An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Equity
- v.6(1); 2022


To Address Women's Health Inequity, It Must First Be Measured
Kathryn godburn schubert.
1 Society for Women's Health Research, Washington, District of Columbia, USA.
Chloe E. Bird
2 Tufts Medical Center, Boston, Massachusetts, USA.
3 Tufts University School of Medicine, Boston, Massachusetts, USA.
4 RAND Corporation, Santa Monica, California, USA.
Katy Kozhimmanil
5 University of Minnesota School of Public Health, Twin Cities, Minnesota, USA.
Susan F. Wood
6 George Washington University Milken Institute School of Public Health, Washington, District of Columbia, USA.
Research and data collection related to what is historically known as “women's health” is consistently underfunded and marginalizes the health risks and experiences of women of color and transgender people. In the wake of the pandemic, the United States has an opportunity to redesign and reimagine a modern public health data infrastructure that centers equity and elevates the health and well-being of under-represented communities, including the full spectrum of gender identities. This piece offers a blueprint for transformational change in how the United States collects, interprets, and shares critical data to deliver greater health justice for all.
Introduction
It is time to acknowledge that the United States needs a dramatic reset when it comes to “women's health” and how we measure it. For decades, our public health system has not only marginalized women's health but also viewed it through a flawed monolithic exclusionary lens. Research and data collection related to women's health have been consistently underfunded and excluded the health risks and lived experiences of important populations, 1 such as women of color and transgender people. In this piece, we intend to instigate a conversation on the urgent need for transformational reform in the United States public health data infrastructure that centers equity by including sex assigned at birth, gender identity, race, ethnicity, and other statuses, to achieve more inclusive health policies.
The scarcity of real-time disaggregated data—across variables such as sex and gender identity, race, ethnicity, geographic location, age, and disability—contributed 2 to the devastating toll of COVID-19 and systemic disparities in health outcomes 3 among minority and marginalized populations. The lesson is clear: we cannot fix what we do not accurately measure. This country's data infrastructure must be fundamentally redesigned to center equity and elevate the health and well-being of marginalized populations.
To address our nation's enduring and chronic data failures, the Robert Wood Johnson Foundation 4 created a National Commission to Transform Public Health Data Systems, 5 with the goal of creating recommendations 6 on how to build a modern equity-centered public health data infrastructure that helps policymakers identify problems, target interventions, and allocate resources to those most in need. Informing the Commission's deliberations were five expert panels, which examined population-specific data gaps that contribute to health inequities among American Indians/Alaska Natives, Black people/African Americans, lesbian, gay, bisexual, transgender, queer or questioning, intersex, asexual, and more (LGBTQ+) communities, people living with disabilities, and women.
The women expert panel 7 was tasked with identifying the change needed in data systems to achieve greater sex and gender equity in health outcomes among women. Recognizing the intersectionality among population-specific groups, panelists were selected across race, ethnicity, sex, gender identity, lived experiences, geographic location and backgrounds in women's health research, policy, maternal, and public health. Collectively, participants represented perspectives from government and nongovernment sectors, and public and nonpublic health systems. Central to this expert panel's deliberations were in-depth discussions and analysis of the glaring gaps in women's health equity, across a span of intersecting identities, stemming from the historic lack of inclusion of women in health research and the dearth of accurate, disaggregated sex, and gender data.
We reference studies examining differences between women and men. Most include only cisgender people and/or were not clear as to whether transgender people were included. When we refer to “transgender people,” we mean transgender women and men. Furthermore, we acknowledge the consequences gender identity goes beyond how a person identifies, and includes multiple factors such as access to resources, roles and practices, norms, beliefs, decision-making power and autonomy, laws, policy, and institutions. 8
The Impact of Data Failures on Women's Health Equity
The pandemic provided a stark reminder of how the intersectionality of race, gender identity, and social determinants of health factor into a person's risk for poor health and disease-related outcomes. Although data found that more men than women 9 in the United States died from the COVID-19 virus, critical variables such as race and line of work obscure the risk of death for women from certain communities. * Studies in Georgia and Michigan showed the COVID death rate for Black women three times as high 10 as that for White and Asian men, with disparities further exacerbated by the lack of uniform reporting of race/ethnicity in COVID-19 studies. 11 Without examining the intersections of race and gender, researchers stated, “the blanket claim that women with COVID-19 fare better than men, makes invisible the high death rate among Black women.” *
Women hold 76% 12 of the nation's health care jobs and account for the vast majority of frontline service workers, 13 making them especially vulnerable to exposure. In addition, they are four times more likely 14 to suffer from long COVID. * Alongside longer lifespans 15 and different comorbidities, the ramifications from COVID infections could potentially be more severe and costly for women over time. Without tracking and measuring these data points, we cannot fully understand who is at the greatest risk and the potential lifelong debilitating impacts.
Cisgender women—especially women of color—have been historically and contemporarily to be excluded from biomedical research. Only as recently as 2016 did the National Institutes of Health (NIH) institute a policy that sex as a biological variable be factored into its funded research. This policy aimed to ensure that differences according to sex assigned at birth are considered, but one unintended effect is erasure of transgender people in research. Research institutes and organizations continue to consistently underfund research 16 on women, even when it comes to diseases that have the greatest impact on women's health. A recent analysis of NIH research funding patterns reveals there are roughly three times as many diseases 17 as female-favored diseased in the NIH portfolio.
Furthermore, male-favored diseases are significantly more likely to be overfunded and female-favored diseases more likely to be underfunded. * Nationwide, only one-third 18 of cardiovascular disease clinical trial subjects are assigned female at birth, despite the fact that it is the number one killer of women in the United States. * These glaring inequities are all the more irrational considering the immense societal return on investment that could be achieved through greater women's health research. Another study 19 examining NIH's 2019 funding decisions revealed that a mere 4.5% of funding on coronary artery disease (CAD) addressed questions related to how the disease impacts women, but that doubling NIH funding for research on CAD in women would produce a return on investment of 9500% over 30 years. *
Gender, race, and age biases persist in clinical trials for life-saving vaccines and drugs. Although the FDA's 2020 Drug Trials Snapshots 20 report shows that women made up >50% of drug trial participants, overall—among both women and men—only 8% of all trial participants were Black or African American, 11% were Hispanic, and 30% were over the age of 65. Pregnant people were excluded from COVID vaccine trials, leading to vaccine hesitancy 21 among this population—even though global studies 22 showed that they face significantly higher mortality rates from COVID-19. Unfortunately, it is difficult to determine the true extent of health inequities and impact of the pandemic due to the lack of data on minorities and marginalized populations, including cisgender women of color and transgender people.
Standardizing Data Collection Around Sex and Gender Identity
Developing intentional consistent definitions of sex and gender data and establishing routine data collection are essential to identifying health disparities and achieving health equity. Data collection efforts must recognize evolving terminology related to the spectrum of gender identity, and the range of ways in which people—both cisgender and trans—experience health and the health care system, to capture a holistic understanding of health and its impact over time.
A 2022 report 23 from the National Academies of Sciences, Engineering, and Medicine calls on the NIH to standardize language and practices used for data collection on sex and gender, “including collecting gender data by default, and not conflating gender with sex as a biological variable.” The report argues that, in most contexts, collecting data on gender is more relevant than collecting data on sex as a biological variable, and offers the following five guiding principles 24 for data collection ( Table 1 ).
National Academies of Science, Engineering, and Medicine's Guiding Principles for data collection on sex, gender, and sexual orientation
As inclusive language practices evolve around sex and gender identity in the scientific and medical communities, we must proceed with intention on the use of language and definitions, to center equity in the approach to data collection, and to continually reassess definitions to ensure findings are correctly interpreted, shared, and compared across community-based and national data systems.
Building Women's Health Equity Through Data Systems Transformation
Research and data on women's health are inextricably linked to many facets of identity and other social determinants, impacting health outcomes. Yet our outdated data systems are ill-equipped to capture this vital information. Health care systems that are designed to routinely collect and report a standardized and comprehensive set of essential data points must be structured to allow for intersectional analysis between variables and remain nimble as data are collected over time. The ability to pull data by sex or gender identity, as well as by race, ethnicity, disability, employment, and socioeconomic status, and other variables, will help identify the biggest health gaps and prioritize areas of focus.
After thoughtful deliberations, the women expert panel reached unanimous agreement on four overarching recommendations and calls-to-action to reinvent America's public health data systems, with an eye toward women's health equity ( Table 2 ).
Recommendations and Calls-to-Action
Now is the time to widen our lens on “women's health” to include research and data across the full spectrum of gender identities, sex, race, ethnicity, and other variables to address systemic health disparities. The United States has an unprecedented opportunity—and obligation—to rebuild a modern public health data infrastructure, cemented in a foundation of equity and inclusion. The recommendations outlined earlier by the women expert panel on population-specific data gaps, convened by the Robert Wood Johnson Foundation, offer a blueprint for transformational change in how the United States collects, interprets, and shares critical data on sex and gender that is inclusive of all numerical gender minorities. This disruptive model for data systems reform has enormous potential to transform care, enhance equity, and create empowerment through better health outcomes for generations to come.
Acknowledgments
All persons who have made substantial contributions to the study reported in the article, but who do not meet the criteria for authorship, have given us their written permission to be mentioned here. The authors thank the following individuals: additional members of the women expert panel Wanda D. Barfield, MD, MPH; Juanita Chinn, PhD; Andria Cornell, MPH; Joia Crear-Perry, MD; Georgian Dukes, MHA; Janet Hamilton, MPH, Mara Kiesling; Giannina Ong, MA; and Karen Ellis, MMS Education, expert panel coordinator.
Abbreviations Used
Authors' contributions.
Conceptualization, project administration, writing—original draft, and writing—review and editing by K.G.S. Conceptualization and writing—review and editing by C.E.B., K.K., and S.F.W.
Authorship Statement
All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the study to take a public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the article. Furthermore, each author certifies that this material or similar materials has not been and will not be submitted to or published in any other publication before its appearance in Health Equity .
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Funding for the women's panel convening and findings provided by the Robert Wood Johnson Foundation.
Cite this article as: Schubert KG, Bird CE, Kozhimmanil K, Wood SF (2022) To address women's health inequity, it must first be measured , Health Equity 6:1, 881–886, DOI: 10.1089/heq.2022.0107.
* This research article uses the term “men” and “women” although they do not indicate whether this was inclusive of trans men, trans women or only cis men and cis women.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Science & Research
- Science and Research Special Topics
Women's Health Research
From the fda office of women's health.
OWH promotes and conducts research initiatives that facilitate FDA regulatory decision-making and advance the understanding of sex differences and health conditions unique to women. Learn more about women’s health research in the Women’s Health section, including links below.

About OWH research
OWH scientific programs support research, workshops, and initiatives that advance understanding of women’s health issues.

OWH-funded research
Learn more about research funded by OWH, including how to apply for extramural research funding, and a searchable list of projects.

Peer-reviewed scientific publications
OWH staff and OWH-funded researchers are working to advance the science of sex differences. View peer-reviewed publications.

Women's health education and training
Find continuing education opportunities, upcoming events, and subscribe to receive the latest information about future opportunities from OWH.
RELATED INFORMATION

Pregnancy exposure registries
Information collected can help health care providers and others who are pregnant learn more about the safety of medicines and vaccines used during pregnancy.

Bench to Bedside: Sex as a Biological Variable (SABV)
Free self-paced training on sex and gender differences that impact health, disease, and treatment, developed by OWH in collaboration with the National Institutes of Health.

Free publications for women
Download or order free copies of more than 40 fact sheets on women’s health topics.
Follow Office of Women's Health
X (formerly twitter).
Follow FDA Office of Women's Health @FDAWomen
Watch videos from Office of Women's Health on YouTube's FDA Channel
OWH Newsletter
The OWH newsletter highlights women's health initiatives, meetings, and regulatory safety information from FDA.
Paragraph Header Contact the FDA Office of Women's Health
(301) 796-9440 Phone (301) 847-8601 fax
Hours Available
Office of Women's Health
FDA Office of Women's Health Newsletter
The Office of Women's Health newsletter highlights women's health initiatives, meetings, and regulatory safety information from FDA.
- Annual Awards
- Mission and Vision
- Share Your Story
- Women’s Health Research
- Board of Directors
- Collaborations
- Partner with SWHR
- Philanthropy
- Job Opportunities
- Alzheimer’s Disease
- Endometriosis and Fibroids
- Roundtables
- Science Events
- Advisory Council
- Women’s Health Policy Agenda
- Position Statements
- Policy Letters
- Legislation
- Policy Events
- Read My Lips
- Women’s Health Equity Initiative
- Coronavirus
- Publications
- Peer-Reviewed Articles
- Guides & Toolkits
- SWHR in the News
- Read Women’s Health Stories
- Annual Awards 2024
- Annual Awards 2023
- Annual Awards 2018-2022
Home » Blog » The Evolution of Women’s Health Research
The Evolution of Women’s Health Research

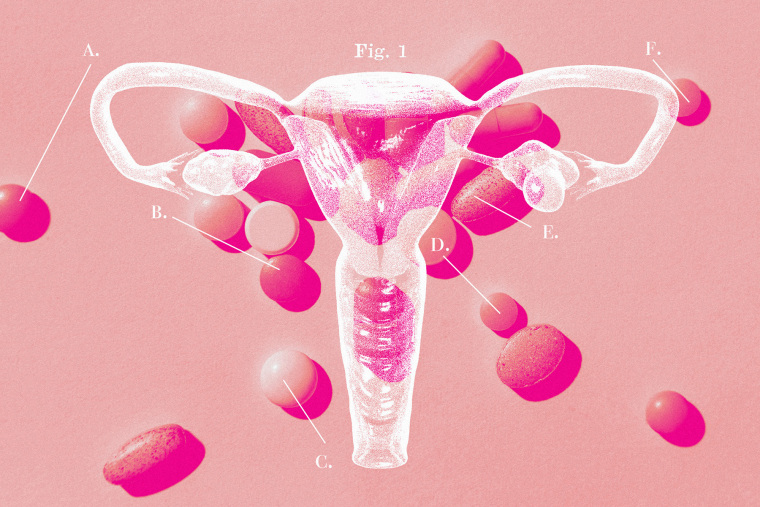
Our current understanding of women’s health research—the study of health across a woman’s lifespan in order to preserve wellness and to prevent, diagnose, and treat disease, for the full range of health conditions for which women are disproportionately or differently affected by—did not exist until about 30 years ago.
Where Women’s Health Research Started
Up until the 1990s, essentially all health research was conducted exclusively or predominantly on men and by men .
For decades, women were actively excluded from participating in most clinical trials because of the belief that female hormonal cycles were too difficult to manage in experiments and a fear that the inclusion of women in trials may harm women’s reproductive health , including potential pregnancies. Additionally, the assumption that using only one sex would reduce variation in trial results meant that research also did not incorporate female animals, cells, and tissue. Researchers, therefore, often assumed that results from all-male studies could be extrapolated to females—compromising women’s health care.
The Society for Women’s Health Research (SWHR) was founded in 1990 by Dr. Florence Haseltine to correct this balance and bring attention to the space of women’s health research. Soon after its founding, SWHR joined other advocacy groups to encourage Congress to pass the National Institutes of Health (NIH) Revitalization Act of 1993 , mandating the inclusion of women and minorities in NIH-funded clinical trials. In the same year, the Food and Drug Administration (FDA) required the inclusion of women in efficacy studies and in the analysis of data on sex differences. Two decades later, in 2016, the NIH implemented a policy stating that sex as a biological variable should be factored into preclinical research and study reporting. Today, all NIH-funded researchers must either include both female and male research subjects or explain why they do not.
Continuing to Close the Gaps
Throughout the years, SWHR has actively educated on and promoted the growth of women’s health research. SWHR helped found the Organization for the Study of Sex Differences (OSSD) in 2006 and launch the Biology of Sex Differences journal in 2010. With each new program, SWHR is helping close gaps by promoting research on biological sex differences in disease and improving women’s health through science, policy, and education:
- SWHR regularly convenes interdisciplinary stakeholders to discuss women’s health topics and identify research gaps and unmet needs for women’s health across the lifespan. For example, SWHR is hosting “ The Impact of Narcolepsy on Women’s Health Across the Lifespan”, a closed roundtable on March 31, 2022 with experts in psychiatry, sleep, pediatrics, and more, to better understand sleep conditions in women. SWHR will publish conversation insights on its blog in early April.
- SWHR continues to act as a resource for policymakers and pushes for the improved inclusion and representation of women from diverse backgrounds across all levels of science. SWHR continually responds to policy initiatives concerning women’s health, such as providing comments on the recent draft NIH Chief Officer for Scientific Workforce Diversity Strategic Plan and supporting the creation, work, and implementation of recommendations of the Task Force on Research Specific to Pregnant and Lactating Women (PRGLAC).
- SWHR serves as a trusted source for women’s health information and raises awareness about women’s health issues for women, their families, and their providers, particularly through the creation of resources, such as fact sheets, policy roadmaps, and patient toolkits. SWHR’s recent resources range from a Genetic Screening Poster made for use in health offices to a Migraine Matters Fact Sheet to help people living with migraine, 3 in 4 of whom are women.
Women’s Health Research in 2022
While SWHR has been excited to witness and support the expansion of women’s health research to new heights, much remains to be done to close knowledge and care gaps. As we celebrate International Women’s Day, SWHR remains invigorated about the task of advancing women’s health research and the prospect of improved care for women everywhere.
Recent improvements in women’s health provide encouragement for the future: expanded COVID-19 vaccine research on pregnant women, from the Centers for Disease Control and Prevention (CDC) has shown the vaccine to be safe for mothers and infants when administered during pregnancy; the Stephanie Tubbs Jones Uterine Fibroid Research and Education Act has been introduced in Congress and, if passed, will advance research and care for uterine fibroids; and the Protecting Moms Who Served Act , the first bill of the Black Maternal Health Momnibus to be enacted, was signed into law in November 2021, taking us one step closer to ending maternal mortality in the United States and closing disparities in maternal health outcomes.
This year’s International Women’s Day theme of # BreakTheBias reminds us that in working together we can eliminate bias, whether it is across the scientific workforce, in funding research awards, in health care innovation, or within scientific research and clinical trials. Together, we can achieve women’s equality and advance women’s health research for decades to come.
Join SWHR in helping make women’s health mainstream. Learn more about the history of women’s health research here and SWHR’s role in it here .
This article was also reposted on SWHR’s LinkedIn account.
Recent Posts
- Latest Updates on the White House Initiative on Women’s Health Research: Executive Order, SWHR Thank You Letter to First Lady
- Closing Gaps in Physician Endometriosis Education
- Statement from the Society for Women’s Health Research on President Biden’s 2024 State of the Union Address
- Menopause Resource Guides Aim to Create Menopause-Friendly Workplaces for All
- Menopause, Perimenopause, and Migraine
Putting science to work for the health of women
White House Establishes Women’s Health Research Initiative

The White House has announced the establishment of the Women’s Health Research Initiative within the Office of the First Lady. The initiative aims to improve women’s health in the United States by accelerating research on the unique health needs of women across their lifespans and therefore fundamentally change how we approach and fund women’s health research.
In alignment with our mission and values, ORWH is honored to serve alongside NIH and various federal agencies and offices to transform the research landscape and close gaps to improve the health of women. ORWH Director, Janine A. Clayton, M.D., FARVO states, “Women’s health research is critical to NIH’s mission to seek fundamental knowledge about the nature and behavior of living systems and to apply that knowledge to enhance health. Incorporating women’s lived experiences, identities, and other social determinants of health into the research enterprise will lead to science advancements. We look forward to collaborating with the White House to promote research that involves women across the lifespan, considers the influence of sex and gender, and fosters health equity to ensure that all women receive evidence-based disease prevention and treatment tailored to their unique needs and circumstances.”
Deputy Director for Program Coordination, Planning, and Strategic Initiatives (DPCPSI) in the NIH Office of the Director, Tara A. Schwetz, Ph.D. also states, "Tackling issues critical to understanding and supporting women's health is core to the NIH Mission. Our team looks forward to continued collaboration with the White House to advance women's health research across the biomedical enterprise."
This new initiative will be led by First Lady Jill Biden, who has long championed women’s health, and the White House Gender Policy Council. The initiative will be chaired by Dr. Carolyn Mazure, an esteemed leader in the field of women’s health research, who will coordinate the initiative on behalf of the Office of the First Lady and the Gender Policy Council. To spur innovation, unleash transformative investment to close research gaps, and to improve women's health, the President directs his Administration to:
- Establish an Initiative consisting of executive departments and agencies across the Federal government
- Deliver concrete recommendations to advance women’s health research
- Take a targeted, high-impact approach
- Engage the scientific, private sector, and philanthropic communities
Visit the White House Briefing Room for more information on the initiative and the First Lady’s remarks .
Director’s Messages
March 27, 2024
February 27, 2024
January 25, 2024
November 30, 2023
- Share full article
Advertisement
Supported by
Biden Signs Executive Order to Expand Research on Women’s Health
The president said that improving women’s health was crucial to ensuring a healthy, stable economy.
Biden Signs Executive Order to Boost Women’s Health Research
The executive order is aimed at addressing the underrepresentation of women in health research..
We’ve launched the first ever White House initiative on women’s health research to pioneer the next generation of scientific research and discovery in women’s health. Think of all the breakthroughs we’ve made in medicine across the board, but women have not been the focus. And today — [applause] today, we’re jumpstarting that investment by dedicating $200 million in the National Institutes of Health to tackle some of the most pressing health problems facing women today. With the executive order I’m about to sign, I’m directing the most comprehensive set of executive actions ever taken to improve women’s health — ever taken. And I’m going to ensure that women’s health is integrated and prioritized across the entire federal government. It’s not just in women’s health, not just at N.I.H., the National Science Foundation or the Defense Department, the Environmental Protection Agency. I mean, across the board. This is really serious.

By Zolan Kanno-Youngs
Reporting from Washington
President Biden on Monday signed an executive order to expand the federal government’s research into women’s health, including midlife conditions like menopause, arthritis and heart disease, as well as issues specifically affecting women in the military.
In what the White House described as the “most comprehensive” action by a president on women’s health research, Mr. Biden directed federal agencies to ensure that they are using federal funds to research health conditions and diseases that disproportionately affect women.
Standing alongside the first lady, Jill Biden, and Vice President Kamala Harris, Mr. Biden said improving women’s health was crucial to guaranteeing a healthy, stable economy.
“There’s not a damn thing a man can do a woman can’t do,” Mr. Biden said. “To state the obvious, if you want to have the strongest economy in the world, you can’t leave half of the country behind.”
Carolyn M. Mazure, a psychologist and a professor at the Yale School of Medicine, who is the chairwoman of the White House initiative on Women’s Health Research, told reporters on Sunday night that health conditions like heart disease, Alzheimer’s, menopause and fibroids would be a focus of the expanded research effort.
“I’m not even a betting woman,” said Maria Shriver, the former first lady of California, who also attended the event, “but I’ll bet today that this is the first time a president of the United States has ever signed an executive order that mentions the words ‘menopause’ and ‘women’s midlife health’ in it.”
After the U.S. Supreme Court overturned Roe v. Wade in 2022 and the Alabama Supreme Court ruled last month that frozen embryos should be considered children , threatening in vitro fertilization, the Biden campaign has increasingly accused Republicans of undermining women’s health. During his State of the Union address this month, Mr. Biden said such decisions would motivate women to vote in the November election, while also saying his White House would commit to investing in women’s health in the year ahead.
“You can’t lead America with old ideas and take us backwards,” Mr. Biden said, adding, “To lead the land of possibilities, you need a vision for the future laying out what we can and should do and what we’re going to do.”
Mr. Biden’s executive order will require agencies to report annually their investments in women’s health research and to study ways that artificial intelligence can be used to advance such research. The National Institutes of Health will increase by 50 percent investments in small businesses focused on women’s health. The Defense Department also plans to invest $10 million to learn more about cancers and mental health issues affecting women in active military service.
The White House has called on Congress to pass a plan to invest $12 billion to create a new fund for women’s health research at the National Institutes of Health. In the meantime, the executive order signed on Monday directed the N.I.H. to spend $200 million on women’s health research. Dr. Biden traveled to Cambridge, Mass., last month to announce the first step of the women’s health initiative: $100 million to support women’s health researchers and start-up companies.
Zolan Kanno-Youngs is a White House correspondent, covering President Biden and his administration. More about Zolan Kanno-Youngs
- Open access
- Published: 01 April 2024
Midwives’ lived experiences of caring for women with mobility disabilities during pregnancy, labour and puerperium in Eswatini: a qualitative study
- Annie M. Temane 1 ,
- Fortunate N. Magagula 2 &
- Anna G. W. Nolte 1
BMC Women's Health volume 24 , Article number: 207 ( 2024 ) Cite this article
Metrics details
Midwives encounter various difficulties while aiming to achieve excellence in providing maternity care to women with mobility disabilities. The study aimed to explore and describe midwives’ experiences of caring for women with mobility disabilities during pregnancy, labour and puerperium in Eswatini.
A qualitative, exploratory, descriptive, contextual research design with a phenomenological approach was followed. Twelve midwives working in maternal health facilities in the Hhohho and Manzini regions in Eswatini were interviewed. Purposive sampling was used to select midwives to participate in the research. In-depth phenomenological interviews were conducted, and Giorgi’s descriptive phenomenological method was used for data analysis.
Three themes emerged from the data analysis: midwives experienced physical and emotional strain in providing maternity care to women with mobility disabilities, they experienced frustration due to the lack of equipment to meet the needs of women with mobility disabilities, and they faced challenges in providing support and holistic care to women with mobility disabilities during pregnancy, labour and puerperium.
Conclusions
Midwives experienced challenges caring for women with mobility disabilities during pregnancy, labour and the puerperium in Eswatini. There is a need to develop and empower midwives with the knowledge and skill to implement guidelines and enact protocols. Moreover, equipment and infrastructure are required to facilitate support and holistic maternity care for women with mobility disabilities.
Peer Review reports
Globally, few studies have focused on midwives’ views of providing maternity care to women with mobility disabilities during pregnancy, labour and the puerperium [ 1 ]. In The Disabled World [ 2 ], the World Health Organisation (WHO) defines ‘disability’ as an umbrella term covering impairments, activity limitations, and participation restrictions. Furthermore, the WHO defines an ‘impairment’ as a problem in bodily function or structure; an ‘activity limitation’ as a difficulty encountered by an individual in executing a task or action; and ‘participation restriction’ as a problem experienced by an individual in various life situations [ 2 ]. In this study, mobility disabilities refer to an impairment in the functioning of the upper and lower extremities as experienced by women during pregnancy, labour and the puerperium.
Midwives, as frontline workers in the delivery of maternity care [ 3 ] responsible for the lives of the mother and the baby, are accountable for providing competent and holistic care for women during pregnancy, labour and puerperium. As part of healthcare provision, midwives play an important role in ensuring that every woman, including women with mobility disabilities, receives the best maternity care during pregnancy, labour and puerperium. Moridi et al. [ 4 ] state that women with mobility disabilities are entitled to feel safe, respected and well cared for by midwives, who must be sufficiently prepared to care for these women.
According to the Global Population Report, [ 5 ] more than one billion people have some form of disability. Eswatini is classified as a middle-income setting in the southern African region, measuring 17 000 square kilometres with a population of 1 093 238. Of the population, 76.2% reside in rural areas (833 472), and 23.8% (259 766) reside in urban areas [ 6 ]. The economy is largely agricultural as most industries manufacture agricultural products [ 7 ]. Of the Eswatini population, 146 554 (13%) live with disabilities, with most being women (87 258; 16%), 22,871 (14.1%) and 26,270 (14.3%) of them reside in the Hhohho and Manzini regions respectively [ 8 ]. 15% (125 545) of people with disabilities live in rural areas, and 85% of the disabled population is unemployed [ 8 ], which means most of these individuals are economically disadvantaged. Furthermore, according to the Eswatini Central Statistics Office, 8 26.5% of people with disabilities have a mobility (walking) disability, with 63.5% of these being women.
Midwives may encounter difficulties while aiming to achieve excellence in providing maternity care to women with mobility disabilities in what may be challenging circumstances [ 9 ]. The WHO [ 10 ] claims people with disabilities do not receive the health services they need and are thus likely to find healthcare providers have inadequate skills. Lawler et al. [ 11 ] argue that ineffective interactions and poor communication with women needing care, particularly among health professionals engaged in providing maternity services, limit these women’s opportunities to participate in decision-making processes during pregnancy, childbirth, and postpartum care. According to the University of Johannesburg, [ 12 ] the midwife, together with the mother, have to engage collaboratively in order to come up with opportunities to promote health while removing any challenges that could impede the achievement thereof.
Walsh-Gallagher et al. [ 13 ] postulate that healthcare professionals tend to view women with disabilities as liabilities and regard them as high risk; they often exclude them from the individualised plan of care, which leads to an increase in these women’s fears about their maternity care. These challenges frequently result in health disparities and prevent women with mobility disabilities from receiving optimal maternity care. By exploring midwives’ experiences of this phenomenon, guidelines for support can be developed to extend available knowledge on maternity care for women with mobility disabilities during pregnancy, labour and puerperium.
Study design
The aim of the study was to explore and describe midwives’ experiences of caring for women with mobility disabilities during pregnancy, labour and puerperium in the Hhohho and Manzini regions of Eswatini. A qualitative, [ 14 ] exploratory, [ 15 ] descriptive, [ 16 ] contextual [ 17 ] research design with a phenomenological approach [ 18 ] was applied for this study to gain insight and understanding of the research phenomenon [ 19 ]. The phenomenon under study was midwives’ lived experiences caring for women with mobility disabilities during pregnancy, labour and puerperium. The participants were approached face-to-face to participate in the study. The researchers followed the Consolidated Criteria for Reporting Qualitative Research (COREQ) to report on this qualitative study [ 20 ].
The setting for the study was the Hhohho and Manzini regions of Eswatini. The researcher collected data at the site where participants experienced the phenomenon, as emphasised by Yildiz, [ 21 ] within the context in which they were comfortable to be interviewed [ 22 ]. This setting included maternal health facilities in hospitals and public health units.
Population and sampling
The study’s population comprised midwives working in maternal health facilities in hospitals and public health units, that is, one referral hospital and one public health unit in the Hhohho region and two referral hospitals and one public health unit in the Manzini region of Eswatini. Purposive sampling was used to select midwives to participate in the study; [ 16 ] 12 midwives from both regions were included. The midwives were between the ages of 35 and 55, and all midwives were black in race and identified as females. The years of experience in the field ranged between 5 and 15 years. The criteria for inclusion were midwives who had provided maternity care to women with mobility disabilities during pregnancy, labour and puerperium for a period of not more than two to three years, willing to participate in the study. The sample size was determined by repetitions of key statements about the research phenomenon during data collection, termed data saturation [ 23 ]. None of the participants refused to participate in the study.
Table 1 summarises the participants’ demographic characteristics.
Data collection
In-depth phenomenological, face-to-face, individual interviews were conducted to collect data [ 17 ]. The researcher who was a Midwifery lecturer held a Master’s Degree in Maternal and Neonatal science at the time of the study requested approval from the Unit manager to seek permission from the midwives to take part in the study. The midwives were given an information letter which included objectives of the study and the reasons for conducting the study. After recruiting midwives and obtaining their written consent to participate in the study and permission to audio-record the interviews, the researcher set up appointments with them for the interviews, and the data collection process commenced. The central question posed to participants was: How was it for you to care for a woman with a mobility disability during pregnancy, labour and puerperium? A pilot of the tool was performed on the first participant who met the inclusion criteria and possessed the same characteristics as those of the study sample. The pre-testing question yielded positive results, the participant responded to the question asked and there was no need to rephrase it or further test it.
The interviews were conducted from March 2019 to July 2019 and lasted 30–45 min. The researcher conducted interviews until the data became redundant and repetitive, reflecting that saturation had been reached, in congruence with Fouché et al. [ 25 ] In addition, field notes were recorded in a notebook after each in-depth phenomenological interview. No repeat interviews were held. The researcher ensured bracketing by omitting any perceptions from her past experiences that were likely to influence her interpretation of the research findings.
Data analysis
Before data analysis commenced, data were organised in computer files after being transcribed and translated into narrative form. Data from each participant were coded and stored in the relevant file and kept in a safe place; only the researcher could access the information. Back-up copies were made of all the data, and the master copies were stored in a safe to which only the researcher had access.
Data collection and analysis occurred concurrently. The researcher was guided by Giorgi et al.’s [ 26 ] five-step method of data analysis. This entailed the researcher reading all the transcribed data and the entire ‘naïve description’ provided by the participants during the interviews. The demarcation of ‘meaning units’ within narratives followed. In addition, the researcher marked where meaning shifts occurred and transformed meaning units into descriptive expressions. The researcher laid out the general structure of midwives’ experiences. Moreover, an independent coder was provided with the raw data (after signing a confidentiality agreement) to analyse the findings. The researcher and independent coder analysed the data separately and met for a consensus discussion. Both agreed on all the units of analysis, with an inter-coder reliability of 100%.
Measures of trustworthiness
The research was informed by Guba and Lincoln’s [ 27 ] model in relation to credibility, transferability, dependability and confirmability. For credibility, the researcher ensured prolonged engagement in the field [ 28 ], peer debriefing, [ 29 ] member checking, and an external auditor was used [ 25 ]. The study was also presented at a national conference. Transferability refers to the ability to extend the findings of one’s study to comparable environments or participants, as stated by Pitney et al. [ 30 ] The researcher ensured the study’s transferability by providing a richly documented account and in-depth description of all aspects and processes of the study protocol. Data saturation also confirmed transferability [ 23 ]. Dependability is evident in a study when other researchers are able to follow the researcher’s decision trail [ 31 ]. The researcher ensured dependability by densely describing the research process in congruence with Fouché et al.’s [ 25 ] guidelines, so that other researchers can follow similar steps of the same research methodology. Confirmability occurs when the research is judged by the way in which the findings and conclusions achieve their aim and are not the result of the researcher’s prior assumptions and preconceptions [ 32 ]. The researcher ensured this by remaining true to the research process through reflexivity and not compromising the research process in any way [ 28 ]. In addition, the researcher engaged an independent coder and provided a chain of evidence of the entire research process to enable an audit. Therefore, all forms of collected data, including raw data, reflexive journals, [ 29 ] notes and transcriptions, were recorded.
Ethical clearance to conduct this study was obtained from the University of Johannesburg Faculty of Health Sciences Higher Degrees Committee (ref. no. HDC-01-50-2018), University of Johannesburg Faculty of Health Research Ethics Committee (ref. no. REC-01-82-2018), and the Eswatini National Health Research Review Board (ref. no. NHRRB982/2018). The researcher applied and adhered to the four principles to be considered when conducting research: autonomy, beneficence, non-maleficence and justice [ 33 ]. Autonomy was adhered to by affording the participants the right to choose to participate in the study and by signing a written informed consent form a week after it was given to them before the interviews commenced. Beneficence was ensured through doing good and doing no harm to participants by prioritising the participants’ interests above those of the researcher, and did not engage in any practice that jeopardised their rights. Non-maleficence was observed by eradicating any possible harmful risks in the study; the researcher ensured the safety of the participants by conducting interviews in a familiar, private environment where they felt free and safe from harm. Furthermore, justice was observed by treating all participants equally regardless of their biographical, social and economic status.
Three themes and categories emerged from the data analysis. Table 2 summarises the themes and categories of midwives’ lived experiences caring for women with mobility disabilities during pregnancy, labour and puerperium in Eswatini.
Theme 1: physical and emotional efforts required from midwives to provide maternity care to women with mobility disabilities
Category 1.1: midwives experienced that woman with mobility disabilities needed assistance getting onto the bed during labour and delivery.
According to the participants, caring for women with mobility disabilities weighed heavily on them physically as they were required to assist the women onto delivery beds, which were too high for the women to climb up on their own:
“The beds are too high, they need to be adjustable…unless you change her to another room, we only have one in the other room…but to be honest she delivered on the same high bed with the help…It’s uncomfortable even with me who is normal, how about someone who has a disability? Getting the woman onto the bed is also uncomfortable for us we end up having pain on our backs.” (M3) . “The challenge is that I couldn’t help her to climb on to the bed, because I needed someone to assist when she came for postnatal care as she was even carrying 3 babies, I didn’t know what to do…I eventually went out and asked for assistance from my colleague…” (M10) . “I believe that the equipment should accommodate the women with disability, however, ours is not accommodative to the women…there are no special delivery beds, specifically designed for them because in my opinion the beds have to be shorter so they can be able to get on to them easily…yes so that they can be able to climb on the beds” (M1) .
Category 1.2: midwives experienced challenges in manoeuvring women with mobility disabilities during labour
Midwives reported it was difficult to perform some procedures while progressing these women during labour and delivery. This situation called for some adjustment and improvisation on their part, and they were unsure if it was the right thing to do.
“Even though she was a bit uncomfortable and anxious because the leg was just straight and could not bend, I reassured her…She had to remove the artificial leg and remain with the stump. I placed her on the lithotomy position. With the other hand she had to hold on to the ankle of the normal foot, even though it was awkward and difficult to manoeuvre, she managed to deliver the baby.” (M1) . “Luckily for us, she didn’t sustain a tear and we were saved from suturing her cause we foresaw difficulties as how we could have done it as she couldn’t open her thighs well due to the disability…yes I had to get a partner to assist, since she couldn’t even open her thighs. She also couldn’t cooperate possibly because of the pain that is also more reason I asked for my colleague to assist.” (M6) . “…yes…let me make an example, in my case she had a fracture, even if the pelvis was gynaecoid, there were problems of finding the right position for her during delivery, when she had to push the baby out…” (M8) . “The one that I saw did not have one leg. She had come for her postnatal care. We assisted and her on the couch, with my colleague. Since she couldn’t keep her legs open, I asked my colleague to keep one of her legs open whilst I examined her.” (M12) .
Category 1.3: midwives experienced anxiety and the need to exercise patience when caring for women with mobility disabilities
The participants experienced an emotional and psychological burden when caring for women with mobility disabilities. They felt unqualified and foresaw difficulties that triggered anxiety, which led to them not knowing what to do and how to handle these women.
“It was during labour…the woman was limping the woman she was on crutches. The moment she came into the ward I am a human being I just felt sorry for her kutsi (as to) how is she going to take care of the baby, and the hand was somehow deformed.” (M3) . “At first its emotionally draining as an individual you cause you start sympathising…(other midwife chips in)…yes you even find yourself saying things just because you pity her, and in the process they get hurt.” (M6) . “It came as a shock and it was my first experience, it came as a shock as to how I was going to help her as even my experience was limited in that area.” (M7) . “As I was taking care of her it became necessary for me to put myself into her shoes and to bear with her considering her situation….When you see her for the first time you would pity her yet she is now used to it.” (M1) .
Theme 2: lack of equipment to meet the needs of women with mobility disabilities
Category 2.1: midwives reported a lack of special beds and infrastructure to meet the needs of women with mobility disabilities.
Midwives reported their frustration at the lack of sufficient equipment like special beds and examination tables, tailored for women with mobility disabilities. It was a challenge to provide maternity care for women without this equipment.
“I believe that the infrastructure and equipment should accommodate the women with mobility disability, however, ours is not accommodative to the women…Usually we don’t have the prenatal ward in the maternity, most women who come in the latent phase have to ambulate, or go to the waiting huts and come back when the labour pains are stronger…There are no special delivery beds, specifically designed for them because in my opinion the beds have to be shorter so they can be able to get on to them easily. We do not even have toilets meant for them.” (M1) . “I was anxious as to how was she going to push how to push cause we do not have the right beds when it was time for pushing I asked for assistance…” (M2) . “The challenge is that I couldn’t help her to climb on to the bed, because I needed someone to assist when she came for postnatal care…the beds need to be adjustable so that they are able to be pushed lower for the mother to move from wheel chair to the bed and we pull the bed up again to examine her.” (M11) .
Theme 3: challenges in providing holistic care to women with mobility disabilities during pregnancy, labour, and puerperium
Category 3.1: midwives reported a lack of guidelines and protocols in caring holistically for women with mobility disabilities.
Midwives emphasised a lack of guidelines, protocols and knowledge about caring holistically for women with mobility disabilities. This resulted in everyone making their own decisions and doing as they saw fit in caring for these women:
“I think during antenatal care they (the women with mobility disabilities) need to be prepared for labour cause for others the pain is extraordinary, apart from the pain threshold, they also face self-esteem issues, they are looked down upon…I only saw that she was disabled during assessment cause nothing was recorded on the antenatal care card.” (M2) . “I was not aware of the disability at first, I only discovered when she was pushing…she was admitted and progressed by another midwife, I only attended to her when she was pushing… there was nothing written on the nurse’s notes/ handover notes about her disability.” (M5) . “There is no normal practice for a woman with mobility disability when they come and they are in labour, I usually admit regardless of the stage of labour or dilatation…It is not a protocol, it’s a midwife’s prerogative.” (M1) . “We assess and come up with our own discretion even in terms of admitting them (women with mobility disability). Some midwives will admit them regardless of the stage of labour and disregard the protocol that women who come into labour have to ambulate if they are in the latent phase.” (M8) . “There is one that came the past 3 days she has 3 children now and we just scheduled her for c/section because we know that she has been having c/section since she started. Just from looking at the way she walked, we could tell that she couldn’t deliver normally.” (M9) .
Category 3.2: midwives experienced challenges in allowing significant others to support women with mobility disabilities during labour and delivery
Consequent to the challenges in providing holistic care to women with mobility disabilities, midwives experienced challenges in allowing significant others to support these women during labour and delivery.
“It can depend on the patients themselves, they should decide and we need to be flexible for it to happen…as you can see our labour room also has the issue of privacy…we would need to restructure cause we have beds for 5 or more women in labour room…and then bringing someone from outside could be tricky” (M6) . “Maybe…not sure though, that they can bring their relatives, but maybe, considering staffing limitation…also the issue of discrimination and privacy, they (the women with disabilities) might feel we discriminate against them because they are disabled we now treat them differently.” (M7) . “Maybe if she can (bring her relative) but that’s not necessary, because I can always ask my colleague to assist, unless there is no one…” (M12) .
Childbirth is a special experience that requires a personal connection between the midwife and the woman giving birth, characterised by successful communication and respect [ 34 ]. However, the themes identified in the study indicated that midwives experienced challenges caring for women with mobility disabilities during pregnancy, labour and puerperium based on their limited capacity and preparedness, and lack of protocols to care for these women. They also reported a lack of supportive equipment for women with mobility disabilities. This posed a challenge for them in attending to these women’s specific needs, and they did not always know how to handle the situation appropriately.
One of the themes centred on midwives’ experiences of the physical and emotional efforts required of them to provide maternity care to women with mobility disabilities. They explained women with mobility disabilities required assistance getting onto the bed during labour and delivery, and more manoeuvring was expected of them (as midwives) as they had to adjust their performance and some procedures. The midwives also reported challenges in providing holistic care to women with mobility disabilities during pregnancy, labour and puerperium. Konig-Bachmann et al. [ 35 ] reiterate that caring for women with disabilities requires a level of flexibility, adaptation beyond routine procedures, and demands a high degree of improvisation from healthcare providers to ensure high-quality care. Morrison et al. [ 36 ] also found that healthcare providers reported difficulties with equipment when providing healthcare for women with physical disabilities; particularly the beds being too high for them to access. Smeltzer et al. [ 37 ] similarly allude to the importance of educating and training clinicians to equip them with knowledge and technical skills to provide more effective care to women with physical disabilities.
The midwives also shared that labour and deliveries were further complicated by some women with mobility disabilities not being able to cooperate due to the pain they experienced; others could not change position due to their disability. In a study by Sonalkar et al., [ 38 ] healthcare providers described the gynaecologic examination as challenging to complete as it required patience and the ability to be adaptable to different methods and positioning. Similarly, Konig-Bachmann et al. [ 35 ] indicate that in order to provide high-quality care for women with disabilities, healthcare providers need to exercise strong flexibility, adapt beyond routine procedures, and engage in a high degree of improvisation. Byrnes and Hickey [ 39 ] concur with this study’s findings and state that due to mobility restrictions, it may be difficult to assess the fundal height and foetal growth in women with physical disabilities.
Some midwives reported their caregiving role was emotionally draining as they felt sorry and pitied the women with mobility disabilities; thus, they needed to show compassion and reassure them. According to Mgwili et al., [ 40 ] psychoanalytic thinkers associate pity among staff members upon first contact with a physically disabled person as being instigated by personal feelings, stimulated by the disability. The midwives in this study stated they needed to be more patient and adjust their approach to caring for these women. Tarasoff [ 41 ] and Schildberger et al. [ 42 ] reiterated that healthcare providers seemed uncomfortable with women’s disability, consequently failing to offer needed support. According to Sonalkar et al., [ 38 ] healthcare providers reported there would be less fear and concern about hurting women with disabilities if midwives had increased training. Similarly, Mitra et al. [ 43 ] mentioned that healthcare providers had a general lack of confidence in their ability to provide adequate maternity care for women with physical disabilities.
Another theme was midwives’ challenges in providing competent and quality care for women with mobility disabilities due to a lack of equipment, including special beds and examination tables to meet these women’s needs. The examination, labour and delivery beds were too high and could not be adjusted for the women to get on by themselves, or even with the assistance of a midwife. In addition, the midwives reported there was no prenatal ward or waiting huts where they could place these women during the latent phase of labour. The midwives further emphasised there were no special toilets for women with mobility disabilities, which made it hazardous and difficult for them. Mitra et al. [ 43 ] concur on the barriers to providing maternity care to women with physical disabilities presented from health professionals’ perspectives. The authors indicated that participants from their study reported inaccessible equipment, including examination tables, as a barrier, making it more difficult and time-consuming to care for women with physical disabilities. In addition, Sonalkar et al. [ 38 ] said healthcare providers shared their concern about the lack of adjustable examination tables and transfer equipment, thus presenting a barrier to equitable care for women with disabilities.
Midwives further reported a lack of guidelines and protocols. This resulted in everyone making their own decisions and doing as they saw fit in caring for these women, and, in most instances, not recording the disability at all during antenatal care and admission into labour records. They often only discovered that the woman had a mobility disability at a later stage, when they were in labour. Sonalkar et al. [ 38 ] reported that healthcare providers felt frustrated and overwhelmed by the uncertainty of whether they made the correct decisions when caring for women with physical disabilities due to the lack of guidelines forcing them to use their own judgement. Mitra et al. [ 43 ] determined that most healthcare providers reported a lack of maternity practice guidelines for women with physical disabilities. Also, healthcare providers highlighted the importance of learning about disabilities and having a better understanding of a condition, particularly if it is likely to be exacerbated during pregnancy [ 44 ]. The need to make and read the notes on these women’s antenatal care cards or reports was emphasised.
Due to the lack of clear guidelines and protocols in caring for women with mobility disabilities, the midwives reported they sometimes admitted the woman into the labour ward regardless of the stage of labour, while other midwives did not and wanted them to walk around and come back for admission once they are in the active phase of labour. Furthermore, the midwives explained they often referred these women for caesarean sections right away, regardless of whether the woman could deliver normally due to mere panic from just seeing the disability or based on a previous record of surgery. Smeltzer et al. [ 45 ] researched obstetric clinicians’ experiences and educational preparation in caring for pregnant women with physical disabilities, and they agree on the lack of knowledge among health professionals caring for women with mobility disability.
Devkota et al. [ 46 ] also agree regarding midwives’ inefficiency in providing quality care for women with mobility disabilities. They claim healthcare providers often struggle to understand women with disabilities’ needs as they are not formally trained to provide services to this population. These healthcare providers were found to be undertrained in specific skills that would equip them to provide better and more targeted services for women with disabilities.
Consequent to the challenges in providing holistic care to women with mobility disabilities during pregnancy, labour and puerperium, midwives experienced challenges in allowing significant others to support these women. They reported that as much as they needed assistance caring for these women, and as much as the women would prefer to have their family members or significant others assisting them, this is not possible due to the lack of privacy, especially in public health facilities. Walsh-Gallager et al.’s [ 13 ] study on the ambiguity of disabled women’s experiences of pregnancy, childbirth and motherhood resonate with this study’s findings. The authors reported that women with disabilities’ partners were denied access or had their visits curtailed on several occasions due to inflexible hospital visiting policies. Redshaw et al. [ 47 ] reiterated the same in their study; disabled women were less likely to say their companion or partner was welcome to visit, let alone provide any form of assistance. In addition, a study by Bassoumah and Mohammad [ 48 ] reported that women with disabilities were denied their spouses’ support while receiving maternity care. Byrnes and Hickey [ 39 ] also concur that every effort should be made to allow women with disabilities who are in labour to receive support from significant others, and they should be active partners in the labour process.
Limitations
The study was limited to two of the four regions of Eswatini, namely Hhohho and Manzini; hence, the results could not be generalised for the whole country. The study also only focused on mobility disabilities due to time constraints and limited funds. Future research could be conducted to cover all other forms of disabilities.
This study focused on midwives’ lived experiences caring for women with mobility disabilities during pregnancy, labour and puerperium in Eswatini. In-depth phenomenological interviews were conducted, the findings were analysed, and themes were established. The findings illustrate that midwives experienced challenges caring for women with mobility disabilities during pregnancy, labour and puerperium in Eswatini. There is a need to develop and implement guidelines to empower midwives with knowledge and skill to provide support and holistic maternity care, and enact protocols. They should also have access to appropriate equipment and infrastructure specifically tailored towards promoting optimal health for women with mobility disabilities.
Data availability
The data analysed is available from the corresponding author upon reasonable request.
González-Timoneda A, Hernández Hernández V, Pardo Moya S, Alfaro Blazquez R. Experiences and attitudes of midwives during the birth of a pregnant woman with COVID-19 infection: a qualitative study. Women Birth. 2021;34(5):467.
Article Google Scholar
Disabled World. Definitions of disability [home page on the internet]. C2009 [updated 2021; cited 2023 July 26]. Available from: https://disabled-world.com/definitions/disability-definitions.php .
Aune I, Tysland T, Vollheim SA. Norwegian midwives’ experiences of relational continuity of midwifery care in the primary health care service: a qualitative descriptive study. Nordic J Nurs Res. 2021;4(1):5–13.
Moridi M, Pazandeh F, Hajian S, Potrata B. Midwives’ perspectives of respectful maternity care during childbirth: a qualitative study. PLoS ONE. 2020;15(3):1–12. https://doi.org/10.1371/journal.pone.0229941 .
Article CAS Google Scholar
United Nations. Background: International Day of Persons with Disabilities. [homepage on the internet]. c2022 [updated 2022 December 1; cited 2023 July 20]. Available from: https://un.org/en/observances/day-of-persons-with-disabilities/background .
Central Statistics Office. Population and housing census: 2017. Volume 3. Mbabane: Swaziland Government Printing Office; 2019a.
Google Scholar
Central Statistics Office. National accounts estimates. Mbabane: Swaziland Government Printing Office; 2018.
Central Statistics Office. Population and housing census: 2017. Volume 6. Mbabane: Swaziland Government Printing Office; 2019b.
Magqadiyane S. Experiences of midwives for caring un-booked pregnant mothers in a maternity unit at a district hospital in the Eastern Cape Province. Advances in reproductive sciences [serial online]. 2020. [cited 2021 August 5];8:186–200. https://doi.org/10.4236/arsci.2020.84016 .
World Health Organisation (WHO). Global report on health equity for persons with disabilities. [homepage on the internet]. c2022 [updated 2022 December 2; cited 2023 July 20]. Available from: https://who.int/health-topics/disability#tab=tab_1 .
Lawler D, Lalor J, Begley C. Access to maternity services for women with physical disability: a systematic review of literature. Int J Childbirth. 2013;3(4):203–17.
University of Johannesburg. Department of nursing paradigm. Johannesburg: University of Johannesburg;2017.
Walsh-Gallagher D, McConkey R, Sinclair M, Clarke R. Normalising birth for women with a disability: the challenges facing practitioners. Midwifery. 2013;29:294–9.
Article PubMed Google Scholar
Silverman D, editor. Qualitative research. 5th ed. Los Angeles: SAGE; 2021.
Nassaji H. Good qualitative research. Language Teaching Research [serial online]. 2020. [cited 2021 August 6];24(4):427–431. Available from: https://journals.sagepub.com/doi/pdf/10.1177/1362168820941288 .
Doyle L, McCabe C, Keogh B, Brady A, McCann M. An overview of the qualitative design within nursing research. Journal of Research in Nursing [serial online]. 2020. [cited 2021 August 6];25(5):444–446. Available from: https://journals.sagepub.com/doi/pdf/10.1177/1744987119880234 .
Hennink M, Hutter I, Bailey A. Qualitative research methods. 2nd ed. London: SAGE; 2020.
Frechette J, Bitzas V, Aubry M, Kilpatrick K, Lavoie-Tremblay M. Capturing lived experience: methodological considerations for interpretive phenomenological inquiry. Int J Qual Meth. 2022;19:2–11.
Flick U. The SAGE handbook of qualitative research design. London: SAGE; 2022.
Book Google Scholar
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. https://doi.org/10.1093/intqhc/mzm042 .
Yildiz A. A discussion on accurate and effective data collection for qualitative research. J Curr Researches Educational Stud. 2020;10(2):17–24.
Papakitsou V. Qualitative research: narrative approaches in sciences. Dialogues Clin Neurosci Mental Health. 2020;3(1):63–70.
Johnson JL, Adkins D, Chauvin S. Qualitative research in pharmacy education: a review of the quality indicators of rigor in qualitative research. Am J Pharm Educ. 2020;84(1):138–46.
Magagula T. The guidelines of maternity care of women with mobility disabilities in the Hhohho and Manzini regions: Eswatini [unpublished thesis]. University of Johannesburg, Johannesburg; 2021.
Fouché CB, Strydom H, Roestenburg WJH, editors. Research at grassroots for social sciences and human services professions. 5th ed. Pretoria: Van Schaik; 2021.
Giorgi A, Giorgi B, Morley J. The descriptive phenomenological psychological method. In: The SAGE handbook of qualitative research in psychology. 2nd edition. Los Angeles: SAGE; 2017.
Guba EG, Lincoln YS. Fourth generation evaluation. Newbury Park, CA: SAGE; 1989.
Rose J, Johnson W. Contextualising reliability and validity in qualitative research: toward more rigorous and trustworthy qualitative social science in leisure research. J Leisure Res. 2020;1:10–3. https://doi.org/10.1080/00222216.2020.1722042 .
Creswell JW, Creswell JD. Research Design: qualitative, quantitative and mixed methods approaches. 5th Ed. California: SAGE; 2018.
Pitney WA, Parker J, Singe SM, Potteiger K. Qualitative research in health professions. Thorofare: SLACK Incorporated; 2020.
Leavy P, editor. The Oxford handbook of qualitative research. New York: Oxford University Press; 2020.
Kyngäs H, Mikkonen K, Kääriäinen M, editors. The application of content analysis in nursing science research. 2020. [cited 2022 April 27]. Available from: https://dl1tarjomac.ir/nursing-ebooks/TPC202203.pdf .
Dhai A, McQuoid-Mason DJ. Bioethics, human rights and health law: principles and practice. Cape Town: Juta; 2020.
Hallam J, Howard C, Locke A, Thomas M. Communicating choice: an exploration of mothers’ experiences of birth. J Reprod Infant Psyc. 2016;34(2):175–84.
König-Bachmann M, Zenzmaier C, Schildberger B. Health professionals’ views on maternity care for women with physical disabilities: a qualitative study. BMC Health Serv Res. 2019;19(551):1–11.
Morrison J, Basnet M, Buthathoki B, et al. Disabled women’s maternal and newborn health care in rural Nepal: a qualitative study. Midwifery. 2014;30:1132–9.
Article PubMed PubMed Central Google Scholar
Smeltzer S, Wint A, Ecker J, Iezzoni L. Labor, delivery, and anaesthesia experiences of women with physical disability. Birth. 2017;44(4):315–24.
Sonalkar S, Chavez V, McClusky J, Hunter TA, Mollen CJ. Gynaecologic care for women with physical disabilities: a qualitative study of patients and providers. Women Health Iss. 2020;30(2):136–41.
Byrnes L, Hickey M. Perinatal care for women with disabilities: clinical considerations. J Nurse Practitioners. 2016;12(8):506–7.
Mgwili VN, Watermayer B. Physically disabled women and discrimination in reproductive health care: Psychoanalytic reflections. In: Disability and Social Change: A South African agenda [serial online]. 2006. [cited 2020 June 01]. Available from: https://www.hsrcpress.ac.za .
Tarasoff LA. Improving perinatal care for women with physical disabilities [Abstract]. J Obstet Gynaecol Can. 2016;38(5):501.
Schildberger B, Zenzmaier C, König-Bachmann M. Experiences of Austrian mothers with mobility or sensory impairments during pregnancy, childbirth and the puerperium: a qualitative study. BMC Pregnancy Childb. 2017;17(201):1–11.
Mitra M, Akobirshoev I, Moring N, et al. Access to and satisfaction with prenatal care among pregnant women with physical disabilities: findings from a national survey. J Womens Health. 2017;26(12):1356–63.
Hall J, Hundley V, Collins B, Ireland J. Dignity and respect during pregnancy and childbirth: a survey of experience of disabled women. BMC Pregnancy Childb. 2018;18(328):1–13.
Smeltzer S, Mitra M, Long-Bellil L, Iezzoni L, Smith L. Obstetric clinicians’ experiences and educational preparation for caring for pregnant women with physical disabilities: a qualitative study. Disabil Health J. 2018;11(1):8–13.
Devkota HR, Murray EA, Kett M, Groce N. Health care provider’s attitude towards disability and experience of women with disabilities in the use of maternal healthcare service in rural Nepal. Reprod Health. 2017;14(79):1–14.
Redshaw M, Malouf R, Gao H, Gray R. Women with disability: the experience of maternity care during pregnancy, labour and birth and the postnatal period. BMC Pregnancy Childb. 2013;13(174):1–14.
Bassoumah B, Mohammed A. The socio-cultural challenges to maternal and neonatal care: the views of women with disabilities receiving maternity care in the Chereponi district of Northern Ghana. Sci Afr. 2020;7:1–10.
Download references
Acknowledgements
The authors would like to acknowledge the midwives in the Hhohho and Manzini regions of Eswatini who participated in the study and provided their own experiences of providing maternity care to women with mobility disabilities during pregnancy, labour and puerperium.
The research received funding from the University of Johannesburg Postgraduate Supervisor-linked Bursary.
Author information
Authors and affiliations.
Health Sciences, University of Johannesburg, Johannesburg, South Africa
Annie M. Temane & Anna G. W. Nolte
Mother and Child Nursing, University of Eswatini, Kwaluseni, Eswatini
Fortunate N. Magagula
You can also search for this author in PubMed Google Scholar
Contributions
F.N.M conducted the research and wrote the manuscript. A.M.T supervised, reviewed, and finalised the manuscript. A.G.W.N co-supervised the study and edited the manuscript for final submission.
Corresponding author
Correspondence to Annie M. Temane .
Ethics declarations
Ethical approval and consent to participate.
Ethical clearance to conduct this study was obtained from the University of Johannesburg Faculty of Health Sciences Higher Degrees Committee (ref. no. HDC-01-50-2018), University of Johannesburg Faculty of Health Research Ethics Committee (ref. no. REC-01-82-2018) and the Eswatini National Health Research Review Board (ref. no. NHRRB982/2018). Participation in this study was voluntary, and informed consent was obtained from participants before the interviews commenced.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Temane, A.M., Magagula, F.N. & Nolte, A.G.W. Midwives’ lived experiences of caring for women with mobility disabilities during pregnancy, labour and puerperium in Eswatini: a qualitative study. BMC Women's Health 24 , 207 (2024). https://doi.org/10.1186/s12905-024-03032-z
Download citation
Received : 18 August 2023
Accepted : 18 March 2024
Published : 01 April 2024
DOI : https://doi.org/10.1186/s12905-024-03032-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Experiences
- Maternity care
- Women with mobility disabilities
- Labour and the puerperium
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
BREAKING: Caitlin Clark leads Iowa to women's NCAA Final Four
PCOS symptoms are still difficult for doctors to diagnose and treat. Here’s why
Every morning, Jeni Gutke swallows 12 pills. In the evening, she takes 15 more, then another before bed. She also takes an injectable medication once weekly, and two other medications as needed.
Gutke, of Joliet, Illinois, has polycystic ovary syndrome, or PCOS, and the medications and supplements help the 45-year-old cope with migraines, high blood pressure, diabetes, high cholesterol, anxiety and depression that come with the complex hormonal condition.
Not one of Gutke’s medications are technically “PCOS drugs.”

The Food and Drug Administration has not approved a medication specifically for PCOS, which is often linked to infertility, irregular or missed periods, weight problems, and other debilitating symptoms. Gutke’s array of medications is typical of how many of the estimated 5 million women in the U.S. diagnosed with PCOS deal with it.“It’s such a vast syndrome that affects everything from your head to your toes,” she said. She was diagnosed with endometrial cancer — another risk linked to PCOS — at age 37.
After nearly a century of disagreements over what, exactly, defines the condition, as well as a lack of research, PCOS is still poorly understood. The symptoms vary so widely that any single drug would be unlikely to help all patients, said Dr. Heather Huddleston, a reproductive endocrinologist at the University of California, San Francisco and director of UCSF’s PCOS Clinic.
Women with PCOS and the doctors who care for them say they want better options — treatments for the condition’s root causes rather than bandages for individual symptoms. Even as calls for better treatments grow, the lack of investment in PCOS research has limited doctors’ ability to help their patients.
“It gets very messy to try to identify one treatment that’s going to work for everybody,” Huddleston said.
Many women with the condition end up taking off-label prescriptions — meaning drugs technically approved for other conditions, like diabetes or obesity — to help PCOS-related symptoms. Navigating insurance coverage for off-label prescriptions can be challenging.
“There’s no magic pill,” said Tallene Hacatoryan, 31, a registered dietician from Orange County, California. “There are too many components for there to be a one-size-fits-all treatment.”

Hacatoryan was diagnosed with PCOS at age 18 and now works as a diet and lifestyle coach for women with PCOS. Although research is murky when it comes to the best diet for women with PCOS, the most up-to-date international guidelines recommend exercise and a healthy diet. There’s no evidence that any particular diet improves symptoms, although some women have found lifestyle coaching helpful.
Insufficient funding for research
Among the reported 315 medical conditions that receive federal support from the National Institutes of Health , PCOS ranks near the bottom, with an estimated $10 million earmarked for research in 2024. Until 2022, PCOS was so underfunded that it wasn’t included as a line item in the NIH list. And the condition is not explicitly included in the $100 million the Department of Health and Human Services announced recently to research neglected areas of women’s health. Neither is PCOS mentioned in President Joe Biden’s recent executive order to advance women’s health , which includes $200 million for NIH research grants, or the White House’s calls for Congress to allocate $12 billion to fund women’s health research.
A spokesperson at the NIH said that it’s too early to know which women’s health conditions will receive funding under the new initiative.
“Given how common PCOS is, the amount of funding it’s gotten is proportionately extremely small,” Huddleston said.
Government funding is just one part of the total research budget for a given disease. While it’s tough to pin down a dollar figure for private industry spending, experts say the lack of FDA-approved PCOS treatments reflects a lack of investment from drugmakers, too.
Developing PCOS treatments requires a better understanding of the condition. This, in turn, requires far more research tracking thousands of women over many years, which can be extremely expensive, experts say.
However, there are some promising signs.
Although research is early and only in a few dozen women, there are a handful of small drug companies studying possible PCOS treatments. A Menlo Park, California-based company called May Health , for instance, is developing a one-time surgical procedure it thinks could help with PCOS. Spruce Bio, a San Francisco biotech firm, is running a small clinical trial with a drug called tildacerfont for PCOS. It is not clear yet if the oral drug works. President and CFO Samir Gharib said larger clinical trials will depend on the company’s ability to “secure additional financing” or partner with another drug company.
More women's health news
The fda recently attended a meeting with advocacy group pcos challenge where women shared their experiences with the agency’s scientists and drug companies. no pcos drug trials were announced after the meeting, but the fda’s interest shows a growing push for improved treatment, said william patterson, a spokesperson for pcos challenge.no known cure for pcos.
Doctors recommend hormonal contraceptives — most commonly the birth control pill — to regulate heavy, irregular periods;, acne;, and unwanted hair growth. Others say taking the pill just masks, rather than treats, their PCOS symptoms and the symptoms return as soon as they stop taking it.
“PCOS is unfortunately not curable, so treatment is about managing its symptoms,” said Dr. Jessica Chan, a reproductive endocrinologist at Cedars-Sinai. Chan said birth control can be a good option for some, but not all, of her PCOS patients.
For women with PCOS whose main concerns are insulin resistance or stubborn weight gain, Chan often prescribes off-label diabetes medications like metformin.
Some doctors who treat PCOS, including OB-GYNs or endocrinologists, have also begun prescribing GLP-1 agonists like Ozempic and Wegovy, which have shown promise for some women with PCOS, although studies have been small and early -stage.
Novo Nordisk, the company that makes Ozempic and Wegovy, said it has no plans as of now to seek FDA approval for PCOS. Still, the company mentions PCOS on its Truth About Weight website, part of its marketing campaign for Wegovy
Causes and symptoms of PCOS
“We don’t know the initial spark leading to PCOS or where it arises from,” Chan said.
PCOS affects an estimated 6% to 12% of reproductive-age women in the U.S. The real prevalence is likely higher since an estimated 70% of cases go undetected.
Experts generally agree that PCOS, at its core, is a hormone-related condition. Women with PCOS have higher levels of androgen hormones, which can cause a range of symptoms, including:
Missing, irregular, or heavy periods
Excess hair growth on the face or body
Thinning or balding scalp hair
According to endocrinologist Dr. Andrea Dunaif, some doctors have been pushing to separate PCOS into two different diagnoses: one having more to do with the reproductive cycle and fertility issues and another having more to do with metabolism, high body weight, and diabetes.
“PCOS looks to be at least two or three different conditions we’re lumping together, but they’re genetically distinct,” said Dunaif, the chief of the endocrinology, diabetes and bone disease division of Mount Sinai Health System and the Icahn School of Medicine.
The confusion surrounding PCOS diagnosis is partly why it’s been hard to get large pharmaceutical companies to invest in PCOS treatment, she said.
In Dunaif’s view, it’s not accurate to call the condition “PCOS” at all, because it has more to do with excess hormones than it does with actual cysts on the ovaries. PCOS got its name from the bumps on the ovaries appearing like cysts on an ultrasound image. These are not cysts, but instead egg follicles that are, as Dunaif described them, “arrested in development.”
As it is, many doctors diagnose the condition based on two of three factors:
Irregular periods
High androgen levels
Multiple follicles on the patient’s ovaries
But these three factors don’t account for some of the most challenging symptoms of PCOS: insulin resistance and stubborn weight gain. Excess androgen hormones can spike insulin levels, which interferes with how the body processes sugar. Doctors aren’t sure whether the hormonal dysregulation causes insulin resistance, or whether insulin resistance causes excess androgen hormones.
Either way, women with PCOS have a higher risk of diabetes, excess weight gain, high cholesterol, and high blood pressure. Yet these metabolic conditions aren’t included in the criteria many doctors use to diagnose PCOS. The result? A missed diagnosis.
This was initially the case for Candice Bolden, 35, who started noticing acne and excess facial and body hair several years before she was diagnosed with PCOS in 2021. Bolden, a lifelong dancer, also had unusually low energy.

“The final straw was excess weight gain that I could not take off no matter what I did,” said Bolden, who lives in Los Angeles. “All the other things I had kind of just stuffed under the rug. I’d just chalked it up to being a hairy, Haitian woman.”After gaining 35 pounds, the 5-foot-2-inch Bolden, who exercised twice a day and followed strict diets, saw multiple doctors who she said ignored her symptoms.
“Doctors kept telling me I was fine, and to go home, work out, and eat clean,” she said. “It was the most frustrating thing ever.”
‘We don’t have to live underneath this dark cloud’
Women living with PCOS say the rise of online communities, including on social media apps like TikTok and Instagram, has given them a place to speak out, share the treatment approaches working for them, and meet other women with PCOS.
When Bolden finally got a diagnosis, she wasn’t sure what to do next. Gutke and Hacatoryan had similar experiences.
“I was like, ‘Wait, I have so many questions,’ and the doctor just told me, ‘It is what it is,’” Hacatoryan said.
Hacatoryan calls women in her online community her “cysters.”
Bolden said she’s noticed more women turning to social media to learn how others manage their PCOS and share their own stories.
On her own social media accounts, she’s been trying to change the narrative about PCOS being primarily a fertility problem, which she sees as an outdated perception.
“When I was diagnosed, my doctor mentioned PCOS being the No. 1 reason for infertility, and that shattered me,” said Bolden, who was newly engaged at the time and eager to start a family. “I was happy I was diagnosed, because it showed me something was actually happening and I wasn’t just crazy. But I was heartbroken.”
Things changed after Bolden moved; found a new doctor; and worked closely with her husband and the online PCOS community to find a system that worked to manage her PCOS symptoms.
Bolden is now pregnant and expecting a baby girl.
“I want people diagnosed with PCOS to know there’s hope, and we don’t have to live underneath this dark cloud all the time,” she said.
NBC News contributor Caroline Hopkins is a health and science journalist who covers cancer treatment for Precision Oncology News. She is a graduate of the Columbia University Graduate School of Journalism.
Maternal mental health problems are 'No. 1 complication in pregnancy'
Child and maternal health experts shared the challenge of providing wraparound care and extended research during a panel discussion on women’s health.
Leigh Anne Kelley
- Share on Facebook
- Share on Twitter
- Copy address link to clipboard
A discussion on women’s health in Washington, D.C., represented a collaboration between Children’s National Hospital and Fralin Biomedical Research Institute at VTC. Melissa Schooley (from left) moderated a panel that included Nia Imani Bodrick, Catherine Limperopoulos, and Brittany Howell. Photo by Leigh Anne Kelley for Virginia Tech.

Modern medicine treats patients independently, but when it comes to women’s health, physicians and researchers stressed the need for a holistic approach during a recent panel discussion on maternal health in Washington, D.C.
“Maternal health is children’s health,” said Catherine Limperopoulos , chief and director of the Developing Brain Institute at Children’s National Hospital. “Many people aren’t aware that maternal mental health problems” — such as postpartum depression and anxiety — “are the No. 1 one complication in pregnancy.”
Limperopoulos was one of three featured speakers for the March 7 discussion on maternal health sponsored by Children’s National and the Fralin Biomedical Research Institute at VTC, which has research programs in brain and behavior development in Roanoke on the Virginia Tech Health Sciences and Technology campus and cancer research programs in Roanoke as well the Children’s National Research & Innovation Campus in Washington, D.C.
As a pediatrician with Children’s National, Nia Imani Bodrick is directly involved in caring for patients. She said while women may put off care for themselves, they prioritize pediatric visits for their children — making those regular wellness checks an ideal time to intervene.
Bodrick said there’s a need to support projects such as HealthySteps , which began as a research program and has been integrated into pediatric practices in 25 states, Germany, and Washington, D.C., including Bodrick’s.
“One of the best things we do is we screen for postpartum depression up to six months, and we keep short-term mental health on staff,” Bodrick said, although recruiting and retaining those providers is a challenge. The evidence-based program also is designed to identify and address a child’s developmental delays early and ensure families have the support they need.
At the Fralin Biomedical Research Institute, Assistant Professor Brittany Howell studies factors that influence healthy infant brain development in her Maternal Influence on Neurodevelopment (MIND) Lab. Howell is also an investigator on the national HEALthy Brain and Child Development Study .
She explained the need for more research into factors that influence a child’s early years and said the timelines of budget cycles and the structure of research funding often don’t take into account unique attributes of maternal health and rapid changes that take place during early childhood.
Howell also said maternal health research would benefit from increased funding, giving the example of breast milk and the milk microbiome. “It’s an amazingly dynamic fluid, yet we know next to nothing,” she said. More study could provide evidence-based recommendations to clinicians and families, she said.
Comments during the event resonated with President Joe Biden’s proposal for broader support for women’s health research in general in his State of the Union address, which took place the same day. During the address, he said “women are more than half of our population, but research on women’s health has always been underfunded.”
The event was moderated by Melissa Schooley , a member of Fralin Biomedical Research Institute’s advisory board and vice president of global reimbursement, health policy, and government affairs for Abiomed , a health technology company. Schooley has been a leader in the Abiomed Women’s Initiative to drive awareness of heart failure risks unique to women and the need for broader screening and access to therapy, including therapy to promote heart recovery.
540-526-2002
- Children's National Research & Innovation Campus
- Fralin Biomedical Research Institute at VTC
- Fralin Biomedical Research Institute at VTC - top news
- Friedlander News
- Good Health and Well-Being
Related Content
Dr. Loh: Women have been underrepresented in clinical research
In prior columns I’ve alluded to the inapplicability of clinical trial results to certain populations, often as a result of non-inclusion of those patient groups into the study cohort. Recognition of those disparities has resulted in active efforts by the US Food and Drug Administration to include those underrepresented populations into these projects so that the results actually reflect what can be expected in those patient groups.
There are many barriers to the inclusion of these patients on both sides of the equation, that is, from the research side based on cost and effort, and from the patient side based on ability and trust to allow participation. I am part of an academic proposal to bridge those obstacles, but that is a subject for a future column. For this column, I’d like to focus on a major effort to include about half of our population that has been underrepresented in clinical research and for which more information is absolutely required. Although those barriers have usually been based on racial or ethnic criteria, it turns out that being female has been a bias that has finally been recognized and is being addressed.
This month, the Biden administration announced an executive order proposing a $12 billion fund to improve our long-overdue understanding of women’s health and to strengthen women’s health research standards across federal agencies. In his remarks, President Biden called this first Initiative on Women’s Health Research the “most comprehensive executive actions ever taken to improve women’s health” and said it highlighted the administration’s efforts to enhance economic gains for women. “Our administration has turned around the economy because we focused on women. … If you want to have the strongest economy in the world, you can’t leave half the workforce behind.”
Within this order, the National Science Foundation and Department of Health and Human Services are instructed to research ways to use artificial intelligence (another one of my favorite topics) to advance women’s health research, including a national network of women’s research centers. There certainly are gaps in medical knowledge concerning how to diagnose, manage, and treat diseases that affect women more than men, and evaluate illnesses that affect women differently than men.
So this order will create a Fund for Women’s Heath Research at the National Institutes of Health (NIH). It also directs the HHS to expand data collection on women’s midlife health and launch an agenda that can guide investments toward menopause-related research in heart, brain, and bone health. Menopause, I suspect that’s a word that has never before seen the light of day in an executive order. Employers estimate that the U.S. economy loses $26.6 billion annually due to menopause-related symptoms and many have been promoting menopause benefits to mitigate those losses.
In addition, impactful conditions like endometriosis and fibroids, plus breast cancer, Alzheimer’s disease and autoimmune disorders disproportionately affect women. As a practicing cardiologist for over four decades, I can tell you that we became aware that women present with heart attacks differently that men only because it became apparent the we were taught “classical symptoms” generated by data acquired in studying men and not women.
New topics targeted for investigation will include wider range subjects including computational research, data standardization, engineering biomechanics, and environmental factors. Simplification of the arduous process of getting funding is also part of this initiative. Lest one think that this is yet another governmental bureaucracy, this initiative also calls on public (ARPA-H)-private (SBIR) engagement to meet these goals. I have known and worked with both of those entities and can tell you they are the best of the best when it comes to guiding meaningful projects to successful conclusions.
And since the overturning of Roe v. Wade in June 2022, the ability of women to make decisions about their own healthcare and bodily integrity has also been top of mind for many. This order reminds us all that women’s issues go far beyond abortion, but are also included under the umbrella of women’s health. It’s also about whether one thinks it’s OK for the government to tell you how to manage your family decisions, like whether you should have children, when you should have them, and how to educate them by constraining what they can learn.
Parents should be able to decide whether or not to even become parents, and once they are, be able to make educational decisions with their children. Beyond health and safety of children and the community at large, the government should support and not dictate to women.
To be fair, there is bipartisan support for this endeavor. To paraphrase Jack Harlow in Bloomberg, we must realize there are supporters of he-who-must-not-be-named who believe that women exist to bear children (Handmaid’s, as it were), make dinner (in Katie Britt’s kitchen, I suspect) while pouring a cocktail for the man of the house, do laundry while cleaning the house, and do women’s work (like raising the children) while the men do real work.
Let’s see if the men in the Congress try to cut this funding out of the 2025 federal budget. Some of these men endorsed by HWMNBN who are running for office are even suggesting that women should not be allowed to vote. None of these men have ever met my wife. And God help them if they ever do.
Irving Kent Loh, M.D., is a preventive cardiologist and the director of the Ventura Heart Institute in Thousand Oaks. Email him at [email protected].
More than one alcoholic drink a day raises heart disease risk for women
Young to middle-aged women who drink more than one alcoholic beverage a day, on average, were more likely to develop coronary heart disease than people who drink less, according to new research by Kaiser Permanente Northern California.
Women in the study who reported drinking eight or more alcoholic beverages per week were 33 to 51 percent more likely to develop coronary heart disease. And women who binge drink — three alcoholic beverages per day — were 68 percent more likely to develop coronary heart disease than those who drink in moderation, the research showed.
“There has been an increasing prevalence of alcohol use among young and middle-aged women as women may feel they’re protected against heart disease until they’re older, but this study shows that even in that age group, women who drink more than the recommended amount of one drink per day or tend to binge drink, are at risk for coronary heart disease,” Jamal Rana , a cardiologist with the Permanente Medical Group and the study’s lead author, wrote in an email.
The study will be presented at the American College of Cardiology’s Annual Scientific Session in early April. It was funded by the National Institutes of Health (NIH) and the National Institute on Alcohol Abuse and Alcoholism.
Risk is highest for binge drinking
The study used data from 432,265 adults, ages 18 to 65, who received care in the Kaiser Permanente Northern California integrated health organization. The group was composed of about 243,000 men and 189,000 women who filled out routine assessments between 2014 and 2015 in which they reported their alcohol intake. Researchers then looked at the coronary heart disease diagnoses among participants over the four years that followed.
Get Well+Being tips straight to your inbox

Participants were divided into three groups, according to their alcohol intake: low (one to two drinks per week), moderate (three to 14 drinks per week for men and three to seven drinks per week for women), or high (15 or more drinks per week for men and eight or more drinks per week for women).
Participants were also categorized as either engaging in binge drinking or not, with binge drinking being defined for men as having more than four drinks in a single day and for women as having more than three drinks a day, in the prior three months. Those who reported no alcohol use were not included.
During the four-year follow-up period, 3,108 participants were diagnosed with coronary heart disease. Higher levels of alcohol consumption were associated with a higher incidence of coronary heart disease. Both men and women who reported heavy episodic drinking, or binge drinking, had the highest risk.
The link between alcohol and coronary heart disease proved to be especially strong among women, the data showed.
Coronary heart disease, also known as coronary artery disease, is the most common type of heart disease in the United States, according to the Centers for Disease Control and Prevention . The disease develops when the arteries of the heart are unable to deliver enough oxygen-rich blood to the heart because of plaque buildup.
Heart disease is the No. 1 killer of American women , according to the CDC. Symptoms differ, and often there are none until people suffer from a heart attack or other problem, a NIH report said.
“There has long been this idea that alcohol is good for the heart, but more and more evidence is challenging that notion,” Rana wrote.
Alcohol is a risk factor for many health issues
Alcohol is actually a toxin to the heart, said Nieca Goldberg , a clinical associate professor of medicine at NYU Grossman School of Medicine and medical director of Atria New York City. Alcohol raises blood pressure , increases the risk for heart rhythm problems, especially during times of binge drinking, is associated with an enlarged heart and is a toxin to the heart muscle , she said.
“I think this is an important study to do because for a while, people thought that alcohol was protective against the heart because of earlier studies that were done in the past. But in fact, we don’t prescribe alcohol to fight heart disease,” she said.
Alcohol use is rising among women
The link between alcohol and heart disease for women is cause for concern, given that alcohol use among women is on the rise. While men used to drink more, studies over the past several years show that gap is closing.
Approximately 13 percent of adult women report binge drinking , with 25 percent of those women saying they do so at least weekly, on average, and 25 percent saying they consume at least six drinks during a binge drinking occasion, according to the CDC. A study in July in JAMA Network Open showed the number of alcohol-related deaths among women was rising at a faster rate than those among men, particularly for people 65 and older.
“I think this raises an important issue, because oftentimes, we think of heavy drinkers as men only. But we have to have heightened awareness that women may be heavy alcohol drinkers,” Goldberg said.
Occasional binge drinking can affect heart health
But it wasn’t just heavy drinkers who were affected, said Mary Ann McLaughlin , cardiologist at the Mount Sinai Fuster Heart Hospital. The study is interesting because it showed that even occasional drinking, if it reaches the level of binge drinking, can affect heart health, she said.
There are those who thought just drinking on the weekends was not a big deal, because they weren’t drinking every day, she said. “But the fact is, if they have more than four drinks as a woman or more than five drinks as a man on one day, in the past three months, they were at increased risk,” McLaughlin said.
Women are more adversely affected by alcohol
It is not a surprise that alcohol poses a higher risk for women than men when it comes to heart health, said C. Noel Bairey Merz , director of the Barbra Streisand Women’s Heart Center in the Smidt Heart Institute at Cedars-Sinai.
Women are more adversely affected than men by a lot of things such as cigarettes and pharmaceuticals and a bottle of beer or a glass of wine, where the dosage for men and women is the same and yet women are smaller, she said, referring to women being physically smaller, on average. Women also metabolize differently, their blood pressure is different, their liver function is different, they even deposit fat differently, Merz said.
“Women and men are built differently,” she said, noting she wasn’t even referring to the obvious reproductive differences. “It could be that in addition to body surface area … there are just pure biological differences in how the alcohol is metabolized.”
It’s possible to mitigate some of the ill effects of alcohol, the experts said. For instance, when people reduce or stop drinking, their blood pressure can improve and some lose weight as alcohol is a sugar that is no longer being consumed.
But issues such as enlargement of the heart happen with long-term heavy drinking, and even if the person stops, that may not improve, they said.
“If one stops drinking, some of the risk could reverse,” McLaughlin said. “The degree of improvement would depend on the age of the person and number of years of drinking.”
Read more from Well+Being
Well+Being shares news and advice for living well every day. Sign up for our newsletter to get tips directly in your inbox.
Vitamin B12 for fatigue has no proven benefit unless you have a deficiency that causes anemia.
Flashes, shimmers and blind spots: Here’s what migraine aura looks like.
Sparkling water is a better choice for your teeth than most popular beverages.
You can help your brain form healthy habits and break the bad ones.
Our 7 best tips to build an exercise habit .

- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
How to Thrive as You Age
Women who do strength training live longer. how much is enough.

Allison Aubrey

Strength training is good for everyone, but women who train regularly get a significantly higher boost in longevity than men. Gary Yeowell/Getty Images hide caption
Strength training is good for everyone, but women who train regularly get a significantly higher boost in longevity than men.
Resistance training does more than help us build strong muscles.
A new study finds women who do strength training exercises two to three days a week are more likely to live longer and have a lower risk of death from heart disease, compared to women who do none.
"We were incredibly impressed by the finding," says study author Martha Gulati , who is also the director of preventive cardiology at Cedars Sinai in Los Angeles.
Of the 400,000 people included in the study, only 1 in 5 women did regular weight training. But those who did, saw tremendous benefits.
"What surprised us the most was the fact that women who do muscle strengthening had a reduction in their cardiovascular mortality by 30%," Gulati says. "We don't have many things that reduce mortality in that way."
Strength training is also good for bones, joints, mood and metabolic health. And at a time when many women focus on aerobic activity and hesitate to do weight training, the findings add to the evidence that a combination of both types of exercise is powerful medicine. "Both should be prescribed," Gulati says.

Shots - Health News
Millions of women are 'under-muscled.' these foods help build strength.
The findings are part of a larger study, published in The Journal of the American College of Cardiology, which evaluated the differences in the effects of exercise between men and women.
While the study finds that even small doses of exercise are beneficial for everyone, the data show that women need less exercise than men to get the same gains in longevity.
Women who did moderate intensity exercise, such as brisk walking, five times a week, reduced their risk of premature death by 24%, compared to 18% for men.
"The take home message is – let's start moving," says Eric Shiroma , a prevention-focused researcher at the National Heart, Lung, and Blood Institute, part of the National Institutes of Health, which provided grant support for the research..
It's not exactly clear what drives the variance between sexes, but there are physiological differences between men and women, and differences in heart disease risks , too.
People born female have less muscle and lower aerobic capacity in general. Also, women have more capillaries feeding part of their muscles, Shiroma says. The findings show women need to do less exercise to change their baseline of aerobic and muscular strength. "It might be that this relative increase in strength [in women compared to men] is what's driving this difference in benefit," he says.
The results show a little can go a long way. "The benefits start as soon as you start moving," Shiroma says.
It's increasingly common to see female weight lifters and body builders on social media, and many gyms and work-out studios now incorporate weight training into many of their classes and offerings. But, given that about 80% of women in the study said they don't participate in regular weight training, there's still a lot of hesitancy.

Ann Martin says her mood improves with resistance training. "It gets your blood flowing," she says. "It feels good." Deb Cutler/Ann Martin hide caption
"I was always the awkward one in gym class back in school days," says Ann Martin, 69, of Wilmington, Del. She shied away from gyms and weight-training machines. Martin has always been a walker, but she realized she needed to build more strength, so last year she started working out with a trainer to learn how to use the equipment. "It's fun now," she says. "I can feel my muscles getting stronger."
Strength training can be intimidating, Shiroma says. "But it's not all bodybuilders trying to lift super amounts of weight." He says there are many ways to incorporate resistance training into your life.
All activities that require your muscles to work against a weight or force count as strength training. This includes the use of weight machines, resistance bands or tubes, as well as all the many ways we can use our own body weight, as we do with push-ups and squats.
The findings of this new study fit with the Physical Activity Guidelines for Americans , which recommend that adults get a minimum of 2.5 hours of moderate-intensity exercise a week, that's about 30 minutes, most days of the week. The guidelines also call for doing strength-based activities at least two days a week.

This 22-Minute Workout Has Everything You Need
The increase in lifespan can likely be explained in part, by the well-being that comes from the other hidden benefits. Here are 5 ways building strength can boost good health.
1. Strength training helps protect joints.
Physical therapists often recommend resistance training for patients with knee and hip pain. "Strength training protects joints, resulting in less stress through the body," says Todd Wheeler, a physical therapist at MedStar Health Physical Therapy in Washington, D.C . "If joints could talk, they would say 'It's not my fault I'm irritated," Wheeler says. They'd blame it on weak muscles. He says strong muscles support the joints, which can help decrease joint pain. Wheeler recommends starting small and simply. For instance, try a few squats and table pushups. "Listen to your body and gradually increase intensity over time," he says.

2. Building muscle burns more calories
Aerobic exercise – such as running and cycling – typically burns more calories in real time compared to strength training. But people who weight train can get a boost in calorie burning over the long-term.
"When you're doing resistance training, you're building muscle. That muscle requires energy," says Bryant Johnson , a trainer who wrote The RBJ Workout . So, adding muscle mass can help people burn more calories.
Dr. Gulati also points to research that shows weight lifting and resistance training can help people lose more fat and improve body composition.
3. Resistance training protects against injuries and falls
As we've reported, millions of Americans, especially women, are under-muscled, and muscle mass is a predictor of longevity .
Since muscle mass peaks in our 30s and then starts a long, slow decline, we need to take steps to slow this down. If we don't do strength training exercise, we're more likely to become weak, increasing the risk of falls, which is the top cause of death among older adults in the U.S.
And since muscle loss - also known as sarcopenia - affects more than 45% of older adults in the U.S., "it's important to know about it and take steps to prevent it," says Richard Joseph , a wellness focused physician. He says strength training improves bone density which also protects against injuries and falls.
Joseph says people can get the biggest bang for their buck when they're starting out by focusing on lower body exercises that work big muscle groups in the legs.
4. Strength training helps control blood sugar
About 1 in 3 adults in the U.S. has prediabetes. Strength training can help control blood sugar by clearing glucose out of the bloodstream.
When we use our muscles during exercise, whether it's pushing, pulling, lifting or moving, they require more glucose for energy. This explains why exercise after meals can help control blood sugar.
And a recent study found strength training can be even more effective than aerobic activity in controlling blood sugar in people with diabetes.
5. Muscle building may help boost mood
A meta-analysis published in the medical journal JAMA Psychiatry in 2018, which included the results of more than 30 clinical trials, found a reduction in symptoms of depression among people who did weight training two times a week or more.
Strength training has also been shown to improve depressive symptoms in people at risk of metabolic disease. And, research shows strength training can tamp down anxiety, too.
Ann Martin says it makes sense that our moods improve when we move. "It gets your blood flowing," she says. "It feels good."

Scientists can tell how fast you're aging. Now, the trick is to slow it down
This story was edited by Jane Greenhalgh
- resistance training
- strength training
- weight training
- heart disease
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Environmental Factor
Your online source for niehs news, niehs news in brief.
Earth Day and World Autism Month, Women in Science, Director’s lecture, and Codeathon.
By Ben Richardson
Discover environment and health connections this April

Check out a new video and podcast created with NIEHS support to raise awareness about the environment’s role in health. The multimedia products can be shared with your networks this April in support of Earth Day and World Autism Month.
Together with institutes and individuals across the globe, NIEHS will recognize April 22 as the 54th annual Earth Day. For a quick explanation of how your environment affects your health, check out this short video produced by NIEHS-funded scientists at Oregon State University.
In addition, listen to this NIEHS podcast featuring Staci Bilbo, Ph.D., of Duke University, to learn about her research related to autism spectrum disorder. Bilbo recently published findings on the combined effects of diesel pollution and maternal stress on neurodevelopment and the likelihood of autism characteristics in mice.
NIEHS hosts Women in Science Winter Social

Women in Science (WiS), a cross-divisional NIEHS group, hosted a Winter Social Feb. 27 in Rall Cafeteria. More than 40 people attended the event, which provided an opportunity for participants to network, play games, and recognize Black History Month and Women’s History Month.
Women in Science provides relevant information, support, networking opportunities, and events open to all NIEHS staff interested in topics important for women. The next WiS event will be held April 3 at noon, and it will feature a presentation by Amanda Cravens, Ph.D., a research social scientist at the U.S. Geological Survey. For more information about WiS, contact Vicki Sutherland, Ph.D.
Director outlines environmental health priorities at Yale event
NIEHS Director Rick Woychik, Ph.D. , described his vision for the future of environmental health at a March 6 Yale School of Public Health Dean’s Lecture in New Haven, Connecticut. This lecture was part of a series that brings together public health experts and thought leaders from around the globe to discuss diversity, equity, inclusion, and scientific rigor.
“We’ve been reaching out to the global community and listening to what you all have to say about where we should be going in the environmental health sciences,” said Woychik. “One of the things I’m personally most passionate about is integrating environmental exposures into the very fabric of the way that we study human diseases.”
During the event, Woychik highlighted current environmental justice initiatives at NIEHS, the need for future strategies aimed at reducing health disparities worldwide, and the institute’s emerging scientific priority areas, including climate change and health.
Codeathon explores implications of AI for biological research
More than 100 biologists, data scientists, and programmers participated in a National Center for Biotechnology Information codeathon during the last week in February. Ten teams collaborated to address various challenges in the biological and biomedical research domains using machine learning (ML) and artificial intelligence (AI) approaches.
The projects spanned a wide range of topics, including predicting drug sensitivity in cancer cell lines, visualizing human genome data for CRISPR applications, identifying genomic and omic features associated with traits such as COVID-19 and hypertension, and exploring the use of expert-entrained AI-based systems for toxicological property analysis.
“This week provided an opportunity to work collaboratively rather than competitively with some amazing people,” said Trey Saddler, a data scientist in the Division of Translational Toxicology. “The event demonstrated what can be accomplished when a diverse group of talented people come together to solve difficult problems.”
All presentations and data repositories from each team can be found on the National Library of Medicine website and GitHub.
(Ben Richardson, Ph.D., is a Presidential Management Fellow in the NIEHS Office of Communications and Public Liaison.)
Related Articles
Heather Patisaul selected to lead Division of Translational Toxicology

Scientists talk precision medicine, environmental health at NC event

NIEHS celebrates Earth Day with Green awards and community events

NIEHS seeks input on next strategic plan

Advisory Council considers research questions on aging, exposomics, report back
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 21 November 2023
Only 0.5% of neuroscience studies look at women’s health. Here’s how to change that

- Emily G. Jacobs 0
Emily G. Jacobs is associate professor of psychological and brain sciences at University of California, Santa Barbara, and director of the Ann S. Bowers Women’s Brain Health Initiative.
You can also search for this author in PubMed Google Scholar
Neuroscientists now have unprecedented access to the living brain, thanks to magnetic resonance imaging (MRI). More than 50,000 human-brain-imaging articles have been published since MRI came on the scene in the 1990s. But of those, less than 0.5% consider health factors specific to women.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 623 , 667 (2023)
doi: https://doi.org/10.1038/d41586-023-03614-1
Reprints and permissions
Competing Interests
The author declares no competing interests.
Related Articles

- Neuroscience
- Personalized medicine

Innate immunity in neurons makes memories persist
News & Views 27 MAR 24

Formation of memory assemblies through the DNA-sensing TLR9 pathway
Article 27 MAR 24

A brainstem–hypothalamus neuronal circuit reduces feeding upon heat exposure

Memories are made by breaking DNA — and fixing it
News 27 MAR 24

Ketamine is in the spotlight thanks to Elon Musk — but is it the right treatment for depression?
News Explainer 20 MAR 24

Circulating myeloid-derived MMP8 in stress susceptibility and depression
Article 07 FEB 24

Sustained antidepressant effect of ketamine through NMDAR trapping in the LHb
Article 18 OCT 23
Mental health: The invisible effects of neglected tropical diseases
Outlook 12 OCT 23
Senior Scientist, Research
Be part of something altogether life-changing! Working at Cytiva means being at the forefront of providing new solutions to transform human heal...
Vancouver, British Columbia (CA)
Postdoctoral positions in the integrative structural biology of cancer and immunity
Postdoctoral positions in the integrative structural biology study of signaling complexes important in cancer and the immune system
Farmington, Connecticut (US)
University of Connecticut Health Center (UCHC)
Faculty Positions & Postdocs at Institute of Physics (IOP), Chinese Academy of Sciences
IOP is the leading research institute in China in condensed matter physics and related fields. Through the steadfast efforts of generations of scie...
Beijing, China
Institute of Physics (IOP), Chinese Academy of Sciences (CAS)
Postdoctoral Scholar - PHAST Alzheimer
Memphis, Tennessee
The University of Tennessee Health Science Center (UTHSC)
Postdoctoral Associate- Neurodevelopmental Disease
Houston, Texas (US)
Baylor College of Medicine (BCM)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Turn Your Curiosity Into Discovery
Latest facts.

Facts on Junk Food Marketing and Kids

The Future of Video Game Art Emerging Patterns and CuttingEdge Technologies
35 facts about lyubertsy.
Written by Tate Lewin
Modified & Updated: 02 Mar 2024
Reviewed by Jessica Corbett

Lyubertsy is a fascinating city located in the Moscow Oblast region of Russia. With a rich history and vibrant culture, Lyubertsy has become a prominent destination for both tourists and locals alike. This article will take you on a journey through 35 interesting facts about Lyubertsy, providing you with a comprehensive overview of this enchanting city. From its historical landmarks and architectural wonders to its renowned festivals and local cuisine, Lyubertsy has something to offer for everyone. So, buckle up and get ready to explore the hidden gems and fascinating trivia that make Lyubertsy such a remarkable place to visit.
Key Takeaways:
- Lyubertsy, a city in Russia, is known for its rich history, cultural events, and vibrant community. From museums to parks, it offers something for everyone to explore and enjoy.
- With a population of over 190,000, Lyubertsy boasts a strong sense of community, low crime rate, and warm hospitality. It’s a city with a high standard of living and a rich cultural heritage.
Lyubertsy is a vibrant city located in the Moscow Oblast of Russia.
Nestled in the southeastern part of Moscow , Lyubertsy is known for its rich history, cultural heritage, and beautiful landscapes.
The city is named after the Russian nobleman Dmitry Lyubertsy.
Dmitry Lyubertsy was a prominent figure in the 19th century and played a significant role in the development of the region.
Lyubertsy is home to a population of over 190,000 people.
With a large and diverse community, the city offers a unique blend of traditions, languages, and cultures.
The city is famous for its industrial sector.
Lyubertsy is known for its manufacturing plants, including the production of machinery, electronics, and textiles.
Lyubertsy has a rich cultural heritage.
The city is home to several museums, art galleries, and theaters, showcasing the talent and creativity of its residents.
The Lyubertsy District is dotted with picturesque parks and green spaces.
Residents and visitors can enjoy leisurely walks, picnics, and outdoor activities in the city’s numerous parks and gardens.
Lyubertsy is well-connected to Moscow through an extensive transportation network.
Commuting to and from the city is convenient, thanks to the availability of buses, trains, and metro lines.
The city experiences a continental climate.
Winters in Lyubertsy are cold and snowy, while summers are warm and moderately humid.
Lyubertsy has a rich sporting culture.
The city is home to various sports complexes, arenas, and stadiums, encouraging a healthy and active lifestyle among its residents.
The famous Russian singer, Alla Pugacheva, was born in Lyubertsy.
Alla Pugacheva, often referred to as the “Queen of Russian Pop,” is a beloved figure in the music industry.
The Lyubertsy Railway Station is an important transportation hub.
It connects the city to other parts of Russia, making travel accessible and convenient for residents and visitors.
Lyubertsy is known for its vibrant cultural events and festivals.
Throughout the year, the city hosts various celebrations, showcasing its rich traditions, music, and dance.
The city has a thriving educational system.
Lyubertsy is home to several schools, colleges, and universities, providing quality education to its residents.
Lyubertsy offers a range of recreational activities.
Residents and visitors can enjoy swimming, ice skating, skiing, and other outdoor activities in the city’s sports complexes and recreational centers.
The Lyubertsy History Museum preserves the city’s historical artifacts.
The museum showcases the rich history and heritage of Lyubertsy, allowing visitors to delve into its past.
The city has a variety of shopping centers and markets.
From local boutiques to large malls, Lyubertsy offers plenty of options for shopping enthusiasts.
Lyubertsy has a strong sense of community.
Residents actively participate in local events, volunteer programs, and social initiatives, fostering a close-knit and supportive environment.
The city is known for its delicious Russian cuisine.
Visitors can savor traditional dishes such as borscht, pelmeni, and blini in Lyubertsy’s charming restaurants and cafes.
Lyubertsy is surrounded by picturesque countryside.
Nature lovers can explore the nearby forests, lakes, and rivers, offering tranquility and an escape from the city’s hustle and bustle.
The city has several architectural landmarks.
From historical buildings to modern structures, Lyubertsy boasts a diverse range of architectural styles.
Lyubertsy is a hub for arts and culture.
The city embraces various art forms, including music, theater, painting, and sculpture.
Lyubertsy has a low crime rate.
The city’s focus on security and community well-being contributes to a safe and secure living environment.
Lyubertsy celebrates its rich heritage through folk festivals.
Traditional music, dance, and costumes take center stage during these vibrant celebrations.
The city has a well-developed healthcare system.
Residents have access to modern medical facilities and clinics, ensuring their well-being.
Lyubertsy is a city of historical significance.
It played a crucial role in Russia’s past and preserves its heritage through museums and historical sites.
Lyubertsy is home to many talented artists and musicians.
The city’s vibrant creative scene showcases local talent and promotes artistic expression.
The city has a strong sense of environmental consciousness.
Efforts are made to promote sustainability, green initiatives, and conservation of natural resources.
Lyubertsy hosts various cultural exhibitions and events.
These events provide a platform for artists, craftsmen, and cultural enthusiasts to showcase their work.
The city is known for its warm hospitality.
Visitors can experience the friendly and welcoming nature of the locals during their stay in Lyubertsy.
Lyubertsy is a center for academic research and innovation.
The city promotes scientific development and fosters collaboration between educational institutions and industries.
The Lyubertsy City Park is a popular recreational spot.
With its lush greenery, walking trails, and recreational facilities, the park offers a refreshing escape for residents.
Lyubertsy celebrates its rich history through historical reenactments.
These events allow visitors to step back in time and experience the city’s past firsthand.
The city is known for its impressive Soviet-era architecture.
Visitors can admire the unique architectural style and grandeur of buildings constructed during the Soviet era.
Lyubertsy is well-connected to other major cities in Russia.
Traveling to and from Lyubertsy is convenient due to its excellent transportation infrastructure.
Lyubertsy offers a high standard of living.
The city provides its residents with quality amenities, services, and a favorable quality of life.
With its rich history, cultural heritage, and vibrant community, Lyubertsy offers a unique and compelling experience for residents and visitors alike. Whether it’s exploring the city’s museums, enjoying the scenic beauty of its parks, or immersing oneself in its art and culture, Lyubertsy has something for everyone. Discover the charm and allure of this remarkable city and experience the warmth and hospitality of its residents.
In conclusion, Lyubertsy is a fascinating city with a rich history, vibrant culture, and plenty of attractions to explore. From its beautiful parks and gardens to its impressive architectural landmarks, Lyubertsy offers something for everyone. Whether you’re interested in history, art, or simply enjoying the local cuisine, this city has it all. So, if you’re planning a visit to Russia, be sure to include Lyubertsy in your itinerary. You won’t be disappointed!
Q: What is the population of Lyubertsy?
A: The population of Lyubertsy is around 180,000.
Q: What are some popular tourist attractions in Lyubertsy?
A: Some popular tourist attractions in Lyubertsy include Lyubertsy Museum of Local Lore, Novodevichy Cemetery, and St. Nicholas Cathedral.
Q: Is Lyubertsy a safe city for tourists?
A: Yes, Lyubertsy is generally considered to be a safe city for tourists. However, it is always recommended to exercise caution and take normal safety precautions.
Q: What is the weather like in Lyubertsy?
A: The weather in Lyubertsy can vary depending on the season. Summers are generally mild and warm, while winters can be cold with snowfall.
Q: Are there good transportation options in Lyubertsy?
A: Yes, Lyubertsy is well-connected to Moscow and other nearby cities through public transportation options like buses and trains.
Q: Are there any local specialties or dishes to try in Lyubertsy?
A: Lyubertsy is known for its delicious Russian cuisine, including dishes like borscht, pelmeni, and blini.
Q: Can I find accommodations in Lyubertsy?
A: Yes, there are a variety of accommodations available in Lyubertsy, ranging from hotels to guesthouses and apartments for rent.
Q: Is English widely spoken in Lyubertsy?
A: While English may not be widely spoken, many people in the tourist areas and establishments can understand and communicate in English.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
Share this Fact:
Sales channel built for e-commerce businesses
Create your e-commerce presence yourself from scratch
Find B2B Leads Data
- B2B Database
- Location reports
- All Rentechdigital Products
List of Women's health clinics in Moscow Oblast
Number of women's health clinics in moscow oblast with email address, phone number, geocoded address, and other key details for download., number of women's health clinics, smartscrapers has the most up to date and comprehensive women's health clinics list in moscow oblast. our lists are constantly being verified and our database is constantly being updated..
Trusted by 100k+ Businesses
Download list of Women's health clinics in Moscow Oblast
Find new clients and close more deals with the world’s best business leads provider. You can download Women's health clinics email and phone number lists for your sales teams. Here is a random sample of 10 records for you to look at the fields and the data that we provide.

How Smartscrapers Data Services Helps Businesses
Explore the strategic advantages our web scraping solutions bring to your business.
Email Campaigns
Transform your email campaigns with accurate and up-to-date contact information. Our web scraping services empower you to build targeted email lists, enhance personalization, and boost deliverability, ensuring your messages reach the right audience.
Cold Calling
Revolutionize your cold-calling strategies with our web scraping solutions. Access updated contact information, tailor pitches based on audience insights, and increase conversion rates, turning leads into valuable customers through effective communication.
Mail Campaigns
Enhance your direct mail campaigns with our targeted data solutions. Craft tailored content based on precise insights, increase response rates by delivering resonant content and optimize your budget by targeting the most relevant recipients.
Number of Women's health clinics locations by each city/area
How many women's health clinics are there in moscow oblast .
There are a total of 101 Women's health clinics in Moscow Oblast as of March 15, 2024 .
Download the list of 101 Women's health clinics in Moscow Oblast as of March 15, 2024 based on phone number, email, and both.
Number of Women's health clinics in Moscow Oblast with Phone Number
Number of Women's health clinics in Moscow Oblast with Email
Number of Women's health clinics in Moscow Oblast with Phone Number and Email
Download sales qualified leads of Women's health clinics in the Moscow Oblast
Download this data in CSV, Esri Shapefile, Excel, GeoJSON, or KML (Google Earth) file formats.
Related Women's health clinics Leads By Location
- Women's health clinics Leads in Afghanistan
- Women's health clinics Leads in Algeria
- Women's health clinics Leads in Angola
- Women's health clinics Leads in Argentina
- Women's health clinics Leads in Armenia
- Women's health clinics Leads in Australia
- Women's health clinics Leads in Austria
- Women's health clinics Leads in Azerbaijan
- Women's health clinics Leads in Bahrain
- Women's health clinics Leads in Bangladesh
- Women's health clinics Leads in Amhara Region
- Women's health clinics Leads in Addis Ababa
- Women's health clinics Leads in Ashanti Region
- Women's health clinics Leads in Greater Accra Region
- Women's health clinics Leads in Jambyl Region
- Women's health clinics Leads in Almaty
- Women's health clinics Leads in Nur-Sultan
- Women's health clinics Leads in Kiambu County
- Women's health clinics Leads in Mombasa County
- Women's health clinics Leads in Nakuru District
- Women's health clinics Leads in Ajman City
- Women's health clinics Leads in Al Shamkhah City
- Women's health clinics Leads in Dubai
- Women's health clinics Leads in Ras Al Khaimah City
- Women's health clinics Leads in Sharjah
- Women's health clinics Leads in Yerevan
- Women's health clinics Leads in Paraná
- Women's health clinics Leads in Río Cuarto
- Women's health clinics Leads in Linz Stadt
Data of Women's health clinics in Moscow Oblast with/without Website
Download the list of Women's health clinics in Moscow Oblast as of March 15, 2024 with and without website information.
Number of Women's health clinics in Moscow Oblast with website
Number of Women's health clinics in Moscow Oblast without website
List of Women's health clinics in Moscow Oblast By Ratings
Download the data of the number of star-rated Women's health clinics in Moscow Oblast as of March 15, 2024 .
Number of 1 star-rated Women's health clinics in Moscow Oblast
Number of 2 star-rated Women's health clinics in Moscow Oblast
Number of 3 star-rated Women's health clinics in Moscow Oblast
Number of 4 star-rated Women's health clinics in Moscow Oblast
Number of 5 star-rated Women's health clinics in Moscow Oblast
Newly Opened Business

Recently Closed Business
Monthly Insights for Market Analysis and Growth
Receive monthly updates on business openings and closings across diverse industries.
- Essential data for sales, marketing professionals, investors, and analysts.
- Strategically compiled to inform and guide your marketing and sales tactics.
- Leverage monthly data to refine your sales leads and marketing strategies.
- Stay ahead of market trends with timely, comprehensive business insights.
Special Features
Monthly dispatch of business dynamics in over 5000 categories.
Data sets tailored for impactful sales and marketing applications.
Efficient access to a wide array of business information.
Not Just Leads!
Unlock the complete potential of your marketing, sales, analytics, and other business operations with quality leads found nowhere else on the Internet. Decrease your time spent on finding leads and shift your focus to more productive tasks.
Close Faster

Gain Insights

Attract Customers

What is the total number of Women's health clinics in Moscow Oblast?
Where can i get the women's health clinics in moscow oblast leads database, how to download sales qualified leads database of women's health clinics in moscow oblast, can i download a sample dataset of women's health clinics leads in moscow oblast, in what formats can i download women's health clinics in moscow oblast leads, how much does the women's health clinics in moscow oblast dataset cost, how many women's health clinics in moscow oblast have phone numbers, how many women's health clinics in moscow oblast have email lists, how many women's health clinics in moscow oblast have phone number lists and emails, what is the total count of women's health clinics in moscow oblast with a website, what is the total count of women's health clinics in moscow oblast without a website, how many 5-star rated women's health clinics are there in moscow oblast, what is the total count of 4-star rated women's health clinics in moscow oblast, how many 3-star rated women's health clinics are there in moscow oblast, what is the total count of 2-star rated women's health clinics in moscow oblast, how many 1-star rated women's health clinics are there in moscow oblast, how to target women's health clinics through facebook ad campaigns, how to target women's health clinics through google ad campaigns, how do email addresses of women's health clinics assist in online marketing, how do phone numbers of women's health clinics help businesses, how does the mailing address data of women's health clinics support marketing strategies.

COMMENTS
The National Institutes of Health (NIH) Office of Research on Women's Health (ORWH) was established in 1990. With the completion of the office's 30th anniversary year, we look back and recount some of the key events and overall zeitgeist that led to ORWH's formation, and how it became the focal point at the nation's primary biomedical research agency for coordinating research on science to ...
Correction to: Assessing the survival time of women with breast cancer in Northwestern Ethiopia: using the Bayesian approach. Chalachew Gashu and Aragaw Eshetie Aguade. BMC Women's Health 2024 24 :162. Correction Published on: 6 March 2024. The original article was published in BMC Women's Health 2024 24 :120.
Women's Health is an open access, peer-reviewed international journal that focuses on all aspects of women's healthcare. The aim of the journal is to increase knowledge regarding all issues that specifically affect women. View full journal description. This journal is a member of the Committee on Publication Ethics (COPE).
Women's Health Issues (WHI) is a peer-reviewed, bimonthly, multidisciplinary journal that publishes research and review manuscripts related to women's health care and policy. As the official journal of the Jacobs Institute of Women's Health , it is dedicated to improving the health and health care of all women throughout the lifespan and in ...
The "bottom-up" approach of a wide dissemination of information to clinicians, together with practical incentives for stakeholders with competing interests to collaborate, promise to improve women's healthcare. Keywords: research quality, methodology, evidence-based medicine, systematic review. Go to: 1. Introduction.
Women's health has long been overlooked in both fundamental and clinical research, which, sadly, also holds true for the bioengineering field — albeit things are slowly changing.
BMC Women's Health is an open access, peer-reviewed journal that considers articles on all aspects of the health and wellbeing of adolescent girls and women, with a particular focus on the physical, mental, and emotional health of women in developed and developing nations. The journal welcomes submissions on women's public health issues, health behaviours, breast cancer, gynecological diseases ...
The age at which women experience menopause varies widely — with a range in healthy women of about 20 years — and fertility can decline drastically as much as a decade before its onset. This ...
A focus on women's health research, and the star caught in the act of devouring a planet. Hear the biggest stories from the world of science |03 May 2023.
critical, systematic historical research on women's health. book reviews. Contributors provide the technical and scientific backdrop that women's health issues require. From time to time, special symposium issues on a single theme are published. Publication office: Taylor & Francis, Inc., 530 Walnut Street, Suite 850, Philadelphia, PA 19106.
Preview abstract. Open Access Review article First published March 13, 2024. xml PDF / EPUB. Table of contents for Women's Health, 20, , Jan 01, 2024.
Funding for the women's panel convening and findings provided by the Robert Wood Johnson Foundation. Cite this article as: Schubert KG, Bird CE, Kozhimmanil K, Wood SF (2022) To address women's health inequity, it must first be measured , Health Equity 6:1, 881-886, DOI: 10.1089/heq.2022.0107. * This research article uses the term "men ...
Janine Austin Clayton, M.D., FARVO, was appointed Associate Director for Research on Women's Health and Director of the Office of Research on Women's Health at the National Institutes of Health (NIH) in 2012. Dr. Clayton has strengthened NIH support for research on diseases, disorders, and conditions that affect women.
OWH-Funded Research Projects - The FDA Office of Women's Health (OWH) awards research grants for 1-2 year studies to address regulatory research questions related to women's health issues and ...
March 08, 2022. Our current understanding of women's health research—the study of health across a woman's lifespan in order to preserve wellness and to prevent, diagnose, and treat disease, for the full range of health conditions for which women are disproportionately or differently affected by—did not exist until about 30 years ago.
Date Posted: November 15, 2023. The White House has announced the establishment of the Women's Health Research Initiative within the Office of the First Lady. The initiative aims to improve women's health in the United States by accelerating research on the unique health needs of women across their lifespans and therefore fundamentally ...
Biden traveled to Cambridge, Mass., last month to announce the first step of the women's health initiative: $100 million to support women's health researchers and start-up companies.
Midwives encounter various difficulties while aiming to achieve excellence in providing maternity care to women with mobility disabilities. The study aimed to explore and describe midwives' experiences of caring for women with mobility disabilities during pregnancy, labour and puerperium in Eswatini. A qualitative, exploratory, descriptive, contextual research design with a phenomenological ...
Funding for research on women's health is still a fraction of that available for men's health. Demonstrators in Washington DC last September drew attention to the lack of funding for research ...
Neither is PCOS mentioned in President Joe Biden's recent executive order to advance women's health, which includes $200 million for NIH research grants, or the White House's calls for ...
During the address, he said "women are more than half of our population, but research on women's health has always been underfunded." The event was moderated by Melissa Schooley , a member of Fralin Biomedical Research Institute's advisory board and vice president of global reimbursement, health policy, and government affairs for ...
So this order will create a Fund for Women's Heath Research at the National Institutes of Health (NIH). It also directs the HHS to expand data collection on women's midlife health and launch ...
And women who binge drink — three alcoholic beverages per day — were 68 percent more likely to develop coronary heart disease than those who drink in moderation, the research showed.
Strength training is good for everyone. But women who train regularly, reduce their risk of death from heart disease significantly. And here are 5 other hidden benefits of building muscle.
Women in Science provides relevant information, support, networking opportunities, and events open to all NIEHS staff interested in topics important for women. The next WiS event will be held April 3 at noon, and it will feature a presentation by Amanda Cravens, Ph.D., a research social scientist at the U.S. Geological Survey.
More than 50,000 human-brain-imaging articles have been published since MRI came on the scene in the 1990s. But of those, less than 0.5% consider health factors specific to women. Women's health ...
25x25: At the heart of global health Scientific Sessions 2014 4-7 May 2014 | Melbourne, Australia www.worldcardiocongress.org Global Platform For cardiovascular disease specialists and public health professionals to share knowledge and network with their peers World leadinG exPerts Presenting 150 sessions on cardiology, policy and public health
Experienced Medical Laboratory Technician with a demonstrated history of working in the health wellness and fitness industry. Skilled in Good Laboratory Practice (GLP), Medical Devices, Laboratory Medicine, Laboratory Animal Medicine, and Validation. Strong research professional with a Specialist focused in Veterinary Medicine from Московская Государственная ...
This article will take you on a journey through 35 interesting facts about Lyubertsy, providing you with a comprehensive overview of this enchanting city. From its historical landmarks and architectural wonders to its renowned festivals and local cuisine, Lyubertsy has something to offer for everyone.
Number of Women's health clinics in Moscow OblastList of Women's health clinics in Moscow Oblast with email address, phone number, geocoded address, and other key details for download. Data updated on September 25, 2023. $79. $790 (90% off) PURCHASE DATASET FREE SAMPLE DATASET. Klinika Beregita. 5.0 3 reviews.