Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Collection

Fear, anxiety, and phobias
Fear is an emotional response to a perceived specific threat. Although fear is an essential survival mechanism, when it becomes persistent, it might lead to anxiety, or manifest as a specific phobia, namely, an irrational fear of a specific object, situation, or event. Understanding the cognitive and neural processes underlying these related emotional states is critical for the diagnosis and treatment of a variety of associated anxiety disorders.
This Collection welcomes original research articles investigating the processes underlying fear, anxiety, and specific phobias. Empirical animal and human research that focuses on the diagnosis and treatment of related anxiety disorders is welcome.

Robert M. Sears, PhD
Emotional Brain Institute, Nathan Kline Institute for Psychiatric Research and Child and Adolescent Psychiatry, New York University Grossman School of Medicine, USA
Andras N. Zsido, PhD FPsyS
Institute of Psychology University of Pécs, Hungary
- Collection content
- How to submit
- About the Guest Editors
- Collection policies
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
January 1, 2014
Why Do We Develop Certain Irrational Phobias?
By Andrew Watts
Katherina K. Hauner , a postdoctoral fellow at the Northwestern University Feinberg School of Medicine, answers:
Under normal circumstances, fear triggers a natural fight-or-flight response that allows animals to react quickly to threats in their environment. Irrational and excessive fear, however, is typically a maladaptive response. In humans, an unwarranted, persistent fear of a certain situation or object, known as specific phobia, can cause overwhelming distress and interfere with daily life. Specific phobia is among the more prevalent anxiety disorders, affecting an estimated 9 percent of Americans within their lifetime. Common subtypes include fear of small animals, insects, flying, enclosed spaces, blood and needles.
For fear to escalate to irrational levels, a combination of genetic and environmental factors is very likely at play. Estimates of genetic contributions to specific phobia range from roughly 25 to 65 percent, although we do not know which genes have a leading part. No specific phobia gene has been identified, and it is highly unlikely that a single gene is responsible. Rather variants in several genes may predispose an individual to developing a number of psychological symptoms and disorders, including specific phobia.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
As for the environmental component, a person may develop a phobia after a particularly frightening event, especially if he or she feels out of control. Even witnessing or hearing about a traumatic occurrence can contribute to its development. For instance, watching a devastating airplane crash on the news may trigger a fear of flying. That said, discerning the origin of the disorder can be difficult because people tend to do a poor job of identifying the source of their fears.
Our understanding of how and why phobias crop up remains limited, but we have made great strides in abating them. Exposure therapy, a form of cognitive-behavior therapy, is widely accepted as the most effective treatment for anxieties and phobias, and the vast majority of patients complete treatment within 10 sessions. During exposure therapy, a person engages with the particular fear to help diminish and ultimately overcome it over time. An individual might, for example, look at a photograph of the dreaded object or become immersed in the situation he or she loathes. Fortunately for those plagued by irrational fears, we can treat a phobia rapidly and successfully without necessarily knowing its origin.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Quality of Life in Individuals With Anxiety Disorders
- Mauro V. Mendlowicz , M.D. , and
- Murray B. Stein , M.D.
Search for more papers by this author
OBJECTIVE: Quality-of-life indices have been used in medical practice to estimate the impact of different diseases on functioning and well-being and to compare outcomes between different treatment modalities. An integrated view of the issue of quality of life in patients with anxiety disorders can provide important information regarding the nature and extent of the burden associated with these disorders and may be useful in the development of strategies to deal with it. METHOD: A review of epidemiological and clinical studies that have investigated quality of life (broadly conceptualized) in patients with panic disorder, social phobia, posttraumatic stress disorder, generalized anxiety disorder, and obsessive-compulsive disorder was conducted by searching MEDLINE and PsycLIT citations from 1984 to 1999. A summary of the key articles published in this area is presented. RESULTS: The studies reviewed portray an almost uniform picture of anxiety disorders as illnesses that markedly compromise quality of life and psychosocial functioning. Significant impairment can also be found in individuals with subthreshold forms of anxiety disorders. Effective pharmacological or psychotherapeutic treatment has been shown to improve the quality of life for patients with panic disorder, social phobia, and posttraumatic stress disorder. Limitations in current knowledge in this area are identified, and suggestions for needed future research are provided. CONCLUSIONS: It is expected that a more thorough understanding of the impact on quality of life will lead to increased public awareness of anxiety disorders as serious mental disorders worthy of further investment in research, prevention, and treatment.
Anxiety disorders were described as early as the fourth century B.C. in the writings of Hippocrates (1) , but their importance was not fully appreciated until less than 30 years ago. For complex historical reasons the first specialists in psychiatry, the alienists of the early nineteenth century, were mainly concerned with the description and classification of psychotic disorders. As a result, the development of the field of anxiety disorders (as well as the domains of somatization and conversion disorders) was left to specialists in internal medicine and neurology such as da Silva, Briquet, Beard, Charcot, and Freud (2) . The interest of mainstream psychiatry in anxiety disorders would remain limited throughout the first half of the twentieth century because of the prevailing belief that neurotic disorders were benign conditions with nonorganic causes and that their treatment should necessarily be based on some form of psychotherapy (3) .
The realization that anxiety disorders could be successfully treated by pharmacological means (4) , the development of reliable diagnostic criteria (5) , and the advent of modern psychiatric nosology set the stage for a critical reappraisal of the magnitude of the problem of anxiety disorders. Using the DSM-III criteria, the National Institute of Mental Health (NIMH) Epidemiologic Catchment Area (ECA) study showed that anxiety disorders had the highest overall prevalence rate among the mental disorders, with a 6-month rate of 8.9% and a lifetime rate of 14.6% (1) , and affected 26.9 million individuals in the United States at some point in their lives. The costs associated with anxiety disorders in 1990 were a staggering $46.6 billion, accounting for 31.5% of total expenditures in that year for mental health (6) .
Quality of Life: The Concept
It is often said that the cost of human suffering cannot be measured. This truism may no longer be accurate. Many aspects of human suffering (or its absence) can be reliably measured. One of the approaches to this difficult yet invaluable task makes use of the concept of “quality of life.” This concept, developed in the social sciences, was first applied in medical practice to determine if available cancer treatments could not only increase the survival time of patients but also improve their sense of well-being (7) . The concept of quality of life was later applied to compare several antihypertensive medications in terms of functioning, well-being, and life satisfaction (8) .
According to Patrick and Erickson (9) , life has two dimensions: quantity and quality. Quantity of life is expressed in terms of “hard” biomedical data, such as mortality rates or life expectancy. Quality of life refers to complex aspects of life that cannot be expressed by using only quantifiable indicators; it describes an ultimately subjective evaluation of life in general. It encompasses, though, not only the subjective sense of well-being but also objective indicators such as health status and external life situations (10) . Data about quality of life can be used to estimate the impact of different diseases on functioning and well-being, to compare outcomes between different treatment modalities (such as medication and surgery), and, as in the examples mentioned, to differentiate between two therapies with marginal differences in mortality and/or morbidity (11) .
No single definition of quality of life is universally accepted (12) . There is, however, a degree of consensus regarding the minimal requirements for an operational definition of quality of life for employment in health status assessment and research. First, most experts agree that the scope of the concept of quality of life should be centered on the individual’s subjective perception of the quality of his or her own life. This consensus stems from the findings of several sociological studies that have demonstrated that objective conditions of life such as education and income are only marginally related to the subjective experience of a higher quality of life (13 , 14) . Second, most authors agree that given the difficulties in assessing the relative impact of the complex experiences that ultimately determine one’s perception of quality of life, quality of life is better approached as a multidimensional construct, covering a certain number of conventionally defined domains (15) . Finally, it is recommended that we avoid the vagaries of abstract and philosophical concepts and concentrate on aspects of personal experience that are related to health and health care (health-related quality of life) (16) .
An example of a subjective multidimensional definition of health-related quality of life was proposed by Patrick and Erickson (17) : “the value assigned to the duration of life as modified by the social opportunities, perceptions, functional states, and impairments that are influenced by disease, injuries, treatments, or policies” (p. 6). Aaronson et al. (18) suggested that the assessment of quality of life should comprise at least the following four domains: 1) physical functional status, 2) disease- and treatment-related physical symptoms, 3) psychological functioning, and 4) social functioning. Additional domains that are of particular relevance to specific demographic, cultural, or clinical populations (such as sexual function, body image, or sleep) may sometimes need to be included in the assessment to increase the breadth of coverage (19) .
Approaches to Studying Quality of Life in Individuals With Anxiety Disorders
Data regarding quality of life in mental disorders in general, and in anxiety disorders in particular, derive from two types of sources. The first source is represented by epidemiological studies such as the ECA and the National Comorbidity Survey. Although these studies were not specifically designed to study the association between quality of life and mental disorders in the community, they provide a number of indicators from which quality of life can be inferred. These indicators include a subjective assessment of physical and emotional health, psychosocial functioning, and financial dependency (1 , 20 , 21) .
Clinical studies made by using specifically designed instruments represent the second major source of data concerning quality of life. These instruments may be generic (i.e., attempting to measure multiple important aspects of quality of life) or specific (i.e., focusing on aspects of health status that are specific to the area of primary interest). The latter may be specific to a disease (e.g., panic disorder), to a population (e.g., elderly patients), to a function (e.g., sleep), or to a problem (e.g., pain) (22) . The main advantage of generic measures is that they permit comparisons across conditions and populations. In contrast, specific measures are intended to detect small, meaningful changes in specific conditions to which generic measures may be insensitive.
Although quality-of-life data can be collected in interviews or through patient diaries, most studies now employ self-report questionnaires, the most cost-effective method for obtaining patient-related information (19) . For this report, a review of epidemiological and clinical studies that have investigated quality of life (broadly conceptualized) in patients with panic disorder, social phobia, posttraumatic stress disorder (PTSD), generalized anxiety disorder, and obsessive-compulsive disorder (OCD) was conducted by searching MEDLINE and PsycLIT from Jan. 1984 to Oct. 1999. The key words employed were “quality of life,” “impairment,” and “disability.” With few exceptions (to be discussed later), only clinical studies utilizing self-report instruments based on subjective, multidimensional concepts of health-related quality of life that were properly validated were considered. ( Table 1 briefly summarizes the psychometric properties of these instruments.)
Quality of Life in Individuals With Panic Disorder
Studies in community samples.
The ECA study is an important source of data regarding the epidemiology of panic disorder and the impact of panic disorder on quality of life. This study found a lifetime prevalence for panic disorder of 1.5% (21) . The domains of quality of life assessed were the subjective reporting of health, psychosocial functioning, and financial dependency. Quality-of-life measures in persons with lifetime panic disorder were compared with those of persons with lifetime major depression—a condition whose social morbidity is well documented (41 , 42) —and subjects with neither disorder (21 , 43) .
Among persons with panic disorder in the community, 35% felt they were in fair or poor physical health, and 38% felt they were in poor emotional health (21) . Individuals with major depression showed similar rates (29% and 39%, respectively), whereas those with neither disorder had significantly lower levels of negative perceptions of their physical and mental health (24% and 16%). A total of 27% of the persons with panic disorder were receiving welfare or some form of disability compensation, a significantly higher proportion than that found among persons with major depression (16%) and with neither disorder (12%).
Infrequent Panic Attacks and Quality of Life
Persons with panic attacks that did not meet the full DSM-III criteria for panic disorder because of insufficient frequency of attacks or symptoms (“infrequent” panic attacks: lifetime prevalence=3.6%) also showed substantial impairment in perceived physical and emotional health, occupational functioning, and financial independence. Klerman and colleagues (44) noted that on almost any measure, subjects with panic attacks were intermediate in severity between those who met the full criteria for panic disorder and those with no disorder. These findings were consistent with Gelder’s observation (45) that the difference between subjects with panic disorder and with panic attacks is more quantitative than qualitative. Since the lifetime prevalence of panic attacks in the general population is more than twice as high as that of panic disorder (7.3% and 3.5%, respectively, in the National Comorbidity Survey [46]), panic attacks are more likely to be associated with a higher population-attributable risk of decrements in social and vocational function than panic disorder itself (47) .
Studies in Clinical Samples
The most widely used instrument currently employed to measure quality of life is the Medical Outcomes Study 36-item Short-Form Health Survey (23) . It assesses two broad dimensions—mental health and physical health—each consisting of four specific domains (i.e., eight total): physical functioning, role limitations due to physical health problems, bodily pain, social functioning, general mental health (covering psychological distress and well-being), role limitations due to emotional problems, vitality, and general health perceptions. Norms are available for the general U.S. population as well as for several medical conditions (48) .
Sherbourne and colleagues (49) used the Short-Form Health Survey to compare the quality of life of patients with current panic disorder to that of patients with depression or chronic medical conditions such as hypertension, diabetes (type I or II), heart disease, arthritis, and chronic lung disease. In this study panic disorder emerged as associated with high psychological distress and limitations in role functioning but with relatively preserved physical functioning. In contrast, patients with depression showed limitations in all domains of functioning that were as great as or greater than the limitations associated with most chronic medical diseases.
The findings of Sherbourne and colleagues (49) are consistent with those of several other studies using the Short-Form Health Survey. Numerous investigators (47 , 50 – 54) clearly documented a decreased quality of life in patients with panic disorder compared to normal subjects. Four studies (47 , 50 , 51 , 54) found significant impairment in scores on the physical functioning subscales of the Short-Form Health Survey, as well as in scores on the mental health functioning subscales for patients with panic disorder. Schonfeld and colleagues (51) also found that major depression had a far greater impact on scores for subscales of the Short-Form Health Survey than any anxiety disorder, including panic disorder. These findings, like the epidemiologic findings cited previously, place the quality of life in patients with panic disorder as better than that of patients with major depression but still markedly lower than that of otherwise healthy individuals.
The publication of numerous validation studies, availability of general population norms, and ease of administration make the Short-Form Health Survey a very attractive option for the measurement of quality of life in persons with anxiety disorders. Nonetheless, it should be noted that making statistical comparisons by using the Short-Form Health Survey may not be straightforward (55) . Six of the eight scales of the Short-Form Health Survey have continuous variables, with scores ranging from 0 to 100. Scores on these measures in the general population, however, tend to be skewed to the left, with a majority of individuals showing a relatively high quality of life. The two remaining scales—role limitations due to physical health problems and role limitations due to emotional problems—are categorical. Thus, comparisons of scores on the Short-Form Health Survey in patient groups with population norms may be methodologically complicated, requiring the use of nonparametric tests or logarithmic or z transformations to obtain a more normal distribution. These procedures, however, have been seldom reported in the literature concerning anxiety disorders to date.
Impact of Treatment on Quality of Life in Patients With Panic Disorder
A growing number of clinical trials have incorporated quality-of-life assessment as an outcome measure in the treatment of panic disorder. The measurement of quality of life in clinical trials represents a special situation, imposing specific requirements on the instruments to be employed. For evaluative purposes it is essential to demonstrate that the instrument is capable of measuring the magnitude of the longitudinal changes on the dimension of interest in an individual or group exposed to a specific intervention. This property is called sensitivity to change, or responsiveness. For measures that are to be administered repeatedly, it is important that the instrument have very good reliability. Characteristics such as reliability and responsiveness may be difficult to reconcile in a single instrument, particularly in generic instruments intended to cover extensive domains. As shown in the descriptions of studies to follow, the Short-Form Health Survey seems to perform admirably in these respects. The sensitivity to change of the Sheehan Disability Scale (37) , Social Adjustment Scale (unpublished handbook by Weissman et al.), and Quality of Life Enjoyment and Satisfaction Questionnaire (34) have been demonstrated, which supports their use in clinical trials.
Another important characteristic of an instrument is its interpretability. For evaluative purposes, one should be able to interpret changes in the instrument’s scores in terms of their relevance (or lack thereof) for the health status of a patient. Although clinicians can easily interpret the implications of a change in the number of panic attacks per day or in the percentage of time spent worrying about having a panic attack, the meaning of a change in the score on a quality-of-life instrument may remain obscure unless some standard is provided. To our knowledge, only the Short-Form Health Survey provides standards for comparing clinical changes across several clinical conditions, as seen in the study by Jacobs et al. (56) , to be described. We will summarize results from studies of panic disorder outcomes according to the main quality-of-life measure(s) employed.
Outcome studies using the Short-Form Health Survey
Mavissakalian et al. (57) treated 110 patients with moderate-to-severe panic disorder, including agoraphobia, with a fixed regimen of imipramine, 2.25 mg/day per kg of body weight for 24 weeks. The Short-Form Health Survey was administered at pretreatment and at week 16. A total of 53% of the patients had a marked and stable response. Completers (N=59) and noncompleters (N=51) had equivalent scores on a baseline Short-Form Health Survey, except on the pain subscale, on which completers scored significantly lower than noncompleters. At week 16 the completers showed significant improvements on all subscales, particularly on role limitations (emotional), energy, social functioning, and mental health.
Jacobs et al. (56) examined the effects of clonazepam and placebo on scores for patients with panic disorder on the Short-Form Health Survey in a double-blind, controlled trial. Quality-of-life assessments were made at baseline and after 6 weeks of therapy (or at premature termination from the study). Between-group comparisons showed that clonazepam-treated patients (N=71) had a significant improvement in scores on the Short-Form Health Survey mental health component summary (which aggregates the scores of the four subscales measuring mental and emotional health) compared to placebo-treated subjects (N=68) after 6 weeks of treatment. Scores on the mental health component summary were found to be strongly related to clinical measures, with patients reporting marked improvement in avoidance and fear also showing the strongest mental health component summary score gains. The authors observed that the 8.9-point gain in scores on the mental health component summary observed in the clonazepam group was comparable to the 10.9-point improvement reported for recovered depressive individuals.
Outcome studies using the Quality of Life Enjoyment and Satisfaction Questionnaire
The Quality of Life Enjoyment and Satisfaction Questionnaire is a validated quality-of-life scale that rates eight aspects of quality of life, including physical health, subjective feelings, activities of daily living, and overall life satisfaction (34) .
Pohl et al. (58) and Pollack et al. (59) conducted a 10-week, randomized, double-blind study comparing the effects of sertraline and placebo in over 150 outpatients with a DSM-III-R diagnosis of panic disorder with or without agoraphobia. At the beginning and end of the double-blind phase the patients completed the Quality of Life Enjoyment and Satisfaction Questionnaire. In both studies, in addition to experiencing fewer panic attacks, sertraline-treated patients exhibited a statistically significant increase (change from baseline) in scores on the Quality of Life Enjoyment and Satisfaction Questionnaire for total and overall life satisfaction compared with placebo-treated patients.
Outcome studies using the Sheehan Disability Scale
The Sheehan Disability Scale is a three-item self-report that assesses impairment in work activities, social life and leisure activities, and family life and home responsibilities (38) .
Three studies have compared selective serotonin reuptake inhibitors (SSRIs) to placebo in randomized, controlled studies for the treatment of panic disorder. Hoehn-Saric et al. (60) compared fluvoxamine with placebo in 50 patients with panic disorder over 8 weeks and failed to find statistically significant group differences among scores on the Sheehan Disability Scale. The authors suggested that a longer follow-up period might be needed to detect improvements in social adjustment. Lecrubier et al. (61) compared the effects of placebo, paroxetine, and clomipramine in 367 patients with panic disorder. At week 9, patients treated with paroxetine (N=123) and clomipramine (N=121) showed significantly larger increases from baseline in scores on the three Sheehan Disability Scale items than placebo-treated subjects (N=123); there were no significant differences between scores for groups treated with paroxetine or clomipramine on any Sheehan Disability Scale items. Michelson et al. (62) compared groups receiving 10 mg/day or 20 mg/day of fluoxetine to a placebo group among 243 patients with a diagnosis of panic disorder. After 10 weeks of therapy, functional impairment, as measured by the Sheehan Disability Scale, was significantly more improved on items for family life (for groups receiving 10 or 20 mg/day of fluoxetine) and social life (for the group receiving 10 mg/day of fluoxetine) in the fluoxetine groups than in the placebo group. Reduction in the frequency of panic attacks was found to correlate poorly with ratings on the Sheehan Disability Scale and other secondary outcome measures, which suggests that the impairment associated with panic disorder may result primarily from other symptom domains, such as phobic avoidance and depression.
Outcome studies using the Social Adjustment Scale—Self-Report
The Social Adjustment Scale—Self-Report is a 42-item, self-report instrument measuring either instrumental or expressive role performance over the past 2 weeks in six major areas of functioning. It was originally designed as an outcome measurement to evaluate psychotherapy and drug treatment for depressed patients (35) .
To our knowledge, only one study has employed quality of life as an outcome measure for the treatment of patients with panic disorder with cognitive behavior therapy. Telch et al. (63) randomly assigned 156 outpatients meeting the DSM-III-R criteria for panic disorder with agoraphobia to group cognitive behavioral therapy or to a delayed-treatment control condition. An assessment battery including two measures relevant to the assessment of quality of life, the Social Adjustment Scale—Self-Report and the Sheehan Disability Scale, was administered at baseline (week 0), posttreatment (week 9), and 6-month follow-up. Consistent with results from previous studies, patients with panic disorder showed a significant impairment in quality of life at baseline. Treated subjects displayed significantly less impairment on the Social Adjustment Scale—Self-Report scale measuring work outside and inside the home, social and leisure activities, marital and extended family relationships, and overall functioning and on the Sheehan Disability Scale items measuring family and social functioning, work functioning, and global functioning. Anxiety and phobic avoidance were shown to be significantly associated with quality of life, whereas the frequency of panic attacks was not. The authors hypothesized that the infrequency and transient nature of panic attacks may lead to less impairment than the more chronic and pervasive symptoms of anxiety and agoraphobic avoidance. These conclusions are supported by the findings of other groups that employed the Sheehan Disability Scale to measure impairment in patients with panic disorder, such as Michelson et al. (62) , just mentioned, and Leon et al. (64) , who found that the frequency of panic attacks accounts for no more than 12% of the variance in impairment.
Quality of Life in Individuals With Social Phobia
Although social phobia is not a newly recognized disorder (65) , the magnitude of the problem was not fully appreciated until the late 1980s, leading to social phobia being termed a “neglected anxiety disorder” (66) . Even mental health specialists may have felt at first that this disorder, then just recently included in the DSM-III, represented an undue extension of the medical model into the domain of a naturally occurring phenomenon—shyness. Also, the first clinical studies comparing patients with social phobia and panic disorder reported that patients with social phobia tended to be men with higher educational, intellectual, social, and occupational status (67 – 69) , suggesting that social phobia was a relatively benign condition. It was not until the ECA findings were reported (70) that a different profile emerged, showing social phobia to be a common disorder associated with significant disability and impairment.
Studies in Epidemiologic Samples
Although the ECA study did not include direct measures of quality of life, many of the areas surveyed by the ECA are relevant to this issue. For example, the rate of financial dependency among subjects with uncomplicated social phobia (22.3%) was found to be significantly elevated compared with that of normal subjects (70) .
The National Comorbidity Survey (20) reinforced the perception of social phobia as a major source of disability and suffering. It found a much higher lifetime prevalence for social phobia (13.3%) than the ECA. It showed that social phobia is negatively related to education and income and is significantly elevated among never-married individuals, students, persons who are neither working nor studying, and those who live with their parents. Approximately half of the persons with social phobia reported at least one outcome indicative of severity at some time in their lives (either significant role impairment, professional help seeking, or use of medication more than once); social phobia was also associated with low social support (71) .
Subthreshold Social Phobia
Some studies suggest that the negative impact of social phobia on quality of life may be felt beyond the strict set of diagnostic criteria in DSM-III/DSM-III-R. Davidson and colleagues (72) examined the Duke University site’s ECA data to compare individuals with social phobia, subthreshold social phobia (i.e., phobic avoidance of public speaking and/or meeting strangers or eating in public not associated with significant functional interference), and nonphobic, healthy comparison subjects. Compared with nonphobic normal subjects, persons with noncomorbid subthreshold social phobia were more likely to be female and unmarried and to report less income and fewer years of education. Persons with uncomplicated subthreshold social phobia were also more likely to report poor grades and lack of a close friend—a measure of perceived social support. Davidson and colleagues (72) concluded that subthreshold social phobia, in terms of impairment, closely resembles social phobia diagnosed according to the DSM-III criteria, which is similar to Klerman and colleagues’ conclusions (44) with respect to infrequent panic attacks.
Some studies have investigated the possibility that the subtypes of social phobia may affect quality of life in different ways or degrees. Kessler and colleagues (73) used National Comorbidity Survey data to compare social phobia characterized by pure speaking fears and by other social fears. Overall, social phobia characterized by pure speaking fears was found to be less persistent, less impairing, and less highly comorbid than social phobia characterized by more generalized social fears. Thus, although even subthreshold social phobia may be associated with a reduced quality of life (72) , these findings suggest that the most pervasive functional impairment and reduced quality of life is seen in persons who suffer from generalized social phobia (74) .
Schneier and colleagues (40) examined the nature of impairment of functioning in 32 outpatients with social phobia by comparing their scores on two new rating scales—the Disability Profile and the Liebowitz Self-Rated Disability Scale—with those of 14 normal comparison subjects. The Disability Profile is a clinician-rated instrument with items assessing current (i.e., over the last 2 weeks) and most severe lifetime impairment due to emotional problems in eight domains. The Liebowitz Self-Rated Disability Scale is a patient-rated instrument with 11 items assessing current and most severe lifetime impairment due to emotional problems. More than half of all patients with social phobia reported at least moderate impairment at some time in their lives due to social anxiety and avoidance in areas of education, employment, family relationships, marriage or romantic relationships, friendships or social network, and other interests. A substantial minority reported at least moderate impairment in the areas of activities of daily living (such as shopping and personal care) and suicidal behavior or desire to live. On the Liebowitz scale, more than half of all patients reported at least moderate impairment in self-regulation of alcohol use at some time in their lives due to social phobia. Patients with social phobia were rated more impaired than normal comparison subjects on nearly all items on both measures. These findings on the Liebowitz Self-Rated Disability Scale must be considered preliminary, pending further validation of this instrument.
Wittchen and Beloch (75) measured quality of life and other indices of impairment in a group of 65 subjects with social phobia (with no significant comorbidity) and compared the results with those from a comparison group of individuals with herpes infection. The instruments employed included the Short-Form Health Survey and the Liebowitz Self-Rated Disability Scale. Compared to the matched comparison group, the group with social phobia had significantly lower scores (i.e., worse function) on most of the Short-Form Health Survey scales. Pronounced reductions in self-rated quality of life were found among the patients with social phobia in the domains of role limitation due to emotional problems, social functioning, general mental health, and vitality. Standardized summed scores for the mental health components of the Short-Form Health Survey showed that 23.1% of all subjects with social phobia were severely impaired and 24.6% were significantly impaired compared to only 4.5% of the comparison subjects. The Liebowitz Self-Rated Disability Scale showed that social phobia affected most areas of life but in particular education, career, and romantic relations.
Impact of Treatment on Quality of Life in Patients With Social Phobia
In a 12-week, double-blind, randomized, placebo-controlled trial, Stein et al. (76) had patients with social phobia (91.3% with the generalized subtype of the disorder) treated with fluvoxamine, an SSRI. At the study’s endpoint, patients taking fluvoxamine (N=34) showed a significantly greater improvement in scores on the work functioning and family life and home functioning items of the Sheehan Disability Scale compared to placebo-treated patients (N=34).
Safren and colleagues (77) studied quality of life in a group of treatment-seeking persons with social phobia who underwent cognitive behavioral therapy for anxiety disorders in a university clinic. Subjects with comorbidities were not excluded. The instrument employed to measure quality of life was the Quality of Life Inventory (78) , a 17-item scale that assesses a person’s satisfaction in a particular area of life that he or she deems important (such as health, relationships, and work). Patients with social phobia judged their overall quality of life as lower than that of a normative reference group. Quality of life was inversely associated with various measures of severity of social phobia (especially social interaction anxiety), functional impairment, and depression. Subjects with generalized social phobia had significantly lower scores on the Quality of Life Inventory than those with nongeneralized social phobia. Patients showed significant improvement in scores on the Quality of Life Inventory after completion of cognitive behavioral group therapy for social phobia. However, their posttreatment scores on the Quality of Life Inventory remained lower than those of the normative group.
These studies suggest that there may be merit to the continued inclusion of quality-of-life outcome measures in treatment studies of social phobia, although changes may turn out to be more subtle (and perhaps more difficult to measure) than those seen in panic disorder.
Quality of Life in Individuals With PTSD
Generations of military physicians described PTSD under a variety of rubrics: nostalgia (Civil War), shell shock (World War I), combat fatigue or combat exhaustion (World War II), or post-Vietnam syndrome (79 , 80) . When the diagnosis of PTSD was finally added to the official psychiatric nomenclature with the publication of the DSM-III in 1980, little was known about the role played by the disorder in civilian life. The misconception that PTSD could only result from either combat experiences or some unusually severe traumas in civilian life was incorporated into the DSM-III/DSM-III-R description of a stressor as being “outside the range of usual human experiences.” Recent appreciation of the role played by a wide range of traumas experienced in the community in the genesis of PTSD led to the suppression of this description in the DSM-IV, which in turn emphasizes the subjective experience of intense fear, helplessness, or horror resulting from a person’s exposure to real or threatened death or serious injury or to a threat to the physical integrity of self or others. This major conceptual change extended the scope of the PTSD construct well beyond its original limits. Readers must be aware that the cases defined according to the DSM-III/DSM-III-R criteria represent just part of the universe delineated by those criteria.
Epidemiologic studies (81 – 83) found a lifetime prevalence for PTSD of 7.8% to 9.2%, with the rate in women two times higher than that in men. Zatzick and colleagues (84) undertook an archival analysis of data from the National Vietnam Veterans Readjustment Study to measure the impact of PTSD on functioning and quality of life. Six domains were examined: bed days in the past 2 weeks, role functioning, subjective well-being, self-reported physical health status, current physical functioning, and perpetration of violent interpersonal acts in the past year. The study subjects consisted of a nationally representative sample of 1,200 male Vietnam veterans. Poorer outcomes were significantly more common in subjects with PTSD than in subjects without PTSD in all domains except bed days in the past 2 weeks. Even after adjusting for demographic characteristics as well as for comorbid psychiatric and other medical disorders, subjects with PTSD continued to have a significantly higher risk of diminished well-being, fair or poor physical health, current unemployment, and physical limitations than did veterans without PTSD.
Zatzick and colleagues (85) also investigated the impact of PTSD on the quality of life of female veterans. A total of 432 female veterans of the Vietnam theater, most of whom were nurses, were assessed as part of the National Vietnam Veterans Readjustment Study. Functional impairment and diminished quality of life were assessed by responses to questions covering six domains: bed days in the past 3 months, role functioning, subjective well-being, self-reported physical health status, current physical functioning, and perpetration of violent interpersonal acts in the past year. PTSD was found to be associated with significantly elevated odds of poorer functioning in all domains, except perpetration of violence in the past year. After adjustment for demographic characteristics and medical and psychiatric comorbidities, PTSD remained associated with a statistically significant elevation of the odds of poorer functioning in three domains: role functioning, self-reported physical health status, and bed days in the past 3 months. When these results were compared with their findings in male Vietnam veterans (84) , Zatzick and colleagues (85) found similar patterns of elevated odds across genders, suggesting that sex differences are minimal or absent in the extent to which PTSD is related to functional impairment.
Jordan and colleagues (86) interviewed Vietnam veterans and their spouses or co-resident partners as part of the National Vietnam Veterans Readjustment Study to assess family and marital adjustment, parenting problems, and the presence of violence. Veterans with PTSD were found to be much more likely to report marital, parental, and family adjustment problems than were veterans without PTSD. There was more violence in the families of veterans with PTSD than in the families of veterans without PTSD. The majority of the spouses and partners reported high levels of nonspecific distress, and the children of veterans with PTSD were more likely to have behavioral problems than were the children of veterans without PTSD. These data underscore that PTSD (and, by inference, other anxiety disorders, although this has been little studied) adversely affects the quality of life, not only of individuals with the disorder, but also of their families.
Stein and colleagues (87) studied the impact of full and “partial” PTSD (or subthreshold PTSD—i.e., having fewer than the required number of DSM-IV criterion C or criterion D symptoms) on the social functioning of a community sample. Persons with partial PTSD reported significantly more interference with work or education than did traumatized subjects without PTSD, but they reported significantly less interference than persons with the full disorder. Persons with full and partial PTSD reported comparable levels of interference with social and family functioning. The authors concluded that partial PTSD seems to carry a burden of disability that approaches, if not matches, that produced by full PTSD. These findings remain to be replicated by using more comprehensive and standardized measures of quality of life.
Studies in Clinical Samples and Impact of Treatment
There is presently a dearth of information about quality of life in patients with PTSD. But a study using the Short-Form Health Survey in 16 patients with PTSD who participated in a clinical trial suggests that quality of life is markedly compromised in this disorder (88) . Furthermore, pilot data from this 12-week, double-blind, placebo-controlled study of the SSRI fluoxetine suggest that significant improvement in health-related quality of life can be obtained with pharmacologic treatment (88) . These findings remain to be replicated in larger study groups and extended to other treatment modalities, but they are promising indeed.
Quality of Life in Individuals With OCD
Until 1980 obsessive-compulsive disorder was thought to be rare. The ECA study, however, found lifetime prevalences ranging from 1.94% to 3.29% (89) , although a more recent study places the current prevalence rate in a somewhat lower range (90) . Despite its well-known morbidity, few studies have attempted to measure the impact of OCD on quality of life.
Koran and colleagues (91) studied quality of life in 60 unmedicated patients with moderate-to-severe OCD using the Short-Form Health Survey and compared their scores with published norms for the general U.S. population and with patients with either depression or diabetes. Patients with OCD had higher median scores on all domains of physical health for quality of life (physical functioning, role limitation due to physical problems, and bodily pain) than patients with diabetes and depression and scored near the general population norm. In contrast, in all the domains of mental health (social functioning, role limitation due to emotional problems, and mental health), the OCD patients’ average scores were well below those of the general population. The diabetic patients’ median scores were similar to those of the depressed patients. The severity of OCD was negatively correlated with scores on social functioning (i.e., the more severe the disorder, the lower the scores). This single study, which remains to be replicated, portrayed OCD as a disorder with a marked negative impact on quality of life.
Quality of Life in Individuals With Generalized Anxiety Disorder
Probably none of the categories of anxiety disorder established in DSM-III has been more difficult to ratify than generalized anxiety disorder. After two waves of substantial revisions in the diagnostic criteria and almost 20 years of continuous research, the uncertainties concerning the nature, boundaries, and clinical implications of this nosologic entity remain as strong as ever. As Roy-Byrne and Katon (92) pointed out, “there continues to be considerable debate about whether generalized anxiety disorder is a freestanding primary disorder, a prodromal or residual phase of other disorders, a personality trait, or a comorbid condition that modifies the course, treatment response, and outcome of other diseases” (p. 34). There is increasing recognition that comorbidity is a fundamental feature in the nature and course of generalized anxiety disorder. Judd and colleagues (93) found that 80% of individuals with lifetime generalized anxiety disorder also had a comorbid mood disorder during their lifetime. This finding suggests that the ideal goal of studying “pure,” noncomorbid generalized anxiety disorder may be unattainable.
The ECA study used the DSM-III criteria for generalized anxiety disorder, which emphasize its status as a residual category, and found a reported lifetime prevalence of 4.1% to 6.6% (94) . A total of 58% to 65% of the subjects who had generalized anxiety disorder also had at least one other DSM-III disorder. Persons with generalized anxiety disorder were more often unmarried or divorced. A significantly higher proportion of persons with generalized anxiety disorder than without had received disability benefits during their lifetimes. Even when employed, individuals with generalized anxiety disorder showed indirect evidence of impairment: a significantly higher proportion of them had annual incomes of less than $10,000 (1980 dollars).
The National Comorbidity Survey (95) used the DSM-III-R criteria for generalized anxiety disorder; these emphasize the presence of excessive and/or unrealistic worry, somatic symptoms, and a duration of at least 6 months. The hierarchical exclusion rules of the DSM-III, which preclude the diagnosis of generalized anxiety disorder if a patient meets the criteria for any other mental disorder, were replaced by a less restrictive rule that required only that the diagnosis of generalized anxiety disorder could not be assigned if it occurred during the course of a mood or psychotic disorder. Generalized anxiety disorder was found to be a relatively rare current disorder (current prevalence of 1.6%) but a more frequent lifetime disorder, affecting 5.1% of the U.S. population aged 15–54 years. The vast majority of persons with generalized anxiety disorder also had at least one other disorder (current morbidity, 66.3%; lifetime morbidity, 90.4%). The most frequent comorbid disorders were affective disorder and panic disorder. “Pure” lifetime generalized anxiety disorder was found to be rare, with a lifetime prevalence of 0.5%. Wittchen and colleagues (95) found that comorbidity was associated with a significantly greater likelihood of interference with daily activities (51.2% in comorbid generalized anxiety disorder; 28.1% in “pure” generalized anxiety disorder) and made it more difficult to assess the role played by noncomorbid generalized anxiety disorder.
Massion and colleagues (96) examined the effects of generalized anxiety disorder and panic disorder on the quality of life of a group of patients from the Harvard/Brown Anxiety Disorders Research Program using questions derived from the National Comorbidity Survey. Both groups showed impairment in role functioning and social life as well as low overall life satisfaction. Generalized anxiety disorder was associated with a reduction in overall emotional health. However, the finding that the vast majority of the patients with generalized anxiety disorder had at least one other anxiety disorder led the authors to affirm that “generalized anxiety disorder virtually never occurs in isolation” and made it difficult to assess the role played by noncomorbid generalized anxiety disorder. In summary, these limited data suggest that, although relatively rare, noncomorbid generalized anxiety disorder can be found in a substantial minority of individuals and is associated with important impairment in its own right.
Comparing the Relative Decrements in Quality of Life Attributable to Different Anxiety Disorders
Most, if not all, of the studies reviewed previously involve comparisons between the decrements in quality of life associated with a specific anxiety disorder and with physical disorders or major depression. These studies, part of the first generation of investigations on the impact of anxiety disorders on quality of life, were mainly comparing this impact against well-known “gold standards” of impairment and incapacity such as depression or hypertension. Recently, some studies have shifted the focus of their investigations toward comparing the decrements in quality of life attributable to different anxiety disorders and can be considered the forerunners of a new generation of studies on quality of life in patients with anxiety disorders.
Kessler and Frank (97) used National Comorbidity Survey data to examine relationships between DSM-III-R psychiatric disorders and work impairment in the U.S. labor force. Individuals with anxiety disorders, when compared to persons without them, showed statistically significantly higher rates of work impairment. Among individuals with anxiety disorders, those with panic disorder had the highest number of days on which their productivity was reduced (mean=4.87 days per month, SD=1.56), whereas those with social phobia had the lowest (mean=1.11 days per month, SD=0.47). Data for persons with generalized anxiety disorder and PTSD fell in the intermediate range (mean=3.11 days per month, SD=1.33; mean=2.76 days per month, SD=1.00, respectively).
Schonfeld and colleagues (51) employed the Short-Form Health Survey to investigate the degree to which untreated anxiety disorders and major depressive disorder, occurring either singly or in combination, reduced functioning and well-being among 637 primary-care patients. Trained lay interviewers administered the NIMH Diagnostic Interview Schedule to this group and identified 319 patients meeting the diagnostic criteria for one or more of six anxiety disorders (generalized anxiety disorder, PTSD, simple phobia, social phobia, panic disorder or agoraphobia, and OCD) and major depression. Of this group, 137 (43%) had a single disorder, and 182 (57%) had multiple disorders. Regression models were used to estimate the relative effects of these disorders on quality of life by comparing patients with anxiety disorders to patients without anxiety. Simple phobia and OCD scores were omitted from the analysis because they almost never occurred as single disorders. The estimated effect of each single disorder on all subscales for physical, social, and emotional functioning was substantial. The effects due to major depression were the most negative of any disorder, with reductions in score of more than 20 points (on a 100-point scale) below the predicted scores for the reference group with no disorders on six of eight subscales. Among the anxiety disorders, PTSD had significant negative effects across all functioning scales and was estimated to have the second most negative burden on five of the eight subscales of the Short-Form Health Survey; the main score reductions were observed in the subscales for role limitations (emotional) (42 points), role limitations (physical health) (29.2 points), and vitality (23.1 points). For panic disorder or agoraphobia, the largest score reductions were in the subscales for role limitations (physical health) (29.7 points) and bodily pain (20.1 points). The effects of generalized anxiety disorder were mostly felt in the subscales for role limitations (emotional) (28.2 points) and role limitations (physical health) (21.1 points). The role limitations (emotional) subscale showed the largest score reduction for social phobia (22 points). These findings highlight the value of examining specific domains of functioning across the anxiety disorders, because they appear to vary considerably.
Olfson and colleagues (98 , 99) examined social and occupational disability associated with several DSM-IV mental disorders and groups of subthreshold psychiatric symptoms that did not meet the full criteria for a DSM-IV disorder (including depressive, generalized anxiety, panic, obsessive-compulsive, drug, and alcohol symptoms) in 1,001 adult primary-care outpatients in a large health maintenance organization. The assessment consisted of a structured diagnostic interview for DSM-IV given by telephone, the Sheehan Disability Scale, and three impairment items from the ECA study. After adjusting for the confounding effects of comorbid axis I disorders, other subthreshold symptoms, age, sex, race, marital status, and perceived physical health status, only subthreshold symptoms for depressive and panic disorder were found to be significantly correlated with impairment measures. Although depressive symptoms were significantly correlated with impairment in social, family, and work functioning, impairment associated with panic symptoms was restricted to loss of work and increased utilization of mental health services.
The construct of “illness intrusiveness” was described by Devins (28) as corresponding to “lifestyle disruptions, attributable to an illness and/or its treatment, that interfere with continued involvement in valued activities and interests” (p. 252). The Illness Intrusiveness Ratings Scale (29) is a multidimensional tool that examines 13 domains of functioning, each of which may be specifically affected by an illness or its treatment. Antony and colleagues (30) measured the extent to which anxiety disorders interfere with several domains of functioning by having individuals with panic disorder (N=35), social phobia (N=49), and OCD (N=51) complete the Illness Intrusiveness Ratings Scale. The three groups did not differ on total scores on the Illness Intrusiveness Ratings Scale, but significant differences in particular domains of functioning were observed. Patients with OCD reported more interference with respect to passive recreation (e.g., reading) than did patients with social phobia and more interference with respect to religious expression than did the two other groups. Patients with social phobia reported more impairment with respect to social relationships and self-expression or self-improvement than any other group. Average scores on the Illness Intrusiveness Ratings Scale for the three anxiety disorders were considerably higher than those found in other chronic illnesses. These findings are consistent with the well-known impairment of social life associated with social phobia and with the tendency of obsessions (many of them with religious content) to invade the consciousness and disrupt intentional activities.
Quality-of-Life Studies of Patients With Anxiety Disorders: Limitations and Prospects
Quality-of-life assessment has been instrumental in exposing the extent and seriousness of anxiety disorders. As summarized previously, both epidemiological and clinical studies clearly delineate the extensive reduction in quality of life associated with anxiety disorders and hint at possible differences between anxiety disorders. Significant degrees of impairment can also be found in individuals with subthreshold forms of anxiety disorders, particularly panic disorder. Preliminary evidence suggests that panic disorder and PTSD may exert a heavier toll on quality of life than other anxiety disorders. Effective pharmacological or psychotherapeutic treatments have been shown to improve the quality of life in patients with panic disorder and social phobia but have yet to be demonstrated for other anxiety disorders.
Several validated generic and specific instruments have been shown to adequately measure quality of life in patients with anxiety disorders, raising the issue of how to select the most adequate instrument for a given purpose. It has been suggested that future studies addressing quality of life should employ a combination of generic and specific instruments to maximize both sensitivity and generalizability (100) . The Short-Form Health Survey is the most extensively tested generic measure and would constitute the natural candidate for an all-purpose instrument. The choice of the accompanying specific instrument should be determined by the specific goals of the study. An alternative approach would be the modular system proposed by Aaronson et al. (18) : the Short-Form Health Survey would constitute the “generic core” to which one or several additional “specific” modules with 10–15 questions could be added. These modules would focus on domains of quality of life that are not captured by the Short-Form Health Survey but that are likely to be affected by the presence of anxiety disorders (such as sleep in PTSD) or by the treatment itself (such as the sexual function of patients medicated with SSRIs). A modular instrument, the Hepatitis Quality of Life Questionnaire (101) , has been recently validated for the assessment of quality of life in patients with chronic hepatitis C; similar measures could be developed for anxiety disorders.
Progress in the field of the assessment of quality of life in anxiety disorders has not been homogeneous. Certain areas of knowledge are in need of further scientific investigation. First, although some disorders such as panic disorder have been reasonably well studied, others such as PTSD have been largely neglected. Second, there are disagreements between epidemiological and clinical findings in some areas that need to be clarified. The causes of this disagreement are open to debate and will require further study (102) . Third, to our knowledge, only a handful of studies have attempted to compare the impact of different anxiety disorders on quality of life. Fourth, the original goal for which the concept of quality of life was first adopted in clinical research was to compare outcomes between different treatment modalities. However, we found only 11 studies—eight in panic disorder, two in social phobia, and a small pilot study on PTSD—that attempted to assess the impact of treatment on the quality of life in patients with anxiety disorders. This is surprising considering that unlike other areas of medical research, mental health has few physiological variables to employ as outcome measures and would likely benefit from an approach that has proved successful in oncology and cardiology. It is likely that therapies that are equivalent in terms of the reduction of symptoms may be qualitatively or quantitatively dissimilar with respect to effects on quality of life. Knowledge of these differences may lead to a more informed choice of treatment modality for a particular disorder and, perhaps, for individual patients. In this area, much additional research is needed.
Despite the growing number of studies undertaken during the past 15 years, the investigation of quality of life in individuals with anxiety disorders is still in its infancy. Nevertheless, the studies conducted to date almost uniformly portray a picture of anxiety disorders as illnesses that markedly compromise quality-of-life and psychosocial functioning in several functional domains. It is hoped that these findings will translate into a more accurate public (and health care policy) view of anxiety disorders as serious mental disorders worthy of further research and appropriate health care expenditures. Finally, outcome studies that incorporate quality-of-life indices will further inform us as to the efficacy of existing and new treatments to lessen the burden of illness attributable to these disorders.
Received June 18, 1999, revision received Nov. 5, 1999, accepted Dec. 10, 1999. From the Department of Psychiatry, University of California at San Diego. Address reprint requests to Dr. Stein, Department of Psychiatry, University of California at San Diego, 8950 Villa La Jolla Dr., Suite 2243, La Jolla, CA 92037; [email protected] (e-mail). Supported in part by NIMH grant MH-57835. The authors thank Leslie Wetherell for her review of the manuscript.
1. Regier DA, Boyd JH, Burke JD Jr, Rae DS, Myers JK, Kramer M, Robins LN, George LK, Karno M, Locke BZ: One-month prevalence of mental disorders in the United States: based on five Epidemiologic Catchment Area sites. Arch Gen Psychiatry 1988 ; 45:977–986 Crossref , Medline , Google Scholar
2. Pichot P: Nosological models in psychiatry. Br J Psychiatry 1994 ; 164:232–240 Crossref , Medline , Google Scholar
3. Klerman GL: Approaches to the phenomena of comorbidity, in Comorbidity of Mood and Anxiety Disorders. Edited by Maser JD, Cloninger CR. Washington, DC, American Psychiatric Press, 1990, pp 13–37 Google Scholar
4. Klein DF, Fink M: Psychiatric reaction patterns to imipramine. Am J Psychiatry 1962 ; 119:432–438 Link , Google Scholar
5. Feighner JP, Robins E, Guze SB, Woodruff RA Jr, Winokur G, Mu𮸠R: Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry 1972 ; 26:57–63 Crossref , Medline , Google Scholar
6. DuPont RL, Rice DP, Miller LS, Shiraki SS, Rowland CR, Harwood HJ: Economic costs of anxiety disorders. Anxiety 1996 ; 2:167–172 Crossref , Medline , Google Scholar
7. Spitzer WO, Dobson AJ, Hall J: Measuring the quality of life of cancer patients: a concise QL-index for use by physicians. J Chronic Dis 1981 ; 34:585–597 Crossref , Medline , Google Scholar
8. Croog SH, Levine S, Testa MA, Brown B, Bulpitt CJ, Jenkins CD, Klerman GL, Williams GH: The effects of antihypertensive therapy on the quality of life. N Engl J Med 1986; 314:1657– 1664 Google Scholar
9. Patrick DL, Erickson P: Health Status and Health Policy: Quality of Life in Health Care Evaluation and Resource Allocation. New York, Oxford University Press, 1993 Google Scholar
10. Dimenas ES, Dahlof CG, Jern SC, Wiklund IK: Defining quality of life in medicine. Scand J Prim Health Care Suppl 1990 ; 1:7–10 Medline , Google Scholar
11. Spilker B: Introduction, in Quality of Life and Pharmacoeconomics in Clinical Trials. Edited by Spilker B. Philadelphia, Lippincott-Raven, 1996, pp 1–10 Google Scholar
12. Gill TM, Feinstein AR: A critical appraisal of the quality of quality-of-life measurements. JAMA 1994 ; 272:619–626 Crossref , Medline , Google Scholar
13. Palmore E, Luikart C: Health and social factors related to life satisfaction. J Health Soc Behav 1972, 13:68–80 Google Scholar
14. Larson R: Thirty years of research on the subjective well-being of older Americans. J Gerontol 1978, 33:109–125 Google Scholar
15. Gerin P, Dazord A, Boissel J, Chifflet R: Quality of life assessment in therapeutic trials: rationale for and presentation of a more appropriate instrument. Fundam Clin Pharmacol 1992 ; 6:263–276 Crossref , Medline , Google Scholar
16. Ware JE Jr: Standards for validating health measures: definition and content. J Chronic Dis 1987 ; 40:473–480 Crossref , Medline , Google Scholar
17. Patrick DL, Erickson P: What constitutes quality of life? concepts and dimensions. Clin Nutr 1988, 7:53–63 Google Scholar
18. Aaronson NK, Bullinger M, Ahmedzai S: A modular approach to quality-of-life assessment in cancer clinical trials. Recent Results Cancer Res 1988 ; 111:231–249 Crossref , Medline , Google Scholar
19. Aaronson NK: Quality of life assessment in clinical trials: methodologic issues. Control Clin Trials 1989; 10(4 suppl):195S–208S Google Scholar
20. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994 ; 51:8–19 Crossref , Medline , Google Scholar
21. Markowitz JS, Weissman MM, Ouellette R, Lish JD, Klerman GL: Quality of life in panic disorder. Arch Gen Psychiatry 1989 ; 46:984–992 Crossref , Medline , Google Scholar
22. Guyatt GH, Eagle DJ, Sackett B, Willan A, Griffith L, McIlroy W, Patterson CJ, Turpie I: Measuring quality of life in the frail elderly. J Clin Epidemiol 1993; 46:1433– 1444 Google Scholar
23. Ware JE Jr, Sherbourne CD: The MOS 36-Item Short-Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care 1992 ; 30:473–483 Crossref , Medline , Google Scholar
24. McHorney CA, Ware JE Jr, Raczek AE: The MOS 36-Item Short-Form Health Survey (SF-36), II: psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 1993 ; 31:247–263 Crossref , Medline , Google Scholar
25. McHorney CA, Ware JE Jr, Lu JF, Sherbourne CD: The MOS 36-item Short-Form Health Survey (SF-36), III: tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care 1994 ; 32:40–66 Crossref , Medline , Google Scholar
26. Ware JE Jr, Kosinski M, Gandek B, Aaronson NK, Apolone G, Bech P, Brazier J, Bullinger M, Kaasa S, Leplège A, Prieto L, Sullivan M: The factor structure of the SF-36 Health Survey in 10 countries: results from the IQOLA Project. Med Care 1998; 51:1159– 1165 Google Scholar
27. Bullinger M, Alonso J, Apolone G, Lepl禥 A, Sullivan M, Wood-Dauphine S, Gandek B, Wagner A, Aaronson NK, Bech P, Fukuhara S, Kaasa S, Ware JE Jr: Translating health status questionnaires and evaluating their quality: the IQOLA Project approach. Med Care 1998 ; 51:913–923 Google Scholar
28. Devins GM: Illness intrusiveness and the psychosocial impact of lifestyle disruptions in chronic life-threatening disease. Adv Ren Replace Ther 1994 ; 1:251–263 Crossref , Medline , Google Scholar
29. Devins GM, Binik YM, Hutchinson TA, Hollomby DJ, Barre PE, Guttmann RD: The emotional impact of end-stage renal disease: importance of patients’ perception of intrusiveness and control. Int J Psychiatry Med 1983–1984; 13:327–343 Google Scholar
30. Antony MM, Roth D, Swinson RP, Huta V, Devins GM: Illness intrusiveness in individuals with panic disorder, obsessive-compulsive disorder, or social phobia. J Nerv Ment Dis 1998 ; 186:311–315 Crossref , Medline , Google Scholar
31. Devins GM, Mandin H, Hons RB, Burgess ED, Klassen J, Taub K, Schorr S, Letorneau PK, Buckle S: Illness intrusiveness and quality of life in end-stage renal disease: comparison and stability across treatment modalities. Health Psychol 1990, 9:117–142 Google Scholar
32. Devins GM, Berman L, Shapiro CM: Impact of sleep apnea and other sleep disorders on marital relationships and adjustment (abstract). Sleep Res 1993, 22:550 Google Scholar
33. Robb JC, Cooke RG, Devins GM, Trevor-Young L, Joffe RT: Quality of life and lifestyle in euthymic bipolar disorder. J Psychiatr Res 1997, 31:509–517 Google Scholar
34. Endicott J, Nee J, Harrison W, Blumenthal R: Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacol Bull 1993 ; 29:321–326 Medline , Google Scholar
35. Weissman MM, Prusoff BA, Thompson WD, Harding PS, Myers JK: Social adjustment by self-report in a community sample and in psychiatric outpatients. J Nerv Ment Dis 1978 ; 166:317–326 Crossref , Medline , Google Scholar
36. Weissman MM, Bothwell S: Assessment of social adjustment by patient self-report. Arch Gen Psychiatry 1976, 33:1111– 1115 Google Scholar
37. Leon AC, Shear MK, Portera L, Klerman GL: Assessing impairment in patients with panic disorder: the Sheehan Disability Scale. Soc Psychiatry Psychiatr Epidemiol 1992 ; 27:78–82 Crossref , Medline , Google Scholar
38. Sheehan DV: The Anxiety Disease. New York, Charles Scribner’s Sons, 1983 Google Scholar
39. Leon AC, Olfson M, Portera L, Farber L, Sheehan DV: Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int J Psychiatry Med 1997, 27:93–105 Google Scholar
40. Schneier FR, Heckelman LR, Garfinkel R, Campeas R, Fallon BA, Gitow A, Street L, Del Bene D, Liebowitz MR: Functional impairment in social phobia. J Clin Psychiatry 1994 ; 55:322–331 Medline , Google Scholar
41. Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, Berry S, Greenfield S, Ware J: The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 1989 ; 262:914–919 Crossref , Medline , Google Scholar
42. Johnson J, Weissman MM, Klerman GL: Service utilization and social morbidity associated with depressive symptoms in the community. JAMA 1992; 267:1478– 1483 Google Scholar
43. Weissman MM: Panic disorder: impact on quality of life. J Clin Psychiatry 1991; 52(Feb suppl):6–8 Google Scholar
44. Klerman GL, Weissman MM, Ouellette R, Johnson J, Greenwald S: Panic attacks in the community: social morbidity and health care utilization. JAMA 1991 ; 265:742–746 Crossref , Medline , Google Scholar
45. Gelder MG: Panic disorder: fact or fiction? Psychol Med 1989 ; 19:277–283 Google Scholar
46. Eaton WW, Kessler RC, Wittchen HU, Magee WJ: Panic and panic disorder in the United States. Am J Psychiatry 1994 ; 151:413–420 Link , Google Scholar
47. Katon W, Hollifield M, Chapman T, Mannuzza S, Ballenger J, Fyer A: Infrequent panic attacks: psychiatric comorbidity, personality characteristics and functional disability. J Psychiatr Res 1995 ; 29:121–131 Crossref , Medline , Google Scholar
48. McDowell I, Newell C: Measuring Health: A Guide for Rating Scales and Questionnaires, 2nd ed. New York, Oxford University Press, 1996 Google Scholar
49. Sherbourne CD, Wells KB, Judd LL: Functioning and well-being of patients with panic disorder. Am J Psychiatry 1996 ; 153:213–218 Link , Google Scholar
50. Hollifield M, Katon W, Skipper B, Chapman T, Ballenger JC, Mannuzza S, Fyer AJ: Panic disorder and quality of life: variables predictive of functional impairment. Am J Psychiatry 1997 ; 154:766–772 Link , Google Scholar
51. Schonfeld WH, Verboncoeur CJ, Fifer SK, Lipschutz RC, Lubeck DP, Buesching DP: The functioning and well-being of patients with unrecognized anxiety disorders and major depressive disorder. J Affect Disord 1997 ; 43:105–119 Crossref , Medline , Google Scholar
52. Fyer AJ, Katon W, Hollifield M, Rassnick H, Mannuzza S, Chapman T, Ballenger JC: The DSM-IV panic disorder field trial: panic attack frequency and functional disability. Anxiety 1996 ; 2:157–166 Crossref , Medline , Google Scholar
53. Ettigi P, Meyerhoff AS, Chirban JT, Jacobs RJ, Wilson RR: The quality of life and employment in panic disorder. J Nerv Ment Dis 1997 ; 185:368–372 Crossref , Medline , Google Scholar
54. Candilis PJ, McLean RY, Otto MW, Manfro GG, Worthington JJ III, Penava SJ, Marzol PC, Pollack MH: Quality of life in patients with panic disorder. J Nerv Ment Dis 1999 ; 187:429–434 Crossref , Medline , Google Scholar
55. Rose MS, Koshman ML, Spreng S, Sheldon R: Statistical issues encountered in the comparison of health-related quality of life in diseased patients to published general population norms: problems and solutions. J Clin Epidemiol 1999 ; 52:405–412 Crossref , Medline , Google Scholar
56. Jacobs RJ, Davidson JR, Gupta S, Meyerhoff AS: The effects of clonazepam on quality of life and work productivity in panic disorder. Am J Manag Care 1997; 3:1187– 1196 Google Scholar
57. Mavissakalian MR, Perel JM, Talbott-Green M, Sloan C: Gauging the effectiveness of extended imipramine treatment for panic disorder with agoraphobia. Biol Psychiatry 1998 ; 43:848–854 Crossref , Medline , Google Scholar
58. Pohl RB, Wolkow RM, Clary CM: Sertraline in the treatment of panic disorder: a double-blind multicenter trial. Am J Psychiatry 1998; 155:1189– 1195 Google Scholar
59. Pollack MH, Otto MW, Worthington JJ, Manfro GG, Wolkow R: Sertraline in the treatment of panic disorder: a flexible-dose multicenter trial. Arch Gen Psychiatry 1998; 55:1010– 1016 Google Scholar
60. Hoehn-Saric R, McLeod DR, Hipsley PA: Effect of fluvoxamine on panic disorder. J Clin Psychopharmacol 1993 ; 13:321–326 Crossref , Medline , Google Scholar
61. Lecrubier Y, Judge R: Long-term evaluation of paroxetine, clomipramine and placebo in panic disorder. Collaborative Paroxetine Panic Study Investigators. Acta Psychiatr Scand 1997 ; 95:153–160 Crossref , Medline , Google Scholar
62. Michelson D, Lydiard RB, Pollack MH, Tamura RN, Hoog SL, Tepner R, Demitrack MA, Tollefson GD (Fluoxetine Panic Disorder Study Group): Outcome assessment and clinical improvement in panic disorder: evidence from a randomized controlled trial of fluoxetine and placebo. Am J Psychiatry 1998; 155:1570– 1577 Google Scholar
63. Telch MJ, Schmidt NB, Jaimez TL, Jacquin KM, Harrington PJ: Impact of cognitive-behavioral treatment on quality of life in panic disorder patients. J Consult Clin Psychol 1995 ; 63:823–830 Crossref , Medline , Google Scholar
64. Leon AC, Shear MK, Portera L, Klerman GL: The relationship of symptomatology to impairment in patients with panic disorder. J Psychiatr Res 1993 ; 27:361–367 Crossref , Google Scholar
65. Pelissolo A, Lépine JP: Phobie sociale: perspectives historiques et conceptuèlles. Encéphale 1995 ; 21:15–24 Google Scholar
66. Liebowitz MR, Gorman JM, Fyer AJ, Klein DF: Social phobia: review of a neglected anxiety disorder. Arch Gen Psychiatry 1985 ; 42:729–736 Crossref , Medline , Google Scholar
67. Amies PL, Gelder MG, Shaw PM: Social phobia: a comparative clinical study. Br J Psychiatry 1983 ; 142:174–179 Crossref , Medline , Google Scholar
68. Persson G, Nordlund CL: Agoraphobics and social phobics: differences in background factors, syndrome profiles and therapeutic response. Acta Psychiatr Scand 1985 ; 71:148–159 Crossref , Medline , Google Scholar
69. Solyom L, Ledwidge B, Solyom C: Delineating social phobia. Br J Psychiatry 1986 ; 149:464–470 Crossref , Medline , Google Scholar
70. Schneier FR, Johnson J, Hornig CD, Liebowitz MR, Weissman MM: Social phobia: comorbidity and morbidity in an epidemiologic sample. Arch Gen Psychiatry 1992 ; 49:282–288 Crossref , Medline , Google Scholar
71. Magee WJ, Eaton WW, Wittchen HU, McGonagle KA, Kessler RC: Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch Gen Psychiatry 1996 ; 53:159–168 Crossref , Medline , Google Scholar
72. Davidson JR, Hughes DC, George LK, Blazer DG: The boundary of social phobia: exploring the threshold. Arch Gen Psychiatry 1994 ; 51:975–983 Crossref , Medline , Google Scholar
73. Kessler RC, Stein MB, Berglund P: Social phobia subtypes in the National Comorbidity Survey. Am J Psychiatry 1998 ; 155:613–619 Link , Google Scholar
74. Stein MB, Chavira DA: Subtypes of social phobia and comorbidity with depression and other anxiety disorders. J Affect Disord 1998; 50(suppl 1):S11–S16 Google Scholar
75. Wittchen HU, Beloch E: The impact of social phobia on quality of life. Int Clin Psychopharmacol 1996; 11(suppl 3):15–23 Google Scholar
76. Stein MB, Fyer AJ, Davidson JRT, Pollack MH, Wiita B: Fluvoxamine treatment of social phobia (social anxiety disorder): a double-blind, placebo-controlled study. Am J Psychiatry 1999 ; 156:756–760 Abstract , Google Scholar
77. Safren SA, Heimberg RG, Brown EJ, Holle C: Quality of life in social phobia. Depress Anxiety 1996–1997; 4:126–133 Google Scholar
78. Frisch MB, Cornell J, Villanueva M, Retzlaff PJ: Clinical validation of the Quality of Life Inventory: a measure of life satisfaction for use in treatment planning and outcome assessment. Psychol Assessment 1992 ; 4:92–101 Crossref , Google Scholar
79. Helzer JE, Robins LN, McEvoy L: Post-traumatic stress disorder in the general population: findings of the Epidemiologic Catchment Area survey. N Engl J Med 1987; 317:1630– 1634 Google Scholar
80. Jordan BK, Schlenger WE, Hough RL, Kulka RA, Weiss DS, Fairbank JA, Marmar CR: Lifetime and current prevalence of specific psychiatric disorders among Vietnam veterans and controls. Arch Gen Psychiatry 1991 ; 48:207–215 Crossref , Medline , Google Scholar
81. Breslau N, Davis GC, Andreski P, Peterson E: Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991 ; 48:216–222 Crossref , Medline , Google Scholar
82. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048– 1060 Google Scholar
83. Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P: Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry 1998 ; 55:626–632 Crossref , Medline , Google Scholar
84. Zatzick DF, Marmar CR, Weiss DS, Browner WS, Metzler TJ, Golding JM, Stewart A, Schlenger WE, Wells KB: Posttraumatic stress disorder and functioning and quality of life outcomes in a nationally representative sample of male Vietnam veterans. Am J Psychiatry 1997; 154:1690– 1695 Google Scholar
85. Zatzick DF, Weiss DS, Marmar CR, Metzler TJ, Wells KB, Golding JM, Stewart A, Schlenger WE, Browner WS: Posttraumatic stress disorder and functioning and quality of life outcomes in female Vietnam veterans. Mil Med 1997 ; 162:661–665 Crossref , Medline , Google Scholar
86. Jordan BK, Marmar CR, Fairbank JA, Schlenger WE, Kulka RA, Hough RL, Weiss DS: Problems with families of male Vietnam veterans with posttraumatic stress disorder. J Consult Clin Psychol 1992 ; 60:916–926 Crossref , Medline , Google Scholar
87. Stein MB, Walker JR, Hazen AL, Forde DR: Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry 1997; 154:1114– 1119 Google Scholar
88. Malik ML, Connor KM, Sutherland SM, Smith RD, Davison RM, Davidson JR: Quality of life and posttraumatic stress disorder: a pilot study assessing changes in SF-36 scores before and after treatment in a placebo-controlled trial of fluoxetine. J Trauma Stress 1999 ; 12:387–393 Crossref , Medline , Google Scholar
89. Rasmussen SA, Eisen JL: Epidemiology of obsessive-compulsive disorder. J Clin Psychiatry 1990; 51(suppl 2):10–13 Google Scholar
90. Stein MB, Forde DR, Anderson G, Walker JR: Obsessive-compulsive disorder in the community: an epidemiologic survey with clinical reappraisal. Am J Psychiatry 1997; 154:1120– 1126 Google Scholar
91. Koran LM, Thienemann ML, Davenport R: Quality of life for patients with obsessive-compulsive disorder. Am J Psychiatry 1996 ; 153:783–788 Link , Google Scholar
92. Roy-Byrne PP, Katon W: Generalized anxiety disorder in primary care: the precursor/modifier pathway to increased health care utilization. J Clin Psychiatry 1997; 58(suppl 3):34–38 Google Scholar
93. Judd LL, Kessler RC, Paulus MP, Zeller PV, Wittchen H-U, Kunovac JL: Comorbidity as a fundamental feature of generalized anxiety disorders: results from the National Comorbidity Study (NCS). Acta Psychiatr Scand Suppl 1998 ; 393:6–11 Crossref , Medline , Google Scholar
94. Blazer DG, Hughes D, George LK, Swartz M, Boyer R: Generalized anxiety disorder, in Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press; 1991, pp 180–203 Google Scholar
95. Wittchen H-U, Zhao S, Kessler RC, Eaton WW: DSM-III-R generalized anxiety disorder in the National Comorbidity Study. Arch Gen Psychiatry 1994 ; 51:355–364 Crossref , Medline , Google Scholar
96. Massion AO, Warshaw MG, Keller MB: Quality of life and psychiatric morbidity in panic disorder and generalized anxiety disorder. Am J Psychiatry 1993 ; 150:600–607 Link , Google Scholar
97. Kessler RC, Frank RG: The impact of psychiatric disorders on work loss days. Psychol Med 1997 ; 27:861–873 Crossref , Medline , Google Scholar
98. Olfson M, Broadhead WE, Weissman MM, Leon AC, Farber L, Hoven C, Kathol RG: Subthreshold psychiatric symptoms in a primary care group practice. Arch Gen Psychiatry 1996 ; 53:880–886 Crossref , Medline , Google Scholar
99. Olfson M, Fireman B, Weissman MM, Leon AC, Sheehan DV, Kathol RG, Hoven C, Farber L: Mental disorders and disability among patients in a primary care group practice. Am J Psychiatry 1997; 154:1734– 1740 Google Scholar
100. Eisen GM, Locke GR III, Provenzale D: Health-related quality of life: a primer for gastroenterologists. Am J Gastroenterol 1999; 94:2017– 2021 Google Scholar
101. Bayliss MS, Gandek B, Bungay KM, Sugano D, Hsu MA, Ware JE Jr: A questionnaire to assess the generic and disease-specific health outcomes of patients with chronic hepatitis C. Qual Life Res 1998 ; 7:39–55 Crossref , Medline , Google Scholar
102. Regier DA, Kaelber CT, Rae DS, Farmer ME, Knauper B, Kessler R, Norquist GS: Limitations of diagnostic criteria and assessment instruments for mental disorders: implications for research and policy. Arch Gen Psychiatry 1998 ; 55:109–115 Crossref , Medline , Google Scholar
- Brainwide Mendelian Randomization Study of Anxiety Disorders and Symptoms Biological Psychiatry, Vol. 95, No. 8
- Thirty-year trends of anxiety disorders among adolescents based on the 2019 Global Burden of Disease Study 3 April 2024 | General Psychiatry, Vol. 37, No. 2
- Unconditioned stimulus devaluation decreases the generalization of costly safety behaviors Journal of Anxiety Disorders, Vol. 103
- The Prevalence of Anxiety Among University Students in the United Arab Emirates Following the COVID-19 Lockdown Cureus, Vol. 24
- Anxiety and Quality of Life in College Students with a Chronic Illness Compared to Those Without: The Mediational Roles of Experiential Avoidance and Committed Action 15 March 2024 | International Journal of Mental Health and Addiction, Vol. 95
- Quality of Life in Posttraumatic Stress Disorder: The Role of Posttraumatic Anhedonia and Depressive Symptoms in a Treatment-Seeking Community Sample 20 March 2024 | Trauma Care, Vol. 4, No. 1
- Which clinical factors delay proper treatment in panic disorder? A cross‐sectional multicentric study 15 February 2024 | Early Intervention in Psychiatry, Vol. 1
- Comparison of subjective quality of life domains in schizophrenia, mood, and anxiety disorders; an individual patient data meta-analysis Psychiatry Research, Vol. 332
- Functional impairment in a Spanish Sample of Children and Adolescents with Obsessive–Compulsive Disorder 27 June 2022 | Child Psychiatry & Human Development, Vol. 55, No. 1
- MAUNA CHIKITSA IN COVID-19 INDUCED MANAS ROGA 14 January 2024 | International Ayurvedic Medical Journal, Vol. 12, No. 01
- Clinical and economic burden of anxiety/depression among older adult COPD patients: evidence from the COPD-AD China Registry study 8 January 2024 | Frontiers in Psychiatry, Vol. 14
- Small Steps over time: A longitudinal usability test of an automated interactive text messaging intervention to support self-management of depression and anxiety symptoms Journal of Affective Disorders, Vol. 345
- Grey matter structural alterations in anxiety disorders: a voxel-based meta-analysis 27 December 2023 | Brain Imaging and Behavior, Vol. 527
- Multi-Task Learning Using Facial Features for Mental Health Screening
- DeepScreen: Boosting Depression Screening Performance with an Auxiliary Task
- Ein moderiertes Mediationsmodell zur Erklärung der Beziehung zwischen Risikogruppenzugehörigkeit, Wahrnehmung der Bedrohung, Wissen und Einhaltung der COVID-19-Verhaltensmaßnahmen 3 December 2023
- Naturalistic examination of the anxiolytic effects of medical cannabis and associated gender and age differences in a Canadian cohort 9 June 2023 | Journal of Cannabis Research, Vol. 5, No. 1
- The prevalence of anxiety in adult endocrinology outpatients: A systematic review and meta–analysis Psychoneuroendocrinology, Vol. 158
- The occurrence and extent of anxiety and distress among Dutch travellers after encountering an animal associated injury 15 August 2023 | Tropical Diseases, Travel Medicine and Vaccines, Vol. 9, No. 1
- Psikiyatrik Hastalıklarda İntihar ve Acil Serviste İntihar Girişimine Müdahale: Güncel Bir Gözden Geçirme 1 November 2023 | Phoenix Medical Journal, Vol. 5, No. 3
- The effect of symptomatology and mental wellbeing on quality of life in people with acoustic neuroma Journal of Clinical Neuroscience, Vol. 116
- Multistrain probiotic rescinds quinpirole-induced obsessive-compulsive disorder phenotypes by reshaping of microbiota gut-brain axis in rats Pharmacology Biochemistry and Behavior, Vol. 47
- Characterizing the effects of self-compassion interventions on anxiety: Meta-analytic evidence from randomized controlled studies Journal of Contextual Behavioral Science, Vol. 30
- Stress can affect mitochondrial energy metabolism and AMPK/SIRT1 signaling pathway in rats Brain Research Bulletin, Vol. 203
- Psychiatric Issues in Women Veterans Psychiatric Clinics of North America, Vol. 46, No. 3
- The effect of internet-delivered cognitive behavioral therapy for depression and anxiety on quality of life: A meta-analysis of randomized controlled trials Internet Interventions, Vol. 33
- Expositionstherapie bei Panikstörung und Agoraphobie im Kontext bestehender antidepressiver Medikation 29 August 2023 | Der Nervenarzt, Vol. 94, No. 9
- Trauma Matters: Integrating Genetic and Environmental Components of PTSD 7 September 2022 | Advanced Genetics, Vol. 4, No. 3
- Mental health and quality of life during weight loss in females with clinically severe obesity: a randomized clinical trial 21 November 2022 | Journal of Behavioral Medicine, Vol. 46, No. 4
- Associations between anxiety disorders and depression symptoms are related to 24-hour movement behaviors among Brazilian adolescents Journal of Affective Disorders, Vol. 41
- Sex differences in the prevalence and factors associated with anxiety disorders in Canada: A population-based study Journal of Psychiatric Research, Vol. 63
- Worry, rumination and negative metacognitive beliefs as moderators of outcomes of transdiagnostic group cognitive-behavioural therapy in emotional disorders Journal of Affective Disorders, Vol. 420
- Transdiagnostic computations of uncertainty: towards a new lens on intolerance of uncertainty Neuroscience & Biobehavioral Reviews, Vol. 148
- Implementation of physical exercises in the health restoration program of adolescents aged 8-14 years old with bronchial asthma 30 March 2023 | Scientific Journal of National Pedagogical Dragomanov University. Series 15. Scientific and pedagogical problems of physical culture (physical culture and sports), No. 3(162)
- Contrasting Hygiene-Related Gastrointestinal Infections and Stress-Related Diseases at a Primary Health Care Facility within a Sub-Saharan African City: Before and during the COVID-19 Pandemic 22 December 2022 | Diseases, Vol. 11, No. 1
- Associations of neural error‐processing with symptoms and traits in a dimensional sample recruited across the obsessive–compulsive spectrum 28 August 2022 | Psychophysiology, Vol. 60, No. 2
- Baseline executive functioning moderates treatment‐related changes in quality of life in veterans with posttraumatic stress disorder and comorbid traumatic brain injury 6 October 2022 | Journal of Traumatic Stress, Vol. 36, No. 1
- Posttraumatic Stress Symptoms, Physical Illness, and Social Adjustment Among Disaster Victims 20 May 2022 | Disaster Medicine and Public Health Preparedness, Vol. 17
- Cognitive-behavioral therapy for anxiety disorders in Italian mental health services
- School-based cognitive behavioral interventions for youth with anxiety
- Anxiety Management in Developing Countries 29 April 2023
- Emotional maltreatment
- Yoga Plus Mantram Repetition to Reduce Chronic Pain in Veterans With Post-Traumatic Stress Disorder: A Feasibility Trial 26 December 2023 | Global Advances in Integrative Medicine and Health, Vol. 12
- Divergent presentation of anxiety in high-risk groups within the intellectual disability population 5 October 2022 | Journal of Neurodevelopmental Disorders, Vol. 14, No. 1
- A survey of depression and anxiety disorders in urban and rural Suriname 8 January 2022 | BMC Public Health, Vol. 22, No. 1
- Anxiety disorders in patients with noncardiac chest pain: association with health-related quality of life and chest pain severity 10 January 2022 | Health and Quality of Life Outcomes, Vol. 20, No. 1
- Anxiolytic effect of Anthemis nobilis L. (roman chamomile) and Citrus reticulata Blanco (tangerine) essential oils using the light-dark test in zebrafish (Danio rerio) Journal of Ethnopharmacology, Vol. 298
- Neurobehavioral phenotype of Kabuki syndrome: Anxiety is a common feature 6 October 2022 | Frontiers in Genetics, Vol. 13
- Association of childhood trauma, and resilience, with quality of life in patients seeking treatment at a psychiatry outpatient: A cross-sectional study from Nepal 4 October 2022 | PLOS ONE, Vol. 17, No. 10
- Frequency and Correlates of Fathers' Accommodation in Pediatric Anxiety Disorders 19 May 2021 | Child Psychiatry & Human Development, Vol. 53, No. 5
- The benefits of physical exercise on state anxiety: Exploring possible mechanisms Mental Health and Physical Activity, Vol. 23
- The bidirectional relationship between anxiety disorders and alcohol use disorders in adults: Findings from a longitudinal population-based study Journal of Affective Disorders, Vol. 314
- Continuous Neurophysiologic Data Accurately Predict Mood and Energy in the Elderly 14 September 2022 | Brain Sciences, Vol. 12, No. 9
- Climbing as an Add-On Treatment Option for Patients with Severe Anxiety Disorders and PTSD: Feasibility Analysis and First Results of a Randomized Controlled Longitudinal Clinical Pilot Trial 15 September 2022 | International Journal of Environmental Research and Public Health, Vol. 19, No. 18
- Threat belief determines the degree of costly safety behavior: Assessing rule-based generalization of safety behavior with a dimensional measure of avoidance Behaviour Research and Therapy, Vol. 156
- Internalized stigma in obsessive compulsive disorder: Correlates and associations with quality of life Archives of Psychiatric Nursing, Vol. 39
- Prospective relations between anxiety sensitivity and transdiagnostic anxiety following cognitive-behavioral therapy: Evidence from the Coordinated Anxiety Learning management trial Behaviour Research and Therapy, Vol. 155
- Prevalence and correlates of anxiety symptoms among Black people in Canada: A significant role for everyday racial discrimination and racial microaggressions Journal of Affective Disorders, Vol. 308
- The Effect of Behavioral Inhibition Temperament on Social Anxiety: The Double Mediation Effect of Rejection Sensitivity and Ambivalence over Emotional Expressiveness THE KOREAN JOURNAL OF DEVELOPMENTAL PSYCHOLOGY, Vol. 35, No. 2
- Meaning in life, psychological hardiness and death anxiety: individuals with or without generalized anxiety disorder (GAD) 8 January 2022 | Current Psychology, Vol. 41, No. 6
- The association of general practitioners’ awareness of depression and anxiety with change in quality of life in heart failure patients: results of the prospective observational RECODE-HF cohort study 25 October 2021 | Family Practice, Vol. 39, No. 3
- A Moderated Mediation Model Explaining the Relationship Between Risk-Group Membership, Threat Perception, Knowledge, and Adherence to COVID-19 Behavioral Measures 19 May 2022 | Frontiers in Public Health, Vol. 10
- Psychometric properties of the DSM‐5 social anxiety disorder dimensional scale in an Australian community sample 26 October 2021 | Journal of Clinical Psychology, Vol. 78, No. 5
- Life balance and traumatic txperiences in undergraduate students living near conflict zones 26 March 2020 | Current Psychology, Vol. 41, No. 4
- Health-Related Quality of Life and Psychological Distress in Patients With Hypermobility Type Ehlers-Danlos Syndrome 18 April 2022 | SAGE Open, Vol. 12, No. 2
- Exploring the relationship between the gut microbiome and mental health outcomes in a posttraumatic stress disorder cohort relative to trauma-exposed controls European Neuropsychopharmacology, Vol. 56
- Kub-E: An interactive design device for children with panic disorder International Journal of Child-Computer Interaction, Vol. 31
- A dimensional measure of safety behavior: A non-dichotomous assessment of costly avoidance in human fear conditioning 4 March 2021 | Psychological Research, Vol. 86, No. 1
- Avoiding a feared stimulus: Modelling costly avoidance of learnt fear in a sensory preconditioning paradigm Biological Psychology, Vol. 168
- Avoidance coping mediates the effect of hardiness on mental distress symptoms for both male and female subjects 22 October 2021 | Scandinavian Journal of Psychology, Vol. 63, No. 1
- Physical Activity Prevalence in Caregivers of Children With Different Ages and Its Association With Their Psychological and Physical Health Problems The Asian Journal of Kinesiology, Vol. 24, No. 1
- Video Game to Attenuate Pandemic-Related Stress From an Equity Lens: Development and Usability Study 12 May 2022 | JMIR Formative Research, Vol. 6, No. 5
- Effectiveness of a Web-Based Intervention to Prevent Anxiety in the Children of Parents With Anxiety: Protocol for a Randomized Controlled Trial 10 November 2022 | JMIR Research Protocols, Vol. 11, No. 11
- Recent Insights into the Association between Stress, Anxiety and Hypertension in Adults: A Systematic Review International Journal Of Pharmaceutical And Phytopharmacological Research, Vol. 12, No. 2
- Trends in the incidence and DALYs of anxiety disorders at the global, regional, and national levels: Estimates from the Global Burden of Disease Study 2019 Journal of Affective Disorders, Vol. 297
- Anxiolytic Effect of Anthemis Nobilis L. (Roman Chamomile) and Citrus Reticulata Blanco (Tangerine) Essential Oils Using the Light-Dark Test in Zebrafish (Danio Rerio) SSRN Electronic Journal
- The Role of Posttraumatic Cognitions in Integrated Treatments for Co-Occurring Posttraumatic Stress Disorder and Alcohol Use Disorder SSRN Electronic Journal
- Family Accommodation of Symptoms in Adults With Obsessive-Compulsive Disorder: Factor Structure and Usefulness of the Family Accommodation Scale for OCD–Patient Version 1 January 2022 | Journal of Psychiatric Practice, Vol. 28, No. 1
- COVID-19 Sürecinde Önleyici Davranışlar ile Yaşam Kalitesi Arasındaki İlişkinin İncelenmesi 25 December 2021 | Anemon Muş Alparslan Üniversitesi Sosyal Bilimler Dergisi, Vol. 9, No. 6
- Polygenic risk for obsessive-compulsive disorder (OCD) predicts brain response during working memory task in OCD, unaffected relatives, and healthy controls 23 September 2021 | Scientific Reports, Vol. 11, No. 1
- Cognitive behavioral therapy in 22q11.2 deletion syndrome: A case study of two young adults with an anxiety disorder 10 August 2020 | Journal of Intellectual Disabilities, Vol. 25, No. 4
- Utilisation and predictors of use of exposure therapy in the treatment of anxiety, OCD and PTSD in an Australian sample: a preliminary investigation 27 July 2021 | BMC Psychology, Vol. 9, No. 1
- Therapeutic processes in digital interventions for anxiety: A systematic review and meta-analytic structural equation modeling of randomized controlled trials Clinical Psychology Review, Vol. 90
- Quality of life and its association with psychiatric disorders in outpatients with trauma history in a tertiary hospital in Kathmandu, Nepal: a cross-sectional study 16 February 2021 | BMC Psychiatry, Vol. 21, No. 1
- Association between anxiety and hypertension in adults: A systematic review and meta-analysis Neuroscience & Biobehavioral Reviews, Vol. 131
- Acceptability, effectiveness and cost-effectiveness of blended cognitive-behavioural therapy (bCBT) versus face-to-face CBT (ftfCBT) for anxiety disorders in specialised mental health care: A 15-week randomised controlled trial with 1-year follow-up 12 November 2021 | PLOS ONE, Vol. 16, No. 11
- Correlates of Quality of Life in Anxiety Disorders: Review of Recent Research 6 October 2021 | Current Psychiatry Reports, Vol. 23, No. 11
- A case-control study on physical activity preferences, motives, and barriers in patients with psychiatric conditions Comprehensive Psychiatry, Vol. 111
- Anxiety Status and Coping Strategies in Association with Sociodemographic Factors, Dietary and Lifestyle Habits in Greece Clinical Practice & Epidemiology in Mental Health, Vol. 17, No. 1
- Psychosocial functioning in integrated treatment of co-occurring posttraumatic stress disorder and alcohol use disorder Journal of Psychiatric Research, Vol. 142
- Effects of music therapy on anxiety: A meta-analysis of randomized controlled trials Psychiatry Research, Vol. 304
- Effectiveness of Mindfulness-Based Cognitive Therapy for Positive Clinical Outcome in Panic Disorder: a 5-year Longitudinal Study 2 July 2021 | Mindfulness, Vol. 12, No. 9
- Development and psychometric properties of the Anticipatory Anxiety Inventory 1 September 2021 | Cognition, Brain, Behavior. An interdisciplinary journal, Vol. 25, No. 3
- An Examination of Correlates of Quality of Life in Children and Youth With Mental Health Issues 1 September 2021 | Frontiers in Psychiatry, Vol. 12
- The risk of depression and anxiety in patients with familial mediterranean fever – a cross-sectional study Journal of Affective Disorders, Vol. 292
- The 2019 Universiti Teknologi MARA, Malaysia Staff Survey: Determining the Level and Predictors of Quality of Life 9 August 2021 | Frontiers in Psychiatry, Vol. 12
- Impact of group transdiagnostic cognitive‐behavior therapy for anxiety disorders on comorbid diagnoses: Results from a pragmatic randomized clinical trial in primary care 18 June 2021 | Depression and Anxiety, Vol. 38, No. 7
- Does Self-Disclosure on Social Networking Sites Enhance Well-Being? The Role of Social Anxiety, Online Disinhibition, and Psychological Stress
- Randomized pilot trial of cognitive-behavioral therapy and acceptance-based behavioral therapy in the treatment of Spanish-speaking Latino primary care patients with generalized anxiety disorder Journal of Behavioral and Cognitive Therapy, Vol. 31, No. 2
- Experiential avoidance, committed action and quality of life: Differences between college students with and without chronic illness 12 July 2019 | Journal of Health Psychology, Vol. 26, No. 7
- Emotional processing in panic disorder and its subtypes: An fMRI study using emotional faces Journal of Affective Disorders, Vol. 287
- Review: Inflammation and anxiety‐based disorders in children and adolescents – a systematic review and meta‐analysis 16 November 2020 | Child and Adolescent Mental Health, Vol. 26, No. 2
- Anxiety in Late-Life Depression: Determinants of the Course of Anxiety and Complete Remission The American Journal of Geriatric Psychiatry, Vol. 29, No. 4
- COVID-19 Pandemic and Quality of Life among Romanian Athletes 12 April 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 8
- Duration of anxiety disorder and its associated risk indicators: Results of a longitudinal study of the general population 27 October 2020 | Depression and Anxiety, Vol. 38, No. 3
- Reducing Test Anxiety and Related Symptoms Using a Biofeedback Respiratory Practice Device: A Randomized Control Trial 2 January 2021 | Applied Psychophysiology and Biofeedback, Vol. 46, No. 1
- Off-task thinking among adults with and without social anxiety disorder: an ecological momentary assessment study 19 October 2020 | Cognition and Emotion, Vol. 35, No. 2
- EEG Correlates of Cognitive Functions and Neuropsychiatric Disorders: A Review of Oscillatory Activity and Neural Synchrony Abnormalities Current Psychiatry Research and Reviews, Vol. 16, No. 4
- Depression and the Quality of Life among Filipino Chemotherapy Patients 5 January 2021 | Jurnal Ners, Vol. 16, No. 1
- I’m Not Feeling It: Momentary Experiential Avoidance and Social Anxiety Among Individuals With Social Anxiety Disorder Behavior Therapy, Vol. 52, No. 1
- Individualized Homeopathic Medicines in the Treatment of Generalized Anxiety Disorder: A Double-Blind, Randomized, Placebo-Controlled, Pilot Trial 4 March 2021 | Complementary Medicine Research, Vol. 28, No. 5
- A study on depression, anxiety, stress, and life quality among medical aspirants and medical students of Aligarh City in North India Archives of Medicine and Health Sciences, Vol. 9, No. 1
- Mental Illness 28 March 2021
- The influence of depression-PTSD comorbidity on health-related quality of life in treatment-seeking veterans 4 June 2020 | European Journal of Psychotraumatology, Vol. 11, No. 1
- A randomized controlled trial of a six-session cognitive behavioral treatment of emotional disorders in adolescents 14–17 years old in child and adolescent mental health services (CAMHS) 14 March 2020 | BMC Psychology, Vol. 8, No. 1
- Emotion dysregulation as a maintenance factor for posttraumatic stress symptoms: The role of anxiety sensitivity 11 May 2020 | Journal of Clinical Psychology, Vol. 76, No. 12
- Role of PPARs in Progression of Anxiety: Literature Analysis and Signaling Pathways Reconstruction PPAR Research, Vol. 2020
- Moving Beyond the Negative 9 September 2020 | Journal of Nervous & Mental Disease, Vol. 208, No. 11
- The Use of Evidence-Based Assessment for Anxiety Disorders in an Australian Sample Journal of Anxiety Disorders, Vol. 75
- An integrative contextual behavioral model of intimate relations Journal of Contextual Behavioral Science, Vol. 18
- Anhedonia is Central for the Association between Quality of Life, Metacognition, Sleep, and Affective Symptoms in Generalized Anxiety Disorder: A Network Analysis Journal of Affective Disorders
- Evidence for inhibited temperament as a transdiagnostic factor across mood and psychotic disorders Journal of Affective Disorders, Vol. 274
- Adolescent Endorsement of the “Weak-Not-Sick” Stereotype for Generalised Anxiety Disorder: Associations with Prejudice, Discrimination, and Help-Giving Intentions toward Peers 28 July 2020 | International Journal of Environmental Research and Public Health, Vol. 17, No. 15
- Understanding the aetiology of fear of falling from the perspective of a fear-avoidance model – A narrative review Clinical Psychology Review, Vol. 79
- Costly avoidance triggered by categorical fear generalization Behaviour Research and Therapy, Vol. 129
- Quality of Life in Heterogeneous Anxiety Disorders: Changes Across Cognitive-Behavioral Treatments 7 December 2018 | Behavior Modification, Vol. 44, No. 3
- A mechanistic model for individualised treatment of anxiety disorders based on predictive neural biomarkers 24 March 2020 | Psychological Medicine, Vol. 50, No. 5
- Relative Cost Effectiveness of In‐Person and Internet Interventions for Relationship Distress 10 December 2018 | Family Process, Vol. 59, No. 1
- The Association between Physical Activity and Anxiety Symptoms for General Adult Populations: An Analysis of the Dose-Response Relationship Psychiatry Investigation, Vol. 17, No. 1
- Biobehavioral utility of mindfulness-based art therapy: Neurobiological underpinnings and mental health impacts 21 October 2019 | Experimental Biology and Medicine, Vol. 245, No. 2
- Efficacy and safety of acupuncture combined with western medicine for anxiety 31 July 2020 | Medicine, Vol. 99, No. 31
- Efficacy and cost-effectiveness of an unguided, internet-based self-help intervention for social anxiety disorder in university students: protocol of a randomized controlled trial 25 June 2019 | BMC Psychiatry, Vol. 19, No. 1
- Physical exercise augmented cognitive behaviour therapy for older adults with generalised anxiety disorder (PEXACOG): study protocol for a randomized controlled trial 18 March 2019 | Trials, Vol. 20, No. 1
- Quality of life in children and adolescents with obsessive-compulsive disorder: The Pediatric Quality of Life Enjoyment and Satisfaction Questionnaire (PQ-LES-Q) Bulletin of the Menninger Clinic, Vol. 83, No. 4
- Pro‐neurocognitive and anti‐sarcopenic benefits of one‐year metformin therapy in ovariectomized aged mice 30 August 2019 | Clinical and Experimental Pharmacology and Physiology, Vol. 46, No. 12
- A School-Based Comparison of Positive Search Training to Enhance Adaptive Attention Regulation with a Cognitive-Behavioural Intervention for Reducing Anxiety Symptoms in Children 10 May 2019 | Journal of Abnormal Child Psychology, Vol. 47, No. 11
- The role of the brain–gut–microbiota axis in psychology: The importance of considering gut microbiota in the development, perpetuation, and treatment of psychological disorders 30 September 2019 | Brain and Behavior, Vol. 9, No. 11
- Using self‐report to explore the relationship between anxiety and quality of life in children on the autism spectrum 17 June 2019 | Autism Research, Vol. 12, No. 10
- Generalized anxiety disorder: advances in neuroimaging studies 1 August 2019 | Brazilian Journal of Psychiatry, Vol. 41, No. 4
- An Online- and Mobile-Based Application to Facilitate Exposure for Childhood Anxiety Disorders Cognitive and Behavioral Practice, Vol. 26, No. 3
- Smartphone apps for the treatment of mental disorders: a systematic review. (Preprint) 3 June 2019 | JMIR mHealth and uHealth
- Anxiety moderates the influence of ASD severity on quality of life in adults with ASD Research in Autism Spectrum Disorders, Vol. 62
- Efficacy of an unguided internet‐based self‐help intervention for social anxiety disorder in university students: A randomized controlled trial 27 January 2019 | International Journal of Methods in Psychiatric Research, Vol. 28, No. 2
- The erring brain: Error‐related negativity as an endophenotype for OCD—A review and meta‐analysis 5 March 2019 | Psychophysiology, Vol. 56, No. 4
- Overthinkers, attention-seekers and wallflowers: peer perceptions of clinical anxiety disorders in adolescence Journal of Public Mental Health, Vol. 18, No. 1
- Do P.M. Tromp , Ph.D. ,
- Lisa E. Williams , Ph.D. ,
- Andrew S. Fox , Ph.D. ,
- Jonathan A. Oler , Ph.D. ,
- Patrick H. Roseboom , Ph.D. ,
- Gregory M. Rogers , Ph.D. ,
- Brenda E. Benson , Ph.D. ,
- Andrew L. Alexander , Ph.D. ,
- Daniel S. Pine , M.D. ,
- Ned H. Kalin , M.D.
- Cerebral resting state markers of biased perception in social anxiety 1 December 2018 | Brain Structure and Function, Vol. 224, No. 2
- The effects of Inquiry-Based Stress Reduction (IBSR) on mental health and well-being among a non-clinical sample Complementary Therapies in Clinical Practice, Vol. 34
- Quality of life following treatment for PTSD: Comparison of videoconferencing and in-person modalities 16 November 2017 | Journal of Telemedicine and Telecare, Vol. 25, No. 2
- Depression and Anxiety, Vol. 36, No. 3
- Stakeholder Perceptions of the Barriers to Receiving and Delivering Exposure-Based Cognitive Behavioral Therapy for Anxiety Disorders in Adult Community Mental Health Settings 5 March 2018 | Community Mental Health Journal, Vol. 55, No. 1
- Applied Research in Quality of Life, Vol. 14, No. 1
- Mindfulness, Vol. 10, No. 6
- Journal of Affective Disorders, Vol. 247
- Journal of Environmental Psychology, Vol. 65
- Psychiatry Research: Neuroimaging, Vol. 291
- Safety and Health at Work, Vol. 10, No. 1
- Residential Treatment for Children & Youth, Vol. 36, No. 3
- Frontiers in Psychology, Vol. 10
- Galanin ve Egzersizin Ratlarda Anksiyete Üzerine Etkisinin Açık Alan ve Yükseltilmiş Artı Labirent Testleri ile Değerlendirilmesi 11 December 2018 | Düzce Tıp Fakültesi Dergisi, Vol. 20, No. 3
- Öğrenme Güçlüğü Yaşayan Çocuklarda ve Ebeveynlerinde Yaşam Kalitesi 3 December 2018 | Ankara Üniversitesi Eğitim Bilimleri Fakültesi Özel Eğitim Dergisi
- Children’s Perceptions of Barriers to Session Attendance in School-Based Treatment for Anxiety 9 February 2018 | School Mental Health, Vol. 10, No. 4
- Somatic complaints in children and adolescents with social anxiety disorder 14 September 2018 | neuropsychiatrie, Vol. 32, No. 4
- Validation of the Mental Health Continuum‐Short Form and the dual continua model of well‐being and psychopathology in an adult mental health setting 5 July 2018 | Journal of Clinical Psychology, Vol. 74, No. 12
- An Initial Investigation of the Use of Comparative Referents to Assess Social Anxiety European Journal of Psychological Assessment, Vol. 34, No. 6
- Mental Disorder, Psychological Distress, and Functional Status in Canadian Military Personnel 28 February 2018 | The Canadian Journal of Psychiatry, Vol. 63, No. 9
- Preventing family transmission of anxiety: Feasibility RCT of a brief intervention for parents 25 March 2018 | British Journal of Clinical Psychology, Vol. 57, No. 3
- How to measure monetary losses in gambling disorder? An evidence-based refinement Psychiatry Research, Vol. 263
- Longitudinal Network Stability of the Functional Impairment of Anxiety and Depression 28 December 2017 | Clinical Psychological Science, Vol. 6, No. 3
- Effect of Comorbid Post-Traumatic Stress Disorder and Panic Disorder on Defensive Responding Journal of Psychophysiology, Vol. 32, No. 2
- Factors associated with health-related quality of life in stable ambulatory congestive heart failure patients: Systematic review 31 January 2018 | European Journal of Preventive Cardiology, Vol. 25, No. 5
- Children's anxiety symptoms and salivary immunoglobulin A: A mutual regulatory system? 24 November 2017 | Developmental Psychobiology, Vol. 60, No. 2
- International Urogynecology Journal, Vol. 29, No. 8
- Hernia, Vol. 22, No. 5
- Current Treatment Options in Psychiatry, Vol. 5, No. 1
- Comprehensive Psychiatry, Vol. 80
- Comprehensive Psychiatry, Vol. 87
- Journal of Affective Disorders, Vol. 230
- The American Journal of Geriatric Psychiatry, Vol. 26, No. 2
- Journal of Anxiety Disorders, Vol. 54
- Neural correlates of working memory deficits and associations to response inhibition in obsessive compulsive disorder NeuroImage: Clinical, Vol. 17
- Psychotherapy Research, Vol. 28, No. 6
- Journal of Clinical Child & Adolescent Psychology, Vol. 47, No. 6
- Post-treatment predictors of follow-up status for obsessive-compulsive disorder treated with concentrated exposure therapy 17 April 2018 | Cogent Psychology, Vol. 5, No. 1
- Journal of Diabetes Research, Vol. 2018
- PLOS ONE, Vol. 13, No. 12
- Sao Paulo Medical Journal, Vol. 136, No. 4
- Revista Brasileira de Educação Médica, Vol. 42, No. 4
- Iranian Journal of Psychiatry and Behavioral Sciences, Vol. 12, No. 2
- Poor quality of life and functioning in bipolar disorder 27 March 2017 | International Journal of Bipolar Disorders, Vol. 5, No. 1
- The Relation of Dysfunctional Cognitive Schemas and Personality Dimensions in Generalized Anxiety Disorder Acta Medica Marisiensis, Vol. 63, No. 4
- The development and validation of static and adaptive screeners to measure the severity of panic disorder, social anxiety disorder, and obsessive compulsive disorder 3 April 2017 | International Journal of Methods in Psychiatric Research, Vol. 26, No. 4
- The Microbiome in Posttraumatic Stress Disorder and Trauma-Exposed Controls: An Exploratory Study Psychosomatic Medicine, Vol. 79, No. 8
- Comorbid Social Phobia and Major Depressive Disorder: the Influence of Remission from Depression on Quality of Life and Functioning 3 August 2016 | Applied Research in Quality of Life, Vol. 12, No. 3
- Protective effect of atorvastatin on d-galactose-induced aging model in mice Behavioural Brain Research, Vol. 334
- Cognitive biases among early adolescents with elevated symptoms of anxiety, depression, and co‐occurring symptoms of anxiety‐depression 23 November 2016 | Infant and Child Development, Vol. 26, No. 5
- Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials Journal of Affective Disorders, Vol. 218
- Genome-wide expression and response to exposure-based psychological therapy for anxiety disorders 29 August 2017 | Translational Psychiatry, Vol. 7, No. 8
- Child Anxiety Prevention Study: Impact on Functional Outcomes 8 July 2016 | Child Psychiatry & Human Development, Vol. 48, No. 3
- Treating Social Anxiety Disorder with CBT: Impact on Emotion Regulation and Satisfaction with Life 5 March 2016 | Cognitive Therapy and Research, Vol. 41, No. 3
- Depression and hospital admission in older patients with head and neck cancer: analysis of a national healthcare database 31 August 2016 | Gerodontology, Vol. 34, No. 2
- Separate and combined effects of genetic variants and pre-treatment whole blood gene expression on response to exposure-based cognitive behavioural therapy for anxiety disorders 24 August 2016 | The World Journal of Biological Psychiatry, Vol. 18, No. 3
- The Age of Onset of Anxiety Disorders 24 March 2016 | The Canadian Journal of Psychiatry, Vol. 62, No. 4
- Debate: Are Benzodiazepines Appropriate Treatments for Patients with Substance Use Disorders? Yes Journal of Addiction Medicine, Vol. 11, No. 2
- Examining the Psychometric Properties of the Pediatric Quality of Life Enjoyment and Satisfaction Questionnaire in Two Samples of Youth with OCD 21 June 2016 | Child Psychiatry & Human Development, Vol. 48, No. 1
- Brain Imaging and Behavior, Vol. 11, No. 3
- Applied Nursing Research, Vol. 38
- Journal of Affective Disorders, Vol. 208
- Neuropsychologia, Vol. 96
- Psychiatry Research: Neuroimaging, Vol. 261
- Psychiatry Research, Vol. 249
- Psychological Medicine, Vol. 47, No. 1
- International Journal of Psychiatry in Clinical Practice, Vol. 21, No. 2
- Aging, Neuropsychology, and Cognition, Vol. 24, No. 5
- Expert Opinion on Pharmacotherapy, Vol. 18, No. 3
- Inflammatory Bowel Diseases, Vol. 23, No. 5
- BMC Psychiatry, Vol. 17, No. 1
- Health and Quality of Life Outcomes, Vol. 15, No. 1
- PLOS ONE, Vol. 12, No. 10
- International Journal of Cognitive Therapy, Vol. 10, No. 2
- Journal of Clinical Pediatric Dentistry, Vol. 41, No. 3
- Quality of Life and Functioning in Comorbid Posttraumatic Stress Disorder and Major Depressive Disorder After Treatment With Citalopram Monotherapy Clinical Neuropharmacology, Vol. 40, No. 1
- Sleep Disruption, Safety Learning, and Fear Extinction in Humans: Implications for Posttraumatic Stress Disorder 24 September 2017
- Provision of information leaflet before urodynamic study reduces the pre-examination anxiety level 21 July 2015 | Neurourology and Urodynamics, Vol. 35, No. 7
- Cross-generational influences on childhood anxiety disorders: pathways and mechanisms 4 May 2016 | Journal of Neural Transmission, Vol. 123, No. 9
- Anxiety and diabetes: Innovative approaches to management in primary care 24 July 2016 | Experimental Biology and Medicine, Vol. 241, No. 15
- Anxiety, Gambling Activity, and Neurocognition: A Dimensional Approach to a Non-Treatment-Seeking Sample Journal of Behavioral Addictions, Vol. 5, No. 2
- Treatment of anxiety and depression: medicinal plants in retrospect 4 March 2016 | Fundamental & Clinical Pharmacology, Vol. 30, No. 3
- The progress cascading model: A scalable model for teaching and mentoring graduate trainees in exposure therapy Journal of Obsessive-Compulsive and Related Disorders, Vol. 9
- Depression and Anxiety, Vol. 33, No. 3
- Depression and Anxiety, Vol. 33, No. 12
- Journal of Clinical Psychology in Medical Settings, Vol. 23, No. 3
- Current Treatment Options in Psychiatry, Vol. 3, No. 1
- Asian Journal of Psychiatry, Vol. 23
- Brain Research Bulletin, Vol. 120
- From social anxiety to interpersonal connectedness: Relationship building within face-to-face, phone and instant messaging mediums Computers in Human Behavior, Vol. 54
- Clinical Psychology Review, Vol. 45
- Journal of Anxiety Disorders, Vol. 38
- Psychological Medicine, Vol. 46, No. 5
- Psychological Medicine, Vol. 46, No. 15
- Behavioural and Cognitive Psychotherapy, Vol. 44, No. 2
- Military Behavioral Health, Vol. 4, No. 2
- Journal of Child and Adolescent Psychopharmacology, Vol. 26, No. 3
- Journal of Neurotrauma, Vol. 33, No. 22
- Clinical Psychology: Science and Practice, Vol. 23, No. 3
- BMC Psychiatry, Vol. 16, No. 1
- BMC Urology, Vol. 16, No. 1
- PLOS ONE, Vol. 11, No. 5
- Mindfulness- and Acceptance-Based Interventions in the Treatment of Anxiety Disorders
- Biological predictors of pharmacological therapy in anxiety disorders 1 April 2022 | Dialogues in Clinical Neuroscience, Vol. 17, No. 3
- Propriedades psicométricas da versão portuguesa do Inventário Geriátrico de Ansiedade numa amostra de idosos utentes de estruturas residenciais 30 September 2015 | Revista Portuguesa de Investigação Comportamental e Social, Vol. 1, No. 2
- Health-related quality of life in posttraumatic stress disorder: 4 years follow-up study of individuals exposed to urban violence Psychiatry Research, Vol. 228, No. 3
- Effectiveness of the implementation of guidelines for anxiety disorders in specialized mental health care 22 September 2014 | Acta Psychiatrica Scandinavica, Vol. 132, No. 1
- Elite identity and status anxiety: An interpretative phenomenological analysis of management consultants 16 December 2013 | Organization, Vol. 22, No. 3
- Augmentation of cognitive and behavioural therapies (CBT) with d-cycloserine for anxiety and related disorders 10 May 2015 | Cochrane Database of Systematic Reviews, Vol. 2015, No. 5
- Anxiety Disorders: Panic Disorder and Agoraphobia 20 February 2015
- Sleep Variability in Military‐Related PTSD: A Comparison to Primary Insomnia and Healthy Controls 28 January 2015 | Journal of Traumatic Stress, Vol. 28, No. 1
- Depression and Anxiety, Vol. 32, No. 7
- Social Psychiatry and Psychiatric Epidemiology, Vol. 50, No. 8
- Clinical Child and Family Psychology Review, Vol. 18, No. 3
- Current Hypertension Reports, Vol. 17, No. 8
- Comprehensive Psychiatry, Vol. 58
- EBioMedicine, Vol. 2, No. 10
- Internet Interventions, Vol. 2, No. 4
- Journal of Affective Disorders, Vol. 178
- Journal of Anxiety Disorders, Vol. 34
- Progress in Neurobiology, Vol. 129
- Panic disorder and health-related quality of life: The predictive roles of anxiety sensitivity and trait anxiety Psychiatry Research, Vol. 225, No. 1-2
- Preventive Medicine, Vol. 76
- Psychological Medicine, Vol. 45, No. 5
- International Psychogeriatrics, Vol. 27, No. 4
- Military Psychology, Vol. 27, No. 2
- Psychological Inquiry, Vol. 26, No. 4
- Journal of Women's Health, Vol. 24, No. 11
- Journal of Social and Clinical Psychology, Vol. 34, No. 7
- Jornal Brasileiro de Psiquiatria, Vol. 64, No. 1
- Trends in Psychiatry and Psychotherapy, Vol. 37, No. 4
- JMIR Research Protocols, Vol. 4, No. 4
- Frontiers in Endocrinology, Vol. 5
- International Journal of Environmental Research and Public Health, Vol. 12, No. 9
- The prevalence and burden of subthreshold generalized anxiety disorder: a systematic review 1 May 2014 | BMC Psychiatry, Vol. 14, No. 1
- Predictive accuracy of Edinburgh Postnatal Depression Scale assessment during pregnancy for the risk of developing postpartum depressive symptoms: a prospective cohort study 7 April 2014 | BJOG: An International Journal of Obstetrics & Gynaecology, Vol. 121, No. 13
- Quality of Life Research, Vol. 23, No. 4
- Applied Research in Quality of Life, Vol. 9, No. 4
- The Psychological Record, Vol. 64, No. 4
- Behaviour Research and Therapy, Vol. 59
- Behaviour Research and Therapy, Vol. 62
- Comprehensive Psychiatry, Vol. 55, No. 1
- Comprehensive Psychiatry, Vol. 55, No. 2
- Comprehensive Psychiatry, Vol. 55, No. 3
- Comprehensive Psychiatry, Vol. 55, No. 5
- Drug and Alcohol Dependence, Vol. 145
- Journal of Affective Disorders, Vol. 166
- Journal of Anxiety Disorders, Vol. 28, No. 2
- Journal of Contextual Behavioral Science, Vol. 3, No. 2
- Research in Developmental Disabilities, Vol. 35, No. 1
- Psychological Medicine, Vol. 44, No. 3
- Psychological Medicine, Vol. 44, No. 11
- Journal of Motor Behavior, Vol. 46, No. 4
- Self and Identity, Vol. 13, No. 1
- The Effect of a Combined Versus a Conventional Cognitive-Behavioral Therapy on Quality of Life for Comorbid Panic Disorder With Agoraphobia and Generalized Anxiety Disorder 24 September 2013 | Behavior Modification, Vol. 38, No. 1
- BMC Public Health, Vol. 14, No. 1
- Health and Quality of Life Outcomes, Vol. 12, No. 1
- PLoS ONE, Vol. 9, No. 3
- PLoS ONE, Vol. 9, No. 7
- PLoS ONE, Vol. 9, No. 6
- Korea Journal of Counseling, Vol. 15, No. 4
- Korean Journal of Health Psychology, Vol. 19, No. 4
- Journal of Medical Internet Research, Vol. 16, No. 9
- Ethical Issues and Ethical Therapy Associated with Anxiety Disorders 24 August 2014
- Prediction of childhood ADHD symptoms to quality of life in young adults: Adult ADHD and anxiety/depression as mediators Research in Developmental Disabilities, Vol. 34, No. 10
- Endophänotypen der Zwangsstörung Zeitschrift für Psychiatrie, Psychologie und Psychotherapie, Vol. 61, No. 3
- Psychological Stress and Unruptured Intracranial Aneurysms Neurosurgery, Vol. 73, No. 1
- The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta‐analysis of direct comparisons 4 June 2013 | World Psychiatry, Vol. 12, No. 2
- Impact of panic disorder on quality of life among veterans in a primary care pilot study Comprehensive Psychiatry, Vol. 54, No. 3
- A Pilot Study Examining the Effects of Kouk Sun Do on University Students with Anxiety Symptoms 4 June 2012 | Stress and Health, Vol. 29, No. 2
- The Timing of Exposure in Clinic-Based Treatment for Childhood Anxiety Disorders 2 April 2013 | Behavior Modification, Vol. 37, No. 2
- Depression and Anxiety
- Journal of Neural Transmission, Vol. 120, No. 1
- Journal of Immigrant and Minority Health, Vol. 15, No. 5
- The Journal of Primary Prevention, Vol. 34, No. 6
- Quality of Life Research, Vol. 22, No. 6
- CNS Drugs, Vol. 27, No. 5
- Behavior Therapy, Vol. 44, No. 2
- Journal of Affective Disorders, Vol. 147, No. 1-3
- Journal of Affective Disorders, Vol. 150, No. 3
- Journal of Affective Disorders, Vol. 151, No. 1
- Psychiatry Research, Vol. 206, No. 1
- Psychosomatics, Vol. 54, No. 5
- Psychological Medicine, Vol. 43, No. 7
- The Spanish Journal of Psychology, Vol. 16
- Cognitive Behaviour Therapy, Vol. 42, No. 4
- European Addiction Research, Vol. 19, No. 4
- The Timing of Exposure in Clinic-Based Treatment for Childhood Anxiety Disorders 25 September 2012 | Behavior Modification, Vol. 37, No. 1
- Health and Quality of Life Outcomes, Vol. 11, No. 1
- PLoS ONE, Vol. 8, No. 5
- International Journal of Cognitive Therapy, Vol. 6, No. 1
- World Journal of Psychiatry, Vol. 3, No. 2
- Assessing PTSD-related Functional Impairment and Quality of Life 21 November 2012
- Paula P. Schnurr , Ph.D. , and
- Carole A. Lunney , M.A.
- Anxiety Disorders and Latinos 13 September 2012 | Hispanic Journal of Behavioral Sciences, Vol. 34, No. 4
- Depression and Dysthymic Disorders 25 June 2012
- Social Psychiatry and Psychiatric Epidemiology, Vol. 47, No. 5
- Quality of Life Research, Vol. 21, No. 10
- Asian Journal of Psychiatry, Vol. 5, No. 4
- Gaceta Sanitaria, Vol. 26, No. 1
- Journal of Anxiety Disorders, Vol. 26, No. 1
- Journal of Anxiety Disorders, Vol. 26, No. 3
- Journal of Anxiety Disorders, Vol. 26, No. 7
- Neuroscience & Biobehavioral Reviews, Vol. 36, No. 9
- NeuroImage, Vol. 59, No. 2
- Personality and Individual Differences, Vol. 52, No. 3
- Psychological Medicine, Vol. 42, No. 9
- Journal of Technology in Human Services, Vol. 30, No. 1
- The Journal of Alternative and Complementary Medicine, Vol. 18, No. 6
- BMC Psychiatry, Vol. 12, No. 1
- BMC Medicine, Vol. 10, No. 1
- International Journal of Mental Health Systems, Vol. 6, No. 1
- International Journal of Neuroscience, Vol. 122, No. 4
- Respiratory rehabilitation: a physiotherapy approach to the control of asthma symptoms and anxiety Clinics, Vol. 67, No. 11
- Quality of Life Well-Being in General Medicine, Mental Health and Coaching 2 November 2011
- The Impact of Bulimic Syndromes, Mood and Anxiety Disorders and Their Comorbidity on Psychosocial Impairment: What Drives Impairment in Comorbidity? 13 July 2011 | European Eating Disorders Review, Vol. 20, No. 1
- Anxiety, Health Risk Factors, and Chronic Disease 20 January 2011 | American Journal of Lifestyle Medicine, Vol. 5, No. 6
- Prevention of depressive disorders: towards a further reduction of the disease burden of mental disorders 26 July 2011 | Early Intervention in Psychiatry, Vol. 5, No. 3
- Do measures used in studies of anxiety disorders reflect activities and participation as defined in the WHO International Classification of Functioning, Disability and Health? 22 March 2011 | Clinical Rehabilitation, Vol. 25, No. 7
- The protective effects of resilience and hope on quality of life of the families coping with the criminal traumatisation of one of its members 5 May 2011 | Journal of Clinical Nursing, Vol. 20, No. 13-14
- The psychometric properties of the panic disorder module of the Patient Health Questionnaire (PHQ-PD) in high-risk groups in primary care Journal of Affective Disorders, Vol. 130, No. 1-2
- Psychometrics of a brief measure of anxiety to detect severity and impairment: The overall anxiety severity and impairment scale (OASIS) Journal of Psychiatric Research, Vol. 45, No. 2
- Depression and Anxiety, Vol. 28, No. 5
- 9 Cognitieve therapie ter preventie van terugval bij depressie en angststoornissen
- Der Nervenarzt, Vol. 82, No. 3
- Journal of Psychopathology and Behavioral Assessment, Vol. 33, No. 1
- Asian Journal of Psychiatry, Vol. 4, No. 3
- Behaviour Research and Therapy, Vol. 49, No. 3
- Injury, Vol. 42, No. 3
- Journal of Anxiety Disorders, Vol. 25, No. 3
- Women's Health Issues, Vol. 21, No. 4
- Family Practice, Vol. 28, No. 5
- The American Journal on Addictions, Vol. 20, No. 4
- American Journal of Orthopsychiatry, Vol. 81, No. 2
- BMC Psychiatry, Vol. 11, No. 1
- Yonsei Medical Journal, Vol. 52, No. 3
- Pharmacological Treatment for Phobias and Anxiety Disorders 8 February 2011
- Prevention of Mental Disorders in Late Life 2 December 2010
- Interpersonal Processes in the Anxiety Disorders 16 March 2012
- The Netherlands Mental Health Survey and Incidence Study‐2 (NEMESIS‐2): design and methods 16 July 2010 | International Journal of Methods in Psychiatric Research, Vol. 19, No. 3
- Evolving concepts of anxiety
- Identifying target groups for the prevention of anxiety disorders in the general population 1 June 2010 | Acta Psychiatrica Scandinavica, Vol. 122, No. 1
- Nina A. Sayer, Ph.D.
- Siamak Noorbaloochi, Ph.D.
- Patricia Frazier, Ph.D.
- Kathleen Carlson, Ph.D.
- Amy Gravely, M.A.
- Maureen Murdoch, M.D., M.P.H.
- Through the Lens of Therapeutic Jurisprudence 8 May 2009 | Journal of Interpersonal Violence, Vol. 25, No. 3
- Zebrafish antipredatory responses: A future for translational research? Behavioural Brain Research, Vol. 207, No. 2
- Social Indicators Research, Vol. 97, No. 2
- Psychological Injury and Law, Vol. 3, No. 3
- Social Anxiety in Children and Adolescents
- Changes in quality of life following cognitive-behavioral group therapy for panic disorder 16 April 2020 | European Psychiatry, Vol. 25, No. 1
- NeuroImage, Vol. 53, No. 3
- Behavioural and Cognitive Psychotherapy, Vol. 38, No. 4
- Cyberpsychology, Behavior, and Social Networking, Vol. 13, No. 4
- Revista Brasileira de Psiquiatria, Vol. 33, No. 1
- Rasch model analysis of the Depression, Anxiety and Stress Scales (DASS) 9 May 2009 | BMC Psychiatry, Vol. 9, No. 1
- Impaired spatial navigation in pediatric anxiety 17 September 2009 | Journal of Child Psychology and Psychiatry, Vol. 50, No. 10
- Health-Related Quality of Life in College Undergraduates with Learning Disabilities: The Mediational Roles of Anxiety and Sadness 24 October 2008 | Journal of Psychopathology and Behavioral Assessment, Vol. 31, No. 3
- Translating Effective Web-Based Self-Help for Problem Drinking Into the Real World Alcoholism: Clinical and Experimental Research, Vol. 33, No. 8
- Quality of Life in Treatment-Seeking Patients with Obsessive-Compulsive Disorder with and without Major Depressive Disorder 1 July 2009 | The Canadian Journal of Psychiatry, Vol. 54, No. 7
- Co-occurrence of Insomnia and Anxiety Disorders: A Review of the Literature 20 April 2009 | American Journal of Lifestyle Medicine, Vol. 3, No. 4
- Brook A. Marcks, Ph.D.
- Risa B. Weisberg, Ph.D.
- Martin B. Keller, M.D.
- Impact of Sleep Disturbances on PTSD Symptoms and Perceived Health Journal of Nervous & Mental Disease, Vol. 197, No. 2
- Depression and Anxiety, Vol. 26, No. 9
- Depression and Anxiety, Vol. 26, No. 12
- Indian Journal of Hematology and Blood Transfusion, Vol. 25, No. 2
- Revista Médica de Homeopatía, Vol. 2, No. 3
- Behavior Therapy, Vol. 40, No. 1
- Computers in Human Behavior, Vol. 25, No. 2
- Clinical Psychology Review, Vol. 29, No. 8
- Journal of Affective Disorders, Vol. 112, No. 1-3
- Journal of Anxiety Disorders, Vol. 23, No. 4
- Journal of Anxiety Disorders, Vol. 23, No. 8
- Journal of Substance Abuse Treatment, Vol. 37, No. 4
- Medical Hypotheses, Vol. 73, No. 1
- CNS Spectrums, Vol. 14, No. 12
- Epidemiologia e Psichiatria Sociale, Vol. 18, No. 3
- Epidemiologia e Psichiatria Sociale, Vol. 18, No. 1
- Cognitive Behaviour Therapy, Vol. 38, No. 2
- CNS Drugs, Vol. 23, No. 6
- Anthroposophic Therapy for Anxiety Disorders: A Two-year Prospective Cohort Study in Routine Outpatient Settings 10 June 2009 | Clinical Medicine Insights: Psychiatry, Vol. 2
- Establishing an innovative model of nutrition and dietetic care for a mental health service through collaboration with non‐nutrition healthcare workers 4 November 2008 | Nutrition & Dietetics, Vol. 65, No. 4
- Costs and Cost-Effectiveness of Family CBT Versus Individual CBT in Clinically Anxious Children 1 October 2008 | Clinical Child Psychology and Psychiatry, Vol. 13, No. 4
- Subjective Quality of Life in Psychiatric Patients: Diagnosis and Illness-Specific Profiles 1 September 2008 | The Canadian Journal of Psychiatry, Vol. 53, No. 9
- Posttraumatic Stress Disorder and Health-Related Quality of Life among a Sample of Treatment- and Pension-Seeking Deployed Canadian Forces Peacekeeping Veterans 1 September 2008 | The Canadian Journal of Psychiatry, Vol. 53, No. 9
- The relationship between functional outcomes and the treatment of anxious and painful somatic symptoms in patients with generalized anxiety disorder 23 July 2008 | Current Medical Research and Opinion, Vol. 24, No. 9
- The Netherlands Study of Depression and Anxiety (NESDA): rationale, objectives and methods 3 September 2008 | International Journal of Methods in Psychiatric Research, Vol. 17, No. 3
- Suicidal status during antidepressant treatment in 789 Sardinian patients with major affective disorder 10 July 2008 | Acta Psychiatrica Scandinavica, Vol. 118, No. 2
- Anxiety vulnerability is associated with altered anterior cingulate response to an affective appraisal task NeuroReport, Vol. 19, No. 10
- ‘Laff Yer Heid Aff’: The role of comedy inincreasing public awareness of common mental health problems 1 July 2008 | Clinical Psychology Forum, Vol. 1, No. 187
- Web‐based self‐help for problem drinkers: a pragmatic randomized trial 11 January 2008 | Addiction, Vol. 103, No. 2
- Depression and Anxiety, Vol. 25, No. 3
- Depression and Anxiety, Vol. 25, No. 7
- Social Psychiatry and Psychiatric Epidemiology, Vol. 43, No. 4
- Behavior Genetics, Vol. 38, No. 1
- Journal of Anxiety Disorders, Vol. 22, No. 2
- Journal of Anxiety Disorders, Vol. 22, No. 3
- Journal of Anxiety Disorders, Vol. 22, No. 4
- Journal of Anxiety Disorders, Vol. 22, No. 8
- Neuroscience Letters, Vol. 430, No. 2
- CNS Spectrums, Vol. 13, No. S14
- Journal of College Student Psychotherapy, Vol. 22, No. 3
- Caregiver burden in anxiety disorders Current Opinion in Psychiatry, Vol. 21, No. 1
- International Clinical Psychopharmacology, Vol. 23, No. 5
- Psychosomatics, Vol. 49, No. 5
- BMC Public Health, Vol. 8, No. 1
- Korean Journal of Clinical Psychology, Vol. 27, No. 4
- Revista Brasileira de Psiquiatria, Vol. 30, No. suppl 2
- Internal Medicine, Vol. 47, No. 1
- A New Case-Finding Tool for Anxiety: A Pragmatic Diagnostic Validity Study in Primary Care 4 March 2008 | The International Journal of Psychiatry in Medicine, Vol. 37, No. 4
- Domains of quality of life and symptoms in male veterans treated for posttraumatic stress disorder 21 December 2007 | Journal of Traumatic Stress, Vol. 20, No. 6
- Child Abuse and Health-Related Quality of Life in Adulthood Journal of Nervous & Mental Disease, Vol. 195, No. 10
- History of trauma and dissociative symptoms among patients with obsessive-compulsive disorder and social anxiety disorder 24 April 2007 | Psychiatric Quarterly, Vol. 78, No. 3
- Self-help interventions for anxiety disorders: An overview 11 July 2007 | Current Psychiatry Reports, Vol. 9, No. 4
- Escitalopram in a working population: results from an observational study of 2378 outpatients in Austria 18 April 2007 | Human Psychopharmacology: Clinical and Experimental, Vol. 22, No. 4
- Murray B. Stein, M.D., M.P.H.
- Alan N. Simmons, Ph.D.
- Justin S. Feinstein, B.S.
- Martin P. Paulus, M.D.
- Personality traits and health-related quality of life in patients with mood and anxiety disorders 11 October 2006 | Quality of Life Research, Vol. 16, No. 1
- Mental Health, Quality of Life, and Health Functioning in Women Veterans 2 July 2016 | Journal of Interpersonal Violence, Vol. 22, No. 2
- Cochrane Database of Systematic Reviews
- Depression and Anxiety, Vol. 24, No. 5
- Biological Psychiatry, Vol. 61, No. 3
- Behaviour Research and Therapy, Vol. 45, No. 10
- Behaviour Research and Therapy, Vol. 45, No. 12
- Clinical Psychology Review, Vol. 27, No. 5
- Journal of Anxiety Disorders, Vol. 21, No. 4
- The American Journal of Geriatric Psychiatry, Vol. 15, No. 3
- International Clinical Psychopharmacology, Vol. 22, No. 3
- Health and Quality of Life Outcomes, Vol. 5, No. 1
- British Journal of Psychiatry, Vol. 190, No. 5
- Revista Brasileira de Psiquiatria, Vol. 29, No. 3
- Quality of Life in Obsessive-Compulsive Disorder
- The meaning of self‐perception of health in the UK armed forces 24 December 2010 | British Journal of Health Psychology, Vol. 11, No. 4
- Posttraumatic stress disorder: Examination of what clinicians know 20 August 2006 | Clinical Psychologist, Vol. 10, No. 2
- Social anxiety and obsessive-compulsive spectra: Validation of the SHY-SR and the OBS-SR among the Spanish population Psychiatry Research, Vol. 142, No. 2-3
- Do empirically supported treatments generalize to private practice? A benchmark study of a cognitive‐behavioural group treatment programme for social phobia 24 December 2010 | British Journal of Clinical Psychology, Vol. 45, No. 1
- International Journal of Geriatric Psychiatry, Vol. 21, No. 4
- Social Psychiatry and Psychiatric Epidemiology, Vol. 41, No. 8
- Experimental Brain Research, Vol. 173, No. 2
- The Lancet, Vol. 368, No. 9553
- Comprehensive Psychiatry, Vol. 47, No. 3
- Journal of Affective Disorders, Vol. 96, No. 1-2
- Hormones and Behavior, Vol. 50, No. 4
- Journal of Consulting and Clinical Psychology, Vol. 74, No. 4
- Cost-Utility Analysis of Methadone Maintenance Treatment: A Methodological Approach 3 July 2009 | Substance Use & Misuse, Vol. 41, No. 1
- Psychotherapy and Psychosomatics, Vol. 75, No. 3
- Journal of Family Psychotherapy, Vol. 16, No. 4
- Expert Review of Neurotherapeutics, Vol. 6, No. 2
- PharmacoEconomics, Vol. 24, No. 10
- Functional Impact and Health Utility of Anxiety Disorders in Primary Care Outpatients Medical Care, Vol. 43, No. 12
- The Role of Cognitions in OCD Treatment: Toward Rapprochement Cognitive Behaviour Therapy, Vol. 34, No. 3
- Early Diagnosis Can Decrease the Social and Economic Burden of Social Anxiety Disorder 26 June 2016 | Australian & New Zealand Journal of Psychiatry, Vol. 39, No. 7
- Mark Hyman Rapaport , M.D. ,
- Cathryn Clary , M.D. ,
- Rana Fayyad , Ph.D. , and
- Jean Endicott , Ph.D.
- A Meta-analytic Review of the Efficacy of Drug Treatment in Generalized Anxiety Disorder Journal of Clinical Psychopharmacology, Vol. 25, No. 2
- Predictive and Treatment Validity of Life Satisfaction and the Quality of Life Inventory 26 July 2016 | Assessment, Vol. 12, No. 1
- Comorbidity of depression and anxiety in nursing home patients 16 February 2005 | International Journal of Geriatric Psychiatry, Vol. 20, No. 3
- Social Psychiatry and Psychiatric Epidemiology, Vol. 40, No. 6
- Psychopharmacology, Vol. 177, No. 3
- Journal of Behavioral Medicine, Vol. 28, No. 6
- Cognitive and Behavioral Practice, Vol. 12, No. 1
- Behaviour Research and Therapy, Vol. 43, No. 7
- Comprehensive Psychiatry, Vol. 46, No. 6
- Journal of Affective Disorders, Vol. 88, No. 1
- Journal of Anxiety Disorders, Vol. 19, No. 7
- Journal of Behavior Therapy and Experimental Psychiatry, Vol. 36, No. 2
- Journal of Psychiatric Research, Vol. 39, No. 4
- CNS Spectrums, Vol. 10, No. 3
- CNS Spectrums, Vol. 10, No. S12
- Psychological Assessment, Vol. 17, No. 3
- World Futures, Vol. 61, No. 4
- Substance Use & Misuse, Vol. 40, No. 12
- Australian and New Zealand Journal of Psychiatry, Vol. 39, No. 7
- Acceptance and Commitment Therapy in the Treatment of Posttraumatic Stress Disorder 26 July 2016 | Behavior Modification, Vol. 29, No. 1
- BMC Psychiatry, Vol. 5, No. 1
- Développement et validation d’un questionnaire mesurant le soutien social en situation d’anxiété auprès d’une population universitaire 25 January 2006 | Santé mentale au Québec, Vol. 30, No. 2
- Murray B. Stein , M.D., M.P.H. ,
- Cathy D. Sherbourne , Ph.D. ,
- Michelle G. Craske , Ph.D. ,
- Adrienne Means-Christensen , Ph.D. ,
- Alexander Bystritsky , M.D. ,
- Wayne Katon , M.D. ,
- Greer Sullivan , M.D., M.S.P.H. , and
- Peter P. Roy-Byrne , M.D.
- Quality of Life Assessment in Turkish Patients with Schizophrenia and Their Relatives 31 August 2016 | Psychological Reports, Vol. 95, No. 1
- Anxiety in rheumatoid arthritis 3 June 2004 | Arthritis Care & Research, Vol. 51, No. 3
- Depression and Anxiety, Vol. 19, No. 2
- Depression and Anxiety, Vol. 20, No. 4
- Children and Youth Services Review, Vol. 26, No. 7
- European Neuropsychopharmacology, Vol. 14
- Journal of Anxiety Disorders, Vol. 18, No. 6
- Psychoneuroendocrinology, Vol. 29, No. 8
- International Journal of Forensic Mental Health, Vol. 3, No. 1
- Psychosomatics, Vol. 45, No. 1
- Expert Opinion on Investigational Drugs, Vol. 13, No. 7
- Expert Review of Neurotherapeutics, Vol. 4, No. 5
- Revista do Hospital das Clínicas, Vol. 59, No. 6
- Psychological Reports, Vol. 95, No. 5
- The impairments caused by social phobia in the general population: implications for intervention 29 August 2003 | Acta Psychiatrica Scandinavica, Vol. 108
- Evaluation of the Computerized Assessment System for Psychotherapy Evaluation and Research (CASPER) interview with a psychiatric inpatient population 1 January 2003 | Journal of Clinical Psychology, Vol. 59, No. 9
- Peter P. Roy-Byrne , M.D. ,
- Murray B. Stein , M.D. ,
- Greer Sullivan , M.D. ,
- Adrienne Means-Christensen , Ph.D. , and
- Alexander Bystritsky , M.D.
- Quality of Life in OCD: Differential Impact of Obsessions, Compulsions, and Depression Comorbidity 1 March 2003 | The Canadian Journal of Psychiatry, Vol. 48, No. 2
- Depression and Anxiety, Vol. 18, No. 1
- Journal of Anxiety Disorders, Vol. 17, No. 4
- Epilepsy & Behavior, Vol. 4
- Southern Medical Journal, Vol. 96, No. 6
- Increased Probability of Remaining in Remission from Panic Disorder with Agoraphobia after Drug Treatment in Patients Who Received Concurrent Cognitive-Behavioural Therapy: A Follow-Up Study 16 December 2002 | Psychotherapy and Psychosomatics, Vol. 72, No. 1
- Quality of Life in Anxiety Disorders: A Comparison of Obsessive-Compulsive Disorder, Social Anxiety Disorder, and Panic Disorder 27 October 2003 | Psychopathology, Vol. 36, No. 5
- Social Phobia 2 September 2016 | Journal of the American Psychiatric Nurses Association, Vol. 8, No. 3
- Anxiety Disorders and Disability Secondary to Urinary Incontinence among Adults over Age 50 23 June 2016 | The International Journal of Psychiatry in Medicine, Vol. 32, No. 2
- Journal of Psychosomatic Research, Vol. 53, No. 6
- Urology, Vol. 60, No. 5
- General Hospital Psychiatry, Vol. 24, No. 6
- Journal of General Internal Medicine, Vol. 17, No. 3
- Current Opinion in Psychiatry, Vol. 15, No. 2
- The American Journal of Geriatric Psychiatry, Vol. 10, No. 5
- Open-Label Evaluation of Venlafaxine Sustained Release in Outpatients with Generalized Anxiety Disorder with Comorbid Major Depression or Dysthymia: Effectiveness, Tolerability and Predictors of Response 11 November 2002 | Neuropsychobiology, Vol. 46, No. 3
- Revista Brasileira de Psiquiatria, Vol. 24, No. 1
- Current Psychiatry Reports, Vol. 3, No. 4
- Psychiatric Clinics of North America, Vol. 24, No. 4
- Applied and Preventive Psychology, Vol. 10, No. 3
- New England Journal of Medicine, Vol. 344, No. 17
- The Journal of Alternative and Complementary Medicine, Vol. 7, No. 1
- Clinical Neuropharmacology, Vol. 24, No. 4
- Journal of Couples Therapy, Vol. 10, No. 1
- Expert Opinion on Pharmacotherapy, Vol. 2, No. 10
- Murray B. Stein , M.D., F.R.C.P.C. , and
- Yin M. Kean , M.P.H.
- Depression and Anxiety, Vol. 12, No. S1
- Quality of Life Impairment in Anxiety Disorders

Articles on Phobias
Displaying 1 - 20 of 26 articles.

Biophobia: search trends reveal a growing fear of nature
Ricardo Correia , University of Helsinki and Stefano Mammola , University of Helsinki

Innies, outies and omphalophobia: 7 navel-gazing questions about belly buttons answered
Sarah Leupen , University of Maryland, Baltimore County

Why are we so scared of clowns? Here’s what we’ve discovered
Sophie Scorey , University of South Wales ; James Greville , University of South Wales ; Philip Tyson , University of South Wales , and Shakiela Davies , University of South Wales

Scared of needles? Claustrophobic? One longer session of exposure therapy could help as much as several short ones
Bronwyn Graham , UNSW Sydney and Sophie H Li , UNSW Sydney

CBT? DBT? Psychodynamic? What type of therapy is right for me?
Sourav Sengupta , University at Buffalo

Pictures of COVID injections can scare the pants off people with needle phobias. Use these instead
Holly Seale , UNSW Sydney and Jessica Kaufman , Murdoch Children's Research Institute

Tokophobia is an extreme fear of childbirth. Here’s how to recognise and treat it
Julie Jomeen , Southern Cross University ; Catriona Jones , University of Hull ; Claire Marshall , University of Hull , and Colin Martin , Southern Cross University

Spider home invasion season: why the media may be to blame for your arachnophobia
Mike Jeffries , Northumbria University, Newcastle

Fear can spread from person to person faster than the coronavirus – but there are ways to slow it down
Jacek Debiec , University of Michigan

Anxiety in autistic children – why rates are so high
Keren MacLennan , University of Reading

Curious Kids: where do phobias come from?
Lara Farrell , Griffith University

Fear of the dentist: what is dental phobia and dental anxiety?
Ellie Heidari , King's College London

Get ‘inspidered’ – from fear of spiders to fascination
Gerhard J. Gries , Simon Fraser University and Andreas Fischer , Simon Fraser University

You can’t ‘erase’ bad memories, but you can learn ways to cope with them
Carol Newall , Macquarie University and Rick Richardson , UNSW Sydney

Tokophobia: what it’s like to have a phobia of pregnancy and childbirth
Catriona Jones , University of Hull ; Franziska Wadephul , University of Hull , and Julie Jomeen , University of Hull

Health Check: why are some people afraid of heights?
Bek Boynton , James Cook University and Anne Swinbourne , James Cook University

How virtual reality spiders are helping people face their arachnophobia

Why are some people afraid of cats?
Sally Shuttleworth , University of Oxford

From creepy clowns to the dancing plague – when phobias are contagious
Clare Glennan , Cardiff Metropolitan University

Fear of death underlies most of our phobias
Lisa Iverach , University of Sydney ; Rachel E. Menzies , University of Sydney , and Ross Menzies , University of Sydney
Related Topics
- Arachnophobia
- Exposure therapy
- Mental health
- Neuroscience
Top contributors
Professor of Midwifery and Dean in the Faculty of Health Sciences, Southern Cross University
Senior Research Fellow in Maternal and Reproductive Health, University of Hull
Senior Lecturer, Psychology, James Cook University
Principal Program Officer (Respectful Workplaces), James Cook University
Honorary Associate at Department of Psychology, Macquarie University and Research Fellow, University of Sydney
Associate Professor, McGill University
Associate professor, UNSW Sydney
PhD Candidate, University of Essex
Senior Lecturer in Psychology and Behavioural Medicine, St George's, University of London
Associate Professor, University of Sydney
Professor of Psychology, University of Essex
Postdoctoral research fellow, School of Psychology, University of Sydney
Lecturer of Psychology, Cardiff Metropolitan University
Associate Professor, Ecology, Northumbria University, Newcastle
Professor of Neuropsychology (Hons), Cardiff University
- X (Twitter)
- Unfollow topic Follow topic
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Research Findings on the Genetics of Phobias
Daniel B. Block, MD, is an award-winning, board-certified psychiatrist who operates a private practice in Pennsylvania.
:max_bytes(150000):strip_icc():format(webp)/block-8924ca72ff94426d940e8f7e639e3942.jpg)
Phobias are extreme fears that make it impossible to function normally. Phobias may grow out of really negative experiences, but because they are overwhelming and often irrational, they become disabling. There are many different types of phobias; some of the most common include:
- Fear of specific animals (dogs, spiders, etc.)
- Fear of open spaces, enclosed space, or high places
- Fear of natural events, such as thunderstorms
While fears are an unavoidable part of being human, most fears can be controlled and managed. Phobias, however, cause psychological and physical reactions that are difficult if not impossible to manage. As a result, people with phobias will go to great lengths to avoid the object of their fears.
What Causes Phobias?
Why does someone react to a normal, everyday event — the bark of a dog, for example — with extreme fear and anxiety? Why do other people react to the same experience with mild anxiety or calm?
The causes of phobias are not yet widely understood. Increasingly, however, research shows that genetics may play at least some role.
Studies show that twins who are raised separately have a higher than average rate of developing similar phobias. Other studies show that some phobias run in families, with first-degree relatives of phobia sufferers more likely to develop a phobia.
In “Untangling genetic networks of panic, phobia, fear, and anxiety,” Villafuerte and Burmeister reviewed several earlier studies in an attempt to determine what, if any, genetic causes can be identified for anxiety disorders.
Family Studies Suggest a Genetic Link
If a family member has a phobia, you are at an increased risk for a phobia as well.
In general, relatives of someone with a specific anxiety disorder are most likely to develop the same disorder. In the case of agoraphobia (fear of open spaces), however, first-degree relatives are also at increased risk for panic disorder, indicating a possible genetic link between agoraphobia and panic disorder .
Researchers have found that first-degree relatives of someone suffering from a phobia are approximately three times more likely to develop a phobia.
According to the findings, twin studies showed that when one twin has agoraphobia, the second twin has a 39% chance of developing the same phobia. When one twin has a specific phobia, the second twin has a 30% chance of also developing a specific phobia. This is much higher than the 10% chance of developing an anxiety disorder found in the general population.
Gene Isolation Suggests a Link Between Phobias and Panic Disorder
Although they were unable to specifically isolate the genetic causes of phobias, Villafuerte and Burmeister reviewed several studies that appear to demonstrate genetic anomalies in both mice and humans with anxiety disorders. The early research appears to show that agoraphobia is more closely linked to panic disorder than to the other phobias, but is far from conclusive.
More research will need to be performed in order to isolate the complex genetics involved in the development of phobias and other anxiety disorders. However, this study does support the theory that genetics play a major role.
- Villafuerte, Sandra and Burmeister, Margit. Untangling genetic networks of panic, phobia, fear and anxiety . Genome Biology . July 28, 2003. 4(8):224.
By Lisa Fritscher Lisa Fritscher is a freelance writer and editor with a deep interest in phobias and other mental health topics.
ORIGINAL RESEARCH article
Diagnostic accuracy and clinical utility of the phq-2 and gad-2: a comparison with long-format measures for depression and anxiety.

- 1 Department of Psychology, University of Iceland, Reykjavík, Iceland
- 2 Department of Psychology, Faculty of Social Sciences, Stockholm University, Stockholm, Stockholm, Sweden
The final, formatted version of the article will be published soon.
Select one of your emails
You have multiple emails registered with Frontiers:
Notify me on publication
Please enter your email address:
If you already have an account, please login
You don't have a Frontiers account ? You can register here
Background: Anxiety and depression are highly prevalent and often comorbid mental disorders that are encompassed within the broad category of emotional disorders. The frequent comorbidity of anxiety and depression can pose challenges for accurate diagnosis and treatment which, in turn, highlights the need for reliable measurements that are simultaneously responsive to change and prevent non-response bias. Brief measures of anxiety and depression can potentially increase response rates due to their brevity and ease of administration. This study evaluates the psychometric characteristics, discriminative accuracy, and sensitivity to change of the Generalized Anxiety Disorder 2-item scale (GAD-2) and the Patient Health Questionnaire 2-item scale (PHQ-2) within a clinical population. Method: The sample comprised treatment-seeking participants (n = 3411), screened (n = 2477) to receive an internet-based psychotherapeutic intervention (cognitivebehavioral, psychodynamic, or waitlist). Results: Brief measures can effectively detect individuals who may be eligible for a diagnosis of depression and anxiety, not only prior to but also during and following the completion of psychological treatment. The discriminative ability of the GAD-2 was significantly greater during active treatment and at post-assessment compared with pre-treatment screening, although no such differences were found for the PHQ-2. Finally, endorsing the most severe response option on the GAD-2 and PHQ-2 was associated with a high probability of presenting clinically relevant anxiety and depressive symptoms. Conclusion: Brief measures of anxiety and depression are viable instruments to screen for and monitor anxiety and depressive symptoms.
Keywords: Generalized Anxiety Disorder Questionnaire1, Patient Health Questionnaire2, Psychometric Evaluation3, Internet-Based Psychotherapy4, Receiver Operating Characteristic (ROC) Analysis5, Item-Option Characteristic Analysis6
Received: 17 Jul 2023; Accepted: 23 Apr 2024.
Copyright: © 2024 Hlynsson and Carlbring. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Per Carlbring, Department of Psychology, Faculty of Social Sciences, Stockholm University, Stockholm, SE-106 91, Stockholm, Sweden
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Open access
- Published: 24 April 2024
Association between body mass index and mental health among nurses: a cross-sectional study in China
- Bonan Luan ORCID: orcid.org/0000-0003-2703-3390 1 ,
- Xueyan Tian ORCID: orcid.org/0000-0002-7933-5844 2 ,
- Chao Wang ORCID: orcid.org/0000-0001-6097-7719 2 ,
- Ming Cao ORCID: orcid.org/0009-0001-4858-838X 2 &
- Dongmei Liu ORCID: orcid.org/0000-0003-1822-7580 2
BMC Health Services Research volume 24 , Article number: 506 ( 2024 ) Cite this article
1 Altmetric
Metrics details
To examine the correlation between body mass index (BMI) and mental well-being in Chinese nurses during the COVID-19 epidemic.
This study was conducted in a tertiary hospital using a cross-sectional design. A total of 2,811 nurses were enlisted at Shengjing Hospital in China during the period from March to April, 2022. Information was gathered through a questionnaire that individuals completed themselves. The mental health of the participants was assessed using the Patient Health Questionnaire-9 and the Generalized Anxiety Disorder Assessment-7. Binary logistic regression was used to calculate adjusted odds ratios (ORs) and their corresponding 95% confidence intervals.
The prevalence of nurses experiencing depression and anxiety was 7.8% (219) and 6.7% (189), respectively. Regarding depression after adjustment, the odds ratios (ORs) for each quartile, compared to the lowest quartile, were as follows: 0.91 (95% confidence interval [CI]: 0.53, 1.56), 2.28 (95% CI: 0.98, 3.77), and 2.32 (95% CI: 1.41, 3.83). The p-value for trend was found to be 0.001. The odds ratios (ORs) for anxiety after adjustment were 2.39 (0.83, 4.36), 4.46 (0.51, 7.93), and 2.81 (1.56, 5.08) when comparing the highest quartiles to the lowest quartile. The p -value for trend was 0.009.
This study found a positive association between BMI and poor mental health among nurses during the COVID-19 pandemic, particularly in those who were overweight or obesity. The findings could assist in developing interventions and help policy-makers establish appropriate strategies to support the mental health of frontline nurses, especially those who are overweight or obesity.
Peer Review reports
Introduction
Depression and anxiety are the most common mental health illnesses worldwide [ 1 ]. Depression is a mood disorder that affects an individual’s thoughts and feelings and leads to persistent feelings of sadness and disinterest [ 2 ]. Anxiety is a group of mental disorders characterized by nervousness, apprehension, and fear [ 3 ]. Depression and anxiety disorders are major contributors to the mental health burden of adults [ 4 ]. Poor mental health often affects regular activities and probably results in poor professional performance. Given the detrimental effects of depression and anxiety on physical and mental health, it is important to explore the relevant factors, and to thereby contribute toward preventing the development of mental health disorders [ 5 ].
According to the National Institute of Health of America, body mass index (BMI) is a measure that defines individuals as underweight, normal weight, or overweight, that is calculated using their weight and height [ 6 ]. Recent research indicates that high BMI and obesity continue to relentlessly increase globally, with approximately two billion people being overweight or obese [ 7 ]. In a meta-analysis including 57 prospective studies and 900,000 adults, they found that above 25 kg/m 2 , positive associations between BMI and cardiovascular disease, hypertension, diabetes mellitus, stroke, and cancer were recorded in both sexes. Moreover, each 5 kg/m 2 higher BMI was associated with about 30% higher overall mortality [ 8 ]. Obesity-related diseases have become the fifth leading cause of death worldwide [ 9 ].
A systematic review and meta-analysis on the longitudinal relationship between BMI and mental health, they found that obesity at baseline increased the risk of onset of depression and the unadjusted ORs were 1.55 (including 15 included studies and 58,745 participants) [ 10 ]. Moreover, another meta-analysis of 8 Mendelian randomization studies indicated that obesity is a causal risk factor for elevated risk of depression (OR = 1.33) [ 11 ]. Previous studies also demonstrate a bi-directional relationship between obesity and mental health [ 12 ]. Although these existing studies address the issue of obesity and mental health, none of these studies address this issue among nurses.
As nurses fulfill an essential role among healthcare workers, they experienced a particularly high occupational burden during the peak of coronavirus disease (COVID-19) pandemic [ 13 ]. In a multi-center cross-sectional online survey, among 395 healthcare workers, there were 42.28% and 56.2% were found to have depression, and anxiety during the COVID-19 pandemic, respectively [ 14 ]. A recent study conducted in 2020 from China shows that nurses experienced more unfavorable mental health outcomes than other healthcare workers during the pandemic [ 15 ]. Furthermore, for nurses, poor mental health may influence not only themselves but also their professional performance and the quality of the health care provided, even affecting patient safety [ 16 , 17 ]. A growing body of evidence suggests that individuals with changes in BMI have experienced deteriorating symptoms, such as isolation, anxiety and depression as a result of the COVID-19 pandemic compared to previous timepoints. The increasing obesity rates may have modestly increased the prevalence of depressive symptoms in the general population [ 18 ]. However, there is currently no data to explore the association between BMI and mental health among nurses during the COVID-19 pandemic. To fill this gap, we conducted a large cross-sectional study to explore the association between BMI and mental health among nurses in China during the COVID-19 pandemic.
Study design
The present cross-sectional investigation was carried out at a Chinese hospital throughout the period from March 2022 to April 2022. The survey was conducted by the nursing department, and it included a total of 3,450 nurses who were employed at the hospital. In the end, a grand total of 2,811 individuals supplied valid and useful responses, leading to an effective response rate of 81.49%. An ensemble of web-based surveys that individuals completed themselves was utilized. Participants successfully filled out a well-organized questionnaire within a time frame of 20 to 25 min. Figure 1 provides a visual representation of the specific information using a flow chart.
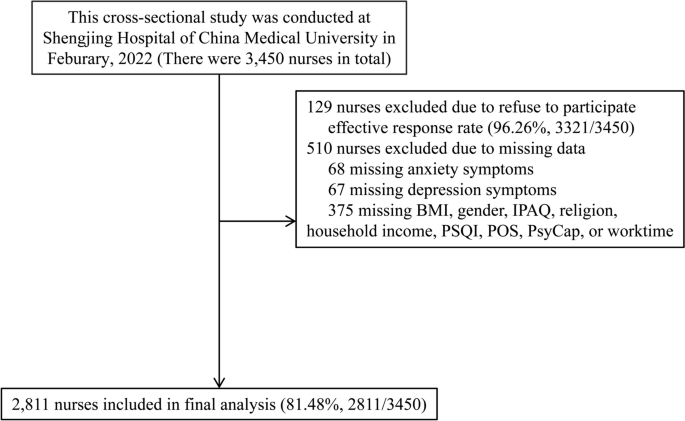
Flowchart of this study
The Ethics Committee of Shengjing Hospital Affiliated China Medical University granted ethical permission (2022PS753K). All participants provided written informed consent. The procedures were carried out in accordance with the ethical guidelines outlined in the 1975 Declaration of Helsinki.
Inclusion and exclusion criteria
The criteria for inclusion were as follows: nurses who were currently employed in hospitals and actively working. The study employed the following exclusion criteria: nurses who had engaged in employment for less than three months or had not completed the psychological questionnaire in its whole were disqualified.
Measurement of covariates characteristics
This study gathered data from the nursing staff on various aspects, including demographic characteristics, dietary habits, life-related factors, work-related factors, experienced important life events, history of physical sickness, exposure to the COVID-19 pandemic, and psychological assessments.
The demographic data encompassed age, gender, and body mass index (BMI), which was self-reported by the participants and measured in kg/m 2 . The individual's dietary habits encompassed their smoking status, alcohol consumption patterns, and coffee consumption patterns. Smoking behavior was classified into three categories: current smokers (those who smoked at least one cigarette per day and had done so for at least six months), former smokers (those who had stopped smoking for at least six months), and non-smokers. Alcohol and coffee consumption patterns are classified into three categories: current drinkers (those who use alcohol or coffee at least once a day and have been doing so for at least six months), former drinkers (those who have stopped consuming alcohol or coffee for at least six months), and non-drinkers (those who do not consume alcohol or coffee).
Life-related factors encompassed various aspects such as sleep quality (measured by PSQI, Pittsburgh Sleep Quality Index scores), physical activity (assessed using IPAQ, International Physical Activity Questionnaire, in terms of Mets × hour/week), religious affiliation, marital status, presence of siblings, monthly household income (in RMB, yuan), occurrence of major life events, history of chronic disease, and frequency of visiting friends.The researchers evaluated the level of physical activity (PA) in the past week using the abbreviated version of the International Physical Activity Questionnaire [ 19 ]. The Pittsburgh sleep quality index (PSQI) [ 20 ] was used to assess sleep quality.
Work-related variables including employment, field of expertise, weekly working hours, and night shifts. Exposure to the COVID-19 pandemic pertains to nurses who may come into touch with patients suspected or confirmed to have COVID-19, or find themselves in a situation that necessitates COVID-19 quarantine.
Measurements of psychological variates
The level of organization support was measured using the Chinese version of the Perceived Organization Support Questionnaire (POS) [ 21 ]. The Cronbach's α coefficient for POS was 0.921. The Chinese version of the 24-item Psychological Capital Questionnaire (PCQ) [ 22 , 23 ] was used to assess PsyCap. The Cronbach's α coefficients for self-efficacy, hope, resilience, and optimism were 0.921, 0.936, 0.920, and 0.900, respectively.
Measurement of depression and anxiety
The assessment of depressive symptoms was conducted using clinically validated measures, specifically the PHQ09 [ 24 ]. The PHQ09 scale consists of nine items, each with a 4-point Likert-type scale answer. These responses indicate the frequency of individuals' feelings during the preceding two weeks, ranging from 0 to 3. The cumulative score spans from 0 to 27, with a higher value denoting a greater intensity of depression symptoms. A PHQ09 score of 10 or more was used to determine the presence of serious depression.
The Chinese version of the GAD07 [ 25 ] was used to assess anxiety symptoms. The GAD07 questionnaire comprises 7 items, with each item being responded to on a 4-point Likert-type scale ranging from 0 (indicating never) to 3 (indicating always). A greater score indicates a higher level of anxiety symptoms. A GAD07 standardized score of 10 or higher was used to characterize the presence of significant anxiety symptoms. The Cronbach's α coefficients for the Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 (GAD-7) were 0.951 and 0.928, respectively.
Sample size calculation
The confidence level (1-α) was 0.95; the proportion of main outcome (depression and anxiety) was 0.1; The confidence interval width (two sided) was 0.03. The confidence interval formula was Exact (Clopper-Pearson); the 2-tailed P value was 0.05. The sample size was 1,603. It was calculated by PASS 11.0 (Power Analysis and Sample Size 11.0, NCSS Inc., USA) [ 8 , 10 , 18 ].
Statistical analysis
The data were analyzed using SPSS 22.0 for Windows, developed by SPSS Inc. in Chicago, IL, USA. The continuous variables were reported as the median together with the interquartile range. The categorical variables were presented as the count (proportion). Discrete sets of data that are neither related or dependent on each other. The mean of two continuous variables that follow a normal distribution was compared using the Student's t-test. The Mann–Whitney U test was employed to compare the average values of two continuous variables that do not follow a normal distribution. On the other hand, the χ2 test or Fisher's exact test were utilized for categorical variables.
The quartiles were determined by categorizing the BMI values of all participants depending on their distribution, and these quartiles were then utilized for subsequent research. The study investigated the association between quartile categories of BMI and the presence of poor mental health, specifically depression and anxiety, using binary unconditional logistic regression analysis. The dependent variable in this study was the individual's mental health state, whereas the independent variable was their BMI. The crude odds ratio (OR) was calculated using crude data, and model 1 was further modified for age and gender. Model 2 further accounted for baseline variables that were deemed clinically significant or had a p -value < 0.10 in the univariate analysis. These variables included alcohol consumption, sleep quality, number of siblings, experience of major life events, frequency of visiting friends, years of employment, duration of work hours, psychological characteristics related to depression, age, physical activity, marital status, history of chronic disease, specialty, and psychological characteristics related to anxiety. The Model 3 was modified to account for all baseline variables. Adjusted OR and their corresponding 95% confidence intervals (95% CI) were calculated using binary unconditional logistic regression, taking into account any confounding factors. The study examined the presence of a linear trend by analyzing the median value of each quartile as a continuous variable. All P values were calculated using a two-tailed test, and the observed difference was considered statistically significant when the P value was less than 0.05.
A total of 2,811 nurses were ultimately enrolled in the study, with a median age of 35 years and a median BMI of 21.83 kg/m 2 . Female participants constituted the majority (94.20%). Out of the total, 69.9% (1,965) of the nurses had a normal weight, 6.3% (177) were underweight, 19.9% (558) were overweight, and 3.9% (111) were obese. The occurrence of depression and anxiety among nurses was 7.8% (219 out of 2,811) and 6.7% (189 out of 2,811), respectively; see details in Table 1 (the distribution of characters by outcome status) and supplementary Table 1 ( the distribution of characters by BMI status ) .
Participants with elevated BMI, impaired sleep quality, and diminished scores in perceived organizational support, efficacy, hope, resiliency, and optimism exhibited an increased likelihood of developing depression, as indicated by the univariate analysis. A greater proportion of individuals with depression exhibited concurrent alcohol consumption, had siblings, encountered significant life events, had infrequent social interactions with friends, had employment tenure exceeding five years, and worked in excess of 40 h per week. Individuals who were older, had a higher BMI, experienced poor sleep quality, engaged in lower levels of weekly physical activity, and had lower scores in perceived organizational support, efficacy, hope, resiliency, and optimism were found to have a higher likelihood of developing anxiety. A greater proportion of individuals with anxiety engaged in marriage or cohabitation, had siblings, experienced significant life events, had a background of chronic illnesses, had infrequent social interactions with friends, had a job history exceeding five years, worked for more than 40 h per week, and were employed in the surgical department. The factors stated above exhibited statistical significance in the univariate analysis, as shown in detail in Table 1 .
In order to investigate the correlation between BMI and depression, the BMI was divided into four categories based on quartiles. In comparison to the lowest quartile, the odds ratios (ORs) for the other quartiles were as follows: 0.91 (0.53, 1.56), 2.28 (0.98, 3.77), and 2.32 (1.41, 3.83) after making adjustments. Additionally, the p-value for the trend was found to be 0.001. In relation to anxiety, the odds ratios (ORs) for each quartile were as follows: 2.39 (0.83, 4.36), 4.46 (0.51, 7.93), and 2.81 (1.56, 5.08) after adjusting for other factors. Furthermore, there was a significant trend with a p -value of 0.009. Refer to the comprehensive information provided in Table 2 . We also did sensitivity analysis by excluding participants who were underweight (BMI < 18.5) and only including participants who exposed to the COVID-19 pandemic, these results were consistent with the main outcome; see details in supplementary Tables 2 and 3 .
Obesity is a major contributor to morbidity and mortality. However, no existing study has focused on the relationship between BMI and mental health among nurses during COVID-19 pandemic. Therefore, we performed a cross-sectional study on a large population of nurses in China. This study showed a positive association between BMI and poor mental health (anxiety and depression) among Chinese nurses during the COVID-19 pandemic, particularly in those who were overweight or obesity.
In line with this, A systematic review and meta-analysis on the longitudinal relationship between BMI and mental health, they found that obesity at baseline increased the risk of onset of depression and the unadjusted ORs were 1.55 (including 15 included studies and 58,745 participants) [ 10 ]. Another population-based cross-sectional study enrolled 4,361 Iranian healthcare staff; their results indicate that abdominal obesity was significantly associated with anxiety among females but not among males. It is worth noting that in the current study, most participants were female. At the same time, no significant association was discovered between abdominal obesity and psychological distress in either gender. There was, however, a weak positive association between BMI and depression [ 26 ]. Further, a meta-analysis reviewed 25 prospective studies and provided solid evidence of the link between obesity and depression, indicating a bi-directional relationship between BMI and depression [ 27 ]. A possible mechanism is the adoption of an unhealthy lifestyle, such as insufficient physical exercise and unhealthy dietary preferences, possibly leading to obesity [ 27 ].
The exact underlying pathophysiological mechanism between being overweight and poor mental health is unknown. It has been shown that immune inflammation disorder plays an essential role in mental health disorders such as depression and anxiety. Moreover, a high BMI status can lead to many pro-inflammatory factors in the peripheral circulation system crossing the blood–brain barrier, subsequently inducing depressive-like behaviors. In such cases, the risk of depression and anxiety gradually increases [ 28 , 29 ]. The association between obesity and disorders such as depression and anxiety may also be explained by hypothalamic–pituitary–adrenal (HPA) axis disorder, leptin, or microbial mechanisms [ 30 , 31 , 32 , 33 , 34 , 35 ]. The obesity might involve HPA-axis dysregulation and HPA-axis dysregulation is also well known to be involved in depression. Through HPA axis dysregulation, obesity might cause development to depression. Leptin play an important role in the signaling pathway of glutamatergic neurons for regulating depression-related behaviors, suggesting a possible association between synaptic depression and behavioral manifestations of depression. Depression is associated with decreased gut microbiota richness and diversity. Fecal microbiota transplantation from depressed patients to microbiota-depleted rats can induce behavioural and physiological features characteristic of depression in the recipient animals, including anhedonia and anxiety-like behaviours, as well as alterations in tryptophan metabolism. This suggests that the gut microbiota may play a causal role in the development of features of depression.
While this study provides interesting insights, it is important to acknowledge its various limitations. First, since this study is cross-sectional, there is a concern for reverse causation, where mental health problems may contribute to increased BMI. Future studies with a longitudinal framework are warranted to address this issue. Second, the data were gathered by self-reported questionnaires, specifically pertaining to measurements such as height and weight. It is important to note that this method may be susceptible to recall bias. In addition, given that the majority of the study sample consists of young women, there is a possibility that they may be tempted to falsely report their height and weight. Therefore, this social desirability bias is another limitation of this study. Third, it is important to note that the GAD-7 and PHQ-9 are screening questionnaires that lack the ability to provide clinical diagnosis. This limitation may have had an impact on the outcomes of our study. However, this study is the first to examine the connection between BMI and mental health in nurses during the COVID-19 epidemic while accounting for several influential factors.
Availability of data and materials
No datasets were generated or analysed during the current study.
Naser AY, Alwafi H, Amara NA, et al. Epidemiology of depression and anxiety among undergraduate students. Int J Clin Pract. 2021;75(9):e14414.
Article PubMed Google Scholar
Durisko Z, Mulsant BH, Andrews PW. An adaptationist perspective on the etiology of depression. J Affect Disord. 2015;172:315–23.
Amu H, Osei E, Kofie P, et al. Prevalence and predictors of depression, anxiety, and stress among adults in Ghana: a community-based cross-sectional study. PLoS ONE. 2021;16(10):e0258105.
Article CAS PubMed PubMed Central Google Scholar
mhGAP: Mental Health Gap Action Programme: Scaling Up Care for Mental, Neurological and Substance Use Disorders. Geneva: World Health Organization; 2008.
Salari N, Khazaie H, Hosseinian-Far A, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. 2020;18(1):100.
Article PubMed PubMed Central Google Scholar
Weir CB, Jan A. BMI Classification Percentile And Cut Off Points. In: In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
Google Scholar
Rothman KJ. BMI-related errors in the measurement of obesity. Int J Obes (Lond). 2008;32(Suppl 3):S56–9.
Prospective Studies Collaboration, Whitlock G, Lewington S, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96.
Article PubMed Central Google Scholar
Lopez-Jimenez F. Speakable and unspeakable facts about BMI and mortality. Lancet. 2009;373(9669):1055–6.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–9.
Jokela M, Laakasuo M. Obesity as a causal risk factor for depression: systematic review and meta-analysis of mendelian randomization studies and implications for population mental health. J Psychiatr Res. 2023;163:86–92.
Hruby A, Lieberman HR, Smith TJ. Symptoms of depression, anxiety, and post-traumatic stress disorder and their relationship to health-related behaviors in over 12,000 US military personnel: bi-directional associations. J Affect Disord. 2021;283:84–93.
Phillips CS, Becker H, Gonzalez E. Psychosocial well-being: an exploratory cross-sectional evaluation of loneliness, anxiety, depression, self-compassion, and professional quality of life in oncology nurses. Clin J Oncol Nurs. 2021;25(5):530–8.
Nayak BS, Sahu PK, Ramsaroop K, Maharaj S, Mootoo W, Khan S, Extravour RM. Prevalence and factors associated with depression, anxiety and stress among healthcare workers of Trinidad and Tobago during COVID-19 pandemic: a cross-sectional study. BMJ Open. 2021;11(4):e044397.
Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976.
Maharaj S, Lees T, Lal S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of australian nurses. Int J Environ Res Public Health. 2018;16(1):61.
Abbas A, Al-Otaibi T, Gheith OA, et al. Sleep quality among healthcare workers during the COVID-19 pandemic and its impact on medical errors: Kuwait experience. Turk Thorac J. 2021;22(2):142–8.
J Devoe D, Han A, Anderson A, Katzman DK, Patten SB, Soumbasis A, Flanagan J, Paslakis G, Vyver E, Marcoux G, Dimitropoulos G. The impact of the COVID-19 pandemic on eating disorders: a systematic review. Int J Eat Disord. 2023;56(1):5–25.
Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95.
Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Article CAS PubMed Google Scholar
Eisenberger R, Stinglhamber F, Vandenberghe C, et al. Perceived supervisor support: contributions to perceived organizational support and employee retention. J Appl Psychol. 2002;87(3):565–73.
Avey JB, Luthans F, Smith RM, et al. Impact of positive psychological capital on employee well-being over time. J Occup Health Psychol. 2010;15(1):17–28.
Wu S, Xu Z, Zhang Y, et al. Relationship among psychological capital, coping style and anxiety of Chinese college students. Riv Psichiatr. 2019;54(6):264–8.
PubMed Google Scholar
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Heidari-Beni M, Azizi-Soleiman F, Afshar H, et al. Relationship between obesity and depression, anxiety and psychological distress among Iranian health-care staff. East Mediterr Health J. 2021;27(4):327–35.
Kasen S, Cohen P, Chen H, Must A. Obesity and psychopathology in women: a three decade prospective study. Int J Obes (Lond). 2008;32(3):558–66.
Valkanova V, Ebmeier KP, Allan CL. CRP, IL-6 and depression: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2013;150(3):736–44.
Amer SAAM, Fouad AM, El-Samahy M, et al. Mental stress, anxiety and depressive symptoms and interleuken-6 level among healthcare workers during the COVID-19 pandemic. J Prim Care Community Health. 2021;12:21501327211027430.
Wang P, Loh KH, Wu M, et al. A leptin-BDNF pathway regulating sympathetic innervation of adipose tissue. Nature. 2020;583(7818):839–44.
Guo M, Lu Y, Garza JC, et al. Forebrain glutamatergic neurons mediate leptin action on depression-like behaviors and synaptic depression. Transl Psychiatry. 2012;2(2):e83.
Martin KA, Mani MV, Mani A. New targets to treat obesity and the metabolic syndrome. Eur J Pharmacol. 2015;763(Pt A):64–74.
Kelly JR, Borre Y, O’ Brien C, et al. Transferring the blues: depression-associated gut microbiota induces neurobehavioural changes in the rat. J Psychiatr Res. 2016;82:109–18.
Choi KW, Kim YK, Jeon HJ. Comorbid anxiety and depression: clinical and conceptual consideration and transdiagnostic treatment. Adv Exp Med Biol. 2020;1191:219–35.
Rosmond R, Dallman MF, Björntorp P. Stress-related cortisol secretion in men: relationships with abdominal obesity and endocrine, metabolic and hemodynamic abnormalities. J Clin Endocrinol Metab. 1998;83(6):1853–9.
CAS PubMed Google Scholar
Download references
Acknowledgements
We give special thanks to all the colleagues of Shengjing Hospital for their help and support. We thank International Science Editing ( http://www.internationalscienceediting.com ) for editing this manuscript. The authors would like to thank all of the study participants.
Conflict of interest
There is no conflict of interest.
This study was financially supported by The 345 Talent Project of Shengjing Hospital (grant number: N/A).
These sponsors had no role in the study design; in the collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and affiliations.
Department of Operating Room, Shengjing Hospital of China Medical University, Shenyang, P.R. China
Department of Urology, Shengjing Hospital of China Medical University, 36 Sanhao Street, Shenyang, Liaoning, 110004, P.R. China
Xueyan Tian, Chao Wang, Ming Cao & Dongmei Liu
You can also search for this author in PubMed Google Scholar
Contributions
B.L and M.C had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. D.L and M.C: Protocol/project development. B.L, C.W, X. T, M.C, and D.L: Data collection or management. B.L, C.W, and X.T: Data analysisBonan Luan: Manuscript writing/editing.
Corresponding author
Correspondence to Dongmei Liu .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval (2022PS753K) was offered by the Ethics Committee of Shengjing hospital Affiliated China Medical University. All informed consent of these patients in this study has been obtained. The research program is in line with the ethical guidelines of the 1975 Declaration of Helsinki.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Luan, B., Tian, X., Wang, C. et al. Association between body mass index and mental health among nurses: a cross-sectional study in China. BMC Health Serv Res 24 , 506 (2024). https://doi.org/10.1186/s12913-024-11006-y
Download citation
Received : 31 January 2024
Accepted : 18 April 2024
Published : 24 April 2024
DOI : https://doi.org/10.1186/s12913-024-11006-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
How parents’ views of their kids’ screen time, social media use changed during COVID-19

When Pew Research Center fielded a survey of U.S. parents at the beginning of March 2020, we knew the conversation around children and technology was at the forefront of many parents’ minds. Yet no one knew just how relevant that conversation would become in the months ahead.
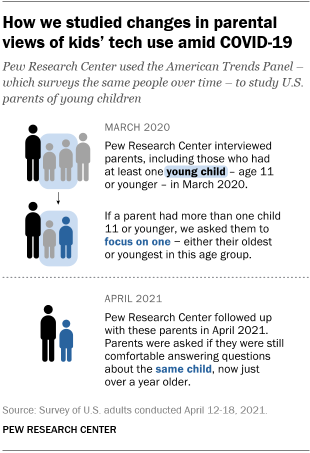
The first year of the coronavirus pandemic brought a variety of challenges for parents, from helping their kids manage technology to increased screen time. Those with young children wrestled with a lack of child care and worried about their kids’ social skills – concerns that are still relevant today as schools navigate changing circumstances, parents manage changes in where and how they work , and families await vaccines for children under 5.
In April 2021, the Center followed up with many of the same parents we surveyed in March 2020 to check in on their children’s use of technology and social media during the pandemic. This second survey focused on parents who had a kid age 11 or younger in 2020, and it was fielded at a time when some schools were temporarily reverting to virtual learning and vaccines were not yet approved for children under 12. Below, we take a closer look at what these parents told us about their young child, including how the experiences they reported in 2021 compared with their responses from 2020.
Pew Research Center has long studied changes in parenting and family dynamics, as well as the adoption of digital technologies. This analysis of parents’ experiences with and attitudes about their children’s tech use is based on data from 1,681 parents who had at least one child age 11 or younger as of March 2020 and participated in two surveys conducted on the Center’s American Trends Panel (ATP) between spring 2020 and 2021 – coinciding with the first year of the coronavirus outbreak. The first survey was conducted March 2-15, 2020, and the second was conducted April 12-18, 2021.
The questions that are the focus of this analysis asked parents to think specifically about one of their children who was age 11 or younger in March 2020. If the parent had more than one child age 11 or younger at the time of the first survey, they were instructed to think about either their oldest or youngest child in this age group.
The following terminology is used in this analysis:
Parents of a young child: Refers to parents who had at least one child age 11 or younger when first interviewed in March 2020.
Parents of a child age 0 to 4: Refers to parents whose randomly assigned child was under age 5 (0 to 4) in March 2020.
Parents of a child age 5 to 11: Refers to parents whose randomly assigned child was age 5 to 11 in March 2020.
Everyone who is part of this analysis is a member of the Center’s American Trends Panel (ATP), an online survey panel that is recruited through national, random sampling of residential addresses. This way, nearly all U.S. adults have a chance of selection. Data from the ATP is weighted to be representative of the U.S. adult population by gender, race, ethnicity, partisan affiliation, education and other categories. Read more about the ATP’s methodology .
The data for this analysis is also adjusted to represent the population of parents with one or more children ages 17 or younger living in their household as of March 2020, and focuses on the subset who had at least one child age 11 or younger at the time, regardless of whether that child lived in their household (referred to as a “young child” in this analysis).
Here are the questions, responses and methodology used for this analysis.

More use of digital devices and some social media sites
Whether a result of the pandemic or simply of other events or changes in a child’s life, the year following our first survey in March 2020 saw a rising share of parents who said their young child had used digital devices and social media.
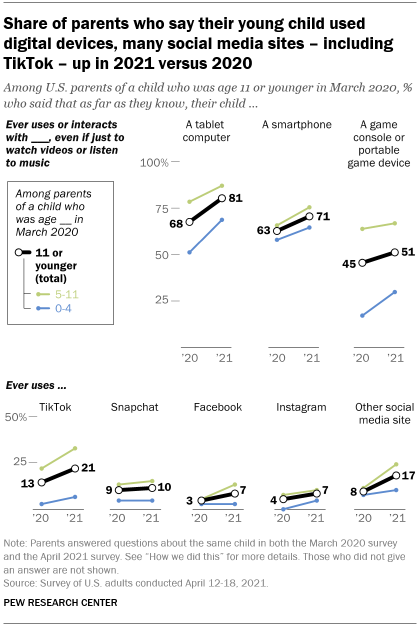
In April 2021, about eight-in-ten parents of a child who was age 11 or younger at the time of the first interview (81%) said their kid ever used or interacted with a tablet computer – even if just to watch videos or listen to music – up from 68% in March 2020. About seven-in-ten (71%) said the same thing about their kid’s use of a smartphone, up from 63% the year before. And 51% of parents with a young child said their child used a game console or portable game device in 2021, up slightly from 2020.
Among the four social media sites the survey covered, the largest share of parents reported that the young child they were asked about used TikTok: 21% said this in April 2021, up from 13% in 2020. There were small changes in the share saying their child used Instagram or Facebook, while Snapchat use stayed virtually the same. And the share who said their young child used a social media site other than TikTok, Snapchat, Facebook and Instagram roughly doubled between 2020 and 2021, from 8% to 17%.
Social media use differed dramatically depending on the age of the child being followed over time; for example, relatively few parents who had a child under 5 when the pandemic began said this child used social media in either 2020 or 2021.
But for some social media sites, there were changes for kids on both ends of this age range. Among parents who had a child age 5 to 11 at the outset of the pandemic, the share who said this child used TikTok rose 11 percentage points (21% in 2020 to 32% in 2021). For parents with a child who was younger than 5 at the time of the first interview, there was a 4-point uptick from 1% to 5%.
There were also double-digit increases in the share of parents answering about a child who was under 5 in March 2020 who said this child used a tablet (51% in 2020 to 69% in 2021) or a game console or portable game device (16% to 29%) over this period. Still, parents of a child this age were far less likely than those whose child was age 5 to 11 at the outset of the pandemic to report use of these digital devices in either year.
Other variations in kids’ use of devices and social media were also apparent. Even as many kids started using tech in 2021, others were not using these things in 2021 when they had in 2020. Among parents with a young child who said their kid had used a smartphone in 2020, for instance, 14% said their child was not using one in 2021. Similarly, 19% of parents who said their young child had used a game console or portable game device in 2020 said that child was not doing so in 2021.
Growing parental concerns about screen time
Amid these changes, parents increasingly expressed worry about the amount of time their child was spending on devices.
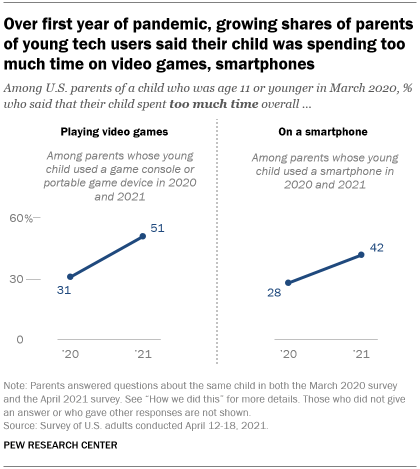
When asked about screen time in April 2021, a quarter of all parents of a young child said that their child spent too much time on a smartphone; about the same share (23%) said their child spent too much time playing video games; and about one-in-ten (8%) said the same about time on social media sites.
For parents whose child used a gaming console or portable game device in both 2020 and 2021, the share who said that child spent too much time playing video games rose 20 points over the first year of the pandemic, from 31% to 51%.
There was also a 14-point jump in the share of parents who said their smartphone-using young child spent too much time on it, from 28% to 42% among those whose child used one in both 2020 and 2021.
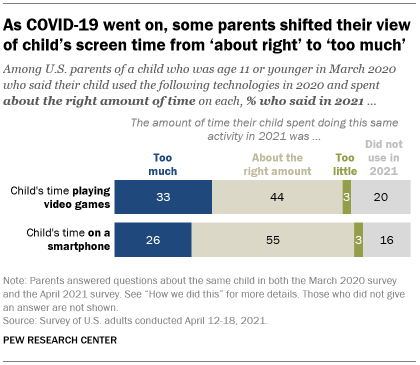
And while majorities of parents whose child used these devices in 2020 initially said their child’s time on them was about right, some parents reported different views on screen time a year later when reinterviewed.
Among parents who thought their child’s time playing video games was appropriate in 2020, 44% said the same in 2021 – but a third said that their child was now spending too much time doing this. Similarly, among those who said their child’s time on smartphones was about right in 2020, about a quarter (26%) said in 2021 that their child was now spending too much time this way; 55% said it was still about right.
Some changes in parents’ management of screen time
In both March 2020 and April 2021, majorities of parents whose child was 5 to 11 at the start of the pandemic said they ever checked the websites their child visits or the mobile apps they use; limited the times of day or length of time when this child can use screens; or took away the child’s smartphone or internet privileges as punishment. But the patterns of change over time also show some movement in parents’ approaches.
Some 16% of parents with a child this age said they did not limit screen time for this child in 2021, despite having said they did so in 2020. Conversely, 8% of these parents reported limiting their child’s screen time in 2021, after having not done this in 2020. There was a similar pattern when it comes to taking away smartphone or internet privileges: 14% of parents who had a 5- to 11-year-old child at the start of the pandemic didn’t do this in 2021 even though they had in 2020, compared with 6% who moved in the opposite direction. The Center’s other work also reflects these changing approaches to screen time – some parents loosened their rules during the pandemic, while others became stricter.
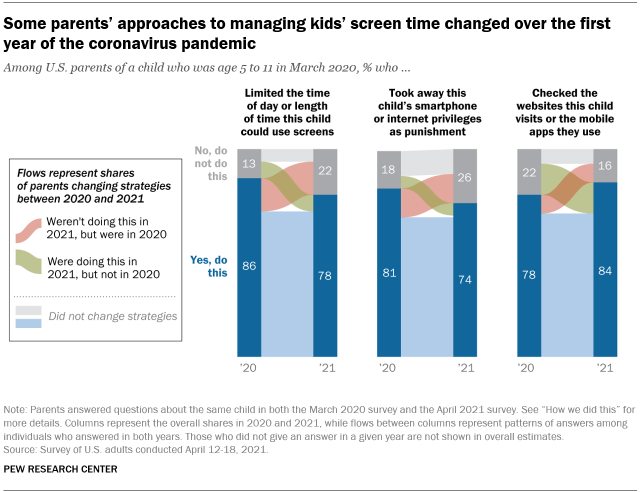
Some parents whose child was 5 to 11 in March 2020, for example, became more attentive to what their child was doing online over time: 15% of these parents said they checked their kid’s website or app usage in 2021 – and that they had not done this in 2020.
Changes in parenting approaches also extended to the times of day children could use screens. For example, about half of parents of a 5- to 11-year-old child in 2020 (48%) said in 2021 that they would allow their child to use mobile devices just before bedtime. Some had loosened their stance from a year prior: 16% reported being OK with this in 2021 after saying the opposite in 2020. On the other hand, 8% tightened their restrictions – they were no longer OK with their child using mobile devices just before bed. Some 43% of parents consistently were not OK with it, while 32% consistently were.
The unique approach of this study – surveying parents about a specific child and looking at how individual parents’ responses changed over time – provides a window into children’s pandemic experiences with technology. Still, parents may not always know what devices their children use or exactly how much time they spend on them. And beyond these findings, it is important to note that screen time can take many forms and that there are healthy debates about whether and how screen time affects children.
Note: Here are the questions, responses and methodology used for this analysis.
- Children & Tech
- Coronavirus (COVID-19)
- COVID-19 & Technology
- Social Media

Colleen McClain is a research associate focusing on internet and technology research at Pew Research Center
59% of U.S. parents with lower incomes say their child may face digital obstacles in schoolwork
Parenting children in the age of screens, a week in the life of popular youtube channels, facts on foreign students in the u.s., the skills americans say kids need to succeed in life, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
Building and construction workers are reporting mental health issues in high numbers, but some are trying to make a difference
Like many people in construction, James Knight is feeling the pressure his industry is under.
In recent times, his Canberra electrical business has been left unpaid for work due to other construction companies collapsing.
"It's affected my kids seeing my wife and I stressed about it," Mr Knight said.
"It's affected our employees with the uncertainty and just having to go by our word that that we'll pull through and we'll be okay."
Mental health challenges among tradies have been common for years, if not always talked about.
The charity MATES in Construction estimates someone from the industry is lost to suicide every two days.
High interest rates, increased costs and a shortage of labour and materials are now adding an extra mental burden.
Mr Knight lives with depression and anxiety, and said the issues the industry is facing have not helped.
"I notice I'm not running at optimum performance, mentally speaking," he said.
"The guys notice it and notice the self-esteem is not always there.
"I've actually been diagnosed with ADHD, which lends itself to [depression and anxiety]"
But his experiences have prompted Mr Knight to take action to prevent others going through the same thing.
He and his wife Nikki run their business a little differently.
They reimburse staff for health-related costs such as gym memberships and supplements to help them maintain positive mental health.
He said he also encouraged his staff to be open about their problems.
"Their general health is very important to us, both mental and physical," Mr Knight said.
"My wife Nikki and I have got an open-door policy. We've definitely had a range of different things brought to us and some surprising, some straight down what we were expecting.
"But I think holistically, everyone is in a lot better place for it."
Industry wide problems
Research conducted by Central Queensland University indicates people who work in the building and construction industry are at a significantly higher risk of mental health problems.
MATES in Construction chief executive Chris Lockwood said it was a combination of long hours and work that could be both dangerous and lonely.
"That's why we do see significantly higher rates of poor mental health and tragically, even suicide in the industry," Mr Lockwood said.
The cost-of-living crisis overlaid on the current problems in the industry has compounded those dangers.
"Those sorts of pressures in terms of the finances that already were an issue for people working construction," Mr Lockwood said.
"[With] the cost of living, the impacts on top of it, we've seen some very direct impacts.
"Some months our call volumes have almost more than doubled, [from] people that are actually calling in distress needing support."
Building in a fix
Like a lot of male-dominated industries, Mr Knight said in decades past there has been a culture of silence when it comes to mental health.
He said things had changed in the industry.
"[It used to be] just go to the pub and write yourself off," he said.
"I think it's a lot easier these days, there's a lot more education around the mental health space and it being okay to not be okay."
Across the industry, mental health charities are improving mental health culture one job site at a time.
Canberra's The Healthy Tradie Project speaks to workers on site about mental health, incorporating breath work and yoga into their outreach.
OzHelp has been helping people in blue collar "high risk and hard to reach" jobs for 20 years.
David Lockwood said the mental health outreach sessions that MATES in Construction have on-site can save lives.
"The blokes and the women are all comfortable to step forward and actually say 'we should look out for our mates and have those honest conversations'."
- X (formerly Twitter)
Related Stories
'bang there goes $120,000': subcontractors struggling to stay afloat after building companies collapse.
Construction workers are more likely to die by suicide than a work accident. Joel wants to change that statistic
Jeff was having suicidal thoughts. Then he met John
- Construction and Real Estate Industry
- Mental Health
This paper is in the following e-collection/theme issue:
Published on 25.4.2024 in Vol 26 (2024)
Digital Therapeutic (Mika) Targeting Distress in Patients With Cancer: Results From a Nationwide Waitlist Randomized Controlled Trial
Authors of this article:

Original Paper
- Franziska Springer 1 * , MSc ;
- Ayline Maier 2 * , PhD ;
- Michael Friedrich 1 , PhD ;
- Jan Simon Raue 2 , PhD ;
- Gandolf Finke 2 , PhD ;
- Florian Lordick 3, 4 , Prof Dr ;
- Guy Montgomery 5 , Prof Dr ;
- Peter Esser 1 , PhD ;
- Hannah Brock 1 , MSc ;
- Anja Mehnert-Theuerkauf 1 , Prof Dr
1 Department of Medical Psychology and Medical Sociology, Comprehensive Cancer Center Central Germany, University Medical Center Leipzig, Leipzig, Germany
2 Fosanis GmbH, Berlin, Germany
3 Department of Medicine II, University Medical Center Leipzig, Leipzig, Germany
4 University Cancer Center Leipzig, Comprehensive Cancer Center Central Germany, Leipzig, Germany
5 Center for Behavioral Oncology, Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York, NY, United States
*these authors contributed equally
Corresponding Author:
Anja Mehnert-Theuerkauf, Prof Dr
Department of Medical Psychology and Medical Sociology, Comprehensive Cancer Center Central Germany, University Medical Center Leipzig
Philipp-Rosenthal-Str. 55, Haus W
Leipzig, 04103
Phone: 49 341 97 18800
Email: [email protected]
Background: Distress is highly prevalent among patients with cancer, but supportive care needs often go unmet. Digital therapeutics hold the potential to overcome barriers in cancer care and improve health outcomes.
Objective: This study conducted a randomized controlled trial to investigate the efficacy of Mika, an app-based digital therapeutic designed to reduce distress across the cancer trajectory.
Methods: This nationwide waitlist randomized controlled trial in Germany enrolled patients with cancer across all tumor entities diagnosed within the last 5 years. Participants were randomized into the intervention (Mika plus usual care) and control (usual care alone) groups. The participants completed web-based assessments at baseline and at 2, 6, and 12 weeks. The primary outcome was the change in distress from baseline to week 12, as measured by the National Comprehensive Cancer Network Distress Thermometer. Secondary outcomes included depression, anxiety (Hospital Anxiety and Depression Scale), fatigue (Functional Assessment of Chronic Illness Therapy-Fatigue), and quality of life (Clinical Global Impression-Improvement Scale). Intention-to-treat and per-protocol analyses were performed. Analyses of covariance were used to test for outcome changes over time between the groups, controlling for baseline.
Results: A total of 218 patients (intervention: n=99 and control: n=119) were included in the intention-to-treat analysis. Compared with the control group, the intervention group reported greater reductions in distress ( P =.03; ηp²=0.02), depression ( P< .001; ηp²=0.07), anxiety ( P= .03; ηp²=0.02), and fatigue ( P= .04; ηp²=0.02). Per-protocol analyses revealed more pronounced treatment effects, with the exception of fatigue. No group difference was found for quality of life.
Conclusions: Mika effectively diminished distress in patients with cancer. As a digital therapeutic solution, Mika offers accessible, tailored psychosocial and self-management support to address the unmet needs in cancer care.
Trial Registration: German Clinical Trials Register (DRKS) DRKS00026038; https://drks.de/search/en/trial/DRKS00026038
Introduction
In addition to somatic symptoms such as pain [ 1 ], patients with cancer report elevated levels of distress, anxiety, and depression [ 2 , 3 ]. Epidemiological data show that the prevalence of clinically substantial psychological distress typically ranges from 30% to 60% among patients with cancer [ 2 , 4 ]. Psychological distress can persist long after the end of treatment and is associated with reduced quality of life (QoL), lower cancer treatment adherence, and lower survival rates [ 5 ].
Supportive care interventions to prevent and manage the adverse psychological and physical effects of cancer across the cancer trajectory effectively improve outcomes such as emotional distress, QoL, and fatigue [ 6 ]. Optimal supportive care is holistic and patient centered, that is, based on the needs of each individual patient [ 7 ]. However, access to supportive care is often limited by a lack of specialist staff, organizational deficiencies, and barriers that cause patients to avoid or delay their treatment [ 8 - 10 ]. Thus, emerging or persistent supportive care needs across the cancer trajectory often go unmet, with detrimental psychosocial and emotional impacts on patients with cancer [ 11 ]. Moreover, the number of patients living with cancer has increased rapidly in recent years [ 12 ] due to improved early detection, diagnosis, and oncological treatments, posing a growing challenge to health systems worldwide to ensure adequate and long-term care for all patients with cancer [ 13 ].
The increasing use of digital health has ushered in a new era of patient-centered cancer care due to its potential for cancer care delivery [ 14 ]. Digital health interventions provide multiple benefits: they facilitate easy and low-threshold access to care, can overcome barriers to care (eg, location, time, and health status), may enhance symptom management through real-time symptom assessment, are scalable, and provide cost-effective and efficient information sharing [ 14 ]. Growing literature suggests that digital therapeutics, a subset of digital health interventions providing evidence-based treatments driven by software, play a useful role in addressing the unmet needs of patients with cancer [ 15 ]. For instance, various mobile apps have proven to be effective in catering to specific needs of patients with cancer, such as pain, anxiety, or QoL, by using different types of interventions, such as psychoeducation, physical exercises, or coping skills training (eg, [ 16 - 19 ]). Moreover, large analyses such as systematic reviews and meta-analyses evaluating the efficacy of app-based interventions for patients with cancer show positive effects on patient-relevant outcomes, such as distress, QoL, anxiety, depression, pain, and fatigue [ 20 - 23 ].
Existing app-based supportive care interventions provide various intervention modules, such as symptom monitoring, psychoeducation, mindfulness exercises, physical exercises, and cognitive behavioral therapy (CBT) techniques [ 24 ]. However, most of these apps are limited in their scope, targeting only specific symptoms (eg, fatigue) [ 25 ] and health behaviors (eg, physical activity) [ 26 ], or provide only a single function (eg, mindfulness training or symptom tracking) [ 27 - 29 ]. Furthermore, some of these apps were originally developed for non–oncology patient populations and have only been slightly adapted for patients with cancer [ 30 ]. Only a few apps offer a broader range of intervention modules [ 25 , 31 ], but they target specific subgroups of patients with cancer (eg, patients with 1 tumor entity or with specific symptoms).
Despite the evident need, there is yet no digital therapeutic that comprehensively addresses the problems faced by all patients with cancer and simultaneously offers tailored support for each individual patient. Therefore, we investigated the efficacy of Mika (developed by Fosanis GmbH), an app-based digital therapeutic that addresses all patients with cancer transdiagnostically and provides a holistic supportive care intervention. The app incorporates evidence-based supportive care elements, such as distress and symptom monitoring [ 32 ], CBT-based coping skills training [ 33 ], mindfulness-based stress reduction (MBSR) [ 34 , 35 ], strength and flexibility training [ 36 ], and patient education [ 37 ], thus targeting different aspects of psychological distress. An artificial intelligence algorithm individually tailors the content of the app to patients’ needs, considering cancer type, cancer treatment stage, and use behavior. A previously conducted pilot study of 70 patients with gynecological cancer indicated Mika’s feasibility and potential efficacy [ 38 ]. Considering the significant prevalence and impact of psychological distress among patients with cancer, this condition was selected as the primary end point of our study. This is underscored by the app’s integrated features for distress tracking and management alongside the widespread recommendation for distress screening in routine clinical care. Distress is recognized as a crucial clinical marker for assessing the efficacy of interventions across various tumor types and catering to the immediate and long-term supportive care needs of this patient group.
The primary aim of this waitlist randomized controlled trial (RCT) was to examine the efficacy of the Mika app for general distress in patients with cancer. The secondary aim was to assess the efficacy of the Mika app on anxiety, depression, fatigue, and QoL. We hypothesized that participants receiving access to the Mika app plus usual care (UC) for 12 weeks would report greater reductions in distress, anxiety, depression, and fatigue and greater improvements in QoL compared to participants receiving UC only.
Study Design
This nationwide unblinded 2-arm waitlist RCT evaluated the efficacy of the app-based digital therapeutic Mika in reducing distress in patients with cancer and was conducted fully decentralized in Germany, that is, participant recruitment, delivery of the study intervention, and outcome data collection were conducted without involving in-person contact between the study team and the participants. In this RCT, participants were assigned to either (1) access to the Mika app plus UC (intervention group [IG]), or (2) UC alone (control group [CG]). Participants were assessed at baseline (t0), 2 weeks (t1), 6 weeks (t2), and 12 weeks (t3) using self-report questionnaires. Once the participants in the CG completed the 12-week questionnaire, they also received access to the Mika app.
Ethical Considerations
The trial was approved by the Ethics Committee of the Medical Faculty of Leipzig University (404/21-ek) and was registered at the German Clinical Trials Register (DRKS00026038) in October 2021. All participants provided written informed consent prior to their participation in the study and retained the autonomy to withdraw from the study at any time. All personal data collected and used for this study underwent deidentification to safeguard the anonymity of participants. Monetary compensation was not provided to participants for their involvement in the study.
Participants
Textbox 1 shows the inclusion and exclusion criteria for this study. We only included patients who had been diagnosed with cancer or relapse within the last 5 years as they are likely to feel burdened by the physical and psychological effects of the disease and its treatment and therefore require supportive care. Epidemiological data indicate that supportive care needs typically decline in the years of long-term survivorship (cancer or relapse diagnosis ≥5 years ago) [ 39 ]. Participants were required to confirm their cancer diagnosis during the course of the study by submitting a letter from their treating physician. The study team enrolled patients after they had provided written informed consent, which had to be completed at home and submitted by email or mail.
Inclusion criteria
- Age≥18 years
- Cancer diagnosis or relapse diagnosis within the last 5 years (10th revision of the International Statistical Classification of Diseases and Related Health Problems: C00-C97)
- Access to a smartphone or tablet
- Ability to provide informed consent
Exclusion criteria
- Insufficient German language skills
- Inability to use a smartphone or tablet
- Prior use of the investigated digital therapeutic
Random Assignment
Participants were randomly assigned (1:1) to either the IG or CG using permuted block randomization with blocks of 4 based on an a priori created randomization list. The allocation sequence was concealed from the study investigators until assignment. Due to the nature of the intervention, it was not feasible to blind participants or the study team to the group assignment.
Recruitment and Procedure
Between September and November 2021, patients were recruited via social media advertising campaigns (Facebook and Instagram, Meta Inc) and informational emails to cancer support groups that directed patients to the trial website with a contact form for study registration. In addition, patients were recruited from a participant pool consisting of participants from previous independent studies at the University Medical Center Leipzig. Patients from the participant pool were approached directly by the study team via phone.
All interested patients were screened by phone to determine eligibility. To identify patients who were already users of the digital therapeutic, the study team asked participants about their use of digital support, however, without referring to the publicly available digital therapeutic by name to prevent CG patients from accessing the digital therapeutic before their enrollment in the study. Eligible patients received study information in the form of a video and text via email. Patients were informed that they were required to submit a physician’s letter confirming their cancer diagnosis via a secure cloud data-sharing service (TeamDrive, Crunchbase) during the course of their study participation. After providing informed consent, the participants were randomized into the IG or CG and completed the baseline questionnaires. Participants were informed about their group assignment following a completed baseline assessment. IG participants received a study access code to activate the app after downloading it from the app stores for either Android or iOS smartphones, allowing free use. The questionnaire battery was administered electronically using LimeSurvey (LimeSurvey GmbH). All participants received email invitations and reminders at 2, 6, and 12 weeks to complete the questionnaire. This RCT focused on changes in outcomes from baseline (t0) to week 12 (t3). The 2 assessments in between (t1 and t2) were not part of the analysis; an analysis of the trajectory of the symptoms is planned for the future. Once the CG participants completed the 12-week questionnaire, they also received a study access code that could be used to activate the app. All the participants received information about the app’s content and technical application via a standardized telephone introduction to the app. All participants were contacted for an exploratively structured telephone interview after completing the 12-week questionnaire. During this interview, the use of psychotherapeutic support during study participation was assessed. Data collection ended in March 2022.
Data monitoring was performed via standardized phone calls following questionnaire completion of each participant across all measurement time points to ensure data validity. These phone calls served to ask participants to provide missing questionnaire data, to allow participants to clarify difficulties in understanding single questionnaire items, and to provide assistance with limited app functionality. Missing questionnaire data were entered directly into the database by the study team, with a study team member reading the unanswered questions and associated response options to participants verbatim, prompting them to select their response option.
Self-reported adverse reactions and side effects of the investigated digital therapeutic were assessed at each measurement time point as part of the web-based questionnaire battery.
Intervention
Mika is an app-based digital therapeutic that provides a personalized supportive intervention aiming to reduce distress associated with cancer and its medical treatment, thus improving patients’ QoL. Mika comprises 3 modules: Check-Up , Discover, and Journeys . The Check-Up module allows for the monitoring of distress and symptom monitoring with electronic patient-reported outcomes that can be shared and discussed with the attending physician. The Discover module delivers coaching via articles and videos on cancer types and medical treatments, psychological well-being, physical activity, diet, and social and financial issues, which are based on scientific evidence and presented in a clear and understandable manner for patients. The Journeys module provides users with evidence-based, resource-activating training courses combining psychoeducation and exercises to help patients cope with the mental and physical effects of cancer, for example, coping with stress and fatigue, making decisions, or living with immunotherapy (for more details on the app modules, refer to Table 1 and Figure 1 ). An artificial intelligence algorithm within the app customizes the content for each patient. This includes personalized recommendations based on cancer type, cancer treatment stage, and crucially; the nature and severity of reported symptoms; and ensuring personalized support for each individual. This customization process not only accounts for general patient information but also actively incorporates real-time symptom tracking data and user reading behavior using an attentional factorization machine that predicts a patient’s likelihood of engaging with specific content. This approach focuses on important feature interactions related to content consumption [ 40 ], ensuring that recommendations are dynamically adjusted as patients report changes in symptoms and interact with the content. In addition, the algorithm uses a Dirichlet loss function to estimate the uncertainty in predictions [ 41 ], allowing the content to be ranked and presented based on the estimated read probability. The model undergoes monthly updates using historical data, optimizing through hyperparameter tuning evaluated by 7-fold time series cross-validation.
It is hypothesized that the digital therapeutic empowers patients with cancer by improving their health literacy and self-management along the cancer trajectory using evidence-based methods, such as symptom monitoring, patient education, MBSR, strength and flexibility training, acceptance and commitment therapy, and CBT-based coping skills training.
The Mika app was developed by Fosanis GmbH in collaboration with leading research institutions, such as the Charité University Hospital Berlin, University Hospital Leipzig, and the National Center for Tumor Diseases Heidelberg. All content of the app was carefully reviewed by experts (eg, oncologists, psychotherapists, nutritionists, and physiotherapists) before publication. The feasibility and preliminary efficacy of Mika were investigated in a previously conducted randomized pilot study involving 70 patients with gynecological cancer [ 38 ]. Mika is available for download free of charge in German and the United Kingdom app stores for Android and iOS smartphones.
IG participants could freely choose the modules to work on. While regular app use was recommended, participants were instructed to use the app at least 3 times a week.
a PRO: patient-reported outcome.

UC Condition
UC consisted of all health care that patients in Germany usually receive. There were no restrictions on health care use.
Outcome Assessment
Primary outcome.
The primary outcome was the change in psychological distress from baseline to 12 weeks, measured using the validated German version of the National Comprehensive Cancer Network Distress Thermometer [ 42 ]. Distress Thermometer is a well-established single-item self-report measure that assesses the global level of distress on a 0 (no distress) to 10 (extreme distress)-point Likert scale. It shows excellent psychometric properties across various cancer populations worldwide and is recommended as a clinical tool for routine clinical care [ 43 ]. A score ≥5 indicates clinically significant levels of distress.
Secondary Outcomes
The secondary outcomes included changes in anxiety and depression symptoms, fatigue from baseline to 12 weeks, and QoL at 12 weeks. Anxiety and depression symptoms were measured using the Hospital Anxiety and Depression Scale [ 44 ], a 14-item self-report measure of anxiety and depression, with 7 items measuring each subscale. Scores for each subscale range from 0 to 21, with a higher score indicating higher levels of anxiety or depression and a cutoff score of ≥8 for each subscale. Fatigue was assessed using the Functional Assessment of Chronic Illness Therapy-Fatigue [ 45 ], a 13-item measure that assesses self-reported tiredness, weakness, and difficulty in performing usual activities due to fatigue. The Functional Assessment of Chronic Illness Therapy-Fatigue score ranges from 0 to 52, with higher scores representing less fatigue. Self-reported QoL was measured using an adapted version of the Clinical Global Impression-Improvement Scale [ 46 ], a single-item 7-point measure that assesses the overall improvement of a patient’s disease relative to a baseline state at the beginning of the intervention. In this trial, the Clinical Global Impression-Improvement Scale measured improvement in QoL relative to the beginning of the study, with a value of 4 indicating no change, <4 indicating improvement, and >4 indicating deterioration in QoL.
Intervention Safety
The safety of the digital therapeutic was assessed by the number and type of self-reported adverse reactions and side effects during the trial duration.
Intervention Adherence and Engagement
Adherence to the intervention was assessed by tracking app activities. IG participants were considered active once they activated the app using the study access code and consented to the Mika app’s privacy terms. Subsequently, their pseudonymized in-app activities were automatically recorded as log data. These log data facilitated the evaluation of intervention adherence, defined as the number of days with ≥1 app activity during each of the three 4-week periods (0-4, 5-8, and 9-12 weeks) within the 12-week intervention. Such an approach enabled us to capture the frequency and diversity of app engagement, thus embodying a comprehensive definition of adherence. In addition, engagement across the app’s 3 modules—Check-Up, Discover, and Journeys—was analyzed.
Statistical Analysis
Given an estimated dropout rate of 20% (50/250), a priori sample calculations showed that a sample of 2×125 (N=250) at baseline was needed to detect a change of 1 scale point (SD 2; α=.05; 1−β=.8) in the primary outcome.
Primary analyses were performed using the intention-to-treat (ITT) principle, which included all randomized participants with a confirmed cancer diagnosis by a physician’s letter. Analyses were also performed per-protocol (PP), which was restricted to participants who (1) completed the self-report questionnaire at all measurement time points, (2) did not receive psychotherapeutic support during study participation, (3) did not use the investigated digital therapeutic before receiving access during study participation, and (4) used the investigated digital therapeutic at least 1 time per period up to the 5- to 8-week period of the 12-week intervention period (only IG).
Analysis of covariance was used to examine changes in distress, depression, anxiety, and fatigue outcomes between the trial arms from baseline to 12 weeks, controlling for baseline scores. Exploratory regression analyses were conducted to investigate potential variables influencing the primary outcome. These analyses focused exclusively on sociodemographic and clinical factors that showed differences between the IG and CG in the initial group comparison. Partial eta–squared was reported as the effect size for all analyses of covariance, with effect sizes interpreted as small, medium, and large at ≥0.01, ≥0.06, and ≥0.14 [ 47 ], respectively. Differences in QoL between trial arms at follow-up (12 weeks) were analyzed with a 2-tailed 2-sample t test, using Hedges g ' as a measure of effect size (≥0.2=small effect, ≥0.5=medium effect, and ≥0.8=large effect [ 47 ]).
Missing outcome data at random were imputed using the expectation-maximization algorithm. For dropouts, the last observation carried forward was used. For deceased participants, the worst possible values were assumed. Dropouts were participants who failed to complete the baseline or follow-up questionnaires or failed to provide a physician’s letter confirming their cancer diagnosis. A dropout analysis was performed to compare the variables of age, sex, and baseline distress between study noncompleters (dropouts) and study completers using chi-square and t tests. Furthermore, to model the robustness of the primary efficacy analysis under different assumptions for missing data mechanisms, an explorative sensitivity analysis using reference-based multiple imputation (jump-to-reference) [ 48 ] was performed in the extended ITT population (all randomized participants). For this purpose, monotone missing values were replaced using the jump-to-reference approach, whereas sporadic missing values were replaced under the assumption of missing at random. For jump-to-control and jump-to-reference imputation, 50 data sets were generated to minimize the loss of statistical power. The results were then aggregated across the imputed data sets [ 49 ].
All statistical tests were 2-tailed, with a significance level of 5%. Analyses were performed using R (version 4.1.0; R Foundation for Statistical Computing) [ 50 ].
Study Sample
Over the 3-month recruitment period, 517 persons were screened for eligibility and 321 were determined eligible. Of the 321 participants, 248 (77.3%) gave informed consent and were randomly assigned to the IG and the CG ( Figure 2 ). Of the 248 participants, 37 (14.9%) were considered dropouts because they did not complete baseline or follow-up assessments (n=7), failed to confirm their cancer diagnosis by submission of a physician’s letter (n=7), or both (n=23). Age and sex of study dropouts and study completers did not differ ( P age =.89 and P sex =.23), but participants who dropped out showed higher distress levels at baseline compared to study completers ( P =.02). Participants without a verified cancer diagnosis (30/248, 12.1%) were excluded from the ITT analysis, resulting in an ITT population of 218 participants (n=99, 45.4% IG and n=119, 54.6% CG). Of the 218 participants, 173 (79%) were recruited via social media advertisements and cancer support groups and 45 (21%) were recruited using the participant pool of prior studies.

Baseline characteristics were balanced between the groups ( Table 2 ), but participants in the IG were younger compared with those in the CG ( P =.02). No baseline differences in the primary and secondary outcome parameters were observed between the groups, with P values as follows: P =.99 (distress), P =.25 (depression), P =.47 (anxiety), and P =.21 (fatigue). On average, participants were 56 (SD 11) years old, and 60.6% (132/218) of the participants were female and had been diagnosed with cancer 25 (SD 17) months earlier. The most frequently reported cancer types were breast cancer (74/218, 33.9%) and hematological cancer (61/218, 28%), with 8.7% (19/218) of participants reporting a diagnosis of relapsed cancer. The PP population comprised 124 participants, following the exclusion of 94 participants. The primary reasons for exclusion were psychotherapeutic support during study participation and prior use of the investigated digital therapeutic.
a Intervention=12-week access to digital therapeutic app intervention+usual care.
b Control=usual care.
c NCCN Distress Thermometer: National Comprehensive Cancer Network Distress Thermometer (at baseline, clinically significant level of distress≥5).
d HADS-A: Hospital Anxiety and Depression Scale, anxiety subscale (German version, at baseline, cutoff score ≥8).
e HADS-D: Hospital Anxiety and Depression Scale, depression subscale (German version, at baseline, cutoff score ≥8).
f Multiple reasons are possible within 1 patient, and cases do not add up to the total number.
After 12 weeks, participants in the IG reported a reduced level of distress compared to participants in the CG in the ITT population ( F 1,215 =4.7; P =.03; ηp²=0.02; Table 3 ). The observed treatment effect was more pronounced in the PP population ( F 1,121 =6.9; P =.01; ηp²=0.05). The analysis revealed that higher levels of baseline distress predicted a greater change in distress after 12 weeks in the IG. An exploratory regression analysis yielded no predictive effect of age on the change in distress. The explorative sensitivity analysis among all randomized participants (n=248) showed comparable treatment effects (jump-to-control: F 1,19375.1 =5.3; P =.02; ηp²=0.02 and jump-to-intervention: F 1,15314.8 =5.9; P =.02; ηp²=0.02).
a An analysis of covariance was used to test for differences in change in distress levels between groups from baseline to follow-up (12 weeks), controlling for baseline. The partial eta–squared is the reported standardized effect size for the mean difference. The effect sizes can be interpreted as small, medium, or large at ≥0.01, ≥0.06, and ≥0.14, respectively. The results of the intention-to-treat and per-protocol analysis are reported.
b Intervention=12-week access to digital therapeutic app intervention+usual care.
c Control=usual care.
d N/A: not applicable.
In the ITT population, symptoms of anxiety ( F 1,215 =4.8; P =.03; ηp²=0.02), depression ( F 1,215 =15.5; P <.001; ηp²=0.07), and fatigue ( F 1,215 =4.4; P =.04; ηp²=0.02) improved in participants in the IG from baseline to 12 weeks compared to participants in the CG ( Table 4 ). The observed treatment effects on anxiety and depression were more pronounced in the PP population (anxiety: F 1,121 =7.2; P =.01; ηp²=0.06 and depression: F 1,121 =14.9; P <.001; ηp²=0.11). A trend-to-significant treatment effect was observed for fatigue symptoms in the PP population ( F 1,121 =3.8; P =.05; ηp²=0.03). QoL did not differ significantly between the groups at 12 weeks (ITT: t 216 =0.88; P =.38; g=0.12 and PP: t 122 =1.63; P =.11; g=0.30).
c HADS-A: Hospital Anxiety and Depression Scale, anxiety subscale (German version, at baseline, cutoff score ≥8).
d ITT: intention-to-treat.
e N/A: not applicable.
f Italicized values are significant at P <.05.
g PP: per-protocol.
h HADS-D: Hospital Anxiety and Depression Scale, depression subscale (German version, at baseline, cutoff score ≥8).
i FACIT-F Functional Assessment of Chronic Illness Therapy–Fatigue.
j CGI-I: Clinical Global Impression Improvement.
Safety Outcomes
IG participants reported no adverse reactions or side effects of digital therapeutic during the study.
Of the 99 participants in the IG (ITT), 98 (99%), 78 (79%), and 67 (68%) used the digital therapeutic intervention at 0- to 4-, 5- to 8-, and 9- to 12-week periods of the 12-week intervention, respectively, demonstrating good initial adherence to the intervention, which decreased moderately over time. App use (module use and days spent on the app) decreased over time ( Table 5 ). IG participants accessed content from various categories at different frequencies. The most accessed categories were cancer therapy, symptoms and side effects, and nutrition in cancer, with 80% (79/99), 83% (82/99), and 80% (79/99) of users accessing the content in these categories, respectively. Conversely, partnership and family, relaxation, and recipes were accessed less, with 29% (28/99), 34% (33/99), and 32% (31/99) of users, respectively.
Principal Findings
This nationwide waitlist RCT examined the efficacy of Mika, an app-based digital therapeutic that provides a personalized supportive intervention for patients with cancer. Participants who had access to the Mika app for 12 weeks showed significant improvements in perceived distress (ie, the primary outcome) and symptoms of anxiety, depression, and fatigue (ie, the secondary outcomes) compared to participants who received UC. The observed treatment effects were similar in the ITT and PP populations but more pronounced in the PP population, indicating the overall robustness of the findings. We observed no group difference in the QoL after 12 weeks. Intervention adherence was good, and no adverse reactions or side effects of the investigated digital therapeutic were reported.
Comparison With Prior Work
While a growing body of research shows evidence of the efficacy of app-based interventions for oncological populations on distress, fatigue, anxiety, and depression [ 20 , 25 , 27 , 31 , 51 ], this is the first study to examine the efficacy of a single holistic app-based digital therapeutic based on multiple intervention modules on these patient-relevant outcomes. Although the improvement in the primary outcome was modest, it reflects the nuanced nature of psycho-oncological interventions, where even modest changes can have significant clinical relevance. Furthermore, we conducted comprehensive testing of the effects of the investigated digital therapeutic on patients with cancer across all tumor entities, using a larger sample size compared to most previous studies [ 25 , 27 , 31 , 51 ].
In contrast to the findings of this study, however, other studies found an effect of app-based supportive interventions on QoL [ 23 , 27 , 31 ]. This difference in findings could be due to differences in the operationalization and measurement of QoL. In this study, participants’ global QoL was assessed using a single-item questionnaire after a 12-week intervention period. However, global QoL has been shown to be less affected in patients with cancer compared to specific components of QoL, such as social or cognitive functioning and symptom burden from fatigue or insomnia [ 52 ]. Further research using different QoL assessment tools could provide more insights into the efficacy of the investigated digital therapeutic on specific aspects of QoL.
A significant level of intervention adherence and engagement with the digital therapeutic, with varying degrees of interaction across the different app modules, indicates good acceptability and perceived subjective benefit of the investigated digital therapeutic and allows for reliable conclusions about its efficacy in oncological settings. The broad range of engagement, as illustrated by the IQRs, underscores the personalized nature of app use, catering to diverse participant needs and preferences. The variability in engagement levels across different app modules highlights the importance of personalizing digital therapeutics to increase adherence and maximize therapeutic effects.
As we evaluated the app intervention holistically, future studies should examine the impact of the app’s individual components.
While the dropout rate in the IG was slightly higher than that in the CG, the dropout rate in the IG as well as the overall dropout rate was low compared to other app-based supportive interventions [ 25 , 30 ]. Considering that patients with cancer have been found to have a positive attitude toward digital health [ 53 , 54 ], the findings of this study add to the notion that digital health interventions have the potential to overcome barriers associated with access to supportive care in oncological populations [ 55 ].
We found a positive effect of the investigated digital therapeutic on general psychological distress and a broad range of specific distress-associated parameters. Importantly, improvements in psychological symptoms, that is, depression and anxiety, can also have a positive tertiary preventive effect on cancer progression [ 5 ]. The effect sizes in this study ranged from small (ηp²=0.02) to medium (ηp²=0.07) in the ITT population and were more pronounced in the PP population (ηp²=0.05-0.11). The primary outcome improvement, while subtle, aligns with the expected outcomes in psycho-oncological interventions, highlighting the importance of considering the broad spectrum of therapeutic impacts. The medium to large effects observed in secondary end points, together with the primary outcome, illustrate the broad therapeutic impact and highlight the digital therapeutic’s capacity to significantly improve key aspects of psychological well-being in patients with cancer. Small-to-medium effect sizes are common in in-person supportive care interventions [ 6 ]. Our results also compare well with other app-based supportive care interventions, such as small effect sizes reported for a CBT and psychoeducation self-management apps on fatigue [ 25 ] or small to medium effects of a web-based mindfulness-based intervention on anxiety and depression [ 56 ]. This is further supported by the results of several systematic reviews [ 20 , 21 ]. The fact that such effect sizes can be achieved with minimal cost and personnel effort via a digital approach further supports the significant potential for accessibility, reach, and impact of digital therapeutics.
Clinical Implications
The multifaceted intervention modules of the investigated digital therapeutic aim to support patients holistically. The investigated digital therapeutic hereby translates widely used evidence-based intervention methods within supportive care, such as symptom monitoring; patient education; modules of CBT, MBSR, and acceptance and commitment therapy; and strength and flexibility training, into a digital format. The intervention modules of the app are designed to help patients learn about their disease and prepare for discussions with clinicians in an informed decision-making process. This may reduce anxiety and insecurities across the cancer trajectory, while empowering patients and strengthening their self-efficacy.
While it is acknowledged that digital therapeutic interventions might not fully replicate the “in-person” experience, the scope and utility of these tools in the realm of oncology are substantial. For instance, a study evaluating a mobile app designed for tracking patient-reported daily activities found that when supervised by a physician, the data collected were more accurate than when used without guidance [ 57 ]. Conversely, a music app was equally effective in alleviating pain and anxiety in emergency department patients irrespective of supervision [ 58 ]. This suggests that certain interventions, such as symptom tracking, might be more prone to inaccuracies without proper guidance than passive activities, such as listening to music. In addition, CBT, which is traditionally the most effective in face-to-face settings, has generated interest in the digital domain. A study on the digital adaptation of mindfulness-based cognitive therapy for patients with cancer experiencing distress found the therapeutic connection between therapist and patient to be as potent as in in-person sessions [ 59 ]. This underlines the evolving role of digital therapeutics and its potential to reshape therapeutic avenues in oncology, thus paving the way for enhanced patient care.
Furthermore, considering the increasing number of patients with cancer experiencing psychosocial distress and the limited availability of health care professionals, digital therapeutics could present scalable and cost-effective solutions. These solutions can address symptoms and bolster the quality and accessibility of supportive care [ 55 , 60 , 61 ]. Recognizing patients’ diverse needs, tools such as the Mika app leverage artificial intelligence to deliver real-time, tailored support. This has the potential to benefit a broad spectrum of patients with cancer globally while also reducing the pressure on health care infrastructure and professionals. Therefore, digital therapeutics offer a patient-focused approach that is adaptable to specific clinical and lifestyle challenges such as disease management, emotional support, and health-related determinants. They might also further enhance medication adherence, tolerance to chemotherapy, and overall survival rate in the cancer care continuum [ 15 ]. Incorporating these digital tools into routine oncological supportive care can augment patient-centric care and enrich patient experience, safety, and interactions with clinicians [ 15 , 61 ]. However, while there is a consensus among medical professionals and stakeholders regarding the revolutionary potential of digital health in addressing cancer treatment challenges, the path to universal adoption remains intricate. Future studies should delve into the assimilation of digital therapeutics, such as Mika, into standard care across varied clinical environments and evaluate hurdles such as digital literacy and the acceptance of digital tools by both patients and health care professionals [ 62 - 64 ].
Strengths and Limitations
The main strength of this study was the app itself. It addresses the overreaching problem areas faced by all patients with cancer while providing tailored support for population-specific areas of burden (ie, cancer type, treatment status, and use behavior). Its flexible and easily accessible use allows for seamless integration into patients’ daily lives and continuity of supportive treatment. In addition, the low overall dropout rate and data monitoring led to very little missing data. Similar findings in the ITT, PP, and extended ITT populations suggest overall robustness of the results.
This study has several limitations. First, the web-based recruitment procedure may have led to study registration from patients with cancer who were particularly motivated, digitally literate, and highly functioning in seeking support during their cancer journey, which may limit the generalizability of the study. However, the use of additional recruitment pathways (support groups and participant pool) likely resulted in the recruitment of a more heterogeneous sample, possibly compensating for potential selection bias. Future studies might investigate the impact of various recruitment channels on the efficacy of digital therapeutics, and thus, which population may be particularly responsive to digital interventions. Second, the higher number of dropouts in the IG compared to the CG may reflect treatment dissatisfaction or lost interest in the treatment of some participants, potentially confounding the study’s results. Dropouts, who are more likely to show elevated levels of distress, may have been made aware of the increased need for support through the intervention modules. Patients with clinically significant levels of distress or mental disorders might have accessed support services with more guidance from a health care professional, such as psychotherapy or psycho-oncological counseling. However, no side effects or adverse events were reported in the IG, and the overall robust pattern of results in the ITT, PP, and extended ITT populations suggests a low risk of attrition bias. The fact that participants who dropped out of the study showed higher baseline distress levels may have led to an underestimation of the intervention effect as higher baseline distress levels predicted a greater change in outcome after treatment. Third, due to the nature of the intervention, the group allocation could not be blinded. While experimenter bias was reduced due to a predefined, standardized monitoring procedure and statistical analysis plan, IG participants may have anticipated potential effects. Fourth, the intervention, along with its adherence, was assessed as a whole, which requires the evaluation of specific modules and any potential dose-response relationship in the future. In addition, there was no specific measure to evaluate the subjective usefulness or satisfaction with the digital therapeutic under investigation. Incorporating such a measure could have provided targeted insights into the participants’ perceptions and experiences with the app. However, the observed use behavior, characterized by participants repeatedly accessing the app and actively engaging with its content, may serve as an indirect indicator of the app’s value to the participants. Future studies should aim to validate this interpretation. Finally, the study sample included participants with a wide variety of cancer diagnoses, which did not allow for the examination of diagnosis-specific intervention effects. However, the sample composition is consistent with the target population of the investigated digital therapeutic, which includes patients with cancer of all entities, and strengthens the study’s generalizability and clinical utility. Moreover, a large body of data shows that while variables such as cancer type, treatment status, disease progression, and sex may influence the magnitude of treatment response to supportive therapy, the beneficial effects of supportive therapy are present across various cancer subpopulations [ 65 - 67 ]. In addition, there is a consensus that psychosocial support needs to be integrated into routine cancer care for all cancer types [ 68 , 69 ].
Conclusions
In summary, this RCT demonstrated that Mika, an app-based digital therapeutic that provides a personalized supportive care intervention, can effectively reduce psychological distress and further alleviate symptoms of anxiety, depression, and fatigue in patients with cancer. Digital therapeutics, such as Mika, deliver easily accessible, patient-centered, and effective psychosocial and self-management support for patients with cancer across the course of the disease. Digital therapeutics may present scalable solutions to support patients with cancer worldwide and thus help fill the supportive care gap. Further research is needed to explore the integration of Mika into routine cancer care and its efficacy in diverse clinical settings.
Acknowledgments
The clinical trial was funded by Fosanis GmbH, Berlin.
Data Availability
The data set generated during and analyzed during this study, including individual participant data that underlie the results reported in this article after deidentification (text, tables, and figures), clinical study report, informed consent form, and analytic code, are available from AMT beginning 3 months and ending 5 years following article publication. Access to the data will be granted to investigators whose proposed use of the data has been approved by an independent review committee identified for this purpose, for individual patient data meta-analysis. Proposals for accessing the data may be submitted up to 36 months following article publication.
Authors' Contributions
JSR and GF provided financial support. FS, AM, and HB provided administrative support, with FS also contributing to the collection and assembly of data. MF contributed to data curation. FS, AM, and MF contributed to data analysis and interpretation. FS and AM equally contributed to writing the original draft. All authors contributed to reviewing and editing the draft and provided final approval of the manuscript. AMT, FS, and JSR contributed to the conception and design.
Conflicts of Interest
FS, MF, and HB received research funding for this trial from Fosanis GmbH, which was paid to their institution. AM is an employee at the company Fosanis GmbH. JSR and GF work for the company Fosanis GmbH. They are the managing directors and board members of Fosanis GmbH and own shares of Fosanis GmbH. All other authors declare no other conflicts of interest.
CONSORT-eHEALTH checklist (V 1.6.1).
- Pachman DR, Barton DL, Swetz KM, Loprinzi CL. Troublesome symptoms in cancer survivors: fatigue, insomnia, neuropathy, and pain. J Clin Oncol. Oct 20, 2012;30(30):3687-3696. [ CrossRef ] [ Medline ]
- Mehnert A, Hartung TJ, Friedrich M, Vehling S, Brähler E, Härter M, et al. One in two cancer patients is significantly distressed: prevalence and indicators of distress. Psychooncology. Jan 16, 2018;27(1):75-82. [ CrossRef ] [ Medline ]
- Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. Feb 2011;12(2):160-174. [ CrossRef ] [ Medline ]
- Meggiolaro E, Berardi MA, Andritsch E, Nanni MG, Sirgo A, Samorì E, et al. Cancer patients' emotional distress, coping styles and perception of doctor-patient interaction in European cancer settings. Pall Supp Care. Jul 09, 2015;14(3):204-211. [ CrossRef ] [ Medline ]
- Brown KW, Levy AR, Rosberger Z, Edgar L. Psychological distress and cancer survival: a follow-up 10 years after diagnosis. Psychosom Med. 2003;65(4):636-643. [ CrossRef ] [ Medline ]
- Faller H, Schuler M, Richard M, Heckl U, Weis J, Küffner R. Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: systematic review and meta-analysis. J Clin Oncol. Feb 20, 2013;31(6):782-793. [ CrossRef ] [ Medline ]
- Epstein RM, Street RL. Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute. 2007. URL: https://cancercontrol.cancer.gov/sites/default/files/2020-06/pcc_monograph.pdf [accessed 2024-03-05]
- Alcalde Castro M, Chavarri Guerra Y, Ramos-Lopez WA, Covarrubias-Gómez A, Sanchez S, Quiroz P, et al. Patient-reported barriers for accessing supportive care among patients with metastatic cancer treated at a public cancer center in Mexico. J Clin Oncol. Dec 01, 2018;36(34_suppl):124. [ CrossRef ]
- Carrieri D, Peccatori FA, Boniolo G. Supporting supportive care in cancer: the ethical importance of promoting a holistic conception of quality of life. Crit Rev Oncol Hematol. Nov 2018;131:90-95. [ CrossRef ] [ Medline ]
- Kumar P, Casarett D, Corcoran A, Desai K, Li Q, Chen J, et al. Utilization of supportive and palliative care services among oncology outpatients at one academic cancer center: determinants of use and barriers to access. J Palliat Med. Aug 2012;15(8):923-930. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bellas O, Kemp E, Edney L, Oster C, Roseleur J. The impacts of unmet supportive care needs of cancer survivors in Australia: a qualitative systematic review. Eur J Cancer Care (Engl). Nov 12, 2022;31(6):e13726. [ CrossRef ] [ Medline ]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. Jan 08, 2019;69(1):7-34. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Atun R, Cavalli F. The global fight against cancer: challenges and opportunities. Lancet. Feb 2018;391(10119):412-413. [ CrossRef ]
- Penedo FJ, Oswald LB, Kronenfeld JP, Garcia SF, Cella D, Yanez B. The increasing value of eHealth in the delivery of patient-centred cancer care. Lancet Oncol. May 2020;21(5):e240-e251. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gussoni G, Ravot E, Zecchina M, Recchia G, Santoro E, Ascione R, et al. Digital therapeutics in oncology: findings, barriers and prospects. A narrative review. Ann Res Oncol. Feb 2022;02(01):55. [ FREE Full text ] [ CrossRef ]
- Yang J, Weng L, Chen Z, Cai H, Lin X, Hu Z, et al. Development and testing of a mobile app for pain management among cancer patients discharged from hospital treatment: randomized controlled trial. JMIR Mhealth Uhealth. May 29, 2019;7(5):e12542. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ghanbari E, Yektatalab S, Mehrabi M. Effects of psychoeducational interventions using mobile apps and mobile-based online group discussions on anxiety and self-esteem in women with breast cancer: randomized controlled trial. JMIR Mhealth Uhealth. May 18, 2021;9(5):e19262. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hou IC, Lin HY, Shen SH, Chang KJ, Tai HC, Tsai AJ, et al. Quality of life of women after a first diagnosis of breast cancer using a self-management support mHealth app in Taiwan: randomized controlled trial. JMIR Mhealth Uhealth. Mar 04, 2020;8(3):e17084. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Keum J, Chung MJ, Kim Y, Ko H, Sung MJ, Jo JH, et al. Usefulness of smartphone apps for improving nutritional status of pancreatic cancer patients: randomized controlled trial. JMIR Mhealth Uhealth. Aug 31, 2021;9(8):e21088. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hernandez Silva E, Lawler S, Langbecker D. The effectiveness of mHealth for self-management in improving pain, psychological distress, fatigue, and sleep in cancer survivors: a systematic review. J Cancer Surviv. Feb 2019;13(1):97-107. [ CrossRef ] [ Medline ]
- Matis J, Svetlak M, Slezackova A, Svoboda M, Šumec R. Mindfulness-based programs for patients with cancer via eHealth and mobile health: systematic review and synthesis of quantitative research. J Med Internet Res. Nov 16, 2020;22(11):e20709. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Adriaans DJ, Dierick-van Daele AT, van Bakel MJ, Nieuwenhuijzen GA, Teijink JA, Heesakkers FF, et al. Digital self-management support tools in the care plan of patients with cancer: review of randomized controlled trials. J Med Internet Res. Jun 29, 2021;23(6):e20861. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Qin M, Chen B, Sun S, Liu X. Effect of mobile phone app-based interventions on quality of life and psychological symptoms among adult cancer survivors: systematic review and meta-analysis of randomized controlled trials. J Med Internet Res. Dec 19, 2022;24(12):e39799. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Springer F, Mehnert-Theuerkauf A. Content features and its implementation in novel app-based psycho-oncological interventions for cancer survivors: a narrative review. Curr Opin Oncol. Jul 01, 2022;34(4):313-319. [ CrossRef ] [ Medline ]
- Spahrkäs SS, Looijmans A, Sanderman R, Hagedoorn M. Beating cancer-related fatigue with the Untire mobile app: results from a waiting-list randomized controlled trial. Psychooncology. Nov 2020;29(11):1823-1834. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mayer DK, Landucci G, Awoyinka L, Atwood AK, Carmack CL, Demark-Wahnefried W, et al. SurvivorCHESS to increase physical activity in colon cancer survivors: can we get them moving? J Cancer Surviv. Feb 9, 2018;12(1):82-94. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lengacher CA, Reich RR, Ramesar S, Alinat CB, Moscoso M, Cousin L, et al. Feasibility of the mobile mindfulness-based stress reduction for breast cancer (mMBSR(BC)) program for symptom improvement among breast cancer survivors. Psychooncology. Feb 2018;27(2):524-531. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mikolasek M, Witt CM, Barth J. Effects and implementation of a mindfulness and relaxation app for patients with cancer: mixed methods feasibility study. JMIR Cancer. Jan 13, 2021;7(1):e16785. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gustafson DH, DuBenske LL, Atwood AK, Chih MY, Johnson RA, McTavish F, et al. Reducing symptom distress in patients with advanced cancer using an e-alert system for caregivers: pooled analysis of two randomized clinical trials. J Med Internet Res. Nov 14, 2017;19(11):e354. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chung IY, Jung M, Park YR, Cho D, Chung H, Min YH, et al. Exercise promotion and distress reduction using a mobile app-based community in breast cancer survivors. Front Oncol. 2019;9:1505. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Greer JA, Jacobs J, Pensak N, MacDonald JJ, Fuh C, Perez GK, et al. Randomized trial of a tailored cognitive-behavioral therapy mobile application for anxiety in patients with incurable cancer. Oncologist. Aug 25, 2019;24(8):1111-1120. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Basch E, Deal AM, Kris MG, Scher HI, Hudis CA, Sabbatini P, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol. Feb 20, 2016;34(6):557-565. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Greer JA, Park ER, Prigerson HG, Safren SA. Tailoring cognitive-behavioral therapy to treat anxiety comorbid with advanced cancer. J Cogn Psychother. Jan 01, 2010;24(4):294-313. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. Nov 2007;21(8):1038-1049. [ CrossRef ] [ Medline ]
- Speca M, Carlson LE, Goodey E, Angen M. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med. 2000;62(5):613-622. [ CrossRef ] [ Medline ]
- Winters-Stone KM, Dobek J, Nail L, Bennett JA, Leo MC, Naik A, et al. Strength training stops bone loss and builds muscle in postmenopausal breast cancer survivors: a randomized, controlled trial. Breast Cancer Res Treat. Jun 19, 2011;127(2):447-456. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Adam R, Bond C, Murchie P. Educational interventions for cancer pain. A systematic review of systematic reviews with nested narrative review of randomized controlled trials. Patient Educ Couns. Mar 2015;98(3):269-282. [ CrossRef ] [ Medline ]
- Wolff J, Stupin J, Olschewski J, Pirmorady Sehouli A, Maier A, Fofana M, et al. Digital therapeutic to improve cancer-related well-being: a pilot randomized controlled trial. Int J Gynecol Cancer. Jul 03, 2023;33(7):1118-1124. [ CrossRef ] [ Medline ]
- Harrison SE, Watson EK, Ward AM, Khan NF, Turner D, Adams E, et al. Primary health and supportive care needs of long-term cancer survivors: a questionnaire survey. J Clin Oncol. May 20, 2011;29(15):2091-2098. [ CrossRef ] [ Medline ]
- Xiao J, Ye H, He X, Zhang H, Wu F, Chua TS. Attentional factorization machines: learning the weight of feature interactions via attention networks. arXiv. Preprint posted online August 15, 2017. 2017. [ FREE Full text ] [ CrossRef ]
- Sensoy M, Kaplan L, Kandemir M. Evidential deep learning to quantify classification uncertainty. In: Proceedings of the 32nd Conference on Neural Information Processing Systems. 2018. Presented at: NeurIPS '18; December 3-8, 2018; Montreal, QC. URL: https://www.proceedings.com/48413.html
- Mehnert A, Müller D, Lehmann C, Koch U. Die Deutsche version des NCCN distress-thermometers. Z Für Psychiatr Psychol Psychother. Jan 2006;54(3):213-223. [ CrossRef ]
- National Comprehensive Cancer Network. Distress management. Clinical practice guidelines. J Natl Compr Canc Netw. Jul 01, 2003;1(3):344-374. [ CrossRef ] [ Medline ]
- Petermann F. Hospital anxiety and depression scale, Deutsche version (HADS-D). Z Für Psychiatr Psychol Psychother. Jul 2011;59(3):251-253. [ CrossRef ]
- Lai J, Cella D, Chang C, Bode RK, Heinemann AW. Item banking to improve, shorten and computerize self-reported fatigue: an illustration of steps to create a core item bank from the FACIT-Fatigue Scale. Qual Life Res. Aug 2003;12(5):485-501. [ CrossRef ] [ Medline ]
- Guy W. Clinical global impressions scale. Psychiatry. 1976. [ CrossRef ]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Oxfordshire, UK. Routledge; 2013.
- Carpenter JR, Roger JH, Kenward MG. Analysis of longitudinal trials with protocol deviation: a framework for relevant, accessible assumptions, and inference via multiple imputation. J Biopharm Stat. Oct 18, 2013;23(6):1352-1371. [ CrossRef ] [ Medline ]
- Enders CK. Applied Missing Data Analysis. New York, NY. The Guilford Press; 2022.
- R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing. 2021. URL: https://www.R-project.org/ [accessed 2024-03-05]
- Ham K, Chin S, Suh YJ, Rhee M, Yu ES, Lee HJ, et al. Preliminary results from a randomized controlled study for an app-based cognitive behavioral therapy program for depression and anxiety in cancer patients. Front Psychol. Jul 25, 2019;10:1592. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hinz A, Mehnert A, Dégi C, Reissmann DR, Schotte D, Schulte T. The relationship between global and specific components of quality of life, assessed with the EORTC QLQ-C30 in a sample of 2019 cancer patients. Eur J Cancer Care (Engl). Mar 16, 2017;26(2):e12416. [ CrossRef ] [ Medline ]
- Jansen F, van Uden-Kraan CF, van Zwieten V, Witte BI, Verdonck-de Leeuw IM. Cancer survivors' perceived need for supportive care and their attitude towards self-management and eHealth. Support Care Cancer. Jun 26, 2015;23(6):1679-1688. [ CrossRef ] [ Medline ]
- Kessel KA, Vogel MM, Kessel C, Bier H, Biedermann T, Friess H, et al. Mobile health in oncology: a patient survey about app-assisted cancer care. JMIR Mhealth Uhealth. Jun 14, 2017;5(6):e81. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Marthick M, McGregor D, Alison J, Cheema B, Dhillon H, Shaw T. Supportive care interventions for people with cancer assisted by digital technology: systematic review. J Med Internet Res. Oct 29, 2021;23(10):e24722. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nissen ER, O'Connor M, Kaldo V, Højris I, Borre M, Zachariae R, et al. Internet-delivered mindfulness-based cognitive therapy for anxiety and depression in cancer survivors: a randomized controlled trial. Psychooncology. Jan 18, 2020;29(1):68-75. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Egbring M, Far E, Roos M, Dietrich M, Brauchbar M, Kullak-Ublick GA, et al. A mobile app to stabilize daily functional activity of breast cancer patients in collaboration with the physician: a randomized controlled clinical trial. J Med Internet Res. Sep 06, 2016;18(9):e238. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chai PR, Schwartz E, Hasdianda MA, Azizoddin DR, Kikut A, Jambaulikar GD, et al. A brief music app to address pain in the emergency department: prospective study. J Med Internet Res. May 20, 2020;22(5):e18537. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bisseling E, Cillessen L, Spinhoven P, Schellekens M, Compen F, van der Lee M, et al. Development of the therapeutic alliance and its association with internet-based mindfulness-based cognitive therapy for distressed cancer patients: secondary analysis of a multicenter randomized controlled trial. J Med Internet Res. Oct 18, 2019;21(10):e14065. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Parikh RB, Basen-Enquist KM, Bradley C, Estrin D, Levy M, Lichtenfeld JL, et al. Digital health applications in oncology: an opportunity to seize. J Natl Cancer Inst. Oct 06, 2022;114(10):1338-1339. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Aapro M, Bossi P, Dasari A, Fallowfield L, Gascón P, Geller M, et al. Digital health for optimal supportive care in oncology: benefits, limits, and future perspectives. Support Care Cancer. Oct 12, 2020;28(10):4589-4612. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rankin NM, Butow PN, Thein T, Robinson T, Shaw JM, Price MA, et al. Everybody wants it done but nobody wants to do it: an exploration of the barrier and enablers of critical components towards creating a clinical pathway for anxiety and depression in cancer. BMC Health Serv Res. Jan 22, 2015;15(1):28. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Leader AE, Capparella LM, Waldman LB, Cammy RB, Petok AR, Dean R, et al. Digital literacy at an urban cancer center: implications for technology use and vulnerable patients. JCO Clinical Cancer Informatics. Dec 2021;(5):872-880. [ CrossRef ]
- den Bakker CM, Schaafsma FG, Huirne JA, Consten EC, Stockmann HB, Rodenburg CJ, et al. Cancer survivors' needs during various treatment phases after multimodal treatment for colon cancer - is there a role for eHealth? BMC Cancer. Dec 04, 2018;18(1):1207. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cillessen L, Johannsen M, Speckens AE, Zachariae R. Mindfulness-based interventions for psychological and physical health outcomes in cancer patients and survivors: a systematic review and meta-analysis of randomized controlled trials. Psychooncology. Dec 11, 2019;28(12):2257-2269. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tauber NM, O'Toole MS, Dinkel A, Galica J, Humphris G, Lebel S, et al. Effect of psychological intervention on fear of cancer recurrence: a systematic review and meta-analysis. J Clin Oncol. Nov 01, 2019;37(31):2899-2915. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Merluzzi TV, Pustejovsky JE, Philip EJ, Sohl SJ, Berendsen M, Salsman JM. Interventions to enhance self-efficacy in cancer patients: a meta-analysis of randomized controlled trials. Psychooncology. Sep 09, 2019;28(9):1781-1790. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jacobsen PB, Wagner LI. A new quality standard: the integration of psychosocial care into routine cancer care. J Clin Oncol. Apr 10, 2012;30(11):1154-1159. [ CrossRef ] [ Medline ]
- Fann JR, Ell K, Sharpe M. Integrating psychosocial care into cancer services. J Clin Oncol. Apr 10, 2012;30(11):1178-1186. [ CrossRef ] [ Medline ]
Abbreviations
Edited by YH Lin; submitted 21.08.23; peer-reviewed by F Denis, A Haussmann, N Schaeffeler, P Chow; comments to author 24.01.24; accepted 23.02.24; published 25.04.24.
©Franziska Springer, Ayline Maier, Michael Friedrich, Jan Simon Raue, Gandolf Finke, Florian Lordick, Guy Montgomery, Peter Esser, Hannah Brock, Anja Mehnert-Theuerkauf. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 25.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Soccer-Period anxiety and white shorts linked to drop in performance - study
- Medium Text

Sign up here.
Reporting by Lori Ewing, Editing by Toby Davis
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab

LaLiga leaders Real Madrid are virtually assured of a record-extending 36th Spanish title after Jude Bellingham's late goal secured a 3-2 comeback win over Barcelona last Sunday.

Sports Chevron

Magic crush Cavaliers to halve series deficit to 2-1
Paolo Banchero collected 31 points and 14 rebounds to fuel the host Orlando Magic to a convincing 121-83 victory over the Cleveland Cavaliers on Thursday in Game 3 of their Eastern Conference first-round series.

Fresh off a resilient victory that changed the course of their first-round Western Conference playoff series, the Los Angeles Kings return home for Game 3 on Friday against the Edmonton Oilers.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.38(1); 2013 Jan
Current Diagnosis and Treatment of Anxiety Disorders
Anxiety disorders are the most prevalent mental health conditions. Although they are less visible than schizophrenia, depression, and bipolar disorder, they can be just as disabling. The diagnoses of anxiety disorders are being continuously revised. Both dimensional and structural diagnoses have been used in clinical treatment and research, and both methods have been proposed for the new classification in the Diagnostic and Statistical Manual of Mental Disorders IV (DSM-5). However, each of these approaches has limitations. More recently, the emphasis in diagnosis has focused on neuroimaging and genetic research. This approach is based partly on the need for a more comprehensive understanding of how biology, stress, and genetics interact to shape the symptoms of anxiety.
Anxiety disorders can be effectively treated with psychopharmacological and cognitive–behavioral interventions. These inter ventions have different symptom targets; thus, logical combinations of these strategies need to be further studied in order to improve future outcomes. New developments are forthcoming in the field of alternative strategies for managing anxiety and for treatment-resistant cases. Additional treatment enhancements should include the development of algorithms that can be easily used in primary care and with greater focus on managing functional impairment in patients with anxiety.
INTRODUCTION
Anxiety disorders are present in up to 13.3% of individuals in the U.S. and constitute the most prevalent subgroup of mental disorders. 1 The extent of their prevalence was first revealed in the Epidemiological Catchments Area study about 26 years ago. 2 Despite their widespread prevalence, these disorders have not received the same recognition as other major syndromes such as mood and psychotic disorders; in addition, the primary care physician is usually the principal assessor and treatment provider. 3 , 4 As a result of this management environment, anxiety disorders can be said to account for decreased productivity, increased morbidity and mortality rates, and the growth of alcohol and drug abuse in a large segment of the population. 5 – 7
Anxiety disorders currently included in the Diagnostic and Statistical Manual of Mental Disorders, 4th ed., text revision (DSM IV-TR) are listed in Table 1 . 8
Anxiety Disorders
Advances in anxiety research over the previous decade are likely to be reflected in modifications of diagnostic criteria in the upcoming DSM-5 , 9 planned for publication in May 2013. For instance, post-traumatic stress disorder (PTSD) and obsessive–compulsive disorder (OCD) have been reclassified in the separate domains of Trauma and Stressor Related Disorders and Obsessive–Compulsive and Related Disorders, respectively. 10 , 11
In this article, we review the challenges to the diagnosis of anxiety disorders, provide a model that explains how anxiety symptoms occur and change over time, highlight the neurotransmitter systems affected by these disorders, and discuss the roles and relative efficacy of pharmacological and non-pharmacological interventions.
DIAGNOSTIC DILEMMAS
Within the past 10 years or so, epidemiological data have been used in the attempt to refine the boundaries of diagnostic categories of anxiety disorders. The results of this approach have been progressively reflected from DSM III to IIIR to DSM IV-TR (see Table 1 ) and, finally, to DSM-5 . However, this effort has been hampered by the extensive presence of comorbidities in patients with anxiety, as revealed by the National Comorbidity Survey (NCS). 11 For instance, in patients with some disorders such as generalized anxiety disorder (GAD) and social anxiety disorder (SAD), the presence of comorbidities is a rule rather than the exception. 12 In clinical practice and in research, it is not unusual to find the coexistence of two or more diagnosable conditions in the same patient or at least symptomatic overlap with several subsyndromal states. This is particularly true for symptom overlap between different anxiety disorders, depression, and alcohol and drug abuse. 13
A related phenomenon is the emergence of different disorders in the same patient over a lifetime. For example, during an initial evaluation, the original diagnosis could be panic disorder that resolves after treatment, and then presents after a few years with symptoms more suitable to a diagnosis of OCD or GAD. Whether this process reflects a primary diathesis or two distinct entities is uncertain.
Another significant problem with the present classification of anxiety disorders is the absence of known etiological factors and of specific treatments for different diagnostic categories. Studying the genetic underpinnings of anxiety disorders using molecular biological techniques has failed to produce a single gene or a cluster of genes implicated as an etiologic factor for any single anxiety disorder, even though some genetic findings exist for OCD and panic disorder. 14 , 15 Despite a lack of specificity, family and twin studies point to the importance of genetic factors that are possibly shared among various anxiety disorders, depression, and alcohol and drug abuse. 16
Despite these diagnostic ambiguities, the emergence of efficacious serotonergic medications that cut across a variety of categorical disorders (e.g., mood and anxiety) has led many to suggest that a dimensional model might be more applicable in the study and treatment of these conditions. 17 In this view, the disorder is seen as a complex set of coexisting symptom dimensions (e.g., panic, social awkwardness, and obsessiveness). Each of these dimensions can vary, depending on hypothetical, biological, or genetic factors, which may dictate separate biological or psychological treatment approaches. 9 The usefulness of the dimensional versus the categorical approach remains a highly debatable topic in research and in clinical practice and is one of the bases for the introduction of DSM-5 . 18 , 19
Within psychiatry, similarities between distinct disorders has led to the emergence of the term “spectrum” disorders, a concept initially developed for OCD. 20 This conceptualization was helpful in evaluating similar responses to pharmacological and psychological treatments and has been expanded to consider many other spectra such as social anxiety, panic–agoraphobia, and post-traumatic disorders. 21 – 23 This approach, although useful, can be overly inclusive and misleading because it sometimes lumps together disorders that have little in common, such as placing pathological gambling and body dysmorphic disorder (BDD) in the same OCD spectrum. So far, few genetic or neuro-circuitry investigations have validated this concept.
Dimensional and categorical diagnosis in the DSM-IV-TR is usually produced by cross-sectional comparisons of distinct subject samples. However, diagnostic presentations in clinical practice occur in individuals treated sequentially and may therefore be better understood as part of a psychopathological process that unfolds over time. For example, although a patient might meet criteria for OCD purely on the basis of obsessions or compulsions, the latter usually arise later in the disorder as if to counteract the threat and anxiety associated with obsessive thoughts. 24
Analogous viewpoints can be found in medical disease, with symptoms usually representing a combination of a noxious agent and the body’s reaction to its presence. For instance, when the lungs are infected with the harmful organism Mycobacterium tuberculosis , they compensate by forming scars around the tissue. In the short run, this may be effective in walling off the infection (and may even elude clinical detection), but the strategy fails when pushed to the extreme, leading to respiratory compromise in some cases.
In recent years, scientists and clinicians have begun to realize that the processes underlying anxiety and fear might be similar among the various disorders. This has resulted in the implementation of uniform treatment regimens in primary care 25 and in the development of the unified theory of anxiety. 26
THE ‘ABC’ MODEL OF ANXIETY
Understanding how emotional reactivity, core beliefs, and coping strategies interact in time should lead to more precise diagnoses and better management of anxiety disorders. We recently applied a mathematical model using nonlinear dynamics to describe these processes 27 and further developed this model to cover diagnostic presentations and their underlying processes. 28 The model that we, for simplicity, call the “ABC model of anxiety” could be viewed as an interaction in space and time of a larms, b eliefs and c oping strategies ( Figure 1 ).

Schematic detailing the “ABC” model of anxiety. In this model, a variety of triggering events can elicit responses at the levels of A larm sensations, B eliefs, and associated C oping (ABC) strategies, including behaviors. Each of these processes originates in discrete brain circuits that are functionally connected. Over time, this perpetuates a vicious circle, shaping the presentation of a variety of anxiety disorders.
Alarms (A) are emotional sensations or physiological reactions to a trigger situation, sensation, or thought. A well-defined set of brain circuits rapidly processes information about the alarm.
The ensuing decision to act is made on the basis of beliefs (B) that rely heavily on previous experiences, personal and cultural background, and the information that is perceived by the sensory organs. Patients with anxiety disorders appear to process information about a supposedly dangerous situation with more focused attention compared with individuals without the disorder. 29 Accurate decision-making regarding beliefs is obscured by a flood of details, which leads to catastrophic thinking and indecision.
This, in turn, leads to coping strategies (C), for example, specific behaviors or mental activity aimed at reducing anxiety and avoiding the perceived “danger.” Coping strategies can be considered adaptive or maladaptive, based on their efficacy in reducing the target anxiety. These processes evolve over time, forming a complex picture of a particular anxiety disorder.
As a clinical example, panic disorder may start as an initial devastating panic attack driven by activation of the brain’s alarm networks. This event activates circuits that process information about danger and, when coupled with personal beliefs about the event, leads to increased concern about personal health and safety. This in turn leads to a specific attempt to decrease the danger of the situation (e.g., a medical workup that initially calms the fear).
These processes often occur in healthy people who might experience an unpleasant or dangerous situation; in patients with panic disorder, however, a regular medical workup is in-sufficient to calm them because they require a 100% assurance of “no danger.” Because this is impossible to provide, worry and anticipation of another impending attack persist. The patient subsequently increases “safety” coping behaviors such as having repeated medical examinations (seeking reassurance) and having a “safe” person around at all times.
Unfortunately, because no absolute safety is to be found, these behaviors become more extensive and chronic in the attempt to alleviate anxiety. The fact that anxiety persists induces more worry and eventually distress, thus perpetuating the vicious circle of the disorder (recurrent panic attacks). If the pattern is uninterrupted, it eventually leads to even more inappropriate coping behavior, such as avoidance of any potential triggers of panic (agoraphobia), and can result in comorbid despair and depression. Most of the anxiety disorders follow this process even though different stages may predominate in different disorders; that is, ritualistic behavior is more characteristic of OCD, and avoidance predominates in social anxiety disorder.
We have found that patients quickly recognize and interpret their symptom patterns within the ABC model. We effectively incorporate this pattern with medication and behavioral techniques, as described in the previous studies. 30 We have also found that conceptualization of clinical cases using the ABC model is particularly helpful in teaching psychiatric residents. Using this model, residents are able to understand and to begin administering cognitive–behavioral therapy (CBT) within relatively few sessions.
Interplay Between Biological and Psychological Factors
In order to treat an anxiety disorder effectively, clinicians should understand how these conditions emerge and which factors are involved in maintaining them. In recent years, we have gained a better understanding of the interplay between genetic, biological, and stress factors that shape the presentation of the disorder, although it is not clear which factors are inherited.
One possibility is that abnormal cognition could be the inherited factor. Cognitive theory assigns a primary importance to abnormal or “catastrophic” cognition as an underlying mechanism of all anxiety disorders. Most cognitive strategies for treatment and research were developed in earlier years.
The ABC model focuses on the interaction of information processing and emotional and cognitive processes that are controlled by overlapping circuits and compete for the same brain resources. 27
In most anxiety disorders, patients usually process fear-inducing information in excessive detail that overwhelms their ability to appraise it properly. They cope by separating the information into “good” and “bad” with no gray area in between. As a result, they consider the worst-case scenario (i.e., by catastrophizing about the situation) and then act to protect themselves against the perceived danger.
Stress also plays a major role in the pathology of anxiety disorders. For example, PTSD is a condition in which stress is considered the main etiological factor, although there is a high degree of co-occurring stress reported by these patients. In other anxiety disorders such as GAD and OCD, the role of stress is less apparent. Nevertheless, patients with any anxiety disorder often pinpoint the onset of their disorder in relation to a striking stressful event or to a continuous persistent stressor. Whether a cause or a consequence, increased stress reactivity sometimes accounts for relapses in chronic anxiety conditions like GAD. According to some studies, a stressful event or a persistent and chronic disorder can even cause secondary biological changes in specific brain structures. 31 , 32
The current DSM-IV-TR system does not adequately address the role of stressors. Although stressors are separately identified along Axis IV of the multiaxial system, the context for the patient is unclear. Perhaps a better way to address the patient’s anxiety would be to indicate the source and rate the persistence (i.e., immediate, intermittent, or constant) and the degree of the stress (i.e., mild, moderate, severe, or catastrophic). With this approach, we might be better able to capture the landscape and dynamic of the stress. For example, panic disorder resulting from exposure to catastrophic combat may differ clinically from panic disorder that results from a persistent work-related stress or separation from family. Exploration of how stress affects biology and the course of anxiety disorders is clearly needed.
Biological Factors
Biological factors are of primary importance in anxiety disorders. Anxiety disorders can occur in the context of medical illness, 33 and the clinician should consider an intricate relationship between medical illnesses and anxiety disorders. This relationship could be manifold.
First, metabolic or autonomic abnormalities caused by the illness can produce the syndrome of anxiety (i.e., hyperthyroidism sometimes results in panic attacks). The symptom of medical illness can be a trigger for anxiety (i.e., sensations of arrhythmia can serve as a trigger for a panic attack). Sometimes medical illness can mimic the anxiety disorder (i.e., when perseverations in mental retardation are mistaken for OCD).
Finally, medical illness and an anxiety disorder can simply coexist in the same patient. One of the most interesting interactions between medical illness and anxiety disorders is pediatric autoimmune neuropsychiatric disorder associated with streptococcal infections (PANDAS), which has been reported in a subset of OCD patients. 34
Over the previous two decades, the main thrust of biological research in anxiety disorders has shifted from peripheral measures of autonomic and neurochemical parameters to identifying reactivity and neurochemistry of the living brain directly through advances in neuroimaging technology. Anxiety disorders are an appropriate target for neuroimaging research because it is easy to provoke specific symptoms in many cases. Much of the research on neural circuits has focused on models of anxiety and fear proposed earlier by basic scientists, 35 , 36 and a synthesis of current data has been attempted for panic disorder 37 and OCD. 38
There have been some excellent reviews of neuroimaging experiments in anxiety, 39 , 40 but the picture remains incomplete, in part because of a lack of clinical trials addressing the long-term integration of threat responses. As in the dynamical model, every anxiety disorder may be viewed as an interplay of anxious feelings, abnormal processing of information, and inadequate coping strategies. In accordance with this model of anxiety, overlapping neuronal circuits are responsible for alarm reactions, processing of perceived threats, and behavioral coping (see Figure 1 ). This model attempts to simplify complex brain circuitry that needs to be studied over the next several decades before we can truly understand how the brain processes threats over time.
For simplicity we identify Alarm circuits (A), in which the amygdala is the structure of primary importance. These circuits also include periaqueductal gray matter and multiple nuclei in the brainstem. 41 The disturbance of anxiety circuits results in a lower threshold for alarm reactions that leads to spontaneous panic attacks. These circuits are possibly responsible for the quick response to a threat.
Circuits associated with Beliefs (B), responsible for processing information related to “threats,” are probably closely associated with the basal ganglia, cingulum, and corticostriatal connections, which are typically affected in OCD.
Abnormalities in Coping (C) should be governed by distributed cortical networks and are difficult to tease apart. Thus, a convenient mnemonic explaining these circuits could be A (Alarm, amygdala), B (Beliefs, basal ganglia), and C (Coping, cortex).
How Anxiety Affects Neurotransmitters
Neuronal circuits are governed by multiple neurotransmitter systems; the most extensive of these are gamma-aminobutyric acid (GABA) and glutamate. The neural systems of the three major neurotransmitter systems—serotonin, dopamine, and norepinephrine—have been extensively studied in normal and pathological anxiety states. 40 , 42 The significance of these systems in anxiety is apparent from the fact that most effective therapies for these disorders affect one or several of them. However, anxiety disorders are not simply a deficiency of one neurotransmitter or another. The networks governed by these transmitters have extensive interrelationships, multiple feedback mechanisms, and complex receptor structures. 43 This complexity helps to explain the unpredictable and sometimes paradoxical responses to medication.
Research involving other neurotransmitter systems has been fruitful in elucidating their function in anxiety but thus far has failed to produce new treatments. The primary neurotransmitter and receptor systems implicated in the pathogenesis of anxiety disorders are discussed next.
The primary serotonergic pathways originate in the raphe nuclei and project widely to numerous targets throughout the forebrain. 44 These circuits play a fundamental role in regulating brain states, including anxiety, and modulate the dopaminergic and noradrenergic pathways as well. 45 Increased serotonergic tone appears to be correlated with a reduction in anxiety; however, the mechanism underlying this correlation is not known.
There are also numerous serotonin receptor subtypes whose roles may vary, depending on location. For example, the serotonin-1a receptor serves as both a mediator and an inhibitor of serotonergic neurotransmission, depending on whether it is located on the presynaptic or the postsynaptic neuron. 46 Furthermore, not all serotonin receptor subtypes mediate anxiolytic effects; this is demonstrated by the fact that serotonin-2a receptor agonism underlies the psychedelic properties of drugs such as lysergic acid (LSD) and mescaline. 47
Despite this complexity, it is recognized that medications that inhibit the reuptake of serotonin, presumably increasing serotonergic neurotransmission, result in a reduction in symptoms of anxiety for many patients. 48
Gamma-aminobutyric Acid
GABA is the main inhibitory neurotransmitter in the central nervous system (CNS). Increases in GABA neurotransmission mediate the anxiolytic effect of barbiturates and benzodiazepines. 49 Medications in these classes do not bind directly to the GABA receptor; instead, they promote the open configuration of an associated chloride channel. Barbiturates do this by increasing the duration of the channels’ open state, whereas benzodiazepines increase the frequency of opening.
Although modulation of GABA-ergic pathways can reduce anxiety almost immediately, compensatory mechanisms associated with these circuits and the use of barbiturates and benzodiazepines can result in tolerance and potentially fatal withdrawal. 50 Further, these drugs impair memory encoding and thus may undermine the efficacy of concomitantly administered psychotherapy.
Anticonvulsant agents also alter GABA transmission and are used to treat anxiety. 51 This class of medications affects GABA transmission indirectly by blocking calcium channels, resulting in a lower potential for withdrawal and addiction. 52
The principal dopaminergic pathways originate from the midbrain in the ventral tegmental area and substantia nigra, with projections to the cortex, striatum, limbic nuclei, and infundibulum. Dopamine’s role in normal and pathological anxiety states is complex, and dopaminergic pathways may affect anxiety states in several ways. 53 It is well known that dopamine D 2 blockade, the characteristic mechanism of antipsychotic medications, is also anxiolytic. 54
This class of medications has been widely used in the treatment of anxiety. However, as a catecholamine, dopamine is up-regulated with norepinephrine in anxiety states, whereas increases in dopaminergic signaling also appear to mediate feelings of self-efficacy and confidence—which can act to reduce anxiety. 55 , 56 The result of this complexity is a variation in responses to medications that increase dopamine. Some patients with anxiety disorder respond well to pro-dopaminergic drugs such as bupropion (Wellbutrin, GlaxoSmithKline); other patients find that such agents exacerbate their symptoms.
Norepinephrine
Noradrenergic neurons originate primarily in the locus coeruleus in the pons and project widely throughout the CNS. 57 Like dopamine, norepinephrine is a catecholamine that is up-regulated in anxiety states, but it has a complex and potentially bidirectional role in mediating normal and pathological anxiety. Many of the physiological symptoms of anxiety are mediated by norepinephrine, and antagonists of various norepinephrine receptor subtypes are used to combat particular aspects of anxiety.
For example, propranolol, an antagonist of the beta 2 -norepinephrine receptor, is used to reduce the rapid heart rate, hand tremor, and quivering voice that might accompany public speaking or other activities associated with performance anxiety. 58 Although propranolol has been useful in targeting these physiological symptoms of normal anxiety, it has not been particularly effective in reducing the emotional or cognitive aspects of anxiety and is not generally used as a therapy for anxiety disorders.
Similarly, prazosin (Minipress, Pfizer), an antagonist of the alpha 1 -norepinephrine receptor, is used to reduce the intensity and frequency of nightmares associated with PTSD but has not been effective in relieving other symptoms of anxiety disorders. 59 , 60 Serotonin–norepinephrine reuptake inhibitors (SNRIs), such as venlafaxine (Effexor, Wyeth/Pfizer) and duloxetine (Cymbalta, Eli Lilly), have been effective in the treatment of anxiety disorders. 61 These medications also help to reduce neuropathic pain and may target the agonal component of anxiety.
Glutamate is the primary excitatory neurotransmitter in the CNS and is involved in virtually every neuronal pathway, including those underlying normal and pathological anxiety states. 62 , 63 The N -methyl- d -aspartate (NMDA) receptor subtype may be particularly important in anxiety disorders, as it is believed to mediate learning and memory. Activation of the NMDA receptor triggers protein synthesis, which appears to strengthen the connection between neurons when they fire concurrently. Therefore, glutamatergic pathways are probably involved in both conditioning and extinction, the processes associated with the development and treatment of anxiety disorders, respectively. 64
Preliminary evidence suggests that both augmentation and antagonism of NMDA-mediated pathways are effective in the treatment of anxiety disorders, although no glutamatergic medications have received an FDA indication for this use. d -cycloserine enhances glutamatergic neurotransmission and has been effective in augmenting the effects of exposure therapy for anxiety disorders. 65 However, the NMDA receptor antagonists memantine (Namenda, Forest) and riluzole (Rilutek, Sanofi) have evidence supporting their efficacy in the treatment of OCD. 66 Interestingly, memantine appears to be much less effective in the treatment of GAD, suggesting that different pathways may underlie different anxiety disorders. 67
Other Neurotransmitters
Many other neurotransmitter systems participate in the biological mechanisms of fear and anxiety. Neuropeptides, including substances P, N, and Y; corticotropin-releasing factor (CRF); cannabinoids; and others, modulate fear in animal models. 68 – 70 However, none of the experimental agents that utilize these systems have been translated into FDA-approved treatments. 71 Stringent criteria for approval, along with high placebo responses typical in anxiety trials, could be responsible. 72
PHARMACOLOGICAL THERAPY
Numerous neurotransmitters play a role in normal states and in pathological anxiety states. Each of these systems is a potential target for pharmacological intervention, but relatively few classes of medications are used in clinical practice for the treatment of anxiety. These drug classes are briefly discussed next.
Selective Serotonin Reuptake Inhibitors
SSRIs, usually indicated in depression, are considered to be the first line of therapy for anxiety disorders. This drug class includes fluoxetine (Prozac, Eli Lilly), sertraline (Zoloft, Pfizer), citalopram (Celexa, Forest), escitalopram (Lexapro, Forest), fluvoxamine (Luvox, Solvay), paroxetine (Paxil, GlaxoSmithKline), and vilazodone (Viibryd, Forest). 72 The essential characteristic of the medications in this class is that they inhibit the serotonin transporter and appear to cause desensitization of postsynaptic serotonin receptors, thus normalizing the activity of serotonergic pathways.
The mechanism by which this leads to amelioration of anxiety symptoms is not fully understood. Vilazodone, the most recently approved medication in this class (although indicated for major depressive disorder), also acts as a partial agonist at the serotonin-1a receptor, which may contribute to anxiolysis. 73 Buspirone (BuSpar, Bristol-Myers Squibb), which is not a serotonin reuptake inhibitor (SRI), is also a 5-HT 1a agonist and is frequently used as a single agent or as augmentation to SSRI therapy. 74
Serotonin–Norepinephrine Reuptake Inhibitors
SNRIs, which inhibit the serotonin and norepinephrine transporters, include venlafaxine, desvenlafaxine (Pristiq, Pfizer), and duloxetine. 75 Milnacipran (Savella, Cypress/Forest) is rarely, if ever, used to treat anxiety because its only FDA-approved indication is for fibromyalgia. 76 SNRIs are typically used after failure or inadequate response to an SSRI. They are used in place of augmentation to SSRIs because the combination of these two drug classes may result in serotonin syndrome.
Patient responses to SNRIs can vary widely; some patients may experience an exacerbation of the physiological symptoms of anxiety as a result of the increased norepinephrine-mediated signaling caused by inhibition of the norepinephrine transporter. For patients who do not experience this effect, the increased noradrenergic tonus may contribute to the anxiolytic efficacy of these medications.
Benzodiazepines
Although benzodiazepines were widely used in the past to treat anxiety conditions, they are no longer considered to be first-line therapies because of the risks associated with their chronic use. 75 They are very effective in reducing acute anxiety but are associated with problematic adverse effects when used for a long time in high doses, including:
- physiological and psychological dependence.
- potential fatalities upon withdrawal.
- impaired cognition and coordination.
- a potentially lethal overdose when they are mixed with alcohol or opioids.
- inhibition of memory encoding, which can interfere with the efficacy of concomitant psychotherapy.
For these reasons, the use of benzodiazepines is often restricted to the short-term treatment of acute anxiety or as therapy for refractory anxiety after failed trials of several other drugs. Of note, some subgroups of patients do well with low doses of benzodiazepines and are able to safely taper from high doses, especially when cognitive–behavioral therapy (CBT) is added. 77
Antiseizure Medications
Because of the side effects of benzodiazepines, antiepileptic agents have been used more extensively for the treatment of anxiety. Antiseizure drugs were initially used for mood stabilization in mood disorders; however, their anxiolytic properties were quickly noted. Many agents in this drug class are being used in an off-label fashion to treat anxiety, especially gabapentin (Neurontin, Pfizer) and pregabalin (Lyrica, Pfizer). 51 , 78 Less information is available for topiramate (Topamax, Janssen), lamotrigine (Lamictal, GlaxoSmithKline), and valproate (Depacon, Abbott). 79 In higher doses, the antiseizure class can produce adverse effects similar to those of the benzodiazepines. 80
Tricyclic Antidepressants
All tricyclic antidepressants (TCAs) function as norepinephrine reuptake inhibitors, and several mediate serotonin reuptake inhibition as well. Although several medications in this drug class are comparable in efficacy to the SSRIs or SNRIs for anxiety disorders, TCAs carry a greater number of adverse effects and are potentially lethal in an overdose. For this reason, TCAs are rarely used in the treatment of anxiety disorders. A notable exception is clomipramine (Anafranil, Malinckrodt), which may be more efficacious than SSRIs or SNRIs in patients with OCD. 81
Additional Medications
Hydroxyzine (Atarax, Pfizer), mirtazapine (Remeron, Organon), nefazodone (Bristol-Myers Squibb), and atypical neuroleptic agents are commonly used to treat anxiety. 82 Although all of these medications are efficacious for anxiety disorders, especially OCD, they are not considered first-line treatments and are typically used as an adjunct to an SSRI or an SNRI. Hydroxyzine is indicated for anxiety and probably achieves anxiolysis by inhibiting the histamine H 1 receptor and the serotonin-2a receptor. 83
TREATMENT STRATEGIES
Initial treatment algorithms.
During the 1990s, mainstream psychological and pharmacological treatments of anxiety disorders were developed and tested, leading to an initial algorithm that is similar for all major anxiety disorders. 84 , 85 The typical algorithm, adapted from Roy-Byrne et al., 25 is presented in Figure 2 .

Stepped-care treatment algorithm. AD = antidepressant therapy; CBT = cognitive–behavioral therapy; MED = medication; rTMS = repetitive transcranial magnetic stimulation; SSRI = selective serotonin reuptake inhibitor. (Adapted from Roy-Byrne, et al. Arch Gen Psychiatry 2005;62[3]:290–298; 3 and Roy-Byrne et al. JAMA 2010;303[19]:1921–1928. 25 )
In general, clinicians must choose between CBT and an SSRI and then try another SSRI if the first one did not work or was not tolerated. None of the SSRIs has shown superiority to another. The choice of an SSRI is usually based on the side-effect profile, pharmacokinetic and pharmacodynamic properties, and potential interactions with coadministered medications.
Several excellent reviews of SSRI therapies for anxiety disorders have been published. 86 A general principle with SSRIs is to “start low and go slow,” starting with approximately half the dose of that used for depression and slowly titrating the dose upward, with no more than a once-weekly change in the dosage.
Antidepressants with broader mechanisms of action (i.e., venlafaxine and clomipramine) have been tried in nonresponders. The rationale for this practice is that these medications affect more than one neurotransmitter system and have some, albeit weak, meta-analytic data supporting their superiority in depression and OCD. 87 Benzodiazepines are generally avoided except in acute states or treatment-resistant chronic conditions.
Few data have been published about what to do after the few initial steps of treatment, such as how long maintenance therapy should last. Based on clinical experience, we generally recommend continuing treatment until the patient has achieved marked symptom reduction for at least 6 months. More research on this topic is needed.
Further testing of combined treatments at the initial and later steps of the typical algorithm was subsequently performed. 88 , 89 In the later stages of anxiety treatment, GABA-ergic anti-epileptic drugs and atypical antipsychotic agents may be tried. Atypical neuroleptic medications have shown even better evidence of efficacy in anxiety disorders, according to some placebo-controlled trials. 90
Side Effect Profiles
Patients and physicians need to be aware of adverse drug reactions. An extensive review of the side effects of SSRIs has been published by Valuck. 91 In other studies, SSRIs and SNRIs were found to increase the risk of suicidality 92 and atypical neuroleptic agents caused tardive dyskinesia and arrhythmias. 93 All of these drugs can cause weight gain and sexual dysfunction. Because polypharmacy is becoming the rule rather than the exception, especially in complex and treatment-resistant anxiety, practitioners should be cognizant of potential drug–drug interactions. 94
Serotonin syndrome and neuroleptic malignant syndromes, although rare, should be kept in mind. Discontinuation of SSRIs has not been well studied, but a withdrawal syndrome upon abrupt discontinuation of SSRIs (and SNRIs) is common. Symptoms may include paresthesias, nonvertiginous dizziness, nausea, diaphoresis, and rebound anxiety. 95 For this reason, stopping SSRIs and SNRIs should involve a gradual tapering and should take place, if possible, in parallel with CBT.
Cognitive–Behavioral Therapy and Medications
CBT has received the greatest amount of empirical support for the psychological treatment of anxiety disorders. 96 In our treatment algorithm, CBT stands with the SSRIs as a first-line treatment choice (see Figure 2 ). Combining drug therapy and CBT has shown mixed results in favoring one approach over the other, depending on the type of anxiety disorder.
A review and meta-analysis approached the question of combination treatment over monotherapy or CBT in anxiety by hypothesizing that CBT would be more successful compared with medications; however, the medication held an advantage over CBT in depression. 97 Within the anxiety disorders, there was great heterogeneity in their responsiveness to either CBT or medication, with CBT holding an advantage over medication in patients with panic disorder. By contrast, patients with social anxiety disorder were more responsive to medication.
The choice of medication or CBT, alone or in combination, is based on several variables, including the availability of a therapist; the affordability of CBT, which costs more than medication, especially if drugs are prescribed in primary care settings; and patient preference.
Cognitive–Behavior Therapy Alone
It is generally acknowledged that the treatment of anxiety disorders is suboptimal because of a lack of CBT therapists or the availability of affordable sessions. There is a great need to distill the essence of good therapy and to bring it into the primary care setting, with an emphasis on education and staff training. 25 Oxford University Press has published many excellent manuals that include both therapist and patient guides. 98 The proliferation of the Internet-based, self-administered therapies calls for further research into the efficacy of this method of dissemination. 99 Complex anxiety disorders might not be able to be self-treated adequately, whereas a specific phobia might be self-treated alone or with the support of a friend of family member.
Koszycki et al. 100 discussed whether self-administered CBT could stand alone or could be optimized with therapist-directed CBT, self-administered CBT, or medication augmented with self-administered CBT. Their work suggested that even self-administered treatment might be an effective addition to the CBT armamentarium.
Although many treatments are effective for anxiety, not all of them can help everyone and not all of them are effective for all anxiety disorders. A simple phobia is easier to treat than a complicated case of PTSD. The most empirically supported treatments are SSRIs and CBT. Relapse rates for CBT, compared with medication, are an understudied area, although our clinical experience suggests that CBT has a longer treatment effect if the patient continues to use the skills and tools learned in therapy.
CBT shares much in common with other more dynamically based forms of psychotherapy. A patient seeks help from an expert caregiver who treats the patient in a warm and nonjudgmental relationship in an attempt to help the patient function and feel better in a reality-oriented setting. However, CBT is directive and collaborative; the therapist establishes clear and specific goals with the patient and uses evidence-based techniques to elicit the patient’s feelings and bodily sensations (Arousal, or Alarm), dysfunctional and irrational thinking (Beliefs), and subsequent behavior (Coping).
The helping relationship is less emphasized in CBT as a curative factor, but it is considered important in building trust and support, serving as a springboard for patients to consider their erroneous beliefs and behaviors that cause them anxiety and fear. The therapist is explicit about conceptualizing the patient’s disorder, with regard to the genesis, evolution, and maintenance of the disorder over time. The therapist often incorporates manuals or other psychoeducational materials and may propose daily homework to help the patient learn more adaptive ways to manage and reduce the alarm (A), change irrational and dysfunctional beliefs (B), and develop adaptive coping (C) mechanisms, often through exposure exercises. To the most appropriate extent possible, patients are taught the ABC model to help them understand the dynamic and reciprocal relationship among feelings, thoughts, and behaviors.
Patient compliance with therapy is directly proportional to the treatment’s effectiveness. Motivational interviewing, which is used to help patients examine the cost–benefit ratio of their maladaptive thoughts and behavior, often increases compliance and, subsequently, effectiveness. 101 Patients are taught self-monitoring and symptom-reduction techniques to increase their motivation to confront their anxiety. Breathing and relaxation techniques can be explained as mental hygiene to raise one’s threshold for the onset of alarm reactivity and for increasing the patient’s ability to notice whether an alarm reaction is mounting over the course of the day.
The linchpin in the CBT model of anxiety is considered to be the patient’s thoughts. 102 Misguided beliefs must change for both the alarm to down-regulate and for subsequent adaptive coping to replace avoidant and escape-based coping. Although beliefs are the linchpin, exposure to the anxiety-producing thought, image, or situation is often the essential CBT component for jogging the linchpin loose. This too is a dynamic process. Cognitive restructuring techniques aimed at reducing catastrophic thinking help to diminish irrational or exaggerated thoughts, thereby allowing patients to become more willing to test those beliefs through exercises involving exposure.
Exposure is the gradual and systematic presentation of the anxiety-inducing thought, image, or situation for a long enough time for patients to see that their anxious feelings can be decreased without engaging in avoidance or escape. For example, a patient who is afraid of dogs might first be shown a picture of a dog, then stand across the street from a pet shop, and finally hold a dog in his or her arms. The patient would engage in each of these steps repeatedly and in a concentrated but not overwhelming way.
Ideally, the patient would experience a gradual lessening of anxiety at each step before moving on to the next. The patient would experience the alarm being reduced, and the exaggerated belief that all dogs are dangerous could be modified to a more accurate belief that most pet dogs are not threatening. The hoped-for outcome would be that the patient would no longer have a phobic avoidance of all dogs.
Mindfulness (The Third Wave)
A final emerging area in the evolution of CBT is the approach based on mindfulness (acceptance). This is the “third wave” in CBT, the first wave being the strict behavioral approach and the second wave emphasizing the cognitive approach. 103
Mindfulness is a type of meditation that has been adapted from Buddhist psychology. One definition is “awareness of present experience with acceptance.” 103 These therapies owe a debt of gratitude to Jon Kabat-Zinn’s Mindfulness-Based Stress Reduction (MBSR) program, which began at the University of Massachusetts in 1979. 104
Mindfulness-based cognitive therapy (MBCT) is one component of the integration of mindfulness into CBT. 105 MBCT has been applied to the treatment of panic disorder and other anxiety disorders, but more carefully controlled research is needed in this area. 106 MBCT emphasizes the prevention of relapse through a meta-cognitive or mindful awareness that leads patients to realize that their current symptoms do not necessarily mean that they are relapsing.
Acceptance and commitment therapy involves a mindful focus; many exercises are aimed at the meta-cognitive level to help patients perceive their thinking and subsequent anxiety to be separate from, and less identified with, their sense of self. Anxiety-causing thoughts are to be observed and accepted, not to be struggled with and changed, as in more traditional CBT and Western psychological approaches. 107
Shifting Treatment to Primary Care
In today’s managed care environment, the treatment of anxiety usually takes place in the primary care setting. Given the increasing limits on primary care physicians’ time, it is not surprising that anxiety disorders are underrecognized and undertreated. At the same time, SSRIs (antidepressants) are increasingly used in primary care, and physicians in fact are the largest group of prescribers. This is a mixed blessing for several reasons:
- SSRIs are often prescribed quickly in response to emotional distress that might not meet criteria for an anxiety disorder.
- The dose and duration of therapy might be inadequate.
- Adverse effects might not be managed by any means other than by discontinuation of the treatment.
This state of affairs may partly explain why psychiatrists are seeing more patients who are disenchanted with numerous failed attempts at pharmacotherapy.
Another problem in primary care is a lack of understanding of behavioral strategies that result in low referral rates to mental health professionals. There has been a trend toward developing comprehensive treatments for panic disorder to be delivered by primary care physicians.
In one study, an algorithm was tested for the treatment of panic disorder. 108 This study reflected the trend of how psychiatrists became more like consultants to primary care physicians, assisting them with correct initial management plans and taking over the management of more severe and treatment-resistant anxiety.
Management of Treatment-Resistant Anxiety
In managing refractory anxiety, it is important to start with a re-evaluation of the patient, including the diagnosis; comorbidities; and the interplay of cognitive, stress-related, and biological factors. Inadequate coping strategies on the part of patients and their family members should be reviewed. Doses and duration of the initial treatments should be assessed.
Initially, more intensive CBT, combined with an adequate trial of SSRIs, SNRIs, or both, may be needed in refractory anxiety. After that, the treatment may progress to a combination of SSRIs with antiepileptic or atypical neuroleptic agents, especially if bipolar disorder or a psychotic disorder is suspected. 109 , 110 Later, partial hospitalization in specialized centers with more extensive CBT and medication management might be recommended. 111
Although other forms of therapy have not demonstrated efficacy in anxiety disorders, they may be helpful for addressing personality issues in chronically anxious patients.
Experimental and Off-Label Nonpharmacological Treatments
Therapies for anxiety disorders, beyond combining conventional treatments, using off-label antiepileptic and antipsychotic agents, and introducing more intensive CBT programs, are mostly experimental. Promising medications have included intravenous clomipramine, citalopram, and morphine. 109 Many other treatments targeting more specific neurotransmitter systems have failed. 72
A handful of invasive therapies have emerged. These options may be considered after several off-label pharmacotherapy and psychotherapeutic approaches have failed or when significant functional impairment remains. They are typically reserved for the most treatment-resistant cases, typically those involving severe OCD. Invasive treatments often target brain circuits implicated in the processing of fear and anxiety.
Electroconvulsive Therapy
Electroconvulsive therapy (ECT) involves the application of brief electrical impulses to the scalp to induce large-scale cortical neuronal discharges, eventually producing generalized seizure activity. Although ECT is effective in treatment-resistant mood disorders, data regarding its efficacy in anxiety disorders are limited. 112 The mechanism and focal targets of ECT have not yet been determined.
Vagal Nerve Stimulation
Initially developed as an antiepileptic treatment, vagal nerve stimulation (VNS) was used in psychiatric patients after sustained mood improvements were noted with this therapy. 113 VNS is thought to stimulate brain networks relevant to anxiety and fear processing (taking place in the amygdala, hippocampus, insula, and orbitofrontal cortex) via the afferent vagal nerve. This modality is not routinely used to treat anxiety, and evidence of its effectiveness in resistant anxiety disorders is limited. 114 To date, no randomized controlled trials have investigated this intervention further.
Repetitive Transcranial Magnetic Stimulation
Focal magnetic stimulation of the scalp is used with the goal of invoking excitation or inhibition of cortical neurons. Repetitive transcranial magnetic stimulation (rTMS) is less invasive than ECT; anesthesia induction is not required, and rTMS does not elicit generalized seizure activity in the brain. It also has the advantage of being able to target brain regions thought to be involved in anxiety disorders.
The main limitations of rTMS include the inability to penetrate deeper brain structures implicated in OCD (the caudate nucleus, thalamus, and anterior capsule fiber tracts) or in panic disorder (the amygdala, hippocampus, and anterior cingulate); there is also a lack of specificity at the site of stimulation.
rTMS has not been approved as a treatment for any anxiety disorder, probably because of the paucity of large-scale studies. There is limited evidence for efficacy in treating OCD, although larger treatment effects have been reported by altering the stimulation site. 115 , 116 rTMS has been reported to improve anxiety symptoms in PTSD and panic disorder, although the approach has not been incorporated into clinical practice. 117
A small study reported significant anxiety reductions in patients with generalized anxiety disorder (GAD) using a symptom-provocation task during functional magnetic resonance imaging (fMRI) to guide individual selection of the rTMS site. 118 No studies have investigated the role of rTMS in social anxiety disorder.
Although psychosurgery has been used for various treatment-resistant anxiety disorders such as GAD, panic disorder, and social phobia, long-term follow-up studies in these patients have revealed adverse cognitive outcomes, including apathy and frontal lobe dysfunction. 119 Consequently, surgical approaches are usually reserved for OCD, given the disproportionate functional deficits that are a hallmark in treatment-refractory cases.
Several surgical approaches have been used, including anterior capsulotomy (which targets the anterior limb of the internal capsule), anterior cingulotomy (which targets the anterior cingulate and cingulum bundle), subcaudate tractotomy (which targets the substantia innominata, just inferior to the caudate nucleus), and limbic leucotomy (which combines anterior cingulotomy with subcaudate tractotomy). 120 , 121
Cingulotomy remains the most commonly used psychosurgical procedure in North America, probably because of its clinical efficacy as well as low morbidity and mortality rates. Postsurgical effects have included transient headache, nausea, or difficulty urinating. Postoperative seizures, the most serious common side effect, have been reported from 1% to 9% of the time.
Patient outcomes cannot be fully assessed until at least 6 months to 2 years after the definitive procedure, suggesting that postoperative neural reorganization plays an important role in recovery. Direct comparisons of each lesion approach within studies are rare.
Overall, the long-term outcomes of these approaches have demonstrated significant therapeutic effects of each procedure. In general, reported response rates vary from 30% to 70% in terms of remission, response, and functional improvements in quality of life.
Deep-Brain Stimulation
Deep-brain stimulation (DBS) involves the insertion of small electrodes under precise stereotactic MRI guidance. The major advantage of DBS over ablative surgery is the ability to adjust and customize neurostimulation. 122 Following implantation, parameters of electrode stimulation (electrode polarity, intensity, frequency, and laterality) can be modified. Parameters can be optimized by a specially trained clinician during long-term follow-up.
Several studies with blinded stimulation have been conducted with moderate-to-fair results. 123 More recently, structures adjacent to the internal capsule have also been targeted. 124 , 125 In all trials, response rates have been consistently reported in the 50% range. 125
Postoperative complications (e.g., infections, lead malfunctions) occur more commonly with DBS because of the prosthetic nature of the procedure. Batteries must also be periodically explanted and replaced. Stimulation-related side effects have been reported, including mood changes (transient sadness, anxiety, euphoria, and hypomania), sensory disturbances (olfactory, gustatory, and motor sensations), and cognitive changes (confusion and forgetfulness). These side effects are typically stimulation-dependent and disappear after the stimulation parameters are altered.
Complementary and Alternative Medicine
During the 1990s, many alternative treatment strategies for anxiety disorders emerged. 126 These included herbal medications (with St. John’s wort the most frequently used), vitamins, nutritional supplements, magnetic and electroencephalographic synchronizing devices, “energy” treatments, and meditation-based therapies (see Mindfulness on page 38).
These treatments may be provided by alternative medicine practitioners within the scope of a health care model, such as acupuncture, homeopathy, Ayurvedic medicine, Reiki, and healing touch. Because of minimal FDA regulation and widespread over-the-counter availability, many of these same treatments are self-selected and used by patients. Herbs are the most commonly used complementary and alternative medicine (CAM) products and are particularly popular with those with psychiatric disorders. Anxiety is one of the strongest predictors of herbal remedy utilization, 127 and patients often use these treatments without the knowledge of their physician. Consequently, clinicians and pharmacists are advised to regularly monitor the full range of treatments used by their patients, including a thorough medication reconciliation of prescription and non-prescription products, herbs, and supplements at each visit.
Results of herbal trials for anxiety disorders have been mixed. The widespread use of Piper methysticum (Kava) for anxiolysis was curtailed by reports of hepatotoxicity, prompting government warnings and withdrawal of the product from the market in many Western countries. 128 , 129 However, a randomized placebo crossover trial using a supposedly benign aqueous formulation reported moderate reductions in anxiety symptoms in a small sample of patients with mixed anxiety disorders. 128 , 130 Both Hypericum perforatum (St. John’s wort) and Silybum marianum (milk thistle) have been used for the treatment of OCD symptoms, although no placebo-controlled trials revealed any significant differences in symptoms or adverse effects between treatment groups. 131 , 132 Lower-quality studies of CAM have reported modest treatment effects for interventions such as mindfulness meditation, yoga, and acupuncture. 133
Despite a lack of data on efficacy, many patients continue to use CAM therapies, prompting a need to monitor use for potential interactions with prescription medications. 134 For instance, St. John’s wort is known to interact with many medications because of the induction of cytochrome P450 (CYP) isoenzymes 3A4 and 2C9. Of relevance in anxiety disorders, CYP3A4 may cause a decrease in serum levels of alprazolam (Xanax, Pfizer) and clonazepam (Klonopin, Roche). Combining St. John’s wort with SSRIs also increases the risk of serotonin syndrome. Milk thistle inhibits CYP3A4 and has the potential to increase levels of other medications metabolized by this pathway. Kava has been linked with inhibition of several CYP isoenzymes, including 1A2, 2D6, 2C9, and 3A4. 135 Further exploration of the efficacy of these alternative strategies for anxiety disorders is needed.
Functional Status
Although many patients with anxiety disorders experience symptom relief with treatment, residual symptoms still have an impact on everyday functions. Even subclinical anxiety can produce disability sometimes exceeding that seen in other severe mental illnesses. 111 , 136 In addition, chronic, persistent anxiety disorders have a significant impact on patients’ lives, often leading to deficits in social and work skills. Yet there are few clear interventions or programs with a focus on rehabilitation and restoration of function in these patients.
Stress is an important factor in the emergence and maintenance of anxiety syndromes. Patients who need to return to the workforce can experience increased stress that in turn may cause re-emergence of the symptoms, again resulting in decreased productivity and even loss of employment. More research is needed to address this problem.
Anxiety disorders are treatable. Effective treatments have been developed, and algorithms have been refined. However, more work needs to be directed toward merging of our knowledge of the biological mechanisms of anxiety with treatment in order to more accurately predict and improve treatment response. Dynamic models of anxiety—such as the ABC model—can be helpful in understanding the interplay between processes responsible for development and maintenance of the symptoms over time and between biological and psychological factors affecting them.
We need to learn how to better administer existing efficacious treatments in real-world health care environments, such as in primary care, and to inform the public via media outlets. We should continue to test alternative therapies for treating and preventing anxiety disorders and to help patients whose anxiety is resistant to conventional treatments.
Finally, we need to consider the patient’s feelings about mental illness and address their responses early in treatment. All of these measures will enhance the care of patients with anxiety.
Disclosure: Dr. Bystritsky reports that he has received honoraria, research grants, and travel reimbursements from AstraZeneca, Takeda, and Brainsway. He has also served as a consultant for UpToDate, John Wiley & Sons, Brainsonix Corp., and Consumer Brands. Dr. Khalsa, Dr. Cameron, and Dr. Schi3man report that they have no financial or commercial relationships in regard to this article. This work was supported in part by a grant from the Saban Family Foundation.
H5N1 bird flu: What threat does it pose?
Dr. Rajesh Gulati at UC Riverside answers some common questions about the virus and its spread
The World Health Organization has raised concerns about the spread of H5N1 bird flu , the disease caused by infection with avian (bird) influenza (flu) Type A viruses. Currently, H5N1 bird flu is causing outbreaks in U.S. poultry and dairy cows.

Dr. Rajesh Gulati , interim chair of internal medicine at the University of California, Riverside School of Medicine , answers some questions about H5N1 bird flu. Gulati is the associate dean of graduate medical education at UCR and a practicing hospitalist at Riverside Community Hospital.
Q: How is this new virus strain behaving differently than strains in earlier outbreaks?
This new strain of avian influenza (H5N1) is different from earlier strains because it has adapted and changed. It has used new genetic material from wild bird genes and infected more wild bird species than previous strains have. It has also been affecting mammals — wild ones, such as bears and foxes, but also domesticated ones, like dairy cattle and cats. We can see this new virus strain is also sticking around longer than previous outbreaks.
Q: How does the virus spread? How might it spread to humans?
The virus initially caused outbreaks in North American poultry species but has now been detected in many types of mammals as well as a few humans. It is spread through droplets or dust from infected animals, which a human can inhale or transfer from hands to the eyes/nose/mouth. We are not sure about the spread from person to person, but viruses are able to adapt and mutate rapidly. It is important to refer to the Center for Disease Control and Prevention for their research and recommendations.
Q: What precautions should people take?
Many precautions need to be taken by those in the dairy industry in direct contact with possibly infected animals, or those who often interact with wild birds. These individuals should be using PPE (such as respirators), creating isolated areas, and monitoring exposures. The virus is affecting dairy cattle; we want to make sure we are not consuming raw milk products, which contain many more dangerous microbes than possibly just H5N1 and are only drinking pasteurized milk.
In addition, for those of us with pet cats or dogs, it’s important to limit their interactions with wild birds to avoid any spread of the virus to our homes. We should also try to limit our interactions with wild birds, including their feathers, feces, or nests.
In general, one of the best ways to protect against viruses is frequent hand washing with soap and water and to avoid touching your hands to your face/mouth/nose/eyes if they are contaminated in any way.
Q: How can the spread be contained?
The current methods of control for H5N1 will likely be quarantining and culling (selective slaughter) of infected animals. If infection is suspected, it’s important to trace it back to the source and see the interactions along the way. If there is a need for a vaccine, COVID has shown us that our research centers can get them made (relatively) quickly and administered to prevent an outbreak from becoming catastrophic. For now, the virus appears to be contained to some domesticated mammals and the individuals who were interacting with them on a frequent basis.
Q: The virus has jumped to livestock and wild animals. How might this pose a danger to humans?
The lives of humans and the animals we consume and acquire products from are tightly linked. We interact frequently with domestic animals for farming, trade, and food production, which increases the opportunity for zoonotic transmission — infections that are spread between people and animals. It has the possibility of seriously disrupting our food supply and leading to significant economic losses.
Due to the rapid mutation, this virus can spread across species. It can lead to strains that are more virulent, that is, extremely severe or harmful, or even adapt itself to person-to-person transmission. This could lead to widespread outbreaks or even a global pandemic.
Header image credit: wildpixel/iStock/Getty Images Plus.
Media Contacts
Related articles.

Physicists solve puzzle about ancient galaxy found by Webb telescope
Small protein plays big role in chronic HIV infection
New center positions UC Riverside as a leader in quantum vibronics

Minoritized groups face high anxiety when taking part in research experiments

IMAGES
VIDEO
COMMENTS
Concerning phobias, nonexperiential, engaging innate fear, and experiential, engaging conditioned fear, disorders can be distinguished. However, so far, we know a lot about how the brain processes fear that is conditioned, while much less is known about innate fear. An increase of research on innate fear is therefore necessary.
Specific phobia, which has a lifetime prevalence of 7.4%, is one of the most common disorders 1. It is defined in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a marked fear or anxiety about a specific object or situation (for example, flying, heights, animals, receiving an injection, or seeing blood) 2.
As many people with specific phobias do not seek treatment, the epidemiological aspects of this Review concentrate on population-based data, focusing on the prevalence, incidence, and natural history of specific phobias. We also discuss research on risk factors (including genetic epidemiology) and treatment modalities for specific phobias.
Introduction. Anxiety disorders, which include generalised anxiety disorder, panic disorder, agoraphobia, social phobia, and specific (simple) phobias, are more prevalent in adults than are other mental disorders. 1 In 1987, Marks 2 reviewed the existing literature and conceptualised the study of anxiety, which led to a surge in research on the epidemiology and natural history of the ...
In various animal phobias, in particular, regard to snake and spider fears, cognitive reappraisal has been identified 31, 32 as a good strategy to regulate negative emotions. In contrast, social ...
Introduction. Evidence shows that specific phobias (SPs) are the most common anxiety- and mental disorders with a lifetime prevalence between 7.4 and 14% among adults with a cumulative incidence ...
This Collection welcomes original research articles investigating the processes underlying fear, anxiety, and specific phobias. Empirical animal and human research that focuses on the diagnosis ...
Anxiety disorders form the most common group of mental disorders and generally start before or in early adulthood. Core features include excessive fear and anxiety or avoidance of perceived threats that are persistent and impairing. Anxiety disorders involve dysfunction in brain circuits that respond to danger. Risk for anxiety disorders is influenced by genetic factors, environmental factors ...
Specific phobia is among the more prevalent anxiety disorders, affecting an estimated 9 percent of Americans within their lifetime. Common subtypes include fear of small animals, insects, flying ...
Anxiety is widely conceptualized as a state of heightened distress, arousal, and vigilance that can be elicited by potential threat (1, 2).When extreme or pervasive, anxiety can be debilitating ().Anxiety disorders are among the leading cause of years lived with disability, afflicting ∼300 million individuals annually ().In the United States, nearly 1 in 3 individuals will experience an ...
Among them, specific phobias are the most common, with a prevalence of 10.3%, then panic disorder (with or without agoraphobia) is the next most common with a prevalence of 6.0%, followed by social phobia (2.7%) and generalized anxiety disorder (2.2%). Evidence is lacking as to whether these disorders have become more prevalent in recent decades.
A specific phobia is a common anxiety-related disorder that can be treated efficiently using different therapies including exposure therapy or cognitive therapy. One of the most famous methods to treat a specific phobia is exposure therapy. Exposure therapy involves exposing the target patient to the anxiety source or its context without the intention to cause any danger. One promising track ...
The ECA study, however, found lifetime prevalences ranging from 1.94% to 3.29% (89), although a more recent study places the current prevalence rate in a somewhat lower range (90). Despite its well-known morbidity, few studies have attempted to measure the impact of OCD on quality of life.
The focus of research on the pharmacotherapy of anxiety disorders has shifted from serotonin, norepinephrine and GABA systems to other neurotransmitters and pathways including glutamate and neuropeptides ( 89 ). Presented below is a review of recent and ongoing studies of medications for GAD, PD, and SAD.
Articles on Phobias. Displaying 1 - 20 of 26 articles. For those suffering from arachnophobia, a harmless spider isn't just a spider. ... Our research shows that coulrophobia, or fear of clowns ...
Fear of specific animals (dogs, spiders, etc.) Fear of open spaces, enclosed space, or high places. Fear of natural events, such as thunderstorms. While fears are an unavoidable part of being human, most fears can be controlled and managed. Phobias, however, cause psychological and physical reactions that are difficult if not impossible to manage.
All phobias are anxiety disorders, lumped in the same class as post-traumatic stress disorder and panic disorder, among others. And anxiety disorders are, fundamentally, based on fear. "What we know about the neurocircuitry and brain basis of fear originally comes from animal research," says psychiatrist Scott Rauch, MD, of Harvard Medical School.
410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. A phobia is an uncontrollable, irrational, and persistent fear of a specific object, situation, or activity. The fear experienced by people with phobias can be so great that some go to extreme lengths to avoid the source of their fear.
More research is needed to confirm exactly why a person develops agoraphobia or social anxiety. Researchers currently believe complex phobias are caused by a combination of life experiences, brain ...
This article is part of the Research Topic Depression: Social Stress, Inflammation, Neuromodulatory, ... discriminative accuracy, and sensitivity to change of the Generalized Anxiety Disorder 2-item scale (GAD-2) and the Patient Health Questionnaire 2-item scale (PHQ-2) within a clinical population. Method: The sample comprised treatment ...
Depression and anxiety are the most common mental health illnesses worldwide [].Depression is a mood disorder that affects an individual's thoughts and feelings and leads to persistent feelings of sadness and disinterest [].]. Anxiety is a group of mental disorders characterized by nervousness, apprehension, and fear [].Depression and anxiety disorders are major contributors to the mental ...
The anxiety disorders, as classified in the International Classification of Diseases (ICD-10) ( ), comprise the phobic disorders, including agoraphobia with (F40.00) or without panic disorder (F40.01), social phobia (F40.1), and the specific phobias (F40.2), as well as other anxiety disorders, including panic disorder (F41.0), generalized ...
Pew Research Center has long studied changes in parenting and family dynamics, as well as the adoption of digital technologies. This analysis of parents' experiences with and attitudes about their children's tech use is based on data from 1,681 parents who had at least one child age 11 or younger as of March 2020 and participated in two surveys conducted on the Center's American Trends ...
Research conducted by Central Queensland University indicates people who work in the building and construction industry are at a significantly higher risk of mental health problems.
Background: Distress is highly prevalent among patients with cancer, but supportive care needs often go unmet. Digital therapeutics hold the potential to overcome barriers in cancer care and improve health outcomes. Objective: This study conducted a randomized controlled trial to investigate the efficacy of Mika, an app-based digital therapeutic designed to reduce distress across the cancer ...
Among them, specific phobias are the most common, with a prevalence of 10.3%, then panic disorder (with or without agoraphobia) is the next most common with a prevalence of 6.0%, followed by social phobia (2.7%) and generalized anxiety disorder (2.2%). Evidence is lacking as to whether these disorders have become more prevalent in recent decades.
Women's soccer teams have been ditching white shorts as part of a growing trend aimed at tackling period anxiety in sport, and new research shows that women's teams who play in white perform worse.
Advances in anxiety research over the previous decade are likely to be reflected in modifications of diagnostic criteria in the upcoming DSM-5, 9 planned for publication in May 2013. For instance, post-traumatic stress disorder (PTSD) and obsessive-compulsive disorder (OCD) have been reclassified in the separate domains of Trauma and Stressor Related Disorders and Obsessive-Compulsive and ...
The World Health Organization has raised concerns about the spread of H5N1 bird flu, the disease caused by infection with avian (bird) influenza (flu) Type A viruses. Currently, H5N1 bird flu is causing outbreaks in U.S. poultry and dairy cows. Dr. Rajesh Gulati. Dr. Rajesh Gulati, interim chair of ...