

Introduction to qualitative nursing research
This type of research can reveal important information that quantitative research can’t.
- Qualitative research is valuable because it approaches a phenomenon, such as a clinical problem, about which little is known by trying to understand its many facets.
- Most qualitative research is emergent, holistic, detailed, and uses many strategies to collect data.
- Qualitative research generates evidence and helps nurses determine patient preferences.
Research 101: Descriptive statistics
Differentiating research, evidence-based practice, and quality improvement
How to appraise quantitative research articles
All nurses are expected to understand and apply evidence to their professional practice. Some of the evidence should be in the form of research, which fills gaps in knowledge, developing and expanding on current understanding. Both quantitative and qualitative research methods inform nursing practice, but quantitative research tends to be more emphasized. In addition, many nurses don’t feel comfortable conducting or evaluating qualitative research. But once you understand qualitative research, you can more easily apply it to your nursing practice.
What is qualitative research?
Defining qualitative research can be challenging. In fact, some authors suggest that providing a simple definition is contrary to the method’s philosophy. Qualitative research approaches a phenomenon, such as a clinical problem, from a place of unknowing and attempts to understand its many facets. This makes qualitative research particularly useful when little is known about a phenomenon because the research helps identify key concepts and constructs. Qualitative research sets the foundation for future quantitative or qualitative research. Qualitative research also can stand alone without quantitative research.
Although qualitative research is diverse, certain characteristics—holism, subjectivity, intersubjectivity, and situated contexts—guide its methodology. This type of research stresses the importance of studying each individual as a holistic system (holism) influenced by surroundings (situated contexts); each person develops his or her own subjective world (subjectivity) that’s influenced by interactions with others (intersubjectivity) and surroundings (situated contexts). Think of it this way: Each person experiences and interprets the world differently based on many factors, including his or her history and interactions. The truth is a composite of realities.
Qualitative research designs
Because qualitative research explores diverse topics and examines phenomena where little is known, designs and methodologies vary. Despite this variation, most qualitative research designs are emergent and holistic. In addition, they require merging data collection strategies and an intensely involved researcher. (See Research design characteristics .)
Although qualitative research designs are emergent, advanced planning and careful consideration should include identifying a phenomenon of interest, selecting a research design, indicating broad data collection strategies and opportunities to enhance study quality, and considering and/or setting aside (bracketing) personal biases, views, and assumptions.
Many qualitative research designs are used in nursing. Most originated in other disciplines, while some claim no link to a particular disciplinary tradition. Designs that aren’t linked to a discipline, such as descriptive designs, may borrow techniques from other methodologies; some authors don’t consider them to be rigorous (high-quality and trustworthy). (See Common qualitative research designs .)
Sampling approaches
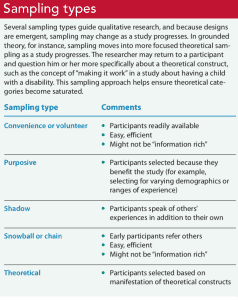
Sampling approaches depend on the qualitative research design selected. However, in general, qualitative samples are small, nonrandom, emergently selected, and intensely studied. Qualitative research sampling is concerned with accurately representing and discovering meaning in experience, rather than generalizability. For this reason, researchers tend to look for participants or informants who are considered “information rich” because they maximize understanding by representing varying demographics and/or ranges of experiences. As a study progresses, researchers look for participants who confirm, challenge, modify, or enrich understanding of the phenomenon of interest. Many authors argue that the concepts and constructs discovered in qualitative research transcend a particular study, however, and find applicability to others. For example, consider a qualitative study about the lived experience of minority nursing faculty and the incivility they endure. The concepts learned in this study may transcend nursing or minority faculty members and also apply to other populations, such as foreign-born students, nurses, or faculty.
Qualitative nursing research can take many forms. The design you choose will depend on the question you’re trying to answer.
A sample size is estimated before a qualitative study begins, but the final sample size depends on the study scope, data quality, sensitivity of the research topic or phenomenon of interest, and researchers’ skills. For example, a study with a narrow scope, skilled researchers, and a nonsensitive topic likely will require a smaller sample. Data saturation frequently is a key consideration in final sample size. When no new insights or information are obtained, data saturation is attained and sampling stops, although researchers may analyze one or two more cases to be certain. (See Sampling types .)
Some controversy exists around the concept of saturation in qualitative nursing research. Thorne argues that saturation is a concept appropriate for grounded theory studies and not other study types. She suggests that “information power” is perhaps more appropriate terminology for qualitative nursing research sampling and sample size.
Data collection and analysis
Researchers are guided by their study design when choosing data collection and analysis methods. Common types of data collection include interviews (unstructured, semistructured, focus groups); observations of people, environments, or contexts; documents; records; artifacts; photographs; or journals. When collecting data, researchers must be mindful of gaining participant trust while also guarding against too much emotional involvement, ensuring comprehensive data collection and analysis, conducting appropriate data management, and engaging in reflexivity.
Data usually are recorded in detailed notes, memos, and audio or visual recordings, which frequently are transcribed verbatim and analyzed manually or using software programs, such as ATLAS.ti, HyperRESEARCH, MAXQDA, or NVivo. Analyzing qualitative data is complex work. Researchers act as reductionists, distilling enormous amounts of data into concise yet rich and valuable knowledge. They code or identify themes, translating abstract ideas into meaningful information. The good news is that qualitative research typically is easy to understand because it’s reported in stories told in everyday language.
Evaluating a qualitative study
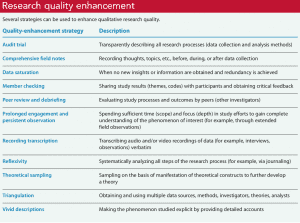
Evaluating qualitative research studies can be challenging. Many terms—rigor, validity, integrity, and trustworthiness—can describe study quality, but in the end you want to know whether the study’s findings accurately and comprehensively represent the phenomenon of interest. Many researchers identify a quality framework when discussing quality-enhancement strategies. Example frameworks include:
- Trustworthiness criteria framework, which enhances credibility, dependability, confirmability, transferability, and authenticity
- Validity in qualitative research framework, which enhances credibility, authenticity, criticality, integrity, explicitness, vividness, creativity, thoroughness, congruence, and sensitivity.
With all frameworks, many strategies can be used to help meet identified criteria and enhance quality. (See Research quality enhancement ). And considering the study as a whole is important to evaluating its quality and rigor. For example, when looking for evidence of rigor, look for a clear and concise report title that describes the research topic and design and an abstract that summarizes key points (background, purpose, methods, results, conclusions).
Application to nursing practice
Qualitative research not only generates evidence but also can help nurses determine patient preferences. Without qualitative research, we can’t truly understand others, including their interpretations, meanings, needs, and wants. Qualitative research isn’t generalizable in the traditional sense, but it helps nurses open their minds to others’ experiences. For example, nurses can protect patient autonomy by understanding them and not reducing them to universal protocols or plans. As Munhall states, “Each person we encounter help[s] us discover what is best for [him or her]. The other person, not us, is truly the expert knower of [him- or herself].” Qualitative nursing research helps us understand the complexity and many facets of a problem and gives us insights as we encourage others’ voices and searches for meaning.
When paired with clinical judgment and other evidence, qualitative research helps us implement evidence-based practice successfully. For example, a phenomenological inquiry into the lived experience of disaster workers might help expose strengths and weaknesses of individuals, populations, and systems, providing areas of focused intervention. Or a phenomenological study of the lived experience of critical-care patients might expose factors (such dark rooms or no visible clocks) that contribute to delirium.
Successful implementation
Qualitative nursing research guides understanding in practice and sets the foundation for future quantitative and qualitative research. Knowing how to conduct and evaluate qualitative research can help nurses implement evidence-based practice successfully.
When evaluating a qualitative study, you should consider it as a whole. The following questions to consider when examining study quality and evidence of rigor are adapted from the Standards for Reporting Qualitative Research.
Jennifer Chicca is a PhD candidate at the Indiana University of Pennsylvania in Indiana, Pennsylvania, and a part-time faculty member at the University of North Carolina Wilmington.
Amankwaa L. Creating protocols for trustworthiness in qualitative research. J Cult Divers. 2016;23(3):121-7.
Cuthbert CA, Moules N. The application of qualitative research findings to oncology nursing practice. Oncol Nurs Forum . 2014;41(6):683-5.
Guba E, Lincoln Y. Competing paradigms in qualitative research . In: Denzin NK, Lincoln YS, eds. Handbook of Qualitative Research. Thousand Oaks, CA: SAGE Publications, Inc.;1994: 105-17.
Lincoln YS, Guba EG. Naturalistic Inquiry . Thousand Oaks, CA: SAGE Publications, Inc.; 1985.
Munhall PL. Nursing Research: A Qualitative Perspective . 5th ed. Sudbury, MA: Jones & Bartlett Learning; 2012.
Nicholls D. Qualitative research. Part 1: Philosophies. Int J Ther Rehabil . 2017;24(1):26-33.
Nicholls D. Qualitative research. Part 2: Methodology. Int J Ther Rehabil . 2017;24(2):71-7.
Nicholls D. Qualitative research. Part 3: Methods. Int J Ther Rehabil . 2017;24(3):114-21.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Acad Med . 2014;89(9):1245-51.
Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice . 10th ed. Philadelphia, PA: Wolters Kluwer; 2017.
Thorne S. Saturation in qualitative nursing studies: Untangling the misleading message around saturation in qualitative nursing studies. Nurse Auth Ed. 2020;30(1):5. naepub.com/reporting-research/2020-30-1-5
Whittemore R, Chase SK, Mandle CL. Validity in qualitative research. Qual Health Res . 2001;11(4):522-37.
Williams B. Understanding qualitative research. Am Nurse Today . 2015;10(7):40-2.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Post Comment

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

Honoring our veterans

Supporting the multi-generational nursing workforce

Vital practitioners

From data to action

Many travel nurses opt for temporary assignments because of the autonomy and opportunities − not just the big boost in pay

Effective clinical learning for nursing students

Nurse safety in the era of open notes

Collaboration: The key to patient care success

Health workers fear it’s profits before protection as CDC revisits airborne transmission

Why COVID-19 patients who could most benefit from Paxlovid still aren’t getting it

Human touch

Leadership style matters

My old stethoscope

Nurse referrals to pharmacy

Lived experience
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 15, Issue 1
- Qualitative data analysis
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Correspondence to Kate Seers RCN Research Institute, School of Health & Social Studies, University of Warwick, Coventry, CV4 7AL, Warwick, UK; kate.seers{at}warwick.ac.uk
https://doi.org/10.1136/ebnurs.2011.100352
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Good qualitative research uses a systematic and rigorous approach that aims to answer questions concerned with what something is like (such as a patient experience), what people think or feel about something that has happened, and it may address why something has happened as it has. Qualitative data often takes the form of words or text and can include images.
Qualitative research covers a very broad range of philosophical underpinnings and methodological approaches. Each has its own particular way of approaching all stages of the research process, including analysis, and has its own terms and techniques, but there are some common threads that run across most of these approaches. This Research Made Simple piece will focus on some of these common threads in the analysis of qualitative research.
So you have collected all your qualitative data – you may have a pile of interview transcripts, field-notes, documents and notes from observation. The process of analysis is described by Richards and Morse 1 as one of transformation and interpretation.
It is easy to be overwhelmed by the volume of data – novice qualitative researchers are sometimes told not to worry and the themes will emerge from the data. This suggests some sort of epiphany, (which is how it happens sometimes!) but generally it comes from detailed work and reflection on the data and what it is telling you. There is sometimes a fine line between being immersed in the data and drowning in it!
A first step is to sort and organise the data, by coding it in some way. For example, you could read through a transcript, and identify that in one paragraph a patient is talking about two things; first is fear of surgery and second is fear of unrelieved pain. The codes for this paragraph could be ‘fear of surgery’ and ‘fear of pain’. In other areas of the transcript fear may arise again, and perhaps these codes will be merged into a category titled ‘fear’. Other concerns may emerge in this and other transcripts and perhaps best be represented by the theme ‘lack of control’. Themes are thus more abstract concepts, reflecting your interpretation of patterns across your data. So from codes, categories can be formed, and from categories, more encompassing themes are developed to describe the data in a form which summarises it, yet retains the richness, depth and context of the original data. Using quotations to illustrate categories and themes helps keep the analysis firmly grounded in the data. You need to constantly ask yourself ‘what is happening here?’ as you code and move from codes, to categories and themes, making sure you have data to support your decisions. Analysis inevitably involves subjective choices, and it is important to document what you have done and why, so a clear audit trail is provided. The coding example above describes codes inductively coming from the data. Some researchers may use a coding framework derived from, for example, the literature, their research questions or interview prompts, (Ritchie and Spencer 2 ) or a combination of both approaches.
Qualitative data, such as transcripts from an interview, are often routed in the interaction between the participant and the researcher. Reflecting on how you, as a researcher, may have influenced both the data collected and the analysis is an important part of the analysis.
As well as keeping your brain very much in gear, you need to be really organised. You may use highlighting pens and paper to keep track of your analysis, or use qualitative software to manage your data (such as NVivio or Atlas Ti). These programmes help you organise your data – you still have to do all the hard work to analyse it! Whatever you choose, it is important that you can trace your data back from themes to categories to codes. There is nothing more frustrating than looking for that illustrative patient quote, and not being able to find it.
If your qualitative data are part of a mixed methods study, (has both quantitative and qualitative data) careful thought has to be given to how you will analyse and present findings. Refer to O’Caithain et al 3 for more details.
There are many books and papers on qualitative analysis, a very few of which are listed below. 4 , – , 6 Working with someone with qualitative expertise is also invaluable, as you can read about it, but doing it really brings it alive.
- Richards L ,
- Ritchie J ,
- O'Cathain ,
- Bradley EH ,
- Huberman AM
Competing interests None.
Read the full text or download the PDF:

Nursing Research Guide
- General Search Strategies
- Searching by Author & Theory
- Searching for Qualitative Studies
- Searching for Systematic Reviews & Controlled Trials
- Health Data & Statistics
- Tutorials & Help
- SoN and APA (7th Ed.)
- NSC 890: PICOT Searches
What is qualitative research?
Qualitative research in Nursing approaches a clinical question from a place of unknowing in an attempt to understand the complexity, depth, and richness of a particular situation from the perspective of the person or persons impacted by the situation (i.e., the subjects of the study).
Study subjects may include the patient(s), the patient's caregivers, the patient's family members, etc. Qualitative research may also include information gleaned from the investigator's or researcher's observations.
While typically more subjective than quantitative research (which focuses on measurements and numbers), qualitative research still employs a systematic approach.
Qualitative research is generally preferred over quantitative research (which on measurements and numbers) when the clinical question centers around life experiences or meaning.
Adapted from:
- Wilson, B., Austria, M.J., & Casucci, T. (2021 March 21). Understanding Quantitative and Qualitative Approaches
- Chicca, J. (2020 June 5). Introduction to qualitative nursing research. American Nurse Journal.
Where can I find qualitative research?
Qualitative research can be found in numerous databases. Some good starting options are:
- CINAHL Ultimate Journal articles and eBooks in nursing and allied health.
- MEDLINE (EBSCOhost Web) Journal articles in medicine, life sciences, health care, and biomedical research.
- APA PsycINFO Articles from journals, newspapers, and magazines, along with eBooks in nearly every social science subject area.
- PubMed Citation search of journal articles and books in health and life sciences.
How can I find qualitative research?
Cinahl and/or medline.
- Start at the Advanced Search screen.
- Add a search term that represents the topic you are interested in into one (or more) of the search boxes.
- Scroll down until you see the Limit your results section.
- Qualitative - High Sensitivity (broadest category/broad search)
- Qualitative - High Specificity (narrowest category/specific search)
- Qualitative - Best Balance (somewhere in between)
- Select or click the search button.

APA PsycINFO
- Start at the Advanced Search screen.
- Use the Methodology menu to select Qualitative .

- Use the drop-down menu next the Enter search term box to set the search to MeSH Terms
- Qualitative Research
- Nursing Methodology Research

How can I use keywords to search for qualitative research?
Try adding adding a keyword that might specifically identify qualitative research. You could add the term qualitative to your search and/or your could add different types of qualitative research according to your specific needs and/or research assignment.
For example, consider the following types of qualitative research in light of the types of questions a researcher might be trying to answer with each qualitative research type:
- Clinical question: What happens to the quality of nursing practice when we implement a peer-mentoring system?
- Clinical question: How is patient autonomy promoted by a unit?
- Clinical question: What is the nursing role in end-of-life decisions?
- Clinical question: What discourses are used in nursing practice and how do they shape practice?
- Clinical question: How does Filipino culture influence childbirth experiences?
- Clinical question: What are the immediate underlying psychological and environmental causes of incivility in nursing?
- Clinical question: How does the basic social process of role transition happen within the context of advanced practice nursing transitions?
- Clinical question: When and why did nurses become researchers?
- Clinical question: How does one live with a diagnosis of scleroderma?
- Clinical question: What is the lived experience of nurses who were admitted as patients on their home practice units?
Adapted from: Chicca, J. (2020 June 5). Introduction to qualitative nursing research . American Nurse Journal.
Need more help?
Finding relevant qualitative research can be both difficult and time consuming. Once you conduct a search, you will need to review your search results and look at individual articles, their subject terms, and abstracts to determine if they are truly qualitative research articles. And that's a determination that only you can make.
If you still need help after trying the search strategies and tips suggested on this research guide, we encourage you to schedule an in-person or Zoom research appointment . Health Services librarian Rachel Riffe-Albright is a great bet, but any librarian would be happy to help!
Additonal resources on qualitative research
The following are research guides created by other academic libraries. While you likely will not have access to any of their linked resources, the tips and tricks shared may be useful to you as you search for qualitative research:
- What is Qualitative Research? from UTA Libraries at University of Texas Arlington
- Finding Qualitative Research Articles from Ashland University Library
- Finding Qualitative Research Articles from the Health Sciences Library at University of Washington
- Advanced Search Guide: Qualitative and Quantitative Studies from Southern Connecticut State University Library
- Finding Qualitative and Quantitative Studies in CINAHL from Southern Connecticut State University Library
- << Previous: Searching by Author & Theory
- Next: Searching for Systematic Reviews & Controlled Trials >>
- Last Updated: Mar 29, 2024 11:04 AM
- URL: https://libguides.eku.edu/nursing
EO/AA Statement | Privacy Statement | 103 Libraries Complex Crabbe Library Richmond, KY 40475 | (859) 622-1790 ©
- Research article
- Open access
- Published: 09 November 2005
A qualitative study of nursing student experiences of clinical practice
- Farkhondeh Sharif 1 &
- Sara Masoumi 2
BMC Nursing volume 4 , Article number: 6 ( 2005 ) Cite this article
356k Accesses
166 Citations
9 Altmetric
Metrics details
Nursing student's experiences of their clinical practice provide greater insight to develop an effective clinical teaching strategy in nursing education. The main objective of this study was to investigate student nurses' experience about their clinical practice.
Focus groups were used to obtain students' opinion and experiences about their clinical practice. 90 baccalaureate nursing students at Shiraz University of Medical Sciences (Faculty of Nursing and Midwifery) were selected randomly from two hundred students and were arranged in 9 groups of ten students. To analyze the data the method used to code and categories focus group data were adapted from approaches to qualitative data analysis.
Four themes emerged from the focus group data. From the students' point of view," initial clinical anxiety", "theory-practice gap"," clinical supervision", professional role", were considered as important factors in clinical experience.
The result of this study showed that nursing students were not satisfied with the clinical component of their education. They experienced anxiety as a result of feeling incompetent and lack of professional nursing skills and knowledge to take care of various patients in the clinical setting.
Peer Review reports
Clinical experience has been always an integral part of nursing education. It prepares student nurses to be able of "doing" as well as "knowing" the clinical principles in practice. The clinical practice stimulates students to use their critical thinking skills for problem solving [ 1 ]
Awareness of the existence of stress in nursing students by nurse educators and responding to it will help to diminish student nurses experience of stress. [ 2 ]
Clinical experience is one of the most anxiety producing components of the nursing program which has been identified by nursing students. In a descriptive correlational study by Beck and Srivastava 94 second, third and fourth year nursing students reported that clinical experience was the most stressful part of the nursing program[ 3 ]. Lack of clinical experience, unfamiliar areas, difficult patients, fear of making mistakes and being evaluated by faculty members were expressed by the students as anxiety-producing situations in their initial clinical experience. In study done by Hart and Rotem stressful events for nursing students during clinical practice have been studied. They found that the initial clinical experience was the most anxiety producing part of their clinical experience [ 4 ]. The sources of stress during clinical practice have been studied by many researchers [ 5 – 10 ] and [ 11 ].
The researcher came to realize that nursing students have a great deal of anxiety when they begin their clinical practice in the second year. It is hoped that an investigation of the student's view on their clinical experience can help to develop an effective clinical teaching strategy in nursing education.
A focus group design was used to investigate the nursing student's view about the clinical practice. Focus group involves organized discussion with a selected group of individuals to gain information about their views and experiences of a topic and is particularly suited for obtaining several perspectives about the same topic. Focus groups are widely used as a data collection technique. The purpose of using focus group is to obtain information of a qualitative nature from a predetermined and limited number of people [ 12 , 13 ].
Using focus group in qualitative research concentrates on words and observations to express reality and attempts to describe people in natural situations [ 14 ].
The group interview is essentially a qualitative data gathering technique [ 13 ]. It can be used at any point in a research program and one of the common uses of it is to obtain general background information about a topic of interest [ 14 ].
Focus groups interviews are essential in the evaluation process as part of a need assessment, during a program, at the end of the program or months after the completion of a program to gather perceptions on the outcome of that program [ 15 , 16 ]. Kruegger (1988) stated focus group data can be used before, during and after programs in order to provide valuable data for decision making [ 12 ].
The participants from which the sample was drawn consisted of 90 baccalaureate nursing students from two hundred nursing students (30 students from the second year and 30 from the third and 30 from the fourth year) at Shiraz University of Medical Sciences (Faculty of Nursing and Midwifery). The second year nursing students already started their clinical experience. They were arranged in nine groups of ten students. Initially, the topics developed included 9 open-ended questions that were related to their nursing clinical experience. The topics were used to stimulate discussion.
The following topics were used to stimulate discussion regarding clinical experience in the focus groups.
How do you feel about being a student in nursing education?
How do you feel about nursing in general?
Is there any thing about the clinical field that might cause you to feel anxious about it?
Would you like to talk about those clinical experiences which you found most anxiety producing?
Which clinical experiences did you find enjoyable?
What are the best and worst things do you think can happen during the clinical experience?
What do nursing students worry about regarding clinical experiences?
How do you think clinical experiences can be improved?
What is your expectation of clinical experiences?
The first two questions were general questions which were used as ice breakers to stimulate discussion and put participants at ease encouraging them to interact in a normal manner with the facilitator.
Data analysis
The following steps were undertaken in the focus group data analysis.
Immediate debriefing after each focus group with the observer and debriefing notes were made. Debriefing notes included comments about the focus group process and the significance of data
Listening to the tape and transcribing the content of the tape
Checking the content of the tape with the observer noting and considering any non-verbal behavior. The benefit of transcription and checking the contents with the observer was in picking up the following:
Parts of words
Non-verbal communication, gestures and behavior...
The researcher facilitated the groups. The observer was a public health graduate who attended all focus groups and helped the researcher by taking notes and observing students' on non-verbal behavior during the focus group sessions. Observer was not known to students and researcher
The methods used to code and categorise focus group data were adapted from approaches to qualitative content analysis discussed by Graneheim and Lundman [ 17 ] and focus group data analysis by Stewart and Shamdasani [ 14 ] For coding the transcript it was necessary to go through the transcripts line by line and paragraph by paragraph, looking for significant statements and codes according to the topics addressed. The researcher compared the various codes based on differences and similarities and sorted into categories and finally the categories was formulated into a 4 themes.
The researcher was guided to use and three levels of coding [ 17 , 18 ]. Three levels of coding selected as appropriate for coding the data.
Level 1 coding examined the data line by line and making codes which were taken from the language of the subjects who attended the focus groups.
Level 2 coding which is a comparing of coded data with other data and the creation of categories. Categories are simply coded data that seem to cluster together and may result from condensing of level 1 code [ 17 , 19 ].
Level 3 coding which describes the Basic Social Psychological Process which is the title given to the central themes that emerge from the categories.
Table 1 shows the three level codes for one of the theme
The documents were submitted to two assessors for validation. This action provides an opportunity to determine the reliability of the coding [ 14 , 15 ]. Following a review of the codes and categories there was agreement on the classification.
Ethical considerations
The study was conducted after approval has been obtained from Shiraz university vice-chancellor for research and in addition permission to conduct the study was obtained from Dean of the Faculty of Nursing and Midwifery. All participants were informed of the objective and design of the study and a written consent received from the participants for interviews and they were free to leave focus group if they wish.
Most of the students were females (%94) and single (% 86) with age between 18–25.
The qualitative analysis led to the emergence of the four themes from the focus group data. From the students' point of view," initial clinical anxiety", "theory-practice gap", clinical supervision"," professional role", was considered as important factors in clinical experience.
Initial clinical anxiety
This theme emerged from all focus group discussion where students described the difficulties experienced at the beginning of placement. Almost all of the students had identified feeling anxious in their initial clinical placement. Worrying about giving the wrong information to the patient was one of the issues brought up by students.
One of the students said:
On the first day I was so anxious about giving the wrong information to the patient. I remember one of the patients asked me what my diagnosis is. ' I said 'I do not know', she said 'you do not know? How can you look after me if you do not know what my diagnosis is?'
From all the focus group sessions, the students stated that the first month of their training in clinical placement was anxiety producing for them.
One of the students expressed:
The most stressful situation is when we make the next step. I mean ... clinical placement and we don't have enough clinical experience to accomplish the task, and do our nursing duties .
Almost all of the fourth year students in the focus group sessions felt that their stress reduced as their training and experience progressed.
Another cause of student's anxiety in initial clinical experience was the students' concern about the possibility of harming a patient through their lack of knowledge in the second year.
One of the students reported:
In the first day of clinical placement two patients were assigned to me. One of them had IV fluid. When I introduced myself to her, I noticed her IV was running out. I was really scared and I did not know what to do and I called my instructor .
Fear of failure and making mistakes concerning nursing procedures was expressed by another student. She said:
I was so anxious when I had to change the colostomy dressing of my 24 years old patient. It took me 45 minutes to change the dressing. I went ten times to the clinic to bring the stuff. My heart rate was increasing and my hand was shaking. I was very embarrassed in front of my patient and instructor. I will never forget that day .
Sellek researched anxiety-creating incidents for nursing students. He suggested that the ward is the best place to learn but very few of the learner's needs are met in this setting. Incidents such as evaluation by others on initial clinical experience and total patient care, as well as interpersonal relations with staff, quality of care and procedures are anxiety producing [ 11 ].
Theory-practice gap
The category theory-practice gap emerged from all focus discussion where almost every student in the focus group sessions described in some way the lack of integration of theory into clinical practice.
I have learnt so many things in the class, but there is not much more chance to do them in actual settings .
Another student mentioned:
When I just learned theory for example about a disease such as diabetic mellitus and then I go on the ward and see the real patient with diabetic mellitus, I relate it back to what I learned in class and that way it will remain in my mind. It is not happen sometimes .
The literature suggests that there is a gap between theory and practice. It has been identified by Allmark and Tolly [ 20 , 21 ]. The development of practice theory, theory which is developed from practice, for practice, is one way of reducing the theory-practice gap [ 21 ]. Rolfe suggests that by reconsidering the relationship between theory and practise the gap can be closed. He suggests facilitating reflection on the realities of clinical life by nursing theorists will reduce the theory-practice gap. The theory- practice gap is felt most acutely by student nurses. They find themselves torn between the demands of their tutor and practising nurses in real clinical situations. They were faced with different real clinical situations and are unable to generalise from what they learnt in theory [ 22 ].
Clinical supervision
Clinical supervision is recognised as a developmental opportunity to develop clinical leadership. Working with the practitioners through the milieu of clinical supervision is a powerful way of enabling them to realize desirable practice [ 23 ]. Clinical nursing supervision is an ongoing systematic process that encourages and supports improved professional practice. According to Berggren and Severinsson the clinical nurse supervisors' ethical value system is involved in her/his process of decision making. [ 24 , 25 ]
Clinical Supervision by Head Nurse (Nursing Unit Manager) and Staff Nurses was another issue discussed by the students in the focus group sessions. One of the students said:
Sometimes we are taught mostly by the Head Nurse or other Nursing staff. The ward staff are not concerned about what students learn, they are busy with their duties and they are unable to have both an educational and a service role
Another student added:
Some of the nursing staff have good interaction with nursing students and they are interested in helping students in the clinical placement but they are not aware of the skills and strategies which are necessary in clinical education and are not prepared for their role to act as an instructor in the clinical placement
The students mostly mentioned their instructor's role as an evaluative person. The majority of students had the perception that their instructors have a more evaluative role than a teaching role.
The literature suggests that the clinical nurse supervisors should expressed their existence as a role model for the supervisees [ 24 ]
Professional role
One view that was frequently expressed by student nurses in the focus group sessions was that students often thought that their work was 'not really professional nursing' they were confused by what they had learned in the faculty and what in reality was expected of them in practice.
We just do basic nursing care, very basic . ... You know ... giving bed baths, keeping patients clean and making their beds. Anyone can do it. We spend four years studying nursing but we do not feel we are doing a professional job .
The role of the professional nurse and nursing auxiliaries was another issue discussed by one of the students:
The role of auxiliaries such as registered practical nurse and Nurses Aids are the same as the role of the professional nurse. We spend four years and we have learned that nursing is a professional job and it requires training and skills and knowledge, but when we see that Nurses Aids are doing the same things, it can not be considered a professional job .
The result of student's views toward clinical experience showed that they were not satisfied with the clinical component of their education. Four themes of concern for students were 'initial clinical anxiety', 'theory-practice gap', 'clinical supervision', and 'professional role'.
The nursing students clearly identified that the initial clinical experience is very stressful for them. Students in the second year experienced more anxiety compared with third and fourth year students. This was similar to the finding of Bell and Ruth who found that nursing students have a higher level of anxiety in second year [ 26 , 27 ]. Neary identified three main categories of concern for students which are the fear of doing harm to patients, the sense of not belonging to the nursing team and of not being fully competent on registration [ 28 ] which are similar to what our students mentioned in the focus group discussions. Jinks and Patmon also found that students felt they had an insufficiency in clinical skills upon completion of pre-registration program [ 29 ].
Initial clinical experience was the most anxiety producing part of student clinical experience. In this study fear of making mistake (fear of failure) and being evaluated by faculty members were expressed by the students as anxiety-producing situations in their initial clinical experience. This finding is supported by Hart and Rotem [ 4 ] and Stephens [ 30 ]. Developing confidence is an important component of clinical nursing practice [ 31 ]. Development of confidence should be facilitated by the process of nursing education; as a result students become competent and confident. Differences between actual and expected behaviour in the clinical placement creates conflicts in nursing students. Nursing students receive instructions which are different to what they have been taught in the classroom. Students feel anxious and this anxiety has effect on their performance [ 32 ]. The existence of theory-practice gap in nursing has been an issue of concern for many years as it has been shown to delay student learning. All the students in this study clearly demonstrated that there is a gap between theory and practice. This finding is supported by other studies such as Ferguson and Jinks [ 33 ] and Hewison and Wildman [ 34 ] and Bjork [ 35 ]. Discrepancy between theory and practice has long been a source of concern to teachers, practitioners and learners. It deeply rooted in the history of nurse education. Theory-practice gap has been recognised for over 50 years in nursing. This issue is said to have caused the movement of nurse education into higher education sector [ 34 ].
Clinical supervision was one of the main themes in this study. According to participant, instructor role in assisting student nurses to reach professional excellence is very important. In this study, the majority of students had the perception that their instructors have a more evaluative role than a teaching role. About half of the students mentioned that some of the head Nurse (Nursing Unit Manager) and Staff Nurses are very good in supervising us in the clinical area. The clinical instructor or mentors can play an important role in student nurses' self-confidence, promote role socialization, and encourage independence which leads to clinical competency [ 36 ]. A supportive and socialising role was identified by the students as the mentor's function. This finding is similar to the finding of Earnshaw [ 37 ]. According to Begat and Severinsson supporting nurses by clinical nurse specialist reported that they may have a positive effect on their perceptions of well-being and less anxiety and physical symptoms [ 25 ].
The students identified factors that influence their professional socialisation. Professional role and hierarchy of occupation were factors which were frequently expressed by the students. Self-evaluation of professional knowledge, values and skills contribute to the professional's self-concept [ 38 ]. The professional role encompasses skills, knowledge and behaviour learned through professional socialisation [ 39 ]. The acquisition of career attitudes, values and motives which are held by society are important stages in the socialisation process [ 40 ]. According to Corwin autonomy, independence, decision-making and innovation are achieved through professional self-concept 41 . Lengacher (1994) discussed the importance of faculty staff in the socialisation process of students and in preparing them for reality in practice. Maintenance and/or nurturance of the student's self-esteem play an important role for facilitation of socialisation process 42 .
One view that was expressed by second and third year student nurses in the focus group sessions was that students often thought that their work was 'not really professional nursing' they were confused by what they had learned in the faculty and what in reality was expected of them in practice.
The finding of this study and the literature support the need to rethink about the clinical skills training in nursing education. It is clear that all themes mentioned by the students play an important role in student learning and nursing education in general. There were some similarities between the results of this study with other reported studies and confirmed that some of the factors are universal in nursing education. Nursing students expressed their views and mentioned their worry about the initial clinical anxiety, theory-practice gap, professional role and clinical supervision. They mentioned that integration of both theory and practice with good clinical supervision enabling them to feel that they are enough competent to take care of the patients. The result of this study would help us as educators to design strategies for more effective clinical teaching. The results of this study should be considered by nursing education and nursing practice professionals. Faculties of nursing need to be concerned about solving student problems in education and clinical practice. The findings support the need for Faculty of Nursing to plan nursing curriculum in a way that nursing students be involved actively in their education.
Dunn SV, Burnett P: The development of a clinical learning environment scale. Journal of Advanced Nursing. 1995, 22: 1166-1173.
Article CAS PubMed Google Scholar
Lindop E: Factors associated with student and pupil nurse wastage. Journal of Advanced Nursing. 1987, 12 (6): 751-756.
Beck D, Srivastava R: Perceived level and source of stress in baccalaureate nursing students. Journal of Nursing Education. 1991, 30 (3): 127-132.
CAS PubMed Google Scholar
Hart G, Rotem A: The best and the worst: Students' experience of clinical education. The Australian Journal of Advanced Nursing. 1994, 11 (3): 26-33.
Sheila Sh, Huey-Shyon L, Shiowli H: Perceived stress and physio-psycho-social status of nursing students during their initial period of clinical practice. International Journal of Nursing Studies. 2002, 39: 165-175. 10.1016/S0020-7489(01)00016-5.
Article Google Scholar
Johnson J: Reducing distress in first level and student nurses. Journal of Advanced Nursing. 2000, 32 (1): 66-74. 10.1046/j.1365-2648.2000.01421.x.
Admi H: Nursing students' stress during the initial clinical experience. Journal of Nursing Education. 1997, 36: 323-327.
Blainey GC: Anxiety in the undergraduate medical-surgical clinical student. Journal of Nursing Education. 1980, 19 (8): 33-36.
Wong J, Wong S: Towards effective clinical teaching in nursing. Journal of Advanced Nursing. 1987, 12 (4): 505-513.
Windsor A: Nursing students' perceptions of clinical experience. Journal of Nursing Education. 1987, 26 (4): 150-154.
Sellek T: Satisfying and anxiety creating incidents for nursing students. Nursing Times. 1982, 78 (35): 137-140.
PubMed Google Scholar
Krueger RA: Focus Groups: A Practical Guide for Applied Research. Sage Publications: California. 1988
Google Scholar
Denzin NK: The Research Act. 1989, Prentice Hall: Englewood Cliffs, New Jersey, 3
Stewart DW, Shamdasani PN: Analysing focus group data. Focus Groups: Theory and Practice. Edited by: Shamdasani PN. 1990, Sage Publications: Newbury Park
Barbour RS, Kitzinger J: Developing focus group research : politics, theory and practice. Sage. 1999
Patton MQ: Qualitative Evaluation and Research Methods. 1990, Sage publications, 2
Graneheim UH, Lundman B: Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004, 24: 105-112. 10.1016/j.nedt.2003.10.001.
Streubert HJ, Carpenter DR: Qualitative Research in Nursing. Advancing the Humanistic Imperative. 1995, J.B. Lippincott Company: Philadelphia
Polit DF, Hungler BP: Nursing research: Principles and Methods. Philadelphia newyork. 1999
Allmark PA: classical view of the theory-practice gap in nursing. Journal of Advanced Nursing. 1995, 22 (1): 18-23. 10.1046/j.1365-2648.1995.22010018.x.
Tolley KA: Theory from practice for practice: Is this a reality?. Journal of Advanced Nursing. 1995, 21 (1): 184-190. 10.1046/j.1365-2648.1995.21010184.x.
Rolfe G: Listening to students: Course evaluation as action research. Nurse Education Today. 1994, 14 (3): 223-227. 10.1016/0260-6917(94)90085-X.
Johns Ch: clinical supervision as a model for clinical leadership. Journal of Nursing Management. 2003, 11: 25-34. 10.1046/j.1365-2834.2002.00288.x.
Article PubMed Google Scholar
Berggren I, Severinsson E: Nurses supervisors'action in relation to their decision-making style and ethical approach to clinical supervision. Journal of Advanced Nursing. 2003, 41 (6): 615-622. 10.1046/j.1365-2648.2003.02573.x.
Begat I, Severinsson E: Nurses' satisfaction with their work environment and the outcomes of clinical nursing supervision on nurses' experiences of well-being. Journal of Nursing Management. 2005, 13: 221-230. 10.1111/j.1365-2834.2004.00527.x.
Bell P: Anxiety in mature age and higher school certificate entry student nurses – A comparison of effects on performance. Journal of Australian Congress of Mental Health Nurses. 1984, 4/5: 13-21.
Ruth L: Experiencing before and throughout the nursing career. Journal of Advanced Nursing. 2002, 39: 119-10.1046/j.1365-2648.2000.02251.x.
Neary M: Project 2000 students' survival kit: a return to the practical room. Nurse Education Today. 1997, 17 (1): 46-52. 10.1016/S0260-6917(97)80078-0.
Jinks A, Pateman B: Nither this nor that: The stigma of being an undergraduate nurse. Nursing Times. 1998, 2 (2): 12-13.
CAS Google Scholar
Stephen RL: Imagery: A treatment for nursing student anxiety. Journal of Nursing Education. 1992, 31 (7): 314-319.
Grundy SE: The confidence scale. Nurse Educator. 1993, 18 (1): 6-9.
Copeland L: Developing student confidence. Nurse Educator. 1990, 15 (1): 7-
Ferguson K, Jinks A: Integrating what is taught with what is practised in the nursing curriculum: A multi-dimensional model. Journal of Advanced Nursing. 1994, 20 (4): 687-695. 10.1046/j.1365-2648.1994.20040687.x.
Hewison A, Wildman S: The theory-practice gap in nursing: A new dimension. Journal of Advanced Nursing. 1996, 24 (4): 754-761. 10.1046/j.1365-2648.1996.25214.x.
Bjork T: Neglected conflicts in the discipline of nursing: Perceptions of the importance and value of practical skill. Journal of Advanced Nursing. 1995, 22 (1): 6-12. 10.1046/j.1365-2648.1995.22010006.x.
Busen N: Mentoring in advanced practice nursing. Journal of Advanced Nursing Practice. 1999, 2: 2-
Earnshaw GP: Mentorship: The students' view. Nurse Education Today. 1995, 15 (4): 274-279. 10.1016/S0260-6917(95)80130-8.
Kelly B: The professional self-concepts of nursing undergraduates and their perceptions of influential forces. Journal of Nursing Education. 1992, 31 (3): 121-125.
Lynn MR, McCain NL, Boss BJ: Socialization of R.N. to B.S.N Image:. Journal of Nursing Scholarship. 1989, 21 (4): 232-237.
Article CAS Google Scholar
Klein SM, Ritti RR: Understanding Organisational Behaviour. 1980, Kent: Boston
Corwin RG: The professional employee: A study of conflict in nursing roles. The American Journal of Sociology. 1961, 66: 604-615. 10.1086/223010.
Lengacher CA: Effects of professional development seminars on role conception, role deprivation, and self-esteem of generic baccalaureate students. Nursing Connections. 1994, 7 (1): 21-34.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1472-6955/4/6/prepub
Download references
Acknowledgements
The author would like to thank the student nurses who participated in this study for their valuable contribution
Author information
Authors and affiliations.
Psychiatric Nursing Department, Fatemeh (P.B.U.H) College of Nursing and Midwifery Shiraz University of Medical Sciences, Zand BlvD, Shiraz, Iran
Farkhondeh Sharif
English Department, Shiraz University, Shiraz, Iran
Sara Masoumi
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Farkhondeh Sharif .
Additional information
Competing interests.
The author(s) declare that they no competing interests.
Authors' contributions
FSH: Initiation and design of the research, focus groups conduction, data collection, analysis and writing the paper, SM: Editorial revision of paper
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Sharif, F., Masoumi, S. A qualitative study of nursing student experiences of clinical practice. BMC Nurs 4 , 6 (2005). https://doi.org/10.1186/1472-6955-4-6
Download citation
Received : 10 June 2005
Accepted : 09 November 2005
Published : 09 November 2005
DOI : https://doi.org/10.1186/1472-6955-4-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Focus Group
- Nursing Student
- Professional Role
- Nursing Education
- Focus Group Session

BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 09 April 2024
A qualitative study of leaders’ experiences of handling challenges and changes induced by the COVID-19 pandemic in rural nursing homes and homecare services
- Malin Knutsen Glette 1 , 2 ,
- Tone Kringeland 2 ,
- Lipika Samal 3 , 4 ,
- David W. Bates 3 , 4 &
- Siri Wiig 1
BMC Health Services Research volume 24 , Article number: 442 ( 2024 ) Cite this article
149 Accesses
2 Altmetric
Metrics details
The COVID-19 pandemic had a major impact on healthcare services globally. In care settings such as small rural nursing homes and homes care services leaders were forced to confront, and adapt to, both new and ongoing challenges to protect their employees and patients and maintain their organization's operation. The aim of this study was to assess how healthcare leaders, working in rural primary healthcare services, led nursing homes and homecare services during the COVID-19 pandemic. Moreover, the study sought to explore how adaptations to changes and challenges induced by the pandemic were handled by leaders in rural nursing homes and homecare services.
The study employed a qualitative explorative design with individual interviews. Nine leaders at different levels, working in small, rural nursing homes and homecare services in western Norway were included.
Three main themes emerged from the thematic analysis: “Navigating the role of a leader during the pandemic,” “The aftermath – management of COVID-19 in rural primary healthcare services”, and “The benefits and drawbacks of being small and rural during the pandemic.”
Conclusions
Leaders in rural nursing homes and homecare services handled a multitude of immediate challenges and used a variety of adaptive strategies during the COVID-19 pandemic. While handling their own uncertainty and rapidly changing roles, they also coped with organizational challenges and adopted strategies to maintain good working conditions for their employees, as well as maintain sound healthcare management. The study results establish the intricate nature of resilient leadership, encompassing individual resilience, personality, governance, resource availability, and the capability to adjust to organizational and employee requirements, and how the rural context may affect these aspects.
Peer Review reports
In 2021, essential healthcare services in 90% of the world’s countries were disrupted by the COVID-19 pandemic [ 1 ]. Healthcare services were heavily stressed and had to address unexpected issues and sudden changes, whilst still providing high quality care over a prolonged period [ 2 , 3 ]. Despite the intense focus on hospitals during this period, other parts of the healthcare system such as nursing homes and homecare services also faced extreme challenges. These included issues such as having to introduce and constantly adapt new infection control routines, as well as being given increased responsibility in caring for infected and seriously ill patients in facilities that were not built for such circumstances [ 4 , 5 , 6 , 7 ]. Mortality rates in nursing homes were especially high [ 8 ].
Resilience in healthcare is about a system’s ability to adapt to challenges and changes at different levels (e.g., organization, leaders, health personnel) to maintain high quality care [ 9 , 10 ]. During the COVID-19 pandemic, leaders and the front line were forced to rapidly adjust to keep healthcare services afloat. It has been demonstrated in previous research that effective leadership is crucial in navigating crises and building resilience within health systems [ 11 , 12 , 13 ]. Furthermore, leaders play key roles in facilitating health personnel resilience, for example, through promoting a positive outlook on change and by developing health personnels’ competencies and strengths [ 12 , 14 , 15 ]. During the COVID-19 pandemic, this role became intensified [ 16 , 17 , 18 ], and leaders’ roles in promoting resilient healthcare services were central, for example safeguarding resources, providing emotional support and organizing systems to cope with extreme stresses [ 3 , 19 ].
Smaller, rural nursing homes and home care services are geographically dispersed and typically remote from specialized healthcare services or other nursing home and homecare services. They also tend to have reduced access to personnel due to low population density, frequently leading to the need to make independent decisions, often in complex situations [ 20 ]. Overall, rural healthcare services face different challenges than their urban counterparts [ 21 , 22 , 23 ]. The COVID-19 pandemic intensified some of these issues and created new ones which needed to be managed [ 21 , 24 , 25 ].
The research base on COVID-19 has expanded extensively the past years [ 26 ], covering areas such as clinical risks and outcomes for healthcare workers [ 27 ] and patients [ 28 ], hospital admissions [ 29 ] and healthcare utilization during the pandemic [ 30 ]. Moreover, areas like healthcare leaders' [ 16 , 17 , 31 ] and healthcare professionals’ [ 2 , 32 ] strategies to handle the pandemic challenges, and COVID related strategies’ effect on quality of care [ 33 , 34 ]. And lastly, but not exhaustively, the COVID-19 pandemic in different healthcare settings such as hospitals [ 35 ], primary healthcare services and [ 36 ] mental healthcare services [ 37 ]. However, research on rural healthcare settings, particularly leaders in rural nursing homes and homecare services, have received less attention [ 38 , 39 , 40 ]. Despite the anticipated importance of primary healthcare services in future healthcare and the prevalence of rural healthcare options [ 41 , 42 ]. Overall, there are still lessons to be learned from the COVID-19 pandemic, specifically identifying resilience promoting and inhibiting factors in different health care settings during crisis, how leaders deal with crisis management, and furthermore, to understand and draw lessons from challenges that were overcome during the pandemic[ 43 , 44 ].
Aim and research question
The aim of this study was to assess how healthcare leaders in rural primary healthcare services managed nursing homes and homecare services during the COVID-19 pandemic. Moreover, the study aimed to explore how adaptations to changes and challenges induced by the pandemic were handled by these leaders.
The research question guiding the study was: How did primary healthcare leaders in rural areas experience their leadership during the COVID-19 pandemic, and how did they adapt to the rapid onset changes demanded by the COVID-19 outbreak?
The study employed a qualitative explorative design to study in-depth, how nursing home and homecare leaders in Norwegian rural primary healthcare services experienced and addressed the extreme challenges and needs for change induced by the COVID-19 pandemic [ 45 , 46 ]. Four rural municipalities of different sizes were included in the study. Nursing home and homecare leaders at different organizational levels participated in individual interviews (See Table 1 ).
Norway is divided into 356 municipalities. These municipalities have the autonomy to administer and manage their primary healthcare services, subject to certain laws and regulations (e.g., Act on municipal health and care services [ 47 ], Act on patient and user rights [ 48 ] and Regulation on quality in nursing and care services for service provision [ 49 ]). All municipalities are obligated to offer specified healthcare services independent of their size and inhabitant number (Se Fig. 1 for a brief overview of healthcare services provided by the Norwegian municipalities, comprising nursing homes and home care services, and included municipalities).
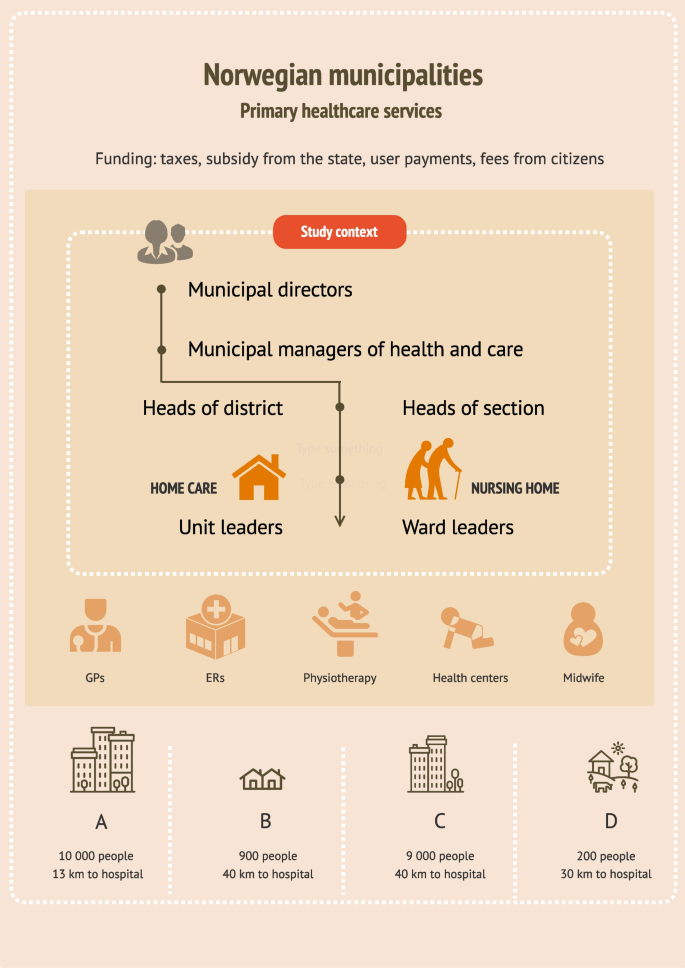
Brief overview of healthcare services provided by the Norwegian municipalities, comprising nursing homes and home care services, and the included municipalities
Recruitment and participants
Recruitment was anchored in the municipal management. The municipal manager of health and care in 11 municipalities across the Norwegian west coast were first contacted via email, then by telephone (se Fig. 1 ). Most managers who responded to our contact were positive, but many had to decline due to time constraints related to pandemic management. Four managers agreed to data collection in their municipality with the stipulation that the nursing home- and homecare leaders wanted to participate. All levels of leaders were eligible for inclusion due to the small size of the healthcare services. We contacted the leaders of nursing homes and home care services in the four municipalities, first by email, then by telephone. Nine leaders agreed to participate. One leader declined. All included leaders were female, registered nurses (RNs), and had long and broad experiences with working as RNs either in the healthcare service they now were leaders in, or in other healthcare settings. Some leaders stated that they had continued education or Master’s degrees, but more leader specific qualifications such as leader education, training or courses were not disclosed (Table 1 . Overview of participants and setting).
Data collection
Individual interviews were conducted from November 2021 to November 2022 by the first author (MKG). Leaders in one of the municipalities (municipality B) wished to do the interview in a group interview (three leaders), which we arranged. All but one interview was conducted at the leaders’ work premises (in their offices or in meeting rooms). One leader was interviewed via Zoom due to a temporary need for increased infection precautions. All interviews were guided by a predeveloped interview guide which was based on resilience in healthcare theory [ 50 , 51 ] and contained subject such as: Success factors and challenges with handling the COVID-19 pandemic; New solutions and how new knowledge and information was handled; and Lessons learned from the pandemic.
Data analysis
The interviews were audio recorded and transcribed. The analysis followed the steps in Braun and Clarkes thematic approach [ 52 ]. This involved reading through the transcripts multiple times to find meanings related to the overall research question. Text with meaning was inserted into a Word table which provided initial codes. After the coding process, which involved creating and continuously revising codes, there were 47 codes. The codes were then organized into categories and categories were sorted into initial main themes. Themes and categories were assessed to determine whether any of them should be merged, refined, split or eliminated [ 52 ] (see Table 2 for example of the analysis process). The author team reviewed and approved categories and themes to ensure that each theme illuminated its essence [ 52 ].
We analyzed the interviews and identified three main themes and eight categories (Table 3 ). The results are presented according to identified main themes.
Navigating the role of a leader during the pandemic
Overall, the leaders seemed to have two primary focuses when they talked about how they had experienced the COVID-19 pandemic. These were their personal coping, and how they managed the organizational challenges arising throughout the pandemic period. Particularly in the beginning, they reported feelings of fear and insecurity. Leaders dreaded the consequences which could result from mistakes, such as providing wrong, or missing essential information.
“Having such a responsibility is a burden, and even though you’re not alone, you still feel like you’re the one responsible for the safety of the employees and the patients. Ensuring the safety of everyone was the priority, which is why it was critical to make sure that the protocols we were distributing were the correct ones…” (L1 nursing home municipality C)
Additionally, several leaders stated that they were concerned about personnel who had contracted COVID-19 (some of whom had serious symptoms), and even felt responsible for their situation. Leaders of two of the municipalities reported feelings of frustration, and despair, and all leaders reported long working hours. Leaders expressed that they felt that they had been “on call” for the last two years, and described long working days, with limited consideration for evenings, nights, weekends, or vacations.
A range of organizational challenges was described (e.g., dealing with a stressed economy, experiencing task overload, working within an unprepared organization and the struggle to get a hold on enough personal protective equipment. One of the most prominent challenges in the data set, was the acquisition, interpretation, and distribution of information issued by the authorities. The leaders described that new information was issued frequently along with constantly changing routines. New routines where developed, distributed, and discarded nonstop in the attempt to “get the organization in line with the state authorities”.
“There was new information issued [from the Norwegian directorate of health] almost hourly… we had more than enough to, in a way, keep up with all these procedures that came, or all the new messages that came, and these [information and routines] had to be issued out to the employees and to the next of kin…” (L1 nursing home municipality A)
Despite the difficulties related to information flow, or lack thereof, the leaders devised a range of solutions to make information more accessible to their staff (e.g., informational e-mails, developing short information sheets, making information binders, and meeting up physically to go through new routines with their employees). The data indicated that it was hard to gauge how much information to make available to their staff, who were eager for knowledge, yet still found it hard to process everything. On occasion, the leaders desired assistance or someone to assume authority, or as one leader articulated: “someone to push the red button” (L1 homecare municipality C), due to their struggles to keep up with information, regulations, and routines in the face of rapid changes.
Not surprisingly, leaders felt a heightened need to take the lead during the COVID-19 pandemic. This was a long-running crisis, and they had to be present, approachable and a source of support for their staff, while also striving to gain the employees’ understanding. For example, in one healthcare service the employees wanted more strict rules than necessary and had strong opinions on how things should be done in “in their healthcare service”, while the leader was stringent with sticking to national regulations which were less strict. Another aspect was handling disagreement with measures among employees. Often measures were not in line with the employees’ wishes, which created friction.
The pandemic highlighted the importance of leaders taking on the task of creating a secure working environment for their employees. The leaders noted considerable anxiety among the staff, particularly in facilities that had not experienced any COVID-19 cases. Leaders came to understand the importance of tending to all wards, regardless of whether they had been affected by the infection, even though it was perceived as taxing. Overall, the leaders worked actively to make the situation in wards with infection outbreaks as best as possible. A leader from a healthcare service which had a major COVID-19 outbreak stated:
“We constantly tried to create new procedures to make it as easy as possible for them [So] that they didn’t have to think about anything. That they [didn’t have to think about] bringing food to work, that they had to [remember] this or that. That they were provided with everything they needed…” (L2 nursing home municipality C)
Another recurring topic in the dataset, was the constant challenges and changes the leaders had to overcome and adapt to during the COVID-19 pandemic. For example, there was a need to plan for all possible scenarios, particularly if they were to have a major infection outbreak among the staff (e.g., how to limit the infection outbreak, how to deal with staffing, how to arrange the wards in case of an outbreak). One healthcare service experienced such a scenario, which demanded a rapid response, when they had a major COVID-19 outbreak with over twenty infected employees almost overnight. The leaders were left with the impossible task of covering a range of shifts, and they were forced to adopt a strategy of reaching out to other healthcare services within their municipality (other wards, nursing homes, the home care services and psychiatric services) asking if they had any nurses “to spare.” Eventually, they managed to cover their staffing needs without using a temp agency.
The leaders of this nursing home also had to deal with numerous small, but important challenges such as how to deal with dirty laundry, what to do with food scraps, where to put decorations and knick-knacks, how to provide wardrobes and lunchrooms, and generally, how to handle an infection outbreak in facilities not designed for this purpose.
Leaders in all primary healthcare services implemented strategies to prevent infection or spread of infection. They introduced longer shifts, split up the personnel in teams, made cleaning routines for lunchrooms and on-call rooms, set up a temporary visiting room for next of kin, developed routines for patient visits, regularly debriefed personnel of infection routines, made temporary wardrobes, and removed unnecessary tasks from the work schedule. New digital tools were introduced, particularly for distributing instructional videos and information among employees, and to keep contact with other leaders.
Although many leaders described the situation as challenging, particularly in the beginning, many found themselves gaining increased control over the situation as time went by.
“Little by little, in some way, the routine of everyday life has become more settled… you can’t completely relax yet, but you can certainly feel a bit more organized, and more confident in your decisions, since we have been doing it for a while [ca 1 year]. (L1 nursing home municipality C)
The aftermath—management of covid-19 in rural primary healthcare services
Despite organizational as well as personal challenges, leaders’ overall impression of the COVID-19 management was positive. The leaders firmly believed that the quality of healthcare services had been preserved, and all the physical healthcare needs of the patients had been properly cared for. According to leaders, there was not a rise in adverse events (e.g., falls, wounds) and patients and next of kin were positive in their feedback. The one main concern regarding quality of care was, however, the aspect of the patients’ sociopsychological state. Patients became isolated and lonely when they could not receive visitors or had to be isolated in their rooms or their homes during COVID. Nevertheless, the leaders expressed admiration for the healthcare personnel's work in addressing psychosocial needs to the best of their capacity. Overall, the leaders were proud of how the front-line healthcare personnel had handled the pandemic, and the extraordinary effort they put in to keeping the healthcare services running.
Several leaders stated that they now felt better prepared for “a next pandemic”, but they also had multiple suggestions for organizational improvements. These suggestions included: set up a visit coordinator, develop a better pandemic plan, be better prepared nationally, develop local PPE storage sites, introduce digital supervision for isolation rooms (for example RoomMate [ 53 ]), provide more psychological help for employees who struggled in the aftermath of an infection outbreak, have designated staff on standby for emergency situations, establish clear communication channels for obtaining information and, when constructing new nursing homes and healthcare facilities, consider infection control measures.
The leaders also discussed the knowledge they had acquired during this period. Many talked about learning how to use digital tools, but mostly they talked about the experience they had gained in handling crisis:
“I believe we are equipped in a whole different way now. There’s no doubt about that. Both employees and leaders and the healthcare service in general, I think… I have no doubt about that… so… there have been lessons learned, no doubt about it….” (L1 nursing home municipality C)
Leaders also talked about what they experienced as success factors in handling the pandemic: Long shifts (11,5 h), with the same shift going 4 days in a row to avoid contacts between different shift, the use of Microsoft Teams and other communication tools to increased and ease intermunicipal cooperation, and the possibility to share experiences, making quick decisions and take action quickly, developing close cooperation with the municipality chief medical officer and the nursing home physician, the involvement of the occupational healthcare service (take the employees’ work situation seriously) and the conduct of “Risk, Vulnerability and Preparedness” analysis (a tool to identify possible threats in order to implement preventive measures and necessary emergency response). The leaders also talked about the advantages of getting input from employees (e.g., through close cooperation with the employee representatives).
The benefits and drawbacks of being small and rural during a pandemic
Aspects of being a small healthcare service within a small municipality were highlighted by several of the leaders. For example, the leader of one the smaller healthcare service included in the study, addressed the challenge of acquiring enough competent staff. To be able to fulfill their requirements for competent staff, the municipality needed to buy healthcare services from neighboring municipalities. Another drawback was that employees who had competence or healthcare education often lacked experience in infection control and infection control routines, because they had rarely or never had infectious outbreaks of any kind. This made it particularly challenging to implement infection control measures. In one of the larger municipalities in this study, they had worked targeted for years to increase the competence in their municipality by focusing on full time positions to all and educating assistants to become Licensed practical nurses (LPN). They benefited from these measures during the pandemic.
Another aspect which was emphasized as essential to survive a pandemic in a small municipality, was intermunicipal cooperation. Leaders of all four healthcare services stated that they built increased cooperation with nearby municipalities during the pandemic. Leaders from the different municipalities met often, sometimes several times a week, and helped each other, shared routines, and methods, asked each other questions, coordinated covid-19 testing and developed intermunicipal corona wards, kept each other updated on infection status locally, and relied on each other’s strengths.
“We established a very good intermunicipal cooperation within the health and care services. We helped each other. Shared both routines and procedures, and actually had Teams meetings twice a week, where I could ask questions…and… we all had different strengths in the roles we held, not all of them [group members] were healthcare personnel either, and they had a lot of questions regarding the practical [handling of the pandemic]. At the same time, they [people who were not healthcare personnel] were good at developing routines and procedures, which they shared with the rest. In other words, the cooperation between the municipalities was very good, and for a small municipality, it was worth its weight in gold”. (L1, nursing home/homecare Municipality D)
The same leader stated that they could not have managed the pandemic without support from other larger municipalities and advised closer cooperation following the pandemic as well. An advantage of being small was the ability to easily track and monitor the virus spread within the municipality. Moreover, it was easy to have close cooperation with the infectious disease physician, the municipal chief medical officer, and the nursing home physician, as one person often held several of these roles. Some leaders also had several roles themselves such as a combination of nursing home leader and homecare leader or a combination of nursing home leader and health and care manager (overseeing all health and care services in the municipality). This was perceived as both an advantage and a disadvantage. This was an advantage because they gained a full overview of the situation due to their multiple areas of responsibility, but a disadvantage because it was demanding for one person to handle everything alone, making the system vulnerable. Another challenging aspect was a lack of people to fill all the necessary roles. For example, in one municipality they did not have a public health officer (a physician in charge of the healthcare services in a municipality, and the municipal management’s medical adviser), and had to hire a private practicing physician, who was not resident in the municipality to take on this role.
The economy was also a continuous source of worry. Running a small healthcare service within a small municipality was stated as expensive because the municipalities were obligated to provide the same healthcare services as the larger municipalities, but with less income (e.g., tax payment per inhabitant). The pandemic led to new expenses such as overtime payment, and wage supplement for changed work hours. Leader had to continuously balance a sound use of resources, and responsible operation.
Table 4 provides and overview of the challenges leaders encountered, how they were handled, and leaders’ suggestions for further improvement.
We assessed how leaders in rural primary healthcare services coped with unprecedented challenges during the COVID-19 pandemic. On one hand, they had to manage personal struggles such as insecurity, guilt, and excessive workload. At the same time, they had to confront major organizational issues such as financial instability, lack of resources, and information overload. Moreover, their roles changed, and the need to lead, make more decisions and be more supportive was heightened. While adapting to these changing roles, the leaders continuously introduced new measures to handle pandemic induced challenges including development of new routines, distilled and distributed information, reorganized staffing plans and rearranged wards. Although patients’ safety and quality of care was perceived as safeguarded throughout the COVID-19 pandemic period, leaders had several suggestions for improvements in case of future crises.
Previous research on primary healthcare services during COVID-19 support several of the findings identified here. Similar challenges requiring leaders to adapt their ways of working such as insufficient contingency plans and infection control, lack of staffing, changing guidelines and routines and challenges related to information flow were found [ 17 , 31 , 54 , 55 , 56 ]. Leader strategies to handle these challenges included reallocation of staff, providing support, provide training and distill and distribute information [ 16 , 31 , 55 , 57 ]. Some findings in this study, particularly related to the rural context, has not been found elsewhere. We found that 1) the leaders’ and healthcare services’ increased their dependency on neighboring municipalities during the pandemic and 2) we identified both the advantages and drawbacks of leaders having to function in multiple roles during the pandemic. The heightened importance of cooperation within municipalities and healthcare services in rural areas as opposed to urban areas, has however, been highlighted both before and during the pandemic [ 17 , 23 ].
The pandemic prompted organizations like the World Health Organization (WHO), International Council of Nurses (ICN), and Organization for Economic Co-operation and Development (OECD) to advocate for the advancement of more resilient healthcare services to be able to overcome current and future health system challenges [ 3 , 58 , 59 ]. To achieve the goal of resilient healthcare services, a multi-focal perspective incorporating both individual, teams and systems, is needed. This is because health system organization and leadership on all levels will impact how resilience can be built on team and individual level and thereby reinforce resilience in organizations [ 12 , 51 , 60 , 61 , 62 ].
The multiple aspects of resilient leadership
Leadership style, leaders’ facilitation for flexibility and leaders’ management of resources, competence, and equipment, will affect the resilience of health personnel and thereby the organizational resilience [ 12 , 15 , 63 ]. However, resilient leadership is affected by multiple aspects. For one, leaders inherent individual resilience will influence how and if, they lead resiliently [ 64 ]. Individual resilience is a multifaceted concept consisting of the person’s determination, persistence, adaptability and recuperative capacity, and is impacted by their personal qualities, conduct and cultural outlook [ 12 ]. Similar to previous literature [ 65 , 66 ], the current study found that leaders had to cope with personal challenges such as fear, guilt, adapting to changed roles and increased workload, while performing their everyday tasks. Literature have shown that leaders' responses to challenges can be influenced by their unique personality traits, ultimately shaping their resilience and leadership style [ 67 , 68 ]. Personal qualities needed to “lead well” have also shown to vary between rural and urban healthcare services. For example, Doshi [ 69 ] found that being social, passionate and extrovert was more important in urban areas than in rural areas. This indicate that leaders’ personality traits affect resilience in healthcare, and that resilience promoting personality traits may vary across urban and rural areas. More research is needed to study these relationships.
Although measures to increase personal resilience can be effective (e.g., mindfulness, workshops/training, therapy) [ 70 , 71 , 72 , 73 ] it is not sufficient to base resilience building on these aspects alone [ 74 ]. There is a need to consider how leaders are influenced and supported by the system they are working within to become, and act more resiliently. This includes the support leaders have in their community (e.g., peer support, leader support and proper guidance), their access to resources and their freedom to make decisions [ 60 , 75 , 76 ]. In the current study, it appeared to be a connection between leaders’ coping and the amount of support they had from colleagues. In our interpretation, leaders who talked about their cooperation with others, also talked more positively of their COVID-19 experiences (e.g., how much they had learned or what they had accomplished, rather than how pressured and anxious they were). Similar results have previously been found. For example, leaders in Marshall and colleagues’ study [ 65 ] felt isolated and struggled to make sense of the situation (COVID-19 induced challenges), while leaders in Seljemo and colleagues’ study stated that support from other managers made it easier to cope with high workloads [ 31 ]. In smaller rural healthcare settings, obtaining support can be challenging due to the limited presence of leader colleagues in close proximity [ 77 ]. Additionally, Gray & Jones [ 78 ] suggests that resilient leaders are leaders who ask for help when needed. This indicates that leaders in more isolated areas may require more effort to form connections beyond their organization, and rural healthcare systems must afford greater attention to enabling peer networking (e.g., by providing time and resources).
Through recurrent intermunicipal, online meetings, leaders in the current study attained to initiate, and preserve contact with other leaders in other healthcare settings, much more than before the COVID-19 pandemic. This was particularly important for the smallest, most rural municipalities, where one leader held many roles, and was by one leader, stated as the main reason they were able to manage the COVID-19 pandemic in their primary healthcare service. The tendency to increase intermunicipal cooperation during this period, and the overall need for smaller, rural healthcare services to cooperate with others is found in other literature [ 23 , 79 ]. However, mostly as collaboration within primary healthcare services, and not across organizations. Although recommended by leaders, it is not clear if this close contact has been maintained after the pandemic.
The governance leaders are working under will affect leaders’ possibility to lead resiliently. The governance allows for effective coordination of financing, resource generation, and service delivery activities, ensuring optimal system performance [ 80 ]. Yet, governing for resilience has proven to be a major challenge, because it requires systems to be both flexible and stable at the same time [ 76 ]. Flexibility presupposes systems’, health personnel’, and leaders’ ability to adapt to current conditions, and is essential for systems to cope with unpredictable, non-linear, and ever-changing social and environmental conditions. Conversely, stability must also be implemented to ensure that new policies are sustained and effective, and to stabilize expectations and promote coordination over time [ 76 ]. This means that leaders need flexibility to make their own decisions, as well as the stability that proper guidelines and direction provides [ 81 ]. In this study, some leaders reported experiencing chaos and loss of control when routines and guidelines lacked in the beginning of the pandemic. Similar results have been found among other healthcare leaders, as well as healthcare personnel [ 32 , 66 ]. In contrast, the leaders’ need for flexibility to be able to adapt to the everchanging work environment brought on by the pandemic (examples in Table 3 ) was demonstrated in this, and other studies [ 16 , 17 ]. It can, however, be argued that the balance between flexibility and stability is often skewed more towards flexibility in rural regions. Rural leaders must make unsupported decisions more often than urban leaders as they face higher demands and fewer available resources (such as competence, staff, and funding) [ 77 ]. This requires rural leaders to be more innovative and adaptable to current circumstances [ 23 , 69 , 77 , 79 ]. That said, the availability of resources have shown to impact a system's flexibility, often by influencing the quality of its adaptations [ 2 ].
In low-resource healthcare settings across the globe, certain adaptations made to combat pandemic challenges ended up causing damage (e.g., reuse or misuse of PPE, overexploitation of healthcare personnel and the use of unconventional treatment methods) [ 2 , 82 ]. In high resource healthcare services, as included in this study, adaptations were often described as beneficial, and potential long-lasting solutions (Table 3 ) [ 16 , 17 , 31 ]. Although not comparable to low resource healthcare services, variation in resource availability and economy between the included healthcare services was also expressed in this study. Norwegian municipalities’ income is closely tied to their tax revenue and population size [ 83 ], and regardless of income, the municipalities are required to provide specific healthcare services to their inhabitants. Thus, the financial foundation of smaller more rural municipalities is not as strong as that of larger municipalities. These inequalities were expressed as notable by both leaders and by healthcare personnel in a preceding study exploring the same primary rural healthcare services as included here [ 32 ]. Since resilience in healthcare is also highly dependent on the competence and experience of employees and leaders, the combination of resource and financial deficiencies, more often experienced in rural healthcare services than in urban healthcare services, may pose particular challenges in resilience building in rural areas [ 23 , 84 ]. This is worth exploring further, along with the rural healthcare services’ particular need to be flexible versus the potential difficulty they may have in making beneficial adaptations because of a weaker financial foundation.
Resilience and leadership style
Providing support to employees was an important leader task during the pandemic [ 55 , 66 ] and have further, been found to be particularly vital in rural areas, where employees have a smaller network of colleagues to turn to [ 84 ]. Other vital leadership tasks, recognizable from crisis leadership literature and also found in this study, were the importance of organizing, directing and implementing actions, forging cooperation, enabling work- arounds or adaptation, direct and guide and the importance of communication and dissemination of information [ 85 , 86 ]. Although charismatic leadership Footnote 1 has been found to be most valuable during crisis [ 87 ], there is an ongoing discussion of what leadership style is best suited to promote resilience in healthcare [ 11 , 14 , 66 , 88 ]. For example, both transformational and transactional leadership 1 [ 89 ] have been stated as resilience promoting leadership styles [ 15 ]. However, as found in other literature [ 66 , 88 ], the results of this study indicated that leaders oscillated between different styles during the COVID-19 pandemic period. For example, in the beginning of the pandemic when uncertainty characterized the healthcare system, leaders became stricter with rules and regulations, demonstrating an authoritative leadership style 1 . Further, stepping in, lecturing about infection control procedures and use of PPE, indicated a coaching leadership 1 style and lastly, when the leaders went against employees wishes to ensure safe maintenance of operation, it showed similarities to a transformational leadership style 1 [ 90 ]. Interestingly, leaders did not speak directly about how their leadership styles changed, and seemed unaware of their leadership style adaptation. Similarly, in Sihvola et al. [ 66 ] leaders found it surprising how novel conditions could influence their leadership style.
On one side, these results, suggest that an adaptive leadership style can be necessary during crisis. On the other side, this and other studies [ 31 , 54 ] indicate that leaders need more knowledge on crisis leadership, for example, to be made aware of the potential need to oscillate between different leadership styles during a crisis, and the possible subsequent challenges. For example, a study conducted by Boyle og Mervin [ 91 ] found that being a “nurse leader” (all leaders in this study were nurses), showed challenging because the leaders were judged as a peer rather than a leader. This can cause challenges, particularly when stepping into an authoritative leadership style. Such conflicts were not reported in this study, however, these are all aspects which should be given more attention when investigating resilience in healthcare and leadership styles [ 88 ]. Furthermore, it is crucial to acquire further understanding on the distinctions between leading in rural and urban areas, and how various leadership approaches may be impacted by managing tight-knit employee teams, which is often the case in small rural nursing home and homecare services. And finally, there is a need to provide a deeper understanding of the factors that promote or impede resilience in rural primary healthcare services, and the influence of the contextual aspects on resilience in healthcare.
Limitations
This study has limitations which need to be addressed. A larger number of included primary healthcare leaders over a wider geographical area and across boarders would have provided a broader view of leader experiences during the COVID-19 pandemic. However, it was very difficult to get leaders to take time to reflect during this crisis. This study does provide insight into a variety of different municipalities of different sizes, organization and locations in the Norwegian context, providing a variety of rural primary healthcare leaders experiences during the pandemic. Interviews were conducted in different ways (focus group, digital and individually) this could have influenced leaders description of their experiences. Furthermore, interviews were held at different points throughout the pandemic phases, leading to a mix of leaders with both current and reflective experiences of navigating the pandemic. This should be taken into consideration when reading the results.
By exploring nursing home and home care leaders’ experiences with the COVID-19 pandemic in rural areas, we found that the leaders met a range of rapid onset challenges of different nature, many of which demanded fast decisions and solutions. Leaders handled these challenges and changes in a variety of ways in their different contexts. In addition to health system challenges, leaders also had to cope with rapidly changing roles, while managing their own and employees’ insecurities. This study’s results demonstrate the intricate nature of resilient leadership, encompassing individual resilience, personality, governance, resource availability, and the capability to adjust to organizational and employee requirements. In addition, there may be differences between how resilience in healthcare is built and progresses in rural healthcare services versus urban contexts. Further research to understand the interplay between these aspects is needed, and it is critical to consider context.
Availability of data and materials
Data are available from the corresponding author upon reasonable request.
Charismatic leadership : influence and persuasion of others to help the fulfill their mandate, also in face of adversity; Transformational leadership: pushing to work and think in new ways; Authoritative leadership : the leader in control, low autonomy; Coaching leadership : the leader support employee’s skill advancement; Transactional leadership : exchange of rewards for fulfilling expectations.
Abbreviations
International Council of Nurses
Licensed practical nurse
Organization for Economic Co-operation and Development
Personal protective equipment
Registered Nurse
The World Health Organization
WHO. COVID-19 continues to disrupt essential health services in 90% of countries WHO2021 [Available from: https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries .
Malin Knutsen G, Kristiana L, Siri W, et al. Resilience perspective on healthcare professionals’ adaptations to changes and challenges resulting from the COVID-19 pandemic: a meta-synthesis. BMJ Open. 2023;13(9):e071828.
Article Google Scholar
OECD. Ready for the Next Crisis? Investing in Health System Resilience. 2023.
Book Google Scholar
Franzosa E, Gorbenko K, Brody AA, et al. “At home, with care”: lessons from New York City home-based primary care practices managing COVID-19. J Am Geriatr Soc. 2021;69(2):300–6.
Article PubMed Google Scholar
Franchini L, Varani S, Ostan R, et al. Home palliative care professionals perception of challenges during the Covid-19 outbreak: a qualitative study. Palliat Med. 2021;35(5):862–74.
Damian AJ, Gonzalez M, Oo M, Anderson D. A national study of community health centers’ readiness to address COVID-19. J Am Board Fam Med. 2021;34(Suppl):S85-s94.
Zhao S, Yin P, Xiao LD, et al. Nursing home staff perceptions of challenges and coping strategies during COVID-19 pandemic in China. Geriatric Nursin. 2021;42(4):887–93.
Aalto UL, Pitkälä KH, Andersen-Ranberg K, et al. COVID-19 pandemic and mortality in nursing homes across USA and Europe up to October 2021. Eur Geriatr Med. 2022;13(3):705–9.
Article PubMed PubMed Central Google Scholar
Wiig S, Aase K, Billett S, et al. Defining the boundaries and operational concepts of resilience in the resilience in healthcare research program. BMC Health Serv Res. 2020;20(1):330.
Wiig S, Fahlbruch B. Exploring Resilience - An Introduction. In: Wiig S, Fahlbruch B, editors. Exploring Resilience : a scientific journey from practice to theory. Springer briefs in applied sciences and technology : safety management. Springer Open: Cham; 2019. p. 1–3.
Google Scholar
Barasa E, Mbau R, Gilson L. What is resilience and how can it be nurtured? A systematic review of empirical literature on organizational resilience. Int J Health Policy Manag. 2018;7(6):491–503.
Bowman A. Leadership and resilience: where the literature stands. J Leadersh Stud. 2022;16(2):33–41.
Akerjordet K, Furunes T, Haver A. Health-promoting leadership: an integrative review and future research agenda. J Adv Nurs. 2018;74(7):1505–16.
Eliot JL. Resilient leadership: the impact of a servant leader on the resilience of their followers. Adv Dev Hum Resour. 2020;22(4):404–18.
Ree E, Ellis LA, Wiig S. Managers’ role in supporting resilience in healthcare: a proposed model of how managers contribute to a healthcare system’s overall resilience. Int J Health Governance. 2021;26(3):266–80.
Lyng HB, Ree E, Wibe T, Wiig S. Healthcare leaders’ use of innovative solutions to ensure resilience in healthcare during the Covid-19 pandemic: a qualitative study in Norwegian nursing homes and home care services. BMC Health Serv Res. 2021;21(1):878.
Ree E, Wiig S, Seljemo C, et al. Managers’ strategies in handling the COVID-19 pandemic in Norwegian nursing homes and homecare services. Leadership in Health Services. (ahead-of-print). 2022;200–18.
Saleem J, Ishaq M, Zakar R, et al. Experiences of frontline Pakistani emigrant physicians combating COVID-19 in the United Kingdom: a qualitative phenomenological analysis. BMC Health Serv Res. 2021;21(1):291.
Glette MK, Bates DW, Dykes PC, et al. A resilience perspective on Healthcare Personnels’ Experiences of Managing the COVID-19 Pandemic: A qualitative study in Norwegian nursing homes and come care services. BMC Health Services Research. 2023 (in review).
Smedt SED, Mehus G. Sykepleieforskning i rurale områder i Norge; en scoping review (English title: Nursing research in rural areas in Norway; a scoping review). Norsk tidsskrift for helseforskning. 2017;13;2:1–27.
W P, L R. Rural, remote and at risk: Why rural health services face a steep climb to recovery from Covid-19. Nuffield Trust; 2020.
van Pijkeren N, Msc P, Wallenburg I, et al. Caring peripheries: How care practitioners respond to processes of peripheralisation. Sociologia Ruralis. 2023;64:64–81.
van de Bovenkamp H, van Pijkeren N, Ree E, et al. Creativity at the margins: a cross-country case study on how Dutch and Norwegian peripheries address challenges to quality work in care for older persons. Health Policy. 2023;127:66–73.
Melvin SC, Wiggins C, Burse N, et al. The role of public health in COVID-19 emergency response efforts from a Rural health perspective. Prev Chronic Dis. 2020;17:E70.
Segel JE, Ross HI, Edwards JL, et al. The unique challenges facing rural providers in the COVID-19 pandemic. Popul Health Manag. 2020;24(3):304–6.
Teixeira da Silva JA, Tsigaris P, Erfanmanesh M. Publishing volumes in major databases related to Covid-19. Scientometrics. 2021;126(1):831–42.
Article CAS PubMed Google Scholar
Gholami M, Fawad I, Shadan S, et al. COVID-19 and healthcare workers: a systematic review and meta-analysis. Int J Infect Dis. 2021;104:335–46.
Article CAS PubMed PubMed Central Google Scholar
Ferguson J, Rosser JI, Quintero O, et al. Characteristics and outcomes of coronavirus disease patients under nonsurge conditions, Northern California, USA, March-April 2020. Emerg Infect Dis. 2020;26(8):1679–85.
Helgeland J, Telle KE, Grøsland M, et al. Admissions to Norwegian hospitals during the COVID-19 pandemic. Scandinavian J Pub Health. 2021;49(7):681–8.
Moynihan R, Sanders S, Michaleff ZA, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11(3):e045343.
Seljemo C, Wiig S, Røise O, Ree E. The role of local context for managers’ strategies when adapting to the COVID-19 pandemic in Norwegian homecare services: a multiple case study. BMC Health Serv Res. 2023;23(1):492.
Glette MK, Bates DW, Dykes PC, et al. A resilience perspective on healthcare personnels’ experiences of managing the COVID-19 pandemic: a qualitative study in Norwegian nursing homes and come care services. BMC Health Serv Res. 2023;23(1):1177.
Iness AN, Abaricia JO, Sawadogo W, et al. The effect of hospital visitor policies on patients, their visitors, and health care providers during the COVID-19 pandemic: a systematic review. Am J Med. 2022;135(10):1158-67.e3.
Füszl A, Bouvier-Azula L, Van den Nest M, et al. Provision of safe patient care during the COVID-19 pandemic despite shared patient rooms in a tertiary hospital. Antimicrob Resist Infect Control. 2022;11(1):61.
Mohammadinia L, Saadatmand V, Khaledi Sardashti H, et al. Hospital response challenges and strategies during COVID-19 pandemic: a qualitative study. Front Public Health. 2023;11:1167411.
Samdal GB, Alpers LM, Sekse RJT, et al. Barriers and facilitators for leading nursing homes through the COVID-19 pandemic: a focus group study in Norway. Nurs Open. 2023;10(11):7154–67.
Abbas MJ, Kronenberg G, McBride M, et al. The early impact of the COVID-19 pandemic on acute care mental health services. Psychiatr Serv. 2021;72(3):242–6.
Nessler K, Van Poel E, Willems S, et al. The response of primary care practices in rural and urban settings in Poland to the challenges of the COVID-19 pandemic. Ann Agric Environ Med. 2022;29(4):575–81.
Anaraki NR, Mukhopadhyay M, Karaivanov Y, et al. Living and working in rural healthcare during the COVID-19 pandemic: a qualitative study of rural family physicians’ lived experiences. BMC Prim Care. 2022;23(1):335.
Pavloff M, Labrecque ME, Bally J, et al. Rural home care nursing during COVID-19. Can J Nurs Res. 2023;55(4):486–93.
OECD. Realising the Potential of Primary Health Care. OECD; 2020.
The World Bank. Rural population (% of total population) 2018. Available from: https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS . Cited 2023 18.12.
Ellis LA, Churruca K, Clay-Williams R, et al. Patterns of resilience: a scoping review and bibliometric analysis of resilient health care. Saf Sci. 2019;118:241–57.
Scott A, Braithwaite J, Melbourne Uo. Is COVID-19 opening the fault lines in our healthcare system? : Institute of Applied Economic and Social Research.; 2020 [Available from: http://nla.gov.au/nla.obj-2931172550 .
Creswell JW. Research design : qualitative, quantitative, and mixed methods approaches. 5th ed. ed. Los Angeles, Calif: SAGE; 2018.
Holloway I, Galvin K. Qualitative research in nursing and healthcare: Wiley Blackwell; 2017.
Lov om kommunal helse-og omsorgstjeneste (english title: Act on municipal health and care services), LOV-2011–06–24–30 (2011).
Lov om pasient- og brukerrettigheter (English title: Act on patient and user rights), LOV-1999-07-02-63.
Forskrift om kvalitet i pleie- og omsorgstjenestene (English title: Regulation on quality in nursing and care services for service provision), FOR-2003–06–27–792 (2003).
Hollnagel E, . Making Healthcare resilient: From safety-I to Safety-II. In: Hollnagel E, Braithwaite J, Wears RL, editors. Resilient health care. Ashgate studies in resilience engineering. 1. Farnham, Surrey, England: Ashgate; 2013.
Wiig S, Fahlbruch B. Exploring Resilience – An Introduction. In: Wiig S, Fahlbruch B, editors. Exploring Resilience: A Scientific Journey from Practice to Theory. Cham: Springer International Publishing; 2019. p. 1–5.
Chapter Google Scholar
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Sensio. RoomMate. Available from: https://www.sensio.io/no/produkter/roommate?utm_term=roommate&utm_campaign=S%C3%B8k+%7C+Produkter&utm_source=adwords&utm_medium=ppc&hsa_acc=5538158809&hsa_cam=20506326432&hsa_grp=159856433744&hsa_ad=672316590141&hsa_src=g&hsa_tgt=kwd-28346982&hsa_kw=roommate&hsa_mt=p&hsa_net=adwords&hsa_ver=3&gclid=EAIaIQobChMI3rHE6qPpgwMVOVKRBR124QjJEAAYASAAEgKR5vD_BwE . Cited 2024 19.01.
Alakeely M, Almutari A, Masud N, Altulaihi B. Preparedness of primary health care leaders during COVID-19 outbreak, Riyadh, Saudi Arabia: a qualitative study. Risk Manag Healthc Policy. 2021;14:4339–51.
Skagerström J, Fernemark H, Nilsen P, et al. Challenges of primary health care leadership during the COVID-19 pandemic in Sweden: a qualitative study of managers’ experiences. Leadersh Health Serv. 2023;36(3):389–401.
Dale JN, Morken T, Eliassen KE, et al. Preparedness and management during the first phase of the COVID-19 outbreak - a survey among emergency primary care services in Norway. BMC Health Serv Res. 2022;22(1):896.
Karreinen S, Paananen H, Kihlström L, et al. Living through uncertainty: a qualitative study on leadership and resilience in primary healthcare during COVID-19. BMC Health Serv Res. 2023;23(1):233.
ICN. ICN President calls for resilient health systems at UN High Level Meeting on Pandemic Prevention, Preparedness and Response: ICN; 2023 [updated 21.09.23. Available from: https://www.icn.ch/news/icn-president-calls-resilient-health-systems-un-high-level-meeting-pandemic-prevention .
World Health Organization. Building health systems resilience for universal health coverage and health security during the COVID-19 pandemic and beyond: a brief on the WHO position. Geneva: WHO; 2021. Available from: https://www.who.int/publications/i/item/WHO-UHL-PHC-SP-2021.02 .
Sagan A, Webb E, Rajan D, et al. Health system resilience during the pandemic: it’s mostly about governance. Eurohealth. 2021;27(1):10–5.
Wiig S, Lyng HB, Greenfield D, Braithwaite J. Care in the future—reconciling health system and individual resilience. Int J Qual Health Care. 2023;35(4):mzad082.
Tsandila-Kalakou F, Wiig S, Aase K. Factors contributing to healthcare professionals’ adaptive capacity with hospital standardization: a scoping review. BMC Health Serv Res. 2023;23(1):799.
Fagerdal B, Lyng HB, Guise V, et al. Exploring the role of leaders in enabling adaptive capacity in hospital teams - a multiple case study. BMC Health Serv Res. 2022;22(1):908.
Gröschke D, Hofmann E, Müller ND, Wolf J. Individual and organizational resilience—Insights from healthcare providers in Germany during the COVID-19 pandemic. Front Psychol. 2022;13:965380.
Marshall F, Gordon A, Gladman JRF, Bishop S. Care homes, their communities, and resilience in the face of the COVID-19 pandemic: interim findings from a qualitative study. BMC Geriatr. 2021;21(1):102.
Sihvola S, Kvist T, Nurmeksela A. Nurse leaders’ resilience and their role in supporting nurses’ resilience during the COVID-19 pandemic: a scoping review. J Nurs Manag. 2022;30(6):1869–80.
Haver A, Akerjordet K, Furunes T. Wise emotion regulation and the power of resilience in experienced hospitality leaders. Scand J Hosp Tour. 2014;14(2):152–69.
Kumari K, Ali SB, Batool M, et al. The interplay between leaders’ personality traits and mentoring quality and their impact on mentees’ job satisfaction and job performance. Front Psychol. 2022;13:937470.
Doshi D. Improving leadership of health services in rural areas: exploring traits and characteristics. Int J Healthcare Manag. 2020;13(sup1):183–91.
McKinley N, Karayiannis PN, Convie L, et al. Resilience in medical doctors: a systematic review. Postgrad Med J. 2019;95(1121):140–7.
Cleary M, Kornhaber R, Thapa DK, et al. The effectiveness of interventions to improve resilience among health professionals: a systematic review. Nurse Educ Today. 2018;71:247–63.
Huey CWT, Palaganas JC. What are the factors affecting resilience in health professionals? A synthesis of systematic reviews. Med Teach. 2020;42(5):550–60.
Joyce S, Shand F, Tighe J, et al. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open. 2018;8(6):e017858.
Khalili H, Lising D, Kolcu G, et al. Advancing health care resilience through a systems-based collaborative approach: Lessons learned from COVID-19. J Interprof Care. 2021;35(6):809–12.
Kaul V, Shah VH, El-Serag H. Leadership during crisis: lessons and applications from the COVID-19 pandemic. Gastroenterology. 2020;159(3):809–12.
Beunen R, Patterson J, Van Assche K. Governing for resilience: the role of institutional work. Curr Opinion Environ Sustainability. 2017;28:10–6.
van de Bovenkamp H, van Pijkeren N, Ree E, et al. Creativity at the margins: a cross-country case study on how Dutch and Norwegian peripheries address challenges to quality work in care for older persons. Health Policy. 2022;127:66–73.
Gray D, Jones K. The resilience and wellbeing of public sector leaders. Int J Pub Leadership. 2018;14(3):138–54.
Bish M, Kenny A, Nay R. A scoping review identifying contemporary issues in rural nursing leadership. J Nurs Scholarsh. 2012;44(4):411–7.
Sagan A, Webb E, Azzopardi-Muscat N, et al. Health systems resilience during COVID-19. Lessons for building back better. Health policy series. 2021; 56:[1–136 pp.]. Available from: https://eurohealthobservatory.who.int/publications/i/health-systems-resilience-during-covid-19-lessons-for-building-back-better .
Grote G. Leadership in Resilient Organizations. In: Wiig S, Fahlbruch B, editors. Exploring Resilience : a scientific journey from practice to theory. 1. Springer Open: Cham; 2019. p. 59–67.
Poon YSR, Lin YP, Griffiths P, et al. A global overview of healthcare workers’ turnover intention amid COVID-19 pandemic: a systematic review with future directions. Human Resources Health. 2022;20(1):70.
NOU: 2022: no 10. Inntektssystemet for kommunene (English title: The revenue system for the municipalities). Oslo: Ministry of Local Government and Rural Affairs
Matheson C, Robertson HD, Elliott AM, et al. Resilience of primary healthcare professionals working in challenging environments: a focus group study. Br J Gen Pract. 2016;66(648):e507–15.
Boin A, Kuipers S, Overdijk W. Leadership in times of crisis: a framework for assessment. Int Rev Pub Administration. 2013;18(1):79–91.
Baker EL, Irwin R, Matthews G. Thoughts on adaptive leadership in a challenging time. J Public Health Manag Pract. 2020;26(4):378–9.
Ali BJ, Anwar G. Administrative crisis: the role of effective leadership styles in crisis management international journal of advanced engineering. Manag Sci. 2021;7(6):31–41.
Tvedt IM, Tommelein ID, Klakegg OJ, Wong J-M. Organizational values in support of leadership styles fostering organizational resilience: a process perspective. Int J Manag Proj Bus. 2023;16(2):258–78.
Grote G. Leadership in Resilient Organizations. In: Wiig S, Fahlbruch B, editors. Exploring Resilience: A Scientific Journey from Practice to Theory. Cham: Springer International Publishing; 2019. p. 59–69.
Jasper L. Building an adaptive leadership style. Strategic Finance. 2018;99(9):54–61.
Boyle TJ, Mervyn K. The making and sustaining of leaders in health care. J Health Organ Manag. 2019;33(2):241–62.
Download references
Acknowledgements
The authors would like to thank participating leaders for their contribution to the study. We would also like to acknowledge Ole-Jørn Borum for graphical design on fig. 1 .
Open access funding provided by University of Stavanger & Stavanger University Hospital The publication processing charge was covered by the University of Stavanger.
Author information
Authors and affiliations.
SHARE – Center for Resilience in Healthcare, Faculty of Health Sciences, University of Stavanger, Stavanger, Norway
Malin Knutsen Glette & Siri Wiig
Department of Health and Caring Sciences, Western Norway University of Applied Sciences, Haugesund, Norway
Malin Knutsen Glette & Tone Kringeland
Division of General Internal Medicine and Primary Care, Department of Medicine, Brigham & Women’s Hospital, Harvard Medical School, Boston, MA, USA
Lipika Samal & David W. Bates
Department of Health Policy and Management, Harvard T. H. Chan School of Public Health, Boston, MA, USA
You can also search for this author in PubMed Google Scholar
Contributions
MKG, SW, TK, and DWB was involved in discussions regarding the project’s development. MKG conducted interviews and led the analysis of the transcribed data. The manuscript was a collaborative effort between MKG, SW, TK, DWB and LS, where all authors provided feedback. The author team approved the manuscript before submission.
Corresponding author
Correspondence to Malin Knutsen Glette .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Norwegian Agency for Shared Services in Education and Research (SIKT) in 2022 and provides the ethical approval, information security and privacy services as a part of the HK-dir (Norwegian Directorate for Higher Education and Skills). An informed consent form was signed by all leaders prior to the interviews, and information about the aim of the study and their right to redraw was repeated immediately before the interviews started.
Consent for publication
Not applicable.
Competing interests
Dr. Bates reports grants and personal fees from EarlySense, personal fees from CDI Negev, equity from ValeraHealth, equity from Clew, equity from MDClone, personal fees and equity from AESOP, personal fees and equity from Feelbet-ter, equity from Guided Clinical Solutions, and grants from IBM Watson Health, outside the submitted work. Dr. Bates has a patent pending (PHC-028564 US PCT), on intraoperative clinical decision support. The other authors report no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Glette, M.K., Kringeland, T., Samal, L. et al. A qualitative study of leaders’ experiences of handling challenges and changes induced by the COVID-19 pandemic in rural nursing homes and homecare services. BMC Health Serv Res 24 , 442 (2024). https://doi.org/10.1186/s12913-024-10935-y
Download citation
Received : 22 January 2024
Accepted : 31 March 2024
Published : 09 April 2024
DOI : https://doi.org/10.1186/s12913-024-10935-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nursing home
- Resilience in healthcare
- Patient safety
- Quality of care
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- NCSBN Member Login Submit
Access provided by
Login to your account
If you don't remember your password, you can reset it by entering your email address and clicking the Reset Password button. You will then receive an email that contains a secure link for resetting your password
If the address matches a valid account an email will be sent to __email__ with instructions for resetting your password
Download started.
- PDF [167 KB] PDF [167 KB]
- Add To Online Library Powered By Mendeley
- Add To My Reading List
- Export Citation
- Create Citation Alert
Qualitative Research in Nursing and Health Professions Regulation
- Allison Squires, PhD, RN, FAAN Allison Squires Search for articles by this author
- Caroline Dorsen, PhD, FNP, RN Caroline Dorsen Search for articles by this author
- Credentialing
- government regulation
- professional autonomy
- qualitative research
- • Explain the importance of qualitative research for studies about regulatory issues in nursing.
- • Discuss the core concepts of qualitative research.
- • Describe common methodological challenges researchers can encounter when conducting qualitative research on professional regulatory issues.
- • Identify solutions that can enhance the quality, rigor, and trustworthiness of the findings for regulatory studies.
- Blackman T.
- Google Scholar
- Bradley E.H.
- Devers K.J.
- Scopus (2269)
- Evans-Agnew R.A.
- Boutain D.M.
- Griffith D.M.
- Shelton R.C.
- Scopus (30)
- Waterfield J.
- Holden M.A.
- Ismail K.M.
- Foster N.E.
- Saunders B.
- Kingstone T.
- Scopus (4861)
- Scopus (709)
- Vandermause R.
- Edmundson L.
- Perfetti A.R.
- Yardley S.J.
- Richardson J.C.
A Review of Core Qualitative Research Concepts
- Bochner A.P.
- Scopus (1409)
- Scopus (3251)
- Open table in a new tab
- Patton M.Q.
- Hennink M.M.
- Kaiser B.N.
- Marconi V.C.
- Scopus (1586)
- Vanstone M.
A Note on Cross-language Qualitative Research on Regulatory Issues
- Scopus (136)
- Scopus (387)
- Ziebland S.
- Chiumento A.
- Barbour R.S.
- Poon M.K.-L.
- Scopus (35)
- Lincoln Y.S.
- Gonzalez y Gonzalez E.M.
- Aroztegui Massera C.
- MacKenzie C.A.
- Santos H.P.O.
- Sandelowski M.
- Scopus (98)
- Suurmond J.
- Woudstra A.
- Essink-Bot M.-L.
- Scopus (190)
- Wong J.P.-H.
- Scopus (110)
An Overview of Qualitative Study Designs Appropriate for Regulatory Studies
- Carter S.M.
- Scopus (411)
- Scopus (265)
- Scopus (115)
- Scopus (76)
- Scopus (180)
- Trinidad S.B.
- Scopus (1325)
- van Manen M.
- Willis D.G.
- Sullivan-Bolyai S.
- Scopus (213)
Underutilized Qualitative Designs in Regulatory Research
- Anderson R.A.
- Crabtree B.F.
- Steele D.J.
- McDaniel R.R.
- Scopus (185)
- Carolan C.M.
- Cresswell K.
- Robertson A.
- Morgan S.J.
- Pullon S.R.H.
- Macdonald L.M.
- McKinlay E.M.
- Anderson R.
- Hardwick R.
- Vowinkel J.
- Fletcher A.
- Scopus (158)
- van Belle S.
- van Olmen J.
- Scopus (296)
- Westhorp G.
- Scopus (111)
- Macintyre Latta M.
- Schnellert L.
- Spector-Mersel G.
- Wolgemuth J.R.
Design Dictates the Analytic Approach
- Castro F.G.
- Kellison J.G.
- Scopus (292)
- Scopus (218)
Samples, Sampling, and Saturation
- Malterud K.
- Siersma V.D.
- Guassora A.D.
- MacPhail C.
- Ranganathan M.
- Nelson L.K.
- Norris A.C.
- Farris A.J.
- Babbage D.R.
- Scopus (97)
- Scopus (10142)
Framing Findings
- Scopus (242)
- • Introducing quotes with a single sentence, rather than establishing the context of the quote and how it links to the theme
- • Inserting overly long quotes to represent experiences or the phenomenon
- • Failing to transition between quotes and the next paragraph without an explanatory or transition sentence
- • Choosing quotes that do not represent the theme
- • Inserting too many quotes
- • Separating every quote, regardless of length (35 words or more should be in a separate paragraph), without integrating them into the paragraph for a seamless reading experience.
Choosing Quotes
Managing word count limitations, avoiding discussion pitfalls and the generalizability trap.
- Carminati L.
Conclusions
Ce posttest, instructions, provider accreditation.
- a. Local and national governmental oversight through health professions regulation is needed for professional practice.
- b. Health professions are regulated in order to avoid a risk of harm to the public.
- c. Congress mandates that all professions are regulated.
- d. Both a and b
- a. There are not enough studies to determine the effectiveness of qualitative research yet.
- b. Quantitative research is more critical because it provides both exploratory and explanatory data.
- c. Qualitative research can play a vital role in ensuring that the stakeholder’s voice is represented and their experiences inform the evaluation of regulations and their associated policies.
- d. None of the above
- a. Identification, modification, or abolition
- b. Creation, modification, or elimination
- c. Oversight, enforcement, or evaluation
- d. Creation, development, or destruction
- c. Data saturation
- d. Reliability
- a. Data saturation
- b. Trustworthiness
- a. Termination
- b. Content closure
- c. Conclusion
- d. Data saturation
- a. Rigorous
- b. Trustworthy
- c. Unbiased
- d. Credible
- a. Grounded theory
- b. Phenomenology
- c. Ethnography
- d. Generic qualitative descriptive
- a. The applicability of the results is immediately apparent and translatable into the real world.
- b. The end goal of the study is to generate a theory from the data.
- c. The study must describe the lived experience of a phenomenon.
- d. Generic approaches offer flexibility for studying regulation and regulatory issues.
- 12. Pragmatic qualitative studies _____
- 13. Case studies _____
- 14. Realist evaluations _____
- a. Might work well exploring a state level analysis of a regulatory change
- b. A way to compare contemporary and historical stakeholder perspectives around the legislative process or similar phenomena
- c. Might be useful for studying how new regulations have affected those subject to them during the early phases of implementation
- d. Contributes to the evidence to support or change a regulation
- a. Recruit a sample size that will achieve data saturation.
- b. Aim for a heterogeneous sample.
- c. Plan to achieve a minimum sample size of 8 as a realistic and achievable goal in most cases.
- d. Sample size has no impact on regulatory research.
- a. Long quote
- b. Strong opening sentence
- d. Phenomenon
- a. Representative of participants’ experiences
- b. Improve the trustworthiness of results
- c. Articulately or succinctly explain a phenomenon
- d. All of the above
- a. The discussion section may end up too “thin” because the authors have left no room in the word count for a robust discussion of the findings
- b. The discussion section uses the first paragraph to summarize the findings from the study and how they are unique from the literature
- c. The authors assume the findings are generalizable to the broader population.
- a. They should include all findings, even if the content does not tie back to the original research question.
- b. They can provide useful direction for others seeking to replicate the study in different contexts or with populations affected by the same regulations.
- c. Suggestions for realistic, existing, measurable variables that might be sensitive to the effects of a regulation cannot be useful for a qualitative study focused on regulation.
- d. Qualitative findings can always be applied to other regional, state, national, or international populations.
Evaluation Form (required)
- • Explain the importance of qualitative research for studies about regulatory issues in nursing. 1 2 3 4 5 ___________________________________
- • Discuss the core concepts of qualitative research. 1 2 3 4 5 ___________________________________
- • Describe common methodological challenges researchers can encounter when conducting qualitative research on professional regulatory issues. 1 2 3 4 5 ___________________________________
- • Identify solutions that can enhance the quality, rigor, and trustworthiness of the findings for regulatory studies. 1 2 3 4 5 ___________________________________
- • Were the authors knowledgeable about the subject? 1 2 3 4 5 ___________________________________
- • Were the methods of presentation (text, tables, figures, etc.) effective? 1 2 3 4 5 ___________________________________
- • Was the content relevant to the objectives? 1 2 3 4 5 ___________________________________
- • Was the article useful to you in your work? 1 2 3 4 5 ___________________________________
- • Was there enough time allotted for this activity? 1 2 3 4 5 ___________________________________
- Krefting L.
- Scopus (1933)
Article info
Identification.
DOI: https://doi.org/10.1016/S2155-8256(18)30150-9
ScienceDirect
- View Large Image
- Download Hi-res image
- Download .PPT
Linked Article
- Preview As is standard in scholarly publishing, NCSBN’s Journal of Nursing Regulation (JNR) requires its authors to disclose any potential conflicts of interest (COI). Although COI information has always been collected by our staff in order to support editors’ review of the paper, it was not our standard practice to publish COI statements in each article. In this issue, JNR is retrospectively publishing the COI statements, which were collected with the below papers at submission, in order to make potential COI’s transparent to readers, as well as editors.
Related Articles
- Access for Developing Countries
- Articles & Issues
- Current Issue
- List of Issues
- Supplements
- For Authors
- Guide for Authors
- Author Services
- Permissions
- Researcher Academy
- Submit a Manuscript
- Journal Info
- About the Journal
- Contact Information
- Editorial Board
- New Content Alerts
- Call for Papers
- January & April 2022 Issues
The content on this site is intended for healthcare professionals.
- Privacy Policy
- Terms and Conditions
- Accessibility
- Help & Contact

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

A qualitative study of nursing student experiences of clinical practice
Farkhondeh sharif.
1 Psychiatric Nursing Department, Fatemeh (P.B.U.H) College of Nursing and Midwifery Shiraz University of Medical Sciences, Zand BlvD, Shiraz, Iran
Sara Masoumi
2 English Department, Shiraz University, Shiraz, Iran
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Nursing student's experiences of their clinical practice provide greater insight to develop an effective clinical teaching strategy in nursing education. The main objective of this study was to investigate student nurses' experience about their clinical practice.
Focus groups were used to obtain students' opinion and experiences about their clinical practice. 90 baccalaureate nursing students at Shiraz University of Medical Sciences (Faculty of Nursing and Midwifery) were selected randomly from two hundred students and were arranged in 9 groups of ten students. To analyze the data the method used to code and categories focus group data were adapted from approaches to qualitative data analysis.
Four themes emerged from the focus group data. From the students' point of view," initial clinical anxiety", "theory-practice gap"," clinical supervision", professional role", were considered as important factors in clinical experience.
The result of this study showed that nursing students were not satisfied with the clinical component of their education. They experienced anxiety as a result of feeling incompetent and lack of professional nursing skills and knowledge to take care of various patients in the clinical setting.
Clinical experience has been always an integral part of nursing education. It prepares student nurses to be able of "doing" as well as "knowing" the clinical principles in practice. The clinical practice stimulates students to use their critical thinking skills for problem solving [ 1 ]
Awareness of the existence of stress in nursing students by nurse educators and responding to it will help to diminish student nurses experience of stress. [ 2 ]
Clinical experience is one of the most anxiety producing components of the nursing program which has been identified by nursing students. In a descriptive correlational study by Beck and Srivastava 94 second, third and fourth year nursing students reported that clinical experience was the most stressful part of the nursing program[ 3 ]. Lack of clinical experience, unfamiliar areas, difficult patients, fear of making mistakes and being evaluated by faculty members were expressed by the students as anxiety-producing situations in their initial clinical experience. In study done by Hart and Rotem stressful events for nursing students during clinical practice have been studied. They found that the initial clinical experience was the most anxiety producing part of their clinical experience [ 4 ]. The sources of stress during clinical practice have been studied by many researchers [ 5 - 10 ] and [ 11 ].
The researcher came to realize that nursing students have a great deal of anxiety when they begin their clinical practice in the second year. It is hoped that an investigation of the student's view on their clinical experience can help to develop an effective clinical teaching strategy in nursing education.
A focus group design was used to investigate the nursing student's view about the clinical practice. Focus group involves organized discussion with a selected group of individuals to gain information about their views and experiences of a topic and is particularly suited for obtaining several perspectives about the same topic. Focus groups are widely used as a data collection technique. The purpose of using focus group is to obtain information of a qualitative nature from a predetermined and limited number of people [ 12 , 13 ].
Using focus group in qualitative research concentrates on words and observations to express reality and attempts to describe people in natural situations [ 14 ].
The group interview is essentially a qualitative data gathering technique [ 13 ]. It can be used at any point in a research program and one of the common uses of it is to obtain general background information about a topic of interest [ 14 ].
Focus groups interviews are essential in the evaluation process as part of a need assessment, during a program, at the end of the program or months after the completion of a program to gather perceptions on the outcome of that program [ 15 , 16 ]. Kruegger (1988) stated focus group data can be used before, during and after programs in order to provide valuable data for decision making [ 12 ].
The participants from which the sample was drawn consisted of 90 baccalaureate nursing students from two hundred nursing students (30 students from the second year and 30 from the third and 30 from the fourth year) at Shiraz University of Medical Sciences (Faculty of Nursing and Midwifery). The second year nursing students already started their clinical experience. They were arranged in nine groups of ten students. Initially, the topics developed included 9 open-ended questions that were related to their nursing clinical experience. The topics were used to stimulate discussion.
The following topics were used to stimulate discussion regarding clinical experience in the focus groups.
1. How do you feel about being a student in nursing education?
2. How do you feel about nursing in general?
3. Is there any thing about the clinical field that might cause you to feel anxious about it?
4. Would you like to talk about those clinical experiences which you found most anxiety producing?
5. Which clinical experiences did you find enjoyable?
6. What are the best and worst things do you think can happen during the clinical experience?
7. What do nursing students worry about regarding clinical experiences?
8. How do you think clinical experiences can be improved?
9. What is your expectation of clinical experiences?
The first two questions were general questions which were used as ice breakers to stimulate discussion and put participants at ease encouraging them to interact in a normal manner with the facilitator.
Data analysis
The following steps were undertaken in the focus group data analysis.
1. Immediate debriefing after each focus group with the observer and debriefing notes were made. Debriefing notes included comments about the focus group process and the significance of data
2. Listening to the tape and transcribing the content of the tape
3. Checking the content of the tape with the observer noting and considering any non-verbal behavior. The benefit of transcription and checking the contents with the observer was in picking up the following:
a. Parts of words
b. Non-verbal communication, gestures and behavior...
The researcher facilitated the groups. The observer was a public health graduate who attended all focus groups and helped the researcher by taking notes and observing students' on non-verbal behavior during the focus group sessions. Observer was not known to students and researcher
The methods used to code and categorise focus group data were adapted from approaches to qualitative content analysis discussed by Graneheim and Lundman [ 17 ] and focus group data analysis by Stewart and Shamdasani [ 14 ] For coding the transcript it was necessary to go through the transcripts line by line and paragraph by paragraph, looking for significant statements and codes according to the topics addressed. The researcher compared the various codes based on differences and similarities and sorted into categories and finally the categories was formulated into a 4 themes.
The researcher was guided to use and three levels of coding [ 17 , 18 ]. Three levels of coding selected as appropriate for coding the data.
Level 1 coding examined the data line by line and making codes which were taken from the language of the subjects who attended the focus groups.
Level 2 coding which is a comparing of coded data with other data and the creation of categories. Categories are simply coded data that seem to cluster together and may result from condensing of level 1 code [ 17 , 19 ].
Level 3 coding which describes the Basic Social Psychological Process which is the title given to the central themes that emerge from the categories.
Table Table1 1 shows the three level codes for one of the theme
Examples of 3 levels of coding
The documents were submitted to two assessors for validation. This action provides an opportunity to determine the reliability of the coding [ 14 , 15 ]. Following a review of the codes and categories there was agreement on the classification.
Ethical considerations
The study was conducted after approval has been obtained from Shiraz university vice-chancellor for research and in addition permission to conduct the study was obtained from Dean of the Faculty of Nursing and Midwifery. All participants were informed of the objective and design of the study and a written consent received from the participants for interviews and they were free to leave focus group if they wish.
Most of the students were females (%94) and single (% 86) with age between 18–25.
The qualitative analysis led to the emergence of the four themes from the focus group data. From the students' point of view," initial clinical anxiety", "theory-practice gap", clinical supervision"," professional role", was considered as important factors in clinical experience.
Initial clinical anxiety
This theme emerged from all focus group discussion where students described the difficulties experienced at the beginning of placement. Almost all of the students had identified feeling anxious in their initial clinical placement. Worrying about giving the wrong information to the patient was one of the issues brought up by students.
One of the students said:
On the first day I was so anxious about giving the wrong information to the patient. I remember one of the patients asked me what my diagnosis is. ' I said 'I do not know', she said 'you do not know? How can you look after me if you do not know what my diagnosis is?'
From all the focus group sessions, the students stated that the first month of their training in clinical placement was anxiety producing for them.
One of the students expressed:
The most stressful situation is when we make the next step. I mean ... clinical placement and we don't have enough clinical experience to accomplish the task, and do our nursing duties .
Almost all of the fourth year students in the focus group sessions felt that their stress reduced as their training and experience progressed.
Another cause of student's anxiety in initial clinical experience was the students' concern about the possibility of harming a patient through their lack of knowledge in the second year.
One of the students reported:
In the first day of clinical placement two patients were assigned to me. One of them had IV fluid. When I introduced myself to her, I noticed her IV was running out. I was really scared and I did not know what to do and I called my instructor .
Fear of failure and making mistakes concerning nursing procedures was expressed by another student. She said:
I was so anxious when I had to change the colostomy dressing of my 24 years old patient. It took me 45 minutes to change the dressing. I went ten times to the clinic to bring the stuff. My heart rate was increasing and my hand was shaking. I was very embarrassed in front of my patient and instructor. I will never forget that day .
Sellek researched anxiety-creating incidents for nursing students. He suggested that the ward is the best place to learn but very few of the learner's needs are met in this setting. Incidents such as evaluation by others on initial clinical experience and total patient care, as well as interpersonal relations with staff, quality of care and procedures are anxiety producing [ 11 ].
Theory-practice gap
The category theory-practice gap emerged from all focus discussion where almost every student in the focus group sessions described in some way the lack of integration of theory into clinical practice.
I have learnt so many things in the class, but there is not much more chance to do them in actual settings .
Another student mentioned:
When I just learned theory for example about a disease such as diabetic mellitus and then I go on the ward and see the real patient with diabetic mellitus, I relate it back to what I learned in class and that way it will remain in my mind. It is not happen sometimes .
The literature suggests that there is a gap between theory and practice. It has been identified by Allmark and Tolly [ 20 , 21 ]. The development of practice theory, theory which is developed from practice, for practice, is one way of reducing the theory-practice gap [ 21 ]. Rolfe suggests that by reconsidering the relationship between theory and practise the gap can be closed. He suggests facilitating reflection on the realities of clinical life by nursing theorists will reduce the theory-practice gap. The theory- practice gap is felt most acutely by student nurses. They find themselves torn between the demands of their tutor and practising nurses in real clinical situations. They were faced with different real clinical situations and are unable to generalise from what they learnt in theory [ 22 ].
Clinical supervision
Clinical supervision is recognised as a developmental opportunity to develop clinical leadership. Working with the practitioners through the milieu of clinical supervision is a powerful way of enabling them to realize desirable practice [ 23 ]. Clinical nursing supervision is an ongoing systematic process that encourages and supports improved professional practice. According to Berggren and Severinsson the clinical nurse supervisors' ethical value system is involved in her/his process of decision making. [ 24 , 25 ]
Clinical Supervision by Head Nurse (Nursing Unit Manager) and Staff Nurses was another issue discussed by the students in the focus group sessions. One of the students said:
Sometimes we are taught mostly by the Head Nurse or other Nursing staff. The ward staff are not concerned about what students learn, they are busy with their duties and they are unable to have both an educational and a service role
Another student added:
Some of the nursing staff have good interaction with nursing students and they are interested in helping students in the clinical placement but they are not aware of the skills and strategies which are necessary in clinical education and are not prepared for their role to act as an instructor in the clinical placement
The students mostly mentioned their instructor's role as an evaluative person. The majority of students had the perception that their instructors have a more evaluative role than a teaching role.
The literature suggests that the clinical nurse supervisors should expressed their existence as a role model for the supervisees [ 24 ]
Professional role
One view that was frequently expressed by student nurses in the focus group sessions was that students often thought that their work was 'not really professional nursing' they were confused by what they had learned in the faculty and what in reality was expected of them in practice.
We just do basic nursing care, very basic . ... You know ... giving bed baths, keeping patients clean and making their beds. Anyone can do it. We spend four years studying nursing but we do not feel we are doing a professional job .
The role of the professional nurse and nursing auxiliaries was another issue discussed by one of the students:
The role of auxiliaries such as registered practical nurse and Nurses Aids are the same as the role of the professional nurse. We spend four years and we have learned that nursing is a professional job and it requires training and skills and knowledge, but when we see that Nurses Aids are doing the same things, it can not be considered a professional job .
The result of student's views toward clinical experience showed that they were not satisfied with the clinical component of their education. Four themes of concern for students were 'initial clinical anxiety', 'theory-practice gap', 'clinical supervision', and 'professional role'.
The nursing students clearly identified that the initial clinical experience is very stressful for them. Students in the second year experienced more anxiety compared with third and fourth year students. This was similar to the finding of Bell and Ruth who found that nursing students have a higher level of anxiety in second year [ 26 , 27 ]. Neary identified three main categories of concern for students which are the fear of doing harm to patients, the sense of not belonging to the nursing team and of not being fully competent on registration [ 28 ] which are similar to what our students mentioned in the focus group discussions. Jinks and Patmon also found that students felt they had an insufficiency in clinical skills upon completion of pre-registration program [ 29 ].
Initial clinical experience was the most anxiety producing part of student clinical experience. In this study fear of making mistake (fear of failure) and being evaluated by faculty members were expressed by the students as anxiety-producing situations in their initial clinical experience. This finding is supported by Hart and Rotem [ 4 ] and Stephens [ 30 ]. Developing confidence is an important component of clinical nursing practice [ 31 ]. Development of confidence should be facilitated by the process of nursing education; as a result students become competent and confident. Differences between actual and expected behaviour in the clinical placement creates conflicts in nursing students. Nursing students receive instructions which are different to what they have been taught in the classroom. Students feel anxious and this anxiety has effect on their performance [ 32 ]. The existence of theory-practice gap in nursing has been an issue of concern for many years as it has been shown to delay student learning. All the students in this study clearly demonstrated that there is a gap between theory and practice. This finding is supported by other studies such as Ferguson and Jinks [ 33 ] and Hewison and Wildman [ 34 ] and Bjork [ 35 ]. Discrepancy between theory and practice has long been a source of concern to teachers, practitioners and learners. It deeply rooted in the history of nurse education. Theory-practice gap has been recognised for over 50 years in nursing. This issue is said to have caused the movement of nurse education into higher education sector [ 34 ].
Clinical supervision was one of the main themes in this study. According to participant, instructor role in assisting student nurses to reach professional excellence is very important. In this study, the majority of students had the perception that their instructors have a more evaluative role than a teaching role. About half of the students mentioned that some of the head Nurse (Nursing Unit Manager) and Staff Nurses are very good in supervising us in the clinical area. The clinical instructor or mentors can play an important role in student nurses' self-confidence, promote role socialization, and encourage independence which leads to clinical competency [ 36 ]. A supportive and socialising role was identified by the students as the mentor's function. This finding is similar to the finding of Earnshaw [ 37 ]. According to Begat and Severinsson supporting nurses by clinical nurse specialist reported that they may have a positive effect on their perceptions of well-being and less anxiety and physical symptoms [ 25 ].
The students identified factors that influence their professional socialisation. Professional role and hierarchy of occupation were factors which were frequently expressed by the students. Self-evaluation of professional knowledge, values and skills contribute to the professional's self-concept [ 38 ]. The professional role encompasses skills, knowledge and behaviour learned through professional socialisation [ 39 ]. The acquisition of career attitudes, values and motives which are held by society are important stages in the socialisation process [ 40 ]. According to Corwin autonomy, independence, decision-making and innovation are achieved through professional self-concept 41 . Lengacher (1994) discussed the importance of faculty staff in the socialisation process of students and in preparing them for reality in practice. Maintenance and/or nurturance of the student's self-esteem play an important role for facilitation of socialisation process 42 .
One view that was expressed by second and third year student nurses in the focus group sessions was that students often thought that their work was 'not really professional nursing' they were confused by what they had learned in the faculty and what in reality was expected of them in practice.
The finding of this study and the literature support the need to rethink about the clinical skills training in nursing education. It is clear that all themes mentioned by the students play an important role in student learning and nursing education in general. There were some similarities between the results of this study with other reported studies and confirmed that some of the factors are universal in nursing education. Nursing students expressed their views and mentioned their worry about the initial clinical anxiety, theory-practice gap, professional role and clinical supervision. They mentioned that integration of both theory and practice with good clinical supervision enabling them to feel that they are enough competent to take care of the patients. The result of this study would help us as educators to design strategies for more effective clinical teaching. The results of this study should be considered by nursing education and nursing practice professionals. Faculties of nursing need to be concerned about solving student problems in education and clinical practice. The findings support the need for Faculty of Nursing to plan nursing curriculum in a way that nursing students be involved actively in their education.
Competing interests
The author(s) declare that they no competing interests.
Authors' contributions
FSH: Initiation and design of the research, focus groups conduction, data collection, analysis and writing the paper, SM: Editorial revision of paper
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/1472-6955/4/6/prepub
Acknowledgements
The author would like to thank the student nurses who participated in this study for their valuable contribution
- Dunn SV, Burnett P. The development of a clinical learning environment scale. Journal of Advanced Nursing. 1995; 22 :1166–1173. [ PubMed ] [ Google Scholar ]
- Lindop E. Factors associated with student and pupil nurse wastage. Journal of Advanced Nursing. 1987; 12 :751–756. [ PubMed ] [ Google Scholar ]
- Beck D, Srivastava R. Perceived level and source of stress in baccalaureate nursing students. Journal of Nursing Education. 1991; 30 :127–132. [ PubMed ] [ Google Scholar ]
- Hart G, Rotem A. The best and the worst: Students' experience of clinical education. The Australian Journal of Advanced Nursing. 1994; 11 :26–33. [ PubMed ] [ Google Scholar ]
- Sheila Sh, Huey-Shyon L, Shiowli H. Perceived stress and physio-psycho-social status of nursing students during their initial period of clinical practice. International Journal of Nursing Studies. 2002; 39 :165–175. doi: 10.1016/S0020-7489(01)00016-5. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnson J. Reducing distress in first level and student nurses. Journal of Advanced Nursing. 2000; 32 :66–74. doi: 10.1046/j.1365-2648.2000.01421.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Admi H. Nursing students' stress during the initial clinical experience. Journal of Nursing Education. 1997; 36 :323–327. [ PubMed ] [ Google Scholar ]
- Blainey GC. Anxiety in the undergraduate medical-surgical clinical student. Journal of Nursing Education. 1980; 19 :33–36. [ PubMed ] [ Google Scholar ]
- Wong J, Wong S. Towards effective clinical teaching in nursing. Journal of Advanced Nursing. 1987; 12 :505–513. [ PubMed ] [ Google Scholar ]
- Windsor A. Nursing students' perceptions of clinical experience. Journal of Nursing Education. 1987; 26 :150–154. [ PubMed ] [ Google Scholar ]
- Sellek T. Satisfying and anxiety creating incidents for nursing students. Nursing Times. 1982; 78 :137–140. [ PubMed ] [ Google Scholar ]
- Krueger RA. Focus Groups: A Practical Guide for Applied Research. Sage Publications: California. 1988.
- Denzin NK. The Research Act. 3. Prentice Hall: Englewood Cliffs, New Jersey; 1989. [ Google Scholar ]
- Stewart DW, Shamdasani PN. Analysing focus group data. In: Shamdasani PN, editor. Focus Groups: Theory and Practice. Sage Publications: Newbury Park; 1990. [ Google Scholar ]
- Barbour RS, Kitzinger J. Developing focus group research : politics, theory and practice. Sage. 1999.
- Patton MQ. Qualitative Evaluation and Research Methods. 2. Sage publications; 1990. [ Google Scholar ]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004; 24 :105–112. doi: 10.1016/j.nedt.2003.10.001. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Streubert HJ, Carpenter DR. Advancing the Humanistic Imperative. J.B. Lippincott Company: Philadelphia; 1995. Qualitative Research in Nursing. [ Google Scholar ]
- Polit DF, Hungler BP. Nursing research: Principles and Methods. Philadelphia newyork. 1999.
- Allmark PA. classical view of the theory-practice gap in nursing. Journal of Advanced Nursing. 1995; 22 :18–23. doi: 10.1046/j.1365-2648.1995.22010018.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tolley KA. Theory from practice for practice: Is this a reality? Journal of Advanced Nursing. 1995; 21 :184–190. doi: 10.1046/j.1365-2648.1995.21010184.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rolfe G. Listening to students: Course evaluation as action research. Nurse Education Today. 1994; 14 :223–227. doi: 10.1016/0260-6917(94)90085-X. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johns Ch. clinical supervision as a model for clinical leadership. Journal of Nursing Management. 2003; 11 :25–34. doi: 10.1046/j.1365-2834.2002.00288.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Berggren I, Severinsson E. Nurses supervisors'action in relation to their decision-making style and ethical approach to clinical supervision. Journal of Advanced Nursing. 2003; 41 :615–622. doi: 10.1046/j.1365-2648.2003.02573.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Begat I, Severinsson E. Nurses' satisfaction with their work environment and the outcomes of clinical nursing supervision on nurses' experiences of well-being. Journal of Nursing Management. 2005; 13 :221–230. doi: 10.1111/j.1365-2834.2004.00527.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bell P. Anxiety in mature age and higher school certificate entry student nurses – A comparison of effects on performance. Journal of Australian Congress of Mental Health Nurses. 1984; 4/5 :13–21. [ Google Scholar ]
- Ruth L. Experiencing before and throughout the nursing career. Journal of Advanced Nursing. 2002; 39 :119. doi: 10.1046/j.1365-2648.2000.02251.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Neary M. Project 2000 students' survival kit: a return to the practical room. Nurse Education Today. 1997; 17 :46–52. doi: 10.1016/S0260-6917(97)80078-0. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jinks A, Pateman B. Nither this nor that: The stigma of being an undergraduate nurse. Nursing Times. 1998; 2 :12–13. [ PubMed ] [ Google Scholar ]
- Stephen RL. Imagery: A treatment for nursing student anxiety. Journal of Nursing Education. 1992; 31 :314–319. [ PubMed ] [ Google Scholar ]
- Grundy SE. The confidence scale. Nurse Educator. 1993; 18 :6–9. [ PubMed ] [ Google Scholar ]
- Copeland L. Developing student confidence. Nurse Educator. 1990; 15 :7. [ PubMed ] [ Google Scholar ]
- Ferguson K, Jinks A. Integrating what is taught with what is practised in the nursing curriculum: A multi-dimensional model. Journal of Advanced Nursing. 1994; 20 :687–695. doi: 10.1046/j.1365-2648.1994.20040687.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hewison A, Wildman S. The theory-practice gap in nursing: A new dimension. Journal of Advanced Nursing. 1996; 24 :754–761. doi: 10.1046/j.1365-2648.1996.25214.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bjork T. Neglected conflicts in the discipline of nursing: Perceptions of the importance and value of practical skill. Journal of Advanced Nursing. 1995; 22 :6–12. doi: 10.1046/j.1365-2648.1995.22010006.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Busen N. Mentoring in advanced practice nursing. Journal of Advanced Nursing Practice. 1999; 2 :2. [ Google Scholar ]
- Earnshaw GP. Mentorship: The students' view. Nurse Education Today. 1995; 15 :274–279. doi: 10.1016/S0260-6917(95)80130-8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kelly B. The professional self-concepts of nursing undergraduates and their perceptions of influential forces. Journal of Nursing Education. 1992; 31 :121–125. [ PubMed ] [ Google Scholar ]
- Lynn MR, McCain NL, Boss BJ. Socialization of R.N. to B.S.N Image: Journal of Nursing Scholarship. 1989; 21 :232–237. [ PubMed ] [ Google Scholar ]
- Klein SM, Ritti RR. Understanding Organisational Behaviour. Kent: Boston; 1980. [ Google Scholar ]
- Corwin RG. The professional employee: A study of conflict in nursing roles. The American Journal of Sociology. 1961; 66 :604–615. doi: 10.1086/223010. [ CrossRef ] [ Google Scholar ]
- Lengacher CA. Effects of professional development seminars on role conception, role deprivation, and self-esteem of generic baccalaureate students. Nursing Connections. 1994; 7 :21–34. [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
Evaluating qualitative research studies can be challenging. Many terms—rigor, validity, integrity, and trustworthiness—can describe study quality, but in the end you want to know whether the study's findings accurately and comprehensively represent the phenomenon of interest. ... Nursing Research: A Qualitative Perspective. 5th ed ...
Significance of Qualitative Research. The qualitative method of inquiry examines the 'how' and 'why' of decision making, rather than the 'when,' 'what,' and 'where.'[] Unlike quantitative methods, the objective of qualitative inquiry is to explore, narrate, and explain the phenomena and make sense of the complex reality.Health interventions, explanatory health models, and medical-social ...
Useful terms. Some of the qualitative approaches used in nursing research include grounded theory, phenomenology, ethnography, case study (can lend itself to mixed methods) and narrative analysis. The data collection methods used in qualitative research include in depth interviews, focus groups, observations and stories in the form of diaries ...
Introduction. Qualitative descriptive approaches to nursing and healthcare research provide a broad insight into particular phenomena and can be used in a variety of ways including as a standalone research design, as a precursor to larger qualitative studies and commonly as the qualitative component in mixed-methods studies.
1.1. Background. Research indicates that there is a potential for patients to improve safety (Davis, Jacklin, Sevdalis, & Vincent, 2007; Vincent & Coulter, 2002) and that patients are willing and able to be involved in safety‐related work (Waterman et al., 2006 Wright et al., 2016).However, several barriers to involving patients in improving patient safety has been identified and organized ...
Global Qualitative Nursing Research. Global Qualitative Nursing Research (GQNR) is an open access, peer-reviewed journal focusing on qualitative research in fields relevant to nursing and other health professionals world-wide. Please see the Aims and Scope tab for … | View full journal description. This journal is a member of the Committee on ...
Data analysis. Data collection and inductive thematic analysis took place iteratively [45, 53].The first author coded the data (i.e. observation reports, interview and focus group transcripts), basing the codes on the research question and theoretical notions on nursing role development and distinctions.
In crit-ically appraising qualitative research, steps need to be taken to ensure its rigour, credibility and trustworthiness. (table 1). Some of the qualitative approaches used in nursing research include grounded theory, phenomenology, ethnography, case study (can lend itself to mixed methods) and narrative analysis.
Good qualitative research uses a systematic and rigorous approach that aims to answer questions concerned with what something is like (such as a patient experience), what people think or feel about something that has happened, and it may address why something has happened as it has. Qualitative data often takes the form of words or text and can include images. Qualitative research covers a ...
Longitudinal qualitative research (LQR) is an emerging methodology in health behavior and nursing research—fields focused on generating evidence to support nursing practices as well as programs, and policies promoting healthy behaviors (Glanz et al., 2008; Polit & Beck, 2017).Because human experiences are rarely comprised of concrete, time-limited events, but evolve and change across time ...
Qualitative Research in Nursing and Healthcare Discover how to conduct qualitative nursing research with confidence Co-authored by experienced researchers, Qualitative Research in Nursing and Healthcare offers practical and applied examples for those who carry out qualitative research in the healthcare arena. With clear explanations of abstract ideas and practical procedures, this updated ...
More specifically, research systematically uses disciplined approaches to complete an inquiry to find answers or solutions. 2 Nursing research is also systematic and seeks to develop or expand knowledge specific to nursing practice. 2, 3 Although a non-nurse may be involved in a nursing research study, the project is nursing research when the ...
Qualitative research methods are increasingly recognized for their importance in healthcare-related research, particularly in contextualizing social and cultural realities that impact human behavior (Al-Busaidi et al., 2008; Renjith et al., 2021).There is a growing interest in and acceptance of qualitative research approaches in the health sciences, both as stand-alone methodologies and ...
Qualitative research is critical for studies about regulatory issues in nursing and across all health professions. When in-depth stakeholder perspectives are needed, qualitative approaches are often the best methodological choice to ensure their viewpoints and experiences are captured when evaluating the consequences of policy implementation or when informing regulation design.
Qualitative research in Nursing approaches a clinical question from a place of unknowing in an attempt to understand the complexity, depth, and richness of a particular situation from the perspective of the person or persons impacted by the situation (i.e., the subjects of the study).. Study subjects may include the patient(s), the patient's caregivers, the patient's family members, etc ...
As the use of qualitative research methods proliferates throughout health care, and specifically nursing research studies, there is a need for Clinical Nurse Specialists (CNSs) to become informed regarding the potential utility of qualitative research findings in practice. In this column, the questions of what qualitative findings mean, how the ...
Qualitative research methods began to appear in nursing in 1960s and 1970s amid cautious and reluctant acceptance. In the 1980s, qualitative health research emerged as a distinctive domain and mode of inquiry. 1 Qualitative research refers to any kind of research that produces findings not arrived at by means of statistical analysis or other means of quantification. 2,3 It uses a naturalistic ...
In study done by Hart and Rotem stressful events for nursing students during clinical practice have been studied. They found that the initial clinical experience was the most anxiety producing part of their clinical experience [ 4 ]. The sources of stress during clinical practice have been studied by many researchers [ 5 - 10] and [ 11 ].
Qualitative research in nursing: Advancing the humanistic imperative. 4th ed. Lippincott Williams & Wilkens, Philadelphia, PA 2007. Google Scholar). Results. ... This qualitative study captured a considerable range of student and faculty experiences with VS. That said, limitations to this study include the small sample size and the possibility ...
This descriptive qualitative study explored nursing students' experiences in participating in a student death doula service-learning program in palliative care settings. Fourteen final-year undergraduate nursing students participated in semi-structured focus group discussions via Zoom. Four focus group discussions were conducted.
In the current study, nursing work is understood as a role that supports adaptation to meet the needs of patients and the healthcare system. The model presented here may frame discussions about appreciating the value of the complex work of nurses. ... a particular problem in qualitative research, because subjects who act as participants or ...
Qualitative research is a type of research that explores and provides deeper insights into real-world problems.[1] Instead of collecting numerical data points or intervene or introduce treatments just like in quantitative research, qualitative research helps generate hypotheses as well as further investigate and understand quantitative data. Qualitative research gathers participants ...
The study employed a qualitative explorative design to study in-depth, how nursing home and homecare leaders in Norwegian rural primary healthcare services experienced and addressed the extreme challenges and needs for change induced by the COVID-19 pandemic [45, 46]. Four rural municipalities of different sizes were included in the study.
Qualitative research is critical for studies about regulatory issues in nursing and across all health professions. When in-depth stakeholder perspectives are needed, qualitative approaches are often the best methodological choice to ensure their viewpoints and experiences are captured when evaluating the consequences of policy implementation or when informing regulation design.
This study aims to understand the perspectives and concerns of family members regarding the recruitment and engagement of their advanced cancer relatives in nursing research through qualitative research. To achieve this objective, the study seeks to address the following research questions:
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Ethical Review Committee for research in human subjects, Chiangrai province, Thailand (No. 35/2565). The data collection procedures were carefully designed to protect confidentiality.
In the 1990s, Sandelowski viewed qualitative methods as the antithesis of clinical research and "far removed from the immediate practical aims of intervention studies and nursing practice" (Sandelowski, 1996, p. 359). However, today we see that such methods not only benefit clinical studies, but are needed to explore, illuminate and ...
@article{Katayama2024HowNS, title={How nursing students' perceptions of people with psychiatric disabilities change when using the strengths model during practicums: A qualitative research study.}, author={Miho Katayama and Ritsuko Aijo and Kazuyo Kitaoka and Megumi Kawaguchi}, journal={Nurse education today}, year={2024}, volume={138}, pages ...
Clinical experience is one of the most anxiety producing components of the nursing program which has been identified by nursing students. In a descriptive correlational study by Beck and Srivastava 94 second, third and fourth year nursing students reported that clinical experience was the most stressful part of the nursing program [ 3 ].