

Keynote webinar | Spotlight on sleep in brain health
LIVE: Thursday 2nd May 2024, 18:00-19:30 (CEST)
Quality sleep is essential for health. But what happens to our brains when sleep patterns are disturbed? Join our experts to explore the interplay between sleep disruption and neurological diseases, and the questions that you need to be asking your patients to help you prevent the harmful effects of sleep deprivation.
Springer Medicine
Neurological research and practice, latest issues, neurological research and practice 1/2024, neurological research and practice 1/2023, neurological research and practice 1/2022, neurological research and practice 1/2021, neurological research and practice 1/2020, neurological research and practice 1/2019.
scroll for more
use your arrow keys for more
scroll or use arrow keys for more
About this journal
Neurological Research and Practice , official journal of the German Neurological Society, is an international publication with a broad scope reflecting all clinical, translational and basic research aspects of neurology and neuroscience. Neurological Research and Practice provides a forum for clinicians and scientists with an interest in all areas of neurology including, but not limited to, genetics, vascular diseases and critical care, disorders of the spine, movement disorders, neuroimmunology, infections, oncology, epilepsy, neuroimaging and neuroradiology, neurodevelopment and degeneration. The journal will publish research articles, reviews, clinical trial protocols, standard operating procedures, letters to the editor and guidelines.
- Medical Journals
- Webcasts & Webinars
- CME & eLearning
- Newsletters
- ESMO Congress 2023
- 2023 ERS Congress
- ESC Congress 2023
- EHA2023 Hybrid Congress
- 2023 ASCO Annual Meeting Coverage
- Advances in Alzheimer’s
- About Springer Medicine
- Diabetology
- Endocrinology
- Gastroenterology
- Geriatrics and Gerontology
- Gynecology and Obstetrics
- Infectious Disease
- Internal Medicine
- Respiratory Medicine
- Rheumatology

Springer Medizin
Neurological research and practice.
- Alle Ausgaben
Ausgabe 1/2022
Inhalt (62 artikel), therapy development for spinal muscular atrophy: perspectives for muscular dystrophies and neurodegenerative disorders.
Sibylle Jablonka, Luisa Hennlein, Michael Sendtner
Neurological management and work-up of neurotoxicity associated with CAR T cell therapy
Nora Möhn, Viktoria Bonda, Lea Grote-Levi, Victoria Panagiota, Tabea Fröhlich, Christian Schultze-Florey, Mike P. Wattjes, Gernot Beutel, Matthias Eder, Sascha David, Sonja Körner, Günter Höglinger, Martin Stangel, Arnold Ganser, Christian Koenecke, Thomas Skripuletz
The special role of CXCL13 in Lyme neuroborreliosis: a case report
Deborah K. Erhart, Vera Bracknies, Susanne Lutz-Schuhbauer, Sonja Wigand, Hayrettin Tumani
Early vigabatrin augmenting GABA-ergic pathways in post-anoxic status epilepticus (VIGAB-STAT) phase IIa clinical trial study protocol
Carolina B. Maciel, Fernanda J. P. Teixeira, Katie J. Dickinson, Jessica C. Spana, Lisa H. Merck, Alejandro A. Rabinstein, Robert Sergott, Guogen Shan, Guanhong Miao, Charles A. Peloquin, Katharina M. Busl, Lawrence J. Hirsch
Heterozygous POLG variant Ser1181Asn co-segregating in a family with autosomal dominant axonal neuropathy, proximal muscle fatigability, ptosis, and ragged red fibers
Maike F. Dohrn, Corina Heller, Diana Zengeler, Carolin D. Obermaier, Saskia Biskup, Joachim Weis, Stefan Nikolin, Kristl G. Claeys, Ulrike Schöne, Danique Beijer, Natalie Winter, Pascal Achenbach, Burkhard Gess, Jörg B. Schulz, Lejla Mulahasanovic
Guillain-Barré syndrome and fulminant encephalomyelitis following Ad26.COV2.S vaccination: double jeopardy
Maria Ioanna Stefanou, Eleni Karachaliou, Maria Chondrogianni, Christos Moschovos, Eleni Bakola, Aikaterini Foska, Konstantinos Melanis, Elisabeth Andreadou, Konstantinos Voumvourakis, Matilda Papathanasiou, Eleni Boutati, Georgios Tsivgoulis
SOP: thrombolysis in ischemic stroke under oral anticoagulation therapy
Pawel Kermer, Peter D. Schellinger, Peter A. Ringleb, Martin Köhrmann
Intra-arterial application of nimodipine in reversible cerebral vasoconstriction syndrome: a neuroradiological method to help differentiate from primary central nervous system vasculitis
Daniel Strunk, Roland Veltkamp, Sven G. Meuth, René Chapot, Markus Kraemer
Characterization of advanced Parkinson’s disease in Germany: results of the non-interventional OBSERVE-PD study
David J. Pedrosa, Florin Gandor, Wolfgang H. Jost, Carolin Arlt, Koray Onuk, Lars Timmermann
Diagnosing SARS-CoV-2 vaccination associated rhombencephalitis requires comprehensive work-up and exclusion of differentials
Josef Finsterer, Fulvio A. Scorza, Carla A. Scorza, Ana C. Fiorini
Polyradiculitis and encephalomyelitis in the same patient following a SARS-CoV-2 vaccination
Josef Finsterer
Transcranial Doppler sonography and the effect of haematopoietic stem cell transplantation in sickle cell disease
Sylvia Thurn, Katharina Kleinschmidt, Irena Kovacic, Christina Wendl, Ralf A. Linker, Selim Corbacioglu, Felix Schlachetzki
A mobile battery-powered brain perfusion ultrasound (BPU) device designed for prehospital stroke diagnosis: correlation to perfusion MRI in healthy volunteers
Mustafa Kilic, Fabien Scalzo, Chandler Lyle, Dobri Baldaranov, Maximilian Dirnbacher, Tristan Honda, David S. Liebeskind, Felix Schlachetzki
A multicenter, randomized, double-blind, placebo-controlled trial to test efficacy and safety of transcranial direct current stimulation to the motor cortex after stroke (NETS): study protocol
Christian Gerloff, Kirstin-Friederike Heise, Robert Schulz, Friedhelm C. Hummel, Silke Wolf, Antonia Zapf, Diana Cordes, Christian Gerloff, Kirstin-Friederike Heise, Friedhelm Hummel, Robert Schulz, Silke Wolf, Kerstin Haevernick, Heike Krüger, Linda Krause, Anna Suling, Karl Wegscheider, Antonia Zapf, Jürgen Dressnandt, Barbara Schäpers, Christoph Schrödl, Björn Hauptmann, Anja Kirchner, Anna Brault, Alexander Gutschalk, Constanze Richter, Dennis A. Nowak, Jitka Veldema, Giacomo Koch, Michele Maiella, Christian Dohle, Katrin Jettkowski, Mario Pilz, Farsin Hamzei, Lydia Olischer, Caroline Renner, Marcus Groß, Michael Jöbges, Bernhard Voller
On the quest for hidden ovarian teratomas in therapy-refractory anti-NMDA receptor encephalitis: a case report
Christoph Cirkel, Anna Cirkel, Georg Royl, Alex Frydrychowicz, Lars Tharun, Steffen Deichmann, Achim Rody, Thomas F. Münte, Björn Machner
Intracranial bleeding under vitamin K antagonists or direct oral anticoagulants: results of the RADOA registry
Waltraud Pfeilschifter, Edelgard Lindhoff-Last, Ali Alhashim, Barbara Zydek, Simone Lindau, Stavros Konstantinides, Oliver Grottke, Ulrike Nowak-Göttl, Christian von Heymann, Ingvild Birschmann, Jan Beyer-Westendorf, Patrick Meybohm, Andreas Greinacher, Eva Herrmann
Residents as teachers in Neurology: a Germany-wide survey on the involvement of neurological residents in clinical teaching
Anne-Sophie Biesalski, Lars Tönges, Isabelle von Kirchbauer, Eileen Gülke, Hanna Eisenberg, Franziska Maria Ippen, Friederike Schmidt-Graf
Recovery of intracranial stenoses in varicella zoster virus vasculitis after long-term treatment with valacyclovir and prednisolone
Markus Kraemer, Daniel Strunk, Jana Becker, Roland Veltkamp, Peter Berlit
A look back at 3 years of neurological research and practice (NRP)
Werner Hacke
AMPLIFY-NEOVAC: a randomized, 3-arm multicenter phase I trial to assess safety, tolerability and immunogenicity of IDH1-vac combined with an immune checkpoint inhibitor targeting programmed death-ligand 1 in isocitrate dehydrogenase 1 mutant gliomas
Lukas Bunse, Anne-Kathleen Rupp, Isabel Poschke, Theresa Bunse, Katharina Lindner, Antje Wick, Jens Blobner, Martin Misch, Ghazaleh Tabatabai, Martin Glas, Oliver Schnell, Jens Gempt, Monika Denk, Guido Reifenberger, Martin Bendszus, Patrick Wuchter, Joachim P Steinbach, Wolfgang Wick, Michael Platten
Long-term benefit of pallidal deep brain stimulation in a patient with VPS16-associated dystonia
Jan Niklas Petry-Schmelzer, Joohyun Park, Tobias B. Haack, Veerle Visser-Vandewalle, Michael T. Barbe, Gilbert Wunderlich
Exploring the relationships between composite scores of disease severity, seizure-freedom and quality of life in Dravet syndrome
Adam Strzelczyk, Gerhard Kurlemann, Thomas Bast, Ulrich Bettendorf, Gerhard Kluger, Thomas Mayer, Bernd A. Neubauer, Tilman Polster, Sarah von Spiczak, Regina Trollmann, Markus Wolff, Toby Toward, Jens Gruenert, Eddie Gibson, Clive Pritchard, Joe Carroll, Felix Rosenow, Susanne Schubert-Bast
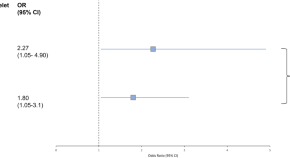
Antiplatelets or anticoagulants? Secondary prevention in cervical artery dissection: an updated meta-analysis
Ei Zune The, Ne Naing Lin, Ching Jocelyn Chan, Jason Cher Wei Loon, Benjamin Yong-Qiang Tan, Chee Seong Raymond Seet, Hock Luen Teoh, Joy Vijayan, Leong Litt Leonard Yeo
LGI-1 encephalopathy following ChAdOx1 nCov-19 vaccination
Tamara Garibashvili, Josef Georg Heckmann
External ventricular drain use is associated with functional outcome in aneurysmal subarachnoid hemorrhage
Sarah E. Nelson, Jose I. Suarez, Alexander Sigmon, Jun Hua, Casey Weiner, Haris I. Sair, Robert D. Stevens
Historical review: the German Neurological Society and its honorary members (1952–1982)
Michael Martin, Heiner Fangerau, Axel Karenberg
COVID-19 outcomes in hospitalized Parkinson’s disease patients in two pandemic waves in 2020: a nationwide cross-sectional study from Germany
Raphael Scherbaum, Dirk Bartig, Daniel Richter, Eun Hae Kwon, Siegfried Muhlack, Ralf Gold, Christos Krogias, Lars Tönges
Neurological manifestations of post-COVID-19 syndrome S1-guideline of the German society of neurology
Christiana Franke, Peter Berlit, Harald Prüss
Anti-Homer-3 antibodies in cerebrospinal fluid and serum samples from a 58-year-old woman with subacute cerebellar degeneration and diffuse breast adenocarcinoma
Christof Klötzsch, Matthias Böhmert, Ruxandra Hermann, Bianca Teegen, Kristin Rentzsch, Andreas Till
Current diagnosis and treatment practice of central retinal artery occlusion: results from a survey among German stroke units
Carolin Hoyer, Simon Winzer, Egbert Matthé, Ida Heinle, Vesile Sandikci, Darius Nabavi, Michael Platten, Volker Puetz, Kristina Szabo
New concepts in neurology education: successful implementation of flipped classroom lectures
Katharina Mosene, Henrik Heitmann, Dennis Pötter, Friederike Schmidt-Graf
Single-center experience of induction therapy in non-systemic vasculitic neuropathy
Christian Schneider, Meike K. Wassermann, Gereon R. Fink, Helmar C. Lehmann
Carriers of POLG1 variants require investigations for multisystem disease and for mtDNA variations
Josef Finsterer, Sinda Zarrouk
Heterozygous POLG variant Ser1181Asn is associated with autosomal dominant neuro-myopathy in one family with no further specific manifestations of mitochondrial syndrome
Maike F. Dohrn, Danique Beijer, Lejla Mulahasanovic
Super-refractory status epilepticus in adults
Michael P Malter, Janina Neuneier
Regional computed tomography perfusion deficits in patients with hypoglycemia: two case reports
Jennifer Sartor-Pfeiffer, Mirjam Lingel, Maria-Ioanna Stefanou, Tobias Lindig, Benjamin Bender, Sven Poli, Ulf Ziemann, Andreas Fritsche, Katharina Feil, Annerose Mengel
Management of medication overuse (MO) and medication overuse headache (MOH) S1 guideline
Hans-Christoph Diener, Peter Kropp, Thomas Dresler, Stefan Evers, Stefanie Förderreuther, Charly Gaul, Dagny Holle-Lee, Arne May, Uwe Niederberger, Sabrina Moll, Christoph Schankin, Christian Lampl
Multifocal leukoencephalopathy associated with intensive use of cocaine and the adulterant levamisole in a 29-year old patient
Nadine Tollens, Philip Post, Michael Martins Dos Santos, Pascal Niggemann, Melanie Warken, Joachim Wolf
ADCY5-related dyskinesia: a case report
Shih-Ying Chen, Chen-Jui Ho, Yan-Ting Lu, Chih-Hsiang Lin, Meng-Han Tsai
Sudden vision loss and neurological deficits after facial hyaluronic acid filler injection
Alexandra Lucaciu, Patrick Felix Samp, Elke Hattingen, Roxane-Isabelle Kestner, Petra Davidova, Thomas Kohnen, Jasmin Rudolph, Andreas Dietz, Helmuth Steinmetz, Adam Strzelczyk
Essen transition model for neuromuscular diseases
Michael Fleischer, Bayram Coskun, Benjamin Stolte, Adela Della-Marina, Heike Kölbel, Hildegard Lax, Michael Nonnemacher, Christoph Kleinschnitz, Ulrike Schara-Schmidt, Tim Hagenacker
Antithrombotic treatment and outcome after endovascular treatment and acute carotid artery stenting in stroke patients with atrial fibrillation
Johannes M. Weller, Franziska Dorn, Julius N. Meissner, Sebastian Stösser, Niklas M. Beckonert, Julia Nordsiek, Christine Kindler, Christoph Riegler, Fee Keil, Gabor C. Petzold, Felix J. Bode, A. Reich, O. Nikoubashman, J. Röther, B. Eckert, M. Braun, G. F. Hamann, E. Siebert, C. H. Nolte, G. Bohner, R. M. Eckert, J. Borggrefe, P. Schellinger, J. Berrouschot, A. Bormann, C. Kraemer, H. Leischner, M. Petersen, F. Stögbauer, T Boeck-Behrens, S. Wunderlich, A. Ludolph, K. H. Henn, C. Gerloff, J. Fiehler, G. Thomalla, A. Alegiani, J. H. Schäfer, S. Tiedt, L. Kellert, C. Trumm, U. Ernemann, S. Poli, J. Liman, M. Ernst, K. Gröschel, T. Uphaus
Anti-flotillin-1/2 antibodies in a patient with neurogenic muscle atrophy and mild neuropsychological impairment
Tobias A. Wagner-Altendorf, Klaus-Peter Wandinger, Robert Markewitz, Anna Antufjew, Tobias Boppel, Thomas F. Münte
Impact of COVID-19 pandemic on physical and mental health status and care of adults with epilepsy in Germany
Kimberly Körbel, Felix Rosenow, Margarita Maltseva, Heiko Müller, Juliane Schulz, Panagiota-Eleni Tsalouchidou, Lisa Langenbruch, Stjepana Kovac, Katja Menzler, Mario Hamacher, Felix von Podewils, Laurent M. Willems, Catrin Mann, Adam Strzelczyk
Brain tumor related epilepsy: pathophysiological approaches and rational management of antiseizure medication
Sabine Seidel, Tim Wehner, Dorothea Miller, Jörg Wellmer, Uwe Schlegel, Wenke Grönheit
The impact of apraxia and neglect on early rehabilitation outcome after stroke
S. Latarnik, J. Stahl, S. Vossel, C. Grefkes, G. R. Fink, P. H. Weiss
Why cognitive training is important for the health status in Parkinson’s disease: preliminary evidence from a clinical three-weeks multidisciplinary intervention
Jennifer Michels, Cornelius J. Werner, Beate Schumann-Werner, Jörg B. Schulz, Ana S. Costa, Kathrin Reetz
Long-term efficacy with deep brain stimulation of the globus pallidus internus in cervical dystonia: a retrospective monocentric study
Clemens Jacksch, Kirsten E. Zeuner, Ann-Kristin Helmers, Karsten Witt, Günther Deuschl, Steffen Paschen
PET-MRI in idiopathic inflammatory myositis: a comparative study of clinical and immunological markers with imaging findings
Manu Santhappan Girija, Ravindu Tiwari, Seena Vengalil, Saraswati Nashi, Veeramani Preethish-Kumar, Kiran Polavarapu, Karthik Kulanthaivelu, Arpana Arbind, Mainak Bardhan, Akshata Huddar, Gopikrishnan Unnikrishnan, Valasani Ravi Kiran, Tanushree Chawla, Bevinahalli Nandeesh, Chandana Nagaraj, Atchayaram Nalini
Sex differences in etiology and short-term outcome in young ischemic stroke patients receiving mechanical thrombectomy
Ralph Weber, Evgenia Winezki, Aristeidis H. Katsanos, Melissa Cueillette, Karim Hajjar, Elif Yamac, Roland Veltkamp, Rene Chapot
Isolated slow orthostatic tremor of the trunk
N. Ahmad Aziz, Marcus Grobe-Einsler, Oliver Kaut
Does diabetes mellitus affect the safety profile of valproic acid for the treatment of status epilepticus? A retrospective cohort study
Annekatrin Müller, Judith von Hofen-Hohloch, Carolin Awissus, Jens Przybilla, Achmed Mrestani, Joseph Classen
No serological evidence for neuronal damage or reactive gliosis in neuro-COVID-19 patients with long-term persistent headache
Laura de Boni, Alexandru Odainic, Natalie Gancarczyk, Luisa Kaluza, Christian P. Strassburg, Xenia A. K. Kersting, Joseph M. Johnson, Ullrich Wüllner, Susanne V. Schmidt, Jacob Nattermann, Gabor C. Petzold
Anti-SEZ6L2 antibodies in paraneoplastic cerebellar syndrome: case report and review of the literature
Annika Kather, Florian Holtbernd, Robert Brunkhorst, Dimah Hasan, Robert Markewitz, Klaus-Peter Wandinger, Martin Wiesmann, Jörg B. Schulz, Simone C. Tauber
Real-world evidence on siponimod treatment in patients with secondary progressive multiple sclerosis
Liesa Regner-Nelke, Marc Pawlitzki, Alice Willison, Leoni Rolfes, Sinem-Hilal Oezalp, Christopher Nelke, Tristan Kölsche, Melanie Korsen, Matthias Grothe, Sergiu Groppa, Felix Luessi, Sinah Engel, Gereon Nelles, Eckhard Bonmann, Holger Roick, Anke Friedrich, Philipp Knorn, Harald Landefeld, Zoltan Biro, Michael Ernst, Antonios Bayas, Martina Menacher, Katja Akgün, Christoph Kleinschnitz, Tobias Ruck, Tjalf Ziemssen, Refik Pul, Sven G. Meuth
Teaching distinguishing semiological features improves diagnostic accuracy of seizure-like events by emergency physicians
Wenke Grönheit, Vanessa Behrens, Tatjana Liakina, Christoph Kellinghaus, Soheyl Noachtar, Stoyan Popkirov, Tim Wehner, Eva Brammen, Jörg Wellmer
Side matters: differences in functional outcome and quality of life after thrombectomy in left and right hemispheric stroke
Milani Deb-Chatterji, Fabian Flottmann, Lukas Meyer, Caspar Brekenfeld, Jens Fiehler, Christian Gerloff, Götz Thomalla, C. Gerloff, J. Fiehler, G. Thomalla, A. Alegiani, Boeckh-Behrens, Silke Wunderlich, Ulrike Ernemann, Sven Poli, Eberhard Siebert, Christian H. Nolte, Sarah Zweynert, Georg Bohner, Alexander Ludolph, Karl-Heinz Henn, Jan Hendrik Schäfer, Fee Keil, Joachim Röther, Bernd Eckert, Jörg Berrouschot, Albrecht Bormann, Franziska Dorn, Gabor Petzold, Christoffer Kraemer, Hannes Leischner, Christoph Trumm, Steffen Tiedt, Lars Kellert, Martina Petersen, Florian Stögbauer, Michael Braun, Gerhard F. Hamann, Klaus Gröschel, Timo Uphaus, Arno Reich, Omid Nikoubashman, Peter Schellinger, Jan Borggrefe, Jörg Hattingen, Jan Liman, Marielle Ernst
The gut-brain axis in ischemic stroke: its relevance in pathology and as a therapeutic target
Corinne Benakis, Arthur Liesz
Prognostic markers of post-stroke depression (PROMoSD): study protocol of a prospective single-center observational study on raphe hypoechogenicity as a predictor of post-stroke depression
Daniel Richter, Andreas Ebert, Lisa Mazul-Wach, Quirin Ruland, Jeyanthan Charles-James, Ralf Gold, Georgios Tsivgoulis, Georg Juckel, Christos Krogias
ALSFRS-R-SE: an adapted, annotated, and self-explanatory version of the revised amyotrophic lateral sclerosis functional rating scale
André Maier, Matthias Boentert, Peter Reilich, Simon Witzel, Susanne Petri, Julian Großkreutz, Moritz Metelmann, Paul Lingor, Isabell Cordts, Johannes Dorst, Daniel Zeller, René Günther, Tim Hagenacker, Torsten Grehl, Susanne Spittel, Joachim Schuster, Albert Ludolph, Thomas Meyer
Intravenous thrombolysis for acute ischemic stroke associated with known left ventricular thrombus: safe or not?
Sofia Kitmeridou, Dimitrios Tsiptsios, Dimos Tsalkidis, Evlampia A. Psatha, Ioannis Iliopoulos, Nikolaos Aggelousis, Konstantinos Vadikolias
Myositis in Germany: epidemiological insights over 15 years from 2005 to 2019
Marc Pawlitzki, Laura Acar, Lars Masanneck, Alice Willison, Liesa Regner-Nelke, Christopher Nelke, Helmut L’hoest, Ursula Marschall, Jens Schmidt, Sven G. Meuth, Tobias Ruck
Aktuelle Ausgaben
Neurological research and practice 1/2024, neurological research and practice 1/2023, neurological research and practice 1/2022, neurological research and practice 1/2021, neurological research and practice 1/2020, neurological research and practice 1/2019.
Scrollen für mehr
Benutzen Sie die Pfeiltasten für mehr
Scrollen oder Pfeiltasten für mehr
Neu in den Fachgebieten Neurologie und Psychiatrie
08.04.2024 | Posttraumatische Belastungsstörung | Nachrichten
Perinatale PTBS: Signifikanter Anstieg der Diagnoserate
05.04.2024 | Parkinson-Krankheit | Nachrichten
Parkinsonschutz durch Kaffee: Es liegt wohl am Koffein
03.04.2024 | Angeborene Herzfehler | Nachrichten
Angeborene Herzfehler: Viele sind später körperlich oder kognitiv eingeschränkt
02.04.2024 | Vorhofflimmern | Nachrichten
Antikoagulation plus SSRI-Antidepressiva: Kombi erhöht das Blutungsrisiko!
- Facharzt-Training
- Zeitschriften
- Springer Medizin Podcast – der Talk für Gesundheitsprofis
- Info & Hilfe
- Anästhesiologie
- Allgemeinmedizin
- Arbeitsmedizin
- Augenheilkunde
- Dermatologie
- Gynäkologie und Geburtshilfe
- Innere Medizin
- Kardiologie
- Onkologie und Hämatologie
- Orthopädie und Unfallchirurgie
- Psychiatrie
- Rechtsmedizin
- Zahnmedizin
- Klimawandel und Gesundheit
- Neues aus dem Markt
- Praxis und Beruf
- Seltene Erkrankungen
- GOÄ & EBM
- Kasuistiken
- Algorithmen & Infografiken
- Blickdiagnosen
- Arthropedia
- Kongressberichterstattung
- Medizin für Apothekerinnen und Apotheker
- Für Ärztinnen und Ärzte in Weiterbildung
- Für Medizinstudierende
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Neurol Res Pract

ORIGINAL RESEARCH article
Interrater reliability of the fugl-meyer motor assessment in stroke patients: a quality management project within the estrel study.

- 1 Neurorehabilitation and Neurology, University Department of Geriatric Medicine FELIX PLATTER, University of Basel, Basel, Switzerland
- 2 Department of Health Professions, Bern University of Applied Sciences, Bern, Switzerland
- 3 Division of Vascular Neurology and Neurorehabilitation, Department of Neurology, University of Zurich and University Hospital Zurich, Zurich, Switzerland
- 4 Department of Neurology and Department of Clinical Research, University of Basel and University Hospital Basel, Basel, Switzerland
- 5 Cereneo Center of Neurology and Rehabilitation, Zurich, Switzerland
- 6 Valens Clinics, Reha Center Triemli, Vitznau, Switzerland
Introduction: The Fugl-Meyer Motor Assessment (FMMA) is recommended for evaluating stroke motor recovery in clinical practice and research. However, its widespread use requires refined reliability data, particularly across different health professions. We therefore investigated the interrater reliability of the FMMA scored by a physical therapist and a physician using video recordings of stroke patients.
Methods: The FMMA videos of 50 individuals 3 months post stroke (28 females, mean age 71.64 years, median National Institutes of Health Stroke Scale score 3.00) participating in the ESTREL trial (Enhancement of Stroke Rehabilitation with Levodopa: a randomized placebo-controlled trial) were independently scored by two experienced assessors (i.e., a physical therapist and a physician) with specific training to ensure consistency. As primary endpoint, the interrater reliability was calculated for the total scores of the entire FMMA and the total scores of the FMMA for the upper and lower extremities using intraclass correlation coefficients (ICC). In addition, Spearman’s rank order correlation coefficients (Spearman’s rho) were calculated for the total score and subscale levels. Secondary endpoints included the FMMA item scores using percentage agreement, weighted Cohen’s kappa coefficients, and Gwet’s AC1/AC2 coefficients.
Results: ICCs were 0.98 (95% confidence intervals (CI) 0.96–0.99) for the total scores of the entire FMMA, 0.98 (95% CI 0.96–0.99) for the total scores of the FMMA for the upper extremity, and 0.85 (95% CI 0.70–0.92) for the total scores of the FMMA for the lower extremity. Spearman’s rho ranged from 0.61 to 0.94 for total and subscale scores. The interrater reliability at the item level of the FMMA showed (i) percentage agreement values with a median of 77% (range 44–100%), (ii) weighted Cohen’s kappa coefficients with a median of 0.69 (range 0.00–0.98) and (iii) Gwet’s AC1/AC2 coefficients with a median of 0.84 (range 0.42–0.98).
Discussion and conclusion: The FMMA appears to be a highly reliable measuring instrument at the overall score level for assessors from different health professions. The FMMA total scores seem to be suitable for the quantitative measurement of stroke recovery in both clinical practice and research, although there is potential for improvement at the item level.
Introduction
Motor impairment is one of the most important disabilities associated with stroke and can significantly affect the quality of life ( 1 ). Muscle weakness, abnormal synergy, and spasticity are among the motor deficits commonly assessed in stroke patients ( 2 ). Considering the repair processes, measuring motor recovery after stroke is very important. The Fugl-Meyer Motor Assessment (FMMA) ( 3 ) is strongly recommended as a clinical and research tool for the evaluation of changes in motor impairment after stroke ( 4 ). It was a key component of the assessment recommendations for improving the methodology of adult rehabilitation and recovery trials ( 5 ) and clinical motor rehabilitation ( 6 ), which should be repeated at different measurement time points. The inclusion of the upper extremity FMMA (FMMA-UE) in further recommendations for outcome measurement after stroke has confirmed its importance ( 7 , 8 ).
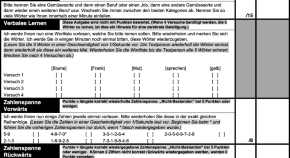
The maximum total score per side is 66 points for the FMMA-UE and 34 points for the lower extremity FMMA (FMMA-LE) ( 4 ). The FMMA items are rated on an ordinal scale with the scores 0 = cannot perform, 1 = performs partially and 2 = performs fully ( 4 ). The practical implementation of the test and the assessment of its individual items require standardized, sound training as well as routine. These aspects can be promoted by a uniform test version in the different languages of the respective countries of application. Upon completion of the present project, standardized FMMA test forms translated into more than 10 different languages were available [e.g., at https://www.gu.se/en/neuroscience-physiology/fugl-meyer-assessment ( 9 )]. However, to the best of our knowledge, no standardized, validated German version of the test is currently available. Therefore, we developed an adapted German version of the assessment, based on the original article and protocols of the University of Gothenburg ( 3 , 10 , 11 ). The corresponding assessment forms can be found in the Supplementary Table S1 . The interprofessional application of this German version of the FMMA into clinical trials requires good psychometric properties in terms of the validation process.
A high interrater reliability of the German version of the FMMA across different health professions is essential for the use of the assessment in clinical studies, but also for its application in daily rehabilitation practice. The English version of the FMMA showed excellent intra- and interrater reliability ( 4 ). Platz et al. ( 12 ) found a very high interrater reliability of the FMMA-UE with intraclass correlation coefficients (ICC) based on video recordings. In the Sullivan et al. ( 13 ) study, interrater agreement between expert and therapist raters using video recordings was high for the FMMA total scores with an ICC value of 0.98 as well as for total scores of the FMMA-UE with 0.99 and moderate to high for the FMMA-LE total scores with 0.91. Based in part on the strong evidence for validity, reliability, responsiveness, and clinical utility, the FMMA-UE was incorporated into the core set of European evidence-based recommendations for Clinical Assessment of Upper Limb In Neurorehabilitation (CAULIN) ( 7 ).
In this context, refined reliability data and the availability of transculturally adapted, validated FMMA versions in different languages are even more important. Investigating the interrater reliability of new FMMA versions using sufficiently large samples is a relevant component in this regard. Therefore, we aimed to investigate (i) the interrater reliability of the German FMMA across health professions and (ii) the comparability of the psychometric properties of the German FMMA with those of the English version.
Materials and methods
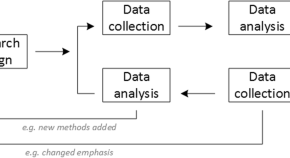
Project objectives and design.
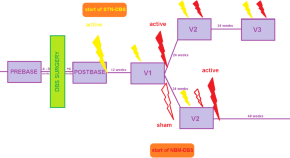
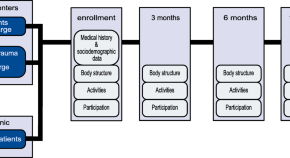
The aim of this research project was to study the interrater reliability of the German version of the FMMA in terms of its consistent and accurate application across health professions. The FMMA is used in the ongoing Swiss multicentre ESTREL trial (Enhancement of Stroke Rehabilitation with Levodopa: a randomized placebo-controlled trial, BASEC-number 2018–02021, ClinicalTrials.gov NCT03735901) ( 14 ), in which the current reliability study with a cross-sectional design was embedded.
Study population and procedure
All patients in this study had a video recorded FMMA at their regular three-month visit as part of their participation in ESTREL ( 14 , 15 ). In brief, ESTREL investigates whether Levodopa, compared to placebo, given in addition to standardized rehabilitation based on the principles of motor learning, is associated with a patient-relevant enhancement of functional recovery in acute ischemic or haemorrhagic stroke patients, as measured by the FMMA after 3 months ( 14 , 15 ).
The present project followed the Guidelines for Reporting Reliability and Agreement Studies (GRRAS) ( 16 ). As a preparatory step, an extensive literature research on relevant FMMA publications in the English-speaking world was conducted. After the selection of adequate reference literature, different FMMA versions were analyzed in detail and their contents were precisely compared. Between December 2019 and May 2021, FMMA video recordings of the three-month visit of ESTREL stroke patients were performed at the two best recruiting centres, Basel and Zurich, Switzerland. The FMMA was applied in an outpatient visit setting, in most cases by the first author (KW).
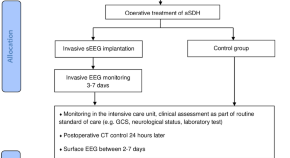
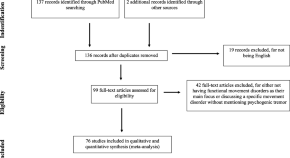
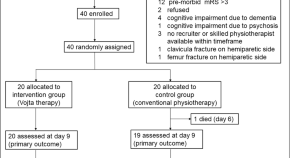
The sampling method of the recordings was consecutive, following a standardized procedure. Eligibility criteria: We took the first 72 available FMMA videos from ESTREL participants who were eligible for the trial ( 14 ). Of these, 62 videos were identified in Basel and 10 in Zurich. The first author (KW) performed a quality check of all collected videos based on the criteria of (i) completeness, (ii) visibility of the entire examination, and (iii) potential source of bias. Video recordings were excluded, if (a) the FMMA was incomplete, (b) a FMMA subscale was not fully visible, and (c) the evaluation sheet with the FMMA ratings was visible on the video. In addition, recordings were excluded if one of the assessors of the videos was the FMMA examiner being videotaped. A flowchart of the video selection process is presented in Figure 1 .
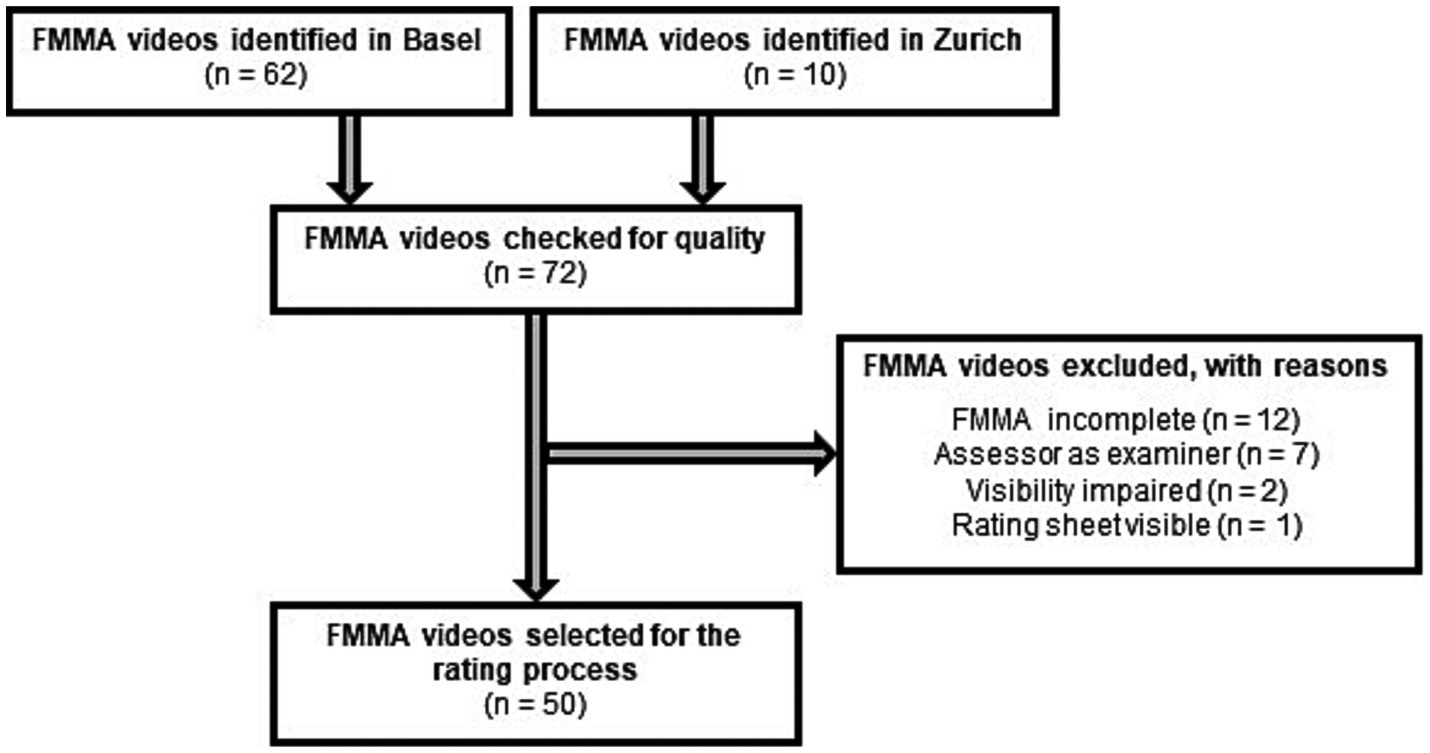
Figure 1 . Flow chart of the selection process for FMMA video recordings. FMMA, Fugl-Meyer Motor Assessment; n, number of subjects.
Independent assessors
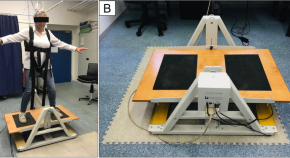
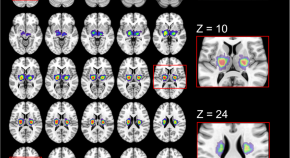
Two independent assessors – one from each participating centre – rated the FMMA videos. Rating was limited to the hemiparetic side in each case. The assessors consisted of one research physician (LM) and one research physiotherapist (AS) from the two different centres, each with a master’s degree and clinical experience – who met the following criteria: First, both assessors had participated at least twice in a standardized, four-hour in-person FMMA training course by an FMMA expert (JH), based on the German version of the FMMA (see Figure 2 , FMMA training). Second, both assessors had applied the German version at least 50 times on stroke patients in a standardized setting.
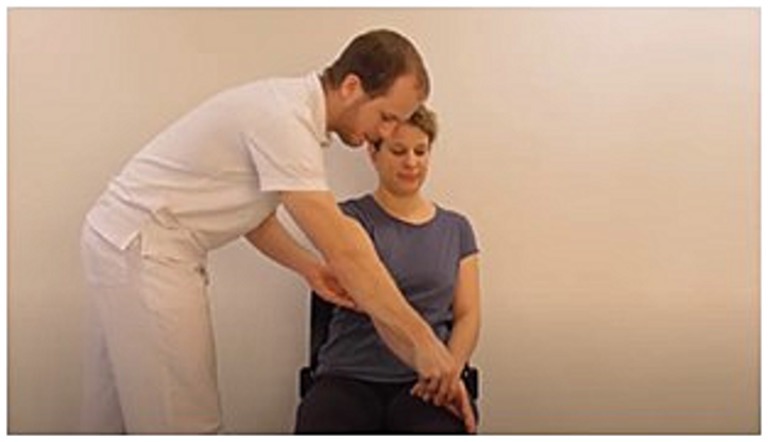
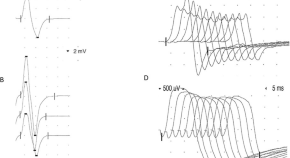
Figure 2 . Example illustration from FMMA training for assessors: FMMA-UE. FMMA-UE, Fugl-Meyer motor assessment upper extremity.
The assessors scored the videos separately in space and time, and independently of each other and other study personnel. The scores were directly entered in coded electronic case report forms (eCRF) of the German version of the FMMA within the secure web application REDCap (Research Electronic Data Capture) ( 17 ). Regarding clinical information, the assessors were unaware of the initial stroke severity, including the FMMA scores at baseline, but were not blinded to the medical history of the subjects in the video recordings. Both assessors had the same access to on-site training and additional video tutorials for recapitulation. They were given additional guidance and explanation on how to proceed in special situations where FMMA items could not be completed for non-stroke-related reasons (e.g., due to pain) or where items were incomplete on video. The flow chart of the study procedure can be found in Figure 3 .
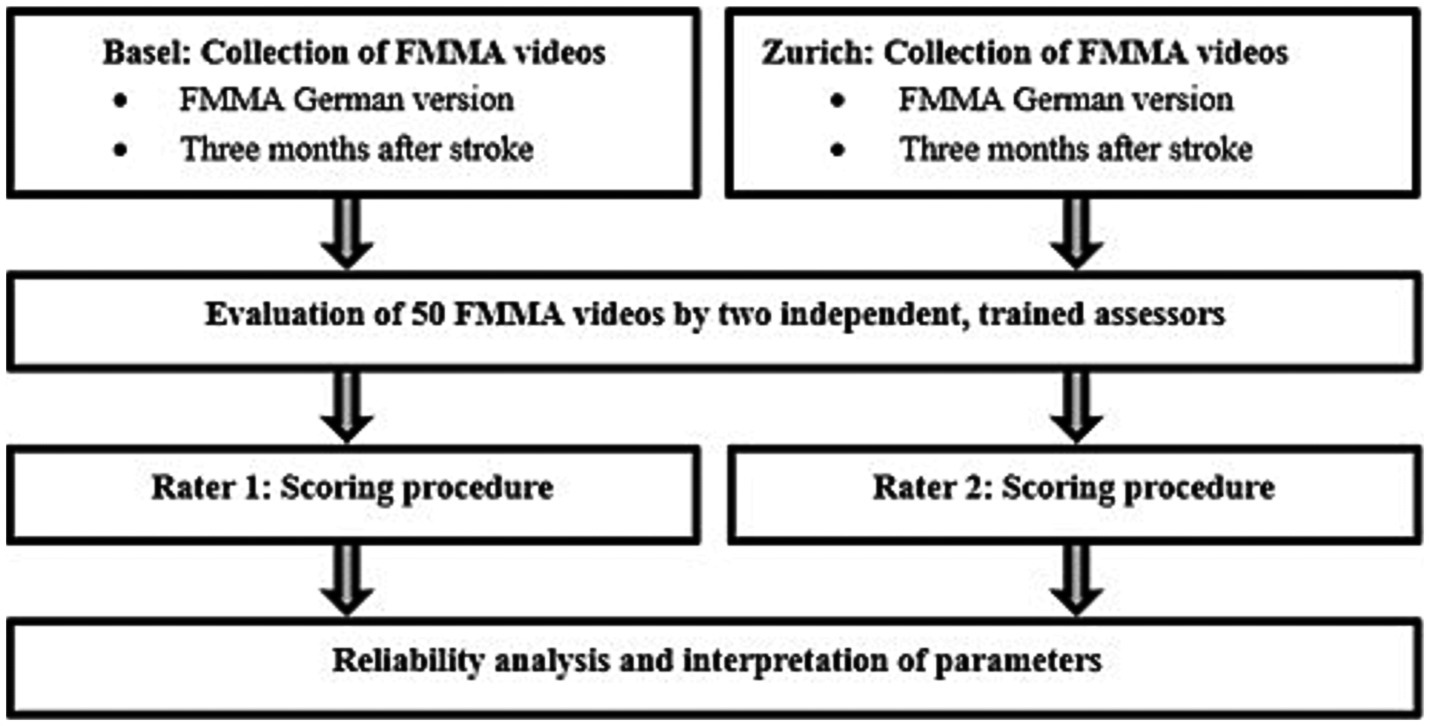
Figure 3 . Flow chart of the study procedure. FMMA, Fugl-Meyer Motor assessment.
Data recording and confidentiality
The videos were recorded with a GoPro camera, GoPro Incorporation (San Mateo, California, US). Camera positions (heights, distances) were exactly defined in written form for the FMMA-UE and the FMMA-LE and are presented in the Supplementary Figure S1 . The storage of all health-related personal data was protected by appropriate operational and organizational measures in accordance with Article 18 of the Ordinance on Clinical Trials in Human Research of the Swiss Confederation ( 18 ).
The informed consent form for the ESTREL trial specifies that the FMMA tests may only be recorded and used for internal research purposes in order to conduct a thorough evaluation.
Statistical reliability analysis
A sample size of 50 subjects was recommended for reliability studies in order to reasonably determine kappa values ( 19 ). In our project, we followed this recommendation, as well as appropriate reference studies that included between 10 and 60 individuals after stroke in their reliability analyses ( 12 , 13 , 20 – 26 ).
Our primary endpoint was the interrater reliability of the FMMA, calculated for the total scores of the entire FMMA and the total scores of the FMMA for the affected extremities using ICCs with the corresponding 95% confidence intervals (CI). The following ICC form fitted the model best: Two-way mixed effects, absolute agreement, multiple raters/measurements ( 27 , 28 ). ICC values were also calculated for the FMMA subscales, as these parameters were recommended for use with continuous variables ( 19 ). For comparison with the reference literature, ICCs were calculated for all FMMA subscales. Since it is questionable whether the ICC – as a parameter for continuous variables ( 19 ) – is suitable for variables with few levels, the ICC was not considered as the only parameter for the coordination subscales (three items/0–6 levels) of the FMMA and for the wrist (five items/0–10 levels) and hand (seven items/0–14) subscales of the FMMA-UE. For these subscales, weighted Cohen’s kappa values with associated CIs were calculated. Since the data were non-parametric, Spearman’s rank-order correlation coefficients (Spearman’s rho values) with appropriate p -values and 95% CI were calculated to document the strength of association for total and subscale evaluations between assessor 1 and assessor 2.
Several statistical procedures formed the secondary endpoints for assessing the reliability of the FMMA at the item level: (i) Percentage agreement values between the two ratings were calculated for all 50 FMMA individual tasks of the affected extremities. (ii) Weighted Cohen’s kappa ( 29 , 30 ) values and corresponding 95% CI were obtained from the FMMA ordinal variables. (iii) Gwet’s AC1/AC2 coefficients with corresponding 95% CIs were calculated at the item level in addition to the weighted Cohen’s kappa values.
Statistical procedures to determine all end points were performed using RStudio software, version 1.2.1335.
Evaluation of parameters
Reliability parameters were categorized according to appropriate classifications (see Supplementary Tables S2, S3 ): We applied the 95% CIs of the ICC estimates for interpretation instead of the ICC estimates themselves ( 27 ) and used the Landis and Koch ( 31 ) classification for the weighted Cohen’s kappa and the Gwet’s AC1/AC2 values to compare the results of the German FMMA with those of previously published studies.
Fifty video recordings were eligible to study the interrater reliability of the German FMMA version ( Figure 1 ). There were no missing data that affected the statistical analysis.
Patient characteristics
50 individuals with stroke were recorded 3 months ±14 days after randomization in the ESTREL trial. 28 of the participants were female, the mean age was 71.64 years, and the median National Institutes of Health Stroke Scale (NIHSS) score was 3.00. All patient demographic and clinical characteristics are presented in Table 1 .

Table 1 . Patient demographic and clinical characteristics.
Descriptive findings of the Fugl-Meyer Motor assessment
Between June and September 2021, 50 FMMA ratings were carried out by both assessors. The difference in median total scores between assessors was less than three points for the FMMA-UE and one point for the FMMA-LE. The median values with the corresponding first and third quantiles of the two assessors’ total FMMA scores are shown in Table 2 .
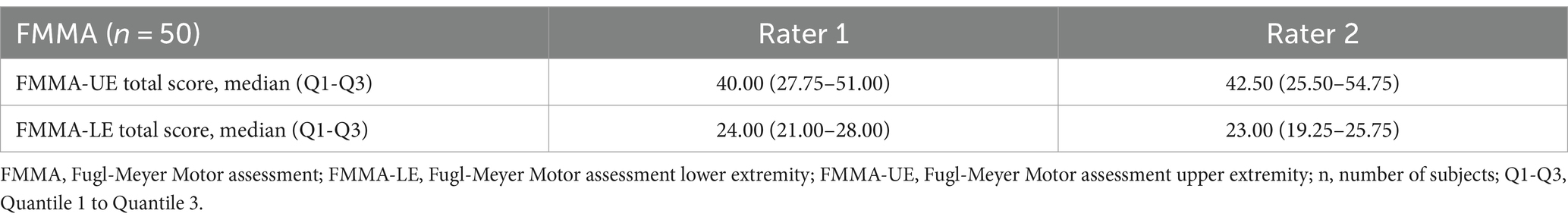
Table 2 . FMMA median and quantile values of the two assessors.
Primary endpoint
All interrater reliability parameters at the overall score and subscale levels of the FMMA are shown in Table 3 .
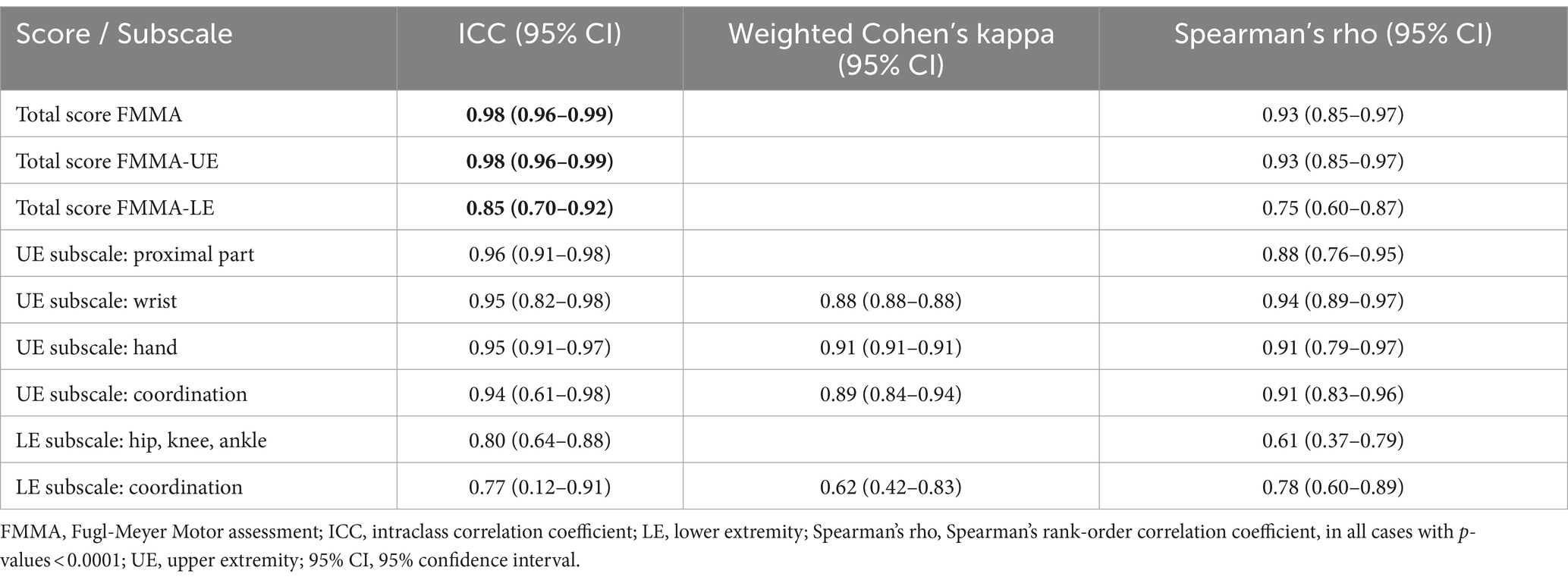
Table 3 . Interrater reliability parameters of the German version of the FMMA at the overall score level.
For all total scores (FMMA-UE, FMMA-LE and entire FMMA) as well as for the proximal part subscale of the FMMA-UE and the hip, knee, ankle subscale of the FMMA-LE, the ICC values were between 0.80 (95% CI 0.64–0.88) for volitional movement within flexor and extensor synergies of the lower extremity and 0.98 (95% CI 0.96–0.99) for the total scores of the FMMA-UE. The total scores of the entire FMMA were very similar at 0.98 (95% CI 0.96–0.99). Using Koo and Li′s ( 27 ) classification for the 95% CI of the ICC values, the reliability of the meaningful subscales as well as that of the total scores (values written bold in Table 3 ) was classified as moderate to excellent.
Weighted Cohen’s kappa values ranged from 0.62 (95% CI 0.42–0.83) for the coordination subscales of the FMMA-LE to 0.91 (95% CI 0.91–0.91) for the hand subscales of the FMMA-UE. Using Landis & Koch (1979) ( 31 ) benchmarking for kappa statistics, the strength of agreement was found to be moderate to almost perfect.
The Spearman’s rank-order correlation coefficients for the total score and subscale levels ranged from 0.61 to 0.94 (median 0.91), with the lowest value for the hip, knee, ankle subscales of the FMMA-LE (values <0.7). The highest values were obtained for the FMMA-UE total scores, the total scores of the entire FMMA, and the wrist, hand, and the coordination subscales of the FMMA-UE (values >0.9). All p -values of Spearman’s rank-order correlation coefficients were smaller than 0.001.
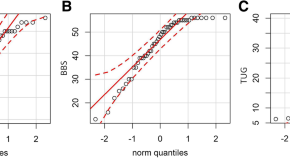
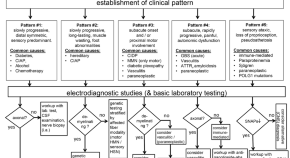
Secondary endpoints
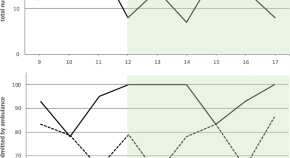
All item-based interrater reliability parameters of the German version of the FMMA-UE are summarized in Table 4 and those of the FMMA-LE in Table 5 . A graphical representation comparing all three item-level measures of the FMMA is shown in Figure 4 .
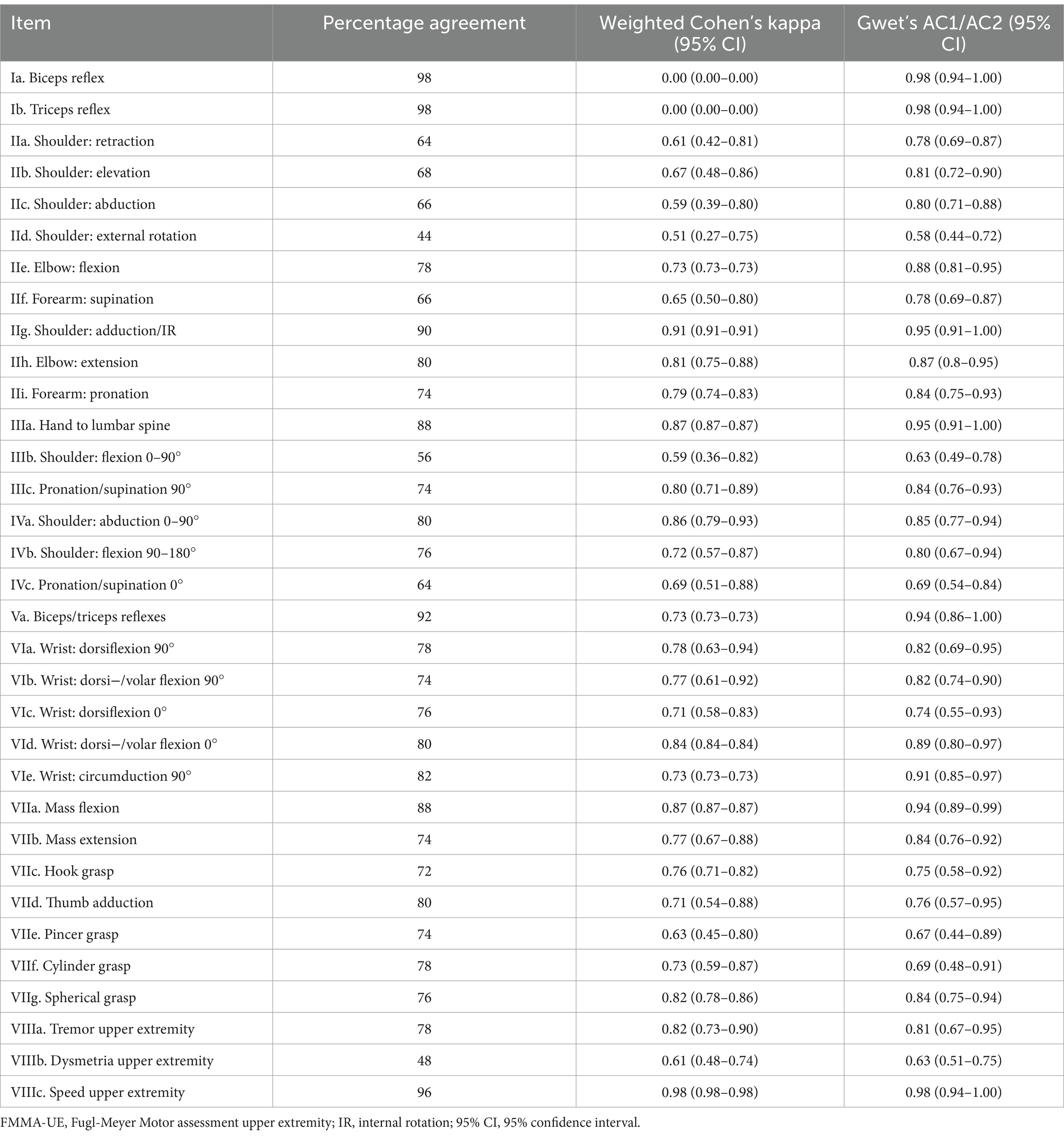
Table 4 . Item-based interrater reliability parameters of the German version of the FMMA-UE.
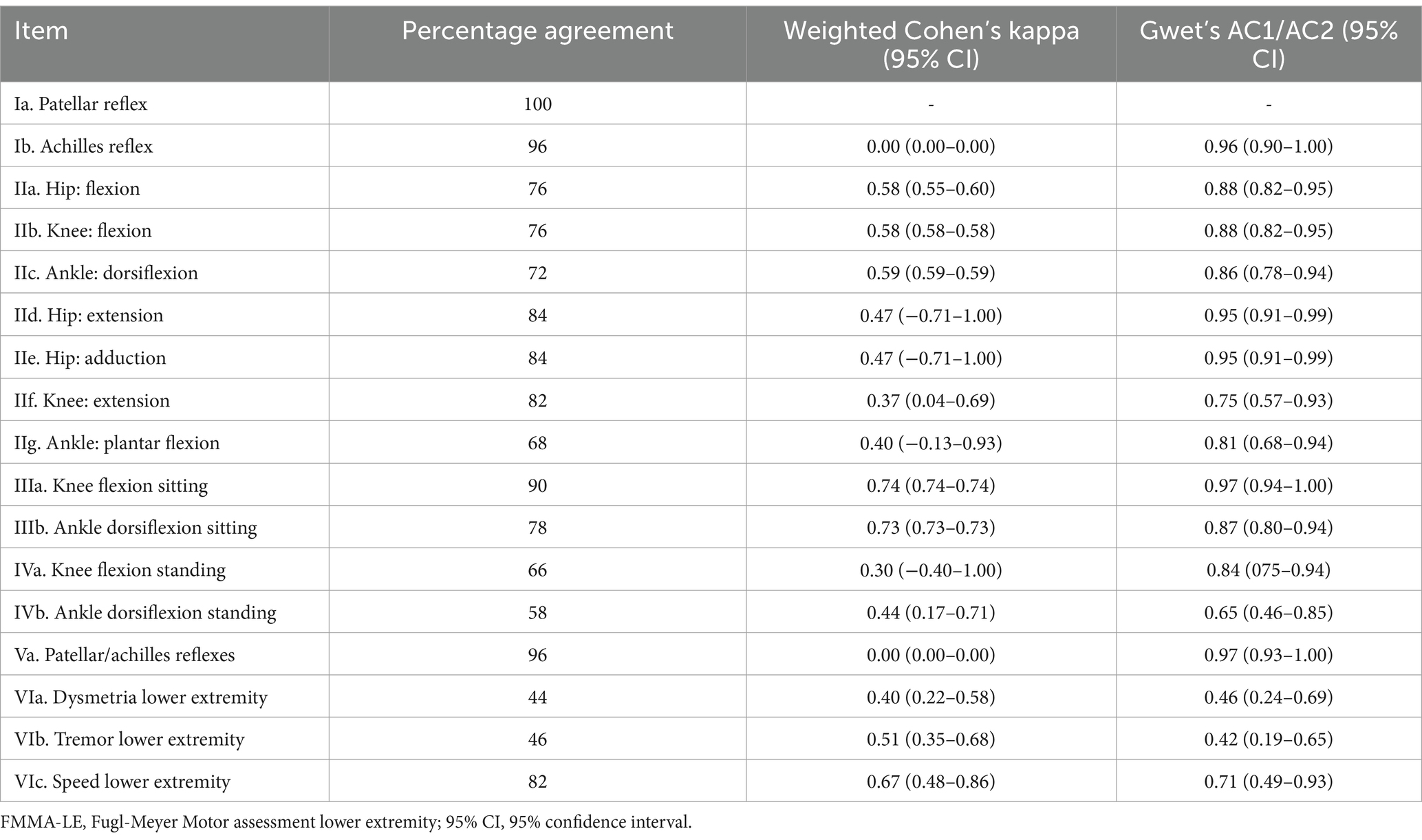
Table 5 . Item-based interrater reliability parameters of the German version of the FMMA-LE.
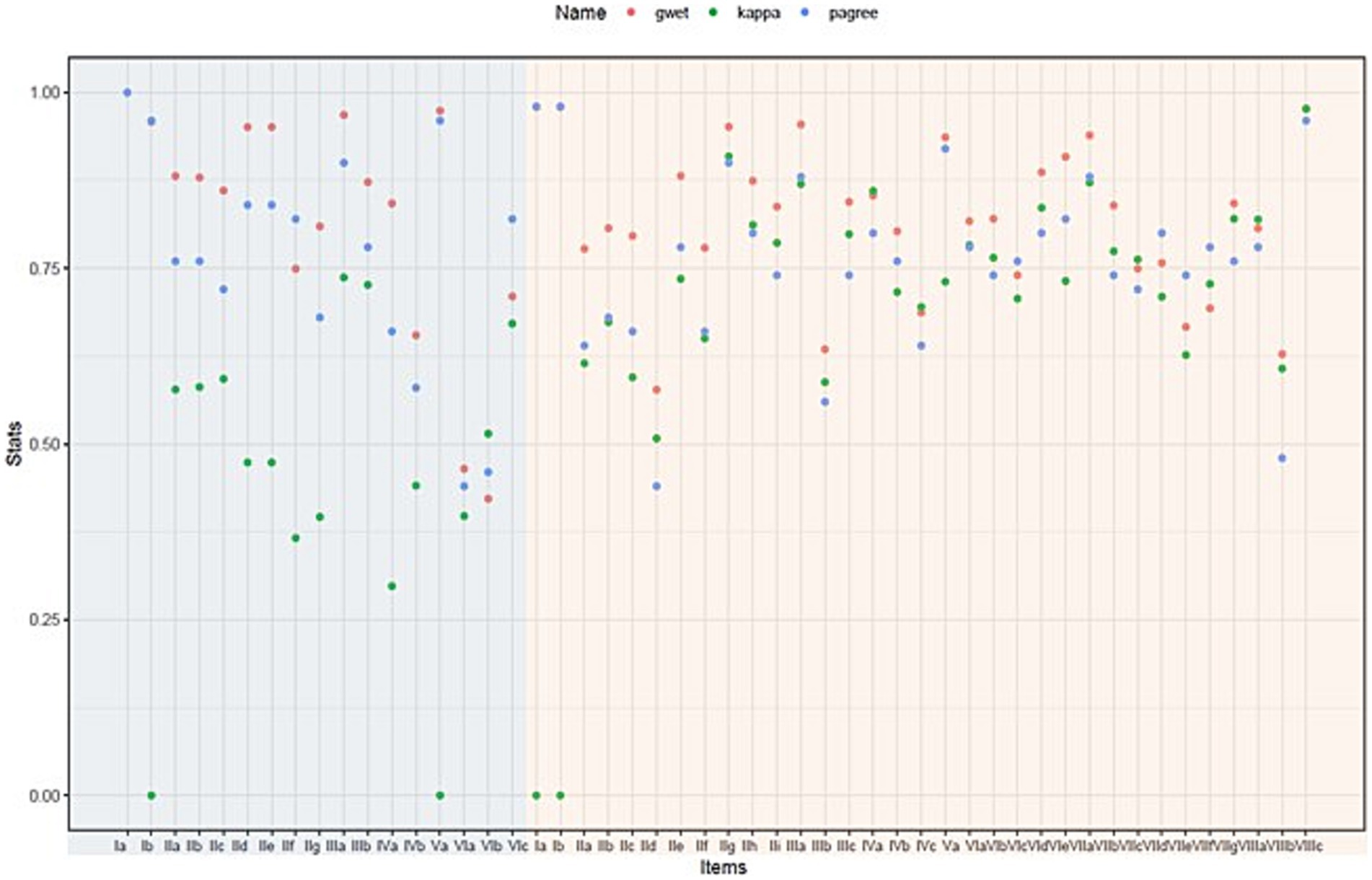
Figure 4 . Graphical representation comparing percentage agreement, weighted Cohen’s kappa, and Gwet’s AC2 for each item. The items on light blue background are part of the FMMA-LE, those on light red of the FMMA-UE. Individual measurement points overlap for item Ib of the FMMA-LE and items Ia, Ib, VIa, and VIIIc of the FMMA-UE. FMMA-LE, Fugl-Meyer Motor assessment lower extremity; FMMA-UE, Fugl-Meyer Motor assessment upper extremity; gwet, Gwet’s AC1/AC2 coefficient; kappa, weighted Cohen’s kappa coefficient; pagree, percentage agreement.
Most of the assessor agreements were above 0.75 for most of the items. The three different statistical parameters (percentage agreement, weighted Cohen’s kappa coefficients, Gwet’s AC1/AC2 coefficients) shown in the graph were far apart for some items, indicating a high heterogeneity, while they were close for others. It can also be seen that the parameter distances were generally larger for the lower extremity items than for the upper extremity items.
Percentage agreement values for upper extremity items ranged from 44 to 98% (median 77%), with the highest data for reflex activities (values >95%) and the lowest for one component each of the flexor synergy and the coordination subscale (values <50%). Agreement values for the FMMA-LE were generally similar to those of the FMMA-UE and ranged from 44 to 100%. The highest agreement was found for the presence or absence as well as the quality of reflex activity (values >95%) and the lowest for two components of the coordination subscale (values <50%).
As presented in Table 4 , weighted Cohen’s kappa coefficients of the upper extremity items ranged from 0.00 (95% CI 0.00–0.00) to 0.98 (95% CI 0.98–0.98) with a median of 0.73. Based on the benchmarking of Landis & Koch (1977) ( 31 ), the strength of the agreement could be classified as slight to almost perfect. For the FMMA-LE (see Table 5 ), the lowest kappa values were 0.00 (95% CI 0.00–0.00) for item Ib. as well as for item Va. and the highest was 0.74 (95% CI 0.74–0.74) for one component of the tasks performed in a sitting position. The median was 0.47. Thus, the degree of agreement was slight to substantial.
In most cases, the Gwet’s AC1/AC2 coefficients were higher than the weighted Cohen’s kappa coefficients. Based on these Gwet’s AC1/AC2 values (median for the items of the entire FMMA 0.84, range 0.42–0.98; median for the items of the FMMA-UE 0.82, range 0.58–0.98; median for the items of the FMMA-LE 0.87, range 0.42–0.97), moderate to almost perfect agreement according to the classification of Landis and Koch (1977) ( 31 ) was found for the FMMA-UE, while it was also moderate to almost perfect for the lower extremity.
The results indicate the following key findings: (i) The total scores of the entire FMMA show excellent interrater reliability of the German FMMA version across different health professions. This makes it suitable for quantitative measurement of stroke recovery in both clinical practice and research. (ii) Interrater reliability at the item level was lower than in comparable studies with FMMA versions in other languages, leaving room for potential improvement in this area.

Interrater reliability at the overall score level
For the total scores of the entire FMMA, which includes both the FMMA-UE and FMMA-LE, the ICC was 0.98 (95% CI 0.96–0.99), which is considered excellent ( 27 ). This finding is consistent with studies that investigated the interrater reliability of the English version of the FMMA in different settings ( 12 , 13 , 26 ).
Item-level interrater reliability
The percentage agreement values in the present study, which ranged from 44 to 98% for the FMMA-UE and from 44 to 100% for the FMMA-LE, were lower than those of the Colombian Spanish version of Hernández et al. (2019, 2020) ( 24 , 25 ), which ranged from 88 to 100% for the FMMA-UE and FMMA-LE. The level of agreement for the items of the FMMA-UE and FMMA-LE in the transculutural/cross-cultural translation and validation studies was above 70% for an Italian version ( 23 ) and for a Danish version ( 22 ). Both working groups classified an agreement of ≥70% as satisfactory ( 22 , 23 ). In contrast, the agreement values for our German version were below 70% for eight items of the FMMA-UE (seven of them within the proximal part subscale) and five items of the FMMA-LE (two of them within the coordination subscale).
Particularly noticeable are the lower percentage agreement values of the respective three items from the coordination subscales of the FMMA-UE and FMMA-LE compared to the data of the above-mentioned articles. In this study, the FMMA-UE coordination item values ranged from 48 to 96% (with the lowest value for dysmetria followed by tremor) and FMMA-LE values ranged from 44 to 82%, whereas the reference studies reported FMMA-UE coordination item values of at least 80% and FMMA-LE values of at least 70% ( 22 – 25 ). These discrepancies raise the question of whether the items of the coordination subscale of the German FMMA should be defined more specifically.
Another explanation for the lower interrater reliability values at the item level in the present project could be that the assessors of the reference studies were therapists ( 22 – 25 ). In the present project the assessors consisted of a physician and a physiotherapist. At the item level, profession-specific differences in rating may well be apparent.
Implications for research and clinical practice
According to expert recommendations ( 5 , 6 , 8 ), the FMMA should be implemented as important assessment for the body function and structure domain of the International Classification of Functioning, Disability and Health (ICF) throughout the continuum of stroke care to optimize the quality of the rehabilitation pathway. The results of the present project make a small but important contribution on this way.
To ensure a consistent and uniform application of the FMMA, a clear, standardized training and refresher training structure as well as a lively exchange between assessors during the training process are of great importance. These elements are largely similar to the procedures used in our training setting. Therefore, and in line with See et al. ( 26 ), we recommend the creation of instructional videos as well as test patient videos to compare scoring as a supplement to FMMA presence training in small groups with an expert and standardized assessment forms.
Based on the proposed measures, the assessment forms of the German version of the FMMA can be further developed and the training structure can be adapted. In the future, international standardization and harmonization of FMMA protocols might be useful.
To the best of our knowledge, this is the first reliability study with a cross-sectional design at a predefined measurement time point in which two assessors evaluated the interrater reliability of a German FMMA version using video recordings of 50 individuals after stroke. Except for the studies by Hernández et al. ( 24 , 25 ) with 60 stroke patients, all selected reference studies with similar populations had smaller sample sizes ( 12 , 13 , 21 – 23 , 26 , 32 ). Furthermore, the consistency of the ICC values across different calculation methods indicated the robustness of our key findings.
The assessors of the current project belong to two different health professions (a physician and a physical therapist), which can be seen as a strength considering that the FMMA is meant to be used more widely in the future. Therefore, and for the envisioned higher acceptance of the FMMA as key motor recovery assessment tool, a high reliability across different professions is essential. Another strength was that the video recordings could be evaluated remotely, avoiding repetitions of the FMMA, which would have introduced the risk of bias due to learning effects. Furthermore, the video approach may allow centralized adjudication within the multicentre ESTREL trial and could improve the quality of future stroke recovery and rehabilitation studies.
Limitations
We are aware of the following limitations of our project. Firstly, the generalisability of the findings based on video recordings with only two assessors has not been demonstrated. A future statistical reliability analysis should incorporate the original FMMA scores from the ESTREL database obtained from real measurements at the time of videotaping in the presence of patients. In this way, the original on-site FMMA ratings might be compared with the ratings of the two assessors based on the videotaped FMMA. This would allow additional comparison of interrater reliability with that reported in the literature based on FMMA ratings in the presence of patients.
Secondly, different statistical approaches to calculating interrater reliability were described in the literature. The parallel calculation of Gwet’s AC1/AC2 coefficients for the item level of the FMMA can be considered a useful complement to the weighted Cohen-Kappa coefficients. The statistic of Gwet, in turn, is not well known because studies of interrater reliability in the current research field rarely report these coefficients. The comparability of study results is important in this context, which is why the use of Svensson’s method ( 33 ), for example, should be considered in future cross-cultural translations and adaptations. Likewise, the determination of systematic disagreement would be an interesting approach. For example, the tasks actively performed by patients with combined movement levels and directions, which are difficult to assess from only one perspective, tended to reflect more systematic inconsistencies. This was evident in some large movement tasks as well as in the evaluation of dysmetria of the FMMA-UE, but also in the standing items and coordination tasks (dysmetria and tremor) of the FMMA-LE. Thirdly, the results of our study are not necessarily applicable to populations other than stroke patients and to assessors from other health professions (e.g., study nurses).
The FMMA appears to be a highly reliable measuring instrument at the overall score level for assessors from different health professions. The FMMA total scores seem to be suitable for the quantitative measurement of stroke recovery in both clinical practice and research, although there is potential for improvement at the item level.
Data availability statement
The datasets generated for this study are available on request to the corresponding author.
Ethics statement
All participants had provided their informed consent to participate in ESTREL, in which videotaping of the FMMA is mentioned. Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements (BASEC-Nr. Req.-2020–00443). Written informed consent was obtained from the individuals for the publication of any potentially identifiable images or data included in this article.
Author contributions
KW: Writing – review & editing, Writing – original draft. AS: Writing – review & editing. LM: Writing – review & editing. JK: Writing – review & editing. CT: Writing – review & editing. AL: Writing – review & editing. JH: Writing – review & editing, Writing – original draft. SE: Writing – review & editing, Writing – original draft.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Swiss National Science Foundation (project number 179667), and the P&K Puehringer Foundation.
Acknowledgments
We would like to thank all experts for their participation: Nathanael Lutz, Sabine Schaedelin, Jan Taeymans, and Amir Tal.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1335375/full#supplementary-material
1. Dimyan, MA, and Cohen, LG. Neuroplasticity in the context of motor rehabilitation after stroke. Nat Rev Neurol . (2011) 7:76–85. doi: 10.1038/nrneurol.2010.200
PubMed Abstract | Crossref Full Text | Google Scholar
2. Pandian, S, and Arya, KN. Stroke-related motor outcome measures: do they quantify the neurophysiological aspects of upper extremity recovery? J Bodyw Mov Ther . (2014) 18:412–23. doi: 10.1016/j.jbmt.2013.11.006
3. Fugl-Meyer, AR, Jääskö, L, Leyman, I, Olsson, S, and Steglind, S. The post-stroke hemiplegic patient. 1. A method for evaluation of physical performance. Scand J Rehabil Med . (1975) 7:13–31.
Google Scholar
4. Gladstone, DJ, Danells, CJ, and Black, SE. The fugl-meyer assessment of motor recovery after stroke: a critical review of its measurement properties. Neurorehabil Neural Repair . (2002) 16:232–40. doi: 10.1177/154596802401105171
5. Kwakkel, G, Lannin, NA, Borschmann, K, English, C, Ali, M, Churilov, L, et al. Standardized measurement of sensorimotor recovery in stroke trials: consensus-based core recommendations from the stroke recovery and rehabilitation roundtable. Int J Stroke . (2017) 12:451–61. doi: 10.1177/1747493017711813
6. Pohl, J, Held, JPO, Verheyden, G, Alt Murphy, M, Engelter, S, Flöel, A, et al. Consensus-based Core set of outcome measures for clinical motor rehabilitation after stroke-A Delphi study. Front Neurol . (2020) 11:875. doi: 10.3389/fneur.2020.00875
Crossref Full Text | Google Scholar
7. Prange-Lasonder, GB, Alt Murphy, M, Lamers, I, Hughes, AM, Buurke, JH, Feys, P, et al. European evidence-based recommendations for clinical assessment of upper limb in neurorehabilitation (CAULIN): data synthesis from systematic reviews, clinical practice guidelines and expert consensus. J Neuroeng Rehabil . (2021) 18:162. doi: 10.1186/s12984-021-00951-y
8. Duncan Millar, J, Van Wijck, F, Pollock, A, and Ali, M. International consensus recommendations for outcome measurement in post-stroke arm rehabilitation trials. Eur J Phys Rehabil Med . (2021) 57:61–8. doi: 10.23736/S1973-9087.20.06575-2
9. Alt, Murphy M. Fugl-Meyer assessment: university of Gothenburg, Institute of Neuroscience and Physiology; (2023). Available at: https://www.gu.se/en/neuroscience-physiology/fugl-meyer-assessment .
10. University of Gothenburg RM . Fugl-Meyer Assessment - Lower Extremity (FMA-LE) English (2019). Available at: https://www.gu.se/en/neuroscience-physiology/fugl-meyer-assessment .
11. University of Gothenburg RM . Fugl-Meyer Assessment - Upper Extremity (FMA-UE) English (2019). Available at: https://www.gu.se/en/neuroscience-physiology/fugl-meyer-assessment .
12. Platz, T, Pinkowski, C, van Wijck, F, Kim, IH, di Bella, P, and Johnson, G. Reliability and validity of arm function assessment with standardized guidelines for the Fugl-Meyer test, action research arm test and box and block test: a multicentre study. Clin Rehabil . (2005) 19:404–11. doi: 10.1191/0269215505cr832oa
13. Sullivan, KJ, Tilson, JK, Cen, SY, Rose, DK, Hershberg, J, Correa, A, et al. Fugl-Meyer assessment of sensorimotor function after stroke: standardized training procedure for clinical practice and clinical trials. Stroke . (2011) 42:427–32. doi: 10.1161/STROKEAHA.110.592766
14. Engelter, ST, and Traenka, C. Enhancement of Stroke Rehabilitation With Levodopa (ESTREL) (2023). Available at: https://clinicaltrials.gov/ct2/show/study/NCT03735901
15. Engelter, ST, Traenka, C, Held, JPO, Lyrer, PA, Michel, P, Müri, R, et al. Pharmakologische Unterstützung der Neurorehabilitation nach Schlaganfall mit Levodopa. Psychiatr Neurol . (2019) 4:14–7.
16. Kottner, J, Audigé, L, Brorson, S, Donner, A, Gajewski, BJ, Hróbjartsson, A, et al. Guidelines for reporting reliability and agreement studies (GRRAS) were proposed. J Clin Epidemiol . (2011) 64:96–106. doi: 10.1016/j.jclinepi.2010.03.002
17. Vanderbilt University . Research Electronic Data Capture (REDCap) (2004). Available at: https://www.project-redcap.org/
18. Swiss Confederation . Ordinance on Clinical Trials in Human Research (2013). Available at: https://www.fedlex.admin.ch/eli/cc/2013/643/en#fn-d6e1721 .
19. de Vet, HCW, Terwee, CB, Mokkink, LB, and Knol, DL. Measurement in medicine: a practical guide . Cambridge: Cambridge University Press (2011).
20. Amano, S, Umeji, A, Uchita, A, Hashimoto, Y, Takebayashi, T, Takahashi, K, et al. Clinimetric properties of the Fugl-Meyer assessment with adapted guidelines for the assessment of arm function in hemiparetic patients after stroke. Top Stroke Rehabil . (2018) 25:500–8. doi: 10.1080/10749357.2018.1484987
21. Barbosa, NE, Forero, SM, Galeano, CP, Hernández, ED, Landinez, NS, Sunnerhagen, KS, et al. Translation and cultural validation of clinical observational scales - the Fugl-Meyer assessment for post stroke sensorimotor function in Colombian Spanish. Disabil Rehabil . (2019) 41:2317–23. doi: 10.1080/09638288.2018.1464604
22. Busk, H, Alt Murphy, M, Korsman, R, Skou, ST, and Wienecke, T. Cross-cultural translation and adaptation of the Danish version of the Fugl-Meyer assessment for post stroke sensorimotor function. Disabil Rehabil . (2021) 1-8 doi: 10.1080/09638288.2021.1919215
23. Cecchi, F, Carrabba, C, Bertolucci, F, Castagnoli, C, Falsini, C, Gnetti, B, et al. Transcultural translation and validation of Fugl-Meyer assessment to Italian. Disabil Rehabil . (2021) 43:3717–22. doi: 10.1080/09638288.2020.1746844
24. Hernández, ED, Galeano, CP, Barbosa, NE, Forero, SM, Nordin, Å, Sunnerhagen, KS, et al. Intra- and inter-rater reliability of Fugl-Meyer assessment of upper extremity in stroke. J Rehabil Med . (2019) 51:652–9. doi: 10.2340/16501977-2590
25. Hernández, ED, Forero, SM, Galeano, CP, Barbosa, NE, Sunnerhagen, KS, and Alt, MM. Intra- and interrater reliability of Fugl-Meyer assessment of lower extremity early after stroke. Braz. J Phys Ther . (2020). doi: 10.1016/j.bjpt.2020.12.002
26. See, J, Dodakian, L, Chou, C, Chan, V, McKenzie, A, Reinkensmeyer, DJ, et al. A standardized approach to the Fugl-Meyer assessment and its implications for clinical trials. Neurorehabil Neural Repair . (2013) 27:732–41. doi: 10.1177/1545968313491000
27. Koo, TK, and Li, MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med . (2016) 15:155–63. doi: 10.1016/j.jcm.2016.02.012
28. McGraw, KO, and Wong, S. Forming inferences about some intraclass correlation coefficients. Psychol Methods . (1996) 50:30–46.
29. Cohen, J . A coefficient of agreement for nominal scales. Educ Psychol Meas . (1960) 20:37–46. doi: 10.1177/001316446002000104
30. Cohen, J . Weighted kappa: nominal scale agreement provision for scaled disagreement or partial credit. Psychol Bull . (1968) 70:213. doi: 10.1037/h0026256
31. Landis, JR, and Koch, GG. The measurement of observer agreement for categorical data. Biometrics . (1977) 33:159–74. doi: 10.2307/2529310
32. Amano, S, Umeji, A, Uchita, A, Hashimoto, Y, Takebayashi, T, Kanata, Y, et al. Reliability of remote evaluation for the Fugl-Meyer assessment and the action research arm test in hemiparetic patients after stroke. Top Stroke Rehabil . (2018) 25:432–7. doi: 10.1080/10749357.2018.1481569
33. Svensson, E . Different ranking approaches defining association and agreement measures of paired ordinal data. Stat Med . (2012) 31:3104–17. doi: 10.1002/sim.5382
Keywords: Fugl-Meyer assessment, stroke, motor disorders, recovery, rehabilitation, reliability, training
Citation: Wiesner K, Schwarz A, Meya L, Kaufmann JE, Traenka C, Luft AR, Held JPO and Engelter S (2024) Interrater reliability of the Fugl-Meyer Motor assessment in stroke patients: a quality management project within the ESTREL study. Front. Neurol . 15:1335375. doi: 10.3389/fneur.2024.1335375
Received: 08 November 2023; Accepted: 04 March 2024; Published: 08 April 2024.
Reviewed by:
Copyright © 2024 Wiesner, Schwarz, Meya, Kaufmann, Traenka, Luft, Held and Engelter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Karin Wiesner, [email protected]
† These authors have contributed equally to this work and share last authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

Volume 2, issue 1, December 2020
52 articles in this issue
Immunoglobulins to mitigate paraneoplastic Lambert Eaton Myasthenic Syndrome under checkpoint inhibition in Merkel cell carcinoma
Authors (first, second and last of 7).
- Maike F. Dohrn
- Ulrike Schöne
- Simone Tauber
- Content type: Letter to the editor
- Open Access
- Published: 09 December 2020
- Article: 52
“Neurological manifestations of COVID-19” - guideline of the German society of neurology
Authors (first, second and last of 11).
- Peter Berlit
- Julian Bösel
- Thomas Hummel
- Content type: Guidelines
- Published: 02 December 2020
- Article: 51
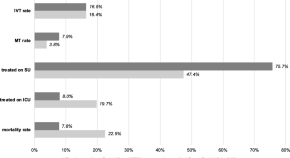
DIagnostic Subdural EEG electrodes And Subdural hEmatoma (DISEASE): a study protocol for a prospective nonrandomized controlled trial
Authors (first, second and last of 10).
- Sae-Yeon Won
- Thomas M. Freiman
- Juergen Konczalla
- Content type: Clinical trial protocol
- Published: 15 December 2020
- Article: 50
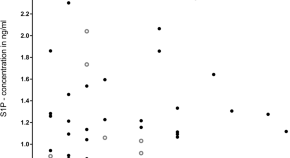
Sphingosine 1-phosphate levels in cerebrospinal fluid after subarachnoid hemorrhage
- Anika Männer
- Dominique Thomas
- Waltraud Pfeilschifter
- Content type: Research article
- Published: 23 November 2020
- Article: 49
Comparison of stroke care parameters in acute ischemic stroke patients with and without concurrent Covid-19. A Nationwide analysis
Authors (first, second and last of 6).
- Daniel Richter
- Christos Krogias
- Ralph Weber
- Published: 19 November 2020
- Article: 48
Decreased admissions and change in arrival mode in patients with cerebrovascular events during the first surge of the COVID-19 pandemic
- Carolin Hoyer
- Lenja Weber
- Kristina Szabo
- Published: 16 November 2020
- Article: 47
A machine learning-based classification approach on Parkinson’s disease diffusion tensor imaging datasets
Authors (first, second and last of 4).
- Jannik Prasuhn
- Marcus Heldmann
- Norbert Brüggemann
- Published: 10 November 2020
- Article: 46
Outcome measures and treatment effectiveness in late onset myasthenia gravis
Authors (first, second and last of 5).
- Francesca Pasqualin
- Silvia V. Guidoni
- Domenico M. Bonifati
- Published: 30 October 2020
- Article: 45
Impact of the COVID-19-pandemic on thrombectomy services in Germany
- Steffen Tiedt
- Felix J. Bode
- for the GSR-ET investigators
- Article: 44
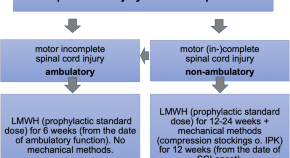
Prevention of thromboembolism in spinal cord injury -S1 guideline
Authors (first, second and last of 12).
- Norbert Weidner
- Oliver J. Müller
- Oswald Marcus
- Published: 10 December 2020
- Article: 43
Comprehensive approaches for diagnosis, monitoring and treatment of chronic inflammatory demyelinating polyneuropathy
- Anna Lena Fisse
- Jeremias Motte
- Content type: Review
- Published: 08 December 2020
- Article: 42

Combined subthalamic and nucleus basalis of Meynert deep brain stimulation for Parkinson’s disease with dementia (DEMPARK-DBS): protocol of a randomized, sham-controlled trial
- Christine Daniels
- Frank Steigerwald
- Jens Volkmann
- Published: 19 October 2020
- Article: 41
Safety and efficacy of intravenous thrombolysis in stroke patients on prior antiplatelet therapy in the WAKE-UP trial
Authors (first, second and last of 24).
- Benedikt M. Frey
- Florent Boutitie
- on behalf of the WAKE-UP investigators
- Published: 20 November 2020
- Article: 40
Validation of a German version of the Cerebellar Cognitive Affective/ Schmahmann Syndrome Scale: preliminary version and study protocol
Authors (first, second and last of 19).
- Andreas Thieme
- Sandra Roeske
- Dagmar Timmann
- Published: 29 September 2020
- Article: 39
Lack of cerebellar tDCS effects on learning of a complex whole body dynamic balance task in middle-aged (50–65 years) adults
Authors (first, second and last of 8).
- M. Rauscher
- K. M. Steiner
- Published: 22 September 2020
- Article: 38
Printed by Parkinson’s: a neurological art project linking patient stories and biosignals
- Lucia K. Feldmann
- Andrea A. Kühn
- Published: 04 November 2020
- Article: 37

Dural tear from diagnostic lumbar puncture followed by long-term morbidity: a case report
- Aleksander Fjeld Haugstvedt
- Inger Birgitte Havsteen
- Hanne Christensen
- Published: 08 October 2020
- Article: 36

Diagnosis and therapy of functional tremor a systematic review illustrated by a case report
- Michael Bartl
- Rebekka Kewitsch
- Walter Paulus
- Published: 03 December 2020
- Article: 35
Historic review: select chapters of a history of stroke
- Axel Karenberg
- Published: 01 December 2020
- Article: 34

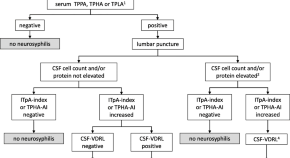
German guidelines on the diagnosis and treatment of neurosyphilis
- Matthias Klein
- Klemens Angstwurm
- Published: 17 November 2020
- Article: 33
Collateral damages in the SARS-CoV-2 pandemia– two cases
- Christian Urbanek
- Jana Kötteritzsch
- Armin J. Grau
- Published: 11 November 2020
- Article: 32
Disease modifying treatment trials in Parkinson’s disease: how to balance expectations and interests of patients, physicians and industry partners?
- K. E. Zeuner
- Content type: Position statement
- Published: 02 November 2020
- Article: 31
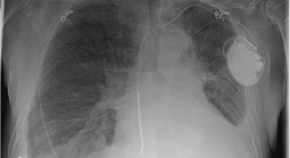
Severe pneumonia with formation of a pulmonary cavity associated with long-term rituximab therapy in multiple sclerosis
- Carolin Schwake
- Published: 12 October 2020
- Article: 30
Bridging therapy is associated with improved cognitive function after large vessel occlusion stroke – an analysis of the German Stroke Registry
- Philipp Ettelt
- Ilko L. Maier
- on behalf of the GSR-ET Collaborators
- Published: 27 July 2020
- Article: 29
Historic review: the foundation-period and the first 15 years of the “Gesellschaft fuer Neuropaediatrie” (GNP) between 1950 and 1990
- Hans Michael Strassburg
- Published: 06 October 2020
- Article: 28
Cross-cultural adaption and validation of the German version of the Mini-BESTest in individuals after stroke: an observational study
- Elena Cramer
- Franziska Weber
- Dörte Zietz
- Published: 01 October 2020
- Article: 27
Increased incidence of transient global amnesia during the Covid-19 crisis?
- Ralph Werner
- Moritz Keller
- Johannes C. Woehrle
- Published: 16 September 2020
- Article: 26
Gene specific therapies – the next therapeutic milestone in neurology
- David Brenner
- Albert C. Ludolph
- Jochen H. Weishaupt
- Published: 08 September 2020
- Article: 25
Historic review: a short history of neuropediatrics in Germany between 1850 and 1950
- Published: 01 September 2020
- Article: 24

Vojta therapy improves postural control in very early stroke rehabilitation: a randomised controlled pilot trial
- Corina Epple
- Barbara Maurer-Burkhard
- Thorsten Steiner
- Published: 20 August 2020
- Article: 23
Letter to the editor: risk comorbidities of COVID-19 in Parkinson’s disease patients in Germany
- Dirk Bartig
- Lars Tönges
- Published: 11 August 2020
- Article: 22
Symptoms and probabilistic anatomical mapping of lacunar infarcts
Authors (first, second and last of 18).
- Ewgenia Barow
- Hans Pinnschmidt
- Published: 03 August 2020
- Article: 21
Diagnosis of peripheral neuropathy
- Helmar C. Lehmann
- Gilbert Wunderlich
- Claudia Sommer
- Content type: Standard operating procedure
- Published: 15 July 2020
- Article: 20
Guillain-Barré syndrome and SARS-CoV-2
- Alexander Winschel
- Published: 08 July 2020
- Article: 19
German hospital capacities for prolonged mechanical ventilator weaning in neurorehabilitation – results of a representative survey
- Thomas Platz
- Andreas Bender
- Michael Sailer
- Published: 01 July 2020
- Article: 18
Recovery from stroke: current concepts and future perspectives
- Christian Grefkes
- Gereon R. Fink
- Published: 16 June 2020
- Article: 17
Guideline “diagnosis and non interventional therapy of neuropathic pain” of the German Society of Neurology (deutsche Gesellschaft für Neurologie)
- Tanja Schlereth
- Published: 10 June 2020
- Article: 16
PIMIDES I: a pilot study to assess the feasibility of patient-controlled neurostimulation with the EASEE® system to treat medically refractory focal epilepsy
- Kristina Kravalis
- Andreas Schulze-Bonhage
- Published: 02 June 2020
- Article: 15

How to use and assess qualitative research methods
- Loraine Busetto
- Wolfgang Wick
- Christoph Gumbinger
- Published: 27 May 2020
- Article: 14
Optical coherence tomography-based assessment of retinal vascular pathology in cerebral small vessel disease
Authors (first, second and last of 13).
- A. Abdelhak
- H. Neugebauer
- Published: 15 May 2020
- Article: 13
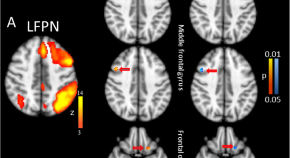
Changed functional connectivity at rest in functional illiterates after extensive literacy training
- Bahram Mohammadi
- Thomas F. Münte
- Jascha Rüsseler
- Published: 12 May 2020
- Article: 12
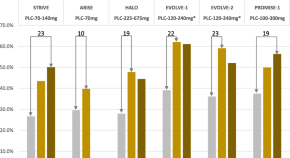
Prevention of migraine with monoclonal antibodies against CGRP or the CGRP receptor
Authors (first, second and last of 14).
- Hans-Christoph Diener
- Stefanie Förderreuther
- Peer Tfelt-Hansen
- Content type: Guideline
- Published: 13 April 2020
- Article: 11
Protocol for a multicenter observational prospective study of functional recovery from stroke beyond inpatient rehabilitation - The Interdisciplinary Platform for Rehabilitation Research and Innovative Care of Stroke Patients (IMPROVE)
- Gunnar Birke
- Götz Thomalla
- Published: 06 April 2020
- Article: 10
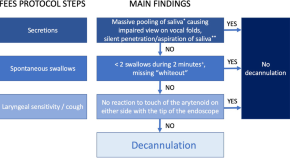
Inter-rater and test-retest reliability of the “standardized endoscopic swallowing evaluation for tracheostomy decannulation in critically ill neurologic patients”
- Tobias Warnecke
- Rainer Dziewas
- Published: 30 March 2020
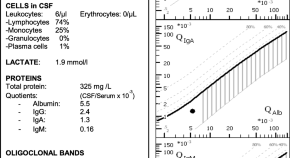
S1 guidelines “lumbar puncture and cerebrospinal fluid analysis” (abridged and translated version)
Authors (first, second and last of 29).
- H. F. Petereit
- T. Zimmermann
- Published: 16 March 2020
Verum versus sham tDCS in the treatment of stroke-induced apraxia: study protocol of the randomized controlled trial RAdiCS -“Rehabilitating (stroke-induced) Apraxia with direct Current Stimulation”
- Nina N. Kleineberg
- Monika K. Richter
- Published: 04 March 2020
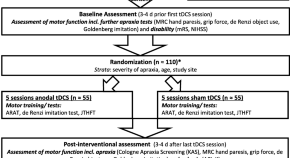
Antibody-related movement disorders – a comprehensive review of phenotype-autoantibody correlations and a guide to testing
- Felix Gövert
- Frank Leypoldt
- Bettina Balint
- Published: 20 February 2020

Neurological research and practice: the first year
- Werner Hacke
- Content type: Editorial
- Published: 28 February 2020
Autoimmune encephalitis in children and adolescents
- Published: 03 January 2020
Remarkable improvement of primary orthostatic tremor using perampanel
- Marcus Grobe-Einsler
- Oliver Kaut
- Published: 29 January 2020
For authors
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 11 April 2024
Guillain-barré syndrome (GBS) with antecedent chikungunya infection: a case report and literature review
- Sreelakshmi V. 1 na1 ,
- Amrita Pattanaik ORCID: orcid.org/0000-0002-1562-0347 1 na1 ,
- Srilatha Marate 1 ,
- Reeta S Mani 2 ,
- Aparna R. Pai 3 &
- Chiranjay Mukhopadhyay 1
Neurological Research and Practice volume 6 , Article number: 21 ( 2024 ) Cite this article
Metrics details
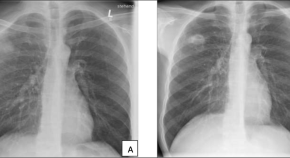
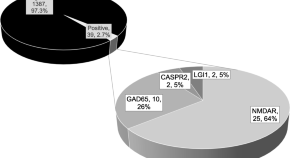
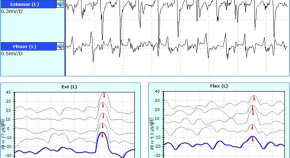
Guillain-Barré Syndrome (GBS) is an autoimmune neuropathy. Antecedent infections have been seen to be significant triggering factors for developing GBS. Among them, arboviral infections are rapidly gaining importance as significant triggers, especially in the areas where they are endemic. Chikungunya, an arboviral infection that usually causes a self-limiting acute febrile illness can lead to GBS as one its severe complications. Herein, we describe a case of a 21-year-old female who presented with weakness in all four limbs and paresthesia. Nerve conduction study and cerebrospinal fluid (CSF) analysis showed axonal, demyelinating motor and sensory neuropathy with albuminocytological dissociation indicating Acute Motor and Sensory Axonal Neuropathy (AMSAN) variant of GBS. Serum IgM antibodies against ganglioside GM1 were detected. Anti-Chikungunya IgM antibodies were found in both serum and CSF samples. The patient was initiated with Intravenous Immunoglobulin (IVIG) therapy. In view of hypoxia, she was intubated and was on mechanical ventilation. After 2 weeks of being comatose, the patient gradually improved and was discharged with no sequelae.
A literature review on antecedent infections in GBS is presented alongside the case report to better understand the association of GBS with antecedent infections, especially the endemic arboviral infections like Chikungunya, Dengue and Zika. This will help in reinforcing the significance of having robust surveillance and public health control measures for infectious diseases.
Guillain-Barré Syndrome (GBS) is a rare but serious autoimmune disorder, affecting the peripheral nervous system (PNS). Highlighting the magnitude of the problem, globally, it has an annual incidence of 1–2 cases per 100,000 people [ 1 ]. However, regional differences in the incidence rate has been observed. As per the prevalence surveys done in Europe, Asia, America, and Australia, 0.4 to 4 GBS cases per 100,000 people have been reported annually [ 2 ]. In Asia, an annual incidence of 1.71, 1.82, 0.42 GBS cases per 100,000 people have been observed in China, South Korea, and Japan respectively [ 3 , 4 ]. These cases have been more frequently reported during the monsoon season in some regions [ 2 , 5 ]. However, contradicting this, in other geographical locations, studies have reported the peak of GBS cases in summer and winter, thus pointing towards a regional variation in the seasonality of the cases. Some studies also suggest that there is no discernible seasonal fluctuation [ 6 , 7 ]. Increased incidence in GBS is also observed during outbreaks and pandemics. A recent instance is the significant rise in GBS cases following the COVID-19 pandemic [ 8 , 9 , 10 ]. Although the exact cause of GBS is still unknown, it is speculated to be a post-infectious condition since 2/3rd of the patients suffer from some form of infectious disease before the neurological condition sets in [ 11 , 12 ]. Many bacterial and viral infections have been implicated in triggering the immune system against nerves, damaging it. As a consequence, weakness and tingling sensation in the extremities progressing to acute flaccid paralysis is seen [ 12 , 13 ]. Less than one-third of the patients with GBS require mechanical ventilation due to respiratory muscle weakness. A mortality rate of 1–18% has been reported in such patients [ 14 , 15 ]. Early diagnosis and treatment with intravenous immunoglobulin or plasmapheresis are effective in reducing the severity of the illness and aid in the recovery of the patients [ 12 ]. GBS is mostly a monophasic condition, but recurrence is observed in about 3–10% of the patients. It may occur at any age, however, higher incidences have been observed in adults compared to children with a predominance seen in males [ 16 , 17 ].
GBS is a heterogeneous disorder having regional variation with respect to the clinical presentation, electrophysiological subtype, and outcome [ 18 ]. The lack of definitive cause and effective treatment is a major challenge that clinicians are facing even after 100 years since the reporting of the first case of GBS. Herein, we present a clinical case of fulminant GBS with antecedent Chikungunya infection. Chikungunya infection is an acute febrile illness usually associated with rashes and arthralgia, transmitted through Aedes aegypti and Aedes albopictus mosquitoes [ 19 , 20 ]. Although meningitis, encephalitis, and GBS have been documented as consequences of a severe acute Chikungunya infection, neurological complications are uncommon [ 21 ]. Neurological complications of Chikungunya infection, including one case of GBS were first observed during the outbreak of 1964 in Madras, India [ 22 ].
The objectives of this review include: (i) reviewing the antecedent infections in GBS, (ii) illustrating the pathogenesis of GBS, (iii) describing the clinical features, and (iv) summarizing the treatment and management.
Case presentation
A 21-year-old female presented with rapid progressive weakness involving all four limbs associated with sensory symptoms in the form of paraesthesia followed by numbness. A month prior, she suffered from high-grade fever, chills, rigors with no other symptoms. There was no laboratory confirmed etiological diagnosis. No other premorbid conditions were found as well.
On initial examination, patient had respiratory distress with hypoxia, in view of which she was intubated and was put on control mode of ventilation. Neurological examination revealed tetraparesis, with paraesthesia of the extremities. There was bilateral but asymmetric facial palsy. Deep tendon reflexes were abolished. Pupils were sluggishly reactive. Routine blood examination revealed hyponatremia (126 mEq/L), anaemia with Vitamin B12 and folate deficiency, mild hypokalaemia (3.4 mmol/L), and elevated inflammatory markers. Nerve conduction study and CSF analysis identified axonal, demyelinating motor and sensory neuropathy with albuminocytological dissociation which indicated the Acute Motor Sensory Axonal Neuropathy (AMSAN) variant of GBS. Patient’s serum was positive for IgM antibodies against GM1 ganglioside; IgM antibodies against Chikungunya virus were found to be present in both serum and CSF. IgM antibodies against other prevalent arboviruses like Dengue, Zika, Japanese encephalitis virus, West Nile virus were not detected in both serum and CSF samples.
IVIG therapy (0.4 g/kg/day for 5 days) along with other supportive measures were immediately initiated in the patient. Nevertheless, she continued to deteriorate and 2 days later, ocular movements were lost with power in limbs worsening to zero. The EEG demonstrated severe encephalopathy with theta waves, suggestive of deep coma attributed to hyponatremia and sedation during intubation. She remained comatose with Glasgow Coma Scale score of 3 even after the completion of one course of IVIG therapy. Therefore, another cycle of IVIG therapy was administered. Despite a normal MRI report, a diagnosis of Bickerstaff brainstem encephalitis was considered because of the clinical picture that was presented.
After 10 days, the patient could move her lip, jaw, shoulders, proximal limbs and showed distal flickering. She was eventually removed from ventilatory support. Even with protective measures in place, due to facial weakness, exposure keratitis occurred and was managed by lid taping by the ophthalmology consultant. While intubated, the patient developed paralytic ileus for a few hours which was managed conservatively with bowel rest and intravenous fluid therapy. Physiotherapy and swallowing exercises were started along with iron, vitamin B12, and folate supplementation and continued after discharge. At discharge, she was hemodynamically stable with power of 4/5 in all four limbs, she was able to swallow semi- solids, and maintained saturation in room air.
Literature review: antecedent infections in GBS
Methodology.
We conducted the literature search through multiple search engines such as PubMed, Scopus, Medline, Google Scholar, and ScienceDirect using the search terms: “Guillain-Barré Syndrome”, “GBS”, “autoimmunity”, “antecedent infection”, “bacteria”, “viruses”, “molecular mimicry”, “arboviruses in GBS”, “Chikungunya infection in GBS”, “intravenous immunoglobulins”, “plasmapheresis”. Thereafter, the search was limited to observational and interventional studies on Guillain-Barré Syndrome with antecedent infections. Only articles published in English language were considered. Additionally, relevant studies were identified through reference analysis. The articles available from 1st January 1990 until 31st December 2023, under the above-mentioned criteria were scanned and relevant studies were included in this narrative review. The results are presented under four headings: Antecedent infections causing GBS, Pathogenesis of GBS, Clinical manifestations and Diagnosis, and Treatment and Prognosis.
In addition, all the published cases of GBS with antecedent Chikungunya were included in this literature review. Up to 31st December, 2023, nine papers were published and a total of 33 cases have been described (Table 1 ). There was no gender prevalence, and the average age of patients studied was 51.
Antecedent infections causing GBS
Though the definitive cause of GBS is still unknown, it has been noted that antecedent infections within two to four weeks were present in 2-3rd of the GBS patients before the onset of neurological symptoms [ 11 , 12 ]. A wide spectrum of infectious agents including bacteria and viruses have been reported to cause GBS. Among them, the commonest agent is the Campylobacter jejuni , a Gram-negative bacteria causing gastroenteritis which accounts for 33% of GBS cases in the western countries, and 45–60% in China and Japan [ 11 , 23 , 24 , 25 , 26 , 27 , 28 ]. Other bacteria like Mycoplasma pneumoniae and Haemophilus influenzae have also been reported to trigger GBS [ 11 , 29 ].
Several viral infections have been associated with triggering GBS and have been reported worldwide. A case-control study conducted in Netherlands in 154 GBS patients reported antecedent infections with CMV, EBV, Parainfluenza 1 virus, Influenza A, Influenza B, Adenovirus, Herpes simplex virus (HSV), Varicella zoster virus (VZV) [ 11 ]. Another study conducted in China with 150 GBS patients reported antecedent infections with Influenza A virus, Influenza B virus, Hepatitis E virus (HEV), Hepatitis A virus (HAV), Dengue virus, Cytomegalovirus (CMV), Epstein- Barr virus (EBV), Herpes simplex virus (HSV), Varicella- zoster virus (VZV), and Rubella virus [ 29 ]. Cytomegalovirus has been found to be the most common viral infection which triggers the immune system leading to GBS [ 11 , 29 , 30 , 31 ]. Following CMV, Epstein Barr virus is found to be the next common antecedent viral infection causing approximately 10% of total GBS cases [ 11 , 29 , 32 ]. GBS cases in children are mostly due to antecedent respiratory viral infections [ 33 ]. Antecedent infection with HEV, HAV, and Hepatitis B virus were also reported to cause GBS [ 34 , 35 , 36 ]. Rarely, infections with Adenovirus, Rubella were also observed as antecedent event in GBS patients [ 37 ].
Among the arboviruses, antecedent Zika virus infection has been widely studied in GBS. The 2013 Zika virus outbreak in French Polynesia was followed by an increased number of GBS cases [ 38 ]. The Zika virus epidemic that started in Brazil in 2016 and disseminated to 15 countries and territories increased the GBS global incidence rate 2.6 times [ 39 , 40 ]. Other arboviral infections including Dengue, Chikungunya, and Japanese Encephalitis have also been implicated in the pathogenesis of GBS. In a multinational case-control study conducted in Brazil, Argentina, and Malaysia during 2017–2019 to understand the association of GBS with antecedent arboviral infections, it was found that 55% (27/49) of patients had recent infections. Arboviral infections caused due to Dengue and Chikungunya virus were found in 4% of these cases [ 41 ]. Another study conducted in Mexico to predict the incidence of GBS owing to arboviral infections reported antecedent Zika and Dengue infections in GBS but intriguingly, GBS was not associated with antecedent Chikungunya infection [ 42 ]. Among studies conducted in India, one done in the northern region reported 11.5% (3/26) antecedent Dengue infection in GBS [ 43 ]. In another study conducted in southern India, it was found that 79.3% of GBS patients studied had antecedent infections, of which viral infections with Chikungunya virus, Japanese Encephalitis virus, and Dengue virus were prominent [ 44 ].
While the occurrence of GBS following Chikungunya infection is uncommon, it is recognised as a potential trigger for GBS, particularly during outbreaks and in regions where the virus is endemic. During the Chikungunya outbreak at Reunion Island, France in 2005–2006, Lebrun et al. reported 2 cases of GBS with antecedent Chikungunya infection. In both the patients, Chikungunya infection was confirmed by the presence anti-Chikungunya IgM and IgG antibodies in serum and CSF [ 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 ]. Antecedent Chikungunya infections in GBS reported globally in the last two decades are depicted in ( Table 1 ) .
Pathogenesis of GBS
Th pathophysiology of GBS has been the subject of numerous studies, and research is still ongoing. The most accepted mechanism of pathogenesis is “molecular mimicry” at the B-cell level, particularly in the axonal variant ( Fig. 1 ) . Previous studies found a structural similarity between lipopolysaccharide on the cell membrane of C. jejuni and the glycan molecule in the ganglioside, and the antibody produced against the bacteria led to nerve cell damage through cross-reactive immunological responses [ 54 , 55 , 56 ]. Supporting this, the animal studies carried out in “acute motor axonal neuropathy rabbit model” observed molecular mimicry in acute motor axonal neuropathy (AMAN) type of GBS [ 57 ]. Anti-ganglioside antibodies have been recorded in 36% of GBS patients [ 58 ]. These antibodies have been shown to have different peripheral nerve targets. Anti-GD1a antibodies bind to paranodal myelin, nodes of Ranvier, and neuromuscular junction. Anti-GM1 and anti-GQ1B antibodies bind to a peripheral nerve or neuromuscular junction [ 59 ]. This anti-ganglioside antibody mediated disease progression through complement cascade activation and formation of membrane attack complex plays a major role in the degeneration of nerve components [ 60 ].
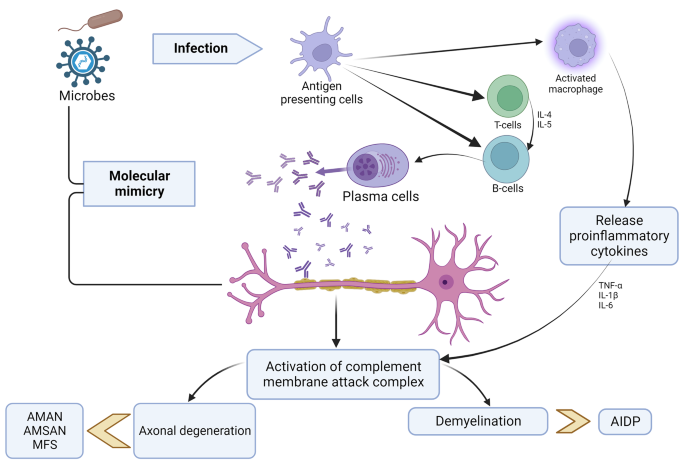
AIDP- “Acute Inflammatory Demyelinating Polyneuropathy,” AMAN- “Acute Motor Axonal Neuropathy,” AMSAN- “Acute Motor and Sensory Axonal Neuropathy,” MFS- “Miller Fisher Syndrome,” TNF- “Tumor Necrosis Factor,” IL- “Interleukin”.
There are a few studies done in arboviral infections that have demonstrated anti-ganglioside antibodies. Dutta et al. observed an increase in anti-GD1a, GD1b, GT1b, and GQ1b antibodies in GBS patients with antecedent Japanese Encephalitis infection [ 61 ]. In a study conducted in immunocompetent mice, an increase in anti-GD1a and GD1b antibodies was observed in Zika virus associated GBS [ 62 ]. In another study involving GBS patients with antecedent Zika virus infection, antibody against GD3 ganglioside was found to be in high [ 63 ]. In GBS patients who had a prior COVID-19 infection, antibodies against GM1, GM2, GD1a, and GQ1b have been identified [ 64 , 65 , 66 ]. In the AIDP variant, autoantibodies against cell adhesion proteins like neurofascin, NRCAM, and contactin-2 localized at Ranvier’s nodes have been suggested as possible targets [ 67 ]. Similar evidence is not well documented for Chikungunya infection. Anti-ganglioside screening has been sparsely done in GBS cases associated with antecedent Chikungunya infection. Although molecular mimicry is speculated to be the most likely mechanism for such cases, there is a lack of evidence that demonstrates viral structure mimicking neural structures. There are two pathways of pathogenesis of Neuro-Chikungunya proposed. One is the direct viral CNS infection which may explain the quick onset of neurological symptoms in GBS patients with antecedent Chikungunya infection (as short as 2 or 3 days) and the second is the PNS affection by autoimmune mechanisms. However, there is a need to generate more evidence on it as well as on the possibility of viral mutations leading to neurological complications [ 68 , 69 ].
Apart from anti-ganglioside antibodies, the epineurium and endoneurium of the nerves have demonstrated infiltration of T lymphocytes in GBS. CD4 + and CD8 + T lymphocytes, as well as macrophages, are observed in greater numbers. It is suggested that the activated T lymphocytes in infections release proinflammatory cytokines, that further activate the complement system leading to demyelination and axonal degeneration. TNF-α produced by the infiltrating T cells has a direct myelinotoxic effect on myelinated fibers, causing demyelination [ 70 ]. The exact mechanisms of pathogenesis, however, still remains unclear.
Clinical manifestations and diagnosis
GBS is caused by the autoimmune attack of peripheral nerves. After the onset of symptoms, it may take 24 hours to four weeks to reach the nadir. The clinical symptoms involved in GBS include weakness and tingling sensation of upper and/or lower limbs which may progress to paralysis of leg, arm, or facial muscles if left untreated [ 12 ].. Some patients may suffer from facial nerve palsy, oculomotor weakness, or oropharyngeal weakness. 10 to 30% GBS patients suffer from severe respiratory muscle weakness within 2 to 4 weeks and require mechanical ventilation [ 71 ]. Keesen et al. observed that in well-characterised GBS patients, respiratory involvement was more distinctively associated with antecedent Chikungunya infection as compared to other arboviral etiology [ 72 ]. Autonomic manifestations like ileus, urinary retention, fever, tachycardia or bradycardia, hypertension or hypotension are also reported in the GBS patients [ 73 , 74 , 75 ].. Fulminant GBS cases reported are characterized by the “absence of brainstem reflexes, complete tetraplegia, and respiratory arrest” [ 76 ]. Rarely, papilledema, facial myokymia, hearing loss, meningeal signs, change in mental status, vocal cord paralysis are also seen in GBS patients [ 77 ]. (Fig. 2 ) shows the clinical features seen in the different variants of GBS.
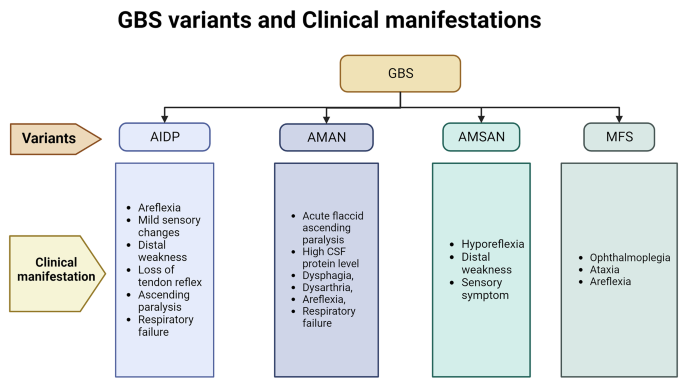
GBS variant and Clinical manifestation
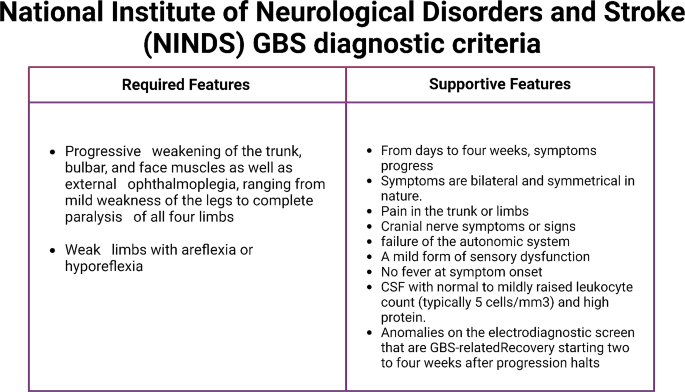
National Institute of Neurological Disorders and Stroke (NINDS) GBS diagnostic criteria
AIDP- “Acute Inflammatory Demyelinating Polyneuropathy,” AMAN- “Acute Motor Axonal Neuropathy,” AMSAN- “Acute Motor and Sensory Axonal Neuropathy,” MFS- “Miller Fisher Syndrome”.
A diagnosis of GBS is mostly based on the clinical history and physical examination. “National Institute of Neurological Disorders and Stroke (NINDS)” has published the GBS diagnostic criteria that is being widely followed (Fig. 3 ) [ 78 ]. The CSF examination and electrophysiological studies provide additional details about the condition. Routine laboratory investigations such as complete blood count, tests for blood glucose, electrolyte estimation, kidney and liver function tests are done in order to exclude other underlying pathologies. Anti-ganglioside antibodies found in the serum aid in identifying the GBS variant. In GBS, CSF protein level is elevated with a normal cell count. CSF examination is also done to find albumin-cytological dissociation [ 78 ]. The severity of the symptoms can be assessed by nerve conduction studies (NCS) and electromyography, which can aid in distinguishing between the axonal and demyelinating forms. Radiological studies can aid in cases where CSF and nerve conduction studies are inconclusive. Spine Magnetic Resonance Imaging (MRI) can exclude other conditions like compressive polyradiculopathy and transverse myelitis [ 79 ].
Treatment and prognosis
Primarily IVIg (0.4 g/kg for 5 days) and plasma exchange (200–250 ml plasma/kg body weight in five sessions) are the recommended treatments for GBS which are quite effective. Due to better availability and ease of administration, IVIg is preferred over plasma exchange. Despite therapy, there is a significant mortality of 3–10% [ 78 , 80 ].
ICU admission is warranted in about 22% of the patients with GBS due to increasing respiratory insufficiency, as was the case here; severe dysfunction in swallowing, cardiac abnormalities and in rapid progression of weakness. Respiratory distress requiring mechanical ventilation has been reported in cases with antecedent Chikungunya infection. In such cases, both acute and long-term mortality are low [ 78 , 81 ].
Antiviral treatment can be considered in patients with GBS who have an ongoing treatable viral infection; however, preceding infections have usually resolved before the onset of weakness [ 78 ]. Arboviral infections including Chikungunya infection is managed by supportive measures. A few novel antiviral compounds and monoclonal antibodies are being evaluated against Chikungunya virus [ 82 , 83 , 84 ]..
Severe disability is seen in 20% of cases which require neurorehabilitation. Some of the delayed complications of GBS include neuropathic pain, postural hypotension, and fatigue. These may persist for months together [ 80 ].
In conclusion, although GBS is considered as a rare disease, there is a perceptible increase in the incidence, especially during outbreaks and pandemics of infectious disease. Many studies mentioned in the literature review have concurred the same. Here we have reported a case of GBS associated with antecedent Chikungunya infection. Chikungunya infection most often causes a self-limiting disease; however, severe complications have been reported occasionally. The case described in this paper adds to the few cases of Chikungunya infection preceding GBS reported globally. This will help physiciansunderstand the clinical course and managesuch cases better. As per the evidence in literature, it is worth noting that acute Arboviral infections including Chikungunya infection lead to GBS in a short period of time that usually ranges from a few days to a few weeks. Most of these cases require ICU support due to frequently associated respiratory insufficiency. Documentation of such cases can help public health policy makers to undertake more surveillance programs and implement appropriate control measures to reduce the burden of Arboviral infections. Along with it, an understanding of the pathogenesis may lead to the development of more directed preventive and therapeutic interventions.
Data availability
Not applicable.
Abbreviations
Guillain Barré Syndrome
Acute Inflammatory Demyelinating Polyneuropathy
Acute Motor Axonal Neuropathy
Acute Motor and Sensory Axonal Neuropathy
Miller Fisher Syndrome
Pharyngeal Cervical Brachial
Bickerstaff’s brainstem encephalitis
Intravenous Immunoglobulin
Lower Motor Neuron
Magnetic Resonance Imaging
Endotracheal tube
Electroencephalogram
Polymerase Chain Reaction
Antigen-presenting cells
Cytomegalovirus
Epstein Barr virus
Cluster of differentiation
Real-time reverse transcriptase polymerase chain reaction
Bragazzi, N. L., Kolahi, A. A., Nejadghaderi, S. A., Lochner, P., Brigo, F., Naldi, A., et al. (2021). Global, regional, and national burden of Guillain–Barré syndrome and its underlying causes from 1990 to 2019. J Neuroinflammation , 18 (1), 264. https://doi.org/10.1186/s12974-021-02319-4 .
Article PubMed PubMed Central Google Scholar
Kuwabara, S. (2004). Guillain-Barré syndrome: Epidemiology, pathophysiology and management. Drugs , 64 (6), 597–610. https://doi.org/10.2165/00003495-200464060-00003 .
Article PubMed Google Scholar
Zheng, P., Tian, D. C., Xiu, Y., Wang, Y., & Shi, F. D. (2021). Incidence of Guillain-Barré syndrome (GBS) in China: A national population-based study. The Lancet Regional Health Western Pacific , 18 , 100302. https://doi.org/10.1016/j.lanwpc.2021.100302 .
Matsui, N., Nodera, H., Kuzume, D., Iwasa, N., Unai, Y., et al. (2018). Guillain-Barré syndrome in a local area in Japan, 2006–2015: An epidemiological and clinical study of 108 patients. European Journal of Neurology , 25 (5), 718–724. https://doi.org/10.1111/ene.13569 .
Article CAS PubMed Google Scholar
Mathew, T., Srinivas, M., Nadig, R., Arumugam, R., & Sarma, G. R. (2014). Seasonal and monthly trends in the occurrence of Guillain-Barre syndrome over a 5-year period: A tertiary care hospital-based study from South India. Annals of Indian Academy of Neurology , 17 (2), 239–241. https://doi.org/10.4103/0972-2327.132662 .
Boucquey, D., Sindic, C. J., Lamy, M., Delmée, M., Tomasi, J. P., & Laterre, E. C. (1991). Clinical and serological studies in a series of 45 patients with Guillain-Barré syndrome. Journal of the Neurological Sciences , 104 (1), 56–63. https://doi.org/10.1016/0022-510x(91)90216-t .
Meshram, R. M., Merchant, S., Bokade, C. M., Bhongade, S., Patil, S., et al. (2016). Seasonal Variation in Childhood Guillain- Barre Syndrome in Central India. J Pediatr Neonatal Care , 5 (6), 00201. https://doi.org/10.15406/jpnc.2016.05.00201 .
Article Google Scholar
Pimentel, V., Luchsinger, V. W., Carvalho, G. L., Alcará, A. M., Esper, N. B., Marinowic, D., Zanirati, G., & da Costa, J. C. (2023). Guillain-Barré syndrome associated with COVID-19: A systematic review. Brain, behavior, & immunity - health , 28 , 100578. https://doi.org/10.1016/j.bbih.2022.100578 .
Bueso, T., Montalvan, V., Lee, J., Gomez, J., Ball, S., Shoustari, A., Julayanont, P., & Jumper, C. (2021). Guillain-Barre Syndrome and COVID-19: A case report. Clinical Neurology and Neurosurgery , 200 , 106413. https://doi.org/10.1016/j.clineuro.2020.106413 .
Chakraborty, U., Hati, A., & Chandra, A. (2021). Covid-19 associated Guillain-Barré syndrome: A series of a relatively uncommon neurological complication. Diabetes & Metabolic Syndrome , 15 (6), 102326. https://doi.org/10.1016/j.dsx.2021.102326 .
Article CAS Google Scholar
Jacobs, B. C., Rothbarth, P. H., van der Meché, F. G., Herbrink, P., Schmitz, P. I., de Klerk, M. A., & van Doorn, P. A. (1998). The spectrum of antecedent infections in Guillain-Barré syndrome: A case-control study. Neurology , 51 (4), 1110–1115. https://doi.org/10.1212/wnl.51.4.1110 .
Guillain–Barré syndrome (2023). https://www.who.int/news-room/fact-sheets/detail/guillain-barré-syndrome . Accessed 08 Aug 2023.
Jasem, J., Marof, K., Nawar, A., Khalaf, Y., Aswad, S., Hamdani, F., Islam, M., & Kalil, A. (2013). Guillain-Barré syndrome as a cause of acute flaccid paralysis in Iraqi children: A result of 15 years of nation-wide study. BMC Neurology , 13 , 195. https://doi.org/10.1186/1471-2377-13-195 .
Melone, M. A., Heming, N., Meng, P., Mompoint, D., Aboab, J., Clair, B., Salomon, J., Sharshar, T., Orlikowski, D., Chevret, S., & Annane, D. (2020). Early mechanical ventilation in patients with Guillain-Barré syndrome at high risk of respiratory failure: A randomized trial. Annals of Intensive care , 10 (1), 128. https://doi.org/10.1186/s13613-020-00742-z .
Article CAS PubMed PubMed Central Google Scholar
Netto, A. B., Taly, A. B., Kulkarni, G. B., Rao, U. G., & Rao, S. (2011). Mortality in mechanically ventilated patients of Guillain Barré Syndrome. Annals of Indian Academy of Neurology , 14 (4), 262–266. https://doi.org/10.4103/0972-2327.91942 .
Arami, M. A., Yazdchi, M., & Khandaghi, R. (2006). Epidemiology and characteristics of Guillain-Barré syndrome in the northwest of Iran. Annals of Saudi Medicine , 26 (1), 22–27. https://doi.org/10.5144/0256-4947.2006.22 .
Nagappa, M., Rahul, W., Sinha, S., Bindu, P. S., Mathuranath, P. S., Rao, S., et al. (2017). Guillain Barre Syndrome in the elderly: Experience from a tertiary-care hospital in India. Journal of Clinical Neuroscience: Official Journal of the Neurosurgical Society of Australasia , 46 , 45–49. https://doi.org/10.1016/j.jocn.2017.08.048 .
Doets, A. Y., Verboon, C., van den Berg, B., Harbo, T., Cornblath, & IGOS Consortium. (2018). Regional variation of Guillain-Barré syndrome. Brain: A Journal of Neurology , 141 (10), 2866–2877. https://doi.org/10.1093/brain/awy232 .
Chikungunya virus| CDC (2023). https://www.cdc.gov/chikungunya/index.html . Accessed 14 Jun 2023.
Ojeda Rodriguez, J. A., Haftel, A., & Walker, I. I. I. (2023). Chikungunya Fever. In: StatPearls. Treasure Island (FL): StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK534224/ . Accessed 14 Jun 2023.
Gonçalves Júnior, J., de Oliveira Bringel, M., Rodrigues de Morais, L. (2022). Chikungunya Neurological Manifestations: A Systematic Literature Review IntechOpen . doi: https://doi.org/10.5772/intechopen.95525 .
Thiruvengadam, K. V., Kalyanasundaram, V., & Rajgopal, J. (1965). Clinical and pathological studies on chikungunya fever in Madras city. The Indian Journal of Medical Research , 53 (8), 729–744.
CAS PubMed Google Scholar
Guillain-Barré Syndrome| Campylobacter| CDC (2022). https://www.cdc.gov/campylobacter/guillain-barre.html . Accessed 09 Aug 2023.
Hao, Q., Saida, T., Kuroki, S., Nishimura, M., Nukina, M., Obayashi, H., & Saida, K. (1998). Antibodies to gangliosides and galactocerebroside in patients with Guillain-Barré syndrome with preceding Campylobacter jejuni and other identified infections. Journal of Neuroimmunology , 81 (1–2), 116–126. https://doi.org/10.1016/s0165-5728(97)00166-5 .
Constant, O. C., Bentley, C. C., Denman, A. M., Lehane, J. R., & Larson, H. E. (1983). The Guillain-Barré syndrome following Campylobacter enteritis with recovery after plasmapheresis. The Journal of Infection , 6 (1), 89–91. https://doi.org/10.1016/s0163-4453(83)95881-4 .
Molnar, G. K., Mertsola, J., & Erkko, M. (1982). Guillain-Barré syndrome associated with campylobacter infection. British Medical Journal (Clinical Research ed) , 285 (6342), 652. https://doi.org/10.1136/bmj.285.6342.652 .
Pryor, W. M., Freiman, J. S., Gillies, M. A., & Tuck, R. R. (1984). Guillain-Barré syndrome associated with Campylobacter infection. Australian and New Zealand Journal of Medicine , 14 (5), 687–688. https://doi.org/10.1111/j.1445-5994.1984.tb05033.x .
Speed, B., Kaldor, J., & Cavanagh, P. (1984). Guillain-Barré syndrome associated with Campylobacter jejuni enteritis. The Journal of Infection , 8 (1), 85–86. https://doi.org/10.1016/s0163-4453(84)93516-3 .
Hao, Y., Wang, W., Jacobs, B. C., Qiao, B., Chen, M., Liu, D., Feng, X., & Wang, Y. (2019). Antecedent infections in Guillain-Barré syndrome: A single-center, prospective study. Annals of Clinical and Translational Neurology , 6 (12), 2510–2517. https://doi.org/10.1002/acn3.50946 .
Mamishi, S., Ashrafi, M. R., Mohammadi, M., Zamani, G., Pourakbari, B., Mahmoudi, S., & Aziz-Ahari, S. (2021). Cytomegalovirus infection and Guillain-Barré syndrome: The First Case-Control Study in Iran. Iranian Journal of Child Neurology , 15 (4), 35–41. https://doi.org/10.22037/ijcn.v15i4.31285 .
Leung, J., Sejvar, J. J., Soares, J., & Lanzieri, T. M. (2020). Guillain-Barré syndrome and antecedent cytomegalovirus infection, USA 2009–2015. Neurological Sciences: Official Journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology , 41 (4), 885–891. https://doi.org/10.1007/s10072-019-04156-z .
Abidoye, O., Raybon-Rojas, E., & Ogbuagu, H. (2022). A rare case of Epstein-Barr Virus: Infectious mononucleosis complicated by Guillain-Barré Syndrome. Cureus , 14 (1), e21085. https://doi.org/10.7759/cureus.21085 .
Gupta, M., Monjazeb, S., Rosser, T., Santoro, J. D., & Ahsan, N. (2023). A case of Pediatric Guillain-Barré Syndrome after respiratory syncytial virus infection. Pediatric Neurology , 146 , 129–131. https://doi.org/10.1016/j.pediatrneurol.2023.06.013 .
Zheng, X., Yu, L., Xu, Q., Gu, S., & Tang, L. (2018). Guillain-Barre syndrome caused by hepatitis E infection: Case report and literature review. BMC Infectious Diseases , 18 (1), 50. https://doi.org/10.1186/s12879-018-2959-2 .
Blecker, E., & Ehtsham, M. (2021). Guillain-Barré Syndrome Likely due to Relapsing Hepatitis A. Case reports in hepatology , 2021 , 5570027. https://doi.org/10.1155/2021/5570027 .
Wei, J., & Duan, S. (2021). Severe Guillain-Barré syndrome associated with chronic hepatitis B: A case report and literature review. Medicine , 100 (48), e27989. https://doi.org/10.1097/MD.0000000000027989 .
Figueiredo, C. A., Klautau, G. B., Afonso, A. M., Castrignano, S. B., Oliveira, M. I., et al. (2008). Isolation and genotype analysis of Rubella virus from a case of Guillain-Barré syndrome. Journal of Clinical Virology: The Official Publication of the Pan American Society for Clinical Virology , 43 (3), 343–345. https://doi.org/10.1016/j.jcv.2008.07.015 .
Cao-Lormeau, V. M., Blake, A., Mons, S., Lastère, S., Roche, C., Vanhomwegen, J., Dub, T., et al. (2016). Guillain-Barré syndrome outbreak associated with Zika virus infection in French polynesia: A case-control study. Lancet (London England) , 387 (10027), 1531–1539. https://doi.org/10.1016/S0140-6736(16)00562-6 .
Koike, H., Chiba, A., & Katsuno, M. (2021). Emerging infection, vaccination, and Guillain-Barré syndrome: A review. Neurology and Therapy , 10 (2), 523–537. https://doi.org/10.1007/s40120-021-00261-4 .
Assesssment and management of Guillain-Barré syndrome in the context of Zika virus infection: interim guidance update (2016). https://www.who.int/publications-detail-redirect/WHO-ZIKV-MOC-16.4-Rev.1 . Accessed 8 Jun 2023.
Leonhard, S. E., Tan, C. Y., van der Eijk, A. A., Reisin, R. R., Franken, S. C., Huizinga, R., et al. (2021). Antecedent infections in Guillain-Barré syndrome in endemic areas of arbovirus transmission: A multinational case-control study. Journal of the Peripheral Nervous System: JPNS , 26 (4), 449–460. https://doi.org/10.1111/jns.12469 .
Arriaga-Nieto, L., Hernández-Bautista, P. F., Vallejos-Parás, A., Grajales-Muñiz, C., et al. (2022). Predict the incidence of Guillain Barré Syndrome and Arbovirus infection in Mexico, 2014–2019. PLOS Global Public Health , 2 (3), e0000137. https://doi.org/10.1371/journal.pgph.0000137 .
Verma, R., Sharma, P., Garg, R. K., Atam, V., Singh, M. K., & Mehrotra, H. S. (2011). Neurological complications of dengue fever: Experience from a tertiary center of north India. Annals of Indian Academy of Neurology , 14 (4), 272–278. https://doi.org/10.4103/0972-2327.91946 .
Dutta, D., Debnath, M., Nagappa, M., Das, S. K., Wahatule, R., Sinha, S., Taly, A. B., & Ravi, V. (2021). Antecedent infections in Guillain-Barré syndrome patients from south India. Journal of the Peripheral Nervous System: JPNS , 26 (3), 298–306. https://doi.org/10.1111/jns.12459 .
Lebrun, G., Chadda, K., Reboux, A. H., Martinet, O., & Gaüzère, B. A. (2009). Guillain-Barré syndrome after chikungunya infection. Emerging Infectious Diseases , 15 (3), 495–496. https://doi.org/10.3201/eid1503.071482 .
Lemant, J., Boisson, V., Winer, A., Thibault, L., André, H., Tixier, F., Lemercier, M., Antok, E., Cresta, M. P., Grivard, P., et al. (2008). Serious acute Chikungunya virus infection requiring intensive care during the Reunion Island outbreak in 2005–2006. Critical care Medicine , 36 (9), 2536–2541. https://doi.org/10.1097/CCM.0b013e318183f2d2 .
Balavoine, S., Pircher, M., Hoen, B., Herrmann-Storck, C., Najioullah, F., Madeux, B., Signate, A., Valentino, R., Lannuzel, A., Saint Louis, M., Cassadou, S., Cabié, A., & Schepers, K. (2017). Guillain-Barré Syndrome and Chikungunya: Description of all cases diagnosed during the 2014 outbreak in the French West Indies. The American Journal of Tropical Medicine and Hygiene , 97 (2), 356–360. https://doi.org/10.4269/ajtmh.15-0753 .
Villamil-Gómez, W., Silvera, L. A., Páez-Castellanos, J., & Rodriguez-Morales, A. J. (2016). Guillain-Barré syndrome after Chikungunya infection: A case in Colombia. Enfermedades Infecciosas y Microbiologia Clinica , 34 (2), 140–141. https://doi.org/10.1016/j.eimc.2015.05.012 .
Matos, A. M. B., Carvalho, M., Malta, F. M., Rodrigues, D. L., Félix, C. L., Pannuti, A. C., Lima, C. S., Espósito, A. D. D. R., Santos, D. L. A. D., von Glehn, L. M. B., Colares, F., da Fonseca, J. K. B., de Oliveira, B. A. L., A. C. P., & Romano, C. M. (2020). High proportion of Guillain-Barré syndrome associated with chikungunya in Northeast Brazil. Neurology(R) Neuroimmunology & Neuroinflammation , 7 (5), e833. https://doi.org/10.1212/NXI.0000000000000833 .
do Rosário, M. S., de Jesus, P. A. P., Farias, D. S., Novaes, M. A. C., Francisco, M. V. L. O., Santos, C. S., Moura, D., Lima, F. W. M., Alcantara, L. C. J., & de Siqueira, I. C. (2022). Guillain-Barré Syndrome and Miller Fisher Syndrome in Association with an arboviral outbreak: A Brazilian Case Series. Frontiers in Medicine , 9 , 911175. https://doi.org/10.3389/fmed.2022.911175 .
Agarwal, A., Vibha, D., Srivastava, A. K., Shukla, G., & Prasad, K. (2017). Guillain-Barre syndrome complicating Chikungunya virus infection. Journal of Neurovirology , 23 (3), 504–507. https://doi.org/10.1007/s13365-017-0516-1 .
Mahto, S. K., Gupta, P. K., Singh, A., & Meena, R. C. (2018). Atypical neurological manifestations of Chikungunya Fever: Two case reports. Indian Journal of Critical care Medicine: peer-reviewed Official Publication of Indian Society of Critical Care Medicine , 22 (4), 306–308. https://doi.org/10.4103/ijccm.IJCCM_459_17 .
Hameed, S., & Khan, S. (2019). Rare variant of Guillain-Barré syndrome after chikungunya viral fever. BMJ case Reports , 12 (4), e228845. https://doi.org/10.1136/bcr-2018-228845 .
van den Berg, B., Walgaard, C., Drenthen, J., Fokke, C., Jacobs, B. C., & van Doorn, P. A. (2014). Guillain-Barré syndrome: Pathogenesis, diagnosis, treatment and prognosis. Nature Reviews Neurology , 10 (8), 469–482. https://doi.org/10.1038/nrneurol.2014.121 .
Nyati, K. K., & Nyati, R. (2013). Role of Campylobacter jejuni infection in the pathogenesis of Guillain-Barré syndrome: An update. BioMed Research International , 2013 , 852195. https://doi.org/10.1155/2013/852195 .
Finsterer, J. (2022). Triggers of Guillain-Barré Syndrome: Campylobacter jejuni predominates. International Journal of Molecular Sciences , 23 (22), 14222. https://doi.org/10.3390/ijms232214222 .
Shahrizaila, N., & Yuki, N. (2011). Guillain-barré syndrome animal model: the first proof of molecular mimicry in human autoimmune disorder. Journal of biomedicine & biotechnology , 2011 , 829129. https://doi.org/10.1155/2011/829129 .
Saeed, M. L., Baloch, K., Mahmud, B., Khan, S. N., Qureshi, M. T., Shad, M. S. S., Hussain, Z. S., Munawar, S. W., Qadeer, K., A., & Abdullah, A. (2019). Role of anti-ganglioside antibodies in the diagnosis of Guillain-Barré Syndrome as an alternate investigation. Cureus , 11 (5), e4625. https://doi.org/10.7759/cureus.4625 .
Goodfellow, J. A., Bowes, T., Sheikh, K., Odaka, M., Halstead, S. K., Humphreys, P. D., Wagner, E. R., Yuki, N., Furukawa, K., Furukawa, K., Plomp, J. J., & Willison, H. J. (2005). Overexpression of GD1a ganglioside sensitizes motor nerve terminals to anti-GD1a antibody-mediated injury in a model of acute motor axonal neuropathy. The Journal of Neuroscience: The Official Journal of the Society for Neuroscience , 25 (7), 1620–1628. https://doi.org/10.1523/JNEUROSCI.4279-04.2005 .
Susuki, K., Rasband, M. N., Tohyama, K., Koibuchi, K., Okamoto, S., Funakoshi, K., Hirata, K., Baba, H., & Yuki, N. (2007). Anti-GM1 antibodies cause complement-mediated disruption of sodium channel clusters in peripheral motor nerve fibers. The Journal of Neuroscience: The Official Journal of the Society for Neuroscience , 27 (15), 3956–3967. https://doi.org/10.1523/JNEUROSCI.4401-06.2007 .
Dutta, D., Debnath, M., Seshagiri, D. V., Nair, B. V. S., Das, S. K., Wahatule, R., Sinha, S., Ravi, V., Taly, A. B., & Nagappa, M. (2022). Impact of antecedent infections on the antibodies against gangliosides and Ganglioside complexes in Guillain-Barré syndrome: A correlative study. Annals of Indian Academy of Neurology , 25 (3), 401–406. https://doi.org/10.4103/aian.aian_121_22 .
Beaver, J. T., Mills, L. K., Swieboda, D., Lelutiu, N., Esser, E. S., Antao, O. Q., Scountzou, E., Williams, D. T., Papaioannou, N., Littauer, E. Q., & Skountzou, I. (2020). Zika virus-induced neuro-ocular pathology in immunocompetent mice correlates with anti-ganglioside autoantibodies. Human Vaccines & Immunotherapeutics , 16 (9), 2092–2108. https://doi.org/10.1080/21645515.2020.1775459 .
Nico, D., Conde, L., Rivera-Correa, J. L., Vasconcelos-Dos-Santos, A., et al. (2018). Prevalence of IgG autoantibodies against GD3 Ganglioside in Acute Zika Virus infection. Frontiers in Medicine , 5 , 25. https://doi.org/10.3389/fmed.2018.00025 .
Simões, J. L. B., & Bagatini, M. D. (2021). Purinergic Signaling of ATP in COVID-19 Associated Guillain-Barré Syndrome. Journal of Neuroimmune Pharmacology: The Official Journal of the Society on NeuroImmune Pharmacology , 16 (1), 48–58. https://doi.org/10.1007/s11481-020-09980-1 .
Dufour, C., Co, T. K., & Liu, A. (2021). GM1 ganglioside antibody and COVID-19 related Guillain Barre Syndrome - a case report, systemic review and implication for vaccine development. Brain Behavior & immunity - health , 12 , 100203. https://doi.org/10.1016/j.bbih.2021.100203 .
Chan, M., Han, S. C., Kelly, S., Tamimi, M., Giglio, B., & Lewis, A. (2021). A Case Series of Guillain-Barré Syndrome after COVID-19 infection in New York. Neurology Clinical Practice , 11 (4), e576–e578. https://doi.org/10.1212/CPJ.0000000000000880 .
Ziganshin, R. H., Ivanova, O. M., Lomakin, Y. A., Belogurov, A. A. Jr, Kovalchuk, S. I., Azarkin, I. V., Arapidi, G. P., Anikanov, N. A., Shender, V. O., Piradov, M. A., Suponeva, N. A., Vorobyeva, A. A., Gabibov, A. G., Ivanov, V. T., & Govorun, V. M. (2016). The pathogenesis of the demyelinating form of Guillain-Barre Syndrome (GBS): Proteo-peptidomic and immunological profiling of physiological fluids. Molecular & Cellular Proteomics: MCP , 15 (7), 2366–2378. https://doi.org/10.1074/mcp.M115.056036 .
Article CAS PubMed Central Google Scholar
Ferreira da Silva, I. R., Frontera, J. A., Moreira, & Nascimento, O. J. (2016). News from the battlefront: Zika virus-associated Guillain-Barré syndrome in Brazil. Neurology , 87 (15), e180–e181. https://doi.org/10.1212/WNL.0000000000003024 .
Cerny, T., Schwarz, M., Schwarz, U., Lemant, J., Gérardin, P., & Keller, E. (2017). The range of neurological complications in Chikungunya Fever. Neurocritical care , 27 (3), 447–457. https://doi.org/10.1007/s12028-017-0413-8 .
Nyati, K. K., & Prasad, K. N. (2014). Role of cytokines and toll-like receptors in the immunopathogenesis of Guillain-Barré syndrome. Mediators of Inflammation , 2014 , 758639. https://doi.org/10.1155/2014/758639 .
Fokke, C., van den Berg, B., Drenthen, J., Walgaard, C., van Doorn, P. A., & Jacobs, B. C. (2014). Diagnosis of Guillain-Barré syndrome and validation of Brighton criteria. Brain: A Journal of Neurology , 137 (Pt 1), 33–43. https://doi.org/10.1093/brain/awt285 .
Keesen, T. S. L., de Almeida, R. P., Gois, B. M., Peixoto, R. F., Pachá, A. S. C., Vieira, F. C. F., Paixão, M., Cazzaniga, R., Boyton, R. J., & Altmann, D. M. (2017). Guillain-Barré syndrome and arboviral infection in Brazil. The Lancet Infectious Diseases , 17 (7), 693–694. https://doi.org/10.1016/S1473-3099(17)30333-X .
Ho, T. W., Hsieh, S. T., Nachamkin, I., Willison, H. J., Sheikh, K., Kiehlbauch, J., Flanigan, K., McArthur, J. C., Cornblath, D. R., McKhann, G. M., & Griffin, J. W. (1997). Motor nerve terminal degeneration provides a potential mechanism for rapid recovery in acute motor axonal neuropathy after Campylobacter infection. Neurology , 48 (3), 717–724. https://doi.org/10.1212/wnl.48.3.717 .
Lehmann, H. C., Jangouk, P., Kierysch, E. K., Meyer zu Hörste, G., Hartung, H. P., & Kieseier, B. C. (2010). Autoantibody-mediated dysfunction of sympathetic neurons in guillain-barre syndrome. Archives of Neurology , 67 (2), 203–210. https://doi.org/10.1001/archneurol.2009.331 .
van Doorn, P. A., Ruts, L., & Jacobs, B. C. (2008). Clinical features, pathogenesis, and treatment of Guillain-Barré syndrome. The Lancet Neurology , 7 (10), 939–950. https://doi.org/10.1016/S1474-4422(08)70215-1 .
Nakamura, Y., Motoki, M., Hirose, T., Hosokawa, T., Ishida, S., & Arawaka, S. (2019). Fulminant Guillain-Barré syndrome showing severe pharyngeal-cervical-brachial weakness in the recovery phase: A case report. BMC Neurology , 19 (1), 145. https://doi.org/10.1186/s12883-019-1376-5 .
Mustafa, A., Adio, B., & Yarahmadi, A. (2021). Descending paralysis as an atypical presentation of Guillain-Barré Syndrome. SAGE open Medical case Reports , 9 , 2050313X20986662. https://doi.org/10.1177/2050313X20986662 .
Leonhard, S. E., Mandarakas, M. R., Gondim, F. A. A., Bateman, K., Ferreira, M. L. B., Cornblath, D. R., van Doorn, P. A., Dourado, M. E., Hughes, R. A. C., Islam, B., Kusunoki, S., Pardo, C. A., Reisin, R., Sejvar, J. J., Shahrizaila, N., Soares, C., Umapathi, T., Wang, Y., Yiu, E. M., Willison, H. J., & Jacobs, B. C. (2019). Diagnosis and management of Guillain-Barré syndrome in ten steps. Nature Reviews Neurology , 15 (11), 671–683. https://doi.org/10.1038/s41582-019-0250-9 .
Singh, G., Bell, D., Rasuli, B., et al. (2021). Guillain-Barré syndrome. Reference Article Radiopaedia org . https://doi.org/10.53347/rID-7533 . https://radiopaedia.org/articles/guillain-barre-syndrome-2 Accessed on 05 Oct 2023.
Head, V. A., & Wakerley, B. R. (2016). Guillain-Barré syndrome in general practice: Clinical features suggestive of early diagnosis. The British Journal of General Practice: The Journal of the Royal College of General Practitioners , 66 (645), 218–219. https://doi.org/10.3399/bjgp16X684733 .
Witsch, J., Galldiks, N., Bender, A., Kollmar, R., Bösel, J., Hobohm, C., Günther, A., Schirotzek, I., Fuchs, K., & Jüttler, E. (2013). Long-term outcome in patients with Guillain-Barré syndrome requiring mechanical ventilation. Journal of Neurology , 260 (5), 1367–1374. https://doi.org/10.1007/s00415-012-6806-x .
Abdelnabi, R., Kovacikova, K., Moesslacher, J., Donckers, K., Battisti, V., Leyssen, P., Langer, T., Puerstinger, G., Quérat, G., Li, C., Decroly, E., Tas, A., Marchand, A., Chaltin, P., Coutard, B., van Hemert, M., Neyts, J., & Delang, L. (2020). Novel class of Chikungunya Virus small molecule inhibitors that targets the viral Capping Machinery. Antimicrobial Agents and Chemotherapy , 64 (7), e00649–e00620. https://doi.org/10.1128/AAC.00649-20 .
Feibelman, K. M., Fuller, B. P., Li, L., LaBarbera, D. V., & Geiss, B. J. (2018). Identification of small molecule inhibitors of the Chikungunya virus nsP1 RNA capping enzyme. Antiviral Research , 154 , 124–131. https://doi.org/10.1016/j.antiviral.2018.03.013 .
Kovacikova, K., & van Hemert, M. J. (2020). Small-molecule inhibitors of Chikungunya Virus: Mechanisms of Action and Antiviral Drug Resistance. Antimicrobial Agents and Chemotherapy , 64 (12), e01788–e01720. https://doi.org/10.1128/AAC.01788-20 .
Download references
Acknowledgements
Author information.
V Sreelakshmi and Amrita Pattanaik contributed equally to this work and share first authorship.
Authors and Affiliations
Manipal Institute of Virology, Manipal Academy of Higher Education, Manipal, 576104, Karnataka, India
Sreelakshmi V., Amrita Pattanaik, Srilatha Marate & Chiranjay Mukhopadhyay
Department of Neurovirology, National Institute of Mental Health and Neurosciences (NIMHANS), Karnataka, Bengaluru, India
Reeta S Mani
Department of Neurology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, 576104, Karnataka, India
Aparna R. Pai
You can also search for this author in PubMed Google Scholar
Contributions
SV prepared the first draft of the manuscript and performed the virological laboratory investigations. AP was involved in conceptualisation, literature research, and manuscript editing and review. SM was responsible for literature search and manuscript editing. ARP was responsible for patient recruitment, interpretation of clinical data, manuscript editing and review. RSM and CM were responsible for critically revising the paper for important intellectual content and overall supervision. All authors have read and approved the final manuscript.
Corresponding authors
Correspondence to Amrita Pattanaik or Aparna R. Pai .
Ethics declarations
Ethics approval and consent to participate.
The additional virological investigations done were a part of the study titled, ‘Screening for antecedent viral infections in Guillain Barre Syndrome’ that was approved by the Institutional Ethical Committee (IEC), Kasturba Medical College, and Kasturba Hospital (Approval ID: 167/2022).
Consent for publication
Written informed consent was obtained from the patient for the publication of this report.
Competing interests
The authors declare that they have no competing interests.
Authors’ information
Manipal Institute of Virology, Manipal Academy of Higher Education, Manipal, Karnataka, India.
Sreelakshmi V, Amrita Pattanaik, Srilatha Marate, Chiranjay Mukhopadhyay.
Department of Neurovirology, National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru, Karnataka, India.
Reeta S Mani.
Department of Neurology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
Aparna R Pai.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
V., S., Pattanaik, A., Marate, S. et al. Guillain-barré syndrome (GBS) with antecedent chikungunya infection: a case report and literature review. Neurol. Res. Pract. 6 , 21 (2024). https://doi.org/10.1186/s42466-024-00315-6
Download citation
Received : 02 December 2023
Accepted : 04 March 2024
Published : 11 April 2024
DOI : https://doi.org/10.1186/s42466-024-00315-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Guillain-Barré Syndrome
- Antecedent infections
- Arboviral infections
- Chikungunya
- Molecular mimicry
- Intravenous immunoglobulin
Neurological Research and Practice
ISSN: 2524-3489
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Neurological Research and Practice, official journal of the German Neurological Society, is an international publication with a broad scope reflecting all clinical, translational and basic research aspects of neurology and neuroscience.Neurological Research and Practice provides a forum for clinicians and scientists with an interest in all areas of neurology including, but not limited to ...
Almost 2 years ago, on February 28, 2019, the first set of articles appeared in the new peer-reviewed open access online-only scientific Journal "Neurological Research and Practice" (NRP). The journal is published jointly by Biomed Central (BMC, a division of Springer-Nature Publishers) and the German Neurological Society (Deutsche ...
Neurological Research and Practice, official journal of the German Neurological Society, is an international publication with a broad scope reflecting all clinical, translational and basic research aspects of neurology and neuroscience.Neurological Research and Practice provides a forum for clinicians and scientists with an interest in all areas of neurology including, but not limited to ...
Volumes and issues. Volume 6 December 2024. December 2024, issue 1. Volume 5 December 2023. December 2023, issue 1. Volume 4 December 2022. December 2022, issue 1. Volume 3 December 2021. December 2021, issue 1.
Neurological Research and Practice. Volumes and issues. Volume 3, issue 1. Search within journal. Search. Volume 3, issue 1, December 2021. 66 articles in this issue. Long-term recovery of upper limb motor function and self-reported health: results from a multicenter observational study 1 year after discharge from rehabilitation
Neurological Research and Practice. Volumes and issues. Volume 5, issue 1. Search within journal. Search. Volume 5, issue 1, December 2023. 67 articles in this issue. Outcome of endovascular stroke therapy in a large mandatory stroke-registry Authors (first, second and last of 7) Sonja Hyrenbach;
A peer-reviewed, open access journal in neurology, neurosciences & neurodevelopment. This website uses cookies to ensure you get the best experience. ... Neurological Research and Practice 2524-3489 (Online) Website ISSN Portal About Articles ...
Neurological Research and Practice 2019 1:16: 4186: Research: Open in a separate window. In December 2020, NRP was included into Pubmed in a record-breaking time of less than 2 years after the publication of the first articles.This is a great breakthrough and the first milestone on our way to a widely accepted international scientific journal ...
Neurological Research and Practice is the official Journal of the German Neurological Society (Deutsche Gesellschaft für Neurologie (DGN)), one of the largest national neurological societies worldwide with more than 10,000 members. NRP was created by the leadership of the DGN as an international, English language publication with a broad ...
Neurological Research and Practice is different from other new open access journals. Firstly, this journal is owned and edited by the German Neurological Society and not by a commercial publishing company. Secondly, although we will provide open access, there will be no costs for authors in the first few years of establishing the journal; all ...
Neurological long-term sequelae are increasingly considered an important challenge in the recent COVID-19 pandemic. However, most evidence for neurological symptoms after SARS-CoV-2 infection and ...
Neurological Research and Practice 1/2020 Neurological Research and Practice 1/2019 Scrollen für mehr Benutzen Sie die Pfeiltasten für mehr Scrollen oder Pfeiltasten für mehr Anzeige. Neu in den Fachgebieten Neurologie und Psychiatrie 19.03.2024 | Burn-out | Nachrichten ...
Neurological Research and Practice. Volumes and issues. Volume 4, issue 1. Search within journal. Search. Volume 4, issue 1, December 2022. 62 articles in this issue. Myositis in Germany: epidemiological insights over 15 years from 2005 to 2019 Authors (first, second and last of 11) Marc Pawlitzki;
Neurological Research and Practice is the official Journal of the German Neurological Society (Deutsche Gesellschaft für Neurologie (DGN)), one of the largest national neurological societies worldwide with more than 10,000 members. NRP was created by the leadership of the DGN as an international, English language publication with a broad ...
Current diagnosis and treatment practice of central retinal artery occlusion: results from a survey among German stroke units. Carolin Hoyer, Simon Winzer, Egbert Matthé, Ida Heinle, Vesile Sandikci, Darius Nabavi, Michael Platten, Volker Puetz, Kristina Szabo. Open Access COVID-19 Letter to the editor.
Neurology ® Clinical Practice Value-Based Care Series; ... By requesting research collaboration via email, we quickly received more than 60 responses. Following one in-person meeting and more than 30 teleconferences, a grant was submitted for a multi-site CADASIL study. In preparation, several neurologists with active cohorts submitted ...
The use of a dedicated neurological triage system improves process times and resource utilization: a prospective observational study from an interdisciplinary emergency department. Carolin Hoyer. Patrick Stein. Kristina Szabo. Research article. Open Access. Published: 25 October 2019. Article: 29.
Neurological Research and Practice Vols. 1 to 6; 2019 to 2024; 2024: v.6 2024: 2019 to 2023: v.1 2019: v.2 2020: v.3 2021: v.4 2022: v.5 2023: Articles from Neurological Research and Practice are provided here courtesy of Deutsche Gesellschaft für Neurologie e.V. Follow NCBI. Connect with NLM
In March 2019, we launched Neurological Research and Practice (NRP), the official English language, open access, online journal of the German Society of Neurology (Deutsche Gesellschaft für Neurologie) [].Each year, I have reported on the new journal's progress [2, 3].In our third year, it's time again to summarize what we've achieved and what's about to come.
5 Cereneo Center of Neurology and Rehabilitation, Zurich, Switzerland; 6 Valens Clinics, Reha Center Triemli, Vitznau, Switzerland; Introduction: The Fugl-Meyer Motor Assessment (FMMA) is recommended for evaluating stroke motor recovery in clinical practice and research. However, its widespread use requires refined reliability data ...
Neurological Research and Practice. Volumes and issues. Volume 2, issue 1. Search within journal. Search. Volume 2, issue 1, December 2020. 52 articles in this issue. Immunoglobulins to mitigate paraneoplastic Lambert Eaton Myasthenic Syndrome under checkpoint inhibition in Merkel cell carcinoma
Neurological Research and Practice offers a place for the dissemination of current research contributions in the quickly growing fields of Clinical Neurology and Neurology. Neurological Research and Practice provides high-quality, original articles where all submitted articles are peer reviewed to provide top quality. The journal welcomes ...
Guillain-Barré Syndrome (GBS) is an autoimmune neuropathy. Antecedent infections have been seen to be significant triggering factors for developing GBS. Among them, arboviral infections are rapidly gaining importance as significant triggers, especially in the areas where they are endemic. Chikungunya, an arboviral infection that usually causes a self-limiting acute febrile illness can lead to ...