- Open access
- Published: 21 June 2021

A review of research-supported group treatments for drug use disorders
- Gabriela López 1 ,
- Lindsay M. Orchowski ORCID: orcid.org/0000-0001-9048-3576 2 ,
- Madhavi K. Reddy 3 ,
- Jessica Nargiso 4 &
- Jennifer E. Johnson 5
Substance Abuse Treatment, Prevention, and Policy volume 16 , Article number: 51 ( 2021 ) Cite this article
27k Accesses
8 Citations
3 Altmetric
Metrics details
This paper reviews methodologically rigorous studies examining group treatments for interview-diagnosed drug use disorders. A total of 50 studies reporting on the efficacy of group drug use disorder treatments for adults met inclusion criteria. Studies examining group treatment for cocaine, methamphetamine, marijuana, opioid, mixed substance, and substance use disorder with co-occurring psychiatric conditions are discussed. The current review showed that cognitive behavioral therapy (CBT) group therapy and contingency management (CM) groups appear to be more effective at reducing cocaine use than treatment as usual (TAU) groups. CM also appeared to be effective at reducing methamphetamine use relative to standard group treatment. Relapse prevention support groups, motivational interviewing, and social support groups were all effective at reducing marijuana use relative to a delayed treatment control. Group therapy or group CBT plus pharmacotherapy are more effective at decreasing opioid use than pharmacotherapy alone. An HIV harm reduction program has also been shown to be effective for reducing illicit opioid use. Effective treatments for mixed substance use disorder include group CBT, CM, and women’s recovery group. Behavioral skills group, group behavioral therapy plus CM, Seeking Safety, Dialectical behavior therapy groups, and CM were more effective at decreasing substance use and psychiatric symptoms relative to TAU, but group psychoeducation and group CBT were not. Given how often group formats are utilized to treat drug use disorders, the present review underscores the need to understand the extent to which evidence-based group therapies for drug use disorders are applied in treatment settings.
Drug use disorders are a significant public health concern in the United States. According to the National Epidemiologic Survey of Alcohol and Related Conditions-III, the lifetime prevalence rate of DSM-5 drug use disorders is 9.9%, which includes amphetamine, cannabis, club drug, cocaine, hallucinogen, heroin, opioid, sedative/tranquilizer, and solvent/inhalant use disorders [ 1 ]. Drug use disorders are defined in terms of eleven criteria including physiological, behavioral and cognitive symptoms, as well as consequences of criteria, any two of which qualify for a diagnosis [ 2 , 3 ]. The individual and community costs of drug use are estimated at over $193 billion [ 4 , 5 ] and approximately $78.5 billion [ 6 ] for opioids alone. Consequences include overdose [ 7 ], mental health problems [ 8 ], and a range of medical consequences such as human immunodeficiency virus [ 9 , 10 ], hepatitis C virus [ 9 ], and other viral and bacterial infections [ 11 ].
Evidence-based practice was formally defined by Sackett et al. [ 12 ] in 1996 to refer to the “conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients” (p. 71). In 2006, the American Psychological Association [ 13 ] developed a policy on evidence-based practice (EBP) of psychotherapy, which emphasized the integration of best research evidence (i.e., data from meta-analyses, randomized controlled trials, effectiveness trials, and other forms of systematic case studies and reviews) with clinical expertise and judgment to deliver treatment in the context of a patient’s individual needs, preferences and culture. The shift towards EBP for substance use disorders has multiple benefits for practitioners and patients, including an increased focus on the implementation of treatments that are safe and cost-effective [ 14 ]. A recent survey of clinicians’ practices with substance use treatment found that clinicians often conducted therapy in groups [ 15 ]. While most clinicians who completed the survey reported use of evidence-based treatment practices (EBT) some also reported the use of non-EBT practices [ 15 ]. Ensuring that clinicians can readily access information regarding the current state of evidence regarding group-based therapies for substance use disorders is critical for fostering increased use of EBTs.
Although any effort to summarize a literature as large and complex as the psychological treatment literature is useful, there are several limitations. With few exceptions, research-supported treatment lists categorize treatments by formal change theory (e.g., cognitive-behavioral, interpersonal) and describe little about the context, format, or setting in which treatments were conducted and tested [ 16 ]. As a result, it is often difficult to ascertain from existing resources whether research supported treatments were conducted in group or individual format. A group format is often used in substance use treatment [ 17 ] and aftercare programs [ 18 , 19 , 20 , 21 , 22 ] . The discrepancy between the wide-spread use of group therapy in clinical practice and the relative paucity of research on the efficacy of group treatments has been noted by treatment researchers [ 23 ] and clinicians [ 24 ]. According to Lundahl’s [ 25 ] 2010 meta-analysis of studies evaluating the efficacy of motivational interviewing (MI), a commonly used treatment for substance use disorders, examination of the 119 studies concluded that studies of MI in a group format were too rare to draw solid conclusions about the efficacy of group MI. Also, it is possible that efficacy of treatments developed for individual delivery will be altered when delivered in a group format and vice versa. Given the limited empirical inquiry on group treatments for substance use, a framework organizing the literature on the efficacy of group therapy to treat substance use disorders would be useful. There is also a need for a more recent rigorous review of the empirical evidence to support group-based treatments for substance use disorders. Over 15 years ago, Weiss and colleagues conducted a review of 24 treatment outcome studies within the substance use disorder intervention literature comparing group therapy to other treatments conditions (i.e., no group therapy, individual therapy, group therapy plus individual therapy), and found no differences between group and individual therapy [ 26 ].
Given the importance of understanding the current evidence base for group-delivered treatments for substance use disorders, the present review sought to provide a summary of the literature on the benefits of group treatments for drug use disorders. Group treatments are potentially cost-effective, widely disseminable, and adaptable to a variety of populations but are lagging individual treatments in terms of research attention. Thus, highlighting characteristics of group treatments that are potentially efficacious is of import to stimulate further empirical inquiry. The review is organized by drug type (cocaine, methamphetamine, marijuana, opiate, mixed substance use disorders; SUD) and co-occurring SUD and psychiatric problems. We excluded studies focused on alcohol use disorder alone as this literature is summarized elsewhere (see Orchowski & Johnson, 2012). Given research suggesting that several factors impact outcomes of group treatments, including formal change theory driving the treatment approach (i.e., cognitive-behavioral, motivational interviewing), as well as patient factors [ 27 ], the review begins by first reviewing each theory of change (i.e., type of treatment), and then concludes by summarizing the research examining the extent to which patient factors influence the efficacy of group treatments for SUD.
To locate studies that evaluated a group treatment for SUD that met review inclusion criteria, the authors conducted a comprehensive literature search of PsycINFO and MedLine through 2020. Three individuals then examined abstracts of the articles for relevance. In addition, the authors utilized the reference lists of review studies and meta-analyses of SUD- treatments to locate additional studies that might meet the review inclusion criteria. The authors and a research assistant then reviewed full articles with relevance to the current study and excluded any studies that did not meet the review inclusion criteria (see Fig. 1 ).
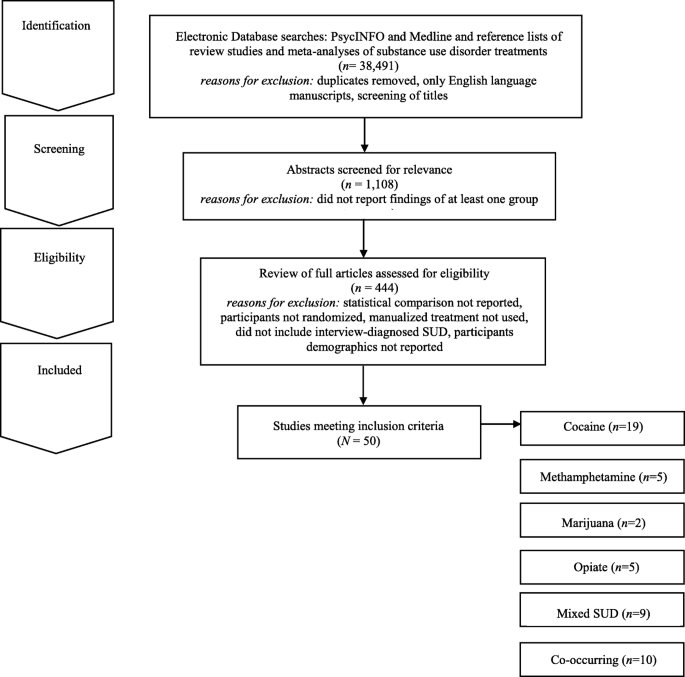
Electronic Search Strategy Flowchart
For inclusion in the review, studies needed to meet the following criteria: 1) report the findings of at least one group treatment; 2) provide at least one statistical comparison between the group treatment and a control condition; 3) randomize participants between the group treatment and control condition; 4) utilize a manualized treatment; 5) include patients with an interview-diagnosed SUD; and 6) provide information regarding the demographic characteristics of the participants in the study. Studies’ methods and results were used for data extraction. Studies which maintained a primary focus on the treatment of SUD, but also included treatment of a co-occurring psychiatric condition, were included in the review. Studies which included alcohol use as a comorbid diagnosis along another substance use were included. Studies examining the efficacy of group treatment for only alcohol use were excluded. The final set of articles included were 50 research studies that utilized a group treatment modality for the treatment of SUD, including separately examining cocaine, methamphetamine, marijuana, opioid, mixed substance, or SUD with comorbid psychiatric problems in adults.
It should be noted that several studies that met inclusion criteria were not reported in the present review because they did not report the use of a specific screening instrument for SUD as a part of the study inclusion/exclusion criteria. These studies are as follows and include these comparisons: group-based relational therapy [ 28 ] two studies by Guydish et al. [ 29 , 30 ] comparing a day treatment program to residential treatment (RT) program, a day treatment program to a coping skills group [ 31 ], standard care to a harm reduction group [ 32 ], 12 step group to a CBT group [ 33 ], medical management treatment (MMT) with CBT group to an MMT plus treatment reinforcement plan [ 34 ], treatment as usual to contingency management (CM) [ 35 ], professionally led recovery training group to treatment as usual (TAU) [ 36 ], two 4 month residential treatment programs [ 37 ], varying lengths of therapeutic community program (TPC) with and without relapse prevention [ 38 ], and Information and Referral plus peer advocacy to a Motivational group with CBT group [ 39 ].
Review of evidence-based theories of change
The 50 research studies meeting inclusion criteria tested the following group treatment modalities: contingency management (CM), motivational interviewing (MI), relapse prevention (RP), social support (SS), cognitive-behavioral (CBT), coping skills (CS), harm reduction (HR), cognitive therapy (CT), drug counseling (DC), recovery training (RT), standard group therapy (SGT), family therapy (FT), intensive group therapy (IGT), 12 step facilitation group therapy (12SG), relational psychotherapy mothers’ group (RPMG), psychoeducational therapy group (PET), behavioral skills (BS), and seeking safety (SS). Below, we briefly review the theory of change that drives each of these treatments.
Several treatment approaches are grounded in behavioral therapies and/or cognitive therapies. Broadly, cognitive therapy is an approach that focuses exclusively on targeting thoughts that are identified as part of a diagnosis or behavioral problem [ 28 ]. Cognitive-behavioral (CBT) therapy is an approach that targets specific symptoms, thoughts, and behaviors that are identified as part of a diagnosis or presenting problem [ 28 ]. Under the umbrella of CBT several other treatment modalities exist. For example, relapse prevention is a CBT treatment that hypothesizes that there are cognitive, behavioral, and affective mechanism that underlie the process of relapse [ 40 ]. Recovery training is a more specific form of relapse prevention, including education on addiction and recovery and reinforcing relapse prevention skills (e.g., understanding triggers, coping with cravings etc.) [ 41 , 42 ]. Other treatments focus on coping skills more broadly. For example, coping skills treatments include a focus on components of adaptability in interpersonal relationships, thinking and feeling, as well as approaches to self and life [ 28 ]. Some treatment approaches also recognize that individuals may not be ready to change their substance use. For example, motivational interviewing is often described as a therapy guiding technique in which the therapist is a helper in the behavior change process and expressed acceptance of the patient [ 43 ]. Standard group therapy includes 90 min sessions approximately twice a week in a group setting, [ 44 ] whereas intensive group therapy is a heavier dose of standard group therapy that includes 120-min sessions up to five times a week [ 44 ]. Psychoeducational therapy group focused on providing information on the immediate and delayed problems of substance use disorders to patients [ 45 ]. Lastly, dialectical behavior therapy (DBT) is a type of CBT therapy that focuses on helping regulate intense emotional states and provides skills to reduce arousal levels, and increase mindfulness, emotional regulation, and interpersonal skills [ 46 ].
Grounded within behavioral therapies, are behavioral skills training which focused on developing behaviors that are adaptive [ 28 ]. Contingency management is a type of behavioral therapy in which patients are reinforced or rewarded for positive behavioral change [ 47 ]. Harm reduction is a term for interventions aiming to reduce the problematic effects of behaviors [ 48 ]. Several treatment approaches also focus on interpersonal networks and building interpersonal skills. For example, social support is any psychological resources provided by a social network to help patients cope with stress [ 49 ]. Twelve-step facilitation group therapy is a more specific form of social support, which focuses on introducing patients to the 12 steps of alcoholics anonymous or related groups (i.e., cocaine or narcotics anonymous) to encourage 12-step meeting attendance in their community [ 33 , 50 ]. Seeking Safety is a present-focused and empowerment-based intervention focused on coping skills that emphasizes the importance of safety within interpersonal relationships [ 51 ]. Drug counseling describes treatment that aims to facilitate abstinence, encourage mutual support, and provide coping skills [ 52 ]. Finally, family therapy is a family-based intervention that aims to change, parenting behaviors and family interactions [ 53 ]. Overall, there are many overlapping components and skill sets in the models discussed above (See Table 1 ).
Group-based cocaine use treatments for adults
Nineteen studies were identified that targeted cocaine use and utilized some form of group therapy, the most of any drug in this review (see Table 2 ). Overall, the studies showed that all of the group therapy modalities included in this review generally reduced cocaine use when compared to treatment as usual (TAU), including day hospital groups [ 54 ]. Two studies, Magura et al. (1994) and Magura et al. (2002) did not find group differences between 8 months CBT and 8 months of TAU that consisted of methadone maintenance therapy among 141 patients with cocaine disorder [ 60 , 69 ]. When compared directly, individuals in CBT groups achieved longer abstinence than individuals in 12 step facilitation groups [ 33 ] or low intensity groups [ 64 , 65 ]. However, in another study, individuals with cocaine dependence receiving 12-step based Group Drug Counseling (GDC; similar to 12-step facilitation) had similar cocaine abstinence outcomes with or without additional individual CBT [ 41 ]. This may suggest that group 12-step facilitation is an effective intervention for cocaine dependence. Two studies demonstrated the superiority of CM groups for reducing cocaine use as compared to CBT [ 62 ] or TAU groups [ 61 , 62 ] at 12 weeks [ 54 ], 17 weeks [ 53 ], 26 weeks [ 53 ] and 52 weeks follow up [ 51 ]. Therefore, CBT group therapy and contingency management groups appear to be more effective at reducing cocaine use than TAU groups.
Group-based methamphetamine use treatments for adults
Only five treatment studies were identified that examined group treatments for methamphetamine use (see Table 3 ). Three studies found longer periods of abstinence for the group treatment (CM or drug+CM) than for TAU or non-CM conditions. The first study conducted by Rawson and colleagues compared matrix model (MM) with TAU in eight community outpatient settings [ 71 ]. The MM consisted of CBT groups, family education groups, social support groups, and individual counseling sessions along with weekly urine screens for 16 weeks. Participants in the MM condition attended more sessions, stayed in treatment longer, had more than twice as many contacts, evidence longer abstinence and greater self-reported psychosocial functioning relative to the TAU group. However, these significant differences did not persist 6 months later at follow-up.
Shoptaw et al. (2006) [ 73 ] compared four groups for treating methamphetamine dependence sertraline + CM, sertraline only, placebo + CM, and placebo [ 73 ]. Additionally, all participants attended a relapse prevention group conducted three times a week over a 14-week period. Findings provided support for the efficacy of CM for amphetamine use disorders. Group treatment (CM or drug + CM) was more effective for sustaining longer periods of abstinence relative to TAU or non-CM conditions. Roll et al. [ 72 ] found that effects of CM relative to TAU became larger as the duration of CM increased. Jaffe et al. [ 70 ] evaluated a culturally tailored intervention for 145 methamphetamine dependent gay and bisexual males. Participants in the Gay Specific CBT condition reported the most rapid decline in levels of methamphetamine use relative to standard CBT, CBT + CM, suggesting benefits for culturally appropriate group methamphetamine interventions.
Group-based marijuana use treatments for adults
Two studies examining group treatments for adults with marijuana use disorders were identified (see Table 4 ). Both studies were conducted by the same research group, utilizing the same inclusion criteria for marijuana use (50 times in 90 days). The studies examined group relapse prevention (RP) [ 76 ], specifically designed for adult marijuana users. The first trial [ 75 ] ( n = 212) comparing relapse prevention to a social support group found participants in both group treatment conditions did well overall, with two-thirds (65%) reporting abstinence of marijuana use for 2 weeks after session 4 or the quit date and 63% reporting abstinence during the last 2 weeks of treatment. Gender differences emerged; no differences between group treatments were found for women, but men in the relapse prevention group reported reduced marijuana use at the 3-month follow-up compared to men in the social support group.
A second trial [ 74 ] randomized participants to 14 sessions of group RP enhanced with cognitive behavioral skills training, two sessions of motivational interviewing (MI) with feedback and advice on cognitive behavioral skills (modeled after the Drinkers Check-up) [ 77 ], or a 4-month delayed treatment control (DTC) group which consisted of the RP group or individual MI treatment of the participants choosing. Compared to individuals randomly assigned to the DTC condition, participants in the group RP and individual MI conditions evidenced a significantly greater reduction in marijuana use and related problems over 16-month follow-up. However, examination of participants’ reactions to DTC assignment indicated that participants who felt that changing their marijuana use was their own responsibility were more likely than those who did not to change their use patterns without treatment engagement.
Group-based opiate use treatments for adults
Five group treatment studies for opioid use were identified (see Table 5 ). Two studies compared the effectiveness of pharmacotherapy plus group therapies [ 79 , 80 , 81 ] to pharmacotherapy alone in samples of opioid dependent persons, and both found that adding group treatment improved outcomes. The first study compared Naltrexone with monthly medical monitoring visits to an enhanced group condition (EN) consisting of Naltrexone plus a Matrix Method (MM) [ 79 ]. MM consisted of hourly individual sessions, 90-min CBT group, and 60 min of cue-exposure weekly for weeks 1–12; hourly individual sessions and CBT group sessions for weeks 13–26; and 90-min social support group sessions for weeks 27–52. Results found that EN participants took more study medication, were retained in treatment longer, used less opioids while in treatment, and showed greater improvement on psychological and affective dimensions than Naltrexone only participants. No difference by treatment condition was found at 6- and 12-month follow-ups. Similarly, Scherbaum et al. [ 80 ] compared routine Methadone Maintenance Therapy (MMT) with routine MMT plus group CBT psychotherapy (20 90-min sessions for 20 weeks). MMT plus group CBT participants showed less drug use than participants in the MMT group (i.e., control group). In contrast, a higher dose of group therapy provided without methadone maintenance was less effective for heroin use than was a lower dose of group therapy with methadone maintenance (Sees et al. [ 81 ]. This suggests that the combination of pharmacotherapy and group therapy for opioid use is optimal.
Shaffer et al. [ 22 ] compared psychodynamic group therapy with a hatha yoga group. All participants received methadone maintenance and individual therapy. No differences between two treatment conditions were found. For all participants, longer participation in treatment was associated with reduction in drug use and criminal activity. Lastly, Des Jarlais et al. [ 78 ] compared a group social learning AIDS/drug injection treatment program (4 sessions, 60–90 min, over 2 weeks) to a control condition. All participants received information about AIDS and HIV antibody test counseling. Compared to control participants, intervention participants reported lower rates of drug injection over time.
Group treatments for mixed SUD for adults
Nine treatment studies were identified that targeted mixed substance use with group treatments (see Table 6 ). Three involved CBT. Downey et al. [ 82 ] compared group CBT plus individual CBT to group CBT plus vouchers in a sample of 14 polysubstance users (cocaine and heroin) maintained on buprenorphine. The study was significantly underpowered and they found no significant differences on treatment outcomes. Marques and Formiogioni [ 84 ] compared individual CBT to group CBT in a sample of 155 participants with alcohol and/or drug dependence. They found that both formats resulted in similar outcomes, with higher compliance in the group CBT participants (66.7% compliance with treatment). Rawson et al. [ 87 ] compared three 16-week treatments: CM, group CBT, and CM plus group CBT, among 171 participants with cocaine disorder or methamphetamine abuse. They found that CM produced better retention and lower rates of stimulant use than CBT during treatment, but CBT produced comparable longer-term outcomes.
Two studies involved Group Drug Counseling (GDC). Greenfield et al. [ 52 ] compared a group drug counseling (GDC) (mixed gender) to a women’s recovery group (WRG) that both met weekly, for 12 weeks, for 90-min sessions among 44 participants that had a substance use disorder other than nicotine. WRG evidenced significantly greater reductions in drug and alcohol use over the follow up compared with GDC. Schottenfeld et al. [ 88 ] compared GDC (weekly, 1-h group sessions) to a community reinforcement approach (CRA; twice weekly sessions for the first 12 weeks and then weekly the following 12 weeks) among 117 patients with an opioid and cocaine use disorder. There were no differences in retention or drug use.
Remaining studies examined other interventions. Margolin et al. [ 83 ] compared an HIV Harm reduction program (HHRP) that met twice weekly for 2 h to an active control group that met six times in a sample of 90 HIV-seropositive methadone-maintained injection drug users with opioid dependence, and abuse or dependence on cocaine. At follow up, they had lower addiction severity scores and were less likely to have engaged in high risk behaviors compared to control. McKay et al. [ 85 ] compared weekly phone monitoring and counseling plus a support group in the first 4 weeks (TEL), twice-weekly individualized relapse prevention, and twice-weekly standard group counseling (STND) among 259 referred participants with alcohol use disorder or cocaine disorder. STND resulted in more days abstinent than TEL. Nemes et al. [ 86 ] compared a 12-month group program (10 months inpatient and 2 months outpatient) to an abbreviated group program (6 months inpatient, 6 months outpatient) among 412 patients with multiple drug/alcohol use disorders. Results indicated that both groups had reduction in arrests and drug use. There were no significant difference between groups. Lastly, Smith et al. [ 89 ] compared a standard treatment program (STP, daily group counseling, family outreach, 12-step program introduction, four 2 h sessions for family) to an enhanced treatment program (ETP; twice weekly group on relapse prevention and interpersonal violence in additional to all STP components) among 383 inpatient veterans meeting for an alcohol, cocaine, or amphetamine use disorder. Results indicated that ETP had enhanced abstinence rates at 3-month and 12-month follow up compared to STP, regardless of type of drug use.
Group Treatments for SUD and Co-Occurring Psychiatric Problems
Individuals with psychiatric distress are at high risk for comorbid SUD [ 90 ]. Ten randomized controlled studies meeting our inclusion criteria examined the efficacy of group therapy for SUD and co-occurring psychiatric problems (see Table 7 ). Three studies described group treatment of SUD and co-occurring DSM-IV Axis II disorders [ 18 , 91 , 96 ], three studies examined group treatment of drug abuse and co-occurring DSM-IV classified Axis I disorders [ 92 , 93 , 99 ], one study explored group drug abuse treatment and co-occurring psychiatric problems among homeless individuals without limiting to DSM-IV Axis I or Axis II diagnoses [ 97 ], and one study focused on group drug treatment among individuals testing positive for HIV [ 98 ]. Within this diverse set of RCTs, participants generally included individuals diagnosed with any form of SUD; however, some studies focused specifically on individuals using cocaine [ 91 , 97 ] or cocaine/opioids [ 98 ].
A range of group treatment approaches are represented, including group psychoeducational therapy, group CBT approaches, group DBT, Seeking Safety and CM. DiNitto and colleagues [ 92 ] evaluated the efficacy of adding a group-based psychoeducational program entitled “Good Chemistry Groups” to standard inpatient SUD treatment services among 97 individuals with a dual diagnosis of SUD and a DSM-IV Axis I psychological disorder. The nine 60-min Good Chemistry Group sessions were offered 3 times per week for 3 weeks. When compared to standard inpatient treatment, the addition of the psychoeducational group was not associated with any changes in medical, legal, alcohol, drug, psychiatric or family/social problems among participants.
The efficacy of adding a psychoeducational group treatment to standard individual therapy to address HIV risk among cocaine users has also been examined [ 91 ]. Participants were randomly assigned to complete the following: 1) individually-administered Standard Intervention developed by the NIDA Cooperative Agreement Final Cohort sites [ 100 ] including HIV testing, and pre- and post-HIV testing counseling on risks relating to cocaine use, transmission of STDs/HIV, condom use, cleaning injection equipment, and the benefits of treatment; or) Standard Intervention plus four 2-h peer-delivered psychoeducational groups addressing stress management, drug awareness, risk reduction strategies, HIV education and AIDS. Among the sample of 966 individuals completing the 3-month follow-up, the group psychoeducational treatment was not differentially effective in reducing drug use and HIV risk behavior in comparison to standard treatment alone at 3-months post-baseline, regardless of treatment type, individuals with antisocial personality disorder (ASPD) demonstrated less improvement in crack cocaine use compared to individuals without ASPD or depression.
The following types of group CBT have sustained research evaluation meeting our inclusion criteria to address co-occurring SUD and Axis I or Axis II disorders: 1) group behavioral skills training; 2) group cognitive behavioral therapy; 3) group-based Seeking Safety [ 51 ], and 4) group dialectical behavioral therapy. Specifically, Jerrell and Ridgely [ 93 ] examined the efficacy of group behavioral skills (BS) training, group-based 12-step facilitation (TS) treatment, and intensive case management among 132 individuals with a dual diagnosis of SUD and another Axis I psychiatric problem over the course of 24-months. Based on the Social and Independent Living Skills program [ 101 ], the BS group included one group per week addressing self-management skills designed to enhance abstinence, including medication management, relapse prevention, social skills, leisure activities and symptom monitoring. Relative to participants in TS groups, participants in the BS groups evidenced increased psychosocial functioning and decreased psychiatric symptoms (i.e., schizophrenia, depressive symptoms, mania, drug use and alcohol use) across the 6-, 12- and 18-month follow-up assessments after treatment entry.
Lehman and colleagues’ [ 95 ] examination of the efficacy of group CBT for substance abuse compared to TAU among 54 individuals with SUD and either schizophrenia or a major affective disorder revealed no differences between treatment groups over the course of a 1-year follow-up period. More promising findings were reported in Fisher and Bentley’s [ 18 ] evaluation of a group CBT and group therapy based in the disease and recovery model (DRM) among 38 individuals with dual diagnosis of SUD and a personality disorder. Groups met three times per week for 12 weeks and were compared to TAU. Individuals in group CBT and group DRM indicated improved social and family functioning compared to TAU, and among those who completed the group in an outpatient setting, CBT was more effective in reducing alcohol use, enhancing psychological functioning and improving social and family functioning compared to DRM and TAU.
Group behavioral therapy plus abstinence contingent housing and work administered in the context of a day treatment program was compared to behavioral group treatment alone among individuals with cocaine abuse/dependence, non-psychotic psychiatric conditions, and homelessness [ 97 , 102 ]. The group behavioral therapy included 8 weeks of daily treatment (4 h and 50 min per day) of groups addressing relapse prevention training, assertiveness training, AIDS education, 12-step facilitation, relaxation, recreation development, goal setting, and goal planning. Participants also engaged in a process-oriented group as well as individual counseling and urine monitoring and engaged in a weekly 90 min psychoeducational group therapy during months 3–6 following treatment enrollment. Individuals who received contingency-based work and housing were provided with rent-free housing and employment in construction or food service industries after 2 consecutive weeks of abstinence [ 103 ]. Relative to BS groups alone, group behavioral day treatment plus contingency management was associated with greater abstinence at 2- and 6-month follow-ups [ 102 ] and were less likely to relapse [ 97 ], although gains were not maintained at 12-months [ 104 ]. Both groups evidenced positive changes in drug use overtime compared to baseline [ 104 ].
Zlotnick, Johnston and Najavits [ 99 ] evaluated the efficacy of Seeking Safety (SS), in comparison to treatment as usual (TAU) among 49 incarcerated women with substance use disorder (SUD) and full or subthreshold posttraumatic stress disorder (PTSD). SS aims to decrease PTSD and SUD through psychoeducational and present-focused and empowerment-based instruction on coping skills that emphasize abstinence and safety [ 51 ]. The SS group treatment included 90-min group sessions held three times per week, that were completed in addition to the 180 to 240 h of group and individual therapy provided in TAU. All participants showed similar improvement on assessments of PSTD, SUD, legal problems and other psychiatric concerns at 12-week, 3- and 6-month follow-ups following prison release. Nonetheless, there was a trend for improved PTSD and continued improvements in psychiatric symptoms at follow-up among participants completing SS compared to TAU. Greater completion of SS sessions was associated with increased improvement in PTSD as well as drug use among women [ 99 ].
Dialectical behavioral group therapy (DBT), a CBT-focused treatment for individuals with borderline personality disorder (BPD), has also been evaluated in comparison to TAU among individuals with BPD and co-occurring SUD [ 96 ]. Core elements of DBT are manualized [ 105 ], and have been evaluated in prior research [ 106 , 107 , 108 ]. Techniques center on providing the participant with acceptance and validation while maintaining a continual focus on behavior change, and include the following: mindfulness skills training, behavioral analysis of dysfunctional behavior, cognitive restructuring, coping skills training, exposure-based strategies addressing maladaptive emotions, and behavioral management skills training. DBT was administered through 2 ¼ hour weekly group sessions administered in combination with 60 min of weekly individual therapy and the opportunity for skills-coaching phone calls. Relative to TAU, participants randomly assigned to DBT demonstrated greater reductions in drug use during the 12-month treatment and at the 16-month follow-up assessment, as well as greater gains in adjustment at the 16-month follow-up assessment.
Although contingency management is commonly administered individually, Petry and colleagues [ 98 ] examined the efficacy of weekly 60-min group-based contingency management (CM) for reinforcing health behaviors and HIV-positive individuals with cocaine or opioid disorders ( N = 170) in comparison to 12-step facilitation (TS) over the course of a 24-week period. Overall, participants in CM were more likely than those in TS to submit consecutive drug-free urine specimens, although the overall proportion of drug-free specimens did not vary between groups during treatment or over the follow-up period. Notably, during treatment, group CM was associated with greater reductions in HIV-risk behaviors as well as overall viral load compared to TS; although effects were not maintained over the follow-up period.
Across these studies, many trials showed positive gains for both group treatments examined [ 18 , 97 , 98 ], or no difference between groups when examining the benefit of adding group treatment to existing TAU [ 91 , 92 , 95 , 99 ]. However, one study demonstrated greater reductions in drug use among individuals with BPD and SUD who completed group DBT in comparison to TAU [ 96 ]. Further, BS groups were more effective than TS groups in improving psychosocial functioning and decreasing substance use [ 93 ]. Finally, CBT was more effective than DRM in reducing alcohol use, enhancing psychological functioning and improving social and family functioning compared to DRM and TAU among individuals dually diagnosed with SUD and a personality disorder [ 18 ].
Factors associated with treatment efficacy
Gender and treatment efficacy.
Five of the studies included in the present review examined whether treatment was differentially effective for men and women. Although Jarrell and Ridgely’s [ 93 ] evaluation of group BS, group TS and individual case management for individuals with SUD and co-occurring Axis I disorders did not examine whether group treatment types were differentially effective for men and women, data indicated that women—regardless of treatment group—reported higher role functioning (i.e.., independent living, work productivity, as well as immediate and extended social relationships), increased psychiatric symptomatology (depression, mania, drug use, alcohol use) across the follow-up periods compared to men.
Race and ethnicity and treatment efficacy
Among the studies included in the present review, only three examined whether treatment efficacy varied as a function of race and ethnicity. A secondary examination of the efficacy of group BS in comparison to group TS and individual case management [ 93 ] suggested that outcomes in each group treatment among ethnic and racial minority clients were equivalent to White participants during the 6-month follow [ 94 ]. The initial evaluation indicated that—regardless of group treatment type—racial/ethnic minority participants reported lower scores in personal well-being, lower life satisfaction (i.e., satisfaction with living), worse role functioning (i.e., independent living, work productivity, immediate and extended social relationships) over the follow-up periods compared to White participants [ 93 ].
Conclusions
In general, participants in group treatment for drug use disorders exhibit more improvement on typical measures of outcome (e.g., abstinence & use rates, objective measures, urinalysis) when compared to standard care without group [ 18 , 109 ] and those who refuse or drop out of treatment [ 110 ]. Specifically, CBT and CM appear to be more effective at reducing cocaine use than TAU groups. CM is effective in increasing periods of abstinence among users of methamphetamine. Both relapse prevention and social support group therapy were effective for marijuana use although relapse prevention was more helpful for men than for women. Brief MI and relapse prevention were both effective at reducing marijuana use. CBT and CBT-related treatments (including the matrix model) when added to pharmacotherapy were more effective for opioid use disorder than pharmacotherapy alone. Effective treatments for Mixed SUD include group CBT, CM, and women’s recovery group. Longer relapse prevention periods appear to be more helpful in reducing mixed SUD. Behavioral skills and behavioral skills plus contingency management helped decreased psychiatric symptoms and drug use behaviors. Psychoeducation groups alone, a commonly used intervention, were not effective at addressing SUD and co-occurring psychiatric problems. Additionally, it is important to note that there is potential for risk of bias in the studies included across four domains: participants, predictors, outcome, and analysis [ 111 ]. The current study did not comprehensively assess for risk of bias and this is a study limitation. Future research could assess for risk of bias by following the guidelines suggested by the Cochrane Handbook [ 112 ].
The current literature offers a wide variety of group treatments with varying goals and based on varying formal change theories. Overall, studies that reported between-group effect size ( n = 7) reported small to medium effect sizes potentially suggesting differences were moderate but of potential theoretical interest. Of those seven studies, only two studies reported large effect sizes (both comparing an active treatment to a delayed treatment/untreated condition). In order to better characterize magnitude of intervention effects, future studies should report effect sizes and their confidence intervals [ 113 , 114 ]. Moreover, groups based on cognitive-behavioral theory [ 35 ], motivational enhancement theory [ 43 ], stages of change theory [ 115 ], 12-step theory [ 41 ] and psychoeducational group models [ 116 ] have all been the subject of recent studies. Steps of treatment have also been used to classify groups for acutely ill individuals with SUD versus middle stage (recovering) or after care groups, with the latter mainly focusing on relapse prevention. Group therapy is provided – at least as an augment to multimodal interventions – in most of the outpatient and inpatient programs in English speaking and European countries [ 17 , 117 ]. Therefore, continued efforts to implement and scale up group-based treatments for SUD known to be effective are needed. CM appears to be effective at addressing various drug use problems and further research should evaluate whether it would also be useful for marijuana use.
Future Research Questions
Studies of other group treatments for SUD that use rigorous, interview-based diagnosis, use control groups, randomly assign participants to condition, report the ethnic and racial composition of the sample, are adequately powered, implement a treatment manual, and compare outcomes to individual treatment as well are necessary.
Little is known regarding the possible mediators and moderators of treatment outcome in group interventions for SUD
Key Learning Objectives
Group treatment approaches are widely utilized and are often less costly to implement than individual treatments, currently we know very little whether one group approach is superior to another in the treatment of SUD.
Group treatment approaches seem to be more effective at improving positive outcomes (e.g., abstinence, use rates, objective measures, urinalysis) when compared to standard care without group [ 18 , 109 ], and those who refuse and drop out of treatment
More thorough randomized controlled trials of group SUD treatments are needed [ 110 ].
Availability of data and materials
Not applicable. The present study does not include original data. However, the authors of the study have listed all articles reviewed in this study in the reference section.
Abbreviations
Twelve Step Facilitation Group Therapy
Alcohol Dependence
Acquired Immunodeficiency Syndrome
Addiction Severity Index
Antisocial Personality Disorder
Abbreviated Program
Behavioral Skills
Borderline Personality Disorder
Cognitive Behavioral Therapy
Cocaine Dependence
Composite Diagnostic Interview Schedule
Contingency Management
Community Reinforcement Approach
Coping Skills
Cognitive Therapy
Dialectical Behavioral Therapy
Day Treatment
Drug Counseling
Diagnostic Interview Schedule
Diagnostic and Statistical Manual
Disease and Recovery Model
Delayed to Control
Evidence-Based Practice
Evidence-Based Treatment Practice
Enhanced Group Condition
Enhanced Treatment Program
Family Therapy
Group Drug Counseling
Human Immunodeficiency Virus
HIV Harm Reduction
Harm Reduction
Intensive Group Therapy
Individual Therapy
Motivational Interviewing
Matrix Model
Methadone Maintenance Therapy
National Institute of Drug Abuse
Psychoeducational Therapy Group
Pre-Post with Comparison Group (matched or otherwise)
Post Traumatic Stress Disorder
Random Assignment with Control
Relapse Prevention
Recovery Training
Random Assignment to Active Treatment
Relational Psychotherapy Mothers’ Group
Structured Clinical Interview for Diagnosis
Social Support
Standard Group Therapy
Substance Use Disorder
Seeking Safety
Standard Group Counseling
Standard Treatment Program
Treatment as Usual
Phone Monitoring and Counseling, with Support Group
Therapeutic Community Program
Twelve Step
Women’s Recovery Group
Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, et al. Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on alcohol and related conditions-III. JAMA Psychiatry. 2016;73(1):39–47.
Article PubMed PubMed Central Google Scholar
Edition F. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed; 2013.
Google Scholar
Rehm J, Marmet S, Anderson P, Gual A, Kraus L, Nutt DJ, et al. Defining substance use disorders: do we really need more than heavy use? Alcohol Alcohol. 2013;48(6):633–40.
Article CAS PubMed Google Scholar
Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011;12(4):657–67.
Article PubMed Google Scholar
Center NDI. National Drug Threat Assessment. Washington: United States Department of Justice; 2011.
Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54(10):901–6.
Kamal R, Cox C, Rousseau D, Foundation ftKF. Costs and outcomes of mental health and substance use disorders in the US. JAMA. 2017;318(5):415.
Hall WD, Patton G, Stockings E, Weier M, Lynskey M, Morley KI, et al. Why young people's substance use matters for global health. Lancet Psychiatry. 2016;3(3):265–79.
Khalsa JH, Treisman G, McCance-Katz E, Tedaldi E. Medical consequences of drug abuse and co-occurring infections: research at the National Institute on Drug Abuse. Subst Abus. 2008;29(3):5–16.
McCoy CB, Lai S, Metsch LR, Messiah SE, Zhao W. Injection drug use and crack cocaine smoking: independent and dual risk behaviors for HIV infection. Ann Epidemiol. 2004;14(8):535–42.
Contoreggi, md C, Rexroad, rph VE, Lange, md, et al. Current Management of Infectious Complications in the injecting drug user. J Subst Abus Treat. 1998;15(2):95–106.
Article Google Scholar
Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312(7023):71–2.
Article CAS PubMed PubMed Central Google Scholar
American Psychological Association PTFoE-BP. Evidence-based practice in psychology. Am Psychol. 2006;61:271–85.
Pope C. Resisting evidence: the study of evidence-based medicine as a contemporary social movement. Health. 2003;7(3):267–82.
Wendt D. Group therapy for substance use disorders: a survey of clinician practices. J Groups Addict Recover. 2017;12(4):243 EOA.
Johnson J. Using research-supported group treatments. J Clin Psychol In Session. 2008;64(11):1206–24.
Stinchfield RD, Owen P, Winters K. Group therapy for substance abuse: A review of the empirical research. In: Burlingame AFG, editor. Handbook of group psychotherapy. New York: Wiley; 1994. p. 458–88.
Fisher MS Sr, Bentley KJ. Two group therapy models for clients with a dual diagnosis of substance abuse and personality disorder. Psychiatr Serv. 1996;47(11):1244–50.
Kaminer Y, Burleson JA, Blitz C, Sussman J, Rounsaville BJ. Psychotherapies for adolescent substance abusers: a pilot study. J Nerv Ment Dis. 1998;186(11):684–90.
McKay JR, Alterman AI, Cacciola JS, O'Brien CP, Koppenhaver JM, Shepard DS. Continuing care for cocaine dependence: comprehensive 2-year outcomes. J Consult Clin Psychol. 1999;67(3):420–7.
McKay JR, Alterman AI, Cacciola JS, Rutherford MJ, O'Brien CP, Koppenhaver J. Group counseling versus individualized relapse prevention aftercare following intensive outpatient treatment for cocaine dependence: initial results. J Consult Clin Psychol. 1997;65(5):778–88.
Shaffer HJ, LaSalvia TA, Stein JP. Comparing hatha yoga with dynamic group psychotherapy for enhancing methadone maintenance treatment: a randomized clinical trial. Altern Ther Health Med. 1997;3(4):57–66.
CAS PubMed Google Scholar
Morgan-Lopez AA, Fals-Stewart W. Analytic methods for modeling longitudinal data from rolling therapy groups with membership turnover. J Consult Clin Psychol. 2007;75(4):580–93.
Weiss RD. Treating patients with bipolar disorder and substance dependence: lessons learned. J Subst Abus Treat. 2004;27(4):307–12.
Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A meta-analysis of motivational interviewing: twenty-five years of empirical studies. Res Soc Work Pract. 2010;20(2):137–60.
Weiss RD, Jaffee WB, de Menil VP, Cogley CB. Group therapy for substance use disorders: what do we know? Harvard Rev Psychiatry. 2004;12(6):339–50.
Burlingame GM, MacKenzie KR, Strauss B. Bergin & Garfields Handbook Of Psychotherapy And Behavior Change. Small group treatment: Evidence for effectiveness and mechanisms of change. In: Lambert M, editor. Handbook of psychotherapy and behavior change. 5th ed. New York: Wiley; 2003. p. 647–96.
Beck AT. Cognitive therapy: nature and relation to behavior therapy. Behav Ther. 1970;1(2):184–200.
Guydish J, Sorensen JL, Chan M, Werdegar D, Bostrom A, Acampora A. A randomized trial comparing day and residential drug abuse treatment: 18-month outcomes. J Consult Clin Psychol. 1999;67(3):428–34.
Guydish J, Werdegar D, Sorensen JL, Clark W, Acampora A. Drug abuse day treatment: a randomized clinical trial comparing day and residential treatment programs. J Consult Clin Psychol. 1998;66(2):280–9.
Avants SK, Margolin A, Sindelar JL, Rounsaville BJ, Schottenfeld R, Stine S, et al. Day treatment versus enhanced standard methadone services for opioid-dependent patients: a comparison of clinical efficacy and cost. Am J Psychiatry. 1999;156(1):27–33.
Avants SK, Margolin A, Usubiaga MH, Doebrick C. Targeting HIV-related outcomes with intravenous drug users maintained on methadone: a randomized clinical trial of a harm reduction group therapy. J Subst Abus Treat. 2004;26(2):67–78.
Maude-Griffin PM, Hohenstein JM, Humfleet GL, Reilly PM, Tusel DJ, Hall SM. Superior efficacy of cognitive-behavioral therapy for urban crack cocaine abusers: main and matching effects. J Consult Clin Psychol. 1998;66(5):832–7.
Rohsenow DJ, Monti PM, Martin RA, Michalec E, Abrams DB. Brief coping skills treatment for cocaine abuse: 12-month substance use outcomes. J Consult Clin Psychol. 2000;68(3):515–20.
Beck ATW, F. D.; Newman, C. F.; Liese, B. S. Cognitive therapy of substance abuse. New York: Guilford; 1993.
McAuliffe WE. A randomized controlled trial of recovery training and self-help for opioid addicts in New England and Hong Kong. J Psychoactive Drugs. 1990;22(2):197–209.
Czuchry M, Dansereau DF. Node-link mapping and psychological problems. Perceptions of a residential drug abuse treatment program for probationers. J Subst Abus Treat. 1999;17(4):321–9.
Article CAS Google Scholar
McCusker J, Bigelow C, Frost R, Garfield F, Hindin R, Vickers-Lahti M, et al. The effects of planned duration of residential drug abuse treatment on recovery and HIV risk behavior. Am J Public Health. 1997;87(10):1637–44.
Rosenblum A, Magura S, Kayman DJ, Fong C. Motivationally enhanced group counseling for substance users in a soup kitchen: a randomized clinical trial. Drug Alcohol Depend. 2005;80(1):91–103.
Marlatt GA, Donovan DM. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. 2nd ed. New York: The Guilford Press; 2005. p. xiv, 416-xiv
Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken LS, et al. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse collaborative cocaine treatment study. Arch Gen Psychiatry. 1999;56(6):493–502.
Luthar SSS, N.E.; Altomare, M. Relational psychotherapy Mother’s group: A randomized clinical trial for substance abusing mothers. Dev Psychopathol. 2007;19:243–61.
Miller WRR, S. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford Press; 1991.
Hoffman JA, Caudill BD, Koman JJ 3rd, Luckey JW, Flynn PM, Mayo DW. Psychosocial treatments for cocaine abuse. 12-month treatment outcomes. J Subst Abus Treat. 1996;13(1):3–11.
Kaminer Y, Burleson JA, Goldberger R. Cognitive-behavioral coping skills and psychoeducation therapies for adolescent substance abuse. J Nerv Ment Dis. 2002;190(11):737–45.
Linehan M. DBT skills training manual. 2nd ed. London: The Guilford Press; 2015.
Petry NM. Contingency management: what it is and why psychiatrists should want to use it. Psychiatrist. 2011;35(5):161–3.
Logan DE, Marlatt GA. Harm reduction therapy: a practice-friendly review of research. J Clin Psychol. 2010;66(2):201–14.
PubMed PubMed Central Google Scholar
Ellis B, Bernichon T, Yu P, Roberts T, Herrell JM. Effect of social support on substance abuse relapse in a residential treatment setting for women. Eval Program Plan. 2004;27(2):213–21.
Nowinski J, Baker S. The twelve-step facilitation handbook: A systematic approach to early recovery from alcoholism and addiction. San Francisco: Jossey-Bass; 1992. p. xxii. 215-xxii
Najavits LM. Seeking safety: a treatment manual for PTSD and substance abuse. New York: Guilford; 2002.
Greenfield SF, Trucco EM, McHugh RK, Lincoln M, Gallop RJ. The Women's recovery group study: a stage I trial of women-focused group therapy for substance use disorders versus mixed-gender group drug counseling. Drug Alcohol Depend. 2007;90(1):39–47.
Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, Tejeda M. Multidimensional family therapy for adolescent drug abuse: results of a randomized clinical trial. Am J Drug Alcohol Abuse. 2001;27(4):651–88.
Coviello DM, Alterman AI, Rutherford MJ, Cacciola JS, McKay JR, Zanis DA. The effectiveness of two intensities of psychosocial treatment for cocaine dependence. Drug Alcohol Depend. 2001;61(2):145–54.
Crits-Christoph P, Siqueland L, McCalmont E, Weiss RD, Gastfriend DR, Frank A, et al. Impact of psychosocial treatments on associated problems of cocaine-dependent patients. J Consult Clin Psychol. 2001;69(5):825–30.
Siqueland L, Crits-Christoph P, Gallop R, Barber JP, Griffin ML, Thase ME, et al. Retention in psychosocial treatment of cocaine dependence: predictors and impact on outcome. Am J Addict. 2002;11(1):24–40.
Mercer D, Carpenter G, Daley D. The adherence and competence scale for group addiction counseling for TCACS: Center for Psychotherapy Research, Department of Psychiatry, University of Pennsylvania Medical School; 1994.
Luborsky L. Principles of psychoanalytic psychotherapy a manual for supportive-expressive treatment; 1984.
Epstein DH, Hawkins WE, Covi L, Umbricht A, Preston KL. Cognitive-behavioral therapy plus contingency management for cocaine use: findings during treatment and across 12-month follow-up. Psychol Addict Behav. 2003;17(1):73–82.
Magura S, Rosenblum A, Lovejoy M, Handelsman L, Foote J, Stimmel B. Neurobehavioral treatment for cocaine-using methadone patients: a preliminary report. J Addict Dis. 1994;13(4):143–60.
Petry NM, Alessi SM, Hanson T. Contingency management improves abstinence and quality of life in cocaine abusers. J Consult Clin Psychol. 2007;75(2):307–15.
Rawson RA, Huber A, McCann M, Shoptaw S, Farabee D, Reiber C, et al. A comparison of contingency management and cognitive-behavioral approaches during methadone maintenance treatment for cocaine dependence. Arch Gen Psychiatry. 2002;59(9):817–24.
Rohsenow DJ, Monti PM, Rubonis AV, Gulliver SB, Colby SM, Binkoff JA, et al. Cue exposure with coping skills training and communication skills training for alcohol dependence: 6- and 12-month outcomes. Addiction. 2001;96(8):1161–74.
Rosenblum A, Magura S, Foote J, Palij M, Handelsman L, Lovejoy M, et al. Treatment intensity and reduction in drug use for cocaine-dependent methadone patients: a dose-response relationship. J Psychoactive Drugs. 1995;27(2):151–9.
Rosenblum A, Magura S, Palij M, Foote J, Handelsman L, Stimmel B. Enhanced treatment outcomes for cocaine-using methadone patients. Drug Alcohol Depend. 1999;54(3):207–18.
Volpicelli JR, Markman I, Monterosso J, Filing J, O'Brien CP. Psychosocially enhanced treatment for cocaine-dependent mothers: evidence of efficacy. J Subst Abus Treat. 2000;18(1):41–9.
Weinstein SP, Gottheil E, Sterling RC. Randomized comparison of intensive outpatient vs. individual therapy for cocaine abusers. J Addict Dis. 1997;16(2):41–56.
Gottheil E, Weinstein SP, Sterling RC, Lundy A, Serota RD. A randomized controlled study of the effectiveness of intensive outpatient treatment for cocaine dependence. Psychiatr Serv. 1998;49(6):782–7.
Magura S, Rosenblum A, Fong C, Villano C, Richman B. Treating cocaine-using methadone patients: predictors of outcomes in a psychosocial clinical trial. Subst Use Misuse. 2002;37(14):1927–55.
Jaffe A, Shoptaw S, Stein J, Reback CJ, Rotheram-Fuller E. Depression ratings, reported sexual risk behaviors, and methamphetamine use: latent growth curve models of positive change among gay and bisexual men in an outpatient treatment program. Exp Clin Psychopharmacol. 2007;15(3):301–7.
Rawson RA, Marinelli-Casey P, Anglin MD, Dickow A, Frazier Y, Gallagher C, et al. A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction. 2004;99(6):708–17.
Roll JM, Chudzynski J, Cameron JM, Howell DN, McPherson S. Duration effects in contingency management treatment of methamphetamine disorders. Addict Behav. 2013;38(9):2455–62.
Shoptaw S, Huber A, Peck J, Yang X, Liu J, Jeff D, et al. Randomized, placebo-controlled trial of sertraline and contingency management for the treatment of methamphetamine dependence. Drug Alcohol Depend. 2006;85(1):12–8.
Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000;68(5):898–908.
Stephens RS, Roffman RA, Simpson EE. Treating adult marijuana dependence: a test of the relapse prevention model. J Consult Clin Psychol. 1994;62(1):92–9.
Marlatt GAG, J.R. Relapse prevention (unpublished manuscript). In: Luther SSS, Boltas D, editors. Relational parenting Mother’s group: A therapist’s manual. New York: Guilford Press; 1985.
Miller WR, Benefield RG, Tonigan JS. Enhancing motivation for change in problem drinking: a controlled comparison of two therapist styles. J Consult Clin Psychol. 1993;61(3):455–61.
Des Jarlais DC, Casriel C, Friedman SR, Rosenblum A. AIDS and the transition to illicit drug injection--results of a randomized trial prevention program. Br J Addict. 1992;87(3):493–8.
Rawson RA, McCann MJ, Shoptaw SJ, Miotto KA, Frosch DL, Obert JL, et al. Naltrexone for opioid dependence: evaluation of a manualized psychosocial protocol to enhance treatment response. Drug Alcohol Rev. 2001;20(1):67–78.
Scherbaum N, Kluwig J, Specka M, Krause D, Merget B, Finkbeiner T, et al. Group psychotherapy for opiate addicts in methadone maintenance treatment--a controlled trial. Eur Addict Res. 2005;11(4):163–71.
Sees KL, Delucchi KL, Masson C, Rosen A, Clark HW, Robillard H, et al. Methadone maintenance vs 180-day psychosocially enriched detoxification for treatment of opioid dependence: a randomized controlled trial. JAMA. 2000;283(10):1303–10.
Downey KK, Helmus TC, Schuster CR. Treatment of heroin-dependent poly-drug abusers with contingency management and buprenorphine maintenance. Exp Clin Psychopharmacol. 2000;8(2):176–84.
Margolin A, Avants SK, Warburton LA, Hawkins KA, Shi J. A randomized clinical trial of a manual-guided risk reduction intervention for HIV-positive injection drug users. Health Psychol. 2003;22(2):223–8.
Marques AC, Formigoni ML. Comparison of individual and group cognitive-behavioral therapy for alcohol and/or drug-dependent patients. Addiction. 2001;96(6):835–46.
McKay JR, Lynch KG, Shepard DS, Morgenstern J, Forman RF, Pettinati HM. Do patient characteristics and initial progress in treatment moderate the effectiveness of telephone-based continuing care for substance use disorders? Addiction. 2005;100(2):216–26.
Nemes S, Wish ED, Messina N. Comparing the impact of standard and abbreviated treatment in a therapeutic community. Findings from the district of Columbia treatment initiative experiment. J Subst Abus Treat. 1999;17(4):339–47.
Rawson RA, McCann MJ, Flammino F, Shoptaw S, Miotto K, Reiber C, et al. A comparison of contingency management and cognitive-behavioral approaches for stimulant-dependent individuals. Addiction. 2006;101(2):267–74.
Schottenfeld RS, Pantalon MV, Chawarski MC, Pakes J. Community reinforcement approach for combined opioid and cocaine dependence. Patterns of engagement in alternate activities. J Subst Abus Treat. 2000;18(3):255–61.
Smith TL, Volpe FR, Hashima JN, Schuckit MA. Impact of a stimulant-focused enhanced program on the outcome of alcohol- and/or stimulant-dependent men. Alcohol Clin Exp Res. 1999;23(11):1772–9.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the epidemiologic catchment area (ECA) study. JAMA. 1990;264(19):2511–8.
Compton WM, Cottler LB, Ben-Abdallah A, Cunningham-Williams R, Spitznagel EL. The effects of psychiatric comorbidity on response to an HIV prevention intervention. Drug Alcohol Depend. 2000;58(3):247–57.
DiNitto DM, Webb DK, Rubin A. Gender differences in dually-diagnosed clients receiving chemical dependency treatment. J Psychoactive Drugs. 2002;34(1):105–17.
Jerrell JM, Ridgely MS. Comparative effectiveness of three approaches to serving people with severe mental illness and substance abuse disorders. J Nerv Ment Dis. 1995;183(9):566–76.
Jerrell JM, Wilson JL. Ethnic differences in the treatment of dual mental and substance disorders. A preliminary analysis. J Subst Abus Treat. 1997;14(2):133–40.
Lehman AF, Herron JD, Schwartz RP, Myers CP. Rehabilitation for adults with severe mental illness and substance use disorders. A clinical trial. J Nerv Ment Dis. 1993;181(2):86–90.
Linehan MM, Schmidt H 3rd, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. Am J Addict. 1999;8(4):279–92.
Milby JB, Schumacher JE, Vuchinich RE, Wallace D, Plant MA, Freedman MJ, et al. Transitions during effective treatment for cocaine-abusing homeless persons: establishing abstinence, lapse, and relapse, and reestablishing abstinence. Psychol Addict Behav. 2004;18(3):250–6.
Petry NM, Weinstock J, Alessi SM, Lewis MW, Dieckhaus K. Group-based randomized trial of contingencies for health and abstinence in HIV patients. J Consult Clin Psychol. 2010;78(1):89–97.
Zlotnick C, Johnson J, Najavits LM. Randomized controlled pilot study of cognitive-behavioral therapy in a sample of incarcerated women with substance use disorder and PTSD. Behav Ther. 2009;40(4):325–36.
Wechsberg WM, MacDonald BR, Dennis ML, Inciardi JA, Surratt HL, Leukefeld CG, et al. The standard intervention for reduction in HIV risk behavior; protocol changes suggested by the continuing HIV/AIDS epidemic. Bloomington: Lighthouse Institute; 1997.
Liberman RP, Massel HK, Mosk MD, Wong SE. Social skills training for chronic mental patients. Hosp Community Psychiatry. 1985;36(4):396–403.
Milby JB, Schumacher JE, McNamara C, Wallace D, Usdan S, McGill T, et al. Initiating abstinence in cocaine abusing dually diagnosed homeless persons. Drug Alcohol Depend. 2000;60(1):55–67.
Milby JB, Schumacher JE, Raczynski JM, Caldwell E, Engle M, Michael M, et al. Sufficient conditions for effective treatment of substance abusing homeless persons. Drug Alcohol Depend. 1996;43(1–2):39–47.
Milby JB, Schumacher JE, Wallace D, Frison S, McNamara C, Usdan S, et al. Day treatment with contingency management for cocaine abuse in homeless persons: 12-month follow-up. J Consult Clin Psychol. 2003;71(3):619–21.
Linehan MMD, L.A. Dialectical behavior therapy manual of treatment interventions for drug abusers with borderline personality disorder. Seattle: University of Washington; 1997.
Linehan MM, Heard HL, Armstrong HE. Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1993;50(12):971–4.
Linehan MM, Tutek DA, Heard HL, Armstrong HE. Interpersonal outcome of cognitive behavioral treatment for chronically suicidal borderline patients. Am J Psychiatry. 1994;151(12):1771–6.
Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48(12):1060–4.
Burtscheidt W, Schwarz R, Redner C, Gaebel W. Behavioral therapeutic methods in ambulatory treatment of alcoholism. Early results of an experimental study. Fortschr Neurol Psychiatr. 1999;67(6):274–80.
Sandahl C, Herlitz K, Ahlin G, Rönnberg S. Time-limited group psychotherapy for moderately alcohol dependent patients: A randomized controlled clinical trial. Psychother Res. 1998;8(4):361–78.
Wolff RF, Moons KG, Riley RD, Whiting PF, Westwood M, Collins GS, et al. PROBAST: a tool to assess the risk of bias and applicability of prediction model studies. Ann Intern Med. 2019;170(1):51–8.
Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. In: Cochrane handbook for systematic reviews of interventions; 2019. p. 205–28.
Chapter Google Scholar
Diener MJ. The Corsini Encyclopedia of Psychology; 2010. p. 1.
Book Google Scholar
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Trials. 2010;11(1):1–8.
Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviors. Prog Behav Modif. 1992;28:183–218.
Drake RE, McLaughlin P, Pepper B, Minkoff K. Dual diagnosis of major mental illness and substance disorder: an overview. New Dir Ment Health Serv. 1991;1991(50):3–12.
Kunzke D, Strauss B, Burtscheidt W. The effectiveness of psychodynamic group therapy in the treatment of alcohol abuse. A review. Gruppenpsychotherapie und Gruppendynamik. 2002;38:53–70.
Download references
Acknowledgements
The authors have no acknowledgements.
The study is not supported through funding.
Author information
Authors and affiliations.
Center for Alcohol and Addiction Studies, Brown University, Providence, RI, 02912, USA
Gabriela López
Alpert Medical School of Brown University, Department of Psychiatry and Human Behavior, Providence, RI, 02904, USA
Lindsay M. Orchowski
Walter Reed Army Institute of Research, Silver Spring, MD, 20910, USA
Madhavi K. Reddy
Massachusetts General Hospital, Harvard Medical School, Boston, MA, 02115, USA
Jessica Nargiso
Division of Public Health, Michigan State University, Flint, MI, 48502, USA
Jennifer E. Johnson
You can also search for this author in PubMed Google Scholar
Contributions
All authors participated in the review of manuscripts included in the study, writing of sections of the manuscript, as well as final editing of the paper. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Lindsay M. Orchowski .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
López, G., Orchowski, L.M., Reddy, M.K. et al. A review of research-supported group treatments for drug use disorders. Subst Abuse Treat Prev Policy 16 , 51 (2021). https://doi.org/10.1186/s13011-021-00371-0
Download citation
Accepted : 03 April 2021
Published : 21 June 2021
DOI : https://doi.org/10.1186/s13011-021-00371-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Substance use disorders
- Group therapy
Substance Abuse Treatment, Prevention, and Policy
ISSN: 1747-597X
- General enquiries: [email protected]

Increasing patient safety due to an implemented ward pharmacist in an interprofessional cancer care team evaluated in a prospective, controlled intervention study
- Svenja Dierkes
- Annette Freidank
- Roland Radziwill

Correction to: Buprenorphine extended-release injection (Brixadi ® ) in the management of opioid use disorder: a profile of its use in the USA
- Hannah A. Blair
Determine and remove the drug trigger, usually antibiotics, that causes acute generalised exanthematous pustulosis
- Esther S. Kim
- Connie Kang
Adjust antimicrobial agent regimens in older patients to correct for changes in pharmacokinetics and to avoid adverse events
Assessment of rational antibiotic use among children being treated in primary care facilities in punjab, pakistan: findings and implications.
- Zia Ul Mustafa
- Amer Hayat Khan
- Brian Godman
Sparsentan in immunoglobulin A nephropathy: a profile of its use
- Young-A Heo
What is the role of pioglitazone for patients with type 2 diabetes in value-based care settings?
- Andrea Bush
- Matthew Seamon

Treating paediatric Crohn’s disease is challenging but new treatments hold promise
Correction to: efanesoctocog alfa in hemophilia a: a profile of its use, correction to: nadofaragene firadenovec in high-risk bacillus calmette guérin unresponsive non-muscle invasive bladder cancer: a profile of its use, be aware of the risks of nephrotoxicity when prescribing amoxicillin and third-generation cephalosporins.
- Amy Zhuang-Yan
Treat bipolar depression with atypical antipsychotics and mood stabilisers; new therapies require further study
Get on top of gout with a fresh look at treatment options.
- Caroline Fenton
Evaluation of diclofenac utilization patterns before and after digital risk minimization intervention in outpatient settings in Montenegro
- Maja Stankovic
- Nemanja Turkovic
- Nemanja Rancic

Multisite primary care led amoxicillin challenge pathway to safely remove penicillin allergy label
- David C. Mari
- Kelley M. Henson
- Taylor A. Banks

Administer antidepressants during pregnancy on a case-by-case basis
- Yvette N. Lamb
Metformin reduces the complications of gestational diabetes mellitus but its long-term effects on offspring require further study
Buprenorphine extended-release injection (brixadi ® ) in the management of opioid use disorder: a profile of its use in the usa, mirvetuximab soravtansine in folate receptor alpha-positive, platinum-resistant ovarian cancers: a profile of its use.
- Yahiya Y. Syed


Pirtobrutinib in relapsed or refractory mantle cell lymphoma: a profile of its use
Preferably pre-empt pathological scars, or pick from a plethora of therapies, correction to: tezepelumab in severe asthma: a profile of its use, platelet-rich plasma therapy for chronic cutaneous wounds stratified by etiology: a systematic review of randomized clinical trials.
- Verónica Salgado-Pacheco
- Montserrat Serra-Mas
- Marta Otero-Viñas

Expand the treatment horizon of premenstrual dysphoric disorder with targeted therapeutic approaches
Treat borderline personality disorder with psychotherapy and concomitant psychiatric disorders with adjuvant pharmacotherapy, efanesoctocog alfa in hemophilia a: a profile of its use.

Nadofaragene firadenovec in high-risk Bacillus Calmette Guérin unresponsive non-muscle invasive bladder cancer: a profile of its use
Nirsevimab in the prevention of respiratory syncytial virus lower respiratory tract disease: a profile of its use.
- Matt Shirley
The PHASTER Study: Economic and Organizational Impact of Subcutaneous (SC) Pertuzumab and Trastuzumab Fixed-Dose Combination (PH FDC SC) for Treatment of HER2+ Breast Cancer Patients
- Elisabetta Munzone
- Alessandra Fabi
- Michelino De Laurentiis

Acknowledgement to Referees
Understand the benefits and risks of intravenous methadone for perioperative and chronic cancer pain management, tezepelumab in severe asthma: a profile of its use, spesolimab in generalised pustular psoriasis flares: a profile of its use, correction to: rbx2660 (rebyota ® ) in preventing recurrence of clostridioides difficile infection: a profile of its use in the usa, manage vitiligo with a personalised approach: consider old and new treatments.
- Nicole L. France

The role of belzutifan, an inhibitor of hypoxia-inducible factor, for renal cell carcinoma in adults with Von Hippel–Lindau disease: a review
- Anne M. Schwartz
- Waddih Fakhre
- Alan D. Kaye
Ublituximab in relapsing forms of multiple sclerosis: a profile of its use
Deucravacitinib in plaque psoriasis: a profile of its use.

Towards intra-articular therapies for more than just symptom management in osteoarthritis
Manage idiopathic hypersomnia with a combination of non-pharmacological and pharmacological treatments, first reports of adverse drug reactions, go with your gut: targeting the microbiome for treatment of irritable bowel syndrome, rbx2660 (rebyota ® ) in preventing recurrence of clostridioides difficile infection: a profile of its use in the usa, prescribe colchicine with care and be aware of colchicine drug interactions, addressing the opioid epidemic in pakistan: urgent need for opioid stewardship and comprehensive solutions.
- Adeel Siddiqui
- Sunil Shrestha
- Omar Akhlaq Bhutta
Nails blue? Don’t be sad, the cause may be discoverable

Treat functional constipation in children with conventional options first and consider alternatives if needed
Linzagolix in moderate to severe symptoms of uterine fibroids: a profile of its use.

Manage truncal acne and scarring the same as for facial acne, but more trunk-specific therapies are warranted

- Find a journal
- Publish with us
- Track your research
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
April 23, 2024
Research in Context: Treating depression
Finding better approaches.
While effective treatments for major depression are available, there is still room for improvement. This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs.

Everyone has a bad day sometimes. People experience various types of stress in the course of everyday life. These stressors can cause sadness, anxiety, hopelessness, frustration, or guilt. You may not enjoy the activities you usually do. These feelings tend to be only temporary. Once circumstances change, and the source of stress goes away, your mood usually improves. But sometimes, these feelings don’t go away. When these feelings stick around for at least two weeks and interfere with your daily activities, it’s called major depression, or clinical depression.
In 2021, 8.3% of U.S. adults experienced major depression. That’s about 21 million people. Among adolescents, the prevalence was much greater—more than 20%. Major depression can bring decreased energy, difficulty thinking straight, sleep problems, loss of appetite, and even physical pain. People with major depression may become unable to meet their responsibilities at work or home. Depression can also lead people to use alcohol or drugs or engage in high-risk activities. In the most extreme cases, depression can drive people to self-harm or even suicide.
The good news is that effective treatments are available. But current treatments have limitations. That’s why NIH-funded researchers have been working to develop more effective ways to treat depression. These include finding ways to predict whether certain treatments will help a given patient. They're also trying to develop more effective drugs or, in some cases, find new uses for existing drugs.
Finding the right treatments
The most common treatments for depression include psychotherapy, medications, or a combination. Mild depression may be treated with psychotherapy. Moderate to severe depression often requires the addition of medication.
Several types of psychotherapy have been shown to help relieve depression symptoms. For example, cognitive behavioral therapy helps people to recognize harmful ways of thinking and teaches them how to change these. Some researchers are working to develop new therapies to enhance people’s positive emotions. But good psychotherapy can be hard to access due to the cost, scheduling difficulties, or lack of available providers. The recent growth of telehealth services for mental health has improved access in some cases.
There are many antidepressant drugs on the market. Different drugs will work best on different patients. But it can be challenging to predict which drugs will work for a given patient. And it can take anywhere from 6 to 12 weeks to know whether a drug is working. Finding an effective drug can involve a long period of trial and error, with no guarantee of results.
If depression doesn’t improve with psychotherapy or medications, brain stimulation therapies could be used. Electroconvulsive therapy, or ECT, uses electrodes to send electric current into the brain. A newer technique, transcranial magnetic stimulation (TMS), stimulates the brain using magnetic fields. These treatments must be administered by specially trained health professionals.
“A lot of patients, they kind of muddle along, treatment after treatment, with little idea whether something’s going to work,” says psychiatric researcher Dr. Amit Etkin.
One reason it’s difficult to know which antidepressant medications will work is that there are likely different biological mechanisms that can cause depression. Two people with similar symptoms may both be diagnosed with depression, but the causes of their symptoms could be different. As NIH depression researcher Dr. Carlos Zarate explains, “we believe that there’s not one depression, but hundreds of depressions.”
Depression may be due to many factors. Genetics can put certain people at risk for depression. Stressful situations, physical health conditions, and medications may contribute. And depression can also be part of a more complicated mental disorder, such as bipolar disorder. All of these can affect which treatment would be best to use.
Etkin has been developing methods to distinguish patients with different types of depression based on measurable biological features, or biomarkers. The idea is that different types of patients would respond differently to various treatments. Etkin calls this approach “precision psychiatry.”
One such type of biomarker is electrical activity in the brain. A technique called electroencephalography, or EEG, measures electrical activity using electrodes placed on the scalp. When Etkin was at Stanford University, he led a research team that developed a machine-learning algorithm to predict treatment response based on EEG signals. The team applied the algorithm to data from a clinical trial of the antidepressant sertraline (Zoloft) involving more than 300 people.

EEG data for the participants were collected at the outset. Participants were then randomly assigned to take either sertraline or an inactive placebo for eight weeks. The team found a specific set of signals that predicted the participants’ responses to sertraline. The same neural “signature” also predicted which patients with depression responded to medication in a separate group.
Etkin’s team also examined this neural signature in a set of patients who were treated with TMS and psychotherapy. People who were predicted to respond less to sertraline had a greater response to the TMS/psychotherapy combination.
Etkin continues to develop methods for personalized depression treatment through his company, Alto Neuroscience. He notes that EEG has the advantage of being low-cost and accessible; data can even be collected in a patient’s home. That’s important for being able to get personalized treatments to the large number of people they could help. He’s also working on developing antidepressant drugs targeted to specific EEG profiles. Candidate drugs are in clinical trials now.
“It’s not like a pie-in-the-sky future thing, 20-30 years from now,” Etkin explains. “This is something that could be in people's hands within the next five years.”
New tricks for old drugs
While some researchers focus on matching patients with their optimal treatments, others aim to find treatments that can work for many different patients. It turns out that some drugs we’ve known about for decades might be very effective antidepressants, but we didn’t recognize their antidepressant properties until recently.
One such drug is ketamine. Ketamine has been used as an anesthetic for more than 50 years. Around the turn of this century, researchers started to discover its potential as an antidepressant. Zarate and others have found that, unlike traditional antidepressants that can take weeks to take effect, ketamine can improve depression in as little as one day. And a single dose can have an effect for a week or more. In 2019, the FDA approved a form of ketamine for treating depression that is resistant to other treatments.
But ketamine has drawbacks of its own. It’s a dissociative drug, meaning that it can make people feel disconnected from their body and environment. It also has the potential for addiction and misuse. For these reasons, it’s a controlled substance and can only be administered in a doctor’s office or clinic.
Another class of drugs being studied as possible antidepressants are psychedelics. These include lysergic acid diethylamide (LSD) and psilocybin, the active ingredient in magic mushrooms. These drugs can temporarily alter a person’s mood, thoughts, and perceptions of reality. Some have historically been used for religious rituals, but they are also used recreationally.
In clinical studies, psychedelics are typically administered in combination with psychotherapy. This includes several preparatory sessions with a therapist in the weeks before getting the drug, and several sessions in the weeks following to help people process their experiences. The drugs are administered in a controlled setting.
Dr. Stephen Ross, co-director of the New York University Langone Health Center for Psychedelic Medicine, describes a typical session: “It takes place in a living room-like setting. The person is prepared, and they state their intention. They take the drug, they lie supine, they put on eye shades and preselected music, and two therapists monitor them.” Sessions last for as long as the acute effects of the drug last, which is typically several hours. This is a healthcare-intensive intervention given the time and personnel needed.
In 2016, Ross led a clinical trial examining whether psilocybin-assisted therapy could reduce depression and anxiety in people with cancer. According to Ross, as many as 40% of people with cancer have clinically significant anxiety and depression. The study showed that a single psilocybin session led to substantial reductions in anxiety and depression compared with a placebo. These reductions were evident as soon as one day after psilocybin administration. Six months later, 60-80% of participants still had reduced depression and anxiety.
Psychedelic drugs frequently trigger mystical experiences in the people who take them. “People can feel a sense…that their consciousness is part of a greater consciousness or that all energy is one,” Ross explains. “People can have an experience that for them feels more ‘real’ than regular reality. They can feel transported to a different dimension of reality.”
About three out of four participants in Ross’s study said it was among the most meaningful experiences of their lives. And the degree of mystical experience correlated with the drug’s therapeutic effect. A long-term follow-up study found that the effects of the treatment continued more than four years later.
If these results seem too good to be true, Ross is quick to point out that it was a small study, with only 29 participants, although similar studies from other groups have yielded similar results. Psychedelics haven’t yet been shown to be effective in a large, controlled clinical trial. Ross is now conducting a trial with 200 people to see if the results of his earlier study pan out in this larger group. For now, though, psychedelics remain experimental drugs—approved for testing, but not for routine medical use.
Unlike ketamine, psychedelics aren’t considered addictive. But they, too, carry risks, which certain conditions may increase. Psychedelics can cause cardiovascular complications. They can cause psychosis in people who are predisposed to it. In uncontrolled settings, they have the risk of causing anxiety, confusion, and paranoia—a so-called “bad trip”—that can lead the person taking the drug to harm themself or others. This is why psychedelic-assisted therapy takes place in such tightly controlled settings. That increases the cost and complexity of the therapy, which may prevent many people from having access to it.
Better, safer drugs
Despite the promise of ketamine or psychedelics, their drawbacks have led some researchers to look for drugs that work like them but with fewer side effects.
Depression is thought to be caused by the loss of connections between nerve cells, or neurons, in certain regions of the brain. Ketamine and psychedelics both promote the brain’s ability to repair these connections, a quality called plasticity. If we could understand how these drugs encourage plasticity, we might be able to design drugs that can do so without the side effects.

Dr. David Olson at the University of California, Davis studies how psychedelics work at the cellular and molecular levels. The drugs appear to promote plasticity by binding to a receptor in cells called the 5-hydroxytryptamine 2A receptor (5-HT2AR). But many other compounds also bind 5-HT2AR without promoting plasticity. In a recent NIH-funded study, Olson showed that 5-HT2AR can be found both inside and on the surface of the cell. Only compounds that bound to the receptor inside the cells promoted plasticity. This suggests that a drug has to be able to get into the cell to promote plasticity.
Moreover, not all drugs that bind 5-HT2AR have psychedelic effects. Olson’s team has developed a molecular sensor, called psychLight, that can identify which compounds that bind 5-HT2AR have psychedelic effects. Using psychLight, they identified compounds that are not psychedelic but still have rapid and long-lasting antidepressant effects in animal models. He’s founded a company, Delix Therapeutics, to further develop drugs that promote plasticity.
Meanwhile, Zarate and his colleagues have been investigating a compound related to ketamine called hydroxynorketamine (HNK). Ketamine is converted to HNK in the body, and this process appears to be required for ketamine’s antidepressant effects. Administering HNK directly produced antidepressant-like effects in mice. At the same time, it did not cause the dissociative side effects and addiction caused by ketamine. Zarate’s team has already completed phase I trials of HNK in people showing that it’s safe. Phase II trials to find out whether it’s effective are scheduled to begin soon.
“What [ketamine and psychedelics] are doing for the field is they’re helping us realize that it is possible to move toward a repair model versus a symptom mitigation model,” Olson says. Unlike existing antidepressants, which just relieve the symptoms of depression, these drugs appear to fix the underlying causes. That’s likely why they work faster and produce longer-lasting effects. This research is bringing us closer to having safer antidepressants that only need to be taken once in a while, instead of every day.
—by Brian Doctrow, Ph.D.
Related Links
- How Psychedelic Drugs May Help with Depression
- Biosensor Advances Drug Discovery
- Neural Signature Predicts Antidepressant Response
- How Ketamine Relieves Symptoms of Depression
- Protein Structure Reveals How LSD Affects the Brain
- Predicting The Usefulness of Antidepressants
- Depression Screening and Treatment in Adults
- Serotonin Transporter Structure Revealed
- Placebo Effect in Depression Treatment
- When Sadness Lingers: Understanding and Treating Depression
- Psychedelic and Dissociative Drugs
References: An electroencephalographic signature predicts antidepressant response in major depression. Wu W, Zhang Y, Jiang J, Lucas MV, Fonzo GA, Rolle CE, Cooper C, Chin-Fatt C, Krepel N, Cornelssen CA, Wright R, Toll RT, Trivedi HM, Monuszko K, Caudle TL, Sarhadi K, Jha MK, Trombello JM, Deckersbach T, Adams P, McGrath PJ, Weissman MM, Fava M, Pizzagalli DA, Arns M, Trivedi MH, Etkin A. Nat Biotechnol. 2020 Feb 10. doi: 10.1038/s41587-019-0397-3. Epub 2020 Feb 10. PMID: 32042166. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. Ross S, Bossis A, Guss J, Agin-Liebes G, Malone T, Cohen B, Mennenga SE, Belser A, Kalliontzi K, Babb J, Su Z, Corby P, Schmidt BL. J Psychopharmacol . 2016 Dec;30(12):1165-1180. doi: 10.1177/0269881116675512. PMID: 27909164. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. Agin-Liebes GI, Malone T, Yalch MM, Mennenga SE, Ponté KL, Guss J, Bossis AP, Grigsby J, Fischer S, Ross S. J Psychopharmacol . 2020 Feb;34(2):155-166. doi: 10.1177/0269881119897615. Epub 2020 Jan 9. PMID: 31916890. Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors. Vargas MV, Dunlap LE, Dong C, Carter SJ, Tombari RJ, Jami SA, Cameron LP, Patel SD, Hennessey JJ, Saeger HN, McCorvy JD, Gray JA, Tian L, Olson DE. Science . 2023 Feb 17;379(6633):700-706. doi: 10.1126/science.adf0435. Epub 2023 Feb 16. PMID: 36795823. Psychedelic-inspired drug discovery using an engineered biosensor. Dong C, Ly C, Dunlap LE, Vargas MV, Sun J, Hwang IW, Azinfar A, Oh WC, Wetsel WC, Olson DE, Tian L. Cell . 2021 Apr 8: S0092-8674(21)00374-3. doi: 10.1016/j.cell.2021.03.043. Epub 2021 Apr 28. PMID: 33915107. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ, Singh NS, Dossou KS, Fang Y, Huang XP, Mayo CL, Wainer IW, Albuquerque EX, Thompson SM, Thomas CJ, Zarate CA Jr, Gould TD. Nature . 2016 May 26;533(7604):481-6. doi: 10.1038/nature17998. Epub 2016 May 4. PMID: 27144355.
Connect with Us
- More Social Media from NIH
FDA drafts two guidances on safety testing for cell and gene therapy products
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 04 October 2021
Psychedelic therapy: a roadmap for wider acceptance and utilization
- Mason Marks 1 , 2 &
- I. Glenn Cohen ORCID: orcid.org/0000-0002-0223-3305 1 , 3
Nature Medicine volume 27 , pages 1669–1671 ( 2021 ) Cite this article
64k Accesses
24 Citations
338 Altmetric
Metrics details
- Drug development
- Drug regulation
Psychedelics have shown great promise in treating mental-health conditions, but their use is severely limited by legal obstacles, which could be overcome.
The COVID-19 pandemic has exacerbated a national mental-health crisis in the United States. For two decades, drug-overdose deaths have risen exponentially, and suicide rates have steadily increased. These trends reflect deep-seated problems with the healthcare system, including low investment in preventative mental healthcare and a lack of innovation in psychiatry. In search of more effective treatments, clinicians are exploring the therapeutic use of psychedelic compounds, a promising avenue for addressing the mental-health crisis. However, there are social and legal obstacles to making psychedelics a viable treatment option 1 .

Schedule I controlled substances
Psychedelics are a class of natural and synthetic compounds that includes psilocybin, MDMA (3,4-methylenedioxymethamphetamine), ibogaine and DMT (dimethyltryptamine). Some psychedelics have been used by Indigenous communities for hundreds or thousands of years. Others were first synthesized in the early 20th century. By the middle of the 20th century, clinicians used psychedelics as adjuncts to psychotherapy, reporting a variety of benefits. However, in the 1970s they were categorized as schedule I controlled substances, which are said to have “no currently accepted medical use and a high potential for abuse”; this blocked mainstream research on these compounds for decades.
In the late 1990s, the US Drug Enforcement Administration (DEA) permitted some researchers to study limited amounts of psychedelics, which allowed research to resume. Clinical trials have now been conducted at leading universities, and a growing body of evidence supports the use of psychedelics, such as psilocybin and MDMA, in the treatment of depression 2 , post-traumatic stress disorder 3 and anxiety toward the end of life 4 .
The schedule I status of most psychedelics imposes a ceiling on many policy recommendations. The evidence in support of rescheduling is strong, particularly for psilocybin, which is derived from fungi 5 . Unlike other schedule I substances such as heroin, and schedule II compounds, including cocaine and fentanyl, psilocybin exhibits a low risk of toxicity and a very low potential for dependence or addiction 6 . Psilocybin use is not criminalized in several countries, including Portugal and the Netherlands, and a study commissioned by the Dutch Ministry of Health found that over-the-counter sales posed minimal risk to individual people and the public 7 .
Acknowledging its therapeutic benefits, the Canadian government made psilocybin available to people with life-threatening illness through compassionate-use regulation. On the basis of clinical-trial data, the US Food and Drug Administration (FDA) designated psilocybin a breakthrough therapy for major depressive disorder and treatment-resistant depression 8 .
Rescheduling can occur through several means. The US Congress can amend the Controlled Substances Act, changing the categorization of any controlled substance 9 . Alternatively, the president or the federal attorney general could command the DEA to reschedule a substance. Finally, any person from within or outside the government can petition the DEA to reschedule substances, which may trigger FDA review of available evidence.
The FDA is obligated to protect the public and ensure the dissemination of accurate medical information, and it has spontaneously opined on potential scheduling of unregulated substances, such as the dietary supplement kratom. Similarly, it could recommend the rescheduling of psilocybin because the available evidence no longer supports its current classification.
Limits on federal funding and research
Due to the schedule I status of most psychedelics, federal funding for research is nearly non-existent.
More directly, a federal appropriations rider — a provision inserted into a funding bill that may effectuate public policy by limiting how funds are spent — creates a considerable obstacle to such research. First enacted in 1996, the rider prohibits federal funds from supporting “any activity that promotes the legalization of any drug or other substance included in schedule I.” 10 This rider has been renewed in every appropriations process since then. Because research on psychedelics could advance scientific knowledge and provide evidence that supports rescheduling, a form of legalization, the rider arguably prohibits the use of federal funds to support research on psychedelics, so long as they remain in schedule I.
Bills to eliminate the rider, in 2019 and 2021, both failed. However, as this Comment was going to print, the National Institute on Drug Abuse funded a trial to investigate the use of psilocybin for smoking cessation, possibly reflecting an encouraging policy shift.
Under existing regulation, well-capitalized private companies fund most research and, to a large extent, they control the agenda and shape federal drug policies. Instead, the goal should be a psychedelics industry in which patients and marginalized communities have seats at the table. Achieving this goal will require more-inclusive clinical trials and unbiased regulatory review of psychedelics by the FDA.
The FDA currently oversees phase 3 trials of MDMA for the treatment of post-traumatic stress disorder and phase 2 trials of psilocybin for the treatment of drug-resistant depression 11 . In addition to being funded by private donors, existing trials often lack diversity and exclude populations who may benefit from psychedelics, such as people with histories of severe trauma and self-harm 12 . An infusion of federal funds could be used to make psychedelics research more equitable and inclusive.
Patents may limit access
Given promising clinical-trial results, many stakeholders are attempting to patent psychedelic compounds and methods of producing and administering them.
Patents entitle their holders to exclude others from making, using or selling patented inventions for approximately 20 years 13 . The public-policy justification for patents rests on the theory that the right to exclude incentivizes drug development, an expensive endeavor, made riskier when other companies can copy an invention. Accordingly, companies such as the British pharmaceutical firm Compass Pathways have sought patents on psilocybin compounds and methods of treating a variety of mental-health conditions with psychedelics 14 . They argue that patents are necessary to protect their investments not only in drug discovery but also in commercialization, which may involve expensive clinical trials and other requirements to obtain approval from the FDA and other regulators and buy-in from the medical community 15 .
At the same time, the sudden interest in patenting psychedelics has prompted criticism from stakeholders, including patient advocates, scientists, journalists, lawyers and Indigenous communities 16 . Some claim patenting psychedelics exploits the traditional knowledge of Indigenous communities without acknowledgment or compensation, a practice called ‘biopiracy’.
Others argue that patents make a small number of companies gatekeepers for the emerging psychedelics industry, which could inhibit research, stifle innovation and restrict access to needed therapies.
These concerns are not unique to psychedelics. Patents on genetic technologies, cancer therapies and other innovations have engendered similar debates 17 . However, some features of psychedelics, including their long and complicated history, raise unique concerns that could exacerbate pre-existing problems with patenting medical products.
Novelty and non-obviousness are two conditions for patentability. However, because psychedelics are often derived from natural products that have been used in traditional practices for centuries, psychedelic inventions may lack novelty or would have been obvious to people experienced in the field. Nevertheless, the US Patent and Trademark Office (PTO) has issued psychedelic patents of questionable validity 18 .
Weak psychedelic patents could potentially be invalidated in court, but that does not make them harmless, because patent holders can still wield them offensively. Defending against patent-infringement claims is expensive, and the prospect discourages action by smaller startups and non-profit research organizations, even when they are in the right.
One explanation for the issuance of problematic patents for psychedelics may be a lack of expertise at the PTO. Because psychedelics were criminalized for decades, the agency lacks personnel adept at evaluating novelty and non-obviousness in this field. To address this concern, a group called ‘Porta Sophia’ created a library of existing psychedelic technologies to help patent applicants and PTO examiners assess the novelty of inventions 19 .
Other potential solutions include encouraging inventors to sign patent pledges — promises not to enforce patent rights under certain conditions. During the COVID-19 pandemic, some companies took the Open COVID Pledge, promising not to enforce their rights against competitors using their technologies to address the pandemic. Impressive advancements have been seen in the psychedelics space without patents. Two leading non-profits, the Multidisciplinary Association for Psychedelic Studies and the Usona Institute, conduct clinical trials with psychedelics while eschewing patent rights.
Restricting patents on psychedelics may be necessary to promote their role in the meaningful advancement of mental healthcare. US law prohibits patents on products of nature, including human genes; abstract ideas, such as those expressed by mathematical formulas; and natural phenomena, including the laws of nature. Some might also think of psychedelics as tools of discovery that should be free to all and reserved exclusively to none. Psychiatrist Stanislav Grof once said that when psychedelics are used responsibly, they may do for psychiatry what the microscope achieved for biology and the telescope accomplished for astronomy 20 .
Improving access and acceptance
As the evidence base for psychedelic therapies grows, it is essential that payers expand coverage.
Many who might benefit from psychedelics may be on Medicaid, and even if private insurers begin coverage, many patients will be unable to access these therapies. Coverage should therefore be central to policy-reform efforts in federal and state governments, or the liberalization of psychedelics may leave those most in need without access.
Many physicians who wish to incorporate psychedelics into their practices need training, and it will be essential to create evidence-based clinical-practice guidelines. Standards may help reduce fear among some healthcare professionals about medical malpractice liability if patients have bad outcomes while using these therapies. But litigation may be necessary to shape the boundaries here.
A final looming issue is the question of which healthcare or para-medical professionals will be empowered to help patients. It is not only licensed physicians who are interested in psychedelics practice, and it remains unclear who else may play leading roles and what licensure regimes might look like.
One approach would center psychedelics within a prescription model that requires licensed prescribers, typically physicians. This model has benefits, but it may raise challenges in a setting in which many patients already use psychedelics, either alone or with the assistance of healthcare professionals or spiritual healers. A prescription model may not be the best approach for everyone.
The Oregon model
The state of Oregon is pursuing an alternative model in which trained facilitators licensed by the Oregon Health Authority will administer psilocybin 21 . Clients seeking access to ‘psilocybin services’, as they are called in Oregon, need not have a medical diagnosis to participate. Because clinical-trial participants often report sustained feelings of wellbeing 22 , some believe psilocybin services could help fill the current gap in preventative mental healthcare.
The Oregon model of psilocybin services envisions the facilitator as new type of professional trained in Western scientific knowledge as well as Indigenous uses of plant medicines. The Oregon Psilocybin Advisory Board, appointed by Governor Kate Brown in March, is advising the Oregon Health Authority on rules for this emerging industry 23 .
Given the worsening mental-health crisis, and a lack of innovation in psychopharmacology, it is urgent that the US Congress make funds available for psychedelics research, which is currently sustained mainly by corporate and private donors. As with cannabis regulation, there will be challenges and opportunities when a medical model is introduced over a preexisting less-regulated model. This, however, is a good problem for the medico-legal community to face, compared with the status quo, in which the answer is firmly ‘just say no’.
Marks, M. N. Y. Univ. J. Legis. Public Policy 21 , 69–140 (2018).
Google Scholar
Davis, A. K. et al. JAMA Psychiatry 78 , 481–489 (2021).
Article Google Scholar
Mithoefer, M. C. et al. Psychopharmacol. 236 , 2735–2745 (2019).
Article CAS Google Scholar
Griffiths, R. R., Johnson, M. W. & Carducci, M. A. J. Psychopharmacol. 30 , 1181–1197 (2016).
Johnson, M. W., Griffiths, R. R. & Hendricks, P. S. Neuropharmacol. 142 , 143–166 (2018).
De Veen, B. T. H. Expert Rev. Neurother. 17 , 203–212 (2016).
van Amsterdam, J., Opperhuizen, A. & van den Brink, W. Regul. Toxicol. Pharmacol. 59 , 423–429 (2011).
Brooks, M. Medscape https://www.medscape.com/viewarticle/921789 (2019).
Marks, M. M. Adm. Law Rev. 72 , 649–718 (2020).
National Institutes of Health. https://grants.nih.gov/grants/policy/nihgps/html5/section_4/4.2.7_promotion_or_legalization_of_controlled_substances.htm (2021).
McCall, B. Nat. Med . https://www.nature.com/articles/d41591-020-00001-5 (2020).
Michaels, T. I., Purdon, J., Collins, A. & Williams, M. T. BMC Psychiatry 18 , 245–259 (2018).
Hickey, K.J. Congress. Res. Serv . https://crsreports.congress.gov/product/details?prodcode=R46525 (2020).
US Patent 10,947,257 (filed 9 October 2018).
Angermayer, C. LinkedIn https://www.linkedin.com/pulse/open-letter-tim-ferriss-value-patents-psychedelic-angermayer/ (2021).
Love, S. Motherboard https://www.vice.com/en/article/m7amw4/is-it-possible-to-create-an-ethical-psychedelics-company (2021).
Lidsky, L. STAT First Opinion https://www.statnews.com/2019/07/23/patent-reform-protect-access-lifesaving-drugs/ (2019).
Love, S. Motherboard https://www.vice.com/en/article/g5gdzy/can-lsd-treat-food-allergies-we-dont-know-but-its-already-been-patented (2021).
Richert, L. Psychology Today https://www.psychologytoday.com/us/blog/hygieias-workshop/202107/the-complicated-patenting-our-psychedelic-future (2021).
Schreck, M. MAPS Bulletin 21 , 26–28 (2011).
Marks, M. Gizmodo https://gizmodo.com/inside-the-fight-to-legalize-psilocybin-therapy-in-oreg-1845450885 (2020).
Agin-Liebes, G. I. et al. J. Psychopharmacol. 34 , 155–166 (2020).
Acker, L. The Oregonian https://www.oregonlive.com/pacific-northwest-news/2021/03/governor-appoints-board-to-oversee-oregons-new-psychedelic-mushroom-program.html (2021).
Download references
Acknowledgements
We are grateful for the support of the Saisei Foundation and thank E. Wright Clayton and R. Sachs for helpful comments on an earlier draft of this article.
Author information
Authors and affiliations.
Project on Psychedelics Law and Regulation (POPLAR) at the Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics at Harvard Law School, Cambridge, MA, USA
Mason Marks & I. Glenn Cohen
University of New Hampshire Franklin Pierce School of Law, Concord, NH, USA
- Mason Marks
Harvard Law School, Cambridge, MA, USA
I. Glenn Cohen
You can also search for this author in PubMed Google Scholar
Contributions
M.M. and I.G.C. drafted the manuscript.
Corresponding author
Correspondence to Mason Marks .
Ethics declarations
Competing interests.
I.G.C. and M.M.’s work was supported by the Project on Psychedelics Law and Regulation (POPLAR), which itself receives funding from the Saisei Foundation, a non-profit organization based in Austin, Texas. M.M. is a governor-appointed member of the Oregon Psilocybin Advisory Board and chairs its licensing subcommittee.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Marks, M., Cohen, I.G. Psychedelic therapy: a roadmap for wider acceptance and utilization. Nat Med 27 , 1669–1671 (2021). https://doi.org/10.1038/s41591-021-01530-3
Download citation
Published : 04 October 2021
Issue Date : October 2021
DOI : https://doi.org/10.1038/s41591-021-01530-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Drug scheduling limits access to essential medicines and should be reformed.
- Carmel Shachar
Nature Medicine (2023)
Great Expectations: recommendations for improving the methodological rigor of psychedelic clinical trials
- Jacob S. Aday
- Boris D. Heifets
- Joshua D. Woolley
Psychopharmacology (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
How to Thrive as You Age
Got tinnitus a device that tickles the tongue helps this musician find relief.

Allison Aubrey

After using the Lenire device for an hour each day for 12 weeks, Victoria Banks says her tinnitus is "barely noticeable." David Petrelli/Victoria Banks hide caption
After using the Lenire device for an hour each day for 12 weeks, Victoria Banks says her tinnitus is "barely noticeable."
Imagine if every moment is filled with a high-pitched buzz or ring that you can't turn off.
More than 25 million adults in the U.S., have a condition called tinnitus, according to the American Tinnitus Association. It can be stressful, even panic-inducing and difficult to manage. Dozens of factors can contribute to the onset of tinnitus, including hearing loss, exposure to loud noise or a viral illness.
There's no cure, but there are a range of strategies to reduce the symptoms and make it less bothersome, including hearing aids, mindfulness therapy , and one newer option – a device approved by the FDA to treat tinnitus using electrical stimulation of the tongue.
The device has helped Victoria Banks, a singer and songwriter in Nashville, Tenn., who developed tinnitus about three years ago.
"The noise in my head felt like a bunch of cicadas," Banks says. "It was terrifying." The buzz made it difficult for her to sing and listen to music. "It can be absolutely debilitating," she says.

Shots - Health News
Tinnitus bothers millions of americans. here's how to turn down the noise.
Banks tried taking dietary supplements , but those didn't help. She also stepped up exercise, but that didn't bring relief either. Then she read about a device called Lenire, which was approved by the FDA in March 2023. It includes a plastic mouthpiece with stainless steel electrodes that electrically stimulate the tongue. It is the first device of its kind to be approved for tinnitus.
"This had worked for other people, and I thought I'm willing to try anything at this point," Banks recalls.
She sought out audiologist Brian Fligor, who treats severe cases of tinnitus in the Boston area. Fligor was impressed by the results of a clinical trial that found 84% of participants who tried Lenire experienced a significant reduction in symptoms. He became one of the first providers in the U.S. to use the device with his patients. Fligor also served on an advisory panel assembled by the company who developed it.
"A good candidate for this device is somebody who's had tinnitus for at least three months," Fligor says, emphasizing that people should be evaluated first to make sure there's not an underlying medical issue.
Tinnitus often accompanies hearing loss, but Victoria Banks' hearing was fine and she had no other medical issue, so she was a good candidate.
Banks used the device for an hour each day for 12 weeks. During the hour-long sessions, the electrical stimulation "tickles" the tongue, she says. In addition, the device includes a set of headphones that play a series of tones and ocean-wave sounds.
The device works, in part, by shifting the brain's attention away from the buzz. We're wired to focus on important information coming into our brains, Fligor says. Think of it as a spotlight at a show pointed at the most important thing on the stage. "When you have tinnitus and you're frustrated or angry or scared by it, that spotlight gets really strong and focused on the tinnitus," Fligor says.
"It's the combination of what you're feeling through the nerves in your tongue and what you're hearing through your ears happening in synchrony that causes the spotlight in your brain to not be so stuck on the tinnitus," Fligor explains.

A clinical trial found 84% of people who used the device experienced a significant reduction in symptoms. Brian Fligor hide caption
A clinical trial found 84% of people who used the device experienced a significant reduction in symptoms.
"It unsticks your spotlight" and helps desensitize people to the perceived noise that their tinnitus creates, he says.
Banks says the ringing in her ears did not completely disappear, but now it's barely noticeable on most days.
"It's kind of like if I lived near a waterfall and the waterfall was constantly going," she says. Over time, the waterfall sound fades out of consciousness.
"My brain is now focusing on other things," and the buzz is no longer so distracting. She's back to listening to music, writing music, and performing music." I'm doing all of those things," she says.
When the buzz comes back into focus, Banks says a refresher session with the device helps.
A clinical trial found that 84% of people who tried Lenire , saw significant improvements in their condition. To measure changes, the participants took a questionnaire that asked them to rate how much tinnitus was impacting their sleep, sense of control, feelings of well-being and quality of life. After 12 weeks of using the device, participants improved by an average of 14 points.
"Where this device fits into the big picture, is that it's not a cure-all, but it's quickly become my go-to," for people who do not respond to other ways of managing tinnitus, Fligor says.
One down-side is the cost. Banks paid about $4,000 for the Lenire device, and insurance doesn't cover it. She put the expense on her credit card and paid it off gradually.
Fligor hopes that as the evidence of its effectiveness accumulates, insurers will begin to cover it. Despite the cost, more than 80% of participants in the clinical trial said they would recommend the device to a friend with tinnitus.
But, it's unclear how long the benefits last. Clinical trials have only evaluated Lenire over a 1-year period. "How durable are the effects? We don't really know yet," says audiologist Marc Fagelson, the scientific advisory committee chair of the American Tinnitus Association. He says research is promising but there's still more to learn.
Fagelson says the first step he takes with his patients is an evaluation for hearing loss. Research shows that hearing aids can be an effective treatment for tinnitus among people who have both tinnitus and hearing loss, which is much more common among older adults. An estimated one-third of adults 65 years of age and older who have hearing loss, also have tinnitus.
"We do see a lot of patients, even with very mild loss, who benefit from hearing aids," Fagelson says, but in his experience it's about 50-50 in terms of improving tinnitus. Often, he says people with tinnitus need to explore options beyond hearing aids.
Bruce Freeman , a scientist at the University of Pittsburgh Medical Center, says he's benefitted from both hearing aids and Lenire. He was fitted for the device in Ireland where it was developed, before it was available in the U.S.
Freeman agrees that the ringing never truly disappears, but the device has helped him manage the condition. He describes the sounds that play through the device headphones as very calming and "almost hypnotic" and combined with the tongue vibration, it's helped desensitize him to the ring.
Freeman – who is a research scientist – says he's impressed with the results of research, including a study published in Nature, Scientific Reports that points to significant improvements among clinical trial participants with tinnitus.
Freeman experienced a return of his symptoms when he stopped using the device. "Without it the tinnitus got worse," he says. Then, when he resumed use, it improved.
Freeman believes his long-term exposure to noisy instruments in his research laboratory may have played a role in his condition, and also a neck injury from a bicycle accident that fractured his vertebra. "All of those things converged," he says.
Freeman has developed several habits that help keep the high-pitched ring out of his consciousness and maintain good health. "One thing that does wonders is swimming," he says, pointing to the swooshing sound of water in his ears. "That's a form of mindfulness," he explains.
When it comes to the ring of tinnitus, "it comes and goes," Freeman says. For now, it has subsided into the background, he told me with a sense of relief. "The last two years have been great," he says – a combination of the device, hearing aids and the mindfulness that comes from a swim.
This story was edited by Jane Greenhalgh
- ringing in ears
- hearing loss

IMAGES
VIDEO
COMMENTS
This paper reviews methodologically rigorous studies examining group treatments for interview-diagnosed drug use disorders. A total of 50 studies reporting on the efficacy of group drug use disorder treatments for adults met inclusion criteria. Studies examining group treatment for cocaine, methamphetamine, marijuana, opioid, mixed substance ...
Drug Alcohol Depend 2019; 205: 107648 Crossref, Medline, Google Scholar. 7 Center for Drug Evaluation and Research, US Food and Drug Administration: The Voice of the Patient: A Series of Reports From the US Food and Drug Administration's (FDA's) Patient-Focused Drug Development Initiative: Opioid Use Disorder. Rockville, Md, Center for Drug ...
Drug therapy (or pharmacotherapy) involves the administration of drugs to treat or prevent disease. In some cases - often in the treatment of disease such as cancer, HIV infection and diabetes ...
To combat this growing health threat and its cardiac, renal, and neurologic comorbidities, new and more effective diabetes drugs and treatments are essential. As the last several years have seen many new developments in the field of diabetes pharmacology and therapy, we determined that a new and up to date review of these advances was in order.
Mental disorders represent a worldwide public health concern1, 2.Psychotherapies and pharmacotherapies are recommended as first line treatments3, 4.However, evidence has recently emerged suggesting that the efficacy of both types of treatment may have been overestimated, due to several shortcomings of clinical trials, such as publication bias, researcher allegiance, or use of weak comparison ...
Results from a phase 3, double-blind, randomized, placebo-controlled trial demonstrate that MDMA-assisted therapy is safe and effective in treating severe post-traumatic stress disorder.
A review of drug resistance in cancer analyses each biological determinant of resistance separately and discusses existing and new therapeutic strategies to combat the problem as a whole.
Targeted drug therapy, immunotherapy, and personalized medicines are now largely being employed, which were not common a few years back. ... hormones and interfere with the body's overall metabolism. 32, 33 The 2018 Nobel Prize attributed to immune checkpoint therapy research has highlighted the importance of immunotherapy, ...
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
In this systematic review and meta-analysis, we show that advanced cancer patients who have exhausted standard of care treatments and participate in a randomized clinical trial with a control arm without any anticancer drug overall benefited from the experimental treatment when randomized into the experimental arms with a 42% decrease in the risk of disease progression and a 18% decrease in ...
This review explores the current conventional drugs used in the treatment of type 2 DM, the associated limitations related to their usage and the cutting edge novel nanoformulations that are under continual research for circumventing the stated drawbacks of the conventional drug use. 2. Pathophysiology of diabetes.
Research will also be limited by the fact that there is not currently a rigorous definition of some of the clinical techniques used in these trials (e.g., psychedelic-assisted psychotherapy) and that expectations and the participants' prior drug experiences are important variables in the response to psychedelic-assisted therapy . Future ...
This paper reviews methodologically rigorous studies examining group treatments for interview-diagnosed drug use disorders. A total of 50 studies reporting on the efficacy of group drug use disorder treatments for adults met inclusion criteria. Studies examining group treatment for cocaine, methamphetamine, marijuana, opioid, mixed substance, and substance use disorder with co-occurring ...
Drugs & Therapy Perspectives supports healthcare professionals working in clinical settings by publishing concise, authoritative review articles to aid drug formulary and treatment decisions, and original research articles on all aspects of pharmacological treatment to promote optimal patient outcomes.. As a hybrid journal, Drugs & Therapy Perspectives does not charge authors to publish using ...
Drugs & Therapy Perspectives. Publishing model: Hybrid. Submit your manuscript (this opens in a new tab) ... Original Research Article Open access 21 December 2023 Pages: 432 - 446 ... This journal's calls for papers. Collections this journal is participating in.
This article reviews group psychotherapy research published within the past 30 years, predominantly focusing on outcomes of group treatments for patients with various mental disorders. Additionally, meta-analyses on the efficacy of group treatments for patients with cancer or chronic pain are summarized. Results strongly support the use of group therapy and demonstrate outcomes equivalent to ...
The first BCR-ABL1 tyrosine-kinase inhibitor was discovered through drug screens in 1992, and in 2001 it became the first-line therapy with long-term remission rates for BCR-ABL-driven chronic ...
Abstract. Drug discovery is a dynamic field constantly evolving with the aim of identifying novel. therapeutic agents to combat various diseases. In this review, we present an overview of recent ...
Finding better approaches. While effective treatments for major depression are available, there is still room for improvement. This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs.
A research team co-led by UCLA investigators has shown that an immunotherapy drug combination can be an effective second-line therapy for patients with an aggressive and deadly type of melanoma that is resistant to the widely used immunotherapy drugs known as PD-1 inhibitors.
Monoamine oxidase inhibitors. Iproniazid was the first drug defined as an antidepressant; it was later classified as a monoamine oxidase inhibitor (MAOI)[6,7].Several other MAOIs have been introduced since 1957[].Due to their irreversible inhibition of monoamine oxidase, MOAIs have numerous side effects, such as hepatotoxicity and hypertensive crises, that can lead to lethal intracranial ...
PROVIDENCE, R.I. [Brown University] — A team of Brown University researchers is launching a study to test the combined use of the drug MDMA and talk therapy as a treatment for post-traumatic stress disorder and alcohol use disorder in military veterans. The study is the first at Brown on MDMA-assisted therapy and the first anywhere to test the treatment's effectiveness for dual disorders ...
The research team is currently working to develop an integrated biochip which can potentially be commercialised for use in drug screening and bio-assays on a single chip. Paper titled "Autonomous Microlasers for Profiling Extracellular Vesicles from Cancer Spheroids", published in Nano Letters, 16 March 2023. DOI: 10.1021/acs.nanolett.2c04123
The US Food and Drug Administration@s (FDA) Center for Biologics Evaluation and Research (CBER) on Tuesday issued two draft guidances related to cell and gene therapy testing: one addresses safety testing products derived of human allogeneic cells expanded for use in cell-based products and the other addresses testing animal- and human-derived materials in the manufacturing of cell and gene ...
A research consortium conducting a 10-year study of exercise biology released its first paper, working to map exercise benefits on the molecular level in rats.
On the basis of clinical-trial data, the US Food and Drug Administration (FDA) designated psilocybin a breakthrough therapy for major depressive disorder and treatment-resistant depression 8 ...
More than 25 million adults in the U.S. have tinnitus, a condition that causes ringing or buzzing in the ears. An FDA approved device that stimulates the tongue, helped 84% of people who tried it.
Colorectal cancer research is eligible for funding through the military's Peer Reviewed Cancer Research Program, where it must compete against dozens of other cancers for a limited amount of ...
Fortunately, the prospect of regenerative medicine as an alternative to conventional drug-based therapies is becoming a tangible reality by the day owing to the vigorous commitment of the research communities in studying the potential applications across a wide range of diseases like neurodegenerative diseases and diabetes, among many others .
Reshaping the MLR to appropriately include spending on social drivers of health interventions will enable more health plans to offer these vital services and enable states to cover more ...