Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

68 templates


cybersecurity
6 templates
19 templates

58 templates

18 templates

physiotherapy
14 templates
Bipolar Disorder Case Report
Bipolar disorder case report presentation, free google slides theme and powerpoint template.
Bipolar disorder can be a challenging condition to manage, but with the right support and treatment, individuals living with bipolar disorder can lead fulfilling lives. At the heart of managing this complex condition lies effective communication between mental health professionals and their patients. So, when it comes to presenting a case report on bipolar disorder, creating a workable and engaging slideshow is crucial. With the help of this template, you can tailor a visual narrative that not only enhances comprehension but also showcases the unique nuances of each case. By incorporating eye-catching graphics and compelling case studies, you can share your findings with confidence, knowing that you have conveyed the information in an unforgettable way.
Features of this template
- 100% editable and easy to modify
- 28 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Greek and Roman Papyrology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Agriculture
- History of Education
- History of Emotions
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Variation
- Language Families
- Language Evolution
- Language Reference
- Lexicography
- Linguistic Theories
- Linguistic Typology
- Linguistic Anthropology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Culture
- Music and Media
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Oncology
- Medical Toxicology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Neuroscience
- Cognitive Psychology
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business History
- Business Ethics
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic Methodology
- Economic History
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Political Behaviour
- Political Economy
- Political Institutions
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >
5 Psychiatric Treatment of Bipolar Disorder: The Case of Janice
- Published: February 2013
- Cite Icon Cite
- Permissions Icon Permissions
Chapter 5 covers the psychiatric treatment of bipolar disorder, including a case history, key principles, assessment strategy, differential diagnosis, case formulation, treatment planning, nonspecific factors in treatment, potential treatment obstacles, ethical considerations, common mistakes to avoid in treatment, and relapse prevention.
Signed in as
Institutional accounts.
- Google Scholar Indexing
- GoogleCrawler [DO NOT DELETE]
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Real Life Bipolar Disorder: A Case Study of Susan
Bipolar disorder is a complex and often misunderstood mental health condition that affects millions of individuals worldwide. For those living with bipolar disorder, the highs and lows of life can be dizzying, as they navigate through periods of intense mania and debilitating depression. To truly grasp the impact of this disorder, it’s crucial to explore real-life experiences and the stories of those who have dealt firsthand with its challenges.
In this article, we delve into the fascinating case study of Susan, a woman whose life has been profoundly shaped by her bipolar disorder diagnosis. By examining Susan’s journey, we aim to shed light on the realities of living with this condition and the strategies employed to manage and treat it effectively.
But before we plunge deeper into Susan’s story, let’s first gain a comprehensive understanding of bipolar disorder itself. We’ll explore the formal definition, the prevalence of the condition, and its impact on both individuals and society as a whole. This groundwork will set the stage for a more insightful exploration of Susan’s experience and provide valuable context for the subsequent sections of this article.
Bipolar disorder is more than just mood swings; it is a condition that can significantly disrupt an individual’s life, relationships, and overall well-being. By studying a real-life case like Susan’s, we can gain a personal insight into the multifaceted challenges faced by those with bipolar disorder and the importance of effective treatment and support systems. In doing so, we hope to foster empathy, inspire early diagnosis, and contribute to the advancement of knowledge about bipolar disorder’s complexities.
The Case of Susan: A Real Life Experience with Bipolar Disorder
Susan’s story provides a compelling illustration of the impact that bipolar disorder can have on an individual’s life. Understanding her background, symptoms, and the effects of the disorder on her daily life can provide valuable insights into the challenges faced by those with bipolar disorder.
Background Information on Susan
Susan, a thirty-eight-year-old woman, was diagnosed with bipolar disorder at the age of twenty-five. Her early experiences with the disorder were characterized by periods of extreme highs and lows, often resulting in strained relationships and an inability to maintain steady employment. Susan’s episodes of mania frequently led to impulsive decision-making, excessive spending sprees, and risky behaviors. On the other hand, her depressive episodes left her feeling hopeless, fatigued, and unmotivated.
Symptoms and Diagnosis of Bipolar Disorder in Susan
To receive an accurate diagnosis, Susan underwent a thorough examination by mental health professionals. The criteria for diagnosing bipolar disorder include significant and persistent mood swings, alternating between periods of mania and depression. Susan exhibited classic symptoms of bipolar disorder, such as elevated mood, increased energy, racing thoughts, decreased need for sleep, and reckless behavior during her manic episodes. These episodes were interspersed with periods of deep sadness, loss of interest in activities, and changes in appetite and sleep patterns during depressive phases.
Effects of Bipolar Disorder on Susan’s Daily Life
Living with bipolar disorder presents unique challenges for Susan. The unpredictable shifts in her mood and energy levels significantly impact her ability to function in both personal and professional spheres. During manic phases, Susan experiences heightened productivity, creativity, and confidence, often leading her to take on excessive responsibilities and projects. However, these periods are eventually followed by crashes into depressive episodes, leaving her unable to complete tasks, maintain relationships, or even perform routine self-care. The constant fluctuations in her emotional state make it difficult for Susan to establish a sense of stability and predictability in her life.
Susan’s struggle with bipolar disorder is not uncommon. Many individuals with this condition face similar obstacles in their daily lives, attempting to manage the debilitating highs and lows while striving for a sense of normalcy. By understanding the real-life implications of bipolar disorder, we can more effectively tailor our support systems and treatment options to address the needs of individuals like Susan. In the next section, we will explore the various approaches to treating and managing bipolar disorder, providing potential strategies for improving the quality of life for those living with this condition.
Treatment and Management of Bipolar Disorder in Susan
Managing bipolar disorder requires a multifaceted approach that combines psychopharmacological interventions, psychotherapy, counseling, and lifestyle modifications. Susan’s journey towards finding effective treatment and management strategies highlights the importance of a comprehensive and tailored approach.
Psychopharmacological Interventions
Pharmacological interventions play a crucial role in stabilizing mood and managing symptoms associated with bipolar disorder. Susan’s treatment plan involved medications such as mood stabilizers, antipsychotics, and antidepressants. These medications aim to regulate the neurotransmitters in the brain associated with mood regulation. Susan and her healthcare provider closely monitored her medication regimen and made adjustments as needed to achieve symptom control.
Psychotherapy and Counseling
Psychotherapy and counseling provide individuals with bipolar disorder a safe space to explore their thoughts, emotions, and behaviors. Susan engaged in cognitive-behavioral therapy (CBT), which helped her identify and challenge negative thought patterns and develop healthy coping mechanisms. Additionally, psychoeducation in the form of group therapy or support groups allowed Susan to connect with others facing similar challenges, fostering a sense of community and reducing feelings of isolation.
Lifestyle Modifications and Self-Care Strategies
In addition to medical interventions and therapy, lifestyle modifications and self-care strategies play a vital role in managing bipolar disorder. Susan found that maintaining a stable routine, including regular sleep patterns, exercise, and a balanced diet, helped regulate her mood. Avoiding excessive stressors and implementing stress management techniques, such as mindfulness meditation or relaxation exercises, also supported her overall well-being. Engaging in activities she enjoyed, nurturing her social connections, and setting realistic goals further enhanced her quality of life.
Striving for stability and managing bipolar disorder is an ongoing process. What works for one individual may not be effective for another. It is crucial for individuals with bipolar disorder to work closely with their healthcare providers and engage in open communication about treatment options and progress. Fine-tuning the combination of psychopharmacological interventions, therapy, and self-care strategies is essential to optimize symptom control and maintain stability.
Understanding the complexity of treatment and management helps foster empathy for individuals like Susan, who face the daily challenges associated with bipolar disorder. It underscores the importance of early diagnosis, accessible mental health care, and ongoing support systems to enhance the lives of individuals living with this condition. In the following section, we will explore the various support systems available to individuals with bipolar disorder, including family support, peer support groups, and the professional resources that contribute to their well-being.
Support Systems for Individuals with Bipolar Disorder
Navigating the challenges of bipolar disorder requires a strong support system that encompasses various sources of assistance. From family support to peer support groups and professional resources, these networks play a significant role in helping individuals manage their condition effectively.
Family Support
Family support is vital for individuals with bipolar disorder. Understanding and empathetic family members can provide emotional support, monitor medication adherence, and help identify potential triggers or warning signs of relapse. In Susan’s case, her family played a crucial role in her recovery journey, providing a stable and nurturing environment. Education about bipolar disorder within the family helps foster empathy, reduces stigma, and promotes open communication.
Peer Support Groups
Peer support groups provide individuals with bipolar disorder an opportunity to connect with others who share similar experiences. Sharing personal stories, strategies for coping, and offering mutual support can be empowering and validating. In these groups, individuals like Susan can find solace in knowing that they are not alone in their struggles. Peer support groups may meet in-person or virtually, allowing for easier access to support regardless of physical proximity.
Professional Support and Resources
Professional support is crucial in the management of bipolar disorder. Mental health professionals, such as psychiatrists, psychologists, and therapists, provide expertise and guidance in developing comprehensive treatment plans. Regular therapy sessions allow individuals like Susan to explore emotional challenges and develop healthy coping mechanisms. Psychiatrists closely monitor medication effectiveness and make necessary adjustments. Additionally, case managers or social workers can assist with navigating the healthcare system, accessing resources, and connect individuals with other community services.
Beyond direct professional support, there are resources and organizations dedicated to bipolar disorder education, advocacy, and support. Online forums, websites, and helplines provide information, guidance, and a sense of community. These platforms allow individuals to access information at any time and connect with others who understand their unique experiences.
Support systems for bipolar disorder are crucial in empowering individuals and enabling them to lead fulfilling lives. They contribute to reducing stigma, providing emotional support, and ensuring access to resources and education. Through these support systems, individuals with bipolar disorder can gain self-confidence, develop effective coping strategies, and improve their overall well-being.
In the next section, we explore the significance of case studies in understanding bipolar disorder and how they contribute to advancing research and knowledge in the field. Specifically, we will examine how Susan’s case study serves as a valuable contribution to furthering our understanding of this complex disorder.
The Importance of Case Studies in Understanding Bipolar Disorder
Case studies play a vital role in advancing our understanding of bipolar disorder and its complexities. They offer valuable insights into individual experiences, treatment outcomes, and the overall impact of the condition on individuals and society. Susan’s case study, in particular, provides a unique perspective that contributes to broader research and knowledge in the field.
How Case Studies Contribute to Research
Case studies provide an in-depth examination of specific individuals and their experiences with bipolar disorder. They allow researchers and healthcare professionals to observe patterns, identify commonalities, and gain valuable insights into the factors that influence symptom presentation, treatment response, and prognosis. By analyzing various case studies, researchers can generate hypotheses and refine treatment approaches to optimize outcomes for individuals with bipolar disorder.
Case studies are particularly helpful in documenting rare or atypical presentations of bipolar disorder. They shed light on lesser-known subtypes, such as rapid-cycling bipolar disorder or mixed episodes, contributing to a more comprehensive understanding of the condition. Case studies also provide opportunities for clinicians and researchers to discuss unique challenges and discover innovative interventions to improve treatment outcomes.
Susan’s Case Study in the Context of ATI Bipolar Disorder
Susan’s case study is an example of how individual experiences can inform the development of Assessment Technologies Institute (ATI) for bipolar disorder. By examining her journey, researchers can analyze treatment approaches, evaluate the effectiveness of various interventions, and develop evidence-based guidelines for managing bipolar disorder.
Susan’s case study provides rich information about the impact of medication, psychotherapy, and lifestyle modifications on symptom control and overall well-being. It offers valuable insights into the benefits and limitations of specific interventions, highlighting the importance of personalized treatment plans tailored to individual needs. Additionally, Susan’s case study can contribute to ongoing discussions about the role of support systems and the integration of peer support groups in managing and enhancing the lives of individuals with bipolar disorder.
The detailed documentation of Susan’s experiences serves as a powerful tool for healthcare providers, researchers, and individuals living with bipolar disorder. It highlights the complexities and challenges associated with the condition while fostering empathy and understanding among various stakeholders.
Case studies, such as Susan’s, play a crucial role in enhancing our understanding of bipolar disorder. They provide insights into individual experiences, treatment approaches, and the impact of the condition on individuals and society. Through these case studies, we can cultivate empathy for individuals with bipolar disorder, advocate for early diagnosis and effective treatment, and contribute to advancements in research and knowledge.
By illuminating the realities of living with bipolar disorder, we acknowledge the need for accessible mental health care, support systems, and evidence-based interventions. Susan’s case study exemplifies the importance of a comprehensive approach to managing bipolar disorder, integrating psychopharmacological interventions, psychotherapy, counseling, and lifestyle modifications.
Moving forward, it is essential to continue studying cases like Susan’s and explore the diverse experiences within the bipolar disorder population. By doing so, we can foster empathy, encourage early intervention and personalized treatment, and contribute to advancements in understanding bipolar disorder, ultimately improving the lives of individuals affected by this complex condition.
Empathy and Understanding for Individuals with Bipolar Disorder
Developing empathy and understanding for individuals with bipolar disorder is crucial in fostering a supportive and inclusive society. By recognizing the unique challenges they face and the complexity of their experiences, we can better advocate for their needs and provide the necessary resources and support.
It is important to understand that bipolar disorder is not simply a matter of mood swings or being “moody.” It is a chronic and often debilitating mental health condition that affects individuals in profound ways. The extreme highs of mania and the lows of depression can disrupt relationships, employment, and overall quality of life. Developing empathy means acknowledging that these struggles are real and offering support and understanding to those navigating them.
Encouraging Early Diagnosis and Effective Treatment
Early diagnosis and effective treatment are key factors in managing bipolar disorder and reducing the impact of its symptoms. Encouraging individuals to seek help and reducing the stigma associated with mental illness are crucial steps toward achieving early diagnosis. Increased awareness campaigns and education can empower individuals to recognize the signs and symptoms of bipolar disorder in themselves or their loved ones, facilitating timely intervention.
Once diagnosed, providing access to quality mental health care and ensuring individuals receive appropriate treatment is essential. Bipolar disorder often requires a combination of pharmacological interventions, psychotherapy, and lifestyle modifications. By advocating for comprehensive treatment plans and promoting ongoing care, we can help individuals with bipolar disorder achieve symptom control and improve their overall well-being.

The Role of Case Studies in Advancing Knowledge about Bipolar Disorder
Case studies, like Susan’s, play a significant role in advancing knowledge about bipolar disorder. They provide unique insights into individual experiences, treatment outcomes, and the wider impact of the condition. Researchers and healthcare providers can learn from these individual cases, developing evidence-based guidelines and refining treatment approaches.
Additionally, case studies contribute to reducing stigma by providing personal narratives that humanize the disorder. They showcase the challenges faced by individuals with bipolar disorder and highlight the importance of support systems, empathy, and understanding. By sharing these stories, we can help dispel misconceptions and promote a more compassionate approach toward mental health as a whole.
In conclusion, developing empathy and understanding for individuals with bipolar disorder is essential. By recognizing the complexity of their experiences, advocating for early diagnosis and effective treatment, and valuing the insights provided by case studies, we can create a society that supports and uplifts those with bipolar disorder. It is through empathy and education that we can reduce stigma, promote accessible mental health care, and improve the lives of those affected by this condition.In conclusion, gaining a comprehensive understanding of bipolar disorder is crucial in order to support individuals affected by this complex mental health condition. Through the real-life case study of Susan, we have explored the numerous facets of bipolar disorder, including its background, symptoms, and effects on daily life. Susan’s journey serves as a powerful reminder of the challenges individuals face in managing the highs and lows of bipolar disorder and emphasizes the importance of effective treatment and support systems.
We have examined the various approaches to treating and managing bipolar disorder, including psychopharmacological interventions, psychotherapy, and lifestyle modifications. Understanding the role of these treatments and the need for personalized care can significantly improve the quality of life for individuals like Susan.
Support systems also play a crucial role in helping those with bipolar disorder navigate the complexities of the condition. From family support to peer support groups and access to professional resources, fostering a strong network of assistance can provide the necessary emotional support, education, and guidance needed for individuals to effectively manage their symptoms.
Furthermore, case studies, such as Susan’s, contribute to advancing our knowledge about bipolar disorder. By delving into individual experiences, researchers gain valuable insights into treatment outcomes, prognosis, and the impact of the condition on individuals and society as a whole. These case studies foster empathy, reduce stigma, and contribute to the development of evidence-based guidelines and interventions that can improve the lives of individuals with bipolar disorder.
In fostering empathy and promoting early diagnosis, effective treatment, and ongoing support, we create a society that actively embraces and supports individuals with bipolar disorder. By encouraging understanding, reducing stigma, and prioritizing mental health care, we can ensure that those affected by bipolar disorder receive the support and resources necessary to lead fulfilling and meaningful lives. Through empathy, education, and continued research, we can work towards a future where individuals with bipolar disorder are understood, valued, and empowered to thrive.
Similar Posts

Vraylar for Bipolar: A Comprehensive Guide
Bipolar disorder is a complex and challenging mental health condition that affects millions of people worldwide. Dealing with the extreme highs and lows of this disorder can be overwhelming and disrupt all aspects of life. While…

Understanding the Concept of Mundo Bipolar
Imagine a world painted with the brightest hues of yellow, where laughter echoes through the streets, and an abundance of energy electrifies every passing moment. Now, contrast that with a world drowned in shades of gray,…
Adderall Withdrawal and Depression: Causes, Symptoms, and Coping Strategies
Imagine feeling a surge of energy and focus like you’ve never experienced before, only to be followed by a deep void of fatigue and despair. This rollercoaster of emotions is all too familiar to those who…

What Anxiety Disorder is Most Common?
Imagine feeling an overwhelming sense of unease creeping up on you like a shadow, ready to engulf your every thought and action. Your heart races, palms sweat, and your mind spins out of control. This is…

Understanding Bipolar Withdrawal from Loved Ones: Causes, Symptoms, and Coping Strategies
Living with bipolar disorder can be a rollercoaster ride, not just for the individual experiencing it, but also for their loved ones. The intense highs and lows characteristic of this mental health condition can take a…

Understanding Attention Seeking Behavior and its Connection to Depression
Imagine a crowded room filled with people. Amongst the chatter and laughter, there is always that one person who craves attention, their every action designed to captivate those around them. They may engage in dramatic displays,…
Difficult-to-Diagnose Case Studies of Bipolar Demonstrating Wide Variations in Presentations
- First Online: 06 October 2023
Cite this chapter

- C. Raymond Lake 2
71 Accesses
Seventy case studies help in the recognition of Bipolar across a wide range of severity from successful Bipolar II clients to grandiose, paranoid, and psychotic Bipolar individuals. Mental health workers and families of severe Bipolars are at risk, and recommendations of steps for increased safety are offered. The severely mentally ill are at highest risk for violence against themselves and others.
Psychotic Bipolar killers have been inappropriately found sane and guilty of murder by the legal community.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Aaro D. Michigan mom who killed her children used fake doctor’s note to get them out of school, investigators say. FOX News. 2019 Feb 24.
Google Scholar
Adler E. Spade’s father: death could shed light on mental illness. K C Star. 2018a June 7.
Adler E. Kate Spade suffered years of mental illness, sister says. KC Star. 2018b June 8.
Adler E, Smith J, Osterheldt J, Williams MR, Saffo R. Kate Spade, dead at 55, always said Kansas City helped shape her life and career. Kansas City Star. 2018 June 5.
Amsterdam Telegraph. Van Gogh was not psychotic or bipolar when he cut off his ear, medical experts decide. Amsterdam Telegraph. 2016 16 Sept.
Anderson J. Witness testifies Yates was insane. Assoc Press. www.beliefnet.com/news/2002/03/Witness-Testifies-Yates-Was-Insane.aspx . 2002.
Anonymous Children Murdered by their Christian Parents, Memorial Page, 2006.
Armour N, Allen K. AAF Teams will need answers from Johnny Manziel. USA Today. 2019 Mar 1.
Baker S. 20 years ago Marilyn Lemak killed her three children in their Naperville home. The case still haunts law enforcement. Naperville Sun. 2019 Mar 2.
BBC. Timeline: how Norway’s terrorist attacks unfolded. 2012 Apr 17. On line.
Becker J, Kovaleski SF, Lou M, Barry D. Jigsaw picture of an accused killer. NY Times. 2011 Jan 16.
Berger J, Gross J. From mental illness to Yale to murder charge. NY Times. 1998 June 19.
Blinder A. Waffle House suspect once had his guns taken away. NY Times. 2018 Apr 23.
Blumer JD. The illness of Vincent van Gogh. Am J Psychiatry. 2002;59(4):519–26.
Article Google Scholar
Brezosky L. Jury sentences Brownsville man to death. San Antonio Express News. 2010 July 29.
Carlson GA, Goodwin FK. The stages of mania: a longitudinal analysis of the manic episode. Arch Gen Psychiatry. 1973;28:221–8.
Article PubMed Google Scholar
Chan M. Revisiting Andrea Yates 15 years after she drowned her children. Time. 2016 June 20.
CNN.com/Justice. Yates sentenced to life in prison. CNN. 2002 Mar 15.
Dupree D. Navy Yard shooter had mind control group contact. Examiner.com . 2013 Oct 26.
Duwe G. Opinion: the rise and decline of mass shootings. AOL News. 2010 May 1.
Fawcett J, Golden B, Rosenfeld N. New hope for people with bipolar disorder. New York: Three Rivers Press; 2007.
Fazel S, Lichtenstein P, Grann M, Goodwin GM, Langstrom N. Bipolar disorder and violent crime: new evidence from population-based longitudinal studies and systematic review. Arch Gen Psychiatr. 2010;67:931–8.
Fletcher K. Schizophrenia drove Okie to murder, psychiatrist says. Lincoln County News, Augusta, MA, 12/17/2008.
Foderaro LW. Man who killed fiancée is sent to mental hospital. NY Times. 2000 May 12.
Friedman SH, Hrouda D, Holden C, Noffsinger S, Resnick P. Filicide-suicide: common factors in parents who kill their children and themselves. J Am Acad Psychiatry Law. 2005;33(4):496–504.
Gann C, Parkinson J. Stress of life in the public eye might have fueled Jackson’s mood disorder, doctors say. ABC News Medical Unit. 2012 July 12.
Gardner A, Fahrenhold DA, Fisher M. Loughner’s descent into a world of fantasy. Wash Post. 2011 Jan 13.
German J. Las Vegas’ shooter’s autopsy gives no clues. Las Vegas Review-Journal. 2018 Feb 9.
Gladstone R. The Richest, Says Forbes, Got 41% Richer. Forbes Magazine. 1987 Oct 13. On Line.
Glenn C, Peter J, Johnson K, Madhani A. Who is Steven Paddock? Police say he killed 59 in Las Vegas rampage. USA Today. 2018 Oct 2.
Glover S, O’Neill A, Lah K, Ortega B. Sources: Vegas killer paid cash for property and privacy. CNN. 2017 Oct 5.
Goldstein DB, Schmidt S. Genic intolerance to functional variation and the interpretation of personal genomes. PLOS genetics on line. 2013 Aug 22.
Goodstein L, Glaberson W. The well-marked roads of homicidal rage. NY Times. 2000 Apr 9.
Goodwin FK. The biology of recurrence: new directions for the pharmacologic bridge. J Clin Psychiatry. 1989;50:40–4.
PubMed Google Scholar
Klein A, Williams C, Weil M. 2 officers shot at pentagon’s main entrance. Wash Post. 2010 Mar 5.
Kleinfield NR, Rashbaum WK. Miriam Carey was in car when police fired, official says. NY Times. 2013 Oct 4.
Kraepelin E. Dementia Praecox and Paraphrenia , E & S Livingstone, Edinburgh Scotland 1919 Thoemmes Press, 2002.
Kraepelin E. Manic depressive insanity and paranoia. 1921/1976.
Kransz M. Mother who killed 3 kids was hospitalized with paranoid delusions months before shooting. [email protected] 2018, updated Feb 20 2019.
Kroft S. Untreated mental illness an imminent danger? [transcript] 60 minutes. 2013 Sept 29.
Lake CR. Psychotic rampage killers: Mania, not schizophrenia—psychiatry’s role in prevention. Psychiatr Ann. 2014a;44:213–4.
Lake CR. Rampage murderers, part I: psychotic versus non-psychotic and a role for psychiatry in prevention. Psychiatr Ann. 2014b;44(5):217–25.
Lake CR. Personal interview with Mr. Andy Loya. Jan 22 and 29, 2014c.
Lambert R. Was Anders Breivik a psychotic spree killer or a calculating terrorist? RUSI Analysis. 2011 Aug 18.
Longman J. John E du Pont, 72, dies; killed athlete. NY Times 2010 Dec 10.
Lucey C. Kanye West delivers jaw-dropping performance in oval office. Assoc Press. 2018 Oct 12.
Mandal V. Families of mentally ill pay terrible toll: psychiatric patients are killing and assaulting their families at an alarming rate. Vancouver Sun. 2002 Oct 7.
Mann D. The case of Otty Sanchez: StandDown Texas Project. 2009 Dec 1.
Mann D. Gone baby gone. Texas Observer. 2010 Jan 13.
McLean H. James Holmes – schizophrenia could be a game changer. HarryMcLean.com . 2012 July 28.
Medina J, Burns A, Goldman A. No manifesto, no phone calls: Las Vegas killer left only cryptic clues. NY Times. 2017 Oct 5.
NBC News. Mother confesses to severing baby’s arms. 2004 Nov 23. On line.
Olmstead M. What we know about the Las Vegas shooter. Slate.com . 2017a Oct 2. Online.
Olmstead M. Las Vegas gunman’s brother describes a high-roller life at the casinos. Slate.com . 2017b Oct 4. Online.
Osterheldt J. Superwomen like Kate Spade smile to hide the pain. Time to hang up the cape and live. Kansas City Star. 2018a June 5.
Osterheldt J. Time to hang up the cape, seek help and live. KC Star. 2018b June 7.
Puente N. Case reopened for Brownsville man convicted of killing three children. Valley Central.com . 2022 Mar 2.
Rivera K. What is Johnny Manziel up to now? 2022 Feb 23. NickiSwift.com on line.
Rosack J. Patient charged with murder of schizophrenia expert. Psychiatr News. 2006;41:1.
Sable. 2002 Sable K. Parents who murder. http://karisable.com/Parentmur.htm . Captured 3/20/20.
Serna J, Winton R. Carrie Fisher’s autopsy reveals cocktail of drugs, including cocaine,opiates, and ecstasy. Chicago Trib. 2017 June 19.
Shear MD, Schmidt MS. Gunman and 12 victims killed in shooting at D.C. Navy Yard NY Times. 2013 Sept 16.
Sontag D. A mental patient, a slain worker, troubling questions. NY Times. 2011 June 17.
Sulzberger AG, Carey B. Getting someone to treatment can be difficult and inconclusive, experts say. NY Times. 2011 Jan 19.
Tucker E, Christoffersen J. Slain motorist reportedly suffered delusions. Associated Press, KC Star. 2013 Oct 5.
Vera A. Waffle house shooter was once arrested by secret service for trespassing near White House. CNN. 2018 Apr 22.
Walsh D. The murder conviction of Andrea Yates: a tragic case, a barbaric verdict. World Socialist Web Site. 2002 Mar 15.
Ward B. Dr. Astrid Desrosiers talking to investigators at MGH. Boston.com/news . 2009 Oct 27.
Wehr TA, Goodwin FK. Can antidepressants cause mania and worsen the course of affective illness? Am J Psychiatry. 1987;144(11):1403–11.
Woodruff J. How did Aaron Alexis get security clearance to be a defense contractor? PBS Newshour. 2013 Sept 17.
Writer. 2001.
Zapotosky M, Horwitz S, Morello C. Miriam Carey, driver shot near U.S. Capitol, likely struggled with mental illness, police say. Wash Post. 2013 Oct 4.
Download references
Author information
Authors and affiliations.
Department of Psychiatry and Behavioral Sciences, University of Kansas Health System, Kansas City, KS, USA
C. Raymond Lake
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Lake, C.R. (2023). Difficult-to-Diagnose Case Studies of Bipolar Demonstrating Wide Variations in Presentations. In: Bipolar for Psychotherapists and Their Clients. Springer, Cham. https://doi.org/10.1007/978-3-031-38750-0_4
Download citation
DOI : https://doi.org/10.1007/978-3-031-38750-0_4
Published : 06 October 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-38749-4
Online ISBN : 978-3-031-38750-0
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

Patient Case: 30-Year-Old Male With Bipolar Disorder
Nidal Moukaddam, MD, PhD, presents the case of a 30-year-old male diagnosed with bipolar 1 disorder and shares her initial impressions on diagnosis.
EP: 1 . Patient Case: 30-Year-Old Male With Bipolar Disorder
Ep: 2 . approaching the treatment of bipolar disorder, ep: 3 . treatment selection for bipolar disorder, ep: 4 . takeaways for bipolar disorder management.
Nidal Moukaddam, MD, PhD: Today, we’re going to talk about a new case. A 30-year-old man has taken short-term disability leave from work due to the progression of a depressive episode. He received a diagnosis of bipolar I disorder about 10 years ago. He had his first episode of mania at the age of 20 and 2 subsequent episodes of mania between the ages of 21 and 29. He was treated with lithium, which was highly effective, but he experienced excessive thirst and developed hyperthyroidism. His lithium level at the time was in the therapeutic range of 0.8 mEq/L. He was switched to valproate; however, valproate lacked the efficacy of lithium and caused adverse effects of sedation and weight gain. During his third manic episode, he started on olanzapine but experienced excessive weight gain. He was then cross-titrated to quetiapine, which improved his manic symptoms. However, weight gain again became an adverse effect, and he also complained of sedation. The patient reported sleeplessness and made unnecessary online purchases when unable to sleep, but the quetiapine sleepiness was unacceptable. Despite these adverse effects, he continued taking] quetiapine until he decompensated into his third depressive episode. The quetiapine was then augmented with lamotrigine, which was titrated up to 300 mg per day but demonstrated no efficacy. At the time of presentation, the patient was adhering to the medications. He did not have a substance use disorder, which was confirmed by a negative toxicology screen. His TSH [thyroid-stimulating hormone] level was in the middle of the normal range, and he had no suicidal ideations or psychotic symptoms.
I think the most important thing to do when somebody comes to you, even if they tell you they have a diagnosis, is to confirm the diagnosis. You want to start by making up your own mind, and sometimes the patient is not a good source of information. But in the case of bipolar disorder without psychosis, you expect the patient to be able to give you a solid history. Typically, the part of the history that’s hardest to nail down is mania. When people experience mania, they have excessive energy and excessive activation that creates the need for sleep, and sometimes they like it. They feel that this is the way it should be, so they don’t point it out as pathological. Now, the DSM-5 [ Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition ] criteria tell us that mania that leads to hospitalization or some negative consequence like incarceration is problematic no matter what the duration is. Assuming the patient did not end up in the hospital or in prison, we want to verify the story of mania. In the current case presentation, I can see many of my colleagues saying, “Hey, you’re not giving us enough symptoms of mania. He’s a bit sleepless. He makes frivolous purchases. That’s bipolar disorder but not bipolar I; maybe it’s bipolar II.”
Thus, my first step would be to explain that this patient had at least a week without sleep. During that week, he was spacing, had pressured speech, and was talking fast to the point that others around him commented about it. He became more impulsive, and buying things was the tip of the iceberg. He also became more sexual to the point where it got him in trouble in his relationships, he spent more money than he had planned, etc. These examples of impulsivity often nail down the diagnosis of bipolar disorder. Of course, these symptoms change with the time that we live in. For example, before unlimited plans on cell phones, you would have been taught to ask: “Do you get a very high bill on your phone when you’re manic?” Because patients with mania talk a lot, and the bills would be higher when they call across state lines or internationally. First, I would recommend verifying the diagnosis. My impression of the patient is that this is somebody with a set diagnosis of bipolar I. Three manic episodes is a lot. He has impairment because of it, and it’s affected his job. Thus, my first step is confirming the diagnosis. My second would be a lot of psychoeducation; make sure that the patient understands what he’s up against and why he needs treatment.
Transcript Edited for Clarity

The Week in Review: April 1-5

Blue Light Blockers: A Behavior Therapy for Mania

An Update on Bipolar I Disorder

Blue Light, Depression, and Bipolar Disorder

Recap: Mood Disorders 2024
Evidence-Based Novel Therapies for Bipolar Depression: Top 5 Takeaways
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Can Acad Child Adolesc Psychiatry
- v.22(4); 2013 Nov
Language: English | French
First Manic Episode in an 11 Year-old Girl
Don quang tran.
1 Centre Hospitalier Universitaire de Sherbrooke, University of Sherbrooke, Department of Psychiatry, Sherbrooke, Quebec
Vincent Beaudry
Yves lajoie.
We present the case of an 11 year-old girl admitted to the Centre hospitalier universitaire de Sherbrooke for a first manic episode.
Differential diagnoses of adjustment disorder, attention-deficit/hyperactivity disorder, oppositional defiant disorder, and conduct disorder were considered but eliminated.
No organic etiology was detected. Her condition rapidly remitted with aripiprazole 3mg. After her discharge, she suffered a relapse due to instability of her living conditions and was rehospitalized.
Conclusion:
Mania is a difficult diagnosis in youths due to its nonspecific symptoms, rare prepubertal occurrence, and diagnostic complexity. Despite ongoing research, there is little conclusive information on the impact of psychosocial stressors on the evolution of early-onset bipolar disorder.
Résumé
Nous présentons le cas d’une fillette de 11 ans hospitalisée au Centre hospitalier universitaire de Sherbrooke pour un premier épisode de manie.
Méthode:
Les diagnostics différentiels du trouble d’adaptation, du trouble de déficit de l’attention avec hyperactivité, du trouble oppositionnel avec provocation et du trouble des conduites ont été envisagés mais rejetés.
Résultats:
Aucune étiologie organique n’a été détectée. La rémission de son affection a été rapide avec 3 mg d’aripiprazole. Après son congé, elle a souffert d’une rechute attribuable à l’instabilité de ses conditions de vie et a été réhospitalisée.
La manie est un diagnostic difficile chez les adolescents en raison de ses symptômes non spécifiques, d’une rare occurrence pré-pubère, et de la complexité diagnostique. Malgré la recherche en cours, il y a peu d’information concluante sur l’effet des stresseurs psychologiques sur l’évolution du trouble bipolaire d’apparition précoce.
“Ansa” is an eleven year-old girl who lives with Mrs. J, her mother; her parents have been divorced for years, and she has little contact with her father. Ansa’s early childhood history was marked by her mother’s numerous unstable relationships which led to the mother and daughter moving many times before Ansa was seven. Ansa was unknown to any child psychiatry service. From age six to eight, Ansa was on methylphenidate for suspected attention-deficit/hyperactivity disorder (ADHD); there were no beneficial effects, and the medication was discontinued. Otherwise, Ansa’s past psychiatric history is negative. She has never had physical illnesses, has never taken drugs, alcohol, or medication. Family history is positive for Mrs. J’s borderline personality disorder and her uncle’s possible but unconfirmed diagnosis of bipolar disorder.
Ansa was admitted to our service for grandiosity, agitation, and distractibility that had appeared in the last two days. She had no sleep, spending the nights cleaning her room. She had excessive projects, including becoming a rock star. These symptoms rendered her totally unable to attend school and even take care of her basic needs, such as hygiene. There were no recent stressors. The mental status examination showed a child unable to remain seated (spending the whole interview moving from object to object), an irritable and labile affect, logorrhea, accelerated speech, and flight of thoughts. She expressed countless projects although there was no delusional grandiosity. She denied hallucinations and suicidal ideations. Baseline metabolic tests were negative, including complete blood count, electrolytes, thyroid levels, and urinalysis. A physical evaluation by the pediatrician yielded no significant findings. An electroencephalogram and brain magnetic resonance imaging (MRI) were negative. Ansa was diagnosed with acute manic episode with no identifiable organic etiology but with a possible biological vulnerability for emotional dysregulation, given the mother’s borderline personality disorder.
After no improvement with quetiapine 12.5mg and olanzapine 5mg trials, Ansa was given aripiprazole 5mg. With the medication and strong presence of nurses and psychoeducators, her condition was stabilized in less than five days. Due to sedation, aripiprazole was lowered to 2mg, resulting in a manic relapse. Aripiprazole was increased to 3mg, and the manic symptoms quickly resolved, again in less than five days. The hospitalisation lasted one month in order to monitor Ansa’s symptoms and level of functioning during progressive returns to school. They were ultimately successful, and Ansa was discharged.
The following week, despite compliance to medication, Ansa suffered a relapse of the identical symptoms and was readmitted. This coincided perfectly with turbulent changes in her environment. Indeed, Ansa and her mother had just moved in with family friends: there were frequent unexpected visits from various acquaintances, accompanied by daily verbal violence. Mrs. J admitted to her fragile emotional state and that Ansa would usually internalize her mother’s feelings. Since no other cause was identified, the manic relapse was attributed mainly to the unstable environment with a child in a symbiotic relationship with her mother, who suffers from borderline personality disorder but whose parental capacities were considered preserved. Given the apparently clear temporal relationship of the symptomatic relapse with the stressors, an adjustment disorder was considered as part of the differential diagnosis. However, the clinical presentation – especially the mental status examination as previously described – clearly corresponded to the severity of a mood disorder. In addition, the patient’s personal and longitudinal history revealed no signs of conduct disorder or oppositional defiant disorder. The relapse also heightened the prior hypothesis of Ansa’s biological vulnerability to emotional dysregulation.
No pharmacological change was made and with the presence of the multidisciplinary team, Ansa’s condition remitted in four days. The total hospital stay lasted three weeks in order to once again observe Ansa’s evolution during progressive returns to school, which were successful. Ansa was then discharged with a follow-up by a social worker and psychiatrist. After a year of follow-up, she is doing well, and the family situation remains stable.
Early-onset Bipolar Disorder
Studies have shown that bipolar disorder usually begins with an index episode of depression: positive family history ( Pavuluri, Birmaher, & Naylor, 2005 ), clinical severity, psychotic symptoms, and psychomotor retardation are well documented predictors of bipolarity. Approximately 20% of youths with a first major depressive episode will develop a manic episode. Prodromal symptoms of bipolar disorder – hyperactivity, anxiety, dysphoria – have been identified but remain nonspecific (American Academy of Child and Adolescent Psychiatry – AACAP, 2007 ). Ansa’s case illustrates this diagnostic complexity since prodromal symptoms must be taken in the context of environmental instability.
Early-onset bipolar disorder is often considered atypical because of the fluctuating course of symptoms and lack of clear episodes, which defines the classic phenotype ( AACAP, 2007 ). Some authors have introduced the concept of “broad phenotype” of bipolar disorder for youths with extreme irritability, explosiveness, mood variability, and functional impairment. In bipolar disorder literature, one particularity for the pediatric population is the introduction of the concepts of “ultrarapid cycling” (hours to days) and “ultradian cycling” (minutes to hours). Geller et al. (2000) described a prepubertal and early adolescent bipolar disorder (PEA-BP) phenotype which includes both types of cycles.
Although continuity between this “juvenile mania” and adult bipolar disorder has not been established ( Duffy, 2007 ), the prevalence of bipolar disorder diagnoses in children and adolescents is increasing dramatically, with a fortyfold increase in 1993–2004 in the USA ( AACAP, 2007 ). The prevalence of the classic phenotype in prepubertal children is unknown but is considered rare. Ansa represents our service’s earliest manic episode and one of the few prepubertal cases.
The rate of comorbidity between juvenile bipolar disorder and ADHD has been previously described as high in numerous studies. However, a recent review by Anne Duffy (2012) stated that ADHD is not a reliable predictor for the development of juvenile bipolar disorder. The strong overlap of symptoms between the two conditions (distractibility, hyperactivity, talkativeness) raises questions about diagnostic specificity. Thus, DSM-V work groups for bipolar disorder have proposed specifying in the “B” criteria of (hypo)mania that symptoms must absolutely represent a change from baseline ( American Psychiatric Association, 2012b ). This proposal could help reduce the double-counting of symptoms towards ADHD and bipolarity. “Disruptive Mood Dysregulation Disorder” is a proposed additional diagnosis to target youths suffering from sustained irritability ( American Psychiatric Association, 2012a ; Margulies, Weintraub, Basile, Grover, & Carlson 2012 ).
In our opinion, the debate on early-onset bipolar disorder remains important. The AACAP states in its most recent practice parameters that “caution must be taken before applying this diagnosis in preschool children” ( AACAP, 2007 ). The stigma of psychiatric diagnoses and the consequences of mislabeling juveniles should not be minimized. Iatrogenic risks must be weighed against risks of inappropriately treating ill juveniles especially since mood stabilizers are associated with potential serious adverse effects ( Parens & Johnston, 2010 ). Nonetheless, a recent meta-analysis concluded in the efficacy and safety of antipsychotics in early-onset bipolar disorder, leading to the US Food and Drug Administration’s approval of several antipsychotics in juveniles, including aripiprazole ( Liu et al., 2011 ).
Ansa’s case is striking in her fragility to psychosocial stressors and quick improvement with environmental stability and medication. There is little conclusive information on the impact of the environment on the evolution of early-onset bipolar disorder. This is a crucial point since the therapeutic approach might have to target better psychosocial follow-ups with the entire family rather than focus on individual treatments. Ultimately, these issues illustrate the need for more scientific research to better identify and treat patients with bipolar disorder.
The patient and parent have both given written consent to the publication of this paper following an explanation of the procedure. Patient anonymity has been protected.
Acknowledgements/Conflicts of Interest
The authors have no financial relationships to disclose.
- American Academy of Child and Adolescent Psychiatry Practice parameters for the assessment and treatment of children and adolescents with bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2007; 36 (1):138–157. [ PubMed ] [ Google Scholar ]
- American Psychiatric Association DSM-5 Development: D 00 Disruptive Mood Dysregulation Disorder. 2012a Retrieved April 10, 2012 from http://www.dsm5.org/proposedrevision/pages/proposedrevision.aspx?rid=397 . [ Google Scholar ]
- American Psychiatric Association DSM-5 Development: Manic Episode. 2012b Retrieved April 10, 2012 from http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=425 . [ Google Scholar ]
- Duffy A. Does bipolar disorder exist in children? A selected review. Canadian Journal of Psychiatry. 2007; 52 (7):409–417. [ PubMed ] [ Google Scholar ]
- Duffy A. The nature of the association between childhood ADHD and the development of bipolar disorder: A review of prospective high-risk studies. American Journal of Psychiatry. 2012; 169 (12):1247–1255. [ PubMed ] [ Google Scholar ]
- Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL, Delbello MP, Soutullo CA. Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid attention deficit hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology. 2000; 10 (3):157–164. [ PubMed ] [ Google Scholar ]
- Liu HY, Potter MP, Woodworth KY, Yorks DM, Petty CR, Wozniak JR, Biederman J. Pharmacologic treatments for pediatric bipolar disorder: A review and meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry. 2011; 50 (8):749–762. [ PubMed ] [ Google Scholar ]
- Margulies DM, Weintraub S, Basile J, Grover PJ, Carlson GA. Will disruptive mood dysregulation disorder reduce false diagnosis of bipolar disorder in children? Bipolar Disorders. 2012; 14 (5):488–496. [ PubMed ] [ Google Scholar ]
- Parens E, Johnston J. Controversies concerning the diagnosis and treatment of bipolar disorder in children. Child Adolescent Psychiatry Mental Health. 2010; 10 :4–9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pavuluri MN, Birmaher B, Naylor MW. Pediatric bipolar disorder: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 2005; 44 (9):846–871. [ PubMed ] [ Google Scholar ]
- Case report
- Open access
- Published: 14 June 2014
Case report: bipolar disorder as the first manifestation of CADASIL
- Soyeon Park 1 ,
- Boram Park 1 ,
- Min Kyung Koh 2 &
- Yeon Ho Joo 1
BMC Psychiatry volume 14 , Article number: 175 ( 2014 ) Cite this article
18k Accesses
22 Citations
1 Altmetric
Metrics details
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is an inherited cerebrovascular disease, clinically characterized by variable manifestations of migraine, recurrent transient ischemic attack or lacunar strokes, cognitive decline, and mood disturbances. However, manic episodes have rarely been documented as an initial symptom of CADASIL and bipolar disorder presenting as the first manifestation in CADASIL has not been reported previously from evaluations by psychiatrists or psychological testing by psychologists.
Case presentation
A 53 year old woman developed symptoms of mania in her 50s leading to a personality change involving a continuously labile mood and irritability over a number of years. Neuropsychological testing revealed an intact memory, but impairment in attention and executive function. In the Rorschach test, she showed a high level of cognitive rigidity. Magnetic resonance imaging findings were very consistent with a diagnosis of CADASIL, which was confirmed by genetic testing for NOTCH3 mutations. Atypical antipsychotics proved to be helpful in treating her manic symptoms and for behavior control.
We present a novel case of CADASIL that first presented as bipolar disorder. We contend that when patients show a late onset personality change or chronically irritable mood that deteriorates over many years, an organic cause such as CADASIL must be considered. Further studies are needed to better understand the exact impacts of cerebral tissue lesions and psychiatric symptoms in CADASIL patients.
Peer Review reports
The genetic contributions to bipolar disorder (BD) have been well characterized, with an increased risk, estimated to be 8-fold higher than the prevalence in the general population, in siblings with affected probands [ 1 ]. It is believed that BD is a complex genetic disease that is caused by various interactions between the environment and by multiple genes [ 1 ]. Although a high degree of heritability is known for BD, the mode of inheritance for this disorder appears complex, indicating that it is non-Mendelian in nature and involves genes that have yet to be identified [ 2 ]. One of the suggestions for why BD has not been clarified as a single genetic disease is heterogeneity. Research on BD subtypes is still at an early stage, and the concepts being developed to explain this disease are changing continuously. Recently, the concept of a bipolar spectrum disorder was introduced to try to understand BD from a continuous line into the past. Hence, there have been attempts to distinguish between BD subtypes to better understand the etiology of this disorder.
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is a rare hereditary disease caused by mutations in the NOTCH3 gene on chromosome 19p13.1 [ 3 ]. CADASIL is a systemic angiopathy and it is characterized by recurrent transient ischemic attacks (TIA), strokes, vascular dementia, mood disturbances and motor disability. If CADASIL arises at an age below 20, the most common first symptom is migraine. However, if the first symptoms of CADASIL occur in persons over 50, they can rapidly progress to a more serious condition such as depression [ 4 ]. Because these cases do not show neurological abnormalities, they are commonly diagnosed as a mood disorder only. The diagnosis of CADASIL is therefore often delayed or missed in psychiatric clinics.
Although there has been considerable neurological research on CADASIL, there have been fewer studies of the mood disorders associated with this disease. Psychiatric disturbances have been mentioned by almost all previous studies of CADASIL, but most of these reports have only addressed the presence of psychiatric disorders among the symptoms of the disease and have not focused specifically on the psychiatric aspects of CADASIL [ 5 ]. Hence, prior CADASIL studies have not incorporated a psychiatric evaluation or provided any detailed descriptions of psychiatric symptoms. In our current report, we present a case of CADASIL that first presented as BD. Through our analysis of this case, we provide new insights into the issues around the initial differential diagnosis of CADASIL and also the appropriate interventions for these patients.
A 53-year-old woman visited our out-patient psychiatric clinic in March 2013. Her daughter reported that she had become excessively talkative, impulsive, and verbally aggressive. The changes in her personality had begun to appear in 2008 and her symptoms of hostility had become more severe recently. Her premorbid personality was described as reserved, diligent, frugal, and calm and she had worked in a market for more than 20 years. However, during the previous 5 years, she had begun to speak garrulously and often lost the thread of a conversation and included many irrelevant details when providing an explanation. She had become much more easily irritable and angry, which took the form of yelling and throwing objects. She had also begun to argue over seemingly unimportant matters with her neighbors. She had also begun to impulse buy multiple items also make many unnecessary purchases for her family. She had also become very hyperactive in her work life and social life. She did not display any sleep or eating disorders at the time of her visit.
The patient’s husband had an explosive temperament and alcohol problems which were a source of great stress and concern for her. Since 2000, she had begun to irregularly attend a local psychiatric clinic to receive medications for a depressed mood and insomnia. At the time of these visits, she was taking both antidepressants and sleeping pills. However, she and her family denied that she had experienced any depressive episodes or had ever been diagnosed with a mood disorder. She had no history of head trauma but had hypertension and diabetes, both of which are cardiovascular risk factors. There was also no history of migraine, a prior TIA, or stroke reported by the patient.
Her family history further revealed that her father had died at 76 years of age after having suffered a stroke and that he had hypertension, diabetes and a history of depression including a suicide attempt. However, her mother is 76 years old and in good health. She has three younger brothers, the oldest of whom is 51 years old and has been diagnosed with cerebellar atrophy. He also has dysarthira and cerebellar ataxia. Those symptoms had gradually developed within the previous 2 years. Her second brother had suffered from depression and had committed suicide 20 years previously. Her youngest brother had no health issues, but his 17-year-old son had been diagnosed with epilepsy. She also has a son and a daughter. Her son suffers from migraine attacks but her daughter is healthy.
When her mental condition was assessed she showed no evidence of delusions or hallucinations, but she did have pressured speech, circumstantiality, labile moods, poor impulse control, and made grandiose plans. She demonstrated no insights into the changes in her personality and behavior. Bedside neuropsychological testing revealed total scores that were within the normal range (K-MMSE 29/30). However, a Montreal Cognitive Assessment test (MOCA-K 25/30) revealed a failure to perform the trail making test (TMT) and copy cube. In the attention subtest, she tapped on the wrong letters and failed to correct this. In the language subtest, she could speak more than 11 words in 60 seconds but the all of the words began with the same sound with a different suffix, for example, like, liked, likely, look, looked, looking. In a delayed recall subtest, she recalled only two words correctly out of five. She was successful with Clock drawing, the Luria’s fist-edge-palm test and the loop test.
Due to a suspected late-onset bipolar disorder with chronic manic features in this case, neuropsychological testing was performed by a clinical psychologist. To evaluate this patient’s comprehensive cognitive function, we performed the following tests: BGT, Clock Drawing Test, Color Trail Test (CTT) 1/2, Korean Auditory Verbal Learning Test (K-AVLT), Stroop Test, Word/Figural Fluency Test, Executive Complex Figure Test, Grooved Pegboard Test, Finger Tapping Test, Hand Dynamometer, MMPI-II, Sentence Completion Test (SCT), Wisconsin Card Sorting Test (WCST) and Rorschach Test.
The K-AVLT findings showed that the patient had a normal ability to encode and retrieve verbal information. However her abilities in terms of tracking sequential stimulations, dividing her attention and inhibitory control function were found to be severely impaired, with a poor score in terms of attention and executive function in the CTT tests (<1% percentile). Cognitive productivity was also poor as reflected in impaired word/figure fluency. In the WCST, the patient showed 18 perseverative responses (50% percentile) and 47 non-perseverative responses (<1% percentile). Her potential for perseveration was therefore low, and she showed an impaired efficient sorting tendency. The results of the Rorschach test indicated a strong cognitive rigidity in this patient as she only responded to the same content repetitively. Finally, the results of the MMPI-II showed that scales 1 and 9 were all higher than 65 T, indicating that this patient was complaining of physical pain or discomfort and making efforts to cope with difficulties in her cognitive function.
In conclusion, neuropsychological testing of our current case revealed an intact memory, but impairment in both attention and executive function. Although the patient’s perseveration tendency was not clear, she revealed a high level of cognitive rigidity in the Rorschach test. The results of the neurological examination of this case were unremarkable and other systemic examinations showed no abnormalities. The results of routine laboratory tests including VDRL, HIV antibodies and thyroid function were also unremarkable apart from hyperlipidemia. MRI analysis of the brain was performed and revealed severe leukoencephalopathy. There was a high signal intensity found by T2 weighted images (T2W1) and low signal intensity in the left pons. In fluid-attenuated inversion-recovery (FLAIR) images, a high signal intensity was prominent on the periventricular white matter, both basal ganglia, thalamus, and the external capsule. These magnetic resonance imaging (MRI) findings are very consistent with a diagnosis of CADASIL. Since the clinical and MRI findings for this patient were highly suggestive of CADASIL, genetic testing for NOTCH3 mutations was performed. As expected, a heterogeneous mutation was detected in this patient that causes an arginine to proline substitution in exon 3 of chromosome 19 p13.2-13.1 (c.224G > C).
During her hospital treatment, her manic symptoms, including a labile mood, talkativeness and impulsivity, partially responded to atypical antipsychotics (quetiapine, 800 mg) and benzodiazepine (bromazepam, 6 mg) treatment. She was also prescribed with amlodipine (novasc), metformin (diabex), and atorvastatin (lipitor) for the management of the vascular risk factors, hypertension, diabetes, and hyperlipidemia, respectively. She was able to be discharged after two weeks in hospital. At the time of discharge, she was no longer hostile or aggressive but still showed slight impulsivity and mood instability symptoms. Her initial Montgomery-Asberg Depression Scale (MADRS) and Young Mania Rating Scale (YMRS) scores were 24 and 37, respectively. Two weeks after treatment, these values were lowered to 17 and 25, respectively. Her Clinical Global Impression-Severity Scale (CGI-S) score was 6 (severely ill) at initial presentation and 4 (moderately ill) at hospital discharge. Her Global Assessment of Functioning (GAF) score also slightly improved from 50 to 60 after treatment.
Conclusions
CADASIL is an example of pleiotropism i.e. single gene effects on multiple phenotypic traits. CASASIL is a monogenic disease caused by a dysfunction in the NOTCH3 gene localized on chromosome 19p13.1, but shows a wide variety of clinical symptoms. This disease is characterized by five main symptoms: migraine with aura, subcortical ischemic events, mood disturbance, apathy, and cognitive impairment [ 6 ]. Psychiatric symptoms, mainly episodes of mood disturbances, are seen in 23% of CADASIL cases [ 5 ].
Our current case of a bipolar clinical presentation of CADASIL without remarkable neurologic deficits provides some important new insights into this disorder. Our patient was interviewed and described by a psychiatrist. Psychiatric disturbances in patients with CADASIL are usually reported to occur during the course of the disease [ 5 ], and are often the first recorded symptoms because the affected patients will first be admitted to a psychiatric clinics. The initial symptoms of CADASIL vary with the age of onset, but migraine and TIA are the most commonly reported initial symptoms [ 4 ]. Depression is the second most common first symptom in patients who first present with CADASIL at an age of over 50 [ 4 ]. However, manic episodes have rarely been documented as an initial symptom of CADASIL [ 4 , 7 ]. A recent CADASIL review article, has highlighted that personality and behavioral disorders, such as irritability and aggressiveness, were reported in only 7 cases (2%) of a previous 454 patient cohort and that BD was documented in 9 cases (2%) of a 451 patient series [ 5 ]. However, these studies were limited by the fact that clinical manifestations were mainly defined by medical specialists or medical records and not through psychiatric evaluations. Also, manic symptoms appear to be uncommon in CADASIL patients and may therefore have generated less interest among clinicians.
Few studies have investigated mood disorder with a more specific focus on psychiatric disorders in CADASIL. Layhe et al. [ 8 ] reported two CADASIL cases who had been admitted to a gerontopsychiatric hospital with psychopathological manifestations at the onset of the disorder. One of these patients had experienced a submanic episode who had become impulsive, verbally aggressive, irritable, and sexually preoccupied. Taylor et al. [ 9 ] have described a male CADASIL patient who showed persistent behavioral disturbances, irritability, and angry outbursts that lasted for 4years. Gamakaranage et al. [ 10 ] have also described a CADASIL case with a changed personality involving mood swings, aggressive behavior, and cognitive deficit [ 10 ]. Although this patient seemed to show symptoms of mania, this was considered to be just a personality problem as the causes were attributed to the persistence of manic symptoms for many years. This patient was not interviewed by psychiatrist. Only one previous report has described a case of CADASIL with mania [ 11 ]. However, it had not included detailed descriptions of neuropsycholocial evaluations or psychiatric treatment.
In our present case report, the symptoms of BD which had begun when our patient was aged in her 50s seemed for many years to be a personality change due to a continuously labile mood and irritability. She had specific findings on a cerebral MRI and did not respond well to medication. She showed an intact memory, but neuropsychological testing revealed impairment of both attention and executive function. However, detailed descriptions of psychiatric symptoms, neuropsychological testing and treatments are available for this patient. We propose several clinical characteristics of CADASIL presenting as BD. All CADASIL cases for which manic symptoms have been reported including our current case have been documented with a labile mood, irritability, and verbal aggression, with no euphoria or elated mood. All CADASIL patients show a first manifestation of late-onset disease after reaching the age of 50. In addition, as they show a chronic symptom course which has progressed for years, they have often been diagnosed with a personality problem. We contend therefore that when patients show a late onset personality change, and a chronically labile or irritable mood that deteriorates over many years, an organic cause like CADASIL must be considered.
The most prominent neurologic deficits reported in CADASIL patients to date manifest as a reduced processing speed as assessed, for example, by the timed measurements in the TMT and the symbol digit tests. Indeed, abnormalities that are revealed by the TMT B, which measures processing speeds and set shifting, are remarkably consistent across all published studies on CADASIL including our current case [ 12 ]. Cognitive decline predominantly affects frontal lobe functions and is characterized by impaired executive function and poor concentration. Cognitive decline may also commence insidiously before the onset of symptomatic ischemic episodes in CADASIL [ 13 ]. These impairments are suggestive of dysfunction in the subcortical-frontal network [ 12 , 14 ]. Memory and other cognitive functions are relatively preserved at the early stages of CADASIL [ 12 ].
Patients presenting with psychiatric symptoms should undergo a brain MRI if they have a history of headache, stroke-like episodes, or cognitive changes and a positive family history of these manifestations [ 15 ]. Hyperintensities of the external capsule and the anterior pole of the temporal lobe are highly suggestive of CADASIL [ 16 ]. Hyperintense lesions have been found in both subcortical white matter and gray nuclei and occur more frequently in BD subjects than in age-matched controls [ 17 ]. Abnormalities converge in the prefrontal white matter and, in particular, in the tracts that connect prefrontal regions and subcortical gray matter structures known to be involved in emotion [ 17 ]. It is noteworthy that the MRI changes previously known in BD are strikingly similar to those reported in CADASIL. It might be postulated that psychiatric manifestations in CADASIL depend on the extent of the damage the cortical-subcortical circuits, as evidenced by white matter lesions and lacunar infarcts [ 18 ]. Recently, ischemic subcortical lesions are reputed to be important risk factors for the onset of mood disorders [ 19 ]. However, information is still lacking regarding the relationship between mood disorders and lesions detected on MRI. The NOTCH pathways have been postulated as a cause of white matter changes in BD [ 17 ].
Although some studies of CADASIL have described phenotype-genotype correlations, the genotype cannot be used to predict the phenotype in this disease [ 20 ]. The R75P mutation identified in our current case is a novel mutation in a CADASIL patient but is relatively common in Koreans [ 21 ]. In addition, this mutation is related to arginine, whereas previous CADASIL case reports have frequently described the involvement of a cysteine residue. However, several mutations at arginine residues in EGF-like repeats have been identified previously in other proteins that are functionally related to NOTCH3 [ 21 ]. Whilst anterior temporal hyperintensities have been commonly observed in 75% of CADASIL cases without an R75P mutation, they have not been observed in any patients with this mutation [ 21 ]. Consistently, our current patient did not show prominent anterior temporal hyperintensities (Figure 1 D).
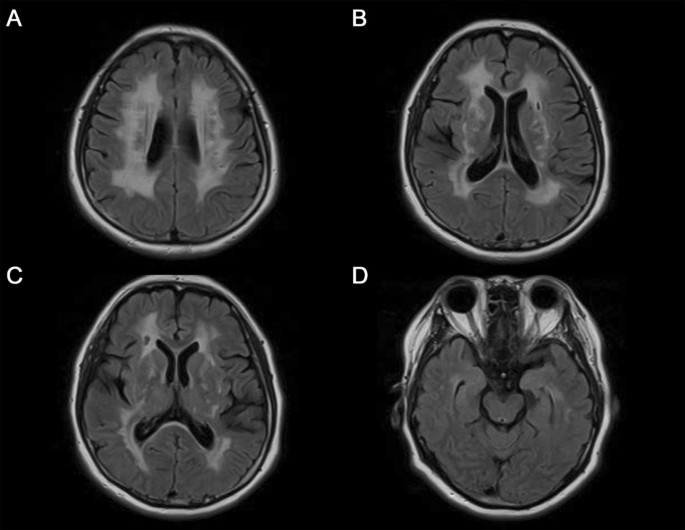
Cerebral MRI with fluid-attenuated inversion-recovery (FLAIR) showing high-signal intensity lesions in the periventricular white matter, both basal ganglia, thalamus, and external capsule (A-C), but not prominent in the anterior temporal poles (D).
However, this study was retrospective and has some limitations. This was not confirmed GOM by a skin biopsy, and we investigated exon 2–11, 18 of NOTCH3 which was known as mutation of CASASIL. Because we did not survey other exons from 12 to 15 or 20–23 have been reported [ 22 ] expressing NOTCH3 and exclude the possibility of other mutations related to cysteine.
CADASIL is likely to be an underdiagnosed disease, particularly in psychiatric patients. It is therefore important to highlight CADASIL to psychiatrists as a potential differential diagnosis. When BD patients show different clinical features such as resistance to antipsychotics, and late onset and chronic progression, the neurological signs and detection of white-matter MRI abnormalities, as well as a positive family history of stroke, are helpful for diagnosing CADASIL [ 23 ]. Testing which is particularly sensitive for the detection of the early cognitive changes can then be performed such as digit span back-forwards, TMT-B, Stroop, and WCST tests. These tests have revealed that patients with CADASIL show preservation of encoding processes even though memory retrieval is impaired [ 23 ].
There is currently no treatment with a proven efficacy for CADASIL. Because CADASIL is a vascular disorder responsible for cerebral ischemic events, treatment of vascular risk factors is needed for secondary prevention in affected patients. Hypertension, hypercholesterolemia and diabetes should also be treated very strictly in these cases. Donepezil can be prescribed for improving executive function, and other symptoms should be treated symptomatically in CADASIL patients [ 24 ]. Yuan et al., have reported that valproate (VPA), an anticonvulsant and mood stabilizer activates the NOTCH3/c-FLIP cascade, conferring cytoprotective effects on vascular smooth muscle cells [ 25 ]. Thus, VPA may be useful in the treatment of CADASIL, particularly in patients showing BD. In our current case, atypical antipsychotics proved to be helpful in behavior control. Further studies are needed to better understand the exact impacts of cerebral tissue lesions and psychiatric symptoms in CADASIL patients.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Craddock N, Sklar P: Genetics of bipolar disorder. Lancet. 2013, 381 (9878): 1654-1662. 10.1016/S0140-6736(13)60855-7.
Article CAS PubMed Google Scholar
Muller-Oerlinghausen B, Berghofer A, Bauer M: Bipolar disorder. Lancet. 2002, 359 (9302): 241-247. 10.1016/S0140-6736(02)07450-0.
Article PubMed Google Scholar
Joutel A, Corpechot C, Ducros A, Vahedi K, Chabriat H, Mouton P, Alamowitch S, Domenga V, Cecillion M, Marechal E, Maciazek J, Vayssiere C, Cruaud C, Cabanis EA, Ruchoux MM, Weissenbach J, Bach JF, Bousser MG, Tournier-Lasserve E: Notch3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature. 1996, 383 (6602): 707-710. 10.1038/383707a0.
Desmond DW, Moroney JT, Lynch T, Chan S, Chin SS, Mohr JP: The natural history of CADASIL: a pooled analysis of previously published cases. Stroke. 1999, 30 (6): 1230-1233. 10.1161/01.STR.30.6.1230.
Valenti R, Poggesi A, Pescini F, Inzitari D, Pantoni L: Psychiatric disturbances in CADASIL: a brief review. Acta Neurol Scand. 2008, 118 (5): 291-295. 10.1111/j.1600-0404.2008.01015.x.
Chabriat H, Vahedi K, Iba-Zizen MT, Joutel A, Nibbio A, Nagy TG, Krebs MO, Julien J, Dubois B, Ducrocq X, Levasseur M, Mas JL, Dubois B, Homeyer P, Lyon-Caen O: Clinical spectrum of CADASIL: a study of 7 families. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Lancet. 1995, 346 (8980): 934-939. 10.1016/S0140-6736(95)91557-5.
Dichgans M, Mayer M, Uttner I, Bruning R, Muller-Hocker J, Rungger G, Ebke M, Klockgether T, Gasser T: The phenotypic spectrum of CADASIL: clinical findings in 102 cases. Ann Neurol. 1998, 44 (5): 731-739. 10.1002/ana.410440506.
Leyhe T, Wiendl H, Buchkremer G, Wormstall H: CADASIL: underdiagnosed in psychiatric patients?. Acta Psychiatr Scand. 2005, 111 (5): 392-396. 10.1111/j.1600-0447.2004.00452.x. Discussion 396–397
Taylor MH, Doody GA: CADASIL: a guide to a comparatively unrecognised condition in psychiatry. Adv Psychiatr Treat. 2008, 14 (5): 350-357. 10.1192/apt.bp.107.004655.
Article Google Scholar
Gamakaranage C, Chang T: CADASIL presenting as a change in personality. Journal of the Ceylon College of Physicians. 2011, 42: 33-34.
Google Scholar
Lalith Kumar SK, Mahr G: CADASIL Presenting as Bipolar Disorder. Psychosomatics. 1997, 38 (4): 397-398. 10.1016/S0033-3182(97)71452-X.
Dichgans M: Cognition in CADASIL. Stroke. 2009, 40 (3 Suppl): S45-47.
Amberla K, Waljas M, Tuominen S, Almkvist O, Poyhonen M, Tuisku S, Kalimo H, Viitanen M: Insidious cognitive decline in CADASIL. Stroke. 2004, 35 (7): 1598-1602. 10.1161/01.STR.0000129787.92085.0a.
Peters N, Opherk C, Danek A, Ballard C, Herzog J, Dichgans M: The pattern of cognitive performance in CADASIL: a monogenic condition leading to subcortical ischemic vascular dementia. Am J Psychiatry. 2005, 162 (11): 2078-2085. 10.1176/appi.ajp.162.11.2078.
Dericioglu N, Vural A, Agayeva N, Basar K, Anil Yagcioglu AE, Gursoy-Ozdemir Y: Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy (CADASIL) in Two Siblings with Neuropsychiatric Symptoms. Psychosomatics. 2013, 54 (6): 594-598. 10.1016/j.psym.2012.12.002.
Markus HS, Martin RJ, Simpson MA, Dong YB, Ali N, Crosby AH, Powell JF: Diagnostic strategies in CADASIL. Neurology. 2002, 59 (8): 1134-1138. 10.1212/WNL.59.8.1134.
Mahon K, Burdick KE, Szeszko PR: A role for white matter abnormalities in the pathophysiology of bipolar disorder. Neurosci Biobehav Rev. 2010, 34 (4): 533-554. 10.1016/j.neubiorev.2009.10.012.
Starkstein SE, Robinson RG: Depression following cerebrovascular lesions. Semin Neurol. 1990, 10 (3): 247-253. 10.1055/s-2008-1041275.
Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M: ‘Vascular depression’ hypothesis. Arch Gen Psychiatry. 1997, 54 (10): 915-922. 10.1001/archpsyc.1997.01830220033006.
Singhal S, Bevan S, Barrick T, Rich P, Markus HS: The influence of genetic and cardiovascular risk factors on the CADASIL phenotype. Brain. 2004, 127 (Pt 9): 2031-2038.
Kim Y, Choi EJ, Choi CG, Kim G, Choi JH, Yoo HW, Kim JS: Characteristics of CADASIL in Korea: a novel cysteine-sparing Notch3 mutation. Neurology. 2006, 66 (10): 1511-1516. 10.1212/01.wnl.0000216259.99811.50.
Tikka S, Mykkanen K, Ruchoux MM, Bergholm R, Junna M, Poyhonen M, Yki-Jarvinen H, Joutel A, Viitanen M, Baumann M, Kalimo H: Congruence between NOTCH3 mutations and GOM in 131 CADASIL patients. Brain. 2009, 132 (Pt 4): 933-939.
PubMed PubMed Central Google Scholar
Chabriat H, Bousser MG: Neuropsychiatric manifestations in CADASIL. Dialogues Clin Neurosci. 2007, 9 (2): 199-208.
Chabriat H, Joutel A, Dichgans M, Tournier-Lasserve E, Bousser MG: Cadasil. Lancet Neurol. 2009, 8 (7): 643-653. 10.1016/S1474-4422(09)70127-9.
Yuan P, Salvadore G, Li X, Zhang L, Du J, Chen G, Manji HK: Valproate activates the Notch3/c-FLIP signaling cascade: a strategy to attenuate white matter hyperintensities in bipolar disorder in late life?. Bipolar Disord. 2009, 11 (3): 256-269. 10.1111/j.1399-5618.2009.00675.x.
Article CAS PubMed PubMed Central Google Scholar
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-244X/14/175/prepub
Download references
Author information
Authors and affiliations.
Department of Psychiatry, University of Ulsan College of Medicine, Asan Medical Center, 88 Olympic-ro 43-gil, Songpa-gu, Seoul, 136-736, South Korea
Soyeon Park, Boram Park & Yeon Ho Joo
Department of Psychology, Asan Medical Center, 88 Olympic-ro 43-gil, Songpa-gu, Seoul, 136-736, South Korea
Min Kyung Koh
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Yeon Ho Joo .
Additional information
Competing interests.
All authors disclose no potential conflicts of interest include employment, consultancies, stock ownership, honoraria, paid expert testimony, patient applications/registrations, and grants or other funding.
Authors’ contributions
S Park participated in the design of the study and drafted the manuscript. BR Park made acquisition and interpretation of a psychiatric history of a case report part and helped to draft the manuscript. MKK made acquisition and interpretation of psychological tests of a case report part and helped to draft the manuscript. YHJ conceived of the study, and participated in its design and coordination and helped to draft the manuscript. Each author has participated sufficiently in the work to take public responsibility for appropriate portions of the content. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Park, S., Park, B., Koh, M.K. et al. Case report: bipolar disorder as the first manifestation of CADASIL. BMC Psychiatry 14 , 175 (2014). https://doi.org/10.1186/1471-244X-14-175
Download citation
Received : 21 August 2013
Accepted : 11 June 2014
Published : 14 June 2014
DOI : https://doi.org/10.1186/1471-244X-14-175
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Bipolar disorder
- Mood disorder
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
16 likes • 8,499 views. A. asifiqbal545. clinical case presentation -bipolar disorder. an excellent case of bipolar disorder by dr Asif iqbal . Health & Medicine. 1 of 18. Download now. clinical case presentation -bipolar disorder - Download as a PDF or view online for free.
This is an interesting case, as we take a look at this 23-year-old female who first comes in to see her psychiatrist with moderate depressive symptoms. At the time of the interview, her chief complaint included feeling like she's lacking energy, she's feeling depressed. She's also reporting difficulty in paying attention, organizing her ...
We're going to go ahead to patient case No. 1. This is a 27-year-old woman who's presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode.
So, when it comes to presenting a case report on bipolar disorder, creating a workable and engaging slideshow is crucial. With the help of this template, you can tailor a visual narrative that not only enhances comprehension but also showcases the unique nuances of each case. By incorporating eye-catching graphics and compelling case studies ...
DIAGNOSIS. BIPOLAR DISORDER. Formerly referred to as manic depressive illness, with two distinct aspects; mania and depression. During mania an individual feels or acts abnormally happy, energetic, or irritable. They often make poorly thought out decisions with little regard to the consequences. The need for sleep is usually reduced.
Case Study Details. Sarah is a 42-year-old married woman who has a long history of both depressive and hypomanic episodes. Across the years she has been variable diagnoses as having major depression, borderline personality disorder, and most recently, bipolar disorder. Review of symptoms indicates that she indeed have multiple episodes of ...
CASE STUDY Gary (bipolar disorder) Case Study Details. Gary is a 19-year-old who withdrew from college after experiencing a manic episode during which he was brought to the attention of the Campus Police ("I took the responsibility to pull multiple fire alarms in my dorm to ensure that they worked, given the life or death nature of fires"). ...
Chapter 5 covers the psychiatric treatment of bipolar disorder, including a case history, key principles, assessment strategy, differential diagnosis, case formulation, treatment planning, nonspecific factors in treatment, potential treatment obstacles, ethical considerations, common mistakes to avoid in treatment, and relapse prevention.
Through the real-life case study of Susan, we have explored the numerous facets of bipolar disorder, including its background, symptoms, and effects on daily life. Susan's journey serves as a powerful reminder of the challenges individuals face in managing the highs and lows of bipolar disorder and emphasizes the importance of effective ...
Bipolar clients with psychotic or depressive symptoms are at high risk for misdiagnoses of "Schizophrenia" and Major Depressive Disorder (MDD) and then getting mismedicated with drugs that do not address a Bipolar Disorder, have an unfavorable risk-to-benefit ratio, or make it worse (Sects. 6.2 and 6.3).
The terms "soft bipolar" or "bipolar spectrum" were first proposed by Akiskal and Mallya ( 4) to describe psychopathological states that could not be easily diagnosed. It has been reported that soft bipolar cases may be prevalent up to 5.1%-23.7% ( 5 ). Cyclothymia and unspecified type of bipolar disorder are suggested to be present ...
Pediatric Bipolar Disorder: A Case Presentation and Discussion Gretchen Weeks, RN, BSN, & Regena Spratling, PhD, RN, APRN, CPNP KEY WORDS Behavior, depression, mania, mood, pediatric bipolar ... Department Case Study www.jpedhc.org March-April 2018 201. bipolar disorder. A 10-year-old boy presented to his primary care provider (PCP) for unusual ...
Bipolar Disorder - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. A Case study about Bipolar disorders.
A 30-year-old man has taken short-term disability leave from work due to the progression of a depressive episode. He received a diagnosis of bipolar I disorder about 10 years ago. He had his first episode of mania at the age of 20 and 2 subsequent episodes of mania between the ages of 21 and 29. He was treated with lithium, which was highly ...
Perform a thorough clinical assessment for patients with a manic, hypomanic, or mixed episode, or those with a bipolar depression episode, including information about the patient's clinical and psychosocial status, medical and psychiatric comorbidities, current and past medications as well as medication compliance, and substance use. [ 3]
Case Presentation Pbl 12 (Bipolar Disorder) - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. Case Presentation Pbl 12 (Bipolar Disorder
Early-onset Bipolar Disorder. Studies have shown that bipolar disorder usually begins with an index episode of depression: positive family history (Pavuluri, Birmaher, & Naylor, 2005), clinical severity, psychotic symptoms, and psychomotor retardation are well documented predictors of bipolarity.Approximately 20% of youths with a first major depressive episode will develop a manic episode.
Case Report on Bipolar Affective Disorder: Mania with Psychotic Symptoms Kounassegarane Deepika AbstrAct Bipolar affective disorder (BPAD) is a major psychiatric disorder all around the world, which is mainly characterized by frequent and recurrent episodes of mania, hypomania, and depression. A majority of complete etiology or pathogenesis of ...
Bipolar disorder is a mood disorder characterized by periods of mania, hypomania, and depression that interfere with the child's daily functioning (American Psychiatric Association, 2013; Birmaher, 2013). There are subtypes of bipolar disorder, such as bipolar I disorder, bipolar II disorder, cyclothymic disorder, and other specified bipolar and related disorders (American Psychiatric ...
Case presentation. A 53-year-old woman visited our out-patient psychiatric clinic in March 2013. Her daughter reported that she had become excessively talkative, impulsive, and verbally aggressive. The changes in her personality had begun to appear in 2008 and her symptoms of hostility had become more severe recently.