We will keep fighting for all libraries - stand with us!

Internet Archive Audio

- This Just In
- Grateful Dead
- Old Time Radio
- 78 RPMs and Cylinder Recordings
- Audio Books & Poetry
- Computers, Technology and Science
- Music, Arts & Culture
- News & Public Affairs
- Spirituality & Religion
- Radio News Archive

- Flickr Commons
- Occupy Wall Street Flickr
- NASA Images
- Solar System Collection
- Ames Research Center

- All Software
- Old School Emulation
- MS-DOS Games
- Historical Software
- Classic PC Games
- Software Library
- Kodi Archive and Support File
- Vintage Software
- CD-ROM Software
- CD-ROM Software Library
- Software Sites
- Tucows Software Library
- Shareware CD-ROMs
- Software Capsules Compilation
- CD-ROM Images
- ZX Spectrum
- DOOM Level CD

- Smithsonian Libraries
- FEDLINK (US)
- Lincoln Collection
- American Libraries
- Canadian Libraries
- Universal Library
- Project Gutenberg
- Children's Library
- Biodiversity Heritage Library
- Books by Language
- Additional Collections

- Prelinger Archives
- Democracy Now!
- Occupy Wall Street
- TV NSA Clip Library
- Animation & Cartoons
- Arts & Music
- Computers & Technology
- Cultural & Academic Films
- Ephemeral Films
- Sports Videos
- Videogame Videos
- Youth Media
Search the history of over 866 billion web pages on the Internet.
Mobile Apps
- Wayback Machine (iOS)
- Wayback Machine (Android)
Browser Extensions
Archive-it subscription.
- Explore the Collections
- Build Collections
Save Page Now
Capture a web page as it appears now for use as a trusted citation in the future.
Please enter a valid web address
- Donate Donate icon An illustration of a heart shape
Research methods and organization studies
Bookreader item preview, share or embed this item, flag this item for.
- Graphic Violence
- Explicit Sexual Content
- Hate Speech
- Misinformation/Disinformation
- Marketing/Phishing/Advertising
- Misleading/Inaccurate/Missing Metadata
![[WorldCat (this item)] [WorldCat (this item)]](https://archive.org/images/worldcat-small.png)
plus-circle Add Review comment Reviews
2 Favorites
DOWNLOAD OPTIONS
No suitable files to display here.
IN COLLECTIONS
Uploaded by station23.cebu on January 8, 2020
SIMILAR ITEMS (based on metadata)
- Find My Rep
You are here
The SAGE Handbook of Organizational Research Methods
- David Buchanan - Cranfield University, UK
- Alan Bryman - University of Leicester, UK
- Description
Buchanan & Bryman have gathered together many of the world's leading writers on theory, method and analysis in organizational research and have made this the most comprehensive and cutting-edge volume in this ever-growing field. The handbook aims to:
- Provide a comprehensive critical review of contemporary issues, debates, field practice, and trends across the domain of organizational research;
- Locate current thinking, debates, and methods in the history of organizational research;
- Identify trends, theories, and issues which have the potential to shape the underpinning epistemologies, theories and methodologies of future organizational research;
- Explore strategies for bridging the gap between researchers and those who are in a position to act on research findings to influence organizational practice
'This handbook provides a rich resource for organizational researchers, locating the technical aspects of organizational research in the wider context of personal, epistemological, theoretical, historical, ethical, and political issues. The editors have gathered together many of the world's leading writers on methodological issues in organizational research, and have made this the most comprehensive and cutting edge volume in this growing field' - Public Administration, Development, and Environment
Short chapters allow selective study of concepts in organizational research (grounded theory or specific methods like interviewing). The amount of information provided is sufficient, but short enough to be processed by small student teams and presented to classmates/fellow students. Beyond that, the handbook is an ideal reference for students to catch up on topics that weren't taught in former courses. At some points, illustrations or diagrams could leaven the reading. In a new edition, digital elements (online surveys, Big Data, smartphone and diary studies) should be included/gain more attention.
A few chapters of the handbook are suggested for deeper understanding of the logics of sampling and some design aspects.
I highly recommend this book
A diverse and detailed insight into different perspectives and experiences of organisational research - not at introductory text but good for those with some knowledge of organisational research.
It is a very good qualitative research book. It contains a coherent topics e.g. Grounded theory and practical guidelines for QR
Individual chapters are useful assignments for undergraduate working groups within an introductory course on social science methodology. Very accessible for students with a strong focus on practical applicability.
I consider the book very useful for student who want to obtain deeper knowledge of a specific research method, as well as get fammiliar with new and yet not commonly known approaches to organizational research.
Too much reading for students
MBA to be relaunched in 2013. This book will be reviewed for this new MBA course later this year 2012.
Preview this book
Sample materials & chapters.
Chapter One
For instructors
Select a purchasing option, related products.

- Technical Support
- Find My Rep
You are here
Organization Studies
Preview this book.
- Description
Aims and Scope
- Editorial Board
- Abstracting / Indexing
- Submission Guidelines
Organization Studies (OS), published in collaboration with the European Group for Organization Studies (EGOS), is a global, peer-reviewed journal that promotes the understanding of organizations, organizing and the organized, and the societal relevance of that understanding. OS prompts engagement with organizations and organizing as psychological, social, economic, cultural, political, historical and philosophical phenomena, and is the leading journal in the development of relevant and impactful knowledge of how organizations and organizing shape and are shaped by societies.
OS welcomes innovative, high-quality research from all paradigms and disciplines that advance organization research. It promotes multidisciplinarity through research that engages across disciplinary boundaries; it invites all social science methodologies and methods that provide insights into organizations, organizing and the organized in and between societies. It encourages studies that reflect on the broader implications of their results. + Follow Organization Studies on Facebook - click here. + Follow Organization Studies on Twitter - click here. + Follow Organization Studies on LinkedIn - click here. Organization Studies Guidelines for Reviewers .
"Organization Studies goes to the top of the stack because it is such a reliable source of thoughtful scholarship. Authors get into the pages of this journal by reflecting deeply on issues. There is less running after transient 'mainstreams', and more willingness to enact meaningful discourse that people should take seriously. Organization Studies features 'seasoned inquiry' in the best sense of that phrase. It dominates that niche hands down." Karl E Weick
" I am a great admirer of Organization Studies . Its issues contain articles with new ideas, analysis that is rigorous, empirical methodologies that are sound and helpful ideas relevant to thoughtful practitioners." Chris Argyris
"Organization Studies is an exemplar of quality publishing in organization theory. Its success has helped enormously to build the more creative and confident European management research community we now have. I am confident OS will retain its European distinctiveness while becoming a premier publishing outlet for the best scholarship from throughout the world. OS can make a difference both in intellectual and policy terms and I have great hopes it will". Andrew Pettigrew
All issues of Organization Studies are available to browse online . This journal is a member of the Committee on Publication Ethics (COPE) .
Organization Studies (OS) is a highly ranked and globally respected, multidisciplinary journal with over 40 years history of publishing excellent organization research. OS aims at advancing our knowledge of organizations, organizing, the organized, the disorganized and the unsettled. It is broadly rooted in the social sciences and promotes an understanding of these phenomena as shaping, and shaped by, the societies of which they are part.
OS invites innovative high-quality research from a wide range of philosophical traditions, disciplines, and methodological approaches. It encourages the interplay between theorizing and empirical research, in the belief that they are mutually informative.
OS welcomes articles that push organization theory forward through research that fully or partly draws on empirical data to research studies based on qualitative, quantitative or mixed methods. Further, we accept conceptual articles that develop theory without reliance on empirical data. In the medium term, OS will focus on empirical manuscripts and will advise authors of manuscripts that do not draw on empirical data in any form to submit to Organization Theory (OT) instead.
If you would like to know more about the Aims & Scope, please read the most recent editorial here. If you would like to learn more about the historical intellectual signature of OS , please click here.
Our commitment
We are committed to OS being the leading hub of a community of scholars – authors, reviewers, editors and readers –, whose defining characteristics are a passion for ideas, open-minded intellectual curiosity, collegiate critique, and uncompromising adherence to the highest scholarly standards.
We expect every article published in OS to provide meaningful insights that challenge and exceed existing knowledge in the area of organization studies. We encourage bold research, driven by academic curiosity that crosses existing boundaries and dares to explore novel ground. We are looking for original research, but do not seek novelty as an end in itself, but rather as the result of the passion to advance our scholarly community and move our journal entrepreneurially ahead.
We are open to paradigmatic plurality and multidisciplinary research, but each article must have a solid theoretical grounding and must strive to develop further the tradition to which it adheres. We are committed to the accumulation of knowledge and demand that all articles engage seriously with existing literature. Submissions need to clearly communicate which conversations they wish to be part of or challenge, and what the novel theoretical insights are that their research contributes in relation to existing organizational literatures.
We are open to a wide range of epistemologies, methodologies and methods and expect empirical submissions to account for and motivate the approach chosen. Empirical studies must display professional rigour in data collection and analysis appropriate for the specific approach.
Types of Submissions
OS welcomes the following types of submissions: (a) empirical or conceptual ‘Research articles’; (b) shorter, essay-style ‘X and Organization Studies’; (c) ‘Perspectives articles’ that serve as introductions to Virtual Special Issues; (d) ‘Method/ology articles; (e) ‘Agora’ opinion pieces, and (f) ‘Media reviews’.
Empirical or conceptual papers, 'X and Organization Studies,' "Perspective articles' and Method/ology article are all peer-reviewed and benefit from our rigorous and developmental review process
Empirical or conceptual research articles
We welcome empirical and conceptual research articles. Manuscripts must be original in style and content (not under review, accepted and/or published elsewhere). The maximum length of submitted manuscripts is 13,000 words (including references and appendices).
‘X and Organization Studies’ essays
‘X and OS’ are essay-style articles that draw attention to unexplored, unthought, or marginalized topics in order to revitalize research and inspire the field of organization studies more broadly. Articles in this section will have to contribute to both the ‘X’ and the ‘OS’. ‘X and OS’ are written prior to when a full empirical or conceptual research article can address a topic, but also, importantly, they accomplish their objective in the style of an essay (please see here for our expectations concerning this article type; recent examples can be found here ). The maximum length of X and OS essays is 7.500 words (including references). Authors are asked to discuss preliminary ideas with the Editors-in-Chief. After initial green light from the EiC, developed manuscripts will go through a regular peer review process."
Perspectives articles
Perspectives articles are introductions to Virtual Special Issues, which cover a set of articles (five to six) previously published in Organization Studies . Perspectives pieces provide a focused overview of the evolution of a topic over time, the contribution of selected prior articles to the development and ongoing debate, and, most importantly, raise concerns about missing insights and knowledge, in order to outline fruitful avenues for future research. The Perspectives article is published in a regular OS issue, and also published online together with the previously published OS articles as part of a Virtual Special Issue. Interested authors should discuss their ideas with the Editors-in-Chief. The maximum length of a Perspectives article is 13,000 words (including references). Previous Virtual Special Issues can be found here . After initial green light from the EiC, developed manuscripts will go through a regular peer review process.
Method/ology articles
Method/ology articles address questions of methodology and method broadly (including philosophy of science, ontology, epistemology, study design, novel analytical methods, and writing). Method/ology articles should situate themselves firmly within organization studies and tackle issues or problems directly related to the “doing” of organization studies research. They must address topics of interest to readers of OS and make clear the connection to research conducted in OS . The maximum length for Method/ology articles is 13.000 words (including references).
In line with the idea of knowledge emerging from gathering together in spaces like assemblies and squares, OS publishes short opinion pieces in the form of single contributions or as dialogues in essay style (all in all no longer than 2,000 words including references). In the Agora , we deal with the big issues of our times and their organizational dimensions. With this format, we wish to offer a forum for debating contemporary matters of academic interest to the readers of Organization Studies , in the hope that this triggers discussion or sets off reflections that lead to empirical studies and theorizing. Agora pieces are single-authored: (please see here for our expectations concerning this article type; recent examples can be found here ). Those interested in contributing to the Agora section should contact the Editors-in-Chief in advance, briefly sketching the issue and their personal views, the organizational relevance, why the issue deserves sparking an urgent debate, and the kind of research required.
Authors who have published an Agora piece, cannot resubmit for the three years following the date of acceptance of their published Agora. This is to guarantee variety and fairness in access to this section of the Journal.
Media Reviews
Books are and remain at the heart and centre of scholarly formats. However, in order to account for the relevance of and inspiration from other forms of media in the process of defining, producing, and diffusing knowledge, we have broadened the scope of reviews and OS now offers a Media Reviews section. Proposals should be directed towards our Media Review Editors (email: [email protected] ).
If you are interested in proposing a Special Issue, please click here .
- Abstracts in Anthropology Online
- Academic Search Premier
- All-Russian VINITI Abstracts Journal
- Applied Social Sciences Index & Abstracts (ASSIA)
- Bibliography of Asian Studies
- British Education Index
- British Humanities Index
- Business Index ASAP
- Business Source Corporate
- Business Source Elite
- Business Source Premier
- CSA Environmental Sciences & Pollution Management
- Cab Abstracts
- Child Development Abstracts & Bibliography (Ceased 2001)
- Communication Abstracts
- Criminology, Penology and Police Science Abstracts
- Cumulative Index to Nursing and Allied Health Literature CINAHL
- Current Contents / Social and Behavioral Sciences
- Current Contents/ Social and Behavioral Sciences
- Current Literature on Science of Science
- Current Management Literature
- DELNET - Developing Libraries Network (Members Only)
- Documentation in Public Administration
- EBSCO: Educational Administration Abstracts
- EBSCO: Human Resources Abstracts
- ERIC Database (Science/Maths/Environ. Educ.)
- Educational Management Abstracts
- Educational Research Abstracts Online - e-Psyche
- Educational Technology Abstracts
- Emerald Management Reviews
- Environmental Science & Pollution Management
- Focus On: Industrial and Organizational Psychology
- Global Health (Previously CAB Health)
- Health & Safety Science Abstracts
- ISI Alerting Services
- International Bibliography of the Social Sciences
- International Political Science Abstracts
- MLA International Bibliography
- MasterFILE Premier
- Mental Health Abstracts (online through DIALOG)
- Psychological Abstracts
- Research Alert
- Research into Higher Education Abstracts
- Risk Abstracts
- Social SciSearch
- Social Science Source
- Social Sciences Citation Index (SSCI)
- Social Services Abstracts
- Sociological Abstracts
- Sociology of Education Abstracts
- Studies on Women & Gender Abstracts
- Technical Education and Training Abstracts
- Urban Affairs Abstracts
- VINITI Abstracts Journal
- Work Related Abstracts
- World Agricultural Economics and Rural Sociology Abstracts
- Worldwide Political Science Abstracts
- e-Psyche (Ceased)
Please read the guidelines below carefully before visiting Organization Studies ’ ScholarOne submission site https://mc.manuscriptcentral.com/orgstudies to upload your manuscript. In addition, we ask you to have a close look into our and Sage’s general Editorial and Publishing Policies that are to be found here . Manuscripts not conforming to these guidelines and policies may be returned.
- What do we publish? 1.1 Aims & Scope 1.2 Article types
- Preparing your manuscript 2.1 Title, Keywords, and Abstract 2.2 Manuscript formatting 2.3 Reference style
- Submitting a manuscript
- After acceptance 4.1 Author Accepted Manuscripts (AAM) 4.2 Online First publication
- Further information
1. What do we publish?
1.1 Aims & Scope
OS welcomes innovative, high-quality research from all paradigms and disciplines that advance organization research; it invites all social science methodologies and methods, and encourages studies that reflect on the broader implications of their results.
Before submitting your manuscript to OS, please ensure you have read our Aims & Scope . Only manuscripts of sufficient quality that meet the OS aims and scope will be reviewed.
1.2 Article Types
OS welcomes the following types of submissions:
(a) empirical or conceptual ‘Research articles’; (b) shorter, essay-style ‘X and Organization Studies’; (c) ‘Perspectives articles’ that serve as introductions to Virtual Special Issues; (d) ‘Method/ology articles; (e) ‘Agora’ opinion pieces, and (f) ‘Media reviews’.
‘X and OS’ are essay-style articles that draw attention to unexplored, unthought, or marginalized topics in order to revitalize research and inspire the field of organization studies more broadly. Articles in this section will have to contribute to both the ‘X’ and the ‘OS’. ‘X and OS’ are written prior to when a full empirical or conceptual research article can address a topic, but also, importantly, they accomplish their objective in the style of an essay (please see here for our expectations concerning this article type; recent examples can be found here). The maximum length of X and OS essays is 7.500 words (including references). Authors are asked to discuss preliminary ideas with the Editors-in-Chief. After initial green light from the EiC, developed manuscripts will go through a regular peer review process."
Perspectives articles are introductions to Virtual Special Issues, which cover a set of articles (five to six) previously published in Organization Studies. Perspectives pieces provide a focused overview of the evolution of a topic over time, the contribution of selected prior articles to the development and ongoing debate, and, most importantly, raise concerns about missing insights and knowledge, in order to outline fruitful avenues for future research. The Perspectives article is published in a regular OS issue, and also published online together with the previously published OS articles as part of a Virtual Special Issue. Interested authors should discuss their ideas with the Editors-in-Chief. The maximum length of a Perspectives article is 13,000 words (including references). Previous Virtual Special Issues can be found here . After initial green light from the EiC, developed manuscripts will go through a regular peer review process.
Method/ology articles address questions of methodology and method broadly (including philosophy of science, ontology, epistemology, study design, novel analytical methods, and writing). Method/ology articles should situate themselves firmly within organization studies and tackle issues or problems directly related to the “doing” of organization studies research. They must address topics of interest to readers of OS and make clear the connection to research conducted in OS. The maximum length for Method/ology articles is 13.000 words (including references).
In line with the idea of knowledge emerging from gathering together in spaces like assemblies and squares, OS publishes short opinion pieces in the form of single contributions or as dialogues in essay style (all in all no longer than 2,000 words including references). In the Agora, we deal with the big issues of our times and their organizational dimensions. With this format, we wish to offer a forum for debating contemporary matters of academic interest to the readers of Organization Studies, in the hope that this triggers discussion or sets off reflections that lead to empirical studies and theorizing. Agora pieces are single-authored: (please see here for our expectations concerning this article type; recent examples can be found here . Those interested in contributing to the Agora section should contact the Editors-in-Chief in advance, briefly sketching the issue and their personal views, the organizational relevance, why the issue deserves sparking an urgent debate, and the kind of research required.
Books are and remain at the heart and centre of scholarly formats. However, in order to account for the relevance of and inspiration from other forms of media in the process of defining, producing, and diffusing knowledge, we have broadened the scope of reviews and OS now offers a Media Reviews section. Proposals should be directed towards our Media Review Editors (email: [email protected] ).
Back to top
2. Preparing your manuscript
2.1 Title, Keywords, and Abstract
The title, keywords and abstract are key to ensuring readers find your article online. Submissions of articles and essays should be accompanied by
- an informative abstract of 300 words (maximum): Good abstracts describe the material presented in the paper, including the question or focus, the type of study reported (e.g., conceptual, empirical, qualitative, field, network study, etc.), the context, the main data source, and the most significant findings and contributions. The better your abstract, the easier it is for others to identify, read, and build upon your work;
- 5 to 7 keywords: Four keywords must be selected from the OS ScholarOne keyword list, the remaining keywords may be freely chosen.
Authors should explain any background information about the submission that the acting editor should be aware of in a cover letter (see also under 3. Submitting a manuscript).
2.2 Manuscript formatting
Manuscripts submitted to OS must be in an editable (e.g. Word) format, we do not accept manuscripts as PDF file.
Organize the manuscript by using primary, secondary, and tertiary headings, rather than numbered headings (see recent OS issues for examples).
Within the manuscript, text should be typed double-spaced in 12-point Times New Roman. Tables may be single-spaced and in smaller fonts.
When submitting a paper and during the review process, tables and figures should be inserted in the text to facilitate reading of the manuscript. Ensure that figures and tables are inserted in editable formats (Word, Excel, PowerPoint). Before acceptance, you will have to upload all tables and figures in separate files. Figures supplied in colour will appear in colour online regardless of whether or not these illustrations are reproduced in colour in the printed version. For specifically requested colour reproduction in print, you will receive information regarding the costs from Sage after receipt of your accepted article.
2.3 Reference style
References to articles, books, and other source works cited in the text and listed in the references section should follow the OS Style and Reference Guide (see here for details).
3. Submitting a manuscript
Authors should not re-submit a manuscript that OS has rejected at an earlier time, unless they are doing so at the explicit invitation of one of the editors.
Ordinarily, the editors will only consider up to a maximum of three submissions at a time from an author (regardless of single- or co-author status). Should an author believe there are exceptional circumstances to consider when it comes to this policy, we ask the author to contact us for a consultation.
OS is hosted on Sage track, a web based online submission and peer review system powered by ScholarOne. Authors need to submit their manuscripts (in editable format) to the OS ScholarOne submission site https://mc.manuscriptcentral.com/orgstudies
On the site, you will be asked to upload a title page , with contact information for all authors. Please include acknowledgements and funding information on the title page.
Please also make sure that you answer all the manuscript- and author-related questions in the system, and that all authors’ names are entered into the manuscript submission form.
Every submission must name a corresponding author who will be involved in all correspondence regarding the manuscript. Provide full contact details for the corresponding author on the OS ScholarOne site. Academic affiliations are required for all co-authors.
Please add an author b iography of no more than 100 words on each author’s personal history and current interests (1 st step of your submission under the header “Type, Title, & Abstract”).
When authors submit a manuscript for consideration, they must certify that the manuscript is not at the same time under review for publication in another outlet (e.g., book chapter, journal) nor that it, or a closely related version of the manuscript, has previously been published in another outlet.
Please indicate in your cover letter people who have already viewed the paper, members of thesis committees and colleagues who would have a conflict of interest in reviewing the paper, and any other circumstances that might affect the integrity of the anonymize review process. It is not useful to include a description or summary of the paper in the cover letter. Use the cover letter to tell the editor whether any of the data in a submitted manuscript have been published elsewhere or are used in manuscripts under review in other outlets and how the submitted manuscript differs. (Please see our Editorial and Publishing Policies for further information.)
Authors should prepare their manuscripts in such a way that they cannot be identified. To preserve anonymity in the anonymize review process, authors should avoid revealing their identity in text through obvious and/or multiple self-references to previous work or in footnotes. If authors cite their own published work or work in progress, however, these references must be included in the references with full bibliographic information. Authors should reference their own work as they would the work of any other scholar. Reviewers will ask what the contribution of a manuscript is above what has already been published and must have this information.
Any acknowledgements and funding information should be provided in the respective fields on the OS ScholarOne site and on the title page, but not in the main text of the manuscript. (In manuscripts accepted for OS publication any acknowledgements will appear at the end of the article prior to the Declaration of Conflicting Interests (if applicable), any notes and the References).
Authors are responsible for obtaining permission from copyright holders for reproducing any illustrations, pictures, tables, figures or lengthy quotations previously published elsewhere.
For further information including guidance on fair dealing for criticism and review, please see the Journal Permission Guidelines . More information is also available on the Copyright and Permissions page on the Sage Author Gateway .
4. After acceptance
4.1 Author Accepted Manuscripts (AAM)
OS makes accepted manuscripts available to subscribers online as rapidly as possible. Author Accepted Manuscripts (AAM) are the final author-created accepted version before they have gone through Sage’s copy editing, formatting and proofing process. Author Accepted Manuscripts are posted online in PDF format and clearly identified as unedited manuscript by the bar “Author Accepted” across the pages. Authors can correct last minor errors within their article when reviewing proofs during the copy-editing process but no changes can be made to the AAM PDF.
AAMs can be cited by the Digital Object Identifier (DOI). Once the manuscript has gone through copy-editing, typesetting, and review of the resulting proof, the AAM is replaced by the OnlineFirst version. All versions of the article have the same DOI as the Author Accepted Manuscript.
To view the list of AAMs, visit the journal’s homepage and click on the Accepted Manuscripts link at the top of the page (see landing page here ).
4.2 Online First publication
OS benefits from OnlineFirst, a feature offered through Sage’s electronic journal platform, Sage Journals Online. It allows final revision articles (completed articles in queue for assignment to an upcoming issue) to be hosted online prior to their inclusion in a final print and online journal issue which significantly reduces the lead time between submission and publication. For more information, please visit the Sage OnlineFirst Fact Sheet .
5. Further information
Any correspondence, queries or additional requests for information on the Manuscript Submission process should be sent to the Editorial Office as follows:
Sophia Tzagaraki, Managing Editor E-mail: [email protected]
- Read Online
- Sample Issues
- Current Issue
- Email Alert
- Permissions
- Foreign rights
- Reprints and sponsorship
- Advertising
Individual Subscription, E-access
Individual Subscription, Print Only
Institutional Subscription, E-access
Institutional Subscription & Backfile Lease, E-access Plus Backfile (All Online Content)
Institutional Subscription, Print Only
Institutional Subscription, Combined (Print & E-access)
Institutional Subscription & Backfile Lease, Combined Plus Backfile (Current Volume Print & All Online Content)
Institutional Backfile Purchase, E-access (Content through 1998)
Individual, Single Print Issue
Institutional, Single Print Issue
To order single issues of this journal, please contact SAGE Customer Services at 1-800-818-7243 / 1-805-583-9774 with details of the volume and issue you would like to purchase.

Qualitative Methodologies in Organization Studies
Volume II: Methods and Possibilities
- © 2018
- Malgorzata Ciesielska 0 ,
- Dariusz Jemielniak 1
Teesside University Business School, Teesside University, Middlesbrough, United Kingdom
You can also search for this editor in PubMed Google Scholar
Akademia Leona Koźmińskiego, Warsaw, Poland
Addresses new and experimental research methods
Provides contributions from internationally renowned authors from across business and management fields
Includes case studies, holistic literature reviews and secondary data analysis
64k Accesses
83 Citations
7 Altmetric
- Table of contents
About this book
Editors and affiliations, about the editors, bibliographic information.
- Publish with us
This is a preview of subscription content, log in via an institution to check access.
Access this book
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Other ways to access
Licence this eBook for your library
Institutional subscriptions
Table of contents(11 chapters)
Front matter.
- Marta Strumińska-Kutra, Izabela Koładkiewicz
Observation Methods
- Malgorzata Ciesielska, Katarzyna W. Boström, Magnus Öhlander
Fieldwork Techniques for Our Times: Shadowing
- Barbara Czarniawska
Interviewing in Qualitative Research
- Svetlana Gudkova
Focus Group Interviews
- Katarzyna Gawlik
The Repertory Grid Technique
- Dorota Bourne, Devi A. Jankowicz
Relational Methods in Organization Studies: A Critical Overview
- Mustafa Özbilgin, Joana Vassilopoulou
Template Analysis in Business and Management Research
- Nigel King, Joanna Brooks, Saloomeh Tabari
Discourse Analysis
- Aylin Kunter
Designing a Qualitative Research Project
- Agata Stasik, Adam Gendźwiłł
What Should Be Avoided During Qualitative Research?
- Beata Glinka, Przemysław Hensel
Back Matter
- research methods
- data collection
- reflective analysis
- action research
- repertory grid technique
This book provides a thorough review of tested qualitative methods often used in organization studies, and outlines the challenges and essential requirements of designing a qualitative research project. The methods examined include case studies, observation, interviewing and the repertory grid technique. By highlighting certain key ‘rules’ for carrying out qualitative research and describing issues that should be avoided, this second volume of Qualitative Methodologies in Organization Studies is essential reading for academics and researchers who wish to understand the current state of qualitative data gathering within organization studies. Those exploring organization studies will find this two-volume collection extremely valuable as it contains robust contributions from highly-skilled authors who are actively researching in this field.
Malgorzata Ciesielska
Dariusz Jemielniak
M algorzata Ciesielska is Senior Lecturer in Organization Studies & HRM at Teesside University, UK, and Associate Editor of Tamara – Journal for Critical Organization Inquiry .
Dariusz Jemielniak is Professor of Management, Head of the Center for Research on Organizations and Workplaces, and Founder of the New Research on Digital Societies group at Kozminski University, Poland.
Book Title : Qualitative Methodologies in Organization Studies
Book Subtitle : Volume II: Methods and Possibilities
Editors : Malgorzata Ciesielska, Dariusz Jemielniak
DOI : https://doi.org/10.1007/978-3-319-65442-3
Publisher : Palgrave Macmillan Cham
eBook Packages : Business and Management , Business and Management (R0)
Copyright Information : The Editor(s) (if applicable) and The Author(s) 2018
Hardcover ISBN : 978-3-319-65441-6 Published: 17 January 2018
Softcover ISBN : 978-3-319-88030-3 Published: 06 June 2019
eBook ISBN : 978-3-319-65442-3 Published: 11 December 2017
Edition Number : 1
Number of Pages : XXI, 264
Number of Illustrations : 1 b/w illustrations
Topics : Organization , Project Management , Operations Research/Decision Theory , Market Research/Competitive Intelligence
Policies and ethics
- Find a journal
- Track your research

- Business & Money
- Management & Leadership

Enjoy fast, free delivery, exclusive deals, and award-winning movies & TV shows with Prime Try Prime and start saving today with fast, free delivery
Amazon Prime includes:
Fast, FREE Delivery is available to Prime members. To join, select "Try Amazon Prime and start saving today with Fast, FREE Delivery" below the Add to Cart button.
- Cardmembers earn 5% Back at Amazon.com with a Prime Credit Card.
- Unlimited Free Two-Day Delivery
- Streaming of thousands of movies and TV shows with limited ads on Prime Video.
- A Kindle book to borrow for free each month - with no due dates
- Listen to over 2 million songs and hundreds of playlists
- Unlimited photo storage with anywhere access
Important: Your credit card will NOT be charged when you start your free trial or if you cancel during the trial period. If you're happy with Amazon Prime, do nothing. At the end of the free trial, your membership will automatically upgrade to a monthly membership.
Buy new: $170.00
Return this item for free.
Free returns are available for the shipping address you chose. You can return the item for any reason in new and unused condition: no shipping charges
- Go to your orders and start the return
- Select the return method

Download the free Kindle app and start reading Kindle books instantly on your smartphone, tablet, or computer - no Kindle device required .
Read instantly on your browser with Kindle for Web.
Using your mobile phone camera - scan the code below and download the Kindle app.

Image Unavailable

- To view this video download Flash Player
Follow the author

Research Methods and Organization Studies 1st Edition
Purchase options and add-ons.
- ISBN-10 1138138517
- ISBN-13 978-1138138513
- Edition 1st
- Publisher Routledge
- Publication date December 22, 2015
- Language English
- Dimensions 5.5 x 8.5 inches
- Print length 300 pages
- See all details

Editorial Reviews
About the author, product details.
- Publisher : Routledge; 1st edition (December 22, 2015)
- Language : English
- Hardcover : 300 pages
- ISBN-10 : 1138138517
- ISBN-13 : 978-1138138513
- Item Weight : 16 ounces
- Dimensions : 5.5 x 8.5 inches
About the author
Alan bryman.
Discover more of the author’s books, see similar authors, read author blogs and more
Customer reviews
Customer Reviews, including Product Star Ratings help customers to learn more about the product and decide whether it is the right product for them.
To calculate the overall star rating and percentage breakdown by star, we don’t use a simple average. Instead, our system considers things like how recent a review is and if the reviewer bought the item on Amazon. It also analyzed reviews to verify trustworthiness.
- Sort reviews by Top reviews Most recent Top reviews
Top review from the United States
There was a problem filtering reviews right now. please try again later..
- Amazon Newsletter
- About Amazon
- Accessibility
- Sustainability
- Press Center
- Investor Relations
- Amazon Devices
- Amazon Science
- Start Selling with Amazon
- Sell apps on Amazon
- Supply to Amazon
- Protect & Build Your Brand
- Become an Affiliate
- Become a Delivery Driver
- Start a Package Delivery Business
- Advertise Your Products
- Self-Publish with Us
- Host an Amazon Hub
- › See More Ways to Make Money
- Amazon Visa
- Amazon Store Card
- Amazon Secured Card
- Amazon Business Card
- Shop with Points
- Credit Card Marketplace
- Reload Your Balance
- Amazon Currency Converter
- Your Account
- Your Orders
- Shipping Rates & Policies
- Amazon Prime
- Returns & Replacements
- Manage Your Content and Devices
- Recalls and Product Safety Alerts
- Conditions of Use
- Privacy Notice
- Consumer Health Data Privacy Disclosure
- Your Ads Privacy Choices
- University of Michigan Library
- Research Guides
Organizational Studies
- Research Methods
- Getting Started
- Reference and Background
- Journal Articles
Best Bet: Research Methods
- Sage Research Methods This link opens in a new window Searches across a large body of the social and behavioral sciences literature from Sage Publications on topics such as designing research projects, understanding methods or identifying new methods, conducting research, and writing up findings.
Finding Information About Research Methods
Literature on research methods can be found in books and journal articles, so searching in the library catalog and databases will turn up relevant sources.
Some relevant subjects to search on in the Library Catalog include:
- Organization Research -- Methodology
- Organizational sociology -- Research
- Organizational behavior -- Research
- Social sciences -- Research
- Social sciences -- Research -- Methodology
- Social sciences -- Statistical methods
- Sociology -- Research
Many publishers distribute books on research methods. Sage is among the most prolific and offers Sage Research Methods: a database devoted specifically to the research methods literature.
This paper is in the following e-collection/theme issue:
Published on 29.3.2024 in Vol 26 (2024)
Usability of Health Care Price Transparency Data in the United States: Mixed Methods Study
Authors of this article:

Original Paper
- Negar Maleki 1 , PhD ;
- Balaji Padmanabhan 2 , PhD ;
- Kaushik Dutta 1 , PhD
1 School of Information Systems and Management, Muma College of Business, University of South Florida, Tampa, FL, United States
2 Decision, Operations & Information Technologies Department, Robert H. Smith School of Business, University of Maryland, College Park, MD, United States
Corresponding Author:
Negar Maleki, PhD
School of Information Systems and Management
Muma College of Business
University of South Florida
4202 E Fowler Avenue
Tampa, FL, 33620
United States
Phone: 1 8139742011
Email: [email protected]
Background: Increasing health care expenditure in the United States has put policy makers under enormous pressure to find ways to curtail costs. Starting January 1, 2021, hospitals operating in the United States were mandated to publish transparent, accessible pricing information online about the items and services in a consumer-friendly format within comprehensive machine-readable files on their websites.
Objective: The aims of this study are to analyze the available files on hospitals’ websites, answering the question—is price transparency (PT) information as provided usable for patients or for machines?—and to provide a solution.
Methods: We analyzed 39 main hospitals in Florida that have published machine-readable files on their website, including commercial carriers. We created an Excel (Microsoft) file that included those 39 hospitals along with the 4 most popular services—Current Procedural Terminology (CPT) 45380, 29827, and 70553 and Diagnosis-Related Group (DRG) 807—for the 4 most popular commercial carriers (Health Maintenance Organization [HMO] or Preferred Provider Organization [PPO] plans)—Aetna, Florida Blue, Cigna, and UnitedHealthcare. We conducted an A/B test using 67 MTurkers (randomly selected from US residents), investigating the level of awareness about PT legislation and the usability of available files. We also suggested format standardization, such as master field names using schema integration, to make machine-readable files consistent and usable for machines.
Results: The poor usability and inconsistent formats of the current PT information yielded no evidence of its usefulness for patients or its quality for machines. This indicates that the information does not meet the requirements for being consumer-friendly or machine readable as mandated by legislation. Based on the responses to the first part of the experiment (PT awareness), it was evident that participants need to be made aware of the PT legislation. However, they believe it is important to know the service price before receiving it. Based on the responses to the second part of the experiment (human usability of PT information), the average number of correct responses was not equal between the 2 groups, that is, the treatment group (mean 1.23, SD 1.30) found more correct answers than the control group (mean 2.76, SD 0.58; t 65 =6.46; P <.001; d =1.52).
Conclusions: Consistent machine-readable files across all health systems facilitate the development of tools for estimating customer out-of-pocket costs, aligning with the PT rule’s main objective—providing patients with valuable information and reducing health care expenditures.
Introduction
From 1970 to 2020, on a per capita basis, health care expenditures in the United States have increased sharply from US $353 per person to US $12,531 per person. In constant 2020 dollars, the increase was from US $1875 in 1970 to US $12,531 in 2020 [ 1 ]. The significant rise in health care expenses has put policy makers under enormous pressure to find ways to contain these expenditures. Price transparency (PT) in health care is 1 generally proposed strategy for addressing these problems [ 2 ] and has been debated for years [ 3 ]. Some economists believe that PT in health care will cut health care prices in the same way it has in other industries, while others argue that owing to the specific characteristics of the health care market, PT would not ameliorate rising health care costs. Price elasticity also does not typically apply in health care, since, if a problem gets severe, people will typically seek treatment regardless of cost, with the drawback that individuals learn of their health care costs after receiving treatment [ 4 ]. Complex billing processes, hidden insurer-provider contracts, the sheer quantity of third-party payers, and substantial quality differences in health care delivery are other unique aspects of health care that complicate the situation considerably.
The Centers for Medicare & Medicaid Services (CMS) mandated hospitals to post negotiated rates, including payer-specific negotiated costs, for 300 “shoppable services” beginning in January 2021. The list must include 70 CMS-specified services and an additional 230 services each hospital considers relevant to its patient population. Hospitals must include each third-party payer and their payer-specific fee when negotiating multiple rates for the same care. The data must be displayed simply, easily accessible (without requiring personal information from the patient), and saved in a machine-readable manner [ 5 ]. These efforts aim to facilitate informed patient decision-making, reduce out-of-pocket spending, and decrease health care expenditures. Former Secretary of Health and Human Services, Alex Azar, expressed a vision of hospital PT when declaring the new legislation “a patient-centered system that puts you in control and provides the affordability you need, the options and control you want, and the quality you deserve. Providing patients with clear, accessible information about the price of their care is a vital piece of delivering on that vision” [ 6 ].
Despite the legislation, it is not clear if people are actually engaging in using PT tools. For example, in 2007, New Hampshire’s HealthCost website was established, providing the negotiated price and out-of-pocket costs for 42 commonly used services by asking whether the patient is insured or their insurer and the zip code to post out-of-pocket costs in descending order. Mehrotra et al [ 7 ] examined this website over 3 years to understand how often and why these tools have mainly been used. Their analysis suggested that despite the growing interest in PT, approximately 1% of the state’s population used this tool. Low PT tool usage was also seen in other studies [ 8 - 10 ], suggesting that 3% to 12% of individuals who were offered the tool used it during the study period, and in all studies, the duration was at least 12 months. Thus, offering PT tools does not in itself lead to decreased total spending, since few people who have access to them use them to browse for lower-cost services [ 7 , 11 ].
In a recent paper, researchers addressed 1 possible reason for low engagement—lack of awareness. They implemented an extensive targeted online advertising campaign using Google Advertisements to increase awareness and assessed whether it increased New Hampshire’s PT website use. Their findings suggested that although lack of awareness is a possible reason for the low impact of PT tools in health care spending, structural factors might affect the use of health care information [ 12 ]. Individuals may not be able to exactly determine their out-of-pocket expenses from the information provided.
Surprisingly, there is little research on the awareness and usability of PT information after the current PT legislation went into effect. A recent study [ 13 ] highlighted the nonusability of existing machine-readable files for employers, policy makers, researchers, or consumers, and this paper adds to this literature by answering the question—is PT information as provided usable for patients or machines? Clearly, if it is of value to patients, it can be useful; the reason to take the perspective of machines was to examine whether this information as provided might also be useful for third-party programs that can extract information from the provided data (to subsequently help patients through other ways of presenting this information perhaps). We address this question through a combination of user experiments and data schema analysis. While there are recent papers that have also argued that PT data have deficiencies [ 13 , 14 ], ours is the first to combine user experiments with analysis of data schema from several hospitals in Florida to make a combined claim on value for patients and machines. We hope this can add to the discourse on PT and what needs to be done to extract value for patients and the health care system as a whole.
Impact of PT Tools
The impact of PT tools on consumers and health care facilities has been investigated in the literature. Some studies showed that consumers with access to PT tools are more likely to reduce forgone needed services over time. Moreover, consumers who use tools tend to find the lowest service prices [ 8 , 15 - 17 ]. A few studies investigated the impact of PT tools on the selection of health care facilities. They illustrated that some consumers tend to change health care facilities pursuing lower prices, while some others prefer to stay with expensive ones, although they are aware of some other facilities that offer lower prices [ 9 , 18 ]. Finally, some research studied the impact of PT tools on cost and showed that some consumers experienced no effect, while others experienced decreases in average consumer expenses [ 8 , 17 , 18 ]. However, the impact of PT tools on health care facilities is inconclusive, meaning different studies concluded different effects. Some stated that PT tools decrease the prices of imaging and laboratory services, while others said that although public charge disclosure lowers health care facility charges, the final prices remained unchanged [ 17 , 18 ].
Legislation Related Works
In a study, researchers considered 20 leading US hospitals to assess provided chargemasters to understand to what extent patients can obtain information from websites to determine the out-of-pocket costs [ 19 ]. Their findings showed that although all hospitals provided chargemasters on their websites, they rarely offered transparent information, making it hard for patients to determine out-of-pocket costs. Their analysis used advanced diagnostic imaging services to assess hospitals’ chargemasters since these are the most common services people look for. Mehrotra et al [ 7 ] also mentioned that the most common searches belonged to outpatient visits, magnetic resonance imaging (MRI), and emergency department visits. To this end, we used “MRI scan of the brain before and after contrast” as one of the shoppable services in our analysis. Another study examined imaging services in children’s hospitals (n=89), restricting the analysis to hospitals (n=35) that met PT requirements—published chargemaster rates, discounted cash prices, and payer-negotiated prices in a machine-readable file, and published costs for 300 common shoppable medical services in a consumer-friendly format. Their study revealed that, in addition to a broad range of imaging service charges, most hospitals lack the machine-readable file requirement [ 20 ].
Arvisais-Anhalt et al [ 21 ] identified 11 hospitals with available chargemasters in Dallas County to compare the prices of a wide range of available services. They observed significant variations for a laboratory test: partial thromboplastin time, a medication: 5 mg tablet of amlodipine, and a procedure: circumcision. Reddy et al [ 22 ] focus on New York State to assess the accessibility and usability of hospitals’ chargemasters from patients’ viewpoint. They found that 189 out of 202 hospitals had a locatable chargemaster on their home page. However, only 37 hospitals contain the Current Procedural Terminology (CPT) code, which makes those without the CPT code unusable due to the existence of many different descriptions for the same procedure; for example, an elective heart procedure had 34 entries. We add to this considerable literature by examining a subset of Florida hospitals.
In a competitive market, higher-quality goods and services require higher prices [ 23 ]. Based on this, Patel et al [ 24 ] examined the relationship between the Diagnosis-Related Group (DRG) chargemaster and quality measures. Although prior research found no convincing evidence that hospitals with greater costs also delivered better care [ 25 ], they discovered 2 important quality indicators that were linked to standard charges positively and substantially—mortality rate and readmission rates—which both are quality characteristics that are in line with economic theory. Moreover, Patel et al [ 24 ] studied the variety of one of the most commonly performed services (vaginal delivery) as a DRG code, which motivated us to select “Vaginal delivery without sterilization or D&C without CC/MCC” as another shoppable service in our analysis.
Ethical Considerations
All data used in this study, including the secondary data set obtained from hospitals’ websites and the data collected during the user experiment, underwent a thorough anonymization process. The study was conducted under protocols approved by the University of South Florida institutional review board (STUDY004145: “Effect of price transparency regulation (PTR) on the public decisions”) under HRP-502b(7) Social Behavioral Survey Consent. This approval encompassed the use of publicly available anonymized secondary data from hospitals’ websites, as well as a user experiment aimed at assessing awareness of the PT rule and the usability of hospitals’ files. No individual-specific data were collected during the experiment, which solely focused on capturing subjects’ awareness and opinions regarding the PT rule and associated files. At the onset of the experiment, participants were provided with a downloadable consent form and were allowed to withdraw their participation at any time. Survey participants were offered a US $2 reward, and their involvement was entirely anonymous.
Data Collection
According to CMS, “Starting January 1, 2021, each hospital operating in the United States will be required to provide clear, accessible pricing information online about the items and services they provide in two ways: 1- As a comprehensive machine-readable file with all items and services. 2- In a display of shoppable services in a consumer-friendly format.” As stated, files available on hospitals’ websites should be consumer-friendly, so the question of whether these files are for users arises. On the other hand, as stated, files should be machine-readable, so again the question of whether these files are for machines arises. Below we try to answer both questions in detail, respectively.
Value for Users: User Experiments
When a public announcement is disseminated, its efficacy relies on ensuring widespread awareness and facilitating practical use during times of necessity. Previous research on PT announcements has highlighted the challenges faced by patients in accurately estimating out-of-pocket expenses. However, a fundamental inquiry arises—are individuals adequately informed about the availability of tools that enable them to estimate their out-of-pocket costs for desired services? To address this, we conducted a survey to assess public awareness of PT legislation. The survey encompassed a range of yes or no and multiple-choice questions aimed at gauging participants’ familiarity with the PT rule in health care and their entitlement to obtain cost information prior to receiving a service. Additionally, we inquired about participants’ knowledge of resources for accessing pricing information and whether they were aware of the PT rule. Furthermore, we incorporated follow-up questions to ensure that the survey responses were not provided arbitrarily, thereby securing reliable and meaningful outcomes.
Moreover, considering the previously established evidence of subpar usability associated with the currently available files, we propose streamlining the existing files and developing a user-friendly and comprehensive document for conducting an A/B test. This test aims to evaluate which file better facilitates participants in accurately estimating their out-of-pocket costs. In collaboration with Florida Blue experts during biweekly meetings throughout the entire process outlined in this paper, the authors determined the optimal design for the summary table. This design, which presents prices in a more user-friendly format, enhancing overall participant comprehension, was used during the A/B testing. Participants were randomly assigned to either access the hospitals’ files or a meticulously constructed summary table, manually created in Excel, prominently displaying cost information (Please note that all files, including the hospitals’ files and our Excel file, are made available in the same format [Excel] on a cloud-based platform to eliminate any disparities in accessing the files. This ensures equitable ease of finding, downloading, and opening files, as accessing the hospitals’ files typically requires significant effort.). The experiment entailed presenting 3 distinct health-related scenarios and instructing participants to locate the price for the requested service. Subsequently, participants were asked to provide the hospital name, service price, insurer name, and insurance plan. Additionally, we sought feedback on the perceived difficulty of finding the requested service and their priority for selecting hospitals [ 26 ], followed by Likert scale questions to assess participants’ evaluation of the provided file’s efficacy in facilitating price retrieval.
The experiments were conducted to investigate the following questions: (1) Are the individuals aware of the PT legislation? and (2) Is the information provided usable for patients? To evaluate the usability of files found on websites, we selected 2 prevalent services based on existing literature and 2 other services recommended as high-demand ones by Florida Blue experts, Table 1 . Furthermore, meticulous efforts were made to ensure that both the control and treatment groups encountered identical circumstances, thus allowing for a systematic examination of the disparities solely attributable to variations in data representation.
a DRG: Diagnosis-Related Group.
b D&C: dilation and curettage.
c CC/MCC: complication or comorbidity/major complication or comorbidity.
d CPT: Current Procedural Terminology.
e MRI: magnetic resonance imaging.
Participants
A total of 67 adults (30 female individuals; mean 41.43, SD 12.39 years) were recruited on the Amazon Mechanical Turk platform, with no specific selection criteria other than being located in the United States.
We focused on 75 main hospitals (ie, the main hospital refers to distinguish a hospital from smaller clinics or specialized medical centers within the same health system) in the state of Florida. When we searched their websites for PT files (machine-readable files), only 89% (67/75) of hospitals included machine-readable files. According to the PT legislation, these files were supposed to contain information about 300 shoppable services. However, only 58% (39/67) of hospitals included information such as insurer prices in their files. Therefore, for the rest of the analysis, we only included the 39 hospitals that have the required information in their machine-readable files on their websites. We created an Excel file that included those 39 hospitals along with the 4 services—CPT 45380, 29827 and 70553 and DRG 807—mentioned in the literature ( Table 1 ) for 4 popular (suggested by Florida Blue experts) commercial carriers (Health Maintenance Organization [HMO] or Preferred Provider Organization [PPO] plans)—Aetna, Florida Blue, Cigna, and UnitedHealthcare.
Participants were recruited for the pilot and randomly assigned by the Qualtrics XM platform to answer multiple-choice questions and fill in blanks based on the given scenarios. First, participants responded to questions regarding the awareness of PT and then were divided into 2 groups randomly to answer questions regarding the usability of hospital-provided PT information. One group was assigned hospitals’ website links (control group), while the other group was given an Excel file with the same information provided in files on hospitals’ websites, but in a manner that was designed to allow easier comparison of prices across hospitals ( Multimedia Appendix 1 ). Participants were given 3 scenarios that asked them to find a procedure’s price based on their hospital and insurer selection to compare hospital-provided information with Excel. We provide some examples of hospitals’ files and our Excel file in Multimedia Appendix 1 and the survey experiment questions in Multimedia Appendix 2 .
Value for Machines: Schema Integration—Machine-Readable Files Representation
Through meticulous investigation of machine-readable files from 39 hospitals, we discovered that these files may vary in formats such as CSV or JSON, posing a challenge for machines to effectively manage the data within these files. Another significant obstacle arises from the lack of uniformity in data representation across these files, rendering them unsuitable for machine use without a cohesive system capable of processing them collectively. Our analysis revealed that hospitals within a single health system exhibit consistent data representation, although service prices may differ (we include both the same and different chargemaster prices in our study), while substantial disparities in data representation exist between hospitals affiliated with different health systems.
Moving forward, we will use the terms “data representation” and “schema” interchangeably, with “schema” denoting its database management context. In this context, a schema serves as a blueprint outlining the structure, organization, and relationships of data within a database system. It encompasses key details such as tables, fields, data types, and constraints that define the stored data. To systematically illustrate schema differences among hospitals associated with different health systems, we adopted the methodology outlined in reference [ 27 ] for schema integration, which offers a valid approach for comparing distinct data representations. The concept of schema integration encompasses four common categories: (1) identical: hospitals within the same health system adhere to this concept as their representations are identical; (2) equivalent: while hospitals in health system “A” may present different representations from those in health system “B,” they possess interchangeable columns; (3) compatible: in cases where hospitals across different health systems are neither identical nor equivalent, the modeling constructs, designer perception, and integrity constraints do not contradict one another; and (4) incompatible: in situations where hospitals within different health systems demonstrate contradictory representations, distinct columns exist for each health system due to specification incoherence.
Our analysis focused on health systems in Florida that encompassed a minimum of 4 main hospitals, using the most up-to-date data available on their respective websites. Within this scope, we identified 8 health systems with at least 4 main hospitals, of which 88% (7/8) of health systems had published machine-readable files on their websites. Consequently, our analysis included 65% (36/55) of hospitals that possessed machine-readable files available on their websites. To facilitate further investigation by interested researchers, we have made the analyzed data accessible on a cloud-based platform. During our analysis, we meticulously extracted the schema of each health system by closely scrutinizing the hospitals associated with each health system, capturing key details such as tables, fields, and data types. Subsequently, we compiled a comprehensive master field name table trying to have the same data type and field names that make it easier for machines to retrieve information. We elaborate on the master field names table in greater detail within the results section.
Value for Users
Question 1 (pt awareness).
Based on the responses, it is evident that participants need to be made aware of the PT legislation. Among the participants, 64% (49/76) reported that they had not heard about the legislation. However, they believe it is important to know the service price before receiving it—response charts are provided in Multimedia Appendix 3 .
Question 2 (Human Usability of PT Information)
Based on the responses to scenarios, the average number of correct responses is not equal between the 2 groups, that is, the treatment group (mean 1.23, SD 1.30) found more correct answers than the control group (mean 2.76, SD 0.58; t 65 =6.46; P <.049; d =1.52). The t tests (2-tailed) for the other questions in the experiment are in Multimedia Appendix 4 .
These suggest that current files on hospitals’ websites are not consumer-friendly, and participants find it challenging to estimate out-of-pocket costs for a desired service. For this reason, in addition to making the files easier to use, this information should also include thorough documentation that explains what each column represents, up to what amount an insurer covers for a specific service, or the stated price covers up to how many days of a particular service, that is, “contracting method.” For example, based on consulting with one of the senior network analysts of Florida Blue, some prices for a service like DRG 807 are presented as per diem costs, and based on the current information on these files, it cannot be recognizable without having comprehensive documentation for them.
Value for Machines
After carefully reviewing all machine-readable file schemas, we create a master field name table, including the available field names in machine-readable files ( Table 2 ). According to Table 2 , the first column represents master field names that we came up with, and the following columns each represent hospitals within a health system. The “✓” mark shows that hospitals within a health system have identical field names as we consider as master field names and the “written” cells show equivalent field names, meaning that hospitals within that health system use different field names—we write what they use in their representation—while the content is equivalent to what we select as the master field name. The “❋” mark means that although hospitals within health system #2 provide insurer names and plans in their field names, some codes make those columns unusable for machines to recognize them the same as master field names. We also include the type of field names for all representations in parentheses.
a As noted previously, since we focus on the health system level instead of the hospital level, our schema does not have hospital-level information; however, it would be beneficial to add hospital information to the table.
b ✓: it means the given master field name in that row appears on the given health system file in that column.
c str: shows “string” as the data type.
d int: shows “integer” as the data type.
e CPT: Current Procedural Terminology.
f HCPCS: Health care Common Procedure Coding System.
g Not applicable.
h Apr: all patients refined.
i DRG: Diagnosis-Related Group.
j Ms: Medicare severity.
k CDM: charge description master.
l UB: uniform billing.
m float: it shows “float” as the data type.
n ❋: it means that although hospitals within health system #2 provide insurer names and plans in their field names, some codes make those columns unusable for machines to recognize them the same as master field names.
We did reverse engineering and drew entity-relationship diagrams (ERDs) for each hospital based on their data representation. However, as hospitals within the same health system have the same ERDs, we only include 1 ERD for each health system ( Figure 1 ). According to Figure 1 , although hospitals have tried to follow an intuitive structure, we can still separate them into three groups: (1) group I: all hospitals within this group have several columns for different insurers. As shown in the ERDs, we decided to have a separate entity, called “Insurance” for this group; (2) group II: all hospitals within this group have many sheets, and each sheet belongs to a specific insurer with a specific plan. As shown in the ERDs, we decided to create an “Insurance_Name” entity for this group’s ERD to show the difference in data representation; and (3) group III: all hospitals within this system have a “payer” column which includes the names of insurers without their plans. As shown in the ERDs, we decided to put this column as an attribute in the “Service” entity, and do not have an “Insurance” entity for this group’s ERD.
In conclusion, although most hospitals have adopted group I logic for data representation, for full similarity, a standard representation with the same intuitive field names (like what we suggest as the master field name; Table 2 ) should be proposed so that it can cover all systems’ data representations and be used as machine-readable file, for at least machine benefits. Mainly, standardization in the format and semantics of the provided data can help substantially in making the data more machine friendly.

Comparison With New CMS Guidelines
Recently, CMS has published guidelines regarding the PT legislation [ 28 ]. The most recent CMS guideline is a step forward in ensuring standardization but is still only recommended and is not mandatory. These guidelines exhibit overlaps with our fields in Table 2 , with slight differences attributed to granularities. Our observation reveals that hospitals within the same health system adopt a uniform schema. Therefore, our suggested schema operates on the granularity of health systems rather than individual hospitals.
The recent CMS guidelines allocate 24% (6/25) of field names specifically to hospital information, encompassing details such as “Hospital Name,” “Hospital File Date,” “Version,” “Hospital Location,” “Hospital Financial Aid Policy,” and “Hospital Licensure Information.” These details, absent in current hospital files, are crucial for informed decision-making. As noted previously, since we focus on the health system level instead of the hospital level, our schema does not have hospital-level information; however, it would be beneficial to add hospital information to the tables.
Our analysis reveals that the 11 field names in Table 2 align with the field names in the new CMS guidelines, demonstrating a substantial overlap of 58% (11/19). The corresponding CMS field names (compatible with our schema) include “Item or Service Description (Description or CDM Service Description),” “Code (Code),” “Code Type (Code Type),” “Setting (Patient Class),” “Gross Charge (Gross Charge),” “Discounted Cash Price (Discounted Cash Price),” “Payer Name (Insurer Name),” “Plan Name (Insurer Plan),” “Payer Specific Negotiated Charge: Dollar Amount (Price),” “De-identified Minimum Negotiated Charge (Min Negotiated Rate),” and “De-identified Maximum Negotiated Charge (Max Negotiated Rate).” Additionally, both our schema and the new CMS guidelines propose data types for each field name.
In our schema, which represents current hospitals’ files, there are 5 field names absent in the new CMS guidelines “Revenue Description,” “Revenue Code,” “Package/Line Level,” “Procedure ID,” and “Self Pay.” Conversely, the new CMS guidelines introduce 8 additional field names “Billing Class,” “Drug Unit of Measurement,” “Drug Type of Measurement,” “Modifiers,” “Payer Specific Negotiated Charge: Percentage,” “Contracting Method,” “Additional Generic Notes,” and “Additional Payer-Specific Notes.” We regard these new field names as providing further detailed information and enhancing consumer decision-making. If hospitals within a health system adopt consistent formats and can map their formats to the new CMS guidelines clearly in a mapping document they also provide, this can be more useful than the current optional guideline that is suggested.
In summary, since our analysis is based on the current data schema that hospitals have in place, we believe the schema we put out is easier to implement with minimal change to what the hospitals are currently doing. However, given the recent CMS guidelines, we recommend adding 8 additional fields as well as hospital-specific information.
Implications
The PT legislation aims to enable informed decision-making, reduce out-of-pocket expenses, and decrease overall health care expenditures. This study investigates the usage of current files by individuals and machines. Our results, unfortunately, suggest that PT data—as currently reported—appear to be neither useful for patients nor machines, raising important questions as to what these appear to be achieving today. Moreover, the findings indicate that even individuals with basic computer knowledge struggle with the usability of these files, highlighting the need for significant revisions to make them consumer-friendly and accessible to individuals of all technical proficiency levels. Additionally, inconsistencies in data representation between hospitals affiliated with different health systems pose challenges for machines, necessitating schema design improvements and the implementation of a standardized data representation. By addressing these concerns, PT legislation can achieve consistency and enhance machine readability, thus improving its effectiveness in promoting informed decision-making and reducing health care costs.
Although the official announcement of PT legislation is recent, prior studies [ 15 - 17 ] have attempted to evaluate the usability of PT, while subsequent studies [ 19 - 22 ] have examined the effectiveness of PT tools following the announcement. However, despite the introduction of PT rules, it appears that the usability of these files has not undergone significant improvements, indicating the necessity for proactive measures from responsible executives to ensure the effectiveness of this legislation. Our analysis of this matter emphasizes 2 primary factors—a lack of awareness among stakeholders and the challenges associated with using files due to inconsistencies in their format and representation.
As of April 2023, the CMS has issued over 730 warning notices and 269 requests for Corrective Action Plans. A total of 4 hospitals have faced Civil Monetary Penalties for noncompliance, and these penalties are publicly disclosed on the CMS website. The remaining hospitals subjected to comprehensive compliance reviews have either rectified their deficiencies or are actively engaged in doing so. While we acknowledge these efforts to comply with PT rules, our research revealed a notable disparity in data representation among hospitals affiliated with different health systems. Consequently, we focused on schema design and proposed the implementation of a master field name that encompasses a comprehensive data representation derived from an analysis of 36 hospitals. Standardizing the data representation across all health systems’ machine-readable files will effectively address concerns about consistency. Therefore, significant modifications are required for the PT legislation to enhance machine readability and provide clearer guidance on the design and structure of the files’ schema. If the hospital-provided information is consistent and of high quality, PT tools provided by health insurers may be able to estimate an individual’s total expenses more accurately.
Limitations
Our objective was to have an equal number in both groups. However, in the case of the group tasked with obtaining information from the hospitals’ websites, most did not finish the task and dropped out without completing it. This occurred because the task of retrieving the cost from the hospitals’ websites in its current form is complex, as indicated by feedback from some participants. Only 19% (13/67) completed the task in that group (control group). Although this is a limitation of the study, it also highlights the complexity of obtaining cost information from hospitals’ websites in the current form. In the treatment group, 81% (54 out of 67) of participants completed the task of retrieving the data, and the completion percentage was much higher.
Conclusions
Due to the poor usability and inconsistency of the formats, we, unfortunately, did not find evidence that the PT rule as implemented currently is useful to consumers, researchers, or policy makers (despite the legislation’s goals that files are “consumer-friendly” and “machine-readable”). As 1 solution, we suggest a master field name for the data representation of machine-readable files to make them consistent, at least for the machines. Building tools that enable customers to estimate out-of-pocket costs is facilitated by having consistent machine-readable files across all health systems, which can be considered as future work for researchers and companies to help the PT rule reach its main goal, which is providing useful information for patients and reducing health care expenditures. In addition, another worthwhile approach to reducing some of the exorbitant health care costs in the United States would be to integrate clinical decision support tools into the providers’ workflow, triggered by orders for medications, diagnostic testing, and other billable services. In this regard, Bouayad et al [ 29 ] conducted experiments with physicians to demonstrate that PT, when included as part of the system they interact with, such as clinical decision support integrated into electronic health record systems, can significantly aid in cost reduction. This is a promising direction for practice but needs to be implemented carefully to avoid unanticipated consequences, such as scenarios where cost is incorrectly viewed as a proxy for quality, or where the use of this information introduces new biases for physicians and patients.
Conflicts of Interest
None declared.
Example of Excel format of hospitals’ files and our created Excel file.
Survey questions and experiment scenarios.
Participants’ responses chart regarding price transparency awareness.
The t test analysis regarding human usability of price transparency information based on participants’ responses.
- McGough M, Winger A, Rakshit S, Amin K. How has U.S. spending on healthcare changed over time? Health System Tracker. 2022. URL: https://www.healthsystemtracker.org/chart-collection/u-s-spending-healthcare-changed-time/ [accessed 2024-03-13]
- Christensen HB, Floyd E, Maffett M. The only prescription is transparency: the effect of charge-price-transparency regulation on healthcare prices. Manag Sci. 2020;66(7):2861-2882. [ CrossRef ]
- Muir MA, Alessi SA, King JS. Clarifying costs: can increased price transparency reduce healthcare spending? UC Hastings Research Paper No. 38 (SSRN). Feb 26, 2013.:319-367. [ FREE Full text ] [ CrossRef ]
- Reinhardt UE. Health care price transparency and economic theory. JAMA. 2014;312(16):1642-1643. [ CrossRef ] [ Medline ]
- CY 2020 hospital Outpatient Prospective Payment System (OPPS) policy changes: hospital price transparency requirements (CMS-1717-F2). CMS.gov. 2020. URL: https://tinyurl.com/mrafxtvd [accessed 2024-03-13]
- Secretary Azar statement on proposed rule for hospital price transparency. HHS.gov. 2020. URL: https://tinyurl.com/yc4dx2vx [accessed 2024-03-13]
- Mehrotra A, Brannen T, Sinaiko AD. Use patterns of a state health care price transparency web site: what do patients shop for? Inquiry. 2014;51:0046958014561496. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Desai S, Hatfield LA, Hicks AL, Sinaiko AD, Chernew ME, Cowling D, et al. Offering a price transparency tool did not reduce overall spending among California public employees and retirees. Health Aff (Millwood). 2017;36(8):1401-1407. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sinaiko AD, Joynt Maddox KE, Rosenthal MB. Association between viewing health care price information and choice of health care facility. JAMA Intern Med. 2016;176(12):1868-1870. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Desai S, Hatfield LA, Hicks AL, Chernew ME, Mehrotra A. Association between availability of a price transparency tool and outpatient spending. JAMA. 2016;315(17):1874-1881. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sinaiko AD, Rosenthal MB. Examining a health care price transparency tool: who uses it, and how they shop for care. Health Aff (Millwood). 2016;35(4):662-670. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Desai SM, Shambhu S, Mehrotra A. Online advertising increased New Hampshire residents' use of provider price tool but not use of lower-price providers. Health Aff (Millwood). 2021;40(3):521-528. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kona M, Corlette S. Hospital and insurer price transparency rules now in effect but compliance is still far away. Health Affairs Forefront. 2022. URL: hhttps://tinyurl.com/3x6ymxf2 [accessed 2024-03-13]
- Wheeler C, Taylor R. New year, new CMS price transparency rule for hospitals. Health Affairs Forefront. 2021. URL: https://www.healthaffairs.org/content/forefront/new-year-new-cms-price-transparency-rule-hospitals [accessed 2024-03-13]
- Chernew M, Cooper Z, Larsen-Hallock E, Morton FS. Are health care services shoppable? Evidence from the consumption of lower-limb MRI scans. National Bureau of Economic Research. 2021. URL: https://www.nber.org/papers/w24869 [accessed 2024-03-13]
- Mehrotra A, Dean KM, Sinaiko AD, Sood N. Americans support price shopping for health care, but few actually seek out price information. Health Aff (Millwood). 2017;36(8):1392-1400. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Brown ZY. Equilibrium effects of health care price information. Rev Econ Stat. 2019;101(4):699-712. [ FREE Full text ] [ CrossRef ]
- Wu SJ, Sylwestrzak G, Shah C, DeVries A. Price transparency for MRIs increased use of less costly providers and triggered provider competition. Health Aff (Millwood). 2014;33(8):1391-1398. [ CrossRef ] [ Medline ]
- Glover M, Whorms DS, Singh R, Almeida RR, Prabhakar AM, Saini S, et al. A radiology-focused analysis of transparency and usability of top U.S. hospitals' chargemasters. Acad Radiol. 2020;27(11):1603-1607. [ CrossRef ] [ Medline ]
- Hayatghaibi SE, Alves VV, Ayyala RS, Dillman JR, Trout AT. Transparency and variability in pricing for pediatric outpatient imaging in US children's hospitals. JAMA Netw Open. 2022;5(3):e220736. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Arvisais-Anhalt S, McDonald S, Park JY, Kapinos K, Lehmann CU, Basit M. Survey of hospital chargemaster transparency. Appl Clin Inform. 2021;12(2):391-398. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Reddy S, Daly G, Baban S, Kadesh A, Block AE, Grimes CL. Accessibility and usability of hospital chargemasters in New York state. J Gen Intern Med. 2022;37(8):2130-2131. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Robinson JC. Hospital quality competition and the economics of imperfect information. Milbank Q. 1988;66(3):465-481. [ Medline ]
- Patel KN, Mazurenko O, Ford E. Analysis of hospital quality measures and web-based chargemasters, 2019: cross-sectional study. JMIR Form Res. 2021;5(8):e26887. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Batty M, Ippolito B. Mystery of the chargemaster: examining the role of hospital list prices in what patients actually pay. Health Aff (Millwood). 2017;36(4):689-696. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Muhlestein DB, Wilks CEA, Richter JP. Limited use of price and quality advertising among American hospitals. J Med Internet Res. 2013;15(8):e185. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Batini C, Lenzerini M, Navathe SB. A comparative analysis of methodologies for database schema integration. ACM Comput Surv. 1986;18(4):323-364. [ FREE Full text ] [ CrossRef ]
- Voluntary hospital price transparency machine-readable file sample format data dictionary (version 1.1). CMS.gov. URL: https://www.cms.gov/files/document/hospital-price-transparency-machine-readable-data-dictionary-tall.pdf [accessed 2024-03-13]
- Bouayad L, Padmanabhan B, Chari K. Can recommender systems reduce healthcare costs? the role of time pressure and cost transparency in prescription choice. MIS Q. 2020;44(4):1859-1903. [ CrossRef ]
Abbreviations
Edited by S He; submitted 07.07.23; peer-reviewed by KN Patel, R Marshall, G Deckard; comments to author 03.12.23; revised version received 21.01.24; accepted 26.02.24; published 29.03.24.
©Negar Maleki, Balaji Padmanabhan, Kaushik Dutta. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 29.03.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
- Study Protocol
- Open access
- Published: 29 March 2024
Evaluation of heroin-assisted treatment in Norway: protocol for a mixed methods study
- Lars Henrik Myklebust 1 ,
- Desiree Eide 1 ,
- Espen A. Arnevik 4 ,
- Omid Dadras 2 ,
- Silvana De Pirro 1 , 6 ,
- Rune Ellefsen 4 ,
- Lars T. Fadnes 2 , 3 ,
- Morten Hesse 5 ,
- Timo L. Kvamme 5 ,
- Francesca Melis 1 ,
- Ann Oldervoll 1 ,
- Birgitte Thylstrup 5 ,
- Linda E.C. Wusthoff 1 , 4 &
- Thomas Clausen 1
BMC Health Services Research volume 24 , Article number: 398 ( 2024 ) Cite this article
Metrics details
Opioid agonist treatment (OAT) for patients with opioid use disorder (OUD) has a convincing evidence base, although variable retention rates suggest that it may not be beneficial for all. One of the options to include more patients is the introduction of heroin-assisted treatment (HAT), which involves the prescribing of pharmaceutical heroin in a clinical supervised setting. Clinical trials suggest that HAT positively affects illicit drug use, criminal behavior, quality of life, and health. The results are less clear for longer-term outcomes such as mortality, level of function and social integration. This protocol describes a longitudinal evaluation of the introduction of HAT into the OAT services in Norway over a 5-year period. The main aim of the project is to study the individual, organizational and societal effects of implementing HAT in the specialized healthcare services for OUD.
The project adopts a multidisciplinary approach, where the primary cohort for analysis will consist of approximately 250 patients in Norway, observed during the period of 2022–2026. Cohorts for comparative analysis will include all HAT-patients in Denmark from 2010 to 2022 ( N = 500) and all Norwegian patients in conventional OAT ( N = 8300). Data comes from individual in-depth and semi-structured interviews, self-report questionnaires, clinical records, and national registries, collected at several time points throughout patients’ courses of treatment. Qualitative analyses will use a flexible inductive thematic approach. Quantitative analyses will employ a wide array of methods including bi-variate parametric and non-parametric tests, and various forms of multivariate modeling.
The project’s primary strength lies in its comprehensive and longitudinal approach. It has the potential to reveal new insights on whether pharmaceutical heroin should be an integral part of integrated conventional OAT services to individually tailor treatments for patients with OUD. This could affect considerations about drug treatment even beyond HAT-specific topics, where an expanded understanding of why some do not succeed with conventional OAT will strengthen the knowledge base for drug treatment in general. Results will be disseminated to the scientific community, clinicians, and policy makers.
Trial registration
The study was approved by the Norwegian Regional Committee for Medical and Health Research Ethics (REK), ref.nr.:195733.
Peer Review reports
Opioid use disorder (OUD) is a major global health concern with an estimated caseload of 31.5 million in 2022 [ 1 ]. It is frequently related to infectious diseases from injection-based drug use, psychiatric disorders, deterioration of social relations, reduced workforce participation, and a tenfold increase in crude all-cause rate of mortality [ 2 ]. The treatment and care for patients with OUD has gradually developed from an initial emphasis on abstinence and withdrawal management, to regular prescriptions of opioid agonists for maintenance treatment (OAT) [ 3 ].
Half a century after the first initiatives of prescribing methadone for OUD in a regular manner [ 4 , 5 ] OAT now has a strong evidence-base [ 6 ]. Overall, it contributes to a substantial reduction in mortality, general health benefits, and reduced use of illicit drugs and criminal activity [ 6 , 7 , 8 , 9 ]. Still, not all individuals find conventional OAT sufficiently attractive over time, and cycles of dropout and re-entering are ongoing challenges in these programs [ 10 , 11 , 12 ]. A variable retention rate of 20–84% has been observed [ 13 ]. Among the efforts to improve the inclusion of patients in OAT is the introduction of more diverse medication options, such as rapid-onset, short-acting injectable pharmaceutical opioids such as heroin [ 14 ].
The use of medical grade heroin (diacetylmorphine) in treating OUD has been applied in England since the 1920s, originally as hand-out prescriptions to take home [ 15 , 16 ]. Initiatives to incorporate it into more regular OAT started in Switzerland in 1994, with promising results [ 17 , 18 ]. Now, three decades later and after clinical trials from several European countries and Canada, the body of research suggests that heroin-assisted treatment (HAT) is beneficial for a sub-selection of patients in regard to health outcomes and reductions in use of illicit drugs and criminal behavior [ 19 , 20 , 21 ]. The results are less clear for longer-term outcomes such as mortality [ 6 , 19 ].
Still, HAT remains politically controversial [ 22 ], and reduced illicit heroin use and criminal behavior may not be compelling arguments for its efficacy. Rather, as for any other medical treatment its impact may better be assessed by patients’ improvement in quality of life, everyday level of function, and mortality [ 23 ].
Although newer studies suggests that take home doses are a feasible and safe alternative for patients deemed suitable [ 24 , 25 ], medical heroin is typically administered under rigorous and comprehensive medical supervision due to the risk of serious adverse events and diversion [ 26 ]. Studies on cost effectiveness suggest both excessive expenses and inconclusive results when compared with methadone treatment, which are possibly dependent on methodological issues and poor consideration of the mechanisms involved [ 20 , 27 , 28 ].
Additionally, most of the research on the effectiveness of HAT originates from randomized clinical trials which may have limitations concerning the understanding of long-term outcomes and the mechanisms behind [ 23 ]. Thus, the main contribution of HAT may lie in the engagement of a high-risk population in utilization of health- and social services over time, like the more conventional options of OAT [ 23 , 29 ]. A more comprehensive view of outcomes beyond the mere quantity and frequency of drug use and criminal behaviour can provide crucial information about the mechanisms responsible for treatment effectiveness, and its possible impact on other clinically and socially relevant parameters [ 30 ].
The current Norwegian HAT study is presented in this context. The study is part of a clinical project by the Norwegian Directorate of Health, with the aim to evaluate the implementation of HAT into the national OAT services. It is based on a model from Denmark where the use of medical heroin was introduced in 2010, following the British “RIOTT” line of test trials from 2005 [ 31 ]. Denmark currently has five clinics as permanent parts of the national healthcare system, although a limited amount of research has been published from this model [ 32 ].
The Norwegian HAT-project
OAT programs based on prescription of methadone and buprenorphine has in various forms been integrated into the Norwegian health and social services-system since 1997 [ 33 ]. In the spring of 2020, the Norwegian Directorate of Health introduced a time-limited, clinically based project on the use of pharmaceutical heroin in the specialist healthcare services. Based on a day-center model, treatment is offered at two designated clinics in the largest Norwegian cities of Oslo and Bergen. The clinics consist of injection sites and medical personnel for the administration of pharmaceutical heroin twice a day, in combination with a take-home oral overnight dose of slow-releasing opioid-agonist such as methadone or morphine. Take-home doses of heroin are not granted, and patients must attend daily all year around. Psychosocial services and support are also offered [ 34 ]. Patients are referred from other services of substance use disorder treatment, specialist healthcare services or general practitioners. Criteria for admission are ongoing OUD with at least one former attempt of conventional OAT, being over 18 years of age and with general competency of consent. Exclusion criteria are severe mental disorders with reduced competency of consent, pregnancy, or repeated violent behavior.
The Norwegian Centre for Addiction Research (SERAF) at the University of Oslo was granted the research-based evaluation of the HAT project in 2021. The study will be conducted together with Section for Clinical Addiction Research (RusForsk) at Oslo University Hospital, Bergen Addiction Research Group (BAR) at Haukeland University Hospital in Bergen, Centre for Alcohol and Drug Research (CRF) at Aarhus University in Denmark, and the Norwegian user organization proLARNett.
The primary aim of the research project is to examine the effects from implementing HAT in Norway for individual patients and for the health services organization. A secondary aim is to compare these findings with the Danish HAT program.
Based on the Norwegian Directorate of Health’s specifications in the project proposal, the study will cover the following thematic areas:
Explore the attitudes, experiences and challenges of HAT as perceived by patients, their relatives, and clinical staff.
Describe changes in mental and physical health among patients receiving HAT, and in what way it is associated with outcomes such as quality of life, utilization of health- and social services, social reintegration, criminal behavior and use of illicit drugs.
Report any serious adverse events and incidents at treatment initiation, during treatment, and after discharge from HAT.
Perform an economic evaluation of the program with associated clinical benefits and societal costs.
Evaluate the organizational processes involved in the implementation of HAT in Norwegian specialist healthcare services, and the eventual impact from HAT on OUD patients’ utilization of conventional OAT.
Additional research relevant to HAT that is not explicitly outlined in the proposal (may require additional approvals from the Norwegian Regional Committee for Medical and Health Research Ethics.)
The themes were operationalized into six work packages, with corresponding research questions and data sources (shown in Table 1 ).
Methods and design
The project is a multi-dimensional study, involving an array of methodological approaches and data sources. The main part is a prospective cohort study of all Norwegian HAT patients, compared with the cohorts of all Danish HAT patients and Norwegian patients in conventional OAT.
Study populations and size
The primary target group is all patients enrolled in the two HAT clinics in Oslo and Bergen during the period 2022–2026, with an expected total sample size of N = 250. Based on earlier findings, the ratio of men to women is expected to be 4:1, with an age distribution of 27–60, presenting multiple substance use disorders. As the study is based on the total clinical population, representation will be determined by its demographics, with no exclusion of genders or ethnic minorities. The patients who have applied to but have not been accepted for HAT will be used for comparison, with an expected sample size of 100.
Comparative data from the Danish cohort will be drawn from the comprehensive dataset at Aarhus University from 2010 and onwards, with a sample size of approximately 500 [ 35 ]. Likewise, the comprehensive dataset at SERAF on the cohort of Norwegian patients in conventional OAT from 2003 has an approximate sample size of 8300.
Data sources
Data on the primary cohort of Norwegian HAT patients will be based on a prospective collection of both qualitative and quantitative variables from treatment inclusion and throughout the project period. For the cohorts of Danish patients, of Norwegian patients that have been referred to but not granted HAT, and of Norwegian patients in conventional OAT, data are mainly based on national registries.
In-depth and semi-structured interviews and observation
The qualitative part of the project includes individual in-depth and semi-structured interviews with patients and relatives on their views and experiences with HAT, and focus group interviews with staff concerning implementation, clinical and legal aspects of the project. Semi-structured interview protocols have been developed by the project group and user representatives. Interviews will include 25–35 patients and 10–20 family members, conducted by a team of researchers and user representatives at 1, 6, 18 months after patients enter treatment, and with relatives after 4 and 12 months. Focus group interviews with staff will be conducted at 3, 9 and 18 months. Further, the clinic managers are being interviewed at several timepoints from the planning of the clinics and throughout the duration of the project.
For insights into clinic aspects not identified through interviews, researchers will conduct participant observation in the clinics over several periods of 1–2 weeks throughout the study.
Questionnaires
The quantitative part of the project will use similar questionnaires to preceding projects involving patients in conventional OAT. These will evaluate changes in physical and mental health, personal economy, utilization of social services, criminal behavior and illegal drug use by repeated measures administered at inclusion, by 3, 6 and 12 months of treatment, and thereafter yearly (24, 36 and 48 months). Staff are asked to complete a separate questionnaire if a patient leaves treatment.
Clinical records
Information will also be obtained from the individual patient’s routine clinical records on variables such as main vital signs, nutritional status, cognitive function and mental health, medication, and comorbidities, as well as more HAT-specific variables such as adverse events, dosage, and administration routes of the pharmaceutical heroin.
Central register databases
Nordic national registers are an important and useful source for epidemiological and healthcare services research, including the study of substance use disorders [ 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ]. The project will utilize databases from national registries in both Norway and Denmark to describe the cohorts and to monitor the changes and outcomes in a wider context. Currently, one study has explored the use of the Short Form (SF-36) Health Survey in patients enrolled in the Danish HAT database, finding support for the structural and external validity for its use in HAT [ 44 ].
Table 2 gives an overview of the relevant Norwegian and Danish register databases along with their relevant variables.
Additional studies
Currently, the only planned sub-study is on the pharmacokinetics of heroin and its metabolites, and its subjective effects on patients. Despite its widespread use, the pharmacology of heroin remains poorly understood [ 45 , 46 , 47 ]. A subsample of patients will therefore be invited to participate in this observational study with post-administration blood samples collected at different time points, with analysis of the concentration of heroin and its metabolites together with scales of subjective experience. The study has been granted separate approvals from Norwegian Regional Committee for Medical and Health Research Ethics.
Analysis strategy
Exploration and analysis of data will be both by qualitative and quantitative strategies, for individual patients and at the organizational level.
Qualitative
Treatment satisfaction of patients is particularly significant to the project and is often dependent on the context of factors such as staff, management, and clinical environment [ 48 , 49 ]. Qualitative analyses are widely considered valuable for description of phenomena and hypothesis generation, taking into consideration the natural context in which people and organizations function [ 50 ]. Transcribed interviews will be coded following the principles of a flexible inductive thematic analysis and multidimensional approach [ 51 ].
Quantitative
Given the large amount and comprehensive nature of the data, variables of interest will vary in levels of measurement and distribution, so parametric and non-parametric tests will be used accordingly.
Presentation of cohorts will include descriptive statistics by basic parameters such as mean or medians, standard deviations and ratios, and bivariate analyses by ANOVA and Chi-Square tests. Various advanced methods such as survival analysis and logistic and linear regression modeling will be applied based on the type and distribution of dependent variables and co-variates. To avoid ecological fallacy and nested dimensions, multi-level methods will be applied for analyses of patients in relation to services’ organization [ 52 ]. Given the longitudinal design and to address the repeated measurements and correlated data, linear mixed models (LMM) (random intercepts or random slope models) will be used for person-specific effects, and marginal models like Generalized Estimating Equations (GEE) for population effects.
A theoretical sample size for statistical power will not be calculated because the study is based on the total clinical population available. For analyses of discrete and possible repeated events such as the number of criminal acts or medical prescriptions, statistical power will most likely be sufficient even with a restricted number of individuals. For analyses where the proportion of patients to number of variables may imply low statistical power, stratification of the study-population and restrictions to the number of covariates in the multivariate models will be applied.
Economic evaluations
Health economics and methods of cost-effectiveness analysis can guide decision makers, but at the same time they intrinsically rely on sets of politically and administratively determined rules and contexts [ 53 ]. In general, the cost-effectiveness of a treatment is intended to reflect the difference between the recourse’s opportunity costs (medical heroin) and those of the foregone or conventional alternative, to capture a broader set of values beyond the scope of mere financial costs [ 54 ].
Initially, for operating costs a three-step, top-down methodology used and refined by a former healthcare services project will be applied, where total costs are distributed on service units and units of treatment for individual patients [ 55 ].
For cost-effectiveness analyses of healthcare interventions, outcome is often measured in quality-adjusted life years (QALYs) for individual patients, in number of accidents or fatal incidents, or as societal costs associated with patients’ level of functioning and societal (criminal) behavior [ 56 ]. This will readily apply to the project and is in line with the national Norwegian recommendations for evaluation of new health interventions [ 57 , 58 ]. The relationships between HAT and various forms of criminal behavior (both property crime and illegal drug offences), labor market attachment, income and drug expenditures are also unclear and possible subjects for investigation during the project [ 20 ].
The data for all analyses will come from key account figures and relevant variables already obtained in the project.
The main strength of the study comes from its clinical and longitudinal approaches. The use of patient-interviews combined with clinical records, self-report data and register-based information will enhance the analyses and may uncover important associations between the individual patients, treatment, and the organizational level of healthcare services. The results are therefore expected to address aspects of HAT that may contribute to the development of clinical services and individually tailored treatments for OUD.
Study limitations are mainly related to the designs’ limitation for isolation of the effects from HAT on the outcome variables. Although valuable associations often have been suggested by longitudinal ecological studies, this limited possibility of unbiased causal inference remains a major weakness of both epidemiological and cohort designs [ 59 ]. Consequently, analyses will be cautiously interpreted within the context of previous findings, as well as patient and staff experiences. The triangulation of different types of data sources and cohorts, with the use of multivariate analysis and modeling might nevertheless provide more nuanced insights than currently exist.
Also, socially desirable bias concerning self-report questionnaires may be inherent in all self-reported outcomes [ 60 ]. This will apply to the study, as patients in the Norwegian cohort are possibly aware that the prospects of HAT may depend on the results from the study.
The sample of patients in the main cohort might also not be representative of individuals with OUD who do not seek the HAT option for reasons related to the study outcomes, such as social deprivation and isolation, behavioral misconduct, and incarceration [ 61 , 62 ]. Comparison with patients not granted access to the HAT-treatment may partly address this, although not to a full extent.
Lastly, the results will emerge in the context of a Nordic cultural and political system with healthcare reimbursements, insurance models and legal aspects that may limit their generalizability to other countries and societies. Given a cautious interpretation, the project may nonetheless be considered relevant to populations where OAT is used, and a wide range of medications are potentially provided.
Results from this project have the potential to identify new insights of value to patients, healthcare personnel, service administrators and policy makers as to whether an option for pharmaceutical heroin could be implemented as a conventional part of OAT services. We believe that the results will suggest future themes for research within the field of HAT with a potential for individually tailored treatment and care for individuals with OUD. This could affect considerations about drug treatment even beyond HAT-specific topics, where an expanded understanding of why some patients do not succeed with conventional OAT or specific OAT medications will strengthen the knowledge base for drug treatment in general.
Data availability
Data sharing is not applicable to this article as no datasets are currently completed or analyzed. The data that support the eventual findings of this study are available from both national registries, individual health journals and the project-specific database, but restrictions apply to the availability which are under license for the current study. Data may be available from the authors upon reasonable request and dependent on permissions from the Norwegian Regional Committee for Medical and Health Research Ethics. All information on subjects will be stored in the University of Oslo's secure services for sensitive data (TSD). Files for analysis will not contain directly identifying information of patients. Data will be stored in a non-identifiable way for 15 years after the end of the project.

Abbreviations
Opioid agonist treatment
Opioid use disorder
- Heroin assisted treatment
Generalized Estimating Equations
Linear mixed models
Quality-Adjusted Life Years
Norwegian Regional Committee for Medical and Health Research Ethics
Norwegian Centre for Addiction Research, Oslo
Section for Clinical Addiction Research, Oslo
Bergen Addiction Research Group, Bergen
Centre for Alcohol and Drug Research, Aarhus
Norwegian User-union
United Nations Office on Drugs and Crime (UNODC). World Drug Report 2023. 2023.
Degenhardt L, Grebely J, Stone J, Hickman M, Vickerman P, Marshall BDL, et al. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. Lancet. 2019;394(10208):1560–79.
Article CAS PubMed PubMed Central Google Scholar
Babor TF, Caulkins J, Fischer B, Foxcroft D, Medina-Mora ME, Obot I, et al. Drug Policy and the Public Good: a summary of the second edition. Addiction. 2019;114(11):1941–50.
Article Google Scholar
Dole VP, Nyswander M. A Medical treatment for Diacetylmorphine (Heroin) addiction. A clinical trial with Methadone Hydrochloride. JAMA. 1965;193:646–50.
Article CAS PubMed Google Scholar
Isbell H, Vogel VH. The addiction liability of methadon (amidone, dolophine, 10820) and its use in the treatment of the morphine abstinence syndrome. Am J Psychiatry. 1949;105(12):909–14.
Strang J, Volkow ND, Degenhardt L, Hickman M, Johnson K, Koob GF et al. Opioid use disorder. Nat Rev Dis Primers. 2020;6(1).
Chaillon A, Bharat C, Stone J, Jones N, Degenhardt L, Larney S, et al. Modeling the population-level impact of opioid agonist treatment on mortality among people accessing treatment between 2001 and 2020 in New South Wales, Australia. Addiction. 2022;117(5):1338–52.
Article PubMed Google Scholar
Havnes I, Bukten A, Gossop M, Waal H, Stangeland P, Clausen T. Reductions in convictions for violent crime during opioid maintenance treatment: a longitudinal national cohort study. Drug Alcohol Depend. 2012;124(3):307–10.
Clausen T, Anchersen K, Waal H. Mortality prior to, during and after opioid maintenance treatment (OMT): a national prospective cross-registry study. Drug Alcohol Depend. 2008;94(1–3):151–7.
Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357:j1550.
Article PubMed PubMed Central Google Scholar
Bukten A, Skurtveit S, Waal H, Clausen T. Factors associated with dropout among patients in opioid maintenance treatment (OMT) and predictors of re-entry. A national registry-based study. Addict Behav. 2014;39(10):1504–9.
Bukten A, Roislien J, Skurtveit S, Waal H, Gossop M, Clausen T. A day-by-day investigation of changes in criminal convictions before and after entering and leaving opioid maintenance treatment: a national cohort study. BMC Psychiatry. 2013;13:262.
Klimas J, Hamilton MA, Gorfinkel L, Adam A, Cullen W, Wood E. Retention in opioid agonist treatment: a rapid review and meta-analysis comparing observational studies and randomized controlled trials. Syst Rev. 2021;10(1):216.
Timko C, Schultz NR, Cucciare MA, Vittorio L, Garrison-Diehn C. Retention in medication-assisted treatment for opiate dependence: a systematic review. J Addict Dis. 2016;35(1):22–35.
Strang J, Sheridan J. Heroin prescribing in the British system of the mid 1990s: data from the 1995 national survey of community pharmacies in England and Wales. Drug Alcohol Rev. 1997;16(1):7–16.
Berridge V. Heroin prescription and history. N Engl J Med. 2009;361(8):820–1.
van den Brink W, Hendriks VM, Blanken P, Koeter MW, van Zwieten BJ, van Ree JM. Medical prescription of heroin to treatment resistant heroin addicts: two randomised controlled trials. BMJ. 2003;327(7410):310.
Rehm J, Gschwend P, Steffen T, Gutzwiller F, Dobler-Mikola A, Uchtenhagen A. Feasibility, safety, and efficacy of injectable heroin prescription for refractory opioid addicts: a follow-up study. Lancet. 2001;358(9291):1417–23.
Strang J, Groshkova T, Uchtenhagen A, van den Brink W, Haasen C, Schechter MT, et al. Heroin on trial: systematic review and meta-analysis of randomised trials of diamorphine-prescribing as treatment for refractory heroin addictiondagger. Br J Psychiatry. 2015;207(1):5–14.
Smart R, Reuter P. Does heroin-assisted treatment reduce crime? A review of randomized-controlled trials. Addiction. 2022;117(3):518–31.
Oviedo-Joekes E, Brissette S, Marsh DC, Lauzon P, Guh D, Anis A, et al. Diacetylmorphine versus methadone for the treatment of opioid addiction. N Engl J Med. 2009;361(8):777–86.
Farrell M, Hall W. Heroin-assisted treatment: has a controversial treatment come of age? Br J Psychiatry. 2015;207(1):3–4.
Bell J, van der Waal R, Strang J. Supervised Injectable Heroin: a clinical perspective. Can J Psychiat. 2017;62(7):451–6.
Meyer M, Strasser J, Kock P, Walter M, Vogel M, Dursteler KM. Experiences with take-home dosing in heroin-assisted treatment in Switzerland during the COVID-19 pandemic-Is an update of legal restrictions warranted? Int J Drug Policy. 2022;101:103548.
Oviedo-Joekes E, Dobischok S, Carvajal J, MacDonald S, McDermid C, Klakowicz P, et al. Clients’ experiences on North America’s first take-home injectable opioid agonist treatment (iOAT) program: a qualitative study. BMC Health Serv Res. 2023;23(1):553.
Ferri M, Davoli M, Perucci CA. Heroin maintenance for chronic heroin-dependent individuals. Cochrane Database Syst Rev. 2011;2011(12):CD003410.
PubMed PubMed Central Google Scholar
Dijkgraaf MG, van der Zanden BP, de Borgie CA, Blanken P, van Ree JM, van den Brink W. Cost utility analysis of co-prescribed heroin compared with methadone maintenance treatment in heroin addicts in two randomised trials. BMJ. 2005;330(7503):1297.
Byford S, Barrett B, Metrebian N, Groshkova T, Cary M, Charles V, et al. Cost-effectiveness of injectable opioid treatment v. oral methadone for chronic heroin addiction. Br J Psychiatry. 2013;203(5):341–9.
Poulter HL, Walker T, Ahmed D, Moore HJ, Riley F, Towl G, et al. More than just ‘free heroin’: caring whilst navigating constraint in the delivery of diamorphine assisted treatment. Int J Drug Policy. 2023;116:104025.
Tiffany ST, Friedman L, Greenfield SF, Hasin DS, Jackson R. Beyond drug use: a systematic consideration of other outcomes in evaluations of treatments for substance use disorders. Addiction. 2012;107(4):709–18.
Groshkova T, Metrebian N, Hallam C, Charles V, Martin A, Forzisi L, et al. Treatment expectations and satisfaction of treatment-refractory opioid-dependent patients in RIOTT, the Randomised Injectable Opiate Treatment Trial, the UK’s first supervised injectable maintenance clinics. Drug Alcohol Rev. 2013;32(6):566–73.
Sundhetsstyrelsen. Evaluering af ordningen med lægeordineret heroin til opioidafhængige patienter. Opgørelse over årene 2013–2020. København; 2021.
Waal H. Merits and problems in high-threshold methadone maintenance treatment. Evaluation of medication-assisted rehabilitation in Norway 1998–2004. Eur Addict Res. 2007;13(2):66–73.
Ellefsen R, Wusthoff LEC, Arnevik EA. Patients’ satisfaction with heroin-assisted treatment: a qualitative study. Harm Reduct J. 2023;20(1):73.
Gabrhelik R, Handal M, Mravcik V, Nechanska B, Tjagvad C, Thylstrup B et al. Opioid maintenance treatment in the Czech Republic, Norway and Denmark: a study protocol of a comparative registry linkage study. Bmj Open. 2021;11(5).
Arendt M, Munk-Jorgensen P, Sher L, Jensen SO. Mortality among individuals with cannabis, cocaine, amphetamine, MDMA, and opioid use disorders: a nationwide follow-up study of Danish substance users in treatment. Drug Alcohol Depend. 2011;114(2–3):134–9.
PubMed Google Scholar
Bukten A, Lokdam NT, Skjaervo I, Ugelvik T, Skurtveit S, Gabrhelik R et al. PriSUD-Nordic-diagnosing and treating Substance Use disorders in the Prison Population: protocol for a mixed methods study. Jmir Res Protoc. 2022;11(3).
Bukten A, Stavseth MR, Clasuen T. From restrictive to more liberal: variations in moratlity among patients in opioid maintenance treament over a 12-year period. BMC Health Serv Res. 2019;19(1):553.
Mortensen LH, Rehnberg J, Dahl E, Diderichsen F, Elstad JI, Martikainen P, et al. Shape of the association between income and mortality: a cohort study of Denmark, Finland, Norway and Sweden in 1995 and 2003. Bmj Open. 2016;6(12):e010974.
Munk-Jorgensen P, Ostergaard SD. Register-based studies of mental disorders. Scand J Public Health. 2011;39(7 Suppl):170–4.
Lassemo E, Myklebust LH. Changes in patterns of coercion during a nine-year period in a Norwegian psychiatric service area. Int J Methods Psychiatr Res. 2021;30(4):e1889.
Myklebust LH, Sorgaard KW, Bjorbekkmo S, Eisemann MR, Olstad R. Time-trends in the utilization of decentralized mental health services in Norway - A natural experiment: the VELO-project. Int J Ment Health Syst. 2010;4:5.
Myklebust LH, Lassemo E. The role of local inpatient psychiatric units and general practitioner on continuity of care in Northern Norway: a case-register study. Int J Methods Psychiatr Res. 2021;30(2):e1866.
Kvamme T, Thylstrup B, Hesse M. Quality of life assessment in Danish Heroin Assisted Treatment Patients: Validity of the SF-36 Survey. submitted.
De Pirro S, Galati G, Pizzamiglio L, Badiani A. The affective and neural correlates of Heroin versus Cocaine Use in Addiction are influenced by environmental setting but in Opposite directions. J Neurosci. 2018;38(22):5182–95.
De Pirro S, Lush P, Parkinson J, Duka T, Critchley HD, Badiani A. Effect of alcohol on the sense of agency in healthy humans. Addict Biol. 2020;25(4):e12796.
Milella MS, D’Ottavio G, De Pirro S, Barra M, Caprioli D, Badiani A. Heroin and its metabolites: relevance to heroin use disorder. Translational Psychiatry. 2023;13(1):120.
Kelly SM, O’Grady KE, Brown BS, Mitchell SG, Schwartz RP. The role of patient satisfaction in methadone treatment. Am J Drug Alcohol Abuse. 2010;36(3):150–4.
Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39–48.
Korstjens I, Moser A, Series. Practical guidance to qualitative research. Part 2: context, research questions and designs. Eur J Gen Pract. 2017;23(1):274–9.
Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual Res Psychol. 2021;18(3):328–52.
Dyjack D. Ecological fallacies. J Environ Health. 2019;81(9):50–.
Google Scholar
Gold MR, Russell JES, Weinstein LB. MC. Cost-Effectiveness in Health and Medicine: Oxford University Press; 1996 1996.
Turner HC, Sandmann FG, Downey LE, Orangi S, Teerawattananon Y, Vassall A, et al. What are economic costs and when should they be used in health economic studies? Cost Eff Resour Alloc. 2023;21(1):31.
Lassemo E, Myklebust L, Sorgaard K. Patient cost and treatment unit cost comparison in the VELO-Study. Psychiat Prax. 2011;38.
Yates BT. Cost-inclusive evaluation: a banquet of approaches for including costs, benefits, and cost-effectiveness and cost-benefit analyses in your next evaluation. Eval Program Plann. 2009;32(1):52–4.
The Directorate of Health. Recommendations for the economic evaluation of new interventions in the Norwegian health sector. Oslo2012.
Meld. St. 34. Principles for priority settings in health care. Summary of a white paper on priority setting in the Norwegian health care sector. In: Servces NMoHaC, editor. Oslo2017.
Jekel JF, Katz DL, Elmpre JG. Epideimology, biostatisticvcs and preventive medicine. Pennsylvania, USA: B.W.Saunders; 2001.
Latkin CA, Edwards C, Davey-Rothwell MA, Tobin KE. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addict Behav. 2017;73:133–6.
Hosseinbor M, Yassini Ardekani SM, Bakhshani S, Bakhshani S. Emotional and social loneliness in individuals with and without substance dependence disorder. Int J High Risk Behav Addict. 2014;3(3):e22688.
Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: improving public health and safety. JAMA. 2009;301(2):183–90.
Cho HL, Danis M, Grady C. Post-trial responsibilities beyond post-trial access. Lancet. 2018;391(10129):1478–9.
Cook K, Snyder J, Calvert J. Attitudes toward Post-trial Access to Medical interventions: a review of academic literature, legislation, and International guidelines. Dev World Bioeth. 2016;16(2):70–9.
Download references
Acknowledgements
We would like to thank the representatives from proLARNett for inputs on the design and aims of the study. Also thanks to associate professor Eva Lassemo at SINTEF-Helse, Norway for inputs on economical analysis.
The project is funded by the Norwegian Directorate of Health for the duration of 4.5 years with an annual limit of 5 million NOK (assignment No.20/00546). No remuneration is planned for the subjects’ participation in the project.
Open access funding provided by University of Oslo (incl Oslo University Hospital)
Author information
Authors and affiliations.
Norwegian Centre for Addiction Research, Faculty of Medicine, University of Oslo, Kirkevegen 166, Building 45, NO-0407, Oslo, Norway
Lars Henrik Myklebust, Desiree Eide, Silvana De Pirro, Francesca Melis, Ann Oldervoll, Linda E.C. Wusthoff & Thomas Clausen
Bergen Addiction Research Group, Department of Addiction Medicine, Haukeland University Hospital, P.b 1400, NO-5021, Bergen, Norway
Omid Dadras & Lars T. Fadnes
Department of Global Public Health and Primary Care, University of Bergen, P.b 7804, NO-5020, Bergen, Norway
Lars T. Fadnes
Section for Clinical Addiction Research, Oslo University Hospital, P.b 4950 Nydalen, NO-0424, Oslo, Norway
Espen A. Arnevik, Rune Ellefsen & Linda E.C. Wusthoff
Centre for Alcohol and Drug Research, Aarhus University, Bartholins Allé 10, DK-8000, Aarhus, Denmark
Morten Hesse, Timo L. Kvamme & Birgitte Thylstrup
Department of Physiology and Pharmacology “V. Erspamer,” La Sapienza, University of Rome, P. Ie Aldo Moro 5, 00185, Rome, Italy
Silvana De Pirro
You can also search for this author in PubMed Google Scholar
Contributions
LHM wrote and drafted the manuscript with critical input from all the authors. The study was planned and designed by TC, DE, LTF and LECW. The statistical section had essential inputs from FM and LHM, the section on economic evaluation had substantial inputs from OD, FM and LHM. The litterature search was conducted LHM, with inputs from TC and LECW. Authors OD, SDP, RE, MH, BT, TLK, EAA and AO read the manuscript and had substantial contributions on data-aquisition and corresponding background material.
Corresponding author
Correspondence to Lars Henrik Myklebust .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Norwegian Regional Committee for Medical and Health Research Ethics (REK 195733). Informed consent was obtained from all participants. A particular revision of the Helsinki declaration on eventual continued post-trial provisions of clinical care and treatment [ 63 , 64 ] does not apply as the project solely observes the outcomes from already provided treatment and does not initiate any research interventions. No specific insurances for subjects are taken out for the study. In case of injury or complications despite all precautions, patients have the right to apply for compensation through the Norwegian System of Patient Injury Compensation (NPE).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Myklebust, L.H., Eide, D., Arnevik, E.A. et al. Evaluation of heroin-assisted treatment in Norway: protocol for a mixed methods study. BMC Health Serv Res 24 , 398 (2024). https://doi.org/10.1186/s12913-024-10767-w
Download citation
Received : 24 November 2023
Accepted : 21 February 2024
Published : 29 March 2024
DOI : https://doi.org/10.1186/s12913-024-10767-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Opioid maintenance treatment
- Health services
- Mixed methods
- Longitudinal
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Read our research on: Abortion | Podcasts | Election 2024
Regions & Countries
What the data says about abortion in the u.s..
Pew Research Center has conducted many surveys about abortion over the years, providing a lens into Americans’ views on whether the procedure should be legal, among a host of other questions.
In a Center survey conducted nearly a year after the Supreme Court’s June 2022 decision that ended the constitutional right to abortion , 62% of U.S. adults said the practice should be legal in all or most cases, while 36% said it should be illegal in all or most cases. Another survey conducted a few months before the decision showed that relatively few Americans take an absolutist view on the issue .
Find answers to common questions about abortion in America, based on data from the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, which have tracked these patterns for several decades:
How many abortions are there in the U.S. each year?
How has the number of abortions in the u.s. changed over time, what is the abortion rate among women in the u.s. how has it changed over time, what are the most common types of abortion, how many abortion providers are there in the u.s., and how has that number changed, what percentage of abortions are for women who live in a different state from the abortion provider, what are the demographics of women who have had abortions, when during pregnancy do most abortions occur, how often are there medical complications from abortion.
This compilation of data on abortion in the United States draws mainly from two sources: the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, both of which have regularly compiled national abortion data for approximately half a century, and which collect their data in different ways.
The CDC data that is highlighted in this post comes from the agency’s “abortion surveillance” reports, which have been published annually since 1974 (and which have included data from 1969). Its figures from 1973 through 1996 include data from all 50 states, the District of Columbia and New York City – 52 “reporting areas” in all. Since 1997, the CDC’s totals have lacked data from some states (most notably California) for the years that those states did not report data to the agency. The four reporting areas that did not submit data to the CDC in 2021 – California, Maryland, New Hampshire and New Jersey – accounted for approximately 25% of all legal induced abortions in the U.S. in 2020, according to Guttmacher’s data. Most states, though, do have data in the reports, and the figures for the vast majority of them came from each state’s central health agency, while for some states, the figures came from hospitals and other medical facilities.
Discussion of CDC abortion data involving women’s state of residence, marital status, race, ethnicity, age, abortion history and the number of previous live births excludes the low share of abortions where that information was not supplied. Read the methodology for the CDC’s latest abortion surveillance report , which includes data from 2021, for more details. Previous reports can be found at stacks.cdc.gov by entering “abortion surveillance” into the search box.
For the numbers of deaths caused by induced abortions in 1963 and 1965, this analysis looks at reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. In computing those figures, we excluded abortions listed in the report under the categories “spontaneous or unspecified” or as “other.” (“Spontaneous abortion” is another way of referring to miscarriages.)
Guttmacher data in this post comes from national surveys of abortion providers that Guttmacher has conducted 19 times since 1973. Guttmacher compiles its figures after contacting every known provider of abortions – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, and it provides estimates for abortion providers that don’t respond to its inquiries. (In 2020, the last year for which it has released data on the number of abortions in the U.S., it used estimates for 12% of abortions.) For most of the 2000s, Guttmacher has conducted these national surveys every three years, each time getting abortion data for the prior two years. For each interim year, Guttmacher has calculated estimates based on trends from its own figures and from other data.
The latest full summary of Guttmacher data came in the institute’s report titled “Abortion Incidence and Service Availability in the United States, 2020.” It includes figures for 2020 and 2019 and estimates for 2018. The report includes a methods section.
In addition, this post uses data from StatPearls, an online health care resource, on complications from abortion.
An exact answer is hard to come by. The CDC and the Guttmacher Institute have each tried to measure this for around half a century, but they use different methods and publish different figures.
The last year for which the CDC reported a yearly national total for abortions is 2021. It found there were 625,978 abortions in the District of Columbia and the 46 states with available data that year, up from 597,355 in those states and D.C. in 2020. The corresponding figure for 2019 was 607,720.
The last year for which Guttmacher reported a yearly national total was 2020. It said there were 930,160 abortions that year in all 50 states and the District of Columbia, compared with 916,460 in 2019.
- How the CDC gets its data: It compiles figures that are voluntarily reported by states’ central health agencies, including separate figures for New York City and the District of Columbia. Its latest totals do not include figures from California, Maryland, New Hampshire or New Jersey, which did not report data to the CDC. ( Read the methodology from the latest CDC report .)
- How Guttmacher gets its data: It compiles its figures after contacting every known abortion provider – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, then provides estimates for abortion providers that don’t respond. Guttmacher’s figures are higher than the CDC’s in part because they include data (and in some instances, estimates) from all 50 states. ( Read the institute’s latest full report and methodology .)
While the Guttmacher Institute supports abortion rights, its empirical data on abortions in the U.S. has been widely cited by groups and publications across the political spectrum, including by a number of those that disagree with its positions .
These estimates from Guttmacher and the CDC are results of multiyear efforts to collect data on abortion across the U.S. Last year, Guttmacher also began publishing less precise estimates every few months , based on a much smaller sample of providers.
The figures reported by these organizations include only legal induced abortions conducted by clinics, hospitals or physicians’ offices, or those that make use of abortion pills dispensed from certified facilities such as clinics or physicians’ offices. They do not account for the use of abortion pills that were obtained outside of clinical settings .
(Back to top)
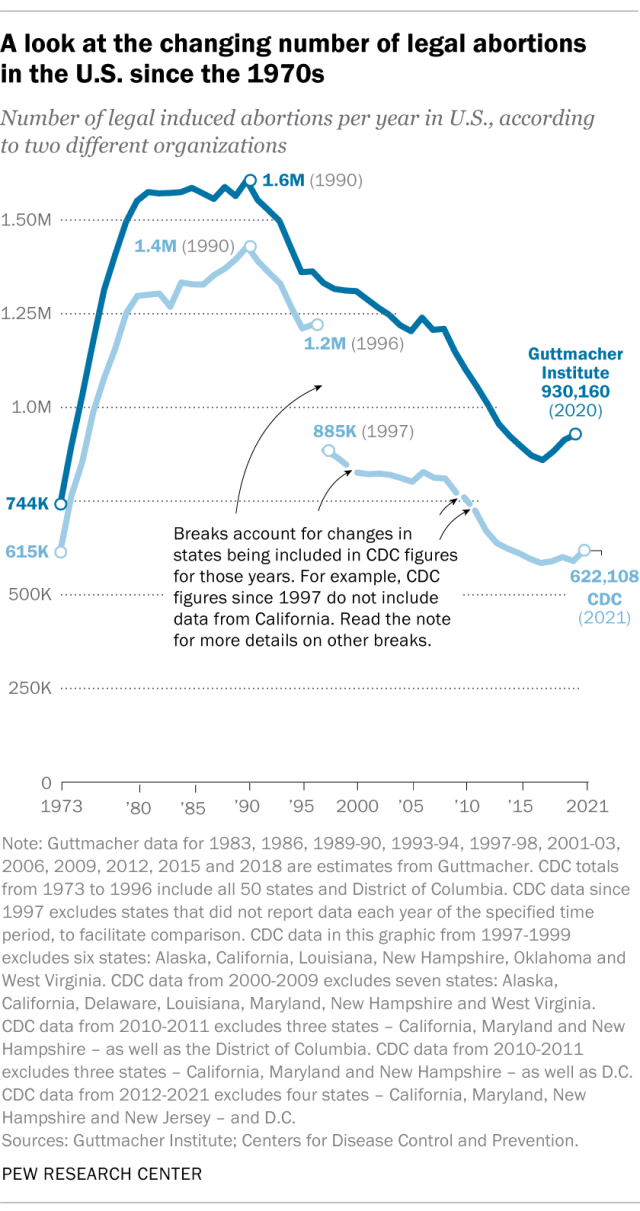
The annual number of U.S. abortions rose for years after Roe v. Wade legalized the procedure in 1973, reaching its highest levels around the late 1980s and early 1990s, according to both the CDC and Guttmacher. Since then, abortions have generally decreased at what a CDC analysis called “a slow yet steady pace.”
Guttmacher says the number of abortions occurring in the U.S. in 2020 was 40% lower than it was in 1991. According to the CDC, the number was 36% lower in 2021 than in 1991, looking just at the District of Columbia and the 46 states that reported both of those years.
(The corresponding line graph shows the long-term trend in the number of legal abortions reported by both organizations. To allow for consistent comparisons over time, the CDC figures in the chart have been adjusted to ensure that the same states are counted from one year to the next. Using that approach, the CDC figure for 2021 is 622,108 legal abortions.)
There have been occasional breaks in this long-term pattern of decline – during the middle of the first decade of the 2000s, and then again in the late 2010s. The CDC reported modest 1% and 2% increases in abortions in 2018 and 2019, and then, after a 2% decrease in 2020, a 5% increase in 2021. Guttmacher reported an 8% increase over the three-year period from 2017 to 2020.
As noted above, these figures do not include abortions that use pills obtained outside of clinical settings.
Guttmacher says that in 2020 there were 14.4 abortions in the U.S. per 1,000 women ages 15 to 44. Its data shows that the rate of abortions among women has generally been declining in the U.S. since 1981, when it reported there were 29.3 abortions per 1,000 women in that age range.
The CDC says that in 2021, there were 11.6 abortions in the U.S. per 1,000 women ages 15 to 44. (That figure excludes data from California, the District of Columbia, Maryland, New Hampshire and New Jersey.) Like Guttmacher’s data, the CDC’s figures also suggest a general decline in the abortion rate over time. In 1980, when the CDC reported on all 50 states and D.C., it said there were 25 abortions per 1,000 women ages 15 to 44.
That said, both Guttmacher and the CDC say there were slight increases in the rate of abortions during the late 2010s and early 2020s. Guttmacher says the abortion rate per 1,000 women ages 15 to 44 rose from 13.5 in 2017 to 14.4 in 2020. The CDC says it rose from 11.2 per 1,000 in 2017 to 11.4 in 2019, before falling back to 11.1 in 2020 and then rising again to 11.6 in 2021. (The CDC’s figures for those years exclude data from California, D.C., Maryland, New Hampshire and New Jersey.)
The CDC broadly divides abortions into two categories: surgical abortions and medication abortions, which involve pills. Since the Food and Drug Administration first approved abortion pills in 2000, their use has increased over time as a share of abortions nationally, according to both the CDC and Guttmacher.
The majority of abortions in the U.S. now involve pills, according to both the CDC and Guttmacher. The CDC says 56% of U.S. abortions in 2021 involved pills, up from 53% in 2020 and 44% in 2019. Its figures for 2021 include the District of Columbia and 44 states that provided this data; its figures for 2020 include D.C. and 44 states (though not all of the same states as in 2021), and its figures for 2019 include D.C. and 45 states.
Guttmacher, which measures this every three years, says 53% of U.S. abortions involved pills in 2020, up from 39% in 2017.
Two pills commonly used together for medication abortions are mifepristone, which, taken first, blocks hormones that support a pregnancy, and misoprostol, which then causes the uterus to empty. According to the FDA, medication abortions are safe until 10 weeks into pregnancy.
Surgical abortions conducted during the first trimester of pregnancy typically use a suction process, while the relatively few surgical abortions that occur during the second trimester of a pregnancy typically use a process called dilation and evacuation, according to the UCLA School of Medicine.
In 2020, there were 1,603 facilities in the U.S. that provided abortions, according to Guttmacher . This included 807 clinics, 530 hospitals and 266 physicians’ offices.
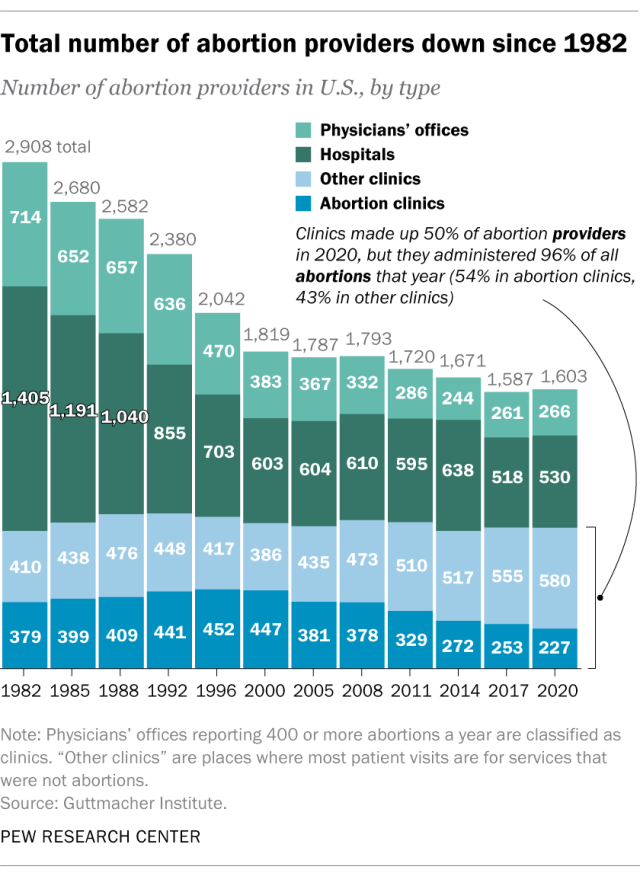
While clinics make up half of the facilities that provide abortions, they are the sites where the vast majority (96%) of abortions are administered, either through procedures or the distribution of pills, according to Guttmacher’s 2020 data. (This includes 54% of abortions that are administered at specialized abortion clinics and 43% at nonspecialized clinics.) Hospitals made up 33% of the facilities that provided abortions in 2020 but accounted for only 3% of abortions that year, while just 1% of abortions were conducted by physicians’ offices.
Looking just at clinics – that is, the total number of specialized abortion clinics and nonspecialized clinics in the U.S. – Guttmacher found the total virtually unchanged between 2017 (808 clinics) and 2020 (807 clinics). However, there were regional differences. In the Midwest, the number of clinics that provide abortions increased by 11% during those years, and in the West by 6%. The number of clinics decreased during those years by 9% in the Northeast and 3% in the South.
The total number of abortion providers has declined dramatically since the 1980s. In 1982, according to Guttmacher, there were 2,908 facilities providing abortions in the U.S., including 789 clinics, 1,405 hospitals and 714 physicians’ offices.
The CDC does not track the number of abortion providers.
In the District of Columbia and the 46 states that provided abortion and residency information to the CDC in 2021, 10.9% of all abortions were performed on women known to live outside the state where the abortion occurred – slightly higher than the percentage in 2020 (9.7%). That year, D.C. and 46 states (though not the same ones as in 2021) reported abortion and residency data. (The total number of abortions used in these calculations included figures for women with both known and unknown residential status.)
The share of reported abortions performed on women outside their state of residence was much higher before the 1973 Roe decision that stopped states from banning abortion. In 1972, 41% of all abortions in D.C. and the 20 states that provided this information to the CDC that year were performed on women outside their state of residence. In 1973, the corresponding figure was 21% in the District of Columbia and the 41 states that provided this information, and in 1974 it was 11% in D.C. and the 43 states that provided data.
In the District of Columbia and the 46 states that reported age data to the CDC in 2021, the majority of women who had abortions (57%) were in their 20s, while about three-in-ten (31%) were in their 30s. Teens ages 13 to 19 accounted for 8% of those who had abortions, while women ages 40 to 44 accounted for about 4%.
The vast majority of women who had abortions in 2021 were unmarried (87%), while married women accounted for 13%, according to the CDC , which had data on this from 37 states.
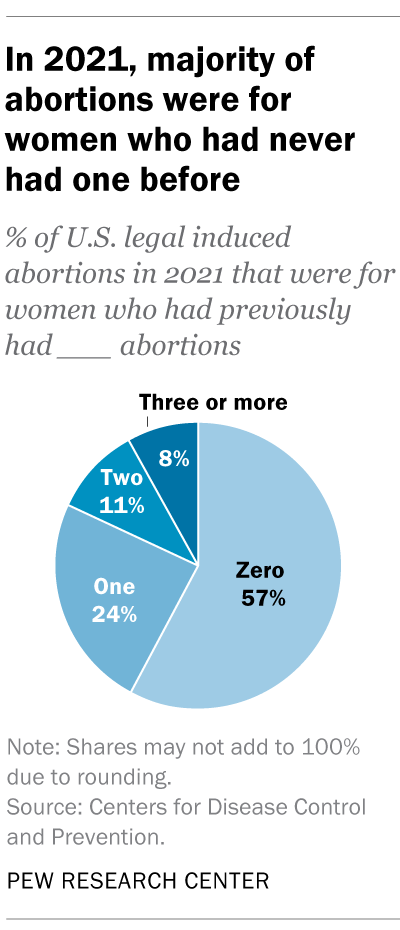
In the District of Columbia, New York City (but not the rest of New York) and the 31 states that reported racial and ethnic data on abortion to the CDC , 42% of all women who had abortions in 2021 were non-Hispanic Black, while 30% were non-Hispanic White, 22% were Hispanic and 6% were of other races.
Looking at abortion rates among those ages 15 to 44, there were 28.6 abortions per 1,000 non-Hispanic Black women in 2021; 12.3 abortions per 1,000 Hispanic women; 6.4 abortions per 1,000 non-Hispanic White women; and 9.2 abortions per 1,000 women of other races, the CDC reported from those same 31 states, D.C. and New York City.
For 57% of U.S. women who had induced abortions in 2021, it was the first time they had ever had one, according to the CDC. For nearly a quarter (24%), it was their second abortion. For 11% of women who had an abortion that year, it was their third, and for 8% it was their fourth or more. These CDC figures include data from 41 states and New York City, but not the rest of New York.
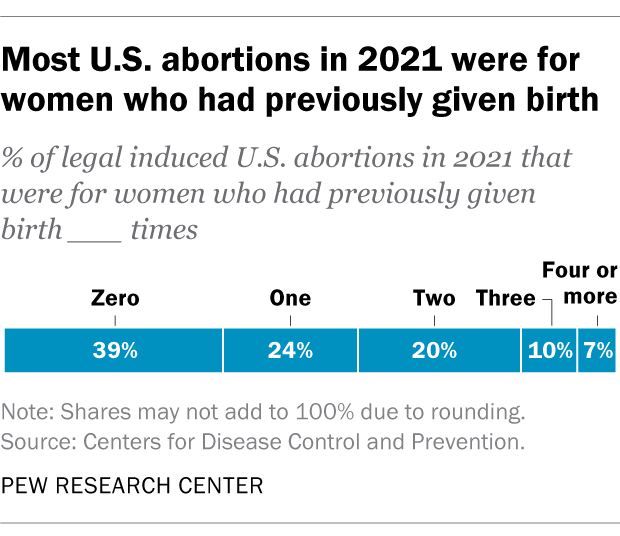
Nearly four-in-ten women who had abortions in 2021 (39%) had no previous live births at the time they had an abortion, according to the CDC . Almost a quarter (24%) of women who had abortions in 2021 had one previous live birth, 20% had two previous live births, 10% had three, and 7% had four or more previous live births. These CDC figures include data from 41 states and New York City, but not the rest of New York.
The vast majority of abortions occur during the first trimester of a pregnancy. In 2021, 93% of abortions occurred during the first trimester – that is, at or before 13 weeks of gestation, according to the CDC . An additional 6% occurred between 14 and 20 weeks of pregnancy, and about 1% were performed at 21 weeks or more of gestation. These CDC figures include data from 40 states and New York City, but not the rest of New York.
About 2% of all abortions in the U.S. involve some type of complication for the woman , according to an article in StatPearls, an online health care resource. “Most complications are considered minor such as pain, bleeding, infection and post-anesthesia complications,” according to the article.
The CDC calculates case-fatality rates for women from induced abortions – that is, how many women die from abortion-related complications, for every 100,000 legal abortions that occur in the U.S . The rate was lowest during the most recent period examined by the agency (2013 to 2020), when there were 0.45 deaths to women per 100,000 legal induced abortions. The case-fatality rate reported by the CDC was highest during the first period examined by the agency (1973 to 1977), when it was 2.09 deaths to women per 100,000 legal induced abortions. During the five-year periods in between, the figure ranged from 0.52 (from 1993 to 1997) to 0.78 (from 1978 to 1982).
The CDC calculates death rates by five-year and seven-year periods because of year-to-year fluctuation in the numbers and due to the relatively low number of women who die from legal induced abortions.
In 2020, the last year for which the CDC has information , six women in the U.S. died due to complications from induced abortions. Four women died in this way in 2019, two in 2018, and three in 2017. (These deaths all followed legal abortions.) Since 1990, the annual number of deaths among women due to legal induced abortion has ranged from two to 12.
The annual number of reported deaths from induced abortions (legal and illegal) tended to be higher in the 1980s, when it ranged from nine to 16, and from 1972 to 1979, when it ranged from 13 to 63. One driver of the decline was the drop in deaths from illegal abortions. There were 39 deaths from illegal abortions in 1972, the last full year before Roe v. Wade. The total fell to 19 in 1973 and to single digits or zero every year after that. (The number of deaths from legal abortions has also declined since then, though with some slight variation over time.)
The number of deaths from induced abortions was considerably higher in the 1960s than afterward. For instance, there were 119 deaths from induced abortions in 1963 and 99 in 1965 , according to reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. The CDC is a division of Health and Human Services.
Note: This is an update of a post originally published May 27, 2022, and first updated June 24, 2022.

Sign up for our weekly newsletter
Fresh data delivered Saturday mornings
Key facts about the abortion debate in America
Public opinion on abortion, three-in-ten or more democrats and republicans don’t agree with their party on abortion, partisanship a bigger factor than geography in views of abortion access locally, do state laws on abortion reflect public opinion, most popular.
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
- Study Protocol
- Open access
- Published: 27 March 2024
The effects of individual music therapy in nursing home residents with dementia to improve general well-being: study protocol of a randomized controlled trial
- Vanusa M. Baroni Caramel ORCID: orcid.org/0000-0002-1921-0951 1 , 2 ,
- Jenny T. van der Steen ORCID: orcid.org/0000-0002-9063-7501 3 , 4 ,
- Annemieke C. Vink ORCID: orcid.org/0000-0003-4242-4314 5 ,
- Sarah I. M. Janus ORCID: orcid.org/0000-0003-0419-4407 1 ,
- Jos W. R. Twisk ORCID: orcid.org/0000-0001-9617-1020 6 ,
- Erik J. A. Scherder ORCID: orcid.org/0000-0003-1203-3208 2 &
- Sytse U. Zuidema ORCID: orcid.org/0000-0002-4991-9507 1
BMC Geriatrics volume 24 , Article number: 290 ( 2024 ) Cite this article
48 Accesses
Metrics details
Dementia is often associated with Neuropsychiatric Symptoms (NPS) such as agitation, depression, hallucinations, anxiety, that can cause distress for the resident with dementia in long-term care settings and can impose emotional burden on the environment. NPS are often treated with psychotropic drugs, which, however, frequently cause side effects. Alternatively, non-pharmacological interventions can improve well-being and maintain an optimal quality of life (QoL) of those living with dementia. Other QoL related outcomes, such as pain, discomfort and sleep disruption are relevant outcomes in music trials as well. Music therapy is a non-pharmacological intervention that can reduce NPS and improve well-being, and its associated symptoms in dementia.
The research will be conducted at eight nursing home facilities of a health care organization in the Netherlands. A sample size of 30 in each group (experimental and control group) is required, totalling 60 residents increased to 80 when considering expected drop out to follow up. The participants in the intervention group receive 30 min of individual music therapy (MT) in their own room by a music therapist twice a week for 12 weeks. The participants in the control group will receive 30 min of individual attention in their own room by a volunteer twice a week for 12 weeks. Assessments will be done at baseline, 6 weeks and 12 weeks. An independent observer, blinded for the intervention or control condition, will assess directly observed well-being (primary outcome) and pain (secondary outcome) before and after the sessions. Nurses will assess other secondary outcomes unblinded, i.e., perceived quality of life and NPS, both assessed with validated scales. The sleep duration will be indirectly assessed by a wrist device called MotionWatch. Information about psychotropic drug use will be derived from electronic medical chart review.
The main purpose of this study is to assess the effects of individual music therapy on directly observed well-being controlled for individual attention in nursing home residents with dementia with NPS. The outcomes refer to both short-term and long-term effects consistent with therapeutic goals of care for a longer term. We hope to overcome limitations of previous study designs such as not blinded designs and music facilitators that were not only music therapists but also occupational therapists and nurses. This study should lead to more focused recommendations for practice and further research into non-pharmacological interventions in dementia such as music therapy.
Trial registration
The trial is registered at the International Clinical Trials Registry Platform (ICTRP) search portal in the Netherlands Trial Registration number NL7708, registration date 04-05-2019.
Peer Review reports
Introduction
Background and rationale.
Dementia is a common disease and in 2021, the World Health Organization estimated that around 55 million people have dementia worldwide [ 1 ]. Dementia is a neurodegenerative syndrome characterized by a progressive deterioration of cognitive function, in particular memory but other cognitive domains such as language, praxis, visual perception and most notably executive functions are also often affected [ 2 ]. Personality and behavior changes, together with a decline in the ability to perform activities of daily living, may result in a loss of independence. The personality and behavioral changes are often reflected in Neuropsychiatric Symptoms (NPS). More specifically, NPS may express itself in, for example, agitation, disinhibition, irritability, delusions, hallucinations, depression, anxiety and apathy. These symptoms are ubiquitous in nursing home patients with dementia, with overall rates of more than 80% [ 3 ].
As there are no curative treatments for dementia yet, it is important to focus on interventions that may have beneficial effects on well-being and maintain an optimal quality of life. Quality of life is defined by the WHO as “individuals’ perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” [ 4 ]. Well-being is defined in terms of a state of equilibrium existing between personal resources and life challenges that, when achieved, gives rise to positive emotions and psychological health [ 5 ]. The constructs of QoL and well-being have often been used inter-changeably in dementia research [ 6 ].
There is a growing consensus that quality of life is an important outcome for assessing the effectiveness of interventions for dementia in clinical trials even though it concerns a multidimensional construct influenced by a variety of factors [ 7 , 8 ]. An observational study in 288 nursing home residents with dementia, showed that NPS such as agitation and depression were particularly strong predictors of poor QoL [ 9 ]. These results underline the growing awareness that NPS independently decreases QoL in moderate and severe stages of dementia [ 9 ]. Pain is highly prevalent in nursing home residents [ 10 , 11 ] and can also cause NPS and influences their quality of life directly [ 12 ]. Nursing home residents with severe cognitive impairment who have difficulty expressing pain may manifest it through agitation, aggression, or withdrawal [ 10 ]. Pain in dementia may express itself also through vocalizations (e.g., crying, screaming, noisy breathing), specific facial expressions (e.g. grimacing) and body language such as restless behaviour [ 13 , 14 ].
Another factor that may reduce QoL of people with dementia is a deterioration of sleep quality. Sleep disturbances include poor sleep efficiency and increased night awakenings. Petrovsky [ 15 ] used domains of Lawton’s framework for quality of life in persons with dementia to synthesize current knowledge on the association between sleep disruption and quality of life in persons with dementia. Sleep disruption was negatively associated with all of four QoL domains (physical functioning, social/behavioral functioning, emotional well-being and cognitive function). In sum, neuropsychiatric symptoms, in relation to or provoked by pain and sleep disturbances, reduces QoL in people with dementia.
Consequently, the question arises if adequate strategies are available for treating this triad of symptoms, i.e. NPS, pain, and sleep disturbances, and hence, improving QoL, in people with dementia. NPS are often treated pharmacologically with psychotropic drugs, which frequently cause unwanted side effects, such as somnolence and extrapyramidal symptoms [ 16 ]. Psychosocial interventions, however, may obviate the indication for antipsychotic drug prescriptions [ 17 ]. Moreover, therapies such as validation, reminiscence, psychomotor therapy, multisensory stimulation and music therapy can increase QoL of people with dementia and their caregivers [ 18 ]. Sikkes et al. reviewed the evidence and found that various non-pharmacologic treatments such as music therapy effectively improve behavior [ 19 ].
Music therapy is a non-pharmacological intervention which is used as a treatment for NPS in patients with dementia [ 20 , 21 , 22 ]. In the USA, music therapy is defined by the American Music Therapy Association (AMTA) as “the clinical and evidence-based use of music interventions within a therapeutic relationship to accomplish individualized goals by a credentialed professional who has completed an approved music therapy program” [ 23 ]. This definition of music therapy and the accompanying AMTA Standards of Practice recommend an individualized treatment process, including referral, building a therapeutic relationship, assessment, observation, targeting individualized goals and objectives, treatment planning, protocol selection and implementation, termination and evaluation [ 24 ]. The number of studies examining the effects of music therapy for people with dementia has increased over time [ 25 ]. A Cochrane review in 2011 [ 26 ] included 10 studies mostly of poor quality and could not draw firm conclusions about the effects of music therapy in the treatment of behavioral, social, cognitive and emotional problems of older people with dementia. In an update of the Cochrane review [ 27 ] twenty-two studies were included. The results from the review suggest that music therapy may also improve emotional well-being including quality of life. However, outcomes could be based on recall or direct observation, and not all outcomes are assessed blinded. The results of the review further suggest that providing institutionalized people with dementia with at least five sessions of a music-based therapeutic intervention might reduce NPS. Moreover, individual therapy, compared with group therapy, had larger effects on behavioral outcomes (agitation, aggression and overall behavioral problems).
Indeed, music therapy can be offered via individual treatment, as well as through a group approach [ 28 ]. The group approach benefits engagement and social interaction but in advanced stages of dementia, individual music therapy can better reach the residents with communicative limitations. Personalized interventions with music or music therapy may be a predictor of success [ 20 ].
In 2010, we conducted a randomized pilot study on individual music therapy in a nursing home in the Netherlands. The intervention group received individual music therapy from a qualified music therapist who used a person-centered approach. The results pointed to possible reduction of NPS in patients who received individual music therapy compared to patients in the control condition who received usual care [ 29 ]. The sample size of the pilot study was very small and the outcome assessments were not blinded. Sakamoto [ 30 ] conducted an RCT in 2013 with blinded outcome assessment and individual intervention sessions carried out by music facilitators. The study indicated that interactive individualized interventions reduce stress and increase relaxation in individuals with severe dementia immediately after the intervention.
The main purpose of the present study is to build on the earlier pilot study with an improved design, in which we blindly assess the effects of individual music therapy delivered by an accredited music therapist on directly observed well-being and related outcomes such as NPS, agitation, depression, quality of life and pain controlled for individual attention in nursing home residents with dementia who also have NPS.
Trial design
The design involves an individual randomized controlled trial (RCT) employing longitudinal repeated measurements in nursing home residents with dementia and NPS. The study is single blinded. The research assistant who assesses the primary outcome well-being and the secondary outcome pain through observation does not know whether residents participate in the experimental group or the control group. The music therapist and the patients themselves cannot be blinded to the condition they are assigned to. Nursing staff that performs the measurements as part of the secondary outcomes is not blinded either. The research takes place at eight nursing homes facilities of a health care organization in the Netherlands. Music therapy is provided in 30-minutes sessions, twice a week for 12 weeks, in their own room. The control group receives a ‘social’ visit with individual attention with the same frequency and of the same duration.
A process evaluation is performed according to an approach developed by Saunders [ 31 ], using components from Linnan and Steckler’s [ 32 ]. The process evaluation is based on mixed methods, collecting quantitative and qualitative data. Qualitative data collection comprises a focus group discussion with participants of health care professionals to evaluate barriers and facilitators influencing the implementation of research protocol. Quantitative data is gathered with questionnaires about reach, dose delivered, dose received, fidelity, recruitment and participant engagement. Quantitative data is gathered with questionnaires at 1, 2, 6 and 12 weeks after the baseline assessment completed by music therapists (intervention) or attendants (control). The questionnaires include items about participation in the sessions, fidelity, dose, engagement and about levels of implementation. Nurses and a research assistant will fill a questionnaire at the end of treatment to evaluate the process of implementation. Quantitative data will be analyzed with descriptive statistics.
Study setting
The study population consist of a sample of residents with dementia and NPS, residing on psychogeriatric units in one of eight nursing homes facilities of a health care organization (Amstelring) in the Netherlands.
Participants’ eligibility
Inclusion criteria.
First, potentially eligible participants of psychogeriatric units in eight nursing homes are screened for eligibility according to the following criteria:
Candidate has a charted diagnosis of dementia, which is in general according to Diagnostic and Statistical Manual of Mental Disorders IV criteria (American psychiatric association, 2001).
Display a clinically relevant NPS measured with the Neuropsychiatric Inventory Nursing Home Version (NPI-NH) [ 33 , 34 ] with the Frequency X Severity item score for at least one individual item rated 4 (Wood, 2000 [ 35 ]; Margallo, 2001 [ 36 ], Zuidema, 2007 [ 3 ], Zuidema, 2010 [ 37 ].
Exclusion criteria
Candidate having received individual music therapy before or having participated in a music therapy group in the past 3 months.
Candidate has major comorbid psychiatric diagnosis (i.e., schizophrenia, psychosis, anxiety disorder). Due to an overlap between depression and dementia [ 38 ], candidate participants with a history of depression will not be excluded.
Candidate has a hearing impairment that hampers the listening to music at a moderately volume. We use item 1a of the Severe Dual Sensory Loss in old age screening tool (SDSL) [ 39 ]. SDSL was found a valid and reliable tool [ 40 ].
Demographic variables
Demographic variables such as age and gender will be assessed at baseline from the electronical medical chart review.
At baseline, nurses will register whether the resident has any background in music with questions about their experiences with music before entering the nursing home. The relatives of participants are asked closed-ended questions if the participant:
Has no experience with music in the past.
Played an instrument before or was involved in singing activities or made music in some other way.
Has served as a professional musician.
Material and procedure
Intervention.
The participants of the intervention group (music therapy) receive 30 min of individual music therapy twice a week for 12 weeks in their own room. Music therapists use music experiences to promote health [ 41 ]. In this trial, music therapy consists of individual active music therapy sessions with also receptive techniques. Individual music therapy implies a one-to-one contact between the music therapist and the patient using a person-centered approach. Receptive and active music therapy are often combined [ 42 ]. Receptive therapeutic interventions consist of listening to music by the therapist who sings, plays, or selects recorded music for the recipients. In active music therapy, recipients are actively involved in the music-making, for instance by playing on small instruments. The participants may be encouraged to participate in musical improvisation with instruments or voices, movements activities or singing.
To determine the precise content of the intervention and to standardize procedures amongst all music therapists of Amstelring we conducted a focus group with 7 music therapists working at the nursing home facilities of Amstelring. We used a group interview because reaching a consensus is best achieved in a group setting. The focus group established a therapy protocol that comprised six steps for this study purpose:
All participating music therapists are employed by the nursing home organization. The music therapists are qualified and credentialed professionals by the federations for music therapy in the Netherlands (NVvMT), indicating that they have all been trained at an acknowledged and certified music therapy study program.
The music therapist will ask, before the start, the participant or a legal representative about the musical preferences of the participant with a questionnaire (Gerdner, 2010 [ 43 ], Raven-de Vries, 2018 [ 44 ]). Based on this information, the music therapist will develop an individual music therapy session for the participants.
Music therapists start each session trying to connect with the patient by eye contact, calling the name or giving a hand, to build trust.
Music therapists use an observation list between 4 and 6 weeks. This observation list is based on the improvisational music therapy guideline of Kurstjens [ 45 ] and has been used to identify which important musical elements are of help in the approach of the problem.
The music therapists will adapt the therapy continuously to needs and wishes of the participants. Participants receive an individual session tailored to the musical preferences of the participant.
The participant will be invited to make a choice out of different musical instruments such as a guitar, keyboard, drums, maracas, etc. The therapist will aim at using active techniques mainly, for example improvisation where participants will try to play the instruments, sing together, clap the hands, move the body or face with the music. Also, receptive techniques will be used such as listening to live or pre-recorded music. The music therapist provides a safe environment, in which the participant can experience contact, interaction, atonement, structure and a natural finishing of the session.
In case of refusal of the session of adverse reactions such as fatigue or traumatic memory during the sessions, music therapists inform the researcher (VMBC). The music therapists then stop immediately. Music therapists fill in questionnaires at 1, 2, 6 and 12 weeks after the intervention starts to gather information for the process evaluation. During the Covid-19 outbreak, the music therapists (intervention group) use gloves and face masks during the sessions.
Control condition
The control group receives 30 min of individual attention twice a week for 12 weeks with no therapeutic basis. Individual attention will take place through a social visit, during which an attendant will drink coffee or tea with the participant. The individual attention will be given in the resident’s room by one attendant, who will have a conversation with the participant, drink coffee without an intervention goal such as cognitive training and without any musical intervention. The person who is doing the social visits is an informal care support company employee or volunteer. The attendants are students who work for an informal care support company and had a workshop about dementia. This is on top of the regular usual care delivered. The attendant starts every session by trying to connect with the patient via eye contact, calling his/her name or giving a hand, to build trust.
The attendants from the informal care support company or care support volunteer who provide the individual attention report attended sessions in the participants forms. In case of refusal of the session, the attendants inform the researcher (VMBC). The individual attention will then stop immediately. Attendants fill in questionnaires at 1, 2, 6 and 12 weeks after the individual attention starts to gather information for the process evaluation. During the Covid-19 outbreak, the attendants (control group) use gloves and face masks through the sessions.
Primary outcome measure
Observed well-being is the primary outcome measure rather than multidimensional quality of life with proxy estimation of domain ratings based on recall. Lawton has most extensively explored the concept of QoL concerning dementia and described QoL in dementia in terms of four sectors: psychological well-being, behavioral competence, objective environment (response to surroundings) and perceived QoL [ 46 , 47 , 48 ]. Jonker et al. reviewed conceptual developments in QoL research concerning dementia and based on the dimensions presented by Lawton, they identified psychological well-being as the core dimension of QoL of patients with dementia. Patients with severe dementia cannot always self-report their psychological well-being [ 49 ] but indicators of wellbeing of persons with dementia can be observed with validated instruments. We assess well-being with an objective observational instrument−the Discomfort Scale - Dementia of Alzheimer Type (DS-DAT) where discomfort is defined as a negative emotional and/or physical state subject to variation in magnitude in response to internal or environmental conditions. It is a scale for direct observation of behavior of a patient and is applicable also in later phases of dementia [ 50 ]. The Dutch translation is characterized by a good reliability (Hoogendoorn. 2001) [ 51 ] and validity (van der Steen, 2002) [ 52 , 53 ]. The scale consists of 9 items measuring 7 negative and 2 positive items regarding vocalization, breathing, facial expression, and body movements. The nine 4-point items are summed for a total score ranging from 0 (no observed discomfort) to 27 (highest possible level of observed discomfort). Well-being will be assessed by a blinded research assistant at baseline (T0), six weeks (T1) and twelve weeks (T2). Well-being is assessed during 5 min before and after the music therapy sessions or individual attention sessions. The research assistant will be trained in using the DS-DAT trough an instructional video and practice completion of the DS-DAT with videotaped patients. Feedback is provided against the scores of the scale’s developer (Dr Hurley) who had rated the patient video clips.
Secondary outcomes measures
Secondary outcomes are also assessed in all /participating residents and include pain, quality of life, neuropsychiatric symptoms (agitation, anxiety, symptoms of depression), quality of sleep and psychotropic drug use.
Pain will be assessed by a blinded research assistant at baseline, six weeks and twelve weeks during 2 min before and after the intervention session or individual attention with the PAIC-15 (Pain Assessment in Impaired Cognition) [ 54 , 55 ] which is an observational assessment instrument that lists 15 items and uses scores from 0 to 3 for each item. PAIC-15 comprises three domains: facial expression, body movements and verbalizations/vocalizations. Each domain has 5 items and the total score is the sum of all items, ranging from 0 to 45. The research assistant will be trained in using the PAIC-15.
Quality of life will be rated by non-blinded nurses at baseline (T0), at six weeks (T1) and at twelve weeks (T2) with the Quality of Life in Late-Stage Dementia Scale (QUALID) [ 56 ] that can be used with late-stage dementia patients in institutional settings and has been designed for proxy-rating by nurses. Responses reflect patient behavior over the past seven days. The QUALID consists of eleven items that are short and simple and is characterized by a good reliability and validity and the Dutch translation was a valid measure for quality of life in patients with advanced dementia [ 57 ]. The total score is the sum of all items, ranging from 11 to 55. Lower scores indicate a higher quality of life.
Neuropsychiatric symptoms (NPS) will be assessed by non-blinded nurses at baseline (T0), at six weeks (T1) and at twelve weeks (T2) with the Neuropsychiatric Inventory Nursing Home Version (NPI-NH), a scale originally developed by Cummings [ 33 , 34 ] to assess NPS in outpatients with dementia. The nursing home version was developed for use of professional caregivers in institutions and proved to be valid and reliable for trained nursing staff [ 58 , 59 ]. The NPI-NH is the only nursing home instrument to assess NPS that occurred in the past four weeks that has been translated into Dutch [ 60 ]. The NPI is a structured interview that includes 12 neuropsychiatric symptoms: delusions, hallucinations, agitation, depression, anxiety, euphoria, apathy, disinhibition, irritability, aberrant motor behavior, night-time disturbances and appetite/eating change. Frequency (F) and severity (S) of each symptom are rated on a four (1–4) and three (1–3) point scale respectively. A separate score can be calculated for each symptom by multiplying the frequency and severity (FxS score), resulting values range from zero to 12 for each symptom. Summing all FxS scores results in a total score that ranges from 0 to 144. Interview also includes a caregiver distress questions using a 5-point scale.
Agitation and aggression will be assessed by non-blinded nurses at baseline (T0), 6 weeks (T1) and 12 weeks (T2) using the caregiver rated questionnaire Cohen-Mansfield Agitation Inventory (CMAI). This instrument, developed by Cohen-Mansfield and Billig [ 61 ] and validated by Miller [ 62 ] is an instrument that specifically addresses agitation or aggression that has been translated into Dutch. The Dutch translation of the CMAI (CMAI-D) has been validated by De Jonghe [ 63 ] and rated agitated behaviors occurred during last two weeks. The frequency of each symptom is rated on a seven-point scale (1–7) ranging from ‘never’ to ‘several times an hour’. Summing all symptom scores results in a total score that ranges from 29 to 203.
Depression will be rated by non-blinded nurses at baseline (T0), at six weeks (T1) and twelve weeks (T2) with the Cornell Scale for Depression in Dementia (CSDD) [ 64 ], which has good internal consistency [ 65 ]. Responses reflect symptoms of depression in the week before. The CSDD is a 19-item instrument, with scores for each item ranging from 0 to 2 (total score range 0–38). The CSDD has been translated into Dutch [ 66 ].
Physical activity : rest-activity data will be collected by a MotionWatch (CamNtech Ltd, Cambridge, UK). The MotionWatch measures the arm movements of the participant; based on these movements, the rest-activity and physical activity are determined. It quantifies accelerations due to motor activity of the arm and integrates these over I-minute periods. The MotionWatch has the size and shape of a watch, is worn on the dominant wrist. The participants will be asked to wear the MotionWatch twenty-four hours a day for 1 week in the week before the intervention starts (T0) and the week directly after the last intervention session (T2). Nurses are asked to temporarily take off the MotionWatch when the participant takes a shower, performs another activity in which the MotionWatch could be exposed to too much water. Nurses will report the time that devices are taken off. Five parameters are calculated: Interdaily Stability (IS), Intradaily Variability (IV), Relative Amplitude (RA), most active period of 10 h and least active period of five hours. First, the IS variable that quantifies the strength of coupling between the rest-activity rhythm and supposedly stable Zeitgebers (e.g., meals) is calculated. IV, which quantifies the fragmentation of the rhythm, that is, the frequency and extent of transitions between rest and activity. RA quantifies the difference between the main activity (day) and rest (night) periods. The parameter of 10 most active hours (M10) is used to determine the amount of physical activity. The parameter (L5) are least active periods of five hours to determine rest activity.
Data on chronic psychotropic drug use will be derived from the electronic medical chart. Psychotropic drugs will be categorized into antipsychotics, anxiolytics, hypnotics, antidepressants and anti-dementia drugs according to the Anatomical Therapeutic Classification (ATC) system.
Any attrition or adverse effects of the interventions will be documented. The interventions will be discontinued if, in consultation with the physician or psychologists, harmful effects are observed and are expected to continue with exposure to any of the two interventions.
The nurses will determine the stage of dementia, measured with the Global Deterioration Scale (GDS) [ 67 , 68 ] at baseline. The DS describes seven stages: ‘no global impairment’ (1), ‘very mild cognitive decline’ (2), ‘mild cognitive decline’ (3), ‘moderate cognitive decline’ (4), ‘moderately severe’ (5), ‘severe’ (6) and ‘very severe global impairment’ (7).
Participants timeline
All eligible residents for whom consent have been provided will be randomly allocated to the intervention group (individual music therapy) or control group (individual attention). Randomization will take place with a statistician using randomization software. The outcomes variables are measured at baseline (T0) one week before individual attention of music therapy starts (pre-treatment), after 6 weeks of intervention (T1) and after 12 weeks of intervention (T2). Figure 1 shows the participant’s flow.
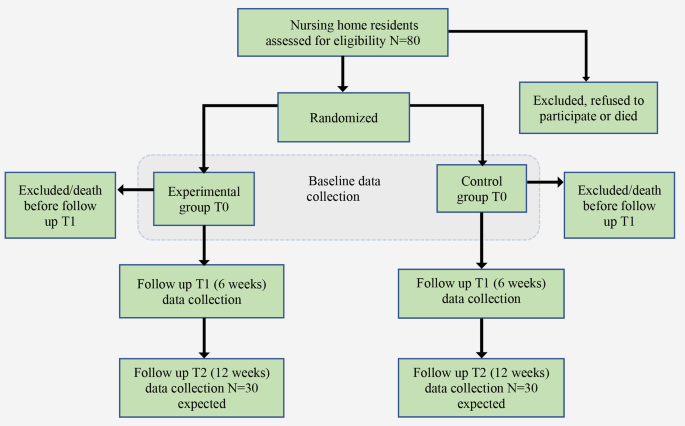
Participant flow: T0 baseline data collection, T1 follow up assessment at 6 weeks and T2 the follow up after 12 weeks. Participants who are lost to follow-up at the T2 assessment can still be included in the analyses, due to the use of mixed models analyses
Measurements (DS-DAT and PAIC-15) will be done at baseline T0, just shortly before (T1a and T2a) and shortly after the intervention (T1b and T2b); to assess overall effects, cumulative and immediate effects ( see Table 1 ). An independent research assistant performs the blinded direct observations and complies the primary outcome well-being (measured with the DS-DAT) and secondary outcome pain (measured with the PAIC-15). The nursing staff will complete the unblinding observations scales concerning the various stages of dementia at baseline T0 and they will fill in the unblinding questionnaires about QoL, NPS, agitation and symptoms of depression at T1b and T2b.
Data prescription records concerning medication use, among which psychotropic drugs, will be extracted from the electronic medical charts by VMBC, physician employed by the participating organization.
Sample size
The sample size calculation is based on the study’s primary outcome measure, the Discomfort Scale – Dementia of Alzheimer type (DS-DAT) [ 51 ] for F-tests ANOVA repeated measures. To determine the sample size required to assess relevant effects, we used data from the Cochrane review on music-based therapeutic interventions [ 27 ]; the effect size for emotional well-being and quality of life (SMD 0.32, 95%CI 0.02 to 0.62). The correlation between multiple assessments of the DS-DAT was calculated with the data of Schalkwijk et al. [ 57 ] as 0.6. Using a type I error of 0.05, a power of 0.80, two follow-up measurements and 2 groups, a sample size of 30 in each group is required, totaling 60 participants to achieve 0.81 power. According to the availability of music therapists we estimated that the study would take approximately 3 years. The mortality rate in the nursing home setting is high. Moore [ 58 ] stated that the length of stay in long-term care facilities in Europe countries is almost 2 years. It is estimated that about a one third (20 of 60 residents) may die or will be lost to follow up for other reasons during the study period, so we need to enroll a total of around 70 till 80 residents for this study.
Recruitment
First, the medical staff is informed about the goal and procedure of the study. Second, the medical staff (physicians) of each psychogeriatric unit of the eight nursing homes selects eligible residents with dementia and NPS who have a referral for individual music therapy. Third the researcher provides an information letter with informed consent form to competent residents and to legal representatives of non-competent residents. After informed consent or proxy informed consent has been given and the participant has been recruited, the participants are randomly allocated to the intervention group (individual music therapy) or control group (individual attention).
Assignment of interventions
Participants will be randomly assigned to either the control or the experimental group with a 1:1 allocation as per a computer-generated randomisation schedule. Randomization is performed by a statistician who is not involved in carrying out the study in the facilities, using randomization software.
The study is single blinded, i.e. that the therapist and the patients themselves are not blinded. Trained research assistants who are blinded to intervention assignment, conduct the well-being (primary outcome) and pain (secondary outcome) measurements. The nursing staff completes the scales concerning the stage of dementia, QoL, NPS, agitation and symptoms of depression. Blinding to these measurements is not possible because these measurements require familiarity with the person’s usual behavior in the previous week(s). The nursing staff who complete the questionnaires are not blinded to intervention assignment, but they are not informed about the hypothesis and specific research questions.
Data analysis
Immediate effects are defined as the difference in change between outcomes 15 min before and after the intervention sessions. Cumulative effects are effects over time not including those immediately after the session (i.e., built-up effect over time and measured before the session in order not to include possible immediate effects of the session). Overall effects are effects over time including those immediately after the session. Immediate, cumulative and overall effects are analyzed with mixed model analysis to consider the dependency of the repeated observations within the patient.
For the immediate effects, the outcome will be the post-test (T1b, T2b) and adjustment will be made for the pre-test (T1a, T2a). For the cumulative effect, the outcome will be the pre-test and an adjustment will be made for the baseline. For overall effects, the outcome will be post-test and adjustment will be made for the baseline.
For all treatment effects, effects at the different time-points will be analyzed by adding a time x treatment interaction to the mixed model analysis. Furthermore, both crude and adjusted (adjustments for gender, age, cognitive deterioration and for medication use, which will be added as a time-dependent covariate) will be performed. In the mixed-model analysis, we will also evaluate whether an adjustment for the correlated observations within facilities is necessary. There is no need to impute missing data because mixed models can handle missing assessments.
In explorative post-hoc analysis we will evaluate whether the intervention effects will be different for patients with a musical background by adding the interaction between the intervention variable and presence of musical background.
Sleep quality data of the MotionWatch (CamNtech Ltd, Cambridge, UK) will be analyzed with Motionware software version 1.2.1. Five parameters will be calculated: Interdaily stability, Intradaily variability, Relative Amplitude, most active period of 10 h and least active period of five hours. The 5 parameters will be analyzed with linear regression analyses with the values measured after the intervention period as outcome with an adjustment for the baseline vale of particular outcome.
Study monitoring
This clinical trial does not involve a high-risk intervention. We do not expect adverse events or significant unintended effects of the intervention. However, the participants of this study are vulnerable subjects and monitoring, and quality assurance will be necessary according to national legislation (WMO). The Department of anesthesiology (an independent department of UMCG) will be responsible for the data monitoring.
Over recent decades, the care offered in nursing homes has expanded to include various types of psychosocial interventions such as music therapy, validation, gentle care, psychomotor therapy and movement activation [ 69 ]. Music therapy is a non-pharmacological intervention which is also used as a treatment for NPS in patients with dementia and can improve quality of life [ 70 ].
Quality of life (QoL) is a multi-dimensional concept that includes well-being and has objective and subjective effects [ 49 , 50 , 51 ]. Psychological well-being is considered to be the central indicator for QoL of patients with dementia [ 52 ]. This study aims to show if individual music therapy leads to improved well-being of nursing home residents with dementia and NPS. NPS result in a lower QoL for people with dementia and their caregivers and affect the quality of the relationship with the caregivers [ 71 ]. Efforts aiming at preventing low or decreasing well-being and QoL at any stage of dementia should, therefore, target the factors associated with lower QoL such as psychotropic drug use [ 17 ], NPS [ 9 ], pain [ 10 ] and sleep disturbances [ 15 ] as well as keeping a person-centered approach open to the individual perceptions of QoL [ 71 ]. Music-based interventions can be effective in alleviating the NPS of dementia, such as agitation, depression, and anxiety [ 72 , 73 , 74 ]. Recently, a systematic review concluded that non-pharmacological interventions such as music therapy show a positive impact on pain [ 75 ]. Further, a recent review of 8 studies identified 6 studies showing a positive effect of music interventions on sleep outcomes. There were decreases in nighttime sleep disturbance, increases in daytime alertness, and improvements in sleep quality [ 76 ].
Further, in patients unable to self-report, directly observed well-being is an expression of their emotional and physical state an important indicator of comfort and quality of life, in addition to impressions of quality of life assessed over a specific time window such as the previous week. Quality of life is an important outcome of different care approaches, including palliative care. Improving quality of life and maximizing comfort are goals of palliative care in dementia [ 77 ]. With this design and specific analyses, we can ensure blinding and allow estimation of short and long-term effects.
Participants receive either individual music therapy or a social visit for individual attention, in their own room. This is because the room represents a safe place for the resident. Moving residents to another room may lead unnecessary to more restless behavior during the already short duration of the therapy session.
Research often lacks methodological rigor and continues to produce mixed results. A recent Cochrane review [ 27 ] included 22 studies with 1097 randomized participants to assess the effects of music-based therapeutic interventions for people with dementia. This review showed modest positive effects in meta-analyses of 9 studies on emotional well-being and quality of life of interventions that included group and individual interventions. Only seven studies out of the 22 studies received individual music therapy treatment. Sensitivity analyses indicated that the SMDs for individual therapy were similar to those for the main analyses with individual and group therapy, except for behavioral problems (both agitation or aggression and overall), for which SMDs for individual therapy were clearly larger. In this Cochrane review, many studies did not used blinded outcome assessment. We use blinded assessment for the primary outcome (well-being) and one of the secondary outcome (pain) but possible limitations of this study will be the unblinded assessment of secondary outcomes (with the QUALID, NPI-NH, CMAI, CSDD) assessed by nurses of the department.
During the Covid-19 outbreak, the music therapists (intervention group) and the attendants (control group) used gloves and mouth masks through the sessions that may complicate the relation between participants and music therapists or attendants. Residents who participate in the study during Covid-19 period might receive substandard quality sessions because of the difficulties in the verbal and non-verbal contact. Sensitivity analysis will be done to examine whether this period with wearing of face masks and gloves yields a negative effect on treatment outcome, compared to the period before (or after) the outbreak of COVID-19.
The present study aims to make a next step in the field of music therapy and address the limitations of earlier research by including a larger number of participants and investigating if individual music therapy influences well-being of people with dementia and on NPS and other outcomes. Major strengths of the current study design are, first, the blinded primary outcome assessments and second, the comparison between intervention group with the control group receiving enhanced usual care to rule out effects of extra individual attention. The residents of the intervention group receive individual music therapy from qualified and certified music therapists with knowledge and skills that are clinically relevant to personalized care delivery. This study will help to clarify the effects of individual music therapy in dementia care.
Data availability
The handling of personal data is conducted according to the EU General Data Protection Regulation and the Dutch Act of Implementation of the General Data Protection Regulation (in Dutch: AVG, UAVG).
Abbreviations
- Neuropsychiatric symptoms
- Music therapy
American Music Therapy Association
Dutch association of music therapists:DS-DAT:Discomfort Scale - Dementia of Alzheimer Type
Pain Assessment in Impaired Cognition
Quality of Life in Late-Stage Dementia Scale
Neuropsychiatric Inventory Nursing Home Version
Cohen-Mansfield Agitation Inventory
Cornell Scale for Depression in Dementia
Global Deterioration scale
Medical research involving human subjects act
World Health Organization Dementia. https://www.who.int/news-room/fact-sheets/detail/dementia (accessed 04 October 2021).
Kester M, Scheltens P. Dementia. Practical neurology v9 n4 2009; 9:241–51.
Zuidema SU, Verhey FRJ, Derksen E, Koopmans RTCM. Prevalence of neuropsychiatric symptoms in a large sample of Dutch nursing home patients with dementia. Int J Geriatr Psychiatry. 2007;22:632–8.
Article PubMed Google Scholar
WHOQOL. Measuring Quality of Life. World Health Organization: https://www.who.int/publications/i/item/WHO-HIS-HSI-Rev .2012.03 (accessed 2 November 2022).
Dodge R, Daly A, Huyton J, Sanders L. The challenge of defining wellbeing. Int J Wellbeing. 2012;2(3):222–35.
Article Google Scholar
Clark C, Woods B, Moniz-Cook E, Mountain G, Øksnebjerg, Chattat R, Diaz A, Gove D, Vernooij-Dassen M, Wolverson E. Measuring the well-being of people with dementia: a conceptual scoping review. BMC. 2020;18:249.
Google Scholar
Naglie G. Quality of life in dementia. Can J Neurol Sci. 2007;34(Suppl):S57–61.
Ettema TP, Droes R-M, de Lange J, Mellenbergh GJ, Ribbe. M. W: A review of quality-of-life instruments used in dementia. Qual Life Res. 2005; 14, 67 5–686.
Wetzels RB, Zuidema SU, Jonghe JFM, Verhey FRJ, Koopmans RTC. Determinants of quality of life in Nursing Home residents with dementia. Dement Geriatr Cogn Disord. 2010;29:189–97.
Article CAS PubMed Google Scholar
Boerlage AA, van Dijk M, Stronks DL, de Wit R, van der Rijt CC. Pain prevalence and characteristics in three Dutch residential homes. Eur J pain. 2008;12(7):910–6.
Achterberg WP, Gambassi G, Finne-Soveri H, Liperoti R, Noro A, Frijters DH, Cherubini A, Dell’ Aquila G, Ribbe MW. Pain in European long-term care facilities: cross-national study in Finland, Italy and the Netherlands. Pain. 2010;148:70–4.
American Geriatrics Society Panel on Chronic Pain in Older Persons. The management of chronic pain in older persons. J Am Geriatric Soc. 1998;46:635–51.
Cipher DJ, Clifford PA. Dementia, pain, depression, behavioural disturbances and ADLs: toward a comprehensive conceptualization of quality of life in long-term care. Int J Geriatr Psychiatry. 2004;19:741–8.
Pieper MJ, van Dalen-Kok AH, Francke AL, van der Steen JT, Scherder EJ, Husebø BS, Achterberg WP. Interventions targeting pain or behaviour in dementia: a systematic review. Ageing Res Rev. 2013;12(4):1042–55. https://doi.org/10.1016/j.arr.2013.05.002 .
Petrovsky DV, McPhillips MV, Li J, Caffee L, Hodgson NA. Sleep disruption and quality of life in persons with dementia: a state-of-the-art review. Geriatr nurs (New York). 2018;11(6):640–5.
van Iersel MB, Zuidema SU, Koopmans RT, Verhey FR, Olde Rikkert MG. Antipsychotics for behavioural and psychological problems in elderly people with dementia: a systematic review of adverse events. Drugs Aging. 2005;22(10):845–58.
Birkenhager-Gilesse EG, Kollen Bj, Achterberg WP, Boersma F, Jongman L, Zuidema SU. Effects of Psychosocial interventions for behavioral and psychological symptoms in dementia on the prescription of psychotropic drugs: a systematic review and Meta analyses. J Am Med Dir Assoc. 2018;19(3):276.
Olazaran J, Reisberg B, Clare L, Cruz I, Pena-Casanova J, Del ST, Woods B, Beck C, Auer S, Lai C, Spector A, Fazio S, Bond J, Kivipelto M, Brodaty H, Rojo JM, Collins H, Teri L, Mittelman M, Orrel M, Feldman HH, Muniz R. Nonpharmacological therapies in Alzheimer’s disease: a systematic review of efficacy. Dement Geriatr Cogn Disord. 2010;30:161–78.
Sikkes AMS, Tang Y, Jutten RJ, Wesselman LMP, Turkstra LS, Brodaty H, Clare L, Cassidy-Eagle E, Cox KL, Chételat G, Dautricourt S, Dhana K, Dodge H, Dröes RM, Hampstead BM, Holland T, Lampit A, Laver K, Lutz A, Lautenschlager NT, McCurry SM, Meiland FJM, Moris MC, Mueller KD, Peters R, Ridel G, Spector A, van der Steen JT, Tamplin J, Thompson Z, Bahar-Fuchs A. Toward a theory-based specification of non-pharmacological treatments in aging and dementia: focused reviews and methodological recommendations. J Alzheimer’s Association2021 02; 17(2): 255–70.
Raglio A, Bellelli G, Mazzola P, Bellandi D, Giovagnoli AR, Farina E, et al. Music, music therapy and dementia: a review of literature and the recommendations of the Italian Psychogeriatric Association. Maturitas. 2012;72(4):305–10.
Hsu MH, Flowerdew R, Parker M. Jörg Fachner and Helen Odell-Miller. Individual music therapy for managing neuropsychiatric symptoms for people with dementia and their carers: a cluster randomised controleed feasibility study. BMC Geriatr. 2015;15:84.
Article PubMed PubMed Central Google Scholar
Ueda T, Suzukamo Y, Sato M, Izumi S. Effects of music therapy on behavioral and psychological symptoms of dementia: a systematic reviwu and meta-analysis. Ageing Res Reviwua. 2013;12:628–41.
American Music Therapy Association. Definition of Music Therapy. 2018. Available online: https://www.musictherapy.org/about/quotes/ Accessed on 11 September 2018.
Hanser SB. The New Music Therapist’s Handboek. 3rd ed. Boston, UK: Berklee; 2018.
Gold C, Eickholt J, Assmus J, Stige B, Wake JD, Baker FA, Tamplin J, Clark I, Lee YC, Jacobsen SL, Ridder HMO, Kretz G, Muthesius D, Wosch T, Ceccato E, Raglio A, Ruggeri M, Vink A, Zuidema S, Odell-Miller H, Orrell M, Scheneider J, Kubiak C, Romeo R, Geretsegger M. Music Interventions for Dementia and Depression in Elderly care (MIDDEL): protocol and statistical analysis plan for a multinational cluster-randomised trial. BMJ open 2019 03 30;9(3): e023436.
Vink AC, Bruinsma MS, Scholten RJPM. Music therapy for people with dementia Cochrane database. Syst Rev. 2004;(3).CD003477.
Van der Steen JT, Smaling HJA, van der Wouden JC, Bruinsma MS, Scholten R, Vink AC. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. 2018;7:CD003477.
PubMed Google Scholar
Hanser SB. Integrative Health through Music Therapy: accompanying the Journey from Illness to Wellness. London, UK: Palgrave Macmillan; 2016.
Book Google Scholar
Baroni Caramel V, Broersen M. Music therapy in dementia. Pilot about effect at neuropsychiatric symptoms Muziektherapie Bij dementia. Pilot naar het effect op neuropsychiatrische symptomen. [in Dutch] Tijdschrift voor Ouderengeneeskunde 2014,1:9–13.
Sakamoto M, Ando H, Tsutou A. Comparing the effects of different individualized music interventions for elderly individuals with severe dementia. Int Psychogeriatr. 2013;25(5):775–84.
Saunders RP, Evans MH, Joshi P. Developing a process-evaluation plan for assessing health promotion program implementation: a how-to guide. Health Promot Pract. 2005;6:134–47.
Linnan L, Steckler A. Process Evaluation for Public Health Interventions and Research: an overview. Jossey-Bass: San Francisco; 2002.
Cummings JL, Mega M, Gray K, et al. The neuropsychiatric inventory:comprehensive assessment of psychopathology in dementia. Neurology. 1994;44:2308–14.
Cummings JL. The neuropsychiatric inventory: assessing psychopathology in dementia patients. Neurology. 1997;48(suppl 6):S10–16.
CAS PubMed Google Scholar
Wood S, Cummings JL, Hsu MA, et al. The use of the neuropsychiatric inventory in nursing home residents. Characterization and measurement. Am J Geriatr Psychiatry. 2000;8:75–83.
Margallo M, Swann A, O’Brien J, Fairbairn A, Reichelt K, Potkins D, Mynt P, Ballard C. Prevalence of the pharmacological and psychological symptoms amongst dementia suffers Iiving in care environments. Int J Geriatric Psychiatry. 2001;16:39–44.
Zuidema SU, de Jonghe JFM, Verhey FRJ, Koopmans RTC. Environmental correlates of neuropsychiatric symptoms in nursing home patients with dementia. Int J Geriatr Psychiatry. 2010;25:14–22.
Leyhe T. July: Classification and overlap of depression and dementia. Alzheimer ‘s & Dementia v; 13 n7S_Part_28 (2017): P1346.
Lyng K, Svingen E. Kartlegging av alvorlig, kombinerte sasetap hos eldre. Evaluering av en sjekklisterbasert screeingingmetodikk. Rapport 9/01. NOVA, Oslo, pp6.
Roets-Merken LM, Zuidema ZU, Vernooij-Dassen MJFJ, Kempen GIJM. Screening for hearing, visual and dual sensory impairment in older adults using behavioural cues: a validation study. Int J Nurs Stud v51 nl 1 (2014): 1434–40.
Bruscia KE. Defining music therapy. 2nd ed. Gilsum, NH: Barcelona; 1998.
Guetin S, Charras K, Berard A, Arbus C, Berthelon P, Blanc F, Blayac JP, Bonte F, Bouceffa JP, Clement S, Ducourneau G, Gzill F, Laeng N, Lecourt E, Ledoux S, Plate) H, Thomas-Anterion C, Touchon J, Vrait FX, leger JM. An overview of the use of music therapy in the context of Alzheimer’s disease: a report of a French expert group. Dementia. 2013;12(5):619–34.
Gerdner LA, Schoenfelder DP. Individualized music for elders with dementia. J Gerontol nurs. 2010;36(6):7–15.
Raven-De Vries A, Verkerk M, Akse M, Denkbeeld. 2018, v30 n2 (201804):25–6.
Kurstjens H. Observatieleidraad muzikale vormgeving, 2009.
Lawton MP. Environment and other determinants of well-being in older people. Gerontologist. 1983;4:349–57.
Lawton MP. A multidimensional view of quality of life in frail elders; in Birren JE. In: Lubben JE, Rowe JC, Deutchman DE, editors. Quality of life in the frail Elderly. San Diego: Academic; 1991. pp. 3–27.
Lawton MP. Quality of life in Alzheimer disease. Alzheimer Dis Assoc Disord. 1994;8(suppl 3):138–50.
Jonker C, Gerritsen DL, Bosboom PR, van der Steen JT. A model for quality-of-life measures in patients with dementia: Lawton’s next step. Dement Geriatr Cogn Disord. 2004;18:159–64.
Hurley AC, Volicer BJ, Hanrahan PA, et al. Assessment of discomfort in advanced Alzheimer patients. Res Nurs Health. 1992;15:369–77.
Hoogendoorn LI, Kamp Svd, Ader SMCA, Ooms HJ, van der Steen ME. De Rol Van De Observator in De Betrouwbaarheid Van De Nederlandse Versie Van De Discomfort Scale- Dementia of Alzheimer Type (OS-DAT). Tijdschr Gerontol Geriatr. 2001;32:117–21.
Van der Steen JT, Ooms ME, van der Wal G, Ribe MW. Het meten van (on)welbevinden bij demente patienten. Tidschr Gerontol Geriatr. 2002;33(6):257–63.
Van der Steen JT, Ooms ME, van der Wal G, Ribbe MW. Het meten van (on)welbevinden bij dementia patienten - validiteit Van De Nederlandse Versie Van De Discomfort Scale- Dementia of Alzheimer Type (OS-DAT). Tijdschr Gerontol Geriatr. 2002;33:248–54.
Corbett A, Achterberg W, Husebo B, Lobbezoo F, de Vet H, Kunz M, Strand L, Constantinou M, Tudose C, Kappesser J, de Waal M, Lautenbacher S. An international road map to improve pain assessment in people with impaired cognition: the development of the Pain Assessment in Impaired Cognition (PAIC) meta-tool. BMC Neurol; EU-COST action td I 005 Pain Assessment in Patients with Impaired Cognition, especially Dementia Collaborators: http://www.cost-tdl005.net/ . 2014; 14:229.
Van Dalen-Kok AH, Achterberg WP, Rijkmans WE, Tukker-van Vuuren SA, Delwel S, de Vet HC, Lobbezoo F, de Waal MW. Pain Assessment in impaired cognition (PAIC): content validity of the Dutch version of a new and universal tool to measure pain in dementia. Clin Interv Aging. 2017;13:25–34.
Weiner MF, Martin-Cook K, Svetlik DA, Saine K, Foster B, Fontaone CS. The quality of life in late-stage dementia (QUALID) scale. J Am Med Dir Assoc. 2000;1(3):114116.
Schalkwijk D, Verlare LR, Muller MT, Knol DL, van der Steen JT. Het meten van kwaliteit van leven bij ernstig demente verpleeghuisbewoners: psychometrisch eigenschappen Van De Qualid-Schaal. Tijdschr Gerontol Geriatr. 2009;40(5):184–92.
Moore DC, Payne S, Keegan T, Block L, Deliens L, Gambassi G, Heikkila R, Kijowska V, Pasman HR, Pivodic L, Froggatt K. Length of stay in long-term care facilities: a comparison of residents in six European countries. Results of the PACE cross-sectional study. BMJ Open. 2020;10:e033881. https://doi.org/10.1136/bmjopen-2019-033881 .
Lange RT, Hopp GA, Kang N. Psychometric properties and factor structure of the neuropsychiatric inventory nursing home version in an elderly neuropsychiatric population. Int J Geriatr Psychiatry. 2004;19:440–8.
Kat MG, de Jonghe JFM, Aalten P, et al. Neuropsychiatric symptoms of dementia: psychometric aspects of the neuropsychiatric inventory (NPI) Dutch version. Tijdschr Gerontolol Geriatr. 2002;33:150–5.
CAS Google Scholar
Cohen-Mansfield J, Billig N. Agitated behaviour in the elderly 1. Conceptual review. J Am Geriatr Soc. 1986;34:711–21.
Miller RJ, Snowdon J, Vaughan R. The use of the Cohen-Mansfield Agitation Inventory in the assessment of behavioural disorders in nursing homes. J Am Geriatr Soc. 1995;43:546–9.
De Jonghe JFM. Factor structure and validity of the Dutch version of the Cohen Mansfield Agitation Inventory (CMAI-D). J Am Geriatr Soc. 1996;44:888–9.
Alexopoulos GS, Abrams RC, Young RC, et al. Cornell Scale for Depression in Dementia. Biol Psychiatry. 1988;23:271–84.
Muller-Thomsen T, Arlt S, Mann U, Mass R, Ganzer S. Detecting depression in Alzheimer’s disease: evaluation of four different scales. Arch Clin Neuropsychol. 2005;20(2):27 l-6.
Droes RM. Cornell Scale for Depression in Dementia. Nederlandse vertaling. Interne publication. Amsterdam: vakgroep Psychiatrie, Vrije Universiteit; 1993.
Reisberg B, Ferris SH, de Leon MJ, Crook T. The global deterioration scale foe assessment of primary degenerative dementia. Am J Psychiatrie. 1982;139:I1361139.
Reisberg B, Ferris SH, Franssen E. An ordinal functional assessment tool for Alzheimer’s-type dementia. Hosp Community Psychiatry. 1985;36:593–5.
Dröes RM, Boelens-van der Knoop E, Bos J, Meihuizen L, Ettema T, Gerritsen D, Hoogeveen F, De Lange J, Schölzel-Dorenbos C. Quality of life in dementia in perspective. An explorative study of variations in opinions among people with dementia and their professional caregivers, and in literature. 2006, Dementia, 5, 4: pp. 533–58.
Vasionnytė I, Madison G. May: Musical interventions for patients with dementia: a meta-analysis. Journal of clinical nursing v22 n9-10 (2013): 1203–16.
Shin IS, Masterman D, Fairbanks L, Cummings JL. Neuropsychiatric symptoms and quality of life in Alzheimer disease. Am J Geriatric Psychiatry. 2005;13(6):469–74.
Ydstebø AE, Bergh S, Selbæk G, Šaltyte Benth J, Brønnick K, Vossius C, Haapala I, Biggs S, Kurrle S. Longitudinal changes in quality of life among elderly people with and without dementia. Int Psychogeriatr. 2018;30(11):1607–18.
Guetin S, Portet F, Picot M, Pommié C, Messoudi M, Djabelkir L, Olsen AL, Cano MM, Lecourt E, Touchon J. Effect of music therapy on anxiety and depression in patients with Alzheimer’s type dementia: Randomized, controlled study. Dementia and geriatric cognitive disorders, v28 n1 (2009): 36–46.
Raglio A, Bellelli G, Traficante D, Gianotti M, Ubezio MC, Villani D, Trabucchi M. Efficacy of music therapy in treatment of behavioral and psychiatric symptoms of dementia. Alzheimer Disease and Associated disorders v22 n2 (2008):158–62.
Liao YJ, Parajuli J, Jao YL, Kitko L, Berish D. Non-pharmacological interventions for pain in people with dementia: a systemic review. Int J Nurs Stud (2021), v124, 104082.
Mu CX, Lee S, Boddupalli S, Meng H. Effects of music interventions on sleep in people with dementia: a systematic review. Dementia. 2022;v21(n6):2053–71.
van der Steen JT, Radbruch L, Hertogh CMPM, de Boer ME, Hughes JC, Larkin P, Francke AL, Jünger S, Gove D, Firth G, Koopmans RTCM, Volicer L. White paper defining optimal palliative care in older people with dementia: a Delphi study and recommendations from the European Association for Palliative Care. Palliat Med. 201403;v28(n3):197–209.
Download references
Acknowledgements
The authors want to acknowledge the nursing home residents who voluntarily participated in this study. We thank all the music therapists and nurses of Amstelring who contributed to this study. We thank the research assistant Marianne Pruis who did all the blinded observations.
Amstelring Care Institution (RVB U-9109-2019 IB/RR/lw) support this study. This study has also Alzheimer Nederland as subsiding party (Project number: WE.09-2018-06). The funders had no role in the study design, data collection and analysis of data.
Author information
Authors and affiliations.
Department of primary and long-term care, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands
Vanusa M. Baroni Caramel, Sarah I. M. Janus & Sytse U. Zuidema
Faculty of Behavioral and Movement Sciences, Clinical Neuropsychology, Amsterdam, The Netherlands
Vanusa M. Baroni Caramel & Erik J. A. Scherder
Department of Public Health and Primary Care, Leiden University Medical Center, Leiden, The Netherlands
Jenny T. van der Steen
Department of Primary and Community Care, Radboud university medical center, Nijmegen, The Netherlands
Department of Music Therapy, ArtEZ University of The Arts, Academy of Music, Enschede, The Netherlands
Annemieke C. Vink
Department of epidemiology & data science of Amsterdam UMC, Amsterdam, The Netherlands
Jos W. R. Twisk
You can also search for this author in PubMed Google Scholar
Contributions
The first author wrote the main manuscript text and the other authors reviewed the manuscript several times. All authors reviewed the manuscript.
Corresponding author
Correspondence to Vanusa M. Baroni Caramel .
Ethics declarations
Access to data.
The first (VMBC) and fourth (SIMJ) authors will have access to the full dataset in Redcap. The anonymized data that support the findings of this study will be available upon reasonable request from the corresponding author. The data will not be publicity available due to privacy or ethical restrictions.
Ethical approval
“This study was conducted according to the guidelines laid down in the declaration of Helsinki. Ethical approval was obtained from the Medical Ethics Review Board of the university medical center of Groningen (UMCG) in the context of the Medical Research Involving Human Subjects Act (WMO). The review board reference number is METc 2019/021. An informed (proxy) consent is obtained for all participants. Participation in the study will be voluntary. Participants or legal representatives can withdraw consent at any time. Any attrition or adverse effects of the intervention or control group will be documented. In addition to sessions immediately stopped in the case of adverse reactions, the interventions will be discontinued if, in consultation with the physician or psychologists, harmful effects are observed and are expected to continue with exposure to any of the two interventions. The trial is registered at the International Clinical Trials Registry Platform (ICTRP) search Trial Registration number NL 7708 ( https://trialsearch.who.int/Trial2.aspx?TrialID=NL7708) ” in the Ethics approval and consent to participate section.
Consent for publication
Not Applicable.
Conflict of interest
The authors declare that they have no competing interests.
Informed consent
The first author (VMBC) provides an information letter with informed consent form to competent residents and to the legal representatives of non-competent eligible residents. All information sheets and consent forms were be written in Dutch. First author will discuss the trial with patients or legal representatives and then obtain consent when willing to participate in the trial.
Confidentiality
All study-related information will be stored securely at the study site. All participant information will be stored in locked file cabinets in areas with limited access. All files are confidential and coded with a 5-number code. The coding list is stored in a record cabinet with a key that only the first author can access.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Baroni Caramel, V.M., van der Steen, J.T., Vink, A.C. et al. The effects of individual music therapy in nursing home residents with dementia to improve general well-being: study protocol of a randomized controlled trial. BMC Geriatr 24 , 290 (2024). https://doi.org/10.1186/s12877-024-04863-z
Download citation
Received : 08 December 2022
Accepted : 01 March 2024
Published : 27 March 2024
DOI : https://doi.org/10.1186/s12877-024-04863-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality of life
- Psychosocial intervention
- Behavioral symptoms
- Randomized controlled trial
- Nursing homes
American Journal of Neuroradiology
Advanced Search
Imaging Genomics of Glioma Revisited: Analytic Methods to Understand Spatial and Temporal Heterogeneity
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Cymon N. Kersch
- ORCID record for Minjae Kim
- ORCID record for Jared Stoller
- ORCID record for Ramon F. Barajas Jr
- ORCID record for Ji Eun Park
- Figures & Data
- Info & Metrics
An improved understanding of the cellular and molecular biologic processes responsible for brain tumor development, growth, and resistance to therapy is fundamental to improving clinical outcomes. Imaging genomics is the study of the relationships between microscopic, genetic, and molecular biologic features and macroscopic imaging features. Imaging genomics is beginning to shift clinical paradigms for diagnosing and treating brain tumors. This article provides an overview of imaging genomics in gliomas, in which imaging data including hallmarks such as IDH -mutation, MGMT methylation, and EGFR -mutation status can provide critical insights into the pretreatment and posttreatment stages. This article will accomplish the following: 1) review the methods used in imaging genomics, including visual analysis, quantitative analysis, and radiomics analysis; 2) recommend suitable analytic methods for imaging genomics according to biologic characteristics; 3) discuss the clinical applicability of imaging genomics; and 4) introduce subregional tumor habitat analysis with the goal of guiding future radiogenetics research endeavors toward translation into critically needed clinical applications.
- ABBREVIATIONS:
Imaging genomics is the study of the relationships between microscopic, genetic, and molecular biologic features and macroscopic imaging features. Imaging genomics is important in CNS pathologies because tissue sampling faces challenges, including invasiveness in a critically functioning organ, the feasibility of intraoperative imaging, technical difficulties in site-specific tissue sampling, and requirements for study team coordination among neurosurgeons, radiologists, and pathologists. Through the use of imaging genomics, we seek to improve the clinical care of patients by predicting risk and patient outcomes with identification of noninvasive imaging biomarkers. 1 Imaging features can be divided into 2 categories: first, low-dimensional imaging features that include semantic or qualitative features comprising a standardized lexicon for the description of tumors (Visually AcceSAble Rembrandt Images [VASARI]; https://radiopaedia.org/articles/vasari-mri-feature-set ) or a description of tumor morphology (ie, T2-FLAIR mismatch sign). Second, radiomics features include high-throughput data that completely cover the range of quantitative features that can be extracted from images such as texture, shape, and margin gradient. 2 Radiomics can be derived from either handcrafted or deep learning techniques. 3 Radiogenomics is a subcategory of imaging genomics that is based on radiomics. 1 , 2 In radiogenomics, imaging features are extracted automatically and with high throughput, and radiogenomics often requires the use of a machine learning algorithm for model development. 2 , 4
Imaging genomics is technology-heavy and incorporates some combination of clinical imaging, “-omic” tissue analyses with “big data” bioinformatics, and artificial intelligence (AI) through machine learning algorithms. Imaging genomics has different methodologic approaches and uses low-dimensional semantic features and high-dimensional radiomics features. During cancer development, a few genes undergo distinct changes in specific locations, 5 and identifying these with imaging biomarkers requires distinct radiomics techniques. For instance, an IDH mutation is an ideal tumor-specific neoantigen that can be assessed with low-dimensional imaging features because it is uniform in a given tumor and does not change with time. 6 On the other hand, epidermal growth factor receptor ( EGFR ) amplification and MGMT promoter methylation status are distributed heterogeneously within a given tumor, and loss of EGFR amplification 7 and alterations of the MGMT promoter methylation status occur during treatment. 8 These results necessitate using high-dimensional imaging features including radiomics and deep learning–based features to spatially discern these heterogeneous biologic expression patterns. AI is particularly helpful to handle high-dimensional imaging features as well as large-scale transcriptomics and genomics data.
Imaging genomics can be applicable to many clinical scenarios from diagnosis to treatment-planning and evaluating the treatment response. For example, it may be applied when tumor diagnostics are incomplete due to challenges with tissue sampling or when noninvasively subtyping gliomas on the basis of known gene expression or mutation patterns, including those associated with IDH , MGMT , EGFR , and others. 9 ⇓ - 11 Moreover, imaging genomics and radiomics have applicability in prognostication, which can support decision-making of patients and clinicians. Its applications also extend into evaluating the tumor microenvironment and determining how this microenvironment changes with time in response to treatment. Finally, imaging genomics and especially radiomics may provide novel tools to evaluate the response to these therapies when it is challenging to distinguish posttreatment changes such as pseudoprogression, tumor progression, and treatment complications such as radionecrosis.
This article will achieve the following: 1) review the methods used in imaging genomics including visual analysis, quantitative analysis, and radiomics analysis; 2) recommend suitable analytic methods for imaging genomics according to biologic characteristics; 3) discuss the clinical applicability of imaging genomics; and 4) introduce subregional tumor habitat analysis with the goal of guiding future radiogenetics research endeavors toward translation into critically needed clinical applications.
- PART 1: METHODOLOGY OVERVIEW
An overview of the methodology and clinical utility of imaging genomics is shown in Fig 1 . Imaging genomics studies are usually based on 3 main methodologies: First, physiologic information from multiparametric MR imaging, usually based on low-dimensional features, can be used. Second, modeling and validation using high-dimensional data including radiomics and deep learning can be performed. Third, voxelwise spatial mapping and clustering using voxels from multiparametric MR imaging can be used. The main role of imaging genomics is prediction of genomics, including depiction of intratumoral heterogeneity, prediction of molecular subtypes, or colocalization and in situ validation. Depiction of intratumoral heterogeneity, which is often achieved with radiomics, facilitates understanding of microscopic genetic features. Prediction of molecular and genetic mutations in individuals or groups facilitates understanding of molecular and biologic features. Colocalization and in situ validation, which are often achieved with voxel-wise clustering and spatial mapping, facilitate understanding of macroscopic features to predict tumor aggressiveness, tumor infiltration, and vascularity. Further clinical utilities for imaging genomics include prognostication for patient consultation and determination of the therapeutic implications of treatment-planning for chemotherapy and radiation therapy. A detailed process of structuring an imaging genomics study is summarized as follows.
- Download figure
- Open in new tab
- Download powerpoint
Sample workflow for imaging genomics studies to integrate glioma imaging phenotypes with molecular features. In imaging genomics studies of glioma, pretreatment MR imaging sequences are typically obtained. Next, tumor tissue is collected, sometimes under image guidance in relation to specific imaging features, and then subjected to various types of genomics, transcriptomics, and proteomics analyses. Both the imaging and molecular data require preprocessing and normalization steps before they are integrated to assess the associations between imaging phenotypes and genomic and molecular features. Finally, these associations are interpreted in the context of the clinical disease and known complex biologic processes and pathways.
Data Collection
Imaging data are collected through standard and specialized protocols that provide detailed information about the size, shape, location, and other imaging characteristics of the tumor, while biologic data collected from tissue samples reveal the genomic/transcriptomic profile of the tumor. Imaging data variability must be considered and harmonized across different imaging vendors and institutions because it greatly affects the reproducibility of imaging features. Imaging-acquisition protocols need to be unified across multiple centers to conduct a prospective study. For retrospective analysis, a phantom study, test-retest analysis, quantitative maps, or value normalization can be used. The detailed methodology is explained elsewhere. 12 For tumor characteristics that are binary (such as the presence or absence of an IDH mutation) and that do not change across a tumor, tumor tissue samples do not need to be spatially colocalized with the specific imaging features with which they are being correlated. Publicly available databases of genomics and transcriptomic data and their correlated clinical radiographs have resulted in some of the first large number of cohort studies in this field, for instance, the National Cancer Institute’s large The Cancer Genomic Atlas was expanded to include a companion imaging database, The Cancer Imaging Archive, which has led to hundreds of publications in oncology exploring radiogenomics ( https://www.cancerimagingarchive.net ). However, for biologic features that vary over regions of a single tumor, spatially colocalized data (imaging and biologic) need to be collected from brain tumors. Precise colocalization of the tissue and imaging data is critical to permit these correlates, and this can be achieved through intraoperative stereotactic tissue sampling. 13 , 14
Imaging Data Preprocessing
Once the data are collected, they undergo preprocessing steps to ensure their quality and suitability for postprocessing. These may involve tasks such as resizing the images to a consistent resolution, normalizing the intensity values, removing artifacts or noise, and aligning the images in a standardized orientation.
ROI Segmentation
Once the images are acquired, an ROI is defined. The ROI is typically used as a bounding method (manual or automated segmentation) that prevents analytic extension into normal brain structures. This step ensures that subsequent analyses are specifically conducted on the tumor region.
Image Processing and Feature Extraction (especially, radiomics)
Once the imaging data are collected, they can undergo any number of image-processing steps to extract relevant features from the precise location of the colocalized tissue sample. Imaging features can be obtained from anatomic images (T1, T2-weighted, FLAIR), diffusion-weighted images, perfusion-weighted images, and metabolic images. Relevant imaging features according to genetic/molecular features are demonstrated in Part 2. In radiomics, these include intensity-based features (voxel intensities), shape-based features (geometric properties), texture-based features (spatial patterns), and spatial-based features (relationships between different regions).
Biologic Analysis
The tissue data are simultaneously processed and analyzed to identify genetic mutations, gene-expression patterns, methylation patterns, and other biologic alterations. This direct tissue analysis provides information about the molecular characteristics and nuanced tumor biology, which can include potential therapeutic targets. Further subanalyses of the gene-expression profile can provide additional tissue features such as an estimation of the abundance of member cell types in a mixed cell population with cellular deconvolution techniques.
Data Integration and Analysis
The extracted imaging features and biologic data are then integrated and analyzed together to define biologic processes that are correlated with imaging features or phenotypes. The detailed integration analysis is explained in Part 2 regarding molecular features. Supervised learning including modeling is the most common method to predict 1 or 2 genomic mutations and molecular features. In radiomics, statistical and machine learning techniques including dimensionality reduction methods, feature selection techniques, or modeling approaches are used. When one uses AI, the choice of model depends on the specific task and available data. For example, convolutional neural networks can achieve image-analysis tasks by learning patterns and features from the input training images. The training process adjusts the internal parameters of the model to minimize the differences between the predicted and ground truth tumor annotations. After training, the model is evaluated using a separate validation data set. This step assesses the performance and generalizability of the model and may involve adjusting hyperparameters (eg, learning rate, regularization), exploring different model architectures, or augmenting the training data with transformations or variations. For validation, external validation is highly recommended to achieve the generalizability of the model. The detailed radiologic and statistical perspectives are summarized elsewhere. 12 Other analytic methods are as follows: Correlation plots or unsupervised learning methods including clustering are adopted to demonstrate heterogeneity to demonstrate correlation among multiple different genomic mutations and molecular features. To perform a prognostication or outcome study using imaging genomics, one can perform time-to-event analysis.
- PART 2: ANALYTIC METHODOLOGY FOR DIFFERENT MOLECULAR FEATURES OF GLIOMAS
The spatial distribution of tumor molecular features has a substantial influence on the choice of analytic methodology ( Fig 2 ). The biologic background of the molecular features of gliomas is summarized with a review of current analytic methodologies (Online Supplemental Data). 4 , 15 , 16 The analytic approaches that best reflect the spatial distribution of given molecular features are proposed. Ubiquitously expressed biologic features such as IDH mutations may be assessed using low-dimensional, lesion-wide analysis. Conversely, for molecular features with fractional mutation (ie, CDKN2A/B) or different subtypes of molecular alterations (ie, H3K27-altered), a histogram analysis or high-dimensional analysis using imaging-based computational techniques such as radiomics and deep learning with a supervised approach may be the most appropriate. For heterogeneous and dynamic molecular features (ie, MGMT promoter methylation, EGFR amplification), radiomics and deep learning with an unsupervised approach may best reflect spatial and temporal heterogeneity.
Differences in the biologic distribution of genes and molecular subtypes in glioma and suggested analytic methods of imaging genomics. For genes and molecular subtypes that are stable and ubiquitous, imaging genomics using averaged values or a simple imaging phenotype such as T2-FLAIR mismatch sign is applicable. For genes and molecular subtypes with a skewed distribution or those that include different subtypes, a histogram analysis or supervised learning using AI or radiomics is applicable. For genes and molecular subtypes that are dynamic and heterogeneous, pattern-wise analysis using unsupervised learning or subregional analysis to explain intratumoral heterogeneity needs to be applied.
Imaging Genomics for Ubiquitously Expressed Biologic Features
Biologic features of idh mutations..
IDH mutation in glioma is ubiquitously expressed in all tumor cells in the IDH -mutant type. 16 In the World Health Organization (WHO) CNS5 edition published in 2021, secondary glioblastoma or IDH- mutant glioblastoma is no longer listed. 16 Regardless of the histologic grade, tumors with IDH wild-type are now assigned as “(molecular) glioblastoma, IDH -wild-type, CNS grade grade 4.” Thus, distinguishing IDH -mutational status becomes more important because it is a strong prognostic factor for survival. 17
Review of Current Analytic Methodologies.
Visual analysis of various imaging features has been shown to differ according to IDH1 -mutation status as characterized by standardized imaging lexicons such as VASARI. 18 In addition, the T2-FLAIR mismatch sign is a validated imaging sign for IDH -mutant status in patients with diffuse adult-type glioma, specifically in diffuse astrocytoma, IDH -mutant type without the 1p/19q codeletion. The T2-FLAIR mismatch sign is expressed in the entire tumor, which shows entirely homogeneous high signal intensity on T2-weighted images and low signal intensity in the internal portion on FLAIR images. The T2-FLAIR mismatch sign has been previously described in detail. 19 ⇓ - 21 Imaging genomics clinicopathologic analysis suggests that the presence of tumor microcystic change is a causative etiology of FLAIR suppression. 22 The positive predictive value of the T2-FLAIR mismatch sign for IDH -mutation status was 100% in retrospective cohort studies of diffuse adult-type gliomas. 19 , 20 There are false-positives for the T2-FLAIR mismatch sign when it is observed in other tumors such as dysplastic embryogenic tumors 23 and pilocytic astrocytoma. 24 When a study design includes all gliomas, both the positive predictive value and specificity of the T2-FLAIR mismatch sign for IDH -mutation may decrease.
Advanced physiologic imaging has also been shown to predict IDH -mutation status such as DSC, 25 dynamic contrast-enhancement (DCE), 26 intravoxel incoherent motion (IVIM), 26 and metabolic imaging such as amide proton transfer–weighted imaging. 27 While CBF is not useful in distinguishing IDH -mutation status, the medians of the parameters derived from DSC and IVIM such as the CBV, microcirculation perfusion coefficient, and simplified perfusion fraction were lower in IDH -mutant gliomas. 25 In addition, the median lower fractional volume of intravascular space using a distributed parameter model showed the highest diagnostic performance among DCE-derived parameters, including those based on the Tofts model. 26 Such findings may support the lower vascularity, permeability, and flow in the tumor microenviroment of IDH -mutant gliomas due to resistance to neoangiogenesis by regulation of hypoxia-inducible factor α. 28 In terms of chemical exchange saturation transfer (CEST) imaging metrics, the median amide/amine signal ratio and levels of amine signal differentiated IDH wild-type from the pooled IDH -mutant gliomas, supporting the relevance of tumor acidity in differentiating gliomas. 27
Supervised learning approaches with radiomics features and deep learning features have been used to predict IDH -mutation status with multiparametric MR imaging. 29 This approach often requires large, highly curated data sets. On the basis of the glioma The Cancer Genomic Atlas cohort, a prediction model of IDH -mutation status using multiple machine learning classifiers exhibited a preoperative accuracy of up to 88.9%. 30 In terms of AI, use of convolutional neural networks has demonstrated an accuracy of 94% for IDH -1 mutation status and 92% for 1p/19q codeletion status. 31
Proposed Analytic Methodology.
For ubiquitously expressed biologic features such as IDH mutations, a lesion-wide visual analytic approach that captures the whole tumor and provides direct and intuitive information is proposed. The ubiquitous expression of IDH mutations in all tumor cells negates the need to reflect intratumoral heterogeneity, making histogram or radiomics approaches excessive.
The T2-FLAIR mismatch sign, when applied appropriately, is a representative visual analytic approach that is simple to use and has been extensively validated in real-world clinical settings. For physiologic imaging, the median or mean values from physiologic imaging modalities including DSC, DCE, IVIM, and amide proton transfer–weighted imaging from the entire tumor ROI are suitable for analyzing this ubiquitous expression of genetic mutation. Supervised learning using high-dimensional imaging features to classify IDH -mutant tumors is feasible, but future research should be directed to proposing and validating a simple, visual, or statistical analytic approach that enables lesion-wide reflection of ubiquitously expressed biologic features.
Imaging Genomics for Subtypes with a Skewed Distribution
Intratumoral heterogeneity of cdkn2a/b..
Certain molecular features of gliomas are characterized by fractional mutations or different subtypes of molecular alterations. CDKN2A/B is a tumor-suppressor gene that, when homozygously deleted, promotes biologic aggressiveness in IDH -mutant gliomas. 32 In the WHO CNS classification published in 2021, a CDKN2A/B homozygous deletion results in a CNS WHO grade of 4 for IDH- mutant tumors, even without microvascular proliferation or necrosis. 16 Thus, grading is no longer entirely histologic, and CDKN2A/B status becomes important. The percentage of cells with homozygous deletion across all IDH -mutant tumors is bimodal, with a median value of <10%. 33 However, this distribution is skewed toward histologically high-grade tumors having >50% deletion.
Intertumoral Heterogeneity of Histone H3 Lysine 27-Altered Diffuse Midline Glioma.
Histone H3 lysine 27-altered diffuse midline glioma (H3K27-DMG) is a unique molecular subgroup that includes subtypes with an alternative mechanism for the loss of H3K27 trimethylation, such as additional somatic genetic alterations of receptor tyrosine kinases, cell cycle regulators, mediators of DNA repair, and/or phosphoinositide 3-kinase/protein kinase B/mammalian target of rapamycin signaling. 34 The 2021 WHO classification adopted the revised designation “diffuse midline glioma, H3K27-altered” to include subtypes of diffuse midline glioma (DMG) with an alternative mechanism for the loss of H3K27 trimethylation. These include 4 subtypes of DMGs: 1) H3.3 p.K28M ( K27M )-mutant, 2) H3.1 or 3.2 p.K28M ( K27M )-mutant, 3) H3-wild-type with EZHIP overexpression, and 4) EGFR -mutant, which mainly includes bithalamic diffuse gliomas that present H3K27M or EZHIP overexpression together with strong enrichment in EGFR alterations. The H3K27-altered type is characterized by low intratumoral heterogeneity because the K27M -mutant variant causes a global reduction in levels of H3 lysine 27 trimethylation (H3K27me3). 35 In addition, EZHIP overexpression results in H3K27me3 global reduction. 36
There are a limited number of studies predicting CDKN2A/B status, and most have used supervised learning approaches. 37 , 38 A recent study of imaging genomics for CDKN2A/B showed a trend toward an infiltrative pattern, a larger maximal diameter, and a higher value of the 95th percentile of normalized CBV being independent predictors of CDKN2A/B . 39 Imaging features of CDKN2A/B deletion may overlap with those implying tumor aggressiveness.
For H3K27M-DMG, imaging features have been characterized by comparing the mean values or histogram parameters of ADC or relative CBV (rCBV). 40 , 41 Imaging features of H3K27-altered tumors have various presentations (high intertumoral heterogeneity), but most tumors show relatively uniform signals (low intratumoral heterogeneity). 42 Metabolic imaging with MRS has demonstrated significantly higher citrate and glutamine levels in H3K27-DMG tumors. 43
For fractional mutation of CDKN2A/B , the proposed analytic methodology is histogram analysis. To depict intratumoral heterogeneity of CDKN2A/B , histogram parameters of skewness, kurtosis, and percentile values are useful. By means of radiomics, intratumoral heterogeneity can be captured, and CDKN2A/B can be diagnosed using supervised learning. Using the median or mean value derived from histograms of physiologic imaging biomarkers, imaging prediction of CDKN2A/B may be difficult because there is no clear technical cutoff, and IDH -mutant tumors evolve toward homozygous deletion across time.
For H3K27-altered DMG, the imaging features have various presentations (high intertumoral heterogeneity), but most tumors show relatively uniform signals (low intratumoral heterogeneity). 42 Pattern-wise diagnosis is helpful to depict intertumoral heterogeneity of H3K27-altered DMG. Metabolic imaging with MRS has demonstrated significantly higher citrate and glutamine levels in H3K27-DMG tumors. 43 On the basis of the low intratumoral heterogeneity of metabolic/cell signaling alterations, noninvasive metabolic imaging may provide a method for improved preoperative diagnosis of tumors with H3K27 alterations.
Imaging Genomics for Subtypes with Dynamic and Heterogeneous Biologic Features
Biologic background of mgmt methylation and egfr -mutation status..
Some molecular features of gliomas have spatial and temporal heterogeneity with evolution of the mutational status with treatment. DNA promoter methylation of the MGMT gene is a clinically important feature that is predictive of temozolomide sensitivity, which is the standard-of-care chemotherapeutic agent used in the treatment of glioblastoma. Prior investigations have demonstrated MGMT methylation to be heterogeneous, with heterogeneity of methylation patterns across the MGMT 5′ CpG island, and capable of changing through the course of therapy.
EGFR amplification and EGFR variant III ( EGFRvIII ) mutations have both temporal and spatial heterogeneity. EGFRvIII mutations were detectable only in subclones of the tumor in EGFR amplification samples of individual patients, which suggested that EGFRvIII mutations are late events in tumor development. 44 Heterogeneity of EGFRvIII has also been observed at the protein level. In contrast, wild-type EGFR expression is much more abundant and lacks the profound heterogeneity observed with EGFRvIII . This finding indicates that both the occurrence and disappearance of EGFR mutations are frequent processes that significantly contribute to tumor heterogeneity.
Radiomics and deep learning–based approaches involve the extraction of hundreds of quantitative features from images. 4 Typically, machine-learning techniques are subsequently applied to the extracted radiomics features. These techniques use 2 main methods: 45 1) dimensionality reduction and feature selection via unsupervised approaches, and 2) association analysis with ≥1 specific outcome via supervised approaches.
MGMT Promoter Methylation Status
Using supervised learning methods, numerous studies have assessed the correlation of conventional MR imaging features from T1-weighted, T2-weighted, FLAIR, and T1-weighted gadolinium contrast-enhanced (CE-T1WI) images with MGMT methylation status. Published studies have reported a wide range of predictive accuracy ranging from 60% to >80%. 46 ⇓ ⇓ - 49 For dimensionality reduction and feature selection, algorithms such as maximum redundancy and maximum relevance 46 or least absolute shrinkage and selection operator (LASSO) have been used. Fusion radiomics signatures determined by logistic regression modeling of single radiomics signatures selected from each sequence and habitat have been shown to predict survival. 46 In particular, convolutional neural networks–based architectures have been validated or further developed with transfer learning to determine MGMT promoter methylation status. 48 , 49
EGFR Amplification Status
Histogram analysis and supervised learning approaches (machine learning) with radiomics have been used to predict EGFR amplification in glioblastomas and have achieved a diagnostic accuracy of up to 78%. 50 ⇓ ⇓ - 53 Measures such as the maximum rCBV, relative peak height, and percentage signal recovery from DSC have been correlated with EGFR mutation status. 53 Logistic regression models with or without dimensionality reduction and feature selection via LASSO using conventional images such as T2WI, CE-T1WI, FLAIR, and DWI have been most commonly used. 51 , 52
For genes exhibiting both spatial and temporal heterogeneity, unsupervised approaches to dimensionality reduction and feature selection are more beneficial than supervised approaches. The 2 most commonly used unsupervised approaches are cluster analysis and principal component analysis (PCA). 2 Genomics data are often multidimensional. Cluster analysis is a method that sorts through genomics data and allows better visualization through heatmaps. 54 A heatmap can readily display trends in data by simultaneously accounting for each dimension of the genomic data fed into the computational pipeline. PCA also explores multidimensional genomics data and determines the impact a specific dimension of the data has on variation in the data set as a whole. This process shows the likelihood of contribution from a specific attribute compared with the contributions of other dimensions in the data. 55 Both cluster analysis and PCA allow the analysis of contributions from individual vectors within an extensive basis of vectors.
One good example of unsupervised learning for MGMT promoter methylation status is a study that used dimensionality reduction with unsupervised learning to account for the intra- and intertumoral heterogeneity of MGMT . By means of anatomic FLAIR and CE-T1WI features, K-means clustering of radiomics features obtained 3 distinct and reproducible imaging subtypes of glioblastoma with molecular characteristics, including MGMT promoter methylation status. 47
For EGFR amplification status, unsupervised learning using regional information has been studied. Intratumoral heterogeneity can be depicted by conducting separate regional-based analyses of imaging biomarkers, including enhancing tumors, nonenhancing tumors, necrosis, and edema. In a multiparametric MR imaging and multisegmentation study, the spatial tumor pattern (location) and intensity distribution obtained from histograms of T2-FLAIR, ADC, and rCBV values were compared between EGFR variant III -positive ( EGFRVIII+) versus EGFR variant III -negative ( EGFRvIII −) tumors. EGFRvIII + tumors displayed a higher rCBV, lower ADC, higher fractional anisotropy, lower T2-FLAIR, and a distinctive spatial pattern ( Fig 3 ). 56 EGFRvIII + tumors had a more isotropic distribution of rCBV in enhancing and nonenhancing tumors and a low rCBV in perinecrotic tissue. This finding was observed with PCA of complex time-signal-intensity curves from DSC imaging of the peritumoral region. 57 This unsupervised learning approach showed that EGFRvIII+ tumors had more homogeneity in time-signal-intensity curve–based features between immediate and distant peritumoral ROIs, while greater heterogeneity was observed in EGFRvIII tumors.
Illustration of the use of an unsupervised learning method and a subregional analysis to account for an EGFRvIII mutation. A , Histogram analysis of multiparametric MR imaging enables depiction of the differences between the EGFRvIII- mutant and wild group (reproduced with permission from Bakas et al 57 ). B , For EGFRvIII -mutant tumors, there is no heterogeneity in the perfusion pattern distribution between the far and near ROIs, while there is considerable heterogeneity between the far and near ROIs for patients who have EGFRvIII – tumors (reproduced with permission from Akbari et al 56 ).
- PART 3: ADVANCING PERSONALIZED MEDICINE USING IMAGING GENOMICS AND RADIOMICS
The standard-of-care treatment for glioblastoma includes upfront maximal safe resection followed by concurrent radiation therapy and temozolomide and then adjuvant temozolomide. 58 For patients with a good performance status, their treatment often includes the use of tumor-treating fields after concurrent chemoradiation. With this treatment paradigm, patients with glioblastoma have a median survival of 20.9 months. 59 However, there is substantial variation in individual outcomes, with survival ranging from a few weeks to many years. Imaging genomics has demonstrated clinical feasibility in selecting subgroups of patients who are likely to benefit from specific therapies, including immunotherapies and targeted molecular therapies, and in improving our ability to assess treatment responses.
Maximal safe surgical cytoreduction is unequivocally linked to improved clinical outcomes for patients with glioblastoma. However, the highly infiltrative growth pattern often leads to involvement of eloquent brain regions and challenges discerning areas with the highest risk of tumor recurrence. This feature makes achieving “negative” surgical margins difficult, if not impossible. Assessing tumor infiltration by using imaging genomics is an important issue and needs to be validated with spatial mapping. A colocalization study demonstrated imaging correlates of tumor infiltration using anatomic, perfusion, diffusion images and O-(2-[18F]-fluoroethyl)-L-tyrosine ([ 18 F] FET) PET and subsequent multiregion stereotactic biopsies. 14 In nonenhancing gliomas, FLAIR had the highest diagnostic accuracy. Recently, an optical imaging technique and fiber laser-based stimulated Raman histology showed the potential to noninvasively predict residual infiltrative glioma. 60 This finding has the potential to assist in personalizing resection plans on the basis of the individual risk of local recurrence, while concurrently minimizing the risk of neurologic deficits and preserving function status. Although radiomics has begun to explore imaging correlates of tumor cellularity 61 and the extent of infiltration, 62 spatial mapping and colocalization are difficult to achieve for radiomics because this technique demonstrates heterogeneity and complexity, and spatial information is lost.
Temozolomide
Temozolomide is used in glioblastoma treatment alongside radiation therapy. However, response to this agent varies among patients and depends on individual tumor biology. Patients with methylated MGMT promoters show an enhanced response to temozolomide. 9 , 10 Therefore, noninvasive determination of MGMT methylation status using imaging genomic applications can predict temozolomide sensitivity. Imaging genomics methodologies to assess MGMT promoter methylation have been previously discussed herein. Similarly, the gene telomerase reverse transcriptase ( TERT ), which is sometimes mutated in glioblastoma, impacts temozolomide and radiation sensitivity. A recent study created an optimized radiomics score using a LASSO regression model and multivariate analysis to predict TERT promoter mutations. 63 This model, which combines the radscore with patient characteristics, demonstrated high prediction accuracy.
Radiation Therapy
Radiation, a standard treatment for glioblastoma and many gliomas, may be optimized through radiomics. A recent review article 64 demonstrated that a radiomics-guided radiation therapy approach may aid radiation therapy planning by using radiomics volumetric signature maps and radiomics subvolumes. This approach would further enable personalization of radiation treatment plans based on patient-specific anatomic and tumor characteristics using radiomics. Radiomics and imaging genomics could offer novel biomarkers for variable inter- and intratumoral radiation sensitivity, guiding individualized dose/fractionation plans and dose painting across a tumor.
Immunotherapy
Immunotherapies, primarily targeting programmed cell death protein 1/programmed death-ligand 1, or anti-cytotoxic T-lymphocyte-associated protein 4, use the adaptive immune system against tumor cells. Unfortunately, these therapies have shown little benefit in improving survival of patients with glioblastoma to date. Two recently published international randomized Phase III trials evaluating the efficacy of adding nivolumab to the treatment of newly diagnosed glioblastoma with and without MGMT promoter methylation showed no benefit over the standard-of-care treatment. 65 , 66 The ineffectiveness of immune checkpoint blockade in glioblastoma could be due to decreased CNS immune surveillance, low tumor mutation burden, poor BBB penetration, or insufficient immunologic response to glioblastomas. However, some glioblastoma subtypes may respond better to immune-modulating therapeutics. One randomized control study showed that patients who received neoadjuvant and/or adjuvant therapy with pembrolizumab had significantly extended overall survival among patients with recurrent glioblastoma. 67 Imaging genomics and radiomics may provide insight into more immunogenic glioblastomas that could have heightened sensitivity to immune-modulating therapies. One imaging study used radiomics to characterize tumor macrophage infiltration within the tissue microenvironment, which plays a critical role in the tumor-immune interface. 68 A recent review elaborated on how radiomics and imaging phenotypes correlate with the immune microenvironment of gliomas, their applications in immunotherapy era, and ongoing challenges in the field. 69
PART 4: POTENTIAL POWERFUL IMAGING GENOMICS TOOL FOR ENABLING BOTH SPATIAL MAPPING AND DEPICTING HETEROGENEITY—TUMOR HABITAT ANALYSIS
When assessing the translational utility of imaging genomics to the previously discussed clinical diagnostic and treatment pathways, it is critically important at the methodologic level to account for the vast intratumoral heterogeneity that these tumors exhibit. Imaging analyses that use supervised learning with radiomics or deep learning features are limited for biologic validation for 3 reasons: First, the end point of the classifier is singular for radiomics using supervised learning, which does not consider any heterogeneity. Second, there is a danger of overfitting or overinterpreting the derived models for supervised learning. 70 Third, radiomics depicts heterogeneity and complexity within a given ROI, in which any spatial information is lost. Pattern-wise analysis using unsupervised learning may reduce dimensionality and the risks of overfitting, but regional biologic validation is ultimately needed. 70
Tumor habitat analysis uses spatially oriented “voxels.” Grouping “similar” voxels together (parcellation) may define multiple subregions with a common biology that respond differentially to therapy or drive progression. 71 Parcellation methods include either an a priori assumption of a binary threshold, a geographic assumption, or a data-driven analysis using a clustering method. Tumor habitat analysis is in line with existing methods of imaging genomics, including subregions or subvolumes of a tumor or signature map. This method enables depiction of intratumoral heterogeneity similar to that of radiomics as well as spatial mapping and colocalization for further biologic validation. By means of subregions or subvolumes, tumor habitat analysis may guide imaging-guided treatment-planning and predict localization of tumor recurrence site. Below is a description of studies demonstrating use cases (specific situations or scenarios) of tumor habitat analysis are utilized.
Depiction of the Tumor Microenvironment Using Tumor Habitat Analysis
A data-driven analysis of clustering demonstrated tumor subregions with distinct biology and pathologic correlations with the tumor microenvironment (TME). 71 Figure 4 explains the difference between radiomics-based supervised learning methods and voxelwise unsupervised learning (clustering) methods for tumor habitat analysis. These data-driven approaches have successfully distinguished viable tumors from nonviable tumors using multiparametric MR imaging and validated the method against H&E histology. 72 , 73
Limitations of radiomics with supervised learning for explaining intratumoral heterogeneity. The TME interacts with genes, and subregions evolve and develop certain genomic mutations. Tumor habitat (subregional) analysis is an analytic method using voxelwise clustering of multiparametric MR imaging data that maintains the spatial information.
In glioblastoma, tumor habitat analysis using multiparametric MR imaging with diffusion-weighted and perfusion-weighted imaging has been conducted with a voxel-based clustering method. 74 The process is assisted by deep learning–based segmentation, which enables reproducible tumor delineation, and the voxels containing physiologic information—the ADC reflecting cellularity and the rCBV reflecting vascular density—can be extracted within the ROI.
Potential Utility of Tumor Habitat Analysis
Virtual biopsy and radiogenomics..
Voxelwise clustering and tumor habitat analysis enable the establishment of distinct functional regions with spatial information and the spatial coregistration of the images and corresponding histologic findings. 70 In breast cancer, multiparametric MR imaging habitat analysis and coregistered histology identified biologically validated subregions of hypoxia, necrosis, and other conditions. 75 This result suggests the possibility that virtual biopsies can depict the most aggressive tumor portion of the glioma as well as help to predict genetic mutations under different TMEs. In terms of radiogenomics, tumor heterogeneity is shaped by both genetic differences and the local microenvironment. 76 Due to differences in the tissue architecture and nutrient and oxygen levels, regional differences in the TME lead to different selection of subpopulation of tumor cells (clonal selection). For example, late development of EGFRvIII is correlated with a TME promoting anabolic metabolism in glioblastoma cells, leading to alterations in the levels of EGFRvIII expression. 76 Depiction of tumor habitats based on hypoxic regions enables investigation of genetic/molecular alterations per subregion that may enhance the prediction of certain mutations.
Treatment Monitoring.
The most promising clinical application of tumor habitat analysis is assessing the treatment response. 70 Temporal changes in the tumor habitat, the “spatiotemporal habitat,” occur during and after treatment with both spatial and temporal variation. Following treatment, outcomes can include tumor response, tumor progression, pseudoprogression, and radiation necrosis or other adverse effects of the anticancer therapies, all of which could be evaluated with habitat analysis.
Pseudoprogression
Pseudoprogression is thought to represent an inflammatory response to treatment but radiographically mimics tumor growth and thus poses a dilemma for the clinician when considering a treatment change or pursuing close surveillance. The feasibility of subregional analysis was shown in differentiating pseudoprogression on the basis of a voxelwise clustering method that exhibited better performance than the single parameters of the ADC or CBV. 74 By means of spatiotemporal habitat analysis on the ADC and CBV, 3 spatial habitats of a hypervascular cellular (high CBV and low ADC), a hypovascular cellular (low CBV and low ADC), and a nonviable tissue habitat (low CBV and high ADC) were identified, and an increase in the hypervascular cellular (OR, 4.55, P = .002) and hypovascular cellular (OR, 1.22, P < .001) habitats was predictive of tumor progression. 77
Prediction of Treatment Response
Spatiotemporal habitats also assist in monitoring treatment responses in patients with glioblastoma. 77 On the basis of a spatiotemporal habitat analysis of the ADC and CBV, a short-term increase in the hypervascular cellular habitat (hazard ratio, 40.0; P = .001) and hypovascular cellular habitat was significantly associated with shorter progression-free survival (hazard ratio, 3.78; P < . 001) after concurrent chemoradiation therapy. Validation using a prospective cohort showed that an immediate increase in hypovascular cellular tumors after concurrent chemoradiation therapy was strongly associated with shorter progression-free survival. 77
Comparative Assessment with Current Methodology.
By means of spatially oriented voxels and learning methods, tumor habitat analysis has the potential to become a powerful tool for imaging genomics. While traditional radiomics methods offer valuable insights into tumor heterogeneity, they often fail to account for spatial information, an area in which habitat analysis excels. Therefore, tumor habitat analysis is likely to be most beneficial for accurately distinguishing various intratumoral regions, thereby enhancing our ability to differentiate between viable and nonviable tumor areas as well as to discern treatment-induced changes such as pseudoprogression. However, comparisons with traditional radiomics methods indicate the need for further studies to establish the role of habitat analysis, because the specificity and sensitivity of the latter can be influenced by factors such as the choice of clustering methods, the quality of input imaging data, and the presence of overlapping imaging features. Despite these hurdles, its potential for improving therapeutic decision-making, predicting prognosis, and monitoring treatment response makes tumor habitat analysis a promising avenue in neuro-oncology.
- PART 5. LIMITATIONS, CHALLENGES TO BE ADDRESSED, AND FUTURE OPPORTUNITIES
Imaging genomics is not aimed at replacing actual genomics. There are features that are only attainable through direct tissue analysis of genetic data and molecular characteristics that lack specific imaging features. Furthermore, imaging features overlap among high-grade gliomas with increased cellularity showing a low ADC and increased vascularity exhibiting a high rCBV. Nonetheless, imaging genomics is useful in patients with brainstem glioma or deep-located tumors in the pretreatment stage. With spatial mapping, imaging genomics can become a powerful noninvasive tool for guiding treatment and treatment monitoring. Surgery and radiation therapy can be guided by demonstrating an infiltrative tumor component. Timely and noninvasive diagnosis is possible for the posttreatment stage by enabling localization of viable tumor or tumor progression that requires subsequent treatment.
For future studies, different analytic approaches for biologic features that are ubiquitously expressed, demonstrate skewed distribution, or display temporal or spatial heterogeneity are proposed. Biologic validation, when possible and appropriate, should be encouraged, and analytic techniques such as molecular imaging and tumor habitat analysis that enable colocalization will prove promising.
- CONCLUSIONS
Imaging genomics not only identifies genomic and molecular alterations noninvasively but also can help with prognostication, assessing and predicting tumor progression, and guiding therapy by spatial mapping and localization. In the pretreatment and diagnostic stage, different analytic approaches should be applied for imaging genomics. For ubiquitously expressed genomics features such as IDH -mutation status, a simple visual evaluation is sufficient. For skewed distribution or intra-/intertumoral heterogeneity including CDKN2A/B homozygous deletion or H3K27-altered status, histogram analysis of physiologic imaging biomarkers or radiomics with supervised learning methods are suitable. For dynamic alterations of MGMT promoter methylation or EGFR -mutation status, unsupervised learning of high-dimensional data is suitable. In the posttreatment stage, spatial mapping of imaging genomics has greater clinical implications through tumor habitat analysis to localize and predict tumor progression and guide therapy. Ultimately, colocalization of imaging genomics and actual pathology will improve this technique and broaden its utility in patients with glioma.
- Acknowledgments
We thank Bethany Barajas, MSN, for her helpful comments regarding this article and the many wonderful patients who selflessly contribute their time to undergo research medical imaging while confronting a deadly disease.
C.N. Kersch and M. Kim are co-first authors.
Ji Eun Park was supported by the National Research Foundation of Korea grant funded by the Korean government (grant No.: RS-2023-00305153) and Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare: HI22C0471. Ramon F. Barajas, Jr was supported by the National Institutes of Health, National Cancer Institute K08CA237809, KL2TR002370, and L30CA220897 and Jonathan D + Mark C. Lewis Foundation.
Disclosure forms provided by the authors are available with the full text and PDF of this article at www.ajnr.org .
- Nardini C ,
- Wang DS , et al
- Basu S , et al
- Quackenbush J , et al
- Gillies RJ ,
- Kinahan PE ,
- de Bruin EC ,
- McGranahan N , et al
- Waitkus MS ,
- Diplas BH ,
- van den Bent MJ ,
- Kerkhof M , et al
- Brandes AA ,
- Franceschi E ,
- Tosoni A , et al
- Esteller M ,
- Garcia-Foncillas J ,
- Andion E , et al
- Diserens AC ,
- Gorlia T , et al
- Parsons DW ,
- Jin G , et al
- Kim HJ , et al
- Eberhart CG ,
- Zhang Y , et al
- Verburg N ,
- Koopman T ,
- Yaqub MM , et al
- Kickingereder P ,
- Wesseling P , et al
- Ramos-Fresnedo A ,
- Pullen MW ,
- Perez-Vega C , et al
- Ahn SS , et al
- Poisson LM ,
- Brat DJ , et al
- Wijnenga MM , et al
- Johnson DR ,
- Patel SH , et al
- Deguchi S ,
- Mitsuya K , et al
- Amatya VJ ,
- Kolakshyapati M , et al
- Kaufmann TJ ,
- He B , et al
- Mancini L ,
- Casagranda S ,
- Gautier G , et al
- Kempa S , et al
- Chang JH , et al
- Hsieh KL , et al
- Grinband J ,
- Weinberg BD , et al
- Marker DF ,
- Broniscer A ,
- Qu C , et al
- Gan H , et al
- Vallero SG ,
- Bertero L ,
- Morana G , et al
- Gao J , et al
- Pan H , et al
- Park JE , et al
- Lin HZ , et al
- Kurokawa R ,
- Kurokawa M ,
- Baba A , et al
- Aboian MS ,
- Solomon DA ,
- Felton E , et al
- Pratt D , et al
- Eskilsson E ,
- Røsland GV ,
- Solecki G , et al
- Raimondi S , et al
- Hao X , et al
- Rathore S ,
- Rozycki M , et al
- Yogananda CG ,
- Nalawade SS , et al
- Choi KS , et al
- Hawkins-Daarud A , et al
- Xu K , et al
- Tsankova NM ,
- Bauer A , et al
- Shah AD , et al
- Schlesner M
- Pisapia JM , et al
- Pisapia J , et al
- Nabors LB ,
- Portnow J ,
- Ahluwalia M , et al
- Taillibert S ,
- Kanner A , et al
- Pekmezci M ,
- Morshed RA ,
- Chunduru P , et al
- Malone HR ,
- Bowden SG , et al
- Macyszyn L ,
- Da X , et al
- Wu G , et al
- Abdollahi H ,
- Clark H , et al
- Idbaih A , et al
- Carpentier AF , et al
- Cloughesy TF ,
- Mochizuki AY ,
- Orpilla JR , et al
- Chang K , et al
- Khalili N ,
- Kazerooni AF ,
- Familiar A , et al
- Tomaszewski MR ,
- O’Connor JP ,
- Waterton JC , et al
- Henning EC ,
- Sotak CH , et al
- Carano RA ,
- Ross J , et al
- Goh MJ , et al
- Jardim-Perassi BV ,
- Dominguez-Viqueira W , et al
- Furnari FB ,
- Cavenee WK , et al
- Kim HS , et al
- Received July 28, 2023.
- Accepted after revision November 9, 2023.
- © 2024 by American Journal of Neuroradiology
Thank you for your interest in spreading the word on American Journal of Neuroradiology.
NOTE: We only request your email address so that the person you are recommending the page to knows that you wanted them to see it, and that it is not junk mail. We do not capture any email address.
Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager

- Tweet Widget
- Facebook Like
- Google Plus One
Jump to section
- PART 4: POTENTIAL POWERFUL IMAGING GENOMICS TOOL FOR ENABLING BOTH SPATIAL MAPPING AND DEPICTING HETEROGENEITY—TUMOR HABITAT ANALYSIS
Related Articles
- No related articles found.
- Google Scholar
Cited By...
- No citing articles found.
This article has not yet been cited by articles in journals that are participating in Crossref Cited-by Linking.
More in this TOC Section
- Imaging Findings Post Stereotactic Radiosurgery for Vestibular Schwannoma: A Primer for the Radiologist
- Radiologic Classification of Hippocampal Sclerosis in Epilepsy
Similar Articles

COMMENTS
First published in 2004. 'Bryman has given researchers who study organizations and people in organizations just what they need, a source book on how such research is done, written for them on them by one of them. There are research methods books aplenty, but not for this particular field. Bryman's compendious knowledge enables him to review ...
Organizational Research Methods (ORM), peer-reviewed and published quarterly, brings relevant methodological developments to a wide range of researchers in organizational and management studies and promotes a more effective understanding of current and new methodologies and their application in organizational settings.ORM is an elite scholarly journal, known for high-quality, from the ...
Research Methods and Organization Studies. Alan Bryman. Routledge, Sep 2, 2003 - Business & Economics - 300 pages. First published in 2004. 'Bryman has given researchers who study organizations and people in organizations just what they need, a source book on how such research is done, written for them on them by one of them.
Organization Studies (OS) publishes top quality theoretical and empirical research with the aim of promoting the understanding of organizations, organizing and the organized in and between societies. OS is a multidisciplinary journal with global reach, rooted in the social sciences, comparative in outlook and open to paradigmatic plurality.
The SAGE Handbook of Organizational Research Methods provides a rich resource for organizational researchers, locating the technical aspects of organizational research in the wider context of the relevant personal, epistemological, theoretical, historical, ethical, and political issues.. David Buchanan and Alan Bryman have gathered together many of the world's leading writers on theory, method ...
Designed for those who study organizations and the people within them, this valuable source book of research contains analysis and discussion of research methods (both quantitative and qualitative), in terms of their uses and limitations.
Research methods and organization studies by Bryman, Alan. Publication date 1989 Topics Organisation -- Recherche, Organizational sociology -- Research, Organisatieonderzoek, Organisationsforschung, Onderzoeksmethoden, Organizational sociology Research Publisher London ; Boston : Unwin Hyman
Research Methods and Organization Studies Issue 20 of Contemporary social research series Volume 20 of Special Study of the Kennan Institute for Advanced Russian S: Author: Alan Bryman: Publisher: Unwin Hyman, 1989: Original from: the University of Michigan: Digitized: Jul 16, 2009: ISBN: 0044452128, 9780044452126:
The SAGE Handbook of Organizational Research Methods. provides a rich resource for organizational researchers, locating the technical aspects of organizational research in the wider context of the relevant personal, epistemological, theoretical, historical, ethical, and political issues.. Buchanan & Bryman have gathered together many of the world's leading writers on theory, method and ...
Method/ology articles should situate themselves firmly within organization studies and tackle issues or problems directly related to the "doing" of organization studies research. They must address topics of interest to readers of OS and make clear the connection to research conducted in OS. The maximum length for Method/ology articles is 13 ...
Method/ology articles should situate themselves firmly within organization studies and tackle issues or problems directly related to the "doing" of organization studies research. They must address topics of interest to readers of OS and make clear the connection to research conducted in OS. The maximum length for Method/ology articles is 13 ...
Research Methods and Organization Studies. Alan Bryman. Unwin Hyman, 1989 - Organisation - Recherche - 283 pages. This text has been designed to contribute towards the effective practice and evaluation of organizational research through enhanced understanding of methodological issues and problems. It is tailored for the needs of management ...
The methods examined include case studies, observation, interviewing and the repertory grid technique. By highlighting certain key 'rules' for carrying out qualitative research and describing issues that should be avoided, this second volume of Qualitative Methodologies in Organization Studies is essential reading for academics and ...
Amazon.com: Research Methods and Organization Studies: 9781138138513: Bryman, Alan: Books. Skip to main content.us. Delivering to Lebanon 66952 Update location Books. Select the department you want to search in. Search Amazon. EN. Hello, sign in. Account & Lists ...
This revision of a best selling research methods textbook introduces social science methods as applied broadly to the study of issues that arise as part of organizational life. These include issues involving organizational participants such as managers, teachers, customers, patients and clients, and transactions within and between organizations.In this new edition, chapter 19 now focuses on ...
Finding Information About Research Methods. Literature on research methods can be found in books and journal articles, so searching in the library catalog and databases will turn up relevant sources. Some relevant subjects to search on in the Library Catalog include: Organization Research -- Methodology. Organizational sociology -- Research.
Chunhu Jeon. Kristen Raney. Wookyung Lee. Preview abstract. Restricted access Research article First published October 11, 2022 pp. 140-166. xml GET ACCESS. Table of contents for Organizational Research Methods, 27, 1, Jan 01, 2024.
Research methods are specific procedures for collecting and analyzing data. Developing your research methods is an integral part of your research design. When planning your methods, there are two key decisions you will make. First, decide how you will collect data. Your methods depend on what type of data you need to answer your research question:
Background: Increasing health care expenditure in the United States has put policy makers under enormous pressure to find ways to curtail costs. Starting January 1, 2021, hospitals operating in the United States were mandated to publish transparent, accessible pricing information online about the items and services in a consumer-friendly format within comprehensive machine-readable files on ...
Books. Research Methods and Organization Studies. Alan Bryman. Routledge, 1989 - Social Science - 283 pages. Heinrich Schenker: A Research and Information Guide is an annotated bibliography concerning both the nature of primary sources related to the composer and the scope and significance of the secondary sources which deal with him, his ...
The main strength of the study comes from its clinical and longitudinal approaches. The use of patient-interviews combined with clinical records, self-report data and register-based information will enhance the analyses and may uncover important associations between the individual patients, treatment, and the organizational level of healthcare services.
The report includes a methods section. In addition, this post uses data from StatPearls, an online health care resource, on complications from abortion. ... About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling ...
Organizational Research Methods (ORM) was established to bring relevant methodological developments to researchers working in organizational sciences. ORM's goal is to enhance the use of current and new methodologies to advance theory and research practice. Articles should be understandable to readers with background knowledge consistent with ...
Background and rationale. Dementia is a common disease and in 2021, the World Health Organization estimated that around 55 million people have dementia worldwide [].Dementia is a neurodegenerative syndrome characterized by a progressive deterioration of cognitive function, in particular memory but other cognitive domains such as language, praxis, visual perception and most notably executive ...
Research Methods for Organizational Studies. Beautifully written and thoroughly class-tested, this practical text provides students of management and organizational studies with clear guidelines for conducting real-world research. Unusually applied, it provides tools with which to do research (data sets and statistical software) and discusses ...
An improved understanding of the cellular and molecular biologic processes responsible for brain tumor development, growth, and resistance to therapy is fundamental to improving clinical outcomes. Imaging genomics is the study of the relationships between microscopic, genetic, and molecular biologic features and macroscopic imaging features. Imaging genomics is beginning to shift clinical ...