- Technical Support
- Find My Rep

You are here
Research Design Qualitative, Quantitative, and Mixed Methods Approaches
- John W. Creswell - Department of Family Medicine, University of Michigan
- J. David Creswell - Carnegie Mellon University, USA
- Description
See what’s new to this edition by selecting the Features tab on this page. Should you need additional information or have questions regarding the HEOA information provided for this title, including what is new to this edition, please email [email protected] . Please include your name, contact information, and the name of the title for which you would like more information. For information on the HEOA, please go to http://ed.gov/policy/highered/leg/hea08/index.html .
For assistance with your order: Please email us at [email protected] or connect with your SAGE representative.
SAGE 2455 Teller Road Thousand Oaks, CA 91320 www.sagepub.com
Supplements
“A long time ago, I participated in one of Dr. Creswell’s workshops on mixed methods research.... I am still learning from Dr. Creswell. I appreciate how he takes complex topics and makes them accessible to everyone. But I must caution my students that Dr. Creswell’s easygoing cadence and elegant descriptions sometimes mask the depth of the material. This reminds me of why he is such a highly respected researcher and teacher.”
“I always have enjoyed using Creswell's books (as a student and as an instructor) because the writing is straightforward.”
“This book is based around dissertation chapters, and that's why I love it using in my class. Practical, concise, and to the point!”
“This book is easy to use. The information and additional charts are also helpful.”
Clear material, student support website, and faculty resources.
The book provides a comprehensive overview and does well at demystifying the research philosophy. I have recommended it to my level 7 students for their dissertation project.
This book will be added to next academic year's reading list.
I am fed up with trying to get access to this "inspection copy". You don't respond to emails (and the email addresses you provide do not work). I get regular emails from you saying my ebook order is ready, but it does not appear in VitalSource and I cannot access it through any link on this web page. I am not willing to waste any more time on this. There are good alternatives.
Excellent introduction for research methods.
Creswell has always had excellent textbooks. Sixth Edition is no exception!
- Fully updated for the 7th edition of the Publication Manual of the American Psychological Association.
- More inclusive and supportive language throughout helps readers better see themselves in the research process.
- Learning Objectives provide additional structure and clarity to the reading process.
- The latest information on participatory research, evaluating literature for quality, using software to design literature maps, and additional statistical software types is newly included in this edition.
- Chapter 4: Writing Strategies and Ethical Considerations now includes information on indigenous populations and data collection after IRB review.
- An updated Chapter 8: Quantitative Methods now includes more foundational details, such as Type 1 and Type 2 errors and discussions of advantages and disadvantages of quantitative designs.
- A restructured and revised Chapter 10: Mixed Methods Procedures brings state-of-the-art thinking to this increasingly popular approach.
- Chapters 8, 9, and 10 now have parallel structures so readers can better compare and contrast each approach.
- Reworked end-of-chapter exercises offer a more straightforward path to application for students.
- New research examples throughout the text offer students contemporary studies for evaluation.
- Current references and additional readings are included in this new edition.
- Compares qualitative, quantitative, and mixed methods research in one book for unparalleled coverage.
- Highly interdisciplinary examples make this book widely appealing to a broad range of courses and disciplines.
- Ethical coverage throughout consistently reminds students to use good judgment and to be fair and unbiased in their research.
- Writing exercises conclude each chapter so that readers can practice the principles learned in the chapter; if the reader completes all of the exercises, they will have a written plan for their scholarly study.
- Numbered points provide checklists of each step in a process.
- Annotated passages help reinforce the reader's comprehension of key research ideas.
Sample Materials & Chapters
Chapter 1: The Selection of a Research Approach
Chapter 2: Review of the Literature
For instructors
Select a purchasing option, related products.

Quantitative, Qualitative, Mixed Methods, and Triangulation Research Simplified
- PMID: 38567919
- DOI: 10.3928/00220124-20240328-03
For the novice nurse researcher, identifying a clinical researchable problem may be simple, but discerning an appropriate research approach may be daunting. What are the differences among quantitative, qualitative, mixed methods, and triangulation research? Which method is applicable for the study one wants to conduct? This article discusses the two main research traditions (quantitative and qualitative) and the differences and similarities in methods for front-line nurses. It simplifies and clarifies how the reader might enhance the rigor of the research study by using mixed methods or triangulation. The four types of research are described, and examples are provided to support readers to plan projects, use the most appropriate method, and effectively communicate findings. [ J Contin Educ Nurs. 202x;5x(x):xx-xx.] .

- Kindle Store
- Kindle eBooks
- Education & Teaching
Promotions apply when you purchase
These promotions will be applied to this item:
Some promotions may be combined; others are not eligible to be combined with other offers. For details, please see the Terms & Conditions associated with these promotions.
- Highlight, take notes, and search in the book
- In this edition, page numbers are just like the physical edition
Rent $35.71
Today through selected date:
Rental price is determined by end date.
Buy for others
Buying and sending ebooks to others.
- Select quantity
- Buy and send eBooks
- Recipients can read on any device
These ebooks can only be redeemed by recipients in the US. Redemption links and eBooks cannot be resold.

Download the free Kindle app and start reading Kindle books instantly on your smartphone, tablet, or computer - no Kindle device required .
Read instantly on your browser with Kindle for Web.
Using your mobile phone camera - scan the code below and download the Kindle app.

Image Unavailable

- To view this video download Flash Player
Follow the author

Research Design: Qualitative, Quantitative, and Mixed Methods Approaches 6th Edition, Kindle Edition
- ISBN-13 978-1071817940
- Edition 6th
- Sticky notes On Kindle Scribe
- Publisher SAGE Publications, Inc
- Publication date October 24, 2022
- Language English
- File size 22105 KB
- See all details
- Kindle (5th Generation)
- Kindle Keyboard
- Kindle (2nd Generation)
- Kindle (1st Generation)
- Kindle Paperwhite
- Kindle Paperwhite (5th Generation)
- Kindle Touch
- Kindle Voyage
- Kindle Oasis
- Kindle Scribe (1st Generation)
- Kindle Fire HDX 8.9''
- Kindle Fire HDX
- Kindle Fire HD (3rd Generation)
- Fire HDX 8.9 Tablet
- Fire HD 7 Tablet
- Fire HD 6 Tablet
- Kindle Fire HD 8.9"
- Kindle Fire HD(1st Generation)
- Kindle Fire(2nd Generation)
- Kindle Fire(1st Generation)
- Kindle for Windows 8
- Kindle for Windows Phone
- Kindle for BlackBerry
- Kindle for Android Phones
- Kindle for Android Tablets
- Kindle for iPhone
- Kindle for iPod Touch
- Kindle for iPad
- Kindle for Mac
- Kindle for PC
- Kindle Cloud Reader
Customers who bought this item also bought

Editorial Reviews
About the author.
John W. Creswell, PhD, is a professor of family medicine and senior research scientist at the Michigan Mixed Methods Program at the University of Michigan. He has authored numerous articles and 30 books on mixed methods research, qualitative research, and research design. While at the University of Nebraska-Lincoln, he held the Clifton Endowed Professor Chair, served as Director of the Mixed Methods Research Office, founded SAGE’s Journal of Mixed Methods Research , and was an adjunct professor of family medicine at the University of Michigan and a consultant to the Veterans Administration health services research center in Ann Arbor, Michigan. He was a Senior Fulbright Scholar to South Africa in 2008 and to Thailand in 2012. In 2011, he co-led a National Institute of Health working group on the “best practices of mixed methods research in the health sciences,” and in 2014 served as a visiting professor at Harvard’s School of Public Health. In 2014, he was the founding President of the Mixed Methods International Research Association. In 2015, he joined the staff of Family Medicine at the University of Michigan to Co-Direct the Michigan Mixed Methods Program. In 2016, he received an honorary doctorate from the University of Pretoria, South Africa. In 2017, he co-authored the American Psychological Association “standards” on qualitative and mixed methods research. In 2018 his book on “Qualitative Inquiry and Research Design” (with Cheryl Poth) won the Textbook and Academic Author’s 2018 McGuffey Longevity Award in the United States. He currently makes his home in Ashiya, Japan and Honolulu, Hawaii.
Product details
- ASIN : B0B5HJGW31
- Publisher : SAGE Publications, Inc; 6th edition (October 24, 2022)
- Publication date : October 24, 2022
- Language : English
- File size : 22105 KB
- Text-to-Speech : Enabled
- Screen Reader : Supported
- Enhanced typesetting : Enabled
- X-Ray : Not Enabled
- Word Wise : Enabled
- Sticky notes : On Kindle Scribe
- Print length : 320 pages
- Page numbers source ISBN : 1071817949
- #3 in Social Science Methodology
- #3 in Education Theory Research
- #6 in Social Science Research
About the author
John w. creswell.
John W. Creswell is a Professor of Educational Psychology at Teachers College, University of Nebraska-Lincoln. He is affiliated with a graduate program in educational psychology that specializes in quantitative and qualitative methods in education. In this program, he specializes in qualitative and quantitative research designs and methods, multimethod research, and faculty and academic leadership issues in colleges and universities.
Customer reviews
Customer Reviews, including Product Star Ratings help customers to learn more about the product and decide whether it is the right product for them.
To calculate the overall star rating and percentage breakdown by star, we don’t use a simple average. Instead, our system considers things like how recent a review is and if the reviewer bought the item on Amazon. It also analyzed reviews to verify trustworthiness.
Reviews with images

- Sort reviews by Top reviews Most recent Top reviews
Top reviews from the United States
There was a problem filtering reviews right now. please try again later..
Top reviews from other countries
- Amazon Newsletter
- About Amazon
- Accessibility
- Sustainability
- Press Center
- Investor Relations
- Amazon Devices
- Amazon Science
- Sell on Amazon
- Sell apps on Amazon
- Supply to Amazon
- Protect & Build Your Brand
- Become an Affiliate
- Become a Delivery Driver
- Start a Package Delivery Business
- Advertise Your Products
- Self-Publish with Us
- Become an Amazon Hub Partner
- › See More Ways to Make Money
- Amazon Visa
- Amazon Store Card
- Amazon Secured Card
- Amazon Business Card
- Shop with Points
- Credit Card Marketplace
- Reload Your Balance
- Amazon Currency Converter
- Your Account
- Your Orders
- Shipping Rates & Policies
- Amazon Prime
- Returns & Replacements
- Manage Your Content and Devices
- Recalls and Product Safety Alerts
- Conditions of Use
- Privacy Notice
- Consumer Health Data Privacy Disclosure
- Your Ads Privacy Choices
- Open access
- Published: 11 April 2024
The role of champions in the implementation of technology in healthcare services: a systematic mixed studies review
- Sissel Pettersen 1 ,
- Hilde Eide 2 &
- Anita Berg 1
BMC Health Services Research volume 24 , Article number: 456 ( 2024 ) Cite this article
229 Accesses
Metrics details
Champions play a critical role in implementing technology within healthcare services. While prior studies have explored the presence and characteristics of champions, this review delves into the experiences of healthcare personnel holding champion roles, as well as the experiences of healthcare personnel interacting with them. By synthesizing existing knowledge, this review aims to inform decisions regarding the inclusion of champions as a strategy in technology implementation and guide healthcare personnel in these roles.
A systematic mixed studies review, covering qualitative, quantitative, or mixed designs, was conducted from September 2022 to March 2023. The search spanned Medline, Embase, CINAHL, and Scopus, focusing on studies published from 2012 onwards. The review centered on health personnel serving as champions in technology implementation within healthcare services. Quality assessments utilized the Mixed Methods Appraisal Tool (MMAT).
From 1629 screened studies, 23 were included. The champion role was often examined within the broader context of technology implementation. Limited studies explicitly explored experiences related to the champion role from both champions’ and health personnel’s perspectives. Champions emerged as promoters of technology, supporting its adoption. Success factors included anchoring and selection processes, champions’ expertise, and effective role performance.
The specific tasks and responsibilities assigned to champions differed across reviewed studies, highlighting that the role of champion is a broad one, dependent on the technology being implemented and the site implementing it. Findings indicated a correlation between champion experiences and organizational characteristics. The role’s firm anchoring within the organization is crucial. Limited evidence suggests that volunteering, hiring newly graduated health personnel, and having multiple champions can facilitate technology implementation. Existing studies predominantly focused on client health records and hospitals, emphasizing the need for broader research across healthcare services.
Conclusions
With a clear mandate, dedicated time, and proper training, health personnel in champion roles can significantly contribute professional, technological, and personal competencies to facilitate technology adoption within healthcare services. The review finds that the concept of champions is a broad one and finds varied definitions of the champion role concept. This underscores the importance of describing organizational characteristics, and highlights areas for future research to enhance technology implementation strategies in different healthcare settings with support of a champion.
Peer Review reports
Digital health technologies play a transformative role in healthcare service systems [ 1 , 2 ]. The utilization of technology and digitalization is essential for ensuring patient safety, delivering high quality, cost-effective, and sustainable healthcare services [ 3 , 4 ]. The implementation of technology in healthcare services is a complex process that demands systematic changes in roles, workflows, and service provision [ 5 , 6 ].
The successful implementation of new technologies in healthcare services relies on the adaptability of health professionals [ 7 , 8 , 9 ]. Champions have been identified as a key factor in the successful implementation of technology among health personnel [ 10 , 11 , 12 ]. However, they have rarely been studied as an independent strategy; instead, they are often part of a broader array of strategies in implementation studies (e.g., Hudson [ 13 ], Gullslett and Bergmo [ 14 ]). Prior research has frequently focused on determining the presence or absence of champions [ 10 , 12 , 15 ], as well as investigating the characteristics of individuals assuming the champion role (e.g., George et al. [ 16 ], Shea and Belden [ 17 ]).
Recent reviews on champions [ 18 , 19 , 20 ] have studied their effects on adherence to guidelines, implementation of innovations and facilitation of evidence-based practice. While these reviews suggest that having champions yields positive effects, they underscore the importance for studies that offer detailed insights into the champion’s role concerning specific types of interventions.
There is limited understanding of the practical role requirements and the actual experiences of health personnel in performing the champion role in the context of technology implementation within healthcare services. Further, this knowledge is needed to guide future research on the practical, professional, and relational prerequisites for health personnel in this role and for organizations to successfully employ champions as a strategy in technology implementation processes.
This review seeks to synthesize the existing empirical knowledge concerning the experiences of those in the champion role and the perspectives of health personnel involved in technology implementation processes. The aim is to contribute valuable insights that enhance our understanding of practical role requirements, the execution of the champion role, and best practices in this domain.
The term of champions varies [ 10 , 19 ] and there is a lack of explicit conceptualization of the term ‘champion’ in the implementation literature [ 12 , 18 ]. Various terms for individuals with similar roles also exist in the literature, such as implementation leader, opinion leader, facilitator, change agent, superuser and facilitator. For the purpose of this study, we have adopted the terminology utilized in the recent review by Rigby, Redley and Hutchinson [ 21 ] collectively referring to these roles as ‘champions’. This review aims to explore the experiences of health personnel in their role as champions and the experiences of health personnel interacting with them in the implementation of technology in the healthcare services.
Prior review studies on champions in healthcare services have employed various designs [ 10 , 18 , 19 , 20 ]. In this review, we utilized a comprehensive mixed studies search to identify relevant empirical studies [ 22 ]. The search was conducted utilizing the Preferred Reporting Items for Systematic and Meta-Analysis (PRISMA) guidelines, ensuring a transparent and comprehensive overview that can be replicated or updated by others [ 23 ]. The study protocol is registered in PROSPERO (ID CRD42022335750), providing a more comprehensive description of the methods [ 24 ]. A systematic mixed studies review, examining research using diverse study designs, is well-suited for synthesizing existing knowledge and identifying gaps by harnessing the strengths of both qualitative and quantitative methods [ 22 ]. Our search encompassed qualitative, quantitative, and mixed methods design to capture experiences with the role of champions in technology implementation.
Search strategy and study selection
Search strategy.
The first author, in collaboration with a librarian, developed the search strategy based on initial searches to identify appropriate terms and truncations that align with the eligibility criteria. The search was constructed utilizing a combination of MeSH terms and keywords related to technology, implementation, champion, and attitudes/experiences. Conducted in August/September 2022, the search encompassed four databases: Medline, Embase, CINAHL, and Scopus, with an updated search conducted in March 2023. The full search strategy for Medline is provided in Appendix 1 . The searches in Embase, CINAHL and Scopus employed the same strategy, with adopted terms and phrases to meet the requirements of each respective database.
Eligibility criteria
We included all empirical studies employing qualitative, quantitative, and mixed methods designs that detailed the experiences and/or attitudes of health personnel regarding the champions role in the implementation of technology in healthcare services. Articles in the English language published between 2012 and 2023 were considered. The selected studies involved technology implemented or adapted within healthcare services.
Conference abstract and review articles were excluded from consideration. Articles published prior 2012 were excluded as a result of the rapid development of technology, which could impact the experiences reported. Furthermore, articles involving surgical technology and pre-implementation studies were also excluded, as the focus was on capturing experiences and attitudes from the adoption and daily use of technology. The study also excluded articles that involved champions without clinical health care positions.
Study selection
A total of 1629 studies were identified and downloaded from the selected databases, with Covidence [ 25 ] utilized as a software platform for screening. After removing 624 duplicate records, all team members collaborated to calibrate the screening process utilizing the eligibility criteria on the initial 50 studies. Subsequently, the remaining abstracts were independently screened by two researchers, blinded to each other, to ensure adherence to the eligibility criteria. Studies were included if the title and abstract included the term champion or its synonyms, along with technology in healthcare services, implementation, and health personnel’s experiences or attitudes. Any discrepancies were resolved through consensus among all team members. A total of 949 abstracts were excluded for not meeting this inclusion condition. During the initial search, 56 remaining studies underwent full-text screening, resulting in identification of 22 studies qualified for review.
In the updated search covering the period September 2022 to March 2023, 64 new studies were identified. Of these, 18 studies underwent full-text screening, and one study was included in our review. The total number of included studies is 23. The PRISMA flowchart (Fig. 1 ) illustrates the process.
Flow Chart illustrating the study selection and screening process
Data extraction
The research team developed an extraction form for the included studies utilizing an Excel spreadsheet. Following data extraction, the information included the Name of Author(s) Year of publication, Country/countries, Title of the article, Setting, Aim, Design, Participants, and Sample size of the studies, Technology utilized in healthcare services, name/title utilized to describe the Champion Role, how the studies were analyzed and details of Attitude/Experience with the role of champion. Data extraction was conducted by SP, and the results were deliberated in a workshop with the other researchers AB, and HE until a consensus was reached. Any discrepancies were resolved through discussions. The data extraction was categorized into three categories: qualitative, quantitative, and mixed methods, in preparation for quality appraisal.
Quality appraisal
The MMAT [ 26 ] was employed to assess the quality of the 23 included studies. Specifically designed for mixed studies reviews, the MMAT allows for the appraisal of the methodological quality of studies falling into five categories. The studies in our review encompassed qualitative, quantitative descriptive, and mixed methods studies. The MMAT begins with two screening questions to confirm the empirical nature of this study. Subsequently, all studies were categorized by type and evaluated utilizing specific criteria based on their research methods, with ratings of ‘Yes,’ ‘No’ or ‘Can’t tell.’ The MMAT discourages overall scores in favor of providing a detailed explanation for each criterion. Consequently, we did not rely on the MMAT’s overall methodical quality scores and continued to include all 23 studies for our review. Two researchers independently scored the studies, and any discrepancies were discussed among all team members until a consensus was reached. The results of the MMAT assessments are provided in Appendix 2 .
Data synthesis
Based on discussions of this material, additional tables were formulated to present a comprehensive overview of the study characteristics categorized by study design, study settings, technology included, and descriptions/characteristics of the champion role. To capture attitudes and experiences associated with the champion role, the findings from the included studies were translated into narrative texts [ 22 ]. Subsequently, the reviewers worked collaboratively to conduct a thematic analysis, drawing inspiration from Braun and Clarke [ 27 ]. Throughout the synthesis process, multiple meetings were conducted to discern and define the emerging themes and subthemes.
The adopting of new technology in healthcare services can be perceived as both an event and a process. According to Iqbal [ 28 ], experience is defined as the knowledge and understanding gained after an event or the process of living through or undergoing an event. This review synthesizes existing empirical knowledge regarding the experiences of occupying the champion role, and the perspectives of health personnel interacting with champions in technology implementation processes.
Study characteristics
The review encompassed a total of 23 studies, and an overview of these studies is presented in Table 1 . Of these, fourteen studies employed a qualitative design, four had quantitative design, and five utilized a mixed method design. The geographical distribution revealed that the majority of studies were conducted in the USA (8), followed by Australia (5), England (4), Canada (2), Norway (2), Ireland (1), and Malaysia (1). In terms of settings, 11 studies were conducted in hospitals, five in primary health care, three in home-based care settings, and four in a mixed settings where two or more settings collaborated. Various technologies were employed across these studies, with client health records (7) and telemedicine (5) being the most frequently utilized. All studies included experiences from champions or health personnel collaborating with champions in their respective healthcare services. Only three studies had the champion role as a main objective [ 29 , 30 , 31 ]. The remaining studies described champions as one of the strategies in technology implementation processes, including 10 evaluation studies (including feasibility studies [ 32 , 33 , 34 ] and one cost-benefit study [ 30 ]).
Several studies underscored the importance of champions for successful implementation [ 29 , 30 , 31 , 34 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 49 ]. Four studies specifically highlighted champions as a key factor for success [ 34 , 36 , 37 , 43 ], and one study went further to describe champions as the most important factor for successful implementation [ 39 ]. Additionally, one study associated champions with reduced labor cost [ 30 ].
Thin descriptions, yet clear expectations for technology champions’ role and -attributes
The analyses revealed that the concept of champions in studies pertaining to technology implementation in healthcare services varies, primarily as a result of the diversity of terms utilized to describe the role combined with short role descriptions. Nevertheless, the studies indicated clear expectations for the champion’s role and associated attributes.
The term champion
The term champion was expressed in 20 different forms across the 23 studies included in our review. Three studies utilized multiple terms within the same study [ 32 , 47 , 48 ] and 15 different authors [ 29 , 32 , 33 , 35 , 36 , 37 , 39 , 40 , 41 , 42 , 43 , 44 , 46 , 47 , 50 ] employed the term with different compositions (Table 1 ). Furthermore, four authors utilized the term Super user [ 30 , 31 , 49 , 51 ], while four authors employed the terms Facilitator [ 38 ], IT clinician [ 48 ], Leader [ 45 ], and Manager [ 34 ], each in combination with more specific terms (such as local opinion leaders, IT nurse, or practice manager).
Most studies associated champion roles with specific professions. In seven studies, the professional title was explicitly linked to the concept of champions, such as physician champions or clinical nurse champions, or through the strategic selection of specific professions [ 29 , 33 , 36 , 40 , 43 , 47 , 50 ]. Additionally, some studies did not specify professions, but utilized terms like clinicians [ 45 ] or health professionals [ 41 ].
All included articles portray the champion’s role as facilitating implementation and daily use of technology among staff. In four studies, the champion’s role was not elaborated beyond indicating that the individual holding the role is confident with an interest in technology [ 35 , 41 , 42 , 44 ]. The champion’s role was explicitly examined in six studies [ 29 , 30 , 31 , 33 , 46 , 50 ]. Furthermore, seven studies described the champion in both the methods and results [ 32 , 36 , 38 , 47 , 48 , 49 , 51 ]. In ten of the studies, champions were solely mentioned in the results [ 34 , 35 , 37 , 39 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ].
Eight studies provided a specific description or definition of the champion [ 29 , 30 , 31 , 32 , 38 , 48 , 49 , 50 ]. The champion’s role was described as involving training in the specific technology, being an expert on the technology, providing support and assisting peers when needed. In some instance, the champion had a role in leading the implementation [ 50 ], while in other situations, the champion operated as a mediator [ 48 ].
The champions tasks
In the included studies, the champion role encompassed two interrelated facilitators tasks: promoting the technology and supporting others in adopting the technology in their daily practice. Promoting the technology involved encouraging staff adaptation [ 32 , 34 , 35 , 37 , 40 , 41 , 49 ], generally described as being enthusiastic about the technology [ 32 , 35 , 37 , 41 , 48 ], influencing the attitudes and beliefs of colleagues [ 42 , 45 ] and legitimizing the introduction of the technology [ 42 , 46 , 48 ]. Supporting others in technology adaption involved training and teaching [ 31 , 35 , 38 , 40 , 51 ], as well as providing technical support [ 30 , 31 , 39 , 43 , 49 ] and social support [ 49 ]. Only four studies reported that the champions received their own training to enable them able to support their colleagues [ 30 , 31 , 39 , 48 ]. Furthermore, eight studies [ 32 , 34 , 38 , 40 , 48 , 49 , 50 , 51 ], specified that the champion role included leadership and management responsibilities, mentioning tasks such as planning, organizing, coordinating, and mediating technology adaption without providing further details.
Desirable champion attributes
To effectively fulfill their role, champions should ideally possess clinical expertise and experience [ 29 , 35 , 38 , 40 , 48 ], stay professionally updated [ 37 , 48 ], and possess knowledge of the organization and workflows [ 29 , 34 , 46 ]. They should have the ability to understand and communicate effectively with healthcare personnel [ 31 , 32 , 46 , 49 ] and be proficient in IT language [ 51 ]. Moreover, champions should demonstrate a general technological interest and competence, and competence, along with specific knowledge of the technology to be implemented [ 32 , 37 , 49 ]. It is also emphasized that they should command formal and/or informal respect and authority in the organization [ 36 , 45 ], be accessible to others [ 39 , 43 ], possess leadership qualities [ 34 , 37 , 38 , 46 ], and understand and balance the needs of stakeholders [ 43 ]. Lastly, the champions should be enthusiastic promoters of the technology, engaging and supporting others [ 31 , 32 , 33 , 34 , 37 , 39 , 40 , 41 , 43 , 49 ], while also effectively coping with cultural resistance to change [ 31 , 46 ].
Anchoring and recruiting for the champion role
The champions were organized differently within services, holding various positions in the organizations, and being recruited for the role in different ways.
Anchoring the champion role
The champion’s role is primarily anchored at two levels: the management level and/or the clinical level, with two studies having champions at both levels [ 34 , 49 ]. Those working with the management actively participated in the planning of the technology implementation [ 29 , 36 , 40 , 41 , 45 ]. Serving as advisors to management, they leveraged their clinical knowledge to guide the implementation in alignment with the necessities and possibilities of daily work routines in the clinics. Champions in this capacity experienced having a clear formal position that enabled them to fulfil their role effectively [ 29 , 40 ]. Moreover, these champions served as bridge builders between the management and department levels [ 36 , 45 ], ensuring the necessary flow of information in both directions.
Champions anchored at the clinic level played a pivotal role in the practical implementation and facilitation of the daily use of technology [ 31 , 33 , 35 , 37 , 38 , 43 , 48 , 51 ]. Additionally, these champions actively participated in meetings with senior management to discuss the technology and its implementation in the clinic. This position conferred potential influence over health personnel [ 33 , 35 ]. Champions at the clinic level facilitated collaboration between employees, management, and suppliers [ 48 ]. Fontaine et al. [ 36 ] identified respected champions at the clinical level, possessing authority and formal support from all leadership levels, as the most important factor for success.
Only one study reported that the champions received additional compensation for their role [ 36 ], while another study mentioned champions having dedicated time to fulfil their role [ 46 ]. The remaining studies did not provide this information.
Recruiting for the role as champion
Several studies have reported different experiences regarding the management’s selection of champions. A study highlighted the distinctions between a volunteered role and an appointed champion’s role [ 31 ]. Some studies underscored that appointed champions were chosen based on technological expertise and skills [ 41 , 48 , 51 ]. Moreover, the selection criteria included champions’ interest in the specific technology [ 42 ] or experiential skills [ 40 ]. The remaining studies did not provide this information.
While the champion role was most frequently held by health personnel with clinical experience, one study deviated by hiring 150 newly qualified nurses as champions [ 30 ] for a large-scale implementation of an Electronic Health Record (EHR). Opting for clinical novices assisted in reducing implementation costs, as it avoided disrupting daily tasks and interfering with daily operations. According to Bullard [ 30 ], these super-user nurses became highly sought after post-implementation as a result of their technological confidence and competence.
Reported experiences of champions and health personnel
Drawing from the experiences of both champions and health personnel, it is essential for a champion to possess a combination of general knowledge and specific champion characteristics. Furthermore, champions are required to collaborate with individuals both within and outside the organization. The subsequent paragraphs delineate these experiences, categorizing them into four subsets: champions’ contextual knowledge and expertise, preferred performance of the champion role, recognizing that a champion alone is insufficient, and distinguishing between reactive and proactive champions.
Champions’ contextual knowledge and know-how
Health personnel with experience interacting with champions emphasized that a champion must be familiar with the department and its daily work routines [ 35 , 40 ]. Knowledge of the department’s daily routines made it easier for champions to facilitate the adaptation of technology. However, there was a divergence of opinions on whether champions were required to possess extensive clinical experience to fulfil their role. In most studies, having an experienced and competent clinician as a champion instilled a sense of confidence among health personnel. Conversely, Bullard’s study [ 30 ] exhibited that health personnel were satisfied with newly qualified nurses in the role of champion, despite their initial skepticism.
It is a generally expected that champions should possess technological knowledge beyond that of other health professionals [ 37 , 41 ]. Some health personnel perceived the champions as uncritical promoters of technology, with the impression that health personnel were being compelled to utilize technology [ 46 ]. Champions could also overestimate the readiness of health personnel to implement a technology, especially during the early phases of the implementation process [ 32 ]. Regardless of whether the champion is at the management level or the clinic level, champions themselves have acknowledged the importance of providing time and space for innovation. Moreover, the recruitment of champions should span all levels of the organization [ 34 , 46 ]. Furthermore, champions must be familiar with daily work routines, work tools, and work surfaces [ 38 , 40 , 43 ].
Preferable performance of the champion role
The studies identified several preferable characteristics of successful champions. Health personnel favored champions utilizing positive words when discussing technology and exhibiting positive attitudes while facilitating and adapting it [ 33 , 34 , 37 , 38 , 41 , 46 ]. Additionally, champions who were enthusiastic and engaging were considered good role models for the adoption of technology. Successful champions were perceived as knowledgeable and adept problem solvers who motivated and supported health personnel [ 41 , 43 , 44 , 48 ]. They were also valued for being available and responding promptly when contacted [ 42 ]. Health professionals noted that champions perceived as competent garnered respect in the organization [ 40 ]. Moreover, some health personnel felt that some certain champions wielded a greater influence based on how they encouraged the use of the system [ 48 ]. It was also emphasized that health personnel needed to feel it was safe to provide feedback to champions, especially when encountering difficulties or uncertainties [ 49 ].
A champion is not enough
The role of champions proved to be more demanding than expected [ 29 , 31 , 38 ], involving tasks such as handling an overwhelming number of questions or actively participating in the installation process to ensure the technology functions effectively in the department [ 29 ]. Regardless of the organizational characteristics or the champion’s profile, appointing the champion as a “solo implementation agent” is deemed unsuitable. If the organization begins with one champion, it is recommended that this individual promptly recruits others into the role [ 42 ].
Health personnel, reliant on champions’ expertise, found it beneficial to have champions in all departments, and these champions had to be actively engaged in day-to-day operations [ 31 , 33 , 34 , 37 ]. Champions themselves also noted that health personnel increased their technological expertise through their role as champions in the department [ 39 ].
Furthermore, the successful implementation of technology requires the collaboration of various professions and support functions, a task that cannot be solely addressed by a champion [ 29 , 43 , 48 ]. In Orchard et. al.‘s study [ 34 ], champions explicitly emphasized the necessity of support from other personnel in the organization, such as those responsible for the technical aspects and archiving routines, to provide essential assistance.
According to health personnel, the role of champions is vulnerable in case they become sick or leave their position [ 42 , 51 ]. In some of the included studies, only one or a few hold the position of champion [ 37 , 38 , 42 , 48 ]. Two studies observed that their implementations were not completed because champions left or reassigned for various reasons [ 32 , 51 ]. The health professionals in the study by Owens and Charles [ 32 ] expressed that champions must be replaced in such cases. Further, the study of Olsen et al., 2021 [ 42 ] highlights the need for quicky building a champion network within the organization.
Reactive and proactive champions
Health personnel and champions alike noted that champions played both a reactive and proactive role. The proactive role entailed facilitating measures such as training and coordination [ 31 , 32 , 33 , 34 , 37 , 39 , 40 , 41 , 43 , 48 , 49 ] as initiatives to generate enthusiasm for the technology [ 31 , 32 , 33 , 34 , 35 , 37 , 39 , 40 , 41 , 43 , 49 ]. On the other hand, the reactive role entailed hands-on support and troubleshooting [ 30 , 31 , 39 , 43 , 49 ].
In a study presenting experiences from both health personnel and champions, Yuan et al. [ 31 ] found that personnel observed differences in the assistance provided by appointed and self-chosen champions. Appointed champions demonstrated the technology, answered questions from health personnel, but quickly lost patience and track of employees who had received training [ 31 ]. Health personnel perceived that self-chosen champions were proactive and well-prepared to facilitate the utilization of technology, communicating with the staff as a group and being more competent in utilizing the technology in daily practice [ 31 ]. Health personnel also noted that volunteer champions were supportive, positive, and proactive in promoting the technology, whereas appointed champions acted on request and had a more reactive approach [ 31 ].
This review underscores the breadth of the concept of champion and the significant variation in the champion’s role in implementation of technology in healthcare services. This finding supports the results from previous reviews [ 10 , 18 , 19 , 20 ]. The majority of studies meeting our inclusion criteria did not specifically focus on the experiences of champions and health personnel regarding the champion role, with the exception of studies by Bullard [ 30 ], Gui et al. [ 29 ], Helmer-Smith et al. [ 33 ], Hogan-Murphy et al. [ 46 ], Rea et al. [ 50 ], and Yuan et al. [ 31 ].
The 23 studies encompassed in this review utilized 20 different terms for the champion role. In most studies, the champion’s role was briefly described in terms of the duties it entailed or should entail. This may be linked to the fact that the role of champions was not the primary focus of the study, but rather one of the strategies in the implementation process being investigated. This result reinforces the conclusions drawn by Miech et al. [ 10 ] and Shea et al. [ 12 ] regarding the lack of united understandings of the concept. Furthermore, in Santos et al.‘s [ 19 ] review, champions were only operationalized through presence or absence in 71.4% of the included studies. However, our review finds that there is a consistent and shared understanding that champions should promote and support technology implementation.
Several studies advocate for champions as an effective and recommended strategy for implementing technology [ 30 , 31 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 42 , 43 , 45 , 46 ]. However, we identified that few studies exclusively explore health personnel`s experiences within the champion role when implementing technology in healthcare services.
This suggests a general lack of information essential for understanding the pros, cons, and prerequisites for champions as a strategy within this field of knowledge. However, this review identifies, on a general basis, the types of support and structures required for champions to perform their role successfully from the perspectives of health personnel, contributing to Shea’s conceptual model [ 12 ].
Regarding the organization of the role, this review identified champions holding both formal appointed and informal roles, working in management or clinical settings, being recruited for their clinical and/or technological expertise, and either volunteering or being hired with specific benefits for the role. Regardless of these variations, anchoring the role is crucial for both the individuals holding the champion role and the health personnel interacting with them. Anchoring, in this context, is associated with the clarity of the role’s content and a match between role expectations and opportunities for fulfilment. Furthermore, the role should be valued by the management, preferably through dedicated time and/or salary support [ 34 , 36 , 46 ]. Additionally, our findings indicate that relying on a “solo champion” is vulnerable to issues such as illness, turnover, excessive workload, and individual champion performance [ 32 , 37 ]. Based on these insights, it appears preferable to appoint multiple champions, with roles at both management and clinical levels [ 33 ].
Some studies have explored the selection of champions and its impact on role performance, revealing diverse experiences [ 30 , 31 ]. Notably, Bullard [ 30 ], stands out for emphasizing long clinical experience, and hiring newly trained nurses as superusers to facilitate the use of electronic health records. Despite facing initial reluctance, these newly trained nurses gradually succeeded in their roles. This underscores the importance of considering contextual factors in the champion selection [ 30 , 52 ]. In Bullard’s study [ 30 ], the collaboration between newly trained nurses as digital natives and clinical experienced health personnel proved beneficial, highlighting the need to align champion selection with the organization’s needs based on personal characteristics. This finding aligns with Melkas et al.‘s [ 9 ] argument that implementing technology requires a deeper understanding of users, access to contextual know-how, and health personnel’s tacit knowledge.
To meet role expectations and effectively leverage their professional and technological expertise, champions should embody personal qualities such as the ability to engage others, take a leadership role, be accessible, supportive, and communicate clearly. These qualities align with the key attributes for change in healthcare champions described by Bonawitz et al. [ 15 ]. These attributes include influence, ownership, physical presence, persuasiveness, grit, and a participative leadership style (p.5). These findings suggest that the active performance of the role, beyond mere presence, is crucial for champions to be a successful strategy in technology implementation. Moreover, the recruitment process is not inconsequential. Identifying the right person for the role and providing them with adequate training, organizational support, and dedicated time to fulfill their responsibilities emerge as an important factor based on the insights from champions and health personnel.
Strengths and limitations
While this study benefits from identifying various terms associated with the role of champions, it acknowledges the possibility of missing some studies as a result of diverse descriptions of the role. Nonetheless, a notable strength of the study lies in its specific focus on the health personnel’s experiences in holding the champion role and the broader experiences of health personnel concerning champions in technology implementation within healthcare services. This approach contributes valuable insights into the characteristics of experiences and attitudes toward the role of champions in implementing technology. Lastly, the study emphasizes the relationship between the experiences with the champion role and the organizational setting’s characteristics.
The champion role was frequently inadequately defined [ 30 , 33 , 34 , 35 , 36 , 37 , 39 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 51 ], aligning with previous reviews [ 17 , 19 , 21 ]. As indicated by van Laere and Aggestam [ 52 ], this lack of clarity complicates the identification and comparison of champions across studies. Studies that lacking a distinct definition of the champion’s role were consequently excluded. Only studies written in English were included, introducing the possibility of overlooking relevant studies based on our chosen terms for identifying the champion’s role. Most of the included studies focused on technology implementation in a general context, with champions being just one of several measures. This approach resulted in scant descriptions, as champions were often discussed in the results, discussion, or implications sections rather than being the central focus of the research.
As highlighted by Hall et al. [ 18 ]., methodological issues and inadequate reporting in studies of the champion role create challenges for conducting high-quality reviews, introducing uncertainty around the findings. We have adopted a similar approach to Santos et al. [ 19 ], including all studies even when some issues were identified during the quality assessment. Our review shares the same limitations as previous review by Santos et al. [ 19 ] on the champion role.
Practical implications, policy, and future research
The findings emphasize the significance of the relationship between experiences with the champion role and characteristics of organizational settings as crucial factors for success in the champion role. Clear anchoring of the role within the organization is vital and may impact routines, workflows, staffing, and budgets. Despite limited evidence on the experience of the champion’s role, volunteering, hiring newly graduated health personnel, and appointing more than one champion are identified as facilitators of technology implementation. This study underscores the need for future empirical research including clear descriptions of the champion roles, details on study settings and the technologies to be adopted. This will enable the determination of outcomes and success factors in holding champions in technology implementation processes, transferability of knowledge between contexts and technologies as well as enhance the comparability of studies. Furthermore, there is a need for studies to explore experiences with the champion role, preferably from the perspective of multiple stakeholders, as well as focus on the champion role within various healthcare settings.
This study emphasizes that champions can hold significant positions when provided with a clear mandate, dedicated time, and training, contributing their professional, technological, and personal competencies to expedite technology adoption within services. It appears to be an advantage if the health personnel volunteer or apply for the role to facilitate engaged and proactive champions. The implementation of technology in healthcare services demands efforts from the entire service, and the experiences highlighted in this review exhibits that champions can play an important role. Consequently, empirical studies dedicated to the champion role, employing robust designs based current knowledge, are still needed to provide solid understanding of how champions can be a successful initiative when implementing technology in healthcare services.
Data availability
This review relies exclusively on previously published studies. The datasets supporting the conclusions of this article are included within the article and its supplementary files: Description and characteristics of included studies in Table 1 , Study characteristics. The search strategy is provided in Appendix 1 , and the Critical Appraisal Summary of included studies utilizing MMAT is presented in Appendix 2 .
Abbreviations
Electronic Health Record
Implementation Outcomes Framework
Preferred Reporting Items for Systematics and Meta-Analysis
Meskó B, Drobni Z, Bényei É, Gergely B, Győrffy Z. Digital health is a cultural transformation of traditional healthcare. mHealth. 2017;3:38. https://doi.org/10.21037/mhealth.2017.08.07 .
Article PubMed PubMed Central Google Scholar
Pérez Sust P, Solans O, Fajardo JC, Medina Peralta M, Rodenas P, Gabaldà J, et al. Turning the crisis into an opportunity: Digital health strategies deployed during the COVID-19 outbreak. JMIR Public Health Surveill. 2020;6:e19106. https://doi.org/10.2196/19106 .
Alotaibi YK, Federico F. The impact of health information technology on patient safety. Saudi MedJ. 2017;38:117380. https://doi.org/10.15537/smj.2017.12.20631 .
Article Google Scholar
Kuoppamäki S. The application and deployment of welfare technology in Swedish municipal care: a qualitative study of procurement practices among municipal actors. BMC Health Serv Res. 2021;21:918. https://doi.org/10.1186/s12913-021-06944-w .
Kraus S, Schiavone F, Pluzhnikova A, Invernizzi AC. Digital transformation in healthcare: analyzing the current state-of-research. J Bus Res. 2021;123:557–67. https://doi.org/10.1016/j.jbusres.2020.10.030 .
Frennert S. Approaches to welfare technology in municipal eldercare. JTechnolHum. 2020;38:22646. https://doi.org/10.1080/15228835.2020.1747043 .
Konttila J, Siira H, Kyngäs H, Lahtinen M, Elo S, Kääriäinen M, et al. Healthcare professionals’ competence in digitalisation: a systematic review. Clin Nurs. 2019;28:74561. https://doi.org/10.1111/jocn.14710 .
Jacob C, Sanchez-Vazquez A, Ivory C. Social, organizational, and technological factors impacting clinicians’ adoption of mobile health tools: systematic literature review. JMIR mHealth uHealth. 2020;8:e15935. https://doi.org/10.2196/15935 .
Melkas H, Hennala L, Pekkarinen S, Kyrki V. Impacts of robot implementation on care personnel and clients in elderly-care institutions. Int J Med Inf. 2020;134:104041. https://doi.org/10.1016/j.ijmedinf.2019.104041 .
Miech EJ, Rattray NA, Flanagan ME, Damschroder L, Schmid AA, Damush TM. Inside help: an integrative review of champions in healthcare-related implementation. SAGE Open Med. 2018;6. https://doi.org/10.1177/2050312118773261 .
Foong HF, Kyaw BM, Upton Z, Tudor Car L. Facilitators and barriers of using digital technology for the management of diabetic foot ulcers: a qualitative systematic review. Int Wound J. 2020;17:126681. https://doi.org/10.1111/iwj.13396 .
Shea CM. A conceptual model to guide research on the activities and effects of innovation champions. Implement Res Pract. 2021;2. https://doi.org/10.1177/2633489521990443 .
Hudson D. Physician engagement strategies in health information system implementations. Healthc Manage Forum. 2023;36:86–9. https://doi.org/10.1177/08404704221131921 .
Article PubMed Google Scholar
Gullslett MK, Strand Bergmo T. Implementation of E-prescription for multidose dispensed drugs: qualitative study of general practitioners’’ experiences. JMIR HumFactors. 2022;9:e27431. https://doi.org/10.2196/27431 .
Bonawitz K, Wetmore M, Heisler M, Dalton VK, Damschroder LJ, Forman J, et al. Champions in context: which attributes matter for change efforts in healthcare? Implement Sci. 2020;15:62. https://doi.org/10.1186/s13012-020-01024-9 .
George ER, Sabin LL, Elliott PA, Wolff JA, Osani MC, McSwiggan Hong J, et al. Examining health care champions: a mixed-methods study exploring self and peer perspectives of champions. Implement Res Pract. 2022;3. https://doi.org/10.1177/26334895221077880 .
Shea CM, Belden CM. What is the extent of research on the characteristics, behaviors, and impacts of health information technology champions? A scoping review. BMC Med Inf Decis Mak. 2016;16:2. https://doi.org/10.1186/s12911-016-0240-4 .
Hall AM, Flodgren GM, Richmond HL, Welsh S, Thompson JY, Furlong BM, Sherriff A. Champions for improved adherence to guidelines in long-term care homes: a systematic review. Implement Sci Commun. 2021;2(1):85–85. https://doi.org/10.1186/s43058-021-00185-y .
Santos WJ, Graham ID, Lalonde M, Demery Varin M, Squires JE. The effectiveness of champions in implementing innovations in health care: a systematic review. Implement Sci Commun. 2022;3(1):1–80. https://doi.org/10.1186/s43058-022-00315-0 .
Wood K, Giannopoulos V, Louie E, Baillie A, Uribe G, Lee KS, Haber PS, Morley KC. The role of clinical champions in facilitating the use of evidence-based practice in drug and alcohol and mental health settings: a systematic review. Implement Res Pract. 2020;1:2633489520959072–2633489520959072. https://doi.org/10.1177/2633489520959072 .
Rigby K, Redley B, Hutchinson AM. Change agent’s role in facilitating use of technology in residential aged care: a systematic review. Int J Med Informatics. 2023;105216. https://doi.org/10.1016/j.ijmedinf.2023.105216 .
Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health. 2014;35:29–45. https://doi.org/10.1146/annurev-publhealth-032013-182440 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71 .
Pettersen S, Berg A, Eide H. Experiences and attitudes to the role of champions in implementation of technology in health services. A systematic review. PROSPERO. 2022. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022335750 . Accessed [15 Feb 2023].
Covidence. Better Syst Rev Manag. https://www.covidence.org/ . 2023;26.
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34:285–91. https://doi.org/10.3233/EFI-180221 .
Braun V, Clarke V. Thematic analysis: a practical guide. 1st ed. SAGE; 2022.
Iqbal MP, Manias E, Mimmo L, Mears S, Jack B, Hay L, Harrison R. Clinicians’ experience of providing care: a rapid review. BMC Health Serv Res. 2020;20:1–10. https://doi.org/10.1186/s12913-020-05812-3 .
Gui X, Chen Y, Zhou X, Reynolds TL, Zheng K, Hanauer DA. Physician champions’ perspectives and practices on electronic health records implementation: challenges and strategies. JAMIA open. 2020;3:5361. https://doi.org/10.1093/jamiaopen/ooz051 .
Bullard KL. Cost effective staffing for an EHR implementation. Nurs Econ. 2016;34:726.
Google Scholar
Yuan CT, Bradley EH, Nembhard IM. A mixed methods study of how clinician ‘super users’ influence others during the implementation of electronic health records. BMC Med Inf Decis Mak. 2015;15:26. https://doi.org/10.1186/s12911-015-0154-6 .
Owens C, Charles N. Implementation of a text-messaging intervention for adolescents who self-harm (TeenTEXT): a feasibility study using normalisation process theory. Child Adolesc Psychiatry Ment Health. 2016;10:14. https://doi.org/10.1186/s13034-016-0101-z .
Helmer-Smith M, Fung C, Afkham A, Crowe L, Gazarin M, Keely E, et al. The feasibility of using electronic consultation in long-term care homes. JAm Med Dir Assoc. 2020;21:11661170e2. https://doi.org/10.1016/j.jamda.2020.03.003 .
Orchard J, Lowres N, Freedman SB, Ladak L, Lee W, Zwar N, et al. Screening for atrial fibrillation during influenza vaccinations by primary care nurses using a smartphone electrocardiograph (iECG): a feasibility study. Eur J Prev Cardiol. 2016;23:13–20. https://doi.org/10.1177/2047487316670255 .
Bee P, Lovell K, Airnes Z, Pruszynska A. Embedding telephone therapy in statutory mental health services: a qualitative, theory-driven analysis. BMC Psychiatry. 2016;16:56. https://doi.org/10.1186/s12888-016-0761-5 .
Fontaine P, Whitebird R, Solberg LI, Tillema J, Smithson A, Crabtree BF. Minnesota’s early experience with medical home implementation: viewpoints from the front lines. J Gen Intern Med. 2015;30(7):899–906. https://doi.org/10.1007/s11606-014-3136-y .
Kolltveit B-CH, Gjengedal E, Graue M, Iversen MM, Thorne S, Kirkevold M. Conditions for success in introducing telemedicine in diabetes foot care: a qualitative inquiry. BMC Nurs. 2017;16:2. https://doi.org/10.1186/s12912-017-0201-y .
Salbach NM, McDonald A, MacKay-Lyons M, Bulmer B, Howe JA, Bayley MT, et al. Experiences of physical therapists and professional leaders with implementing a toolkit to advance walking assessment poststroke: a realist evaluation. Phys Ther. 2021;101:1–11. https://doi.org/10.1093/ptj/pzab232 .
Schwarz M, Coccetti A, Draheim M, Gordon G. Perceptions of allied health staff of the implementation of an integrated electronic medical record across regional and metropolitan settings. Aust Health Rev. 2020;44:965–72. https://doi.org/10.1071/AH19024 .
Stewart J, McCorry N, Reid H, Hart N, Kee F. Implementation of remote asthma consulting in general practice in response to the COVID-19 pandemic: an evaluation using extended normalisation process theory. BJGP Open. 2022;6:1–10. https://doi.org/10.3399/BJGPO.2021.0189 .
Bennett-Levy J, Singer J, DuBois S, Hyde K. Translating mental health into practice: what are the barriers and enablers to e-mental health implementation by aboriginal and Torres Strait Islander health professionals? JMed. Internet Res. 2017;19:e1. https://doi.org/10.2196/jmir.6269 .
Olsen J, Peterson S, Stevens A. Implementing electronic health record-based National Diabetes Prevention Program referrals in a rural county. Public Health Nurs (Boston Mass). 2021;38(3):464–9. https://doi.org/10.1111/phn.12860 .
Yang L, Brown-Johnson CG, Miller-Kuhlmann R, Kling SMR, Saliba-Gustafsson EA, Shaw JG, et al. Accelerated launch of video visits in ambulatory neurology during COVID-19: key lessons from the Stanford experience. Neurology. 2020;95:305–11. https://doi.org/10.1212/WNL.0000000000010015 .
Article CAS PubMed Google Scholar
Buckingham SA, Sein K, Anil K, Demain S, Gunn H, Jones RB, et al. Telerehabilitation for physical disabilities and movement impairment: a service evaluation in South West England. JEval Clin Pract. 2022;28:108495. https://doi.org/10.1111/jep.13689 .
Chung OS, Robinson T, Johnson AM, Dowling NL, Ng CH, Yücel M, et al. Implementation of therapeutic virtual reality into psychiatric care: clinicians’ and service managers’’ perspectives. Front Psychiatry. 2022;12:791123. https://doi.org/10.3389/fpsyt.2021.791123 .
Hogan-Murphy D, Stewart D, Tonna A, Strath A, Cunningham S. Use of normalization process theory to explore key stakeholders’ perceptions of the facilitators and barriers to implementing electronic systems for medicines management in hospital settings. Res SocialAdm Pharm. 2021;17:398405. https://doi.org/10.1016/j.sapharm.2020.03.005 .
Moss SR, Martinez KA, Nathan C, Pfoh ER, Rothberg MB. Physicians’ views on utilization of an electronic health record-embedded calculator to assess risk for venous thromboembolism among medical inpatients: a qualitative study. TH Open. 2022;6:e33–9. https://doi.org/10.1055/s-0041-1742227 .
Yusof MM. A case study evaluation of a critical Care Information System adoption using the socio-technical and fit approach. Int J Med Inf. 2015;84:486–99. https://doi.org/10.1016/j.ijmedinf.2015.03.001 .
Dugstad J, Sundling V, Nilsen ER, Eide H. Nursing staff’s evaluation of facilitators and barriers during implementation of wireless nurse call systems in residential care facilities. A cross-sectional study. BMC Health Serv Res. 2020;20:163. https://doi.org/10.1186/s12913-020-4998-9 .
Rea K, Le-Jenkins U, Rutledge C. A technology intervention for nurses engaged in preventing catheter-associated urinary tract infections. Comput Inf Nurs. 2018;36:305–13. https://doi.org/10.1097/CIN.0000000000000429 .
Bail K, Davey R, Currie M, Gibson J, Merrick E, Redley B. Implementation pilot of a novel electronic bedside nursing chart: a mixed-methods case study. Aust Health Rev. 2020;44:672–6. https://doi.org/10.1071/AH18231 .
van Laere J, Aggestam L. Understanding champion behaviour in a health-care information system development project – how multiple champions and champion behaviours build a coherent whole. Eur J Inf Syst. 2016;25:47–63. https://doi.org/10.1057/ejis.2015.5 .
Download references
Acknowledgements
We would like to thank the librarian Malin E. Norman, at Nord university, for her assistance in the development of the search, as well as guidance regarding the scientific databases.
This study is a part of a PhD project undertaken by the first author, SP, and funded by Nord University, Norway. This research did not receive any specific grant from funding agencies in the public, commercial, as well as not-for-profit sectors.
Open access funding provided by Nord University
Author information
Authors and affiliations.
Faculty of Nursing and Health Sciences, Nord university, P.O. Box 474, N-7801, Namsos, Norway
Sissel Pettersen & Anita Berg
Centre for Health and Technology, Faculty of Health Sciences, University of South-Eastern Norway, PO Box 7053, N-3007, Drammen, Norway
You can also search for this author in PubMed Google Scholar
Contributions
The first author/SP has been the project manager and was mainly responsible for all phases of the study. The second and third authors HE and AB have contributed to screening, quality assessment, analysis and discussion of findings. Drafting of the final manuscript has been a collaboration between the first/SP and third athor/AB. The final manuscript has been approved by all authors.
Corresponding author
Correspondence to Sissel Pettersen .
Ethics declarations
Ethics approval and consent to participate.
This review does not involve the processing of personal data, and given the nature of this study, formal consent is not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pettersen, S., Eide, H. & Berg, A. The role of champions in the implementation of technology in healthcare services: a systematic mixed studies review. BMC Health Serv Res 24 , 456 (2024). https://doi.org/10.1186/s12913-024-10867-7
Download citation
Received : 19 June 2023
Accepted : 14 March 2024
Published : 11 April 2024
DOI : https://doi.org/10.1186/s12913-024-10867-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Technology implementation
- Healthcare personnel
- Healthcare services
- Mixed methods
- Organizational characteristics
- Technology adoption
- Role definitions
- Healthcare settings
- Systematic review
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 16 April 2024
‘Enough is enough’: a mixed methods study on the key factors driving UK NHS nurses’ decision to strike
- Daniel Sanfey 1
BMC Nursing volume 23 , Article number: 247 ( 2024 ) Cite this article
61 Accesses
5 Altmetric
Metrics details
The UK National Health Service (NHS) is one of the largest employers in the world and employs around 360,000 registered nurses. Following a protracted pay dispute in December 2022 NHS nurses engaged in industrial action resulting in the largest nurse strikes in the 74-year history of the NHS. Initially it appeared these strikes were a direct consequence of pay disputes but evidence suggests that the situation was more complex. This study aimed to explore what the key factors were in driving UK NHS nurses’ decision to strike.
A convergent parallel mixed methods design was used. The study was conducted throughout the UK and involved participants who were nurses working for the NHS who voted in favour of strike action. Data collection involved the use of an online survey completed by 468 nurses and 13 semi-structured interviews. Descriptive and inferential statistics were used for quantitative data analysis and a process of inductive thematic analysis for the qualitative data. The quantitative and qualitative data were analysed separately and then integrated to generate mixed methods inferences.
The quantitative findings showed that patient safety, followed by staff shortages, pay, and unmanageable work demands were the most important factors encouraging nurses’ decision to strike. The qualitative findings served to further the understanding of these factors particularly in relation to participants’ perception of the NHS and the consequences of inadequate pay and staff shortages. Three overarching and overlapping themes represented the qualitative findings: Save our NHS, Money talks, and It’s untenable. Integration of the findings showed a high level of concordance between the two data sets and suggest that the factors involved are interconnected and inextricably linked.
Conclusions
The UK NHS is a challenging and demanding work environment in which the well-being of its patients is dependent on the well-being of those who care for them. Concerns relating to patient welfare, the nursing profession and the NHS played a large part in driving UK NHS nurses’ decision to strike. In order to address these concerns a focus on recruitment and retention of nurses in the NHS is needed.
Peer Review reports
The United Kingdom National Health Service (NHS) is the seventh largest employer in the world [ 1 ] providing public health services for a population of around 67 million people [ 2 ]. Of the 1.4 million staff working for the NHS approximately a quarter of these are registered nurses [ 3 ]. Nurses are the backbone of the NHS providing hospital and community services and are often patients’ first and last point of contact when accessing care.
Nurses working for the NHS are paid according to a pre agreed pay and grading system decided upon by the UK Government with recommendations from an independent NHS pay review body. Research has shown that when taking inflation into account the average pay of NHS nurses has fallen in real terms by 8% between 2010/11 and 2021/22 [ 4 ], with the figure estimated at closer to 20% for more experienced nurses [ 5 ].
The Royal College of Nurses (RCN) is the largest nursing union in the world and represents around 405,000 registered nurses working in the UK [ 6 ]. Following a protracted pay dispute with the UK government, in October 2022 the RCN balloted its members working for the NHS on whether to take industrial action in the form of strikes. Despite the high threshold for success, with all ballots needing to be conducted by post and a 50% turnout and 40% vote in favour, the ballot was conclusive. NHS nurses voted in favour of strike action in the majority of NHS Trusts throughout the UK. Footnote 1 In December 2022, for the first time in the RCN’s 106-year history their members engaged in strike action. The largest nursing strike in the 74-year history of the NHS.
On the surface it appears clear. NHS nurses were striking to secure better pay. This is supported by the most recent NHS staff survey [ 7 ] which found that only 25.6% of staff were satisfied with their level of pay. However, the staff survey also highlighted a number of other factors that indicate a high level of discontent, portraying the NHS as a stressful, demanding and unsatisfactory work environment. Furthermore, increasing numbers of nurses are leaving the profession due to health reasons, burnout and exhaustion [ 8 ], with additional nurses voicing their intent to leave because of high workload pressures and feeling undervalued [ 9 ]. This leads to the question: what are the key factors that have driven UK NHS nurses’ decision to strike?
Answering this research question is particularly pertinent at this time as the UK NHS is currently experiencing some of the greatest pressures in its history [ 10 ]. Waiting times are at an all-time high and record numbers of patients are waiting for treatment [ 11 ]. Not only are nurses engaging in strike action but also a plethora of other professions within the NHS including doctors, radiologists and physiotherapists; all of which only serves to exacerbate what is widely considered as an NHS in crisis [ 12 ]. At a time of widespread industrial action throughout the UK in which 2022 saw the highest number of working days lost to strikes for more than 30 years [ 13 ], determining the key factors driving UK NHS nurses’ decision to strike may serve to inform those concerned with prolonged and future industrial action, not just within the nursing profession and the NHS, but also the wider UK workforce.
Literature review
A strike has been defined as ‘A temporary stoppage of work by a group of employees in order to express a grievance or enforce a demand’ (p.3) [ 14 ], Hyman [ 15 ] highlights that it is predominantly a calculated act and that the complete stoppage of work and its temporary and collective nature distinguish it from other forms of work-based protest.
Nursing strikes are a global phenomenon with incidences occurring in a diverse range of countries including America, Japan, Kenya, India, Australia and throughout Europe. In the UK nurses have a rich history of protest, but the incidences of strikes within the profession are few and far between. A limited number of empirical studies exist identifying factors that have driven nurses to go on strike. These include quantitative [ 16 , 17 , 18 ], qualitative [ 19 , 20 , 21 ], and mixed methods designs [ 22 , 23 ]. Within these, issues relating to pay and working conditions predominate, but other factors such as intimidation from unions, failures of healthcare systems and addressing public perceptions of nurses were also found. What is notable is that none of these studies focus solely on factors driving nurses’ decision to strike, instead collecting data on a broad range of topics. This diverse approach may explain to some extent why they fail to facilitate a thorough understanding of the key factors driving nurses’ decision to strike. At present, it appears that there are no existing empirical studies focusing on nurse strikes within the UK, signifying a gap in the literature.
In addition to existing empirical studies there is a wide body of literature in the form of retrospective accounts that document and provide theoretical interpretations of individual and country specific nurse strikes [ 24 , 25 , 26 , 27 , 28 , 29 , 30 ]. By depicting the nurse strike within a historical, political, and professional context these accounts help to further illuminate the phenomenon and facilitate a much richer and deeper understanding. With this, we begin to appreciate the nurse strike as distinct from those within industrialised settings and as much a form of advocacy as that of self-preservation.
For any strike there are consequences. Whether they be for employers, workers, service users, the government, or for society at large. Within the healthcare environment there are concerns that a strike may have the additional consequence of compromising patient care. This has led some to denounce strikes by nurses citing them as immoral, unjustifiable [ 31 ] and wholly inappropriate [ 32 ]. Yet, it has been argued that such a stance fails to see the bigger picture and puts too much emphasis on the nurse/patient relationship [ 33 ].
Healthcare provision is a collective endeavour and whilst nurses have a professional responsibility to prioritise patient care and put the safety and wellbeing of those requiring care at the forefront of all they do [ 34 , 35 ]; governments, employers and health policy makers also have a responsibility to facilitate an environment conducive to such an approach [ 36 ]. In situations where this does not happen it can be argued that to not stand up and take appropriate action would in itself be unethical [ 37 ] and antithetical to the standards required. It has therefore been posited that concerns around patient safety and standards of care can now be seen as one of the key driving factors for nurse strikes [ 26 ].
The aim of this study is to explore what the key factors are driving UK NHS nurses’ decision to strike. The findings of this study can be used to inform government, employers, unions and health policy makers concerned with prolonged and future industrial action and stimulate a wider discussion around the demands of contemporary nursing and the challenges of working for the UK NHS.

Study design
A convergent parallel mixed methods design was used for the study to facilitate a detailed inquiry into the research question and enhance the validity of any inferences made. Quantitative and qualitative data were collected concurrently but separately, with equal importance given to each. The two data sets were then analysed independently, after which the results were merged and interpreted [ 38 ]. This approach helped to better understand the statistical trends associated with the nurse strikes whilst gaining a contextual understanding of the motivation and experiences that lay behind them. A summary of the study design can be seen in Fig. 1 . The study is deemed exploratory in nature due to the lack of previous research on the topic within the UK and also to allow a certain amount of creativity and flexibility within the research methods used [ 39 ].
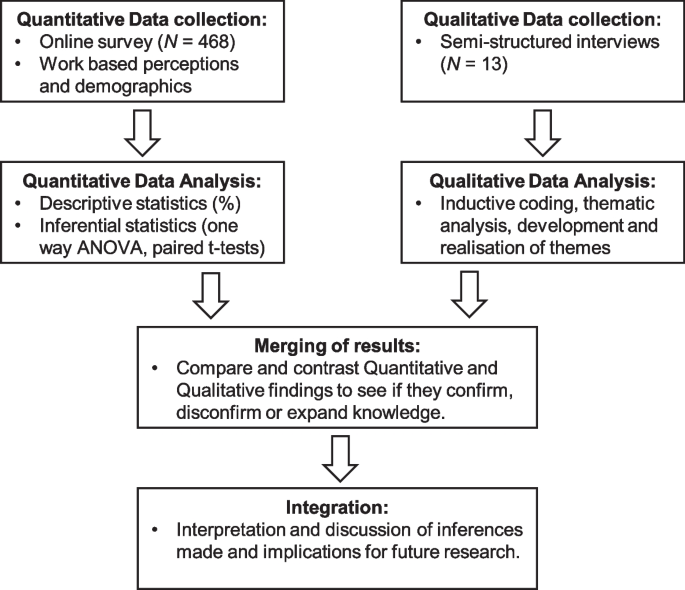
Convergent parallel mixed methods design used for study
Study setting and sampling
The study took place within the United Kingdom across all four nations of England, Wales, Scotland and Northern Ireland. The eligibility criteria included registered nurses working for the UK NHS who were also members of the RCN and voted in favour of strike action in the ballots conducted in October/November 2022 and/or May June 2023.
Participants were recruited for the quantitative methods through a combination of voluntary and convenience sampling. Nurses were notified of the study and invited to participate via the use of online nursing forums related to the RCN, social media sites (including Facebook, Twitter and LinkedIn), networking, and word of mouth. In addition, following approval from the local research and development (R&D) boards the study was advertised within two large NHS trusts in the south of England. This was achieved by distributing flyers and posters amongst the hospital wards. An email notification was also sent by the R&D department in one of the trusts. Further sampling was achieved on the picket lines outside two hospitals in Wales during the strikes in June 2023 with nurses informed of the study in person and provided with a QR code to access a survey.
Over 300,000 nurses were balloted in the first ballot on strike action in October/November 2022 [ 40 ]. The number of ballots completed and the proportion of nurses who voted in favour of strike action were not released and were not provided on request. However, with UK law [ 41 ] requiring a 50% response rate and a minimum of 40% voting ‘yes’ for strike action to happen we can assume that the actual population of nurses voting for strike action was at the very least 60,000 Footnote 2 nurses. A sample size of 384 participants was therefore deemed necessary in order for the sample to be representative. This was calculated using a basic prevalence sample size calculator with a confidence level of 95% and a margin of error at 5% [ 42 ].
Purposive and voluntary sampling was used for the qualitative methods. Potential participants were identified by scanning social media platforms for posts by nurses that implied they were in favour of and passionate about the strikes. Those nurses were then contacted, informed of the study and invited to participate ( n 8). In addition, on hearing of the study a number of nurses came forward and volunteered their participation ( n 5).
Quantitative data collection and analysis
An online cross-sectional survey was designed and administered for the study (Additional file 1 ) and was made available via the digital survey platform Lamapoll [ 43 ]. Data was collected between the 21st April and 1st July 2023 and was analysed using IBM SPSS Statistics software v.29. Prior to data collection the survey was piloted and reviewed by 8 nurses who provided feedback. This resulted in minor adjustments in the wording for a single question and the subsequent removal of a sub-scale which was deemed unclear and lacking relevance.
The survey asked participants to select which factors they felt encouraged their decision to vote for strike action from a predetermined list. The list included seven factors which were compiled to reflect the most relevant points from the literature review, the stance of the RCN, and the current political climate within the UK. Descriptive statistics were used to depict how frequently each of the factors were chosen. In addition, participants were asked to rank those factors in order of importance. Means were calculated and compared. A one-way repeated measures ANOVA test was performed to determine whether the difference between the ranked levels of importance between factors was significant.
A number of the factors (staff shortages, pay and unmanageable work demands) were singled out for further exploration. This was done to try and gain an insight into the motivation lying behind each of those factors; that is, were those nurses more concerned with self-preservation and their own individual well-being ( self-motivation ), or were they more concerned with the well-being of the profession and the patients it cares for ( professional motivation ).
To determine the weighting towards the two constructs of self-motivation and professional motivation a series of Likert items were designed using a 5-point bipolar scale, ranging from strongly disagree to strongly agree . The items were divided into three subscales relating to each of the chosen factors. The three sub-scales combined had good reliability [ 44 , 45 ] for both the Professional motivation construct (Cronbach’s α = .88; 6 items) and the Self-motivation construct (Cronbach’s α = .86; 6 items). Measures of internal consistency for the individual sub-scales can be found in Table 1 . The order of questions within each sub-scale were varied to minimise acquiescent response bias [ 46 ]. The scales were numerically coded into interval data and grouped under their corresponding constructs. Paired t-tests were performed to determine whether the difference between the two constructs was statistically significant for each sub-scale.
Demographic data was obtained to inform what type of nurses participated in the survey and presented in tabular form using descriptive statistics.
Qualitative data collection and analysis
Semi-structured interviews were conducted using an interview guide consisting of a range of questions and probes designed to elicit rich and insightful responses (Additional file 2 ). An additional set of probes were used for responses that complimented the factors listed within the survey so as to facilitate congruence between the data sets (Additional file 3 ). To allow the inclusion of participants from a broad geographical range interviews took place online via the video conferencing platform Zoom. They were conducted between the 23rd May and the 23rd June 2023. Interviews were conducted until it was felt that saturation of data was achieved; meaning, new data appeared to be repeating what was previously collected and thus, it was felt that further data collection was unlikely to add to the findings. The mean length of the interviews was exactly 50 minutes.
Thematic analysis of the data was conducted using the methods outlined by Braun and Clarke [ 47 ] with the help of MAXQDA 2022 data analysis software. These methods involved a 6-phase process. Phase 1 – familiarisation, began by a single researcher conducting the interviews and transcribing them verbatim. This helped to facilitate familiarity with and immersion of the data. An inductive approach was used for phase 2 - generating initial codes, in which coding of the transcripts was guided by the content of the data rather than any preconceived theoretical or epistemological perspectives. This phase generated over 90 interrelated and often overlapping codes which were sorted and organised using a mind map. Organising the codes in this way helped to see the relations between them and formed the beginnings of phase 3 – searching for themes. Initially this phase took on a rather positivist approach that saw the inception of themes based on the prevalence of codes and their semantic level context. However, a more interactive and organic approach developed in phase 4 – reviewing themes, where the initial set of themes were revised to ensure they really represented the coded extracts, as well as the story being told across the entire data set. It is here that the researcher’s subjective interpretation began to play a more influential role. Themes developed not just based on the data within the codes but on how they were perceived and understood by the researcher. This process gained momentum in phase 5 – defining and naming themes where the essence of each theme, how they related to one another and the story that they told was fully realised. Phase 6 – producing the report saw the outcome of this process in which the qualitative results tell a story that reflects the coming together of the experiences, meaning and reality of participants with that of the understanding, values and skills of the researcher.
Mixed methods analysis
Quantitative and qualitative data were integrated at the interpretation and reporting level. The key findings of the quantitative data were presented alongside qualitative data using a joint display table. This approach helped to merge the data in a more direct way and facilitate a better understanding of the mixed methods meta-inferences [ 48 ].
Ethical considerations
Ethical approval was granted by the University of Freiburg’s ethical research committee (Application no. 23–1126-S2). All surveys were completed anonymously and informed consent gained from all participants. Participants who partook in the interviews were provided with a participant information sheet and asked to sign a consent form prior to being interviewed. The interviews were anonymised during transcription with all identifiable data subsequently deleted. All data was held and stored in accordance with the UK Data Protection Act of 2018. Participation was completely voluntary, and no financial incentives made.
Five hundred forty-four nurses responded to the survey. Those that did not fulfil the eligibility criteria or provided an insufficient amount of data were discarded, resulting in 468 completed surveys included in the analysis. Thirteen participants were recruited for the semi-structured interviews. The demographics and work-based characteristics for the quantitative and qualitative samples are displayed in Tables 2 and Table 3 respectively. Female nurses working in hospital settings with adult patients predominated. There was a broad range of experience across the two data sets with the majority of nurses having trained in the UK. Demographics for RCN membership were not available to draw comparisons with; however, the sample is broadly proportional to that of the UK nursing register with regards to age, gender and type of nursing. It is underrepresented by mental health nurses and those who trained outside of the UK [ 49 ].
Quantitative results
The factors that encouraged nurses’ decision to strike are displayed in Fig. 2 . The mode number of factors chosen was 5, in which Staff shortages and Patient safety were the most frequently cited.
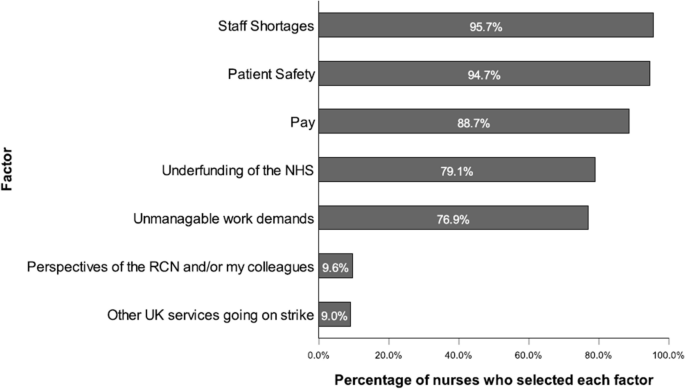
Factors that encouraged participants’ decision to strike. Note . N = 468
Nurses indicated that patient safety, followed by staff shortages were the most important factors that encouraged their decision to strike. The ranked means and standard deviations for the level of importance ascribed to each factor are presented in Table 4 . A one-way repeated measures ANOVA found that the difference between the level of importance for the factors was significant at the .05 alpha level. Wilks’ Lambda = .04, F (6, 462) = 2149.69, p < .001, multivariate partial eta squared = .97. However, post-hoc pairwise comparisons with a Bonferroni adjustment indicate that the difference was not significant between each level of ranking. Those that were significant are highlighted in Table 4 .
Responses to the Likert sub-scales and the level of agreement that nurses had to the individual items are presented in Fig. 3 . The results of the paired t-tests (Table 5 ) indicate that those who cited pay and unmanageable work demands as factors that encouraged their decision to strike were significantly more professionally motivated than self-motivated ( α = .05). However, it should be noted that the effect size, whilst moderate for pay was small for unmanageable work demands. The difference between the level of professional motivation and self-motivation for those who cited staff shortages as a factor that encouraged their decision to strike was not statistically significant.
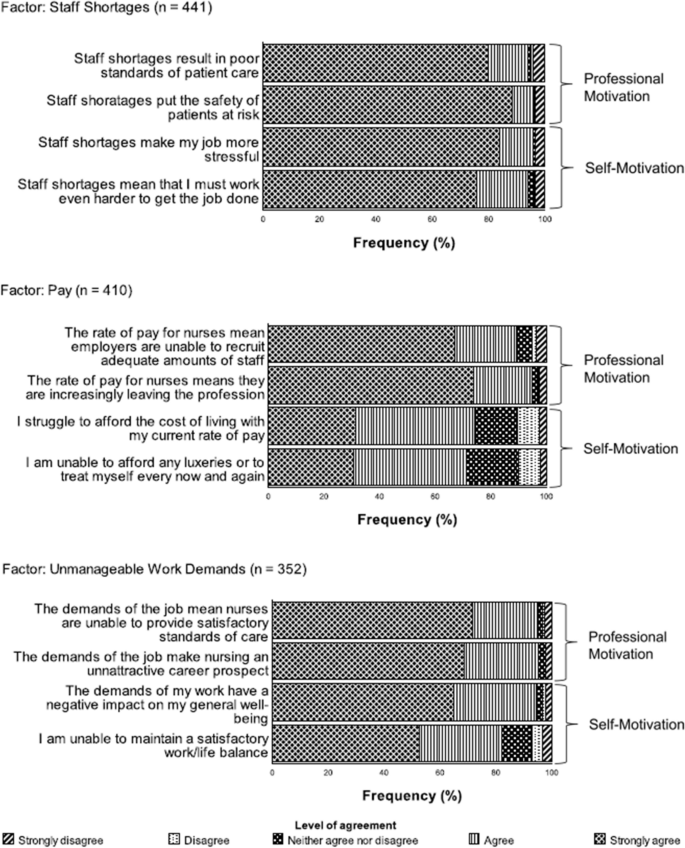
Likert sub-scales showing individual items and their relation to the constructs professional motivation and self-motivation. Note . Order of items presented to facilitate easy understanding of how the items relate to the constructs of Professional Motivation and Self-motivation. The order of items within the survey was different
Qualitative results
The process of thematic analysis identified three overarching and overlapping themes which were selected to represent the data. These themes included: Save our NHS, Money talks, and It’s untenable.
Save our NHS
The state of the NHS was reflected upon throughout the interviews. Participants were passionate about the NHS and its ability to provide high standards of safe and effective care, free at the point of need. However, there was a recognition that the NHS was failing as an institution, the injustice of which was palpable and articulated by the following comment:
I don't understand, genuinely don't understand why people aren't rioting because of the state of the NHS. We are going to lose this incredible thing… It's just, I mean, I feel quite emotional. It’s just shocking. It's just shocking that it's happening. Participant 2
Witnessing the decline of the NHS seemed to elicit a sense of loss and foreboding in participants. One nurse explained how this had evolved into a sense of shame at what it has become.
I was very proud going back years ago to put on a uniform, to enter that building and start my shift. And I was proud to tell people that I worked for the NHS. And I'm not anymore. I'm embarrassed by it. I'm embarrassed by the care that we give. I’m embarrassed by the treatment that some of the patients get. It's heart breaking, it really is. Participant 10.
And yet, these feelings seemed to stem, not from an idealistic view of what the NHS should be or how it should be run, but rather from the lived experience of providing frontline care on a day-to-day basis. This results in a visceral understanding that nurses are not just the providers of care but also the recipients of care, along with their families, loved ones, and the nation as a whole. For example, on reflecting on caring for a dying patient participant 6 acknowledged “That could be me one day.” In addition, whilst talking about the poor standards of care she had witnessed, participant 13 expressed “I’m worried about the care my parents are going to receive, I’m worried about the care I’m going to receive in the future!” Participant 5 spoke about living with a congenital heart condition, needing regular specialist review, extensive surgery and a costly hospital stay. He concluded “I’ve really benefited from the NHS, as an end user and also as an employee. I think it’s a great institution and I think it needs to continue.”
Nurses’ decision to strike could therefore be seen as a call to arms in response to the witnessed decline of the NHS and all that it entailed. The value and appreciation that nurses hold for the NHS comes with a real sense that it is worth fighting for. The decision to strike was seen to play an important part in that fight. Participant 12 highlighted this point in saying:
It really is about the health of all people in the UK and the future of what that's going to look like. And it's not looking good, you know, from where we're at just now. If we don't fight, I believe there's a real possibility we could lose the NHS.
Money talks
It was widely felt throughout the interviews that the rate of pay that nurses receive does not reflect their level of expertise, professional development, and the responsibility that comes with the job. The following nurse discussed this in relation to her own professional development.
If I did my nurse prescribing in a couple of years, which is a possibility, it's not going to get me any more pay. And the level of responsibility that comes with that… We're a very responsible profession, you know, breaking bad news, seeing things that the ordinary general public wouldn't even dream to see… And yet, we're not recognised financially, or with the respect as a profession that we deserve. Participant 11
Participants throughout the interviews felt that the nursing profession was undervalued and underappreciated, especially by the government and thus, their decision to strike was an attempt to highlight this. This sentiment was particularly pertinent in relation to the recent COVID pandemic. Participants reflected upon the sacrifices they made during the pandemic and the discrepancy of being hailed as heroes by the government one day, to receiving yet another below inflation pay rise the next. This served to exacerbate the feeling of being undervalued as highlighted in the following excerpts:
My husband had a heart attack during the pandemic, I couldn't visit him. But I was still going to work. I was in this building. But I couldn't go and see him. There are huge, huge sacrifices made by all of us. Four of my colleagues died, and we're not even worth a real time pay increase! Participant 2.
Yes, let's all stand out on our doorsteps and clap and bang our pans for the wonderful people who are doing a wonderful job. But actually, when you want a decent wage, we're not going to give that to you. Participant 5
The level of pay that nurses receive was therefore perceived as a measure of the value and appreciation ascribed to the profession. In addition, better pay was viewed as a vital tool in incentivising people to become nurses and to work in the NHS. This point was made by Participant 4 who explained:
I don't personally care about the pay. For me at least as an individual… But I do care about pay for my colleagues and the wider NHS, is it 47,000 nursing vacancies? They're not going to get filled with shoddy pay. There needs to be an incentive to be a nurse at the moment.
The pursuit of better pay was a key factor driving nurses’ decision to strike because better pay was seen as integral to addressing the ongoing recruitment and retention crisis of nurses within the NHS.
It’s untenable
The recruitment and retention crisis, and it’s resulting staff shortages was frequently cited by participants as being the root of the problem and fundamental to their decision to strike. Staff shortages result in nurses having to take on an additional workload to meet the needs of patients. As participant 7 explains, “It’s not doable. You’re having to work twice as hard… You’re having to do several people’s jobs.” Participants spoke of how staying late after work and working through their breaks to try and keep on top of the workload was an everyday occurrence. The relentless pressure and responsibility of the job is at times overwhelming and the impact on individual nurses seen as untenable. As participant 13 pointed out.
We're not designed to be in flight mode all the time, are we? And if we don't get respite, then we're in trouble and that's what we're seeing on our work force right now in terms of how people feel, burnout, wanting to leave, going off sick….
This was also reflected upon by participant 10 who spoke about her own experiences of being burnt out from work and how this impacted her.
I ended up being off for three months… I was at the point where I didn’t want to be a nurse anymore, I didn’t want to be in my marriage. I wanted to walk out of my home, my children, my…. I just wanted to pick-up and walk out of my life.
With this we see that the morale of nurses working in an environment that is chronically understaffed is persistently under threat. As participant 1 lamented, “it makes you feel inadequate. It makes you feel that you’re not doing your job as well as you should be.” A point further elaborated on by participant 11 who noted: “nurses can’t be the nurses that they want to be. You know, they’re feeling disappointed with themselves, they’re feeling let down, they feel that they have failed.” All of this results in more and more nurses leaving the NHS or the profession completely, which only serves to exacerbate the problem of staff shortages. The decision to strike was effectively a way of nurses saying, “enough is enough, this cannot go on!”
Despite the strains of the job, it is interesting to note however that participants largely considered the real consequences of staff shortages to be suffered by patients. With increasing workloads and high patient to nurse ratios nurses’ ability to provide even the most basic standards of care are compromised. They are often faced with difficult decisions on prioritising and allocating care; things get missed, mistakes happen, and treatments and care are not provided in a timely fashion. This compromises the safety of patients and results in them coming to harm. A point stressed by participant 13.
I have seen, and I have experienced patients having poor health outcomes, or poor experiences as a result of not being able to deliver the care that we know we can deliver. And that's because of circumstances such as short staffing, and people being off long-term sick with stress.
It seems then that nurses’ decision to strike was a cry for help, not just for nurses working within the NHS, but for the very patients it aims to serve.
Integration of quantitative and qualitative results
Integration of the quantitative and qualitative findings show a high level of concordance between the two data sets. Table 6 provides examples of how the qualitative findings not only confirmed the key quantitative findings ( confirmation ) but also served to expand the understanding of them ( expansion ). No incidences were found where the two sets of findings contradicted each other ( disconfirm ).
This mixed methods study offers valuable insights into the key factors driving UK NHS nurses’ decision to strike. The quantitative findings identify that patient safety, followed by staff shortages and pay were the most important factors. The qualitative findings support these findings and further enhance our understanding of them. Mixed methods inferences suggest that the factors driving UK NHS nurses’ decision to strike are complex, interconnected and inextricably linked.
What is notable from the findings was that two factors: perspectives of the RCN and/or my colleagues and other UK services going on strike were deemed the least important factors and cited by less than 10% of participants. In addition, they did not arise within the qualitative data. This suggests that the decision to strike by participants was made with a high level of autonomy and was largely independent of the widespread industrial action taking place within the UK during that time.
In contrast to other empirical studies conducted on nurse strikes outside of the UK [ 16 , 17 , 18 , 21 , 22 , 23 ] this study found that pay was not the most cited factor encouraging nurses’ decision to strike. Due to these studies varying considerably in their aims, context and methodological profiles it is difficult to draw any definitive conclusions as to why this difference occurs; however, it suggests that factors driving nurses’ decision to strike are context specific and reflective of differing cultural and economic environments.
Although pay was not found to be the most important factor, the qualitative findings indicate that it still plays an integral role in encouraging nurses’ decision to strike. In part, this is because it was seen as an indicator of how valued and appreciated the nursing profession is. West et al. [ 50 ] argue that this sense of value is essential for nurses’ well-being and their ability to deliver high-quality care. The finding that nurses perceive pay as a measure of value is supported by Clayton-Hathway et al. [ 51 ] who go on to suggest that the lack of value ascribed to the nursing profession, and its resulting low pay is rooted in the perception of nursing as ‘women’s work’ and indicative of the patriarchal society historically found within the UK. This concept of gender disparities in relation to pay is compelling and challenges the assumption that low pay is simply to do with a lack of funds. It suggests that further research on the qualitative determinants of nurses pay would be valuable.
Within this study it was found that there was a high level of both self and professional motivation behind the factors driving participants’ decision to strike, but it was the latter that predominated. The concept of professional motivation being a driving force in nurses’ decision to strike is supported by accounts of nurse strikes both within the UK [ 25 , 52 ] and outside [ 19 , 24 , 26 , 28 ]. Briskin [ 24 ] referred to it as ‘the politicisation of caring’, a theory closely aligned to Hart’s [ 25 ] ‘clinical militancy’. However, there is a danger in adopting such terminology that we are merely conforming to the stereotypes around industrial action and failing to adequately reflect the nuances of the nurse strike. The findings of this study indicate a softer, more considered approach by nurses that is deeply rooted in a sense of moral justice and duty of care. With this understanding one is compelled to rethink the depiction of the strike as a form of self-gratifying militancy, to that of a legitimate act of compassionate care [ 53 ].
The finding that professional motivation plays a significant role behind the factors driving UK NHS nurses’ decision to strike is important as it can be used to garner public support for future nurse strikes and better inform those in opposition to them. In addition, it can be used by the RCN to reflect upon their communication strategies and ensure they adequately reflect the perceptions of their membership; furthermore, it may serve to challenge those accounts by media outlets that portray the strikes to be driven solely by individual monetary gain. A suggestion for further research could therefore be to conduct a content analysis on the media coverage of the strikes and compare the findings with that of this study. This could provide valuable insights into the validity of the mainstream media’s interpretation of strikes and the role it plays in influencing public opinion.
The mixed methods inferences of this study help us to understand that the factors driving UK NHS nurses’ decision to strike are complex, multifaceted and inextricably linked. Figure 4 provides a conceptual model of these inferences and summarises the interconnected nature of the factors.
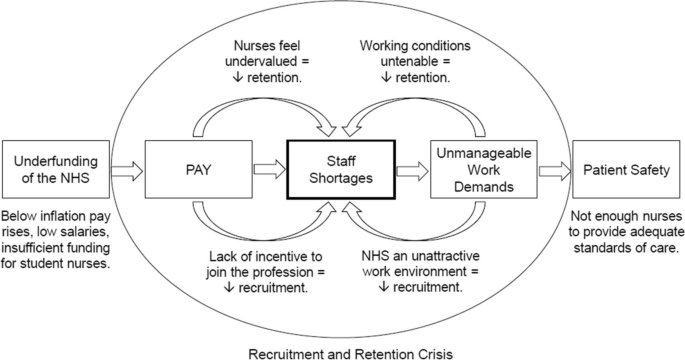
Interconnectedness of factors drawn from mixed methods inferences. Note . This model shows how factors encouraging nurses’ decision to strike lead into one another and are centred around staff shortages. The interplay of pay, staff shortages and unmanageable work demands creates a vicious cycle that manifests as a recruitment and retention crisis, resulting in compromised patient safety
Limitations
The findings of this study should be judged within the context of its limitations. First of all, it should be noted that this study was conducted by a single lone researcher who is also a registered nurse working for the UK NHS and a member of the RCN. Whilst every attempt was made to reduce bias and provide a true representation of participants perspectives the lack of investigator triangulation leaves the study susceptible to observer bias. In particular, the validity of the qualitative findings would have been enhanced by a second reviewer confirming the selection of and allocation of codes, and the generation of themes.
A further limitation can be found in the sampling methods used. The use of voluntary sampling means that the findings are likely to be subject to self-selection bias and thus less representative of those nurses who were less forthright about their decision to strike. Furthermore, a large proportion of participants were recruited via social media meaning that the study may not adequately reflect the views of those nurses who do not use social media. Data collection began approximately 5 months after the initial ballot in which nurses first voted to strike. It may have been that by this time there was an element of strike fatigue resulting in an unwillingness to participate and engage with the study. Had the data collection happened sooner it may have helped to minimise response bias and encourage greater participation.
This notion of strike fatigue may also explain to some extent why the RCN failed to secure a further strike mandate following the completion of this study. In focusing on the key factors that drove nurses’ decision to strike this study fails to adequately portray how those decisions, and the volition to strike may change over time.
Although the results of this study are compelling it is important to recognise that an element of social desirability bias may have played a part. Participants may have felt drawn toward emphasising those factors that portrayed them as striking for the greater good so as to uphold the reputation of the profession and justify the act. Although it is not possible to quantify to what extent social desirability bias played a role it should be taken into consideration when interpreting the results.
In keeping with the exploratory nature of this study a novel approach was used in the survey design. Due to the lack of previous research in this area and the absence of a strong theoretical foundation in relation to the constructs used, there is a danger that the survey lacks construct validity. The survey would therefore benefit from greater scrutiny in the form of expert opinion review, further research and refinement with the use of factor analysis.
This mixed methods study has facilitated an exploration into the key factors driving UK NHS nurses’ decision to strike leading up to and during the industrial action of 2022/23. The findings identify that factors relating to patient safety, staff shortages, pay and unmanageable work demands were key, and that there was a strong sense of professional motivation lying behind them; that is, participants concerns around the welfare of patients, the nursing profession and the NHS often came before that of their own.
In adopting a mixed methods design this study helps to highlight that the factors driving UK NHS nurses’ decision to strike do not stand in isolation and therefore, a holistic and multifactorial approach to addressing them is required. Nurses’ concerns around recruitment and retention and the implications of staff shortages need to be taken into consideration. Perhaps more importantly however, this study demonstrates that the NHS is a challenging and demanding work environment, and that the well-being of its patients is dependent on the well-being of those who care for them. If nobody cares for the carers the process of healthcare delivery breaks down. Thus, one can consider these nurse strikes as a movement, a movement toward putting the care back into care .
This study paves the way for future research on nurse strikes and could also be used to inform research into other healthcare related professions engaged in industrial action. Further research looking at the factors driving nurses’ decision to strike is required to confirm the validity of these findings and also to develop the constructs of self and professional motivation in relation to strikes. In addition, research looking into the perspectives of the mainstream media on nurse strikes and the determinants of nurses’ pay would offer valuable insights and increase our understanding of the nurse strike.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
NHS Trusts are organisations that provide healthcare services on behalf of the NHS within a given specialisation or geographical area. The majority of nurses working for the UK NHS are employed directly by an NHS Trust.
The actual figure is likely to be far higher but a further increase in population size does not influence the sample size calculation.
Abbreviations
Research and Development
Royal College of Nursing
- National Health Service
- United Kingdom
Armstrong M. The World's biggest employers. [online]. Statista: Hamburg; 2022. [Accessed 3 Aug 2023]. Available from: https://www.statista.com/chart/3585/the-worlds-biggest-employers/ .
ONS. Estimates of the population for the UK, England, Wales, Scotland and Northern Ireland. [online]. Office for National Statistics: Newport; 2022. [Accessed 3 Aug 2023]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/mid2021 .
NHS Digital. NHS workforce statistics - April 2023 (including selected provisional statistics for may 2023). [online]. NHS Digital: Leeds; 2022. [Accessed 3 Aug 2023]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics/april-2023 .
Charlesworth A, Buchan J. NHS pay: new seeds of division? 25th March. Health Foundation Blog [online]. 2023. [Accessed 3 Aug 2023]. Available from: https://www.health.org.uk/news-and-comment/blogs/nhs-pay-new-seeds-of-division .
Cannings J, Halterbeck M, Conlon G, Guglielmi P. A decade of pay erosion: the destructive effect on UK nursing staff earnings and retention. A report for the Royal College of nursing. [online]. London Economics: London; 2022. [Accessed 3 Aug 2023]. Available from: https://londoneconomics.co.uk/blog/publication/a-decade-of-pay-erosion-the-destructive-effect-on-uk-nursing-staff-earnings-and-retention-october-2022/ .
RCN. Annual review of the year 2021. [online]. Royal College of Nursing: London; 2022. [Accessed 3 Aug 2023]. Available from: https://www.rcn.org.uk/Professional-Development/publications/annual-review-of-the-year-2021-uk-pub-010-097 .
NHS Staff Survey. NHS staff survey 2022: national results briefing. [online]. Picker Institute: Oxford; 2023. [Accessed 3rd Aug 2023]. Available from: https://www.nhsstaffsurveys.com/results/national-results/ .
NMC. 2023 NMC Register Leavers Survey: Summary report. [online]. Nursing and Midwifery Council: London; 2023. [Accessed 3rd Aug 2023]. Available from: https://www.nmc.org.uk/globalassets/sitedocuments/data-reports/may-2023/annual-data-report-leavers-survey-2023.pdf .
RCN. Employment Survey 2021 . [online]. Royal College of Nursing: London; 2021. [Accessed 3rd Aug 2023]. Available from: https://www.rcn.org.uk/Professional-Development/publications/employment-survey-2021-uk-pub-010-075 .
BMA. An NHS Under Pressure. [online]. British Medical Association: London; 2023. [Accessed: 6th Sept 2023]. Available from: https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/an-nhs-under-pressure .
NHS England. Consultant-led referral to treatment waiting times data 2022–23 . [online]. NHS England: Redditch; 2023. [Accessed 6th Sept 2023]. Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/rtt-data-2022-23/ .
Freedman, S. and Wolf, R. The NHS productivity puzzle: why has hospital activity not increased in line with funding and staffing? [online]. Institute for Government: London; 2023. [Accessed 6th Sept 2023]. Available from: https://www.instituteforgovernment.org.uk/publication/nhs-productivity .
ONS. The impact of strikes in the UK: June 2022 to February 2023 . [online]. Office for National Statistics: Newport; 2023. [Accessed 26th Aug 2023]. Available from: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/workplacedisputesandworkingconditions/articles/theimpactofstrikesintheuk/june2022tofebruary2023 .
Peterson, F. Strikes in the United States 1880–1936. [online]. Bureau of Labor Statistics: Washington; 1937. [Accessed 3rd Aug 2023]. Available from: https://fraser.stlouisfed.org/files/docs/publications/bls/bls_0651_1938.pdf .
Hyman R. Strikes. London: Fontana/Collins; 1974.
Google Scholar
Binkowska-Bury M, Marc M, Nagorska M, Januszewicz P, Ryzko J. The opinions of polish nurses and patients on nursing protests. Coll Antropol. 2013;37(3):691–9. PMID: 24308205
PubMed Google Scholar
Kravitz RL, Leake B, Zawacki BE. Nurses’ views of a public hospital nurses’ strike. West J Nurs Res. 1992;14(5):645–61. https://doi.org/10.1177/019394599201400507 .
Article CAS PubMed Google Scholar
El-Fatah IMA, Sleem WF, Ata AA. Role of the nurse managers during nursing personnel strikes. IOSR-JNHS. 2018;7(1):77–86. https://doi.org/10.9790/1959-0701067786 .
Article Google Scholar
Brown GD, Greaney AM, Kelly-Fitzgibbon ME, McCarthy J. The 1999 Irish nurses’ strike: nursing versions of the strike and self-identity in a general hospital. J Adv Nurs. 2006;56(2):200–8. https://doi.org/10.1111/j.1365-2648.2006.03998.x .
Article PubMed Google Scholar
Catlin A. Nursing strike, America, 2019: concept analysis to guide practice. Nurs Outlook. 2020;68(4):468–75. https://doi.org/10.1016/j.outlook.2020.03.002 .
Mabange E, Muller M. Strike actions by nurses/midwives in a nursing service. Health SA Gesondheid. 2000;5(1):22–37. https://doi.org/10.4102/hsag.v5i1.24 .
Kunene PJ. Strikes by nursing personnel: a challenge for nurse managers in KwaZulu-Natal Province. Ph. D. Thesis. University of Zululand; 1995.
Nala NP. Strategies for curbing strike action by nurses in public institutions, South Africa. Ph. D. Thesis. University of Zululand; 2014.
Briskin L. Resistance, mobilization and militancy: nurses on strike. Nurs Inq. 2011;19(4):285–96. https://doi.org/10.1111/j.1440-1800.2011.00585.x .
Hart C. Behind the mask: nurses, their unions and nursing policy. London: Bailliere Tindall; 1994.
Hayes L. Nurses on strike. In: Brenner A, Day B, Ness I, editors. The encyclopedia of strikes in American history. New York: M.E. Sharpe; 2009. p. 707–15.
Hayward S, Fee E. More in sorrow than in anger: the British nurses’ strike of. Int J Health Serv. 1988;1992:397–415. https://doi.org/10.2190/CKJC-UGCX-DTFN-W9AK .
Katsuragi S. Better working conditions won by ‘nurse wave’ action: Japanese nurses’ experience of getting a new law by their militant campaign. Nurs Ethics. 1997;4(4):313–22. https://doi.org/10.1177/096973309700400407 .
Mckeown M. Alliances in action: Opportunities and threats to solidarity between workers and service users in health and social care disputes. Soc Theory Health. 2009;7(2):148–69. https://doi.org/10.1057/sth.2009.8 .
Strachan G. Not just a labour of love: industrial action by nurses in Australia. Nurs Ethics. 1997;4(4):294–302. https://doi.org/10.1177/096973309700400405 .
Tabak N, Wagner N. Professional solidarity versus responsibility for the health of the public: is a nurses’ strike morally defensible? Nurs Ethics. 1997;4(4):283–93. https://doi.org/10.1177/096973309700400404 .
Clay T. Nurses, power, and politics. London: Heinemann Nursing; 1987.
Neiman P. Nursing strikes: an ethical perspective on the US healthcare community. Nurs Ethics. 2011;18(4):596–605. https://doi.org/10.1177/0969733011408050 .
ICN. The ICN code of ethics for nurses. [online]. International Council of Nurses: Geneva; 2021. [Accessed 3rd Aug 2023]. Available from: https://www.icn.ch/node/1401 .
NMC. The code: professional standards of practice and behaviour for nurses, midwives and nursing associates. [online]. Nursing and Midwifery Council: London; 2018. [Accessed 3rd Aug 2023]. Available from: https://www.nmc.org.uk/standards/code/ .
Essex R, Weldon SM. The justification for strike action in healthcare: a systematic critical interpretive synthesis. Nurs Ethics. 2022;29(5):1152–73. https://doi.org/10.1177/09697330211022411 .
Article PubMed PubMed Central Google Scholar
Jennings K, Western G. A right to strike? Nurs Ethics. 1997;4(4):277–82. https://doi.org/10.1177/096973309700400403 .
Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. 3rd ed. Los Angeles: SAGE; 2018.
Swedberg R. Exploratory research. In: Elman C, Gerring J, Mahoney J, editors. The production of knowledge: enhancing Progress in social science. Cambridge: Cambridge University Press; 2020. p. 17–41.
Chapter Google Scholar
RCN. RCN’s biggest ever strike ballot now open. [online]. Royal College of Nursing: London; 2022. [Accessed 6th Jan 2023]. Available from: https://www.rcn.org.uk/news-and-events/news/uk-rcns-biggest-ever-strike-ballot-now-open-061022 .
Great Britain. Trade Union Act 2016. Chapter 15. London: The Stationery Office.
Conroy RM. The RCSI sample size handbook: a rough guide may 2021 version. [online]. Royal College of Surgeons Ireland: Dublin; 2021. [Accessed 6th Jan 2023]. Available from: https://www.beaumontethics.ie/docs/application/samplesize2021.pdf .
LamaPoll LamaPoll. [online]. LamaPoll: Frankfurt; 2023. [Accessed 26th Feb 2023]. Available from: https://www.lamapoll.de/ .
Bland JM, Altman DG. Statistics notes: Cronbach’s alpha. BMJ. 1997;314:572. https://doi.org/10.1136/bmj.314.7080.572 .
Article CAS PubMed PubMed Central Google Scholar
DeVellis RF. Scale development: theory and applications. 4th ed. Los Angeles: Sage; 2017.
Rattray J, Jones MC. Essential elements of questionnaire design and development. J Clin Nurs. 2007;16(2):234–43. https://doi.org/10.1111/j.1365-2702.2006.01573.x .
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa .
Guetterman TC, Fetters MD, Creswell JW. Integrating quantitative and qualitative results in health science mixed methods research through joint displays. Ann Fam Med. 2015;13(6):554–61. https://doi.org/10.1370/afm.1865 .
NMC. The NMC register: 1 April 2022–31 March 2023. [online]. Nursing and Midwifery Council: London; 2023. [Accessed 26th Aug 2023]. Available from: https://www.nmc.org.uk/about-us/reports-and-accounts/registration-statistics/ .
West M, Bailey S, Williams E. The courage of compassion: supporting nurses and midwives to deliver high-quality care. The King’s Fund: London; 2020. [Accessed 16th Aug 2023]. Available from: https://www.kingsfund.org.uk/publications/courage-compassion-supporting-nurses-midwives .
Clayton-Hathway K, Griffiths H, Schutz S, Humbert AL, Mcllroy, R. Gender and nursing as a profession: valuing nurses and paying them their worth. Royal College of Nursing: London; 2020. [Accessed 16th Aug 2023]. Available from: https://www.rcn.org.uk/Professional-Development/publications/pub-007954 .
Sullivan T, Christenson I, Wan D. Nurses in the National Health Service: reflections on recent industrial unrest. Health Manpow Manage. 1991;13(3):3–9. PMID: 10116147
McKeown M, Stowell-Smith M, Foley B. Passivity vs. militancy: a Q methodological study of nurses’ industrial relations on Merseyside (England). J Adv Nurs. 1999;30(1):140–9. https://doi.org/10.1046/j.1365-2648.1999.01058.x .
Download references
Acknowledgements
Many thanks to Dr. Ercüment Çelik for overseeing this project and for his comments and suggestions relating to protocol development and write-up of the study. Thank you also to Urs A. Fichtner from University Hospital Freiburg Institute for Medical Biometry and Statistics for his advice and suggestions regarding the statistical analysis for the study. This study formed part of a Master’s in Global Urban Health at the University of Freiburg, Germany. Many thanks to Sonia Diaz-Monslave and the GUH master’s team for facilitating the process. Thank you also to the reviewers of the manuscript for their thoughtful and valuable comments and suggestions.
Open Access funding enabled and organized by Projekt DEAL. The author received no financial support for the research or authorship.
Author information
Authors and affiliations.
Centre for Medicine and Society, University of Freiburg, Fahnenbergplatz, 79085, Freiburg im Breisgau, Germany
Daniel Sanfey
You can also search for this author in PubMed Google Scholar
Contributions
D.S. took full responsibility for the conception, design, data collection, analysis, interpretation, figure preparation and write-up of the study.
Corresponding author
Correspondence to Daniel Sanfey .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted in accordance with the Declaration of Helsinki. Informed consent was gained from all participants partaking in both the quantitative and qualitative methods. Ethical approval was granted by the University of Freiburg’s ethical research committee (Application no. 23–1126-S2). All data was held and stored in accordance with the UK Data Protection Act of 2018.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sanfey, D. ‘Enough is enough’: a mixed methods study on the key factors driving UK NHS nurses’ decision to strike. BMC Nurs 23 , 247 (2024). https://doi.org/10.1186/s12912-024-01793-4
Download citation
Received : 03 October 2023
Accepted : 09 February 2024
Published : 16 April 2024
DOI : https://doi.org/10.1186/s12912-024-01793-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Industrial action
- Mixed methods
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
METHODS article
A multiphase study protocol of identifying, and predicting cancer-related symptom clusters: applying a mixed-method design and machine learning algorithms.

- 1 Department of Nursing, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
- 2 Nursing Care Research Center in Chronic Diseases, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
- 3 Department of Biostatistics, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
- 4 Department of Medical Oncology, School of Medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Objectives: In recent years, there has been increasing attention on the cluster approach to symptom management. Two significant challenges in the symptom cluster (SC) approach are identifying and predicting these clusters. This multiphase protocol aims to identify SCs in patients with advanced cancer as the primary objective, with the secondary objective of developing machine learning algorithms to predict SCs identified in the first phase.
Methods: The 2-MIXIP study consists of two main phases. The first phase involves identifying SCs, and the second phase focuses on developing predictive algorithms for the identified SCs. The identification of SCs involves a parallel mixed-method design (quantitative and qualitative). Quantitative and qualitative methods are conducted simultaneously and given equal importance. The data are collected and analyzed independently before being integrated. The quantitative part is conducted using a descriptive-analytical method. The qualitative analysis is conducted using a content analysis approach. Then, the identified SCs from both parts are integrated to determine the final clusters and use them in the second phase. In the second phase, we employ a tree-based machine learning method to create predictive algorithms for SCs using key demographic and clinical patient characteristics.
Conclusion: The findings of the 2-MIXIP study can help manage cancer patients' symptoms more effectively and enhance clinical decision-making by using SCs prediction. Furthermore, the results of this study can provide guidance for clinical trials aimed at managing symptoms.
1 Introduction
Patients with cancer typically experience multiple concurrent symptoms, which can make their management challenging and impact their quality of life ( 1 ). The term “symptom cluster” has been proposed to describe this phenomenon ( 2 ). This concept suggests that concurrent symptoms do not exist independently but interact with each other through mechanisms. A symptom cluster (SC) is defined as “two or more symptoms that appear simultaneously and are related to each other, which may have a common underlying cause or mechanism”. The connections between symptoms within a cluster are typically stronger than those between symptoms in other clusters ( 3 , 4 ), and symptoms within a cluster mutually influence each other synergistically ( 5 ). A cluster of symptoms works cooperatively to increase patient suffering, and reduce treatment compliance, which may even affect patient survival compared with a single symptom. Consequently, in recent years, SC approach has received more attention in efforts to manage symptoms ( 6 – 8 ). SC research is an emerging field in symptom management that aims to enhance the understanding and treatment of cancer-related symptoms.
Identification of symptom clusters (SCs) is important for predicting other symptoms within a cluster, discovering possibly overlooked symptoms, making decisions to design an appropriate care plan, and individualizing interventions ( 9 – 11 ). There are two significant clinical advantages of SC approach. One reason is that when interventions are performed to improve a specific symptom in a cluster, other symptoms within that cluster may also be alleviated. In fact, by improving one symptom, the entire cluster can be improved. Another benefit of the patient care program is the ability to select interventions that address multiple symptoms within a cluster, rather than focusing on individual symptoms ( 8 , 12 , 13 ).
There are several challenges in the supply cluster approach. The primary challenge is to identify these clusters ( 8 ). Both quantitative and qualitative methods can be used for this purpose. With a quantitative approach, clusters can be identified using statistical clustering methods, although they may be subject to bias. The use of various definitions, diverse data collection tools, and different data analysis approaches has led to data sets that are challenging to interpret ( 8 , 14 ). It is also important to note that current research focuses on clusters defined using statistical relationships between symptoms rather than those derived from patient experiences. An alternative approach to examining symptom clusters is through qualitative studies of symptom experience. Using a qualitative approach to identify SCs can overcome the limitations of statistical methods because it captures the unique experiences of patients ( 15 , 16 ) and can lead to a deeper understanding of SCs from a patient-centered perspective rather than a statistics-based one. In fact, the use of both quantitative and qualitative methods can complement each other for a more comprehensive and accurate investigation of clusters. To our knowledge, no study has used the combination of both methods to identify SCs. The 2-MIXIP study is the first to simultaneously employ quantitative and qualitative methods to identify SCs in patients with advanced cancer. The second challenge is that the clusters of symptoms identified are obtained from a population of patients, and we need to determine how many clusters exist and what combinations are present in our target population. Until this point, they have more restricted clinical use. In a real clinical setting, identifying the cluster(s) our patient belongs to is a very challenging, time-consuming, and complex task that can sometimes exceed the capabilities of nurses and the healthcare team. Furthermore, the patient's condition may change at any moment, including changes in the disease stage, severity of symptoms, and so on, which can result in alterations to the cluster's condition, making continuous assessments unfeasible. Therefore, to address this clinical gap, the method of predicting SCs can be used. However, the main challenge in this field is to use methods that yield the highest prediction accuracy ( 8 ). One of the most powerful methods is machine learning techniques ( 17 ). To the best of our knowledge, no study has been conducted to predict cancer-related symptom clusters using advanced methods.
1.1 Objectives
According to the challenges mentioned, the primary goal of the 2-MIXIP multiphase study is to identify SCs in patients with advanced cancer undergoing active treatment. The secondary objective is to develop machine learning algorithms to predict symptom clusters identified in the initial phase. This makes the clinical application of these clusters in symptom management more practical for nurses and palliative care teams.
2.1 Design and setting
This study employs a multiphase design to investigate advanced cancer in adults. It consists of two main phases (see Figure 1 ). The first phase involves identifying SCs, whereas the second phase focuses on developing predictive algorithms for the identified SCs using machine learning methods. The study is conducted at three academic centers: Baghai 2 Teaching Hospital, the Clinical Oncology Department of Golestan Hospital, and Shafa Oncology Clinic, all affiliated with Ahvaz Jundishapur University of Medical Sciences (AJUMS), Ahvaz, Iran. This study has been approved by the Institutional Review Board affiliated with AJUMS (IR.AJUMS.REC.1402.046). Written informed consent is obtained from all participants.
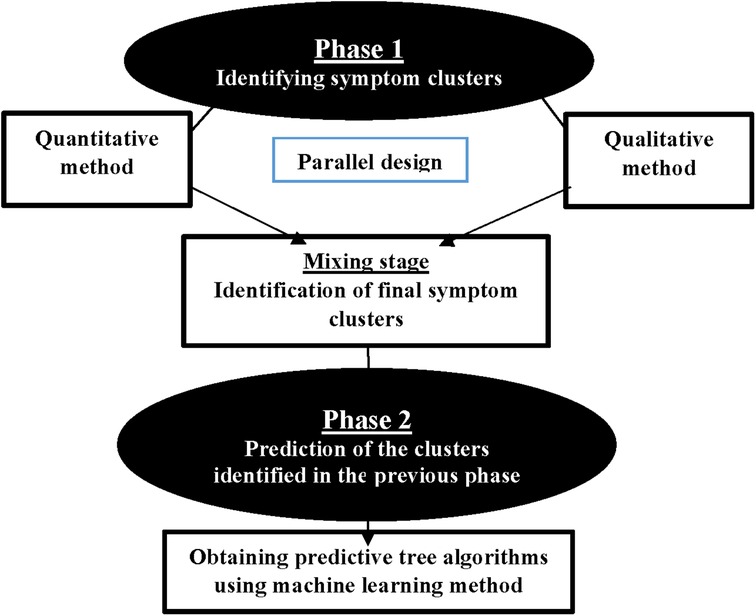
Figure 1 . Study phases.
2.2 Phase 1 (identifying symptom clusters)
The main objective of the initial phase of the study is to identify symptom clusters. The identification of clusters is conducted using a parallel mixed-method design, incorporating both quantitative and qualitative approaches. Two quantitative and qualitative stages are conducted simultaneously and given equal importance. The data are collected and analyzed independently before being combined.
2.2.1 Quantitative stage
The quantitative stage is conducted using a descriptive-analytical method. A convenience sampling method is used in the quantitative phase. The inclusion criteria comprised the following: (1) being in an advanced stage of cancer; (2) undergoing active treatment; (3) adults aged 18 years and older; and (4) ability to communicate effectively. Exclusion criteria include: (1) a history of mental illness or cognitive impairment; (2) unstable clinical condition; (3) concurrent serious medical conditions.
Quantitative Data Collection: Data are collected using a demographic characteristics form and the Memorial Symptom Assessment Scale (MSAS) questionnaire. The MSAS is a self-report questionnaire designed by Portenoy et al. in 1994 to measure multidimensional symptom experience. The MSAS contains 32 common symptoms divided into two parts. The first part contains 24 symptoms, including three aspects of occurrence (frequency), intensity, and distress for each symptom. The second part includes 8 symptoms that are assessed solely based on their intensity and distress. Using the MSAS, patients are asked to indicate whether they have experienced any of the symptoms in the past week (i.e., symptom occurrence). If individuals have experienced these symptoms, they are asked to assess their frequency, intensity, and distress. The MSAS is scored using the Likert scale. It also includes an open-ended question at the end that asks patient to list any additional symptoms beyond the 32 specified ( 18 ). The reliability and validity of the MSAS have been well established in oncology patients ( 19 – 22 ). In Bahrami et al.'s study, the MSAS demonstrated good validity and reliability among cancer patients in Iran. The Cronbach's alpha coefficient was 0.77 ( α = 0.77) ( 23 ).
2.2.1.1 Sample size
In factor analysis studies with numerous variables, one method for estimating the sample size is to apply a general rule (rule of thumb), which suggests that a minimum of 3–20 subjects per item should be considered necessary to avoid calculation problems ( 24 – 28 ). As the MSAS examines 32 symptoms in general, with 20 samples considered for each item, the estimated sample size for the quantitative stage of this study is 640 people.
Quantitative Data Analysis: Data are analyzed using R software Version 4.2.2. Descriptive statistics are presented as frequency/percentage, as well as mean and standard deviation (SD). One powerful method that can be used to identify clusters of symptoms is network analysis (NA). In general, networks are defined as a set of interconnected components, such as symptoms in this research. NA is a graph-based method that can identify the relationships between symptoms and various clusters of symptoms experienced by patients, and visualize and interpret them quantitatively. Network analysis (NA) can be helpful in identifying key symptoms that affect other concurrent symptoms or clusters, which are potential targets for therapeutic interventions ( 19 ). The primary function, estimateNetwork, employs the least absolute shrinkage and selection operator (LASSO) with extended Bayesian information criterion (EBIC) model selection, utilizing a hypertuning parameter ( γ ) to determine model sparsity. Polychoric correlations are computed for ordinal data, establishing a Gaussian graphical model with nodes representing items and edges denoting partial correlations. Four centrality indices (strength, betweenness, closeness, and expected influence) are identified as pivotal nodes in the network. The study also explores bridge nodes connecting different communities, using bridge-expected influence metrics to identify nodes likely to activate nearby communities. Overall, this study employs advanced network estimation techniques, centrality indices, and bridge node analysis to comprehensively investigate the interconnectedness within the network.
2.2.2 Qualitative stage
In this stage, the qualitative method of content analysis is used to identify SCs, and it is conducted simultaneously with the quantitative stage. The participants for the qualitative phase are selected from the participants in the quantitative phase who experience three or more co-occurring symptoms upon entering the study and are willing to share their experiences. In the qualitative stage, the purposive sampling method is used. Also, we will strive to achieve maximum diversity in our sampling to capture a wide range of experiences.
2.2.2.1 Sample size
Sampling continues until data saturation is reached. Data saturation occurs when no additional data are available to further expand the information. The criterion for reaching this stage is the repetition of previous data, ensuring that the researcher consistently encounters data that confirms the previous findings. This process aims to ensure that the arrival of new people does not alter the researcher's decision and final summary. At this stage, the researcher concludes the selection of new participants ( 29 ).
2.2.2.2 Qualitative data collection
When conducting research, the researcher identifies suitable participants and obtains their consent to participate. The time and place of the interview are then determined. The data collection method involves individual face-to-face semi-structured interviews. The interview process follows a general guide and begins with a broad question, such as “How have you been feeling physically in the past week?” This is followed by questions about the psychological symptoms experienced by the patient and how these symptoms relate to their physical experiences. After addressing these broad questions, the interview process continues with probing questions. Participants' experiences of symptoms are thoroughly explored in the interviews, and each mention of multiple symptoms is examined in greater detail. Participants are not asked about specific symptoms, as the interview questions are broad enough to capture important aspects of each participant's symptom experience. During the interview, probing and clarifying questions such as “Can you explain more?” were asked. “Can you give an example?” etc. are done for further investigation. Any new issues identified during the initial interviews are incorporated into the interview guide for subsequent interviews. In addition, field notes and reflexive reports are maintained after each interview to aid subsequent interviews and data analysis.
The interview is conducted in a location with appropriate environmental conditions. The main factors that determine the duration of the interview include the interviewee's tolerance, the volume of information, and the willingness of the participants. Multiple interviews may be conducted for each participant if necessary, as they facilitate in-depth reflection for both the participant and the researcher throughout the data collection process. All interviews are recorded with the participants' consent, and they are assured of the confidentiality of the information and restricted access to the recorded voice. Noted that participants have the option to decline audio recording of their speech. In such cases, the audio recorder device is turned off, and the required information is documented in writing. After each interview, the recorded material is transcribed verbatim into text.
2.2.2.3 Qualitative data analysis
Qualitative data are analyzed concurrently with data collection using conventional content analysis, following the steps outlined by Elo and Kyngas ( 30 ). Data analysis ideally begins after the first interview and continues throughout the research process. This iterative process of moving back and forth between data collection and analysis enables researchers to explore relevant concepts and their dimensions ( 31 ). Analyzing data during the initial stages of collection can guide subsequent data collection to obtain relevant information ( 32 ). The categories are compared by two researchers, as well as the project's lead researcher. The analyzed categories are compared and discussed until a consensus is reached. If more than two participants independently mentioned an association between at least two symptoms, they were grouped together. Quotations are provided for each code and category of data in preparation for reporting findings. Depending on the study's purpose, researchers may opt to identify relationships between categories and subcategories based on their concurrence, antecedents, or consequences. Additionally, MAXQDA software is used for data management.
2.2.2.4 Trustworthiness of qualitative data
The trustworthiness and authenticity of qualitative data are evaluated based on the criteria outlined by Lincoln and Guba ( 33 – 35 ). To ensure confirmability, the research team reviews the data, acting as a peer review process to verify that the analyzed data represent true findings and are free from potential bias. Additionally, the method of returning the data to the participants and obtaining their approval are used, known as member checking. The reliability of the research is determined by the researcher's consistent involvement with the research data, dedicating sufficient time collecting the data, checking the extracted data, and analyzing them. All interviews are recorded, and exact quotes from participants are provided to illustrate identified categories, thereby reducing the risk of researchers selectively filtering data through recall or summarization and ensuring greater reliability. Credibility is achieved through a wide variety of samples. To enhance validity, the identified SCs are reviewed by a specialized group comprising an oncologist, an oncology nurse, and the research team. They use their clinical experiences to review and confirm the data. Also, a group meeting is held with several patients to discuss the identified SCs and compare them with their experiences once again. To enhance replicability, all stages of research, particularly data analysis and category formation, are thoroughly documented. This allows other researchers to review the available documentation in the respective field. The researcher thoroughly describes the features and characteristics of the participants, and the findings are presented in the form of articles at international conferences.
2.2.3 Mixing/integration stage
In this stage, the findings from both the quantitative and qualitative parts are integrated. The identified SCs from both parts are combined for use in the second phase of the study, which involves predicting clusters. In this study, we adhere to Creswell's approach ( 36 ). Creswell argues that the parallel combination method is the most suitable approach for comparing different perspectives derived from quantitative and qualitative data. The expected outcome involves integrating two databases to demonstrate how the data converge or diverge (Creswell, 53). In this study, quantitative and qualitative methods complement each other, with each method identifying clusters based on its strengths to provide a more comprehensive view of symptom clusters. In the first step of integration, the identified clusters are placed against each other. In the second step, we compare the two to identify similarities and differences. In the third and final step, we determine the ultimate clusters by identifying the number of clusters and the symptoms contained in each cluster. During the integration stage of SCs, we encounter three modes. Table 1 displays the modes and the research team's approach.
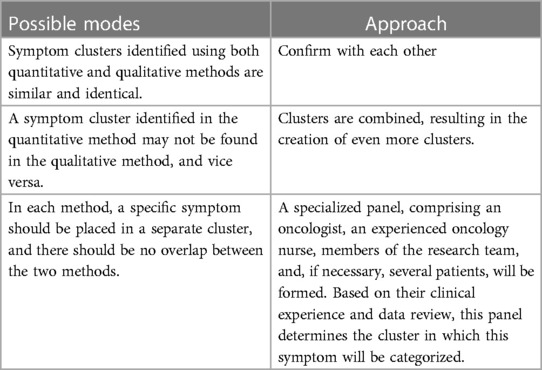
Table 1 . Integration stage of qualitative and quantitative data.
2.3 Phase 2 (predicting symptom clusters)
The main objective of the second phase is to predict SCs identified in the first phase of the study. In this phase, we use machine learning (ML) methods to develop predictive algorithms for SCs based on key demographic and clinical characteristics such as age, sex, type of cancer, and type of treatment. Machine learning encompasses various techniques. In this study, we focus on tree-based machine learning algorithms (decision trees) to predict clusters within different patient subgroups.
To develop predictive machine learning algorithms, various steps must be taken. The main steps include ( 37 ): (1) Training: a process during which the system is provided with both the input data and the correct outcome (answer) to learn from initially. (2) Testing: To evaluate the performance of trained algorithms, it is essential to compare the predictions made by the algorithm on a separate dataset from the one used for training, with the actual results for that dataset, which were known but not disclosed during training. (3) Tuning: The process of optimizing the parameters that affect the model to enable the algorithm to perform at its best. (4) Determining the accuracy, sensitivity, and specificity of the predictive algorithm. (5) Production of the final algorithm.
For prediction, we input important demographic and clinical variables as predictor variables, and SCs as the outcome, into the model. This allows the prediction algorithm to be generated based on these variables for homogeneous subgroups of patients. The samples in the second phase of the study are identical to those in the first phase. As a result, 70% of the samples from the first phase are used for machine training, while the remaining 30% will be used for testing. The R programing software is used to generate the algorithm.
3 Discussion
The 2-MIXIP study consists of two main phases: identifying and predicting cancer-related symptom clusters. In the first phase, we use both quantitative and qualitative approaches simultaneously to identify clusters. Using a qualitative approach to identify symptom clusters can offer valuable insights into the types of clusters that patients experience, as well as uncover clusters that may go undetected by statistical methods. Additionally, the qualitative approach can help prioritize the clusters based on their significance for patients and identify the predominant symptom in each cluster that holds great clinical importance. Qualitative methods may provide valuable data on how patients perceive, prioritize, and evaluate symptom clusters, which may aid in making decisions about more effective symptom management ( 2 ). In fact, the qualitative method provides an opportunity to explore the breadth and complexity of related symptoms. Qualitative methods have been used in fewer studies than quantitative methods to examine SC in oncology patients ( 16 , 38 ). More studies with a qualitative approach are needed to comprehensively understand SC in this patient population.
In the second phase of the study, tree-based machine learning algorithms are used to predict the identified SCs from the first phase. Tree-based algorithms enable the creation of predictive models that offer accuracy, stability, and ease of interpretation. Unlike linear models, nonlinear models depict nonlinear relationships well and can simultaneously consider several variables for prediction. Tree algorithms can handle both categorical and continuous variables ( 39 ). Although the process of generating these tree algorithms is complex, they are actually very simple to understand. Machine learning algorithms can greatly enhance prediction accuracy compared with conventional statistical regression models by capturing complex and nonlinear relationships in the data. In general, decision trees offer several advantages, including easy understanding, powerful data exploration, minimal need for data cleaning, resilience to outliers and missing values, no requirement for data normalization during processing, and no restrictions on data type ( 40 , 41 ).
The implementation of this study faces several limitations. This study also has several limitations. Participation is limited to patients who speak Farsi. It is not possible to interview patients who experience numerous symptoms but are in a serious physical condition. The variables are subjective in nature, which makes them vulnerable to the influence of cultural differences, individual variations, and family, social, and personal challenges. Additionally, this study was only conducted in one city, so it may not account for cultural, social, racial differences, etc., which could impact the generalizability of the results to some extent.
4 Conclusion
The findings of the 2-MIXIP study help to effectively manage symptoms in patients with advanced cancer, thereby improving their quality of life. The clinical decision-making authority of the care team, particularly nurses, is enhanced by predicting symptom clusters. This enables them to select more effective interventions that address a group of symptoms rather than a single symptom. Identifying SCs can also help individualize interventions ( 10 , 11 ). Furthermore, the results of this study serve as the foundation for future research, such as clinical trials for managing symptoms and the creation of clinical instruments for evaluating clusters of cancer-related symptoms.
Data availability statement
The final dataset and the code for statistical analysis will be available upon reasonable request.
Ethics statement
The protocol approved by the Institutional Review Board (IRB) of Ahvaz Jundishapur University of Medical Sciences (Ref. ID: IR.AJUMS.REC.1402.046). Written informed consent will be obtained from all participants.
Author contributions
MM: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. KZ: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. MG: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing. MJ: Data curation, Formal Analysis, Methodology, Software, Writing – original draft, Writing – review & editing. HK: Data curation, Investigation, Project administration, Resources, Writing – original draft, Writing – review & editing. DR: Data curation, Investigation, Project administration, Resources, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research including data collection and staff.
This study is funded by a research grant from the Ahvaz Jundishapur University of Medical Sciences [grant number: NCRCCD-0202]. Funder have no roles in data collection, analysis, interpretation, writing and publishing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Snijders RAH, Brom L, Theunissen M, van den Beuken-van Everdingen MHJ. Update on prevalence of pain in patients with cancer 2022: a systematic literature review and meta-analysis. Cancers (Basel) . (2023) 15(3):591. doi: 10.3390/cancers15030591
PubMed Abstract | Crossref Full Text | Google Scholar
2. Dodd M, Janson S, Facione N, Faucett J, Froelicher ES, Humphreys J, et al. Advancing Science of symptom management. J Adv Nurs . (2001) 33(5):668–76. doi: 10.1046/j.1365-2648.2001.01697.x
3. Harris CS, Kober K, Cooper B, Conley YP, Hammer MJ, Dhruva AA, et al. Symptom clusters in oncology outpatients: stability and consistency across a cycle of chemotherapy. BMJ Support Palliat Care . (2022) 13(e3):bmjspcare-2022-003785. doi: 10.1136/spcare-2022-003785
Crossref Full Text | Google Scholar
4. Shin H, Dudley WN, Bhakta N, Horan MR, Wang Z, Bartlett TR, et al. Associations of symptom clusters and health outcomes in adult survivors of childhood cancer: a report from the st jude lifetime cohort study. J Clin Oncol . (2023) 41(3):497–507. doi: 10.1200/JCO.22.00361
5. Lin DM, Yin XX, Wang N, Zheng W, Wen YP, Meng LM, et al. Consensus in identification and stability of symptom clusters using different symptom dimensions in newly diagnosed acute myeloid leukemia patients undergoing induction therapy. J Pain Symptom Manage . (2019) 57(4):783–92. doi: 10.1016/j.jpainsymman.2018.12.329
6. Guo M, Wang C, Yin X, Nie L, Wang G. Symptom clusters and related factors in oesophageal cancer patients 3 months after surgery. J Clin Nurs . (2019) 28(19–20):3441–50. doi: 10.1111/jocn.14935
7. Kim HJ, McGuire DB, Tulman L, Barsevick AM. Symptom clusters: concept analysis and clinical implications for cancer nursing. Cancer Nurs . (2005) 28(4):270–82; quiz 283–4. doi: 10.1097/00002820-200507000-00005
8. Miaskowski C, Barsevick A, Berger A, Casagrande R, Grady PA, Jacobsen P, et al. Advancing symptom science through symptom cluster research: expert panel proceedings and recommendations. J Natl Cancer Inst . (2017) 109(4):djw253. doi: 10.1093/jnci/djw253
9. Kim HJ, Barsevick AM, Beck SL, Dudley W. Clinical subgroups of a psychoneurologic symptom cluster in women receiving treatment for breast cancer: a secondary analysis. Oncol Nurs Forum . (2012) 39(1):E20–30. doi: 10.1188/12.ONF.E20-E30
10. Miladinia M, Voss JG, Molavynejad S, Malehi AS, Zarea K, Nouri EM, et al. Slow-stroke back massage compared with music therapy for leukemia-related pain and fatigue: a randomized controlled trial. JCO Oncology Practice . (2021) 17(11):e1614–21. doi: 10.1200/OP.21.00156
11. Ghafoor I, Hafeez H, Naz F, Abubakar M, Jamshed A. Prevalence of symptom clusters in cancer patients at first presentation in palliative care clinic as per different disease groups. J Cancer Immunol . (2019) 1(1):1–11. doi: 10.33696/cancerimmunol.1.001
12. Miladinia M, Jahangiri M, Kennedy AB, Fagerström C, Tuvesson H, Safavi SS, et al. Determining massage dose-response to improve cancer-related symptom cluster of pain, fatigue, and sleep disturbance: a 7-arm randomized trial in palliative cancer care. Palliat Med . (2023) 37(1):108–19. doi: 10.1177/02692163221129158
13. Dodd MJ, Miaskowski C, Lee KA. Occurrence of symptom clusters. J Natl Cancer Inst Monogr . (2004) 32:76–8. doi: 10.1093/jncimonographs/lgh008
14. Aktas A, Walsh D, Rybicki L. Symptom clusters: myth or reality? Palliat Med . (2010) 24(4):373–85. doi: 10.1177/0269216310367842
15. Barsevick AM. The elusive concept of the symptom cluster. Oncol Nurs Forum . (2007) 34(5):971–80. doi: 10.1188/07.ONF.971-980
16. Maguire R, Stoddart K, Flowers P, McPhelim J, Kearney N. An interpretative phenomenological analysis of the lived experience of multiple concurrent symptoms in patients with lung cancer: a contribution to the study of symptom clusters. Eur J Oncol Nurs . (2014) 18(3):310–5. doi: 10.1016/j.ejon.2014.02.004
17. Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J . (2019) 6(2):94–8. doi: 10.7861/futurehosp.6-2-94
18. Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlander-Klar H, Kiyasu E, et al. The memorial symptom assessment scale: an instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer . (1994) 30A(9):1326–36. doi: 10.1016/0959-8049(94)90182-1
19. Papachristou N, Barnaghi P, Cooper B, Kober KM, Maguire R, Paul SM, et al. Network analysis of the multidimensional symptom experience of oncology. Sci Rep . (2019) 9(1):2258. doi: 10.1038/s41598-018-36973-1
20. Browall M, Brandberg Y, Nasic S, Rydberg P, Bergh J, Rydén A, et al. A prospective exploration of symptom burden clusters in women with breast cancer during chemotherapy treatment. Support Care Cancer . (2017) 25(5):1423–9. doi: 10.1007/s00520-016-3527-1
21. Özalp G, Uysal N, Oğuz G, Koçak N, Karaca Ş, Kadıoğulları N. Identification of symptom clusters in cancer patients at palliative care clinic. Asia Pac J Oncol Nurs . (2017) 4(3):259–64. doi: 10.4103/apjon.apjon_17_17
22. Kenne Sarenmalm K, Browall M, Gaston-Johansson F. Symptom burden clusters: a challenge for targeted symptom management. A longitudinal study examining symptom burden clusters in breast cancer. J Pain Symptom Manage . (2014) 47(4):731–41. doi: 10.1016/j.jpainsymman.2013.05.012
23. Bahrami M, Assarroudi M, Mahmoodzadeh M. Investigation of symptoms’ frequency, severity, and distress in patients with leukemia admitted to hematology-oncology wards of selected hospitals in Isfahan, Iran, in 2016. HSR%J Health Syst Res . (2017) 13(2):140–5. doi: 10.22122/jhsr.v13i2.2919 [in Persian].
24. Carmen Y, Betsy M, Morgan BL, Voorhis CRWV. Understanding power and rules of thumb for determining sample sizes. Tutor Quant Methods Psychol . (2007) 3(2):43–50. doi: 10.20982/tqmp.03.2.p043
25. Pett MA, Lackey NR, Sullivan JJ. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrument Development in Health Care Research . Thousand Oaks: SAGE Publications (2003). doi: 10.4135/9781412984898
Google Scholar
26. Chaiviboontham S, Phinitkhajorndech N, Tiansaard J. Symptom clusters in patients with end-stage renal disease undergoing hemodialysis. Int J Nephrol Renovasc Dis . (2020) 28(13):297–305. doi: 10.2147/IJNRD.S271619
27. Bentler PM, Chou C-P. Practical issues in structural modeling. Sociol Methods Res . (1987) 16(1):78–117. doi: 10.1177/0049124187016001004
28. Mundfrom DJ, Shaw DG, Ke TL. Minimum sample size recommendations for conducting factor analyses. Int J Testing . (2005) 5:159–68. doi: 10.1207/s15327574ijt0502_4
29. Ranjbar H, Haghdoost AA, Salsali M, Khoshdel A, Soleimani M, Bahrami N. Sampling in qualitative research: a guide for beginning. J Army Univ Med Sci . (2012) 10(3):238–50. https://sid.ir/paper/96654/fa2012
30. Kyngäs HA, Mikkonen K, Kääriäinen M. The Application of Content Analysis in Nursing Science Research . Switzerland: Springer Cham (2020). doi: 10.1007/978-3-030-30199-6
31. Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory . 4th ed. Los Angeless: Sage (2015).
32. Erlingsson C, Brysiewicz P. A hands-on guide to doing content analysis. Afr J Emerg Med . (2017) 7(3):93–9. doi: 10.1016/j.afjem.2017.08.001
33. Lincoln YS, Guba EG. Naturalistic Inquiry . Thousand Oaks: SAGE (1985). p. 289–331. doi: 10.1016/0147-1767(85)90062-8
34. Colorafi KJ, Evans B. Qualitative descriptive methods in health science research. Herd . (2016) 9(4):16–25. doi: 10.1177/1937586715614171
35. Miles M, Huberman M, Saldana J. Qualitative Data Analysis: A Methods Sourcebook . 3rd ed. Thousand Oaks, CA: Sage (2014).
36. Creswell JW, Clark VLP. Designing and Conducting Mixed Methods Research . Thousand Oaks, CA: Sage publications (2017).
37. Sidey-Gibbons JAM, Sidey-Gibbons CJ. Machine learning in medicine: a practical introduction. BMC Med Res Methodol . (2019) 19(1):64. doi: 10.1186/s12874-019-0681-4
38. Lopez V, Copp G, Brunton L, Molassiotis A. Symptom experience in patients with gynecological cancers: the development of symptom cIusters through patient narratives. J Support Oncol . (2011) 9(2):64–71. doi: 10.1016/j.suponc.2011.01.005
39. Hu L, Li L. Using tree-based machine learning for health studies: literature review and case series. Int J Environ Res Public Health . (2022) 19(23):16080. doi: 10.3390/ijerph192316080
40. Chen JH, Asch SM. Machine learning and prediction in medicine—beyond the peak of inflated expectations. N Engl J Med . (2017) 376(26):2507–9. doi: 10.1056/NEJMp1702071
41. Gibbons C, Richards S, Valderas JM, Campbell J. Supervised machine learning algorithms can classify open-text feedback of doctor performance with human-level accuracy. J Med Internet Res . (2017) 19(3):e65. doi: 10.2196/jmir.6533
Keywords: nursing care, palliative care, qualitative research, quality of life, symptom management
Citation: Miladinia M, Zarea K, Gheibizadeh M, Jahangiri M, Karimpourian H and Rokhafroz D (2024) A multiphase study protocol of identifying, and predicting cancer-related symptom clusters: applying a mixed-method design and machine learning algorithms. Front. Digit. Health 6:1290689. doi: 10.3389/fdgth.2024.1290689
Received: 15 September 2023; Accepted: 5 April 2024; Published: 19 April 2024.
Reviewed by:
© 2024 Miladinia, Zarea, Gheibizadeh, Jahangiri, Karimpourian and Rokhafroz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kourosh Zarea [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

- Request new password
- Create a new account
Research Design: Qualitative, Quantitative, and Mixed Methods Approaches
You are here, student resources, welcome to the companion website.
Welcome to the SAGE edge site for Research Design, Fifth Edition .
The SAGE edge site for Research Design by John W. Creswell and J. David Creswell offers a robust online environment you can access anytime, anywhere, and features an array of free tools and resources to keep you on the cutting edge of your learning experience.

This best-selling text pioneered the comparison of qualitative, quantitative, and mixed methods research design. For all three approaches, John W. Creswell and new co-author J. David Creswell include a preliminary consideration of philosophical assumptions, key elements of the research process, a review of the literature, an assessment of the use of theory in research applications, and reflections about the importance of writing and ethics in scholarly inquiry.
The Fifth Edition includes more coverage of: epistemological and ontological positioning in relation to the research question and chosen methodology; case study, PAR, visual and online methods in qualitative research; qualitative and quantitative data analysis software; and in quantitative methods more on power analysis to determine sample size, and more coverage of experimental and survey designs; and updated with the latest thinking and research in mixed methods.
Acknowledgments
We gratefully acknowledge John W. Creswell and J. David Creswell for writing an excellent text. Special thanks are also due to Tim Guetterman of the University of Michigan, Shannon Storch of the University of Creighton, and Tiffany J. Davis of the University of Houston for developing the ancillaries on this site.
Comparative investigations of aftersintering of UO 2 fuel pellets
- Theory and Processes of Formation and Sintering of Powdered Materials
- Published: 06 May 2010
- Volume 51 , pages 173–176, ( 2010 )
Cite this article
- V. V. Basov 1
23 Accesses
Explore all metrics
The basic parameters of comparative tests of UO 2 fuel pellets produced by the technology of powder metallurgy for aftersinterability using their repeated thermal treatment (aftersintering) in different gas media, namely, with and without humidification, are presented. The results of an evaluation of the level of aftersinterability of these pellets by different procedures is presented, they are analyzed, and a substantiation of the expediency of using this operation manual for evaluating afersintering without the humidification of the gas medium developed at the OAO Machine Building Works (MSZ), Elektrostal’, Moscow oblast, is presented.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Fuel pellets based on uranium dioxide and alloyed with nanodispersed additives of Al(OH)3 and TiO2
V. S. Panov, V. Yu. Lopatin, … V. V. Martynov
Effects of Dual Oxidizers on the Properties of Composite Solid Rocket Propellants

Development Background and Research Progress of UN-U3Si2 Composite Fuel
An Acceptable Model and Related Statistical Methods for the Analysis of Fuel Densification , US Nuclear Regulatory Commission, Regulatory Guide 1.126.1978.
Freshley, M.D., Brite, D.M., Daniel, I.L., and Hart, P.E., J. Nucl. Mater , 1976, vol. 62, pp. 138–166.
Article CAS ADS Google Scholar
Radford, K. and Pope, I., J. Nucl. Mater , 1977, vol. 64, pp. 289–299.
Radford, K., et al., US Patent 4430276, 1984.
Basov, V.V., Metodika provedeniya ispytanii tabletok is dioksida urana na “dospekaemost’ “ (Procedure for Performance of the Tests of the Pellets made of Uranium Dioxide for Aftersinterability), Electrostal’: PO MSZ, 1994.
Google Scholar
Bakhteev, A.N., Opredelenie termicheskoi stabil’nosti geometricheskikh razmerov toplivnykh tabletok tipa “V” i “R”: Metodika vypolneniya izmerenii (Determination of Thermal Stability of Geometric Sizes for Fuel Pellets of Types “V” and “R”: Procedure of Carrying out the Measurements), Moscow: VNIINM, 1992.
Basov, V.V., Opredelenie kharacteristik termicheskoi stabil’nosti toplivnykh tabletok tipov “R”, “R-E”, “V”: Metodika (tekhnologicheskaya instruktsiya) (Determination of Characteristics of Thermal Stability of Fuel Pellets of Types “R”, “R-E”, and “V”: Procedure (Technological Instruction), Electrostal’: OAO MSZ, 1999.
Kotel’nikov, R.B., Bashlykov, S.N., Kashtanov, A.I., et al., Vysokotemperaturnoe yadernoe toplivo (HighTemperature Nuclear Fuel), Moscow: Metallurgiya, 1978.
Download references
Author information
Authors and affiliations.
OAO Machine Building Works, ul. K. Marksa 12, Elektrostal’, Moscow oblast, 144001, Russia
V. V. Basov
You can also search for this author in PubMed Google Scholar
Additional information
Original Russian Text © V.V. Basov, 2009, published in Izvestiya VUZ. Poroshkovaya Metallurgiya i Funktsional’nye Pokrytiya, 2009, No. 3, pp. 27–30.
About this article
Basov, V.V. Comparative investigations of aftersintering of UO 2 fuel pellets. Russ. J. Non-ferrous Metals 51 , 173–176 (2010). https://doi.org/10.3103/S1067821210020185
Download citation
Published : 06 May 2010
Issue Date : April 2010
DOI : https://doi.org/10.3103/S1067821210020185
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- fuel pellets
- model of fuel compaction
- repeated thermal treatment
- aftersintering
- aftersinterability
- procedure of carrying out aftersintering
- aftersintering installation
- stoichiometric composition
- isothermal sintering
- thermal shrinkage
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
The Sixth Edition of the bestselling Research Design: Qualitative, Quantitative, and Mixed Methods Approaches provides clear and concise instruction for designing research projects or developing research proposals. This user-friendly text walks readers through research methods, from reviewing the literature to writing a research question and stating a hypothesis to designing the study.
This bestselling text pioneered the comparison of qualitative, quantitative, and mixed methods research design. For all three approaches, John W. Creswell and new co-author J. David Creswell include a preliminary consideration of philosophical assumptions; key elements of the research process; a review of the literature; an assessment of the use of theory in research applications, and ...
The Third Edition of John W. Creswell's best-selling Research Design enables readers to compare three approaches to research—qualitative, quantitative, and mixed methods—in a single research methods text. The book examines these methodologies side by side within the process of research, from the beginning steps of philosophical assumptions to the writing and presenting of research. Written ...
Students, researchers, and practitioners in many fields have relied on Creswells' Research Design: Qualitative, Quantitative, and Mixed Methods Approaches for a long time as their go-to textbook on research design. The sixth edition, published in 2022, builds on the strengths of its predecessors while also addressing some of the challenges and limitations of conducting research in a complex ...
The Sixth Edition of the bestselling Research Design: Qualitative, Quantitative, and Mixed Methods Approaches provides clear and concise instruction for designing research projects or developing research proposals. This user-friendly text walks readers through research methods, from reviewing the literature to writing a research question and stating a hypothesis to designing the study.
A mixed-method approach has emerged from an integrated view of quantitative and qualitative research (Maarouf, 2019) and is acknowledged as the third methodological movement over the last two ...
For a quarter of a century, John Creswell's Research Design: Qualitative, Quantitative, and Mixed Methods Approaches had been a leader in the field of social science research methods.
Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, by John Creswell and J. David Creswell. Thousand Oaks, CA: Sage Publication, Inc. 275 pages, $67.00 (Paperback). ... Track citation; Share Share. Give access. Share full text access. ... Wiley Research DE&I Statement and Publishing Policies; Developing World Access; Help ...
"This best-selling text pioneered the comparison of qualitative, quantitative, and mixed method research design. For all three approaches, John W. Creswell and new co-author J. David Creswell include a preliminary consideration of philosophical assumptions, key elements of the research process, a review of the literature, an assessment of the use of theory in research applications, and ...
The sixth edition of the best-selling text, Research Design: Qualitative, Quantitative, and Mixed Methods Approaches by John W. Creswell and J. David Creswell, continues to provide clear and concise instruction for designing research projects or developing research proposals.This user-friendly text walks readers through research methods, from reviewing the literature to writing a research ...
This bestselling text pioneered the comparison of qualitative, quantitative, and mixed methods research design. For all three approaches, John W. Creswell and new co author J. David Creswell include a preliminary consideration of philosophical assumptions; key elements of the research process; a review of the literature; an assessment of the use of theory in research applications, and ...
A mixed methods design is useful when an exclusively quantitative or qualitative approach is inadequate to fully understand a research problem. The combined strengths of both quantitative and qualitative methods can provide the most robust results.
This article discusses the two main research traditions (quantitative and qualitative) and the differences and similarities in methods for front-line nurses. It simplifies and clarifies how the reader might enhance the rigor of the research study by using mixed methods or triangulation.
This best-selling text pioneered the comparison of qualitative, quantitative, and mixed methods research design. For all three approaches, John W. Creswell and new co-author J. David Creswell include a preliminary consideration of philosophical assumptions, key elements of the research process, a review of the literature, an assessment of the use of theory in research applications, and ...
Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 5th Edition by John W. Creswell and J. David Creswell, Los Angeles, CA: SAGE, 2018, $38.34 ...
The eagerly anticipated Fourth Edition of the title that pioneered the comparison of qualitative, quantitative, and mixed methods research design is here! For all three approaches, Creswell includes a preliminary consideration of philosophical assumptions, a review of the literature, an assessment of the use of theory in research approaches, and refl ections about the importance of writing and ...
The Sixth Edition of the bestselling Research Design: Qualitative, Quantitative, and Mixed Methods Approaches provides clear and concise instruction for designing research projects or developing research proposals. This user-friendly text walks readers through research methods, from reviewing the literature to writing a research question and stating a hypothesis to designing the study.
A systematic mixed studies review, examining research using diverse study designs, is well-suited for synthesizing existing knowledge and identifying gaps by harnessing the strengths of both qualitative and quantitative methods . Our search encompassed qualitative, quantitative, and mixed methods design to capture experiences with the role of ...
Study design. A convergent parallel mixed methods design was used for the study to facilitate a detailed inquiry into the research question and enhance the validity of any inferences made. Quantitative and qualitative data were collected concurrently but separately, with equal importance given to each.
Method: The study employed a parallel mixed methods design, with a Phase 1 qualitative stage (N = 30) and a Phase 2 quantitative stage (Model 1: N = 320; Model 2: N = 319). In both phases, participants were sexual minority men, equally stratified as those with versus without recent tanning exposure and were recruited from across the United States.
The main objective of the initial phase of the study is to identify symptom clusters. The identification of clusters is conducted using a parallel mixed-method design, incorporating both quantitative and qualitative approaches. Two quantitative and qualitative stages are conducted simultaneously and given equal importance.
This study aims to fill the gap by testing the mediating role of positive emotions (enjoyment, pride, and hope) between future L2 writing selves (ideal L2 self and ought-to L2 self) and SRL strategy use in the Chinese English as a foreign language (EFL) writing context with a mixed method design incorporating both quantitative and qualitative ...
The Challenges of Conducting Qualitative Research in Quantitative Culture: Saudi Arabia as a Case Study . Abstract . In the Kingdom of Saudi Arabia (KSA), qualitative research methods are infrequently employed, as researchers in the region are more accustomed to quantitative approaches, with a certain hesitancy to embrace qualitative methodology.
This best-selling text pioneered the comparison of qualitative, quantitative, and mixed methods research design. For all three approaches, John W. Creswell and new co-author J. David Creswell include a preliminary consideration of philosophical assumptions, key elements of the research process, a review of the literature, an assessment of the ...
Thus, this research explores experiences of parents facing perinatal loss in 2020-2021, further focusing on the pandemic's impact. Using a mixed-methods design with self-reports and qualitative interviews, this paper presents results from the quantitative protocol, involving an update and follow-up of a previous study.
The Bestselling Text is Completely Updated and Better than Ever!Praise for the Third Edition:"I have used the older edition with great success. The new one is even better." —Kathleen Duncan, University of La Verne The Third Edition of the bestselling text Research Design by John W. Creswell enables readers to compare three approaches to research—qualitative, quantitative, and mixed ...
The methods, techniques, and results of comparative studies of VVER and PWR fuel tested in the HBWR reactor (Norway) are presented. Experimental VVER fuel elements with uranium dioxide fuel were fabricated at the Machine Building Plant (MSZ) (in Elektrostal) using standard technology; the experimental PWR fuel elements were fabricated according to the model specifications. The results obtained ...
More research is required to investigate the experiences and perspectives of these additional groups. Our study had several notable strengths. First, we successfully integrated qualitative results into the design of the quantitative survey, creating an integrated mixed methods study.
The basic parameters of comparative tests of UO2 fuel pellets produced by the technology of powder metallurgy for aftersinterability using their repeated thermal treatment (aftersintering) in different gas media, namely, with and without humidification, are presented. The results of an evaluation of the level of aftersinterability of these pellets by different procedures is presented, they are ...