An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Med Surg (Lond)
- v.79; 2022 Jul


Successful medical management of diabetic ketoacidosis at first presentation in a child with type 1 diabetes: A case report
Shriya sharma.
a Nepalese Army Institute of Health Sciences, Kathmandu, Nepal
Aakriti Adhikari
Samikshya adhikari, sabin poudel, gaurab mainali, sumit kumar yadav.
b Shree Birendra Hospital, Kathmandu, Nepal
Associated Data
Introduction and importance.
Diabetic ketoacidosis (DKA) is considered to be a common presentation of type 1 diabetes mellitus in children. It occurs when absolute or relative insulin insufficiency prevents glucose from entering the cells for use as metabolic fuel, causing the liver to quickly break down fat into ketones for use as fuel source. As a result, ketones are overproduced, accumulating in the blood and urine making the blood acidic.
Case presentation
A 4 years and 8 months old child presented with the complaint of abdominal pain and vomiting along with polyurea, polydipsia and polyphagia. Routine examination of blood revealed that increased random blood glucose level. Once diagnosed, DKA was managed with fluid and insulin therapy with close monitoring and supervision.
Clinical discussion
DKA can be easily diagnosed. Proper management should be done on time to prevent complications like hypokalemia, hyponatremia leading to cerebral edema and shock.
Conclusions
Diabetic awareness programs and school educational tutorials are beneficial for community awareness of the signs and symptoms of diabetes.
- • Diabetic ketoacidosis (DKA) is considered to be a common presentation of type 1 diabetes mellitus in children.
- • Severe fall in insulin levels leads to increase in lipolysis which will lead to increase in level of ketone bodies resulting metabolic acidosis and compensatory respiratory alkalosis.
- • DKA is diagnoses on the basis of hyperglycemia, metabolic acidosis and ketonuria and severity is categorized on the basis of acid-base status.
- • Early medical management and close monitoring could prevent complications like cerebral edema, mental confusion, shock and death.
1. Introduction
Type 1 diabetes is due to autoimmune destruction of pancreatic beta cells which leads to insufficient insulin production resulting in hyperglycemia [ 1 ].The common symptoms presenting in type 1 diabetes are polyurea, polydipsia, and weight loss [ 2 ]. Severe fall in insulin levels leads to increase in lipolysis which will lead to increase in level of ketone bodies resulting metabolic acidosis and compensatory respiratory alkalosis [ 3 ]. Diabetes ketoacidosis (DKA) is the common presentation of type 1 diabetes mellitus in children. The prevalence of onset of diabetic ketoacidosis among type 1 diabetes mellitus was found to be 26.3% in one of the studies [ 4 ]. Common complications observed due to ketoacidosis are electrolyte abnormalities like hypokalemia, hyponatremia leading to cerebral edema and shock [ 5 ].
If Diabetic ketoacidosis is not treated on time, the compensatory mechanism will fail soon and lead to cerebral edema, mental confusion, unconsciousness, coma and death [ 3 , 6 ]. DKA is the most common cause of death in children and adolescents with type 1 diabetes and cause of half of all deaths in diabetic patients under the age of 24 years [ 7 ]. Immediate and aggressive intervention is required. Early medical management could prevent complications like cerebral edema, mental confusion, shock and death. Here, we present a successful medical management of a diabetic ketoacidosis as a first presentation in a child with type 1 Diabetes mellitus. This case has been reported accordingly in line with SCARE 2020 criteria [ 8 ].
2. Case presentation
A 4 years 8 months old school going male child presented to the Emergency department of Shree Birendra Hospital with complaints of abdominal pain in periumbilical region for 1 day. Pain was mild, acute on onset, non-radiating associated with irritability. He also had a history of multiple episodes of vomiting for the last 3 days. Vomitus was non-projectile consisting of partially digested food particles and water. It was non-bile stained, was not mixed with blood, and was non-foul smelling. He also had a history of polyuria, polydipsia, and polyphagia for 7 days. Day by day there was an increase in frequency of urine which was associated with increased water intake. There is a history of a 2 kgs weight loss within a week. He was born healthy at term following an uncomplicated pregnancy and was the second child of a non-consanguineous marriage. There was no any family history of type I DM and any chronic illness.
On physical examination, the child was irritable and dehydrated with a dry tongue and mucosa. Vitals recorded at the time of admission were as follows; blood pressure of 80/50 mmHg, pulse rate of 128 beats/min and were low volume, respiratory rate of 24 breaths/minute, oxygen saturation of 95% on room air, and body temperature were 98 °F. Systemic examinations were normal.
Routine examination of blood revealed an increase in random blood glucose level with value of 448 mg/dl (ref. 140 mg/dl) and hyponatremia with value of 130 mEq/L (ref. 136–145 mEq/L), however serum potassium, urea and creatinine levels were normal. Urine examination revealed that the urine was acidic, acetone positive and sugar was present in urine. Arterial blood gas analysis showed pH 7.23 (ref. 7.35–7.45), pCO 2 31 (ref. 35–45 mmHg), HCO 3 − 13.21 (ref. 22–26mmoL/l), and PO 2 102 (80–105 mmHg). Hematological examination was unremarkable.
Based on hyperglycemia, metabolic acidosis, and ketonuria a diagnosis of DKA was made and management was initiated. The child was shifted to Pediatrics intensive care unit (PICU) where he was given intravenous fluid of 320 ml normal saline IV over 1 hour at the rate of 20 ml/kg. Similarly, regular insulin 0.5 ml hourly at the rate of 0.05 unit/kg hr (1ml insulin in 23ml NS) and injection ceftriaxone 500 mg IV 12 hourly at the rate of 63 mg/kg/day were administered for the next 23 hours. The child was kept in N/2 IV Fluid 100 ml/hourly with 1mEq KCl in each 100 ml IV fluid. If random blood sugar fell below 250 mg/dl, N/2 IV fluid and 5% dextrose at 100ml/hourly with 1mEq KCl in each ml of 100 ml IV fluid was indicated. We kept our patient on nil per oral. Similarly, if random blood sugar falls below 200 mg/dl, N/2 IV fluid and 10% dextrose at 100 ml/hourly was indicated.
Further, the vitals were monitored hourly; random blood sugar and neurological assessment were done 2 hourly; renal function test, electrolyte were monitored 6 hourly. X-ray of chest to rule out pulmonary infections such as pneumonia, ultrasonography of abdomen to rule out any organ damage, ophthalmology consultations to rule out papilloedema were done. There were no significant findings on any one of them. After 5 days on PICU, our patient's symptoms gradually improved. He was started on an oral fluid and liquid diet. The random blood glucose levels monitored at different time intervals were in the normal range. We discharged the patient after 7 days of admission with advice of Insulin Glargine 6 units sc once a day and Insulin Lispro 4 units before breakfast, lunch and dinner. The patient was properly instructed to follow up after 1 week for insulin management as per glucose report.
3. Clinical discussion
DKA is life threatening complications of uncontrolled diabetes mellitus if proper intervention is not done on time [ 9 ]. Risk of developing DKA at manifestation of diabetes is high in young children (<2 years), girls, children of ethnic minority status, low socio-economic status [ [10] , [11] , [12] ]. Successful management of diabetic ketoacidosis depends upon swift diagnosis, regular monitoring of clinical and biochemical parameters with prompt intervention. The diagnosis of DKA can be made on the basis of biochemical criteria of random blood glucose level greater than 200mg/dl with a venous pH of level <7.3 and/or a bicarbonate (HCO3) level of <15 mmol/L; ketonemia and ketonuria [ 11 ]. Early detection of diabetic ketoacidosis in our case led to proper medical management of a patient preventing him from complications like cerebral edema. However, diagnosis of DKA should not be confused with asthma, hypokalemia, metabolic acidosis, respiratory acidosis, pneumonia, salicylate poisoning, acute abdomen, gastroenteritis etc. [ 13 ].
Muktan et al. in their retrospective study found that polyurea, polydipsia, weight loss, abdominal pain, vomiting as the most common symptoms of DKA [ 14 ]. Our patient also presented with similar symptoms from which we made a provisional diagnosis of DKA after physical examination which was later confirmed by biochemical examination. DKA can be managed in any hospital/private unit or in a pediatric inpatient ward in case of children by trained nursing and medical personnel.
Rosenbloom et al. in his study had described the management of Diabetic Ketoacidosis depends on the severity of DKA. The severity of DKA is categorized by acid-base status in which mild DKA has pH 7.2 to <7.3; bicarbonate 10 to <15 mEq/L, moderate DKA has pH 7.1 to <7.2; bicarbonate 5 to 9 mEq/L and severe DKA has pH < 7.1; bicarbonate <5 mEq/L [ 15 ]. Our patient had pH level of 7.23 and bicarbonate level at 13.21. Thus, he had a mild DKA and was treated accordingly.
The child presented with DKA should be closely monitored in the unit. Blood glucose, electrolyte level, neurological assessment, vitals, and urine routine examination should be monitored on hourly basis [ 16 ]. We monitored our patient's vitals hourly; random blood glucose level and neurological assessment 2 hourly; electrolyte, input/output charting, and urine routine examination 6 hourly.
The patient with DKA is treated with intravenous fluids and intravenous insulin if the child is nauseated/vomiting, clinically dehydrated or is not alert [ 17 ]. We managed our patient as per his symptoms. We used normal saline for the first 24 hours to treat and manage dehydration and mild sodium depletion. We kept our patient on Insulin to control increased random blood glucose level. KCL along with intravenous fluids was given to manage the impending hypokalemia. In order to treat and prevent possible bacterial infections, ceftriaxone was given. Since we kept our patient nil per oral, dextrose in intravenous fluids was introduced the next day.
4. Conclusion
We present a case of diabetic ketoacidosis in a child with type 1 diabetic mellitus. It is a life threatening complications if timely intervention is not done. Timely management with fluid therapy along with insulin should be done. Regular monitoring and neurological observation are equally important to prevent complications like cerebral edema. Educational programs, diabetes awareness campaigns, and school educational tutorials can be beneficial for community awareness of the signs and symptoms of diabetes.
Author agreement statement
We the undersigned declare that this manuscript is original, has not been published before and is not currently being considered for publication elsewhere.
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
We understand that the Corresponding Author is the sole contact for the Editorial process. He/she is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs.
Ethical approval
This is a case report, therefore, it did not require ethical approval from the ethics committee.
Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review by the editor-in-chief of this journal on request.
Registration of research studies
Not applicable
The study did not receive any grant from funding agencies in the public, commercial or not-for-profit sectors.
Author contribution
All authors: writing the paper, collection of Data, revising it critically for important intellectual content, reviewing, and editing.
Shriya Sharma, Nepalese Army Institute of Health Sciences, Kathmandu, Nepal E-mail: [email protected]
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
The authors report no conflicts of interest.
Acknowledgment
Appendix A Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.103981 .
Appendix A. Supplementary data
The following is the Supplementary data to this article:

- Blood gases/acid-base
- Cardiac markers
- Coagulation/fibrinolysis
- Infection/sepsis
- Information management
- Kidneys/fluids
- Neonatology
- Point-of-care testing
- Process optimization
- Quality assurance
- Preanalytical phase
- Creatinine/urea
- Electrolytes
- Hemoglobins
- Natriuretic peptide
- About this site
- Journal scanner Explore selected articles curated by biochemist and journalist Chris Higgins
Sign up for our quarterly newsletter and get the newest articles from acutecaretesting.org

- Journal scans >
Printed from acutecaretesting.org
Severe diabetic ketoacidosis – a remarkable case study

Summarized from Van de Vyver C, Damen J, Haentjens C et al . An exceptional case of diabetic ketoacidosis. Case Reports in Emergency Medicine 2017.
Diabetic ketoacidosis (DKA) is a potentially life-threatening acute complication of type 1 diabetes caused by insulin deficiency. It is characterized by raised blood glucose (hyperglycemia), metabolic acidosis, and increased blood/urine ketones. Dehydration and electrolyte disturbance are common and affected patients may develop some degree of acute kidney injury (AKI) consequent on fluid loss (hypovolemia) due to osmotic diuresis associated with severe hyperglycemia. DKA evolves rapidly over a short time frame (hours rather than days) and can occur (rarely) in those with type 2 diabetes. This DKA case study is particularly noteworthy because of the severity of the hyperglycemia and acid-base disturbance, and the fact that the patient survived such profound metabolic disturbance and associated life-threatening hemodynamic changes. The case concerns a 33-year-old woman with ”brittle” type 1 diabetes treated with continuous subcutaneous insulin infusion (insulin pump). She had, in common with many brittle diabetics, a history of gastroparesis (delayed stomach emptying). Some 36 hours prior to emergency hospital admission she complained of abdominal pain and vomiting after attending a party. Her condition deteriorated before transfer to hospital. The ambulance team reported a rapid decline in Glasgow Coma Score (GCS) from 13 to 3 in only 10 minutes, sinus tachycardia, undetectable peripheral pulse, and hypotension (BP 99/52 mmHg).
Clinical examination revealed severe dehydration and respiratory distress (respiration rate 40 breaths/min). Urgent intubation was necessary and systolic blood pressure dropped further to 55 mmHg. Initial (fingerstick) blood glucose was above the upper detection limit of the analyzer and blood ketones were >8.0 mmol/L. Blood gas analysis revealed severe metabolic acidosis (pH 6.74, bicarbonate 5 mmol/L, p CO 2 39.9 mmHg (5.3 kPa) and hypoxemia ( p O 2 50.2 mmHg, 6.7 kPa). Among other abnormal laboratory test results, perhaps the most remarkable was serum glucose 107 mmol/L (1924 mg/dL). (Serum glucose >33 mmol/L (600 mg/dL) is rarely seen in patients with DKA.) White blood count (32.8x10 9 /L), C-reactive protein (789 nmol/L) and lactate (4.6 mmol/L) were also grossly elevated. Other laboratory testing revealed severe hyponatremia (sodium 113 mmol/L), severe hyperkalemia (6.7 mmol/L) and acute kidney failure (serum creatinine 332 µmol/L). Following presumptive diagnosis of DKA, sepsis and acute renal failure, the patient was treated with aggressive IV fluids, norepinephrine, bicarbonate, and insulin, IV bolus and drip. Intensive investigation for evidence of infection proved fruitless. With treatment, the patient’s condition improved over the following days and she was extubated. Normal renal function was restored after 2 days. In discussion of this case history, the authors briefly review the pathogenesis and treatment of DKA in general terms. They also highlight some interesting features of this case. One aspect discussed relates to the blood gas results on admission, in particular the curiously normal p CO 2 (39.9 mmHg, 5.3kPa).
Metabolic acidosis usually provokes compensatory hyperventilation and reduced p CO 2 . The authors propose plausible theories to explain the much higher than expected p CO 2 in this case. They also propose that the remarkably high blood glucose in this case is the result of the combined effect of reduced glucose elimination consequent on renal failure and the presence of gastroparesis.
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info .

has a master's degree in medical biochemistry and he has twenty years experience of work in clinical laboratories.

Acute care testing handbook
Get the acute care testing handbook.
Your practical guide to critical parameters in acute care testing.

Scientific webinars
Check out the list of webinars.
Radiometer and acutecaretesting.org present free educational webinars on topics surrounding acute care testing presented by international experts.
Sign up for the Acute Care Testing newsletter
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
On March 6th, 2019, Maria Fernandez, a 19-year-old female, presented to the Emergency Department with complaints of nausea, vomiting, abdominal pain, and lethargy. She reveals a recent diagnosis of type 1 diabetes but admits to noncompliance with treatment. At the time of admission, Maria’s vital signs were as follows: BP 87/50, HR 118, RR 28, O2 95% on room air, diffuse abdominal pain at a level of 5, on a verbal numeric 1-10 scale, with non-radiating pain beginning that morning. She was A&O x3, oriented to self, place, and situation, but sluggish. Upon assessment it is revealed that she is experiencing blurry vision, Kussmaul respirations, dry, flushed skin, poor skin turgor, weakness, and a fruity breath smell. Labs were drawn. During the first hour of admission, Maria requested water four times and urinated three times.
Code status: Full code
Medical hx : Type 1 Diabetes
Insurance : None
Allergies : NKA
Significant Lab Values
- Blood glucose 388
- ABGs: pH 7.25, Bicarb 12 mEq/L, paCO2 30 mm Hg, anion gap 20 mEq/L, paO2 94%
- Urinalysis: Ketones and acetone present, BUN 25 mL/dL, Cr 2.1 ml/dL
- Chemistry: sodium 111 mEq/L, potassium 5.5 mEq/L, chloride 90 mEq/L, phosphorus 2.5 mg/dL, Magnesium 2.0 mg/dL
- CBC: WBC 13,000 mcL, RBC 4.7 mcL, Hgb 12.6 g/dL , Hct 37% (Wolters Kluwer, 2018).
Diagnosis: Diabetes Ketoacidosis
- Oxygen administration by nasal cannula on 2L and airway management
- Establish IV access
- IV fluid administration with 0.9% NS; prepare to titrate to 0.45% normal saline as needed
- Monitor blood glucose levels
- Administer 0.1-0.15 unit/kg IV bolus of regular insulin
- IV drip infusion at 0.1 unit/kg/hr of regular insulin to hyperglycemia after bolus,
- Addition of Dextrose to 0.9% NS as glucose levels decreases to 250 mg/dL
- Monitor potassium levels
- Potassium replacement via IV when the potassium level is 5.0 mg/dL or less and urine output is adequate
- Assess for signs of hypokalemia or hyperkalemia
- Monitor vital signs and cardiac rhythm
- Q1-2hr fingerstick blood glucose checks initially, then q4-6hr once stabilized
- Monitor blood pH, I&O
- Assess level of consciousness; provide seizure and safety precautions (Henry et al., 2016)
- Notify MD of any critical changes
Maria Fernandez was then transferred to the ICU unit for close observation, maintenance of IV insulin drip, cardiac monitoring, fluid resuscitation, and correction for metabolic acidosis.
Upon discharge, Maria was reeducated on Type 1 Diabetes Mellitus through the use of preferred learning materials.
- What is the priority assessment data that supports DKA diagnosis?
- What education strategies would you consider implementing to improve treatment adherence after discharge?
- What considerations, services, or resources would you anticipate to be offered by case management or social services?
Henry, N.J., McMichael, M., Johnson, J., DiStasi, A., Ball, B.S., Holman, H.C., Elkins, C.B., Janowski, M.J., Hertel, R.A., Barlow, M.S., Leehy, P., & Lemon, T. (2016). RN adult medical surgical nursing: Review module (10 th ed.). Leawood, KS: Assessment Technologies Institute.
Wolters Kluwer. (2018). Lippincott Nursing Advisor (Version 4.1.0) [Mobile application software]. Retrieved from http://itunes.apple.com
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
- Publications
- Conferences & Events
- Professional Learning
- Science Standards
- Awards & Competitions
- Daily Do Lesson Plans
- Free Resources
- American Rescue Plan
- For Preservice Teachers
- NCCSTS Case Collection
- Partner Jobs in Education
- Interactive eBooks+
- Digital Catalog
- Regional Product Representatives
- e-Newsletters
- Bestselling Books
- Latest Books
- Popular Book Series
- Prospective Authors
- Web Seminars
- Exhibits & Sponsorship
- Conference Reviewers
- National Conference • Denver 24
- Leaders Institute 2024
- National Conference • New Orleans 24
- Submit a Proposal
- Latest Resources
- Professional Learning Units & Courses
- For Districts
- Online Course Providers
- Schools & Districts
- College Professors & Students
- The Standards
- Teachers and Admin
- eCYBERMISSION
- Toshiba/NSTA ExploraVision
- Junior Science & Humanities Symposium
- Teaching Awards
- Climate Change
- Earth & Space Science
- New Science Teachers
- Early Childhood
- Middle School
- High School
- Postsecondary
- Informal Education
- Journal Articles
- Lesson Plans
- e-newsletters
- Science & Children
- Science Scope
- The Science Teacher
- Journal of College Sci. Teaching
- Connected Science Learning
- NSTA Reports
- Next-Gen Navigator
- Science Update
- Teacher Tip Tuesday
- Trans. Sci. Learning
MyNSTA Community
- My Collections
Diabetic Ketoacidosis Upon Diagnosis
A Biochemistry Case Study
By Ali Chaari, Aisha Kafoud
Share Start a Discussion

This directed case study is designed to help students integrate biochemical and physiological concepts with clinical aspects of disease. The case tells the story of a little girl who experiences diabetic ketoacidosis and is diagnosed with type 1 diabetes mellitus (T1DM). The story is based on an actual patient and the presented data are authentic. The case can be delivered as an individual assignment by using the case study handout or displayed in class with optional role play by using the PowerPoint presentation (see Supplemental Materials). Both versions of the case cover the same basic content, but the questions are somewhat different. Upon successful completion of the case, students should understand the basics of metabolic acidosis in T1DM, differences between T1DM and T2DM, and the behavior of the blood buffer equilibrium in response to physiological change. The case was originally written for an intermediate biochemistry course, but it could also be used in a physiology or an advanced biology course.
Download Case
Date Posted
- Discuss the basics of metabolic acidosis in T1DM.
- Distinguish T1DM from T2DM.
- Predict the behavior of the blood buffer equilibrium in response to a physiological change.
- Use Winter’s formula to perform calculations with real patient data.
- Correlate real clinical data with biochemical tests.
- Explain the role of insulin and how ketoacidosis can occur due to insulin insufficiency.
Diabetes; type 1 diabetes; T1DM; ketoacidosis; blood buffer; acidosis; Winter’s formula; insulin insufficiency
Subject Headings
EDUCATIONAL LEVEL
Undergraduate lower division, Undergraduate upper division, Clinical education
TOPICAL AREAS
TYPE/METHODS
Teaching Notes & Answer Key
Teaching notes.
Case teaching notes are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Teaching notes are intended to help teachers select and adopt a case. They typically include a summary of the case, teaching objectives, information about the intended audience, details about how the case may be taught, and a list of references and resources.
Download Notes
Answer Keys are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Download Answer Key
Materials & Media
Supplemental materials.
The PowerPoint presentation below offers an alternative way to deliver the case in class.
- PowerPoint Presentation (~3.9 MB)
You may also like
Web Seminar
Join us on Thursday, June 13, 2024, from 7:00 PM to 8:00 PM ET, to learn about the science and technology of firefighting. Wildfires have become an e...
Join us on Thursday, October 10, 2024, from 7:00 to 8:00 PM ET, for a Science Update web seminar presented by NOAA about climate science and marine sa...
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Research Gaps Around Type 1 Diabetes
A large body of research on Type 2 diabetes has helped to develop guidance, informing how patients are diagnosed, treated, and manage their lifestyle. In contrast, Type 1 diabetes, often mistakenly associated only with childhood, has received less attention.
In this Q&A, adapted from the April 17 episode of Public Health On Call , Stephanie Desmon speaks to Johns Hopkins epidemiologists Elizabeth Selvin , PhD '04, MPH, and Michael Fang , PhD, professor and assistant professor, respectively, in the Department of Epidemiology, about recent findings that challenge common beliefs about type 1 diabetes. Their conversation touches on the misconception that it’s solely a childhood condition, the rise of adult-onset cases linked to obesity, and the necessity for tailored approaches to diagnosis and care. They also discuss insulin prices and why further research is needed on medications like Ozempic in treating Type 1 diabetes.
I want to hear about some of your research that challenges what we have long understood about Type 1 diabetes, which is no longer called childhood diabetes.
MF: Type 1 diabetes was called juvenile diabetes for the longest time, and it was thought to be a disease that had a childhood onset. When diabetes occurred in adulthood it would be type 2 diabetes. But it turns out that approximately half of the cases of Type 1 diabetes may occur during adulthood right past the age of 20 or past the age of 30.
The limitations of these initial studies are that they've been in small clinics or one health system. So, it's unclear whether it's just that particular clinic or whether it applies to the general population more broadly.
We were fortunate because the CDC has collected new data that explores Type 1 diabetes in the U.S. Some of the questions they included in their national data were, “Do you have diabetes? If you do, do you have Type 1 or Type 2? And, at what age were you diagnosed?”
With these pieces of information, we were able to characterize how the age of diagnosis of Type 1 diabetes differs in the entire U.S. population.
Are Type 1 and Type 2 diabetes different diseases?
ES: They are very different diseases and have a very different burden. My whole career I have been a Type 2 diabetes epidemiologist, and I’ve been very excited to expand work with Type 1 diabetes.
There are about 1.5 million adults with Type 1 diabetes in the U.S., compared to 21 million adults with Type 2 diabetes. In terms of the total cases of diabetes, only 5 to 10 percent have Type 1 diabetes. Even in our largest epidemiologic cohorts, only a small percentage of people have Type 1 diabetes. So, we just don't have the same national data, the same epidemiologic evidence for Type 1 diabetes that we have for Type 2. The focus of our research has been trying to understand and characterize the general epidemiology and the population burden of Type 1 diabetes.
What is it about Type 1 that makes it so hard to diagnose?
MF: The presentation of symptoms varies by age of diagnosis. When it occurs in children, it tends to have a very acute presentation and the diagnosis is easier to make. When it happens in adulthood, the symptoms are often milder and it’s often misconstrued as Type 2 diabetes.
Some studies have suggested that when Type 1 diabetes occurs in adulthood, about 40% of those cases are misdiagnosed initially as Type 2 cases. Understanding how often people get diagnosed later in life is important to correctly diagnose and treat patients.
Can you talk about the different treatments?
MF: Patients with Type 1 diabetes are going to require insulin. Type 2 diabetes patients can require insulin, but that often occurs later in the disease, as oral medications become less and less effective.
ES: Because of the epidemic of overweight and obese in the general population, we’re seeing a lot of people with Type 1 diabetes who are overweight and have obesity. This can contribute to issues around misdiagnosis because people with Type 1 diabetes will have signs and will present similarly to Type 2 diabetes. They'll have insulin resistance potentially as a result of weight gain metabolic syndrome. Some people call it double diabetes—I don't like that term—but it’s this idea that if you have Type 1 diabetes, you can also have characteristics of Type 2 diabetes as well.
I understand that Type 1 used to be considered a thin person's disease, but that’s not the case anymore. MF: In a separate paper, we also explored the issue of overweight and obesity in persons with Type 1 diabetes. We found that approximately 62% of adults with Type 1 diabetes were either overweight or obese, which is comparable to the general U.S. population.
But an important disclaimer is that weight management in this population [with Type 1 diabetes] is very different. They can't just decide to go on a diet, start jogging, or engage in rigorous exercise. It can be a very, very dangerous thing to do.
Everybody's talking about Ozempic and Mounjaro—the GLP-1 drugs—for diabetes or people who are overweight to lose weight and to solve their diabetes. Where does that fit in with this population?
ES: These medications are used to treat Type 2 diabetes in the setting of obesity. Ozempic and Mounjaro are incretin hormones. They mediate satiation, reduce appetite, slow gastric emptying, and lower energy intake. They're really powerful drugs that may be helpful in Type 1 diabetes, but they're not approved for the management of obesity and Type 1 diabetes. At the moment, there aren't data to help guide their use in people with Type 1 diabetes, but I suspect they're going to be increasingly used in people with Type 1 diabetes.
MF: The other piece of managing weight—and it's thought to be foundational for Type 1 or Type 2—is dieting and exercising. However, there isn’t good guidance on how to do this in persons with Type 1 diabetes, whereas there are large and rigorous trials in Type 2 patients. We’re really just starting to figure out how to safely and effectively manage weight with lifestyle changes for Type 1 diabetics, and I think that's an important area of research that should continue moving forward.
ES: Weight management in Type 1 diabetes is complicated by insulin use and the risk of hypoglycemia, or your glucose going too low, which can be an acute complication of exercise. In people with Type 2 diabetes, we have a strong evidence base for what works. We know modest weight loss can help prevent the progression and development of Type 2 diabetes, as well as weight gain. In Type 1, we just don't have that evidence base.
Is there a concern about misdiagnosis and mistreatment? Is it possible to think a patient has Type 2 but they actually have Type 1?
MF: I think so. Insulin is the overriding concern. In the obesity paper, we looked at the percentage of people who said their doctors recommended engaging in more exercise and dieting. We found that people with Type 1 diabetes were less likely to receive the same guidance from their doctor. I think providers may be hesitant to say, “Look, just go engage in an active lifestyle.”
This is why it's important to have those studies and have that guidance so that patients and providers can be comfortable in improving lifestyle management.
Where is this research going next?
ES: What's clear from these studies is that the burden of overweight and obesity is substantial in people with Type 1 diabetes and it's not adequately managed. Going forward, I think we're going to need clinical trials, clear clinical guidelines, and patient education that addresses how best to tackle obesity in the setting of Type 1 diabetes.
It must be confusing for people with Type 1 diabetes who are hearing about people losing all this weight on these drugs, but they go to their doctor who says, “Yeah, but that's not for you.”
ES: I hope it's being handled more sensitively. These drugs are being used by all sorts of people for whom they are not indicated, and I'm sure that people with Type 1 diabetes are accessing these drugs. I think the question is, are there real safety issues? We need thoughtful discussion about this and some real evidence to make sure that we're doing more good than harm.
MF: Dr. Selvin’s group has published a paper, estimating that about 15% of people with Type 1 diabetes are on a GLP-1. But we don't have great data on what potentially can happen to individuals.
The other big part of diabetes that we hear a lot about is insulin and its price. Can you talk about your research on this topic?
MF: There was a survey that asked, “Has there been a point during the year when you were not using insulin because you couldn’t afford it?” About 20% of adults under the age of 65 said that at some point during the year, they couldn't afford their insulin and that they did engage in what sometimes is called “cost-saving rationing” [of insulin].
Medicare is now covering cheaper insulin for those over 65, but there are a lot of people for whom affordability is an issue. Can you talk more about that?
MF: The fight is not over. Just because there are national and state policies, and now manufacturers have been implementing price caps, doesn't necessarily mean that the people who need insulin the most are now able to afford it.
A recent study in the Annals of Internal Medicine looked at states that adopted or implemented out-of-pocket cost caps for insulin versus those that didn't and how that affected insulin use over time. They found that people were paying less for insulin, but the use of insulin didn't change over time. The $35 cap is an improvement, but we need to do more.
ES: There are still a lot of formulations of insulin that are very expensive. $35 a month is not cheap for someone who is on insulin for the rest of their lives.
- Overweight and Obesity in People With Type 1 Diabetes Nearly Same as General Population
- The Impacts of COVID-19 on Diabetes and Insulin
- Why Eli Lilly’s Insulin Price Cap Announcement Matters
Related Content

To Protect Human Health, We Must Protect the Earth’s Health

New Grant Enables Johns Hopkins Researchers to Implement Community Health Worker-Led Health Interventions for Noncommunicable Diseases in Nepal

The Omnipresence of PFAS—and What We Can Do About Them


Summer Institute in Data to Policy

Filters and Digital Health Program Reduced Participants' Arsenic Levels by Nearly Half in American Indian Households Relying on Well Water
- Introduction
- Article Information
HR indicates hazard ratio.
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
- CME & MOC
Kendall EK , Olaker VR , Kaelber DC , Xu R , Davis PB. Association of SARS-CoV-2 Infection With New-Onset Type 1 Diabetes Among Pediatric Patients From 2020 to 2021. JAMA Netw Open. 2022;5(9):e2233014. doi:10.1001/jamanetworkopen.2022.33014
Manage citations:
© 2024
- Permissions
Association of SARS-CoV-2 Infection With New-Onset Type 1 Diabetes Among Pediatric Patients From 2020 to 2021
- 1 Center for Artificial Intelligence in Drug Discovery, Case Western Reserve University School of Medicine, Cleveland, Ohio
- 2 The Center for Clinical Informatics Research and Education, The MetroHealth System, Cleveland, Ohio
- 3 Center for Community Health Integration, Case Western Reserve University School of Medicine, Cleveland, Ohio
Incidence of new-onset type 1 diabetes (T1D) increased during the COVID-19 pandemic, 1 and this increase has been associated with SARS-CoV-2 infection. 2 The US Centers for Disease Control and Prevention reported that pediatric patients with COVID-19 were more likely to be diagnosed with diabetes after infection, although types 1 and 2 were not separated. 3 Therefore, whether COVID-19 was associated with new-onset T1D among youths remains unclear. This cohort study assessed whether there was an increase in new diagnoses of T1D among pediatric patients after COVID-19.
Data were obtained using TriNetX Analytics Platform, a web-based database of deidentified electronic health records of more than 90 million patients, from the Global Collaborative Network, which includes 74 large health care organizations across 50 US states and 14 countries with diverse representation of geographic regions, self-reported race, age, income, and insurance types. 4 The MetroHealth System institutional review board deemed the study exempt because it was determined to be non–human participant research. The study followed the STROBE reporting guideline.
The study population comprised pediatric patients in 2 cohorts: (1) patients aged 18 years or younger with SARS-CoV-2 infection between March 2020 and December 2021 and (2) patients aged 18 years or younger without SARS-CoV-2 infection but with non–SARS-CoV-2 respiratory infection during the same period. SARS-CoV-2 infection was defined as described in prior studies. 5 These cohorts were subdivided into groups aged 0 to 9 years and 10 to 18 years.
Cohorts were propensity score matched (1:1 using nearest-neighbor greedy matching) for demographics and family history of diabetes ( Table ). Risk of new diagnosis of T1D within 1, 3, and 6 months after infection were compared between matched cohorts using hazard ratios (HRs) and 95% CIs. Statistical analyses were conducted in the TriNetX Analytics Platform. Further details and analyses from the TriNetX database are given in the eMethods in the Supplement .
The Table shows population characteristics before and after matching. The study population included 1 091 494 pediatric patients: 314 917 with COVID-19 and 776 577 with non–COVID-19 respiratory infections. The matched cohort included 571 256 pediatric patients: 285 628 with COVID-19 and 285 628 with non–COVID-19 respiratory infections. By 6 months after COVID-19, 123 patients (0.043%) had received a new diagnosis of T1D, but only 72 (0.025%) were diagnosed with T1D within 6 months after non–COVID-19 respiratory infection. At 1, 3, and 6 months after infection, risk of diagnosis of T1D was greater among those infected with SARS-CoV-2 compared with those with non–COVID-19 respiratory infection (1 month: HR, 1.96 [95%CI, 1.26-3.06]; 3 months: HR, 2.10 [95% CI, 1.48-3.00]; 6 months: HR, 1.83 [95% CI, 1.36-2.44]) and in subgroups of patients aged 0 to 9 years, a group unlikely to develop type 2 diabetes, and 10 to 18 years ( Figure ). Similar increased risks were observed among children infected with SARS-CoV-2 compared with other control cohorts at 6 months (fractures: HR, 2.09 [95% CI, 1.41- 3.10]; well child visits: HR, 2.10 [95% CI, 1.61- 2.73]).
In this study, new T1D diagnoses were more likely to occur among pediatric patients with prior COVID-19 than among those with other respiratory infections (or with other encounters with health systems). Respiratory infections have previously been associated with onset of T1D, 6 but this risk was even higher among those with COVID-19 in our study, raising concern for long-term, post–COVID-19 autoimmune complications among youths. Study limitations include potential biases owing to the observational and retrospective design of the electronic health record analysis, including the possibility of misclassification of diabetes as type 1 vs type 2, and the possibility that additional unidentified factors accounted for the association. Results should be confirmed in other populations. The increased risk of new-onset T1D after COVID-19 adds an important consideration for risk-benefit discussions for prevention and treatment of SARS-CoV-2 infection in pediatric populations.
Accepted for Publication: August 6, 2022.
Published: September 23, 2022. doi:10.1001/jamanetworkopen.2022.33014
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2022 Kendall EK et al. JAMA Network Open .
Corresponding Author: Rong Xu, PhD, Sears Tower T303, Center for Artificial Intelligence in Drug Discovery ( [email protected] ); Pamela B. Davis, MD, PhD, Sears Tower T402, Center for Community Health Integration ( [email protected] ), Case Western Reserve University, 10900 Euclid Ave, Cleveland, OH 44106.
Author Contributions : Ms Kendall and Ms Olaker had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Kendall, Xu, Davis.
Acquisition, analysis, or interpretation of data: Kendall, Olaker, Kaelber, Xu.
Drafting of the manuscript: Kendall, Olaker.
Critical revision of the manuscript for important intellectual content: Kendall, Kaelber, Xu, Davis.
Statistical analysis: Kendall, Olaker, Xu.
Obtained funding: Xu.
Administrative, technical, or material support: All authors.
Supervision: Kaelber, Xu, Davis.
Conflict of Interest Disclosures: Dr Kaelber reported receiving grants from the National Institutes of Health during the conduct of the study. No other disclosures were reported.
Funding/Support : This study was supported by grants AG057557 (Dr Xu), AG061388 (Dr Xu), AG062272 (Dr Xu), and AG076649 (Drs Xu and Davis) from the National Institute on Aging; grant R01AA029831 (Drs Xu and Davis) from the National Institute on Alcohol Abuse and Alcoholism; grant UG1DA049435 from the National Institute on Drug Abuse, and grant 1UL1TR002548-01 from the Clinical and Translational Science Collaborative of Cleveland.
Role of the Funder/Sponsor : The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
The use of FreeStyle libre improves glycaemic control along with reducing diabetes burden and hospital admissions in a socially deprived Northwest English population
- Research article
- Published: 23 April 2024
Cite this article

- Giovanni Cucinotta 1 ,
- Zeeshan Tariq 1 ,
- Adhithya Sankar 1 ,
- Francis L. Martin 2 &
- Stephen Nyangoma 2
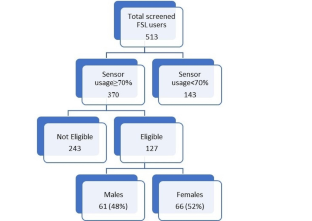
This retrospective study aimed to use mixed (qualitative and quantitative) methods to evaluate the role of FSL in reducing hospital admissions due to all causes, HbA1c, and reported hypoglycaemic episodes in people with diabetes living in a socially deprived region of Northwest England.
Data were collected retrospectively from previous consultations, which coincided with the 6th -week, 6th -month and annual review including blood tests, hospital admissions due to any cause and reported hypoglycaemia. Also, FSL assessment and satisfaction semi-structured questionnaire was done to assess the impact of FSL on diabetes management and quality of life. Mixed-effects models were used to assess glycaemic control and reductions in hospital admissions and reported hypoglycaemic episodes.
Just 127 patients met the inclusion criteria. A multivariate linear mixed model method that analyses HbA1c data longitudinally revealed mean differences (mmol/mol) between baseline and post-FSL measurements, estimated by restricted maximum likelihood method (REML) of 9.64 (six weeks), 7.68 (six months) and 7.58 (annual review); all with a corresponding p -value of < 0.0001. For DKA patients, the bootstrap method revealed a significant reduction in mean HbA1c of 25.5, 95% confidence interval (CI) [8.8, 42.6] mmol/mol. It is demonstrated that FSL use for one year resulted in 59% reduction in hospital admissions and 46% reduction in reported hypoglycaemic episodes.
The use of FSL resulted in statistically significant reductions in hospital admissions, HbA1c and reported hypoglycaemic episodes among diabetics in a socially deprived Northwest region of England. These outcomes show a direct association with a higher questionnaire score.
Key message
• FreeStyle Libre (FSL) users in deprived areas are likely to have a reduction in: all diabetes and non-diabetes related hospital admissions; diabetic ketoacidosis (DKA); and, hypoglycaemia and glycated haemoglobin (HbA1c) levels.
• Most FSL users perceive a reduction in their diabetes burden and more in control of their diabetes and this is directly associated with improved care outcomes. Patients with a higher questionnaire score present with the greatest improvements.
• More than one-third of the total FSL users reported a sensor usage <70% which suggests that compliance remains a significant issue and this raises questions on the cost-effectiveness of this technology in this type of population.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Data availability
The data that support the findings of this study are available on request from the corresponding author, [GC]. The data are not publicly available due to restrictions as their containing information could compromise the privacy of research participants.
Abbreviations
Ambulatory Glucose Profile
Clinical Commissioning Groups
Continuous Glucose Monitoring System
confidence interval
Diabetic Keto-Acidosis
English Index of Multiple Deprivation
- FreeStyle Libre
glycated haemoglobin
interquartile range
Incidence Rate-Ratios
intermittently scanned continuous glucose monitoring
Latent Autoimmune Diabetes in Adults
Lower-layer Super Output Areas
Maturity-onset diabetes of the young
restricted maximum likelihood method
Standard Deviation
Time In Range
Lancashire County Council. 2019 deprivation analysis. 2019. https://www.lancashire.gov.uk/lancashire-insight/deprivation/indices-of-deprivation-2019/2019-deprivation-analysis/ . Accessed 1 January 2022.
Public Health England. Blackpool Local Authority Health Profile 2019. 2020. https://fingertips.phe.org.uk/static-reports/health-profiles/2019/e06000009.html?area-name=blackpool . Accessed 2 January 2022.
Lancashire County Council. Diabetes. 2021. https://www.lancashire.gov.uk/lancashire-insight/health-and-care/health/long-term-conditions/diabetes/ . Accessed 18 November 2023.
Diabetes.co.uk. Cost of Diabetes. 2019. https://www.diabetes.co.uk/cost-of-diabetes.html . Accessed 6 February 2022.
Lameijer A, Fokkert MJ, Edens MA, et al. Two-year use of flash glucose monitoring is associated with sustained improvement of glycemic control and quality of life (FLARE-NL-6)BMJ Open Diabetes. Res Care. 2021;9:e002124. https://doi.org/10.1136/bmjdrc-2021-002124 .
Article Google Scholar
Al Hayek AA, Al Dawish MA. Frequency of Diabetic Ketoacidosis in patients with type 1 diabetes using FreeStyle Libre: a Retrospective Chart Review. Adv Ther. 2021;38(6):3314–24. https://doi.org/10.1007/s12325-021-01765-z .
Article CAS PubMed PubMed Central Google Scholar
Lameijer A, Fokkert MJ, Edens MA, Slingerland RJ, Bilo HJG, van Dijk PR. Determinants of HbA1c reduction with FreeStyle Libre flash glucose monitoring (FLARE-NL 5). J Clin Transl Endocrinol. 2020;22:100237. https://doi.org/10.1016/j.jcte.2020.100237 .
Ministry of Housing, Communities & Local Government. The English Indices of Deprivation 2019 (IoD2019). https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/835115/IoD2019_Statistical_Release.pdf Accessed 1 February 2024.
Gibb FW, Jennings P, Leelarathna L, Wilmot EG. AGP in daily clinical practice: a guide for use with the FreeStyle Libre flash glucose monitoring system. British Journal of Diabetes. 2020;20(1):32–40. https://doi.org/10.15277/bjd.2020.240 .
Green JA. Too many zeros and/or highly skewed? A tutorial on modelling health behaviour as count data with Poisson and negative binomial regression. Health Psychol Behav Med. 2021;9(1):436–55. https://doi.org/10.1080/21642850.2021.1920416 .
Article PubMed PubMed Central Google Scholar
Wagner JA, Bermudez-Millan A, Berthold SM, et al. Risk factors for drug therapy problems among Cambodian americans with complex needs: a cross-sectional, observational study. Health Psychol Behav Med. 2022;10(1):145–59. https://doi.org/10.1080/21642850.2021.2021917 .
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2023. URL https://www.R-project.org/ .
Wickham H. (2016). ggplot2: Elegant Graphics for Data Analysis . Springer-Verlag New York. ISBN 978-3-319-24277-4, https://ggplot2.tidyverse.org .
NICE. Recommendations| Type 2 diabetes in adults: management| Guidance| NICE. www.nice.org.uk.2015. https://www.nice.org.uk/guidance/ng28/chapter/Recommendations#hbA1c-measurement-and-targets . Accessed 10 July 2023.
NICE. Recommendations| Type 1 Diabetes in Adults: Diagnosis and Management| Guidance| NICE. www.nice.org.uk.2015. https://www.nice.org.uk/guidance/ng17/chapter/Recommendations Accessed 10 July 2023.
Overend L, Simpson E, Grimwood T. Qualitative analysis of patient responses to the ABCD FreeStyle Libre audit questionnaire. Practical Diabetes. 2019;36(2):45–50.
Download references
Acknowledgements
We acknowledge the help of Natasya Atherton, Simone Johnston and the rest of the DSN team for supporting the data collection of this study. F.L.M. and S.N. received funding from the NIHR Manchester Biomedical Research Centre (Grant number: NIHR203308). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
Adult Diabetes Department, Blackpool Teaching Hospitals NHS Foundation Trust, Whinney Heys Road, FY3 8NR, Blackpool, UK
Giovanni Cucinotta, Zeeshan Tariq & Adhithya Sankar
Research & Development, Blackpool Teaching Hospitals NHS Foundation Trust, Whinney Heys Road, FY3 8NR, Blackpool, UK
Francis L. Martin & Stephen Nyangoma
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Giovanni Cucinotta .
Ethics declarations
There are no conflicts of interest to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cucinotta, G., Tariq, Z., Sankar, A. et al. The use of FreeStyle libre improves glycaemic control along with reducing diabetes burden and hospital admissions in a socially deprived Northwest English population. J Diabetes Metab Disord (2024). https://doi.org/10.1007/s40200-024-01424-4
Download citation
Received : 04 January 2024
Accepted : 20 March 2024
Published : 23 April 2024
DOI : https://doi.org/10.1007/s40200-024-01424-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Socially deprived population
- Hospital admissions
- Hypoglycaemia
- Find a journal
- Publish with us
- Track your research

- Follow UNSW on LinkedIn
- Follow UNSW on Instagram
- Follow UNSW on Facebook
- Follow UNSW on WeChat
- Follow UNSW on TikTok
$5.7m for clinical trials
2024-04-17T10:03:00+10:00

Photo: Getty Images.
Three UNSW Sydney projects have been awarded funding under the government’s Medical Research Future Fund’s clinical trials activity initiative.
UNSW Sydney researchers have been awarded more than $5.7 million under the Australian government’s Medical Research Future Fund (MRFF) clinical trials activity initiative, with projects spanning spinal cord injury, stroke, and diabetic ketoacidosis.
Interim Dean of UNSW Medicine & Health Professor Adrienne Torda congratulated the UNSW researchers who received funding.
“These grants will help UNSW researchers and our partners improve the quality of life and health outcomes for many. I am so proud the teams who were successful in this round of funding and look forward to supporting their studies,” Prof. Torda said.
Reducing spinal cord injury pain
UNSW Professor Sylvia Gustin from UNSW Science and NeuRA was awarded $2.22 million for a randomised placebo-controlled trial to investigate the efficacy of an interactive brain-computer interface neuromodulation treatment combined with transcranial direct current stimulation for people with spinal cord injury neuropathic pain.
The team of Prof. Gustin will conduct a randomised clinical trial to examine the efficacy and mechanisms of an advanced interactive Brain-Computer Interface Neuromodulation (BCI-N) treatment combined with transcranial direct current stimulation (tDCS). The study has the potential to inform patient care across the spectrum of initial hospitalisation to home-based self-management.
“Given the deleterious impact of spinal cord injury neuropathic pain on the quality of life and the easy translation of our novel brain-technology intervention into accessible home use, the results of this clinical trial are expected to provide a sustainable advance in spinal cord injury pain management,” Prof. Gustin said.
Improving outcomes for people with a debilitating form of stroke
Professor Jeremy Cohen from The George Institute for Global Health and UNSW Medicine & Health has received $1.9 million for a project that aims to improve the outcomes for younger people with a debilitating form of stroke, subarachnoid haemorrhage.
“A subarachnoid haemorrhage is a devastating type of stroke affecting around 2000 Australians a year, a third of whom will die from the condition with the remainder at risk of permanent disability. Up to 40 per cent of this often young and previously fit population are unable to return to their previous occupation,” Prof. Cohen said.
A common complication in this type of stroke is low blood levels of sodium (or hyponatremia) which occurs in up to two thirds of hospitalised patients. Hyponatremia is associated with a twofold increase in duration of hospital and ICU stay in these patients.
Previous work by Dr Jeremy Cohen, Director of the Wesley Hospital Intensive Care Unit and Honorary Professorial Fellow at The George Institute, confirmed that hyponatraemia during ICU admission is also significantly associated with worse levels of disability six months later.
This study will investigate if fludrocortisone, a low cost and well-established corticosteroid that regulates salt and water balance in the body, can prevent this fall in sodium and therefore improve outcomes in these patients.
Fluid therapy for diabetic ketoacidosis
Professor Mahesh Ramanan from The George Institute for Global Health and UNSW Medicine & Health has received $1.6 million for a fluid therapy trial for patients presenting with diabetic ketoacidosis.
Diabetic ketoacidosis (DKA) is a life-threatening complication of diabetes in which the body produces excess blood acids known as ketones. It occurs when there isn't enough insulin in the body and can be triggered by infection or other illness.
Fluid therapy is a vital component of the treatment of DKA, but which fluid provides the best outcomes is unknown. Saline is widely recommended in national and international guidelines despite a lack of high-quality evidence to support its use. It can lead to complications associated with worse outcomes in critically ill patients.
An alternative fluid, Plasma-Lyte 148 – a balanced salt solution that more closely matches the biochemistry of human blood – has theoretical advantages over saline and is recommended in some DKA guidelines.
“It is hoped that the results will provide definitive guidance on the best choice of fluid therapy in DKA and reduce healthcare costs by reducing the time patients need to spend in ICU and hospital,” Prof. Ramanan said.
Media enquiries
For enquiries about this story and interview requests please contact Yolande Hutchinson.
Tel: 0420 845 023 Email: [email protected]

Share this story
- Share this page on Email
- Share this page on Facebook
- Share this page on Twitter
- Share this page on LinkedIn
- Share this page on WhatsApp
- Share this page on FacebookMessenger
- Share this page on WeChat
- Share this page on Copy
Related stories

UNSW awarded over $17m in NHMRC clinical trials funding

UNSW researchers awarded $33m for medical research

UNSW receives $20m to support medical breakthroughs

- Previous Article
- Next Article
Presentation
Clinical pearls, case study: type 1 and type 2, too.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Heidi L. Gassner , Stephen E. Gitelman; Case Study: Type 1 and Type 2, Too?. Clin Diabetes 1 July 2003; 21 (3): 140–141. https://doi.org/10.2337/diaclin.21.3.140
Download citation file:
- Ris (Zotero)
- Reference Manager
R.M. is a 17-year-old African-American girl with new-onset diabetes, presumed to be type 2 diabetes. She presented to her pediatrician during the winter months with the classic symptoms of polyuria and polydipsia. She reported weight loss over the preceding weeks, but was otherwise well. Her family history was positive for type 2 diabetes in grandparents and some distant relatives and negative for autoimmune diseases.
Physical examination revealed a blood pressure of 103/53 mmHg, pulse of 79, and temperature of 38°C. Her weight was 60 kg (132 lb, 50–75th percentile), height was 155 cm (61 inches, 10th percentile), and body mass index (BMI) was 25 kg/m 2 (85th percentile). She had acanthosis nigricans and was at Tanner V stage of sexual development.
Urinalysis revealed a glucose level of >1,000 mg/dl and ketones of 40 mg/dl. Her initial laboratory studies included a blood glucose measurement of 726 mg/dl, bicarbonate of 21 mmol/l (normal range 23–32 mmol/l), venous pH of 7.37, hemoglobin A 1c (A1C) of 8.6%, and C-peptide of 1.0 ng/ml (normal range 0.6–3.2 ng/ml).
R.M. was admitted to the hospital for subcutaneous insulin therapy, fluids, and diabetes education. She was discharged to her home on metformin, 500 mg twice daily, and a split-mixed insulin regimen of NPH and lispro at ∼1 unit/kg/day, with two-thirds being taken in the morning and one-third in the evening. She was also started on a fixed carbohydrate, reduced-fat meal plan.
At her first follow-up visit 1 month later, R.M. was found to be positive for islet cell autoantibodies (ICAs), glutamic acid decarboxylase (GAD) antibodies, and ICA-512 antibodies. Her A1C was 7.8%. Her insulin doses had been slowly decreased, with glucose levels consistently <150 mg/dl and total daily insulin requirements of ∼0.5 units/kg/day. Her metformin was discontinued given her positive antibody studies and near-euglycemic blood glucose range.
At another follow-up 3 months later, R.M. was still off metformin, and her blood glucose levels were in a euglycemic range on <0.4 units/kg/day (10 units of NPH with 4 units of lispro at breakfast and 6 units of NPH with 3 units of lispro at dinner). Her A1C was 5.9%. She had not required any adjustments for high blood glucose levels.
How does one distinguish between type 1 diabetes and type 2 diabetes?
When should autoantibodies be measured?
In patients who have type 1 diabetes with evidence of insulin resistance, what treatment options are available?
Most practitioners today would have assumed that this adolescent had recent-onset type 2 diabetes. The risk factors include non-Caucasian ancestry, positive family history, presence of acanthosis in someone with an elevated BMI, and hyperglycemia without ketoacidosis. 1
In the past, type 1 diabetes would account for the majority of diabetes seen in this age-group. Yet, the national obesity epidemic has changed the types of diabetes being seen, especially in pediatrics. The most recent National Health and Nutrition Examination Survey noted that 30% of adolescents are now overweight, 2 and there has been a commensurate rise in the number of cases of type 2 diabetes found in adolescents. 3 Recently, in a cohort of obese adolescents, 20% were noted to have impaired glucose tolerance, and 4% had undiagnosed type 2 diabetes. 4 In some pediatric diabetes practices, type 2 diabetes now accounts for 25–50% of the patient population, and this continues to increase. 1
The incidence of type 2 diabetes in American adolescents is highest among African-Americans, Latinos, and Asians. 1 For the African American population, this increased risk for type 2 diabetes results at least in part from the fact that African-American prepubertal children and adolescents have greater insulin resistance than their Caucasian counterparts, even when matched for BMI. 5 , 6
Given the increase of obesity in our society, we expect that many children who present with new-onset diabetes will have evidence of obesity and acanthosis, which are strongly suggestive of type 2 diabetes. Yet, rather than assume that they have type 2 diabetes, clinicians must test for autoantibodies to clarify the underlying etiology.
R.M. was found to have positive antibodies directed against the β-cells and thus, clearly, has autoimmune-mediated type 1 diabetes. However, she also has evidence of insulin resistance, which is found in type 2 diabetes. Some have referred to this condition as “double diabetes,” or “type 1.5 diabetes.”
Multiple studies have shown that up to 90% of new-onset type 1 diabetic patients will have evidence of at least one antibody at diagnosis, and ∼40–50% will have two or more. 7 Tests for four autoantibodies are now available through commercial laboratories. The traditional assay to measure ICAs involves incubating a patient’s serum with a section of normal pancreas and assessing reactivity via indirect immunoflurosence. The other three antibody tests now available are for GAD, ICA-512 (also known as IA-2 or tyrosine phosphatase), and insulin autoantibodies (IAAs). The IAA measurement must be obtained within 10 days to 2 weeks from the initiation of exogenous insulin therapy, because exogenous insulin may induce antibody positivity.
Although most patients with type 1 diabetes are autoantibody-positive, ethnicity confers notable differences and may make confirmation of type 1 diabetes more difficult. African-American adolescents with new-onset type 1 diabetes have up to a fourfold greater chance of exhibiting no autoantibodies compared to their Caucasian counterparts (17.4 vs. 4.6%, respectively). 8 Thus, African-American adolescents with type 1 diabetes may initially present as antibody-negative, which may prove misleading in making therapy decisions.
The presence of autoantibodies has important implications for patient care. In the U.K. Prospective Diabetes Study, subjects presumed to have type 2 diabetes, yet who were noted to have one or more autoantibodies, progressed more rapidly to β-cell failure and required insulin therapy. 9 Up to 90% of patients who were positive for ICA and GAD antibodies required insulin within 6 years. 9
In this case, had one assumed that this was a case of type 2 diabetes and treated R.M. solely with metformin, the patient may have done well initially, during her honeymoon phase. However, she would have been at high risk for progression to diabetic ketoacidosis as her honeymoon period waned or when faced with an intercurrent illness or stress. Furthermore, intensive insulin therapy is one potential means to prolong the honeymoon phase and protect endogenous insulin secretion, 10 and she would have been denied this potential benefit.
Despite the evidence that R.M. has type 1 diabetes, we must return to considerations about type 2 diabetes. Although she tested positive for autoantibodies, she did present with acanthosis nigricans, an elevated BMI, a positive family history, and was from a higher-risk ethnic group. If we had studied her formally, she would almost certainly have exhibited increased insulin resistance, and she may have ultimately developed type 2 diabetes later in life if she had not had earlier autoimmune destruction of her β-cells.
One question to consider is whether there is a role for insulin sensitizers in such a situation. Metformin may be a useful addition to insulin for adolescents with type 1 diabetes and insulin resistance. 11 Preliminary studies have found that metformin lowered A1C, decreased insulin dosage, and caused no weight gain in adolescents with type 1 diabetes and poor metabolic control. 11 Clinicians initiating such therapy must carefully inform the patient and family about the risks of lactic acidosis and the increased risk for hypoglycemia with combined therapy. Further studies with metformin and other insulin sensitizers (such as thiazolidinediones) are needed before this will become established therapy.
For R.M., we elected to continue her subcutaneous low-dose insulin regimen at 0.4 units/kg/day during the honeymoon phase, but we may consider adding metformin therapy in the future.
With the surge in obesity, we are witnessing a rise in type 2 diabetes, especially among children and adolescents. These patients often present in puberty, at a time of increased insulin resistance.
All pediatric patients who are diagnosed with new-onset diabetes need antibody studies obtained to distinguish type 1 from type 2 diabetes in order to provide appropriate therapies. Autoantibodies may not always be positive in African Americans with new-onset type 1 diabetes.
Patients who have type 1 diabetes and evidence of insulin resistance may benefit from the addition of metformin as an insulin-sensitizing agent. However, the use of metformin in these patients is still under investigation and has not yet gained approval from the Food and Drug Administration.
Heidi L. Gassner, MD, is a pediatric endocrine fellow, and Stephen E. Gitelman, MD, is an associate professor of clinical pediatrics in the Department of Pediatric Endocrinology at the University of California, San Francisco.
Email alerts
- Online ISSN 1945-4953
- Print ISSN 0891-8929
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account

IMAGES
VIDEO
COMMENTS
We present a case of diabetic ketoacidosis in a child with type 1 diabetic mellitus. It is a life threatening complications if timely intervention is not done. Timely management with fluid therapy along with insulin should be done. Regular monitoring and neurological observation are equally important to prevent complications like cerebral edema.
Diabetic ketoacidosis (DKA) is a cardinal feature of type 1 diabetes. However, there is a strong, almost dogmatic, errant perception by physicians that DKA is a complication that only occurs in patients with type 1 diabetes. This is not true. DKA does occur in type 2 diabetes; however, it rarely occurs in the absence of a precipitating event.
Case Reports in Emergency Medicine 2017. Diabetic ketoacidosis (DKA) is a potentially life-threatening acute complication of type 1 diabetes caused by insulin deficiency. It is characterized by raised blood glucose (hyperglycemia), metabolic acidosis, and increased blood/urine ketones. Dehydration and electrolyte disturbance are common and ...
Despite advances in medical management, type 1 diabetes remains a burdensome disease with everyday challenges and substantial medical costs. In addition, most youth with type 1 diabetes do not meet the American Diabetes Association guidelines for glycemic control and are likely to experience excess morbidity and premature mortality (17-19).The objective of this study was to test the ...
Case Study: Hyperglycemia, concern for diabetic ketoacidosis, and type 1 diabetes History of present illness The patient is a 36-year-old man who has had type 1 diabetes for 15 years.
** The data in Tables 1 and 2 (following page) and the description of the patient's condition and treatment have been modified from a case reported by A.N. Cebeci and A. G. Üven ("Delirium in Diabetic Ketoacidosis: A Case Report," The Journal of Clinical Research in Pediatric Endo-crinology . 4(1): 39-41, 2012).
Further work revealed a patient with type 1 diabetes who was being treated with oral agents indicated for type 2 diabetes, all of which may have contributed to and precipitated EDKA. This case highlights the importance of accurately diagnosing diabetes subclasses and emphasizes the need to consider dietary risk factors in addition to ...
Results of hospital laboratory studies (Table 1-1) revealed that the patient's initial blood glucose level was 1192 mg/dL and clinical presentation and laboratory findings were consistent with a diagnosis of diabetic ketoacidosis (DKA). The patient reported no family history of diabetes. His father died at age 35 of renal failure.
Diabetic Ketoacidosis Upon Diagnosis: A Biochemistry Case Study. Diabetes mellitus is a metabolic disorder characterised by hyperglycemia. The two main types of diabetes mellitus are type 1 diabetes mellitus (T1DM) and type 2 (T2DM), which exhibit similar symptoms while having two very difer-ent pathophysiologies (Alam et al., 2014).
On March 6th, 2019, Maria Fernandez, a 19-year-old female, presented to the Emergency Department with complaints of nausea, vomiting, abdominal pain, and lethargy. She reveals a recent diagnosis of type 1 diabetes but admits to noncompliance with treatment. At the time of admission, Maria's vital signs were as follows: BP 87/50, HR 118, RR 28 ...
A case-control study conducted psychiatric assessments on people described as having 'brittle diabetes', a study population having frequent admissions with Type 1 diabetes. 8 However, the study did not quantify numbers of people with recurrent DKA only describing them as having 'glycaemic instability'. Therefore, their finding of an ...
Background: Diabetic ketoacidosis (DKA) is a common consequence of electrolyte and dehydration abnormalities that affect individuals with type-1 diabetes. DKA is a major diabetic complication ...
Case Study: Hyperglycemia, concern for diabetic ketoacidosis, and type 1 diabetes. Hospital course. In the emergency room, the patient's lab work was obtained, and he was determined to not have ...
People with type 1 diabetes who take a GLP-1 drug for weight loss or other health benefits may see unexpected low blood sugar levels, as well as a higher risk of diabetic ketoacidosis. While GLP-1 agonists have become a staple for weight ... A case study. In a 2023 case report, a person with type 1 arrived at an emergency room with ...
The patient's history of present illness on admission includes type I diabetes and missing insulin administration, which led to diabetic ketoacidosis (Bedaso, Oltaye, Geja, & Ayalew, 2019). Past and current medical history: Type I diabetes since she was 9 years old, hypothyroidism, hypertension, and asthma.
Abstract. This directed case study is designed to help students integrate biochemical and physiological concepts with clinical aspects of disease. The case tells the story of a little girl who experiences diabetic ketoacidosis and is diagnosed with type 1 diabetes mellitus (T1DM). The story is based on an actual patient and the presented data ...
Severe hypertriglyceridemia (HTG) is a rare complication of insulin resistance. Its presentation with diabetic ketoacidosis (DKA) has been reported in a few cases, where most patients have type-1 diabetes mellitus (DM). Our case represents a unique presentation of DKA associated with severe HTG above 10,000 mg/dL in an adult with type-2 DM.
There are about 1.5 million adults with Type 1 diabetes in the U.S., compared to 21 million adults with Type 2 diabetes. In terms of the total cases of diabetes, only 5 to 10 percent have Type 1 diabetes. Even in our largest epidemiologic cohorts, only a small percentage of people have Type 1 diabetes. So, we just don't have the same national ...
Incidence of new-onset type 1 diabetes (T1D) increased during the COVID-19 pandemic, 1 and this increase has been associated with SARS-CoV-2 infection. 2 The US Centers for Disease Control and Prevention reported that pediatric patients with COVID-19 were more likely to be diagnosed with diabetes after infection, although types 1 and 2 were not separated. 3 Therefore, whether COVID-19 was ...
We conducted a cohort study using nationwide registers from 1996 to 2020 to identify individuals with diabetes, ascertain SMI status (namely, schizophrenia, bipolar disorder, or major depression) and identify the outcomes: hospitalization for hypoglycemia and diabetic ketoacidosis (DKA).
Aims/hypothesis This study compares the efficacy and safety of a tubeless, on-body automated insulin delivery (AID) system with that of a tubeless, on-body sensor-augmented pump (SAP). Methods This multicentre, parallel-group, RCT was conducted at 13 tertiary medical centres in South Korea. Adults aged 19-69 years with type 1 diabetes who had HbA1c levels of <85.8 mmol/mol (<10.0%) were ...
Aim This retrospective study aimed to use mixed (qualitative and quantitative) methods to evaluate the role of FSL in reducing hospital admissions due to all causes, HbA1c, and reported hypoglycaemic episodes in people with diabetes living in a socially deprived region of Northwest England. Methods Data were collected retrospectively from previous consultations, which coincided with the 6th ...
Professor Mahesh Ramanan from The George Institute for Global Health and UNSW Medicine & Health has received $1.6 million for a fluid therapy trial for patients presenting with diabetic ketoacidosis. Diabetic ketoacidosis (DKA) is a life-threatening complication of diabetes in which the body produces excess blood acids known as ketones.
The most recent National Health and Nutrition Examination Survey noted that 30% of adolescents are now overweight, 2 and there has been a commensurate rise in the number of cases of type 2 diabetes found in adolescents. 3 Recently, in a cohort of obese adolescents, 20% were noted to have impaired glucose tolerance, and 4% had undiagnosed type 2 ...