Skip to content
Read the latest news stories about Mailman faculty, research, and events.

Departments
We integrate an innovative skills-based curriculum, research collaborations, and hands-on field experience to prepare students.
Learn more about our research centers, which focus on critical issues in public health.
Our Faculty
Meet the faculty of the Mailman School of Public Health.
Become a Student
Life and community, how to apply.
Learn how to apply to the Mailman School of Public Health.
New Research Highlights Inequities in Diagnosis, Treatment of Postpartum Depressive Symptoms
Pregnancy and childbirth can be significant stressors on mental health. Nearly one in eight people who have given birth develop postpartum depression, according to the Centers for Disease Control and Prevention. More than just the “baby blues,” postpartum depressive symptoms can lead to adverse outcomes for birthing people and families, and treatment requires effective screening, diagnosis and management.
New research from Columbia University Mailman School of Public Health and the UNC Gillings School of Global Public Health, published online and in the April print issue of Health Affairs , has uncovered significant underdiagnosis and undertreatment of postpartum depressive symptoms as well as stark racial and ethnic inequities in diagnosis and treatment for those with postpartum depressive symptoms. The research was led by senior author Jamie Daw , PhD, assistant professor of Health Policy and Management at Columbia Mailman School in collaboration with Sarah Haight, first author and doctoral candidate in epidemiology at the Gillings School as part of her dissertation.
The research drew on data from a novel survey led by Daw at Columbia that followed up with 4,542 postpartum people who had a live birth in 2020 in seven jurisdictions: Kansas, Michigan, New Jersey, Pennsylvania, Utah, Virginia and New York City. The researchers found that 11.8 percent of those sampled reported postpartum depressive symptoms at 2-6 months postpartum. However, only 1 in 4 individuals with depressive symptoms received a perinatal mood and anxiety disorder (PMAD) diagnosis, and one in two reported receiving some form of mental health care in the first year postpartum.
The study found that while there were no statistical differences in PMAD diagnoses based on race or ethnicity, among those with depressive symptoms, 67 percent of white respondents received postpartum mental health treatment compared to only 37 percent of Hispanic and Black respondents and 19.7 percent of respondents who identified as Asian, Native Hawaiian, Pacific Islander, Southwest Asian, Middle Eastern or North African.
“Our study in concert with existing work shows that Asian, Black and Latine birthing people, who may be at the greatest risk of postpartum depression, are the least likely to receive any form of postpartum mental health care—illustrating stark racial inequities in how postpartum depression is identified and managed in the U.S.,” said Haight.
“Previous studies on PMAD symptoms, diagnosis and treatment have typically focused only on the early postpartum period. By following people through the postpartum year, our findings elucidate how many individuals with mental health symptoms fall through the cracks and don’t ever receive the care they need,” said Daw.
The study findings suggest that policies that require and reimburse universal mental health screening at postpartum visits, ensure connections to care, reduce gaps in postpartum insurance coverage, and require clinician training in culturally responsive resources could improve equity of postpartum depression diagnosis and care in the U.S.
Birthing people undergo physical, mental and social upheaval during the perinatal and postpartum periods. Caring for a newborn, managing hormonal changes, and navigating existing social, financial or relational situations—each can place a burden on mental health that PMAD can magnify, according to authors Haight and Daw. PMAD is linked to low social support, less closeness and warmth with partners, stunted infant growth, delayed infant cognitive and language development, poor infant sleep, compromised maternal-infant attachment, and difficulty initiating or maintaining breastfeeding. “Half of pregnancy-related deaths in the U.S. occur in the postpartum year and mental health conditions are the second leading cause of deaths in the late postpartum period. Improving equitable access to PMAD diagnosis and treatment is thus critical to addressing the maternal health crisis in the U.S.,” said Daw.
“Our findings document disparities in care, but future work is needed to investigate how structural and interpersonal racism may explain these observed inequities and what efforts are needed to address these mechanisms and their harmful effects,” said Haight.
The study is part of the Health Affairs April 2024 issue on perinatal mental health and well-being, which explores the impacts of perinatal mental health on parents, infants and children and how policies can intervene to help. Daw and Haight, along with fellow experts and co-authors, will be part of a virtual symposium on Wednesday, April 3 at 1:00 pm, ET.
Co-authors are Chantel Martin, Brian Wells Pence, and Joanna Maselko, Gillings School; Karen Sheffield-Abdullah, UNC School of Nursing; Sarah Verbiest, UNC School of Social Work, School of Medicine and Gillings School.
Media Contact
Stephanie Berger, [email protected]
Related Information
Meet our team, jamie daw, phd.
- Affiliate, Columbia Population Research Center
New research highlights inequities in treatment of postpartum depressive symptoms
April 1, 2024
Pregnancy and childbirth can be significant stressors on mental health. Nearly one in eight people who have given birth develop postpartum depression , according to the Centers for Disease Control and Prevention. More than just the “baby blues,” postpartum depressive symptoms can lead to adverse outcomes for birthing people and families, and treatment requires effective screening, diagnosis and management.
New research from the UNC Gillings School of Global Public Health and the Columbia University Mailman School of Public Health, published today online and in the April print issue of Health Affairs , has uncovered significant underdiagnosis and undertreatment of postpartum depressive symptoms. As part of her dissertation, this study was led by Sarah Haight, MPH, doctoral candidate in epidemiology at the Gillings School in collaboration with Jamie Daw, PhD, assistant professor of health policy and management at the Mailman School. The researchers also found stark racial and ethnic inequities in treatment for those with postpartum depressive symptoms.
The research drew on data from a novel survey led by Daw at Columbia University that followed up with 4,542 postpartum people who had a live birth in 2020 in seven jurisdictions: Kansas, Michigan, New Jersey, Pennsylvania, Utah, Virginia and New York City. The researchers found that 11.8% of those sampled reported postpartum depressive symptoms at 2-6 months postpartum. However, only one in four individuals with depressive symptoms received a perinatal mood and anxiety disorder (PMAD) diagnosis, and one in two reported receiving some form of mental health care in the first year postpartum.
The study found that while there were no statistical differences in PMAD diagnoses based on race or ethnicity, among those with depressive symptoms, 67% of white respondents received postpartum mental health treatment compared to only 37% of Hispanic and Black respondents and 19.7% of respondents who identified as Asian, Native Hawaiian, Pacific Islander, Southwest Asian, Middle Eastern or North African.

Sarah Haight
“Our study in concert with existing work shows that Asian, Black and Latine birthing people, who may be at the greatest risk of postpartum depression, are the least likely to receive any form of postpartum mental health care – illustrating stark racial and ethnic inequities in how postpartum depression is identified and managed in the U.S.,” said Haight.
“Previous studies on PMAD symptoms, diagnosis and treatment have typically focused only on the early postpartum period. By following people through the postpartum year, our findings elucidate how many individuals with mental health symptoms fall through the cracks and don’t ever receive the care they need,” said Daw.
The study findings suggest that policies that require and reimburse universal mental health screening at postpartum visits, ensure connections to care, reduce gaps in postpartum insurance coverage, and require clinician training in culturally responsive resources could improve equity of postpartum depression diagnosis and care in the U.S.
Birthing people undergo physical, mental and social upheaval during the perinatal and postpartum periods. Caring for a newborn, managing hormonal changes, and navigating existing social, financial or relational situations – each can place a burden on mental health that PMAD can magnify, according to the researchers. PMAD is linked to low social support, less closeness and warmth with partners, stunted infant growth, delayed infant cognitive and language development, poor infant sleep, compromised maternal-infant attachment, and difficulty initiating or maintaining breastfeeding.
“Half of pregnancy-related deaths in the U.S. occur in the postpartum year and mental health conditions are the second leading cause of deaths in the late postpartum period. Improving equitable access to PMAD diagnosis and treatment is thus critical to addressing the maternal health crisis in the U.S.,” said Daw.
“Our findings document disparities in care, but more work is needed to investigate how structural and interpersonal racism may explain these observed inequities and what efforts are needed to address these mechanisms and their harmful effects,” said Haight.
The study is part of the Health Affairs April 2024 issue on perinatal mental health and well-being, which explores the impacts of perinatal mental health on parents, infants and children and how policies can intervene to help. Haight and Daw, along with fellow experts and co-authors, will be part of a virtual symposium on Wednesday, April 3, at 1:00 p.m. ET
Join the conversation and register for this FREE event: https://www.healthaffairs.org/do/10.1377/he20240312.862836/full/
Additional co-authors on this study include Chantel Martin, PhD (Gillings School), Karen Sheffield-Abdullah, PhD, RN, CNM (UNC School of Nursing), Sarah Verbiest, DrPH (UNC School of Social Work, School of Medicine and Gillings School), Brian Wells Pence, PhD (Gillings School), and Joanna Maselko, ScD (Gillings School).
Contact the UNC Gillings School of Global Public Health communications team at [email protected] .
Use this form to submit news, events and announcements to be shared via our newsletter and digital screens.
View and download the visual elements associated with the Gillings School.
For the use of our faculty, staff and students, the School offers the following PowerPoint template, which can be modified as needed.
This form allows faculty and staff to create a new web profile or update a current one.
This form enables Gillings School representatives to submit requests for website edits.
Garcia wins the 2024 Gertrude M. Cox Award
Information for:.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 12 April 2021
Predicting women with depressive symptoms postpartum with machine learning methods
- Sam Andersson 1 ,
- Deepti R. Bathula 2 ,
- Stavros I. Iliadis 1 ,
- Martin Walter 3 , 4 , 5 &
- Alkistis Skalkidou 1
Scientific Reports volume 11 , Article number: 7877 ( 2021 ) Cite this article
10k Accesses
42 Citations
2 Altmetric
Metrics details
- Machine learning
- Risk factors
Postpartum depression (PPD) is a detrimental health condition that affects 12% of new mothers. Despite negative effects on mothers’ and children’s health, many women do not receive adequate care. Preventive interventions are cost-efficient among high-risk women, but our ability to identify these is poor. We leveraged the power of clinical, demographic, and psychometric data to assess if machine learning methods can make accurate predictions of postpartum depression. Data were obtained from a population-based prospective cohort study in Uppsala, Sweden, collected between 2009 and 2018 (BASIC study, n = 4313). Sub-analyses among women without previous depression were performed. The extremely randomized trees method provided robust performance with highest accuracy and well-balanced sensitivity and specificity (accuracy 73%, sensitivity 72%, specificity 75%, positive predictive value 33%, negative predictive value 94%, area under the curve 81%). Among women without earlier mental health issues, the accuracy was 64%. The variables setting women at most risk for PPD were depression and anxiety during pregnancy, as well as variables related to resilience and personality. Future clinical models that could be implemented directly after delivery might consider including these variables in order to identify women at high risk for postpartum depression to facilitate individualized follow-up and cost-effectiveness.
Similar content being viewed by others
Postpartum depression: a developed and validated model predicting individual risk in new mothers
Trine Munk-Olsen, Xiaoqin Liu, … Merete L. Maegbaek

Individualized prediction of psychiatric readmissions for patients with major depressive disorder: a 10-year retrospective cohort study
Ting Zhu, Jingwen Jiang, … Wei Zhang
Predicting change in diagnosis from major depression to bipolar disorder after antidepressant initiation
Melanie F. Pradier, Michael C. Hughes, … Roy H. Perlis
Introduction
Postpartum depression (PPD), defined as having an episode of minor or major depression during pregnancy or up to one year after giving birth, is a relatively common condition that affects 8–15% of new mothers in Sweden every year 1 , 2 . The etiology of PPD is not well understood, but the condition likely arises from a combination of psychological, psychosocial and biological factors 3 , 4 . The most well documented biological risk factors for PPD are hypothalamic–pituitary–adrenal axis dysregulation, inflammatory processes, genetic vulnerability, and allopregnanolone withdrawal 4 . The strongest psychosocial factors are previous depression, severe life events, some forms of chronic stress and relationship struggles 4 , 5 . The role of resilience and personality have been lately also gaining attention 6 , 7 .
PPD is a condition that can have devastating effects on the mothers, as well as their children 8 , 9 . Mothers may experience persistent doubts about their ability to care for the child, have difficulties bonding with their child, and also have thoughts about hurting the child 2 . Moreover, PPD can affect a child’s development by interfering with the mother-infant relationship 10 , 11 . For instance, children of mothers with PPD have greater cognitive, behavioral and interpersonal problems compared to children of mothers without PPD 12 , 13 . Despite PPD being a detrimental health condition for many women, numerous affected women fail to receive adequate care 14 . There exist several effective treatments and interventions for PPD 14 , 15 , 16 , but they are only cost-effective among high-risk women. The idea of prenatal prediction of PPD has existed for several years and early studies using more traditional methods attempted to predict women at risk by prenatal assessment of critical variables 17 . However, to date, there has been no effective way to predict women at risk for the development of depressive symptoms postpartum.
Traditional statistical methods allow researchers to estimate risks by sequentially analysing the associations mainly between two variables, often controlling for the effect of others. Further, machine learning (ML) methods enable researchers to iteratively and simultaneously analyse multiple interacting associations between variables 18 as well as to devise data-driven predictive models that then can be evaluated by quantifying the performance metrics across all models in order to find the best predictive model. The power of ML allows for the analysis of complex non-linear relationships and even the integration and pooling of multiple different data-types from several sources 19 , 20 , 21 . Over the last decade, there has been a steady increase in the use of ML in medicine and its effects can be observed in many fields including oncology 22 , 23 , 24 , 25 , cardiology and hematology 26 , 27 , critical care 28 , 29 , and psychiatry 30 , 31 , 32 , 33 , 34 , 35 . Importantly, PPD represents a unique case in which a moderately high chance to develop a serious psychiatric condition is coupled with a very precise temporal prediction of when such symptoms are to be expected. As such, and considering PPDs substantial societal burden, ML-based risk classification can be applied in an ideal situation with high expected societal benefit. With approximately 120,000 annual births in Sweden and the typical prevalence of PPD at 12% among women who nearly in their entirety present with a multitude of adaptations after childbirth, close monitoring of the whole population for early depressive sentinels after childbirth seems hardly feasible in reality. In contrast, close follow-up among high risk groups during midwife or nurse-led postpartum assessments may strongly contribute to more tailored and cost-efficient maternal perinatal mental care services.
However, despite promising results in other fields, relatively few studies have been performed using ML in the field of perinatal mental health. An early study in the field could predict PPD with an accuracy of 84% by use of multilayer perceptrons and assessment of 16 variables 36 . A recent pilot study used ML algorithms applied to data extracted from electronic health records to show that ML models can be utilized to predict PPD and identify critical variables that conform with known risk variables such as race, demographics, threatened abortion, prenatal mental disorder, anxiety, and an earlier episode of major depression 34 . Another study also developed models to predict PPD, which were then integrated into a mobile application platform to be used by pregnant women 37 , while a recently published study compared four PPD prediction models that comprised demographic, social and mental health data 38 . In the latter study, psychological resilience was pointed out as an important predictive factor. However, these studies have been limited by either sample size or richness of data. Finally, in a recently published study, Zhang et al. proposed a machine learning based framework for PPD risk prediction in pregnancy, using electronic health record data 39 .
To date, our study is the first using a population-based, large and rich dataset, including a wide range of clinical and psychometric self-report and medical journal-derived variables and evaluating a range of different ML algorithms against each other, and also after stratification for earlier or pregnancy depression, to provide a robust screening tool, at discharge from the delivery ward, for predicting women at risk for developing depressive symptoms later in the postpartum period.
Hence, we aim to predict women at risk for depressive symptoms at 6 weeks postpartum, from clinical, demographic, and psychometric questionnaire data available after childbirth, by use of machine learning methods.
Descriptive statistics
Table 1 shows summary statistics of the study population by depressive symptom status at 6 weeks postpartum. Results are presented as frequencies and relative frequencies within EPDS status [N (%)] or median (interquartile range) for sociodemographic, clinical and questionnaire variables. Of the 4313 participants in the study, 577 had depressive symptoms at 6 weeks postpartum. The mean age for both groups was 31 years. Differences were seen among women with depressive symptoms and women without depressive symptoms across sociodemographic variables like education, employment, and country of origin, as well as many other variables known as risk factors for postpartum depression. A greater proportion of women with depressive symptoms postpartum did not receive adequate support from their partner and were not breastfeeding.
Classification graphs
To evaluate whether ML can predict women with depressive symptoms, two datasets were used, namely the BP variables and the combined dataset, that includes the BP variables and three psychometric questionnaires (RS, SOC, and VPSQ). Performance of different ML models was first evaluated for the BP data (Fig. 1 ). The performance metrics for Ridge Regression, LASSO Regression, Gradient Boosting Machines, Distributed Radom Forests (DRF), Extreme Randomized Forests (XRT), Naïve Bayes and Stacked Ensembles models are shown. Balanced accuracy, NPV and AUC were quite similar across the models, with accuracy reaching 72% and AUC 79% for XRT. NPV was over 92% for all models. Sensitivity was quite low and together with specificity and PPV, they varied between the models. Sensitivity was highest for DRF at 84%, while only 65% for XRT; DRF had though the lowest specificity and PPV. The highest PPV was observed for Ridge Regression and Stacked Ensemble, at 41%.
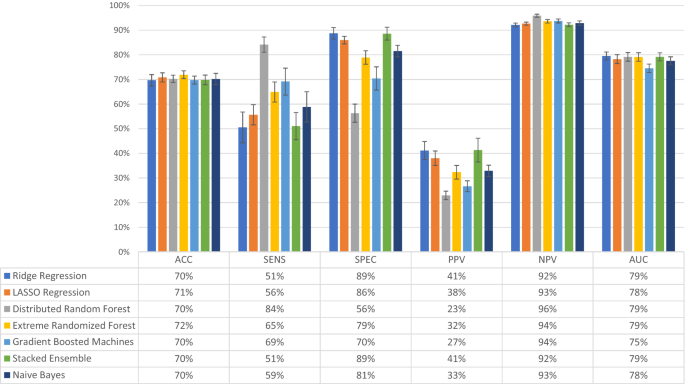
Evaluation of model performance in the dataset containing only background, medical and pregnancy-related variables (n = 4277 women). The models tested were Ridge Regression, LASSO Regression, Distributed Random Forest, Extremely Randomized Trees, Gradient Boosted Machines, Stacked Ensemble, and Naïve Bayes. Models were assessed for accuracy (ACC), sensitivity (SENS), specificity (SPEC), positive predictive value (PPV), negative predictive value (NPV), and area under the curve (AUC), the outcome being depressive symptoms at 6 weeks postpartum. The bars represent the level of performance measures (in percent) and the table below the bar plot presents the exact numerical values. Error bars represent one standard deviation from the mean.
Performance of different ML models was then evaluated for the combined dataset, even including psychometric measures (Fig. 2 ). Performance metrics for the same models showed that NPV was still over 90% for all models, but otherwise, similar levels of accuracy and AUC were observed. More variability among the models was observed for sensitivity, specificity and PPV. XTR had the highest accuracy (at 73%) and AUC (at 81%) among all models, with a balance in sensitivity at 72% and specificity at 75%; PPV was at 33% and NPV at 94%. As this balancing act is an essential attribute of predictive models based on imbalanced datasets the subsequent experimental analysis was provided using only XRT.
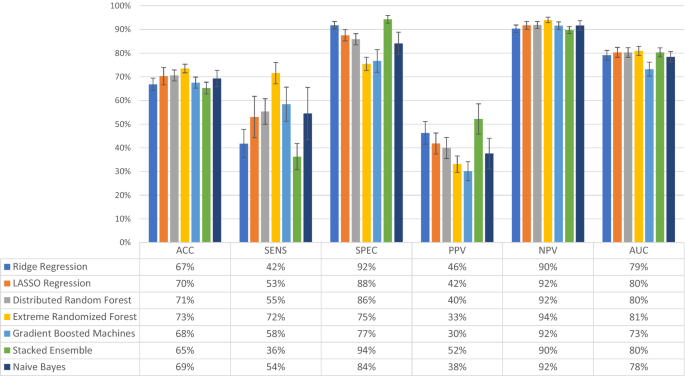
Evaluation of model performance in the total combined dataset (n = 2385 women). The combined dataset contained the background, medical and pregnancy-related variables, as well as answers to the questionnaires Resilience-14, Sense of Coherence-29 and Vulnerable Personality Scale Questionnaire. The models tested were Ridge Regression, LASSO Regression, Distributed Random Forest, Extremely Randomized Trees, Gradient Boosted Machines, Stacked Ensemble, and Naïve Bayes. Models were assessed for accuracy (ACC), sensitivity (SENS), specificity (SPEC), positive predictive value (PPV), negative predictive value (NPV), and area under the curve (AUC), the outcome being depressive symptoms at 6 weeks postpartum. The bars represent the level of performance measures (in percent) and the table below the bar plot presents the exact numerical values. Error bars represent one standard deviation from the mean.
Comparative performance of the XRT model using all variables, the top 50%, and the top 25% variables, for both the BP and the combined dataset is shown in Fig. 3 . There was an apparent trade-off between model sensitivity and specificity, which were both affected by dataset used and percent of variables included (Fig. 3 ). Sensitivity was highest with use of only 25% of the combined dataset, while specificity was highest with the use of the top 50% of the BP dataset. None among the other measures were greatly affected by either dataset used or percent of variables included (a trend to lower PPV when 25% of variables used was noted). The AUC curves corresponding to Figs. 2 and 3 are available in the supplementary material (Supplementary Figure 1 ).
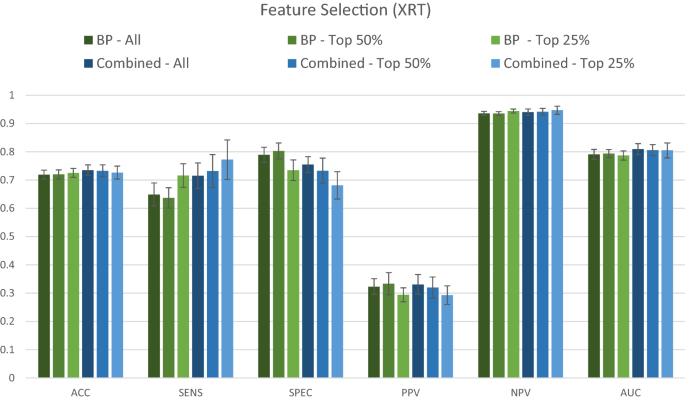
Comparative performance of the dataset containing only background, medical history and pregnancy-related variables (BP) and the combined dataset (BP + RS + SOC + VPSQ). The Extremely Randomized Trees (XRT) algorithm was used to compare the performance of the two datasets for predicting depression at 6 weeks postpartum. Models were assessed for accuracy (ACC), sensitivity (SENS), specificity (SPEC), positive predictive value (PPV), negative predictive value (NPV), and area under the curve (AUC). The variable selection procedure shows results when All (100%), Top 50%, and Top 25% of variables were retained, ranked according to Mean Decrease in Impurity (MDI) relevance.
The results for the performance of the XRT models after stratification for previous depression are shown in Fig. 4 . For all women, XRT achieved a balanced accuracy of 73%, a sensitivity of 72%, a specificity of 75%, a positive predictive value of 33%, a negative predictive value of 94% and an AUC of 81%. For women with depression in pregnancy or earlier in life, XRT achieved a balanced accuracy of 69%, a sensitivity of 76%, a specificity of 61%, a positive predictive value of 44%, a negative predictive value of 87% and an AUC of 77%. For women without any previous depressive episode, balanced accuracy was 64%, sensitivity 52%, specificity 76%, positive predictive value of 13%, negative predictive value 97% and AUC of 73% (Fig. 4 ). Among the results from analyses of the individual questionnaires, no single one achieved an accuracy of more than 70% (Supplementary Figure 2 ).
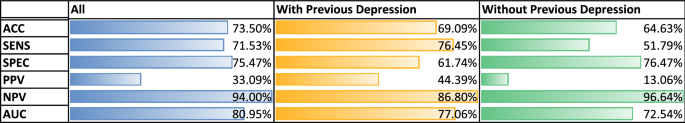
Stratified classification graphs for Extreme Randomized Forest (XRT) model, by pregnancy/previous depression status. Results presented for all women (All, n = 2385, of which 14% had postpartum depression, PPD), women with depression during current pregnancy or earlier in life (With Previous Depression, n = 971, of which 27% had PPD), and women without any previous depression episode (Without Previous Depression, n = 1414, of which 6% had PPD). For each category, models were assessed for accuracy (ACC), sensitivity (SENS), specificity (SPEC), positive predictive value (PPV), negative predictive value (NPV), and area under the curve (AUC).
Variable importance
The 25 most important variables by MDI based on Distributed Random Forests (DRF) models, considering the women with different previous depression status are shown in Fig. 5 . For all women, Anxiety During Pregnancy and Depressive During Pregnancy stand out as the two most important variables (importance level above 0.7) (Fig. 5 A). The variables following in importance were questions included in the psychometric instruments, except for history of depression. Similarly, for women with previous depression, Anxiety During Pregnancy and Depressive During Pregnancy stand out as important variables for the presence of depression postpartum (importance level above 0.9) (Fig. 5 B). Finally, for women without depression, Anxiety During Pregnancy was the absolutely most important variable (importance level of 1) (Fig. 5 C). Even here, variables relating to resilience, sense of coherence and personality followed, but interestingly, variables such as breastfeeding, BMI, traumatic events in childhood, mode of delivery, hypoxia in the newborn and age place among the top 25 variables.
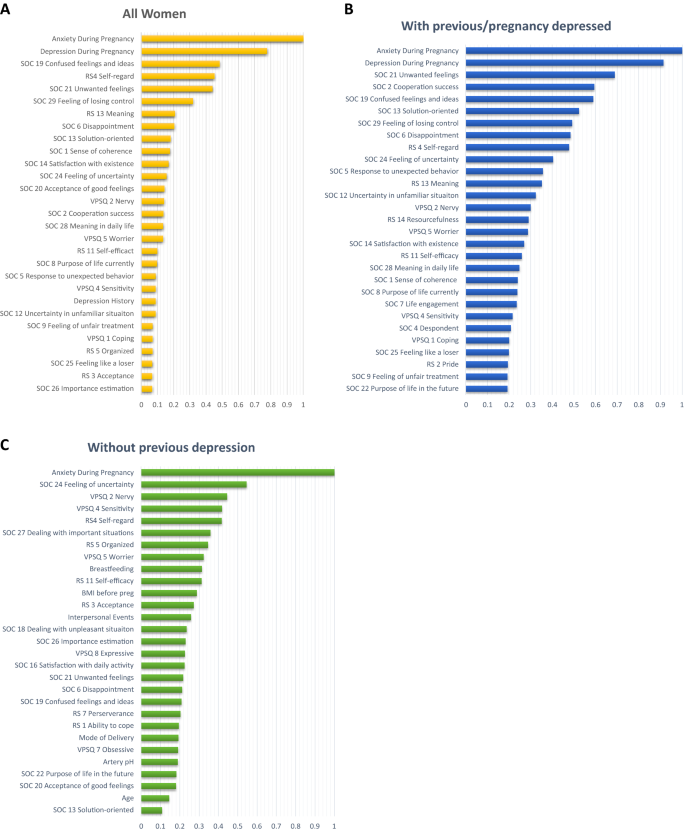
Ranked importance of the assessed variables using the Extremely Randomized Trees (XRT) models in the combined dataset, considering the women with different previous depression status. Results presented for all women ( A ), All women (n = 2385), ( B ) women with depression during current pregnancy or earlier in life (Previous/pregnancy depression, n = 971), and ( C ) women without any previous depression episode (No previous depression, n = 1414). The graphs depict the variable importance as a relative measure that is scaled to a maximum of 1.0. The x-axis represents the relative contribution to the classification algorithm of the corresponding feature on the y-axis.
The 25 most important variables based only on BP variables for all women (n = 4313) can be found in Fig. 6 . The two variables that have an importance level above 0.9 are again Depression During Pregnancy and Anxiety During Pregnancy. The next variable with an importance level above 0.3 is Depression History, while the remaining rate below 0.2.

Ranked importance of the assessed background, medical history and pregnancy variables for all women (n = 4277) using Extremely Randomized Trees (XRT) models. The top 25% of the variables are reported . The x-axis represents the relative contribution of the corresponding variable to the classification algorithm.
Including only the top 20 variables, the AUC is only reduced by 1% to 0.79, including just 10 variables reduced the AUC by 2% to ~ 0.78, while after including just 5 variables reduced the AUC by 3% to ~ 0.77. For the previously non-depressed group, including 10 variables gives an AUC of 0.72, and 5 variables an AUC of 0.71.
In this study, we evaluated a range of different machine learning (ML) methods to predict pregnant women at risk for postpartum depressive (PPD) symptoms. The classification performance of the chosen ML algorithms was not significantly different in regard to accuracy, NPV, AUC measures. However, variations were more pronounced in regard to sensitivity, specificity and PPV. In general, as expected, an inverse relationship is observed in performance with respect to sensitivity and specificity. Furthermore, PPV is considerably lower than NPV due to low prevalence of PPD, as expected.
Overall, XRT provides robust performance with highest accuracy and well-balanced sensitivity and specificity. Addition of resilience and personality self-reported variables to the background, medical history and pregnancy-related variables provides marginal improvement in both accuracy and AUC. It is nevertheless of note that these extra variables boost the sensitivity of the XRT model substantially for only a slight drop in specificity. As this does not depend on the lower sample size used for the second step of analyses involving personality and resilience measures, it could be hypothesized that there is either a certain redundancy between variables, e.g. that low resilience is a core feature among depressed patients during pregnancy, or that anxiety and depression measures, available for all patients, have such a strong predictive value that the further addition of variables does not greatly improve accuracy.
These results suggest a possible benefit of using ML to screen new mothers at discharge from the delivery ward in order to identify those at high risk for postpartum depressive symptoms. However, because of the low PPV across all models, due to the relatively low prevalence of PPD at 12%, one would expect that many women identified at high risk would in the end not get depressed. On the other hand, these methods may nevertheless permit the identification of a high-risk group, to which preventive interventions would be offered in a cost-effective way, mainly by avoiding large costs related to full-blown depressive episodes postpartum. These could include the provision of extra support as well as more focused and longitudinal assessments in these mothers. Furthermore, the variables included in the BASIC study refer to easily acquired web-based self-reports, which support their use for screening purposes. Because of the high NPV, we would not expect many women not identified as high risk to develop depression postpartum. As such, the application of our classification algorithms would boost cost-effectiveness, allowing for a tailored resource allocation towards the mothers initially identified at risk versus a more widespread follow up of all mothers; in the low-risk group, assessments could be limited to single timepoints, as is praxis today. As PPD affects more than 16,000 families every year in Sweden alone, with high associated costs, estimated at $30,000 per mother-infant pair for untreated peripartum mood disorders, preventive efforts would have substantial societal benefits 40 .
It is interesting that performance metrics, especially accuracy and AUC, remain stable even when the number of variables used in the models is reduced from 100 to 50% and even to 25% of all variables available, and AUC is relatively stable even at 5–10 variables. As discussed above, this is in line with the thought that there is some redundancy when it comes to the variables included, with depression and anxiety during pregnancy being highly correlated with some background and medical history variables, and possibly mediating their association with PPD. It is thus intriguing to observe that only among non-previously depressed, variables such as breastfeeding, BMI, traumatic interpersonal events in childhood, mode of delivery, infant hypoxia and age are emerging as important for prediction, along with resilience and personality variables, which are otherwise more prominent among those earlier depressed. This is important to have in mind when developing screening strategies; the variables used might need to be adjusted for the group of women with previous depression. Anxiety during pregnancy continues to be very predictive in both groups. The stability of the performance measures however, indicates that an abbreviated survey can be used to screen without significantly affecting predictive power.
Among possible explanations for the somewhat lower accuracy in both the depressed group (earlier or during pregnancy) (n = 971, accuracy = 69%) and never-depressed subgroups (n = 1414, accuracy = 64%) are the lower sample sizes as well as a relatively decreased variability in the data (the algorithms did not have a big number of examples of alternatives to learn from). Sensitivity is the same in the earlier depressed group, but drops to 52% in the never depressed group, underlining the difficulty in identifying women at high risk for having their first ever depressive episode after childbirth. In general, the high NPV figure in the never earlier depressed group means that women with a negative screening in that group do not need tighter follow-up; NPV nonetheless drops to 86% in the earlier depressed group, suggesting that further screening in the postpartum period might still benefit this high-risk group of women.
Our study showed a slightly higher AUC than most earlier studies’ best prediction models (79% by Wang et al. and 78% by Zhang et al.), though our accuracy of 73% is lower than the 84% reported by Tortajada et al. 34 , 36 , 38 . However, in the latter study, the main outcome was depression at 32 weeks and not at 6 weeks postpartum, genetic data was included and the study sample was more homogeneous since it consisted of SSRI-free Caucasian women. Moreover, a lower EPDS cut-off was used followed by clinical interviews, possibly reducing the risk of misclassification of study cases and controls. Nevertheless, in our study, a clinical evaluation was not possible for practical reasons, due to the much larger study population. Finally, in addition to clinical and environmental variables, information on related gene polymorphisms was also utilized in that study.
Furthermore, Wang et al. identified race, obesity, anxiety, depression, different types of pain, and antidepressant and anti-inflammatory drug use during pregnancy as the most important variables for their prediction models 34 . These variables differed somewhat from the ones we identified as being most important with the caveat that our model also indicated that anxiety during pregnancy and depression history or depressive symptoms during pregnancy were overwhelmingly the most significant predictors for PPD. It has to be noted that we included many psychometric measures, which followed in importance, e.g. the question 19 on the SOC scale “Do you have very mixed up feelings and ideas?” and question 4 on RS, which measures self-regard (“I am friends with myself”). The population in the BASIC study is quite homogeneous, most participants having a high education, are quite healthy and born in the Nordic countries. Further, the BASIC dataset has no information on race. BMI was also identified in our study as an important variable, both in the BP dataset analysis and the sub-analysis among women without previous depression. Rates of antidepressant use are low. Differences in the analytical approach might also account for some differences in the results.
These findings further illuminate the difficulties in predicting which women will go on to develop postpartum depressive symptoms after childbirth. From the variable importance plots, the most predictive variables for postpartum depressive symptoms, available at the time of discharge from the delivery ward, is to either have anxiety or depressive symptoms during pregnancy. In fact, these two variables are by far the most predictive, along nevertheless with distinct variables related to resilience, sense of coherence and personality. The predictive algorithms reach an accuracy for the whole group of 73% and AUC of 81%, which is at the limit for possible use in clinical settings. The algorithms might need to be different according to whether women had experience depression before in life. Further studies, possibly using more advanced methods and bigger samples, are warranted.
Very recently, Zhang et al. also proposed a machine learning based framework for PPD risk prediction using electronic health record (EHR) data 39 . While the techniques employed are comparable to our study with similar processing pipeline, they report higher AUC. This increment can be attributed majorly to the substantially larger cohort used in their study. Several ML studies have demonstrated that large datasets lead to lower estimation variance and hence provide better predictive performance. Furthermore, the top predictors also differ between our study due to differences in data sources. Additionally, a PPV higher than that reported in our study would significantly increase the clinical utility of our proposed framework. However, PPV is directly related to the prevalence of PPD in the population studied, which is only about 12%. While the classification threshold of the model can be adjusted to improve PPV, it does not ensure the expected benefit as other evaluation metrics, like sensitivity, specificity and NPV, would be adversely affected. Even Zhang et al. that reported higher AUC values, only report a PPV of ~ 27% for the validation site with prevalence of 6.5%, highlighting the issue 39 .
The lack of effective ways that would allow for early prediction of women at risk for depressive symptoms in the postpartum period has been addressed in the Introduction. In fact, the Edinburgh Postnatal Depression Scale is nowadays used as a screening tool for current depression 41 . National guidelines in several countries recommend screening for PPD at 6 to 8 weeks postpartum; however, the suggested target groups of women to be screened vary between countries 42 , 43 , 44 . Also, the use of the EPDS at this time is used to screen for concurrent depression. In contrast, the role of EPDS in pregnancy, in combination with other variables, for early identification of women at risk for development of depressive symptoms later in the postpartum period has not been studied. In our study we do show that high EPDS scores in pregnancy are highly predictive of postpartum depression.
This study had numerous strengths. First, it addresses a novel field, as there are very few studies in the area, none from the Nordic countries, and none of earlier algorithms is being widely used in clinical practice. The large sample size allowed us to train a robust range of different ML algorithms. The richness of the BASIC dataset provided us with the opportunity to investigate the predictive power of a large number of background, medical history, pregnancy and delivery related variables, as well as psychometric questionnaires; the last ones both as total scores but also at individual item level. A key novelty feature of the study in the inclusion of many resilience and personality-related variables, that have been identified in the literature but not included in previous models. We also explore the importance of variables in terms of their predictive power of PPD, an effort directed towards to designing a compact survey to screen for PPD. Finally, the analysis of clinically relevant sub-groups such as women with previous depression or depression during pregnancy gave clinically useful insights.
Some limitations of the study include the non-representative sample in that women born in Scandinavia, with a high education and cohabitating with the child’s father were over-represented in the cohort, which makes the findings difficult to generalize to the background population. Sources of selection bias are the exclusion of non-Swedish speaking women as the questionnaires were only offered in the Swedish language, and the fact that more healthy women are more prone to participate in studies of this kind. Not all women self-reported on all variables, but we addressed this problem of missing values with exclusions and imputations where appropriate. Class imbalance in the outcome made the training stages of the algorithms challenging but were also addressed appropriately. Lastly, theoretically, some items from the scales on personality (SSP), and attachment (ASQ) might have had a more prominent role in prediction if they would have been available for a larger proportion of the women in this study. The study by Zhang et al., published after our study was conducted, reported higher AUC and included some predictors lacking in our study 39 . Future studies should make sure to include these important predictive variables for further evaluation.
Depressive symptoms and anxiety during pregnancy are highly predictive factors for women who go on and develop postpartum depressive symptoms, while variables relating to resilience, sense of coherence and personality also play a modest role. The predictive algorithms have relatively good accuracy and AUC, with XRT performing best.
Data sources
Data for the development of the prediction models were obtained from the “Biology, Affect, Stress, Imaging and Cognition during Pregnancy and the Puerperium” (BASIC) study. BASIC is a population-based prospective cohort study at the Department of Obstetrics and Gynaecology at Uppsala University Hospital, Uppsala, Sweden 7 . Between September 2009 and November 2018 all pregnant women who were 18 years of age or older, did not have their identities concealed, had sufficient ability to read and understand Swedish and did not have known bloodborne infections and/or non-viable pregnancy as diagnosed by routine ultrasound were invited to participate in the study 45 . Data acquisition in the BASIC study was mainly based on online surveys and questionnaires that the women were asked to fill out during pregnancy at the 17th and 32nd gestational week and at 6 weeks, 6 months and 12 months postpartum. The surveys included questions about background characteristics, such as sociodemographic variables, psychological measures, medical information, information on reproductive history, lifestyle and sleep. All questionnaires were self-reported and web-based. Data are also retrieved from the medical journals. The participation rate for the study was 20% but the cohort had a relatively low attrition rate, with 71% of the participants remaining in the study at 12 months follow-up 45 .
This study focuses on two subsets of variables from the BASIC study: and (i) background, medical history and pregnancy/delivery variables (BP) and (ii) further psychometric questionnaires (information on exact assessment methods and coding is provided in Table 1 for the background variables and Supplementary Table 1 for the exact questions in the different questionnaires). The BP variables consisted of sociodemographic and lifestyle information, self-reported health, medical history and variables relating to pregnancy and childbirth. This dataset included even information on depression and anxiety symptoms during pregnancy. Depression symptoms were assessed by a score of 12 or more on the Edinburg Postnatal Depression Scale (EPDS) in pregnancy weeks 17, 32 or 38, while anxiety during pregnancy was defined as ratings in the highest quartile on either the State Trait Anxiety Inventory (STAI) 46 , the Beck Anxiety Inventory or the anxiety subscale of the EPDS (EPDS-3A). These variables were available for the majority of the BASIC participants. The total number of interpersonal and non-interpersonal events in the Lifetime Instances of Traumatic Events Scale (LITE) 47 was also included among BP variables. The BP variables consisted of continuous, discrete, nominal and ordinal categorical variables, measured at various time points during the study.
The extra psychometric scales used were the Attachment Style Questionnaire (ASQ) 48 , the Resilience-14 scale (RS) 49 , 50 , the Sense of Coherence Scale-29 (SOC) 51 , the Vulnerable Personality Style Questionnaire (VPSQ) 52 , 53 , and the Swedish Scale of Personalities (SSP) 54 . ASQ, RS, SOC, VPSQ, and SSP were filled out at gestational week 17 or 32, VPSQ and LITE assessments were conducted at 12 months postpartum. All variables were assessed on a Likert scale and coded as ordinal variables. These scales were used for only specific period of time during the course of the BASIC project, different for each scale, and are thus available for different number of women (Table 1 ) 45 .
Additionally, the participants of BASIC study were also asked to fill out the EPDS at different time-points during and after pregnancy. The outcome in this study was EPDS score at 6 weeks postpartum, assessing the degree of self-reported depressive symptoms in the early postpartum period. The discrete scores for this timepoint were then aggregated and a cut-off of a score of 12 or higher was used to indicate women with depressive symptoms, in accordance to validation studies for the Swedish population 55 . The number of women in the BASIC study who had completed the EPDS at 6 weeks postpartum and were thus included was 4313.
Ethics declarations
The study has been approved by the Research Ethics Board in Uppsala (Dnr 2009/171, with amendments). All participating women gave written informed consent before being included in the study. All methods were carried out in accordance with relevant guidelines and regulations.
Data pre-processing
The pre-processing consisted of splitting the original BASIC dataset into different subsets. Two subsets were retained for our study, i.e. background & pregnancy (BP) data and psychometric questionnaire data. Data for twins and women with multiple pregnancies were removed from the dataset, as these are relatively rare, are followed very closely during and after childbirth, and are associated with higher risk for PPD 56 , 57 . Explorative data analyses were conducted on individual variables to check their distributions and to identify and remove outliers that were assessed to be non-informative. Psychometric questionnaires and BP variables that contained information about the women after the time point of the outcome, namely 6 weeks postpartum, were also excluded to avoid inadvertent biases of the results.
SSP was omitted from the analysis due to large number of missing observations, as this survey was used only for few years during recruitment for the BASIC study 45 . Its inclusion would have resulted in a much smaller sample size for the final analysis.
The dataset consists of continuous, nominal and ordinal variables. As continuous variables in the dataset have varying scales, normalization is performed to transform all the variables to a common range from 0 to 1. Furthermore, nominal and ordinal variables that represent non-numerical values are encoded using binary numerical representations for improving the performance of the ML algorithms.
Data imputation
As missing values can drastically impact the performance of ML models, a conservative approach was adopted to handle them. Firstly, samples (rows, corresponding to one pregnancy) with more than 50% missing values in the included variables were eliminated, and the final number of pregnancies in the ML analyses was 4277. Next, variables (columns, corresponding to a distinct variable) with more than 25% missing data were also eliminated. Finally, the remaining missing values were imputed from the available data. While continuous variables were imputed using multivariate imputation by chained equations (MICE) 58 , categorical and ordinal variables were imputed with K nearest neighbors’ imputation 59 .
Classification techniques
With ML algorithms, there is no one-size-fits-all solution, making it imperative to try multiple alternatives. Consequently, this study explored different ML algorithms for supervised classification that modeled data in different ways. In order to present a comprehensive comparison, the following algorithms were implemented: Ridge Regression, LASSO Regression, Gradient Boosting Machines, Distributed Radom Forests, Extreme Randomized Forest, Naïve Bayes, and Stacked Ensembles. Ridge Regression specializes in analysing multiple regression data with multicollinearity, while LASSO Regression is a type of linear regression that shrinks data values towards a central point, and results in simple, sparse models (i.e. models with fewer parameters). Gradient Boosting Machines (GBM) and Random Forests are ensemble learners. In Distributed Radom Forests (DRF), a subset of features is used to determine the most discriminative thresholds to split the trees on. However, unlike DRF, where one builds an ensemble of deep independent trees, in GBM, we specify an ensemble of weak, shallow successive trees, where each tree is learning and improving on the previous tree. In Extremely Randomized Trees (XRT), instead of using the most discriminative thresholds for the splits, thresholds are drawn at random for each feature and the best of these random thresholds are used as the splitting rule, resulting in lower variance but more bias. XRT are similar to DRF with the caveat of more randomness. Naïve Bayes (NB) is a probabilistic classifier based on Bayes’ Theorem. The NB works under the assumption that the presence of any particular feature for a certain outcome is unrelated to the presence of any other feature for that outcome. Thus, despite if the features depend on each other or upon the existence of other features, the NB assumes that all of the features independently contribute to the outcome probability. Stacked Ensemble learns a new model by combining predictions of existing models. Stacked Ensembles are a class of supervised learning algorithms that work by training a meta-learner to find the optimal combination of base learners. Unlike bagging and boosting were the goal is to stack a number of weak learners together, the goal is to stack a number of diverse and strong learners together to optimize learning 60 .
For all the classification algorithms, the outcome measure was the participants’ EPDS score at 6 weeks postpartum represented as a binary variable with 12 as cut-off, while predictor variables included the BP variables and psychometric data described above.
Class imbalance
The BASIC dataset, as a population-based sample and in accordance to clinical situations, is predominantly composed of data from women who did not experience PPD at 6 weeks postpartum (less than 10% of the women representing PPD cases), consequently leading to extreme data class imbalance. ML classifiers trained on such imbalanced datasets usually generate biased results. To mitigate this imbalance, the minority class consisting of women with PPD was oversampled during ML training. Unlike under sampling of majority class consisting of women without PPD, this approach avoids loss of information and leverages all the samples from both classes.
Evaluation metrics
The performance of model prediction of the ML classification algorithms was evaluated using a variety of performance metrics. The performance of each classification model was captured by the Confusion Matrix that formed the basis for other metrics. In addition to the most commonly used classification accuracy, sensitivity (true positive rate) and specificity (false positive rate) are also reported. The positive predictive value (PPV) and negative predictive value (NPV) are also reported. Additionally, a Receiver Operating Characteristic (ROC) curve was specified for each classification to show the relation between the true positive rate and false positive rate. The performance of the classifiers was then summarized by the total area under the ROC curve (AUC), with the higher the AUC (between 0 and 1) indicating a better performance of the classification.
Variable (feature) importance/selection
The success of a ML algorithm does not only depend on good predictive performance but also on generalizability and easy interpretability. Identifying variables that have significant impact on the outcome is valuable, especially in the medical domain. Variable importance using Random Forests models can be calculated using Gini Importance or Mean Decrease in Impurity (MDI) 61 . The MDI relevance of a variable is obtained by calculating how effective the variable is at reducing the uncertainty when creating decision trees. The variable that is most effective and used the most will be ranked as most important.
Analytic strategy
The analytical strategy consisted of breaking the analysis down into steps and iteratively building towards a final classification model, all the while being cognizant of any potential biases introduced by the approach. The workflow is presented in Fig. 7 . First, the raw data was split into the BP and the different psychometric questionnaires datasets in order to build predictive models independently on each psychometric questionnaire and to identify the ones with the highest accuracy for classification of PPD. Second, the psychometric questionnaires that yielded the highest accuracies were combined with the BP dataset. Predictions were then performed with the aggregate data (combined dataset). Additional models were trained with reduced datasets resulting from variable selection. Top 50% and top 25% variables with MDI were used to train separate classification models to determine the relative contribution of those variables to the prediction. Additionally, stratified analyses were performed, where participants were stratified by a previous history of depression (defined as earlier depression, earlier contact with psychiatrist/psychologist, or depression during pregnancy).
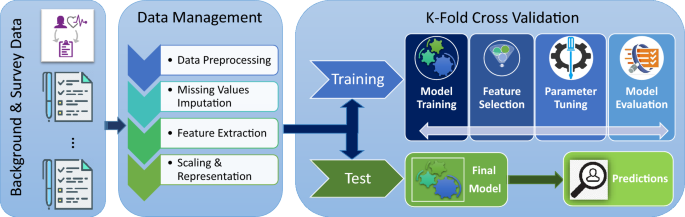
Study workflow and analytical strategy. Data were obtained from the “Biology, Affect, Stress, Imaging and Cognition during Pregnancy and the Puerperium” (BASIC) study, a population-based prospective cohort study in Uppsala, Sweden. Data included in our study comprised (i) background, medical history and pregnancy-related variables (BP) from women, and (ii) further psychometric questionnaires, available at discharge from the delivery ward. The data were processed and either were used to test models or train the machine learning algorithms, to predict depressive symptoms at 6 weeks postpartum.
Based on preliminary analyses, SSP and ASQ did not provide any information gain relative to BP data. Hence, only RS, SOC and VPSQ variables that provided predictive performances comparable to BP variables were included in the aggregate analysis.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request and after data transfer agreements are in place, according to current regulations.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5 5th edn. (American Psychiatric Association, 2013).
Book Google Scholar
Fitelson, E., Kim, S., Baker, A. S. & Leight, K. Treatment of postpartum depression: clinical, psychological and pharmacological options. Int. J. Womens Health 3 , 1–14. https://doi.org/10.2147/IJWH.S6938 (2010).
Article PubMed PubMed Central Google Scholar
Patel, M. et al. Postpartum depression: a review. J. Health Care Poor Underserved 23 , 534–542. https://doi.org/10.1353/hpu.2012.0037 (2012).
Article PubMed Google Scholar
Yim, I. S., Tanner Stapleton, L. R., Guardino, C. M., Hahn-Holbrook, J. & Dunkel Schetter, C. Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu. Rev. Clin. Psychol. 11 , 99–137. https://doi.org/10.1146/annurev-clinpsy-101414-020426 (2015).
Bloch, M., Daly, R. C. & Rubinow, D. R. Endocrine factors in the etiology of postpartum depression. Compr. Psychiatry 44 , 234–246. https://doi.org/10.1016/S0010-440X(03)00034-8 (2003).
Asif, S. et al. Severe obstetric lacerations associated with postpartum depression among women with low resilience—a Swedish birth cohort study. BJOG https://doi.org/10.1111/1471-0528.16271 (2020).
Iliadis, S. I. et al. Personality and risk for postpartum depressive symptoms. Arch. Womens Ment. Health 18 , 539–546. https://doi.org/10.1007/s00737-014-0478-8 (2015).
Article CAS PubMed Google Scholar
Committee on Obstetric Practice. American College of Obstetricians and Gynecologists Committee opinion no. 630: screening for perinatal depression. Obstet. Gynecol. 125 , 1268–1271 (2015).
Article Google Scholar
Ko, J. Y., Rockhill, K. M., Tong, V. T., Morrow, B. & Farr, S. L. Trends in postpartum depressive symptoms—27 States, 2004, 2008, and 2012. MMWR Morb. Mortal Wkly. Rep. 66 , 153–158. https://doi.org/10.15585/mmwr.mm6606a1 (2017).
Dennis, C. L. & McQueen, K. The relationship between infant-feeding outcomes and postpartum depression: a qualitative systematic review. Pediatrics 123 , e736–e751. https://doi.org/10.1542/peds.2008-1629 (2009).
Slomian, J., Honvo, G., Emonts, P., Reginster, J.-Y. & Bruyère, O. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health 15 , 174550651984404. https://doi.org/10.1177/1745506519844044 (2019).
Article CAS Google Scholar
Moore Simas, T. A. et al. Matched cohort study of healthcare resource utilization and costs in young children of mothers with postpartum depression in the United States. J. Med. Econ. 23 , 174–183. https://doi.org/10.1080/13696998.2019.1679157 (2020).
Murray, L., Woolgar, M., Cooper, P. & Hipwell, A. Cognitive vulnerability to depression in 5-year-old children of depressed mothers. J. Child Psychol. Psychiatry 42 , 891–899. https://doi.org/10.1111/1469-7610.00785 (2001).
Nguyen, J. A literature review of alternative therapies for postpartum depression. Nurs. Womens Health 21 , 348–359. https://doi.org/10.1016/j.nwh.2017.07.003 (2017).
The Management of Depression During Pregnancy. A report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Obstet. Gynecol. 114 , 703–713. https://doi.org/10.1097/AOG.0b013e3181ba0632 (2009).
Dennis, C.-L. & Hodnett, E. D. Psychosocial and psychological interventions for treating postpartum depression. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD006116.pub2 (2007).
Righetti-Veltema, M., Conne-Perréard, E., Bousquet, A. & Manzano, J. Risk factors and predictive signs of postpartum depression. J. Affect. Disord. 49 , 167–180. https://doi.org/10.1016/s0165-0327(97)00110-9 (1998).
Lee, Y. et al. Applications of machine learning algorithms to predict therapeutic outcomes in depression: a meta-analysis and systematic review. J. Affect. Disord. 241 , 519–532. https://doi.org/10.1016/j.jad.2018.08.073 (2018).
Bzdok, D. & Meyer-Lindenberg, A. Machine learning for precision psychiatry: opportunities and challenges. Biol. Psychiatry Cognit. Neurosci. Neuroimaging 3 , 223–230. https://doi.org/10.1016/j.bpsc.2017.11.007 (2018).
Friston, K. J., Redish, A. D. & Gordon, J. A. Computational nosology and precision psychiatry. Comput. Psychiatry 1 , 2–23. https://doi.org/10.1162/CPSY_a_00001 (2017).
Rohart, F., Gautier, B., Singh, A. & Lê Cao, K.-A. mixOmics: an R package for ‘omics feature selection and multiple data integration. PLOS Comput. Biol. 13 , e1005752. https://doi.org/10.1371/journal.pcbi.1005752 (2017).
Article CAS PubMed PubMed Central ADS Google Scholar
Ahmed, F. E. Artificial neural networks for diagnosis and survival prediction in colon cancer. Mol. Cancer 4 , 29 (2005).
Anagnostou, T., Remzi, M., Lykourinas, M. & Djavan, B. Artificial neural networks for decision-making in urologic oncology. Eur. Urol. 43 , 596–603 (2003).
Jerez, J. et al. Improvement of breast cancer relapse prediction in high risk intervals using artificial neural networks. Breast Cancer Res. Treat. 94 , 265–272 (2005).
Suzuki, K., Li, F., Sone, S. & Doi, K. Computer-aided diagnostic scheme for distinction between benign and malignant nodules in thoracic low-dose CT by use of massive training artificial neural network. IEEE Trans. Med. Imaging 24 , 1138–1150 (2005).
Baxt, W. G., Shofer, F. S., Sites, F. D. & Hollander, J. E. A neural computational aid to the diagnosis of acute myocardial infarction. Ann. Emerg. Med. 39 , 366–373 (2002).
Zini, G. Artificial intelligence in hematology. Hematology 10 , 393–400 (2005).
Bent, P. et al. Early and intensive continuous hemofiltration for severe renal failure after cardiac surgery. Ann. Thorac. Surg. 71 , 832–837 (2001).
Huang, L., Yu, P., Ju, F. & Cheng, J. Prediction of response to incision using the mutual information of electroencephalograms during anaesthesia. Med. Eng. Phys. 25 , 321–327 (2003).
Choi, J., Choi, J. & Jung, H.-T. Applying machine-learning techniques to build self-reported depression prediction models. CIN Comput. Inform. Nurs. 36 , 317–321. https://doi.org/10.1097/CIN.0000000000000463 (2018).
Gao, S., Calhoun, V. D. & Sui, J. Machine learning in major depression: from classification to treatment outcome prediction. CNS Neurosci. Ther. 24 , 1037–1052. https://doi.org/10.1111/cns.13048 (2018).
Graham, S. et al. Artificial intelligence for mental health and mental illnesses: an overview. Curr. Psychiatry Rep. 21 , 1–18. https://doi.org/10.1007/s11920-019-1094-0 (2019).
Helbich, M., Hagenauer, J. & Roberts, H. Relative importance of perceived physical and social neighborhood characteristics for depression: a machine learning approach. Soc. Psychiatry Psychiatr. Epidemiol. https://doi.org/10.1007/s00127-019-01808-5 (2019).
Wang, S., Pathak, J. & Zhang, Y. Using electronic health records and machine learning to predict postpartum depression. Stud. Health Technol. Inform. 264 , 888–892. https://doi.org/10.3233/SHTI190351 (2019).
Tai, A. M. Y. et al. Machine learning and big data: implications for disease modeling and therapeutic discovery in psychiatry. Artif. Intell. Med. 99 , 101704. https://doi.org/10.1016/j.artmed.2019.101704 (2019).
Tortajada, S. et al. Prediction of postpartum depression using multilayer perceptrons and pruning. Methods Inf. Med. 48 , 291–298. https://doi.org/10.3414/ME0562 (2009).
Jiménez-Serrano, S., Tortajada, S. & García-Gómez, J. M. A mobile health application to predict postpartum depression based on machine learning. Telemed. e-Health 21 , 567–574. https://doi.org/10.1089/tmj.2014.0113 (2015).
Zhang, W., Liu, H., Silenzio, V. M. B., Qiu, P. & Gong, W. Machine learning models for the prediction of postpartum depression: application and comparison based on a cohort study. JMIR Med. Inform. 8 , e15516. https://doi.org/10.2196/15516 (2020).
Zhang, Y., Wang, S., Hermann, A., Joly, R. & Pathak, J. Development and validation of a machine learning algorithm for predicting the risk of postpartum depression among pregnant women. J. Affect. Disord. 279 , 1–8. https://doi.org/10.1016/j.jad.2020.09.113 (2021).
Luca, D. L., Garlow, N., Staatz, C., Margiotta, C. & Zivin, K. Societal Costs of Untreated Perinatal Mood and Anxiety Disorders in the United States (Mathematica Policy Research, 2019).
Google Scholar
Levis, B., Negeri, Z., Sun, Y., Benedetti, A. & Thombs, B. D. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. BMJ 371 , m4022. https://doi.org/10.1136/bmj.m4022 (2020).
Siu, A. L. & Force, A. T. U. P. S. T. Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA 315 , 380–387. https://doi.org/10.1001/jama.2015.18392 (2016).
National Collaborating Centre for Mental Health (UK). Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance: Updated Edition (NICE Clinical Guidelines, No. 192. 5, CASE IDENTIFICATION AND ASSESSMENT, British Psychological Society, 2014).
Austin, M. P., Highet, N. & Group, E. W. Mental Health Care in the Perinatal Period: Australian Clinical Practice Guideline (Centre of Perinatal Excellence, 2017).
Axfors, C. et al. Cohort profile: the Biology, Affect, Stress, Imaging and Cognition (BASIC) study on perinatal depression in a population-based Swedish cohort. BMJ Open 9 , e031514. https://doi.org/10.1136/bmjopen-2019-031514 (2019).
Spielberger, C. D. State‐trait anxiety inventory. In The Corsini Encyclopedia of Psychology , 1. https://doi.org/10.1002/9780470479216.corpsy0943 (2010).
Greenwald, R. & Rubin, A. Assessment of posttraumatic symptoms in children: development and preliminary validation of parent and child scales. Res. Soc. Work Pract. 9 , 61–75. https://doi.org/10.1177/104973159900900105 (1999).
Feeney, J., Noller, P. & Hanrahan, M. Assessing adult attachment. In Attachment in Adults: Clinical and Developmental Perspectives (eds Sperling, M. B. & Berman, W. H.) 128–151 (The Guilford Press, New York, 1994).
Aiena, B. J., Baczwaski, B. J., Schulenberg, S. E. & Buchanan, E. M. Measuring resilience with the RS–14: a tale of two samples. J. Pers. Assess. 97 , 291–300 (2015).
Wagnild, G. M. & Young, H. M. Development and psychometric evaluation of the resilience scale. J. Nurs. Meas. 1 , 165–178 (1993).
CAS PubMed Google Scholar
Antonovsky, A. The structure and properties of the sense of coherence scale. Soc. Sci. Med. 36 , 725–733. https://doi.org/10.1016/0277-9536(93)90033-Z (1993).
Boyce, P., Hickey, A., Gilchrist, J. & Talley, N. J. The development of a brief personality scale to measure vulnerability to postnatal depression. Arch. Womens Ment. Health 3 , 147–153. https://doi.org/10.1007/s007370170012 (2001).
Gelabert, E. et al. The vulnerable personality style questionnaire: psychometric properties in Spanish postpartum women. Arch. Womens Ment. Health 14 , 115–124 (2011).
Gustavsson, J. P. et al. Swedish universities Scales of Personality (SSP): construction, internal consistency and normative data. Acta Psychiatr. Scand. 102 , 217–225. https://doi.org/10.1034/j.1600-0447.2000.102003217.x (2000).
Wickberg, B. & Hwang, C. P. The Edinburgh Postnatal Depression Scale: validation on a Swedish community sample. Acta Psychiatr. Scand. 94 , 181–184. https://doi.org/10.1111/j.1600-0447.1996.tb09845.x (1996).
Vilska, S. et al. Mental health of mothers and fathers of twins conceived via assisted reproduction treatment: a 1-year prospective study. Hum. Reprod. 24 , 367–377. https://doi.org/10.1093/humrep/den427 (2009).
Wenze, S. J., Battle, C. L. & Tezanos, K. M. Raising multiples: mental health of mothers and fathers in early parenthood. Arch. Womens Ment. Health 18 , 163–176. https://doi.org/10.1007/s00737-014-0484-x (2015).
Azur, M. J., Stuart, E. A., Frangakis, C. & Leaf, P. J. Multiple imputation by chained equations: what is it and how does it work?: Multiple imputation by chained equations. Int. J. Methods Psychiatr. Res. 20 , 40–49. https://doi.org/10.1002/mpr.329 (2011).
Beretta, L. & Santaniello, A. Nearest neighbor imputation algorithms: a critical evaluation. BMC Med. Inform. Decis. Mak. 16 (Suppl 3), 74. https://doi.org/10.1186/s12911-016-0318-z (2016).
van der Laan, M. J., Polley, E. C. & Hubbard, A. E. Super learner. Stat. Appl. Genet. Mol. Biol. https://doi.org/10.2202/1544-6115.1309 (2007).
Article MathSciNet PubMed PubMed Central MATH Google Scholar
Hastie, T., Tibshirani, R. & Friedman, J. H. The Elements of Statistical Learning: Data Mining, Inference, and Prediction 2nd edn. (Springer, 2009).
Download references
Acknowledgements
The authors would like to acknowledge Anastasia Kollia, Hanna Henriksson and Emma Bränn for valuable insights and help with data collection and management in the BASIC study. Marina Krylova, Nils Kroemer, and Hamidreza Jamalabadi for valuable insights and assistance in the initial phase of the analyses planning. Dr. Narayanan Chatapuram Krishnan for his excellent machine learning course. Subhranil Bagchi for time spent aiding in coding and students at IIT Ropar for their insights and help with coding and theoretical discussions. Prof. Inger Sundström Poromaa, Ass. Prof. Fotios Papadopoulos and all colleagues working in the BASIC research group for their contribution with critical comments and discussions. Finally, the authors would like to sincerely thank Dr. Diem Nguyen for language editing and comments.
Open access funding provided by Uppsala University. This study has been supported by the municipality of Uppsala and Akademiska University Hospital in Sweden, the Swedish Research foundation (523-2014-2342 and 523-2014-07605), Marianne and Marcus Wallenberg foundation and the Swedish Medical Association.
Author information
Authors and affiliations.
Department of Women’s and Children’s Health, Uppsala University, 751 85, Uppsala, Sweden
Sam Andersson, Stavros I. Iliadis & Alkistis Skalkidou
Department of Computer Science and Engineering, Indian Institute of Technology Ropar, Rupnagar, Punjab, 140001, India
Deepti R. Bathula
Department of Psychiatry and Psychotherapy, University Hospital Jena, Jena, Germany
Martin Walter
Department of Psychiatry and Psychotherapy, Eberhardt Karls University, Tübingen, Germany
Department of Behavioral Neurology, Leibniz Institute for Neurobiology, Magdeburg, Germany
You can also search for this author in PubMed Google Scholar
Contributions
A.S. conceived and designed the study. The analysis plan was decided on with the contribution of all authors. Analyses were performed by D.R.B., S.A., and S.I.I. S.A., D.R.B., and S.I.I. prepared the figures and tables. All authors made substantial contributions to the interpretation of results. S.A. wrote the first draft and all authors critically revised the manuscript and approved the final version.
Corresponding author
Correspondence to Alkistis Skalkidou .
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary informations., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Andersson, S., Bathula, D.R., Iliadis, S.I. et al. Predicting women with depressive symptoms postpartum with machine learning methods. Sci Rep 11 , 7877 (2021). https://doi.org/10.1038/s41598-021-86368-y
Download citation
Received : 16 September 2020
Accepted : 15 March 2021
Published : 12 April 2021
DOI : https://doi.org/10.1038/s41598-021-86368-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Enhancing explainability in predicting mental health disorders using human–machine interaction.
- Inderpreet Kaur
- Umesh Gupta
Multimedia Tools and Applications (2024)
Unveiling the prevalence and risk factors of early stage postpartum depression: a hybrid deep learning approach
- Umesh Kumar Lilhore
- Surjeet Dalal
- Arshad Hashmi
Wife-Mother Role Conflict at the Critical Child-Rearing Stage: A Machine-Learning Approach to Identify What and How Matters in Maternal Depression Symptoms in China
- Liuzhi Hong
Prevention Science (2023)
Prenatal and Childbirth Risk Factors of Postpartum Pain and Depression: A Machine Learning Approach
- McClain Sampson
Maternal and Child Health Journal (2023)
- Trine Munk-Olsen
- Xiaoqin Liu
- Merete L. Maegbaek
Translational Psychiatry (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Kujawa leads study to predict postpartum depression by examining brain function throughout pregnancy

Media Inquiries
- 615-322-6397 Email
Latest Stories
- Limited Submission Opportunity: 2024 Creating Equitable Pathways to STEM Graduate Education Program
- Vanderbilt Law announces launch of Undergraduate Minor in Legal Studies
- Two A&S psychology faculty receive prestigious awards in vision sciences
Jan 30, 2024, 12:02 PM
By Jenna Somers

A five-year, nearly $3.6 million grant from the National Institute of Mental Health will support Autumn Kujawa , associate professor of psychology and human development at Vanderbilt Peabody College of education and human development , and her team in examining changes in brain processes throughout pregnancy to understand whether and to what extent these changes predict postpartum depression. Establishing an understanding of the early predictors for postpartum depression could support the development of timely and targeted treatments for high-risk patients during pregnancy to address symptoms before they develop or when they begin to appear.
Postpartum depression has profound negative effects on mothers, their children, and the mother-child relationship, creating an urgent need to better understand risk and to help to inform prevention efforts. Previous research by Kujawa and others demonstrates that, outside of pregnancy, low activation of positive emotions systems and reward responsiveness in the brain predict future depressive symptoms. When functioning normally, these systems also support social motivation in mother-infant relationships. However, pregnancy can greatly affect the function of positive emotions systems and reward responsiveness due to rapid hormonal fluctuations and increased stress associated with dramatic changes in roles, expectations, and relationships. With this understanding, Kujawa theorizes that low positive emotions systems functioning during pregnancy could predict increased risk for postpartum depression.
“If we can better understand some of these mechanisms of peripartum depression, we might be able to adapt interventions from our study with mothers and older children for pregnant and postpartum people to focus on increasing positive emotions, particularly in the context of caregiving and establishing a relationship with a new baby,” Kujawa said. “We’re also interested in the timing for predicting risk—how early in pregnancy can we observe markers of risk for later symptoms? That could help to determine when to administer assessments and intervene.”
Kujawa and her team will conduct longitudinal assessments with 300 pregnant participants across the peripartum period (15 weeks gestation to five weeks postpartum) to examine trajectories of positive emotions systems function, whether it influences mother-infant interactions, and explore biological and social processes shaping risk for postpartum depression. At 15 weeks postpartum, mothers and infants will participate in an observed free play interaction to assess mutual enjoyment. Depressive symptoms and diagnoses will be assessed from 15 weeks gestation through 25 weeks postpartum.
Importantly, Kujawa’s work could add valuable insight to current mental health practices during the prenatal and postpartum periods and inform novel treatment methods. Traditionally, during these periods, depressive symptoms are screened using the Edinburgh Postnatal Depression Scale. While useful for assessing symptoms and referring patients for treatment, the screening does not offer information about underlying causes and personalized approaches to intervention. Kujawa’s work aims to do both, which could possibly allow mental health professionals to intervene before depressive symptoms develop or become severe.
Keep Reading

Vanderbilt Peabody researcher receives grant to study depression link in mothers and children

Kujawa receives $1.45 million grant to study new intervention for child mental health

Study reveals brain function predictors of treatment outcomes for adolescent depression
Explore story topics.
- Education and Psychology
- Autumn Kujawa
- Department of Psychology and Human Development
- Ideas In Action
- Ideas in Action Featured
- Peabody College
- peabody-home
- Psychology and Human Development
Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
- Download PDF
- CME & MOC
- Share X Facebook Email LinkedIn
- Permissions
Postpartum Depression—New Screening Recommendations and Treatments
- 1 University of Massachusetts Chan Medical School, Worcester
- 2 UMass Memorial Health, Worcester, Massachusetts
- Medical News & Perspectives What to Know About the First Pill Approved for Postpartum Depression Rita Rubin, MA JAMA
- Comment & Response Screening Recommendations and Treatments for Postpartum Depression—Reply Tiffany A. Moore Simas, MD, MPH, MEd; Anna Whelan, MD; Nancy Byatt, DO, MS, MBA JAMA
- Comment & Response Screening Recommendations and Treatments for Postpartum Depression Itamar Nitzan, MD; Raylene Philips, MD; Robert D. White, MD JAMA
Perinatal mental health conditions are those that occur during pregnancy and the year following childbirth, whether onset of the condition(s) predates pregnancy or occurs in the perinatal period. Perinatal mental health conditions are the leading cause of overall and preventable maternal mortality and include a wide array of mental health conditions including anxiety, depression, and substance use disorders. 1 , 2 Perinatal depression specifically affects 1 in 7 perinatal individuals. 3 While commonly referred to as postpartum depression, it is more accurately called perinatal depression because its onset corresponds with prepregnancy (27%), pregnancy (33%), and postpartum (40%) time frames. 3
Read More About
Moore Simas TA , Whelan A , Byatt N. Postpartum Depression—New Screening Recommendations and Treatments. JAMA. 2023;330(23):2295–2296. doi:10.1001/jama.2023.21311
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Subscribe or renew today
Every print subscription comes with full digital access
Science News
Depression among new mothers is finally getting some attention.
Why is a happy time of life a dark time for some women?

JOY TO ANGUISH Depression in new mothers remains a mystery, but new views into the brain and a potential drug offer fresh hope.
Gaiamoments/iStockphoto
Share this:
By Laura Beil
March 11, 2018 at 5:00 am
On the hormonal roller coaster of life, the ups and downs of childbirth are the Tower of Power. For nine long months, a woman’s body and brain absorb a slow upwelling of hormones, notably progesterone and estrogen. The ovaries and placenta produce these two chemicals in a gradual but relentless rise to support the developing fetus.
With the birth of a baby, and the immediate expulsion of the placenta, hormone levels plummet. No other physiological change comes close to this kind of free fall in both speed and intensity. For most women, the brain and body make a smooth landing, but more than 1 in 10 women in the United States may have trouble coping with the sudden crash. Those new mothers are left feeling depressed, isolated or anxious at a time society expects them to be deliriously happy.
This has always been so. Mental struggles following childbirth have been recognized for as long as doctors have documented the experience of pregnancy. Hippocrates described a woman’s restlessness and insomnia after giving birth. In the 19th century, some doctors declared that mothers were suffering from “insanity of pregnancy” or “insanity of lactation.” Women were sent to mental hospitals.
Modern medicine recognizes psychiatric suffering in new mothers as an illness like any other, but the condition, known as postpartum depression, still bears stigma. Both depression and anxiety are thought to be woefully underdiagnosed in new mothers, given that many women are afraid to admit that a new baby is anything less than a bundle of joy. It’s not the feeling they expected when they were expecting.
Treatment — when offered — most commonly involves some combination of antidepression medication, hormone therapy, counseling and exercise. Still, a significant number of mothers find these options wanting. Untreated, postpartum depression can last for years, interfering with a mother’s ability to connect with and care for her baby.
Although postpartum depression entered official medical literature in the 1950s, decades have passed with few new options and little research.
Even as brain imaging has become a common tool for looking at the innermost workings of the mind, its use to study postpartum depression has been sparse. A 2017 review in Trends in Neurosciences found only 17 human brain imaging studies of postpartum depression completed through 2016. For comparison, more than four times as many have been conducted on a problem called “internet gaming disorder” — an unofficial diagnosis acknowledged only five years ago.
Rise and fall
The hormone progesterone rises far above typical levels during pregnancy, then plummets after childbirth. Researchers are investigating how this and other changes contribute to postpartum depression.

Source: K.D. Pennell, M.A. Woodlin and P.B. Pennell/ Steroids 2015
Now, however, more researchers are turning their attention to this long-neglected women’s health issue, peering into the brains of women to search for the root causes of the depression. At the same time, animal studies exploring the biochemistry of the postpartum brain are uncovering changes in neural circuitry and areas in need of repair.
And for the first time, researchers are testing an experimental drug designed specifically for postpartum depression. Early results have surprised even the scientists.
Women’s health experts hope that these recent developments signal a new era of research to help new moms who are hurting.
“I get this question all the time: Isn’t it just depression during the postpartum period? My answer is no,” says neuroscientist Benedetta Leuner of Ohio State University. “It’s occurring in the context of dramatic hormonal changes, and that has to be impacting the brain in a unique way. It occurs when you have an infant to care for. There’s no other time in a woman’s life when the stakes are quite as high.”
Brain drain
Even though progesterone and estrogen changes create hormonal whiplash, pregnancy wouldn’t be possible without them. Progesterone, largely coming from the ovaries, helps orchestrate a woman’s monthly menstrual cycle. The hormone’s primary job is to help thicken the lining of the uterus so it will warmly welcome a fertilized egg. In months when conception doesn’t happen, progesterone levels fall and the uterine lining disintegrates. If a woman becomes pregnant, the fertilized egg implants in the uterine wall and progesterone production is eventually taken over by the placenta, which acts like an extra endocrine organ.
Like progesterone, estrogen is a normal part of the menstrual cycle that kicks into overdrive after conception. In addition to its usual duties in the female body, estrogen helps encourage the growth of the uterus and fetal development, particularly the formation of the hormone-producing endocrine system.
These surges in estrogen and progesterone, along with other physiological changes, are meant to support the fetus. But the hormones, or chemicals made from them, cross into the mother’s brain, which must constantly adapt. When it doesn’t, signs of trouble can appear even before childbirth, although they are often missed. Despite the name “postpartum,” about half of women who become ill are silently distressed in the later months of pregnancy.
Decades ago, controversy churned over whether postpartum depression was a consequence of fluctuating hormones alone or something else, says neuroscientist Joseph Lonstein of Michigan State University in East Lansing. He studies the neurochemistry of maternal caregiving and postpartum anxiety. Lonstein says many early studies measured hormone levels in women’s blood and tried to determine whether natural fluctuations were associated with the risk of postpartum depression. Those studies found “no clear correlations with [women’s] hormones and their susceptibility to symptoms,” he says. “While the hormone changes are certainly thought to be involved, not all women are equally susceptible. The question then became, what is it about their brains that makes particular women more susceptible?”
Brain changes
Research in rodents, along with imaging studies in new mothers, are finding areas of the brain that could be involved in postpartum depression. Among them:

1. Amygdalae Sometimes called the body’s “emotional thermostat,” these two structures are deep in the brain, one on each side. Studies suggest that, among other things, depressed mothers have heightened amygdala responses to an unfamiliar baby, perhaps blunting the response to their own child.
2. Nucleus accumbens Famous for its role in reward, pleasure and addiction, this area showed less ability to change in a study of rats with symptoms of postpartum depression.
3. Hippocampus This region contains receptors for neurosteroids, potent products of the hormone progesterone. During pregnancy, the number of neurosteroid receptors typically drops, presumably to protect the brain from high levels of progesterone and estrogen circulating at the same time. When progesterone drops immediately following loss of the placenta after birth, the receptors repopulate. But depressed women may not experience this rebound.
Seeking answers, researchers have examined rodent brains and placed women into brain scanners to measure the women’s responses to pictures or videos of babies smiling, babbling or crying. Though hormones likely underlie the condition, many investigations have led to the amygdalae. These two, almond-shaped clumps of nerve cells deep in the brain are sometimes referred to as the emotional thermostat for their role in the processing of emotions, particularly fear.
The amygdalae are entangled with many structures that help make mothers feel like mothering, says neuroscientist Alison Fleming of the University of Toronto Mississauga. The amygdalae connect to the striatum, which is involved in experiencing reward, and to the hippocampus, a key player in memory and the body’s stress response. And more: They are wired to the hypothalamus, the interface between the brain and the endocrine system (when you are afraid, the endocrine system produces adrenaline and other chemicals that get your heart racing and palms sweating). The amygdalae are also connected to the prefrontal cortex and insula, involved in decision making, motivation and other functions intertwined with maternal instinct.
Fleming and colleagues have recently moved from studies in postpartum rodents to human mothers. In one investigation, reported in 2012 in Social Neuroscience , women were asked to look at pictures of smiling infants while in a functional MRI, which images brain activity. In mothers who were not depressed, the researchers found a higher amygdala response, more positive feelings and lower stress when women saw their own babies compared with unfamiliar infants.
But an unexpected pattern emerged in mothers with postpartum depression, as the researchers reported in 2016 in Social Neuroscience . While both depressed and not-depressed mothers showed elevated amygdala activity when viewing their own babies, the depressed mothers also showed heightened responses to happy, unknown babies , suggesting reactions to the women’s own children were blunted and not unique. This finding may mean that depressed women had less inclination to emotionally attach to their babies.
Mothers with postpartum depression also showed weaker connectivity between the amygdalae and the insula. Mothers with weaker connectivity in this area had greater symptoms of depression and anxiety. Women with stronger connectivity were more responsive to their newborns.
While there’s still no way to definitely know that the amygdalae are responding to postpartum chemical changes, “it’s very likely,” Lonstein says, pointing out that the amygdalae are influenced by the body’s reaction to hormones in other emotional settings.
Maternal rewards
While important, the amygdalae are just part of the puzzle that seems to underlie postpartum depression. Among others is the nucleus accumbens, famous for its role in the brain’s reward system and in addiction, largely driven by the yin and yang of the neurotransmitters dopamine and serotonin. In studies, mothers who watched films of their infants (as opposed to watching unknown infants) experienced increased production of feel-good dopamine. The women also had a strengthening of the connection between the nucleus accumbens, the amygdalae and other structures, researchers from Harvard Medical School and their collaborators reported in February 2017 in Proceedings of the National Academy of Sciences .
That’s not entirely surprising given that rodent mothers find interacting with their newborn pups as neurologically rewarding as addictive drugs, says Ohio State’s Leuner. Rodent mothers that are separated from their offspring “will press a bar 100 times an hour to get to a pup. They will step across electrified grids to get to their pups. They’ve even been shown in some studies to choose the pups over cocaine.” Mothers find their offspring “highly, highly rewarding,” she says.
When there are postpartum glitches in the brain’s reward system, women may find their babies less satisfying, which could increase the risk for impaired mothering. Writing in 2014 in the European Journal of Neuroscience , Leuner and colleagues reported that in rats with symptoms of postpartum depression (induced by stress during pregnancy, a major risk factor for postpartum depression in women), nerve cells in the nucleus accumbens atrophied and showed fewer protrusions called dendritic spines — suggesting weaker connections to surrounding nerve cells compared with healthy rats. This is in contrast to other forms of depression, which show an increase in dendritic spines.
Cuddle chemical
In one study, women with depressive symptoms in the first two weeks after delivery had lower levels of the hormone oxytocin in the third trimester than women without depression. (Each circle is one woman; horizontal lines are means.) But the story is complicated because other studies have shown that giving artificial oxytocin during labor does not alleviate symptoms.

Unpublished follow-up experiments conducted by Leuner’s team also point to a role for oxytocin, a hormone that spikes with the birth of a baby as estrogen and progesterone fall. Sometimes called the “cuddle chemical,” oxytocin is known for its role in maternal bonding ( SN Online: 4/16/15 ). Leuner hypothesizes that maternal depression is associated with deficits in oxytocin receptors that enable the hormone to have its effects as part of the brain’s reward system.
If correct, the idea may help explain why oxytocin treatment failed women in some studies of postpartum depression. The hormone may simply not have the same potency in some women whose brains are short on receptors the chemical can latch on to. The next step is to test whether reversing the oxytocin receptor deficits in rodents’ brains relieves symptoms.
Leuner and other scientists emphasize that the oxytocin story is complex. In 2017, in a study reported in Depression & Anxiety , women without a history of depression who received oxytocin — which is often given to promote contractions or stem bleeding after delivery — had a 32 percent higher likelihood of developing postpartum depression than women who did not receive the hormone. In more than 46,000 births, 5 percent of women who did not receive the hormone were diagnosed with depression, compared with 7 percent who did.
“This was the opposite of what we predicted,” says Kristina Deligiannidis, a neuroscientist and perinatal psychiatrist at the Feinstein Institute for Medical Research in Manhasset, N.Y. After all, oxytocin is supposed to enhance brain circuits involved in mothering. “We had a whole group of statisticians reanalyze the data because we didn’t believe it,” she says. While the explanation is unknown, one theory is that perhaps the women who needed synthetic oxytocin during labor weren’t making enough on their own — and that could be why they are more prone to depression after childbirth.
But postpartum depression can’t be pinned to any single substance or brain malfunction — it doesn’t reside in one tidy nest of brain cells, or any one chemical process gone haywire. Maternal behavior is based on complex neurological circuitry. “Multiple parts of the brain are involved in any single function,” Deligiannidis says. “Just to have this conversation, I’m activating several different parts of my brain.” When any kind of depression occurs, she says, multiple regions of the brain are suffering from a communication breakdown.
Looking further, Deligiannidis has also examined the role of certain steroids synthesized from progesterone and other hormones and known to affect maternal brain circuitry. In a 2016 study in Psychoneuroendocrinology involving 32 new mothers at risk for postpartum depression and 24 healthy mothers, Deligiannidis and colleagues reported that concentrations of some steroids that affect the brain, also called neurosteroids, were higher in women at risk for developing depression (because of their past history or symptoms), compared with women who were not. The higher levels suggest a system out of balance — the brain is making too much of one neurosteroid and not enough of another, called allopregnanolone, which is thought to protect against postpartum depression and is being tested as a treatment.
Treating pregnancy withdrawal

Postpartum depression doesn’t weigh down just mom. Research suggests it might have negative effects on her offspring that can last for years. Risks include:
- Higher levels of cortisol and other stress hormones
- More time fussing and crying
- More “indeterminate sleep,” hovering between deep and active sleep
Infants and children
- Increased risk of developmental problems
- Slower growth
- Lower cognitive function
- Elevated cortisol levels
Adolescents
- Higher risk of depression
Tufts University neuroscientist Jamie Maguire, based in Boston, got interested in neurosteroids during her postgraduate studies in the lab of Istvan Mody at UCLA. Maguire and Mody reported in 2008 in Neuron that during pregnancy, the hippocampus has fewer receptors for neurosteroids , presumably to protect the brain from the massive levels of progesterone and estrogen circulating at that time. When progesterone drops after birth, the receptors repopulate.
But in mice genetically engineered to lack those receptors, something else happened: The animals were less interested in tending to their offspring, failing to make nests for them.
“We started investigating. Why are these animals having these abnormal postpartum behaviors?” Maguire recalls. Was an inability to recover these receptors making some women susceptible? Interestingly, similar receptors are responsible for the mood-altering and addictive effects of some antianxiety drugs, suggesting that the sudden progesterone drop after childbirth could be leaving some women with a kind of withdrawal effect.
Further experiments demonstrated that giving the mice a progesterone-derived neurosteroid — producing levels close to what the mice had in pregnancy — alleviated the symptoms.
Today, Maguire is on the scientific advisory board of Boston area–based Sage Therapeutics, which is testing a formulation of allopregnanolone called brexanolone. Results of an early clinical trial published last July in The Lancet assessed whether brexanolone would alleviate postpartum symptoms in women with severe postpartum depression. The study involved 21 women randomly assigned to receive a 60-hour infusion of the drug or a placebo within six months after delivery.
At the end of treatment, the women who received the drug reported a 21-point reduction on a standard scale of depression symptoms, compared with about 9 points for the women on a placebo. “These women got better in about a day,” says Deligiannidis, who is on the study’s research team. “The results were astonishing.”
In November, Sage Therapeutics announced the results of two larger studies, although neither has been published. Combined, the trials involved 226 women with severe or moderate postpartum depression. Both groups showed similar improvements that lasted for the month the women were followed. The company has announced plans to request approval from the U.S. Food and Drug Administration to market brexanolone in the United States. This is an important first step, researchers say, toward better treatments.
“We are just touching on one small piece of a bigger puzzle,” says Jodi Pawluski, a neuroscientist at the Université de Rennes 1 in France who coauthored the 2017 review in Trends in Neurosciences . She was surprised at the dearth of research, given how common postpartum depression is. “This is not the end, it’s the beginning.”
This story appears in the March 17, 2018 issue of Science News with the headline, “From Joy to Anguish: Depression among new mothers gets much-needed attention.”
Editor’s note: This article was updated on March 13, 2018, to correct measurements on the graph, Progesterone levels during pregnancy and after. The amounts are plasma progesterone in ng/ml.
More Stories from Science News on Neuroscience

Chickadees use memory ‘bar codes’ to find their hidden food stashes

Here’s how magnetic fields shape desert ants’ brains

Dogs know words for their favorite toys

Ancient viruses helped speedy nerves evolve

How do babies learn words? An AI experiment may hold clues

A new device let a man sense temperature with his prosthetic hand

Under very rare conditions, Alzheimer’s disease may be transmitted

Handwriting may boost brain connections more than typing does
Subscribers, enter your e-mail address for full access to the Science News archives and digital editions.
Not a subscriber? Become one now .

I Took the New Postpartum Depression Pill—Here’s What Happened
T he introduction of zuranolone by the Food and Drug Administration (FDA) in August 2023 marked a pivotal moment in the treatment of postpartum depression (PPD) . Distinct from the mild and brief "baby blues" that many new child-bearers experience, experts say postpartum depression involves deeper, persistent feelings of sadness, anxiety, fatigue, irritability and more that can significantly impact a parent's ability to care for herself and her newborn.
With one in eight or almost 13%, of new mothers reporting symptoms of postpartum depression according to the Centers for Disease Control and Prevention (CDC) —and acknowledging that this number is likely higher due to cases that go unreported—zuranolone's approval introduces an essential option for those seeking relief.
Unlike traditional interventions that rely on psychotherapy and conventional antidepressants, zuranolone promises a faster response, easing symptoms in as little as three days with a treatment course of only two weeks.
Katrina Furey, MD, a psychiatrist from Yale , points out the significance of zuranolone amidst the broader context of maternal mental health, noting that mental health issues are the most prevalent complications following childbirth, even more than conditions related to gestational diabetes or hypertension.
This innovative medication addresses postpartum depression at its source as it is a synthetic form of allopregnanolone, a crucial neurosteroid for mood balance that is often found in low levels in women with postpartum depression. Allopregnanolone specifically targets malfunctioning GABA-A receptors in the brain, which are key to managing mood and behavior that malfunction without sufficient allopregnanolone, leading to symptoms. Along with healthcare providers' growing dedication to screening for postpartum depression, this treatment marks a major advance in providing new mothers with prompt and effective care.
If you find yourself experiencing any of the following signs of postpartum depression—
- An increase in tears or a feeling of constant sadness.
Growing irritability or feelings of anger.
Withdrawing from loved ones and friends.
Feeling disconnected or indifferent towards your baby.
Worrying about harming your child.
Continuous self-doubt about your ability to be a good mother or concerns over not caring properly for your baby.
—remember, you're not navigating this alone. Support and resources are readily available. Don't hesitate to seek assistance by talking to your healthcare provider.
Ahead, we share the personal story of Samantha M., a 31-year-old from New York who navigated through the challenges of postpartum depression. As a wife and mother of three, participating in a phase three clinical trial—the final phase before market approval—for zuranolone was a turning point for her and her family.
Get The Healthy by Reader's Digest newsletter
Taking the new postpartum depression drug
By Samantha M., as told to Dr. Patricia Varacallo, DO
After the birth of my third child, I found myself in a place I had never anticipated. I've experienced low moments in the past, but never to the point of receiving a diagnosis. While I was familiar with the term "postpartum depression," facing it was an entirely different story. Instead of the joy and bonding after childbirth—a feeling I fondly remembered with my first two—I was engulfed by an overwhelming sadness and a deep sense of detachment, affecting not just my relationship with my newborn but also with my husband. My mind was a tangled mess of confusion, guilt, and a yearning for the normalcy I once knew, leaving me to wonder: Why can't I just enjoy these moments?
It never got to the point of harming myself, but I felt like I was just existing.
No. Motivation. whatsoever.
I distinctly remember my two little ones and my husband joking around the dinner table and I just couldn't feel the same happiness they were feeling…and that was not like me.
Healing My Gut with Probiotics Relieved My Depression: I Tried It
Seeking help for postpartum depression
I remember the turning point came about two months postpartum early spring 2021, during a conversation with one of my best friends from college who is now working in women's health. She mentioned a clinical trial for a new postpartum depression drug called zuranolone.
Having discussed the standard postpartum depression treatment options with my OBGYN six weeks after giving birth, I was all too aware of the lengthy wait—often weeks or months—for traditional antidepressants to possibly start working. Then there was brexanolone, the first FDA-approved drug specifically for postpartum depression, requiring a 60-hour continuous IV infusion. It was good to know that this existed if the circumstances warranted it, but in my case the thought of being hospitalized and away from my family for three nights made me hesitant.
I learned zuranolone was different—it was a daily pill taken for just two weeks. No hospital stays, no IVs.
My husband and I had a thorough conversation. I reflected on the requirement to discontinue breastfeeding for the clinical trial, since zuranolone could be present in breast milk and its effects on a baby are unknown. I struggled with this decision, as I didn't want to lose another precious bonding opportunity with my baby, but I knew my condition was getting worse. I chose to enroll.
The catch with many clinical trials is the uncertainty of possibly being given a placebo (a substance with no therapeutic effect, used as a control in testing new drugs) instead of the real drug. Despite this risk of not getting the actual medication, I still believed the chance to potentially improve my condition was too significant to pass up.
What to Know About CBD and Depression
I took the new postpartum depression drug
Zurualonone may not be right for every patient, and you'll need to discuss it with your doctor. But when I tell you that I started to feel a little bit better after taking just the second dose of the drug...I am not exaggerating. Right away, I felt something shift and I started to feel more like myself than I had in months. I dared to hope it was the zuranolone working.
For 14 days, I took the 50-milligram dose, each day feeling progressively more grounded, more connected to my life and the people in it. My husband noticed the change, too. We began to reconnect in ways that had felt lost for some time.
I'd been cautioned about possible side effects, like fatigue, digestive issues, cold symptoms, and increased risk of urinary tract infections. I experienced only some slight drowsiness in the beginning, but it never hindered my daily activities.
Following the treatment, I had check-ins at approximately one month and then again at six weeks, and the positive feelings persisted—I still felt closer to my former self than I had in a long time. The heavy fog of depression had lifted, allowing me to fully engage with my family and enjoy the precious moments with my newborn that I had been missing.
10 Vitamins for Depression That Could Boost Your Mood
Life after taking the postpartum depression pill
Today, a little more than three years since participating in the trial, the drug is now available to other new moms and my own sense of wellbeing remains intact.
For any woman, life is not without its challenges—juggling the responsibilities of being a mother to three and a wife certainly has its moments—but genuinely, I continue to feel good. To maintain my balance, I've discovered that therapy is beneficial for me, and I also made a commitment to myself to manage my mental health by practicing yoga twice a week.
Sharing my personal experience isn't easy, (and believe me, I was hesitant to do so) but I do it in the hope that it might help someone else feeling lost with postpartum depression. The path through is different for everyone, but options and support are available.
Whether it's traditional treatments or new ones like zuranolone, the first step is reaching out for help. For me, that step was a conversation with a friend that led to a clinical trial and a medication that changed my life. For someone else, it just might be this story that makes all the difference.
For the latest in wellness delivered to you daily, subscribe to The Healthy @ Reader's Digest newsletter and follow The Healthy on Facebook and Instagram . Keep reading:
- "Here's How I Knew I Had Uterine Cancer": One Patient's Story After Spotting a Tell-Tale Sign
- 4 Postpartum Yoga Poses To Strengthen Your Core, From a Certified Yoga & Postnatal Instructor
- What Is 'Vaginal Seeding'? Medical Doctors Explain
- I Ate an Avocado Every Day for a Week—Here's What Happened
The post I Took the New Postpartum Depression Pill—Here’s What Happened appeared first on The Healthy .


Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Science News
- Meetings and Events
- Social Media
- Press Resources
- Email Updates
- Innovation Speaker Series
Population Study Finds Depression Is Different Before, During, and After Pregnancy
May 15, 2023 • Research Highlight
Perinatal depression is a common but serious mood disorder. The DSM-5, which is the classification system used to diagnose mental disorders, defines perinatal depression as a depressive episode with onset either during pregnancy or in the first 4 weeks after pregnancy (postpartum). However, pregnancy and postpartum are associated with different hormonal, behavioral, and emotional changes. Combining them into a single disorder may make studying and treating depression more difficult. Additionally, restricting the postpartum period to the first month after childbirth may miss many women who continue to experience depressive symptoms beyond this time point.
New research funded by the National Institute of Mental Health examined the current classification of perinatal depression by looking at population-level rates of depression over an extended period. The study, led by Veerle Bergink, M.D., Ph.D. , at the Icahn School of Medicine at Mount Sinai and the Erasmus Medical Center, compared depressive episodes among new mothers before, during, and after pregnancy.
The researchers used data from population registries in Denmark to identify 392,287 women who had given birth for the first time between 1999 and 2015. Only first-child births were included to avoid counting the same woman more than once. Then, the researchers calculated the number of first-time and repeat depressive episodes women experienced during each of the following months, reflecting three separate periods:
- 12 months before pregnancy (preconception)
- 9 months before to birth (pregnancy)
- 12 months after birth (postpartum)
First-time and repeat depressive episodes were classified based on the number of times women sought psychiatric care for a new depressive episode or after having previously received depression treatment. The researchers calculated these rates separately for treatment at outpatient and inpatient psychiatric facilities. In this study, most treatment took place at outpatient facilities, reflecting care for moderate to severe depression, with only the most severe episodes treated at inpatient facilities.
Overall, treatment rates for first-time depressive episodes exceeded rates for repeat depressive episodes, regardless of the period (preconception, pregnancy, or postpartum). This was especially true during the postpartum period. First-time depressive episodes treated in outpatient and inpatient facilities rose substantially after childbirth and peaked at 2 months postpartum. The number of outpatient visits for first-time depression was also higher during pregnancy (especially in the second trimester) than before pregnancy.
Outpatient and inpatient visits for repeat depression were relatively consistent from month to month in both the preconception and postpartum periods. However, women who had previously received depression treatment sought more outpatient care for depression during pregnancy than they had before becoming pregnant. Unlike first-time depressive episodes, for which treatment rates were highest in the postpartum period, for repeat depressive episodes, the most outpatient visits were received during the second trimester of pregnancy.
This study’s findings support the idea that pregnancy and postpartum are risk periods for maternal mental health. The results also point to a change in depressive episodes from pregnancy to after birth, specifically, a high onset of new depressive episodes in the second trimester of pregnancy and the first 5 months postpartum. This finding may have important implications for clinical care. A high rate of depressive episodes during pregnancy and after delivery underscores the vulnerabilities of both periods for new mothers and the need for access to readily available and comprehensive mental health care.
Moreover, the data showed a significant rise in depression treatment well into the postpartum period with rates higher than during pregnancy or preconception for several months after delivery. Because this is outside the clinical window in which perinatal depression can officially be diagnosed, the authors suggest extending the assessment of depression beyond 4 weeks postpartum, which may identify many more women who could benefit from treatment. Distinguishing between depression with pregnancy onset and depression with postpartum onset could also refine the diagnoses to better capture differences in their rates and presentation.
Although the findings add to our knowledge of depression that occurs before, during, and after pregnancy, the study has a few limitations. For example, the researchers analyzed population data from Denmark—a country with specific perceptions around and systems of mental health care—and the results may not generalize to other countries. In addition, the sample was limited to women who had given birth for the first time and were experiencing depressive episodes at the severe end of the spectrum (those treated in psychiatric facilities). The incidence and recurrence of depression may differ for women who have already given birth or with milder forms of depression.
More research is needed to understand how rates of depression vary in different locations and for different groups. Population-level studies that systematically explore depression and other mental health disorders can provide insights that lead to improved diagnosis and treatment.
Molenaar, N. M., Maegbaek, M. L., Rommel, A.-S., Ibroci, E., Liu, X., Munk-Olsen, T., & Bergink, V. (2023). The incidence of depressive episodes is different before, during, and after pregnancy: A population-based study. Journal of Affective Disorders , 322 , 273–276. https://doi.org/10.1016/j.jad.2022.11.031
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
November 10, 2020
Postpartum depression may last for years
At a glance.
- About 5% of women reported persistently high levels of postpartum depression symptoms for three years after giving birth.
- Longer screening periods after birth may be needed to help more women with postpartum depression get treatment.

Many women develop symptoms of postpartum depression after giving birth. These include anxiety, sadness, difficulty sleeping, exhaustion, or disturbing thoughts.
Postpartum depression can make it difficult for new mothers to take care of themselves and their babies. But many women don’t recognize its symptoms, or don’t know that treatments are available.
Current guidelines recommend that pediatricians screen mothers for postpartum depression at their children’s well visits for up to 6 months after birth. Using pediatrician visits in this way may help identify more women with the condition and guide them to resources and treatment.
Postpartum depression isn’t the same for everyone. Researchers have found many differences in symptoms between individual women, as well as how early it starts and how long it lasts.
To better understand the different trajectories for postpartum depression, a research team led by Dr. Diane Putnick from NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) used data from a study that tracked more than 4,500 women and their children for 3 years after birth.
The study asked women about symptoms of postpartum depression 4 months and 1, 2, and 3 years after birth. The researchers also looked at factors that might influence the length or severity of postpartum depression. These included age, race, education, marital status, gestational diabetes or high blood pressure, and preexisting mental health conditions. Results were published on November 1, 2020, in Pediatrics .
The women’s experiences with postpartum depression fell into four main trajectories. In the most common, women had levels of symptoms that remained low over time. Almost three-quarters of the participants fell into this category.
A second group, making up 8% of participants, had low levels of symptoms at four months after birth that grew worse over time. Another 13% had moderate symptoms that decreased over time. And about 5% experienced high levels of depressive symptoms that stayed higher than the other groups, even years after giving birth in some women.
Women with a previous mood disorder diagnosis and those who experienced gestational diabetes were the most likely to fall into the group with persistently high symptoms. Women with persistently high symptoms were also more likely to be younger and have less education.
More work is needed to better understand the factors that influence the trajectory of postpartum depression for different women. Improved screening could eventually help doctors identify more women who are struggling with the condition.
“Our study indicates that six months may not be long enough to gauge depressive symptoms,” Putnick says. “These long-term data are key to improving our understanding of mom’s mental health, which we know is critical to her child’s well-being and development.”
Related Links
- Factors That Affect Depression Risk
- Depression Screening and Treatment in Adults
- When a Bundle of Joy Brings Sorrow
- What Should I Know About Postpartum Depression?
- Perinatal Depression
References: Trajectories of Maternal Postpartum Depressive Symptoms. Putnick DL, Sundaram R, Bell EM, Ghassabian A, Goldstein RB, Robinson SL, Vafai Y, Gilman SE, Yeung E. Pediatrics . 2020 Nov;146(5):e20200857. doi: 10.1542/peds.2020-0857. PMID: 33109744.
Funding: NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
Connect with Us
- More Social Media from NIH
New Study IDs Moms at Highest Risk for Postpartum Depression

The risk for postpartum depression is highest among first-time mothers, mothers younger than 25 years old and mothers of twins, according to a survey of more than 1.1 million moms worldwide.
Moms older than 40 years old having twins are at the highest risk, researchers from the University of Virginia School of Medicine, Johns Hopkins University and Flo Health found.
“The size of this study, in over 1 million new mothers, make the findings highly significant and definitive. Most studies on postpartum depression are small and confined to a small region. This study answers questions about risk factors for postpartum depression from a worldwide sample,” said Jennifer L. Payne, MD , the study’s senior author and director of the Reproductive Psychiatry Research Program at the UVA School of Medicine.
Better Understanding Postpartum Depression Risk Factors
It is vital to better identify the risk factors for postpartum depression, the researchers said, because of the potential health effects on both moms and their children. For example, the researchers highlight that women are twice as likely as men to experience depression during their childbearing years. Women are also at increased risk of experiencing major depression after giving birth.
Children of women who experience postpartum depression are more likely to develop major depression and other psychiatric disorders, the researchers note. Having a mother who experiences postpartum depression is also associated with developmental challenges for children, including lower IQs and slower language development.
“There is a growing necessity to identify risk factors that place women at elevated risk, prior to the onset of affective illness, during this vulnerable time-period so that preventive measures can be instituted,” the researchers write.
To better understand the risk factors for postpartum depression, the researchers analyzed responses from more than 1.1 million new mothers to the “After Childbirth Survey” on the Flo app, which helps women track their period and menstrual cycle.
By age group, the percentage of women self-reporting postpartum depression symptoms was highest among 18- to 24-year-olds, at 10%. The rate of postpartum depression then steadily declined by increasing age, dropping to 6.5% for 35- to 39-year-olds, before increasing slightly to 6.9% among women 40 and older. Across all age groups, postpartum depression was significantly lower among women who had previously had children compared with first-time moms.
Women who had twins were more likely to report postpartum depression – 11.3% of mothers of twins reported symptoms, compared with 8.3% of mothers of a single child. This difference was especially pronounced among moms ages 40 and older; 15% of moms in this age group having twins reported postpartum depression symptoms, compared with 6.6% of mothers of one baby. Women older than 40 having twins, the researchers concluded, are at “markedly high risk” for postpartum depression.
The researchers found no significant difference in the rates of postpartum depression between mothers of boys or girls.
“Most women with postpartum depression are not diagnosed or treated. Clinicians caring for new mothers can be aware of factors like age, first pregnancy and twin pregnancies that put women at a higher risk of developing postpartum depression and screen and intervene early,” Payne said. “Early intervention can prevent the negative outcomes associated with postpartum depression for both mothers and their children.”
Findings Published
The findings have been published in the Journal of Affective Disorders. The research team consisted of Helen Bradshaw, Julia N. Riddle, Rodion Salimgaraev, Liudmila Zhaunova and Payne.
To keep up with the latest medical research news from UVA, subscribe to the Making of Medicine blog at http://makingofmedicine.virginia.edu.
Categories: All Releases , Children's Hospital , Neurosciences & Behavioral Health , Women's Health

Public Information Officer
Email | [email protected]
Phone | 434.924.5770
Latest News

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Womens Health (Lond)
Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes
Justine slomian.
1 Department of Public Health, Epidemiology and Health Economics, University of Liège, Liège, Belgium
Germain Honvo
Patrick emonts.
2 Department of Obstetrics and Gynaecology, CHU Liège, Liège, Belgium
Jean-Yves Reginster
Olivier bruyère.
3 Department of Sport Science, University of Liège, Liège, Belgium
Introduction:
The postpartum period represents the time of risk for the emergence of maternal postpartum depression. There are no systematic reviews of the overall maternal outcomes of maternal postpartum depression. The aim of this study was to evaluate both the infant and the maternal consequences of untreated maternal postpartum depression.
We searched for studies published between 1 January 2005 and 17 August 2016, using the following databases: MEDLINE via Ovid, PsycINFO, and the Cochrane Pregnancy and Childbirth Group trials registry.
A total of 122 studies (out of 3712 references retrieved from bibliographic databases) were included in this systematic review. The results of the studies were synthetized into three categories: (a) the maternal consequences of postpartum depression, including physical health, psychological health, relationship, and risky behaviors; (b) the infant consequences of postpartum depression, including anthropometry, physical health, sleep, and motor, cognitive, language, emotional, social, and behavioral development; and (c) mother–child interactions, including bonding, breastfeeding, and the maternal role.
Discussion:
The results suggest that postpartum depression creates an environment that is not conducive to the personal development of mothers or the optimal development of a child. It therefore seems important to detect and treat depression during the postnatal period as early as possible to avoid harmful consequences.
Introduction
Pregnancy and childbirth are two major events in a woman’s life. The birth of a baby induces sudden and intense changes in a woman’s roles and responsibilities. Thus, the postpartum period represents the time of risk for the emergence of maternal postpartum depression (PPD). 1 PPD is a serious mental health problem. The Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV) defines PPD as a specifier for major depressive disorder (MDD). 2 PPD is also defined symptomatically as exceeding a given threshold on a screening measure, such as the Edinburgh Postnatal Depression Scale (EPDS). 3 , 4 In general, PPD occurs within 4 to 6 weeks after childbirth, and symptoms similar to MDD that may be present include depressed mood, loss of interest or pleasure in activities, sleep disturbance, appetite disturbance, loss of energy, feelings of worthlessness or guilt, diminished concentration, irritability, anxiety, and thoughts of suicide. 5
The prevalence of PPD varies substantially depending on the definition of the disorder, country, diagnostic tools used, threshold of discrimination chosen for the screening measure, and period over which the prevalence is determined. 3 , 6 For example, Halbreich and Karkun 7 performed a review of the literature and found a PPD prevalence that varied between 0.5% and 60% among countries, as estimated by the self-reported 10-item EPDS questionnaire. The prevalence of PPD varies from 1.9% to 82.1% in developed countries, with the lowest prevalence reported in Germany and the highest prevalence in the United States. 7 , 8 In developing countries, the prevalence varies from 5.2% to 74.0%, with the lowest prevalence reported in Pakistan and the highest prevalence in Turkey. 8 This tremendous variation in the prevalence of PPD could be explained by heterogeneous study designs or the use of different diagnostic tools (e.g. the EPDS, Center for Epidemiologic Studies Depression Scale (CES-D), or Beck Depression Inventory (BDI)). 9
Untreated PPD seems to have negative consequences for both infants and mothers. Nonsystematic reviews have indicated that the risks to children of untreated depressed mothers (compared to mothers without PPD) include problems such as poor cognitive functioning, behavioral inhibition, emotional maladjustment, violent behavior, externalizing disorders, and psychiatric and medical disorders in adolescence. 5 , 10 – 17 These nonsystematic reviews reported the outcomes of these children from birth to adolescence. Other nonsystematic and systematic reviews have also explored specific maternal risks when mothers’ PPD is untreated, including more weight problems, 18 , 19 alcohol and illicit drug use, 20 social relationship problems, 21 breastfeeding problems, 22 or persistent depression 23 compared with women who have received treatment. Nevertheless, there are no well-established systematic reviews of the overall maternal and/or infant outcomes of maternal PPD. Thus, the aim of this study was to evaluate all the maternal consequences of untreated PPD and its effects on children between 0 and 3 years of age.
To the extent possible, this research adhered to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement. 24
Search strategy
We searched for all studies published between 1 January 2005 and 17 August 2016, using the following databases: MEDLINE via Ovid, PsycINFO, and the Cochrane Pregnancy and Childbirth Group trials registry. The following keywords were applied in the databases during the literature search: “postpartum depression” OR “postnatal depression” OR “puerperal depression.” The research was limited to human studies published in the English language. The search strategy and search terms used for this research are detailed in Appendix 1 . Additional studies were identified through a manual search of the bibliographic references of the relevant articles and existing reviews.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (a) cohort and cross-sectional epidemiological and qualitative individual studies; (b) studies that included mothers of all ages who suffered from PPD (all combinations of comparison groups were possible: PPD vs no PPD, severe PPD vs mild PPD, etc.); and (c) studies that included health (physical or psychological) or social outcomes of PPD in the results.
The exclusion criteria were as follows: (a) meta-analyses, systematic and nonsystematic reviews, randomized controlled trials, and case studies; and (b) studies that included mothers who received treatment for PPD. Meta-analyses and systematic and nonsystematic reviews were only accessed to review their bibliographic references.
It is also important to note that there are many factors (e.g. comorbid conditions (anxiety, posttraumatic stress disorder, or substance abuse), socioeconomic status, education level, co- or single-parenting, and number of previous pregnancies) that could play an important role in the experience of PPD. Nevertheless, in the present systematic review, these factors were not considered as exclusion criteria; instead, they were treated as potential confounding factors. Moreover, because these confounding factors are difficult to account for in a systematic review, the adjusted results were used and discussed in this article when available.
After duplicates were removed, studies identified by the search strategy were exported to an Excel spreadsheet for study selection.
Study selection
In the first step, two investigators performed the study selection and assessed the titles and abstracts of the studies to exclude articles that were immaterial to the systematic review based on the inclusion criteria. In the second step, the same two investigators selected, read and evaluated the full-text studies that met the inclusion criteria. Given the large number of abstracts and full-text articles that needed to be read, the two investigators selected the studies independently.
Data extraction
The studies were divided between the two investigators for data extraction. However, if there was doubt regarding an article, the article was discussed by the two investigators, and a consensus was reached. The two investigators extracted the data from the selected studies according to a standardized data extraction form. The following data were isolated for each study: authors; journal name; year of publication; country of origin; objective of the study; study population data (type of population, mean age, sex ratio of the children, and age, if provided); sample size; design (length of intervention, number of groups, and description of groups); tools used to assess maternal PPD; reported prevalence of maternal PPD; types of infant and/or maternal outcomes and main (adjusted) results; and conclusion. To ensure that as many studies as possible were included in our systematic review, we systematically contacted the authors or co-authors when the full-text paper was not available.
Analysis and synthesis of the results
To facilitate data extraction, the included studies were initially grouped according to three types of outcomes: physical (e.g. weight, length, anthropometric indices, motor development, and physical health); psychological (e.g. mental health, cognitive development, language development, and bonding); or “other” (e.g. social relationships, quality of life, breastfeeding, and risky behaviors). Each outcome group was then thematically analyzed, coded by topic, and divided into more appropriate subgroups. The outcome subgroups were based on information obtained from the studies included in this review. In terms of the studies’ outcomes, key words were labeled and classified into groups with similar consequences. For example, the subcategories “weight,” “length,” and “anthropometric indices” were combined into the more general category of “anthropometry.”
This systematic review of the literature used a narrative synthesis methodology. Each included study was described in a commentary that reported the findings. Similarities and differences among the studies were also synthesized to draw conclusions within the subgroups.
Included studies
Of the 3712 references retrieved from the bibliographic databases ( Figure 1 ), we identified 122 eligible studies that evaluated the consequences of PPD: 68 that evaluated the maternal consequences and 73 that evaluated the infant consequences. Among the included studies, 19 examined both the infant and the maternal consequences of PPD.

Flowchart of the selection of relevant literature.
The group of studies that evaluated the maternal consequences of PPD included 46 cohort studies 25 – 72 and 21 cross sectional studies 73 – 92 (including 1 qualitative study). 93 The majority of the studies were performed in the United States (28 of 68) and Europe (22 of 68), 10 studies were performed in Asia, and 8 studies were performed in Australia and New Zealand. All studies included women aged between 13 and 45 years. The number of participants ranged from 15 93 to 22,118, 28 and the duration of follow-up varied from 2 weeks 32 to 6 years 33 for the cohort studies.
PPD was mainly diagnosed according to the 10-item EPDS (46 studies); however, there were studies that used the BDI (6 studies), the World Health Organization Composite International Diagnostic Interview—Short Form (CIDI-SF; 3 studies), the Mini International Neuropsychiatric Interview (MINI; 3 studies), the Postpartum Depression Screening Scale (PDSS; 4 studies), and the CES-D (2 studies). To assess PPD, other studies used other questionnaires (e.g. the Patient Health Questionnaire depression module (PHQ-9 42 or PHQ-8 74 ), the Brief Symptom Inventory (BSI), 31 or the Hamilton Depression Rating Scale (HDRS) 30 ). The prevalence of PPD varied from 4.5% in a population of Canadian mothers at 6 weeks postpartum 89 to 68.8% in a population of Australian mothers at 4 months postpartum. 64
The group of studies that evaluated the infant consequences of PPD included 61 cohort studies 31 , 34 , 37 , 45 , 48 , 49 , 52 , 53 , 56 , 64 – 66 , 69 – 72 , 94 – 138 and 12 cross-sectional studies. 90 – 92 , 139 – 147 Most of the studies were performed in the United States (27 of 73) and Europe (20 of 73), 12 studies were performed in Asia, 10 studies were performed in Africa, and 4 studies were performed in Australia and New Zealand. All studies included women aged between 14 and 49 years and a percentage of baby girls that varied between 37.7% 49 and 57.5%. 147 The number of participants ranged from 28 123 to 24,263, 98 and the duration of follow-up varied from 2 months 31 , 118 , 123 to 5 years 96 for the cohort studies.
PPD was mainly diagnosed according to the 10-item EPDS (37 studies); however, there were studies that used the CES-D (9 studies), the BDI (7 studies), and the depression section of the Structured Clinical Interview for DSM-IV (SCID; 4 studies). To assess PPD, other studies used various types of questionnaires (e.g. the PHQ-9 135 , 136 or the BSI 100 ). Only one study did not specify the questionnaire that was used to detect PPD. 98 The prevalence of PPD varied from 2.7% in a population of Pakistani mothers at 18 months postpartum 94 to 68.8% in a population of Australian mothers at 4 months postpartum. 64
The outcomes were separated into three sections: “maternal consequences of PPD,” “infant consequences of PPD,” and “mother–child interactions.” The first section, “maternal consequences of PPD,” reported results for 5 different types of outcomes: physical health (3 studies), 35 , 67 , 88 including health care practices and utilization measures (2 studies); 63 , 78 psychological health, including anxiety and depression (6 studies); 36 , 37 , 42 , 44 , 66 , 88 quality of life (8 studies); 27 , 37 , 39 , 48 , 66 , 85 , 86 , 88 relationships, including social relationships and relationships with the partner and sexuality (7 studies); 37 , 38 , 44 , 66 , 73 , 74 , 85 and risky behaviors, including addictive behavior (smoking behavior and alcohol consumption: 4 studies) 55 , 68 , 84 , 87 and suicidal ideation (7 studies). 28 , 30 , 33 , 76 , 81 , 85 , 93 The second section, “infant consequences of PPD,” reported results for 9 different types of outcomes: anthropometry, including weight, length, and anthropometric indices (13 studies); 97 , 100 , 104 , 109 , 110 , 112 , 113 , 119 , 125 , 126 , 131 , 140 , 142 infant health (10 studies); 48 , 104 , 119 , 122 – 124 , 135 , 136 , 138 , 142 infant sleep (3 studies); 104 , 108 , 130 motor development (7 studies); 66 , 94 , 95 , 97 , 103 , 107 , 141 cognitive development (11 studies); 94 , 95 , 99 , 101 – 103 , 107 , 134 , 139 , 141 , 147 language development (13 studies); 66 , 94 , 95 , 102 , 103 , 105 , 116 , 117 , 129 , 131 , 132 , 139 , 141 emotional development (5 studies); 94 – 96 , 115 , 121 social development (4 studies); 66 , 115 , 141 , 143 and behavioral development (12 studies). 49 , 52 , 96 , 110 , 111 , 114 , 115 , 120 , 121 , 131 , 133 , 141 Finally, the third section, “mother–child interactions,” reported results for 3 different types of outcomes: bonding and attachment, including mother-to-infant and infant-to-mother bonding (15 studies); 29 , 31 , 34 , 37 , 43 , 44 , 47 , 52 , 54 , 56 , 61 , 64 , 82 , 106 , 127 breastfeeding (22 studies); 25 , 26 , 32 , 41 , 45 , 59 , 60 , 62 , 65 , 69 – 72 , 77 , 89 – 92 , 118 , 119 , 130 , 137 and maternal role, including maternal behaviors (9 studies), 26 , 40 , 49 , 52 , 53 , 62 , 79 , 83 , 85 maternal competence (2 studies), 51 , 75 maternal care for the infant (6 studies), 37 , 53 , 130 , 137 , 145 , 146 infant health care practices or utilization measures (8 studies), 26 , 37 , 57 , 63 , 98 , 128 , 130 , 142 maternal perception of the infant’s patterns (5 studies), 40 , 46 , 50 , 58 , 80 and the risk of maltreatment (2 studies). 130 , 144
Maternal consequences of PPD
Physical health.
Only three studies evaluated the physical health of depressed mothers ( Table 1 ). One study found that compared to the general population of women, depressed mothers scored significantly lower on the 36-Item Short Form Health Survey (SF-36) physical component summary score (assessed based on physical functioning, role limitations due to physical health, bodily pain, and general health perceptions). 88 However, this study indicated that the severity of the depressed mood was not associated with a worse physical health status, whereas a worse aerobic capacity emerged as a significant independent contributor to physical health status. The two last studies evaluated postpartum weight retention (PPWR) and found that significantly more women with PPWR had higher scores on the PPD scale. 35 , 67
Characteristics of the studies included in the evaluation of maternal physical health.
PPD: postpartum depression; PPWR: postpartum weight retention; EPDS: Edinburgh Postnatal Depression Scale; SD: standard deviation; SF-36: 36-Item Short Form Health Survey; OR: odds ratio; CI: confidence interval.
Health care practices and utilization measures
Two studies 63 , 78 demonstrated an effect of maternal PPD on health care practices and utilization measures ( Table 1 ). One of these studies demonstrated that women with worse depressive symptoms were more likely to consult a general practitioner or mental health professional than women with milder depressive symptoms. 78 The other study showed that women with PPD consulted with family physicians more often than nondepressed mothers did. 63
Psychological health
Six studies ( Table 2 ) evaluated the association between PPD and psychological health; five studies focused on overall psychological health, 37 , 42 , 44 , 66 , 88 two studies focused on anxiety, 36 , 37 and three studies focused on depression. 36 , 37 , 66
Characteristics of the studies included in the evaluation of the maternal psychological health.
GAD: generalized anxiety disorder; MDD: major depressive disorder; PPD: postpartum depression; EPDS: Edinburgh Postnatal Depression Scale; DSM-IV: Diagnostic and Statistical Manual of Mental Disorders (4th ed.); PHQ-9: Patient Health Questionnaire depression module; QIDS-SR: Quick Inventory of Depressive Symptomatology (Self-Report); BDI-II: Beck Depression Inventory-II; GLM: general linear models; SD: standard deviation.
Overall psychological health
Several studies showed that depressed mothers presented lower mood scores in the long term (1 year after childbirth) than mothers without depression. One study highlighted that compared to the general population of women, depressed mothers scored significantly lower on the SF-36 mental component summary score (based on vitality, social functioning, role limitations due to emotional problems, and mental health). 88 This study also showed that depressed mood was a significant predictor of mental health status in the future (explaining 18% of its variance). 88 Another study showed that women with PPD had lower self-esteem than mothers without depression. 66 Depressed mothers also reported being less happy, more dysphoric, and sadder than mothers without depression. 44 In addition, women with high depression scores had significantly higher levels of anger, lower scores for anger control, and lower levels of positive affect than mothers with low depression scores. 37 Finally, mothers with PPD were generally less responsive to negative stimuli, with lower ratings for intensity and reactions to negative pictorial stimuli, than mothers without PPD. 42
One study showed that depressed mothers had significantly elevated levels of state and trait anxiety at 1 year and 3.5 years after childbirth compared with nondepressed mothers. 37 Another study highlighted that depressed mothers at 3 months postpartum were more likely to exhibit an anxiety disorder than nondepressed mothers at 6 months postpartum, but not after this time point. 36
Compared to nondepressed women, women who were diagnosed with depression in the first weeks after childbirth continued to suffer from depression at 1 year after childbirth. 36 , 37 , 66 However, one study underlined that although mothers continued to suffer from depression, the symptoms appeared to improve, progressing from moderate-to-severe depression at 6 weeks to mild-to-moderate depression at 1 year. 66 Therefore, there appeared to be a slight improvement in the severity of depression over time with or without treatment. 66 Another study used a life history calendar method and found that compared to currently nondepressed mothers, mothers who were depressed at follow-up (3.5 years) did not have more depressive episodes; however, they had longer depressive episodes, received more psychotherapy after hospitalization, and experienced more negative life events during the follow-up period. 37
Quality of life
Eight studies 27 , 37 , 39 , 48 , 66 , 85 , 86 , 88 examined the overall quality of life of depressed mothers compared with nondepressed mothers ( Table 3 ). Three studies 48 , 86 , 88 demonstrated a significantly negative association between maternal depressive symptoms and quality of life. Women with PPD had lower scores on all dimensions of quality of life (e.g. SF-36 or a generic Health-Related Quality of Life (HRQoL) questionnaire) than women without PPD. However, one of the three studies showed that after controlling for mental health-related quality of life earlier in the postpartum period, there was no difference in the subsequent mental health-related quality of life according to the presence of significant depressive symptoms later in the postpartum period. 48
Characteristics of the studies included in the evaluation of the maternal quality of life.
PPD: postpartum depression; CIDI-SF: Composite International Diagnostic Interview—Short Form; EPDS: Edinburgh Postnatal Depression Scale; CES-D: Center for Epidemiologic Studies Depression Scale; MINI: Mini International Neuropsychiatric Interview; BDI-II: Beck Depression Inventory-II; OR: odds ratio; CI: confidence interval.
Studies also showed that PPD was associated with greater perceived stress, 66 more negative life events (indicating greater distress and discontinuity), more financial problems, and more illness among close relatives. 37 Depressive symptoms were also associated with fatigue during the first week but not at 6 weeks, 3 months, and 6 months after childbirth. 39
Regarding the life environment, one study showed that PPD predicted lower levels of household functioning (household care). 85 Another study demonstrated that mothers who experienced depression were twice as likely to become homeless and approximately 1.5 times more likely to be at risk for homelessness than nondepressed mothers. 27
Relationships
Seven studies evaluated social and couple relationships in relation to maternal depressive symptoms ( Table 4 ); four studies were related to social relationships, 37 , 66 , 73 , 85 and four studies were related to relationships with partners and sexuality. 37 , 38 , 44 , 74
Characteristics of the studies included in the evaluation of the maternal social and couple relationship.
FSD: female sexual dysfunction; PPD: postpartum depression; PDSS-SF: Postpartum Depression Screening Scale—Short Form; SRQ-20: Self-Reporting Questionnaire-20; PHQ-8: Patient Health Questionnaire depression module; EPDS: Edinburgh Postnatal Depression Scale; MINI: Mini International Neuropsychiatric Interview; BDI-II: Beck Depression Inventory-II; RR: risk ratio; CI: confidence interval; OR: odds ratio.
Social relationships
PPD was associated with more relationship difficulties 37 and therefore with lower social function. 85 Depressed mothers also presented lower (perceived) social support scores than nondepressed mothers. 66 Regarding the probability of returning to paid work, one study showed that there was no difference between depressed and nondepressed mothers. 73 The authors of this study specified that most mothers experienced depressive symptoms during the first year after childbirth; thus, depression was not an independent predictor of how quickly mothers would return to work.
Partner relationships and sexuality
Depressed mothers rated their relationship with their partner as more distant, cold and difficult, and felt less confident than nondepressed mothers over the first year after childbirth. 44 Depressed mothers also reported having more relationship difficulties, including romantic break-ups, than nondepressed mothers; however, this difference was not significant. 37 Regarding sexual life during the first year after childbirth, mothers who had resumed sexual activity had lower depression scores than mothers who did not resume sexual activity during the postpartum period. 38 In addition, depression appeared to cause nearly three times more sexual dysfunction during the first year after childbirth. 74
Risky behaviors
Addictive behavior.
Three studies 55 , 84 , 87 evaluated the influence of PPD on smoking behavior ( Table 5 ). One study showed that smoking and depression often co-occurred among mothers during the postpartum period. 87 The prevalence of PPD was higher among smokers than nonsmokers; conversely, smoking was also more common among mothers with a major depressive episode. The two other studies demonstrated that women who quit smoking during pregnancy might be more likely to relapse if they experience negative emotions or depressive symptoms. 55 , 84 In addition, one study evaluated the influence of PPD on postpartum “risky” drinking at 3 months among women who were frequent drinkers before pregnancy. 68 This study emphasized that there was no significant association between maternal PPD and risky drinking.
Characteristics of the studies included in the evaluation of the maternal risky behavior.
PPD: postpartum depression; EPDS: Edinburgh Postnatal Depression Scale; BDI: Beck Depression Inventory; CIDI-SF: Composite International Diagnostic Interview—Short Form; ICD-9-CM: International Classification of Diseases, Ninth Revision, Clinical Modification; PDSS: Postpartum Depression Screening Scale; HDRS: Hamilton Depression Rating Scale; MINI: Mini International Neuropsychiatric Interview; MDD: maternal major depressive disorder; OR: odds ratio; CI: confidence interval; SD: standard deviation.
Suicidal ideation
Five studies showed that higher levels of depressive symptoms were associated with an increased prevalence of suicidal ideation 30 , 33 , 76 , 81 , 85 ( Table 5 ). Mothers with high suicidality risks experienced greater mood disturbances and more severe postpartum symptomatology than mothers with low suicidality risks. 81 One of the five studies also demonstrated that women who reported higher levels of depression were also significantly more likely to report thoughts of self-harm than women with low levels of depression. 30 The sixth study 28 showed a significant association between PPD and suicidal ideation in an unadjusted analysis, but not in adjusted analysis. An additional study demonstrated that mothers who experienced PPD could imagine acts of infanticide. 93 The authors of this study explained that many mothers preferred to describe their suicidal thoughts rather than their infanticidal thoughts when seeking health care.
Infant consequences of PPD
Anthropometry.
The characteristics and main results of the studies included in the evaluation of anthropometric parameters are presented in Table 6 .
Characteristics of the studies included in the evaluation of infant anthropometric outcomes.
PPD: postpartum depression; CES-D: Center for Epidemiologic Studies Depression Scale; SCID-NP: Structured Clinical Interview for DSM-IV, Non-Patient edition; EPDS: Edinburgh Postnatal Depression Scale; BSI: Brief Symptom Inventory; SRQ-20: Self-Reporting Questionnaire-20; BMI: body mass index; WHZ: weight-for-height z-score; SS: subscapular; TR: triceps; OR: odds ratio; CI: confidence interval.
A total of 11 studies reported weight as an outcome. Among them, five studies 97 , 104 , 131 , 140 , 142 demonstrated a significant effect of maternal PPD on the child’s weight; infants of depressed mothers gained less weight than infants of nondepressed mothers. Four studies were conducted in low-resource countries (India, 131 Nigeria, 140 Zambia, 142 and Bangladesh 97 ), and one study was conducted in the United States with a very low-income population. 104 Two other studies (one in the United Kingdom 125 and one in Nigeria 119 ) showed that while there were differences in infant weight in the first months of life, they did not persist. Finally, four studies demonstrated that maternal PPD had no effect 100 , 113 , 126 or a very small effect 112 on the child’s weight. Two studies were conducted in high-income countries (a multicountry study that included Belgium, Germany, Italy, Poland, and Spain 113 and one study conducted in the Netherlands 100 ). The third study 126 was conducted in South Africa; however, the authors stated that they were unable to test their hypothesis due to a lack of statistical power.
Eight studies identified in this systematic review reported infant length as an outcome. Three of the studies 110 , 140 , 142 showed a significant effect of maternal PPD on stunting. The three studies were conducted in low-resource countries (Nigeria, 140 Zambia, 142 and South Africa 110 ). One other study 119 showed differences in length in the first months of life; however, it was determined that these differences did not persist over time (Nigeria). Three other studies 97 , 113 , 126 demonstrated that maternal PPD had no effect on stunting. One multicountry study 113 evaluated high-income countries (Belgium, Germany, Italy, Poland, and Spain), and two studies were conducted in low-income countries, including Bangladesh 97 and South Africa. 126 The authors of the South African study stated that they were unable to test their hypothesis due to a lack of statistical power. Another study 109 conducted in a high-income country (the United States) showed the opposite effect: exposure to PPD was associated with a greater height-for-age z-score and a longer leg length.
Anthropometric indices
Four studies evaluated anthropometric indices, and two of them showed no effect of maternal PPD. One study 140 found that maternal PPD was not associated with head circumference (Nigeria). Two studies demonstrated that the triceps and subscapular skinfold thicknesses did not differ between infants of depressed and nondepressed mothers (one study was conducted in Belgium, Germany, Italy, Poland, and Spain; 113 the other was from the United States 112 ). In contrast, one study from the United States 109 showed that PPD was associated with higher subscapular and triceps skinfold thickness scores, which indicated overall adiposity.
Infant health
Of the 10 cohort studies, 9 indicated a significant association between maternal PPD and health concerns in infants ( Table 7 ). Maternal depressive symptoms at 5 months seemed to predict more overall physical health concerns for infants at 9 months 104 and a greater proportion of childhood illnesses. 119 Three studies showed that infants of depressed mothers had significantly more diarrheal episodes per year than those of nondepressed mothers, 119 , 122 , 138 and one study reported that infants of depressed mothers had more days of illness with diarrhea. 138 Harriet et al. specified that these associations with diarrheal episodes were accurate only within the first 3 months. One study also associated maternal depressive symptoms with infant colic. 124 Two studies reported greater overall pain in the infants of depressed mothers 48 and a stronger infant pain response during routine vaccinations. 123 One study demonstrated that maternal PPD at 4 months predicted worse health-related quality of life for the infant in the following months. 48 One study indicated a robust and predictive association between maternal PPD and febrile disease in children. 135 Another study 136 showed that probable postnatal depression was associated with an approximately three-fold increased risk of mortality in infants up to 6 months of age, with an approximately two-fold increased risk of mortality up to 12 months of age. This study also showed that probable postnatal depression was associated with an increased risk of infant morbidity. Only one cross-sectional study reported a nonsignificant association between a high risk of maternal depression and serious illness or diarrheal episodes after adjusting for infant age and other possible confounders. 142 Nevertheless, the occurrence of these two outcomes was proportionally higher among infants of depressed mothers.
Characteristics of the studies included in the evaluation of infant health.
PPD: postpartum depression; CES-D: Center for Epidemiologic Studies Depression Scale; SCID-NP: Structured Clinical Interview for DSM-IV, Non-Patient edition; EPDS: Edinburgh Postnatal Depression Scale; PHQ-9: Patient Health Questionnaire depression module; SRQ-20: Self-Reporting Questionnaire-20; WHO: World Health Organization; SD: standard deviation; CI: confidence interval; SES: socioeconomic status; PND: postnatal depression; RR: risk ratio.
Infant sleep
Three studies evaluated the association between maternal depressive symptoms and infant sleep patterns ( Table 8 ). Two studies showed that higher depressive symptoms were associated with an increased incidence of infant night-time awakenings and predicted more problematic infant sleep patterns. 104 , 108 One of the two studies demonstrated that children whose mothers had severe and/or chronic depressive symptoms had a higher risk of sleep disorders than those with mothers who had mild depressive symptoms. 108 The third study reported that significantly fewer children of mothers with depressive symptoms were placed in the recommended back-to-sleep position compared with children of women who had not experienced depression. 130
Characteristics of the studies included in the evaluation of infant sleep.
PPD: postpartum depression; CES-D: Center for Epidemiologic Studies Depression Scale; EPDS: Edinburgh Postnatal Depression Scale; PHQ: Patient Health Questionnaire; CI: confidence interval; RR: risk ratio.
Motor development
Three of seven studies showed a significant effect of maternal PPD on the motor development of infants ( Table 9 ). The first study, 97 conducted in Bangladesh, showed that symptoms of maternal PPD that were present at 2–3 months predicted impaired motor development in infants at 6–8 months. The second study 95 included Greek mothers in Crete and demonstrated that symptoms of maternal PPD were associated with lower fine motor scores in infants at 18 months of age (a 5-unit decrease on the scale of fine motor development). The third study 94 showed a nonsignificant impact of maternal depression on the fine and gross motor development of children at 2 and 6 months that became significant at 12 months for gross motor development and at 18 months for fine motor development (Pakistan). The fourth study 141 underlined the indirect effect of maternal PPD on motor development as a consequence of the effects of maternal depressive symptoms on the quality of the home environment. This mechanism had a direct effect on early child development. Three studies 66 , 103 , 107 demonstrated that maternal PPD had no effect on motor development ( Table 9 ). Two studies 66 , 107 explained the nonsignificant results by stating that most of the mothers in the depressed group had moderate-to-severe depression symptoms that were similar to a general description of psychological difficulty during the postnatal period and were less severe than a psychiatric diagnosis of a depressive illness (France and Taiwan). The third study 103 emphasized that the home environment remained a significant predictor of infant development in Australia.
Characteristics of the studies included in the evaluation for motor development in children.
PPD: postpartum depression; AKUADS: Aga Khan University Anxiety and Depression Scale; EPDS: Edinburgh Postnatal Depression Scale; BDI-II: Beck Depression Inventory-II; CI: confidence interval; OR: odds ratio; PND: postnatal depression.
Cognitive development
Of the 11 studies, 7 94 , 95 , 99 , 101 , 102 , 107 , 147 indicated a significant and negative association between maternal postpartum depressive symptoms and cognitive development in children ( Table 10 ). One of the studies 147 specifically emphasized the important role of maternal insensitivity in delays in children’s cognitive development. The eighth study 141 underlined the indirect effect of maternal PPD on cognitive development, which occurred as a result of maternal depressive symptoms that impacted the quality of the home environment and had a direct effect on early child development. Three studies 103 , 134 , 139 showed that maternal PPD was not significantly correlated with children’s cognitive development. One of the studies found a nonsignificant effect of maternal PPD and indicated that the home environment was a more important predictor of infant cognitive development in Australia. 103
Characteristics of the studies included in the evaluation of child cognitive development.
PPD: postpartum depression; AKUADS: Aga Khan University Anxiety and Depression Scale; CES-D: Center for Epidemiologic Studies Depression Scale; EPDS: Edinburgh Postnatal Depression Scale; BDI-II: Beck Depression Inventory-II; DSM-IV: Diagnostic and Statistical Manual of Mental Disorders (4th ed.);
OR: odds ratio; CI: confidence interval; MSEL: Mullen Scales of Early Learning; PND: postnatal depression.
Language development
A series of different variables may be used to assess language development. Across all studies included in the review ( Table 11 ), language development was evaluated using the following measures: overall language development, 94 , 103 , 105 , 117 expressive and receptive communication, 66 , 95 , 102 , 139 parent-to-child reading, 116 composite speech, 131 and literacy and enrichment literacy activities combined with an understanding of vocabulary and production. 132
Characteristics of the studies included in the evaluation of child language development.
PPD: postpartum depression; AKUADS: Aga Khan University Anxiety and Depression Scale; EPDS: Edinburgh Postnatal Depression Scale; CES-D: Center for Epidemiologic Studies Depression Scale; BDI-II: Beck Depression Inventory-II; DSM-IV: Diagnostic and Statistical Manual of Mental Disorders (4th ed.); MINI: Mini International Neuropsychiatric Interview; OR: odds ratio; CI: confidence interval; CSBS-DP: Communication and Symbolic Behavior Scales Developmental Profile.
Of 13 studies, 6 102 , 105 , 116 , 131 , 132 , 139 demonstrated a significant effect of maternal PPD on the language development of infants. Four studies demonstrated an indirect effect on language development; in particular, one study 117 showed that maternal depressive symptomatology in the postnatal year was indirectly associated with worse child language skills at 36 months. Moreover, depression was associated with worse caregiving, and maternal caregiving was positively associated with language. In addition, the effects of depression on caregiving were stronger in less-advantaged socioeconomic groups. Another study 141 underlined the indirect effect of maternal PPD on language development via maternal depressive symptoms that impacted the quality of the home environment and had a direct effect on early child development. The third study, 94 conducted in Pakistan, showed that a child’s language development was affected by maternal PPD only when the father’s income was high. The fourth study 129 reported that maternal PPD was a predictor of less silence and of neutral, positive, and high positive infant vocalizations. This study also found that infants of depressed mothers were more likely to maintain high positive vocalizations than infants of nondepressed mothers, which is a rare vocal quality affective behavior.
The last three studies 66 , 95 , 103 showed that maternal PPD had no effect on the language development of infants. One study 66 justified the nonsignificant results because the majority of the mothers in the depressed group suffered from moderate-to-severe depressive symptoms that were less severe than a psychiatric diagnosis of a depressive illness (Taiwan). The third study 103 highlighted that the home environment remained the significant predictor of infant development in Australia.
Emotional development
Four of five studies 94 , 96 , 115 , 121 demonstrated a significant effect of maternal PPD on the emotional development of infants ( Table 12 ). Infants of depressed mothers also had a significantly higher fear score 115 , 121 and higher degrees of emotional disorders that included anxiety 96 than infants of nondepressed mothers. In addition, one study showed that mothers with a low depression score after birth and a high depression score after several months postpartum had children with significantly higher fear scores than women with decreasing or stable depressive symptomatology. 121 One study indicated a nonsignificant effect of maternal PPD on the social-emotional development of children at 18 months of age. 95 The last study showed that maternal PPD was not associated with separation anxiety. 96
Characteristics of the studies included in the evaluation of child emotional development.
PPD: postpartum depression; AKUADS: Aga Khan University Anxiety and Depression Scale; BDI-II: Beck Depression Inventory-II; EPDS: Edinburgh Postnatal Depression Scale; OR: odds ratio; CI: confidence interval.
Social development
The results of the four studies included in the evaluation of social development are presented in Table 13 . One study indicated that the infants of depressed mothers had lower social engagement scores at 9 months than infants of nondepressed mothers. 115 In this study, the effect of MDD on social engagement was moderated by maternal sensitivity. Another study showed the indirect effect of maternal PPD on social development via the impact of maternal depressive symptoms on the quality of the home environment, which directly affected early child development. 141
Characteristics of the studies included in the evaluation of child social development.
PPD: postpartum depression; EPDS: Edinburgh Postnatal Depression Scale; BDI-II: Beck Depression Inventory-II; m-ADBB: Modified Alarm Distress Baby Scale.
One study did not find differences between infants of depressed or nondepressed mothers in the area of social development, 66 and another study showed that maternal PPD did not predict infant social withdrawal (in infants of HIV-infected mothers). 143

Behavioral development
Of 12 studies, 10 demonstrated a significant effect of maternal postpartum depressive symptoms on negative behavior in infants ( Table 14 ). Studies described multiple behavioral traits in children with depressed mothers, including an increase in child behavioral problems at age 2 years, 110 more mood disorders and a more difficult temperament, 114 more internalizing of problems, 111 , 120 lower scores on the Communication and Symbolic Behavior Scales Developmental Profile, 131 less mature regulatory behaviors, 115 and higher fear scores that increased behavioral inhibition. 121 One study examined the bidirectional effect of depressed maternal mood on mother–infant engagement using a picture book activity and found that infants of mothers with a depressed mood tended to push away and close books more often. 49 Another study showed a detrimental effect of maternal PPD on dysregulated behavior in infants only when PPD was associated with a comorbid personality disorder. 133 Another study demonstrated that depression explained a significant portion of children’s warmth-seeking behavior toward their mothers (for all mothers) and infant attention and arousal (only for adolescent mothers). 52
Characteristics of the studies included in the evaluation of child behavioral development.
PPD: postpartum depression; K-SADS: Kiddie Schedule for Affective Disorders and Schizophrenia; EPDS: Edinburgh Postnatal Depression Scale; SCID: Structured Clinical Interview for DSM-IV; BDI-II: Beck Depression Inventory-II; MMD: maternal mood disorder; CBCL: Child Behavior Checklist; PD: personality disorders; MDD: major depressive disorder; MDI: Major Depression Inventory; OR: odds ratio; CI: confidence interval; CSBS-DP: Communication and Symbolic Behavior Scales Developmental Profile.
One study 141 reported the indirect effect of maternal PPD on self-regulatory behaviors via maternal depressive symptoms, which had an impact on the quality of the home environment and directly affected early child development.
Only one study explored hyperactivity with inattention and physical aggression in the form of opposition; it did not identify an association between maternal PPD and children’s behavioral outcomes. 96
Mother–child interactions
Bonding and attachment, mother-to-infant bonding.
A total of 11 studies 29 , 31 , 34 , 37 , 43 , 44 , 47 , 52 , 56 , 61 , 82 demonstrated a negative effect of maternal depression on mother-to-infant bonding ( Table 15 ). These studies showed that maternal depression might be a risk factor in the development of the mother–infant relationship. For example, O’Higgins et al. 34 demonstrated that women who scored ⩾13 on the EPDS at week 4 were five times more likely to be experiencing poor bonding at the same time as women who scored <13 on the EPDS. Despite these results, Muzik et al. 43 concluded that all women, regardless of whether they are depressed, showed increased bonding with their infant over the first 6 months postpartum. Unfortunately, depressed women showed consistently greater impairment in bonding scores at all time points than nondepressed mothers. However, one study showed that mother–infant bonding appeared to be negatively affected by maternal PPD only in the first months; 61 these studies did not identify an effect of PPD on maternal bonding at 14 months, despite finding negative effects at 2 weeks, 6 weeks, and 4 months postnatally.
Characteristics of the studies included in the evaluation of bonding/attachment between mother and infant.
PPD: postpartum depression; EPDS: Edinburgh Postnatal Depression Scale; BDI: Beck Depression Inventory; CIDI: Composite International Diagnostic Interview; SCL-90-R: Symptom Checklist-90—Revised; PDSS: Postpartum Depression Screening Scale; BSI: Brief Symptom Inventory; SCID: Structured Clinical Interview for DSM-IV; MFAS: Maternal–Fetal Attachment Scale; PRAQ-R: Pregnancy Related Anxiety Questionnaire—Revised; STAI-T: State-Trait Anxiety Inventory—Trait version; PBQ-16: Postpartum Bonding Questionnaire-16; PCERA: Parent–Child Early Relational Assessment; OR: odds ratio; SD: standard deviation; PTSD: posttraumatic stress disorder; MIBQ: Mother–Infant Bonding Questionnaire; MIBS: Mother-to-Infant Bonding Scale.
In addition, women with depressive symptoms showed less closeness, 44 warmth, 44 , 52 and sensitivity 44 , 52 and a significantly lower level of mutual attunement (with regard to emotional availability) 37 and experienced more difficulties in their relationships with their child 44 during the first year than women without depressive symptoms. Lower emotional involvement with the newborn was observed among mothers who suffered from PPD. 82
Finally, mothers who were diagnosed as depressed were more likely to have an insecure state of mind regarding attachment; they had more negative perceptions of their relationship with their infant than nondepressed mothers. 54 , 64 McMahon et al. 64 highlighted that chronically depressed mothers were more likely to be classified as feeling insecure about their attachment, whereas briefly depressed mothers did not differ from mothers who had never been depressed.
Infant-to-mother bonding
Four studies 31 , 34 , 52 , 64 demonstrated a significantly negative effect of maternal PPD on infant–mother bonding ( Table 15 ). One study showed that infants of chronically depressed mothers were more likely to be insecurely attached, while infants of briefly depressed mothers did not differ from infants of mothers who had never been depressed. 64 Another study reported that as maternal depression increased, babies scored less favorably with respect to seeking warmth from their mothers. 52
One study showed that scores on both the maternal positive affective involvement scale and the positive communication scale were lower in mothers with depressive symptoms than in mothers who did not have symptoms of depression. 56 Nevertheless, this study showed that the number of depressive features did not affect infant scale scores (for preterm babies). Another study found that maternal PPD at 2 months was associated with insecure infant attachment at 2 and 18 months. 127 However, this study noted that when concurrent maternal sensitivity was considered, the quality of the early mother–infant relationship remained important, although maternal depression was no longer predictive. Two studies showed that postnatal depressive symptoms were not related to attachment insecurity 106 or disorganization 64 , 106 at 14 months.
Breastfeeding
A total of 22 studies evaluated the association between maternal PPD and breastfeeding, 25 , 26 , 32 , 41 , 45 , 59 , 60 , 62 , 65 , 69 – 72 , 77 , 89 – 92 , 118 , 119 , 130 , 137 ( Table 16 ). Of which, 16 studies found a significant negative effect of maternal depressive symptoms on breastfeeding and/or its parameters. Mothers with depressive symptoms were significantly more likely to discontinue breastfeeding (early interruption of exclusive breastfeeding in the first months), 41 , 59 , 69 , 71 , 90 , 91 , 118 , 119 , 137 engage in less-healthy feeding practices with their infant 25 , 62 , 130 (e.g. significantly more depressed women fed their children prematurely and inappropriately compared with nondepressed women), 130 be unsatisfied with their infant feeding method, 59 experience significant breastfeeding problems, 59 report lower levels of breastfeeding self-efficacy, 59 , 92 and exhibit a lack of breastfeeding confidence 91 and bottle feed 45 , 62 , 65 than mothers without depressive symptoms. Higher depression scores were also associated with early weaning. 89
Characteristics of the studies included in the evaluation of breastfeeding.
PPD: postpartum depression; SCID-NP: Structured Clinical Interview for DSM-IV, Non-Patient edition; EPDS: Edinburgh Postnatal Depression Scale; BDI: Beck Depression Inventory; POMS: Profile of Mood States; GHQ: General Health Questionnaire; CES-D: Center for Epidemiologic Studies Depression Scale; PHQ: Patient Health Questionnaire; PDSS: Postpartum Depression Screening Scale; OR: odds ratio; CI: confidence interval; RR: risk ratio; MDD: major depressive disorder; TGF: transforming growth factor; CRF: corticotropin-releasing factor; FT4: plasma free thyroxine; SD: standard deviation; BSES-SF: Breastfeeding Self-Efficacy Scale—Short Form.
Hatton et al. 65 showed conflicting results; they reported a significant inverse relationship between depressive symptoms and breastfeeding at 6 weeks postpartum, but not at 12 weeks.
The four remaining studies did not find a difference between depressed mothers and nondepressed mothers with respect to feeding practices; 26 , 60 , 70 , 72 one study showed that a delayed onset of lactation within the first 48 h, methodological breastfeeding problems, and nipple pain were significantly predictive of breastfeeding cessation. 70
Breast milk concentration and endocrine response to breastfeeding
Three studies evaluated the association between PPD and breast milk concentration and/or the endocrine response to breastfeeding. Maternal depressive symptoms appeared to be correlated with lower oxytocin, 41 total T4 41 concentrations, and higher TGF-β2 concentrations. 77 Kawano and Emori 32 identified weak negative correlations between breast milk secretory immunoglobulin A levels (breast milk SigA level) and all negative profile of mood states (POMS: tension–anxiety, depression–dejection, anger–hostility, fatigue, and confusion); however, there was no correlation between breast milk SigA level and positive POMS state.
Maternal role
Studies that evaluated the association between PPD and the maternal role are presented in Table 17 . Nine studies focused on maternal behaviors and PPD, 26 , 40 , 49 , 52 , 53 , 62 , 79 , 83 , 85 two studies focused on PPD and maternal competence, 51 , 75 six studies focused on PPD and maternal care for infants, 37 , 53 , 130 , 137 , 145 , 146 eight studies focused on PPD and infant health care practices or utilization measures, 26 , 37 ,57,63, 98 , 128 , 130 , 142 five studies focused on maternal perceptions of the infant’s patterns and depression, 40 , 46 , 50 , 58 , 80 and two studies focused on PPD and the risk of maltreatment. 130 , 144
Characteristics of the studies included in the evaluation of the maternal role.
PPD: postpartum depression; MDD: major depressive disorder; GAD: generalized anxiety disorder; EPDS: Edinburgh Postnatal Depression Scale; BDI: Beck Depression Inventory; CES-D: Center for Epidemiologic Studies Depression Scale; MINI: Mini International Neuropsychiatric Interview; PHQ: Patient Health Questionnaire; SRQ-20: Self-Reporting Questionnaire-20; GAD-Q: Generalized Anxiety Disorder Questionnaire; ZSDS: Zung Self-Rating Depression Scale; SOC: sense of coherence; IFSAC: Inventory of Functional Status after Childbirth; OR: odds ratio; CI: confidence interval; SD: standard deviation; RR: risk ratio; ED: emergency department; ICQ: Infant Care Questionnaire.
Maternal behaviors
Depressed mothers appeared to be more likely to engage in less-healthy practices with their infant compared to nondepressed mothers ( Table 17 ). They were less likely to place their infant in the back-to-sleep position, 26 , 62 to use a car seat, 26 and to have a working smoke alarm in the home. 26 A higher proportion of the mothers with self-scored depressive symptoms had a poor sense of coherence (comprehensibility, manageability, and meaningfulness) compared with mothers without depressive symptoms. 40 Depressive symptoms were also negatively associated with participation in positive enrichment activities with the child. 52 , 53 , 62 Mothers with PPD were less likely to tell their child stories every day 62 and played games less often 62 than nondepressed mothers. One study found no significant differences in mother–infant engagement with a picture book between depressed and nondepressed mothers. 49 However, this study noted that the infants of these two groups of mothers showed significant differences in their nonverbal behaviors. Depressed mothers also tended to sing faster to their infants than nondepressed mothers. 79 Reissland et al. 83 demonstrated that depressed mothers preferred to cradle their infant to the left, similar to stressed mothers; nondepressed mothers showed right-sided cradling, similar to nonstressed mothers. Nevertheless, the authors added that the left-sided cradling bias might be due to stress rather than depression experienced by mothers. In addition, as depression increased, mothers scored less favorably on positive affect, contingent responsiveness, physical intrusiveness, punitive tone, verbal content, and general verbalness. 52 Low nurturance (defined as behaviors that promotes a child’s psychological growth) and high discipline scores were significantly associated with postnatal depression. 53 Finally, one study showed that functional status, an evaluation of overall functional status, household function, social function, personal function, and infant care activities, was negatively correlated with PPD, with the exception of infant care activities. 85
Maternal competence
Two studies showed that depressed mothers had a lower perception of their competence than nondepressed mothers ( Table 17 ). The first study highlighted that women with lower parenting self-efficacy were more likely to report depressive symptoms than women with higher parenting self-efficacy. 75 The second study concluded that maternal depression was an important factor (32.3% of the total variance) that affected perceived maternal role competence and satisfaction at 6 weeks postpartum. 51
Maternal care for infant
All six studies indicated a significant association between maternal PPD and the care that mothers provided to their child ( Table 17 ). Studies showed that EPDS scores were significantly correlated with increased difficulty with infant care 145 and that significantly more depressed women had poor parenting practices than women who had not experienced PPD. 130 One study highlighted that children of depressed mothers experienced more interruptions and breaks in parental care. 37 Another study indicated that mothers with depressive symptoms showed books, played with or talked to the infant and followed routines significantly less often than nondepressed mothers. 137 A further study demonstrated that low nurturance and high discipline scores were significantly associated with PPD (higher scores were indicative of greater nurturance and a greater use of discipline behaviors). 53 Another study 146 reported that children with a depressed mother had a greater mean number of hours of household television exposure during both weekdays and weekends. Bank et al. 146 also showed that infants of depressed mothers were exposed to significantly more children’s programming than infants of nondepressed mothers.
Infant health care practices and utilization measures
Six out of eight studies demonstrated an effect of maternal PPD on infant health care practices and utilization ( Table 17 ). The first study 128 showed that children whose mothers had depressive symptoms at 2 to 4 months had a reduced probability of receiving age-appropriate vaccinations or age-appropriate well-child visits between 6 and 24 months. This study also showed that these children had an increased likelihood of visiting the emergency department between 1.5 and 2.5 years of age. Mothers who had depressive symptoms also had an increased probability of reporting that their children had sustained injuries. The second study 130 highlighted that depressed women differed significantly from women who had not experienced depression in their use of health services for their child. Depressed women were less likely to complete expected well-health visits for their child. The relative risk (RR) of inadequate well-child visits was two times greater for depressed women than for women who had never experienced depression. Children of depressed women were also less likely to complete immunizations within the expected time frame, and they had significantly more visits to the emergency department for acute care. The third study 98 demonstrated that infants of mothers with PPD were more likely to have ⩾6 sick or emergency visits and had an increased risk of hospitalization compared to infants of mothers without depression. The fourth study 37 reported that most depressed women sought some form of professional help for their child compared to nondepressed women. The fifth study showed that women with PPD consulted more with family physicians and pediatricians than nondepressed mothers did. 63 In addition, the rate of PPD was significantly higher in women who consulted health services for medical reasons (nonroutine care) than for those who visited for routine care only. 57
Another study 26 demonstrated that women with PPD had an increased likelihood of bringing their babies for emergency room visits than women without PPD; however, this association was no longer significant in the adjusted model. Finally, one study 142 did not demonstrate a significant effect of maternal PPD on infant health care practices and utilization measures. This study showed that a high risk of maternal depression did not have a negative impact on the completion of routine immunizations in Zambia. However, clinic location and older infant age were significantly associated with incomplete vaccinations.
Maternal perceptions of infants’ patterns
Postpartum depressive symptoms appear to lead to negative maternal perceptions of infant patterns ( Table 17 ). One study showed that mothers with depressive symptoms had a higher perception of their children’s temperament as “more difficult” than nondepressed mothers. 40 Another study highlighted that mothers with elevated depressive symptoms were more inclined to report infant crying/fussing, sleeping and temperament problems than mothers without PPD. 58 The third study reported that mothers who suffered from PPD were more likely to rate negative infant faces shown for a longer period more negatively than mothers without PPD. 50 The authors of this third study concluded that their results highlighted the difficulties that these mothers have in responding to their own infants’ signals. A fourth study demonstrated that the only difference between mothers with and without PPD was their assessment of babies’ faces; neutral baby faces were judged to be less neutral by depressed mothers than by nondepressed mothers. 80 Mothers with PPD were also less likely to accurately identify happy infant faces (no differences regarding sad faces were identified) than mothers without PPD. 46
Risk of maltreatment
The studies included in the evaluation of the risk of maltreatment are presented in Table 17 . One study found that depressed women had a significantly higher risk (4.2 times greater) for spanking their child compared with nondepressed women. 130 Another study did not identify a direct effect of maternal PPD on abusive behaviors; however, it demonstrated that PPD strongly influenced worries about how to parent and concerns about how their parenting affected the fear of being abusive. 144 This study also highlighted that poor maternal care influenced difficulty with bonding, which also affected abusive behaviors.
The purpose of this study was to evaluate the maternal and infant consequences of maternal PPD.
First, as expected, maternal PPD was associated with more negative maternal physical and psychological health and with a worse quality of life. Surprisingly, there were very few results regarding maternal physical health. Only three studies included in the present systematic review showed that depressed mothers presented more PPWR 35 , 67 and lower scores on all SF-36 domains, 88 while a systematic review conducted in 2014 evaluated the impact of sleep, stress, and depression on PPWR and found conflicting results, as follows: of seven studies that examined PPD and weight retention, three studies reported nonsignificant associations and four studies reported positive associations. 18 As it was decided to reject the systematic and nonsystematic review of this research, this previous systematic review 18 was not included. In addition, based on the inclusion criteria of our systematic review, only one 67 of the studies included in this previous systematic review 18 could be considered in our results (of seven studies, two were published before 2005 and four were rejected based on the title and abstract). Indeed, this study excluded treated PPD, while the previous systematic review 18 did not. This is an important difference between the two studies, and it could explain many of the discrepancies between our findings and those of this previous review. The two studies included in the examination of PPWR were both cohort studies and seemed to be of good quality: one study included 75 women followed for 14 months, 35 and the other study included 850 women followed for 18 months. 67 In addition, both studies used the EPDS to screen for PPD. However, they did not use the same cut-off values: one study used a cut-off value of ⩾10 35 and the other study used a cut-off of >12. 67 Given this information, we can assert that our results seem to support the risk of PPWR among depressed mothers. As previously observed in cases of women’s health, depressed mothers appeared to be more likely to consult general practitioners, pediatricians, or mental health professionals for medical reasons (nonroutine care) than for routine care. 57 , 63 , 78 These results suggest that depressed women had more health expenditures than nondepressed women.
Depressed mothers also seemed to experience more difficulties in their social relationships (including relationships with their partners) 37 , 44 and to feel that they received lower quality social support 85 than nondepressed mothers. These results are consistent with the qualitative study of Rodrigues et al., 148 who reported poor marital relationships and a lack of practical help and emotional support among depressed mothers. Depressed mothers seemed to have more risky behaviors (including the risk of start smoking again after pregnancy 55 , 84 and an increased prevalence of suicidal ideations). 30 , 33 , 76 , 81 , 85 These results are consistent with a review conducted in 2013, which showed that women who had high depressive symptom scores were also more likely than those with lower scores to engage in risky behaviors (alcohol, illicit drug, or other substances use). 20 Nevertheless, according to the inclusion criteria of our systematic review, none of the studies included in this previous review 20 could be considered in our analyses (of 12 studies, 5 were published before 2005 and 7 were rejected after reading the title and abstract). PPD therefore appeared to be associated with higher risk behaviors, regardless of whether the women were treated for these symptoms.
Concerning the outcomes of children aged 0 to 3 years, it seemed that the anthropometric consequences of maternal PPD differed between high- and low-income countries. Maternal PPD seemed to have few associations with the weight and length of infants in high-income countries 100 , 113 except during the transient period at the beginning of the newborn’s life. 125 However, in low-income populations, maternal PPD seemed to be associated with less infant weight gain and stunting. 97 , 104 , 110 , 131 , 140 , 142 Moreover, many studies indicated significant and negative associations between maternal postpartum depressive symptoms and infant cognitive development, 94 , 95 , 99 , 101 , 102 , 107 , 141 , 147 language development, 94 , 102 , 105 , 116 , 117 , 131 , 132 , 139 infant behaviors, 49 , 52 , 110 , 114 , 120 , 121 , 131 , 133 overall infant health concerns, 48 , 104 , 119 , 122 – 124 , 135 , 136 , 138 and quality of sleep. 104 , 108
In contrast, the impact of maternal PPD on infant motor development seemed to be controversial: some studies 94 , 95 , 97 demonstrated a clear effect of PPD on children’s gross and fine motor development, while other studies 66 , 103 , 107 did not demonstrate this effect. Regardless of whether they showed an effect, all but one study (60 subjects) 66 that evaluated the effect of PPD on child motor development were cohort studies and included large samples of subjects (from 360 103 to 652 subjects). 97 Four of the six studies used the EPDS as a screening tool for depression; the two other studies used the Aga Khan University Anxiety and Depression Scale (AKUADS) or the BDI-II. The studies that used the EPDS did not use the same cut-off values: the two studies that used the EPDS that did not find an effect of PPD on motor development used a cut-off value of ⩾12, 103 , 107 while the two studies that used the EPDS and found evidence in favor of this relationship used cut-off values of ⩾13 95 and ⩾10. 97 Regarding these conflicting results, there may be a confounding factor. We suggest that PPD could affect the life and home environments 66 , 94 , 103 , 117 , 141 of the infants, which could impact their development, particularly through a lack of caregiving from the mother. Similarly, maternal PPD did not seem to have a direct effect on child social development. 66 , 143
Concerning mother–infant interaction, the majority of studies found a significant association between maternal PPD and the care that mothers provide their children. Therefore, it is reasonable to assume that maternal PPD has a real impact on how a mother cares for her child. Maternal PPD seemed to be associated with poor maternal care, which influenced bonding difficulties and insecure attachments. 31 , 34 Although physical contact does not appear to be necessary for the development of a healthy bond, 149 , 150 difficulty with mother–infant bonding could originate from (early) physical separation or a lack of maternal emotional availability. 151 In addition, difficulties in mother-to-infant bonding could reduce the quality of parenting practices 37 , 53 , 130 , 137 , 145 , 146 and could affect the rates of abusive behavior. 144 The quality of the mother–infant relationship seemed to have an influence on the overall development of these infants; however, it was also affected by the way mothers cared for their child. Maternal PPD seemed to have a negative effect on these parameters, which created a vicious circle around the mother–child couple. It is interesting to note that successful treatment of PPD may not be sufficient to improve infants’ attachment, temperament, and cognitive development. 5 In addition, many studies identified a significantly negative effect of maternal depressive symptoms on breastfeeding and/or its parameters (e.g. discontinued breastfeeding, less-healthy feeding practices, breastfeeding problems, lower satisfaction, or reduced confidence). 25 , 41 , 45 , 59 , 62 , 77 , 89 , 90 , 118 , 119 , 137 These results are consistent with a systematic review published in 2014 that also showed negative effects of PPD on breastfeeding. 22 In this systematic review, PPD was associated with a shorter breastfeeding duration in almost all studies; therefore, PPD appeared to be associated with more breastfeeding problems, regardless of whether women were treated for PPD symptoms. The authors of several studies noted that PPD predicted and was predicted by breastfeeding cessation. 22 Many studies found a significant and negative association between maternal PPD and the duration of breastfeeding and a positive association between maternal PPD and breastfeeding problems. The Dias and Figueiredo’s 22 systematic review included 48 studies, 14 which were included in the present systematic review (the other studies were published before 2005 (n = 17) or rejected based on the title and abstract (n = 17)).
Some studies 64 , 108 , 121 compared the impact of chronic depression versus transient depression on child development and found that chronic maternal depression seemed to have a more serious impact on child development. In addition, some studies highlighted the importance of other environmental factors on the delay in child development, such as the infants’ life environment 66 , 94 , 103 , 117 , 141 or maternal sensitivity. 115 , 127 , 147 Therefore, maternal PPD could also indirectly impact a child’s development via a demonstrated lack of caregiving. The quality of the mother–infant relationship is critical for infant development, and maternal PPD could have a negative effect. Moreover, the relationship a mother develops with her child is dependent on the mother’s own emotional health. 94 One study explained that a potential implication of the results was that the infants of mothers with PPD reacted to negative maternal nonverbal engagement by displaying negative behaviors, and they showed less interest in interacting. 49 Infants’ dissatisfaction with their environment or their relationship with their mothers could explain their more difficult temperaments, greater display of internalization or communication problems, more problems relating to their mothers, and more difficulties in social development, particularly in their ability to relate to other individuals. In addition, lower socioeconomic groups seemed to be at a higher risk. Thus, an unfavorable environment should be a warning signal for caregivers. Therefore, in these subgroups (including populations from low-income countries), the prevention and early recognition of maternal PPD may improve the optimal development of children and the care their mothers provide.
In conclusion, maternal PPD seems to have many negative effects on both child and maternal health; however, it is important to highlight that the studies included were heterogeneous in their designs, the tools they used to assess PPD and the large group of confounding factors that was considered (even though adjusted results were used when they were available). Nevertheless, efforts to screen and prevent maternal PPD are critical.
Need for a consensus regarding PPD diagnosis
A difficulty emerged during the evaluation of the maternal and infant consequences of untreated PPD as a result of the heterogeneity of the PPD diagnosis. While PPD is not a recent pathology, a consensus regarding the “best diagnostic tool” does not exist. The prevalence of maternal depression therefore depends on the definition and/or the tool used to diagnose PPD. 3 , 6 – 8 In addition, the prevalence of PPD may depend on the cut-off values used with the same diagnostic tool.
The 122 studies included in this systematic review also used different diagnostic tools. PPD was mainly diagnosed using the EPDS (68 studies); however, it was also assessed using various other questionnaires, such as the BDI (10 studies), the CES-D (10 studies), the MINI (4 studies), the SCID (4 studies), the DSM-IV (2 studies), the PHQ-9 (3 studies), the PHQ-8 (1 study), the PHQ-D (1 study), the CIDI (3 studies), the PDSS (3 studies), the BSI (2 studies), the SQR-20 (2 studies), the GAD-Q (2 studies), and the HDRS (1 study). Therefore, the prevalence of PPD varied among these studies, from 2.7% in a population of Pakistani mothers at 18 months postpartum 94 to 68.8% in a population of Australian mothers at 4 months postpartum. 64
Concerning the cut-off values, there were also several disparities. For example, as shown Tables 1 1 – 17 , among the studies that used the EPDS, the authors used different cut-off values to establish the diagnosis of PPD; cut-off values of 8, 57 9, 40 10, 44 11, 132 12, 31 13, 34 or 14 65 were used to screen for postnatal depression. Cox et al. 4 showed that a cut-off point of 13 or more on the EPDS indicates a probable depression with a sensitivity of 86% and a specificity of 78% in the postnatal period. Another study indicated that the optimal cut-off for probable major depression during the antenatal period may be higher (15 or more). 152 Some authors used different cut-off values to classify depression as mild/moderate (e.g. EPDS ⩾ 8 86 or EPDS ⩾ 10 and ⩽12 108 ) or severe (EPDS ⩾ 12 86 or EPDS ⩾ 13 108 ). Other authors considered the EPDS a screening tool that measures probable depression and does not provide a clinical diagnosis of depression; these authors considered an EPDS score of 13 indicative of PPD. 112
Although previous research conducted a receiver operating characteristic curve (ROC) analysis comparing the EPDS, BDI, and HRSD scores with the SCID Mood Module and showed that these scales were highly predictive of a major depressive episode, 153 future studies should develop a consensus to standardize the tools researchers use to diagnose depression during the postpartum period. The EPDS 4 seems to be the most commonly used PPD diagnostic tool. Nevertheless, researchers must agree on cut-off values to ensure the validity and reliability of the tool. For example, in 2006, Matthey et al. 154 recommended the use of a validated score of 13 or higher on the EPDS when reporting probable major depression during the postnatal period and a score of 15 or higher during the antenatal period (particularly for English-speaking women). However, it seems that these recommendations are not always followed. In any case, it is sometimes difficult to compare the outcomes of PPD because of the heterogeneity of its diagnosis. It is important to be careful given that in some cases, the results of this systematic review combined results from studies that were heterogeneous in terms of design (cross-sectional vs cohort studies) and methodology (e.g. screening tools used for PPD or length of follow-up).
Implications for practice
Social support seems to have a protective effect against postnatal depression. 8 , 155 , 156 However, depressed mothers presented lower perceived social support than nondepressed mothers. 66 Social support also seems to stimulate maternal self-efficacy, 157 which plays a key role in the process of constructing parenthood. 158 A study showed that mothers who had a strong belief in their maternal abilities had better outcomes in terms of emotional well-being, attachment to the child and adaptation to their new role. 159 In addition, maternal self-efficacy is positively associated with the mothers’ coping strategies.
Even when everything seems to be going well, the majority of women seem to feel fears or anxiety at the beginning of maternity given the sudden changes in their role. 160 It is normal for mothers to be worried about the safety and well-being of their child. Nevertheless, given all the identity disturbances related to the arrival of a baby, it is not uncommon for women to encounter episodes of psychological distress of varying duration and degrees of severity during the postnatal period. Childbirth may be a traumatic experience for a woman. 161 A lack of social support, pain during the first stage of labor, feelings of powerlessness, unfulfilled expectations, and negative interactions with medical personnel are examples of factors that can influence the perception of a traumatic experience following childbirth. These findings suggest several intervention points for health care practitioners, including opportunities to discuss the birth during the postpartum period. 161
Nevertheless, one study indicated a discrepancy between professionals’ perceptions of maternal needs and the needs that mothers actually had. 162 Professionals seemed to be more concerned about needs during pregnancy than during the postpartum period. Moreover, they seemed to identify very few unmet needs during the postnatal period, while the mothers tend to feel neglected during this period. 162 However, many studies have shown that mothers have important physical and emotional needs during the year after childbirth. 155 , 158 , 160 , 162 – 179 In addition, the present systematic review shows that the health of infants and children is intimately associated with the health of their mothers.
These elements suggest that the promotion of maternal health by professionals cannot end at the birth of the newborn or at the 6-week postpartum visit. 164 The needs of mothers take longer than 6 weeks to resolve. Fahey and Shenassa 164 noted that a healthy postnatal period depends on a woman’s ability to effectively employ her own skills to satisfy her own needs and those of her family. Thus, postnatal care providers must understand that women’s health needs during this transition period are not limited to physical recovery, and they must identify care strategies that will help women develop the required skills to appropriately meet their needs.
The recommendations in terms of maternal health promotion are increasingly moving toward a holistic vision of women’s health. It is necessary to go beyond health care itself to meet the complete needs of mothers; 164 , 180 – 182 this is even more true as maternity leave is increasingly shortened, thus presenting additional risks of insufficient education and health promotion models for mothers. 183 It is important that professionals implement rigorous follow-up procedures outside the hospital to continue to support parents during this life event. 184
Strengths and limitations of the study
To our knowledge, this study is the first systematic review in several decades to evaluate the consequences of untreated maternal PPD in both mothers and their children from 0 to 3 years of age. Our study included 122 studies and encompassed all outcomes for mothers and children that have been described since January 2005. The limitations of this study are that given the number of abstracts initially included in the review, study selection and data extraction were not performed using a double-blinded method, and an assessment of the studies’ methodological quality was not performed. Nevertheless, the inclusion and exclusion criteria were rigorously discussed and defined at the beginning of the study by the two researchers who performed the review. In addition, if there was doubt regarding an abstract or an article, the article was discussed, and the researchers reached a consensus regarding its inclusion or exclusion. Another limitation of this study is that given the substantial number of maternal PPD outcomes, the present review compares heterogeneous studies that used various designs (cohort vs cross-sectional studies) and tools to assess PPD. Therefore, it is important to consider that potential confounding factors could be present.
We conclude that maternal postnatal depression has negative consequences for both mothers who suffer from this pathology and their children up to 3 years of age. PPD has important impacts, mainly on mothers’ psychological health, quality of life, and interactions with their infant, partner, and relatives. Depressed women are caught in a vicious circle in which they become sadder and angrier and have increasingly lower perceptions of their competence. The accumulation of these elements creates an environment that is not conducive to the personal development of mothers or the optimal development of a child. The present systematic review shows that the health of infants and children is intimately associated with the health of their mothers. In addition, severe or chronic maternal depression seems to present a higher risk to children’s development than milder depression. Thus, maternal PPD has many direct and indirect negative effects on the development of a child, including lower quality of the home environment and decreased maternal sensitivity and caregiving. It therefore seems important to detect and treat depression in the postnatal period as early as possible to avoid harmful consequences. The risks are greater for children in low-income populations. Consequently, more attention should be paid to these areas.
Acknowledgments
The author would like to thank all the co-authors of this article, especially Germain Honvo for helping in the data extraction.
Appendix 1.
Search strategy and search terms used for this systematic research.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.


Extending Medicaid Coverage After Birth May Increase Postpartum Treatment for Depression, Anxiety

Reducing Late-Night Alcohol Sales Curbed Violent Crimes by 23% Per Year in a Baltimore Neighborhood
Extending medicaid coverage after birth may increase postpartum treatment for depression, anxiety ..

Extending Medicaid Coverage After Birth May Increase Postpartum Treatment for Depression, Anxiety
A new study found that extending medicaid eligibility for birthing people increase treatment for perinatal mood and anxiety disorder by more than 20 percentage points, compared to birthing people with commercial insurance. , jillian mckoy.
Extending postpartum Medicaid eligibility extensions may increase treatment for perinatal mood and anxiety disorders (PMADs), a leading cause of perinatal illness and mortality, according to a new study led by School of Public Health and Brown University researchers.
Published in the journal Health Affairs , the study found that retaining Medicaid coverage after birth increased outpatient mental health and medication treatment for PMADs by 20.5 percentage points, compared to birthing people who received commercial coverage. Retaining postpartum Medicaid also appeared to significantly lower patients’ out-of-pocket spending for mental healthcare.
The majority of US states have now extended postpartum Medicaid coverage to 12 months through the American Rescue Plan Act , but the new findings provide critical data and insight into the role of Medicaid coverage on perinatal mental health, and why Medicaid extensions are so important for the health of low-income birthing people postpartum. Without this coverage, many people would otherwise become uninsured or struggle to pay for high-cost commercial insurance and medical care. Untreated PMADs can increase birthing people’s risk of substance use, depression, anxiety, and suicide, as well as developmental delays among their newborns. Estimates show that one in three pregnancy-related deaths occur between six weeks and one year after childbirth.
“We know that maternal mental health conditions are a leading cause of maternal morbidity and mortality, and postpartum mood and anxiety disorders are the most commonly occurring maternal mental health condition,” says study lead and corresponding author Sarah Gordon , assistant professor of health law, policy & management, and who served as a senior advisor on health policy for the US Department of Health and Human Services from 2021-2024. “Evidence-based treatments are available and effective, but underutilized. Insufficient health insurance coverage is one reason for low treatment rates among the postpartum population that extending postpartum Medicaid coverage can address.”
For the study, Gordon and colleagues utilized data on insurance claims and income, as well as birth records in Colorado between 2014-2019, before Colorado extended Medicaid eligibility. The researchers compared postpartum PMAD treatment among patients with incomes at or below 138 percent of the federal poverty level (FPL) and who were eligible to remain in Medicaid after 60 days postpartum, to patients with incomes above 138 percent of the FPL, who were ineligible to receive Medicaid beyond 60 days postpartum and enrolled in commercial insurance.
Compared to birthing people with commercial health insurance, remaining on Medicaid for 12 months postpartum was alsolinked to a 16 percentage point increase in patients filling a prescription medication for depression or anxiety, and a 7.3 percentage point increase in patients receiving at least one outpatient mental health visit. Retaining Medicaid beyond 60 days postpartum was associated with almost a 20 percentage point increase in “continuous” postpartum treatment, which is considered three or more outpatient mental health visits or prescription refills.
This extended Medicaid coverage alsoalleviated healthcare costs for birthing people, lowering out-of-pocket costs by $40.84 for outpatient mental health visits, and by $3.24 for each prescription refill, compared to costs for commercially insured birthing people.
Medicaid-insured birthing people may have higher PMAD treatment rates because of more affordable care, and fewer gaps in coverage that likely occur among birthing people who became ineligible for Medicaid. The researchers say these findings underscore the fact that commercial insurance is not an equal alternative for low-income postpartum people, and losing Medicaid eligibility can be detrimental to both health and finances.
“Our findings suggest that postpartum Medicaid extensions are likely an important policy lever to promote postpartum maternal mental health by lowering barriers to accessing treatment,” Gordon says. “However, mental health screening and referrals, availability of providers, and quality of mental healthcare are also critical to supporting the mental health of postpartum people.”
Gordon recently joined the Health Affairs podcast A Health Podyssey to speak about another recent Health Affairs paper she led that explores lessons from the continuous enrollment provision of the Families First Coronavirus Response Act of 2020. Click here to listen to the episode .
Explore Related Topics:
- health policy
- maternal and child health
- maternal health
- postpartum depression
- pregnancy complications
- strategic direction
- Share this story
- 0 Comments Add
Senior Writer and Editor
Jillian McKoy is the senior writer and editor at the School of Public Health. Profile
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.
Post a comment. Cancel reply
Your email address will not be published. Required fields are marked *
Researchers Delve Into New Moms’ Depression
By Melissa Glim
Tuesday, May 10, 2022

Many women develop symptoms of depression after giving birth. IRP research is helping to characterize the course of those symptoms and the risk factors that may contribute to them.
Fresh off celebrating Mother’s Day this past Sunday, as well as Women’s Health Week this week, it’s important to acknowledge that being a new mom isn’t easy. As joyful and exciting as a new baby might be, it can be exhausting and worrisome, too. Many new moms experience some level of baby blues, but for some women, those blues can take a downward turn into symptoms of more serious depression.
Approximately one out of every eight women in the U.S. experiences symptoms of postpartum depression, according to the U.S. Centers for Disease Control and Prevention. What’s more, a recent study led by IRP staff scientist Diane Putnick, Ph.D. , has shown that the course of postpartum depression can differ significantly among women. The study of nearly 5,000 women not only showed that 25 percent of them experienced symptoms of postpartum depression, but it also found that depression symptoms followed several different patterns and could persist for at least three years after giving birth. 1 Understanding these different patterns of symptoms and some of the risk factors associated with them may help physicians recognize and monitor mothers who are at higher risk for persistent depression.
Good mental health is important not only for the mothers’ well-being, but for their children as well. Dr. Putnick points out that there’s a great deal of research that shows a mother’s mental health has a direct impact on her child’s cognitive, emotional, and behavioral development. Moreover, while obstetricians and mental health professionals are the traditional healthcare providers that diagnose and treat postpartum depression, the doctor most new moms see most consistently is their child’s pediatrician.
“The American Academy of Pediatrics recommends depression screening for new moms at well-child visits, but only up to six months after the birth of the child,” Dr. Putnick says. “I hope this study, and others like it, will show that period needs to be extended. Six months isn’t long enough to know if the mom is getting better.”

Dr. Diane Putnick
To map out the different trajectories of postpartum depression, Dr. Putnick and her colleagues in the lab of IRP senior investigator Edwina Yeung, Ph.D. , analyzed data from a study of mothers and children from upstate New York that began in 2008. The mothers were given regular assessments, including a brief screening for depression at intervals beginning four months after their children were born and continuing until the children were 3 years old.
The good news was that about three quarters of the women had very low depression symptoms throughout the study. Another 13 percent of women had medium-level depressive symptoms that got better over time. However, about 8 percent of mothers had depressive symptoms that actually worsened over time, and another 4 percent experienced depressive symptoms that remained consistently high throughout the study.
“A lot of people think postpartum depression is something that will go away if they just wait long enough,” Dr. Putnick says, “but when the study came out, people reached out to me from the public to say, ‘Hey, this is me. This happened to me, and my doctor didn’t believe that it could still be postpartum depression.’”
To get a clearer picture of why women might fall into these various depression patterns, Dr. Putnick and her colleagues also looked at the medical histories and sociodemographic traits of the women in the study. The researchers found that women who had had a mood disorder in the past were more likely to experience postpartum depression, as were younger mothers and women with lower levels of education. In addition, women with gestational diabetes were more likely to experience symptoms of postpartum depression. Exactly why these factors may contribute to a higher risk for depression is still a mystery, but Dr. Putnick is continuing her studies to get to the bottom of it.
“The fact that younger mothers and mothers with less education were more likely to be in the persistently depressed group indicates that stress might be a factor,” she explains. “These are women who are having babies relatively young and women who maybe haven't completed the education they wanted to or who have fewer resources, for example. I think that there's also very likely a genetic component to this, as well as the effects of hormone changes.”

Because kids whose mothers are depressed are more likely to experience cognitive and behavioral problems, better understanding postpartum depression is critical for improving the lives of both women and children.
Because the children of mothers with depression are at higher risk for cognitive, behavioral, and developmental delays, Dr. Putnick is currently looking at how mothers’ depression affects kids’ fine and gross motor skills, communications, cognition, and interpersonal and social skills. It’s still early, but she says it appears that postpartum depression may be associated with children’s social skills.
“If you think about it in terms of a mom who is depressed in those early years, one of the major ways depression manifests is fatigue and lack of energy,” says Dr. Putnick, “so she may not have the energy to play with her child or take them out where they can experience different stimuli and situations.”
By identifying the factors that influence mothers’ depression and children’s development, researchers like Dr. Putnick can help physicians and mental healthcare providers be better equipped to help both moms and kids. Moving forward, Dr. Putnick is excited to share these findings and translate them directly into regular practice.
“We’ve focused on questions that parents and pediatricians really want to know the answers to,” Dr. Putnick says. “I think one of the reasons this study has gotten so much attention is that it was really easy to talk about it with people and show the impact of the work quickly.”
References:
[1] Putnick DL, Sundaram R, Bell EM, Ghassabian A, Goldstein RB, Robinson SL, Vafai Y, Gilman SE, Yeung E. Trajectories of maternal postpartum depressive symptoms. Pediatrics. 2020 Nov 1;146(5):e20200857. doi: 10.1542/peds.2020-0857.
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
Related Blog Posts
- Wearable Tech Tracks Ebbs and Flows of Bipolar Disorder
- Gender Differences in Emotional Responses May Start in the Womb
- Moms’ Caffeine Consumption May Affect Babies’ Brains
- Rare Genetic Variants Underlie Susceptibility to Reproductive Disruption
- Genes Contribute to Population-Based Differences in Antidepressant Response
This page was last updated on Wednesday, May 24, 2023
- Share full article

Life in the Throes of Postpartum Depression
Four new mothers open up about the common yet isolating struggle.
Credit... Travis Dove for The New York Times
Supported by

By Catherine Pearson
- June 27, 2023
If you give birth to a baby in the United States in 2023, odds are you will learn something about postpartum depression along the way — maybe from your doctor or midwife, maybe from a celebrity or on social media .
But for many women, postpartum depression is shockingly isolating — a mix of sadness, hopelessness and overwhelm that stems not just from the hormonal tumult of pregnancy and the postpartum period, but from many other stressors, like a lack of paid leave, insufficient child care, and the staggering responsibility of caring for a new and helpless human.
The condition, which can arise at any point during the first year postpartum — and is distinct from the relatively short-lived “ baby blues ” most women experience soon after delivery — is now recognized as one of the most common complications of childbirth. It affects one in eight new moms , and mental health struggles are a leading cause of pregnancy-related death in the United States, primarily from suicide and drug overdose.
There are more treatment options for postpartum depression now than ever before, including the first medication designed specifically to treat it. But factors like stigma and inadequate screening keep many mothers from getting help. The Centers for Disease Control and Prevention estimates that about 20 percent of women were not asked about depression during a prenatal visit, and more than half of women with postpartum depression continue to go untreated.
This spring, The New York Times spent time with four mothers who were then in the grips of postpartum depression. They offered a stark, intimate glimpse into their experiences, in their own words.
Conversations have been edited and condensed for clarity.
Allie’s Story
“If I looked at the baby for too long, I’d start crying. If I had to hand the baby to my husband so I could go to the bathroom, I’d start crying.” — Allie Strickland, 28, Charleston, S.C. Her son, August, was 8 months old when she spoke to The Times.

My son was due at the end of September , but in late August, I started having contractions. I think I just went into denial, like, no, he couldn’t possibly be showing up this early. The birth itself was not a great experience. They set him on my chest and I only had time to touch his back and for me to realize: “Oh. That’s my baby right there.” Then he was gone. I was so out of it that I kept asking: “Where is he? What’s going on?” My whole body was filled with panic. But they did give him back to me, and we were able to do skin-to-skin.
On our second day in the hospital, I got hit with the baby blues. If I looked at the baby for too long, I’d start crying. If I had to hand the baby to my husband so I could go to the bathroom, I’d start crying. Once we got home, I put the baby’s bassinet as close to our bed as I could, and even then, I would stay awake and just stare at him. Nighttime was the worst. As soon as the sun set, I would feel this intense doom: How much sleep will we get tonight? What if we do get sleep and something happens? We had the Owlet monitor sock and the Nanit video monitor, and even then, I would lay there listening to him breathe. I couldn’t look away.
I started working with a therapist before becoming pregnant, and I knew I was at a higher risk for postpartum mental health disorders because I had a history of anxiety and depression. At three weeks postpartum, I had my medication adjusted. It helped a little, but there was always something for me to feel scared about. Is he getting enough milk? What if something happens while we’re out and about?
At his one-month appointment with the pediatrician, I filled out one of those questionnaires that checks for postpartum mental health issues, and I knew that my answers were going to be a big red flag. Like, oh, we definitely need to talk to this lady. But they never said anything.
Two months ago, I found a new therapist who works specifically with postpartum moms. I see her twice a month and her office is baby-friendly, so I can bring him. It has not been a cure-all or anything close to it, but she has given me some tools to help me manage my anxiety. One is a list of questions I can ask myself to try and identify: Is this thought coming from a place of logic? A place of emotion? How likely is it for this thing to actually happen?
It has helped me a lot to know, OK, other moms also experience intrusive thoughts — they’re worried when they go to the top of the stairs that they’re going to fall and drop their baby, or that something is going to happen while they’re driving. But she has helped me understand that just because certain feelings are common, they are not “normal.”
Carrie’s Story
“Depression feels like a physical weight.” — Carrie Keefe, 39, Turners Falls, Mass. She has a 10-year-old and 7-year-old, and her baby, Lily, was 4 months old when she spoke to The Times.
We struggled for about five years to get pregnant with Lily. I had multiple miscarriages and more chemical pregnancies than I can count. I do think secondary infertility caused a kind of trauma. I went into this pregnancy feeling like: I am so grateful for this . I have to soak up every second of it. And for the first month after she was born, I was euphoric. But then, and I hate saying it, it felt like the magic of it just kind of died off. It all started to feel really, really heavy.
I started to see a therapist who specializes in loss and infertility about four or five months into my pregnancy. It was online, through BetterHelp. Our insurance didn’t cover it, but I had a coupon code to get a percentage off for seven sessions. In hindsight, I should have pushed to keep going, but I remember asking my husband: “Can we afford $350 a month?” It was like having another car payment.
I run a business making baby bonnets, and I never really stopped working. I took three weeks off after the baby was born — if I don’t show up, my husband and I don’t pay our mortgage. I had this vision that I would take the baby to work with me, but I didn’t think about the fact that once I’m done for the day, I go home and have two very energetic kids who need me, too.
I feel exhausted, like I am unworthy of this life that I used to love. At work, I feel like I am doing the bare minimum. It’s as if my passion for doing what I love is entirely lost. At home, I feel like a zombie. My 7-year-old loves to do craft projects with me, which when I was pregnant I really enjoyed. But they feel more like a chore when dealing with the postpartum depression. The fact that I feel like I can’t fully show up for my family, or for the job I love, kind of adds another level of depression, on top of the hormonal stuff.
A few weeks ago, I was really swimming in my head: Like, I have this baby here who is making it so I can’t work, but if I could work, I could make more money . It was this snowballing frustration and rage. I called my husband and told him: “I need you to come home from work right now.” He dropped everything and did. I was screaming and crying, and he took the baby away to give me a break. I slept for, like, five hours. After that, I spoke to my mom and she told me she thought I needed to talk to somebody.
I met with my OB-GYN and he prescribed Zoloft, and connected me to a social worker who said she’s going to get me placed with a therapist, but it is going to take four to six weeks. I was shocked but I also kind of felt like: Well, maybe I am not really deserving of this help. If it’s going to take six weeks, then clearly there are people out there who need it more than I do.
To me, the depression feels like a physical weight — like, if I could just take it off of me. If I could just reach into my chest and pull it out.
Janelle’s Story
“One fear you have is: Are they going to take my children away?” — Janelle Jones, 27, Brooklyn, N.Y. She has a 4-year-old and her baby, Ava, was 8 months when she spoke to The Times.
I had some depression when I became a parent the first time around. I got treatment, but I feel like it kind of lingered — and with the second pregnancy it came back full force. I don’t think I knew I was feeling it again until around six weeks postpartum. My partner actually noticed before I did — he was like, “Janelle, I think it’s happening again.”
That’s also when I started to realize, Oh my god, I’m going to have to go back to work soon. I’m a nurse, and I had always tied that to my identity, but I started feeling like, I don’t want to be a nurse anymore. Forget this license.
I couldn’t concentrate on things. I was overstimulated and I was so irritable — with my partner and with my family. I felt like: This is a lot . Did I really want this? It just felt overwhelming. I would sit on the couch and just watch Netflix. I’d try and get up and do something, but it felt like I was stuck.
I started seeing a therapist who works with my OB-GYN’s clinic. It was not a good fit, but she told me about a place called The Motherhood Center that offers a more intensive level of care. You go for full days, from 10 a.m. to 3 p.m. I knew I needed help, but I also felt like, Am I really that bad, that I need that type of assistance? It was hard to come to terms with: I need mental health help. I was in the program from December to February.
A few months after the baby was born, I did have feelings of not wanting to be here anymore. It was this feeling of impending doom, like something bad was going to happen. I never spoke about that when it was happening, because you feel so ashamed. How do you say that out loud? One fear you have is, Are they going to take my children away? There’s such a stigma to all of this — even doing this interview.
I’m taking Prozac and I am continuing to go to therapy — and I am doing better, though I still have hard weeks. I want people to know that motherhood is so complex, and it’s beautiful. I think that getting treatment and being vulnerable is so important. Because it’s in the vulnerability that you’re able to move forward.
Shivani’s Story
“Every time I had Rishav at the breast, I started to cry. ” — Shivani Hiralal, 29, Phoenix. Her baby, Rishav, was just turning 1 when she spoke to The Times.
I struggled a lot with fertility : We tried for a year, and then I suffered a miscarriage. After that, I had an ectopic pregnancy that essentially took three months to diagnose, and then it took us a whole year after that to get pregnant again. Then a month before our son was born, my husband developed fungal pneumonia. I had to resuscitate him, and he had to be hospitalized and intubated. I think all of that contributed to what I experienced postpartum.
I was in a lot of pain after the birth, to the point where I couldn’t really sit up in bed, and I was just really, really exhausted. I was also having a hard time breastfeeding — he wasn’t really latching. When it was time for our son’s first pediatrician’s appointment, I had my husband and my mom take him because I couldn’t move, I couldn’t sit, everything was uncomfortable. I cried the entire time they were gone. I felt like such a failure of a mother.
Every time I had Rishav at the breast, I started to cry. I dreaded feeding him every two hours. I knew he was relying on me for food, but it was hurting me and he wasn’t getting enough, and it just felt like too much. I switched to exclusive pumping, but I had a lot of guilt, pain and shame around breastfeeding. I didn’t feel that immediate, instant connection to him. I did have moments — not long periods, and not anything I ever felt like I would act on — when I wondered whether my son was better off without me. Was I just not a good mom? Was I not made to be a good mom?
When I was around four or five weeks postpartum, I met with my therapist (I had been in therapy before, and scheduled the appointment when I was still pregnant) and told her: “I am crying all the time. I do not think this is the baby blues.”
At my six-week postpartum checkup, something still felt wrong physically. I still felt a lot of pressure, and I didn’t know if it was my stitches or something else. My OB-GYN referred me to a pelvic floor physical therapist and urogynecologist. Then she started getting ready to leave the room, and I was like: “Wait! Before you go, there’s something I really want to speak to you about, which is my mental health.” And that’s when I just started crying. She thanked me for bringing it up, and told me that because of how busy things are she’s not always able to.
I had a urinary tract infection, and the urogynecologist diagnosed me with prolapse , both of the uterus and the rectum. Thankfully, my husband has great health insurance so I was able to see a pelvic floor physical therapist .
At around nine months, I started feeling a lot better emotionally. I think a lot of that had to do with the fact that I was finally doing much better physically. I’m definitely still healing, but now that my son is turning 1, I kind of look back at that whole experience in awe. I’m like, Wow. I made a lot of progress . I guess there’s a message of hope in here.
If you are having thoughts of suicide, call or text 988 to reach the 988 Suicide and Crisis Lifeline or go to SpeakingOfSuicide.com/resources for a list of additional resources. Go here for resources outside the United States.
An earlier version of this article misstated the given name of Janelle Jones’s baby. She is Ava, not Eva.
How we handle corrections
Catherine Pearson is a reporter for the Well section of The Times, covering families and relationships. More about Catherine Pearson
Pregnancy, Childbirth and Postpartum Experiences
‘A Chance to Live’: Cases of trisomy 18 may rise as many states restrict abortion. Some women have chosen to have these babies , love them tenderly and care for them devotedly.
Teen Pregnancies: A large study in Canada found that women who were pregnant as teenagers were more likely to die before turning 31 .
Weight-Loss Drugs: Doctors say they are seeing more women try weight-loss medications in the hopes of having a healthy pregnancy. But little is known about the impact of those drugs on a fetus.
Premature Births: After years of steady decline, premature births rose sharply in the United States between 2014 and 2022. Experts said the shift might be partly the result of a growing prevalence of health complications among mothers .
Depression and Suicide: Women who experience depression during pregnancy or in the year after giving birth have a greater risk of suicide and attempted suicide .
A Long Awaited Breakthrough: Scientists said they had pinpointed the cause of severe morning sickness — a discovery could lead to better treatments for severe nausea and vomiting during pregnancy.
Advertisement

Postpartum Depression
What postpartum depression looks like in new dads, new study of 2,500 fathers fills critical gaps in the research..
Posted December 31, 2021 | Reviewed by Devon Frye
- What Is Depression?
- Find a therapist to overcome depression
- Postpartum depression and anxiety are better studied for mothers than fathers.
- Prior research has show that fathers are also at-risk for postpartum psychiatric illness, but there are gaps in the research.
- The current study of a large group of fathers looks at rates of anxiety and depression, and risk factors, during the two years following birth.
- Rates of co-occurring paternal postnatal depression and anxiety are as high as 25 percent, representing a significant concern.
By Grant H. Brenner
Pregnancy , and the time following the birth of a child, is for many a time of joy, great expectation, and of course also increased stress and anxiety . The strain placed on the family is considerable, and is a time of increased risk for a variety of problems. Postpartum depression and anxiety are better studied in women than men, as authors Dennis, Marini, Dol, Vigod, Grigoriadis, and Brown note in their recent article in Depression and Anxiety (2021) investigating paternal postpartum difficulties.
Scope of the Problem
They report that approximately 17 percent of women develop postpartum depression, and 15 percent anxiety, with almost 10 percent experiencing both. Risk factors included prior history of mental illness, low support, higher levels of fatigue, and disrupted infant sleep.
For fathers, research has been less robust, though as we recognize the importance of fatherhood, this is shifting. Recent research highlighting the role of father-child attachment and the development of paternal identity , for instance, has outlined how men become fathers—from the moment when they realize the baby is actually real, rather than an abstract idea, to recognizing how much responsibility they have, to taking on the role of father, to navigating complex and often conflicting emotions.
The study authors note that the existing literature finds variable rates of paternal postpartum problems, with depression ranging from 8 percent shortly following childbirth, rising over 25 percent with the first 6 months, and then falling again toward the end of the first year. Rates of anxiety range from 2 to 18 percent, with risk factors including paternal history of mental illness, maternal postpartum problems, economic strain, and newborn health problems.
Postpartum Depression and Anxiety in the First Two Years Following Childbirth
However, no study has systematically looked at anxiety and depression, along with related risk factors, together. To address these questions, Dennis and colleagues used long-term data collected between 2015 and 2019 with over 2,500 fathers, 75 percent of whom completed time points over the two years of the study. Questionnaires were sent every three months for the first year, and then twice a year for the second year to develop a longitudinal view. Although not all fathers completed all time points, the pooled data were analyzed to draw valid conclusions about the overall population.
Measures included the Edinburgh Postnatal Depression Scale, subscales of the State-Trait Anxiety Inventory, and six domains potential risk factors based on existing research:
- demographic factors
- pregnancy-related factors
- psychiatric and substance/ alcohol use problems
- paternal childhood adversity
- perceived quality of relationship and support with their partners
- parent and baby-related factors.
Each of these six domains included a number of relevant sub-factors—for example, under "parent-child relationship," there was breastfeeding quality, co- sleeping , parental sleep quality, parental satisfaction, parental role orientation, and outside childcare support.
They found that in the first year, 569 fathers reported mild to moderate co-occurring anxiety and depression. In the second year, 323 fathers reported mild to moderate depression and anxiety. Three percent of fathers reported more severe symptoms, which tended to start within the first year and persist into the second year. Depression rates started at 4 percent, rose to over 11 percent within 3 months, and then leveled off to around 10 percent over the remainder of the study period. Anxiety followed a similar pattern, starting lower at 8.8 percent, rising to over 20 percent over 3-6 months, and then leveling out at 20.4 percent at the 24-month study endpoint.
Risk factors for co-occurring depression and anxiety included low or fair perceived infant health within the first 4 weeks, a prior paternal depression history, elevated paternal anxiety during the pregnancy, a history of intimate partner violence , a need for greater guidance, and prior history of paternal attention -deficit/hyperactivity disorder ( ADHD ). Protective factors included better partner alliance and adjustment, better social integration, greater attachment, more hours of uninterrupted sleep, and higher paternal satisfaction. Risk and protective factors were similar for the first and second years, with differences in the second year including financial strain as a risk factor, and loss of significance of uninterrupted sleep as a protective factor.
Lessons Learned
Postpartum paternal depression and anxiety occur together for a significant percentage of fathers—almost 25 percent in the first year and almost 10 percent continuing into the second year following childbirth, on par with rates of maternal depression and anxiety. Many of the risk factors identified could be addressed through psychosocial interventions, including quality of relationship with mother and baby, treatment of prior anxiety, depression and ADHD, support- and sleep-related factors, and recognition of the role of fathers’ own childhood adversity during the postpartum period.
Biological, psychological, and relationship factors play a role, and providing good support and possibly therapeutic interventions for fathers would be expected to reduce rates of depression and anxiety. Prior psychiatric conditions should be identified and treated, and fathers who experienced maltreatment during their own childhoods likely would benefit from addressing how these issues get stirred up when they have children of their own, as such adverse childhood experiences may both predispose to anxiety and depression.

Paternal developmental trauma may also interfere with father-infant bonding, leading to emotional detachment, feelings of inadequacy, and disruption of protective attachment to mother and child. Interventions to help fathers experiencing depression and anxiety also would be expected to reduce maternal depression and anxiety, and strengthen the overall family system. Future research will look at what interventions are most effective, and how to integrate them into healthcare settings both to identify and assist at-risk fathers, as well as to bolster the overall effectiveness of parent education and preparation for pregnancy, childbirth, and the postpartum period.
Facebook image: Elnur/Shutterstock
LinkedIn image: christinarosepix/Shutterstock
Dennis, C.-L., Marini, F., Dol, J., Vigod, S. N., Grigoriadis, S., & Brown, H. K. (2021). Paternal prevalence and risk factors for comorbid depression and anxiety across the first 2 years postpartum: A nationwide Canadian cohort study. Depression and Anxiety, 1– 13. https://doi.org/10.1002/da.23234
Note: A Psychiatry for the People post ("Our Blog Post") is not intended to be a substitute for professional advice. We will not be liable for any loss or damage caused by your reliance on information obtained through Our Blog Post. Please seek the advice of professionals, as appropriate, regarding the evaluation of any specific information, opinion, advice, or other content. We are not responsible and will not be held liable for third party comments on Our Blog Post. Any user comment on Our Blog Post that in our sole discretion restricts or inhibits any other user from using or enjoying Our Blog Post is prohibited and may be reported to Sussex Publishers/Psychology Today. Neighborhood Psychiatry. All rights reserved.

SOL Mental Health is a practice of medical professionals, therapists, wellness experts, and administrative support staff dedicated to providing compassionate, conscientious care. We strive to constantly improve patient experience and raise the overall standard of what patients seeking mental health care receive.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Perinatal depression linked with premenstrual mood disorders – new research
Associate Professor of Epidemiology, Karolinska Institutet
Disclosure statement
Donghao Lu receives funding from the Swedish Research Council, Swedish Research Council for Health, Working Life and Welfare, and Karolinska Institutet.
Karolinska Institutet provides funding as a member of The Conversation UK.
View all partners

Changes in mood are a common experience for many women throughout their reproductive years. Menstruation, pregnancy and menopause are all punctuated by hormonal fluctuations – and these fluctuations can affect a person’s mood.
But for the millions of women who have a premenstrual disorder , such as severe premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD), these mood changes can be far more severe than normal. Symptoms are typically confined to the days before menstruation – yet the chronic and cyclical nature of premenstrual disorders, particularly PMDD, can profoundly affect a person’s life.
Premenstrual disorders manifest through a range of symptoms – including mood swings, irritability and fatigue. PMS is generally regarded as a milder variant of PMDD.
Premenstrual disorders affect millions of women of reproductive age around the world. It’s estimated that anywhere from 1-6% of women have PMDD, and between 20% and 30% of women experience moderate-to-severe PMS. Mild PMS is a common experience and would not necessarily be considered a disease.
Despite their prevalence, there’s a dire lack of awareness and understanding, both among the public and healthcare providers, about premenstrual disorders and the affect they can have on quality of life and health.
But recent research, conducted by myself and colleagues, has just shed more light on these conditions and the possible mechanisms underlying them. Our study found that women who have a premenstrual disorder may also be at greater risk of depression during or after pregnancy .
Read more: Premenstrual dysphoric disorder: the frightening psychological condition suffered by Dixie D'Amelio
Previous research by us has illustrated a link between premenstrual disorders and a higher risk of subsequent suicidal behaviour , early menopause and severe menopause symptoms , and even premature death. Having a premenstrual disorder may also partly explain why mental health problems may be more common in young women .
Perinatal depression
Amid this backdrop of chronic struggle, pregnancy offers a temporary respite from the cyclical torment of premenstrual disorders, as it pauses menstruation – and its accompanying symptoms.
But compelling evidence shows premenstrual disorders are probably caused by an abnormal response to normal hormone fluctuations – meaning this break may not be without its challenges.
The hormonal fluctuations that happen during and after pregnancy can also precipitate a unique form of turmoil: perinatal depression . This condition affects 10-20% of birthing women. It shares a significant symptom overlap with depression – characterised by extreme sadness, low energy and irritability.
Historically, the threads connecting premenstrual disorders and perinatal depression have been recognised anecdotally. However, there has been a lack of good evidence proving this link.

But our latest study, which looked at data from over 1 million mothers in Sweden, is the first of its kind to demonstrate a strong relationship between premenstrual disorders and perinatal depression .
We revealed that women with a history of premenstrual disorders are five times more susceptible to developing perinatal depression if they become pregnant. This connection persists even after adjusting for various factors – including history of previous psychiatric disorders. This indicates that the two conditions may share an underlying cause – possibly rooted in an abnormal response to hormonal changes.
Read more: Maternal mental health problems – the impact in numbers
Moreover, our study is the first to draw connections not just to postnatal depression (depression after childbirth) but also antenatal depression (depression during pregnancy). We found that women with premenstrual disorders were around four-and-a-half times more likely to experience antenatal depression. This insight may suggest it’s time to reevaluate antenatal depression, and investigate whether it’s also closely linked to hormonal fluctuations.
We also showed that women who experience perinatal depression are at a higher risk of encountering premenstrual disorders later on.
Advocate for mental health
The causes of perinatal depression are complex. But our research highlights how premenstrual disorders and postnatal depression appear to be interconnected for some. This suggests that understanding and treating one condition could help with managing the other.
Our latest study serves as a call for heightened awareness and a more nuanced understanding of the hormonal underpinnings of mood disorders across different stages of a woman’s life. It also suggests that women with a history of premenstrual disorders should be closely screened for perinatal depression, and provided with the help and resources they may need for their mental health before and during pregnancy, and just after giving birth.
Moreover, it encourages women themselves to advocate for their mental health, armed with the understanding that their experiences before and during pregnancy are not isolated – but part of a broader hormonal narrative that needs addressing.
- Mental health
- Premenstrual dysphoric disorder
- Maternal mental health
- perinatal depression

Audience Development Coordinator (fixed-term maternity cover)

Data and Reporting Analyst

Lecturer (Hindi-Urdu)

Director, Defence and Security

Opportunities with the new CIEHF
Helping Women with Postpartum Depression
What is Postpartum Depression?
Postpartum depression (PPD) is a serious mood disorder. Women who develop PPD have feelings of intense sadness, worry and exhaustion following childbirth.
Postpartum Depression Statistics
Statistics on Postpartum Depression
Postpartum depression is a condition that takes many forms and can remain undiagnosed for long periods of time.
Awareness of postpartum depression first arose in the late 1980s. Since then, many studies have been conducted on its incidence, risk factors, and successful treatment rates among the world’s population.
Sadly, it’s believed that postpartum depression is much more common than the data reveals. Some healthcare providers believe the condition’s prevalence could be at least twice as much as what is actually reported and diagnosed. If postpartum depression symptoms go unreported and untreated, they cannot be accounted for in public health statistics.
Regardless, the numerous studies conducted on this condition have provided important statistics that shed light on the pervasiveness and magnitude of a global mental health issue.
Quick Postpartum Depression Facts and Statistics
- Approximately 1 in 10 women will experience postpartum depression after giving birth, with some studies reporting 1 in 7 women.
- Postpartum depression generally lasts 3 to 6 months. However, this varies based on several factors.
- It is estimated that nearly 50% of mothers with postpartum depression are not diagnosed by a health professional.
- 80% of women with postpartum depression will achieve a full recovery.
Postpartum Depression Statistics in the U.S.
While exact postpartum depression rates are unknown, there are some generally agreed-upon figures about the number of women who experience postpartum depression annually.
One recent study found that 1 in 7 women may experience postpartum depression in the year after giving birth. With approximately 4 million live births occurring annually in the United States, this equates to almost 600,000 postpartum depression diagnoses .
It’s important to understand that these numbers only account for live births.
Many women who miscarry or have stillbirths experience postpartum depression symptoms as well. When including women who have miscarried or have had a stillbirth, around 900,000 women suffer from postpartum depression annually in the U.S.
International Postpartum Depression Statistics Worldwide
Postpartum depression is a global issue as well. The condition affects tens if not hundreds of millions annually if all countries are accounted for.
Postpartum Depression Statistics in Canada
- Data released in 2019 indicates that 23% of new mothers in Canada experienced symptoms of postpartum depression or anxiety after childbirth.
- Younger mothers — ages 25 and below — were more likely to develop postpartum depression or anxiety. The prevalence for this group was 30% compared to 23% for other age groups.
- Over 30% of new mothers with postpartum depression or anxiety also had a depressive disorder or mood disorder before pregnancy and delivery.
Postpartum Depression Statistics in the UK
- Similar to the U.S., the number of new mothers in the UK who experience postpartum depression, also called perinatal depression, is around 1 in 10.
- Approximately 1 in 8 British women also experience depression during pregnancy (antenatal depression).
- The Royal College of Psychiatrists reports that around 25% of women with postpartum depression still experience symptoms after their new baby turns one.
Postpartum Depression Statistics in Australia
- According to data from the 2010 Australian National Infant Feeding Survey, approximately 56,000 new mothers reported having a postpartum depression diagnosis.
- In Australia, around 1 in 5 women do not receive proper prenatal and postnatal follow-up screenings. This includes high-risk groups of women, such as those with reported emotional distress and a family history of depression.
- Postpartum depression symptoms began during pregnancy for roughly 40% of Australian women.
Postpartum Depression Statistics in the Philippines
- A multicenter study published in 2019 reported that 16.4% of new mothers in the Philippines experienced postpartum depression at the 6-week mark following delivery.
- In 2007, the Thirteenth Congress of the Republic of the Philippines introduced the Postpartum Depression Research Act of 2007, designed to conduct and support research surrounding postpartum conditions.
Postpartum Depression Statistics by Race
Another important fact to consider about postpartum depression is that it can affect people from all races, ethnicities, cultures, and educational or economic backgrounds.
The chart below details the percentages of women of various ethnicities who have been diagnosed with postpartum depression.
Postpartum Depression in New Mothers by Ethnicity/Race
The following data displays the percentages of women with symptoms of postpartum depression among various different ethnic groups.
Postpartum Depression Statistics: Special Circumstances
Postpartum depression doesn’t only affect new mothers. Below, learn more about the rates of postpartum depression among new fathers and adoptive parents.
Statistics on Postpartum Depression in Men
Studies have found that around 50% of men who have partners diagnosed with postpartum depression will go on to develop depression themselves.
Statistics on Postpartum Depression in Adoptive Parents
Some studies have shown that rates of postpartum depression in adoptive parents can be comparable to rates in biological mothers.
On the other hand, one 1995 study found that roughly 8% of adoptive parents experienced severe postpartum depression. This significantly contrasts the condition’s prevalence in biological mothers in the same study, 16.5%.
Additionally, according to a study published in the journal Archives of Women’s Mental Health , “adoptive women reported significantly greater well-being than postpartum women.”
The stressors that adoptive parents face differ from those faced by biological parents, which may contribute to these differing rates. For example, adoptive parents tend to be characterized by higher income levels and occupational status, as well as a lack of delivery complications and hormonal changes following childbirth.
Despite the disparities between postpartum biological mothers and adoptive mothers, the stressful life events that accompany new parenthood can be extremely difficult to navigate. New parents — mothers, fathers, biological, or adoptive — who are struggling with major depression or anxiety deserve support and assistance.
Statistics on Postpartum Depression Types
Part of spreading awareness about postpartum depression is understanding that this condition can take many forms. Here are some statistics regarding the rates and risk factors of specific types of postpartum depression .
Postpartum Blues Statistics
- Also called ‘ baby blues ,’ postpartum blues impacts approximately 50% to 75% of new mothers, according to the Cleveland Clinic. Many of these women will experience the more severe condition of postpartum depression or a related condition.
- Baby blues tends to set in around 1 to 4 days after giving birth.
- Without treatment, postpartum blues usually lasts only 1 to 2 weeks after delivery.
Postpartum Anxiety Statistics
- Roughly 75% of women with maternal depression also had signs of postpartum anxiety disorder, according to a study published in the journal Acta Clinica Croatica.
- According to a 2016 study, 17% of postpartum women experienced anxiety and similar mental disorders within the first 3 months after giving birth.
Postpartum OCD Statistics
- Postpartum obsessive-compulsive disorder (OCD) is believed to occur in 3% to 5% of childbearing women.
- For women with a past history of OCD, the likelihood that they will experience recurrent OCD following childbirth is 25% to 75%.
- When OCD symptoms develop in postpartum women after delivery, they tend to persist for at least 6 months.
Postpartum Panic Disorder Statistics
- Approximately 7% of new mothers develop postpartum panic disorder after childbirth.
- The symptoms of postpartum panic disorder typically appear only a few days after giving birth. However, some women experience symptoms for the first time later, anytime during the first year of motherhood.
- In many cases, postpartum panic attacks last between 20 and 30 minutes.
Postpartum PTSD Statistics
- Almost 1 in 10 women will experience postpartum post-traumatic stress disorder (PTSD) after delivery.
- Around 30% of new mothers experiencing complications during pregnancy or delivery meet partial criteria for PTSD.
Postpartum Psychosis Statistics
- Between 1 and 2 women out of every 1,000 will develop postpartum psychosis , a severe and potentially deadly disorder.
- Women who have a history of bipolar disorder are 40% more likely to develop postpartum psychosis.
- Tragically, 10% of postpartum psychosis cases result in suicide or infanticide.
Postpartum Depression Suicide Rates
- According to a Canadian study, the most at-risk time for suicide among postpartum women was 9 to 12 months after giving birth.
- Over 60% of women who took their own life during the postpartum period had not seen a mental health care provider within the month leading up to their death.
- Over the past decade, suicide attempts during and after pregnancy have nearly tripled.
Statistics on Postpartum Depression Risk Factors
There is no known cause of postpartum depression. Instead, there are a number of risk factors — such as health problems occurring during labor and a lack of social support — that increase your likelihood of developing it.
Here are some statistics regarding specific potential causes and risk factors for postpartum depression .
Medical History Risk Factors
- Women with a history of depression, anxiety disorders, or serious mood disorders are 30% to 35% more likely to develop postpartum depression.
- If a pregnant woman has experienced postpartum depression with previous births, she has an increased risk (10% to 50%) of experiencing it again.
- It is believed that 50% of women who develop postpartum depression begin experiencing symptoms during pregnancy. This proves the case for early symptom recognition, depression screening, and access to treatment options.
Environmental Risk Factors
- While postpartum depression can affect people of all backgrounds, people in poverty or who have poor access to education and health care may run a higher risk.
- Data suggests that 25% of people with a lower income level and lack access to quality health care and education will develop postpartum depression.
- One study found that new moms of low socioeconomic status were 11 times more likely to develop postpartum depression symptoms than women of higher socioeconomic status.
Postpartum Depression and Breastfeeding Statistics
A 2021 study conducted by researchers at Florida Atlantic University found that current breastfeeding status played a role in the risk of postpartum depression among new mothers.
In fact, breastfeeding women had a significantly lower risk of postpartum depression than women not breastfeeding. Further, the longer a mother breastfed, the lower her risk of postpartum depression.
More research is needed to understand the relationship between postpartum depression and breastfeeding across various subgroups of women.
Statistics of Postpartum Depression Treatment
From these facts and statistics, it’s easy to see how prevalent postpartum depression is globally. Awareness, screening tools, risk prediction, and early diagnosis and treatment can all help improve these concerning numbers regarding women’s health.
As with all forms of mental illnesses, early recognition and treatment of postpartum depression can lead to better symptom management and faster recovery rates. Treatment for this condition may include psychiatry, psychotherapy, support groups , and/or antidepressants. Regardless, it’s never too late to seek help.
Consult with your doctor immediately if you’re experiencing symptoms of postpartum depression. Get started on the path toward treatment today.
Medical Editor
- Fact-Checked
Kimberly Langdon is a Doctor of Medicine and graduated from The Ohio State University in 1991. She completed her residency in Obstetrics and Gynecology at The Ohio State University Hospitals, Department of OB/GYN. Board-Certified in 1997, she is now retired from clinical practice after a long and successful career. Currently, she is the Founder and Chief Medical Officer of a Medical Device Company that is introducing patented products to treat vaginal microbial infections without the need for drugs. She is an expert in Vaginal Infections, Menstrual disorders, Menopause, and Contraception.
Jenna Carberg was diagnosed with postpartum depression following the birth of her daughter in 2016. It was a healthy birth but in the following days, Jenna's mood changed quickly. Doctors suggested that it might be the "baby blues", but her husband Chris suggested she seek a second opinion. Jenna was diagnosed with postpartum depression and began a journey that lasted 9 long months with significant ups and downs. Jenna's mental health care and her experiences became a passion for her to share with the world. She and her husband Chris founded PostpartumDepression.org as a support website designed to help women suffering in silence and their loved ones.
- Postpartum Depression. (n.d.). Retrieved from https://www.apa.org/pi/women/resources/reports/postpartum-depression.aspx
- Genetic Predictors of Postpartum Depression Uncovered by Johns Hopkins Researchers – 05/21/2013. (2013, May 21). Retrieved from https://www.hopkinsmedicine.org/news/media/releases/genetic_predictors_of_postpartum_depression_uncovered_by_johns_hopkins_researchers
- Goyal, D., Gay, C., & Lee, K. A. (2010). How much does low socioeconomic status increase the risk of prenatal and postpartum depressive symptoms in first-time mothers?. Women’s health issues: official publication of the Jacobs Institute of Women’s Health , 20 (2), 96-104.
- Baby Blues: Causes, Symptoms and Treatment. (2016, May 18). Retrieved from https://americanpregnancy.org/first-year-of-life/baby-blues/
- New Study Reveals Disturbing PPD Statistics. Retrieved on April 1, 2024, from http://www.seleni.org/advice-support/2018/3/16/new-study-reveals-disturbing-ppd-statistics
- Postpartum Mood Disorders. A Couples Guide. Dr. Christina G. Hibbert, Psy.D. Retrieved on April 1, 2024, from https://psychotherapy.com/mom.html
- Postpartum depression: Types, symptoms, treatment & prevention. Cleveland Clinic. (n.d.). Retrieved April 1, 2024, from https://my.clevelandclinic.org/health/diseases/9312-postpartum-depression
- Mott, S. L., Schiller, C. E., Richards, J. G., O’Hara, M. W., & Stuart, S. (2011, August). Depression and anxiety among postpartum and adoptive mothers. Archives of women’s mental health. Retrieved April 1, 2024, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3433270/
- Nakić Radoš, S., Tadinac, M., & Herman, R. (2018, March). Anxiety during pregnancy and postpartum: Course, predictors and comorbidity with postpartum depression. Acta clinica Croatica. Retrieved April 1, 2024, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6400346/
- Menkedick, S. (2020, March 19). Postpartum anxiety is an epidemic among American mothers. Time. Retrieved April 1, 2024, from https://time.com/5806230/postpartum-anxiety-epidemic/
- Miller, E. S., Chu, C., Gollan, J., & Gossett, D. R. (2013). Obsessive-compulsive symptoms during the postpartum period. A prospective cohort. The Journal of reproductive medicine. Retrieved April 1, 2024, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5705036/
- PTSD after pregnancy: When a doctor becomes a patient: Your pregnancy matters: UT southwestern medical center. Your Pregnancy Matters | UT Southwestern Medical Center. (n.d.). Retrieved April 1, 2024, from https://utswmed.org/medblog/ptsd-after-pregnancy-when-doctor-becomes-patient/
- How rates of perinatal mental … – Wiley Online Library. (n.d.). Retrieved April 1, 2024, from https://onlinelibrary.wiley.com/doi/10.1111/1753-6405.12999
- Professor Jeannette Milgrom FAPS MCHP MCCLP. (n.d.). Professor Jeannette Milgrom FAPS MCHP MCCLP, parent-Infant Research Institute and the University of Melbourne. APS. Retrieved April 1, 2024, from https://psychology.org.au/inpsych/2017/february/milgrom
- Government of Canada, S. C. (2019, June 24). Maternal Mental Health in Canada, 2018/2019. The Daily – . Retrieved April 1, 2024, from https://www150.statcan.gc.ca/n1/daily-quotidien/190624/dq190624b-eng.htm
- Postnatal depression key facts: Royal College of Psychiatrists. RC PSYCH ROYAL COLLEGE OF PSYCHIATRISTS. (n.d.). Retrieved April 1, 2024, from https://www.rcpsych.ac.uk/mental-health/problems-disorders/postnatal-depression-key-facts
- Labrague LJ;McEnroe-Petitte D;Tsaras K;Yboa BC;Rosales RA;Tizon MM;D’souza MS; (n.d.). Predictors of postpartum depression and the utilization of postpartum depression services in rural areas in the Philippines. Perspectives in psychiatric care. Retrieved April 1, 2024, from https://pubmed.ncbi.nlm.nih.gov/31355473/#:~:text=One%20hundred%20sixty%2Dfive%20women,significant%20direct%20influences%20on%20PPD.
- Mughal, S. (2021, July 2). Postpartum depression. StatPearls [Internet]. Retrieved April 1, 2024, from https://www.ncbi.nlm.nih.gov/books/NBK519070/
- Perinatal suicide: Highest risk occurs at 9 to 12 months postpartum. MGH Center for Women’s Mental Health. (2019, March 21). Retrieved April 1, 2024, from https://womensmentalhealth.org/posts/perinatal-suicide-highest-risk-occurs-at-9-to-12-months-postpartum/
- The significance of breastfeeding practices on postpartum … (n.d.). Retrieved April 1, 2024, from https://onlinelibrary.wiley.com/doi/epdf/10.1111/phn.12969
Get Answers to Your Postpartum Depression Questions
- Patient Care & Health Information
- Diseases & Conditions
- Postpartum depression
The birth of a baby can start a variety of powerful emotions, from excitement and joy to fear and anxiety. But it can also result in something you might not expect — depression.
Most new moms experience postpartum "baby blues" after childbirth, which commonly include mood swings, crying spells, anxiety and difficulty sleeping. Baby blues usually begin within the first 2 to 3 days after delivery and may last for up to two weeks.
But some new moms experience a more severe, long-lasting form of depression known as postpartum depression. Sometimes it's called peripartum depression because it can start during pregnancy and continue after childbirth. Rarely, an extreme mood disorder called postpartum psychosis also may develop after childbirth.
Postpartum depression is not a character flaw or a weakness. Sometimes it's simply a complication of giving birth. If you have postpartum depression, prompt treatment can help you manage your symptoms and help you bond with your baby.
Products & Services
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- A Book: Mayo Clinic Guide to Your Baby's First Years
- A Book: Obstetricks
Symptoms of depression after childbirth vary, and they can range from mild to severe.
Baby blues symptoms
Symptoms of baby blues — which last only a few days to a week or two after your baby is born — may include:
- Mood swings
- Irritability
- Feeling overwhelmed
- Reduced concentration
- Appetite problems
- Trouble sleeping
Postpartum depression symptoms
Postpartum depression may be mistaken for baby blues at first — but the symptoms are more intense and last longer. These may eventually interfere with your ability to care for your baby and handle other daily tasks. Symptoms usually develop within the first few weeks after giving birth. But they may begin earlier — during pregnancy — or later — up to a year after birth.
Postpartum depression symptoms may include:
- Depressed mood or severe mood swings
- Crying too much
- Difficulty bonding with your baby
- Withdrawing from family and friends
- Loss of appetite or eating much more than usual
- Inability to sleep, called insomnia, or sleeping too much
- Overwhelming tiredness or loss of energy
- Less interest and pleasure in activities you used to enjoy
- Intense irritability and anger
- Fear that you're not a good mother
- Hopelessness
- Feelings of worthlessness, shame, guilt or inadequacy
- Reduced ability to think clearly, concentrate or make decisions
- Restlessness
- Severe anxiety and panic attacks
- Thoughts of harming yourself or your baby
- Recurring thoughts of death or suicide
Untreated, postpartum depression may last for many months or longer.
Postpartum psychosis
With postpartum psychosis — a rare condition that usually develops within the first week after delivery — the symptoms are severe. Symptoms may include:
- Feeling confused and lost
- Having obsessive thoughts about your baby
- Hallucinating and having delusions
- Having sleep problems
- Having too much energy and feeling upset
- Feeling paranoid
- Making attempts to harm yourself or your baby
Postpartum psychosis may lead to life-threatening thoughts or behaviors and requires immediate treatment.
Postpartum depression in the other parent
Studies show that new fathers can experience postpartum depression, too. They may feel sad, tired, overwhelmed, anxious, or have changes in their usual eating and sleeping patterns. These are the same symptoms that mothers with postpartum depression experience.
Fathers who are young, have a history of depression, experience relationship problems or are struggling financially are most at risk of postpartum depression. Postpartum depression in fathers — sometimes called paternal postpartum depression — can have the same negative effect on partner relationships and child development as postpartum depression in mothers can.
If you're a partner of a new mother and are having symptoms of depression or anxiety during your partner's pregnancy or after your child's birth, talk to your health care provider. Similar treatments and supports provided to mothers with postpartum depression can help treat postpartum depression in the other parent.
When to see a doctor
If you're feeling depressed after your baby's birth, you may be reluctant or embarrassed to admit it. But if you experience any symptoms of postpartum baby blues or postpartum depression, call your primary health care provider or your obstetrician or gynecologist and schedule an appointment. If you have symptoms that suggest you may have postpartum psychosis, get help immediately.
It's important to call your provider as soon as possible if the symptoms of depression have any of these features:
- Don't fade after two weeks.
- Are getting worse.
- Make it hard for you to care for your baby.
- Make it hard to complete everyday tasks.
- Include thoughts of harming yourself or your baby.
If you have suicidal thoughts
If at any point you have thoughts of harming yourself or your baby, immediately seek help from your partner or loved ones in taking care of your baby. Call 911 or your local emergency assistance number to get help.
Also consider these options if you're having suicidal thoughts:
- Seek help from a health care provider.
- Call a mental health provider.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential. The Suicide & Crisis Lifeline in the U.S. has a Spanish language phone line at 1-888-628-9454 (toll-free).
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
Helping a friend or loved one
People with depression may not recognize or admit that they're depressed. They may not be aware of signs and symptoms of depression. If you suspect that a friend or loved one has postpartum depression or is developing postpartum psychosis, help them seek medical attention immediately. Don't wait and hope for improvement.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
There is no single cause of postpartum depression, but genetics, physical changes and emotional issues may play a role.
- Genetics. Studies show that having a family history of postpartum depression — especially if it was major — increases the risk of experiencing postpartum depression.
- Physical changes. After childbirth, a dramatic drop in the hormones estrogen and progesterone in your body may contribute to postpartum depression. Other hormones produced by your thyroid gland also may drop sharply — which can leave you feeling tired, sluggish and depressed.
- Emotional issues. When you're sleep deprived and overwhelmed, you may have trouble handling even minor problems. You may be anxious about your ability to care for a newborn. You may feel less attractive, struggle with your sense of identity or feel that you've lost control over your life. Any of these issues can contribute to postpartum depression.
Risk factors
Any new mom can experience postpartum depression and it can develop after the birth of any child, not just the first. However, your risk increases if:
- You have a history of depression, either during pregnancy or at other times.
- You have bipolar disorder.
- You had postpartum depression after a previous pregnancy.
- You have family members who've had depression or other mood disorders.
- You've experienced stressful events during the past year, such as pregnancy complications, illness or job loss.
- Your baby has health problems or other special needs.
- You have twins, triplets or other multiple births.
- You have difficulty breastfeeding.
- You're having problems in your relationship with your spouse or partner.
- You have a weak support system.
- You have financial problems.
- The pregnancy was unplanned or unwanted.
Complications
Left untreated, postpartum depression can interfere with mother-child bonding and cause family problems.
- For mothers. Untreated postpartum depression can last for months or longer, sometimes becoming an ongoing depressive disorder. Mothers may stop breastfeeding, have problems bonding with and caring for their infants, and be at increased risk of suicide. Even when treated, postpartum depression increases a woman's risk of future episodes of major depression.
- For the other parent. Postpartum depression can have a ripple effect, causing emotional strain for everyone close to a new baby. When a new mother is depressed, the risk of depression in the baby's other parent may also increase. And these other parents may already have an increased risk of depression, whether or not their partner is affected.
- For children. Children of mothers who have untreated postpartum depression are more likely to have emotional and behavioral problems, such as sleeping and eating difficulties, crying too much, and delays in language development.
If you have a history of depression — especially postpartum depression — tell your health care provider if you're planning on becoming pregnant or as soon as you find out you're pregnant.
- During pregnancy, your provider can monitor you closely for symptoms of depression. You may complete a depression-screening questionnaire during your pregnancy and after delivery. Sometimes mild depression can be managed with support groups, counseling or other therapies. In other cases, antidepressants may be recommended — even during pregnancy.
- After your baby is born, your provider may recommend an early postpartum checkup to screen for symptoms of postpartum depression. The earlier it's found, the earlier treatment can begin. If you have a history of postpartum depression, your provider may recommend antidepressant treatment or talk therapy immediately after delivery. Most antidepressants are safe to take while breastfeeding.
- Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision DSM-5-TR. American Psychiatric Association; 2022. https://dsm.psychiatryonline.org. Accessed May 9, 2022.
- Postpartum depression. Office on Women's Health. https://www.womenshealth.gov/mental-health/mental-health-conditions/postpartum-depression. Accessed May 5, 2022.
- Depression among women. Centers for Disease Control and Prevention. https://www.cdc.gov/reproductivehealth/depression/index.htm. Accessed May 5, 2022.
- What is peripartum depression (formerly postpartum)? American Psychiatric Association. https://www.psychiatry.org/patients-families/postpartum-depression/what-is-postpartum-depression. Accessed Nov. 18, 2022.
- Viguera A. Postpartum unipolar depression: Epidemiology, clinical features, assessment, and diagnosis. https://www.uptodate.com/contents/search. Accessed Nov. 18, 2022.
- Viguera A. Mild to moderate postpartum unipolar major depression: Treatment. https://www.uptodate.com/contents/search. Accessed May 6, 2022.
- Viguera A. Severe postpartum unipolar major depression: Choosing treatment. https://www.uptodate.com/contents/search. Accessed May 6, 2022.
- Faden J, et al. Intravenous brexanolone for postpartum depression: What it is, how well does it work, and will it be used? Therapeutic Advances in Psychopharmacology. 2020; doi:10.1177/2045125320968658.
- FAQs. Postpartum depression. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/postpartum-depression. Accessed May 6, 2022.
- Suicide prevention. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/suicide-prevention. Accessed May 6, 2022.
- Postpartum depression. Merck Manual Professional Version. https://www.merckmanuals.com/professional/gynecology-and-obstetrics/postpartum-care-and-associated-disorders/postpartum-depression#. Accessed May 6, 2022.
- AskMayoExpert. Depression in pregnancy and postpartum. Mayo Clinic; 2022.
- American Academy of Pediatrics. Postpartum care of the mother. In: Guidelines for Perinatal Care. 8th ed. American Academy of Pediatrics; American College of Obstetricians and Gynecologists; 2017.
- Kumar SV, et al. Promoting postpartum mental health in fathers: Recommendations for nurse practitioners. American Journal of Men's Health. 2018; doi:10.1177/1557988317744712.
- Scarff JR. Postpartum depression in men. Innovations in Clinical Neuroscience. 2019;16:11.
- Bergink V, et al. Postpartum psychosis: Madness, mania, and melancholia in motherhood. American Journal of Psychiatry. 2016; doi:10.1176/appi.ajp.2016.16040454.
- Yogman M, et al. Fathers' roles in the care and development of their children: The role of pediatricians. Pediatrics. 2016; doi:10.1542/peds.2016-1128.
- FDA approves first treatment for post-partum depression. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-post-partum-depression. Accessed May 6, 2022.
- Deligiannidis KM, et al. Effect of zuranolone vs placebo in postpartum depression: A randomized clinical trial. JAMA Psychiatry. 2021; doi:10.1001/jamapsychiatry.2021.1559.
- Betcher KM (expert opinion). Mayo Clinic. May 10, 2022.
- 988 Suicide & Crisis Lifeline. https://988lifeline.org/. Accessed Nov. 18, 2022.
Associated Procedures
- Electroconvulsive therapy (ECT)
News from Mayo Clinic
- Mayo Clinic Minute: Postpartum depression is more than baby blues Feb. 02, 2023, 03:00 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 5, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
written by researcher(s)
New research links perinatal depression with premenstrual mood disorders
by Donghao Lu, The Conversation

Changes in mood are a common experience for many women throughout their reproductive years. Menstruation, pregnancy and menopause are all punctuated by hormonal fluctuations—and these fluctuations can affect a person's mood.
But for the millions of women who have a premenstrual disorder , such as severe premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD), these mood changes can be far more severe than normal. Symptoms are typically confined to the days before menstruation—yet the chronic and cyclical nature of premenstrual disorders, particularly PMDD, can profoundly affect a person's life.
Premenstrual disorders manifest through a range of symptoms—including mood swings, irritability and fatigue. PMS is generally regarded as a milder variant of PMDD.
Premenstrual disorders affect millions of women of reproductive age around the world. It's estimated that anywhere from 1-6% of women have PMDD, and between 20% and 30% of women experience moderate-to-severe PMS. Mild PMS is a common experience and would not necessarily be considered a disease.
Despite their prevalence, there's a dire lack of awareness and understanding, both among the public and health care providers, about premenstrual disorders and the effect they can have on quality of life and health.
But recent research, conducted by myself and colleagues, has just shed more light on these conditions and the possible mechanisms underlying them. Our study found that women who have a premenstrual disorder may also be at greater risk of depression during or after pregnancy .
Previous research by us has illustrated a link between premenstrual disorders and a higher risk of subsequent suicidal behavior , early menopause and severe menopause symptoms , and even premature death. Having a premenstrual disorder may also partly explain why mental health problems may be more common in young women .
Perinatal depression
Amid this backdrop of chronic struggle, pregnancy offers a temporary respite from the cyclical torment of premenstrual disorders, as it pauses menstruation—and its accompanying symptoms.
But compelling evidence shows premenstrual disorders are probably caused by an abnormal response to normal hormone fluctuations —meaning this break may not be without its challenges.
The hormonal fluctuations that happen during and after pregnancy can also precipitate a unique form of turmoil: perinatal depression . This condition affects 10–20% of birthing women. It shares a significant symptom overlap with depression —characterized by extreme sadness, low energy and irritability.
Historically, the threads connecting premenstrual disorders and perinatal depression have been recognized anecdotally. However, there has been a lack of good evidence proving this link.
But our latest study, which looked at data from over 1 million mothers in Sweden, is the first of its kind to demonstrate a strong relationship between premenstrual disorders and perinatal depression .
We revealed that women with a history of premenstrual disorders are five times more susceptible to developing perinatal depression if they become pregnant. This connection persists even after adjusting for various factors—including history of previous psychiatric disorders. This indicates that the two conditions may share an underlying cause—possibly rooted in an abnormal response to hormonal changes.
Moreover, our study is the first to draw connections not just to postnatal depression (depression after childbirth) but also antenatal depression (depression during pregnancy). We found that women with premenstrual disorders were around four-and-a-half times more likely to experience antenatal depression. This insight may suggest it's time to reevaluate antenatal depression, and investigate whether it's also closely linked to hormonal fluctuations.
We also showed that women who experience perinatal depression are at a higher risk of encountering premenstrual disorders later on.
Advocate for mental health
The causes of perinatal depression are complex. But our research highlights how premenstrual disorders and postnatal depression appear to be interconnected for some. This suggests that understanding and treating one condition could help with managing the other.
Our latest study serves as a call for heightened awareness and a more nuanced understanding of the hormonal underpinnings of mood disorders across different stages of a woman's life. It also suggests that women with a history of premenstrual disorders should be closely screened for perinatal depression , and provided with the help and resources they may need for their mental health before and during pregnancy, and just after giving birth.
Moreover, it encourages women themselves to advocate for their mental health, armed with the understanding that their experiences before and during pregnancy are not isolated—but part of a broader hormonal narrative that needs addressing.
Explore further
Feedback to editors

How do wildfires affect mental health? A new study examines the connection
4 minutes ago

Radiation before mastectomy found to cut time delays for reconstructive surgery in breast cancer patients
13 minutes ago

Platform tracks SARS-CoV-2 mutational impact on disease severity, identifies effective therapeutic inhibitors
58 minutes ago

The architectural role of p53: Early 3D chromatin remodeling to trigger cellular stress response

Researchers discuss the unseen community effects of COVID-19 stay-at-home orders

Untangling the threads of early onset dementia

Study finds many younger people from high income neighborhoods jumped the eligibility queue for COVID-19 vaccines in NYC
11 hours ago

New report presents a global plan to combat prostate cancer
16 hours ago

Suicides among US college student athletes have doubled over past 20 years: Study

Prairie voles display signs of human-like depression, show promise as animal model
17 hours ago
Related Stories

Positive associations found between premenstrual disorders and perinatal depression
Mar 28, 2024

New data show prevalence of premenstrual dysphoric disorder
Jan 30, 2024

Higher childhood BMI may increase risk for premenstrual disorders
Mar 16, 2022

Premenstrual disorders tied to earlier natural menopause
Sep 21, 2023
Women's wellness: Understanding depression and the gender gap
Apr 17, 2018

Women's wellness: Understanding the depression gender gap
Feb 13, 2019
Recommended for you

Study finds lonely women experience increased activation in regions of the brain associated with food cravings
Apr 4, 2024

Body mapping links responses to music with degree of uncertainty and surprise

Study questions effectiveness of brain stimulation for memory enhancement

Mistreatment in childbirth is common in the US especially among the disadvantaged, study finds
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

Subscribe Follow Watch
Director's Messages
Addressing the maternal health crisis.
Dr. David Murray is joined in this message by Dr. Janine Clayton, Director of the NIH Office of Research on Women's Health (ORWH) ; Dr. Diana Bianchi , Director of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) ; Dr. Eliseo J. Pérez-Stable , Director of the National Institute on Minority Health and Health Disparities (NIMHD) ; and Dr. Gary Gibbons , Director of the National Heart, Lung, and Blood Institute (NHLBI) .
The United States is experiencing a maternal health crisis with rising rates of pregnancy-related complications and deaths, also called maternal morbidity and mortality. While many research efforts have focused on understanding pregnancy and newborn outcomes, the majority of severe pregnancy-related complications and maternal deaths occur during the year immediately after pregnancy, also known as the postpartum period. More than 80% of these complications and deaths are preventable.
To identify gaps in research on postpartum health and support evidence-based improvements in maternal health care, our five institutes and offices came together to organize a Pathways to Prevention (P2P) Workshop on Identifying Risks and Interventions to Optimize Postpartum Health . Our hope is that this will be a catalyst for rapid changes and greatly broaden the research lens.
Speakers at the workshop included researchers, health care professionals, and people impacted by pregnancy-related health complications. They spoke about the need to consider women’s health across the lifespan, including long before and long after pregnancy. They also highlighted how structural disparities, like differences in local infrastructure and access to care, increase the risk of morbidity and mortality experienced by Black or African American and American Indian/Alaska Native women. A theme that permeated the workshop was the need to listen to patients and their families and engage them in research efforts.
Each of us brings a different perspective and set of resources to addressing this crisis:
- As outlined in our new strategic plan , ODP seeks to promote and support preventive intervention research that addresses risk factors for illness, injury, and the leading causes of death, many of which also lead to poor postpartum health outcomes. Our office is also working to mobilize collaborative NIH-wide efforts to enhance prevention research that addresses health disparities.
- ORWH promotes the life course perspective—the consideration of how biological, social, and environmental factors intersect and interact with each other over a woman's entire life—when studying the health of women. Not only is pregnancy a stress test affecting women’s health later in life, but the postpartum period is also a time of considerable stress and health concerns. As Dr. Clayton said during the workshop, we need to “bridge the chasm,” where entering the postpartum period should not mean leaving maternal care, but rather entering postpartum care. Extending holistic team-based care with wraparound services to the postpartum period and aligning research with women’s lived experiences is necessary to improve postpartum health.
- NICHD is interested in disparities in maternal health including those for people with disabilities and those stemming from limited access to high quality health care including mental health. NICHD will use the outcomes of the P2P workshop to inform the NIH-wide Implementing a Maternal health and PRegnancy Outcomes Vision for Everyone (IMPROVE) initiative .
- NIMHD-supported research explores how bias infiltrates so many aspects of medical care. African American and American Indian/Alaska Native women have maternal death rates that are nearly four times that of White women in the United States; these death rates stem from many different social and structural disparities arising from less access to high quality care rather than from intrinsic, biological, or behavioral health differences.
- NHLBI is focused on advancing health equity through the improvement of maternal cardiovascular health. Cardiovascular factors are a leading cause of death, both during and after pregnancy. Bias and structural disparities clearly affect psychological and biological risk factors and directly impact maternal illness and death. Identification and treatment of these factors need to be considered in any efforts to improve not only maternal health but also future cardiovascular health. The Chronic Hypertension and Pregnancy (CHAP) Trial showed that treating chronic hypertension during early pregnancy reduces adverse pregnancy outcomes, informing clinical guidance and representing a pathway toward prevention of maternal morbidity and mortality. The CHAP study will inform future implementation and dissemination efforts centered on improving maternal health.
We encourage you to review the following workshop publications to identify ways you or your organization can help address the postpartum health crisis.
- A report from the independent panel identifying research gaps and making recommendations to move the field forward
- A systematic evidence review
- A portfolio review data snapshot (PDF) describing NIH research activities in maternal health and maternal morbidity and mortality
- A report highlighting opportunities and resources (PDF) to help federal agencies and the research community address the independent panel’s recommendations
There is an urgent need for a national effort to support research, dissemination, and implementation of postpartum health initiatives. By taking a life course perspective, curbing bias, and elevating the voices of patients and their families, we will move toward making the United States the best country in the world to give birth.

IMAGES
COMMENTS
New research from Columbia University Mailman School of Public Health and the UNC Gillings School of Global Public Health, published online and in the April print issue of Health Affairs, ... Black and Latine birthing people, who may be at the greatest risk of postpartum depression, are the least likely to receive any form of postpartum mental ...
"After years of dedicated research and collaboration with other scientists around the country, women living with postpartum and perinatal depression have a new, at-home, easy-to-use treatment ...
The rapid therapeutic effects of zuranolone or brexanolone support the hypothesis of an excitation-inhibition imbalance and GABAergic signalling dysfunction in postpartum depression. But the story is certainly more complex. In a 2023 longitudinal study published in eBioMedicine, blood levels of inflammatory mediators, including TNF-α and IL ...
The research drew on data from a novel survey led by Daw at Columbia University that followed up with 4,542 postpartum people who had a live birth in 2020 in seven U.S. jurisdictions: Kansas ...
The researchers also found stark racial and ethnic inequities in treatment for those with postpartum depressive symptoms. The research drew on data from a novel survey led by Daw at Columbia University that followed up with 4,542 postpartum people who had a live birth in 2020 in seven jurisdictions: Kansas, Michigan, New Jersey, Pennsylvania ...
This article reviews novel neurosteroid therapeutics for post-partum depression, with a focus on their development, clinical trial data, current practices, and future directions in this exciting ...
Postpartum depression (PPD) is a serious health issue that can affect about 15% of the female population within after giving birth. It often conveys significant negative consequences to the offsprings. The symptoms and risk factors are somewhat similar to those found in non-postpartum depression. The main difference resides in the fact that PPD ...
Postpartum depression (PPD) is a detrimental health condition that affects 12% of new mothers. Despite negative effects on mothers' and children's health, many women do not receive adequate care.
Kujawa and her team will conduct longitudinal assessments with 300 pregnant participants across the peripartum period (15 weeks gestation to five weeks postpartum) to examine trajectories of ...
Moore Simas TA, Whelan A, Byatt N. Postpartum Depression—New Screening Recommendations and Treatments. JAMA. 2023;330(23):2295-2296. doi:10 ... Archive JAMA Network Audio JAMA Network Video JAMA Network Conferences JAMA Surgery Guide to Statistics and Methods Medical News Mpox (Monkeypox) Research Ethics Topics and Collections Visual ...
Research in rodents, along with imaging studies in new mothers, are finding areas of the brain that could be involved in postpartum depression. Among them: Alila Medical Media/Shutterstock ...
Postpartum depression (PPD) is a significant health issue for many new mothers in the weeks and months following a child's birth. Quantitative data suggest that a mother's PPD negatively impacts healthcare decision-making for the child via routine well-baby visits and pediatric care.
The estimated prevalence of postpartum depression ranges from 6.5 to 12.9% or even higher in lower-income and middle-income countries. 1,4,5 Some studies have shown increased rates of depression ...
A new mom shares how the recently approved two-week postpartum depression drug was a game-changer to combat a notably common condition during a tender phase of life. The post I Took the New ...
May 15, 2023 • Research Highlight. Perinatal depression is a common but serious mood disorder. The DSM-5, which is the classification system used to diagnose mental disorders, defines perinatal depression as a depressive episode with onset either during pregnancy or in the first 4 weeks after pregnancy (postpartum).
Postpartum depression can be prevented when parents are given positive parenting lessons and when the maternal-infant bond is promoted and increased. This can be achieved through social support from family and healthcare providers. ... New insights into perinatal depression: pathogenesis and treatment during pregnancy and postpartum. Dialogues ...
At a Glance. About 5% of women reported persistently high levels of postpartum depression symptoms for three years after giving birth. Longer screening periods after birth may be needed to help more women with postpartum depression get treatment. Depression and other mental health conditions that surface after the baby is born can have ...
The risk for postpartum depression is highest among first-time mothers, mothers younger than 25 years old and mothers of twins, according to a survey of more than 1.1 million moms worldwide. Moms older than 40 years old having twins are at the highest risk, researchers from the University of Virginia School of Medicine, Johns Hopkins University ...
Results: A total of 122 studies (out of 3712 references retrieved from bibliographic databases) were included in this systematic review. The results of the studies were synthetized into three categories: (a) the maternal consequences of postpartum depression, including physical health, psychological health, relationship, and risky behaviors; (b) the infant consequences of postpartum depression ...
All News Extending Medicaid Coverage After Birth May Increase Postpartum Treatment for Depression, Anxiety A new study found that extending Medicaid eligibility for birthing people increase treatment for perinatal mood and anxiety disorder by more than 20 percentage points, compared to birthing people with commercial insurance.
To map out the different trajectories of postpartum depression, Dr. Putnick and her colleagues in the lab of IRP senior investigator Edwina Yeung, Ph.D., analyzed data from a study of mothers and children from upstate New York that began in 2008.The mothers were given regular assessments, including a brief screening for depression at intervals beginning four months after their children were ...
This spring, The New York Times spent time with four mothers who were then in the grips of postpartum depression. They offered a stark, intimate glimpse into their experiences, in their own words ...
About two-thirds of white women (67%) said they received mental health treatment for their diagnosed depression or anxiety during pregnancy or in their first year of motherhood, researchers found. Comparatively, fewer than two out of five (37%) Black and Hispanic received treatment for their pregnancy-related mood disorders, results show.
Postpartum depression and anxiety are better studied for mothers than fathers. Prior research has show that fathers are also at-risk for postpartum psychiatric illness, but there are gaps in the ...
DOI: 10.1377/hlthaff.2023.01441. Extending postpartum Medicaid eligibility extensions may increase treatment for perinatal mood and anxiety disorders (PMADs), a leading cause of perinatal illness ...
The new study is the first to show a link between premenstrual disorders and perinatal depression. Impact Photography/ Shutterstock. But our latest study, which looked at data from over 1 million ...
Postpartum Depression Statistics in Canada. Data released in 2019 indicates that 23% of new mothers in Canada experienced symptoms of postpartum depression or anxiety after childbirth. Younger mothers — ages 25 and below — were more likely to develop postpartum depression or anxiety. The prevalence for this group was 30% compared to 23% for ...
Studies show that new fathers can experience postpartum depression, too. They may feel sad, tired, overwhelmed, anxious, or have changes in their usual eating and sleeping patterns. These are the same symptoms that mothers with postpartum depression experience. Fathers who are young, have a history of depression, experience relationship ...
Premenstrual disorders manifest through a range of symptoms—including mood swings, irritability and fatigue. PMS is generally regarded as a milder variant of PMDD. Premenstrual disorders affect ...
As outlined in our new strategic plan, ODP seeks to promote and support preventive intervention research that addresses risk factors for illness, injury, and the leading causes of death, many of which also lead to poor postpartum health outcomes. Our office is also working to mobilize collaborative NIH-wide efforts to enhance prevention ...