healthinquire.com
Rn vati: navigating mental health trends in 2019, seeking mental health support understand rn vati mental health 2019 and available resources.
These days, mental health issues are more prevalent than ever before. It's become imperative to prioritize mental well-being and address challenges promptly. In this blog post, we'll explore RN Vati Mental Health 2019, focusing on key aspects, pain points, and resources for mental health support.
Navigating Mental Health Challenges: Key Aspects and Pain Points
The mental health landscape has evolved significantly, and we face many challenges. One major concern is the stigma associated with mental illness. People often hesitate to seek help due to fear of judgment or social isolation. Moreover, mental health services are often underfunded, leading to limited accessibility and long wait times for treatment.
RN Vati Mental Health 2019: A Glimmer of Hope in Addressing Mental Health Issues
RN Vati Mental Health 2019 aims to address the aforementioned challenges head-on. The initiative focuses on providing comprehensive mental health support to individuals, communities, and healthcare professionals. By raising awareness, reducing stigma, and advocating for improved mental health services, RN Vati Mental Health 2019 aims to create a positive change.
Key Elements and Resources Highlighted During RN Vati Mental Health 2019
The campaign highlighted several key elements and resources to support mental well-being. A key focus was on promoting mental health education and awareness through workshops, seminars, and public campaigns. Additionally, resources like helplines, support groups, and online platforms were introduced to provide accessible and timely support to individuals seeking assistance.
Moving Forward: Embracing Mental Health Support and Creating Positive Change
RN Vati Mental Health 2019 served as an eye-opening reminder of the importance of mental well-being. The initiative highlighted the need for increased awareness, reduced stigma, and improved access to mental health services. By embracing the support available through resources like helplines, support groups, and online platforms, we can foster a healthier and more supportive environment for individuals struggling with mental health concerns.

RN Vati Mental Health 2019 Report
Introduction.
The RN Vati Mental Health 2019 report provides valuable insights into the current state of mental health among registered nurses (RNs) in the United States. With its comprehensive data and analysis, this report sheds light on the unique challenges and concerns faced by RNs, highlighting the need for greater attention and support for their mental well-being.
Key Findings
Prevalence of mental health conditions.
The report reveals that a significant proportion of RNs are struggling with mental health conditions. Approximately one in four RNs reported experiencing symptoms of depression, anxiety, or PTSD in the past year. This prevalence rate is notably higher than the general population, indicating a concerning trend among healthcare professionals.
Impact on Work Performance
Mental health conditions can have a profound impact on RNs' work performance and overall job satisfaction. The report found that RNs with mental health conditions are more likely to experience burnout, reduced job satisfaction, and impaired job performance. This not only affects the quality of care provided to patients but also contributes to the ongoing nursing shortage.
Contributing Factors
The report identifies several factors that contribute to the high prevalence of mental health conditions among RNs. These include:
- Work-Related Stressors: RNs often work in demanding and stressful environments, with long hours, shift work, and exposure to traumatic events.
- Lack of Resources and Support: Many RNs lack access to adequate resources and support to cope with the stressors of their job. This includes limited access to mental health services and a lack of organizational support for mental well-being.
- Stigma and Discrimination: Mental health conditions are often stigmatized in society, and RNs may face discrimination or negative attitudes from colleagues or patients. This can prevent them from seeking help or disclosing their mental health struggles.
Call for Action
The RN Vati Mental Health 2019 report calls for urgent action to address the mental health crisis among RNs. This includes:
- Increased Funding for Mental Health Services: Governments and healthcare organizations need to increase funding for mental health services, making them more accessible and affordable for RNs.
- Workplace Interventions: Employers should implement workplace interventions to reduce stress and promote mental well-being among RNs. This can include providing mental health training, flexible work arrangements, and peer support programs.
- Eliminating Stigma: Efforts must be made to eliminate stigma and discrimination associated with mental health conditions. This can be achieved through education campaigns and by creating a more supportive and understanding environment in healthcare settings.
The RN Vati Mental Health 2019 report serves as a wake-up call, highlighting the urgent need to address the mental health crisis among RNs. By taking action to improve access to mental health services, reduce stigma, and create supportive workplace environments, we can help ensure that RNs have the tools and resources they need to thrive both personally and professionally.
What is the prevalence of mental health conditions among RNs? Approximately one in four RNs reported experiencing symptoms of depression, anxiety, or PTSD in the past year.
How does mental health affect RNs' work performance? Mental health conditions can lead to burnout, reduced job satisfaction, and impaired job performance, negatively impacting both the quality of care provided to patients and the nursing shortage.
What factors contribute to the high prevalence of mental health conditions among RNs? Work-related stressors, lack of resources and support, and stigma and discrimination are key factors contributing to the high prevalence of mental health conditions among RNs.
What can be done to address the mental health crisis among RNs? Increased funding for mental health services, workplace interventions to reduce stress and promote mental well-being, and efforts to eliminate stigma and discrimination are essential steps in addressing the mental health crisis among RNs.
Why is it important to address the mental health crisis among RNs? Addressing the mental health crisis among RNs is crucial to ensure quality patient care, address the nursing shortage, and promote the overall well-being of healthcare professionals.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- VA Author Manuscripts

Veterans’ Experiences Initiating VA-Based Mental Health Care
Michelle j. bovin.
National Center for PTSD at Veterans Affairs Boston Healthcare System, Boston, Massachusetts, and Boston University School of Medicine
Christopher J. Koenig
San Francisco State University and Palo Alto Healthcare system, Palo Alto, California
Kara A. Zamora
San Francisco Veterans Affairs Healthcare system, San Francisco, California
Jeffrey M. Pyne
Central Arkansas Veterans Healthcare System, North Little Rock, Arkansas, and University of Arkansas for Medical Sciences
Christopher J. Miller
Veterans Affairs Boston Healthcare System, Boston, Massachusetts, and Harvard Medical School
Jessica M. Lipschitz
Patricia b. wright.
University of Arkansas for Medical Sciences
James F. Burgess, Jr.
Veterans Affairs Boston Healthcare System, Boston, Massachusetts, and Boston University School of Public Health
Michelle J. Bovin, National Center for PTSD at Veterans Affairs Boston Healthcare System, Boston, Massachusetts, and Department of Psychiatry, Boston University School of Medicine; Christopher J. Miller, Center for Healthcare Organization and Implementation Research, Veterans Affairs Boston Healthcare System, and Department of Psychiatry, Harvard Medical School; Christopher J. Koenig, Department of Communication Studies, San Francisco State University and Palo Alto Healthcare system, Palo Alto, California; Jessica M. Lipschitz, Center for Healthcare Organization and Implementation Research, Veterans Affairs Boston Healthcare System, and Department of Psychiatry, Harvard Medical School; Kara A. Zamora, San Francisco Veterans Affairs Healthcare System, San Francisco, California; Patricia B. Wright, College of Nursing, University of Arkansas for Medical Sciences; Jeffrey M. Pyne, Center for Mental Healthcare and Outcomes Research and South Central Mental Illness Research, Education and Clinical Center, Central Arkansas Veterans Healthcare System, North Little Rock, Arkansas, and Division of Health Services Research, Department of Psychiatry, College of Medicine, University of Arkansas for Medical Sciences; James F. Burgess Jr., Center for Healthcare Organization and Implementation Research, Veterans Affairs Boston Healthcare System, and Health Law, Policy and Management Department, Boston University School of Public Health.
Military veterans who could benefit from mental health services often do not access them. Research has revealed a range of barriers associated with initiating United States Department of Veterans Affairs (VA) care, including those specific to accessing mental health care (e.g., fear of stigmatization). More work is needed to streamline access to VA mental health-care services for veterans. In the current study, we interviewed 80 veterans from 9 clinics across the United States about initiation of VA mental health care to identify barriers to access. Results suggested that five predominant factors influenced veterans’ decisions to initiate care: (a) awareness of VA mental health services; (b) fear of negative consequences of seeking care; (c) personal beliefs about mental health treatment; (d) input from family and friends; and (e) motivation for treatment. Veterans also spoke about the pathways they used to access this care. The four most commonly reported pathways included (a) physical health-care appointments; (b) the service connection disability system; (c) non-VA care; and (d) being mandated to care. Taken together, these data lend themselves to a model that describes both modifiers of, and pathways to, VA mental health care. The model suggests that interventions aimed at the identified pathways, in concert with efforts designed to reduce barriers, may increase initiation of VA mental health-care services by veterans.
Over the last two decades, the United States Department of Veterans Affairs (VA) has identified improving access to health care as a priority area (e.g., Kehle, Greer, Rutks, & Wilt, 2011 ; Miller, 2001 ). This focus on access has intensified since the VA waitlist crisis in 2014 ( Oppel & Shear, 2014 ). In response, the VA established the MyVA Access Initiative to strengthen veteran access to both VA and non-VA care ( U.S. Department of Veterans Affairs, 2014a ). Research consistent with this focus has identified a range of barriers to care including: lack of knowledge of VA eligibility and services ( Wagner, Dichter, & Mattocks, 2015 ; Washington, Yano, Simon, & Sun, 2006 ), trouble navigating the health-care system ( Gorman, Blow, Ames, & Reed, 2011 ; Johnson, Carlson, & Hearst, 2010 ), and logistical difficulties associated with traveling to appointments ( Gorman et al., 2011 ; Johnson et al., 2010 ; Washington, Bean-Mayberry, Riopelle, & Yano, 2011 ). Some of these barriers may be particularly relevant for specific veteran groups. For example, the need to travel long distances for care is particularly pertinent to the 36% of VA users located in rural areas ( Goins, Williams, Carter, Spencer, & Solovieva, 2005 ; United States Department of Veterans Affairs, Veterans Health Administration, Office of Rural Health, 2008 ).
Veterans in need of mental health care may face additional challenges in accessing care. For example, symptoms such as lack of motivation and trouble concentrating may further complicate veterans’ abilities to traverse an already challenging system. Indeed, research has found that more severe psychiatric symptoms are associated with increased access barriers ( Drapalski, Milford, Goldberg, Brown, & Dixon, 2008 ). In addition, veterans may avoid seeking treatment based on negative beliefs about mental health care ( Pietrzak, Johnson, Goldstein, Malley, & Southwick, 2009 ), or fear of negative consequences associated with seeking help ( Gorman et al., 2011 ; Hoge et al., 2004 ; Stecker, Fortney, Hamilton, & Ajzen, 2007 ).
Veterans new to the VA system may have an especially difficult time accessing services. Specifically, they may lack knowledge of VA eligibility and services and have difficulty navigating the VA health-care system. These barriers also may limit access for veterans who have been ensconced in VA care for a long time (e.g., through primary care), but who are attempting to access a new type of service (e.g., mental health services).
Although the literature includes explorations of veterans’ perceptions of VA mental health-care access (including studies using data from the Veterans Health Administration (VHA) Survey of Health Care Experience of Patients (SHEP), e.g., Burnett-Zeigler, Zivin, Ilgen, & Bohnert 2011 ; Budzi, Lurie, Singh, & Hooker 2010 ; Prentice, Davies, & Pizer 2014 ) and has detailed a number of facilitators and barriers that may influence the initiation of care (e.g., Elbogen et al., 2013 ; Ouimette et al., 2011 ; Spoont et al., 2014 ), the vast majority of these investigations have used quantitative approaches. These approaches are limited, however, in instances in which the structured-answer choices do not adequately capture the experiences of the participant ( Duffy, 1987 ). In the case of facilitators and barriers to mental health care, a deeply personal topic for many veterans, providing an opportunity for veterans to expand upon how they made the decision to initiate (or not initiate) care provides a forum for gaining additional, richer, data. Further, confirmation of the themes already identified in the literature through this method would provide additional support for conclusions drawn from quantitative methods.
Relatedly, whereas the literature has focused on identifying factors that influence the initiation of care, there may be other aspects of access that have not been examined because of a primarily quantitative approach to the question. Indeed, a better understanding of the ways that veterans first get connected to VA mental health care is still needed. Accurately conceptualizing initiation of care is crucial to streamlining access and improving receipt of timely and appropriate services, including mental health services, for veterans.
In the current study, we used qualitative methods to develop a more complete understanding of veterans’ initial experiences accessing VA mental health care. These analyses were conducted as part of a larger, mixed-methods study that aimed to develop a veteran-centered measure of perceptions of access to health care: the Perceived Access Inventory (PAI; Pyne et al., 2018 ). Whereas the PAI represents a generalizable measure of perceived access, for the current article, we used qualitative methods to explore experiences by veterans initially accessing VA mental health care.
Study Population
Eligible participants were United States military veterans between the ages of 18 and 70 years, with at least one positive screen for posttraumatic stress disorder (PTSD), alcohol-use disorder (AUD), or major depressive disorder (MDD) documented in their VA medical record during the previous year. These screening measures are typically conducted in primary care settings. Veterans who screen positive for these disorders do not necessarily receive services for them, or are even aware that they screened positive for a mental health problem. Therefore, our sample included veterans with and without a history of using VA-based mental health services or being aware of what was in their medical record regarding these screens. However, we excluded veterans who screened positive but denied any distress related to the condition for which they screened positive, because they were unlikely to need mental health services. We also excluded veterans with documented psychosis or dementia in their VA medical records, as these conditions could potentially interfere with the informed-consent process and/or completion of the qualitative interview. We recruited participants from nine clinics: three separate clinics within each of three Veterans Integrated Service Networks (VISNs; VISN 1 in the Northeast, VISN 16 in the Central South, and VISN 21 in the West).
Recruitment Procedures
We mailed recruitment packets to 585 eligible veterans across all three study VISNs. Recruitment packets included a letter briefly describing the study and stating that recipients would receive a call from the study team, unless they opted out by either calling study personnel or returning an enclosed, self-addressed, stamped response form. Veterans who did not opt out within 2 weeks ( n = 496) were called by trained study staff to discuss study participation and confirm eligibility. Of these, 258 veterans were reached and 72 of these veterans (27.9% of those reached by phone; 12.3% of those sent a study packet) were included in the study. These 72 veterans, plus eight additional veterans recruited onsite, made up the final study sample ( n = 80). Sampling was purposive, and intended to ensure adequate numbers of women and members of racial/ethnic minorities, as well as a mixture of veterans living in rural and urban areas, older and younger veterans, and veterans with and without a history of mental health-service access. All study procedures were approved by the VA Central Institutional Review Board (CIRB). Additional detail on this study’s opt-out design and recruitment procedures can be found in a previous peer-reviewed article from this study ( Miller et al., 2017 ).
Study Sample
A total of 80 veterans participated in the study, approximately equally distributed across the three VISNs. Participants were mostly between 30 and 60 years old ( M = 45.8 years; SD = 13.7 years), White (62.5%), non-Hispanic (71.3%), and male (75%), with approximately half living in rural areas (46.2%; see Table 1 ). As described in the previous article from this study ( Miller et al., 2017 ), our recruitment strategy was generally successful in obtaining our desired sample, although study participants were more likely to have accessed VA-based mental health services in the past year than those who did not participate.
Study-Sample Characteristics
In addition to a self-report demographic questionnaire, participating veterans completed a semistructured qualitative interview, designed in part based on the state-of-the-art (SOTA) access model ( Fortney, Burgess, Bosworth, Booth, & Kaboli, 2011 ). The SOTA access model describes five dimensions of access to care, including Geographical (e.g., travel distance), Temporal (e.g., wait times for the next appointment), Financial (e.g., costs associated with getting care), Cultural (e.g., stigma associated with getting care), and Digital (e.g., connectivity to allow remote access to healthcare services). In addition to questions regarding these domains, the qualitative interview guide also included open-ended questions regarding the process of accessing VA medical and mental health services more generally (e.g., overall experience of receiving care at the VA).
Study Procedures
Interviews generally were conducted in person at the veteran’s local VA community-based outpatient clinic, with a small subset ( n = 6) conducted over the telephone. Written informed consent was obtained for in-person participants, and CIRB-approved verbal consent was obtained for telephone participants. Study sessions involved administration of the aforementioned demographics questionnaire and semistructured qualitative interview, as well as additional measures unrelated to this article. Interviews were conducted by the qualitative team, which consisted of four researchers experienced in conducting qualitative interviews and analyses, including one communication scientist, one applied anthropologist, one nurse scientist, and one clinical psychologist. Study sessions took about 1.5–2 hr each, and veterans were provided with financial compensation for participating.
Analytic Plan
Qualitative interviews were audio recorded and professionally transcribed verbatim. The qualitative team (described in the previous section) undertook the coding and analysis of the resulting transcripts. Using a subset of transcribed interviews, the qualitative team used a modified form of directed content analysis to develop an original codebook to characterize interview content ( Hsieh & Shannon, 2005 ). Directed content analysis was used to generate deductive codes from the SOTA Access Model. While reading transcripts, the team noticed other features of veterans’ experiences that could not be captured in the existing deductive codes; inductive codes were generated to capture this content. The resulting codebook therefore combined both deductive and inductive codes to describe interview content.
An iterative process was used to determine which deductive and inductive codes would comprise the final codebook. The qualitative team first read one transcript every 2 weeks to discuss deductive code application and inductive codes that may have been generated. All code definitions were discussed and refined orally, circulated via e-mail for written clarification, and incorporated into the next round of coding. After three months, no new inductive codes were proposed, and the codebook was finalized with 49 substantive codes grouped into six domains ( Pyne et al., 2018 ).
In preparation for coding, one team member segmented all transcripts into a coding unit consisting of a question asked by the interviewer and the participant’s answer to that question. Once transcripts were segmented into units, qualitative team members coded interviews using ATLAS.ti qualitative management software ( Muhr, 2017 ). To assess intercoder reliability, 20% of interviews were reviewed and discussed during periodic reliability meetings, with discrepancies in coding resolved by consensus.
The current article focuses on interview segments assigned a single code, entitled “Getting the Ball Rolling,” an inductive code describing factors influencing veterans access to VA mental health care for the first time. We used qualitative thematic analysis ( Braun & Clarke, 2006 ) for this article. Specifically, we first exported all coded segments of interview text to which the “Getting the Ball Rolling” code had been applied from the ATLAS.ti software into a separate text file. Next, Christopher J. Miller reviewed all segments in the text file and developed an analytic summary that described common themes within the data. This summary was first discussed among the full qualitative team and revised according to comments to take into consideration the relationship between the summary and results of other codes and analytic summaries. Then, it was presented before the full study team, who also offered comments in light of the overall research project concerning access to VA mental health care. Finally, Michelle J. Bovin reviewed the coded segments and resulting themes to create a model that accounted for the data and thematic findings.
In total, the “Getting the Ball Rolling” code was applied to 299 interview segments. Examination of these segments suggested three superordinate themes: (a) onset or worsening of symptoms, which was the motivation for seeking treatment; (b) facilitators and barriers to getting help; and (c) the actual pathways that veterans followed that led them to initiate mental health services (see Figure 1 ). These themes and associated subthemes are discussed below.

Schematic representation of the modifiers of and pathways to initial VA mental health-care access. The circles represent the modifiers of access to specialty mental health care, whereas the truncated squares represent commonly reported pathways to this care.
Onset/Worsening of Symptoms
The veterans in our sample noted that they did not think about accessing VA mental health services until they experienced, recognized, or saw a worsening of their mental health symptoms. Sometimes the onset/increase in symptoms was tied to a triggering event. One veteran noted the following.
I would say getting married was [the tipping point]. The stressors of experiencing something new when I was—I didn’t realize that I was depressed and angry and trying to learn to live with another person, even though we had been living together already it was more—it was a change of environment. (Participant 3028)
In other cases, veterans noticed that their symptoms were affecting their daily lives: “All I knew was I was very angry and I wanted to take somebody I work with and throw them in a trash can, which was my red flag, ‘Need help!’” (Participant 2009).
Although this symptom exacerbation was often not enough to prompt the veteran to contact VA mental health immediately, it served as the beginning of the pathway toward care for all the veterans who eventually did decide to seek services.
Barriers and Facilitators to Initiating Mental Health Treatment
Although onset or worsening of symptoms was the initial step in the pathway toward initiating care, not all veterans who experienced this onset or worsening eventually sought care. Veterans reported a number of barriers and facilitators which affected their decision to seek (or not to seek) help. In particular, five common subthemes, or factors, were identified during interviews: (a) Awareness of VA Mental Health Services; (b) Fear of Negative Consequences of Seeking Care; (c) Personal Beliefs About Mental Health Treatment; (d) Input From Family and Friends; and (e) Motivation for Treatment.
Awareness of VA mental health services or processes for obtaining them.
Many veterans reported not being provided with information about when, or how, to access VA mental health services. This frequently was discussed in the context of separating from the military. A number of veterans in our sample reported that they were not given any information about how to access VA services after separation, or if they were, these instructions were vague or unhelpful. Some veterans were also given incorrect information about access, such as being told they were not eligible for services based on noncombat status. Other veterans indicated that, although they were provided with some information about accessing services, they were overwhelmed by their other out-processing duties and were therefore unable to focus on this information at the time. Many participants commented that after separation, they got the impression that the focus of the military was to get them out as quickly as possible, rather than to ensure that they were aware of the services they were eligible for, should they need them.
Because I, I, there’s a process when you get discharged and they speed that process up. I do not know if you’re going to be working with veterans [but if you do] you’ll hear that a lot. They do not give you any information when they’re getting you out, they just want you stamped out and gone as fast as possible. (Participant 3009)
Fear of negative consequences of seeking care.
Several veterans reported that they did not seek mental health services, in some cases for years, because of concerns about negative consequences. While study participants were still in the military, these issues were of particular concern, because they feared that seeking care might risk their military careers. One veteran, who noticed psychiatric symptoms prior to separation, discussed his fear of seeking help.
It was difficult to seek that kind of treatment … it could have potentially affected my career had I decided to stay in. I mean depending on what you disclose in seeking treatment like that it can make you nondeployable. And if you’re nondeployable then you get kicked out of the service. (Participant 1019)
Personal beliefs about mental health treatment.
Internal stigmatization (i.e., negative beliefs about mental health treatment and the people who seek it) also served as a barrier to accessing care. Even if veterans were hearing from others that they should seek help, these personal beliefs were often powerful deterrents to care.
Well I was out of control, couldn’t keep no job, and I was not sleeping at night. And I had lost a lot of weight and my mother told me to go get me some help. … I really didn’t want to come because I always heard [mental health clinic] it was crazy people up here so I was not wanting to come up here [to the mental health clinic]. (Participant 1002)
Input from family and friends.
Veterans often mentioned interactions with family and friends as the impetus for seeking treatment. These interactions frequently came in the form of demands that the veteran get help (from spouses or partners), or suggestions that accessing services might help the veteran feel better (from other veterans). For example, when asked why he decided to seek help, one veteran commented:
… basically it was my wife told me I needed to get help or they were leaving. ‘Cause I, she would wake up I would be, you know, in the corner, you know, with a knife in my hand crying ah, you know, where the slightest little thing with my kids I would just explode at them. You know so … I was starting to drink more and … you know, just accumulation of things … [but] the biggest thing was her saying get help or we’re gone. (Participant 2015)
Another reported it was not his wife, but a fellow veteran who influenced him to seek treatment.
My uncle he was … he’s a veteran and told me I just needed to come up here and he just kept telling me I needed to come to the VA. He was like, boy you’ve got problems you need to come up there. (Participant 1004)
Motivation for treatment.
Whether because of fear of how they would be perceived if they sought treatment, internalized stigma about mental health issues, lack of motivation as a result of depression, or other factors, several veterans we interviewed noted that they had not sought services despite knowing both that they were struggling with mental health issues and that VA mental health care was accessible. Paradoxically, increases in symptom severity sometimes reduced motivation for seeking treatment. As one veteran noted, “Well, what I think initially makes it hard, is like you’re in this crisis mode of depression. It’s hard to get out of bed. So seeking help is way beyond that” (Participant 2029).
Pathways to Mental Health Care
In discussing their initiation of VA mental health treatment, many veterans in our sample went beyond discussing why they chose to access (or not access) care, and spoke about how they eventually became enrolled in this care. Overwhelmingly, veterans reported that, even after experiencing an onset or worsening of symptoms, and with facilitators in place, they did not initiate mental health care by contacting VA specialty mental health clinics directly. Instead, participants indicated that initial contact with these clinics was generally made through four pathways: (a) VA physical health appointments, usually in primary care; (b) the service connected disability system; (c) non-VA services (including vet centers); and (d) mandated treatment.
VA physical health appointments.
One of the main pathways discussed as an entry point to VA mental health services was through VA physical health appointments (especially—but not exclusively—through primary care). Whereas in some cases this was based on a formal referral process, in other cases it was more serendipitous (e.g., a veteran decided to investigate mental health services while he was already at the VA for an audiology appointment). Veterans noted that having mental health services offered at the same location as their physical health treatments was a facilitator for initiating psychiatric treatment:
And then once I found [the local VA clinic] I was like oh! Ok! I can come here for both my physical and my mental? Because when I first started coming here, it was for my pain to get a new doctor. And then I started with the mental health services and I went “Sweet!” It was very, very helpful to have them both collocated. (Participant, 2009)
The service-connected disability system.
Several veterans reported that their initial contact with the VA was related to seeking service-connected disability status rather than treatment. During or after the process of seeking such disability, which can include paid cash benefits ( Department of Veterans Affairs, 2017 ), these veterans ended up receiving mental health services they would not have sought otherwise.
I didn’t even really know too much about the VA … my uncle just kept telling me I needed to come to the VA … I went up there and I didn’t know what to do … so they sent me through a few things and I filled out some papers and the next thing you know I had to go see a doctor. You know he did a physical and all that stuff … I ended up coming out with like 70% disability and stuff like that so I think 50% of it was PTSD, and that’s how I ended up getting connected with the psychiatrist. And they made an appointment for me and I went in and saw some guy and then the next thing you know he was like, “You really need to talk to a psychiatrist.” So I ended up going and talking with her and then she made some appointments and it just went from there. (Participant 1002)
Non-VA services.
A number of veterans noted that non-VA services ultimately introduced them to VA mental health services. In our sample, both vet centers and private sector care facilitated these connections, which could be made through direct referrals (e.g., one veteran was receiving suboxone treatment in the private sector and was referred to the VA because the medications would be more affordable). However, the connections were often more indirect, with the non-VA settings providing veterans with information about how to navigate the VA system. One veteran described how the vet center staff eased his transition to the VA.
[Initially I didn’t know how to navigate the VA] … there’s the fliers on the walls, but, there’s no standard way of “this is where you go.” They have a kiosk but if you have no idea what you’re doing with it, then you do not even know how to check in, so you go to the lady at the front, whomever’s there is their receptionist, and they ask you who you are and what you’re there for and you go “I don’t know what I’m here for,” and that’s the first thing, you actually have to find your way in. [But the vet center] gave me all kinds of, any information that I needed, they assisted me with getting, they told me where to go, they got me directions, they were really helpful with that because, like I said it’s vets treating vets, so they understand more. (Participant 2009)
Mandated treatment.
A small number of veterans noted that they initially entered the VA mental health system as an alternative to jail or more intensive inpatient services. For example, one veteran reported that he initiated VA substance-abuse treatment in lieu of jail time after receiving a citation for driving under the influence of alcohol. Another veteran described his choice between initiating outpatient mental health care or submitting to involuntary hospitalization: “They ended up admitting me into the psych ward, and they let me out and told me a week later I had to seek [outpatient] counseling … to stay out of the hospital” (Participant 2032).
Our qualitative investigation into the initiation of VA mental health treatment provided rich data on what influences veterans to access this care, as well as the pathways to achieving access. These data lend themselves to a model of mental health-care access highlighting the facilitators and barriers that may encourage or impede a given veteran’s decision ultimately to engage in treatment. The model also includes common pathways to initiating this care (see Figure 1 ). Although other models have explored the sociocultural factors that influence care initiation (e.g., the network-episode model; Pescosolido, 2006 ), it is this additional attention to specific pathways that sets our model apart.
Many of our findings are consistent with previous literature on barriers and facilitators to accessing care ( Fischer et al., 2016 ). Specifically, our findings emphasize the importance of personal motivation ( Schultz, Martinez, Cucciare, & Timko, 2016 ), input from family and friends ( Spoont et al., 2014 ), knowledge of available services ( Wagner et al., 2015 ; Washington et al., 2006 ), internalized stigma ( Pietrzak et al., 2009 ), and fear about the consequences of seeking care ( Gorman et al., 2011 ; Hoge et al., 2004 ; Stecker, Fortney, Hamilton, & Ajzen, 2007 ) as impacting the initiation of VA mental health care.
In other areas, however, our findings appear to be at odds with the previous literature—or at least to not emphasize facets of access to care that have been emphasized consistently in the literature. For example, veteran interview segments in this analysis did not cite travel difficulties frequently as a barrier to initiating VA mental health care, which is particularly surprising because nearly half of our sample was comprised of rural veterans, for whom travel is often described as a primary barrier to accessing care (e.g., Buzza et al., 2011 ; Goins et al., 2005 ). This may not have been the case in our study because travel distance may be a more important barrier to continuing, rather than initiating, care. Consistent with this, separate codes (not part of this analysis) did suggest that travel difficulties were seen as barriers to ongoing care. However, it also may be that the factors influencing the initiation of mental health care are somewhat different from those associated with initiating other types of care.
One of the benefits of using a qualitative approach is the ability to uncover unexpected findings by capturing veterans’ lived experiences of accessing care. Although we set out to investigate factors that influence the initiation of care, many veterans took the opportunity to also discuss their pathways to accessing VA mental health care. Although it is possible for veterans to directly contact VA specialty mental health clinics for services, this was not the case for our sample. Instead, veterans in our sample consistently indicated that they became connected with VA mental health services through one of four pathways: VA physical health care, service-connection disability services, non-VA services including vet centers, and mandates to receive treatment. The VA already has begun to capitalize on these pathways; one component of the VA’s large-scale quality-improvement initiative for veteran access was the introduction of VA Primary Care Mental Health Integration (PC-MHI), a program that embeds mental health providers into primary care teams ( Zeiss & Karlin, 2008 ). Since their initial inception in the late 2000s, PC-MHI services have already demonstrated improvements in facilitating mental health diagnoses and treatment engagement for veterans ( Bohnert, Sripada, Mach, & McCarthy, 2016 ). Our findings—that primary care appointments may serve as an important gateway to mental health treatment—are therefore consistent with this body of literature on PC-MHI.
Other pathways to mental health treatment revealed in this study have been subject to less attention in previous research. For example, we were surprised to find that the service-connected disability system served as the de facto entry point to mental health treatment for some veterans in our sample. Currently, staff conducting compensation and pension examinations that help determine a veteran’s eligibility for disability compensation are instructed to inform the veterans they interview of available treatment options. However, staff who conduct these examinations are often required to conduct back-to-back comprehensive diagnostic evaluations in very short time frames, which may limit the time they have to pursue these discussions. Our results suggest that additional efforts to increase the frequency with which compensation and pension examiners discuss treatment options may help more veterans seek and receive appropriate mental health services.
Another pathway that has received less attention in the literature is that of non-VA services. In particular, in the current study, vet centers often served as a pathway to VA mental health care. Although technically part of the Veterans Health Administration, vet centers—which were established in 1979 to assist veterans and their families with adjustment difficulties—historically have maintained a degree of independence from VA medical centers to ensure confidential counseling ( Department of Veterans Affairs, 2015 ). Although known to provide additional services (i.e., counseling, outreach, and referral) to veterans outside of the VA, little research has focused on the content of these services. Our findings suggest that both the vet centers themselves and the veterans who use their services, can provide immeasurable assistance to veterans hoping to transition to mental health care at the VA. It is possible that not all veterans who take advantage of vet centers would wish to transition to the VA. Because there is no shared medical record between the VA and the vet centers, accessing services at the latter is a method for compartmentalizing treatment. However, our findings suggest that some veterans do wish to make this transition. Therefore, working with vet-center staff may be another avenue to explore in an effort to provide these veterans with the support they need to access care.
Finally, several veterans in our study indicated that their pathway to VA mental health care was through the legal system or similar requirements. The idea of court-mandated mental health treatment for certain behaviors (e.g., partner battering, substance abuse) is not new; offenders are often assigned to treatment as a component of their sentence. Our findings suggest that, above and beyond such mandated treatment, strengthening the ability of the legal system’s representatives to connect veterans with VA mental health care may be helpful. Effectively leveraging this pathway, however, would need to account for the fact that some veterans might see such referrals as punitive even if they were not court-mandated.
Our findings should be considered within the context of the enormous strides VA has already made to improve veterans’ access to mental health care. Efforts including the introduction of PC-MHI, the mandating of regular mental health screenings (e.g., Department of Veterans Affairs, 2007 ), the passage of legislation aimed at reducing wait times (e.g., the Veterans Access, Choice and Accountability Act of 2014; Department of Veterans Affairs, 2014b ); and targeted campaigns within VA hospitals designed to reduce stigma around mental health treatment ( Department of Veterans Affairs, 2011 ) all have served to facilitate the initiation of services. Despite this, there are still veterans who would benefit from mental health care who do not initiate treatment. Our results provide guidance on what additional interventions may further facilitate mental health access for these veterans. For example, the importance of family and friends in veterans’ decisions to initiate care suggests that interventions that target the nonveteran community might be beneficial. Furthermore, organizations and individuals that provide VA mental health-care referrals (e.g., lawyers who regularly work with veterans; compensation and pension examiners) may help connect more veterans with VA mental health care if they are provided information packets that describe the mental health services VA offers, as well as the best way to access them. Although effective interventions to improve access are already in place, our findings suggest that additional outreach may be effective at further reducing the gap between veterans who could benefit from mental health treatment and those who initiate this care.
Our findings have implications for public sector mental health services outside of the VA system, as well. First, the facilitators and barriers to receiving help that we identified generally align well with previous literature (e.g., Gorman et al., 2011 ; Pietrzak et al., 2009 ; Wagner et al., 2015 ), suggesting that our findings are likely generalizable. Therefore, interventions geared toward improving access suggested by our results (e.g., those designed to provide psychoeducation about the availability and purpose of mental health services and to normalize help seeking) may be effective in non-VA as well as VA settings. Second, the pathways to care identified in the current study may be relevant to any health system that aims to ensure that all patients needing mental health services have access to them. This would include, but would not be limited to, outpatient mental health clinics within accountable care organizations, which are ultimately incentivized not only to treat patients who are actively seeking their services, but also to make it easier for patients who are suffering from mental illness symptoms to seek treatment before a mental health crisis occurs (e.g., Bao, Casalino, & Pincus, 2013 ). For such clinics, partnering more closely with representatives of the legal system and physical health-care providers may be essential to streamlining access to their services.
This study has several limitations. First, our sample consisted mostly of White males. Therefore, the results may not be generalizable to other veteran groups. Second, we limited our sample only to veterans who had a positive screen for PTSD, AUD, or MDD. Veterans with other mental health disorders may not report the same barriers, facilitators, and pathways to mental health care. Third, because of our small sample size, it was impossible to estimate which of the pathways we identified would be the most promising to pursue to improve VA mental health access for the greatest number of veterans, and/or whether certain pathways would better suited for particular subsets of veterans (e.g., those at urban vs. rural sites). Additional research is needed to explore this possibility. Fourth, our sample consisted of veterans who were already in the VA system, and had therefore overcome existing barriers sufficiently to be using VA at least for physical health concerns. It is possible that veterans who have not been involved in the system at all may face additional access barriers that are not represented here. Finally, because our investigation focused purely on initiation of care, we cannot speak to the factors that encourage veterans to maintain engagement in care. Understanding both initiation and continued access is essential because initial access is only as good as available follow-up services. Getting people into the system, but not providing sufficient resources to treat them effectively, ultimately does them a disservice. Future research is encouraged to explore both aspects of access, as well as their interaction.
Despite these limitations, this article provides rich information about the barriers and facilitators veterans encounter when deciding whether to initiate VA mental health care. In addition, it provides information about the pathways veterans take to access this care. The findings serve to reinforce the current VA efforts (e.g., PC-MHI; the antistigmatization campaign), and suggest additional avenues to pursue. In particular, providing compensation and pension examiners, vet center staff, and representatives of the legal system detailed information about the services VA provides, as well as the methods through which these services can be accessed, may benefit a myriad of veterans who are not currently receiving VA mental health care. Future work should be undertaken to explore novel entry points to care to ensure that all veterans are able to receive the help they need and deserve.
Acknowledgments
This research was funded by United States Department of Veterans Affairs, Health Services Research & Development, CRE 12-300 (“Development and Validation of a Perceived Access Measure,” principal investigator: Jeffrey M. Pyne). James F. Burgess Jr., who passed away during the revision of this article, was an inspirational leader of this project and we are grateful to have had the opportunity to work with him. The authors would also like to thank Ellen P. Fischer and Regina L. Stanley for their invaluable contributions to this article.
Contributor Information
Michelle J. Bovin, National Center for PTSD at Veterans Affairs Boston Healthcare System, Boston, Massachusetts, and Boston University School of Medicine.
Christopher J. Koenig, San Francisco State University and Palo Alto Healthcare system, Palo Alto, California.
Kara A. Zamora, San Francisco Veterans Affairs Healthcare system, San Francisco, California.
Jeffrey M. Pyne, Central Arkansas Veterans Healthcare System, North Little Rock, Arkansas, and University of Arkansas for Medical Sciences.
Christopher J. Miller, Veterans Affairs Boston Healthcare System, Boston, Massachusetts, and Harvard Medical School.
Jessica M. Lipschitz, Veterans Affairs Boston Healthcare System, Boston, Massachusetts, and Harvard Medical School.
Patricia B. Wright, University of Arkansas for Medical Sciences.
James F. Burgess, Jr., Veterans Affairs Boston Healthcare System, Boston, Massachusetts, and Boston University School of Public Health.
- Bao Y, Casalino LP, & Pincus HA (2013). Behavioral health and health-care reform models: Patient-centered medical home, health home, and accountable care organization . The Journal of Behavioral Health Services & Research , 40 , 121–132. 10.1007/s11414-012-9306-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bohnert KM, Sripada RK, Mach J, & McCarthy JF (2016). Same-day integrated mental health care and PTSD diagnosis and treatment among VHA primary care patients with positive PTSD screens . Psychiatric Services , 67 , 94–100. 10.1176/appi.ps.201500035 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Braun V, & Clarke V (2006). Using thematic analysis in psychology . Qualitative Research in Psychology , 3 , 77–101. 10.1191/1478088706qp063oa [ CrossRef ] [ Google Scholar ]
- Budzi D, Lurie S, Singh K, & Hooker R (2010). Veterans’ perceptions of care by nurse practitioners, physician assistants, and physicians: A comparison from satisfaction surveys . Journal of the American Academy of Nurse Practitioners , 22 , 170–176. 10.1111/j.1745-7599.2010.00489.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Burnett-Zeigler I, Zivin K, Ilgen MA, & Bohnert AS (2011). Perceptions of quality of health care among veterans with psychiatric disorders . Psychiatric Services , 62 , 1054–1059. 10.1176/ps.62.9.pss6209_1054 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buzza C, Ono SS, Turvey C, Wittrock S, Noble M, Reddy G, … Reisinger HS (2011). Distance is relative: Unpacking a principal barrier in rural healthcare . Journal of General Internal Medicine , 26 , 648–654. 10.1007/s11606-011-1762-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Drapalski AL, Milford J, Goldberg RW, Brown CH, & Dixon LB (2008). Perceived barriers to medical care and mental health care among veterans with serious mental illness . Psychiatric Services , 59 , 921–924. 10.1176/ps.2008.59.8.921 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Duffy ME (1987). Quantitative and qualitative research: Antagonistic or complementary? Nursing & Health Care , 8 , 356–357. [ PubMed ] [ Google Scholar ]
- Elbogen EB, Wagner HR, Johnson SC, Kinneer P, Kang H, Vasterling JJ, … Beckham JC (2013). Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey . Psychiatric Services , 64 , 134–141. 10.1176/appi.ps.004792011 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fischer EP, McSweeney JC, Wright P, Cheney A, Curran GM, Henderson K, & Fortney JC (2016). Overcoming barriers to sustained engagement in mental health care: Perspectives of rural veterans and providers . The Journal of Rural Health , 32 , 429–438. 10.1111/jrh.12203 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fortney JC, Burgess JFJ Jr., Bosworth HB, Booth BM, & Kaboli PJ (2011). A re-conceptualization of access for 21st century healthcare . Journal of General Internal Medicine , 26 , 639–647. 10.1007/s11606-011-1806-6 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goins RT, Williams KA, Carter MW, Spencer SM, & Solovieva T (2005). Perceived barriers to health care access among rural older adults: A qualitative study . The Journal of Rural Health , 21 , 206–213. 10.1111/j.1748-0361.2005.tb00084.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gorman LA, Blow AJ, Ames BD, & Reed PL (2011). National Guard families after combat: Mental health, use of mental health services, and perceived treatment barriers . Psychiatric Services , 62 , 28–34. 10.1176/ps.62.1.pss6201_0028 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, & Koffman RL (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care . The New England Journal of Medicine , 351 , 13–22. 10.1056/NEJMoa040603 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hsieh HF, & Shannon SE (2005). Three approaches to qualitative content analysis . Qualitative Health Research , 15 , 1277–1288. 10.1177/1049732305276687 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnson PJ, Carlson KF, & Hearst MO (2010). Healthcare disparities for American Indian veterans in the United States: A population-based study . Medical Care , 48 , 563–569. 10.1097/MLR.0b013e3181d5f9e1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kehle SM, Greer N, Rutks I, & Wilt T (2011). Interventions to improve veterans’ access to care: A systematic review of the literature . Journal of General Internal Medicine , 26 ( Suppl. 2 ), 689–696. 10.1007/s11606-011-1849-8 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Miller CJ, Burgess JF Jr., Fischer EP, Hodges DJ, Belanger LK, Lipschitz JM, … Pyne JM (2017). Practical application of opt-out recruitment methods in two health services research studies . BMC Medical Research Methodology , 17 , 57 10.1186/s12874-017-0333-5 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Miller LJ (2001). Improving access to care in the VA Health System: A progress report FORUM . Washington, DC: VA Health Services Research & Development. [ Google Scholar ]
- Muhr T (2017). ATLAS.ti [Computer software] . Berlin, Germany: Scientific Software Development. [ Google Scholar ]
- Oppel RA Jr., & Shear MD (2014, May 28). Severe report finds VA hid waiting lists at hospitals . New York Times . Retrieved from http://www.nytimes.com/2014/05/29/us/va-report-confirms-improper-waiting-lists-at-phoenix-center.html [ Google Scholar ]
- Ouimette P, Vogt D, Wade M, Tirone V, Greenbaum MA, Kimerling R, … Rosen CS (2011). Perceived barriers to care among Veterans Health Administration patients with posttraumatic stress disorder . Psychological Services , 8 , 212–223. 10.1037/a0024360 [ CrossRef ] [ Google Scholar ]
- Pescosolido BA (2006). Of pride and prejudice: The role of sociology and social networks in integrating the health sciences . Journal of Health and Social Behavior , 47 , 189–208. 10.1177/002214650604700301 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, & Southwick SM (2009). Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans . Psychiatric Services , 60 , 1118–1122. 10.1176/ps.2009.60.8.1118 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prentice JC, Davies ML, & Pizer SD (2014). Which outpatient wait-time measures are related to patient satisfaction? American Journal of Medical Quality , 29 , 227–235. 10.1177/1062860613494750 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pyne JM, Kelly PA, Fischer EP, Miller CJ, Wright PB, Zamora K, … Fortney JC (2018). Perceived Access Inventory: Development of a preliminary version . Manuscript submitted for publiccation . [ Google Scholar ]
- Schultz NR, Martinez R, Cucciare MA, & Timko C (2016). Patient, program, and system barriers and facilitators to detoxification services in the U.S. Veterans Health Administration: A qualitative study of provider perspectives . Substance Use & Misuse , 51 , 1330–1341. 10.3109/10826084.2016.1168446 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Spoont MR, Nelson DB, Murdoch M, Rector T, Sayer NA, Nugent S, & Westermeyer J (2014). Impact of treatment beliefs and social network encouragement on initiation of care by VA service users with PTSD . Psychiatric Services , 65 , 654–662. 10.1176/appi.ps.201200324 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stecker T, Fortney JC, Hamilton F, & Ajzen I (2007). An assessment of beliefs about mental health care among veterans who served in Iraq . Psychiatric Services , 58 , 1358–1361. 10.1176/ps.2007.58.10.1358 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- United States Department of Veteran Affairs. (2007). Vista Clinical Reminder user manual . Retrieved from https://www.va.gov/vdl/documents/Clinical/CPRS-Clinical_Reminders/pxrm_2_6_um.pdf
- United States Department of Veterans Affairs. (2014a). Accelerating access to care initiative: Fact sheet . Retrieved from https://www.va.gov/health/docs/052714AcceleratingAccessFactSheet.PDF
- United States Department of Veterans Affairs. (2014b). Choice Act summary . Retrieved from https://www.va.gov/opa/choiceact/documents/Choice-Act-Summary.pdf
- United States Department of Veterans Affairs. (2015). Vet Center Program . Retrieved from https://www.vetcenter.va.gov/index.asp
- United States Department of Veterans Affairs. (2017). Veterans Benefits Administration: Compensation . Retrieved from http://www.benefits.va.gov/compensation/
- United States Department of Veterans Affairs & Military Suicide Research Consortium. (2011). VA launches awareness campaign to reduce stigma . Retrieved from https://msrc.fsu.edu/news/va-launches-awareness-campaign-reduce-stigma
- United States Department of Veterans Affairs, Veterans Health Administration, Office of Rural Health. (2008). Veterans rural health: Perspective and opportunities . Rockville, MD: Booz Allen Hamilton. [ Google Scholar ]
- Wagner C, Dichter ME, & Mattocks K (2015). Women veterans’ pathways to and perspectives on Veterans Affairs health care . Women’s Health Issues , 25 , 658–665. 10.1016/j.whi.2015.06.009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Washington DL, Bean-Mayberry B, Riopelle D, & Yano EM (2011). Access to care for women veterans: Delayed healthcare and unmet needs . Journal of General Internal Medicine , 26 , 655–661. 10.1007/s11606-011-1772-z [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Washington DL, Yano EM, Simon B, & Sun S (2006). To use or not to use: What influences why women veterans choose VA health care . Journal of General Internal Medicine , 21 , S11–S18. 10.1111/j.1525-1497.2006.00369.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zeiss AM, & Karlin BE (2008). Integrating mental health and primary care services in the Department of Veterans Affairs health-care system . Journal of Clinical Psychology in Medical Settings , 15 , 73–78. 10.1007/s10880-008-9100-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
Study Tracks Shifts in Student Mental Health During College
Dartmouth study followed 200 students all four years, including through the pandemic.

Phone App Uses AI to Detect Depression From Facial Cues
A four-year study by Dartmouth researchers captures the most in-depth data yet on how college students’ self-esteem and mental health fluctuates during their four years in academia, identifying key populations and stressors that the researchers say administrators could target to improve student well-being.
The study also provides among the first real-time accounts of how the coronavirus pandemic affected students’ behavior and mental health. The stress and uncertainty of COVID-19 resulted in long-lasting behavioral changes that persisted as a “new normal” even as the pandemic diminished, including students feeling more stressed, less socially engaged, and sleeping more.
The researchers tracked more than 200 Dartmouth undergraduates in the classes of 2021 and 2022 for all four years of college. Students volunteered to let a specially developed app called StudentLife tap into the sensors that are built into smartphones. The app cataloged their daily physical and social activity, how long they slept, their location and travel, the time they spent on their phone, and how often they listened to music or watched videos. Students also filled out weekly behavioral surveys, and selected students gave post-study interviews.
The study—which is the longest mobile-sensing study ever conducted—is published in the Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies .
The researchers will present it at the Association of Computing Machinery’s UbiComp/ISWC 2024 conference in Melbourne, Australia, in October.
These sorts of tools will have a tremendous impact on projecting forward and developing much more data-driven ways to intervene and respond exactly when students need it most.
The team made their anonymized data set publicly available —including self-reports, surveys, and phone-sensing and brain-imaging data—to help advance research into the mental health of students during their college years.
Andrew Campbell , the paper’s senior author and Dartmouth’s Albert Bradley 1915 Third Century Professor of Computer Science, says that the study’s extensive data reinforces the importance of college and university administrators across the country being more attuned to how and when students’ mental well-being changes during the school year.
“For the first time, we’ve produced granular data about the ebb and flow of student mental health. It’s incredibly dynamic—there’s nothing that’s steady state through the term, let alone through the year,” he says. “These sorts of tools will have a tremendous impact on projecting forward and developing much more data-driven ways to intervene and respond exactly when students need it most.”
First-year and female students are especially at risk for high anxiety and low self-esteem, the study finds. Among first-year students, self-esteem dropped to its lowest point in the first weeks of their transition from high school to college but rose steadily every semester until it was about 10% higher by graduation.
“We can see that students came out of high school with a certain level of self-esteem that dropped off to the lowest point of the four years. Some said they started to experience ‘imposter syndrome’ from being around other high-performing students,” Campbell says. “As the years progress, though, we can draw a straight line from low to high as their self-esteem improves. I think we would see a similar trend class over class. To me, that’s a very positive thing.”
Female students—who made up 60% of study participants—experienced on average 5% greater stress levels and 10% lower self-esteem than male students. More significantly, the data show that female students tended to be less active, with male students walking 37% more often.
Sophomores were 40% more socially active compared to their first year, the researchers report. But these students also reported feeling 13% more stressed during their second year than during their first year as their workload increased, they felt pressure to socialize, or as first-year social groups dispersed.
One student in a sorority recalled that having pre-arranged activities “kind of adds stress as I feel like I should be having fun because everyone tells me that it is fun.” Another student noted that after the first year, “students have more access to the whole campus and that is when you start feeling excluded from things.”
In a novel finding, the researchers identify an “anticipatory stress spike” of 17% experienced in the last two weeks of summer break. While still lower than mid-academic year stress, the spike was consistent across different summers.
In post-study interviews, some students pointed to returning to campus early for team sports as a source of stress. Others specified reconnecting with family and high school friends during their first summer home, saying they felt “a sense of leaving behind the comfort and familiarity of these long-standing friendships” as the break ended, the researchers report.
“This is a foundational study,” says Subigya Nepal , first author of the study and a PhD candidate in Campbell’s research group. “It has more real-time granular data than anything we or anyone else has provided before. We don’t know yet how it will translate to campuses nationwide, but it can be a template for getting the conversation going.”
The depth and accuracy of the study data suggest that mobile-sensing software could eventually give universities the ability to create proactive mental-health policies specific to certain student populations and times of year, Campbell says.
For example, a paper Campbell’s research group published in 2022 based on StudentLife data showed that first-generation students experienced lower self-esteem and higher levels of depression than other students throughout their four years of college.
“We will be able to look at campus in much more nuanced ways than waiting for the results of an annual mental health study and then developing policy,” Campbell says. “We know that Dartmouth is a small and very tight-knit campus community. But if we applied these same methods to a college with similar attributes, I believe we would find very similar trends.”
Weathering the pandemic
When students returned home at the start of the coronavirus pandemic, the researchers found that self-esteem actually increased during the pandemic by 5% overall and by another 6% afterward when life returned closer to what it was before. One student suggested in their interview that getting older came with more confidence. Others indicated that being home led to them spending more time with friends talking on the phone, on social media, or streaming movies together.
The data show that phone usage—measured by the duration a phone was unlocked—indeed increased by nearly 33 minutes, or 19%, during the pandemic, while time spent in physical activity dropped by 52 minutes, or 27%. By 2022, phone usage fell from its pandemic peak to just above pre-pandemic levels, while engagement in physical activity had recovered to exceed the pre-pandemic period by three minutes.
Despite reporting higher self-esteem, students’ feelings of stress increased by more than 10% during the pandemic. By the end of the study in June 2022, stress had fallen by less than 2% of its pandemic peak, indicating that the experience had a lasting impact on student well-being, the researchers report.
In early 2021, as students returned to campus, their reunion with friends and community was tempered by an overwhelming concern about the still-rampant coronavirus. “There was the first outbreak in winter 2021 and that was terrifying,” one student recalls. Another student adds: “You could be put into isolation for a long time even if you did not have COVID. Everyone was afraid to contact-trace anyone else in case they got mad at each other.”
Female students were especially concerned about the coronavirus, on average 13% more than male students. “Even though the girls might have been hanging out with each other more, they are more aware of the impact,” one female student reported. “I actually had COVID and exposed some friends of mine. All the girls that I told tested as they were worried. They were continually checking up to make sure that they did not have it and take it home to their family.”
Students still learning remotely had social levels 16% higher than students on campus, who engaged in activity an average of 10% less often than when they were learning from home. However, on-campus students used their phones 47% more often. When interviewed after the study, these students reported spending extended periods of time video-calling or streaming movies with friends and family.
Social activity and engagement had not yet returned to pre-pandemic levels by the end of the study in June 2022, recovering by a little less than 3% after a nearly 10% drop during the pandemic. Similarly, the pandemic correlates with students sticking closer to home, with their distance traveled nearly cut in half during the pandemic and holding at that level since then.
Campbell and several of his fellow researchers are now developing a smartphone app known as MoodCapture that uses artificial intelligence paired with facial-image processing software to reliably detect the onset of depression before the user even knows something is wrong.
Morgan Kelly can be reached at [email protected] .
- Mental Health and Wellness
- Innovation and Impact
- Arts and Sciences
- Class of 2021
- Class of 2022
- Department of Computer Science
- Guarini School of Graduate and Advanced Studies
- Mental Health
Class of 2028 Draws Record Number of Applicants

Writing about important events in our lives, not just ‘I had a coffee today,’ but ‘I had this deep discussion with my mom,’ generally provides more benefit therapeutically.

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- About the Director
- Advisory Boards and Groups
- Strategic Plan
- Offices and Divisions
- Careers at NIMH
- Staff Directories
- Getting to NIMH

Decoding the Mind: Basic Science Revolutionizes Treatment of Mental Illnesses
By Linda Brady, Margaret Grabb, Susan Koester, Yael Mandelblat-Cerf, David Panchision, Jonathan Pevsner, Ashlee Van’t-Veer, and Aleksandra Vicentic on behalf of the NIMH Division of Neuroscience and Basic Behavioral Science
March 21, 2024 • 75th Anniversary
Follow the NIMH Director on
For 75 years, NIMH has transformed the understanding and treatment of mental illnesses through basic and clinical research—bringing hope to millions of people. This Director’s Message, guest written by NIMH’s Division of Neuroscience and Basic Behavioral Science , is part of an anniversary series celebrating this momentous milestone.
The Division of Neuroscience and Basic Behavioral Science (DNBBS) at the National Institute of Mental Health (NIMH) supports research on basic neuroscience, genetics, and basic behavioral science. These are foundational pillars in the quest to decode the human mind and unravel the complexities of mental illnesses.
At NIMH, we are committed to supporting and conducting genomics research as a priority research area . As the institute celebrates its 75th Anniversary , we are spotlighting DNBBS-supported efforts connecting genes to cells to circuits to behavior that have led to a wealth of discoveries and knowledge that can improve the diagnosis, treatment, and prevention of mental illnesses.
Making gene discoveries
Medical conditions often run in families. For instance, if someone in your immediate family has high blood pressure, you are more likely to have it too. It is the same with mental disorders—often they run in families. NIMH is supporting research into human genetics to better understand why this occurs. This research has already led to the discovery of hundreds of gene variants that make us more or less likely to develop a mental disorder.
There are two types of genetic variation: common and rare. Common variation refers to DNA changes often seen in the general population, whereas rare variation is DNA changes found in only a small proportion of the population. Individually, most common gene variants have only a minor impact on the risk for a mental disorder. Instead, most disorders result from many common gene variants that, together, contribute to the risk for and severity of that disorder.
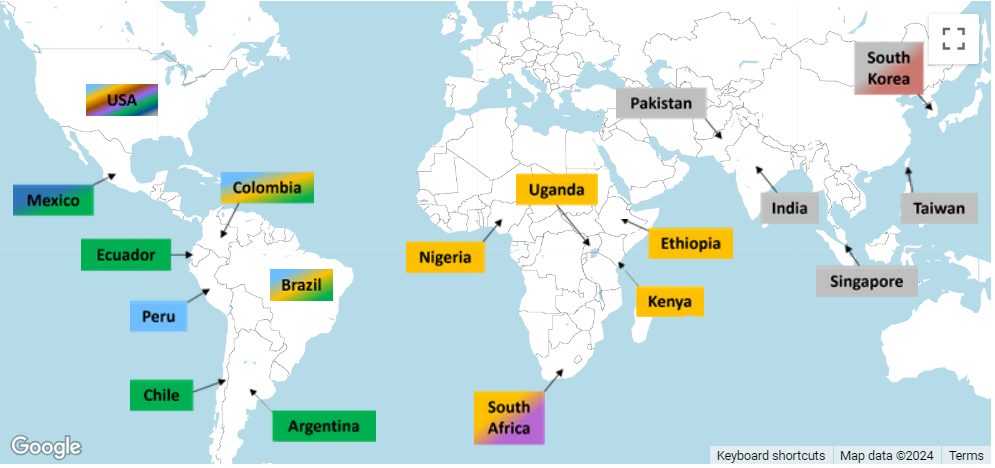
NIMH is committed to uncovering the role of genes in mental disorders with the aim of improving the lives of people who experience them. One of the many ways NIMH contributes to the discovery of common gene variants is by supporting the Psychiatric Genomics Consortium (PGC) . The consortium of almost 1,000 scientists across the globe, including ones in the NIMH Intramural Research Program and others conducting NIMH-supported research, is one of the largest and most innovative biological investigations in psychiatry.
Global collaborations such as the PGC are critical to amassing the immense sample sizes needed to identify common gene variants. Data from the consortium’s almost one million participants have already led to transformative insights about genetic contributors to mental illnesses and the genetic relationships of these illnesses to each other. To date, studies conducted as part of the consortium have uncovered common variation in over a dozen mental illnesses.
In contrast to common gene variants, rare gene variants are very uncommon in the general population. When they do occur, they often have a major impact on the occurrence of an illness, particularly when they disrupt gene function or regulation. Rare variants involving mutations in a single gene have been linked to several mental disorders, often through NIMH-supported research. For instance, a recent NIMH-funded study found that rare variation in 10 genes substantially increased the risk for schizophrenia. However, it is important to note that genetics is not destiny; even rare variants only raise the risk for mental disorders, but many other factors, including your environment and experiences, play important roles as well.
Because of the strong interest among researchers and the public in understanding how genes translate to changes in the brain and behavior, NIMH has developed a list of human genes associated with mental illnesses. These genes were identified through rare variation studies and are meant to serve as a resource for the research community. The list currently focuses on rare variants, but NIMH plans to continue expanding it as evidence accumulates for additional gene variants (rare or common).
Moreover, mental illnesses are a significant public health burden worldwide . For this reason, NIMH investments in genomics research extend across the globe. NIMH has established the Ancestral Populations Network (APN) to make genomics studies more diverse and shed light on how genetic variation contributes to mental disorders across populations. APN currently includes seven projects with more than 100 researchers across 25 sites worldwide.
Connecting biology to behavior
While hundreds of individual genes have been linked to mental illnesses, the function of most of these genes in the brain remains poorly understood. But high-tech advances and the increased availability of computational tools are enabling researchers to begin unraveling the intricate roles played by genes.
In addition to identifying genetic variation that raises the risk for mental illnesses, NIMH supports research that will help us understand how genes contribute to human behavior. This information is critical to discovering approaches to diagnose, treat, and ultimately prevent or cure mental illnesses.
An NIMH-funded project called the PsychENCODE consortium focuses on understanding how genes impact brain function. PsychENCODE is furthering knowledge of how gene risk maps onto brain function and dysfunction by cataloging genomic elements in the human brain and studying the actions of different cell types. The PsychENCODE dataset currently includes multidimensional genetic data from the postmortem brains of thousands of people with and without mental disorders.
Findings from the first phase of PsychENCODE were published as a series of 11 papers examining functional genomics in the developing and adult brains and in mental disorders. A second batch of PsychENCODE papers will be published later this year. These findings help clarify the complex relationships between gene variants and the biological processes they influence.
PsychENCODE and other NIMH-supported projects are committed to sharing biospecimens quickly and openly to help speed research and discovery.

Facilitating these efforts is the NIMH Repository and Genomics Resource (NRGR) , where samples are stored and shared. NRGR includes hundreds of thousands of samples, such as DNA, RNA, and cell lines, from people with and without mental disorders, along with demographic and diagnostic information.

Another NIMH initiative to connect risk genes to brain function is Scalable and Systematic Neurobiology of Psychiatric and Neurodevelopmental Disorder Risk Genes (SSPsyGene) . This initiative uses cutting-edge techniques to characterize the biological functions of 250 mental health risk genes—within the cells where they are expressed—to better understand how those genes contribute to mental illnesses. By systematically characterizing the biological functions of risk genes in cells, SSPsyGene will empower researchers to learn about biological pathways that may serve as new targets for treatment.
Genes also affect behavior by providing the blueprint for neurons, the basic units of the nervous system. Neurons communicate with each other via circuits in the brain, which enables us to process, integrate, and convey information. NIMH supports many initiatives to study the foundational role of neural networks and brain circuits in shaping diverse mental health-related behaviors like mood, learning, memory, and motivation.
For instance, studies supported through a basic-to-translational science initiative at NIMH focus on modifying neural activity to improve cognitive, emotional, and social processing . Similarly, another new funding opportunity encourages studies in humans and animals examining how emotional and social cues are represented across brain circuits to help address a core deficit in many mental disorders. These studies will increase understanding of the biological mechanisms that support behavior throughout life and offer interventions to improve these functions in healthy and clinical populations.
Developing treatments and therapeutics
The gene discovery and biology-to-behavior programs described here will lay the foundation for delivering novel therapeutics. To be prepared to rapidly implement findings from this research, NIMH supports several initiatives to identify behavioral and biological markers for use in clinical studies and increase our ability to translate research into practice.
Through its therapeutics discovery research programs , NIMH advances early stage discovery and development studies in humans and early efficacy trials for mental disorders. Taking these efforts a step further, NIMH supports the National Cooperative Drug Discovery/Development Groups for the Treatment of Mental Disorders , which encourage public–private partnerships to accelerate the discovery and development of novel therapeutics and new biomarkers for use in human trials. Moreover, NIMH is one of several institutes and centers in the NIH Blueprint Neurotherapeutics Network , launched to enable neuroscientists in academia and biotechnology companies to develop new drugs for nervous system disorders.
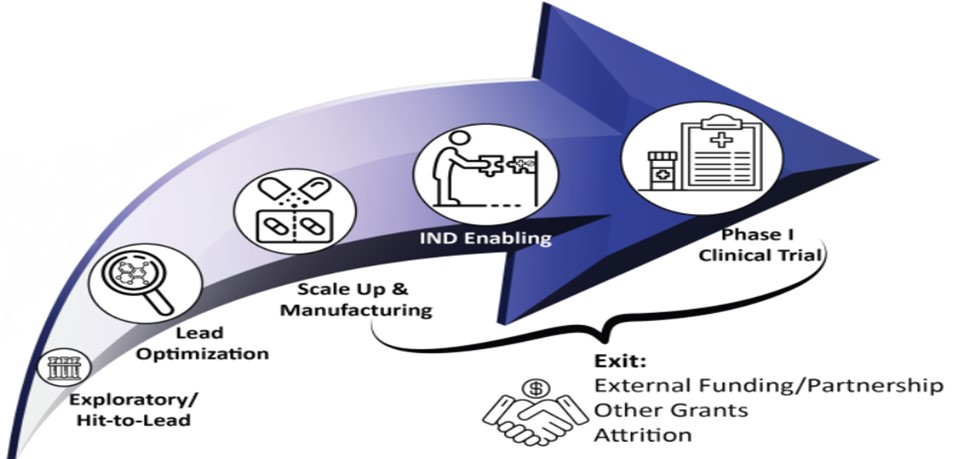
For the treatments of tomorrow, NIMH is building a new research program called Pre-Clinical Research on Gene Therapies for Rare Genetic Neurodevelopmental Disorders , which encourages early stage research to optimize gene therapies to treat disorders with prominent cognitive, social, or affective impairment. In parallel, NIMH’s Planning Grants for Natural History Studies of Rare Genetic Neurodevelopmental Disorders encourage the analysis of pre-existing data from people with rare disorders to learn about disease progression and enable future clinical trials with these populations.
NIMH's Division of Neuroscience and Basic Behavioral Science supports many different research projects that help us learn about genes and gene functions, how the brain develops and works, and impacts on behavior. By investing in basic neuroscience, genetics, and behavioral research, we're trying to find new targets for treatment and develop better therapies for mental disorders. We're hopeful these efforts will lead to new ways to treat and prevent mental illnesses in the near future and, ultimately, improve the lives of people in this country and across the globe.
- Share full article
Advertisement
Supported by
When Teens Visit Doctors, Increasingly the Subject is Mental Health

By Matt Richtel
Increasingly, doctor visits by adolescents and young adults involve mental health diagnoses, along with the prescription of psychiatric medications.
That was the conclusion of a new study that found that in 2019, 17 percent of outpatient doctor visits for patients ages 13 to 24 in the United States involved a behavioral or mental health condition, including anxiety, depression, suicidal ideation, self-harm or other issues. That figure rose sharply from 2006, when just 9 percent of doctor’s visits involved psychiatric illnesses.
The study , published Thursday in JAMA Network Open, also found a sharp increase in the proportion of visits involving psychiatric medications. In 2019, 22.4 percent of outpatient visits by the 13-24 age group involved the prescription of at least one psychiatric drug, up from 13 percent in 2006.
The Big Picture
The study is the latest evidence in a shift in the kinds of ailments affecting children, adolescents and young adults. For many decades, their health care visits involved more bodily ailments, such as broken bones, viruses and drunken-driving injuries. Increasingly, however, doctors are seeing a wide variety of behavioral and mental health issues.

The reasons are not entirely clear. Some experts have said that modern life presents a new kind of mental pressure, even as society has limited the risks of physical ailments.
The latest study does not posit a reason for the shift. But the pandemic alone was not to blame, it noted. “These findings suggest the increase in mental health conditions seen among youth during the pandemic occurred in the setting of already increasing rates of psychiatric illness,” wrote the authors, a pediatrician and psychiatrist at Harvard Medical School. “Treatment and prevention strategies will need to account for factors beyond the direct and indirect effects of the pandemic.”

The Numbers
The analysis was drawn from the National Ambulatory Care Survey, which asks a sample of clinicians from across the country about the reasons for patient visits. Between 2006 and 2019, patients aged 13 to 24 made 1.1 billion health care visits, of which 145 million involved mental health issues. But the share of mental-health-related visits rose each year, the study found, as did the prescription of psychiatric medications, including stimulants, antipsychotics, mood stabilizers and anti-anxiety drugs.
The study found that antidepressants had the greatest increase, but it did not specify the exact level, said Dr. Florence T. Bourgeois, a pediatrician at Boston Children’s Hospital, an associate professor of pediatrics at Harvard Medical School and a co-author of the paper.
The prescription patterns leave an open question, she said.
“We can’t differentiate whether this speaks to the severity of conditions or changes in prescribing attitudes and trends,” she said. Either way, she added, “We are treating these conditions aggressively.”
Matt Richtel is a health and science reporter for The Times, based in Boulder, Colo. More about Matt Richtel
Managing Anxiety and Stress
Stay balanced in the face of stress and anxiety with our collection of tools and advice..
How are you, really? This self-guided check-in will help you take stock of your emotional well-being — and learn how to make changes .
These simple and proven strategies will help you manage stress , support your mental health and find meaning in the new year.
First, bring calm and clarity into your life with these 10 tips . Next, identify what you are dealing with: Is it worry, anxiety or stress ?
Persistent depressive disorder is underdiagnosed, and many who suffer from it have never heard of it. Here is what to know .
If you notice drastic shifts in your mood during certain times of the year, you could have seasonal affective disorder. Here are answers to your top questions about the condition .
How much anxiety is too much? Here is how to establish whether you should see a professional about it .
This paper is in the following e-collection/theme issue:
Published on 28.3.2024 in Vol 11 (2024)
Translating Suicide Safety Planning Components Into the Design of mHealth App Features: Systematic Review
Authors of this article:

- Kim Gryglewicz 1 * , MSW, PhD ;
- Victoria L Orr 2 * , BS ;
- Marissa J McNeil 2 * , MA ;
- Lindsay A Taliaferro 3 , MPH, PhD, CHES ;
- Serenea Hines 2 , MSW ;
- Taylor L Duffy 2 , BS ;
- Pamela J Wisniewski 4 * , PhD
1 School of Social Work, University of Central Florida, Orlando, FL, United States
2 Center for Behavioral Health Research & Training, University of Central Florida, Orlando, FL, United States
3 Department of Population Health Sciences, University of Central Florida, Orlando, FL, United States
4 Department of Computer Science, Vanderbilt University, Nashville, TN, United States
*these authors contributed equally
Corresponding Author:
Kim Gryglewicz, MSW, PhD
School of Social Work
University of Central Florida
12805 Pegasus Drive HS I
Orlando, FL, 32816
United States
Phone: 1 14078232954
Email: [email protected]
Background: Suicide safety planning is an evidence-based approach used to help individuals identify strategies to keep themselves safe during a mental health crisis. This study systematically reviewed the literature focused on mobile health (mHealth) suicide safety planning apps.
Objective: This study aims to evaluate the extent to which apps integrated components of the safety planning intervention (SPI), and if so, how these safety planning components were integrated into the design-based features of the apps.
Methods: Following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, we systematically analyzed 14 peer-reviewed studies specific to mHealth apps for suicide safety planning. We conducted an analysis of the literature to evaluate how the apps incorporated SPI components and examined similarities and differences among the apps by conducting a comparative analysis of app features. An independent review of SPI components and app features was conducted by downloading the available apps.
Results: Most of the mHealth apps (5/7, 71%) integrated SPI components and provided customizable features that expanded upon traditional paper-based safety planning processes. App design features were categorized into 5 themes, including interactive features, individualized user experiences, interface design, guidance and training, and privacy and sharing. All apps included access to community supports and revisable safety plans. Fewer mHealth apps (3/7, 43%) included interactive features, such as associating coping strategies with specific stressors. Most studies (10/14, 71%) examined the usability, feasibility, and acceptability of the safety planning mHealth apps. Usability findings were generally positive, as users often found these apps easy to use and visually appealing. In terms of feasibility, users preferred using mHealth apps during times of crisis, but the continuous use of the apps outside of crisis situations received less support. Few studies (4/14, 29%) examined the effectiveness of mHealth apps for suicide-related outcomes. Positive shifts in attitudes and desire to live, improved coping strategies, enhanced emotional stability, and a decrease in suicidal thoughts or self-harm behaviors were examined in these studies.
Conclusions: Our study highlights the need for researchers, clinicians, and app designers to continue to work together to align evidence-based research on mHealth suicide safety planning apps with lessons learned for how to best deliver these technologies to end users. Our review brings to light mHealth suicide safety planning strategies needing further development and testing, such as lethal means guidance, collaborative safety planning, and the opportunity to embed more interactive features that leverage the advanced capabilities of technology to improve client outcomes as well as foster sustained user engagement beyond a crisis. Although preliminary evidence shows that these apps may help to mitigate suicide risk, clinical trials with larger sample sizes and more robust research designs are needed to validate their efficacy before the widespread adoption and use.
Introduction
Suicide is one of the leading causes of death in the United States, accounting for >45,000 deaths annually [ 1 ]. Over the last decade, suicide rates have doubled for youth aged 10 to 24 years [ 2 ] and have steadily increased for racial and ethnic minority youth [ 1 , 3 , 4 ]. Suicide ideation and attempt rates have also risen [ 5 , 6 ], especially among youth and minoritized populations [ 5 , 7 - 11 ]. Numerous studies have shown that untreated mental illness, limited or lack of available care, and low perceived need for mental health treatment are common, yet preventable, suicide risk antecedents [ 12 - 19 ]. Moreover, stigma, difficulties recognizing suicide warning signs, preferences for self-reliance and autonomy, fear of burdening others, and negative treatment experiences can negatively affect help-seeking intentions and engagement in mental health services [ 20 - 24 ].
Researchers have identified various suicide prevention strategies to reduce the public health problem of suicide [ 25 , 26 ]. Safety planning is an integral component of suicide care [ 27 ] and has been empirically validated for reducing suicidality [ 28 , 29 ]. The process of safety planning involves collaboration between a clinical and client, as well as with the at-risk individual and their support network. This means that the support network could also be part of the safety planning process [ 30 ]. Safety planning involves jointly identifying, problem-solving, and communicating strategies to keep an individual safe if a crisis arises. Core strategies focus on uncovering warning signs or triggers that precede an emotional event, identifying and reinforcing the use of healthful self-management strategies to cope with distress, encouraging the use of positive socialization strategies for distraction and support, creating a network of external support and professional contacts to solicit assistance and support, and reducing access to lethal means [ 31 ]. The individualized nature of creating a safety plan (ie, a written document detailing the plan to keep an individual safe during a crisis) allows the person at risk of suicide the ability to incorporate culturally relevant and meaningful strategies, thereby making these plans useful and relevant for diverse populations [ 30 , 32 ].
Suicide safety planning is a brief intervention that has been used in both acute and clinical settings [ 31 , 33 , 34 ] and as a self-help tool [ 35 ]. Overall, researchers have found this intervention to be feasible, acceptable, and useful to facilitate support and reduce suicide risk [ 32 , 33 , 35 - 37 ]. Researchers have found safety plans and related interventions, such as crisis response planning [ 38 ], to be effective in reducing the risk of hospitalization, increasing engagement in mental health treatment, and promoting the use of healthful coping strategies when used alongside other therapeutic approaches [ 33 , 34 , 36 , 39 , 40 ]. Although safety planning has shown initial success in reducing suicidal urges and offering a sense of hope to individuals in crisis [ 41 ], some clinicians and researchers have criticized this process [ 42 , 43 ]. For example, safety planning encourages clinicians to revisit and update safety plans with their clients over time [ 44 ], which can prove challenging if service use barriers prevent clients from reaccessing care or if clients misplace or throw away their paper-based safety plan.
Considering these challenges, mobile health (mHealth) technologies could offer a timely and effective solution to address some of the criticisms directed at traditional safety planning methods. mHealth, particularly the use of apps, represents a common tool used by consumers with access to mobile phones [ 45 , 46 ]. In addition, mHealth has garnered attention as a practical and convenient method for implementing mental health interventions [ 47 ], with increase in the quantity and functionality of applications and tools resulting in increased use [ 48 ]. In general, mHealth apps have been used to effectively help individuals identify and manage symptoms of various mental health problems and conditions such as depression, anxiety, substance abuse, posttraumatic stress, and eating disorders [ 49 , 50 ]. Thus, incorporating mHealth apps into mental health treatment and adjunctive interventions may prove beneficial.
Furthermore, incorporating mHealth apps into established evidence-based interventions may also serve as a culturally inclusive way of disseminating treatment to younger, more technologically savvy generations who also happen to demonstrate higher rates of suicidal thoughts and behaviors than adults [ 6 ]. mHealth apps may also help address service use barriers and risk factors (eg, stigma) that hinder individuals from seeking help and participating in treatment for suicidality. Combining suicide safety planning practices with mHealth apps may combat accessibility concerns as well, including a commonly reported flaw of the traditional intervention—the reliance on a paper format [ 35 ]. Given the widespread proliferation of mHealth apps for suicide prevention, there is a need to examine the components and features that have been incorporated into the design of suicide safety planning apps.
The purpose of this systematic literature review was to first assess the extent to which suicide safety planning mHealth apps integrated the 6 steps or components of a widely used safety planning intervention (SPI) developed by Stanley and Brown [ 31 ] (research question [RQ] 1). Next, we independently reviewed available mHealth suicide safety planning apps via download from iOS and Android app stores to assess the integration of SPI components and to categorize different app design features used to personalize the end users’ experience (RQ2). We also examined the evidence on the effectiveness of these apps in terms of usability, acceptability, app engagement, and suicide-related outcomes (RQ3). This review aims to synthesize the extant research to inform suicide prevention efforts, clinical practice, and future development of suicide safety planning mHealth apps.
In accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 statement guidelines ( Multimedia Appendix 1 [ 51 ]), a comprehensive systematic review of existing literature on suicide safety planning via mHealth apps was conducted. The process is described in the following sections.
Systematic Literature Review
Eligibility criteria.
The inclusion criteria for the reviewed research studies were as follows: (1) a primary focus on suicide safety planning involving the use of a mHealth app, (2) publication in a peer-reviewed article written in English, and (3) availability of the full text of the article. Studies were excluded if (1) the word suicide, safety plan, or app was not included in the title; (2) they included other forms of mHealth technologies as the primary focus (eg, web-based applications); (3) the apps were designed with safety planning as a secondary focus (ie, not exclusively for suicide safety planning, not intended as a crisis intervention, or use of safety planning as a secondary tool to other treatment modalities); and (4) they were part of other systematic reviews or meta-analyses. We included studies across the entire system development life cycle (eg, formative evaluations and 1 group pre-posttest designs) owing to limited research on the topic and the relatively recent emergence of such research.
Information Sources
The following 5 bibliographic databases were used to systematically review the literature: PsycINFO, PubMed, ACM Digital Libraries, Academic Search Premier, and ERIC. We limited our results to articles published between January 2000 and May 2023. All databases were last searched on July 2, 2023.
Search Strategy
We used the following keywords to search for the topic of interest in each scientific database: “Safety Plan*” AND (“Applications” OR “Apps”); (“Suicide” OR “Safety Plan*”) AND (“Applications” OR “Apps”); “Suicide Interven*” AND (“Applications” OR “Apps”); “Suicide Prevent*” AND (“Applications” OR “Apps”); “Suicide Contract” AND (“Applications” OR “Apps”); “mHealth” AND “Suicide”; “Crisis Response” AND “Plan*.” Asterisks were added to search for words that began with the preceding letters (eg, prevent*: prevent, prevention, and preventing). An example of the search strategy outlined above is provided in Multimedia Appendix 2 .
Selection Process
Citations obtained from electronic databases were imported into Zotero (version 6.0.16). Two reviewers (KG and VLO) independently screened the articles to remove duplicates and assessed inclusion and exclusion criteria by title and abstract. For articles about which the reviewers were uncertain after the title and abstract review, 4 reviewers independently analyzed the full-text articles to determine whether they met the inclusion criteria. The reviewers discussed discrepancies until they reached a consensus. The references of all articles that met the inclusion criteria were reviewed and cross-referenced for additional relevant articles. We included all eligible studies (N=14) in this systematic review ( Figure 1 [ 51 ]).

Data Collection Process
Data from eligible studies were analyzed using the Cochrane Collaboration’s data extraction template for included studies (version 1.8) [ 52 ]. We added study-specific items to the template to answer RQ1 and RQ2. Specifically, to answer RQ1, we reviewed articles describing each mHealth app and coded, using a dichotomous (yes or no) coding scheme, for the following SPI components: (1) personal warning signs, (2) coping strategies, (3) ways to distract oneself through social activities, (4) identification of and ways to access trusted individuals (eg, family and friends) for support, (5) identification of and ways to access community supports (eg, mental health professionals, nonmental health adult supports, crisis, or emergency services), and (6) information about keeping the environment safe (eg, restricting access to lethal means). To answer RQ2, we downloaded available mHealth apps via the Apple App Store or Google Play Store or contacted app developers to conduct an independent review of SPI components and app features described in the articles. Next, we created codes to describe app features, organized and categorized codes based on similarities, and generated 5 themes to capture the core aspects of features. To answer RQ3, we extracted both qualitative and quantitative findings reported on primary and secondary outcomes. We categorized the study outcomes into 3 main research themes.
Two reviewers coded 2 research articles to assess interrater reliability based on the coding template and made refinements as necessary (eg, added operational definitions to describe SPI components and provided examples of app features). Once finalized, the reviewers used the template to extract the data from the remaining studies. Data items included (1) general article information (eg, author, publication year, and country); (2) study methods (eg, aims and research design); (3) study characteristics (eg, sample size, sample demographics, and setting); (4) SPI intervention characteristics (RQ1); (5) mHealth app design features (RQ2) and primary and secondary outcomes (RQ3); and (6) study implications and future directions ( Multimedia Appendix 3 [ 42 , 43 , 53 - 64 ]). A similar process was used to independently code the SPI components and app features of the mHealth apps available for download.
Risk of Bias Assessment
The risk of bias for each study was assessed by 2 independent reviewers (KG and VLO) using Joanna Briggs Institute (JBI) appraisal tools for quasi-experimental [ 65 ] and qualitative research study designs [ 66 ]. For studies that included mixed methods designs, we used both tools as recommended by the JBI. Each appraisal tool used a rating scale with yes, no, unclear, and nonapplicable responses. The overall appraisal rating was based on the following categories: include, exclude, and seek further information. Disagreements between the reviewers were discussed until they reached a consensus ( Multimedia Appendix 4 [ 65 , 66 ]).
Synthesis of Results
Owing to the heterogeneity of the study designs, participants, and outcomes collected, we could not perform a meta-analysis of the identified studies in this review. Therefore, we present a narrative synthesis of the study findings.
Study Selection
The initial search of electronic databases and hand-searched references resulted in a total of 46,397 peer-reviewed articles. After duplicate records were removed, 21,151 studies remained. Titles were screened for relevancy (eg, relating to suicide, suicide safety planning, and mHealth apps), and 20,970 articles were excluded. A total of 181 abstracts were reviewed. Following full-text reviews of 54 articles, 40 articles were removed (15 studies did not include an mHealth app and 25 were not intended as a suicide safety planning app). A total of 14 articles met the inclusion criteria (refer to Figure 1 for breakdown).
Study Characteristics
The detailed study characteristics of the selected articles (N=14) are presented in Multimedia Appendix 3 . Most studies (12/14, 86%) were conducted outside the United States [ 42 , 53 - 63 ]. The year range of the selected articles was between 2015 and 2023.
Study Design
As shown in Tables 1 and 2 , a total of 7 mHealth suicide safety planning apps were studied across the 14 articles in our data set ( Multimedia Appendix 3 ). We classified the articles based on the research design (ie, formative feedback, usability assessment, single cohort pre-posttest, and random control trial protocol). Formative designs assessed SPI components and features to guide app development [ 43 , 56 , 61 , 64 ], whereas usability designs assessed interface design issues and functionality (eg, task difficulty and time to complete tasks) [ 55 , 60 , 61 , 64 ]. Other studies evaluated the acceptability or feasibility of a fully developed mHealth app [ 54 , 58 - 60 , 62 , 63 ]. Across these studies, participants rated the frequency and duration of app use; ease of navigation; and level of satisfaction, comfort, confidence, or engagement in using the app.
a N/A: not applicable.
Sample Characteristics
Across studies, the study sample varied in age, type of participant (eg, youth or adults at risk of suicide and clinicians collaborating with suicidal clients), and setting (eg, suicide prevention clinic and pediatric inpatient facility). Among studies that recruited participants to inform or evaluate mHealth suicide safety planning apps [ 43 , 54 - 56 , 58 - 64 ], the sample size ranged from 11 to 36 participants. However, after reporting dropout rates, sample sizes dropped to as low as 2 participants and as high as 22 participants.
Integration of SPI Components Within mHealth Apps
Most articles (5/7, 71%) describing the mHealth apps incorporated SPI components into the design of their apps [ 54 , 58 , 61 , 63 , 64 ] ( Table 3 ). Creating a safe environment from lethal means was the missing component in 29% (2/7) of the apps [ 55 , 56 ].
a BoMM: Brake of My Mind.
b SPC: safety planning component.
c SPC or app feature included in the app.
d MHP: mental health professional.
e SPC or app feature missing in the app.
f Denotes innovative app features aligned with SPI components.
g Feature included in the app that was not mentioned in the article.
We used the JBI quasi-experimental appraisal tool [ 65 ] to assess the risk of bias across 5 studies [ 55 , 58 - 60 , 63 ]. These studies did not include a control or comparison group, increasing the threat to internal validity. Pre- and posttest measures were used to assess the immediate effects of the mHealth apps. However, the lack of repeated outcome measures over time, selection bias (nonrandom samples), and small sample sizes pose a risk of bias within and across these studies.
The qualitative appraisal checklist tool [ 66 ] was used to assess the risk of bias in 4 studies [ 43 , 54 , 56 , 62 ]. Across 2 studies [ 43 , 54 ], the cultural or theoretical orientation of the researchers and their influence on the research process was unclear. These issues were noted in the other 2 studies [ 56 , 62 ] as well. In these studies [ 56 , 62 ], it was also difficult to identify the philosophical perspective and congruity between the research methods, data analysis, and interpretation. The studies included more of a description of the design of the apps and included general perceptions from stakeholders.
The remaining studies [ 61 , 64 ] were assessed using both the quasi-experimental and qualitative appraisal tools owing to their mixed methods designs. In both studies, it was unclear whether the researchers’ cultural or theoretical orientation, their influence on the research, and the adequate representation of the participants and their voices were addressed. Other key issues included the lack of a control or comparison group, nonrandom and small sample sizes, and the use of posttest measures to assess usability at only 1 time point. JBI appraisal results are included in Multimedia Appendix 4 .
On the basis of our independent review of available mHealth suicide safety planning apps, SPI components described in each article were verified in 71% (5/7) of the apps [ 54 , 56 , 58 , 61 , 63 ]. The app features described in the articles were also confirmed in these apps. App features not highlighted in the articles but found within the apps are listed in Table 3 . We were unable to verify SPI components and app features in 2 of the reviewed apps in the literature [ 55 , 64 ].
Comparative Analysis of SPI Components and App Features
In our analysis of the literature and available mHealth apps for download, we synthesized the commonalities of app features and categorized them into 5 broad themes: interactive features, individualized user experience, interface design, guidance and training, and privacy and sharing. These features are described in the following sections.
Interactive Features
Three of the suicide safety planning mHealth apps [ 54 , 56 , 61 ] allowed users to associate suicide warning signs or precipitating stressors with their personalized coping strategies (aligns with SPI 1 and 2 in Table 3 ). O’Grady et al [ 61 ] stressed the importance of including this feature in apps, as this functionality can serve to preemptively address an impending crisis before it fully manifests. Most of the suicide safety planning mHealth apps (6/7, 86%) also included social distractor features in which users had access to their phone’s camera with the ability to upload or view media content (eg, pictures, quotes, music, activities, videos, and inspirational stories; SPI 3) [ 54 , 55 , 58 , 61 , 63 , 64 ]. In the BackUp app [ 63 ], loved ones, trusted supports, and suicidal users were able to upload media and share content to inspire hope and distract users from negative thinking.
Each mHealth app also included a built-in feature for users to save and contact trusted individuals within their social support networks (SPI 4). Typically, users entered contact information into the mHealth app directly or linked to their contact directories. A unique feature of the MYPLAN app [ 54 ] allowed users to create prewritten messages that they could send to their social supports during times of distress. Although this feature was created to inform loved ones of the app user’s emotional state during a crisis, participants (ie, app users) noted concerns about messages being misunderstood, whereas relatives felt that messages could minimize emotional states or provide inaccurate information about the app user’s safety. All apps included the ability to access community supports such as mental health professionals (SPI 5). Three apps [ 54 , 55 , 61 ] included GPS capabilities, which enabled users to search for nearby counseling agencies or emergency services, and, after selecting a search result, users received directions for quick access (SPI 5 and 6). The ED-SAFE app [ 64 ] included a referral search engine that allowed users to find behavioral health care by specialty and zip code. Emergency service numbers, mostly displayed via a phone icon or brief words (eg, “Crisis”), were clearly visible (listed on all pages) in 57% (4/7) of the mHealth apps [ 56 , 58 , 61 , 63 ], which is the suggested ethical guideline from prior work [ 67 ]. Three apps did not include access to emergency service numbers on all pages but provided them somewhere else within the app [ 54 , 55 , 64 ].
Individualized User Experience
All apps (7/7, 100%) allowed users to continually add to or revise their safety plans. Examples included the addition of new warning signs, reasons for living, and identifying coping strategies. None of the apps maintained a historical record of the previous safety plans or provided a visual mechanism to track daily, weekly, or monthly patterns based on stressors encountered or coping strategies used. Other personalization aspects included the ability to enable or disable therapeutic modalities [ 61 ], the inclusion of web-based resources to take an aptitude and personality test [ 55 ], exercises to express moods [ 55 ], and mood tracking [ 55 , 56 , 61 ]. In addition, all apps had built-in features to make esthetic customizations, such as personalizing the home screen, changing the color palate, and adding background pictures [ 54 - 56 , 58 , 61 , 63 ]. In 57% (4/7) of the apps, notifications were enabled to remind users about using their safety plan or skills to practice [ 54 , 56 , 61 , 63 ].
Interface Design
Several studies used iterative feedback from content and app design experts to create easy-to-navigate interfaces [ 58 , 61 , 63 ]. To enhance the navigation experience, a simple layout, clear or user-friendly language, and accessibility features were important design considerations included in some mHealth apps [ 54 , 58 , 61 , 64 ]. For example, SafePlan ’s layout mimicked the paper version of the safety plan to better transition users from using the paper version to the app [ 61 ].
Guidance and Training
In-app tutorials or instructional videos were included in 86% (6/7) of the suicide safety planning mHealth apps [ 54 - 56 , 58 , 63 , 64 ]. Some of these tutorials focused on how to use the app, whereas others explained the safety planning process. For example, the BeyondNow app [ 58 ] included a video outlining the process of safety planning and links to other helpful information. The most extensive tutorials were seen in the companion app to ED-SAFE [ 64 ], where tutorials could be received from a female provider, a male community member, or an avatar. The mHealth suite of apps also included self-care education materials about suicidality, safety plans, and life plans. In addition, the BackUp app [ 63 ] provided supportive contacts with web-based information on ways to identify warning signs and strategies to talk with suicidal individuals. The Brake of My Mind app [ 55 ] included an introduction from the developer with additional web-based resources to increase app usability.
Privacy and Sharing
Researchers also highlighted app privacy and sharing capabilities as important features to consider when designing mHealth suicide safety planning apps. Given the personal nature of the information saved, most mHealth apps required a username and password to log in [ 54 - 56 , 61 , 63 , 64 ]. For example, ED-SAFE [ 64 ] used the username and password feature to verify user identity and connect information collected in the emergency department setting to the mHealth app. Other apps disabled GPS for location tracking or did not use external servers to store users’ information for privacy and security concerns [ 61 , 63 ]. Several apps (5/7, 71%) included features allowing users to share self-monitoring data or share safety plans with clinicians or trusted individuals [ 54 , 56 , 58 , 61 , 64 ]. For instance, ED-SAFE [ 64 ] allowed users to share safety plans as well as appointment information, self-care education, helplines, referrals, and distractions through password-protected privileges given to authorized family members.
mHealth App Evidence of Effectiveness
The qualitative and quantitative findings were categorized into 3 main research themes: app usability and acceptability, app use and engagement, and suicide-related outcomes.
App Usability and Acceptability Findings
Across 71% (10/14) of the studies [ 54 - 56 , 58 - 64 ] that assessed the initial usability or acceptability of mHealth suicide safety planning apps, stakeholders’ experiences testing the mHealth apps were generally positive. Four studies [ 55 , 60 , 61 , 64 ] included standard rating scales (ie, System Usability Scale [ 68 ]) to assess the perceived usability of their apps, and scores exceeded the minimum usability standards (ie, >70). The remaining studies used qualitative feedback from focus groups, case reports, and open-ended questionnaires. For example, in the study by Buus et al [ 54 ], participants found the MYPLAN safety planning app useful in recognizing patterns of impending crises and for reinforcing personalized strategies to cope with distress. In describing the benefits of the BeyondNow safety planning app, participants in the study by Melvin et al [ 58 ] reported developing a sense of hope and connection from using the app. Researchers have attributed these findings to the accessibility of the app and its customizable features. According to the authors, stakeholders regarded apps as highly intuitive, easy to use, and visually appealing interface in terms of the design [ 59 , 61 , 62 , 64 ].
App Use and App Engagement
Five studies examined app use over time [ 58 - 60 , 63 , 64 ]. Overall app engagement and use were minimal. Across 3 studies, >70% of the participants used the apps at least once during the testing period, which ranged from 1 to 10 weeks [ 58 , 59 , 63 ]. In the study by Melvin et al [ 58 ], 77% (17/22) of the participants reported using the mHealth app “occasionally” or “a lot,” including to make changes to safety plans. Most participants also reported using the mHealth app during a suicidal crisis (15/22, 68%) or when experiencing suicidal ideation (18/22, 82%). Increased frequency of app use during a crisis or among participants with high levels of suicide ideation was reported in studies by Pauwels et al [ 63 ] and Muscara et al [ 59 ]. Larkin et al [ 64 ] reported that 2 (40%) out of 5 participants reported downloading the ED-SAFE patient mHealth app after discharge. Low uptake rates were mostly attributed to the participants’ forgetfulness to download the app. Although most participants acknowledged the benefits of using mHealth suicide safety planning apps during times of crisis [ 58 , 63 ], participant feedback from the study by Muscara et al [ 59 ] suggested that participants did not believe or were unsure whether the use of the BeyondNow safety planning app could help them manage their symptoms or keep individuals safe during a crisis. Only 35% (6/17) of the participants favored using the app in the future. Conversely, participants in the study by Nuij et al [ 60 ] noted that easy access to the Backup mHealth app provided a sense of reassurance and helped to deter suicidal thoughts.
Suicide-Related Outcomes
Suicide-related outcomes were examined across 29% (4/14) of the small-scale pilot studies (with sample sizes ranging between 3 and 22) [ 55 , 58 , 59 , 63 ]. The study by Jeong et al [ 55 ] assessed the Theory of Planned Behavior constructs, including attitudes, subjective norms, perceived behavioral control, and intentions toward engaging in suicide attempts, using a pre-posttest design with a small (N=3) sample of adolescent survivors of suicide attempts. The results showed statistically significant changes in attitudes, perceived behavioral control, and intentions, suggesting that the suicide safety planning app helped to positively shift attitudes toward life and reduce beliefs and intentions to engage in self-harm behavior.
Suicide coping or resilience was evaluated in 2 studies using pre-posttest designs [ 58 , 59 ]. Both studies used the same safety planning app (ie, BeyondNow ) to examine the changes in protective factors. Melvin et al [ 58 ] found a statistically significant increase in suicide-related coping among youth and adult participants (n=22). This finding suggests an increase in knowledge and confidence to use internal coping strategies and external resources to manage suicide ideation. However, the researchers did not observe statistically significant changes in suicide resilience (ie, the perceived ability to manage suicidal thoughts and feelings). In contrast, Muscara et al [ 59 ] found a significant increase in 1 subscale of suicide resilience, emotional stability (ie, the ability to regulate emotions), among youth participants (N=17) in their study.
Suicidal ideation or self-harm behavior were measured in 3 studies [ 58 , 59 , 63 ]. In an open-label, single-group design, Melvin et al [ 58 ] found statistically significant reductions in both the severity and intensity of suicide ideation following exposure to an 8-week trial that evaluated the clinical effectiveness of using the BeyondNow suicide safety planning app as an adjunct to treatment as usual (ie, existing mental health services). In an evaluation of the same mHealth app, but with the addition of a personalized toolbox app (ie, BlueIce ), instead of treatment as usual, Muscara et al [ 59 ] also found a reduction in suicide ideation and self-harm behaviors (ie, attempts to harm oneself with and without suicidal intent). However, these findings were not conclusive or statistically significant owing to the small sample size and lack of a control group. Pauwels et al [ 63 ] found a similar, nonsignificant decrease in suicide ideation scores in a study examining pre-posttest changes following exposure to the BackUp suicide safety planning app. Although these studies provide some evidence of clinical utility, these researchers noted study limitations and the need for further evaluation using randomized controlled trials (RCTs).
Principal Findings
The primary aim of this study was to conduct a comprehensive analysis of the integration and inclusion of the SPI components developed by Stanley and Brown [ 31 ] in the design of mHealth suicide safety planning apps. The secondary aim was to synthesize and assess the research methods of studies that reported on the effectiveness of these apps. Implications of these findings and practical recommendations for future directions in mHealth suicide safety planning research are described in the following sections.
Integrating Components of Suicide Safety Planning Into mHealth Apps
Overall, most apps included the core components of the SPI developed by Stanley and Brown [ 31 ], such as the identification of suicide warning signs, coping strategies, and supportive persons. Therefore, the results from this review provide evidence of some level of successful integration of SPI components into mHealth suicide safety planning apps (RQ1). Lethal means safety was 1 component that was not incorporated in 2 of the apps reviewed. Reducing access to lethal means is a critical part of suicide safety planning [ 31 ] and warrants inclusion in mHealth apps as it brings attention to methods that could be used to attempt or die by suicide if not removed from a user’s environment.
An important aspect of suicide safety planning is access to one’s safety plan. In this review, having access to safety plans at any time [ 54 , 55 , 58 , 60 , 61 ] and being able to continually revise the plan were considered benefits over traditional paper-based safety planning. In some apps, users could create associations between different suicide safety planning components (SPCs; eg, triggers and coping strategies) to better contextualize their experiences and create actional plans for mitigating crises [ 54 , 56 , 61 ]. We recommend that additional linkages between the SPCs be included to further personalize users’ experiences.
Despite the integration of SPI components within mHealth suicide safety planning app designs, we also identified important gaps in the literature that warrant the attention of app designers, researchers, and mental health professionals who may use this type of technology within their clinical practice. For instance, researchers have consistently emphasized the importance of completing the initial safety plan alongside a knowledgeable clinician [ 42 , 54 , 58 , 61 ] to ensure that at-risk users and loved ones understand the components and purpose of a safety plan. However, many of the analyzed apps allowed users to complete the safety plan without the recommended clinical support, and in some cases, they lacked disclaimers. Therefore, additional guidance from a professional when using mHealth suicide safety planning apps would further serve to assist users and ensure that the safety planning process is carried out as intended.
This review also found that most of the apps did not go beyond the traditional SPCs of paper-based protocols to integrate more interactive features that could potentially improve adherence or engagement. For instance, daily or weekly check-ins have been shown to improve adherence in other mHealth contexts, such as for smoking cessation [ 69 ] and the management of schizophrenia [ 70 ]. Visualization graphs of patterns or trends in suicide warning signs, triggers, and coping behaviors logged over time may serve to increase engagement and improve outcomes, as visualizing behavior change over time has been recommended in other mHealth contexts [ 71 ], such as alcohol reduction [ 72 ]. Furthermore, other meaningful ways to actively and continuously engage one’s support contacts (eg, clinicians, parents, and family members) and to reinforce the use of healthful coping strategies would be an advantageous direction for future exploration in mHealth app design. Beyond general support contacts, prior research has found that parental support is a significant protective factor against youth suicide [ 73 , 74 ]. For youth, in particular, it may be advantageous to include parents, family members, or other trusted adults in the mHealth suicide safety planning process to increase uptake, enhance help-seeking and coping behaviors, and reinforce ways to keep one’s environment safe. However, future research would need to carefully design and evaluate such interventions to ensure they are effective before making these interventions widely available through the dissemination of mHealth apps for suicide safety planning.
Another variation across the apps was that some apps provided default values for suicide SPCs (eg, suggested coping strategies), whereas others did not. Therefore, an area of future research could be to study whether providing default values is beneficial or detrimental to the safety planning process. Finally, rather than training focused on the technical aspects of using the mHealth app, there is a need to include psychoeducation for suicide safety planning [ 75 ], especially related to coping strategies and lethal means restriction, which should be modeled as a collaborative process between at-risk users and their support systems [ 76 ].
Usability and Design Considerations for mHealth Suicide Safety Planning Apps
Overall, our review highlights three important recommendations to consider when designing safety planning mHealth apps (RQ2): the need to (1) encourage end user collaboration in the design and implementation of the intervention, (2) incorporate personalization or customization capabilities, and (3) develop appropriate privacy safeguards to prevent liability and address other safety concerns that may arise when integrating mental health care and technology. A key strength of most studies in our review was the interdisciplinary collaboration between app developers, computer scientists, and clinical researchers that facilitated the design, development, and evaluation of the various mHealth suicide safety planning apps. In addition, multiple stakeholders were included in the design process, including individuals at risk of suicide, clinicians, usability experts, parents, and extended family members. Only in 1 instance, end users engaged who were not considered part of the target population of at-risk users (eg, students). We strongly recommend that future research continue to include researchers from across multiple disciplines (eg, psychology, public health, social work, medicine, computer science, and human-computer interaction), intended end users, and mental health professionals across each stage of the research process. For instance, researchers from different disciplines may be able to raise important threats to validity during the research design process that could lead to more robust study designs.
A key weakness highlighted within several studies was limited uptake or sustained use of the mHealth suicide safety planning apps over time. Such findings shed suspicion on the feasibility of this type of intervention being effective outside of research, regardless of the high usability and acceptability ratings. Some studies attributed lack of use to the reduction of suicidal behaviors over time, but others suggested that the suicide safety planning process, as designed to be carried out within the apps, was only suited for in-crisis situations and not appropriate for sustained use over time. Although this may be the case, it is also possible that the lack of interactive or engaging features within the apps made them less appealing to users. Being able to customize and personalize app features may help to enhance the user’s experience and increase app engagement. Many of the apps included social distractions (ie, music and pictures) or other features, such as diary cards, which might help increase overall app engagement during noncrisis periods. However, as suicidality is episodic, future research should be conducted to understand how different modalities or features (eg, mood tracking, journaling, mindfulness, and art) could be combined with suicide safety planning in a complementary way for long-term use and engagement. Future work should also consider leveraging advanced technologies and assessments, such as artificial intelligence and ecological momentary assessments [ 77 , 78 ], that could be used to anticipate heightened suicide risk and prompt users to engage in the mHealth app suicide safety planning process when they need it most.
Threats to Validity and Inconclusive Clinical Outcomes Associated With the Use of mHealth Suicide Safety Planning Apps
This review provides some preliminary evidence suggesting that suicide safety planning via mHealth apps could be an easy-to-use mechanism to provide individualized care to those who may otherwise go unserved due to common treatment barriers (RQ3), such as poor accessibility to service providers, lack of knowledge about suicide, and stigmatizing beliefs about help seeking [ 20 - 24 ]. At the same time, several threats to validity were uncovered by our assessment of risk bias, which can inform directions for future research. First, the robustness of the qualitative studies could be improved by stating the positionality of the researchers as well as a clear justification for the design of the mHealth apps. In some cases, articles were published by interdisciplinary teams, whereas in other cases, authors appeared to be from a single discipline (eg, computer science). Details about the composition and expertise of the research team are important, as well-implemented mHealth apps require interdisciplinary skill sets that span clinical, design-based, and technical expertise. Furthermore, the quantitative studies analyzed in our review were constrained by small sample sizes and no published RCTs. Among the pre-posttest studies conducted thus far, the clinical outcomes were inconclusive.
As such, RCTs with control groups, random assignment, and repeated measure outcomes assessed over time are needed in the future to evaluate the efficacy of using suicide safety planning mHealth apps compared with traditional paper-based safety plans [ 54 , 57 ], specifically related to reducing suicidal urges and behaviors and increasing use of coping strategies, as well as increased engagement in crisis and mental health services after the crisis. When doing so, researchers should recruit larger samples to ensure that the results are conclusive and can be generalized to the populations of interest. Furthermore, additional use metrics collected by the apps to track behavioral data associated with using different app features, such as user engagement with the 6 components of the SPI developed by Stanley and Brown [ 31 ], should be considered to better understand the potential mediating factors and behaviors that may influence clinical outcomes. Although the usability of the apps would be an important consideration to control for in future studies, it is necessary to move beyond such measures to determine the efficacy of mHealth apps in reducing suicide-related outcomes. In summary, the inclusion of more advanced study design methodologies and recommendations from lessons learned in future mHealth apps could serve to mitigate suicide risk and promote overall safety.
Limitations and Future Research
This systematic review included 14 peer-reviewed articles that designed, developed, and evaluated mHealth apps for suicide safety planning. There are several limitations of this study that should be addressed in future research. First, although our search process was comprehensive, it is possible that our keywords missed relevant articles and mHealth apps that should have been included in the review. Second, as many of the apps described in the articles were not publicly available for download, we requested access from the corresponding authors to conduct our review. In 2 cases, we were unable to gain access to the apps; therefore, our analysis was based on the description of those apps based on the published paper. As such, it may be possible that some features were not described in the original papers; thus, they were not included in our review. Future research should also consider conducting a systematic feature analysis of mHealth suicide safety planning apps that are publicly available for download but not studied within the peer-reviewed literature. Finally, a limited number of published RCTs at the time of the review restricted our ability to report on app use and suicide-related outcomes. As such, the main call-to-action from this review is the need to move beyond usability studies of newly developed mHealth suicide safety planning apps to robust clinical research designs to examine their efficacy in reducing suicidality among at-risk user populations.
Conclusions
Overall, most articles included in this review did little to evaluate the efficacy of mHealth suicide safety planning apps beyond usability assessments, signaling that these apps and corresponding research are still in their infancy in terms of validating clinical outcomes. Although most of the mHealth safety planning apps included in our review are not yet downloadable and broadly available for public use, the prevalence and popularity of mHealth suicide prevention and mental health support apps on the open market that have been deployed without rigorous peer-reviewed research is a concern. As such, there is a critical need for future research to ensure that mHealth apps for suicide safety planning integrate the lessons learned from empirical user-based and clinical research, are upheld to high ethical mental health care standards, and show clinical efficacy for reducing suicidality before the apps are released to end users. This is especially true given the delicate and important goal of preventing suicide among at-risk populations. It is promising to see that future randomized clinical trials have been registered to build upon this important preliminary work on mHealth suicide safety planning apps.
Acknowledgments
The authors would like to thank the following authors who provided access to their apps to conduct this feature analysis: Niels Buus and JL Stovgaard Larsen (MYPLAN); Glenn Melvin (BeyondNow); James Duggan (SafePlan); and Lea Meier, Caroline Gurtner, and François von Kaenel (SERO).
Conflicts of Interest
None declared.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist.
Example search strategy.
Detailed summary of the selected articles and key findings (N=14).
Critical appraisal results.
- WISQARS™ — web-based injury statistics query and reporting system. Centers for Disease Control and Prevention. URL: https://www.cdc.gov/injury/wisqars/index.html [accessed 2023-01-11]
- Curtin SC, Heron M. Death rates due to suicide and homicide among persons aged 10-24: United States, 2000-2017. NCHS Data Brief. Oct 2019.(352):1-8. [ Medline ]
- Congressional Black Caucus. Ring the alarm: the crisis of black youth suicide in America. The National Action Alliance for Suicide Prevention. Dec 2019. URL: https://theactionalliance.org/resource/ring-alarm-crisis-black-youth-suicide-america [accessed 2023-06-05]
- Ramchand R, Gordon JA, Pearson JL. Trends in suicide rates by race and ethnicity in the United States. JAMA Netw Open. May 03, 2021;4(5):e2111563. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gaylor EM, Krause KH, Welder LE, Cooper AC, Ashley C, Mack KA, et al. Suicidal thoughts and behaviors among high school students - youth risk behavior survey, United States, 2021. MMWR Suppl. Apr 28, 2023;72(1):45-54. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Plemmons G, Hall M, Doupnik S, Gay J, Brown C, Browning W, et al. Hospitalization for suicide ideation or attempt: 2008-2015. Pediatrics. Jun 2018;141(6):e20172426. [ CrossRef ] [ Medline ]
- Johns MM, Lowry R, Haderxhanaj LT, Rasberry CN, Robin L, Scales L, et al. Trends in violence victimization and suicide risk by sexual identity among high school students - youth risk behavior survey, United States, 2015-2019. MMWR Suppl. Aug 21, 2020;69(1):19-27. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Peña JB, Wyman PA, Brown CH, Matthieu MM, Olivares TE, Hartel D, et al. Immigration generation status and its association with suicide attempts, substance use, and depressive symptoms among latino adolescents in the USA. Prev Sci. Dec 2008;9(4):299-310. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Johns MM, Lowry R, Andrzejewski J, Barrios LC, Demissie Z, McManus T, et al. Transgender identity and experiences of violence victimization, substance use, suicide risk, and sexual risk behaviors among high school students - 19 states and large urban school districts, 2017. MMWR Morb Mortal Wkly Rep. Jan 25, 2019;68(3):67-71. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stone DM, Jones CM, Mack KA. Changes in suicide rates - United States, 2018-2019. MMWR Morb Mortal Wkly Rep. Feb 26, 2021;70(8):261-268. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jin SS, Dolan TM, Cloutier AA, Bojdani E, DeLisi L. Systematic review of depression and suicidality in child and adolescent (CAP) refugees. Psychiatry Res. Aug 2021;302:114025. [ CrossRef ] [ Medline ]
- Fortune S, Stewart A, Yadav V, Hawton K. Suicide in adolescents: using life charts to understand the suicidal process. J Affect Disord. Jun 2007;100(1-3):199-210. [ CrossRef ] [ Medline ]
- Moskos M, Olson L, Halbern S, Keller T, Gray D. Utah youth suicide study: psychological autopsy. Suicide Life Threat Behav. Oct 2005;35(5):536-546. [ CrossRef ] [ Medline ]
- Pagura J, Fotti S, Katz LY, Sareen J, Swampy Cree Suicide Prevention Team. Help seeking and perceived need for mental health care among individuals in Canada with suicidal behaviors. Psychiatr Serv. Jul 2009;60(7):943-949. [ CrossRef ] [ Medline ]
- Sankey M, Lawrence R. Brief report: classification of adolescent suicide and risk-taking deaths. J Adolesc. Dec 2005;28(6):781-785. [ CrossRef ] [ Medline ]
- Pisani AR, Wyman PA, Petrova M, Schmeelk-Cone K, Goldston DB, Xia Y, et al. Emotion regulation difficulties, youth-adult relationships, and suicide attempts among high school students in underserved communities. J Youth Adolesc. Jun 2013;42(6):807-820. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rajappa K, Gallagher M, Miranda R. Emotion dysregulation and vulnerability to suicidal ideation and attempts. Cogn Ther Res. Nov 9, 2011;36:833-839. [ CrossRef ]
- Hung P, Busch SH, Shih YW, McGregor AJ, Wang S. Changes in community mental health services availability and suicide mortality in the US: a retrospective study. BMC Psychiatry. Apr 25, 2020;20(1):188. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hester RD. Lack of access to mental health services contributing to the high suicide rates among veterans. Int J Ment Health Syst. Aug 18, 2017;11:47. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Curtis C. Youth perceptions of suicide and help-seeking: ‘they'd think I was weak or “mental”’. J Youth Stud. Jul 28, 2010;13(6):699-715. [ CrossRef ]
- Aguirre Velasco A, Cruz IS, Billings J, Jimenez M, Rowe S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? A systematic review. BMC Psychiatry. Jun 11, 2020;20(1):293. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Czyz EK, Horwitz AG, Eisenberg D, Kramer A, King CA. Self-reported barriers to professional help seeking among college students at elevated risk for suicide. J Am Coll Health. 2013;61(7):398-406. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hom MA, Stanley IH, Joiner TE. Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: a review of the literature. Clin Psychol Rev. Aug 2015;40:28-39. [ CrossRef ] [ Medline ]
- Wilson CJ, Deane FP. Adolescent opinions about reducing help-seeking barriers and increasing appropriate help engagement. J Educ Psychol Consult. 2001;12(4):345-364. [ CrossRef ]
- Ougrin D, Tranah T, Stahl D, Moran P, Asarnow JR. Therapeutic interventions for suicide attempts and self-harm in adolescents: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. Feb 2015;54(2):97-107.e2. [ CrossRef ] [ Medline ]
- Pfeiffer PN, King C, Ilgen M, Ganoczy D, Clive R, Garlick J, et al. Development and pilot study of a suicide prevention intervention delivered by peer support specialists. Psychol Serv. Aug 2019;16(3):360-371. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Evidence. Zero Suicide. URL: https://zerosuicide.edc.org/evidence [accessed 2023-10-25]
- Ferguson M, Rhodes K, Loughhead M, McIntyre H, Procter N. The effectiveness of the safety planning intervention for adults experiencing suicide-related distress: a systematic review. Arch Suicide Res. 2022;26(3):1022-1045. [ CrossRef ] [ Medline ]
- Nuij C, van Ballegooijen W, de Beurs D, Juniar D, Erlangsen A, Portzky G, et al. Safety planning-type interventions for suicide prevention: meta-analysis. Br J Psychiatry. Aug 2021;219(2):419-426. [ CrossRef ] [ Medline ]
- Conti EC, Jahn DR, Simons KV, Edinboro LP, Jacobs ML, Vinson L, et al. Safety planning to manage suicide risk with older adults: case examples and recommendations. Clin Gerontol. 2020;43(1):104-109. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stanley B, Brown GK. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn Behav Pract. May 2012;19(2):256-264. [ CrossRef ]
- Chesin MS, Stanley B, Haigh EA, Chaudhury SR, Pontoski K, Knox KL, et al. Staff views of an emergency department intervention using safety planning and structured follow-up with suicidal veterans. Arch Suicide Res. Jan 02, 2017;21(1):127-137. [ CrossRef ] [ Medline ]
- Stanley IH, Hom MA, Joiner TE. A systematic review of suicidal thoughts and behaviors among police officers, firefighters, EMTs, and paramedics. Clin Psychol Rev. Mar 2016;44:25-44. [ CrossRef ] [ Medline ]
- Stanley B, Brown GK, Brenner LA, Galfalvy HC, Currier GW, Knox KL, et al. Comparison of the safety planning intervention with follow-up vs usual care of suicidal patients treated in the emergency department. JAMA Psychiatry. Sep 01, 2018;75(9):894-900. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Labouliere CD, Stanley B, Lake AM, Gould MS. Safety planning on crisis lines: feasibility, acceptability, and perceived helpfulness of a brief intervention to mitigate future suicide risk. Suicide Life Threat Behav. Feb 2020;50(1):29-41. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Czyz EK, King CA, Biermann BJ. Motivational interviewing-enhanced safety planning for adolescents at high suicide risk: a pilot randomized controlled trial. J Clin Child Adolesc Psychol. 2019;48(2):250-262. [ CrossRef ] [ Medline ]
- Stewart KL, Darling EV, Yen S, Stanley B, Brown GK, Weinstock LM. Dissemination of the safety planning intervention (SPI) to university counseling center clinicians to reduce suicide risk among college students. Arch Suicide Res. 2020;24(sup1):75-85. [ CrossRef ] [ Medline ]
- Rudd MD, Joiner TE, Rajab MH. Treating Suicidal Behavior: An Effective, Time-Limited Approach. New York City, NY. Guilford Publications; 2001.
- Asarnow JR, Berk M, Hughes JL, Anderson NL. The SAFETY program: a treatment-development trial of a cognitive-behavioral family treatment for adolescent suicide attempters. J Clin Child Adolesc Psychol. 2015;44(1):194-203. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bryan CJ, Mintz J, Clemans TA, Leeson B, Burch TS, Williams SR, et al. Effect of crisis response planning vs. contracts for safety on suicide risk in U.S. Army Soldiers: a randomized clinical trial. J Affect Disord. Apr 01, 2017;212:64-72. [ CrossRef ] [ Medline ]
- Little V, Neufeld J, Cole AR. Integrating safety plans for suicidal patients into patient portals: challenges and opportunities. Psychiatr Serv. Jun 01, 2018;69(6):618-619. [ CrossRef ] [ Medline ]
- Nuij C, van Ballegooijen W, Ruwaard J, de Beurs D, Mokkenstorm J, van Duijn E, et al. Smartphone-based safety planning and self-monitoring for suicidal patients: rationale and study protocol of the CASPAR (Continuous Assessment for Suicide Prevention And Research) study. Internet Interv. May 05, 2018;13:16-23. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kennard BD, Biernesser C, Wolfe KL, Foxwell AA, Craddock Lee SJ, Rial KV, et al. Developing a brief suicide prevention intervention and mobile phone application: a qualitative report. J Technol Hum Serv. Oct 01, 2015;33(4):345-357. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Moscardini EH, Hill RM, Dodd CG, Do C, Kaplow JB, Tucker RP. Suicide safety planning: clinician training, comfort, and safety plan utilization. Int J Environ Res Public Health. Sep 04, 2020;17(18):6444. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Czyz EK, Arango A, Healy N, King CA, Walton M. Augmenting safety planning with text messaging support for adolescents at elevated suicide risk: development and acceptability study. JMIR Ment Health. May 25, 2020;7(5):e17345. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Anderson M, Jiang J. Teens, social media and technology 2018. Pew Research Center. May 31, 2018. URL: https://www.pewresearch.org/internet/2018/05/31/teens-social-media-technology-2018/ [accessed 2024-02-28]
- Comer JS. Introduction to the special series: applying new technologies to extend the scope and accessibility of mental health care. Cogn Behav Pract. Aug 2015;22(3):253-257. [ CrossRef ]
- Lal S. E-mental health: promising advancements in policy, research, and practice. Healthc Manage Forum. Mar 2019;32(2):56-62. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Turvey CL, Roberts LJ. Recent developments in the use of online resources and mobile technologies to support mental health care. Int Rev Psychiatry. 2015;27(6):547-557. [ CrossRef ] [ Medline ]
- Shingleton RM, Richards LK, Thompson-Brenner H. Using technology within the treatment of eating disorders: a clinical practice review. Psychotherapy (Chic). Dec 2013;50(4):576-582. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. Mar 29, 2021;372:n71. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ryan R, Horey D, Oliver S, McKenzie J, Prictor M, Santesso N, et al. Cochrane Consumers and Communication Group Standard protocol text and additional guidance for review authors. La Trobe University. Mar 2019. URL: https://opal.latrobe.edu.au/articles/journal_contribution/Standard_Protocol_Text_and_Additional_Guidance_for_Review_Authors/6692969 [accessed 2023-05-19]
- Andreasson K, Krogh J, Bech P, Frandsen H, Buus N, Stanley B, et al. MYPLAN -mobile phone application to manage crisis of persons at risk of suicide: study protocol for a randomized controlled trial. Trials. Apr 11, 2017;18(1):171. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Buus N, Erlangsen A, River J, Andreasson K, Frandsen H, Larsen JL, et al. Stakeholder perspectives on using and developing the MYPLAN suicide prevention mobile phone application: a focus group study. Arch Suicide Res. 2020;24(1):48-63. [ CrossRef ] [ Medline ]
- Jeong YW, Chang HJ, Kim JA. Development and feasibility of a safety plan mobile application for adolescent suicide attempt survivors. Comput Inform Nurs. Aug 2020;38(8):382-392. [ CrossRef ] [ Medline ]
- Meier L, Gurtner C, Nuessli S, Miletic M, Bürkle T, Durrer M. SERO - a new mobile app for suicide prevention. Stud Health Technol Inform. May 16, 2022;292:3-8. [ CrossRef ] [ Medline ]
- Melia R, Francis K, Duggan J, Bogue J, O'Sullivan M, Young K, et al. Using a safety planning mobile app to address suicidality in young people attending community mental health services in Ireland: protocol for a pilot randomized controlled trial. JMIR Res Protoc. Feb 21, 2023;12:e44205. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Melvin GA, Gresham D, Beaton S, Coles J, Tonge BJ, Gordon MS, et al. Evaluating the feasibility and effectiveness of an Australian safety planning smartphone application: a pilot study within a tertiary mental health service. Suicide Life Threat Behav. Jun 2019;49(3):846-858. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Muscara F, Ng O, Crossley L, Lu S, Kalisch L, Melvin G, et al. The feasibility of using smartphone apps to manage self-harm and suicidal acts in adolescents admitted to an inpatient mental health ward. Digit Health. Nov 26, 2020;6:2055207620975315. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nuij C, van Ballegooijen W, de Beurs D, de Winter RF, Gilissen R, O'Connor RC, et al. The feasibility of using smartphone apps as treatment components for depressed suicidal outpatients. Front Psychiatry. Sep 27, 2022;13:971046. [ FREE Full text ] [ CrossRef ] [ Medline ]
- O'Grady C, Melia R, Bogue J, O'Sullivan M, Young K, Duggan J. A mobile health approach for improving outcomes in suicide prevention (SafePlan). J Med Internet Res. Jul 30, 2020;22(7):e17481. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Skovgaard Larsen JL, Frandsen H, Erlangsen A. MYPLAN - a mobile phone application for supporting people at risk of suicide. Crisis. May 2016;37(3):236-240. [ CrossRef ] [ Medline ]
- Pauwels K, Aerts S, Muijzers E, De Jaegere E, van Heeringen K, Portzky G. BackUp: development and evaluation of a smart-phone application for coping with suicidal crises. PLoS One. Jun 21, 2017;12(6):e0178144. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Larkin C, Djamasbi S, Boudreaux ED, Varzgani F, Garner R, Siddique M, et al. ReachCare mobile apps for patients experiencing suicidality in the emergency department: development and usability testing using mixed methods. JMIR Form Res. Jan 27, 2023;7:e41422. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Chapter 3: systematic reviews of effectiveness. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. Adelaide, South Australia. Joanna Briggs Institute; 2020.
- Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. Sep 2015;13(3):179-187. [ CrossRef ] [ Medline ]
- De Jaegere E, Portzky G, van den Berg M. Ethical guidelines for technology-based suicide prevention programmes. European Regions Enforcing Actions against Suicide. 2014. URL: https://www.researchgate.net/publication/260297369_Ethical_Guidelines_for_Technology-Based_Suicide_Prevention_Programmes [accessed 2024-02-28]
- Brooke J. SUS: a 'quick and dirty' usability scale. In: Usability Evaluation In Industry. Boca Raton, FL. CRC Press; 1996.
- McClure JB, Anderson ML, Bradley K, An LC, Catz SL. Evaluating an adaptive and interactive mHealth smoking cessation and medication adherence program: a randomized pilot feasibility study. JMIR Mhealth Uhealth. Aug 03, 2016;4(3):e94. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stubbe DE. Enhancing adherence: using mobile health technology to improve self-management for individuals with schizophrenia. Focus (Am Psychiatr Publ). Oct 2020;18(4):424-427. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Short CE, DeSmet A, Woods C, Williams SL, Maher C, Middelweerd A, et al. Measuring engagement in eHealth and mHealth behavior change interventions: viewpoint of methodologies. J Med Internet Res. Nov 16, 2018;20(11):e292. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bell L, Garnett C, Qian T, Perski O, Williamson E, Potts HW. Engagement with a behavior change app for alcohol reduction: data visualization for longitudinal observational study. J Med Internet Res. Dec 11, 2020;22(12):e23369. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hatchel T, Merrin GJ, Espelage AD. Peer victimization and suicidality among LGBTQ youth: the roles of school belonging, self-compassion, and parental support. J LGBT Youth. 2019;16(2):134-156. [ CrossRef ]
- Flouri E, Buchanan A. The protective role of parental involvement in adolescent suicide. Crisis. 2002;23(1):17-22. [ CrossRef ] [ Medline ]
- Abbott-Smith S, Ring N, Dougall N, Davey J. Suicide prevention: what does the evidence show for the effectiveness of safety planning for children and young people? - a systematic scoping review. J Psychiatr Ment Health Nurs. Oct 2023;30(5):899-910. [ CrossRef ] [ Medline ]
- Asarnow JR, Zullo L, Ernestus SM, Venables CW, Goldston DB, Tunno AM, et al. "Lock and protect": development of a digital decision aid to support lethal means counseling in parents of suicidal youth. Front Psychiatry. Oct 6, 2021;12:736236. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Auerbach RP, Lan R, Galfalvy H, Alqueza KL, Cohn JF, Crowley RN, et al. Intensive longitudinal assessment of adolescents to predict suicidal thoughts and behaviors. J Am Acad Child Adolesc Psychiatry. Sep 2023;62(9):1010-1020. [ CrossRef ] [ Medline ]
- Bhatt P, Liu J, Gong Y, Wang J, Guo Y. Emerging artificial intelligence-empowered mHealth: scoping review. JMIR Mhealth Uhealth. Jun 09, 2022;10(6):e35053. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by J Torous; submitted 14.09.23; peer-reviewed by HL Tam, B Leckning; comments to author 06.10.23; revised version received 19.12.23; accepted 31.12.23; published 28.03.24.
©Kim Gryglewicz, Victoria L Orr, Marissa J McNeil, Lindsay A Taliaferro, Serenea Hines, Taylor L Duffy, Pamela J Wisniewski. Originally published in JMIR Mental Health (https://mental.jmir.org), 28.03.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Mental Health, is properly cited. The complete bibliographic information, a link to the original publication on https://mental.jmir.org/, as well as this copyright and license information must be included.
University of South Florida
Main Navigation

From midwife to researcher: USF Nursing PhD student wins awards for perinatal health studies
- March 28, 2024
Research , Student Success
There are three shared experiences among humans across the globe: life, death, and mental health. Unfortunately, some young mothers may experience all three in one perinatal cycle. One nursing PhD student is investigating ways to improve the mental health and morbidity outcomes of perinatal adolescents.
Olajumoke “Jummy” Ojeleye is a third-year PhD student at the University of South Florida (USF). Born and raised in Nigeria, West Africa, Ojeleye was eager to enhance the field of maternal care. She became a nurse-midwife and practiced in various settings, including clinical care, academia, and non-governmental organizations in Nigeria before starting her PhD program at USF. It was as a midwife that she began recognizing that maternal morbidity and mortality were global issues

Olajumoke Ojeleye prepares to present her research.
“According to the World Health Organization, midwives educated to international standards can prevent over 80% of maternal mortality including perinatal depression,” says Ojeleye. “I am committed to making an impact through research and supporting the next generation of nurses and midwives.”
Ojeleye’s goal is to use her experience and skills as a nurse-midwife to address pressing problems in perinatal mental health, an underserved aspect of maternity care. Her research into perinatal mental health was first recognized with a monetary award at the 2023 USF Health Research Day. The recognition continued as her studies progressed. During the 2024 USF Health Research Day, Ojeleye presented findings from her integrative review titled, “Perinatal Depression and Anxiety Among Adolescents: Knowledge, Perception, Care Preferences, and Access to Perinatal Mental Health Care.” Her presentation captured the current state of the science on perinatal depression and perinatal anxiety among adolescents across diverse geographical and cultural contexts and was awarded The USF Health Deans’ Interprofessional Research Award.
This study was foundational to further develop Ojeleye’s understanding of perinatal mental health and the existing gaps, which is a growing area of research among adolescents. The findings helped her identify the specific research gaps and areas to focus on in her follow-up dissertation titled, “The Lived Experiences of Pregnant and Parenting Adolescents With Perinatal Depression and Perinatal Anxiety in the Tampa Bay Area of Florida.” This ongoing study aims to explore pregnant and parenting adolescents' knowledge of mental health, identify their unique mental health needs, understand their care preferences, and determine the factors that motivate or hinder them from utilizing existing perinatal mental health services.

Dr. Ukamaka Oruche and Olajumoke Ojeleye pose together outside the USF Health College of Nursing.
Recently receiving the ISPN Foundational Mental Health Research Grant by the International Society of Psychiatric-Mental Health Nurses for this project, Ojeleye expresses gratitude for all those who mentored her in this process, including Dr. Ukamaka Oruche, USF Health College of Nursing Senior Associate Dean of Research and PhD Program Director.
“I helped Jummy by analyzing and synthesizing her literature review, then refining her manuscript, and identifying the best journal for submission and publication,” says Oruche. "I loved the aha moment in her face when the findings became crystal clear.”
Ojeleye will begin collecting data for this study later this summer.
Return to article listing
Explore More Categories
- Student Success
About Department News
USF Health College of Nursing News highlights the great work of our trailblazing faculty, staff, and students! The College of Nursing is an integral part of USF Health and the University of South Florida. USF Health College of Nursing -- Where Nursing Trailblazers Belong!

IMAGES
VIDEO
COMMENTS
Mental Health Case Study. 1 is Bipolar I disorder? How does it differ from Bipolar II? Bipolar I disorder: The client has at least one episode of mania alternating with major depression. Bipolar II disorder: The client has one or more hypomanic episodes alternating with major depressive episodes. 2 behaviors are exhibited during a manic episode?
A charge nurse on a mental health unit is discussing legal issue with a newly licensed nurse. If a client threatens to seriously harm someone, the provider should notify that person of threat A nurse in an acute care mental health facility is preparing a client for discharge. Make appropriate referrals
Nutrition outline - homework. Lab Exercise 1 - homework. Disorders Associated with Leukocytes. ACOG - information. Week Six Communicable Disease Online Assignment. Exam 4 Burn study guide. Assessment study 22. 23. vati mental health assessment 2019 nurse is planning care for client following suicide attempt. provide the client with plastic eating.
a nurse is contributing to the plan of care for a client who is experiencing acute alcohol withdrawal. which of the following interventions should the nurse recommend. initiate seizure precautions for the client. ATI assessment Learn with flashcards, games, and more — for free.
Mental health case study A female client, diagnosed with Bipolar I, recently stopped taking her lithium. She has not slept, eaten or bathed in days. She is dressing in brightly-colored, flamboyant, and sexually suggestive clothing. She has been spending money freely and buying things she does not need and cannot afford. She recently purchased a trip to Tahiti as well as a motorcycle that she ...
a dissociative disorder characterized by persistent or recurrent feelings of detachment from one's mental processes or body. Medications used for anxiety disorder. 1) Benzodiazepines. 2) Antidepressants (TCAs, SSRIs, MAOIs) Amitriptyline. TCA. Venlafaxine. SNRI. Phenelzine.
VATI Mental Health - Alternate Item Format Quiz. The family of a 14-year-old client with Attention-Deficit Hyperactivity Disorder (ADHD) is requesting the nurse's assistance in implementing strategies in the client's management of ADHD.
The RN Vati Mental Health 2019 report serves as a wake-up call, highlighting the urgent need to address the mental health crisis among RNs. By taking action to improve access to mental health services, reduce stigma, and create supportive workplace environments, we can help ensure that RNs have the tools and resources they need to thrive both ...
View VATI PSYCH CASE STUDY.docx from PSYC 111 at Bryant & Stratton College. 1. What is Bipolar I disorder? How does it differ from Bipolar II? ... mental health case study.docx. Solutions Available. Carrington College, Sacramento. NURS 4435. Mental health case study.docx. Solutions Available. Beckfield College. NUR 201.
Virtual-ATI is a guaranteed, 12-week NCLEX preparation review. Each participant has access to an expert ATI Nurse Educator who works with you one-on-one to verify you're ready for success. The self-paced nature allows educators to provide content assessments and study plans based on individual needs. After the 12-week period, you can earn ...
Learning System. Learning System is a rich bank made up of 34 quizzes covering ten content areas, including a comprehensive cumulative quiz. Perfect for formative quizzing, Learning System helps educators determine if students understand specific content areas. Learn More.
RN VATI Mental Health Case Study. A female client, diagnosed with Bipolar I, recently stopped taking her lithium. She has not slept, eaten or bathed in days. She is dressing in brightly-colored, flamboyant, and sexually suggestive clothing. She has been spending money freely and buying things she does not need and cannot afford.
View VATI Mental Health remediation.docx from NURS MISC at Lamar University. 1. Complete an ATI Focused Review® and send a detailed summary (23 sentences each) of 4 concepts that you learned from the ... Please complete the case study for this mental health module. A female client, diagnosed with Bipolar I, recently stopped taking her lithium.
Mental health and psychiatric management has been elaborately dealt in Ayurveda. ... Brahmi vati has anxiolytic, antidepressant, sleep promoting effect and improves quality of life and decreases blood pressure of prehypertensive stages and disease severity. Further studies on Brahmi vati are needed to get better understanding of the drug ...
Serum creatinine 2.1 mg/dL. -Reference range of 0.5-1.2 mg/dL. The greatest risk to this client is decreased kidney function, which can cause an increase in the client's lithium level; therefore, this value is the priority for the nurse to report to the provider. The clients lithium dosage might need to be modified based on this lab value.
2x sold. 8 items. 1. Exam (elaborations) - Ati mental health proctored exam 2023 with correct answers. 2. Exam (elaborations) - Mental health proctored ati questions and answers. 3. Exam (elaborations) - Rn vati mental health 2023 assessment. 4.
Research has revealed a range of barriers associated with initiating United States Department of Veterans Affairs (VA) care, including those specific to accessing mental health care (e.g., fear of stigmatization). More work is needed to streamline access to VA mental health-care services for veterans. In the current study, we interviewed 80 ...
The team made their anonymized data set publicly available—including self-reports, surveys, and phone-sensing and brain-imaging data—to help advance research into the mental health of students during their college years.. Andrew Campbell, the paper's senior author and Dartmouth's Albert Bradley 1915 Third Century Professor of Computer Science, says that the study's extensive data ...
RN VATI MENTAL HEALTH ASSESSMENT REMEDIATION (latest 2022/2023) RN VATI MENTAL HEALTH ASSESSMENT REMEDIATION (latest 2022/2023) 100% satisfaction guarantee Immediately available after payment Both online and in PDF No strings attached. Previously searched by you. Previously searched by you. Sell. Where do you study.
23. vati mental health assessment 2019 nurse is planning care for client following suicide attempt. provide the client with plastic eating utensils. Skip to document. University; High School. ... GI Case Study; Respiratory system case study 2022; Case Study 5 - Reproductive; NURS 6160 Case Study 1-Genetics-2; Exam Chapter Study Material;
The Division of Neuroscience and Basic Behavioral Science (DNBBS) at the National Institute of Mental Health (NIMH) supports research on basic neuroscience, genetics, and basic behavioral science. These are foundational pillars in the quest to decode the human mind and unravel the complexities of mental illnesses. At NIMH, we are committed to supporting and conducting genomics research as a ...
Between 2006 and 2019, patients aged 13 to 24 made 1.1 billion health care visits, of which 145 million involved mental health issues. But the share of mental-health-related visits rose each year ...
Abdominal pain. The nurse should instruct the client that abdominal pain can indicate hepatoxicity or pancreatitis, both adverse effects of valproic acid; therefore, the client should report this to the provider. A nurse is establishing a therapeutic relationship with a client who has generalized anxiety disorder.
Like the new study suggests, Texas has seen general stability in maternal mortality rates in recent years. "From 2013 to 2019, we're looking at fluctuation between 17 deaths per 100,000 live ...
Advances in mobile and wearable technologies have enabled the potential to passively monitor a person's mental, behavioral, and affective health. These approaches typically rely on longitudinal collection of self-reported outcomes, e.g., depression, stress, and anxiety, to train machine learning (ML) models. However, the need to continuously self-report adds a significant burden on the ...
mental health mental health vati remediation nurse is caring for client who is experiencing anxiety attack. what actions should the nurse take? the nurse should. ... Chapter 10 06-1[35330 ] Cystic Fibrosis case study; Transition to Parenthood Class 16 overall notes; Related documents. Uterine Adaptations overall notes and so much more.
Background: Suicide safety planning is an evidence-based approach used to help individuals identify strategies to keep themselves safe during a mental health crisis. This study systematically reviewed the literature focused on mobile health (mHealth) suicide safety planning apps. Objective: This study aims to evaluate the extent to which apps integrated components of the safety planning ...
20 Multiple choice questions. Term. A nurse is assessing the health status of an older adult client. Although the client denies a problem, the caregiver explains that the client is alert and oriented but consistently has an unkempt appearance, body odor, and soiled clothing. The nurse understands that the client's behavior is likely related to ...
From midwife to researcher: USF Nursing PhD student wins awards for perinatal health studies. March 28, 2024. Research, Student Success. There are three shared experiences among humans across the globe: life, death, and mental health. Unfortunately, some young mothers may experience all three in one perinatal cycle.
Review Mental Health Module Checklist Activities to Complete PREPARE Spend 1 ... Mental Health 1 Mental Health 2 Communication TAKE ASSESSMENT Complete the RN VATI Mental Health Assessment Message Coach upon completion of assessment via the messaging system Review your results and complete an ATI Focused ReviewÆ REMEDIATE Read the ...