- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games

Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
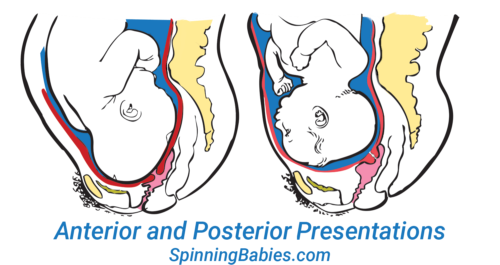
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

What happens to your baby right after birth

How your twins’ fetal positions affect labor and delivery

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Make twice the impact
Your gift can go twice as far to advance cancer research and care!

- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
- Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
- Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History
- Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Abnormal Fetal lie, Malpresentation and Malposition
Original Author(s): Anna Mcclune Last updated: 1st December 2018 Revisions: 12
- 1 Definitions
- 2 Risk Factors
- 3.2 Presentation
- 3.3 Position
- 4 Investigations
- 5.1 Abnormal Fetal Lie
- 5.2 Malpresentation
- 5.3 Malposition
The lie, presentation and position of a fetus are important during labour and delivery.
In this article, we will look at the risk factors, examination and management of abnormal fetal lie, malpresentation and malposition.
Definitions
- Longitudinal, transverse or oblique
- Cephalic vertex presentation is the most common and is considered the safest
- Other presentations include breech, shoulder, face and brow
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) – this is ideal for birth
- Other positions include occipito-posterior and occipito-transverse.
Note: Breech presentation is the most common malpresentation, and is covered in detail here .
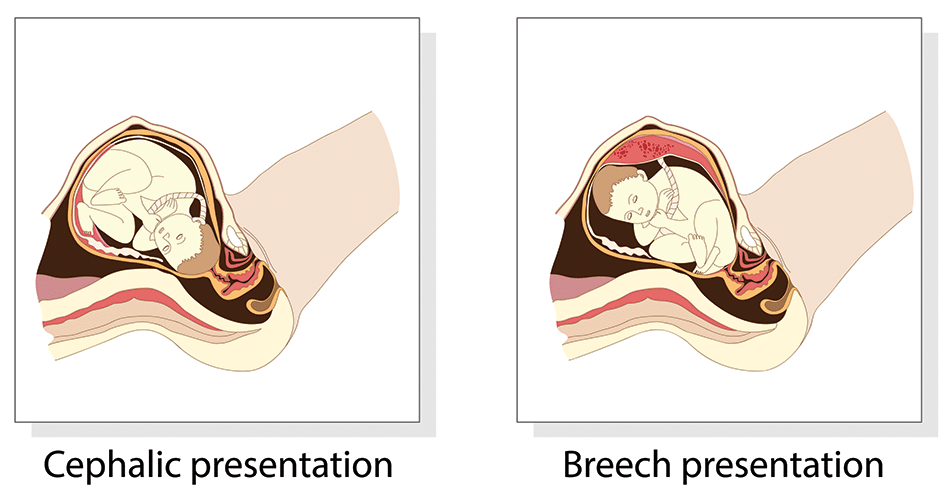
Fig 1 – The two most common fetal presentations: cephalic and breech.
Risk Factors
The risk factors for abnormal fetal lie, malpresentation and malposition include:
- Multiple pregnancy
- Uterine abnormalities (e.g fibroids, partial septate uterus)
- Fetal abnormalities
- Placenta praevia
- Primiparity
Identifying Fetal Lie, Presentation and Position
The fetal lie and presentation can usually be identified via abdominal examination. The fetal position is ascertained by vaginal examination.
For more information on the obstetric examination, see here .
- Face the patient’s head
- Place your hands on either side of the uterus and gently apply pressure; one side will feel fuller and firmer – this is the back, and fetal limbs may feel ‘knobbly’ on the opposite side
Presentation
- Palpate the lower uterus (above the symphysis pubis) with the fingers of both hands; the head feels hard and round (cephalic) and the bottom feels soft and triangular (breech)
- You may be able to gently push the fetal head from side to side
The fetal lie and presentation may not be possible to identify if the mother has a high BMI, if she has not emptied her bladder, if the fetus is small or if there is polyhydramnios .
During labour, vaginal examination is used to assess the position of the fetal head (in a cephalic vertex presentation). The landmarks of the fetal head, including the anterior and posterior fontanelles, indicate the position.
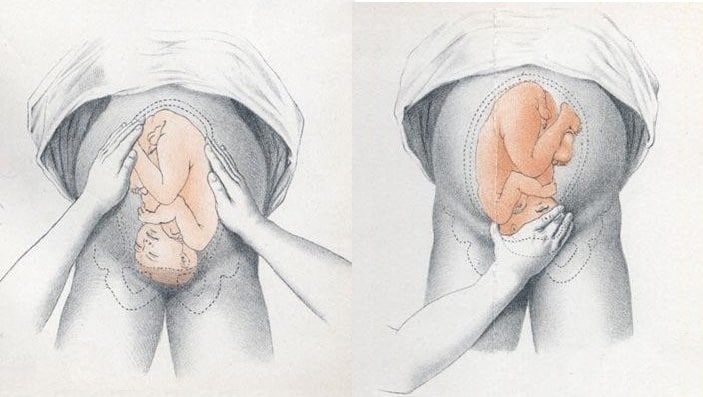
Fig 2 – Assessing fetal lie and presentation.
Investigations
Any suspected abnormal fetal lie or malpresentation should be confirmed by an ultrasound scan . This could also demonstrate predisposing uterine or fetal abnormalities.
Abnormal Fetal Lie
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted – ideally between 36 and 38 weeks gestation.
ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen.
It has an approximate success rate of 50% in primiparous women and 60% in multiparous women. Only 8% of breech presentations will spontaneously revert to cephalic in primiparous women over 36 weeks gestation.
Complications of ECV are rare but include fetal distress , premature rupture of membranes, antepartum haemorrhage (APH) and placental abruption. The risk of an emergency caesarean section (C-section) within 24 hours is around 1 in 200.
ECV is contraindicated in women with a recent APH, ruptured membranes, uterine abnormalities or a previous C-section .
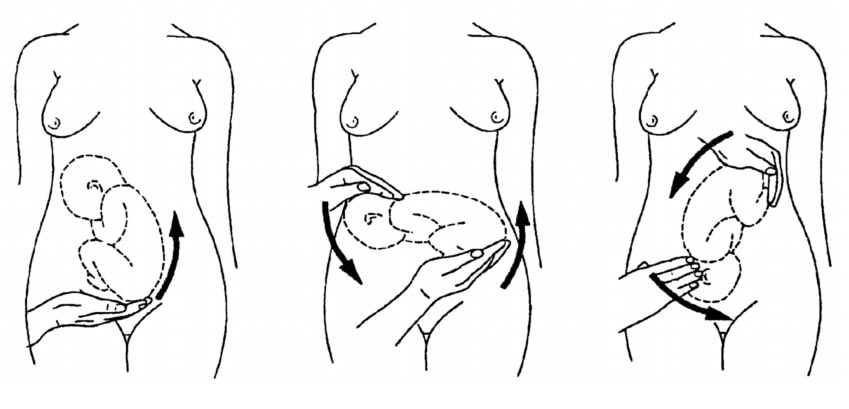
Fig 3 – External cephalic version.
Malpresentation
The management of malpresentation is dependent on the presentation.
- Breech – attempt ECV before labour, vaginal breech delivery or C-section
- Brow – a C-section is necessary
- If the chin is anterior (mento-anterior) a normal labour is possible; however, it is likely to be prolonged and there is an increased risk of a C-section being required
- If the chin is posterior (mento-posterior) then a C-section is necessary
- Shoulder – a C-section is necessary
Malposition
90% of malpositions spontaneously rotate to occipito-anterior as labour progresses. If the fetal head does not rotate, rotation and operative vaginal delivery can be attempted. Alternatively a C-section can be performed.
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) - this is ideal for birth
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation.
- Breech - attempt ECV before labour, vaginal breech delivery or C-section
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Presentation and position of baby through pregnancy and at birth
9-minute read
If you are concerned about your baby’s movements, contact your doctor or midwife for advice immediately.
- If you baby is in a breech presentation, your doctor may recommend trying a technique called an external cephalic version to try and move your baby while they are still in the uterus for an easier birth.
What does presentation and position mean?
Presentation refers to the part of your baby’s body that is facing downwards in the direction of the birth canal.
Position refers to where your baby’s occiput (the bottom part of the back of their head) is in relation to your body.
If your baby is in a breech presentation , then position refers to where your baby’s sacrum (lower back) is in relation to your body.
People — including medical professionals — sometimes use these terms incorrectly. Sometimes when speaking about babies in breech presentation, the word ‘position’ will be used to refer to their presentation. For example, you may read information or hear people say ‘breech position’ instead of ‘breech presentation’.
What are the different types of presentation my baby could be in during pregnancy and birth?
Most babies present headfirst, also known as cephalic presentation. Most babies that are headfirst will be vertex presentation. This means that the crown of their head sits at the opening of your birth canal.
In rare cases, your baby can be headfirst but in face or brow presentation, which may not be suitable for vaginal birth.

If your baby is in a breech presentation, their feet or bottom will be closest to your birth canal. The 3 most common types of breech presentation are:
- frank or extended breech — where your baby’s legs are straight up in front of their body, with their feet up near their face
- complete or flexed breech — where your baby is in a sitting position with their legs crossed in front of their body and their feet near their bottom
- footling breech — where one or both of your baby’s feet are hanging below their bottom, so the foot or feet are coming first
Read more on breech presentation .
What are the different positions my baby could be in during pregnancy and birth?
If your baby is headfirst, the 3 main types of presentation are:
- anterior – when the back of your baby’s head is at the front of your belly
- lateral – when the back of your baby’s head is facing your side
- posterior – when the back of your baby’s head is towards your back

How will I know what presentation and position my baby is in?
Your doctor or midwife can usually work out your baby’s presentation by feeling your abdomen. They may also double check it with a portable ultrasound. Your baby’s presentation is usually checked around 36 weeks .
Your doctor or midwife will also confirm your baby’s head position in labour by examining your belly and using an ultrasound , and they may also do a vaginal examination . During the vaginal examination they are feeling for certain ridges on your baby’s head called sutures and fontanelles that help them work out which way your baby is positioned.
What is the ideal presentation and position for baby to be in for a vaginal birth?
For a vaginal birth, your baby will ideally be headfirst with the back of their head at the front of your belly, also known as being in the anterior position. This position is best for labour and birth since it means that the smallest part of your baby’s head goes down the birth canal first.

When does a baby usually get in the ideal presentation and position for birth?
Your baby will usually be in a headfirst position by 37 weeks of pregnancy. Around 3 in every 100 babies will be in breech presentation after 37 weeks.
Your baby’s position can change with your contractions during labour as they move down the birth canal, so their exact position can change during labour.
What are my options if baby isn't in the ideal presentation or position for a vaginal birth?
If your baby is in a breech presentation, your doctor may recommend a technique called an external cephalic version (ECV) to try and move your baby while they are still in the uterus . An ECV involves your doctor using their hands to apply pressure on your belly and help turn your baby to a headfirst position. It has a 1 in 2 chance of success and is a safe option in most pregnancies.
There is no evidence to show that alternative therapies, such as exercises, acupuncture or chiropractic treatments, help your baby change from a breech presentation to headfirst.
If your baby remains breech, your doctor may discuss having a breech vaginal birth. Not all doctors and hospitals offer this option. They may also suggest you birth your baby with a planned caesarean section .
If your baby’s presentation is headfirst but the position of your baby’s head is not ideal for labour, it can lead to a longer labour, and potential complications . The position of your baby’s head will often change as your labour progresses. If it doesn’t, sometimes you can still give birth without assistance, or you may need your doctor to help turn your baby’s head or help your birth with a vacuum or forceps .
Any procedure or decision for a type of birth will only go ahead with your consent . You will be able to discuss all the options with your doctor, and based on your preferences for yourself and your baby’s safety, make a decision together .
Resources and support
The Royal Australian and New Zealand College of Obstetrics and Gynaecology has a factsheet about the options available to you if your baby is in a breech presentation at the end of your pregnancy .
Mercy Perinatal has information on external cephalic version (ECV) safety and benefits if your baby is in a breech presentation at the end of your pregnancy.
The Women’s Hospital has information about the different presentations and positions your baby could be in, and how it can affect your birthing experience.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: October 2023
Related pages
External cephalic version (ecv), malpresentation, breech pregnancy, search our site for.
- Foetal Version
- Breech Presentation
Need more information?
Top results
Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

When a baby is positioned bottom-down late in pregnancy, this is called the breech position. Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website

Malpresentation is when your baby is in an unusual position as the birth approaches. Sometimes it’s possible to move the baby, but a caesarean maybe safer.
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
ECV is a procedure to try to move your baby from a breech position to a head-down position. This is performed by a trained doctor.
Having a baby
The articles in this section relate to having a baby – what to consider before becoming pregnant, pregnancy and birth, and after your baby is born.
Anatomy of pregnancy and birth - pelvis
Your pelvis helps to carry your growing baby and is tailored for vaginal births. Learn more about the structure and function of the female pelvis.
Planned or elective caesarean
There are important things to consider if you are having a planned or elective caesarean such as what happens during and after the procedure.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.

When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
- Pregnancy Week By Week
- Ovulation Calculator
Malpresentation and Malposition of the Fetus
A malpresentation or malposition of the fetus is when the fetus is in any abnormal position, other than vertex (head down) with the occiput anterior or posterior.
The following are considered malpresentations or malpositions:
Unstable lie
- Transverse presentation
- Oblique presentation
Face presentation
Brow presentation
Shoulder presentation
High head at term
- Prolapsed arm
The cause of a malpresentation can often not be clearly identified but it can be associated with the following:
- Preterm pregnancy
- Uterine anomalies
- Pelvic tumors eg f ibroids
- Placenta previa
- Grandmultiparty
- Contracted maternal pelvis
- Multiple gestation
- Too much amniotic fluyid (polyhydramnios)
- Short umbilical cord
- Fetal anomalies (e.g. anencephaly, hydro-cephalus)
- Abnormal fetal motor ability
There is an increased risk of neonatal and maternal complications associated with a malpresentation including neonatal and maternal trauma. If delivery is indicated, doing a cesarean delivery can significantly decrease the risk of complications.
Transverse lie
Oblique lie
In most cases of a normal vertex (head down) presentation, the baby's head is flexed with the chin close to the baby's chest. In these cases, the presenting part is the occiput, the posterior part of the baby's head. If the baby's head is more but not completekly extended then the baby's brow presents towards the vagina. A brow presentation is rare, maybe happening in about 1 in 2,000 births, more likely in pwomen with their second or subsequent births. A baby with a brow presentation can only deliver vaginally if the head flexes or extends.
Prolapsed arm
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Why would posterior position matter in labor? The head is angled so that it measures larger. The top of the head molds less than the crown.
Baby’s spine is extended, not curled, so the crown of the head is not leading the way. Baby can’t help as much during the birth process to the same degree as the curled up baby.
Some posteriors are easy, while others are long and painful, and there are several ways to tell how your labor will be beforehand. After this, you may want to visit What to do when….in Labor .
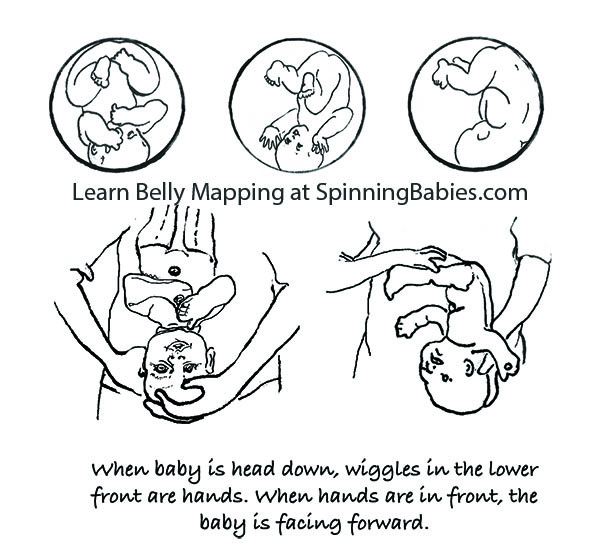
Belly Mapping ® Method tips: The Right side of the abdomen is almost always firmer, but the direct OP baby may not favor one side or the other. Baby’s limbs are felt in front, on both sides of the center line. A knee may slide past under the navel.

The OP position (occiput posterior fetal position) is when the back of the baby’s head is against the mother’s back. Here are drawings of an anterior and posterior presentation.
- When is Breech an Issue?
- Belly Mapping® Breech
- Flip a Breech
- When Baby Flips Head Down
- Breech & Bicornuate Uterus
- Breech for Providers
- What if My Breech Baby Doesn't Turn?
- Belly Mapping ®️ Method
- After Baby Turns
- Head Down is Not Enough
- Sideways/Transverse
- Asynclitism
- Oblique Lie
- Left Occiput Transverse
- Right Occiput Anterior
- Right Occiput Posterior
- Right Occiput Transverse
- Face Presentation
- Left Occiput Anterior
- OP Truths & Myths
- Anterior Placenta
- Body Balancing

Look at the above drawing. The posterior baby’s back is often extended straight or arched along the mother’s spine. Having the baby’s back extended often pushes the baby’s chin up.
Attention: Having the chin up is what makes the posterior baby’s head seem larger than the same baby when it’s in the anterior position.
Because the top of the head enters (or tries to enter) the pelvis first, baby seems much bigger by the mother’s measurements. A posterior head circumference measures larger than the anterior head circumference.
A large baby is not the same issue, however. The challenge with a posterior labor is that the top of the head, not the crown of the head leads the way.
A baby with their spine straight has less ability to wiggle and so the person giving birth has to do the work of two. This can be long and challenging or fast and furious. Also, there are a few posterior labors that are not perceived different than a labor with a baby curled on the left.
Why? Anatomy makes the difference. Learn to work with birth anatomy to reduce the challenge of posterior labor by preparing with our Three Balances SM and more.
What to do?
- Three Balances SM
- Dip the Hip
- Psoas Release
- Almost everything on this website except Breech Tilt
In Labor, do the above and add,
- Abdominal Lift and Tuck
- Other positions to Open the Brim
- Open the Outlet during pushing
There are four posterior positions
The direct OP is the classic posterior position with the baby facing straight forward. Right Occiput Transverse (ROT) is a common starting position in which the baby has a bit more likelihood of rotating to the posterior during labor than to the anterior. Right Occiput Posterior usually involves a straight back with a lifted chin (in the first-time mother). Left Occiput Posterior places the baby’s back opposite the maternal liver and may let the baby flex (curl) his or her back and therefore tuck the chin for a better birth. These are generalities, of course. See a bit more about posterior positions in Belly Mapping ® on this website. Want to map your baby’s position? Learn how with the Belly Mapping ® Workbook .
Pregnancy may or may not show symptoms. Just because a woman’s back doesn’t hurt in pregnancy doesn’t mean the baby is not posterior. Just because a woman is quite comfortable in pregnancy doesn’t mean the baby is not posterior. A woman can’t always feel the baby’s limbs moving in front to tell if the baby is facing the front.
The four posterior fetal positions
Four starting positions often lead to (or remain as) direct OP in active labor. Right Occiput Transverse (ROT), Right Occiput Posterior (ROP), and Left Occiput Posterior (LOP) join direct OP in adding labor time. The LOP baby has less distance to travel to get into an LOT position.
As labor begins, the high-riding, unengaged Right Occiput Transverse baby slowly rotates to ROA , working past the sacral promontory at the base of the spine before swinging around to LOT to engage in the pelvis. Most babies go on to OA at the pelvic floor or further down on the perineal floor.
If a baby engages as a ROT, they may go to OP or ROA by the time they descend to the midpelvis. The OP baby may stay OP. For some, once the head is lower than the bones and the head is visible at the perineum, the baby rotates and helpers may see the baby’s head turn then! These babies finish in the ROA or OA positions.
Feeling both hands in front, in two separate but low places on the abdomen, indicates a posterior fetal position. This baby is Left Occiput Posterior.
Studies estimate 15-30% of babies are OP in labor. Jean Sutton in Optimal Fetal Positioning states that 50% of babies trend toward posterior in early labor upon admission to the hospital. Strong latent labor swings about a third of these to LOT before dilation begins (in “pre-labor” or “false labor”).
Recent research shows about 50% of babies are in a posterior position when active labor begins, but of these, 3/4 of them rotate to anterior (or facing a hip in an occiput transverse, head down position.
Jean Sutton’s observations, reported in her 1996 book, indicates that some babies starting in a posterior position will rotate before arriving to the hospital. Ellice Lieberman observed most posteriors will rotate out of posterior into either anterior or to facing a hip throughout labor. Only 5-8% of all babies emerge directly OP (13% with an epidural in Lieberman’s study). At least 12% of all cesareans are for OP babies that are stuck due to the larger diameter of the OP head in comparison to the OA head. It’s more common for ROT, ROP, and OP babies to rotate during labor and to emerge facing back (OA). Some babies become stuck halfway through a long-arc rotation and some will need a cesarean anyway.
The three anterior starting positions for labor

Why not ROA? ROA babies may have their chins up and this deflexed position may lengthen the course of labor. Less than 4% of starting positions are ROA, according to a Birmingham study. This might not be ideal for first babies, but is not a posterior position either.
The spectrum of ease across posterior labors

Purchase Parent Class
Baby’s posterior position may matter in labor
With a posterior presentation, labor may or may not be significantly affected. There is a spectrum of possibilities with a posterior baby. Some women will not know they had a posterior baby because no one mentions it. Either the providers didn’t know, or didn’t notice. If labor moved along, they may not have looked at fetal position clues since there was no reason to figure out why labor wasn’t progressing. If a woman didn’t have back labor (more pain in her back than in her abdomen), the provider may not have been “clued into” baby’s position.
Some posterior babies are born in less than 8 hours and position did not slow down labor. Some posterior babies are born in less than 24 hours and position did not slow down labor enough to be out of the norm. Some posterior babies are born in less than 36-48 hours without the need for interventions.
Some posterior labors are manageable when women are mobile, supported, and eat and drink freely, as needed. Some posterior labor needs extra support that a well-trained and experienced doula may provide, but that typically a mate or loved one would not have the skills or stamina to keep up with. Some posterior labors progress only with the help of a highly-trained pregnancy bodyworker or deep spiritual, or otherwise a non-conventional model of care. Or, they seem only able to finish with medical intervention.
Some posterior labors are served by an epidural, meaning the pelvic floor relaxes enough for the baby to rotate and come out. Some epidurals, on the other hand, make it so that a woman can not finish the birth vaginally.
NOTE: Parents should know — some birth researchers, like Pediatrician John Kennell, are seriously asking whether a mother’s epidural turns off her body’s release of pain-relieving hormones which a baby relies on during childbirth. Some babies can’t turn and can’t be born vaginally and must be born by cesarean. This is a spectrum of possibilities. I’ve seen every one of the above possibilities several times and can add the wonderful experience of seeing a woman laughing pleasurably and squatting while her posterior baby slid out on to her bedroom floor.
Possible posterior effects, some women will have one or two and some will have many of these:

The forehead that overlaps the pubic bone after labor starts must turn and drop into the pelvis to allow the birth to happen naturally. A cesarean finish of the labor is possible. Look at Abdominal Lift and Tuck in Techniques to guide you to solutions for easier engagement and progress.
- Longer pregnancy (some research shows this and some doesn’t)
- The amniotic sac breaking (water breaks, membranes open, rupture of membranes) before labor (1 in 5 OP labors)
- Not starting in time before induction is scheduled
- Labor is longer and stronger and less rhythmic than expected
- Start and stop labor pattern
- The baby may not engage, even during the pushing stage
- Longer early labor
- Longer active labor
- Back labor (in some cases)
- Pitocin may be used when labor stalls (but a snoring good rest followed by oatmeal may restore a contraction pattern, too)
- Longer pushing stage
- Maybe a woman has all three phases of labor lengthened by the OP labor or one or two of the three phases listed
- Sometimes the baby’s head gets stuck turned halfway to anterior – in the transverse diameter. This may be called a transverse arrest (not a transverse lie ).
- More likely to tear
- More likely to need a vacuum (ventouse) or forceps
- More likely to need a cesarean
These effects are in comparison to a baby in the left occiput anterior or left occiput transverse fetal position at the start of labor.
Who might have a hard time with a posterior baby?
This family just had a fast posterior birth of their second child! Ease in labor includes other factors beyond baby position.
- A first-time mom
- A first-time mom whose baby hasn’t dropped into the pelvis by 38 weeks gestation (two weeks before the due date)
- A woman with an android pelvis (“runs like a boy,” often long and lanky, low pubis with narrow pubic arch and/or sitz bones close together, closer than or equal to the width of a fist)
- A woman whose baby, in the third trimester, doesn’t seem to change position at all, over the weeks. He or she kicks in the womb and stretches, but whose trunk is stationary for weeks. This mother’s broad ligament may be so tight that she may be uncomfortable when baby moves.
- A woman who has an epidural early in labor (data supports this), before the baby has a chance to rotate and come down.
- A woman who labors lying in bed
- Low-thyroid, low-energy woman who has gone overdue (this is my observation)
- A woman who lacks support by a calm and assured woman who is calming and reassuring to the birthing mother (a doula)
- A woman put on the clock
- A woman who refuses all help when the labor exceeds her ability to physically sustain her self (spilling ketones, dehydration, unable to eat or rest in a labor over X amount of hours which might be 24 for some or 48 for others)
- A woman whose birth team can’t match an appropriate technique to the needs of the baby for flexion, rotation, and/or descent from the level of the pelvis where the baby is currently at when stuck
Who is likely to have an easy time with a posterior baby?
- A second-time mom who’s given birth readily before (and pushing went well)
- A posterior baby with a tucked chin on his or her mama’s left side with a round pelvic brim
- An average-sized or smaller baby
- Someone whose posterior baby changes from right to left after doing inversions and other balancing work , though the baby is still posterior
- A woman with a baby in the Left Occiput Posterior, especially if the baby’s chin is tucked or flexed
- A woman who gets bodywork, myofascial release, etc.
- A woman whose posterior baby engages, and does not have an android (triangular) pelvis or a small outlet
- And of all of these, what is necessary is a pelvis big enough to accommodate the baby’s extra head size
- A woman who uses active birthing techniques — vertical positions, moves spontaneously and instinctively or with specific techniques from Spinning Babies ® , and other good advice
- A woman in a balanced nervous state, not so alert and “pumped up,” on guard, etc.
Any woman may also have an easier time than public opinion might indicate, too, just because she isn’t on this list. Equally, just because she is on the “hard” list doesn’t mean she will have a hard time for sure. These are general observations. They are neither condemnations nor promises. Overall, some posterior babies will need help getting born, while some posterior babies are born easily (easy being a relative term).
Let’s not be ideological about posterior labors.
While most posterior babies do eventually rotate, that can still mean there is quite a long wait – and a lot of physical labor during that wait. Sometimes it means the doula, midwife, nurse, or doctor is asking the mother to do a variety of position changes, techniques, and even medical interventions to help finish the labor. Patience works for many, but for some a cesarean is really the only way to be born. Read What To Do When…in Labor .
What causes a baby to be posterior?
There is a rising incidence of posterior babies at the time of birth. We know now that epidural anesthesia increases the rate of posterior position at the time of birth from about 4% (for women who don’t choose an epidural in a university birth setting) up to about 13% (Lieberman, 2005). Low thyroid function is associated with fetal malposition such as posterior or breech. (See Research & References .)
Most babies who are posterior early in labor will rotate to anterior once labor gets going. Some babies rotate late in labor, even just before emerging. Studies such as Lieberman’s show that at any given phase of labor, another 20% of posterior babies will rotate so that only a small number are still posterior as the head emerges.
My observations are that the majority of babies are posterior before labor. The high numbers of posterior babies at the end of pregnancy and in the early phase of labor is a change from what was seen in studies over ten years old. Perhaps this is from our cultural habits of sitting at desks, sitting in bucket seats (cars), and leaning back on the couch (slouching). Soft tissues such as the psoas muscle pair or the broad ligament also seem to be tight more often from these postures, from athletics (quick stops, jolts, and falls), from accidents, and from emotional or sexual assault.
Being a nurse or bodyworker who turns to care for people in a bed or on a table will also twist the lower uterine segment (along with some of the previously mentioned causes). This makes the baby have to compensate in a womb that is no longer symmetrical. Less often, the growing baby settles face-forward over a smaller pelvis, or a triangular-shaped pelvis (android). At the end of pregnancy, the baby’s forehead has settled onto a narrower than usual pubic bone, and if tight round ligaments hold the forehead there, the baby may have a tough time rotating. These are the moms and babies that I’m most concerned with in my work at Spinning Babies®. A baby that was breech beyond week 30 – 34 of pregnancy will flip head down in the posterior position. A woman with a history of breech or posterior babies is more likely to have a breech or posterior baby in the next pregnancy. However, she may not have an as long labor.
The best way to tell if your baby is OP or not, usually, is if you feel little wiggles in the abdomen right above your pubic bone. These are the fingers. They’d feel like little fingers wiggling, not like a big thunk or grinding from the head, though you might feel that, too. The little fingers will be playing by the mouth. This is the easiest indication of OP. The wiggles will be centered in the middle of your lower abdomen, close to the pubic bone. If you feel wiggles far to the right, near your hip, and kicks above on the right, but not near the center and none on the left, then those signal an OA or LOT baby (who will rotate to the OA easily in an active birth). After this, you might go to What to do when…in Labor.
Check out our current references in the Research & References section.

Pin It on Pinterest
Vertex Presentation: How does it affect your labor & delivery?
Medically Reviewed by: Dr. Veena Shinde (M.D, D.G.O, PG – Assisted Reproductive Technology (ART) from Warick, UK) Mumbai, India
- >> Post Created: February 11, 2022
- >> Last Updated: April 19, 2024
Vertex Position - Table of Contents
As you approach the due date for your baby’s delivery, the excitement and apprehensions are at their peak! What probably adds to the anxieties are the medical terms describing the baby, its ‘position’ and ‘presentation.’ Let’s strike that out from the list now!
In simple words, ‘ position ’ of the baby is always in reference to the mother ; on what side of the mother’s pelvis does the baby lean more (left or right) and if the baby is facing the mother’s spine or belly (anterior or posterior) – for eg.: Left Occiput Anterior , Right Occiput Anterior , Right Occiput Posterior and so on.
On the other hand, ‘ presentation’ is the body part of baby (head, shoulder, feet, and buttocks) that will enter the mother’s pelvic region first at the beginning of labor.
As ‘ presentation’ depends on the ‘ position’ of the baby, the terms cannot be used interchangeably, which is often mistakenly done. If you are told by your doctor that your baby is in a head-down position , which means its head will enter the pelvic region first , then it means the baby is in ‘vertex’ presentation or even sometimes loosely referred to as vertex position of baby though its conceptually incorrect however it means the same.
With this article, we aim to explain how exactly vertex presentation affects your labor and delivery.
Understanding Vertex Presentation
If your baby is in the head-down position by the third trimester, then you are one of the 95% mothers who have a vertex baby or a vertex delivery. When the baby enters the birth canal head first, then the top part of the head is called the ‘vertex.’
In exact medical terms, we give you the definition of vertex presentation by the American College of Obstetrics and Gynecologists (ACOG) – “a fetal presentation where the head is presenting first in the pelvic inlet.”
Besides vertex presentation (also sometimes referred to as vertex position of baby or vertex fetal position also), the other occasional presentations (non-vertex presentations) include –
- Breech – baby’s feet or buttocks are down and first to enter the mother’s pelvic region. Head is near the mother’s ribs
- Transverse – baby’s shoulder, arm or even the trunk are the first to enter the pelvis, as the baby is laying on the side and not in a vertical position
It is common that babies turn to a particular position (hence, affecting the presentation) by 34 -36 weeks of pregnancy. Nevertheless, some babies have ‘unstable lies’ ; – wherein the baby keeps changing positions towards the end of the pregnancy and not remaining in any one position for long.
Should you be worried if the baby is in vertex presentation?
Absolutely not! The vertex presentation is not only the most common, but also the best for a smooth delivery. In fact, the chances of a vaginal delivery are better if you have a vertex fetal position.
By 36 weeks into pregnancy, about 95% of the babies position themselves to have the vertex presentation. However, if your baby hasn’t come into the vertex fetal position by this time, then you can talk to your doctor about the options.
You may be suggested a cephalic version procedure also known as the version procedure /external cephalic version (ECV procedure) – which is used to turn the baby/ fetus from a malpresentation – like breech, oblique or transverse (which occur just about 3-4% times) to the cephalic position (head down).
This is how your doctor will try to turn your baby manually by pushing on your belly to get the baby into the vertex presentation. But it is necessary for you to know that this procedure does involve some risk and is successful only 60-70% of the time.
Continue reading below ↓
Read this next

Everything you need to know about Placenta Position & Placenta Health – with FAQs

The Ultimate List of Baby Must Haves

Looking for Diapers on Sale? Here’s where you can get great diaper deals on buying bulk diapers
Risks of vertex position of baby: can there be any complications for the baby in the vertex presentation.
As discussed above, the vertex fetal position/presentation is the best for labor and delivery, but there can be some complications as the baby makes its way through the birth canal. One such complication can arise if the baby is on the larger side. The baby can face difficulty while passing through the birth canal even if it is in the head-down position because of the size.
Babies who weigh over 9 to 10 pounds are called ‘ macrosomic’ or even referred to as fetal macrosomia , and they are at a higher risk of getting their shoulders stuck in the birth canal during delivery, despite being in the head-down position.
In such cases, to avoid birth trauma for the baby, the American College of Obstetricians and Gynecologists (ACOG) suggests that cesarean deliveries should be limited to estimated fetal weights of at least 11 pounds in women without diabetes and about 9 pounds in women with diabetes.
In case of fetal macrosomia, your doctor will monitor your pregnancy more often and work out a particular birth plan for you subject to your age (mothers age) and size of your baby.
How will I deliver a baby in the vertex fetal position?
Even unborn human babies can astonish you if you observe the way they make their way through the birth canal during delivery.
A vertex baby may be in the optimal position ( head-down first in pelvis) for labor and delivery, but it does its own twisting and turning while passing through the birth canal to fit through. In humans, unlike other mammals, the ratio of the baby’s head to the space in the birth canal is quite limited.
The baby has to flex and turn its head in different positions to fit through and ultimately arrive in this world. And it does so successfully! It is a wonder how they know how to do this so naturally.
And to answer the question ‘how will I deliver a baby in the vertex position?’ – Simply NATURALLY i.e. vaginal delivery. Don’t worry, follow your doctor’s instructions, do your breathing and PUSH.
FAQs to keep ready: How can my doctor help me prepare as I approach my due date?
As your due date nears, apart from bodily discomfort, you may experience nervousness about the big day. Your doctor can help by clearing your doubts and putting you at ease. You can ask them the following questions to understand the process better.
Q1) How will I know if my baby is in vertex fetal position?
A doctor can confidently tell you whether or not your baby is in the vertex presentation. Many medical professionals will be able to determine your baby’s position merely by using their hands; this is called ‘Leopold’s maneuvers.’
However, in case they aren’t very confident about the baby’s position even after this, then an ultrasound can confirm the exact position of the baby.
You can also understand this through belly mapping . You are sure to feel the kicks towards the top of your stomach and head (distinct hard circular feel) towards your pelvis.
Q2)Is there any risk of my vertex baby turning and changing positions?
Yes, in case of some women, the baby who has a vertex presentation may turn at the last moment.
What may cause this? Women who have extra amniotic fluid (polyhydramnios) have increased chances of a vertex baby turning into a breech baby at the last minute.
Discuss this with your doctor to understand what are the chances this might happen to you and what all you can do to keep the baby in the vertex presentation for delivery.
Q3) Is there need to be worried if my baby has a breech presentation?
Not really! There are loads of exercises which you which can help you get your baby in the right position.
Then there are the ECV (external cephalic version) procedure which can help in changing the position of your baby into the desired vertex position. Speak with your doctor.
Having a baby in breech position just before labor will require you to have a C-section . Let your doctor guide you. But there is nothing to worry about.
Q4) What may cause babies to come into breech position?
A few circumstances may cause the baby to come into breech position even after 36 weeks into pregnancy.
- If you are carrying twins or multiple babies , in which case there is limited space for each baby to move around.
- Low levels of amniotic fluid which restricts the free movement of the baby or even high levels of amniotic fluid that does not permit the baby to remain in any one position.
- If there are abnormalities in the uterus or other conditions like low-lying placenta or large fibroids in the lower part of the uterus.
Chances of breech babies are higher in births that are pre-term as the baby does not get enough time to flip into a head-down position – cephalic position – vertex presentation (vertex position of baby/ vertex fetal position).
Q5) Can a baby turn from breech position to vertex presentation?
Yes, a baby can turn from a breech position to vertex position / vertex fetal position over time with exercises and sometimes through ECV.
If an ultrasound has confirmed you have a breech baby, then you can do the following to turn it to a vertex baby. Try the following –
- Do not underestimate the wonders of daily walks of about 45-60 mins when it comes to bringing your baby in vertex presentation from breech presentation.
- Talk to your doctor about certain exercises that can help turn your baby in the head-down position. Exercises like ‘ high bridge’ or ‘cat and camel’ can help here. We recommend you to learn and try this only in the presence of a professional.
- External Cephalic Version (ECV ) is a way to manually maneuver the baby to vertex presentation. It is done with the help of an ultrasound and generally after 36 weeks into pregnancy. However, it has the success rate of just 50%. Discuss the risks, if any, with your gynecologist before opting for this procedure.
There are a couple of other unscientific methods that may not be safe to try –
- Light : Placing a torch near your vagina may guide the baby toward the light, and hence, get it in the vertex presentation.
- Music : Playing music near your belly’s bottom may urge the baby to move itself in the head-down position.
Q6) What all can I do to ensure I have a healthy delivery?
A healthy delivery requires the mother to be active, eating well, and staying happy. For any apprehensions regarding labor and delivery, do not hesitate to talk to your doctor and clarify your doubts.
Your doctor can help you understand your baby’s position and presentation, and then based on that they can plan your delivery to ensure your baby’s birth will happen in the safest possible way.
Try and maintain a healthy lifestyle which will also help in overall of your child and placenta health .
Key Takeaway
Yes, vertex presentation or vertex position of baby and vertex delivery are very common, normal, safe, and the best for labor and delivery of the baby. There is probability of complications sometimes, but that is only subject to certain conditions that we discussed above.
However, understand that any other baby position is also safe. The only thing with other positions and presentations is that the chances of a cesarean delivery goes up. Nevertheless, know what matters at the end of it all is a happy and healthy baby in your arms!
Happy pregnancy!
Khushboo Kirale
You may also be interested in.

Sequential Screening – Why is it so important for you to get it done?

Placenta Previa or Low Lying Placenta: How much should you be concerned?
Lateral Placenta: How does this placenta position impact pregnancy and delivery?

hCG levels twins vs. singleton – What’s the difference?

Fundal Placenta: Does Placenta on Top Make Pregnancy Difficult?
Anterior Placenta Position – How It Affects Pregnancy, Labor and Delivery
Subscribe to get our latest posts on parenting and we will make sure you don’t miss a thing!
Privacy Policy - Terms and Conditions
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection
- PMC10248753

Telehealth in the Prenatal and Postpartum Periods
The range and use of telehealth technologies in the prenatal and postpartum periods have exploded since the COVID-19 pandemic. Many of the previous barriers to telehealth have been temporarily removed, which allows for the evaluation of new flexible care models and research on telehealth applications to address pressing clinical outcomes. But what will happen if these exceptions expire? In this column, I describe the scope of telehealth technologies in the prenatal and postpartum periods, the policy changes that have contributed to this growth, and research findings and recommendations from professional organizations that support the integration of telehealth into maternity care.
The author provides current evidence on telehealth in the prenatal and postpartum periods, including new hybrid care models and the application of telehealth modalities on clinical outcomes.

Summer Sherburne Hawkins, PhD, MS
If there is a silver lining of the COVID-19 pandemic, it is the delivery of health care remotely, beyond the confines of traditional clinic settings. In one study of commercially-insured patients who gave birth ( N = 45,203), researchers found that approximately 1% of participants had a telehealth prenatal visit from 2018 through January 2020; this number rose to a high of 17.3% in November 2020 and then declined to 9.9% by October 2021 ( Acharya et al., 2023 ). These trends mirror outpatient visits via telehealth more broadly ( Lo et al., 2022 ). Is telehealth here to stay?
The prenatal and postpartum periods present unique opportunities and challenges to incorporate telehealth: increasing appointment adherence balanced against essential screening, monitoring, and treatment that is well-suited to in-person visits. These issues are even more pressing during a time of increasing maternal mortality, particularly among women of color ( Hoyert, 2023 ). Thus, it is important to review the changes in telehealth that have occurred in recent years and consider the future of telehealth for the prenatal and postpartum periods as we emerge from the COVID-19 pandemic.
The Health Resources & Services Administration (2022) defined telehealth as “the use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, health administration, and public health (para. 1).” Telehealth encompasses a broader array of services than telemedicine and includes non-clinical and clinical services. The four main types of telehealth technologies include the following: 1) live, two-way interactions used for consultative, diagnostic, and treatment services, primarily videoconferencing but also audio-only interactions; 2) store-and-forward imaging, the electronic transmission of medical information such as digital images; 3) remote patient monitoring, the electronic collection and transmission of individual health and medical data to a provider; and 4) mobile health or mHealth, health care and public health practice and education supported by mobile devices ( Health Resources & Services Administration, 2022 ; Presidential Task Force on Telehealth, 2020 ). A range of pregnancy-related services can be offered via telehealth technologies ( Society for Maternal-Fetal Medicine, 2023 ; Weigel, 2020 ). In the prenatal period, telehealth can be used for routine prenatal care, such as remote patient monitoring, screening, consultation with specialists, genetic counseling, and ultrasound reading. In the postpartum period, continuity of care can be improved through virtual follow-up visits, lactation support, and counseling on contraception. Services can also be rendered during the entire perinatal period, including screening and treatment for mental health concerns and monitoring for diabetes and hypertension.
Telehealth Before COVID-19
Telehealth services have been shown to increase access to care, particularly for populations in underserved areas and with fewer resources, and to produce comparable or better outcomes than in-person care ( DeNicola et al., 2020 ; Society for Maternal-Fetal Medicine, 2023 ; Wu et al., 2022 ). DeNicola et al. (2020) conducted a systematic review of 32 studies on the effectiveness of telehealth interventions for improving obstetric outcomes. While they did not examine birth outcomes specifically, they found that text-based interventions increased smoking cessation while text- and web-based interventions increased exclusive breastfeeding and breastfeeding continuation. In one of the included studies, a text-based intervention increased the number of blood pressure measurements in the postpartum period. Wu et al. (2022) conducted an integrative review of 13 studies on virtual prenatal care visits (articles published through 2020), including five studies in which researchers changed protocols in response to the COVID-19 pandemic; they found no differences in birth outcomes between in-person and virtual care models. They also found high patient and clinician satisfaction with telehealth services, high patient confidence in the care they received, and favorable ratings of patient-provider interactions. All five of the studies that included timelines of prenatal visits had varied schedules that ranged from five to nine in-person visits and four to six virtual visits. During the virtual appointments, patients reported their weight and blood pressure, and fetal heart rate was collected through a Doppler while the provider listened remotely ( Wu et al., 2022 ). Carrandi et al. (2023) conducted a systematic review and found some evidence that mHealth interventions during pregnancy, including a range of telehealth technologies, may be cost-effective and “low cost,” but more evidence is needed regarding the cost-effectiveness of mHealth interventions related to improvements in health outcomes and longer-term health service use.
While professional organizations have endorsed the integration of telehealth into obstetric services to increase access to services ( American College of Nurse-Midwives, 2022 ; Presidential Task Force on Telehealth, 2020 ; Society for Maternal-Fetal Medicine, 2023 ), the online nature of telehealth itself and related policies have created their own barriers ( Gajarawala & Pelkowski, 2021 ; Society for Maternal-Fetal Medicine, 2023 ). Telehealth practitioners can provide services across geographic borders, but the lack of multistate licensure limits the scope of delivery. Health care providers must comply with licensure and be appropriately credentialed to deliver services. Physicians need the necessary hardware, software, and secure internet connection to guarantee quality care, patient safety, and privacy, and technologies must be HIPAA compliant. In addition, patients need high-speed broadband internet and hardware to engage in telehealth services. Health care providers need to ensure that the patient-physician relationship is valued in the telehealth treatment plan and their practices are compliant with state laws. When information is transmitted electronically versus in-person, risks exist regarding the potential for inaccuracy of data transmission and misdiagnosis. Malpractice insurance may not cover telehealth, and health care providers need to ensure their liability insurance policies cover telehealth malpractice. Lastly, reimbursement for telehealth services is often less than in-person visits and varies by insurance providers and by state.
Telehealth During COVID-19
COVID-19 was declared a global pandemic in March 2020, and telehealth as we knew it changed almost overnight. The Centers for Medicare & Medicaid Services (2022) issued a waiver, effective March 1, 2020, to expand reimbursement for telehealth services, and many commercial insurers followed suit. To maintain access to care and social distancing, governments, states, and health insurance programs suspended restrictions on services covered and the geographic location of services, increased payment for services, changed or suspended licensing rules, allowed prescriptions based on virtual visits, eliminated cost-sharing for telehealth services, and increased reimbursement for providers ( Lo et al., 2022 ).
Not only did telehealth subsequently expand during the pandemic, but also research on telehealth on obstetric care increased precipitously. Using a database of commercially insured patients ( N = 35,112), Kern-Goldberger et al. (2023) found that telehealth visits during pregnancy increased to 17.2% in 2020, but the number of prenatal care visits did not change. The rate of severe maternal morbidities and stillbirths remained consistent over time, and the preterm birth rate decreased significantly compared to prior years. Boguslawski et al. (2022) compared prenatal care use and outcomes between patients in a telehealth-supplemented prenatal care model during the pandemic to a cohort of patients immediately before the pandemic. They found that patients in the telehealth-exposed cohort were more likely to initiate prenatal care in the first trimester and to receive recommended diabetes screening and ultrasounds; they found no differences in the number of prenatal care visits or pregnancy-related complications.
It is also important to monitor the potential unintended consequences of telehealth. In a retrospective cohort study, Zafman et al. (2023) found that women who gave birth to neonates who were small for gestational age during COVID-19 were more likely to have undetected fetal growth restriction than a cohort who gave birth to neonates who were small for gestational age before COVID-19 but had more telehealth visits and fewer fundal height measurements and growth ultrasounds. The authors suggested that additional self-assessments or third trimester ultrasounds may need to be incorporated in prenatal care schedules ( Zafman et al., 2023 ).
While national guidelines recommend a total of 12 to 14 prenatal visits throughout pregnancy ( Kilpatrick et al., 2017 ) and a comprehensive postpartum visit no later than 12 weeks after birth ( McKinney et al., 2018 ), perhaps telehealth technologies can modify this paradigm. Despite the focus on the quantity of visits, debate also exists about what constitutes adequate and quality prenatal care. Michel and Fontenot (2023) proposed that the current prenatal care structure based on the number of in-person visits without discussions of quality of care does not address barriers to access related to socioeconomic, employment, or other circumstances. New, hybrid, prenatal care models have the potential to increase uptake, but they also need to address other barriers to access, including internet and equipment availability. In a review of 42 studies, Cantor et al. (2022) found evidence that a reduced in-person prenatal care schedule supplemented with telehealth for women with low-risk pregnancies was associated with similar clinical outcomes as in-patient care and had higher patient satisfaction.
While evidence grows on the feasibility and safety of hybrid prenatal models, it is still unclear how to best deliver this modified care schedule. Peahl et al. (2021) presented guidelines for a model of care based on two principles: care related to essential services that is delivered in-person when required and video visits for other services and flexible services that allow patients to tailor support to meet their needs through opt-in programs. They developed a 4-1-4 prenatal plan that included four in-person contacts, one obstetric ultrasound, four virtual contacts, and flexible opt-in options for psychosocial support. This flexible, patient-centered care model is being evaluated. Butler Tobah et al. (2019) conducted a randomized controlled trial (RCT) to test a hybrid care model consisting of eight in-person visits, six virtual visits (phone or online communication) with fetal Doppler and sphygmomanometer home monitoring devices, and access to an online community of pregnant women versus usual care with 12 in-person prenatal visits. They found that patients in the hybrid prenatal care group had higher reported satisfaction and lower pregnancy-related stress but no differences in perceived quality of care, maternal and fetal clinical outcomes, or adherence to recommended prenatal services. The latter hybrid care model had fewer appointments but was considered more favorable by patients without compromising safety or adherence to clinical guidelines ( Butler Tobah et al., 2019 ).
The use of telehealth to address three of the most pressing maternal health outcomes in the prenatal and postpartum periods, hypertension, gestational diabetes mellitus, and mental health issues, has been a recent focus of research/ Kalafat et al. (2020) found that home blood pressure monitoring in the prenatal period was associated with reductions in prenatal visits, prenatal hospital admissions, and diagnosis of preeclampsia, with no differences in maternal, fetal or neonatal outcomes between home monitoring and conventional care. Telehealth-related interventions for monitoring, managing, and treating hypertension in the postpartum period have also expanded through innovative advances ( Kumar et al., 2022 ). Xie et al. (2020) found that telehealth interventions for pregnant women with gestational diabetes mellitus were associated with improvements in glycemic control and reductions in cesarean, macrosomia, pregnancy-induced hypertension or preeclampsia, and preterm birth compared to women in standard care. There is rising interest and an increase in research being conducted on mobile health technologies, including mobile apps, to self-manage blood glucose during pregnancy (fewer for the postpartum period) and interventions to improve clinical outcomes such as glycemic control ( Edwards et al., 2022 ). Hanach et al. (2021) found that telehealth-based interventions that were web- or phone-based were associated with improvements in symptoms of postpartum depression compared to standard care, and participants had high levels of completion and satisfaction with the technology-based interventions. Despite the widespread availability of mobile apps aimed at addressing symptoms of depression and/or anxiety in the prenatal and postpartum periods, few have been clinically tested, and among those that have, there is no evidence of their effectiveness in reducing symptoms compared to usual care ( Tsai et al., 2022 ).
While the pandemic shifted much of our health care out of necessity, it is important to consider whether providers and patients would choose to use telehealth technologies in the prenatal and postpartum periods. In a systematic review, Ghimire et al. (2023) identified 23 studies on the implications of virtual, synchronous prenatal care on the experiences, needs, and preferences for care. They found that pregnant women and health care professionals reported higher satisfaction with virtual than in-person care, and women with low- and high-risk pregnancies preferred a hybrid model of care. They also found that virtual prenatal care reduced travel time, time away from work, clinic wait time, and no-shows, actors that likely contributed to higher satisfaction. Marshall et al. (2023) surveyed women ( N = 1,978) who sought telehealth visits in the prenatal or postpartum periods during the first year of the COVID-19 pandemic. More than half of women who received care in either period had at least one telehealth visit, and among those who used telehealth, more than 80% reported a high quality of care defined as convenient, easy, safe, and with good information. In this study, approximately one-third of women reported being open to telehealth visits in the future ( Marshall et al., 2023 ). Together, these findings suggest that women and health care providers are willing to continue to use a hybrid model of virtual and in-person care in a post-COVID-19 world.
Telehealth After COVID-19
While the COVID-19 public health emergency ended on May 11, 2023, the Consolidated Appropriations Act of 2023 extended many of the telehealth flexibilities authorized during the public health emergency through December 31, 2024 ( Health Resources & Services Administration, 2023 ). The United States Centers for Medicare & Medicaid Services (2023) encouraged states to continue covering telehealth services through Medicaid, but coverage varies by state. Private health insurance coverage of telehealth also varies by commercial plan now that the public health emergency has ended. Many of the barriers to telehealth that were identified before COVID-19 will return if these measures do not extend beyond 2024 and become permanent. Health care providers must continue to be vigilant about changes in coverage of telehealth technologies across insurance providers to help their patients navigate this rapidly evolving landscape. The flexible integration of telehealth will truly support a patient-centered model of quality care in the prenatal and postpartum periods.
The exploding field of telehealth is exciting but presents challenges in synthesizing research because of the breadth of what is considered telehealth. Research is needed on emerging telehealth technologies and evaluations of hybrid care models. While not truly distinct, both streams of research will help inform the other. Ultimately, more focused reviews of the evidence will inform what technology or care model works best for what populations, for what outcome(s), and under what circumstances.
Stepping back, there is a need to document the heterogeneity of telehealth technologies and interventions and to develop and hone the scope as findings emerge. For example, a plethora of mHealth apps in mental health are available, but few have been clinically tested ( Tsai et al., 2022 ), and knowledge is limited about emerging technologies more broadly, including wearable devices and apps ( DeNicola et al., 2020 ). Rigorous evaluations, particularly through RCTs, will help evaluate the effectiveness of new technologies and modified care models on clinical outcomes, safety, and patient and provider satisfaction. A gap in research also exists regarding telehealth technologies and care models for the postpartum period, which is a critical time to facilitate continuity of care to help address maternal morbidities that continue after birth.
Put simply, telehealth emerged to increase access to care. However, inequities in maternity care exist across the United States related to geography, health insurance status, socioeconomic circumstances, and race and ethnicity, among others. Telehealth in the prenatal and postpartum periods has the potential to reduce disparities in care and clinical outcomes but needs to be thoughtfully executed to prevent increasing disparities ( Ukoha et al., 2021 ). Studies designed with a health equity lens will be critical to evaluate the availability, accessibility, and uptake of telehealth services and identify who is benefitting (and who is not). Policies can also support the equitable implementation of telehealth by mandating payment parity, expanding insurance coverage for at-home monitoring, increasing access to broadband internet, and increasing funds for telehealth research ( Presidential Task Force on Telehealth, 2020 ; Society for Maternal-Fetal Medicine, 2023 ; Ukoha et al., 2021 ). Although the idea of returning to a pre-COVID-19 era might seem appealing, it is crucial to recognize that the pandemic transformed telehealth. The adaptations and flexibilities that were introduced during the COVID-19 crisis need to be permanently implemented. If this transition takes place, it is undeniable that telehealth will become a lasting fixture in health care.
Summer Sherburne Hawkins, PhD, MS, is an associate professor, School of Social Work, Boston College, Chestnut Hill, MA.
- Acharya M., Ali M.M., Hayes C.J., Bogulski C.A., Magann E.F., Eswaran H. Trends in telehealth visits during pregnancy, 2018 to 2021. JAMA Network Open. 2023; 6 (4) https://doi:10.1001/jamanetworkopen.2023.6630 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- American College of Nurse-Midwives Position statement: The use of telehealth in midwifery. 2022. https://www.midwife.org/acnm/files/acnmlibrarydata/uploadfilename/000000000331/2022_ps-the-use-of-telehealth-in-midwifery%20.pdf
- Boguslawski S.M., Joseph N.T., Stanhope K.K., Ti A.J., Geary F.H., Boutlet S.L. Impact of the COVID-19 pandemic on prenatal care utilization at a public hospital. American Journal of Perinatology. Advance online publication. 2022. https://doi:10.1055/a-1877-7951 [ PubMed ]
- Butler Tobah Y.S., LeBlanc A., Branda M.E., Inselman J.W., Morris M.A., Ridgeway J.L., Famuyide A. Randomized comparison of a reduced-visit prenatal care model enhanced with remote monitoring. American Journal of Obstetrics and Gynecology. 2019; 221 (6):638.e1–638.e8. https://doi:10.1016/j.ajog.2019.06.034 [ PubMed ] [ Google Scholar ]
- Cantor A.G., Jungbauer R.M., Totten A.M., Tilden E.L., Holmes R., Ahmed A., McDonagh M.S. Telehealth strategies for the delivery of maternal health care: A rapid review. Annals of Internal Medicine. 2022; 175 (9):1285–1297. https://doi:10.7326/M22-0737 [ PubMed ] [ Google Scholar ]
- Carrandi A., Hu Y., Karger S., Eddy K.E., Vogel J.P., Harrison C.L., Callander E. Systematic review on the cost and cost-effectiveness of mHealth interventions supporting women during pregnancy. Women and Birth. 2023; 36 (1):3–10. https://doi:10.1016/j.wombi.2022.03.007 [ PubMed ] [ Google Scholar ]
- Centers for Medicare & Medicaid Services COVID-19 emergency declaration blanket waivers for health care providers. 2022. https://www.cms.gov/files/document/covid-19-emergency-declaration-waivers.pdf
- DeNicola N., Grossman D., Marko K., Somalkar S., Tobah Y.S.B., Ganju N., Lowery C. Telehealth interventions to improve obstetric and gynecologic health outcomes: A systematic review. Obstetrics & Gynecology. 2020; 135 (2):371–372. https://doi: 10.1097/AOG.0000000000003646 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Edwards K.J., Maslin K., Andrade J., Jones R.B., Shawe J. Mobile health as a primary mode of intervention for women at risk of or diagnosed with gestational diabetes mellitus: a scoping review. JBI Evidence Synthesis. 2022; 20 (9):2195–2243. https://doi:10.11124/JBIES-21-00294 [ PubMed ] [ Google Scholar ]
- Gajarawala S.N., Pelkowski J.N. Telehealth benefits and barriers. Journal for Nurse Practitioners. 2021; 17 (2):218–221. https://doi:10.1016/j.nurpra.2020.09.013 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ghimire S., Martinez S., Hartvigsen G., Gerdes M. Virtual prenatal care: A systematic review of pregnant women's and healthcare professionals' experiences, needs, and preferences for quality care. International Journal of Medical Informatics. 2023; 170 https://doi:10.1016/j.ijmedinf.2022.104964 [ PubMed ] [ Google Scholar ]
- Hanach N., de Vries N., Radwan H., Bissani N. The effectiveness of telemedicine interventions, delivered exclusively during the postnatal period, on postpartum depression in mothers without history or existing mental disorders: A systematic review and meta-analysis. Midwifery. 2021; 94 https://doi:10.1016/j.midw.2020.102906 [ PubMed ] [ Google Scholar ]
- Health Resources & Services Administration What is telehealth? 2022. https://www.hrsa.gov/rural-health/topics/telehealth/what-is-telehealth
- Health Resources & Services Administration . 2023. Telehealth policy changes after the COVID-19 public health emergency. https://telehealth.hhs.gov/providers/policy-changes-during-the-covid-19-public-health-emergency/policy-changes-after-the-covid-19-public-health-emergency#:∼:text=The%20Consolidated%20Appropriations%20Act%20of,Medicaid%20Services%20(CMS)%20website [ Google Scholar ]
- Hoyert D.L. National Center for Health Statistics; Health E-Stats: 2023. Maternal mortality rates in the United States, 2021. [ CrossRef ] [ Google Scholar ]
- Kalafat E., Benlioglu C., Thilaganathan B., Khalil A. Home blood pressure monitoring in the antenatal and postpartum period: A systematic review meta-analysis. Pregnancy Hypertension. 2020; 19 :44–51. doi: 10.1016/j.preghy.2019.12.001. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kern-Goldberger A.R., Sheils N.E., Ventura M.E.M., Paderanga A.J.A., Janer C.D., Donato P.R.B., Srinivas S.K. Patterns of prenatal care delivery and obstetric outcomes before and during the COVID-19 pandemic. American Journal of Perinatology. 2023; 40 (6):582–588. http://doi:10.1055/a-1960-2682 [ PubMed ] [ Google Scholar ]
- Kilpatrick S.J., Papile L., Macones G.A., Watterberg K.L. 8 th ed. American Academy of Pediatrics & American College of Obstetricians and Gynecologists; 2017. Guidelines for perinatal care. [ Google Scholar ]
- Kumar N.R., Hirshberg A., Srinivas S.K. Best practices for managing postpartum hypertension. Current Obstetrics and Gynecology Reports. 2022; 11 (3):159–168. https://doi:10.1007/s13669-022-00343-6 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lo J., Rae M., Amin K., Cox C. Outpatient telehealth use soared early in the COVID-19 pandemic but has since receded. 2022. https://www.healthsystemtracker.org/brief/outpatient-telehealth-use-soared-early-in-the-covid-19-pandemic-but-has-since-receded/
- Marshall C., Gutierrez S., Hecht H., Logan R., Kerns J., Diamond-Smith N. Quality of prenatal and postpartum telehealth visits during COVID-19 and preferences for future care. American Journal of Obstetrics and Gynecology Global Reports. 2023; 3 (1) https://doi:10.1016/j.xagr.2022.100139 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McKinney J., Keyser L., Clinton S., Pagliano C. ACOG committee opinion no. 736: Optimizing postpartum care. Obstetrics & Gynecology. 2018; 132 (3):784–785. http://doi:10.1097/AOG.0000000000002849 [ PubMed ] [ Google Scholar ]
- Michel A., Fontenot H. Adequate prenatal care: An integrative review. Journal of Midwifery & Women’s Health. 2023; 68 (2):233–247. https://doi:10.1111/jmwh.13459 [ PubMed ] [ Google Scholar ]
- Peahl A.F., Howell J.D. The evolution of prenatal care delivery guidelines in the United States. American Journal Obstetrics and Gynecology. 2021; 224 (4):339–347. https://doi:10.1016/j.ajog.2020.12.016 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Presidential Task Force on Telehealth Implementing telehealth in practice: ACOG committee opinion summary, number 798. Obstetrics & Gynecology. 2020; 135 (2):493–494. https://doi:10.1097/AOG.0000000000003672 [ PubMed ] [ Google Scholar ]
- Society for Maternal-Fetal Medicine, Healy, A., Davidson, C., Allbert, J., Bauer, S., Toner, L., Combs, C. A., & Patient Safety and Quality Committee. (2023). Society for Maternal-Fetal Medicine Special Statement: Telemedicine in obstetrics—quality and safety considerations. American Journal of Obstetrics & Gynecology, 228(3), B8-B17. 10.1016/j.ajog.2022.12.002 [ PubMed ] [ CrossRef ]
- Tsai Z., Kiss A., Nadeem S., Sidhom K., Owais S., Faltyn M., Lieshout R.J.V. Evaluating the effectiveness and quality of mobile applications for perinatal depression and anxiety: A systematic review and meta-analysis. Journal of Affective Disorders. 2022; 296 :443–453. https://doi:10.1016/j.jad.2021.09.106 [ PubMed ] [ Google Scholar ]
- Ukoha E.P., Davis K., Yinger M., Butler B., Ross T., Crear-Perry J., Nijagal M.A. Ensuring equitable implementation of telemedicine in perinatal care. Obstetrics & Gynecology. 2021; 137 (3):487–492. https://doi:10.1097/AOG.0000000000004276 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- U.S. Centers for Medicare & Medicaid Services CMS waivers, flexibilities, and the transition forward from the COVID-19 public health emergency. 2023. https://www.cms.gov/newsroom/fact-sheets/cms-waivers-flexibilities-and-transition-forward-covid-19-public-health-emergency
- Weigel G., Frederiksen B., Ranji U. Telemedicine and pregnancy care. 2020. https://www.kff.org/womens-health-policy/issue-brief/telemedicine-and-pregnancy-care/
- Wu K.K., Lopez C., Nichols M. Virtual visits in prenatal care: An integrative review. Journal of Midwifery & Women’s Health. 2022; 67 (1):39–52. https://doi:10.1111/jmwh.13284 [ PubMed ] [ Google Scholar ]
- Xie W., Dai P., Qin Y., Wu M., Yang B., Yu X. Effectiveness of telemedicine for pregnant women with gestational diabetes mellitus: An updated meta-analysis of 32 randomized controlled trials with trial sequential analysis. BMC Pregnancy Childbirth. 2020; 20 (1):198. https://doi:10.1186/s12884-020-02892-1 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zafman K.B., Cudjoe E., Levine L.D., Srinivas S.K., Schwartz N. Undetected fetal growth restriction during the Coronavirus Disease 2019 (COVID-19) pandemic. Obstetrics & Gynecology. 2023; 141 (2):414–417. https://doi:10.1097/AOG.0000000000005052 [ PubMed ] [ Google Scholar ]
Butler Tobah, Y. S., LeBlanc, A., Branda, M. E., Inselman, J. W., Morris, M. A., Ridgeway, J. L.,…Famuyide, A. (2019). Randomized comparison of a reduced-visit prenatal care model enhanced with remote monitoring. American Journal of Obstetrics and Gynecology, 221 (6), 638.e1-638.e8. https://doi:10.1016/j.ajog.2019.06.034
Butler Tobah et al. (2019) conducted a RCT to test a hybrid care model in pregnant women recruited from an outpatient obstetric, tertiary, academic center in the Midwest. The program, called OB Nest, consisted of eight in-person visits with an obstetric provider, six virtual visits (phone or online communication) with a nurse, fetal Doppler and sphygmomanometer home monitoring devices, and access to an online community of pregnant women. This program was tested against usual care, which consisted of 12 in-person prenatal visits with obstetric providers. They enrolled 150 pregnant women at less than 13 weeks gestation into each arm of the trial.
Butler Tobah et al. found that patients in the OB Nest group had higher reported satisfaction and lower pregnancy-related stress at 14- and 36-weeks gestation. In contrast, they found no differences in perceived quality of care, maternal and fetal clinical outcomes, and adherence to the recommended prenatal services recommended by the American College of Obstetricians and Gynecologists. The OB Nest model had fewer appointments but was considered more favorable by patients without compromising safety or adherence to clinical guidelines. The authors compared total nursing time for each study arm and found that nursing time was higher in the OB Nest group versus usual care, which may be one reason for higher patient satisfaction, but the researchers did not conduct a cost-effectiveness analysis. They acknowledged that the study population primarily consisted of White, college-educated women of high socioeconomic status. While the two study groups were comparable in terms of demographic characteristics, including race, a limitation of the study was that the authors were not able to examine differential effects of the intervention by participant demographics.
Peahl, A. F., & Howell, J. D. (2021). The evolution of prenatal care delivery guidelines in the United States. American Journal Obstetrics and Gynecology, 224 (4), 339-347. https://doi:10.1016/j.ajog.2020.12.016
Peahl et al. (2021) described the creation of a flexible, patient-centered prenatal care model for 4000 patients served by more than 150 maternity care providers at 12 ambulatory care sites. This care model was initially developed before COVID-19 but continued throughout the pandemic. With input from a variety of stakeholders, systematic literature reviews, patient surveys, and national experts, they created guidelines based on two principles: care related to essential services that is delivered in-person when required and video visits for other services and flexible services that allow patients to tailor support to meet their needs through opt-in programs. During COVID-19, they modified guidelines further as outpatient care was limited to urgent visits only. For the first principle, critical care, including ultrasounds, vaccinations, laboratory tests, and physical exams, could only be completed during in-person visits. Services were grouped based on recommended timing during pregnancy. In-person contacts focused on medical care, and virtual visits were interspersed to include screening and guidance. They developed a 4-1-4 prenatal plan that included four in-person contacts, one obstetric ultrasound, and four virtual contacts. For the second principle, they recognized that some patients want additional anticipatory guidance and psychosocial support, so they created flexible opt-in options that allowed women to attend online group sessions, private online chatrooms, and classes. This flexible, patient-centered care model is currently being evaluated for clinical outcomes and patient safety and is being modified as needed. Since the study team did not provide information on the demographics of the patient population, it remains uncertain whether and how they are addressing the requirements of underserved groups or monitoring how the model affects different populations.
Cantor, A. G., Jungbauer, R. M., Totten, A. M., Tilden, E. L., Holmes, R., Ahmed,…McDonagh, M. S. (2022). Telehealth strategies for the delivery of maternal health care: A rapid review. Annals of Internal Medicine, 175 (9), 1285-1297. https://doi:10.7326/M22-0737
Cantor et al. (2022) conducted a rapid review of the effectiveness and harms of telehealth strategies based on telehealth strategies, particularly on those that arose during the COVID-19 pandemic. They identified 28 RCTs and 14 observational studies published from January 2015 through April 2022. The authors summarized findings on the following clinical outcomes: mental health issues; general maternal care; gestational diabetes hypertension, and weight gain; breastfeeding; smoking cessation; and asthma. Cantor et al. found that a reduced in-person prenatal care schedule supplemented with telehealth for women with low-risk pregnancies was associated with similar clinical and obstetric outcomes as in-patient care. They found that telehealth use across a range of modalities was studied most extensively to treat postpartum depression, monitor diabetes or hypertension during pregnancy, or as an alternative to prenatal care visits during COVID-19. The authors noted higher patient satisfaction with telehealth overall across all clinical outcomes.
Cantor et al. (2022) recognized a number of limitations to the current evidence base. First, the authors noted that none of the studies specifically evaluated access to care or the effects of the interventions on health disparities. Second, researchers in only a few studies examined the use of telehealth in specific clinical areas, including gestational hypertension, breastfeeding, smoking cessation, gestational weight gain, and asthma, which suggests that more research is needed. Third, the authors noted that few studies reported potential harms of telehealth, defined as missed or incorrect diagnoses or delayed treatment. Fourth, a challenge in synthesizing the findings is the heterogeneity in telehealth interventions.
DeNicola, N., Grossman, D., Marko, K., Somalkar, S., Tobah, Y. S. B., Ganju, N.,… Lowery, C. (2020). Telehealth interventions to improve obstetric and gynecologic health outcomes: A systematic review. Obstetrics & Gynecology, 135 (2), 371-372. https://doi: 10.1097/AOG.0000000000003646
DeNicola et al. (2020) conducted a systematic review in which they examined the effectiveness of telehealth interventions for improving obstetric outcomes. They identified 32 articles published through 2017. In 19 of the studies related to low-risk obstetrics (17 RCTs, 1 retrospective cohort study, 1 case-control study), text-based interventions increased smoking cessation while text- and web-based interventions increased exclusive breastfeeding and breastfeeding continuation. However, telehealth interventions had no effects on vaccination uptake or physical wellness (e.g., healthy eating, gestational weight gain). In 13 studies related to high-risk obstetrics (11 RCTs, 1 non-RCT, 1 retrospective cohort study), researchers reported some evidence of an increase in insulin therapy adherence but no other diabetes-related outcomes. The authors of three included studies conducted in Europe found that telehealth-related interventions reduced unscheduled visits, meaning that health-related issues were better managed, but the findings are not directly applicable to the United States context. Authors of one RCT in the United States found that a text-based intervention increased the number of blood pressure measurements in 10 days after birth.
DeNicola et al. concluded that text messaging-based interventions may be beneficial to reinforce certain health behaviors, such as smoking cessation or breastfeeding, and remote monitoring and virtual visits were associated with fewer outpatient visits likely by improving management. They also noted that RCTs are needed to test new telehealth modalities, such as wearable devices and apps. Limitations of this body of research are that researchers have not tested who may benefit from telehealth or the effects of telehealth on disparities. As many of the health behaviors and clinical outcomes examined vary by socioeconomic circumstances and race and ethnicity, it is imperative to understand whether and how the use of telehealth interventions may be shrinking these gaps.
Ghimire, S., Martinez, S., Hartvigsen, G., & Gerdes, M. (2023). Virtual prenatal care: A systematic review of pregnant women's and healthcare professionals' experiences, needs, and preferences for quality care. International Journal of Medical Informatics, 170 , 104964. https://doi:10.1016/j.ijmedinf.2022.104964
Ghimire et al. (2023) conducted a systematic review of virtual prenatal care, defined as the synchronous communication between pregnant women and health care providers, on women’s and providers’ experiences, needs, and preferences. They identified 23 articles published from 2011 to 2021: 13 of the articles were published in 2020 and 2021 and 15 of the studies were conducted in the United States. Ghimire et al. found no differences in maternal and perinatal clinical outcomes, including birth weight, preterm birth, NICU admission, and mode of delivery, between virtual and in-person prenatal care. Home-based virtual prenatal care was the primary modality of hybrid care, consisting of a combination of in-person prenatal visits and virtual visits, which did not necessarily decrease the total number of visits but reduced in-person appointments. Ghimire et al. found that pregnant women and health care professionals reported higher satisfaction with virtual care, and women with low- and high-risk pregnancies preferred the hybrid model of virtual than in-person care. Virtual prenatal care reduced travel time, missed work, clinic wait time, and no-show rate. Ghimire et al. (2023) concluded that training on equipment and ease of use for the consultation system and equipment for home-based monitoring were essential.
Ghimire et al. noted the overall theme related to the importance of communication and technology. While the flexibility of virtual care was preferable, available and seamless technology and equipment were necessary to access care. Video conferencing was preferred, but audio-only virtual care was acceptable for women when necessary. A strength of this review is the inclusion of studies on the practical aspects of telehealth, including internet access and equipment. Patient-provider communication and adequate systems are necessary to support the continuity of care between virtual and in-person appointments. Limitations of the selected studies included small sample sizes and the inability to examine differences by subgroups.
Wu, K. K., Lopez, C., & Nichols, M. (2022). Virtual visits in prenatal care: An integrative review. Journal of Midwifery & Women’s Health, 67 (1), 39-52. https://doi:10.1111/jmwh.13284
Wu et al. (2022) conducted an integrative review of virtual prenatal care visits on patient, health care provider, and organizational experiences. They identified 13 articles (11 studies conducted in the United States) published from 2010 through 2020. In five of the included studies, models were changed in response to the COVID-19 pandemic. The studies had varying methodological designs: most were observational studies, and eight focused on low-risk pregnancies or did not specify risk. Wu et al. noted that among the studies that compared outcome between care models, the authors reported no differences in clinical outcomes, including screening for depression, cesarean, and birth weight, between in-person and virtual visit care models.
Wu et al. also found high patient and clinician satisfaction with telehealth services, in patient confidence in the care they received, and favorable ratings of patient-provider interactions. Patients also appreciated time and cost savings from not having to take time off work or find childcare. The authors found that overall clinic wait times, missed appointments, and cancellations decreased, but no differences were reported in one study. Patients and providers noted the need for training, access to technology, and familiarity with online platforms. Patients and providers expressed limited negative feedback about telehealth, but any difficulties were generally related to discomfort or malfunctions with technology.
In all five of the studies that included timelines of prenatal visits, authors reported varied schedules that ranged from five to nine in-person visits and four to six virtual visits. In seven studies in which researchers described the components of the virtual appointments, patients reported their weight and blood pressure, and fetal heart rate was collected through a Doppler while the provider listened remotely. Laboratory testing and ultrasound were performed during in-patient visits.
Wu et al. noted there was limited research on virtual prenatal care visits related to community-level and policy-related factors. The authors suggest one example could be addressing limited community access to the internet by testing the feasibility and acceptance of audio-only visits. Another example is examining the role of insurance coverage on choice and flexibility with hybrid prenatal care models. While there was a health equity focus in this review, it was not noted whether the researchers specifically examined the differential effect of interventions or how experiences with telehealth varied across subgroups.
Professional Resources
American Academy of Pediatrics. Curfman, A. L., Hackell, J. M., Herendeen, N. E., Alexander, J. J., Marcin, J. P., Moskowitz, W. B.,…Committee on Pediatric Workforce. (2021). Telehealth: Improving access to and quality of pediatric health care. Pediatrics, 148 (3), e2021053129. https://doi:e2021053129. 10.1542/peds.2021-053129
This policy statement included an emphasis on the role of telehealth in improving access and quality of care and services, particularly for under-resourced populations. While the focus is on telehealth for the pediatric population, care for women and infants after birth includes providers across the obstetric and pediatric periods. A series of recommendations is included: 1) Telehealth can increase health equity by expanding access to services; 2) Telehealth can increase access to medical and surgical specialties; 3) Payment parity will allow providers and patients to decide on the most appropriate services regardless of location; 4) Telehealth within the medical home offers continuity of care; 5) Standards of quality should apply equally to telehealth and in-person visits; 6) Geographical, economic, and administrative barriers to telehealth must be addressed to increase access to and continuity of care; 7) Lack of high-speed broadband internet access and adequate equipment are essential to deliver services via telehealth to reduce health care disparities; 8) Research is needed to develop the evidence base on best practices, workforce needs, patient access, quality of care, reduction of costs, and patient/provider satisfaction. These recommendations are not specific to pediatric care and relevant to telehealth more broadly.
American College of Nurse-Midwives. American College of Nurse-Midwives. (2022). Position statement: The use of telehealth in midwifery. https://www.midwife.org/acnm/files/acnmlibrarydata/uploadfilename/000000000331/2022_ps-the-use-of-telehealth-in-midwifery%20.pdf
The American College of Nurse-Midwives recommended the “blending” of traditional care and telehealth, particularly in response to the COVID-19 pandemic, and highlighted the benefits and challenges of telehealth. The use of telehealth should be based on patient preference and access; informed consent, privacy, and confidentiality are paramount; and informed consent and decision-making about the use of telehealth must be communicated to patients. The American College of Nurse-Midwives also presented a series of telehealth-related practice issues; highlighted the need for increased access to high speed internet and HIPAA-compliant platforms; and addressed issues related to licensure, insurance reimbursement, and malpractice insurance.
American College of Obstetricians and Gynecologists. Presidential Task Force on Telehealth. (2020). Implementing telehealth in practice: ACOG committee opinion summary, number 798. Obstetrics & Gynecology, 135 (2), 493-494. https://doi: 10.1097/AOG.0000000000003672
The American College of Obstetricians and Gynecologists (ACOG) endorsed the integration of telehealth into obstetrics and gynecology as technologies that “enhance, not replace, the current standard of care” (abstract). In this committee opinion, ACOG provided a series of recommendations and conclusions related to telehealth. First, obstetrician-gynecologists and other physicians should become familiar with new telehealth technologies. Second, physicians, nurses, and other health care providers must comply with licensure and be appropriately credentialed to deliver services. Third, physicians should have clear guidelines from insurance providers about coverage for telehealth visits and services. Fourth, the patient-physician relationship should be valued in the telehealth treatment plan, and physicians should ensure their practices are compliant with state laws. Fifth, physicians should request proof in writing that their liability insurance policies cover telehealth malpractice. Lastly, physicians should have the necessary hardware, software, and secure internet connection to guarantee quality care and patient safety; sites and equipment should be assessed; and physicians who provide telehealth must be HIPAA compliant.
Although the committee opinion was published in February 2020, ACOG provided a summary of considerations for telehealth that are relevant today. Obstetrician-gynecologists should know the law related to telehealth, ensure security through HIPAA compliance, check licensure requirements and credentialing and privileging , check reimbursement for telehealth services, ensure connectivity and a secure internet connection, and obtain malpractice insurance for telehealth (emphasis from article).
Society for Maternal-Fetal Medicine. Society for Maternal-Fetal Medicine, Healy, A., Davidson, C., Allbert, J., Bauer, S., Toner, L., Combs, C. A., & Patient Safety and Quality Committee. (2023). Society for Maternal-Fetal Medicine special statement: Telemedicine in obstetrics—quality and safety considerations. American Journal of Obstetrics & Gynecology, 228 (3), PB8-B17. https://doi.org/10.1016/j.ajog.2022.12.002
The Society for Maternal-Fetal Medicine published a special statement on telemedicine in obstetrics in which applications of telemedicine for obstetric care and the current evidence on the safety and quality of telemedicine for pregnancy-related services were summarized. With regards to the prenatal and postpartum periods, telehealth can be used for routine prenatal care (e.g., remote patient monitoring and universal screening for intimate partner violence), postpartum care (e.g., screening for postpartum clinical outcomes, such as mental health issues), diabetes mellitus (cell phone-enabled glucose meters integrated with electronic medical records), breastfeeding, hypertension monitoring, genetic counseling, ultrasound reading, postpartum counseling on contraception, and mental health screening and treatment.
The Society for Maternal-Fetal Medicine emphasized the importance of developing protocols and metrics to establish and monitor the quality and safety of telemedicine and noted six quality domains: 1) safe (potential for communication errors, breech of confidentiality, diagnosis inaccuracies); 2) effective (ability to monitor and modify medication regimens and to observe patients performing personal assessments); 3) patient-centered (effect on traditional clinician-patient-staff relationship); 4) timely (avoidance of delays for conditions of home monitoring that may not be available at in-person visits); 5) efficient (reduction in time and cost of travel to in-person visits); 6) equitable (access to broadband internet in the home, low digital literacy, access to language interpretation services, payment parity, health insurance coverage for at-home monitoring). The statement also included a series of potential quality metrics to evaluate telemedicine programs. Overall, there was an emphasis on evaluation and closing the feedback loop in terms of finding out what is working (and what is not), modifying protocols, and evaluating again.
Health Resources & Services Administration. Health Resources & Services Administration. (2022). Best practice guide: Telehealth for maternal health services. https://telehealth.hhs.gov/providers/best-practice-guides/telehealth-for-maternal-health-services
The Health Resources & Services Administration has published best practice guides for providers related to telehealth; one guide is specifically focused on telehealth for maternal health services. This guide includes websites with links and resources dedicated to issues related to billing, preparing patients and providers to use telehealth, telehealth for high-risk pregnancies, and care in the postpartum period.
Implications for Diversity, Equity, and Inclusion
If the telehealth flexibilities authorized during the pandemic become permanent after 2024 ( Health Resources & Services Administration, 2023 ), then many but not all of the pre-COVID-19 barriers to telehealth will be removed. In the face of a rising maternal mortality rate ( Hoyert, 2023 ), it is crucial to implement and assess telehealth technologies to prevent the exacerbation of disparities ( Ukoha et al., 2021 ). A prominent issue that gained national attention during the COVID-19 pandemic was the unequal availability of broadband internet infrastructure throughout the United States. The absence of reliable internet coverage or access to necessary equipment, coupled with limited health and digital literacy, poses a significant challenge to the potential for telehealth to increase access and reduce disparities.
Innovative telehealth programs were developed before the COVID-19 pandemic with the aim to engage marginalized populations. One of the first was the Text4baby program, which was launched in 2010 as a public-private partnership in conjunction with the U.S. Department of Health and Human Services to demonstrate the potential for mobile health technology to address maternal and infant health among underserved populations (Whittaker et al., 2012). This free texting service provides 117 prenatal messages and 147 postnatal messages that cover a range of topics, including symptoms, emotional support, health behaviors; some messages include toll-free numbers to connect women with state or local maternal and children’s health services. In the first 2 years, more than 320,000 women enrolled. Initial results indicated that 95% of women would recommend the program to a friend, and approximately 40% of all text4baby enrollees came from medically underserved areas (Whittaker et al., 2012). Subsequent evaluations have shown that more than one million women enrolled through 2016, and the has reached intended populations as enrollees were more likely to be from low-income households and live in zip codes from high poverty areas (Text4baby, 2017). Evidence also suggests that the program increased health literacy, increased appointment attendance, and improved health behaviors (Text4baby, 2017). While promising, concerns remains about continued funding and partner engagement to sustain enrollment and benefits of the program.
Other telehealth programs were created because health care was forced to change during the pandemic. Kumar et al. (2023) noted that in response to COVID-19, most postpartum visits were transitioned online via video or audio starting in mid-March 2020. In a retrospective cohort study, they found that before the pandemic, Black patients were less likely to attend the postpartum visit after birth and to participate in postpartum depression screening than non-Black patients. After implementation of virtual telehealth visits, racial differences were eliminated. In another study, Khosla et al. (2022) described a rapid switch to telehealth with audio-based visits during the pandemic for hypertension follow-up in the postpartum period. Using a similar retrospective cohort design, Khosla et al. (2022) found that hypertension follow-up via telehealth increased attendance by almost 30 percentage points for Black patients and only three percentage points for White patients, thereby removing the racial gap. However, the authors noted that Black women were still less likely to attend the general 6-week postpartum visit than White women and that appointments were offered in-person or via telehealth. Both of these studies highlight that it is essential to evaluate whether changes in care models have differential effects across marginalized populations and the extent to which they are closing gaps in care and outcomes.
In the aftermath of the pandemic, it is imperative to thoroughly examine different telehealth care models to assess their effect on maternal and infant outcomes, safety, and satisfaction. Studies need to have sufficient sample sizes to determine the effectiveness of programs and to identify variances among subgroups, including those defined by race, ethnicity, and age and the intersection of these identities. Telehealth, with its diverse range of applications, is a promising modality to increase access to care and mitigate health disparities. However, it is essential to ensure that access is not limited to certain individuals while excluding others.
Text4baby. (2017). Text4baby research and evaluation . https://www.text4baby.org/about/data-and-evaluation
Khosla, K., Suresh, S., Mueller, A., Perdigao, J. L., Stewart, K., Duncan, C.,…Rana, S. (2022) Elimination of racial disparities in postpartum hypertension follow-up after incorporation of telehealth into a quality bundle. American Journal of Obstetrics and Gynecology MFM, 4 (3), 100580. https://doi:10.1016/j.ajogmf.2022.100580
Kumar, N. R., Arias, M. P., Leitner, K., Wang, E., Clement, E. G., & Hamm, R. F. (2023). Assessing the impact of telehealth implementation on postpartum outcomes for Black birthing people. American Journal of Obstetrics and Gynecology MFM, 5 (2), 100831. https://doi:10.1016/j.ajogmf.2022.100831
Whittaker, R., Matoff-Stepp, S., Meehan, J., Kendrick, J., Jordan, E., Stange, P.,…Rhee, K. (2012). Text4baby: development and implementation of a national text messaging health information service. American Journal of Public Health, 102 (12), 2207-13. https://doi:10.2105/AJPH.2012.300736
CONFLICT OF INTEREST
The author reports no conflicts of interest or relevant financial relationships.
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
49 templates
18 templates
40 templates
american football
16 templates

41 templates
tropical rainforest
29 templates
Pregnancy Care Theme
Pregnancy care theme presentation, premium google slides theme and powerpoint template.
Pregnancy is a significant phase in a woman's life, and proper care during this period is crucial for both the mother and the baby. Fortunately for them (and for you), we have an editable template about this topic. Since you're a medical professional, we think it's the ideal choice for you to prepare a slideshow with information and tips. Thanks to the pink backgrounds and the nice illustrations, it will help convey your message with ease.
Features of this template
- 100% editable and easy to modify
- 35 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
What are the benefits of having a Premium account?
What Premium plans do you have?
What can I do to have unlimited downloads?
Don’t want to attribute Slidesgo?
Gain access to over 22600 templates & presentations with premium from 1.67€/month.
Are you already Premium? Log in
Related posts on our blog

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access

Zoo preparing for ‘baby boom’ announces fifth elephant pregnancy
WICHITA, Kan. ( KWCH /Gray News) - A zoo in Kansas already expecting an “elephant baby boom” in 2025 announced a fifth elephant is pregnant.
Last year, Sedgwick County Zoo announced that four of its elephants are expecting calves in 2025. On Wednesday, the zoo announced that a fifth is pregnant.
The first birth is expected in early spring 2025.
The zoo said all of the herd’s females except for Stephanie, who is post-reproductive, are now expecting. Among the expectant mothers, Simunye, who is the mother of Titan, a beloved male elephant at the zoo, brings maternal experience to the upcoming births. Talia, Xolani, Arusi and Zuberi are all pregnant with their first offspring.
Lauren Ripple, the elephant manager for the Sedgwick County Zoo, said the process the zoo took to end up with successful pregnancies was not easy.
“We have been trying for several years,” Ripple said. “Just like humans can have problems with fertility, we weren’t getting any pregnancies. But last year we did bring in another adult bull. He was very successful at another zoo, and we will technically have to do a paternity test since we had three bulls at one time. But it’s more than likely Callie is the dad to all these potential calves.”
The elephant care team at the zoo is prioritizing the well-being of the herd during these pregnancies. The care provided includes monitoring body condition and hormones, vitamin and mineral intake and routine bloodwork to ensure optimal health.
These pregnancies hold significance for the sustainability of African elephants in North America. With the species facing challenges in the wild, the zoo said that each birth in an Association of Zoos & Aquariums accredited institution plays a pivotal role in safeguarding the future of the species.
According to the Sedgwick County Zoo, it’s highly unlikely they’ll see twins, with the chances of that happening at less than 1%. Zoo officials said they are hoping for all healthy calves; however, they would like to have the majority be females.
“Elephants, they live in a (matriarchal) society,” Ripple said. “The female calves will live with their moms their whole lives. The bulls when they turn 8 to 12 years of age will, and when hormones start increasing, they naturally get kicked out of their herd. So, here we can mimic a bachelor herd until a certain extent, and the bulls may have to move into another facility.”
Copyright 2024 KWCH via Gray Media Group, Inc. All rights reserved.

Pastor of Our Savior Church arrested, Archdiocese of Mobile confirms

Shocking video shows young men dancing with guns in west Mobile gas station parking lot, sheriff says

Mobile PD: Burglary suspect dead after shots fired by apartment resident

Mobile PD: Woman demands that 2 people pay for her meal, shoots into occupied vehicle

Fate of 350 Jan 6 defendants, Donald Trump, in Supreme Court’s hands
Latest news.

Iran fires air defense batteries at Isfahan air base and nuclear site after drones spotted

School bus hits DMV building, injures driver and 2 students, officials say

School bus hits DMV building

Rapper GloRilla arrested for DUI

Las Vegas pre-K teacher couldn’t afford insulin and lost both legs
Mobile Menu Overlay
The White House 1600 Pennsylvania Ave NW Washington, DC 20500
A Proclamation on Black Maternal Health Week, 2024
During Black Maternal Health Week, we recommit to ending the maternal health crisis that is taking the lives of far too many of our Nation’s mothers.
Women in America are dying at a higher rate from pregnancy-related causes than women in any other developed nation. Black women face even more risk and are three times more likely to die from pregnancy-related causes than white women. That is in no small part because of a long history of systemic racism and bias. Studies show that when Black women suffer from severe injuries or pregnancy complications or simply ask for assistance, they are often dismissed or ignored in the health care settings that are supposed to care for them. People of color — including expecting mothers — also bear the brunt of environmental injustices like air and water pollution, which worsen health outcomes. Too often, Black mothers lack access to safe and secure housing, affordable transportation, and affordable, healthy food. This is unjust and unacceptable.
That is why my Administration has worked to address this crisis from the very beginning. Vice President Kamala Harris came into office as a key leader on maternal health and continues to fight for improved maternal health outcomes, elevating the issue nationally and convening experts and activists to find solutions. My Administration’s first piece of historic legislation — the American Rescue Plan — gave States the option to provide a full year of postpartum coverage to women on Medicaid, increasing it from just 60 days previously. Now, 45 States, Washington, D.C., and the United States Virgin Islands provide a full year of this critical care. We also made coverage under the Affordable Care Act more affordable, saving millions of families an average of $800 per year on health insurance premiums.
My Administration also released the Blueprint for Addressing the Maternal Health Crisis, which outlines actions the Federal Government will take to combat maternal mortality and improve maternal health. To start, we created a new “Birthing-Friendly” hospital designation that highlights hospitals and health systems that offer high-quality maternal care — ensuring that expecting mothers know where to go to get the help they need. To find out which facilities are “Birthing-Friendly,” go to medicare.gov/care-compare/.
Mental health care is health care — it is so important that women have access to it throughout pregnancy and beyond. My Administration launched the Maternal Mental Health Hotline so that the one in five women in America who experience maternal mental health conditions like depression, anxiety, or substance use disorder can get the support they need. New and expecting mothers can call 1-833-TLC-MAMA — a confidential, 24-hour, toll-free number — to connect with professional counselors. Tens of thousands of women have already taken advantage of this valuable hotline, and we know that being able to access support in times of need literally saves lives. Additionally, we are supporting and expanding maternal mental health screening programs, including for postpartum depression. We are partnering with community-based organizations to help pregnant women access services that treat substance use disorder and support victims of domestic violence.
My Administration is working to grow and diversify the maternal health workforce to better serve expecting mothers by helping health care providers hire and train physicians, certified midwives, doulas, and community health workers. I also signed legislation to ensure employers make reasonable accommodations for pregnant and nursing mothers, who deserve job security and to have their workplace rights respected by expanding the use of break time and access to private spaces for millions of nursing parents. I also remain committed to addressing the long-standing inequities that Black communities have faced and that continue to damage the health and wellness of Black mothers. For example, we have been working to end discrimination in housing, make public transit more accessible to everyone no matter where they live, expand access to healthy and affordable food, and tackle dangerous environmental injustices that take the biggest toll on families from communities of color.
There is still so much to do to ensure safety and dignity in pregnancy and childbirth. This week, we extend our gratitude to all the maternal health care workers, who are on the frontlines of this work. Together, I know that we can make America the best country in the world to have a baby.
NOW, THEREFORE, I, JOSEPH R. BIDEN JR., President of the United States of America, by virtue of the authority vested in me by the Constitution and the laws of the United States, do hereby proclaim April 11 through April 17, 2024, as Black Maternal Health Week. I call upon all Americans to raise awareness of the state of Black maternal health in the United States by understanding the consequences of institutional racism; recognizing the scope of this problem and the need for urgent solutions; amplifying the voices and experiences of Black women, families, and communities; and committing to building a world in which Black women do not have to fear for their safety, well-being, dignity, or lives before, during, and after pregnancy.
IN WITNESS WHEREOF, I have hereunto set my hand this tenth day of April, in the year of our Lord two thousand twenty-four, and of the Independence of the United States of America the two hundred and forty-eighth.
JOSEPH R. BIDEN JR.
Stay Connected
We'll be in touch with the latest information on how President Biden and his administration are working for the American people, as well as ways you can get involved and help our country build back better.
Opt in to send and receive text messages from President Biden.

Comscore's 2024 State of Digital Commerce Report
Comscore has released its annual, research-based overview of key insights and trends from 2023 on digital e-commerce, mobile shopping, social and how brands are engaging consumers throughout the consumer journey.
Download the report to see the latest analysis on emerging trends and ways that brands are leveraging a cross-platform strategy to drive total awareness and engagement.
Key takeaways include:
- Record $1.3 Trillion spend in 2023
- Desktop growth outpaced mobile growth
- Q4 2023 achieved the highest quarter since Comscore reporting began
Download Report
To get in touch with our team about this report and how we can support your e-commerce growth, click on this link .
The 2024 State of Digital Commerce report was unveiled at ARF Shopper 2024 in Chicago on April 18.
Multi-Platform Content Measurement
Comscore MMX® Multi-Platform provides an deduplicated view of total audience behavior across desktops, smartphones and tablets.
Request a demo
Multi-Platform Video Measurement
Comscore Video Metrix® Multi-Platform delivers a total view of consumer digital video consumption across desktops, smartphones, tablets and CTV devices.

IMAGES
VIDEO
COMMENTS
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. ... Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie ...
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant patient's spine) with the face and body angled to one side and the neck flexed. Abnormal presentations include face, brow, breech, and shoulder.
Malpresentation can mean your baby's face, brow, buttocks, foot, back, shoulder, arms or legs or the umbilical cord are against the cervix. It's safest for your baby's head to come out first. If any other body part goes down the birth canal first, the risks to you and your baby may be higher. Malpresentation increases the chance that you ...
Possible fetal positions can include: Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left.
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Lie - the relationship between the long axis of the fetus and the mother. Presentation - the fetal part that first enters the maternal pelvis. Position - the position of the fetal head as it exits the birth canal. Other positions include occipito-posterior and occipito-transverse. Note: Breech presentation is the most common ...
If your baby is headfirst, the 3 main types of presentation are: anterior - when the back of your baby's head is at the front of your belly. lateral - when the back of your baby's head is facing your side. posterior - when the back of your baby's head is towards your back. Top row: 'right anterior — left anterior'.
Fetal malpresentation and fetal malposition are frequently interchanged; however, fetal malpresentation refers to a fetus with a fetal part other than the head engaging the maternal pelvis. Fetal malposition in labor includes occiput posterior and occiput transverse positions. Both fetal malposition and malpresentation are associated with significant maternal and neonatal morbidity, which have ...
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
Introduction. Cephalic presentation is the most physiologic and frequent fetal presentation and is associated with the highest rate of successful vaginal delivery as well as with the lowest frequency of complications 1.Studies on the frequency of breech presentation by gestational age (GA) were published more than 20 years ago 2, 3, and it has been known that the prevalence of breech ...
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the ...
Twin pregnancy, cephalic and breech Determining fetal lie, position, presentation and attitude Follow the 4 steps of the Leopold Maneuver for abdominal palpation to determine fetal lie and presentation. Diagnose Count for 60 seconds to have the fetal heart rate bpm (beats per minute) or count for 15 seconds and multiply by 4.
By: Amos Grünebaum. Updated on March 25, 2019. A malpresentation or malposition of the fetus is when the fetus is in any abnormal position, other than vertex (head down) with the occiput anterior or posterior. The following are considered malpresentations or malpositions: Unstable lie. Breech.
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant person's spine) and with the face and body angled to one side and the neck flexed. Variations in fetal presentations include face, brow, breech, and shoulder.
In pregnancy, normal vaginal delivery is possible if the baby is in a favorable position. In clinical terms, it is called presentation. It refers to the anatomic part of the baby that first proceeds to the pelvic inlet or the birth canal. Any position other than the head down or head down with the head extended can be an unfavorable position ...
Pregnancy may or may not show symptoms. Just because a woman's back doesn't hurt in pregnancy doesn't mean the baby is not posterior. Just because a woman is quite comfortable in pregnancy doesn't mean the baby is not posterior. A woman can't always feel the baby's limbs moving in front to tell if the baby is facing the front.
Absolutely not! The vertex presentation is not only the most common, but also the best for a smooth delivery. In fact, the chances of a vaginal delivery are better if you have a vertex fetal position. By 36 weeks into pregnancy, about 95% of the babies position themselves to have the vertex presentation. However, if your baby hasn't come into ...
Telehealth Before COVID-19. Telehealth services have been shown to increase access to care, particularly for populations in underserved areas and with fewer resources, and to produce comparable or better outcomes than in-person care (DeNicola et al., 2020; Society for Maternal-Fetal Medicine, 2023; Wu et al., 2022).DeNicola et al. (2020) conducted a systematic review of 32 studies on the ...
Pregnancy Presentation templates. The day you give birth to a child is the best of your entire life. Nine months living as one, and then a lifetime of pure parent-child love! Check out these Google Slides themes & PowerPoint templates about pregnancy, obstetrics and babies. Easily customizable for everyone!
Pregnancy - Download as a PDF or view online for free. 2. Pregnancy • It is the period from fertilization to birth. • It starts when a male's sperm fertilizes a female's egg (ovum) in the woman's fallopian tube, making a (Zygote) with 46 chromosomes.
Pregnancy Care Theme Presentation . Medical . Premium Google Slides theme and PowerPoint template . Pregnancy is a significant phase in a woman's life, and proper care during this period is crucial for both the mother and the baby. Fortunately for them (and for you), we have an editable template about this topic.
Lauren Ripple, the elephant manager for the Sedgwick County Zoo, said the process the zoo took to end up with successful pregnancies was not easy.
Studies show that when Black women suffer from severe injuries or pregnancy complications or simply ask for assistance, they are often dismissed or ignored in the health care settings that are ...
Desktop growth outpaced mobile growth ; Q4 2023 achieved the highest quarter since Comscore reporting began ; Download Report. To get in touch with our team about this report and how we can support your e-commerce growth, click on this link. The 2024 State of Digital Commerce report was unveiled at ARF Shopper 2024 in Chicago on April 18.