- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

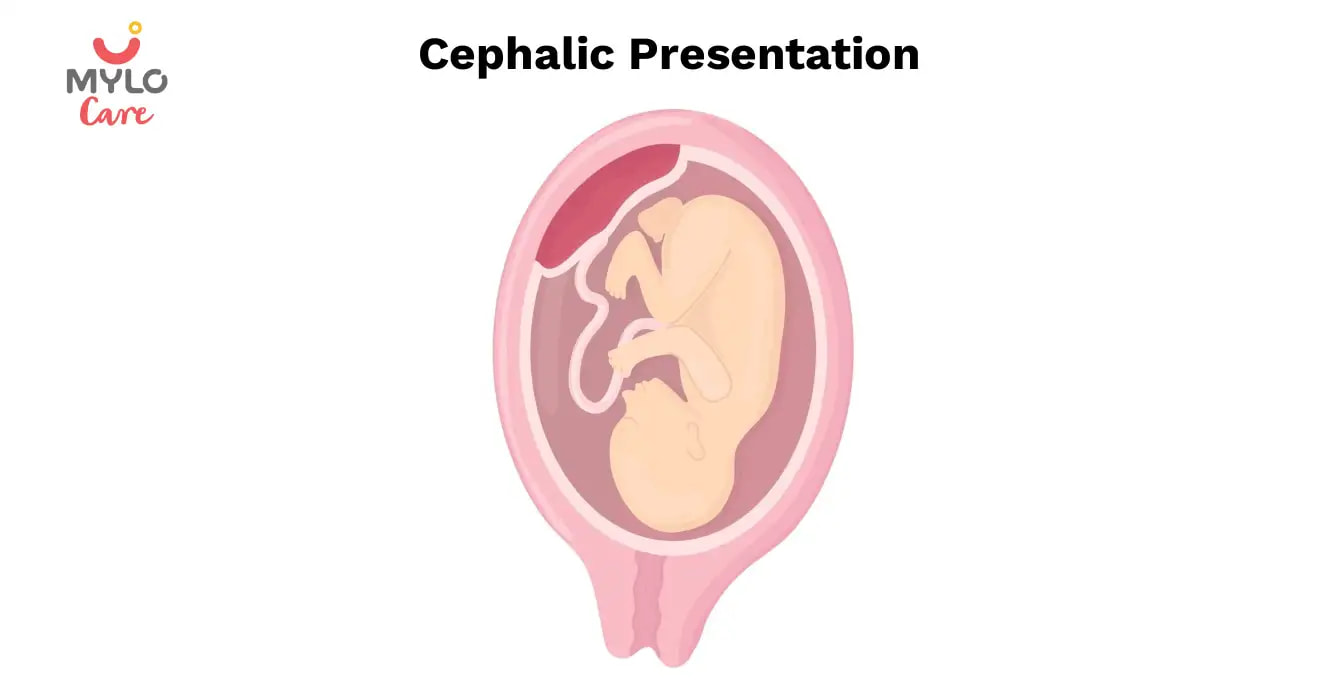
What Is Cephalic Position?
The ideal fetal position for labor and delivery
- Why It's Best
Risks of Other Positions
- Determining Position
- Turning a Fetus
The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery.
About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of pregnancy . Your healthcare provider will monitor the fetus's position during the last weeks of gestation to ensure this has happened by week 36.
If the fetus is not in the cephalic position at that point, the provider may try to turn it. If this doesn't work, some—but not all—practitioners will attempt to deliver vaginally, while others will recommend a Cesarean (C-section).
Getty Images
Why Is the Cephalic Position Best?
During labor, contractions dilate the cervix so the fetus has adequate room to come through the birth canal. The cephalic position is the easiest and safest way for the baby to pass through the birth canal.
If the fetus is in a noncephalic position, delivery becomes more challenging. Different fetal positions have a range of difficulties and varying risks.
A small percentage of babies present in noncephalic positions. This can pose risks both to the fetus and the mother, and make labor and delivery more challenging. It can also influence the way in which someone can deliver.
A fetus may actually find itself in any of these positions throughout pregnancy, as the move about the uterus. But as they grow, there will be less room to tumble around and they will settle into a final position.
It is at this point that noncephalic positions can pose significant risks.
Cephalic Posterior
A fetus may also present in an occiput or cephalic posterior position. This means they are positioned head down, but they are facing the abdomen instead of the back.
This position is also nicknamed "sunny-side up."
Presenting this way increases the chance of a painful and prolonged delivery.
There are three different types of breech fetal positioning:
- Frank breech: The legs are up with the feet near the head.
- Footling breech: One or both legs is lowered over the cervix.
- Complete breech: The fetus is bottom-first with knees bent.
A vaginal delivery is most times a safe way to deliver. But with breech positions, a vaginal delivery can be complicated.
When a baby is born in the breech position, the largest part—its head—is delivered last. This can result in them getting stuck in the birth canal (entrapped). This can cause injury or death.
The umbilical cord may also be damaged or slide down into the mouth of the womb, which can reduce or cut off the baby's oxygen supply.
Some providers are still comfortable performing a vaginal birth as long as the fetus is doing well. But breech is always a riskier delivery position compared with the cephalic position, and most cases require a C-section.
Likelihood of a Breech Baby
You are more likely to have a breech baby if you:
- Go into early labor before you're full term
- Have an abnormally shaped uterus, fibroids , or too much amniotic fluid
- Are pregnant with multiples
- Have placenta previa (when the placenta covers the cervix)
Transverse Lie
In transverse lie position, the fetus is presenting sideways across the uterus rather than vertically. They may be:
- Down, with the back facing the birth canal
- With one shoulder pointing toward the birth canal
- Up, with the hands and feet facing the birth canal
If a transverse lie is not corrected before labor, a C-section will be required. This is typically the case.
Determining Fetal Position
Your healthcare provider can determine if your baby is in cephalic presentation by performing a physical exam and ultrasound.
In the final weeks of pregnancy, your healthcare provider will feel your lower abdomen with their hands to assess the positioning of the baby. This includes where the head, back, and buttocks lie
If your healthcare provider senses that the fetus is in a breech position, they can use ultrasound to confirm their suspicion.
Turning a Fetus So They Are in Cephalic Position
External cephalic version (ECV) is a common, noninvasive procedure to turn a breech baby into cephalic position while it's still in the uterus.
This is only considered if a healthcare provider monitors presentation progress in the last trimester and notices that a fetus is maintaining a noncephalic position as your delivery date approaches.
External Cephalic Version (ECV)
ECV involves the healthcare provider applying pressure to your stomach to turn the fetus from the outside. They will attempt to rotate the head forward or backward and lift the buttocks in an upward position. Sometimes, they use ultrasound to help guide the process.
The best time to perform ECV is about 37 weeks of pregnancy. Afterward, the fetal heart rate will be monitored to make sure it’s within normal levels. You should be able to go home after having ECV done.
ECV has a 50% to 60% success rate. However, even if it does work, there is still a chance the fetus will return to the breech position before birth.
Natural Methods For Turning a Fetus
There are also natural methods that can help turn a fetus into cephalic position. There is no medical research that confirms their efficacy, however.
- Changing your position: Sometimes a fetus will move when you get into certain positions. Two specific movements that your provider may recommend include: Getting on your hands and knees and gently rocking back and forth. Another you could try is pushing your hips up in the air while laying on your back with your knees bent and feet flat on the floor (bridge pose).
- Playing stimulating sounds: Fetuses gravitate to sound. You may be successful at luring a fetus out of breech position by playing music or a recording of your voice near your lower abdomen.
- Chiropractic care: A chiropractor can try the Webster technique. This is a specific chiropractic analysis and adjustment which enables chiropractors to establish balance in the pregnant person's pelvis and reduce undue stress to the uterus and supporting ligaments.
- Acupuncture: This is a considerably safe way someone can try to turn a fetus. Some practitioners incorporate moxibustion—the burning of dried mugwort on certain areas of the body—because they believe it will enhance the chances of success.
A Word From Verywell
While most babies are born in cephalic position at delivery, this is not always the case. And while some fetuses can be turned, others may be more stubborn.
This may affect your labor and delivery wishes. Try to remember that having a healthy baby, and staying well yourself, are your ultimate priorities. That may mean diverting from your best laid plans.
Speaking to your healthcare provider about turning options and the safest route of delivery may help you adjust to this twist and feel better about how you will move ahead.
Glezerman M. Planned vaginal breech delivery: current status and the need to reconsider . Expert Rev Obstet Gynecol. 2012;7(2):159-166. doi:10.1586/eog.12.2
Cleveland Clinic. Fetal positions for birth .
MedlinePlus. Breech birth .
UT Southwestern Medical Center. Can you turn a breech baby around?
The American College of Obstetricians and Gynecologists. If your baby is breech .
Roecker CB. Breech repositioning unresponsive to Webster technique: coexistence of oligohydramnios . Journal of Chiropractic Medicine . 2013;12(2):74-78. doi:10.1016/j.jcm.2013.06.003
By Cherie Berkley, MS Berkley is a journalist with a certification in global health from Johns Hopkins University and a master's degree in journalism.
Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
When Will Your Baby Turn Head Down?

During pregnancy, your baby’s position can change frequently. One of the most important changes occurs when the baby turns to a headfirst, head-down position in the uterus, which often happens toward the end of your pregnancy. Wondering when “should” your baby be head down, or how to tell if your baby is head down? Get these answers as well as more information on the baby’s head-down position, the symptoms of a baby turning head down, and the optimal baby position for birth.
Why Does a Baby Turn to a Head-Down Position for Birth?
So, what does it mean when a baby is head down? Babies generally turn head down toward the birth canal as a part of their natural instinct to get into the best possible position for birth. This is known as the vertex or cephalic presentation . A baby may settle into the optimal position, which is head down and facing the mother's back ( occiput anterior position ), but occasionally they may position themselves head down and face forward ( occiput posterior position ). The face-forward position may cause more discomfort during delivery.
Remember, each pregnancy is unique. If you have any concerns about your baby's position, it's always best to consult your healthcare provider.
When Does a Baby Turn Head Down?
Curious about when a baby “should” be head down? It’s important to remember that the exact timing of when a baby turns head down can vary from pregnancy to pregnancy. Generally, babies turn head down during the third trimester (which ranges from 28 to 40 weeks), a few weeks before birth.
How to Tell if Your Baby Is Head Down
To determine your baby’s position, your healthcare provider will usually perform a physical exam during the final few weeks of your pregnancy, feeling your abdomen to locate your baby’s head. They may also perform an ultrasound to confirm the position, especially if your baby is suspected of being in breech presentation, meaning your baby’s feet or buttocks are positioned downward, lower than the head.
So, how to tell if your baby is head down without an ultrasound? And can you feel when your baby turns head down? You may notice signs and symptoms indicating your baby is turning head down. These could include:
Pressure on your bladder, which may cause frequent urination
Pressure in your pelvis and hips
A reduction of pressure against your diaphragm and lungs, making it easier to breathe
The area where you feel kicks when your baby is head down. You may feel kicks higher in your belly or under your ribs when your baby is head down, whereas in the breech position, you may feel kicks lower in your belly.
These symptoms may be more evident when your baby “drops” lower into your pelvis in preparation for labor. This process is known as lightening .
Remember, every pregnancy is different, and you may not experience any sensation or signs that your baby is head down.
If you're unsure if your baby is head down, your healthcare provider can confirm the position during a prenatal checkup.
What if Your Baby Doesn’t Move Head Down?
When a baby is not head down, they might be in what's known as a breech position or a sideways transverse lie position . In a breech position, the baby's buttocks or feet are positioned to descend down the birth canal first, instead of the head. This position can pose certain risks during vaginal birth , as the baby's head is the last part to emerge. Three main types of breech positions include frank breech, complete breech, and footling breech.
If you're getting closer to your due date and your baby is still not head down, there are a few options that your healthcare provider may consider:
External cephalic version (ECV), a procedure in which a healthcare provider gently manipulates the baby's position from outside the belly. This procedure is usually performed if your baby isn’t in the head-down position after 36 weeks of pregnancy.
A planned cesarean birth ( cesarean section or c-section ) , if the baby's position cannot be changed or poses risks during vaginal delivery.
It's important to discuss these options with your healthcare provider to determine the best course of action for you and your baby. In some cases, your little one may continue to move around and switch positions in the weeks before birth. Again, keep in mind that every pregnancy and birth is unique and your healthcare team will work with you to ensure a safe delivery for both you and your little one.
Can You Help Your Baby Move to a Head-Down Position?
If your baby is not yet in a head-down position and your due date is approaching, you may be wondering how to “get” your baby to turn head down. While you can’t actually make your little one do something, there are some gentle things you can try to encourage them to move, after checking with your healthcare provider. It's important to note that these methods are not guaranteed to work. They include:
Spending time on all fours and rocking back and forth gently
Doing pelvic tilts or rotating your hips in a circular motion
Swimming or walking in water, which can provide buoyancy and help the baby move into a head-down position
Talking to your baby and using gentle and stimulating sounds, such as music, may also encourage them to turn.
Remember to always consult your provider before attempting any exercises or techniques to help your baby move.
The Bottom Line
In the final weeks of pregnancy, you could be concerned about your baby's positioning and wondering “When do babies turn head down?” if your little one hasn't settled into this position yet. But rest assured, your baby still has time to turn head down, and even if they don't do this, there are safe delivery options available. Remember to stay in close communication with your healthcare provider and reach out if you have any questions or concerns. You're doing a great job—keep up the good work!
How We Wrote This Article The information in this article is based on the expert advice found in trusted medical and government sources, such as the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. You can find a full list of sources used for this article below. The content on this page should not replace professional medical advice. Always consult medical professionals for full diagnosis and treatment.
- American College of Obstetricians and Gynecologists, Your Pregnancy and Childbirth: Month to Month, 7th ed. (Washington, DC: American College of Obstetricians and Gynecologists, 2021).
- ACOG. “If Your Baby is Breech.”
- Cleveland Clinic. “Breech Baby.”
- Cleveland Clinic. “Fetal Positions for Birth.”
- Cleveland Clinic. “Vertex Presentation.”
- Mayo Clinic. “Fetal Presentation Before Birth.”
Review this article:
Read more about pregnancy.
- Giving Birth
- Pregnancy Announcement
- Pregnancy Calendar
- Pregnancy Symptoms
- Baby Shower & Registry
- Prenatal Health and Wellness
- Preparing For Your New Baby
- Due Date Calculator
Join a World of Support
through Pregnancy and Parenthood.

Where You Already Belong
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Fetal Presentation, Position, and Lie (Including Breech Presentation)
, MD, Children's Hospital of Philadelphia
Variations in Fetal Position and Presentation
- 3D Models (0)
- Calculators (0)
- Lab Test (0)

Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).

The fetus has a birth defect Overview of Birth Defects Birth defects, also called congenital anomalies, are physical abnormalities that occur before a baby is born. They are usually obvious within the first year of life. The cause of many birth... read more .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
Sometimes the doctor can turn the fetus to be head first before labor begins by doing a procedure that involves pressing on the pregnant woman’s abdomen and trying to turn the baby around. Trying to turn the baby is called an external cephalic version and is usually done at 37 or 38 weeks of pregnancy. Sometimes women are given a medication (such as terbutaline ) during the procedure to prevent contractions.
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

Was This Page Helpful?

Test your knowledge
Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada)—dedicated to using leading-edge science to save and improve lives around the world. Learn more about the MSD Manuals and our commitment to Global Medical Knowledge .
- Permissions
- Cookie Settings
- Terms of use
- Veterinary Edition

- IN THIS TOPIC
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Fetal Presentation, Position, and Lie (Including Breech Presentation)
, MD, Children's Hospital of Philadelphia
Variations in Fetal Position and Presentation
- 3D Models (0)
- Calculators (0)
- Lab Test (0)

Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).

The fetus has a birth defect Overview of Birth Defects Birth defects, also called congenital anomalies, are physical abnormalities that occur before a baby is born. They are usually obvious within the first year of life. The cause of many birth... read more .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
Sometimes the doctor can turn the fetus to be head first before labor begins by doing a procedure that involves pressing on the pregnant woman’s abdomen and trying to turn the baby around. Trying to turn the baby is called an external cephalic version and is usually done at 37 or 38 weeks of pregnancy. Sometimes women are given a medication (such as terbutaline ) during the procedure to prevent contractions.
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.
Drugs Mentioned In This Article

Was This Page Helpful?

Test your knowledge
Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada)—dedicated to using leading-edge science to save and improve lives around the world. Learn more about the Merck Manuals and our commitment to Global Medical Knowledge .
- Permissions
- Cookie Settings
- Terms of use
- Veterinary Edition

- IN THIS TOPIC
- Find in topic
INTRODUCTION
Diagnosis and management of face and brow presentations will be reviewed here. Other cephalic malpresentations are discussed separately. (See "Occiput posterior position" and "Occiput transverse position" .)
Prevalence — Face and brow presentation are uncommon. Their prevalences compared with other types of malpresentations are shown below [ 1-9 ]:
● Occiput posterior – 1/19 deliveries
● Breech – 1/33 deliveries
To continue reading this article, you must sign in . For more information or to purchase a personal subscription, click below on the option that best describes you:
- Medical Professional
- Resident, Fellow or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
Print Options

Home » Child Birth » Cephalic Presentation: All You Need To Know
Cephalic Presentation: All You Need To Know
- By Adeola Adebo
An exciting experience for many expectant mothers is the moment when they feel their baby’s first kick or a change in his/her position.
You may not feel your baby move for the first time until you are about 14-20weeks gone. Many more kicks will surely come after that as your little bean explores his/her temporary home.

Feeling your baby bounce or turn around in your womb is a good sign.
Of course, a bouncing baby is a healthy baby, especially in the third trimester. This is because the third trimester is the time when your baby flips over to assume the birthing position.
This is very important as the position your baby takes in the womb makes all the difference in how you give birth. The final position most babies (about 96%) assume just before birth is the head-first (cephalic) position.
In This Article:
I) cephalic occiput anterior, ii) cephalic occiput posterior, breech (bottom-first) position:, how do you determine your baby’s position, can you change your baby’s position, a final note, what is cephalic position.
You’d most likely begin to hear the term “cephalic position” or “cephalic presentation” as you get closer to your delivery date.

Let us break it down for you; this simply means that your baby’s feet are up with his head down near your birth canal, or vagina. This head-first position is the safest way for your baby to come into this world.
Your doctor will closely keep track of your baby’s position as you get closer to your delivery date. This should begin around weeks 34-36 of your pregnancy. If your baby is not in the cephalic position by the 36 th week, your doctor might try to gently nudge your baby into position.
There are two ways your baby may assume the head-first position:
In this position, your baby’s head is downwards and facing your back. This is the position most babies assume and is the best for a smooth delivery. This is because this position makes it very easy for your baby to come out or crown.
In this position, your baby’s head is also downwards but facing your belly. Only about 5% of cephalic babies are born this way and it is harder for your baby to come out.

Are There Other Positions?
Other positions your baby may assume asides the head-first position are:
About 4% of babies are born in this bottom-first position.
However, this position can cause complications for both mother and baby because the birth canal will have to open wider. There is also an increased risk of your baby’s arms and legs getting tangled. The different breech positions are:
- Frank Breech : This breech position is where your baby’s bottom is facing downwards with legs straight up in such a way that her feet are close to her face.
- Complete Breech: In this position, your baby’s bottom is facing downwards with legs in a crossed position.
- Incomplete Breech: An incomplete breech position is one where one of your baby’s legs is bent in a cross-legged position while the other leg is directed towards the head.
- Footling Breech: Like the name implies, in this position, your baby’s feet are down near the birth canal in such a way that they will exit feet-first.
- Transverse (Sideways): This is a position where your baby is in a sideways position-lying horizontally in your stomach. Some babies who start off in this position eventually shift completely into a head-first position. Rarely, a baby remains in this position till the time of birth. In these cases, your doctor might recommend a Cesarean section (C-section) for safe delivery.
Your doctor can find out your baby’s position through:
- A physical exam
- An ultrasound scan
- Listening to your baby’s heartbeat
You may guess your baby’s position on your own through their kicks. Kicking in your lower stomach or groin may show that your baby is in a breech (bottom-first) position. On the other hand, a baby in the cephalic (head-first) position will kick around your ribs or upper stomach.
A way to get your baby to move is by stroking, massaging or tapping your belly.
You could also try some home exercises like inversions or yoga to encourage your baby to turn. Your doctor may also recommend some medications that will relax your muscles to allow your baby to turn in the right direction.
It is also possible for your baby to be in a cephalic position but still not be facing the right way. During labor, your baby might turn by itself or can be gently assisted to turn by your doctor through your vagina. However, this turning largely depends on your size and your baby’s size.
The best position for a smooth and safe delivery is the cephalic position (head-first). Fortunately, most babies assume this position before birth.
However, even if your baby does not assume this position, there is absolutely no need to worry. Your midwife or doctor will be there to guide you and help you decide what is best for you and your baby.
- Sabrina Rogers-Anderson 2020, 6 Baby Positions In The Womb And What They Mean , The Tot,Viewed on Sept22, 2020,<https://www.thetot.com/pregnancy-and-fertility/6-baby-positions-in-the-womb-and-what-they-mean/>.
- Noreen Iftikhar 2020, Cephalic Position: Getting Baby in The Right Position For Birth , Healthline Parenthood, Viewed on Sept 22, 2020, <https://www.healthline.com/health/pregnancy/cephalic-position>.
- Shutterstock
edie.amy.co
RECENT POSTS
All you need to know about prenatal yoga, how to choose the best healthcare provider for your pregnancy and childbirth, baby proofing your home: newborn safety essentials, baby skin care basics: everything you need to know, how to successfully manage colic in babies.

- Learn /
Why Is Cephalic Presentation Ideal For Childbirth?

5 Dec 2017 | 8 min Read
During labour, contractions stretch your birth canal so that your baby has adequate room to come through during birth. The cephalic presentation is the safest and easiest way for your baby to pass through the birth canal.
If your baby is in a non-cephalic position, delivery can become more challenging. Different fetal positions pose a range of difficulties and varying risks and may not be considered ideal birthing positions.
Two Kinds of Cephalic Positions
There are two kinds of cephalic positions:
- Cephalic occiput anterior , where your baby’s head is down and is facing toward your back.
- Cephalic occiput posterior , where your baby is positioned head down, but they are facing your abdomen instead of your back. This position is also nicknamed ‘sunny-side-up’ and can increase the chances of prolonged and painful delivery.
How to Know if Your Baby is In a Cephalic Position?
You can feel your baby’s position by rubbing your hand on your belly. If you feel your little one’s stomach in the upper stomach, then your baby is in a cephalic position. But if you feel their kicks in the lower stomach, then it could mean that your baby is in a breech position.
You can also determine whether your baby is in the anterior or posterior cephalic position. If your baby is in the anterior position, you may feel their movement underneath your ribs and your belly button could also pop out. If your baby is in the posterior position, then you may feel their kicks in their abdomen, and your stomach may appear rounded up instead of flat.
You can also determine your baby’s position through an ultrasound scan or a physical examination at your healthcare provider’s office.
Benefits of Cephalic Presentation in Pregnancy
Cephalic presentation is one of the most ideal birth positions, and has the following benefits:
- It is the safest way to give birth as your baby’s position is head-down and prevents the risk of any injuries.
- It can help your baby move through the delivery canal as safely and easily as possible.
- It increases the chances of smooth labour and delivery.
Are There Any Risks Involved in Cephalic Position?
Conditions like a cephalic posterior position in addition to a narrow pelvis of the mother can increase the risk of pregnancy complications during delivery. Some babies in the head-first cephalic presentation might have their heads tilted backward. This may, in some rare cases, cause preterm delivery.
What are the Risks Associated with Other Birth Positions?
A small percentage of babies may settle into a non-cephalic position before their birth. This can pose risks to both your and your baby’s health, and also influence the way in which you deliver.
In the next section, we have discussed a few positions that your baby can settle in throughout pregnancy, as they move around the uterus. But as they grow old, there will be less space for them to tumble around, and they will settle into their final position. This is when non-cephalic positions can pose a risk.
Breech Position
There are three types of breech fetal positioning:
- Frank breech : Your baby’s legs stick straight up along with their feet near their head.
- Footling breech: One or both of your baby’s legs are lowered over your cervix.
- Complete breech: Your baby is positioned bottom-first with their knees bent.
If your baby is in a breech position , vaginal delivery is considered complicated. When a baby is born in breech position, the largest part of their body, that is, their head is delivered last. This can lead to injury or even fetal distress. Moreover, the umbilical cord may also get damaged or get wrapped around your baby’s neck, cutting off their oxygen supply.
If your baby is in a breech position, your healthcare provider may recommend a c-section, or they may try ways to flip your baby’s position in a cephalic presentation.
Transverse Lie
In this position, your baby settles in sideways across the uterus rather than being in a vertical position. They may be:
- Head-down, with their back facing the birth canal
- One shoulder pointing toward the birth canal
- Up with their hands and feet facing the birth canal
If your baby settles in this position, then your healthcare provider may suggest a c-section to reduce the risk of distress in your baby and other pregnancy complications.
Turning Your Baby Into A Cephalic Position
External cephalic version (ECV) is a common, and non-invasive procedure that helps turn your baby into a cephalic position while they are in the womb. However, your healthcare provider may only consider this procedure if they consider you have a stable health condition in the last trimester, and if your baby hasn’t changed their position by the 36th week.
You can also try some natural remedies to change your baby’s position, such as:
- Lying in a bridge position: Movements like bridge position can sometimes help move your baby into a more suitable position. Lie on your back with your feet flat on the ground and your legs bent. Raise your pelvis and hips into a bridge position and hold for 5-10 minutes. Repeat several times daily.
- Chiropractic care: A chiropractor can help with the adjustment of your baby’s position and also reduce stress in them.
- Acupuncture: After your doctor’s go-ahead, you can also consider acupuncture to get your baby to settle into an ideal birthing position.
While most babies settle in a cephalic presentation by the 36th week of pregnancy, some may lie in a breech or transverse position before birth. Since the cephalic position is considered the safest, your doctor may recommend certain procedures to flip your baby’s position to make your labour and delivery smooth. You may also try the natural methods that we discussed above to get your baby into a safe birthing position and prevent risks or other pregnancy complications.
When Should A Baby Be In A Cephalic Position?
Your baby would likely naturally drop into a cephalic position between weeks 37 to 40 of your pregnancy .
Is Cephalic Position Safe?
Research shows that 95% of babies take the cephalic position a few weeks or days before their due date. It is considered to be the safest position. It ensures a smooth birthing process.
While most of the babies are in cephalic position at delivery, this is not always the case. If you have a breech baby, you can discuss the available options for delivery with your doctor.
Does cephalic presentation mean labour is near?
Head-down is the ideal position for your baby within your uterus during birth. This is known as the cephalic position. This posture allows your baby to pass through the delivery canal more easily and safely.
Can babies change from cephalic to breech?
The external cephalic version (ECV) is the most frequent procedure used for turning a breech infant.
How can I keep my baby in a cephalic position?
While your baby naturally gets into this position, you can try some exercises to ensure that they settle in cephalic presentation. Exercises such as breech tilt, forward-leaning position (spinning babies program), cat and camel pose can help.
Stitches after a normal delivery : How many stitches do you need after a vaginal delivery? Tap this post to know.
Vaginal birth after caesarean delivery : Learn all about the precautions to consider before having a vaginal delivery after a c-section procedure.
How many c-sections can you have : Tap this post to know the total number of c-sections that you can safely have.
Cover Image Credit: Freepik.com


Related Topics for you
babychakraenglish
cephalicposition
cephalicpresentation
fetaldevelopment
fetalmovement
preganancycare
Suggestions offered by doctors on BabyChakra are of advisory nature i.e., for educational and informational purposes only. Content posted on, created for, or compiled by BabyChakra is not intended or designed to replace your doctor's independent judgment about any symptom, condition, or the appropriateness or risks of a procedure or treatment for a given person.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

How your twins’ fetal positions affect labor and delivery

What happens to your baby right after birth

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

Is cephalic presentation normal at 21 weeks?
You May Also Like
Planning visitors during hospital stay, you’re pregnant how these moms reacted, jump to your week of pregnancy, trending on what to expect, moms share home remedies for pregnancy morning sickness, 8 expensive products moms say are worth the money, ⚠️ you can't see this cool content because you have ad block enabled., 14 moms on what labor really feels like, what are your go-to healthy snacks, things they don't tell you about: mom edition, pregnancy brain moments let's have a laugh, help keep our community safe, to create a safe place, please, on our end, we will.
In this Article
The ABCs of Cephalic Presentation: A Comprehensive Guide for Moms-to-Be
Updated on 24 November 2023
As expectant mothers eagerly anticipate the arrival of their little ones, understanding the intricacies of pregnancy becomes crucial. One term that frequently arises in discussions about childbirth is "cephalic presentation." In this article, we will understand its meaning, types, benefits associated with it, the likelihood of normal delivery and address common concerns expectant mothers might have.
What is the meaning of cephalic presentation in pregnancy?
Cephalic presentation means the baby's head is positioned down towards the birth canal, which is the ideal fetal position for childbirth. This position is considered optimal for a smoother and safer delivery. In medical terms, a baby in cephalic presentation is said to be in a "vertex" position.
The majority of babies naturally assume a cephalic presentation before birth. Other presentations, such as breech presentation (where the baby's buttocks or feet are positioned to enter the birth canal first) or transverse presentation (where the baby is lying sideways), may complicate the delivery process and may require medical intervention.
Cephalic presentation types
There are different types of cephalic presentation, each influencing the birthing process. The primary types include:
1. Vertex Presentation
The most common type where the baby's head is down, facing the mother's spine.
2. Brow Presentation
The baby's head is slightly extended, and the forehead presents first.
3. Face Presentation
The baby is positioned headfirst, but the face is the presenting part instead of the crown of the head.
Understanding these variations is essential for expectant mothers and healthcare providers to navigate potential challenges during labor.
You may also like: How to Get Baby in Right Position for Birth?
What are the benefits of cephalic presentation?
In order to understand whether cephalic presentation is good or bad, let’s take a look at its key advantages:
1. Easier Engagement
This presentation facilitates the baby's engagement in the pelvis, aiding in a smoother descent during labor.
2. Reduced Risk of Complications
Babies in head-first position typically experience fewer complications during delivery compared to other presentations.
3. Faster Labor Progression
This position is associated with quicker labor progression, leading to a potentially shorter and less stressful birthing process.
4. Lower Cesarean Section Rates
The chances of a cesarean section are significantly reduced when the baby is in cephalic presentation in pregnancy.
5. Optimal Fetal Oxygenation
The head-first position allows for optimal oxygenation of the baby as the head can easily pass through the birth canal, promoting a healthy start to life.
What are the chances of normal delivery in cephalic presentation?
The chances of a normal delivery are significantly higher when the baby is in cephalic or head-first presentation. Vaginal births are the natural outcome when the baby's head leads the way, aligning with the natural mechanics of childbirth.
While this presentation increases the chances of a normal delivery, it's important to note that individual factors, such as the mother's pelvic shape, the size of the baby, and the progress of labor, can also influence the delivery process. Sometimes complications may arise during labor and medical interventions or a cesarean section may be necessary.
You may also like: Normal Delivery Tips: An Expecting Mother's Guide to a Smooth Childbirth Experience
How to achieve cephalic presentation in pregnancy?
While fetal positioning is largely influenced by genetic and environmental factors, there are strategies to encourage head-first fetal position:
1. Regular Exercise
Engaging in exercises such as pelvic tilts and knee-chest exercises may help promote optimal fetal positioning.
2. Correct Posture
Maintaining good posture, particularly during the third trimester , can influence fetal positioning.
3. Hands and Knees Position
Spend some time on your hands and knees. This position may help the baby settle into the pelvis with the head down.
4. Forward-leaning Inversion
Under the guidance of a qualified professional, some women try forward-leaning inversions to encourage the baby to move into a head-down position. This involves positioning the body with the hips higher than the head.
5. Prenatal Yoga
Prenatal yoga focuses on strengthening the pelvic floor and promoting flexibility, potentially aiding in cephalic presentation.
6. Professional Guidance
Seeking guidance from a healthcare provider or a certified doula can provide personalized advice tailored to individual needs.
1. Cephalic presentation is good or bad?
Cephalic position is generally considered good as it aligns with the natural process of childbirth. It reduces the likelihood of complications and increases the chances of a successful vaginal delivery . However, it's essential to note that the overall health of both the mother and baby determines its appropriateness.
2. How to increase the chances of normal delivery in cephalic presentation?
Increasing the chances of normal delivery in cephalic presentation involves adopting healthy practices during pregnancy, such as maintaining good posture, engaging in appropriate exercises, and seeking professional guidance. However, individual circumstances vary, and consultation with a healthcare provider is paramount.
Final Thoughts
Navigating the journey of pregnancy involves understanding various aspects, and cephalic presentation plays a crucial role in determining the birthing experience. The benefits of a head-first position, coupled with strategies to encourage it, empower expectant mothers to actively participate in promoting optimal fetal positioning. As always, consulting with healthcare professionals ensures personalized care and guidance, fostering a positive and informed approach towards childbirth.
1. Makajeva J, Ashraf M. Delivery, Face and Brow Presentation. (2023). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing
2. Boos R, Hendrik HJ, Schmidt W. (1987). Das fetale Lageverhalten in der zweiten Schwangerschaftshälfte bei Geburten aus Beckenendlage und Schädellage [Behavior of fetal position in the 2d half of pregnancy in labor with breech and vertex presentations]. Geburtshilfe Frauenheilkd

Anupama Chadha
Anupama Chadha, born and raised in Delhi is a content writer who has written extensively for industries such as HR, Healthcare, Finance, Retail and Tech.
Get baby's diet chart, and growth tips
Related Articles

The Ultimate Guide on Cabbage During Pregnancy Benefits and Precautions

The Pros and Cons of Consuming Brinjal in Pregnancy

A Mom-to-Be's Handbook to Safely Savoring Momos in Pregnancy

The Dos and Don'ts of Drinking Alcohol During Breastfeeding
Related questions, hello frnds..still no pain...doctor said head fix nhi hua hai..bt vagina me pain hai aur back pain bhi... anyone having same issues, kon kon c chije aisi hai jo pregnancy mei gas acidity jalan karti hain... koi btayega plz bcz mujhe aksar khane ke baad hi samagh aata hai ki is chij se gas acidity jalan ho gyi hai. please share your knowledge, i am 13 week pregnancy. anyone having storione-xt tablet. it better to have morning or night , hlo to be moms....i hv a query...in my 9.5 wk i feel body joint pain like in ankle, knee, wrist, shoulder, toes....pain intensity is high...i cnt sleep....what should i do pls help....cn i cosult my doc., influenza and boostrix injection kisiko laga hai kya 8 month pregnancy me and q lagta hai ye plz reply me, related topics, labour & delivery, baby movements, tips for normal delivery, recently published articles, our most recent articles.

Diet & Nutrition
The Ultimate Guide to Consuming Chia Seeds in Pregnancy

Essential Tips for Normal Delivery After Cesarean

Crab During Pregnancy: Benefits, Risks and Smart Choices

Normal Delivery Tips: An Expecting Mother's Guide to a Smooth Childbirth Experience

Top 10 Panchatantra Stories in English You Must Read to Your Children

Health & Wellness
What Helps in Improving Mental Health of Women
- Childhood Disorders: Meaning, Symptoms & Treatment
- Bleeding During Pregnancy 8 Weeks: Should You See a Doctor?
- The Ultimate Guide to Having Sex After C Section
- The Ultimate Guide to Baby Brain Development Food During Pregnancy
- Nappy Rash: Your Ultimate Guide to Symptoms and Quick Relief
- How to Get Periods Immediately to Avoid Pregnancy?
- Loss of Appetite During Pregnancy: Causes and Solutions
- How to Increase Newborn Baby Weight: Expert Tips and Tricks
- Fertisure M: The Comprehensive Solution to Male Infertility and Reproductive Health
- All You Need to Know About the New COVID Variant: Pirola
- Endometrial Polyp and Pregnancy: How Uterine Polyps Can Affect Your Chances of Conception
- How to Stop Heavy Bleeding During Periods: Home Remedies (Part 2)
- How Many Times Should You Have Sex to Get Pregnant?
- A Guide to Planning the Perfect Godh Bharai for the Mom-to-Be
Start Exploring
- Mylo Care: Effective and science-backed personal care and wellness solutions for a joyful you.
- Mylo Baby: Science-backed, gentle and effective personal care & hygiene range for your little one.
- Mylo Community: Trusted and empathetic community of 10mn+ parents and experts.
Product Categories
baby carrier | baby soap | baby wipes | baby shampoo | baby lotion | baby powder | baby body wash | stretch marks cream | stretch marks oil | baby cream | baby massage oil | baby hair oil |

- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
- Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
- Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History
- Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Abnormal Fetal lie, Malpresentation and Malposition
Original Author(s): Anna Mcclune Last updated: 1st December 2018 Revisions: 12
- 1 Definitions
- 2 Risk Factors
- 3.2 Presentation
- 3.3 Position
- 4 Investigations
- 5.1 Abnormal Fetal Lie
- 5.2 Malpresentation
- 5.3 Malposition
The lie, presentation and position of a fetus are important during labour and delivery.
In this article, we will look at the risk factors, examination and management of abnormal fetal lie, malpresentation and malposition.
Definitions
- Longitudinal, transverse or oblique
- Cephalic vertex presentation is the most common and is considered the safest
- Other presentations include breech, shoulder, face and brow
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) – this is ideal for birth
- Other positions include occipito-posterior and occipito-transverse.
Note: Breech presentation is the most common malpresentation, and is covered in detail here .
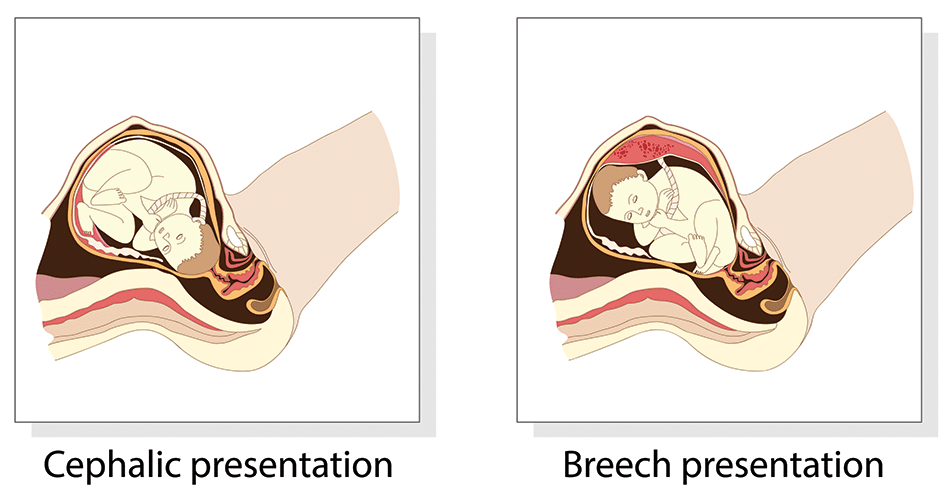
Fig 1 – The two most common fetal presentations: cephalic and breech.
Risk Factors
The risk factors for abnormal fetal lie, malpresentation and malposition include:
- Multiple pregnancy
- Uterine abnormalities (e.g fibroids, partial septate uterus)
- Fetal abnormalities
- Placenta praevia
- Primiparity
Identifying Fetal Lie, Presentation and Position
The fetal lie and presentation can usually be identified via abdominal examination. The fetal position is ascertained by vaginal examination.
For more information on the obstetric examination, see here .
- Face the patient’s head
- Place your hands on either side of the uterus and gently apply pressure; one side will feel fuller and firmer – this is the back, and fetal limbs may feel ‘knobbly’ on the opposite side
Presentation
- Palpate the lower uterus (above the symphysis pubis) with the fingers of both hands; the head feels hard and round (cephalic) and the bottom feels soft and triangular (breech)
- You may be able to gently push the fetal head from side to side
The fetal lie and presentation may not be possible to identify if the mother has a high BMI, if she has not emptied her bladder, if the fetus is small or if there is polyhydramnios .
During labour, vaginal examination is used to assess the position of the fetal head (in a cephalic vertex presentation). The landmarks of the fetal head, including the anterior and posterior fontanelles, indicate the position.
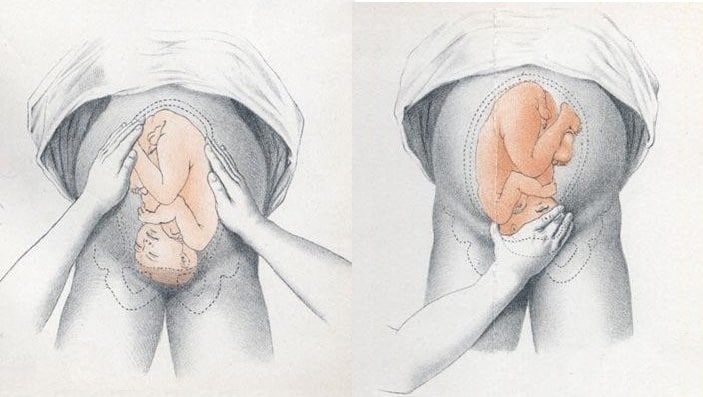
Fig 2 – Assessing fetal lie and presentation.
Investigations
Any suspected abnormal fetal lie or malpresentation should be confirmed by an ultrasound scan . This could also demonstrate predisposing uterine or fetal abnormalities.
Abnormal Fetal Lie
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted – ideally between 36 and 38 weeks gestation.
ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen.
It has an approximate success rate of 50% in primiparous women and 60% in multiparous women. Only 8% of breech presentations will spontaneously revert to cephalic in primiparous women over 36 weeks gestation.
Complications of ECV are rare but include fetal distress , premature rupture of membranes, antepartum haemorrhage (APH) and placental abruption. The risk of an emergency caesarean section (C-section) within 24 hours is around 1 in 200.
ECV is contraindicated in women with a recent APH, ruptured membranes, uterine abnormalities or a previous C-section .
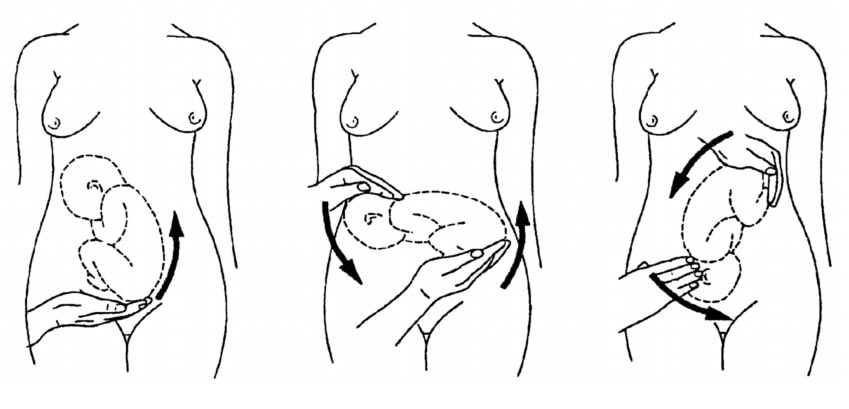
Fig 3 – External cephalic version.
Malpresentation
The management of malpresentation is dependent on the presentation.
- Breech – attempt ECV before labour, vaginal breech delivery or C-section
- Brow – a C-section is necessary
- If the chin is anterior (mento-anterior) a normal labour is possible; however, it is likely to be prolonged and there is an increased risk of a C-section being required
- If the chin is posterior (mento-posterior) then a C-section is necessary
- Shoulder – a C-section is necessary
Malposition
90% of malpositions spontaneously rotate to occipito-anterior as labour progresses. If the fetal head does not rotate, rotation and operative vaginal delivery can be attempted. Alternatively a C-section can be performed.
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) - this is ideal for birth
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation.
- Breech - attempt ECV before labour, vaginal breech delivery or C-section
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Delivery, face and brow presentation.
Julija Makajeva ; Mohsina Ashraf .
Affiliations
Last Update: January 9, 2023 .
- Continuing Education Activity
Face and brow presentation is a malpresentation during labor when the presenting part is either the face or, in the case of brow presentation, it is the area between the orbital ridge and the anterior fontanelle. This activity reviews the evaluation and management of these two presentations and explains the role of the interprofessional team in managing delivery safely for both the mother and the baby.
- Describe the mechanism of labor in the face and brow presentation.
- Summarize potential maternal and fetal complications during the face and brow presentations.
- Review different management approaches for the face and brow presentation.
- Outline some interprofessional strategies that will improve patient outcomes in delivery cases with face and brow presentation issues.
- Introduction
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common presentation in term labor is the vertex, where the fetal neck is flexed to the chin, minimizing the head circumference.
Face presentation – an abnormal form of cephalic presentation where the presenting part is mentum. This typically occurs because of hyperextension of the neck and the occiput touching the fetal back. Incidence of face presentation is rare, accounting for approximately 1 in 600 of all presentations. [1] [2] [3]
In brow presentation, the neck is not extended as much as in face presentation, and the leading part is the area between the anterior fontanelle and the orbital ridges. Brow presentation is considered the rarest of all malpresentation with a prevalence of 1 in 500 to 1 in 4000 deliveries. [3]
Both face and brow presentations occur due to extension of the fetal neck instead of flexion; therefore, conditions that would lead to hyperextension or prevent flexion of the fetal neck can all contribute to face or brow presentation. These risk factors may be related to either the mother or the fetus. Maternal risk factors are preterm delivery, contracted maternal pelvis, platypelloid pelvis, multiparity, previous cesarean section, black race. Fetal risk factors include anencephaly, multiple loops of cord around the neck, masses of the neck, macrosomia, polyhydramnios. [2] [4] [5]
These malpresentations are usually diagnosed during the second stage of labor when performing a digital examination. It is possible to palpate orbital ridges, nose, malar eminences, mentum, mouth, gums, and chin in face presentation. Based on the position of the chin, face presentation can be further divided into mentum anterior, posterior, or transverse. In brow presentation, anterior fontanelle and face can be palpated except for the mouth and the chin. Brow presentation can then be further described based on the position of the anterior fontanelle as frontal anterior, posterior, or transverse.
Diagnosing the exact presentation can be challenging, and face presentation may be misdiagnosed as frank breech. To avoid any confusion, a bedside ultrasound scan can be performed. [6] The ultrasound imaging can show a reduced angle between the occiput and the spine or, the chin is separated from the chest. However, ultrasound does not provide much predicting value in the outcome of the labor. [7]
- Anatomy and Physiology
Before discussing the mechanism of labor in the face or brow presentation, it is crucial to highlight some anatomical landmarks and their measurements.
Planes and Diameters of the Pelvis
The three most important planes in the female pelvis are the pelvic inlet, mid pelvis, and pelvic outlet.
Four diameters can describe the pelvic inlet: anteroposterior, transverse, and two obliques. Furthermore, based on the different landmarks on the pelvic inlet, there are three different anteroposterior diameters, named conjugates: true conjugate, obstetrical conjugate, and diagonal conjugate. Only the latter can be measured directly during the obstetric examination. The shortest of these three diameters is obstetrical conjugate, which measures approximately 10.5 cm and is a distance between the sacral promontory and 1 cm below the upper border of the symphysis pubis. This measurement is clinically significant as the fetal head must pass through this diameter during the engagement phase. The transverse diameter measures about 13.5cm and is the widest distance between the innominate line on both sides.
The shortest distance in the mid pelvis is the interspinous diameter and usually is only about 10 cm.
Fetal Skull Diameters
There are six distinguished longitudinal fetal skull diameters:
- Suboccipito-bregmatic: from the center of anterior fontanelle (bregma) to the occipital protuberance, measuring 9.5 cm. This is the presenting diameter in vertex presentation.
- Suboccipito-frontal: from the anterior part of bregma to the occipital protuberance, measuring 10 cm
- Occipito-frontal: from the root of the nose to the most prominent part of the occiput, measuring 11.5cm
- Submento-bregmatic: from the center of the bregma to the angle of the mandible, measuring 9.5 cm. This is the presenting diameter in face presentation where the neck is hyperextended.
- Submento-vertical: from the midpoint between fontanelles and the angle of the mandible, measuring 11.5cm
- Occipito-mental: from the midpoint between fontanelles and the tip of the chin, measuring 13.5 cm. It is the presenting diameter in brow presentation.
Cardinal Movements of Normal Labor
- Neck flexion
- Internal rotation
- Extension (delivers head)
- External rotation (Restitution)
- Expulsion (delivery of anterior and posterior shoulders)
Some of the key movements are not possible in the face or brow presentations.
Based on the information provided above, it is obvious that labor will be arrested in brow presentation unless it spontaneously changes to face or vertex, as the occipito-mental diameter of the fetal head is significantly wider than the smallest diameter of the female pelvis. Face presentation can, however, be delivered vaginally, and further mechanisms of face delivery will be explained in later sections.
- Indications
As mentioned previously, spontaneous vaginal delivery can be successful in face presentation. However, the main indication for vaginal delivery in such circumstances would be a maternal choice. It is crucial to have a thorough conversation with a mother, explaining the risks and benefits of vaginal delivery with face presentation and a cesarean section. Informed consent and creating a rapport with the mother is an essential aspect of safe and successful labor.
- Contraindications
Vaginal delivery of face presentation is contraindicated if the mentum is lying posteriorly or is in a transverse position. In such a scenario, the fetal brow is pressing against the maternal symphysis pubis, and the short fetal neck, which is already maximally extended, cannot span the surface of the maternal sacrum. In this position, the diameter of the head is larger than the maternal pelvis, and it cannot descend through the birth canal. Therefore the cesarean section is recommended as the safest mode of delivery for mentum posterior face presentations.
Attempts to manually convert face presentation to vertex, manual or forceps rotation of the persistent posterior chin to anterior are contraindicated as they can be dangerous.
Persistent brow presentation itself is a contraindication for vaginal delivery unless the fetus is significantly small or the maternal pelvis is large.
Continuous electronic fetal heart rate monitoring is recommended for face and brow presentations, as heart rate abnormalities are common in these scenarios. One study found that only 14% of the cases with face presentation had no abnormal traces on the cardiotocograph. [8] It is advised to use external transducer devices to prevent damage to the eyes. When internal monitoring is inevitable, it is suggested to place monitoring devices on bony parts carefully.
People who are usually involved in the delivery of face/ brow presentation are:
- Experienced midwife, preferably looking after laboring woman 1:1
- Senior obstetrician
- Neonatal team - in case of need for resuscitation
- Anesthetic team - to provide necessary pain control (e.g., epidural)
- Theatre team - in case of failure to progress and an emergency cesarean section will be required.
- Preparation
No specific preparation is required for face or brow presentation. However, it is essential to discuss the labor options with the mother and birthing partner and inform members of the neonatal, anesthetic, and theatre co-ordinating teams.
- Technique or Treatment
Mechanism of Labor in Face Presentation
During contractions, the pressure exerted by the fundus of the uterus on the fetus and pressure of amniotic fluid initiate descent. During this descent, the fetal neck extends instead of flexing. The internal rotation determines the outcome of delivery, if the fetal chin rotates posteriorly, vaginal delivery would not be possible, and cesarean section is permitted. The approach towards mentum-posterior delivery should be individualized, as the cases are rare. Expectant management is acceptable in multiparous women with small fetuses, as a spontaneous mentum-anterior rotation can occur. However, there should be a low threshold for cesarean section in primigravida women or women with large fetuses.
When the fetal chin is rotated towards maternal symphysis pubis as described as mentum-anterior; in these cases further descend through the vaginal canal continues with approximately 73% cases deliver spontaneously. [9] Fetal mentum presses on the maternal symphysis pubis, and the head is delivered by flexion. The occiput is pointing towards the maternal back, and external rotation happens. Shoulders are delivered in the same manner as in vertex delivery.
Mechanism of Labor in Brow Presentation
As this presentation is considered unstable, it is usually converted into a face or an occiput presentation. Due to the cephalic diameter being wider than the maternal pelvis, the fetal head cannot engage; thus, brow delivery cannot take place. Unless the fetus is small or the pelvis is very wide, the prognosis for vaginal delivery is poor. With persistent brow presentation, a cesarean section is required for safe delivery.
- Complications
As the cesarean section is becoming a more accessible mode of delivery in malpresentations, the incidence of maternal and fetal morbidity and mortality during face presentation has dropped significantly. [10]
However, there are still some complications associated with the nature of labor in face presentation. Due to the fetal head position, it is more challenging for the head to engage in the birth canal and descend, resulting in prolonged labor.
Prolonged labor itself can provoke foetal distress and arrhythmias. If the labor arrests or signs of fetal distress appear on CTG, the recommended next step in management is an emergency cesarean section, which in itself carries a myriad of operative and post-operative complications.
Finally, due to the nature of the fetal position and prolonged duration of labor in face presentation, neonates develop significant edema of the skull and face. Swelling of the fetal airway may also be present, resulting in respiratory distress after birth and possible intubation.
- Clinical Significance
During vertex presentation, the fetal head flexes, bringing the chin to the chest, forming the smallest possible fetal head diameter, measuring approximately 9.5cm. With face and brow presentation, the neck hyperextends, resulting in greater cephalic diameters. As a result, the fetal head will engage later, and labor will progress more slowly. Failure to progress in labor is also more common in both presentations compared to vertex presentation.
Furthermore, when the fetal chin is in a posterior position, this prevents further flexion of the fetal neck, as browns are pressing on the symphysis pubis. As a result, descend through the birth canal is impossible. Such presentation is considered undeliverable vaginally and requires an emergency cesarean section.
Manual attempts to change face presentation to vertex, manual or forceps rotation to mentum anterior are considered dangerous and are discouraged.
- Enhancing Healthcare Team Outcomes
A multidisciplinary team of healthcare experts supports the woman and her child during labor and the perinatal period. For a face or brow presentation to be appropriately diagnosed, an experienced midwife and obstetrician must be involved in the vaginal examination and labor monitoring. As fetal anomalies, such as anencephaly or goiter, can contribute to face presentation, sonographers experienced in antenatal scanning should also be involved in the care. It is advised to inform the anesthetic and neonatal teams in advance of the possible need for emergency cesarean section and resuscitation of the neonate. [11] [12]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Julija Makajeva declares no relevant financial relationships with ineligible companies.
Disclosure: Mohsina Ashraf declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Makajeva J, Ashraf M. Delivery, Face and Brow Presentation. [Updated 2023 Jan 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. [Am J Obstet Gynecol MFM. 2020] Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. Bellussi F, Livi A, Cataneo I, Salsi G, Lenzi J, Pilu G. Am J Obstet Gynecol MFM. 2020 Nov; 2(4):100217. Epub 2020 Aug 18.
- Review Sonographic evaluation of the fetal head position and attitude during labor. [Am J Obstet Gynecol. 2022] Review Sonographic evaluation of the fetal head position and attitude during labor. Ghi T, Dall'Asta A. Am J Obstet Gynecol. 2022 Jul 6; . Epub 2022 Jul 6.
- Stages of Labor. [StatPearls. 2024] Stages of Labor. Hutchison J, Mahdy H, Hutchison J. StatPearls. 2024 Jan
- Leopold Maneuvers. [StatPearls. 2024] Leopold Maneuvers. Superville SS, Siccardi MA. StatPearls. 2024 Jan
- Review Labor with abnormal presentation and position. [Obstet Gynecol Clin North Am. ...] Review Labor with abnormal presentation and position. Stitely ML, Gherman RB. Obstet Gynecol Clin North Am. 2005 Jun; 32(2):165-79.
Recent Activity
- Delivery, Face and Brow Presentation - StatPearls Delivery, Face and Brow Presentation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Getting pregnant
- Life as a parent
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How long will it take to conceive?
- When to take a pregnancy test
- Best positions to conceive
- Top signs of pregnancy
- How to use ovulation kits
- How age affects fertility
- When can I get pregnant after c-section?
- What fertile cervical mucus looks like
- Late period but no pregnancy
- Faint line on pregnancy test
- See all in Getting Pregnant
- How big is my baby?
- Due Date Calculator
- Painful baby movements
- Symptoms you should never ignore
- Hospital bag packing checklist
- How your baby's developing
- Signs of labour
- How to tell baby position by kicks
- Baby movements: boy or girl?
- How to count pregnancy months & weeks
- Nuchal Translucency (NT) scan
- Baby Weight Chart
- See all in Pregnancy
- Baby Name Finder
- Modern Indian Baby Names
- Most Popular Names in India
- Baby Names inspired by the Quran
- Baby Names inspired by Lord Shiva
- Sanskrit Baby Names
- See all in Baby Names
- Your baby week by week
- Baby milestones by month
- Baby Rashes
- Baby skin colour
- Worms in babies and toddlers
- Sleep training methods
- Baby teething remedies
- How to do steaming for a baby
- See all in Baby
- Your toddler month by month
- How much water should toddlers drink?
- When your toddler gets frustrated
- Vegetarian meals for toddlers
- When your toddler won't eat
- Potty training
- Help your toddler sleep
- Bottle to cup
- Games & activities
- What to feed a sick toddler
- See all in Toddler
- गर्भवती होने के लिए संभोग
- प्रेगनेंसी टेस्ट में हल्की रेखा का मतलब
- गर्भावस्था के लक्षण
- गर्भावस्था में खून के धब्बे (ब्लीडिंग)
- गर्भावस्था में शिशु की हलचल
- प्रसव पीड़ा (लेबर पेन) के लक्षण
- शिशु के नक्षत्र पर आधारित नाम
- शिशु को कितनी मात्रा में फॉर्मूला दूध देना है?
- बच्चे के पेट में कीड़े: लक्षण व इलाज
- हिंदी अनुभाग देखें
- Postnatal symptoms to watch out for
- Pain and stitches after delivery
- Postnatal massage
- Postnatal diet
- Post-delivery confinement
- See all in Life as a parent
- Astrology names
- Goddess Lakshmi names
- Baby names by date of birth
- Conjunctivitis
- Combination baby names
- Goddess Durga names
- Sikh baby names
- Bengali baby names
- Eclipses and pregnancy
- Name numerology
- Lord Vishnu names
- What to feed baby with a fever
- Traditional Indian names
- Gestational age vs fetal age
- South Indian baby names
- Mythological baby names
- Pregnancy food chart
- Names that rhyme
- Goddess Saraswati names
- Are air conditioners safe for babies?
- Annaprashan rice ceremony
- Nature names
- Godh bharai: baby shower
- Sesame seeds in pregnancy
cephalic position at 22 weeks normal?
- b BabyCenter__member Posted 05-09-15 Please consult your doctor to clear off the doubt. ... if the overall scan report is good then there shouldn't be anything to worry about. . do not wait. .consult immediately for the symptoms. ..
- l lovely1233 Posted 05-09-15 I asked the same question to the doctor few days back she said baby keeps moving so any position is ok
- s sfk4 Original Poster Posted 10-09-15 BabyCenter__member said: Hi sfk... today only I visited my doctor and asked whether cepha… Thnks for the concern soma_b....I also went for a checkup and nd my gynec said its all normal but adviced me to rest for my lower abdominal pain :)

IMAGES
VIDEO
COMMENTS
Most babies settle into their final position somewhere between 32 to 36 weeks gestation. Head Down, Facing Down (Cephalic Presentation) This is the most common position for babies in-utero. In the cephalic presentation, the baby is head down, chin tucked to chest, facing their mother's back. This position typically allows for the smoothest ...
The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery. About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of pregnancy.
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
This is known as the vertex or cephalic presentation. ... Generally, babies turn head down during the third trimester (which ranges from 28 to 40 weeks), ... especially if your baby is suspected of being in breech presentation, meaning your baby's feet or buttocks are positioned downward, lower than the head. ...
Fetal Presentation, Position, and Lie (Including Breech Presentation) - Learn about the causes, symptoms, diagnosis & treatment from the MSD Manuals - Medical Consumer Version. ... Trying to turn the baby is called an external cephalic version and is usually done at 37 or 38 weeks of pregnancy. Sometimes women are given a medication ...
Cephalic presentation, occiput anterior. This is the best position for labor. Your baby is head-down, their face is turned toward your back, and their chin is tucked to their chest. This allows the back of your baby's head to easily enter your pelvis when the time is right. Most babies settle into this position by week 36 of pregnancy.
This is called cephalic presentation. This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries. There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
Fetal Presentation, Position, and Lie (Including Breech Presentation) - Learn about the causes, symptoms, diagnosis & treatment from the Merck Manuals - Medical Consumer Version. ... Trying to turn the baby is called an external cephalic version and is usually done at 37 or 38 weeks of pregnancy. Sometimes women are given a medication ...
The vast majority of fetuses at term are in cephalic presentation. Approximately 5 percent of these fetuses are in a cephalic malpresentation, such as occiput posterior or transverse, face (figure 1A-B), or brow . Diagnosis and management of face and brow presentations will be reviewed here. Other cephalic malpresentations are discussed separately.
Cephalic presentation means a fetus is in a head-down position. Vertex refers to the fetus's neck being tucked in. There are other types of cephalic presentations like brow and face. These mainly describe how the fetus's neck is flexed. ... It's possible for a fetus to rotate into a cephalic presentation after 36 weeks.
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation, where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations ...
This should begin around weeks 34-36 of your pregnancy. If your baby is not in the cephalic position by the 36 th week, your doctor might try to gently nudge your baby into position. There are two ways your baby may assume the head-first position: i) Cephalic Occiput Anterior . In this position, your baby's head is downwards and facing your back.
Cephalic presentation is one of the most ideal birth positions, and has the following benefits: It is the safest way to give birth as your baby's position is head-down and prevents the risk of any injuries. It can help your baby move through the delivery canal as safely and easily as possible.
This presentation is called occiput anterior and is considered the best position for a vaginal delivery. This position is considered best because this position typically leads to the easiest navigation of the baby through the birth canal. Around 5% of babies are delivered in the occiput posterior position, where the back of the baby's head is ...
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation).
I think they flip so much at this stage because there is so much room. I can feel pressure sometimes and think he must be head down during those times. I see a high risk and he's never said it was an issue. Baby was head down for my ultrasound at 20 week they asked me to come 2 weeks later baby had flipped.
Cephalic presentation means the baby's head is positioned down towards the birth canal, which is the ideal fetal position for childbirth. This position is considered optimal for a smoother and safer delivery. In medical terms, a baby in cephalic presentation is said to be in a "vertex" position. The majority of babies naturally assume a ...
Abnormal Fetal Lie. If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation. ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen. It has an approximate success rate of 50% in primiparous women and 60% in multiparous women.
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common ...
s. sfk4. Posted 05-09-15. I had me scan n ot was cephalic position. Is this position normal at 22 weeks? I'm also having a lower abdominal pain from last 2-3 days n kind of white milky discharge from my vagina which keeps my vagina wet from last 2 days...though the discharge is not much but still m worried.