FACT CHECK: Is The Rate Of Regret After Gender-Affirming Surgery Only 1%?
A post shared on social media claims only 1% of people regret their gender-affirmation surgery.
View this post on Instagram A post shared by matt bernstein (@mattxiv)
Verdict: Misleading
While the study cited does find a 1% regret rate, it and other subsequent studies share disclaimers and the limitations of research, suggesting the rate may actually be higher.
Fact Check:
The Instagram post claims that only 1% of patients regret their gender transition surgeries. The source used is “Regret after Gender-affirmation Surgery: A systematic Review and Meta-analysis of Prevalence” from the National Library of Medicine (NLM).
The caption is misleading, due to several factors and lack of research that were identified by the study itself and other subsequent papers. (RELATED: Did Canada Release A New Passport That Features Pride Flags?)
This study did not conduct original research, but rather compiled research done in many different places which resulted in a disclaimer warning of the danger of generalizing the results. “There is high subjectivity in the assessment of regret and lack of standardized questionnaires,” which varies from study to study, according to the NLM document.
The study quotes a 2017 study published in the Journal of Sex and Marital Therapy , which conducted a follow-up survey of regret among patients after their transition. The study notes a major limitation was that few patients followed up after surgery.
“This study’s main limitation was the sample representativeness. With a response rate of 37%, similar to the attrition rates of most follow-up studies,” according to the study. Out of the response rate, six percent reported dissatisfaction or regret with the surgery, the study claims.
Additional data found in a Cambridge University Press study showed subjects on average do not express regret in the transition until an average of 10 years after their surgery. The study also claimed twelve cases out of the 175 selected, or around seven percent, had expressed detransitioning.
“There is some evidence that people detransition on average 4 or 8 years after completion of transition, with regret expressed after 10 years,” the study suggests. It also states that the actual rate is unknown, with some ranging up to eight percent.
Another study published in 2007 from Sweden titled, “ Factors predictive of regret in sex reassignment ,” found that around four percent of patients who underwent sex reassignment surgery between 1972-1992 regretted the measures taken. The research was done over 10 years after the the procedures.
The National Library of Medicine study only includes individuals who underwent transition surgery and does not take into account regret rates among individuals who took hormone replacement. Research from The Journal of Clinical Endocrinology and Metabolism (JCEM) found that the hormone continuation rate was 70 percent, suggesting nearly 30 percent discontinued their hormone treatment for a variety of reasons.
“In the largest surgery study, approximately 1% of patients regretted having gender-confirmation surgery,” Christina Roberts, M.D, a professor of Pediatrics at the University of Missouri-Kansas City School of Medicine and a participant for the study for the JCEM, told Check Your Fact via email.
Roberts stated that while there were multiple major factors in regards to those regretting the surgery, including poor cosmetic outcome and lack of social support, she claimed discontinuation of hormone therapies and other treatment are “not the same thing as regret.”
“This is an apples to oranges comparison,” Roberts added. (RELATED: Is Disney World Replacing The American Flag With The LGBTQ+ Pride Flag In June 2023?)
Check Your Fact reached out to multiple doctors and researchers associated with the above and other studies and will update this piece if responses are provided.

Joseph Casieri
Fact check reporter.

FactCheck Q&A: was Lyle Shelton right about transgender people and a higher suicide risk after surgery?
Senior Research Fellow, Australian Institute for Suicide Research and Prevention, National Centre of Excellence in Suicide Prevention, Griffith University
Interviewed

Clinical sexologist, Gender team Stockholm, Centre for Andrology and Sexual Medicine, Karolinska Institutet
Professor of Clinical Neuroscience, University of Gothenburg
Research Fellow, Dementia Collaborative Research Centre, School of Psychiatry, University of New South Wales, UNSW Sydney
Disclosure statement
Kairi Kõlves receives funding from the Australian Research Council (currently ARC DP14012567, ARC LP120100021); Commonwealth Department of Health; beyondblue (2013-2015 project Fatal Suicidal Behaviours in LGBT Populations).
Karolina Krysinska does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Griffith University provides funding as a member of The Conversation AU.
View all partners
The Conversation is fact-checking claims made on Q&A, broadcast Mondays on the ABC at 9:35pm. Thank you to everyone who sent us quotes for checking via Twitter using hashtags #FactCheck and #QandA, on Facebook or by email .
Studies that have been done of transgendered people who have had sex reassignment surgery, people who have been followed for 20 or so years have found that after 10 years from the surgery, that their suicide mortality rate was actually 20 times higher than the non-transgendered population. So I’m very concerned that here we are encouraging young people to do things to their bodies … like chest binding for young girls … [and] penis tucking … Now this is taking kids on a trajectory that may well cause them to want to take radical action, such as gender reassignment surgery… – Lyle Shelton, managing director of the Australian Christian Lobby, speaking on Q&A on February 29, 2016.
Australia’s Safe Schools Coalition program has been accused of “promoting a radical view of gender and sexuality” in schools.
The program’s architects say it aims to boost acceptance of same sex attracted, intersex and gender diverse students, staff and families.
Critics have said that the program directs children to groups such as Minus18 , a youth-led network for lesbian, gay, bisexual, transgender and intersex people. Among the resources on Minus18’s website is information about appearance modification for transgender people such as:
Changing your appearance is another way you can express your gender. Things like makeup, the clothes or school uniform you wear, binding your chest, tucking/packing your pants, or the way you do your hair can all help you better express yourself.
Speaking on Q&A, the Australian Christian Lobby’s Lyle Shelton stressed that respect is essential and that no one should be bullied at school. He said that in Victoria, the Bully Stoppers program does address homophobic bullying .
However, Shelton said he would prefer anti-bullying programs didn’t include “contested gender ideology” that may lead to gender reassignment surgery.
He also said research showed that people who had undergone sex reassignment surgery were 20 times more likely to suicide than the general population a decade after their surgery.
Let’s take a closer look at what the research says.
Checking the research
Shelton did not respond to The Conversation’s request for comment and clarification. However, later in the program he referred to a Swedish study of over 300 people over about 30 years between 1973 and about 2003 that found that the suicide mortality rate was 20 times higher than the non transgendered population – so it seems likely he is referring to a 2011 published in the journal PLOS ONE .
That study, led by researcher Cecilia Dhejne, tracked 324 sex-reassigned people in Sweden between 1973 and 2003 to estimate their mortality, morbidity, and criminal rate after surgery. The researchers also included a comparison group. In that group, for every transgender person studied, the researchers included a non-transgendered person the same age and the same sex as the transgender person was before surgery.
The researchers found that:
Persons with transsexualism, after sex reassignment, have considerably higher risks for mortality, suicidal behaviour, and psychiatric morbidity than the general population.
The authors did not find that surgery was the cause of increased suicide risk, writing in their paper that:
the results should not be interpreted such as sex reassignment per se increases morbidity and mortality. Things might have been even worse without sex reassignment.
Why are post-surgery transgender people at higher risk of suicide than the general population?
It is possible that Shelton was not implying any causal relationship between sex reassignment surgery and a higher suicide risk. The Conversation asked him to clarify what he wanted to convey by mentioning the study, but he did not reply.
It is also possible some viewers may have been left with the impression that the study showed sex reassignment surgery causes a higher risk of suicide later in life. That is not the case.
The Conversation asked the authors of that study how they felt about the way Shelton had represented their findings. One of the authors, Mikael Landén from the Department of Clinical Neuroscience at Stockholm’s Karolinska Institutet medical university, told The Conversation that:
As Mr Shelton phrases it, it may sound as if sex reassignment increased suicide risk 20 times. That is not the case. The risk of suicide was increased 19 times compared to the general population, but that is because gender dysphoria is a distressing condition in itself. Our study does not inform us whether sex reassignment decreases (which is likely) or increases (which is unlikely) that risk.
When asked why people who have had sex reassignment surgery may be more prone than the general population to suicide later in life, Landén said:
Gender dysphoria is a distressing condition. We have known for a long time that it is associated with other psychiatric disorders (such as depression) and increased rate of suicide attempts. Sex reassignment is the preferred treatment and outcome studies suggest that gender dysphoria (the main symptom) decreases. But it goes without saying that the procedure is a stressful life event. And that the surgery and medical treatment is not perfect. It is thus not surprising that this group of patients will continue to suffer from stress-related psychiatric disorders. There might be lingering professional and relational problems. It is also possible (but unproven) that gender dysphoria is somehow etiologically related to depression. In that case, fixing the first with a cure would not automatically fix the latter.
As some Q&A viewers, including @BayneMacGregor, pointed out on Twitter as the program aired, the lead author of the study has been asked about this before.
In November 2015, Cecilia Dhejne told the website The TransAdvocate that, “Medical transition alone won’t resolve the effects of crushing social oppression: social anxiety, depression and post-traumatic stress.”
(Dhejne also confirmed to The Conversation that the transcript of her interview on The TransAdvocate website is accurate).
What does other research say?
Recent literature reviews, including a literature review colleagues and I conducted reviewing Australian literature until the end of 2012, found a greater prevalence of suicidal behaviours among sexual minorities in general.
Risk factors for suicidal behaviours specific to LGBTI people include “coming out” in adolescence and early adulthood, prejudice, discrimination, shame, hostility, and self-hatred.
A recent review of literature focused on suicidal behaviours – including suicidal thought, suicide attempts and suicide rates – among trans people (the term used by the authors of that review) between 1966 and April 2015. The authors concluded that the prevalence of suicidal behaviours differs depending on the different stages of transition, but they are still overall greater than the general population.
A 2011 Dutch study found that male-to-female transsexuals had a risk of suicide 5.7 times higher than the general population.
However, suicide risk was found not to be significantly higher in female-to-male transsexuals compared to the general population in an 18 year follow-up of 996 male-to-female and 365 female-to-male transexuals.
Again, those studies do not indicate the cause of increased suicide risk.
It’s possible that a number of other lifestyle factors, combined with lack of social support, discrimination and stigmatisation increase the risk of suicidal behaviour in the trans population.
Shelton was correct to say that research shows that transgendered people who have had sex reassignment surgery had a suicide mortality rate later in life that was roughly 20 times higher than the non-transgendered population.
However, it is also possible some viewers may have been left with the impression that the study showed sex reassignment surgery causes a higher risk of suicide later in life. That is not what the Swedish study showed. In fact, the researchers wrote that things might have been even worse without sex reassignment.
Nevertheless, there is lack of research on the topic and his comment appears to be based on one study from Sweden. – Kairi Kõlves
This FactCheck a good overview of the current research literature. It looks at both international literature on suicide risk and suicidal behaviours in sexual minority populations and, importantly, results of Australian studies.
Three conclusions spring to mind. First, we still have limited insight into the actual causes of the increased suicide risk in the sexual minority groups. Secondly, we need more Australian studies on suicide in the transgender people, ideally designed in close collaboration with people with the lived experience of suicidality. Last, we should remember that despite the higher statistical risk, the majority of transgender people do not attempt suicide or die by suicide .
A better understanding of resilience and protective factors could significantly contribute to improved quality of life and well-being. – Karolina Krysinska
• Lifeline 13 11 14 • Suicide Call Back Service 1300 659 467
- Transgender
- FactCheck Q&A
- Suicide prevention
- Gender identity
- Gender roles
- Suicide rates
- Homophobia in schools
- Transgender students
- Safe Schools Coalition
- australian christian lobby
- Gender studies

Program Manager, Teaching & Learning Initiatives

Lecturer/Senior Lecturer, Earth System Science (School of Science)

Sydney Horizon Educators (Identified)

Deputy Social Media Producer

Associate Professor, Occupational Therapy
- Share on Twitter
- Share on Facebook
- Share on LinkedIn
Female-to-male genital reconstruction surgery has a high negative outcome rate, including urethral compromise and worsened mental health.
The results of a 2021 international survey [1] of 129 female-to-male patients who underwent genital reconstruction surgery support anecdotal reports that complication rates following genital reconstruction are higher than are commonly reported in the surgical literature.
Complication rates, including urethral compromise, and worsened mental health outcomes remain high for gender affirming penile reconstruction. In total, the 129 patients reported 281 complications requiring 142 revisions.
Another paper [2] found a 70% complication rate in one type of female-to-male genital reconstruction surgery.
Even with the “radial forearm free flap” method of creating a synthetic penis — “considered by many as the gold standard for phalloplasty” [3] — there are high rates of complications, with up to 64% urethroplasty related complications [4] .
[1] Robinson, I.S., Blasdel, G., Cohen, O., Zhao, L.C. & Bluebond-Langner, R. (2021). Surgical Outcomes Following Gender Affirming Penile Reconstruction: Patient-Reported Outcomes From a Multi-Center, International Survey of 129 Transmasculine Patients. J Sex Med 18 (4): 800-811. [ Link ]
[2] Bettocchi, C., Ralph, D.J. & Pryor, J.P. (2005). Pedicled pubic phalloplasty in females with gender dysphoria. BJU Int. 95:120–4. [ Link ]
[3] Rashid, M. & Tamimy, M. S. (2013). Phalloplasty: The dream and the reality. Indian J Plast Surg 46 (2): 283-293. [Link]
[4] Fang, R.H., Lin, J.T. & Ma S. (1994). Phalloplasty for female transsexuals with sensate free forearm flap. Microsurgery 15: 349–52. [ Link ]
Medical transition puts both males and females at risk of infertility.
A wide-ranging study [1] found that gender-related drug regimens place patients at risk of infertility:
Suppression of puberty with gonadotropin-releasing hormone agonist analogs (GnRHa) in the pediatric transgender patient can pause the maturation of germ cells, and thus, affect fertility potential. Testosterone therapy in transgender men can suppress ovulation and alter ovarian histology, while estrogen therapy in transgender women can lead to impaired spermatogenesis and testicular atrophy. The effect of hormone therapy on fertility is potentially reversible, but the extent is unclear.
On surgeries, the study noted that cross-sex surgery that includes hysterectomy and oophorectomy in transmen or orchiectomy in transwomen results in permanent sterility.
[1] Cheng, P.J., Pastuszak, A.W., Myers, J.B., Goodwin, I.A. & Hotaling, J.M. (2019). Fertility concerns of the transgender patient. Transl Androl Urol. 8 (3): 209-218. [ Link ]
Genital surgeries tend to reduce the capacity for orgasm in males, and may do so in females.
One study showed that around 30% of male-to-female genital surgeries result in the inability to orgasm [1] .
Figures on female-to-male transitioners are less clear. However, a clinical follow-up study [2] of 38 transmen – 29 of whom had received phalloplasty, and 9 metoidioplasty – found that reported loss of orgasmic capacity was more marginally common than reported gain of orgasmic capacity.
The negative intrapsychic and interpersonal consequences of anorgasmia (the inability to climax) is well-documented, and applies equally to transgender individuals [3] .
[1] Manrique, O., Adabi, K., Martinez-Jorge, J., Ciudad, P., Nicoli, F. and Kiranantawat, K. (2018). Complications and Patient-Reported Outcomes in Male-to-Female Vaginoplasty—Where We Are Today. Annals of Plastic Surgery 80 (6): 684-691. [ Link ]
[2] van de Grift, T., Pigot, G., Kreukels, B., Bouman, M., & Mullender, M. (2019). Transmen’s Experienced Sexuality and Genital Gender-Affirming Surgery: Findings From a Clinical Follow-Up Study. Journal Of Sex & Marital Therapy 45 (3): 201-205. [ Link ]
[3] Levine, S. (2018). Informed Consent for Transgendered Patients. Journal Of Sex & Marital Therapy, 45(3), 218-229. [ Link ]
Vaginoplasty can result in fistula, stenosis, necrosis, prolapse and even death.
Male-to-female genital surgery (vaginoplasty) is associated with significant long-term complications: there is a 2% risk of fistula, 14% risk of stenosis (abnormal narrowing), 1% risk of necrosis (tissue death) and 4% risk of prolapse [1] .
One systematic review [2] found an overall complication rate of 32.5%.
A Dutch study [3] of 55 (out of an original 70) adolescents treated with puberty blockers, cross sex hormones, and genital surgery, showed that among 22 male-to-female patients who underwent vaginoplasty, one adolescent died as a result of necrotizing fasciitis after the surgery.
[2] Dreher, P.C., Edwards, D., Hager, S., Dennis, M., Belkoff, A., Mora, J., Tarry, S. & Rumer, K.L. (2018). Complications of the neovagina in male-to-female transgender surgery: A systematic review and meta-analysis with discussion of management. Clin Anat. 31 (2):191-199. [ Link ]
[3] de Vries, A., McGuire, T., Steensma, E., Wagenaar, T., Doreleijers, P. & Cohen-Kettenis, P. (2014). Young adult psychological outcome after puberty suppression and gender reassignment . [ Link ]
Around 1 in 5 vaginoplasty surgeries lead to corrective surgery.
A systematic review [1] of neo-vagina surgeries found a re-operation rate of 21.7% for non-esthetic reasons.
A Brazilian paper [2] found a somewhat lower, but similar, reoperation rate of 16.8%.
[1] Dreher, P.C., Edwards, D., Hager, S., Dennis, M., Belkoff, A., Mora, J., Tarry, S. & Rumer, K.L. (2018). Complications of the neovagina in male-to-female transgender surgery: A systematic review and meta-analysis with discussion of management. Clin Anat. 31 (2):191-199. [ Link ]
[2] Moisés da Silva, G.V., Lobato, M.I.R., Silva, D.C., Schwarz, K., Fontanari, A.M.V., Costa, A.B., Tavares, P.M., Gorgen, A.R.H., Cabral, R.D. & Rosito, T.E. (2021). Male-to-Female Gender-Affirming Surgery: 20-Year Review of Technique and Surgical Results. Frontiers in Surgery 8. [ Link ]
There is evidence that up to a quarter of transgender genital surgeries result in incontinence.
A systematic literature review [1] found that 21% of male-to-female patients and 25% of female-to-male patients suffered from incontinence as a result of transgender genital surgery.
One recent study [2] estimates the number of post-operative transsexuals suffering stress incontinence to be 23%. This study was not a literature review, and almost all of the participants were male-to-female.
[1] Nassiri, N., Maas, M., Basin, M., Cacciamani, G.E. & Doumanian, L.R. (2020). Urethral complications after gender reassignment surgery: a systematic review. Int J Impot Res. [ Link ]
[2] Kuhn, A., Santi, A. & Birkhäuser, M. (2011). Vaginal prolapse, pelvic floor function, and related symptoms 16 years after sex reassignment surgery in transsexuals. Fertil Steril. 95: 2379-82. [ Link ]
- Introduction
- Conclusions
- Article Information
eAppendix. Supplemental Methods
eTable 1. Read Codes and Terms to Identify Transgender and Gender Diverse Individuals in CPRD GOLD
eTable 2. SNOMED Codes and Terms to Identify Transgender and Gender Diverse Individuals in CPRD Aurum
eTable 3. Read Codes and Terms to Exclude Individuals With Variations of Sex Characteristics in CPRD GOLD
eTable 4. SNOMED Codes and Terms to Exclude Individuals With Variations of Sex Characteristics in CPRD Aurum
eTable 5. Medications Extracted From the Medical Record Used to Identify Sex Assigned at Birth Among Transgender and Gender Diverse Participants in CPRD Aurum and GOLD
eTable 6. Read Codes and Terms to Identify Sex Assigned at Birth for Transgender and Gender Diverse Individuals in CPRD GOLD
eTable 7. SNOMED Codes and Terms to Identify Sex Assigned at Birth for Transgender and Gender Diverse Individuals in CPRD Aurum
eTable 8. Sex-Specific Procedures Extracted From the Hospital Episode Statistics Admitted Patient Care and Outpatient Care Files Used to Identify Sex Assigned at Birth Among Transgender and Gender Diverse Individuals
eTable 9. Characteristics of Transgender and Gender Diverse Individuals and Cisgender Individuals in the United Kingdom’s Clinical Practice Research Datalink 1988–2019 (Without Imputation)
eTable 10. Overall and Cause-Specific Mortality Rate Ratios for Transgender and Gender Diverse Individuals Compared to Cisgender Individuals in the United Kingdom’s Clinical Practice Research Datalink (Without Imputation)
eTable 11. Overall and Cause-Specific Mortality Rate Ratios for Transgender and Gender Diverse Individuals Compared to Cisgender Individuals in the United Kingdom’s Clinical Practice Research Datalink (Only Patients Who Could Have Died During or After 1998)
eTable 12. Mortality Rate Ratios for Deaths Due to Select Causes of Death Among Transgender and Gender Diverse Individuals Compared to Cisgender Individuals in the United Kingdom’s Clinical Practice Research Datalink (Without Imputation)
eTable 13. Mortality Rate Ratios for Deaths Due to Select Causes Among Transgender and Gender Diverse Individuals Compared to Cisgender Individuals in the United Kingdom’s Clinical Practice Research Datalink (Only Patients Who Could Have Died During or After 1998)
eFigure. Flow Chart of Final Analysis Cohort Combining CPRD GOLD and CPRD Aurum
Data Sharing Statement
- Transgender Identity and Suicide Attempts and Mortality in Denmark JAMA Original Investigation June 27, 2023 This nationwide cohort study in Denmark examines the association between individuals who identify as transgender and rates of suicide attempt and mortality (suicide, unrelated, and all cause). Annette Erlangsen, PhD; Anna Lund Jacobsen, BSc; Anne Ranning, PhD; Alex Lauridsen Delamare, MSc; Merete Nordentoft, DMSc; Morten Frisch, MD, PhD
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Jackson SS , Brown J , Pfeiffer RM, et al. Analysis of Mortality Among Transgender and Gender Diverse Adults in England. JAMA Netw Open. 2023;6(1):e2253687. doi:10.1001/jamanetworkopen.2022.53687
Manage citations:
© 2024
- Permissions
Analysis of Mortality Among Transgender and Gender Diverse Adults in England
- 1 Infections and Immunoepidemiology Branch, Division of Cancer Epidemiology and Genetics, National Cancer Institute, National Institutes of Health, Rockville, Maryland
- 2 Department of Medical Education, Brighton & Sussex Medical School, Brighton, United Kingdom
- 3 Live Through This Charity, London, United Kingdom
- 4 Barts Cancer Institute, Queen Mary University of London, London, United Kingdom
- 5 Gender Identity Clinic, Tavistock and Portman NHS Foundation Trust, London, United Kingdom
- Original Investigation Transgender Identity and Suicide Attempts and Mortality in Denmark Annette Erlangsen, PhD; Anna Lund Jacobsen, BSc; Anne Ranning, PhD; Alex Lauridsen Delamare, MSc; Merete Nordentoft, DMSc; Morten Frisch, MD, PhD JAMA
Question Do transgender and gender diverse (TGD) individuals have increased overall and cause-specific morality compared with cisgender people?
Findings In this cohort study of 139 484 individuals, TGD people had elevated overall mortality compared with cisgender people, specifically deaths from external causes (suicides, homicides, and accidental poisonings), endocrine disorders, and other ill-defined and unspecified causes. Transfeminine individuals had a decreased cancer mortality risk compared with cisgender women but the same risk as cisgender men, whereas transmasculine individuals had the same cancer mortality risk as cisgender people.
Meaning These findings highlight the need to develop interventions to prevent suicide, homicide, and accidental poisonings to reduce mortality for TGD individuals.
Importance Limited prior research suggests that transgender and gender diverse (TGD) people may have higher mortality rates than cisgender people.
Objective To estimate overall and cause-specific mortality among TGD persons compared with cisgender persons.
Design, Setting, and Participants This population-based cohort study used data from general practices in England contributing to the UK’s Clinical Practice Research Datalink GOLD and Aurum databases. Transfeminine (assigned male at birth) and transmasculine (assigned female at birth) individuals were identified using diagnosis codes for gender incongruence, between 1988 and 2019, and were matched to cisgender men and women according to birth year, practice, and practice registration date and linked to the Office of National Statistics death registration. Data analysis was performed from February to June 2022.
Main Outcomes and Measures Cause-specific mortality counts were calculated for categories of disease as defined by International Statistical Classification of Diseases and Related Health Problems, Tenth Revision chapters. Overall and cause-specific mortality rate ratios (MRRs) were estimated using Poisson models, adjusted for index age, index year, race and ethnicity, Index of Multiple Deprivation, smoking status, alcohol use, and body mass index.
Results A total of 1951 transfeminine (mean [SE] age, 36.90 [0.34] years; 1801 White [92.3%]) and 1364 transmasculine (mean [SE] age, 29.20 [0.36] years; 1235 White [90.4%]) individuals were matched with 68 165 cisgender men (mean [SE] age, 33.60 [0.05] years; 59 136 White [86.8%]) and 68 004 cisgender women (mean [SE] age, 33.50 [0.05] years; 57 762 White [84.9%]). The mortality rate was 528.11 deaths per 100 000 person-years (102 deaths) for transfeminine persons, 325.86 deaths per 100 000 person-years (34 deaths) for transmasculine persons, 315.32 deaths per 100 000 person-years (1951 deaths) for cisgender men, and 260.61 deaths per 100 000 person-years (1608 deaths) for cisgender women. Transfeminine persons had a higher overall mortality risk compared with cisgender men (MRR, 1.34; 95% CI, 1.06-1.68) and cisgender women (MRR, 1.60; 95% CI, 1.27-2.01). For transmasculine persons, the overall MMR was 1.43 (95% CI, 0.87-2.33) compared with cisgender men and was 1.75 (95% CI, 1.08-2.83) compared with cisgender women. Transfeminine individuals had lower cancer mortality than cisgender women (MRR, 0.52; 95% CI, 0.32-0.83) but an increased risk of external causes of death (MRR, 1.92; 95% CI, 1.05-3.50). Transmasculine persons had higher mortality from external causes of death than cisgender women (MRR, 2.77; 95% CI, 1.15-6.65). Compared with cisgender men, neither transfeminine nor transmasculine adults had a significantly increased risk of deaths due to external causes.
Conclusions and Relevance In this cohort study of primary care data, TGD persons had elevated mortality rates compared with cisgender persons, particularly for deaths due to external causes. Further research is needed to examine how minority stress may be contributing to deaths among TGD individuals to reduce mortality.
Transgender and gender diverse (TGD) individuals have gender identities that differ from their assigned birth sex. In the UK, approximately 200 000 to 500 000 persons older than 16 years (1% of the population) consider themselves to be TGD. 1 Mortality among TGD persons may be higher than that of cisgender persons (individuals whose assigned birth sex matches their gender identity) because of increased risk of external causes of death and deaths due to illness. The murder of TGD people has been increasing globally, particularly for transgender women, who account for 96% of homicides among TGD people. 2 In the UK, transphobic hate crimes reported to the police have quadrupled over the past 6 years. 3 Research from the US 4 , 5 suggests that TGD people are likely to experience violence and that self-harm is common among these individuals, with 41% reporting at least 1 suicide attempt in their lifetimes.
The minority stress model posits that chronic stress due to repeated exposure to violence, discrimination, and economic and social marginalization results in greater vulnerability to poor health outcomes and mortality among TGD individuals globally. 6 The prevalence of alcohol abuse and tobacco use has been reported to be higher among TGD individuals than cisgender individuals. 7 , 8 The global HIV prevalence among transgender women is 19%, nearly 50 times that of cisgender people. 9 Cancer mortality for specific sites has also been reported to be higher among transgender individuals than cisgender individuals. 10 , 11 TGD persons may also be at increased risk of mortality because of the long-term use of gender-affirming hormone therapy. Limited evidence 12 , 13 suggests that estrogen use may increase the risk of myocardial infarction and ischemic stroke in transgender women. Research 14 , 15 indicates that transgender men have a 2-fold and 4-fold increased rate of myocardial infarction compared with cisgender men and cisgender women, respectively, likely due to testosterone therapy and chronic stress resulting from discrimination and minoritized status.
Previous analyses 11 , 16 , 17 have focused on TGD people who use gender-affirming hormone therapy, thereby excluding those who do not use hormones but may have poorer health outcomes associated with marginalized group status. Many prior analyses were either based on small sample size 18 , 19 or did not adjust for important risk factors for mortality (eg, smoking, body mass index, or alcohol use). 11 , 20 , 21 We sought to examine overall and cause-specific mortality in a cohort of TGD individuals compared with a matched cohort of cisgender people.
This cohort study used 2 primary care databases, Clinical Practice Research Datalink (CPRD) GOLD and CPRD Aurum. CPRD GOLD was established in 1987 and contains the primary care data from approximately 9% of the UK, whereas CPRD Aurum was established in 1995 and covers only English practices (approximately 13% of England). 22 , 23 Both databases are representative of the general population in terms of age and sex. 22 , 23 In CPRD, patient demographics, clinical diagnoses, symptoms, medications, and specialist referrals are recorded by general practitioners using either Read (GOLD) or SNOMED (Aurum) codes. 22 , 23
This study is based on data from the February 2020 CPRD GOLD and Aurum database releases (obtained under license from the UK Medicines and Healthcare products Regulatory Agency; the data are provided by patients and collected by the National Health Service as part of their care and support) and the Office of National Statistics (ONS) and Hospital Episode Statistics (HES) releases (Linkage Set 18; reused with the permission of The Health & Social Care Information Centre). The study was approved by the Independent Scientific Advisory Committee of the CPRD. Informed consent of individual patients was not required because anonymized information was obtained from medical records. This study follows Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline for cohort studies. 24
We used diagnosis codes for gender incongruence (previously coded as gender dysphoria or gender identity disorder) to identify 7151 TGD patients in CPRD who were aged 18 years or older (eTables 1, 2, 3, and 4 in Supplement 1 ). The date of the first qualifying gender incongruence term was set to the later of the index date or date of 18th birthday. Identified TGD individuals were then individually matched to 20 cisgender men and 20 cisgender women who were alive on the TGD person’s index date on the following variables: year of birth (within 1 year), practice, and date of practice registration (within 5 years). Inclusion criteria for both groups must have been recorded after the date CPRD identified the practice recording to be up to standard. 23 All individuals with diagnostic codes for variations of sex characteristics (formerly differences of sex development) were excluded.
In CPRD, sex assigned at birth and gender identity are not collected separately. For TGD individuals, sex assigned at birth was determined from documentation of gender-affirming therapies and surgical procedures, sex-specific procedures listed in the primary care database, and the linked HES files (eAppendix and eTables 5, 6, 7, and 8 in Supplement 1 ). We classified TGD individuals as transfeminine (assigned male at birth), transmasculine (assigned female at birth), or TGD, unknown sex assigned at birth, with the understanding that some individuals, particularly those with nonbinary identities, may not identify with these classifications.
Only patients from consenting English practices were eligible to be linked to several registries including the ONS death registration and the HES files. Patients could be represented in the death registry more than once if their practice switched from GOLD to Aurum (all patient data were backfilled from GOLD to Aurum if this occurred). CPRD deduplicated the linked ONS and HES files before analysis to prevent double counting these patients. The death registry records all deaths, including underlying cause of and date of death, occurring in England and covers the period January 2, 1998, to May 31, 2019. Causes of deaths were coded using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision . Fifty-two percent of the individuals from CPRD (33% from GOLD and 79% from Aurum) were eligible to be linked to the ONS death registry. After data cleaning and exclusions, the final analytic data set consisted of 139 486 individuals, including 3317 TGD and 136 169 cisgender individuals (eAppendix and eFigure in Supplement 1 ).
Data analysis was performed from February to June 2022. We calculated the distribution of cohort characteristics by gender identity as frequencies and percentages, means and SDs, and medians and IQRs. Absolute numbers and proportions for counts of 5 or fewer were suppressed because of privacy concerns. We used Poisson regression models to estimate the mortality rate ratios (MRRs) and 95% CIs for overall and cause-specific mortality in TGD individuals (transfeminine, transmasculine, or TGD unknown sex assigned at birth) compared with cisgender men and cisgender women separately. All models were adjusted for continuous index age, continuous index year, race and ethnicity (White, Black, Asian, or another or unknown race and ethnicity), Index of Multiple Deprivation (socioeconomic status measure, in quintiles), smoking status (current, former, or never), alcohol use (current, former, never), body mass index, calculated as weight in kilograms divided by height in meters squared (underweight or healthy weight [<18.5-24.9], overweight [25.0-29.9], or obese [≥30.0]), including the log of person-years as an offset term and a random intercept for practice to account for the correlation between patients from the same practice. Race and ethnicity were identified in the HES database and were assessed in this study because mortality rates vary by racial and ethnic group. Because death dates are also recorded in the CPRD primary care database and have been confirmed to be complete and accurate, 25 person-time was calculated as the time from the index date to the date of death (recorded in CPRD or the death registry) or end of the death registry coverage period (May 31, 2019). Cause-specific mortality counts were calculated for categories of disease as defined by International Statistical Classification of Diseases and Related Health Problems, Tenth Revision chapters (eg, infection, cancer, and nonnatural causes of death), and MRRs were calculated for categories with deaths among TGD persons. Mortality risks were estimated for the 10 chapters that had more than 0 deaths among TGD people. Where the sample size was sufficient, we further divided categories of diseases into the individual cause of death categories suicide or homicide, accidental poisonings, gastrointestinal and lung cancers (the 2 most common cancers among TGD people), endocrine disorders, and other ill-defined and unspecified causes of mortality. Because we identified TGD persons from diagnosis codes related to gender incongruence but were not required to have a record of gender-affirming care (hormones or surgery), we could not determine the sex assigned at birth for 33% of TGD individuals. Therefore, we used multiple imputation with chained equations to impute missing values for sex assigned at birth and other variables with missing values (eAppendix in Supplement 1 ). 26 The imputed results are presented as our main analysis. The results without imputation for sex assigned at birth and other missing data are presented in eTables 9 and 10 in Supplement 1 .
We also conducted a sensitivity analysis restricted to individuals who were alive and enrolled in a CPRD practice as of January 2, 1998 (the start of ONS death registry coverage). In this analysis, person-time was calculated from the later of the index date or January 2, 1998, to the date of death or May 31, 2019 (end of ONS death registry coverage), using multiple imputation. All analyses were conducted using SAS statistical software version 9.4 (SAS Institute).
After imputing missing sex assigned at birth, the cohort consisted of 1951 transfeminine (1801 White [92.3%]) and 1364 transmasculine individuals (1235 White [90.4%]) matched to 68 165 cisgender men (59 136 White [86.8%]) and 68 004 cisgender women (57 762 White [84.9%]) ( Table 1 ). Transmasculine adults were younger (mean [SE] age at index date, 29.20 [0.36] years) than transfeminine individuals (mean [SE], 36.90 [0.34] years), cisgender men (mean [SE], 33.60 [0.05] years), and cisgender women (mean [SE], 33.50 [0.05] years). Transmasculine adults were less likely to be current alcohol users and more likely to be obese than other gender identities. Transfeminine individuals were more likely to be White and current smokers than cisgender people.
During follow-up, the mortality rates were 528.11 deaths per 100 000 person-years (102 deaths) for transfeminine persons and 325.86 deaths per 100 000 person-years (34 deaths) for transmasculine persons. In comparison, the mortality rates were 315.32 deaths per 100 000 person-years (1951 deaths) for cisgender men and 260.61 deaths per 100 000 person-years (1608 deaths) for cisgender women ( Table 1 ). As shown in Table 2 , TGD people had an overall increased risk of mortality compared with cisgender people. Compared with cisgender men, there was an increased risk of overall mortality for transfeminine (MRR, 1.34; 95% CI, 1.06-1.68) and transmasculine (MRR, 1.43; 95% CI, 0.87-2.33) adults. Compared with cisgender women, there was an increased risk of overall mortality among transfeminine (MRR, 1.60; 95% CI, 1.27-2.01) and transmasculine (MRR, 1.75; 95% CI, 1.08-2.83) adults. In the nonimputed analysis (eTable 10 in Supplement 1 ), TGD individuals with unknown sex assigned at birth had the highest risk of death compared with cisgender men (MRR, 1.71; 95% CI, 1.31-2.23) and cisgender women (MRR, 2.11; 95% CI, 1.61-2.78). The results were not materially different when the analysis was restricted to those with follow-up after January 2, 1998 (eTable 11 in Supplement 1 ).
Cause-specific mortality is presented in Table 2 . The risk of cancer death was decreased for transfeminine adults compared with cisgender women (MRR, 0.52; 95% CI, 0.32-0.83) but not when compared with cisgender men or for transmasculine adults compared with either cisgender group. Compared with cisgender women, there was an increased risk of death from external causes for transfeminine (MRR, 1.92; 95% CI, 1.05-3.50) and transmasculine (MRR, 2.77; 95% CI, 1.15-6.65) adults. Compared with cisgender men, neither transfeminine adults nor transmasculine adults had a significantly increased risk of deaths due to external causes. Transfeminine adults had a significantly increased of mortality risk from diseases with symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified, compared with cisgender men (MRR, 4.87; 95% CI, 1.71-13.89) but not cisgender women (MRR, 3.49; 95% CI, 0.47-25.79). The risk of mortality in this classification was elevated for transmasculine adults compared with cisgender men (MRR, 9.27; 95% CI, 2.93-29.30) but was not significant when compared with cisgender women (MRR, 6.83; 95% CI, 0.88-52.74). Results from the nonimputed analysis were similar to the main findings (eTable 10 in Supplement 1 ), with the exception that TGD persons with unknown sex assigned at birth had increased mortality due to external causes compared with cisgender men (MRR, 1.82; 95% CI, 1.31-2.23) and cisgender women (MRR, 2.11; 95% CI, 1.61-2.78). These results did not differ when we restricted follow-up time (eTable 11 in Supplement 1 ).
We investigated deaths due to external causes; neoplasms; endocrine, nutritional, and metabolic diseases; and symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified, by comparing all TGD individuals combined with cisgender men and cisgender women separately ( Table 3 ). Compared with cisgender men, TGD people were 3 times as likely to die from suicide or homicide (MRR, 3.34; 95% CI, 1.70-6.54) and more than twice as likely to die from accidental poisonings (MRR, 2.28; 95% CI, 1.04-5.02). Compared with cisgender women, TGD people were more than 5 times as likely to die from suicide or homicide (MRR, 5.62; 95% CI, 2.65-11.91) and from accidental poisonings (MRR, 5.20; 95% CI, 2.22-12.18). We examined the most common cancer deaths occurring among TGD people: gastrointestinal (consisting of esophagus, stomach, colorectal, and pancreas cancers) and lung cancer. We found no difference in mortality from these 2 cancers between TGD people and cisgender people. In contrast, there were 51 prostate cancer deaths in cisgender men and none among transfeminine adults, and there were 116 breast cancer deaths among cisgender women but none among transmasculine adults. TGD individuals combined had increased mortality from endocrine diseases compared with cisgender women (MRR, 2.95; 95% CI, 1.08-8.07), but not cisgender men (MRR, 1.80; 95% CI, 0.69-4.66). TGD people were more likely to have their deaths classified as symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified than cisgender men (MRR, 5.27; 95% CI, 1.95-14.26) and cisgender women (MRR, 18.63; 95% CI, 5.39-64.37). These results did not differ when we excluded those with missing data (eTable 12 in Supplement 1 ) or restricted follow-up time (eTable 13 in Supplement 1 ).
This cohort study found that TGD individuals have an increased risk of overall mortality, ranging from 34% to 75%, compared with cisgender people. We found an increased mortality due to external causes, with nearly 2-fold increased risk of death among transfeminine adults and almost a 3-fold risk of death among transmasculine adults compared with cisgender women. Research from the Netherlands 11 found the risk of mortality for transgender women was 1.6 times that of cisgender men and 2.4 times that of cisgender women. In that analysis, transgender men had 1.6 times the mortality risk of cisgender women but a nonsignificant increased risk of death that was 1.1 times that of cisgender men. 11 In our analysis, we found TGD persons with unknown sex assigned at birth had mortality rates 1.71 to 2.11 times higher than those for cisgender men and women, respectively. Similarly, Hughes et al 27 found that individuals for whom they were unable to determine sex assigned at birth had the highest mortality rates. This group, which consists of nonbinary persons who may not seek gender-affirming care, those who access hormone therapy outside the medical system, or those with limited access to medical care because of fears of discrimination and other barriers to health care, may experience higher levels of minority stress than TGD persons with a record of gender-affirming care. 7
Previous research 11 , 16 - 18 , 20 , 21 , 28 has found mortality from external causes is 2 to 19 times higher in TGD persons than cisgender persons. When we compared all TGD people combined with cisgender people, we saw 3 to 5 times greater increased mortality from suicide or homicide and 2 to 5 times increased mortality from accidental poisonings. However, when we separately compared transfeminine individuals and transmasculine individuals with cisgender persons, we found an increased risk of external causes of death compared with cisgender women only. Historically, across all age groups, cisgender women have had lower mortality rates due to external causes of death compared with cisgender men. 29 De Blok et al 11 found a 3- to 7-fold increased risk of suicide among transgender women compared with cisgender people, but no significant increase among transgender men. Forty-one percent of TGD respondents in the US National Transgender Discrimination Survey reported attempting suicide, a proportion much greater than the 5% of US adults and the 10% to 20% of lesbian, gay, and bisexual adults who reported ever attempting suicide. 4 Factors associated with suicide attempts included experiencing minority stress related to comorbid health conditions, alienation from family, and experiencing discrimination or marginalization at school or work or when accessing health care. 4
The rate of deaths coded as symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified, were 5 to 19 times higher among TGD individuals compared with cisgender persons. These codes are used when the physician completing the death certificate has insufficient knowledge of the disease that caused the death. These codes are often temporary, because an autopsy can determine cause of death to update the death certificate. 30 In the present study, all these deaths occurred well before the end of the death registry. Previous research 30 , 31 has shown that these codes are more commonly used among minoritized ethnic groups and those from marginalized populations. However, given the small number of events in our study, it is difficult to make inferences about these results.
We did not find increased deaths from cardiovascular infectious diseases among TGD persons in our analysis, contrary to previous research. 11 , 32 Our TGD cohort is young, and cardiovascular deaths in these age groups are rare. Furthermore, we included TGD persons without documentation of gender-affirming hormone therapy, so cardiovascular risk may be lower in our cohort than if we had restricted to those taking therapy. Because we used a primary care database of people receiving medical care, the individuals living with HIV in our study may be more likely to be receiving treatment than individuals sampled in other studies. 11 , 16 , 17 Furthermore, the median index year in our study was 2011, when the use of highly active antiretroviral therapy was widespread, resulting in greatly reduced HIV-related mortality. 33 Indeed, in previous studies, 11 HIV-related deaths decreased among TGD people over time owing to improved HIV treatment. However, mortality from endocrine disorders was more common among TGD individuals compared with cisgender women, which, to our knowledge, has not been reported before. 11 , 17 Further research is needed to understand this increased risk.
We found that TGD persons had no increased risk of cancer death, with transfeminine adults having half the mortality risk of cisgender men. When we examined the most common cancer-specific deaths among TGD people (gastrointestinal and lung cancers), we did not find differences in mortality between TGD individuals and cisgender individuals. Lower rates of cancer-specific mortality among transfeminine people compared with cisgender men may be due to deaths from prostate cancer. There were 51 prostate cancer deaths in cisgender men, and none among transfeminine adults, who have a substantially lower risk of prostate cancer owing to the use of antiandrogen and estrogen hormone therapy. 34 Similarly, there were 116 breast cancer deaths among cisgender women but none among transmasculine adults, for whom risk is lower because of gender-affirming chest surgery. 35 However, as noted already, our cohort is young, and more longitudinal data are needed to understand how long-term hormone use may affect cancer risk at older ages.
This study has limitations. CPRD does not collect gender identity from self-report, which is the criterion standard for ascertaining TGD status. 36 Instead, we used diagnosis codes for gender incongruence to identify TGD patients, which may have missed individuals and underestimated mortality among TGD persons. We used multiple imputation to fill in missing sex assigned at birth for approximately 1000 TGD individuals, which is an imperfect solution and highlights the need for the collection of self-reported gender identity in medical systems. Hormone therapy prescribed by the gender identity clinics was not consistently updated in the patient’s chart. Missing information on hormone therapy prevented us from elucidated sex assigned at birth for many patients and prevented us from examining associations between hormone use and some causes of death (eg, endocrine disorders). We were not able to able to analyze individuals of Asian ethnicity or another race separately because of a limited sample size. In addition, although this is one of the largest mortality studies of TGD persons, the number of deaths was small, thus limiting its statistical power.
To our knowledge, this cohort study is the first report on mortality among TGD persons in England. We found that transfeminine and transmasculine individuals had higher mortality rates than cisgender individuals. Furthermore, we found that those without a record of gender-affirming care and nonbinary individuals may be at highest risk of mortality, underscoring the need for customized care for this population. Our results highlight the need to understand the factors leading to minority stress and to develop interventions for suicide, homicide, and accidental poisonings to reduce mortality for TGD individuals. Future work should follow this cohort as they age to estimate the incidence of conditions like cardiovascular disease and cancer.
Accepted for Publication: December 11, 2022.
Published: January 30, 2023. doi:10.1001/jamanetworkopen.2022.53687
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Jackson SS et al. JAMA Network Open .
Corresponding Author: Sarah S. Jackson, PhD, MPH, Infections and Immunoepidemiology Branch, Division of Cancer Epidemiology and Genetics, National Cancer Institute, National Institutes of Health, 9609 Medical Center Dr, Rm 6-E210, Rockville, MD 20850 ( [email protected] ).
Author Contributions: Dr Jackson had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Jackson, Pfeiffer, Shiels.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Jackson, Brown, Pfeiffer.
Critical revision of the manuscript for important intellectual content: Jackson, Brown, Shrewsbury, O’Callaghan, Berner, Gadalla, Shiels.
Statistical analysis: Jackson, Brown, Pfeiffer, Shiels.
Obtained funding: Jackson.
Administrative, technical, or material support: Gadalla.
Supervision: Jackson.
Conflict of Interest Disclosures: Ms Berner reported receiving personal fees from Pfizer Oncology and Eisai for working on nonpromotional educational materials and serving as a speaker outside the submitted work. No other disclosures were reported.
Funding/Support: This work was supported by the Intramural Research Program, Division of Cancer Epidemiology and Genetics, National Cancer Institute, National Institutes of Health.
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Postoperative complications of male to female sex reassignment surgery: A 10-year French retrospective study
Affiliations.
- 1 Department of plastic, reconstructive and aesthetic surgery, Saint-Louis hospital, avenue Claude-Vellefaux, 75475 Paris cedex 10, France; Paris Diderot university, Sorbonne Paris, Paris, France; Plastic and aesthetic surgery department, hôpital Tenon, Paris, France.
- 2 Plastic and reconstructive surgery, Conception hospital, 147, boulevard Baille, 13005 Marseille, France.
- 3 Department of plastic, reconstructive and aesthetic surgery, Saint-Louis hospital, avenue Claude-Vellefaux, 75475 Paris cedex 10, France.
- 4 Department of plastic, reconstructive and aesthetic surgery, Saint-Louis hospital, avenue Claude-Vellefaux, 75475 Paris cedex 10, France; Paris Diderot university, Sorbonne Paris, Paris, France.
- 5 Plastic and aesthetic surgery department, hôpital Tenon, Paris, France.
- 6 Department of plastic, reconstructive and aesthetic surgery, Saint-Louis hospital, avenue Claude-Vellefaux, 75475 Paris cedex 10, France; Plastic and reconstructive surgery, François-Mitterand hospital, 14, rue Paul-Gaffarel, 21079 Dijon, France. Electronic address: [email protected].
- PMID: 30269882
- DOI: 10.1016/j.anplas.2018.08.002
In primary male to female (MTF) sex reassignment surgery (SRS), the most frequent postoperative functional complications using the penoscrotal skin technique remain neovaginal stenosis, urinary meatal stenosis and secondary revision surgery. We aimed to retrospectively analyze postoperative functional and anatomical complications, as well as secondary procedures required after MTF SRS by penile skin inversion. All patients operated on for MTF SRS, using the inverted technique, from June 2006 to July 2016, were retrospectively reviewed. The minimum follow-up was one year (five-years maximum follow-up). Soft postoperative dilationprotocol was prescribed until complete healing of the vagina. We did not prescribe long-term hard dilation systematically. Possible short-depth neovaginas were primarily treated with further temporary dilation using a hard bougie. Among the 189 included patients, we reported a 2.6% of rectovaginal wall perforations. In 37% of patients we had repeated compressive dressings and 15% of them required blood transfusions. Eighteen percent of patients presented with hematoma and 27% with early infectious complications. Delayed short-depth neovagina occurred in 21% of patients, requiring additional hard dilatation, with a 95.5% success rate. Total secondary vaginoplasty rate was 6.3% (4.7% skin graft and 3.7% bowel plasty). Secondary functional meatoplasty occurred in 1% of cases. Other secondary cosmetic surgery rates ranged between 3 to 20%. A low rate of secondary functional meatoplasty was showed after MTF SRS by penile skin inversion. Hard dilation was prescribed in case of healed short-depth vagina, with good efficiency in most of cases. Secondary vaginoplasty was required in cases of neovagina stenosis or persisting short-depth neovagina after failure of hard dilation protocol.
Keywords: Chirurgie de changement de sexe; Complications postopératoires; Follow-up; Postoperative complications; Sex reassignment surgery; Suivi.
Copyright © 2018 Elsevier Masson SAS. All rights reserved.
- Blood Transfusion / statistics & numerical data
- Middle Aged
- Postoperative Complications
- Retrospective Studies
- Sex Reassignment Surgery / adverse effects*
- Young Adult
- International edition
- Australia edition
- Europe edition

April Ashley, model, actor and transgender activist, dies aged 86
Performer and campaigner was one of the first Britons to undergo gender reassignment surgery
Tributes have been paid to the “true trailblazer” transgender activist April Ashley, who has died aged 86.
One of the first Britons to undergo gender assignment surgery, the model and actor was made an MBE in 2012 for her campaigning work for the transgender community.
Born to a working-class family in Liverpool in 1935, Ashley joined the merchant navy as a teenager. After repeated suicide attempts and a stint in a psychiatric unit, she moved to London in 1955 and then to Paris.
In Paris, she performed at the Le Carrousel nightclub, which was famous for its drag acts, where she was able to save up money for her gender assignment procedure.
In 1960, Ashley became only the second Briton to undergo male to female transition surgery when she had the operation in Casablanca, Morocco. She said in later interviews the procedure made her the happiest she had ever been.
Back in England, she obtained a national insurance card, passport and driving licence that identified her as female.
She went on to have a successful modelling career and was photographed for Vogue magazine and appeared in films including Road to Hong Kong with Bob Hope, Bing Crosby and Joan Collins.
Her career was abruptly cut short in 1961 when the Sunday People outed her as transgender.
In 1963, she married aristocrat Arthur Cameron Corbett in Gibraltar. Their divorce in 1970 marked a landmark legal ruling when the judge ruled it was not possible to legally change sex, and that the marriage was therefore invalid.
Left with nothing, Ashley emigrated to the US west coast to escape the prejudice and discrimination she faced at home. She returned to Britain in 2005, when she was legally recognised as female thanks to the Gender Recognition Act.
The singer Boy George tweeted: “R.I.P April Ashley! A force of nature and transgender high priestess!”
Peter Tatchell, the LGBTQ+ rights campaigner, called her “the GREAT trans trailblazer for decades” and “hero”.
“I was so honoured to know & support her in a past era when she was reviled after being outed as trans,” he said.
Trans activist and actor Jake Graf wrote: “A true trailblazer of the trans community has left us. April Ashley MBE was the definition of grace and humility, despite having fought hard throughout her life for her place in society.
“A true queen. Gone, but never forgotten. Rest in power.”
- Transgender
Most viewed
Court orders first gender-affirming surgery for a transgender federal prisoner
In a first, the Federal Bureau of Prisons has been ordered to secure gender-affirming surgery for a transgender prisoner.
A federal judge in the U.S. District Court for the Southern District of Illinois ordered the bureau on Monday to undergo a nationwide search for a qualified surgeon to perform the surgery for the inmate, Cristina Nichole Iglesias.
The directive will bring Iglesias — who has been imprisoned since 1994 for threatening to use a weapon of mass destruction — a step closer to receiving the procedure, which she has been fighting to get for six years, the last three in the courts.
“I am hopeful that I will finally get the care I need to live my life fully as the woman I am,” Iglesias said in a statement provided to NBC News by her legal representative, the American Civil Liberties Union. “BOP has denied me gender-affirming surgery for years — and keeps raising new excuses and putting new obstacles in my way. I am grateful that the court recognized the urgency of my case and ordered BOP to act.”
Monday's court order could pave the way for other transgender prisoners to receive gender-affirming surgeries as well. LGBTQ advocates have called these procedures "life-saving," and Monday's decision could bolster the Biden administration's goal of improving the lives of incarcerated transgender people.
A 2015 report by the Justice Department estimated that 35 percent of trans prisoners surveyed had reported being sexually assaulted behind bars within the last year. Under the Trump administration, the Bureau of Prisons was required to “use biological sex as the initial determination” for housing trans prisoners.
A 2020 NBC News investigation that tracked 45 states and Washington, D.C., found that out of 4,890 transgender inmates in state prisons, only 15 were confirmed to being housed according to their lived gender.
In January, the Biden administration restored Obama-era guidelines for federal prisons to house transgender inmates by their gender identity "when appropriate." The guidelines also require prison staff to refer to trans inmates by their lived name and pronouns.
The ACLU estimates that the Federal Bureau of Prisons has more than 1,200 transgender people currently in its custody.
Iglesias has been in federal prison for roughly 28 years and currently lives in a bureau-run residential re-entry center in Florida, according to the ACLU.
Although she identified herself as a woman upon her incarceration, she has been housed in men's facilities for over two decades, and during that time has experienced physical and sexual violence, the ACLU said. In May, her lawsuit to seek gender-affirming surgery resulted in her being one of the few transgender federal prisoners moved to a facility that corresponds with her gender identity.
Iglesias then became the first transgender prisoner to be evaluated for gender-affirming surgery, which the Bureau of Prisons recommended in January. However, the ACLU said in a statement that the bureau had "sought to postpone any referral to a surgeon for months."
In Monday's ruling , Judge Nancy Rosenstengel slammed the prison bureau's handling of Iglesias' case and compared its "tactics" to a game of “whack-a-mole.” Rosenstengel also ordered the bureau to provide the court with weekly updates and a detailed plan to ensure that Iglesias gets the surgery before her release in December.
The Bureau of Prisons told NBC News in a statement that it does not comment on “pending litigation or matters subject to legal proceedings,” nor on “the conditions of confinement for any individual or group of inmates.”
“For years, Cristina has fought to receive the health care the Constitution requires," Joshua Blecher-Cohen, an ACLU of Illinois staff attorney who represents Ms. Iglesias, said in a statement.
"The court’s order makes clear that she needs gender-affirming surgery now and that BOP cannot justify its failure to provide this medically necessary care," he said. "We hope this landmark decision will help secure long-overdue health care for Cristina — and for the many other transgender people in federal custody who have been denied gender-affirming care.”
Follow NBC Out on Twitter , Facebook & Instagram
Reporter, NBC OUT
Do I need a referral to see a specialist? Learn more here . Explore the Department Directory Learn more about Telehealth Appointments Protect Yourself from West Nile Virus
How to schedule your APPOINTMENT at Denver Health: CURRENT PATIENTS: Login to MyChart to schedule appointments or call 303-436-4949 . NEW PATIENTS: Schedule an appointment online or call 303-436-4949 . NEED CARE? Schedule a Virtual Urgent Care appointment or click here to find an Urgent Care clinic .
MyChart Login
Login to MyChart
MyChart for Mobile
Download the MyChart mobile app for access to your healthcare information. Managing your healthcare has never been more simple. Download for iPhone and Android .
MyChart Sign Up
Learn about MyChart features , and sign up for an account .
Virtual Urgent Care Now Available for Denver Health MyChart Users
Denver Health MyChart users can now have a virtual urgent care visit with one of our expert providers. It’s easy and convenient to get the urgent care you need from the comfort of your home, using your smartphone, tablet or computer.
Click here for more details

- Departments & Services
- Conditions & Treatments
- Our Locations
- Find a Provider
- Pharmacy / Prescriptions
- Pay my bill
- Main Campus (303) 436-6000
- Appointments (303) 436-4949
- Lean Academy 855-888-5326
- Nurseline (303) 739-1211
- Pharmacy (303) 389-1390
- Telehealth (303) 436-4949
Contact LGBTQ Patient Navigator
Hours of operation, vaginoplasty.
Learn more about gender affirmation surgery:
Interested in this surgery?
Please complete the following surgical interest form and submit it to our LGBTQ+ Services team.
Surgical Interest Form
Overview of Vaginoplasty
Vaginoplasty is a gender-affirming, feminizing, lower surgery to create a vagina* and vulva (including mons, labia, clitoris, and urethral opening) and remove the penis, scrotal sac and testes.
What is the procedure for vaginoplasty?
- The scrotum and testes are removed.
- The glans is made into a clitoris.
- Space for the vagina is dissected between the bladder and the rectum.
- Skin from the shaft of the penis* is inverted to create the inner walls of your vagina.
- Extra skin may be taken from the scrotum* to line your vagina. The hair roots on the skin graft will be cauterized.
- The urethra is shortened.
- Vulva are created using scrotal and urethral tissue.
- A temporary urinary catheter is inserted into the bladder.
- A temporary prosthesis/stent is inserted in the vagina.
Do I need to have hair removal before vaginoplasty ?
Hair removal is highly encouraged and recommended prior to penile inversion vaginoplasty (full depth vaginoplasty). The scrotal skin will be used to make the neo vagina. If you do not do hair removal, there will be hair inside the vagina. This can make post operative care more difficult and place you at increased risk for post op infection. The surgeon will not do any hair removal during the surgical procedure. Ask an LGBTQ+ Patient Advocate about resources for hair removal.
** Hair removal is not required for minimal depth vaginoplasty.
Do I need to stop taking hormones before vaginoplasty?
Your surgeon will discuss this with you at your pre-visit.
How long will my hospital stay be?
You will be admitted to the hospital for 3 days following your surgery.
What medications will I be prescribed after surgery?
You will likely receive painkillers and antibiotics to prevent infection. Your surgeon will provide you with a list of medications to avoid for the first month. Do not resume taking hormones until your surgeon has advised you to do so.
What should I expect during the healing process?
- Bleeding during the first 48 hours following surgery
- Itchiness and small shooting electrical sensations as nerve endings heal
- Bruising can spread from your belly to your thighs and takes 3-4 weeks to settle down
- A bit of spraying when you urinate which usually improves over time
- Swelling of your labia which can take up to 6 weeks to resolve
- Brown/yellow vaginal discharge for the first 6-8 weeks
- Your vulva will approach its final appearance at 4 months
- Numbness that will improve over the first few months, and can take up to 18 months to resolve
- Red, dark pink or purple scars that take up to one year to fade
What will my post-operative routine look like?
A urinary catheter will be in place for the first five days after surgery to allow you to pass urine while your urethra heals. Sometimes people still aren’t able to urinate when the catheter comes out, due to swelling around the urethra. This situation can easily be resolved with a second catheter that will remain in place for a week and be removed by your physician when you go home. You’ll be encouraged to drink lots of fluids to prevent urinary tract infections.
A prosthesis/stent will be placed in your vagina during surgery and will remain there for 5 days to make sure the skin grafts stay in place. When it’s removed, you will begin dilating and douching. A vaginal douche is a process of rinsing the vagina by forcing water or another solution into the vagina to flush away vaginal discharge or other contents. You will be given a set of vaginal dilators of different sizes. You’ll use them to maintain vaginal depth and width and promote healing.
Initially, you’ll dilate several times a day and over the first year the amount of time spent dilating will be gradually reduced. After you have completely healed, you will only need to dilate about once a week. The frequency depends on how much penetrative sex you have. For the first two months after surgery, you will take sitz baths. A sitz bath is a way to soak your surgical site to keep it clean. You’ll want to wear thin maxi pads for about one month to manage post-operative bleeding and discharge.
What check-ups will be needed after my hospital stay?
The number of check-ups needed varies from person to person. If possible, see your primary care provider about a week after and then every 2-4 weeks for the first few months. When you visit your surgeon or primary care provider, they should check your surgical sites to make sure there are no infections or wound healing problems. They will ask questions about dilating, bleeding, vaginal discharge, fever, pain and how you are feeling emotionally and physically.
How long will it take for me to get back to my usual activities?
Recovery time varies from person to person, so always follow the advice of your surgeon. Many people begin to feel more comfortable during the second week after their surgery. You’ll need plenty of rest in the first two weeks. It’s common to be back to your usual activities, including work, in six to eight weeks. Some activities, such as driving, heavy lifting, exercise, sex and soaking in hot tubs, may be restricted in the post-operative period. Your surgeon will give you advice about when it is okay to resume these activities. Complete recovery can take up to one year.
What complications are associated with vaginoplasty?
All surgical procedures involve some risks, including negative reactions to anesthesia, blood loss, blood clots and infection. These complications can, in extreme cases, result in death. It’s important to discuss these risks in detail with your surgeon. Your surgical care team will take a wide variety of steps to prevent these problems, detect them if they arise and respond to them appropriately.
They will also inform you about what you can do to minimize your risks. The list below includes some of the complications associated with vaginoplasty in particular. It does not replace a thorough consultation with your surgeon.
This is when blood collects in the surgical site, causing pain, swelling and redness. Smaller hematomas can be drained, but larger ones require removal through surgery.
Abscess Formation
An abscess is a collection of pus. It’s caused by a bacterial infection. It can be treated with antibiotics or drained by the surgeon.
This is when clear fluid accumulates in the surgical site. Small seromas may need to be aspirated, or sucked out, once or more by the surgeon.
Loss of Sensation
You may have small areas of numbness. Your ability to achieve orgasm could decrease. Loss of clitoris is a remote possibility.
Rectovaginal fistula
This is when an abnormal path between the rectum and vagina is created. Surgery would be needed to correct this.
May be correctable with various treatments, including additional surgery.
Injury to the Nerves or Muscles in the Legs
Can lead to numbness or a change of sensation in the skin of the legs. In very rare cases, it can lead to difficulty moving the leg which needs correction through surgery.
Unsatisfactory Size or Shape of the Vagina, Clitoris or Labia
Outcomes that are quite different from what was expected may require surgical revision.
Urological Complications
Examples include:
- fistulas (flow of urine to areas other than urethra opening)
- stenosis (narrowing of the urethra, causing difficulties urinating)
- strictures (blockage of the urethra, causing difficulty urinating).
It is common to have spraying or dribbling when urinating until your swelling settles down. If these problems don’t resolve on their own, they may require additional surgery.
- 0 && newsLoaded" class="" data-id="{044698B9-FA04-4636-994D-47662155601F}" ref="news"> News
- 0 && blogLoaded" class="" data-id="{9AB9C6CB-06BD-4D71-867F-FAB69D88F93C}" ref="blog"> Blog Articles
- 0 && storiesLoaded" class="" data-id="{71E64EA2-1956-4F7C-A67D-579E0BB54378}" ref="stories"> Patient Stories
- Apr 27 Boot Camp for New Dads ®
- May 1 Labor and Delivery Tour for Expectant Families
- May 8 Labor and Delivery Tour for Expectant Families
- May 11 Labor and Delivery Tour for Expectant Families
- Skip to main content
- Keyboard shortcuts for audio player

Heated arguments at the Supreme Court in newest abortion case

Nina Totenberg

The Supreme Court heard arguments in a case examining a federal-state conflict over emergency abortions. Catie Dull/NPR hide caption
The Supreme Court heard arguments in a case examining a federal-state conflict over emergency abortions.
Inscrutable. That is the only word to accurately describe the Supreme Court's latest abortion argument Thursday.
At issue is a clash between federal and state law about how pregnant women must be treated in the emergency room. Specifically, whether a state may ban medical termination of a pregnancy if the woman's health, but not her life, is in grave danger.

Supreme Court to examine a federal-state conflict over emergency abortions
The case centers on a law enacted in 1986 to stop hospitals from turning away uninsured patients or dumping them on other hospitals. It's known as the Emergency Medical Treatment and Labor Act, or EMTALA. The law says that as a condition for receiving Medicare funds, hospital emergency departments must stabilize a patient whose life or health is at risk. If the hospital can't do that, it must provide safe transport to a facility that can.
But Idaho and a few other states have now enacted laws that ban emergency abortions unless the mother's life, but not her health, is at risk.

Shots - Health News
What's at stake as the supreme court hears idaho case about abortion in emergencies.
At the Supreme Court lectern Thursday, Idaho Solicitor General Joshua Turner defended the restrictive law, declaring that the state is entitled to make decisions about the practice of medicine within its borders. But he faced some unusually angry questions from the court's three liberal justices, all women, with an occasional assist from conservative Justice Amy Coney Barrett, who is firmly opposed to abortion.
Justice Sonia Sotomayor hammered Turner with a series of real-life examples of women in dire health circumstances, who would be denied a medically necessary abortion under the Idaho law. She interrupted him so often that Chief Justice John Roberts at one point intervened to lower the temperature and get an answer from Turner.
Drawing an analogy not involving abortion, Sotomayor, a diabetic, observed that "no state licensing law" would permit the state to tell doctors, "don't treat diabetics with insulin, treat them only with [far less effective] pills.... Federal law would say you can't do that."

Supreme Court allows Idaho abortion ban to be enacted, first such ruling since Dobbs
Justice Elena Kagan asked Turner what in EMTALA says that a woman has to be at "death's door" before doctors treat her with a necessary emergency abortion to stabilize her condition.
"That understanding is a humble one with respect to the federalism role of the states as the primary care provider for the citizens, not the federal government," Turner answered.
"It may be too humble for women's health, you know," Kagan observed, caustically.
And Justice Ketanji Brown Jackson said that EMTALA established a "federal mandate" that preempts state laws.
Pummeled with questions, Idaho's Turner refused to commit to which health-threatening conditions could be legally treated with abortions under state law. Could an abortion take place to preserve a woman's organs? Her fertility? To save her from future debilitating kidney disease or strokes?
Turner's ambiguous answers prompted surprise from Justice Barrett, a mother of seven who has herself had miscarriages. "Counsel, I'm kind of shocked actually because I thought your own expert had said below that these kinds of cases were covered. And you're now saying they're not? Turner's replay clearly didn't satisfy her. She accused him of "hedging."
Chief Justice Roberts asked who would make the decision, other than the doctor, as to what constitutes a permissible emergency abortion and what the standard would be.
Turner replied that there is no objective standard, just a subjective one. The doctor's decision would not be judged based on what a "reasonable doctor" would do, only on whether he personally acted in good faith.
Arguing the other side of the case on behalf of the Biden administration, Solicitor General Elizabeth Prelogar faced an equal barrage of questions, mainly from the court's conservative justices.
Could a woman's psychological health be justification for an emergency abortion? No, replied Prelogar.
Three justices—Roberts, Barrett, and Neil Gorsuch—all asked if EMTALA provides exceptions for doctors or hospitals with religious objections to abortion.
Prelogar replied that conscience objections exempt both from performing abortions under EMTALA, but she added that the Department of Health and Human Services "had never come across a hospital that had a blanket objection to providing life-preserving and health-preserving pregnancy termination care."
Several conservative justices also sought to flesh out what limits there might be to laws that condition federal aid, such as the funding to hospitals governed by EMTALA. Barrett and Gorsuch, for instance, asked if gender-reassignment surgery could be banned at hospitals as a condition for receiving federal money.
Prelogar replied that in her view Congress has that power.
And Justice Samuel Alito, author of the decision overturning Roe v. Wade, looked up at the clock at one point and observed that an hour and a half into the argument, "one potentially very important phrase in EMTALA has hardly been mentioned...and that is EMTALA's reference to the woman's 'unborn child.'"
"The statute did nothing to displace the woman herself as an individual with an emergency medical condition," Prelogar replied. "In many of the cases you're thinking about, there is no possible way to stabilize the unborn child...it's inevitable that the pregnancy is going to be lost, but Idaho would deny women treatment in that circumstance even though it's senseless."
A decision in the case is expected in the summer.
- Supreme Court
- Election Integrity
- Immigration
Political Thought
- American History
- Conservatism
- Progressivism
International
- Global Politics
- Middle East
Government Spending
- Budget and Spending
Energy & Environment
- Environment
Legal and Judicial
- Crime and Justice
- Second Amendment
- The Constitution
National Security
- Cybersecurity
Domestic Policy
- Government Regulation
- Health Care Reform
- Marriage and Family
- Religious Liberty
- International Economies
- Markets and Finance
Sex Reassignment Doesn’t Work. Here Is the Evidence.

Ryan T. Anderson, Ph.D.
Former Visiting Fellow, DeVos Center

Key Takeaways
McHugh points to the reality that because sex change is physically impossible, it frequently does not provide the long-term wholeness and happiness that people seek.
Unfortunately, many professionals now view health care—including mental health care—primarily as a means of fulfilling patients’ desires, whatever those are.
Our brains and senses are designed to bring us into contact with reality, connecting us with the outside world and with the reality of ourselves.
Sex “reassignment” doesn’t work. It’s impossible to “reassign” someone’s sex physically, and attempting to do so doesn’t produce good outcomes psychosocially.
As I demonstrate in my book, “ When Harry Became Sally: Responding to the Transgender Moment ,” the medical evidence suggests that sex reassignment does not adequately address the psychosocial difficulties faced by people who identify as transgender. Even when the procedures are successful technically and cosmetically, and even in cultures that are relatively “trans-friendly,” transitioners still face poor outcomes.
Dr. Paul McHugh, the university distinguished service professor of psychiatry at the Johns Hopkins University School of Medicine, explains :
Transgendered men do not become women, nor do transgendered women become men. All (including Bruce Jenner) become feminized men or masculinized women, counterfeits or impersonators of the sex with which they ‘identify.’ In that lies their problematic future.
When ‘the tumult and shouting dies,’ it proves not easy nor wise to live in a counterfeit sexual garb. The most thorough follow-up of sex-reassigned people —extending over 30 years and conducted in Sweden, where the culture is strongly supportive of the transgendered—documents their lifelong mental unrest. Ten to 15 years after surgical reassignment, the suicide rate of those who had undergone sex-reassignment surgery rose to 20 times that of comparable peers.
Indeed, the best scientific research supports McHugh’s caution and concern.
Here’s how The Guardian summarized the results of a review of “more than 100 follow-up studies of post-operative transsexuals” by Birmingham University’s Aggressive Research Intelligence Facility:
[The Aggressive Research Intelligence Facility], which conducts reviews of health care treatments for the [National Health Service], concludes that none of the studies provides conclusive evidence that gender reassignment is beneficial for patients. It found that most research was poorly designed, which skewed the results in favor of physically changing sex. There was no evaluation of whether other treatments, such as long-term counseling, might help transsexuals, or whether their gender confusion might lessen over time.
“There is huge uncertainty over whether changing someone’s sex is a good or a bad thing,” said Chris Hyde, the director of the facility . Even if doctors are careful to perform these procedures only on “appropriate patients,” Hyde continued, “there’s still a large number of people who have the surgery but remain traumatized—often to the point of committing suicide.”
Of particular concern are the people these studies “lost track of.” As The Guardian noted, “the results of many gender reassignment studies are unsound because researchers lost track of more than half of the participants.” Indeed, “Dr. Hyde said the high drop-out rate could reflect high levels of dissatisfaction or even suicide among post-operative transsexuals.”
Hyde concluded: “The bottom line is that although it’s clear that some people do well with gender reassignment surgery, the available research does little to reassure about how many patients do badly and, if so, how badly.”
The facility conducted its review back in 2004, so perhaps things have changed in the past decade?
Not so. In 2014, a new review of the scientific literature was done by Hayes, Inc., a research and consulting firm that evaluates the safety and health outcomes of medical technologies. Hayes found that the evidence on long-term results of sex reassignment was too sparse to support meaningful conclusions and gave these studies its lowest rating for quality:
Statistically significant improvements have not been consistently demonstrated by multiple studies for most outcomes. … Evidence regarding quality of life and function in male-to-female adults was very sparse. Evidence for less comprehensive measures of well-being in adult recipients of cross-sex hormone therapy was directly applicable to [gender dysphoric] patients but was sparse and/or conflicting. The study designs do not permit conclusions of causality and studies generally had weaknesses associated with study execution as well. There are potentially long-term safety risks associated with hormone therapy but none have been proven or conclusively ruled out.
The Obama administration came to similar conclusions. In 2016, the Centers for Medicare and Medicaid Services revisited the question of whether sex reassignment surgery would have to be covered by Medicare plans. Despite receiving a request that its coverage be mandated, it refused, on the ground that we lack evidence that it benefits patients.
Here’s how the June 2016 “ Proposed Decision Memo for Gender Dysphoria and Gender Reassignment Surgery ” put it:
Based on a thorough review of the clinical evidence available at this time, there is not enough evidence to determine whether gender reassignment surgery improves health outcomes for Medicare beneficiaries with gender dysphoria. There were conflicting (inconsistent) study results—of the best designed studies, some reported benefits while others reported harms. The quality and strength of evidence were low due to the mostly observational study designs with no comparison groups, potential confounding, and small sample sizes. Many studies that reported positive outcomes were exploratory type studies (case-series and case-control) with no confirmatory follow-up.
The final August 2016 memo was even more blunt. It pointed out:
Overall, the quality and strength of evidence were low due to mostly observational study designs with no comparison groups, subjective endpoints, potential confounding (a situation where the association between the intervention and outcome is influenced by another factor such as a co-intervention), small sample sizes, lack of validated assessment tools, and considerable lost to follow-up.
That “lost to follow-up,” remember, could be pointing to people who committed suicide.
And when it comes to the best studies, there is no evidence of “clinically significant changes” after sex reassignment:
The majority of studies were non-longitudinal, exploratory type studies (i.e., in a preliminary state of investigation or hypothesis generating), or did not include concurrent controls or testing prior to and after surgery. Several reported positive results but the potential issues noted above reduced strength and confidence. After careful assessment, we identified six studies that could provide useful information. Of these, the four best designed and conducted studies that assessed quality of life before and after surgery using validated (albeit non-specific) psychometric studies did not demonstrate clinically significant changes or differences in psychometric test results after [gender reassignment surgery].
In a discussion of the largest and most robust study—the study from Sweden that McHugh mentioned in the quote above—the Obama Centers for Medicare and Medicaid Services pointed out the 19-times-greater likelihood for death by suicide, and a host of other poor outcomes:
The study identified increased mortality and psychiatric hospitalization compared to the matched controls. The mortality was primarily due to completed suicides (19.1-fold greater than in control Swedes), but death due to neoplasm and cardiovascular disease was increased 2 to 2.5 times as well. We note, mortality from this patient population did not become apparent until after 10 years. The risk for psychiatric hospitalization was 2.8 times greater than in controls even after adjustment for prior psychiatric disease (18 percent). The risk for attempted suicide was greater in male-to-female patients regardless of the gender of the control. Further, we cannot exclude therapeutic interventions as a cause of the observed excess morbidity and mortality. The study, however, was not constructed to assess the impact of gender reassignment surgery per se.
These results are tragic. And they directly contradict the most popular media narratives, as well as many of the snapshot studies that do not track people over time. As the Obama Centers for Medicare and Medicaid pointed out, “mortality from this patient population did not become apparent until after 10 years.”
So when the media tout studies that only track outcomes for a few years, and claim that reassignment is a stunning success, there are good grounds for skepticism.
As I explain in my book , these outcomes should be enough to stop the headlong rush into sex reassignment procedures. They should prompt us to develop better therapies for helping people who struggle with their gender identity.
And none of this even begins to address the radical, entirely experimental therapies that are being directed at the bodies of children to transition them.
Sex Change Is Physically Impossible
We’ve seen some of the evidence that sex reassignment doesn’t produce good outcomes psychosocially. And as McHugh suggested above, part of the reason why is because sex change is impossible and “it proves not easy nor wise to live in a counterfeit sexual garb.”
But what is the basis for the conclusion that sex change is impossible?
Contrary to the claims of activists , sex isn’t “assigned” at birth—and that’s why it can’t be “reassigned.” As I explain in “When Harry Became Sally,” sex is a bodily reality that can be recognized well before birth with ultrasound imaging. The sex of an organism is defined and identified by the way in which it (he or she) is organized for sexual reproduction.
This is just one manifestation of the fact that natural organization is “the defining feature of an organism,” as neuroscientist Maureen Condic and her philosopher brother Samuel Condic explain. In organisms, “the various parts … are organized to cooperatively interact for the welfare of the entity as a whole. Organisms can exist at various levels, from microscopic single cells to sperm whales weighing many tons, yet they are all characterized by the integrated function of parts for the sake of the whole.”
Male and female organisms have different parts that are functionally integrated for the sake of their whole, and for the sake of a larger whole—their sexual union and reproduction. So an organism’s sex—as male or female—is identified by its organization for sexually reproductive acts. Sex as a status—male or female—is a recognition of the organization of a body that can engage in sex as an act.
That organization isn’t just the best way to figure out which sex you are. It’s the only way to make sense of the concepts of male and female at all. What else could “maleness” or “femaleness” even refer to, if not your basic physical capacity for one of two functions in sexual reproduction?
The conceptual distinction between male and female based on reproductive organization provides the only coherent way to classify the two sexes. Apart from that, all we have are stereotypes.
This shouldn’t be controversial. Sex is understood this way across sexually reproducing species. No one finds it particularly difficult—let alone controversial—to identify male and female members of the bovine species or the canine species. Farmers and breeders rely on this easy distinction for their livelihoods. It’s only recently, and only with respect to the human species, that the very concept of sex has become controversial.
And yet, in an expert declaration to a federal district court in North Carolina concerning H.B. 2 (a state law governing access to sex-specific restrooms), Dr. Deanna Adkins stated, “From a medical perspective, the appropriate determinant of sex is gender identity.” Adkins is a professor at Duke University School of Medicine and the director of the Duke Center for Child and Adolescent Gender Care (which opened in 2015).
Adkins argues that gender identity is not only the preferred basis for determining sex, but “the only medically supported determinant of sex.” Every other method is bad science, she claims: “It is counter to medical science to use chromosomes, hormones, internal reproductive organs, external genitalia, or secondary sex characteristics to override gender identity for purposes of classifying someone as male or female.”
In her sworn declaration to the federal court, Adkins called the standard account of sex—an organism’s sexual organization—“an extremely outdated view of biological sex.”
Dr. Lawrence Mayer responded in his rebuttal declaration: “This statement is stunning. I have searched dozens of references in biology, medicine and genetics—even Wiki!—and can find no alternative scientific definition. In fact, the only references to a more fluid definition of biological sex are in the social policy literature.”
Just so. Mayer is a scholar in residence in the Department of Psychiatry at the Johns Hopkins University School of Medicine and a professor of statistics and biostatistics at Arizona State University.
Modern science shows that our sexual organization begins with our DNA and development in the womb, and that sex differences manifest themselves in many bodily systems and organs, all the way down to the molecular level. In other words, our physical organization for one of two functions in reproduction shapes us organically, from the beginning of life, at every level of our being.
Cosmetic surgery and cross-sex hormones can’t change us into the opposite sex. They can affect appearances. They can stunt or damage some outward expressions of our reproductive organization. But they can’t transform it. They can’t turn us from one sex into the other.
“Scientifically speaking, transgender men are not biological men and transgender women are not biological women. The claims to the contrary are not supported by a scintilla of scientific evidence,” explains Mayer.
Or, as Princeton philosopher Robert P. George put it, “Changing sexes is a metaphysical impossibility because it is a biological impossibility.”
The Purpose of Medicine, Emotions, and the Mind
Behind the debates over therapies for people with gender dysphoria are two related questions: How do we define mental health and human flourishing? And what is the purpose of medicine, particularly psychiatry?
Those general questions encompass more specific ones: If a man has an internal sense that he is a woman, is that just a variety of normal human functioning, or is it a psychopathology? Should we be concerned about the disconnection between feeling and reality, or only about the emotional distress or functional difficulties it may cause?
What is the best way to help people with gender dysphoria manage their symptoms: by accepting their insistence that they are the opposite sex and supporting a surgical transition, or by encouraging them to recognize that their feelings are out of line with reality and learn how to identify with their bodies?
All of these questions require philosophical analysis and worldview judgments about what “normal human functioning” looks like and what the purpose of medicine is.
Settling the debates over the proper response to gender dysphoria requires more than scientific and medical evidence. Medical science alone cannot tell us what the purpose of medicine is.
Science cannot answer questions about meaning or purpose in a moral sense. It can tell us about the function of this or that bodily system, but it can’t tell us what to do with that knowledge. It cannot tell us how human beings ought to act. Those are philosophical questions, as I explain in “ When Harry Became Sally .”
While medical science does not answer philosophical questions, every medical practitioner has a philosophical worldview, explicit or not. Some doctors may regard feelings and beliefs that are disconnected from reality as a part of normal human functioning and not a source of concern unless they cause distress. Other doctors will regard those feelings and beliefs as dysfunctional in themselves, even if the patient does not find them distressing, because they indicate a defect in mental processes.
But the assumptions made by this or that psychiatrist for purposes of diagnosis and treatment cannot settle the philosophical questions: Is it good or bad or neutral to harbor feelings and beliefs that are at odds with reality? Should we accept them as the last word, or try to understand their causes and correct them, or at least mitigate their effects?
While the current findings of medical science, as shown above, reveal poor psychosocial outcomes for people who have had sex reassignment therapies, that conclusion should not be where we stop. We must also look deeper for philosophical wisdom, starting with some basic truths about human well-being and healthy functioning.
We should begin by recognizing that sex reassignment is physically impossible. Our minds and senses function properly when they reveal reality to us and lead us to knowledge of truth. And we flourish as human beings when we embrace the truth and live in accordance with it. A person might find some emotional relief in embracing a falsehood, but doing so would not make him or her objectively better off. Living by a falsehood keeps us from flourishing fully, whether or not it also causes distress.
This philosophical view of human well-being is the foundation of a sound medical practice. Dr. Michelle Cretella, the president of the American College of Pediatricians—a group of doctors who formed their own professional guild in response to the politicization of the American Academy of Pediatrics—emphasizes that mental health care should be guided by norms grounded in reality, including the reality of the bodily self.
“The norm for human development is for one’s thoughts to align with physical reality, and for one’s gender identity to align with one’s biologic sex,” she says. For human beings to flourish, they need to feel comfortable in their own bodies, readily identify with their sex, and believe that they are who they actually are. For children especially, normal development and functioning require accepting their physical being and understanding their embodied selves as male or female.
Unfortunately, many professionals now view health care—including mental health care—primarily as a means of fulfilling patients’ desires, whatever those are. In the words of Leon Kass, a professor emeritus at the University of Chicago, today a doctor is often seen as nothing more than “a highly competent hired syringe”:
The implicit (and sometimes explicit) model of the doctor-patient relationship is one of contract: the physician—a highly competent hired syringe, as it were—sells his services on demand, restrained only by the law (though he is free to refuse his services if the patient is unwilling or unable to meet his fee). Here’s the deal: for the patient, autonomy and service; for the doctor, money, graced by the pleasure of giving the patient what he wants. If a patient wants to fix her nose or change his gender, determine the sex of unborn children, or take euphoriant drugs just for kicks, the physician can and will go to work—provided that the price is right and that the contract is explicit about what happens if the customer isn’t satisfied.
This modern vision of medicine and medical professionals gets it wrong, says Kass. Professionals ought to profess their devotion to the purposes and ideals they serve. Teachers should be devoted to learning, lawyers to justice, clergy to things divine, and physicians to “healing the sick, looking up to health and wholeness.” Healing is “the central core of medicine,” Kass writes—“to heal, to make whole, is the doctor’s primary business.”
To provide the best possible care, serving the patient’s medical interests requires an understanding of human wholeness and well-being. Mental health care must be guided by a sound concept of human flourishing. The minimal standard of care should begin with a standard of normality. Cretella explains how this standard applies to mental health:
One of the chief functions of the brain is to perceive physical reality. Thoughts that are in accordance with physical reality are normal. Thoughts that deviate from physical reality are abnormal—as well as potentially harmful to the individual or to others. This is true whether or not the individual who possesses the abnormal thoughts feels distress.
Our brains and senses are designed to bring us into contact with reality, connecting us with the outside world and with the reality of ourselves. Thoughts that disguise or distort reality are misguided—and can cause harm. In “ When Harry Became Sally ,” I argue that we need to do a better job of helping people who face these struggles.
This piece originally appeared in The Daily Signal
Neither federal lawmakers nor courts should have the power to redefine what it is to be a man or a woman for all Americans. Learn more about policies that curb government overreach with Solutions .
COMMENTARY 3 min read
Subscribe to email updates
© 2024, The Heritage Foundation
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley-Blackwell Online Open

Trends in suicide death risk in transgender people: results from the Amsterdam Cohort of Gender Dysphoria study (1972–2017)
C. m. wiepjes.
1 Department of Endocrinology, Amsterdam UMC, VU University Medical Center, Amsterdam the Netherlands
2 Center of Expertise on Gender Dysphoria, Amsterdam UMC, VU University Medical Center, Amsterdam the Netherlands
M. den Heijer
M. a. bremmer.
3 Department of Psychiatry, Amsterdam UMC, VU University Medical Center, Amsterdam the Netherlands
C. J. M. de Blok
B. j. g. coumou.
4 Department of Medical Psychology, Amsterdam UMC, VU University Medical Center, Amsterdam the Netherlands
T. D. Steensma
Associated data.
Author elects to not share data.
This study explored the overall suicide death rate, the incidence over time, and the stage in transition where suicide deaths were observed in transgender people.
A chart study, including all 8263 referrals to our clinic since 1972. Information on death occurrence, time, and cause of death was obtained from multiple sources.
Out of 5107 trans women (median age at first visit 28 years, median follow‐up time 10 years) and 3156 trans men (median age at first visit 20 years, median follow‐up time 5 years), 41 trans women and 8 trans men died by suicide. In trans women, suicide deaths decreased over time, while it did not change in trans men. Of all suicide deaths, 14 people were no longer in treatment, 35 were in treatment in the previous two years. The mean number of suicides in the years 2013–2017 was higher in the trans population compared with the Dutch population.
Conclusions
We observed no increase in suicide death risk over time and even a decrease in suicide death risk in trans women. However, the suicide risk in transgender people is higher than in the general population and seems to occur during every stage of transitioning. It is important to have specific attention for suicide risk in the counseling of this population and in providing suicide prevention programs.
Significant outcomes
- Suicide death risk in trans people did not increase over time.
- Suicide deaths occurred during every stage of transitioning.
- Suicide death risk is higher in trans people than in the general population.
Limitations
- Psychological comorbidity was not known.
- No data were available for people on the waiting list for their first appointment.
Introduction
Gender dysphoria (GD) refers to the distress related to a marked incongruence between one’s assigned gender at birth and the experienced gender ( 1) . Trans people are diverse in the intensity of experienced GD ( 2) , their needs for medical transition ( 3) , and the impairment that GD can have on their life. Studies focusing on the wellbeing of trans people show a greater vulnerability for experiencing mental health problems compared with the non‐trans (cis) population ( 4) . Most prevalent are affective and anxiety problems ( 5 , 6 , 7 , often accompanied by feelings, thoughts, or behaviours linked to suicidality ( 8 , 9 .
The prevalence of suicidality in trans people in suicidal ideation, suicidal attempts, and suicide death rates is studied in varying degrees and shows high variability in findings. A systematic review by McNeil et al ( 9) . reported suicidal ideation rates across 17 identified studies, ranging from 37% ( 10) up to 83% ( 11) . Prevalence rates on suicidal attempts in trans people, which are generally observed to be lower than suicidal ideation, showed to be lower but also with a wide variation in reported rates, ranging from 9.8% ( 12) up to 44% ( 13) . Since structured prevalence studies on suicide deaths are lacking in the transgender literature, an estimation comes from a limited number of studies reporting on suicide death rates in small study samples. Derived from a systematic review on suicidality in trans people by Marshall et al. ( 8) , suicide death rates varied from 0% ( 14) to 4.2% in a sample of 24 post‐treatment trans people from Sweden ( 15) . Six of these studies only included postsurgical people ( 14 , 15 , 16 , 17 , 18 , 19 , whereas two studies also included trans people who were only using hormones without surgery ( 20 , 21 . However, studies differentiating the treatment stage during which death by suicide occurred are lacking. In addition, studies differentiating between suicide in trans women and trans men are scarce. While some studies found that trans men have a higher risk of suicide attempts than trans women ( 22 , 23 , other studies reported no differences in suicide attempts between trans women and trans men ( 24 , 25 . Only one cohort distinguished suicide death risk in trans women and trans men and found that trans women had an increased risk of suicide death compared with trans men ( 20 , 21 .
Aims of the study
The aim of the current study is to explore the overall suicide death rate in trans women and trans men in the largest clinical cohort of gender‐referred people seen at the Center of Expertise on Gender Dysphoria of the Amsterdam University Medical Centers between 1972 and 2017 the Netherlands ( 26) . In addition, the change in incidence of suicide death rate over time and at what stage in transition (pretreatment, during hormonal treatment and/or surgical phase, or post‐treatment) suicide deaths were observed was explored. The relevance of such information is to get a greater understanding of how large the risk is in clinically referred transgender people and whether suicide prevention interventions should focus on specific stages in transition or not.
Material and methods
Study design.
A retrospective chart study was performed, including all people who once visited the Center of Expertise on Gender Dysphoria of the Amsterdam UMC, Vrije Universiteit Amsterdam, the Netherlands, between 1972 and 2017. The selection of the study population is described previously ( 26) . A total of 8263 adults, adolescents, and children were included, with a median age at first visit of 25 years (range 4 to 81 years) and a median follow‐up time of 7.5 years (range 0.0 to 45.5 years). Information on death occurrence, time, and cause of death was obtained by cross‐checking multiple sources: the National Civil Record Registry ( 21) , which contains date of birth and date of death of all inhabitants of the Netherlands, and the hospital registration system, medical, and psychological files for cause of death.
The Medical Ethics Review Committee of the Amsterdam UMC, Vrije Universiteit Amsterdam, reviewed this study and determined that the Medical Research Involving Human Subjects Act (WMO) did not apply to this study. Therefore, and because of the retrospective design, necessity for informed consent was waived.
After an initial visit to the endocrinologist (for adults) or child psychiatrist (for children and adolescents), all people were referred to the psychology department for the diagnostic phase. In this phase, people were seen to gain insight into their experienced gender identity, to verify whether they fulfill the diagnosis gender dysphoria, to explore their treatment desires, and to prepare them for possible medical interventions. After this phase, people may start with hormonal treatment. Trans women received treatment with anti‐androgens and estrogens. Trans men were treated with testosterone. In adolescents, treatment first started with a period of puberty suppression, followed by estrogens of testosterone around the age of 16 years ( 27) .
Surgical interventions can be offered to people aged 18 years or older. Depending on the desired treatment, the surgery is preceded after at least one year of hormonal treatment (genital surgery) or can be offered after the diagnostic phase (e.g., breast removal). After surgery, all people were usually seen every 2 years for medical check‐up.
Statistical analyses
Characteristics of the population were shown as median with range due to the non‐normal distribution. The total number of people seen at our center and the total number of suicide deaths were counted and were expressed as percentages as well as incidence per 100 000 person years. For each year, the number of people at risk and the number of people who died by suicide were calculated. Cox regression analyses were performed to calculate hazard ratios (HR) with corresponding 95% confidence intervals (95% CI). Date of first visit was used as start date of follow‐up. The end date of follow‐up was either date of death or date of closing the database (December 31, 2017). Suicide death was analyzed as event. To analyze whether the incidence of suicide deaths changed over time, the year of first visit was added as determinant to the analyses. Analyses were adjusted for age at first visit as age might be related to suicide death risk. Time between date of suicide death and first visit, and between date of suicide death and start of hormonal treatment, if applicable, were calculated. All analyses were performed for the total population and were stratified for trans women and trans men.
All analyses were performed using STATA Statistical software (Statacorp, College Station, TX, USA), version 15.1.
The characteristics of the study population are shown in Table 1 . In total, 8263 people attended the gender identity clinic, of which 5107 were trans women (median age at first visit 28 years, range 4 to 81 years) and 3156 were trans men (median age at first visit 20 years, range 4 to 73 years). The median follow‐up time was 7.5 years (range 0.0–45.5 years), which was longer in trans women (10.2 years, range 0.0–45.5 years) than in trans men (4.8 years, range 0.0–45.5 years). The total follow‐up time was 92 227 person years (64 287 in trans women and 27 940 in trans men).
Characteristics of the study population (A) and the people who died by suicide (B)
Data are shown as number or median (range).
Forty‐nine people died by suicide: 41 trans women (0.8%) and 8 trans men (0.3%), which is 64 per 100 000 person years in trans women and 29 per 100 000 person years in trans men. The median follow‐up time between first visit and suicide death was 6.7 years (range 0.6 to 32.7 years) in trans women and 6.7 years (range 0.6 to 23.1 years) in trans men. Trans women had a higher overall suicide death risk than trans men (per year: HR 2.26, 95% CI 1.06–4.82). Four suicide deaths occurred in individuals who were referred to the clinic before the age of 18 (0.2%), which is a lower risk than in adults (0.7%, P = 0.010).
The course of number of people at risk and the number of people who died by suicide over the years is shown in Fig. 1 . Overall suicide deaths did not increase over the years: HR per year 0.97 (95% CI 0.94–1.00). In trans women, suicide death rates decreased slightly over time (per year: HR 0.96, 95% CI 0.93–0.99), while it did not change in trans men (per year: HR 1.10, 95% CI 0.97–1.25). Adjustment for age at the first visit did not change these numbers.

Number of people at risk (left y ‐axis) and the number of suicides (right y ‐axis), between 1972 and 2017.
As the median follow‐up time between first visit and suicide death was 6.7 years, subgroup analyses were performed in those who had their first visit before 2011. This did not change the outcomes: trans women ( n = 3115) HR 0.94, 95% CI 0.91–0.98; trans men ( n = 1269) HR 1.02, 95% CI 0.90–1.16).
Of the 49 people who died by suicide, 35 had a face‐to‐face contact with the endocrinologist or psychologist of the gender identity clinic in the previous two years, while the other 14 people were no longer in active counseling with the clinic. Sixteen of the 35 people who recently had visited the clinic, only came for a medical check‐up, as they were postsurgery (vaginoplasty or phalloplasty). Two people were in the surgery trajectory, and 17 were still in the diagnostic or hormonal phase at time of suicide. The transition phases separately for trans women and trans men who died by suicide are shown in Table 2 .
The occurrence of suicide deaths distinguished for transition stage, and trans women or trans men
Data are shown as number. In active counseling is defined as a face‐to‐face contact with the endocrinologist or psychologist of the gender identity clinic in the previous two years.
The mean number of suicides in the years 2013–2017 was higher in the trans population (40 per 100 000 person years; 43 per 100 000 trans women and 34 per 100 000 trans men) compared with the Dutch population in this time frame (11 per 100 000 person years; 15 per 100 00 registered men and 7 per 100 000 registered women) ( 28) .
The current study investigated the suicide death risk in the largest clinical cohort of gender‐referred individuals to the Center of Expertise on Gender Dysphoria at the Amsterdam UMC, the Netherlands, between 1972 and 2017. Findings from the chart reviews showed us a decrease in suicide death risk over time in trans women and no change in suicide death risk in trans men. Trans women, however, showed a higher suicide death risk than trans men. Between 2013 and 2017, the suicide risk in Dutch referred transgender people (40 per 100 000 person years) showed to be three to four times higher than the general Dutch population (11 per 100 000 person years) ( 28) . Evaluation of transition stage in relation to suicide deaths showed that approximately two‐third of the observed suicides occurred in those who were still in active treatment (diagnostic, hormonal, or surgical phase). The incidence of suicide deaths and transition stage was similar in trans women and trans men.
Suicidal behaviour is a complex phenomenon that is a result of many individual (age, male sex assigned at birth, previous suicide attempts, mental health history, substance abuse) as well as more distant environmental factors. A recent literature review clearly demonstrates the specific risk factors for suicide in sexual minority youth, which includes negative social environments, inadequate support within the closest social network, and an absence of lesbian, gay, bisexual, and transgender (LGBT) movements in communities ( 29) . In our cohort, both trans women and trans men show a three‐ to four‐fold elevated risk of suicide compared with the population rate in the Netherlands and can therefore be considered a high‐risk group. Although the Netherlands is known for its tolerance toward sexual minority groups in comparison to most countries in the world ( 30) , the societal position of trans people is generally less favorable compared with the lesbian, gay, bisexual, and cis‐gender population. Furthermore, compared with trans men, the societal position of trans women is lower ( 31 , 32 .
In the Netherlands, between 1972 and 2017 suicide rates showed a fluctuating course. Our finding of a slightly decreasing suicide risk in Dutch trans women may confer some hope. Recent studies showed an increase in societal acceptance toward lesbian, gay, bisexual, and transgender people ( 31) , and indications of an increase in social‐economic status over the years ( 33) . Although specific information on trans men and trans women is unavailable, it is conceivable that the improvement of societal position may have effect on the psychological functioning and the prevention of suicidal risk in trans women. The cause of this increase in tolerance seems largely to be the effect of a national and international increase in visibility and attention for trans people in media and society. Another explanation may be that, with the increase in attention and acceptance, the threshold for transgender people to seek treatment or professional help has become lower over the years. This is also reflected by the increase in referrals each year ( 26) . Lastly, with the increase of knowledge in this field and the literature about the vulnerability of the transgender population for suicidal ideation, suicidal attempts, and suicide death rates, it is conceivable to assume that the attention to these risks has increased in clinical counseling and may have its effect on prevention of suicide deaths over the years.
Although the incidence of suicide deaths in trans women decreased over the years, the overall incidence still showed to be higher in trans women compared with trans men. Conflicting results in literature are reported about the risk of suicide attempts between trans women and trans men. Some studies reported that trans men had a higher risk of suicide attempts than trans women ( 22 , 23 , while in other studies no differences in suicide attempts between trans women and trans men were found ( 24 , 25 . Only two studies looked at the differences in the risk of death by suicide between trans women and trans men and found that trans women had an increased risk compared with trans men ( 20 , 21 . However, these two studies were earlier studies performed in our center and therefore include a smaller part of our current study population.
An important finding was that the incidence for observed suicide deaths was almost equally distributed over the different stages of treatment. Although the distribution showed that one‐third of the suicides occurred in people who were no longer in active treatment in our center, the other two‐third of the people who died by suicide still visited our center in the previous two years. About half of these last two‐third people were still in active diagnostic or medical treatment, while the other half completed their transition and only came for a medical check‐up. This indicates that vulnerability for suicide occurs similarly in the different stages of transition. Although the literature on suicide risk factors is comprehensive, and particular suicidal risk factors like verbal victimization, physical and sexual violence, and the absence of social support ( 9 , 34 , may apply for transgender people in all stages of transitioning, it seems clinically highly relevant to understand and explore possible differences in motives and risk factors in the different stages of treatment. Therefore, future research on suicide deaths and suicide risk factors in transgender people should have a greater focus on transition status in relation to these motives and risk factors.
This study is performed in the largest cohort of gender‐referred people from the Netherlands, consisting of a large population of both adult and adolescent trans women and trans men at different stages of their transition with a long follow‐up time. However, this study has also some limitations. First, this study is a retrospective chart study. Although we used multiple strategies to obtain data about date of death, it is possible that we missed some data. Second, we did not have information about psychological comorbidities or other psychological information, such as social support. Third, we only had information about people who actually visited our gender identity clinic. Information about people on the waiting list for their first appointment was lacking.
To conclude, in our clinic we observed no increase in suicide death risk over time and even a decrease over time in suicide death risk in trans women was found. Since the suicide risk in the transgender population is higher than the general population and seems to occur during every stage of transitioning, it is important that (mental) health practitioners pay attention to this risk and create a safe environment in which these feelings can be discussed at all stages of treatment and counseling. Further research is necessary to investigate the motives behind the suicides, as input in the development of adequate suicide prevention programs.
Conflicts of interests
Wiepjes CM, den Heijer M, Bremmer MA, Nota NM, de Blok CJM, Coumou BJG, Steensma TD. Trends in suicide death risk in transgender people: results from the Amsterdam Cohort of Gender Dysphoria study (1972–2017) . [ PMC free article ] [ PubMed ]
Data availability statement

- Weather
Search location by ZIP code
Nh senate committee hears testimony on bill to ban some gender-confirmation surgery for children.
- Copy Link Copy {copyShortcut} to copy Link copied!

GET OUR POLITICS NEWSLETTER
Stay up to speed on all the latest local and national political news.
Lawmakers in Concord heard testimony Thursday on a bill to ban genital gender-confirmation surgery for children under the age of 18.
The Senate Judiciary Committee heard hours of testimony on House Bill 619, amended legislation that would ban genital gender-confirmation surgery for children under 18. The bill has already passed the New Hampshire House.
The legislation would also class referrals for reassignment surgery outside the state as "unprofessional conduct."
"Children are, by definition, immature," said Jennifer Black, of Windham. "We don't allow them to vote, enter into contracts, get a tattoo or smoke, because we know they lack the capacity to understand what they are doing."
>> Download the free WMUR app to get updates on the go: Apple | Google Play <<
Some argued that allowing children, with parental consent, to get an irreversible surgery at such a young age is a form of cruelty. Others noted that such procedures are only being performed on a small number of older teens nationwide.
"Twenty times per year in the United States, never in New Hampshire, and virtually all of these surgeries are vaginoplasty for 17-year-old transgender girls right before heading off to college, while they can still recover in their parents' home with their parents' love and support, rather than in a college dorm with other students who may not even know they're transgender," said Chris Erchull, of GLAD Legal Advocates & Defenders.
There is a battle over data in the debate. Lawmakers who sponsored the bill said there isn't enough data for patients or families to give informed consent with a full understanding of the risks involved.
"I'm not trying to say that to trivialize this, but if you have to wait until you're 18 to use a tanning bed with those known risks, why would be endorsing something with completely unknown risks that have many people talking about the challenges they never knew or expected from these surgeries?" said state Rep. Erica Layon, R-Derry.
Dr. Ketih Loud, chairman of the Dartmouth Health Department of Pediatrics, urging senators to reject the bill.
"We prefer to use scalpels, and this statute feels a little more like a machete and does not allow for the nuance that we need in clinical practice," Loud said.
Breaking News
ARGUMENT ANALYSIS
Supreme court divided over federal-state conflict on emergency abortion ban.
The Supreme Court on Wednesday was divided over whether a federal law requiring hospitals that participate in Medicare to provide “necessary stabilizing treatment” in an emergency overrides an Idaho law that bars most abortions.
The court’s ruling could affect health care in emergency rooms in the 22 states that have imposed restrictions on abortions, particularly in the six states that – like Idaho – lack exemptions to the general ban to protect the health of the mother.
The federal law at the center of the case is known as the Emergency Medical Treatment and Labor Act. Passed in 1986, the law was intended to ensure that all patients have access to emergency services without regard to their ability to pay for those services. And in particular, EMTALA provides that when someone with an “emergency medical condition” comes to a hospital that participates in Medicare, the hospital must offer the treatment necessary to stabilize that condition.
Shortly after the Supreme Court’s 2022 decision in Dobbs v. Jackson Women’s Health Organization , overturning the constitutional right to an abortion, the Biden administration went to federal court in Idaho. It argued that EMTALA trumps an Idaho law that generally makes it a crime to provide an abortion except in a handful of circumstances, such as to save the life of the mother or in cases of rape or incest.
A federal judge agreed with the Biden administration and barred the state from enforcing its abortion ban to the extent that it conflicted with EMTALA. After a divided U.S. Court of Appeals for the 9th Circuit declined to put that order on hold, the state and its Republican-controlled legislature came to the Supreme Court, which agreed earlier this year to allow Idaho to enforce the law and to weigh in on the merits of the dispute.
Representing the state, Idaho Solicitor General Joshua Turner told the justices that nothing in EMTALA requires doctors to provide treatments that violate state law. Turner urged the court to reject the federal government’s “unlimited” reading of EMTALA – which, he contended, would apply not only to abortion but also to laws regulating opioid treatments and to informed consent laws, among others.
U.S. Solicitor General Elizabeth Prelogar offered a very different view of EMTALA, characterizing it as a law whose “promise is simple but profound.” The law was intended to ensure that hospitals do not deny treatment to any patients who arrive at the emergency room. In cases in which there is no other way to stabilize a pregnant woman and prevent her health from deteriorating, Prelogar said, abortion is the appropriate care that hospitals must provide – even if Idaho can enforce its ban in virtually every other circumstance.
The court’s three liberal justices repeatedly pressed Turner on the state’s interpretation of EMTALA, emphasizing a variety of scenarios in which Idaho would not allow a pregnant woman to obtain an abortion. Justice Ketanji Brown Jackson described what she saw as a direct conflict between EMTALA and Idaho’s abortion ban. EMTALA, she said, provides that hospitals must provide treatment to stabilize a patient’s health, but – if abortion is involved – Idaho prohibits such treatment unless it is necessary to prevent death.
Justice Elena Kagan echoed Jackson’s concerns, asking Turner about a scenario in which a pregnant woman arrives at the emergency room with a serious health condition that will not lead to her death, but – without an abortion – will result in her being unable to have more children. A variety of scenarios exist, Kagan and her liberal colleagues repeatedly stressed, in which a pregnant patient, though not at risk of dying, could be in a state of medical distress that, without receiving an abortion, might lead to loss of organs, loss of fertility, or a need for lifelong treatments like dialysis. EMTALA, Kagan stressed, would require the hospital to perform an abortion, but Idaho would not permit it.
Turner conceded that such a situation would be “very difficult” and raise “tough medical questions.” But Kagan was not mollified by that response, countering that federal law already addresses the question, providing that doctors don’t have to wait until the pregnant woman is ready to die.
Justice Sonia Sotomayor asked Turner to address a series of rapid-fire hypotheticals involving pregnant women, including a patient whose problems began during her 14th week of pregnancy but were not sufficiently serious to warrant an abortion, leading to her delivery of the baby at 27 weeks and a hysterectomy, so that she could not have any more children.
Turner posited that doctors in Idaho could perform abortions in some of the circumstances that Sotomayor outlined, telling the court that physicians would not need “medical certainty” that a patient would die to perform an abortion.
Turner’s assurances led to a series of questions from the court’s conservative justices. Some of them, like Justice Amy Coney Barrett and Chief Justice John Roberts, focused on how the law would actually operate in practice under Turner’s description. Would doctors who make the decision to perform an abortion, Barrett asked, be prosecuted under Idaho law? And has Idaho issued any kind of guidance to assist doctors in making these kinds of decisions?
Roberts shared Barrett’s concerns, asking Turner who makes decisions about whether an abortion would be covered under Idaho law under this standard.
Turner explained that the state’s Board of Medicine oversees the licensing of Idaho physicians, and that the board looks at whether a doctor made the decision in good faith.
Other justices looked at a broader issue: whether there is in practice any real conflict between EMTALA and the Idaho ban in light of a ruling by the Idaho Supreme Court that narrowed the scope of the law, so that EMTALA would not override it. Justice Brett Kavanaugh asked Turner to focus on “the actual dispute as it exists now.” For each of the conditions that the federal government identifies as requiring abortion as a stabilizing treatment, Kavanaugh observed, the state now contends that Idaho law actually would permit an abortion. Is there any condition, Kavanaugh queried, where Idaho law would not allow an abortion? And if not, Kavanaugh continued, what would that mean for this case?
Turner responded that although the federal government maintains that abortion is not the only stabilizing care for mental health conditions, the American Psychiatric Association indicates that abortions are “imperative for mental health conditions.”
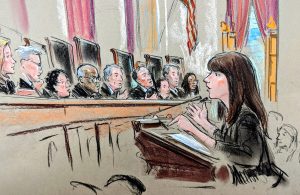
U.S. Solicitor General Elizabeth Prelogar argues for the government. (William Hennessy)
Prelogar pushed back against any suggestion that there is no gap between the care that EMTALA requires and what Idaho law allows. She told the justices that “the situation on the ground in Idaho is showing the devastating consequences of that gap,” as emergency rooms in Idaho are faced with the unpalatable choice of waiting for a pregnant woman’s condition to deteriorate enough so that they can provide abortions or transferring her to another state entirely – which, she said, hospitals in the state are currently doing once every other week.
Addressing Turner’s contention that mental health conditions would not be covered by Idaho law, Prelogar insisted that in grave mental health emergencies providing an abortion would not be the proper medical practice and further would not do anything to address the underlying mental health condition, which would be treated with psychiatric medication. A patient in a mental health emergency may not be able to provide informed consent to an abortion. So although an “emergency medical condition” can include mental health problems, she said, it would not be the government’s practice to include abortion as care that would be required in such a situation.
Prelogar faced a barrage of questions from the court’s conservative justices about whether the government can supersede Idaho’s general abortion ban by imposing conditions on the recipients of federal funds – here, the hospitals that entered into Medicare contracts. Both Justice Clarence Thomas and Alito raised this question, with Thomas asking Prelogar to identify other legislation under the Constitution’s spending clause that preempts criminal law. Thomas and Alito also questioned whether the federal government can supersede a state’s laws when the state did not enter into the contract with the federal government (and therefore did not agree to the conditions imposed by the government).
Justice Neil Gorsuch expressed concern about the scope of the government’s power to place conditions on federal spending. Could the federal government, Gorsuch asked, condition the receipt of funds by hospitals on their compliance with federal medical malpractice and licensing requirements?
Barrett suggested that it was “odd” that a private entity could circumvent state law though a side agreement with the federal government. Could Congress use its authority under the spending clause to regulate or prohibit other kinds of medical care, she asked, such as gender reassignment surgery, or to ban abortion across the country?
Prelogar acknowledged that Congress has “broad authority through the spending clause.”
Gorsuch then appeared doubtful about the federal government’s need to seek an injunction barring Idaho from enforcing its ban at all. He told Prelogar that EMTALA is a “reticulated statute” that allows the government to seek remedies such as fines for noncomplicance. “Congress has given you lots of tools,” he told Prelogar.
Alito complained, with about 30 minutes left in the nearly two-hour argument, that the attorneys and the justices had “hardly” mentioned EMTALA’s reference to the “unborn child,” suggesting that it was an odd phrase to put in a statute that, on the government’s reading, is supposed to require abortions? In Alito’s view, the inclusion of the phrase indicated that the statute imposes a duty not only to the pregnant woman, but also to the unborn child. But the government, he said, was asking the justices to interpret “a statute signed by Ronald Reagan” as imposing a duty to perform an abortion even when doing so would be contrary to state law.
Barrett and Roberts both asked about the interaction between EMTALA and “conscience objections” – whether either doctors or hospitals could decline to perform abortions based on their religious or moral beliefs.
Prelogar told the court that both hospitals and physicians could assert a conscience objection, and that “EMTALA does not override either set of conscience protections.” In response to a follow-up question from Roberts, she explained that hospitals make their staffing decisions to ensure that someone who is able to provide care is on call. “[I]f the question is could you force an individual doctor to step in then over a conscience objection, the answer is no.” However, she acknowledged, if a hospital repeatedly did not have someone available to run its emergency room, including providing abortions in an emergency, it was possible that the federal government could eventually “terminate the Medicare funding agreement.”
A decision in the case is expected by summer.
This article was originally published at Howe on the Court .
Posted in Featured , Merits Cases
Cases: Moyle v. United States , Idaho v. United States
Recommended Citation: Amy Howe, Supreme Court divided over federal-state conflict on emergency abortion ban , SCOTUSblog (Apr. 24, 2024, 3:45 PM), https://www.scotusblog.com/2024/04/supreme-court-divided-over-federal-state-conflict-on-emergency-abortion-ban/
Privacy Overview
Friday, April 26, 2024
Tax payer funded gender reassignment surgeries prompt questions about military readiness.
- by: Tracy Beanz

Read our latest news on any of these social networks!
Get the latest news delivered daily!
We will send you breaking news right to your inbox
Recent Articles


IMAGES
VIDEO
COMMENTS
This observational study showed an increased mortality risk in transgender people using hormone treatment, regardless of treatment type. This increased mortality risk did not decrease over time. The cause-specific mortality risk because of lung cancer, cardiovascular disease, HIV-related disease, and suicide gives no indication to a specific effect of hormone treatment, but indicates that ...
Fact Check: The Instagram post claims that only 1% of patients regret their gender transition surgeries. The source used is "Regret after Gender-affirmation Surgery: A systematic Review and Meta-analysis of Prevalence" from the National Library of Medicine (NLM). The caption is misleading, due to several factors and lack of research that ...
Background: Gender dysphoria is a condition that often leads to significant patient morbidity and mortality. Although gender-affirming surgery (GAS) has been offered for more than half a century with clear significant short-term improvement in patient well-being, few studies have evaluated the long-term durability of these outcomes.
Studies of mortality and somatic well-being after sex-reassignment surgery (SRS) of transsexual individuals are equivocal. Accordingly, the present study investigated mortality and somatic morbidity using a sample of transsexual individuals who comprised 98% (n = 104) of all surgically reassigned transsexual individuals in Denmark.
Adolescents with gender identity disorder who were accepted or rejected for sex reassignment surgery: a prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 2001; 40:472-481 [Google Scholar] 43. Judge C, O'Donovan C, Callaghan G, et al.. Gender dysphoria - prevalence and co-morbidities in an Irish adult population. ...
Gender-affirming treatment remains a topic of controversy; of particular concern is whether gender-affirming treatment reduces suicidality. A narrative review was undertaken evaluating suicide-related outcomes following gender-affirming surgery, hormones, and/or puberty blockers. Of the 23 studies that met the inclusion criteria, the majority ...
Excerpt from Q&A, February 29, 2016. Studies that have been done of transgendered people who have had sex reassignment surgery, people who have been followed for 20 or so years have found that ...
Expand. Medical transition puts both males and females at risk of infertility. Expand. Genital surgeries tend to reduce the capacity for orgasm in males, and may do so in females. Expand. Vaginoplasty can result in fistula, stenosis, necrosis, prolapse and even death. Expand. Around 1 in 5 vaginoplasty surgeries lead to corrective surgery. Expand.
Key Points. Question What are the temporal trends in gender-affirming surgery (GAS) in the US?. Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
Patterns in age and cause of death contribution to the sex gap in life expectancy: a comparison among ten countries. Genus. Published online August 2, ... Hald GM. Long-term follow-up of individuals undergoing sex reassignment surgery: psychiatric morbidity and mortality. Nord J Psychiatry. 2016;70(4) :241-247 ...
In primary male to female (MTF) sex reassignment surgery (SRS), the most frequent postoperative functional complications using the penoscrotal skin technique remain neovaginal stenosis, urinary meatal stenosis and secondary revision surgery. We aimed to retrospectively analyze postoperative functional and anatomical complications, as well as ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Sex and sexual health tips for transgender women after gender-affirming surgery. Sex after surgery. Achieving orgasm. Libido. Vaginal depth and lubrication. Aftercare. Contraceptions and STIs ...
Performer and campaigner was one of the first Britons to undergo gender reassignment surgery. Léonie Chao-Fong and agency. Tue 28 Dec 2021 18.20 EST Last modified on Wed 29 Dec 2021 00.15 EST.
The study, published in 2011, estimated the "mortality, morbidity, and criminal rate after surgical sex reassignment of transsexual persons" of "324 "sex-reassigned persons" in Sweden for 30 years.
April 21, 2022, 8:29 PM UTC. By Matt Lavietes. In a first, the Federal Bureau of Prisons has been ordered to secure gender-affirming surgery for a transgender prisoner. A federal judge in the U.S ...
Please tell your medical provider the words you use to describe your body. Vaginoplasty is a gender-affirming, feminizing, lower surgery (transgender surgery; gender reassignemnt surgery; sex change surgery) to create a vagina and vulva (including mons, labia, clitoris, and urethral opening) and remove the penis, scrotal sac and testes.
Barrett and Gorsuch, for instance, asked if gender-reassignment surgery could be banned at hospitals as a condition for receiving federal money. Prelogar replied that in her view Congress has that ...
Lili Ilse Elvenes (28 December 1882 - 13 September 1931), better known as Lili Elbe, was a Danish painter, transgender woman, and one of the earliest recipients of sex reassignment surgery (gender-affirming surgery).. She was a painter under her birth name Einar Wegener. After transitioning in 1930, she changed her legal name to Lili Ilse Elvenes, stopped painting, and later adopted the ...
Cosmetic surgery and cross-sex hormones can't change us into the opposite sex. They can affect appearances. They can stunt or damage some outward expressions of our reproductive organization.
Introduction. Studies of mortality and somatic well-being after sex-reassignment surgery (SRS) of transsexual individuals are equivocal. Accordingly, the present study investigated mortality and somatic morbidity using a sample of transsexual individuals who comprised 98% (n = 104) of all surgically reassigned transsexual individuals in Denmark.
Introduction. Gender dysphoria (GD) refers to the distress related to a marked incongruence between one's assigned gender at birth and the experienced gender (1).Trans people are diverse in the intensity of experienced GD (2), their needs for medical transition (3), and the impairment that GD can have on their life.Studies focusing on the wellbeing of trans people show a greater ...
Political Director. CONCORD, N.H. —. Lawmakers in Concord heard testimony Thursday on a bill to ban genital gender-confirmation surgery for children under the age of 18. The Senate Judiciary ...
Transgender Teen Dies After Surgery Goes Wrong (images via Pexels/Anna) In 2016, a medical article revealed that one of the study participants in the Dutch linchpin transgender experiment had died.
The Supreme Court on Wednesday was divided over whether a federal law requiring hospitals that participate in Medicare to provide "necessary stabilizing treatment" in an emergency overrides an Idaho law that bars most abortions. The court's ruling could affect health care in emergency rooms in the 22 states that have imposed restrictions ...
Countries recognising gender self-identification for legal gender; sub-national entities are not marked World map of non-binary gender recognition. Legal gender, or legal sex, is a sex or gender that is recognized under the law. Biological sex, sex reassignment and gender identity are used to determine legal gender. The details vary by jurisdiction. Legal gender identity is fundamental to many ...
The US Government is providing gender reassignment surgery for active-duty military, and this article will detail our military readiness. Everything in this article should be viewed through the lens of military readiness. Could an ADSM ever be combat-ready based on DoD standards if they have gender reassignment surgery? The answer is NO.
Zoey -Credit:Dawn Womack. A mum is raising money to help pay for her "amazing" daughter's gender reassignment surgery following massive waiting lists for treatment on the NHS. Dawn Womack, from Wakefield, is raising the money to help her daughter Zoey, who has been transitioning since she was 16. Now 19, she faces long waiting lists on the NHS ...
Criminalization: The law criminalized consensual same-sex sexual activity, which was punishable by death, flogging, or a lesser punishment. There were no reports of such punishments being enforced during the year. ... and NGOs reported that authorities sometimes pressured LGBTQI+ persons to undergo gender reassignment surgery. Reports indicated ...