group moderators need experience, as do those tasked with the analysis of the resulting data. Focus groups can be less appropriate for discussing sensitive topics that participants might be reluctant to disclose in a group setting [ 13 ]. Moreover, attention must be paid to the emergence of “groupthink” as well as possible power dynamics within the group, e.g. when patients are awed or intimidated by health professionals.
Choosing the “right” method
As explained above, the school of thought underlying qualitative research assumes no objective hierarchy of evidence and methods. This means that each choice of single or combined methods has to be based on the research question that needs to be answered and a critical assessment with regard to whether or to what extent the chosen method can accomplish this – i.e. the “fit” between question and method [ 14 ]. It is necessary for these decisions to be documented when they are being made, and to be critically discussed when reporting methods and results.
Let us assume that our research aim is to examine the (clinical) processes around acute endovascular treatment (EVT), from the patient’s arrival at the emergency room to recanalization, with the aim to identify possible causes for delay and/or other causes for sub-optimal treatment outcome. As a first step, we could conduct a document study of the relevant standard operating procedures (SOPs) for this phase of care – are they up-to-date and in line with current guidelines? Do they contain any mistakes, irregularities or uncertainties that could cause delays or other problems? Regardless of the answers to these questions, the results have to be interpreted based on what they are: a written outline of what care processes in this hospital should look like. If we want to know what they actually look like in practice, we can conduct observations of the processes described in the SOPs. These results can (and should) be analysed in themselves, but also in comparison to the results of the document analysis, especially as regards relevant discrepancies. Do the SOPs outline specific tests for which no equipment can be observed or tasks to be performed by specialized nurses who are not present during the observation? It might also be possible that the written SOP is outdated, but the actual care provided is in line with current best practice. In order to find out why these discrepancies exist, it can be useful to conduct interviews. Are the physicians simply not aware of the SOPs (because their existence is limited to the hospital’s intranet) or do they actively disagree with them or does the infrastructure make it impossible to provide the care as described? Another rationale for adding interviews is that some situations (or all of their possible variations for different patient groups or the day, night or weekend shift) cannot practically or ethically be observed. In this case, it is possible to ask those involved to report on their actions – being aware that this is not the same as the actual observation. A senior physician’s or hospital manager’s description of certain situations might differ from a nurse’s or junior physician’s one, maybe because they intentionally misrepresent facts or maybe because different aspects of the process are visible or important to them. In some cases, it can also be relevant to consider to whom the interviewee is disclosing this information – someone they trust, someone they are otherwise not connected to, or someone they suspect or are aware of being in a potentially “dangerous” power relationship to them. Lastly, a focus group could be conducted with representatives of the relevant professional groups to explore how and why exactly they provide care around EVT. The discussion might reveal discrepancies (between SOPs and actual care or between different physicians) and motivations to the researchers as well as to the focus group members that they might not have been aware of themselves. For the focus group to deliver relevant information, attention has to be paid to its composition and conduct, for example, to make sure that all participants feel safe to disclose sensitive or potentially problematic information or that the discussion is not dominated by (senior) physicians only. The resulting combination of data collection methods is shown in Fig. 2 .

Possible combination of data collection methods
Attributions for icons: “Book” by Serhii Smirnov, “Interview” by Adrien Coquet, FR, “Magnifying Glass” by anggun, ID, “Business communication” by Vectors Market; all from the Noun Project
The combination of multiple data source as described for this example can be referred to as “triangulation”, in which multiple measurements are carried out from different angles to achieve a more comprehensive understanding of the phenomenon under study [ 22 , 23 ].
Data analysis
To analyse the data collected through observations, interviews and focus groups these need to be transcribed into protocols and transcripts (see Fig. 3 ). Interviews and focus groups can be transcribed verbatim , with or without annotations for behaviour (e.g. laughing, crying, pausing) and with or without phonetic transcription of dialects and filler words, depending on what is expected or known to be relevant for the analysis. In the next step, the protocols and transcripts are coded , that is, marked (or tagged, labelled) with one or more short descriptors of the content of a sentence or paragraph [ 2 , 15 , 23 ]. Jansen describes coding as “connecting the raw data with “theoretical” terms” [ 20 ]. In a more practical sense, coding makes raw data sortable. This makes it possible to extract and examine all segments describing, say, a tele-neurology consultation from multiple data sources (e.g. SOPs, emergency room observations, staff and patient interview). In a process of synthesis and abstraction, the codes are then grouped, summarised and/or categorised [ 15 , 20 ]. The end product of the coding or analysis process is a descriptive theory of the behavioural pattern under investigation [ 20 ]. The coding process is performed using qualitative data management software, the most common ones being InVivo, MaxQDA and Atlas.ti. It should be noted that these are data management tools which support the analysis performed by the researcher(s) [ 14 ].

From data collection to data analysis
Attributions for icons: see Fig. Fig.2, 2 , also “Speech to text” by Trevor Dsouza, “Field Notes” by Mike O’Brien, US, “Voice Record” by ProSymbols, US, “Inspection” by Made, AU, and “Cloud” by Graphic Tigers; all from the Noun Project
How to report qualitative research?
Protocols of qualitative research can be published separately and in advance of the study results. However, the aim is not the same as in RCT protocols, i.e. to pre-define and set in stone the research questions and primary or secondary endpoints. Rather, it is a way to describe the research methods in detail, which might not be possible in the results paper given journals’ word limits. Qualitative research papers are usually longer than their quantitative counterparts to allow for deep understanding and so-called “thick description”. In the methods section, the focus is on transparency of the methods used, including why, how and by whom they were implemented in the specific study setting, so as to enable a discussion of whether and how this may have influenced data collection, analysis and interpretation. The results section usually starts with a paragraph outlining the main findings, followed by more detailed descriptions of, for example, the commonalities, discrepancies or exceptions per category [ 20 ]. Here it is important to support main findings by relevant quotations, which may add information, context, emphasis or real-life examples [ 20 , 23 ]. It is subject to debate in the field whether it is relevant to state the exact number or percentage of respondents supporting a certain statement (e.g. “Five interviewees expressed negative feelings towards XYZ”) [ 21 ].
How to combine qualitative with quantitative research?
Qualitative methods can be combined with other methods in multi- or mixed methods designs, which “[employ] two or more different methods [ …] within the same study or research program rather than confining the research to one single method” [ 24 ]. Reasons for combining methods can be diverse, including triangulation for corroboration of findings, complementarity for illustration and clarification of results, expansion to extend the breadth and range of the study, explanation of (unexpected) results generated with one method with the help of another, or offsetting the weakness of one method with the strength of another [ 1 , 17 , 24 – 26 ]. The resulting designs can be classified according to when, why and how the different quantitative and/or qualitative data strands are combined. The three most common types of mixed method designs are the convergent parallel design , the explanatory sequential design and the exploratory sequential design. The designs with examples are shown in Fig. 4 .

Three common mixed methods designs
In the convergent parallel design, a qualitative study is conducted in parallel to and independently of a quantitative study, and the results of both studies are compared and combined at the stage of interpretation of results. Using the above example of EVT provision, this could entail setting up a quantitative EVT registry to measure process times and patient outcomes in parallel to conducting the qualitative research outlined above, and then comparing results. Amongst other things, this would make it possible to assess whether interview respondents’ subjective impressions of patients receiving good care match modified Rankin Scores at follow-up, or whether observed delays in care provision are exceptions or the rule when compared to door-to-needle times as documented in the registry. In the explanatory sequential design, a quantitative study is carried out first, followed by a qualitative study to help explain the results from the quantitative study. This would be an appropriate design if the registry alone had revealed relevant delays in door-to-needle times and the qualitative study would be used to understand where and why these occurred, and how they could be improved. In the exploratory design, the qualitative study is carried out first and its results help informing and building the quantitative study in the next step [ 26 ]. If the qualitative study around EVT provision had shown a high level of dissatisfaction among the staff members involved, a quantitative questionnaire investigating staff satisfaction could be set up in the next step, informed by the qualitative study on which topics dissatisfaction had been expressed. Amongst other things, the questionnaire design would make it possible to widen the reach of the research to more respondents from different (types of) hospitals, regions, countries or settings, and to conduct sub-group analyses for different professional groups.
How to assess qualitative research?
A variety of assessment criteria and lists have been developed for qualitative research, ranging in their focus and comprehensiveness [ 14 , 17 , 27 ]. However, none of these has been elevated to the “gold standard” in the field. In the following, we therefore focus on a set of commonly used assessment criteria that, from a practical standpoint, a researcher can look for when assessing a qualitative research report or paper.
Assessors should check the authors’ use of and adherence to the relevant reporting checklists (e.g. Standards for Reporting Qualitative Research (SRQR)) to make sure all items that are relevant for this type of research are addressed [ 23 , 28 ]. Discussions of quantitative measures in addition to or instead of these qualitative measures can be a sign of lower quality of the research (paper). Providing and adhering to a checklist for qualitative research contributes to an important quality criterion for qualitative research, namely transparency [ 15 , 17 , 23 ].
Reflexivity
While methodological transparency and complete reporting is relevant for all types of research, some additional criteria must be taken into account for qualitative research. This includes what is called reflexivity, i.e. sensitivity to the relationship between the researcher and the researched, including how contact was established and maintained, or the background and experience of the researcher(s) involved in data collection and analysis. Depending on the research question and population to be researched this can be limited to professional experience, but it may also include gender, age or ethnicity [ 17 , 27 ]. These details are relevant because in qualitative research, as opposed to quantitative research, the researcher as a person cannot be isolated from the research process [ 23 ]. It may influence the conversation when an interviewed patient speaks to an interviewer who is a physician, or when an interviewee is asked to discuss a gynaecological procedure with a male interviewer, and therefore the reader must be made aware of these details [ 19 ].

Sampling and saturation
The aim of qualitative sampling is for all variants of the objects of observation that are deemed relevant for the study to be present in the sample “ to see the issue and its meanings from as many angles as possible” [ 1 , 16 , 19 , 20 , 27 ] , and to ensure “information-richness [ 15 ]. An iterative sampling approach is advised, in which data collection (e.g. five interviews) is followed by data analysis, followed by more data collection to find variants that are lacking in the current sample. This process continues until no new (relevant) information can be found and further sampling becomes redundant – which is called saturation [ 1 , 15 ] . In other words: qualitative data collection finds its end point not a priori , but when the research team determines that saturation has been reached [ 29 , 30 ].
This is also the reason why most qualitative studies use deliberate instead of random sampling strategies. This is generally referred to as “ purposive sampling” , in which researchers pre-define which types of participants or cases they need to include so as to cover all variations that are expected to be of relevance, based on the literature, previous experience or theory (i.e. theoretical sampling) [ 14 , 20 ]. Other types of purposive sampling include (but are not limited to) maximum variation sampling, critical case sampling or extreme or deviant case sampling [ 2 ]. In the above EVT example, a purposive sample could include all relevant professional groups and/or all relevant stakeholders (patients, relatives) and/or all relevant times of observation (day, night and weekend shift).
Assessors of qualitative research should check whether the considerations underlying the sampling strategy were sound and whether or how researchers tried to adapt and improve their strategies in stepwise or cyclical approaches between data collection and analysis to achieve saturation [ 14 ].
Good qualitative research is iterative in nature, i.e. it goes back and forth between data collection and analysis, revising and improving the approach where necessary. One example of this are pilot interviews, where different aspects of the interview (especially the interview guide, but also, for example, the site of the interview or whether the interview can be audio-recorded) are tested with a small number of respondents, evaluated and revised [ 19 ]. In doing so, the interviewer learns which wording or types of questions work best, or which is the best length of an interview with patients who have trouble concentrating for an extended time. Of course, the same reasoning applies to observations or focus groups which can also be piloted.
Ideally, coding should be performed by at least two researchers, especially at the beginning of the coding process when a common approach must be defined, including the establishment of a useful coding list (or tree), and when a common meaning of individual codes must be established [ 23 ]. An initial sub-set or all transcripts can be coded independently by the coders and then compared and consolidated after regular discussions in the research team. This is to make sure that codes are applied consistently to the research data.
Member checking
Member checking, also called respondent validation , refers to the practice of checking back with study respondents to see if the research is in line with their views [ 14 , 27 ]. This can happen after data collection or analysis or when first results are available [ 23 ]. For example, interviewees can be provided with (summaries of) their transcripts and asked whether they believe this to be a complete representation of their views or whether they would like to clarify or elaborate on their responses [ 17 ]. Respondents’ feedback on these issues then becomes part of the data collection and analysis [ 27 ].
Stakeholder involvement
In those niches where qualitative approaches have been able to evolve and grow, a new trend has seen the inclusion of patients and their representatives not only as study participants (i.e. “members”, see above) but as consultants to and active participants in the broader research process [ 31 – 33 ]. The underlying assumption is that patients and other stakeholders hold unique perspectives and experiences that add value beyond their own single story, making the research more relevant and beneficial to researchers, study participants and (future) patients alike [ 34 , 35 ]. Using the example of patients on or nearing dialysis, a recent scoping review found that 80% of clinical research did not address the top 10 research priorities identified by patients and caregivers [ 32 , 36 ]. In this sense, the involvement of the relevant stakeholders, especially patients and relatives, is increasingly being seen as a quality indicator in and of itself.
How not to assess qualitative research
The above overview does not include certain items that are routine in assessments of quantitative research. What follows is a non-exhaustive, non-representative, experience-based list of the quantitative criteria often applied to the assessment of qualitative research, as well as an explanation of the limited usefulness of these endeavours.
Protocol adherence
Given the openness and flexibility of qualitative research, it should not be assessed by how well it adheres to pre-determined and fixed strategies – in other words: its rigidity. Instead, the assessor should look for signs of adaptation and refinement based on lessons learned from earlier steps in the research process.
Sample size
For the reasons explained above, qualitative research does not require specific sample sizes, nor does it require that the sample size be determined a priori [ 1 , 14 , 27 , 37 – 39 ]. Sample size can only be a useful quality indicator when related to the research purpose, the chosen methodology and the composition of the sample, i.e. who was included and why.
Randomisation
While some authors argue that randomisation can be used in qualitative research, this is not commonly the case, as neither its feasibility nor its necessity or usefulness has been convincingly established for qualitative research [ 13 , 27 ]. Relevant disadvantages include the negative impact of a too large sample size as well as the possibility (or probability) of selecting “ quiet, uncooperative or inarticulate individuals ” [ 17 ]. Qualitative studies do not use control groups, either.
Interrater reliability, variability and other “objectivity checks”
The concept of “interrater reliability” is sometimes used in qualitative research to assess to which extent the coding approach overlaps between the two co-coders. However, it is not clear what this measure tells us about the quality of the analysis [ 23 ]. This means that these scores can be included in qualitative research reports, preferably with some additional information on what the score means for the analysis, but it is not a requirement. Relatedly, it is not relevant for the quality or “objectivity” of qualitative research to separate those who recruited the study participants and collected and analysed the data. Experiences even show that it might be better to have the same person or team perform all of these tasks [ 20 ]. First, when researchers introduce themselves during recruitment this can enhance trust when the interview takes place days or weeks later with the same researcher. Second, when the audio-recording is transcribed for analysis, the researcher conducting the interviews will usually remember the interviewee and the specific interview situation during data analysis. This might be helpful in providing additional context information for interpretation of data, e.g. on whether something might have been meant as a joke [ 18 ].
Not being quantitative research
Being qualitative research instead of quantitative research should not be used as an assessment criterion if it is used irrespectively of the research problem at hand. Similarly, qualitative research should not be required to be combined with quantitative research per se – unless mixed methods research is judged as inherently better than single-method research. In this case, the same criterion should be applied for quantitative studies without a qualitative component.
The main take-away points of this paper are summarised in Table Table1. 1 . We aimed to show that, if conducted well, qualitative research can answer specific research questions that cannot to be adequately answered using (only) quantitative designs. Seeing qualitative and quantitative methods as equal will help us become more aware and critical of the “fit” between the research problem and our chosen methods: I can conduct an RCT to determine the reasons for transportation delays of acute stroke patients – but should I? It also provides us with a greater range of tools to tackle a greater range of research problems more appropriately and successfully, filling in the blind spots on one half of the methodological spectrum to better address the whole complexity of neurological research and practice.
Take-away-points
Acknowledgements
Abbreviations, authors’ contributions.
LB drafted the manuscript; WW and CG revised the manuscript; all authors approved the final versions.
no external funding.
Availability of data and materials
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The qualitative research interview
Affiliation.
- 1 Department of Family Medicine, University of Medicine and Dentistry at Robert Wood Johnson Medical School, Somerset, New Jersey 08873, USA. [email protected]
- PMID: 16573666
- DOI: 10.1111/j.1365-2929.2006.02418.x
Background: Interviews are among the most familiar strategies for collecting qualitative data. The different qualitative interviewing strategies in common use emerged from diverse disciplinary perspectives resulting in a wide variation among interviewing approaches. Unlike the highly structured survey interviews and questionnaires used in epidemiology and most health services research, we examine less structured interview strategies in which the person interviewed is more a participant in meaning making than a conduit from which information is retrieved.
Purpose: In this article we briefly review the more common qualitative interview methods and then focus on the widely used individual face-to-face in-depth interview, which seeks to foster learning about individual experiences and perspectives on a given set of issues. We discuss methods for conducting in-depth interviews and consider relevant ethical issues with particular regard to the rights and protection of the participants.
Publication types
- Research Support, N.I.H., Extramural
- Research Support, Non-U.S. Gov't
- Data Collection / methods
- Ethics, Research
- Interpersonal Relations
- Interviews as Topic / methods*
- Qualitative Research*
Grants and funding
- 1D12HP00167/PHS HHS/United States
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
Semi-Structured Interview | Definition, Guide & Examples
Published on January 27, 2022 by Tegan George . Revised on June 22, 2023.
A semi-structured interview is a data collection method that relies on asking questions within a predetermined thematic framework. However, the questions are not set in order or in phrasing.
In research, semi-structured interviews are often qualitative in nature. They are generally used as an exploratory tool in marketing, social science, survey methodology, and other research fields.
They are also common in field research with many interviewers, giving everyone the same theoretical framework, but allowing them to investigate different facets of the research question .
- Structured interviews : The questions are predetermined in both topic and order.
- Unstructured interviews : None of the questions are predetermined.
- Focus group interviews : The questions are presented to a group instead of one individual.
Table of contents
What is a semi-structured interview, when to use a semi-structured interview, advantages of semi-structured interviews, disadvantages of semi-structured interviews, semi-structured interview questions, how to conduct a semi-structured interview, how to analyze a semi-structured interview, presenting your results (with example), other interesting articles, frequently asked questions about semi-structured interviews.
Semi-structured interviews are a blend of structured and unstructured types of interviews.
- Unlike in an unstructured interview, the interviewer has an idea of what questions they will ask.
- Unlike in a structured interview, the phrasing and order of the questions is not set.
Semi-structured interviews are often open-ended, allowing for flexibility. Asking set questions in a set order allows for easy comparison between respondents, but it can be limiting. Having less structure can help you see patterns, while still allowing for comparisons between respondents.
Semi-structured interviews are best used when:
- You have prior interview experience. Spontaneous questions are deceptively challenging, and it’s easy to accidentally ask a leading question or make a participant uneasy.
- Your research question is exploratory in nature. Participant answers can guide future research questions and help you develop a more robust knowledge base for future research.
Just like in structured interviews, it is critical that you remain organized and develop a system for keeping track of participant responses. However, since the questions are less set than in a structured interview, the data collection and analysis become a bit more complex.
Differences between different types of interviews
Make sure to choose the type of interview that suits your research best. This table shows the most important differences between the four types.
Semi-structured interviews come with many advantages.
Best of both worlds
No distractions, detail and richness.
However, semi-structured interviews also have their downsides.
Low validity
High risk of research bias, difficult to develop good semi-structured interview questions.
Since they are often open-ended in style, it can be challenging to write semi-structured interview questions that get you the information you’re looking for without biasing your responses. Here are a few tips:
- Define what areas or topics you will be focusing on prior to the interview. This will help you write a framework of questions that zero in on the information you seek.
- Write yourself a guide to refer to during the interview, so you stay focused. It can help to start with the simpler questions first, moving into the more complex ones after you have established a comfortable rapport.
- Be as clear and concise as possible, avoiding jargon and compound sentences.
- How often per week do you go to the gym? a) 1 time; b) 2 times; c) 3 times; d) 4 or more times
- If yes: What feelings does going to the gym bring out in you?
- If no: What do you prefer to do instead?
- If yes: How did this membership affect your job performance? Did you stay longer in the role than you would have if there were no membership?
Once you’ve determined that a semi-structured interview is the right fit for your research topic , you can proceed with the following steps.
Step 1: Set your goals and objectives
You can use guiding questions as you conceptualize your research question, such as:
- What are you trying to learn or achieve from a semi-structured interview?
- Why are you choosing a semi-structured interview as opposed to a different type of interview, or another research method?
If you want to proceed with a semi-structured interview, you can start designing your questions.
Step 2: Design your questions
Try to stay simple and concise, and phrase your questions clearly. If your topic is sensitive or could cause an emotional response, be mindful of your word choices.
One of the most challenging parts of a semi-structured interview is knowing when to ask follow-up or spontaneous related questions. For this reason, having a guide to refer back to is critical. Hypothesizing what other questions could arise from your participants’ answers may also be helpful.
Step 3: Assemble your participants
There are a few sampling methods you can use to recruit your interview participants, such as:
- Voluntary response sampling : For example, sending an email to a campus mailing list and sourcing participants from responses.
- Stratified sampling of a particular characteristic trait of interest to your research, such as age, race, ethnicity, or gender identity.
Step 4: Decide on your medium
It’s important to determine ahead of time how you will be conducting your interview. You should decide whether you’ll be conducting it live or with a pen-and-paper format. If conducted in real time, you also need to decide if in person, over the phone, or via videoconferencing is the best option for you.
Note that each of these methods has its own advantages and disadvantages:
- Pen-and-paper may be easier for you to organize and analyze, but you will receive more prepared answers, which may affect the reliability of your data.
- In-person interviews can lead to nervousness or interviewer effects, where the respondent feels pressured to respond in a manner they believe will please you or incentivize you to like them.
Step 5: Conduct your interviews
As you conduct your interviews, keep environmental conditions as constant as you can to avoid bias. Pay attention to your body language (e.g., nodding, raising eyebrows), and moderate your tone of voice.
Relatedly, one of the biggest challenges with semi-structured interviews is ensuring that your questions remain unbiased. This can be especially challenging with any spontaneous questions or unscripted follow-ups that you ask your participants.
After you’re finished conducting your interviews, it’s time to analyze your results. First, assign each of your participants a number or pseudonym for organizational purposes.
The next step in your analysis is to transcribe the audio or video recordings. You can then conduct a content or thematic analysis to determine your categories, looking for patterns of responses that stand out to you and test your hypotheses .
Transcribing interviews
Before you get started with transcription, decide whether to conduct verbatim transcription or intelligent verbatim transcription.
- If pauses, laughter, or filler words like “umm” or “like” affect your analysis and research conclusions, conduct verbatim transcription and include them.
- If not, you can conduct intelligent verbatim transcription, which excludes fillers, fixes any grammatical issues, and is usually easier to analyze.
Transcribing presents a great opportunity for you to cleanse your data . Here, you can identify and address any inconsistencies or questions that come up as you listen.
Your supervisor might ask you to add the transcriptions to the appendix of your paper.
Coding semi-structured interviews
Next, it’s time to conduct your thematic or content analysis . This often involves “coding” words, patterns, or recurring responses, separating them into labels or categories for more robust analysis.
Due to the open-ended nature of many semi-structured interviews, you will most likely be conducting thematic analysis, rather than content analysis.
- You closely examine your data to identify common topics, ideas, or patterns. This can help you draw preliminary conclusions about your participants’ views, knowledge or experiences.
- After you have been through your responses a few times, you can collect the data into groups identified by their “code.” These codes give you a condensed overview of the main points and patterns identified by your data.
- Next, it’s time to organize these codes into themes. Themes are generally broader than codes, and you’ll often combine a few codes under one theme. After identifying your themes, make sure that these themes appropriately represent patterns in responses.
Analyzing semi-structured interviews
Once you’re confident in your themes, you can take either an inductive or a deductive approach.
- An inductive approach is more open-ended, allowing your data to determine your themes.
- A deductive approach is the opposite. It involves investigating whether your data confirm preconceived themes or ideas.
After your data analysis, the next step is to report your findings in a research paper .
- Your methodology section describes how you collected the data (in this case, describing your semi-structured interview process) and explains how you justify or conceptualize your analysis.
- Your discussion and results sections usually address each of your coded categories.
- You can then conclude with the main takeaways and avenues for further research.
Example of interview methodology for a research paper
Let’s say you are interested in vegan students on your campus. You have noticed that the number of vegan students seems to have increased since your first year, and you are curious what caused this shift.
You identify a few potential options based on literature:
- Perceptions about personal health or the perceived “healthiness” of a vegan diet
- Concerns about animal welfare and the meat industry
- Increased climate awareness, especially in regards to animal products
- Availability of more vegan options, making the lifestyle change easier
Anecdotally, you hypothesize that students are more aware of the impact of animal products on the ongoing climate crisis, and this has influenced many to go vegan. However, you cannot rule out the possibility of the other options, such as the new vegan bar in the dining hall.
Since your topic is exploratory in nature and you have a lot of experience conducting interviews in your work-study role as a research assistant, you decide to conduct semi-structured interviews.
You have a friend who is a member of a campus club for vegans and vegetarians, so you send a message to the club to ask for volunteers. You also spend some time at the campus dining hall, approaching students at the vegan bar asking if they’d like to participate.
Here are some questions you could ask:
- Do you find vegan options on campus to be: excellent; good; fair; average; poor?
- How long have you been a vegan?
- Follow-up questions can probe the strength of this decision (i.e., was it overwhelmingly one reason, or more of a mix?)
Depending on your participants’ answers to these questions, ask follow-ups as needed for clarification, further information, or elaboration.
- Do you think consuming animal products contributes to climate change? → The phrasing implies that you, the interviewer, do think so. This could bias your respondents, incentivizing them to answer affirmatively as well.
- What do you think is the biggest effect of animal product consumption? → This phrasing ensures the participant is giving their own opinion, and may even yield some surprising responses that enrich your analysis.
After conducting your interviews and transcribing your data, you can then conduct thematic analysis, coding responses into different categories. Since you began your research with several theories about campus veganism that you found equally compelling, you would use the inductive approach.
Once you’ve identified themes and patterns from your data, you can draw inferences and conclusions. Your results section usually addresses each theme or pattern you found, describing each in turn, as well as how often you came across them in your analysis. Feel free to include lots of (properly anonymized) examples from the data as evidence, too.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Student’s t -distribution
- Normal distribution
- Null and Alternative Hypotheses
- Chi square tests
- Confidence interval
- Quartiles & Quantiles
- Cluster sampling
- Stratified sampling
- Data cleansing
- Reproducibility vs Replicability
- Peer review
- Prospective cohort study
Research bias
- Implicit bias
- Cognitive bias
- Placebo effect
- Hawthorne effect
- Hindsight bias
- Affect heuristic
- Social desirability bias
A semi-structured interview is a blend of structured and unstructured types of interviews. Semi-structured interviews are best used when:
- You have prior interview experience. Spontaneous questions are deceptively challenging, and it’s easy to accidentally ask a leading question or make a participant uncomfortable.
The four most common types of interviews are:
- Structured interviews : The questions are predetermined in both topic and order.
- Semi-structured interviews : A few questions are predetermined, but other questions aren’t planned.
Social desirability bias is the tendency for interview participants to give responses that will be viewed favorably by the interviewer or other participants. It occurs in all types of interviews and surveys , but is most common in semi-structured interviews , unstructured interviews , and focus groups .
Social desirability bias can be mitigated by ensuring participants feel at ease and comfortable sharing their views. Make sure to pay attention to your own body language and any physical or verbal cues, such as nodding or widening your eyes.
This type of bias can also occur in observations if the participants know they’re being observed. They might alter their behavior accordingly.
The interviewer effect is a type of bias that emerges when a characteristic of an interviewer (race, age, gender identity, etc.) influences the responses given by the interviewee.
There is a risk of an interviewer effect in all types of interviews , but it can be mitigated by writing really high-quality interview questions.
Inductive reasoning is a bottom-up approach, while deductive reasoning is top-down.
Inductive reasoning takes you from the specific to the general, while in deductive reasoning, you make inferences by going from general premises to specific conclusions.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
George, T. (2023, June 22). Semi-Structured Interview | Definition, Guide & Examples. Scribbr. Retrieved March 30, 2024, from https://www.scribbr.com/methodology/semi-structured-interview/
Is this article helpful?
Tegan George
Other students also liked, structured interview | definition, guide & examples, unstructured interview | definition, guide & examples, what is a focus group | step-by-step guide & examples, "i thought ai proofreading was useless but..".
I've been using Scribbr for years now and I know it's a service that won't disappoint. It does a good job spotting mistakes”
- Open access
- Published: 27 March 2024
Choosing and accessing COVID-19 treatment options: a qualitative study with patients, caregivers, and health care providers in Lebanon
- Reem Hoteit ORCID: orcid.org/0000-0001-8139-9321 1 ,
- Aya Hassoun 2 ,
- Elie Bou Sanayeh 3 ,
- Marie Christelle Saade 3 ,
- Gladys Honein-AbouHaidar 4 &
- Elie A. Akl ORCID: orcid.org/0000-0002-3444-8618 3 , 5
Health Research Policy and Systems volume 22 , Article number: 38 ( 2024 ) Cite this article
15 Accesses
4 Altmetric
Metrics details
The coronavirus disease 2019 (COVID-19) pandemic has strained healthcare systems globally, particularly in terms of access to medicines. Lebanon has been greatly affected by the pandemic, having faced concomitant financial and economic crises. The objective of the study was to understand the experiences of patients with COVID-19 in Lebanon, as well as those of their families, and healthcare providers, with regards to their treatment decisions and accessibility to COVID-19 medicines.
For this qualitative study, we conducted 28 semi-structured interviews. We used purposive sampling to recruit participants with a diverse range of perspectives. The data collection phase spanned from August to November 2021 and was conducted virtually. After transcribing and translating the interviews, we employed thematic analysis to identify recurring themes and patterns.
In total, 28 individuals participated in this study. Participants highlighted challenges owing to the COVID-19 pandemic and economic crisis. Accessing COVID-19 medicines posed major hurdles for physicians and patients, given limited availability, global shortages, local circumstances, community hoarding and stockpiling by pharmacies. Providers based treatment decisions on research, local and international practice guidelines, experiences and expert feedback. Patients sought information from social media, community members and physicians, as well as through word of mouth. Accessing medicines involved navigating the healthcare system, the black market, charities, personal networks and political parties and sourcing from abroad. The medicines were either free, subsidized or at inflated costs.
Conclusions
This study highlights the diversity and complexity of factors influencing decision-making and accessing medicines during the COVID-19 pandemic in Lebanon. Future research should explore strategies for ensuring medicine access during crises, drawing insights from comparative studies across different countries.
Peer Review reports
Introduction
The emergence of the coronavirus disease 2019 (COVID-19) instigated a global health crisis, presenting formidable challenges to healthcare systems and economies across the world [ 1 , 2 ]. Since its first appearance in December 2019 in China, severe acute respiratory coronavirus 2 (SARS-CoV-2) has infected around 700 million individuals, resulting in a staggering death toll exceeding 6.9 million by November 2023 [ 3 , 4 ]. Owing to COVID-19-related lockdowns and the heightened demand for essential medications, drug shortages have become a significant global problem [ 5 , 6 ].
Prior to the pandemic, healthcare systems in low- and middle-income countries (LMICs) suffered from limited financial resources, healthcare workforce shortages and unavailability of medications [ 7 , 8 , 9 ]. The pandemic further strained these already fragile health systems [ 2 ]. For example, the strong demand for medications to treat COVID-19 patients, including analgesics, sedatives, antibiotics, hydroxychloroquine and remdesivir, considerably affected medication accessibility and inadvertently encouraged black market activity [ 10 , 11 , 12 , 13 ]. Escalating medication prices rendered these crucial medications unaffordable for many patients, particularly in LMICs [ 13 , 14 , 15 ].
The economic and financial crises in Lebanon, coupled with the Beirut Port’s destruction, severely impacted the entire healthcare sector, affecting hospitals, healthcare providers and the pharmaceutical and medical supply industry [ 16 ]. The COVID-19 pandemic worsened this situation, posing two major challenges: the selection of appropriate therapies and ensuring access to these treatments [ 17 , 18 ]. This shortage of prescription drugs in Lebanon peaked during the COVID-19 pandemic [ 19 ].
Factors influencing decisions regarding COVID-19 treatment can be complicated and multidimensional. They encompass an individual patient’s medical history, comorbidities and risk factors, as well as the availability and efficacy of various therapeutic options [ 20 ]. Therapeutic management in the early stages of the pandemic was challenging owing to uncertainty and continuously evolving evidence [ 21 ]. Clinicians attempted to manage COVID-19 using a variety of treatments that targeted numerous possible mechanisms, such as antiviral, anti-inflammatory and immunomodulatory drugs [ 22 ]. There was also misinformation in various media outlets about the benefits of some medications for either preventing or treating COVID-19 [ 23 ]. This resulted in an increase in risky self-medication with several over-the-counter medications [ 2 , 24 ].
The objective of the study is to understand the experiences of patients with COVID-19 in Lebanon, as well as those of their families, and healthcare providers, with regards to their treatment decisions and accessibility to COVID-19 medicines.
Study design
This study adopted a descriptive qualitative research design using semi-structured individual interviews (refer to Appendix 1 for the interview guide). The qualitative approach utilized is rooted in naturalistic inquiry and offers a wide array of theoretical or philosophical orientations, sampling techniques and data-gathering strategies [ 25 ].
Participants
We recruited participants from different regions in Lebanon. Eligible participants belonged to one of the following groups:
physicians and nurses directly involved in caring for patients diagnosed with COVID-19
hospital and community pharmacists involved in dispensing medications for patients diagnosed with COVID-19
patients previously diagnosed with COVID-19
family members or caregivers of patients previously diagnosed with COVID-19.
We excluded patients who were psychologically unable to participate or provide coherent and clear descriptions of their experiences.
Sampling and recruitment
We used purposeful sampling by approaching individuals belonging to the groups of interest. We also used snowballing sampling by asking participants to refer us to other eligible individuals. Additionally, physicians and pharmacists assisted in the recruitment of potential former patients and caregivers. The Institutional Review Board (IRB) at the American University of Beirut (AUB) approved the study. All participants provided oral consent prior to participation. The interviewers took all precautions to guarantee participants’ anonymity and confidentiality. Participants were informed that their participation was entirely voluntary and that they could opt-out at any time.
Data collection
Following an explanation of the study’s objectives, we interviewed participants virtually in either English or Arabic, depending on their preferences. We audio-recorded interviews following participants’ consent. We conducted a total of 28 interviews, and we ceased to collect data when thematic saturation was reached, that is, no new themes emerged from the data analysis [ 26 ].
Two team members (AH and EBS) conducted the interviews between August and November of 2021. The individuals received thorough training on conducting interviews, focusing on techniques to remain neutral and nonjudgemental and to sustain the interviewees’ engagement in the subject matter. To enhance the quality of data collection, we held regular debriefing meetings following the initial interviews. These meetings provided an opportunity for reflection on the data collection process and identification of areas of improvement.
Data analysis
The interviewers transcribed the audio-recorded interviews, and translated them into English when applicable. Another team member (RH) verified transcript accuracy by checking them against the audio recordings. We employed Quirkos, a qualitative analysis software, for coding and organizing the data. We applied Braun and Clarke’s six-step thematic analysis approach [ 27 ]. In phase 1, GHA and RH read a few transcripts independently to familiarize themselves with the information and established a preliminary framework for data coding. In phase 2, they independently annotated the transcripts line by line. They assigned labels to each idea (coding), leaving room for new codes as they emerged. In phase 3, GHA, EAA and RH reviewed the coded transcripts and identified emerging themes, along with quotes that illustrated each theme. In phase 4, GHA, EAA and RH reviewed and refined the list of emerging themes, and created a thematic map. In phase 5, they outlined the final thematic framework. Finally, in phase 6, we developed a complete narrative of the findings and selected interviewee quotes for each theme and sub-theme.
Increasing rigour
All interviewers received training in interviewing skills, maintaining consistency and rigour [ 28 ]. We also made sure that interviewers had no prior relationship with participants, fostering objectivity and minimizing bias [ 28 ]. We interviewed participants in their preferred language as a way to ensure their understanding of the questions and their ability to easily express their thoughts [ 28 , 29 ]. To ensure transferability, we employed triangulation by compiling viewpoints of various population groups [ 29 ]. We halted data collection upon reaching saturation [ 30 ], ensuring comprehensive data coverage and depth. We verified transcript accuracy by checking them against the audio recordings [ 31 ]. Three members of our research team (GHA, EAA and RH) actively participated in the analysis and the generation of codes, themes and subthemes. In reporting this study, we adhered to the highest standards by following the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist [ 32 ].
Demographics
We recruited 28 participants: 3 community pharmacists, 4 hospital pharmacists, 8 physicians, 1 nurse, 3 patients and 9 caregivers. The interviews lasted about 40 min on average.
Emerging themes
The following themes emerged in relation to the experiences of participants with regards to treatment decisions and accessibility to COVID-19 medicines: country crises, access challenges, cost challenges, drivers for providers’ decision-making, drivers for patients and caregivers’ decision-making and accessing medicines (Fig. 1 ).
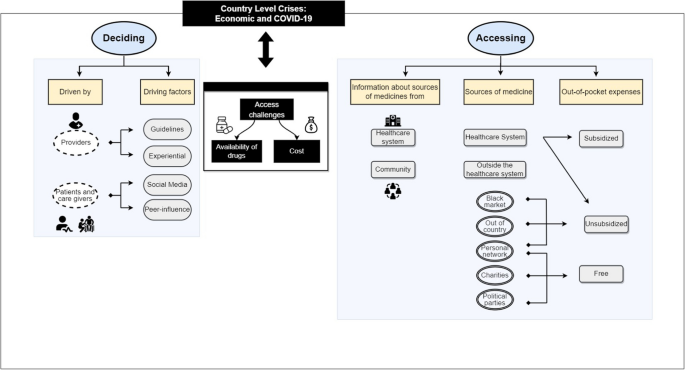
Factors influencing decision-making and accessing medicines during the COVID-19 pandemic in Lebanon
When the majority of participants expressed the same opinions, we used the term “most participants”; otherwise, we used the terms “many” or “few” as appropriate. When citing quotes from participants, we used the following acronyms: physicians (Phys), nurses (Nurse), community pharmacists (C-Pharm), hospital pharmacists (H-Pharm), patients (Pt) and caregivers (Cg).
Country crises
Most participants discussed current events in the country, including the COVID-19 pandemic, the economic crisis and the financial crisis. “Because of the current situation in Lebanon, we’re seeing things we never thought we would” (H-Pharm 02). “COVID-19 came around in March 2020, and Lebanon had already started its economic crisis” (H-Pharm 04).
Participants noted their experiences with the financial crisis and the closure of banks. “I woke up in the morning at 6:45 am, wore my clothes and went down to the bank but found it closed […], I went down to [..], same thing, it closed as I was on my way so I said, ‘where should I get them the money now?; they asked for money for the tests” (Cg 08).
One caregiver also mentioned that the economic crisis had forced them to work multiple jobs. “I work two jobs but now if you work in Lebanon the salaries are not enough” (Cg 08).
In addition to this, participants complained about how the country’s financial situation impacted access to medicines. “The purchasing power of the patients had already decreased. And like all countries when it comes to medication and the healthcare system, which was already collapsing in Lebanon, it’s common that in the end, the patient has to self-fund their treatment. And patients in low economical standing will have no access to treatment” (H-Pharm 04).
Access challenges
The crisis impacted the supply of COVID-19 medications. First, there were drug shortages directly related to the COVID-19 medicines, similar to the global crisis “… we saw that everyone is facing this, worldwide… Then we went into shortages, we didn’t have anymore because the consumption had increased” (H-Pharm 02). “Even the Colchicine, we heard about it, and we went around and looked for it and it was very hard for us to find it easily” (Cg 02).
“For example, remdesivir they used for my mother-in-law we got six injections, and the first day we tried to get it we called the pharmacies they told us they don’t have it. In the hospital, there was no remdesivir because it was getting brought based on an order from the company and it needed a prescription from the doctor to obtain” (Cg 01).
Second, the challenging circumstances in Lebanon had an additional impact on the accessibility of medicines. “The effect of the medications is unrelated to COVID-19. I mean, the availability of the medications. Now, even after COVID-19 has decreased, we have shortages in medications that are unrelated to COVID-19, it has to do with the economic situation. So, it’s not COVID-19 that made the crisis in medications, not at all” (Phys 08). “It was hard to provide medications because of the terrible situation of Lebanon” (Nurse 01).
Many pharmacists discussed community hoarding. “People were running to the pharmacies to secure one of these medications even if they did not need it at the time, just for the sake of keeping it at home just in case, which led to a huge shortage of supply” (C-Pharm 02).
However, patients were concerned about pharmacies stockpiling medications. “Exactly, because of the economic crisis selling the drug was not beneficial for the pharmacies so they started keeping it for emergency cases and selling it at the black market rate. After all the demand was very high” (Cg 07).
Few physicians mentioned lack of availability of medicines specifically in the hospitals, particularly for the new medications. “They had to get the medications outside of the hospital…the shortage was due to the fact that basically, this is a new medication, and it hasn’t been brought to Lebanon yet.” (Phys 08).
A few pharmacists stated that they always had a backup plan. “To be honest we never had really bad shortages, we never fully ran out, we always had a plan B. When there was no more dexamethasone for IV, we prepared other corticoids, even if it wasn’t mentioned in any studies or guidelines. We used to prepare them and keep them as backups in case they were ever needed” (H-Pharm 04).
Cost challenges
Both providers and patients noted unaffordable costs as another factor affecting access to medications, considering the devaluation of the currency. “The single pill got to about 50 USD, it was very expensive. So, it was really expensive for most people. Its actual price was 5000 Lira” [H-Pharm 04; note that at the time 5000 Lira was worth less than 5 US dollars (USD)]. “Even tablets like vitamins are available but they are very expensive, not everyone can afford them” (Cg 04).
Patients complained about price manipulation. “The prices were definitely manipulated because when I would buy a medication I would find more than one price tag… The lozenges for her throat used to cost 19 000 Lira and now it costs 45 000 Lira. They put more than one label on the box of medication, there are about three price tags on it” (Cg 06).
Additionally, it was mentioned that the pricing of medications was changed to the US currency. “Yes, most of the time they were fresh dollar” (Phys 08).
Drivers of decision-making for providers
During the COVID-19 pandemic, several factors influenced decisions by providers, patients and caregivers about which medicines to use or not use.
Owing to the rapid development of evidence, providers were compelled to rely on research to prescribe certain medications. “There was a committee that used to review the data available and to review all the evidence at the time and make the decisions.” (Phys 04). “… the COVID-19 protocol changed every couple of days. Every once in a while, a new study would appear, a new update, and it would change again” (H-Pharm 01).
Providers also relied on clinical practice guidelines developed either locally or internationally, for example, by the WHO. “The medications we were prescribing were based on WHO” (Phys 03). Although they relied on those guidelines, some providers expressed hesitations about them. “Yes, we were following the guidelines of treatment of COVID-19, we would tell this is the medication that needs to be taken because this is what the guidelines say. We are not sure of the guidelines, but this is what is needed now” (Phys 09).
Additionally, the providers’ prior experience or trial and error played a role in the decision-making process. “At first, personally, I did not have much experience with this disease but later on and after I acquired some experience, I was finally able to give my own opinion on the matter” (C-Pharm 01).
Reliance on local peers with different specialities played a significant role in decision-making. “Because we had several specialities – cardiovascular, internal medicine, and others – everyone did their research and every week we would meet and explain to each other… Everyone gave their inputs and propositions, in their own specialities, about which drugs might be good, and which drugs were used in which cases” (H-Pharm 04).
International expertise was also sought during the pandemic. “We also had video conferences with hospitals and ICUs in France and the United States, because we had physicians that went and studied in those countries and still had contacts, we did one video conference with France, and one with the US to ask about their protocols. And there were discussions about what’s best. And when Actemra was first being used by the ones we talked to somewhere in Houston, we weren’t using it yet in our hospital. After the video conference, they found that their patients are showing good results, so it was added to our protocol..” (H-Pharm 04).
It is of note that the country’s situation and drug availability influenced the decision-making process. As expressed by many doctors: “We were following the new guidelines, taking into consideration the situation of the country and the availability of the drugs and imaging” (Phys 02).
Drivers of decision-making for patients and caregivers
Patients and caregivers relied on social media to decide on drug purchases. “Yes. Honestly, they saw me crying and I had posted on Instagram that if anyone please could help with their experience because there were no studies at that time” (Cg 03). “At first people used to wait for what the media says and then come running to the pharmacies to buy these medications, it happened first with vitamin C then 2 weeks later with vitamin D then it was the zinc 25 mg and then zinc 50 mg turns” (C-Pharm 01). “Even the colchicine, we heard about it on social media, and we went around and looked for it and it was very hard for us to find easily” (Cg 02).
Patients and caregivers were also influenced by people in their communities, some of whom had experience with COVID-19. “Other people around us who also had corona, everyone that got corona would say take this and do this” (Pt 02). “My dad caught it in the beginning, so I started asking people to see what we could do. One of my friends told me that there was a person who took this medicine, and they told me to try it, so I decided to do that” (Cg 03).
Patients reported different attitudes about consulting with their doctors. “We heard about remdesivir and asked the doctor, he told us he can’t advise us to take it or not, if we would like to try it based on other patients and not on medical research then go ahead” (Cg 07). Some made decisions on their own on the basis of word of mouth. “My friend called me and told to me not listen to the doctors and to take zithromax. I bought it and took one pill” (Pt 08).
Accessing medicines
We have identified two subthemes under the theme of “accessing medicines”: information about how to get the medicines and the sources of medicines.
Information about how to get the medicines
Typically, patients obtained information about how to get the medicines from healthcare providers, including nurses, physicians and pharmacists. “Yes sure!… [local charities] used to give those medications (remdesivir, Actemra, etc.) for free. And there were some other providers. We used to indicate the providers to the families of the patients” (Nurse 01).
Patients also inquired about the source of medicines from recovered COVID-19 patients: “From other people around us who also had corona” (Pt 02).
Sources of medicines
Patients and their caregivers obtained the medicines either through the healthcare system or from outside the healthcare systems, including the black market, nongovernmental organizations (NGOs), personal networks, political parties and outside of the country.
- Healthcare system
When patients were admitted, few reported that COVID-19 medicines were available in the hospital. “They were all found in the hospital” (Cg 05). However, for several patients, their family members had to seek medicines from community pharmacies. “We got them from the pharmacy” (Cg 01).
Medicines were obtained at no cost thanks to a subsidy by the Lebanese government. “So, it was for free if it was from the Ministry” (Cg 02). However, some other medicines were purchased on an unsubsidized basis and at high cost. “A few pills were for 1 300 000 Lebanese Lira in the pharmacy” (Cg 02).
- Black market
Owing to the limited supply and urgent need for COVID-19 medications, the black market flourished. “There were two more weeks, and the Ministry was supposed to secure it, but we needed it urgently, so they gave us the number of someone who sells it in the black market and he got it for us” (Pt 03).
The black market was viewed as a double-edged sword because it allowed access but at an inflated cost. “They gave us five remdesivir and one Actemra for US$ 1200” (Cg 07). “The remdesivir is like. So, he made us pay US$ 700 for one,.. So, US$ 4200 for six pills” (Pt 03).
Because of the country’s financial crisis, inflated black market prices presented a major challenge for patients. “… it was a challenge for us to financially secure the medicine. And of course, him asking for US$ 4200 cash was not something easy for someone to get and pay, but if it is the only solution of course we would do it” (Pt 03).
Charities supported patients in accessing their medicines either for free or through financial support. “Suppose I were to get COVID-19 now, my name would go down at the municipality and they get you vitamin C and vitamin D – a charity organization, not from the government” (Cg 08). “I paid 1 million and the rest was on the charity organization” (Cg 08); “For ivermectin there were a lot of organizations trying to supply it, it’s a very cheap drug… that costs US$ 4. There were also a lot of organizations trying to supply remdesivir, ‘Hariri’ (a local charity) was trying to help with it since hospitals did not have it, people were going to her villa to get it, it costs I think about US$ 4000” (Phys 02).
Personal network
Caregivers of patients with COVID-19 used their personal networks, including family and friends: “Also, from a person who knows a pharmacist he’s friends with, they got them for us” (Cg 02). “We had to get the baricitinib from someone we know, who got it for us from the Ministry” (Cg 02).
Political parties
Political parties also supplied medicines to their supporters. “There were parties that were obtaining them, like [name of political parties]. Those were for free as a donation from [name of political party]” (Pt 02).
From outside of the country
Typically, family or friends helped by purchasing medicines while travelling. “At the time, an Iraqi who is friends with my relative got it and he paid US$ 400” (Pt 08).
Out-of-country purchases were driven by either lack of local supply or inflated costs. “The ivermectin was still not in Lebanon, so we got it elsewhere, from a woman who lives in Africa, she got it for us and sent it. And we started with cortisone, this is from day 1” (Cg 02). “My cousin sent it from Sweden, she sent zinc and vitamin C because vitamin C here now costs 60 000 Lira, before it cost 14 000 Lira and now it costs 60 000” (Cg 06).
This study aimed to to understand the experiences of patients with COVID-19 in Lebanon, as well as those of their families, physicians, nurses and pharmacists, with regards to their treatment decisions and accessibility to COVID-19 medicines.
The participants highlighted the country’s difficulties, especially the severe impact of COVID-19 pandemic and the economic crisis. Access to COVID-19 medicines and their costs were major challenges according to the three groups interviewed. Limited access related to global shortage of medicines, the local challenging circumstances, community hoarding (according to pharmacists) and stockpiling by pharmacies (according to patients). For providers, the decision-making process for COVID-19 treatments was shaped by research evidence, local and international practice guidelines, previous experiences and feedback from both local and international experts. Patients and their caregivers relied on social media, community members, physicians and word of mouth. Information on how to get the medicines was obtained from either healthcare providers or patients who recovered from COVID-19. Accessing medicines involved navigating through the healthcare system (hospitals and pharmacies), as well as outside that system, including the black market, charities, personal networks, political parties and outside of the country. Across these different sources, the medicines were either free, subsidized or at inflated costs.
Comparison to similar studies
A major finding in our study was the accessibility of patients and healthcare providers to needed medicines. This is corroborated by other studies conducted in Lebanon [ 33 , 34 ] and low-and middle-income countries [ 35 ]. The global impact of lockdowns on medicine manufacturing, supply and distribution contributed to shortages during the high-demand period of the COVID-19 pandemic [ 36 , 37 ]. Furthermore, Lebanon has faced severe economic and financial crises starting in 2019, which severely hindered the capacity to import vital healthcare equipment and medicines [ 38 , 39 ]. Indeed, the World Bank characterized the crisis as “among the world’s worst since the 1850s” [ 40 ]. The lack of government reimbursement further hindered hospitals in procuring necessary medications and medical supplies [ 41 ]. Consequently, individuals affected by COVID-19 in Lebanon resorted to unregulated sources, including the black market, often resulting in inflated prices and the risk of expired or counterfeit drugs [ 13 , 14 , 15 , 42 ].
Moreover, in line with our findings, other studies found that healthcare providers followed both international and national guidelines when deciding on potential treatments for COVID-19 patients [ 43 , 44 ]. However, in the absence of effective medications, discussion on various social media platforms encouraged self-medication and the use of herbal medicines [ 45 , 46 ]. In addition, a recent study conducted in Jordan assessing the usage of medications and natural products amidst the second wave of COVID-19 revealed that individuals primarily sought guidance from family and friends, with social media platforms serving as significant sources of advice concerning the use of these medications [ 47 ]. The same study showed that pharmacists notably played a significant role in guiding individuals on choosing these treatments compared with other healthcare providers [ 47 ].This highlights the impact of social media on treatment choices and emphasizes the need for disseminating accurate and evidence-based information.
Strengths and limitations
To our knowledge, this is the first study in Lebanon to comprehensively explore the interplay between country crises and medication accessibility during the COVID-19 pandemic, offering valuable insights into the unique challenges faced by the country. We explored in-depth the lived experiences of our participants, ensuring the representation of the perspectives of healthcare providers, patients and caregivers. Also, we used a rigorous qualitative methodology (please refer to the “Increasing rigour” section).
There are several limitations to consider. Firstly, the study focuses primarily on Lebanon, which may limit the findings’ generalizability to other countries with distinct settings and healthcare systems. Moreover, there is a possibility of recall bias among participants, as their recollections of events and experiences concerning medication accessibility during the crisis might be influenced by subjective interpretations or memory lapses. Additionally, the sampling technique employed might introduce selection bias, as participants were recruited through purposive sampling. Furthermore, it is important to note that this study is based on a specific snapshot in time during the COVID-19 pandemic. Consequently, its findings may not fully encapsulate the dynamic and evolving nature of the crisis or account for potential shifts in medication accessibility and decision-making processes over time.
This study sheds light on the wide range of factors influencing treatment decisions during the COVID-19 pandemic in Lebanon. It also unveils how patients and their families had to access medications either through the formal healthcare systems or through black markets and other channels. Plans are needed to address medicine availability, affordability and equitable distribution during similar future crises. There is an urgent need for collaborative efforts involving stakeholders, policy-makers and key systems such as Meditrack and AMAN within the Ministry of Public Health [ 48 , 49 ]. These initiatives are intended to establish resilient and sustainable drug supply chains and to ensure timely and equitable access to medications for all individuals, particularly in times of crisis. Furthermore, improving collaboration among healthcare providers, expediting medication access and creating patient support programs can alleviate the difficulties that people seeking treatment confront. For example, streamlining communication between hospitals, pharmacies and primary care doctors could speed up the prescription and dispensing processes.
Future research should focus on effective strategies to ensure medicine access during crises. Comparative research across different countries can provide valuable insights into successful tactics that can be tailored across different countries.
What is already known on this topic
global healthcare systems have been strained owing to the COVID-19 pandemic, leading to challenges in medicine access; and
Lebanon’s healthcare system has been significantly impacted by the pandemic and financial crises, affecting the availability of medicines.
What this study adds
it uncovers key factors influencing both healthcare providers and patients in their treatment decisions, providing a comprehensive perspective; and
it describes varied sources for medicines, including informal networks and the black market.
How this study might affect research, practice or policy
the findings emphasize the necessity for strategies that ensure continuous medicine access, particularly during times of crises and economic instability.
Availability of data and materials
The datasets analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
American University of Beirut
Consolidated Criteria for Reporting Qualitative Research
Coronavirus disease 2019
Community pharmacists
Hospital pharmacists
Institutional review board
Low- and middle-income countries
Lebanese Ministry of Public Health
Nongovernmental organizations
Severe acute respiratory syndrome coronavirus 2
Legido-Quigley H, Asgari N, Teo YY, Leung GM, Oshitani H, Fukuda K, et al. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet. 2020;395(10227):848–50.
Article CAS PubMed PubMed Central Google Scholar
Kretchy IA, Asiedu-Danso M, Kretchy J-P. Medication management and adherence during the COVID-19 pandemic: perspectives and experiences from low-and middle-income countries. Res Social Adm Pharm. 2021;17(1):2023–6.
Article PubMed Google Scholar
WHO. WHO Coronavirus (COVID-19) Dashboard: World Health Organization; 2022. https://covid19.who.int/ .
Hoteit R, Yassine HM. Biological properties of SARS-CoV-2 variants: epidemiological impact and clinical consequences. Vaccines. 2022;10(6):919.
Badreldin HA, Atallah B. Global drug shortages due to COVID-19: Impact on patient care and mitigation strategies. Res Social Adm Pharm. 2021;17(1):1946–9.
Sánchez DIR, Vogler S. Shortages of medicines to treat COVID-19 symptoms during the first wave and fourth wave: analysis of notifications reported to registers in Austria, Italy, and Spain. Pharmacy (Basel). 2023;11(4).
Agampodi TC, Agampodi SB, Glozier N, Siribaddana S. Measurement of social capital in relation to health in low and middle income countries (LMIC): a systematic review. Soc Sci Med. 2015;128:95–104.
Adam T, de Savigny D. Systems thinking for strengthening health systems in LMICs: need for a paradigm shift. Health Policy Plan. 2012;27(suppl 4):iv1-iv3.
Reeves A, Gourtsoyannis Y, Basu S, McCoy D, McKee M, Stuckler D. Financing universal health coverage – effects of alternative tax structures on public health systems: cross-national modelling in 89 low-income and middle-income countries. Lancet. 2015;386(9990):274–80.
Article PubMed PubMed Central Google Scholar
Farmer KC. Stress and strain on the US drug supply: the intersection of shortages, globalization, counterfeit products, and throw in a global COVID-19 pandemic. J Am Pharm Assoc. 2021;61(1):e85–6.
Article CAS Google Scholar
Martin AJ, Shulder S, Dobrzynski D, Quartuccio K, Pillinger KE. Antibiotic use and associated risk factors for antibiotic prescribing in COVID-19 hospitalized patients. J Pharm Pract. 2021:08971900211030248.
Dagrou A, Chimhutu V. I Buy medicines from the streets because i am poor: a qualitative account on why the informal market for medicines thrive in ivory coast. Inquiry. 2022;59:00469580221086585.
Plata GG. The black market for COVID-19 antiviral drugs. Br Med J. 2022;377.
Shuchman M. Low-and middle-income countries face up to COVID-19. Nat Med. 2020.
White CM. Counterfeit drugs: a major issue for vulnerable citizens throughout the world and in the United States. J Am Pharm Assoc. 2021;61(1):e93–8.
Article Google Scholar
El-Harakeh A, Haley SJ. Improving the availability of prescription drugs in Lebanon: a critical analysis of alternative policy options. Health Res Policy Syst. 2022;20(1):106.
Filip R, Gheorghita Puscaselu R, Anchidin-Norocel L, Dimian M, Savage WK. Global challenges to public health care systems during the COVID-19 pandemic: a review of pandemic measures and problems. J Personal Med. 2022;12(8):1295.
Patrucco F, Gavelli F, Fagoonee S, Solidoro P, Undas A, Pellicano R. Current treatment challenges in the COVID-19 pandemic. 2021.
Das M. Lebanon faces critical shortage of drugs. Lancet Oncol. 2021;22(8):1063.
Robinson PC, Liew DF, Tanner HL, Grainger JR, Dwek RA, Reisler RB, et al. COVID-19 therapeutics: challenges and directions for the future. Proc Natl Acad Sci. 2022;119(15): e2119893119.
Siemieniuk RA, Bartoszko J, Ge L, Zeraatkar D, Izcovich A, Kum E, et al. Drug treatments for COVID-19: living systematic review and network meta-analysis. Br Med J. 2021;373: n967.
Google Scholar
Dixit SB, Zirpe KG, Kulkarni AP, Chaudhry D, Govil D, Mehta Y, et al. Current approaches to COVID-19: therapy and prevention. Indian J Crit Care Med. 2020;24(9):838.
El Mikati IK, Hoteit R, Harb T, El Zein O, Piggott T, Melki J, et al. Defining misinformation and related terms in health-related literature: scoping review. J Med Internet Res. 2023;25: e45731.
Jirjees F, Ahmed M, Sayyar S, Amini M, Al-Obaidi H, Aldeyab MA. Self-medication with antibiotics during COVID-19 in the eastern Mediterranean region countries: a review. Antibiotics. 2022;11(6):733.
Colorafi KJ, Evans B. Qualitative descriptive methods in health science research. HERD. 2016;9(4):16–25.
Strauss A, Corbin J. Basics of qualitative research techniques. 1998.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Mays N, Pope C. Qualitative research: rigour and qualitative research. Br Med J. 1995;311(6997):109–12.
Tobin GA, Begley CM. Methodological rigour within a qualitative framework. J Adv Nurs. 2004;48(4):388–96.
Varpio L, Ajjawi R, Monrouxe LV, O’Brien BC, Rees CE. Shedding the cobra effect: problematising thematic emergence, triangulation, saturation and member checking. Med Educ. 2017;51(1):40–50.
Long T, Johnson M. Rigour, reliability and validity in qualitative research. Clin Eff Nurs. 2000;4(1):30–7.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Khattar G, Hallit J, El Chamieh C, Bou SE. Cardiovascular drug shortages in Lebanon: a broken heart. Health Econ Rev. 2022;12(1):24.
Osman M, Kasir D, Kassem II, Hamze M. Shortage of appropriate diagnostics for antimicrobial resistance in Lebanese clinical settings: a crisis amplified by COVID-19 and economic collapse. J Glob Antimicrob Resist. 2021;27:72.
Boro E, Stoll B. Barriers to COVID-19 health products in low-and middle-income countries during the COVID-19 pandemic: a rapid systematic review and evidence synthesis. Front Public Health. 2022;10: 928065.
EMA. Availability of medicines during COVID-19 pandemic European Medicines Agency; 2023 https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/availability-medicines-during-covid-19-pandemic .
Newton PN, Bond KC, Adeyeye M, Antignac M, Ashenef A, Awab GR, et al. COVID-19 and risks to the supply and quality of tests, drugs, and vaccines. Lancet Glob Health. 2020;8(6):e754–5.
Bou Sanayeh E, El Chamieh C. The fragile healthcare system in Lebanon: sounding the alarm about its possible collapse. Health Econ Rev. 2023;13(1):21.
HRW. Lebanon: COVID-19 Worsens Medical Supply Crisis: Human Rights Watch; 2021. https://www.hrw.org/news/2020/03/24/lebanon-covid-19-worsens-medical-supply-crisis .
WorldBank. The World Bank In Lebanon 2022. https://www.worldbank.org/en/country/lebanon/overview . Accessed 17 Nov 2023.
Shallal A, Lahoud C, Zervos M, Matar M. Lebanon is losing its front line. J Glob Health. 2021;11.
AmnestyInternational. Lebanon: Government must address medication shortages and healthcare crisis 2023. https://www.amnesty.org/en/latest/news/2023/02/lebanon-government-must-address-medication-shortages-and-healthcare-crisis/ .
Pan H, Peto R, Henao-Restrepo A, Preziosi M, Sathiyamoorthy V, Abdool Karim Q, et al. Consortium WST (2021) repurposed antiviral drugs for COVID-19-Interim WHO solidarity trial results. N Engl J Med. 2021;384:497–511.
Article CAS PubMed Google Scholar
Lamontagne F, Agoritsas T, Siemieniuk R, Rochwerg B, Bartoszko J, Askie L, et al. A living WHO guideline on drugs to prevent COVID-19. Br Med J. 2021;372.
Roman YM, Burela PA, Pasupuleti V, Piscoya A, Vidal JE, Hernandez AV. Ivermectin for the treatment of coronavirus disease 2019: a systematic review and meta-analysis of randomized controlled trials. Clin Infect Dis. 2022;74(6):1022–9.
Garegnani LI, Madrid E, Meza N. Misleading clinical evidence and systematic reviews on ivermectin for COVID-19. BMJ Evid Based Med. 2022;27(3):156–8.
Thiab SH, Nassar RI, Thiab S, Basheti IA. Medications and natural products used in Jordan for prevention or treatment of COVID-19 infection during the second wave of the pandemic: a cross-sectional online survey. Saudi Pharm J. 2022;30(6):856–62.
MOPH. MediTrack Project - Track & Trace System for Pharmaceuticals: Ministry of Public Health; 2020. https://www.moph.gov.lb/en/Drugs/index/0/15088 .
MOPH. Steps to Obtain a Unique Health ID, Enter the Medical Record into AMAN Program and Follow Up Through the Hotline 1214: Ministry of Public Health; 2023. https://www.moph.gov.lb/en/Pages/0/22862/moph-mobile-application-#/en/Pages/0/68151/steps-to-obtain-a-unique-health-id-enter-the-medical-record-into-aman-program-and-follow-up-through -.
Download references
Acknowledgements
Not applicable.
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and affiliations.
Clinical Research Institute, American University of Beirut, Riad-El-Solh, P.O. Box: 11-0236, Beirut, 1107 2020, Lebanon
Reem Hoteit
School of Public Health, University of Saskatchewan, Saskatoon, SK, S7N 5A2, Canada
Aya Hassoun
Department of Internal Medicine, American University of Beirut Medical Center, Beirut, Lebanon
Elie Bou Sanayeh, Marie Christelle Saade & Elie A. Akl
Rafic Hariri School of Nursing, American University of Beirut, Beirut, Lebanon
Gladys Honein-AbouHaidar
Department of Health Research Methods, Evidence, and Impact (HEI), McMaster University, Hamilton, Canada
Elie A. Akl
You can also search for this author in PubMed Google Scholar
Contributions
Concept and design: AH and EAA. Data collection: EBS, AH and MCS. Data analysis: RH, GHA and EAA. Data interpretation: RH, GHA and EAA. Drafting of the manuscript: RH, AH and EAA . All authors reviewed and approved the submitted version of the manuscript.
Corresponding author
Correspondence to Elie A. Akl .
Ethics declarations
Ethics approval and consent to participate.
The Institutional Review Board (IRB) at the American University of Beirut (AUB) approved the study.
Consent for publication
All participants provided oral consent prior to participation.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hoteit, R., Hassoun, A., Bou Sanayeh, E. et al. Choosing and accessing COVID-19 treatment options: a qualitative study with patients, caregivers, and health care providers in Lebanon. Health Res Policy Sys 22 , 38 (2024). https://doi.org/10.1186/s12961-024-01131-9
Download citation
Received : 15 August 2023
Accepted : 09 March 2024
Published : 27 March 2024
DOI : https://doi.org/10.1186/s12961-024-01131-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medication accessibility
- Medication shortages
- Treatment decisions
- Economic crisis
- Healthcare professionals
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 25 March 2024
A great way to bring up health behaviour topics at playgroup: a qualitative evaluation of the Healthy Conversations @ Playgroup program
- Georgia Middleton 1 ,
- Brittany J. Johnson 1 ,
- Dimity Dutch 1 ,
- Stewart G. Trost 2 ,
- Rebecca Byrne 3 ,
- Hayley E. Christian 4 , 5 ,
- Anna Henry 4 ,
- Caroline O. Terranova 3 ,
- Kate E. Williams 6 ,
- Li Kheng Chai 3 , 7 ,
- Denise S. K. Brookes 3 ,
- Kate Simon 3 &
- Rebecca K. Golley 1
BMC Public Health volume 24 , Article number: 890 ( 2024 ) Cite this article
163 Accesses
Metrics details
The early years is a critical stage to establish optimal nutrition and movement behaviours. Community playgroups are a relaxed environment for parents with a focus on social connection and supporting parents in their role as ‘First Teachers’. Playgroups are therefore an opportunistic setting to promote health behaviours in the early years. To support parents with young children around healthy lifestyle behaviours, the Healthy Conversations @ Playgroup program was delivered in urban and regional areas, across three Australian jurisdictions between 2021–2023.
This qualitative evaluation aimed to understand how the Healthy Conversations @ Playgroup program was experienced by parents, playgroup coordinators and peer facilitators.
Semi-structured virtual interviews and focus groups were conducted with parents, playgroup coordinators (i.e., person responsible for coordinating the playgroup) and peer facilitators (i.e., trained facilitator for the program) that participated in the Healthy Conversations @ Playgroup study. Transcripts were analysed following a thematic analysis approach.
Twenty-eight playgroup parents, coordinators or peer facilitators participated in one of 8 focus groups or 5 interviews. Four themes were developed: Program strengths and challenges; Setting strengths and challenges; Factors that impact program delivery; Participant’s suggestions for future program delivery.
Conclusions
The Healthy Conversations @ Playgroup program was valued by parents, providing validation and normalisation of parenting practices, and fostering a shared experience of parenting. Playgroups are a convenient setting for families to attend. The dynamic and distracting nature of the playgroup setting were carefully considered when designing the program. Strategies to further enhance program engagement could include use of coordinator or parent champions, tailored delivery, and extending the reach to other family members.
Trial registration
Australian New Zealand Clinical Trials Registry ACTRN12621000055808, registered 22 January 2021, https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=380890
Peer Review reports
The early years of life are critical for establishing health-promoting behaviours to support optimal health, growth, and development [ 1 , 2 ]. Health-promoting behaviours include regular physical activity, limited screen time, healthy eating, and adequate sleep [ 1 ]. However, recent population-level surveys indicate that only 28% of Australian children aged 2–3 years are meeting both fruit and vegetable recommendations [ 3 ], and only 17% of Australian children aged 2–5 years are meeting both physical activity and sedentary behaviour recommendations [ 4 ]. Health behaviours established in the early years can track into adolescence and adulthood, influencing health across the life course [ 2 , 5 , 6 ]. Therefore, it is important to intervene early and establish healthy behaviours in childhood [ 7 , 8 , 9 , 10 , 11 ].
Parents are children’s first teachers, and their parenting practices are instrumental in shaping children’s eating, movement, and sleep behaviours [ 12 , 13 , 14 ]. Parenting practices are specific, observable parenting actions such as creating a safe, interesting environment, setting limits and rules, having realistic expectations, and using appropriate feedback and consequences [ 15 , 16 ]. Supportive parenting practices and the family environment are integral for developing child autonomy [ 17 ]. Autonomy supporting parenting practices, where parents encourage thoughtful child decision-making, have been shown to support the development of healthy behaviours in children [ 18 ]. However, previous research has indicated that parents require knowledge, skills, and confidence to effectively use autonomy supportive practices to promote child health behaviours [ 14 , 19 ].
Parent involvement has been recognised as integral for improving child health behaviour outcomes that support healthy growth [ 20 , 21 , 22 ]. However, programs delivered through Early Childhood Education and Care settings, while suitable for reaching a large proportion of preschool-aged children, are not necessarily conducive to parental participation and engagement as parents time at the setting is limited [ 23 , 24 ]. Programs delivered in community settings where parents already attend with their child may have a higher likelihood of success, particularly where there are existing mechanisms for parent support [ 25 ]. Community playgroups are one such setting, offering a unique model of informal family support by bringing together groups of families with young children in local settings for shared play and socialising. Community playgroups offer a low- or no-cost, safe, and relaxed environment where existing social networks exist among attending parents, they enable shared learning and support, and are facilitated by a playgroup coordinator who is often a parent volunteer [ 26 ]. Despite playgroups existing internationally, including in the United Kingdom and United States, few child health promotion programs have been delivered and evaluated in community settings such as playgroups [ 27 ].
In 2018, Fuller and colleagues conducted focus groups with parents attending community playgroups in Brisbane, Australia, to determine what parents would find acceptable in a program delivered in playgroups [ 28 ]. The findings indicated that parents did not want to be ‘educated’ but desired strategies and support for dealing with parenting challenges. This aligns with previous reports that programs supporting parents commonly provide education, advice, and strategies [ 16 , 29 , 30 ] but parents also require support for increased capability and confidence [ 7 , 28 , 31 , 32 ]. Additionally, parents did not want to lose their valuable playgroup time to an external program and felt the support and guidance received from other parents at playgroup facilitated autonomy supporting parenting practices [ 28 ].
The Healthy Conversations @ Playgroup program was designed to support parents to use autonomy promoting parenting practices to improve children’s eating, movement, screen time and sleep behaviours [ 26 ]. The program was designed to be suitable to embed in the universal care system. The program was evaluated in community playgroups, hereafter referred to as playgroups, in three Australian jurisdictions (South Australia, Western Australia, Queensland; urban and regional areas) as a multi-site randomised controlled trial (ACTRN12621000055808) [ 26 ]. Recruitment, program delivery and evaluation occurred between 2021–2023, over three waves (due to COVID-19). Playgroup associations in each state promoted the program to all registered playgroups, who self-selected to participate ( n = 51 total playgroups participated in the evaluation). In brief, the H ealthy Conversations @ Playgroup program comprises 10 conversations delivered by a peer facilitator (a parent external to the playgroup, employed and trained to deliver the program) over five fortnightly sessions within the usual playgroup schedule [ 26 ]. The conversations were designed to increase parents’ capability and self-efficacy to implement autonomy-supportive parenting practices . Conversation topics included: reducing stress at mealtimes, limiting screens without tantrums, supporting movement skills in children, bedtime activities and routines to support sleep, and celebrating achievements. Further details of the program design and quantitative evaluation are reported in Trost et al. [ 26 ]. This qualitative study aimed to understand how the Healthy Conversations @ Playgroup program was experienced by parents, playgroup coordinators, and peer facilitators.
Study design
This study aligns with a critical qualitative approach, informed by critical realism ontology and an epistemological orientation of contextualism [ 33 ]. Through this position, we acknowledge that human practices shape the way we experience and know about reality and the world, and that human experiences cannot be studied in isolation from the contexts in which they exist [ 33 ]. This is well suited to understanding the shared experiences of participating in or delivering the Healthy Conversations @ Playgroup program. A thematic analysis approach guided the collection and analysis of data for this study [ 33 , 34 ].
Recruitment
Parents who participated in the Healthy Conversations @ Playgroup trial were eligible to participate in this qualitative study. As contact information of participating parents was collected for the broader program, this information was available to recruit parents into this qualitative study. Parents were invited via phone by a member of the research team to participate in a virtual focus group, between November 2022 to February 2023. Each playgroup in the program had a playgroup coordinator, a contact person who was typically a parent or community volunteer. Their contact information was also collected for the broader program and thus available to the research team to recruit into the qualitative study. Playgroup coordinators were invited via email or phone by a member of the research team to participate in a virtual focus group. Contact details of the peer facilitators who were responsible for delivering the Healthy Conversations @ Playgroup program were also available to the research team for this qualitative study. Peer facilitators were invited via email by a member of the research team to participate in a virtual one-on-one interview. Potential participants were provided with an information sheet, allocated to a suitable focus group or interview time, and asked to provide verbal (parents) or written consent (peer facilitators and playgroup coordinators) to participate.
Data collection
Two semi-structured focus group/interview guides were developed, one for parents, and one for playgroup coordinators and peer facilitators (Additional file 1 ). Both guides were pilot tested with participants, and as they required no major changes their data were used in analysis. The guides were designed based on those used in Fuller et al.’s focus groups [ 28 ], and other qualitative explorations of parenting practices [ 35 , 36 ]. The questions aimed to explore participants’ experiences of the program, what they perceived as program strengths and weaknesses, and what they would recommend for future iterations. Focus groups were chosen because they encourage group reflection and exploration of potentially sensitive issues by creating a safe space where similar experiences or views can be shared, and a shared experience can be created [ 37 ]. One-on-one interviews were chosen for the peer facilitators to encourage depth of responses, and to maintain their confidentiality as they were known to one another [ 37 ]. Peer facilitators were offered copies of their transcripts for review; none took up the offer. Due to the nature of focus groups, this was not possible for other participants.
All focus groups and interviews were conducted via video call using Microsoft Teams Version 1.6.00.11166, and were audio recorded and transcribed verbatim by professional transcription agency OutScribe Transcription, a human transcription service. GM (PhD), an experienced qualitative researcher, conducted all focus groups and interviews, and another member of the research team acted as notetaker (DD or research assistant). GM conducted the qualitative exploration as an independent party to the Healthy Conversations @ Playgroup program. They were not involved in the design, delivery, or evaluation of the program, and had no prior relationship to participants. This potentially helped reduce social desirability bias and protected participants from feeling pressured to provide a socially acceptable response to the designers or deliverers of the program.
The data collection and analysis team, comprising of GM, DD, BJJ, and a research assistant are white females with no children and approached this research from a background in public health and dietetics. All work in the space of child and family health and nutrition and have varying degrees of experience and knowledge working with this population group and researching childhood health behaviours and related parenting practices. GM had no prior experience with playgroups; however, BJJ, DD and the research assistant were involved in other aspects of the broader program, excluding program delivery. DD and the research assistant had minimal qualitative research experience prior to this study, but were supported and guided by GM.
Data analysis
The basic principles of thematic analysis were followed, as seen in Fig. 1 . This involved following the six steps of thematic analysis as laid out by Braun and Clarke [ 33 , 34 ]. GM coded all transcripts, and DD coded 70% of the transcripts, to familiarise themselves with the data and the coding structure, and to incorporate alternative perspectives. NVivo 12Pro qualitative analysis software (QSR International Pty Ltd. 2018) was used for organisation and management. Team analysis meetings were held regularly (GM, DD, BJJ), and DD and GM maintained reflexive journals across all stages of data analysis to bracket assumptions, reflect on findings and document analytical queries for future discussion. This study was limited to sampling participants from the Healthy Conversations @ Playgroup trial, and thus data saturation did not guide recruitment. However, the themes developed through analysis were analytically robust and well supported by the data, and the team are confident that saturation of the themes presented in this article was achieved, as new data was not producing new or conflicting findings.
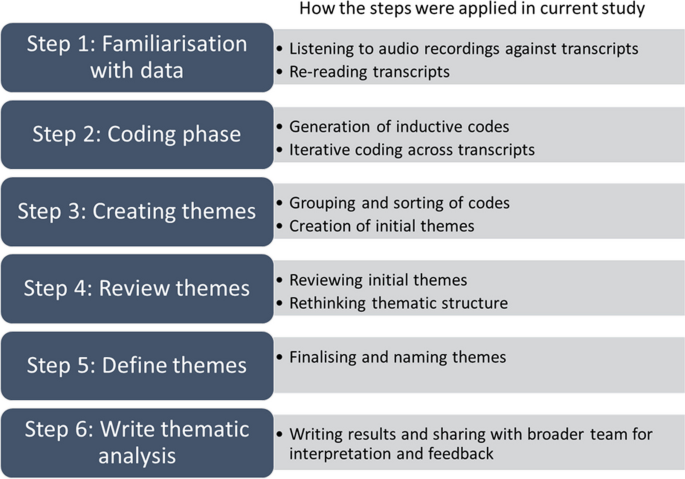
The six steps of thematic analysis [ 33 , 34 ] and how they were applied in the current study
Sample and participant characteristics
Twenty-eight individuals participated in this qualitative evaluation: 17 parents, 6 playgroup coordinators, and 5 peer facilitators (Additional Fig. 1 ). Six focus groups were conducted with parents ( n = 2–5 per group), two focus groups were conducted with playgroup coordinators ( n = 3 per group), and five individual interviews were conducted with peer facilitators, lasting approximately 46 min (range 36–60 min). Participants were from South Australia ( n = 10), Western Australia ( n = 10), and Queensland ( n = 8). Full demographic characteristics of participants are described in Table 1 . Peer facilitators were parents themselves, often familiar with the playgroup setting from personal or professional experience.
Four main themes were derived across parent, playgroup coordinator, and peer facilitator transcript data: 1) Program strengths and challenges, 2) Setting strengths and challenges, 3) Factors impacting program delivery, and 4) Participant’s suggestions for future program delivery. All participants have been given pseudonyms. See Additional Fig. 2 for analysis coding tree.
Theme 1: Program strengths and challenges
Within this theme, there are four subthemes: 1) Relevant, helpful conversations, 2) Reducing parenting pressures, 3) Fostering peer support, and 4) Ever-changing challenges of parenting. See Table 2 for participant quotes against each subtheme.
Relevant, helpful conversations
Parents described their involvement in the Healthy Conversations @ Playgroup program as a positive experience and described the opportunity to have conversations about relevant topics as a strength of the program. Parents commented that while it is not unusual for these topics to be discussed between parents at playgroup, they welcomed the dedicated time to have these conversations. Peer facilitators and playgroup coordinators echoed these sentiments and noted the importance of having the peer facilitator start the conversation and keep it on track. They reflected on the importance of the conversational, rather than stand-and-deliver style.
Reducing parenting pressures
Parents described not feeling judged by peer facilitators and other parents in the program and felt the program fostered an environment of open-mindedness. There was a shared understanding at the playgroups that what works for one family may not work for another, and that no parent is perfect. Parents also described that the program reaffirmed their choice of parenting practices and boosted their confidence. This sentiment was echoed by peer facilitators, who described intentionally approaching the conversations in a way that would not increase pressure on parents. Both peer facilitators and playgroup coordinators described the program facilitated a safe environment for parents to share their experiences and fostered an understanding that all families were different.
Fostering peer support
Participants identified peer support as a core strength of the program, fostered by peer facilitators and other parents. The value of having a ‘peer’ facilitate the conversations, as someone who had ‘been through it’ and could speak to their own experiences, was evident across participant responses and viewed as a strength of the program. Parents provided peer support through connecting with one another and sharing their own experiences and strategies. This was particularly helpful for first-time parents who could learn from parents who had older children and had dealt with similar challenges in the past. The peer-sharing provided an opportunity for parents to identify with one another and learn from each other. The program normalised the challenges parents often face at this stage of child development, and a common shared parenting experience was fostered.
Ever-changing challenges of parenting
Although the program topics were thought to be relevant, participants noted that some topics were of more interest than others. Some parents felt that they had already overcome the challenges associated with some topics, and others did not find the topics of relevance to their child at the time of the program. The ever-changing nature of the challenges parents face as children grow was generally cited as why topics were not always viewed as relevant for parents.
Theme 2: Setting strengths and challenges
Within this theme, there are three subthemes: 1) Playgroups are a suitable setting for programs supporting parents, 2) Playgroup environments can be distracting, and 3) Playgroups have varied attendance. See Table 3 for participant quotes against each subtheme.
Playgroups are a suitable setting for programs supporting parents
Playgroups were described as a suitable setting for a child health promotion program supporting parents, as they were familiar, casual, relaxed, and safe environments. Peer facilitators and playgroup coordinators described playgroups as providing a receptive audience with the potential for broad reach in the community. Aligning with the design and intention of the program, attending playgroup was already part of parents’ routine, and therefore attendance at the program was viewed by many as convenient. Parents valued not having to make additional time to attend the program outside of their existing activities and appreciated being able to attend with their children, thus confirming the thinking behind the program design.
Playgroup environments can be distracting
Although playgroups were identified as a suitable and convenient setting for delivery of the program, participants acknowledged the playgroup environment as one with frequent distractions for parents and peer facilitators, due to competing demands on attention. Distractions largely came from children requesting their parent’s attention. This could pose a challenge for parents attempting to engage in the conversations, and for peer facilitators trying to facilitate the conversations. Peer facilitators and playgroup coordinators also noted the challenges of different layouts of playgroups. The way the playgroups were set-up in the space, and the way they were coordinated were noted as impacting parents’ ability to engage with the conversations.
Playgroups have varied attendance
Another challenge presented by the playgroup setting was the varied attendance of parents from week to week. This could impact parents’ ability to engage in conversations not just through their own attendance, but through the inconsistent presence of others. The varied attendance meant group size and dynamics changed frequently, which impacted the engagement of parents and the quality of conversations. The COVID-19 pandemic further exacerbated issues with attendance at the time.
Theme 3: Factors that impact program delivery
Within this theme, there are five subthemes: 1) Each playgroup is unique, 2) Timing of and between sessions, 3) Group dynamics, 4) Perceived engagement with the program, and 5) Competence of peer facilitator. This theme is composed exclusively of peer facilitator and playgroup coordinator data, as it relates to how the program was run and the questions that were asked of these population groups. See Table 4 for participant quotes against each subtheme.
Each playgroup is unique
It was evident from participant descriptions that each playgroup runs differently, depending on the parents, the playgroup coordinators, and the physical space and environment. Peer facilitators noted that these components impacted their delivery of the program, and how easy it was for parents to engage. From peer facilitator’s perspectives, the playgroup coordinators were integral to the program’s success. If playgroup coordinators were supportive and valued the program, and set-up the playgroup to be conducive to participation, this increased the likelihood that parents could engage.
Timing of and between sessions
Sessions were intended to be delivered every two weeks, but because of personal illness, or COVID-19 disruptions, some peer facilitators ran sessions weekly or had longer breaks between sessions. The shorter distance between sessions was viewed positively by some peer facilitators, who found it easier to engage parents when sessions were delivered in close succession. The timing of the sessions over the year also appeared to impact parents’ engagement, with peer facilitators noting better parental participation when the program was provided further along in the school term compared to the first weeks of term, where parents were more likely wanting to ‘catch up’ after the break from playgroups over the holidays.
Group dynamics
Peer facilitators and program coordinators described group dynamics impacting parents’ engagement in the program. Peer facilitators described conversations as easier to facilitate when parents were confident and relaxed with each other. When the dynamics were not as constructive, facilitating the conversations was more challenging, particularly when parents were not as open to sharing or contributing to discussion. Playgroups with an established group of parents led to constructive conversations, especially compared with new groups where parents were not as familiar with one another. However, peer-facilitators observed established friendship groups within a playgroup could make it difficult for those who were not part of the friendship group to contribute.
Perceived engagement with the program
Playgroup coordinators and peer facilitators noted that a number of the parents who were involved in the program appeared to already be very confident and familiar with the topics, and thus were not as interested in participating in the conversations. Some parents were also more interested in catching up with one another or spending time with their child(ren) than engaging in the conversations. Peer facilitators noted that parents’ interest or engagement in the topics often determined how easy or challenging the conversations were to facilitate. When parents were engaged, facilitators felt they barely had to drive the conversation at all, but when parents were not interested, facilitators could feel as though they were talking to an empty room. Playgroup coordinators and peer facilitators also observed the opportunity the conversations brought to engage newer parents or those with minimal established connections at playgroup, noting that engagement could change over time from passively observing, to more actively contributing as time went on.
Competence of peer facilitator
Due to the dynamic nature of playgroups, it was important that the person delivering the program could adapt to each playgroup environment. The importance of peer facilitators being competent, flexible, and confident in their delivery to accommodate the playgroup environment was acknowledged in participant’s responses. As anticipated in the design of Healthy Conversations @ Playgroup , this was integral to program delivery, due to the varied nature of playgroups, and factors that impacted parents’ engagement in the conversations.
Theme 4: Participant’s suggestions for future program delivery
Within this theme, there are three subthemes: 1) Who and how of program delivery, 2) Program content, and 3) Tailoring to meet playgroup needs. These are participant’s suggestions for the program based on their perceptions and experiences, and many sit in contradiction to the strengths and benefits of the program they expressed. See Table 5 for participant quotes against each subtheme.
Who and how of program delivery
Due to the distracting nature of playgroups, participants suggested offering the program in a setting that more easily allows parents to concentrate, such as at a time and place away from children, or where child-supervision was provided. Participants described flexibility for delivery, including drop-in, once-off or follow-up sessions, virtual delivery of sessions, and increased opportunities for co-parent involvement. These suggestions sit in contrast to the benefits and strengths of the current delivery and setting of the Healthy Conversations @ Playgroup program described by participants, and it is clear that there needs to be balance between the benefits of the playgroup setting against its challenges.
These participants were asked how they envisioned long-term program delivery. Playgroup coordinators and peer facilitators suggested that support from playgroups at the jurisdiction level was required to ensure delivery of the program could be maintained through playgroups on an ongoing basis. Alternatively, they suggested other service providers who could potentially deliver the program instead. For sustainable delivery of the program, peer facilitators discussed the option for the program to be delivered by playgroup coordinators or champions.
Program content
Participants suggested additional topics for the program. Common suggestions were behaviour management and regulation, child development, sibling relationships, speech and language development, and toileting. Parents also suggested topics related to engaging with specialists, parenting roles and support, child developmental transitions, and further information on using screen time positively. Playgroup coordinators and peer facilitators also suggested introduction of solids, parent self-care, and toothbrushing.
Peer facilitators and playgroup coordinators suggested providing more practical tips, more resources or handouts for parents to revisit, and opportunities for notetaking. However, these suggestions contradict the strength of the relaxed, informal conversation-style format of the program, which parents explicitly preferred over stand-and-deliver lecture-style programs. Participants also suggested providing practical activities for children and/or parents during the conversations that aligned with the conversation topics for each session, to keep the children busy and parents engaged.
Tailoring to meet playgroup needs
Some participants suggested splitting the program by child age, so that only information relevant to child age and stage was being discussed. Others disputed this suggestion, as they felt this would negatively impact the peer support provided by parents with different experiences. Peer facilitators indicated that it would be helpful to have more involvement with the playgroup prior to delivering the program, to support specific tailoring of the program to individual playgroup environments and parent characteristics.
The study aim was to understand how the Healthy Conversations @ Playgroup program was experienced by parents, playgroup coordinators, and peer facilitators. Through qualitative analysis of focus group and interview data, peer support and normalising parenting challenges were found to be key program strengths. Playgroups were suitable for delivering this type of program, but the setting presented a dynamic environment that required flexibility and cooperation for successful program delivery.
Social support was a strength of the Healthy Conversations @ Playgroup program. The support provided by peers helped to normalise and create a shared experience of parenting. Peer support was facilitated by having parents of children of different ages and stages and having a ‘peer’ facilitate the sessions. The program helped parents feel more confident and assured in their parenting practices, which is an important aspect of parent capacity and likelihood of participating in positive parenting practices [ 38 ]. Research has shown that capacity building is an integral component of successful behaviour change [ 31 ], and without this feeling of confidence and capability, it is less likely parents would make behaviour changes at home [ 7 , 28 , 32 ]. Many programs in the child health promotion space provide education, advice and strategies, and the fostering of parenting support and capacity is often overlooked [ 7 , 28 , 31 , 32 ]. For parents to be able to effectively support health behaviours in children, they need to feel supported themselves.
The Healthy Conversations @ Playgroup program was unique in using an existing community setting with social connection. It has been established that the health and wellbeing of caregivers, including parents, is integral to being able to care for others [ 39 ]. This sentiment was discussed by parents in the present study, “for the kids to be healthy, their mummy’s need to be healthy as well”. Parenting is challenging and too often parents feel alone in the challenges they face [ 40 ], especially first-time parents [ 41 ]. Mothers in particular bear the brunt of social expectation for their children’s health status [ 42 , 43 ], and feelings of shame and stigma at not being ‘good enough’ can lead to poor outcomes for both parents and children [ 43 ]. The Healthy Conversations @ Playgroup program drew on the strengths of the playgroup setting, as an environment that provides social support, a sense of belonging and feelings of reassurance and validation [ 44 , 45 ]. The finding that the program was able to provide this support to parents as a novel way to improve child health behaviours was reassuring, as it was an intention of the program as informed by the focus groups that preceded the program design [ 28 ].
The playgroup setting provided an optimal environment for fostering support and was considered convenient and comfortable for parents and children. Delivering the program in a setting where parents already attend is another core strength of Healthy Conversations @ Playgroup , and a facilitator to parental engagement in a program such as this, as it did not require transport or attendance to an additional setting [ 20 , 46 ]. However, playgroups were also described as a dynamic and potentially distracting environment by all participant groups. The dynamic and distracting nature of playgroups was anticipated [ 28 ] and strategies were incorporated into the program design by having facilitators who could embrace the complexity of the environment, work constructively with enthusiastic playgroup coordinators, and engage in flexible delivery to ensure the conversations suited parents in their playgroup environment. This flexibility of delivery aligns with the emphasis on effective facilitation for successful program implementation [ 47 ]. To further strengthen program delivery in the playgroup setting, participants suggested the facilitator attend each playgroup prior to the program to understand the contexts, parent needs, and group dynamics and tailor their delivery accordingly.
While the program was viewed positively by most participants in this study, some parents felt that they were already addressing the topics presented in the Healthy Conversations @ Playgroup program at home. However, population-representative health survey data indicates that majority of households are still not meeting recommendations for these health behaviours [ 3 , 4 , 48 , 49 , 50 ], presenting an incongruence between what parents say they do at home, and what actually occurs. Additionally, parents valued hearing other’s experiences, but few acknowledged their role in helping others through sharing their own experiences. Playgroups pose a convenient, safe, and supportive environment for programs that aim to foster parent capacity building for promoting health behaviours in children. Program champions could be used to enhance the delivery of these programs through playgroups, helping to increase participation, reach and engagement, and motivate change.
Strengths and considerations
This qualitative study allowed an in-depth evaluation of the Healthy Conversations @ Playgroup program and is one of the first qualitative evaluations of a health promotion program set in a community playgroup setting. GM, who conducted the focus groups and interviews, was independent to the program and had no part in its design or delivery, reducing the potential for social desirability bias to impact the findings. Most transcripts were coded by two members of the research team, which strengthened the interpretation of the findings and the depth of the analytical discussions with the broader team. Participants were sampled from those already attending playgroups, and had self-selected to both be a part of the Healthy Conversations @ Playgroup program, and this qualitative evaluation, therefore may not reflect the views and profiles of broader parent population. Finally, as this was an opportunistic evaluation of the program, many parents had received the program over 12 months prior to participating in the focus group and therefore the results presented in this study may be impacted by recall bias.
Implications for research and practice
The Healthy Conversations @ Playgroup program is a first step in supporting positive child health behaviours in a playgroup setting. Many of the program strengths aligned with the intention of the program design, as informed by the focus groups with parents [ 28 ], confirming consultation with the target population as an integral step in program design. Building from these strengths, future iterations of the program could look at reach and engagement with support networks such as co-parents and other caregivers to strengthen practices at home. The use of champions to increase reach and engagement is also worth exploring. Some parents in this study did not recognise the value they had in supporting others who were struggling, which is an underutilised opportunity in the supportive environment fostered at playgroups. The scalability of the program, including how it’s delivered, and how much it’s tailored to the individual setting, is an area for future research.
The Healthy Conversations @ Playgroup program was valued by participants and provided social support, confidence, reassurance, validation of parenting practices, and fostered normalisation and a shared experience of parenting. It provided opportunities for sharing strategies and learning from others on how to engage in autonomy supporting parenting practices at home. Playgroups are a convenient and safe setting for children and their families and are ideal for delivering health promotion programs such as Healthy Conversations @ Playgroup . Potential opportunities to support future delivery of the program in playgroups to help reach a broader parent population include engaging broader support networks including co-parents and grandparents, and enlisting program champions, to increase reach and engagement, motivate change, and strengthen practices at home.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to the nature of the data, the conditions of ethics approval, and privacy concerns, but are available from the corresponding author on reasonable request.
Kuzik N, Poitras VJ, Tremblay MS, Lee EY, Hunter S, Carson V. Systematic review of the relationships between combinations of movement behaviours and health indicators in the early years (0–4 years). BMC Public Health. 2017;17(Suppl 5):849.
Article PubMed PubMed Central Google Scholar
Birch L, Fisher J. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101(2):539–49.
Article CAS PubMed Google Scholar
Australian Bureau of Statistics (ABS). National Health Survey: Dietary behaviour 2020–21 financial year: ABS; 2022 [Available from: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/dietary-behaviour/2020-21 .
Australian Institute of Health and Welfare (AIHW). Physical activity across the life stages. Canberra: AIHW; 2018.
Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas. 2011;70(3):266–84.
Article PubMed Google Scholar
Nicklaus S. Development of food variety in children. Appetite. 2009;52(1):253–5.
Campbell KJ, Hesketh KD. Strategies which aim to positively impact on weight, physical activity, diet and sedentary behaviours in children from zero to five years. A systematic review of the literature. Obes Rev. 2007;8(4):327–38.
Kaikkonen JE, Mikkilä V, Magnussen CG, Juonala M, Viikari JS, Raitakari OT. Does childhood nutrition influence adult cardiovascular disease risk? - Insights from the Young Finns Study. Ann Med. 2013;45(2):120–8.
Ness AR, Maynard M, Frankel S, Smith GD, Frobisher C, Leary SD, et al. Diet in childhood and adult cardiovascular and all cause mortality: the Boyd Orr cohort. Heart. 2005;91(7):894–8.
Article CAS PubMed PubMed Central Google Scholar
Hardy L, King L, Hector D, Lloyd B. Weight status and weight-related behaviors of children commencing school. Prev Med. 2012;55(5):433–7.
Lobstein T, Baur L, Uauy R, IASO International Obesity TaskForce. Obesity in children and young people: A crisis in public health. Obesity Reviews. 2004;5:4–85.
Lindsay AS, KM, Kim J, Gortmaker S. The role of parents in preventing childhood obesity. Future Child. 2006;16(1):169–86.
Yee A, Lwin M, Ho S. The influence of parental practices on child promotive and preventive food consumption behaviors: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14(1):47.
Xu H, Wen LM, Rissel C. Associations of parental influences with physical activity and screen time among young children: a systematic review. J Obes. 2015;2015: 546925.
Power TG, Sleddens EF, Berge J, Connell L, Govig B, Hennessy E, et al. Contemporary research on parenting: conceptual, methodological, and translational issues. Child Obes. 2013;9(Suppl 1):S87–94.
Golley RK, Perry RA, Magarey A, Daniels L. Family-focused weight management program for five- to nine-year-olds incorporating parenting skills training with healthy lifestyle information to support behaviour modification. Nutr Diet. 2007;64(3):144–50.
Article Google Scholar
Jungert T, Landry R, Joussemet M, Mageau G, Gingras I, Koestner R. Autonomous and controlled motivation for parenting: associations with parent and child outcomes. J Child Fam Stud. 2015;24(7):1932–42.
Côté-Lecaldare M, Joussemet M, Dufour S. How to support toddlers’ autonomy: a qualitative study with child care educators. Early Educ Dev. 2016;27(6):822–40.
Paes VM, Ong KK, Lakshman R. Factors influencing obesogenic dietary intake in young children (0–6 years): systematic review of qualitative evidence. BMJ Open. 2015;5(9): e007396.
Mehdizadeh A, Nematy M, Vatanparast H, Khadem-Rezaiyan M, Emadzadeh M. Impact of parent engagement in childhood obesity prevention interventions on anthropometric indices among preschool children: A systematic review. Child Obes. 2020;16(1):3–19.
Morris H, Skouteris H, Edwards S, Rutherford L. Obesity prevention interventions in early childhood education and care settings with parental involvement: a systematic review. Early Child Dev Care. 2014;185(8):1283–313.
van de Kolk I, Verjans-Janssen SRB, Gubbels JS, Kremers SPJ, Gerards S. Systematic review of interventions in the childcare setting with direct parental involvement: effectiveness on child weight status and energy balance-related behaviours. Int J Behav Nutr Phys Act. 2019;16(1):110.
Bell L, Golley R. Interventions for improving young children’s dietary intake through early childhood settings: A systematic review. Int J Child Health Nutr. 2015;4(1):14–32.
Hesketh KD, Campbell KJ. Interventions to prevent obesity in 0–5 year olds: an updated systematic review of the literature. Obesity (Silver Spring). 2010;18(Suppl 1):S27-35.
PubMed Google Scholar
Strange C, Fisher C, Howat P, Wood L. Fostering supportive community connections through mothers’ groups and playgroups. J Adv Nurs. 2014;70(12):2835–46.
Trost SG, Byrne R, Williams KE, Johnson BJ, Bird A, Simon K, et al. Study protocol for Healthy Conversations @ Playgroup: a multi-site cluster randomized controlled trial of an intervention to promote healthy lifestyle behaviours in young children attending community playgroups. BMC Public Health. 2021;21(1):1757.
Brown T, Moore TH, Hooper L, Gao Y, Zayegh A, Ijaz S, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2019;7(7):CD001871.
Fuller AB, Byrne RA, Golley RK, Trost SG. Supporting healthy lifestyle behaviours in families attending community playgroups: parents’ perceptions of facilitators and barriers. BMC Public Health. 2019;19(1):1740.
Gerards SM, Sleddens EF, Dagnelie PC, de Vries NK, Kremers SP. Interventions addressing general parenting to prevent or treat childhood obesity. Int J Pediatr Obes. 2011;6(2–2):e28-45.
Magarey AM, Perry RA, Baur LA, Steinbeck KS, Sawyer M, Hills AP, et al. A parent-led family-focused treatment program for overweight children aged 5 to 9 years: the PEACH RCT. Pediatrics. 2011;127(2):214–22.
Johnson BJ, Zarnowiecki D, Hendrie GA, Mauch CE, Golley RK. How to reduce parental provision of unhealthy foods to 3- to 8-year-old children in the home environment? A systematic review utilizing the Behaviour Change Wheel framework. Obes Rev. 2018;19(10):1359–70.
Golley R, Hendrie G, Slater A, Corsini N. Interventions that involve parents to improve children’s weight-related nutrition intake and activity patterns - What nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness? Obes Rev. 2011;12(2):114–30.
Braun V, Clarke V. Thematic Analysis: A Practical Guide. Los Angeles: SAGE Publications Ltd; 2022.
Book Google Scholar
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2).
Litterbach EK, Russell CG, Taki S, Denney-Wilson E, Campbell KJ, Laws RA. Factors influencing engagement and behavioral determinants of infant feeding in an mhealth program: qualitative evaluation of the growing healthy program. JMIR Mhealth Uhealth. 2017;5(12): e196.
Russell CG, Taki S, Azadi L, Campbell KJ, Laws R, Elliott R, et al. A qualitative study of the infant feeding beliefs and behaviours of mothers with low educational attainment. BMC Pediatr. 2016;16:69.
Liamputtong P. Qualitative research methods. 4th ed. Oxford, UK: Oxford University Press; 2013.
Google Scholar
Vance AJ, Brandon DH. Delineating among parenting confidence, parenting self-efficacy and competence. ANS Adv Nurs Sci. 2017;40(4):E18.
Kitson A, Feo R, Lawless M, Arciuli J, Clark R, Golley RK, et al. Towards a unifying caring life-course theory for better self-care and caring solutions: A discussion paper. J Adv Nurs. 2021;78:e6–20.
PubMed PubMed Central Google Scholar
Bäckström C, Larsson T, Wahlgren E, Golsäter M, Mårtensson LB, Thorstensson S. ‘It makes you feel like you are not alone’: Expectant first-time mothers’ experiences of social support within the social network, when preparing for childbirth and parenting. Sex Reproduct Healthcare. 2017;12:51–7.
Campbell K, Hesketh K, Crawford D, Salmon J, Ball K, McCallum Z. The Infant Feeding Activity and Nutrition Trial (INFANT) an early intervention to prevent childhood obesity: Cluster-randomised controlled trial. BMC Public Health. 2008;8(1):103.
Maher J, Fraser S, Wright J. Framing the mother: childhood obesity, maternal responsibility and care. J Gend Stud. 2010;19(3):233–47.
Liss M, Schiffrin HH, Rizzo KM. Maternal Guilt and Shame: The Role of Self-discrepancy and Fear of Negative Evaluation. J Child Fam Stud. 2013;22(8):1112–9.
Hancock K, Cunningham N, Lawrence D, Zarb D, Zubrick S. Playgroup participation and social support outcomes for mothers of young children: a longitudinal cohort study. PLoS ONE. 2015;10(7): e0133007.
Harman B, Guilfoyle A, O’Connor M. Why mothers attend playgroup. Australas J Early Childhood. 2014;39(4):131–7.
Ash T, Agaronov A, Young T, Aftosmes-Tobio A, Davison KK. Family-based childhood obesity prevention interventions: a systematic review and quantitative content analysis. Int J Behav Nutr Phys Act. 2017;14(1):113.
Harvey G, Kitson A. PARIHS re-visited: introducing the i-PARIHS framework. Implementing Evidence-Based Practice in Healthcare: A Facilitation Guide. 1st edition ed. United Kingdom: Routledge; 2015: 22–46.
Johnson B, Bell L, Zarnowiecki D, Rangan A, Golley R. Contrbition of discretionary foods and drinks to Australian Children’s intake of energy, saturated fat, Added Sugars and Salt. Children. 2017;4(12):104.
Armstrong G, Maitland C, Lester L, Trost S, Trapp G, Boruff B, et al. Associations between the home yard and preschoolers’ outdoor play and physical activity. Public Health Res Pract. 2019;29(1): e2911907.
Active Healthy Kids Australia. Reboot! Reimagining Physically Active Lives: 2022 Australian Report Card on Physical Activity for Children and Young People. Melbourne, Victoria; 2022.
Download references
Acknowledgements
The authors would like to thank playgroup partners including Play Matters Australia (in Queensland), Playgroup South Australia and Playgroup Western Australia for their collaboration and assistance with recruiting playgroups and facilitating recruitment of participants and delivery of the program. We especially wish to acknowledge the work and support of Penny Allen, Alana Hitchcock, Nicole Walker, Melissa Luhrman and Andrew McMahon from Play Matters Australia; Craig Bradbrook, Rebecca Blunn, and Alicia Beames from Playgroup SA; and David Zarb and Caroline Ince from Playgroup WA.
We would also like to thank the parents, peer facilitators and playgroup coordinators who participated in this qualitative evaluation, for their time and sharing their experiences. Finally, we would like to thank Samantha Morgillo, Research Assistant at Flinders University, who supported this work.
This project is funded by the Australian Government Medical Research Future Fund Preventative Public Health Research Initiative (2019; GNT1200764). HC is supported by a National Heart Foundation Future Leader Fellowship (#102549) and partially by the Australian Government through the Australian Research Council's Centre of Excellence for Children and Families over the Life Course (Project ID CE200100025). BJJ is supported by an Early- Mid Career Researcher Fellowship from The Hospital Research Foundation Group (2022-CF-EMCR-008-QA25323). RB is supported by an Australian Research Council Discovery Early Career Researcher Award (DE230101053). No funders contributed to the design of the study, nor had a role in data collection, management, analysis, and interpretation, nor in the dissemination of findings.
Author information
Authors and affiliations.
Flinders University, College of Nursing and Health Sciences, Caring Futures Institute, Adelaide, SA, Australia
Georgia Middleton, Brittany J. Johnson, Dimity Dutch & Rebecca K. Golley
School of Human Movement and Nutrition Sciences, The University of Queensland Australia, Brisbane, QLD, Australia
Stewart G. Trost
Faculty of Health, School of Exercise and Nutrition Science, Queensland University of Technology, Brisbane, QLD, Australia
Rebecca Byrne, Caroline O. Terranova, Li Kheng Chai, Denise S. K. Brookes & Kate Simon
Telethon Kids Institute, The University of Western Australia, Perth, WA, Australia
Hayley E. Christian & Anna Henry
School of Population and Global Health, The University of Western Australia, Perth, WA, Australia
Hayley E. Christian
Centre for Child and Family Studies, School of Early Childhood and Inclusive Education, Queensland University of Technology, Brisbane, QLD, Australia
Kate E. Williams
Health and Wellbeing Queensland, Queensland Government, Brisbane, QLD, Australia
Li Kheng Chai
You can also search for this author in PubMed Google Scholar
Contributions
GM, BJJ, RKG and SGT conceived the study, with assistance from LKC, COT, HEC, KEW, AH and DSKB. DD and GM recruited participants with assistance from BJJ, HEC, SGT, and AH. GM conducted focus groups and interviews and DD supported as note-taker. GM led data analysis and BJJ and DD assisted, with support from all co-authors. GM drafted the manuscript, with assistance from DD, BJJ, and RKG. All authors contributed to synthesis of results, reviewing, editing, and approving the final version of the paper.
Corresponding authors
Correspondence to Brittany J. Johnson or Rebecca K. Golley .
Ethics declarations
Ethics approval and consent to participate.
This project was performed in accordance with the ethical standards laid down in the Declaration of Helsinki and was approved by the Human Research Ethics Committee of Children’s Health Queensland (HREC/19/QCHQ/66486), The Queensland University of Technology (2000000576), Flinders University (2586) and The University of Western Australia (RA/4/20/6386). All participants provided informed consent prior to participating.
Consent for publication
Not applicable.
Competing interests
AH and KS were site coordinators for the Healthy Conversations @ Playgroup trial and acted as peer facilitators in some instances. All other authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Interview/focus group schedules. Interview/focus group schedules containing the questions that guided the focus group and interview discussions.
Additional file 2.
Participant flow through Healthy Conversations @ Playgroup qualitative evaluation study. Figure of the flow through the study of the three population groups included in the qualitative evaluation.
Additional file 3.
Coding tree for thematic analysis of interview and focus group data. Description: Figure of the coding tree that sits behind the results presented in the paper
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Middleton, G., Johnson, B.J., Dutch, D. et al. A great way to bring up health behaviour topics at playgroup: a qualitative evaluation of the Healthy Conversations @ Playgroup program. BMC Public Health 24 , 890 (2024). https://doi.org/10.1186/s12889-024-17703-x
Download citation
Received : 05 October 2023
Accepted : 08 January 2024
Published : 25 March 2024
DOI : https://doi.org/10.1186/s12889-024-17703-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Early childhood
- Peer-led program
- Healthy eating
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 28 March 2024
Using the consolidated Framework for Implementation Research to integrate innovation recipients’ perspectives into the implementation of a digital version of the spinal cord injury health maintenance tool: a qualitative analysis
- John A Bourke 1 , 2 , 3 ,
- K. Anne Sinnott Jerram 1 , 2 ,
- Mohit Arora 1 , 2 ,
- Ashley Craig 1 , 2 &
- James W Middleton 1 , 2 , 4 , 5
BMC Health Services Research volume 24 , Article number: 390 ( 2024 ) Cite this article
Metrics details
Despite advances in managing secondary health complications after spinal cord injury (SCI), challenges remain in developing targeted community health strategies. In response, the SCI Health Maintenance Tool (SCI-HMT) was developed between 2018 and 2023 in NSW, Australia to support people with SCI and their general practitioners (GPs) to promote better community self-management. Successful implementation of innovations such as the SCI-HMT are determined by a range of contextual factors, including the perspectives of the innovation recipients for whom the innovation is intended to benefit, who are rarely included in the implementation process. During the digitizing of the booklet version of the SCI-HMT into a website and App, we used the Consolidated Framework for Implementation Research (CFIR) as a tool to guide collection and analysis of qualitative data from a range of innovation recipients to promote equity and to inform actionable findings designed to improve the implementation of the SCI-HMT.
Data from twenty-three innovation recipients in the development phase of the SCI-HMT were coded to the five CFIR domains to inform a semi-structured interview guide. This interview guide was used to prospectively explore the barriers and facilitators to planned implementation of the digital SCI-HMT with six health professionals and four people with SCI. A team including researchers and innovation recipients then interpreted these data to produce a reflective statement matched to each domain. Each reflective statement prefaced an actionable finding, defined as alterations that can be made to a program to improve its adoption into practice.
Five reflective statements synthesizing all participant data and linked to an actionable finding to improve the implementation plan were created. Using the CFIR to guide our research emphasized how partnership is the key theme connecting all implementation facilitators, for example ensuring that the tone, scope, content and presentation of the SCI-HMT balanced the needs of innovation recipients alongside the provision of evidence-based clinical information.
Conclusions
Understanding recipient perspectives is an essential contextual factor to consider when developing implementation strategies for healthcare innovations. The revised CFIR provided an effective, systematic method to understand, integrate and value recipient perspectives in the development of an implementation strategy for the SCI-HMT.
Trial registration
Peer Review reports
Injury to the spinal cord can occur through traumatic causes (e.g., falls or motor vehicle accidents) or from non-traumatic disease or disorder (e.g., tumours or infections) [ 1 ]. The onset of a spinal cord injury (SCI) is often sudden, yet the consequences are lifelong. The impact of a SCI is devastating, with effects on sensory and motor function, bladder and bowel function, sexual function, level of independence, community participation and quality of life [ 2 ]. In order to maintain good health, wellbeing and productivity in society, people with SCI must develop self-management skills and behaviours to manage their newly acquired chronic health condition [ 3 ]. Given the increasing emphasis on primary health care and community management of chronic health conditions, like SCI, there is a growing responsibility on all parties to promote good health practices and minimize the risks of common health complications in their communities.
To address this need, the Spinal Cord Injury Health Maintenance Tool (SCI-HMT) was co-designed between 2018 and 2023 with people living with SCI and their General Practitioners (GPs) in NSW, Australia [ 4 ] The aim of the SCI-HMT is to support self-management of the most common and arguably avoidable potentially life-threatening complications associated with SCI, such as mental health crises, autonomic dysreflexia, kidney infections and pressure injuries. The SCI-HMT provides comprehensible information with resources about the six highest priority health areas related to SCI (as indicated by people with SCI and GPs) and was developed over two phases. Phase 1 focused on developing a booklet version and Phase 2 focused on digitizing this content into a website and smartphone app [ 4 , 5 ].
Enabling the successful implementation of evidence-based innovations such as the SCI-HMT is inevitably influenced by contextual factors: those dynamic and diverse array of forces within real-world settings working for or against implementation efforts [ 6 ]. Contextual factors often include background environmental elements in which an intervention is situated, for example (but not limited to) demographics, clinical environments, organisational culture, legislation, and cultural norms [ 7 ]. Understanding the wider context is necessary to identify and potentially mitigate various challenges to the successful implementation of those innovations. Such work is the focus of determinant frameworks, which focus on categorising or classing groups of contextual determinants that are thought to predict or demonstrate an effect on implementation effectiveness to better understand factors that might influence implementation outcomes [ 8 ].
One of the most highly cited determinant frameworks is the Consolidated Framework for Implementation Research (CFIR) [ 9 ], which is often posited as an ideal framework for pre-implementation preparation. Originally published in 2009, the CFIR has recently been subject to an update by its original authors, which included a literature review, survey of users, and the creation of an outcome addendum [ 10 , 11 ]. A key contribution from this revision was the need for a greater focus on the place of innovation recipients, defined as the constituency for whom the innovation is being designed to benefit; for example, patients receiving treatment, students receiving a learning activity. Traditionally, innovation recipients are rarely positioned as key decision-makers or innovation implementers [ 8 ], and as a consequence, have not often been included in the application of research using frameworks, such as the CFIR [ 11 ].
Such power imbalances within the intersection of healthcare and research, particularly between those receiving and delivering such services and those designing such services, have been widely reported [ 12 , 13 ]. There are concerted efforts within health service development, health research and health research funding, to rectify this power imbalance [ 14 , 15 ]. Importantly, such efforts to promote increased equitable population impact are now being explicitly discussed within the implementation science literature. For example, Damschroder et al. [ 11 ] has recently argued for researchers to use the CFIR to collect data from innovation recipients, and that, ultimately, “equitable population impact is only possible when recipients are integrally involved in implementation and all key constituencies share power and make decisions together” (p. 7). Indeed, increased equity between key constituencies and partnering with innovation recipients promotes the likelihood of sustainable adoption of an innovation [ 4 , 12 , 14 ].
There is a paucity of work using the updated CFIR to include and understand innovation recipients’ perspectives. To address this gap, this paper reports on a process of using the CFIR to guide the collection of qualitative data from a range of innovation recipients within a wider co-design mixed methods study examining the development and implementation of SCI-HMT. The innovation recipients in our research are people living with SCI and GPs. Guided by the CFIR domains (shown in the supplementary material), we used reflexive thematic analysis [ 16 ]to summarize data into reflective summaries, which served to inform actionable findings designed to improve implementation of the SCI-HMT.
The procedure for this research is multi-stepped and is summarized in Fig. 1 . First, we mapped retrospective qualitative data collected during the development of the SCI-HMT [ 4 ] against the five domains of the CFIR in order to create a semi-structured interview guide (Step 1). Then, we used this interview guide to collect prospective data from health professionals and people with SCI during the development of the digital version of the SCI-HMT (Step 2) to identify implementation barriers and facilitators. This enabled us to interpret a reflective summary statement for each CFIR domain. Lastly, we developed an actionable finding for each domain summary. The first (RESP/18/212) and second phase (2019/ETH13961) of the project received ethical approval from The Northern Sydney Local Health District Human Research Ethics Committee. The reporting of this study was conducted in line with the consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines [ 17 ]. All methods were performed in accordance with the relevant guidelines and regulations.
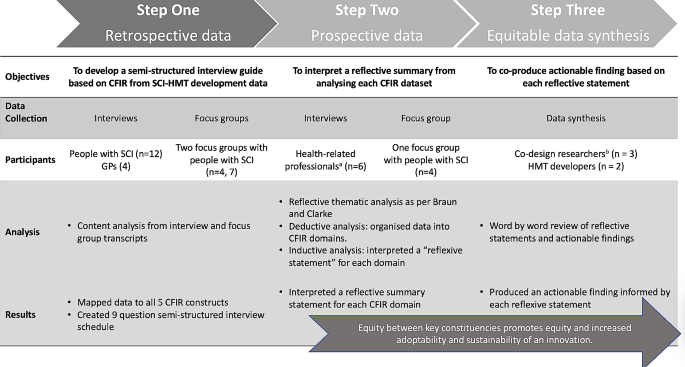
Procedure of synthesising datasets to inform reflective statements and actionable findings. a Two health professionals had a SCI (one being JAB); b Two co-design researchers had a SCI (one being JAB)
Step one: retrospective data collection and analysis
We began by retrospectively analyzing the data set (interview and focus group transcripts) from the previously reported qualitative study from the development phase of the SCI-HMT [ 4 ]. This analysis was undertaken by two team members (KASJ and MA). KASJ has a background in co-design research. Transcript data were uploaded into NVivo software (Version 12: QSR International Pty Ltd) and a directed content analysis approach [ 18 ] was applied to analyze categorized data a priori according to the original 2009 CFIR domains (intervention characteristics, outer setting, inner setting, characteristics of individuals, and process of implementation) described by Damschroder et al. [ 9 ]. This categorized data were summarized and informed the specific questions of a semi-structured interview guide. The final output of step one was an interview guide with context-specific questions arranged according to the CFIR domains (see supplementary file 1). The interview was tested with two people with SCI and one health professional.
Step two: prospective data collection and analysis
In the second step, semi-structured interviews were conducted by KASJ (with MA as observer) with consenting healthcare professionals who had previously contributed to the development of the SCI-HMT. Healthcare professionals included GPs, Nurse Consultants, Specialist Physiotherapists, along with Health Researchers (one being JAB). In addition, a focus group was conducted with consenting individuals with SCI who had contributed to the SCI-HMT design and development phase. The interview schedule designed in step one above guided data collection in all interviews and the focus group.
The focus group and interviews were conducted online, audio recorded, transcribed verbatim and uploaded to NVivo software (Version 12: QSR International Pty Ltd). All data were subject to reflexive, inductive and deductive thematic analysis [ 16 , 19 ] to better understand participants’ perspectives regarding the potential implementation of the SCI-HMT. First, one team member (KASJ) read transcripts and began a deductive analysis whereby data were organized into CFIR domains-specific dataset. Second, KASJ and JAB analyzed this domain-specific dataset to inductively interpret a reflective statement which served to summarise all participant responses to each domain. The final output of step two was a reflective summary statement for each CFIR domain.
Step three: data synthesis
In the third step we aimed to co-create an actionable finding (defined as tangible alteration that can be made to a program, in this case the SCI-HMT [ 20 ]) based on each domain-specific reflective statement. To achieve this, three codesign researchers (KAS and JAB with one person with SCI from Step 2 (deidentified)) focused on operationalising each reflective statement into a recommended modification for the digital version of the SCI-HMT. This was an iterative process guided by the specific CFIR domain and construct definitions, which we deemed salient and relevant to each reflective statement (see Table 2 for example). Data synthesis involved line by line analysis, group discussion, and repeated refinement of actionable findings. A draft synthesis was shared with SCI-HMT developers (JWM and MA) and refinement continued until consensus was agreed on. The final outputs of step three were an actionable finding related to each reflective statement for each CFIR domain.
The characteristics of both the retrospective and prospective study participants are shown in Table 1 . The retrospective data included data from a total of 23 people: 19 people with SCI and four GPs. Of the 19 people with SCI, 12 participated in semi-structured interviews, seven participated in the first focus group, and four returned to the second focus group. In step 2, four people with SCI participated in a focus group and six healthcare professionals participated in one-on-one semi-structured interviews. Two of the healthcare professionals (a GP and a registrar) had lived experience of SCI, as did one researcher (JAB). All interviews and focus groups were conducted either online or in-person and ranged in length between 60 and 120 min.
In our overall synthesis, we actively interpreted five reflective statements based on the updated CFIR domain and construct definitions by Damschroder et al. [ 11 ]. Table 2 provides a summary of how we linked the updated CFIR domain and construct definitions to the reflective statements. We demonstrate this process of co-creation below, including illustrative quotes from participants. Importantly, we guide readers to the actionable findings related to each reflective statement in Table 2 . Each actionable statement represents an alteration that can be made to a program to improve its adoption into practice.
Participants acknowledged that self-management is a major undertaking and very demanding, as one person with SCI said, “ we need to be informed without being terrified and overwhelmed”. Participants felt the HMT could indeed be adapted, tailored, refined, or reinvented to meet local needs. For example, another person with SCI remarked:
“Education needs to be from the get-go but in bite sized pieces from all quarters when readiness is most apparent… at all time points , [not just as a] a newbie tool or for people with [long-term impairment] ” (person with SCI_02).
Therefore, the SCI-HMT had to balance complexity of content while still being accessible and engaging, and required input from both experts in the field and those with lived experience of SCI, for example, a clinical nurse specialist suggested:
“it’s essential [the SCI-HMT] is written by experts in the field as well as with collaboration with people who have had a, you know, the lived experience of SCI” (healthcare professional_03).
Furthermore, the points of contact with healthcare for a person with SCI can be challenging to navigate and the SCI-HMT has the potential to facilitate a smoother engagement process and improve communication between people with SCI and healthcare services. As a GP suggested:
“we need a tool like this to link to that pathway model in primary health care , [the SCI-HMT] it’s a great tool, something that everyone can read and everyone’s reading the same thing” (healthcare professional_05).
Participants highlighted that the ability of the SCI-HMT to facilitate effective communication was very much dependent on the delivery format. The idea of digitizing the SCI-HMT garnered equal support from people with SCI and health care professionals, with one participant with SCI deeming it to be “ essential” ( person with SCI_01) and a health professional suggesting a “digitalized version will be an advantage for most people” (healthcare professional_02).
Outer setting
There was strong interest expressed by both people with SCI and healthcare professionals in using the SCI-HMT. The fundamental premise was that knowledge is power and the SCI-HMT would have strong utility in post-acute rehabilitation services, as well as primary care. As a person with SCI said,
“ we need to leave the [spinal unit] to return to the community with sufficient knowledge, and to know the value of that knowledge and then need to ensure primary healthcare provider [s] are best informed” (person with SCI_04).
The value of the SCI-HMT in facilitating clear and effective communication and shared decision-making between healthcare professionals and people with SCI was also highlighted, as shown by the remarks of an acute nurse specialist:
“I think this tool is really helpful for the consumer and the GP to work together to prioritize particular tests that a patient might need and what the regularity of that is” (healthcare professional_03).
Engaging with SCI peer support networks to promote the SCI-HMT was considered crucial, as one person with SCI emphasized when asked how the SCI-HMT might be best executed in the community, “…peers, peers and peers” (person with SCI_01). Furthermore, the layering of content made possible in the digitalized version will allow for the issue of approachability in terms of readiness for change, as another person with SCI said:
“[putting content into a digital format] is essential and required and there is a need to put summarized content in an App with links to further web-based information… it’s not likely to be accessed otherwise” (person with SCI_02).
Inner setting
Participants acknowledged that self-management of health and well-being is substantial and demanding. It was suggested that the scope, tone, and complexity of the SCI-HMT, while necessary, could potentially be resisted by people with SCI if they felt overwhelmed, as one person with SCI described:
“a manual that is really long and wordy, like, it’s [a] health metric… they maybe lack the health literacy to, to consume the content then yes, it would impede their readiness for [self-management]” (person with SCI_02).
Having support from their GPs was considered essential, and the HMT could enable GP’s, who are under time pressure, to provide more effective health and advice to their patients, as one GP said:
“We GP’s are time poor, if you realize then when you’re time poor you look quickly to say oh this is a patient tool - how can I best use this?” (healthcare professional_05).
Furthermore, health professional skills may be best used with the synthesis of self-reported symptoms, behaviors, or observations. A particular strength of a digitized version would be its ability to facilitate more streamlined communication between a person with SCI and their primary healthcare providers developing healthcare plans, as an acute nurse specialist reflected, “ I think that a digitalized version is essential with links to primary healthcare plans” (healthcare professional_03).
Efficient communication with thorough assessment is essential to ensure serious health issues are not missed, as findings reinforce that the SCI-HMT is an educational tool, not a replacement for healthcare services, as a clinical nurse specialist commented, “ remember, things will go wrong– people end up very sick and in acute care “ (healthcare professional_02).
The SCI-HMT has the potential to provide a pathway to a ‘hope for better than now’ , a hope to ‘remain well’ and a hope to ‘be happy’ , as the informant with SCI (04) declared, “self-management is a long game, if you’re keeping well, you’ve got that possibility of a good life… of happiness”. Participants with SCI felt the tool needed to be genuine and
“acknowledge the huge amount of adjustment required, recognizing that dealing with SCI issues is required to survive and live a good life” (person with SCI_04).
However, there is a risk that an individual is completely overwhelmed by the scale of the SCI-HMT content and the requirement for lifelong vigilance. Careful attention and planning were paid to layering the information accordingly to support self-management as a ‘long game’, which one person with SCI reflected in following:
“the first 2–3 year [period] is probably the toughest to get your head around the learning stuff, because you’ve got to a stage where you’re levelling out, and you’ve kind of made these promises to yourself and then you realize that there’s no quick fix” (person with SCI_01).
It was decided that this could be achieved by providing concrete examples and anecdotes from people with SCI illustrating that a meaningful, healthy life is possible, and that good health is the bedrock of a good life with SCI.
There was universal agreement that the SCI-HMT is aspirational and that it has the potential to improve knowledge and understanding for people with SCI, their families, community workers/carers and primary healthcare professionals, as a GP remarked:
“[different groups] could just read it and realize, ‘Ahh, OK that’s what that means… when you’re doing catheters. That’s what you mean when you’re talking about bladder and bowel function or skin care” (healthcare professional_04).
Despite the SCI-HMT providing an abundance of information and resources to support self-management, participants identified four gaps: (i) the priority issue of sexuality, including pleasure and identity, as one person with SCI remarked:
“ sexuality is one of the biggest issues that people with SCI often might not speak about that often cause you know it’s awkward for them. So yeah, I think that’s a that’s a serious issue” (person with SCI_03).
(ii) consideration of the taboo nature of bladder and bowel topics for indigenous people, (iii) urgent need to ensure links for SCI-HMT care plans are compatible with patient management systems, and (iv) exercise and leisure as a standalone topic taking account of effects of physical activity, including impact on mental health and wellbeing but more especially for fun.
To ensure longevity of the SCI-HMT, maintaining a partnership between people with SCI, SCI community groups and both primary and tertiary health services is required for liaison with the relevant professional bodies, care agencies, funders, policy makers and tertiary care settings to ensure ongoing education and promotion of SCI-HMT is maintained. For example, delivery of ongoing training of healthcare professionals to both increase the knowledge base of primary healthcare providers in relation to SCI, and to promote use of the tools and resources through health communities. As a community nurse specialist suggested:
“ improving knowledge in the health community… would require digital links to clinical/health management platforms” (healthcare professional_02).
In a similar vein, a GP suggested:
“ our common GP body would have continuing education requirements… especially if it’s online, in particular for the rural, rural doctors who you know, might find it hard to get into the city” (healthcare professional_04).
The successful implementation of evidence-based innovations into practice is dependent on a wide array of dynamic and active contextual factors, including the perspectives of the recipients who are destined to use such innovations. Indeed, the recently updated CFIR has called for innovation recipient perspectives to be a priority when considering contextual factors [ 10 , 11 ]. Understanding and including the perspectives of those the innovation is being designed to benefit can promote increased equity and validation of recipient populations, and potentially increase the adoption and sustainability of innovations.
In this paper, we have presented research using the recently updated CFIR to guide the collection of innovation recipients’ perspectives (including people with SCI and GPs working in the community) regarding the potential implementation barriers and facilitators of the digital version of the SCI-HMT. Collected data were synthesized to inform actionable findings– tangible ways in which the SCI-HMT could be modified according of the domains of the CFIR (e.g., see Keith et al. [ 20 ]). It is important to note that we conducted this research using the original domains of the CFIR [ 9 ] prior to Damschroder et al. publishing the updated CFIR [ 11 ]. However, in our analysis we were able to align our findings to the revised CFIR domains and constructs, as Damschroder [ 11 ] suggests, constructs can “be mapped back to the original CFIR to ensure longitudinal consistency” (p. 13).
One of the most poignant findings from our analyses was the need to ensure the content of the SCI-HMT balanced scientific evidence and clinical expertise with lived experience knowledge. This balance of clinical and experiential knowledge demonstrated genuine regard for lived experience knowledge, and created a more accessible, engaging, useable platform. For example, in the innovation and individual domains, the need to include lived experience quotes was immediately apparent once the perspective of people with SCI was included. It was highlighted that while the SCI-HMT will prove useful to many parties at various stages along the continuum of care following onset of SCI, there will be those individuals that are overwhelmed by the scale of the content. That said, the layering of information facilitated by the digitalized version is intended to provide an ease of navigation through the SCI-HMT and enable a far greater sense of control over personal health and wellbeing. Further, despite concerns regarding e-literacy the digitalized version of the SCI-HMT is seen as imperative for accessibility given the wide geographic diversity and recent COVID pandemic [ 21 ]. While there will be people who are challenged by the technology, the universally acceptable use of the internet is seen as less of a barrier than printed material.
The concept of partnership was also apparent within the data analysis focusing on the outer and inner setting domains. In the outer setting domain, our findings emphasized the importance of engaging with SCI community groups, as well as primary and tertiary care providers to maximize uptake at all points in time from the phase of subacute rehabilitation onwards. While the SCI-HMT is intended for use across the continuum of care from post-acute rehabilitation onwards, it may be that certain modules are more relevant at different times, and could serve as key resources during the hand over between acute care, inpatient rehabilitation and community reintegration.
Likewise, findings regarding the inner setting highlighted the necessity of a productive partnership between GPs and individuals with SCI to address the substantial demands of long-term self-management of health and well-being following SCI. Indeed, support is crucial, especially when self-management is the focus. This is particularly so in individuals living with complex disability following survival after illness or injury [ 22 ], where health literacy has been found to be a primary determinant of successful health and wellbeing outcomes [ 23 ]. For people with SCI, this tool potentially holds the most appeal when an individual is ready and has strong partnerships and supportive communication. This can enable potential red flags to be recognized earlier allowing timely intervention to avert health crises, promoting individual well-being, and reducing unnecessary demands on health services.
While the SCI-HMT is an educational tool and not meant to replace health services, findings suggest the current structure would lead nicely to having the conversation with a range of likely support people, including SCI peers, friends and family, GP, community nurses, carers or via on-line support services. The findings within the process domain underscored the importance of ongoing partnership between innovation implementers and a broad array of innovation recipients (e.g., individuals with SCI, healthcare professionals, family, funding agencies and policy-makers). This emphasis on partnership also addresses recent discussions regarding equity and the CFIR. For example, Damschroder et al. [ 11 ] suggests that innovation recipients are too often not included in the CFIR process, as the CFIR is primarily seen as a tool intended “to collect data from individuals who have power and/or influence over implementation outcomes” (p. 5).
Finally, we feel that our inclusion of innovation recipients’ perspectives presented in this article begins to address the notion of equity in implementation, whereby the inclusion of recipient perspectives in research using the CFIR both validates, and increases, the likelihood of sustainable adoption of evidence-based innovations, such as the SCI-HMT. We have used the CFIR in a pragmatic way with an emphasis on meaningful engagement between the innovation recipients and the research team, heeding the call from Damschroder et al. [ 11 ], who recently argued for researchers to use the CFIR to collect data from innovation recipients. Adopting this approach enabled us to give voice to innovation recipient perspectives and subsequently ensure that the tone, scope, content and presentation of the SCI-HMT balanced the needs of innovation recipients alongside the provision of evidence-based clinical information.
Our research is not without limitations. While our study was successful in identifying a number of potential barriers and facilitators to the implementation of the SCI-HMT, we did not test any implementation strategies to impact determinants, mechanisms, or outcomes. This will be the focus of future research on this project, which will investigate the impact of implementation strategies on outcomes. Focus will be given to the context-mechanism configurations which give rise to particular outcomes for different groups in certain circumstances [ 7 , 24 ]. A second potential concern is the relatively small sample size of participants that may not allow for saturation and generalizability of the findings. However, both the significant impact of secondary health complications for people with SCI and the desire for a health maintenance tool have been established in Australia [ 2 , 4 ]. The aim our study reported in this article was to achieve context-specific knowledge of a small sample that shares a particular mutual experience and represents a perspective, rather than a population [ 25 , 26 ]. We feel our findings can stimulate discussion and debate regarding participant-informed approaches to implementation of the SCI-HMT, which can then be subject to larger-sample studies to determine their generalisability, that is, their external validity. Notably, future research could examine the interaction between certain demographic differences (e.g., gender) of people with SCI and potential barriers and facilitators to the implementation of the SCI-HMT. Future research could also include the perspectives of other allied health professionals working in the community, such as occupational therapists. Lastly, while our research gave significant priority to recipient viewpoints, research in this space would benefit for ensuring innovation recipients are engaged as genuine partners throughout the entire research process from conceptualization to implementation.
Employing the CFIR provided an effective, systematic method for identifying recipient perspectives regarding the implementation of a digital health maintenance tool for people living with SCI. Findings emphasized the need to balance clinical and lived experience perspectives when designing an implementation strategy and facilitating strong partnerships with necessary stakeholders to maximise the uptake of SCI-HMT into practice. Ongoing testing will monitor the uptake and implementation of this innovation, specifically focusing on how the SCI-HMT works for different users, in different contexts, at different stages and times of the rehabilitation journey.
Data availability
The datasets supporting the conclusions of this article are available available upon request and with permission gained from the project Steering Committee.
Abbreviations
spinal cord injury
HMT-Spinal Cord Injury Health Maintenance Tool
Consolidated Framework for Implementation Research
Kirshblum S, Vernon WL. Spinal Cord Medicine, Third Edition. New York: Springer Publishing Company; 2018.
Middleton JW, Arora M, Kifley A, Clark J, Borg SJ, Tran Y, et al. Australian arm of the International spinal cord Injury (Aus-InSCI) Community Survey: 2. Understanding the lived experience in people with spinal cord injury. Spinal Cord. 2022;60(12):1069–79.
Article PubMed PubMed Central Google Scholar
Craig A, Nicholson Perry K, Guest R, Tran Y, Middleton J. Adjustment following chronic spinal cord injury: determining factors that contribute to social participation. Br J Health Psychol. 2015;20(4):807–23.
Article PubMed Google Scholar
Middleton JW, Arora M, Jerram KAS, Bourke J, McCormick M, O’Leary D, et al. Co-design of the Spinal Cord Injury Health Maintenance Tool to support Self-Management: a mixed-methods Approach. Top Spinal Cord Injury Rehabilitation. 2024;30(1):59–73.
Article Google Scholar
Middleton JW, Arora M, McCormick M, O’Leary D. Health maintenance Tool: how to stay healthy and well with a spinal cord injury. A tool for consumers by consumers. 1st ed. Sydney, NSW Australia: Royal Rehab and The University of Sydney; 2020.
Google Scholar
Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019;19(1):189.
Jagosh J. Realist synthesis for Public Health: building an Ontologically Deep understanding of how Programs Work, for whom, and in which contexts. Annu Rev Public Health. 2019;40(1):361–72.
Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10(1):53.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):50.
Damschroder LJ, Reardon CM, Opra Widerquist MA, Lowery JC. Conceptualizing outcomes for use with the Consolidated Framework for Implementation Research (CFIR): the CFIR outcomes Addendum. Implement Sci. 2022;17(1):7.
Damschroder LJ, Reardon CM, Widerquist MAO, Lowery JC. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022;17(1):75.
Plamondon K, Ndumbe-Eyoh S, Shahram S. 2.2 Equity, Power, and Transformative Research Coproduction. Research Co-Production in Healthcare2022. p. 34–53.
Verville L, Cancelliere C, Connell G, Lee J, Munce S, Mior S, et al. Exploring clinicians’ experiences and perceptions of end-user roles in knowledge development: a qualitative study. BMC Health Serv Res. 2021;21(1):926.
Gainforth HL, Hoekstra F, McKay R, McBride CB, Sweet SN, Martin Ginis KA, et al. Integrated Knowledge Translation Guiding principles for conducting and Disseminating Spinal Cord Injury Research in Partnership. Arch Phys Med Rehabil. 2021;102(4):656–63.
Langley J, Knowles SE, Ward V. Conducting a Research Coproduction Project. Research Co-Production in Healthcare2022. p. 112– 28.
Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qualitative Research in Psychology. 2020:1–25.
Tong A, Sainsbury p, Craig J. Consolidated criteria for reporting qulaitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016;2:8–14.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101.
Keith RE, Crosson JC, O’Malley AS, Cromp D, Taylor EF. Using the Consolidated Framework for Implementation Research (CFIR) to produce actionable findings: a rapid-cycle evaluation approach to improving implementation. Implement Science: IS. 2017;12(1):15.
Choukou M-A, Sanchez-Ramirez DC, Pol M, Uddin M, Monnin C, Syed-Abdul S. COVID-19 infodemic and digital health literacy in vulnerable populations: a scoping review. Digit HEALTH. 2022;8:20552076221076927.
PubMed PubMed Central Google Scholar
Daniels N. Just Health: Meeting Health needs fairly. Cambridge University Press; 2007. p. 397.
Parker SM, Stocks N, Nutbeam D, Thomas L, Denney-Wilson E, Zwar N, et al. Preventing chronic disease in patients with low health literacy using eHealth and teamwork in primary healthcare: protocol for a cluster randomised controlled trial. BMJ Open. 2018;8(6):e023239–e.
Salter KL, Kothari A. Using realist evaluation to open the black box of knowledge translation: a state-of-the-art review. Implement Sci. 2014;9(1):115.
Sebele-Mpofu FY. The Sampling Conundrum in qualitative research: can Saturation help alleviate the controversy and alleged subjectivity in Sampling? Int’l J Soc Sci Stud. 2021;9:11.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by Information Power. Qual Health Res. 2015;26(13):1753–60.
Download references
Acknowledgements
Authors of this study would like to thank all the consumers with SCI and healthcare professionals for their invaluable contribution to this project. Their participation and insights have been instrumental in shaping the development of the SCI-HMT. The team also acknowledges the support and guidance provided by the members of the Project Steering Committee, as well as the partner organisations, including NSW Agency for Clinical Innovation, and icare NSW. Author would also like to acknowledge the informant group with lived experience, whose perspectives have enriched our understanding and informed the development of SCI-HMT.
The SCI Wellness project was a collaborative project between John Walsh Centre for Rehabilitation Research at The University of Sydney and Royal Rehab. Both organizations provided in-kind support to the project. Additionally, the University of Sydney and Royal Rehab received research funding from Insurance and Care NSW (icare NSW) to undertake the SCI Wellness Project. icare NSW do not take direct responsibility for any of the following: study design, data collection, drafting of the manuscript, or decision to publish.
Author information
Authors and affiliations.
John Walsh Centre for Rehabilitation Research, Northern Sydney Local Health District, St Leonards, NSW, Australia
John A Bourke, K. Anne Sinnott Jerram, Mohit Arora, Ashley Craig & James W Middleton
The Kolling Institute, Faculty of Medicine and Health, The University of Sydney, Sydney, NSW, Australia
Burwood Academy Trust, Burwood Hospital, Christchurch, New Zealand
John A Bourke
Royal Rehab, Ryde, NSW, Australia
James W Middleton
State Spinal Cord Injury Service, NSW Agency for Clinical Innovation, St Leonards, NSW, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Project conceptualization: KASJ, MA, JWM; project methodology: JWM, MA, KASJ, JAB; data collection: KASJ and MA; data analysis: KASJ, JAB, MA, JWM; writing—original draft preparation: JAB; writing—review and editing: JAB, KASJ, JWM, MA, AC; funding acquisition: JWM, MA. All authors contributed to the revision of the paper and approved the final submitted version.
Corresponding author
Correspondence to John A Bourke .
Ethics declarations
Ethics approval and consent to participate.
The first (RESP/18/212) and second phase (2019/ETH13961) of the project received ethical approval from The Northern Sydney Local Health District Human Research Ethics Committee. All participants provided informed, written consent. All data were to be retained for 7 years (23rd May 2030).
Consent for publication
Not applicable.
Competing interests
MA part salary (from Dec 2018 to Dec 2023), KASJ part salary (July 2021 to Dec 2023) and JAB part salary (Jan 2022 to Aug 2022) was paid from the grant monies. Other authors declare no conflicts of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bourke, J.A., Jerram, K.A.S., Arora, M. et al. Using the consolidated Framework for Implementation Research to integrate innovation recipients’ perspectives into the implementation of a digital version of the spinal cord injury health maintenance tool: a qualitative analysis. BMC Health Serv Res 24 , 390 (2024). https://doi.org/10.1186/s12913-024-10847-x
Download citation
Received : 14 August 2023
Accepted : 11 March 2024
Published : 28 March 2024
DOI : https://doi.org/10.1186/s12913-024-10847-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Spinal Cord injury
- Self-management
- Innovation recipients
- Secondary health conditions
- Primary health care
- Evidence-based innovations
- Actionable findings
- Consolidated Framework for implementation research
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 25 March 2024
Long-acting injectable depot buprenorphine from a harm reduction perspective in patients with ongoing substance use and multiple psychiatric comorbidities: a qualitative interview study
- Björn Johnson 1 ,
- Bodil Monwell 2 , 3 &
- Andrea Johansson Capusan 4 , 5
Harm Reduction Journal volume 21 , Article number: 68 ( 2024 ) Cite this article
185 Accesses
Metrics details
Long-acting injectable depot buprenorphine may increase access to opioid agonist treatment (OAT) for patients with opioid use disorder in different treatment phases. The aim of this study was to explore the experiences of depot buprenorphine among Swedish patients with ongoing substance use and multiple psychiatric comorbidities.
Semi-structured qualitative interviews were conducted with OAT patients with experience of depot buprenorphine. Recruitment took place at two OAT clinics with a harm reduction focus, specializing in the treatment of patients with ongoing substance use and multiple comorbidities. Nineteen participants were included, 12 men and seven women, with a mean age of 41 years (range 24–56 years), and a mean of 21 years (5–35 years) of experience with illicit substance use. All participants had ongoing substance use and psychiatric comorbidities such as ADHD, anxiety, mood, psychotic and eating disorders. Interviews were transcribed verbatim. Thematic content analysis was conducted both manually and using qualitative data analysis software.
Participants reported social benefits and positive changes in self-perception and identity. In particular, depot buprenorphine contributed to a realization that it was possible to make life changes and engage in activities not related to substance use. Another positive aspect that emerged from the interviews was a noticeable relief from perceived pressure to divert OAT medication, while some expressed the lack of income from diverted oral/sublingual OAT medication as a negative, but still acceptable, consequence of the depot buprenorphine. Many participants considered that the information provided prior to starting depot buprenorphine was insufficient. Also, not all patients found depot buprenorphine suitable, and those who experienced coercion exhibited particularly negative attitudes towards the medication.
Conclusions
OAT patients with ongoing substance use and multiple psychiatric comorbidities reported clear benefits of depot buprenorphine, including changes in self-perception which has been theorized to play an important role in recovery. Clinicians should consider the specific information needs of this population and the extensive diversion of traditional OAT medications in this population to improve the treatment experience and outcomes. Overall, depot buprenorphine is a valuable treatment option for a population in need of harm reduction and may also contribute to psychological changes that may facilitate recovery in those with the greatest need.
Novel treatment options with long-acting injectable depot buprenorphine (hereafter: depot buprenorphine) for opioid use disorder have increased access to opioid agonist treatment (OAT) in recent years. In pivotal trials, depot injections have shown similar efficacy to sublingual buprenorphine/naloxone [ 1 ] and superior efficacy to placebo [ 2 ]. The first depot injection was approved in the USA in 2017 [ 3 ] and since 2019, weekly [ 1 ] and/or monthly [ 1 , 2 ] subcutaneous buprenorphine injections are available for the treatment of moderate to severe opioid use disorder (OUD) in the EU, UK, Canada, Australia, New Zealand and several countries in the Middle East and North Africa. Patient-reported outcomes from RCTs and observational studies indicate long-term safety and increased patient satisfaction with depot injections [ 4 , 5 ].
Patient perspectives on depot buprenorphine
Interestingly, the introduction of depot buprenorphine has also led to a renewed research interest in patient perceptions and attitudes towards OAT in general and depot buprenorphine in particular.In recent years, several studies have investigated how depot buprenorphine affects patients’ lives, their treatment, and their relationships with treatment staff [ 6 , 7 , 8 , 9 ]. Our research group conducted a stratified qualitative interview study [ 7 ] to explore reasons for choosing depot buprenorphine and reasons for discontinuing or declining this treatment. Qualitative studies describe benefits in terms of practical factors, an increased sense of freedom, psychological benefits such as a reshaping of self-identity to feel “normal” [ 6 , 7 ], and a reduction in the stigma associated with daily supervised OAT [ 8 ]. Loss of contact with staff, the need for a daily routine, and concerns about medication effects and side effects are reasons for choosing to discontinue depot buprenorphine or continue with sublingual treatment [ 9 ]. A trusting relationship with treatment staff and adequate information are important for successful induction of depot buprenorphine [ 7 ]. In contrast, mistrust and coercion could lead to a “polluted pharmaceutical atmosphere”, similar to that described during the clinical introduction of sublingual buprenorphine/naloxone combinations, which negatively affected patients’ perceptions of medication effects and side effects [ 10 ].
In the early stages of clinical implementation, depot buprenorphine was predominantly offered to more stable patients, which explains why early qualitative studies [ 6 , 7 , 8 ] did not capture how depot buprenorphine affected patients at the most severe end of the OUD spectrum with ongoing polysubstance use and multiple comorbidities. This perspective is important for the use of buprenorphine depot injections. Firstly, research from other medical fields such as the treatment of schizophrenia, with decades of experience in depot injections, suggests that the most unstable patients may benefit most from these formulations [ 11 ]. In addition, unstable patients may face several barriers to accessing care, including poor treatment adherence and clinicians’ concerns that treatment may be harmful [ 12 , 13 ] which must be balanced against the considerable harms of untreated OUD. It is therefore important to explore how unstable patients themselves experience the potential benefits and disadvantages associated with depot buprenorphine.
The setting
In Sweden, national regulations require OAT to be provided in a specialised psychiatric or addiction care setting, registered with the Health and Social Care Inspectorate [ 14 , 15 ]. The treatment must include both medication and, for those patients who need it, psychological or psychosocial treatment and support, either provided by the unit or in collaboration with the municipal social services or other care providers [ 15 ].
The availability of OAT is low compared to many Western European countries. The contrast with neighbouring Denmark and Norway, with more than twice as many OAT patients per 100 000 inhabitants than Sweden, is stark [ 16 , 17 ]. Access to treatment also varies considerably across the country [ 16 ]. There are no current estimates of the prevalence of opioid dependence in the Swedish population, but drug-related deaths increased steadily over the period 2000–2017 and are among the highest in Europe [ 18 ]. However, there has been a slight decrease in deaths since 2017, in parallel with an expansion of harm reduction interventions such as naloxone distribution, needle exchange programs and an increased access to OAT.
The number of OAT patients in Sweden has increased continuously over the last decades, from about 1000 patients in 2000 to about 7500 patients in 2022 [ 16 ]. The most common OAT medication is still methadone, followed by sublingual buprenorphine and sublingual buprenorphine-naloxone combination. Since 2007, the Swedish National Board of Health and Welfare has recommended buprenorphine-naloxone as the first-line medication in OAT, but in many local settings, implementation of these recommendations has been hampered by local traditions and patient resistance. Depot buprenorphine was introduced in 2019. In 2022 about 10% of Swedish OAT patients were prescribed depot formulations.
For many years OAT was a controversial treatment modality in Sweden. Access was strictly regulated, with high thresholds for entry, a strong focus on abstinence and rehabilitation [ 19 ], and an emphasis on the potential harms caused by the treatment itself, while disregarding the harms of untreated OUD. Harm reduction-oriented OAT did not exist, and patients with repeated relapses into illicit substance use were discharged from treatment according to earlier national guidelines [ 20 ]. This led, among other things, to the emergence of a significant illicit market for OAT medicines [ 21 ].
Since 2015, however, the national regulatory framework for OAT has been brought in line with modern research, with lower thresholds for entering treatment [ 19 ] and no longer recommending involuntary discharge, while emphasizing harm reduction measures such as naloxone distribution [ 22 ]. The metropolitan areas now have clinics with a strong harm-reduction profile, with units specialising in clients with ongoing substance use and multiple somatic and psychiatric co-morbidities. However, there are considerable variations across the country, and in some healthcare regions involuntary discharge is still a common practice [ 16 ].
Swedish OAT has traditionally had a strong focus on control and medical safety. According to the current national regulations, which have not yet been adapted to the depot formulations, the prescribed medication must be taken daily under clinic supervision for the first three months. After that, if the treatment outcome is stable, the doctor can gradually allow the patient to manage their own medication [ 23 , 24 ].
In this study, we aimed to investigate the experiences of patients with ongoing, severe substance use and multiple comorbidities who are receiving long-acting injectable depot buprenorphine within a harm reduction setting in Sweden. Our goal was to generate new insights into the potential benefits and challenges associated with depot buprenorphine in this specific patient population. Specifically, we explored how the adoption of depot buprenorphine impacts various aspects of patients’ lives, including their treatment experiences, relationships with treatment staff, and perspectives on their future opioid agonist treatment (OAT). By focusing on this subgroup, we aimed to contribute valuable knowledge to enhance the understanding and optimization of depot buprenorphine use in the context of harm reduction for patients with complex needs.
The study is based on qualitative, semi-structured interviews with OAT patients with ongoing substance use and multiple comorbidities.
Sampling and recruitment
Participants were recruited between December 2021 and May 2022 from two harm reduction units specializing in the treatment of patients with ongoing, severe polysubstance use and multiple comorbidities. The units were part of two larger OAT clinics, each serving approximately 600–700 patients, located in two large cities (> 300,000 inhabitants). In the first clinic, around 100 patients, of whom just under half were treated with depot buprenorphine, had contact with the harm reduction unit. In the second clinic, about 150 patients had contact with the harm reduction unit, but only about ten of them were treated with depot buprenorphine. The treatment staff included doctors specialized in psychiatry or addiction medicine, nurses, and mental health workers. Additionally, the clinics could provide access to medical workups and hepatitis C treatment, as well as services from psychologists and occupational therapists.
Inclusion criteria for the study were having (1) OAT at one of the two units with harm reduction profile included in the study, (2) ongoing substance use and (3) multiple comorbidities (such as, but not limited to, substance use disorders other than OUD, psychiatric disorders including affective, anxiety or psychotic disorder, somatic comorbidities including hepatitis C); and (4) willingness to participate. Exclusion criteria were the inability to give informed consent, either because of poor language skills or because they were too impaired by substances and/or mental illness at the time of the information. Excluded participants were given the opportunity to return at a later date if they wished to participate in the study.
Posters, flyers and information to clinical staff were used to inform patients who were part of the target group about the opportunity to participate. Interested patients were given a date and time for the interview, which usually coincided with a visit for their depot injection or other medication collection. As patients with ongoing substance use and/or mental illness may find it difficult to attend scheduled appointments, the interviewer was also available in the reception area of the clinics, without prior booking, allowing for the opportunity to meet with respondents who missed their scheduled appointments.
All interviews were conducted by BM, a clinical researcher with extensive experience in conducting qualitative interviews with patients who use psychoactive substances and have severe psychiatric comorbidities. BM had previously worked as healthcare counsellor at another OAT clinic but had no previous relationship with the clinics or patients in question. Recruitment and interviews continued until BM deemed that data saturation had been achieved.
Ethical considerations
Interviewing patients with active use and comorbidities poses several ethical challenges. Patients may be too affected by substances or by mental illness to give informed consent or to participate in the interview at a given time. This could limit the possibility of the most vulnerable patients to have their voices heard. We chose to handle this dilemma by conducting an individual clinical assessment of potential participants prior to the interviews. BM conducted a clinical assessment to evaluate the participants’ degree of influence of psychoactive substances, potential cognitive impairment, and current psychiatric status. Assessments were recorded in field notes.
Another aspect was that many patients had experience of involuntary discharge and it was important to ensure confidentiality. Participants received both verbal and written information about the study. They were informed that the interviews would be confidential, that they could discontinue the interview at any time, that all data would be pseudonymized before publication, and that their participation would not affect their treatment in any way. Subsequently, the patients signed an informed consent form. In the case of patients interviewed by telephone, staff at the clinic provided written information and obtained written consent before the interview. Participant characteristics are reported only at the group level, to avoid the risk of individual participants being identified.
The study was reviewed and approved by the Swedish Ethical Review Authority (Ref. No. 2020 − 00796).
Interview procedure
Semi-structured interviews were conducted using an interview guide covering the following themes: (a) background and history of substance use, (b) previous treatment experiences, (c) experiences with and views on OAT, (d) relationships with treatment staff, (e) views on control and support in ongoing treatment, (f) thoughts on the choice of drug formulation, (g) perceptions of the information provided by staff about depot buprenorphine, and (h) thoughts about the future.
The data consist of nineteen interviews. Eighteen were conducted face-to-face, in a secluded room at the clinic in question, and one was conducted by telephone [ 7 , 25 ]. Seven participants were perceived to be affected by substance intake (six of them confirmed this) and a further two were experiencing withdrawal symptoms. None of them were disoriented or considered so substance-impaired that they were unable to give informed consent or that it would be impossible to conduct an interview. However, four other people were excluded from the study: three did not meet the inclusion criteria (two were stable and in remission, one did not speak sufficient Swedish) and one was excluded due to agitated, aggressive behavior at the clinic. After the interviews, the participants received a shopping voucher worth SEK 200 (about €20).
The interviews lasted on average 37 min (range 21–55 min). They were recorded on a digital voice recorder and then transcribed verbatim by BM.
Thematic analysis [ 26 ] was carried out in two ways. The material was thoroughly read and coded by BM and AJC based on the themes outlined in the interview guide. This was followed by a detailed coding, in which different patterns in the interview responses were identified. The themes and sub-themes were then compiled in an Excel spreadsheet. In parallel, and blinded to the above findings, BJ conducted a computer-assisted thematic analysis using NVivo (Release 1.7, QSR International 2022). Initially, an inductive coding was carried out manually in NVivo. This coding was then carefully reviewed, with some codes modified and others merged. Subsequently, more general categories and subcategories were created. The parallel categorizations in Excel and NVivo were then compared and found to be largely consistent. In the final step of the analysis, the categories and codes were reviewed once more in NVivo and illustrative quotes were selected from the relevant text passages. The selection was made by BJ, who also wrote the first draft of the results section. The quotes were translated into English using ChatGPT 3.5 and then proofread by a native English translator.
The participants
Nineteen participants, 12 men and 7 women, mean age 41 years (range 24–56 years) were included. Eighteen had ongoing depot buprenorphine treatment, 12 with weekly injections and 5 with monthly injections. One participant had recently discontinued depot buprenorphine treatment and switched back to sublingual mono-buprenorphine.
Study participants had a diagnosed opioid use disorder and extensive experience of polydrug use. The mean duration of illicit drug use was 21 years (5–35 years). Before starting OAT, nine participants had used heroin as their primary drug, two had mainly used other opioids, and six had switched between heroin and other opioids. Two reported primary drugs other than opioids. Many had started using drug in their early teens and spoke of a childhood spent in difficult circumstances, including parents with drug problems, lack of care, and traumatic experiences.
All participants had received some treatment prior to starting OAT. Nine had extensive treatment experience for substance use disorders, including compulsory treatment, while the rest had more limited treatment experience prior to OAT. Most had been in OAT for a relatively short time, three years or less, but some had long experience and had been involuntarily discharged from OAT several times. As mentioned above, involuntary discharge used to be common practice in Sweden.
As the interviews were conducted in clinics for unstable patients, almost all participants had ongoing illicit substance use. At the time of the interview, nine participants reported extensive use, eight had more limited use, and one reported short-time abstinence, of less than three months. In one case, the participant did not provide information on drug status. There was a high level of psychiatric comorbidity in the group, with ADHD or other neurodevelopmental disorders, current or lifetime anxiety disorders, mood disorders, trauma and/or psychosis. Experiences of eating disorders and intentional self-harm were also reported.
Freedom of choice and information
Participants were offered depot injections due to their ongoing instability, with the intention of improving adherence and/or reducing the risk of overdose. Several patients reported that they had been advised by staff to try depot buprenorphine, because of inadequate effectiveness or side effects from previous medication. Some had asked to try depot buprenorphine themselves, having been recommended to do so by peers or having otherwise come across positive information. Most participants reported that the decision to try depot buprenorphine was voluntary. However, some reported feeling that the staff had effectively forced them to choose between depot buprenorphine and involuntary discharge from OAT, either because they were suspected of selling medication, or because they missed scheduled appointments or otherwise mismanaged their treatment. One participant reported being presented with a fait accompli:
“When I came [to the clinic] before Christmas, there was only one bottle and one syringe here when I was supposed to get my dose. […] They just said I would get this [a depot injection] instead, something about it being Christmas and New Year and they couldn’t dispense tablets daily, so I got this instead. They said it was the same dose as the tablets.” (Male participant #3) .
In addition to exploring participants’ opinions about voluntariness, we also inquired about the adequacy of the information they had received before starting depot buprenorphine treatment. While some participants felt that they had been adequately informed, others had gained knowledge by observing friends or partners who had tried depot buprenorphine. Nevertheless, a significant number of participants, including some who were enthusiastic about depot buprenorphine, reported that they had not received enough information. For instance, one participant stated:
“No, I didn’t get so much information other than that it [the dose] would last for a week. That it was in injection form, I wouldn’t have to come every day. And that it works just like usual.” (Female participant #6) .
Effects and side effects of depot buprenorphine
The perceived effects and side effects of the medication were a topic that was addressed in all interviews. A clear majority of the participants reported being satisfied with depot buprenorphine and described the depot effect as more even and stable than treatment with sublingual tablets.
“On Subs [buprenorphine tablets], I felt worse in the evenings and in the morning, when you wake up and so on. It feels like the “sub” wears off when you sleep. Then it takes a while before it starts working again. You dip quickly. Now it’s even.” (Male participant #14) .
Participants described feeling good, harmonious, and/or more “normal”. Some who had previously supplemented their medication with heroin or other illicit opioids, reported that they no longer needed to do so. The craving was gone, and so were the thoughts of heroin.
“I have no craving for heroin anymore, it’s completely insane. Because I had it on the tablets all the time, for all those years. I had to work with the craving all the time. But the depot buprenorphine, they kind of just cut it off.” (Female participant #19) .
Some participants said that they felt that the medication was right for them from the start, while others reported that the effect had varied during the first few weeks. The latter reported decreasing effects and withdrawal symptoms that became noticeable or significant towards the end of the week. Some said that they sometimes bought illicit buprenorphine to balance the effect. During the titration phase, many patients reported being offered earlier refills or extra doses in the form of sublingual tablets to counter withdrawal symptoms.
“I think it’s going great. Except on the weekends… I have it weekly, so on Saturday afternoon it starts to run out. You get cold sweats. (…) I have to run out to buy Subs on the street. I just have to.” (#15, Woman, 56 years) .
Use of illicit substances – mainly benzodiazepines or other sedatives or hypnotics – was common among the patients but notably the participants did not relate this to the depot buprenorphine. Instead, they described it as something they chose to do because they enjoyed it, or to cope with anxiety and poor mental health, or as a habit they had had for a long time and did not think they could stop. However, most participants reported that their use of illicit substances decreased when they started with the depot buprenorphine.
There were also some participants who were dissatisfied with the depot buprenorphine. They reported that the medication was not effective enough against drug cravings, or that the effect wore off after a few days, resulting in cravings and gradually increasing withdrawal symptoms. All of these people had an extensive use of illicit substances, which they described as a way of boosting their medication. Several of the dissatisfied participants stated that they had been negative towards depot buprenorphine from the beginning and had felt coerced by the staff. One person had switched back to sublingual tablets and two others said that they wanted to do so.
Just over half of the participants reported side effects, mostly described as temporary or mild. Pain, tenderness or “lumps” at the injection site were the most common. Some also described side effects such as tingling, numbness, dry mouth, brief nausea and headache after the injection which they related to temporary too high dose exposure. These side effects resolved over time or after dose adjustment. Several participants mentioned typical opioid-related side effects such as constipation, stomach problems, and sweating, but these problems were described as milder than with sublingual buprenorphine or methadone. Overall, participants described more side effects and negative experiences with other formulations than with depot buprenorphine.
Social benefits of depot buprenorphine
All the participants who had a positive view of depot buprenorphine talked about various social benefits that the injections had given them. The most commonly reported benefit was that depot buprenorphine meant that the patients no longer had to follow the “traditional” Swedish OAT structure (see background section), which was perceived as time-consuming and/or uncomfortable. Often, this was about avoiding the stress and anxiety that could result from having to get up early and go to the clinic every day.
“You don’t have to rush and feel anxiety about coming here. Otherwise, you must get up every morning, feel bad [due to early withdrawal symptoms] and take the bus all the way here. Meet a load of people everywhere to get your dose. With all that anxiety the whole time, which starts the night before. Damn. But when I got [the depot buprenorphine], I felt good, was just… healthy all the time… you know, I could wake up at 8 in the morning and feel that everything was fine… and then I could go back to sleep for a while.” (Male participant #3) .
Avoiding meeting other patients who were under the influence of drugs, or from whom they had other reasons to stay away, was also mentioned as a benefit by several people.
“Before, when I picked up my [buprenorphine tablets], I picked them up in the afternoon because it affected me a lot to come in the morning and see everything that was going on here… yes, how they [the other patients] are. It’s tough seeing them when they’re under the influence.” (Female participant #22) .
As well as highlighting what they did not have to do, some participants emphasized the increased freedom that depot buprenorphine gave them – the freedom to travel and see relatives, and to have more control over their own time. “No, but still, my ambition is to get monthly injections. To get this higher degree of freedom. I think it’s not only beneficial for me, it’s beneficial for all individuals after a time.” (Male participant #7) .
Positive changes in self-perception and identity
In addition to the social benefits of depot buprenorphine, many patients also reported more profound changes in perspective and daily life – that depot buprenorphine could help you to “shift the focus in life […], to self-realization instead of destructiveness” (Male participant #12) as one participant put it. This type of benefit was described mainly by patients who did not have an extensive use of illicit substances. “You don’t have to think about the fact that you are, like, a former junkie. You don’t have to think about your life as a drug addict. That’s not what you are, you’re a human being.” (Male participant #12) .
Participants reported that depot buprenorphine had helped them realize that they could make positive changes in their lives. “I can do things in my life. I’m not tied down anymore. I’m tied to this place [the clinic], but not in the same way. Not tied to addiction… and not tied to medication either.” (Male participant #7) Several also mentioned engaging in other activities to fill their day, such as dating, working out, or cooking, after starting depot buprenorphine treatment.
Some participants described the opportunity to shift focus as an almost life-changing transformation of their self-image and identity. They no longer lived as people with addiction, and therefore did not need to identify as such.
“The biggest lifestyle difference between the tablets and [depot buprenorphine], I think, is that I can feel more like a normal… um… normal person. I don’t have to identify as a… as the addicted person in the same way now that I get the injections (…) This is the person I want to be. The person I am today, who can stand for their decisions and be a good fellow human being. Make good decisions for myself and others.” (Male participant #21) .
However, changing one’s identity could also be a challenging or even frightening experience. One person, who had experienced severe drug problems since her early teens, described it as a strange feeling to suddenly be able to be someone else, but at the same time not knowing what to do with the rest of one’s life.
“I have a disability pension. I don’t know if I’ll get a job or something… I don’t have anyone [to talk to]. But I thought I would start talking to my contact person. So maybe I could start with some kind of activity. To pass the time. (…) Because I am alone during the days now. I just sit, sit at home.” (Female participant #6) .
Diversion and the illicit buprenorphine market
One of the obvious advantages of depot buprenorphine is that it cannot be diverted, i.e., sold to or shared with people outside of treatment. In the interviews, we asked questions about the illicit buprenorphine market and what depot buprenorphine could mean for this market.
Many patients testified to a relatively extensive illicit trade in buprenorphine tablets associated with OAT programs. There was often “a damn pestering ” (Male participant #16) from people wanting to buy. “As soon as I walk out of this door here, if you go to the regular [clinic] and pick up [tablets] during the day, then there are at least thirty people asking to buy.” (Female participant #22) The costumers are other people with opioid dependence, “those who have dropped out of [treatment] or who were our friends when we were still using.” (Female participant #15) .
Several participants said that it was nice to be able to avoid the hassle by referring to receiving depot buprenorphine. In fact, some of them described this as one of the greatest benefits of this treatment. “It’s great! I’m so happy to be able to say it: ‘You can’t suck out my Subutex because it’s in my arm’” [laughs and taps his arm]. (Male participant #15) Another participant stated: “Even today, people who don’t know I’m on depot call me. But it [the medication] is in my stomach, it’s not on the table, I have nothing to sell [chuckles].” (Female participant #6) .
That patients who receive sublingual tablets often sell part of their dose was a common perception among the patients we interviewed. An eight-milligram tablet can be sold for 150–300 kronor [approx. 13–26 €] in the city where we conducted most of the interviews. Such sales can therefore provide a significant extra income. “It’s very common. […] If you think about it, three hundred kronor a day… that’s 9,000 [800 €] a month.” (Male participant #13) .
Several participants suggested that economic motives often played a decisive role for patients who declined or discontinued depot buprenorphine treatment.
“[They would say], ‘No, this [depot buprenorphine] doesn’t work for me, it’s crap.’ But I think that’s bullshit. 99% of it has to do with either using other substances and wanting to keep the option to do so, or to sell a part of their medication.” (Male participant #21) .
Participants also shared their own experiences of selling tablets. One person said that he had previously sold a part of his dose for economic reasons, but that he did not regret starting depot buprenorphine treatment.
“It certainly changed my financial situation a little bit. But based on the stability and well-being I get from [depot buprenorphine], it’s priceless. So [depot buprenorphine], for me, it’s the holy grail. There’s nothing I would choose over [depot buprenorphine], I wouldn’t even choose heroin.” (Male participant #21) .
In this study we explored the experiences of depot buprenorphine treatment in unstable OAT patients with severe ongoing polysubstance use and multiple psychiatric comorbidities.
While the positive and negative aspects reported by this group of patients were similar to those reported in previous Australian and Swedish studies of more stable OAT patients [ 6 , 7 , 8 ], several treatment aspects emerged that were more specific to this treatment group.
It is particularly interesting that this group of unstable patients describe similar positive changes in self-perception and identity as shown in studies with more unselected groups of OAT patients [ 6 , 7 ]. People with long-term problems with illicit drugs often develop a lifestyle with particular values, skills and livelihoods associated with drug use. Over time, many lose their networks and anchorage in “normal” society and develop an identity as a “deviant” or “outsider” [ 27 , 28 , 29 ]. It is in the drug subculture that they are rooted, have most of their social relationships and feel a sense of belonging. Many studies emphasise the importance of changing one’s identity in order to move away from drug use and bring about lasting change [ 27 , 28 , 30 , 31 ]. For this to be successful, individuals need to break with their previous lifestyle and resume or establish social relationships outside the drug-using subculture. The stories of the participants in this study suggest that depot buprenorphine can be an important facilitator in such a process of change. It can free up time, allow a change of focus in life, and reduce exposure to people and environments associated with the drug subculture.
Diversion to the illicit market is a well-documented problem in OAT [ 21 , 32 ] and has been a primary motivation for the development of buprenorphine-naloxone combinations. The practical impossibility of diversion has been emphasized as a major advantage of depot buprenorphine. It is therefore rather surprising that previous studies on depot buprenorphine have not explored patients’ views on this issue. Our study is the first to explicitly examine the importance of the illicit buprenorphine market in patients’ decision-making regarding sublingual versus depot buprenorphine.
As in previous research [ 21 ], our interviews revealed a significant illicit market for buprenorphine tablets. Many participants recounted their own experiences of using illicit buprenorphine prior to starting OAT. This use usually took the form of low doses administered intranasally or intravenously, although sublingual use of illicit buprenorphine also occurred. Such use often had pseudo-therapeutic motives, for example when patients had difficulty obtaining or retaining a place in regular treatment [ 33 ].
It can be difficult to obtain reliable information about sensitive topics through interviews, particularly in relation to prohibited or stigmatizing behaviors that the participants may have engaged in themselves [ 21 ]. However, the participants in this study were unexpectedly candid about diversion, including the negative impact of decreased diversion on their income. Pressure to sell their medication appeared to be part and parcel of their daily lives. Several participants also shared their own experiences of selling medication before starting depot buprenorphine treatment. This is consistent with previous research describing patients with ongoing use, whose social contacts include others with active use, as most likely to engage in diversion [ 21 ].
Drug subcultures often develop what the anthropologist Philippe Bourgois [ 34 ] has called a “moral economy of sharing”, i.e. a system of norms in which it is considered unethical not to share drugs with friends who are “drug sick”. In this moral economy, economic and altruistic motives often go hand in hand [ 35 , 36 ]. Breaking with such a norm system is difficult and does not happen automatically simply by starting treatment where different rules are supposed to apply. As noted above, successful disengagement often requires breaking away from your old network in the drug culture and creating a new, drug-free social network. The accounts of participants in this study suggest that depot buprenorphine may facilitate such disengagement.
Although they may continue to use other drugs, these unstable patients clearly experienced reduced opioid craving and increased stability. When treated with sublingual formulations, both missing doses and diversion are common, potentially leading to suboptimal medication levels. The positive effects of depot buprenorphine may in fact reflect unstable patients receiving a sufficient dose of buprenorphine, which is necessary for effective treatment retention [ 37 ]. Additionally, depot buprenorphine may increase access to treatment, which is particularly important given that this group of patients may not be offered OAT to the same extent as more stable patients with better adherence [ 12 , 13 ].
Conversely, insufficient medication effects towards the end of the dose periods (in our population mostly weekly injections) may contribute to relapse and continued substance use among unstable patients, who are close to the illicit market. Insufficient effects were particularly evident during titration, but the problem may persist in some patients. It is important to take patients’ experiences into account and make appropriate dose adjustments or use monthly formulations to increase stability.
Like previous research [ 7 , 9 ], this study suggests that depot buprenorphine is not suitable for all patients. People who are skeptical before trying depot buprenorphine often remain so, and many in this group seem to discontinue the treatment. It is therefore necessary and appropriate to offer patients a choice of different formulations. New patients and unstable patients can be offered depot buprenorphine or a buprenorphine-naloxone combination as alternatives for buprenorphine treatment. Both earlier findings [ 21 ] and the findings of this study indicate that mono-buprenorphine tablets entail a higher risk of diversion.
Changing medications can cause frustration and anxiety for patients in OAT, particularly when information about the new medication is insufficient or when patients feel coerced to make the change [ 7 , 10 ]. Although patients expressed trust in treatment staff and reported receiving information from both staff and peers, overall we found that patients perceived information about depot buprenorphine to be insufficient. One possible explanation may be that the information provided might not reflect patients’ experiences at different stages of their treatment. A recent study of patients’ early experiences of treatment highlighted shifting negative and positive states [ 38 ] and emphasized the need for staff to inform patients about this and to help them manage their emotions and anxiety during the induction phase. Another factor to consider is the potential cognitive impairment due to ongoing substance use and comorbidities, suggesting that information may need to be adapted and repeated to meet the needs of this unstable patient population.
In conclusion, this study delves into the experiences of depot buprenorphine treatment among unstable patients with severe polysubstance use and psychiatric comorbidities. While echoing both positive and negative aspects observed in stable and unselected groups of patients, it highlights the potential of depot buprenorphine in facilitating identity change, decreasing diversion to the illicit market, and enhancing treatment retention. However, challenges such as insufficient medication effects and inadequate information dissemination warrant careful consideration, emphasizing the importance of individualized treatment options and targeted communication for this patient population.
Data availability
Permission to share data is controlled by the ethics permission. Queries regarding the permission to obtain data can be made to the Swedish Ethics Authority, +46 10 475 0800 (email: [email protected]).
Abbreviations
Opioid agonist treatment
- Opioid use disorder
Lofwall MR, Walsh SL, Nunes EV, Bailey GL, Sigmon SC, Kampman KM, et al. Weekly and monthly subcutaneous buprenorphine depot formulations vs daily sublingual buprenorphine with naloxone for treatment of opioid use disorder: a randomized clinical trial. JAMA Intern Med. 2018;178:764–773.
Haight BR, Learned SM, Laffont CM, Fudala PJ, Zhao Y, Garofalo AS, et al. Efficacy and safety of a monthly buprenorphine depot injection for opioid use disorder: A multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2019;393(10173):778–790.
Heidbreder C, Fudala PJ, Greenwald MK. History of the discovery, development, and FDA-approval of buprenorphine medications for the treatment of opioid use disorder. Drug Alcohol Depend Rep. 2023;6:100133.
Frost M, Bailey GL, Lintzeris N, Strang J, Dunlop A, Nunes EV, et al. Long-term safety of a weekly and monthly subcutaneous buprenorphine depot (CAM2038) in the treatment of adult out-patients with opioid use disorder. Addiction. 2019;114(8):1416–1426.
Lintzeris N, Dunlop AJ, Haber PS, Lubman DI, Graham R, Hutchinson S, et al. Patient-reported outcomes of treatment of opioid dependence with weekly and monthly subcutaneous depot vs daily sublingual buprenorphine: A randomized clinical trial. JAMA Netw Open. 2021;4(5):e219041.
Barnett A, Savic M, Lintzeris N, Bathish R, Arunogiri S, Dunlop AJ, et al. Tracing the affordances of long-acting injectable depot buprenorphine: a qualitative study of patients’ experiences in Australia. Drug Alcohol Depend. 2021;227:108959.
Johnson B, Flensburg OL, Capusan AJ. Patient perspectives on depot buprenorphine treatment for opioid addiction: a qualitative interview study. Subst Abuse Treat Prev Policy. 2022;17:40.
Treloar C, Lancaster K, Gendera S, Rhodes T, Shahbazi J, Byrne M, et al. Can a new formulation of opiate agonist treatment alter stigma? Place, time and things in the experience of extended-release buprenorphine depot. Int J Drug Policy. 2022;107:103788.
Clay S, Treloar C, Degenhardt L, Grebely J, Christmas M, Gough C, et al. “I just thought that was the best thing for me to do at this point”: Exploring patient experiences with depot buprenorphine and their motivations to discontinue. Int J Drug Policy. 2023;115:104002.
Bartoszko A. Polluting pharmaceutical atmospheres: compulsion, resistance, and symbolism of buprenorphine in Norway. Nord Stud Alcohol Drugs. 2019;36(3):267–285.
Tiihonen J, Mittendorfer-Rutz E, Majak M, Mehtala J, Hoti F, Jedenius E, et al. Real-world effectiveness of antipsychotic treatments in a nationwide cohort of 29823 patients with schizophrenia. JAMA Psychiatry. 2017;74(7):686–693.
Hudgins A, Uzwiak B, Pizzicato L, Viner K. Barriers to effective care: specialty drug treatment in Philadelphia. J Subst Abuse Treat. 2017;131:108639.
Aronowitz SV, Hudgins A. Problematizing “patient stability” in opioid use disorder care: Flexible definitions, (in) flexible treatment. Int J Drug Policy. 2022;108:103804.
Socialstyrelsens föreskrifter och allmänna råd om läkemedelsassisterad behandling vid opioidberoende (HSLF-FS 2016:1). 2016. Stockholm: Socialstyrelsen.
Socialstyrelsen. Nationella riktlinjer för vård och stöd vid missbruk och beroende. 2019. Stockholm: Socialstyrelsen.
Drug Commission of Inquiry. We can do better! Knowledge-based drugs policy focused on life and health. Swedish Government Official Reports SOU 2023;62:2023.
Gedeon C, Sandell M, Birkemose I, Kakko J, Rúnarsdóttir V, Simojoki K, et al. Standards for opioid use disorder care: an assessment of Nordic approaches. Nord Stud Alcohol Drugs. 2019;36(3):286–298.
EMCDDA. European drug report 2022: Trends and developments. Luxembourg: Publications Office of the European Union; 2022.
Andersson L, Håkansson A, Krantz P, Johnson B. Investigating opioid-related fatalities in southern Sweden: contact with care-providing authorities and comparison of substances. Harm Reduct J. 2020;17:5.
Andersson L, Johnson B. Patient choice as a means of empowerment in opioid substitution treatment: a case from Sweden. Drugs: Educ Prev Policy. 2020;27(2):105–117.
Johnson B, Richert T. Diversion of methadone and buprenorphine by patients in opioid substitution treatment in Sweden: prevalence estimates and risk factors. Int J Drug Policy. 2015;26(2):183–190.
Socialstyrelsen. Nationella riktlinjer för vård och stöd vid missbruk och beroende [National guidelines for care and support in substance abuse and dependence]. Stockholm: Socialstyrelsen; 2019.
Socialstyrelsen. Läkemedelsassisterad behandling vid opioidberoende: Kunskapsstöd – i hälso- och sjukvård och socialtjänst [Medication-assisted treatment for opioid dependence: Knowledge support – in healthcare and social services]. Stockholm: Socialstyrelsen; 2020.
HSLF-FS 2016:1. Socialstyrelsens föreskrifter och allmänna råd om läkemedelsassisterad behandling vid opioidberoende [The National Board of Health and Welfare’s regulations and general advice on medicationassisted treatment for opioid dependence]. https://www.socialstyrelsen.se/kunskapsstod-och-regler/regler-ochriktlinjer/foreskrifter-och-allmanna-rad/konsoliderade-foreskrifter/20161-om-lakemedelsassisterad-behandling-vidopioidberoende/ . Accessed 6 Dec 2023.
Sturges JE, Hanrahan KJ. Comparing telephone and face-to-face qualitative interviewing: a research note.Qual Res. 2004;4(1):107–118.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Svensson B. Pundare, jonkare och andra [Speed-freaks, junkies and others]. Stockholm: Carlssons; 2007.
McIntosh J, McKeganey N. Addicts’ narratives of recovery from drug use: Constructing a non-addict identity. Soc Sci Med. 2000;50(10):1501–1510.
Moshier SJ, McHugh RK, Calkins AW, Hearon BA, Rosellini AJ, Weitzman ML, Otto MW. The role of perceived belongingness to a drug subculture among opioid-dependent patients. Psychol Addict Behav. 2012;26(4):812–820.
Dingle GA, Cruwys T, Frings D. Social identities as pathways into and out of addiction. Front Psychol. 2015;6(1795):1–12.
Lalander P. Illegal street economies and drugs: Getting involved, skilled and trying to quit. In: Kolind T, Hunt G, Thon B, editors. The SAGE Handbook of Drug and Alcohol Studies: Social Science Approaches. London: Sage Publications; 2017.
Lofwall MR, Walsh SL. A review of buprenorphine diversion and misuse: the current evidence base and experiences from around the world. J Addict Med. 2014;8(5):315–326.
Richert T, Johnson B. Long-term self-treatment with methadone or buprenorphine as a response to barriers to opioid substitution treatment: The case of Sweden. Harm Reduct J. 2015;12:12.
Bourgois P. The moral economies of homeless heroin addicts: confronting ethnography, HIV risk, and everyday violence in San Francisco shooting encampments. Subst Use Misuse. 1998;33(11):2323–2351.
Havnes IA, Clausen T, Middelthon AL. “Diversion” of methadone or buprenorphine: “Harm” versus “helping”. Harm Reduct J. 2013;10:24.
Johnson B, Richert T. Diversion of methadone and buprenorphine from opioid substitution treatment: Patients who regularly sell or share their medication. J Addict Dis. 2015;34(1):1–17.
Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Sys Rev. 2014;2:CD002207.
Neale J, Parkin S, Strang J. How do patients feel during the first 72 h after initiating long-acting injectable buprenorphine? An embodied qualitative analysis. Addiction. 2023;118(7):1329–1339.
Download references
Acknowledgements
We would like to thank the participants who generously shared their experiences in the interviews. We also thank the clinical staff at the two participating OAT clinics for their help in informing participants about the study and providing logistical help to facilitate the interviews.
Open access funding provided by Lund University. (1) Swedish Research Council for Health, Working Life and Welfare, project number: FORTE 2022 − 228 (2) Medical Research Council of Southeast Sweden, project number: FORSS-931904, -940502, -969130, -982042. Funding providers had no role in the actual work with any part of this study or the current manuscript.
Open access funding provided by Lund University.
Author information
Authors and affiliations.
School of Social Work, Lund University, Lund, Sweden
Björn Johnson
Department of Psychiatry, County Hospital Jönköping, Jönköping, Sweden
Bodil Monwell
Department of Social Work, Jönköping University, Jönköping, Sweden
Department of Psychiatry in Linköping, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Andrea Johansson Capusan
Center for Social and Affective Neuroscience, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: AJC, BJ, BMData collection: BM. Funding acquisition: AJC, BJ, BM. Methodology: AJC, BJ, BM. Project administration: AJC. Qualitative analysis: AJC, BJ, BM. Resources: AJC. Writing – original draft: AJC, BJ. Writing – review & editing: AJC, BJ, BM.
Corresponding author
Correspondence to Björn Johnson .
Ethics declarations
Ethics approval.
This study is part of a research project studying the introduction of depot buprenorphine in Sweden, approved by the Swedish Ethical Review Authority (reference no. 2020 − 00796).
Consent for publication
Not applicable.
Competing interests
Andrea J Capusan has received speaker’s fees, and/or scientific advisory board compensation from Lundbeck, Indivior, Camurus, and DNE Pharma, all outside the scope of the current project.Björn Johnson has no competing interests to declare.Bodil Monwell has no competing interests to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Johnson, B., Monwell, B. & Capusan, A.J. Long-acting injectable depot buprenorphine from a harm reduction perspective in patients with ongoing substance use and multiple psychiatric comorbidities: a qualitative interview study. Harm Reduct J 21 , 68 (2024). https://doi.org/10.1186/s12954-024-00984-1
Download citation
Received : 06 December 2023
Accepted : 07 March 2024
Published : 25 March 2024
DOI : https://doi.org/10.1186/s12954-024-00984-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Polydrug use
- Psychiatric comorbidity
- Long-acting injectable depot buprenorphine
- Qualitative interviews.
Harm Reduction Journal
ISSN: 1477-7517
- Submission enquiries: [email protected]

VIDEO
COMMENTS
Revised on June 22, 2023. A structured interview is a data collection method that relies on asking questions in a set order to collect data on a topic. It is one of four types of interviews. In research, structured interviews are often quantitative in nature. They can also be used in qualitative research if the questions are open-ended, but ...
An interview is a qualitative research method that relies on asking questions in order to collect data. Interviews involve two or more people, one of whom is the interviewer asking the questions. ... Semi-structured interviews are often open-ended, allowing for flexibility, but follow a predetermined thematic framework, giving a sense of order ...
Open-ended questions are common in structured interviews. However, researchers use them when conducting qualitative research and looking for in-depth information about the interviewee's perceptions or experiences. These questions take longer for the interviewee to answer, and the answers take longer for the researcher to analyze.
Interviewing. This is the most common format of data collection in qualitative research. According to Oakley, qualitative interview is a type of framework in which the practices and standards be not only recorded, but also achieved, challenged and as well as reinforced.[] As no research interview lacks structure[] most of the qualitative research interviews are either semi-structured, lightly ...
A qualitative research interview is a one-to-one data collection session between a researcher and a participant. Interviews may be carried out face-to-face, over the phone or via video call using a service like Skype or Zoom. There are three main types of qualitative research interview - structured, unstructured or semi-structured.
Introduction. Qualitative researchers are used to dealing with unstructured data in social settings that are often dynamic and unpredictable. That said, there are research methods that can provide some more control over this unpredictable data while collecting insightful data.. The structured interview is one such method. Researchers can conduct a structured interview when they want to ...
Qualitative interviewing provides a method for collecting rich and detailed information about how individuals experience, understand and explain events in their lives. ... structure should reflect the goals and stage of your research. Less structured interviews are most appropriate for early stages of research because they
Semi-structured interviews are typically organized around a topic guide comprised of an ordered set of broad topics (usually 3-5). ... This article argues that, in qualitative interview research ...
Qualitative interview is a broad term uniting semi-structured and unstructured interviews. Quali-tative interviewing is less structured and more likely to evolve as a natural conversation; it is of-ten conducted in the form of respondents narrating their personal experiences or life histories. Qualitative interviews can be part of ethnography ...
Overview of the structured interview for qualitative research, including defining characteristics, things to know, and reflexive exercises. Chapter 1: Overview of the Structured Interview for Qualitative Research icon angle down. Start time: 00:00:00; End time: 00:04:12;
Nicholls, 2009), and choosing the right type of interview is critical in qualitative research. Types of interviews Mason (2002) defines "qualitative interviewing" as "in-depth, semi-structured or loosely structured forms of interviewing" (p.62). This type of interview requires a number of open-ended questions related to the
If you need 10 interviews, it is a good idea to plan for 15. Likely, a few will cancel, delay, or not produce useful data. 5. Not keeping your golden thread front of mind. We touched on this a little earlier, but it is a key point that should be central to your entire research process.
A structured interview is a quantitative research method where the interviewer a set of prepared closed-ended questions in the form of an interview schedule, which he/she reads out exactly as worded. ... Qualitative Research in Psychology, 8(4), 333-353. Maryudi, A., & Fisher, M. (2020). The power in the interview: A practical guide for ...
Semi-Structured: Semi-Structured Interview. Entry in The SAGE Encyclopedia of Qualitative Research Methodsby Lioness Ayres; Editor: Lisa M. Given The semi-structured interview is a qualitative data collection strategy in which the researcher asks informants a series of predetermined but open-ended questions.The researcher has more control over the topics of the interview than in unstructured ...
Introduction. In medical education research, the qualitative research interview is a viable and highly utilized data-collection tool (DiCicco-Bloom and Crabtree Citation 2006; Jamshed Citation 2014).There are a range of interview formats, conducted with both individuals and groups, where semi-structured interviews are becoming increasingly prevalent in medical education research.
Research interviews are a fundamental qualitative research method 15 and are utilised across methodological approaches. Interviews enable the researcher to learn in depth about the perspectives ...
Kinds of qualitative interviews - we will discuss each, in turn. Unstructured interviews can help a researcher LEARN MORE about an entire phenomenon set - to THEN go back and refine his/her research. • unstructured interview is a type of interview that does not make use of a set of standardized questions.
Benefits. Structured interviews can be conducted efficiently by interviewers trained only to follow the instructions on the interview guide or questionnaire. Structured interviews do not require the development of rapport between interviewer and interviewee, and they can produce consistent data that can be compared across a number of respondents.
The methods of qualitative data collection most commonly used in health research are document study, observations, semi-structured interviews and focus groups [1, 14, 16, 17]. Document study These can include personal and non-personal documents such as archives, annual reports, guidelines, policy documents, diaries or letters.
Abstract. Background: Interviews are among the most familiar strategies for collecting qualitative data. The different qualitative interviewing strategies in common use emerged from diverse disciplinary perspectives resulting in a wide variation among interviewing approaches. Unlike the highly structured survey interviews and questionnaires ...
182 DOING RESEARCH Learning how to design and use structured interviews, questionnaires and observation instruments is an important skill for research-ers. Such survey instruments can be used in many types of research, from case study, to cross-sectional survey, to experiment. A study of this sort can involve anything from a short
The study used a structured interview and Focused Group Discussion (FGD) guide for data collection. A structured interview also called a standardized interview, interview schedule, or researcher ...
A semi-structured interview is a data collection method that relies on asking questions within a predetermined thematic framework. However, the questions are not set in order or in phrasing. In research, semi-structured interviews are often qualitative in nature. They are generally used as an exploratory tool in marketing, social science ...
This study adopted a descriptive qualitative research design using semi-structured individual interviews (refer to Appendix 1 for the interview guide). The qualitative approach utilized is rooted in naturalistic inquiry and offers a wide array of theoretical or philosophical orientations, sampling techniques and data-gathering strategies [ 25 ].
Semi-structured virtual interviews and focus groups were conducted with parents, playgroup coordinators (i.e., person responsible for coordinating the playgroup) and peer facilitators (i.e., trained facilitator for the program) that participated in the Healthy Conversations @ Playgroup study. ... Liamputtong P. Qualitative research methods. 4th ...
Semi-structured interviews were conducted between 31 January 2023 and 16 February 2023, and ranged from 53 to 82 min (M = 68 min) and were recorded with consent from the participants for further analysis. All the interviews were conducted by the first author, who was a female undergraduate research student. ... Qualitative Health Research, 26 ...
Procedure. The procedure for this research is multi-stepped and is summarized in Fig. 1.First, we mapped retrospective qualitative data collected during the development of the SCI-HMT [] against the five domains of the CFIR in order to create a semi-structured interview guide (Step 1).Then, we used this interview guide to collect prospective data from health professionals and people with SCI ...
The study is based on qualitative, semi-structured interviews with OAT patients with ongoing substance use and multiple comorbidities. Sampling and recruitment Participants were recruited between December 2021 and May 2022 from two harm reduction units specializing in the treatment of patients with ongoing, severe polysubstance use and multiple ...