Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- What Is Qualitative Research? | Methods & Examples

What Is Qualitative Research? | Methods & Examples
Published on June 19, 2020 by Pritha Bhandari . Revised on June 22, 2023.
Qualitative research involves collecting and analyzing non-numerical data (e.g., text, video, or audio) to understand concepts, opinions, or experiences. It can be used to gather in-depth insights into a problem or generate new ideas for research.
Qualitative research is the opposite of quantitative research , which involves collecting and analyzing numerical data for statistical analysis.
Qualitative research is commonly used in the humanities and social sciences, in subjects such as anthropology, sociology, education, health sciences, history, etc.
- How does social media shape body image in teenagers?
- How do children and adults interpret healthy eating in the UK?
- What factors influence employee retention in a large organization?
- How is anxiety experienced around the world?
- How can teachers integrate social issues into science curriculums?
Table of contents
Approaches to qualitative research, qualitative research methods, qualitative data analysis, advantages of qualitative research, disadvantages of qualitative research, other interesting articles, frequently asked questions about qualitative research.
Qualitative research is used to understand how people experience the world. While there are many approaches to qualitative research, they tend to be flexible and focus on retaining rich meaning when interpreting data.
Common approaches include grounded theory, ethnography , action research , phenomenological research, and narrative research. They share some similarities, but emphasize different aims and perspectives.
Note that qualitative research is at risk for certain research biases including the Hawthorne effect , observer bias , recall bias , and social desirability bias . While not always totally avoidable, awareness of potential biases as you collect and analyze your data can prevent them from impacting your work too much.
Prevent plagiarism. Run a free check.
Each of the research approaches involve using one or more data collection methods . These are some of the most common qualitative methods:
- Observations: recording what you have seen, heard, or encountered in detailed field notes.
- Interviews: personally asking people questions in one-on-one conversations.
- Focus groups: asking questions and generating discussion among a group of people.
- Surveys : distributing questionnaires with open-ended questions.
- Secondary research: collecting existing data in the form of texts, images, audio or video recordings, etc.
- You take field notes with observations and reflect on your own experiences of the company culture.
- You distribute open-ended surveys to employees across all the company’s offices by email to find out if the culture varies across locations.
- You conduct in-depth interviews with employees in your office to learn about their experiences and perspectives in greater detail.
Qualitative researchers often consider themselves “instruments” in research because all observations, interpretations and analyses are filtered through their own personal lens.
For this reason, when writing up your methodology for qualitative research, it’s important to reflect on your approach and to thoroughly explain the choices you made in collecting and analyzing the data.
Qualitative data can take the form of texts, photos, videos and audio. For example, you might be working with interview transcripts, survey responses, fieldnotes, or recordings from natural settings.
Most types of qualitative data analysis share the same five steps:
- Prepare and organize your data. This may mean transcribing interviews or typing up fieldnotes.
- Review and explore your data. Examine the data for patterns or repeated ideas that emerge.
- Develop a data coding system. Based on your initial ideas, establish a set of codes that you can apply to categorize your data.
- Assign codes to the data. For example, in qualitative survey analysis, this may mean going through each participant’s responses and tagging them with codes in a spreadsheet. As you go through your data, you can create new codes to add to your system if necessary.
- Identify recurring themes. Link codes together into cohesive, overarching themes.
There are several specific approaches to analyzing qualitative data. Although these methods share similar processes, they emphasize different concepts.
Qualitative research often tries to preserve the voice and perspective of participants and can be adjusted as new research questions arise. Qualitative research is good for:
- Flexibility
The data collection and analysis process can be adapted as new ideas or patterns emerge. They are not rigidly decided beforehand.
- Natural settings
Data collection occurs in real-world contexts or in naturalistic ways.
- Meaningful insights
Detailed descriptions of people’s experiences, feelings and perceptions can be used in designing, testing or improving systems or products.
- Generation of new ideas
Open-ended responses mean that researchers can uncover novel problems or opportunities that they wouldn’t have thought of otherwise.
Receive feedback on language, structure, and formatting
Professional editors proofread and edit your paper by focusing on:
- Academic style
- Vague sentences
- Style consistency
See an example

Researchers must consider practical and theoretical limitations in analyzing and interpreting their data. Qualitative research suffers from:
- Unreliability
The real-world setting often makes qualitative research unreliable because of uncontrolled factors that affect the data.
- Subjectivity
Due to the researcher’s primary role in analyzing and interpreting data, qualitative research cannot be replicated . The researcher decides what is important and what is irrelevant in data analysis, so interpretations of the same data can vary greatly.
- Limited generalizability
Small samples are often used to gather detailed data about specific contexts. Despite rigorous analysis procedures, it is difficult to draw generalizable conclusions because the data may be biased and unrepresentative of the wider population .
- Labor-intensive
Although software can be used to manage and record large amounts of text, data analysis often has to be checked or performed manually.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Chi square goodness of fit test
- Degrees of freedom
- Null hypothesis
- Discourse analysis
- Control groups
- Mixed methods research
- Non-probability sampling
- Quantitative research
- Inclusion and exclusion criteria
Research bias
- Rosenthal effect
- Implicit bias
- Cognitive bias
- Selection bias
- Negativity bias
- Status quo bias
Quantitative research deals with numbers and statistics, while qualitative research deals with words and meanings.
Quantitative methods allow you to systematically measure variables and test hypotheses . Qualitative methods allow you to explore concepts and experiences in more detail.
There are five common approaches to qualitative research :
- Grounded theory involves collecting data in order to develop new theories.
- Ethnography involves immersing yourself in a group or organization to understand its culture.
- Narrative research involves interpreting stories to understand how people make sense of their experiences and perceptions.
- Phenomenological research involves investigating phenomena through people’s lived experiences.
- Action research links theory and practice in several cycles to drive innovative changes.
Data collection is the systematic process by which observations or measurements are gathered in research. It is used in many different contexts by academics, governments, businesses, and other organizations.
There are various approaches to qualitative data analysis , but they all share five steps in common:
- Prepare and organize your data.
- Review and explore your data.
- Develop a data coding system.
- Assign codes to the data.
- Identify recurring themes.
The specifics of each step depend on the focus of the analysis. Some common approaches include textual analysis , thematic analysis , and discourse analysis .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Bhandari, P. (2023, June 22). What Is Qualitative Research? | Methods & Examples. Scribbr. Retrieved March 27, 2024, from https://www.scribbr.com/methodology/qualitative-research/
Is this article helpful?

Pritha Bhandari
Other students also liked, qualitative vs. quantitative research | differences, examples & methods, how to do thematic analysis | step-by-step guide & examples, unlimited academic ai-proofreading.
✔ Document error-free in 5minutes ✔ Unlimited document corrections ✔ Specialized in correcting academic texts
- Privacy Policy
Buy Me a Coffee

Home » Qualitative Research – Methods, Analysis Types and Guide
Qualitative Research – Methods, Analysis Types and Guide
Table of Contents

Qualitative Research
Qualitative research is a type of research methodology that focuses on exploring and understanding people’s beliefs, attitudes, behaviors, and experiences through the collection and analysis of non-numerical data. It seeks to answer research questions through the examination of subjective data, such as interviews, focus groups, observations, and textual analysis.
Qualitative research aims to uncover the meaning and significance of social phenomena, and it typically involves a more flexible and iterative approach to data collection and analysis compared to quantitative research. Qualitative research is often used in fields such as sociology, anthropology, psychology, and education.
Qualitative Research Methods

Qualitative Research Methods are as follows:
One-to-One Interview
This method involves conducting an interview with a single participant to gain a detailed understanding of their experiences, attitudes, and beliefs. One-to-one interviews can be conducted in-person, over the phone, or through video conferencing. The interviewer typically uses open-ended questions to encourage the participant to share their thoughts and feelings. One-to-one interviews are useful for gaining detailed insights into individual experiences.
Focus Groups
This method involves bringing together a group of people to discuss a specific topic in a structured setting. The focus group is led by a moderator who guides the discussion and encourages participants to share their thoughts and opinions. Focus groups are useful for generating ideas and insights, exploring social norms and attitudes, and understanding group dynamics.
Ethnographic Studies
This method involves immersing oneself in a culture or community to gain a deep understanding of its norms, beliefs, and practices. Ethnographic studies typically involve long-term fieldwork and observation, as well as interviews and document analysis. Ethnographic studies are useful for understanding the cultural context of social phenomena and for gaining a holistic understanding of complex social processes.
Text Analysis
This method involves analyzing written or spoken language to identify patterns and themes. Text analysis can be quantitative or qualitative. Qualitative text analysis involves close reading and interpretation of texts to identify recurring themes, concepts, and patterns. Text analysis is useful for understanding media messages, public discourse, and cultural trends.
This method involves an in-depth examination of a single person, group, or event to gain an understanding of complex phenomena. Case studies typically involve a combination of data collection methods, such as interviews, observations, and document analysis, to provide a comprehensive understanding of the case. Case studies are useful for exploring unique or rare cases, and for generating hypotheses for further research.
Process of Observation
This method involves systematically observing and recording behaviors and interactions in natural settings. The observer may take notes, use audio or video recordings, or use other methods to document what they see. Process of observation is useful for understanding social interactions, cultural practices, and the context in which behaviors occur.
Record Keeping
This method involves keeping detailed records of observations, interviews, and other data collected during the research process. Record keeping is essential for ensuring the accuracy and reliability of the data, and for providing a basis for analysis and interpretation.
This method involves collecting data from a large sample of participants through a structured questionnaire. Surveys can be conducted in person, over the phone, through mail, or online. Surveys are useful for collecting data on attitudes, beliefs, and behaviors, and for identifying patterns and trends in a population.
Qualitative data analysis is a process of turning unstructured data into meaningful insights. It involves extracting and organizing information from sources like interviews, focus groups, and surveys. The goal is to understand people’s attitudes, behaviors, and motivations
Qualitative Research Analysis Methods
Qualitative Research analysis methods involve a systematic approach to interpreting and making sense of the data collected in qualitative research. Here are some common qualitative data analysis methods:
Thematic Analysis
This method involves identifying patterns or themes in the data that are relevant to the research question. The researcher reviews the data, identifies keywords or phrases, and groups them into categories or themes. Thematic analysis is useful for identifying patterns across multiple data sources and for generating new insights into the research topic.
Content Analysis
This method involves analyzing the content of written or spoken language to identify key themes or concepts. Content analysis can be quantitative or qualitative. Qualitative content analysis involves close reading and interpretation of texts to identify recurring themes, concepts, and patterns. Content analysis is useful for identifying patterns in media messages, public discourse, and cultural trends.
Discourse Analysis
This method involves analyzing language to understand how it constructs meaning and shapes social interactions. Discourse analysis can involve a variety of methods, such as conversation analysis, critical discourse analysis, and narrative analysis. Discourse analysis is useful for understanding how language shapes social interactions, cultural norms, and power relationships.
Grounded Theory Analysis
This method involves developing a theory or explanation based on the data collected. Grounded theory analysis starts with the data and uses an iterative process of coding and analysis to identify patterns and themes in the data. The theory or explanation that emerges is grounded in the data, rather than preconceived hypotheses. Grounded theory analysis is useful for understanding complex social phenomena and for generating new theoretical insights.
Narrative Analysis
This method involves analyzing the stories or narratives that participants share to gain insights into their experiences, attitudes, and beliefs. Narrative analysis can involve a variety of methods, such as structural analysis, thematic analysis, and discourse analysis. Narrative analysis is useful for understanding how individuals construct their identities, make sense of their experiences, and communicate their values and beliefs.
Phenomenological Analysis
This method involves analyzing how individuals make sense of their experiences and the meanings they attach to them. Phenomenological analysis typically involves in-depth interviews with participants to explore their experiences in detail. Phenomenological analysis is useful for understanding subjective experiences and for developing a rich understanding of human consciousness.
Comparative Analysis
This method involves comparing and contrasting data across different cases or groups to identify similarities and differences. Comparative analysis can be used to identify patterns or themes that are common across multiple cases, as well as to identify unique or distinctive features of individual cases. Comparative analysis is useful for understanding how social phenomena vary across different contexts and groups.
Applications of Qualitative Research
Qualitative research has many applications across different fields and industries. Here are some examples of how qualitative research is used:
- Market Research: Qualitative research is often used in market research to understand consumer attitudes, behaviors, and preferences. Researchers conduct focus groups and one-on-one interviews with consumers to gather insights into their experiences and perceptions of products and services.
- Health Care: Qualitative research is used in health care to explore patient experiences and perspectives on health and illness. Researchers conduct in-depth interviews with patients and their families to gather information on their experiences with different health care providers and treatments.
- Education: Qualitative research is used in education to understand student experiences and to develop effective teaching strategies. Researchers conduct classroom observations and interviews with students and teachers to gather insights into classroom dynamics and instructional practices.
- Social Work : Qualitative research is used in social work to explore social problems and to develop interventions to address them. Researchers conduct in-depth interviews with individuals and families to understand their experiences with poverty, discrimination, and other social problems.
- Anthropology : Qualitative research is used in anthropology to understand different cultures and societies. Researchers conduct ethnographic studies and observe and interview members of different cultural groups to gain insights into their beliefs, practices, and social structures.
- Psychology : Qualitative research is used in psychology to understand human behavior and mental processes. Researchers conduct in-depth interviews with individuals to explore their thoughts, feelings, and experiences.
- Public Policy : Qualitative research is used in public policy to explore public attitudes and to inform policy decisions. Researchers conduct focus groups and one-on-one interviews with members of the public to gather insights into their perspectives on different policy issues.
How to Conduct Qualitative Research
Here are some general steps for conducting qualitative research:
- Identify your research question: Qualitative research starts with a research question or set of questions that you want to explore. This question should be focused and specific, but also broad enough to allow for exploration and discovery.
- Select your research design: There are different types of qualitative research designs, including ethnography, case study, grounded theory, and phenomenology. You should select a design that aligns with your research question and that will allow you to gather the data you need to answer your research question.
- Recruit participants: Once you have your research question and design, you need to recruit participants. The number of participants you need will depend on your research design and the scope of your research. You can recruit participants through advertisements, social media, or through personal networks.
- Collect data: There are different methods for collecting qualitative data, including interviews, focus groups, observation, and document analysis. You should select the method or methods that align with your research design and that will allow you to gather the data you need to answer your research question.
- Analyze data: Once you have collected your data, you need to analyze it. This involves reviewing your data, identifying patterns and themes, and developing codes to organize your data. You can use different software programs to help you analyze your data, or you can do it manually.
- Interpret data: Once you have analyzed your data, you need to interpret it. This involves making sense of the patterns and themes you have identified, and developing insights and conclusions that answer your research question. You should be guided by your research question and use your data to support your conclusions.
- Communicate results: Once you have interpreted your data, you need to communicate your results. This can be done through academic papers, presentations, or reports. You should be clear and concise in your communication, and use examples and quotes from your data to support your findings.
Examples of Qualitative Research
Here are some real-time examples of qualitative research:
- Customer Feedback: A company may conduct qualitative research to understand the feedback and experiences of its customers. This may involve conducting focus groups or one-on-one interviews with customers to gather insights into their attitudes, behaviors, and preferences.
- Healthcare : A healthcare provider may conduct qualitative research to explore patient experiences and perspectives on health and illness. This may involve conducting in-depth interviews with patients and their families to gather information on their experiences with different health care providers and treatments.
- Education : An educational institution may conduct qualitative research to understand student experiences and to develop effective teaching strategies. This may involve conducting classroom observations and interviews with students and teachers to gather insights into classroom dynamics and instructional practices.
- Social Work: A social worker may conduct qualitative research to explore social problems and to develop interventions to address them. This may involve conducting in-depth interviews with individuals and families to understand their experiences with poverty, discrimination, and other social problems.
- Anthropology : An anthropologist may conduct qualitative research to understand different cultures and societies. This may involve conducting ethnographic studies and observing and interviewing members of different cultural groups to gain insights into their beliefs, practices, and social structures.
- Psychology : A psychologist may conduct qualitative research to understand human behavior and mental processes. This may involve conducting in-depth interviews with individuals to explore their thoughts, feelings, and experiences.
- Public Policy: A government agency or non-profit organization may conduct qualitative research to explore public attitudes and to inform policy decisions. This may involve conducting focus groups and one-on-one interviews with members of the public to gather insights into their perspectives on different policy issues.
Purpose of Qualitative Research
The purpose of qualitative research is to explore and understand the subjective experiences, behaviors, and perspectives of individuals or groups in a particular context. Unlike quantitative research, which focuses on numerical data and statistical analysis, qualitative research aims to provide in-depth, descriptive information that can help researchers develop insights and theories about complex social phenomena.
Qualitative research can serve multiple purposes, including:
- Exploring new or emerging phenomena : Qualitative research can be useful for exploring new or emerging phenomena, such as new technologies or social trends. This type of research can help researchers develop a deeper understanding of these phenomena and identify potential areas for further study.
- Understanding complex social phenomena : Qualitative research can be useful for exploring complex social phenomena, such as cultural beliefs, social norms, or political processes. This type of research can help researchers develop a more nuanced understanding of these phenomena and identify factors that may influence them.
- Generating new theories or hypotheses: Qualitative research can be useful for generating new theories or hypotheses about social phenomena. By gathering rich, detailed data about individuals’ experiences and perspectives, researchers can develop insights that may challenge existing theories or lead to new lines of inquiry.
- Providing context for quantitative data: Qualitative research can be useful for providing context for quantitative data. By gathering qualitative data alongside quantitative data, researchers can develop a more complete understanding of complex social phenomena and identify potential explanations for quantitative findings.
When to use Qualitative Research
Here are some situations where qualitative research may be appropriate:
- Exploring a new area: If little is known about a particular topic, qualitative research can help to identify key issues, generate hypotheses, and develop new theories.
- Understanding complex phenomena: Qualitative research can be used to investigate complex social, cultural, or organizational phenomena that are difficult to measure quantitatively.
- Investigating subjective experiences: Qualitative research is particularly useful for investigating the subjective experiences of individuals or groups, such as their attitudes, beliefs, values, or emotions.
- Conducting formative research: Qualitative research can be used in the early stages of a research project to develop research questions, identify potential research participants, and refine research methods.
- Evaluating interventions or programs: Qualitative research can be used to evaluate the effectiveness of interventions or programs by collecting data on participants’ experiences, attitudes, and behaviors.
Characteristics of Qualitative Research
Qualitative research is characterized by several key features, including:
- Focus on subjective experience: Qualitative research is concerned with understanding the subjective experiences, beliefs, and perspectives of individuals or groups in a particular context. Researchers aim to explore the meanings that people attach to their experiences and to understand the social and cultural factors that shape these meanings.
- Use of open-ended questions: Qualitative research relies on open-ended questions that allow participants to provide detailed, in-depth responses. Researchers seek to elicit rich, descriptive data that can provide insights into participants’ experiences and perspectives.
- Sampling-based on purpose and diversity: Qualitative research often involves purposive sampling, in which participants are selected based on specific criteria related to the research question. Researchers may also seek to include participants with diverse experiences and perspectives to capture a range of viewpoints.
- Data collection through multiple methods: Qualitative research typically involves the use of multiple data collection methods, such as in-depth interviews, focus groups, and observation. This allows researchers to gather rich, detailed data from multiple sources, which can provide a more complete picture of participants’ experiences and perspectives.
- Inductive data analysis: Qualitative research relies on inductive data analysis, in which researchers develop theories and insights based on the data rather than testing pre-existing hypotheses. Researchers use coding and thematic analysis to identify patterns and themes in the data and to develop theories and explanations based on these patterns.
- Emphasis on researcher reflexivity: Qualitative research recognizes the importance of the researcher’s role in shaping the research process and outcomes. Researchers are encouraged to reflect on their own biases and assumptions and to be transparent about their role in the research process.
Advantages of Qualitative Research
Qualitative research offers several advantages over other research methods, including:
- Depth and detail: Qualitative research allows researchers to gather rich, detailed data that provides a deeper understanding of complex social phenomena. Through in-depth interviews, focus groups, and observation, researchers can gather detailed information about participants’ experiences and perspectives that may be missed by other research methods.
- Flexibility : Qualitative research is a flexible approach that allows researchers to adapt their methods to the research question and context. Researchers can adjust their research methods in real-time to gather more information or explore unexpected findings.
- Contextual understanding: Qualitative research is well-suited to exploring the social and cultural context in which individuals or groups are situated. Researchers can gather information about cultural norms, social structures, and historical events that may influence participants’ experiences and perspectives.
- Participant perspective : Qualitative research prioritizes the perspective of participants, allowing researchers to explore subjective experiences and understand the meanings that participants attach to their experiences.
- Theory development: Qualitative research can contribute to the development of new theories and insights about complex social phenomena. By gathering rich, detailed data and using inductive data analysis, researchers can develop new theories and explanations that may challenge existing understandings.
- Validity : Qualitative research can offer high validity by using multiple data collection methods, purposive and diverse sampling, and researcher reflexivity. This can help ensure that findings are credible and trustworthy.
Limitations of Qualitative Research
Qualitative research also has some limitations, including:
- Subjectivity : Qualitative research relies on the subjective interpretation of researchers, which can introduce bias into the research process. The researcher’s perspective, beliefs, and experiences can influence the way data is collected, analyzed, and interpreted.
- Limited generalizability: Qualitative research typically involves small, purposive samples that may not be representative of larger populations. This limits the generalizability of findings to other contexts or populations.
- Time-consuming: Qualitative research can be a time-consuming process, requiring significant resources for data collection, analysis, and interpretation.
- Resource-intensive: Qualitative research may require more resources than other research methods, including specialized training for researchers, specialized software for data analysis, and transcription services.
- Limited reliability: Qualitative research may be less reliable than quantitative research, as it relies on the subjective interpretation of researchers. This can make it difficult to replicate findings or compare results across different studies.
- Ethics and confidentiality: Qualitative research involves collecting sensitive information from participants, which raises ethical concerns about confidentiality and informed consent. Researchers must take care to protect the privacy and confidentiality of participants and obtain informed consent.
Also see Research Methods
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

Questionnaire – Definition, Types, and Examples

Case Study – Methods, Examples and Guide

Observational Research – Methods and Guide

Quantitative Research – Methods, Types and...

Qualitative Research Methods

Explanatory Research – Types, Methods, Guide
Qualitative Research : Definition
Qualitative research is the naturalistic study of social meanings and processes, using interviews, observations, and the analysis of texts and images. In contrast to quantitative researchers, whose statistical methods enable broad generalizations about populations (for example, comparisons of the percentages of U.S. demographic groups who vote in particular ways), qualitative researchers use in-depth studies of the social world to analyze how and why groups think and act in particular ways (for instance, case studies of the experiences that shape political views).
- Next: Choose an approach >>
- Choose an approach
- Find studies
- Learn methods
- Get software
- Get data for secondary analysis
- Network with researchers

- Last Updated: Jan 31, 2024 9:21 AM
- URL: https://guides.library.stanford.edu/qualitative_research
No internet connection.
All search filters on the page have been cleared., your search has been saved..
- All content
- Dictionaries
- Encyclopedias
- Expert Insights
- Foundations
- How-to Guides
- Journal Articles
- Little Blue Books
- Little Green Books
- Project Planner
- Tools Directory
- Sign in to my profile My Profile
- Sign in Signed in
- My profile My Profile
The SAGE Encyclopedia of Qualitative Research Methods
- Edited by: Lisa M. Given
- Publisher: SAGE Publications, Inc.
- Publication year: 2008
- Online pub date: December 27, 2012
- Discipline: Anthropology
- Methods: Artistic inquiry , Action research
- DOI: https:// doi. org/10.4135/9781412963909
- Keywords: art , inquiry Show all Show less
- Print ISBN: 9781412941631
- Online ISBN: 9781412963909
- Buy the book icon link
Reader's guide
Entries a-z, subject index.
Qualitative research is designed to explore the human elements of a given topic, while specific qualitative methods examine how individuals see and experience the world. Qualitative approaches are typically used to explore new phenomena and to capture individuals' thoughts, feelings, or interpretations of meaning and process. Such methods are central to research conducted in education, nursing, sociology, anthropology, information studies, and other disciplines in the humanities, social sciences, and health sciences. Qualitative research projects are informed by a wide range of methodologies and theoretical frameworks.
The SAGE Encyclopedia of Qualitative Research Methods presents current and complete information as well as ready-to-use techniques, facts, and examples from the field of qualitative research in a very accessible style. In taking an interdisciplinary approach, these two volumes target a broad audience and fill a gap in the existing reference literature for a general guide to the core concepts that inform qualitative research practices. The entries cover every major facet of qualitative methods, including access to research participants, data coding, research ethics, the role of theory in qualitative research, and much more—all without overwhelming the informed reader.
Key Features
Defines and explains core concepts, describes the techniques involved in the implementation of qualitative methods, and presents an overview of qualitative approaches to research; Offers many entries that point to substantive debates among qualitative researchers regarding how concepts are labeled and the implications of such labels for how qualitative research is valuedl; Guides readers through the complex landscape of the language of qualitative inquiry; Includes contributors from various countries and disciplines that reflect a diverse spectrum of research approaches from more traditional, positivist approaches, through postmodern, constructionist ones; Presents some entries written in first-person voice and others in third-person voice to reflect the diversity of approaches that define qualitative work
Approaches and Methodologies; Arts-Based Research, Ties to; Computer Software; Data Analysis; Data Collection; Data Types and Characteristics; Dissemination; History of Qualitative Research; Participants; Quantitative Research, Ties to; Research Ethics; Rigor; Textual Analysis, Ties to; Theoretical and Philosophical Frameworks
The SAGE Encyclopedia of Qualitative Research Methods is designed to appeal to undergraduate and graduate students, practitioners, researchers, consultants, and consumers of information across the social sciences, humanities, and health sciences, making it a welcome addition to any academic or public library.
Front Matter
- Editorial Board
- List of Entries
- Reader's Guide
- About the Editor
- Contributors
- Introduction
Reader’s Guide
- A/r/tography
- Action Research
- Advocacy Research
- Applied Research
- Appreciative Inquiry
- Artifact Analysis
- Arts-Based Research
- Arts-Informed Research
- Autobiography
- Autoethnography
- Basic Research
- Clinical Research
- Collaborative Research
- Community-Based Research
- Comparative Research
- Content Analysis
- Conversation Analysis
- Covert Research
- Critical Action Research
- Critical Arts-Based Inquiry
- Critical Discourse Analysis
- Critical Ethnography
- Critical Hermeneutics
- Critical Research
- Cross-Cultural Research
- Discourse Analysis
- Document Analysis
- Duoethnography
- Ecological Research
- Emergent Design
- Empirical Research
- Empowerment Evaluation
- Ethnography
- Ethnomethodology
- Evaluation Research
- Evidence-Based Practice
- Explanatory Research
- Exploratory Data Analysis
- Feminist Research
- Field Research
- Foucauldian Discourse Analysis
- Genealogical Approach
- Grounded Theory
- Hermeneutics
- Heuristic Inquiry
- Historical Discourse Analysis
- Historical Research
- Historiography
- Indigenous Research
- Institutional Ethnography
- Institutional Research
- Interdisciplinary Research
- Internet in Qualitative Research
- Interpretive Inquiry
- Interpretive Phenomenology
- Interpretive Research
- Market Research
- Meta-Analysis
- Meta-Ethnography
- Meta-Synthesis
- Methodological Holism Versus Individualism
- Methodology
- Mixed Methods Research
- Multicultural Research
- Narrative Analysis
- Narrative Genre Analysis
- Narrative Inquiry
- Naturalistic Inquiry
- Observational Research
- Oral History
- Orientational Perspective
- Para-Ethnography
- Participatory Action Research (PAR)
- Performance Ethnography
- Phenomenography
- Phenomenology
- Place/Space in Qualitative Research
- Playbuilding
- Portraiture
- Program Evaluation
- Q Methodology
- Readers Theater
- Social Justice
- Social Network Analysis
- Survey Research
- Systemic Inquiry
- Theatre of the Oppressed
- Transformational Methods
- Unobtrusive Research
- Value-Free Inquiry
- Virtual Ethnography
- Virtual Research
- Visual Ethnography
- Visual Narrative Inquiry
- Bricolage and Bricoleur
- Connoisseurship
- Dance in Qualitative Research
- Ethnopoetics
- Fictional Writing
- Film and Video in Qualitative Research
- Literature in Qualitative Research
- Multimedia in Qualitative Research
- Music in Qualitative Research
- Photographs in Qualitative Research
- Photonovella and Photovoice
- Poetry in Qualitative Research
- Researcher as Artist
- Storytelling
- Visual Research
- Association for Qualitative Research (AQR)
- Center for Interpretive and Qualitative Research
- International Association of Qualitative Inquiry
- International Institute for Qualitative Methodology
- ResearchTalk, Inc.
- ATLAS.ti"(Software)
- Computer-Assisted Data Analysis
- Diction (Software)
- Ethnograph (Software)
- Framework (Software)
- HyperRESEARCH (Software)
- MAXqda (Software)
- NVivo (Software)
- Qualrus (Software)
- SuperHyperQual (Software)
- TextQuest (Software)
- Transana (Software)
- Analytic Induction
- ATLAS.ti" (Software)
- Audience Analysis
- Axial Coding
- Categorization
- Co-Constructed Narrative
- Codes and Coding
- Coding Frame
- Comparative Analysis
- Concept Mapping
- Conceptual Ordering
- Constant Comparison
- Context and Contextuality
- Context-Centered Knowledge
- Core Category
- Counternarrative
- Creative Writing
- Cultural Context
- Data Analysis
- Data Management
- Data Saturation
- Descriptive Statistics
- Discursive Practice
- Diversity Issues
- Embodied Knowledge
- Emergent Themes
- Emic/Etic Distinction
- Emotions in Qualitative Research
- Ethnographic Content Analysis
- Ethnostatistics
- Evaluation Criteria
- Everyday Life
- Experiential Knowledge
- Explanation
- Gender Issues
- Heteroglossia
- Historical Context
- Horizonalization
- Imagination in Qualitative Research
- In Vivo Coding
- Indexicality
- Interpretation
- Intertextuality
- Liminal Perspective
- Literature Review
- Lived Experience
- Marginalization
- Membership Categorization Device Analysis (MCDA)
- Memos and Memoing
- Meta-Narrative
- Negative Case Analysis
- Nonverbal Communication
- Open Coding
- Peer Review
- Psychological Generalization
- Rapid Assessment Process
- Reconstructive Analysis
- Recursivity
- Reflexivity
- Research Diaries and Journals
- Research Literature
- Researcher as Instrument
- Researcher Sensitivity
- Response Groups
- Rhythmanalysis
- Rigor in Qualitative Research
- Secondary Analysis
- Selective Coding
- Situatedness
- Social Context
- Systematic Sociological Introspection
- Tacit Knowledge
- Textual Analysis
- Thematic Coding and Analysis
- Theoretical Memoing
- Theoretical Saturation
- Thick Description
- Transcription
- Typological Analysis
- Understanding
- Video Intervention/Prevention Assessment
- Visual Data
- Visual Data Displays
- Writing Process
- Active Listening
- Audiorecording
- Captive Population
- Closed Question
- Cognitive Interview
- Convenience Sample
- Convergent Interviewing
- Conversational Interviewing
- Covert Observation
- Critical Incident Technique
- Data Archive
- Data Collection
- Data Generation
- Data Security
- Data Storage
- Diaries and Journals
- Email Interview
- Focus Groups
- Free Association Narrative Interview
- In-Depth Interview
- In-Person Interview
- Interactive Focus Groups
- Interactive Interview
- Interview Guide
- Interviewing
- Leaving the Field
- Life Stories
- Narrative Interview
- Narrative Texts
- Natural Setting
- Naturalistic Data
- Naturalistic Observation
- Negotiating Exit
- Neutral Question
- Neutrality in Qualitative Research
- Nonparticipant Observation
- Nonprobability Sampling
- Observation Schedule
- Open-Ended Question
- Participant Observation
- Peer Debriefing
- Pilot Study
- Probes and Probing
- Projective Techniques
- Prolonged Engagement
- Psychoanalytically Informed Observation
- Purposive Sampling
- Quota Sampling
- Random Sampling
- Recruiting Participants
- Research Problem
- Research Question
- Research Setting
- Research Team
- Researcher Roles
- Researcher Safety
- Sample Size
- Sampling Frame
- Secondary Data
- Semi-Structured Interview
- Sensitizing Concepts
- Serendipity
- Snowball Sampling
- Stratified Sampling
- Structured Interview
- Structured Observation
- Subjectivity Statement
- Telephone Interview
- Theoretical Sampling
- Triangulation
- Unstructured Interview
- Unstructured Observation
- Videorecording
- Virtual Interview
- Ethnography (Journal)
- Field Methods (Journal)
- Forum: Qualitative Social Research (Journal)
- International Journal of Qualitative Methods
- Journal of Contemporary Ethnography
- Journal of Mixed Methods Research
- Narrative Inquiry (Journal)
- Oral History Review (Journal)
- Qualitative Health Research (Journal)
- Qualitative Inquiry (Journal)
- Qualitative Report, The (Journal)
- Qualitative Research (Journal)
- Advances in Qualitative Methods Conference
- Ethnographic and Qualitative Research Conference
- First-Person Voice
- Interdisciplinary Qualitative Studies Conference
- International Congress of Qualitative Inquiry
- International Human Science Research Conference
- Publishing and Publication
- Qualitative Health Research Conference
- Representational Forms of Dissemination
- Research Proposal
- Education, Qualitative Research in
- Evolution of Qualitative Research
- Health Sciences, Qualitative Research in
- Humanities, Qualitative Research in
- Politics of Qualitative Research
- Qualitative Research, History of
- Social Sciences, Qualitative Research in
- Confidentiality
- Conflict of Interest
- Disengagement
- Disinterestedness
- Empowerment
- Informed Consent
- Insider/Outsider Status
- Intersubjectivity
- Key Informant
- Marginalized Populations
- Member Check
- Over-Rapport
- Participant
- Participants as Co-Researchers
- Reciprocity
- Researcher–Participant Relationships
- Secondary Participants
- Virtual Community
- Vulnerability
- Generalizability
- Objectivity
- Probability Sampling
- Quantitative Research
- Reductionism
- Reliability
- Replication
- Ethics Review Process
- Project Management
- Qualitative Research Summer Intensive
- Research Design
- Research Justification
- Theoretical Frameworks
- Thinking Qualitatively Workshop Conference
- Accountability
- Authenticity
- Ethics and New Media
- Ethics Codes
- Institutional Review Boards
- Integrity in Qualitative Research
- Relational Ethics
- Sensitive Topics
- Audit Trail
- Confirmability
- Credibility
- Dependability
- Inter- and Intracoder Reliability
- Observer Bias
- Subjectivity
- Transferability
- Translatability
- Transparency
- Trustworthiness
- Verification
- Discursive Psychology
- Chaos and Complexity Theories
- Constructivism
- Critical Humanism
- Critical Pragmatism
- Critical Race Theory
- Critical Realism
- Critical Theory
- Deconstruction
- Epistemology
- Essentialism
- Existentialism
- Feminist Epistemology
- Grand Narrative
- Grand Theory
- Nonessentialism
- Objectivism
- Postcolonialism
- Postmodernism
- Postpositivism
- Postrepresentation
- Poststructuralism
- Queer Theory
- Reality and Multiple Realities
- Representation
- Social Constructionism
- Structuralism
- Subjectivism
- Symbolic Interactionism
Sign in to access this content
Get a 30 day free trial, more like this, sage recommends.
We found other relevant content for you on other Sage platforms.
Have you created a personal profile? Login or create a profile so that you can save clips, playlists and searches
- Sign in/register
Navigating away from this page will delete your results
Please save your results to "My Self-Assessments" in your profile before navigating away from this page.
Sign in to my profile
Sign up for a free trial and experience all Sage Learning Resources have to offer.
You must have a valid academic email address to sign up.
Get off-campus access
- View or download all content my institution has access to.
Sign up for a free trial and experience all Sage Research Methods has to offer.
- view my profile
- view my lists
Research Methodologies
- Quantitative Research Methodologies
Qualitative Research Methodologies
- Systematic Reviews
- Finding Articles by Methodology
- Design Your Research Project
Library Help
What is qualitative research.
Qualitative research methodologies seek to capture information that often can't be expressed numerically. These methodologies often include some level of interpretation from researchers as they collect information via observation, coded survey or interview responses, and so on. Researchers may use multiple qualitative methods in one study, as well as a theoretical or critical framework to help them interpret their data.
Qualitative research methods can be used to study:
- How are political and social attitudes formed?
- How do people make decisions?
- What teaching or training methods are most effective?
Qualitative Research Approaches
Action research.
In this type of study, researchers will actively pursue some kind of intervention, resolve a problem, or affect some kind of change. They will not only analyze the results but will also examine the challenges encountered through the process.
Ethnography
Ethnographies are an in-depth, holistic type of research used to capture cultural practices, beliefs, traditions, and so on. Here, the researcher observes and interviews members of a culture — an ethnic group, a clique, members of a religion, etc. — and then analyzes their findings.
Grounded Theory
Researchers will create and test a hypothesis using qualitative data. Often, researchers use grounded theory to understand decision-making, problem-solving, and other types of behavior.
Narrative Research
Researchers use this type of framework to understand different aspects of the human experience and how their subjects assign meaning to their experiences. Researchers use interviews to collect data from a small group of subjects, then discuss those results in the form of a narrative or story.
Phenomenology
This type of research attempts to understand the lived experiences of a group and/or how members of that group find meaning in their experiences. Researchers use interviews, observation, and other qualitative methods to collect data.
Often used to share novel or unique information, case studies consist of a detailed, in-depth description of a single subject, pilot project, specific events, and so on.
- Hossain, M.S., Runa, F., & Al Mosabbir, A. (2021). Impact of COVID-19 pandemic on rare diseases: A case study on thalassaemia patients in Bangladesh. Public Health in Practice, 2(100150), 1-3.
- Nožina, M. (2021). The Czech Rhino connection: A case study of Vietnamese wildlife trafficking networks’ operations across central Europe. European Journal on Criminal Policy and Research, 27(2), 265-283.
Focus Groups
Researchers will recruit people to answer questions in small group settings. Focus group members may share similar demographics or be diverse, depending on the researchers' needs. Group members will then be asked a series of questions and have their responses recorded. While these responses may be coded and discussed numerically (e.g., 50% of group members responded negatively to a question), researchers will also use responses to provide context, nuance, and other details.
- Dichabeng, P., Merat, N., & Markkula, G. (2021). Factors that influence the acceptance of future shared automated vehicles – A focus group study with United Kingdom drivers. Transportation Research: Part F, 82, 121–140.
- Maynard, E., Barton, S., Rivett, K., Maynard, O., & Davies, W. (2021). Because ‘grown-ups don’t always get it right’: Allyship with children in research—From research question to authorship. Qualitative Research in Psychology, 18(4), 518–536.
Observational Study
Researchers will arrange to observe (usually in an unobtrusive way) a set of subjects in specific conditions. For example, researchers might visit a school cafeteria to learn about the food choices students make or set up trail cameras to collect information about animal behavior in the area.
- He, J. Y., Chan, P. W., Li, Q. S., Li, L., Zhang, L., & Yang, H. L. (2022). Observations of wind and turbulence structures of Super Typhoons Hato and Mangkhut over land from a 356 m high meteorological tower. Atmospheric Research, 265(105910), 1-18.
- Zerovnik Spela, Kos Mitja, & Locatelli Igor. (2022). Initiation of insulin therapy in patients with type 2 diabetes: An observational study. Acta Pharmaceutica, 72(1), 147–157.
Open-Ended Surveys
Unlike quantitative surveys, open-ended surveys require respondents to answer the questions in their own words.
- Mujcic, A., Blankers, M., Yildirim, D., Boon, B., & Engels, R. (2021). Cancer survivors’ views on digital support for smoking cessation and alcohol moderation: a survey and qualitative study. BMC Public Health, 21(1), 1-13.
- Smith, S. D., Hall, J. P., & Kurth, N. K. (2021). Perspectives on health policy from people with disabilities. Journal of Disability Policy Studies, 32(3), 224–232.
Structured or Semi-Structured Interviews
Researchers will recruit a small number of people who fit pre-determined criteria (e.g., people in a certain profession) and ask each the same set of questions, one-on-one. Semi-structured interviews will include opportunities for the interviewee to provide additional information they weren't asked about by the researcher.
- Gibbs, D., Haven-Tang, C., & Ritchie, C. (2021). Harmless flirtations or co-creation? Exploring flirtatious encounters in hospitable experiences. Tourism & Hospitality Research, 21(4), 473–486.
- Hongying Dai, Ramos, A., Tamrakar, N., Cheney, M., Samson, K., & Grimm, B. (2021). School personnel’s responses to school-based vaping prevention program: A qualitative study. Health Behavior & Policy Review, 8(2), 130–147.
- Call : 801.863.8840
- Text : 801.290.8123
- In-Person Help
- Email a Librarian
- Make an Appointment
- << Previous: Quantitative Research Methodologies
- Next: Systematic Reviews >>
- Last Updated: Mar 23, 2024 6:39 PM
- URL: https://uvu.libguides.com/methods
What is Qualitative Research? Definition, Types, Examples, Methods, and Best Practices
By Nick Jain
Published on: June 21, 2023

Table of Contents
What is Qualitative Research?
5 key types of qualitative research, examples of qualitative research, qualitative research methods: the top 4 techniques, qualitative research best practices.
Qualitative research is defined as an exploratory metho d that aims to understand complex phenomena, often within their natural settings, by examining subjective experiences, beliefs, attitudes, and behaviors.
Unlike quantitative research , which focuses on numerical measurements and statistical analysis, qualitative research employs a range of data collection methods to gather detailed, non-numerical data that can provide in-depth insights into the research topic.
Here are the key characteristics of Qualitative Research:
- Subjectivity : Qualitative research acknowledges the subjective nature of human experiences and perceptions. It recognizes that individuals interpret and construct meaning based on their unique perspectives, cultural backgrounds, and social contexts. Researchers using qualitative methods aim to capture this subjectivity by engaging in detailed qualitative observations , interviews, and analyses that capture the nuances and complexities of human behavior.
- Contextualization : Qualitative research places a strong emphasis on the context in which social phenomena occur. It seeks to understand the interconnectedness between individuals, their environments, and the broader social structures that shape their experiences. Researchers delve into the specific settings and circumstances that influence the behavior and attitudes of participants, aiming to unravel the intricate relationships between different variables.
- Flexibility : Qualitative research is characterized by its flexibility and adaptability. Researchers have the freedom to modify their research design and methods during the course of the study based on emerging insights and new directions. This flexibility allows for iterative and exploratory research, enabling researchers to delve deeper into the subject matter and capture unexpected findings.
- Interpretation and meaning-making : Qualitative research recognizes that meaning is not fixed but constructed through social interactions and interpretations. Researchers engage in a process of interpretation and meaning-making to make sense of the data collected. This interpretive approach allows researchers to explore multiple perspectives, cultural influences, and social constructions that shape participants’ experiences and behaviors.
- Richness and depth : One of the key strengths of qualitative research is its ability to generate rich and in-depth data. Through methods such as interviews, focus groups , and participant observation, researchers can gather detailed narratives and descriptions that go beyond surface-level information. This depth of data enables a comprehensive understanding of the research topic, including the underlying motivations, emotions, and social dynamics at play.
- Inductive reasoning : Qualitative research often employs an inductive reasoning approach. Instead of starting with preconceived hypotheses or theories, researchers allow patterns and themes to emerge from the data. They engage in iterative cycles of data collection and analysis to develop theories or conceptual frameworks grounded in the empirical evidence gathered. This inductive process allows for new insights and discoveries that may challenge existing theories or offer alternative explanations.
- Naturalistic setting : Qualitative research frequently takes place in naturalistic settings, where participants are observed and studied in their everyday environments. This setting enhances the ecological validity of the research, as it allows researchers to capture authentic behaviors, interactions, and experiences. By observing individuals in their natural contexts, researchers can gain a deeper understanding of how social phenomena unfold in real-world situations.
Learn more: What is Qualitative Observation?
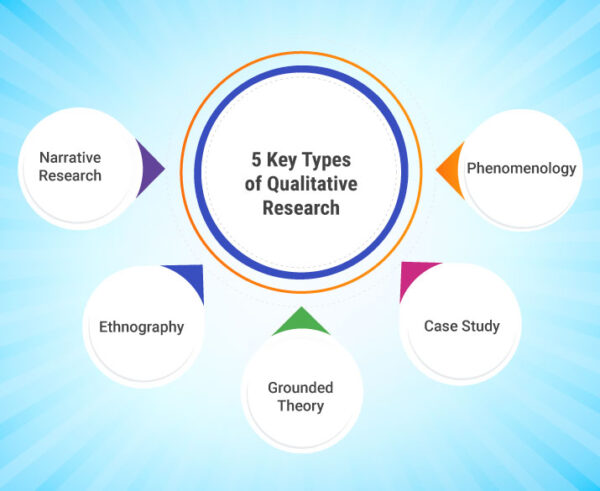
Here are the 5 key qualitative research types that are employed in studies:
1. Phenomenology : This type of research focuses on understanding the essence and meaning of a particular phenomenon or experience as perceived by individuals who have lived through it. It seeks to capture the subjective experiences and perspectives of participants.
2. Ethnography : Ethnographic research involves immersing oneself in a specific cultural or social group to observe and understand its practices, customs, beliefs, and values. Researchers spend extended periods of time within the community to gain a holistic view of its way of life.
3. Grounded Theory: Grounded theory aims to generate new theories or conceptual frameworks based on the analysis of data collected from interviews, observations, or documents. It involves systematically coding and categorizing data to identify patterns and develop theoretical explanations.
4. Case Study : In a case study, researchers conduct an in-depth examination of a single individual, group, or event to gain a detailed understanding of the subject of study. This approach allows for rich contextual information and can be particularly useful in exploring complex and unique cases.
5. Narrative Research: Narrative research focuses on analyzing the stories and personal narratives of individuals to gain insights into their experiences, identities, and sense-making processes. It emphasizes the power of storytelling in constructing meaning.
Example 1. A researcher conducting a phenomenological study might explore the lived experiences of individuals who have survived a natural disaster to understand the psychological and emotional impact of such events.
Example 2. An ethnographer might immerse themselves in a remote indigenous community to study their cultural practices, rituals, and social dynamics.
Example 3. A grounded theory study might investigate the coping mechanisms employed by cancer patients by conducting interviews and analyzing their experiences.
Example 4. A case study could involve examining a specific company’s organizational culture to understand its impact on employee performance and job satisfaction.
Example 5. A narrative research project might analyze the personal narratives of individuals who have experienced significant life transitions, such as migration or career changes, to understand the underlying meaning-making processes.
Learn more: What is Qualitative Market Research?

Here are the best qualitative research methods that offer unique advantages in capturing rich data, facilitating in-depth analysis, and generating comprehensive findings:
1. In-Depth Interviews
One of the most widely used qualitative research techniques is in-depth interviews. This method involves conducting one-on-one interviews with participants to gather rich, detailed information about their experiences, perspectives, and opinions. In-depth interviews allow researchers to explore a participant’s thoughts, emotions, and motivations, providing deep insights into their behavior and decision-making processes. The flexibility of this method allows for the exploration of individual experiences in great detail, making it particularly suitable for sensitive topics or complex phenomena. Through careful probing and open-ended questioning, researchers can develop a comprehensive understanding of the participant’s worldview, uncovering hidden patterns, and generating new hypotheses.
2. Focus Groups
Focus group research involves the gathering of a small group of individuals (typically 6-10) who share common characteristics or experiences. This method encourages participants to engage in open discussions facilitated by a skilled moderator. Focus groups offer a dynamic environment that allows participants to interact, share their perspectives, and build upon each other’s ideas. This method is particularly useful for exploring group dynamics, collective opinions, and societal norms. By observing interactions within the group, researchers can gain valuable insights into how social influences shape individual attitudes and behaviors. Focus groups also allow for the exploration of diverse viewpoints, enabling researchers to identify patterns, contradictions, and shared experiences.
3. Observational Research
Observational research involves systematically observing and documenting participants’ behaviors and interactions within their natural environments. This method provides researchers with a direct window into real-life contexts, allowing for a comprehensive understanding of social interactions, cultural practices, and behavioral patterns. Whether conducted through participant observation or unobtrusive observation, this method eliminates the potential biases associated with self-reporting, as participants’ actions speak louder than words. Observational research is especially valuable in studying nonverbal communication, contextual factors, and complex social systems. It can also provide insights into unarticulated behaviors or experiences that may be difficult to capture through other methods. However, careful planning, ethical considerations, and the need for prolonged engagement are crucial for conducting successful observational research .
4. Case Studies
Case studies involve an in-depth examination of a specific individual, group, organization, or event. Researchers collect data through various sources, such as interviews, observations, documents, and artifacts, to construct a holistic understanding of the case under investigation. This method allows for an exploration of complex social phenomena in their real-life context, uncovering rich, detailed insights that may not be accessible through other methods. Case studies provide an opportunity to examine unique or rare cases, delve into historical contexts, and generate context-specific knowledge. The findings from case studies are often highly detailed and context-bound, offering rich descriptions and contributing to theory development or refinement.
Qualitative research methods offer a range of powerful tools for exploring subjective experiences, meanings, and interpretations. In-depth interviews allow for the exploration of individual perspectives, while focus groups illuminate group dynamics. Observational research provides a direct view of participants’ behaviors, and case studies offer a holistic understanding of specific cases. By leveraging these qualitative methods, researchers can unveil deep insights, capture complex phenomena, and generate context-specific knowledge.
- Clear Research Objectives: Clearly define the qualitative research objectives, questions, or hypotheses that guide the study. This helps maintain focus and ensures that data collection and analysis are aligned with the research goals.
- Sampling Strategy: Select participants or cases that are relevant to the qualitative research questions and provide diverse perspectives. Purposeful sampling techniques, such as maximum variation or snowball sampling, can help ensure the inclusion of a wide range of experiences and viewpoints.
- Data Collection Rigor: Employ rigorous qualitative data collection techniques to ensure the accuracy, credibility, and depth of the findings. This may involve conducting multiple interviews or qualitative observations , using multiple sources of data, and taking detailed field notes.
- Ethical Considerations: Adhere to ethical guidelines and obtain informed consent from participants. Protect the privacy, confidentiality, and anonymity of participants and ensure their voluntary participation throughout the qualitative research process.
- Data Analysis: Utilize systematic and rigorous approaches to analyze qualitative research data. This may involve coding, categorizing, and identifying patterns or themes within the data. Software tools like NVivo or ATLAS.ti can assist in organizing and analyzing large datasets.
- Triangulation: Enhance the validity and reliability of the findings by employing triangulation. Triangulation involves using multiple data sources, methods, or researchers to corroborate and validate the results, reducing the impact of researcher bias.
- Member Checking: Share the preliminary findings with participants to verify the accuracy and interpretation of their data. Member checking allows participants to provide feedback and corrections, enhancing the trustworthiness of the research.
- Reflexive Journaling: Maintain a reflexive journal throughout the research process to record reflections, insights, and decisions made during data collection and analysis. This journal can serve as a valuable tool for ensuring transparency and traceability in the research process.
- Clear and Transparent Reporting: Present the research findings in a clear, coherent, and transparent manner. Clearly describe the research methodology, data collection, and analysis processes. Provide rich and thick descriptions of the findings, supported by direct quotations and examples from the data.
By following these best practices, qualitative researchers can enhance the rigor, credibility, and trustworthiness of their research, leading to valuable and meaningful insights into the complex phenomena under investigation.
Learn more: What is Customer Experience (CX) Research?
Enhance Your Research
Collect feedback and conduct research with IdeaScale’s award-winning software
Elevate Research And Feedback With Your IdeaScale Community!
IdeaScale is an innovation management solution that inspires people to take action on their ideas. Your community’s ideas can change lives, your business and the world. Connect to the ideas that matter and start co-creating the future.
Copyright © 2024 IdeaScale
Privacy Overview

Qualitative Research Using R: A Systematic Approach pp 1–19 Cite as
Qualitative Research: An Overview
- Yanto Chandra 3 &
- Liang Shang 4
- First Online: 24 April 2019
3670 Accesses
5 Citations
Qualitative research is one of the most commonly used types of research and methodology in the social sciences. Unfortunately, qualitative research is commonly misunderstood. In this chapter, we describe and explain the misconceptions surrounding qualitative research enterprise, why researchers need to care about when using qualitative research, the characteristics of qualitative research, and review the paradigms in qualitative research.
- Qualitative research
- Gioia approach
- Yin-Eisenhardt approach
- Langley approach
- Interpretivism
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Qualitative research is defined as the practice used to study things –– individuals and organizations and their reasons, opinions, and motivations, beliefs in their natural settings. It involves an observer (a researcher) who is located in the field , who transforms the world into a series of representations such as fieldnotes, interviews, conversations, photographs, recordings and memos (Denzin and Lincoln 2011 ). Many researchers employ qualitative research for exploratory purpose while others use it for ‘quasi’ theory testing approach. Qualitative research is a broad umbrella of research methodologies that encompasses grounded theory (Glaser and Strauss 2017 ; Strauss and Corbin 1990 ), case study (Flyvbjerg 2006 ; Yin 2003 ), phenomenology (Sanders 1982 ), discourse analysis (Fairclough 2003 ; Wodak and Meyer 2009 ), ethnography (Geertz 1973 ; Garfinkel 1967 ), and netnography (Kozinets 2002 ), among others. Qualitative research is often synonymous with ‘case study research’ because ‘case study’ primarily uses (but not always) qualitative data.
The quality standards or evaluation criteria of qualitative research comprises: (1) credibility (that a researcher can provide confidence in his/her findings), (2) transferability (that results are more plausible when transported to a highly similar contexts), (3) dependability (that errors have been minimized, proper documentation is provided), and (4) confirmability (that conclusions are internally consistent and supported by data) (see Lincoln and Guba 1985 ).
We classify research into a continuum of theory building — > theory elaboration — > theory testing . Theory building is also known as theory exploration. Theory elaboration refers to the use of qualitative data and a method to seek “confirmation” of the relationships among variables or processes or mechanisms of a social reality (Bartunek and Rynes 2015 ).
In the context of qualitative research, theory/ies usually refer(s) to conceptual model(s) or framework(s) that explain the relationships among a set of variables or processes that explain a social phenomenon. Theory or theories could also refer to general ideas or frameworks (e.g., institutional theory, emancipation theory, or identity theory) that are reviewed as background knowledge prior to the commencement of a qualitative research project.
For example, a qualitative research can ask the following question: “How can institutional change succeed in social contexts that are dominated by organized crime?” (Vaccaro and Palazzo 2015 ).
We have witnessed numerous cases in which committed positivist methodologists were asked to review qualitative papers, and they used a survey approach to assess the quality of an interpretivist work. This reviewers’ fallacy is dangerous and hampers the progress of a field of research. Editors must be cognizant of such fallacy and avoid it.
A social enterprises (SE) is an organization that combines social welfare and commercial logics (Doherty et al. 2014 ), or that uses business principles to address social problems (Mair and Marti 2006 ); thus, qualitative research that reports that ‘social impact’ is important for SEs is too descriptive and, arguably, tautological. It is not uncommon to see authors submitting purely descriptive papers to scholarly journals.
Some qualitative researchers have conducted qualitative work using primarily a checklist (ticking the boxes) to show the presence or absence of variables, as if it were a survey-based study. This is utterly inappropriate for a qualitative work. A qualitative work needs to show the richness and depth of qualitative findings. Nevertheless, it is acceptable to use such checklists as supplementary data if a study involves too many informants or variables of interest, or the data is too complex due to its longitudinal nature (e.g., a study that involves 15 cases observed and involving 59 interviews with 33 informants within a 7-year fieldwork used an excel sheet to tabulate the number of events that occurred as supplementary data to the main analysis; see Chandra 2017a , b ).
As mentioned earlier, there are different types of qualitative research. Thus, a qualitative researcher will customize the data collection process to fit the type of research being conducted. For example, for researchers using ethnography, the primary data will be in the form of photos and/or videos and interviews; for those using netnography, the primary data will be internet-based textual data. Interview data is perhaps the most common type of data used across all types of qualitative research designs and is often synonymous with qualitative research.
The purpose of qualitative research is to provide an explanation , not merely a description and certainly not a prediction (which is the realm of quantitative research). However, description is needed to illustrate qualitative data collected, and usually researchers describe their qualitative data by inserting a number of important “informant quotes” in the body of a qualitative research report.
We advise qualitative researchers to adhere to one approach to avoid any epistemological and ontological mismatch that may arise among different camps in qualitative research. For instance, mixing a positivist with a constructivist approach in qualitative research frequently leads to unnecessary criticism and even rejection from journal editors and reviewers; it shows a lack of methodological competence or awareness of one’s epistemological position.
Analytical generalization is not generalization to some defined population that has been sampled, but to a “theory” of the phenomenon being studied, a theory that may have much wider applicability than the particular case studied (Yin 2003 ).
There are different types of contributions. Typically, a researcher is expected to clearly articulate the theoretical contributions for a qualitative work submitted to a scholarly journal. Other types of contributions are practical (or managerial ), common for business/management journals, and policy , common for policy related journals.
There is ongoing debate on whether a template for qualitative research is desirable or necessary, with one camp of scholars (the pluralistic critical realists) that advocates a pluralistic approaches to qualitative research (“qualitative research should not follow a particular template or be prescriptive in its process”) and the other camps are advocating for some form of consensus via the use of particular approaches (e.g., the Eisenhardt or Gioia Approach, etc.). However, as shown in Table 1.1 , even the pluralistic critical realism in itself is a template and advocates an alternative form of consensus through the use of diverse and pluralistic approaches in doing qualitative research.
Alvesson, M., & Kärreman, D. (2007). Constructing mystery: Empirical matters in theory development. Academy of Management Review, 32 (4), 1265–1281.
Article Google Scholar
Bartunek, J. M., & Rynes, S. L. (2015). Qualitative research: It just keeps getting more interesting! In Handbook of qualitative organizational research (pp. 41–55). New York: Routledge.
Google Scholar
Brinkmann, S. (2018). Philosophies of qualitative research . New York: Oxford University Press.
Bucher, S., & Langley, A. (2016). The interplay of reflective and experimental spaces in interrupting and reorienting routine dynamics. Organization Science, 27 (3), 594–613.
Chandra, Y. (2017a). A time-based process model of international entrepreneurial opportunity evaluation. Journal of International Business Studies, 48 (4), 423–451.
Chandra, Y. (2017b). Social entrepreneurship as emancipatory work. Journal of Business Venturing, 32 (6), 657–673.
Corley, K. G., & Gioia, D. A. (2004). Identity ambiguity and change in the wake of a corporate spin-off. Administrative Science Quarterly, 49 (2), 173–208.
Cornelissen, J. P. (2017). Preserving theoretical divergence in management research: Why the explanatory potential of qualitative research should be harnessed rather than suppressed. Journal of Management Studies, 54 (3), 368–383.
Denis, J. L., Lamothe, L., & Langley, A. (2001). The dynamics of collective leadership and strategic change in pluralistic organizations. Academy of Management Journal, 44 (4), 809–837.
Denzin, N. K., & Lincoln, Y. S. (2011). Introduction. In N. K. Denzin & Y. S. Lincoln (Eds.), The Sage handbook of qualitative research (4th ed.). Thousand Oaks: Sage.
Doherty, B., Haugh, H., & Lyon, F. (2014). Social enterprises as hybrid organizations: A review and research agenda. International Journal of Management Reviews, 16 (4), 417–436.
Dubé, L., & Paré, G. (2003). Rigor in information systems positivist case research: Current practices, trends, and recommendations. MIS Quarterly, 27 (4), 597–636.
Easton, G. (2010). Critical realism in case study research. Industrial Marketing Management, 39 (1), 118–128.
Eisenhardt, K. M. (1989a). Building theories from case study research. Academy of Management Review, 14 (4), 532–550.
Eisenhardt, K. M. (1989b). Making fast strategic decisions in high-velocity environments. Academy of Management Journal, 32 (3), 543–576.
Fairclough, N. (2003). Analysing discourse: Textual analysis for social research . Abingdon: Routledge.
Book Google Scholar
Flyvbjerg, B. (2006). Five misunderstandings about case-study research. Qualitative Inquiry, 12 (2), 219–245.
Friese, S. (2011). Using ATLAS.ti for analyzing the financial crisis data [67 paragraphs]. Forum Qualitative Sozialforschung/Forum: Qualitative Social Research, 12 (1), Art. 39. http://nbn-resolving.de/urn:nbn:de:0114-fqs1101397
Garfinkel, H. (1967). Studies in ethnomethodology . Malden: Blackwell Publishers.
Geertz, C. (1973). Interpretation of cultures . New York: Basic Books.
Gehman, J., Glaser, V. L., Eisenhardt, K. M., Gioia, D., Langley, A., & Corley, K. G. (2017). Finding theory–method fit: A comparison of three qualitative approaches to theory building. Journal of Management Inquiry, 27 , 284–300. in press.
Gioia, D. A. (1992). Pinto fires and personal ethics: A script analysis of missed opportunities. Journal of Business Ethics, 11 (5–6), 379–389.
Gioia, D. A. (2007). Individual epistemology – Interpretive wisdom. In E. H. Kessler & J. R. Bailey (Eds.), The handbook of organizational and managerial wisdom (pp. 277–294). Thousand Oaks: Sage.
Chapter Google Scholar
Gioia, D. (2019). If I had a magic wand: Reflections on developing a systematic approach to qualitative research. In B. Boyd, R. Crook, J. Le, & A. Smith (Eds.), Research methodology in strategy and management . https://books.emeraldinsight.com/page/detail/Standing-on-the-Shoulders-of-Giants/?k=9781787563360
Gioia, D. A., & Chittipeddi, K. (1991). Sensemaking and sensegiving in strategic change initiation. Strategic Management Journal, 12 (6), 433–448.
Gioia, D. A., Price, K. N., Hamilton, A. L., & Thomas, J. B. (2010). Forging an identity: An insider-outsider study of processes involved in the formation of organizational identity. Administrative Science Quarterly, 55 (1), 1–46.
Gioia, D. A., Corley, K. G., & Hamilton, A. L. (2013). Seeking qualitative rigor in inductive research: Notes on the Gioia methodology. Organizational Research Methods, 16 (1), 15–31.
Glaser, B. G., & Strauss, A. L. (2017). Discovery of grounded theory: Strategies for qualitative research . New York: Routledge.
Graebner, M. E., & Eisenhardt, K. M. (2004). The seller’s side of the story: Acquisition as courtship and governance as syndicate in entrepreneurial firms. Administrative Science Quarterly, 49 (3), 366–403.
Grayson, K., & Shulman, D. (2000). Indexicality and the verification function of irreplaceable possessions: A semiotic analysis. Journal of Consumer Research, 27 (1), 17–30.
Hunt, S. D. (1991). Positivism and paradigm dominance in consumer research: Toward critical pluralism and rapprochement. Journal of Consumer Research, 18 (1), 32–44.
King, G., Keohane, R. O., & Verba, S. (1994). Designing social inquiry: Scientific inference in qualitative research . Princeton: Princeton University Press.
Kozinets, R. V. (2002). The field behind the screen: Using netnography for marketing research in online communities. Journal of Marketing Research, 39 (1), 61–72.
Langley, A. (1988). The roles of formal strategic planning. Long Range Planning, 21 (3), 40–50.
Langley, A., & Abdallah, C. (2011). Templates and turns in qualitative studies of strategy and management. In Building methodological bridges (pp. 201–235). Bingley: Emerald Group Publishing Limited.
Langley, A., Golden-Biddle, K., Reay, T., Denis, J. L., Hébert, Y., Lamothe, L., & Gervais, J. (2012). Identity struggles in merging organizations: Renegotiating the sameness–difference dialectic. The Journal of Applied Behavioral Science, 48 (2), 135–167.
Langley, A. N. N., Smallman, C., Tsoukas, H., & Van de Ven, A. H. (2013). Process studies of change in organization and management: Unveiling temporality, activity, and flow. Academy of Management Journal, 56 (1), 1–13.
Lin, A. C. (1998). Bridging positivist and interpretivist approaches to qualitative methods. Policy Studies Journal, 26 (1), 162–180.
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry . Beverly Hills: Sage.
Mair, J., & Marti, I. (2006). Social entrepreneurship research: A source of explanation, prediction, and delight. Journal of World Business, 41 (1), 36–44.
Nag, R., Corley, K. G., & Gioia, D. A. (2007). The intersection of organizational identity, knowledge, and practice: Attempting strategic change via knowledge grafting. Academy of Management Journal, 50 (4), 821–847.
Ozcan, P., & Eisenhardt, K. M. (2009). Origin of alliance portfolios: Entrepreneurs, network strategies, and firm performance. Academy of Management Journal, 52 (2), 246–279.
Prasad, P. (2018). Crafting qualitative research: Beyond positivist traditions . New York: Taylor & Francis.
Pratt, M. G. (2009). From the editors: For the lack of a boilerplate: Tips on writing up (and reviewing) qualitative research. Academy of Management Journal, 52 (5), 856–862.
Ramoglou, S., & Tsang, E. W. (2016). A realist perspective of entrepreneurship: Opportunities as propensities. Academy of Management Review, 41 (3), 410–434.
Sanders, P. (1982). Phenomenology: A new way of viewing organizational research. Academy of Management Review, 7 (3), 353–360.
Sobh, R., & Perry, C. (2006). Research design and data analysis in realism research. European Journal of Marketing, 40 (11/12), 1194–1209.
Stake, R. E. (2010). Qualitative research: Studying how things work . New York: Guilford Press.
Strauss, A., & Corbin, J. M. (1990). Basics of qualitative research: Grounded theory procedures and techniques . Thousand Oaks: Sage.
Vaccaro, A., & Palazzo, G. (2015). Values against violence: Institutional change in societies dominated by organized crime. Academy of Management Journal, 58 (4), 1075–1101.
Weick, K. E. (1989). Theory construction as disciplined imagination. Academy of Management Review, 14 (4), 516–531.
Welch, C. L., Welch, D. E., & Hewerdine, L. (2008). Gender and export behaviour: Evidence from women-owned enterprises. Journal of Business Ethics, 83 (1), 113–126.
Welch, C., Piekkari, R., Plakoyiannaki, E., & Paavilainen-Mäntymäki, E. (2011). Theorising from case studies: Towards a pluralist future for international business research. Journal of International Business Studies, 42 (5), 740–762.
Wodak, R., & Meyer, M. (Eds.). (2009). Methods for critical discourse analysis . London: Sage.
Yin, R. K. (1981). Life histories of innovations: How new practices become routinized. Public Administration Review, 41 , 21–28.
Yin, R. (2003). Case study research: Design and methods . Thousand Oaks: Sage.
Young, R. A., & Collin, A. (2004). Introduction: Constructivism and social constructionism in the career field. Journal of Vocational Behavior, 64 (3), 373–388.
Download references
Author information
Authors and affiliations.
The Hong Kong Polytechnic University, Hong Kong, Kowloon, Hong Kong
Yanto Chandra
City University of Hong Kong, Hong Kong, Kowloon, Hong Kong
Liang Shang
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter.
Chandra, Y., Shang, L. (2019). Qualitative Research: An Overview. In: Qualitative Research Using R: A Systematic Approach. Springer, Singapore. https://doi.org/10.1007/978-981-13-3170-1_1
Download citation
DOI : https://doi.org/10.1007/978-981-13-3170-1_1
Published : 24 April 2019
Publisher Name : Springer, Singapore
Print ISBN : 978-981-13-3169-5
Online ISBN : 978-981-13-3170-1
eBook Packages : Social Sciences Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An Overview of Qualitative Research Methods
Direct Observation, Interviews, Participation, Immersion, Focus Groups
- Research, Samples, and Statistics
- Key Concepts
- Major Sociologists
- News & Issues
- Recommended Reading
- Archaeology
Qualitative research is a type of social science research that collects and works with non-numerical data and that seeks to interpret meaning from these data that help understand social life through the study of targeted populations or places.
People often frame it in opposition to quantitative research , which uses numerical data to identify large-scale trends and employs statistical operations to determine causal and correlative relationships between variables.
Within sociology, qualitative research is typically focused on the micro-level of social interaction that composes everyday life, whereas quantitative research typically focuses on macro-level trends and phenomena.
Key Takeaways
Methods of qualitative research include:
- observation and immersion
- open-ended surveys
- focus groups
- content analysis of visual and textual materials
- oral history
Qualitative research has a long history in sociology and has been used within it for as long as the field has existed.
This type of research has long appealed to social scientists because it allows the researchers to investigate the meanings people attribute to their behavior, actions, and interactions with others.
While quantitative research is useful for identifying relationships between variables, like, for example, the connection between poverty and racial hate, it is qualitative research that can illuminate why this connection exists by going directly to the source—the people themselves.
Qualitative research is designed to reveal the meaning that informs the action or outcomes that are typically measured by quantitative research. So qualitative researchers investigate meanings, interpretations, symbols, and the processes and relations of social life.
What this type of research produces is descriptive data that the researcher must then interpret using rigorous and systematic methods of transcribing, coding, and analysis of trends and themes.
Because its focus is everyday life and people's experiences, qualitative research lends itself well to creating new theories using the inductive method , which can then be tested with further research.
Qualitative researchers use their own eyes, ears, and intelligence to collect in-depth perceptions and descriptions of targeted populations, places, and events.
Their findings are collected through a variety of methods, and often a researcher will use at least two or several of the following while conducting a qualitative study:
- Direct observation : With direct observation, a researcher studies people as they go about their daily lives without participating or interfering. This type of research is often unknown to those under study, and as such, must be conducted in public settings where people do not have a reasonable expectation of privacy. For example, a researcher might observe the ways in which strangers interact in public as they gather to watch a street performer.
- Open-ended surveys : While many surveys are designed to generate quantitative data, many are also designed with open-ended questions that allow for the generation and analysis of qualitative data. For example, a survey might be used to investigate not just which political candidates voters chose, but why they chose them, in their own words.
- Focus group : In a focus group, a researcher engages a small group of participants in a conversation designed to generate data relevant to the research question. Focus groups can contain anywhere from 5 to 15 participants. Social scientists often use them in studies that examine an event or trend that occurs within a specific community. They are common in market research, too.
- In-depth interviews : Researchers conduct in-depth interviews by speaking with participants in a one-on-one setting. Sometimes a researcher approaches the interview with a predetermined list of questions or topics for discussion but allows the conversation to evolve based on how the participant responds. Other times, the researcher has identified certain topics of interest but does not have a formal guide for the conversation, but allows the participant to guide it.
- Oral history : The oral history method is used to create a historical account of an event, group, or community, and typically involves a series of in-depth interviews conducted with one or multiple participants over an extended period.
- Participant observation : This method is similar to observation, however with this one, the researcher also participates in the action or events to not only observe others but to gain the first-hand experience in the setting.
- Ethnographic observation : Ethnographic observation is the most intensive and in-depth observational method. Originating in anthropology, with this method, a researcher fully immerses themselves into the research setting and lives among the participants as one of them for anywhere from months to years. By doing this, the researcher attempts to experience day-to-day existence from the viewpoints of those studied to develop in-depth and long-term accounts of the community, events, or trends under observation.
- Content analysis : This method is used by sociologists to analyze social life by interpreting words and images from documents, film, art, music, and other cultural products and media. The researchers look at how the words and images are used, and the context in which they are used to draw inferences about the underlying culture. Content analysis of digital material, especially that generated by social media users, has become a popular technique within the social sciences.
While much of the data generated by qualitative research is coded and analyzed using just the researcher's eyes and brain, the use of computer software to do these processes is increasingly popular within the social sciences.
Such software analysis works well when the data is too large for humans to handle, though the lack of a human interpreter is a common criticism of the use of computer software.
Pros and Cons
Qualitative research has both benefits and drawbacks.
On the plus side, it creates an in-depth understanding of the attitudes, behaviors, interactions, events, and social processes that comprise everyday life. In doing so, it helps social scientists understand how everyday life is influenced by society-wide things like social structure , social order , and all kinds of social forces.
This set of methods also has the benefit of being flexible and easily adaptable to changes in the research environment and can be conducted with minimal cost in many cases.
Among the downsides of qualitative research is that its scope is fairly limited so its findings are not always widely able to be generalized.
Researchers also have to use caution with these methods to ensure that they do not influence the data in ways that significantly change it and that they do not bring undue personal bias to their interpretation of the findings.
Fortunately, qualitative researchers receive rigorous training designed to eliminate or reduce these types of research bias.
- Definition of Idiographic and Nomothetic
- Pilot Study in Research
- Social Surveys: Questionnaires, Interviews, and Telephone Polls
- Definition and Overview of Grounded Theory
- A Review of Software Tools for Quantitative Data Analysis
- Macro- and Microsociology
- The Difference Between Descriptive and Inferential Statistics
- How to Conduct a Sociology Research Interview
- Understanding Path Analysis
- Understanding Purposive Sampling
- The Different Types of Sampling Designs in Sociology
- 3 Surveys for Student Feedback to Improve Instruction
- Probability and Chance
- Definition of Aggregate and Social Aggregate
- Scientific Method Lesson Plan
- Definition of a Hypothesis
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Methodology
- What Is Qualitative Research? | Methods & Examples
What Is Qualitative Research? | Methods & Examples
Published on 4 April 2022 by Pritha Bhandari . Revised on 30 January 2023.
Qualitative research involves collecting and analysing non-numerical data (e.g., text, video, or audio) to understand concepts, opinions, or experiences. It can be used to gather in-depth insights into a problem or generate new ideas for research.
Qualitative research is the opposite of quantitative research , which involves collecting and analysing numerical data for statistical analysis.
Qualitative research is commonly used in the humanities and social sciences, in subjects such as anthropology, sociology, education, health sciences, and history.
- How does social media shape body image in teenagers?
- How do children and adults interpret healthy eating in the UK?
- What factors influence employee retention in a large organisation?
- How is anxiety experienced around the world?
- How can teachers integrate social issues into science curriculums?
Table of contents
Approaches to qualitative research, qualitative research methods, qualitative data analysis, advantages of qualitative research, disadvantages of qualitative research, frequently asked questions about qualitative research.
Qualitative research is used to understand how people experience the world. While there are many approaches to qualitative research, they tend to be flexible and focus on retaining rich meaning when interpreting data.
Common approaches include grounded theory, ethnography, action research, phenomenological research, and narrative research. They share some similarities, but emphasise different aims and perspectives.
Prevent plagiarism, run a free check.
Each of the research approaches involve using one or more data collection methods . These are some of the most common qualitative methods:
- Observations: recording what you have seen, heard, or encountered in detailed field notes.
- Interviews: personally asking people questions in one-on-one conversations.
- Focus groups: asking questions and generating discussion among a group of people.
- Surveys : distributing questionnaires with open-ended questions.
- Secondary research: collecting existing data in the form of texts, images, audio or video recordings, etc.
- You take field notes with observations and reflect on your own experiences of the company culture.
- You distribute open-ended surveys to employees across all the company’s offices by email to find out if the culture varies across locations.
- You conduct in-depth interviews with employees in your office to learn about their experiences and perspectives in greater detail.
Qualitative researchers often consider themselves ‘instruments’ in research because all observations, interpretations and analyses are filtered through their own personal lens.
For this reason, when writing up your methodology for qualitative research, it’s important to reflect on your approach and to thoroughly explain the choices you made in collecting and analysing the data.
Qualitative data can take the form of texts, photos, videos and audio. For example, you might be working with interview transcripts, survey responses, fieldnotes, or recordings from natural settings.
Most types of qualitative data analysis share the same five steps:
- Prepare and organise your data. This may mean transcribing interviews or typing up fieldnotes.
- Review and explore your data. Examine the data for patterns or repeated ideas that emerge.
- Develop a data coding system. Based on your initial ideas, establish a set of codes that you can apply to categorise your data.
- Assign codes to the data. For example, in qualitative survey analysis, this may mean going through each participant’s responses and tagging them with codes in a spreadsheet. As you go through your data, you can create new codes to add to your system if necessary.
- Identify recurring themes. Link codes together into cohesive, overarching themes.
There are several specific approaches to analysing qualitative data. Although these methods share similar processes, they emphasise different concepts.
Qualitative research often tries to preserve the voice and perspective of participants and can be adjusted as new research questions arise. Qualitative research is good for:
- Flexibility
The data collection and analysis process can be adapted as new ideas or patterns emerge. They are not rigidly decided beforehand.
- Natural settings
Data collection occurs in real-world contexts or in naturalistic ways.
- Meaningful insights
Detailed descriptions of people’s experiences, feelings and perceptions can be used in designing, testing or improving systems or products.
- Generation of new ideas
Open-ended responses mean that researchers can uncover novel problems or opportunities that they wouldn’t have thought of otherwise.
Researchers must consider practical and theoretical limitations in analysing and interpreting their data. Qualitative research suffers from:
- Unreliability
The real-world setting often makes qualitative research unreliable because of uncontrolled factors that affect the data.
- Subjectivity
Due to the researcher’s primary role in analysing and interpreting data, qualitative research cannot be replicated . The researcher decides what is important and what is irrelevant in data analysis, so interpretations of the same data can vary greatly.
- Limited generalisability
Small samples are often used to gather detailed data about specific contexts. Despite rigorous analysis procedures, it is difficult to draw generalisable conclusions because the data may be biased and unrepresentative of the wider population .
- Labour-intensive
Although software can be used to manage and record large amounts of text, data analysis often has to be checked or performed manually.
Quantitative research deals with numbers and statistics, while qualitative research deals with words and meanings.
Quantitative methods allow you to test a hypothesis by systematically collecting and analysing data, while qualitative methods allow you to explore ideas and experiences in depth.
There are five common approaches to qualitative research :
- Grounded theory involves collecting data in order to develop new theories.
- Ethnography involves immersing yourself in a group or organisation to understand its culture.
- Narrative research involves interpreting stories to understand how people make sense of their experiences and perceptions.
- Phenomenological research involves investigating phenomena through people’s lived experiences.
- Action research links theory and practice in several cycles to drive innovative changes.
Data collection is the systematic process by which observations or measurements are gathered in research. It is used in many different contexts by academics, governments, businesses, and other organisations.
There are various approaches to qualitative data analysis , but they all share five steps in common:
- Prepare and organise your data.
- Review and explore your data.
- Develop a data coding system.
- Assign codes to the data.
- Identify recurring themes.
The specifics of each step depend on the focus of the analysis. Some common approaches include textual analysis , thematic analysis , and discourse analysis .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
Bhandari, P. (2023, January 30). What Is Qualitative Research? | Methods & Examples. Scribbr. Retrieved 25 March 2024, from https://www.scribbr.co.uk/research-methods/introduction-to-qualitative-research/
Is this article helpful?

Pritha Bhandari
- Skip to main content
- Skip to primary sidebar
- Skip to footer
- QuestionPro

- Solutions Industries Gaming Automotive Sports and events Education Government Travel & Hospitality Financial Services Healthcare Cannabis Technology Use Case NPS+ Communities Audience Contactless surveys Mobile LivePolls Member Experience GDPR Positive People Science 360 Feedback Surveys
- Resources Blog eBooks Survey Templates Case Studies Training Help center
Home Market Research
Qualitative Research Methods: Types, Analysis + Examples

Qualitative research is based on the disciplines of social sciences like psychology, sociology, and anthropology. Therefore, the qualitative research methods allow for in-depth and further probing and questioning of respondents based on their responses. The interviewer/researcher also tries to understand their motivation and feelings. Understanding how your audience makes decisions can help derive conclusions in market research.
What is qualitative research?
Qualitative research is defined as a market research method that focuses on obtaining data through open-ended and conversational communication .
This method is about “what” people think and “why” they think so. For example, consider a convenience store looking to improve its patronage. A systematic observation concludes that more men are visiting this store. One good method to determine why women were not visiting the store is conducting an in-depth interview method with potential customers.
For example, after successfully interviewing female customers and visiting nearby stores and malls, the researchers selected participants through random sampling . As a result, it was discovered that the store didn’t have enough items for women.
So fewer women were visiting the store, which was understood only by personally interacting with them and understanding why they didn’t visit the store because there were more male products than female ones.
Gather research insights
Types of qualitative research methods with examples
Qualitative research methods are designed in a manner that helps reveal the behavior and perception of a target audience with reference to a particular topic. There are different types of qualitative research methods, such as in-depth interviews, focus groups, ethnographic research, content analysis, and case study research that are usually used.
The results of qualitative methods are more descriptive, and the inferences can be drawn quite easily from the obtained data .
Qualitative research methods originated in the social and behavioral research sciences. Today, our world is more complicated, and it is difficult to understand what people think and perceive. Online research methods make it easier to understand that as it is a more communicative and descriptive analysis .
The following are the qualitative research methods that are frequently used. Also, read about qualitative research examples :
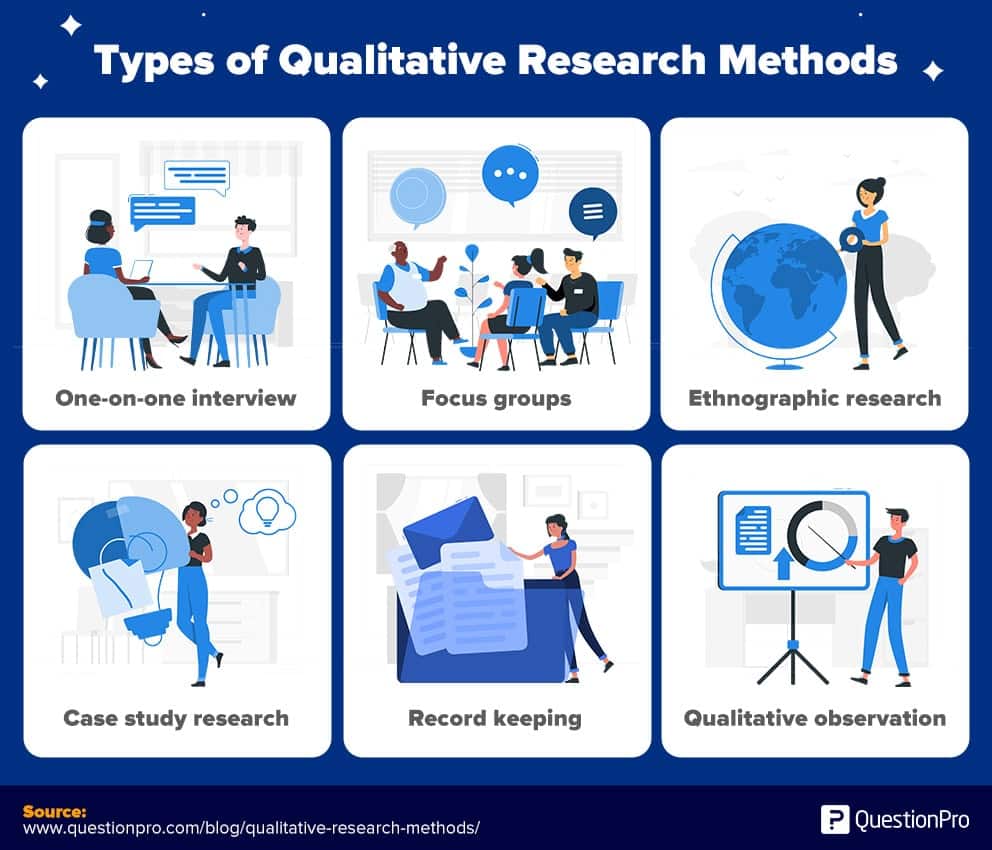
1. One-on-one interview
Conducting in-depth interviews is one of the most common qualitative research methods. It is a personal interview that is carried out with one respondent at a time. This is purely a conversational method and invites opportunities to get details in depth from the respondent.
One of the advantages of this method is that it provides a great opportunity to gather precise data about what people believe and their motivations . If the researcher is well experienced, asking the right questions can help him/her collect meaningful data. If they should need more information, the researchers should ask such follow-up questions that will help them collect more information.
These interviews can be performed face-to-face or on the phone and usually can last between half an hour to two hours or even more. When the in-depth interview is conducted face to face, it gives a better opportunity to read the respondents’ body language and match the responses.
2. Focus groups
A focus group is also a commonly used qualitative research method used in data collection. A focus group usually includes a limited number of respondents (6-10) from within your target market.
The main aim of the focus group is to find answers to the “why, ” “what,” and “how” questions. One advantage of focus groups is you don’t necessarily need to interact with the group in person. Nowadays, focus groups can be sent an online survey on various devices, and responses can be collected at the click of a button.
Focus groups are an expensive method as compared to other online qualitative research methods. Typically, they are used to explain complex processes. This method is very useful for market research on new products and testing new concepts.
3. Ethnographic research
Ethnographic research is the most in-depth observational research method that studies people in their naturally occurring environment.
This method requires the researchers to adapt to the target audiences’ environments, which could be anywhere from an organization to a city or any remote location. Here, geographical constraints can be an issue while collecting data.
This research design aims to understand the cultures, challenges, motivations, and settings that occur. Instead of relying on interviews and discussions, you experience the natural settings firsthand.
This type of research method can last from a few days to a few years, as it involves in-depth observation and collecting data on those grounds. It’s a challenging and time-consuming method and solely depends on the researcher’s expertise to analyze, observe, and infer the data.
4. Case study research
T he case study method has evolved over the past few years and developed into a valuable quality research method. As the name suggests, it is used for explaining an organization or an entity.
This type of research method is used within a number of areas like education, social sciences, and similar. This method may look difficult to operate; however , it is one of the simplest ways of conducting research as it involves a deep dive and thorough understanding of the data collection methods and inferring the data.
5. Record keeping
This method makes use of the already existing reliable documents and similar sources of information as the data source. This data can be used in new research. This is similar to going to a library. There, one can go over books and other reference material to collect relevant data that can likely be used in the research.
6. Process of observation
Qualitative Observation is a process of research that uses subjective methodologies to gather systematic information or data. Since the focus on qualitative observation is the research process of using subjective methodologies to gather information or data. Qualitative observation is primarily used to equate quality differences.
Qualitative observation deals with the 5 major sensory organs and their functioning – sight, smell, touch, taste, and hearing. This doesn’t involve measurements or numbers but instead characteristics.
Explore Insightfully Contextual Inquiry in Qualitative Research
Qualitative research: data collection and analysis
A. qualitative data collection.
Qualitative data collection allows collecting data that is non-numeric and helps us to explore how decisions are made and provide us with detailed insight. For reaching such conclusions the data that is collected should be holistic, rich, and nuanced and findings to emerge through careful analysis.
- Whatever method a researcher chooses for collecting qualitative data, one aspect is very clear the process will generate a large amount of data. In addition to the variety of methods available, there are also different methods of collecting and recording the data.
For example, if the qualitative data is collected through a focus group or one-to-one discussion, there will be handwritten notes or video recorded tapes. If there are recording they should be transcribed and before the process of data analysis can begin.
- As a rough guide, it can take a seasoned researcher 8-10 hours to transcribe the recordings of an interview, which can generate roughly 20-30 pages of dialogues. Many researchers also like to maintain separate folders to maintain the recording collected from the different focus group. This helps them compartmentalize the data collected.
- In case there are running notes taken, which are also known as field notes, they are helpful in maintaining comments, environmental contexts, environmental analysis , nonverbal cues etc. These filed notes are helpful and can be compared while transcribing audio recorded data. Such notes are usually informal but should be secured in a similar manner as the video recordings or the audio tapes.
B. Qualitative data analysis
Qualitative data analysis such as notes, videos, audio recordings images, and text documents. One of the most used methods for qualitative data analysis is text analysis.
Text analysis is a data analysis method that is distinctly different from all other qualitative research methods, where researchers analyze the social life of the participants in the research study and decode the words, actions, etc.
There are images also that are used in this research study and the researchers analyze the context in which the images are used and draw inferences from them. In the last decade, text analysis through what is shared on social media platforms has gained supreme popularity.
Characteristics of qualitative research methods
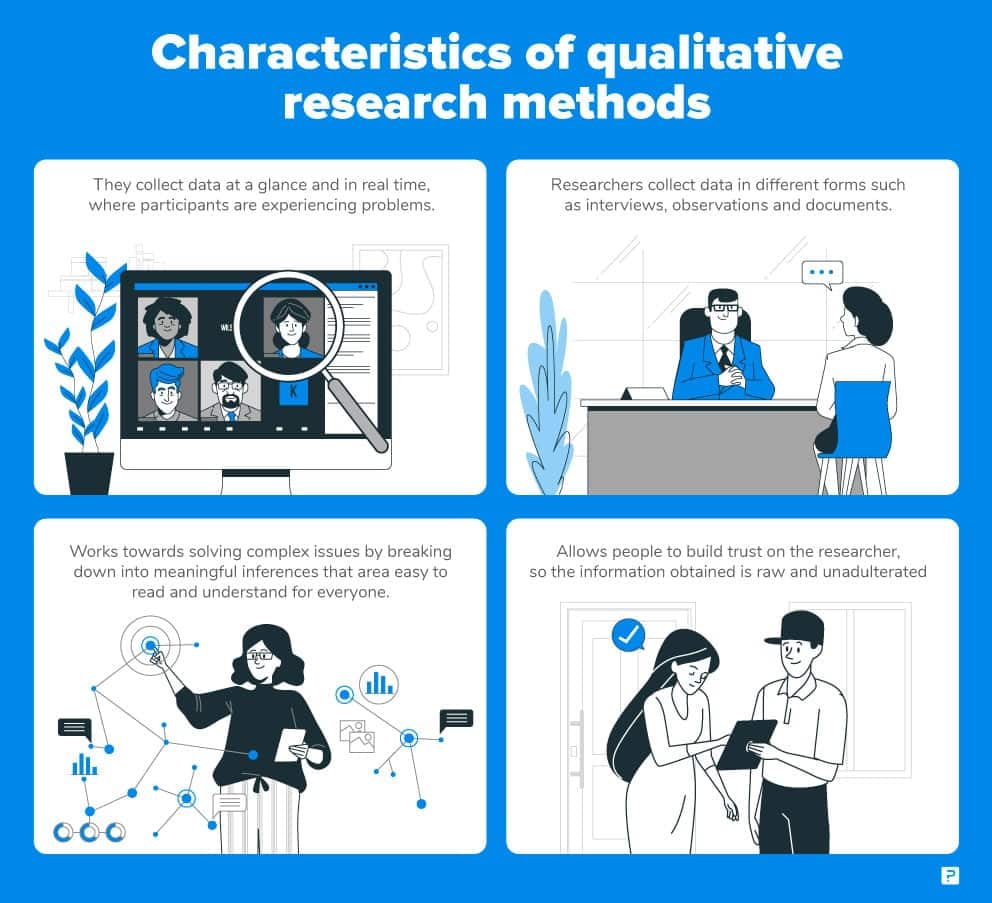
- Qualitative research methods usually collect data at the sight, where the participants are experiencing issues or research problems . These are real-time data and rarely bring the participants out of the geographic locations to collect information.
- Qualitative researchers typically gather multiple forms of data, such as interviews, observations, and documents, rather than rely on a single data source .
- This type of research method works towards solving complex issues by breaking down into meaningful inferences, that is easily readable and understood by all.
- Since it’s a more communicative method, people can build their trust on the researcher and the information thus obtained is raw and unadulterated.
Qualitative research method case study
Let’s take the example of a bookstore owner who is looking for ways to improve their sales and customer outreach. An online community of members who were loyal patrons of the bookstore were interviewed and related questions were asked and the questions were answered by them.
At the end of the interview, it was realized that most of the books in the stores were suitable for adults and there were not enough options for children or teenagers.
By conducting this qualitative research the bookstore owner realized what the shortcomings were and what were the feelings of the readers. Through this research now the bookstore owner can now keep books for different age categories and can improve his sales and customer outreach.
Such qualitative research method examples can serve as the basis to indulge in further quantitative research , which provides remedies.
When to use qualitative research
Researchers make use of qualitative research techniques when they need to capture accurate, in-depth insights. It is very useful to capture “factual data”. Here are some examples of when to use qualitative research.
- Developing a new product or generating an idea.
- Studying your product/brand or service to strengthen your marketing strategy.
- To understand your strengths and weaknesses.
- Understanding purchase behavior.
- To study the reactions of your audience to marketing campaigns and other communications.
- Exploring market demographics, segments, and customer care groups.
- Gathering perception data of a brand, company, or product.
LEARN ABOUT: Steps in Qualitative Research
Qualitative research methods vs quantitative research methods
The basic differences between qualitative research methods and quantitative research methods are simple and straightforward. They differ in:
- Their analytical objectives
- Types of questions asked
- Types of data collection instruments
- Forms of data they produce
- Degree of flexibility
LEARN MORE ABOUR OUR SOFTWARE FREE TRIAL
MORE LIKE THIS

Resident Experience: What It Is and How to Improve It
Mar 27, 2024

11 Best Employee Onboarding and Training Software in 2024
Top 11 Team Engagement Software in 2024
8 Leading Brand Health Tracker to Track Your Brand Reputation
Mar 26, 2024
Other categories
- Academic Research
- Artificial Intelligence
- Assessments
- Brand Awareness
- Case Studies
- Communities
- Consumer Insights
- Customer effort score
- Customer Engagement
- Customer Experience
- Customer Loyalty
- Customer Research
- Customer Satisfaction
- Employee Benefits
- Employee Engagement
- Employee Retention
- Friday Five
- General Data Protection Regulation
- Insights Hub
- Life@QuestionPro
- Market Research
- Mobile diaries
- Mobile Surveys
- New Features
- Online Communities
- Question Types
- Questionnaire
- QuestionPro Products
- Release Notes
- Research Tools and Apps
- Revenue at Risk
- Survey Templates
- Training Tips
- Uncategorized
- Video Learning Series
- What’s Coming Up
- Workforce Intelligence
- Open access
- Published: 27 May 2020
How to use and assess qualitative research methods
- Loraine Busetto ORCID: orcid.org/0000-0002-9228-7875 1 ,
- Wolfgang Wick 1 , 2 &
- Christoph Gumbinger 1
Neurological Research and Practice volume 2 , Article number: 14 ( 2020 ) Cite this article
686k Accesses
268 Citations
89 Altmetric
Metrics details
This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions, and focussing on intervention improvement. The most common methods of data collection are document study, (non-) participant observations, semi-structured interviews and focus groups. For data analysis, field-notes and audio-recordings are transcribed into protocols and transcripts, and coded using qualitative data management software. Criteria such as checklists, reflexivity, sampling strategies, piloting, co-coding, member-checking and stakeholder involvement can be used to enhance and assess the quality of the research conducted. Using qualitative in addition to quantitative designs will equip us with better tools to address a greater range of research problems, and to fill in blind spots in current neurological research and practice.
The aim of this paper is to provide an overview of qualitative research methods, including hands-on information on how they can be used, reported and assessed. This article is intended for beginning qualitative researchers in the health sciences as well as experienced quantitative researchers who wish to broaden their understanding of qualitative research.
What is qualitative research?
Qualitative research is defined as “the study of the nature of phenomena”, including “their quality, different manifestations, the context in which they appear or the perspectives from which they can be perceived” , but excluding “their range, frequency and place in an objectively determined chain of cause and effect” [ 1 ]. This formal definition can be complemented with a more pragmatic rule of thumb: qualitative research generally includes data in form of words rather than numbers [ 2 ].
Why conduct qualitative research?
Because some research questions cannot be answered using (only) quantitative methods. For example, one Australian study addressed the issue of why patients from Aboriginal communities often present late or not at all to specialist services offered by tertiary care hospitals. Using qualitative interviews with patients and staff, it found one of the most significant access barriers to be transportation problems, including some towns and communities simply not having a bus service to the hospital [ 3 ]. A quantitative study could have measured the number of patients over time or even looked at possible explanatory factors – but only those previously known or suspected to be of relevance. To discover reasons for observed patterns, especially the invisible or surprising ones, qualitative designs are needed.
While qualitative research is common in other fields, it is still relatively underrepresented in health services research. The latter field is more traditionally rooted in the evidence-based-medicine paradigm, as seen in " research that involves testing the effectiveness of various strategies to achieve changes in clinical practice, preferably applying randomised controlled trial study designs (...) " [ 4 ]. This focus on quantitative research and specifically randomised controlled trials (RCT) is visible in the idea of a hierarchy of research evidence which assumes that some research designs are objectively better than others, and that choosing a "lesser" design is only acceptable when the better ones are not practically or ethically feasible [ 5 , 6 ]. Others, however, argue that an objective hierarchy does not exist, and that, instead, the research design and methods should be chosen to fit the specific research question at hand – "questions before methods" [ 2 , 7 , 8 , 9 ]. This means that even when an RCT is possible, some research problems require a different design that is better suited to addressing them. Arguing in JAMA, Berwick uses the example of rapid response teams in hospitals, which he describes as " a complex, multicomponent intervention – essentially a process of social change" susceptible to a range of different context factors including leadership or organisation history. According to him, "[in] such complex terrain, the RCT is an impoverished way to learn. Critics who use it as a truth standard in this context are incorrect" [ 8 ] . Instead of limiting oneself to RCTs, Berwick recommends embracing a wider range of methods , including qualitative ones, which for "these specific applications, (...) are not compromises in learning how to improve; they are superior" [ 8 ].
Research problems that can be approached particularly well using qualitative methods include assessing complex multi-component interventions or systems (of change), addressing questions beyond “what works”, towards “what works for whom when, how and why”, and focussing on intervention improvement rather than accreditation [ 7 , 9 , 10 , 11 , 12 ]. Using qualitative methods can also help shed light on the “softer” side of medical treatment. For example, while quantitative trials can measure the costs and benefits of neuro-oncological treatment in terms of survival rates or adverse effects, qualitative research can help provide a better understanding of patient or caregiver stress, visibility of illness or out-of-pocket expenses.
How to conduct qualitative research?
Given that qualitative research is characterised by flexibility, openness and responsivity to context, the steps of data collection and analysis are not as separate and consecutive as they tend to be in quantitative research [ 13 , 14 ]. As Fossey puts it : “sampling, data collection, analysis and interpretation are related to each other in a cyclical (iterative) manner, rather than following one after another in a stepwise approach” [ 15 ]. The researcher can make educated decisions with regard to the choice of method, how they are implemented, and to which and how many units they are applied [ 13 ]. As shown in Fig. 1 , this can involve several back-and-forth steps between data collection and analysis where new insights and experiences can lead to adaption and expansion of the original plan. Some insights may also necessitate a revision of the research question and/or the research design as a whole. The process ends when saturation is achieved, i.e. when no relevant new information can be found (see also below: sampling and saturation). For reasons of transparency, it is essential for all decisions as well as the underlying reasoning to be well-documented.
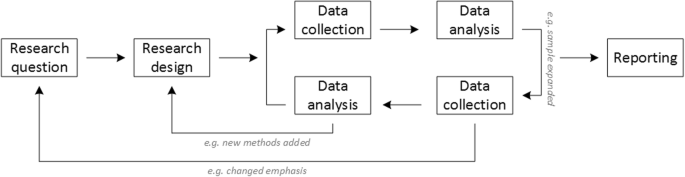
Iterative research process
While it is not always explicitly addressed, qualitative methods reflect a different underlying research paradigm than quantitative research (e.g. constructivism or interpretivism as opposed to positivism). The choice of methods can be based on the respective underlying substantive theory or theoretical framework used by the researcher [ 2 ].
Data collection
The methods of qualitative data collection most commonly used in health research are document study, observations, semi-structured interviews and focus groups [ 1 , 14 , 16 , 17 ].
Document study
Document study (also called document analysis) refers to the review by the researcher of written materials [ 14 ]. These can include personal and non-personal documents such as archives, annual reports, guidelines, policy documents, diaries or letters.
Observations
Observations are particularly useful to gain insights into a certain setting and actual behaviour – as opposed to reported behaviour or opinions [ 13 ]. Qualitative observations can be either participant or non-participant in nature. In participant observations, the observer is part of the observed setting, for example a nurse working in an intensive care unit [ 18 ]. In non-participant observations, the observer is “on the outside looking in”, i.e. present in but not part of the situation, trying not to influence the setting by their presence. Observations can be planned (e.g. for 3 h during the day or night shift) or ad hoc (e.g. as soon as a stroke patient arrives at the emergency room). During the observation, the observer takes notes on everything or certain pre-determined parts of what is happening around them, for example focusing on physician-patient interactions or communication between different professional groups. Written notes can be taken during or after the observations, depending on feasibility (which is usually lower during participant observations) and acceptability (e.g. when the observer is perceived to be judging the observed). Afterwards, these field notes are transcribed into observation protocols. If more than one observer was involved, field notes are taken independently, but notes can be consolidated into one protocol after discussions. Advantages of conducting observations include minimising the distance between the researcher and the researched, the potential discovery of topics that the researcher did not realise were relevant and gaining deeper insights into the real-world dimensions of the research problem at hand [ 18 ].
Semi-structured interviews
Hijmans & Kuyper describe qualitative interviews as “an exchange with an informal character, a conversation with a goal” [ 19 ]. Interviews are used to gain insights into a person’s subjective experiences, opinions and motivations – as opposed to facts or behaviours [ 13 ]. Interviews can be distinguished by the degree to which they are structured (i.e. a questionnaire), open (e.g. free conversation or autobiographical interviews) or semi-structured [ 2 , 13 ]. Semi-structured interviews are characterized by open-ended questions and the use of an interview guide (or topic guide/list) in which the broad areas of interest, sometimes including sub-questions, are defined [ 19 ]. The pre-defined topics in the interview guide can be derived from the literature, previous research or a preliminary method of data collection, e.g. document study or observations. The topic list is usually adapted and improved at the start of the data collection process as the interviewer learns more about the field [ 20 ]. Across interviews the focus on the different (blocks of) questions may differ and some questions may be skipped altogether (e.g. if the interviewee is not able or willing to answer the questions or for concerns about the total length of the interview) [ 20 ]. Qualitative interviews are usually not conducted in written format as it impedes on the interactive component of the method [ 20 ]. In comparison to written surveys, qualitative interviews have the advantage of being interactive and allowing for unexpected topics to emerge and to be taken up by the researcher. This can also help overcome a provider or researcher-centred bias often found in written surveys, which by nature, can only measure what is already known or expected to be of relevance to the researcher. Interviews can be audio- or video-taped; but sometimes it is only feasible or acceptable for the interviewer to take written notes [ 14 , 16 , 20 ].
Focus groups
Focus groups are group interviews to explore participants’ expertise and experiences, including explorations of how and why people behave in certain ways [ 1 ]. Focus groups usually consist of 6–8 people and are led by an experienced moderator following a topic guide or “script” [ 21 ]. They can involve an observer who takes note of the non-verbal aspects of the situation, possibly using an observation guide [ 21 ]. Depending on researchers’ and participants’ preferences, the discussions can be audio- or video-taped and transcribed afterwards [ 21 ]. Focus groups are useful for bringing together homogeneous (to a lesser extent heterogeneous) groups of participants with relevant expertise and experience on a given topic on which they can share detailed information [ 21 ]. Focus groups are a relatively easy, fast and inexpensive method to gain access to information on interactions in a given group, i.e. “the sharing and comparing” among participants [ 21 ]. Disadvantages include less control over the process and a lesser extent to which each individual may participate. Moreover, focus group moderators need experience, as do those tasked with the analysis of the resulting data. Focus groups can be less appropriate for discussing sensitive topics that participants might be reluctant to disclose in a group setting [ 13 ]. Moreover, attention must be paid to the emergence of “groupthink” as well as possible power dynamics within the group, e.g. when patients are awed or intimidated by health professionals.
Choosing the “right” method
As explained above, the school of thought underlying qualitative research assumes no objective hierarchy of evidence and methods. This means that each choice of single or combined methods has to be based on the research question that needs to be answered and a critical assessment with regard to whether or to what extent the chosen method can accomplish this – i.e. the “fit” between question and method [ 14 ]. It is necessary for these decisions to be documented when they are being made, and to be critically discussed when reporting methods and results.
Let us assume that our research aim is to examine the (clinical) processes around acute endovascular treatment (EVT), from the patient’s arrival at the emergency room to recanalization, with the aim to identify possible causes for delay and/or other causes for sub-optimal treatment outcome. As a first step, we could conduct a document study of the relevant standard operating procedures (SOPs) for this phase of care – are they up-to-date and in line with current guidelines? Do they contain any mistakes, irregularities or uncertainties that could cause delays or other problems? Regardless of the answers to these questions, the results have to be interpreted based on what they are: a written outline of what care processes in this hospital should look like. If we want to know what they actually look like in practice, we can conduct observations of the processes described in the SOPs. These results can (and should) be analysed in themselves, but also in comparison to the results of the document analysis, especially as regards relevant discrepancies. Do the SOPs outline specific tests for which no equipment can be observed or tasks to be performed by specialized nurses who are not present during the observation? It might also be possible that the written SOP is outdated, but the actual care provided is in line with current best practice. In order to find out why these discrepancies exist, it can be useful to conduct interviews. Are the physicians simply not aware of the SOPs (because their existence is limited to the hospital’s intranet) or do they actively disagree with them or does the infrastructure make it impossible to provide the care as described? Another rationale for adding interviews is that some situations (or all of their possible variations for different patient groups or the day, night or weekend shift) cannot practically or ethically be observed. In this case, it is possible to ask those involved to report on their actions – being aware that this is not the same as the actual observation. A senior physician’s or hospital manager’s description of certain situations might differ from a nurse’s or junior physician’s one, maybe because they intentionally misrepresent facts or maybe because different aspects of the process are visible or important to them. In some cases, it can also be relevant to consider to whom the interviewee is disclosing this information – someone they trust, someone they are otherwise not connected to, or someone they suspect or are aware of being in a potentially “dangerous” power relationship to them. Lastly, a focus group could be conducted with representatives of the relevant professional groups to explore how and why exactly they provide care around EVT. The discussion might reveal discrepancies (between SOPs and actual care or between different physicians) and motivations to the researchers as well as to the focus group members that they might not have been aware of themselves. For the focus group to deliver relevant information, attention has to be paid to its composition and conduct, for example, to make sure that all participants feel safe to disclose sensitive or potentially problematic information or that the discussion is not dominated by (senior) physicians only. The resulting combination of data collection methods is shown in Fig. 2 .
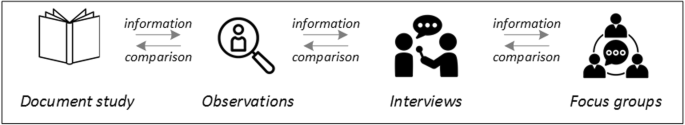
Possible combination of data collection methods
Attributions for icons: “Book” by Serhii Smirnov, “Interview” by Adrien Coquet, FR, “Magnifying Glass” by anggun, ID, “Business communication” by Vectors Market; all from the Noun Project
The combination of multiple data source as described for this example can be referred to as “triangulation”, in which multiple measurements are carried out from different angles to achieve a more comprehensive understanding of the phenomenon under study [ 22 , 23 ].
Data analysis
To analyse the data collected through observations, interviews and focus groups these need to be transcribed into protocols and transcripts (see Fig. 3 ). Interviews and focus groups can be transcribed verbatim , with or without annotations for behaviour (e.g. laughing, crying, pausing) and with or without phonetic transcription of dialects and filler words, depending on what is expected or known to be relevant for the analysis. In the next step, the protocols and transcripts are coded , that is, marked (or tagged, labelled) with one or more short descriptors of the content of a sentence or paragraph [ 2 , 15 , 23 ]. Jansen describes coding as “connecting the raw data with “theoretical” terms” [ 20 ]. In a more practical sense, coding makes raw data sortable. This makes it possible to extract and examine all segments describing, say, a tele-neurology consultation from multiple data sources (e.g. SOPs, emergency room observations, staff and patient interview). In a process of synthesis and abstraction, the codes are then grouped, summarised and/or categorised [ 15 , 20 ]. The end product of the coding or analysis process is a descriptive theory of the behavioural pattern under investigation [ 20 ]. The coding process is performed using qualitative data management software, the most common ones being InVivo, MaxQDA and Atlas.ti. It should be noted that these are data management tools which support the analysis performed by the researcher(s) [ 14 ].
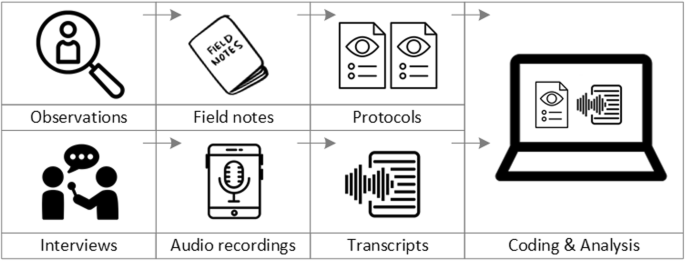
From data collection to data analysis
Attributions for icons: see Fig. 2 , also “Speech to text” by Trevor Dsouza, “Field Notes” by Mike O’Brien, US, “Voice Record” by ProSymbols, US, “Inspection” by Made, AU, and “Cloud” by Graphic Tigers; all from the Noun Project
How to report qualitative research?
Protocols of qualitative research can be published separately and in advance of the study results. However, the aim is not the same as in RCT protocols, i.e. to pre-define and set in stone the research questions and primary or secondary endpoints. Rather, it is a way to describe the research methods in detail, which might not be possible in the results paper given journals’ word limits. Qualitative research papers are usually longer than their quantitative counterparts to allow for deep understanding and so-called “thick description”. In the methods section, the focus is on transparency of the methods used, including why, how and by whom they were implemented in the specific study setting, so as to enable a discussion of whether and how this may have influenced data collection, analysis and interpretation. The results section usually starts with a paragraph outlining the main findings, followed by more detailed descriptions of, for example, the commonalities, discrepancies or exceptions per category [ 20 ]. Here it is important to support main findings by relevant quotations, which may add information, context, emphasis or real-life examples [ 20 , 23 ]. It is subject to debate in the field whether it is relevant to state the exact number or percentage of respondents supporting a certain statement (e.g. “Five interviewees expressed negative feelings towards XYZ”) [ 21 ].
How to combine qualitative with quantitative research?
Qualitative methods can be combined with other methods in multi- or mixed methods designs, which “[employ] two or more different methods [ …] within the same study or research program rather than confining the research to one single method” [ 24 ]. Reasons for combining methods can be diverse, including triangulation for corroboration of findings, complementarity for illustration and clarification of results, expansion to extend the breadth and range of the study, explanation of (unexpected) results generated with one method with the help of another, or offsetting the weakness of one method with the strength of another [ 1 , 17 , 24 , 25 , 26 ]. The resulting designs can be classified according to when, why and how the different quantitative and/or qualitative data strands are combined. The three most common types of mixed method designs are the convergent parallel design , the explanatory sequential design and the exploratory sequential design. The designs with examples are shown in Fig. 4 .
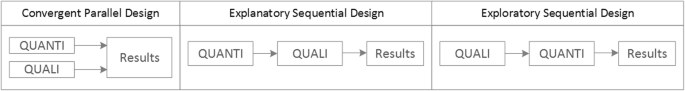
Three common mixed methods designs
In the convergent parallel design, a qualitative study is conducted in parallel to and independently of a quantitative study, and the results of both studies are compared and combined at the stage of interpretation of results. Using the above example of EVT provision, this could entail setting up a quantitative EVT registry to measure process times and patient outcomes in parallel to conducting the qualitative research outlined above, and then comparing results. Amongst other things, this would make it possible to assess whether interview respondents’ subjective impressions of patients receiving good care match modified Rankin Scores at follow-up, or whether observed delays in care provision are exceptions or the rule when compared to door-to-needle times as documented in the registry. In the explanatory sequential design, a quantitative study is carried out first, followed by a qualitative study to help explain the results from the quantitative study. This would be an appropriate design if the registry alone had revealed relevant delays in door-to-needle times and the qualitative study would be used to understand where and why these occurred, and how they could be improved. In the exploratory design, the qualitative study is carried out first and its results help informing and building the quantitative study in the next step [ 26 ]. If the qualitative study around EVT provision had shown a high level of dissatisfaction among the staff members involved, a quantitative questionnaire investigating staff satisfaction could be set up in the next step, informed by the qualitative study on which topics dissatisfaction had been expressed. Amongst other things, the questionnaire design would make it possible to widen the reach of the research to more respondents from different (types of) hospitals, regions, countries or settings, and to conduct sub-group analyses for different professional groups.
How to assess qualitative research?
A variety of assessment criteria and lists have been developed for qualitative research, ranging in their focus and comprehensiveness [ 14 , 17 , 27 ]. However, none of these has been elevated to the “gold standard” in the field. In the following, we therefore focus on a set of commonly used assessment criteria that, from a practical standpoint, a researcher can look for when assessing a qualitative research report or paper.
Assessors should check the authors’ use of and adherence to the relevant reporting checklists (e.g. Standards for Reporting Qualitative Research (SRQR)) to make sure all items that are relevant for this type of research are addressed [ 23 , 28 ]. Discussions of quantitative measures in addition to or instead of these qualitative measures can be a sign of lower quality of the research (paper). Providing and adhering to a checklist for qualitative research contributes to an important quality criterion for qualitative research, namely transparency [ 15 , 17 , 23 ].
Reflexivity
While methodological transparency and complete reporting is relevant for all types of research, some additional criteria must be taken into account for qualitative research. This includes what is called reflexivity, i.e. sensitivity to the relationship between the researcher and the researched, including how contact was established and maintained, or the background and experience of the researcher(s) involved in data collection and analysis. Depending on the research question and population to be researched this can be limited to professional experience, but it may also include gender, age or ethnicity [ 17 , 27 ]. These details are relevant because in qualitative research, as opposed to quantitative research, the researcher as a person cannot be isolated from the research process [ 23 ]. It may influence the conversation when an interviewed patient speaks to an interviewer who is a physician, or when an interviewee is asked to discuss a gynaecological procedure with a male interviewer, and therefore the reader must be made aware of these details [ 19 ].

Sampling and saturation
The aim of qualitative sampling is for all variants of the objects of observation that are deemed relevant for the study to be present in the sample “ to see the issue and its meanings from as many angles as possible” [ 1 , 16 , 19 , 20 , 27 ] , and to ensure “information-richness [ 15 ]. An iterative sampling approach is advised, in which data collection (e.g. five interviews) is followed by data analysis, followed by more data collection to find variants that are lacking in the current sample. This process continues until no new (relevant) information can be found and further sampling becomes redundant – which is called saturation [ 1 , 15 ] . In other words: qualitative data collection finds its end point not a priori , but when the research team determines that saturation has been reached [ 29 , 30 ].
This is also the reason why most qualitative studies use deliberate instead of random sampling strategies. This is generally referred to as “ purposive sampling” , in which researchers pre-define which types of participants or cases they need to include so as to cover all variations that are expected to be of relevance, based on the literature, previous experience or theory (i.e. theoretical sampling) [ 14 , 20 ]. Other types of purposive sampling include (but are not limited to) maximum variation sampling, critical case sampling or extreme or deviant case sampling [ 2 ]. In the above EVT example, a purposive sample could include all relevant professional groups and/or all relevant stakeholders (patients, relatives) and/or all relevant times of observation (day, night and weekend shift).
Assessors of qualitative research should check whether the considerations underlying the sampling strategy were sound and whether or how researchers tried to adapt and improve their strategies in stepwise or cyclical approaches between data collection and analysis to achieve saturation [ 14 ].
Good qualitative research is iterative in nature, i.e. it goes back and forth between data collection and analysis, revising and improving the approach where necessary. One example of this are pilot interviews, where different aspects of the interview (especially the interview guide, but also, for example, the site of the interview or whether the interview can be audio-recorded) are tested with a small number of respondents, evaluated and revised [ 19 ]. In doing so, the interviewer learns which wording or types of questions work best, or which is the best length of an interview with patients who have trouble concentrating for an extended time. Of course, the same reasoning applies to observations or focus groups which can also be piloted.
Ideally, coding should be performed by at least two researchers, especially at the beginning of the coding process when a common approach must be defined, including the establishment of a useful coding list (or tree), and when a common meaning of individual codes must be established [ 23 ]. An initial sub-set or all transcripts can be coded independently by the coders and then compared and consolidated after regular discussions in the research team. This is to make sure that codes are applied consistently to the research data.
Member checking
Member checking, also called respondent validation , refers to the practice of checking back with study respondents to see if the research is in line with their views [ 14 , 27 ]. This can happen after data collection or analysis or when first results are available [ 23 ]. For example, interviewees can be provided with (summaries of) their transcripts and asked whether they believe this to be a complete representation of their views or whether they would like to clarify or elaborate on their responses [ 17 ]. Respondents’ feedback on these issues then becomes part of the data collection and analysis [ 27 ].
Stakeholder involvement
In those niches where qualitative approaches have been able to evolve and grow, a new trend has seen the inclusion of patients and their representatives not only as study participants (i.e. “members”, see above) but as consultants to and active participants in the broader research process [ 31 , 32 , 33 ]. The underlying assumption is that patients and other stakeholders hold unique perspectives and experiences that add value beyond their own single story, making the research more relevant and beneficial to researchers, study participants and (future) patients alike [ 34 , 35 ]. Using the example of patients on or nearing dialysis, a recent scoping review found that 80% of clinical research did not address the top 10 research priorities identified by patients and caregivers [ 32 , 36 ]. In this sense, the involvement of the relevant stakeholders, especially patients and relatives, is increasingly being seen as a quality indicator in and of itself.
How not to assess qualitative research
The above overview does not include certain items that are routine in assessments of quantitative research. What follows is a non-exhaustive, non-representative, experience-based list of the quantitative criteria often applied to the assessment of qualitative research, as well as an explanation of the limited usefulness of these endeavours.
Protocol adherence
Given the openness and flexibility of qualitative research, it should not be assessed by how well it adheres to pre-determined and fixed strategies – in other words: its rigidity. Instead, the assessor should look for signs of adaptation and refinement based on lessons learned from earlier steps in the research process.
Sample size
For the reasons explained above, qualitative research does not require specific sample sizes, nor does it require that the sample size be determined a priori [ 1 , 14 , 27 , 37 , 38 , 39 ]. Sample size can only be a useful quality indicator when related to the research purpose, the chosen methodology and the composition of the sample, i.e. who was included and why.
Randomisation
While some authors argue that randomisation can be used in qualitative research, this is not commonly the case, as neither its feasibility nor its necessity or usefulness has been convincingly established for qualitative research [ 13 , 27 ]. Relevant disadvantages include the negative impact of a too large sample size as well as the possibility (or probability) of selecting “ quiet, uncooperative or inarticulate individuals ” [ 17 ]. Qualitative studies do not use control groups, either.
Interrater reliability, variability and other “objectivity checks”
The concept of “interrater reliability” is sometimes used in qualitative research to assess to which extent the coding approach overlaps between the two co-coders. However, it is not clear what this measure tells us about the quality of the analysis [ 23 ]. This means that these scores can be included in qualitative research reports, preferably with some additional information on what the score means for the analysis, but it is not a requirement. Relatedly, it is not relevant for the quality or “objectivity” of qualitative research to separate those who recruited the study participants and collected and analysed the data. Experiences even show that it might be better to have the same person or team perform all of these tasks [ 20 ]. First, when researchers introduce themselves during recruitment this can enhance trust when the interview takes place days or weeks later with the same researcher. Second, when the audio-recording is transcribed for analysis, the researcher conducting the interviews will usually remember the interviewee and the specific interview situation during data analysis. This might be helpful in providing additional context information for interpretation of data, e.g. on whether something might have been meant as a joke [ 18 ].
Not being quantitative research
Being qualitative research instead of quantitative research should not be used as an assessment criterion if it is used irrespectively of the research problem at hand. Similarly, qualitative research should not be required to be combined with quantitative research per se – unless mixed methods research is judged as inherently better than single-method research. In this case, the same criterion should be applied for quantitative studies without a qualitative component.
The main take-away points of this paper are summarised in Table 1 . We aimed to show that, if conducted well, qualitative research can answer specific research questions that cannot to be adequately answered using (only) quantitative designs. Seeing qualitative and quantitative methods as equal will help us become more aware and critical of the “fit” between the research problem and our chosen methods: I can conduct an RCT to determine the reasons for transportation delays of acute stroke patients – but should I? It also provides us with a greater range of tools to tackle a greater range of research problems more appropriately and successfully, filling in the blind spots on one half of the methodological spectrum to better address the whole complexity of neurological research and practice.
Availability of data and materials
Not applicable.
Abbreviations
Endovascular treatment
Randomised Controlled Trial
Standard Operating Procedure
Standards for Reporting Qualitative Research
Philipsen, H., & Vernooij-Dassen, M. (2007). Kwalitatief onderzoek: nuttig, onmisbaar en uitdagend. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Qualitative research: useful, indispensable and challenging. In: Qualitative research: Practical methods for medical practice (pp. 5–12). Houten: Bohn Stafleu van Loghum.
Chapter Google Scholar
Punch, K. F. (2013). Introduction to social research: Quantitative and qualitative approaches . London: Sage.
Kelly, J., Dwyer, J., Willis, E., & Pekarsky, B. (2014). Travelling to the city for hospital care: Access factors in country aboriginal patient journeys. Australian Journal of Rural Health, 22 (3), 109–113.
Article Google Scholar
Nilsen, P., Ståhl, C., Roback, K., & Cairney, P. (2013). Never the twain shall meet? - a comparison of implementation science and policy implementation research. Implementation Science, 8 (1), 1–12.
Howick J, Chalmers I, Glasziou, P., Greenhalgh, T., Heneghan, C., Liberati, A., Moschetti, I., Phillips, B., & Thornton, H. (2011). The 2011 Oxford CEBM evidence levels of evidence (introductory document) . Oxford Center for Evidence Based Medicine. https://www.cebm.net/2011/06/2011-oxford-cebm-levels-evidence-introductory-document/ .
Eakin, J. M. (2016). Educating critical qualitative health researchers in the land of the randomized controlled trial. Qualitative Inquiry, 22 (2), 107–118.
May, A., & Mathijssen, J. (2015). Alternatieven voor RCT bij de evaluatie van effectiviteit van interventies!? Eindrapportage. In Alternatives for RCTs in the evaluation of effectiveness of interventions!? Final report .
Google Scholar
Berwick, D. M. (2008). The science of improvement. Journal of the American Medical Association, 299 (10), 1182–1184.
Article CAS Google Scholar
Christ, T. W. (2014). Scientific-based research and randomized controlled trials, the “gold” standard? Alternative paradigms and mixed methodologies. Qualitative Inquiry, 20 (1), 72–80.
Lamont, T., Barber, N., Jd, P., Fulop, N., Garfield-Birkbeck, S., Lilford, R., Mear, L., Raine, R., & Fitzpatrick, R. (2016). New approaches to evaluating complex health and care systems. BMJ, 352:i154.
Drabble, S. J., & O’Cathain, A. (2015). Moving from Randomized Controlled Trials to Mixed Methods Intervention Evaluation. In S. Hesse-Biber & R. B. Johnson (Eds.), The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry (pp. 406–425). London: Oxford University Press.
Chambers, D. A., Glasgow, R. E., & Stange, K. C. (2013). The dynamic sustainability framework: Addressing the paradox of sustainment amid ongoing change. Implementation Science : IS, 8 , 117.
Hak, T. (2007). Waarnemingsmethoden in kwalitatief onderzoek. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Observation methods in qualitative research] (pp. 13–25). Houten: Bohn Stafleu van Loghum.
Russell, C. K., & Gregory, D. M. (2003). Evaluation of qualitative research studies. Evidence Based Nursing, 6 (2), 36–40.
Fossey, E., Harvey, C., McDermott, F., & Davidson, L. (2002). Understanding and evaluating qualitative research. Australian and New Zealand Journal of Psychiatry, 36 , 717–732.
Yanow, D. (2000). Conducting interpretive policy analysis (Vol. 47). Thousand Oaks: Sage University Papers Series on Qualitative Research Methods.
Shenton, A. K. (2004). Strategies for ensuring trustworthiness in qualitative research projects. Education for Information, 22 , 63–75.
van der Geest, S. (2006). Participeren in ziekte en zorg: meer over kwalitatief onderzoek. Huisarts en Wetenschap, 49 (4), 283–287.
Hijmans, E., & Kuyper, M. (2007). Het halfopen interview als onderzoeksmethode. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [The half-open interview as research method (pp. 43–51). Houten: Bohn Stafleu van Loghum.
Jansen, H. (2007). Systematiek en toepassing van de kwalitatieve survey. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Systematics and implementation of the qualitative survey (pp. 27–41). Houten: Bohn Stafleu van Loghum.
Pv, R., & Peremans, L. (2007). Exploreren met focusgroepgesprekken: de ‘stem’ van de groep onder de loep. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Exploring with focus group conversations: the “voice” of the group under the magnifying glass (pp. 53–64). Houten: Bohn Stafleu van Loghum.
Carter, N., Bryant-Lukosius, D., DiCenso, A., Blythe, J., & Neville, A. J. (2014). The use of triangulation in qualitative research. Oncology Nursing Forum, 41 (5), 545–547.
Boeije H: Analyseren in kwalitatief onderzoek: Denken en doen, [Analysis in qualitative research: Thinking and doing] vol. Den Haag Boom Lemma uitgevers; 2012.
Hunter, A., & Brewer, J. (2015). Designing Multimethod Research. In S. Hesse-Biber & R. B. Johnson (Eds.), The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry (pp. 185–205). London: Oxford University Press.
Archibald, M. M., Radil, A. I., Zhang, X., & Hanson, W. E. (2015). Current mixed methods practices in qualitative research: A content analysis of leading journals. International Journal of Qualitative Methods, 14 (2), 5–33.
Creswell, J. W., & Plano Clark, V. L. (2011). Choosing a Mixed Methods Design. In Designing and Conducting Mixed Methods Research . Thousand Oaks: SAGE Publications.
Mays, N., & Pope, C. (2000). Assessing quality in qualitative research. BMJ, 320 (7226), 50–52.
O'Brien, B. C., Harris, I. B., Beckman, T. J., Reed, D. A., & Cook, D. A. (2014). Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine : Journal of the Association of American Medical Colleges, 89 (9), 1245–1251.
Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., Burroughs, H., & Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality and Quantity, 52 (4), 1893–1907.
Moser, A., & Korstjens, I. (2018). Series: Practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. European Journal of General Practice, 24 (1), 9–18.
Marlett, N., Shklarov, S., Marshall, D., Santana, M. J., & Wasylak, T. (2015). Building new roles and relationships in research: A model of patient engagement research. Quality of Life Research : an international journal of quality of life aspects of treatment, care and rehabilitation, 24 (5), 1057–1067.
Demian, M. N., Lam, N. N., Mac-Way, F., Sapir-Pichhadze, R., & Fernandez, N. (2017). Opportunities for engaging patients in kidney research. Canadian Journal of Kidney Health and Disease, 4 , 2054358117703070–2054358117703070.
Noyes, J., McLaughlin, L., Morgan, K., Roberts, A., Stephens, M., Bourne, J., Houlston, M., Houlston, J., Thomas, S., Rhys, R. G., et al. (2019). Designing a co-productive study to overcome known methodological challenges in organ donation research with bereaved family members. Health Expectations . 22(4):824–35.
Piil, K., Jarden, M., & Pii, K. H. (2019). Research agenda for life-threatening cancer. European Journal Cancer Care (Engl), 28 (1), e12935.
Hofmann, D., Ibrahim, F., Rose, D., Scott, D. L., Cope, A., Wykes, T., & Lempp, H. (2015). Expectations of new treatment in rheumatoid arthritis: Developing a patient-generated questionnaire. Health Expectations : an international journal of public participation in health care and health policy, 18 (5), 995–1008.
Jun, M., Manns, B., Laupacis, A., Manns, L., Rehal, B., Crowe, S., & Hemmelgarn, B. R. (2015). Assessing the extent to which current clinical research is consistent with patient priorities: A scoping review using a case study in patients on or nearing dialysis. Canadian Journal of Kidney Health and Disease, 2 , 35.
Elsie Baker, S., & Edwards, R. (2012). How many qualitative interviews is enough? In National Centre for Research Methods Review Paper . National Centre for Research Methods. http://eprints.ncrm.ac.uk/2273/4/how_many_interviews.pdf .
Sandelowski, M. (1995). Sample size in qualitative research. Research in Nursing & Health, 18 (2), 179–183.
Sim, J., Saunders, B., Waterfield, J., & Kingstone, T. (2018). Can sample size in qualitative research be determined a priori? International Journal of Social Research Methodology, 21 (5), 619–634.
Download references
Acknowledgements
no external funding.
Author information
Authors and affiliations.
Department of Neurology, Heidelberg University Hospital, Im Neuenheimer Feld 400, 69120, Heidelberg, Germany
Loraine Busetto, Wolfgang Wick & Christoph Gumbinger
Clinical Cooperation Unit Neuro-Oncology, German Cancer Research Center, Heidelberg, Germany
Wolfgang Wick
You can also search for this author in PubMed Google Scholar
Contributions
LB drafted the manuscript; WW and CG revised the manuscript; all authors approved the final versions.
Corresponding author
Correspondence to Loraine Busetto .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Busetto, L., Wick, W. & Gumbinger, C. How to use and assess qualitative research methods. Neurol. Res. Pract. 2 , 14 (2020). https://doi.org/10.1186/s42466-020-00059-z
Download citation
Received : 30 January 2020
Accepted : 22 April 2020
Published : 27 May 2020
DOI : https://doi.org/10.1186/s42466-020-00059-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative research
- Mixed methods
- Quality assessment
Neurological Research and Practice
ISSN: 2524-3489
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

Quantitative and Qualitative Research
- I NEED TO . . .
- What is Quantitative Research?
- What is Qualitative Research?
- Quantitative vs Qualitative
- Step 1: Accessing CINAHL
- Step 2: Create a Keyword Search
- Step 3: Create a Subject Heading Search
- Step 4: Repeat Steps 1-3 for Second Concept
- Step 5: Repeat Steps 1-3 for Quantitative Terms
- Step 6: Combining All Searches
- Step 7: Adding Limiters
- Step 8: Save Your Search!
- What Kind of Article is This?
- More Research Help This link opens in a new window
What is qualitative research?
Qualitative research is a process of naturalistic inquiry that seeks an in-depth understanding of social phenomena within their natural setting. It focuses on the "why" rather than the "what" of social phenomena and relies on the direct experiences of human beings as meaning-making agents in their every day lives. Rather than by logical and statistical procedures, qualitative researchers use multiple systems of inquiry for the study of human phenomena including biography, case study, historical analysis, discourse analysis, ethnography, grounded theory, and phenomenology.
University of Utah College of Nursing, (n.d.). What is qualitative research? [Guide] Retrieved from https://nursing.utah.edu/research/qualitative-research/what-is-qualitative-research.php#what
The following video will explain the fundamentals of qualitative research.
- << Previous: What is Quantitative Research?
- Next: Quantitative vs Qualitative >>
- Last Updated: Dec 8, 2023 10:05 PM
- URL: https://libguides.uta.edu/quantitative_and_qualitative_research
University of Texas Arlington Libraries 702 Planetarium Place · Arlington, TX 76019 · 817-272-3000
- Internet Privacy
- Accessibility
- Problems with a guide? Contact Us.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 41, Issue 4
- Perceived barriers and opportunities to improve working conditions and staff retention in emergency departments: a qualitative study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-3067-9416 Jo Daniels 1 , 2 ,
- http://orcid.org/0000-0002-8013-3297 Emilia Robinson 1 ,
- http://orcid.org/0000-0001-5686-5132 Elizabeth Jenkinson 3 ,
- http://orcid.org/0000-0002-2064-4618 Edward Carlton 4 , 5
- 1 Department of Psychology , University of Bath , Bath , UK
- 2 Psychology , North Bristol NHS Trust , Westbury on Trym , Bristol , UK
- 3 Department of Health and Social Sciences , University of the West of England , Bristol , UK
- 4 Emergency Department, Southmead Hospital , North Bristol NHS Trust , Westbury on Trym , UK
- 5 Bristol Medical School , University of Bristol , Bristol , UK
- Correspondence to Dr Jo Daniels, Department of Psychology, University of Bath, Bath, UK; j.daniels{at}bath.ac.uk
Background Staff retention in Emergency Medicine (EM) is at crisis level and could be attributed in some part to adverse working conditions. This study aimed to better understand current concerns relating to working conditions and working practices in Emergency Departments (EDs).
Methods A qualitative approach was taken, using focus groups with ED staff (doctors, nurses, advanced care practitioners) of all grades, seniority and professional backgrounds from across the UK. Snowball recruitment was undertaken using social media and Royal College of Emergency Medicine communication channels. Focus group interviews were conducted online and organised by profession. A semi-structured topic guide was used to explore difficulties in the work environment, impact of these difficulties, barriers and priorities for change. Data were analysed using a directive content analysis to identify common themes.
Results Of the 116 clinical staff who completed the eligibility and consent forms, 46 met criteria and consented, of those, 33 participants took part. Participants were predominantly white British (85%), females (73%) and doctors (61%). Four key themes were generated: ‘culture of blame and negativity’, ‘untenable working environments’, ‘compromised leadership’ and ‘striving for support’. Data pertaining to barriers and opportunities for change were identified as sub-themes. In particular, strong leadership emerged as a key driver of change across all aspects of working practices.
Conclusion This study identified four key themes related to workplace concerns and their associated barriers and opportunities for change. Culture, working environment and need for support echoed current narratives across healthcare settings. Leadership emerged more prominently than in prior studies as both a barrier and opportunity for well-being and retention in the EM workplace. Further work is needed to develop leadership skills early on in clinical training, ensure protected time to deliver the role, ongoing opportunities to refine leadership skills and a clear pathway to address higher levels of management.
- qualitative research
- staff support
Data availability statement
Data are available upon reasonable request. Requests go to the corresponding author - Jo Daniels ([email protected], University of Bath, UK). De-identified participant data can be made available upon reasonable request.
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/emermed-2023-213189
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Retention of staff in emergency medicine is at crisis level and has been a high priority area for over a decade.
Multiple guidelines have been published to outline improvements that need to be made to retain staff; however, little improvement has been seen on the ground in EDs.
Key factors such as staff burnout and poor working conditions are known to influence intention to leave; however, it is unclear why change has not taken place despite knowledge of these problems and existing guidelines seeking to address these issues.
WHAT THIS STUDY ADDS
This qualitative study assessed perceived barriers that may be inhibiting the implementation to working conditions and working practices in EDs.
Leadership is identified as an important driver of change in working practices and can play an important role in workplace well-being and retention.
Key recommendations for avenues of improvement are made, identifying key actions at government, professional, organisational and personal level.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This study identifies leadership as a key opportunity for change and as a result makes specific recommendations for policy and practice regarding leadership in emergency medicine.
Introduction
Emergency Medicine (EM) is facing a global staffing crisis. 1 Record numbers of staff continue to leave the UK NHS with EM the most affected specialty. 2 EM reports the highest work intensity of all medical specialties, 3 with ‘intensity’ recognised as one of the leading factors in job dissatisfaction, attrition and career burnout. 3–5 These factors are amplified in an already stretched workforce. 2 Psychological well-being of the EM workforce is compromised, with working conditions recognised as playing a key role. 6 7 Staff attrition has a systemic impact: lower staff ratios lead to higher workloads, reduced quality of care, 8 higher levels of medical errors 9 and poorer staff well-being, 10 all factors associated with staff absence and intention to leave. 11 The landscape of EM has also changed; increased prevalence of high patient acuity, multimorbidity and an ageing population all bear considerable impact.
Key sector stakeholder initiatives and policy recommendations relating to retention and well-being 12–14 are largely generic and forfeit relevance to the specialty due to the lack of specificity to the clinical context within which these guidelines need to be implemented. Retention improvement programmes suggest approaches should be tailored per organisation, 12 however, this assumes that the challenges faced by staff across specialities and disciplines are homogeneous. In a specialty which reports the highest pressured environment, highest attrition and rates of burnout, 15 considerations of workplace context and specificity of policy recommendations are likely to be crucial. Interventions or initiatives must take account of the unique demands of the EM working environment, and how feasible it is to implement recommendations.
The James Lind Alliance (JLA) priority setting partnership in EM 16 identified initiatives to improve staff retention as research priorities in 2017 and again in the 2022 JLA refresh, 17 signalling the need for further research in this area due to a deepening workforce crisis. Current guidelines and initiatives target working conditions which are known to be associated with retention; however, these initiatives have been poorly implemented or enforced, with few formal evaluations of such interventions. 5 Moreover, current research is limited to the perspectives of specific professional groups and most are survey-based studies. 18
In order to better address current working conditions, with a view to improving retention, this research was aimed at determining practical barriers and opportunities for change in the ED working environment as perceived by professional staff working in this environment. This will tooffer insight into the shared experiences, constraints and priorities of those working within the ED.
Enhanced understanding of these issues can provide a firm basis from which to shape, inform and underpin future policies and workplace initiatives, ensuring that practical barriers and opportunities for change are embedded in a way that optimises relevance and feasibility of implementation in the ED working environment.
Study aims and objectives
This study sought to engage three core professional groups (doctors, nurses, advanced care practitioners; ACPs) who work within an EM context to better understand (a) primary concerns relating to working conditions; (b) perceived barriers to implementing change and (c) perceived opportunities and targets for change. Findings will be used to underpin key recommendations that are tailored to the needs of an over-burdened and under-resourced ED.
This qualitative study forms part of a larger collaborative project between the University of Bath and the Royal College of Emergency Medicine (RCEM), funded by a UKRI Policy Fund. The full recommendations relating to the four core themes are available on the RCEM website (Psychologically Informed Practice and Policy (PIPP) | RCEM).
Methodology
This study uses a qualitative approach involving online focus groups in order to gain a rich and detailed understanding of participant perspectives and views, unrestricted by closed question responses. Focus groups offer the opportunity to gain an understanding of shared experiences and narratives, using a dynamic approach to the subject matter, allowing further probing for clarification and participant interaction for deeper insights. The COVID Clinicians Cohort (CoCCo) study 19 was used to organise data into key categories; this model mirrors Maslow’s Hierarchy of Needs 20 from a workplace perspective.
Participants
To be eligible for participation, ED staff must have been currently employed in a UK NHS ED as either a doctor, nurse or ACP.
ACPs are a recently developed workforce of accredited clinicians who have received advanced training to expand the scope of their usual role (eg, paramedic, nurse), permitting them to take on additional clinical responsibility in the ED.
These three groups are core affiliates of the RCEM and represent the majority of the workforce in the ED. The ED setting was used as the focus (rather than all acute care settings) as this represents the core and central setting for EM.
Recruitment and procedure
Online adverts and qualtrics survey links were distributed through social media (ie, Twitter) and RCEM communication channels using snowball recruitment methods. Profession-specific focus group interviews were conducted online using MS teams by two study researchers (JD, ER) using a semi-structured topic guide (see online supplemental materials ). The guide was shaped by the scope of study aims and the current evidence base and explored difficulties in the work environment, impact of these difficulties, barriers and priorities for change. Focus groups were 60–90 min in duration and were recorded using encrypted audio recorders, transcribed and stored securely. Participants were given debrief information sheets following the focus group. Transcripts were not returned to participants and no repeat focus groups were carried out.
Supplemental material
Directive content analysis was applied to the data. 21 This analysis strategy was used to identify common themes from participant responses, using deductive codes by identifying key concepts from existing theory 19 and prior research. Two researchers (ER, JD) read through each transcript, highlighting passages that could be categorised in the pre-determined codes. Any passages that could not be categorised within the initial coding theme were given new codes. Further coding was then conducted and this iteration was reviewed and updated. After coding was completed, initial notes from the focus groups were revisited to ensure all reflective notes were incorporated where relevant. Final themes were refined through an iterative process between JD, ER and EJ (qualitative analysis expert), with all stages of analysis reaching consensus agreement with regard to the content and labelling of codes and themes.
Patient and public involvement
As this study focused on staff experiences in an EM workplace, a Clinical Advisory Group (CAG) was used in place of patient or public involvement. The CAG comprised of five clinicians working in the ED who advised on the scope and priorities of the study. This included two medical consultants, one charge nurse, one trainee and one specialty grade doctor. Of those, three were males and two were females. All CAG members were offered renumeration for their time.
Of the 117 total responses to the study advert, 16 respondents were eligible but not available to attend focus groups and 55 either did not consent or were not eligible based on their role and/or department. From the remaining 46 respondents, 13 of these could not attend or cancelled, leaving a final sample of N=33 (28% of total responses). Due to higher response rates from doctors, these focus groups were further grouped by grade; nurses and ACPs were grouped by profession only and were organised base on availability. There were 11 groups in total (see table 1 ). Participants were mostly female, and from a white British background. Ages were spread fairly evenly across the categories, except ages 35–44 which included substantially fewer participants.
- View inline
Participant and focus group characteristics
Following analysis of the qualitative data, four key themes were generated. These were termed: ‘culture of blame and negativity’, ‘untenable working environments’, ‘compromised leadership’ and ‘striving for support’. Data within these themes that were identified as ‘barriers’ or ‘opportunities’ for change were extracted ( table 2 ). Illustrative participant quotes are identified by researcher codes, which reflect the profession and a recoded group number, to preserve anonymity.
Primary concerns, barriers and opportunities for change
Culture of blame and negativity
When asked about the most difficult aspects of their working conditions, participants commonly reported a culture of blame and negativity in the ED. The work culture not only felt unsupportive and ‘toxic’ but had a marked effect on well-being. Participants described a culture which was quick to blame rather than support:
You worry about making a mistake, and if you did make a mistake who would have your back. (ACP, G7) You very rarely get anyone saying that was a good job. (SAS doctor, G8)
This was particularly felt top-down, where those in management position were perceived to take an unsympathetic view of extended waiting times and unmet targets, despite the tangible constraints of operating at overcapacity and ‘exit block’, problems that participants perceived to be out of their control. Participants in all groups indicated that the negative culture instils anxiety over how they might be perceived by peers, but particularly by senior colleagues:
That’s a classic example… she’s a senior member of the team, really knows her job…. She was quite critical really, in a very negative way about how you managed that patient. (Nurse, G11)
Some participants reported senior colleagues having unrealistic expectations of the more junior staff, with little consideration of the increased pressures that have arisen in recent years:
It’s ridiculous to compare the needs, even for our senior colleagues who were registrars five years ago, the reality of running the department overnight is not the same as it was then. (SAS doctor, G1)
Existing structures and working practices of the NHS were described as ‘archaic’ and ‘old fashioned’, leading staff to feel blamed if they could not cope with the pressures and disempowered to seek support due to the expectation that they should be ‘unbreakable’ (Trainee, G9). Participants also voiced that they were unclear on lines of accountability, who to approach for what problem. This barrier to escalating their concerns was further compounded by the belief that both clinical leadership and higher management were generally overburdened and unreceptive to discussions on workplace concerns.
Increasing pressure and longer waiting times were described as driving antisocial behaviour from patients, exposing staff to risks to physical and psychological well-being:
So the long wait causes verbal or physical violence and aggression, which has a massive impact on staff well-being. (Nurse, G11)
Participants highlighted the desire to be supported to learn from difficult experiences and develop in light of them, suggesting that a simple checking in on how individual staff members are progressing would be well received and beneficial to well-being:
We have intermittent debriefs… but it’s not every time. It doesn’t necessarily need to be every time, but it’s not as frequent as it should be. Even if it is just ask are you okay? (Trainee, G5)
Interprofessional respect and development of a more empathic culture of shared responsibility were flagged as key opportunities for change that would support better team cohesion:
We need to change how we speak and respect each group, and we need to try and understand each other’s point of view, and if we could get better ways of working, but just talking to each other about what are my problems, what are your problems, why is this stressing you, what’s stressing us, how can we work together to do that. (ACP, G2)
Findings suggest that EM professionals are confronted with outdated perceptions of clinical demand from within teams and systems, with unrealistic expectations which compound a blame and shame culture when expectations are not met. Operating within this chronically under-resourced system was framed as compromising workforce well-being and risking burnout, yet participants indicated that simple interventions such as check-ins, clearer lines of accountability and a more civil and respectful culture would offer key opportunities for growth and sustainability even in the face of a staffing crisis.
Untenable work environments
The complex work environment within the ED was described as being of significant concern, compromising care and leaving staff feeling undervalued due to basic needs being unmet. Participants frequently reported poor quality or inadequate facilities, such as provision of toilets, lockers and changing rooms, hot food only available within limited hours, poorly functioning IT systems and rest spaces being in a different building.
So you’re just basically sharing (toilets) with the patients. In the urgent care centre there’s two toilets for the whole of the department in there, often one of those is broken…and not enough lockers for every member of staff. (ACP, G2) Stuff like working computers, a consistently working POD system… those little things I think make a bigger impact on your life than how many people come in through the front door. (Trainee, G5)
A lack of physical space for administrative tasks was highlighted by many clinical staff, being described as ‘woefully inadequate’ (ACP, G2). Wards were described as ‘unfit for purpose ’ (Nurse, G11), which was attributed, in part, to higher management lacking understanding of the needs and practices of the ED. One example highlighted the long-term impact of ED workspace changes that were not fit for purpose:
…it was clear that no clinical staff had been involved. Doors were in the wrong space, no sinks in the right place, not enough storage, poor flow, poor layout (ACP, G2)
Existing rest spaces or staff rooms were reported to be taken over to provide more clinical room, limiting the space for staff to change, rest and decompress.
The nurses were getting changed in a corridor, now they seem to have a cubicle they can get changed in. But the facilities for the same trust are really very different. (Nurse, G10)
This was perceived to be particularly important due to working in the high-pressure environments of a crowded ED, where staff voiced concerns regarding the sustainability of working with a high workload safely without private spaces.
EDs were perceived to be more busy, for reasons associated with shifts in societal expectations and perceptions of the scope and role of ED:
Go back ten years ago in the emergency department and people would try their best at home, would take painkillers, will see how it goes, not wanting to trouble A&E, but seems like now it seems like A&E is the open door for everybody just to come in with everything. (ACP, G7)
Participants used emotionally laden language when describing the intensity of the workload itself, with parallels drawn between being at war and working on the NHS frontline, where staff worked under similar levels of intensity but longer term and without rest.
…when people are deployed (in the forces) they are deployed for 6 months…because that 6 months is intense, it’s intense on your body, it’s intense on your mind, it’s intense on your family, it’s intense on everything about you, and that’s while you were deployed for 6 months, and then there’s some recovery time coming back. (Consultant, G4)
Comparisons were also made to the sinking of ‘the Titanic’:
There is the jollying everybody along, being the redcoat on the shift, cheering everybody up, saying everything is going to be okay, but feeling like you’re just rearranging the deckchairs on the Titanic (Nurse, G10)
The impact of a consistently high workload was described as being compacted by a lack of agency and autonomy over working patterns, which was perceived to be related to non-clinical staff making decisions about shifts without understanding the inherent pressures:
The people who control our rotas are… her job is a rota co-ordinator, she works in an office, she is administrative, and the person who signs that off is the manager for the department, again non-clinical, and getting leave is a nightmare, it’s awful. (Trainee doctor, G5)
Consultants identified that there were limited options to reduce workload when approaching retirement, and they did not necessarily feel well-equipped to continue operating under high pressure and for long hours. Those in training posts reported insufficient time to meet requirements or study due to workload, influencing both career progression and confidence in the role.
You are getting no progression because you’re not getting your training, and I know that personally in the last year I made my decision that I will not continue to work clinically, I will step back in the next few years because there’s… why would I stay doing something that there’s no reward for? (Nurse, G11)
Participants agreed that there was both a need and an opportunity for the ED to be a ‘nicer place to work’ (ACP, G2). Specific suggestions included a full staffing quota, ensuring staff are adequately rested to return to work and the opportunity for peer support:
My top three things would be coming on with a full staffing quote so you know there’s no gaps in the rota, so you’re all there. Everyone is well rested and ready for the shift, just being able to talk to each other on the shop floor and being quite open with each other on how everyone is feeling. (ACP, G7)
Many of the suggested changes directed at making working conditions in the ED more sustainable related to basic needs such as being able to take breaks, access healthy food and functioning IT when needed:
…having those opportunities to go off and have a five minutes when you need to, to be able to continue your shift. (ACP, G7) It would be really nice to be able to have some healthy nice food in the department. (Nurse, G11) As more and more of our job goes electronic, electronic notes, electronic prescribing, actually having IT systems that are fit for purpose, everyone has access to (Trainee doctor, G9)
Self-rostering was frequently mentioned as a positive experience for participants and a useful avenue to help participants to deliver better care and improve well-being:
One day off between a set of shifts is not enough to decompress and be re-energised to start back on your next set of shifts. So I think the rota, we have moved to a more self-rostering method now, and I think that’s helping with staff well-being, especially in our team. (A7)
Overall, working in existing ED environments was described as ‘untenable’ and ‘unsustainable’ in terms of both the working environment and the lack of agency and autonomy over high-intensity workloads. Many of the problems and solutions relate to provision of resources to meet basic needs, many of which are subject to professional and NHS regulations; however, due to pressures this is not being implemented.
Compromised leadership
Clinical leads in the ED were perceived to hold responsibility for setting the tone for culture and behaviour in the ED, leading by example:
And you lead by example as well, so if your consultant in charge is not taking a break you feel like you can’t ask to take a break. It’s the same with the nurses, if the nurse in charge is not taking a break then a lot of the junior nurses won’t come and ask for a break because again you’re guided by the leadership aren’t you? (A7)
The clinical lead in the ED is a key conduit for change, from a cultural and environmental perspective especially. However, participants expressed frustration about feeling that their voices were not heard or valued outside of the department, in part due to clinical leads being reluctant to escalate their concerns due to the discrepancies between clinical priorities within the ED and the priorities expressed by trust level executive management:
You’ve got the clinical side, and we are to one degree or another worried about the patients, and then you have got the management side and they are worried about figures, times or money, and those two things don’t really mesh together (ACP, G2)
Yet, within the EDs, leadership was described as being poorly supported in terms of protected time to train and deliver the role fully. Consultants voiced reluctance to take on a leadership role due to lack of ‘visible leaders’ to provide inspiration or exemplar: ‘There is no one for us to look up to, to lead us’ (Consultant, G4), ‘We need compassionate leadership’ (SAS doctor, G1).
A lack of definition or clear understanding of what the clinical role entailed was reported to make it difficult for clinical leads to be effective in their role:
People tell you that you’re there to lead, and you’re like I know but what does that mean? And then you don’t know if you’ve got to go to all these meetings, which ones you really need to go to, which ones can I not go to, also for me I do the job on my own. (Clinical lead, G6)
Participants emphasised they need a ‘clear definition of what the college would see the role to be, and how much time they would expect it to take of your job ’ (Clinical lead, G6). Any possibility for growth was hampered by a lack of training or support from colleagues to help with even the practicalities of the role (such as recruitment and personnel management):
I have literally started last week on a leadership course that’s been for other clinical leads in the organisation. But I feel a bit could have done with this maybe earlier. But that’s more about your leadership qualities and conflict resolution, it’s all that side of it as opposed to the actual practicalities of the job. (Clinical Lead, G6)
When considering possible solutions to these difficulties, participants suggested that an accessible time to do the job and an online repository may offer an opportunity to share resources, learn from one another and foster development:
I think sharing all the stuff we shared on the WhatsApp, trying to share stuff, so how to write a business case, what you need to do. (Clinical lead, G6) I should be doing work at a time I am getting paid, so you need to give me that time. (Trainee doctor, G9)
Mentorship was also deemed to be important for successful delivery of the role:
I think personally as leads and stuff we should all have some kind of mentoring type…Supervision, that’s the thing, we don’t get any. (Nurses, G10)
Participants described having difficulties feeding into emerging issues to address unmet need, blocked from communication with leaders by ‘layers of bureaucratic sediment’. This was compounded by the career trajectory of NHS management, where often those in post would swiftly move on for promotion.
Overall, clinical leadership within the ED was described as compromised, unsupported and, ultimately, a key barrier or missed opportunity for change in culture and working practices in the ED. However, there were clear indications of opportunities for growth and change, including a need for compassionate leadership, shared resources, time to do the job and mentorship.
Striving for support
This final theme encompasses the concerns raised by participants regarding well-being and staff support, specifically the barriers to accessing well-being support and their preferences in relation to what changes are likely to improve their well-being. Common barriers included having to attend support or well-being services during time off, with the scheduling of support geared to a ‘nine to five’ non-clinical workforce (ACP, G2). Mental health stigma in the ED was also cited as a key barrier.
I think for me it still feels like a bit of a stigma about saying I am struggling what should I do next. (Nurses, G11) There’s nowhere that I can express how I am feeling or even understand how I am feeling. (Consultant, G4)
This was reinforced by well-being not being viewed as a priority, with team check-ins or formal appraisals described as having ‘nothing in there about wellbeing’ (Clinical lead, G6), despite suggestions that simple well-being check-ins would suffice.
Participants suggested that support should not be purely accessed after the fact but something that should be prioritised and routinely available to staff to safeguard mental health:
… psychological support…it shouldn’t be something that we access when there is a problem, it should be something where we go well every month on a Friday at this time I go and talk to someone about what I have seen. (Trainee, G9)
Participants’ lack of understanding about which services were being offered was raised by many, with participants often able to list services available, or where the staff support centre was based, but not how or when one might access them. This offers a key opportunity for collaboration between staff support services and the ED to develop clearer pathways or a clear role for a departmental well-being lead.
Peer support was consistently highlighted as a highly valued resource that should be considered part of supportive culture ‘gives you somebody else to share the load with, and not be that single voice’ (Trainee doctor, G9). However, limited physical space and time to engage in peer activities were cited as barriers:
Well yeah it would be lovely to sit down and chat with my peers, apart from the fact that 1) we’re constantly busy, 2) we don’t have anywhere where we can sit and have a confidential gas. (SAS doctor, G8)
Overall, accounts suggested that existing support was largely unfit for purpose, and where it was easy to access (such as peer support) and available, it was often incompatible with ED working practices and within a culture where seeking support was often stigmatised.
Some participants expressed that having a psychologist embedded within the department was highly valued as a resource, particularly the different levels of support dependent on need:
…(during the pandemic) we setup weekly drop-in sessions with the psychologist… and it was really great for a lot of people to be able to drop-in, and then that led on to having one to one for people who felt they needed that, and also within ED we had a psychologist come round to our supervision when we needed them. (ACP, G7)
Participants reflected that psychological input introduced in response to the impact of the COVID-19 pandemic was highly valued. While many were open to discussion about their mental health and well-being, for many, stigma still permeates the ED culture and is further compounded by poor understanding and communication of available resources. Appointment of well-being leads, more value placed on well-being (including informal peer support) and routine access to psychology are suggested as opportunities to make strides towards improved well-being.
This study identified four key themes describing the difficulties in the ED work place. Working culture, physical working environment, pathways to care and leadership represent the core workplace concerns within our sample. These issues were perceived to play an instrumental role in their ability to sustain good working practices, well-being and, importantly, their intention to leave. Participants identified key barriers and opportunities within their work contexts which resonate with existing research and policy and can be used to shape the future policy and research development. 22 , 2 5 These findings act as a basis for the development of specialty-specific targets for change that are aligned with the views and voices of those working in this working environment and also take account the barriers and opportunities faced in the fast-paced unique environment of the ED. For a full set of EM-specific recommendations to underpin change across all of these four areas, see the Psychologically Informed Practice and Policy (PIPP) recommendations ( https://rcem.ac.uk/workforce/psychologically-informed-practice-and-policy-pipp/ )
Several of our findings have been noted in previous studies, particularly the role of culture, environment and access to support. 22 Most of the research examining factors associated with working conditions and retention in EM are profession specific 3 6 18 19 and are not readily generalisable to other professional groups in the ED. However, our study included doctors, nurses and ACPs from which emerged common cross-cutting themes affecting all of these professions working in the ED, themes which are consistent with the broader literature 9 10 but specific to the EM working environment.
As reflected in the work by Darbyshire et al , 5 the nature of the problems described were systemic; the workplace challenges were interrelated and appeared reciprocal in influence, arguably maintaining one another. The cyclical nature itself proves a key barrier to change, which raises the question: which is the primary target to effect most change? Leadership has a pivotal influence across these themes and is unequivocally vital to workforce transformation; however, this is an area that has been largely neglected in EM, with very little research seeking to develop or evaluate leadership interventions in this environment. Indeed, there is an assumption that leadership naturally develops over time and is fully formed on appointment to the role. 23 However, leadership within the ED is particularly complex and demanding due to the range of competencies required (clinical, managerial and administrative) 23 and the high-pressured environment within which this role needs to be delivered. This warrants tailored training and support to fully succeed. In settings where the nature of the work is unpredictable and at times clinically critical, leadership is pivotal to patient outcomes and team functioning, 23 24 which are particularly crucial in the ED setting. Leadership has the potential to be a powerful driver in workforce transformation, cultural change 25 and team functioning within these highly skilled, professionally interdependent teams. 26 To fully harness the capacity of leaders as agents of change, those in leadership positions must be sufficiently skilled, 27 feel supported to act on important issues 27 and have time to do the job. Yet, participants in this study reported poor role definition, lack of training and absence of protected time to deliver the role. This was compounded by blurred lines of accountability that led to impotence to effect change.
Implications
The development of leadership in EM should now be a primary focus. There are clear steps that can be taken to begin to mobilise and maximise the pivotal influence of leadership in effecting change, across government, professional, organisational and individual levels.
On a public policy level, there has been a rapid growth of government level publications and resources to recognise the role of leadership as a conduit to better patient and team health. 28 However, recommended leadership training is often generic and never mandated. This is surprising given the clear links with patient safety and team functioning. 23 24 Leadership training in healthcare should be mandated by government bodies, not least due to links with patient safety. 29
Significant work has been undertaken by RCEM to integrate and embed mandatory leadership training into the training curriculum for EM trainees, without which they cannot progress. While this demonstrates forward thinking and some future-proofing for the medical profession, it cannot cease at this point, it must be supported with continuing professional development post-training. The relevant professional bodies provide access to good quality leadership training such as the RCEM EM Leaders Programme and the RCN Leadership Programme, however, this is largely online without protected time to access or support development. More work is needed to ensure leadership training is visible, supported as part of a workplan, and a priority area championed by all relevant professional bodies.
Further work is needed to ensure that leadership competencies are introduced at an early stage of training 23 so the necessary skills are embedded and cultivated on the pathway towards and within leadership roles, rather than ad hoc when necessity dictates. This falls to both training and professional bodies to work together to ensure that theory-driven leadership is a core part of the teaching curriculum, with mentorship and practical resources (such as role definition, a personal development plan, human resource support) to complement and facilitate the necessary continuing professional development throughout a clinical career. Responsibility then moves to the employing local NHS trusts to support the development of those individuals within leadership positions. It is at this level that ED clinical leads and their teams can harness their influence; local NHS trust policies are driven by guidance from government and professional bodies, however, they have the power to shape local policy and mandate change in view of the needs of a service. We summarise key recommendations to underpin change at a local NHS level in Box 1 .
Key leadership recommendations for local NHS trust level commissioning
Those in leadership positions should be supported to attend leadership training as part of their workplan, within their workplace hours. This would include top-up training and training assignments.
Support to engage with a leadership mentorship or coaching programme as part of their workplan, with a view to continuing professional leadership development and creating safe spaces to problem-solve, reflect and seek support.
Access to the consultation service within the local NHS staff support services.
Appointment of a designated ‘Wellbeing Lead’ with protected time and support to deliver the role.
Clear description of roles and responsibilities, to include protected time dedicated to undertaking additional responsibilities associated with a leadership role and a professional development plan that is reviewed annually.
Support to engage with the EM clinical lead network in order to access resources to support the delivery of the role and access peer support when necessary.
Clear lines of accountability at an NHS organisational level with identified pathways to escalate concerns.
EM, emergency medicine.
Appointment of well-being leads within the ED, as outlined in the RCEM PIPP recommendations 30 and other key documents, 22 is also a key step towards workplace transformation through leadership; however, it is imperative this role is also supported with protected time and development. A well-being lead with a clearly defined remit and role would play a pivotal gatekeeper role in encouraging attitudes towards well-being in the ED by delivering ‘warm handovers’ and well-being initiatives, such as informal check-ins, staff team activities (ie, safety huddles), and well-being surveys.
On an individual level, those in leadership positions are more likely to succeed by harnessing the influence and opportunity that accompanies the role, identifying and taking inventory of challenges and barriers, clarifying lines of accountability to drive forward change and advocating for the needs of their team. Two mechanisms by which leadership bears the greatest influence include leading and prioritising a continuous cycle of quality improvement (eg, autonomy over work patterns, access to rest spaces, patient flow, taking steps to address the diversity gap) and role modelling of positive professional behaviours. 26 The latter includes compassionate and inclusive attributes but also speaks to the necessity to meet basic needs: taking breaks, adhering to annual leave, destigmatising views on mental health and openness to learning and change. Those in leadership roles should be encouraged to engage with the leadership networks, broadened to encompass a platform or virtual environment (ie, repository) to share and access resources and be granted access to leadership consultation with the well-being team as and when necessary. Those in leadership positions should also be provided with clear referral processes and internal professional standards to help address any incivility, including bullying, harassment and issues of inclusion. This would help promote a culture of care and interprofessional valuing and respect, improving team cohesion.
Finally, it is imperative that lines of accountability are clear for those in a leadership position. While many NHS trusts differ in their management structures, each trust will have communication pathways to divisional and executive management leadership teams. In order to drive the full potential of leaders to action change through these mechanisms, it is fundamental that pathways from ‘shop floor’ to the chief executive are clear and opinions and concerns of ED leadership are welcomed.
Flow through the ED, staff ratios, pay and pension structures are of course prime targets for change and where the current high-profile focus lies. However, leadership is a key conduit to change and those with mandatory powers must now move to recognise this in order to unlock the full potential of this role.
Limitations and future directions
There are inherent limitations in the small size of some of the participant groups, and as such the views and opinions expressed cannot be considered transferable across their respective professions. While many prospective participants did not proceed to focus group meetings due to last minute requests to cover shifts, the participant pool was comfortably within the bounds of what is acceptable for a qualitative study.
Findings should be interpreted in light of the sample consisting mainly of white women, therefore the views of males and minority groups may not be fully represented. Doctors made up a higher proportion of the final sample; this may be a consequence of using RCEM communication channels as a primary recruitment method, which has more members registered as doctors than nurses. As not all professions working in ED were included (eg, physiotherapy, psychology) it is possible that additional themes or differences might have been missed.
The geographical spread reflects a broad reach; however, there was a preponderance towards the South West, where the research was conducted. While none of the interviewees were known to the research team, those in the South West may have been more exposed to recruitment drives through mutual connections.
The development and testing of leadership training and packages should be a priority for professional bodies and at organisational level. This should take account of the overlapping and competing competencies required of ED leadership, including managerial, administrative and clinical components and the high-pressured context within which these skills are required.
This study identified key themes in understanding workplace concerns in the ED, and their associated barriers and opportunities for change. Leadership in EM should now be a primary focus, with further investment and support to target the development of leadership skills early on in training and provide protected time to refine these leadership skills and qualities across the working lifetime. This will serve to harness the pivotal influence of leadership in EM, which, if properly supported, holds the potential to act as a conduit for change across all areas of focus.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants and was approved by University of Bath Psychology Research Ethics Committee (22-039). The Health Research Authority toolkit confirmed further approval was not required. Participants gave informed consent to participate in the study before taking part.
Acknowledgments
The study authors would like to extend thanks to all who contributed to this project including participants and the clinical advisory group. The authors would also like to acknowledge and thank RCEM President (AB) and policy advisor (SMcI) who advised on the policy priorities of RCEM and wellbeing clinical leads (Dr Jo Poitier, Consultant Clinical Psychologist at Alder Hey Children's NHS Foundation Trust; Dr Olivia Donnelly, Consultant Clinical Psychologist at North Bristol NHS Trust) who were consulted on their respective areas of expertise. They also thank Rita De Nicola for help in preparing the manuscript.
- World Health Organisation
- Royal College of Emergency Medicine
- General Medical Council
- Darbyshire D ,
- Brewster L ,
- Isba R , et al
- Fitzgerald K ,
- Benger J , et al
- Roberts T ,
- Daniels J ,
- Hulme W , et al
- Kanavaki AM ,
- Lightfoot CJ ,
- Palmer J , et al
- Johnson J ,
- Watt I , et al
- Hofmeyer A ,
- National Health Service
- Royal College of Nursing
- Chen CC , et al
- James Lind Alliance
- McDermid F ,
- Pease A , et al
- Health Education England
- Husebø SE ,
- Thomas CS ,
- Tersigni A , et al
- Poorkavoos M
- Chaudry J ,
- McKenzie S , et al
- Brittain AC ,
- Carrington JM
- Robinson E ,
- Jenkinson E , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
Handling editor Caroline Leech
Twitter @drjodaniels
Contributors The original concept for the paper was developed by JD and shaped in consultation with EC and the RCEM President AB. JD was the primary contributor, guarantor and lead for the content and refinement of the paper. EJ gave expert methodological advice and contributed to the reporting and refinement of results. ER and JD performed the analysis, both contributing to the reporting of the results. ER prepared the manuscript for publication. EC gave expert advice on all aspects of the study from an Emergency Medicine standpoint and also contributed to the write-up of the paper. All authors contributed to the final version of the paper and approved for publication.
Funding This research has been carried out through funding from the UK Research and Innovation Policy (UKRI) Support Fund. The funder did not provide a grant number for this project, it is part of block 'UKRI Policy Support' funding from UKRI directly to Universities who distribute within their institutions. The funders had no role in considering the study design or in the collection, analysis or interpretation of data; the writing of the report or the decision to submit the article for publication.
Competing interests None declared.
Patient and public involvement Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:

2024 Workshops

- 2024 Homepage
- Registration
- Featured Speakers
- Invited Programs
- Teaching Sessions
- Student Programming
- Flash Talks
- Code of Conduct
- Reserve Your Room
- Plan Your Trip
- APS 2024 FAQs
- Program Committee
- Exhibits & Sponsorships
- Press Information
The APS Annual Convention includes these extended educational sessions that offer attendees the opportunity to learn research methods and techniques from prominent psychological scientists.
Workshops are open to Convention registrants only and require additional registration fees. Workshops can be added when you register for the APS Convention. If you’ve finalized your registration, please follow these instructions to add a workshop .
Registration Fees:
THURSDAY, MAY 23
Introduction to Structural Equation Modeling in the Psychological Sciences
Presenter: Tim Hayes, Florida International University
Thursday, May 23, 9:00 AM – 12:50 PM
Structural Equation Modeling (SEM) combines common factor analysis with multiple regression to allow researchers to assess true score relations among constructs of theoretical interest. This workshop presents an overview of the logic, implementation, and interpretation of SEMs. Topics covered include: path analysis, confirmatory factor analysis, and structural regression analysis.
Prerequisite :
- A standard graduate course in linear regression analysis
- Software packages: lavaan (R) and Mplus.
- Bring a laptop (fully charged).
Measurement, Not Schmeasurement
Presenter: Jessica Flake, McGill University
We assume that psychological measures produce meaningful numbers: higher satisfaction scores indeed represent more satisfaction. Measurement is a fundamental part of psychological research, and our scores require thorough and transparent evaluation of their validity. This workshop will cover how to evaluate and refine scales using psychometric methods and open science practices.
- An introductory and intermediate courses in statistics with knowledge of regression.
Understanding Bayesian: An Introduction to Key Concepts
Presenter: Brian Leventhal, Jame Madison University
This workshop introduces steps of Bayesian analysis:
- specifying a prior
- using a likelihood
- forming a posterior
- making inferences
Attendees will be able to articulate major considerations of a Bayesian analysis, contrast Bayesian and Frequentist approaches, and identify components of Bayesian research.
Prerequisite:
- Participants should have an understanding of basic descriptive and inferential statistics (e.g., hypothesis testing, p-values, confidence intervals).
- Familiarity with linear regression and maximum likelihood estimation will be beneficial, but not required.
Data Visualization in R for Researchers Who Do Not Use R
Presenters: Emily Nordmann, University of Glasgow and Wilhelmiina Toivo, University of Glasgow
Thursday, May 23, 1:00 PM – 3:50 PM
In this session we’ll cover why you should use R for data visualization followed by an introduction to boxplots, histograms, violin-plots, density plots, bar charts, scatterplots, and more complex layered plots using ggplot. No prior knowledge of R is required.
- Please work through the workshop prep at https://emilynordmann.github.io/aps-dataviz/index.html . This will include installing R and the necessary packages to run the workshop, as well as introducing some basic terminology to help support the session.
Dynamic Structural Equation Modeling (DSEM) in Mplus
Presenter: Ellen Hamaker, Utrecth University
Thursday, May 23, 1:00 PM – 4:50 PM
This workshop provides a first introduction—both theoretically and practically—into dynamic structural equation modeling (DSEM). DSEM combines time series analysis, multilevel modeling, and structural equation modeling, and allows for a flexible and elegant approach to intensive longitudinal data such as obtained with daily diaries, experience sampling, and ambulatory assessments.
- Bring a laptop (fully charged) with Mplus installed or use the demo version of Mplus to participate in the practical portion.
Power Analysis in Structural Equation Modeling (SEM)
Presenter: Y. Andre Wang, University of Toronto
Thursday, May 23, 1:00 PM – 4:50 PM
This workshop will introduce attendees to power analysis in SEM and offer a hands-on tutorial. Attendees will learn how to connect power considerations (e.g., to detect specific target effects, to assess model fit) to their research goals, and how to conduct power analysis on their own models using R or pwrSEM, a point-and-click web application.
- Bring a laptop (fully charged) with the following software installed: R, R Studio.
- Working knowledge of R is not necessary but preferred.
- Familiarity with structural equation modelling is recommended.
FRIDAY, MAY 24
Introduction to Generalized Linear Models in the Psychological Sciences
Presenter : Connor McCabe, University of Washington
Friday, May 24, 10:30 AM – 11:50 AM
This workshop provides a comprehensive introduction to generalized linear models (GLMs), a popular approach for modeling binary and count dependent variables in psychological science. It will provide accessible coverage of both theory and application, including hands-on demonstrations for data analysis and visualization in R and state-of-the-science methods for moderation analysis.
- Bring a laptop (fully charged) with R and Rstudio. (optional)
- A working knowledge of linear regression principles and at least some familiarity with the R statistical software language.
Experience Sampling Methods and Implementation
Presenter: Sabrina Thai, Brock University
Friday, May 24, 10:30 AM – 12:20 PM
Learn how to create your own experience-sampling smartphone app using ExperienceSampler, and how to integrate ExperienceSampler with existing survey software. We will also discuss issues related to conducting experience sampling studies: design decisions, best practices, data organization, and data analysis.
Prerequisite :
- Bring your laptops (fully charged) to follow along with the workshop slides.
A Beginner’s Guide to Qualitative Research
Presenter : Jaclyn Siegel, The University of Chicago
Friday, May 24, 10:30 AM – 12:20 PM
This beginner-friendly workshop will lead researchers through some of the basics of conducting qualitative research (e.g., different analytic methods, positionality), including practical elements of qualitative work (e.g., sample sizes). The workshop will end with a deep dive into thematic analysis, a popular approach to analyzing qualitative data in psychology.
Prerequisite : none
Creating Computationally Reproducible Manuscripts
Presenter : Jason Geller, Princeton University
Friday, May 24, 1:00 PM – 2:20 PM
Open Science practices, which emphasize transparency, reproducibility, and accessibility, are indeed becoming increasingly important in the psychological community. In this workshop, you will learn to set up a reproducible workflow to create a publication-ready manuscript that combines data, R or Python code, text, and references.
Prerequisites :
- R/Rstudio
- Basic knowledge of R or Python
Introduction to Multilevel Modeling
Presenter : Jason Rights, The University of British Columbia
Friday, May 24, 1:00 PM – 2:50 PM
Multilevel modeling (MLM) is widely used in psychology and other fields to analyze nested data structures (e.g., students nested within schools or repeated measures nested within individuals). This workshop will provide a brief introduction to MLM, including both theoretical foundations as well as tools for practical application.
- Knowledge of regression modeling
- Bring a laptop (fully charged) with R & Rstudio installed
SATURDAY, MAY 25
Writing for a Popular Audience to Disseminate Your Work and Broaden Your Impact
Presenter : Andrew Devendorf, University of South Florida
Saturday, May 25, 10:30 AM – 11:50 AM
Although psychologists can benefit society by sharing their research with the public, most lack training on translating ideas into an accessible, engaging, and meaningful package. This workshop will overview the process of writing for, and pitching to, the popular press. Strategies and challenges related to scientific communication will be discussed.
Data Storytelling Training
Presenter : Lisa Cantrell, Stories of Science
Saturday, May 25, 1:00 PM – 2:20 PM
How do you make a research presentation compelling? One of the biggest secrets in science communication is this: the same narrative strategies that Hollywood uses for creating compelling movies are those that we should be using to talk about our research findings. In this workshop, participants experience demos of research presentations told with and without storytelling components and then discuss how a story format pushes the audience’s thinking forward about the research.
Participants will have the opportunity to practice sharing their data story in small groups and by the end of the session, participants will have a draft of their own research data story and a method for turning their future studies into data stories for presentations at conferences, job talks, and speaking engagements.
The Art of the Elevator Pitch
Presenter: Tammy Spence, Stories of Science
Saturday, May 25, 2:30 PM – 3:50 PM
The elevator pitch. We talk about it often. We say it is important for networking and sharing our research. And yet when it comes to actually doing it, we find ourselves using jargon, spending too much time on details that aren’t important, or not giving the right context for our audience. The elevator pitch is, at its core, a story that should be compelling, focused, and clear.
This workshop is intended to guide participants step by step through building their own compelling, clear, and focused elevator pitch—specifically around their research—and then honing it to 60 seconds. By the end of the session, participants will have a draft of a 60-second elevator pitch and 1-2 short anecdotes that they can use to illustrate their research.
Privacy Overview
- Open access
- Published: 27 March 2024
Evaluation of a peer-support, ‘mentor mother’ program in Gaza, Mozambique; a qualitative study
- Leila Katirayi 1 ,
- Sozinho Ndima 2 ,
- Amgad Farah 3 ,
- Whitney Ludwig 4 ,
- Atanásio Mabote 5 ,
- Ismail Chiposse 6 ,
- Ana Muteerwa 7 ,
- Jessica Greenberg Cowan 7 &
- Ivete Meque 2
BMC Health Services Research volume 24 , Article number: 382 ( 2024 ) Cite this article
Metrics details
Retention in prevention of mother-to-child transmission of HIV programs is critical to reduce vertical transmission. To addresses challenges with retention, Mozambique launched a peer-support program in 2018, in which HIV-positive mothers provide adherence support as mentor mothers (MMs) for HIV-positive pregnant and lactating women and HIV-exposed and infected children.
A descriptive qualitative evaluation was conducted across nine facilities in Gaza Province to assess the acceptability and barriers to implementation of the mentor mother program (MMP) among those receiving services and providing services. In-depth interviews and focus group discussions were conducted with MMs, MM supervisors, health care workers (HCWs), HIV-positive mothers enrolled in the MMP, HIV-positive mothers who declined MMP enrollment, and key informants involved in the implementation of the program. Thematic analysis identified emerging recurrent themes and patterns across the participants’ responses. Data were collected between November-December 2020.
There were initial challenges with acceptability of the MMP, especially regarding confidentiality concerns and MM roles. Sharing additional information about MMs and making small changes during the beginning of the MMP resulted in generally high acceptance of the MMP. HIV-positive mothers reported that counseling from MMs improved their understanding of the importance of anti-retroviral treatment (ART) and how to take and administer ART. HIV-positive mothers reported having reduced guilt and shame about their HIV-status, feeling less alone, and having more control over their health. MMs shared that their work made them feel valued and decreased their self-stigmatization. However, MMs also reported feeling that they had inadequate resources to perform optimal job functions; they listed inadequate transportation, insufficient stipends, and false addresses of clients among their constraints. Overall, HCWs felt that their workload was significantly reduced with MM support and wanted more MMs in the community and health facility.
Conclusions
This study found that the MMP was considered a substantive and highly valued support to HIV-positive mothers, resulting in increased ART literacy among patients, improved self-reported well-being and sense of community and reduced feelings of isolation. Recommendations include strengthening MM training, increasing financial and materiel resources, additional information provided to newly enrolled mothers and support for the male partners.
Peer Review reports
In the past decade, significant progress has been made in the prevention of mother-to-child transmission (PMTCT) of HIV [ 1 , 2 ]. Nevertheless, each year, more than 700,000 pregnant women and women of reproductive age contract HIV worldwide. More than 70% of these women live in just 23 countries, most of which are in sub-Saharan Africa [ 1 , 3 ]. In the absence of treatment, the risk of mother-to-child transmission of HIV during pregnancy, childbirth, and breastfeeding can be as high as 45% [ 1 ]. In Mozambique, approximately 150,000 children ages 0–14 are living with HIV [ 4 ], the national HIV prevalence is 12.4% % among adults aged 15–49 and the country’s highest prevalence is Gaza Province at 20.9% [ 5 ]. At the time the national mentor mother strategy was launched in 2018, the government of Mozambique reported that retention rates in HIV care and treatment among pregnant women were 65% in Gaza Province versus 81% nationally [ 6 ]. Strengthening retention among HIV-positive pregnant and lactating women is a priority both because improved retention improves the health of women, and it reduces vertical transmission and infant morbidity and mortality.
Challenges with PMTCT
Poor retention of mothers and children in care, inadequate social support, transportation costs, and stigma have been identified as barriers that impede the success of PMTCT strategies [ 7 ]. Delays at the facilities, overcrowding, long wait times, and privacy concerns during counseling sessions result in women discontinuing PMTCT interventions. The success of PMTCT interventions may also be hindered by poor motivation among pregnant and lactating women and health care workers (HCWs), inadequate support systems, and low adherence to medication and appointments [ 7 , 8 , 9 ].
Mentor mother program - a peer-led approach to HIV programming
One potential approach to overcoming challenges to PMTCT programs is by providing peer support, such as Mentor Mothers (MMs). MMs are HIV-positive mothers who have completed the PMTCT cascade, the clinical program intended to prevent HIV transmission during pregnancy, labor, delivery, and breastfeeding [ 7 , 8 , 9 , 10 , 11 , 12 ]. The MM model strengthens the PMTCT cascade by optimizing HCWs’ time by shifting tasks from the HCWs to the MMs and empowering individuals living with HIV to support one another via a formal mentoring and counseling strategy. The MMs provide psychosocial support and education to HIV-positive pregnant and lactating mothers and serve as role models, thereby promoting retention [ 13 ].
Mentor Mothers are trained to provide group and one-on-one support to HIV-positive pregnant and lactating women. They encourage enrollment, adherence, and retention in HIV care and treatment and share their own experiences as HIV-positive mothers. Their scope of work includes tracing women who miss their clinic visits via phone calls and home visits and counseling HIV-positive mothers on PMTCT [ 14 , 15 ]. By 2017, MM programs (MMPs) had supported over two million women living with HIV in sub-Saharan Africa in countries such as South Africa, Uganda, Ethiopia, Malawi, and Nigeria. The programs have resulted in reported decreases in mother-to-child transmission rates, increased ART adherence, improved uptake of early infant HIV diagnosis, and reduced workloads for HCWs [ 14 ].
Igumbor et al. used secondary data obtained from a Uganda MMP to assess the influence of MMs on the retention of mother-infant pairs in HIV-care by comparing mother-infant pairs attending the standard care of PMTCT services to the PMTCT services received through the MMP [ 7 ]. They found an increase in the number of mother-baby pairs retained at six weeks after birth (96.7% versus 65.8%), six weeks after cessation of breastfeeding (81.5%versus 42%), and 18 months after birth (71.2% versus 20.6%) when supported by the MMs [ 7 ].
Mentor mother program in Mozambique
In 2016, the Elizabeth Glaser Pediatric AIDS Foundation (EGPAF), in collaboration with the Mozambique Ministry of Health launched the MMP (originally called “Educator Mothers”) in Gaza province. The MMP was launched in 100 high-volume facilities with high-HIV prevalence, including health centers and rural hospitals. The program trained HIV-positive mothers to provide support as MMs who then conducted home visits for HIV-positive pregnant and lactating women and HIV-exposed and infected children. To be eligible to be a MM, the HIV-positive mothers had to have been compliant in care and treatment. The introductory five-day training included guidance on conducting home visits, adherence counseling, screening for tuberculosis and malnutrition, screening for other sexual transmissible infections, completing program forms, and additional topics regarding pregnancy and the postpartum period. Depending on their individual performance during the training, MMs were assigned to one of the following positions: MM focal point, MM supervisor, or MM. The MM focal points were based at health facilities and were responsible for the coordination of the MMP, demand creation, and follow-up for referrals. The MM supervisors performed home visits and provided technical support and supervision for a maximum of 10 MMs and MMs only performed the home visits.
Previous research has found that MMPs are associated with improved retention in prevention of vertical transmission services and higher viral suppression rates among pregnant and postpartum women [ 16 ]. However, initial feedback from EGPAF program staff at the facilities reported challenges with the MMP program, including women not accepting MM visits in their homes, MMs facing challenges with male partners during home visits, HCWs not accepting the MMs at the facility, confidentiality concerns and lack of sufficient stipends for MMs. This study was conducted to better understand the challenges of implementing the MMP program, and how these challenges can be addressed. This paper explores the acceptability of the MMP, barriers to implementation and provides recommendations for improvement.
Study design
A qualitative descriptive study [ 17 ] was conducted using data collected through in-depth interviews (IDIs) and focus group discussions (FGDs).
Study population
The study population was comprised of MMs, MM supervisors, HCWs from the antenatal care and child at-risk units, HIV-positive mothers enrolled in the MMP, HIV-positive mothers who refused MMP enrollment, and key informants including MMP managers, MMP coordinators, and district mother focal points.
Eligibility criteria for MMs and MM supervisors to participate in the study required that they had provided services in their role in the selected sites for at least six months in the previous year. Eligible HCWs were nurses who worked in antenatal care and child at-risk units at the health facilities where the study took place for at least six months in the previous year. Eligible HIV-positive mothers were 18 years of age, pregnant or postpartum and had been invited to join the MMP; subjects included (study those who accepted and those who declined participation). Eligible Key informants were EGPAF staff, responsible for the MMP design, implementation, and monitoring. All participants were at least 18 years old. See Table 1 for an overview of data collected.
Site selection
The MMP was implemented by EGPAF in 12 of the 14 districts in Gaza province (the second most southern province of Mozambique, bordering South Africa and Zimbabwe). Nine health facilities were selected for the study based on the presence of a focal point for the MMP. Seven sites were health centers located in Bilene, Xai-Xai, Chongoene, Chibuto, Guijá, Chockwé, and Mabalane, and two rural hospitals were selected in Manjakazi and Chicumbane.
Data collection
EGPAF hired short-term staff located in Gaza called Evaluation Assistants (EAs), to collect the data. The EAs had research experience and held undergraduate degrees in social sciences. They were from Gaza province and familiar with the local culture. The EAs had no prior relationship to the MMP or the study. EAs introduced themselves and the study objectives to all study participants prior to obtaining informed consent.
Data were collected between November- December 2020. EAs conducted IDIs and FGDs using semi-structured guides designed for this study (see Appendix A - G in the supplementary material). Because data collection took place during the peak of the COVID-19 pandemic, the data collection guides were not piloted. Instead, the data collection training had an extended role-playing section for the EAs to become intimately familiar with the guides.
IDIs lasted 30–40 min on average, while FGDs lasted approximately one hour and twenty minutes. EAs were instructed to take notes regarding all non-verbal communications or behaviors (referred to as ‘field notes.’) All interviews and FGDs were conducted at the health facilities in private rooms where conversations could not be heard. All interviews were completed and no repeat interviews were needed. All IDIs and FGDs were audio-recorded.
The guides were designed in English and translated into Portuguese and Changana, which is one local language in Southern Mozambique. These data collection tools were back-translated into participants’ languages by those fluent in Portuguese and Changana to ensure accuracy and comprehensibility. Demographic data for the IDI and FGD participants were also collected. FGDs were comprised of 5–12 participants, led by a moderator RA and assisted by a notetaker RA. Individual interviews consisted of one participant and one interviewer. The tools asked about experiences with the MMP since its inception in 2016. See supplemental material for guides. Audio-recordings were transcribed by the EAs and translated from Changana to Portuguese and then to English. A total of 92 IDIs and eight FGDs were conducted with respective groups. Please see Table 1 for an overview of data collected.
For each of the nine sites, we aimed to conduct one FGD with MMs and interview one MM supervisor, two HCWs, up to five HIV-positive mothers and one HIV-positive mother who did not enroll. We aimed to interview all eligible key informants. Sample sizes were based on previous literature that indicated that saturation is reached at 10–12 interviews and 3–6 FGDs per a homogenous group [ 18 , 19 ].
HIV-positive mothers were divided into two subgroups, those who enrolled in the MMP and those who did not. Three to five mothers enrolled in the program were selected using simple random sampling from a list of eligible HIV-positive mothers. EAs obtained a list of those who did not accept participation in the MMP from HCWs, and they were contacted in the order of most recent refusal. All of the HIV-positive mothers were contacted over the phone by health facility staff. The interviews were set on a day that the HIV-positive mother was already scheduled to return to the health facility for an appointment to avoid any inconvenience.
EAs randomly selected a MM and an MM supervisor from each district to participate by placing eligible MM and MM supervisors’ names in a bag. If any selected individuals refused to participate, additional participants were selected. The MMs and MM supervisors were contacted on the phone by the MM District Supervisors. Similarly, EAs asked the head nurse or the HCW in-charge of the facility in each district to provide a list of all eligible HCWs who were working during the weeks of data collection. Once this list was obtained, HCWs for each district were randomly selected by the EAs. All eligible key informants working in the program were invited to participate in the study. All health facility staff (including MM supervisors) were contacted by the head nurse in person or over the phone to schedule the interview when they were already scheduled to be at the health facility. All recruited participants agreed to participate. Reporting for this study adheres to the consolidated criteria for reporting qualitative research (COREQ) guidelines.
Thematic analysis was employed using a combined inductive and deductive approach. Using an inductive approach, two RAs trained in qualitative analysis and one of the principal investigators (the qualitative lead) reviewed transcripts and individually identified potential codes from the data. The RAs and the PI agreed as a group which codes best reflected the data. Codes were naturally grouped into over-arching topic areas, referred to as ‘themes,’ creating the first code list. Next the PI and RAs reviewed all the IDI and FGD guides to see if the code list would cover all of the topics raised in the guides, adding new codes as needed (using a deductive approach). The two RAs trained in qualitative analysis coded the same transcripts, compared the assigned codes for similar text segments, and resolved any discrepancies by refining or introducing new codes. Once the code list was finalized, the two RAs coded the transcripts individually. Data were analyzed by a thematic analysis approach by study population group: HIV-positive mothers who enrolled in MMP, HIV-positive mothers who refused MMP, MM supervisors, key informants and HCWs. Coding was conducted using the qualitative analysis software, MAXQDA, v.18.
Once all transcripts were coded, code reports were generated for each code. Data reduction and summary tables were generated from the code reports. These tables summarized data into descriptive, text-based summaries that also included text excerpts representative of the identified themes to provide a comprehensive overview of the results.
The frequency in which findings were expressed among participants have been summarized in statements such as a couple (two), a few (max of 4 or 35-40%), half (50%), some (60–65%), most, many/majority (80-85%) of the total number. Some statements may have been less common because they were not directly asked about in the data collection tool, but participants felt that the issue was important and raised it. Participants did not provide feedback on the findings.
The mean age for HIV-positive mothers was approximately 30 years and 62% of those participating in the MMP were married. Across both groups of mothers, all women reported they had disclosed their HIV status to at least one person in their home. At the time of enrollment in the study, mothers who were enrolled in the MMP reported having known their HIV status and been on ART for a median of 72 months, compared to women who did not accept MMP enrollment, who reported having known their status and being on ART for a median of 45 months (Table 2 ).
A total of 70 MMs participated in the eight FGDs. The mean age was 35 years old. All of them had completed some formal education, with 60% ( n = 42) having secondary education; 76% ( n = 53) had been an MM for three or more years.
Among the individuals who participated in the IDIs, 11 were MM supervisors with a mean age of 36 years. Eight of the MM supervisors had a secondary education, seven had been a supervisor for at least three years, and one had been in the role for one year. Additionally, 15 HCWs participated in the study, all of whom were female and had been in their position for at least 12 months. The majority of the HCWs were nurses.
A total of 12 key informants were interviewed, which included one MM program manager, two MM program coordinators, and nine MM focal points. Data not shown.
Theme 1: acceptability of the mentor mother program
Many MMs reported that at the beginning of MMP implementation they struggled with acceptance from the HIV-positive women and were often treated poorly. One MM Supervisor reported that prior to the MMP many patients had abandoned treatment. HIV-positive mothers feared ART treatment and believed that they had to endure this illness alone. However, perceptions changed with more exposure to the MMP and MMs began to experience fewer difficult cases.
…while in the past treatment was full of abandonment because there were no mentor mothers who supported this issue. So many people were afraid and abandoned it. So, the advantage is that people go back to the hospital… It is no longer full of people who have defaulted. Because, in the old days, people were afraid of like, hey… this disease is just me… so, now they know that, hey… we all live in it. So, the advantage is this… that I see her, that there are mentor mothers here in the hospital. (MM Supervisors, 09SM0013)
The MMP came to be generally accepted by the HIV-positive mothers receiving MMs. One of the aspects that contributed significantly to the acceptance of the program was the increased understanding about ART and its importance through messages about how to take ART, how ART protects women and their children and how ART can allow one to live a longer life. HIV-positive mothers also reported that they had a better understanding of why they should return to the health facility and the health benefits they could expect.
What I really like about this program is to be sensitized, encouraged to take medication, not to drop out of treatment, take medication at the same time every day… It is important because I feel so good in my life when complying with the treatment, and when they (MMs) also help me in giving advice to continue with the medication… (HIV-positive mother– enrolled, 02MI0008).
HIV-positive mothers enrolled in the MMP reported feeling very comfortable with MMs. This feeling of comfort may have been due to HIV-positive mothers knowing that the MMs had shared similar experiences with their patients. A few HCWs and a key informant stated that HIV-positive mothers felt more at ease speaking with MMs in comparison to health care professionals. An enrolled HIV-positive mother indicated that there are things she might feel too scared to discuss with a HCW, but she would ask questions and talk with the MM during a home visit. Many of the enrolled HIV-positive mothers expressed feeling better and less worried about treatment after MMs shared their experiences.
I feel good in my heart and I feel good in my body too. While I’m worried about taking the pills… So that I too can live and be able to raise my children…This is where they [MMs] encourage me… I follow the rules, because I know that the [MMs], encourage me and I also realize that life is not bought, so I have to comply with everything they tell me. I also give my heart… Because that person who encourages you considers you as a mother and father would. (HIV-positive mothers enrolled, 06MI0005)
Many HIV-positive mothers found it helpful to have MMs attend clinical appointments with them, stating that MMs provided moral support and advocated for HIV-positive mothers if conflict arose with the HCWs (such as HCWs being upset with women for not returning earlier). Additionally, HIV-positive mothers presenting with an MM at the health facility were guaranteed to be seen first, saving them time in the queue.
We sometimes find people who do not accept going to the hospital… if they are afraid we will accompany them… They say they are afraid of the delay in attending the hospital. And we have sensitized them to facilitate their care at the hospital. . (MM, 04MM0001)
Both key informants and enrolled HIV-positive mothers discussed how MMs alleviate feelings of fear and shame among the HIV-positive mothers; this leads to the HIV-positive mothers feeling empowered to disclose their HIV status to other members of the family. This included MMs assisting with partner counseling and, sometimes, having a male mentor from a program similar to the MMP come to HIV-positive mothers’ homes to talk to their male partners.
They adapted a way to test us all so that it looks like we’re testing for the first time, so that he [male partner] doesn’t discover that I take pills and so that we learn our HIV status together… But my husband said, hey… I don’t believe it. I’ll go to another hospital in Xin. (HIV-positive mother– refused enrollment, 05MR0009).
Many MMs shared that their work in the MMP made them feel valued and important, with decreased self-stigmatization towards themselves. MMs explained they experienced feelings of satisfaction due to having an impact on others’ lives and discussed no longer feeling ‘alone’, as the MMP provided a sense of community.
What I like most is that when I’m with the group I feel good; my heart is not poor. Because when I see the sisters [other HIV-positive mothers], I see myself too, and I feel very happy . (MM, 08MM0001).
HCWs reported that their workload was significantly reduced with the MMs’ support, and they wanted more MMs in the community and within more units at the facilities. HCWs strongly valued MMs bringing HIV-positive who were lost to follow-up back to the facility. They also noted a that MMs improved HCWs’ insight to their patients’ health conditions.
…Because they [MMs} help us. They help us, they do a wonderful job, they also reduce what is our burden… (Key informant, 01CP0001).
Theme 2: implementation challenges with the MMP
One of the initial challenges was lack of communication around the role of the MMs. MM Supervisors reported that when the MMP was first implemented most HCWs did not understand the purpose of MMs, their duties, or how they could be helpful. Key informants reported that HCWs did not understand how MMs could help facilitate messages regarding medication adherence, the importance of returning to the health facility and other key messages. Initially MMs were excluded from health unit meetings, HCWs refused to see MMP patients, and MMs were called derogatory names. A couple of MM Supervisors stated that there was pushback from HCWs at the beginning of the MMP, but after a few meetings the situation was resolved. HCWs started to appreciate and value the work of the MMs. Once HCWs started to understand how MMs could help them retain HIV-positive mothers as patients, health visits were revised to accommodate a patient’s time with the nurse and the MM.
…And what was a little challenging for me was because of the rotation of the nurses and to make the nurses understand that the MMs are there to work directly… the nurse did not know what was the role of the mentor mother. (Key informant, 03PF0002)
It wasn’t only the HCWs that didn’t fully understand the MMP. Some MMs reported being unsure of their roles, how to handle certain situations and generally needing more ongoing support. Individuals who were promoted to a new role in the MMP also reported wanting more transitional training.
I entered without a clue. I went to training, of course. But I entered without the notion of where and how to start. But I had people there to support me… (Key informant, 05PF0002).
There were also challenges with HIV-positive mothers understanding the roles of the MMs. Many MMs reported at the onset of the MMP, HIV-positive mothers were fearful and non-trusting of the MMs during their first home visit. HIV-positive mothers were very concerned that the MM might disclose their HIV status to others in the home.
Initially there were concerns about MMs visiting homes, but this was mostly resolved by removing materials that could identify MMs, such as uniforms, bicycles, and folders, and by introducing MMs to community leaders and members to address concerns of ‘strangers’ wandering around neighborhoods.
What really screwed us up, were the T-shirts…they hate the T-shirts because, the T-shirts, even the neighbor can see that that one is the one she works with, they say that these T-shirts are AIDS…For that reason, they rejected us… (MM, 03MM0001).
Male partners were also a challenge cited by most respondents because some male partners would reportedly not allow MMs to enter their homes or interact with their wives. Some participants reported that male partners threatened MMs.
Sometimes the husband does not accept for the mother mentor to visit, and sometimes even with a machete he threatens MMs saying, ‘I’m going to cut you if you don’t want to leave my house’… (MM supervisor, 07SM0003).
One of the main challenges expressed by the MMs was inadequate resources to do their job, such as insufficient stipends, not enough phone credits to call patients and/or supervisors, and having to use their own resources (such as soap and masks during COVID-19).
… mentor mothers work a lot, but the subsidy it is not suitable, it should improve a little bit in the subsidy part… (MM supervisor, 07SM0003).
MMs also felt their workloads were unrealistic and there were not enough MMs to meet the number of women who required support. This was especially problematic when MMs would have to travel long distances in order to reach HIV-positive mothers in peripheral communities.
Maybe if the MM’s leadership could afford at least a little time for the MMs to rest because as far as I know, the MMs have no right to vacation. Sometimes I think it’s suffocating to be working every day from January to December, from Monday to Friday and a little difficult. (HCW, 01PS0007)
Many MMs noted challenges locating HIV-positive mothers in the community due to incorrect addresses, not having a phone number, and many of the women working during the day.
So, this job is very difficult to find people, because addresses are not clear…you go but you just don’t find the home…we don’t know why they give fake addresses… (MM, 02MM0001).
A number of respondents also reported that they did not have enough space at the facilities to counsel women, which led to counseling sessions in which patients were uncomfortable speaking while other people were in the room.
Theme 3: recommendations to improve the MM program
HIV-positive mothers enrolling in the MMP requested clearer communication about what happens when an MM makes a home visit and what confidentiality practices are in-place to protect them.
One HCW recommended that MM training be extended for more than a week. A key informant suggested that MMs attend the training provided to new recruits as it would be a refresher and will boost their confidence in supporting HIV-positive mothers. Likewise, continuous training was requested, including refresher sessions, be provided to the MMs as the program continues to evolve.
MMs and HCWs recommended improvements to the MM training and support, including enhanced training to help prepare MMs for their first visit to an HIV-positive woman’s home and more training when entering a new role. Providing an adequate support system to help them handle problems in the field was also suggested.
… we would like to continue learning … renew knowledge and continuing to learn new things that we didn’t learn in the first training. There was a time that we had a training to work with phones… (MM, 07MM0001).
Among HCWs, MM Supervisors, and key informants, a stronger link with the community was reported as being important for continued MMP implementation. One suggestion was having a community member partner with the MMP to help identify the homes of women. This community member would not need to be informed that the MMP is providing HIV services.
Additionally, HCWs, MMs and HIV-positive mothers recognized that more support is needed for male partners to help educate HIV-positive mothers’ partners. HIV-positive mothers suggested the need for male mentors to talk to men and encourage them to test for HIV, since it may be difficult for men to speak to a MM.
“…it is men who understand each other in the way they speak… the result, he knows what his sero-state is. He only denies going to the hospital because he is stubborn; he has, he says, they are lying. So, that requires a man to come and have a conversation until he understands .” (HIV-positive mother– refused enrollment, 05MR0009).
A key informant and a couple of HCWs suggested increasing the means of transportation due to the weather and long travel distances. One of the HCWs suggested providing protective material against COVID-19. Several MMs asked for folders, pens, notebooks, pens, and a couple requested that the folders be water-resistant and able to withstand wear and tear. One request was made for raincoats as well.
All study participant groups recommended recruiting more MMs. An HIV-positive mother said increasing the number of MMs can help improve awareness. While a few HCWs said recruiting MMs will reduce workload, improve the support provided to HIV-positive mothers living in large districts and give MMs the opportunity to take some annual leave. Moreover, a key informant suggested recruiting more MMs to reach HIV-positive mothers in districts located far from the health facility.
I feel that we need more mentor mothers. We have peripheries that are very distant from the health unit, that the mentor mothers cannot reach, but that we have mothers there, who need our support…Yes, we feel that the number [of MMs] we have is still… it is little. (Key-Informant, 09PF0015).
The MMP came to be generally well accepted among HIV-positive mothers, MMs and the HCWs. The increased understanding about ART among HIV-positive mothers, positive and supportive relationships between MMs and HIV-positive mothers, support through disclosure and attending the health facility, job satisfaction among MMs, and reduced workload for HCWs all contributed to a general acceptance and appreciation for the MMP.
Through participation I n the MMP, HIV-positive mothers reported gaining a better understanding of why ART was taken daily and the importance of continuing on ART. Previous literature has demonstrated that peer models help HIV-positive mothers understand the risk of HIV transmission during breastfeeding, the importance of disclosing one’s status to at least one person, how to properly administer medication to babies, and the importance of family planning [ 13 , 20 ]. Improving retention along the PMTCT cascade helps to ensure HIV-exposed infants receive prophylactic ART and helps to increase the rate of mothers following safe infant feeding practices [ 14 , 21 , 22 ].
Previous studies evaluating MM programs have highlighted the strong and trusting relationship between HIV-positive mothers and their MMs. A few studies discussed how MMs’ engagement in attentive listening and making HIV-positive mothers feel like they were ‘on an equal level,’ assisted in reducing self-stigma [ 23 , 24 ]. Similarly, the Mozambique MMP study had many HIV-positive mothers discuss how they felt more compassion for themselves by having someone to talk to who understood what they were going through. Many HIV-positive mothers reported that their self-stigma was lessened, they felt less isolated and alone, and they felt they had more control over their health status.
MMPs in other locations also reported HIV-positive mothers feeling more comfortable disclosing their HIV status to their families or partners after listening to other HIV-positive mothers tell their disclosure stories during peer-support groups or after forming a close relationship with their peer mentor [ 25 , 26 ]. Similarly, HIV-positive mothers involved in the Mozambique MMP reported that MMs provided support to help them disclose their HIV-status, including MMs aiding in partner counseling. Disclosing one’s HIV status allowed the mothers to be more involved in PMTCT activities by increasing their ability to attend program activities without fearing that their involvement would lead to the unintended disclosure of their HIV status.
HIV-positive mothers enrolled in other peer-led programs also reported feeling more at ease in the health unit with the presence of MMs because the MMs were viewed as people they could trust [ 7 , 10 ]. Within the MMP, HIV-positive mothers found it helpful to have MMs attend their health unit appointments with them because they felt their MM could advocate for them with the HCWs.
MMs highly valued their role as MM, discussing at length the strong sense of purpose and satisfaction in helping others. Many MMs and HIV-positive mothers reported appreciating the supportive relationships and community built through the MMP. Previous literature has also identified MM’s devotion to being a MM and enjoyment of their work, also citing the satisfaction of the learning that their patient delivered an HIV-negative baby [ 27 ].
Most HCWs participating in the MMP felt their workload was significantly reduced with the support of MMs and they valued the MM’s ability to bring HIV-positive mothers back to the health unit. Previous literature has reported that HCWS have a high workload and less time for patient care and follow-up, making peer-support interventions critical in decreasing cases of lost-to-follow-up [ 10 , 14 , 22 ].
Theme 2: implementations challenges with the MM program
This study identified many implementation challenges that influenced the initial acceptability of the MMP. The challenges included lack of clarity of the MM roles among HCWs, confidentiality concerns among HIV-positive mothers, MMs need for more clarity regarding their roles and ongoing support for their work, insufficient compensation, and challenges with male partners of HIV-positive mothers.
One of the primary challenges with the MMP was the initial lack of clarity around the MM roles. At the onset of the MMP, HCWs did not understand the role of the MMs, MMs were excluded from health facility meetings and were treated poorly by HCWs. A study in Nigeria reported many challenges between HCWs and MMs due to the non-formal work status, unclear scope of work at the facility level and assignment of non-relevant tasks [ 27 ]. The Nigeria study partly attributed the challenge between HCWs and MMs as due to HCW concerns about MM legitimacy and training. This study went on to note that because MM recruitment and engagement process lies outside the formal health sector (often supported by foreign funded donor programs), it is not always recognized as a valid program by government employed HCWs. Other studies have discussed formalizing the MM structure within national health systems in order to provide a sense of continuity and stable income for MMs [ 28 ].
Another initial challenge with the MMP was HIV-positive mothers not wanting to receive MMs in their homes due to confidentiality concerns. Some HIV-positive mothers felt apprehensive about receiving home visits, since the MMs were identifiable in the community. These anxieties were further aggravated by the lack of knowledge of the MMs’ confidentiality practices. Findings from other peer programs have highlighted overall acceptance of MM support, while also echoing concerns about privacy and confidentiality due to fear of HIV-status disclosure and consequent stigma and discrimination [ 3 , 26 , 29 ]. The lack of knowledge around confidentiality may have resulted in HIV-positive mothers being hesitant to provide their true addresses to the MMs, resulting in MMs struggling to locate some of the mothers. False addresses and challenges locating the women in the community were not reported in any of the other MM studies reviewed.
Another challenge that affected the program’s success was the MM’s own lack of clarity around their roles. Some MMs reported being unsure of their roles, how to handle certain situations and generally needing more ongoing support than was provided. Previous research has discussed the challenges of MMs having an unclear scope of work and how it may limit their impact [ 25 ].
MMs struggled with insufficient compensation and discussed at length having insufficient stipends to do their job, not enough phone credits to call patients and having to use their own resources. Ensuring adequate compensation is critical for the success of peer-support programs, including increased salary or stipend [ 3 , 27 , 30 ].
Many MMs participating in the Mozambique MMP reported male partners being a challenge for MMP implementation. In other peer-led programs, many women reported not being able to take their ART medication properly out of fear of their partner finding the medication and, in turn, knowing their serostatus. This concern has also affected many HIV-positive mothers’ ability to attend health unit visits [ 25 ]. To help mitigate this issue, during the home visits, the MMs sometimes utilized male mentors from the Male Champions program at the health facility to help educate and support male-partners of the HIV-positive mothers.
Theme 3: opportunities to improve the MM program
Study participants shared many recommendations on how to strengthen the MMP and support the development of new MMPs. The main recommendations included greater clarity regarding the roles of MMs, lengthening the MM training and providing refresher training opportunities, ensuring that MMs are not easily identifiable in the community, and providing adequate compensation and resources to the MMs.
Ensuring that the role of the MMP is clear to HIV-positive mothers and HCWs would avoid many of the initial challenges that MMs faced. In order to alleviate fears of unintended HIV status disclosure study participants recommended providing additional information to HIV-positive mothers, specifically explaining the confidentiality practices when visiting homes. HCWs also need to be informed of the role of MM’s in the community and at the facility, and understand the benefits of the MMP. A multi-country study reported that peer mother support recognition and acceptance will be maximized if their role within the health systems is better defined, before and during implementation [ 31 ].
Within the Mozambique MMP, there were concerns of MMP staff not retaining previous training. Key informants suggested that all staff attend the new recruits’ trainings since they could serve as refresher courses and boost staff confidence. This suggestion was supported by the HCWs, who suggested that MM trainings be extended beyond five days. Similarly, additional training and refresher courses were successful in the Eswatini peer-support mother program [ 32 ]. Previous literature has also recommended providing a training certificate, to legitimize the role of the MM [ 31 ].
Future MMP programs should also ensure that MMs are not identifiable with uniforms or any other indicators (such as bicycles or folders) that they are coming from the health facility. A study in Kenya recommended the use of a small identification card instead of uniforms or printed T-shirts [ 14 ].
Acknowledging the work that MMs do within these programs and providing them with adequate resources and compensation will promote program sustainability and strengthen MM support, satisfaction, and performance. Ensuring adequate resources may require moving the MMP into the national health care system. One recommendation is to absorb MMs as routine facility staff, provide MMs with more stable employment, and ideally give the MMP more credibility and respect when establishing a MMP in other facilities [ 31 ].
The challenge of false addresses suggests that MMs and their patients are not always able to engage in candid discussions about whether patients accept home visits. In addition to building support for the MMP, the MMP in Gaza would benefit from clear training in communicating choice to potential patients and ensuring patients that they may opt out of visits until they are ready to accept a home visit by a mentor mother. Ideally such communication would leave the door open for facility-based adherence support and ongoing discussion of the patient’s willingness to accept a home visit.
Study strengths and limitations
A significant strength of the study is that data were gathered from many different groups, providing the opportunity to triangulate data and share a more comprehensive understanding of the acceptability and challenges with the MMP. We hope that the data from this study can be helpful when expanding the MMP or developing other MMPs.
A limitation of this study is that women who started the MMP and dropped out and MM’s who resigned were not included in the study population due to limited funding and resources. While these populations were small, they may have offered additional perspectives about the MMP, including additional challenges in receiving and providing services. To address this limitation, questions were included in the data collection tools specifically asking about the challenges that HIV-positive mothers experienced in the MMP and challenges MM’s faced in their role.
This study highlights that the MMP in Gaza Province provided critical support to HIV-positive mothers in Gaza, resulting in increased understanding of ART and how to take medication, a sense of community, reduced feelings of loneliness, and decreased pressure on the HCWs at health facilities. The study also highlights many opportunities to strengthen the MMP, including the need to provide additional resources to MMs and increase the number of MMs serving the prescribed patient population in order to decrease the workload of existing MMs. This study builds upon an existing evidence base that peer-support programs can be impactful behavior change interventions. While not necessarily generalizable to all settings, the study provides insight for future MMPs working to strengthen ART adherence for HIV-positive mothers within low to middle income communities in Mozambique, sub-Saharan Africa and beyond.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
evaluation assistant
Elizabeth Glaser Pediatric AIDS Foundation
focus group discussion
health care worker
in-depth interview
mentor mother
mentor mother program
prevention of mother-to-child transmission of HIV
Kharsany AB, Karim QA. HIV infection and AIDS in sub-saharan Africa: current status, challenges and opportunities. Open AIDS J. 2016;10:34–48. https://doi.org/10.2174/1874613601610010034
Article CAS PubMed PubMed Central Google Scholar
Vrazo AC, Sullivan D, Ryan Phelps B. Eliminating mother-to-child transmission of HIV by 2030: 5 strategies to ensure continued progress. Glob Health Sci Pract. 2018;6(2):249–56. https://doi.org/10.9745/GHSP-D-17-00097
Article PubMed PubMed Central Google Scholar
Odiachi A, Al-Mujtaba M, Torbunde N, Erekaha S, Afe AJ, Adejuyigbe E, et al. Acceptability of mentor mother peer support for women living with HIV in North-Central Nigeria: a qualitative study. BMC Pregnancy Childbirth. 2021;21(1):545. https://doi.org/10.1186/s12884-021-04002-1
UN country fact sheet, Mozambique. https://aidsinfo.unaids.org/ . Accessed January 15th 2023.
ICAP PHIA report. https://phia.icap.columbia.edu/mozambique-final-report-2021-en-port/ . Accessed January 15th 2023.
MISAU. Estratégia Nacional das Mães Mentoras e Grupos de Mães para Mães.(2018a). Accessed July 10th 2023.
Igumbor JO, Ouma J, Otwombe K, Musenge E, Anyanwu FC, Basera T, et al. Effect of a mentor mother programme on retention of mother-baby pairs in HIV care: a secondary analysis of programmme data in Uganda. PLoS ONE. 2019;14(10):e0223332. https://doi.org/10.1371/journal.pone.0223332
Sam-Agudu NA, Cornelius LJ, Okudaye JN, Adeyemi OA, Isah HO, Wiwa OM, et al. The impact of mentor mother programs on PMTCT service uptake and retention-in-care at primary health care facilities in Nigeria: a prospective cohort study (MoMent Nigeria). J Acquir Immune Defic Syndr. 2014;67(Suppl 2):S132–1388. https://doi.org/10.1097/QAI.0000000000000331
Article PubMed Google Scholar
McNairy ML, Teasdale CA, El-Sadr WM, Mave V, Abrams EJ. Mother and child both matter: reconceptualizing the prevention of mother-to-child transmission care continuum. Curr Opin HIV AIDS. 2015;10(6):403–10. https://doi.org/10.1097/COH.0000000000000199
Phiri S, Tweya H, van Lettow M, Rosenberg NE, Trapence C, Kapito-Tembo A, et al. Impact of facility and community-based peer support models on maternal uptake and retention in Malawi’s option B + HIV prevention of mother-to-child transmission program: a 3-arm cluster randomized controlled trial (PURE Malawi). J Acquir Immune Defic Syndr. 2017;75(Suppl 2):S140–8. https://doi.org/10.1097/qai.0000000000001357
Rosenberg NE, van Lettow M, Tweya H, Kapito-Tembo A, Bourdon CM, Cataldo F, et al. Improving PMTCT uptake and retention services through novel approaches in peer-based family-supported care in the clinic and community: a 3-arm cluster randomized trial (PURE Malawi). J Acquir Immune Defic Syndr. 2014;67(Suppl 2):S114–9. https://doi.org/10.1097/QAI.0000000000000319
Onono M, Kwena Z, Turan J, Bukusi E, Cohen CR, Gray GE. You know you are sick, why do you carry a pregnancy again? Applying the socio-ecological model to understand barriers to PMTCT service utilization in Western Kenya. J AIDS Clin Res. 2015;6(6):467. https://doi.org/10.4172/2155-6113.1000467
Shroufi A, Mafara E, Saint-Sauveur JF, Taziwa F, Vinoles MC. Mother to Mother (M2M) peer support for women in prevention of mother to child transmission (PMTCT) programmes: a qualitative study. PLoS ONE. 2013;8(6):e64717. https://doi.org/10.1371/journal.pone.0064717
Wanga I, Helova A, Abuogi LL, Bukusi EA, Nalwa W, Akama E, et al. Acceptability of community-based mentor mothers to support HIV-positive pregnant women on antiretroviral treatment in western Kenya: a qualitative study. BMC Pregnancy Childbirth. 2019;19(1):288. https://doi.org/10.1186/s12884-019-2419-z
Kaufman MR, Cornish F, Zimmerman RS, Johnson BT. Health behavior change models for HIV prevention and AIDS care: practical recommendations for a multi-level approach. J Acquir Immune Defic Syndr. 2014;66(Suppl 3):S250–8. https://doi.org/10.1097/QAI.0000000000000236
Carlucci JG, Yu Z, González P, Bravo M, Amorim G, das Felicidades Cugara C, Guambe H, Mucanhenga J, Silva W, Tique JA, Sardella Alvim MF, Graves E, De Schacht C, Wester CW. The effect of a Mentor Mothers program on prevention of vertical transmission of HIV outcomes in Zambézia Province, Mozambique: a retrospective interrupted time series analysis. J Int AIDS Soc. 2022;25(6):e25952. https://doi.org/10.1002/jia2.25952 . PMID: 35718940; PMCID: PMC9207359.
Kim H, Sefcik JS, Bradway C. Characteristics of qualitative descriptive studies: a systematic review. Res Nurs Health. 2017;40(1):23–42. https://doi.org/10.1002/nur.21768 . Epub 2016 Sep 30. PMID: 27686751; PMCID: PMC5225027.
Article CAS PubMed Google Scholar
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Sage. 2006;18(1):59–82.
Google Scholar
Guest G, Namey E, McKenna K. How many focus groups are enough? Building an evidence base for nonprobability sample sizes. Sage. 2016;29(1):3–22.
Teasdale CA, Besser MJ. Enhancing PMTCT programmes through psychosocial support and empowerment of women: the Mothers2mothers model of care. S Afr J HIV Med. 2008;29:60.
National AIDS, and STI Control Program. National guidelines for PMTCT peer educationpsychosocial support in Kenya– The Kenya Mentor Mother Program. Ministry of Health, Kenya. 2012. http://guidelines.health.go.ke:8000/media/National_Guidelines__for__PMTCT_Peer_Education_and_Psychosocial_Support_in_Kenya_KMMP.pdf . Accessed 15th June, 2022.
Larson BA, Bii M, Tsikhutsu I, Halim N, Wolfman V, Coakley P, et al. The enhanced Mentor Mother ProgrAm (EMMA) for the prevention of mother-to-child transmission of HIV in Kenya: study protocol for a cluster randomized controlled trial. Trials. 2018;19(1):594. https://doi.org/10.1186/s13063-018-2975-y
Loeffen MJ, Daemen J, Wester FP, Laurant MG, Lo Fo Wong SH, Lagro-Janssen AL. Mentor mother support for mothers experiencing intimate partner violence in family practice: a qualitative study of three different perspectives on the facilitators and barriers of implementation. Eur J Gen Pract. 2017;23(1):27–34. https://doi.org/10.1080/13814788.2016.1267724
McLeish J, Redshaw M. Peer support during pregnancy and early parenthood: a qualitative study of models and perceptions. BMC Pregnancy Childbirth. 2015;15:257. https://doi.org/10.1186/s12884-015-0685-y . PMID: 26459281; PMCID: PMC4603913.
Mphonda SM, Rosenberg NE, Kamanga E, Mofolo I, Mwale G, Boa E, et al. Assessment of peer-based and structural strategies for increasing male participation in an antenatal setting in Lilongwe, Malawi. Afr J Reprod Health. 2014;18(2):97–104.
PubMed PubMed Central Google Scholar
Carbone NB, Njala J, Jackson DJ, Eliya MT, Chilangwa C, Tseka J, et al. I would love if there was a young woman to encourage us, to ease our anxiety which we would have if we were alone: adapting the Mothers2Mothers Mentor Mother Model for adolescent mothers living with HIV in Malawi. PLoS ONE. 2019;14(6):e0217693. https://doi.org/10.1371/journal.pone.0217693
Sam-Agudu NA, Odiachi A, Bathnna MJ, Ekwueme CN, Nwanne G, Iwu EN, Cornelius LJ. They do not see us as one of them: a qualitative exploration of mentor mothers’ working relationships with healthcare workers in rural North-Central Nigeria. Hum Resour Health. 2018;16(1):47. https://doi.org/10.1186/s12960-018-0313-9 . PMID: 30200969; PMCID: PMC6131877.
Ibu JM, Mhlongo EM. The Mentor Mothers Program in the Department of Defense in Nigeria: an Evaluation of Healthcare Workers, Mentor Mothers, and patients’ experiences. Healthc (Basel). 2021;9(3):328. https://doi.org/10.3390/healthcare9030328 . PMID: 33799489; PMCID: PMC8001623.
Article Google Scholar
Thomson KA, Telfer B, Opondo Awiti P, Munge J, Ngunga M, Reid A. Navigating the risks of prevention of mother to child transmission (PMTCT) of HIV services in Kibera, Kenya: barriers to engaging and remaining in care. PLoS ONE. 2018;13(1):e0191463. https://doi.org/10.1371/journal.pone.0191463
Kane S, Kok M, Ormel H, Otiso L, Sidat M, Namakhoma I, et al. Limits and opportunities to community health worker empowerment: a multi-country comparative study. Soc Sci Med. 2016;164:27–34. https://doi.org/10.1016/j.socscimed.2016.07.019
Cataldo F, Sam-Agudu N, Phiri S, Shumba B, Cornelius LJ, Foster G. The roles of expert mothers engaged in prevention of mother-to-child transmission (PMTCT) programs: a commentary on the INSPIRE studies in Malawi, Nigeria, and Zimbabwe. J Acquir Immune Defic Syndr. 2017;75(Suppl 2):S224–32. https://doi.org/10.1097/QAI.0000000000001375
Geldsetzer P, De Neve JW, Bordeaux C, Bärnighausen T, Bossert TJ. Improving the performance of community health workers in Swaziland: findings from a qualitative study. Hum Resour Health. 2017;15(1):68. https://doi.org/10.1186/s12960-017-0236-x
Download references
Acknowledgements
The authors would like to thank the study participants, research assistants that collected the data, and the patient advisors.
This study has been supported by the United States President’s Emergency Plan for AIDS Relief (PEPFAR) through the United State CDC under the terms of #NU2GGH001945. The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the funding agencies.
Author information
Authors and affiliations.
Research Department, Elizabeth Glaser Pediatric AIDS Foundation, Washington, DC, USA
Leila Katirayi
Research Department, Elizabeth Glaser Pediatric AIDS Foundation, Maputo, Mozambique
Sozinho Ndima & Ivete Meque
Milken Institute School of Public Health, Department of Prevention and Community Health, George Washington University, Washington, DC, USA
Amgad Farah
Milken Institute School of Public Health, Department of Public Health, George Washington University, Washington, DC, USA
Whitney Ludwig
XX Department, Elizabeth Glaser Pediatric AIDS Foundation, Maputo, Mozambique
Atanásio Mabote
Ministry of Health, Provincial Director for Gaza, Gaza, Mozambique
Ismail Chiposse
Division of Global HIV & TB, Centers for Disease Control and Prevention, Maputo, Mozambique
Ana Muteerwa & Jessica Greenberg Cowan
You can also search for this author in PubMed Google Scholar
Contributions
LK, SN, and AM designed the study. SN and AM oversaw data collection in the field. LK, SN, AF, and WL drafted the manuscript. All authors were involved in reading and approving the final manuscript.
Corresponding author
Correspondence to Leila Katirayi .
Ethics declarations
Ethics approval and consent to participate.
Ethical clearance was obtained from the Mozambican National Health Science Research Committee on June 1st 2020, protocol number IRB00002657, and approval reference number 238/CNBS/20. The study was also reviewed and approved by the Advarra Institutional Review Board on October 26th 2020, protocol number Pro00046844. This activity was reviewed by the United States Centers for Disease Control and Prevention (CDC) and was conducted consistent with applicable federal law and CDC policy. The CDC co-investigators provided technical support and did not engage in data collection. Informed consent was obtained from all study participants and from the legal guardians of the Illiterate participants. All study methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, supplementary material 4, supplementary material 5, supplementary material 6, supplementary material 7, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Katirayi, L., Ndima, S., Farah, A. et al. Evaluation of a peer-support, ‘mentor mother’ program in Gaza, Mozambique; a qualitative study. BMC Health Serv Res 24 , 382 (2024). https://doi.org/10.1186/s12913-024-10833-3
Download citation
Received : 11 August 2023
Accepted : 06 March 2024
Published : 27 March 2024
DOI : https://doi.org/10.1186/s12913-024-10833-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Peer support
- Mentor mothers
- HIV-positive mothers
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Grad Med Educ
- v.7(4); 2015 Dec
Choosing a Qualitative Research Approach
Associated data.
Editor's Note: The online version of this article contains a list of further reading resources and the authors' professional information .
The Challenge
Educators often pose questions about qualitative research. For example, a program director might say: “I collect data from my residents about their learning experiences in a new longitudinal clinical rotation. If I want to know about their learning experiences, should I use qualitative methods? I have been told that there are many approaches from which to choose. Someone suggested that I use grounded theory, but how do I know this is the best approach? Are there others?”
What Is Known
Qualitative research is the systematic inquiry into social phenomena in natural settings. These phenomena can include, but are not limited to, how people experience aspects of their lives, how individuals and/or groups behave, how organizations function, and how interactions shape relationships. In qualitative research, the researcher is the main data collection instrument. The researcher examines why events occur, what happens, and what those events mean to the participants studied. 1 , 2
Qualitative research starts from a fundamentally different set of beliefs—or paradigms—than those that underpin quantitative research. Quantitative research is based on positivist beliefs that there is a singular reality that can be discovered with the appropriate experimental methods. Post-positivist researchers agree with the positivist paradigm, but believe that environmental and individual differences, such as the learning culture or the learners' capacity to learn, influence this reality, and that these differences are important. Constructivist researchers believe that there is no single reality, but that the researcher elicits participants' views of reality. 3 Qualitative research generally draws on post-positivist or constructivist beliefs.
Qualitative scholars develop their work from these beliefs—usually post-positivist or constructivist—using different approaches to conduct their research. In this Rip Out, we describe 3 different qualitative research approaches commonly used in medical education: grounded theory, ethnography, and phenomenology. Each acts as a pivotal frame that shapes the research question(s), the method(s) of data collection, and how data are analyzed. 4 , 5
Choosing a Qualitative Approach
Before engaging in any qualitative study, consider how your views about what is possible to study will affect your approach. Then select an appropriate approach within which to work. Alignment between the belief system underpinning the research approach, the research question, and the research approach itself is a prerequisite for rigorous qualitative research. To enhance the understanding of how different approaches frame qualitative research, we use this introductory challenge as an illustrative example.
The clinic rotation in a program director's training program was recently redesigned as a longitudinal clinical experience. Resident satisfaction with this rotation improved significantly following implementation of the new longitudinal experience. The program director wants to understand how the changes made in the clinic rotation translated into changes in learning experiences for the residents.
Qualitative research can support this program director's efforts. Qualitative research focuses on the events that transpire and on outcomes of those events from the perspectives of those involved. In this case, the program director can use qualitative research to understand the impact of the new clinic rotation on the learning experiences of residents. The next step is to decide which approach to use as a frame for the study.
The table lists the purpose of 3 commonly used approaches to frame qualitative research. For each frame, we provide an example of a research question that could direct the study and delineate what outcomes might be gained by using that particular approach.
Methodology Overview

How You Can Start TODAY
- 1 Examine the foundations of the existing literature: As part of the literature review, make note of what is known about the topic and which approaches have been used in prior studies. A decision should be made to determine the extent to which the new study is exploratory and the extent to which findings will advance what is already known about the topic.
- 2 Find a qualitatively skilled collaborator: If you are interested in doing qualitative research, you should consult with a qualitative expert. Be prepared to talk to the qualitative scholar about what you would like to study and why . Furthermore, be ready to describe the literature to date on the topic (remember, you are asking for this person's expertise regarding qualitative approaches—he or she won't necessarily have content expertise). Qualitative research must be designed and conducted with rigor (rigor will be discussed in Rip Out No. 8 of this series). Input from a qualitative expert will ensure that rigor is employed from the study's inception.
- 3 Consider the approach: With a literature review completed and a qualitatively skilled collaborator secured, it is time to decide which approach would be best suited to answering the research question. Questions to consider when weighing approaches might include the following:
- • Will my findings contribute to the creation of a theoretical model to better understand the area of study? ( grounded theory )
- • Will I need to spend an extended amount of time trying to understand the culture and process of a particular group of learners in their natural context? ( ethnography )
- • Is there a particular phenomenon I want to better understand/describe? ( phenomenology )
What You Can Do LONG TERM
- 1 Develop your qualitative research knowledge and skills : A basic qualitative research textbook is a valuable investment to learn about qualitative research (further reading is provided as online supplemental material). A novice qualitative researcher will also benefit from participating in a massive online open course or a mini-course (often offered by professional organizations or conferences) that provides an introduction to qualitative research. Most of all, collaborating with a qualitative researcher can provide the support necessary to design, execute, and report on the study.
- 2 Undertake a pilot study: After learning about qualitative methodology, the next best way to gain expertise in qualitative research is to try it in a small scale pilot study with the support of a qualitative expert. Such application provides an appreciation for the thought processes that go into designing a study, analyzing the data, and reporting on the findings. Alternatively, if you have the opportunity to work on a study led by a qualitative expert, take it! The experience will provide invaluable opportunities for learning how to engage in qualitative research.
Supplementary Material
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Uniformed Services University of the Health Sciences, the Department of the Navy, the Department of Defense, or the US government.
References and Resources for Further Reading
This paper is in the following e-collection/theme issue:
Published on 27.3.2024 in Vol 26 (2024)
Assessment of the Barriers and Enablers of the Use of mHealth Systems in Sub-Saharan Africa According to the Perceptions of Patients, Physicians, and Health Care Executives in Ethiopia: Qualitative Study
Authors of this article:

Original Paper
- Genet Tadese Aboye 1, 2 , BSc, MSc, PGD ;
- Gizeaddis Lamesgin Simegn 2 , BSc, MSc, PhD ;
- Jean-Marie Aerts 1 , BSc, MSc, PhD
1 M3-BIORES (Measure, Model & Manage Bioreponses), Division of Animal and Human Health Engineering, Department of Biosystems, KU Leuven, Leuven, Belgium
2 School of Biomedical Engineering, Jimma Institute of Technology, Jimma University, Jimma, Ethiopia
Corresponding Author:
Genet Tadese Aboye, BSc, MSc, PGD
M3-BIORES (Measure, Model & Manage Bioreponses)
Division of Animal and Human Health Engineering, Department of Biosystems
kasteelpark Arenberg 30
Leuven, 3001
Phone: 32 489304866
Email: [email protected]
Background: Digital technologies are increasingly being used to deliver health care services and promote public health. Mobile wireless technologies or mobile health (mHealth) technologies are particularly relevant owing to their ease of use, broad reach, and wide acceptance. Unlike developed countries, Sub-Saharan Africa experiences more challenges and obstacles when it comes to deploying, using, and expanding mHealth systems. In addition to barriers, there are enabling factors that could be exploited for the design, implementation, and scaling up of mHealth systems. Sub-Saharan Africa may require tailored solutions that address the specific challenges facing the region.
Objective: The overall aim of this study was to identify the barriers and enablers for using mHealth systems in Sub-Saharan Africa from the perspectives of patients, physicians, and health care executives.
Methods: Multi-level and multi-actor in-depth semistructured interviews were employed to qualitatively explore the barriers and enablers of the use of mHealth systems. Data were collected from patients, physicians, and health care executives. The interviews were audio recorded, transcribed verbatim, translated, and coded. Thematic analysis methodology was adopted, and NVivo software was used for the data analysis.
Results: Through this rigorous study, a total of 137 determinants were identified. Of these determinants, 68 were identified as barriers and 69 were identified as enablers. Perceived barriers in patients included lack of awareness about mHealth systems and language barriers. Perceived enablers in patients included need for automated tools for health monitoring and an increasing literacy level of the society. According to physicians, barriers included lack of available digital health systems in the local context and concern about patients’ mHealth capabilities, while enablers included the perceived usefulness in reducing workload and improving health care service quality, as well as the availability of mobile devices and the internet. As perceived by health care executives, barriers included competing priorities alongside digitalization in the health sector and lack of interoperability and complete digitalization of implemented digital health systems, while enablers included the perceived usefulness of digitalization for the survival of the highly overloaded health care system and the abundance of educated manpower specializing in technology.
Conclusions: mHealth systems in Sub-Saharan Africa are hindered and facilitated by various factors. Common barriers and enablers were identified by patients, physicians, and health care executives. To promote uptake, all relevant stakeholders must actively mitigate the barriers. This study identified a promising outlook for mHealth in Sub-Saharan Africa, despite the present barriers. Opportunities exist for successful integration into health care systems, and a user-centered design is crucial for maximum uptake.
Introduction
eHealth, or the secure and cost-effective application of information and communication technology (ICT) to support health and health-related sectors, includes, but is not limited to, the use of mobile wireless technologies for public health or mobile health (mHealth) [ 1 , 2 ]. Digital technologies are increasingly being used to deliver health care services and promote public health. mHealth technologies are particularly relevant due to their ease of use, broad reach, and wide acceptance [ 3 ]. Global health service delivery could change as a result of the use of mHealth to support the accomplishment of health objectives. This transformation is being fueled by a potent confluence of different elements. These include the quick development of mobile technologies and apps, the rise of new chances for incorporating mHealth into already existing eHealth services, and the ongoing expansion of mobile cellular network coverage [ 4 , 5 ].
In the literature, it has been shown that mHealth systems in the form of SMS text messages, apps, and telemedicine projects are being used efficiently in the developed world. mHealth solutions are advancing rapidly in these regions [ 6 - 8 ]. The reason for this is the fact that there are a number of enabling factors that facilitate or encourage the use and implementation of such systems. Today, a wide variety of barriers and enablers are present in the developing world that influence the use and implementation of mHealth systems [ 9 - 11 ].
The prevalence and exploitation of mHealth technologies are steadily rising, presenting a significant opportunity for their incorporation into clinical services as a means to enhance the provision of high-quality medical care. Recent data on mobile phone usage in Sub-Saharan Africa revealed that 51% of residents possess a mobile device [ 12 ]. The latest statistics on mobile service subscriptions suggest an ongoing upward trajectory, with expectations of further increases. As of the end of 2020, 495 million individuals, equivalent to 46% of the population in Sub-Saharan Africa, held active mobile service subscriptions. Projections anticipate that this figure will rise, with an estimated 50% of the population (equivalent to 619 million individuals) anticipated to subscribe to mobile services by the end of 2025. Presently, there are 303 million internet users in Sub-Saharan Africa, constituting 28% of the population, and this number is projected to increase to 474 million by 2025 [ 12 , 13 ]. These data underscore the widespread penetration of mobile technology in the region and lay a solid foundation for exploring the potential advantages and challenges associated with its integration into health care services.
Even though the mass penetration of mobile phones is a fact and a very substantial condition to adopt mHealth systems in such countries, there are a number of factors that need to be considered when designing and developing mHealth systems in developing countries. Most mHealth systems initiated in such countries remain in the proof of concept or pilot testing stage. The large implementation of such systems is not widely documented [ 14 , 15 ].
mHealth approaches are widely embraced, and the health care system heavily relies on them in developed regions. From patient management systems to individual patient-centered mobile apps, these initiatives have been operational for a considerable period, in contrast to their counterparts in developing nations. A minor portion of Sub-Saharan African countries, less than half of the total [ 16 , 17 ], are currently endeavoring to incorporate mHealth platforms into their health care systems. This underscores the requirement for additional development of mHealth technology in the region. Ethiopia is currently focusing on strengthening its health care system and aligning it with the Sustainable Development Goals [ 18 ]. With a largely rural population, the nation encounters difficulties in accessing essential services like health care among others. A potential path for improvement lies in the digitalization of health care services, offering the opportunity to enhance efficiency, accessibility, and overall health care outcomes [ 19 ].
The implementation of digital health systems may encounter various challenges, and these challenges are generally context-specific. There is no universal solution that can address these challenges in all circumstances. Given the variation in challenges and the absence of a one-size-fits-all solution, success factors center on designing an mHealth platform that is specific to the context and the target population. This involves identifying these determining factors and incorporating sensitive design considerations to address unique needs [ 13 ]. Various studies have been performed for understanding technology adaption factors using various frameworks such as the Technology Acceptance Model (TAM) and the Unified Theory of Acceptance and Use of Technology (UTAUT) [ 20 - 22 ]. The research conducted by Liu et al [ 21 ] using the UTAUT indicated that users’ intentions to adopt mHealth systems are positively influenced by factors such as effort expectancy, performance expectancy, subjective norm, and perceived ubiquitousness. Notably, privacy concerns exhibited a significantly negative impact only on perceived ubiquity, with no significant effects observed on effort expectancy, performance expectancy, subjective norm, and intention to adopt [ 21 ]. The study by Yang et al [ 20 ] examined consumers’ intentions and behaviors related to the use of digital applications based on the UTAUT and provided valuable guidance for broadening the use of mHealth apps among consumers.
A systematic research study by Jacob et al [ 23 ] comprehending the sociotechnical factors influencing patients’ acceptance of mHealth tools proposed adopting a patient-centric strategy by ensuring that the tools seamlessly integrate into the overall patient journey and treatment plan. This involves giving priority to inclusive design and ensuring thorough patient education and support. Different frameworks have been used to evaluate the implementation of mHealth approaches, but they fall short of addressing all aspects comprehensively. In response, researchers have put forth a consolidated framework to address this limitation by incorporating various factors such as organizational and policy factors, social and personal factors, and technical and material factors [ 24 ].
The digital divide, characterized by unequal access to digital technology, is another factor that may be worsened or improved through the adoption of mHealth [ 25 - 27 ]. Despite evidence showing increased access to mobile devices, there is insufficient implementation of mHealth in Sub-Saharan Africa. Accelerating the integration of digitalization into the heavily burdened health care system could help address the challenges associated with inadequate health care and contribute to narrowing the digital divide in the region. Sub-Saharan Africa presents a unique challenge when it comes to the implementation and scaling up of mHealth systems. In contrast to developed countries, the region faces significant barriers that hinder the adoption and effective use of these systems. However, despite the numerous obstacles facing mHealth adoption in Sub-Saharan Africa, there are also opportunities and enabling factors. Consequently, the design and implementation of mHealth interventions in Sub-Saharan Africa must be tailored to address these specific challenges. Ethiopia, a representative country of Sub-Saharan Africa, is considered as one of these nations with limited implementation and consumption of mHealth systems. Thus, there is a pressing need for a comprehensive study of the barriers and enablers for mHealth adoption in Sub-Saharan Africa in order to help guide the development of tailored mHealth interventions that are suited to the local context and can effectively address the unique challenges facing the region. For this, it is vital to investigate the determinants that could affect the use of mHealth approaches. mHealth strategies are tailored to diverse end users, with certain approaches adapted for organizational use, while others target health care professionals or patients, and sometimes both. The factors influencing each of these populations may exhibit overlaps, yet they are varied and complex, necessitating a comprehensive and separate investigation for each category.
The overall aim of this study was to identify the barriers and enablers from the perspectives of patients, physicians, and health care executives for using mHealth systems in Sub-Saharan Africa and to provide recommendations on mHealth system design and policy-making. The study’s anticipated outcome is a description of the elements that encourage or inhibit the use of mHealth approaches, along with suggestions for resolving these barriers and exploring the enablers. This study can be used as a primary step in undertaking a user-centered design study of mHealth platforms in the Sub-Saharan African context.
Study Design
A multi-level and multi-actor in-depth semistructured interview was employed in order to identify the barriers and enablers of the use of mHealth systems.
Study Area and Sampling
The sample areas for this study included 1 city administration and 2 regions in Ethiopia, namely, Addis Ababa city administration, Oromia region, and Harari region. The study locations were selected based on the Human Development Index (HDI), which serves as a composite measure of a region’s average achievements in 3 fundamental aspects of human development, namely, health, knowledge, and standard of living [ 28 ]. Participants were recruited through nonprobability sampling, with a specific emphasis on purposive sampling techniques. For recruiting individuals, the snowball sampling technique [ 29 ] was used by means of colleagues, organizational contacts, and initial participants.
Participants
Data were collected from patients, physicians, and health care executives. For the health care executive group, individuals eligible for participation included decision-making persons and managers of health offices, hospitals, or similar organizations. For the physician group, individuals eligible for participation included health care professionals working at chronic disease outpatient departments (OPDs), who possessed the ability to communicate in Amharic. Lastly, for the patient group, individuals eligible for participation included chronic disease patients aged between 17 and 50 years who could communicate effectively in Amharic. These criteria were carefully defined to ensure that the selection of participants aligned with the specific characteristics and roles of each group within the study.
The participants in the health care executive group had a variety of positions, including office and hospital directors, coordinators, and ICT heads in federal offices, health bureaus, and hospitals. Additionally, in-depth interviews were conducted with physicians working at chronic disease OPDs. Furthermore, patients who visited the selected health facilities for chronic disease follow-ups were involved in the study.
Data Collection and Analysis
Semistructured interviews [ 30 , 31 ] were selected for this study as they provide the required balance between flexibility and structure for our research. This approach offers the necessary room to explore a subject while maintaining sufficient structure to accomplish the objectives of the study. The interview guides for patients, physicians, and executives are presented in Multimedia Appendix 1 , Multimedia Appendix 2 , and Multimedia Appendix 3 , respectively. The interview guides were structured based on the consolidated framework of the factors impacting clinicians’ adaptation of mHealth [ 24 ]. All interviews were conducted in-person with the participants. Prior to conducting the interviews, participants received an information letter explaining the overall goal of the PhD research and this specific study. An oral explanation was also provided where necessary. Informed consent was obtained from each participant in written form, and their participation was voluntary. When confidentiality and privacy could be assured, interviews with patients were conducted in the waiting area of the hospital. Interviews with physicians and executives were conducted at their offices. No monetary compensation was provided to any of the participants. All of the interviews were carried out by a female researcher (author GTA), who is a biomedical engineer and a PhD student with a focus on the design and development of mHealth systems for Sub-Saharan Africa. The researcher has experience and training in various research methodologies, including qualitative study. The interviews were conducted in Amharic and were audio recorded. The audio recordings from the interviews were first transcribed verbatim and then translated to English. No automatic tool was used for transcription. Google Translate was used for translation, and the information was checked manually for correctness. The thematic analysis methodology described by Braun et al [ 32 ] was employed for this study. The author GTA coded the interview transcripts and revised them with the 2 researchers JMA and GLS. NVivo software (QSR International) was used during the data analysis to code and categorize the data and to create a thematic framework. To report the study, we used the COREQ (Consolidated Criteria for Reporting Qualitative Research) checklist [ 33 ], which has been provided in Multimedia Appendix 4 .
Ethical Considerations
Ethical clearance was obtained from the KU Leuven Social and Societal Ethics Committee (SMEC) (G-2022-5491-R3(MIN)) and from the Jimma University Institute of Health Institutional Review Board (IRB) (JUIH/IRB/311/23).
A total of 48 interviewees participated in the one-to-one interviews. In the patient group, 17 patients (10 men and 7 women) were interviewed. Eight additional patients were approached, but they declined to be interviewed as they were in a hurry, were not willing to be interviewed, or were already frustrated with the system. The mean patient age was 33.9 years, and the mean interview duration was 6.25 minutes.
In the physician group, 19 physicians (12 men and 7 women) were interviewed. Six additional physicians were approached, but they declined to be interviewed as they had hectic schedules. The physicians included in the study were general practitioners who worked in chronic disease OPDs and had an average of 5 years of experience. In this group of individuals, the mean interview duration was 15.7 minutes.
In the health care executive group, 12 health care executives (10 men and 2 women) were interviewed. Owing to a scheduling conflict, 1 additional executive declined to be interviewed. In this group, the mean interview duration was 19.34 minutes. The executives had a variety of positions, including directors in the country’s health minister’s office, directors in city health administrative offices at the zonal and regional levels, hospital chief clinical officers, and ICT heads at hospitals. Owing to the limited number of key respondents in the health care executive group, the number of participants in our study was restricted. Nonetheless, we ensured that the interview process was comprehensive enough to address all crucial aspects, and we included all key informants while also exploring any new viewpoints that emerged.
The total sample size was established based on data saturation, which occurs when new data no longer provide additional perspectives or insights after a certain point. In this study, data saturation was reached following 48 interviews (17 patients, 19 physicians, and 12 health care executives), indicating that an adequate sample size had been achieved. Table 1 provides an overview of the interview characteristics.
a N/A: not applicable.
b ICT: information and communication technology.
A total of 137 determinants for using mHealth systems in Sub-Saharan Africa were identified from the perspectives of patients, physicians, and health care executives. Of the 137 determinants, 68 were barriers and 69 were enablers. Themes were derived from the data. Further categorization of these aspects in the study resulted in the identification of 3 major categories: organizational and policy, social and personal, and technical and material. These categories were based on the consolidated framework of the factors impacting clinicians’ adaptation of mHealth [ 24 ], which takes into account the numerous factors influencing adoption of mHealth systems. The organizational and policy factors pertain to health care organizations’ internal workings, workflow, policies, regulations, patient-related factors, and user engagement. The technical and material factors pertain to system design, system usefulness, IT capabilities, compatibility, data management, user experiences, monetary factors, and ease of use. The social and personal factors include personal characteristics, social and cultural factors, and moderating factors.
Perspectives of Patients
Among patients, after a detailed examination of the data, we identified 10 unique factors that could impede progress, which were referred to as barriers, and 8 unique factors that could facilitate progress, which were referred to as enablers. Figure 1 provides a comprehensive list of these barriers and enablers. Patients were assigned a code based on the study area as follows: those from Addis Ababa were coded “AP,” those from Harari were coded “HP,” and those from Jimma were coded “JP.”

Among the 10 barriers hindering the adoption of mHealth systems, 6 were under the technical and material category. These challenges included system design, system usefulness, IT capabilities, compatibility, data management, user experiences, monetary factors, and ease of use. The remaining 4 barriers were under the social and personal category, which included personal characteristics, social and cultural factors, and moderating factors.
The majority of patients reported that they have never used mHealth systems. However, most of them reported that they would use mHealth systems if they had awareness and if they could access these systems in an affordable way.
More than half of the participants had no awareness about mHealth systems and how they could benefit them. However, upon a detailed explanation about mHealth systems and their importance, they reported that they recognize the usefulness of such tools. They reported that they would use these systems if they could get trustable systems and if recommended by their doctors.
Regarding the barriers associated with using mHealth approaches, the most frequently cited theme was a lack of awareness about mHealth systems.
I don't have the information about such things either. Apart from seeing the texts that come to me, I never installed the application and tried nothing. [AP4]
To be honest... I have never heard or seen health practitioners recommending this to me. I have no idea about such systems. [AP6]
I don't know much about that, but I think it is useful for monitoring my diet and sugar levels. [HP3]
The knowledge gap… For example, when I see my friends using such things, I don't know the source of it. And I learn from them, but for example, when I am talking about this idea with my friends with whom I have the same interest like me they ask me from where I get it from. [JP2]
I don't have the information about this. [JP6]
Patients also perceived the fact that mHealth systems are not readily available as a barrier to not using them. They reported that they browse Google or YouTube when they need to obtain information related to health.
I will download some stuff on YouTube. Video… I see…. I am downloading some video. [JP4]
The only thing I've used so far is Walk Exercise. It is by just browsing. [AP2]
The affordability of smart mobile phones, the requirement for a paid subscription, and the high cost of smart systems were identified as economic factors that can impede the adoption of mHealth systems. These factors are believed to create obstacles for individuals who may not have access to the necessary technology or cannot afford the associated costs.
Because this information is from the internet. It is not possible to access the internet if it is not purchased. Again, you can find that if you go to a place with internet. Even if I have a cell phone, it costs money. [HP1]
But the affordability... I can't afford that mobile so I won't use it. [HP1]
But with the systems, the smart ones are a little expensive, so the cost of the sensors is a barrier. [AP6]
A lack of trustworthy mHealth systems is a significant obstacle to their adoption. Patients feared that the information and services provided by these systems may not be based on reliable evidence. This concern arose from the potential harm caused by inaccurate information or ineffective treatments.
I want it to be something secure. First is the issue of medication. Medical information is not something you can just throw away. Therefore, they have a question of credibility. [AP4]
The reason I don't use it is because most of them are not desirable. Because I hear things that are not trustworthy; I won't take advantage of it. [AP5]
The application must be supported by evidence. [JP4]
Inconvenient features (presentation) of mHealth systems were also perceived as an obstacle to the use of these systems.
I think that a lot of data frustrates people. When you read more data, it is like an education. It needs your time. It needs your opinion. Anyone who is not in the health field may not have an interest in such things. [JP2]
The presentation is a biggest barrier... even if it is translated... there are some words that are cultural and from our community language... there is, isn't it... I think there is a small barrier. Medical terms... because it's a bit difficult to how interpret them. [AP6]
Digital illiteracy, which refers to the lack of ability to effectively use digital technologies, such as computers, smartphones, and the internet, is a recognized barrier to the adoption of mHealth technologies. This challenge is believed to limit the ability to take advantage of the benefits provided by mHealth tools.
Lack of skill in using mobile phones. Configuring systems specially in IOS it is also same for android is difficult. Like Entering Personal Details. And because the app won't start without you doing it. [AP6]
I don't know how to use this kind of thing. I don’t have the knowledge of how to use such systems. So, I never used it. [HP4]
Among the 8 enablers facilitating the adoption of mHealth systems, 5 were under the technical and material category and the remaining 3 were under the social and personal category.
Patients with chronic diseases had a need for easy and automated tools for health monitoring.
It's a matter of health. To control my blood sugar level, there are mandatory things that I have to do. So if there are things installed on my phone to help me with this, it helps. [AP2]
I am suffering from hemorrhoids. Some say wash with cold water; Some say to wash with warm water; not to be confused it will be good if there is a tool to use in my phone. [AP3]
One of the things that inspired me to use it was to find out how many calories I burned in a day; It reminds me how much I should move, if I don't move, I will be exposed to other related diseases. It means it has health benefit for myself. [AP6]
It will be very good. I may not always in need to go to the hospital. I am able to adjust myself from that information; Use the medicine on time. Adjusting the food system; doing activities; There are also recommendations. I have arrived to that conclusion. And it's good. And it's important to have. [HP1]
I think it would be helpful to have more of information, especially to monitor my health. [HP4]
I think it makes things easier for us. If I use it, it will be beneficial. The usefulness is very high. [JP1]
Patients recognized the availability of the internet as one of the facilitating factors of the use of mHealth systems as it could help them access such platforms.
At home, I have Wi-Fi, so it's easy. [AP2]
Now there is telephone, there is Internet, there is Wi-Fi, now there is internet even in a pool house, there is even in a tea house. [JP2]
There is a big difference between where there is internet and where there is no internet. Internet is a way to get many new technologies. We have it now more than ever. [JP4]
Another enabler was the perceived usefulness of mHealth as a convenient tool to access health information.
…. And it helps you to be proactive about your health. It means it prevents you from going to the hospital after something happens. [AP6]
Perspectives of Physicians
Among physicians, we identified a total of 54 factors that were perceived to influence the adoption of mHealth systems. Of the 54 factors, 27 were identified as barriers that hinder the use of mHealth systems and 27 were identified as enablers that facilitate their adoption. The study further classified these factors into 3 main categories, namely, organizational and policy, social and personal, and technical and material. Physicians were assigned a code based on the study area as follows: those from Addis Ababa were coded “AD,” those from Harari were coded “HD,” and those from Jimma were coded “JD.”
Specifically, among the 27 identified barriers, 7 were under the organizational and policy category, 11 were under the social and personal category, and 9 were under the technical and material category. Figure 2 displays the obstacles to the use of mHealth systems from the viewpoint of physicians.

Physicians identified the lack of established mHealth systems as the primary reason for not using them. They acknowledged that their lack of exposure to these systems has prevented them from gaining experience in their use.
Actually, there is no such system or application based health care at the organization where I work. [HD3]
For example, a patient comes to us and we ask about the patient's problem, then we ask and investigate to do a case diagnosis, and at the end we write an investigation paper to investigate and send it to the patient. And we give them hard paper. And we have not prepared them in a computerized way. There is none. [HD6]
The main thing is that this type of system does not exist here. [JD2]
According to physicians, certain types of mHealth systems have been implemented in some organizations they work for. However, these systems are often interrupted and lack continuity. Physicians considered the discontinuity of established mHealth systems as one of the key barriers to the effective use of mHealth tools.
Around two years ago, this program was being popularized, but nobody in the middle was using it. It is not waited until we become experts. It was interrupted in the middle. [JD5]
Sometimes, due to the data and various factors, the system encounters some errors. So we will go back to the manual paperwork at that time. Therefore, when we report using a digital system, if there is an interruption, we often go back to paperwork. [HD7]
Another barrier preventing the use of mHealth systems was the required extra time amidst an overloaded work schedule, especially for recommending such systems to patients.
And again, just because there is high patient load here; I don't have that kind of time. It does not allow to say use this or not. As one patient leaves, another enters. There is a load, and it doesn't allow us to have much contact with the patient. We are going to send by diagnosing and treating with what we already have. [AD1]
A further barrier to the adoption of mHealth systems was the lack of physicians’ awareness about mHealth systems for patients. Some physicians reported that they are not well-informed about these systems, and even for their own personal health and wellness, they rely on browsing the internet rather than using stand-alone health systems. This lack of knowledge and personal use can limit their ability to confidently recommend and implement mHealth tools in their practice, which in turn can hinder patient adoption and engagement. To overcome this barrier, there is a need for greater education and training programs for physicians on the benefits and effective use of mHealth systems, as well as efforts to increase physician engagement with these tools to help build their confidence and understanding.
Now, for example, I don't know anything personally, but for example, I don't know an app for diet. Honestly, now, in terms of exercise, I use YouTube downloads even for myself. [AD2]
Some physicians claimed that they have never given these systems any consideration.
From my point of view, there were no situations where we would recommend using this to my patients. Maybe, I have never thought about it. [JD4]
I don't have the knowledge. I mean, I didn't know there was anything like that about mHealth that you just told me about. To tell you the truth, I only found out about Mobile Health Solution today. [AD5]
Another barrier was physicians’ concerns about patients’ mHealth capability. They acknowledged being worried that their patients do not have the necessary skills or access to technology to make the most of mHealth tools.
But as I said, it's not that the applications have problems; As I told you before, I don't think anyone will use it. It just doesn't feel like that to me. [AD1]
Most of them are illiterate. It is uneducated and I don't think they will use this app. [AD5]
As I mentioned earlier, the problem is that the demographics of the patients are too old to use such systems. They may have a little trouble. [AD6]
What I would consider being the biggest obstacle... Most of the chronic follow-ups have a low level of education. So they may find it very difficult to use applications. [AD7]
I think they are less literate and less qualified. Because the majority cannot read a book. So I think that will be like a gap. [JD2]
Physicians mentioned a further obstacle in the adoption of mHealth systems, namely, lack of trustworthy systems, which raises concerns about the potential risks of recommending them to patients.
People with chronic conditions are very bitter, so they search for something to escape. Sometimes there is information that takes you to stop taking medicine. So, this is the side effect of modern digital. It's not even called a limitation. [JD4]
Another barrier was the lack of readily available mHealth systems in the local context.
But it is not prepared at the app level in our country. It is better if we use this application prepared like this. We tell patients that they will find it on Google because it is not set up like that. [AD7]
The first and most important thing that we can't do is we see it from our country's perspective, if we see it like Ethiopia, there are no rich digital applications for that. Not being able to provide us with that information is the number one factor. [HD7]
Most of the time, because those data are based on foreign populations, those findings have nothing to do with the population of our country. [HD1]
Security and data confidentiality concerns were also perceived as barriers to the use of mHealth systems.
I usually log in with my Google account. I have already accepted my Google account. And I have doubts. I am not sure. As I don't have details about the system. I don't know much about server security. Some app says you can accept or not about personal issue when you open an app. It may be exposed. I'm not sure about the data security and confidentiality. [HD4]
Another barrier was the inconvenient features of some mHealth systems. Most mHealth systems that physicians can use do not have an offline option, and many of these systems work online.
The biggest problem is that they are all online. They don't have offline. And you absolutely need data. [HD4]
A lack of reliable internet and electricity was an additional obstacle.
After all, if there is no internet, we cannot get this information. The main obstacle is the internet. Most mHealth applications are internet-based, so information cannot be accessed when the internet is down. [HD7]
Among the 27 enablers that facilitate the adoption of mHealth systems, 14 were under the organizational policy category. These factors pertain to health care organizations’ internal workings, workflow, policies, regulations, patient-related factors, and user engagement. Moreover, 4 enablers were under the personal and social category involving personal characteristics, cultural factors, and moderating factors. Furthermore, 16 enablers were under the technical and material category encompassing mHealth system design, IT capability, compatibility, user experience, data-related factors, ease of use, and monetary aspects. Physicians’ perspectives on factors that facilitate the use of mHealth systems are depicted in Figure 3 .

Physicians perceived usefulness in promoting easy information storage, access, and retrieval as one of the enablers of the use of mHealth systems. Despite limited exposure to these systems, physicians believed that they represent a convenient way to manage patient data, with the advantages of avoiding loss of information and enabling reliable information retrieval.
On the positive side, there is no such thing as loss of information such as manual cards and paper, papers can be torn and lost. Patients can also be abused. But if we use mHealth systems such as EMR, it will not disappear because we will simply be here and send all the investigations. Whether the data is from this year or before, I can check many things about the patient. It makes it easier for me because I have everything I need there. [AD1]
You will not lose the file, it is well recorded. What did they have before? Or what medication were they taking? Even if the patients don't know what medicine they are taking, how much dose they are prescribed, how many times a day they are taking, so I can get a record from this. [AD2]
Therefore, getting reliable information and then delivering that information to the concerned patient is of great importance. Using mHealth in general allows us to get better information and updated information. [HD7]
You will find information in applications in a very easy and understandable manner. There are books in hard copy. Sometimes when you read those hard copies, you don't understand them, when you go with those applications, they are very encouraging because they are easy to understand. [HD3]
Knowledge is not a big deal as it used to be. Knowledge is cheap. Knowledge is what you can find anywhere by Googling. It is a matter of reading and not reading. But everything is up in the air. And it's not like you used to go to the library to look for a book and get a book. Everything is on your phone. You can open and use it even during operation. Whenever you want. It's very easy. [HD4]
Another enabler was the perceived usefulness in reducing workload and improving health care quality. According to physicians, using mHealth systems has the potential to lessen the strain of health care personnel while also raising the standard of care.
The first reason for not providing quality service is the workload and if something reduces that load, if there are supportive things like this, I think the quality will improve. [AD1]
The timing itself. If you have a current patient, what time did she take her medicine? Did she take it or not? She will be evaluated strictly on time. She takes her medicine on time. A professional can't lie if he skips it knowingly or unknowingly. He cannot say that he gave it to her. When you record what you just did, it will record the time. [AD4]
You can treat your patient in an international standard way. [HD4]
Physicians mentioned that mHealth systems allow for better access to health information for patients. Some believed that providing patients with access to various health-related information at their fingertips will empower them.
Using mHealth in general allows to get better information and updated information. Especially when it comes to health. It helps to live a healthy life by getting new information every day. [HD7]
If the patients have it on their hands, I think it will be a daily experience for them too. It will be easily accessible and it will save our time for the patients as well. [HD2]
Our patients, who have been treated, do not come back with any complications. Because they can get health information and monitor theirs case. Because they may be able to get every detail on the system. [HD6]
Another enabler was the need for a chronic disease management support tool. Physicians recognized the potential benefits of digital automated tools for patients having chronic diseases, as consultations and visits to their office alone may not suffice. To promote healthy lifestyle changes and provide necessary support, it is imperative to equip patients with user-friendly tools that can be integrated into their daily routine.
First, when there is a patient like this... there are chronic ones, for example, diabetic, hypertensive, heart failure. Because they need not only medication but also life modification, they may not achieve what we have told them in one day. But everything how to modify their lifestyle detail is there, so when they get access, they can easily remember what we told them and continue their life. Beyond medication, by the way, also cares about their lifestyle. [HD6]
Availability of phones and the internet was also perceived as a facilitator. According to physicians, availability of phones and the internet has tremendously facilitated the adoption of mHealth systems in a variety of ways. First, regardless of location or the time of day, users may readily access health information and services via their mobile phones. Second, health professionals can use digital tools to gather, preserve, and share patient data, which can improve the quality and efficiency of health care services. The increasing use of mobile phones and the internet in Sub-Saharan Africa has created an opportunity to use these platforms to deliver health information and services to individuals who may have limited access to traditional health care services.
This is because there is internet access and broadband, so everyone works connected to the network. Without that, this simple system wouldn't exist. [AD1]
Now, for medical and other purposes, because of this technology, because of the advent of smartphones, the spread of Wi-Fi, the advent of the Internet, I think that it has made everything easier even the medical education. [HD4]
Having a mobile phone and the internet makes things easier. [HD5]
Physicians who have experienced mHealth systems recognized that these systems are easy to understand and operate. They declared that for users who are familiar with technology, these systems are easy to use.
So you need to know how to access the systems. They are mostly easy. There is nothing difficult unless you are someone who is not familiar with technology to use it. You can search. You can log in and access what you want. I don't have anyone who says it's a challenge. [AD6]
Perspectives of Health Care Executives
Among health care executives, we identified 65 factors that were perceived to influence the adoption of mHealth systems. Of these 65 factors, 31 were classified as barriers and the remaining 34 were classified as enablers. Further categorization of these aspects in the study resulted in the identification of 3 major categories: organizational and policy, social and personal, and technical and material. Health care executives were assigned a code based on the study area as follows: those from Addis Ababa were coded “AA,” those from Harari were coded “HA,” and those from Jimma were coded “JA.”
Among the 31 barriers, 14 were under the organizational and policy category involving elements like the internal working environment of health care organizations, workflow-related challenges, policies and regulations, patient-related factors, and user engagement issues. Moreover, 6 barriers were under the social and personal category involving aspects like social and cultural norms, personal traits, and moderating factors. Furthermore, 11 barriers were under the technical and material category involving difficulties with usefulness, IT capability, compatibility, data-related factors, user experiences, financial factors, and ease of use of mHealth systems. Health care executives’ viewpoints on obstacles to the use of mHealth systems are presented in Figure 4 .

From the perspectives of executives, one of the challenges of implementing mHealth systems in Sub-Saharan Africa is the availability of competing priorities alongside digitalization in the health sector. There are competing demands for resources and attention, such as investing in health care infrastructure, improving health care workforce capacity, and addressing immediate health needs.
We are facing multiple health challenges, including infectious diseases as well as non-communicable diseases like diabetes and hypertension. Additionally, the health sector faces critical issues such as inadequate infrastructure, a shortage of skilled healthcare workers, and limited financial resources. Because there are competing priority areas in the sector that require money. From all of them, it is assigned to this sector and these are taken as a challenge not to work completely with hands. [AA5]
High initial investment required for mHealth technologies was also perceived as a barrier by executives. The cost of implementing mHealth systems includes not only the purchase of hardware and software, but also the cost of training health care workers, adapting existing health care workflows, and establishing new data management and privacy protocols.
As a problem in supply, mHealth technology is expensive. Not being able to avail of all of them is an issue. [HA3]
These start-ups require financing. Although the return is high, the initial investment is also high. mHealth activities require so much investment. [JA2]
Another barrier was that some donor-initiated mHealth systems previously implemented in health care facilities lack government takeover plans after contract expiry. These mHealth systems involving donor support do not have clear take over and exit strategies for ensuring sustainability of the projects.
A project has a lifecycle. It comes up with a project by donors and be started that way.. It won't be owned when it is done. It will not be owned by the government. [AA34]
Skill gap in basic computer literacy was also perceived as a barrier. These skill gaps can be partly attributed to limited exposure or access to digital devices such as computers.
Computer access is limited. The smaller the access, the less likely it is to use mHealth activities. So there is an obvious skill gap. So does the professional. [JA2]
Another barrier was inefficient use of technology.
Efficiently manipulating those technologies if we had them; Proper use of data; One of the challenges is not using technologies properly. We should use them properly and take the appropriate value from them. [AA5]
The absence of individual patient–focused mHealth system implementation was perceived as another barrier to the adoption and implementation of mHealth systems in health care.
While some health care facilities have implemented mHealth initiatives, these initiatives are more focused on the institution rather than the individual patient.
The one that we are using on ART is not to be used by the individual patients. It is an application more with professionals on the periphery than with patients. [JA2]
A further barrier was that implemented mHealth systems lack interoperability and full digitalization. Although attempts to implement mHealth are sparse in health care facilities, lessons can be borrowed from implementation challenges in other areas, such as electronic medical records (EMRs). Some facilities have deployed EMR systems. EMR systems are not fully digitized, with most of them involving a combination of manual and digital systems. Some health care executives also reported that due to mismatch or lack of integration between some medical devices, they are unable to deploy fully digital systems.
There is a lot of fragmented stuff. [AA34]
It is half and half... It is only for reporting, but to make our work more active, it is very good if the facility is fully digital and the delivery points pass through the system through the network. [HA1]
Interoperability is not yet implemented. The two systems are not interoperable. The interoperability is being tested for the country. [JA1]
We have implemented about 80% of the Laboratory Information System (LIS) in our hospital. [JA2]
Another barrier was the difficulty of staff to quickly and easily adapt to mHealth systems.
First of all, sometimes when new things come, there are problems of getting used to that digital thing quickly and not keeping up with it. [JA1]
Another barrier was the lack of awareness among staff members. Going fully digital requires a great deal of work to create awareness, as mHealth technologies are relatively new in the region and many health care workers may not be familiar with them.
As a challenge, we still need a lot of attention for technology in general by the government. We are still in the early stages of our own user experience. [AA2]
There is an opportunity created by technology. However, creating awareness of the work at all levels, from the leadership to health institutions or to the community should be done. Therefore, one of the biggest tasks is to make the awareness. From top to bottom, the importance needs to be well inculcated. This is the lack of awareness of the decision makers from the community level to the top level. [AA5]
The above issue is further exacerbated by the fact that the barrier is related with staff’s reluctance to transition from traditional to digital systems. This lack of awareness and knowledge can lead to resistance or hesitancy in adopting mHealth systems, even if they have the potential to improve patient outcomes and operational efficiency. Health care staff may be unsure of how to use mHealth tools and systems, or they may not understand the benefits of using them.
People who are used to paper work often don't want to be told that we are going to do digital work. [JA2]
The biggest thing I have seen is that there is a problem of commitment. It means that it is very challenging for a person to leave what he used to and come to something new. [JA3]
Among the 34 factors that facilitate the adoption of mHealth systems, 14 were under the organizational and policy category. These factors pertain to health care organizations’ internal workings, workflow, policies, regulations, patient-related factors, and user engagement. Moreover, 4 enablers were under the personal and social category involving personal characteristics, cultural factors, and moderating factors. Additionally, 16 enablers were under the technical and material category encompassing mHealth system design, IT capability, compatibility, user experiences, data-related factors, ease of use, and monetary aspects. Health care executives’ viewpoints on enablers of the use of mHealth systems are presented in Figure 5 .

From the perspectives of executives, the health ministry’s plan to digitalize the health care system is one of the main facilitators or enablers of the use of mHealth systems.
There is a direction according to the government. To use such technologies in most cases; It is for online use. The ministry itself has a strategic plan. To digitalize the healthcare system. It is a priority. [AA1]
The executives emphasized that the plan is not just a matter of execution but also of giving priority and actively pursuing it.
And now technology is making a big contribution to the health sector. And the ministry understands what a great advantage we have; Departments in the Ministry of Health are working with great initiative using mobile technology. [AA5]
Another factor that enables the implementation of mHealth systems is the existence of governance frameworks. Such frameworks were nonexistent a few years ago. However, now, in order to regulate and promote the adoption of mHealth systems, the health ministry has developed a framework that is currently being deployed. Furthermore, a dedicated directorate office has been established to oversee and manage the adoption and implementation of mHealth systems.
Therefore, it is mandatory to create favorable conditions. Facilitating conditions on the ground such as governance frameworks are required. We are working on it. Standards guidelines are required. In addition to this, data standards have also been developed. Now, for example, there are disease codes. A standardized health data access policy has been developed. All these guides the mobile health and govern mHealth as a whole. [AA5]
Now, for example, during the time of Covid, There were mandatory situations to initiate telehealth teleconsultation, but if you ask how it works, there was nothing. But now, there is this direction at the level of the Ministry of Health. They have a directorate office. [JA2]
Another enabler is the recognition that digitalization is crucial for the survival of the heavily burdened health care system in Sub-Saharan Africa. Hospital executives strongly believed that the failure to digitalize the entire health care system within the facility will ultimately lead to its downfall.
But now, considering the complexity of the treatment and the number of patients we see, the staff is now demanding digital solutions. It is understood that we cannot survive if we do not digitize. We have to digitize the entire operation of the hospital. As I said before, it is a matter of survival. It is a hospital where three thousand four thousand people come and go every day. We have 250,000 to 300,000 outpatients per year. We treat about 20000 people. About 170,000 to 180,000 people will come for emergency. We perform surgery on 15000 people. So this process it is huge process. If this process is not digitized, we cannot provide a smooth service. Because it is causing problems for the patient. As a hospital, we have an assessment that it is increasing the number of deaths. [JA2]
According to the executives, another enabler is efforts made toward maximizing the necessary infrastructure provision required for the implementation of mHealth systems. Executives at all levels within the organization realized the importance of providing the required infrastructure, such as ICT and hardware or software resources, to support the deployment of mHealth systems.
In terms of infrastructure... the main thing for digitalization is the internet. They have been given internet access in all nine districts. In terms of computers, they have computers. All adequate internet access to the DHIS health information system, capable computers, and PCs are available at all health centers in the district. [HA2]
For example, they can be computers. Servers. It is not directly from the office but it is fulfilled by different partners as they work together with us. [HA3]
Along with training, tablets are distributed along with resources such as tablets in areas where they are needed. [JA1]
We have invested a lot in infrastructure. Especially our hospital as a health institute has a large ICT infrastructure. We deployed computers. We are working on servers and databases. We trained people and experts for that purpose... It is itself strategically supported and supported by infrastructure. [JA2]
Another enabler is the growing societal familiarity with digital technologies, including social media and financial systems. As more individuals become comfortable with using digital technologies in their daily lives, they may also be more open to using mHealth systems.
At the same time, the opportunity is also very profitable because the number of users of social media is increasing from time to time. [HA3]
Mobile is now used by many people for money transfer. A lot of things... even if a mHealth system doesn't expand, in the finances... a lot... you sit at home and pay. You can withdraw without an ATM machine. It's simple, a person in finance has experience elsewhere. Mobile is now used by many people for money transfers. It is one exposure to general digital systems. [JA2]
The abundance of educated manpower specialized in technology was also perceived as an enabling factor for the adoption of mHealth systems in Sub-Saharan Africa. With a growing pool of technology professionals in the region, there is a greater capacity to develop and implement mHealth solutions that are tailored to the specific needs of the region. This includes the development of innovative technologies, such as mHealth systems and telemedicine platforms, which can improve access to health care services and support patient care. In addition, the presence of a skilled technology workforce can support the deployment, maintenance, and troubleshooting of mHealth systems, which can improve the overall reliability and sustainability of these systems.
… there are many educated young people who can do a lot of creative work; Universities have expanded significantly. [AA2]
… Because educational institutions at the national level can easily produce graduates who can easily design and develop these emerging technology applications. [AA5]
We also have an ICT director with us. We have teams working on software development. So, as a university, as a health institute, as a medical center, we are doing this work. Second, we are building human capacity. Many students are studying. Despite the quality, I think we have that capacity human power. [JA2]
Executives perceived that mHealth solutions are capable of reaching remote and underserved areas where traditional health care services are not readily available, which is a significant enabler for the adoption of mHealth systems in Sub-Saharan Africa. Furthermore, mHealth solutions were thought to aid in overcoming the scarcity of health care personnel by providing remote consultation, training, and education to health care workers, as well as assisting in the delivery of health care services in places with limited resources.
In terms of accessibility, the technology is generally accessible to all communities. The community of our country is located in a very remote place and access to health facilities is very limited. Therefore, mobile technology can be used to make these sections of society that are accessible at different distances easily accessible. Secondly, as mentioned, we have a shortage of health professionals. It is very important to make the service available remotely even if our experts are very limited. From this perspective, it is very important for a society like Ethiopia where there is a shortage of health professionals and the most accessible health facilities are few. [AA5]
Executives perceived mHealth solutions as useful tools for enhancing health care service quality, which is a significant enabler for the adoption of mHealth systems in the region. Health care providers can improve the quality and efficiency of health care services by embracing mHealth technologies, such as electronic health records, clinical decision support systems, and telemedicine platforms. Real-time data collection, monitoring, and analysis enabled by mHealth technologies can also influence evidence-based decision-making and assist health care providers in providing fast and accurate diagnoses and treatment plans.
For example, the patient can take advice without coming to the facility. Alerts can go be sent to him. You will find a lot of information. It means that they will not be abused by looking for their doctors. And it generally makes things easier. [AA1]
It's easy. It's very simple. It makes it easier. It will be easy for everything in time and for the number of people. So it is very good if we use and serve. It is from two sides. Client side and provider side. It also reduces other errors. Another thing is that it reduces time. So it's very good. [HA1]
It will help us gain efficiency. As mentioned earlier, efficiency gains for the health care system are linked to access, mortality, and quality. [JA2]
Another enabler perceived by executives is the availability of mobile phones and the internet. The increasing availability of mobile phones and the internet in Sub-Saharan Africa has created an opportunity to use these platforms to deliver health information and services to individuals who may have limited access to traditional health care services.
The fact that the majority of the society is using mobile technology gives the ministry a great opportunity to implement the system. Second, mobile accessibility is expanding. In Ethiopia, it is said that quite a large number of people have mobile phones in their hands. Therefore, the service can be accessed without coming to the health facility. [AA5]
For example, if you visit the OPD in a hospital, you will find very few people without a smartphone. If you want to buy a laptop and buy a tablet, It is easy. It is available. [JA2]
The overlapping barriers and enablers among the various stakeholders are summarized in Tables 2 and 3 , respectively.
a mHealth: mobile health.
Principal Findings
The barriers and enablers of the implementation of mHealth solutions in Sub-Saharan Africa were identified and explored in detail in this study. All interviewees (patients, physicians, and health care executives) recognized the potential benefits of mHealth. Several overlapping barriers and enablers were identified among the 3 participant groups.
Lack of awareness about mHealth solutions was highlighted as a common barrier to implementing mHealth systems by patients and physicians. They claimed that it was preventing them from experiencing and using mHealth services. They emphasized the importance of raising awareness among stakeholders. Developers and advocates of mHealth solutions must give outreach and education efforts top priority in order to overcome these issues and increase public knowledge of the potential advantages of these solutions. This might entail collaborations with health care institutions, neighborhood-based outreach initiatives, and population-specific marketing plans. Additionally, in order for health care professionals to use mHealth solutions efficiently and explain the advantages to their patients, they need to receive proper training and support. Finally, overcoming cultural barriers will call for sensitivity to the distinctive cultural perspectives and beliefs of various populations, as well as the customization of outreach and education initiatives [ 11 , 34 ].
Another overlapping challenge noted by patients and physicians is digital illiteracy, which refers to a lack of competency or expertise in using digital technologies, such as computers, the internet, and other digital devices or tools. The good news is that an improving literacy level in the society was also viewed as a facilitator by patients and clinicians. According to physicians, the younger generation’s strong digital literacy level is a tremendous opportunity to leverage and apply mHealth systems. The perspective of executives that supports this view is their observation that society is becoming increasingly accustomed to digital technologies, including social media and financial applications. A study involving cancer survivors reported that low digital literacy may hinder information acquisition and technology-enabled cancer care. The study recommended that digital interventions should be adaptable to varying levels of digital health literacy. Policymakers in health care should acknowledge digital disparities and create targeted initiatives to narrow the digital divide while also meeting the pressing demand for the digitization of health care services [ 25 ]. Using digital health information resources and engaging in digital interactions with health care providers offer significant advantages, holding the potential to enhance the efficiency, quality, and accessibility of health care systems, all while empowering patients [ 26 , 35 ].
Another hindrance mentioned is the lack of incorporation of local languages and contextual factors, such as demography, culture, and population, in mHealth systems. Physicians reported that while they are willing to use mHealth systems developed in foreign languages, they prefer those available in the local language. In contrast, all patients interviewed expressed a preference for mHealth systems that incorporate one or more local languages. Studies have also reported the positive impact of user-centric design and local contextualization of mHealth approaches for improved uptake [ 36 , 37 ].
The challenge in engaging patients for accessing diverse patient populations for education or engagement remains an issue. The study by Martin [ 38 ] described barriers for patient engagement, including literacy, access to hard-wired technologies, and understanding of an increasingly complex network of medical care. Developers of mHealth systems need to concentrate more on patient-centered design, involve users in the development process, and work to deliver a customized user experience in order to overcome these difficulties. This can make mHealth systems more usable, effective, and accessible for patients, which will ultimately improve patient outcomes. Additionally, by educating patients on the use of mHealth systems, offering support for their use, and highlighting the advantages of these systems for patient care, health care organizations and providers can encourage patients to use them.
Aside from not being aware of mHealth systems, those who have been exposed to the technology are concerned about the availability of trustworthy systems. Because health is a sensitive issue, patients mentioned that if doctors recommend it during their follow-up, they could use it. However, the majority of doctors said that they had never recommended such systems to their patients. This is due to 2 major reasons. First, physicians have little expertise with mHealth systems, which limits their capacity to use them. Second, because of a lack of understanding of patient-focused mHealth systems, physicians are often unaware of mHealth systems that they could recommend to their patients. According to recent research conducted in developed countries, the findings indicate that health care professionals do not endorse the use of mHealth systems to their patients [ 39 ]. Nonetheless, the aforementioned study revealed that while health care professionals do not recommend mHealth systems to their patients, they do inform them about the existence of these systems should they express a desire to use them. In contrast to the notion that health care professionals solely remind their patients about the availability of mHealth systems, the findings of this study suggest that physicians harbor a degree of skepticism regarding the ability of their patients, particularly those who are elderly or possess limited education, to effectively use such technologies. Consequently, these physicians generally do not recommend mHealth systems to individuals having chronic diseases. The other reason, as perceived by physicians, is that they could not find trustworthy health care systems to prescribe to patients confidently. The lack of adequate regulation and control is one of the key reasons for the unreliability of mHealth systems. Numerous systems make efficacy claims without any supporting data from the scientific community [ 21 , 40 ]. This may cause consumers to rely on incorrect or partial information, which could be harmful to their health.
Even though security issues were mentioned as common barriers by all the stakeholders in the study, some respondents also expressed different beliefs regarding data confidentiality and security. Some of the participants in both patient and physician groups were not worried about security. Some believed that the system they are using has security features, and some mentioned that they are not worried at all whether the system is secured. However, some patients mentioned that they are not sure whether data confidentiality will be maintained during the use of such systems and said that they are skeptical about it. They recommended better security features while designing such systems. The potential for data privacy violations is another problem. Some systems collect users’ private health information but fail to adequately safeguard it from unauthorized access by outside parties. Users may experience serious repercussions as a result, such as discrimination and identity theft. It is crucial to set precise standards and guidelines for mHealth systems in order to address these problems. Researchers have also suggested ways to underpin a radical rethinking of information privacy, confidentiality, security, and integrity to unlock the potential of mHealth and ensure verified access to often sensitive data [ 41 ]. Given the rapid pace of technological development, the protection of personal health information stored in mHealth solutions is an important consideration. In order to protect people’s privacy, it is essential to ensure the confidentiality of such data. This is especially important in light of laws like the Global Data Protection Regulation (GDPR) [ 42 , 43 ].
All patients, physicians, and health care executives perceived the widespread availability of the internet, mobile phones, and digital devices as creating a favorable opportunity to integrate mHealth systems. Though the Sub-Saharan African region is way behind other regions in employing mHealth activities, there is now a high level of commitment and a strong strategic plan to benefit from this opportunity. Furthermore, there is a high need for an individualized patient-focused mHealth system for managing chronic conditions such as diabetes and hypertension. A study conducted by Doyle et al [ 27 ] concluded that implementing mobile phone–based interventions is viable; however, there is a risk of exacerbating inequities, particularly if these interventions necessitate internet access. Internet-based mHealth approaches should carefully assess potential risks for participants and include skill-building sessions on secure internet and phone usage.
The Sub-Saharan African region’s population is growing at an alarming rate, and the region is facing the double burden of communicable and noncommunicable diseases. As a result of these, access to high-quality health care systems may be jeopardized. To make problems worse, social distancing necessitated by the COVID-19 outbreak made face-to-face consulting and care-taking difficult in many cases. According to health care executives, integrating digitalization in health care systems is becoming increasingly important for the health care sector, which is under high pressure. Sub-Saharan Africa faces numerous health care challenges, including limited access to health care services, inadequate health care infrastructure, and a shortage of health care professionals. The COVID-19 pandemic has also highlighted the need for mHealth solutions that can help provide care remotely [ 44 ].
Digitalization can help address these challenges by improving access to health care services, enabling remote consultation and telemedicine, and improving the accuracy and completeness of patient records. This can help reduce the burden on health care facilities and make it easier for patients to access care, especially in remote or underserved areas. Physicians believed that employing a mHealth system can help to reduce workload and also help to achieve quality health care services. Other scholarly works have also affirmed that digital technologies contribute to improved efficiency and the streamlining of health care services. The potential of mHealth to provide health information to patients and the accessibility of patient data through EHRs make the situation easier for health care practitioners, reducing administrative tasks and enhancing care coordination [ 10 , 45 , 46 ].
According to patients, a lack of easily available mHealth systems is also a hindrance. This viewpoint was also shared by both physicians and executives. Physicians reported some experience in using mHealth systems such as reference guidelines, gestational age calculators, etc. These mHealth systems, however, lack local context. Furthermore, physicians reported that they were unable to find standalone systems in the form of apps that would allow them easy access to vital information to update their knowledge and fill knowledge gaps. Despite the fact that the integration of mHealth in health care facilities is not widespread, it is possible to draw on the experiences and obstacles encountered during the implementation of other technologies, such as EMR systems. EMR systems deployed in some health facilities have a lot of challenges for use to the full extent possible. However, owing to discontinuity and nonmaturity of the systems, they are not fully functional and some of them have stopped working. This is also perceived as another hindering factor. Despite efforts to launch mHealth systems, health care executives indicated that most launched mHealth systems so far are for health care personnel. Governments, health care organizations, and technology firms must collaborate to develop infrastructure, raise money, lower regulatory barriers, and encourage user adoption of mHealth systems in order to address these issues. By doing this, we can guarantee that mHealth systems are made more accessible to individuals around the world and contribute to improving access to health care services. A body of literature indicated that health care providers face challenges in improving digital health applications, and collaborating with stakeholders for value creation remains a significant obstacle. Despite these challenges, involving stakeholders and addressing their needs could promote the sustainable development of digital health services [ 47 ].
According to reports from executive stakeholders, many attempts were made to implement mHealth systems in various health care facilities, but most of them were unsuccessful due to a range of issues such as inadequate government ownership, insufficient budget for recurring operational costs, lack of training, insufficient infrastructure, and lack of interoperability. A recent systematic review of systematic reviews indicated that infrastructure, lack of equipment, and technology gaps together accounted for barriers to the use of mHealth systems in developing countries [ 48 ]. Despite these challenges, there were several valuable lessons, such as the need for allocating a sufficient operational budget, proper takeover of projects, and engaging well-matured systems through learning from failed projects. As a result, there is now a renewed focus on digitalization in health care, and mHealth solutions are viewed as valuable tools for addressing complex health care challenges from multiple angles.
A multitude of analogous studies have examined the obstacles hindering the adoption of mHealth systems within health care facilities. Many studies reported lack of knowledge of mHealth systems, infrastructure, lack of equipment, and technology gaps as barriers, and identified the ubiquity of smartphones and apps as a facilitator, especially for the younger generation [ 39 , 48 ]. Absence of a national policy on mHealth, poor internet connectivity, and shortage of electricity were also highlighted as important inhibiting factors for mHealth adoption in low and middle income countries [ 49 ]. The perceived usefulness of mHealth approaches among patients has been reported [ 50 ]. Some of the enablers identified in this study were introduced by previous studies, such as perceived usefulness in improving health service quality and perceived ease of use [ 51 ].
One of the common barriers as perceived by all the stakeholders is security concerns. The results of this study are consistent with the findings of other studies reporting that mHealth app users have security and privacy concerns. The study reported that lack of security features in mHealth apps was a barrier for adoption [ 52 , 53 ].
In the literature, knowledge and limited literacy were presented as barriers for mHealth adoption. However, in this study, an increasing literacy level of the society was identified as one of the enablers. This same factor was reported as a barrier in another similar study [ 53 ]. Consistent with the results in this study, a prior study reported that limited digital literacy and the unreliability of health information from mHealth platforms are barriers for mHealth use [ 25 ].
Developing mHealth solutions that are suited to the local environment, raising awareness, offering adequate training, assigning adequate funding, incorporating various security features, and putting in place and implementing simple governance principles are a few ways to tackle the challenges.
This study is the first of its kind to provide a comprehensive exploration of the barriers and enablers of the use of mHealth systems in Sub-Saharan Africa, with a focus on the multi-level and multi-actor perspectives of patients, physicians, and health care executives. The barriers identified in this study highlight the challenges and limitations that must be overcome in order to successfully implement mHealth systems in Sub-Saharan Africa. Understanding these barriers can help inform the design and implementation of mHealth solutions that are tailored to the specific needs and context of the region. Addressing these challenges necessitates increased investment in mHealth infrastructure, health care worker training programs, and financial sustainability methods for mHealth initiatives. If these barriers are effectively addressed, it may become possible to overcome the challenges associated with implementing mHealth systems in the region, thereby unlocking the full potential of mHealth to enhance health care outcomes for patients, health care providers, and policy makers. The identified enablers will be further investigated and considered in the design of future mHealth platforms for studies in Sub-Saharan Africa.
Limitations of the Study
This study is subject to certain limitations, notably the relatively modest sample size, which may restrict the extent to which the findings can be extrapolated to the broader population. Nonetheless, efforts were made to address this concern by selectively recruiting participants from diverse age cohorts and employment backgrounds. Other limitations include a small patient population (the disease may have influenced the patients’ perceptions). Future investigations could benefit from expanding the sample size to enhance the representativeness of the outcomes. Another potential limitation of this study is the absence of triangulation of results. However, steps were taken to mitigate this shortcoming by collecting sufficient data to comprehensively comprehend the phenomenon, thereby enhancing the validity and reliability of the findings.
The use of mHealth systems in Sub-Saharan Africa has been hindered by a range of factors and has also been facilitated by various enabling factors. Patients, physicians, and health care executives identified common barriers and enablers to the uptake of mHealth systems. The identified barriers must be actively mitigated through the involvement of all relevant stakeholders. Despite the existing barriers, the findings of this study provide a promising outlook for the implementation of mHealth systems in Sub-Saharan Africa. The study highlights the numerous opportunities that exist for the successful integration of mHealth systems into the region’s health care systems. To ensure maximum uptake, it is crucial to adopt a user-centered design approach in mHealth system design and development.
The results of this study have important implications for both mHealth system design and policy-making. The identified barriers and enablers can serve as a guide for the design of mHealth systems that are tailored to meet the needs and preferences of patients, physicians, and health care executives. Additionally, the study findings can inform policy makers on the necessary steps to be taken to facilitate the successful integration of mHealth systems into health care systems in Sub-Saharan Africa.
In conclusion, some of the barriers and enablers of the uptake of mHealth systems in Sub-Saharan Africa are interconnected and require the active involvement of all stakeholders to be addressed. The study provides valuable insights that can inform mHealth system design and policy-making, with the aim of facilitating the successful integration of mHealth systems into health care systems in Sub-Saharan Africa.
Acknowledgments
We extend our gratitude to the Network for Advancement of Sustainable Capacity in Education and Research in Ethiopia (NASCERE). We would also like to thank Eyerusalem Tadese for assisting in interview transcription.
Conflicts of Interest
None declared.
Interview guide for patients.
Interview guide for physicians.
Interview guide for health care executives.
COREQ (Consolidated Criteria for Reporting Qualitative Research) checklist.
- mHealth: use of mobile wireless technologies for public health. World Health Organization. URL: https://tinyurl.com/yc82pnty [accessed 2024-03-05]
- eHealth: Report by the Secretariat. World Health Organization. URL: https://tinyurl.com/ya3xwjua [accessed 2024-03-05]
- mHealth: Use of appropriate digital technologies for public health. World Health Organization. URL: https://apps.who.int/gb/ebwha/pdf_files/EB142/B142_20-en.pdf [accessed 2024-03-05]
- mHealth: New horizons for health through mobile technologies. World Health Organization. URL: https://iris.who.int/bitstream/handle/10665/44607/9789241564250_eng.pdf [accessed 2024-03-05]
- Bradway M, Carrion C, Vallespin B, Saadatfard O, Puigdomènech E, Espallargues M, et al. mHealth Assessment: Conceptualization of a Global Framework. JMIR Mhealth Uhealth. May 02, 2017;5(5):e60. [ FREE Full text ] [ CrossRef ] [ Medline ]
- STOA Workshop eHealth in Europe: Reality and challenges ahead. European Parliament. URL: https://www.europarl.europa.eu/cmsdata/149015/Booklet.pdf [accessed 2024-03-05]
- United States Mhealth App Market Report 2021: Market is Projected to Grow at a CAGR of 26.15% to Reach $5.139 Billion by 2026 from $1.011 Billion in 2019. GlobeNewswire. URL: https://tinyurl.com/36f2yz4v [accessed 2023-04-30]
- mHealth in an mWorld How mobile technology is transforming health care. Deloitte Center for Health Solutions. URL: https://tinyurl.com/mtpk3npk [accessed 2024-03-05]
- Alghamdi M, Gashgari H, Househ M. A Systematic Review of Mobile Health Technology Use in Developing Countries. Stud Health Technol Inform. 2015;213:223-226. [ Medline ]
- Medhanyie AA, Little A, Yebyo H, Spigt M, Tadesse K, Blanco R, et al. Health workers' experiences, barriers, preferences and motivating factors in using mHealth forms in Ethiopia. Hum Resour Health. Jan 15, 2015;13(1):2. [ FREE Full text ] [ CrossRef ] [ Medline ]
- O’Connor Y, O’Connor S, Heavin C, Gallagher J, O’Donoghue J. Chapter 10 - Sociocultural and Technological Barriers Across all Phases of Implementation for Mobile Health in Developing Countries. In: Al-Jumeily D, Hussain A, Mallucci C, Oliver C, editors. Applied Computing in Medicine and Health A volume in Emerging Topics in Computer Science and Applied Computing. Burlington, MA. Morgan Kaufmann; 2016;212-230.
- The Mobile Economy Sub-Saharan Africa 2021. GSM Association. URL: https://tinyurl.com/yf684tsx [accessed 2024-03-05]
- The mHealth Planning Guide: Key Considerations for Integrating Mobile Technology into Health Programs. K4Health. URL: https://pdf.usaid.gov/pdf_docs/PA00MDPV.pdf [accessed 2024-05-03]
- Latif S, Rana R, Qadir J, Ali A, Imran MA, Younis MS. Mobile Health in the Developing World: Review of Literature and Lessons From a Case Study. IEEE Access. 2017;5:11540-11556. [ CrossRef ]
- Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health. Feb 21, 2014;14:188. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Aboye G, Vande Walle M, Simegn G, Aerts J. Current evidence on the use of mHealth approaches in Sub-Saharan Africa: A scoping review. Health Policy and Technology. Dec 2023;12(4):100806. [ CrossRef ]
- Betjeman TJ, Soghoian SE, Foran MP. mHealth in Sub-Saharan Africa. Int J Telemed Appl. 2013;2013:482324. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sustainable Development. United Nations. URL: https://sdgs.un.org/goals [accessed 2024-03-15]
- Ethiopia - Country Commercial Guide. International Trade Administration. URL: https://www.trade.gov/country-commercial-guides/ethiopia-healthcare [accessed 2024-01-29]
- Yang M, Al Mamun A, Gao J, Rahman MK, Salameh AA, Alam SS. Predicting m-health acceptance from the perspective of unified theory of acceptance and use of technology. Sci Rep. Jan 03, 2024;14(1):339. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Liu Y, Lu X, Zhao G, Li C, Shi J. Adoption of mobile health services using the unified theory of acceptance and use of technology model: Self-efficacy and privacy concerns. Front Psychol. Aug 11, 2022;13:944976. [ CrossRef ] [ Medline ]
- Rahimi B, Nadri H, Lotfnezhad Afshar H, Timpka T. A Systematic Review of the Technology Acceptance Model in Health Informatics. Appl Clin Inform. Jul 15, 2018;9(3):604-634. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jacob C, Sezgin E, Sanchez-Vazquez A, Ivory C. Sociotechnical Factors Affecting Patients' Adoption of Mobile Health Tools: Systematic Literature Review and Narrative Synthesis. JMIR Mhealth Uhealth. May 05, 2022;10(5):e36284. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jacob C, Sanchez-Vazquez A, Ivory C. Understanding Clinicians' Adoption of Mobile Health Tools: A Qualitative Review of the Most Used Frameworks. JMIR Mhealth Uhealth. Jul 06, 2020;8(7):e18072. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Melhem SJ, Nabhani-Gebara S, Kayyali R. Digital Trends, Digital Literacy, and E-Health Engagement Predictors of Breast and Colorectal Cancer Survivors: A Population-Based Cross-Sectional Survey. Int J Environ Res Public Health. Jan 13, 2023;20(2):1472. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Arias López M, Ong BA, Borrat Frigola X, Fernández A, Hicklent RS, Obeles AJT, et al. Digital literacy as a new determinant of health: A scoping review. PLOS Digit Health. Oct 2023;2(10):e0000279. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Doyle AM, Bandason T, Dauya E, McHugh G, Grundy C, Dringus S, et al. Mobile Phone Access and Implications for Digital Health Interventions Among Adolescents and Young Adults in Zimbabwe: Cross-Sectional Survey. JMIR Mhealth Uhealth. Jan 13, 2021;9(1):e21244. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Human Development Index (HDI). United Nations Development Program. URL: https://tinyurl.com/4vhpfhnn [accessed 2024-03-05]
- Nikolopoulou K. What Is Snowball Sampling? Scribbr. URL: https://tinyurl.com/52ndd2p4 [accessed 2023-05-10]
- Semi-Structured Interviews. KnowFife Hub. Mar 2018. URL: https://tinyurl.com/ex5prr8s [accessed 2024-03-05]
- George T. Semi-Structured Interview. Scribbr. URL: https://www.scribbr.com/methodology/semi-structured-interview/ [accessed 2023-05-10]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. Jan 2006;3(2):77-101. [ CrossRef ]
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. Dec 2007;19(6):349-357. [ CrossRef ] [ Medline ]
- Addotey-Delove M, Scott R, Mars M. Review of patients’ perspectives of m-health adoption factors in the developing world. Development of a proposed conceptual framework. Informatics in Medicine Unlocked. 2020;21:100460. [ FREE Full text ] [ CrossRef ]
- Busse TS, Nitsche J, Kernebeck S, Jux C, Weitz J, Ehlers JP, et al. Approaches to Improvement of Digital Health Literacy (eHL) in the Context of Person-Centered Care. Int J Environ Res Public Health. Jul 07, 2022;19(14):8309. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Koumpouros Y. User-Centric Design Methodology for mHealth Apps: The PainApp Paradigm for Chronic Pain. Technologies. Jan 31, 2022;10(1):25. [ CrossRef ]
- Gong E, Gu W, Luo E, Tan L, Donovan J, Sun C, et al. Development and Local Contextualization of Mobile Health Messages for Enhancing Disease Management Among Community-Dwelling Stroke Patients in Rural China: Multimethod Study. JMIR Mhealth Uhealth. Dec 17, 2019;7(12):e15758. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Martin T. Assessing mHealth: opportunities and barriers to patient engagement. J Health Care Poor Underserved. Aug 2012;23(3):935-941. [ CrossRef ] [ Medline ]
- Byambasuren O, Beller E, Hoffmann T, Glasziou P. Barriers to and Facilitators of the Prescription of mHealth Apps in Australian General Practice: Qualitative Study. JMIR Mhealth Uhealth. Jul 30, 2020;8(7):e17447. [ FREE Full text ] [ CrossRef ] [ Medline ]
- The Business Case For Rigorous Evaluation Of Mobile Health Apps. Health Affairs. URL: https://tinyurl.com/56e494ny [accessed 2024-03-05]
- Weiss M, Botha A, Herselman M, Loots G. Blockchain as an enabler for public mHealth solutions in South Africa. 2017. Presented at: 2017 IST-Africa Week Conference (IST-Africa); May 30-June 02, 2017; Windhoek, Namibia. [ CrossRef ]
- Galvin HK, DeMuro PR. Developments in Privacy and Data Ownership in Mobile Health Technologies, 2016-2019. Yearb Med Inform. Aug 2020;29(1):32-43. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hernández-Álvarez L, de Fuentes JM, González-Manzano L, Hernández Encinas L. Privacy-Preserving Sensor-Based Continuous Authentication and User Profiling: A Review. Sensors (Basel). Dec 25, 2020;21(1):92. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gruson D. Controlling Reliability, Interoperability and Security of Mobile Health Solutions. EJIFCC. Jun 2021;32(2):118-123. [ FREE Full text ] [ Medline ]
- Digitalization in Healthcare: Benefits and Challenges. CareCloud. URL: https://tinyurl.com/28zfazyh [accessed 2024-01-30]
- Can digital healthcare solutions reduce clinician workload? siHealth. URL: https://tinyurl.com/tr6dtf7n [accessed 2024-01-30]
- Nipa NS, Alam M, Haque MS. Identifying Relevant Stakeholders in Digital Healthcare. In: Mahmud M, Kaiser MS, Kasabov N, Iftekharuddin K, Zhong N, editors. Applied Intelligence and Informatics. AII 2021. Communications in Computer and Information Science, vol 1435. Cham. Springer; 2021;349-357.
- Kruse C, Betancourt J, Ortiz S, Valdes Luna SM, Bamrah IK, Segovia N. Barriers to the Use of Mobile Health in Improving Health Outcomes in Developing Countries: Systematic Review. J Med Internet Res. Oct 09, 2019;21(10):e13263. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Aamir J, Ali SM, Kamel Boulos MN, Anjum N, Ishaq M. Enablers and inhibitors: A review of the situation regarding mHealth adoption in low- and middle-income countries. Health Policy and Technology. Mar 2018;7(1):88-97. [ CrossRef ]
- Place J, Farret A, Del Favero S, Bruttomesso D, Renard E. Assessment of Patient Perceptions About Web Telemonitoring Applied to Artificial Pancreas Use at Home. J Diabetes Sci Technol. Mar 02, 2014;8(2):225-229. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Said GRE. Factors Affecting mHealth Technology Adoption in Developing Countries: The Case of Egypt. Computers. Dec 28, 2022;12(1):9. [ CrossRef ]
- Zhou L, Bao J, Watzlaf V, Parmanto B. Barriers to and Facilitators of the Use of Mobile Health Apps From a Security Perspective: Mixed-Methods Study. JMIR Mhealth Uhealth. Apr 16, 2019;7(4):e11223. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zakerabasali S, Ayyoubzadeh SM, Baniasadi T, Yazdani A, Abhari S. Mobile Health Technology and Healthcare Providers: Systemic Barriers to Adoption. Healthc Inform Res. Oct 2021;27(4):267-278. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by A Mavragani; submitted 28.06.23; peer-reviewed by L Guo, H Pilabré; comments to author 11.10.23; revised version received 01.11.23; accepted 13.02.24; published 27.03.24.
©Genet Tadese Aboye, Gizeaddis Lamesgin Simegn, Jean-Marie Aerts. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 27.03.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

IMAGES
VIDEO
COMMENTS
Qualitative research methods. Each of the research approaches involve using one or more data collection methods.These are some of the most common qualitative methods: Observations: recording what you have seen, heard, or encountered in detailed field notes. Interviews: personally asking people questions in one-on-one conversations. Focus groups: asking questions and generating discussion among ...
Qualitative Research. Qualitative research is a type of research methodology that focuses on exploring and understanding people's beliefs, attitudes, behaviors, and experiences through the collection and analysis of non-numerical data. It seeks to answer research questions through the examination of subjective data, such as interviews, focus ...
Qualitative research is the naturalistic study of social meanings and processes, using interviews, observations, and the analysis of texts and images. In contrast to quantitative researchers, whose statistical methods enable broad generalizations about populations (for example, comparisons of the percentages of U.S. demographic groups who vote in particular ways), qualitative researchers use ...
Qualitative research is a type of research that aims to gather and analyse non-numerical (descriptive) data in order to gain an understanding of individuals' social reality, including understanding their attitudes, beliefs, and motivation. This type of research typically involves in-depth interviews, focus groups, or observations in order to collect data that is rich in detail and context.
While many books and articles guide various qualitative research methods and analyses, there is currently no concise resource that explains and differentiates among the most common qualitative approaches. We believe novice qualitative researchers, students planning the design of a qualitative study or taking an introductory qualitative research course, and faculty teaching such courses can ...
Qualitative research gathers participants' experiences, perceptions, and behavior. It answers the hows and whys instead of how many or how much. It could be structured as a stand-alone study, purely relying on qualitative data or it could be part of mixed-methods research that combines qualitative and quantitative data.
Abstract. This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions ...
Qualitative research methods should not be seen as tools that can be applied independently of theory. It is important for these tools to be based on more than just method. In their research, social scientists and scholars in the humanities emphasize social theory. Departing from a reductionist psychological model of individual behavior that ...
Qualitative research projects are informed by a wide range of methodologies and theoretical frameworks. The SAGE Encyclopedia of Qualitative Research Methods presents current and complete information as well as ready-to-use techniques, facts, and examples from the field of qualitative research in a very accessible style. In taking an ...
Qualitative research is a method of inquiry used in various disciplines, including social sciences, education, and health, to explore and understand human behavior, experiences, and social phenomena. It focuses on collecting non-numerical data, such as words, images, or objects, to gain in-depth insights into people's thoughts, feelings, motivations, and perspectives.
Qualitative research methodologies seek to capture information that often can't be expressed numerically. These methodologies often include some level of interpretation from researchers as they collect information via observation, coded survey or interview responses, and so on.
Qualitative research is defined as an exploratory method that aims to understand complex phenomena, often within their natural settings, by examining subjective experiences, beliefs, attitudes, and behaviors. Unlike quantitative research, which focuses on numerical measurements and statistical analysis, qualitative research employs a range of ...
Qualitative research Footnote 1 —research that primarily or exclusively uses non-numerical data—is one of the most commonly used types of research and methodology in the social sciences. Unfortunately, qualitative research is commonly misunderstood. It is often considered "easy to do" (thus anyone can do it with no training), an "anything goes approach" (lacks rigor, validity and ...
Updated on February 02, 2020. Qualitative research is a type of social science research that collects and works with non-numerical data and that seeks to interpret meaning from these data that help understand social life through the study of targeted populations or places. People often frame it in opposition to quantitative research, which uses ...
Qualitative research methods. Each of the research approaches involve using one or more data collection methods.These are some of the most common qualitative methods: Observations: recording what you have seen, heard, or encountered in detailed field notes. Interviews: personally asking people questions in one-on-one conversations. Focus groups: asking questions and generating discussion among ...
Qualitative research methods originated in the social and behavioral research sciences. Today, our world is more complicated, and it is difficult to understand what people think and perceive. Online research methods make it easier to understand that as it is a more communicative and descriptive analysis. The following are the qualitative ...
Similarly, qualitative research should not be required to be combined with quantitative research per se - unless mixed methods research is judged as inherently better than single-method research. In this case, the same criterion should be applied for quantitative studies without a qualitative component.
Qualitative research is a process of naturalistic inquiry that seeks an in-depth understanding of social phenomena within their natural setting. It focuses on the "why" rather than the "what" of social phenomena and relies on the direct experiences of human beings as meaning-making agents in their every day lives.
Qualitative Methods. Qualitative research methods are most appropriate in situations in which little is known about a phenomenon or when attempts are being made to generate new theories or revise preexisting theories. Qualitative research is inductive rather than deductive and is used to describe phenomena in detail, without answering questions ...
Although qualitative research does not appear to be defined in terms of a specific method, it is certainly common that fieldwork, i.e., research that entails that the researcher spends considerable time in the field that is studied and use the knowledge gained as data, is seen as emblematic of or even identical to qualitative research.
QD is a valuable method for master's-level students and research trainees as it provides a practical, accessible, and flexible approach to qualitative research (Bradshaw et al., 2017), fostering the development of important research skills and contributing to the scientific integrity of their work. The disciplines in which QD research fits ...
1 METHOD. A qualitative research approach was used, involving in-depth semi-structured online and telephone interviews, to support people with SMI to share their experiences of blue space and blue care in their own terms, at their own pace, focusing on people who considered blue spaces to play a role in their well-being. ...
Background Staff retention in Emergency Medicine (EM) is at crisis level and could be attributed in some part to adverse working conditions. This study aimed to better understand current concerns relating to working conditions and working practices in Emergency Departments (EDs). Methods A qualitative approach was taken, using focus groups with ED staff (doctors, nurses, advanced care ...
This beginner-friendly workshop will lead researchers through some of the basics of conducting qualitative research (e.g., different analytic methods, positionality), including practical elements of qualitative work (e.g., sample sizes).
Qualitative research methodology is not a single method, but instead offers a variety of different choices to researchers, according to specific parameters of topic, research question, participants, and settings. The method is the way you carry out your research within the paradigm of quantitative or qualitative research.
Mixed methods research (MMR) has the potential to be a powerful tool to expand the ways early intervention/early childhood special education (EI/ECSE) scholarship understands and informs practice. Integration, or the purposeful combination of quantitative and qualitative research approaches, is central for rigorous MMR. However, it can be challenging to identify and enact integration because ...
Methods. A descriptive qualitative evaluation was conducted across nine facilities in Gaza Province to assess the acceptability and barriers to implementation of the mentor mother program (MMP) among those receiving services and providing services. ... Research Department, Elizabeth Glaser Pediatric AIDS Foundation, Washington, DC, USA.
In this Rip Out, we describe 3 different qualitative research approaches commonly used in medical education: grounded theory, ethnography, and phenomenology. Each acts as a pivotal frame that shapes the research question (s), the method (s) of data collection, and how data are analyzed. 4, 5. Go to:
Methods: Multi-level and multi-actor in-depth semistructured interviews were employed to qualitatively explore the barriers and enablers of the use of mHealth systems. ... Mobile Health (mhealth) (2576) Focus Groups and Qualitative Research for Human Factors Research (690) E-Health Policy and Health Systems Innovation (187 ...