Experiences of implementing hospital management information system (HMIS) at a tertiary care hospital, India
Vilakshan - XIMB Journal of Management
ISSN : 0973-1954
Article publication date: 19 November 2021
Issue publication date: 2 February 2023
Mumbai needs to be transformed into a world-class city as stated in the 2005–2025 development plan of Municipal Corporation. For this initiative, hospital management information system (HMIS) has to be implemented across 400+ health facilities in the city.

Design/methodology/approach
A case study methodology was adopted to study HMIS implementation. Wave 1 of Phase 1 implementation of HMIS is carried out as a pilot project at Film City’s Hospital, Mumbai, which “go-live” on 21st June 2018. The work for hardware and software implementation was awarded to HardSystems and Solutions Limited and SoftSolutions India Private Limited, respectively, through e-tender.
Provision of inadequate quantity of hardware, slowness of network or system, non-satisfactory training after observation confirmation and sign-off process, lack of data entry operators, mismatch in numbering systems in blood bank and many other challenges concerned with the specific departments had become a major impediment in the efforts to maximize number of patients registered into HMIS.
Practical implications
Even after providing many clinical and managerial benefits, being the first cloud-based centrally located HMIS in any of the hospitals in the city, it imposes a major challenge for the management in terms of resistance of employees toward technology and need for the adoption of theoretical models for implementing change for the overall organizational development.
Originality/value
To the best of the authors’ knowledge, no other teaching case study is conducted to study the HMIS implementation in large-scale public health-care services. This is a dummy case study for teaching exercises. The identity of the stakeholders, organizations and events has been masked to maintain confidentiality.
- Change management
- Organizational development
- Health-care services management
- Hospital management information systems
- Pilot project
Arora, L. and Ikbal, F. (2023), "Experiences of implementing hospital management information system (HMIS) at a tertiary care hospital, India", Vilakshan - XIMB Journal of Management , Vol. 20 No. 1, pp. 59-81. https://doi.org/10.1108/XJM-09-2020-0111
Emerald Publishing Limited
Copyright © 2021, Lakshya Arora and Feroz Ikbal.
Published in Vilakshan – XIMB Journal of Management . Published by Emerald Publishing Limited. This article is published under the Creative Commons Attribution (CC BY 4.0) licence. Anyone may reproduce, distribute, translate and create derivative works of this article (for both commercial and non-commercial purposes), subject to full attribution to the original publication and authors. The full terms of this licence maybe seen at http://creativecommons.org/licences/by/4.0/legalcode
It was a dewy evening of Mumbai in July 2018 and a biscuit falls into the hot coffee which Medical Superintendent of Film City’s Hospital, Mumbai was dunking into his huge vintage cup.
Deputy Medical Superintendent and hospital management information system (HMIS) Nodal Officer at Film City’s Hospital bought a letter sent by one of the Heads of a Clinical Department to his office. It was mentioned in the letter that in most domains of the HMIS, the providers have not completed the modules and required integration which they have requested them to make as per the departments’ clinical and documentation requirements. The letter added that the training team was helping them only with cursory skills which they could learn by themselves once the modules would be effectively designed and given. Hence, the representatives of SoftSolutions India Private Limited were suggested to be called in a meeting along with Heads of all the Departments and other users of the system in the presence of Medical Superintendent and Director to avoid financial losses to the health-care system.
The Deputy Medical Superintendent and the HMIS Nodal Officer discussed with the Medical Superintendent that it was only one among many letters received by HOD of many departments of the hospital where HMIS was implemented as a pilot project by the Director in the past few months.
Informatics involves information acquisition, organization, validation, storage, retrieval, integration, analysis, communication and presentation, using IT as a key resource ( Lifshitz et al. , 2007 ; Sinard, 2006 ). HMIS is defined as the “computer system designed to ease the management of all the hospital’s medical and administrative information and to improve the quality of healthcare” ( Degoulet and Fieschi, 1997 ). An EHR system comprises “the longitudinal collection of electronic health information for and about persons, where health information is defined as information pertaining to the health of an individual or health care provided to an individual. Critical building blocks of an EHR system are the electronic health records (EHR) maintained by provider…and by individuals” ( National Institutes of Health, 2003 ).
At present, most of the Indian hospitals are adopting HMIS as a way of automation and digitalization of their health-care records.
Film City’s Hospital, Mumbai
Bombay, the very first possession of Britishers in India, came to King Charles II of England in 1661, when he married the Portuguese queen, as part of the royal dowry. Through Corporation Resolution No. 512 which was dated August 12, 1996 under Maharashtra Act, XXV, 1996, the name “Bombay” has been changed as “Mumbai.”
Greater Mumbai is presently a metropolitan aggregation of around 18 million residents (world’s six largest and largest in India). The port city accounts for most of foreign trade in India as well as government revenues, being one of the major hubs for education, research, development and technology in India ( MCGM, 2019 ).
The Film City’s Hospital situated in the heart of Mumbai is a 1,000-bedded tertiary care facility with around 30 clinical departments where every year more than 55,400 patients are admitted and more than 280,000 patients (new and old) are treated in out-patient department. More than 21,000 operations (major and minor) are performed and 4,200 deliveries are done every year.
In addition to the routine medical services, it also offers various super-specialty services in nephrology, neurosurgery, endocrinology, gastroenterology, cardiology and cardiac vascular and thoracic surgery. This hospital has well-equipped intensive care units for medical, surgical, cardiac and neonate patients. The hospital has its own blood bank and component therapy unit, which provides services round the clock. A whole body CT scanner, cardiac catheterization system and spect camera, etc. are also installed at the hospital. It also has independent hyperbaric oxygen therapy chambers.
The hospital levies fees from the patients at subsidies rate and efforts are made to provide the best and excellent patient care ( MCGM Health Department, 2019 ).
Why hospital management information system…?
India’s 12th 5-year plan highlights the need to improve HMIS throughout the nation and a possible investment in health IT in the public health system (Twelfth Five year Plan Draft 2012, 2017). Multiple findings have reported the advantages of HMIS implementation ( Hillestad R et al. , 2005 ; Wang et al. , 2003 ; Frisse and Holmes, 2007 ; Shekelle et al. , 2006 ).
HMIS is considered to be the most promising instrument to improve the overall efficiency, safety and efficacy of the health service (Basit et al. , 2006). Wide and effective use of HMIS improves the quality of health care ( Frere, 1987 ); minimize adverse events; reduce the cost of medical care ( Lun, 1995 ); increase administrative productivity improvements ( Kuruvilla et al. , 2004 ); reduce documentation as well as enhance access to affordable treatment (Basit et al. , 2006; Yasnoff et al. , 2000 ).
Municipal Corporation aspires Mumbai to be transformed into a millennium and world-class city as stated in the development plan 2005–2025. For this to happen, Mumbai requires to be distinguished about the quality of life aspect by improving the quality of citizen welfare services. As part of this initiative, the HMIS has to be implemented across 400+ health facilities across the city.
There is the availability of digital access original data through HMIS which can be used as a strong tool in the decision support system for the Film City’s Hospital management. The HMIS data can be used for analysis as well as for forecasting purposes. The electronic medical records (EMRs) as well as picture archiving and communication system (PACS) generated can be of great use for the clinical purposes for better diagnosis and treatment. The HMIS data can also be used for drug calculations and better scientific inventory management practices at the hospital.
Hospital management information system implementation at Film City’s Hospital
Literature have shown that implementation and improvement in HMIS to guide policy and management decisions has found essential space in countries such as Peru, Tanzania, Solomon Islands, Caribbean, Lesotho, Honduras, India (Uttar Pradesh) and Kryragya Republic (World Bank Reports , 1993 , 1999, 2000, 2001; Commission on Health Research for Development, 1990 ).
The work of software implementation and post-implementation of HMIS in the film city covering 4 major hospitals, 1 dental hospital, 18 peripheral hospitals, 5 specialty hospitals, 28 maternity homes, 161 dispensaries and 183 health posts was awarded to SoftSolutions India Private Limited.
As per the directives, Wave 1 of Phase 1 implementation of HMIS is carried out at Film City’s Hospital as a pilot project. Wave 2 of Phase 1 was planned to be implemented at other three major hospitals in the city and thereafter at balance health-care locations ( Mukul, 2018 ).
It was decided to form a committee to commence the viability and feasibility of Wi-Fi services project at Film City’s Hospital and the standing committee sanction was received for awarding the work for hardware and network implementation at the Phase I Hospitals and the LOI of worth Rs. 50+ crores for the prestigious project is issued to HardSystems and Solutions Limited. Further, a pilot implementation is planned to be carried out at few departments in Film City’s Hospital which “go-live” on 21st June 2018 ( MCGM IT Department, 2019 ).
Bid document for hospital management information system
The HMIS software pilot project at Film City’s Hospital was awarded to SoftSolutions Private Limited through evaluation of technical and commercial bids by e-tender process, initiated in July 2016. SoftSolutions, also as part of their scope, conducted a site survey for hardware infrastructure for all health-care institutions in the city. The exact quantity and minimum specifications for various hardware and infrastructure have been provided by SoftSolutions post site survey.
The purpose of this bid document is to select an agency for not only the supply but also the hardware and network components’ installation, testing, commissioning and maintenance for the health institutions.
A Bid Evaluation Committee (BEC) was appointed to examine and assess the submitted technical as well as commercial bids. The BEC reviewed the bids to decide if they’re really complete, able to respond and if the bid format complies with the bid specifications. In a bid that does not represent a material variance, it was waived for any informality or nonconformity and the bidder with the lowest cost submitted (L1 rate) in the commercial bid opening was awarded the contract.
Submission of inception report.
Supply, installation and commission of various hardware and network components along with required accessories at health institution.
Undertake required passive structured cabling (including patch chord, faceplate with input/output connector, laying of LAN and fiber cable (if required) with proper labeling, testing certificate and others).
The device should be tested before mass-installation (operating system compatibility, software, drivers, etc.).
The supplier should take care of all installation and support issues that are faced by the end-user, for all hardware and software supplied as part of the purchase order. This would include installation and support for security functions, user configuration, LAN configuration, etc.
Addition of a desktop PC to the security device is to be done by the implementation agency.
In-warranty annual technical support for hardware and network components services for a period of five years.
The following are additional points for the scope of the implementation agency:
The Wi-Fi/network device shall be connected to the local area network.
The supplier shall disable unnecessary services, protocols and ports.
When installing software, ensure that only required software is installed and the latest versions of all software including all recommended security patches are updated.
Disable or remove redundant software/services (including program, machine utilities and network services).
Pre-requisites for hospital management information system pilot project
The Assistant Medical Officer (AMO) of the hospital was appointed as the HMIS implementation nodal person from Film City’s Hospital for coordinating with the internet service provider and hardware supplier appointed by HardSystems and Solutions Limited, implementation of software by SoftSolutions and coordinating with various departments for providing solutions to any challenges faced.
Site readiness – the representative of SoftSolutions visited each department of the hospital for finalizing the network points, in consultation with the Head of Departments (HODs).
For the implementation of HMIS, one server room and one room for hardware and software support staff for the hospital and UPS room per building were identified and subsequently handed over to HardSystems and Solutions Limited, as per the specification ( The Hindu, 2018 ).
The support staff room was used by HardSystems and Solutions Limited for storing the equipment during the installation.
The civil work, if any, required for the network installation, server room and UPS room readiness was carried out by the Hospital Assistant Engineer (AE), Civil Department.
The furniture, if any, required for the HMIS hardware was identified and procurement was carried out by the Hospital M&E department.
The electrical work for HMIS implementation was carried out through the Chief Engineer (M&E) department. The concerned M&E engineer from the hospital coordinated with the representative of SoftSolutions and HardSystems and Solutions Limited.
Hardware and software implementation
As the number of patients was increasing in the waiting areas of the clinical departments, Deputy Medical Superintendent took a round with HMIS nodal officer to locate any patient-free area or store rooms in IPD building.
After the functional requirement study and the hardware survey did from June to September, 2016, the Digital Laboratory and Security room on ground floor of IPD building of the Film City’s Hospital was allotted for hardware storage. A 24 × 7 helpdesk was also created to give instant solutions to the arising issues in the software or hardware.
As per directives, 200 customized portable computer trolleys (to be used for computer-on-wheels) were provided as per the requirements and storage area in the departments.
Under Software Research Survey (SRS) up to September 2016, software customization for medical specialties was done after studying the workflow of major hospitals of Mumbai, for surgical specialties, radiology and central sterile services. Sub-committees were formed in each of these hospitals to monitor the process of customization of software, and sessions to sensitize nursing staff, technicians, pharmacists, registration attendants, etc. were conducted across all the hospitals. Weekly or sometimes fortnightly review meetings were held at the Film City’s Hospital. Also, various teams visited multiple public, private and trust hospitals across the city to study already existing HMIS implemented in these hospitals ( MCGM IT Department, 2019 ).
User acceptance tests and finalization of hospital management information system modules
Documented literature suggests that the degree of end-user satisfaction is a pivotal factor of an information system’s success ( Bailey and Pearson, 1983 ). Many other studies have stressed the significance of levels of end-user satisfaction ( Doll and Torkzadeh, 1988 ; DeLone and McLean, 1992 ).
During the user acceptance test-1 (UAT-1), there were 517 observations noted in module testing which was carried out up to March 21, 2017, by the doctors and other representatives.
Thereafter, in April 2017, a UAT observation confirmation process (also known as system requirement specification reconfirmation) was carried out by SoftSolutions with representatives from various health-care facilities who were assigned for each module so as to prepare SRS 1.1 with more precise information and requirement to aid the development of HMIS.
With reference to the OPD module, about 318 proformas from 29 departments were handed over to SoftSolutions on 9th June 2017 for developing the EMR for the OPD module. Considering each proforma was unique and also an easy-to-use system is to be developed, SoftSolutions has developed a solution and the same was shown to a team of doctors of each department concerned with the OPD module to check the functionality and provide their inputs for the same, so that the precise requirement can be incorporated in the SRS 1.1.
Further, SoftSolutions have documented the information provided during and after the UAT 1 and UAT/SRS reconfirmation in the latest SRS version 1.1 and the same was ascertained by the team of representatives who had provided the information during the UAT/SRS reconfirmation and corrected the same if necessary and provided the sign-off for the respective module SRS 1.1. On completion of the activity, UAT-2 (inter-module) and thereafter UAT-3 (integrated) were planned to be conducted.
On the basis of all the three UAT and UAT observation confirmation processes conducted for different modules, there were a number of change requests made by concerned HODs/departments which after approval from nodal officers were incorporated through some policy decisions for requirements which were taken by the administration.
It was finalized by the management that the short message service (SMS) would be used for registration and inpatient referral only. It is not necessary to send SMS for every activity. For easy workflow of IT services, digital signatures were assigned for important decisions, for legal, medico-legal cases, birth and death certificates.
Recruitment of data entry operators and training of hospital staffs
Deployment of data entry operators (DEOs) for assisting the hospital staff related to the implementation of HMIS was done through prescribed norms of recruitment for different departments for three working shifts.
The training was well planned by a team of SoftSolutions and all the requirements including space and other resources were allocated. Training was done in two parts, which involved orientation lectures and hands-on session conducted in the first and second weeks of February 2018, respectively.
It was decided to use India’s first indigenous Web-based PACS Medsynapse for training doctors and staff of radiology department. It is developed on advanced technologies and provided a full range of features and tools for image processing, distribution and archival. It is very user-friendly, scalable and affordable PACS with more than 20,000 installations in 40 countries.
A training completion certificate on specific HMIS module was awarded to each employee after successful completion of training.
For the purpose of logging into HMIS computers and application, employee’s ID-based default login and password systems were generated, which were later allowed to reset by the users. Thus, all the resident doctors and other staff got access to the HMIS system.
An HMIS refreshment training with proper consultation with Team SoftSolutions was provided once again in October 2018 after proper implementation of all the 32 modules in the system.
Dry run and go-live
A dry run was conducted in the selected clinical and supportive services departments of Film City’s Hospital in Phase 1 from April to June 2018. After the required improvements needed the pilot project “go-live” for Phase 1 of Wave 1 from 21st June 2018 ( MCGM RTI, 2019 ).
Overcoming hospital management information system challenges
Provision of an inadequate quantity of hardware either because of lack of storage space or because of unavailability of furniture and computer trolleys had become a major impediment in the efforts to maximize the number of patients registered into HMIS at Film City’s Hospital, e.g. super-specialties such as nephrology and gastroenterology have an average outpatient load of around 100–150 patients per OPD. But only three computers have been provided for doctors and one for the nursing staff in the OPD of super-specialties.
Because of the slowness of the network or the system, particularly after 11:00 a.m., patients are inconvenienced as they have to wait for long periods till the EMRs are filled and prescriptions and laboratory/radiology requisitions are generated. At times, patients are reluctant to wait for the procedure to be completed. Consequently, only a few requisitions of laboratory and radiology investigations had been processed through the system. It was decided to put more LAN cables but when the issues persist, new Wi-Fi dongles were thought to be procured for every department in the future ( DNA, 2019 ).
Also, a major challenge is that integration of HMIS with various government and insurance schemes is to be undertaken and also a separate budget is to be allocated for HMIS consumables.
HMIS Nodal Officer conducted an immediate evaluation and the following challenges were reported to be faced by some important clinical and supportive services departments.
Department of gastroenterology
One of the issues of the gastroenterology was that all the hospitals in the film city were using different systems for capturing endoscopy reports. Also other investigations such as manometry, PH, fibroscan and breath hydrogen were intended to be managed well so that different reports and PDF can be uploaded in HMIS. The report’s structure given in HMIS was discussed with concerned IT team to check for the network link to the system.
Department of psychiatry
As soon as the recreational activities started for the admitted patients, the HOD of Psychiatry Department entered the IPD area. HMIS Nodal Officer was waiting for him to ask for required modifications.
He said, “Wires need to be covered to protect against damage by the psychiatric patients. Sub-departments like Psychology, Social worker and EEG are also to be included in the system.” HMIS Nodal Officer carefully noted the desired changes. When inquired about the psychiatric OPD, implementation of electronic queue management system monitor was suggested.
Pediatrics department
On meeting with the Professor of Pediatrics while he was checking the nutritional chart for a three-year-old child, the Nodal Officer asks her to raise the concerns regarding HMIS implementation. She swiftly enumerated that the weight, age and height data have to be integrated for making relevant WHO charts and growth curves for classifying patients with severe acute malnutrition or moderate acute malnutrition. She added, immunization record is also to be included in IPD paper. If a vaccine is missing as per national immunization program, a warning has to come on the system. Automatic calculation of surface area is required for prescribing certain drugs. Integration with certain government schemes is also required.
Opening her smart tablet, the HMIS Nodal Officer checked the relevant schemes available in the Film City’s Hospital and asked, “Should Janani Suraksha Scheme also be integrated?” for which she got the affirmative response.
Professor of Pediatrics explained to the Nodal Officer that daily reporting/monthly data have to be available disaggregated in terms of age, gender, notifiable diseases and monsoon-related illness. In addition, the multiple diagnoses have to get sited separately because they are not mutually exclusive. Also, referral list has to be made comprehensive to include physiotherapy, occupational therapy, dietetics and speech therapy in addition to clinical/lab departments.
Radiology department
With the use of Digital Imaging and Communications in Medicine standard and Health Level 7 communication protocol, vendors communicate with the radiology imaging management system termed PACS. Undoubtedly, a major concern in radiology department is to combine the images of each analysis with other important patient records and enhance interoperability with radiology information system and HMIS ( Cummings, 1995 ; Offenmuller, 1997 ).
According to recommendations of PACS Support Engineer given to HMIS Nodal Officer of Film City’s Hospital, “open office” does not support PACS reporting. In addition, the automatic transfer of stored images from USG machine to HMIS was not taking place. Therefore, the HOD of Radiology requested that the licensed access to 3D-MPR viewing be provided to all the radiology employees, including CT/MRI technicians. Furthermore, with the view of additional CT and MRI machines being instilled with additional workload in the near future, approximately 70 licensed accesses needed to be made available to increase the ease, efficiency and speed of reporting. The licensed MS office is also preferred to maintain the integrity and uniformity of the departmental work.
Also, while reporting the patient on PACS, considerable time was consumed in logging in as well as in opening a particular patient. It was difficult to interpret whether the slowness could be attributed to the slow speed of the network or slowness of the operating software.
In addition to this, there was the need for early integration of revenue counter and the central laboratory with the HMIS system for the better functioning.
Laboratory and diagnostics services
Diagnostics is a data-intensive specialty, and laboratory data is often used in addition to patient services to record continuous improvement, performance management, outcome analyses and research studies ( Cowan, 2005 ; Young, 2000 ). At the center of most laboratory activities is the laboratory information system. Workflow management, specimen monitoring, data entry and reporting, regulatory enforcement assistance, code acquisition, interfacing with several other applications, archiving, inventory management and provision of billing information are its features (Eleveitch and Spackman, 2001; Pearson et al. , 2006 ).
For appointment generation counter: token generation facility for the same-day blood collection of patients has to be incorporated in the system. For the token generation, a fast printer device was required as a large number of patients need to be handed over in a short period of time.
For labeling counter
Quality of bar code labels need to be improved. Printouts sometimes are not readable and may face problem in scanning. The problem was discussed with the Project Director, HMIS.
Consumables such as printer roll, appropriate sized labels are not easily available in the hospital.
For collection table: It was discussed with the IT in charge, SoftSolutions, that wall-mounted all-in-one PC units with bar code scanner facility or tablets with in-built scanner need to be installed in OPD for scanning the collected blood samples.
Blood sample processing: Appropriate diagnostic equipment such as blood cell counter and automated biochemistry analyzer have to be procured, which can be integrated with HMIS.
Blood bank services
The blood bank system consists of an autonomous blood center responsible for human blood procurement, storage and distribution ( Li et al. , 2007 ). Because blood bank services are vital segment of the Film City’s Hospital and there were major concerns raised by the employees in the department, Medical Superintendent called for an urgent board meeting ( Tables 1 ).
A unique number was given to each blood bag in the blood bank. This number is followed through the life of that blood bag, i.e. the same number applies at blood group, serological tests, stock taking, cross-matching and issue of blood bag to patients. As on 30th July 2018, the blood bank numbers were at “Indoor 905,” “Outdoor 9888” and “Brought from i.e. BF 1186.”
The HMIS data entries in Blood Bank were attempted since 26th July 2018; however, the HMIS software is unable to match the actual bag numbers because it begins by default 001, 002, 003, etc. Because of this error, the outdoor bag number 8434 may be entered in HMIS as bag number 0004, indoor bag number 894 entered in HMIS as bag number 0005 and so on.
This numbering system, if continued, could have created utter chaos at all levels. Online bloodstock will show wrong bag numbers available to technicians for a cross-match. Issued bags will not correspond to the actual blood bag issued, thus resulting in confusion at a blood bank and clinician level.
In addition, serious mistakes in identifying and discarding of seropositive bags (HIV, Hepatitis B, etc.) can occur because of an incorrect numbering system.
Given the sensitive nature of blood bank work, the slightest error in numbering can cause disastrous results for the patient’s life. Any kind of dual numbering system, as suggested by the HMIS technical team, will further compound the problem, double the workload and invite severe adverse remarks from the FDA.
Because Film City’s Hospital is stationed for the pilot study, any errors can get carried forward and adversely affect the working of other hospitals and other blood banks too. In view of this serious medico-legal and ethical implications, it is essential that HMIS number entries have to categorically match with available numbering for blood bags.
Pharmacy prescriptions and dispensary services
In outpatient health care, the drug management process is a multifaceted relationship between patients, prescribers and pharmacists, which is also enabled by HMIS ( Tamblyn, 2004 ). Electronic medication management has the ability to allow a secure process, but errors may also be created ( Bates et al. , 2001 ).
At Film City’s Hospital, after consultation with head pharmacist, HMIS Nodal Officer noted that a standard prescription format should include name of the drug, preparation, strength, dose, route of administration, frequency and number of days. The route of drug administration should be comprehensive and must also include intradermal, intra-thecal and intra-ocular routes.
It was recommended that the prescriptions need to be in terms of both generic and brand names. Allergies must be a mandatory field, which needs to be pop out during prescriptions. Starting and end dates should be integrated especially for drugs with progressive decreasing doses. At once, no medicines should be prescribed for more than one month.
It was suggested to improvise the SAP system, based on the positive features of government’s “e-Aushadi program” which includes:
Need for surplus and shortage alerts.
Rigorous quality control of medicines should be mandatory and built-in using impaneled NABL-accredited laboratory.
Achieving the milestones
The HMIS is being implemented to improve the quality and responsiveness of health-care services in health-care network in the film city ( Tables 2 and 3 ).
Features of hospital management information system implementation at Film City’s Hospital
The unique features of the HMIS system at Film City’s Hospital are that this system is first of its kind in any of the city’s hospitals that uses a cloud-based centrally located system in which as much as 32 clinical and supportive services HMIS modules are covered. It is made possible to achieve inter-departmental and intra-departmental connectivity in Film City’s Hospital through this system. In addition, this cloud-based system also allows central access to data through any city’s health-care systems, thus enhancing inter-hospitals connectivity ( MCGM RTI, 2019 ).
Hospital management information system implementation – the road ahead
There is a lack of DEOs in some departments. To enhance the time and cost-effectiveness and to achieve digitization through increasing reach to more number of patients, it was decided to implement “Speech to Text” software in the OPDs based on the principle of “machine learning.” The SoftSolutions team has already started taking voice samples of the doctors in the OPDs, and to test the effectiveness of the software, the trial run has been started in the Psychiatry and General Medicine OPD of Film City’s Hospital.
Also, at the registration department, issue of digitalized health card to every patient with Unique Hospital Identification Number and bar coding on it has been started. In the future, the bar scanners will be incorporated to save time at various points in the hospital.
Most of the users are still very resistant in the use of technology in the hospital as they are adapted to traditional manual data entry and calculation methods. The percentage of EMR completion still has to be improved.
Deputy Medical Superintendent along with the HMIS Nodal Officer discussed with the Medical Superintendent, Film City’s Hospital that there is a need for adoption of “John Kotter’s Eight-Step Plan” for implementing change for user acceptability for the overall organizational development and to reinforce the future dream which she had seen of digitalized health-care systems in digitalized India.
Several studies on implementation of HMIS in developed countries ( Ash et al. , 2003 ; Ball, 2003 ; Berg, 2001 ; Benson, 2002 ; Little Johns et al. , 2003 , Joel Rodrigues, 2009 ; Lippeveld et al. , 1992 ; Dudeck et al. , 1997 ) had reported various challenges, including those in managing infrastructure, integration, inter-departmental issues, technical requirements, data and software issues, end-user contribution, standardization of terminologies, training needs and ignorance of hospital administration. In developing nations, numerous health-care professionals associate information systems with filling of infinite registers, collecting information and submitting reports without sufficient input, making HMIS “data-driven” instead of “action-driven” ( Sandiford et al. , 1992 ; Smith et al. , 1988 ). Similarly, in this case study, although being an Indian hospital, managing infrastructure in terms of space for computers, trolleys and other accessories became a major challenge. Allocating areas for installing LAN and rooms for information technologist in a crowded hospital was not that easy task. In this case study, the hospital also faced inter-departmental and inter-hospitals issues with respect to integration and standardization of clinical domains and report structures, respectively. Even after adopting the HMIS principles in several trainings, many employees, especially elder age, felt the need for technical assistance. In addition, the poor doctor–patient ratio and the downtime of the server made the work more complicated as in some of the departments, employees started doing dual entries (both in register and computer) to prevent loss of any data.
Several issues have been identified in the review of reports and studies in low-income countries ( Gladwin, 1999 ), such as general organizational and management difficulties ( Campbell et al. , 1996 ; Braa et al. , 1997 ; Azubuike and Ehiri, 1999 ); data acquisition and processing concerns ( Robey and Lee, 1990 ; Jayasuiriya, 1999 ; Lippeveld et al. , 2000 ); inadequate use of information (WHO, 1994b, 1999; Braa et al. , 1997 ); over-reliance on epidemiological data or specific surveys ( Husein et al. , 1993 ; Sapirie and Orzeszyna, 1995 ); and paucity of an integrated information strategy for the organization ( Van Der Lei et al. , 1993 ). In a similar way, in this case study also, many departments in the hospitals faced challenges around complexity, inconsistency and poor integrity of the system. Although the management tried to ensure the effectiveness, incidents such as mismatch in blood bag numbering in HMIS posed a major ethical issue. There were multiple concerns around data acquisition at revenue and cost centers of the hospital. Although management took corrective and preventive actions, it was reflective of a strategy which would have been well integrated prior with clinical understanding and principles of change management.
Several studies have been conducted on interface design methodologies ( Shearer et al. , 1997 ; Arreola et al. , 1997 ), and among the unidirectional, bidirectional and integrated workstations ( Levine, 1990 ), the interface with more consistent information base is most preferred ( Veader, 1997 ). Studies have reported that an integrated radiology network enhances the efficacy of physicians, minimizes costs, decreases the amount of repetitive or unnecessary tests and increases the quality of care ( Gibby and Mciff, 1997 ). In addition, owing to the extensive adoption of electronic radiology reporting systems, filmless radiology systems and speech recognition, there have also been considerable radiology workflow efficiency improvements ( Mariani et al. , 2006 ; Gay et al. , 2002 ; White, 2005 ; Ralston et al. , 2004 ). Similarly, in this case study, it was observed that with administrative efforts and understanding employee training needs, the number of repetitive tests was reduced. There was a direct benefit in lowering turnaround time and publishing more reports. The better integration and consistency of the PACS will help in increasing the profit per unit volume for the radiology department.
HMIS is important in its ability to resolve issues such as increasing laboratory volume with outreach programs; intensified EMRs integration; and the subsequent need to combine fragmented information systems, laboratory resource shortages, patient safety, cost control, central control of subspecialties, rising demand for laboratory diagnostics and customized intervention ( Becich et al. , 2004 ; Sinard and Morrow, 2001 ). In this case study also, HMIS-integrated EMR played a significant role in decreasing the average waiting time for the patients for receiving the laboratory reports.
Child clinicians frequently feel that there is little utility of health information systems in pediatrics because they tend to be structured for adult services ( Johnson, 2001 ). There are several functional areas, such as immunization records ( Smith, 1988 ), growth monitoring ( Rosenbloom et al. , 2006 ), drug dosing ( American Academy of Pediatrics, 2004 ), patient recognition ( Kuther, 2003 ) and decision support systems ( Miller et al. , 2001 ), which are so vital to the treatment of children and adolescents that their omission contributes to the system hindering quality pediatric care. In this case study, with the discussion with HMIS Nodal Officer, the pediatric department was able to design a customized module which had unique characteristics as compared to any adult-based systems. Drug dosage and calculations, immunizations and growth-monitoring systems were integrated successfully.
Literatures have shown that implementation of computerized blood bank inventory and emergency services ( Catassi and Petersen, 1967 ) and blood bag system ( Ali et al. , 2017 ) plays a significant part in hospital’s decision-making systems ( Li et al. , 2008 ). Similar results were observed in this case study also.
Mohapatra (2009) notes that combining in-patient, pathological and inventory management of hospital pharmaceutical stores enables to enhance the quality of service and efficiency while reducing operating costs. This economic benefits can be reflected in the price, which gives customers more good value. The use of HMIS has been proposed as a way to minimize prescription errors by increasing the readability, standardization and availability of information or providing automatic controls for possible drug-related issues, but the findings are inconsistent ( Huckvale et al. , 2010 ; McKibbon et al. , 2011 , 2012 ). In this case study, the findings suggested that the use of HMIS was helpful in inventory management once the employee got well trained in inventory modules and it generated profitability for the hospital.
Literature shows that during the process of automation, important performance variables involved in the phase of change management are organizational structure, technology infrastructure and implementation approach ( Galliers and Sutherland, 1991 ; Lubitz and Wickramasinghe, 2006 ; Nolan, Norton and CO, 1992 ). Emergent philosophy is more complex ( Markus and Robey, 1988 ) than imperative perspectives ( Robey and Boudreau, 1999 ), stressing a reciprocal instead of a one-way relationship involving technology and organization. Findings of this case study suggest that the management should have strategically thought about the change management perspectives in a visionary sense before taking the step for HMIS implementation. Most of the elder employees were resistant to change and found the system more complex. In terms of ease of use of HMIS, more than half of the employees were either neutral or disagreed in their responses.
Mumbai city map
Picture showing patient health card with UHID and bar coding
Discussion in the meeting conducted at Medical Superintendent’s office, Film City’s Hospital between authorities and the users on the HMIS challenges of blood bank
Progress of HMIS implementation at Film City’s Hospital up to February 2019
Digitization through electronic medical records (EMRs) at Film City’s Hospital
Table showing distribution of customized computer trolleys at Film City’s Hospital
Changes in key performance indicators (KPIs) at Film City’s Hospital after HMIS implementation
Average time spent per service
Average gain per unit volume of the services
Employees ( n = 75) responses for HMIS
Ali , R.S. , Hafez , T.F. , Ali , A.B. and Abd-Alsabour , N. ( 2017 ), “ Blood bag: a web application to manage all blood donation and transfusion processes ”, Paper presented at the 2017 International Conference on Wireless Communications, Signal Processing and Networking (WiSPNET) .
American Academy of Pediatrics ( 2004 ), “ Committee on fetus and newborn. Age terminology during the perinatal period. Pediatrics ”, Vol. 114 , pp. 1362 - 1364 .
Arreola , M. , Neiman , H.L. , Sugarman , A. , et al. ( 1997 ), “ Implementation of a radiology electronic imaging network: the community teaching hospital experience ”, Journal of Digital Imaging , Vol. 10 No. S1 , pp. 146 - 149 .
Ash , J.S. , Gorman , P.N. , Lavelle , M. , et al. , ( 2003 ), “ A Cross-Site qualitative study of physician order entry ”, Journal of American Medical Informatics Association ,
Azubuike , M.C. and Ehiri , J.E. ( 1999 ), “ Health information systems in developing countries: benefits, problems and prospects ”, Journal of the Royal Society for the Promotion of Health , Vol. 119 No. 3 , pp. 180 - 184 .
Bailey , J.E. and Pearson , S.W. ( 1983 ), “ Development of a tool for measuring and analyzing computer user satisfaction ”, Management Science , Vol. 29 No. 5 , pp. 530 - 545 .
Ball , M.J. ( 2003 ), “ Hospital information systems: Perspectives on problems and prospects ”, International Journal of Medical Informatics , Vol. 69 Nos 2/3 .
Bates , D.W. , Cohen , M. , Leape , L.L. , Overhage , J.M. , Shabot , M.M. and Sheridan , T. ( 2001 ), “ White paper – reducing the frequency of errors in medicine using information technology ”, Journal of the American Medical Informatics Association , Vol. 8 No. 4 , pp. 299 - 308 .
Benson , T. ( 2002 ), “ Why general practitioners use computers and hospital physicians do not – part 1: Incentives ”, British Medical Journal ,
Berg , M. ( 2001 ), “ Implementing information systems in health care organizations: myths and challenges ”, International Journal of Medical Informatics , Vol. 64 No. 2-3 .
Becich , M.J. , Gilbertson , J.R. , Gupta , D. , et al. ( 2004 ), “ Pathology and patient safety: the critical role of pathology informatics in error reduction and quality initiatives ”, Clinics in Laboratory Medicine , Vol. 24 No. 4 , pp. 913 - 943 .
Braa , J. , Heywood , A. and Shung King , M. ( 1997 ), “ District level information systems: two cases from South Africa ”, Methods of Information in Medicine , Vol. 36 No. 02 , pp. 115 - 121 .
Campbell , B. , Adjei , S. and Heywood , A. ( 1996 ), From Data to Decision Making in Health: The Evolution of a Health Management Information System , Royal Tropical Institute , Amsterdam .
Catassi , C.A. and Petersen , E.L. ( 1967 ), “ The blood inventory control SystemHelping blood bank management through computerized inventory control ”, Transfusion , Vol. 7 No. 1 , p. 196 .
Commission on Health Research for Development ( 1990 ), Health Research: essential Link to Equity in Development , Oxford University Press , New York, NY .
Cowan , D.F. ( 2005 ), “ Laboratory informatics and the laboratory information system ”, in Cowan , D.F. (Ed.), Informatics for the Clinical Laboratory , Springer , New York, NY , p. 1 - 20 .
Cummings , B.A. ( 1995 ), “ RIS integration strengthens PACS. PACS under managed care ”, Diagn Imaging , Vol. 17 , pp. 13 - 14 .
Degoulet , P. and Fieschi , M. ( 1997 ), Introduction to Clinical Informatics , Springer , New York, NY .
DeLone , W. and McLean , E. ( 1992 ), “ Information systems success: the quest for the dependent variable ”, Information Systems Research , Vol. 3 No. 1 , pp. 60 - 95 .
DNA ( 2019 ), “ HMIS delayed: Mumbaikars won't get rid of hospital queues soon ”, available at: www.dnaindia.com/mumbai/report-hmis-delayed-mumbaikars-won-t-get-rid-of-hospital-queues-soon-2710654 (accessed 7 March 2019 ).
Doll , W.J. and Torkzadeh , G. ( 1988 ), “ The measurement of end-user computing satisfaction ”, MIS Quarterly , Vol. 12 No. 2 , pp. 259 - 274 .
Eleveitch , F.R. and ( 2001 ), Spackman , KA. “ Clinical laboratory informatics ”, in Burtis , C.A. and Ashwood , E.R. (Eds), ( 2001 ), Tietz Fundamentals of Clinical Chemistry , 5th ed. , WB Saunders Company , pp. 262 - 271 .
Frere , J.J. ( 1987 ), Health and Management Information System for Child Survival Project in Pakistan , Technologies for Primary Health Care Project, United States Agency for International Development , Washington, DC , 1 - 23 .
Frisse , M.E. and Holmes , R.L. ( 2007 ), “ Estimated fi nancial savings associated with health information exchange and ambulatory care referral ”, Journal of Biomedical Informatics , Vol. 40 No. 6 , pp. S27 - 32 .
Galliers , R.D. and Sutherland , A.R. ( 1991 ), “ Information systems management and strategy formulation: the ‘stages of growth’ model revisited ”, Information Systems Journal , Vol. 1 No. 2 , pp. 89 - 114 .
Gay , S.B. , Sobel , A.H. , Young , L.Q. and Dwyer , S.J. ( 2002 ), “ Processes involved in reading imaging studies: workflow analysis and implications for workstation development ”, Journal of Digital Imaging , Vol. 15 No. 3 , pp. 171 - 177 .
Gibby , W.A. and Mciff , E.B. ( 1997 ), “ Lnformactics: Radiology networking fosters quality services: Diagn lmaging ”, Vol. 19 , pp. 145 - 159 .
Gladwin , J. ( 1999 ), “ An informational approach to health management in low-income countries ”, Ph.D. Thesis, University of Sheffield .
Hillestad , R. , Bigelow , J. , Bower , A. , Girosi , F. , Meili , R. , Scoville , R. , et al. ( 2005 ), “ Can electronic medical record systems transform health care? Potential health benefits, savings, and costs ”, Health Affairs) , Vol. 24 No. 5 , pp. 1103 - 1117 .
Huckvale , C. , Car , J. , Akiyama , M. , et al. ( 2010 ), “ Information technology for patient safety ”, Quality and Safety in Health Care , Vol. 19 No. S2 , pp. i25 - 33 .
Husein , K. , Adeyi , O. , Bryant , J. and Cara , N.B. ( 1993 ), “ Developing a primary health care management information system that supports the pursuit of equity, effectiveness and affordability ”, Social Science and Medicine (1982) , Vol. 36 No. 5 , pp. 585 - 596 .
Dudeck , J. , Blobel , B. and Lordieck , W. ( 1997 ), New Technologies in Hospital Information Systems , IOS Press .
Jayasuiriya , R. ( 1999 ), “ Managing information systems for health services in a developing country: a case study using a contextualist framework ”, International Journal of Information Management , Vol. 19 , pp. 335 - 349 .
Rodrigues , J. ( 2009 ), “ Health information systems: Concepts, methodologies, tools, and applications, volume 1. Medical information science reference ”,
Johnson , K.J. , Ravert , R.D. and Avertan , A. ( 2001 ), “ Hopkins teen central: assessment of an internet based support system for children with cystic fibrosis ”, PEDIATRICS , Vol. 107 No. 2 , pp. E24 .
Johnson , K.B. ( 2001 ), “ Barriers that impede the adoption of pediatric information technology ”, Archives of Pediatrics and Adolescent Medicine , Vol. 155 No. 12 , pp. 1374 - 1379 .
Kuruvilla , S. , Dzenowagis , J. , Pleasant , A. , Dwivedi , R. , Murthy , N. , Samuel , R. and Scholtz , M. ( 2004 ), “ Digital bridges need concrete foundations: lessons from the health internetwork India ”, BMJ , Vol. 328 No. 7449 , pp. 1193 - 1196 .
Kuther , T.L. ( 2003 ), “ Medical decision-making and minors: issues of consent and assent ”, Adolescence , Vol. 38 No. 150 , pp. 343 - 358 .
Levine , B. ( 1990 ), “ A tilo of interfaces pilots communication networks ”, Diagn Imaging Focus on PACS 12: I .
Li , B.N. , Chao , S. and Dong , M.C. ( 2007 ), “ SIBAS: a blood bank information system and its 5-year implementation at Macau ”, Computers in Biology and Medicine , Vol. 37 No. 5 , pp. 588 - 597 .
Li , B.N. , Dong , M.C. and Chao , S. ( 2008 ), “ On decision making support in blood bank information systems ”, Expert Systems with Applications , Vol. 34 No. 2 , pp. 1522 - 1532 .
Lifshitz , M.S. , Blank Ge . and Schexneider , K. ( 2007 ), “ Clinical laboratory informatics ”, in McPherson , R.A. and Pincus , M.R. (Eds), Henry’s Clinical Diagnosis and Management by Laboratory Methods , 21st ed. , WB Saunders Elsevier . pp. 112 - 121 .
Lippeveld , T.J. , Foltz , A. and Mahouri , Y.M. ( 1992 ), “ Transforming health facility-based reporting systems into management information systems: lessons from the Chad experience ”, Development Discussion Papers, No. 430 , Harvard Institute of International Development , Cambridge, MA , pp. 1 - 27 .
Lippeveld , T. , Sauerborn , R. and Bodart , C. ( 2000 ), Design and Implementation of Health Information Systems , World Health Organization , Geneva .
Little Johns , P. Wyatt , J.C. and Garvican , L. ( 2003 ), “ Evaluating computerized health information systems: Hard lessons still to be learnt ”, BMJ Publishing Group Ltd. BMJ.com .
Lubitz , D.V. and Wickramasinghe , N. ( 2006 ), “ Healthcare and technology: the doctrine of network centric healthcare ”, International Journal of Electronic Healthcare , Vol. 2 No. 4 , pp. 322 - 344 .
Lun , K.C. ( 1995 ), “ The role of information technology in health care cost containment ”, Singapore Med J , Vol. 36 No. 1 , pp. 32 - 34 .
Mariani , C. , Tronchi , A. , Oncini , L. , Pirani , O. and Murri , R. ( 2006 ), “ Analysis of the x-ray work flow in two diagnostic imaging departments with and without a RIS/PACS system ”, Journal of Digital Imaging , Vol. 19 , No. S1 , pp. 18 - 28 .
Markus , M.L. and Robey , D. ( 1988 ), “ Information technology and organizational change: causal structure in theory and research ”, Management Science , Vol. 34 No. 5 , pp. 583 - 598 .
McKibbon , K.A. , Lokker , C. , Handler , S.M. , et al. ( 2012 ), “ The effectiveness of integrated health information technologies across the phases of medication management: a systematic review of randomized controlled trials ”, Journal of the American Medical Informatics Association , Vol. 19 No. 1 , pp. 22 - 30 .
McKibbon , K.A. Lokker , C. Handler , S.M. et al. ( 2011 ),. “ Enabling medication management through health information technology (health IT) ”, Evid Rep Technol Assess (Full Rep) , 1 - 951 .
MCGM ( 2019 ), “ History of municipal corporation of greater mumbai ”, available at: https://portal.mcgm.gov.in/irj/portal/anonymous?NavigationTarget=navurl://e73b30fff440950441693f945ad3cba7 (accessed 7 March 2019 ).
MCGM Health Department ( 2019 ), “ Municipal corporation of greater Mumbai- Health department ”, available at: https://portal.mcgm.gov.in/irj/portal/anonymous?NavigationTarget=navurl://0a06009b86958aea412e367434b40c52 (accessed 7 March 2019 ).
MCGM IT Department ( 2019 ), “ Municipal corporation of greater Mumbai- Information technology department ”, available at: https://portal.mcgm.gov.in/irj/portal/anonymous/qlitdp?guest_user=english (accessed 7 March 2019 ).
MCGM RTI ( 2019 ), “ Municipal corporation of greater Mumbai- Citizen forum (right to information) department manuals ”, available at: https://portal.mcgm.gov.in/irj/portal/anonymous?NavigationTarget=navurl://14ebe3fd2ffb65c2dd97ceeda2158e11 (accessed 7 March 2019 ).
MCGM Bid Document ( 2018 ), “ Bid notification no.: 7100134255: Bid document for supply, installation, testing, commissioning and maintenance of hardware and network components for MCGM’s hospital management information system.’ law insider ”, available at: https://www.lawinsider.com/documents/lHp622wvpZJ (accessed 7 March 2019 ).
Miller , P.L. , Frawley , S.J. and Sayward , F.G. ( 2001 ), “ Issues in computer-based decision support in public health illustrated using projects involving childhood immunization ”, Journal of Public Health Management and Practice : Jphmp , Vol. 7 No. 6 , pp. 75 - 86 .
Mohapatra , S. ( 2009 ), Cases in Management Information System , PHI , New Delhi .
Mukul ( 2018 ), “ MCGM leveraging technology to boost healthcare delivery system ”, available at: https://ehealth.eletsonline.com/2019/02/mcgm-leveraging-technology-to-boost-healthcare-delivery-system/ (accessed 7 March 2019 ).
National Institutes of Health ( 2003 ), “ Committee on data standards for patient safety. Key capabilities of an electronic health record system: Letter report ”, National Academies Press , Washington, DC .
Nolan, Norton and CO ( 1992 ), Ondernemingsstrategie eninformatie technologie. (NNC and VSB) , The Hague .
Offenmuller , W. ( 1997 ), “ Expectations and solutions for HIS/R1S/PACS dataflow and workflow ”, J Digit Imaging , Vol. 10 , pp. 95 - 98 .
Pearson , S. , Balis , U.J. , Fuller , J. , et al. ( 2006 ), “ Managing and validating laboratory information systems; approved guideline ”, Clinical and Laboratory Standards Institute Document AUTO8-A , Vol. 26 No. 36 .
Ralston , M.D. , Coleman , R.M. , Beaulieu , D.M. , Scrutchfield , K. and Perkins , T. ( 2004 ), “ Progress toward paperless radiology in the digital environment: planning, implementation, and benefits ”, Journal of Digital Imaging , Vol. 17 No. 2 , pp. 134 - 143 .
Robey , D. and Boudreau , M.-C. ( 1999 ), “ Accounting for the contradictory organizational consequences of information technology: theoretical directions and methodological implications ”, Information Systems Research , Vol. 10 No. 2 , pp. 167 - 185 .
Robey , J.M. and Lee , S.H. ( 1990 ), “ Information system development in support of national health programme monitoring and evaluation: the case of the Philippines ”, World Health Statistical Quarterly , Vol. 43 , pp. 37 - 46 .
Rosenbloom , S.T. , Qi , X. , Riddle , W.R. , et al. ( 2006 ), “ Implementing pediatric growth charts into an electronic health record system ”, Journal of the American Medical Informatics Association , Vol. 13 No. 3 , pp. 302 - 308 .
Sandiford , P. , Annett , H. and Cibulskis , R. ( 1992 ), “ What can information systems do for primary health care? An international perspective ”, Social Science and Medicine , Vol. 34 No. 10 , pp. 1077 - 1087 .
Sapirie , S.A. and Orzeszyna , S. ( 1995 ), “ Selecting and defining national health indicators. Strengthening country health information unit, division of epidemiological surveillance and health situation and trend assessment ”, World Health Organization , Geneva , available at: www.who.int/healthservices-delivery/information/20000629d.htm
Shearer , S.O. , Miller , T. and Gillen , S. ( 1997 ), “ Picture archiving and communication system implementation: the practical considerations of adapting the technology to the real world of health care operations ”, Journal of Digital Imaging , Vol. 10 , No. S1 , pp. 158 - 160 .
Shekelle , P. Morton , S.C. and Keeler , E.B. ( 2006 ), “ Costs and benefits of health information technology ”, Rockville (MD): Agency for Healthcare Research and Quality (US); (Evidence Reports/Technology Assessments, No. 132) .
Sinard , J.H. and Morrow , J.S. ( 2001 ), “ Informatics and anatomic pathology: meeting challenges and charting the future ”, Human Pathology , Vol. 32 No. 2 , pp. 143 - 148 .
Sinard , J.H. ( 2006 ), “ Practical pathology informatics ”, Demystifying Informatics for the Practicing Anatomic Pathologist , Springer . New York, NY , pp. 1 - 380 .
Smith , D.L. , Hansen , H. , ( 1988 ), and., and Karim , M.S. “ Management information support for district health systems based on primary health care ”, in Wilson RG et al. (Eds), Management Information Systems and Microcomputers in Primary Health Care , Aga Khan Foundation , Geneva , 89 - 110 .
Smith , M.H. ( 1988 ), “ National childhood vaccine injury compensation act ”, Pediatrics , Vol. 82 No. 2 , pp. 264 - 269 .
Tamblyn , R. ( 2004 ), “ Improving patient safety through computerized drug management: the devil is in the details ”, HealthcarePapers , Vol. 5 No. 3 , pp. 52 - 68 .
The Hindu ( 2018 ), “ Dynacons systems bags contract worth ₹58 cr ”, available at: www.thehindubusinessline.com/markets/stock-markets/dynacons-systems-solutions/article24856706.ece (accessed 7 March 2019 ).
Twelfth Five year Plan Draft 2012 ( 2017 ), “ Social sectors, vol. 3.Govt. of India ”, available at: http://planningcommissiongov.in/plans/planrel/12thplan/welcome.html
Van Der Lei , J. , Duisterhout , J.S. , Westerhof , H. , Boon , W. , Cromme , P.V.M. and Van Bammel , J.H. ( 1993 ), “ The introduction of computer based patient records in The Netherlands ”, Annals of Internal Medicine , Vol. 119 No. 10 , pp. 1036 - 1041 .
Van Hartevelt , J.H.W. ( 1993 ), “ Information management in international development as an area for information services with a case in the field of health care in Ghana ”, International Forum on Information and Documentation , Vol. 18 , pp. 32 - 36 .
Veader , P.C. ( 1997 ), “ The missing links ”, February 16, 1997; Online: Peter C. Veader: Internet: August , Vol. 30, 1997
Wang , S.J. , Middleton , B. , Prosser , L.A. , Bardon , C.G. , Spurr , C.D. , Carchidi , P.J. , et al. ( 2003 ), “ A cost-benefit analysis of electronic medical records in primary care ”, The American Journal of Medicine , Vol. 114 No. 5 , pp. 397 - 402 .
White , K.S. ( 2005 ), “ Speech recognition implementation in radiology ”, Pediatric Radiology , Vol. 35 No. 9 , pp. 841 - 846 .
World Bank ( 1993 ), World Development Report 1993: Investing in Health , Oxford University Press , New York, NY .
World Bank ( 1999 ), World Development Indicators 1999 , The World Bank , Washington, DC .
Yasnoff , W.A. , O’Carroll Patrick , W. , Koo , D. , Linkins Robert , W. and Kilbourne , E.M. ( 2000 ), “ Public health informatics: Improving and transforming public health in the information age ”, Journal of Public Health Management and Practice : Jphmp , Vol. 6 No. 6 , pp. 67 - 75 .
Young , K.M. ( 2000 ), The World of Informatics: informatics for Healthcare Professionals , F.A. Davis Company , Philadelphia , p. 11 - 24 .
Further reading
Chaudhry , B. , Wang , J. , Wu , S. , Maglione , M. , Mojica , W. , Roth , E. , Morton , S.C. and Shekelle , P.G. ( 2006 ), “ Systematic review: Impact of health information technology on quality, efficiency and costs of medical care, improving patient care ”, Annals of Internal Medicine , Vol. 144 No. 10 , pp. 742 - 752 .
Connelly , D.P. , Sielaff , B.H. and Willard , K.E. ( 1996 ), “ The clinical workstation as the means of improving laboratory use ”, Clinica Chimica Acta , Vol. 248 No. 1 , pp. 51 - 64 .
Kallinikos , J. ( 2005 ), “ The order of technology: Complexity and control in a connected world ”, Information and Organization , Vol. 15 No. 3 , pp. 185 - 202 .
Kallinikos , J Contini and Lanzara , ( 2008 ), “ Institutional complexity and functional simplification: the case of money claim online service in England and Wales ”, in (Eds) ICT and Innovation in the Public Sector. European Studies in the Making of E-Governmen , Palgrave Macmillan , Basingstoke , pp. 174 - 210 .
Lanzara , G.F. ( 2008 ), “ Building digital institutions: ICT and the rise of assemblages in government ”, in Contini and Lanzara (Eds) , ICT and Innovation in the Public Sector. European Studies in the Making of E-Government , Palgrave Macmillan , Basingstoke , pp. 9 - 48 .
Margolis , C.Z. , Warshawsky , S.S. , Goldman , L. , Dagan , O. , Wirtschafter , T. and Pliskin , J.S. ( 1992 ), “ Computerized algorithms and pediatricians management of common problems in a community clinic ”, Acad Med , Vol. 67 , pp. 282 - 284 .
Schoenbaum , S.C. and Barnett , G.O. ( 1992 ), “ Automated ambulatory medical records systems: an orphan technology ”, International Journal of Technology Assessment in Health Care , Vol. 8 No. 4 , pp. 598 - 609 .
Schriger , D.L. , Baraff , L.J. , Buller , K. , et al. ( 2000 ), “ Implementation of clinical guidelines via a computer charting system: effect on the care of febrile children less than three years of age ”, Journal of the American Medical Informatics Association , Vol. 7 No. 2 , pp. 186 - 195 .
Scott , J.C. ( 1988 ), Seeing like a State: How Certain Schemes to Improve the Human Condition Have Failed , Yale University Press .
Corresponding author
Related articles, we’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

CASE STUDY OF HOSPITAL MANAGEMENT SYSTEM (HMS

Related Papers
International Journal of Clinical Monitoring and Computing
International Journal for Research in Applied Science & Engineering Technology (IJRASET)
IJRASET Publication
Hospital Management System includes registration of patients, storing the details into the system and appointing doctors online. Our software has the facility to give a unique id for every patient and stores the details of every patient and list of all the doctors which work in the hospital. It includes a search availability of a doctor and the details of a patient using the id. Our system gives each doctor a unique code due to which patients can book their appointments online. The Hospital Management System can be entered using a username and a password. It is accessible by an administrator, doctor and the patient as well. Each doctor has their unique username and password which can be logged in by their correspond email-id , like the doctor patient also have their unique username and pass. But the admin has access to both the doctors and patients details and everything which would help the admin to keep an eye over its hospital management. The interface is simple and userfriendly. The data are well protected for personal use and makes the data processing very fast.
Ijaems Journal
— Health institution requires quality data and information management to function effectively and efficiently. It is an understatement to say that many organizations, institutions or government agencies have become critically dependent on the use of database system for their successes especially in the hospital. This work aims at developing an improved hospital information management system using a function-based approach. An efficient HIMS that can be used to manage patient information and its administration is presented in this work. This is with the goal of eradicating the problem of improper data keeping, inaccurate reports, wastage of time in storing, processing and retrieving information faced by the existing hospital information system in order to improve the overall efficiency of the health institution. The system was developed with Hypertext Markup Language (HTML), Cascading Style Sheets (CSS), Hypertext Preprocessor (PHP), and My Structured Query Language (MySQL). The new system was tested using data collected from Renewal Clinic, Ibadan, Nigeria was used as case study were the data for the research was collected and the system was tested. The system provides a vital platform of information storage and retrieval in hospitals.
The paper developed an automated system that is used to manage patient information and its administration. This was with a view to eliminate the problem of inappropriate data Keeping, inaccurate reports, time wastage in storing, processing and retrieving information encountered by the traditional hospital system in order to improve the overall efficiency of the organization. The tools used to implement the system are Hypertext Markup Language (HTML), Cascading Style Sheets (CSS), Hypertext Preprocessor (PHP), and My Structured Query Language(MySQ).The Proposed system was tested using the information collected from Murab Hospital, Ilorin, kwara State , Nigeria and compared with the existing traditional hospital system. The design provides excellent patient services and improved information infrastructure.
Mohammed Aman
OBJECTIVE : Hospitals currently use a manual system for the management and maintenance of critical information. The current system requires numerous paper forms, with data stores spread throughout the hospital management infrastructure. Often information (on forms) is incomplete, or does not follow management standards. Forms are often lost in transit between departments requiring a comprehensive auditing process to ensure that no vital information is lost. Multiple copies of the same information exist in the hospital and may lead to inconsistencies in data in various data stores. A significant part of the operation of any hospital involves the acquisition, management and timely retrieval of great volumes of information. This information typically involves; patient personal information and medical history, staff information, room and ward scheduling, staff scheduling, operating theater scheduling and various facilities waiting lists. All of this information must be managed in an efficient and cost wise fashion so that an institution's resources may be effectively utilized HMS will automate the management of the hospital making it more efficient and error free. It aims at standardizing data, consolidating data ensuring data integrity and reducing inconsistencies. PROJECT OVERVIEW : The Hospital Management System (HMS) is designed for Any Hospital to replace their existing manual, paper based system. The new system is to control the following information; patient information, room availability, staff and operating room schedules, and patient invoices. These services are to be provided in an efficient, cost effective manner, with the goal of reducing the time and resources currently required for such tasks. A significant part of the operation of any hospital involves the acquisition, management and timely retrieval of great volumes of information. This information typically involves; patient personal information and medical history, staff information, room and ward scheduling, staff scheduling, operating theater scheduling and various facilities waiting lists. All of this
International Journal of Computer Theory and Engineering
Ezenwa Nwawudu
emeka ajoku
ABSTRACT This study investigated online hospital management system as a tool to revolutionize medical profession. With many writers decrying how patients queue up for hours in order to receive medical treatment, and some end-up being attended to as „spillover‟, the analyst investigated the manual system in detail with a view to finding out the need to automate the system. Subsequently, a computer-aided program was designed to bring about improvement in the care of individual patients, taking the advantage of computer speed, storage and retrieved facilities. The software designed will take care of patient‟s registration, billing, treatment and payments. The programming language employed in this work was Microsoft C#.
RELATED PAPERS
GERMAN ANDRÉS GIL LOVERA
IOSR Journals
Siti Chairani
British journal of cancer
J. Ciccolini
Nuclear Engineering and Design
Thomas GELAIN
Eduardo Campazzo
Lecture Notes in Computer Science
Mike Brayshaw
2019 27th Iranian Conference on Electrical Engineering (ICEE)
Ali Poureslami
Luca Iandoli
Ryan Hayhurst
Henk Bloemhoff
خالد ي ح ي محمد
Biochimica et Biophysica Acta (BBA) - Biomembranes
Martial Ruat
The Handbook of Environmental Chemistry
Journal of digital imaging
Andreas Brühschwein
arXiv: Number Theory
Mariusz Skałba
Central European Journal of Public Health
Revista Española de Enfermedades Digestivas
José Antonio Rodríguez Montes
Applied Sciences
Rafael Jiménez Castañeda
Acta Neurochirurgica
Gilles Perrin
HERNAN ALEJANDRO OLANO GARCIA
Yaron Dagan
Aziz A Elfazziki
Corinna Nicosia
Wahana Fisika
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to present patient...
How to present patient cases
- Related content
- Peer review
- Mary Ni Lochlainn , foundation year 2 doctor 1 ,
- Ibrahim Balogun , healthcare of older people/stroke medicine consultant 1
- 1 East Kent Foundation Trust, UK
A guide on how to structure a case presentation
This article contains...
-History of presenting problem
-Medical and surgical history
-Drugs, including allergies to drugs
-Family history
-Social history
-Review of systems
-Findings on examination, including vital signs and observations
-Differential diagnosis/impression
-Investigations
-Management
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1
The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the patient’s condition and further management can be planned accordingly. 2 To give a high quality presentation you need to take a thorough history. Consultants make decisions about patient care based on information presented to them by junior members of the team, so the importance of accurately presenting your patient cannot be overemphasised.
As a medical student, you are likely to be asked to present in numerous settings. A formal case presentation may take place at a teaching session or even at a conference or scientific meeting. These presentations are usually thorough and have an accompanying PowerPoint presentation or poster. More often, case presentations take place on the wards or over the phone and tend to be brief, using only memory or short, handwritten notes as an aid.
Everyone has their own presenting style, and the context of the presentation will determine how much detail you need to put in. You should anticipate what information your senior colleagues will need to know about the patient’s history and the care he or she has received since admission, to enable them to make further management decisions. In this article, I use a fictitious case to show how you can structure case presentations, which can be adapted to different clinical and teaching settings (box 1).
Box 1: Structure for presenting patient cases
Presenting problem, history of presenting problem, medical and surgical history.
Drugs, including allergies to drugs
Family history
Social history, review of systems.
Findings on examination, including vital signs and observations
Differential diagnosis/impression
Investigations
Case: tom murphy.
You should start with a sentence that includes the patient’s name, sex (Mr/Ms), age, and presenting symptoms. In your presentation, you may want to include the patient’s main diagnosis if known—for example, “admitted with shortness of breath on a background of COPD [chronic obstructive pulmonary disease].” You should include any additional information that might give the presentation of symptoms further context, such as the patient’s profession, ethnic origin, recent travel, or chronic conditions.
“ Mr Tom Murphy is a 56 year old ex-smoker admitted with sudden onset central crushing chest pain that radiated down his left arm.”
In this section you should expand on the presenting problem. Use the SOCRATES mnemonic to help describe the pain (see box 2). If the patient has multiple problems, describe each in turn, covering one system at a time.
Box 2: SOCRATES—mnemonic for pain
Associations
Time course
Exacerbating/relieving factors
“ The pain started suddenly at 1 pm, when Mr Murphy was at his desk. The pain was dull in nature, and radiated down his left arm. He experienced shortness of breath and felt sweaty and clammy. His colleague phoned an ambulance. He rated the pain 9/10 in severity. In the ambulance he was given GTN [glyceryl trinitrate] spray under the tongue, which relieved the pain to 5/10. The pain lasted 30 minutes in total. No exacerbating factors were noted. Of note: Mr Murphy is an ex-smoker with a 20 pack year history”
Some patients have multiple comorbidities, and the most life threatening conditions should be mentioned first. They can also be categorised by organ system—for example, “has a long history of cardiovascular disease, having had a stroke, two TIAs [transient ischaemic attacks], and previous ACS [acute coronary syndrome].” For some conditions it can be worth stating whether a general practitioner or a specialist manages it, as this gives an indication of its severity.
In a surgical case, colleagues will be interested in exercise tolerance and any comorbidity that could affect the patient’s fitness for surgery and anaesthesia. If the patient has had any previous surgical procedures, mention whether there were any complications or reactions to anaesthesia.
“Mr Murphy has a history of type 2 diabetes, well controlled on metformin. He also has hypertension, managed with ramipril, and gout. Of note: he has no history of ischaemic heart disease (relevant negative) (see box 3).”
Box 3: Relevant negatives
Mention any relevant negatives that will help narrow down the differential diagnosis or could be important in the management of the patient, 3 such as any risk factors you know for the condition and any associations that you are aware of. For example, if the differential diagnosis includes a condition that you know can be hereditary, a relevant negative could be the lack of a family history. If the differential diagnosis includes cardiovascular disease, mention the cardiovascular risk factors such as body mass index, smoking, and high cholesterol.
Highlight any recent changes to the patient’s drugs because these could be a factor in the presenting problem. Mention any allergies to drugs or the patient’s non-compliance to a previously prescribed drug regimen.
To link the medical history and the drugs you might comment on them together, either here or in the medical history. “Mrs Walsh’s drugs include regular azathioprine for her rheumatoid arthritis.”Or, “His regular drugs are ramipril 5 mg once a day, metformin 1g three times a day, and allopurinol 200 mg once a day. He has no known drug allergies.”
If the family history is unrelated to the presenting problem, it is sufficient to say “no relevant family history noted.” For hereditary conditions more detail is needed.
“ Mr Murphy’s father experienced a fatal myocardial infarction aged 50.”
Social history should include the patient’s occupation; their smoking, alcohol, and illicit drug status; who they live with; their relationship status; and their sexual history, baseline mobility, and travel history. In an older patient, more detail is usually required, including whether or not they have carers, how often the carers help, and if they need to use walking aids.
“He works as an accountant and is an ex-smoker since five years ago with a 20 pack year history. He drinks about 14 units of alcohol a week. He denies any illicit drug use. He lives with his wife in a two storey house and is independent in all activities of daily living.”
Do not dwell on this section. If something comes up that is relevant to the presenting problem, it should be mentioned in the history of the presenting problem rather than here.
“Systems review showed long standing occasional lower back pain, responsive to paracetamol.”
Findings on examination
Initially, it can be useful to practise presenting the full examination to make sure you don’t leave anything out, but it is rare that you would need to present all the normal findings. Instead, focus on the most important main findings and any abnormalities.
“On examination the patient was comfortable at rest, heart sounds one and two were heard with no additional murmurs, heaves, or thrills. Jugular venous pressure was not raised. No peripheral oedema was noted and calves were soft and non-tender. Chest was clear on auscultation. Abdomen was soft and non-tender and normal bowel sounds were heard. GCS [Glasgow coma scale] was 15, pupils were equal and reactive to light [PEARL], cranial nerves 1-12 were intact, and he was moving all four limbs. Observations showed an early warning score of 1 for a tachycardia of 105 beats/ min. Blood pressure was 150/90 mm Hg, respiratory rate 18 breaths/min, saturations were 98% on room air, and he was apyrexial with a temperature of 36.8 ºC.”
Differential diagnoses
Mentioning one or two of the most likely diagnoses is sufficient. A useful phrase you can use is, “I would like to rule out,” especially when you suspect a more serious cause is in the differential diagnosis. “History and examination were in keeping with diverticular disease; however, I would like to rule out colorectal cancer in this patient.”
Remember common things are common, so try not to mention rare conditions first. Sometimes it is acceptable to report investigations you would do first, and then base your differential diagnosis on what the history and investigation findings tell you.
“My impression is acute coronary syndrome. The differential diagnosis includes other cardiovascular causes such as acute pericarditis, myocarditis, aortic stenosis, aortic dissection, and pulmonary embolism. Possible respiratory causes include pneumonia or pneumothorax. Gastrointestinal causes include oesophageal spasm, oesophagitis, gastro-oesophageal reflux disease, gastritis, cholecystitis, and acute pancreatitis. I would also consider a musculoskeletal cause for the pain.”
This section can include a summary of the investigations already performed and further investigations that you would like to request. “On the basis of these differentials, I would like to carry out the following investigations: 12 lead electrocardiography and blood tests, including full blood count, urea and electrolytes, clotting screen, troponin levels, lipid profile, and glycated haemoglobin levels. I would also book a chest radiograph and check the patient’s point of care blood glucose level.”
You should consider recommending investigations in a structured way, prioritising them by how long they take to perform and how easy it is to get them done and how long it takes for the results to come back. Put the quickest and easiest first: so bedside tests, electrocardiography, followed by blood tests, plain radiology, then special tests. You should always be able to explain why you would like to request a test. Mention the patient’s baseline test values if they are available, especially if the patient has a chronic condition—for example, give the patient’s creatinine levels if he or she has chronic kidney disease This shows the change over time and indicates the severity of the patient’s current condition.
“To further investigate these differentials, 12 lead electrocardiography was carried out, which showed ST segment depression in the anterior leads. Results of laboratory tests showed an initial troponin level of 85 µg/L, which increased to 1250 µg/L when repeated at six hours. Blood test results showed raised total cholesterol at 7.6 mmol /L and nil else. A chest radiograph showed clear lung fields. Blood glucose level was 6.3 mmol/L; a glycated haemoglobin test result is pending.”
Dependent on the case, you may need to describe the management plan so far or what further management you would recommend.“My management plan for this patient includes ACS [acute coronary syndrome] protocol, echocardiography, cardiology review, and treatment with high dose statins. If you are unsure what the management should be, you should say that you would discuss further with senior colleagues and the patient. At this point, check to see if there is a treatment escalation plan or a “do not attempt to resuscitate” order in place.
“Mr Murphy was given ACS protocol in the emergency department. An echocardiogram has been requested and he has been discussed with cardiology, who are going to come and see him. He has also been started on atorvastatin 80 mg nightly. Mr Murphy and his family are happy with this plan.”
The summary can be a concise recap of what you have presented beforehand or it can sometimes form a standalone presentation. Pick out salient points, such as positive findings—but also draw conclusions from what you highlight. Finish with a brief synopsis of the current situation (“currently pain free”) and next step (“awaiting cardiology review”). Do not trail off at the end, and state the diagnosis if you are confident you know what it is. If you are not sure what the diagnosis is then communicate this uncertainty and do not pretend to be more confident than you are. When possible, you should include the patient’s thoughts about the diagnosis, how they are feeling generally, and if they are happy with the management plan.
“In summary, Mr Murphy is a 56 year old man admitted with central crushing chest pain, radiating down his left arm, of 30 minutes’ duration. His cardiac risk factors include 20 pack year smoking history, positive family history, type 2 diabetes, and hypertension. Examination was normal other than tachycardia. However, 12 lead electrocardiography showed ST segment depression in the anterior leads and troponin rise from 85 to 250 µg/L. Acute coronary syndrome protocol was initiated and a diagnosis of NSTEMI [non-ST elevation myocardial infarction] was made. Mr Murphy is currently pain free and awaiting cardiology review.”
Originally published as: Student BMJ 2017;25:i4406
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed
- ↵ Green EH, Durning SJ, DeCherrie L, Fagan MJ, Sharpe B, Hershman W. Expectations for oral case presentations for clinical clerks: opinions of internal medicine clerkship directors. J Gen Intern Med 2009 ; 24 : 370 - 3 . doi:10.1007/s11606-008-0900-x pmid:19139965 . OpenUrl CrossRef PubMed Web of Science
- ↵ Olaitan A, Okunade O, Corne J. How to present clinical cases. Student BMJ 2010;18:c1539.
- ↵ Gaillard F. The secret art of relevant negatives, Radiopedia 2016; http://radiopaedia.org/blog/the-secret-art-of-relevant-negatives .
- Log In / Register
- Education Platform
- Newsletter Sign Up
Case Studies

- How to Improve
- Improvement Stories
- Publications
- IHI White Papers
- Audio and Video
Case studies related to improving health care.
first < > last
- An Extended Stay A 64-year-old man with a number of health issues comes to the hospital because he is having trouble breathing. The care team helps resolve the issue, but forgets a standard treatment that causes unnecessary harm to the patient. A subsequent medication error makes the situation worse, leading a stay that is much longer than anticipated.
- Mutiny The behavior of a superior starts to put your patients at risk. What would you do? The University of Rochester’s Dr. Paul Griner presents the final installment in a series of case studies for the IHI Open School.
- On Being Transparent You are the CEO and a patient in your hospital dies from a medication error. What do you do next? The University of Rochester’s Dr. Paul Griner presents the fourth in a series of case studies.
- Locked In A cancer diagnosis leads to tears and heartache. But is it correct? Dr. Paul Griner, Professor Emeritus of Medicine at the University of Rochester, presents the third in a series of case studies for the IHI Open School.
- Confidentiality and Air Force One A difficult patient. A difficult decision. The University of Rochester’s Dr. Paul Griner presents the second in a series of case studies.
- The Protective Parent During a 50-year career in medicine, Dr. Paul Griner accumulated hundreds of patient stories. Most of his stories – including this case study "The Protective Parent" - are from the 1950s and 1960s, prior to what we now refer to as “modern medicine.”
- Advanced Case Study Between Sept. 30th and Oct. 14th, 2010, students and residents all over the world gathered in interprofessional teams and analyzed a complex incident that resulted in patient harm. Selected teams presented their work to IHI faculty during a series of live webinars in October.
- A Downward Spiral: A Case Study in Homelessness Thirty-six-year-old John may not fit the stereotype of a homeless person. Not long ago, he was living what many would consider a healthy life with his family. But when he lost his job, he found himself in a downward spiral, and his situation dramatically changed. John’s story is a fictional composite of real patients treated by Health Care for the Homeless. It illustrates the challenges homeless people face in accessing health care and the characteristics of high-quality care that can improve their lives.
- What Happened to Alex? Alex James was a runner, like his dad. One day, he collapsed during a run and was hospitalized for five days. He went through lots of tests, but was given a clean bill of health. Then, a month later, he collapsed again, fell into a deep coma, and died. His father wanted to know — what had gone wrong? Dr. John James, a retired toxicologist at NASA, tells the story of how he uncovered the cause of his son’s death and became a patient safety advocate.
- Improving Care in Rural Rwanda When Dr. Patrick Lee and his teammates began their quality improvement work in Kirehe, Rwanda, last year, the staff at the local hospital was taking vital signs properly less than half the time. Today, the staff does that task properly 95% of the time. Substantial resource and infrastructure inputs, combined with dedicated Rwandan partners and simple quality improvement tools, have dramatically improved staff morale and the quality of care in Kirehe.

How to make an oral case presentation to healthcare colleagues
The content and delivery of a patient case for education and evidence-based care discussions in clinical practice.

BSIP SA / Alamy Stock Photo
A case presentation is a detailed narrative describing a specific problem experienced by one or more patients. Pharmacists usually focus on the medicines aspect , for example, where there is potential harm to a patient or proven benefit to the patient from medication, or where a medication error has occurred. Case presentations can be used as a pedagogical tool, as a method of appraising the presenter’s knowledge and as an opportunity for presenters to reflect on their clinical practice [1] .
The aim of an oral presentation is to disseminate information about a patient for the purpose of education, to update other members of the healthcare team on a patient’s progress, and to ensure the best, evidence-based care is being considered for their management.
Within a hospital, pharmacists are likely to present patients on a teaching or daily ward round or to a senior pharmacist or colleague for the purpose of asking advice on, for example, treatment options or complex drug-drug interactions, or for referral.
Content of a case presentation
As a general structure, an oral case presentation may be divided into three phases [2] :
- Reporting important patient information and clinical data;
- Analysing and synthesising identified issues (this is likely to include producing a list of these issues, generally termed a problem list);
- Managing the case by developing a therapeutic plan.

Specifically, the following information should be included [3] :

Patient and complaint details
Patient details: name, sex, age, ethnicity.
Presenting complaint: the reason the patient presented to the hospital (symptom/event).
History of presenting complaint: highlighting relevant events in chronological order, often presented as how many days ago they occurred. This should include prior admission to hospital for the same complaint.
Review of organ systems: listing positive or negative findings found from the doctor’s assessment that are relevant to the presenting complaint.
Past medical and surgical history
Social history: including occupation, exposures, smoking and alcohol history, and any recreational drug use.
Medication history, including any drug allergies: this should include any prescribed medicines, medicines purchased over-the-counter, any topical preparations used (including eye drops, nose drops, inhalers and nasal sprays) and any herbal or traditional remedies taken.
Sexual history: if this is relevant to the presenting complaint.
Details from a physical examination: this includes any relevant findings to the presenting complaint and should include relevant observations.
Laboratory investigation and imaging results: abnormal findings are presented.
Assessment: including differential diagnosis.
Plan: including any pharmaceutical care issues raised and how these should be resolved, ongoing management and discharge planning.
Any discrepancies between the current management of the patient’s conditions and evidence-based recommendations should be highlighted and reasons given for not adhering to evidence-based medicine ( see ‘Locating the evidence’ ).
Locating the evidence
The evidence base for the therapeutic options available should always be considered. There may be local guidance available within the hospital trust directing the management of the patient’s presenting condition. Pharmacists often contribute to the development of such guidelines, especially if medication is involved. If no local guidelines are available, the next step is to refer to national guidance. This is developed by a steering group of experts, for example, the British HIV Association or the National Institute for Health and Care Excellence . If the presenting condition is unusual or rare, for example, acute porphyria, and there are no local or national guidelines available, a literature search may help locate articles or case studies similar to the case.
Giving a case presentation
Currently, there are no available acknowledged guidelines or systematic descriptions of the structure, language and function of the oral case presentation [4] and therefore there is no standard on how the skills required to prepare or present a case are taught. Most individuals are introduced to this concept at undergraduate level and then build on their skills through practice-based learning.
A case presentation is a narrative of a patient’s care, so it is vital the presenter has familiarity with the patient, the case and its progression. The preparation for the presentation will depend on what information is to be included.
Generally, oral case presentations are brief and should be limited to 5–10 minutes. This may be extended if the case is being presented as part of an assessment compared with routine everyday working ( see ‘Case-based discussion’ ). The audience should be interested in what is being said so the presenter should maintain this engagement through eye contact, clear speech and enthusiasm for the case.
It is important to stick to the facts by presenting the case as a factual timeline and not describing how things should have happened instead. Importantly, the case should always be concluded and should include an outcome of the patient’s care [5] .
An example of an oral case presentation, given by a pharmacist to a doctor, is available here .
A successful oral case presentation allows the audience to garner the right amount of patient information in the most efficient way, enabling a clinically appropriate plan to be developed. The challenge lies with the fact that the content and delivery of this will vary depending on the service, and clinical and audience setting [3] . A practitioner with less experience may find understanding the balance between sufficient information and efficiency of communication difficult, but regular use of the oral case presentation tool will improve this skill.
Tailoring case presentations to your audience
Most case presentations are not tailored to a specific audience because the same type of information will usually need to be conveyed in each case.
However, case presentations can be adapted to meet the identified learning needs of the target audience, if required for training purposes. This method involves varying the content of the presentation or choosing specific cases to present that will help achieve a set of objectives [6] . For example, if a requirement to learn about the management of acute myocardial infarction has been identified by the target audience, then the presenter may identify a case from the cardiology ward to present to the group, as opposed to presenting a patient reviewed by that person during their normal working practice.
Alternatively, a presenter could focus on a particular condition within a case, which will dictate what information is included. For example, if a case on asthma is being presented, the focus may be on recent use of bronchodilator therapy, respiratory function tests (including peak expiratory flow rate), symptoms related to exacerbation of airways disease, anxiety levels, ability to talk in full sentences, triggers to worsening of symptoms, and recent exposure to allergens. These may not be considered relevant if presenting the case on an unrelated condition that the same patient has, for example, if this patient was admitted with a hip fracture and their asthma was well controlled.
Case-based discussion
The oral case presentation may also act as the basis of workplace-based assessment in the form of a case-based discussion. In the UK, this forms part of many healthcare professional bodies’ assessment of clinical practice, for example, medical professional colleges.
For pharmacists, a case-based discussion forms part of the Royal Pharmaceutical Society (RPS) Foundation and Advanced Practice assessments . Mastery of the oral case presentation skill could provide useful preparation for this assessment process.
A case-based discussion would include a pharmaceutical needs assessment, which involves identifying and prioritising pharmaceutical problems for a particular patient. Evidence-based guidelines relevant to the specific medical condition should be used to make treatment recommendations, and a plan to monitor the patient once therapy has started should be developed. Professionalism is an important aspect of case-based discussion — issues must be prioritised appropriately and ethical and legal frameworks must be referred to [7] . A case-based discussion would include broadly similar content to the oral case presentation, but would involve further questioning of the presenter by the assessor to determine the extent of the presenter’s knowledge of the specific case, condition and therapeutic strategies. The criteria used for assessment would depend on the level of practice of the presenter but, for pharmacists, this may include assessment against the RPS Foundation or Pharmacy Frameworks .
Acknowledgement
With thanks to Aamer Safdar for providing the script for the audio case presentation.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal . You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
[1] Onishi H. The role of case presentation for teaching and learning activities. Kaohsiung J Med Sci 2008;24:356–360. doi: 10.1016/s1607-551x(08)70132–3
[2] Edwards JC, Brannan JR, Burgess L et al . Case presentation format and clinical reasoning: a strategy for teaching medical students. Medical Teacher 1987;9:285–292. doi: 10.3109/01421598709034790
[3] Goldberg C. A practical guide to clinical medicine: overview and general information about oral presentation. 2009. University of California, San Diego. Available from: https://meded.ecsd.edu/clinicalmed.oral.htm (accessed 5 December 2015)
[4] Chan MY. The oral case presentation: toward a performance-based rhetorical model for teaching and learning. Medical Education Online 2015;20. doi: 10.3402/meo.v20.28565
[5] McGee S. Medicine student programs: oral presentation guidelines. Learning & Scholarly Technologies, University of Washington. Available from: https://catalyst.uw.edu/workspace/medsp/30311/202905 (accessed 7 December 2015)
[6] Hays R. Teaching and Learning in Clinical Settings. 2006;425. Oxford: Radcliffe Publishing Ltd.
[7] Royal Pharmaceutical Society. Tips for assessors for completing case-based discussions. 2015. Available from: http://www.rpharms.com/help/case_based_discussion.htm (accessed 30 December 2015)
You might also be interested in…

How to demonstrate empathy and compassion in a pharmacy setting

Be more proactive to convince medics, pharmacists urged

How pharmacists can encourage patient adherence to medicines

- Customer Favourites
Healthcare Case Study
Powerpoint Templates
Icon Bundle
Kpi Dashboard
Professional
Business Plans
Swot Analysis
Gantt Chart
Business Proposal
Marketing Plan
Project Management
Business Case
Business Model
Cyber Security
Business PPT
Digital Marketing
Digital Transformation
Human Resources
Product Management
Artificial Intelligence
Company Profile
Acknowledgement PPT
PPT Presentation
Reports Brochures
One Page Pitch
Interview PPT
All Categories

- You're currently reading page 1

Stages // require(['jquery'], function ($) { $(document).ready(function () { //removes paginator if items are less than selected items per page var paginator = $("#limiter :selected").text(); var itemsPerPage = parseInt(paginator); var itemsCount = $(".products.list.items.product-items.sli_container").children().length; if (itemsCount ? ’Stages’ here means the number of divisions or graphic elements in the slide. For example, if you want a 4 piece puzzle slide, you can search for the word ‘puzzles’ and then select 4 ‘Stages’ here. We have categorized all our content according to the number of ‘Stages’ to make it easier for you to refine the results.
Category // require(['jquery'], function ($) { $(document).ready(function () { //removes paginator if items are less than selected items per page var paginator = $("#limiter :selected").text(); var itemsperpage = parseint(paginator); var itemscount = $(".products.list.items.product-items.sli_container").children().length; if (itemscount.
- Business Slides (524)
- Circular (23)
- Cluster (1)
- Complete Decks (7)
- Concepts 1 (5)
- Diagrams (517)

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Case study: 33-year-old female presents with chronic sob and cough.
Sandeep Sharma ; Muhammad F. Hashmi ; Deepa Rawat .
Affiliations
Last Update: February 20, 2023 .
- Case Presentation
History of Present Illness: A 33-year-old white female presents after admission to the general medical/surgical hospital ward with a chief complaint of shortness of breath on exertion. She reports that she was seen for similar symptoms previously at her primary care physician’s office six months ago. At that time, she was diagnosed with acute bronchitis and treated with bronchodilators, empiric antibiotics, and a short course oral steroid taper. This management did not improve her symptoms, and she has gradually worsened over six months. She reports a 20-pound (9 kg) intentional weight loss over the past year. She denies camping, spelunking, or hunting activities. She denies any sick contacts. A brief review of systems is negative for fever, night sweats, palpitations, chest pain, nausea, vomiting, diarrhea, constipation, abdominal pain, neural sensation changes, muscular changes, and increased bruising or bleeding. She admits a cough, shortness of breath, and shortness of breath on exertion.
Social History: Her tobacco use is 33 pack-years; however, she quit smoking shortly prior to the onset of symptoms, six months ago. She denies alcohol and illicit drug use. She is in a married, monogamous relationship and has three children aged 15 months to 5 years. She is employed in a cookie bakery. She has two pet doves. She traveled to Mexico for a one-week vacation one year ago.
Allergies: No known medicine, food, or environmental allergies.
Past Medical History: Hypertension
Past Surgical History: Cholecystectomy
Medications: Lisinopril 10 mg by mouth every day
Physical Exam:
Vitals: Temperature, 97.8 F; heart rate 88; respiratory rate, 22; blood pressure 130/86; body mass index, 28
General: She is well appearing but anxious, a pleasant female lying on a hospital stretcher. She is conversing freely, with respiratory distress causing her to stop mid-sentence.
Respiratory: She has diffuse rales and mild wheezing; tachypneic.
Cardiovascular: She has a regular rate and rhythm with no murmurs, rubs, or gallops.
Gastrointestinal: Bowel sounds X4. No bruits or pulsatile mass.
- Initial Evaluation
Laboratory Studies: Initial work-up from the emergency department revealed pancytopenia with a platelet count of 74,000 per mm3; hemoglobin, 8.3 g per and mild transaminase elevation, AST 90 and ALT 112. Blood cultures were drawn and currently negative for bacterial growth or Gram staining.
Chest X-ray
Impression: Mild interstitial pneumonitis
- Differential Diagnosis
- Aspiration pneumonitis and pneumonia
- Bacterial pneumonia
- Immunodeficiency state and Pneumocystis jiroveci pneumonia
- Carcinoid lung tumors
- Tuberculosis
- Viral pneumonia
- Chlamydial pneumonia
- Coccidioidomycosis and valley fever
- Recurrent Legionella pneumonia
- Mediastinal cysts
- Mediastinal lymphoma
- Recurrent mycoplasma infection
- Pancoast syndrome
- Pneumococcal infection
- Sarcoidosis
- Small cell lung cancer
- Aspergillosis
- Blastomycosis
- Histoplasmosis
- Actinomycosis
- Confirmatory Evaluation
CT of the chest was performed to further the pulmonary diagnosis; it showed a diffuse centrilobular micronodular pattern without focal consolidation.
On finding pulmonary consolidation on the CT of the chest, a pulmonary consultation was obtained. Further history was taken, which revealed that she has two pet doves. As this was her third day of broad-spectrum antibiotics for a bacterial infection and she was not getting better, it was decided to perform diagnostic bronchoscopy of the lungs with bronchoalveolar lavage to look for any atypical or rare infections and to rule out malignancy (Image 1).
Bronchoalveolar lavage returned with a fluid that was cloudy and muddy in appearance. There was no bleeding. Cytology showed Histoplasma capsulatum .
Based on the bronchoscopic findings, a diagnosis of acute pulmonary histoplasmosis in an immunocompetent patient was made.
Pulmonary histoplasmosis in asymptomatic patients is self-resolving and requires no treatment. However, once symptoms develop, such as in our above patient, a decision to treat needs to be made. In mild, tolerable cases, no treatment other than close monitoring is necessary. However, once symptoms progress to moderate or severe, or if they are prolonged for greater than four weeks, treatment with itraconazole is indicated. The anticipated duration is 6 to 12 weeks total. The response should be monitored with a chest x-ray. Furthermore, observation for recurrence is necessary for several years following the diagnosis. If the illness is determined to be severe or does not respond to itraconazole, amphotericin B should be initiated for a minimum of 2 weeks, but up to 1 year. Cotreatment with methylprednisolone is indicated to improve pulmonary compliance and reduce inflammation, thus improving work of respiration. [1] [2] [3]
Histoplasmosis, also known as Darling disease, Ohio valley disease, reticuloendotheliosis, caver's disease, and spelunker's lung, is a disease caused by the dimorphic fungi Histoplasma capsulatum native to the Ohio, Missouri, and Mississippi River valleys of the United States. The two phases of Histoplasma are the mycelial phase and the yeast phase.
Etiology/Pathophysiology
Histoplasmosis is caused by inhaling the microconidia of Histoplasma spp. fungus into the lungs. The mycelial phase is present at ambient temperature in the environment, and upon exposure to 37 C, such as in a host’s lungs, it changes into budding yeast cells. This transition is an important determinant in the establishment of infection. Inhalation from soil is a major route of transmission leading to infection. Human-to-human transmission has not been reported. Infected individuals may harbor many yeast-forming colonies chronically, which remain viable for years after initial inoculation. The finding that individuals who have moved or traveled from endemic to non-endemic areas may exhibit a reactivated infection after many months to years supports this long-term viability. However, the precise mechanism of reactivation in chronic carriers remains unknown.
Infection ranges from an asymptomatic illness to a life-threatening disease, depending on the host’s immunological status, fungal inoculum size, and other factors. Histoplasma spp. have grown particularly well in organic matter enriched with bird or bat excrement, leading to the association that spelunking in bat-feces-rich caves increases the risk of infection. Likewise, ownership of pet birds increases the rate of inoculation. In our case, the patient did travel outside of Nebraska within the last year and owned two birds; these are her primary increased risk factors. [4]
Non-immunocompromised patients present with a self-limited respiratory infection. However, the infection in immunocompromised hosts disseminated histoplasmosis progresses very aggressively. Within a few days, histoplasmosis can reach a fatality rate of 100% if not treated aggressively and appropriately. Pulmonary histoplasmosis may progress to a systemic infection. Like its pulmonary counterpart, the disseminated infection is related to exposure to soil containing infectious yeast. The disseminated disease progresses more slowly in immunocompetent hosts compared to immunocompromised hosts. However, if the infection is not treated, fatality rates are similar. The pathophysiology for disseminated disease is that once inhaled, Histoplasma yeast are ingested by macrophages. The macrophages travel into the lymphatic system where the disease, if not contained, spreads to different organs in a linear fashion following the lymphatic system and ultimately into the systemic circulation. Once this occurs, a full spectrum of disease is possible. Inside the macrophage, this fungus is contained in a phagosome. It requires thiamine for continued development and growth and will consume systemic thiamine. In immunocompetent hosts, strong cellular immunity, including macrophages, epithelial, and lymphocytes, surround the yeast buds to keep infection localized. Eventually, it will become calcified as granulomatous tissue. In immunocompromised hosts, the organisms disseminate to the reticuloendothelial system, leading to progressive disseminated histoplasmosis. [5] [6]
Symptoms of infection typically begin to show within three to17 days. Immunocompetent individuals often have clinically silent manifestations with no apparent ill effects. The acute phase of infection presents as nonspecific respiratory symptoms, including cough and flu. A chest x-ray is read as normal in 40% to 70% of cases. Chronic infection can resemble tuberculosis with granulomatous changes or cavitation. The disseminated illness can lead to hepatosplenomegaly, adrenal enlargement, and lymphadenopathy. The infected sites usually calcify as they heal. Histoplasmosis is one of the most common causes of mediastinitis. Presentation of the disease may vary as any other organ in the body may be affected by the disseminated infection. [7]
The clinical presentation of the disease has a wide-spectrum presentation which makes diagnosis difficult. The mild pulmonary illness may appear as a flu-like illness. The severe form includes chronic pulmonary manifestation, which may occur in the presence of underlying lung disease. The disseminated form is characterized by the spread of the organism to extrapulmonary sites with proportional findings on imaging or laboratory studies. The Gold standard for establishing the diagnosis of histoplasmosis is through culturing the organism. However, diagnosis can be established by histological analysis of samples containing the organism taken from infected organs. It can be diagnosed by antigen detection in blood or urine, PCR, or enzyme-linked immunosorbent assay. The diagnosis also can be made by testing for antibodies again the fungus. [8]
Pulmonary histoplasmosis in asymptomatic patients is self-resolving and requires no treatment. However, once symptoms develop, such as in our above patient, a decision to treat needs to be made. In mild, tolerable cases, no treatment other than close monitoring is necessary. However, once symptoms progress to moderate or severe or if they are prolonged for greater than four weeks, treatment with itraconazole is indicated. The anticipated duration is 6 to 12 weeks. The patient's response should be monitored with a chest x-ray. Furthermore, observation for recurrence is necessary for several years following the diagnosis. If the illness is determined to be severe or does not respond to itraconazole, amphotericin B should be initiated for a minimum of 2 weeks, but up to 1 year. Cotreatment with methylprednisolone is indicated to improve pulmonary compliance and reduce inflammation, thus improving the work of respiration.
The disseminated disease requires similar systemic antifungal therapy to pulmonary infection. Additionally, procedural intervention may be necessary, depending on the site of dissemination, to include thoracentesis, pericardiocentesis, or abdominocentesis. Ocular involvement requires steroid treatment additions and necessitates ophthalmology consultation. In pericarditis patients, antifungals are contraindicated because the subsequent inflammatory reaction from therapy would worsen pericarditis.
Patients may necessitate intensive care unit placement dependent on their respiratory status, as they may pose a risk for rapid decompensation. Should this occur, respiratory support is necessary, including non-invasive BiPAP or invasive mechanical intubation. Surgical interventions are rarely warranted; however, bronchoscopy is useful as both a diagnostic measure to collect sputum samples from the lung and therapeutic to clear excess secretions from the alveoli. Patients are at risk for developing a coexistent bacterial infection, and appropriate antibiotics should be considered after 2 to 4 months of known infection if symptoms are still present. [9]
Prognosis
If not treated appropriately and in a timely fashion, the disease can be fatal, and complications will arise, such as recurrent pneumonia leading to respiratory failure, superior vena cava syndrome, fibrosing mediastinitis, pulmonary vessel obstruction leading to pulmonary hypertension and right-sided heart failure, and progressive fibrosis of lymph nodes. Acute pulmonary histoplasmosis usually has a good outcome on symptomatic therapy alone, with 90% of patients being asymptomatic. Disseminated histoplasmosis, if untreated, results in death within 2 to 24 months. Overall, there is a relapse rate of 50% in acute disseminated histoplasmosis. In chronic treatment, however, this relapse rate decreases to 10% to 20%. Death is imminent without treatment.
- Pearls of Wisdom
While illnesses such as pneumonia are more prevalent, it is important to keep in mind that more rare diseases are always possible. Keeping in mind that every infiltrates on a chest X-ray or chest CT is not guaranteed to be simple pneumonia. Key information to remember is that if the patient is not improving under optimal therapy for a condition, the working diagnosis is either wrong or the treatment modality chosen by the physician is wrong and should be adjusted. When this occurs, it is essential to collect a more detailed history and refer the patient for appropriate consultation with a pulmonologist or infectious disease specialist. Doing so, in this case, yielded workup with bronchoalveolar lavage and microscopic evaluation. Microscopy is invaluable for definitively diagnosing a pulmonary consolidation as exemplified here where the results showed small, budding, intracellular yeast in tissue sized 2 to 5 microns that were readily apparent on hematoxylin and eosin staining and minimal, normal flora bacterial growth.
- Enhancing Healthcare Team Outcomes
This case demonstrates how all interprofessional healthcare team members need to be involved in arriving at a correct diagnosis. Clinicians, specialists, nurses, pharmacists, laboratory technicians all bear responsibility for carrying out the duties pertaining to their particular discipline and sharing any findings with all team members. An incorrect diagnosis will almost inevitably lead to incorrect treatment, so coordinated activity, open communication, and empowerment to voice concerns are all part of the dynamic that needs to drive such cases so patients will attain the best possible outcomes.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Histoplasma Contributed by Sandeep Sharma, MD
Disclosure: Sandeep Sharma declares no relevant financial relationships with ineligible companies.
Disclosure: Muhammad Hashmi declares no relevant financial relationships with ineligible companies.
Disclosure: Deepa Rawat declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Sharma S, Hashmi MF, Rawat D. Case Study: 33-Year-Old Female Presents with Chronic SOB and Cough. [Updated 2023 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Palliative Chemotherapy: Does It Only Provide False Hope? The Role of Palliative Care in a Young Patient With Newly Diagnosed Metastatic Adenocarcinoma. [J Adv Pract Oncol. 2017] Review Palliative Chemotherapy: Does It Only Provide False Hope? The Role of Palliative Care in a Young Patient With Newly Diagnosed Metastatic Adenocarcinoma. Doverspike L, Kurtz S, Selvaggi K. J Adv Pract Oncol. 2017 May-Jun; 8(4):382-386. Epub 2017 May 1.
- Review Breathlessness with pulmonary metastases: a multimodal approach. [J Adv Pract Oncol. 2013] Review Breathlessness with pulmonary metastases: a multimodal approach. Brant JM. J Adv Pract Oncol. 2013 Nov; 4(6):415-22.
- A 50-Year Old Woman With Recurrent Right-Sided Chest Pain. [Chest. 2022] A 50-Year Old Woman With Recurrent Right-Sided Chest Pain. Saha BK, Bonnier A, Chong WH, Chenna P. Chest. 2022 Feb; 161(2):e85-e89.
- Suicidal Ideation. [StatPearls. 2024] Suicidal Ideation. Harmer B, Lee S, Duong TVH, Saadabadi A. StatPearls. 2024 Jan
- Review Domperidone. [Drugs and Lactation Database (...] Review Domperidone. . Drugs and Lactation Database (LactMed®). 2006
Recent Activity
- Case Study: 33-Year-Old Female Presents with Chronic SOB and Cough - StatPearls Case Study: 33-Year-Old Female Presents with Chronic SOB and Cough - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
We use essential cookies to make Venngage work. By clicking “Accept All Cookies”, you agree to the storing of cookies on your device to enhance site navigation, analyze site usage, and assist in our marketing efforts.
Manage Cookies
Cookies and similar technologies collect certain information about how you’re using our website. Some of them are essential, and without them you wouldn’t be able to use Venngage. But others are optional, and you get to choose whether we use them or not.
Strictly Necessary Cookies
These cookies are always on, as they’re essential for making Venngage work, and making it safe. Without these cookies, services you’ve asked for can’t be provided.
Show cookie providers
- Google Login
Functionality Cookies
These cookies help us provide enhanced functionality and personalisation, and remember your settings. They may be set by us or by third party providers.
Performance Cookies
These cookies help us analyze how many people are using Venngage, where they come from and how they're using it. If you opt out of these cookies, we can’t get feedback to make Venngage better for you and all our users.
- Google Analytics
Targeting Cookies
These cookies are set by our advertising partners to track your activity and show you relevant Venngage ads on other sites as you browse the internet.
- Google Tag Manager
- Infographics
- Daily Infographics
- Graphic Design
- Graphs and Charts
- Data Visualization
- Human Resources
- Training and Development
- Beginner Guides
Blog Case Study
How to Present a Case Study like a Pro (With Examples)
By Danesh Ramuthi , Sep 07, 2023

Okay, let’s get real: case studies can be kinda snooze-worthy. But guess what? They don’t have to be!
In this article, I will cover every element that transforms a mere report into a compelling case study, from selecting the right metrics to using persuasive narrative techniques.
And if you’re feeling a little lost, don’t worry! There are cool tools like Venngage’s Case Study Creator to help you whip up something awesome, even if you’re short on time. Plus, the pre-designed case study templates are like instant polish because let’s be honest, everyone loves a shortcut.
Click to jump ahead:
What is a case study presentation?
What is the purpose of presenting a case study, how to structure a case study presentation, how long should a case study presentation be, 5 case study presentation examples with templates, 6 tips for delivering an effective case study presentation, 5 common mistakes to avoid in a case study presentation, how to present a case study faqs.
A case study presentation involves a comprehensive examination of a specific subject, which could range from an individual, group, location, event, organization or phenomenon.
They’re like puzzles you get to solve with the audience, all while making you think outside the box.
Unlike a basic report or whitepaper, the purpose of a case study presentation is to stimulate critical thinking among the viewers.
The primary objective of a case study is to provide an extensive and profound comprehension of the chosen topic. You don’t just throw numbers at your audience. You use examples and real-life cases to make you think and see things from different angles.

The primary purpose of presenting a case study is to offer a comprehensive, evidence-based argument that informs, persuades and engages your audience.
Here’s the juicy part: presenting that case study can be your secret weapon. Whether you’re pitching a groundbreaking idea to a room full of suits or trying to impress your professor with your A-game, a well-crafted case study can be the magic dust that sprinkles brilliance over your words.
Think of it like digging into a puzzle you can’t quite crack . A case study lets you explore every piece, turn it over and see how it fits together. This close-up look helps you understand the whole picture, not just a blurry snapshot.
It’s also your chance to showcase how you analyze things, step by step, until you reach a conclusion. It’s all about being open and honest about how you got there.
Besides, presenting a case study gives you an opportunity to connect data and real-world scenarios in a compelling narrative. It helps to make your argument more relatable and accessible, increasing its impact on your audience.
One of the contexts where case studies can be very helpful is during the job interview. In some job interviews, you as candidates may be asked to present a case study as part of the selection process.
Having a case study presentation prepared allows the candidate to demonstrate their ability to understand complex issues, formulate strategies and communicate their ideas effectively.
The way you present a case study can make all the difference in how it’s received. A well-structured presentation not only holds the attention of your audience but also ensures that your key points are communicated clearly and effectively.
In this section, let’s go through the key steps that’ll help you structure your case study presentation for maximum impact.
Let’s get into it.
Open with an introductory overview
Start by introducing the subject of your case study and its relevance. Explain why this case study is important and who would benefit from the insights gained. This is your opportunity to grab your audience’s attention.

Explain the problem in question
Dive into the problem or challenge that the case study focuses on. Provide enough background information for the audience to understand the issue. If possible, quantify the problem using data or metrics to show the magnitude or severity.
Detail the solutions to solve the problem
After outlining the problem, describe the steps taken to find a solution. This could include the methodology, any experiments or tests performed and the options that were considered. Make sure to elaborate on why the final solution was chosen over the others.
Key stakeholders Involved
Talk about the individuals, groups or organizations that were directly impacted by or involved in the problem and its solution.
Stakeholders may experience a range of outcomes—some may benefit, while others could face setbacks.
For example, in a business transformation case study, employees could face job relocations or changes in work culture, while shareholders might be looking at potential gains or losses.
Discuss the key results & outcomes
Discuss the results of implementing the solution. Use data and metrics to back up your statements. Did the solution meet its objectives? What impact did it have on the stakeholders? Be honest about any setbacks or areas for improvement as well.
Include visuals to support your analysis
Visual aids can be incredibly effective in helping your audience grasp complex issues. Utilize charts, graphs, images or video clips to supplement your points. Make sure to explain each visual and how it contributes to your overall argument.
Pie charts illustrate the proportion of different components within a whole, useful for visualizing market share, budget allocation or user demographics.
This is particularly useful especially if you’re displaying survey results in your case study presentation.
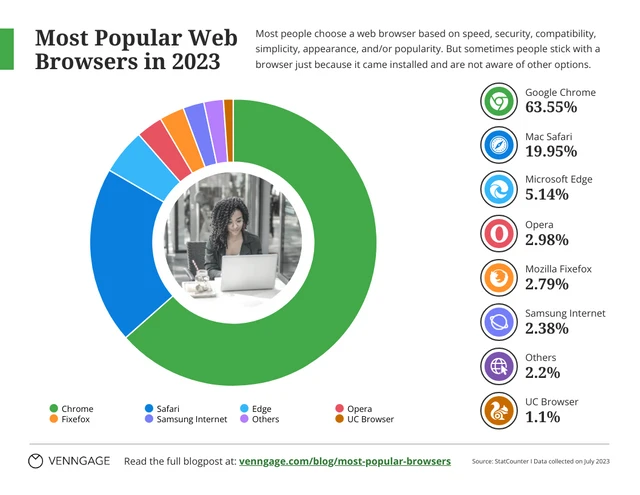
Stacked charts on the other hand are perfect for visualizing composition and trends. This is great for analyzing things like customer demographics, product breakdowns or budget allocation in your case study.
Consider this example of a stacked bar chart template. It provides a straightforward summary of the top-selling cake flavors across various locations, offering a quick and comprehensive view of the data.
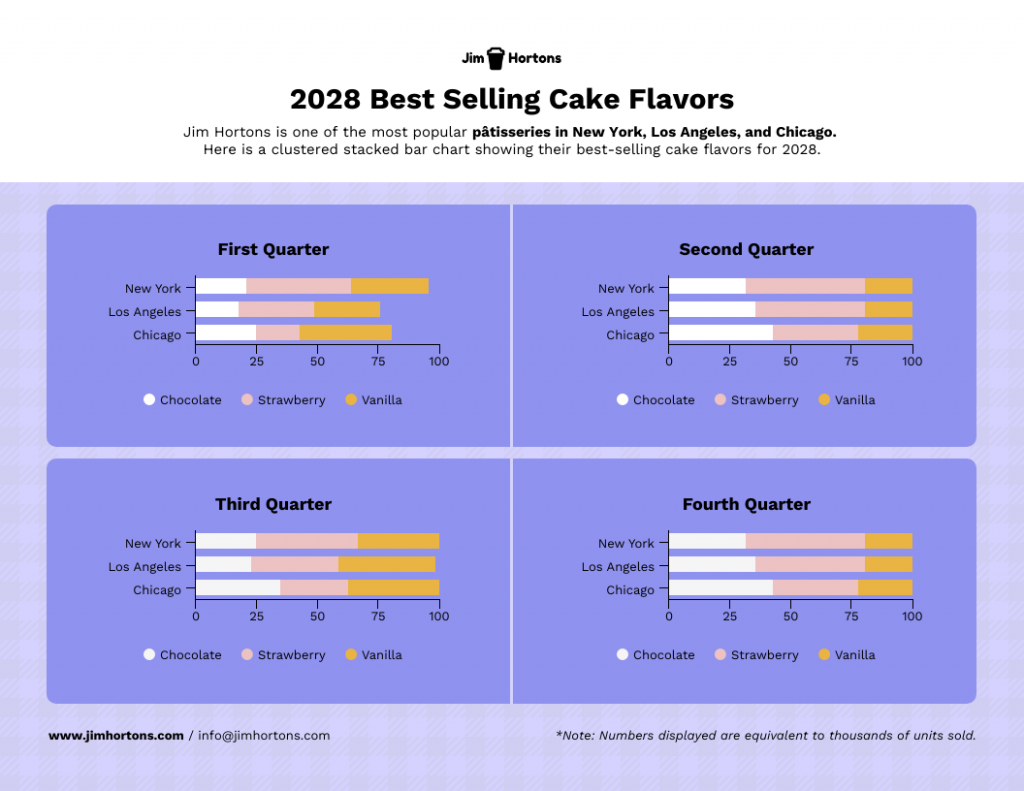
Not the chart you’re looking for? Browse Venngage’s gallery of chart templates to find the perfect one that’ll captivate your audience and level up your data storytelling.
Recommendations and next steps
Wrap up by providing recommendations based on the case study findings. Outline the next steps that stakeholders should take to either expand on the success of the project or address any remaining challenges.
Acknowledgments and references
Thank the people who contributed to the case study and helped in the problem-solving process. Cite any external resources, reports or data sets that contributed to your analysis.
Feedback & Q&A session
Open the floor for questions and feedback from your audience. This allows for further discussion and can provide additional insights that may not have been considered previously.
Closing remarks
Conclude the presentation by summarizing the key points and emphasizing the takeaways. Thank your audience for their time and participation and express your willingness to engage in further discussions or collaborations on the subject.

Well, the length of a case study presentation can vary depending on the complexity of the topic and the needs of your audience. However, a typical business or academic presentation often lasts between 15 to 30 minutes.
This time frame usually allows for a thorough explanation of the case while maintaining audience engagement. However, always consider leaving a few minutes at the end for a Q&A session to address any questions or clarify points made during the presentation.
When it comes to presenting a compelling case study, having a well-structured template can be a game-changer.
It helps you organize your thoughts, data and findings in a coherent and visually pleasing manner.
Not all case studies are created equal and different scenarios require distinct approaches for maximum impact.
To save you time and effort, I have curated a list of 5 versatile case study presentation templates, each designed for specific needs and audiences.
Here are some best case study presentation examples that showcase effective strategies for engaging your audience and conveying complex information clearly.
1 . Lab report case study template
Ever feel like your research gets lost in a world of endless numbers and jargon? Lab case studies are your way out!
Think of it as building a bridge between your cool experiment and everyone else. It’s more than just reporting results – it’s explaining the “why” and “how” in a way that grabs attention and makes sense.
This lap report template acts as a blueprint for your report, guiding you through each essential section (introduction, methods, results, etc.) in a logical order.
Want to present your research like a pro? Browse our research presentation template gallery for creative inspiration!
2. Product case study template
It’s time you ditch those boring slideshows and bullet points because I’ve got a better way to win over clients: product case study templates.
Instead of just listing features and benefits, you get to create a clear and concise story that shows potential clients exactly what your product can do for them. It’s like painting a picture they can easily visualize, helping them understand the value your product brings to the table.
Grab the template below, fill in the details, and watch as your product’s impact comes to life!
3. Content marketing case study template
In digital marketing, showcasing your accomplishments is as vital as achieving them.
A well-crafted case study not only acts as a testament to your successes but can also serve as an instructional tool for others.
With this coral content marketing case study template—a perfect blend of vibrant design and structured documentation, you can narrate your marketing triumphs effectively.

4. Case study psychology template
Understanding how people tick is one of psychology’s biggest quests and case studies are like magnifying glasses for the mind. They offer in-depth looks at real-life behaviors, emotions and thought processes, revealing fascinating insights into what makes us human.
Writing a top-notch case study, though, can be a challenge. It requires careful organization, clear presentation and meticulous attention to detail. That’s where a good case study psychology template comes in handy.
Think of it as a helpful guide, taking care of formatting and structure while you focus on the juicy content. No more wrestling with layouts or margins – just pour your research magic into crafting a compelling narrative.
5. Lead generation case study template
Lead generation can be a real head-scratcher. But here’s a little help: a lead generation case study.
Think of it like a friendly handshake and a confident resume all rolled into one. It’s your chance to showcase your expertise, share real-world successes and offer valuable insights. Potential clients get to see your track record, understand your approach and decide if you’re the right fit.
No need to start from scratch, though. This lead generation case study template guides you step-by-step through crafting a clear, compelling narrative that highlights your wins and offers actionable tips for others. Fill in the gaps with your specific data and strategies, and voilà! You’ve got a powerful tool to attract new customers.
Related: 15+ Professional Case Study Examples [Design Tips + Templates]
So, you’ve spent hours crafting the perfect case study and are now tasked with presenting it. Crafting the case study is only half the battle; delivering it effectively is equally important.
Whether you’re facing a room of executives, academics or potential clients, how you present your findings can make a significant difference in how your work is received.
Forget boring reports and snooze-inducing presentations! Let’s make your case study sing. Here are some key pointers to turn information into an engaging and persuasive performance:
- Know your audience : Tailor your presentation to the knowledge level and interests of your audience. Remember to use language and examples that resonate with them.
- Rehearse : Rehearsing your case study presentation is the key to a smooth delivery and for ensuring that you stay within the allotted time. Practice helps you fine-tune your pacing, hone your speaking skills with good word pronunciations and become comfortable with the material, leading to a more confident, conversational and effective presentation.
- Start strong : Open with a compelling introduction that grabs your audience’s attention. You might want to use an interesting statistic, a provocative question or a brief story that sets the stage for your case study.
- Be clear and concise : Avoid jargon and overly complex sentences. Get to the point quickly and stay focused on your objectives.
- Use visual aids : Incorporate slides with graphics, charts or videos to supplement your verbal presentation. Make sure they are easy to read and understand.
- Tell a story : Use storytelling techniques to make the case study more engaging. A well-told narrative can help you make complex data more relatable and easier to digest.

Ditching the dry reports and slide decks? Venngage’s case study templates let you wow customers with your solutions and gain insights to improve your business plan. Pre-built templates, visual magic and customer captivation – all just a click away. Go tell your story and watch them say “wow!”
Nailed your case study, but want to make your presentation even stronger? Avoid these common mistakes to ensure your audience gets the most out of it:
Overloading with information
A case study is not an encyclopedia. Overloading your presentation with excessive data, text or jargon can make it cumbersome and difficult for the audience to digest the key points. Stick to what’s essential and impactful. Need help making your data clear and impactful? Our data presentation templates can help! Find clear and engaging visuals to showcase your findings.
Lack of structure
Jumping haphazardly between points or topics can confuse your audience. A well-structured presentation, with a logical flow from introduction to conclusion, is crucial for effective communication.
Ignoring the audience
Different audiences have different needs and levels of understanding. Failing to adapt your presentation to your audience can result in a disconnect and a less impactful presentation.
Poor visual elements
While content is king, poor design or lack of visual elements can make your case study dull or hard to follow. Make sure you use high-quality images, graphs and other visual aids to support your narrative.
Not focusing on results
A case study aims to showcase a problem and its solution, but what most people care about are the results. Failing to highlight or adequately explain the outcomes can make your presentation fall flat.
How to start a case study presentation?
Starting a case study presentation effectively involves a few key steps:
- Grab attention : Open with a hook—an intriguing statistic, a provocative question or a compelling visual—to engage your audience from the get-go.
- Set the stage : Briefly introduce the subject, context and relevance of the case study to give your audience an idea of what to expect.
- Outline objectives : Clearly state what the case study aims to achieve. Are you solving a problem, proving a point or showcasing a success?
- Agenda : Give a quick outline of the key sections or topics you’ll cover to help the audience follow along.
- Set expectations : Let your audience know what you want them to take away from the presentation, whether it’s knowledge, inspiration or a call to action.
How to present a case study on PowerPoint and on Google Slides?
Presenting a case study on PowerPoint and Google Slides involves a structured approach for clarity and impact using presentation slides :
- Title slide : Start with a title slide that includes the name of the case study, your name and any relevant institutional affiliations.
- Introduction : Follow with a slide that outlines the problem or situation your case study addresses. Include a hook to engage the audience.
- Objectives : Clearly state the goals of the case study in a dedicated slide.
- Findings : Use charts, graphs and bullet points to present your findings succinctly.
- Analysis : Discuss what the findings mean, drawing on supporting data or secondary research as necessary.
- Conclusion : Summarize key takeaways and results.
- Q&A : End with a slide inviting questions from the audience.
What’s the role of analysis in a case study presentation?
The role of analysis in a case study presentation is to interpret the data and findings, providing context and meaning to them.
It helps your audience understand the implications of the case study, connects the dots between the problem and the solution and may offer recommendations for future action.
Is it important to include real data and results in the presentation?
Yes, including real data and results in a case study presentation is crucial to show experience, credibility and impact. Authentic data lends weight to your findings and conclusions, enabling the audience to trust your analysis and take your recommendations more seriously
How do I conclude a case study presentation effectively?
To conclude a case study presentation effectively, summarize the key findings, insights and recommendations in a clear and concise manner.
End with a strong call-to-action or a thought-provoking question to leave a lasting impression on your audience.
What’s the best way to showcase data in a case study presentation ?
The best way to showcase data in a case study presentation is through visual aids like charts, graphs and infographics which make complex information easily digestible, engaging and creative.
Don’t just report results, visualize them! This template for example lets you transform your social media case study into a captivating infographic that sparks conversation.

Choose the type of visual that best represents the data you’re showing; for example, use bar charts for comparisons or pie charts for parts of a whole.
Ensure that the visuals are high-quality and clearly labeled, so the audience can quickly grasp the key points.
Keep the design consistent and simple, avoiding clutter or overly complex visuals that could distract from the message.
Choose a template that perfectly suits your case study where you can utilize different visual aids for maximum impact.
Need more inspiration on how to turn numbers into impact with the help of infographics? Our ready-to-use infographic templates take the guesswork out of creating visual impact for your case studies with just a few clicks.
Related: 10+ Case Study Infographic Templates That Convert
Congrats on mastering the art of compelling case study presentations! This guide has equipped you with all the essentials, from structure and nuances to avoiding common pitfalls. You’re ready to impress any audience, whether in the boardroom, the classroom or beyond.
And remember, you’re not alone in this journey. Venngage’s Case Study Creator is your trusty companion, ready to elevate your presentations from ordinary to extraordinary. So, let your confidence shine, leverage your newly acquired skills and prepare to deliver presentations that truly resonate.
Go forth and make a lasting impact!

IMAGES
VIDEO
COMMENTS
Jan 14, 2017 •. 177 likes • 73,095 views. Utkarsh Shakya. case study. Design. 1 of 38. hospital case study - Download as a PDF or view online for free.
multi-hospital health system, is currently building a 160-bed hospital in Wexford, Pennsylvania to provide patient-centered care to their communities. The patient-centered design of Wexford Hospital includes a variety of unique facility and technology features such as the rooftop garden, smart television, mobile app, and patient room control.
A case study approach [ 47, 48] was adopted here to understand the deployment of a whole system change in the acute hospital along the four dimensions of STS outlined above. A case study is an approach that is used to generate an in-depth, multi-faceted understanding of a complex issue in its real-life context [ 49 ].
A Case Study on Hospital Management System. Maha. Mahmoud. Under the supervision of Dr Geetha Achuthan. Abstract. Nowadays, the IT system has made many changes in the medical field. Managing a multi-speciality hospital is a challenging task in this fast-paced world of medicine. Therefore, the need for a management type of organization is ...
nity's view of hospital and willingness to pay for services were administered by PAHO staff and steering committee members. Service area surveys included Georgetown and Sandy Bay. 450 questionnaires were admin- istered. Case Study: The SMART Hospital Project 9. Project start date Project end date March 2012 March 2014.
For this initiative, hospital management information system (HMIS) has to be implemented across 400+ health facilities in the city.,A case study methodology was adopted to study HMIS implementation. Wave 1 of Phase 1 implementation of HMIS is carried out as a pilot project at Film City's Hospital, Mumbai, which "go-live" on 21st June 2018.
AI-enhanced title. anup dubey. thesis .. Healthcare. 1 of 10. Download Now. Download to read offline. Healthcare Management Case Study: Patient Suing Hospital - Download as a PDF or view online for free.
CHAPTER FIVE DISCUSSION OF RESULTS 5.0 CONCLUSION The project Hospital Management System (HMS) is for computerizing the working in a hospital. It is a great improvement over the manual system. The computerization of the system has speed up the process. In the current system, the front office managing is very slow.
Hospital Management System Ppt - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online.
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
Slide 25: Case Study Risk Assessment. Images: The Morse Fall Scale is shown with sample patient scores. Slide 26: Assessment of Risk Factors in Your Hospital. The questions for your Team to address are: Which tools will we use to assess fall risk in patients at our hospital? Do unit staff members understand why they are assessing fall risk factors?
The Regional Hospital is a 500-bed hospital in a major metro area of the East Coast and many affiliated clinics. The hospital needs support to effectively meet its ongoing challenges to medical staff and allied clinics due to underfunded and understaffed challenges ; uncertainty in health care legislation; emphasis on extending hospital stays to cut costs that cause the percentage of patients ...
We would like to show you a description here but the site won't allow us.
The case management process. Case management is a collaborative process in which a case manager works with clients to ensure they obtain the proper health care in the most cost-effective manner. This is what the process typically looks like: 1. Screening: The case manager reviews a client's medical records, medical history, and current ...
Presenting our Hospital Management Business Plan PowerPoint Presentation Slides. This is a 100% editable and adaptable PPT slide. You can save it in different formats like PDF, JPG, and PNG. It can be edited with different colors, font, font sizes, and font types of the template as per your requirements.
A case presentation is a narrative of a patient's care, so it is vital the presenter has familiarity with the patient, the case and its progression. The preparation for the presentation will depend on what information is to be included. Generally, oral case presentations are brief and should be limited to 5-10 minutes.
IOT Medical Healthcare Technology Use Cases. Slide 1 of 2. Competitive analysis of abs healthcare company for 2021 ppt infographics templates. Slide 1 of 16. Case Study On Digital Transformation In Healthcare Industry Training Ppt. Slide 1 of 6. Case Study Clinical Medicine Research Company Profile. Slide 1 of 2.
Case Presentation. History of Present Illness: A 33-year-old white female presents after admission to the general medical/surgical hospital ward with a chief complaint of shortness of breath on exertion.She reports that she was seen for similar symptoms previously at her primary care physician's office six months ago.
To save you time and effort, I have curated a list of 5 versatile case study presentation templates, each designed for specific needs and audiences. Here are some best case study presentation examples that showcase effective strategies for engaging your audience and conveying complex information clearly. 1. Lab report case study template.