
Quick Links
- UW HR Resources
Training Videos
The following videos will teach the principles of pregnancy ultrasound, infection control, fetal anatomy, how to date a pregnancy, maternal pelvic anatomy, how to examine amniotic fluid volume, placenta anatomy, fetal presentation, how to identify certain serious complications (such as bleeding, ectopic and multiple gestation pregnancy, and intrauterine growth restriction) and fetal anomalies.
Welcome and Introduction to the Course
This video provides a general introduction and overview of the training course.
How Ultrasound Works
Learning Objectives:
How to use the Ultrasound Machine
Orient the Transducer
Orient the Screen
Rapidly Survey a Pregnant Uterus
Determine Fetal Orientation from a Single Transverse Scan
Infection Control
The Purpose of IPC
How to Keep Equipment Clean and Safe
how to Wash Your Hands Properly
How to Properly Cover Your Cough
2nd & 3rd Trimester Anatomy
How to Identify Normal Fetal Anatomy of the Head, Heart, Abdomen, Spine, Extremities, Skull, Face, and Brain
Fetal Dating: 2nd & 3rd Trimesters
How to Measure the Head, Abdomen, and Femur to find Fetal Age
How to Scan the Correct Level for each Structure
How to Choose the Best Ultrasound Images to Assess Fetal Age in the 2nd and 3rd Trimesters
Pelvic Anatomy
How to Identify Normal Structures
How to Identify Common Problems during Pregnancy
1st Trimester Anatomy
How to Identify the Following Structures on Ultrasound: Gestational Sac, Yolk Sac, Fetus, Corpus Luteum
How to Describe how the Fetus Grows during the First 13 Weeks
1st Trimester Dating
How to Measure "Mean Sac Diameter" to Estimate Fetal Age
How to Measure "Crown Rump Length" to Estimate Fetal Age
How to Choose the Best Ultrasound Images to Assess Fetal Age
Amniotic Fluid
Measure the volume of amniotic fluid.
Provide appropriate care if amniotic fluid levels are too low or too high.
Identify the position of the placenta
Evaluate for placenta previa
Assess for placental abruption
Conduct appropriate follow up and referrals if you suspect either condition
Fetal Lie and Presentation
Why it is important to identify the fetal lie and presentation
How to identify an abnormal fetal lie or presentation
When to perform a follow up ultrasound
1st Trimester Pain and Bleeding
Identify the normal and abnormal gestational sac
Evaluate fetal cardiac activity
Identify the signs of complete and incomplete miscarriage
Identify the signs of molar pregnancy
Perform appropriate ultrasound followup
Ectopic Pregnancy
Identify the signs of an ectopic pregancy on ultrasound
Assess the risk level of ectopic pregnancy and respond appropriately
Multiple Gestation Pregnancy
Identify dizygotic and monozygotic twins on ultrasound
Identify complications that can result in high-risk birth
Properly refer patients with multiple gestation to the hospital
Intrauterine Growth Restriction (IUGR)
Evaluate for IUGR on clinical exam
Evaluate for IUGR with ultrasounds using three different indicators
Make appropriate referrals for IUGR
Fetal Anomalies
Identify some important abnormalities
Many fetal anomalies cannot be seen by ultrasound or are difficult to see
Some babies you scan may be born with abnormalities you did not see on ultrasound
Course Review and Video of Sonographer Scanning a Patient
This video represents a review of what you have learned and shows a sonographer scanning a pregnant woman.
Learn how to make the patient comfortable during the examination
Review how to measure fetal biometry and the amniotic fluid index
Review how to perform the ROBUST scan
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
This topic will provide an overview of major issues related to breech presentation, including choosing the best route for delivery. Techniques for breech delivery, with a focus on the technique for vaginal breech delivery, are discussed separately. (See "Delivery of the singleton fetus in breech presentation" .)
TYPES OF BREECH PRESENTATION
● Frank breech – Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term.
● Complete breech – Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
- Family Planning
- Antenatal Care
- Labor & Delivery
- Newborn Care
- Child Health
- Leadership and Management in Communities
- Country Map
- Add Resource
- How to use ORB
- Resource Guidelines
- Content Review Process
- Creative Commons FAQs
- Español (es)
Fetal Lie and Presentation Ultrasound Training Video
From: University of Washington School of Medicine
Learning Objectives:
- Why it is important to identify the fetal lie and presentation
- How to identify an abnormal fetal lie or presentation
- When to perform a follow up ultrasound
Your Rating/Bookmark
Organisation, health domain, resource type.
Resource viewed 434 times
- Patient Care & Health Information
- Tests & Procedures
Diagnostic ultrasound, also called sonography or diagnostic medical sonography, is an imaging method that uses sound waves to produce images of structures within your body. The images can provide valuable information for diagnosing and directing treatment for a variety of diseases and conditions.
Most ultrasound examinations are done using an ultrasound device outside your body, though some involve placing a small device inside your body.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Assortment of Products for Daily Living from Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Ultrasound is used for many reasons, including to:
- View the uterus and ovaries during pregnancy and monitor the developing baby's health
- Diagnose gallbladder disease
- Evaluate blood flow
- Guide a needle for biopsy or tumor treatment
- Examine a breast lump
- Check the thyroid gland
- Find genital and prostate problems
- Assess joint inflammation (synovitis)
- Evaluate metabolic bone disease
More Information
- Abdominal aortic aneurysm
- Acute kidney failure
- Acute liver failure
- Acute lymphocytic leukemia
- Adenomyosis
- Adult Still disease
- Alcoholic hepatitis
- Ambiguous genitalia
- Anal cancer
- Appendicitis
- Arteriosclerosis / atherosclerosis
- Arteriovenous fistula
- Atelectasis
- Autonomic neuropathy
- Bladder stones
- Blood in urine (hematuria)
- Breast cancer
- Breast pain
- Carotid artery disease
- Cerebral palsy
- Cholestasis of pregnancy
- Chronic exertional compartment syndrome
- Chronic kidney disease
- Cleft lip and cleft palate
- Congenital adrenal hyperplasia
- Conjoined twins
- Deep vein thrombosis (DVT)
- Double uterus
- Down syndrome
- Ductal carcinoma in situ (DCIS)
- Endometrial cancer
- Endometriosis
- Enlarged breasts in men (gynecomastia)
- Enlarged liver
- Epididymitis
- Erectile dysfunction
- Eye melanoma
- Fibroadenoma
- Fibrocystic breasts
- Galactorrhea
- Ganglion cyst
- Glomerulonephritis
- Growth plate fractures
- Hamstring injury
- High blood pressure in children
- Hurthle cell cancer
- Incompetent cervix
- Infant reflux
- Inflammatory breast cancer
- Intussusception
- Invasive lobular carcinoma
- Iron deficiency anemia
- Ischemic colitis
- Kidney cancer
- Knee bursitis
- Liver cancer
- Liver disease
- Liver hemangioma
- Male breast cancer
- Mammary duct ectasia
- Median arcuate ligament syndrome (MALS)
- Menstrual cramps
- Miscarriage
- Morning sickness
- Morton's neuroma
- Multisystem inflammatory syndrome in children (MIS-C)
- Muscle strains
- Muscular dystrophy
- Myelofibrosis
- Neuroblastoma
- Nonalcoholic fatty liver disease
- Osteoporosis
- Ovarian cancer
- Ovarian cysts
- Painful intercourse (dyspareunia)
- Pancreatic cancer
- Patellar tendinitis
- Pelvic inflammatory disease (PID)
- Peripheral artery disease (PAD)
- Peyronie disease
- Placenta previa
- Placental abruption
- Polycystic kidney disease
- Polymyalgia rheumatica
- Post-vasectomy pain syndrome
- Precocious puberty
- Premature birth
- Preterm labor
- Prostate cancer
- Pulmonary embolism
- Pyloric stenosis
- Recurrent breast cancer
- Residual limb pain
- Retinal detachment
- Retinoblastoma
- Rotator cuff injury
- Sacral dimple
- Sacroiliitis
- Scrotal masses
- Secondary hypertension
- Solitary rectal ulcer syndrome
- Spermatocele
- Spina bifida
- Swollen knee
- Takayasu's arteritis
- Tapeworm infection
- Testicular cancer
- Thrombophlebitis
- Thyroid cancer
- Thyroid nodules
- Torn meniscus
- Toxic hepatitis
- Toxoplasmosis
- Tricuspid atresia
- Tuberous sclerosis
- Uterine fibroids
- Uterine prolapse
- Wilms tumor
- Zollinger-Ellison syndrome
Diagnostic ultrasound is a safe procedure that uses low-power sound waves. There are no known risks.
Ultrasound is a valuable tool, but it has limitations. Sound waves don't travel well through air or bone, so ultrasound isn't effective at imaging body parts that have gas in them or are hidden by bone, such as the lungs or head. Ultrasound may also be unable to see objects that are located very deep in the human body. To view these areas, your health care provider may order other imaging tests, such as CT or MRI scans or X-rays.
How you prepare
Most ultrasound exams require no preparation. However, there are a few exceptions:
- For some scans, such as a gallbladder ultrasound, your care provider may ask that you not eat or drink for a certain period of time before the exam.
- Others, such as a pelvic ultrasound, may require a full bladder. Your doctor will let you know how much water you need to drink before the exam. Do not urinate until the exam is done.
- Young children may need additional preparation. When scheduling an ultrasound for yourself or your child, ask your doctor if there are any specific instructions you'll need to follow.
Clothing and personal items
Wear loose clothing to your ultrasound appointment. You may be asked to remove jewelry during your ultrasound, so it's a good idea to leave any valuables at home.
What you can expect
Before the procedure.
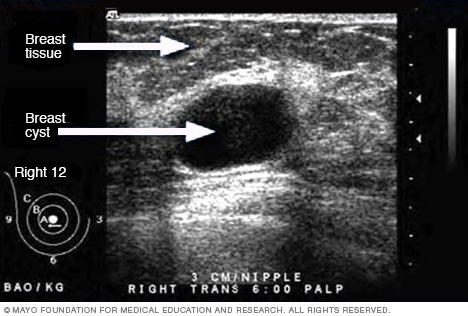
- Ultrasound of breast cyst
This ultrasound shows a breast cyst.
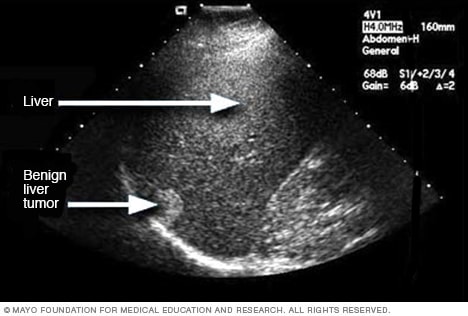
- Liver ultrasound
An ultrasound uses sound waves to make an image. This ultrasound shows a liver tumor that isn't cancer, called benign.

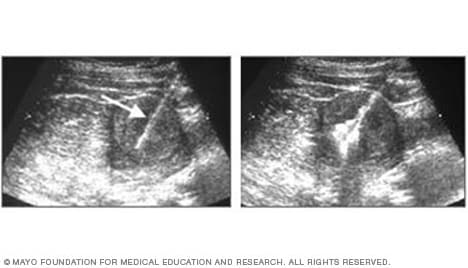
- Ultrasound of gallstones
This ultrasound shows gallstones in the gallbladder.
- Ultrasound of needle-guided procedure
These images show how ultrasound can help guide a needle into a tumor (left), where material is injected (right) to destroy tumor cells.
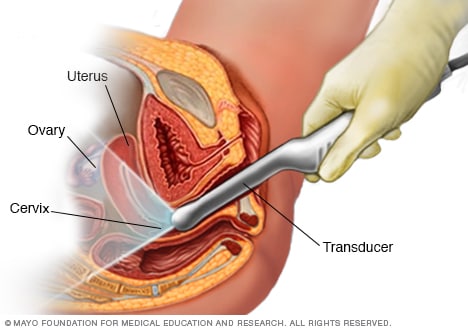
- Transvaginal ultrasound
During a transvaginal ultrasound, you lie on an exam table while a doctor or a medical technician puts a wandlike device, known as a transducer, into the vagina. Sound waves from the transducer create images of the uterus, ovaries and fallopian tubes.
Before your ultrasound begins, you may be asked to do the following:
- Remove any jewelry from the area being examined.
- Remove or reposition some or all of your clothing.
- Change into a gown.
You'll be asked to lie on an examination table.
During the procedure
Gel is applied to your skin over the area being examined. It helps prevent air pockets, which can block the sound waves that create the images. This safe, water-based gel is easy to remove from skin and, if needed, clothing.
A trained technician (sonographer) presses a small, hand-held device (transducer) against the area being studied and moves it as needed to capture the images. The transducer sends sound waves into your body, collects the ones that bounce back and sends them to a computer, which creates the images.
Sometimes, ultrasounds are done inside your body. In this case, the transducer is attached to a probe that's inserted into a natural opening in your body. Examples include:
- Transesophageal echocardiogram. A transducer, inserted into the esophagus, obtains heart images. It's usually done while under sedation.
- Transrectal ultrasound. This test creates images of the prostate by placing a special transducer into the rectum.
- Transvaginal ultrasound. A special transducer is gently inserted into the vagina to look at the uterus and ovaries.
Ultrasound is usually painless. However, you may experience mild discomfort as the sonographer guides the transducer over your body, especially if you're required to have a full bladder, or inserts it into your body.
A typical ultrasound exam takes from 30 minutes to an hour.
When your exam is complete, a doctor trained to interpret imaging studies (radiologist) analyzes the images and sends a report to your doctor. Your doctor will share the results with you.
You should be able to return to normal activities immediately after an ultrasound.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
- Andreas A, et al., eds. Grainger & Allison's Diagnostic Radiology: A Textbook of Medical Imaging. 7th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Jan. 28, 2022.
- General ultrasound. RadiologyInfo.org. https://www.radiologyinfo.org/en/info/genus. Accessed Jan. 28, 2022.
- McKenzie GA (expert opinion). Mayo Clinic. Feb. 1, 2022.
- Chronic pelvic pain
- Ectopic pregnancy
- Fetal macrosomia
- Heavy menstrual bleeding
- Kidney stones
- Molar pregnancy
- Peritonitis
- Rheumatoid arthritis
- Soft tissue sarcoma
- Undescended testicle
- Urinary incontinence
News from Mayo Clinic
- Advancing ultrasound microvessel imaging and AI to improve cancer detection Oct. 13, 2023, 02:01 p.m. CDT
- Doctors & Departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

- Cord presentation
- Report problem with article
- View revision history
Citation, DOI, disclosures and article data
At the time the article was created Yuranga Weerakkody had no recorded disclosures.
At the time the article was last revised Joshua Yap had no financial relationships to ineligible companies to disclose.
- Funic presentation
- Cord (funic) presentation
A cord presentation (also known as a funic presentation or obligate cord presentation ) is a variation in the fetal presentation where the umbilical cord points towards the internal cervical os or lower uterine segment.
It may be a transient phenomenon and is usually considered insignificant until ~32 weeks. It is concerning if it persists past that date, after which it is recommended that an underlying cause be sought and precautionary management implemented.
On this page:
Epidemiology, radiographic features, treatment and prognosis, differential diagnosis.
- Cases and figures
The estimated incidence is at ~4% of pregnancies.
Associations
Recognized associations include:
marginal cord insertion from the caudal end of a low-lying placenta
uterine fibroids
uterine adhesions
congenital uterine anomalies that may prevent the fetus from engaging well into the lower uterine segment
cephalopelvic disproportion
polyhydramnios
multifetal pregnancy
long umbilical cord
Color Doppler interrogation is extremely useful and shows cord between the fetal presenting part and the internal cervical os. However, unlike a vasa previa , the placental insertion is usually normal.
ADVERTISEMENT: Supporters see fewer/no ads
As the complicating umbilical cord prolapse can lead to catastrophic consequences, most advocate an elective cesarean section delivery for persistent cord presentation in the third trimester 3 .
Complications
It can result in a higher rate of umbilical cord prolapse .
For the presence of umbilical cord vessels between the fetal presenting part and the internal cervical os on ultrasound consider:
vasa previa
- 1. Ezra Y, Strasberg SR, Farine D. Does cord presentation on ultrasound predict cord prolapse? Gynecol. Obstet. Invest. 2003;56 (1): 6-9. doi:10.1159/000072323 - Pubmed citation
- 2. Kinugasa M, Sato T, Tamura M et-al. Antepartum detection of cord presentation by transvaginal ultrasonography for term breech presentation: potential prediction and prevention of cord prolapse. J. Obstet. Gynaecol. Res. 2007;33 (5): 612-8. doi:10.1111/j.1447-0756.2007.00620.x - Pubmed citation
- 3. Raga F, Osborne N, Ballester MJ et-al. Color flow Doppler: a useful instrument in the diagnosis of funic presentation. J Natl Med Assoc. 1996;88 (2): 94-6. - Free text at pubmed - Pubmed citation
- 4. Bluth EI. Ultrasound, a practical approach to clinical problems. Thieme Publishing Group. (2008) ISBN:3131168323. Read it at Google Books - Find it at Amazon
Incoming Links
- Variation in fetal presentation
- Vasa praevia
- Umbilical cord prolapse
- Vasa previa
Promoted articles (advertising)
By section:.
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers

Basic Principles of Ultrasound
Jul 20, 2014
720 likes | 1.59k Views
Basic Principles of Ultrasound. Objectives. Define Scope of Practice Understand Principals Understand Physics Understand Transducers Understand Terminology Understand Artifacts. Scope of Practice. eFAST in Trauma Abdomen Chest. Musculoskeletal/Soft tissue Fracture/dislocations.
Share Presentation
- vascular access
- distal shadow
- linear sequential array

Presentation Transcript
Objectives • Define Scope of Practice • Understand Principals • Understand Physics • Understand Transducers • Understand Terminology • Understand Artifacts
Scope of Practice • eFAST in Trauma • Abdomen • Chest • Musculoskeletal/Soft tissue • Fracture/dislocations • Vascular • Access • Blood flow/DVT • Ocular • FB/retinal detachment • Retrobulbar hemorrhage • Genitourinary • Bladder • Ectopic pregnancy • scrotal pain & swelling
3-Tiers • Basic • eFAST, MSK, Skin/Soft Tissue, & Vascular Access • Intermediate • Ocular, Renal, Regional Anesthesia, & DVT • Advanced • OB/Gyn, Testicular, Aorta (AAA), Cardiac (Critical Care), & Pericardiocentesis
Basic Principles • Ultrasound machine and probes create sound waves • Generate waves of vibration from the probe that travel through the tissue of the patient and return to the probe • Received by the machine and interpreted to provide images on screen • Different tissue densities affect the ultrasound beam
Principles • The intensity of the returning echo determines the brightness of the image on the screen • Strong signals = white (hyperechoic) images • Weak signals or lack of signal all together = black (hypoechoic) images • Tissue densities determine the many shades of gray in between
Physics • Diagnostic ultrasound uses sound waves in the frequency range 2-20 MHz • Key properties of sound waves: • Frequency is number of times per second the sound wave is repeated • Wavelength is the distance traveled in 1 cycle • Amplitude is distance between peak and trough
Physics – Parallel Concepts • Conceptually, ultrasound is similar to a laser range finder. • Sound waves sent from the transducer bounce off the object and return. • The ultrasound machine calculates distance to the object from the round-trip time, and creates a grey scale image on the screen.
What does it mean to me? • Lower frequencies image deep structures, but sacrifice resolution. • Higher frequencies provide better resolution, but sacrifice depth. LOWER FREQUENCY Longer wavelength HIGHER FREQUENCY Shorter wavelength
Transducer Function • Ultrasound waves are generated by an electric current -> sent to the crystals -> excites the crystals which vibrate -> creating the resulting wave in the tissue • Beam is ~ 1mm
Transducer Characteristics • The workhorse of the US machine • Sends out sound waves 1% of the time • Listens for echoes 99% of the time • Frequencies are fixed or adjustable • “Footprint” is what touches the patient
Transducer Use • Hold the probe lightly in your hand • Like a pencil • Small movements equal big changes
Transducer Use • Probe marker facing the patient’s right or head • Exceptions: cardiac & procedures
Probe indicator – leading edge Generally to the patient’s head or right side.
Transducer Choices • Curvilinear Array (Curved Probe) • Freq range (5-2 MHz), 30cm depth • Abdomen, FAST, AAA • Linear Sequential Array (Linear Probe) • Freq range (10-5 MHz), 9cm depth • Vascular access, pneumothorax, regional anesthesia • Phased Array (Sector or Cardiac Probe) • Freq range (5-1 MHz), 35cm depth • Cardiac, eFAST, AAA
Transducer directions • Rotating • Fanning/Tilting • Rocking • Sliding • Compression
Transducer directions • Sliding
Transducer directions • Fanning/Tilting • Compression
Transducer directions • Rotation • Rocking
Scanning Planes
Scanning Planes Sagittal Axial
Screen Orientation Near Field Receding Edge Leading Edge Far Field
Image Quality – The 5 P’s • Use Plenty of Gel • Parallel to the table/stretcher • Perpendicular to structure • Pressure (right amount) • Scan in multiple Planes
Gel & Water Stand-offs
Ultrasound transmission gel USE LOTS OF IT!!!
Image Quality - Machine • Depth: Place the object of interest in the center of the screen • Machine will autofocus to the center of the screen giving it the best resolution • Right side markings show depth in cm • Gain: brightness of the image • Can be adjusted for each scan • Be careful not to use too much or too little gain • Autogain
Depth Too Little Too Much
Depth – JUST RIGHT!
Gain Too Little Too Much
Gain – Just Right!
Image Resolution • Spatial Resolution • The ability to distinguish two separate objects close together • Temporal Resolution • The ability to accurately locate structures or events at a specific point in time • Can be improved by decreasing depth & narrowing the sector angle
Spatial Resolution Axial Lateral The ability to distinguish two objects that are laying side-by-side Dependent upon the beam width Two objects cannot be distinguished if they are separated by less than the beam width High freq = narrow width Low freq = wider width • The ability to differentiate two separate objects in the axial plane • Determined by the pulse length • High freq = short length & better axial resolution • Low freq = long length and poor axial resolution
Scanning Modes • B-Mode: • Nearly all of your scans will begin and stay in this mode • Organs appear differently based on their tissue densities
Scanning Modes • M-Mode: • Motion mode provides a reference line on screen • Shows motion towards and away from probe at any depth along that line • Used for detecting fetal heartbeatsand pneumothoracies
Scanning Modes Spectral Doppler Color Flow Doppler Blue – Away : Red – Towards Power Doppler
Attenuation • As the ultrasound beam travels through the body, it looses strength & returns less signal • Certain tissue densities cause this effect: • Slow: Bone, Diaphragm, Pericardium & air = bright (Hyperechoic) images • Moderate: Muscle, Liver, Kidney = gray (Isoechoic) images • Faster: Blood, Ascites, Urine = Darker (Hypoechoic) images
Artifacts • Posterior Enhancement • Reverberation • Edge Artifact • Shadowing • Mirror Image • Comet Tail
Posterior Enhancement Hyperechoic streaking distal to interface of anechoic structure Not a true artifact
Reverberation Bouncing of signal from two reflective surfaces Often seen as a “needle artifact” during procedural ultrasound Called “Ring Down artifact” when seen with air in the bowel or soft tissue
Edge Artifact A distal shadow from the edge of spherical fluid filled structures Scan at different angles to reduce the artifact
Shadowing Anechoic streaking distal to surface with high reflectivity (behaves like light) Stones Bones
Mirror Image Appearance of same image on both sides of highly reflective surface Misinterpretation by machine of signal timing puts image where it thinks it “should be” Often seen on cardiac and around diaphragm
Comet Tail Pathognomonic for excluding pneumothorax
- More by User
BASIC PRINCIPLES
BASIC PRINCIPLES You cannot sell from an empty wagon! Private sector development of industrial/business parks may be adequate. If not, there is a compelling need for local economic development programs to fill the need. STATUTORY AUTHORITY N.C.G.S. §158-7.1(a) provides:
624 views • 19 slides
Basic Principles of GMP
Basic Principles of GMP. Complaints and Recalls. Sections 5 and 6. Complaints and Recalls. Objectives To identify the key issues in product complaint and recall handling To understand the specific requirements for organization, procedures and resources
602 views • 22 slides
Principles of Ultrasound
Types of Ultrasound. Diagnostic (20,000 Hz 750,000 Hz)Therapeutic (.75 MHz 3 MHz)Surgical (3 MHz 10 GHz)Human ear can hear (16-20,000 Hz). Definition. Ultrasound is a deep penetrating modality capable of producing thermal and non-thermal effectsProduced by an alternating current (AC) flow
842 views • 27 slides
Basic Principles of Assessment
Basic Principles of Assessment. Communicating Assessment Results. Feedback Sessions. Oral or written Comprehensible and useful Need to consider: Purposes of assessment What does it mean to the test taker, education, career…. Should be soon after assessment.
475 views • 5 slides
Basic Principles
Basic Principles. Learning objectives. Understand the basic principles undelying A&T techniques Grasp the motivations and applicability of the main principles. Main A&T Principles . General engineering principles: Partition: divide and conquer Visibility: making information accessible
539 views • 10 slides
BASIC ULTRASOUND OF THE KNEE
BASIC ULTRASOUND OF THE KNEE. By Mohamed Hassan Youssef MD Arthritis/ Rehab&Pain Clinic Board certified of ABPM&R. Knee Joint. Knee Bones. Distal end of the F umer Proximal end of the Tibia Head of the Fibula Patella. Knee Bones. Knee Bones. Movement of Patella Upward
968 views • 40 slides
Basic Principles of Ultrasound Imaging
Basic Principles of Ultrasound Imaging. Introduction Ultrasound imaging have different meaning to to different categories of people based on profession or vocation In the Heath Sector- Clinicians, Patients
7.7k views • 17 slides
NMM Dynamic Core and HWRF Zavisa Janjic and Matt Pyle NOAA/NWS/NCEP/EMC , NCWCP, College Park, MD . Basic Principles. Forecast accuracy Fully compressible equations Discretization methods that minimize generation of computational noise and reduce or eliminate need for numerical filters
558 views • 39 slides
Introduction to NMMB Dynamics: How it differs from WRF-NMM Dynamics Zavisa Janjic NOAA/NWS/NCEP/EMC , College Park, MD . Basic Principles. Forecast accuracy Fully compressible equations
781 views • 60 slides
Basic Principles of Learning
Basic Principles of Learning. Basic Principles of Learning. Definition of Learning. Relative permanent change in behavior brought about through experience or interactions with the environment Not all changes result from learning Change in behavior not always immediate
978 views • 39 slides
Principles of Medical Ultrasound
Principles of Medical Ultrasound. Pai-Chi Li Department of Electrical Engineering National Taiwan University. What is Medical Ultrasound?. Prevention : actions taken to avoid diseases.
1.47k views • 81 slides
Basic Principles. No action will occur unless electrical current is flowing No current will flow unless it finds a complete loop out from the source and back to it Current will flow through any and all available loops, although not equally Heating occurs as current flows, due to resistance.
917 views • 46 slides
Basic Principles. We are taking a USER perspective, not a PREPARER perspective. Basic Principles. The Accounting Entity The business unit for which the financial statements are being prepared. Basic Principles. Going Concern
430 views • 13 slides
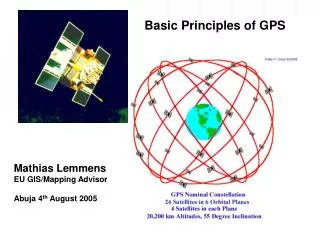
Basic Principles of GPS
Basic Principles of GPS. Mathias Lemmens EU GIS/Mapping Advisor Abuja 4 th August 2005. Contents. Introduction GPS as a surveying tool Methods of Observation Accuracy Aspects Sources of GPS Error. Global Positioning System (GPS).
1.34k views • 43 slides
Basic Principles of Nutriton
Basic Principles of Nutriton. Prof. Dr. Ahmet AYDIN İÜ Cerrahpaşa Tıp Fak. Çocuk Sağlığı ve Hastalıkları ABD Metabolizma ve Beslenme Bilim Dalı Başkanı (www.beslenmebulteni.com) ([email protected]). NUTRITIONAL REQUIREMENTS.
939 views • 73 slides

Basic Principles Of WTO
Non-discriminatory Principle Principle of Tariff Concession Principle of Trade Protection Principle of Trade Facilities,Transparency and Competition Protection. Basic Principles Of WTO. Non-discriminatory Principle. Principle of Most-Favoured-Nation Treatment MFN
1.68k views • 15 slides
Basic Principles of Ultrasound Imaging. Summarized by: Name: AGNES Purwidyantri Student ID number: D0228005 Biomedical Engineering Dept. Ultrasound. Sound waves above 20 KHz are usually called as ultrasound waves.
1.73k views • 22 slides
Basic Physics of Ultrasound
Basic Physics of Ultrasound. WHAT IS ULTRASOUND?. Ultrasound or ultrasonography is a medical imaging technique that uses high frequency sound waves and their echoes. Known as a ‘pulse echo technique’
1.11k views • 17 slides
Principles of Medical Ultrasound. Zahra Kavehvash. Medical Ultrasound Course (25-636). Introduction Acoustic wave propagation Acoustic waves in fluids Acoustic waves in solids Attenuation and dispersion Reflection and Transmission Transducers Beam forming and Diffraction
746 views • 58 slides
Basic Principles of GMP. Equipment. 13. Equipment. Objectives To review the requirements for equipment selection design use maintenance To discuss problems related to issues around selected items of equipment. Equipment. Principle Equipment must be l ocated designed
599 views • 26 slides
Basic Principles of Neuropharmacology
Chapter 12. Basic Principles of Neuropharmacology. Basic Principles of Neuropharmacology. Neuropharmacology is the study of drugs that alter processes controlled by the nervous system. Neuropharmacologic Agents. There are two categories of neuropharmacologic agents
260 views • 7 slides
Basic Principles in Management Accounting
332 views • 8 slides
CME Tracker
Music, Advanced Medicine, and Robotics Merge in Groundbreaking UltraCon 2024 Ultrasound Presentations
Dr. Omar Ishrak and Dr. Gil Weinberg to Headline Medical Tech Conference
AUSTIN, Texas, March 26, 2024 /PRNewswire/ -- The upcoming UltraCon 2024 conference , organized by the American Institute of Ultrasound in Medicine (AIUM), is set to spotlight groundbreaking advancements in medical technology with keynotes from industry luminaries Dr. Omar Ishrak and Dr. Gil Weinberg. This premier event, taking place from April 6–10 in Austin, Texas, will draw professionals from across the medical imaging spectrum to discuss the future of ultrasound technology and its applications.
"With visionaries like Dr. Ishrak and Dr. Weinberg leading our keynote sessions, we're not just looking at the future of ultrasound; we're actively shaping it," said Dr. Richard Hoppmann, MD, FACP, FAIUM, President of the AIUM. "Their groundbreaking work exemplifies the spirit of innovation that drives our field forward, offering new ways to enhance patient care and improve lives."
Known for his transformative leadership at Medtronic and GE Healthcare Systems, Dr. Ishrak has been a central figure in the advancement of medical technology, consistently championing the expansion and integration of ultrasound technology across various facets of healthcare. In his upcoming presentation, "Views on the Future of Ultrasound Technology," Dr. Ishrak will provide a comprehensive overview of ultrasound technology—from technical innovations to its critical role in clinical improvement and its strategic importance in the healthcare ecosystem. He will also highlight the remarkable opportunities it presents for widespread application and accessibility, as well as discuss the expanding use of ultrasound not only in diagnostics but also in enhancing clinical outcomes.
"The future of ultrasound technology lies at the intersection of innovation and patient care," stated Dr. Ishrak. "Ultrasound will play a significant role in shaping the future of healthcare, and at UltraCon 2024, I look forward to exploring how advancements in imaging can redefine what's possible in diagnostics and treatment."
Attendees can also look forward to insights on the application of high-intensity ultrasound as a direct form of therapy, and how the innovative combination of high-intensity ultrasound with pharmaceutical approaches—like liquid biopsy and the increased permeability of the blood-brain barrier—can revolutionize patient care.
Also taking the stage will be Dr. Weinberg, whose keynote, "Sonic Prosthetics: Giving Amputees Robotic Arms That Play By Ear," will explore the intersection of robotics, music, and prosthetics. Dr. Weinberg's pioneering work in developing prosthetic robotic arms for amputees demonstrates a novel use of ultrasound signals to control robotic limbs with unparalleled precision and musicality. This innovative approach not only advances prosthetic technology but also opens new possibilities for amputees to engage in musical creation, showcasing the potential of robotics to enhance human expression and rehabilitation.
"By harnessing the power of ultrasound and machine learning, we aim to provide amputees not just with new limbs, but with new possibilities for expression and interaction," said Dr. Weinberg. "This innovative approach exemplifies the incredible advancements we can achieve when we blend technology with the human spirit of resilience and creativity, and I'm excited to share my learnings with UltraCon attendees in Austin."
As UltraCon 2024 prepares to welcome attendees in Austin, it sets the stage for discussions that will likely shape the trajectory of medical technology in the years to come. With its focus on innovation, the conference is poised to highlight the transformative impact of advanced technologies on medical diagnostics, treatment, and patient care.
For registration and additional information about UltraCon 2024, please visit https://ultracon2024. eventscribe.net/ .
For a list of all UltraCon 2024 exhibitors, please visit this link .
The American Institute of Ultrasound in Medicine is a multidisciplinary medical association of more than 9,000 physicians, sonographers, scientists, students, and other healthcare professionals. Established in the early 1950s, AIUM is dedicated to empowering and cultivating a global multidisciplinary community engaged in the use of medical ultrasound through raising awareness, education, sharing information, and research.
LATEST NEWS
- Mar 26, 2024 Music, Advanced Medicine, and Robotics Merge in Groundbreaking UltraCon 2024 Ultrasound Presentations Dr. Omar Ishrak and Dr. Gil Weinberg to Headline Medical Tech Conference
- Mar 5, 2024 At UltraCon 2024, the Latest Breakthroughs in Ultrasound Technology Take Center Stage The American Institute of Ultrasound in Medicine (AIUM) has announced UltraCon 2024, a gathering that promises to bring together the brightest minds in ultrasound technology.
- Aug 3, 2023 Pulsenmore Wins the AIUM's Shark Tank Competition at UltraCon, Showcasing Revolutionary Patient-Centered Home Ultrasound Solution Pulsenmore, a leading innovator in connected patient-driven home ultrasound, emerged victorious in the American Institute of Ultrasound in Medicine’s first-ever Shark Tank competition held this past March at UltraCon this year in Orlando, Florida.
- Mar 30, 2023 AIUM New Leaders Take Office Members of the American Institute of Ultrasound in Medicine (AIUM) have elected a new slate of leaders to the Executive Committee, Board of Governors, and Communities of Practices. These leaders, from across the country and around the world, will work to support the AIUM’s mission and vision.
- Mar 30, 2023 AIUM Names National Awards Recipients The American Institute of Ultrasound in Medicine (AIUM) is proud to recognize the following doctors, researchers, sonographers, and educators as its 2023 class of national award recipients.
Partner with Us | Press | Privacy Policy | Contact Us
14750 Sweitzer Lane, Suite 100, Laurel, MD 20707 301-498-4100 © American Institute of Ultrasound in Medicine, a 501(c)(3) nonprofit educational organization. All Rights Reserved.
Web Design & Development by Matrix Group International, Inc .
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 2, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
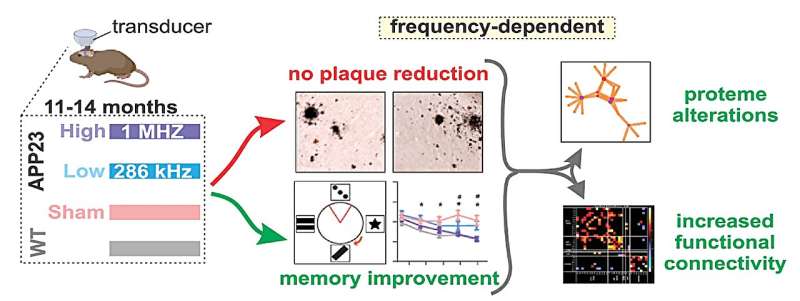
Ultrasound therapy shows promise as a treatment for Alzheimer's disease
by University of Queensland
University of Queensland researchers have found targeting amyloid plaque in the brain is not essential for ultrasound to deliver cognitive improvement in neurodegenerative disorders.
Dr. Gerhard Leinenga and Professor Jürgen Götz from UQ's Queensland Brain Institute (QBI) said the finding challenges the conventional notion in Alzheimer's disease research that targeting and clearing amyloid plaque is essential to improve cognition.
"Amyloid plaques are clumps of protein that can build up in the brain and block communication between brain cells , leading to memory loss and other symptoms of Alzheimer's disease," Dr. Leinenga said.
"Previous studies have focused on opening the blood-brain barrier with microbubbles, which activate the cell type in the brain called microglia which clears the amyloid plaque .
"But we used scanning ultrasound alone on mouse models and observed significant memory enhancement."
Dr. Leinenga said the finding shows that ultrasound without microbubbles can induce long-lasting cognitive changes in the brain, correlating with memory improvement. The research paper has been published in Molecular Psychiatry .
"Ultrasound on its own has direct effects on the neurons, with increased plasticity and improved brain networks," he said.
"We think the ultrasound is increasing the plasticity or the resilience of the brain to the plaques, even though it's not specifically clearing them."
Professor Götz said the study also revealed the effectiveness of ultrasound therapy varied depending on the frequency used.
"We tested two types of ultrasound waves, emitted at two different frequencies," he said. "We found the higher frequency showed superior results, compared to frequencies currently being explored in clinical trials for Alzheimer's disease patients."
The researchers hope to incorporate the findings into Professor Götz's pioneering safety trial using non-invasive ultrasound to treat Alzheimer's disease.
"By understanding the mechanisms underlying ultrasound therapy, we can tailor treatment strategies to maximize cognitive improvement in patients," Dr. Leinenga said.
"This approach represents a significant step toward personalized, effective therapies for neurodegenerative disorders."
Explore further
Feedback to editors

Researchers predict real-world SARS-CoV-2 evolution by monitoring mutations of viral isolates
48 minutes ago

New study targets major risk factor for gastric cancer
57 minutes ago

In people with opioid use disorder, telemedicine for HCV was more than twice as successful as off-site referral

Researchers find genetic variant coding for tubulin protein that may be partially responsible for left-handedness

A molecular route to decoding synaptic specificity and nerve cell communication

Hope for treating autoimmune diseases: Researchers explore diagnostic role of the systemic inflammation index
3 hours ago

Testing environmental water to monitor COVID-19 spread in unsheltered encampments

Dogs may provide new insights into human aging and cognition
18 hours ago

AI's ability to detect tumor cells could be key to more accurate bone cancer prognoses
19 hours ago

Novel pre-clinical models help advance therapeutic development for antibiotic-resistant bacterial infections
Related stories.

Potential noninvasive treatment for Alzheimer's disease
Jun 23, 2021

Ultrasound and drug research holds promise for Alzheimer's disease
Apr 5, 2017

Using focused ultrasound to treat Alzheimer's and Parkinson's
Sep 13, 2023

More evidence ultrasound can help in battle against Alzheimer's disease
Apr 10, 2020

Alzheimer's drugs might get into the brain faster with new ultrasound tool, study shows
Jan 4, 2024

New brain stimulation technique shows promise for treating brain disorders
Feb 23, 2024
Recommended for you

Early cortical remyelination has a neuroprotective effect in multiple sclerosis, study shows
Apr 2, 2024

Novel compound AC102 restores hearing in preclinical models of sudden hearing loss


YKT6 gene variants cause a new neurological disorder, finds study

'Zombie neurons' shed light on how the brain learns

Playtime, being social helps a dog's aging brain, study finds
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Open access
- Published: 29 March 2024
A feasibility study of a handmade ultrasound-guided phantom for paracentesis
- Chien-Tai Huang 1 , 2 ,
- Chih-Hsien Lin 2 ,
- Shao-Yung Lin 2 ,
- Sih‑Shiang Huang 2 &
- Wan-Ching Lien 2 , 3
BMC Medical Education volume 24 , Article number: 351 ( 2024 ) Cite this article
58 Accesses
Metrics details
Simulation-based training is effective for ultrasound (US)-guided procedures. However, commercially developed simulators are costly. This study aims to evaluate the feasibility of a hand-made phantom for US-guided paracentesis.
We described the recipe to prepare an agar phantom. We collected the US performance data of 50 novices, including 22 postgraduate-year (PGY) residents and 28 undergraduate-year (UGY) students, who used the phantom for training, as well as 12 emergency residents with prior US-guided experience. We obtained the feedback after using the phantom with the Likert 5-point scale. The data were presented with medians and interquartile ranges (IQRs) and analyzed by the Wilcoxon rank sum test.
While emergency residents demonstrated superior performance compared to trainees, all trainees exhibited acceptable proficiency (global rating of ≥ 3, 50/50 vs. 12/12, p = 1.000) and comparable needle steadiness [5 (5) vs. 5 (5), p = 0.223]. No significant difference in performance was observed between PGYs [5 (4–5)] and UGYs [5 (4–5), p = 0.825]. No significant differences were observed in terms of image stimulation, puncture texture, needle visualization, drainage simulation, and endurance of the phantom between emergency residents and trainees. However, experienced residents rated puncture texture and draining fluid as “neutral” (3/5 on the Likert scale). The cost of the paracentesis phantom is US$16.00 for at least 30 simulations, reducing it to US$6.00 without a container.
Conclusions
The paracentesis phantom proves to be a practical and cost-effective training tool. It enables novices to acquire paracentesis skills, enhances their US proficiency, and boosts their confidence. Nevertheless, further investigation is needed to assess its long-term impact on clinical performance in real patients.
Trial registration
NCT04792203 at the ClinicalTrials.gov.
Peer Review reports
Introduction
Clinical procedures involve a complex combination of technical skills and cognitive decision-making. Achieving expert performance and sustaining skills necessitate deliberate practice [ 1 ]. Traditionally, procedural skills were acquired, and experience accumulated through direct application on real patients. However, concerns about patient safety and rights have escalated with inexperienced physicians performing procedures directly on patients. Simulation-based medical education provides an alternative for skill proficiency [ 2 ], particularly in ultrasound (US)-guided procedures [ 3 ].
Paracentesis is a commonly encountered procedure in clinical practice. The use of ultrasound guidance diminishes the risk of a dry tap (failure to obtain fluid) during paracentesis and reduces the likelihood of complications such as bleeding, abdominal hematoma, and puncture site infection [ 4 , 5 ]. Additionally, US-guided procedures are integral to emergency medicine training [ 6 ]. However, commercially developed simulators for US-guided procedures are often prohibitively expensive for many emergency departments.
An increasing number of low-cost, handmade phantoms have been developed for US-guided biopsy, thoracocentesis, and pericardiocentesis [ 3 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ]. However, options for paracentesis remain limited [ 18 , 19 , 20 ]. Furthermore, more evidence is needed to assess the learning impact of using handmade phantoms for paracentesis training. This study aims to evaluate the feasibility of a handmade phantom for US-guided paracentesis.
This prospective study was conducted at the Emergency Department of the National Taiwan University Hospital (NTUH) from August 2022 to July 2023. It was approved by the institutional review board of the NTUH (202011111RIND) and registered at ClinicalTrials.gov (NCT04792203). Informed consent was obtained from each participant.
Phantom preparation
Agar substrate
The agar substrate was created by dissolving 10 g of agar powder in 1000 cc of water. After thorough heating to melt the agar powder, the solution underwent filtration to remove impurities. The resulting clear solution was tinted with dark blue food coloring additives.
Paracentesis phantom
A cotton rope, at least 30 cm in length, was inserted into a 10-inch balloon to simulate the bowel. The balloon was then filled with yellowish water dyed with food coloring additives to mimic ascites. After tying the balloon securely, it was affixed to the bottom of the container using super glue (Fig. 1 A). The balloon was covered with the agar substrate, replicating the appearance of human skin and the subcutaneous area. The thickness of the covering could be adjusted based on different body habitus. The phantom was refrigerated for a minimum of 4 h to enhance its longevity (Fig. 1 B).
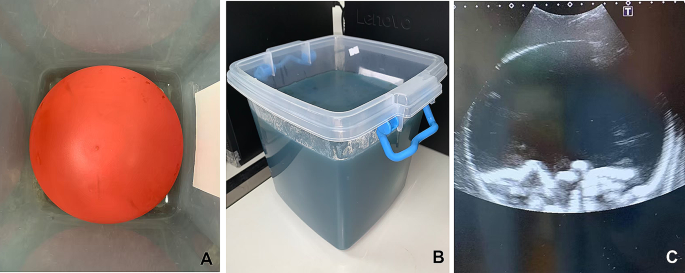
( A ) The balloon was tied in the container; ( B ) The phantom; ( C ) The simulated sonographic image of the phantom
The resulting phantom exhibited easily distinguishable echogenic structures (Fig. 1 C, Supplementary Video ). The balloon effectively delineated boundaries between the peritoneum and the subcutaneous area.
US-guided paracentesis using the hand-made phantom
We recruited 50 trainees, comprising 22 postgraduate-year 1 (PGY-1) residents and 28 undergraduate-year (UGY) students, for participation in a US training curriculum. To assess their experience and confidence in using US, the trainees completed a survey using a 5-point Likert scale (1 = not confident at all; 2 = slightly confident; 3 = somewhat confident; 4 = fairly confident; 5 = completely confident). Subsequently, they attended a 30-minute didactic session covering the theory of US and US-guided paracentesis, followed by small-group hands-on training utilizing the agar phantom. The instructors, were certified by the Taiwan Society of Emergency Medicine.
Following the curriculum, all trainees underwent a skill test, performing paracentesis. The performance was evaluated using an assessment form (Table 1 ) in which the items of the assessment was developed to to encompass the training domains based on expert consensus. Three experts, certified by the Taiwan Society of Emergency Medicine and with over 10 years of US experience, participated in establishing this consensus.
Two independent evaluators, not involved in enrollment and training, graded the performance—one on-site, and the other assessed video recordings with trainee faces masked. Subsequently, trainees provided feedback on the phantom through a survey using a 5-point Likert scale (Supplementary Table 1 ).
Additionally, 12 emergency residents were enrolled to use the phantom without didactics and hands-on training. Their performance was graded, and a survey regarding the phantom was collected.
US machines (Xario 100, Canon, Japan, and Arietta 780, Fujifilm Healthcare, Japan) equipped with a 2–5 MHz curvilinear transducer were used.
Statistical analysis
All data were analyzed by SAS software (SAS 9.4, Cary, North Carolina, USA). Initially, we conducted the Shapiro-Wilk test to assess the normality of continuous data. If the data did not follow a normal distribution, it was presented using medians and interquartile ranges (IQRs). For the comparison between residents and trainees, as well as between PGYs and UGYs, we employed Wilcoxon’s rank-sum test.
To assess inter-rater reliability between two evaluators for the items on the assessment form and global scores, we utilized the intraclass correlation coefficient (ICC) with 95% confidence intervals (CIs). The Spearman correlation coefficient was used to evaluate the relationship between the total score and the global score. The total score represented the sum of each item on the assessment form. The internal reliability of the assessment form was estimated by employing Cronbach’s alpha coefficient [ 21 ]. A p-value less than 0.05 was considered statistically significant.
Following the assessment of normality, it was determined that the scores for each item on the assessment form, the global score, and feedback to the phantom were not normally distributed (all p < 0.0001). Therefore, these data were reported using medians and IQRs.
US performance
The 50 trainees were all considered US novices (Table 2 ). The 12 emergency residents had previous experience with US-guided paracentesis on more than 20 real patients. The ICC for the global score was 0.94 (95% CI, 0.90–0.96), indicating strong inter-rater reliability, as was observed for the items on the checklist (Supplementary Table 2 ). The Spearman correlation coefficient was 0.79 (95% CI, 0.67–0.87) between the total score and the global score, indicative of strong correlation. The standardized Cronbach’s alpha coefficient was 0.75, suggesting good internal reliability.
While the performance of emergency residents surpassed that of trainees, all trainees demonstrated acceptable performance (global rating of ≧ 3). Trainees exhibited less familiarity with US-guided localization, visualization of the needle, and fluid aspiration (Table 2 ). No significant differences were found in the performance between PGYs and UGYs (Supplementary Table 3 ).
There were no significant differences observed in terms of image stimulation, puncture texture, needle visualization, drainage simulation, and endurance of the phantom between emergency residents and trainees. However, it is noteworthy that the residents rated puncture texture and draining fluid as “neutral (Table 3 ). Trainees reported increased confidence in paracentesis after using the phantom, compared with their pre-curriculum survey [4 (3–5) vs. 1 (1), p < 0.0001].
The US phantom could be utilized at least 30 times for practicing paracentesis within one curriculum. The cost of the handmade phantom with a container was approximately $16. Without the container, the cost was reduced to approximately $6.
Commercial US phantoms for paracentesis remain extremely expensive rendering them inaccessible for many training centers. Inexpensive, do-it-yourself phantoms play a crucial role in paracentesis training. In this study, we presented a low-cost, and easily reproducible phantom with echogenicity similar to human tissue and proved its feasibility. Utilizing the phantom facilitates the acquisition of paracentesis skills among novices, enhancing their US abilities and boosting their confidence. While novices demonstrated acceptable performance in paracentesis, it still lags behind that of experienced residents.
Apart from their higher cost, commercial phantoms may degrade with repeated use, requiring an additional fee for fixation. These phantoms typically incorporate polymers, resulting in an excessively firm texture. In contrast, our agar phantom, while having a semi-firm texture that may not perfectly replicate human skin, received a median rating ranging from 3 to 4 from experienced emergency residents in terms of feedback, encompassing image stimulation, puncture texture, needle visualization, and drainage simulation.
Reviewing the literature, some examples of inexpensive, handmade paracentesis phantoms were reported. Wilson et al. documented a gelatin phantom [ 18 ], and Kei et al. employed a water jug covered with pork belly [ 20 ]. Mesquita et al. used multiple gloves filled with various colors to simulate ascites and abdominal organs, elucidating students’ perceptions of the simulator [ 19 ]. In our study, we contribute additional evidence supporting the viability of a handmade phantom, reporting on the performance and feedback of novices in comparison to experienced residents.
Moreover, our phantom exhibited variability and flexibility. For instance, the fluid within the phantom could be altered to appear red or include debris content (such as adding talc), replicating hemoperitoneum or pus, respectively. Additionally, the ratio of fluid to ropes could be adjusted to simulate either a small or a large amount of ascites, depending on the desired training difficulty.
Lower-fidelity modalities are designed to concentrate on a specific learning task and skill acquisition, making them suitable for early learners or novices. In contrast, higher-fidelity simulations are employed for complex tasks, providing cognitive stimuli [ 1 ]. Our handmade phantom is a tool with lower fidelity in external appearance but exhibits high fidelity in ultrasound appearance, making it well-suited for paracentesis training, with novices demonstrating proficiency after completing the curriculum. It is important to note that the long-term impact on skill retention and the translation of acquired skills to proficiency in clinical settings remains unknown.
Gelatin is frequently employed as the primary substrate for homemade phantoms in ultrasound training [ 12 , 18 , 22 ]. However, gelatin necessitates refrigeration to solidify the model. In contrast, agar serves as a vegan-friendly alternative that can set the model without the need for refrigeration. Agar is capable of producing an ultrasound image that closely mimics real tissue and is durable enough to withstand high-volume training [ 23 ]. In this study, we opted for agar as the substrate, and the resulting echogenicity was deemed acceptable.
The assessment form was developed through expert consensus to ensure content validity. Our results also demonstrated good internal and interrater reliability of the assessment form. Research indicates that global rating scales effectively capture various proficiency levels compared to checklists and are user-friendly for examiners [ 24 ]. In this study, the global rating score was utilized to evaluate performance in conjunction with the items on the assessment form.
The main limitation of this study was the inclusion of trainees and emergency residents from a single institution, who voluntarily participated and exhibited high motivation, potentially introducing selection bias. Therefore, caution should be exercised when generalizing these results. Secondly, the study involved a substantial amount of labor and time, approximately 30–60 min for agar preparation and an additional 30 min for phantom assembly, which could limit its feasibility due to time constraints. Third, there may be a potential issue with the image quality of the phantom, as a small amount of air might have been introduced into the balloon during fluid aspiration. However, both trainees and residents reported acceptable image quality. Fourth, while the trainees had prior experience in blood drawing and needle catheterization through routine medical training, feedback concerning human tissue and draining sensation should be interpreted cautiously. Notably, residents with real-world experience rated “neutral” on aspects such as “puncture texture mimics human skin and subcutaneous area” and “draining fluid is realistic.” Lastly, the focus of this study was on evaluating the feasibility of the phantom. Factors such as skill retention and the clinical performance of trainees in real-world scenarios were not investigated. Additionally, the learning effect of using handmade phantoms was not compared with that of using commercial phantoms due to the latter’s high cost. These aspects should be addressed in future studies.
The paracentesis phantom proves to be a practical and cost-effective training tool. It facilitates the acquisition of paracentesis skills among novices, enhancing their US abilities and boosting their confidence. Nevertheless, further investigation is needed to assess its skill retention and long-term impact on clinical performance in real patients.
Data availability
All data analyzed during this study are included in this published article.
Abbreviations
Wang EE, Quinones J, Fitch MT, Dooley-Hash S, Griswold-Theodorson S, Medzon R, Korley F, Laack T, Robinett A, Clay L. Developing technical expertise in emergency medicine–the role of simulation in procedural skill acquisition. Acad Emerg Med. 2008;15(11):1046–57.
Article Google Scholar
Bradley P. The history of simulation in medical education and possible future directions. Med Educ. 2006;40:254–62.
Giannotti E, Jethwa K, Closs S, Sun R, Bhatti H, James J, Clarke C. Promoting simulation-based training in radiology: a homemade phantom for the practice of ultrasound-guided procedures. Br J Radiol. 2022;95(1137):20220354.
Patel PA, Ernst FR, Gunnarsson CL. Evaluation of hospital complications and costs associated with using ultrasound guidance during abdominal paracentesis procedures. J Med Econ. 2012;15(1):1–7.
Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and paracentesis. Chest. 2013;143(2):532–8.
ACEP. Ultrasound guidelines: Emergency, Point-of-care and clinical Ultrasound guidelines in Medicine. Ann Emerg Med. 2017;69(5):e27–54.
James V, Kee CY, Ong GY. A homemade, high-fidelity Ultrasound Model for simulating pneumonia with Parapneumonic Effusion and Empyema. J Emerg Med. 2019;56(4):421–5.
Sullivan A, Khait L, Favot M. A novel low-cost ultrasound-guided Pericardiocentesis Simulation Model: demonstration of feasibility. J Ultrasound Med. 2018;37(2):493–500.
Fredfeldt KE. An easily made ultrasound biopsy phantom. J Ultrasound Med. 1986;5(5):295–7.
McNamara MPJ, McNamara ME. Preparation of a homemade ultrasound biopsy phantom. J Clin Ultrasound. 1989;17(6):456–8.
Silver B, Metzger TS, Matalon TA. A simple phantom for learning needle placement for sonographically guided biopsy. AJR Am J Roentgenol. 1990;154(4):847–8.
Wilson J, Myers C, Lewiss RE. A low-cost, easy to make ultrasound phantom for training healthcare providers in pleural fluid identification and task simulation in ultrasoundguided thoracentesis. Visual J Emerg Med. 2017;8:80–1.
Do HH, Lee S. A low-cost training Phantom for Lung Ultrasonography. Chest. 2016;150(6):1417–9.
Zerth H, Harwood R, Tommaso L, Girzadas DV Jr. An inexpensive, easily constructed, reusable task trainer for simulating ultrasound-guided pericardiocentesis. J Emerg Med. 2012;43(6):1066–9.
Daly R, Planas J, Edens M. Adapting Gel Wax into an ultrasound-guided pericardiocentesis model at low cost. Western J Emerg Med. 2017;18(1):114–6.
Young T, Kuntz H. Modification of Daly’s Do-it-yourself, Ultrasound-guided pericardiocentesis model for added external realism. Western J Emerg Med. 2018;19(3):465–6.
DIY Ultrasound Phantom Compendium. [ https://www.ultrasoundtraining.com.au/resources/diy-ultrasound-phantom-compendium/ )].
Wilson J, Wilson A, Lewiss RE. A low-cost, easy to make ultrasound phantom for training healthcare providers in peritoneal fluid identification and task simulation in ultrasound-guided paracentesis. Visual J Emerg Med. 2017;8:29–30.
de Mesquita DAK, Queiroz EF, de Oliveira MA, da Cunha CMQ, Maia FM, Correa RV. The old one technique in a new style: developing procedural skills in paracentesis in a low cost simulator model. Arq Gastroenterol. 2018;55(4):375–9.
Kei J, Mebust DP. Realistic and Inexpensive Ultrasound Guided Paracentesis Simulator Using Pork Belly with Skin. JETem 2018, 3(3):127–132.
Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334.
Aytaç BG, Ünal S, Aytaç I. A randomized, controlled simulation study comparing single and double operator ultrasound-guided regional nerve block techniques using a gelatine-based home-made phantom. Med (Baltim). 2022;101(35):e30368.
Earle M, Portu G, DeVos E. Agar ultrasound phantoms for low-cost training without refrigeration. Afr J Emerg Med. 2016;6(1):18–23.
Rajiah K, Veettil SK, Kumar S. Standard setting in OSCEs: a borderline approach. Clin Teach. 2014;11(7):551–6.
Download references
Acknowledgements
We thank the Ministry of Science and Technology, Taiwan (MOST 110-2511-H-002-009-MY2) for financial support.
The Ministry of Science and Technology (MOST 110-2511-H-002-009-MY2).
Author information
Authors and affiliations.
Department of Emergency Medicine, National Taiwan University Hospital, Hsin-Chu Branch, Hsin-Chu, Taiwan
Chien-Tai Huang
Department of Emergency Medicine, National Taiwan University Hospital, No.7, Chung-Shan South Road, Taipei, 100, Taiwan
Chien-Tai Huang, Chih-Hsien Lin, Shao-Yung Lin, Sih‑Shiang Huang & Wan-Ching Lien
Department of Emergency Medicine, College of Medicine, National Taiwan University, Taipei, Taiwan
Wan-Ching Lien
You can also search for this author in PubMed Google Scholar
Contributions
CT and WC conceived the study and designed the trial. CT, CH, SY, SS, and WC acquisition of the data. CT and WC analysis and interpretation of the data. CT and WC drafted the manuscript, and all authors contributed substantially to its revision. WC critically revised the manuscript for important intellectual content and took responsibility for the paper as a whole. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Wan-Ching Lien .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Institutional Review Board of the Research Ethics Committee of the National Taiwan University Hospital (202011111RIND). Informed consent was obtained from each participant.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, supplementary material 4, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Huang, CT., Lin, CH., Lin, SY. et al. A feasibility study of a handmade ultrasound-guided phantom for paracentesis. BMC Med Educ 24 , 351 (2024). https://doi.org/10.1186/s12909-024-05339-9
Download citation
Received : 07 October 2023
Accepted : 22 March 2024
Published : 29 March 2024
DOI : https://doi.org/10.1186/s12909-024-05339-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Paracentesis
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.16(4); 2019 Apr

Screening for breech presentation using universal late-pregnancy ultrasonography: A prospective cohort study and cost effectiveness analysis
David wastlund.
1 Cambridge Centre for Health Services Research, Cambridge Institute of Public Health, Cambridge, United Kingdom
2 The Primary Care Unit, Department of Public Health and Primary Care, University of Cambridge, Cambridge, United Kingdom
Alexandros A. Moraitis
3 Department of Obstetrics and Gynaecology, University of Cambridge, NIHR Cambridge Comprehensive Biomedical Research Centre, Cambridge, United Kingdom
Alison Dacey
Edward c. f. wilson.
4 Health Economics Group, Norwich Medical School, University of East Anglia, Norwich, United Kingdom
Gordon C. S. Smith
Associated data.
The terms of the ethical permission for the POP study do not allow publication of individual patient level data. Requests for access to patient level data will usually require a Data Transfer Agreement, and should be made to Mrs Sheree Green-Molloy at the Department of Obstetrics and Gynaecology, Cambridge University, UK ( ku.ca.mac.lhcsdem@dohgdnaoap ).
Despite the relative ease with which breech presentation can be identified through ultrasound screening, the assessment of foetal presentation at term is often based on clinical examination only. Due to limitations in this approach, many women present in labour with an undiagnosed breech presentation, with increased risk of foetal morbidity and mortality. This study sought to determine the cost effectiveness of universal ultrasound scanning for breech presentation near term (36 weeks of gestational age [wkGA]) in nulliparous women.
Methods and findings
The Pregnancy Outcome Prediction (POP) study was a prospective cohort study between January 14, 2008 and July 31, 2012, including 3,879 nulliparous women who attended for a research screening ultrasound examination at 36 wkGA. Foetal presentation was assessed and compared for the groups with and without a clinically indicated ultrasound. Where breech presentation was detected, an external cephalic version (ECV) was routinely offered. If the ECV was unsuccessful or not performed, the women were offered either planned cesarean section at 39 weeks or attempted vaginal breech delivery. To compare the likelihood of different mode of deliveries and associated long-term health outcomes for universal ultrasound to current practice, a probabilistic economic simulation model was constructed. Parameter values were obtained from the POP study, and costs were mainly obtained from the English National Health Service (NHS). One hundred seventy-nine out of 3,879 women (4.6%) were diagnosed with breech presentation at 36 weeks. For most women (96), there had been no prior suspicion of noncephalic presentation. ECV was attempted for 84 (46.9%) women and was successful in 12 (success rate: 14.3%). Overall, 19 of the 179 women delivered vaginally (10.6%), 110 delivered by elective cesarean section (ELCS) (61.5%) and 50 delivered by emergency cesarean section (EMCS) (27.9%). There were no women with undiagnosed breech presentation in labour in the entire cohort. On average, 40 scans were needed per detection of a previously undiagnosed breech presentation. The economic analysis indicated that, compared to current practice, universal late-pregnancy ultrasound would identify around 14,826 otherwise undiagnosed breech presentations across England annually. It would also reduce EMCS and vaginal breech deliveries by 0.7 and 1.0 percentage points, respectively: around 4,196 and 6,061 deliveries across England annually. Universal ultrasound would also prevent 7.89 neonatal mortalities annually. The strategy would be cost effective if foetal presentation could be assessed for £19.80 or less per woman. Limitations to this study included that foetal presentation was revealed to all women and that the health economic analysis may be altered by parity.
Conclusions
According to our estimates, universal late pregnancy ultrasound in nulliparous women (1) would virtually eliminate undiagnosed breech presentation, (2) would be expected to reduce foetal mortality in breech presentation, and (3) would be cost effective if foetal presentation could be assessed for less than £19.80 per woman.
In their cohort study, David Wastlund and colleagues find that universal ultrasound scanning for breech presentation near term is associated with reduced undiagnosed breech presentation and improved pregnancy outcomes, and can be cost-effective.
Author summary
Why was this study done.
- Risks of complications at delivery are higher for babies that are in a breech position, but sometimes breech presentation is not discovered until the time of birth.
- Ultrasound screening could be used to detect breech presentation before birth and lower the risk of complications but would be associated with additional costs.
- It is uncertain if offering ultrasound screening to every pregnancy is cost effective.
What did the researchers do and find?
- This study recorded the birth outcomes of pregnancies that were all screened using ultrasound.
- Economic modelling and simulation was used to compare these outcomes with those if ultrasound screening had not been used.
- Modelling demonstrated that ultrasound screening would lower the risk of breech delivery and, as a result, reduce emergency cesarean sections and the baby’s risk of death.
What do these findings mean?
- Offering ultrasound screening to every pregnancy would improve the health of mothers and babies nationwide.
- Whether the health improvements are enough to justify the increased cost of ultrasound screening is still uncertain, mainly because the cost of ultrasound screening for presentation alone is unknown.
- If ultrasound screening could be provided sufficiently inexpensively, for example, by being used during standard midwife appointments, routinely offering ultrasound screening would be worthwhile.
Introduction
Undiagnosed breech presentation in labour increases the risk of perinatal morbidity and mortality and represents a challenge for obstetric management. The incidence of breech presentation at term is around 3%–4% [ 1 – 3 ], and fewer than 10% of foetuses who are breech at term revert spontaneously to a vertex presentation [ 4 ]. Although breech presentation is easy to detect through ultrasound screening, many women go into labour with an undetected breech presentation [ 5 ]. The majority of these women will deliver through emergency cesarean section (EMCS), which has high costs and increased risk of morbidity and mortality for both mother and child.
In current practice, foetal presentation is routinely assessed by palpation of the maternal abdomen by a midwife, obstetrician, or general practitioner. The sensitivity of abdominal palpation varies between studies (range: 57%–70%) and depends on the skill and experience of the practitioner [ 6 , 7 ]. There is currently no guidance on what is considered an acceptable false negative rate when screening for breech presentation using abdominal palpation. In contrast, ultrasound examination provides a quick and safe method of accurately identifying foetal presentation.
Effective interventions exist for the care of women who have breech presentation diagnosed near term. The Royal College of Obstetricians and Gynaecologists recommends ‘that all women with an uncomplicated breech presentation at term should be offered external cephalic version (ECV)’ [ 2 ]. The rationale for this is to reduce the incidence of breech presentation at term and avoid the risks of vaginal breech birth or cesarean section. The success rate of ECV is considered to be approximately 50% [ 2 , 8 , 9 ], but it differs greatly between nulliparous and parous women (34% and 66%, respectively) [ 9 ]. ECV is overall safe, with less than 1% risk to the foetus and even smaller risk to the mother [ 10 ]; despite this, a significant number of women decline ECV for various reasons [ 11 ]. Should ECV be declined or fail, generally women are offered delivery by planned (elective) cesarean section, as there is level 1 evidence of reduced risk of perinatal death and severe morbidity compared with attempting vaginal breech birth, and it is also associated with lower costs [ 3 , 12 , 13 ]. However, some women may still opt for an attempt at vaginal breech birth if they prioritise nonintervention over managing the relatively small absolute risks of a severe adverse event [ 1 , 14 ].
We sought to assess the cost effectiveness of universal late-pregnancy ultrasound presentation scans for nulliparous women. We used data from the Pregnancy Outcome Prediction (POP) study, a prospective cohort study of >4,000 nulliparous women, which included an ultrasound scan at 36 weeks of gestational age (wkGA) [ 15 ]. Here, we report the outcomes for pregnant nulliparous women with breech presentation in the study and use these data to perform a cost effectiveness analysis of universal ultrasound as a screening test for breech presentation.
Study design
The POP study was a prospective cohort study of nulliparous women conducted at the Rosie Hospital, Cambridge (United Kingdom) between January 14, 2008 and July 31, 2012, and the study has been described in detail elsewhere [ 15 – 17 ]. Ethical approval for the study was obtained from the Cambridgeshire 2 Research Ethics Committee (reference 07/H0308/163), and all participants provided informed consent in writing. Participation in the POP study involved serial phlebotomy and ultrasound at approximately 12 wkGA, 20 wkGA, 28 wkGA, and 36 wkGA [ 16 ]. The outcome of pregnancy was obtained by individual review of all case records by research midwives and by linkage to the hospital’s electronic databases of ultrasonography, biochemical testing, delivery data, and neonatal care data. The research ultrasound at 36 wkGA was performed by sonographers and included presentation, biometry, uteroplacental Doppler, and placental location. The ultrasound findings were blinded except in cases of breech presentation, low lying placenta, or foetal concerns such as newly diagnosed foetal anomaly and an amniotic fluid index (AFI) < 5 cm. This study was not prospectively defined in the POP study protocol paper [ 16 ] but required no further data collection.
If the foetus was in a breech presentation at 36 wkGA, women were counselled by a member of the medical team. In line with guidelines from the National Institute for Health and Care Excellence (NICE), ECV was routinely offered unless there was a clinical indication that contraindicated the procedure, e.g., reduced AFI (<5 cm) [ 18 ]. ECV was performed by 1 of 5 obstetric consultants in the unit between 36–38 wkGA, patients were scanned before the procedure to confirm presentation, and it was performed with ultrasound assessment; 0.25 mg terbutaline SC was given prior to the procedure at the discretion of the clinician. If women refused ECV or the procedure failed, the options of vaginal breech delivery and elective cesarean section (ELCS) were discussed and documented. The local guideline for management of breech presentation, including selection criteria for vaginal breech delivery, was based upon recommendations from the Royal College of Obstetricians and Gynaecologists (RCOG) [ 1 ]. We extracted information about ECV from case records that were individually reviewed by research midwives. Finally, we obtained delivery-related information from our hospital electronic database (Protos; iSoft, Banbury, UK).
Foetal outcomes included mode of delivery (MOD), birth weight, and gestational age at delivery. We used the UK population reference for birthweight, with the 10th and 90th percentile cut-offs for small and large for gestational age, respectively; the centiles were adjusted for sex and gestational age [ 19 ]. Maternal age was defined as age at recruitment. Smoking status, racial ancestry, alcohol consumption, and BMI were taken from data recorded at the booking assessment by the community midwife. Socioeconomic status was quantified using the Index of Multiple Deprivation (IMD) 2007, which is based on census data from the area in the mother’s postcode [ 20 ]. Ethical approval for the study was obtained from the Cambridgeshire 2 Research Ethics Committee (reference 07/H0308/163), and all participants provided informed consent in writing.
This study is reported as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline.
Statistical analysis
Data are presented as median (interquartile range) or n (%), as appropriate. P values are reported for the difference between groups calculated using the two-sample Wilcox rank-sum (Mann–Whitney) test for continuous variables and the Pearson Chi-square test for categorical variables, with trend tests when appropriate. Comparisons were performed using Stata (version 15.1). Missing values were included in the presentation of patient characteristics and outcomes but were excluded from the economic analysis and estimation of parameters.
Economic model and analysis
To evaluate the cost effectiveness of routinely offering late-pregnancy presentation scans, a decision-tree simulation model was constructed using R (version 3.4.1) [ 21 – 24 ]. The time horizon of the economic analysis was from the ultrasound scan (36 wkGA) to infant lifetime, and costs were from the perspective of the English National Health Service (NHS). Costs for modes of delivery were obtained from NHS reference costs [ 25 ]; since these do not list a separate cost for vaginal breech delivery, we assumed that the cost ratio between vaginal breech and ELCS deliveries was the same as in another study (see Supporting information , S1 Text ) [ 12 ].
The population of interest is unselected nulliparous women. The model compares the outcomes at birth for two strategies: ‘universal ultrasound’ and ‘selective ultrasound’ ( Fig 1 ). For universal ultrasound, we assumed that all breech presentations at the time of scanning would be detected (i.e., assumed 100% sensitivity and specificity for the test). For selective ultrasound, the breech presentation was diagnosed either clinically (by abdominal palpation followed by ultrasound for confirmation) or as an incidental finding during a scan for a different indication. These assumptions were based upon current practice and derived from the POP study.

Structure of economic simulation model. ‘Universal ultrasound’ strategy starts in Model A, and patients with breech presentation enter Model C. ‘Selective ultrasound’, i.e., no routine ultrasound, starts in Model B, and only those with a detected breech presentation enter Model C. The letter–number codes for each node are equivalent to the codes in Table 1 . ELCS, elective cesarean section; EMCS, emergency cesarean section.
Compared to a standard antenatal ultrasound for which, typically, multiple measurements are made, an ultrasound scan for foetal presentation alone is technically simple. We theorised that such a scan could be provided by an attending midwife in conjunction with a standard antenatal visit in primary care, using basic ultrasound equipment. Since a specific unit cost for a scan for foetal presentation alone is not included in the national schedule of reference costs [ 25 ], we estimated the cost of ultrasound to include the midwife’s time, the cost of equipment, and room. More details are presented in the Supporting information, S1 Text . The cost of ECV was obtained from James and colleagues [ 26 ] and converted to the 2017 price level using the Hospital and Community Health Services (HCHS) index [ 27 ]. The probability of ECV uptake and success rate as well as MOD were obtained from the POP study. All model inputs are presented in Table 1 and S1 Table , and the calculation of cost inputs is shown in Supporting information, S1 Text .
Abbreviations: CV, cephalic vaginal; ELCS, elective cesarean section; EMCS, emergency cesarean section; MOD, mode of delivery; NHS, National Health Service; POP, Pregnancy Outcome Prediction; SRB, spontaneous reversion to breech; SRC, spontaneous reversion to cephalic; VB, vaginal breech.
Costs given per unit/episode. For probabilities, alpha represent case of event and beta case of no event. MOD shows input values for Dirichlet distribution. Node refers to the chance nodes in Fig 1 .
*Details on how this value was estimated is provided as Supporting information, S1 Text .
†Cost for ECV (high staff cost), converted to 2017 price level using the HCHS index [ 27 ].
‡Weighted average of all complication levels (Total HRGs).
§Due to the small sample size for these parameters in the POP study, the model used inputs for MOD for undetected breech instead.
The end state of the decision tree was the MOD, which was either vaginal, ELCS, or EMCS. Delivery could be either cephalic or breech. EMCS could be either due to previously undiagnosed breech presentation or for other reasons. All cases of breech could spontaneously revert to cephalic presentation. However, we assumed the probability of this to be lower if ECV had been attempted and failed [ 28 ]. If ECV was successful, a reversion back to breech presentation was possible. It is currently unclear whether the probability of MOD varies depending on whether cephalic presentation is the result of successful ECV or spontaneous reversion [ 2 , 10 , 29 – 31 ], but we assumed that the probabilities differed.
Long-term health outcomes were modelled based upon the mortality risk associated with each MOD. The risk of neonatal mortality was taken from the RCOG guidelines. For breech presentation, these risks were 0.05% for delivery through ELCS and 0.20% for vaginal delivery. The risk of neonatal mortality for cephalic presentation with vaginal delivery was 0.10% [ 1 ]. There were no randomised clinical trials that allowed us to compare the outcomes of ELCS versus vaginal delivery for uncomplicated pregnancies with cephalic presentation; however, most observational studies found no significant difference in neonatal mortality and serious morbidity between the two modes [ 32 – 34 ]. For this reason, we assumed the mortality risk for cephalic vaginal and ELCS deliveries to be identical. We also assumed that EMCS would have the same mortality rate as ELCS, both for cephalic and breech deliveries. Studies have found that the MOD for breech presentation affects the risk of serious neonatal morbidity in the short term but not in the long term [ 1 , 3 , 35 ]. For this reason, we focused the economic analysis on the effect from mortality only. The average lifetime quality-adjusted life-years (QALYs) per member of the UK population was estimated using data on quality of life from Euroqol, weighted by longevity indexes from the Office for National Statistics (ONS) [ 36 , 37 ]. Using the annual discount rate of 3.5%, as recommended by NICE, the net present value for the average lifetime QALYs at birth was 24.3 [ 38 ].
The model was probabilistic, capturing how uncertainty in the input parameters affected the outputs by allowing each parameter to vary according to its distribution. Binary and multivariable outcomes were modelled using the beta and the Dirichlet distributions, respectively [ 39 ]. Probabilities of events were calculated from the POP study and presented in Table 1 . On top of the probabilistic sensitivity analysis (PSA), the sensitivity of individual parameters was also explored through one-way sensitivity analyses modifying probabilities by +/− 1 percentage point and costs by +/− £10 to see which parameters had the greatest impact on cost effectiveness estimates.
Total costs depended on the distribution of MOD, the number of expected mortalities, and the cost of ultrasound scanning and ECV. Nationwide costs for each screening strategy were calculated for 585,489 deliveries, i.e., the number of births in England from 2016–2017, assuming 92% occur after 36 wkGA [ 15 , 40 ]. Model parameters were sampled from their respective distributions in a PSA of 100,000 simulations for each strategy. To determine cost effectiveness, we used two different willingness-to-pay thresholds: £20,000 and £30,000 [ 38 ]. A copy of the model code is available from the corresponding author (EW) upon request.
Recruitment to the POP study cohort is shown in Fig 2 and has been previously described [ 17 ]. Information about presentation at the 36-week scan was available for 3,879 women who delivered at the Rosie Hospital, Cambridge, UK; 179 of these had a breech presentation.

Schedule of patient recruitment in the POP study shown by foetal presentation. POP, Pregnancy Outcome Prediction.
We compared maternal and foetal characteristics of the 179 women with breech presentation at 36 weeks to the women with a cephalic presentation ( Table 2 ). Women diagnosed with breech presentation were, on average, a year older than women with a cephalic presentation, but other maternal characteristics did not differ. The babies of women diagnosed breech were smaller and born earlier, but their birth weight centile and the proportions of small for gestational age (SGA) or large for gestational age (LGA) were not markedly different. There were no differences in maternal BMI between the groups. As expected, women with breech presentation were more likely to deliver by ELCS or EMCS.
Abbreviations: AGA, appropriate for gestational age; FTE, full-time education; LGA, large for gestational age; MOD, mode of delivery; POP, Pregnancy Outcome Prediction; SGA, small for gestational age.
Statistics are presented as n (%) for binary outcomes and median (interquartile range) for continuous variables. The "Missing" category was not included in statistical tests. For variables without a "Missing" category, data were 100% complete. P values are reported for the difference between groups using the two-sample Wilcox rank-sum test for continuous variables and the Pearson Chi-square test for categorical variables, with trend test as appropriate (i.e., for deprivation quartile and birth weight centile category).
Breech presentation was suspected before the 36-wkGA scan for 79 (44.1%) of the women with breech presentation through abdominal palpation by the midwife or doctor; out of these, 27 had a clinically indicated scan between 32–36 weeks in which the presentation was reported. For 96 women, the breech presentation was unsuspected before the 36-week scan. Information on suspected breech position was missing for 4 women. There were no differences in BMI between the 79 women with suspected breech and the 96 women misdiagnosed as cephalic prior to the scan (median BMI was 24 in both groups, Wilcoxon rank-sum test P = 0.31).
MOD by ECV status is shown in Table 3 . ECV was performed for 84 women, declined by 45 women, and unsuitable for 23; contraindications included low AFI at screening (18 women), uterine abnormalities (2), and other reasons (3). For 25 women, an ECV was never performed despite consent; 17 babies turned spontaneously, 6 had reduced AFI on the day of the ECV, and 2 went into labour before ECV. When performed, ECV was successful for 12 women; in one case, the baby later reverted to breech presentation before delivery. Information on ECV uptake was missing for 2 women. Foetal presentation and ECV status in the structure of the economic model is shown in Supporting information, S1 Fig .
Abbreviations: ECV, external cephalic version; ELCS, elective cesarean section; EMCS, emergency cesarean section; MOD, mode of delivery.
*Eighteen women were contraindicated due to low AFI at screening, 2 for uterine abnormalities, and 3 for other reasons.
†Seventeen babies turned spontaneously, 6 had reduced AFI on the day of the ECV, and 2 went into labour before ECV.
The results from the economic analysis are presented in Table 4 . On average, universal ultrasound resulted in an absolute decrease in breech deliveries by 0.39%. It also led to fewer vaginal breech deliveries (absolute decrease by 1.04%) and overall EMCS deliveries (0.72%) than selective ultrasound but increased overall deliveries through ELCS (1.51%). Resulting from the more favourable distribution of MOD, the average risk of mortality fell by 0.0013%. On average, 40 women had to be scanned to identify one previously unsuspected breech presentation (95% Credibility Interval [CrI]: 33 to 49); across England, this would mean that 14,826 (95% CrI: 12,048–17,883) unidentified breech presentations could be avoided annually.
Abbreviations: ECV, external cephalic version; ELCS, elective cesarean section; EMCS, emergency cesarean section; MOD, mode of delivery; QALY, quality-adjusted life years; VB, vaginal breech.
Costs (£) are presented per patient, except in column for ‘total population’ ( n = 585,489).
The expected per person cost of universal ultrasound was £2,957 (95% CrI: £2,922–£2,991), compared to £2,949 (95% CrI: £2,915–£2,984) from selective ultrasound, a cost increase of £7.29 (95% CrI: 2.41–11.61). Across England, this means that universal ultrasound would cost £4.27 million more annually than current practice. The increase stems from higher costs of ultrasound scan (£20.3 per person) and ECV (£3.6 per person) but is partly offset by the lower delivery costs (−£16.5 per person). The distribution of differences in costs between the two strategies is shown as Supporting information, S2 Fig . The simulation shows that universal ultrasound would, on average, increase the number of total ELCS deliveries by 8,858 (95% CrI: 7,662–10,068) but decrease the number of EMCS and vaginal breech deliveries by 4,196 (95% CrI: 2,779–5,603) and 6,061 (95% CrI: 6,617–8,670) per year, respectively.
The long-term health outcomes are presented in Table 4 . Nationwide, universal ultrasound would be expected to lower mortality by 7.89 cases annually (95% CrI: 3.71, 12.7). After discounting, this means that universal ultrasound would be expected to yield 192 QALYs annually (95% CrI: 90,308). The cost effectiveness of universal ultrasound depends on the value assigned to these QALYs. The incremental cost effectiveness ratio (ICER) was £23,611 (95% CrI: 8,184, 44,851), which is of borderline cost effectiveness (given NICE’s willingness to pay of £20,000 to £30,000) [ 38 ]. The number needed to scan per prevented mortality was 74,204 (95% CrI: 46,124–157,642).
One-way sensitivity analysis showed that the probability parameter with the greatest impact upon the cost effectiveness of universal ultrasound was the prevalence of breech: increasing this parameter by 1 percentage point was associated with a relative reduction of costs for universal ultrasound by £3.07. The results were less sensitive to the ECV success rate; an increase by 1 percentage point led to a relative reduction in the cost of universal ultrasound by £0.12. The most important cost parameter was the unit cost of ultrasound scan; an increase in this parameter by £10 led to a relative increase for universal ultrasound by £9.79 (see Supporting information , S3 Fig ). Keeping all other parameters equal, universal ultrasound would be cost effective if ultrasound scanning could be provided for less than £19.80 or £23.10 per mother, for a willingness-to-pay threshold of £20,000 or £30,000, respectively. For universal ultrasound to be cost saving, scans would need to cost less than £12.90 per mother.
In a prospective cohort study of >3,800 women having first pregnancies, a presentation scan at approximately 36 wkGA identified the 4.6% of women who had a foetus presenting by the breech, and for more than half of these, breech presentation had not previously been clinically suspected. The majority of these women were ultimately delivered by planned cesarean section, some experienced labour before their scheduled date and were delivered by EMCS, and a small proportion had a cephalic vaginal delivery following either spontaneous cephalic version or ECV. No woman in the cohort had a vaginal breech delivery or experienced an intrapartum cesarean for undiagnosed breech. The low uptake of vaginal breech birth is likely to reflect the fact that this is a nulliparous population, and it is generally accepted that the risks associated with vaginal breech delivery are lower in women who have had a previous normal birth.
Our economic analysis suggests that a universal late-pregnancy presentation scan would decrease the number of foetal mortalities associated with breech presentation and that this is of borderline cost effectiveness, costing an estimated £23,611 per QALY gained. The key driver of cost effectiveness is the cost of the scan itself. In the absence of a specific national unit cost, we have identified the maximum cost at which it would be cost effective. This is £19.80 per scan to yield an ICER of £20,000 per QALY and £23.10 at £30,000. These unit costs may be possible if assessment of presentation could be performed as part of a routine antenatal visit. Portable ultrasound systems adequate for presentation scans are available at low cost, and a presentation scan is technically quite simple, so the required level of skill could be acquired by a large cadre of midwives. This would result in a small fraction of the costs associated with a trained ultrasonographer performing a scan in a dedicated space using a high-specification machine. If universal ultrasound could be provided for less than £12.90 per scan, the policy would also be cost saving.
Our sensitivity analysis shows that the unit cost of ultrasound scans and the prevalence of breech presentation were by far the biggest determinants of the cost and cost effectiveness of universal ultrasound. The detection rate with abdominal palpation (i.e., for selective ultrasound) is the most important parameter aside from these. By contrast, the costs, attempt, and success rates for ECV have modest impact upon the choice of scanning strategy. It appears that the main short-term cost benefit from late-pregnancy screening lies in the possibility of scheduling ELCSs when breech presentation is detected, rather than turning the baby into a cephalic position.
This analysis may have underestimated the health benefits of universal late-pregnancy ultrasound. In the absence of suitable data on long-term outcomes by MOD and foetal presentation, we made the simplifying assumption that mortality rates were equal for ELCSs and EMCSs. Relaxing this assumption would likely favour universal ultrasound, as this strategy would reduce EMCSs, and these are associated with higher risks of adverse outcomes than ELCSs [ 41 – 44 ]; on top of health benefits, this may also reduce long-term NHS costs. It is also possible that an EMCS for a known breech presentation is less expensive and has better health outcomes than one for which breech is detected intrapartum, although lack of separate data for these two scenarios prevented us from pursuing this analysis further.
Our analysis shows that universal late-pregnancy ultrasound screening would increase total number of cesarean sections. Evidence suggests that cesarean delivery may have long-term consequences on the health of the child (increased risk of asthma and obesity), the mother (reduced risk of pelvic organ prolapse and increased risk of subfertility), and future pregnancies (increased risk of placenta previa and stillbirth) [ 45 , 46 ]. There is no evidence that these are related to the type of the cesarean section (elective versus emergency) [ 45 , 46 ]. Our economic modelling has not been able to capture these complex effects due to the model’s endpoints and the focus on the current pregnancy only. However, accounting for these effects, it seems plausible that universal late-pregnancy ultrasound would be more favourable for mothers than children or future pregnancies.
Our results are also driven by vaginal delivery yielding worse long-term health outcomes than ELCS for breech presentation [ 1 ]. However, even though the rate of vaginal breech birth declined after the Term Breech Study, in many cases, the outcomes are not inferior to that of ELCS, and the RCOG guidelines state that vaginal breech delivery may be attempted following careful selection and counselling [ 1 , 3 , 47 ]. It is hard to assess how an increase in vaginal breech delivery would affect the cost effectiveness of universal ultrasound; while decreased mortality risk from vaginal breech delivery would decrease the importance of knowing the foetal presentation, universal screening would facilitate selection for attempted vaginal breech delivery.
One limitation of this study is that foetal presentation was revealed to all women in the POP study. Consequently, this study cannot say what would have happened without routine screening. However, we felt that it was appropriate to reveal the presentation at the time of the 36-wkGA scan, as there is level 1 evidence that planned cesarean delivery reduces the risk of perinatal morbidity and mortality in the context of breech presentation at term [ 44 ]. Another weakness was that the study was being undertaken in a single centre only and that the sample size was too small to avoid substantial parameter uncertainty for rare events. Moreover, less than half of all breech presentations in the POP study were detected by abdominal palpation. It is unclear whether the detection rates were affected by midwives knowing that the women were part of the POP study and, hence, would receive an ultrasound scan at 36 wkGA.
The prevalence of breech presentation in this study (4.6%) appears higher than the 3%–4% that is often reported in literature [ 1 ]. However, this study is unique in that it reports the prevalence at the time of ultrasound scanning, approximately 36 wkGA. Taking into account the number of spontaneous reversions to cephalic and that some cases of successful ECV may have turned spontaneously without intervention, our finding is consistent with the literature. The ECV success rate in the POP study was considerably lower than reported elsewhere in the literature; it was even lower than the 32% success rate that has been reported as the threshold level for when ECV is preferred over no intervention at all [ 48 ]. This might partly reflect the participants in the POP study; they were older and more likely to be obese than in many previous studies, and the cohort consisted of nulliparous women, who have higher rates of ECV failure than parous women [ 9 , 49 , 50 ]. It is also possible that the real-world ECV success rate is lower than in the literature due to publication bias. However, sensitivity analysis indicates that the impact from an increased ECV success rate would be modest (an increase in ECV success rate by 10 percentage points lowers the incremental cost of universal ultrasound by £0.91 per patient).
The findings from this study cannot easily be transferred to another health system due to the differences in healthcare costs and antenatal screening routines. Some countries, e.g., France and Germany, already offer a third-trimester routine ultrasound scan. However, these scans are offered prior to 36 wkGA, and as many preterm breech presentations revert spontaneously, it would have limited predictive value for breech at term [ 51 ]. Whether screening for breech presentation in lower-income settings is likely to be cost effective largely depends on the coverage of the healthcare system; while screening may be relatively more costly, the benefits from avoiding undiagnosed breech presentation may also be relatively larger.
Whether the findings of this study could be extrapolated beyond nulliparous women is hard to assess. The absence of comparable data on screening sensitivity without universal ultrasound for parous women is an important limitation. The risks associated with breech birth also differ between nulliparous and parous women [ 52 , 53 ]. Compared to nulliparous women, parous women have higher success rates for ECV but also higher risk of spontaneous reversion to breech after 36 wkGA [ 9 , 28 ]. Also, the risks associated with vaginal breech delivery are lower in women who have had a previous vaginal birth [ 30 ].
Breech presentation is not the only complication that could be detected through late-pregnancy ultrasound screening. The same ultrasound session could also be used to screen for other indicators of foetal health, such as biometry and signs of growth restriction. Whether also scanning for other complications could increase the benefits from universal ultrasound has been and currently is subject to research [ 54 , 55 ]. Exploring the consequences from such joint screening strategies goes beyond the scope of this paper but has important implications for policy-makers and should therefore be subject to further research.
This study shows that implementation of universal late-pregnancy ultrasound to assess foetal presentation would virtually eliminate undiagnosed intrapartum breech presentation in nulliparous women. If this procedure could be implemented into routine care, for example, by midwives conducting a routine 36-wkGA appointment and using a portable ultrasound system, it is likely to be cost effective. Such a programme would be expected to reduce the consequences to the child of undiagnosed breech presentation, including morbidity and mortality.
Supporting information
S1 strobe checklist.
ECV, external cephalic version; POPs, Pregnancy Outcome Prediction.
PSA, Probabilistic Sensitivity Analysis.
Abbreviations
Funding statement.
This study was funded by the National Institute for Health Research (NIHR) Health Technology Assessment programme, grant number 15/105/01. EW is part funded by the NIHR Cambridge Biomedical Research Centre. US is funded by the NIHR Cambridge Comprehensive Biomedical Research Centre. The views expressed here are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health ( https://www.nihr.ac.uk/ ). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Should all patients with polymyalgia rheumatica have a vascular ultrasound assessment?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-7788-8322 Sharon Cowley 1 , 2 ,
- Patricia Harkins 2 , 3 ,
- Colm Kirby 1 ,
- http://orcid.org/0000-0003-2538-3362 Richard Conway 3 ,
- David J Kane 1 , 2
- 1 Department of Rheumatology , Tallaght University Hospital , Dublin , Ireland
- 2 Trinity College Dublin , Dublin , Ireland
- 3 Department of Rheumatology , St James Hospital , Dublin , Ireland
- Correspondence to Dr Sharon Cowley, Department of Rheumatology, Tallaght University Hospital, Dublin, Ireland; sharoncowley111{at}gmail.com
There is a growing appreciation that both giant cell arteritis (GCA) and polymyalgia rheumatica (PMR) are closely interrelated conditions that have significant overlap in aetiology, clinical characteristics and treatment regimens. Subclinical GCA in PMR is becoming increasingly recognised, and there is evolving evidence that this may be a more aggressive disease phenotype than PMR. Ultrasound (US) lends itself well as a screening tool for GCA in PMR; it is inexpensive, non-invasive, widely available, lacks ionising radiation, may be performed at the bedside and is recommended by EULAR as a first-line investigation for suspected GCA. There is insufficient evidence to currently recommend that all patients with PMR should have a US assessment for vascular involvement. However, as clinical and laboratory parameters alone do not accurately diagnose patients with subclinical GCA, we suggest that vascular US will be increasingly performed by rheumatologists in practice to identify these patients with PMR, preferably as part of larger prospective outcome studies.
- Polymyalgia Rheumatica
- Giant Cell Arteritis
- Ultrasonography
https://doi.org/10.1136/ard-2024-225650
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Giant cell arteritis (GCA) and polymyalgia rheumatica (PMR) are closely interrelated conditions in a common spectrum of inflammatory diseases. Their clinical, epidemiological and immunological overlay has been recently described as GCA-PMR spectrum disease (GPSD). 1 Both diseases can occur separately, simultaneously or in a sequential fashion. Both PMR and GCA are characterised by systemic inflammation, have a predominant interleukin (IL)-6 signature, have evidence of a common pathogenic role of IL-17 in vascular intima 2 and shoulder inflammation, 3 respond excellently to glucocorticoids, affect an older population and tend to relapse. 1 GCA is frequently underdiagnosed in patients with PMR and may explain some cases of glucocorticoid-resistant PMR. 4 5 The lack of evidence guiding risk stratification in GPSD at the time of diagnosis to guide a personalised treatment plan is a major unmet need. Currently, the recommendations for PMR management do not advocate for routine imaging to assess for underlying vasculitis. 6 The presence of ultrasound (US) findings consistent with GCA in patients with newly diagnosed PMR not reporting any clinical cranial GCA symptoms is well established. 7 8 A systematic review that included imaging with US, positron emission tomography (PET) and MRI concluded that more than a quarter of PMR may have subclinical GCA on imaging. 9 Recent US studies have confirmed this finding and suggested that this is a different PMR clinical phenotype, resulting in a different treatment protocol. 10 11 A prospective US study that followed patients with PMR for up to 2 years found that those with US-identified subclinical GCA in PMR were almost four times more likely to relapse compared with isolated PMR. 12 This has raised valid questions about whether rheumatologists should now include vascular imaging in management protocols for PMR to assess for vasculitis to accurately assess risk stratification, guide therapy and optimise patient outcomes.
The recent EULAR imaging guidelines in large vessel vasculitis recommend the US of temporal and axillary arteries to be considered as the first imaging modality to investigate mural inflammatory changes in patients with suspected GCA. 13 US has been shown to have high diagnostic validity, is radiation-free, highly patient-acceptable, widely available and inexpensive. Furthermore, the reliability of findings is high among trained experts and is comparable to that of biopsy readings by pathologists. 14 Professional US practice requires reliable training, sufficient experience, clinician accreditation and adequate equipment to be implemented correctly. The presence of a ‘halo’ on the US, present in GCA, is morphologically defined as a dark hypoechoic ring area around the vessel lumen, which is suggestive of oedema from transmural inflammation. Measurement of the intima-media thickness (IMT) and assessment of vessel compressibility, stenosis and occlusion can also be quantified on US. Axillary arteries can also be measured for thickened IMT, may demonstrate a ‘slope sign’ distinct from atherosclerosis with a smooth thickening continuous up to a transitional point where the IMT gradually slopes downwards back to a normal level 15 and may have visible stenosis or occlusion. The halo score has been developed to quantify the extent of vascular inflammation in GCA. It is based on percentiles of halo thickness, correlates with C reactive protein (CRP) and is shown to be associated with a higher risk of ocular ischaemia. 16 Outcome Measures in Rheumatology (OMERACT) has also defined an ultrasonography score for monitoring disease activity in GCA. 17 This score may be used as a monitoring tool and outcome measure in research, particularly in clinical trials. These tools are an exciting development in GCA and have the potential to stratify patients for personalised treatment and provide objective target organ monitoring during follow-up.
Vascular US studies in PMR
Vascular screening of patients with PMR is not a new concept, with the earliest studies looking at the prevalence of US features of vasculitis in PMR at the time of diagnosis completed over 20 years ago. 7 8 Combined, these studies assessed 110 patients and found a prevalence of 7.3% (eight patients) for subclinical GCA. Biopsies were performed on all US-positive patients (eight) and showed a 50% positivity rate for features of GCA. Among those with a negative biopsy (four), three patients did not have the US-identified positive branch with a halo sign sampled due to anatomical reasons and fear of resultant complications. One further patient had stenosis of the common temporal branch seen on biopsy, which may represent either atherosclerosis or inflammation. It is worth noting that a 3% stenosis rate was seen among their normal controls. Axillary or other vascular territories were not investigated in these earlier studies, which may explain the low incidence rate of US-identified subclinical GCA. In addition, US technology had significantly lower image quality 20 years ago.
There has been significant evolution in US technology and vascular imaging definition in recent years. Vascular scanning techniques for GCA diagnosis have been optimised and standardised, 18 along with the development and validation of a US scoring system by OMERACT for monitoring vascular activity in GCA. 17 These advances have led to two robust studies, which were published in 2023 with a combined population of over 400 patients with PMR. 10 11 Both studies prospectively examined consecutively enrolled patients with newly diagnosed PMR without any clinical symptoms of cranial GCA. An almost identical incidence of subclinical GCA was identified in both studies, at 22% and 22.8%, respectively. This represents a much higher positivity rate than previous studies, which may be explained by the inclusion of more vascular territories. There was a high predilection for the extracranial vessels, with over three-quarters of patients in each study exhibiting axillary involvement. These more recent studies have also provided more clinical information on patients with PMR with subclinical GCA. Older age at the time of diagnosis and higher incidence of hip girdle symptoms were more frequently reported in the subclinical GCA group compared with those with pure PMR. 10 11 CRP levels were significantly higher in the subclinical GCA group in Burg et al ’s study, but this finding was not upheld in De Miguel’s larger multicentre study. The sensitivity and specificity of these clinical and laboratory features for the differentiation of subclinical GCA in PMR from isolated PMR were low by comparison with US, which is a more accurate differentiator than relying solely on clinical characteristics ( table 1 ).
- View inline
Summary of vascular US in PMR studies
Crucial is longer-term follow-up of patients with subclinical GCA in PMR to determine their clinical course, including risk of relapse, rate of progression to GCA, corticosteroid burden and resultant morbidity. To date, there has only been one follow-up study that has reported on the outcomes of subclinical GCA in PMR, with a median follow-up of 22 months from the time US-identified subclinical GCA was observed. 12 150 patients were included, and it was shown that patients with subclinical GCA in PMR were four times more likely to relapse compared with those with PMR. Interestingly, all relapses, apart from one patient, were minor as classified by EULAR 19 without clinical features of ischaemia, aortic or large vessel dilatation, stenosis or occlusion. This higher relapse rate was observed despite those with subclinical GCA being treated with an initial higher glucocorticoid taper (36.6 mg vs 19.8 mg daily of prednisone, p<0.001). 12 An increased requirement for second-line therapies in the subclinical GCA subgroup was also observed, with methotrexate as the most prescribed treatment. It appears from this study that subclinical GCA in PMR has a more severe phenotype than seen in those with PMR ( table 2 ).
Summary of clinical characteristics of patients with US-detected subclinical GCA
Imaging currently plays a major role in the diagnosis of GCA and has an evolving role in PMR. US vascular imaging is an attractive prospect as it has already been implemented as a recommended first-line investigation for GCA, 13 with many centres having established referral pathways. It also has the potential to be incorporated into a fast-track PMR clinic model, as it can be rapidly performed in an outpatient setting, and recent guidelines have advocated for early specialist input in PMR. 20 US requires a trained specialist using appropriate equipment with standardised operational procedures and settings, which requires adequate funding, training time and proficiency. Incorporation of US vascular screening of patients with PMR in an early specialist referral pathway is not currently recommended, but recent studies increasing our understanding of PMR may pave the way for future recommendations in distinct patients with PMR. Given the high disease burden of PMR in the community, targeted screening will likely be most appropriate to ensure equitable use of time and resources in fast-track PMR clinics.
Emerging evidence shows a high prevalence of subclinical GCA in PMR, affecting up to one in four patients. Indeed, this may be a biased estimation, as only a minority of patients with PMR are referred to secondary care currently, with responders to standard glucocorticoid taper being treated in the community. Conversely, it is unknown if there are missed cases affecting large vessels such as the aorta, which is more difficult to assess in its entirety with US alone. A community-based study that recruited patients from primary care regardless of PMR severity reported a lower prevalence of subclinical GCA in PMR at 17.5%. 21 Vascular US has a superior ability to risk stratify patients with PMR when implemented in addition to clinical history, examination and laboratory investigations. It also appears to correlate well with PET studies. US studies have identified that patients with an older age at diagnosis, reporting an increased frequency of hip or pelvic girdle pain and stiffness, are more at risk of having subclinical GCA in PMR. 11 Positive PET/CT studies have also found that patients with PMR with diffuse bilateral lower limb pain, pelvic girdle pain and lower back pain are positive predictors of vascular involvement in this cohort. 22 Whether there is a role for vascular US interrogation in relapsing or glucocorticoid-refractory PMR remains to be elucidated. These patients have more asthenia, weight loss and fever than those with pure PMR, 23 although this cohort requires more studies to determine the prevalence of vascular involvement.
The medium-term clinical outcome of patients with US-identified subclinical GCA in PMR appears to follow a more severe phenotype with an increased rate of relapse and a higher requirement for glucocorticoids and other disease-modifying treatments. 12 Clinicians may have the most yield from scanning patients with PMR that have predominant hip or pelvic girdle pain (which may represent limb claudication), back pain (which can be a manifestation of aortitis), constitutional symptoms (including fever, night sweats, weight loss and/or anaemia), those with very high ESR/CRP at the outset and patients with poor response to initial PMR dose glucocorticoids. Those with relapsing PMR may also benefit from vascular imaging, particularly if these manifestations are also present. It remains unclear how to manage patients with US-identified vascular changes without profound clinical symptoms, as there are currently no longer-term studies on the impact of subclinical GCA on the prognosis of patients with PMR. There are also no consensus recommendations for either routine or targeted vascular screening of patients with PMR. Similarly, there are no studies to determine the minimum glucocorticoid dose to effectively treat PMR both with and without subclinical vasculitis. We believe those who relapse on higher glucocorticoid doses (≥10 mg) with subclinical vasculitis should be given consideration for the early introduction of a steroid-sparing agent. While the vascular US of all patients with PMR is enticing, given the potentially high yield of positive cases, it is clear that further retrospective and prospective international multicentre studies are needed to identify patients most appropriate for screening. Some such studies are underway, and interim findings suggest male patients with a higher ESR at baseline are most likely to have US findings of subclinical vasculitis. 21 We advocate that rheumatology centres that have both the technology and the clinician sonographers should consider including it in the initial assessment of PMR and, preferably, as part of prospective outcome studies. We acknowledge that long-term studies delineating the natural history of PMR and subclinical GCA are required to establish the optimal therapy and cost-effectiveness of this approach.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- Tomelleri A ,
- van der Geest KSM ,
- Khurshid MA , et al
- Corbera-Bellalta M ,
- Audia S , et al
- Reitsema RD ,
- Wekema L , et al
- Duftner C ,
- Buttgereit F , et al
- Chessa E , et al
- Perel P , et al
- Schmidt WA ,
- Gromnica-Ihle E
- Möller DE ,
- Völker L , et al
- Hemmig AK ,
- Gozzoli D ,
- Werlen L , et al
- Karakostas P ,
- Behning C , et al
- De Miguel E ,
- Macchioni P ,
- Conticini E , et al
- Karalilova R ,
- Macchioni P , et al
- Bond M , et al
- Luqmani R ,
- Singh S , et al
- Dasgupta B ,
- Khan AAS , et al
- Kayani A , et al
- Monti S , et al
- Ponte C , et al
- Hellmich B ,
- Keller KK ,
- Mukhtyar CB ,
- Nielsen AW , et al
- Harkins P , et al
- Prieto-Peña D ,
- Martínez-Rodríguez I ,
- Loricera J , et al
- Moya-Alvarado P ,
- Fernandez Leon A ,
- Corica ME , et al
Handling editor Josef S Smolen
Contributors SC is the main author of the article, writing the first draft and making corrections based on co-author feedback. PH, CK, RC and DJK were involved in drafting the manuscript and approving the final version.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests SC: grant support from Novatris, speaker honoria from Janssen and conference attendance support from Abbvie, Janssen and Novartis. CK: conference attendance support from Novartis. PH: grant support from Janssen and Novartis and conference attendance support from Abbvie and Novartis. RC: grant support from Janssen and Novartis and consulting fees/speaker fees from Janssen, Abbvie, Fresenius Kabi, Galapagos, UCB, Viatris, Celltrion, Nordic Pharma and Novartis. DJK: grant support from Novartis and conference attendance support from Abbvie.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Pregnant stingray Charlotte gets another ultrasound as world waits for 'miracle' birth

HENDERSONVILLE - Aquarium and Shark Lab by Team ECCO on Main Street has been giving updates on Charlotte the stingray's asexual pregnancy on social media twice a week on Wednesdays and Saturdays, and the Saturday, March 30 update once again revealed no pups yet from Charlotte.
The California round stingray made national news when it was revealed by Team ECCO staff that she was pregnant with no male stingray in the tank for the past eight years. Staff determined Charlotte became pregnant through a process called parthenogenesis, which is an asexual reproduction where a female can produce an embryo without fertilizing an egg with sperm.
Kady Lyons, a research scientist at the Georgia Aquarium in Atlanta, told the Associated Press in a Feb. 13 article that Charlotte would be the first known round stingray to become pregnant through parthenogenesis.
The average gestation is three to four months for stingrays, but there is no known data for the gestation period for a parthenogenetic pregnancy, according to Team ECCO's March 30 update on Instagram.
"We performed an ultrasound last week and have sent these most recent images to colleagues in other professional marine science programs. We eagerly await their report after this holiday weekend," Team ECCO's Jacob Hensley said in the post. "The aquarium thanks everyone for their continued support, patience and kindness through Charlotte's journey."
More: Answer Man: Why did Charlotte get herself pregnant? 'Mother of Rays' provides insight
More: Still waiting: When will Charlotte the stingray give birth? Too unique to predict.
The Team ECCO staff first noticed a bump on Charlotte in September and performed an ultrasound, worried that it could be a cyst. They sent the results to a contact at a leading aquarium in Australia and a contact from the science department at Arizona State University. Aquarium director B.J. Ramer said both contacts came to the same conclusion: Charlotte was expecting.
The Aquarium has had Charlotte since 2016. Assistant director Kinsley Boyette previously told the Times-News in a previous article that they received the stingray from a private home in Charlotte, and that was how she got her name. There are three cameras in the tank keeping track of Charlotte's every move, Boyette said in the article.
"We are surveilling them all throughout the night and all throughout the day if we are not here. We are on pup watch," she said.
When the pups are born, Boyette said they will be moved to a separate nursing tank the staff has prepared.
Dean Hensley is the news editor for the Hendersonville Times-News. Email him with tips, questions and comments at [email protected]. Please help support this kind of local journalism with a subscription to the Hendersonville Times-News.
Patient Care Solutions
Pharmaceutical Imaging Agents
Digital Solutions
Refurbished Systems
Parts and Accessories
All Services
Medical Technology Advanced Services
MyGEHealthCare Experience
Healthcare Technology Management
Performance Management
Clinical Network Solutions
Cybersecurity
Healthcare Financial Services
Site Planning
Service Shop
AssurePoint Refresh
Medical Affairs - Pharmaceutical Diagnostics
Support and Documentation
Technical Support
Adequacy of Anesthesia
Alzheimer's Disease
Breast Care
Electrophysiology
Federal Health
Intensive Care Unit
Labor and Delivery
Obstetrics and Gynecology
Orthopedics
Ambulatory Surgery Centers
Rural Health
Stroke Solutions
Theranostics
All Insights
Breakthroughs: 2024 Healthcare Trends
Thought Leadership
The Art of Care
Equipment Accessories
Service Shop Parts & Accessories
Contrast Media & Molecular Imaging Agents
Sustainability
Investor Relations
All Imaging
Bone & Metabolic Health
Computed Tomography
Fluoroscopy
Interventional Guided Systems
Invasive Cardiology
Magnetic Resonance Imaging
Mammography
Molecular Imaging
Radiography (X-Ray)
Surgical Imaging
All Ultrasound
LOGIQ General Imaging
Vivid Cardiovascular
Voluson Women's Health
Breast Ultrasound
Surgical Visualization and Guidance
Point of Care
Versana Primary Care
Vscan Handheld
Verisound Digital & AI Ultrasound Solutions
All Patient Care Solutions
Anesthesia Delivery
Diagnostic ECG
Maternal & Infant Care
Patient Monitoring
Ventilators
Clinical Accessories
Contrast Media
Molecular Imaging Agents
Pharma Services
All Digital Solutions
Advanced Visualization
Cardiology IT
Command Center
Digital Health Platform
Enterprise Imaging (VNA)
Imaging Operations
PACS and AI Orchestration
Pharmaceutical IT
Software & Apps Marketplace
Virtual Care
Imaging Accessories
All Cybersecurity
Product Cybersecurity
Skeye Cybersecurity
Product Security Portal
All Education
Clinical Education
Technical Training
Healthcare Learning System
Digital Expert
Cleaner and Disinfectant Compatibility
Core Imaging (CI) Certification
Manuals & Documents
Disinfection of Ultrasound Probes
Interoperability
Press Releases
Ge healthcare introduces caption ai on vscan air sl wireless handheld ultrasound system to help more clinicians capture diagnostic-quality cardiac images.
CHICAGO - Apr 03, 2024
- Caption AI on Vscan Air SL expands access to cardiac care by enabling more medical professionals to feel confident acquiring images for rapid assessments
- AutoEF feature automatically calculates ejection fraction, saving time for clinicians while delivering key information for making their diagnoses
- GE HealthCare to debut new technology at 2024 American College of Cardiology Annual Scientific Session & Expo, April 6 – 8, 2024 in Atlanta
GE HealthCare (Nasdaq: GEHC) today announced the launch of Caption AI artificial intelligence (AI)-driven software for rapid cardiac assessments at the point of care on Vscan Air SL. Now, with Caption AI technology, clinicians using Vscan Air SL handheld ultrasound will have access to real-time, step-by-step guidance to capture diagnostic-quality images and automated ejection fraction estimation to help inform clinical decisions across cardiac settings. Vscan Air SL with Caption AI will debut at the 2024 American College of Cardiology (ACC) Annual Scientific Session & Expo, taking place April 6 – 8, 2024 in Atlanta.
Cardiovascular disease (CVD) is the leading cause of death globally, and the prevalence is expected to continue rising as people live longer and the population increases. 1 Early detection of heart disease is critical to improving patient outcomes, but providing rapid echocardiographic assessments at the point of care can be difficult in resource-constrained facilities and practices. Vscan Air SL with Caption AI is designed to lower the threshold for healthcare professionals to be able to capture cardiac images so that even non-expert ultrasound users can take a quick look at patients’ hearts.
"With the increase of cardiovascular disease and shortage of sonographers around the globe, innovations like the Vscan Air SL with Caption AI are hugely transformative in cardiac care, supporting rapid and confident assessments at the point of care," said cardiologist Jordan B. Strom, M.D., MSc. "AI guidance has enormous potential in ultrasound due to its ability to guide experts and relatively new users in retrieving diagnostic-quality information to make timely and accurate decisions and get patients on the right path sooner."
Caption AI provides real-time visual guidance to prompt users on probe movements and includes a quality meter to ensure the user obtains the best possible images. Once an image is captured, the AutoEF feature automatically calculates a left ventricular ejection fraction (LVEF). In addition, users can efficiently scan with AutoCapture and Save Best Clip features to capture the best quality image from each view.
The ultraportable Vscan Air SL provides high levels of depth, resolution and sensitivity in imaging performance with an industry-leading single crystal transducer technology. The latest integration of Caption AI builds on GE HealthCare’s history and innovation in handheld ultrasound—having introduced the pioneering Vscan in 2010 as the first color, pocket-sized ultrasound device—and is helping to make next-generation ultrasound care accessible to even more patients.
"The integration of Caption AI with the Vscan Air SL handheld ultrasound opens an entirely new chapter for cardiac screening. This technology empowers users with guidance and tools for high quality ultrasound scans and supports earlier detection of cardiac disease," said Roland Rott, president and CEO, Ultrasound, GE HealthCare. "The strategic acquisition of Caption Health in 2023 continues to expand the capabilities of our products and solidifies our leadership in ultrasound and the emerging artificial intelligence landscape."
The launch of Vscan Air SL with Caption AI advances GE HealthCare’s vision and efforts to strengthen precision care, joining the approximately 60 AI-enabled medical device authorizations from GE HealthCare in the United States – more than any other medical device company. Of these, approximately 30 are AI-enabled ultrasound innovations.
In addition to Vscan Air SL, GE HealthCare will also showcase its suite of innovative products and solutions across the cardiology care pathway at ACC 2024, including CardioVisio for Atrial Fibrillation, a digital, patient-centric clinical decision support tool, which includes the most recent ACC guidelines. Telling the story of the heart with integrated cardiology technology, the comprehensive portfolio of cardiovascular solutions delivers across the full continuum of patient care from diagnosis and treatment all the way through post-treatment monitoring.
The Vscan Air SL with Caption AI will be on display in booth #2517. For more information, visit the Vscan Air website here .
About Vscan Air
GE HealthCare's Vscan Air offers two flexible, wireless, dual-probe handheld ultrasound options: the Vscan Air SL, which includes a sector-phased array transducer for rapid cardiac assessments, and the Vscan Air CL, which includes a curved array transducer for abdominal imaging, obstetric assessments, and more. Uniquely, both models also include a linear array transducer bringing shallow and deep scanning together on a single dual probe device suitable for a wide range of assessments. Both models provide a flexible, lightweight, wireless device that delivers crystal clear images anytime, anywhere to help accelerate diagnoses and treatment decisions. The Vscan Air SL now features Caption AI technology, providing clinicians with real-time, step-by-step guidance for confident cardiac assessments at the point of care. The Vscan Air app, available on Android™ and iOS™ devices, allows for the secure viewing of images on a mobile device so clinicians can take Vscan Air with them to every patient.
1 World Health Organization. Cardiovascular diseases (CVDs). June 11, 2021. Available at: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) . Accessed April 2024.
About GE HealthCare Technologies Inc.
GE HealthCare is a leading global medical technology, pharmaceutical diagnostics, and digital solutions innovator, dedicated to providing integrated solutions, services, and data analytics to make hospitals more efficient, clinicians more effective, therapies more precise, and patients healthier and happier. Serving patients and providers for more than 100 years, GE HealthCare is advancing personalized, connected, and compassionate care, while simplifying the patient’s journey across the care pathway. Together our Imaging, Ultrasound, Patient Care Solutions, and Pharmaceutical Diagnostics businesses help improve patient care from diagnosis, to therapy, to monitoring. We are a $19.6 billion business with 51,000 colleagues working to create a world where healthcare has no limits.
Follow us on LinkedIn , X (formerly Twitter) , and Insights for the latest news, or visit our website https://www.gehealthcare.com/ for more information.
- Link Copied
Media contacts
Media Contact
GE HealthCare
+1 312 459 6140
Latest Press Releases
Ge healthcare introduces caption ai on vscan air sl wireless handheld ultrasound system to help more clinicians capture diagnostic-quality cardiac images ....
April 03, 2024
GE HealthCare closes MIM Software acquisition, bolstering its portfolio and advancing its precision care strategy ...
April 01, 2024
JB28833XX April 2024
United States
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
Ultrasound therapy shows promise as a treatment for Alzheimer’s disease
Researchers from UQ's Queensland Brain Institute have found that targeting amyloid plaque in the brain is not essential for ultrasound to deliver cognitive improvement in neurodegenerative disorders.
Dr Gerhard Leinenga and Professor Jürgen Götz said the finding challenges the conventional notion in Alzheimer’s disease research that targeting and clearing amyloid plaque is essential to improve cognition.
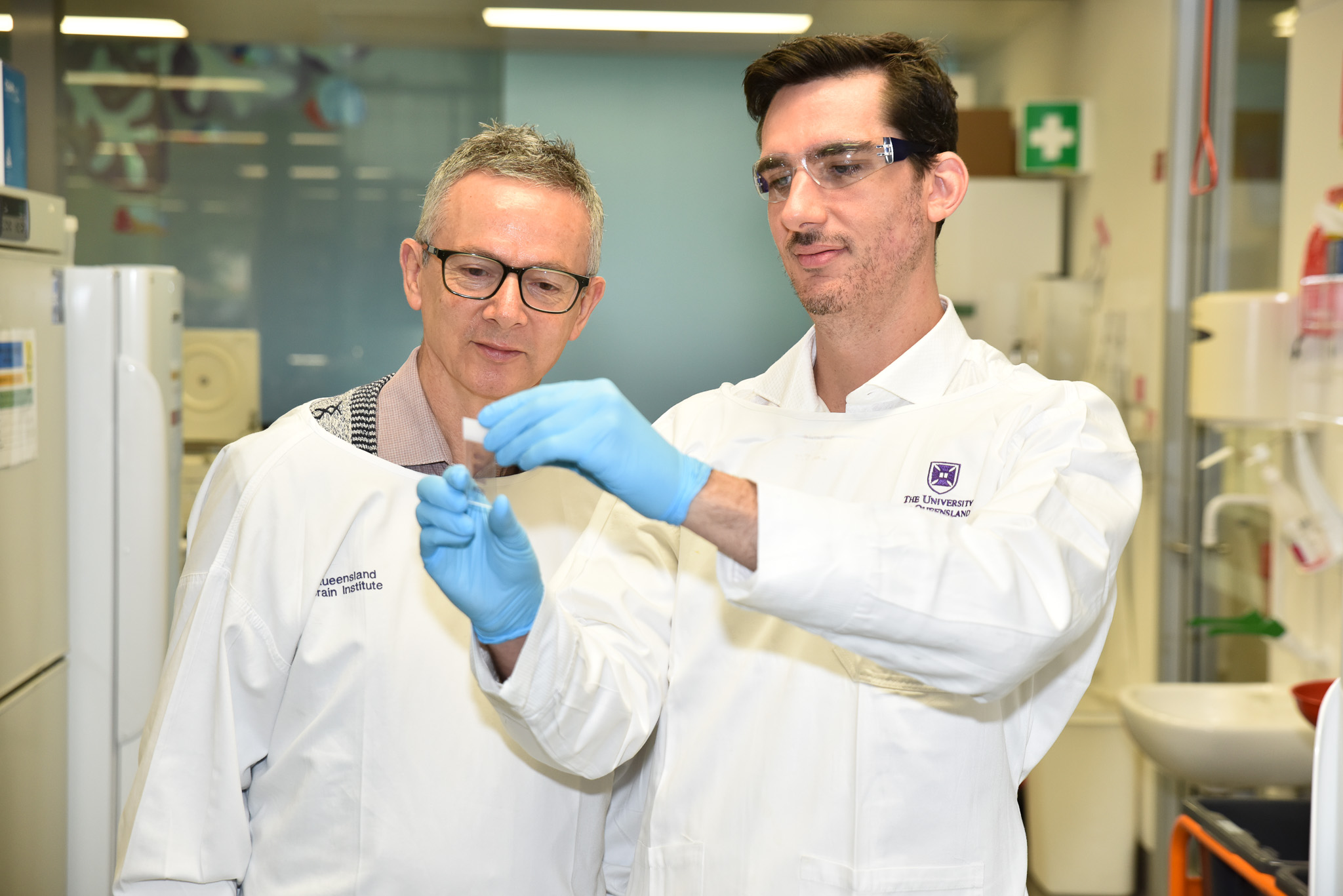
“Amyloid plaques are clumps of protein that can build up in the brain and block communication between brain cells, leading to memory loss and other symptoms of Alzheimer’s disease,” Dr Leinenga said.
“Previous studies have focused on opening the blood-brain barrier with microbubbles, which activate the cell type in the brain called microglia which clears the amyloid plaque.
“But we used scanning ultrasound alone on mouse models and observed significant memory enhancement.”
Dr Leinenga said the finding shows ultrasound without microbubbles can induce long-lasting cognitive changes in the brain, correlating with memory improvement.
“Ultrasound on its own has direct effects on the neurons, with increased plasticity and improved brain networks,” he said.
“We think the ultrasound is increasing the plasticity or the resilience of the brain to the plaques, even though it’s not specifically clearing them.”
Professor Götz said the study also revealed the effectiveness of ultrasound therapy varied depending on the frequency used.
“We tested two types of ultrasound waves, emitted at two different frequencies,” he said.
“We found the higher frequency showed superior results, compared to frequencies currently being explored in clinical trials for Alzheimer’s disease patients.”
The researchers hope to incorporate the findings into Professor Götz’s pioneering safety trial using non-invasive ultrasound to treat Alzheimer’s disease.
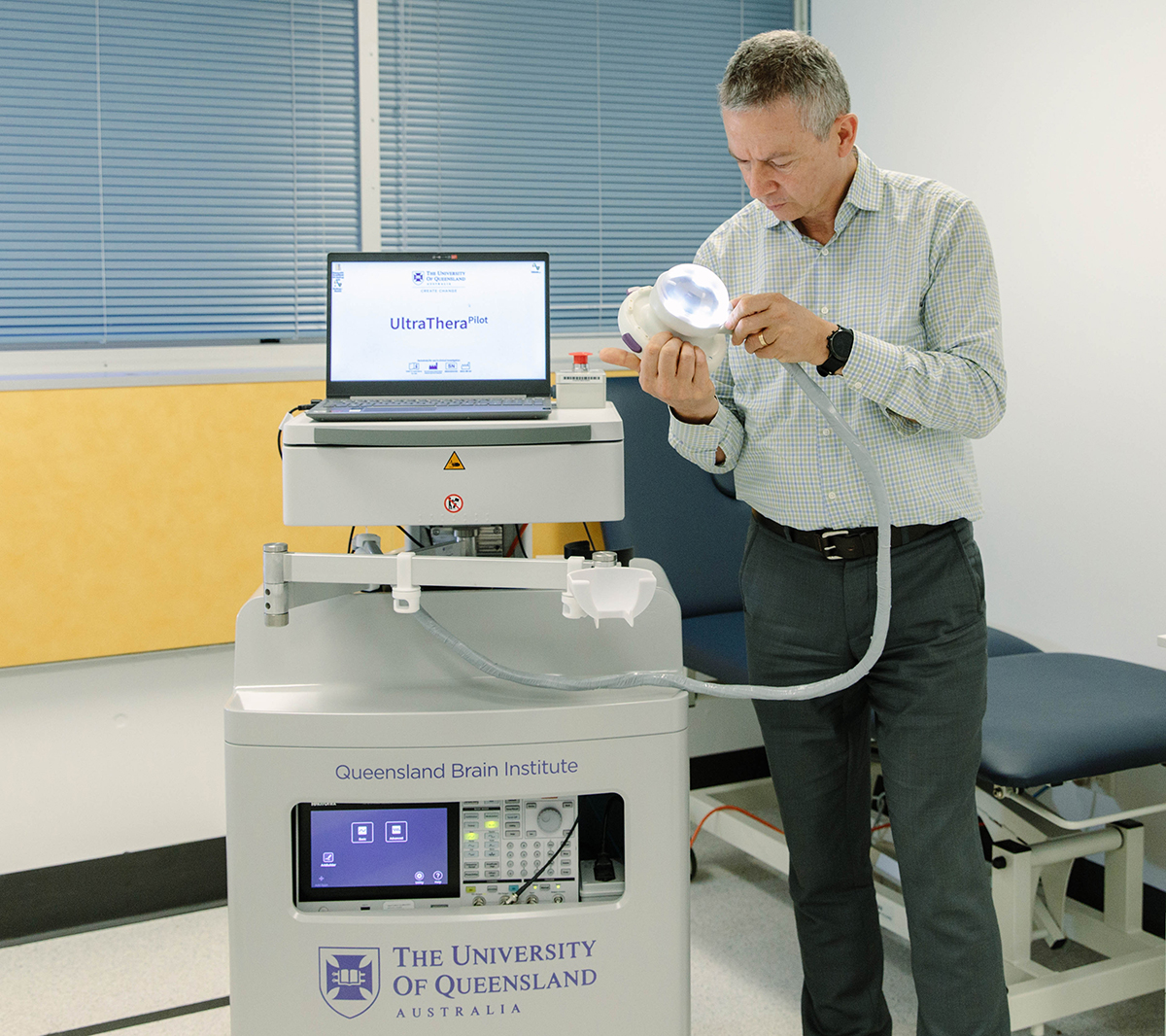
“By understanding the mechanisms underlying ultrasound therapy, we can tailor treatment strategies to maximise cognitive improvement in patients,” Dr Leinenga said.
“This approach represents a significant step towards personalised, effective therapies for neurodegenerative disorders.”
The research paper has been published in Molecular Psychiatry.
Media: QBI Communications, [email protected], Merrett Pye +61 422 096 049; Elaine Pye +61 415 222 606.

Unravelling the mysteries of the presynapse with super resolution microscopy
Mapping potential pathways to MND treatment
- Unravelling the mysteries of the presynapse with super resol...

IMAGES
VIDEO
COMMENTS
Fetal Lie and Presentation. Learning Objectives: Why it is important to identify the fetal lie and presentation. How to identify an abnormal fetal lie or presentation. When to perform a follow up ultrasound. Video 13. 1st Trimester Pain and Bleeding. Learning Objectives: Identify the normal and abnormal gestational sac. Evaluate fetal cardiac ...
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the ...
breech presentation: fetal rump presenting towards the internal cervical os, this has three main types. frank breech presentation (50-70% of all breech presentation): hips flexed, knees extended (pike position) complete breech presentation (5-10%): hips flexed, knees flexed (cannonball position) footling presentation or incomplete (10-30%): one ...
The main types of breech presentation are: Frank breech - Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term. Complete breech - Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
Speaker: Dr. Mahan Mathur, MD.Assistant Professor of Radiology and Biomedical Imaging,Yale University School of Medicine
Intrapartum ultrasound has been found to be more reliable than digital examination in assessing malpresentation and malposition. The use of intrapartum ultrasound to assess fetal position and presentation, in addition to fetal attitude, to predict and aid in decision making regarding delivery can help in improving management decision making.
Part of the POCUS (Point-of-Care UltraSound) curriculum to teach point-of-care ultrasound to medical students, family medicine residents, and other primary c...
Fetal ultrasonography is a standard and vital component of a comprehensive fetal evaluation in pregnancy. There are specific indications for using ultrasound in each trimester and assessing both the fetus and the mother by ultrasonography. Based on maternal and fetal risk factors, ultrasound timing and frequency are individualized to evaluate ...
Fetal Lie and Presentation Ultrasound Training Video. From: University of Washington School of Medicine. Learning Objectives: Why it is important to identify the fetal lie and presentation. How to identify an abnormal fetal lie or presentation. When to perform a follow up ultrasound. Tweet.
Clean the ultrasound probe. 4. Apply a tourniquet. 5. Apply gel to the ultrasound probe. 6. Identify the target vein in the transverse plane: note the depth of the anterior wall of the vein and pay attention to any adjacent structures. 7. Once identified, rotate the probe into the longitudinal plane.
an easy way to make a sterile ultrasound transducer cover in "Ultrasound-Guided Interventions." Once you have enough gel and no bubbles, if you are still not happy with the image try adjusting the gain. Principles: Using the ultrasound machine alone to evaluate a patient is difficult. The images are hard to
Overview. Diagnostic ultrasound, also called sonography or diagnostic medical sonography, is an imaging method that uses sound waves to produce images of structures within your body. The images can provide valuable information for diagnosing and directing treatment for a variety of diseases and conditions. Most ultrasound examinations are done ...
In paediatric patients, ultrasound imaging can have a substantial role in its diagnosis and management. This presentation will explore the ultrasound appearances of the normal pancreas and demonstrate the changes associated with acute and chronic pancreatitis. The role of ultrasound in various treatment options is also discussed.
The use of ultrasound in the third trimester of pregnancy serves a multitude of general and specialized purposes that include but are not limited to the determination of fetal number and presentation, assessment of growth disorders, and characterization of the placenta and amniotic fluid. Thus, the ultrasonographic applications in the third trimester of pregnancy differ from previous ...
Lecture 25b: The basics of gynecological ultrasound. This lecture was delivered by Dr. Shabnam Bobdiwala at ISUOG's Basic Training Course in gynecology in partnership with Erasmus Medical Center, in Rotterdam in 2018. Feel free to download this presentation to support your learning. ISUOG Basic Training by ISUOG is licensed under a Creative ...
Compound presentation means that a fetal hand is coming out with the fetal head. This is a problem because: The amount of baby that must come through the birth canal at one time is increased. There is increased risk of mechanical injury to the arm and shoulder, including fractures, nerve injuries and soft tissue injury.
Citation, DOI, disclosures and article data. A cord presentation (also known as a funic presentation or obligate cord presentation) is a variation in the fetal presentation where the umbilical cord points towards the internal cervical os or lower uterine segment. It may be a transient phenomenon and is usually considered insignificant until ~32 ...
Ultrasound orientation & imaging planes explained clearly by point-of-care ultrasound expert Joshua Jacquet, MD of https://www.medcram.com/?utm_source=Youtub...
Physics • Diagnostic ultrasound uses sound waves in the frequency range 2-20 MHz • Key properties of sound waves: • Frequency is number of times per second the sound wave is repeated • Wavelength is the distance traveled in 1 cycle • Amplitude is distance between peak and trough. Physics - Parallel Concepts • Conceptually ...
Dr. Omar Ishrak and Dr. Gil Weinberg to Headline Medical Tech Conference. AUSTIN, Texas, March 26, 2024 /PRNewswire/ -- The upcoming UltraCon 2024 conference, organized by the American Institute of Ultrasound in Medicine (AIUM), is set to spotlight groundbreaking advancements in medical technology with keynotes from industry luminaries Dr. Omar Ishrak and Dr. Gil Weinberg.
The association of tissue change and treatment success during high-intensity focused ultrasound focal therapy for prostate cancer. Eur Urol Focus 2023; 9(4): 584-591. Crossref. PubMed. Google Scholar. 9. Schultz-Haakh H, Li JK, Welkowitz W, et al. Ultrasonic treatment of varicose veins. Angiology 1989; 40(2): 129-137.
Ultrasound-guided placement of Midlines catheters (MCs) is a standard procedure with many benefits for patients. Even if there are some guidelines worldwide, this invasive technique is still taught at the patient's bed and relies on mentoring in many care centers. The performance of this care by novice practitioners raises ethical and quality ...
University of Queensland researchers have found targeting amyloid plaque in the brain is not essential for ultrasound to deliver cognitive improvement in neurodegenerative disorders.
Simulation-based training is effective for ultrasound (US)-guided procedures. However, commercially developed simulators are costly. This study aims to evaluate the feasibility of a hand-made phantom for US-guided paracentesis. We described the recipe to prepare an agar phantom. We collected the US performance data of 50 novices, including 22 postgraduate-year (PGY) residents and 28 ...
This study shows that implementation of universal late-pregnancy ultrasound to assess foetal presentation would virtually eliminate undiagnosed intrapartum breech presentation in nulliparous women. If this procedure could be implemented into routine care, for example, by midwives conducting a routine 36-wkGA appointment and using a portable ...
There is a growing appreciation that both giant cell arteritis (GCA) and polymyalgia rheumatica (PMR) are closely interrelated conditions that have significant overlap in aetiology, clinical characteristics and treatment regimens. Subclinical GCA in PMR is becoming increasingly recognised, and there is evolving evidence that this may be a more aggressive disease phenotype than PMR. Ultrasound ...
Pregnant stingray Charlotte gets another ultrasound as world waits for 'miracle' birth. HENDERSONVILLE - Aquarium and Shark Lab by Team ECCO on Main Street has been giving updates on Charlotte the stingray's asexual pregnancy on social media twice a week on Wednesdays and Saturdays, and the Saturday, March 30 update once again revealed no pups ...
"The integration of Caption AI with the Vscan Air SL handheld ultrasound opens an entirely new chapter for cardiac screening. This technology empowers users with guidance and tools for high quality ultrasound scans and supports earlier detection of cardiac disease," said Roland Rott, president and CEO, Ultrasound, GE HealthCare.
"But we used scanning ultrasound alone on mouse models and observed significant memory enhancement." Dr Gerhard LEinenga monitoring ultrasound waves with an oscilloscope Dr Leinenga said the finding shows ultrasound without microbubbles can induce long-lasting cognitive changes in the brain, correlating with memory improvement.
We are seeking an experienced ultrasound technician to join our cardiology practice. The ideal candidate will have experience performing vascular and venous studies, and venous ablations. The successful candidate will be responsible for performing diagnostic ultrasound examinations, maintaining equipment, and ensuring quality patient care.