- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Acquisition
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Religion
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business Strategy
- Business History
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Systems
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Politics and Law
- Public Policy
- Public Administration
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment
- < Previous chapter
- Next chapter >

8 Significance of the Problem of Depression
- Published: February 2000
- Cite Icon Cite
- Permissions Icon Permissions
Attempts to define treatment models that work for depression rest on two cardinal assumptions: that the condition(s) being treated is (are) in fact a recognizable and distinctive disorder (or set of disorders) and that the treatment offered for it (them) is reasonably specific to that disorder. However, both of these assumptions have been seriously questioned as they apply to depression. This chapter presents background material that will encourage the exploration of what is known about the first of these assumptions, that depression is a set of distinctive disorders. This exploration leads to consideration of the evidence that bears on the second assumption, that there is a well-defined, specific treatment for depression. In this way, a decision can be made as to whether the guidelines that are presented, based on principles of differential effect, are more or less useful than those based on assumptions about the specificity of depression and its treatment.
Signed in as
Institutional accounts.
- Google Scholar Indexing
- GoogleCrawler [DO NOT DELETE]
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Advertisement
What Do We Know About Depression Among Youth and How Can We Make Progress Toward Improved Understanding and Reducing Distress? A New Hope
- Invited:Review
- Published: 07 June 2023
- Volume 26 , pages 919–942, ( 2023 )
Cite this article
- Benjamin L. Hankin ORCID: orcid.org/0000-0003-2446-0258 1 &
- Julianne M. Griffith ORCID: orcid.org/0000-0002-2414-6245 1
5111 Accesses
3 Citations
8 Altmetric
Explore all metrics
This paper summarizes many findings about depression among children and adolescents. Depression is prevalent, highly distressing, and exerts considerable burden worldwide. Rates surge from childhood through young adulthood and have increased over the last decade. Many risk factors have been identified, and evidence-based interventions exist targeting mostly individual-level changes via psychological or pharmacological means. At the same time, the field appears stuck and has not achieved considerable progress in advancing scientific understanding of depression’s features or delivering interventions to meet the challenge of youth depression’s high and growing prevalence. This paper adopts several positions to address these challenges and move the field forward. First, we emphasize reinvigoration of construct validation approaches that may better characterize youth depression’s phenomenological features and inform more valid and reliable assessments that can enhance scientific understanding and improve interventions for youth depression. To this end, history and philosophical principles affecting depression’s conceptualization and measurement are considered. Second, we suggest expanding the range and targets of treatments and prevention efforts beyond current practice guidelines for evidence-based interventions. This broader suite of interventions includes structural- and system-level change focused at community and societal levels (e.g., evidence-based economic anti-poverty interventions) and personalized interventions with sufficient evidence base. We propose that by focusing on the FORCE (Fundamentals, Openness, Relationships, Constructs, Evidence), youth depression research can provide new hope.
Similar content being viewed by others
Understanding depression in adolescents: a dynamic psychosocial web of risk and protective factors.
Wassilis Kassis, Sibylle Artz & Jennifer White

Protective Mechanisms for Depression among Racial/Ethnic Minority Youth: Empirical Findings, Issues, and Recommendations
Sarah M. Scott, Jan L. Wallander & Linda Cameron
Depressive Disorders
Avoid common mistakes on your manuscript.
Introduction
Over the last several decades, a prodigious literature has amassed on depression in children and adolescents. Major and consequential epidemiological findings show that (1) depression exhibits high prevalence and is associated with substantial distress and burden around the world (World Health Organization [WHO], 2017 ); (2) rates surge six-fold from childhood through late adolescence with steady, persistent rates throughout adulthood (Hankin et al., 1998 , 2015 ); and (3) rates are increasing across generations, with current prevalence rates exceeding those seen just 10 years ago (Daly, 2022 ; Jorm et al., 2017 ). As such, public policy experts recommend annual screening of depression for individuals ages 12 and above (USPSTF, 2022 ). In an effort to better understand (and interrupt) the development of depression across childhood and adolescence, researchers have identified numerous risk and resilience factors that prospectively predict depression (Hankin & Cohen, 2020 ). Indicated or selective preventions can reduce the likelihood of future depression for youth Footnote 1 with elevated symptoms or risk factors (Cuijpers et al., 2021a , 2021b ). Moreover, there exist several evidence-based treatments, including psychotherapies and pharmacotherapies, each of which works generally equally well to relieve youth depression (Weersing et al., 2017 ). Table 1 enumerates what we know regarding risk factors for youth depression, and Table 2 summarizes knowledge of evidence-based interventions (treatments and preventions).
The field has accumulated an impressive corpus of knowledge. At the same time, however, it is an undeniable reality that many young people across the world continue to suffer from and with depression, and there is an urgent and critical need to address this suffering for as many people as possible. Consider global data, for example, which indicate that the age-standardized prevalence of depression increased by 4.2% from 1990 to 2013, whereas the prevalence of anxiety decreased by 0.5% over this same period (Global Burden of Disease Study, 2013 Collaborators, 2015 ). This depression rise has been accompanied by co-occurring increases in rates of treatment; yet, no country included in this global analysis showed diminished depression rates over this time period. Even with many empirically supported treatments, there has been little sustained progress in reducing depression’s burden, or decreasing depression-related distress and suffering since 1980s. What can be done to address clear gaps to reduce the considerable and highly consequential distress and burden associated with youth depression?
The purpose of this paper is to revisit and critically interrogate how and what we think we know about youth depression and its interventions. To this end, we review the sociohistorical context in which the phenomena termed “depression” were conceptualized and highlight the ways in which our academic notions and “best practice” assessment instruments both do and do not align with the symptoms and features of this depression construct. In a similar manner, we consider contemporary prevention and treatment strategies and provide rationale for expanding the range and scope of intervention efforts to more efficiently and effectively respond to youth depression and prioritize structural- and systems-level change.
Ultimately, we strive to provide A New Hope for advancing progress on youth depression. To this end we take some positions (admittedly ours) for what we believe are directions and priorities that hold promise for both improving the scholarly understanding of youth depression and reducing depression-related distress and burden worldwide. We believe meaningful progress can be made without unduly devoting more time, energy, and limited resources investigating primarily unproven biological and technological solutions (e.g., certain biomarkers, Joober, 2022 ; Kapur et al., 2012 ; Winter et al., 2022 ; or innovative pharmacotherapeutics, such as psilocybin or other psychedelics; McClure-Begley & Roth, 2022 ) in the hope that some kind of singular breakthrough will meet massive current needs and close the prevalence-intervention gap.
As Darth Vader famously said in the original Star Wars: A New Hope (episode IV), “Don’t be too proud of this technological terror you’ve constructed. The ability to destroy a planet, or even a whole system, is insignificant next to the power of the Force.” Our perspective and the main points we emphasize can be summarized by focusing on the power of the FORCE: Fundamentals are essential to ground clear thinking informed by humility, history, and philosophy; Openness is needed to explore new ideas with scientific rigor and transparency; Relationships matter for understanding and intervening in youth depression across all levels in social–ecological systems; Constructs are key in the conceptualization, measurement, and classification of depression; and Evidence must be collected and evaluated, grounded in construct validation with epistemic iteration, to ensure accurate, reliable, reproducible knowledge with scientific and practical utility.
In this paper, we have three main goals. First is to provide an overview of what the field knows about depression among youth, via Table 1 for depression risks across ecological levels and Table 2 for interventions. All of this knowledge is grounded in how depression as a construct is currently, and has historically, been conceptualized and measured. Our second goal is to reinvigorate serious academic progress focused on defining and explicating conceptually what depression is among youth as informed by developmental psychopathology. As we summarize in our historical review, necessary and important steps in the construct validation process (content conceptualization; measurement) were minimally engaged in the study of adult depression, and this incomplete conceptual understanding has carried forth in the study of depression among youth. Our final goal is to address immediate needs to reduce the prevalence and distress associated with youth depression. We propose ways for responding to unmet needs of youth at risk for and affected by depression, as well as their families and communities. We begin with an eye toward how we might improve the science of youth depression, with an emphasis on issues of methods, measures, and construct validity. We then propose directions to enhance interventions to alleviate the prevalence and distress of youth depression and suggest efforts that engage multiple ecological systems and stakeholders.
What Is Depression and What Do We Know About It?
For optimal conceptual clarity, we explain and unpack what we mean by specific terms, especially “depression,” among children and adolescents. We define the term “depression” as a construct, i.e., a complex concept intended to synthesize varied components into a cohesive “thing,” one which cannot be directly measured but is inferred from available data. This latent entity is capable of organizing features and processes that cannot be directly observed. We use the terminology of “constructs,” as is typical in psychological science (e.g., Borsboom et al., 2004 ; Cronbach & Meehl, 1955 ; Messick, 1987 ), and these constructs are defined and identified within their nomological networks (Cronbach & Meehl, 1955 ).
Tables 1 and 2 (and other exemplary expert reviews; e.g., Herrman et al., 2022 ; Thapar et al., 2022 ) synthesize the state of knowledge in depression among youth. This summary is based predominantly on modern DSM/ICD perspectives that have primarily conceived of depression as a categorical disorder with philosophical grounding in hard realism. Hard realism states that entities have real essences in nature that provide clear boundaries that separate and can categorize entities (Kendler et al., 2011 ). For example in the periodic table from chemistry, a paradigmatic example is gold as an element, in which gold’s 79 protons (its atomic number) constitute a real essence that separates this element from all other elements. Analogously for psychological disorders, such as depression, hard realism implies the existence of simple, unifying etiological causes (e.g., genetic or brain dysfunctions), and knowing depression’s essential causes enables clear categorization from other psychopathologies. Searching for biomarkers via novel, emerging technologies makes sense when depression is conceptualized through this lens of hard realism in which disorder is believed to be an essential kind. Yet, leading philosophical scholars cogently argue that psychopathological disorders, such as depression, are not essential kinds and do not possess any real essence. Instead, such philosophers assert that depression exhibits characteristics of either soft realism (e.g., as in the case of biological species) with fuzzy boundaries and conflicting conceptualizations, or as a practical kind, based on an instrumentalist approach to science that is pragmatic and avoids deep ontological claims (Kendler, 2022 ).
A Brief History of Depression Over Time: Classification and Its Discontents
What we know about youth depression is grounded in a set of assumptions (e.g., is depression of hard or soft realism, or a practical kind?) and a set of historical events occurring in a particular social–political context. These assumptions and history, both of which are rarely examined, have exerted outsized influence and largely set the mold in which the conceptual contours and measurement of today’s youth depression have been cast. Starting in the mid-late 1970s and persisting into the present, many key notions and assumptions about “what depression is” have largely been determined by particular clinical authorities, and their scholarly conceptions of depression have been concretized and operationalized in an interrelated set of systems and classifications, including the DSM and ICD. These official nosologies dominate how nearly all mental health scholars and applied workers across numerous disciplines think of depression, define it as a syndrome, picture and envision diagnosis, and use assessment instruments. These notions and assumptions then inform the measurements that comprise the data that formatively affect our body of knowledge regarding youth depression. As such, much of what we know about youth depression, including its prevalence and developmental trajectories, comorbidities, risks, and interventions are filtered through a particular contextual lens shaped by philosophical principles and specific historical events. Appreciation for this historical and philosophical undergirding can bring greater understanding of our present knowledge base, as summarized in Tables 1 and 2 .
In this section, we discuss how key historical events over the last century provided a particular context that affected who the field has regarded as primary clinical experts, and shaped how these authorities chose to conceptualize and operationalize depression via particular signs and symptoms. In contemporary research and practice, these authorities’ decisions have largely been uncoupled from the sociohistorical context in which they emerged, yet still these specialists and their beliefs continue to dominate our conceptual and applied understanding of depression (Kendler, 2017 ; Kendler et al., 2010 ). With the dominance of modern DSM in mind, consider the following observation noted by an eminent biological psychiatrist who values ongoing study of phenomenology in psychopathology:
DSM-III and its successors… became universally and uncritically accepted as the ultimate authority on psychopathology and diagnosis. DSM forms the basis for psychiatric teaching to both residents and undergraduates throughout most of the United States…. Because DSM is often used as a primary textbook or the major diagnostic resource in many clinical and research settings, students typically do not know about other potentially important or interesting signs and symptoms that are not included in the DSM…. Validity has been sacrificed to achieve reliability. DSM diagnoses have given researchers a common nomenclature—but probably the wrong one . (emphasis added; Andreasen, 2007 , p. 111).
Our perspective builds on others’ recent work in similar areas, including works emphasizing fundamental philosophical principles (e.g., Aftab et al., 2021 ; Kendler, 2022 ; Kendler and Zachar, 2019 ), historical overviews (e.g., Clark et al., 2017 ; Harrington, 2019 ), constructs (e.g., Bringmann et al., 2022 ; Hayden, 2022 ), and measurement (e.g., Fried et al., 2022 ; Haslbeck et al., 2021 ). We recommend to interested readers these excellent published pieces. Nearly all focus on adults. There exists far less literature pertaining to critical history and philosophy relevant for conceptualizing and measuring depression specifically among children and adolescents. This is a clear gap in the literature and field’s understanding, as such knowledge from adults should not be uncritically adopted in developmental downward extensions to children and adolescents. As we discuss later, these underexamined developmental downward applications of such fundamental concepts and principles can have unintended consequences when principles and practices are applied “top down” with less focus on complementary “bottom up” perspectives from phenomenological and developmental sciences.
The views and perspectives affecting depression’s definition and measurement result from a set of historical conditions that are deeply intertwined with changing political and institutional values and priorities. Funds for research and professional training in clinical psychology and psychiatry were first made possible by the passage of the American Mental Health Act in 1946, shortly after the end of World War II. Shortly thereafter, the National Institute of Mental Health (NIMH) was created with Robert Felix as its founding director, and they emphasized the social roots and consequences of mental health. At the point of its inception, the NIMH concentrated significantly more funds on research connecting mental illness with social determinants of health including poverty, social isolation, poor education, overcrowding, and violence compared with biological or medically focused risks and correlates. This history suggests that the contemporary, medicalized conceptualizations of depression were not a necessary, logical eventuality or even a product of naturalistic scientific progress.
Continuing this history and its impact on classification for psychopathologies, including depression, consider several well-intentioned changes implemented by the United States government and Food and Drug Administration (FDA) during the 1960s–1970s. Specifically, the Kefauver–Harris Amendment of 1962 required that medications needed to demonstrate empirical evidence for their safety and efficacy in terms of treating a specific disease in order to be sold. Then in the 1970s, the FDA mandated that efficacy testing of new drugs required controlled clinical trials. For the growing psychiatric pharmaceutical industry, these novel mandates introduced a new conundrum. If controlled clinical trials required diagnostically homogeneous patients, and no physiological tests existed to definitively establish the presence of psychopathology, how could researchers ensure that participants in a psychiatric clinical trial all share the same disorder? Herein laid the essential problem: No reliable psychiatric diagnostic classification system existed in the 1970s!
A predominant reason for poor reliability in psychiatric diagnosis was the dominance of psychodynamic paradigms in psychology and psychiatry during the 1960s and early 1970s. According to these psychodynamic theories, psychopathology reflects varied intrapsychic conflicts resulting from unconscious drives and impulses and disturbances in early psychosocial development. The leading psychodiagnostics manual in the 1960s–1970s—the Diagnostic and Statistical Manual, Second Edition ( DSM-II ; 1968 )—was an administrative manual grounded in abstract psychodynamic theory. There was little interest in the symptoms themselves and the ways in which they might be organized into coherent syndromes or disorders. Within psychodynamic practice and tradition, depression symptoms were conceptualized and explained as defense against anxiety (the core of all “psychoneurotic disorders”). In other words, psychodynamic conceptual models viewed depression as an expression to cope with underlying anxiety, rather than a phenomenon onto itself that required inquiry and understanding.
Yet, the novel FDA regulations of the 1970s required some simple, straightforward, and reliable way to assign individuals to homogenous groups of “depression” for the purpose of controlled efficacy studies. To continue to sell widely prescribed and used antidepressant medications to adults at that time (e.g., Elavil), pharmaceutical companies needed some means to create groups of homogeneous patients diagnosed with the same disorder (later to be named Major Depression Disorder; MDD, in DSM-III). This urgent press contributed to pressure for a psychiatric diagnostic classification that was first and foremost reliable . That is, clinicians needed to operationalize features of depression to reach adequate consensus on the presence and most observable properties of the phenomena, not its conceptual nature . Accordingly, the developers of the DSM-III endeavored to define mental disorders, including depression, “regardless of the cause,” so uniform diagnostic criteria were created with avowed agnosticism toward potential causal processes or underlying latent constructs that such criteria might be understood to represent. Footnote 2
Instrumental in the early development of an approach toward improving the reliability of classification of psychiatric disorders was a small group of clinical scholars (e.g., psychiatrists, psychologists) from the psychiatry department of the Washington University in St. Louis. This group of scholars, who were named “neo-Kraepelinians,” believed that the development of diagnostic criteria for the classification of mental illness was a valuable and legitimate enterprise. The neo-Kraepelinians thought that the abysmal inter-rater diagnostic agreement noted in voluminous studies from the 1970s could be solved via the creation of operationalized diagnostic criteria and the use of standardized symptom checklists. Feighner led the group in developing diagnostic criteria proposals and checklists (known as Feighner Criteria (Feighner et al., 1972 ), which influenced Research Diagnostic Criteria (RDC; Spitzer et al., 1975 ) and then ultimately the officially approved and recognized DSM-III (APA, 1980 ). In contrast to earlier versions of the DSM (I and II) which were guided by psychodynamic perspectives, the DSM-III aimed to inform the diagnosis of discrete disorders using observable symptom-based criterion, representing a radical shift in clinical approaches to diagnosis and classification. The practical operationalization system formally introduced by the DSM-III permitted researchers and clinicians to use a systematic approach to assemble potentially disparate symptoms into discrete diagnoses with improved reliability.
An important philosophical piece in this history of the early developments leading to DSM-III is that the neo-Kraepelinians intended the symptom criteria they proposed for each disorder (which were then instantiated into DSM-III) to represent a hypothetical diagnostic construct . The psychiatrists at Washington University did not intend nor believe that the symptom lists they proposed for each diagnosis were meant to sufficiently and literally constitute the disorder in an explicit one-to-one manner (Kendler, 2017 ). Rather, the influential neo-Kraepelinians believed that depression and other disorders are hypothetical constructs, so these psychiatrists also developed and proposed an initial set of validity criteria (known as “Robins & Guze criteria”; Robins & Guze, 1970 ). Their underlying assumptions for these validity criteria were grounded in a biological psychiatric medical model, not the psychodynamic theories still predominant in the 1970s, nor other possible conceptual frameworks (e.g., social determinants of health as originally supported by Robert Felix at the start of NIMH). Their views and decisions presumed that depression and other disorders are “essential kinds” in nature and were intended to mirror other medical disorders in other branches of medicine (Blashfield, 1984 ).
What relevance does this history have for the conceptual definition and measurement of the construct of depression today and going forward? This historical context provides the framing in which modern priorities, principles, and beliefs were first set, and understanding these prequels provides important background to explain how and why the dominant DSM/ICD became substantiated as the official classification system. Taken together with its implicit emphasis on essentialism and biological psychiatry, the modern DSM system and this biological framework have driven most basic and applied research since the early 1980s. This forms the bedrock foundation for most of the current knowledge on risks and interventions for depression among adults, adolescents, and children. The neo-Kraepelinians broke new ground by creating consistent symptom checklists intended first to increase reliability of psychopathological disorders conceived as discrete diagnoses. The shifting in the set of assumptions emphasizing biological predominance reflected the neo-Kraepelinians’ beliefs that psychiatry ought to investigate biological causes and treatments of discrete mental illnesses and should position itself as a modern, scientific branch of medicine. This small group of influential authorities at Washington University exerted a tremendous impact on DSM-III and subsequent nosological successors (e.g., currently DSM-5). For these reasons, it behooves us to understand how the neo-Kraepelinians’ assumptions and beliefs affected depression and other disorder definition, conceptualization, measurement, and then interpretation of data for eventual knowledge generation.
Also breaking from the predominant psychodynamic perspective, a few clinical scholars (e.g., Beck, Hamilton) in the mid-late 1960s developed standardized checklists to measure some depression symptoms with adults. These measures (Beck Depression Inventory; Hamilton Depression Rating Scale) reflect each author’s conceptualization of depression based on their observations of particular depression phenomena in different contexts and settings. Hamilton created the HDRS in 1960, for example, drawing on his knowledge and experience with already diagnosed severely depressed hospitalized inpatients, and he emphasized observable indicators such as psychomotor retardation (including slower speech) and weight loss relatively more so than self-reported symptoms. It is notable that the HDRS has remained the gold-standard depression clinical ascertainment for randomized control trials (RCTs) in adults over the last 60 years and is used in about 90% of antidepressant drug trials (Cipriani et al., 2018 ). The development of the HDRS can be contrasted with that of the Beck Depression Inventory (BDI), for instance, which was informed by Aaron Beck’s evolving cognitive theory of depression, and accordingly, placed relatively more emphasis on individuals’ self-reported affective and cognitive experiences.
These and other depression measures offer divergent conceptualizations of what the depression construct is. These differing conceptualizations were grounded in each clinical scholar’s own beliefs, phenomenological observations, and emphases, as well as the larger social and philosophical contexts in which these experts learned and worked. Given such widely divergent conceptual notions and histories, it therefore is not surprising to learn that empirical correlations among these and other depression scales are small to moderate (r’s ranging from 0.2 to 0.5). With this degree of small-to-moderate convergent validity, one cannot assume that different depression instruments equivalently assess the same construct of “depression.” With the discrepant conceptual and substantive content between different measures, the various depression assessments are not interchangeable. It is important to align practical, psychometric, and conceptual practices.
We need to be reminded that the ways in which we construe depression are a product of both the phenomenology and characteristics of depression as well as the limitations imposed by our theories and methods…. This has resulted in a situation where a great deal of what we think we know about depression in children and youth may not be about depression as such. (Hammen & Compas, 1994 , pp. 586–588)
When it comes to assessing depression among youth, the state of knowledge and measurement practice has lagged behind that of adult depression. Prior to Kovacs developing the Children’s Depression Inventory (as a downward extended youth-modification of the BDI) in 1977, for example, few scholars believed that children could be depressed. Indeed, the dominant beliefs and theories of the time held that (1) children are generally happy and show little persistent sadness, (2) youth lack mature social or emotional or cognitive structures deemed necessary for depression, and/or (3) kids manifest behavioral conduct problems (not primary depression-like symptoms as presenting problems or concerns) as a syndrome labeled “masked depression” (e.g., Cantwell, 1982; Strober & Werry, 1986 ). Even as youth depression slowly emerged as a topic of independent inquiry in the late 1970s, few developmental adaptations were considered. Indeed, when it came time to define the content, symptoms and criteria sets for childhood depression for DSM-III, historical writing suggests that key decisions were made based on predominantly entrenched beliefs around adult depression (Strober & Werry, 1986 ). It was largely assumed that youth depression comprised the same symptoms, expressed in the same way, as adult depression, and as a result, diagnostic criteria for depression among children and adolescents in DSM-III were asserted to be nearly the same as those for adults. Once the official psychiatric classification system authoritatively asserted this set of criteria defining depression in youth, the conceptual definition of youth depression as a construct as well as its measurement were established, and later reinforced and reified. Many youth depression assessments were created by translating adult conceptualizations and measurements downward to children and adolescents (e.g., Kendall et al., 1989 ; Klein et al., 2005 ; Weiss & Garber, 2003 ).
So much depends on how scientists conceptualize the problems they work on. Observations lead to interpretations. Interpretations become concepts. And concepts may become dogmas that feel so intuitive, so natural, that they are accepted without question. We should, from time to time, re-evaluate the core beliefs of our fields of study. (Rust & LeDoux, 2023 , p. 4)
We believe it is time to reconsider and revise (to the extent needed) how youth depression is conceptualized, rather than reflexively perpetuate the initial conceptual system of DSM-III that barely questioned and evaluated depression developmentally.
Construct Validity of Currently Oft-Used Depression Measures
As we elaborated in the previous section, the way in which depression is conceptually defined and measured today emerged as a function of a specific set of philosophical principles, scholars’ beliefs, and historical movements and events. In this section, we seek to describe how the field might move forward by re-energizing efforts toward construct validation. We argue that of the three phases of the construct validation process, the first two fundamental primary steps (i.e., defining the construct and operationally translating that conceptualization into reliable measurement, respectively) have historically been, and continue to be, overlooked. Reinvesting in these initial stages, especially of defining clearly the construct, can advance development and implementation of measures that adequately capture what depression is to the youth who experience it.
Implementing psychometrically sound measures starts with sufficient coverage of the key conceptual content. As there exist many ways to gauge construct validity, we focus here on internal structural aspects of depression assessments. Our review considers the degree to which the commonly used instruments may be covering and capturing important content, signs, symptoms, and features of the depression construct as phenomenologically observed and described by youth and other informants (e.g., caregivers, teachers, providers) with most direct access to children’s depression features.
Evidence to date suggests that DSM’s operationalization of the depression construct does not adequately capture and index many features of depression most salient to youth’s phenomenological experiences. For example, in large school-based community samples of Brazilian adolescents aged 14–16 years, researchers used network analyses of self-reported symptoms to evaluate the structure and centrality of depression symptoms to understand which symptoms tend to correlate with other another and are most densely connected with other symptoms (Manfro et al., 2021 ). Certain symptoms that are not captured in current DSM-based criteria, such as loneliness and self-hatred, were among the most interconnected, central, and frequently reported facets of depression, alongside DSM-based symptoms of sadness and worthlessness. These findings among a non-clinical sample of adolescents recruited from the general community align with research examining adult depressed patients, who endorse therapeutic priorities focused on improved self-esteem, as well as reduced loneliness and social isolation (Chevance et al, 2020 ). Manfro and colleagues’ network analysis also showed that hopelessness (not a core DSM MDD feature, but an accessory symptom in ICD-11) served as a highly central symptom of adolescent depression, consistent with adult work finding that hopelessness reliably differentiates depressed from non-depressed participants (McGlinchey et al., 2006 ). Surprisingly, anhedonia, one of the cardinal, criterial symptoms for MDD according to the DSM, was not highly interconnected with other depression symptoms.
This pattern of findings reinforces our proposition that the conceptualization of depression, as described by modern DSM (III through 5), insufficiently reflects the construct of depression as youth experience their symptoms. Moreover, the content of any given depression scale is often quite different from that of another. An analysis of eighteen youth depression instruments found that 52 separate symptoms were included, and these scales only comprised around 50% of the symptoms needed for MDD diagnosis according to DSM. Low content overlap was also observed across the measures, as only 29% of symptoms coincided across scales (Vilar et al., 2022 ). This heterogeneity of assessments extends to RCTs for adolescent depression treatment: 19 different outcome measures were used in 30 trials according to one recent review (Mew et al., 2020 ).
Understanding of the construct of depression as phenomenologically experienced by depressed individuals is underdeveloped. Recent qualitative research conducted among an international sample of depressed adults, as well as their providers and caregivers, indicates that features of mental/psychological pain (described often as “torture,” or “suffering”) were the most frequently endorsed and experienced, followed by anxiety and sadness (Chevance et al., 2020 ). It is notable, however, that none of the most commonly used depression assessments actually measure mental pain as a particularly important feature. Unfortunately, the commonly used depression measures do not cover some of this important phenomenological content that appears to comprise features of depression of primary concern to youth.
Applying the FORCE to Improve Understanding of Youth Depression
The conceptualization and measurement of depression has evolved over time, and contemporary notions of depression as a construct can be understood in the context of the theoretical, social, and political histories from which these notions emerged. Across all current measures of depression, there tends to be a central constellation of specific symptoms and features (e.g., hopelessness, sadness, apathy) that most likely captures core features of the depression construct and explains the moderate intercorrelations among measures. Also, the most used depression measures exhibit considerable heterogeneity in content coverage. Last, the most used measures do not capture important features of depression (e.g., mental pain) that figure prominently in individuals’ phenomenological experience. In our view, the construct of depression should not be defined merely, exclusively, and isomorphically in terms of the scales we use to measure it. Our proposed positions to improve the science of youth depression are organized in terms of the FORCE.
Fundamentals
Meaningful, replicable, and interpretable science, especially in applied areas like youth depression, requires reliable and valid measurement with clinical utility. Before investing further in advanced technologies and biological strategies to provide novel insights into the causes and correlates of youth depression—technologies and strategies that to date have yielded largely unreliable and inconsistent findings (e.g., Joober, 2022 ; Kapur et al., 2012 )—we encourage clinical researchers to consider the assumptions upon which measures and models are built and to re-engage with the fundamental (if often frustrating) challenge of articulating the parameters of the problems we are trying to understand. What are the core features of youth depression? What are the experiences youth describe? What does youth depression look like to parents and caregivers? How can these features inform our efforts to develop measures that facilitate enhanced understanding, as well as early detection and intervention? Meaningful progress can be made by producing and disseminating measures that are optimally valid, reliable, and culturally responsive for the needs of contemporary and future young people and those in their communities .
Revisiting these fundamentals will necessarily require openness. We must be open, for example, to embrace research paradigms that have not been mainstream approaches in clinical psychological science, such as qualitative methods aimed at enriching descriptive understanding of youth depression as observed and experienced by various stakeholders. We agree with Sir Michael Rutter who commented, “I think on the one hand you have to have quantitative analysis, but on the other hand qualitative research has a role to play as well, although I think it would be a mistake to say that simply counting quantities is an answer in itself. Understanding is definitely helped by qualitative studies” (Rutter & Werker, 2021 ). Indeed, as our history highlights, rich descriptive and exploratory work is fundamental to inform testable hypotheses and generate new knowledge that can advance the field.
We also encourage openness to novel conceptualizations of psychopathology that extend beyond current DSM-based nosologies. The Hierarchical Taxonomy of Psychopathology (HiTOP) Consortium (e.g., Kotov et al., 2021 ), for example, provides a promising framework that illustrates how the field can employ stages 1 and 2 of the construct validation process to better understand and organize surface-level signs and symptoms of youth depression, and reimagine the ways in which we conceptualize and structure psychopathology. HiTOP’s approach is focused on descriptive psychopathology and empirical analyses of surface-level phenomenological signs and symptoms. The HiTOP framework is consistent with many proposals in this position paper. HiTOP has begun to develop and test empirical measures using modern construct validation techniques, albeit largely with adults to date (e.g., Clark et al., 2023 ; Simms et al., 2022 ; Watson et al., 2022 ). Last, and importantly, HiTOP contains a committee and structure that formally, openly, and transparently considers and evaluates revisions to the organization and structural model based on ongoing research and evidence (Forbes et al., 2023 ; Kotov et al., 2022 ; Ringwald et al., 2021 ). HiTOP also includes a committee focused on developmental applications and considerations, and work in this developmental HiTOP committee is in progress (e.g., Nelson, et al., 2023 ).
Openness also extends to how we conduct our science. Values of transparency and principled, intentional decision-making are needed to guide construct validation efforts. Moreover, by engaging with science as an iterative, ultimately communal process by which knowledge is shared and collectivized, it is our hope that scholars motivated by open science practices might accelerate progress toward a more valid and reliable science of youth depression.
Relationships
Concretely illustrating such a communal process, the World Health Organizations’ (WHO) international process for depression instrument development provides an excellent example showing how interdisciplinary collaborations and conversations among different working groups can advance fundamental conceptual understanding of what constitutes the depression construct and how best to operationalize such information into measurement (e.g., Fulford & Sartorius, 2009 ; Sartorius et al., 1974 , 1980 ). In the 1970s, the WHO began work to create a standardized assessment that could be used around many countries to estimate adult depression prevalence worldwide. Doing so was an enormous, challenging task, especially because different countries had very different ways of defining and measuring adult depression, as there existed no uniform worldwide psychiatric classification system. As a result, the WHO realized that a necessary first step toward providing these essential epidemiological data was to develop an assessment tool that investigators around the world could agree on and then be used to reliably cover the main depression features across countries and cultures when implemented in the field worldwide. The WHO formalized regular international meetings with expert mental health workers from around the world who provided phenomenological summaries of depressed patients, and reviewed audio and video tapes of clients. These relatively inclusive, regular meetings enabled world-leading clinical scholars to generate the symptoms lists that were eventually included in the WHO’s depression checklist interview measure that was then used in the first international epidemiological study of depression. Also critical in the WHO’s process for creating their Schedule for Standardized Assessment of Depressive Disorders was their inclusion of a companion glossary that defined each symptom and provided clear criteria by which depression features could be rated reliably (Sartorius et al., 1983 ). This rich historical example of the construct validation process illustrates how conceptual content was developed for step 1 by cultivating relationships among experts around the world; it also demonstrates how these world experts invited many viewpoints and considered data to cull down items in step 2 of measure development. We propose that this process can be further enriched by the inclusion and formalization of relationships with non-psychiatric experts, such as youth, families, caregivers, and community partners and providers (broadly defined).
The cultivation and maintenance of collaborative intra- and inter-professional and personal relationships is vital to realizing the goals emphasized in this position paper. To improve content understanding of youth depression, for example, we must meaningfully and reciprocally engage with individuals who have experienced depression (either directly, in the case of youth, or indirectly, in the case of caregivers and providers), and reflect with humility in recognizing the bounds of our own expertise and construct-level understanding. A deeper conceptual understanding of youth depression can be enhanced through conversation and coordination with developmental scientists and others from interdisciplinary, allied fields.
We must also maintain critical and reflective relationships with ourselves and our histories (Rodriguez-Seijas et al., 2023 ). Psychological science and construct conceptualization do not emerge in an intellectual vacuum. They often reflect common sense folk accounts and ideas (Mandler & Kessen, 1959 ), which are then informed by specific theoretical paradigms, philosophical principles, and sociohistorical circumstances. Pausing for such reflection sets the stage to enable clinical scholars to interrogate assumptions undergirding work and examine the role our own preconceptions, paradigms, and positionality play in informing questions asked, methods employed, and interpretations made (Rodriguez-Seijas et al., 2023 ).
At the risk of belaboring the point, the production and dissemination of meaningful and impactful science depend on reliable and valid measures to assess conceptually based constructs. Understanding, detection, prevention, and intervention with respect to youth depression may be improved to the extent that the construct validation process is re-energized, and measurement efforts are reinvigorated. We believe that these goals are aligned with proposals and current efforts to use more ecologically valid digital phenotyping (e.g., sensors, smartphones, experience sampling methods) that enable youth and informants to monitor and rate their experience over time, contexts, and across units of analysis (e.g., Hitchcock et al., 2022 ). Deep phenotyping can provide enhanced information on sleep, various affects and emotions, reports of mental and physical pain, movement, exercise and activity, concentration and distraction, as well as social connection to ascertain what youth are doing (e.g., social media, games, substance use, etc.) and with whom (e.g., peers, family). Such efforts may have dual benefits for the future of the field. Deep phenotyping can both inform construct conceptualization, as well as facilitate the identification of ecologically valid, malleable targets and mechanisms to intervene on youth distress.
Progress in the conceptualization and measurement of youth depression must be based on strong evidence. Moreover, it is important that epistemic iteration drives knowledge generation so that the field’s evidence base dynamically evolves with the production of more developmentally and culturally informed measures. It will be important to engage diverse populations of youth, as well as their caregivers, teachers, and providers at each stage of the construct validation process. All involved should remain reflective and transparent about to whom and the extent to which evidence may generalize.
What Do We Know About Interventions for Youth Depression?
Efforts to improve the conceptualization and measurement of youth depression must occur alongside work to improve its detection, prevention, and treatment. Youth struggle with and from depression, and there continues to be need for better, more accessible interventions. Footnote 3 Thus, we shift attention to review what is known regarding evidence-based interventions for youth depression (see Table 2 ) before describing how the FORCE may be applied to propel the field forward.
In a meta-analysis summarizing treatment effects for youth interventions over the past 50 years, Weisz and colleagues (2017) reported an overall mean effect size (ES) = 0.46 compared to control condition for all youth mental health problems, indicating that treatments yield moderate improvements, on average, in youth mental health. Notably, however, treatments for youth depression, specifically, were found to be generally less effective in yielding symptom improvement (ES = 0.29) relative to interventions for anxiety (ES = 0.61) and other conditions. Moreover, after synthesizing the literature, Weisz and colleagues (2017) concluded that therapy effects have not improved over the past 50 years. Further, estimates indicate that fewer than 50% of depressed adolescents in the United States receive care for their symptoms (Avenevoli et al., 2015 ; Forman-Hoffman et al., 2016 ; Lu, 2019 ), and racial and ethnically minoritized youth encounter disproportionate barriers to mental health care relative to their non-Hispanic white peers (Alegría et al., 2008 ; Lu, 2019 ; Yeh et al., 2003 ). Globally, the WHO ( 2017 ) finds that mental health needs far exceed the availability of mental health workers around the world, with individuals in lower-resourced settings facing particular difficulty accessing adequate care.
Taken together, results of this work paint a sobering picture regarding the field’s present capacity to adequately respond to the challenges of youth depression: Treatments are (at least on average) only modestly effective in reducing symptoms and are only reaching a limited number of youth. Further complicating this picture, there are currently not enough well-trained mental health providers of evidence-based psychotherapy to meet the massive current or anticipated future needs. It is unlikely that the needs of distressed youth can be completely met even with an expanded base of well-trained mental health providers.
Psychopharmacological interventions are also commonly used to treat youth depression, and antidepressant medications have been approved by the FDA for the treatment of depression among adolescents ages 12 and older. The American Association of Child and Adolescent Psychiatry recommends the use of selective serotonin reuptake inhibitors (SSRIs), preferably fluoxetine, as a first-line treatment for depression (Walter et al., 2022 ). It is notable, however, that use of antidepressant medications can be associated with side effects and other risks. For example, the FDA issued a “black box” warning in 2004 cautioning that use of SSRIs among youth may increase the risk of suicidality.
Intervention efforts need not wait until youth experience the onset of a depressive disorder. Preventative interventions aim to reduce the likelihood that youth experience depression in the future and represent one means to proactively reduce youths’ prospective risk for depression-related suffering (Heckman, 2011 ; Lee et al., 2017 ; Mihalopoulos & Chatterton, 2015 ). Systematic and quantitative reviews reveal modest to small effects (pooled SMD = 0.16 [0.07–0.26]; Ormel et al., 2020 ) for psychological or educational interventions for preventing depression across multiple settings (e.g., schools, health care, community) and populations. Generally, effectiveness is higher for preventive interventions targeting youth at risk (selective) or with elevated subsyndromal depression (indicated). Estimates indicate that selective and indicated prevention reduce depression incidence by 20–25% (Ormel et al., 2020 ).
Universal prevention efforts exhibit much smaller effect sizes. Several school-based cognitive behavioral or interpersonal preventions show no meaningful effect on depression risk, on average (Caldwell et al., 2019 ; Cuijpers et al., 2021b ), indicating that some universal prevention efforts are ineffective for reducing risk among unselected youth. A recent large-scale universal prevention trial comparing mindfulness-based training to teaching as usual (TAU) with social–emotional learning among students ( n = 8376) distributed across numerous British schools (84 schools) showed no average prevention effects on primary depression and wellbeing outcomes, and iatrogenic effects were observed in some schools such that TAU did better than mindfulness (Kuyken et al., 2022 ).
This summary illustrates both good and bad news regarding the state of intervention knowledge for youth depression. Encouragingly, some treatments such as cognitive behavioral therapy (CBT) and interpersonal psychotherapy (IPT) demonstrate efficacy as assessed via RCTs, and these have been designated “well-established” treatments for youth depression (see Weersing et al., 2017 ). The bad news is that the field has not progressed in terms of improving effectiveness, dissemination, or implementation of existing preventative and/or treatment interventions to address increasing mental health needs, especially rising prevalence depression rates among youth. One way to shrink depression prevalence is for clinical researchers to reduce the “quality gap” (Jorm et al., 2017 ). This will require providing preventative interventions and treatments that meet minimal standards of clinical practice guidelines and reducing barriers to evidence-based care for youth with highest needs and risk.
Additional gaps and particular limitations in the treatment outcome and prevention literatures also merit attention. Most RCTs, for example, have included predominantly non-Hispanic white youth, and culturally responsive interventions for racial and ethnically minoritized are relatively underfunded and understudied (Pina et al., 2019 ; Polo et al., 2019 ; Walter et al., 2022 ). Further, salient moderators and mediators of treatment response are poorly understood, even among “gold-standard” treatments (Walter et al., 2022 ). Without this knowledge, clinicians are limited in their abilities to select and individualize treatments to most efficiently and effectively meet individual patients’ specific needs. Additionally, many new treatments have been developed and refined over several decades, yet treatment efficacy has not followed suit and has not substantially improved (Holmes et al., 2018 ). Further, with respect to preventative interventions, most prevention trials have relatively short-term follow-ups (less than 1 year), and generally longer-term trials exhibit effect sizes that diminish over time (Caldwell et al., 2019 ; Cuijpers et al., 2021a , 2021b ; Gee et al., 2020 ; Merry et al., 2004 ). So, it remains relatively unclear how long prevention effects last. Overall, despite the field’s best efforts, interventions do not sufficiently map onto the needs of youth experiencing depression. Work remains to further improve interventions to reduce youth depression.
Fortunately, several developments leave us hopeful that significant progress may be made in the coming years. It is increasingly recognized, for instance, that interventions for youth internalizing problems are needed. For example, the Wellcome Trust launched a new priority mental health strategy emphasizing adolescent and young adult (14–24 years) depression and anxiety. Moreover, the United States Office of the Surgeon General ( 2021 ) Advisory on Protecting Youth Mental Health proposes and describes a multipronged, ecologically informed series of recommendations to circumvent youth risk for psychopathology and promote youth wellbeing aimed at both health care specialists (e.g., primary care providers) as well as naturalistic settings and supports (e.g., schools, community organizations, digital media, etc.). As we describe below, this kind of ecological approach is needed in the field of youth depression, as systems- and structure-level change will be essential to augment present evidence-based interventions to address the current prevalence–intervention gap.
There and Back Again: Historical Shifts Between Individual and Relational-Community Mental Health Approaches
We briefly summarize relevant policy and mental health events over the century that illustrate how psychiatry, psychology, and allied disciplines repeatedly (re-)learn the lesson and importance of keeping care within local communities and focusing on relationships. This short history reveals why it can be useful and worthwhile to revisit our field’s history to see what has worked, what has not, and how we can learn from this history and apply these lessons going forward.
Broadly reflecting the back-and-forth shifts emphasizing individually focused care to more relationally based interventions, consider large-scale mental health intervention experiences from military psychiatry. Throughout World War I experts believed the best approach was to move “shell-shocked” soldiers to far-away special hospitals for treatment, yet the affected suffering soldiers did not do well, their recovery was delayed, and some got worse. In contrast during World War 2, military psychiatry adopted more relational help and found that “shell-shocked” soldiers could be rehabilitated and “turned around” more quickly when treated near their platoon or local army communities to which they would then return. These military experiences providing mental health treatment for affected soldiers over decades show that a more locally focused, relational, community-based approach works (Glass, 1971 ).
Robert Felix, NIMH’s first director, was a proponent of this approach. In the Foreword to Caplan’s, 1964 Principles of Preventive Psychiatry emphasizing “community mental health,” Felix wrote, “This book… is a bible. It should be read by every psychiatric resident and mental health worker in training. Footnote 4 ” In 1963, President Kennedy signed the Mental Retardation Facilities and Community Mental Health Centers Construction Act. The idea was that the federal government would release money via block grants to states, which were supposed to build new community mental health centers to replace crumbling, aging, ineffective state mental institutions. However, state governments did not follow through as Congress intended. States did not invest their own funds and instead used federal block grants as a chance to downsize and economize. As a result, there was never sufficient resources and means for mental health system reform as recommended via integration with community mental health.
When major recession and stagflation hit in the 1970s, many adults with severe mental illness had been released from state inpatient hospitals, and numerous released patients faced barriers with the continuation of their psychotropic medication and other supportive therapies. Subsequently, many of these former patients became homeless due to lack of support systems from the community; several were subsequently incarcerated. Indeed, carceral systems, rather than supportive psychotherapeutic care settings, served as a common destination for individuals whose mental health needs remained unmet. Prisons became (and continue to serve) as America’s largest mental hospital system, especially for minoritized individuals and people of color. Today, Illinois Cook County jail, LA County Jail, and NY Rikers Island are the three largest mental health care providers in the United States.
We believe the youth depression field can learn from public health approaches that target modifiable social risk factors and social determinants of health. For example, consider public health efforts aimed at reductions for smoking, cardiovascular disease, and cancer mortality. These public health preventions have included multipronged, intensive programs aimed at both individual and structural targets (e.g., individual, school, curriculum, community) with enduring success (Office of the Surgeon General, 2020 ). Our review of depression facts and findings (Table 1 ) suggests many modifiable risk factors that can be targeted, ranging from the individual level (e.g., cognitive vulnerabilities, poor coping) to environmental and contextual stressors (e.g., peer victimization, childhood maltreatment) to political and structural violence and inequality (e.g., exposure to racism, poverty, armed conflict). Moreover, there exist transactions among individual (e.g., negative emotionality, cognitive vulnerabilities) and contextual risks (e.g., family conflict), such that these risks can mutually reinforce one another over time. As such, interventions can be enhanced by attending to opportunities to intervene at multiple ecological levels by cultivating and leveraging contextual supports to bolster the potential of well-validated individual-level preventions and treatments to allow children, families, and communities to thrive.
“A Matter of Political Will”
Before describing the way in which the FORCE may provide a helpful framework for guiding future work to alleviate youth depression, we echo that reducing mental health problems, including youth depression, is “all a matter of political will” (Jorm, 2014 , p. 800). Mental health workers and clinical scholars across disciplines will need to coordinate, collaborate, and convince politicians and policy makers of the evident truth that investing in proven depression interventions reduces suffering and shrinks disease burden. All too-frequently, the already too-limited funds for mental health services are among the first to be cut during economic challenges of recession or budget problems. Personalized prevention efforts represent one path forward; however, depression interventions will also need to expand beyond only the individual-level focus to effectively target social determinants of health and engage larger-scale, structural system levels. We suggest that additional improvement toward reducing depression can be made by both improving individual interventions and making structural changes.
Applying the FORCE to Improve the Prevention and Treatment of Youth Depression
In order for youth to benefit from depression prevention and treatment efforts, they must first and foremost have access to evidence-based care. Common barriers to care include structural factors (e.g., lack of financial resources or transportation, geographic restrictions, long waitlists, and limited providers), as well as social (e.g., mental health stigmatization) and intrapersonal factors (e.g., lack of confidence in treatment, low perceived need) (Andrade et al., 2014 ; Mojtabai et al., 2011 ). Structural racism and other forms of identity-based oppression as well as lack of provider cultural competence impose additional barriers for individuals with minoritized identities, including LGBTQIA + and transgender individuals, and folks of minoritized racial and ethnic identities (Castro-Ramirez et al., 2021 ; Romanelli & Hudson, 2017 ; Shipherd et al., 2010 ). Thus, addressing barriers to care is fundamental to improving outcomes for children and adolescents.
We are encouraged by several developments that seek to address barriers to care across ecological levels. At the policy level, the Mental Health Parity and Addiction Equity Act of 2008, which was expanded under the Affordable Care Act of 2010, mandated that most health insurance providers guarantee reasonable coverage for mental health care services (Block et al., 2020 ). Project AWARE (Advancing Wellness and Resilience in Education) is a federally funded program that supports the development of school-based prevention, screening, and early intervention services, incentivizing stakeholders to integrate evidence-based services in youths’ naturalistic settings. Moreover, state-level initiatives have been implemented to provide youth with accessible, free services, such as the “I Matter” program in Colorado which provides up to 6 sessions of free psychotherapy for youth 18 and under. Mental Health First Aid, a standardized educational program aimed at increasing mental health literacy and reducing mental health stigma, has been successfully implemented in more than 20 countries worldwide. Meta-analysis shows effectiveness for producing changes in mental health knowledge (ES = 0.56), attitudes (ES = 0.28), and behaviors (ES = 0.25) (Hadlaczky et al., 2014 ).
The growing ubiquity of digital technology also presents exciting opportunities to address barriers to care and increase access to evidence-based treatment. Telehealth technology, such as the use of videoconferencing software to deliver psychotherapy services, may allow providers to reach youth in rural or otherwise hard to reach locations and those youth who face transportation or other physical barriers to care (Myers & Comer, 2016; Nelson et al., 2003 , 2006 ). Text-messaging based interventions have also shown promise to promote treatment engagement and proactively address barriers to care among youth (Ridings et al., 2019 ; Suffoletto et al., 2021 ). Single-session inventions (SSIs) can be delivered asynchronously and in an anonymized manner. They represent another way to provide immediate service access for at-risk youth; SSIs are feasible and effective for reducing depression symptoms among diverse samples of adolescents (Schleider & Weisz, 2017 ). SSI proponents and researchers take care to note that these interventions are meant to motivate and supplement, not replace, comprehensive evidence-based therapies (Dobias et al., 2022 ; Schleider et al., 2022 ).
Addressing the unmet mental health needs of contemporary and future youth will require creativity, flexible thinking, and openness to new approaches and modalities. Doing more and better to address the needs for youth depression will also require openness (and additional training to enhance psychological scientists’ skills) to collaborate and consult with various stakeholders, community members, educational staff, allied health care professionals, and policy makers.
Ecological frameworks for dissemination and implementation emphasize that successful collaboration involves building on existing community strengths, knowledge, and resources to design and refine prevention and treatment strategies that are effective, sustainable, and culturally responsive (Atkins et al., 2015 , 2017 ; Mehta et al., 2019 ). Schools (e.g., Hoover & Bostic, 2021 ) and community mental health centers (e.g., Starin et al., 2014 ) are two clear examples of naturalistic settings in which psychologists can consult and collaborate with multidisciplinary teams to implement evidence-informed interventions for youth. Further, research indicates that digitally facilitated interventions are also enhanced when they feature human support (e.g., coaching) relative to a computer alone (Bennett et al., 2019 ; Ebert et al., 2016 ; Whittaker et al., 2017 ).
Relationships with natural helpers (i.e., non-professionals to whom community members appeal for both social and instrumental support; Israel, 1985 ) may also enhance efforts to respond to the challenge of youth depression, particularly among historically underserved and/or minoritized community members. Trained natural helpers (or “paraprofessionals”) can increase access via increased help-seeking and reduce barriers to care by offering community-based services from community insiders. Such trained natural helpers may be best equipped to respond to the particular cultural values and needs of the children and families they serve. This can be particularly important and valuable in low-resourced and/or historically minoritized settings, in which access to culturally responsive care may be limited and negative experiences within the health care system may be more likely (Jain, 2010 ). Psychologists can partner with community agencies and natural helpers to increase effectiveness of care for historically underserved children and families. These partnerships can improve child outcomes (Garcia et al., 2022 ). For example, psychologists actively collaborated with community agencies to gain insight into community values, norms, and concerns, and used trained natural helpers to provide in-home support to families of young children (age 2–8) enrolled in a course of clinic-based parent–child interaction therapy.
As innovative ways expand the scope and reach of clinical interventions, it will be important to integrate knowledge from ongoing construct validation work. With enhanced and updated understanding of the construct of depression, prevention and treatment strategies need to follow suit. For example, should conceptual and psychometric work show that mental pain is an important feature to include in measures of depression, then new and potentially promising avenues of intervention (e.g., treatments targeting pain alleviation and management for youth across settings and contexts) can be developed and examined. Of course, any enhanced conceptual clarity that may inform expansion or refinement depression interventions will require proper and rigorous evaluation with evidence.
Across ecological levels, prevention and treatment efforts should be informed by empirical evidence and not merely assumed to work. Additionally, applying extant research needs to consider the generalizability of findings and available evidence to samples and the larger population beyond the specific samples (see Simons et al., 2017 for excellent discussion on these “constraints on generalizability”). Interventions involve substantial resources (e.g., time, personnel, money), so knowing from evidence that particular interventions are not superior to control conditions (e.g., school-based cognitive behavioral universal preventions) is important for prioritizing valuable resources and directing policy recommendations toward efforts that do work. More concerningly, even well-intended and conceptualized efforts may be associated with iatrogenic effects. In their large study evaluating universal mindfulness interventions versus TAU in schools, for example, Kuyken et al. ( 2022 ) found iatrogenic effects due to mindfulness training in some schools. These surprising results reinforce the importance of evidence gathering and careful evaluation. In sum, evidence-based care remains essential to promoting wellbeing among youth and their families and prioritizing intervention efforts to those with the highest potential for success.
Next, we illustrate two examples of how principles of the FORCE can be used to advance efforts to reduce youth depression across ecological and structural levels.
Case Example 1: Alleviating Poverty to Alleviate Depression
Poverty, income, and food insecurity represent one key grouping of social determinants of health (cf., Lund et al., 2018 ) with clear implications for youth depression. Highlighting the promise of targeting the economic domain, a compelling recent review states that “we now know that loss of income causes mental illness” (Ridley et al., 2020 , p. 1). Ridley and colleagues’ summary also provides evidence supporting bidirectional causal relationships between poverty and mental illness, including depression.
Quasi-experimental evidence demonstrates the impressive benefits of providing families enhanced economic resources. As part of Covid-19 pandemic relief in July 2021, the US Government expanded temporarily a Child Tax Credit (CTC) so that additional economic funds (up to $3600 maximum per child from the previous CTC of $2000) were provided nearly universally (with few administrative burdens) to families via direct automatic monthly payments to family bank accounts. This expanded CTC was made available to a much wider pool of families relative to previous efforts. The July 2021 expansion made these direct economic benefits available to low-income and unemployed caregivers, who were previously ineligible for this economic support.
The net result of the expanded CTC was that child poverty was cut nearly in half, and food insecurity and insufficiency were reduced (Batra et al., 2023 ). These dramatic results were observed in only two years of increasing financial support to children and families. Comparable findings from another federal program to reduce poverty for low-income families, based on work with Earned Income Tax Credit (EITC), similarly showed outcomes including improved housing, higher family income, and better access to health care. These anti-poverty effects improved mental health especially for Black families (Batra & Hamad, 2021 ).
Results from a large serial cross-sectional study employing a quasi-experimental design showed that the July 2021 expanded CTC was linked with lower depression and anxiety symptoms among lower-income adults with children (Batra et al., 2023 ). More specifically, analyses compared internalizing symptom levels as measured from a baseline (prior to the initiation of the expanded CTC) to after infusion of these additional economic resources. Results showed that low-income caregivers with children reported approximately 13% reduction in clinically significant anxiety symptoms and 6% drop in clinically significant depression.
Additional findings from this expanded CTC study highlight policy implications. With increased financial resources from the expanded CTC, no change was found for average mental health care visits or psychiatric prescriptions. These results suggest that anxiety and depression symptoms can improve without families requiring use of additional mental health services. In other words, changing the circumstances of living can exert meaningful effects for individuals’ psychological symptoms even in the absence of direct psychotherapeutic intervention. Poverty is associated with greater exposure to trauma and violence, increased environmental stressors, worse physical health, and exposure to interpersonal discrimination and structural inequality. Improving safety, economic stability, and physical wellbeing within the family may be reasonably assumed to have downstream effects of lowering depression and co-occurring psychopathologies within families.
In summary, given strong evidence that broader systemic factors and social determinants are linked and appear to causally affect depression and other forms of youth psychopathology, multiple approaches are needed to reduce distress and relieve depression’s burden in addition to improving access to psychological interventions. Social determinants of mental health (e.g., poverty, health care access, food insecurity) are fundamental aspects of youths’ experience that can be addressed by building relationships with community advocates and policymakers to enact higher level economic policy. The recent CTC expansion provides important evidence demonstrating the salutary effects of direct economic interventions for family mental health.
Case Example 2: Personalizing Depression Preventions
Evidence-based reviews demonstrate that indicated and selective preventions are effective for decreasing incidence and risk for anxiety and depression among youth (Breedvelt et al., 2018 ; Caldwell et al., 2019 ; Moreno-Peral et al., 2017 ). While findings are mixed with strength of effectiveness for universal prevention depending on settings, contexts, delivery, and intervention modality, universal interventions can be combined and blended with targeted approaches for anxiety and depression. Parenting programs represent an excellent example of this approach and are among the most efficacious and cost-effective interventions to reduce the prevalence of youth mental health (Prinz & Shapiro, 2018 ). Parenting programs are acceptable to many caregivers, effective across diverse contexts, and can be applied with population-based approaches to achieve high dissemination. Economic analysis shows that parenting programs provide successful impact for family and offspring mental health that result in more savings economically from social service spending relative to the cost of implementing these universal, population-based programs (Washington State Institute for Public Policy, 2019 ).
Systems-contextual approaches, such as the parenting program Triple P, use a tiered approach to flexibly provide contextually sensitive, ecologically engaged, and developmentally appropriate parenting support in a manner that is feasible, scalable, and effective (Sanders & Mazzucchelli, 2022 ). One key explanation for the effectiveness of this program involves the flexible selection of appropriate evidence-based programs emerging from the central, unified theoretical framework to respond to the specific needs and priorities of particular target populations within a broader population-based service model (Sanders & Mazzucchelli, 2022 ). While universal, population-based programs such as Triple P achieve this component via flexible delivery and implementation of teaching particular parenting skills based on varying parenting needs and primary concerns, other options can include personalizing prevention in a manner that matches intervention selection to youth’s particular risks and needs.
Rather than providing a one-size-fits all approach via prevention delivery to all youth regardless of risks or strengths, more precise personalization can occur when evidence-based risk profiles identify individuals or subgroups for whom particular interventions may prove more efficacious. As our risk factor review in Table 1 illustrates, numerous risks could be examined and tested to inform such a risk profile with translation to impact prevention. Here, we provide one example (Hankin, 2020 ). A cognitive and interpersonal risk profile was developed based on foundational research over years of solid, replicable vulnerability research. This algorithm was then tested and evaluated in independent samples and shown to predict future occurrence of MDD (Hankin et al., 2018 ). This risk profile was used in a randomized trial, the Personalized Depression Project (PDP; Young et al., 2021 ), to evaluate the degree to which risk-informed personalized prevention can improve future depression reduction. Youth categorized as exhibiting high or low cognitive and interpersonal risks were randomized to receive an intervention that either matched their risk and best met their needs (e.g., high cognitive risk and low interpersonal risk received a cognitive behavioral program; high interpersonal risk and low cognitive risk received an interpersonal-based program) or mismatched (e.g., high cognitive risk and low interpersonal risk received the interpersonal-based program). Results showed that matched adolescents reported significantly fewer depression symptoms relative to mismatched youth over the 21-month study period, although no significant difference was observed for MDD onset (12% for matched vs 18.3% for mismatched). Additional outcome data for anxiety symptoms revealed that matched youth reported significant decrease in anxiety symptoms compared to mismatched adolescents from postintervention through 18-month follow-up (Jones et al., 2022 ). Last, matched youth experienced significantly fewer dependent stressors compared to non-matched adolescents over follow-up (Jones et al., 2023 ).
In summary, findings from PDP illustrate that openness to new modes of prevention that implement evidence-based approach to personalizing prevention efforts as informed by knowledge of the construct of depression to create health and risk profiles can work to enhance outcomes among youth. Future research is still needed to replicate these PDP findings and extend investigation to evaluate the extent to which the specific cognitive–interpersonal risk classification profile and its categorical cutoffs generalize to other adolescents in other settings and contexts for maximal clinical utility.
Clinical psychological scientific study of youth depression began in earnest in the late 1970s and has seen rapid expansion of inquiry and knowledge accumulation from the mid-1990s to the present. The field has produced impressive facts and findings regarding depression’s prevalence, course, patterning, risk and resilience factors, and interventions. As with all forms of scientific investigation, the validity and utility of this corpus of information on youth depression rests on foundational principles and frameworks that affect, and are affected by, how the construct of depression has been conceptually defined and assessed.
We provided a review of particular sociohistorical events and philosophical principles that help to contextualize how scholars and applied mental health workers have conceptualized and measured youth depression over theses decades. Given particular implicit assumptions affecting how key features of depression have been defined, which signs and symptoms have been predominantly included (as well as excluded), we advocated for a renewal in the refinement, revision, and reconceptualization of the depression construct among children and adolescents especially incorporating a developmentally informed perspective. We discussed modern principles of the construct validation process, including the first two steps of content definition and then measurement development. We encouraged depression experts and important stakeholders to engage in the back-and-forth iterative process involving these two construct validation steps to create living, ongoing measures of the youth depression construct that would be freely available for use and ongoing refinement. Research can then evaluate proposed newer measure(s) via the third step of construct validation in which associations between revitalized measurement instrument(s) and other external constructs (e.g., risk factors, intervention) are evaluated. Because these construct validation steps were not used in the development and testing of most currently and commonly used youth depression measures, our proposal to revisit and reconceptualize the depression construct in a developmentally sensitive manner holds promise for the field of youth depression to improve all aspects of basic scientific and applied knowledge.
At the same time, the considerable number of children and adolescents around the world experiencing elevated depression demands enhanced efforts to reduce the tremendously high distress and burden among youth. The current literature shows that the present suite of evidence-based depression interventions for children and adolescents demonstrate some efficacy and effectiveness in treating and preventing depression. However, these largely individually focused pharmacological and psychological interventions are not enough to meet the massive needs to seriously decrease the gulf between depression’s high prevalence and available implementations provided via trained mental health experts. We proposed more serious attention and focus to broaden interventions beyond the predominant individual level and expand efforts structurally across socio-ecological systems and levels. Such expanded approaches could include more universal efforts with supportive evidence, such as promoting positive parenting (e.g., Triple P), enhancing available resources (e.g., educational, health care), and financial supports to lift children and families out of poverty via government and legislative initiatives. Additionally, expanded universal preventions can be combined with more targeted, selective approaches that personalize depression interventions using risk-informed profiles to guide matching to evidence-based programs.
In closing, the field of youth depression has come a long way, amassed many impressive findings, and found ways to reduce depression symptoms and disorder. At the same time, rates of depression, distress, and burden continue to rise for children and adolescents, and this prevalence–intervention gap is widening. We believe there is a New Hope for the future of youth depression research that can rise to meet these challenges and offer avenues to reduce distress and burden around the world. With a clearer understanding of fundamentals (clear thinking informed by history and philosophy), openness to explore new ideas transparently using the scientific method, relationships with youth, families, and stakeholders most intimately acquainted with depression, constructs to guide conceptualization and measurement of youth depression’s signs and symptoms, and evidence collection and evaluation to ensure accurate and believable knowledge (the FORCE), we look forward to future advances that instill realistic hope and are poised to advance progress on youth depression.
Data Availability
There are no data collected or analyzed for this review, so there are no data to share.
In the context of the present paper, “youth” is used to refer to school-aged children and adolescents, specifically, as much of the evidence and empirical emphasis of the literature to date has focused on these periods of development. We wish to note, however, that the ideas and suggestions promulgated in this paper may provide meaningful directions for efforts to improve research and intervention efforts targeting earlier periods of development (e.g., infancy, preschool age). That is, fundamentals, openness, relationships, constructs, and evidence are essential to improving our understanding of and capacity to respond to the needs of vulnerable young people across the lifespan.
We will proceed to discuss several key events and players involved in the development of the model DSM as it relates to youth depression; however, for more information regarding the history of the DSM, we direct interested readers to several excellent reviews in this area (Blashfield, 1984 ; Blashfield et al., 2014 ; Clark, Cuthbert et al., 2017 ; Frances & Widiger, 2012 ; Horwitz; Kendler, 2016 , 2017 ; Wilson, 1993 ).
We use “intervention” to refer to both prevention and treatment efforts.
Contrast Dr. Felix, as the first NIMH director’s “bible” reference, to the most recent outgoing NIMH Director, Dr. Insel, saying DSM is not the “bible” of psychiatric classification.
Abela, J. R. Z., & Hankin, B. L. (2008). Cognitive vulnerability to depression in children and adolescents: A developmental psychopathology perspective. In J. R. Z. Abela & B. L. Hankin (Eds.), Handbook of depression in children and adolescents (pp. 35–78). The Guilford Press.
Google Scholar
Aftab, A., & Waterman, G. S. (2021). Conceptual competence in psychiatry: Recommendations for education and training. Academic Psychiatry, 45 (2), 203–209.
Article PubMed Google Scholar
Aldao, A., Nolen-Hoeksema, S., & Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30 (2), 217–237. https://doi.org/10.1016/j.cpr.2009.11.004
Alegría, M., Chatterji, P., Wells, K., Cao, Z., Chen, C.-N., Takeuchi, D., Jackson, J., & Meng, X.-L. (2008). Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services, 59 (11), 1264–1272. https://doi.org/10.1176/appi.ps.59.11.1264
American Psychiatric Association. (1968). Diagnostic and statistical manual of mental disorders , 2nd edn. (DSM-II).
American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders , 3rd edn (DSM-III).
Andrade, L. H., Alonso, J., Mneimneh, Z., Wells, J. E., Al-Hamzawi, A., Borges, G., Bromet, E., Bruffaerts, R., de Girolamo, G., de Graaf, R., Florescu, S., Gureje, O., Hinkov, H. R., Hu, C., Huang, Y., Hwang, I., Jin, R., Karam, E. G., Kovess-Masfety, V., et al. (2014). Barriers to mental health treatment: results from the WHO World Mental Health surveys. Psychological Medicine, 44 (6), 1303–1317. https://doi.org/10.1017/S0033291713001943
Andreasen, N. C. (2007). DSM and the death of phenomenology in America: An example of unintended consequences. Schizophrenia Bulletin, 33 (1), 108–112. https://doi.org/10.1093/schbul/sbl054
Atkins, M. S., Cappella, E., Shernoff, E. S., Mehta, T. G., & Gustafson, E. L. (2017). Schooling and children’s mental health: Realigning resources to reduce disparities and advance public health. Annual Review of Clinical Psychology, 13 , 123–147. https://doi.org/10.1146/annurev-clinpsy-032816-045234
Atkins, M. S., Shernoff, E. S., Frazier, S. L., Schoenwald, S. K., Cappella, E., Marinez-Lora, A., Mehta, T. G., Lakind, D., Cua, G., Bhaumik, R., & Bhaumik, D. (2015). Redesigning community mental health services for urban children: Supporting schooling to promote mental health. Journal of Consulting and Clinical Psychology, 83 (5), 839–852. https://doi.org/10.1037/a0039661
Article PubMed PubMed Central Google Scholar
Avenevoli, S., Swendsen, J., He, J.-P., Burstein, M., & Merikangas, K. R. (2015). Major depression in the national comorbidity survey–adolescent supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child & Adolescent Psychiatry, 54 (1), 37–44. https://doi.org/10.1016/j.jaac.2014.10.010
Article Google Scholar
Axelsdóttir, B., Eidet, L. M., Thoner, R., Biedilæ, S., Borren, I., Elvsåshagen, M., Ludvigsen, K. H., & Dahlgren, A. (2022). Research in child and adolescent anxiety and depression: Treatment uncertainties prioritised by youth and professionals. F1000Research, 10 , 1221. https://doi.org/10.12688/f1000research.74205.1
Article PubMed Central Google Scholar
Batra, A., & Hamad, R. (2021). Short-term effects of the earned income tax credit on children’s physical and mental health. Annals of Epidemiology, 58 , 15–21. https://doi.org/10.1016/j.annepidem.2021.02.008
Batra, A., Jackson, K., & Hamad, R. (2023). Effects of the 2021 expanded child tax credit on adults’ mental health: A quasi-experimental study. Health Affairs, 42 (1), 74–82. https://doi.org/10.1377/hlthaff.2022.00733
Beck, A. T. (1962). Reliability of psychiatric diagnoses: 1—A critique of systematic studies. American Journal of Psychiatry, 119 (3), 210–216.
Bendavid, E., Boerma, T., Akseer, N., Langer, A., Malembaka, E. B., Okiro, E. A., Wise, P. H., Heft-Neal, S., Black, R. E., Bhutta, Z. A., BRANCH Consortium Steering Committee. (2021). The effects of armed conflict on the health of women and children. The Lancet, 397 (10273), 522–532. https://doi.org/10.1016/S0140-6736(21)00131-8
Bennett, S. D., Cuijpers, P., Ebert, D. D., Smith, M. M., Coughtrey, A. E., Heyman, I., Manzotti, G., & Shafran, R. (2019). Practitioner review: Unguided and guided self-help interventions for common mental health disorders in children and adolescents: A systematic review and meta-analysis. Journal of Clinical Psychology & Psychiatry, 60 (8), 828–847.
Blashfield, R. K. (1984). The classification of psychopathology: Neo-Kraepelinian and quantitative approaches . Springer. https://doi.org/10.1007/978-1-4613-2665-6
Book Google Scholar
Blashfield, R. K., Keeley, J. W., Flanagan, E. H., & Miles, S. R. (2014). The cycle of classification: DSM-I through DSM-5. Annual Review of Clinical Psychology, 10 , 25–51. https://doi.org/10.1146/annurev-clinpsy-032813-153639
Block, E. P., Xu, H., Azocar, F., & Ettner, S. L. (2020). The mental health parity and addiction equity act evaluation study: Child and adolescent behavioral health service expenditures and utilization. Health Economics, 29 (12), 1533–1548. https://doi.org/10.1002/hec.4153
Borsboom, D., Mellenbergh, G. J., & van Heerden, J. (2004). The concept of validity. Psychological Review, 111 (4), 1061–1071. https://doi.org/10.1037/0033-295X.111.4.1061
Breedvelt, J. J. F., Kandola, A., Kousoulis, A. A., Brouwer, M. E., Karyotaki, E., Bockting, C. L. H., & Cuijpers, P. (2018). What are the effects of preventative interventions on major depressive disorder (MDD) in young adults? A systematic review and meta-analysis of randomized controlled trials. Journal of Affective Disorders, 239 , 18–29. https://doi.org/10.1016/j.jad.2018.05.010
Bringmann, L. F., Elmer, T., & Eronen, M. I. (2022). Back to basics: The importance of conceptual clarification in psychological science. Current Directions in Psychological Science, 31 , 340–346.
Cairns, K. E., Yap, M. B. H., Pilkington, P. D., & Jorm, A. F. (2014). Risk and protective factors for depression that adolescents can modify: A systematic review and meta-analysis of longitudinal studies. Journal of Affective Disorders, 169 , 61–75. https://doi.org/10.1016/j.jad.2014.08.006
Caldwell, D. M., Davies, S. R., Hetrick, S. E., Palmer, J. C., Caro, P., López-López, J. A., Gunnell, D., Kidger, J., Thomas, J., French, C., Stockings, E., Campbell, R., & Welton, N. J. (2019). School-based interventions to prevent anxiety and depression in children and young people: A systematic review and network meta-analysis. The Lancet Psychiatry, 6 (12), 1011–1020. https://doi.org/10.1016/S2215-0366(19)30403-1
Caplan, G. (1964). Principles of preventive psychiatry . Basic Books.
Castro-Ramirez, F., Al-Suwaidi, M., Garcia, P., Rankin, O., Ricard, J. R., & Nock, M. K. (2021). Racism and poverty are barriers to the treatment of youth mental health concerns. Journal of Clinical Child and Adolescent Psychology, 50 (4), 534–546. https://doi.org/10.1080/15374416.2021.1941058
Chevance, A., Ravaud, P., Tomlinson, A., Le Berre, C., Teufer, B., Touboul, S., Fried, E. I., Gartlehner, G., Cipriani, A., & Tran, V. T. (2020). Identifying outcomes for depression that matter to patients, informal caregivers, and health-care professionals: Qualitative content analysis of a large international online survey. The Lancet Psychiatry, 7 (8), 692–702. https://doi.org/10.1016/S2215-0366(20)30191-7
Christina, S., Magson, N. R., Kakar, V., & Rapee, R. M. (2021). The bidirectional relationships between peer victimization and internalizing problems in school-aged children: An updated systematic review and meta-analysis. Clinical Psychology Review, 85 , Article 101979. https://doi.org/10.1016/j.cpr.2021.101979
Cicchetti, D., & Rogosch, F. A. (2002). A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology, 70 (1), 6–20. https://doi.org/10.1037/0022-006X.70.1.6
Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., Leucht, S., Ruhe, H. G., Turner, E. H., Higgins, J. P. T., Egger, M., Takeshima, N., Hayasaka, Y., Imai, H., Shinohara, K., Tajika, A., Ioannidis, J. P. A., & Geddes, J. R. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. The Lancet, 391 (10128), 1357–1366. https://doi.org/10.1016/S0140-6736(17)32802-7
Clark, H. M., Hankin, B.L., Narayan, A. J., & Davis, E. P. (in press). Risk and resilience factors for psychopathology during pregnancy: An application of the Hierarchical Taxonomy of Psychopathology (HiTOP). Development and Psychopathology.
Clark, L. A., Cuthbert, B., Lewis-Fernández, R., et al. (2017). Three approaches to understanding and classifying mental disorder: ICD-11, DSM-5, and the National Institute of Mental Health’s Research Domain Criteria (RDoC). The Journal of Abnormal and Social Psychology, 18 , 72–145.
Colasanto, M., Madigan, S., & Korczak, D. J. (2020). Depression and inflammation among children and adolescents: A meta-analysis. Journal of Affective Disorders, 277 , 940–948. https://doi.org/10.1016/j.jad.2020.09.025
Comer, J. S., & Myers, K. (2016). Future directions in the use of telemental health to improve the accessibility and quality of children’s mental health services. Journal of Child and Adolescent Psychopharmacology, 26 (3), 296–300. https://doi.org/10.1089/cap.2015.0079
Compas, B. E., Connor-Smith, J., & Jaser, S. S. (2004). Temperament, stress reactivity, and coping: Implications for depression in childhood and adolescence. Journal of Clinical Child and Adolescent Psychology, 33 (1), 21–31. https://doi.org/10.1207/S15374424JCCP3301_3
Cronbach, L. J., & Meehl, P. E. (1955). Construct validity in psychological tests. Psychological Bulletin, 52 (4), 281–302. https://doi.org/10.1037/h0040957
Cuijpers, P., Pineda, B. S., Ng, M. Y., Weisz, J. R., Muñoz, R. F., Gentili, C., Quero, S., & Karyotaki, E. (2021a). A meta-analytic review: Psychological treatment of subthreshold depression in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 60 (9), 1072–1084. https://doi.org/10.1016/j.jaac.2020.11.024
Cuijpers, P., Pineda, B. S., Quero, S., Karyotaki, E., Struijs, S. Y., Figueroa, C. A., Llamas, J. A., Furukawa, T. A., & Muñoz, R. F. (2021b). Psychological interventions to prevent the onset of depressive disorders: A meta-analysis of randomized controlled trials. Clinical Psychology Review, 83 , 101955. https://doi.org/10.1016/j.cpr.2020.101955
Daly, M. (2022). Prevalence of depression among adolescents in the U.S. from 2009 to 2019: Analysis of trends by sex, race/ethnicity, and income. Journal of Adolescent Health, 70 (3), 496–499. https://doi.org/10.1016/j.jadohealth.2021.08.026
Dimitry, L. (2012). A systematic review on the mental health of children and adolescents in areas of armed conflict in the Middle East. Child: Care, Health and Development, 38 (2), 153–161. https://doi.org/10.1111/j.1365-2214.2011.01246.x
Dobias, M. L., Morris, R. R., & Schleider, J. L. (2022). Single-Session Interventions Embedded Within Tumblr: Acceptability, Feasibility, and Utility Study. JMIR Formative Research , 6 (7), e39004. https://doi.org/10.2196/39004
Dunn, C., & Sicouri, G. (2022). The relationship between loneliness and depressive symptoms in children and adolescents: A meta-analysis. Behaviour Change, 39 (3), 134–145. https://doi.org/10.1017/bec.2022.13
Dürrbaum, T., & Sattler, F. A. (2020). Minority stress and mental health in lesbian, gay male, and bisexual youths: A meta-analysis. Journal of LGBT Youth, 17 (3), 298–314. https://doi.org/10.1080/19361653.2019.1586615
Ebert, D. D., Donkin, L., Andersson, G., et al. (2016). Does internet-based guided-self-help for depression cause harm? An individual participant data meta-analysis on deterioration rates and its moderators in randomized controlled trials. Psychological Medicine, 46 (13), 2679–2693. https://doi.org/10.1017/S0033291716001562
Eckshtain, D., Kuppens, S., Ugueto, A., Ng, M. Y., Vaughn-Coaxum, R., Corteselli, K., & Weisz, J. R. (2020). Meta-analysis: 13-year follow-up of psychotherapy effects on youth depression. Journal of the American Academy of Child & Adolescent Psychiatry, 59 (1), 45–63. https://doi.org/10.1016/j.jaac.2019.04.002
Exner-Cortens, D., Eckenrode, J., & Rothman, E. (2013). Longitudinal associations between teen dating violence victimization and adverse health outcomes. Pediatrics, 131 (1), 71–78. https://doi.org/10.1542/peds.2012-1029
Feighner, J. P., Robins, E., Guze, S. B., Woodruff, R. A., Jr., Winokur, G., & Munoz, R. (1972). Diagnostic criteria for use in psychiatric research. Archives of General Psychiatry, 26 (1), 57–63. https://doi.org/10.1001/archpsyc.1972.01750190059011
Forbes, M. K., Ringwald, W. R., Allen, T., Cicero, D. C., Clark, L. A., De Young, C. G., Eaton, N. R., Naragon-Gainey, K., Kotov, R., Krueger, R., Latzman, R. D., Martin, E. A., Ruggero, C., Waldman, I., Brandes, C. M., Fried, E. I., Goghari, V., Hankin, B., Sperry, S. H., et al. (2023). Principles and procedures for revising the hierarchical taxonomy of psychopathology. Manuscript submitted.
Forbes, E. E. (2020). Chasing the Holy Grail: Developmentally informed research on frontostriatal reward circuitry in depression. The American Journal of Psychiatry, 177 (8), 660–662. https://doi.org/10.1176/appi.ajp.2020.20060848
Forman-Hoffman, V., McClure, E., McKeeman, J., Wood, C. T., Middleton, J. C., Skinner, A. C., Perrin, E. M., & Viswanathan, M. (2016). Screening for major depressive disorder in children and adolescents: A systematic review for the us preventive services task force. Annals of Internal Medicine, 164 (5), 342–349. https://doi.org/10.7326/M15-2259
Frances, A. J., & Widiger, T. (2012). Psychiatric diagnosis: Lessons from the DSM-IV past and cautions for the DSM-5 future. Annual Review of Clinical Psychology, 8 , 109–130. https://doi.org/10.1146/annurev-clinpsy-032511-143102
Fried, E. I., Flake, J. K., & Robinaugh, D. J. (2022). Revisiting the theoretical and methodological foundations of depression measurement. Nature Reviews Psychology, 1 , 358–368. https://doi.org/10.1038/s44159-022-00050-2
Fulford, K. W. M., & Sartorius, N. (2009). The secret history of ICD and the hidden future of DSM. In M. Broome & L. Bortolotti (Eds.), Psychiatry as cognitive neuroscience: Philosophical perspectives. Oxford University Press.
Garcia, D., Barnett, M. L., Rothenberg, W. A., Tonarely, N. A., Perez, C., Espinosa, N., Salem, H., Alonso, B., San Juan, J., Peskin, A., Davis, E. M., Davidson, B., Weinstein, A., Rivera, Y. M., Orbano-Flores, L. M., & Jent, J. F. (2022). A natural helper intervention to address disparities in parent child-interaction therapy: A randomized pilot study. Journal of Clinical Child and Adolescent Psychology . https://doi.org/10.1080/15374416.2022.2148255
Gee, B., Reynolds, S., Carroll, B., Orchard, F., Clarke, T., Martin, D., Wilson, J., & Pass, L. (2020). Practitioner review: Effectiveness of indicated school-based interventions for adolescent depression and anxiety—A meta-analytic review. Journal of Child Psychology and Psychiatry, 61 (7), 739–756. https://doi.org/10.1111/jcpp.13209
Glass, A. J. (1971). Military psychiatry and changing systems of mental health care. Journal of Psychiatric Research, 8 (3–4), 499–512. https://doi.org/10.1016/0022-3956(71)90039-2
Global Burden of Disease Study 2013 Collaborators. (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 386 (9995), 743–800. https://doi.org/10.1016/S0140-6736(15)60692-4
Hadlaczky, G., Hökby, S., Mkrtchian, A., Carli, V., & Wasserman, D. (2014). Mental health first aid is an effective public health intervention for improving knowledge, attitudes, and behaviour: A meta-analysis. International Review of Psychiatry, 26 (4), 467–475. https://doi.org/10.3109/09540261.2014.924910
Hammen, C. (2005). Stress and depression. Annual Review of Clinical Psychology, 1 (1), 293–319. https://doi.org/10.1146/annurev.clinpsy.1.102803.143938
Hammen, C., & Compas, B. E. (1994). Unmasking unmasked depression in children and adolescents: The problem of comorbidity. Clinical Psychology Review, 14 (6), 585–603. https://doi.org/10.1016/0272-7358(94)90018-3
Hankin, B. L. (2012). Future directions in vulnerability to depression among youth: Integrating risks across multiple levels of analysis. Journal of Child and Adolescent Clinical Psychology, 41 , 695–718.
Hankin, B. L. (2020). Screening for and personalizing prevention of adolescent depression. Current Directions in Psychological Science, 29 , 327–332.
Hankin, B. L., Abramson, L. Y., Moffitt, T. E., Silva, P. A., McGee, R., & Angell, K. E. (1998). Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology, 107 (1), 128–140. https://doi.org/10.1037/0021-843X.107.1.128
Hankin, B. L., & Cohen, J. R. (2020). Assessment of depression in children and adolescents. In M. J. Prinstein, E. A. Young, E. J. Mash, & R. A. Barkley (Eds.), Assessment of childhood disorders (5th ed., pp. 159–191). Guilford Press.
Hankin, B. L., Young, J. F., Abela, J. R. Z., Smolen, A., Jenness, J. L., Gulley, L. D., Technow, J. R., Gottlieb, A. B., Cohen, J. R., & Oppenheimer, C. W. (2015). Depression from childhood into late adolescence: Influence of gender, development, genetic susceptibility, and peer stress. Journal of Abnormal Psychology, 124 (4), 803–816. https://doi.org/10.1037/abn0000089
Hankin, B. L., Young, J. F., Gallop, R., & Garber, J. (2018). Cognitive and interpersonal vulnerabilities to adolescent depression: Classification of risk profiles for a personalized prevention approach. Journal of Abnormal Child Psychology, 46 (7), 1521–1533. https://doi.org/10.1007/s10802-018-0401-2
Harold, G. T., & Sellers, R. (2018). Annual research review: Interparental conflict and youth psychopathology: An evidence review and practice focused update. Journal of Child Psychology and Psychiatry, 59 (4), 374–402. https://doi.org/10.1111/jcpp.12893
Harrington, A. (2019). Mind fixers: Psychiatry’s troubled search for the biology of mental illness . WW Norton & Company.
Haslbeck, J., Ryan, O., Robinaugh, D. J., Waldorp, L. J., & Borsboom, D. (2021). Modeling psychopathology: From data models to formal theories. Psychological Methods . https://doi.org/10.1037/met0000303
Hayden, E. P. (2022). A call for renewed attention to construct validity and measurement in psychopathology research. Psychological Medicine, 52 (14), 2930–2936. https://doi.org/10.1017/S0033291722003221
Heckman, J.J. (2011). Effective child development strategies. The Pre-K debates: Current controversies and issues .
Herrman, H., Patel, V., Kieling, C., Berk, M., Buchweitz, C., Cuijpers, P., Furukawa, T. A., Kessler, R. C., Kohrt, B. A., Maj, M., McGorry, P., Reynolds, C. F., Weissman, M. M., Chibanda, D., Dowrick, C., Howard, L. M., Hoven, C. W., Knapp, M., Mayberg, H. S., et al. (2022). Time for united action on depression: A Lancet-World Psychiatric Association Commission. The Lancet, 399 (10328), 957–1022.
Hitchcock, P. F., Fried, E. I., & Frank, M. J. (2022). Computational psychiatry needs time and context. Annual Review of Psychology, 73 , 243–270. https://doi.org/10.1146/annurev-psych-021621-124910
Holmes, E. A., Ghaderi, A., Harmer, C. J., Ramchandani, P. G., Cuijpers, P., Morrison, A. P., Roiser, J. P., Bockting, C. L. H., O’Connor, R. C., Shafran, R., Moulds, M. L., & Craske, M. G. (2018). The Lancet Psychiatry Commission on psychological treatments research in tomorrow’s science. The Lancet Psychiatry, 5 (3), 237–286. https://doi.org/10.1016/S2215-0366(17)30513-8
Hoover, S., & Bostic, J. (2021). Schools as a vital component of the child and adolescent mental health system. Psychiatric Services, 72 (1), 37–48. https://doi.org/10.1176/appi.ps.201900575
Hulvershorn, L. A., Cullen, K., & Anand, A. (2011). Toward dysfunctional connectivity: A review of neuroimaging findings in pediatric major depressive disorder. Brain Imaging and Behavior, 5 (4), 307–328. https://doi.org/10.1007/s11682-011-9134-3
Infurna, M. R., Reichl, C., Parzer, P., Schimmenti, A., Bifulco, A., & Kaess, M. (2016). Associations between depression and specific childhood experiences of abuse and neglect: A meta-analysis. Journal of Affective Disorders, 190 , 47–55. https://doi.org/10.1016/j.jad.2015.09.006
Israel, B. A. (1985). Social networks and social support: Implications for natural helper and community level interventions. Health Education Quarterly, 12 (1), 65–80. https://doi.org/10.1177/109019818501200106
Jain, S. (2010). The role of paraprofessionals in providing treatment for posttraumatic stress disorder in low-resource communities. JAMA Journal of the American Medical Association, 304 (5), 571–572. https://doi.org/10.1001/jama.2010.1096
Jones, J., Long, E.E., Hankin, B.L. Gallop, R., Davis, M. & Young, J.F. (in press). Personalized depression prevention reduces dependent stressors among adolescents: Results from a randomized controlled trial. Journal of Clinical Child and Adolescent Psychology.
Jones, J. D., Hankin, B. L., Gallop, R., Haraden, D., Sbrilli, M. D., Garber, J., & Young, J. F. (2022). Effects of personalized depression prevention on anxiety through 18-month follow-up: A randomized controlled trial. Behaviour Research and Therapy, 156 , 104156. https://doi.org/10.1016/j.brat.2022.104156
Joober, R. (2022). Psychiatry is the flagship of personalized and precision medicine: Proposing an epistemic horizon to biological psychiatry. Journal of Psychiatry and Neuroscience, 47 (6), E447–E454.
Jorm, A. F. (2014). Why hasn’t the mental health of Australians improved? The need for a national prevention strategy. The Australian and New Zealand Journal of Psychiatry, 48 (9), 795–801. https://doi.org/10.1177/0004867414546387
Jorm, A. F., Patten, S. B., Brugha, T. S., & Mojtabai, R. (2017). Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries. World Psychiatry, 16 (1), 90–99. https://doi.org/10.1002/wps.20388
Kapur, S., Phillips, A. G., & Insel, T. R. (2012). Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Molecular Psychiatry, 17 (12), 1174–1179.
Kendall, P. C., Cantwell, D. P., & Kazdin, A. E. (1989). Depression in children and adolescents: Assessment issues and recommendations. Cognitive Therapy and Research, 13 , 109–146.
Kendler, K. S. (2016). The phenomenology of major depression and the representativeness and nature of DSM criteria. The American Journal of Psychiatry, 173 (8), 771–780. https://doi.org/10.1176/appi.ajp.2016.15121509
Kendler, K. S. (2017). DSM disorders and their criteria: How should they inter- relate? Psychological Medicine, 47 (12), 2054–2060. https://doi.org/10.1017/S0033291717000678
Kendler, K. S. (2022). Potential lessons for DSM from contemporary philosophy of science. JAMA Psychiatry, 79 (2), 99–100. https://doi.org/10.1001/jamapsychiatry.2021.3559
Kendler, K. S., Muñoz, R. A., & Murphy, G. (2010). The development of the Feighner criteria: A historical perspective. The American Journal of Psychiatry, 167 (2), 134–142. https://doi.org/10.1176/appi.ajp.2009.09081155
Kendler, K. S., & Zachar, P. (Eds.). (2019). Toward a philosophical approach to psychiatry: the writings of Kenneth Kendler . Cambridge Scholars Publishing.
Kendler, K. S., Zachar, P., & Craver, C. (2011). What kinds of things are psychiatric disorders? Psychological Medicine, 41 (6), 1143–1150. https://doi.org/10.1017/S0033291710001844
Kerestes, R., Davey, C. G., Stephanou, K., Whittle, S., & Harrison, B. J. (2013). Functional brain imaging studies of youth depression: A systematic review. NeuroImage. Clinical, 4 , 209–231. https://doi.org/10.1016/j.nicl.2013.11.009
Khazanov, G. K., & Ruscio, A. M. (2016). Is low positive emotionality a specific risk factor for depression? A meta-analysis of longitudinal studies. Psychological Bulletin, 142 (9), 991–1015. https://doi.org/10.1037/bul0000059
Klein, D. N., Dougherty, L. R., & Olino, T. M. (2005). Toward guidelines for evidence-based assessment of depression in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34 (3), 412–432.
Kotov, R., Cicero, D. C., Conway, C. C., DeYoung, C. G., Dombrovski, A., Eaton, N. R., First, M. B., Forbes, M. K., Hyman, S. E., Jonas, K. G., Krueger, R. F., Latzman, R. D., Li, J. J., Nelson, B. D., Regier, D. A., Rodriguez-Seijas, C., Ruggero, C. J., Simms, L. J., Skodol, A. E., et al. (2022). The Hierarchical Taxonomy of Psychopathology (HiTOP) in psychiatric practice and research. Psychological Medicine, 52 (9), 1666–1678. https://doi.org/10.1017/S0033291722001301
Kotov, R., Krueger, R. F., Watson, D., Cicero, D. C., Conway, C. C., DeYoung, C. G., Eaton, N. R., Forbes, M. K., Hallquist, M. N., Latzman, R. D., Mullins-Sweatt, S. N., Ruggero, C. J., Simms, L. J., Waldman, I. D., Waszczuk, M. A., & Wright, A. G. C. (2021). The hierarchical taxonomy of psychopathology (HiTOP): A quantitative nosology based on consensus of evidence. Annual Review of Clinical Psychology, 17 , 83–108. https://doi.org/10.1146/annurev-clinpsy-081219-093304
Kuyken, W., Ball, S., Crane, C., Ganguli, P., Jones, B., Montero-Marin, J., Nuthall, E., Raja, A., Taylor, L., Tudor, K., Viner, R. M., Allwood, M., Aukland, L., Dunning, D., Casey, T., Dalrymple, N., De Wilde, K., Farley, E. R., Harper, J., Kappelmann, N., et al. (2022). Effectiveness and cost-effectiveness of universal school-based mindfulness training compared with normal school provision in reducing risk of mental health problems and promoting well-being in adolescence: the MYRIAD cluster randomised controlled trial. Evidence-Based Mental Health, 25 (3), 99–109. https://doi.org/10.1136/ebmental-2021-300396
Lee, Y. Y., Barendregt, J. J., Stockings, E. A., Ferrari, A. J., Whiteford, H. A., Patton, G. A., & Mihalopoulos, C. (2017). The population cost-effectiveness of delivering universal and indicated school-based interventions to prevent the onset of major depression among youth in Australia. Epidemiology and Psychiatric Sciences, 26 (5), 545–564. https://doi.org/10.1017/S2045796016000469
LeMoult, J., Humphreys, K. L., Tracy, A., Hoffmeister, J. A., Ip, E., & Gotlib, I. H. (2020). Meta-analysis: Exposure to early life stress and risk for depression in childhood and adolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 59 (7), 842–855. https://doi.org/10.1016/j.jaac.2019.10.011
Lieb, R., Isensee, B., Höfler, M., Pfister, H., & Wittchen, H. U. (2002). Parental major depression and the risk of depression and other mental disorders in offspring: A prospective-longitudinal community study. Archives of General Psychiatry, 59 (4), 365–374. https://doi.org/10.1001/archpsyc.59.4.365
Loades, M. E., Chatburn, E., Higson-Sweeney, N., Reynolds, S., Shafran, R., Brigden, A., Linney, C., McManus, M. N., Borwick, C., & Crawley, E. (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. Journal of the American Academy of Child & Adolescent Psychiatry, 59 (11), 1218–1239. https://doi.org/10.1016/j.jaac.2020.05.009
Lopez-Duran, N. L., Kovacs, M., & George, C. J. (2009). Hypothalamic-pituitary-adrenal axis dysregulation in depressed children and adolescents: A meta-analysis. Psychoneuroendocrinology, 34 (9), 1272–1283. https://doi.org/10.1016/j.psyneuen.2009.03.016
Lovato, N., & Gradisar, M. (2014). A meta-analysis and model of the relationship between sleep and depression in adolescents: Recommendations for future research and clinical practice. Sleep Medicine Reviews, 18 (6), 521–529. https://doi.org/10.1016/j.smrv.2014.03.006
Lu, W. (2019). Adolescent depression: National trends, risk factors, and healthcare disparities. American Journal of Health Behavior, 43 (1), 181–194. https://doi.org/10.5993/AJHB.43.1.15
Lund, C., Brooke-Sumner, C., Baingana, F., Baron, E. C., Breuer, E., Chandra, P., Haushofer, J., Herrman, H., Jordans, M., Kieling, C., Medina-Mora, M. E., Morgan, E., Omigbodun, O., Tol, W., Patel, V., & Saxena, S. (2018). Social determinants of mental disorders and the sustainable development goals: A systematic review of reviews. The Lancet Psychiatry, 5 (4), 357–369. https://doi.org/10.1016/S2215-0366(18)30060-9
Mandler, G., & Kessen, W. (1959). The language of psychology . John Wiley & Sons.
Manfro, P. H., Pereira, R. B., Rosa, M., Cogo-Moreira, H., Fisher, H. L., Kohrt, B. A., Mondelli, V., & Kieling, C. (2021). Adolescent depression beyond DSM definition: A network analysis. European Child & Adolescent Psychiatry . https://doi.org/10.1007/s00787-021-01908-1
McClure-Begley, T. D., & Roth, B. L. (2022). The promises and perils of psychedelic pharmacology for psychiatry. Nature Reviews Drug Discovery, 21 (6), 463–473.
McGlinchey, J. B., Zimmerman, M., Young, D., & Chelminski, I. (2006). Diagnosing major depressive disorder VIII: Are some symptoms better than others? Journal of Nervous and Mental Disease, 194 (10), 785–790. https://doi.org/10.1097/01.nmd.0000240222.75201.aa
McLeod, B. D., Weisz, J. R., & Wood, J. J. (2007). Examining the association between parenting and childhood depression: A meta-analysis. Clinical Psychology Review, 27 (8), 986–1003. https://doi.org/10.1016/j.cpr.2007.03.001
Mehta, T. G., Lakind, D., Rusch, D., Walden, A. L., Cua, G., & Atkins, M. S. (2019). Collaboration with urban community stakeholders: Refining paraprofessional-led services to promote positive parenting. American Journal of Community Psychology, 63 (3–4), 444–458. https://doi.org/10.1002/ajcp.12316
Merry, S., McDowell, H., Hetrick, S., Bir, J., & Muller, N. (2004). Psychological and/or educational interventions for the prevention of depression in children and adolescents. The Cochrane Database of Systematic Reviews, 1 , CD003380. https://doi.org/10.1002/14651858.CD003380.pub2
Messick, S. (1987). Validity. ETS Research Report Series, 1987 (2), i–208. https://doi.org/10.1002/j.2330-8516.1987.tb00244.x
Mew, E. J., Monsour, A., Saeed, L., Santos, L., Patel, S., Courtney, D. B., Watson, P. N., Szatmari, P., Offringa, M., Monga, S., & Butcher, N. J. (2020). Systematic scoping review identifies heterogeneity in outcomes measured in adolescent depression clinical trials. Journal of Clinical Epidemiology, 126 , 71–79. https://doi.org/10.1016/j.jclinepi.2020.06.013
Mihalopoulos, C., & Chatterton, M. L. (2015). Economic evaluations of interventions designed to prevent mental disorders: A systematic review. Early Intervention in Psychiatry, 9 (2), 85–92. https://doi.org/10.1111/eip.12156
Mojtabai, R., Olfson, M., Sampson, N. A., Jin, R., Druss, B., Wang, P. S., Wells, K. B., Pincus, H. A., & Kessler, R. C. (2011). Barriers to mental health treatment: Results from the national comorbidity survey replication. Psychological Medicine, 41 (8), 1751–1761. https://doi.org/10.1017/S0033291710002291
Moreno-Peral, P., Conejo-Cerón, S., Rubio-Valera, M., Fernández, A., Navas-Campaña, D., Rodríguez-Morejón, A., Motrico, E., Rigabert, A., de Dios Luna, J., Martín-Pérez, C., Rodríguez-Bayón, A., Ballesta-Rodríguez, M. I., Luciano, J. V., & Bellón, J. Á. (2017). Effectiveness of psychological and/or educational interventions in the prevention of anxiety: A systematic review, meta-analysis, and meta-regression. JAMA Psychiatry, 74 (10), 1021–1029. https://doi.org/10.1001/jamapsychiatry.2017.2509
Nelson, B., Wilson, S., Waszczuk, M., Michelini, G., Hankin, B. L., Olino, T., Wagner, N., Haltigan, J. D., Eaton, N., Kotov, R., Shields, A., Tackett, J., Belgrove, M., Hanson, J., Shackman, A., Goulter, N., King, K., Nusslock, R., Kackurkin, A., & Patalay, P. (2023). The hierarchical taxonomy of psychopathology (HiTOP) Framework in child and adolescent psychiatry. Manuscript submitted for publication.
Nelson, E.-L., Barnard, M., & Cain, S. (2003). Treating childhood depression over videoconferencing. Telemedicine Journal and e-Health, 9 (1), 49–55. https://doi.org/10.1089/153056203763317648
Nelson, E.-L., Barnard, M., & Cain, S. (2006). Feasibility of telemedicine intervention for childhood depression. Counselling & Psychotherapy Research, 6 (3), 191–195. https://doi.org/10.1080/14733140600862303
Office of the Surgeon General (2020). Smoking cessation: A Report of the Surgeon General.
Office of the Surgeon General. (2021). Protecting youth mental health: the US surgeon general’s advisory.
Ormel, J., Cuijpers, P., Jorm, A., & Schoevers, R. A. (2020). What is needed to eradicate the depression epidemic, and why. Mental Health & Prevention , 17 , 200177. https://doi.org/10.1016/j.mhp.2019.200177
Paradies, Y., Ben, J., Denson, N., Elias, A., Priest, N., Pieterse, A., Gupta, A., Kelaher, M., & Gee, G. (2015). Racism as a determinant of health: A systematic review and meta-analysis. PLoS ONE, 10 (9), e0138511. https://doi.org/10.1371/journal.pone.0138511
Patel, V., Burns, J. K., Dhingra, M., Tarver, L., Kohrt, B. A., & Lund, C. (2018). Income inequality and depression: A systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry, 17 (1), 76–89. https://doi.org/10.1002/wps.20492
Pellicane, M. J., & Ciesla, J. A. (2022). Associations between minority stress, depression, and suicidal ideation and attempts in transgender and gender diverse (TGD) individuals: Systematic review and meta-analysis. Clinical Psychology Review, 91 , 102113. https://doi.org/10.1016/j.cpr.2021.102113
Pina, A. A., Polo, A. J., & Huey, S. J. (2019). Evidence-based psychosocial interventions for ethnic minority youth: The 10-year update. Journal of Clinical Child and Adolescent Psychology, 48 (2), 179–202. https://doi.org/10.1080/15374416.2019.1567350
Polo, A. J., Makol, B. A., Castro, A. S., Colón-Quintana, N., Wagstaff, A. E., & Guo, S. (2019). Diversity in randomized clinical trials of depression: A 36-year review. Clinical Psychology Review, 67 , 22–35. https://doi.org/10.1016/j.cpr.2018.09.004
Prinz, R. J., & Shapiro, C. J. (2018). Shifting the needle on child maltreatment. In M. R. Sanders & T. G. Mazzucchelli (Eds.), The power of positive parenting: Transforming the lives of children, parents, and communities using the Triple P system (pp. 422–432). Oxford University Press.
Rasic, D., Hajek, T., Alda, M., & Uher, R. (2014). Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: A meta-analysis of family high-risk studies. Schizophrenia Bulletin, 40 (1), 28–38. https://doi.org/10.1093/schbul/sbt114
Ridings, L. E., Anton, M. T., Winkelmann, J., Davidson, T. M., Wray, L., Streck, C. J., & Ruggiero, K. J. (2019). Trauma resilience and recovery program: Addressing mental health in pediatric trauma centers. Journal of Pediatric Psychology, 44 (9), 1046–1056. https://doi.org/10.1093/jpepsy/jsz053
Ridley, M., Rao, G., Schilbach, F., & Patel, V. (2020). Poverty, depression, and anxiety: Causal evidence and mechanisms. Science, 370 (6522), 1–12. https://doi.org/10.1126/science.aay0214
Ringwald, W. R., Forbes, M. K., & Wright, A. G. C. (2021). Meta-analysis of structural evidence for the hierarchical taxonomy of psychopathology (HiTOP) model. Psychological Medicine . https://doi.org/10.1017/S0033291721001902
Robins, E., & Guze, S. B. (1970). Establishment of diagnostic validity in psychiatric illness: Its application to schizophrenia. The American Journal of Psychiatry, 126 (7), 983–986. https://doi.org/10.1176/ajp.126.7.983
Rodriguez-Seijas, C. A., McClendon, J., Wendt, D. C., Novacek, D. M., Ebalu, T., Hallion, L. S., Hassan, N. Y., Huson, K., Spielmans, G. I., Folk, J., Khazem, L., Neblett, E., Cunningham, T., Hampton-Anderson, J., Steinman, S., Hamilton, J. L., & Mekawi, Y. (2023). The next generation of clinical psychological science: Moving toward antiracism. Clinical Psychological Science . https://doi.org/10.31234/osf.io/mhdx8
Romanelli, M., & Hudson, K. D. (2017). Individual and systemic barriers to health care: Perspectives of lesbian, gay, bisexual, and transgender adults. American Journal of Orthopsychiatry, 87 (6), 714–728. https://doi.org/10.1037/ort0000306
Rubens, S. L., Felix, E. D., & Hambrick, E. P. (2018). A meta-analysis of the impact of natural disasters on internalizing and externalizing problems in youth. Journal of Traumatic Stress, 31 (3), 332–341. https://doi.org/10.1002/jts.22292
Rust, N. C., & LeDoux, J. E. (2023). The tricky business of defining brain functions. Trends in Neurosciences, 46 (1), 3–4. https://doi.org/10.1016/j.tins.2022.10.011
Rutter, M., & Sroufe, L. A. (2000). Developmental psychopathology: Concepts and challenges. Development and Psychopathology, 12 (3), 265–296. https://doi.org/10.1017/S0954579400003023
Rutter, M., & Werker, J. (2021). A conversation with Michael Rutter. Annual Review of Developmental Psychology, 3 , 1–14. https://doi.org/10.1146/annurev-devpsych-021821-044256
Samji, H., Wu, J., Ladak, A., Vossen, C., Stewart, E., Dove, N., Long, D., & Snell, G. (2021). Review: Mental health impacts of the covid-19 pandemic on children and youth—A systematic review. Child and Adolescent Mental Health . https://doi.org/10.1111/camh.12501
Sanders, M. R., & Mazzucchelli, T. G. (2022). Mechanisms of change in population-based parenting interventions for children and adolescents. Journal of Clinical Child and Adolescent Psychology, 51 (3), 277–294. https://doi.org/10.1080/15374416.2022.2025598
Sartorius, N., Davidian, H., Ernberg, G., Fenton, F. R., Fujii, I., Gastpar, M., Gulbinat, W., Jablensky, A., Kielholz, P., Lehmann, H. E., & Naraghi, M. (1983). Depressive disorders in different cultures: Including the who schedule FPR Standardized assessment of depressive disorder and a companion glossary. In Depressive disorders in different cultures. Including the who schedule FPR Standardized assessment of depressive disorder and a companion glossary (pp. 156–156).
Sartorius, N., Jablensky, A., Gulbinat, W., & Ernberg, G. (1980). WHO collaborative study: Assessment of depressive disorders. Psychological Medicine, 10 (4), 743–749. https://doi.org/10.1017/S0033291700055033
Sartorius, N., Shapiro, R., & Jablensky, A. (1974). The international pilot study of schizophrenia. Schizophrenia Bulletin, 1 (11), 21–34. https://doi.org/10.1093/schbul/1.11.21
Schleider, J. L., Mullarkey, M. C., Fox, K. R., Dobias, M. L., Shroff, A., Hart, E. A., & Roulston, C. A. (2022). A randomized trial of online single-session interventions for adolescent depression during COVID-19. Nature Human Behaviour, 6 (2), 258–268. https://doi.org/10.1038/s41562-021-01235-0
Schleider, J. L., & Weisz, J. R. (2017). Little treatments, promising effects? Meta-analysis of single-session interventions for youth psychiatric problems. Journal of the American Academy of Child & Adolescent Psychiatry, 56 (2), 107–115. https://doi.org/10.1016/j.jaac.2016.11.007
Schweizer, T. H., & Hankin, B. L. (2020). Cognitive risks: Translating stress into psychopathology. In K. L. Harkness & E. P. Hayden (Eds.), The Oxford handbook of stress and mental health (pp. 371–396). Oxford University Press.
Shipherd, J. C., Green, K. E., & Abramovitz, S. (2010). Transgender clients: Identifying and minimizing barriers to mental health treatment. Journal of Gay & Lesbian Mental Health, 14 (2), 94–108. https://doi.org/10.1080/19359701003622875
Simms, L. J., Wright, A. G. C., Cicero, D., Kotov, R., Mullins-Sweatt, S. N., Sellbom, M., Watson, D., Widiger, T. A., & Zimmermann, J. (2022). Development of measures for the hierarchical taxonomy of psychopathology (HiTOP): A collaborative scale development project. Assessment, 29 (1), 3–16. https://doi.org/10.1177/10731911211015309
Simons, D. J., Shoda, Y., & Lindsay, D. S. (2017). Constraints on generality (COG): A proposed addition to all empirical papers. Perspectives on Psychological Science, 12 (6), 1123–1128.
Slone, M., & Mann, S. (2016). Effects of war, terrorism and armed conflict on young children: A systematic review. Child Psychiatry and Human Development, 47 (6), 950–965. https://doi.org/10.1007/s10578-016-0626-7
Snyder, H. R., Gulley, L. D., Bijttebier, P., Hartman, C. A., Oldehinkel, A. J., Mezulis, A., Young, J. F., & Hankin, B. L. (2015). Adolescent emotionality and effortful control: Core latent constructs and links to psychopathology and functioning. Journal of Personality and Social Psychology, 109 (6), 1132–1149. https://doi.org/10.1037/pspp0000047
Spitzer, R. L., Endicott, J., & Robins, E. (1975). Clinical criteria for psychiatric diagnosis and DSM-III. The American Journal of Psychiatry, 132 (11), 1187–1192. https://doi.org/10.1176/ajp.132.11.1187
Spitzer, R. L., & Fleiss, J. L. (1974). A re-analysis of the reliability of psychiatric diagnosis. The British Journal of Psychiatry, 125 (587), 341–347.
Spruit, A., Goos, L., Weenink, N., Rodenburg, R., Niemeyer, H., Stams, G. J., & Colonnesi, C. (2020). The relation between attachment and depression in children and adolescents: A multilevel meta-analysis. Clinical Child and Family Psychology Review, 23 , 54–69. https://doi.org/10.1007/s10567-019-00299-9
Starin, A. C., Atkins, M. S., Wehrmann, K. C., Mehta, T., Hesson-McInnis, M. S., Marinez-Lora, A., & Mehlinger, R. (2014). Moving science into state child and adolescent mental health systems: Illinois’ evidence-informed practice initiative. Journal of Clinical Child and Adolescent Psychology, 43 (2), 169–178. https://doi.org/10.1080/15374416.2013.848772
Strober, M., & Werry, J. S. (1986). The assessment of depression in children and adolescents. Assessment of Depression . https://doi.org/10.1007/978-3-642-70486-4_28
Suffoletto, B., Goldstein, T., & Brent, D. (2021). A text message intervention for adolescents with depression and their parents or caregivers to overcome cognitive barriers to mental health treatment initiation: Focus groups and pilot trial. JMIR Formative Research, 5 (11), e30580. https://doi.org/10.2196/30580
Thapar, A., Eyre, O., Patel, V., & Brent, D. (2022). Depression in young people. The Lancet, 400 (10352), 617–631. https://doi.org/10.1016/S0140-6736(22)01012-1
Toenders, Y. J., Laskaris, L., Davey, C. G., Berk, M., Milaneschi, Y., Lamers, F., Penninx, B. W. J. H., & Schmaal, L. (2022). Inflammation and depression in young people: A systematic review and proposed inflammatory pathways. Molecular Psychiatry, 27 (1), 315–327. https://doi.org/10.1038/s41380-021-01306-8
US Preventive Services Task Force. (2022). Screening for depression and suicide risk in children and adolescents: US preventive services task force recommendation statement. JAMA, 328 (15), 1534–1542. https://doi.org/10.1001/jama.2022.16946
Vilar, A., Sánchez-Martínez, N., Blasco, M. J., Álvarez-Salazar, S., Batlle Vila, S., & Forero, G. (2022). Content agreement of depressive symptomatology in children and adolescents: A review of eighteen self-report questionnaires. European Child & Adolescent Psychiatry . https://doi.org/10.1007/s00787-022-02056-w
Viner, R., Russell, S., Saulle, R., Croker, H., Stansfield, C., Packer, J., Nicholls, D., Goddings, A. L., Bonell, C., Hudson, L., Hope, S., Ward, J., Schwalbe, N., Morgan, A., & Minozzi, S. (2022). School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the First COVID-19 wave: a systematic review. JAMA Pediatrics, 176 (4), 400–409. https://doi.org/10.1001/jamapediatrics.2021.5840
Wakeling, S., Stukas, A. A., Wright, B. J., & Evans, L. (2020). Negative feedback seeking and excessive reassurance seeking behavior and depression: A meta-analytic review. Journal of Social and Clinical Psychology, 39 (9), 788–823. https://doi.org/10.1521/jscp.2020.39.9.788
Walter, H. J., Abright, A. R., Bukstein, O. G., Diamond, J., Keable, H., Ripperger-Suhler, J., & Rockhill, C. (2022). Clinical practice guideline for the assessment and treatment of children and adolescents with major and persistent depressive disorders. Journal of the American Academy of Child and Adolescent Psychiatry., 62 , 479–502. https://doi.org/10.1016/j.jaac.2022.10.001
Washington State Institute for Public Policy. (2019). Triple P—Positive parenting program.
Watson, D., Forbes, M. K., Levin-Aspenson, H. F., Ruggero, C. J., Kotelnikova, Y., Khoo, S., Bagby, R. M., Sunderland, M., Patalay, P., & Kotov, R. (2022). The development of preliminary HiTOP internalizing spectrum scales. Assessment, 29 (1), 17–33. https://doi.org/10.1177/10731911211003976
Weersing, V. R., Jeffreys, M., Do, M.-C.T., Schwartz, K. T. G., & Bolano, C. (2017). Evidence base update of psychosocial treatments for child and adolescent depression. Journal of Clinical Child and Adolescent Psychology, 46 (1), 11–43. https://doi.org/10.1080/15374416.2016.1220310
Weiss, B., & Garber, J. (2003). Developmental differences in the phenomenology of depression. Development and Psychopathology, 15 (2), 403–430.
Weisz, J. R., Kuppens, S., Ng, M. Y., Eckshtain, D., Ugueto, A. M., Vaughn-Coaxum, R., Jensen-Doss, A., Hawley, K. M., Krumholz Marchette, L. S., Chu, B. C., Weersing, V. R., & Fordwood, S. R. (2017). What five decades of research tells us about the effects of youth psychological therapy: A multilevel meta-analysis and implications for science and practice. American Psychologist, 72 (2), 79–117. https://doi.org/10.1037/a0040360
Whittaker, R., Stasiak, K., McDowell, H., Doherty, I., Shepherd, M., Chua, S., Dorey, E., Parag, V., Ameratunga, S., Rodgers, A., & Merry, S. (2017). MEMO: An mHealth intervention to prevent the onset of depression in adolescents: A double-blind, randomised, placebo-controlled trial. Journal of Child Psychology and Psychiatry, 58 (9), 1014–1022. https://doi.org/10.1111/jcpp.12753
Wilson, M. (1993). DSM-III and the transformation of American psychiatry: A history. American Journal of Psychiatry, 150 , 399–399.
Winter, N. R., Leenings, R., Ernsting, J., Sarink, K., Fisch, L., Emden, D., Blanke, J., Goltermann, J., Opel, N., Barkhau, C., Meinert, S., Dohm, K., Repple, J., Mauritz, M., Gruber, M., Leehr, E. J., Grotegerd, D., Redlich, R., Jansen, A., et al. (2022). Quantifying deviations of brain structure and function in major depressive disorder across neuroimaging modalities. JAMA Psychiatry, 79 (9), 879–888.
World Health Organization. (2017). Depression and other common mental disorders: Global health estimates. World Health Organization. https://apps.who.int/iris/handle/10665/254610 . License: CC BY-NC-SA 3.0 IGO
Yap, M. B. H., Pilkington, P. D., Ryan, S. M., & Jorm, A. F. (2014). Parental factors associated with depression and anxiety in young people: A systematic review and meta-analysis. Journal of Affective Disorders, 156 , 8–23. https://doi.org/10.1016/j.jad.2013.11.007
Yeh, M., McCabe, K., Hough, R. L., Dupuis, D., & Hazen, A. (2003). Racial/ethnic differences in parental endorsement of barriers to mental health services for youth. Mental Health Services Research, 5 (2), 65–77. https://doi.org/10.1023/A:1023286210205
Young, J. F., Jones, J. D., Gallop, R., Benas, J. S., Schueler, C. M., Garber, J., & Hankin, B. L. (2021). Personalized depression prevention: A randomized controlled trial to optimize effects through risk-informed personalization. Journal of the American Academy of Child and Adolescent Psychiatry, 60 (9), 1116-1126.e1. https://doi.org/10.1016/j.jaac.2020.11.004
Zajkowska, Z., Gullett, N., Walsh, A., Zonca, V., Pedersen, G. A., Souza, L., Kieling, C., Fisher, H. L., Kohrt, B. A., & Mondelli, V. (2022). Cortisol and development of depression in adolescence and young adulthood—A systematic review and meta-analysis. Psychoneuroendocrinology, 136 , 105625. https://doi.org/10.1016/j.psyneuen.2021.105625
Zhou, X., Teng, T., Zhang, Y., Del Giovane, C., Furukawa, T. A., Weisz, J. R., Li, X., Cuijpers, P., Coghill, D., Xiang, Y., Hetrick, S. E., Leucht, S., Qin, M., Barth, J., Ravindran, A. V., Yang, L., Curry, J., Fan, L., Silva, S. G., … Xie, P. (2020). Comparative efficacy and acceptability of antidepressants, psychotherapies, and their combination for acute treatment of children and adolescents with depressive disorder: A systematic review and network meta-analysis. The Lancet Psychiatry, 7 (7), 581–601. https://doi.org/10.1016/S2215-0366(20)30137-1
Download references
Acknowledgements
Benjamin L. Hankin acknowledges Grant funding support from NHLBI R01HL155744 and NIMH R01MH109662. Julianne M. Griffith acknowledges grant funding support from NSF GRPF 1000259217.
This work is supported by the National Heart, Lung, and Blood Institute (Grant No. 155744) and National Institute of Mental Health (Grant No. 109662) to Benjamin Hankin and National Science Foundation, 1000259217, Julianne Griffith
Author information
Authors and affiliations.
Department of Psychology, University of Illinois Urbana Champaign, 603 E. Daniel Street, Champaign, IL, 61820, USA
Benjamin L. Hankin & Julianne M. Griffith
You can also search for this author in PubMed Google Scholar
Contributions
For this review and position paper, Benjamin L. Hankin developed the primary ideas, conducted literature searches, wrote the first manuscript draft, and revised the work. Julianne M. Griffith conducted literature searches, and wrote and revised the work. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Benjamin L. Hankin .
Ethics declarations
Conflict of interest.
Neither author has any conflicts of interest nor financial interests to declare. Benjamin L. Hankin is an unpaid member of the HiTOP consortium. He has been on the Editorial Board of this journal.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Hankin, B.L., Griffith, J.M. What Do We Know About Depression Among Youth and How Can We Make Progress Toward Improved Understanding and Reducing Distress? A New Hope. Clin Child Fam Psychol Rev 26 , 919–942 (2023). https://doi.org/10.1007/s10567-023-00437-4
Download citation
Accepted : 08 May 2023
Published : 07 June 2023
Issue Date : December 2023
DOI : https://doi.org/10.1007/s10567-023-00437-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Youth depression
- History and philosophy
- Review and position paper
- Personalized prevention
- Find a journal
- Publish with us
- Track your research
- Research article
- Open access
- Published: 24 August 2020
The experience of loneliness among young people with depression: a qualitative meta-synthesis of the literature
- Louis Achterbergh ORCID: orcid.org/0000-0001-5295-0073 1 , 2 ,
- Alexandra Pitman 1 , 3 ,
- Mary Birken 1 ,
- Eiluned Pearce 1 ,
- Herman Sno 2 &
- Sonia Johnson 1 , 3
BMC Psychiatry volume 20 , Article number: 415 ( 2020 ) Cite this article
48k Accesses
100 Citations
276 Altmetric
Metrics details
Young people have a higher prevalence of loneliness than other age groups, and they are also at risk of depression. Quantitative studies describe a bidirectional association between loneliness and depression, but there is limited understanding of how these influence each other. Little is known about the experience of loneliness among young people with depression. Qualitative approaches may help understand the relationship between loneliness and depression among young people, and how to intervene to improve outcomes. We aimed to conduct a meta-synthesis to understand the complex inter-relationship between loneliness and depression among young depressed people by synthesising evidence from a systematic review of qualitative studies.
We conducted a meta-synthesis of qualitative studies capturing experiences of loneliness among young people with depression. We systematically searched six electronic databases for selected search terms, critically appraised eligible studies, and analysed the data from included studies using the approach of thematic synthesis. We used feedback from an inter-disciplinary research workshop to improve reflexivity.
Our inclusion criteria identified fourteen studies. Our analysis identified four themes: (1) social withdrawal due to poor mental health, (2) non-disclosure of depression contributing to social distance, (3) the desire to connect, and (4) paradoxes of loneliness and depression. These themes illustrated a range of pathways between depression and loneliness, and a sense of how these might be mutually reinforcing. Our findings suggest that where depressed individuals engage in certain behaviours (withdrawing; not confiding) for a range of reasons, this can lead to feelings of loneliness, an awareness of which worsens their mood, thus perpetuating their depression.
Conclusions
Young people with depression experience loneliness as an insurmountable distance between themselves and others. Our findings identified non-disclosure of depression, and the debilitating nature of the depressive symptomatology, as factors perpetuating a vicious cycle of loneliness and depression. They suggest that approaches to tackling the problem might include helping young people communicate about their depression to trusted friends and educating their social networks in how to support them. The wider research literature suggests that cognitive interventions may have a role in shifting maladaptive cognitions about their social world.
Peer Review reports
Loneliness is defined as a negative emotional state that arises when there is a perceived discrepancy between desired and actual social relationships [ 1 ]. The adverse effects of loneliness on mental [ 2 ], and physical health [ 3 ] are now well established. Most work describing the association between loneliness and mental illness has focussed on depression. Depression is the third leading cause of disease worldwide [ 4 ], based on World Health Organisation (WHO) rankings, and its incidence appears to be increasing internationally [ 5 ]. Onset of major depression extends from mid-adolescence to the mid-40s, but almost 40% experience their first episode of depression before age 20 years, with peaks in prevalence in the second and third decades of life [ 4 ]. Cross-sectional work shows that people with depression are ten times more likely to feel lonely than the general population [ 6 ]. Longitudinal studies demonstrate that loneliness not only increases the risk of becoming depressed [ 7 , 8 , 9 ], and worsens depressive symptoms amongst those who are already depressed [ 10 ], but also that loneliness and depression influence each other reciprocally [ 11 ]. This means that people who are lonely are more likely to be become depressed, but also that their depression reinforces their loneliness. The mechanisms underlying this complex inter-relationship between loneliness and depression are unclear and need further investigation, particularly in young people.
Population-based surveys describe a U-shaped age distribution of loneliness, with high rates of loneliness among young people and among the elderly [ 12 ]. However, the majority of epidemiological work on the health impacts of loneliness have been conducted in older age groups [ 7 , 8 , 9 , 13 , 14 ]. Extrapolating the findings of studies in older age groups to younger people is problematic given that experiences of loneliness vary in different demographic and cultural groups [ 15 ]. The social context of loneliness is also very different in young people to later stages of life. Additionally, the experience of depression is also likely to vary by age, with symptoms of irritability and interpersonal difficulties being particularly prominent among adolescents [ 16 ].
The few studies that have been done in young people suggest that social isolation in childhood predicts loneliness in young adulthood [ 17 ] and that chronic peer-related loneliness in childhood predicts adolescent depression [ 18 , 19 , 20 ]. Given the evidence from studies of older age groups, loneliness is likely to be a factor affecting quality of life and prognosis among young people with depression. It is also likely to compound the barriers described by young people in accessing formal or informal help, namely the stigma of mental illness and a reluctance to talk about feelings or emotions [ 21 ]. Adolescence and young adulthood is the greatest risk period for the emergence of depression and also one in which loneliness might be most stigmatising given strong social pressure to appear connected [ 22 ]. In view of the high prevalence of loneliness amongst young people, and the lack of research focussed on this age group, it is important to gain a better understanding of the experience of loneliness among young people with depression, as well as its causes and consequences, to tailor the design of acceptable age-appropriate treatments [ 10 ].
Loneliness is a subjective construct related to the concepts of social isolation [ 23 ], alienation [ 24 ], social connectedness [ 25 ], lack of belonging [ 26 ] and social capital [ 23 ]. Loneliness is distinct from social isolation, which is an objective measure of the absence of relationships with other people [ 27 ]. Loneliness is also distinct from solitude in that loneliness is an unpleasant experience, whereas solitude implies a desire to be alone and is not necessarily a negative experience [ 27 ]. Quantitative work shows that loneliness and social isolation are moderately correlated and both are associated with depression [ 28 , 29 ]. Behavioural genetic analysis finds that young people who are lonely are often depressed, partly because the same genes influence loneliness and depression [ 28 ]. Environmental factors are also important; lonely young adults are more likely to have been bullied and socially isolated as children [ 17 ]. The distinction between loneliness and social isolation is important because socially isolated young adults do not necessarily feel lonely [ 28 ] and young adults who feel lonely do not necessarily spend less time with others in comparison to their less lonely peers [ 30 ].
Available evidence suggests that different age groups experience loneliness differently. Comparison of the social networks of young and middle-aged adults show that young adults reported twice as many days feeling lonely and isolated than late middle-age adults, despite having larger networks [ 31 ]. Interview data from an English community sample show that children and young people aged 10 to 24 years describe loneliness as a sense of exclusion, disconnection from others and unhappiness with relationships [ 32 ]. Children as young as 5 years understand a concept of loneliness, a sadness associated with this, and how it motivates them to make contact with others [ 19 ].
By understanding how loneliness and depression influence each other in young people, there is potential for improving depressive symptoms and depressive outcomes through well-developed and appropriately targeted interventions focused on loneliness. The aim of this meta-synthesis was therefore to summarise qualitative research describing the experience of loneliness and depression among young people, to provide insights into the relationships and pathways between them.
Meta-synthesis is a research method that uses rigorous qualitative methods to synthesize existing qualitative studies, with the aim of constructing greater meaning through an overarching interpretation based on the qualitative studies included [ 33 , 34 , 35 , 36 ]. Thematic synthesis is influenced by the meta-ethnography process and grounded theory [ 35 ] and involves conceptual coding of data to construct an encompassing model providing insights to the phenomenon studied [ 37 ]. The approach identifies patterns across qualitative data and aims to enrich the understanding of a topic, creating new theoretical insights as well as serving as a tool to develop suitable interventions [ 38 ]. It entails an iterative cyclical process comparing and contrasting themes between different studies and attempting to encompass the data using a set of themes that are relevant within each study, constructed as a hierarchical tree structure [ 35 ].
For this study we applied an accepted six step method for conducting a meta-synthesis [ 35 ], consisting of: 1) defining the research question and selection criteria, 2) using those criteria to select studies, 3) undertaking a quality assessment, 4) extracting and presenting formal data, 5) conducting data analysis and 6) reporting the synthesis.
Protocol and search strategy
Before commencing, we registered our meta-synthesis protocol with PROSPERO, the international prospective register for systematic reviews [ 39 ]. We conducted our search using six electronic databases (MEDLINE, PsycINFO, CINAHL, Scopus, ProQuest and Web of Science) from database inception to 21 March 2019. These databases were chosen to capture studies from a range of research disciplines, including medicine, psychology, sociology and anthropology. We developed search terms as a team (see Appendix 1 ), including terms capturing depression and mental ill-health, loneliness and social isolation, and qualitative research. Given the conceptual overlap between loneliness and other constructs such as perceived social support, our search terms also included several other words capturing these concepts [ 10 ]. We also conducted a search of the Ethos British Library database to find any relevant PhD dissertations and hand searched the reference lists of any eligible studies to reduce the chance of missing important studies.
Selection: inclusion & exclusion criteria
We screened titles and abstracts of identified studies for eligibility, followed by full text review where indicated, using the following inclusion criteria to identify studies that:
used a qualitative research design such as semi-structured interviews or focus groups.
sampled adolescents and/or young adults aged 11 to 30 years with a depressive disorder. We chose the age range 11 to 30 years to cover WHO definitions of adolescents (aged 10–19 years), youth (aged 15–24 years), teenagers (aged 15–19 years), and young adults (aged 20–24 years), with a wider margin at the upper limit in order to ensure that we did not exclude studies including young adults as a proportion of those sampled or studies where young people reflected back on their recent adolescence.
explored how young people with depression experience loneliness, both in relation to a current depressive episode and/or in reflecting back on past episodes
included participants with self-reported depression or depression diagnosed by a health professional, regardless of severity of depression or treatment received. We included studies that involved participants with depression, with or without a comorbid anxiety or personality disorder. We also included studies in which the depressive episode was in the context of a diagnosis of bipolar disorder.
Studies were excluded if they:
sampled participants above the age of 30 only, or used a mixed sample of age groups above and below 30
sampled participants without a history of depression.
sampled participants with: a co-morbid chronic physical disability (e.g. rheumatoid arthritis); any co-morbid mental illness other than an anxiety disorder or personality disorder; or a co-morbid neurocognitive disorder (e.g. Alzheimer’s disease). This was to avoid capturing the experience of depression in the context of co-morbid conditions beyond common mental disorders.
presented data mentioning loneliness fleetingly or not at all. For example, a study with data on one participant saying: ‘I feel lonely because I’m depressed’ would not be deemed sufficient in detail to convey anything meaningful about the experience of loneliness.
presented data describing solely the objective presence or absence of social support, rather than subjective feelings about perceived social support, social isolation, or social network size.
used a quantitative research design.
were not written in English or Dutch.
Data screening and extraction
One researcher (LA) conducted the search, removed duplicates, and screened the titles and abstracts of all studies for relevance, before assessing the full text of identified studies for eligibility. Three researchers (MB, EP and AP) were each randomly assigned 10% of these studies for full text assessment to ascertain agreement over inclusion/exclusion, meeting regularly as a group to discuss eligibility.
Quality appraisal
One researcher (LA) appraised all eligible studies for quality using the Critical Appraisal Skills Programme (CASP), a 10-item quality assessment tool for qualitative research [ 40 ], discussing this with the wider team. Studies were appraised on these items grouped under three categories; validity (clarity of research aims, appropriateness of qualitative methodology, research design, recruitment strategy, and data collection, appropriate consideration of researcher reflexivity), results (ethical considerations, appropriateness of data analysis, clarity of findings stated), and utility (the value of the research). Study characteristics and appraisal criteria were summarised in a proforma (Table 1 ). We chose not to exclude studies based on our assessment of low quality. Instead, our synthesis of findings took into account our CASP-based judgements on the quality of included studies, as suggested in methodological guidance [ 35 , 38 ], and can therefore be interpreted in this context.
Data analysis
For each included study, one researcher (LA) identified any text relating to loneliness in the results section (whether quotes or interpretation) and imported relevant passages into a qualitative data analysis software package [ 54 ] to facilitate the process of thematic synthesis. Three researchers (AP, MB, EP) independently assessed a set of studies each to identify which passages to import and compare judgements on which data to include or exclude.
Having established our final database of extracted qualitative data, one researcher (LA) then coded the full dataset, and three researchers (AP, MB, EP) independently coded data from two randomly-allocated studies each. All four researchers then compared their coding to develop an initial coding framework. This was then refined through an iterative process, to develop a taxonomy of analytical themes.
External validity
To improve external validity and reduce researcher subjectivity, we presented the findings of this draft thematic framework at an inter-disciplinary research workshop held in London on 26th June 2019. This formed part of the research activities of the United Kingdom Research and Innovation (UKRI) Loneliness and Social Isolation in Mental Health Research Network (see Acknowledgements). The 58 participants included health and social care practitioners, university and voluntary sector researchers, policy makers, lived experience researchers, and mental health service users. Following an oral presentation of findings, one researcher (LA) led two independent 45-min sessions with 8 attendees in each group to discuss the coding framework in more detail. The comments made were used to revise the coding framework and improve reflexivity.
Reflexivity
Our multidisciplinary research team reduced the dominance of one perspective. This was important, as a meta-synthesis is an overarching interpretation from the joint analysis of primary studies [ 33 ], with a high risk of subjectivity and personal bias. LA is a social scientist and medical student with an interest in the links between mental health and loneliness, AP and SJ are psychiatrists and academics with an interest in sociology and social psychology, EP has a research background in experimental psychology and biological anthropology, with experience of having worked in the voluntary sector, while MB is a mental health occupational therapist and academic. This team approach, and the use of a multidisciplinary research workshop to discuss findings, reduced the focus on loneliness from a medical perspective by including insights from multiple disciplines.
Description of included studies
Our search identified 9188 studies, which was reduced to 6540 after deleting 2648 duplicates (see Fig. 1 ). Following screening of titles/abstracts we excluded 6351 studies for irrelevance. Following full text review of the remaining 188 studies we excluded 177 based on our exclusion criteria, included eleven studies and added three more based on hand searching the references from the selected studies, identifying 14 eligible studies [ 24 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 ], which we included in this meta-synthesis. We achieved 100% agreement on study eligibility between four authors. Characteristics of each study are shown in Table 1 , including an assessment of study quality using CASP criteria.
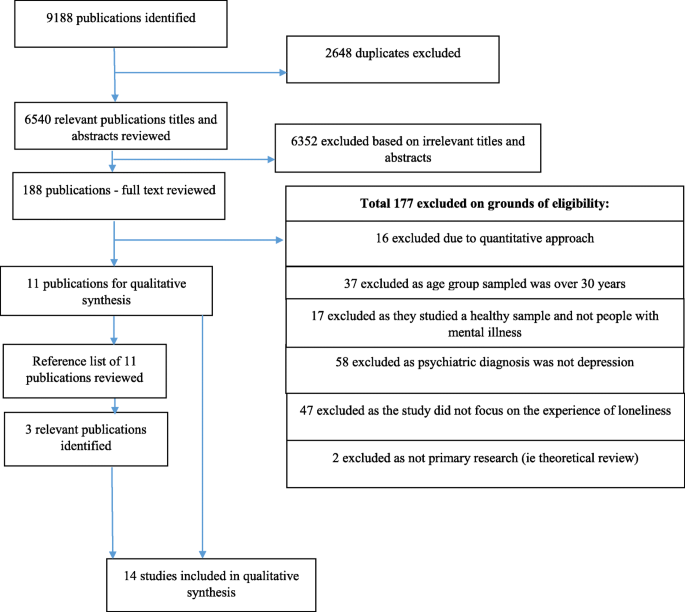
Flow diagram for included studies
The total number of participants was 388, with sample sizes in each study ranging from 5 to 107. Participants’ ages ranged from 11 to 30 years, and roughly three quarters were female ( n = 288). Dates of publication ranged from 2002 to 2019, and studies originated from the United States, United Kingdom, Finland, Belgium, France, Canada, Australia, and Germany. Thirteen studies were published in peer-reviewed journals, while one study was an unpublished PhD dissertation [ 51 ]. One study was a meta-synthesis of six qualitative studies [ 43 ], which included one identified in our own search [ 44 ]. We decided to include this meta-synthesis as a unified whole rather than disaggregating its included studies because a number of those studies were unpublished theses that were unavailable to us.
All studies involved individuals with a history of depression, whilst two studies included participants with depressive episodes in the context of bipolar disorder. In those two studies an unknown proportion had bipolar in one [ 51 ], whilst two out of nine participants had bipolar in the other [ 49 ]. Most studies ( n = 12) collected interview data, while two studies used free text from written self-reports. Included studies used a range of qualitative analytic methods: thematic analysis, interpretative phenomenological analysis, grounded theory, discourse analysis, framework analysis, hermeneutic phenomenology, content analysis, and comparative method analysis.
Thematic synthesis
Our thematic synthesis of 14 eligible studies identified four analytic themes: (1) social withdrawal due to poor mental health, (2) non-disclosure of depression contributing to social distance (with four sub-themes), (3) the desire to connect, and (4) paradoxes of loneliness and depression. Quotes given in italics denote primary data.
Theme 1: social withdrawal due to poor mental health
A key theme we identified related to the debilitating nature of depressive symptoms, which made it very hard for some young people to engage with others. Nearly all studies ( n = 13) described the experience of depression as causing those individuals to withdraw from others, relating this to difficulties in being around others due to low motivation and low energy.
“There would be days that I just couldn’t get out of bed. I didn’t want to face people. I didn’t want to look at anybody, I just wanted to stay there and I guess just sulk by myself, and I just didn’t have any energy.” (Female in her 10s, USA sample) [ 43 ].
Some individuals described feeling better when isolating themselves from peers, because being around others was so emotionally draining . “I come home it’s just kind of like a relief” , explained Lana (teenager, UK sample), who had been bullied at school for reasons unspecified [ 50 ]. Some participants avoided others by spending time in their rooms or going for walks alone. One female participant in her teens from the USA explained , “I just kind of wanted to be by myself.” [ 41 ]
Participants described having stopped participating in activities they had previously enjoyed or not feeling able to fully engage in such activities. A female in her teens from the USA, who had taken an active role in the performing arts since the age of 2 years, explained.
“I was in show choir and throughout that year I just didn’t really enjoy it. I was fine with standing in the back, which really wasn’t like me. My wanting to be in the back just wasn’t normal.” [ 41 ]
Low self-esteem seemed to affect some young people sampled, who felt that their depression had worsened their insecurities, leading them to withdraw socially. The depression had apparently eroded their belief that anyone could find them likeable, resulting in them withdrawing to avoid other people.
“I become even more withdrawn than I normally am, and it’s based on the insecurity, and it came up the unlikeability thing again, that I’m not likable inherently so what’s the use of pretending that I am because eventually they are going to find out.” (Sarah, teenager; Canadian sample) [ 45 ].
Participants also spoke of an inability to feel affection from others: “ When you’re depressed you feel like you don’t have anybody. ” (Tina, teenager, USA sample) [ 44 ]. The syndrome of depression set young people apart from their peers and made them feel different. This change was noted by others, even if they did not necessarily recognise it as depression, and this could lead to others’ withdrawal. The sense of rejection was apparent in young people who coped by isolating themselves, thus compounding their sense of differences between them and others.
People just started drifting away, like they were asking, “What’s wrong with you?” I wanted to ask them, “Why don’t you talk to me anymore?” I felt they were saying “You’re different now!” I just began to hide away a lot and I would say, “I just want to be alone”. (female teenager, USA sample) [ 51 ].
Theme 2: non-disclosure of depression and social distance
The second theme, emerging from 12 studies, was more explicitly related to feelings of loneliness. As young people dealing with depression were hesitant about disclosing their depressed feelings to people in their social networks, they avoided being open about their true selves. This sense of otherness through concealment enhanced participants’ feelings of loneliness. Some individuals described being very aware of putting up a façade and of making extensive efforts to maintain this front to avoid talking about their mental health issues.
“ I would put on a smile for my parents and my siblings. Whenever somebody would leave and I knew I was going to be alone, they would ask me, “Are you going to be alright?” And I would say “Yes, of course,” because I didn’t want them to know what I was dealing with. But, it was a living hell. I put up a really good façade for them, like all cheery and happy, nothing’s wrong.” (Female in her 20s; USA sample) [ 41 ].
A range of reasons were given for the non-disclosure of depressed mood, summarised in the four sub-themes below.
Subtheme 2.1 fear of being judged
Young people in the included studies commonly expressed fear of being judged negatively if they identified themselves as suffering from depression, or of being perceived as unbearable or embarrassing if they vented their feelings. The negative consequences they feared included social exclusion and isolation, as borne out by their experiences:
“ I cannot talk about my sadness, in fact, I don’t dare to talk about it, because then you are considered as a weak person. I see that some people feel pity for me, but they don’t talk to me, they prefer to run away because they are afraid and do not know how to react to someone who is sad.” (Female, teenager, Belgian sample) [ 24 ].
“ If I could talk to them [friends] I would, but I just didn’t feel like I could talk to them. They would keep on going, ‘You’re weird’ or something.” (Sandra, teenager, USA sample) [ 44 ].
Subtheme 2.2 preserving friendships
Another reason for not disclosing their depression was that the young people sampled clearly valued their friendships and wanted to preserve existing networks. They feared losing these connections if they shared their feelings of depression. There was also a fear of burdening others, in that by not disclosing their depressive thoughts they hoped to minimise the negative impact of their depression on others. Many adolescents had experienced negative changes or the ending of friendships as a consequence of mental health problems and this reinforced their reluctance to reveal their feelings to friends.
“I’m afraid that friends and significant others can’t see me the same way as before or something might change between us if I told them all my troubles. I don’t want to bother anybody with my worries.” ( Unknown gender, 15–17 years old; Finnish sample) [ 42 ].
Subtheme 2.3 difficulty explaining oneself
Beyond deliberate efforts to avoid talking about their feelings, young people also found it hard to explain why they felt depressed. Pressure to explain themselves arose from members of their peer group, who struggled to comprehend their experiences, expressing this through intolerance. Their own inability to formulate or articulate an explanation frustrated young people with depression and had the effect of widening the gulf between them and others.
“When you feel bad, you need to have an external explanation for why you have these feelings, because the fact that you feel bad must be caused by something. Participants stated that they often received the question: ‘ Why are you feeling so bad? ’ Adolescents shared that they cannot give a constructive answer because they do not know why they have these feelings. They could not give explanations because there were no specific causes for them. Due to the inability to provide a real explanation regarding the causes, their feelings and depression are not recognized by others.” [ 24 ]
Subtheme 2.4 perceived futility of explaining oneself
Experiencing depression engendered a realisation of being different from one’s peers. This gave rise to the belief that others would not understand one’s situation and that there was therefore no point in discussing it. Young people with depression indicated that they feared others were likely to trivialise, dismiss or ignore their depressive symptoms. Again, their previous negative experiences of others failing to understand them taught some young people not to disclose their feelings. The lack of any incentive or opportunity to confide and feel understood made young people feel very lonely.
“Having others reach out, however, was not always beneficial. Some participants, especially females, did not feel comfortable opening up to those who reached out to them. These participants did not believe the other person would understand what they were going through, believed their problems were ‘ no one else’s business ’ or doubted the person’s motives for reaching out.” [ 41 ]
“Despite the fact that all the individuals in this sample acknowledged social support as an important part of their daily lives, the belief that others cannot understand their experiences often caused individuals to feel alone.” [ 46 ]
Theme 3: the desire to connect
Despite young people reporting a tendency to disengage from certain social interactions, they still expressed a desire for connection and a desire to feel ‘normal’.
“At the same time, the adolescents hoped to have more friends and to be included in their peer group. In addition, they wished to have a good time with the friends and to have somebody to talk to about their problems and feelings.” [ 42 ]
“Most individuals have a strong need to connect and have positive relationships with others especially middle school students.” [ 51 ]
In this sub-theme we identified a conflict with the experiences described in sub-themes 2.3 and 2.4 above, in that although some individuals expressed a wish to talk about their issues, they also experienced difficulties in doing so. Such barriers included a fear of the consequences, particularly the threat of rejection (and perhaps stigmatisation) from peers. To address this, some preferred to share their problems with people who they knew had faced the same mental health issues in preference to their wider peer group, amongst whom it was not always clear who had experienced depression themselves.
Shadow clearly had the wish to disclose to someone, which he expressed in a wish for some kind of group therapy to meet people where he could actually speak about his problems: “ And maybe, that you can talk about it in a group that you can say: “I am [Shadow], I have this and that problem. What do you think, what is your impression, what is your problem?” . . . Because I can’t possibly walk into my classroom and say: “you know what happened to me?” Well, I could, but . . .” (Male, teenager; German sample) [ 52 ].
Theme 4: paradoxes of loneliness and depression
This theme described a number of paradoxes or vicious cycles that were apparent in various forms across a number of studies. Whilst some young people talked about a need or a tendency to withdraw socially, this came with an awareness that such avoidance could create or worsen feelings of loneliness.
“During their depressive experiences, participants felt a distinct separateness from others and often chose solitude over being with others even when feeling lonely” [ 44 ].
“Being around people was, was always a bad thing for me. I constantly felt the need to be alone . . . and I always felt like interacting with other people was difficult for me . . . Ya, that was confusing because I felt lonely but I didn’t feel like being around anyone at the same time” (Jeff, in his 20s, Canadian sample) [ 45 ].
Some young people described their friends showing a form of understanding by not asking too many questions, but then feeling cut off because of an apparent absence of overt concern.
Sometimes when some of my friends are … .. ok with ignoring me, with not asking about it, I feel like kind of I know it’s ridiculous, but unloved. (Female, teenager, UK sample) [ 50 ].
Another trap that some young people described was a vicious cycle of loneliness and depression, was the suggestion that the manner in which they processed feelings about loneliness reinforced their depression.
“They were unable to initiate or sustain relationships because of feelings of severe discomfort around people. They described a cycle of feeling lonely, often as a result of their breakups, and then feeling depressed about the loneliness, causing a self-fulfilling prophecy by further alienating and self-isolating themselves from others.” [ 45 ]
A fear of stigma was also mentioned as a reason for withdrawing from others, but this came at the price of increasing loneliness. Sometimes a yearning to connect with others coexisted with an inability to be with them. However, where they withdrew from others, young people were prevented from getting support from others, thus increasing their sense of alienation from friends.
“While some disclosed their depression to friends, others withdrew, fearful of the perceived stigma and loss of status from being labelled as having mental illness …. However, retreating from others contributed to their loneliness and isolation.” [ 48 ]
The difficult choice that some young people faced, was between withdrawing socially to hide their depression and then feeling excluded, or remaining superficially socially engaged but living behind a façade in not disclosing their depression. In the latter case, the strain of concealing their low mood could create a sense of greater alienation from their peers.
“This process of social isolation was characterized by ambivalent feelings. Participants explained that on the one hand they feel the necessity to share their emotions with others, but on the other hand they felt it was impossible to do this. Consequently, they felt caught up in a vicious circle which made them feel alienated from themselves and from of their social world.” [ 24 ].
No suggestions were made by participants as to how to break such vicious cycles, but a note of optimism was sounded in relation to recovery from depression. During an episode of depression young people characteristically described the experience of yearning for a connection with others, feelings of being very different from others, and a perception that their problems were incomprehensible to their peers; all of which meant that when unwell, gaining a sense of connectedness was out of their reach. However, on recovering from an episode of depression, those who reflected back on those unwell periods had better insight into such traps and were able to see how a lifting of their symptoms removed many of the barriers to connecting with others.
Main findings
This meta-synthesis of fourteen qualitative studies describing the experience of loneliness among young people with depression identified four main themes, conveying the social consequences of both loneliness and depression, and illustrating a range of pathways between them and a sense of how these could be mutually reinforcing. Young people described the symptoms of their depression as leading to social withdrawal. Although they did not name them as such, the symptoms they described match those featuring in diagnostic criteria for depression (low energy, anhedonia, avolition, low self-esteem). The first theme suggests that although debilitating, these symptoms could lead to social isolation but not necessarily feelings of loneliness. Indeed, some young people gained a sense of relief when not having to engage in their usual social roles although this pattern of social withdrawal risked increasing the probability of feeling lonely over the longer term. Our second theme was more explicitly related to loneliness, capturing how non-disclosure of depression made it hard for young people to feel connected because it distanced them from others. Contrary to the experiences of those who preferred to avoid others even at the cost of feeling lonely, data coded under our third theme illustrated a longing to be among others. Our fourth theme described a set of paradoxes faced by young depressed people, including that of yearning for connection, or believing it might help with low mood, yet being unable to tolerate being around others. This theme also described a self-perpetuating cycle of loneliness and depression, providing insights into the cognitive processes underlying this bidirectional relationship. Our data suggest that where depressed individuals engage in certain behaviours (withdrawing and not confiding) this can lead to feelings of loneliness, an awareness of which worsens their mood, thus perpetuating their depression. Again, this process of self-isolation and social alienation builds a sense of one pathway in an apparent bidirectional relationship.
We did not observe any gender or age patterning of themes, but it was hard to rule these out without access to the primary data. Ranging in age from 11 to 30 years, many older subjects reflected back on their previous experiences, but it was not always clear what age they were referring to. We also did not identify any mention of difficulties accessing social contacts or in meeting people, in contrast to the issue of sparse social networks being described as a problem for older age groups [ 55 , 56 ]. In our data psychological aspects of depression were more prominent than social aspects of depression. Although some participants mentioned social anhedonia there was little mention of impaired social communication (for example impaired emotion recognition) or of impaired social perception (for example reduced empathy), as might otherwise be seen in depression [ 57 ]. However, participants may have lacked an awareness of this and we lacked collateral accounts to triangulate their own. We also did not identify overt descriptions of perceived stigma, although this was implied in an avoidance of disclosing depression to peers. Our themes built up a theoretical framework focussed on a dominant pathway of depression leading to loneliness (and loneliness worsening depression) than on loneliness having predated (and/or contributed) to the onset of depression. However, the nature of our study meant that it was impossible to probe individuals’ thoughts about predisposing factors and this warrants further interview work.
Findings in the context of other studies
We believe this to be the first meta-synthesis of qualitative studies describing the experience of loneliness in young people with depression. Quantitative testing of causal models of adolescent depression suggest that loneliness and low self-esteem increase the probability of depression, with low self-esteem having an indirect effect on depression via loneliness [ 58 ]. Our data implied that loneliness was not an antecedent of depression so much as a consequence of it, although none of the included studies probed this. Whilst we did not identify any gender patterning, US survey data suggest that loneliness was one of the most common self-reported features of depression among female adolescents with depression but far less apparent among depressed boys [ 16 ].
Our finding that some young people distance themselves from others through a fear of being rejected is consistent with the interpersonal hostility theory of loneliness [ 30 ]. This theory posits that loneliness generates negative social cognitions through which others can be perceived as threatening, competitive and unwelcoming. This leads to a self-fulfilling prophecy in which social contact is put on hold through fear of negative evaluation [ 30 ]. This process of interpersonal hostility leads to more isolation, which increases the likelihood of feeling lonely, creating a self-reinforcing loneliness cycle accompanied by feelings of low self-esteem [ 59 ].
Empirical studies exploring the responses of young people towards peers suffering from mental illness demonstrate clear stigmatising attitudes towards people with mental health problems and a preference to avoid them [ 60 ]. This would confirm what young people with depression fear: being judged and avoided. Their preference for non-disclosure is therefore unsurprising. Such work also shows that young people’s attitudes towards peers with mental health problems are influenced by their parents’ attitudes and by their previous exposure to people with mental health problems [ 60 ]. This suggests that there is scope to modify attitudes and create more accepting environments for young people with depression.
Adolescence is a time characterized by hormonal, physical, psychological and social change [ 61 ], during which identity formation, role transition, independence and creating relationships are of critical importance [ 62 ]. During this period adolescents become less dependent on parental attachment as peer relationships become more important [ 63 ], but this can mean that the effects of social exclusion by peers are felt more acutely [ 3 , 63 ]. Attachment theory suggests that psychiatric symptoms (such as depression) and feelings of loneliness arise when there is an absence of opportunity to make affectional bonds, or when bonds once made are repeatedly disrupted [ 64 ]. It is also theorised that young people with attachment disorders come to define themselves as outsiders and through this they risk becoming chronically lonely [ 62 ]. It is possible that early experience of unreliable and unresponsive attachment figures can lead to insecure attachment perceptions, including a lack of trust, low self-esteem and difficulties with affect regulation and intimacy [ 63 ]. This is supported by evidence that lonely young adults are more likely to have been bullied and socially isolated as children [ 17 ] and that securely attached adolescents report more emotionally close friendships and greater social acceptance by peers than insecurely attached peers [ 63 ]. Such work suggests that early parenting interventions to improve attachment have the potential to prevent loneliness and depression [ 65 ], although this requires formal testing.
Strengths and limitations
This meta-synthesis used a robust systematic search strategy to identify studies collecting qualitative accounts of loneliness in young people with depression across a range of countries. We followed received guidelines on conducting a meta-synthesis and used an interdisciplinary team approach in conducting our analysis. We addressed threats to validity by presenting preliminary results at a workshop attended by academics, voluntary sector practitioners, and people with lived experience, requesting feedback with which to revise our thematic framework.
The nature of our research question meant that research subjects were hard to reach and it is possible that those willing to participate in included studies are not representative of the wider population of depressed young people. The predominance of female participants from high-income countries, also limits generalisability. Whilst our research question related specifically to the experience of loneliness in the context of depression, our search strategy did not restrict eligibility to studies that had similar aims. Instead, by including studies with the broader remit of understanding the experiences of depression among young people we were able to identify instances where loneliness was mentioned in this context. Whilst this meant that included studies did not necessarily probe the experience of loneliness in depression, restricting the richness and variety in data relevant to our research question, we were able to identify and describe this where it was mentioned. Any meta-synthesis analyses the findings of previously analysed data and is therefore a subjective interpretation of an interpretation [ 34 ]. This could potentially undermine the integrity of individual studies by ignoring the context, leading to superficial interpretations rather than a deeper understanding [ 36 ]. This was a particular threat in our meta-synthesis given the range of analytic approaches used in the constituent fourteen studies. A further limitation of the meta-synthesis approach is that such interpretations are made by a group of researchers with their own perspectives, which might plausibly differ from those of another team. However, we addressed this through our consideration of reflexivity in discussions of the multidisciplinary research team. To address some of these limitations and gain a more in-depth understanding of the pathways between loneliness and depression in young adults, it would be important to conduct qualitative interview studies with a specific focus on these links.
Clinical and policy implications
Our study provides valuable insights for clinicians, teachers, parents, peers and researchers into the social challenges faced by young people with depression, helping them understand how feelings of loneliness might arise in those who feel depressed and how they might compound depressive symptoms, impeding recovery. This is consistent with the evidence that poor subjective social support is associated with poorer recovery from depression [ 10 ].
It was common for research participants to feel that others did not understand them and the distress associated with this was very apparent. Lay dissemination of the findings of this study might help young depressed people feel more understood by those in their social networks and suggest ways in which others can support them appropriately. There is evidence that social media campaigns focussed on mental health awareness and stigma reduction can promote help-seeking for mental illness, but this is thought to be attributable to wider societal awareness in creating environments where it is acceptable to disclose mental illness [ 66 ]. Creating a culture in which it is more acceptable to disclose mental ill-health has the potential to interrupt the vicious cycle of social withdrawal giving rise to loneliness and thereby worsening mood. It may be useful for clinicians to explain to young people with depression that it is common for young patients not to disclose mental health difficulties to their peers, but that this might potentially reduce their sense of connectedness. Clinicians might be able to educate them about the impact of loneliness on the prognosis of their depression and explore appropriate ways to address this.
Early intervention in loneliness would appear to be critical to prevent lonely young adults from being trapped in loneliness as they grow older [ 17 ] and to prevent it from limiting psychosocial functioning and diminishing quality of life at an important stage of social and emotional development. However, whilst this study provides an understanding of the links between loneliness and depression in social terms, it does not detail the psychological processes involved in those pathways. A better understanding of the psychological factors that engender and perpetuate loneliness in young people with depression would help identify those that are modifiable and contribute to developing effective interventions. Combining insights from cognitive neuroscience and social psychology would be helpful in the foundations for this interventional work.
Future research
We have mentioned the need to conduct interview studies directly probing the experience of loneliness in young people with depression, with balanced gender representation. Given the lack of ethnic diversity in our sample and cultural dimensions of social connections, we also need studies conducted in different ethnic groups. Such work might probe, for example, the more extreme phenomenon of hikikomori in Japan where young people with mental health problems engage in extreme self-isolation [ 67 ]. We have also mentioned the need to develop effective interventions. In the wider literature on approaches to addressing loneliness among people with mental health problems, changing cognitions to shift maladaptive cognitions is viewed as most promising, but lacks a robust evidence base [ 68 ]. Amongst trials of interventions to improve subjective and/or objective social isolation for people with mental health problems, again the most promising interventions include cognitive modification for subjective social isolation, as well as interventions with mixed strategies and supported socialisation for objective social isolation [ 69 ]. More research is needed to develop and assess the acceptability of interventions that address cognitions about social engagement among young people with mental health problems, before trialling them rigorously.
Our meta-synthesis of fourteen qualitative studies capturing experiences of loneliness among young people with depression identified four themes revealing the challenges faced by these individuals in their social networks. They described how the symptoms of their depression hampered social engagement, leading to social withdrawal. A preference not to disclose their mental health problems, for a variety of reasons, compounded the perception of differences between depressed young people and their peers. Many longed for a connection with others, but could not tolerate the experience of being with others. Some participants described a self-reinforcing cycle of loneliness and depression, from which it was hard to see a way out. Although participants did not suggest how to intervene to break this cycle, our findings suggest that supporting young people with depression to find appropriate ways to disclose their problems has potential to promote a sense of feeling understood by their peers. The published literature also suggests a role for cognitive interventions to shift maladaptive cognitions about their social world. More widely, a change in societal attitudes towards young people with mental illness would also help promote a sense of feeling accepted and socially connected.
Availability of data and materials
All data are published and in the public domain.
Abbreviations
Academisch Medisch Centrum (Academic Medical Centre)
Critical Appraisal Skills Programme
University College London
World Health Organisation
United Kingdom
United Kingdom Research and Innovation
University Medical Centre
United States of America
Peplau L, Perlman D. Perspectives on loneliness. In: Peplau LA, Perlman D, editors. Loneliness: a sourcebook of current theory, research and therapy. New York: Wiley; 1982. p. 1–8.
Google Scholar
Morrison P, Smith R. Loneliness. An overview. In: Sagan OM, E.D., editor. Narraties of loneliness multidisciplinary perspectives from the 21st century. Oxfordshire: Routledge; 2018.
Spitzer M. Eenzaamheid ('Loneliness'). Amsterdam: Antwerpen: Atlas Contact; 2019.
Malhi G, Mann J. Depression. Lancet. 2018;392(10161):2299–312.
PubMed Google Scholar
Liu Y, Zhang N, Bao G, Huang Y, Ji B, Wu Y, et al. Predictors of depressive symptoms in college students: a systematic review and meta-analysis of cohort studies. J Affect Disord. 2019;244:196–208.
CAS PubMed Google Scholar
Meltzer H, Bebbington P, Dennis M, Jenkins R, McManus S, Brugha T. Feelings of loneliness among adults with mental disorder. Soc Psychiatry Psychiatr Epidemiol. 2013;48(1):5–13.
Smalbrugge M, Jongenelis L, Pot AM, Eefsting JA, Ribbe MW, Beekman ATF. Incidence and outcome of depressive symptoms in nursing home patients in the Netherlands. Am J Geriatr Psychiatry. 2006;14(12):1069–76.
Sjöberg L, Östling S, Falk H, Sundh V, Waern M, Skoog I. Secular changes in the relation between social factors and depression: a study of two birth cohorts of Swedish septuagenarians followed for 5 years. J Affect Disord. 2013;150(2):245–52.
Stessman J, Rottenberg Y, Shimshilashvili I, Ein-Mor E, Jacobs J. Loneliness, health, and longevity. J Gerontol. 2013;69(6):744–50.
Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. 2018;18(1):156.
PubMed PubMed Central Google Scholar
Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. 2006;21(1):140–51.
Lasgaard M, Friis K, Shevlin M. “Where are all the lonely people?” a population-based study of high-risk groups across the life span. Soc Psychiatry Psychiatr Epidemiol. 2016;51(10):1373–84.
Vanhalst J, Goossens L, Luyckx K, Scholte R, Engels R. The development of loneliness from mid- to late adolescence: trajectory classes, personality traits, and psychosocial functioning. J Adolesc. 2013;36(6):1305–12.
Vanhalst J, Klimstra TA, Luyckx K, Scholte R, Engels R, Goossens L. The interplay of loneliness and depressive symptoms across adolescence: exploring the role of personality traits. J Youth Adolescence. 2012;41(6):776–87.
Rokach A. Loneliness of the marginalized. Open J Depression. 2014;3:147–53.
Crowe M, Ward N, Dunnachie B, Roberts M. Characteristics of adolescent depression. Int J Ment Health Nurs. 2006;15(1):10–8.
Matthews T, Danese A, Caspi A, Fisher H, Goldman-Mellor S, Kepa A, et al. Lonely young adults in modern Britain: findings from an epidemiological cohort study. Psychol Med. 2018;49(2):268–77.
Maes M, Van den Noortgate W, Fustolo-Gunnink S, Rassart J, Luyckx K, Goossens L. Loneliness in children and adolescents with chronic physical conditions: a meta-analysis. J Pediatr Psychol. 2017;42(6):622–35.
Qualter P, Brown S, Munn P, Rotenberg K. Childhood loneliness as a predictor of adolescent depressive symptoms: an 8-year longitudinal study. Eur Child Adolesc Psychiatry. 2010;19(6):493–501.
van Winkel M, Wichers M, Collip D, Jacobs N, Derom C, Thiery E, et al. Unraveling the role of loneliness in depression: the relationship between daily life experience and behavior. Psychiatry. 2017;80(2):104–17.
Salaheddin K, Mason B. Identifying barriers to mental health help-seeking among young adults in the UK: a cross-sectional survey. Br J Gen Pract. 2016;66(651):e686–e92.
Pitman A, Mann F, Johnson S. Advancing our understanding of loneliness and mental health problems in young people. Lancet Psychiatry. 2018;5(12):955–6.
Wang J, Lloyd-Evans B, Giacco D, Forsyth R, Nebo C, Mann F, et al. Social isolation in mental health: a conceptual and methodological review. Soc Psychiatry Psychiatr Epidemiol. 2017;52(12):1451–61.
De Mol J, D’Alcantara A, Cresti B. Agency of depressed adolescents: embodiment and social representations. Int J Qual Stud Health Well-Being. 2018;13(sup1):1564516.
Hare-Duke L, Dening T, de Oliveira D, Milner K, Slade M. Conceptual framework for social connectedness in mental disorders: systematic review and narrative synthesis. J Affect Disord. 2018;15(24):188–99.
Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol Bull. 1995;117(3):497–529.
de Jong GJ, van Tilburg T, Dykstra PA. Loneliness and social isolation. In: Perlman DVA, editor. The Cambridge handbook of personal relationships. Cambridge: Cambridge University Press; 2009. p. 485–500.
Matthews T, Danese A, Wertz J, Odgers CL, Ambler A, Moffitt TE, et al. Social isolation, loneliness and depression in young adulthood: a behavioural genetic analysis. Soc Psychiatry Psychiatr Epidemiol. 2016;51(3):339–48.
Ge L, Yap CW, Ong R, Heng BH. Social isolation, loneliness and their relationships with depressive symptoms: A population-based study. PLoS One. 2017;12(8):e0182145.
Cacioppo JT, Patrick W. Loneliness: Human nature and the need for social connection. New York: W W Norton & Co; 2008. p. 317-xiv.
Child S, Lawton L. Loneliness and social isolation among young and late middle-age adults: associations with personal networks and social participation. Aging Ment Health. 2019;23(2):196–204.
ONS (Office for National Statistics) UK. Children’s and young people’s experiences of loneliness: 2018.
Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol. 2009;9(1):59.
Erwin E, Brotherson MJ, Summers JA. Understanding qualitative Metasynthesis: issues and opportunities in early childhood intervention research. J Early Interv. 2011;33(3):186–200.
Lachal J, Revah-Levy A, Orri M, Moro MR. Metasynthesis: An Original Method to Synthesize Qualitative Literature in Psychiatry. Front Psychiatry. 2017;8:269.
Sandelowski M, Docherty S, Emden C. Qualitative metasynthesis: issues and techniques. Res Nurs Health. 1997;20(4):365–71.
Noblit G, Hare R. Meta-ethnography: synthesizing qualitative studies London : SAGE; 1988.
Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol. 2008;8(1):21.
Prospero. International Prospective Register of Systematic Reviews. https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=133569 . Accessed March 2019.
Programme CAS. CASP (Qualitative) Checklist. Available at: https://casp-uk.net/casp-tools-checklists/ . Accessed: March 2019.; 2018.
Al-Khattab H, Oruche U, Perkins D, Draucker C. How African American adolescents manage depression: being with others. J Am Psychiatr Nurs Assoc. 2016;22(5):387–400.
Anttila K, Anttila M, Kurki M, Hätönen H, Marttunen M, Välimäki M. Concerns and hopes among adolescents attending adolescent psychiatric outpatient clinics. Child Adolesc Mental Health. 2015;20(2):81–8.
Dundon E. HS adolescent depression: a Metasynthesis. J Pediatr Health Care. 2006;20(6):384–92.
Farmer TJ. HS the experience of major depression: Adolescents' perspectives. Issues Mental Health Nurs. 2002;23(6):567–85.
Granek L. What’s love got to do with it? The relational nature of depressive experiences. J Humanist Psychol. 2006;46(2):191–208.
Kuwabara S, Van Voorhees B, Gollan J, Alexander G. HS a qualitative exploration of depression in emerging adulthood: disorder, development, and social context. Gen Hosp Psychiatry. 2007;29(4):317–24.
Lachal J, Speranza M, Schmitt A, Spodenkiewicz M, Falissard B, Moro MR, et al. Depression in adolescence: from qualitative research to measurement. Adolesc Psychiatry. 2012;2(4):296–308.
McCann TV, Lubman DI, Clark E. The experience of young people with depression: a qualitative study. J Psychiatr Ment Health Nurs. 2012;19(4):334–40.
Meadus R. Adolescents coping with mood disorder: a grounded theory study. J Psychiatr Ment Health Nurs. 2007;14(2):209–17.
Midgley N, Parkinson S, Holmes J, Stapley E, Eatough V, Target M. Beyond a diagnosis: the experience of depression among clinically-referred adolescents. J Adolesc. 2015;44:269–79.
Rosales L. A phenomenological exploration: the voices of middle school adolescents who suffer from depression [Ph.D.]. Ann Arbor: Texas A&M University - Corpus Christi; 2008.
Weitkamp K, Klein E, Midgley N. The experience of depression: a qualitative study of adolescents with depression entering psychotherapy. Global Qual Nurs Res. 2016;3:2333393616649548.
Woodgate R. Living in the shadow of fear: adolescents’ lived experience of depression. J Adv Nurs. 2006;56(3):261–9.
QSR International Pty Ltd. (2020) NVivo (released in March 2020). https://www.qsrinternational.com/nvivo-qualitative-data-analysissoftware/home .
Domènech-Abella J, Lara E, Rubio-Valera M, Olaya B, Moneta M, Rico-Uribe L, et al. Loneliness and depression in the elderly: the role of social network. Soc Psychiatry Psychiatr Epidemiol. 2017;52(4):381–90.
Rico-Uribe L, Caballero F, Olaya B, Tobiasz-Adamczyk B, Koskinen S, Leonardi M, et al. Loneliness, social networks, and health: a cross-sectional study in three countries. PloS One. 2016;11(1):e0145264–e.
Kupferberg A, Bicks L, Hasler G. Social functioning in major depressive disorder. Neurosci Biobehav Rev. 2016;69:313–32.
Brage D, Meredith W. A causal model of adolescent depression. J Psychol. 1994;128(4):455–68.
Hawkley L, Cacioppo J. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218–27.
Jorm A, Wright AM. Influences on young people's stigmatising attitudes towards peers with mental disorders: national survey of young Australians and their parents. Br J Psychiatry. 2008;192(2):144–9.
Blakemore SJ. Development of the social brain in adolescence. J R Soc Med. 2012;105(3):111–6.
Weiss RS. Loneliness. The Experience of Emotional and Social Isolation. Cambridge (UK) / London (US): the MIT Press; 1973.
Bostik KE, Everall RD. In my mind I was alone: suicidal Adolescents' perceptions of attachment relationships. Int J Adv Couns. 2006;28(3):269–87.
Bowlby J. The making & breaking of Affectional bonds. London: Routledge; 1979.
Wright B, Edginton E. Evidence-based parenting interventions to promote secure attachment: findings from a systematic review and meta-analysis. Glob Pediatr Health. 2016;3:2333794X16661888–2333794X.
Booth RG, Allen BN, Bray Jenkyn KM, Li L, Shariff SZ. Youth mental health services utilization rates after a large-scale social media campaign: population-based interrupted time-series analysis. JMIR Ment Health. 2018;5(2):e27.
Li TM, Wong PW. Youth social withdrawal behavior (hikikomori): a systematic review of qualitative and quantitative studies. Australian New Zealand J Psychiatry. 2015;49(7):595–609.
Mann F, Bone J, Lloyd-Evans B, Frerichs J, Pinfold V, Ma R, et al. A life less lonely: the state of the art in interventions to reduce loneliness in people with mental health problems. Social Psychiatry Psychiatric Epidemiol. 2017;52(6):627–38.
Ma R, Mann F, Wang J, et al. The effectiveness of interventions for reducing subjective and objective social isolation among people with mental health problems: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2020;55:839–76. https://doi.org/10.1007/s00127-019-01800-z .
UCL Event. Understanding Loneliness in people with mental health problems. https:// www.ucl.ac.uk/psychiatry/research/epidemiology-and-applied-clinical-research-department/loneliness-and-social-isolation-11 . Accessed June 2019.
Download references
Acknowledgements
We would like to thank participants in the Loneliness and Social Isolation in Mental Health research network event ‘ Understanding loneliness in people with mental health problems’ at UCL on 26 June 2019 who contributed to a discussion of the emergent thematic framework for this study [ 70 ].
LA conducted this work as part of his mandatory academic internship within the master’s programme in Medicine of the University of Amsterdam, supervised by AP, MB, EP, HS and SJ, and did not receive specific funding. AP, MB, EP, and SJ are supported by a UKRI grant to fund the Loneliness and Social Isolation in Mental Health research network, one of eight Mental Health Networks https://www.ukri.org/research/themes-and-programmes/mental-health-networks/ . AP and SJ are also supported by the University College London Hospitals (UCLH) National Institute for Health Research (NIHR) Biomedical Research Centre (BRC). SJ is additionally supported by the NIHR Mental Health Policy Research Unit and the NIHR Collaboration for Leadership in Applied Health Research and Care (CLAHRC) North Thames. The funders had no role in the design of the study, or in the collection, analysis, or interpretation of data, or in writing or approving the manuscript.
Author information
Authors and affiliations.
UCL Division of Psychiatry, Maple House, 149 Tottenham Court Road, London, W1T 7NF, UK
Louis Achterbergh, Alexandra Pitman, Mary Birken, Eiluned Pearce & Sonia Johnson
Amsterdam UMC, location AMC (University of Amsterdam), Meibergdreef 9, 1105, Amsterdam, AZ, Netherlands
Louis Achterbergh & Herman Sno
Camden and Islington NHS Foundation Trust, St Pancras Hospital, 4 St Pancras Way, London, NW1 0PE, UK
Alexandra Pitman & Sonia Johnson
You can also search for this author in PubMed Google Scholar
Contributions
LA, AP, MB, EP, and SJ conceived the meta-synthesis. LA developed the search strategy and created the review protocol, in collaboration with AP, MB, EP, SJ, and HS. LA conducted the literature search and the initial screen of identified studies, and screened reference lists of included studies. LA, AP, MB, and EP independently contributed to the screening process. LA extracted data, with independent ratings from AP, MB, and EP. LA assessed the methodological quality of each included paper, with input from AP, MB, and EP. LA wrote the first draft, with input from all authors on subsequent drafts. AP co-ordinated the final draft. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Louis Achterbergh .
Ethics declarations
Ethics approval and consent to participate.
We did not seek ethical approval as all data were published and already in the public domain, including dissertations available on Ethos British Library database.

Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Search strategy
To reduce the risk of missing relevant studies our initial search protocol included a term to capture a diagnosis of personality disorder. However, as per our inclusion/exclusion criteria, only studies relating to young people with depression were included.
MeSH terms:
Mood disorder / Affective disorder / Personality disorder / Anxiety disorder /
(and related relevant MeSH depending on database)
OR Depress*
OR Personality disorder**
OR Borderline personality disorder or emotionally-unstable personality disorder or histrionic personality disorder or narcissistic personality disorder
OR Avoidant personality disorder or dependent personality disorder or obsessive/compulsive personality disorder)
AND Loneliness
loneliness [MeSH] OR loneliness OR lonely
(social* adj/2
participation
disconnect*
AND Qualitative research
“Qualitative research”
Interviews as Topic
“Qualitative adj2 (stud* OR method*)”
“Lived experience”
“Mixed?method*”
“Thematic analysis”
“semi-structured” or semistructured or unstructured
(guide*) adj2 (interview* or discussion*))
Focus groups
ethnograph*
group discussion
Patient perspective
NOT (in title)
Mild cognitive impairment
Brain injury
Kidney failure
Renal disease
hemodialysis
Diabetes mellitus
Cystic fibrosis
Coronary heart
We ensured that personality disorder was well-represented in our search terms so that we could conduct two meta-syntheses of qualitative studies with young people based on this search. This article relates only to studies in which the primary diagnosis was depression.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Achterbergh, L., Pitman, A., Birken, M. et al. The experience of loneliness among young people with depression: a qualitative meta-synthesis of the literature. BMC Psychiatry 20 , 415 (2020). https://doi.org/10.1186/s12888-020-02818-3
Download citation
Received : 23 April 2020
Accepted : 12 August 2020
Published : 24 August 2020
DOI : https://doi.org/10.1186/s12888-020-02818-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social isolation
- Meta-synthesis
- Systematic review
- Qualitative research
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Change Password
Your password must have 8 characters or more and contain 3 of the following:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
- Sign in / Register
Request Username
Can't sign in? Forgot your username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
An Exploratory Study of Students with Depression in Undergraduate Research Experiences
- Katelyn M. Cooper
- Logan E. Gin
- M. Elizabeth Barnes
- Sara E. Brownell
*Address correspondence to: Katelyn M. Cooper ( E-mail Address: [email protected] ).
Department of Biology, University of Central Florida, Orlando, FL, 32816
Search for more papers by this author
Biology Education Research Lab, Research for Inclusive STEM Education Center, School of Life Sciences, Arizona State University, Tempe, AZ 85281
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect graduate student depression, we know of no studies that have explored the relationship between depression and undergraduate research. In this study, we sought to understand how undergraduates’ symptoms of depression affect their research experiences and how research affects undergraduates’ feelings of depression. We interviewed 35 undergraduate researchers majoring in the life sciences from 12 research-intensive public universities across the United States who identify with having depression. Using inductive and deductive coding, we identified that students’ depression affected their motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing in undergraduate research experiences. We found that students’ social connections, experiencing failure in research, getting help, receiving feedback, and the demands of research affected students’ depression. Based on this work, we articulate an initial set of evidence-based recommendations for research mentors to consider in promoting an inclusive research experience for students with depression.
INTRODUCTION
Depression is described as a common and serious mood disorder that results in persistent feelings of sadness and hopelessness, as well as a loss of interest in activities that one once enjoyed ( American Psychiatric Association [APA], 2013 ). Additional symptoms of depression include weight changes, difficulty sleeping, loss of energy, difficulty thinking or concentrating, feelings of worthlessness or excessive guilt, and suicidality ( APA, 2013 ). While depression results from a complex interaction of psychological, social, and biological factors ( World Health Organization, 2018 ), studies have shown that increased stress caused by college can be a significant contributor to student depression ( Dyson and Renk, 2006 ).
Depression is one of the top undergraduate mental health concerns, and the rate of depression among undergraduates continues to rise ( Center for Collegiate Mental Health, 2017 ). While we cannot discern whether these increasing rates of depression are due to increased awareness or increased incidence, it is clear that is a serious problem on college campuses. The percent of U.S. college students who self-reported a diagnosis with depression was recently estimated to be about 25% ( American College Health Association, 2019 ). However, higher rates have been reported, with one study estimating that up to 84% of undergraduates experience some level of depression ( Garlow et al. , 2008 ). Depression rates are typically higher among university students compared with the general population, despite being a more socially privileged group ( Ibrahim et al. , 2013 ). Prior studies have found that depression is negatively correlated with overall undergraduate academic performance ( Hysenbegasi et al. , 2005 ; Deroma et al. , 2009 ; American College Health Association, 2019 ). Specifically, diagnosed depression is associated with half a letter grade decrease in students’ grade point average ( Hysenbegasi et al. , 2005 ), and 21.6% of undergraduates reported that depression negatively affected their academic performance within the last year ( American College Health Association, 2019 ). Provided with a list of academic factors that may be affected by depression, students reported that depression contributed to lower exam grades, lower course grades, and not completing or dropping a course.
Students in the natural sciences may be particularly at risk for depression, given that such majors are noted to be particularly stressful due to their competitive nature and course work that is often perceived to “weed students out”( Everson et al. , 1993 ; Strenta et al. , 1994 ; American College Health Association, 2019 ; Seymour and Hunter, 2019 ). Science course instruction has also been described to be boring, repetitive, difficult, and math-intensive; these factors can create an environment that can trigger depression ( Seymour and Hewitt, 1997 ; Osborne and Collins, 2001 ; Armbruster et al ., 2009 ; Ceci and Williams, 2010 ). What also distinguishes science degree programs from other degree programs is that, increasingly, undergraduate research experiences are being proposed as an essential element of a science degree ( American Association for the Advancement of Science, 2011 ; President’s Council of Advisors on Science and Technology, 2012 ; National Academies of Sciences, Engineering, and Medicine [NASEM], 2017 ). However, there is some evidence that undergraduate research experiences can add to the stress of college for some students ( Cooper et al. , 2019c ). Students can garner multiple benefits from undergraduate research, including enhanced abilities to think critically ( Ishiyama, 2002 ; Bauer and Bennett, 2003 ; Brownell et al. , 2015 ), improved student learning ( Rauckhorst et al. , 2001 ; Brownell et al. , 2015 ), and increased student persistence in undergraduate science degree programs ( Jones et al. , 2010 ; Hernandez et al. , 2018 ). Notably, undergraduate research experiences are increasingly becoming a prerequisite for entry into medical and graduate programs in science, particularly elite programs ( Cooper et al. , 2019d ). Although some research experiences are embedded into formal lab courses as course-based undergraduate research experiences (CUREs; Auchincloss et al. , 2014 ; Brownell and Kloser, 2015 ), the majority likely entail working with faculty in their research labs. These undergraduate research experiences in faculty labs are often added on top of a student’s normal course work, so they essentially become an extracurricular activity that they have to juggle with course work, working, and/or personal obligations ( Cooper et al. , 2019c ). While the majority of the literature surrounding undergraduate research highlights undergraduate research as a positive experience ( NASEM, 2017 ), studies have demonstrated that undergraduate research experiences can be academically and emotionally challenging for students ( Mabrouk and Peters, 2000 ; Seymour et al. , 2004 ; Cooper et al. , 2019c ; Limeri et al. , 2019 ). In fact, 50% of students sampled nationally from public R1 institutions consider leaving their undergraduate research experience prematurely, and about half of those students, or 25% of all students, ultimately leave their undergraduate research experience ( Cooper et al. , 2019c ). Notably, 33.8% of these individuals cited a negative lab environment and 33.3% cited negative relationships with their mentors as factors that influenced their decision about whether to leave ( Cooper et al. , 2019c ). Therefore, students’ depression may be exacerbated in challenging undergraduate research experiences, because studies have shown that depression is positively correlated with student stress ( Hish et al. , 2019 ).
While depression has not been explored in the context of undergraduate research experiences, depression has become a prominent concern surrounding graduate students conducting scientific research. A recent study that examined the “graduate student mental health crisis” ( Flaherty, 2018 ) found that work–life balance and graduate students’ relationships with their research advisors may be contributing to their depression ( Evans et al. , 2018 ). Specifically, this survey of 2279 PhD and master’s students from diverse fields of study, including the biological/physical sciences, showed that 39% of graduate students have experienced moderate to severe depression. Fifty-five percent of the graduate students with depression who were surveyed disagreed with the statement “I have good work life balance,” compared to only 21% of students with depression who agreed. Additionally, the study highlighted that more students with depression disagreed than agreed with the following statements: their advisors provided “real” mentorship, their advisors provided ample support, their advisors positively impacted their emotional or mental well-being, their advisors were assets to their careers, and they felt valued by their mentors. Another recent study identified that depression severity in biomedical doctoral students was significantly associated with graduate program climate, a perceived lack of employment opportunities, and the quality of students’ research training environment ( Nagy et al. , 2019 ). Environmental stress, academic stress, and family and monetary stress have also been shown to be predictive of depression severity in biomedical doctoral students ( Hish et al. , 2019 ). Further, one study found that self-esteem is negatively correlated and stress is positively correlated with graduate student depression; presumably research environments that challenge students’ self-esteem and induce stress are likely contributing to depressive symptoms among graduate students ( Kreger, 1995 ). While these studies have focused on graduate students, and there are certainly notable distinctions between graduate and undergraduate research, the research-related factors that affect graduate student depression, including work–life balance, relationships with mentors, research environment, stress, and self-esteem, may also be relevant to depression among undergraduates conducting research. Importantly, undergraduates in the United States have reported identical levels of depression as graduate students but are often less likely to seek mental health care services ( Wyatt and Oswalt, 2013 ), which is concerning if undergraduate research experiences exacerbate depression.
Based on the literature on the stressors of undergraduate research experiences and the literature identifying some potential causes of graduate student depression, we identified three aspects of undergraduate research that may exacerbate undergraduates’ depression. Mentoring: Mentors can be an integral part of a students’ research experience, bolstering their connections with others in the science community, scholarly productivity, and science identity, as well as providing many other benefits ( Thiry and Laursen, 2011 ; Prunuske et al. , 2013 ; Byars-Winston et al. , 2015 ; Aikens et al. , 2016 , 2017 ; Thompson et al. , 2016 ; Estrada et al. , 2018 ). However, recent literature has highlighted that poor mentoring can negatively affect undergraduate researchers ( Cooper et al. , 2019c ; Limeri et al. , 2019 ). Specifically, one study of 33 undergraduate researchers who had conducted research at 10 institutions identified seven major ways that they experienced negative mentoring, which included absenteeism, abuse of power, interpersonal mismatch, lack of career support, lack of psychosocial support, misaligned expectations, and unequal treatment ( Limeri et al. , 2019 ). We hypothesize negative mentoring experiences may be particularly harmful for students with depression, because support, particularly social support, has been shown to be important for helping individuals with depression cope with difficult circumstances ( Aneshensel and Stone, 1982 ; Grav et al. , 2012 ). Failure: Experiencing failure has been hypothesized to be an important aspect of undergraduate research experiences that may help students develop some the most distinguishing abilities of outstanding scientists, such as coping with failure, navigating challenges, and persevering ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, experiencing failure and the stress and fatigue that often accompany it may be particularly tough for students with depression ( Aldwin and Greenberger, 1987 ; Mongrain and Blackburn, 2005 ). Lab environment: Fairness, inclusion/exclusion, and social support within one’s organizational environment have been shown to be key factors that cause people to either want to remain in the work place and be productive or to want to leave ( Barak et al. , 2006 ; Cooper et al. , 2019c ). We hypothesize that dealing with exclusion or a lack of social support may exacerbate depression for some students; patients with clinical depression react to social exclusion with more pronounced negative emotions than do individuals without clinical depression ( Jobst et al. , 2015 ). While there are likely other aspects of undergraduate research that affect student depression, we hypothesize that these factors have the potential to exacerbate negative research experiences for students with depression.
Depression has been shown to disproportionately affect many populations that are underrepresented or underserved within the scientific community, including females ( American College Health Association, 2018 ; Evans et al. , 2018 ), first-generation college students ( Jenkins et al. , 2013 ), individuals from low socioeconomic backgrounds ( Eisenberg et al. , 2007 ), members of the LGBTQ+ community ( Eisenberg et al. , 2007 ; Evans et al. , 2018 ), and people with disabilities ( Turner and Noh, 1988 ). Therefore, as the science community strives to be more diverse and inclusive ( Intemann, 2009 ), it is important that we understand more about the relationship between depression and scientific research, because negative experiences with depression in scientific research may be contributing to the underrepresentation of these groups. Specifically, more information is needed about how the research process and environment of research experiences may affect depression.
Given the high rate of depression among undergraduates, the links between depression and graduate research, the potentially challenging environment of undergraduate research, and how depression could disproportionately impact students from underserved communities, it is imperative to begin to explore the relationship between scientific research and depression among undergraduates to create research experiences that could maximize student success. In this exploratory interview study, we aimed to 1) describe how undergraduates’ symptoms of depression affect their research experiences, 2) understand how undergraduate research affects students’ feelings of depression, and 3) identify recommendations based on the literature and undergraduates’ reported experiences to promote a positive research experience for students with depression.
This study was done with an approved Arizona State University Institutional Review Board protocol #7247.
In Fall 2018, we surveyed undergraduate researchers majoring in the life sciences across 25 research-intensive (R1) public institutions across the United States (specific details about the recruitment of the students who completed the survey can be found in Cooper et al. (2019c) ). The survey asked students for their opinions about their undergraduate research experiences and their demographic information and whether they would be interested in participating in a follow-up interview related to their research experiences. For the purpose of this study, we exclusively interviewed students about their undergraduate research experiences in faculty member labs; we did not consider students’ experiences in CUREs. Of the 768 undergraduate researchers who completed the survey, 65% ( n = 496) indicated that they would be interested in participating in a follow-up interview. In Spring 2019, we emailed the 496 students, explaining that we were interested in interviewing students with depression about their experiences in undergraduate research. Our specific prompt was: “If you identify as having depression, we would be interested in hearing about your experience in undergraduate research in a 30–60 minute online interview.” We did not define depression in our email recruitment because we conducted think-aloud interviews with four undergraduates who all correctly interpreted what we meant by depression ( APA, 2013 ). We had 35 students agree to participate in the interview study. The interview participants represented 12 of the 25 R1 public institutions that were represented in the initial survey.
Student Interviews
We developed an interview script to explore our research questions. Specifically, we were interested in how students’ symptoms of depression affect their research experiences, how undergraduate research negatively affects student depression, and how undergraduate research positively affects student depression.
We recognized that mental health, and specifically depression, can be a sensitive topic to discuss with undergraduates, and therefore we tried to minimize any discomfort that the interviewees might experience during the interview. Specifically, we conducted think-aloud interviews with three graduate students who self-identified with having depression at the time of the interview. We asked them to note whether any interview questions made them uncomfortable. We also sought their feedback on questions given their experiences as persons with depression who had once engaged in undergraduate research. We revised the interview protocol after each think-aloud interview. Next, we conducted four additional think-aloud interviews with undergraduates conducting basic science or biology education research who identified with having depression to establish cognitive validity of the questions and to elicit additional feedback about any questions that might make someone uncomfortable. The questions were revised after each think-aloud interview until no question was unclear or misinterpreted by the students and we were confident that the questions minimized students’ potential discomfort ( Trenor et al. , 2011 ). A copy of the final interview script can be found in the Supplemental Material.
All interviews were individually conducted by one of two researchers (K.M.C. and L.E.G.) who conducted the think-aloud interviews together to ensure that their interviewing practices were as similar as possible. The interviews were approximately an hour long, and students received a $15 gift card for their participation.
Personal, Research, and Depression Demographics
All student demographics and information about students’ research experiences were collected using the survey distributed to students in Fall 2018. We collected personal demographics, including the participants’ gender, race/ethnicity, college generation status, transfer status, financial stability, year in college, major, and age. We also collected information about the students’ research experiences, including the length of their first research experiences, the average number of hours they spend in research per week, how they were compensated for research, who their primary mentors were, and the focus areas of their research.
In the United States, mental healthcare is disproportionately unavailable to Black and Latinx individuals, as well as those who come from low socioeconomic backgrounds ( Kataoka et al. , 2002 ; Howell and McFeeters, 2008 ; Santiago et al. , 2013 ). Therefore, to minimize a biased sample, we invited anyone who identified with having depression to participate in our study; we did not require students to be diagnosed with depression or to be treated for depression in order to participate. However, we did collect information about whether students had been formally diagnosed with depression and whether they had been treated for depression. After the interview, all participants were sent a link to a short survey that asked them if they had ever been diagnosed with depression and how, if at all, they had ever been treated for depression. A copy of these survey questions can be found in the Supplemental Material. The combined demographic information of the participants is in Table 1 . The demographics for each individual student can be found in the Supplemental Material.
a Students reported the time they had spent in research 6 months before being interviewed and only reported on the length of time of their first research experiences.
b Students were invited to report multiple ways in which they were treated for their depression; other treatments included lifestyle changes and meditation.
c Students were invited to report multiple means of compensation for their research if they had been compensated for their time in different ways.
d Students were asked whether they felt financially stable, particularly during the undergraduate research experience.
e Students reported who they work/worked with most closely during their research experiences.
f Staff members included lab coordinators or lab managers.
g Other focus areas of research included sociology, linguistics, psychology, and public health.
Interview Analysis
The initial interview analysis aimed to explore each idea that a participant expressed ( Charmaz, 2006 ) and to identify reoccurring ideas throughout the interviews. First, three authors (K.M.C., L.E.G., and S.E.B.) individually reviewed a different set of 10 interviews and took detailed analytic notes ( Birks and Mills, 2015 ). Afterward, the authors compared their notes and identified reoccurring themes throughout the interviews using open coding methods ( Saldaña, 2015 ).
Once an initial set of themes was established, two researchers (K.M.C. and L.E.G.) individually reviewed the same set of 15 randomly selected interviews to validate the themes identified in the initial analysis and to screen for any additional themes that the initial analysis may have missed. Each researcher took detailed analytic notes throughout the review of an interview, which they discussed after reviewing each interview. The researchers compared what quotes from each interview they categorized into each theme. Using constant comparison methods, they assigned quotes to each theme and constantly compared the quotes to ensure that each quote fit within the description of the theme ( Glesne and Peshkin, 1992 ). In cases in which quotes were too different from other quotes, a new theme was created. This approach allowed for multiple revisions of the themes and allowed the authors to define a final set of codes; the researchers created a final codebook with refined definitions of emergent themes (the final coding rubric can be found in the Supplemental Material). Once the final codebook was established, the researchers (K.M.C. and L.E.G.) individually coded seven additional interviews (20% of all interviews) using the coding rubric. The researchers compared their codes, and their Cohen’s κ interrater score for these seven interviews was at an acceptable level (κ = 0.88; Landis and Koch, 1977 ). One researcher (L.E.G.) coded the remaining 28 out of 35 interviews. The researchers determined that data saturation had been reached with the current sample and no further recruitment was needed ( Guest et al. , 2006 ). We report on themes that were mentioned by at least 20% of students in the interview study. In the Supplemental Material, we provide the final coding rubric with the number of participants whose interview reflected each theme ( Hannah and Lautsch, 2011 ). Reporting the number of individuals who reported themes within qualitative data can lead to inaccurate conclusions about the generalizability of the results to a broader population. These qualitative data are meant to characterize a landscape of experiences that students with depression have in undergraduate research rather than to make claims about the prevalence of these experiences ( Glesne and Peshkin, 1992 ). Because inferences about the importance of these themes cannot be drawn from these counts, they are not included in the results of the paper ( Maxwell, 2010 ). Further, the limited number of interviewees made it not possible to examine whether there were trends based on students’ demographics or characteristics of their research experiences (e.g., their specific area of study). Quotes were lightly edited for clarity by inserting clarification brackets and using ellipses to indicate excluded text. Pseudonyms were given to all students to protect their privacy.
The Effect of Depressive Symptoms on Undergraduate Research
We asked students to describe the symptoms associated with their depression. Students described experiencing anxiety that is associated with their depression; this could be anxiety that precedes their depression or anxiety that results from a depressive episode or a period of time when an individual has depression symptoms. Further, students described difficulty getting out of bed or leaving the house, feeling tired, a lack of motivation, being overly self-critical, feeling apathetic, and having difficulty concentrating. We were particularly interested in how students’ symptoms of depression affected their experiences in undergraduate research. During the think-aloud interviews that were conducted before the interview study, graduate and undergraduate students consistently described that their depression affected their motivation in research, their creativity in research, and their productivity in research. Therefore, we explicitly asked undergraduate researchers how, if at all, their depression affected these three factors. We also asked students to describe any additional ways in which their depression affected their research experiences. Undergraduate researchers commonly described five additional ways in which their depression affected their research; for a detailed description of each way students’ research was affected and for example quotes, see Table 2 . Students described that their depression negatively affected their productivity in the lab. Commonly, students described that their productivity was directly affected by a lack of motivation or because they felt less creative, which hindered the research process. Additionally, students highlighted that they were sometimes less productive because their depression sometimes caused them to struggle to engage intellectually with their research or caused them to have difficulty remembering or concentrating; students described that they could do mundane or routine tasks when they felt depressed, but that they had difficulty with more complex and intellectually demanding tasks. However, students sometimes described that even mundane tasks could be difficult when they were required to remember specific steps; for example, some students struggled recalling a protocol from memory when their depression was particularly severe. Additionally, students noted that their depression made them more self-conscious, which sometimes held them back from sharing research ideas with their mentors or from taking risks such as applying to competitive programs. In addition to being self-conscious, students highlighted that their depression caused them to be overly self-critical, and some described experiencing imposter phenomenon ( Clance and Imes, 1978 ) or feeling like they were not talented enough to be in research and were accepted into a lab by a fluke or through luck. Finally, students described that depression often made them feel less social, and they struggled to socially engage with other members of the lab when they were feeling down.
The Effect of Undergraduate Research Experiences on Student Depression
We also wanted to explore how research impacted students’ feelings of depression. Undergraduates described how research both positively and negatively affected their depression. In the following sections, we present aspects of undergraduate research and examine how each positively and/or negatively affected students’ depression using embedded student quotes to highlight the relationships between related ideas.
Lab Environment: Relationships with Others in the Lab.
Some aspects of the lab environment, which we define as students’ physical, social, or psychological research space, could be particularly beneficial for students with depression.
Specifically, undergraduate researchers perceived that comfortable and positive social interactions with others in the lab helped their depression. Students acknowledged how beneficial their relationships with graduate students and postdocs could be.
Marta: “I think always checking in on undergrads is important. It’s really easy [for us] to go a whole day without talking to anybody in the lab. But our grad students are like ‘Hey, what’s up? How’s school? What’s going on?’ (…) What helps me the most is having that strong support system. Sometimes just talking makes you feel better, but also having people that believe in you can really help you get out of that negative spiral. I think that can really help with depression.”
Kelley: “I know that anytime I need to talk to [my postdoc mentors] about something they’re always there for me. Over time we’ve developed a relationship where I know that outside of work and outside of the lab if I did want to talk to them about something I could talk to them. Even just talking to someone about hobbies and having that relationship alone is really helpful [for depression].”
In addition to highlighting the importance of developing relationships with graduate students or postdocs in the lab, students described that forming relationships with other undergraduates in the lab also helped their depression. Particularly, students described that other undergraduate researchers often validated their feelings about research, which in turn helped them realize that what they are thinking or feeling is normal, which tended to alleviate their negative thoughts. Interestingly, other undergraduates experiencing the same issues could sometimes help buffer them from perceiving that a mentor did not like them or that they were uniquely bad at research. In this article, we use the term “mentor” to refer to anyone who students referred to in the interviews as being their mentors or managing their research experiences; this includes graduate students, postdoctoral scholars, lab managers, and primary investigators (PIs).
Abby: “One of my best friends is in the lab with me. A lot of that friendship just comes from complaining about our stress with the lab and our annoyance with people in the lab. Like when we both agree like, ‘Yeah, the grad students were really off today, it wasn’t us,’ that helps. ‘It wasn’t me, it wasn’t my fault that we were having a rough day in lab; it was the grad students.’ Just being able to realize, ‘Hey, this isn’t all caused by us,’ you know? (…) We understand the stresses in the lab. We understand the details of what each other are doing in the lab, so when something doesn’t work out, we understand that it took them like eight hours to do that and it didn’t work. We provide empathy on a different level.”
Meleana: “It’s great to have solidarity in being confused about something, and it’s just that is a form of validation for me too. When we leave a lab meeting and I look at [another undergrad] I’m like, ‘Did you understand anything that they were just saying?’ And they’re like, ‘Oh, no.’ (…) It’s just really validating to hear from the other undergrads that we all seem to be struggling with the same things.”
Developing positive relationships with faculty mentors or PIs also helped alleviate some students’ depressive feelings, particularly when PIs shared their own struggles with students. This also seemed to normalize students’ concerns about their own experiences.
Alexandra: “[Talking with my PI] is helpful because he would talk about his struggles, and what he faced. A lot of it was very similar to my struggles. For example, he would say, ‘Oh, yeah, I failed this exam that I studied so hard for. I failed the GRE and I paid so much money to prepare for it.’ It just makes [my depression] better, like okay, this is normal for students to go through this. It’s not an out of this world thing where if you fail, you’re a failure and you can’t move on from it.”
Students’ relationships with others in the lab did not always positively impact their depression. Students described instances when the negative moods of the graduate students and PIs would often set the tone of the lab, which in turn worsened the mood of the undergraduate researchers.
Abby: “Sometimes [the grad students] are not in a good mood. The entire vibe of the lab is just off, and if you make a joke and it hits somebody wrong, they get all mad. It really depends on the grad students and the leadership and the mood that they’re in.”
Interviewer: “How does it affect your depression when the grad students are in a bad mood?”
Abby: “It definitely makes me feel worse. It feels like, again, that I really shouldn’t go ask them for help because they’re just not in the mood to help out. It makes me have more pressure on myself, and I have deadlines I need to meet, but I have a question for them, but they’re in a bad mood so I can’t ask. That’s another day wasted for me and it just puts more stress, which just adds to the depression.”
Additionally, some students described even more concerning behavior from research mentors, which negatively affected their depression.
Julie: “I had a primary investigator who is notorious in the department for screaming at people, being emotionally abusive, unreasonable, et cetera. (…) [He was] kind of harassing people, demeaning them, lying to them, et cetera, et cetera. (…) Being yelled at and constantly demeaned and harassed at all hours of the day and night, that was probably pretty bad for me.”
While the relationships between undergraduates and graduate, postdoc, and faculty mentors seemed to either alleviate or worsen students’ depressive symptoms, depending on the quality of the relationship, students in this study exclusively described their relationships with other undergraduates as positive for their depression. However, students did note that undergraduate research puts some of the best and brightest undergraduates in the same environment, which can result in students comparing themselves with their peers. Students described that this comparison would often lead them to feel badly about themselves, even though they would describe their personal relationship with a person to be good.
Meleana: “In just the research field in general, just feeling like I don’t really measure up to the people around me [can affect my depression]. A lot of the times it’s the beginning of a little spiral, mental spiral. There are some past undergrads that are talked about as they’re on this pedestal of being the ideal undergrads and that they were just so smart and contributed so much to the lab. I can never stop myself from wondering like, ‘Oh, I wonder if I’m having a contribution to the lab that’s similar or if I’m just another one of the undergrads that does the bare minimum and passes through and is just there.’”
Natasha: “But, on the other hand, [having another undergrad in the lab] also reminded me constantly that some people are invested in this and meant to do this and it’s not me. And that some people know a lot more than I do and will go further in this than I will.”
While students primarily expressed that their relationships with others in the lab affected their depression, some students explained that they struggled most with depression when the lab was empty; they described that they did not like being alone in the lab, because a lack of stimulation allowed their minds to be filled with negative thoughts.
Mia: “Those late nights definitely didn’t help [my depression]. I am alone, in the entire building. I’m left alone to think about my thoughts more, so not distracted by talking to people or interacting with people. I think more about how I’m feeling and the lack of progress I’m making, and the hopelessness I’m feeling. That kind of dragged things on, and I guess deepened my depression.”
Freddy: “Often times when I go to my office in the evening, that is when I would [ sic ] be prone to be more depressed. It’s being alone. I think about myself or mistakes or trying to correct mistakes or whatever’s going on in my life at the time. I become very introspective. I think I’m way too self-evaluating, way too self-deprecating and it’s when I’m alone when those things are really, really triggered. When I’m talking with somebody else, I forget about those things.”
In sum, students with depression highlighted that a lab environment full of positive and encouraging individuals was helpful for their depression, whereas isolating or competitive environments and negative interactions with others often resulted in more depressive feelings.
Doing Science: Experiencing Failure in Research, Getting Help, Receiving Feedback, Time Demands, and Important Contributions.
In addition to the lab environment, students also described that the process of doing science could affect their depression. Specifically, students explained that a large contributor to their depression was experiencing failure in research.
Interviewer: “Considering your experience in undergraduate research, what tends to trigger your feelings of depression?”
Heather: “Probably just not getting things right. Having to do an experiment over and over again. You don’t get the results you want. (…) The work is pretty meticulous and it’s frustrating when I do all this work, I do a whole experiment, and then I don’t get any results that I can use. That can be really frustrating. It adds to the stress. (…) It’s hard because you did all this other stuff before so you can plan for the research, and then something happens and all the stuff you did was worthless basically.”
Julie: “I felt very negatively about myself [when a project failed] and pretty panicked whenever something didn’t work because I felt like it was a direct reflection on my effort and/or intelligence, and then it was a big glaring personal failure.”
Students explained that their depression related to failing in research was exacerbated if they felt as though they could not seek help from their research mentors. Perceived insufficient mentor guidance has been shown to be a factor influencing student intention to leave undergraduate research ( Cooper et al. , 2019c ). Sometimes students talked about their research mentors being unavailable or unapproachable.
Michelle: “It just feels like [the graduate students] are not approachable. I feel like I can’t approach them to ask for their understanding in a certain situation. It makes [my depression] worse because I feel like I’m stuck, and that I’m being limited, and like there’s nothing I can do. So then I kind of feel like it’s my fault that I can’t do anything.”
Other times, students described that they did not seek help in fear that they would be negatively evaluated in research, which is a fear of being judged by others ( Watson and Friend, 1969 ; Weeks et al. , 2005 ; Cooper et al. , 2018 ). That is, students fear that their mentor would think negatively about them or judge them if they were to ask questions that their mentor thought they should know the answer to.
Meleana: “I would say [my depression] tends to come out more in being more reserved in asking questions because I think that comes more like a fear-based thing where I’m like, ‘Oh, I don’t feel like I’m good enough and so I don’t want to ask these questions because then my mentors will, I don’t know, think that I’m dumb or something.’”
Conversely, students described that mentors who were willing to help them alleviated their depressive feelings.
Crystal: “Yeah [my grad student] is always like, ‘Hey, I can check in on things in the lab because you’re allowed to ask me for that, you’re not totally alone in this,’ because he knows that I tend to take on all this responsibility and I don’t always know how to ask for help. He’s like, ‘You know, this is my lab too and I am here to help you as well,’ and just reminds me that I’m not shouldering this burden by myself.”
Ashlyn: “The graduate student who I work with is very kind and has a lot of patience and he really understands a lot of things and provides simple explanations. He does remind me about things and he will keep on me about certain tasks that I need to do in an understanding way, and it’s just because he’s patient and he listens.”
In addition to experiencing failure in science, students described that making mistakes when doing science also negatively affected their depression.
Abby: “I guess not making mistakes on experiments [is important in avoiding my depression]. Not necessarily that your experiment didn’t turn out to produce the data that you wanted, but just adding the wrong enzyme or messing something up like that. It’s like, ‘Oh, man,’ you know? You can get really down on yourself about that because it can be embarrassing.”
Commonly, students described that the potential for making mistakes increased their stress and anxiety regarding research; however, they explained that how other people responded to a potential mistake was what ultimately affected their depression.
Briana: “Sometimes if I made a mistake in correctly identifying an eye color [of a fly], [my PI] would just ridicule me in front of the other students. He corrected me but his method of correcting was very discouraging because it was a ridicule. It made the others laugh and I didn’t like that.”
Julie: “[My PI] explicitly [asked] if I had the dedication for science. A lot of times he said I had terrible judgment. A lot of times he said I couldn’t be trusted. Once I went to a conference with him, and, unfortunately, in front of another professor, he called me a klutz several times and there was another comment about how I never learn from my mistakes.”
When students did do things correctly, they described how important it could be for them to receive praise from their mentors. They explained that hearing praise and validation can be particularly helpful for students with depression, because their thoughts are often very negative and/or because they have low self-esteem.
Crystal: “[Something that helps my depression is] I have text messages from [my graduate student mentor] thanking me [and another undergraduate researcher] for all of the work that we’ve put in, that he would not be able to be as on track to finish as he is if he didn’t have our help.”
Interviewer: “Why is hearing praise from your mentor helpful?”
Crystal: “Because a lot of my depression focuses on everybody secretly hates you, nobody likes you, you’re going to die alone. So having that validation [from my graduate mentor] is important, because it flies in the face of what my depression tells me.”
Brian: “It reminds you that you exist outside of this negative world that you’ve created for yourself, and people don’t see you how you see yourself sometimes.”
Students also highlighted how research could be overwhelming, which negatively affected their depression. Particularly, students described that research demanded a lot of their time and that their mentors did not always seem to be aware that they were juggling school and other commitments in addition to their research. This stress exacerbated their depression.
Rose: “I feel like sometimes [my grad mentors] are not very understanding because grad students don’t take as many classes as [undergrads] do. I think sometimes they don’t understand when I say I can’t come in at all this week because I have finals and they’re like, ‘Why though?’”
Abby: “I just think being more understanding of student life would be great. We have classes as well as the lab, and classes are the priority. They forget what it’s like to be a student. You feel like they don’t understand and they could never understand when you say like, ‘I have three exams this week,’ and they’re like, ‘I don’t care. You need to finish this.’”
Conversely, some students reported that their research labs were very understanding of students’ schedules. Interestingly, these students talked most about how helpful it was to be able to take a mental health day and not do research on days when they felt down or depressed.
Marta: “My lab tech is very open, so she’ll tell us, ‘I can’t come in today. I have to take a mental health day.’ So she’s a really big advocate for that. And I think I won’t personally tell her that I’m taking a mental health day, but I’ll say, ‘I can’t come in today, but I’ll come in Friday and do those extra hours.’ And she’s like, ‘OK great, I’ll see you then.’ And it makes me feel good, because it helps me take care of myself first and then I can take care of everything else I need to do, which is amazing.”
Meleana: “Knowing that [my mentors] would be flexible if I told them that I’m crazy busy and can’t come into work nearly as much this week [helps my depression]. There is flexibility in allowing me to then care for myself.”
Interviewer: “Why is the flexibility helpful given the depression?”
Meleana: “Because sometimes for me things just take a little bit longer when I’m feeling down. I’m just less efficient to be honest, and so it’s helpful if I feel like I can only go into work for 10 hours in a week. It declutters my brain a little bit to not have to worry about all the things I have to do in work in addition the things that I need to do for school or clubs, or family or whatever.”
Despite the demanding nature of research, a subset of students highlighted that their research and research lab provided a sense of stability or familiarity that distracted them from their depression.
Freddy: “I’ll [do research] to run away from those [depressive] feelings or whatever. (…) I find sadly, I hate to admit it, but I do kind of run to [my lab]. I throw myself into work to distract myself from the feelings of depression and sadness.”
Rose: “When you’re sad or when you’re stressed you want to go to things you’re familiar with. So because lab has always been in my life, it’s this thing where it’s going to be there for me I guess. It’s like a good book that you always go back to and it’s familiar and it makes you feel good. So that’s how lab is. It’s not like the greatest thing in the world but it’s something that I’m used to, which is what I feel like a lot of people need when they’re sad and life is not going well.”
Many students also explained that research positively affects their depression because they perceive their research contribution to be important.
Ashlyn: “I feel like I’m dedicating myself to something that’s worthy and something that I believe in. It’s really important because it contextualizes those times when I am feeling depressed. It’s like, no, I do have these better things that I’m working on. Even when I don’t like myself and I don’t like who I am, which is again, depression brain, I can at least say, ‘Well, I have all these other people relying on me in research and in this area and that’s super important.’”
Jessica: “I mean, it just felt like the work that I was doing had meaning and when I feel like what I’m doing is actually going to contribute to the world, that usually really helps with [depression] because it’s like not every day you can feel like you’re doing something impactful.”
In sum, students highlighted that experiencing failure in research and making mistakes negatively contributed to depression, especially when help was unavailable or research mentors had a negative reaction. Additionally, students acknowledged that the research could be time-consuming, but that research mentors who were flexible helped assuage depressive feelings that were associated with feeling overwhelmed. Finally, research helped some students’ depression, because it felt familiar, provided a distraction from depression, and reminded students that they were contributing to a greater cause.
We believe that creating more inclusive research environments for students with depression is an important step toward broadening participation in science, not only to ensure that we are not discouraging students with depression from persisting in science, but also because depression has been shown to disproportionately affect underserved and underrepresented groups in science ( Turner and Noh, 1988 ; Eisenberg et al. , 2007 ; Jenkins et al. , 2013 ; American College Health Association, 2018 ). We initially hypothesized that three features of undergraduate research—research mentors, the lab environment, and failure—may have the potential to exacerbate student depression. We found this to be true; students highlighted that their relationships with their mentors as well as the overall lab environment could negatively affect their depression, but could also positively affect their research experiences. Students also noted that they struggled with failure, which is likely true of most students, but is known to be particularly difficult for students with depression ( Elliott et al. , 1997 ). We expand upon our findings by integrating literature on depression with the information that students provided in the interviews about how research mentors can best support students. We provide a set of evidence-based recommendations focused on mentoring, the lab environment, and failure for research mentors wanting to create more inclusive research environments for students with depression. Notably, only the first recommendation is specific to students with depression; the others reflect recommendations that have previously been described as “best practices” for research mentors ( NASEM, 2017 , 2019 ; Sorkness et al. , 2017 ) and likely would benefit most students. However, we examine how these recommendations may be particularly important for students with depression. As we hypothesized, these recommendations directly address three aspects of research: mentors, lab environment, and failure. A caveat of these recommendations is that more research needs to be done to explore the experiences of students with depression and how these practices actually impact students with depression, but our national sample of undergraduate researchers with depression can provide an initial starting point for a discussion about how to improve research experiences for these students.
Recommendations to Make Undergraduate Research Experiences More Inclusive for Students with Depression
Recognize student depression as a valid illness..
Allow students with depression to take time off of research by simply saying that they are sick and provide appropriate time for students to recover from depressive episodes. Also, make an effort to destigmatize mental health issues.
Undergraduate researchers described both psychological and physical symptoms that manifested as a result of their depression and highlighted how such symptoms prevented them from performing to their full potential in undergraduate research. For example, students described how their depression would cause them to feel unmotivated, which would often negatively affect their research productivity. In cases in which students were motivated enough to come in and do their research, they described having difficulty concentrating or engaging in the work. Further, when doing research, students felt less creative and less willing to take risks, which may alter the quality of their work. Students also sometimes struggled to socialize in the lab. They described feeling less social and feeling overly self-critical. In sum, students described that, when they experienced a depressive episode, they were not able to perform to the best of their ability, and it sometimes took a toll on them to try to act like nothing was wrong, when they were internally struggling with depression. We recommend that research mentors treat depression like any other physical illness; allowing students the chance to recover when they are experiencing a depressive episode can be extremely important to students and can allow them to maximize their productivity upon returning to research ( Judd et al. , 2000 ). Students explained that if they are not able to take the time to focus on recovering during a depressive episode, then they typically continue to struggle with depression, which negatively affects their research. This sentiment is echoed by researchers in psychiatry who have found that patients who do not fully recover from a depressive episode are more likely to relapse and to experience chronic depression ( Judd et al. , 2000 ). Students described not doing tasks or not showing up to research because of their depression but struggling with how to share that information with their research mentors. Often, students would not say anything, which caused them anxiety because they were worried about what others in the lab would say to them when they returned. Admittedly, many students understood why this behavior would cause their research mentors to be angry or frustrated, but they weighed the consequences of their research mentors’ displeasure against the consequences of revealing their depression and decided it was not worth admitting to being depressed. This aligns with literature that suggests that when individuals have concealable stigmatized identities, or identities that can be hidden and that carry negative stereotypes, such as depression, they will often keep them concealed to avoid negative judgment or criticism ( Link and Phelan, 2001 ; Quinn and Earnshaw, 2011 ; Jones and King, 2014 ; Cooper and Brownell, 2016 ; Cooper et al. , 2019b ; Cooper et al ., unpublished data ). Therefore, it is important for research mentors to be explicit with students that 1) they recognize mental illness as a valid sickness and 2) that students with mental illness can simply explain that they are sick if they need to take time off. This may be useful to overtly state on a research website or in a research syllabus, contract, or agreement if mentors use such documents when mentoring undergraduates in their lab. Further, research mentors can purposefully work to destigmatize mental health issues by explicitly stating that struggling with mental health issues, such as depression and anxiety, is common. While we do not recommend that mentors ask students directly about depression, because this can force students to share when they are not comfortable sharing, we do recommend providing opportunities for students to reveal their depression ( Chaudoir and Fisher, 2010 ). Mentors can regularly check in with students about how they’re doing, and talk openly about the importance of mental health, which may increase the chance that students may feel comfortable revealing their depression ( Chaudoir and Quinn, 2010 ; Cooper et al ., unpublished data ).
Foster a Positive Lab Environment.
Encourage positivity in the research lab, promote working in shared spaces to enhance social support among lab members, and alleviate competition among undergraduates.
Students in this study highlighted that the “leadership” of the lab, meaning graduate students, postdocs, lab managers, and PIs, were often responsible for establishing the tone of the lab; that is, if they were in a bad mood it would trickle down and negatively affect the moods of the undergraduates. Explicitly reminding lab leadership that their moods can both positively and negatively affect undergraduates may be important in establishing a positive lab environment. Further, students highlighted how they were most likely to experience negative thoughts when they were alone in the lab. Therefore, it may be helpful to encourage all lab members to work in a shared space to enhance social interactions among students and to maximize the likelihood that undergraduates have access to help when needed. A review of 51 studies in psychiatry supported our undergraduate researchers’ perceptions that social relationships positively impacted their depression; the study found that perceived emotional support (e.g., someone available to listen or give advice), perceived instrumental support (e.g., someone available to help with tasks), and large diverse social networks (e.g., being socially connected to a large number of people) were significantly protective against depression ( Santini et al. , 2015 ). Additionally, despite forming positive relationships with other undergraduates in the lab, many undergraduate researchers admitted to constantly comparing themselves with other undergraduates, which led them to feel inferior, negatively affecting their depression. Some students talked about mentors favoring current undergraduates or talking positively about past undergraduates, which further exacerbated their feelings of inferiority. A recent study of students in undergraduate research experiences highlighted that inequitable distribution of praise to undergraduates can create negative perceptions of lab environments for students (Cooper et al. , 2019). Further, the psychology literature has demonstrated that when people feel insecure in their social environments, it can cause them to focus on a hierarchical view of themselves and others, which can foster feelings of inferiority and increase their vulnerability to depression ( Gilbert et al. , 2009 ). Thus, we recommend that mentors be conscious of their behaviors so that they do not unintentionally promote competition among undergraduates or express favoritism toward current or past undergraduates. Praise is likely best used without comparison with others and not done in a public way, although more research on the impact of praise on undergraduate researchers needs to be done. While significant research has been done on mentoring and mentoring relationships in the context of undergraduate research ( Byars-Winston et al. , 2015 ; Aikens et al. , 2017 ; Estrada et al. , 2018 ; Limeri et al. , 2019 ; NASEM, 2019 ), much less has been done on the influence of the lab environment broadly and how people in nonmentoring roles can influence one another. Yet, this study indicates the potential influence of many different members of the lab, not only their mentors, on students with depression.
Develop More Personal Relationships with Undergraduate Researchers and Provide Sufficient Guidance.
Make an effort to establish more personal relationships with undergraduates and ensure that they perceive that they have access to sufficient help and guidance with regard to their research.
When we asked students explicitly how research mentors could help create more inclusive environments for undergraduate researchers with depression, students overwhelmingly said that building mentor–student relationships would be extremely helpful. Students suggested that mentors could get to know students on a more personal level by asking about their career interests or interests outside of academia. Students also remarked that establishing a more personal relationship could help build the trust needed in order for undergraduates to confide in their research mentors about their depression, which they perceived would strengthen their relationships further because they could be honest about when they were not feeling well or their mentors might even “check in” with them in times where they were acting differently than normal. This aligns with studies showing that undergraduates are most likely to reveal a stigmatized identity, such as depression, when they form a close relationship with someone ( Chaudoir and Quinn, 2010 ). Many were intimidated to ask for research-related help from their mentors and expressed that they wished they had established a better relationship so that they would feel more comfortable. Therefore, we recommend that research mentors try to establish relationships with their undergraduates and explicitly invite them to ask questions or seek help when needed. These recommendations are supported by national recommendations for mentoring ( NASEM, 2019 ) and by literature that demonstrates that both social support (listening and talking with students) and instrumental support (providing students with help) have been shown to be protective against depression ( Santini et al. , 2015 ).
Treat Undergraduates with Respect and Remember to Praise Them.
Avoid providing harsh criticism and remember to praise undergraduates. Students with depression often have low self-esteem and are especially self-critical. Therefore, praise can help calibrate their overly negative self-perceptions.
Students in this study described that receiving criticism from others, especially harsh criticism, was particularly difficult for them given their depression. Multiple studies have demonstrated that people with depression can have an abnormal or maladaptive response to negative feedback; scientists hypothesize that perceived failure on a particular task can trigger failure-related thoughts that interfere with subsequent performance ( Eshel and Roiser, 2010 ). Thus, it is important for research mentors to remember to make sure to avoid unnecessarily harsh criticisms that make students feel like they have failed (more about failure is described in the next recommendation). Further, students with depression often have low self-esteem or low “personal judgment of the worthiness that is expressed in the attitudes the individual holds towards oneself” ( Heatherton et al. , 2003 , p. 220; Sowislo and Orth, 2013 ). Specifically, a meta-analysis of longitudinal studies found that low self-esteem is predictive of depression ( Sowislo and Orth, 2013 ), and depression has also been shown to be highly related to self-criticism ( Luyten et al. , 2007 ). Indeed, nearly all of the students in our study described thinking that they are “not good enough,” “worthless,” or “inadequate,” which is consistent with literature showing that people with depression are self-critical ( Blatt et al. , 1982 ; Gilbert et al. , 2006 ) and can be less optimistic of their performance on future tasks and rate their overall performance on tasks less favorably than their peers without depression ( Cane and Gotlib, 1985 ). When we asked students what aspects of undergraduate research helped their depression, students described that praise from their mentors was especially impactful, because they thought so poorly of themselves and they needed to hear something positive from someone else in order to believe it could be true. Praise has been highlighted as an important aspect of mentoring in research for many years ( Ashford, 1996 ; Gelso and Lent, 2000 ; Brown et al. , 2009 ) and may be particularly important for students with depression. In fact, praise has been shown to enhance individuals’ motivation and subsequent productivity ( Hancock, 2002 ; Henderlong and Lepper, 2002 ), factors highlighted by students as negatively affecting their depression. However, something to keep in mind is that a student with depression and a student without depression may process praise differently. For a student with depression, a small comment that praises the student’s work may not be sufficient for the student to process that comment as praise. People with depression are hyposensitive to reward or have reward-processing deficits ( Eshel and Roiser, 2010 ); therefore, praise may affect students without depression more positively than it would affect students with depression. Research mentors should be mindful that students with depression often have a negative view of themselves, and while students report that praise is extremely important, they may have trouble processing such positive feedback.
Normalize Failure and Be Explicit about the Importance of Research Contributions.
Explicitly remind students that experiencing failure is expected in research. Also explain to students how their individual work relates to the overall project so that they can understand how their contributions are important. It can also be helpful to explain to students why the research project as a whole is important in the context of the greater scientific community.
Experiencing failure has been thought to be a potentially important aspect of undergraduate research, because it may provide students with the potential to develop integral scientific skills such as the ability to navigate challenges and persevere ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, in the interviews, students described that when their science experiments failed, it was particularly tough for their depression. Students’ negative reaction to experiencing failure in research is unsurprising, given recent literature that has predicted that students may be inadequately prepared to approach failure in science ( Henry et al. , 2019 ). However, the literature suggests that students with depression may find experiencing failure in research to be especially difficult ( Elliott et al. , 1997 ; Mongrain and Blackburn, 2005 ; Jones et al. , 2009 ). One potential hypothesis is that students with depression may be more likely to have fixed mindsets or more likely to believe that their intelligence and capacity for specific abilities are unchangeable traits ( Schleider and Weisz, 2018 ); students with a fixed mindset have been hypothesized to have particularly negative responses to experiencing failure in research, because they are prone to quitting easily in the face of challenges and becoming defensive when criticized ( Forsythe and Johnson, 2017 ; Dweck, 2008 ). A study of life sciences undergraduates enrolled in CUREs identified three strategies of students who adopted adaptive coping mechanisms, or mechanisms that help an individual maintain well-being and/or move beyond the stressor when faced with failure in undergraduate research: 1) problem solving or engaging in strategic planning and decision making, 2) support seeking or finding comfort and help with research, and 3) cognitive restructuring or reframing a problem from negative to positive and engaging in self encouragement ( Gin et al. , 2018 ). We recommend that, when undergraduates experience failure in science, their mentors be proactive in helping them problem solve, providing help and support, and encouraging them. Students also explained that mentors sharing their own struggles as undergraduate and graduate students was helpful, because it normalized failure. Sharing personal failures in research has been recommended as an important way to provide students with psychosocial support during research ( NASEM, 2019 ). We also suggest that research mentors take time to explain to students why their tasks in the lab, no matter how small, contribute to the greater research project ( Cooper et al. , 2019a ). Additionally, it is important to make sure that students can explain how the research project as a whole is contributing to the scientific community ( Gin et al. , 2018 ). Students highlighted that contributing to something important was really helpful for their depression, which is unsurprising, given that studies have shown that meaning in life or people’s comprehension of their life experiences along with a sense of overarching purpose one is working toward has been shown to be inversely related to depression ( Steger, 2013 ).
Limitations and Future Directions
This work was a qualitative interview study intended to document a previously unstudied phenomenon: depression in the context of undergraduate research experiences. We chose to conduct semistructured interviews rather than a survey because of the need for initial exploration of this area, given the paucity of prior research. A strength of this study is the sampling approach. We recruited a national sample of 35 undergraduates engaged in undergraduate research at 12 different public R1 institutions. Despite our representative sample from R1 institutions, these findings may not be generalizable to students at other types of institutions; lab environments, mentoring structures, and interactions between faculty and undergraduate researchers may be different at other institution types (e.g., private R1 institutions, R2 institutions, master’s-granting institutions, primarily undergraduate institutions, and community colleges), so we caution against making generalizations about this work to all undergraduate research experiences. Future work could assess whether students with depression at other types of institutions have similar experiences to students at research-intensive institutions. Additionally, we intentionally did not explore the experiences of students with specific identities owing to our sample size and the small number of students in any particular group (e.g., students of a particular race, students with a graduate mentor as the primary mentor). We intend to conduct future quantitative studies to further explore how students’ identities and aspects of their research affect their experiences with depression in undergraduate research.
The students who participated in the study volunteered to be interviewed about their depression; therefore, it is possible that depression is a more salient part of these students’ identities and/or that they are more comfortable talking about their depression than the average population of students with depression. It is also important to acknowledge the personal nature of the topic and that some students may not have fully shared their experiences ( Krumpal, 2013 ), particularly those experiences that may be emotional or traumatizing ( Kahn and Garrison, 2009 ). Additionally, our sample was skewed toward females (77%). While females do make up approximately 60% of students in biology programs on average ( Eddy et al. , 2014 ), they are also more likely to report experiencing depression ( American College Health Association, 2018 ; Evans et al. , 2018 ). However, this could be because women have higher rates of depression or because males are less likely to report having depression; clinical bias, or practitioners’ subconscious tendencies to overlook male distress, may underestimate depression rates in men ( Smith et al. , 2018 ). Further, females are also more likely to volunteer to participate in studies ( Porter and Whitcomb, 2005 ); therefore, many interview studies have disproportionately more females in the data set (e.g., Cooper et al. , 2017 ). If we had been able to interview more male students, we might have identified different findings. Additionally, we limited our sample to life sciences students engaged in undergraduate research at public R1 institutions. It is possible that students in other majors may have different challenges and opportunities for students with depression, as well as different disciplinary stigmas associated with mental health.
In this exploratory interview study, we identified a variety of ways in which depression in undergraduates negatively affected their undergraduate research experiences. Specifically, we found that depression interfered with students’ motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing. We also identified that research can negatively affect depression in undergraduates. Experiencing failure in research can exacerbate student depression, especially when students do not have access to adequate guidance. Additionally, being alone or having negative interactions with others in the lab worsened students’ depression. However, we also found that undergraduate research can positively affect students’ depression. Research can provide a familiar space where students can feel as though they are contributing to something meaningful. Additionally, students reported that having access to adequate guidance and a social support network within the research lab also positively affected their depression. We hope that this work can spark conversations about how to make undergraduate research experiences more inclusive of students with depression and that it can stimulate additional research that more broadly explores the experiences of undergraduate researchers with depression.
Important note
If you or a student experience symptoms of depression and want help, there are resources available to you. Many campuses provide counseling centers equipped to provide students, staff, and faculty with treatment for depression, as well as university-dedicated crisis hotlines. Additionally, there are free 24/7 services such as Crisis Text Line, which allows you to text a trained live crisis counselor (Text “CONNECT” to 741741; Text Depression Hotline , 2019 ), and phone hotlines such as the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK). You can also learn more about depression and where to find help near you through the Anxiety and Depression Association of American website: https://adaa.org ( Anxiety and Depression Association of America, 2019 ) and the Depression and Biopolar Support Alliance: http://dbsalliance.org ( Depression and Biopolar Support Alliance, 2019 ).
ACKNOWLEDGMENTS
We are extremely grateful to the undergraduate researchers who shared their thoughts and experiences about depression with us. We acknowledge the ASU LEAP Scholars for helping us create the original survey and Rachel Scott for her helpful feedback on earlier drafts of this article. L.E.G. was supported by a National Science Foundation (NSF) Graduate Fellowship (DGE-1311230) and K.M.C. was partially supported by a Howard Hughes Medical Institute (HHMI) Inclusive Excellence grant (no. 11046) and an NSF grant (no. 1644236). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF or HHMI.
- Aikens, M. L., Robertson, M. M., Sadselia, S., Watkins, K., Evans, M., Runyon, C. R. , … & Dolan, E. L. ( 2017 ). Race and gender differences in undergraduate research mentoring structures and research outcomes . CBE—Life Sciences Education , 16 (2), ar34. Link , Google Scholar
- Aikens, M. L., Sadselia, S., Watkins, K., Evans, M., Eby, L. T., & Dolan, E. L. ( 2016 ). A social capital perspective on the mentoring of undergraduate life science researchers: An empirical study of undergraduate–postgraduate–faculty triads . CBE—Life Sciences Education , 15 (2), ar16. Link , Google Scholar
- Aldwin, C., & Greenberger, E. ( 1987 ). Cultural differences in the predictors of depression . American Journal of Community Psychology , 15 (6), 789–813. Medline , Google Scholar
- American Association for the Advancement of Science . ( 2011 ). Vision and change in undergraduate biology education: A call to action . Retrieved November 29, 2019, from http://visionandchange.org/files/2013/11/aaas-VISchange-web1113.pdf Google Scholar
- American College Health Association . ( 2018 ). Undergraduate reference group executive summary, Fall 2018 . Retrieved November 29, 2019, from www.acha.org/documents/ncha/NCHA-II_Fall_2018_Reference_Group_Executive_Summary.pdf Google Scholar
- American College Health Association . ( 2019 ). Retrieved November 29, 2019, from NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf www.acha.org/documents/ncha/NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf Google Scholar
- American Psychiatric Association . ( 2013 ). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing. Google Scholar
- Aneshensel, C. S., & Stone, J. D. ( 1982 ). Stress and depression: A test of the buffering model of social support . Archives of General Psychiatry , 39 (12), 1392–1396. Medline , Google Scholar
- Anxiety and Depression Association of America . ( 2019 ). Home page . Retrieved November 29, 2019, from https://adaa.org Google Scholar
- Armbruster, P., Patel, M., Johnson, E., & Weiss, M. ( 2009 ). Active learning and student-centered pedagogy improve student attitudes and performance in introductory biology . CBE—Life Sciences Education , 8 (3), 203–213. Link , Google Scholar
- Ashford, S. J. ( 1996 ). Working with doctoral students: Rhythms of Academic Life: Personal Accounts of Careers in Academia . In Front, P. J.Taylor, M. S. (Eds.), Rhythms of Academic Life: Personal Accounts of Careers in Academia (pp. 153–158). Thousand Oaks, CA: Sage. Google Scholar
- Auchincloss, L. C., Laursen, S. L., Branchaw, J. L., Eagan, K., Graham, M., Hanauer, D. I. , … & Rowland, S. ( 2014 ). Assessment of course-based undergraduate research experiences: A meeting report . CBE—Life Sciences Education , 13 (1), 29–40. Link , Google Scholar
- Barak, M. E. M., Levin, A., Nissly, J. A., & Lane, C. J. ( 2006 ). Why do they leave? Modeling child welfare workers’ turnover intentions . Children and Youth Services Review , 28 (5), 548–577. Google Scholar
- Bauer, K. W., & Bennett, J. S. ( 2003 ). Alumni perceptions used to assess undergraduate research experience . Journal of Higher Education , 74 (2), 210–230. Google Scholar
- Birks, M., & Mills, J. ( 2015 ). Grounded theory: A practical guide . Thousand Oaks, CA: Sage. Google Scholar
- Blatt, S. J., Quinlan, D. M., Chevron, E. S., McDonald, C., & Zuroff, D. ( 1982 ). Dependency and self-criticism: Psychological dimensions of depression . Journal of Consulting and Clinical Psychology , 50 (1), 113. Medline , Google Scholar
- Brown, R. T., Daly, B. P., & Leong, F. T. ( 2009 ). Mentoring in research: A developmental approach . Professional Psychology: Research and Practice , 40 (3), 306. Google Scholar
- Brownell, S. E., Hekmat-Scafe, D. S., Singla, V., Seawell, P. C., Imam, J. F. C., Eddy, S. L. , … & Cyert, M. S. ( 2015 ). A high-enrollment course-based undergraduate research experience improves student conceptions of scientific thinking and ability to interpret data . CBE—Life Sciences Education , 14 (2), ar21. Link , Google Scholar
- Brownell, S. E., & Kloser, M. J. ( 2015 ). Toward a conceptual framework for measuring the effectiveness of course-based undergraduate research experiences in undergraduate biology . Studies in Higher Education , 40 (3), 525–544. Google Scholar
- Byars-Winston, A. M., Branchaw, J., Pfund, C., Leverett, P., & Newton, J. ( 2015 ). Culturally diverse undergraduate researchers’ academic outcomes and perceptions of their research mentoring relationships . International Journal of Science Education , 37 (15), 2533–2554. Medline , Google Scholar
- Cane, D. B., & Gotlib, I. H. ( 1985 ). Depression and the effects of positive and negative feedback on expectations, evaluations, and performance . Cognitive Therapy and Research , 9 (2), 145–160. Google Scholar
- Ceci, S. J., & Williams, W. M. ( 2010 ). Sex differences in math-intensive fields . Current Directions in Psychological Science , 19 (5), 275–279. Medline , Google Scholar
- Center for Collegiate Mental Health . ( 2017 ). Center for Collegiate Mental Health 2017 Annual Report . State College, PA: Penn State Universit. Google Scholar
- Charmaz, K. ( 2006 ). Constructing grounded theory: A practical guide through qualitative research . Thousand Oaks, CA: Sage. Google Scholar
- Chaudoir, S. R., & Fisher, J. D. ( 2010 ). The disclosure processes model: Understanding disclosure decision making and postdisclosure outcomes among people living with a concealable stigmatized identity . Psychological Bulletin , 136 (2), 236. Medline , Google Scholar
- Chaudoir, S. R., & Quinn, D. M. ( 2010 ). Revealing concealable stigmatized identities: The impact of disclosure motivations and positive first-disclosure experiences on fear of disclosure and well-being . Journal of Social Issues , 66 (3), 570–584. Medline , Google Scholar
- Clance, P. R., & Imes, S. A. ( 1978 ). The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention . Psychotherapy: Theory, Research & Practice , 15 (3), 241. Google Scholar
- Cooper, K. M., Ashley, M., & Brownell, S. E. ( 2017 ). A bridge to active learning: A summer bridge program helps students maximize their active-learning experiences and the active-learning experiences of others . CBE—Life Sciences Education , 16 (1), ar17. Link , Google Scholar
- Cooper, K. M., Blattman, J. N., Hendrix, T., & Brownell, S. E. ( 2019a ). The impact of broadly relevant novel discoveries on student project ownership in a traditional lab course turned CURE . CBE—Life Sciences Education , 18 (4), ar57. Link , Google Scholar
- Cooper, K. M., & Brownell, S. E. ( 2016 ). Coming out in class: Challenges and benefits of active learning in a biology classroom for LGBTQIA students . CBE—Life Sciences Education , 15 (3), ar37. https://doi.org/10.1187/cbe.16-01-0074 Link , Google Scholar
- Cooper, K. M., Brownell, S. E., & Gormally, C. C. ( 2019b ). Coming out to the class: Identifying factors that influence college biology instructor decisions about whether to reveal their LGBQ identity in class . Journal of Women and Minorities in Science and Engineering , 25 (3). Google Scholar
- Cooper, K. M., Downing, V. R., & Brownell, S. E. ( 2018 ). The influence of active learning practices on student anxiety in large-enrollment college science classrooms . International Journal of STEM Education , 5 (1), 23. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., Akeeh, B., Clark, C. E., Hunter, J. S., Roderick, T. B. , … & Brownell, S. E. ( 2019c ). Factors that predict life sciences student persistence in undergraduate research experiences . PLoS ONE , 14 (8). https://doi.org/10.1371/journal.pone.0220186 Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( 2019d ). Diagnosing differences in what introductory biology students in a fully online and an in-person biology degree program know and do regarding medical school admission . Advances in Physiology Education , 43 (2), 221–232. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( In press ). Depression as a concealable stigmatized identity: What influences whether students conceal or reveal their depression in undergraduate research experiences? International Journal of STEM Education , ( in press ). Google Scholar
- Depression and Biopolar Support Alliance . ( 2019 ). Home page . Retrieved November 28, 2019, from www.dbsalliance.org Google Scholar
- Deroma, V. M., Leach, J. B., & Leverett, J. P. ( 2009 ). The relationship between depression and college academic performance . College Student Journal , 43 (2), 325–335. Google Scholar
- Dweck, C. S. ( 2008 ). Mindset: The new psychology of success . New York, NY: Random House Digital. Google Scholar
- Dyson, R., & Renk, K. ( 2006 ). Freshmen adaptation to university life: Depressive symptoms, stress, and coping . Journal of Clinical Psychology , 62 (10), 1231–1244. Medline , Google Scholar
- Eddy, S. L., Brownell, S. E., & Wenderoth, M. P. ( 2014 ). Gender gaps in achievement and participation in multiple introductory biology classrooms . CBE—Life Sciences Education , 13 (3), 478–492. https://doi.org/10.1187/cbe.13-10-0204 Link , Google Scholar
- Eisenberg, D., Gollust, S. E., Golberstein, E., & Hefner, J. L. ( 2007 ). Prevalence and correlates of depression, anxiety, and suicidality among university students . American Journal of Orthopsychiatry , 77 (4), 534–542. Medline , Google Scholar
- Elliott, R., Sahakian, B. J., Herrod, J. J., Robbins, T. W., & Paykel, E. S. ( 1997 ). Abnormal response to negative feedback in unipolar depression: Evidence for a diagnosis specific impairment . Journal of Neurology, Neurosurgery & Psychiatry , 63 (1), 74–82. Medline , Google Scholar
- Eshel, N., & Roiser, J. P. ( 2010 ). Reward and punishment processing in depression . Biological Psychiatry , 68 (2), 118–124. Medline , Google Scholar
- Estrada, M., Hernandez, P. R., & Schultz, P. W. ( 2018 ). A longitudinal study of how quality mentorship and research experience integrate underrepresented minorities into STEM careers . CBE—Life Sciences Education , 17 (1), ar9. Link , Google Scholar
- Evans, T. M., Bira, L., Gastelum, J. B., Weiss, L. T., & Vanderford, N. L. ( 2018 ). Evidence for a mental health crisis in graduate education . Nature Biotechnology , 36 (3), 282. Medline , Google Scholar
- Everson, H. T., Tobias, S., Hartman, H., & Gourgey, A. ( 1993 ). Test anxiety and the curriculum: The subject matters . Anxiety, Stress, and Coping , 6 (1), 1–8. Google Scholar
- Flaherty, C. ( 2018 ). New study says graduate students’ mental health is a “crisis.” Retrieved November 29, 2019, from www.insidehighered.com/news/2018/03/06/new-study-says-graduate-students-mental-health-crisis Google Scholar
- Forsythe, A., & Johnson, S. ( 2017 ). Thanks, but no-thanks for the feedback . Assessment & Evaluation in Higher Education , 42 (6), 850–859. Google Scholar
- Garlow, S. J., Rosenberg, J., Moore, J. D., Haas, A. P., Koestner, B., Hendin, H., & Nemeroff, C. B. ( 2008 ). Depression, desperation, and suicidal ideation in college students: Results from the American Foundation for Suicide Prevention College Screening Project at Emory University . Depression and Anxiety , 25 (6), 482–488. Medline , Google Scholar
- Gelso, C. J., & Lent, R. W. ( 2000 ). Scientific training and scholarly productivity: The person, the training environment, and their interaction . In Brown, S. D.Lent, R. W. (Eds.), Handbook of counseling psychology (pp. 109–139). Hoboken, NJ: John Wiley & Sons Inc. Google Scholar
- Gilbert, P., Baldwin, M. W., Irons, C., Baccus, J. R., & Palmer, M. ( 2006 ). Self-criticism and self-warmth: An imagery study exploring their relation to depression . Journal of Cognitive Psychotherapy , 20 (2), 183. Google Scholar
- Gilbert, P., McEwan, K., Bellew, R., Mills, A., & Gale, C. ( 2009 ). The dark side of competition: How competitive behaviour and striving to avoid inferiority are linked to depression, anxiety, stress and self-harm . Psychology and Psychotherapy: Theory, Research and Practice , 82 (2), 123–136. Medline , Google Scholar
- Gin, L. E., Rowland, A. A., Steinwand, B., Bruno, J., & Corwin, L. A. ( 2018 ). Students who fail to achieve predefined research goals may still experience many positive outcomes as a result of CURE participation . CBE—Life Sciences Education , 17 (4), ar57. Link , Google Scholar
- Glesne, C., & Peshkin, A. ( 1992 ). Becoming qualitative researchers: An introduction . London, England, UK: Longman. Google Scholar
- Grav, S., Hellzèn, O., Romild, U., & Stordal, E. ( 2012 ). Association between social support and depression in the general population: The HUNT study, a cross-sectional survey . Journal of Clinical Nursing , 21 (1–2), 111–120. Medline , Google Scholar
- Guest, G., Bunce, A., & Johnson, L. ( 2006 ). How many interviews are enough? An experiment with data saturation and variability . Field Methods , 18 (1), 59–82. Google Scholar
- Hancock, D. R. ( 2002 ). Influencing graduate students’ classroom achievement, homework habits and motivation to learn with verbal praise . Educational Research , 44 (1), 83–95. Google Scholar
- Hannah, D. R., & Lautsch, B. A. ( 2011 ). Counting in qualitative research: Why to conduct it, when to avoid it, and when to closet it . Journal of Management Inquiry , 20 (1), 14–22. Google Scholar
- Heatherton, T. F., & Wyland, C. L. ( 2003 ). Assessing self-esteem . In Lopez, S. J.Snyder, C. R. (Eds.), Positive psychological assessment: A handbook of models and measures (pp. 219–233). Washington, DC: American Psychological Association. https://doi.org/10.1037/10612-014 . Google Scholar
- Henderlong, J., & Lepper, M. R. ( 2002 ). The effects of praise on children’s intrinsic motivation: A review and synthesis . Psychological Bulletin , 128 (5), 774. Medline , Google Scholar
- Henry, M. A., Shorter, S., Charkoudian, L., Heemstra, J. M., & Corwin, L. A. ( 2019 ). FAIL is not a four-letter word: A theoretical framework for exploring undergraduate students’ approaches to academic challenge and responses to failure in STEM learning environments . CBE—Life Sciences Education , 18 (1), ar11. Link , Google Scholar
- Hernandez, P. R., Woodcock, A., Estrada, M., & Schultz, P. W. ( 2018 ). Undergraduate research experiences broaden diversity in the scientific workforce . BioScience , 68 (3), 204–211. Google Scholar
- Hish, A. J., Nagy, G. A., Fang, C. M., Kelley, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Applying the stress process model to stress–burnout and stress–depression relationships in biomedical doctoral students: A cross-sectional pilot study . CBE—Life Sciences Education , 18 (4), ar51. Link , Google Scholar
- Howell, E., & McFeeters, J. ( 2008 ). Children’s mental health care: Differences by race/ethnicity in urban/rural areas . Journal of Health Care for the Poor and Underserved , 19 (1), 237–247. Medline , Google Scholar
- Hysenbegasi, A., Hass, S. L., & Rowland, C. R. ( 2005 ). The impact of depression on the academic productivity of university students . Journal of Mental Health Policy and Economics , 8 (3), 145. Medline , Google Scholar
- Ibrahim, A. K., Kelly, S. J., Adams, C. E., & Glazebrook, C. ( 2013 ). A systematic review of studies of depression prevalence in university students . Journal of Psychiatric Research , 47 (3), 391–400. Medline , Google Scholar
- Intemann, K. ( 2009 ). Why diversity matters: Understanding and applying the diversity component of the National Science Foundation’s broader impacts criterion . Social Epistemology , 23 (3–4), 249–266. Google Scholar
- Ishiyama, J. ( 2002 ). Does early participation in undergraduate research benefit social science and humanities students? College Student Journal , 36 (3), 381–387. Google Scholar
- Jenkins, S. R., Belanger, A., Connally, M. L., Boals, A., & Durón, K. M. ( 2013 ). First-generation undergraduate students’ social support, depression, and life satisfaction . Journal of College Counseling , 16 (2), 129–142. Google Scholar
- Jobst, A., Sabass, L., Palagyi, A., Bauriedl-Schmidt, C., Mauer, M. C., Sarubin, N. , … & Zill, P. ( 2015 ). Effects of social exclusion on emotions and oxytocin and cortisol levels in patients with chronic depression . Journal of Psychiatric Research , 60 , 170–177. Medline , Google Scholar
- Jones, K. P., & King, E. B. ( 2014 ). Managing concealable stigmas at work: A review and multilevel model . Journal of Management , 40 (5), 1466–1494. Google Scholar
- Jones, M. T., Barlow, A. E., & Villarejo, M. ( 2010 ). Importance of undergraduate research for minority persistence and achievement in biology . Journal of Higher Education , 81 (1), 82–115. Google Scholar
- Jones, N. P., Papadakis, A. A., Hogan, C. M., & Strauman, T. J. ( 2009 ). Over and over again: Rumination, reflection, and promotion goal failure and their interactive effects on depressive symptoms . Behaviour Research and Therapy , 47 (3), 254–259. Medline , Google Scholar
- Judd, L. L., Paulus, M. J., Schettler, P. J., Akiskal, H. S., Endicott, J., Leon, A. C. , … & Keller, M. B. ( 2000 ). Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? American Journal of Psychiatry , 157 (9), 1501–1504. Medline , Google Scholar
- Kahn, J. H., & Garrison, A. M. ( 2009 ). Emotional self-disclosure and emotional avoidance: Relations with symptoms of depression and anxiety . Journal of Counseling Psychology , 56 (4), 573. Google Scholar
- Kataoka, S. H., Zhang, L., & Wells, K. B. ( 2002 ). Unmet need for mental health care among US children: Variation by ethnicity and insurance status . American Journal of Psychiatry , 159 (9), 1548–1555. Medline , Google Scholar
- Kreger, D. W. ( 1995 ). Self-esteem, stress, and depression among graduate students . Psychological Reports , 76 (1), 345–346. Medline , Google Scholar
- Krumpal, I. ( 2013 ). Determinants of social desirability bias in sensitive surveys: A literature review . Quality & Quantity , 47 (4), 2025–2047. Google Scholar
- Landis, J. R., & Koch, G. G. ( 1977 ). An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers . Biometrics , 33 (2), 363–374. Medline , Google Scholar
- Laursen, S., Hunter, A.-B., Seymour, E., Thiry, H., & Melton, G. ( 2010 ). Undergraduate research in the sciences: Engaging students in real science . Hoboken, NJ: Wiley. Google Scholar
- Limeri, L. B., Asif, M. Z., Bridges, B. H., Esparza, D., Tuma, T. T., Sanders, D. , … & Maltese, A. V. ( 2019 ). “Where’s my mentor?” Characterizing negative mentoring experiences in undergraduate life science research . CBE—Life Sciences Education , 18 (4), ar61. Link , Google Scholar
- Link, B. G., & Phelan, J. C. ( 2001 ). Conceptualizing stigma . Annual Review of Sociology , 27 (1), 363–385. Google Scholar
- Luyten, P., Sabbe, B., Blatt, S. J., Meganck, S., Jansen, B., De Grave, C. , … & Corveleyn, J. ( 2007 ). Dependency and self-criticism: Relationship with major depressive disorder, severity of depression, and clinical presentation . Depression and Anxiety , 24 (8), 586–596. Medline , Google Scholar
- Mabrouk, P. A., & Peters, K. ( 2000 ). Student perspectives on undergraduate research (UR) experiences in chemistry and biology . CUR Quarterly , 21 (1), 25–33. Google Scholar
- Maxwell, J. A. ( 2010 ). Using numbers in qualitative research . Qualitative Inquiry , 16 (6), 475–482. Google Scholar
- Mongrain, M., & Blackburn, S. ( 2005 ). Cognitive vulnerability, lifetime risk, and the recurrence of major depression in graduate students . Cognitive Therapy and Research , 29 (6), 747–768. Google Scholar
- Nagy, G. A., Fang, C. M., Hish, A. J., Kelly, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Burnout and mental health problems in biomedical doctoral students . CBE—Life Sciences Education , 18 (2), ar27. Link , Google Scholar
- National Academies of Sciences, Engineering, and Medicine (NASEM) . ( 2017 ). Undergraduate research experiences for STEM students: Successes, challenges, and opportunities . Washington, DC: National Academies Press. https://doi.org/10.17226/24622 Google Scholar
- NASEM . ( 2019 ). The science of effective mentorship in STEMM . Washington, DC: National Academies Press. Retrieved November 29, 2019, from www.nap.edu/download/25568 Google Scholar
- Osborne, J., & Collins, S. ( 2001 ). Pupils’ views of the role and value of the science curriculum: A focus-group study . International Journal of Science Education , 23 (5), 441–467. https://doi.org/10.1080/09500690010006518 Google Scholar
- Porter, S. R., & Whitcomb, M. E. ( 2005 ). Non-response in student surveys: The role of demographics, engagement and personality . Research in Higher Education , 46 (2), 127–152. Google Scholar
- President’s Council of Advisors on Science and Technology . ( 2012 ). Engage to excel: Producing one million additional college graduates with degrees in science, Technology, Engineering, and mathematics . Washington, DC: U.S. Government Office of Science and Technology. Google Scholar
- Prunuske, A. J., Wilson, J., Walls, M., & Clarke, B. ( 2013 ). Experiences of mentors training underrepresented undergraduates in the research laboratory . CBE—Life Sciences Education , 12 (3), 403–409. Link , Google Scholar
- Quinn, D. M., & Earnshaw, V. A. ( 2011 ). Understanding concealable stigmatized identities: The role of identity in psychological, physical, and behavioral outcomes . Social Issues and Policy Review , 5 (1), 160–190. Google Scholar
- Rauckhorst, W. H., Czaja, J. A., & Baxter Magolda, M. ( 2001 ). Measuring the impact of the undergraduate research experience on student intellectual development . Snowbird, UT: Project Kaleidoscope Summer Institute. Google Scholar
- Saldaña, J. ( 2015 ). The coding manual for qualitative researchers . Thousand Oaks, CA: Sage. Google Scholar
- Santiago, C. D., Kaltman, S., & Miranda, J. ( 2013 ). Poverty and mental health: How do low-income adults and children fare in psychotherapy? Journal of Clinical Psychology , 69 (2), 115–126. Medline , Google Scholar
- Santini, Z. I., Koyanagi, A., Tyrovolas, S., Mason, C., & Haro, J. M. ( 2015 ). The association between social relationships and depression: A systematic review . Journal of Affective Disorders , 175 , 53–65. Medline , Google Scholar
- Schleider, J., & Weisz, J. ( 2018 ). A single-session growth mindset intervention for adolescent anxiety and depression: 9-month outcomes of a randomized trial . Journal of Child Psychology and Psychiatry , 59 (2), 160–170. Medline , Google Scholar
- Seymour, E., & Hewitt, N. M. ( 1997 ). Talking about leaving: Why undergraduates leave the sciences . Westview Press. Google Scholar
- Seymour, E., & Hunter, A.-B. ( 2019 ). Talking about leaving revisited . New York, NY: Springer. Google Scholar
- Seymour, E., Hunter, A.-B., Laursen, S. L., & DeAntoni, T. ( 2004 ). Establishing the benefits of research experiences for undergraduates in the sciences: First findings from a three-year study . Science Education , 88 (4), 493–534. Google Scholar
- Smith, D. T., Mouzon, D. M., & Elliott, M. ( 2018 ). Reviewing the assumptions about men’s mental health: An exploration of the gender binary . American Journal of Men’s Health , 12 (1), 78–89. Medline , Google Scholar
- Sorkness, C. A., Pfund, C., Ofili, E. O., Okuyemi, K. S., Vishwanatha, J. K., Zavala, M. E. , … & Deveci, A. ( 2017 ). A new approach to mentoring for research careers: The National Research Mentoring Network . BMC Proceedings , 11 , 22. Medline , Google Scholar
- Sowislo, J. F., & Orth, U. ( 2013 ). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies . Psychological Bulletin , 139 (1), 213. Medline , Google Scholar
- Steger, M. F. ( 2013 ). Experiencing meaning in life: Optimal functioning at the nexus of well-being, psychopathology, and spirituality . In Wong, P. T. P. (Ed.), The human quest for meaning (pp. 211–230). England, UK: Routledge. Google Scholar
- Strenta, A. C., Elliott, R., Adair, R., Matier, M., & Scott, J. ( 1994 ). Choosing and leaving science in highly selective institutions . Research in Higher Education , 35 (5), 513–547. Google Scholar
- Text Depression Hotline . ( 2019 ). Crisis text line . Retrieved November 29, 2019, from www.crisistextline.org/depression Google Scholar
- Thiry, H., & Laursen, S. L. ( 2011 ). The role of student–advisor interactions in apprenticing undergraduate researchers into a scientific community of practice . Journal of Science Education and Technology , 20 (6), 771–784. Google Scholar
- Thompson, J. J., Conaway, E., & Dolan, E. L. ( 2016 ). Undergraduate students’ development of social, cultural, and human capital in a networked research experience . Cultural Studies of Science Education , 11 (4), 959–990. Google Scholar
- Trenor, J. M., Miller, M. K., & Gipson, K. G. ( 2011 ). Utilization of a think-aloud protocol to cognitively validate a survey instrument identifying social capital resources of engineering undergraduates . 118th American Society for Engineering Education Annual Conference and Exposition, Vancouver, BC, Canada . Google Scholar
- Turner, R. J., & Noh, S. ( 1988 ). Physical disability and depression: A longitudinal analysis . Journal of Health and Social Behavior , 29 (1), 23–37. Medline , Google Scholar
- Watson, D., & Friend, R. ( 1969 ). Measurement of social-evaluative anxiety . Journal of Consulting and Clinical Psychology , 33 (4), 448. Medline , Google Scholar
- Weeks, J. W., Heimberg, R. G., Fresco, D. M., Hart, T. A., Turk, C. L., Schneier, F. R., & Liebowitz, M. R. ( 2005 ). Empirical validation and psychometric evaluation of the Brief Fear of Negative Evaluation Scale in patients with social anxiety disorder . Psychological Assessment , 17 (2), 179. Medline , Google Scholar
- World Health Organization . ( 2018 ). Depression . Retrieved November 29, 2019, from www.who.int/news-room/fact-sheets/detail/depression Google Scholar
- Wyatt, T., & Oswalt, S. B. ( 2013 ). Comparing mental health issues among undergraduate and graduate students . American Journal of Health Education , 44 (2), 96–107. Google Scholar
- Carly A. Busch ,
- Tala Araghi ,
- Jingyi He ,
- Katelyn M. Cooper , and
- Colin Harrison, Monitoring Editor
- Emma C. Goodwin ,
- Danielle Pais ,
- Logan E. Gin , and
- Derek Braun, Monitoring Editor
- Baylee A. Edwards ,
- Chloe Bowen ,
- M. Elizabeth Barnes , and
- Tati Russo-Tait, Monitoring Editor
- Sara E. Grineski ,
- Danielle X. Morales , and
- Timothy W. Collins
- Carly A. Busch , and
- Tasneem F. Mohammed ,
- Erika M. Nadile ,
- Madison L. Witt ,
- Cindy Vargas ,
- Missy Tran ,
- Joseph Gazing Wolf ,
- Danielle Brister , and
- Sehoya Cotner, Monitoring Editor
- Katelyn M. Cooper ,
- Sarah L. Eddy , and
- Coping behavior versus coping style: characterizing a measure of coping in undergraduate STEM contexts 14 February 2022 | International Journal of STEM Education, Vol. 9, No. 1
- Lisa A. Corwin ,
- Michael E. Ramsey ,
- Eric A. Vance ,
- Elizabeth Woolner ,
- Stevie Maiden ,
- Nina Gustafson and
- Joseph A. Harsh
- Erin Shortlidge, Monitoring Editor
- K. Supriya ,
- Brian Sato, Monitoring Editor
- Logan E. Gin ,
- Clark Coffman, Monitoring Editor
- Nicholas J. Wiesenthal , and
- Maryrose Weatherton and
- Elisabeth E. Schussler
- Erika Offerdahl, Monitoring Editor
- Eight Recommendations to Promote Effective Study Habits for Biology Students Enrolled in Online Courses Journal of Microbiology & Biology Education, Vol. 23, No. 1
- Fostering professional development through undergraduate research: supporting faculty mentors and student researchers 30 March 2022 | Mentoring & Tutoring: Partnership in Learning, Vol. 30, No. 2
- Jeffrey Maloy ,
- Monika B. Kwapisz , and
- Bryce E. Hughes
- Terrell Morton, Monitoring Editor
- Anxiety and depression among US college students engaging in undergraduate research during the COVID-19 pandemic 14 December 2021 | Journal of American College Health, Vol. 9
- Danielle Brister ,
- Sara E. Brownell ,
- Chade T. Claiborne ,
- Curtis Lunt ,
- Kobe M. Walker ,
- Tamiru D. Warkina ,
- Yi Zheng , and
- Rebecca Price, Monitoring Editor
- Dominant Learning Styles of Interior Design Students in Generation Z 26 July 2021 | Journal of Interior Design, Vol. 46, No. 4
- Linking Emotional Intelligence, Physical Activity and Aggression among Undergraduates 26 November 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 23
- Advancing undergraduate synthetic biology education: insights from a Canadian iGEM student perspective Canadian Journal of Microbiology, Vol. 67, No. 10
- Frank A. Guerrero ,
- Sara E. Brownell , and
- Jennifer Momsen, Monitoring Editor
- Nicholas J. Wiesenthal ,
- Isabella Ferreira , and
- Grant Ean Gardner, Monitoring Editor
- Carolyn E. Clark ,
- Deanna B. Elliott ,
- Travis B. Roderick ,
- Rachel A. Scott ,
- Denisse Arellano ,
- Diana Ramirez ,
- Kimberly Velarde ,
- Allyson Aeschliman ,
- Sarah T. Avalle ,
- Jessica Berkheimer ,
- Rachel Campos ,
- Michael Gerbasi ,
- Sophia Hughes ,
- Julie A. Roberts ,
- Quinn M. White ,
- Ehren Wittekind ,
- Rachelle Spell, Monitoring Editor
- Christine Pfund ,
- Janet L. Branchaw ,
- Melissa McDaniels ,
- Angela Byars-Winston ,
- Steven P. Lee ,, and
- Bruce Birren
- Vladimir Anokhin ,
- MacKenzie J. Gray ,
- Daniel E. Zajic ,
- Jason E. Podrabsky , and
- Erin E. Shortlidge
- Depression as a concealable stigmatized identity: what influences whether students conceal or reveal their depression in undergraduate research experiences? 4 June 2020 | International Journal of STEM Education, Vol. 7, No. 1
Submitted: 4 November 2019 Revised: 24 February 2020 Accepted: 6 March 2020
© 2020 K. M. Cooper, L. E. Gin, et al. CBE—Life Sciences Education © 2020 The American Society for Cell Biology. This article is distributed by The American Society for Cell Biology under license from the author(s). It is available to the public under an Attribution–Noncommercial–Share Alike 3.0 Unported Creative Commons License (http://creativecommons.org/licenses/by-nc-sa/3.0).
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 75, NO. 4 CURRENT ISSUE pp.307-398
- March 01, 2024 | VOL. 75, NO. 3 pp.203-304
- February 01, 2024 | VOL. 75, NO. 2 pp.107-201
- January 01, 2024 | VOL. 75, NO. 1 pp.1-71
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
A Literature Review of Studies of Depression and Treatment Outcomes Among U.S. College Students Since 1990
- Elissa J. Miller M.D., M.P.H.
- Henry Chung M.D.
Search for more papers by this author
According to the fall 2007 American College Health Association-National College Health Assessment ( 1 ), a national survey of approximately 20,500 college students on 39 campuses, 43.2% of the students reported "feeling so depressed it was difficult to function" at least once in the past 12 months. More than 3,200 university students reported being diagnosed as having depression, with 39.2% of those students diagnosed in the past 12 months, 24.2% currently in therapy for depression, and 35.8% taking antidepressant medication. Among the students surveyed, 10.3% admitted "seriously considering attempting suicide" within the past 12 months and 1.9% actually attempted suicide during that period.
Although the above data may seem surprising to some, it is not to most mental health clinicians and administrators at U.S. colleges. According to the 2008 National Survey of Counseling Center Directors, 95% of respondents believe that there has been a trend in recent years of an increase in the number of students with serious psychological problems. In 2008 an estimated 26% of counseling center clients were taking psychiatric medication, up from 20% in 2003, 17% in 2000, and 9% in 1994 ( 2 ). And although the rate of suicide among college students may have decreased in recent decades ( 3 ), suicide remains the third leading cause of death among adolescents and young adults ( 4 ).
Many college administrators have begun to appreciate the effect that a student's depression can have on overall functioning in the college community. Depression has been linked to academic difficulties as well as interpersonal problems at school, with more severe depression correlated with higher levels of impairment ( 5 ). The treatment of depression among college students has been associated with a protective effect on these students' grade point averages ( 6 ). In an effort to diagnose and treat early and effectively, and thus decrease the excess morbidity and risk of suicide associated with depression, some U.S. colleges have even begun to screen students for depression in the primary care setting ( 7 ).
There are unique challenges of providing treatment to college students. These challenges include significant academic pressure in semester-based cycles, extensive semester breaks that result in discontinuities of care, and heavy reliance on community supports that can be inconsistent. Given the prevalence and impact of depression on college campuses and the varying services offered by university mental health centers throughout the United States, there is a significant need to evaluate successful models of treatment and their related outcomes.
The databases PsycINFO, MEDLINE, and CINAHL were searched for studies related to depression among U.S. college students and treatment outcome by using the following terms: "depression," "college or university or graduate or junior college or community college students," "colleges," "community colleges," "treatment and prevention," "empirical study," and "peer reviewed journal." Initially, no limitation was placed on years included in the search. Eighteen relevant publications were read and analyzed closely for method and content, with particular focus on location and inclusion criteria of study participants. Studies were eliminated if participants were students at colleges outside of the United States, if the studies did not have specific depression criteria for inclusion, or if the students included were at risk of depression but did not meet criteria for having depression. Nine remaining articles were reviewed further, and it was decided that the five studies published before 1990 had decreased relevance and would be excluded from this review in light of the growing availability of selective serotonin reuptake inhibitor medications since 1990, which substantially changed the treatment of depression among college students. In addition, the demographic characteristics of U.S. college students may have changed since the early 1990s, with many college counseling center directors noting a trend in recent years of an increase in students with serious psychological problems ( 2 ). Only four articles ( 8 , 9 , 10 , 11 ) remained for this review of depression and treatment outcomes of U.S. college students.
In 2007 Kelly and colleagues ( 8 ) conducted a nonexperimental study that recruited from introductory psychology classes university students with depression who were not currently in treatment, offering both financial compensation and class credit for research involvement. Sixty college students (66% Caucasian, 57% female) with major depression were followed for nine weeks without any treatment to assess for sudden gains (that is, precipitous improvements in depressive symptomatology), remission of depressive symptoms, and reversal of improvements. The authors found that 60% of the college students with major depression experienced sudden gains over the nine weeks of not receiving treatment. However, before the end of the nine-week observation period, more than half of these sudden gains reversed. At the end of the period of not receiving treatment, depression was in remission for 20% of the students. The authors concluded that sudden gains may be part of the natural course of depression for some college students, irrespective of treatment, and that self-evaluation processes may play an important role in recovery.
In 2000 Lara and colleagues ( 9 ) conducted a nonexperimental study in which undergraduate students taking psychology classes who had a recent-onset major depressive episode were paid or received course credit for their research participation. Eighty-four students (51% Caucasian, 86% female) were followed for 26 weeks to assess whether various psychosocial factors predicted the short-term course of major depression. The authors found that within the 26-week period of no treatment, 68% of the college students who were initially depressed recovered. Among those who recovered, 21% relapsed by the end of the 26-week period into another major depressive episode. Lara and colleagues concluded that college students with depression may sometimes spontaneously recover and relapse and that harsh discipline in childhood was significantly associated with higher mean levels of depression at follow-up and relapse but not with recovery.
In 2006 Geisner and colleagues ( 10 ) conducted a four-week randomized controlled trial of depression treatment and recruited undergraduates with depression who were enrolled in psychology courses to participate for course credit. The study enrolled 177 students with depression (49% Caucasian and 48% Asian, 70% female) who were randomly assigned either to an intervention group that received personalized mailed feedback or to a control group. The authors found that depressive symptoms improved for both the intervention and control groups, but in the intervention condition there was a significantly greater improvement of depressive symptoms, as measured by the DSM-IV-Based Depression Scale. There was no significant difference between the intervention and control groups on symptoms measured by the Beck Depression Inventory (BDI). Geisner and colleagues concluded that an intervention using personalized mailed feedback may be useful for reducing depressive symptoms among college students.
In 1993 Pace and Dixon ( 11 ) conducted a four- to seven-week randomized controlled trial to assess the treatment effectiveness of individual cognitive therapy for college students with depressive symptoms. Participating undergraduate students earned course credit for their research involvement. Seventy-four students (100% Caucasian, 81% female) who met strict criteria for study inclusion were randomly assigned to either a group that received individual cognitive therapy or a control condition where participants did not receive treatment and were put on a waiting list for cognitive therapy. Pace and Dixon found that 74% of participants in the cognitive therapy group (versus 33% in control group) were classified as nondepressed with BDI scores of less than 10 after four to seven weeks of treatment. At the one-month follow-up, 81% of participants in the cognitive therapy group (versus 64% of control group) were classified as nondepressed. Outcomes at both time points were statistically significant in favor of cognitive therapy. The authors concluded that brief individual cognitive therapy may effectively reduce mild to moderate depressive symptoms as well as depressive self-schemata among college students.
The current body of literature on depression and treatment outcomes among U.S. college students is sparse, and for the four studies we found, varying inclusion and exclusion criteria, assessment methods, and lengths of treatment make the interpretation of results difficult. Whereas Kelly and colleagues ( 8 ) and Lara and colleagues ( 9 ) used the Structured Clinical Interview for DSM-IV to diagnose participants with major depressive disorder, Geisner and colleagues ( 10 ) and Pace and Dixon ( 11 ) used self-report scales to measure depressive symptoms for study inclusion and Pace and Dixon excluded students with severe levels of depressive symptoms. All four studies recruited students who were not seeking treatment and who were offered course credit for participating, a reward that might have influenced the degree of improvement in outcomes. There was no consistent standard used across studies to define a student with depression, even when using the same assessment tool. In terms of length of treatment, only two of the four reviewed studies followed students for more than nine weeks. The length of time over which students are assessed is especially critical for the college population, where time is defined by a semester calendar, moods are often influenced by exam schedules, and treatments are adjusted to accommodate upcoming vacations ( 12 ). Today's college mental health services tend to employ short-term models of care (eight to 16 sessions), with referral to outside clinicians if longer-term treatment is necessary ( 13 ). Given these dynamics, future research in college mental health will need to establish quality standards for ongoing monitoring and follow-up of students' treatment outcomes.
Unfortunately, the results from these four studies may not be fully applicable to college students today or in the future, particularly in light of the changing demographic characteristics of those attending universities as well as the rapidly evolving role of pharmacology in the treatment of depression. Only two of the four studies reviewed offered any active treatment for depression, and none of the studies included any form of pharmacological treatment. Consistent with current medical literature and best practices, many treatment-seeking college students diagnosed as having depression currently receive psychotherapy and psychopharmacological treatment ( 1 ). Because major depression can be a chronic recurring condition, future research needs to evaluate the effectiveness of the various treatment modalities used to treat college students with depression. This is particularly important in light of the recent addition of a black-box warning for the use of antidepressant medications among young adults aged 18 to 24 years, which recommends the close monitoring of patients taking antidepressant medication for clinical worsening, suicidality, or unusual changes in behavior.
Conclusions
In light of the high prevalence of depression among college students today and the risks and sequelae this illness poses if not diagnosed and treated early and effectively, it is imperative that research funding be increased for both naturalistic and intervention studies of depression and treatment outcomes in the college health setting. First, research documenting depression and treatment outcomes in this cohort should be identified in order to evaluate the adequacy of current care. Second, research should be directed to assessing specific short-term or semester-based interventions for students with depression. Models that explore the effectiveness of integration with primary care, care management, medication, and short-term psychotherapy are all important targets for future study. By conducting such research, effective treatment models and benchmarks of treatment outcome in the college population can be developed and integrated into college mental health practice.
Acknowledgments and disclosures
The authors thank Michael Klein, Ph.D., for his assistance in the development of this brief report.
Dr. Chung has served on advisory boards for Takeda Pharmaceuticals and Lundbeck Pharmaceuticals and has served as a speaker for Pfizer and Jazz Pharmaceuticals. Dr. Miller reports no competing interests.
At the time of this report, Dr. Miller was a Public Psychiatry Fellow at New York State Psychiatric Institute and Columbia University, New York City. Dr. Chung is associate vice-president of student health at New York University Student Heath Center, New York City. Send correspondence to Dr. Miller at the New York State Psychiatric Institute, Columbia University, 1051 Riverside Dr., Box 111, New York, NY 10032 (e-mail: [email protected] ).
1. American College Health Association-National College Health Assessment: Reference Group Report, Fall 2007. Baltimore, American College Health Association, 2008. Available at www.acha-ncha.org/reports_ACHA-NCHAoriginal.html Google Scholar
2. Gallagher R: National Survey of Counseling Center Directors, Alexandria, Va, International Association of Counseling Services, 2008. Available at www.iacsinc.org Google Scholar
3. Schwartz A: Four eras of study of college student suicide in the United States: 1920–2004. Journal of American College Health 54:353–366, 2006 Google Scholar
4. National Center for Injury Prevention and Control: Web-based Injury Statistics Query and Reporting System (WISQARS). Atlanta, Ga, Centers for Disease Control and Prevention, 2005. Available at www.cdc.gov/injury/wisqars/index.html Google Scholar
5. Heiligenstein E, Guenther G, Hsu K, et al: Depression and academic impairment in college students. Journal of American College Health 45:59–64, 1996 Google Scholar
6. Hysenbegasi A, Hass S, Rowland C: The impact of depression on the academic productivity of university students. Journal of Mental Health Policy and Economics 8:145–151, 2005 Google Scholar
7. Chung H, Klein M: Improving identification and treatment of depression in college health. Student Health Spectrum, June 2007, pp 13–19 Google Scholar
8. Kelly M, Roberts J, Bottonari K: Non-treatment related sudden gains in depression: the role of self-evaluation. Behaviour Research and Therapy 45:737–747, 2007 Google Scholar
9. Lara ME, Klein DN, Kasch KL: Psychosocial predictors of the short-term course and outcome of major depression: a longitudinal study of a nonclinical sample with recent-onset episodes. Journal of Abnormal Psychology 109:644–650, 2000 Google Scholar
10. Geisner I, Neighbors C, Larimer M: A randomized clinical trial of a brief, mailed intervention for symptoms of depression. Journal of Consulting and Clinical Psychology 74:393–399, 2006 Google Scholar
11. Pace T, Dixon D: Changes in depressive self-schemata and depressive symptoms following cognitive therapy. Journal of Counseling Psychology 40:288–294, 1993 Google Scholar
12. Lee C: Evidenced-based treatment of depression in the college population. Journal of College Student Psychotherapy 20:23–31, 2005 Google Scholar
13. Stone G, McMichael J: Thinking about mental health policy in university and college counseling centers. Journal of College Student Psychotherapy 10:3–28, 1996 Google Scholar
- Depression and help-seeking behaviors among college students: Findings from the Healthy Minds Study 2018-2019 16 January 2024 | Journal of American College Health, Vol. 11
- Depression recognition in university students based on speech features in social learning environment
- Supporting mental health and wellbeing of university and college students: A systematic review of review-level evidence of interventions 29 July 2022 | PLOS ONE, Vol. 17, No. 7
- Examining Anxiety, Sleep Quality, and Physical Activity as Predictors of Depression among University Students from Saudi Arabia during the Second Wave of the COVID-19 Pandemic 21 May 2022 | International Journal of Environmental Research and Public Health, Vol. 19, No. 10
- Response Actions of Malaysian Universities and Colleges in Managing Student Mental Health: A Systematic Review 16 June 2021 | International Journal of Community Well-Being, Vol. 5, No. 1
- Effects of College Athlete Life Stressors on Baseline Concussion Measures Journal of Sport Rehabilitation, Vol. 29, No. 7
- Effect of Tai Chi on psychological disorder in college students 5 June 2020 | Medicine, Vol. 99, No. 23
- Journal of Rational-Emotive & Cognitive-Behavior Therapy, Vol. 37, No. 1
- Examining the Relationship Between Social Support Satisfaction and Perceived Stress and Depression in Athletic Training Students Athletic Training Education Journal, Vol. 13, No. 2
- Journal of Autism and Developmental Disorders, Vol. 48, No. 3
- Personality and Individual Differences, Vol. 134
- Journal of Evolution of Medical and Dental Sciences, Vol. 5, No. 54
- Mental health first aid training for Australian medical and nursing students: an evaluation study 12 April 2015 | BMC Psychology, Vol. 3, No. 1
- The Cognitive Behaviour Therapist, Vol. 8
- International Journal of Clinical and Health Psychology, Vol. 13, No. 1
- Journal of Affective Disorders, Vol. 125, No. 1-3

Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Empirical Examination of Current Depression Categories in a Population-Based Study: Symptoms, Course, and Risk Factors
- Li-Shiun Chen , M.D., Sc.D. ,
- William W. Eaton , Ph.D. ,
- Joseph J. Gallo , M.D., M.P.H. ,
- Gerald Nestadt , M.D., M.P.H. , and
- Rosa M. Crum , M.D., M.H.S.
Search for more papers by this author
OBJECTIVE: Research studies on the validity of current diagnostic and subthreshold categories of depression that use a population-based follow-up design are rare. The authors examined the validity and utility of four current depression categories by examining subject transition between categories and the symptoms, course, and risk factors of each. METHOD: A general population sample of 1,920 adults from the Baltimore Epidemiologic Catchment Area 13-year follow-up study were examined. Data on diagnoses, symptoms, course, and risk factors were collected by using the National Institute of Mental Health Diagnostic Interview Schedule, the Life Chart Interview, and an office visit. Polychotomous regression was used to examine the heterogeneity of four diagnostic categories: major depressive disorder, depressive syndrome, dysthymia, and a comorbid depression condition (major depressive disorder and dysthymia). RESULTS: Transitions between the four depression categories occurred over the 13 years. Symptom profiles for the four categories were parallel but differed in severity. Course characteristics among the four categories slightly differed. Risk factor profiles showed significant differences. Family history was associated with both depressive syndrome and major depressive disorder. Stressful life events were most strongly associated with depressive syndrome. Female gender was most strongly associated with the comorbid depression category. CONCLUSIONS: The evidence suggests that except for dysthymia, the depression categories are genetically homogeneous and environmentally heterogeneous. Stress is associated with mild depression, and gender is associated with severe depression. The apparent familial transmission of the subthreshold entity, depressive syndrome, needs further investigation.
Lack of consensus as to the heterogeneity of depression is reflected in the evolving diagnostic categories of depressive disorders. Criteria for existing diagnostic categories differ depending on the particular version, and new categories such as minor depressive disorder have been included. For example, the minimal number of symptom groups required for a diagnosis of major depressive disorder changed from DSM-III to DSM-III-R, and distress or impairment caused by symptoms is a new requirement in DSM-IV. There is also a growing interest in subthreshold depression, a classification that requires fewer symptoms than major depressive disorder for diagnosis. The differentiation of dysthymic disorder from major depressive disorder is still an area of intense research (1) . The concept of “double depression,” which captures individuals with both major depressive and dysthymic episodes in specific temporal fashion, poses the question as to whether this classification is a comorbid condition or a separate entity (2) .
Studies on the validity of different depressive disorders have shown inconclusive results. Attempts to distinguish different diagnostic categories have been made by examining symptoms, course, or risk factors. A study by Wells et al. (3) showed that initial depression severity and level of functional status accounted for more of the variance in outcomes than did type of depressive disorder. A comparison of symptoms among cases of major depressive disorder and dysthymic disorder revealed that symptom presentation did not distinguish clearly between the diagnostic groups (4) . The findings by Romanoski et al. (5) , which were based on the 1981 psychiatric assessments of the Baltimore Epidemiologic Catchment Area (ECA) sample, suggested that risk factors differed between the subjects with major depressive disorder and those with nonmajor depression. However, the diagnosis of nonmajor depression comprised several potentially heterogeneous disorders.
Studies have been conducted to examine the diagnostic validity of the distinction between dysthymia and major depressive disorder (1 , 2 , 6) , two disorders with a very high rate of comorbidity (7) . The condition of an index episode of major depressive disorder continuous with a preexisting dysthymia and without an intervening period of euthymia of at least 8 weeks has been coded “double depression” (2) . The poor prognoses for double depressive disorders and dysthymic disorders have been recognized (2) , but there is little conclusive evidence that dysthymia is a separate disease entity from major depressive disorder (6) . In addition, evidence from the Medical Outcomes Study (3) suggests that the outcome for minor depression may be even worse than that for major depressive disorder.
The heterogeneity of minor depression and its separate role from major depressive disorder also have drawn increasing research attention. Family studies suggest that there is a higher risk of minor depression among relatives of probands with major depressive disorder (8) . Epidemiologic evidence suggests that major depressive disorder is more often an exacerbation of a chronic mood disturbance with roots in longstanding vulnerability factors, while in later life minor depression is more often a reaction to commonly experienced stresses (9) . Some researchers have suggested that minor depression is a heterogeneous disorder because some cases of minor depression progress into major depressive disorder while others do not (10 , 11) .
This study uses a prospective and population-based sample to assess the discriminant validity and utility of four subcategories of depression: major depressive disorder, depressive syndrome, dysthymia, and comorbid depression (operationally defined here as meeting criteria for both major depressive disorder and dysthymia). The heterogeneity of these depression categories can be probed from three perspectives: symptoms, natural course, and risk factors.
The ECA study was a series of epidemiologic surveys of the general household population conducted from 1980 to 1983 by collaborators at five sites in the United States (12 , 13) . During 1993–1996, the Baltimore ECA follow-up study interviewed 1,920 adults from the original Baltimore sample of 3,481. Nonresponse was due to mortality, sample loss, or subject refusal. The nonsurvivors were more likely to be older, male, white, less educated, widowed, and unemployed. Subjects lost to follow-up were more likely to be younger, nonwhite, divorced or separated, less educated, and unemployed. Subjects who refused participation were more likely to be white and less educated, but refusal was not associated with baseline psychopathology. Since 24.0% (N=835) of the cohort died, the 1,920 subjects represented 72.6% of survivors (14) . The demographic composition of the follow-up cohort was comparable to that of the original sample in gender and race, but the follow-up group was older and more educated. The follow-up sample was primarily female (63.0%, N=1,209) and Caucasian (67.0%, N=1,286) and ranged in age from 27 to 96 years (median age=48 years) (15) . Depression predicts mortality (16) , but in this sample the effect was not statistically significant. Sample attrition was not associated with depression (14) . After subjects with missing diagnostic information were excluded, 1,856 subjects from the 1993–1996 follow-up were included in the analyses. Subjects signed statements of informed consent in accordance with procedures of the Johns Hopkins School of Public Health Human Subjects Committee.
Symptoms and Diagnoses
The National Institute of Mental Health Diagnostic Interview Schedule (DIS) (17) was used to assess the diagnostic elements, including symptoms, their severity and frequency over time, and whether or not the symptoms were caused by physical illness or injury, use of drugs or alcohol, or the presence of another psychiatric disorder. Several questions targeted at different symptoms were asked for each of the nine depressive symptom groups in the diagnostic criteria. The presence of each symptom in the lifetime and during the worst episode as well as temporal clustering with other symptoms were clarified.
The diagnoses of major depressive disorder and dysthymia were generated from the algorithm based on DSM-III-R criteria. Depressive syndrome was defined by the statement “have had a period of 2 weeks or longer when several (three or more) depressive symptoms occur together including dysphoria or anhedonia” and excluded individuals who met criteria for major depressive disorder (18) . Finally, the comorbid depression group was defined as “meeting criteria for lifetime diagnoses of both major depressive disorder and dysthymia.”
Course Characteristics
Course descriptors were defined operationally following the temporal sequence in disease development and progression. Age at onset was defined as the age in years when the first depressive episode occurred. Depressive episode was defined as a clustering of at least three depressive symptoms, including dysphoria or loss of interest, during a period of 2 weeks or longer. We used the onset age of the first depressive episode as a standard comparison across disorder categories, including the comorbid depression category, which had potentially two different onsets. Prodrome length for depressive syndrome was the duration in years between the onset of the first depressive symptom to the onset of the depressive episode. Number of depressive episodes was the number of lifetime depressive episodes, which indicated the fluctuation of depressive psychopathology over the lifetime.
Impairment was coded present when subjects reported any depression-related interference with working or everyday activities or reported taking medication more than once or being hospitalized for the problem. Depression is known for psychiatric comorbidities, and there is still ongoing debate on the distinction between anxiety and depression (19) . Therefore, we also studied how often each of the four depression categories presented comorbidly with other psychiatric disorders as part of our effort to compare the disease course. Lifetime anxiety disorder comorbidity was defined as meeting DSM-III-R criteria for at least one of the anxiety disorders (phobia, generalized anxiety disorder, panic disorder, obsessive-compulsive disorder) in addition to depression. Lifetime alcohol- or substance-related disorder comorbidity was defined as meeting DSM-III-R criteria for abuse of or dependence on alcohol, cocaine, hallucinogens, marijuana, sedatives, stimulants, or tranquilizers in addition to depression. All these course characteristics were cumulative lifetime measures from all available interviews.
Risk Factors
Family history was assessed in the clinical reappraisal of 810 Baltimore ECA subjects in 1981 (20) and at the wave 2 interview in 1982 as well as during an office visit interview of 349 subjects in 1993–1996 (21) . A positive family history of depression was defined as any first- or second-degree relatives with depression.
Information on stressful life events was collected from administering the DIS at wave 1, wave 2, and wave 3 assessments. The assessed events included separation, divorce, widowhood, life-threatening illnesses, traumatic events, death of loved one(s), children moving out, retirement, losing job, and breakup of love relationships or important friendships. An addition to the interview for the wave 3 follow-up addressed the problem of deterioration of recall with time through a new standardized instrument called the Life Chart Interview (22) . The Life Chart Interview generates age- and calendar-linked personal memory cues for the respondent at the beginning of the interview by means of an interactive visually oriented life calendar that focuses the respondent’s attention on a designated time period. A dichotomous variable to indicate the presence or absence of one or more stressful life events before the onset of the first DIS depressive episode was created. Those who reported any of the above events and also required at least some time for adjustment during the 1 year before onset of the first depressive episode were coded positive for prior stressful life events during the 1 year before onset.
Statistical Analysis
Any overall differences in depressive symptoms, course, and risk factors among the four groups were examined by means of analyses of variance (ANOVAs) for continuous variables and chi-square tests for categorical variables. Nonparametric Kruskal-Wallis tests were used for nonnormally distributed continuous measures. Differences between any two groups were compared by means of two-sample t tests for continuous variables and z tests for categorical variables. Nonparametric Mann-Whitney tests were used for nonnormally distributed continuous measures. We used the Bonferroni method to adjust for type I errors due to multiple comparisons. Both the actual p values and the Bonferroni p values are reported.
We first examined the univariate associations between a set of hypothesized risk factors (female gender, family history of depression, and stressful life events before the onset of the first episode) and each of the four depression categories. The reference group was composed of subjects without major depressive disorder, depressive syndrome, or dysthymia in their lifetime. Next, we used logistic regression models to examine the multivariate associations between hypothesized risk factors and each of the four disorder categories. The interactions between the covariates were also examined. In order to compare the risk factor association profiles across different categories, polychotomous logistic regression models were used to test the homogeneity among these parallel odds ratios. For example, we were able to compare the associations with female gender between the major depressive disorder and the dysthymia categories in the polychotomous regression model. The polychotomous logistic regression model is the natural extension of the binary logistic regression model and can be used to carry out simultaneous analyses of multiple response types (23) . A homogeneity z test was used to test whether two parallel odds ratios for two different response types differed.
Sample Characteristics
Individuals who met criteria for each of the three depression categories (major depressive disorder, dysthymia, and depressive syndrome) were identified first, which resulted in the following lifetime prevalence rates: major depressive disorder: 9.8% (95% confidence interval [CI]=8.2%–11.4%); depressive syndrome: 16.0% (95% CI=14.2%–17.8%); dysthymia: 7.3% (95% CI=6.1%–8.5%). For the purpose of examination among different categories, individuals were assigned to one of four mutually exclusive lifetime categories: major depressive disorder (5.4%, N=100), depressive syndrome (12.0%, N=223), dysthymia (3.7%, N=68), and comorbid depression (major depressive disorder and dysthymia; 2.8%, N=53).
Subject Transition Between Depression Diagnostic Categories
We examined the change of lifetime diagnostic status by cross-tabulating lifetime diagnoses assessed in the wave 1 (1981) interview and lifetime diagnoses summarized from assessments in three waves (1981, 1982, 1993–1996). As seen in table 1 , about 17% of the 59 subjects with major depressive disorder in 1981 developed comorbid dysthymia during the follow-up. About 10% of the 136 subjects with depressive syndrome in 1981 developed major depressive disorder; 5% developed dysthymia; and 8% developed comorbid major depressive disorder and dysthymia. About 19% of the 37 dysthymia subjects in 1981 developed comorbid major depressive disorder.
Symptom Heterogeneity
The proportions of individuals in each of the four categories reporting depressive symptoms during their worst episodes are compared visually in figure 1 and statistically by using polychotomous regression models with homogeneity z tests. Proportions of subjects with depressive syndrome were lower than those of subjects with major depressive disorder for all nine symptom groups. The odds ratio of reporting each symptom group in the major depressive disorder category was significantly higher than it was for the depressive syndrome category (e.g., from the polychotomous regression model for depressed mood, homogeneity z=2.4, N=1,856, p=0.02). For all symptom groups except “feeling worthless,” subjects with dysthymia were significantly less likely than subjects with major depressive disorder to report experiencing the symptoms. Subjects with comorbid depression had significantly higher proportions reporting symptoms of feeling tired, feeling worthless, and suicidal thought/behavior than those with major depressive disorder. To summarize, the associations between each category and the symptom profiles were parallel but significantly differed in the strength of associations (comorbid depression greater than major depressive disorder greater than dysthymia and depressive syndrome), with a few exceptions in the comparison of the major depressive disorder and the comorbid depression categories.
Course Heterogeneity
We compared the means of three continuous course variables (age at onset of first depressive episode, length of prodrome, number of depressive episodes) among the four depression diagnostic categories ( figure 2 shows the distributions of age at first depressive episode). The age-at-onset distributions were similar for the major depressive disorder and depressive syndrome categories. There was more variation in the onset distribution for the dysthymia category, and the age at onset was earlier for the comorbid depression category. Statistical tests for an overall difference across the four depressive categories suggested significant differences in age at onset (Kruskal-Wallis χ 2 =8.84, df=3, p=0.03) and number of episodes (Kruskal-Wallis χ 2 =13.2, df=3, p=0.004), but not in length of prodrome. Next, examination of six paired comparisons by means of Mann-Whitney tests revealed that the comorbid depression category had an earlier onset than the other three categories (versus depressive syndrome: U=3,584, N=236, p=0.004; versus major depressive disorder: U=1,971.5, N=150, p=0.02; versus dysthymia: U=899, N=98, p=0.04). If we used the Bonferroni method to adjust for multiple comparisons by multiplying the above p values by six, only the difference between the comorbid depression and the depressive syndrome categories remained significant.
Next, examination of six paired comparisons again by means of Mann-Whitney tests showed that subjects in the comorbid depression category experienced more episodes than those with major depressive disorder and those with depressive syndrome (versus major depressive disorder: U=1,916, N=148, p=0.03; versus depressive syndrome: U=2,711.5, N=213, p<0.001). If we used the Bonferroni method to adjust for multiple comparisons by multiplying the above p values by six, only the difference between the comorbid depression and the depressive syndrome categories remained significant.
The proportion of subjects reporting dichotomous course variables (impairment, comorbid anxiety disorder, or comorbid alcohol- or substance-related disorder) are compared in table 2 . The chi-square test that compared all four categories suggested an overall difference in the proportion reporting impairment but not in subjects with co-occurring conditions. Subjects in the comorbid depression category reported the highest rate of depression-related impairment (91%), whereas those in the depressive syndrome category reported the lowest rate (63%). Examination of six paired comparisons by means of z tests showed that the impairment rate was higher in the major depressive disorder and comorbid depression categories but lower in the depressive syndrome and dysthymia categories (major depressive disorder versus depressive syndrome: z=4.30, N=323, p<0.00006; major depressive disorder versus dysthymia: z=2.22, N=168, p=0.03; comorbid depression versus depressive syndrome: z=5.36, N=276, p<0.00006; comorbid depression versus dysthymia: z=3.12, N=121, p=0.002). If we used the Bonferroni method to adjust for multiple comparisons by multiplying the above p values by six, all differences except that between the major depressive disorder and the dysthymia categories remained significant.
Risk Factor Heterogeneity Among Four Categories
Results of logistic regressions that compared each of the four depression categories and the reference group are summarized in table 3 . In the univariate regression model, subjects with depressive syndrome, dysthymia, and comorbid depression—but not major depressive disorder—had a significantly higher likelihood of being female; the odds ratio for female gender was much higher in the comorbid depression category than it was in the other three categories. The homogeneity z test of odds ratios between the major depressive disorder and comorbid depression categories indicated that the association between female gender and comorbid depression was significantly stronger than that of female gender and major depressive disorder (z=–2.8, N=1,856, p=0.005). Family history was associated with all four diagnostic categories, but the odds ratio for the dysthymia subjects was lower than those of the other three groups. The homogeneity z test of odds ratios between the major depressive disorder and dysthymia categories indicated that the association between family history and major depressive disorder was significantly stronger than that of family history and dysthymia (z=2.6, N=1,594, p=0.009). Stressful life events had a significantly higher likelihood of occurring with major depressive disorder and depressive syndrome but not with dysthymia or comorbid depression.
In the multivariate regression model, the odds ratio for female gender was significant only for the comorbid depression category. The odds ratio for family history of depressive disorder was significantly associated with all categories except dysthymia. Stressful life events were a significant predictor for major depressive disorder and depressive syndrome but not for dysthymia or comorbid depression. A homogeneity z test comparison of odds ratios between the major depressive disorder and the comorbid depression categories indicated a significantly stronger association between female gender and comorbid depression than between female gender and major depressive disorder (z=–2.02, N=1,160, p=0.04).
Both major depressive disorder and depressive syndrome were associated with family history of depression and stressful life events before onset. Yet, for the subjects with major depressive disorder, family history was a stronger risk factor than a stressful life event; for depressive syndrome, a stressful life event was a stronger risk factor than family history. For subjects with comorbid depression, family history was a prominent risk factor in addition to female gender. Dysthymia was the only category not significantly associated with any of the examined risk factors. There were no significant interactions between the examined risk factors in any of the four categories.
There was a substantial degree of transition among these depression diagnostic categories over time. Symptoms of a substantial proportion of subjects with dysthymia have only intensified with time. The course of some individuals with depressive syndrome or major depressive disorder has become more chronic. The transition from depressive syndrome to major depression is consistent with what has been reported earlier by Broadhead and colleagues (24) . There have been some discrepancies in subject reports of psychopathology in multiple waves of assessments (15) , so we took information from three waves to establish the lifetime diagnoses in wave 3.
The profiles of depressive symptoms were parallel among the four depression diagnostic categories. Proportionally more subjects with comorbid depression or major depressive disorder reported all depression symptom groups than did those with dysthymia or depressive syndrome. The depressive episode was more severe in subjects with comorbid depression than for those with major depressive disorder, especially when reporting symptoms that may be considered more severe in nature, such as suicidality and worthlessness. Individuals with dysthymia presented symptom profiles similar to those with depressive syndrome.
The four depression diagnostic categories were similar in course characteristics except that the earlier onset for comorbid depression might explain its more severe and recurrent nature and the higher proportion of subjects reporting impairment. Our finding of earlier onset for subjects with comorbid depression is consistent with the study by Sorenson et al. (25) . The high rates of impairment associated with all four categories including depressive syndrome are consistent with existing evidence. Wells et al. (3) reported that depressive symptoms in the absence of disorder are associated with limitations in six dimensions of patient well-being and functioning (physical functioning, role functioning, social functioning, number of bed days, current health, and being free of pain) when compared with patients with no chronic conditions in a general medical outpatient sample. Judd et al. (26) found significantly more subjects with depressive symptoms reported high levels of household strain, social irritability, and financial strain as well as limitations in physical or job functioning, restricted activity days, bed days, and poor health status than did subjects without disorder. The lifetime prevalence of major depressive disorder is 5.4%, and in our study 84% of the subjects with major depressive disorder reported impairment. However, the lifetime prevalence of depressive syndrome is 12%, and in our study 63% of the depressive symptom subjects reported impairment. Therefore, we found that more people are impaired by minor depression than by major depressive disorder. This has also been found in prior studies (3, 26). The combination of a higher prevalence and associated impairment of subthreshold or subsyndromal depressive symptoms emphasizes its clinical and public health importance. It has also been demonstrated that individuals with minor depression were associated with 51% more disability days in the community than persons with major depression (24) .
We used the course characteristic onset age for first depressive episode for a standardized comparison of the four depression categories. In this study, the median onset age for subjects with dysthymia was 25 years, while the median onset age for depressive episode was 33 years. Contrary to conclusions based on clinical samples (25) , only a little more than half of the subjects reporting the presence of depressive episode had more than one episode in their lifetime.
Risk factor profiles differed from category to category, and there were linkages between specific risk factors and certain symptom or course characteristics. The association with family history of depressive disorder in episodic forms of depression (major depressive disorder, depressive syndrome, comorbid depression) was strong regardless of symptom severity. The association with stressful life events was stronger for the mild episodic form of depression (depressive syndrome) than it was for major depressive disorder. There was a prominent association between female gender and a more chronic course or more severe symptoms (the comorbid depression category). We used the “stressful life events before the onset of the first depressive episode” as a standardized comparison across disorder categories, in spite of the fact that for the comorbid depression category there are potentially two different onsets. The possibility that different roles might be played by the same risk factor such as stress before the first episodes of different types (depressive versus dysthymic) remain to be investigated.
Not very much is known about the risk factors for depressive syndrome. The existing evidence shows that family history of major depressive disorders and certain type of stressful life events were associated with minor depression (9) , and the association with female gender is still unclear (10) . Our evidence suggests that family history and prior stressful life events, but not female gender, are significant risk factors for depressive syndrome.
The finding that female gender is not a significant risk factor for major depressive disorder has not been reported in earlier studies. We also examined the risk factor profiles for three inclusive categories (all subjects with major depressive disorder, all subjects with depressive syndrome, all subjects with dysthymia), since the four examined categories were mutually exclusive, and the “major depressive disorder” only group did not include those who met criteria for both major depressive disorder and dysthymia. The odds ratio, after adjusting for family history and stressful life events, for female gender among all subjects with major depressive disorder relative to comparison subjects was 3.4 (95% CI=1.5–7.8). In other words, when all major depressive individuals are considered as a group, female gender is more prominent than it is in the group with major depressive disorder only. It is possible that the diagnostic switch between the first and final interviews is captured in the longitudinal study and that the course has been different for female subjects, since more of them have become comorbid, thus changing their diagnostic category and removing them from the major depressive disorder category, while strengthening the association of gender as a risk factor within the comorbid group.
The DIS instrument does not generate the diagnoses of minor depression or double depression. The “depressive syndrome” we used in this study is similar to the category of minor depression (18) . According to current diagnostic concepts, the comorbid depression group of this study consisted of individuals with 1) double depression as defined by Keller and Lavori (2) , or 2) chronic major depressive disorder, or 3) nonconcurrent comorbidity of major depressive disorder and dysthymic disorder. Future research is needed to examine the differences among them. Yet the comorbid depression group represented individuals who were experiencing both an intense and prolonged depressive episode. A limitation of studying a large population sample is the validity of measurements. This study would have been stronger if there were more detailed measures on depression-related impairment. The associations between depressive disorders and the potential risk factors, including family history and stress, could be clarified in future studies with prospectively refined measures. In addition, although three examined risk factors in this study represented potential hormonal, social, genetic, familial, or environmental etiologies for depression, there are still many among the whole spectrum of hypothesized risk factors for depression that were not included.
Since the subthreshold entity, depressive syndrome, is associated with similar etiologic profiles to major depressive disorder and a substantial rate of impairment, we highlight the importance of depressive syndrome in genetic and clinical research. In contrast, the dysthymia category was similar to depressive syndrome regarding symptoms but not risk factor profiles. It did not show a strong relationship to any of the examined risk factors. Its value as a distinct nosologic entity appears to be questionable. The comorbid depression category (lifetime major depressive disorder and dysthymia) has a worse course and is associated with female gender and family history but not with stress. Thus, the evidence suggests a genetic homogeneity and an environmental heterogeneity among three different forms of depression: major depressive disorder, depressive syndrome, and a more severe form of major depressive disorder with chronic and unremitting course.
Received Oct. 1, 1998; revisions received July 27 and Aug. 23, 1999; accepted Sept. 28, 1999. From the Departments of Mental Hygiene and Epidemiology, School of Hygiene and Public Health, Johns Hopkins University; and the Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, Baltimore. Address reprint requests to Dr. Chen, Department of Mental Hygiene, School of Hygiene and Public Health, Johns Hopkins University, 624 North Broadway, Baltimore, MD 21205. Supported by NIMH grant MH-47447.
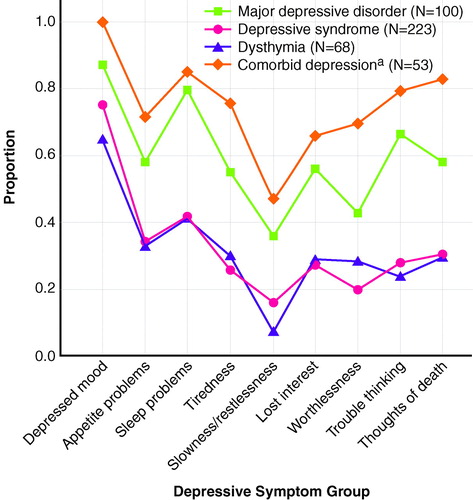
FIGURE 1. Specific Depressive Symptoms During Worst Episodes of Subjects in Four Depression Diagnostic Categories
a Subjects with lifetime diagnoses of both major depressive disorder and dysthymia.
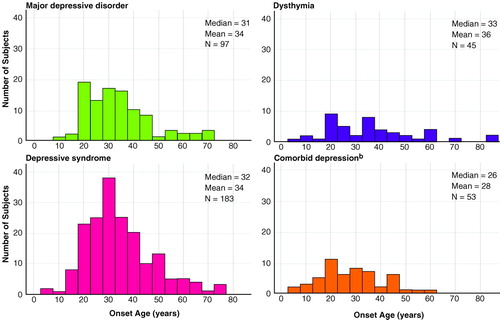
FIGURE 2. Age at First Depressive Episode for Subjects in Four Depression Diagnostic Categories a
a Total numbers for each group are smaller because of missing age-at-onset information.
b Subjects with lifetime diagnoses of both major depressive disorder and dysthymia.
1. Keller MB, Klein DN, Hirschfeld RM, Kocsis JH, McCullough JP, Miller I, First MB, Holzer CP III, Keitner GI, Marin DB, Shea T: Results of the DSM-IV mood disorders field trial. Am J Psychiatry 1995 ; 152:843–849 Link , Google Scholar
2. Keller MB, Lavori PW: Double depression, major depression, and dysthymia: distinct entities or different phases of a single disorder? Psychopharmacol Bull 1984 ; 20:399–402 Google Scholar
3. Wells KB, Burnam MA, Rogers W, Hays R, Camp P: The course of depression in adult outpatients: results from the Medical Outcomes Study. Arch Gen Psychiatry 1992 ; 49:788–794 Crossref , Medline , Google Scholar
4. Spalletta G, Troisi A, Saracco M, Ciani N, Pasini A: Symptom profile, axis II comorbidity and suicidal behaviour in young males with DSM-III-R depressive illnesses. J Affect Disord 1996 ; 39:141–148 Crossref , Medline , Google Scholar
5. Romanoski AJ, Folstein MF, Nestadt G, Chahal R, Merchant A, Brown CH, Gruenberg EM, McHugh PR: The epidemiology of psychiatrist-ascertained depression and DSM-III depressive disorders: results from the Eastern Baltimore Mental Health Survey clinical reappraisal. Psychol Med 1992 ; 22:629–655 Crossref , Medline , Google Scholar
6. Keller MB, Russell CW: Dysthymia, in DSM-IV Sourcebook, vol 2. Edited by Widiger TA, Francis AJ, Pincus HA, Ross R, First MB, Davis WW. Washington, DC, American Psychiatric Association, 1996, pp 21–35 Google Scholar
7. Akiskal HS, King D, Rosenthal TL, Robinson D, Scott-Strauss A: Chronic depressions, part 1: clinical and familial characteristics in 137 probands. J Affect Disord 1981 ; 3:297–315 Crossref , Medline , Google Scholar
8. Maier W, Lichtermann D, Minges J, Heun R, Hallmayer J: The risk of minor depression in families of probands with major depression: sex differences and familiarity. Eur Arch Psychiatry Clin Neurosci 1992 ; 242:89–92 Crossref , Medline , Google Scholar
9. Beekman AT, Deeg DJ, van Tilburg T, Smit JH, Hooijer C, van Tilburg W: Major and minor depression in later life: a study of prevalence and risk factors. J Affect Disord 1995 ; 36:65–75 Crossref , Medline , Google Scholar
10. Beck DA, Koenig HG: Minor depression: a review of the literature. Int J Psychiatry Med 1996 ; 26:177–209 Crossref , Medline , Google Scholar
11. Blazer D: Clinical features in depression in old age: a case for minor depression in later life. Current Opinion in Psychiatry 1991 ; 4:596–599 Crossref , Google Scholar
12. Regier DA, Myers JK, Kramer M, Robins LN, Blazer DG, Hough RL, Eaton WW, Locke BZ: The NIMH Epidemiologic Catchment Area program: historical context, major objectives, and study population characteristics. Arch Gen Psychiatry 1984 ; 41:934–941 Crossref , Medline , Google Scholar
13. Robins LN, Regier DA (eds): Psychiatric Disorders in America: The Epidemiological Catchment Area Study. New York, Free Press, 1991, pp 449 Google Scholar
14. Badawi MA, Eaton WW, Myllyluoma J, Weimer LG, Gallo J: Psychopathology and attrition in the Baltimore ECA 15-year follow-up 1981–1996. Soc Psychiatry Psychiatr Epidemiol 1999 ; 34:91–98 Crossref , Medline , Google Scholar
15. Eaton WW, Anthony JC, Gallo J, Cai G, Tien A, Romanoski A, Lyketsos C, Chen LS: Natural history of Diagnostic Interview Schedule/DSM-IV major depression: the Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry 1997 ; 54:993–999 Crossref , Medline , Google Scholar
16. Bruce ML, Seeman TE, Merrill SS, Blazer DG: The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. Am J Public Health 1994; 84:1796– 1799 Google Scholar
17. Robins LN, Helzer JE, Croughan J, Ratcliff KS: National Institute of Mental Health Diagnostic Interview Schedule (DIS), in Psychiatric Epidemiology: Assessment, Concepts and Methods. Edited by Mezzich JE, Jorge MR, Salloum IM. Baltimore, Johns Hopkins University Press, 1994 Google Scholar
18. Anthony JC, Petronis KR: Suspected risk factors for depression among adults 18–44 years old. Epidemiology 1991 ; 2:123–132 Crossref , Medline , Google Scholar
19. Kendler KS, Heath AC, Martin NG, Eaves LJ: Symptoms of anxiety and symptoms of depression: same genes, different environments? Arch Gen Psychiatry 1987 ; 44:451–457 Google Scholar
20. Anthony JC, Folstein M, Romanoski AJ, Von Korff MR, Nestadt GR, Chahal R, Merchant A, Brown CH, Shapiro S, Kramer M, Gruenberg EM: Comparison of the lay Diagnostic Interview Schedule and a standardized psychiatric diagnosis: experience in eastern Baltimore. Arch Gen Psychiatry 1985 ; 42:667–675 Crossref , Medline , Google Scholar
21. Eaton WW, Anthony JC, Romanoski A, Tien A, Gallo J, Cai G, Neufeld K, Schlaepfer T, Laugharne J, Chen LS: Onset and recovery from panic disorder in the Baltimore Epidemiologic Catchment Area follow-up. Br J Psychiatry 1998 ; 173:501–507 Crossref , Medline , Google Scholar
22. Lyketsos CG, Nestadt G, Cwi J, Heithoff K, Eaton WW: The Life Chart Interview: a standardized method to describe the course of psychopathology. Int J Methods Psychiatr Res 1994 ; 4:143–155 Google Scholar
23. Liang KY, Stewart WF: Polychotomous logistic regression methods for matched case-control studies with multiple case or control groups. Am J Epidemiol 1987 ; 125:720–730 Crossref , Medline , Google Scholar
24. Broadhead WE, Blazer DG, George LK, Tse CK: Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA 1990; 264:2524– 2528 Google Scholar
25. Sorenson SB, Rutter CM, Aneshensel CS: Depression in the community: an investigation into age of onset. J Consult Clin Psychol 1991 ; 59:541–546 Crossref , Medline , Google Scholar
26. Judd LL, Paulus MP, Wells KB, Rapaport MH: Socioeconomic burden of subsyndromal depressive symptoms and major depression in a sample of the general population. Am J Psychiatry 1996; 153:1411– 1417 Google Scholar
- Prevalence of depressive symptoms in patients with advanced schistosomiasis in China: A systematic review and meta-analysis 7 March 2024 | PLOS Neglected Tropical Diseases, Vol. 18, No. 3
- Is melancholia a distinct syndrome? Recurrence, chronicity, and severity give evidence in the 50 year follow-up of the Lundby Study 4 August 2023 | Frontiers in Psychiatry, Vol. 14
- Suicidal behavior in Mexican adolescents: A test of a latent class model using two independent probability samples Preventive Medicine, Vol. 157
- Common and specific determinants of 9-year depression and anxiety course-trajectories: A machine-learning investigation in the Netherlands Study of Depression and Anxiety (NESDA). Journal of Affective Disorders, Vol. 293
- The impact of COVID-19 on subthreshold depressive symptoms: a longitudinal study 15 February 2021 | Epidemiology and Psychiatric Sciences, Vol. 30
- Normal Versus Pathological Mood: Implications for Diagnosis Annual Review of Clinical Psychology, Vol. 15, No. 1
- Neurology, Psychiatry and Brain Research, Vol. 30
- Temporal profiling of depression vulnerability in a preclinical model of sustained depression 17 August 2017 | Scientific Reports, Vol. 7, No. 1
- Smoking Cessation and Electronic Cigarettes in Community Mental Health Centers: Patient and Provider Perspectives 30 November 2016 | Community Mental Health Journal, Vol. 53, No. 6
- A continuum of genetic liability for minor and major depression 16 May 2017 | Translational Psychiatry, Vol. 7, No. 5
- Biological Psychiatry, Vol. 82, No. 5
- Preventive Medicine, Vol. 105
- Social Work Research, Vol. 41, No. 3
- Social Psychiatry and Psychiatric Epidemiology, Vol. 49, No. 6
- Maternal and Child Health Journal, Vol. 18, No. 6
- Journal of Affective Disorders, Vol. 136, No. 3
- Maternal and Child Health Journal, Vol. 15, No. 7
- Journal of Affective Disorders, Vol. 129, No. 1-3
- Psychological Medicine, Vol. 41, No. 6
- Acta Psychiatrica Scandinavica, Vol. 124, No. 4
- Relationship between late‐life depression and life stressors: Large‐scale cross‐sectional study of a representative sample of the Japanese general population 23 July 2010 | Psychiatry and Clinical Neurosciences, Vol. 64, No. 4
- Twenty-five-year course and outcome in anxiety and depression in the Upper Bavarian Longitudinal Community Study 18 November 2009 | Acta Psychiatrica Scandinavica, Vol. 122, No. 1
- Journal of Psychopathology and Behavioral Assessment, Vol. 32, No. 1
- Comprehensive Psychiatry, Vol. 51, No. 3
- Journal of Affective Disorders, Vol. 127, No. 1-3
- Psychiatry Research: Neuroimaging, Vol. 183, No. 3
- Epidemiologic heterogeneity of common mood and anxiety disorders over the lifecourse in the general population: a systematic review 1 June 2009 | BMC Psychiatry, Vol. 9, No. 1
- Binge drinking and depressive symptoms: a 5‐year population‐based cohort study 4 June 2009 | Addiction, Vol. 104, No. 7
- Depression and Anxiety, Vol. 26, No. 4
- Journal of Affective Disorders, Vol. 113, No. 1-2
- Journal of Affective Disorders, Vol. 113, No. 3
- European Archives of Psychiatry and Clinical Neuroscience, Vol. 258, No. 8
- Psychology, Health & Medicine, Vol. 13, No. 1
- Validity of the Concept of Minor Depression in a Developing Country Setting Journal of Nervous & Mental Disease, Vol. 196, No. 1
- Depressed Mood in the Suicidal Population 1 November 2007 | The Canadian Journal of Psychiatry, Vol. 52, No. 11
- Clinically significant non-major depression in a community-dwelling elderly population: epidemiological findings 1 January 2007 | International Journal of Geriatric Psychiatry, Vol. 22, No. 6
- Perceived Reasons for Living at Index Hospitalization and Future Suicide Attempt Journal of Nervous & Mental Disease, Vol. 195, No. 5
- Depression and Anxiety, Vol. 24, No. 1
- Depression and Anxiety, Vol. 24, No. 6
- Journal of Affective Disorders, Vol. 104, No. 1-3
- Context Matters: A Community-Based Study of Maternal Mental Health, Life Stressors, Social Support, and Children's Asthma 1 May 2006 | Pediatrics, Vol. 117, No. 5
- Nordic Journal of Psychiatry, Vol. 60, No. 3
- The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, Vol. 61, No. 6
- Journal of the American Academy of Child & Adolescent Psychiatry, Vol. 45, No. 8
- Minor depression as a predictor of the first onset of major depressive disorder over a 15‐year follow‐up 25 October 2005 | Acta Psychiatrica Scandinavica, Vol. 113, No. 1
- Childhood Adversity and Perceived Need for Mental Health Care Journal of Nervous & Mental Disease, Vol. 193, No. 6
- The Relation between Perceived Need for Mental Health Treatment, DSM Diagnosis, and Quality of Life: A Canadian Population-Based Survey 1 February 2005 | The Canadian Journal of Psychiatry, Vol. 50, No. 2
- Predicting the onset of major depression in subjects with subthreshold depression in primary care: a prospective study 4 October 2004 | Acta Psychiatrica Scandinavica, Vol. 111, No. 2
- Biological Psychiatry, Vol. 58, No. 4
- Disability and Rehabilitation, Vol. 27, No. 3
- Subthreshold depression as a risk indicator for major depressive disorder: a systematic review of prospective studies 28 March 2004 | Acta Psychiatrica Scandinavica, Vol. 109, No. 5
- Patient Education and Counseling, Vol. 54, No. 1
- International Journal of Psychiatry in Clinical Practice, Vol. 8, No. 1
- Chian-Jue Kuo , M.D., M.S. ,
- Hwa-Sheng Tang , M.D. ,
- Charng-Jer Tsay , M.D. ,
- Shi-Kwang Lin , M.D. ,
- Wei-Herng Hu , M.D. , and
- Chiao-Chicy Chen , M.D., Ph.D.
- Journal of Affective Disorders, Vol. 77, No. 1
- Journal of Affective Disorders, Vol. 77, No. 2
- Psychosocial risk factors for depressive disorders in late life Biological Psychiatry, Vol. 52, No. 3
- General Hospital Psychiatry, Vol. 24, No. 2
- Journal of Affective Disorders, Vol. 68, No. 2-3
- Depressive Disorder, Dysthymia, and Risk of Stroke Stroke, Vol. 32, No. 9

- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
7 Depression Research Paper Topic Ideas
Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
In psychology classes, it's common for students to write a depression research paper. Researching depression may be beneficial if you have a personal interest in this topic and want to learn more, or if you're simply passionate about this mental health issue. However, since depression is a very complex subject, it offers many possible topics to focus on, which may leave you wondering where to begin.
If this is how you feel, here are a few research titles about depression to help inspire your topic choice. You can use these suggestions as actual research titles about depression, or you can use them to lead you to other more in-depth topics that you can look into further for your depression research paper.
What Is Depression?
Everyone experiences times when they feel a little bit blue or sad. This is a normal part of being human. Depression, however, is a medical condition that is quite different from everyday moodiness.
Your depression research paper may explore the basics, or it might delve deeper into the definition of clinical depression or the difference between clinical depression and sadness .
What Research Says About the Psychology of Depression
Studies suggest that there are biological, psychological, and social aspects to depression, giving you many different areas to consider for your research title about depression.
Types of Depression
There are several different types of depression that are dependent on how an individual's depression symptoms manifest themselves. Depression symptoms may vary in severity or in what is causing them. For instance, major depressive disorder (MDD) may have no identifiable cause, while postpartum depression is typically linked to pregnancy and childbirth.
Depressive symptoms may also be part of an illness called bipolar disorder. This includes fluctuations between depressive episodes and a state of extreme elation called mania. Bipolar disorder is a topic that offers many research opportunities, from its definition and its causes to associated risks, symptoms, and treatment.
Causes of Depression
The possible causes of depression are many and not yet well understood. However, it most likely results from an interplay of genetic vulnerability and environmental factors. Your depression research paper could explore one or more of these causes and reference the latest research on the topic.
For instance, how does an imbalance in brain chemistry or poor nutrition relate to depression? Is there a relationship between the stressful, busier lives of today's society and the rise of depression? How can grief or a major medical condition lead to overwhelming sadness and depression?
Who Is at Risk for Depression?
This is a good research question about depression as certain risk factors may make a person more prone to developing this mental health condition, such as a family history of depression, adverse childhood experiences, stress , illness, and gender . This is not a complete list of all risk factors, however, it's a good place to start.
The growing rate of depression in children, teenagers, and young adults is an interesting subtopic you can focus on as well. Whether you dive into the reasons behind the increase in rates of depression or discuss the treatment options that are safe for young people, there is a lot of research available in this area and many unanswered questions to consider.
Depression Signs and Symptoms
The signs of depression are those outward manifestations of the illness that a doctor can observe when they examine a patient. For example, a lack of emotional responsiveness is a visible sign. On the other hand, symptoms are subjective things about the illness that only the patient can observe, such as feelings of guilt or sadness.
An illness such as depression is often invisible to the outside observer. That is why it is very important for patients to make an accurate accounting of all of their symptoms so their doctor can diagnose them properly. In your depression research paper, you may explore these "invisible" symptoms of depression in adults or explore how depression symptoms can be different in children .
How Is Depression Diagnosed?
This is another good depression research topic because, in some ways, the diagnosis of depression is more of an art than a science. Doctors must generally rely upon the patient's set of symptoms and what they can observe about them during their examination to make a diagnosis.
While there are certain laboratory tests that can be performed to rule out other medical illnesses as a cause of depression, there is not yet a definitive test for depression itself.
If you'd like to pursue this topic, you may want to start with the Diagnostic and Statistical Manual of Mental Disorders (DSM). The fifth edition, known as DSM-5, offers a very detailed explanation that guides doctors to a diagnosis. You can also compare the current model of diagnosing depression to historical methods of diagnosis—how have these updates improved the way depression is treated?
Treatment Options for Depression
The first choice for depression treatment is generally an antidepressant medication. Selective serotonin reuptake inhibitors (SSRIs) are the most popular choice because they can be quite effective and tend to have fewer side effects than other types of antidepressants.
Psychotherapy, or talk therapy, is another effective and common choice. It is especially efficacious when combined with antidepressant therapy. Certain other treatments, such as electroconvulsive therapy (ECT) or vagus nerve stimulation (VNS), are most commonly used for patients who do not respond to more common forms of treatment.
Focusing on one of these treatments is an option for your depression research paper. Comparing and contrasting several different types of treatment can also make a good research title about depression.
A Word From Verywell
The topic of depression really can take you down many different roads. When making your final decision on which to pursue in your depression research paper, it's often helpful to start by listing a few areas that pique your interest.
From there, consider doing a little preliminary research. You may come across something that grabs your attention like a new study, a controversial topic you didn't know about, or something that hits a personal note. This will help you narrow your focus, giving you your final research title about depression.
Remes O, Mendes JF, Templeton P. Biological, psychological, and social determinants of depression: A review of recent literature . Brain Sci . 2021;11(12):1633. doi:10.3390/brainsci11121633
National Institute of Mental Health. Depression .
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition . American Psychiatric Association.
National Institute of Mental Health. Mental health medications .
Ferri, F. F. (2019). Ferri's Clinical Advisor 2020 E-Book: 5 Books in 1 . Netherlands: Elsevier Health Sciences.
By Nancy Schimelpfening Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Research Council (US) and Institute of Medicine (US) Committee on Depression, Parenting Practices, and the Healthy Development of Children; England MJ, Sim LJ, editors. Depression in Parents, Parenting, and Children: Opportunities to Improve Identification, Treatment, and Prevention. Washington (DC): National Academies Press (US); 2009.

Depression in Parents, Parenting, and Children: Opportunities to Improve Identification, Treatment, and Prevention.
- Hardcopy Version at National Academies Press
1 Introduction and Magnitude of the Problem
- In the United States, 16.2 percent of adults reported major depression in their lifetime, while another 4.1 percent reported meeting a milder but chronic form of depression.
- Certain subpopulations of adults defined by selected population characteristics—such as sex, age, ethnicity, and marital status—indicate disparities in prevalence rates of depression. Female, younger, and divorced adults have higher rates of lifetime depression than their male, older, or married adult counterparts. In general, a positive association has been found between social disadvantage and depression prevalence, except in the case of first generation immigrants.
- Many adults in the United States are parents. Parents (with at least one child under age 18) have similar rates of depression compared to the entire U.S. adult population, including similar disparities in depression rates for selected population characteristics.
- Depression rarely occurs alone; 75 percent of individuals with lifetime or recent major depression also had at least one additional mental health or substance abuse diagnosis.
- Depression, due to its recurrent nature, leads to sustained individual, family, and societal costs.
- 15.6 million children under 18 years of age are living with an adult who had major depression in the past year.
- Depression in parents can have serious biological, psychological, behavioral, and social consequences especially for children who rely on a parent for caregiving, material support, and nurturance.
- Despite this impact, depression is perhaps one of the most effectively treated psychiatric disorders, if recognized and treated early in its onset.
- Individual-, provider-, and system-level barriers exist that decrease the access to and quality of care for depressed adults. These institutional, sociocultural, and linguistic barriers are responsible for causing and maintaining existing disparities. Without a system of care that is culturally and linguistically sensitive and supports a family’s environment, economic resources and relationships with family, coworkers, the community, and society, such disparities may increase. Improving provider-patient-family communication is an important component of addressing differences in quality of care that are associated with patient race, ethnicity, culture, and language.
- The current policy environment does not encourage a two-generation (i.e., parent, child) identification, treatment, and prevention strategy for adults with depression.
Depression is a common, universal, and debilitating public health problem. The Global Burden of Disease study by the World Health Organization (WHO) determined that depression accounts for more disability worldwide than any other condition during the middle years of adulthood (Murray and Lopez, 1996). In fact, major depressive disorder is now the leading cause of disability worldwide (World Health Organization, 2001). For some with depressive episodes, periods of depression may resolve in a few weeks or months. However, it has been estimated that, for 30 to 50 percent of adults, depression is recurrent or chronic or fails to resolve completely (e.g., Depue and Monroe, 1986; Judd et al., 1998; Solomon et al., 2000). Ironically, de pression is perhaps one of the most effectively treated psychiatric disorders and, if recognized early, it can be prevented.
International surveys attest to the universality of depression across cultures. A WHO-based study (using the Composite International Diagnostic Interview 1 ) of 10 countries in North America, Latin America, Europe, and Asia reported a range of lifetime major depression from 3 percent in Japan to 16 percent in the United States (Andrade et al., 2003). More recently, the WHO World Health Surveys, a cross-national study comprised of nearly 250,000 participants in 60 countries across all regions of the world, estimated the overall 1-year prevalence of depressive episode (using criteria of the International Statistical Classification of Diseases and Related Health Problems , 10th revision) alone to be 3.2 percent (Moussavi et al., 2007).
Depression can be disabling for anyone, but the extent of its impact goes beyond the affected individual to the broader family context and especially to the depressed person’s children, who are dependent on their parent for their care and support of their development. Under these circumstances, depression becomes a multigenerational disorder that can have serious biological, psychological, behavioral, and social consequences, especially for children who rely on a parent for caregiving, material support, and nurturance. Effective treatments aimed at reducing or eliminating depression among parents or caregivers may therefore also constitute a significant preventive intervention for children.
Expressed in purely monetary terms, the economic burden of depression is a serious global public health problem as well (Luppa et al., 2007; Moussavi et al., 2007). Estimated costs related to depression in the United States increased in the past decade from $77.4 billion dollars in 1990 to $83.1 billion in 2000 (Greenberg et al., 2003). Of the estimated total amount in 2000, direct treatment costs were $26.1 billion, workplace costs were $51.5 billion (e.g., absenteeism, reduced productivity), and suicide-related costs were $5.4 billion (Greenberg et al., 2003; Muñoz, 2003). There exists, moreover, a strong association between depression and non-adherence to treatment of such medical conditions as diabetes or coronary heart disease, leading to higher treatment costs for their medical care than patients with medical conditions who are not depressed (DiMatteo, Lepper, and Croghan, 2000).
- STUDY CHARGE, APPROACH, AND SCOPE
In May 2006, with support from the Annie E. Casey Foundation, the National Research Council and the Institute of Medicine convened a two-day planning meeting to explore the need for and focus of a future study on maternal depression. Researchers from a variety of disciplines, including pediatrics, policy, and community health, reviewed a small set of studies from the research literature and explored whether the quality of the work was sufficient to support a future comprehensive analysis of the evidence base surrounding maternal depression as well as an exploration of how to improve the application of this knowledge to policy, practice, and program development.
The presentations and discussion resulted in a few key conclusions. The research literature on the treatment and prevention of depression among adults and children is rich with findings about effective interventions. More importantly, there exists a sound knowledge base about the effects of depression in families, the mechanisms of transmission of illness, and the risk and protective factors that either trigger or prevent onset or reduce severity of the disorder. The last 10 years have witnessed an increase in evidence-based prevention in general and the development of promising approaches specific to the identification, treatment, and prevention of depression in families. Aside from presenting and assessing the existing evidence, the meeting also shed light on serious gaps in the synthesis and application of extant findings and interventions in the family setting because of the diffuse and disjointed nature of the prevention, identification, and treatment literatures. Specifically, there exists a need to identify approaches that can highlight ways to translate research knowledge into effective interventions in a broad range of parental support and child health and development strategies.
Study Charge
Concerned about these complex issues, the National Academies’ Board on Children, Youth, and Families formed the Committee on Depression, Parenting Practices, and the Healthy Development of Children, with funding from the Robert Wood Johnson Foundation, the Annie E. Casey Foundation, The California Endowment, and the Substance Abuse and Mental Health Services Administration and the Health Resources and Services Administration of the U.S. Department of Health and Human Services. The National Research Council and the Institute of Medicine appointed the 17-member committee in October 2007 to review the relevant research literature on the identification, prevention, and treatment of parental depression, its interaction with parenting practices, and its effects on children and families. The committee was asked to
clarify what is known about interactions among depression and its co-occurring conditions, parenting practices, and child health and development;
identify the findings, strengths, and limitations of the evidentiary base that support assessment, treatment, and prevention interventions for depressed parents and their children;
highlight disparities in the prevalence, prevention, treatment, and outcomes of parental depression among different sociodemographic populations (e.g., race/ethnicity, socioeconomic status);
examine strategies for widespread implementation of best practice and promising practice programs, given the large numbers of depressed parents; and
identify strategies that can foster the use of effective interventions in different service settings for diverse populations of children and families.
Study Approach
A variety of sources informed the committee’s work. Five formal committee meetings and one public workshop were held during the course of the study. The workshop explored innovative strategies and models that integrate mental health services for depression, parenting, and child development services within various settings for diverse populations of children and families; explored strategies that insure interventions are appropriate for diverse populations; and explored existing opportunities for interventions as well as existing barriers to implementation or replication of promising programs or best practices at regional, state, multi-state, or national levels in a variety of settings.
The committee also reviewed literature from a range of disciplines and sources. Technical reviews were commissioned by experts on a variety of topics including: genetics and the environment; integration and implementation of services and models of care; the economic burden of depression; public-health policy; and vulnerable populations. Data and research on depression in adults, specifically parents, were analyzed. The committee considered research on the causes, comorbidities, and consequences of depression in adults (including parenting and child health outcomes), various health and support services for depression care, the features of interventions and implementation strategies for depression care in diverse populations, and public policies related to implementing promising interventions.
Additionally, the committee visited programs focused on providing mental health services in substance abuse settings to underserviced populations. The limited evaluation of these programs and the lack of a standard against which to study them make it impossible to designate any of them as exemplary models of care. However, these visits provided examples of health services being delivered specifically to vulnerable and underserviced parents, and they helped the committee gain insight into various services, partnerships, approaches, and care models that are used. The sites visited were Entre Familia Program of the Boston Public Health Commission and PROTOTYPES Women’s Center in Pomona, California. Both visits encompassed a tour of the program site and meetings with leaders of the sponsoring institution and other staff and partnering programs.
Study Scope
The committee was charged broadly with an examination of depression in parents and its effects on parenting practices and child development. However, the charge did not specify what “depression” or “parents” should encompass. Therefore, one of the committee’s early tasks was to reach consensus on how to define these terms in reviewing the literature.
Defining Depression
The available literature on depression in adults—and, more specifically, on parents and its effects on parenting practices and children and families—has not measured depression in a consistent manner; it is therefore important to consider these varied approaches. In general, there is continual debate on how to define mental disorders, and specifically for depression there are many tools used in the literature to assess adults for depression.
A review by Frank and Glied (2006) on mental health policy in the United States describes three ways in which epidemiologists generally define who has a mental disorder: (1) those who have symptoms and signs of a particular disorder, (2) those who have mental health-related impairment in daily life, and (3) those who have sought treatment for a mental health condition. A combination of these three is generally preferred over a single one because each selects a distinct subgroup of the population, usually with small overlap. In addition, experts continue to argue about the specific combination of signs and symptoms on which diagnoses should be based.
A variety of methods are used to screen for or diagnose depression, which is reflected in the literature that the committee reviewed. The use of diverse methods for defining depression is a result of restrictions on time and cost, study populations’ sociodemographic characteristics (e.g., race/ethnicity, socioeconomic status), and differences in provider training. Research that defines parental depression by symptoms is more common in the literature than a clinical diagnosis. Literature that discusses effects of depression on parenting practices is based mostly on depressive symptoms or “distress.” In addition, defining depression using symptoms may be more efficient overall from the provider’s perspective but may complicate detection in a person also experiencing conditions resulting from substance use or trauma. For example, substance abuse greatly influences symptoms of mental illness and vice versa. Further, using methods that define depression by symptoms may lead to higher rates among one group over another, for example women compared to men.
The problem with using a clinical definition of parental depression is that it generally identifies only those who are active in the mental health system; people who are isolated or who are disadvantaged are less likely to have access to mental health services and hence are more likely to go undiagnosed. And methods used for clinical diagnosis may vary by type of provider. Generalist physicians provide most of the depression screening and care to the general population, whereas the limited number of available specialty mental health providers (i.e., those with advanced mental health training) may see a more severely ill population.
Given these considerations, in describing this literature on depression in adults who are parents and its effects on parenting practices, children, and families, the committee chose to use both symptoms and a clinical diagnosis of depression whenever the data were available. However, due to the concerns described above, it may be important to distinguish the use of methods that use self-report symptoms compared to clinician-rated depression diagnosis because the method could highlight different outcomes seen across studies of depression, parenting, and child outcomes.
Defining Parents and the Family Unit
Family composition is marked by increased diversity and change. It has been estimated that less than 50 percent of children in the United States live in traditional nuclear families, in which two biological parents are married to each other with full siblings (Brandon and Bumpass, 2001). Instead, children’s living arrangements increasingly include unmarried parents, step-families, foster parents, and multigenerational households. For example, the proportion of cohabitating same-sex and opposite-sex couples who have children is increasing (Bengtson et al., 2005). In addition, the number of grandparents who are raising their grandchildren has increased dramatically over the past few decades (Casper and Bryson, 1998). However a family unit is composed, it still holds true that 70 percent of children under the age of 18 live in two-parent households (Federal Interagency Forum on Child and Family Statistics, 2007).
The committee focused its search of the impact and prevalence of depression, interventions, and strategies of implementation on depression in parents on all individuals who take care of a child or children in a variety of family structures. This definition of a parent allows discussion to include a variety of caregivers of children. However, having decided to focus the study on a variety of caregivers in a variety of family structures, we found limited literature specifically on parents with depression and even more limited information regarding specific groups of caregivers, including fathers and grandparents. The little information that is available for these other caregivers is highlighted throughout the report when available.
- STUDY CONTEXT
Parents and Their Children
In 2004, it was estimated that approximately 148.8 million parents live in the United States (U.S. Census Bureau, 2005a, 2005b). The Current Population Survey, through its household survey data, helps to track the number of mothers, fathers, and other caregivers who take care of children under the age of 18 in the United States. In 2007, it was estimated that there were 36.5 million married parents, single fathers, and single mothers (i.e., households) who care for their own children under the age of 18—that is, approximately 47 percent of households (U.S. Census Bureau, 2008b). Together, these parents take care of approximately 96 percent of almost 74 million children under age 18 in the United States. The remaining 3 percent of children (2.5 million) do not live with either of their parents, but with a grandparent, other relative, or nonrelative or are in the foster care system (U.S. Census Bureau, 2008a).
Prevalence of Depression
In the United States, the 2001 National Comorbidity Survey-Replication (NCS-R) revealed that the prevalence of major depression (defined by syndrome features, impairment, and duration of at least two weeks) in adults in their lifetime was 16.2 percent (over 3 million adults), while another 4.1 percent met the diagnostic criteria for dysthymic disorder, a milder but chronic form of depression (The ESEMeD/MHEDEA 2000 Investigators, 2004; Kessler et al., 2003). Overall, both international and national data support the universal nature of depression. While many studies do not specifically investigate parental depression or even note parental status among their samples, a few national surveys help give insight into the prevalence of depression among adults who are also parents in the United States. For example, a subsample of the National Comorbidity Survey Replication in 2002 reported that 17 percent of parents (with at least one child) had major or severe depression in their lifetime, a prevalence similar to that of the entire U.S. population of 16.2 percent (see Table 1-1 ). Examining rates of parental depression in the past year, the NCS-R found that approximately 7 percent of parents (with at least one child) had major or severe depression in the last 12 months and did not differ by the age of the child (see Table 1-1 ). The Pregnancy Risk Assessment Monitoring System (PRAMS), another national data set that collects self-reported data, offers further insight on the scope of depression, specifically in postpartum women. The survey found that 11 to 20 percent of new mothers were affected by depressive symptoms following childbirth (Centers for Disease Control and Prevention, 2008). One important longitudinal study in the United Kingdom of parents and child outcomes, the Avon Longitudinal Study of Parents and Children, was used to do secondary analyses of paternal peripartum depression (Ramchandani et al., 2008). Father’s depression correlated strongly with maternal depression scores, suggesting that, when fathers are depressed, there may be a high prevalence of both parents being depressed.
Prevalence of Major Depressive Disorder with Hierarchy for Adults with at Least One Child Under the Age of 18 Years, 2002.
Disparities and Vulnerable Populations
Despite its prevalence across cultures, sexes, income strata, and age groups, tremendous differences in depression rates in particular sociodemo graphic categories is noteworthy. For example, women are about twice as likely to be diagnosed with depression as men in nearly all cultures (Andrade et al., 2003; Kessler, 2003; Riolo et al., 2005). Among adults overall, rates of depression are higher among single or divorced people than among their married counterparts (e.g., The ESEMeD/MHEDEA 2000 Investigators, 2004; Kessler et al., 2003). Stratified by age, depression is more common among teenagers and younger adults than among older adults, with apparently increasing rates in more recently born cohorts (e.g., Cross-National Collaborative Group, 1992; The ESEMeD/MHEDEA 2000 Investigators, 2004; Kessler et al., 2005). Similarly, a subsample of the NCS-R reports significant differences in lifetime and past year major depression prevalence rates among parents by gender, marital status, if English was their primary language while they were growing up, if they were born in the United States, and by race/ethnicity (see Tables 1-2 and 1-3 ). Mothers have almost double the prevalence of lifetime major depression than fathers. Parents overall and especially mothers who were divorced, widowed, or separated reported higher lifetime prevalence of major depression than those who were married or never married. Also, parents and mothers born in the United States and raised with English as their primary language report lifetime major depression significantly more than those who were not born in the United States or if English was not their primary language. Unlike the general population of parents and mothers, fathers reported significant differences in lifetime depression rates by current work status. Fathers not in the workforce at all have almost double the prevalence of lifetime depression than fathers who are employed or currently unemployed. Among the general population of parents, poverty status, and educational attainment did not significantly affect the prevalence of lifetime major depression. Although differences in rates by gender and marital status were similar as for prevalence of lifetime major depression, reports of major depression in the past year also found additional differences by current work status. Parents, and in particular fathers, who were employed had approximately half of the prevalence of major depression in the past year compared with parents who were unemployed or not in the workforce (see Table 1-3 ). Finally, similar to the general adult population and specific to the parent population, the Medical Expenditure Panel Survey in 2004 found gender disparities in the prevalence of poor mental health. A total of 4.5 percent of households reported that the mother was the only adult with fair or poor mental health, compared with 2.6 percent of households who reported that the father was the only adult affected. Around 1 percent of households report that both adults (mother and father) had fair or poor mental health (personal communication, Stephen Petterson, Robert Graham Center, February 13, 2008).
Lifetime Prevalence of Major Depression with Hierarchy a by Selected Demographic Characteristics forAdults with at Least One Child Under the Age of 18 Years, 2002 (taking into account weighting and complex survey design).
12-Month Prevalence of Major Depression with Hierarchy by Selected Demographic Characteristics for Adults with at Least One Child Under the Age of 18 Years, 2002 (taking into account weighting and complex survey design).
It is not clear whether certain subgroups of the population are disproportionately affected by depression. For example, differences in (particu larly chronic) depression are reported along the lines of race and ethnicity. However, there seem to be some inconsistencies about whether the prevalence rates for depression in the general adult as well as in the parent population in racial/ethnic minority groups is higher or lower than their white counterparts. Existing national surveys 2 report lower rates in life- time prevalence for adults in these racial/ethnic minority groups (e.g., Asian Americans, African Americans) and similar prevalence rates in a given year to that of non-Hispanic whites (Takeuchi et al., 2007; Williams et al., 2007). The limited available evidence suggests the need for research on this topic (Jackson and Williams, 2006). The subsample of the NCS-R specific to parents shows the highest rates of lifetime and past year major depression specifically among parents who are black immigrants from the Caribbean (about 30 percent), followed by non-Hispanic whites (around 20 percent), African Americans (around 12 percent), non-Mexican Hispanics (around 15 percent), and Mexicans (10 percent). Asians report the lowest prevalence (around 9 percent) (see Tables 1-2 and 1-3 ).
A number of studies have examined depression among groups that are disadvantaged for a variety of reasons, such as poverty. While these studies differ in terms of design, sample size, and specific findings, they all document the same trend: a positive association between depression and social disadvantage , except in the case of first generation immigrants. For example, studies of low-income women found depression rates nearly double those in the general population, ranging between 12 and 27 percent for current (Bassuk et al., 1998; Jesse et al., 2005; Lanzi et al., 1999 ) and 43 percent for lifetime prevalence (Bassuk et al., 1998). A longitudinal population study showed a clear relationship between worsening socioeconomic circumstances and depression, and a meta-analysis of 51 studies found compelling evidence for socioeconomic inequality in depression (Lorant et al., 2003, 2007). Among women participating in state welfare-to-work programs, Siefert and colleagues (2000) recorded current depression among more than a quarter of them. A national survey found homeless women with lifetime prevalence rates of depression around 45 percent and current (i.e., past month) prevalence rates of roughly 10 percent (Bassuk et al., 1998). In their research with incarcerated women, Bloom and colleagues found that 13.7 percent of their sample had been diagnosed with a current episode of depression (Bloom et al., 2003). Research indicates that immigrants from Mexico, the Caribbean, and Africa have lower rates of mental health disorders than their U.S.-born counterparts (Miranda et al., 2005; Vega et al., 1998); however, recent surveys also indicate the mental health status of immigrant populations has been found to deteriorate with the time of tenure in the United States (Grant et al., 2004; Vega et al., 1998).
The scientific literature classifies many of these groups as “vulnerable populations.” The notion of vulnerability is based on the epidemiological concept of risk, which is used to quantify the probability that an individual will become ill or suffer adversity in a given period of time. According to this definition, vulnerable populations are comprised of individuals who have a higher probability of experiencing poor physical, psychological, or social health than others at any point in time due to shared sociodemographic or environmental circumstances (Aday, 1994). Social vulnerability affects health in general and depression specifically via several pathways. For example, such factors as limited access to knowledge and resources as well as increased exposure to such social stressors as marginal neighborhoods, community violence, and discrimination directly affect the genesis, progression, and treatment of depression. In addition, the stigma associated with belonging to a disadvantaged group may increase individuals’ isolation, thus causing or exacerbating depressive symptoms, and it may affect their treatment-seeking behaviors. More generally, the stigma of having a diagnosis of depression among certain disadvantaged and cultural groups may impede depression-related research endeavors (U.S. Surgeon General, 1999).
The concept of vulnerability has important research and policy implications for two main reasons. First, risks may accumulate additively or multiplicatively, depending on the number of high-risk groups to which an individual or family belongs. Second, compared with their normative counterparts, vulnerable populations may require additional medical and social services to meet their multiple, coinciding physical and mental health needs, as well as their children’s developmental needs.
Bearing in mind such vulnerability-related considerations is of particular importance in the context of depression because it is precisely those social environments and characteristics in which depression most commonly occurs—such as poverty, marital status, or disadvantage due to gender, race and ethnicity—that are themselves factors likely to exacerbate or prolong depression. Because of their typically stressful and enduring nature, these conditions may create a constellation of vulnerabilities that overwhelm the person’s coping capabilities and diminish the effectiveness of treatments that have proven successful under less challenging circumstances. Moreover, given the disproportionate incidence of depression among women, particularly those who are poor and single, as well as those who are young and in their prime childbearing and child rearing years, depression poses a concern because of its potential for impairing parenting.
The data from the NCS-R specific to parents reveal similar prevalence rates of depression compared with adults in general, including disparities in gender, race/ethnicity, and marital status, and employment status for fathers. Other demographic disparities that are generally considered a contributor to depression, i.e., income level, was not seen to significantly contribute to depression in parents in this particular subsample of one study (although a difference is still seen). More longitudinal and cross-sectional data are needed to further document and clarify the prevalence, incidence, disparities, causes, and consequences of depression in adults who are parents.
Comorbidities and Correlates of Depression
According to the National Comorbidity Survey, approximately 75 percent of individuals who had lifetime or recent depression also had at least one additional mental health or substance abuse diagnosis (Kessler et al., 2005), as did 60–65 percent of those with current major depression, as reported in both U.S. and international studies (e.g., De Graaf et al., 2002; Rush et al., 2005). Often the depression occurs in part because of difficulties caused by the other disorders, principally substance abuse, anxiety disorders, and conduct and antisocial disorders. In addition, depression is often comorbid with other chronic medical conditions, such as diabetes, hypertension, and arthritis, and can worsen their associated health outcomes (Ciechanowski, Katon, and Russo, 2000; Katon, 1998, 2003; Moussavi et al., 2007). Individuals who are depressed are more likely to amplify physical symptoms and to develop catastrophic ideas about the causes and consequences of their symptoms (Barsky, 1979; Edwards et al., 2006). The social and physical functioning of depressed individuals often is poor, and they are hospitalized more frequently than people with other major chronic medical problems. Such comorbid conditions may greatly complicate the severity, duration, and recurrence of depression and diminish the effectiveness of treatments for it. The reverse is also true: depression may impede individuals’ efforts to find effective treatments or coping strategies for dealing with their co-occurring disorders.
- IMPACT OF DEPRESSION
Adding to the problem that depression rarely occurs alone, a further complication is the recurrent nature of depression as well as its impact on individuals, their families, and society. Although depressed mood or sadness are normal human experiences associated with loss of treasured relationships, disappointments, and failures, most people who experience such states recover quickly within hours or a few days. However, clinically significant depression not only persists but also has detrimental effects on intellectual processes and attitudes about the self, the world, and the future; impedes adaptive behaviors and family and social interactions; erodes en ergy; and disrupts bodily processes—in addition to its effect on mood and emotions.
The National Institute of Mental Health Collaborative Health Program on the Psychobiology of Depression found that, over a 5-year period, depressed persons had lower educational achievement, lower income levels, fewer periods of employment, and decreased occupational status than nondepressed persons matched for age and gender (Coryell, Endicott, and Keller, 1990). The multisite WHO study on the effects of depression on social functioning found that, after 10 years, 25 percent of depressed patients showed poor functioning and about 40 percent exhibited moderate impairment (Thornicroft and Sartorius, 1993). Even with appropriate treatment, depression has the tendency to be episodic and recurrent; that is, after a person has been depressed once and recovers, he or she is likely to experience one or more subsequent episodes; single episodes of depression are the exception (Andrews, 2001; Solomon et al., 2000). This recurrent pattern of illness leads to sustained individual, family, and societal costs.
Consequently, individuals with depression often cannot function in optimal ways in their close relationships or in work, social, and leisure activities. Thus, depression is associated with decrements in work attendance, work quality, and productivity (Kessler et al., 2006; Wang et al., 2004); with unresponsive, harsh, or rejecting parenting (Cummings and Davies, 1999; Goodman and Gotlib, 1999); with dissatisfaction or conflict in close relationships (Kessler, Walters, and Forthofer, 1998; Whisman, 2001); and with medical problems due both to poor self-care and to the effects of depression on neurobiological and immune functioning (Evans et al., 2005; Katon, 2003). Even depression that is considered “subclinical” in severity may, if sufficiently enduring, predict impaired functioning in important roles or disproportionate use of services (Johnson, Weissman, and Klerman, 1992; Wells et al., 1989).
Family and Society
Addressing the charge to the committee, this report describes a large number of traditional clinical and epidemiological approaches documenting the negative impact of depression in parents on parenting and children’s health and development. Using the prevalence data presented above, the number of children under the age of 18 in each household from the NCS-R (i.e., 2.07172), and applying it to U.S. Census data from 2001, the committee estimates that 15.6 million children under 18 years of age are living with an adult who had major depression in the past year (note: the NCS-R public use data does not provide data on depression diagnosis on both parents in a household, so this may be an underestimate of the number of these children). Yet few opportunities currently exist to identify this vulnerable population or to offer prevention and treatment services that can also enhance the parenting practices of a depressed parent in a framework that also offers services for children.
But the focus of the current research literature primarily on symptoms and diagnosis of depression in an adult does not do justice to the larger possible impacts on family development. It is essential to consider both in terms of either difficulties or opportunities for prevention, not just the individuals in the family but the family as a whole. A much broader definition of effects on the family is needed, which the committee introduces here in this report.
This conceptualization considers broadly the environment, economic resources, and relationships with family, coworkers, the community, and society (see Figure 1-1 3 ). The community environment may either contribute to the impacts of parental depression in a family or help to mitigate them. Costs to families are much greater than individual economic costs for the depressed person. The burden of suffering is large for the depressed individual and frequently for other family members as well. The community environment is also likely to directly influence child outcomes. And a family’s current characteristics and financial resources are likely to affect the economic impact of a depressive episode on the family. Once depressed, parents have an effect on their own potential human capital (i.e., decreased employment, earnings, productivity), social capital (i.e., skills, abilities, knowledge, relationships), and their decisions on allocating their resources (i.e., time, money). These characteristics and decisions affect the well-being of family members in both the short term and the long term. They can include the maintenance and development of their children’s physical and mental health (e.g., they cannot take them to the doctor for well-child visits), their development of human capital (e.g., their child dropping out of school, achieving poorer academic performance), and their development of social capital (e.g., their child’s impairment in marital and work relationships). Taking a developmental approach that addresses long-term possible negative consequences of parental depression emphasizes both the magnitude of the costs and the need for action.
Conceptual model of the economic impact of depressed parents on children. NOTES: Employment = unemployment, reduced productivity; Environment = physical—housing quality, rural versus urban; social—crime rates, racial/ethnic representation, (more...)
A parent is central to the family’s functioning. His or her impairments can have dramatic effects on their children and the family. These patterns of impairment in depressed parents and the risks to their families offer natural targets for preventive and treatment interventions at various levels, includ ing, for example, making sure that families with depression have health insurance or recognizing that, with depression, parents will need additional support to get tasks done.
- BARRIERS TO CARE
Like a variety of other health services, access to care for depression may be influenced by geographic, physical, financial, sociocultural, and temporal barriers. Such barriers include transportation issues, physical disabilities, language barriers, cultural customs and beliefs, and health insurance coverage. Furthermore, an individual’s ability to access and use care may be affected by demographic characteristics (i.e., age, gender, education level, occupation, race/ethnicity), need (i.e., perceived health) and enabling characteristics (i.e., language, income, convenience, transportation, health system characteristics like infrastructure, linkages to a variety of providers). Stigma is a major barrier to seeking mental health treatment. Both self-stigma (people’s own responses to depression and help-seeking) and perceived stigma (perceptions of others’ negative responses) partially account for people’s reluctance to seek treatment (Barney et al., 2006; Halter, 2004). Many people are not familiar with treatment options, there is stigma associated with mental health treatments, and many providers are not aware of their patients’ preferences (Dwight-Johnson et al., 2000; Givens et al., 2007; Jaycox et al., 2006).
A number of institutional and sociocultural barriers are responsible for causing and maintaining existing disparities in access to and quality of mental health services received by minority groups. A succinct summary of the complex constellation of barriers is that “disparities result from ongoing interactions among factors at the levels of the health care environment, health care organization, community, provider, and person throughout the course of the depression development and treatment-seeking process” (Chin et al., 2007; Van Voorhees et al., 2007, p. 1617). Social marginalization, which has played a key role in rendering some populations disproportionately vulnerable to and affected by incidence of depression, extends its adverse impact by limiting the engagement of and treatment in historically underserved communities (Aguilar-Gaxiola et al., 2008). These groups’ isolation from mainstream society because of linguistic barriers, geographic isolation, a history of oppression, racism, discrimination, poverty, and immigration status plays a key role in creating and perpetuating many of the barriers to treatment.
In addition to individual and provider barriers to care specific to depression in adults, a body of literature continues to document the system-level limitations in mental health care generally. As described in a 2006 Institute of Medicine report entitled Improving the Quality of Health Care for Mental and Substance-Use Conditions , the “inadequacy of [mental health and substance use] health care is a dimension of the poor quality of all health care” (Institute of Medicine, 2006, p. 8). However, it also points out that care for mental health and substance use problems is also distinct from health care generally. The distinctive features they describe include greater stigma associated with diagnoses, a less developed infrastructure for measuring and improving the quality of care, a need for a greater number of linkages among multiple clinicians, organizations and systems providing care to patients with mental health conditions, less widespread use of information technology, a more educationally diverse workforce, and a differently structured marketplace for the purchase of mental health and substance use health care (Institute of Medicine, 2006). With this in mind, the report recommended using the strategy set forth by another Institute of Medicine report (2001), Crossing the Quality Chasm , as a basic framework to achieve substantial improvements in quality of care, but to tailor it to the distinctive features of mental health and substance use care.
Depression presents a fundamental paradox: it is one of the most prevalent of psychiatric conditions but also one that is highly amenable to treatment, at least in the acute phase. The U.S. Surgeon General, the National Institutes of Health, the Substance Abuse and Mental Health Services Administration, and many others continue to document advances in the understanding of depression, the identification and assessment of depressed individuals, and the development of efficacious treatments, as well as strategies for delivering these interventions effectively. Yet despite recent scientific advances, in 2007, only 64 percent of adults in the United States who had a major depressive episode in the past year received some form of treatment (Office of Applied Studies, 2008). Only approximately 30 percent of depressed adults in community samples reportedly will receive any treatment (Simon et al., 2004). Further, depression in adults is typically discussed as an isolated problem. The focus is rarely on how depression affects parenting and child outcomes; how often it occurs in combination with other parental risks, like substance abuse and trauma; or what kinds of strategies can help to identify, treat, and prevent these negative consequences for parents and their children (Knitzer, Theberge, and Johnson, 2008). The current policy environment does not encourage an identification and treatment strategy with this kind of two-generation developmental lens, nor does it support the dissemination or implementation of the growing body of knowledge about effective interventions.
National surveys exist that describe the rates of depression in adults and indicate disparities as defined by selected population characteristics. A subsample of one such survey specifically identified the parental status of these adults. Parents (with at least one child under age 18) have similar rates of depression compared to the entire U.S. adult population, including similar disparities in depression rates for selected population characteristics such as sex, age, and marital status. In general, social disadvantage has been positively associated with higher prevalence rates of depression in adults except in the case of newly arrived immigrants. Further, a majority of individuals with major depression also had at least one additional mental health or substance abuse diagnosis. Thus, comorbidity between mental disorders tends to be the norm rather than the exception.
Depression, due to its recurrent nature, leads to sustained individual, family, and societal costs. Furthermore, depression in parents or other caregivers can have serious biological, psychological, behavioral, and social consequences especially for children. More longitudinal and cross-sectional data are needed to further document and clarify the prevalence, incidence, disparities, causes, and consequences of depression in adults who are parents. Individual-, provider-, and system-level barriers exist that decrease the access to and quality of care for depressed adults. These institutional and sociocultural barriers are responsible for causing and maintaining existing disparities. Without a system of care that supports a family’s environment, economic resources and relationships with family, coworkers, the community, and society, such disparities may increase.
Ultimately depression is a good and effectively identified indicator of a problem that could trigger a system of care (if it is in place) that intervenes not only by treating depression in the parent but also by enhancing parenting skills and alleviating other stresses, co-occurring conditions, and social contexts, as well as identifying children at risk.
- ORGANIZATION OF THE REPORT
Following this introduction, Chapter 2 describes new approaches to tackling parental depression as well as issues and standards in evaluating this literature. Chapter 3 reviews the causes of depression, and Chapter 4 reviews the effects of depression on parenting and child health and psychological functioning. Chapter 5 reviews strategies to identify and assess depression, and Chapter 6 reviews strategies for the treatment of depression in parents and their families. Chapter 7 reviews strategies for preventing depression in parents, with a special emphasis on the prevention or reduction of adverse outcomes in children of parents who are depressed. Chapter 8 describes an ideal vision of a depression care intervention system, highlighting important components of this system that are emerging in selected service settings as well as through state and European initiatives, and reviewing federal-level initiatives that have supported this knowledge base. Chapter 9 describes systemic, workforce, and fiscal policy challenges that have emerged from current initiatives associated with implementing innovative evidence-based strategies in addressing depression in parents and its impact on children. Chapter 10 describes next steps that can be taken to help contribute to the design and implementation of the ideal prevention and depression system for parental depression, which includes knowledge development and the creation of an organizational culture receptive to new research. To aid the reader, the committee’s summary of the literature is presented at the beginning of the chapter and the conclusions, research gaps, and committee’s recommendations are presented at the end of each chapter, where appropriate. Finally, the role of culture, language, and social determinants of health were identified across the chapters when literature was available when describing vulnerable populations who experience mental health disparities. A list of acronyms is provided in Appendix A . The agenda and participants of the committee’s public workshop are listed in Appendix B , and biographical sketches of the committee members and staff are provided in Appendix C .
- Aday, L.A. (1994). Health status of vulnerable populations . Annual Review of Public Health 15 , 487–509. [ PubMed : 8054096 ]
- Aguilar-Gaxiola, S., Elliott, K., Debb-Sossa, N., King, R.T., Magaña, C.G., Miller, E., Sala, M., Sribney, W.M., and Breslau, J. (2008). Engaging the Underserved: Personal Accounts of Communities on Mental Health Needs for Prevention and Early Intervention Strate gies . Monograph #1, UC Davis Center for Reducing Health Disparities. Sacramento: UC Davis.
- Andrade, L., Caraveo-Anduaga, J.J., Berglund, P., Bijl, R.V., De Graaf, R., Vollebergh, W., Dragomirecka, E., Kohn, R., Keller, M., Kessler, R.C., Kawakami, N., Kilic, C., Offord, D., Ustun, T.B., and Wittchen, H.U. (2003). The epidemiology of major depressive episodes: Results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys . International Journal of Methods in Psychiatric Research , 12 , 3–21. [ PMC free article : PMC6878531 ] [ PubMed : 12830306 ]
- Andrews, G. (2001). Should depression be managed as a chronic disease? British Medical Journal , 322 , 419–421. [ PMC free article : PMC1119639 ] [ PubMed : 11179166 ]
- Barney, L.J., Griffiths, K.M., Jorm, A.F., and Christensen, H. (2006). Stigma about depression and its impact on help-seeking intentions . Australian and New Zealand Journal of Psychiatry , 40 , 51–54. [ PubMed : 16403038 ]
- Barsky, A.J. (1979). Patients who amplify bodily sensations . Annals of Internal Medicine , 91 , 63–70. [ PubMed : 380428 ]
- Bassuk, E.L., Buckner, J.C., Perloff, J.N., and Bassuk, S.S. (1998). Prevalence of mental health and substance use disorders among homeless and low-income housed mothers . American Journal of Psychiatry , 155 , 1561–1564. [ PubMed : 9812118 ]
- Bengtson, V.L., Acock, A.C., Allen, K.R., Dilworth-Anderson, P., and Klein, D.M. (2005). Sourcebook of Family Theory and Research . Thousand Oaks, CA: Sage.
- Bloom, B., Owen, B., Covington, S., and Raeder, M. (2003). Gender-Responsive Strategies: Research, Practice, and Guiding Principles for Women Offenders . Washington, DC: National Institute of Corrections, U.S. Department of Justice.
- Brandon, P.D., and Bumpass, L. (2001). Children’s living arrangement, coresidence of unmarried fathers, and welfare receipt . Journal of Family Issues , 22 , 3–26.
- Casper, L.M., and Bryson, K.R. (1998). CoResident Grandparents and Their Grandchildren: Grandparent Maintained Families . (Current Population Report). Washington, DC: U.S. Bureau of the Census.
- Centers for Disease Control and Prevention. (2008). Prevalence of self-reported postpartum depressive symptoms—17 states, 2004–2005 . Morbidity and Mortality Weekly Report , 57 , 361–366. [ PubMed : 18401329 ]
- Chin, M.H., Walters, A.E., Cook, S.C., and Huang, E.S. (2007). Interventions to reduce racial and ethnic disparities in health care . Medical Care Research and Review , 64 , 7S–28S. [ PMC free article : PMC2366039 ] [ PubMed : 17881624 ]
- Ciechanowski, P.S., Katon, W.J., and Russo, J.E. (2000). Depression and diabetes: Impact of depressive symptoms on adherence, function, and costs . Archives of Internal Medicine , 160 , 3278–3285. [ PubMed : 11088090 ]
- Coryell, W., Endicott, J., and Keller, M.B. (1990). Outcome of patients with chronic affective disorder: A five-year follow-up . American Journal of Psychiatry , 147 , 1627–1633. [ PubMed : 2244640 ]
- Cross-National Collaborative Group. (1992). The changing rate of major depression: Cross-national comparisons . Journal of the American Medical Association , 268 , 3098–3105. [ PubMed : 1433741 ]
- Cummings, E.M., and Davies, P.T. (1999). Depressed parents and family functioning: Interpersonal effects and children’s functioning and development . In T.E. Joiner, editor; and J.C. Coyne, editor. (Eds.), The Interactional Nature of Depression: Advances in Interpersonal Approaches (pp. 299–327). Washington, DC: American Psychological Association.
- De Graaf, R., Bijl, R.V., Smith, F., Vollebergh, W.A.M., and Spijker, J. (2002). Risk factors for 12-month comorbidity of mood, anxiety, and substance use disorders: Findings from the Netherlands Mental Health Survey and Incidence Study . American Journal of Psychiatry , 159 , 620–629. [ PubMed : 11925301 ]
- Depue, R.A., and Monroe, S.M. (1986). Conceptualization and measurement of human disorder and life stress research: The problem of chronic disturbance . Psychological Bulletin , 99 , 36–51. [ PubMed : 3704034 ]
- DiMatteo, M.R., Lepper, H.S., and Croghan, T.W. (2000). Depression is a risk factor for non-compliance with medical treatment . Archives of Internal Medicine , 160 , 2101–2107. [ PubMed : 10904452 ]
- Dwight-Johnson, M., Sherbourne, C.D., Liao, D., and Wells, K.B. (2000). Treatment preferences among depressed primary care patients . Journal of General Internal Medicine , 15 , 527–534. [ PMC free article : PMC1495573 ] [ PubMed : 10940143 ]
- Edwards, R.R., Bingham, C.O. 3rd, Bathon, J., and Haythornewaite, J.A. (2006). Catastrophizing and pain in arthritis, fibromyalgia, and other rheumatic diseases . Arthritis and Rheumatism , 55 , 325–332. [ PubMed : 16583384 ]
- The ESEMeD/MHEDEA 2000 Investigators. (2004). Prevalence of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project . Acta Psychiatrica Scandinavica , 109 , 21–27. [ PubMed : 15128384 ]
- Evans, D.L., Charney, D.S., Lewis, L., Golden, R.N., Gorman, J.M., Krishnan, K.R.R., Nemeroff, C.B., Bremner, J.D., Carney, R.M., Coyne, J.C., Delong, M.R., Frasure-Smith, N., Glassman, A.H., Gold, P.W., Grant, I., Gwyther, L., Ironson, G., Johnson, R.L., Kanner, A.M., Katon, W.J., Kaufmann, P.G., Keefe, F.J., Ketter, T., Laughren, T.P., Leserman, J., Lyketsos, C.G., McDonald, W.M., McEwen, B.S., Miller, A.H., Mussleman, D., O’Connor, C., Petitto, J.M., Pollock, B.G., Robinson, R.G., Roose, S.P., Rowland, J., Sheline, Y., Sheps, D.S., Simon, G., Spiegel, D., Stunkard, A., Sunderland, T., Tibbits, P., Jr., and Valvo, W.J. (2005). Mood disorders in the medically ill: Scientific review and recommendations . Biological Psychiatry , 58 , 175–189. [ PubMed : 16084838 ]
- Federal Interagency Forum on Child and Family Statistics. (2007). America’s Children: Key National Indicators of Well-Being, 2007 . Washington, DC: U.S. Government Printing Office.
- Frank, R.G., and Glied, S. (2006). The population with mental illness . In R.G. Frank, editor; ., S. Glied, editor; , and R. Carter, editor. (Eds.), Better But Not Well: Mental Health Policy in the United States Since 1950 (pp. 8–25). Baltimore, MD: Johns Hopkins University Press.
- Givens, J.L., Katz, I.R., Bellamy, S., and Holmes, W.C. (2007). Stigma and the acceptability of depression treatments among African Americans and whites . Journal of General Medicine , 22 , 1292–1297. [ PMC free article : PMC2219769 ] [ PubMed : 17610120 ]
- Goodman, S., and Gotlib, I. (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission . Psy chological Review , 106 , 458–490. [ PubMed : 10467895 ]
- Grant, B.F., Stinson, F.S., Hasin, D.S., Dawson, D.A., Chou, S.P., and Anderson, K. (2004). Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States . Archives of General Psychiatry , 61 , 1226–1233. [ PubMed : 15583114 ]
- Greenberg, P.E., Kessler, R.C., Birnbaum, H.C., Leong, S.A., Lowe, S.W., Berglund, P.A., and Corey-Lisle, P.K. (2003). The economic burden of depression in the United States: How did it change between 1990 and 2000? Journal of Clinical Psychiatry , 64 , 1465–1475. [ PubMed : 14728109 ]
- Halter, M.J. (2004). The stigma of seeking care and depression . Archives of Psychiatric Nurs ing , 18 , 178–184. [ PubMed : 15529283 ]
- Institute of Medicine. (2001). Crossing the Quality Chasm: A New Health System for the 21st Century . Washington, DC: National Academy Press. [ PubMed : 25057539 ]
- Institute of Medicine. (2006). Improving the Quality of Health Care for Mental and Substance- Use Conditions . Washington, DC: The National Academies Press.
- Jackson, P.B., and Williams, D.R. (2006). Culture, race/ethnicity, and depression . In C.L.M. Keyes, editor; and S.H. Goodman, editor. (Eds.), Women and Depression: A Handbook for the Social, Behavioral, and Biomedical Sciences (pp. 328–359). New York: Cambridge University Press.
- Jaycox, L.H., Asarnow, J.R., Sherbourne, C.D. Rea, M.M., LaBorde, A.P., and Wells, K.B. (2006). Adolescent primary care patients’ preferences for depression treatment . Admin istration and Policy in Mental Health , 33 , 198–207. [ PubMed : 16502131 ]
- Jesse, D.E., Walcott-McQuigg, J., Mariella, A., and Swanson, M.S. (2005). Risks and protective factors associated with symptoms of depression in low-income African American and Caucasian women during pregnancy . Journal of Midwifery and Women’s Health , 50 , 405–410. [ PubMed : 16154068 ]
- Johnson, J., Weissman, M.M., and Klerman, G. (1992). Service utilization and social morbidity associated with depressive symptoms in the community . Journal of the American Medical Association , 267 , 1478–1483. [ PubMed : 1538538 ]
- Judd, L.L., Akiskal, H.S., Maser, J.D., Zeller, P.J., Endicott, J., Coryell, W., Paulus, M.P., Kunovac, J.L., Leon, A.C., Mueller, T.I., Rice, J.A., and Keller, M.B. (1998). A prospective 12-year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders . Archives of General Psychiatry , 55 , 694–700. [ PubMed : 9707379 ]
- Katon, W. (1998). The effect of major depression on chronic medical illness . Seminars in Clinical Neuropsychiatry , 3 , 82–86. [ PubMed : 10085195 ]
- Katon, W.J. (2003). Clinical and health services relationships between major depression, depressive symptoms, and general medical illness . Biological Psychiatry , 54 , 216–226. [ PubMed : 12893098 ]
- Kessler, R.C. (2003). Epidemiology of women and depression . Journal of Affective Disorders , 74 , 5–13. [ PubMed : 12646294 ]
- Kessler, R.C., Akiskal, H.S., Ames, M., Birnbaum, H., Greenberg, P., Hirschfeld, R.M.A., Jin, R., Merikangas, K.R., Simon, G.E., and Wang, P.S. (2006). Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers . American Journal of Psychiatry , 163(9), 1561–1568. [ PMC free article : PMC1924724 ] [ PubMed : 16946181 ]
- Kessler, R.C., Berglund, P., Demler, O., Jin, R., Koretz, D., Merikangas, K.R., Rush, A.J., Walters, E.E., and Wang, P.S. (2003). The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) . Journal of the American Medical Association , 289 , 3095–3105. [ PubMed : 12813115 ]
- Kessler, R.C., Berglund, P., Demler, O., Jin, R., Merikangas, K.R., and Walters, E.E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication . Archives of General Psychiatry , 62 , 593–602. [ PubMed : 15939837 ]
- Kessler, R.C., Walters, E.E., and Forthofer, M.S. (1998). The social consequences of psychiatric disorders, III: Probability of marital stability . American Journal of Psychiatry , 155 , 1092–1096. [ PubMed : 9699699 ]
- Knitzer, J., Theberge, S., and Johnson, K. (2008). Reducing Maternal Depression and Its Impact on Young Children: Toward a Responsive Early Childhood Policy Framework . New York: National Center for Children in Poverty.
- Lanzi, R.G., Pascoe J.M., Keltner B., and Ramey, S.L. (1999). Correlates of maternal depressive symptoms in a National Head Start Program sample . Archives of Pediatrics and Adolescent Medicine , 153(8), 801–807. [ PubMed : 10437751 ]
- Lorant, V., Croux, C., Weich, S., Deliege, D., Mackenbach, J., and Ansseau, M. (2007). Depression and socioeconomic risk factors: 7-year longitudinal population study . British Journal of Psychiatry , 190 , 293–298. [ PubMed : 17401034 ]
- Lorant, V., Deliege, D., Eaton, W., Robert, A., Philippot, P., and Ansseau, M. (2003). Socioeconomic inequalities in depression: A meta-analysis . American Journal of Epidemiology , 157 , 98–112. [ PubMed : 12522017 ]
- Luppa, M., Heinrich, S., Angermeyer, M.C., König, H.H., and Riedel-Heller, S.G. (2007). Cost-of-illness studies of depression: A systematic review . Journal of Affective Disorders , 98 , 29–43. [ PubMed : 16952399 ]
- Miranda, J., Siddique, J., Belin, T.R., and Kohn, L.P. (2005). Depression prevalence in disadvantaged young black women. African and Caribbean immigrants compared to U.S.-born African Americans . Social Psychiatry and Psychiatric Epidemiology , 40 , 253–258. [ PubMed : 15834775 ]
- Moussavi, S., Chatterji, S., Verdes, E., Tandon, A., Patel, V., and Ustun, B. (2007). Depression, chronic diseases, and decrements in health: Results from the World Health Surveys . The Lancet , 370 , 851–858. [ PubMed : 17826170 ]
- Muñoz, S.S. (2003). Cost to treat a depression case falls . The Wall Street Journal , December 31, p. D2.
- Murray, C.J., and Lopez, A.D. (1996). The Global Burden of Disease . Cambridge. MA: Harvard University Press.
- Office of Applied Studies. (2008). Results from the 2007 National Survey on Drug Use and Health: National Findings . (DHHS Pub No. SMA 08-4343). Rockville, MD: Substance Abuse and Mental Health Services Administration.
- Ramchandani, P.G., Stein, A., O’Connor, T.G., Heron, J., Murray, L., and Evans, J. (2008). Depression in men in the postnatal period and later child psychopathology: A population cohort study . Journal of the American Academy of Child and Adolescent Psychiatry , 47 , 390–398. [ PMC free article : PMC2650418 ] [ PubMed : 18388761 ]
- Riolo, S.A., Nguyen, T.A., Greden, J.F., and King, C.A. (2005). Prevalence of depression by race/ethnicity: Findings from the National Health and Nutrition Examination Survey III . American Journal of Public Health , 95 , 998–1000. [ PMC free article : PMC1449298 ] [ PubMed : 15914823 ]
- Rush, A.J., Zimmerman, M., Wisniewski, S.R., Fava, M., Hollon, S.D., Warden, D., Biggs, M.M., Shores-Wilson, K., Shelton, R.C., Luther, J.F., Thomas, B., and Trivedi, M.H. (2005). Comorbid psychiatric disorders in depressed outpatients: Demographic and clinical features . Journal of Affective Disorders , 87 , 43–55. [ PubMed : 15894381 ]
- Siefert, K., Bowman, P.J., Heflin, C.M., Danzger, S., and Williams, D.R. (2000). Social and environmental predictors of maternal depression in current and recent welfare recipients . American Journal of Orthopsychiatry , 70 , 510–522. [ PubMed : 11086529 ]
- Simon, G.E., Fleck, M., Lucas, R., Bushnell, D.M., and the LIDO Group. (2004). Prevalence and predictors of depression treatment in an international primary care study . American Journal of Psychiatry , 161 , 1626–1634. [ PubMed : 15337653 ]
- Solomon, D.A., Keller, M.B., Leon, A.C., Mueller, T.I., Lavori, P.W., Shea, M.T., Coryell, W., Warshaw, M., Turvey, C., Maser, J.D., and Endicott, J. (2000). Multiple recurrences of major depressive disorder . American Journal of Psychiatry , 157 , 229–233. [ PubMed : 10671391 ]
- Takeuchi, D.T., Zane, N., Hong, S., Chae, D.H., Gong, F., Gee, G.C., Walton, E., Sue, S., and Alegria, M. (2007). Immigration-related factors and mental disorders among Asian Americans . American Journal of Public Health , 97 , 84–90. [ PMC free article : PMC1716230 ] [ PubMed : 17138908 ]
- Thornicroft, G., and Sartorius, N. (1993). The course and outcome of depression in different cultures: 10-year follow-up of the WHO Collaborative Study on the Assessment of Depressive Disorders . Psychological Medicine , 23 , 1023–1032. [ PubMed : 8134505 ]
- U.S. Census Bureau. (2005. a). Facts for Features. Father’s Day: June 19, 2005 . Available: http://www .census.gov /Press-Release/www/releases /archives/cb05ff-08.pdf [accessed February 4, 2009].
- U.S. Census Bureau. (2005. b). Facts for Features. Mother’s Day: May 8, 2005 . Available: http://www .census.gov /Press-Release/www/releases /archives/cb05-ff.05-2.pdf [accessed February 4, 2009].
- U.S. Census Bureau. (2008. a). C2. Household Relationship and Living Arrangements of Children/1 Under 18 Years, by Age and Sex: 2007 . Available: http://www .census.gov /population/socdemo /hh-fam/cps2007/tabC2-all.xls [accessed October 29, 2008].
- U.S. Census Bureau. (2008. b). Table F1. Family Households/1, by Type, Age of Own Children, Age of Family Members, and Age, Race and Hispanic Origin/2 of Householder: 2007 . Available: http://www .census.gov /population/socdemo /hh-fam/cps2007/tabF1-all.xls [accessed October 29, 2008].
- U.S. Surgeon General. (1999). Mental Health: A Report of the Surgeon General . Washington, DC: U.S. Department of Health and Human Services.
- Van Voorhees, B.W., Walters, A.E., Prochaska, M., and Quinn, M.T. (2007). Reducing health disparities in depressive disorders outcomes between non-Hispanic whites and ethnic minorities: A call for pragmatic strategies over the life course . Medical Care Research Review , 64 , 157s-194s. [ PubMed : 17766647 ]
- Vega, W.A., Kolody, B., Aguilar-Gaxiola, S., Alderete, E., Catalano, R., and Caraveo-Anduaga, J. (1998). Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California . Archives of General Psychiatry , 55 , 771–778. [ PubMed : 9736002 ]
- Wang, P.S., Beck, A.L., Berglund, P., McKenas, D.K., Pronk, N.P., Simon, G.E., and Kessler, R.C. (2004). Effects of major depression on moment-in-time work performance . Ameri can Journal of Psychiatry , 161 , 1885–1891. [ PubMed : 15465987 ]
- Wells, K.B., Stewart, A., Hays, R.D., Burnam, A., Rogers, W., Daniels, M., Berry, S., Greenfield, S., and Ware, J. (1989). The functioning and well-being of depressed patients . Journal of the American Medical Association , 262 , 914–919. [ PubMed : 2754791 ]
- Whisman, M.A. (2001). The association between depression and marital dissatisfaction . In S.R.H. Beach, editor. (Ed.), Marital and Family Processes in Depression: A Scientific Foundation for Clinical Practice . Washington, DC: American Psychological Association.
- Williams, D.R., Gonzalez, H.M., Neighbors, H., Nesse, R., Abelson, J.M., Sweetman, J., and Jackson, J.S. (2007). Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life . Archives of General Psychiatry , 64 , 305–315. [ PubMed : 17339519 ]
- World Health Organization. (2001). The Global Burden of Disease . Available: http://files .dcp2.org/pdf/GBD/GBD01.pdf [accessed December 2008].
The Composite International Diagnostic Interview is a comprehensive interview designed for the assessment of mental disorders according to the definitions and criteria of the Interna tional Statistical Classification of Diseases and Related Health Problems , 10th revision, and the Diagnostic and Statistical Manual of Mental Disorders , 4th edition.
For example, the National Survey of American Life and the National Latino and Asian American Study.
This concept was developed for the committee through commissioned work by Frances Lynch, Ph.D.
- Cite this Page National Research Council (US) and Institute of Medicine (US) Committee on Depression, Parenting Practices, and the Healthy Development of Children; England MJ, Sim LJ, editors. Depression in Parents, Parenting, and Children: Opportunities to Improve Identification, Treatment, and Prevention. Washington (DC): National Academies Press (US); 2009. 1, Introduction and Magnitude of the Problem.
- PDF version of this title (2.9M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Introduction and Magnitude of the Problem - Depression in Parents, Parenting, an... Introduction and Magnitude of the Problem - Depression in Parents, Parenting, and Children
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
To improve our understanding, some research has been undertaken in which YP themselves are asked about their experience of depression. In a questionnaire study involving adolescents with depression in New Zealand, the researchers identified the aforementioned irritability as the most common characteristic alongside interpersonal problems and ...
Rodent research has shown that there may be a bidirectional association between the gut microbiota and depression: a disordered gut microbiota can play a role in the onset of this mental health problem, but, at the same time, the existence of stress and depression may also lead to a lower level of richness and diversity in the microbiome .
Depression is a prevalent psychiatric disorder that often leads to poor quality of life and impaired functioning. Treatment during the acute phase of a major depressive episode aims to help the patient reach a remission state and eventually return to their baseline level of functioning. Pharmacotherapy, especially selective serotonin reuptake ...
The number of trials that meet inclusion has increased considerably over time. In Fig. 1, we have given a cumulative overview of the included trials over the years and separately across different regions.As can be seen, up to the mid 1990s almost all research was done in North America, since then a growing number of trials has been done in Europe (including the UK) and since 2005 research in ...
Employee Assistance Program (EAP) managers report that depression ranks with family crisis and stress as the most frequent and costly problems that affect the workplace. Reportedly, the negative impact of depression on society ranks even higher than the more widely recognized workplace problem of alcohol abuse (PRNewswire report, 1996).
Introduction. Depression among adolescents and young adults (AYA) is a serious, widespread problem. A striking increase in depressive symptoms is seen in early adolescence [], with rates of depression being estimated to almost double between the age of 13 (8.4%) and 18 (15.4%) [].Research also suggests that the mean age of onset for depressive disorders is decreasing, and the prevalence is ...
Depressive disorders are common, costly, have a strong effect on quality of life, and are associated with considerable morbidity and mortality. Effective treatments are available: antidepressant medication and talking therapies are included in most guidelines as first-line treatments. These treatments have changed the lives of countless patients worldwide for the better and will continue to do ...
Abstract. Three to nine per cent of teenagers meet the criteria for depression at any one time, and at the end of adolescence, as many as 20% of teenagers report a lifetime prevalence of depression. Usual care by primary care physicians fails to recognize 30-50% of depressed patients. Cross-sectional one-time observational study using simple ...
This paper summarizes many findings about depression among children and adolescents. Depression is prevalent, highly distressing, and exerts considerable burden worldwide. Rates surge from childhood through young adulthood and have increased over the last decade. Many risk factors have been identified, and evidence-based interventions exist targeting mostly individual-level changes via ...
The causes of depression are manifold and complex. But biologically definable factors are starting to come to light. One theory that is gaining support is that the culprit might be a slowdown in ...
Design. Meta-synthesis is a research method that uses rigorous qualitative methods to synthesize existing qualitative studies, with the aim of constructing greater meaning through an overarching interpretation based on the qualitative studies included [33,34,35,36].Thematic synthesis is influenced by the meta-ethnography process and grounded theory [] and involves conceptual coding of data to ...
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect ...
university students, found the rate of depression among Nigerian students was only 2.7%. This is much lower compared to the rate of depression among Nigerian outpatients visiting. general clinics ...
According to the fall 2007 American College Health Association-National College Health Assessment ( 1), a national survey of approximately 20,500 college students on 39 campuses, 43.2% of the students reported "feeling so depressed it was difficult to function" at least once in the past 12 months.More than 3,200 university students reported being diagnosed as having depression, with 39.2% of ...
OBJECTIVE: Research studies on the validity of current diagnostic and subthreshold categories of depression that use a population-based follow-up design are rare. The authors examined the validity and utility of four current depression categories by examining subject transition between categories and the symptoms, course, and risk factors of each. METHOD: A general population sample of 1,920 ...
The possible causes of depression are many and not yet well understood. However, it most likely results from an interplay of genetic vulnerability and environmental factors. Your depression research paper could explore one or more of these causes and reference the latest research on the topic. For instance, how does an imbalance in brain ...
Data Availability Statement. ... Peoples R China, as the only developing country, ranks 3rd in the top 10 countries with high production of research papers in the field of depression, and Peoples R China's research in the field of depression has shown a rapid growth trend, and by 2016, it has jumped to become the 2nd largest country in the ...
Depression is a common, universal, and debilitating public health problem. The Global Burden of Disease study by the World Health Organization (WHO) determined that depression accounts for more disability worldwide than any other condition during the middle years of adulthood (Murray and Lopez, 1996). In fact, major depressive disorder is now the leading cause of disability worldwide (World ...
Adolescent depression is a chronic, pervasive, and disabling problem that is often under-recognized and under-treated. The objective of this article is to review recent (over the past 12-18 months ...
population aged 16-85 years, 14.4% have an anxiety. disorder. The pre valence of depression is 6.2%, with the. prevalence of unipolar depressive episodes being 4.1%, dysthymia, 1.3%, and bipolar ...
There is a lack of research in health psychology on the subjective experience of adolescents with mental health disorders. The aim of this study was to explore the experience of depression and the journey into therapy of young people (YP) diagnosed with depression. Semi-structured interviews were carried out with six YP (5 female, aged 15-19).
After applying the inclusion and exclusion criteria, 470 papers were included in this review (Supplementary Table S1). We focused on aspects related to biological, psychological, and social determinants of depression (examples of determinants and related outcomes are provided under each of the following sections. 3.1.
Problem Statement. Research indicates that depression can be associated with both cognitive impairment and dementia, and that depression increases the risk of developing dementia (Steffens et al, 2006). It is not always easy to diagnose depression in a person with Alzheimer's disease, as Alzheimer's itself may mimic the signs of depression.
impoverishment, or depression, or depreciation in activity, strength, amount, quality, force, yield, value, or significance. The second definition states. depression is a period of low general economic activity marked by mass. unemployment, deflation, a decreasing use of resources and a low level of. investment.