- No category

Respiratory Case Study - Asthma Attack - Student handout

Related documents
Study collections
Add this document to collection(s).
You can add this document to your study collection(s)
Add this document to saved
You can add this document to your saved list
Suggest us how to improve StudyLib
(For complaints, use another form )
Input it if you want to receive answer
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMJ Case Rep

Case Report
Conundrum in an asthma exacerbation.
A 66-year-old man, an asthmatic, presented with symptoms suggestive of an acute exacerbation of asthma. His arterial blood gas revealed type 1 respiratory failure (PaO 2 <8 kPa or 60 mm Hg with normal or low PaCO 2 ) with a compensated lactic acidosis. He was treated for an asthma exacerbation and sepsis. Despite treatment, his respiratory rate remained elevated although his hypoxaemia improved. There was progressive worsening of the lactic acidosis. Treatment for sepsis was augmented. Peak flow measurements were not used to assess the severity of his exacerbation nor his response to treatment. An alternate diagnosis of acute coronary syndrome with acute pulmonary oedema was made and his asthma treatment was stopped. This coincided with a decline in his serum lactate. A diagnosis of salbutamol-induced lactic acidosis (SILA) was made. SILA is a relatively common complication of salbutamol therapy in moderate/severe asthma exacerbations. It is caused by a mechanism different from the lactataemia that is associated with septic shock and life-threatening asthma.
Elevated lactate is a marker of severe sepsis and systemic shock. It is also seen in life-threatening asthma when respiratory fatigue and hypoxaemia become overwhelming. However, these are not the only causes. Repeated treatment with nebulised β-2 agonists in otherwise healthy patients can result in hyperlactataemia during a moderate/severe asthma exacerbation.
Acute asthma exacerbations are common medical presentations. Failure to recognise the described scenario can lead to unnecessary escalation of treatment and paradoxical worsening of symptoms ( figure 1 ). Prompt recognition and management lead to dramatic improvement, reducing the risk of iatrogenic harm and prolonged hospital admission.

Flow chart depicting the sequence of events with likely explanations.
Case presentation
The patient, a 66-year-old asthmatic man, had a 3-day history of worsening cough, wheeze and shortness of breath that was not relieved by his salbutamol inhaler. He had purulent sputum but neither fever, chest pain nor haemoptysis. He had been diagnosed with asthma many years ago, but was only treated with a salbutamol inhaler, which he used infrequently. He did not measure his peak flow. He had an admission for an asthma exacerbation 15 years prior, but had never required admission to intensive care. His other comorbidities were atrial fibrillation (AF) and a deep vein thrombosis many years earlier. He had never smoked. He was a retired accountant. He took warfarin in addition to his salbutamol.
On examination, he was able to complete sentences, but was using his accessory muscles to aid respiration. He had a respiratory rate of 23 breaths/min and required 2 L/min of oxygen by nasal cannula to saturate at 94%. His heart rate was 104 bpm and he was normotensive and euvolaemic. Auscultation of the chest revealed a bilateral polyphonic wheeze. The remainder of the examination was normal. A clinical diagnosis of acute infective exacerbation of bronchial asthma was made.
Investigations
The patient's chest radiograph was normal. The white cell count was 11.3 (neutrophils 7.8, eosinophils 0.03×10 9 /L) and C reactive protein was 6 mg/dL. Renal function, serum electrolytes and liver enzymes were normal. Troponin was 8 ng/L. International normalized ratio was 2.2. Arterial blood gas (ABG) at admission ( table 1 ) revealed type 1 respiratory failure and a compensated metabolic acidosis, with a serum lactate of 5.6 mmol/L. Peak flow measurements were not taken. ECG showed AF with a controlled ventricular rate.
Table 1
Timeline of first 10 h of admission, detailing ABG results and medication administration (units and normal ranges for blood gas values given in parenthesis)
ABG, arterial blood gas; BE, base excess; FM, face mask; GTN, glyceryl trinitrate; IV, intravenous; NC, nasal cannula.
Differential diagnosis
Treatment and course.
The patient received repeated doses of 5 mg nebulised salbutamol provided by the ambulance crew. In the emergency department, he received nebulised bronchodilators, parenteral steroids and magnesium. A sepsis care bundle was instituted (intravenous co-amoxiclav, intravenous fluids, blood culture, hourly urine output) because of the lactataemia and he was moved to a monitored bed in the acute medical unit, with instructions to staff to carry out overnight medical review.
He was reviewed 4 h and 6 h after admission. His respiratory rate remained elevated at 24/min but his oxygen saturations had improved to 99%. His heart rate was 105 bpm and he remained normotensive. Urine output was over 150 mL/h. Repeat ABGs revealed worsening lactataemia and metabolic decompensation ( table 1 ). Peak flows were not recorded. Aminophylline infusion was prescribed and intravenous fluids were sped up. Nebulised salbutamol was continued.
After a further 2 h, he developed orthopnoea and worsening hypoxaemia but his wheeze had improved. Clinically, he was thought to have pulmonary oedema, probably precipitated by an acute coronary syndrome. Repeat ECG showed sinus tachycardia without ST changes. Repeat troponin was 40 ng/L. His chest radiograph was unchanged. Aminophylline and salbutamol were stopped. He was treated with fondaparinux, clopidogrel and a glyceryl trinitrate infusion.
At 10 h after admission, the patient showed signs of clinical improvement. His lactate had fallen to 5.9. Over the next few hours, his oxygen was weaned off and a serum lactate level was recorded at 3.3 mmol/L. A diagnosis of salbutamol-induced lactic acidosis and acute exacerbation of asthma was made. He was given prednisolone and a corticosteroid/long-acting β-2 agonist inhaler. Troponin fell to 24 ng/L and treatment for acute coronary syndrome was stopped. Echocardiogram showed a left ventricular ejection fraction of 65%, no regional wall motion abnormalities and no valvular pathology. He was discharged after 24 h.
Outcome and follow-up
At 3-month outpatient follow-up, the patient was well. He had no further asthma exacerbations. He required only infrequent inhaled salbutamol in addition to his salmeterol and fluticasone preventer medication. Infrequent salbutamol usage is not associated with lactic acidosis in otherwise healthy people.
Hyperlactataemia represents a disruption in the homeostatic control of lactate metabolism. It is caused either by increased lactate production or diminished lactate utilisation and clearance. The commonest cause of a raised serum lactate level is type ‘A’ lactic acidosis. This is associated with tissue hypoxia, anaerobic metabolism and increased lactate production. It is seen in profound shock, severe sepsis and life-threatening asthma. However, there are a number of other causes of hyperlactataemia and these are unrelated to tissue hypoxia. Type ‘B’ lactic acidosis has a number of different causes. This topic has been extensively reviewed recently. 1 Table 2 summarises the main causes of lactic acidosis.
Table 2
Causes of lactic acidosis (adapted from Kraut JA et al 1 )
Salbutamol is a selective short acting β-2 agonist that has been used in the treatment of asthma exacerbations since the early 1970's. It has a systemic effect and is recognised as a cause of type ‘B’ lactic acidosis. 2 Intravenous salbutamol is most likely to cause this effect, but it is recognised with nebulised therapy 2 3 and large inhaled doses from a metre-dosed inhaler. 4 5
Since the late 1990s, it has been accepted that adrenergic stimulation of gluconeogenesis, glycogenolysis and glycolysis causes an increased production of lactate, resulting in lactic acidosis. 5 This is not unique to asthma exacerbations and has been reported in acute exacerbations of chronic obstructive pulmonary disease. 2
Figure 1 summarises the physiological response to salbutamol therapy and how this was misinterpreted. The patient took a high frequency of inhaled salbutamol from a metre-dosed inhaler at home and had nebulised treatment before his first ABG, resulting in the high initial value ( table 1 ). He was clinically stable, without signs of sepsis, making type A lactataemia unlikely. His repeat gases at 4 and 5.5 h showed a significantly improved A-a gradient, likely due to an improvement in his asthma. His persistently elevated respiratory rate was compensation for the lactataemia. It is at this point that peak flow measurements are crucial. If, as expected, they showed improvement, it would make it very unlikely that the situation was caused by a worsening of his asthma. Peak flow assessment remains a cornerstone of the assessment of asthma exacerbations. 6 Instead, in this case, the decision was taken to escalate treatment ( table 1 ), leading to further metabolic derangement, confusion over the diagnosis and potential harm to the patient ( figure 1 ).
Increase in lactate secondary to inhaled β agonist therapy is more common than generally recognised. In a prospective study 7 of 18 patients with acute exacerbation of asthma, attending the emergency department, the change in lactate levels after administering 1200 µg of inhaled salbutamol over 120 min was assessed. Fifty per cent of patients had increased lactate levels of over 2.5 mmol/L, and were over 4 mmol/L in four of these. However, none of these patients had acidosis.
Patient's perspective
- I was admitted with a severe asthma attack and was advised that I suffered a small heart attack. This aggravated my asthma problem but I have since learnt that this was a side effect of the nebuliser use.
Learning points
- if there are no signs of shock or hypoperfusion;
- if the lactate rises rapidly after salbutamol therapy;
- if the lactate level rise is associated with an objective improvement in hypoxaemia and peak flow (or forced expiratory volume in 1 s (FEV 1 )).
- Treatment of salbutamol-induced lactic acidosis is to reduce the salbutamol frequency.
- Peak flow or FEV 1 measurement by a peak flow metre or a bedside spirometer is an essential bedside tool that should be used to monitor response to treatment in an asthma exacerbation.
Contributors: Authors BTJI and JS initiated the idea. Author BTJI primarily wrote up the manuscript. All the authors were involved in the care of the patient and helped in the literature search. The manuscript was checked and edited by all the authors and all of them approved the final submission. Author TM was actively involved in rewriting the article during the revision process.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
- Publications
- Conferences & Events
- Professional Learning
- Science Standards
- Awards & Competitions
- Daily Do Lesson Plans
- Free Resources
- American Rescue Plan
- For Preservice Teachers
- NCCSTS Case Collection
- Partner Jobs in Education
- Interactive eBooks+
- Digital Catalog
- Regional Product Representatives
- e-Newsletters
- Bestselling Books
- Latest Books
- Popular Book Series
- Prospective Authors
- Web Seminars
- Exhibits & Sponsorship
- Conference Reviewers
- National Conference • Denver 24
- Leaders Institute 2024
- National Conference • New Orleans 24
- Submit a Proposal
- Latest Resources
- Professional Learning Units & Courses
- For Districts
- Online Course Providers
- Schools & Districts
- College Professors & Students
- The Standards
- Teachers and Admin
- eCYBERMISSION
- Toshiba/NSTA ExploraVision
- Junior Science & Humanities Symposium
- Teaching Awards
- Climate Change
- Earth & Space Science
- New Science Teachers
- Early Childhood
- Middle School
- High School
- Postsecondary
- Informal Education
- Journal Articles
- Lesson Plans
- e-newsletters
- Science & Children
- Science Scope
- The Science Teacher
- Journal of College Sci. Teaching
- Connected Science Learning
- NSTA Reports
- Next-Gen Navigator
- Science Update
- Teacher Tip Tuesday
- Trans. Sci. Learning
MyNSTA Community
- My Collections
Asthma Attack!
By Hollie L. Leavitt
Share Start a Discussion
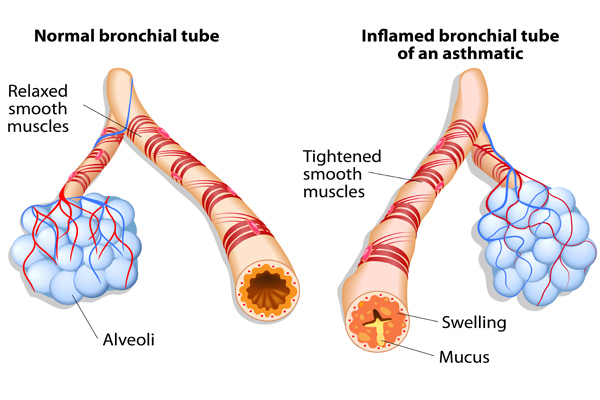
This interrupted case study follows the progress of a pediatric patient who experiences an acute asthma exacerbation brought on by an environmental trigger. Students completing the case will synthesize their understanding of respiratory system anatomy and physiology with the clinical treatment of an obstructive lung disorder. Topics reviewed include bronchoconstriction and dilation, pulmonary ventilation, air flow, gas exchange, respiratory volumes, the oxygen-hemoglobin dissociation curve, pCO2, pO2, and the effects of medications used to treat asthma. Students should have an understanding of the respiratory system before starting the case and thus it is best used at the end of the respiratory system unit as a way for students to apply what they have learned to a real-world situation. The case was developed for an anatomy and physiology class for majors taught through the “flipped” method at a community college, but would also work well for students in a pathophysiology course or in pre-professional programs in health care. It may also be suitable for high school students in an advanced or honors anatomy and physiology program.
Download Case
Date Posted
- Describe the anatomy of the respiratory passageways.
- Understand respiratory system function including air flow and gas exchange.
- Determine the effects of bronchoconstriction and bronchodilation on air flow.
- Describe the pressure gradients required for pulmonary ventilation.
- Understand respiratory volumes and how they are used clinically to assess disease.
- Know how to use the oxygen-hemoglobin dissociation curve.
- Predict how pCO2 and pO2 are affected by an obstructive lung disease.
- Describe pathological changes in the airways and environmental factors that can lead to an acute asthma exacerbation.
- Understand the effects of some of the medications used to treat asthma.
asthma; respiratory anatomy; respiratory physiology; respiratory system; lung pathology; respiratory volumes; oxygen-hemoglobin dissociation;
Subject Headings
EDUCATIONAL LEVEL
High school, Undergraduate lower division, Undergraduate upper division, Professional (degree program)
TOPICAL AREAS
TYPE/METHODS
Teaching Notes & Answer Key
Teaching notes.
Case teaching notes are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Teaching notes are intended to help teachers select and adopt a case. They typically include a summary of the case, teaching objectives, information about the intended audience, details about how the case may be taught, and a list of references and resources.
Download Notes
Answer Keys are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Download Answer Key
Materials & Media
Supplemental materials.
Normal 0 false false false EN-US X-NONE X-NONE MicrosoftInternetExplorer4
The PowerPoint presentation below includes optional slides for in-class review before presenting the case.
- asthma_attack_sup.ppt (~634 KB)
- How Does Asthma Work? This animated video gives an overview of asthma, including why people get it, and how it can be deadly. Running time: 5:09 min. Produced by TED-Ed, 2017.
You may also like
Web Seminar
Join us on Thursday, June 13, 2024, from 7:00 PM to 8:00 PM ET, to learn about the science and technology of firefighting. Wildfires have become an e...
Join us on Thursday, October 10, 2024, from 7:00 to 8:00 PM ET, for a Science Update web seminar presented by NOAA about climate science and marine sa...
Secondary Pre-service Teachers! Join us on Monday, October 21, 2024, from 7:00 to 8:15 PM ET to learn about safety considerations for the science labo...
Elementary Pre-service Teachers! Join us on Monday, October 7, 2024, from 7:00 – 8:15 PM ET to learn about safety considerations for the element...
Case Study: Managing Severe Asthma in an Adult
—he follows his treatment plan, but this 40-year-old male athlete has asthma that is not well-controlled. what’s the next step.
By Kirstin Bass, MD, PhD Reviewed by Michael E. Wechsler, MD, MMSc
This case presents a patient with poorly controlled asthma that remains refractory to treatment despite use of standard-of-care therapeutic options. For patients such as this, one needs to embark on an extensive work-up to confirm the diagnosis, assess for comorbidities, and finally, to consider different therapeutic options.

Case presentation and patient history
Mr. T is a 40-year-old recreational athlete with a medical history significant for asthma, for which he has been using an albuterol rescue inhaler approximately 3 times per week for the past year. During this time, he has also been waking up with asthma symptoms approximately twice a month, and has had three unscheduled asthma visits for mild flares. Based on the National Asthma Education and Prevention Program guidelines , Mr. T has asthma that is not well controlled. 1
As a result of these symptoms, spirometry was performed revealing a forced expiratory volume in the first second (FEV1) of 78% predicted. Mr. T then was prescribed treatment with a low-dose corticosteroid, fluticasone 44 mcg at two puffs twice per day. However, he remained symptomatic and continued to use his rescue inhaler 3 times per week. Therefore, he was switched to a combination inhaled steroid and long-acting beta-agonist (LABA) (fluticasone propionate 250 mcg and salmeterol 50 mcg, one puff twice a day) by his primary care doctor.
Initial pulmonary assessment Even with this step up in his medication, Mr. T continued to be symptomatic and require rescue inhaler use. Therefore, he was referred to a pulmonologist, who performed the initial work-up shown here:
- Spirometry, pre-albuterol: FEV1 79%, post-albuterol: 12% improvement
- Methacholine challenge: PC 20 : 1.0 mg/mL
- Chest X-ray: Within normal limits
Continued pulmonary assessment His dose of inhaled corticosteroid (ICS) and LABA was increased to fluticasone 500 mcg/salmeterol 50 mcg, one puff twice daily. However, he continued to have symptoms and returned to the pulmonologist for further work-up, shown here:
- Chest computed tomography (CT): Normal lung parenchyma with no scarring or bronchiectasis
- Sinus CT: Mild mucosal thickening
- Complete blood count (CBC): Within normal limits, white blood cells (WBC) 10.0 K/mcL, 3% eosinophils
- Immunoglobulin E (IgE): 25 IU/mL
- Allergy-skin test: Positive for dust, trees
- Exhaled NO: Fractional exhaled nitric oxide (FeNO) 53 parts per billion (pbb)
Assessment for comorbidities contributing to asthma symptoms After this work-up, tiotropium was added to his medication regimen. However, he remained symptomatic and had two more flares over the next 3 months. He was assessed for comorbid conditions that might be affecting his symptoms, and results showed:
- Esophagram/barium swallow: Negative
- Esophageal manometry: Negative
- Esophageal impedance: Within normal limits
- ECG: Within normal limits
- Genetic testing: Negative for cystic fibrosis, alpha1 anti-trypsin deficiency
The ear, nose, and throat specialist to whom he was referred recommended only nasal inhaled steroids for his mild sinus disease and noted that he had a normal vocal cord evaluation.
Following this extensive work-up that transpired over the course of a year, Mr. T continued to have symptoms. He returned to the pulmonologist to discuss further treatment options for his refractory asthma.
Diagnosis Mr. T has refractory asthma. Work-up for this condition should include consideration of other causes for the symptoms, including allergies, gastroesophageal reflux disease, cardiac disease, sinus disease, vocal cord dysfunction, or genetic diseases, such as cystic fibrosis or alpha1 antitrypsin deficiency, as was performed for Mr. T by his pulmonary team.
Treatment options When a patient has refractory asthma, treatment options to consider include anticholinergics (tiotropium, aclidinium), leukotriene modifiers (montelukast, zafirlukast), theophylline, anti-immunoglobulin E (IgE) antibody therapy with omalizumab, antibiotics, bronchial thermoplasty, or enrollment in a clinical trial evaluating the use of agents that modulate the cell signaling and immunologic responses seen in asthma.
Treatment outcome Mr. T underwent bronchial thermoplasty for his asthma. One year after the procedure, he reports feeling great. He has not taken systemic steroids for the past year, and his asthma remains controlled on a moderate dose of ICS and a LABA. He has also been able to resume exercising on a regular basis.
Approximately 10% to 15% of asthma patients have severe asthma refractory to the commonly available medications. 2 One key aspect of care for this patient population is a careful workup to exclude other comorbidities that could be contributing to their symptoms. Following this, there are several treatment options to consider, as in recent years there have been several advances in the development of asthma therapeutics. 2
Treatment options for refractory asthma There are a number of currently approved therapies for severe, refractory asthma. In addition to therapy with ICS or combination therapies with ICS and LABAs, leukotriene antagonists have good efficacy in asthma, especially in patients with prominent allergic or exercise symptoms. 2 The anticholinergics, such as tiotropium, which was approved for asthma in 2015, enhance bronchodilation and are useful adjuncts to ICS. 3-5 Omalizumab is a monoclonal antibody against IgE recommended for use in severe treatment-refractory allergic asthma in patients with atopy. 2 A nonmedication therapeutic option to consider is bronchial thermoplasty, a bronchoscopic procedure that uses thermal energy to disrupt bronchial smooth muscle. 6,7
Personalizing treatment for each patient It is important to personalize treatment based on individual characteristics or phenotypes that predict the patient's likely response to treatment, as well as the patient's preferences and practical issues, such as adherence and cost. 8
In this case, tiotropium had already been added to Mr. T's medications and his symptoms continued. Although addition of a leukotriene modifier was an option for him, he did not wish to add another medication to his care regimen. Omalizumab was not added partly for this reason, and also because of his low IgE level. As his bronchoscopy was negative, it was determined that a course of antibiotics would not be an effective treatment option for this patient. While vitamin D insufficiency has been associated with adverse outcomes in asthma, T's vitamin D level was tested and found to be sufficient.
We discussed the possibility of Mr. T's enrollment in a clinical trial. However, because this did not guarantee placement within a treatment arm and thus there was the possibility of receiving placebo, he opted to undergo bronchial thermoplasty.
Bronchial thermoplasty Bronchial thermoplasty is effective for many patients with severe persistent asthma, such as Mr. T. This procedure may provide additional benefits to, but does not replace, standard asthma medications. During the procedure, thermal energy is delivered to the airways via a bronchoscope to reduce excess airway smooth muscle and limit its ability to constrict the airways. It is an outpatient procedure performed over three sessions by a trained physician. 9
The effects of bronchial thermoplasty have been studied in several trials. The first large-scale multicenter randomized controlled study was the Asthma Intervention Research (AIR) Trial , which enrolled patients with moderate to severe asthma. 10 In this trial, patients who underwent the procedure had a significant improvement in asthma symptoms as measured by symptom-free days and scores on asthma control and quality of life questionnaires, as well as reductions in mild exacerbations and increases in morning peak expiratory flow. 10 Shortly after the AIR trial, the Research in Severe Asthma (RISA) trial was conducted to evaluate bronchial thermoplasty in patients with more severe, symptomatic asthma. 11 In this population, bronchial thermoplasty resulted in a transient worsening of asthma symptoms, with a higher rate of hospitalizations during the treatment period. 11 Hospitalization rate equalized between the treatment and control groups in the posttreatment period, however, and the treatment group showed significant improvements in rescue medication use, prebronchodilator forced expiratory volume in the first second (FEV1) % predicted, and asthma control questionnaire scores. 11
The AIR-2 trial followed, which was a multicenter, randomized, double-blind, sham-controlled study of 288 patients with severe asthma. 6 Similar to the RISA trial, patients in the treatment arm of this trial experienced an increase in adverse respiratory effects during the treatment period, the most common being airway irritation (including wheezing, chest discomfort, cough, and chest pain) and upper respiratory tract infections. 6
The majority of adverse effects occurred within 1 day of the procedure and resolved within 7 days. 6 In this study, bronchial thermoplasty was found to significantly improve quality of life, as well as reduce the rate of severe exacerbations by 32%. 6 Patients who underwent the procedure also reported fewer adverse respiratory effects, fewer days lost from work, school, or other activities due to asthma, and an 84% risk reduction in emergency department visits. 6
Long-term (5-year) follow-up studies have been conducted for patients in both the AIR and the AIR-2 trials. In patients who underwent bronchial thermoplasty in either study, the rate of adverse respiratory effects remained stable in years 2 to 5 following the procedure, with no increase in hospitalizations or emergency department visits. 7,12 Additionally, FEV1 remained stable throughout the 5-year follow-up period. 7,12 This finding was maintained in patients enrolled in the AIR-2 trial despite decreased use of daily ICS. 7
Bronchial thermoplasty is an important addition to the asthma treatment armamentarium. 7 This treatment is currently approved for individuals with severe persistent asthma who remain uncontrolled despite the use of an ICS and LABA. Several clinical trials with long-term follow-up have now demonstrated its safety and ability to improve quality of life in patients with severe asthma, such as Mr. T.
Severe asthma can be a challenge to manage. Patients with this condition require an extensive workup, but there are several treatments currently available to help manage these patients, and new treatments are continuing to emerge. Managing severe asthma thus requires knowledge of the options available as well as consideration of a patient's personal situation-both in terms of disease phenotype and individual preference. In this case, the patient expressed a strong desire to not add any additional medications to his asthma regimen, which explained the rationale for choosing to treat with bronchial thermoplasty. Personalized treatment necessitates exploring which of the available or emerging options is best for each individual patient.
Published: April 16, 2018
- 1. National Asthma Education and Prevention Program: Asthma Care Quick Reference.
- 2. Olin JT, Wechsler ME. Asthma: pathogenesis and novel drugs for treatment. BMJ . 2014;349:g5517.
- 3. Boehringer Ingelheim. Asthma: U.S. FDA approves new indication for SPIRIVA Respimat [press release]. September 16, 2015.
- 4. Peters SP, Kunselman SJ, Icitovic N, et al. Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med . 2010;363:1715-1726.
- 5. Kerstjens HA, Engel M, Dahl R. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med . 2012;367:1198-1207.
- 6. Castro M, Rubin AS, Laviolette M, et al. Effectiveness and safety of bronchial thermoplasty in the treatment of severe asthma: a multicenter, randomized, double-blind, sham-controlled clinical trial. Am J Respir Crit Care Med . 2010;181:116-124.
- 7. Wechsler ME, Laviolette M, Rubin AS, et al. Bronchial thermoplasty: long-term safety and effectiveness in patients with severe persistent asthma. J Allergy Clin Immunol . 2013;132:1295-1302.
- 8. Global Initiative for Asthma: Pocket Guide for Asthma Management and Prevention (for Adults and Children Older than 5 Years).
- 10. Cox G, Thomson NC, Rubin AS, et al. Asthma control during the year after bronchial thermoplasty. N Engl J Med . 2007;356:1327-1337.
- 11. Pavord ID, Cox G, Thomson NC, et al. Safety and efficacy of bronchial thermoplasty in symptomatic, severe asthma. Am J Respir Crit Care Med . 2007;176:1185-1191.
- 12. Thomson NC, Rubin AS, Niven RM, et al. Long-term (5 year) safety of bronchial thermoplasty: Asthma Intervention Research (AIR) trial. BMC Pulm Med . 2011;11:8.
Treatable traits and future exacerbation risk in severe asthma, baker’s asthma, the long-term trajectory of mild asthma, age, gender, & systemic corticosteroid comorbidities, ask the expert: william busse, md, challenges the current definition of the atopic march, considering the curveballs in asthma treatment, do mucus plugs play a bigger role in chronic severe asthma than previously thought, an emerging subtype of copd is associated with early respiratory disease.


Case of Acute Severe Asthma
Kane guthrie.
- Dec 2, 2022
A 25-year-old lady Miss. Poor Compliance is rushed into your Emergency Department as a Priority 1. She is a brittle asthmatic and has been given 3x 5mg salbutamol nebs, and 0.5mg of adrenaline IM prehospital. On arrival Miss PC is sitting forward in the tripod position , using her accessory muscles to breath. She is tachypnoeic, agitated and unable to talk.
Vital signs: Pulse 143, BP 138/95, RR 42, Sp02 91% on neb, GCS 14/15.
Past Medical and Medication History
- Smoker. Severe asthmatic. Intubated twice in past 2 years
- Currently taking seritide 250/50mg, salbutamol MDI PRN and prednisolone 50mg PRN
Asthma Epidemiology
- Over 2.2 million Australians have currently diagnosed asthma
- 406 deaths attributed to asthma in 2006
- Highest risk of dying from asthma is in the elderly over 70
- The emergency clinician’s goal in treating acute severe asthma is preventing intubation
- Severe/Critical asthma is a life threatening condition
Asthma Pathophysiology
- Asthma is a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role, in particular, mast cells, eosinophils, T lymphocytes, macrophages, neutrophils, and epithelial cells.
- Smooth muscle hypertrophy and hyperplasia
- Inflammatory cell infiltration and oedema
- Goblet cell and mucous gland hyperplasia with mucous hypersecretion
- Protein deposition including collagen
- Epithelial desquamation
- Most common, responsible for 80-85% of all fatal events is characterised by eosinophilic inflammation associated with gradual deterioration over days-weeks occurring in patients with severe or poorly controlled asthma, and is slow to respond to therapy.
- The second phenotype, with neutrophilic inflammation, has both rapid onset and response to therapy.
Markers of severe asthma:
- Inability to speak in full sentences
- Use of accessory muscles or tracheal tugging
- Cyanosis and sweating
- Pulsus paradoxus (>15mmHg decreased with inspiration). With severe muscle fatigue might be absent
- Quiet chest on auscultation (The “Silent Chest”)
- Confusion or decreased level of consciousness
- Hypotension or bradycardia
- FEV 1<40% predicted
- PEF <40% of predicted or best (<25% in life threatening asthma)
- Oxygen saturation <90-92%
- PaO2 <60mmHg
- PaCO2 >45mmHg
Complications of Asthma :
- Pneumothorax, Pneumomediastinum, Pneumopericardium and Pneumoretroperitoneum
- Cardiac Arrhythmias, Myocardial ischaemia or infarction
- Electrolyte disturbances (hypokalaemia, hypomagnesaemia, hypophosphataemia)
- Lactic Acidosis
- Hyperglycaemia

Conditions that may mimic acute asthma:
- Upper airway obstruction
- Foreign-body aspiration
- Vocal cord dysfunction syndrome
- Pulmonary oedema
- Acute exacerbations of COPD
- Hysterical conversion reaction
- Munchausen syndrome
Diagnostic Test:
- Hyperinflation 5-10%
- Infiltrate 5%
- Pneumothorax <1%
- Pneumomediastinum <1%
- Respiratory alkalosis typical
- Inaccurate predictor of outcome
- Will seldom alter your treatment plan
- An objective measure of lung function
- Useful to assess response to treatment
- Impossible to obtain in the dying patient
- <25% Severe
- 25-50% Moderate
- 50-70% Mild
- >70% Discharge Goal
- Simple, and less painful than ABG
- Provides continuous oxygenation measurements
- Needs to placed on well-perfused site, difficult to obtain readings if global hypoperfusion or peripheral vasoconstriction present.
- Aim to keep sp02 >92%
Management of Acute Severe Asthma
- Hypoxia is the main cause of death in asthma
- Oxygen should be given to keep Sp02 above 92%
- A slight Pco2 rise may occur with oxygen therapy but this is of no clinical significance.
Beta-agonists:
- Rapid acting inhaled beta-agonists (bronchodilators) are the first line therapy for acute asthma.
- Nebulisers should generally be used in acute severe asthma, as provide easier delivery of medication to patient, multi dose inhalers have a role in mild to moderate asthma.
- IV salbutamol gives you the advantage of hitting the beta 2 receptors from the back door, while continuing nebulizer treatment, and should be trialed in patients not responding to nebulisers.
- Continuous nebuliser therapy appears to be more effective than intermittent nebulisers for delivering beta-agonist drugs to relieve airway spasm in acute severe asthma. (Cochrane Review, 2009)
- Salbutamol toxicity can caused a lactic acidosis which is often unrecognized in asthma patients, the lactic acidosis has been hypothesized to adversely affect ventilation by increasing ventilatory demand, increasing dead space ventilation, worsening dynamic hyperinflation and intrinsic PEEP. Management is to discontinue salbutamol at the earliest opportunity.
- Dose: Salbutamol Nebuliser Ampoule 5mg
- Dose: Salbutamol IV 5mg in 500mL of 0.9% sodium chloride or 5% dextrose start at 30mL/hr titrating up to 120mL/hr
Anticholinergics:
- Anticholinergics agents block muscarinic receptors in airway smooth muscles, inhibit vagal cholinergic tone and result in bronchodilation.
- Dose: Ipratropium bromide (Atrovent) 500ug to second dose of salbutamol via neb, can be repeated every 4hours
- Use of corticosteroids within 1 hour of presentation to an ED significantly reduces the need for hospital admission in patients with acute asthma. Benefits appear greatest in patients with more severe asthma, and those not currently receiving steroids
- Dose: Prednisolone 50mg PO
- Dose: IV Hydrocortisone 100-200mg
- Note: Parenteral route is indicated in ventilated patient or patient unable to swallow, eg. Vomiting
Adrenaline:
- Can be give either intravenously or via nebulizer
- Bronchoconstriction is the major pathology in asthma; airway oedema might also make a significant contribution. Both the a-agonist and B-agonist effects of adrenaline might be beneficial, with the alpha effect decreasing oedema and the beta effect responsible for bronchodilation.
- Dose: IV 6mg in 100mls 5% dextrose start at 1-15mLs/hour
- Dose: Nebulizer 1mg in 3ml normal saline
Aminophylline:
- The popularity of aminophylline in asthma exacerbations has diminished in recent years.
- Systematic reviews have shown that IV aminophylline in severe acute asthma does not produce additional bronchodilation above that achieved with beta-agonist and corticosteroids.
- Side effects; cardiac arrhythmia’s, vomiting, toxicity.
- Dose : 5mg/kg over 20min followed by infusion of 500mg aminophyline n 500mL of 5% dextrose at 0.5mg/kg per hour
Magnesium Sulphate:
- Magnesium potential role is asthma may involve a combination of smooth muscle relaxation, inhibition of histamine release and acetylcholine release from nerve endings.
- Most evidence to support the use of magnesium in asthma is in the acute severe asthmatic were it has been shown to be safe and beneficial.
- Dose : IV 2-4g over 30-60mins
- Heliox Mixture 80% helium/20% oxygen
- There is evidence that helium and oxygen mixtures (heliox) may provide additional benefits to patients with acute asthma.
- Heliox mixtures have the potential to decrease airway resistance, and therefore decrease the work of breathing for the severe acute asthma patient.
Antibiotics:
- Antibiotics are not indicated in the management of severe acute asthma.
- Antibiotics should only be used in the setting of an underlying pneumonia, respiratory tract infection or to aid in the prevention of ventilator-associated pneumonia in ICU.
Airway Management
Non-Invasive Positive Pressure Ventilation:
Good quality evidence and trails to support the use of NPPV in asthma are lacking, however it is worth trying when intubation is not immediately indicated. Remember the goal of the emergency clinician’s in treating asthma is to prevent intubation.
- Positive pressure is generally less than 15cmH2O
- Benefit between CPAP vs BiPAP is unknown
- Tachypnea caused by severe asthma can make it difficult for the patient to coordinate they’re breathing with machine making BiPAP uncomfortable
- Need a large randomised control trial to determine the effectives properly of NIV, in acute severe asthma.
“Asthmatic on BiPAP before being Intubated”
Mechanical Ventilation:
1-3% of acute severe asthma requires intubation. Prevention of intubation and mechanical ventilation are the goals of managing acute severe asthma, this can be achieved by maximising pre-intubation therapy, however you don’t want to wait too long or let the severe asthmatic tire before trying to intubate them. Once an asthmatic is intubated and ventilated their morbidity and mortality increasing dramatically, and it can be difficult to wean from the ventilator.
Criteria for Intubation:
- Cardiac or Respiratory arrest
- Altered mental status
- Progressive exhaustion
- Severe hypoxia despite maximal oxygen delivery
- Failure to reverse severe respiratory acidosis despite intensive therapy
- pH <7.2, carbon dioxide pressure increasing by more than 5mmHg/hr or greater than 55 to 70mm/Hg, or oxygen pressure of less than 60mm/Hg.
Challenges:
- Effective pre-oxygenation impossible
- No margin for error or delay
- Need to be intubated by most experienced person available
- High intrathoracic pressure after RSI
Recommendations:
- Fluid bolus before intubation if possible
- RSI preferred
- Ketamine for bronchodilator effects
- Permissive hypercapnea essential
Initial Ventilator settings in paralysed patients:
- FiO2 1.0, then titrate to keep SpO2 >94%
- Tidal Volume 5-6ml/kg
- Ventilator rate 6-8 breaths/min
- Long expiratory time (I:E ratio >1:2)
- Minimal PEEP < 5cmH2O
- Limit peak inspiratory pressure to <40cmH2O
- Target plateau pressure <20cmH2O
- Ensure effective humidification
- Brenner, B. Corbridge, T. & Kazzi, A. (2009). Intubation and mechanical ventilation of the asthmatic patient in respiratory failure. The Journal of Emergency Medicine. 37(2s), s23-s34.
- Camargo, C. Rachelefsky, G. & Schatz, M. (2009). Managing Asthma Exacerbation in the Emergency Department: Summary of the National Asthma Education and Prevention Program Expert Panel Report 3 Guidelines for the Management of Asthma Exacerbation.The Journal of Emergency Medicine. 37 (2S), S6-S17.
- Camargo, C. Spooner, C. & Rowe, B. (2009). Continuous versus intermittent beta-agonist for acute asthma (Review). http://www.thecochranelibrary.com.
- Chua, F. & Lai, D. (2007). Acute severe asthma: Triage, treatment and thereafter. Current Anaesthesia & Critical Care. 18, 61-68.
- Creagh-Brown, B. & Ball, J. (2007). An under-recognized complication of treatment of acute severe asthma. American Journal of Emergency Medicine. 26, 513-515.
- Hodder, R. et al. (2009). Management of acute asthma in adults in the emergency department: nonventilatory management. CMAJ. 182(2), E55-E67.
- Holley, A. & Boots, R.(2009). Review article: Management of acute severe and near-fatal asthma. Emergency Medicine Australasia, (21) 259-268.
- Jones, L. & Goodacre, S. (2009). Magnesium sulphate in the treatment of acute asthma: evaluation of current practice in adult emergency departments. Emergency Medicine Journal. 26, 783-785.
- Melnick, E. & Cottral, J. (2010). Current Guidelines for Management of Asthma in the Emergency Department. http://www.ebmedicine.net. 2(2). 1-13.
- Morris, F. & Fletcher, A. (Ed). (2009). ABC of Emergency Differential Diagnosis. Oxford: Blackwell Publishing
- National Asthma Council of Australia. Asthma management handbook: 2006. Accessed http://www.nationalasthma.org.au/cms/images/stories/amh2006_web_5.pdf, 12/02/2010
- Nowak, R. Corbridge, T. & Brenner, B. (2009). Noninvasive Ventilation. The Journal of Emergency Medicine. 37(2S), S18-S22.
- Peters, S. (2007). Continuous Bronchodilator Therapy. Chest. 131(1),1-5.
- Phipps, P. & Garrard, C. (2003). The pulmonary physician in critical care. 12: Acute severe asthma in the intensive care unit. Thorax. 58, 81-88.
- Ram, F. Wellington, S. Rowe, B. & Wedzicha, J. (2009). Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma (Review)
- Rodrigo, G. Pollack, C. Rodrigo, C. Rowe, B. (2010). Heliox for non-intubated acute asthma patents (Review).
- Rowe, B. Spooner, C. Ducharme, F. Bretzlaff, J. Bota, G. (2008). Early emergency department treatment of acute asthma with systemic corticosteroids (Review). http://www.thecochranelibrary.com.
- Rowe, B. et al. (2009). Magnesium sulfate for treating exacerbations of acute asthma in the emergency department (Review). http://www.thecochranelibrary.com.
Emergency nurse with ultra-keen interest in the realms of toxicology, sepsis, eLearning and the management of critical care in the Emergency Department | LinkedIn |
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Privacy Overview
- Open access
- Published: 03 April 2020
Determinants of Acute Asthma Attack among adult asthmatic patients visiting hospitals of Tigray, Ethiopia, 2019: case control study
- Melaku Negash 1 ,
- Hagos Tsegabrhan 2 ,
- Teklit Meles 3 ,
- Degena Bahrey Tadesse 1 ,
- Gebreamlak Gidey 4 ,
- Yemane Berhane 5 ,
- Kibrom Berhanu 6 &
- Tsgalem Haylemaryam 7
Asthma Research and Practice volume 6 , Article number: 1 ( 2020 ) Cite this article
4848 Accesses
3 Citations
3 Altmetric
Metrics details
Introduction
Acute asthma attack is one of the most common causes of visits to hospital emergency departments in all age groups of the population and accounts for the greater part of healthcare burden from the disease. Despite, Acute asthma attack is an important public health problem that affects not only the patients, but also to the family, health professionals, health care institutions and development of the nation, little is known about the risk factors of acute asthma attack.
Therefore, this study is aimed to investigate the determinants of acute asthma attack among.
The aim of this study was to assess the determinant factors of acute asthma attack among adult asthmatic patients visiting general hospitals of central zone, Tigray, Ethiopia, 2019.
Hospital based unmatched case control study design was conducted in general hospitals of central zone of Tigray, Ethiopia 2019. Data were collected using pretested interviewer administered questionnaire. A total of 289 study subjects (96 cases &193 controls) were selected by systematic random sampling. Data were entered to Epi data version 3.1 then exported to SPSS version 23 for analysis. Bivariate logistic regression was employed to examine the statistical association between dependent and independent variables. Variables with p value < 0.25 in binary logistic regression were entered to multivariable logistic regression model and variables with p value < 0.05 was taken as significant determinants of the outcome variable.
A total of 96 adult asthmatic patients who have acute asthma attack (cases) and 193 adult asthmatic patients without attack (controls)) with 100% response rate were participated in this study. Upper Respiratory tract Infection [AOR = 6.835,95% CI = 3.285,14.222], Season [AOR =2.204,95% CI = 1.011,4.805] kitchen smoke [AOR = 2.307,95%CI1.010,5.272]& sleep apnea [AOR = 9.254, 5%CI =3.563,25.460] were significantly associated with acute asthma exacerbation.
Asthma is a long-term inflammatory disease of the respiratory system which is characterized by wheezing, shortness of breath, chest tightness. Globally it affects approximately 300 million people and is estimated to rise to 400 million by 2025 globally [ 1 , 2 ]. And it is ranked 16th among the leading causes of disability and 28th among the leading causes of burden of disease, as measured by disability adjusted life years (DALYs) [ 3 ].
According to Croatian medical journal 2013, an estimate of asthma prevalence in Africa, was 49.7 million in the age of < 15 years (13.9%), < 45 years 102.9 million (13.8%), and in total population 119.3 million (12.8%) in 2010 [ 4 ].
Asthma exacerbation is defined as a worsening of shortness of breath, cough, wheezing, or chest tightness. If not treated immediately there will be increase in flow resistance causing increased work of breathing, gas exchange inefficiency, respiratory muscle tiredness and finally hypercapnic and hypoxemic respiratory failure [ 5 ]. This implies that acute asthma attack is a significant public health problem that affects patients with their parents or families and the community through labor and school loss, frequent emergency clinic visits, a poor quality of life hospitalizations and finally death [ 6 ]. According to Centers for Disease Control and prevention (CDC) report, More than 11 million people reported having an acute asthma attack [ 7 ].
Despite, in Ethiopia little is known about how risk factors are associated with exacerbation, according to asthma severity and the relative importance of the risk factors. This may be the reason for no policy and strategy to ascertain and acting out of effective intervention in order to reduce the burden of acute asthma attack [ 8 ]. Therefore, this study is aimed to full fill this gap.
Study setting and study design
Hospital based unmatched case control study was conducted in the selected general Hospitals of Central zone of Tigray from November 2018 to July 2019.
Study population and sample size determination
Source population.
All adult asthmatic patients visited to emergency unit who have acute asthma attack.
All adult patients diagnosed as asthma but without acute asthmatic attack who visited the OPD and the regular follow-up unit during the data collection period.
Study population
All selected adult asthmatic patients visited to emergency unit who have acute asthma attack during the data collection period.
All selected adult patients diagnosed as asthma but without acute asthmatic attack who visited the OPD and the regular follow-up unit during the data collection period.
Eligibility criteria
Inclusion criteria.
Adult asthmatic patients who have acute asthma attack during the data collection period.
Adult asthmatic patient without acute asthma attack during the data collection period.
Exclusion criteria
Patients with any history of pulmonary embolism, chronic obstructive pulmonary disease, active pulmonary TB, known congestive heart failure and known mechanical obstruction.

Sample size determination
Sample size was calculated from Previous study conducted in Uganda [ 9 ],using Epi info version 7. sample size was determined based on the assumption of confidence level = 95%; Power = 80%; Odds ratio = 2.132 with case to control ratio = 1:2, proportion of among controls 37.2%, proportion of among cases = 55.8%.
Therefore, the required sample size for cases was =92 where as for the controls =183 and the overall sample size was = 275 then after adding 5% non-response rate, the total sample size was 289. Finally, a sample size for cases was 96 and for controls 193.
Sampling technique and procedure
The total sample size was allocated to each hospital proportionally based on the number of patients who attend in the selected hospitals. A total number of 585(case 165, control.420) patients attended at the selected Hospitals with in 2 months of the previous year (April 1 to May 30–2018). Systematic random sampling method was applied in each hospital to select 289 participants.
Study Variables
Dependent variable.
Acute asthma attack.
Independent variables
Socio-demographic variables.
Age, Gender, Marital status, Residence, Educational level, Employment status and Occupational status.
Behavioral factors
Exercise, vigorous activity Smoking cigarette.
Environmental factors
Humidity, Kitchen smoke, dust, Season.
Medical and Clinical characteristics
URTI, Sleep apnea, Missing follow-up / appointments,
Operational definitions
Those who present with cough, wheezing and difficulty of breathing and diagnosed asthma by physician [ 10 ].
Acute Asthma Attack
Those who present with worsening of wheezing, shortness of breath, cough, chest tightness and diagnosed as acute asthma attack by physician [ 10 ].
Smoker:( daily smoker and non-daily smoker) those who currently smokes or those who quit smoking less than 1 year before the assessment [ 10 ].
Passive smoker: Smoke inhaled involuntarily by non-smokers [ 11 ].
Nonsmoker: Respondents who report never smoke those who quit smoking greater than 1 year before the assessment.
Vigorous activity: participants doing activity more than 10 min continuously, that increases breathing, like carrying or lifting heavy loads, digging or construction work, cutting fire wood [ 11 ].
Data collection tool
Structured questionnaire was used to collect the data which was adapted from different literatures [ 9 , 12 , 13 , 14 ]. The questionnaire contains four parts: socio-demographic, environmental factors, behavioral factors, and Medical &Clinical characteristics.
Data collection procedures
Data were collected from cases and controls using structured questionnaire and checklists through face-to-face interview and from patients chart review respectively.
Twelve BSc nurses as data collectors and three senior nurse supervisors were recruited for the data collection, Then data from cases were collected after they take all the necessary medical care and they recover from their attack whereas from the controls data were collected after they have completed their assessment by physician and at the last record reviews from their chart. Participants were identified as having upper respiratory tract infection and Obstructive sleep apnea from their medical charts which was diagnosed by senior physicians. This is to mean that, it was just suspected clinically by the time of the acute event. The reason we obeyed to use clinically diagnosis for obstructive sleep apnea is that, there is no accesses of modern diagnostic modality like polysomnography in the study area which was Tigray regional state not only in the study area but also in the country Ethiopia as a whole. The evaluation protocol that we use were a single evaluation visit for each case and even those who have follow-up and developed acute asthma attack were included .
Data quality control techniques
Data quality was ensured by training of data collectors and supervisors before data collection period. 5% of the questionnaire was pre-tested in Shire Hospital which was not included in the actual data collection. Based on the findings of the pre-test, questionnaire was modified. The filled questionnaire was checked for completeness and accuracy by data collectors, supervisors and principal investigator each day.. The questionnaire was translated into Tigrigna language for better understanding to both the data collectors and respondents and then back translated into English by another expert to ensure accuracy and consistency.
Data analysis procedures
Data were entered in to Epi data version 3.1 and analyzed using SPSS version 23.0. The degree of association between independent and dependent variables were assessed using adjusted odds ratio with 95% confidence interval. Variables < 0.25 p -value in binary logistic regression were entered to multivariable logistic regression model to control the potential confounding variables. Variables with p-value less than 0.05 in multivariable logistic regression model were taken as significantly associated factors. Variance inflation factor (VIF) was used to assess Multicollinearity between the independent variables. Hosmer and Lemeshow goodness fit model were used to check model fitness.
Ethical consideration
Ethical clearance was obtained from Mekelle University College of health sciences institutional review board (IRB). A subsequent permission was also obtained from Tigray teaching hospitals. Respondents were informed about the purpose of the study and the interview was conducted after receiving the written consent from participants. Confidentiality of the data/information was secured and was not used for other purposes.
Sociodemographic characteristic of study participants
Among the participants, 67.7% (65) of the cases and 60.6% (117) of the controls were females. The median ages of participants were 43 years with interquartile range (IQR) of 26.5 years among cases and 43 median ages with interquartile range (IQR) of 22 for control.
The educational status, one third 33.3% (32) of the cases and 24.9% (48) of the controls were collage and above, where as 14.6% (14) of the cases and 16.6% (32) of the controls were unable to read and write. The majority of the cases 63.5% (61) and 60.1% (116) of the controls were married (Table 1 ).
Behavioral characteristics of study participants
Among the participants, 2.1% (2) of the cases and 1.1% (6) of the controls were smokers.in parallel with this 3.1% of the cases and 4.7% of the control were passive smokers. Regarding vigorous activity 37.5% (36) of the cases and 23.8% (46) of the controls were do vigorous activity. Majority of the participants 72.9% (70) of the cases and 58% (112) of the controls were doing exercise.
Medical & clinical characteristics of study participants
Among the participants, 44.8% (43) of the cases and 13.5% (26) of the controls had Upper Respiratory Tract Infections (URTI) and 29.2% (28) of the cases and few of the controls 5.2% (10) had obstructive sleep apnea.
Among the participants, 31.3% (30) of the cases and 20.7% (40) of the controls had Missing follow up.
Environmental characteristics of study participants
Regarding the seasons of a year, spring season (April, May, June) were the season with high percentage 37.7% (109) of acute asthma attack than the autumn season. Majority of the participants 79.5% (230) were open their window/door while they were cooking. Concerning the kitchen of the participants 32.3% (31) of the cases and 20.2% (39) of the control’s kitchen have no kitchen smoke (chimney) (Table 2 ).
Unmatched case control study with 96 cases and 193 controls was conducted to show the determinants of acute asthma attack among adult asthmatic patients visiting general hospitals of central zone, Tigray, Ethiopia.
Having URTI increases the occurrence of acute asthma attack 6.8 times [AOR = 6.835,95% CI = 3.285,14.222] than those who have not upper respiratory tract infection (URTI) (Table 3 ).
This is consistent with the studies conducted in Gondar, Uganda and Ireland [ 9 , 12 , 15 ].
The association might be due to the mechanism of airway inflammation,mucus hyper secretion, and bronchial hyper responsiveness [ 16 ]. In contrast to this study upper respiratory tract infections was no risk factor for acute asthma exacerbation on the study conduct in Pretoria and New Zealand [ 14 , 17 ]. This difference might be due to difference in health care seeking behavior of the participants in this study.
This study revealed that, sleep apnea was strongly associated with the occurrence of acute asthma exacerbation. Those who have sleep apnea are 9.5 times more likely to run in to acute asthma exacerbation than those who have not sleep apnea [AOR = 9.524, 95% CI = 3.563, 25.460].
This findings is comparable with a study done in Gondar and USA [ 12 , 18 ].
The possible reason is the fact that sleep apnea lead to the worsening of asthma control in patients with concomitant sleep apnea secondary to bronchoconstriction as a result of increase vagal tone while sleeping [ 19 ].
The result of this study shows that the odds of having acute asthma in Spring season was 2.2 times higher than the odds of having acute asthma attack in the autumn season [AOR = 2.204,95% CI = 1.011,4.805]. This is consistent with a study conducted in Canada in which spring season was triggering factor for asthma exacerbation [ 20 ]. Seasonal variation is the risk factors for acute asthma attack especially pollens appearing seasons like spring season exacerbates acute asthma attack. This may be due to the reason that during the spring, tree pollen, mold spores and grass have the power to inflame and narrow the air passages of people who have asthma [ 21 ].
The result of this study was different from a study conducted in Spain which was resulting winter season as higher risk of developing acute asthma attack [ 22 ]. The difference could be arisen from seasonal variation between the study areas, due to the influence of temperature and humidity.
In this study, Kitchen smoke (chimney) is highly associated with risk of acute asthma exacerbation.
Those who have no kitchen smoke in their kitchen were 2.3 times at risk to develop acute asthma exacerbation [AOR = 2.307,95%CI = 1.010,5.2725] than those who have kitchen smoke. This finding is comparable with the study conducted in India [ 13 ]. This is due to the fact that kitchen smoke (chimney) is a way that helps in removing the smokes and fumes from the kitchen and making it clean and smoke free which result in reduction of indoor air pollution and prevents acute asthma exacerbation [ 23 ]. Inhaling harmful smoke can inflame lungs and airway, causing them to swell and block oxygen. This can lead to acute asthma exacerbation [ 24 ]
In this study the determinant factors of acute asthma attack were spring season, presence of upper respiratory tract infection (URTI), having no Kitchen smoke in their kitchen and having obstructive sleep apnea.
Limitations
The diagnosis of respiratory tract infections and sleep apnea was empirical (without laboratory) and all measures used were based on self-reporting, this might end up with social desirability bias. This study may have recall bias, since some of the information was based on the recall of the study participants. Unavailability of studies on acute asthma exacerbation.
Availability of data and materials
The datasets used and analyzed during the current study are presented within the manuscript and available from the corresponding author on reasonable request.
Abbreviations
Adjusted Odds Ratio
Confidence Interval
Crude Odds Ratio
Central Statistical Agency
Interquartile Range
National Health Interview Survey
Out Patient Department
Tigray Region Health Development Agency
Upper Respiratory Tract Infection
Variance Inflation Factor
Adams, JY., Sutter, M.E. & Albertson, T.E. The Patient with Asthma in the Emergency Department. Clinic Rev Alleg Immunol 43, 14-29 (2012). https://doi.org/10.1007/s12016-011-8273-z .
Shah R , Saltoun CA . Chapter 14: Acute severe asthma (status asthmaticus). Allergy and Asthma Proceedings, 2012; 33(Supplement 1):S47-S50. Acute severe asthma. InAllergy and Asthma proceedings 2012 (Vol. 33, No. 3, p. 47). OceanSide Publications..
The Global Asthma Report 2018. Auckland, New Zealand: Global Asthma Network, 2018.
Adeloye D, Chan KY, Rudan I, Campbell H. An estimate of asthma prevalence in Africa: a systematic analysis. Croat Med J. 2013;54(6):519–31.
Article Google Scholar
Park HW, Tantisira KG. Genetic signatures of asthma exacerbation. Allergy, Asthma Immunol Res. 2017;9(3):191–9.
Article CAS Google Scholar
Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: results from the American Productivity Audit. J Occup Environ Med. 2003;45(12):1234–46.
CDC , National Health Interview Survey (NHIS) 2014.
Google Scholar
Jackson DJ, Sykes A, Mallia P, Johnston SL. Asthma exacerbations: Origin, effect and prevention. J Allergy Clin Immunol. 2011;128:1165–74.
Sanya RE, Kirenga BJ, Worodria W, Okot-Nwang M. Risk factors for asthma exacerbation in patients presenting to an emergency unit of a national referral hospital in Kampala, Uganda. Afr Health Sci. 2014;14(3):707–15.
Riley L, Gouda H, Cowan M. Noncommunicable Diseases Progress Monitor, 2017: World Health Organization; 2017.
Ethiopia steps report on risk factors for Chronic Non Communicable Diseases and prevalence of selected NCDs. Ethiopia public Health institute. 2016 . .
Belachew SA, Erku DA, Yimenu DK, Gebresillassie BM. Assessment of predictors for acute asthma attack in asthmatic patients visiting an Ethiopian hospital: are the potential factors still a threat? Asthma Res Pract. 2018;4(1):8.
Sharma GL, Choudhary GS. Assessment of Risk Factors for Acute Asthma Attack in Asthmatic Patients: A Hospital Based Study. Int Arch BioMed Clin Res. 2018;4(4):46–8.
Geyser M, Rheeder P. Risk factors precipitating exacerbations in adult asthma patients presenting at Kalafong Hospital, Pretoria. S Afr Fam Pract. 2008;50(4):67–e.
Nicholson KG, Kent J, Ireland DC. Respiratory viruses and exacerbations of asthma in adults. BMJ. 2003;307(6910):982–6.
Fraenkel DJ, Bardin PG, Sanderson G, et al. Lower airways inflammation during rhinovirus colds in normal and in asthmatic subjects. Am J Respir Crit Care Med. 2009;151(3):879–86.
Kolbe J, Fergusson W, Vamos M, Garrett J. Case-control study of severe life-threatening asthma (SLTA) in adults. Thorax. 2002;57(4):317–22.
De-Lei K, Zheng Q, Hui S, Hong Y. Association of Obstructive Sleep Apnea with Asthma exacerbation; 2017.
Alkhalil M, Schulman E, Getsy J. Obstructive sleep apnea syndrome and asthma: what are the links? J Clin Sleep Med. 2009;5(01):71–8.
Tarlo S, Broder I, Corey P, et al. A case-control study of the role of cold symptoms and other historical triggering factors in asthma exacerbations. Can Respir J. 2000;7(1):42–8.
Surrena H, editor. Handbook for Brunner and Suddarth’s textbook of medical-surgical nursing. Lippincott Williams & Wilkins; 2010.
Pola-Bibian B, et al. Asthma exacerbations in a tertiary hospital: clinical features, triggers, and risk factors for hospitalization. J Investig Allergol Clin Immunol. 2016: 0 . https://doi.org/10.18176/jiaci.0128 .
Eisner M, et al. Exposure to indoor combustion and adult asthma outcomes: environmental tobacco smoke, gas stoves, and woodsmoke. Thorax. 2002;57(11):973–8.
Smeltzer SC, Bare BG, Hinkele JL, Cheever KH. Brunner and Suddath’s Text Book of Medical Surgical 2010. Wolters Kluwer Health:Lippincott Williams & Wilkins. Nursing, vol. 1. 12th ed. p. 622.
Download references
Acknowledgments
Authors thanks to public general hospitals of central zone Tigray, Ethiopia for their co-operation, to data collectors, supervisors, for the health staffs of the hospitals and to the study participants for their valuable information.
Not applicable.
Author information
Authors and affiliations.
Department of adult health nursing ,school of Nursing, Aksum University, Aksum, Ethiopia
Melaku Negash & Degena Bahrey Tadesse
Department of Psychiatric, Mekelle University, Mekelle, Ethiopia
Hagos Tsegabrhan
Adwa General Hospital, Adwa, Ethiopia
Teklit Meles
Department of midwifery, Aksum University, Aksum, Ethiopia
Gebreamlak Gidey
college of medicine and health science, Adigrat university, Adigrat, Ethiopia
Yemane Berhane
Maternity and reproductive health nursing, Mekelle University, Mekelle, Ethiopia
Kibrom Berhanu
Department of Emergency and critical care nursing, Mekelle University, Mekelle, Ethiopia
Tsgalem Haylemaryam
You can also search for this author in PubMed Google Scholar
Contributions
MN: was made substantially contributions to conceived and designed the study, analysis the data, methodology, data interpretation and wrote the final manuscript.TM, DB, GG,YB, had equally contributed to analysis and interpretation of the data. Whereas HT, TH and KB substantial contribution in reviewing overall the study in analysis, interpretation of data, have drafted the manuscript and substantively revised the work. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Melaku Negash .
Ethics declarations
Ethics approval and consent to participate.
Ethical clearance was obtained from Mekelle University College of health sciences institutional review board (IRB). Official supportive letters were obtained from Regional Health Bureau (TRHB) and central zone health office. Respondents were informed about the purpose of the study and the interview was conducted after receiving the written consent from participants. The right of participants to withdraw from the study at any time, without any precondition were secured and participants were informed. Confidentiality of the data/information was secured and was not used for other purposes. No personal identifiers was used on the questionnaire. To maintain confidentiality, data collector was recruited from the study unit.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Annex I: English version structured interview questionnaire.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Negash, M., Tsegabrhan, H., Meles, T. et al. Determinants of Acute Asthma Attack among adult asthmatic patients visiting hospitals of Tigray, Ethiopia, 2019: case control study. asthma res and pract 6 , 1 (2020). https://doi.org/10.1186/s40733-020-00054-w
Download citation
Received : 07 December 2019
Accepted : 17 March 2020
Published : 03 April 2020
DOI : https://doi.org/10.1186/s40733-020-00054-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Acute asthma attack
- Determinants
Asthma Research and Practice
ISSN: 2054-7064
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Campus Directory
- Current Students
- Faculty & Staff

Asthma Case Study
Asthma affects about 6.1 million children in the US under 18 years of age, making it one of the most common chronic childhood disorders (American Lung Association, 2021). Asthma occurs as a result of a stimulus which can range from allergens, cigarette smoke, changes in temperature, stress, or exercise. In this case we’ll experience an asthma attack and subsequent treatment with 16-year-old Ben Mason.
Module 9: Asthma

Review structure and functions of the respiratory system...
Asthma - Page 1

Ben was struggling to breathe when he reached the ER...
Asthma - Page 2
Ben was also given an additional breathing treatment...
Asthma - Page 3
Case Summary
Summary of the Case
Asthma - Summary

Answers to Case Questions
Asthma - Answers

Professionals
Health Professionals Introduced in Case
Asthma - Professionals
Additional Links
Asthma - Links
- Join our Mailing List
Working locally in primary care and collaborating globally to improve respiratory health
Clinical case study - asthma, clinical case study - asthma, resource information.
- Disease management

IMAGES
VIDEO
COMMENTS
1. a. Tidal volume is the volume of air inhaled or exhaled during normal quiet breathing. b. Inspiratory reserve volume is the amount of air that can be inhaled after a normal tidal volume. c. Expiratory reserve volume is the amount of air that can be exhaled after a normal tidal volume.
case study w answers man who lives in small mountain town in colorado, is highly allergic to dust and pollen and has history of mild asthma. wife drove him to ... The provider discusses B.'s asthma management with him; B. says he has had several asthma attacks over the last few weeks. The provider discharges B. with prescriptions for ...
Decreases your immune system's response to reduce symptoms such as swelling and allergic-type reactions such as inflammation. Study with Quizlet and memorize flashcards containing terms like lead to asthma attack, bronchodilator (beta-agonists, anticholinergics, theophylline) medication, Quick relief rescue inhaler mechanism and more.
Figure 1. The respiratory passageways in a non-asthmatic (L) bronchoconstriction can severely decrease the diameter of the. and asthmatic (R) lung. Credit: BruceBlaus, cc by 3.0. already swollen, mucus-producing airways, making it very. difficult to move air into and out of the lungs. The decrease in air flow can range from mild to life ...
may cause a great deal of anxiety for someone actively suffering from an acute asthma exacerbation, or asthma attack. Questions You may need to use the internet or another source to help answer some of the questions in this case study. 1. According to the passage above, what are the three factors involving the airways that lead to an asthma ...
Case presentation. The patient, a 66-year-old asthmatic man, had a 3-day history of worsening cough, wheeze and shortness of breath that was not relieved by his salbutamol inhaler. ... In a prospective study 7 of 18 patients with acute exacerbation of asthma, attending the emergency department, the change in lactate levels after administering ...
Case Study course: training and development chapter the asthma attack case study professor: darlene friesen student: sarah jolicoeur date may 31st, 2021 run the
Asthma Attack - Assignment Training & Development Sarah Glass Hi Laurie, "Asthma Attack" Case Study: In March of 2013, a teenage boy visiting a Tim Hortons franchise in London, Ontario, suffered an asthma attack. The 17-year-old boy was having difficulty breathing and was gasping for air as he tried to get the attention of ...
Abstract. This interrupted case study follows the progress of a pediatric patient who experiences an acute asthma exacerbation brought on by an environmental trigger. Students completing the case will synthesize their understanding of respiratory system anatomy and physiology with the clinical treatment of an obstructive lung disorder.
The majority of adverse effects occurred within 1 day of the procedure and resolved within 7 days. 6. In this study, bronchial thermoplasty was found to significantly improve quality of life, as ...
Chapter 28 :: Patient With Asthma Case Study. Asthma is a chronic inflammatory disorder of the airways. There are 3 components of asthma: inflammation, increased mucous production, and bronchospasm. These components lead to recurrent episodes of wheezing, breathlessness, chest tightness, and cough, particularly at night or in the early morning.
Airflow obstruction in asthma is the result of contraction of the airway smooth muscle and swelling of the airway wall due to: Smooth muscle hypertrophy and hyperplasia. Inflammatory cell infiltration and oedema. Goblet cell and mucous gland hyperplasia with mucous hypersecretion. Protein deposition including collagen.
Acute asthma attack is one of the most common causes of visits to hospital emergency departments in all age groups of the population and accounts for the greater part of healthcare burden from the disease. Despite, Acute asthma attack is an important public health problem that affects not only the patients, but also to the family, health professionals, health care institutions and development ...
Asthma - Page 1. Review structure and functions of the respiratory system in the Case Study Workbook and through the following videos. All of these videos are on the same page. Scroll down to find each video: Respiratory System - Respiration - The Mechanics of Breathing. Sixteen-year-old Ben Mason was warming up for a high school soccer ...
Asthma affects about 6.1 million children in the US under 18 years of age, making it one of the most common chronic childhood disorders (American Lung Association, 2021). Asthma occurs as a result of a stimulus which can range from allergens, cigarette smoke, changes in temperature, stress, or exercise. In this case we'll experience an asthma ...
Clinical case study - asthma . 2019 . Clinical Case Study - Asthma. pdf. Clinical Case Study - Asthma. 6.34 MB. Resource information. Respiratory conditions. Asthma; Respiratory topics. Disease management; Diagnosis; Type of resource. Presentation . Author(s) Jaime Correia de Sousa Ioanna Tsiligianni Miguel Román Rodriguez
SNC4U snc4m case study: asthma attack! national center for case study teaching in science asthma attack! hollie leavitt department of biology college of. Skip to document. University; High School. ... You may need to use the internet or another source to help answer some of the questions in this case study.
Prefers sitting to lying down. SOB with talking. Speaks only in short phrases as a result of breathleseness. Vital Signs. See Patient Case Table 1 2. 1. CASE STUDV 1 2 , ASTHMA. 5 1. Parient Case Question 1. Based on the available clinical evidence, is this patient's asthmatic atiack considered mild, moderate, or bordering on respiratory ...
Jaden Jone Ms. Kolmatiski BIO 20 08/12/20 Part 1: 1. The three factors involving the airways that lead to an asthma attack are exposure to cold and or dry air, being in contact with pollen or other allergens the body is allergic to, having a cold or the flu, certain medications (over the counter or prescribed), certain foods, or even just stress can cause this bronchoconstriction to occur 2.