Overview and General Information about Oral Presentation
- Daily Presentations During Work Rounds
- The New Patient Presentation
- The Holdover Admission Presentation
- Outpatient Clinic Presentations
- The structure of presentations varies from service to service (e.g. medicine vs. surgery), amongst subspecialties, and between environments (inpatient vs. outpatient). Applying the correct style to the right setting requires that the presenter seek guidance from the listeners at the outset.
- Time available for presenting is rather short, which makes the experience more stressful.
- Individual supervisors (residents, faculty) often have their own (sometimes quirky) preferences regarding presentation styles, adding another layer of variability that the presenter has to manage.
- Students are evaluated/judged on the way in which they present, with faculty using this as one way of gauging a student’s clinical knowledge.
- Done well, presentations promote efficient, excellent care. Done poorly, they promote tedium, low morale, and inefficiency.
General Tips:
- Practice, Practice, Practice! Do this on your own, with colleagues, and/or with anyone who will listen (and offer helpful commentary) before you actually present in front of other clinicians. Speaking "on-the-fly" is difficult, as rapidly organizing and delivering information in a clear and concise fashion is not a naturally occurring skill.
- Immediately following your presentations, seek feedback from your listeners. Ask for specifics about what was done well and what could have been done better – always with an eye towards gaining information that you can apply to improve your performance the next time.
- Listen to presentations that are done well – ask yourself, “Why was it good?” Then try to incorporate those elements into your own presentations.
- Listen to presentations that go poorly – identify the specific things that made it ineffective and avoid those pitfalls when you present.
- Effective presentations require that you have thought through the case beforehand and understand the rationale for your conclusions and plan. This, in turn, requires that you have a good grasp of physiology, pathology, clinical reasoning and decision-making - pushing you to read, pay attention, and in general acquire more knowledge.
- Think about the clinical situation in which you are presenting so that you can provide a summary that is consistent with the expectations of your audience. Work rounds, for example, are clearly different from conferences and therefore mandate a different style of presentation.
- Presentations are the way in which we tell medical stories to one another. When you present, ask yourself if you’ve described the story in an accurate way. Will the listener be able to “see” the patient the same way that you do? Can they come to the correct conclusions? If not, re-calibrate.
- It's O.K. to use notes, though the oral presentation should not simply be reduced to reading the admission note – rather, it requires appropriate editing/shortening.
- In general, try to give your presentations on a particular service using the same order and style for each patient, every day. Following a specific format makes it easier for the listener to follow, as they know what’s coming and when they can expect to hear particular information. Additionally, following a standardized approach makes it easier for you to stay organized, develop a rhythm, and lessens the chance that you’ll omit elements.

Specific types of presentations
There are a number of common presentation-types, each with its own goals and formats. These include:
- Daily presentations during work rounds for patients known to a service.
- Newly admitted patients, where you were the clinician that performed the H&P.
- Newly admitted patients that were “handed off” to the team in the morning, such that the H&P was performed by others.
- Outpatient clinic presentations, covering several common situations.
Key elements of each presentation type are described below. Examples of how these would be applied to most situations are provided in italics. The formats are typical of presentations done for internal medicine services and clinics.
Note that there is an acceptable range of how oral presentations can be delivered. Ultimately, your goal is to tell the correct story, in a reasonable amount of time, so that the right care can be delivered. Nuances in the order of presentation, what to include, what to omit, etc. are relatively small points. Don’t let the pursuit of these elements distract you or create undue anxiety.
Daily presentations during work rounds of patients that you’re following:
- Organize the presenter (forces you to think things through)
- Inform the listener(s) of 24 hour events and plan moving forward
- Promote focused discussion amongst your listeners and supervisors
- Opportunity to reassess plan, adjust as indicated
- Demonstrate your knowledge and engagement in the care of the patient
- Rapid (5 min) presentation of the key facts
Key features of presentation:
- Opening one liner: Describe who the patient is, number of days in hospital, and their main clinical issue(s).
- 24-hour events: Highlighting changes in clinical status, procedures, consults, etc.
- Subjective sense from the patient about how they’re feeling, vital signs (ranges), and key physical exam findings (highlighting changes)
- Relevant labs (highlighting changes) and imaging
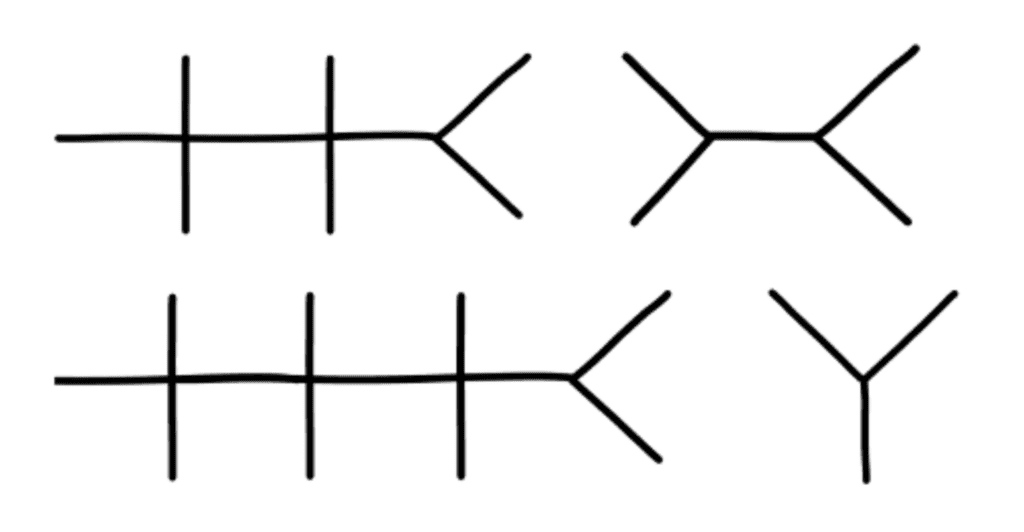
- Assessment and Plan : Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
Example of a daily presentation for a patient known to a team:
- Opening one liner: This is Mr. Smith, a 65 year old man, Hospital Day #3, being treated for right leg cellulitis
- MRI of the leg, negative for osteomyelitis
- Evaluation by Orthopedics, who I&D’d a superficial abscess in the calf, draining a moderate amount of pus
- Patient appears well, states leg is feeling better, less painful
- T Max 101 yesterday, T Current 98; Pulse range 60-80; BP 140s-160s/70-80s; O2 sat 98% Room Air
- Ins/Outs: 3L in (2 L NS, 1 L po)/Out 4L urine
- Right lower extremity redness now limited to calf, well within inked lines – improved compared with yesterday; bandage removed from the I&D site, and base had small amount of purulence; No evidence of fluctuance or undrained infection.
- Creatinine .8, down from 1.5 yesterday
- WBC 8.7, down from 14
- Blood cultures from admission still negative
- Gram stain of pus from yesterday’s I&D: + PMNS and GPCs; Culture pending
- MRI lower extremity as noted above – negative for osteomyelitis
- Continue Vancomycin for today
- Ortho to reassess I&D site, though looks good
- Follow-up on cultures: if MRSA, will transition to PO Doxycycline; if MSSA, will use PO Dicloxacillin
- Given AKI, will continue to hold ace-inhibitor; will likely wait until outpatient follow-up to restart
- Add back amlodipine 5mg/d today
- Hep lock IV as no need for more IVF
- Continue to hold ace-I as above
- Wound care teaching with RNs today – wife capable and willing to assist. She’ll be in this afternoon.
- Set up follow-up with PMD to reassess wound and cellulitis within 1 week
The Brand New Patient (admitted by you)
- Provide enough information so that the listeners can understand the presentation and generate an appropriate differential diagnosis.
- Present a thoughtful assessment
- Present diagnostic and therapeutic plans
- Provide opportunities for senior listeners to intervene and offer input
- Chief concern: Reason why patient presented to hospital (symptom/event and key past history in one sentence). It often includes a limited listing of their other medical conditions (e.g. diabetes, hypertension, etc.) if these elements might contribute to the reason for admission.
- The history is presented highlighting the relevant events in chronological order.
- 7 days ago, the patient began to notice vague shortness of breath.
- 5 days ago, the breathlessness worsened and they developed a cough productive of green sputum.
- 3 days ago his short of breath worsened to the point where he was winded after walking up a flight of stairs, accompanied by a vague right sided chest pain that was more pronounced with inspiration.
- Enough historical information has to be provided so that the listener can understand the reasons that lead to admission and be able to draw appropriate clinical conclusions.
- Past history that helps to shed light on the current presentation are included towards the end of the HPI and not presented later as “PMH.” This is because knowing this “past” history is actually critical to understanding the current complaint. For example, past cardiac catheterization findings and/or interventions should be presented during the HPI for a patient presenting with chest pain.
- Where relevant, the patient's baseline functional status is described, allowing the listener to understand the degree of impairment caused by the acute medical problem(s).
- It should be explicitly stated if a patient is a poor historian, confused or simply unaware of all the details related to their illness. Historical information obtained from family, friends, etc. should be described as such.
- Review of Systems (ROS): Pertinent positive and negative findings discovered during a review of systems are generally incorporated at the end of the HPI. The listener needs this information to help them put the story in appropriate perspective. Any positive responses to a more inclusive ROS that covers all of the other various organ systems are then noted. If the ROS is completely negative, it is generally acceptable to simply state, "ROS negative.”
- Other Past Medical and Surgical History (PMH/PSH): Past history that relates to the issues that lead to admission are typically mentioned in the HPI and do not have to be repeated here. That said, selective redundancy (i.e. if it’s really important) is OK. Other PMH/PSH are presented here if relevant to the current issues and/or likely to affect the patient’s hospitalization in some way. Unrelated PMH and PSH can be omitted (e.g. if the patient had their gall bladder removed 10y ago and this has no bearing on the admission, then it would be appropriate to leave it out). If the listener really wants to know peripheral details, they can read the admission note, ask the patient themselves, or inquire at the end of the presentation.
- Medications and Allergies: Typically all meds are described, as there’s high potential for adverse reactions or drug-drug interactions.
- Family History: Emphasis is placed on the identification of illnesses within the family (particularly among first degree relatives) that are known to be genetically based and therefore potentially heritable by the patient. This would include: coronary artery disease, diabetes, certain cancers and autoimmune disorders, etc. If the family history is non-contributory, it’s fine to say so.
- Social History, Habits, other → as relates to/informs the presentation or hospitalization. Includes education, work, exposures, hobbies, smoking, alcohol or other substance use/abuse.
- Sexual history if it relates to the active problems.
- Vital signs and relevant findings (or their absence) are provided. As your team develops trust in your ability to identify and report on key problems, it may become acceptable to say “Vital signs stable.”
- Note: Some listeners expect students (and other junior clinicians) to describe what they find in every organ system and will not allow the presenter to say “normal.” The only way to know what to include or omit is to ask beforehand.
- Key labs and imaging: Abnormal findings are highlighted as well as changes from baseline.
- Summary, assessment & plan(s) Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- The assessment and plan typically concludes by mentioning appropriate prophylactic considerations (e.g. DVT prevention), code status and disposition.
- Chief Concern: Mr. H is a 50 year old male with AIDS, on HAART, with preserved CD4 count and undetectable viral load, who presents for the evaluation of fever, chills and a cough over the past 7 days.
- Until 1 week ago, he had been quite active, walking up to 2 miles a day without feeling short of breath.
- Approximately 1 week ago, he began to feel dyspneic with moderate activity.
- 3 days ago, he began to develop subjective fevers and chills along with a cough productive of red-green sputum.
- 1 day ago, he was breathless after walking up a single flight of stairs and spent most of the last 24 hours in bed.
- Diagnosed with HIV in 2000, done as a screening test when found to have gonococcal urethritis
- Was not treated with HAART at that time due to concomitant alcohol abuse and non-adherence.
- Diagnosed and treated for PJP pneumonia 2006
- Diagnosed and treated for CMV retinitis 2007
- Became sober in 2008, at which time interested in HAART. Started on Atripla, a combination pill containing: Efavirenz, Tonofovir, and Emtricitabine. He’s taken it ever since, with no adverse effects or issues with adherence. Receives care thru Dr. Smiley at the University HIV clinic.
- CD4 count 3 months ago was 400 and viral load was undetectable.
- He is homosexual though he is currently not sexually active. He has never used intravenous drugs.
- He has no history of asthma, COPD or chronic cardiac or pulmonary condition. No known liver disease. Hepatitis B and C negative. His current problem seems different to him then his past episode of PJP.
- Review of systems: negative for headache, photophobia, stiff neck, focal weakness, chest pain, abdominal pain, diarrhea, nausea, vomiting, urinary symptoms, leg swelling, or other complaints.
- Hypertension x 5 years, no other known vascular disease
- Gonorrhea as above
- Alcohol abuse above and now sober – no known liver disease
- No relevant surgeries
- Atripla, 1 po qd
- Omeprazole 20 mg, 1 PO, qd
- Lisinopril 20mg, qd
- Naprosyn 250 mg, 1-2, PO, BID PRN
- No allergies
- Both of the patient's parents are alive and well (his mother is 78 and father 80). He has 2 brothers, one 45 and the other 55, who are also healthy. There is no family history of heart disease or cancer.
- Patient works as an accountant for a large firm in San Diego. He lives alone in an apartment in the city.
- Smokes 1 pack of cigarettes per day and has done so for 20 years.
- No current alcohol use. Denies any drug use.
- Sexual History as noted above; has sex exclusively with men, last partner 6 months ago.
- Seated on a gurney in the ER, breathing through a face-mask oxygen delivery system. Breathing was labored and accessory muscles were in use. Able to speak in brief sentences, limited by shortness of breath
- Vital signs: Temp 102 F, Pulse 90, BP 150/90, Respiratory Rate 26, O2 Sat (on 40% Face Mask) 95%
- HEENT: No thrush, No adenopathy
- Lungs: Crackles and Bronchial breath sounds noted at right base. E to A changes present. No wheezing or other abnormal sounds noted over any other area of the lung. Dullness to percussion was also appreciated at the right base.
- Cardiac: JVP less than 5 cm; Rhythm was regular. Normal S1 and S2. No murmurs or extra heart sounds noted.
- Abdomen and Genital exams: normal
- Extremities: No clubbing, cyanosis or edema; distal pulses 2+ and equal bilaterally.
- Skin: no eruptions noted.
- Neurological exam: normal
- WBC 18 thousand with 10% bands;
- Normal Chem 7 and LFTs.
- Room air blood gas: pH of 7.47/ PO2 of 55/PCO2 of 30.
- Sputum gram stain remarkable for an abundance of polys along with gram positive diplococci.
- CXR remarkable for dense right lower lobe infiltrate without effusion.
- Monitored care unit, with vigilance for clinical deterioration.
- Hypertension: given significant pneumonia and unclear clinical direction, will hold lisinopril. If BP > 180 and or if clear not developing sepsis, will consider restarting.
- Low molecular weight heparin
- Code Status: Wishes to be full code full care, including intubation and ICU stay if necessary. Has good quality of life and hopes to return to that functional level. Wishes to reconsider if situation ever becomes hopeless. Older brother Tom is surrogate decision maker if the patient can’t speak for himself. Tom lives in San Diego and we have his contact info. He is aware that patient is in the hospital and plans on visiting later today or tomorrow.
- Expected duration of hospitalization unclear – will know more based on response to treatment over next 24 hours.
The holdover admission (presenting data that was generated by other physicians)
- Handoff admissions are very common and present unique challenges
- Understand the reasons why the patient was admitted
- Review key history, exam, imaging and labs to assure that they support the working diagnostic and therapeutic plans
- Does the data support the working diagnosis?
- Do the planned tests and consults make sense?
- What else should be considered (both diagnostically and therapeutically)?
- This process requires that the accepting team thoughtfully review their colleagues efforts with a critical eye – which is not disrespectful but rather constitutes one of the main jobs of the accepting team and is a cornerstone of good care *Note: At some point during the day (likely not during rounds), the team will need to verify all of the data directly with the patient.
- 8-10 minutes
- Chief concern: Reason for admission (symptom and/or event)
- Temporally presented bullets of events leading up to the admission
- Review of systems
- Relevant PMH/PSH – historical information that might affect the patient during their hospitalization.
- Meds and Allergies
- Family and Social History – focusing on information that helps to inform the current presentation.
- Habits and exposures
- Physical exam, imaging and labs that were obtained in the Emergency Department
- Assessment and plan that were generated in the Emergency Department.
- Overnight events (i.e. what happened in the Emergency Dept. and after the patient went to their hospital room)? Responses to treatments, changes in symptoms?
- How does the patient feel this morning? Key exam findings this morning (if seen)? Morning labs (if available)?
- Assessment and Plan , with attention as to whether there needs to be any changes in the working differential or treatment plan. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- Chief concern: 70 yo male who presented with 10 days of progressive shoulder pain, followed by confusion. He was brought in by his daughter, who felt that her father was no longer able to safely take care for himself.
- 10 days ago, Mr. X developed left shoulder pain, first noted a few days after lifting heavy boxes. He denies falls or direct injury to the shoulder.
- 1 week ago, presented to outside hospital ER for evaluation of left shoulder pain. Records from there were notable for his being afebrile with stable vitals. Exam notable for focal pain anteriorly on palpation, but no obvious deformity. Right shoulder had normal range of motion. Left shoulder reported as diminished range of motion but not otherwise quantified. X-ray negative. Labs remarkable for wbc 8, creat 2.2 (stable). Impression was that the pain was of musculoskeletal origin. Patient was provided with Percocet and told to see PMD in f/u
- Brought to our ER last night by his daughter. Pain in shoulder worse. Also noted to be confused and unable to care for self. Lives alone in the country, home in disarray, no food.
- ROS: negative for falls, prior joint or musculoskeletal problems, fevers, chills, cough, sob, chest pain, head ache, abdominal pain, urinary or bowel symptoms, substance abuse
- Hypertension
- Coronary artery disease, s/p LAD stent for angina 3 y ago, no symptoms since. Normal EF by echo 2 y ago
- Chronic kidney disease stage 3 with creatinine 1.8; felt to be secondary to atherosclerosis and hypertension
- aspirin 81mg qd, atorvastatin 80mg po qd, amlodipine 10 po qd, Prozac 20
- Allergies: none
- Family and Social: lives alone in a rural area of the county, in contact with children every month or so. Retired several years ago from work as truck driver. Otherwise non-contributory.
- Habits: denies alcohol or other drug use.
- Temp 98 Pulse 110 BP 100/70
- Drowsy though arousable; oriented to year but not day or date; knows he’s at a hospital for evaluation of shoulder pain, but doesn’t know the name of the hospital or city
- CV: regular rate and rhythm; normal s1 and s2; no murmurs or extra heart sounds.
- Left shoulder with generalized swelling, warmth and darker coloration compared with Right; generalized pain on palpation, very limited passive or active range of motion in all directions due to pain. Right shoulder appearance and exam normal.
- CXR: normal
- EKG: sr 100; nl intervals, no acute changes
- WBC 13; hemoglobin 14
- Na 134, k 4.6; creat 2.8 (1.8 baseline 4 m ago); bicarb 24
- LFTs and UA normal
- Vancomycin and Zosyn for now
- Orthopedics to see asap to aspirate shoulder for definitive diagnosis
- If aspiration is consistent with infection, will need to go to Operating Room for wash out.
- Urine electrolytes
- Follow-up on creatinine and obtain renal ultrasound if not improved
- Renal dosing of meds
- Strict Ins and Outs.
- follow exam
- obtain additional input from family to assure baseline is, in fact, normal
- Since admission (6 hours) no change in shoulder pain
- This morning, pleasant, easily distracted; knows he’s in the hospital, but not date or year
- T Current 101F Pulse 100 BP 140/80
- Ins and Outs: IVF Normal Saline 3L/Urine output 1.5 liters
- L shoulder with obvious swelling and warmth compared with right; no skin breaks; pain limits any active or passive range of motion to less than 10 degrees in all directions
- Labs this morning remarkable for WBC 10 (from 13), creatinine 2 (down from 2.8)
- Continue with Vancomycin and Zosyn for now
- I already paged Orthopedics this morning, who are en route for aspiration of shoulder, fluid for gram stain, cell count, culture
- If aspirate consistent with infection, then likely to the OR
- Continue IVF at 125/h, follow I/O
- Repeat creatinine later today
- Not on any nephrotoxins, meds renaly dosed
- Continue antibiotics, evaluation for primary source as above
- Discuss with family this morning to establish baseline; possible may have underlying dementia as well
- SC Heparin for DVT prophylaxis
- Code status: full code/full care.
Outpatient-based presentations
There are 4 main types of visits that commonly occur in an outpatient continuity clinic environment, each of which has its own presentation style and purpose. These include the following, each described in detail below.
- The patient who is presenting for their first visit to a primary care clinic and is entirely new to the physician.
- The patient who is returning to primary care for a scheduled follow-up visit.
- The patient who is presenting with an acute problem to a primary care clinic
- The specialty clinic evaluation (new or follow-up)
It’s worth noting that Primary care clinics (Internal Medicine, Family Medicine and Pediatrics) typically take responsibility for covering all of the patient’s issues, though the amount of energy focused on any one topic will depend on the time available, acuity, symptoms, and whether that issue is also followed by a specialty clinic.
The Brand New Primary Care Patient
Purpose of the presentation
- Accurately review all of the patient’s history as well as any new concerns that they might have.
- Identify health related problems that need additional evaluation and/or treatment
- Provide an opportunity for senior listeners to intervene and offer input
Key features of the presentation
- If this is truly their first visit, then one of the main reasons is typically to "establish care" with a new doctor.
- It might well include continuation of therapies and/or evaluations started elsewhere.
- If the patient has other specific goals (medications, referrals, etc.), then this should be stated as well. Note: There may well not be a "chief complaint."
- For a new patient, this is an opportunity to highlight the main issues that might be troubling/bothering them.
- This can include chronic disorders (e.g. diabetes, congestive heart failure, etc.) which cause ongoing symptoms (shortness of breath) and/or generate daily data (finger stick glucoses) that should be discussed.
- Sometimes, there are no specific areas that the patient wishes to discuss up-front.
- Review of systems (ROS): This is typically comprehensive, covering all organ systems. If the patient is known to have certain illnesses (e.g. diabetes), then the ROS should include the search for disorders with high prevalence (e.g. vascular disease). There should also be some consideration for including questions that are epidemiologically appropriate (e.g. based on age and sex).
- Past Medical History (PMH): All known medical conditions (in particular those requiring ongoing treatment) are listed, noting their duration and time of onset. If a condition is followed by a specialist or co-managed with other clinicians, this should be noted as well. If a problem was described in detail during the “acute” history, it doesn’t have to be re-stated here.
- Past Surgical History (PSH): All surgeries, along with the year when they were performed
- Medications and allergies: All meds, including dosage, frequency and over-the-counter preparations. Allergies (and the type of reaction) should be described.
- Social: Work, hobbies, exposures.
- Sexual activity – may include type of activity, number and sex of partner(s), partner’s health.
- Smoking, Alcohol, other drug use: including quantification of consumption, duration of use.
- Family history: Focus on heritable illness amongst first degree relatives. May also include whether patient married, in a relationship, children (and their ages).
- Physical Exam: Vital signs and relevant findings (or their absence).
- Key labs and imaging if they’re available. Also when and where they were obtained.
- Summary, assessment & plan(s) presented by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic. This typically concludes with a “health care maintenance” section, which covers age, sex and risk factor appropriate vaccinations and screening tests.
The Follow-up Visit to a Primary Care Clinic
- Organize the presenter (forces you to think things through).
- Accurately review any relevant interval health care events that might have occurred since the last visit.
- Identification of new symptoms or health related issues that might need additional evaluation and/or treatment
- If the patient has no concerns, then verification that health status is stable
- Review of medications
- Provide an opportunity for listeners to intervene and offer input
- Reason for the visit: Follow-up for whatever the patient’s main issues are, as well as stating when the last visit occurred *Note: There may well not be a “chief complaint,” as patients followed in continuity at any clinic may simply be returning for a visit as directed by their doctor.
- Events since the last visit: This might include emergency room visits, input from other clinicians/specialists, changes in medications, new symptoms, etc.
- Review of Systems (ROS): Depth depends on patient’s risk factors and known illnesses. If the patient has diabetes, then a vascular ROS would be done. On the other hand, if the patient is young and healthy, the ROS could be rather cursory.
- PMH, PSH, Social, Family, Habits are all OMITTED. This is because these facts are already known to the listener and actionable aspects have presumably been added to the problem list (presented at the end). That said, these elements can be restated if the patient has a new symptom or issue related to a historical problem has emerged.
- MEDS : A good idea to review these at every visit.
- Physical exam: Vital signs and pertinent findings (or absence there of) are mentioned.
- Lab and Imaging: The reason why these were done should be mentioned and any key findings mentioned, highlighting changes from baseline.
- Assessment and Plan: This is most clearly done by individually stating all of the conditions/problems that are being addressed (e.g. hypertension, hypothyroidism, depression, etc.) followed by their specific plan(s). If a new or acute issue was identified during the visit, the diagnostic and therapeutic plan for that concern should be described.
The Focused Visit to a Primary Care Clinic
- Accurately review the historical events that lead the patient to make the appointment.
- Identification of risk factors and/or other underlying medical conditions that might affect the diagnostic or therapeutic approach to the new symptom or concern.
- Generate an appropriate assessment and plan
- Allow the listener to comment
Key features of the presentation:
- Reason for the visit
- History of Present illness: Description of the sequence of symptoms and/or events that lead to the patient’s current condition.
- Review of Systems: To an appropriate depth that will allow the listener to grasp the full range of diagnostic possibilities that relate to the presenting problem.
- PMH and PSH: Stating only those elements that might relate to the presenting symptoms/issues.
- PE: Vital signs and key findings (or lack thereof)
- Labs and imaging (if done)
- Assessment and Plan: This is usually very focused and relates directly to the main presenting symptom(s) or issues.
The Specialty Clinic Visit
Specialty clinic visits focus on the health care domains covered by those physicians. For example, Cardiology clinics are interested in cardiovascular disease related symptoms, events, labs, imaging and procedures. Orthopedics clinics will focus on musculoskeletal symptoms, events, imaging and procedures. Information that is unrelated to these disciples will typically be omitted. It’s always a good idea to ask the supervising physician for guidance as to what’s expected to be covered in a particular clinic environment.
- Highlight the reason(s) for the visit
- Review key data
- Provide an opportunity for the listener(s) to comment
- 5-7 minutes
- If it’s a consult, state the main reason(s) that the patient was referred as well as who referred them.
- If it’s a return visit, state the reasons why the patient is being followed in the clinic and when the last visit took place
- If it’s for an acute issue, state up front what the issue is Note: There may well not be a “chief complaint,” as patients followed in continuity in any clinic may simply be returning for a return visit as directed
- For a new patient, this highlights the main things that might be troubling/bothering the patient.
- For a specialty clinic, the history presented typically relates to the symptoms and/or events that are pertinent to that area of care.
- Review of systems , focusing on those elements relevant to that clinic. For a cardiology patient, this will highlight a vascular ROS.
- PMH/PSH that helps to inform the current presentation (e.g. past cardiac catheterization findings/interventions for a patient with chest pain) and/or is otherwise felt to be relevant to that clinic environment.
- Meds and allergies: Typically all meds are described, as there is always the potential for adverse drug interactions.
- Social/Habits/other: as relates to/informs the presentation and/or is relevant to that clinic
- Family history: Focus is on heritable illness amongst first degree relatives
- Physical Exam: VS and relevant findings (or their absence)
- Key labs, imaging: For a cardiology clinic patient, this would include echos, catheterizations, coronary interventions, etc.
- Summary, assessment & plan(s) by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic.
- Reason for visit: Patient is a 67 year old male presenting for first office visit after admission for STEMI. He was referred by Dr. Goins, his PMD.
- The patient initially presented to the ER 4 weeks ago with acute CP that started 1 hour prior to his coming in. He was found to be in the midst of a STEMI with ST elevations across the precordial leads.
- Taken urgently to cath, where 95% proximal LAD lesion was stented
- EF preserved by Echo; Peak troponin 10
- In-hospital labs were remarkable for normal cbc, chem; LDL 170, hdl 42, nl lfts
- Uncomplicated hospital course, sent home after 3 days.
- Since home, he states that he feels great.
- Denies chest pain, sob, doe, pnd, edema, or other symptoms.
- No symptoms of stroke or TIA.
- No history of leg or calf pain with ambulation.
- Prior to this admission, he had a history of hypertension which was treated with lisinopril
- 40 pk yr smoking history, quit during hospitalization
- No known prior CAD or vascular disease elsewhere. No known diabetes, no family history of vascular disease; He thinks his cholesterol was always “a little high” but doesn’t know the numbers and was never treated with meds.
- History of depression, well treated with prozac
- Discharge meds included: aspirin, metoprolol 50 bid, lisinopril 10, atorvastatin 80, Plavix; in addition he takes Prozac for depression
- Taking all of them as directed.
- Patient lives with his wife; they have 2 grown children who are no longer at home
- Works as a computer programmer
- Smoking as above
- ETOH: 1 glass of wine w/dinner
- No drug use
- No known history of cardiovascular disease among 2 siblings or parents.
- Well appearing; BP 130/80, Pulse 80 regular, 97% sat on Room Air, weight 175lbs, BMI 32
- Lungs: clear to auscultation
- CV: s1 s2 no s3 s4 murmur
- No carotid bruits
- ABD: no masses
- Ext; no edema; distal pulses 2+
- Cath from 4 weeks ago: R dominant; 95% proximal LAD; 40% Cx.
- EF by TTE 1 day post PCI with mild Anterior Hypokinesis, EF 55%, no valvular disease, moderate LVH
- Labs of note from the hospital following cath: hgb 14, plt 240; creat 1, k 4.2, lfts normal, glucose 100, LDL 170, HDL 42.
- EKG today: SR at 78; nl intervals; nl axis; normal r wave progression, no q waves
- Plan: aspirin 81 indefinitely, Plavix x 1y
- Given nitroglycerine sublingual to have at home.
- Reviewed symptoms that would indicate another MI and what to do if occurred
- Plan: continue with current dosages of meds
- Chem 7 today to check k, creatinine
- Plan: Continue atorvastatin 80mg for life
- Smoking cessation: Doing well since discharge without adjuvant treatments, aware of supports.
- Plan: AAA screening ultrasound
- Log In Username Enter your ACP Online username. Password Enter the password that accompanies your username. Remember me Forget your username or password ?
- Privacy Policy
- Career Connection
- Member Forums
© Copyright 2024 American College of Physicians, Inc. All Rights Reserved. 190 North Independence Mall West, Philadelphia, PA 19106-1572 800-ACP-1915 (800-227-1915) or 215-351-2600
If you are unable to login, please try clearing your cookies . We apologize for the inconvenience.
Presenting a Clinical Vignette: Deciding What to Present
If you are scheduled to make a presentation of a clinical vignette, reading this article will improve your performance. We describe a set of practical, proven steps that will guide your preparation of the presentation. The process of putting together a stellar presentation takes time and effort, and we assume that you will be willing to put forth the effort to make your presentation successful. This and subsequent articles will focus on planning, preparation, creating visual aids (slides), and presentation skills. The intent of this series of articles is to help you make a favorable impression and reap the rewards, personal and professional, of a job well done.
The process begins with the creation of an outline of the topics that might be presented at the meeting. Your outline should follow the typical format and sequence for this type of communication: history, physical examination, investigations, patient course, and discussion. This format is chosen because your audience understands it and uses it every day. If you have already prepared a paper for publication, it can be a rich source of content for the topic outline.
To get you started, we have prepared a generic outline to serve as an example. Look over the generic outline to get a sense of what might be addressed in your presentation. We realize that the generic outline will not precisely fit all of the types of cases; nevertheless, think about the larger principle and ask yourself, "How can I adapt this to my situation?" In order to help you visualize the type of content you might include in the outline, an example of a topic outline for a clinical vignette is presented.
Introduction
The main purpose of the introduction is to place the case in a clinical context and explain the importance or relevance of the case. Some case reports begin immediately with the description of the case, and this is perfectly acceptable.
1. Describing the clinical context and relevance
i. Ergotism is characterized by intense, generalized vasoconstriction of small and large blood vessels. ii. Ergotism is rare and therefore difficult to diagnose. iii. Failure to diagnose can lead to significant morbidity.
Case Presentation
The case report should be chronological and detail the history, physical findings, and investigations followed by the patient's course. At this point, you may wish to include more details than you might have time to present, prioritizing the content later.
i. A 34-year-old female smoker has chronic headaches, dyspnea, and burning leg pain. ii. Clinical diagnosis of mitral valve stenosis is made. iii. She returns in one week because of burning pain in the legs. iv. One month after presentation, cardiac catheterization demonstrates severe mitral valve stenosis. v. Elective mitral valve commisurotomy is scheduled, but the patient is admitted to hospital early because of increased burning pain in her feet and a painful right leg.
2. Physical Examination
i. Normal vital signs. ii. No skin findings. iii. Typical findings of mitral stenosis, no evidence of heart failure. iv. Cool, pulseless right leg. v. Normal neurological examination.
3. Investigations
i. Normal laboratory studies. ii. ECG shows left atrial enlargement. iii. Arteriogram of right femoral artery shows subtotal stenosis, collateral filling of the popliteal artery, and pseudoaneurysm formation.
4. Hospital Course
i. Mitral valve commisurotomy is performed, as well as femoral artery thombectomy, balloon dilation, and a patch graft repair. ii. On the fifth postoperative day, the patient experienced a return of burning pain in the right leg. The leg was pale, cool, mottled, and pulseless. iii. The arteriogram of femoral arteries showed smooth segmental narrowing and bilateral vasospasm suggesting large-vessel arteritis complicated by thrombosis. iv. Treatment was initiated with corticosteroids, anticoagulants, antiplatelet drugs, and oral vasodilators. v. The patient continued to deteriorate with both legs becoming cool and pulseless. vi. Additional history revealed that the patient abused ergotamine preparations for years (headaches). She used 12 tables daily for the past year and continued to receive ergotamine in hospital on days 2, 6, and 7. vii. Ergotamine preparations were stopped, intravenous nitroprusside was begun, and she showed clinical improvement within 2 hours. Nitroprusside was stopped after 24 hours, and the symptoms did not return. viii. The remainder of hospitalization was uneventful.
The main purpose of the discussion section is to articulate the lessons learned from the case. It should describe how a similar case should be approached in the future. It is sometimes appropriate to provide background information to understand the pathophysiological mechanisms associated with the patient's presentation, findings, investigations, course, or therapy.
1. Discussion
i. The most common cause of ergotism is chronic poisoning found in young females with chronic headaches. ii. Manifestations can include neurological, gastrointestinal, and vascular (list each in a table). iii. Ergotamine poisoning induces intense vasospasm, and venous thrombosis may occur from direct damage to the endothelium. iv. Vasospasm is due primarily to the direct vasoconstrictor effects on the vascular smooth muscle. v. Habitual use of ergotamine can lead to withdrawal headaches leading to a cycle of greater levels of ingestion. vi. In addition to stopping ergotamine, a direct vasodilator is usually prescribed. vii. Lesson 1: Physicians should be alert to the potential of ergotamine toxicity in young women with chronic headaches that present with neurological, gastrointestinal, or ischemic symptoms. viii. Lesson 2: The value of a complete history and checking the medication list.
Creating a topic outline will provide a list of all the topics you might possibly present at the meeting. Since you will have only ten minutes, you will prioritize the topics to determine what to keep and what to cut.
How do you decide what to cut? First, identify the basic information in the three major categories that you simply must present. This represents the "must-say" category. If you have done your job well, the content you have retained will answer the following questions:
What happened to the patient? What was the time course of these events? Why did management follow the lines that it did? What was learned?
After you have identified the "must-say" content, identify information that will help the audience better understand the case. Call this the "elaboration" category. Finally, identify the content that you think the audience would like to know, provided there is enough time, and identify this as the "nice-to-know" category.
Preparing a presentation is an iterative process. As you begin to "fit" your talk into the allotted time, certain content you originally thought of as "elaboration" may be dropped to the "nice-to-know" category due to time constraints. Use the following organizational scheme to efficiently prioritize your outline.
Prioritizing Topics in the Topic Outline
1. Use your completed topic outline.
2. Next to each entry in your outline, prioritize the importance of content.
3. Use the following code system to track your prioritization decisions:
A = Must-Say B = Elaboration C = Nice-to-Know
4. Remember, this is an iterative process; your decisions are not final.
5. Review the outline with your mentor or interested colleagues, and listen to their decisions.
Use the Preparing the Clinical Vignette Presentation Checklist to assist you in preparing the topic outline.

- Free Study Planner
- Residency Consulting
- Free Resources
- Med School Blog
- 1-888-427-7737
The Ultimate Patient Case Presentation Template for Med Students
- by Neelesh Bagrodia
- Apr 06, 2024
- Reviewed by: Amy Rontal, MD

Knowing how to deliver a patient presentation is one of the most important skills to learn on your journey to becoming a physician. After all, when you’re on a medical team, you’ll need to convey all the critical information about a patient in an organized manner without any gaps in knowledge transfer.
One big caveat: opinions about the correct way to present a patient are highly personal and everyone is slightly different. Additionally, there’s a lot of variation in presentations across specialties, and even for ICU vs floor patients.
My goal with this blog is to give you the most complete version of a patient presentation, so you can tailor your presentations to the preferences of your attending and team. So, think of what follows as a model for presenting any general patient.
Here’s a breakdown of what goes into the typical patient presentation.

7 Ingredients for a Patient Case Presentation Template
1. the one-liner.
The one-liner is a succinct sentence that primes your listeners to the patient.
A typical format is: “[Patient name] is a [age] year-old [gender] with past medical history of [X] presenting with [Y].
2. The Chief Complaint
This is a very brief statement of the patient’s complaint in their own words. A common pitfall is when medical students say that the patient had a chief complaint of some medical condition (like cholecystitis) and the attending asks if the patient really used that word!
An example might be, “Patient has chief complaint of difficulty breathing while walking.”
3. History of Present Illness (HPI)
The goal of the HPI is to illustrate the story of the patient’s complaint.
I remember when I first began medical school, I had a lot of trouble determining what was relevant and ended up giving a lot of extra details. Don’t worry if you have the same issue. With time, you’ll learn which details are important.
The OPQRST Framework
In the beginning of your clinical experience, a helpful framework to use is OPQRST:
Describe when the issue started, and if it occurs during certain environmental or personal exposures.
P rovocative
Report if there are any factors that make the pain better or worse. These can be broad, like noting their shortness of breath worsened when lying flat, or their symptoms resolved during rest.
Relay how the patient describes their pain or associated symptoms. For example, does the patient have a burning versus a pressure sensation? Are they feeling weakness, stiffness, or pain?
R egion/Location
Indicate where the pain is located and if it radiates anywhere.
Talk about how bad the pain is for the patient. Typically, a 0-10 pain scale is useful to provide some objective measure.
Discuss how long the pain lasts and how often it occurs.
A Case Study
While the OPQRST framework is great when starting out, it can be limiting.
Let’s take an example where the patient is not experiencing pain and comes in with altered mental status along with diffuse jaundice of the skin and a history of chronic liver disease. You will find that certain sections of OPQRST do not apply.
In this event, the HPI is still a story, but with a different framework. Try to go in chronological order. Include relevant details like if there have been any changes in medications, diet, or bowel movements.
Pertinent Positive and Negative Symptoms
Regardless of the framework you use, the name of the game is pertinent positive and negative symptoms the patient is experiencing.
I’d like to highlight the word “pertinent.” It’s less likely the patient’s chronic osteoarthritis and its management is related to their new onset shortness of breath, but it’s still important for knowing the patient’s complete medical picture. A better place to mention these details would be in the “Past Medical History” section, and reserve the HPI portion for more pertinent history.
As you become exposed to more illness scripts, experience will teach you which parts of the history are most helpful to state. Also, as you spend more time on the wards, you will pick up on which questions are relevant and important to ask during the patient interview.
By painting a clear picture with pertinent positives and negatives during your presentation, the history will guide what may be higher or lower on the differential diagnosis.
Some other important components to add are the patient’s additional past medical/surgical history, family history, social history, medications, allergies, and immunizations.
The HEADSSS Method
Particularly, the social history is an important time to describe the patient as a complete person and understand how their life story may affect their present condition.
One way of organizing the social history is the HEADSSS method:
– H ome living situation and relationships – E ducation and employment – A ctivities and hobbies – D rug use (alcohol, tobacco, cocaine, etc.) Note frequency of use, and if applicable, be sure to add which types of alcohol consumption (like beer versus hard liquor) and forms of drug use. – S exual history (partners, STI history, pregnancy plans) – S uicidality and depression – S piritual and religious history
Again, there’s a lot of variation in presenting social history, so just follow the lead of your team. For example, it’s not always necessary/relevant to obtain a sexual history, so use your judgment of the situation.
4. Review of Symptoms
Oftentimes, most elements of this section are embedded within the HPI. If there are any additional symptoms not mentioned in the HPI, it’s appropriate to state them here.
5. Objective
Vital signs.
Some attendings love to hear all five vital signs: temperature, blood pressure (mean arterial pressure if applicable), heart rate, respiratory rate, and oxygen saturation. Others are happy with “afebrile and vital signs stable.” Just find out their preference and stick to that.
Physical Exam
This is one of the most important parts of the patient presentation for any specialty. It paints a picture of how the patient looks and can guide acute management like in the case of a rigid abdomen. As discussed in the HPI section, typically you should report pertinent positives and negatives. When you’re starting out, your attending and team may prefer for you to report all findings as part of your learning.
For example, pulmonary exam findings can be reported as: “Regular chest appearance. No abnormalities on palpation. Lungs resonant to percussion. Clear to auscultation bilaterally without crackles, rhonchi, or wheezing.”
Typically, you want to report the physical exams in a head to toe format: General Appearance, Mental Status, Neurologic, Eyes/Ears/Nose/Mouth/Neck, Cardiovascular, Pulmonary, Breast, Abdominal, Genitourinary, Musculoskeletal, and Skin. Depending on the situation, additional exams can be incorporated as applicable.
Now comes reporting pertinent positive and negative labs. Several labs are often drawn upon admission. It’s easy to fall into the trap of reading off all the labs and losing everyone’s attention. Here are some pieces of advice:
You normally can’t go wrong sticking to abnormal lab values.
One qualification is that for a patient with concern for acute coronary syndrome, reporting a normal troponin is essential. Also, stating the normalization of previously abnormal lab values like liver enzymes is important.
Demonstrate trends in lab values.
A lab value is just a single point in time and does not paint the full picture. For example, a hemoglobin of 10g/dL in a patient at 15g/dL the previous day is a lot more concerning than a patient who has been stable at 10g/dL for a week.
Try to avoid editorializing in this section.
Save your analysis of the labs for the assessment section. Again, this can be a point of personal preference. In my experience, the team typically wants the raw objective data in this section.
This is also a good place to state the ins and outs of your patient (if applicable). In some patients, these metrics are strictly recorded and are typically reported as total fluid in and out over the past day followed by the net fluid balance. For example, “1L in, 2L out, net -1L over the past 24 hours.”
6. Diagnostics/Imaging
Next, you’ll want to review any important diagnostic tests and imaging. For example, describe how the EKG and echo look in a patient presenting with chest pain or the abdominal CT scan in a patient with right lower quadrant abdominal pain.
Try to provide your own interpretation to develop your skills and then include the final impression. Also, report if a diagnostic test is still pending.
7. Assessment/Plan
This is the fun part where you get to use your critical thinking (aka doctor) skills! For the scope of this blog, we’ll review a problem-based plan.
It’s helpful to begin with a summary statement that incorporates the one-liner, presenting issue(s)/diagnosis(es), and patient stability.
Then, go through all the problems relevant to the admission. You can impress your audience by casting a wide differential diagnosis and going through the elements of your patient presentation that support one diagnosis over another.
Following your assessment, try to suggest a management plan. In a patient with congestive heart failure exacerbation, initiating a diuresis regimen and measuring strict ins/outs are good starting points.
You may even suggest a follow-up on their latest ejection fraction with an echo and check if they’re on guideline-directed medical therapy. Again, with more time on the clinical wards you’ll start to pick up on what management plan to suggest.
One pointer is to talk about all relevant problems, not just the presenting issue. For example, a patient with diabetes may need to be put on a sliding scale insulin regimen or another patient may require physical/occupational therapy. Just try to stay organized and be comprehensive.
A Note About Patient Presentation Skills
When you’re doing your first patient presentations, it’s common to feel nervous. There may be a lot of “uhs” and “ums.”
Here’s the good news: you don’t have to be perfect! You just need to make a good faith attempt and keep on going with the presentation.
With time, your confidence will build. Practice your fluency in the mirror when you have a chance. No one was born knowing medicine and everyone has gone through the same stages of learning you are!
Practice your presentation a couple times before you present to the team if you have time. Pull a resident aside if they have the bandwidth to make sure you have all the information you need.
One big piece of advice: NEVER LIE. If you don’t know a specific detail, it’s okay to say, “I’m not sure, but I can look that up.” Someone on your team can usually retrieve the information while you continue on with your presentation.
Example Patient Case Presentation Template
Here’s a blank patient case presentation template that may come in handy. You can adapt it to best fit your needs.
Chief Complaint:
History of Present Illness:
Past Medical History:
Past Surgical History:
Family History:
Social History:
Medications:
Immunizations:
Vital Signs : Temp ___ BP ___ /___ HR ___ RR ___ O2 sat ___
Physical Exam:
General Appearance:
Mental Status:
Neurological:
Eyes, Ears, Nose, Mouth, and Neck:
Cardiovascular:
Genitourinary:
Musculoskeletal:
Most Recent Labs:
Previous Labs:
Diagnostics/Imaging:
Impression/Interpretation:
Assessment/Plan:
One-line summary:
#Problem 1:
Assessment:
#Problem 2:
Final Thoughts on Patient Presentations
I hope this post demystified the patient presentation for you. Be sure to stay organized in your delivery and be flexible with the specifications your team may provide.
Something I’d like to highlight is that you may need to tailor the presentation to the specialty you’re on. For example, on OB/GYN, it’s important to include a pregnancy history. Nonetheless, the aforementioned template should set you up for success from a broad overview perspective.
Stay tuned for my next post on how to give an ICU patient presentation. And if you’d like me to address any other topics in a blog, write to me at [email protected] !
Looking for more (free!) content to help you through clinical rotations? Check out these other posts from Blueprint tutors on the Med School blog:
- How I Balanced My Clinical Rotations with Shelf Exam Studying
- How (and Why) to Use a Qbank to Prepare for USMLE Step 2
- How to Study For Shelf Exams: A Tutor’s Guide
About the Author
Hailing from Phoenix, AZ, Neelesh is an enthusiastic, cheerful, and patient tutor. He is a fourth year medical student at the Keck School of Medicine of the University of Southern California and serves as president for the Class of 2024. He is applying to surgery programs for residency. He also graduated as valedictorian of his high school and the USC Viterbi School of Engineering, obtaining a B.S. in Biomedical Engineering in 2020. He discovered his penchant for teaching when he began tutoring his friends for the SAT and ACT in the summer of 2015 out of his living room. Outside of the academic sphere, Neelesh enjoys surfing at San Onofre Beach and hiking in the Santa Monica Mountains. Twitter: @NeeleshBagrodia LinkedIn: http://www.linkedin.com/in/neelesh-bagrodia

Related Posts

My Success Story: Passing Step 1 and Shelf Exams During Third Year with Med School Tutors

What Happens if I Fail Step 1 (Now That It’s Pass/Fail)?

What is a Fellow Doctor? A Guide on Fellowships for Eager Medical Students
Search the blog, try blueprint med school study planner.
Create a personalized study schedule in minutes for your upcoming USMLE, COMLEX, or Shelf exam. Try it out for FREE, forever!
Could You Benefit from Tutoring?
Sign up for a free consultation to get matched with an expert tutor who fits your board prep needs
Find Your Path in Medicine
A side by side comparison of specialties created by practicing physicians, for you!
Popular Posts

Need a personalized USMLE/COMLEX study plan?
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to present...
How to present clinical cases
- Related content
- Peer review
- Ademola Olaitan , medical student 1 ,
- Oluwakemi Okunade , final year medical student 1 ,
- Jonathan Corne , consultant physician 2
- 1 University of Nottingham
- 2 Nottingham University Hospitals
Presenting a patient is an essential skill that is rarely taught
Clinical presenting is the language that doctors use to communicate with each other every day of their working lives. Effective communication between doctors is crucial, considering the collaborative nature of medicine. As a medical student and later as a doctor you will be expected to present cases to peers and senior colleagues. This may be in the setting of handovers, referring a patient to another specialty, or requesting an opinion on a patient.
A well delivered case presentation will facilitate patient care, act a stimulus for timely intervention, and help identify individual and group learning needs. 1 Case presentations are also used as a tool for assessing clinical competencies at undergraduate and postgraduate level.
Medical students are taught how to take histories, examine, and communicate effectively with patients. However, we are expected to learn how to present effectively by observation, trial, and error.
Principles of presentation
Remember that the purpose of the case presentation is to convey your diagnostic reasoning to the listener. By the end of your presentation the examiner should have a clear view of the patient’s condition. Your presentation should include all the facts required to formulate a management plan.
There are no hard and fast rules for a perfect presentation, rather the content of each presentation should be determined by the case, the context, and the audience. For example, presenting a newly admitted patient with complex social issues on a medical ward round will be very different from presenting a patient with a perforated duodenal ulcer who is in need of an emergency laparotomy.
Whether you’re presenting on a busy ward round or during an objective structured clinical examination (OSCE), it is important that you are concise yet get across all the important points. Start by introducing patients with identifiers such as age, sex, and occupation, and move on to the complaint that they presented with or the reason that they are in hospital. The presenting complaint is an important signpost and should always be clearly stated at the start of the presentation.
Presenting a history
After you’ve introduced the patient and stated the presenting complaint, you can proceed in a chronological approach—for example, “Mr X came in yesterday with worsening shortness of breath, which he first noticed four days ago.” Alternatively you can discuss each of the problems, starting with the most pertinent and then going through each symptom in turn. This method is especially useful in patients who have several important comorbidities.
The rest of the history can then be presented in the standard format of presenting complaint, history of presenting complaint, medical history, drug history, family history, and social history. Strictly speaking there is no right or wrong place to insert any piece of information. However, in some instances it may be more appropriate to present some information as part of the history of presenting complaints rather than sticking rigidly to the standard format. For example, in a patient who presents with haemoptysis, a mention of relevant risk factors such as smoking or contacts with tuberculosis guides the listener down a specific diagnostic pathway.
Apart from deciding at what point to present particular pieces of information, it is also important to know what is relevant and should be included, and what is not. Although there is some variation in what your seniors might view as important features of the history, there are some aspects which are universally agreed to be essential. These include identifying the chief complaint, accurately describing the patient’s symptoms, a logical sequence of events, and an assessment of the most important problems. In addition, senior medical students will be expected to devise a management plan. 1
The detail in the family and social history should be adapted to the situation. So, having 12 cats is irrelevant in a patient who presents with acute appendicitis but can be relevant in a patient who presents with an acute asthma attack. Discerning the irrelevant from the relevant is not always easy, but it comes with experience. 2 In the meantime, learning about the diseases and their associated features can help to guide you in the things you need to ask about in your history. Indeed, it is impossible to present a good clinical history if you haven’t taken a good history from the patient.
Presenting examination findings
When presenting examination findings remember that the aim is to paint a clear picture of the patient’s clinical status. Help the listener to decide firstly whether the patient is acutely unwell by describing basics such as whether the patient is comfortable at rest, respiratory rate, pulse, and blood pressure. Is the patient pyrexial? Is the patient in pain? Is the patient alert and orientated? These descriptions allow the listener to quickly form a mental picture of the patient’s clinical status. After giving an overall picture of the patient you can move on to present specific findings about the systems in question. It is important to include particular negative findings because they can influence the patient’s management. For example, in a patient with heart failure it is helpful to state whether the patient has a raised jugular venous pressure, or if someone has a large thyroid swelling it is useful to comment on whether the trachea is displaced. Initially, students may find it difficult to know which details are relevant to the case presentation; however, this skill becomes honed with increasing knowledge and clinical experience.
Presenting in an exam
Although the same principles as presenting in other situations also apply in an exam setting, the exam situation differs in the sense that its purpose is for you to show your clinical competence to the examiner.
It’s all about making a good impression. Walk into the room confidently and with a smile. After taking the history or examining the patient, turn to the examiner and look at him or her before starting to present your findings. Avoid looking back at the patient while presenting. A good way to avoid appearing fiddly is to hold your stethoscope behind your back. You can then wring to your heart’s content without the examiner sensing your imminent nervous breakdown.
Start with an opening statement as you would in any other situation, before moving on to the main body of the presentation. When presenting the main body of your history or examination make sure that you show the examiner how your findings are linked to each other and how they come together to support your conclusion.
Finally, a good summary is just as important as a good introduction. Always end your presentation with two or three sentences that summarise the patient’s main problem. It can go something like this: “In summary, this is Mrs X, a lifelong smoker with a strong family history of cardiovascular disease, who has intermittent episodes of chest pain suggestive of stable angina.”
Improving your skills
The RIME model (reporter, interpreter, manager, and educator) gives the natural progression of the clinical skills of a medical student. 3 Early on in clinical practice students are simply reporters of information. As the student progresses and is able to link together symptoms, signs, and investigation results to come up with a differential diagnosis, he or she becomes an interpreter of information. With further development of clinical skills and increasing knowledge students are actively able to suggest management plans. Finally, managers progress to become educators. The development from reporter to manager is reflected in the student’s case presentations.
The key to improving presentation skills is to practise, practise, and then practise some more. So seize every opportunity to present to your colleagues and seniors, and reflect on the feedback you receive. 4 Additionally, by observing colleagues and doctors you can see how to and how not to present.
Remember the purpose of the presentation
Be flexible; the context should dictate the content of the presentation
Always include a presenting complaint
Present your findings in a way that shows understanding
Have a system
Use appropriate terminology
Additional tips for exams
Start with a clear introductory statement and close with a brief summary
After your summary suggest a working diagnosis and a management plan
Practise, practise, practise, and get feedback
Present with confidence, and don’t be put off by an examiner’s poker face
Be honest; do not make up signs to fit in with your diagnosis
Originally published as: Student BMJ 2010;18:c1539
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
See “Medical ward rounds” ( Student BMJ 2009;17:98-9, http://archive.student.bmj.com/issues/09/03/life/98.php ).
- ↵ Green EH, Durning SJ, DeCherrie L, Fagan MJ, Sharpe B, Hershman W. Expectations for oral case presentations for clinical clerks: Opinions of internal medicine clerkship directors. J Gen Intern Med 2009 ; 24 : 370 -3. OpenUrl CrossRef PubMed Web of Science
- ↵ Lingard LA, Haber RJ. What do we mean by “relevance”? A clinical and rhetorical definition with implications for teaching and learning the case-presentation format. Acad Med 1999 ; 74 : S124 -7. OpenUrl CrossRef PubMed Web of Science
- ↵ Pangaro L. A new vocabulary and other innovations for improving descriptive in-training evaluations. Acad Med 1999 ; 74 : 1203 -7. OpenUrl CrossRef PubMed Web of Science
- ↵ Haber RJ, Lingard LA. Learning oral presentation skills: a rhetorical analysis with pedagogical and professional implications. J Gen Intern Med 2001 ; 16 : 308 -14. OpenUrl CrossRef PubMed Web of Science

Presenting Your Case
A Concise Guide for Medical Students
- © 2019
- Clifford D. Packer 0
Professor of Medicinem, Department of Medicine, Case Western Reserve University School of Medicine, Louis Stokes Cleveland VA Medical Center, Cleveland, USA
You can also search for this author in PubMed Google Scholar
- Provides a comprehensive guide to case presentation and related activities
- Covers various types of oral case presentations on the wards, including the traditional new patient presentation, transfers, night float admissions, and brief SOAP presentations on daily rounds
- Prepares medical students for their clerkship evaluations, which depend largely on the quality of their oral presentations
11k Accesses
1 Citations
1 Altmetric
This is a preview of subscription content, log in via an institution to check access.
Access this book
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Other ways to access
Licence this eBook for your library
Institutional subscriptions
Table of contents (14 chapters)
Front matter, the importance of a good case presentation and why students struggle with it.
Clifford D. Packer
Organization of the Oral Case Presentation
Variations on the oral case presentation, the hpi: a timeline, not a time machine, pertinent positives and negatives, the diagnostic power of description, the assessment and plan, approaches to differential diagnosis, searching and citing the literature, adding value to the oral presentation, teaching rounds: speaking up, getting involved, and learning to accept uncertainty, the art of the 5-minute talk, future directions of the oral case presentation, back matter.
- Oral case presentation
- Differential Diagnosis
- Five-Minute-Talk
About this book
Medical students often struggle when presenting new patients to the attending physicians on the ward. Case presentation is either poorly taught or not taught at all in the first two years of medical school. As a result, students are thrust into the spotlight with only sketchy ideas about how to present, prioritize, edit, and focus their case presentations. They also struggle with producing a broad differential diagnosis and defending their leading diagnosis. This text provides a comprehensive guide to give well-prepared, focused and concise presentations. It also allows students to discuss differential diagnosis, incorporate high-value care, educate their colleagues, and participate actively in the care of their patients.
Linking in-depth discussion of the oral presentation with differential diagnosis and high value care, Presenting Your Case is a valuable resource for medical students, clerkship directors and others who educatestudents on the wards and in the clinic.
Authors and Affiliations
About the author.
Clifford D. Packer, MD
Professor of Medicine
Department of Medicine
Case Western Reserve University School of Medicine
Louis Stokes Cleveland VA Medical Center
Cleveland, OH, USA
Bibliographic Information
Book Title : Presenting Your Case
Book Subtitle : A Concise Guide for Medical Students
Authors : Clifford D. Packer
DOI : https://doi.org/10.1007/978-3-030-13792-2
Publisher : Springer Cham
eBook Packages : Medicine , Medicine (R0)
Copyright Information : Springer Nature Switzerland AG 2019
Softcover ISBN : 978-3-030-13791-5 Published: 14 May 2019
eBook ISBN : 978-3-030-13792-2 Published: 29 April 2019
Edition Number : 1
Number of Pages : XIV, 196
Number of Illustrations : 8 b/w illustrations, 9 illustrations in colour
Topics : General Practice / Family Medicine
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- UNC Chapel Hill
Case Presentation Skills
Communicating patient care information to colleagues and other health professionals is an essential skill regardless of specialty. Internists have traditionally given special attention to case presentation skills because of the comprehensive nature of patient evaluations and the various settings in which internal medicine is practiced. Students should develop facility with different types of case presentation: written and oral, new patient and follow-up, inpatient and outpatient.
Prerequisite
Basic written and oral case presentation skills, obtained in physical diagnosis courses.
Specific Learning Objectives
- components of comprehensive and abbreviated case presentations (oral and written) and the settings appropriate for each.
- present illness organized chronologically, without repetition, omission, or extraneous information.
- a comprehensive physical examination with detail pertinent to the patient’s problem.
- a succinct and, where appropriate, unified list of all problems identified in the history and physical examination.
- a differential diagnosis for each problem (appropriate to level of training).
- a diagnosis/treatment plan for each problem (appropriate to level of training).
- orally present a new patient’s case in a logical manner, chronologically developing the present illness, summarizing the pertinent positive and negative findings as well as the differential diagnosis and plans for further testing and treatment.
- orally present a follow-up patient’s case, in a focused, problem-based manner that includes pertinent new findings and diagnostic and treatment plans.
- select the appropriate mode of presentation that is pertinent to the clinical situation.
- demonstrate a commitment to improving case presentation skills by regularly seeking feedback on presentations. accurately and objectively record and present data.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
The purpose of the oral case presentation is:
- To concisely communicate the findings of your history and exam to other members of your team
- To formulate and address the clinical questions that are important to your patient’s care
On completion of Foundations of Clinical Medicine, students should be able to perform an accurate, complete and well organized comprehensive oral case presentation for a new clinic or hospital patient, and adapt the case presentation to different clinical settings. A comprehensive OCP includes each of these sections:
The oral case presentation is a mechanism for communicating with your team, which may include residents, attending physicians, nurses, social workers, pharmacists. Your audience may also include the patient and family if it is presented at the hospital bedside.
An oral case presentation includes only a SUBSET of the information that you record in your write-up, the information the team needs to provide care. The write-up contains ALL the facts while the OCP includes the facts needed to understand and address the current issues.
Purpose and format of each section
Identifying information & chief concern (id/cc).
Purpose: Sets the stage and gives a brief synopsis of the patient’s major problem.
Format: Same as in your writeup!
- Identify the patient by name and age. You can also include gender identity, if confirmed.
- Include no more than four medical problems (sometimes there are zero) that are highly relevant to the chief concern. List only the diagnoses here, and elaborate on them in the HPI or PMH.
- Report the chief concern and duration of symptoms
Template: “___ is a ___ year-old with a history of ___ who presents with ___ of ___ duration.”
History of present illness (HPI)
Purpose: Provides a complete account of the presenting problem, including any information from the past medical, family and social history related to that problem.
Content: The same as the HPI in the write up! Most new diagnoses are made based on the HPI so this is the most important part. It should take up 1/3 to 1/2 of your presentation time.
- Background health. If the presenting problem is related to a chronic illness, summarize that illness here.
- Detailed, chronologic description of the presenting problem
- Predisposing conditions and risk factors (a.k.a ‘pertinent positives’)
- Pertinent negatives. Symptoms from the affected organ system and risk factors that the patient doesn’t have
- Optional: Evaluation or hospital course to date
Past Medical History (PMH)
Purpose: To provide a succinct overview of other important medical and surgical history that will aid in the care of the patient.
Format: Report ONLY active medical problems and other medical history that is pertinent to evaluation or ongoing management. Medical or surgical history that is relevant to the chief concern should be included in the HPI.
If a past diagnosis or surgery is not active or relevant, it is included in the write-up but NOT in the OCP.
Template: Include a brief synopsis of each active major problem – remember POTS
- S ymptoms and control
Medications and Allergies
- List all prescribed medications (by generic name if possible) and doses
- List all non-prescription medications and complementary/alternative therapies
- Report any drug allergies and the type of reaction
Social History
Purpose: To provide your listener with the social context of the illness and its impact on ongoing care
Format: In 2-3 sentences summarize the patient’s living situation and support systems, occupation, identity, and any social issues that could impact care.
Health Related Behaviors
- Summarize substance use not already mentioned in HPI, including tobacco, alcohol, drug use
- Risk factors relevant to the presenting concern should be included in the HPI
Physical Examination
Purpose: Succinctly and accurately describe the patient’s physical examination, emphasizing pertinent findings
Format: Begin with general appearance and vital signs. Name each organ system in order, and report the relevant exam:
- HEENT and Neck
- Musculoskeletal
Report all pertinent physical examination findings, both normal and abnormal:
- Complete exam of the organ system(s) relevant to the chief concern
- Other findings (normal or abnormal) that help your listener answer a clinical question.
Use concise but complete descriptions of positive findings.
- Report all abnormal findings regardless of organ system.
- If the examination of a system NOT relevant to the chief concern was normal, you may say “Normal”.
Summary Statement: The lead in to your assessment
Purpose: To synthesize the important history and exam findings, to frame the clinical problem and to lead your listener into your assessment. This is NOT simply a restatement of the ID chief concern.
Format: Restate the identifying data and summarize the key features from the patient’s history and physical exam.
Template: “In summary, NAME is a AGE year old patient who presents with a history of PRESENTING CONCERN AND MAJOR ASSOCIATED SYMPTOMS . Their history is notable for KEY ELEMENTS OF HISTORY THAT IMPACT YOUR ASSESSMENT . Physical exam is notable for KEY FINDINGs THAT IMPACT YOUR ASSESSMENT .
Purpose: Address the clinical problem and demonstrate your clinical reasoning. The clinical problem may range from a new and undiagnosed problem to routine follow-up of a chronic problem. The format varies for each.
For an undiagnosed problem.
Your assessment would address the top 3-4 items on the differential diagnosis suggested by your patient’s history and exam findings
Example: The most likely reason for Lily’s rash is eczema. Her skin dryness and pruritis, and her family history of atopy are all consistent with eczema, as is the history of worsening in the winter and after frequent swimming. She also has a classic distribution on the hands and elbow creases. A less likely possibility is scabies, which frequently affects the hands. However, Lily’s skin between the wrists and elbows is spared, which would be atypical for scabies.
For an exacerbation of a chronic problem.
Your assessment would address the most likely reasons for the exacerbation, as suggested by your patient’s history and exam findings.
Example: The most likely reason for Mr. C’s CHF exacerbation is medication nonadherence due to both costs and confusion. He reports filling his medications less often than monthly because even the co-pay is expensive, which is confirmed by his pharmacy. Although he manages his own medications, he is unable to accurately describe what each is for, or his dosing schedule. A second possibility is new ischemia; however, he’s had no chest pain or tightness, and initial ECG and enzymes were negative. Finally, a URI could have precipitated this exacerbation, as he had low grade fever, cough, and rhinorrhea last week. However, those symptoms have resolved as his edema and shortness of breath have progressed, making this possibility less likely.
Routine follow-up of a chronic problem.
Your assessment would address current control of the problem, evidence of complications, and adequacy of current education and treatment.
Example: Ms. B’s type 2 diabetes is well controlled, with most recent HgbA1c of 6.8. She reports excellent adherence to diet and exercise, as well as metformin. She has no evidence of retinopathy or neuropathy on exam and urine for microalbumin was negative.
Purpose: To outline your next steps in addressing your patient’s clinical problem(s).
Format: The plan is usually presented as a bulleted list, and may include interventions in these categories:
Delivery Tips for Oral Case Presentations:
- At the bedside, introduce your patient and any family members to all members of your team.
- Establish eye contact with your team and your patient, glancing at your notes only as necessary.
- Present with a clear, energetic, and interested voice.
- When presenting at the bedside, recognize the impact of your choice of words on your patient. Avoid medical language that might frighten your patient, unless he has used it. Examples: “ End-stage liver disease ” and “ Another possibility is lung cancer… ”
- Avoid language your patient might find insulting. Examples: “O bese” and “Pleasantly confused elderly woman. ”
- Follow the standard format of the OCP precisely.
- Orient your listeners to the next section of the OCP with a brief pause followed by the title of that section.
- Use precise language.
- Do not rationalize, editorialize, or justify as you present. Just present the “facts”.
- Be aware of your patient’s confidentiality, especially if the patient is in a shared room.
References & resources
The FCM OCP Benchmark is adapted from Dr. Steve McGee’s Guidelines for OCPs on the Third Year Internal Medicine Clerkship. These guidelines are too advanced for what you know at the beginning of medical school but by the time you reach the Patient Care Phase, you should be able to follow them. Current version is available here. Oral Case Presentation (uw.edu)
The Foundations of Clinical Medicine Copyright © by Karen McDonough. All Rights Reserved.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Heart Views
- v.18(3); Jul-Sep 2017
Guidelines To Writing A Clinical Case Report
What is a clinical case report.
A case report is a detailed report of the symptoms, signs, diagnosis, treatment, and follow-up of an individual patient. Case reports usually describe an unusual or novel occurrence and as such, remain one of the cornerstones of medical progress and provide many new ideas in medicine. Some reports contain an extensive review of the relevant literature on the topic. The case report is a rapid short communication between busy clinicians who may not have time or resources to conduct large scale research.
WHAT ARE THE REASONS FOR PUBLISHING A CASE REPORT?
The most common reasons for publishing a case are the following: 1) an unexpected association between diseases or symptoms; 2) an unexpected event in the course observing or treating a patient; 3) findings that shed new light on the possible pathogenesis of a disease or an adverse effect; 4) unique or rare features of a disease; 5) unique therapeutic approaches; variation of anatomical structures.
Most journals publish case reports that deal with one or more of the following:
- Unusual observations
- Adverse response to therapies
- Unusual combination of conditions leading to confusion
- Illustration of a new theory
- Question regarding a current theory
- Personal impact.
STRUCTURE OF A CASE REPORT[ 1 , 2 ]
Different journals have slightly different formats for case reports. It is always a good idea to read some of the target jiurnals case reports to get a general idea of the sequence and format.
In general, all case reports include the following components: an abstract, an introduction, a case, and a discussion. Some journals might require literature review.
The abstract should summarize the case, the problem it addresses, and the message it conveys. Abstracts of case studies are usually very short, preferably not more than 150 words.
Introduction
The introduction gives a brief overview of the problem that the case addresses, citing relevant literature where necessary. The introduction generally ends with a single sentence describing the patient and the basic condition that he or she is suffering from.
This section provides the details of the case in the following order:
- Patient description
- Case history
- Physical examination results
- Results of pathological tests and other investigations
- Treatment plan
- Expected outcome of the treatment plan
- Actual outcome.
The author should ensure that all the relevant details are included and unnecessary ones excluded.
This is the most important part of the case report; the part that will convince the journal that the case is publication worthy. This section should start by expanding on what has been said in the introduction, focusing on why the case is noteworthy and the problem that it addresses.
This is followed by a summary of the existing literature on the topic. (If the journal specifies a separate section on literature review, it should be added before the Discussion). This part describes the existing theories and research findings on the key issue in the patient's condition. The review should narrow down to the source of confusion or the main challenge in the case.
Finally, the case report should be connected to the existing literature, mentioning the message that the case conveys. The author should explain whether this corroborates with or detracts from current beliefs about the problem and how this evidence can add value to future clinical practice.
A case report ends with a conclusion or with summary points, depending on the journal's specified format. This section should briefly give readers the key points covered in the case report. Here, the author can give suggestions and recommendations to clinicians, teachers, or researchers. Some journals do not want a separate section for the conclusion: it can then be the concluding paragraph of the Discussion section.
Notes on patient consent
Informed consent in an ethical requirement for most studies involving humans, so before you start writing your case report, take a written consent from the patient as all journals require that you provide it at the time of manuscript submission. In case the patient is a minor, parental consent is required. For adults who are unable to consent to investigation or treatment, consent of closest family members is required.
Patient anonymity is also an important requirement. Remember not to disclose any information that might reveal the identity of the patient. You need to be particularly careful with pictures, and ensure that pictures of the affected area do not reveal the identity of the patient.
- Open access
- Published: 24 May 2023
Comparing oral case presentation formats on internal medicine inpatient rounds: a survey study
- Brendan Appold 1 ,
- Sanjay Saint 1 , 2 ,
- David Ratz 2 &
- Ashwin Gupta 1 , 2
BMC Medical Education volume 23 , Article number: 377 ( 2023 ) Cite this article
2723 Accesses
11 Altmetric
Metrics details
Oral case presentations – structured verbal reports of clinical cases – are fundamental to patient care and learner education. Despite their continued importance in a modernized medical landscape, their structure has remained largely unchanged since the 1960s, based on the traditional Subjective, Objective, Assessment, Plan (SOAP) format developed for medical records. We developed a problem-based alternative known as Events, Assessment, Plan (EAP) to understand the perceived efficacy of EAP compared to SOAP among learners.
We surveyed (Qualtrics, via email) all third- and fourth-year medical students and internal medicine residents at a large, academic, tertiary care hospital and associated Veterans Affairs medical center. The primary outcome was trainee preference in oral case presentation format. The secondary outcome was comparing EAP and SOAP on 10 functionality domains assessed via a 5-point Likert scale. We used descriptive statistics (proportion and mean) to describe the results.
The response rate was 21% (118/563). Of the 59 respondents with exposure to both the EAP and SOAP formats, 69% ( n = 41) preferred the EAP format as compared to 19% ( n = 11) who preferred SOAP ( p < 0.001). EAP outperformed SOAP in 8 out of 10 of the domains assessed, including advancing patient care, learning from patients, and time efficiency.
Conclusions
Our findings suggest that trainees prefer the EAP format over SOAP and that EAP may facilitate clearer and more efficient communication on rounds, which in turn may enhance patient care and learner education. A broader, multi-center study of the EAP oral case presentation will help to better understand preferences, outcomes, and barriers to implementation.
Peer Review reports
Excellent inter-physician communication is fundamental to both providing high-quality patient care and promoting learner education [ 1 ], and has been recognized as an important educational goal by the Clerkship Directors in Internal Medicine, the Association of American Medical Colleges, and the Accreditation Council for Graduate Medical Education [ 2 ]. Oral case presentations, structured verbal reports of clinical cases [ 3 ], have been referred to as the “currency with which clinicians communicate” [ 4 ]. Oral case presentations are a key element of experiential learning in clinical medicine, requiring learners to synthesize, assess, and convey pertinent patient information and to formulate care plans. Furthermore, oral case presentations allow supervising clinicians to identify gaps in knowledge or clinical reasoning and enable team members to learn from one another. Despite modernization in much of medicine, oral case presentation formats have remained largely unchanged, based on the traditional Subjective, Objective, Assessment, Plan (SOAP) format developed by Dr. Lawrence Weed in his Problem Oriented Medical Record in 1968 [ 5 ].
Given that the goals of a medical record are different than those of oral case presentations, it should not be assumed that they should share the same format. While Dr. Weed sought to make the medical record as “complete as possible,” [ 6 ] internal medicine education leaders have expressed desire for oral case presentations that are succinct, with an emphasis on select relevant details [ 2 ]. Using a common SOAP format between the medical record and oral case presentations risks conflating the distinct goals for each of these communication methods. Indeed, in studying how learners gain oral case presentation skills, Haber and Lingard [ 7 ] found differences in understanding of the fundamental purpose of oral case presentations between medical students and experienced physicians. While students believed the purpose of oral case presentations was to organize the large amount of data they collected about their patients, experienced physicians saw oral case presentations as a method of telling a story to make an argument for a particular conclusion [ 7 ].
In accordance with Dr. Weed’s “problem-oriented approach to data organization,” [ 6 ] but with an eye toward optimizing for oral case presentations, we developed an alternative to SOAP known as the Events, Assessment, Plan (EAP) format. The EAP format is used for patients who are already known to the inpatient team, and may also be utilized for newly admitted patients for whom the attending physician already has context (e.g., via handoff or review of an admission note). As the EAP approach is utilized by a subset of attending physicians at our academic hospital, we sought to understand the perceived effectiveness of the EAP format in comparison to the traditional SOAP format among learners (i.e., medical students and resident physicians).
EAP is a problem-based format used at the discretion of the attending physician. In line with suggested best practices [ 8 ], the EAP structure aims to facilitate transmission of data integrated within the context of clinical problem solving. In this format, significant interval events are discussed first (e.g., a fall, new-onset abdominal pain), followed by a prioritized assessment and plan for each relevant active problem. Subjective and objective findings are integrated into the assessment and plan as relevant to a particular problem. This integration of subjective and objective findings by problem is distinct from SOAP, where subjective and objective findings are presented separately as their own sections, with each section often containing information that is relevant to several problems (Fig. 1 , Additional file 1 : Appendix A).
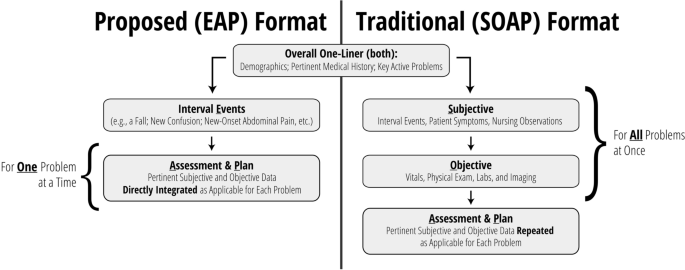
Overview: comparing EAP to SOAP
Settings and participants
We surveyed third- and fourth-year medical students, and first- through fourth-year internal medicine and internal medicine-pediatrics residents, caring for patients at a large, academic, tertiary care hospital and an affiliated Veterans Affairs medical center. Internal medicine is a 12-week core clerkship for all medical students in their second year, with 8 weeks spent on the inpatient wards. All student participants had completed their internal medicine clerkship rotation at the time of the survey. We did not conduct a sample size calculation at the outset of this study.
Data collection methods and processes
An anonymous, electronic survey (Qualtrics, Provo, UT) was created to assess student and resident experience with and preference between EAP and SOAP oral case presentation formats during inpatient internal medicine rounds (Additional file 2 : Appendix B). Ten domains were assessed via 5-point Likert scale (1 [strongly disagree] to 5 [strongly agree]), including the ability of the format to incorporate the patient’s subjective experience, the extent to which the format encouraged distillation and integration of information, the extent to which the format focused on the assessment and plan, the format’s ability to help trainees learn from their own patients and those of their peers, time efficiency, and ease of use. Duration of exposure to each format was also assessed, as were basic demographic data for the purposes of understanding outcome differences among respondents (e.g., students versus residents). For those who had experienced both formats, preference between formats was recorded as a binary choice. Participants additionally had the opportunity to provide explanation via free text. For participants with experience in both formats, the order of evaluation of EAP and SOAP formats were randomized by participant. For questions comparing EAP and SOAP formats directly, choice order was randomized.
The survey was distributed via official medical school email in October 2021 and was available to be completed for 20 days. Email reminders were distributed approximately one week after distribution and again 48 h prior to survey conclusion.
The primary outcome was trainee preference in oral case presentation format. Secondary outcomes included comparison between EAP and SOAP on content inclusion/focus, data integration, learning, time efficiency, and ease of use.
Statistical analyses
Descriptive statistics were used to describe the results (proportion and mean). For comparative analysis between EAP and SOAP, responses from respondents who had experience with both formats were compared using the Wilcoxon Signed Rank Test to evaluate differences. All statistical analyses were done using SAS V9.4 (SAS Institute, Cary, NC). We considered p < 0.05 to be statistically significant.
The overall response rate was 21% (118/563). The response rate was 14% ( n = 62/441) among medical students and 46% ( n = 56/122) among residents. Respondents were 61% ( n = 72) female. A total of 98% ( n = 116) and 52% ( n = 61) of respondents reported experience with SOAP and EAP formats, respectively. Among medical students, 60% ( n = 37) reported experience with SOAP only while 39% ( n = 24) had experience with both formats. Among residents, 36% ( n = 20) and 63% ( n = 35) had experience with SOAP only and both formats, respectively (Table 1 ). Most students (93%) and residents (96%) reported > 8 weeks of exposure to the SOAP format. Duration of exposure to the EAP format varied (0 to 2 weeks [32% of students, 17% of residents], 2 to 4 weeks [36% of students, 47% of residents], 4 to 8 weeks [16% of students, 25% of residents], and > 8 weeks [16% of students, 11% of residents]).
Of the 59 respondents with exposure to both the SOAP and EAP formats, 69% ( n = 41) preferred the EAP format as compared to 19% ( n = 11) preferring SOAP ( p < 0.001). The remainder ( n = 7, 12%) indicated either no preference between formats or indicated another preference. Among residents, 66% ( n = 23) favored EAP, whereas 20% ( n = 7) and 14% ( n = 5) preferred SOAP or had no preference, respectively ( p < 0.001). Among students, 75% ( n = 18) favored EAP, whereas 17% ( n = 4) and 8% ( n = 2) favored SOAP or had no preference, respectively ( p < 0.001).
Likert scale ratings for domains assessed by trainees who had experience in either format are shown in Table 2 . In general, scores for each domain were higher for EAP than SOAP, with the exception of perceived ease of use among students. Among those with experience using both formats, EAP outperformed SOAP most prominently in time efficiency (mean 4.39 vs 2.59, p < 0.001) and encouragement to: focus on assessment and plan (4.64 vs 3.05, p < 0.001), distill pertinent information (4.63 vs 3.17, p < 0.001), and integrate data (4.58 vs 3.31, p < 0.001) (Table 3 ). Respondents also ranked EAP higher in its effectiveness at advancing patient care (4.31 vs 3.71, p < 0.001), its capacity to convey one’s thinking (4.53 vs 3.95, p < 0.001), and its ability to facilitate learning from peers (4.10 vs 3.58, p < 0.001) and one’s own patients (4.24 vs 3.78, p = 0.003). There were no significant differences in the amount of time allotted for discussing the patient’s subjective experience or in ease of use.
Evaluation of trainee free text responses regarding oral case presentation preference revealed several general themes (Table 4 ). First, respondents generally felt that EAP was more time efficient and less repetitive, allowing for additional time to be spent discussing pertinent patient care decisions. Second, several respondents indicated that EAP aligns well with how trainees consider problems naturally (as a single problem in completion). Finally, respondents generally believed that EAP allowed learners to effectively communicate their thinking and demonstrate their knowledge. Those preferring SOAP most often cited format familiarity and the difficulty in switching between formats in describing their preference, though some also believed SOAP was more effective in describing a patient’s current status.
Our single site survey comparing 2 oral case presentation formats revealed a preference among respondents for EAP over SOAP for those medical students and internal medicine residents who had experience with both formats. Furthermore, EAP outperformed SOAP in 8 out of 10 of the functionality domains assessed, including areas such as advancing patient care, learning from patients, and, particularly, time efficiency. Such a constellation of findings implies that EAP may not only be a more effective means to accomplish the key goals of oral case presentations, but it may also provide an opportunity to save time in the process. In line with SOAP’s current de facto status as an oral case presentation format, almost all respondents reported exposure to the SOAP format. Still, indicative of EAP’s growing presence at our academic system, more than one third of medical students and more than one half of residents also reported having experience with the EAP format.
While limited data exist that compare alternative oral case presentations to SOAP on inpatient medicine rounds, such alternatives have been previously trialed in other clinical venues. One such format, the multiple mini-SOAP, developed for complex outpatient visits, encourages each problem to be addressed “in its entirety” before presenting subsequent problems, and emphasizes prioritization by problem pertinency [ 9 ]. The creators suggest that this approach encourages more active trainee participation in formulating the assessment and plan for each problem, by helping the trainee to avoid getting lost in an “undifferentiated jumble of problems and possibilities” [ 9 ] that accumulate when multiple problems are presented all at once. On the receiving end, the multiple mini-SOAP enables faculty to assess student understanding of specific clinical problems one at a time and facilitates focused teaching accordingly.
Another approach has been assessed in the emergency department. Specifically, Maddow and colleagues explored assessment-oriented oral case presentations to increase efficiency in communication between residents and faculty at the University of Chicago [ 10 ]. In the assessment-oriented format, instead of being presented in a stylized order, pertinent information was integrated into the analysis. The authors found that assessment-oriented oral case presentations were about 40% faster than traditional presentations without significant differences in case presentation effectiveness.
Prior to our study, the nature of the format for inpatient medicine oral case presentations had thus far escaped scrutiny. This is despite the fact that oral case presentations are time (and therefore resource) intensive, and that they play an integral role in patient care and learner education. Our study demonstrates that learners favor the EAP format, which has the potential to increase both the effectiveness and efficiency of rounding.
Still, it should be noted that a transition to EAP does present challenges. Implementing this problem-based presentation format requires a conscious effort to ensure a continued holistic approach to patient care: active problems should be defined and addressed in accordance with patient preferences, and the patient’s subjective experience should be meaningfully incorporated into the assessment and plan for each problem. During initial implementation, attending physicians and learners must internalize this new format, often through trial and error.
From there, on an ongoing basis, EAP may require more upfront preparation by attending physicians as compared to SOAP. While chart review by attendings in advance of rounding is useful regardless of the format utilized, this practice is especially important for the EAP format, where trainees are empowered to interpret and distill – rather than simply report a complete set of – information. Therefore, the attending physician must be aware of pertinent data prior to rounds to ensure that key information is not neglected. Specifically, attendings should pre-orient themselves with laboratory values, imaging, and other studies completed, and new suggestions from consultants. More extensive pre-work may be required if teams wish to employ the EAP format for newly admitted patients, as attending physicians must also familiarize themselves with a patient’s medical history and their current presentation prior to initial team rounds.
Our findings should be interpreted within the context of specific limitations. First, low response rates may have led to selection bias within our surveyed population. For instance, learners who desired change in the oral case presentation format may have been more motivated to engage with our survey. Second, there could be unmeasured confounding variables that could have skewed our results in favor of the EAP format. For example, attendings who utilized the EAP format may have been more likely to innovate in other ways to create a more positive experience for learners, which may have influenced the scoring of the oral case presentation format. Third, our findings were largely based on subjective experience. Objective measurement (e.g., duration of rounds, patient care outcomes) may lend additional credibility to our findings. Lastly, our study included only a single site, limiting our ability to generalize our findings.
Our study also had several strengths. Our learner participant pool was broad and included all third- and fourth-year medical students and all internal medicine residents at a major academic hospital. Participation was encouraged regardless of the nature of a participant’s prior exposure to different oral case presentation formats. Our survey was anonymous with randomization to mitigate order bias, and we focused our comparison analysis on those who had exposure to both the EAP and SOAP formats. We collected data to compare EAP with SOAP in 2 distinct ways: head-to-head preference and numeric ratings amongst key domains. Both of these methods demonstrated a significant preference for EAP among learners in aggregate, as well as for students and residents analyzed independently.
Our findings suggest a preference for the EAP format over SOAP, and that EAP may facilitate clearer and more efficient communication on rounds. These improvements may in turn enhance patient care and learner education. While our preliminary data are compelling, a broader, multi-center study of the EAP oral case presentation is necessary to better understand preferences, outcomes, and barriers to implementation. Further studies should seek to improve response rates, for the data to represent a larger proportion of trainees. One potential strategy to improve response rates among medical students and residents is to survey them directly at the end of each internal medicine clerkship period or rotation, respectively. Ultimately, EAP may prove to be a much-needed update to the “currency with which clinicians communicate.”
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, AG, upon reasonable request.
Kihm JT, Brown JT, Divine GW, Linzer M. Quantitative analysis of the outpatient oral case presentation: piloting a method. J Gen Intern Med. 1991;6(3):233–6.
Article Google Scholar
Green EH, Durning SJ, DeCherrie L, Fagan MJ, Sharpe B, Hershman W. Expectations for oral case presentations for clinical clerks: opinions of internal medicine clerkship directors. J Gen Intern Med. 2009;24(3):370–3.
Daniel M, Rencic J, Durning SJ, Holmboe E, Santen SA, Lang V, et al. Clinical Reasoning Assessment Methods: A Scoping Review and Practical Guidance. Acad Med. 2019;94(6):902–12.
Lewin LO, Beraho L, Dolan S, Millstein L, Bowman D. Interrater reliability of an oral case presentation rating tool in a pediatric clerkship. Teach Learn Med. 2013;25(1):31–8.
Wright A, Sittig DF, McGowan J, Ash JS, Weed LL. Bringing science to medicine: an interview with Larry Weed, inventor of the problem-oriented medical record. J Am Med Inform Assoc. 2014;21(6):964–8.
Weed LL. Medical records that guide and teach. New Engl J Med. 1968;278(12):652–7.
Haber RJ, Lingard LA. Learning oral presentation skills: a rhetorical analysis with pedagogical and professional implications. J Gen Intern Med. 2001;16(5):308–14.
Wiese J, Saint S, Tierney LM. Using clinical reasoning to improve skills in oral case presentation. Semin Med Pract. 2002;5(3):29–36.
Google Scholar
Schillinger E, LeBaron S. The multiple mini-SOAP format for student presentations of complex patients. Fam Med. 2003;35(1):13–4.
Maddow CL, Shah MN, Olsen J, Cook S, Howes DS. Efficient communication: assessment-oriented oral case presentation. Acad Emerg Med. 2003;10(8):842–7.
Download references
Acknowledgements
The authors would like to thank Jason M. Engle, MPH, who helped edit, prepare, format, and submit this manuscript and supporting files.
Author information
Authors and affiliations.
University of Michigan Medical School, Ann Arbor, MI, USA
Brendan Appold, Sanjay Saint & Ashwin Gupta
VA Ann Arbor Healthcare System, 2215 Fuller Road, Ann Arbor, MI, 48105, USA
Sanjay Saint, David Ratz & Ashwin Gupta
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: BA SS AG. Data curation: BA DR AG. Formal Analysis: BA SS DR AG. Funding acquisition: SS AG. Investigation: BA SS AG. Methodology: BA SS AG. Project administration: BA SS AG. Resources: SS AG. Software: DR. Supervision: SS AG. Validation: BA SS DR AG. Visualization: BA SS DR AG. Writing – original draft: BA AG. Writing – review & editing: BA SS DR AG. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Ashwin Gupta .
Ethics declarations
Ethics approval and consent to participate.
All methods were carried out in accordance with relevant guidelines and regulations. The need for ethical approval was waived by the ethics committee/Institutional Review Board of the University of Michigan Medical School. The need for informed consent was waived by the ethics committee/Institutional Review Board of the University of Michigan Medical School.
Consent for publication
Not applicable.
Competing interests
Dr. Saint, Mr. Ratz, and Dr. Gupta are employed by the US Department of Veterans Affairs. Dr. Saint reports receiving grants from the Department of Veterans Affairs and personal fees from ISMIE Mutual Insurance Company, Jvion, and Doximity. Dr. Appold, Mr. Ratz, and Dr. Gupta report no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Appendix A. Exemplar Transcripts (EAP, SOAP).
Additional file 2:
Appendix B. Survey Instrument.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Appold, B., Saint, S., Ratz, D. et al. Comparing oral case presentation formats on internal medicine inpatient rounds: a survey study. BMC Med Educ 23 , 377 (2023). https://doi.org/10.1186/s12909-023-04292-3
Download citation
Received : 24 August 2022
Accepted : 22 April 2023
Published : 24 May 2023
DOI : https://doi.org/10.1186/s12909-023-04292-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Oral case presentations

BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Researched by Consultants from Top-Tier Management Companies

Powerpoint Templates
Icon Bundle
Kpi Dashboard
Professional
Business Plans
Swot Analysis
Gantt Chart
Business Proposal
Marketing Plan
Project Management
Business Case
Business Model
Cyber Security
Business PPT
Digital Marketing
Digital Transformation
Human Resources
Product Management
Artificial Intelligence
Company Profile
Acknowledgement PPT
PPT Presentation
Reports Brochures
One Page Pitch
Interview PPT
All Categories
Top 7 Medical Case Presentation Templates with Samples and Examples

Sarojit Hazra
How does information expand beyond essential recollection? Facts alone can diminish in value over time. Context and implementation are crucial to form deep connections and roots. Here comes the role of case studies for clinical personnel in the medical field.
In the always-growing healthcare industry, medical case presentation is essential as it is a suggestion for new researchers. A medical case study is a report where a medical practitioner shares a patient's case. It comprises every detail related to patients. It is beneficial for describing a new medical condition, management options, or treatment for diseases.
Medical case presentations contribute significantly to the evolution of medical knowledge and research.
Case study analysis is essential for every business or industry, like the medical industry. It helps in managing the twists and turns of the industry. Want to take some ideas? Have a look at SlideTeam’s blog Case Analysis Templates .
Let us highlight some significant benefits of medical case presentation:
- Case study presentations are extremely good at depicting realistic clinical frameworks.
- It helps to enhance student participation alongside the joy of learning.
- These are ideal for sharing the latest information on the clinical landscape.
- It promotes critical thinking.
- It can also make better clinical outcomes.
If you are in the healthcare sector, another important tool is the medical dashboard. For a deeper insight, quickly take a look at Medical dashboard Templates .
Each of the slides is 100% editable and customizable. The 100% customizable nature of the templates allows you to edit your presentations. The content-ready slides give you the much-needed structure. Below, let’s explore a wide array of ready to use, content ready medical case presentation templates fit for your organization.
Template 1: Case Study on Blockchain Application in Healthcare: Medical Staff Credential Verification
Blockchain is becoming a potential solution to verify medical credentials. Though these are open to the public, they can be restricted through permissions. Are you finding it difficult to understand and implement? SlideTeam introduces this PPT Template that highlights how to operationalize medical staff verification process using blockchain technology. It explains that healthcare-based systems can also be used to verify the credentials of medical staff. Solutions-based blockchain to track the experiences of medical professionals. The PPT slides are designed with suitable icons, designs, graphs and other relevant material. Grab it quickly and draft your case study as per the client’s requirements.
Click to Download
Template 2: Cost Benefits IOT Digital Twins Implementation Use Cases in the Medical Domain
This PPT template is designed to focus on the use cases in the medical domain, including research and development, diagnosis, surgery, medical equipment, etc. The slide offers a brief description of the mentioned use cases to understand the scenario better. Use it as an essential tool and captivate your audience. Get it Now!
Template 3: Major Use Cases for Tracking Medical Assets Asset Tracking and Management IoT
Want to simplify medical complexities? The asset tracking solution is here to accompany you. It enables the medical sector to locate patients, clinicians, and medications more accurately and quickly. IoT development has made this task much more accessible by guiding you through every significant aspect of a medical asset-tracking solution. Introducing our slide exhibiting use cases of medical tools that can be tracked with IoT technology . Medical assets, including medical tools, medical equipment tracking, medications , etc., are shown in the layout with their use cases and impacts. Each topic is depicted in separate tables with appropriate icons.
Template 4: AIoT Healthcare Applications in Medical Imaging
AIoT is making the medical sector smarter and wiser to improve data management and human-machine interaction. When AIoT is applied to healthcare, enables virtual monitoring and accurate diagnosis of patients to develop a personalized patient experience. Here, we introduce our premium PPT Templates showcasing applications of Artificial Intelligence of Things (AIoT) in radiology. You can provide detailed information about remote diagnosis , personalized treatment , and real-time monitoring. Adapt it now to increase your presentation threshold and educate your audience.
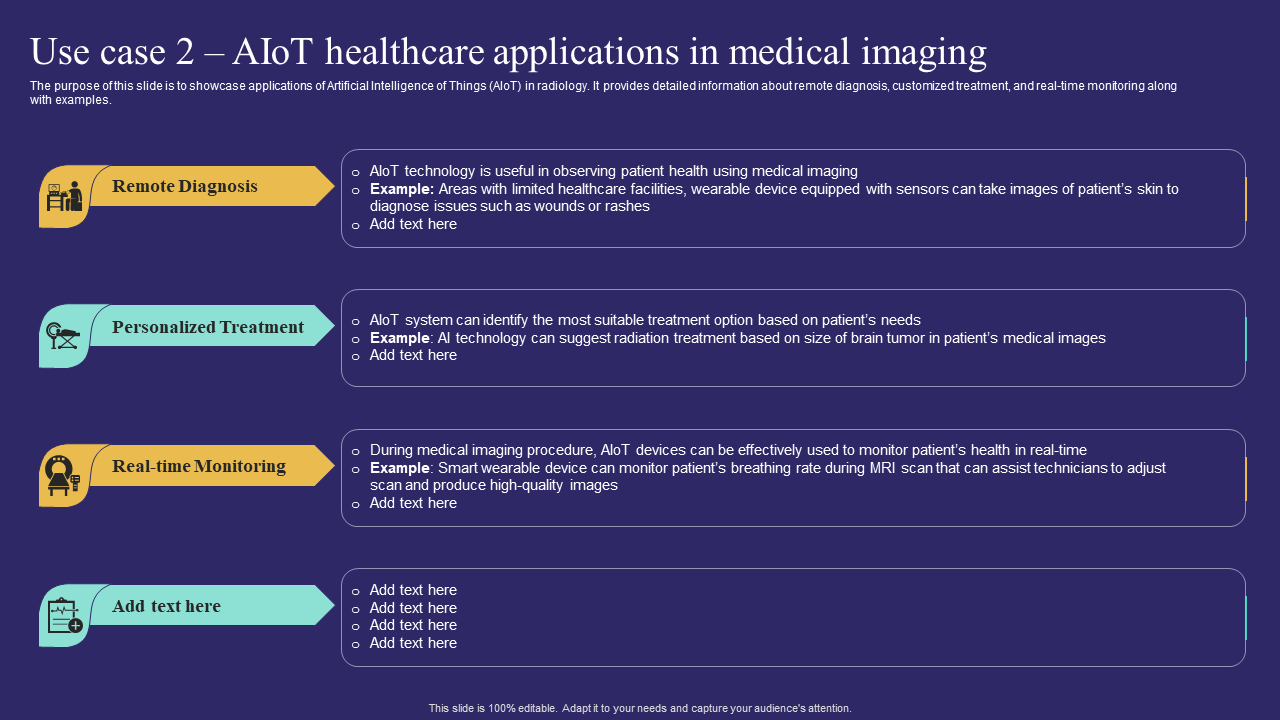
Template 5: Case Study of Leading Medical Devices Manufacturing Organization
An array of disruptive themes is shaping the medical device industry, and cloud computing is one of them. Soon, cloud computing will have a more significant impact on this industry. So, for your convenience, we are presenting our slide covering a case study of blue cloud with lending medical devices manufacturing organization. It covers significant topics like client objective, problem, our solution, and results chronologically. Consisting of three essential stages, this template is excellent for educating and enticing your audience.

Template 6: IoT Technology Use Case for Medical Treatment
IoT, or the Internet of Things, is gaining significance across industries, and the medical sector is no exception. It has taken medical treatment to a new level. This custom-built PowerPoint Template exhibits the use of IoT technology in domains of the healthcare industry. It provides a digital solution for patient treatment. The key elements are primary care, acute care, virtual hospital, etc., which are depicted along with descriptions, benefits, and additional comments. Each illustration is highlighted, colored and has a relevant icon for instantaneous identification.
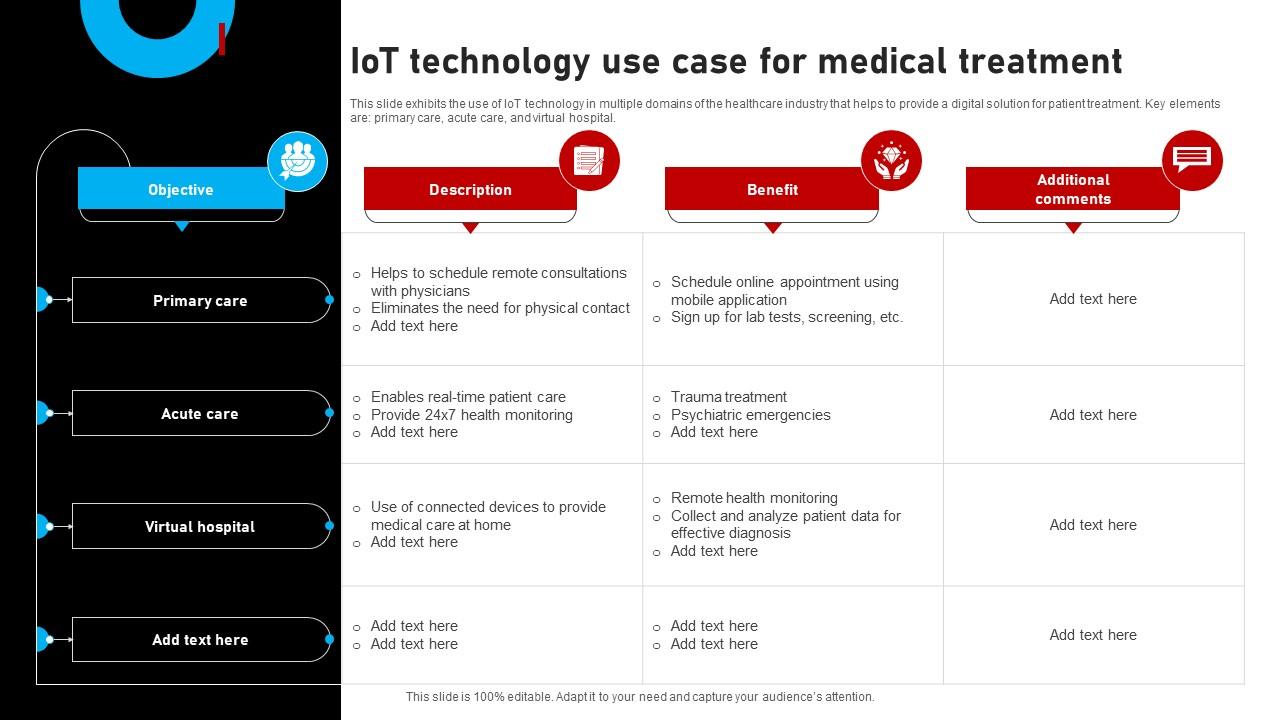
Template 7: IoT Medical Healthcare Technology Use Cases
The transformation of healthcare into digital healthcare has resulted in the rise of IoMT, or medical IoT . It refers to connected devices in medical healthcare and has become one of the fastest-growing industries in the IoT market. It would help if you dived deeper to manage, monitor, and preserve IoT devices in medical healthcare. This PPT presentation demonstrates uses of IoT Medical Healthcare Technology in monitoring patient health. Moreover, the slide includes remote patient monitoring, reduced waiting time, identifying chronic diseases, and drug management. Download this template design and present your case study with ultimate professionalism.
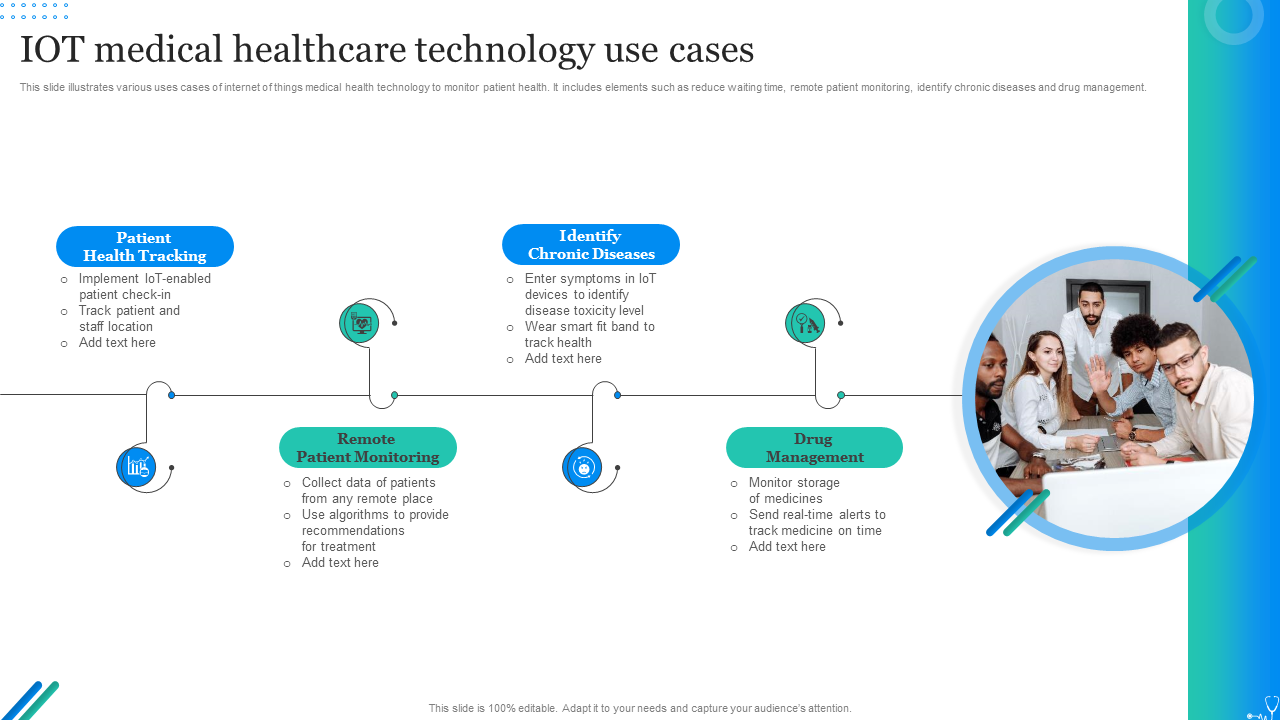
HEALTH CONSULTATION WILL BE QUICKER, SAFER AND SECURE
Case studies have a great history as an educational tool for clinicians. These are highly beneficial for nurturing deeper insights and learning. Access to such visually appealing and comprehensively presented Top 7 Medical Case Presentation Templates enables medical professionals to quickly present their patients' case studies. Be it tracking of medical assets, application of IoT in the clinical field, IoT medical healthcare technology uses, and so on, these templates serve as essential equipment in implementing all.
P.S. For perfection and success, you should dig into SlideTeam's fantastic blog, Medical Report Templates .
Related posts:
- How to Design the Perfect Service Launch Presentation [Custom Launch Deck Included]
- Quarterly Business Review Presentation: All the Essential Slides You Need in Your Deck
- [Updated 2023] How to Design The Perfect Product Launch Presentation [Best Templates Included]
- 99% of the Pitches Fail! Find Out What Makes Any Startup a Success
Liked this blog? Please recommend us

Top 10 Training Framework Templates with Examples and Samples

Top 5 Product Strategy Framework Templates with Samples and Examples
This form is protected by reCAPTCHA - the Google Privacy Policy and Terms of Service apply.

Digital revolution powerpoint presentation slides

Sales funnel results presentation layouts
3d men joinning circular jigsaw puzzles ppt graphics icons
Business Strategic Planning Template For Organizations Powerpoint Presentation Slides
Future plan powerpoint template slide

Project Management Team Powerpoint Presentation Slides

Brand marketing powerpoint presentation slides

Launching a new service powerpoint presentation with slides go to market

Agenda powerpoint slide show
Four key metrics donut chart with percentage

Engineering and technology ppt inspiration example introduction continuous process improvement

Meet our team representing in circular format

CanadiEM MVP Infographic Series
Hiquips (quality improvement), the ‘top five changes’ project: 2015 aha guidelines on cpr + ecc update infographic series.
- CaRMS Guide
Basic Airway Assessment: It’s as easy as… 1-2-3?

- Editorial Board
- Terms of Use Agreement
- Privacy Policy
- Great Evidence in MedEd (GEMeS)
- Featured Education Innovations (FEI)
- TipsForEMExams
- Chalk Talks
- Clinical Questions
- Infographics
- Knowledge Translation
- Physicians as Humans
- Counterpoint
- Arts PRN Gallery
- General Submissions
- Arts PRN Project

How to Present a Case in the Emergency Department
In Education & Quality Improvement , Infographics , Mentorship by Sophie Ramsden September 1, 2020 Leave a Comment
Presenting a case in the ED is important for a number of reasons. Not only does better communication result in better patient care, but it’s also a great learning opportunity and your chance as a clerk to impress your attending. Presenting a case well conveys your level of knowledge and understanding to an attending, which allows them to accurately assess and teach to your weaknesses. It also illustrates that you can create a complete diagnostic and management plan for a patient, while prioritizing dangerous diagnoses and critical next steps. Even if you know everything there is to know about abdominal pain and asked all of the right questions, if you can’t present a case thoroughly but concisely, your attending won’t be able to appreciate that.
Whether you’re brand new to the ED or a well-oiled emergency medicine machine, check out our essential resources for key tips on presenting a case. If you’re interested in a deeper dive into case presentations and some of the evidence supporting different teaching styles, scroll a little further.
To find the resources for this post, referrals from key experts were used, as well as a search on foamsearch.net. It’s also a great idea to use your preceptor as a resource! Ask them at the start of the shift if they have a preference for how you present a case. Being flexible in your presentation style will allow you to accommodate their preferences accordingly.
Essential Resources
- Listen to ClerkCast Episode 1: a podcast for clerks, by clerks. In their first episode, they give a broad overview of life in the ED for clerks, which is especially useful when you are just starting out in the emergency department. They include tips for developing your differential diagnosis, assessing sick patients, and the RAPID mnemonic for discussing next steps with your preceptor. It also goes into a bit more depth (with good and bad examples) on presenting a case. As they explain in the podcast, structuring your HPI around pertinent positives and negatives for dangerous diagnoses will make it easier for your listener to rule in or rule out those diagnoses, as well as neatly convey to them that you’re thinking like an EM doc and prioritizing threats to life and limb.
ClerkCast Episode 1: Introduction to the ED
- Watch these videos on The 3-Minute Emergency Medicine Presentation ( see Going Further for more details). The first video takes you through how to think like an EM doc in generating your differentials and approaching the patient history, and goes through some examples. The second video covers the 3 minute case presentation in detail with an example. They’ve also included an attachment with key red flags for common presentations, which might be a useful resource to have with you on shift!
- Save our 3 Minute EM Presentation Infographic as a handy on-shift reference:

Going Further
The 3-minute emergency medicine medical student presentation: a variation on a theme.
This paper is the key resource for mastering case presentations. It goes over the differences between emergency medicine and other specialties, and how these differences impact the best way to present a case. If you’re looking to get straight into the meat of how to present a case, read the appendix or check out our handy infographic (above), which summarizes the key points. The paper itself is also useful to understand the rationale for the sections included or omitted from the presentation, as well as some common medical student pitfalls. 1
A caveat: case presentations are inherently subjective, and the authors acknowledge that the best presenters are flexible to match the needs of their audience. There are a few areas that I think require extra flexibility. First, the Review of Systems mainly exists as a placeholder for any additional complaints unrelated to the chief complaint, so don’t feel the need to include it if there are none. Second, the authors omit the formal headings of Past Medical History, Social History, etc. This does not mean these are not important – it just means that pertinent details from those headings should be folded into your HPI. If you’re unable to integrate them into your HPI when you’re just starting out, it’s better to go through them systematically than to forget them entirely.
Finally, as they discuss in the paper, your Summary Statement may be combined with your Impression. It’s good to start getting in the habit of committing to a provisional diagnosis and plan even as a medical student. As long as you’re keeping in mind the whole differential and the key rule-out conditions, most preceptors will appreciate you clearly stating your working diagnosis. If you’re feeling confident, it may even be appropriate to start the presentation with it. Here’s an example: “ This is a 32 year old female with a likely peritonsillar abscess. She presented with a sore throat…” .
SNAPPS Framework
S – Summarize the history and physical
N – Narrow the differential to 2-3 possibilities
A – Analyze the differential – give evidence for or against each possibility based on your H&P
P – Probe the preceptor on any points of confusion or uncertainty in the workup
P – Plan the management
S – Select a topic for self-directed learning.
This framework may also be useful for practicing emergency physicians looking for a way to give feedback and structure teaching. To see the SNAPPS framework demonstrated, check out these two videos:
Part 1: https://www.youtube.com/watch?v=rywuzkm8nmY
Part 2: https://www.youtube.com/watch?v=BPNOdPKUFDE
The original paper on the SNAPPS framework, which discusses its evidence and development, can be found here. 2
As a contrast to SNAPPS, some practitioners in a teaching role may favour the One Minute Preceptor model, which is demonstrated here: https://www.youtube.com/watch?v=P0XgABFzcgE
If you’re interested in the evidence around different case presentation styles or teaching strategies, check out this paper . The bottom-line is the SNAPPS framework was preferred over the One Minute Preceptor model by the study participants in the learner role:
Present Your Plan RAPID-ly:
As you get more experienced your case presentations should incorporate your initial plan, in addition to simply presenting the cases. To scaffold this approach, Dr Rob Woods (USask RCPSC program director) did a project to define the components of a good initial management plan a few years ago. Read his staff review below find out how to best present your plans to your attendings too!
This post was edited by Megan Chu and Julia Heighton.
- 1. Davenport C, Honigman B, Druck J. The 3-Minute Emergency Medicine Medical Student Presentation: A Variation on a Theme. Academic Emergency Medicine . Published online July 2008:683-687. doi: 10.1111/j.1553-2712.2008.00145.x
- 2. Wolpaw TM, Wolpaw DR, Papp KK. SNAPPS. Academic Medicine . Published online September 2003:893-898. doi: 10.1097/00001888-200309000-00010
Reviewing with the Staff
The 3 minute clinical presentation is a great tool to start out with. It really organizes the patient information, gets you to commit to a differential diagnosis and justify why. It really brings your thought processes out, forcing you to use the skill of elaboration, which is a key skill in learning. Once this becomes quite familiar, you can start to take on more complex patients. The RAPID approach was developed to have an overall assessment and management plan for more complex ED patients. It serves as a checklist for ensuring key management issues are not missed.
Resuscitation Analgesia & Assessment Patient Needs Interventions (Diagnostic & Therapeutic) Disposition
The RAPID approach makes you consider time sensitive illness in every case. Chest pain (MI, Dissection, PE), unilateral symptoms (CVA), Fever (Severe Sepsis) and Hypotension/shock can all be identified with a scan of the vitals and the chief complaint. Analgesia before assessment but after Resuscitation ensures patients in severe pain don’t provide their family history and social history before you get them some intravenous analgesia (like in renal colic, severe abdominal pain or a deformed limb). Addressing patient needs before interventions ensures you have considered patient values in the diagnostic and treatment plan, and that you look after their basic needs of comfort/warmth/hunger/thirst and social supports. Emergency Physicians are primary experts in DISPOSITION. Can your patient go home or not? Finding this out early in the encounter really helps your efficiency and decision making when you present a patient to your attending.
- Latest Posts
Sophie Ramsden
Latest posts by sophie ramsden ( see all ).
- Vicious Cycles: Management of the Tricyclic Antidepressant Overdose - April 13, 2021
- How to Present a Case in the Emergency Department - September 1, 2020
- Blood & Clots
- Case Series
- CJEM Audio Summary Podcast
- Education & Quality Improvement
- Great Evidence in Medical education Summary (GEMeS)
- Medical Concepts
- National Rounds
- Sirens to Scrubs
- Uncategorized
- Working in EM
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
suicide prevention
8 templates
46 templates
tropical rainforest
29 templates

spring season
34 templates
american football
16 templates

32 templates
Case Report Presentation templates
Free medical google slides themes and powerpoint templates to present a concise, organized clinical case report. customize them with the easy-to-edit graphic resources included, and create an effective presentation..

Clinical Case 01-2023
Present your clinical case to the medical community with this dynamic and engaging presentation by Slidesgo. Who said science can’t be creative and fun?

Maternal Stroke Clinical Case
Download the "Maternal Stroke Clinical Case" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals to...

Cycle Diagrams Theme for a Case Report
Download the "Cycle Diagrams Theme for a Case Report" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for...

Cranioencephalic Trauma Case Report
Download the "Cranioencephalic Trauma Case Report" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals to...

Phosphate Toxicity Case Report
Download the "Phosphate Toxicity Case Report" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals to...

Premium template
Unlock this template and gain unlimited access
Pain Clinical Case
This clinical case template has some geometrical aspects that help you organize your content, but what really helps is the inclusion of tables, infographics, maps and other slides to review the patient history, the case timeline and other essential data.

Clinical Case 03-2023
Clinical cases are very important and serve as a good source of reliable information, since they present a detailed report of things such as symptoms, diagnosis and treatment of a patient. This new free medical template by Slidesgo will help you with the hard task of creating an effective presentation...

Clinical Case 02-2023
Clinical cases are an important reference in the medical community, since they are a trustworthy source of information for doctors. This SlidesGo template will help you explain all the data in an interesting way.

Anatomy & Physiology Case Report
Download the "Anatomy & Physiology Case Report" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals...

Clinical Case in Neurology
Neurology is one of the most complex branches there is in the field of medicine. Dealing with all sorts of disorders and conditions related to the nervous system, clinical cases can often be complicated and as such require a deeper analysis for better understanding. This medical presentation template for neurology...
Endometrial Cancer Case Report
Download the "Endometrial Cancer Case Report" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals to...

Clinical Case 05-2023
We know how useful clinical case presentations are within the medical community. This new free template by Slidesgo will help you create an effective presentation and impress your audience.

Clinical Case 06-2023
Slidesgo is back with a new free medical template, perfect for a presentation about a clinical case. The design is very appealing, so these slides are a nice tool to provide a lot of useful information for doctors and researchers.

Implantation of Hearing Aids in Children Case Report
Download the "Implantation of Hearing Aids in Children Case Report" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity...

Pastel Blue Clinical Case
If you are a doctor and you are working on a clinical case, we have a proposal that will be great for you to present the results of your research. The main color is pastel blue, which is related to health and trust. In addition, we have included many photos...
Clinical Case 04-2023
When trying to prevent diseases, information is key, and if it’s reliable, all the better. With this new free medical template, you can show the results of a clinical case, including the symptoms, the patient monitoring, the treatment and all the important data. Its design will help you grab your...

Clinical Case 07-2019
Here at Slidesgo we’re increasing our catalogue of medical presentation templates with this new design, fresh from the operating room. It’s so original and professional it will help you focus on the important data you need to show to other doctors and physicians.

Rare Disease Clinical Case
2020 is quite special because it’s a leap year, but what could happen on February 29 that makes it particular? It’s when Rare Disease Day is held, whose goal is to raise awareness for lesser-known diseases. The design of our free clinical case presentation template focuses on this topic.
- Page 1 of 29
New! Make quick presentations with AI
Slidesgo AI presentation maker puts the power of design and creativity in your hands, so you can effortlessly craft stunning slideshows in minutes.

- Grand Rounds
Bone & Soft Tissue Sarcoma Conference Tumor Board
Case presentations, wednesday, april 24, 2024 at 7:00 am.
This grand round has been canceled.
Description
- Case presentations
- Additional Info
Accreditation
Dates and times.
Start: 4/24/2024 7:00 AM End: 4/24/2024 8:30 AM
-Discuss the diagnosis and management of orthopedic oncology cases by presenting patient symptoms, medical history, radiologic findings, medical/surgical intervention, and pathologic findings
-Facilitate discussion between attendings, residents, and fellows in the departments of Orthopaedics, MSK Radiology, and Pathology
The School of Medicine, State University of New York at Stony Brook, is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
The School of Medicine, State University of New York at Stony Brook designates this live activity for a maximum of 1.50 AMA PRA Category 1 Credit(s) ™ . Physicians should only claim the credit commensurate with the extent of their participation in the activity.
Need help with this Grand Round Session?
Please contact the Grand Round coordinator listed below:
Kaitlyn Compitello Department: Orthopaedics Phone: (631) 444-9107 Email: [email protected]
American Society for Microbiology
- Case Studies
- A Resistant Foe in Medicine and Agriculture
Case Studies A Resistant Foe in Medicine and Agriculture
April 18, 2024
Submit a Case Study Presentation
A 71-year-old male develops acute respiratory distress 4 weeks after a bone marrow transplant. The patient experiences fever, tachycardia and worsening mentation. Blood and respiratory cultures reveal a gram-negative bacillus, which was not identified by rapid respiratory and blood culture molecular panels. The microorganism is a non-lactose fermenter, and colonies are smooth and slightly raised on blood agar. There is also a notable dirt-like smell.
Did you guess the diagnosis?
Author Information
Asm microbe 2024 registration now open, discover asm membership, get published in an asm journal.
- Open access
- Published: 16 April 2024
Clinical presentation and management of methanol poisoning outbreaks in Riyadh, Saudi Arabia: a retrospective analysis
- Faisal Alhusain 1 , 2 ,
- Mohammed Alshalhoub 1 , 2 ,
- Moath Bin Homaid 3 ,
- Laila Carolina Abu Esba 2 , 4 ,
- Mohammad Alghafees 2 , 5 &
- Mohammad Al Deeb 1 , 2
BMC Emergency Medicine volume 24 , Article number: 64 ( 2024 ) Cite this article
193 Accesses
5 Altmetric
Metrics details
Acute methanol intoxication, whether unintentional or deliberate, necessitates prompt intervention to prevent severe morbidity and mortality. Homemade alcoholic beverages are a frequent source of such poisoning. This retrospective analysis examined two outbreaks of methanol intoxication in Saudi Arabia. It investigated the clinical presentation, implemented management strategies, and any lasting complications (sequelae) associated with these cases. The aim was to assess the potential impact of different treatment modalities and the timeliness of their initiation on patient outcomes.
This was a retrospective case series of methanol poisoning cases which presented to the adult emergency department (ED) at King Abdulaziz Medical City (KAMC) in Riyadh, Saudi Arabia. There were two separate outbreaks in the city, the first one was from September 1 to September 10, 2020 and the second one was from May 14 to May 20, 2021. Electronic charts were reviewed, and data were extracted to previously prepared data extraction sheets.
From the 22 patients who arrived in the ED alive, the most common complaints were nausea or vomiting followed by altered level of consciousness. About 9% from the patient were hypotensive, 36% were tachycardic, 41% were tachypneic and 4% were having SpO2 < 94%. Brain CT was abnormal in 6 patients. Vision impairment was the most common sequalae of methanol poisoning (7 out of 12 patients who were assessed by ophthalmologist, 58%). When the patients were divided based on severity (mild, moderate, severe), nausea or vomiting and loss of consciousness were the most common complaints among the moderate group while loss of consciousness predominated in the severe group. Two patients presented with low blood pressure and were in the sever group. The severe group had a mean Glasgow Coma Scale (GCS) of 8. Most of the patients in the severity groups underwent the same management apart from those who died or deposited. Eight patients in the severe group had to be intubated.
This study demonstrates the multifaceted clinical presentation of methanol poisoning, culminating in a 17.4% mortality rate. Notably, our findings emphasize the critical role of prompt diagnosis and swift initiation of combined fomepizole therapy and hemodialysis in mitigating mortality and minimizing the potential for chronic visual sequelae associated with methanol poisoning.
Peer Review reports
Introduction
Methanol is one of the poisonous alcohols frequently used as a solvent in automobiles, paint thinners and other industrial applications. Poisoning often arises from consumption of illicit or non-commercially produced alcoholic beverages, sometimes referred to as “moonshine.” These beverages inadvertently produce methanol during their synthesis [ 1 ]. Methanol poisoning, either accidental or intentional, is very harmful if not managed rapidly and may lead to significant morbidity and even mortality [ 2 ]. Methanol has a depressant effect on the central nervous system (CNS) when ingested or inhaled but the toxicity of methanol is attributed to its metabolite -formic acid- formed from the oxidation of methanol to formaldehyde and then to formic acid. Formic acid is toxic to the optic nerve, the CNS and the mitochondria and its concentration is directly related to the risk of morbidity and mortality [ 3 ]. Ingesting 50–100 milliliter of pure methanol can cause perpetual blindness and neurological deterioration resulting in death [ 4 ]. The clinical presentation of methanol poisoning varies according to the route of exposure, the amount ingested, and the elapsed time after ingestion. Early symptoms of methanol poisoning include nausea, vomiting, dizziness along with epigastric pain. Later -after a period of 12 to 48 h since ingestion- methanol poisoning can lead to neurologic dysfunction, blindness and even death. Metabolic acidosis with a high anion gap is the most prominent laboratory abnormality [ 5 ]. Various case studies have reported complications ranging from ischemia and necrosis to hypotension and coma [ 6 , 7 ].
Managing methanol toxicity depends on the extent of exposure and requires close monitoring of laboratory parameters. Therapy with an antidote and/or extracorporeal treatment is the mainstay of treatment [ 8 , 9 ]. The treatment approach is directed towards interrupting methanol breakdown to formic acid using a competitive alcohol dehydrogenase enzyme inhibitor, such as fomepizole or ethanol. In addition to directly eliminating the toxic metabolites through hemodialysis [ 4 ]. Administration of sodium bicarbonate is recommended to tackle metabolic acidosis and to reduce formic acid penetration into the CNS and optic nerve [ 3 ]. The use of folic acid is also recommended to accelerate the breakdown of formate [ 10 ]. Early administration of fomepizole has shown to reduce mortality and prevent the need for dialysis. In a multicenter prospective trial, fomepizole administration to 11 patients with methanol poisoning resulted in a fall in concentration of formic acid and an improvement in metabolic acidosis in all patients [ 11 ]. None of the 7 surviving patients that initially presented with visual abnormalities had any decrements in visual acuity at the end of the trial [ 11 ]. Dialysis is also required in severe cases to eliminate the toxic metabolite from the body, however a retrospective study reported a survival of 5 out of 15 patients (33.3%) who were treated with dialysis [ 9 , 12 ].
The global significance of methanol toxicity has been underscored during the COVID-19 pandemic. Some regions witnessed methanol poisoning surges due to sanitizer consumption or misconceptions about alcohol’s protective effects against the virus. Notably, the outbreaks we describe, while coinciding with the pandemic, were linked to the illegal distribution of adulterated alcohol [ 12 ]. Given the profound health implications, including coma and death, early diagnosis and intervention are paramount. This study aimed to describe the clinical presentation, treatment strategies, and outcomes of patients from two distinct methanol poisoning outbreaks in Riyadh, Saudi Arabia, thereby filling existing knowledge gaps and underscoring the importance of timely public health interventions.
Study design
This study was a single center retrospective case series of methanol poisoning cases. It focused on patients that presented to the adult emergency department (ED) at King Abdulaziz Medical City (KAMC), a tertiary care academic hospital in Riyadh, Saudi Arabia. KAMC provides services to a rapidly growing patient population and houses 1,973 beds. The ED at KAMC offers care for national guard employees, their families, and critically ill or injured individuals. The study period encompassed two outbreaks between September 2020 and June 2021.
Data collection
Data for this study were extracted from the electronic medical records at KAMC. The two documented outbreaks occurred from September 1 to September 10, 2020, and May 14 to May 20, 2021. Given the prohibition on the sale, purchase, and consumption of alcohol in Saudi Arabia [ 13 ]. As a result, some might resort to “illicit or non-commercially” alcohol produced illegally by local individuals in the country. For the scope of this study, 5 patients were considered from the first outbreak and 18 from the second. Diagnosis criteria depended on a positive methanol serum concentration exceeding 20 mg/dL. Details such as demographic information, symptoms upon arrival, initial vital signs, laboratory results, GCS, brain computed tomography (CT) findings, and treatment (encompassing fomepizole, sodium bicarbonate, dialysis, folate, and mechanical ventilation) were compiled. Additionally, assessments by ophthalmologist and/or neurologist were conducted for patients presenting with vision or neurological complaints.
Data analysis
The gathered data were subjected to analysis using the Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, Version 22.0). Demographic data and baseline characteristics were summarized and presented as frequencies and proportions.
Based on the severity and clinical presentation, patients were categorized into three groups. A brief rationale for the grouping is: methanol poisoning’s severity can be gauged through clinical manifestations such as coma or seizures and laboratory indicators like blood pH levels. A lower pH often indicates acidosis, a common consequence of methanol poisoning. The severity groups were defined as: Mild: patients not in a coma, no seizures, and an initial pH > 7.2, Moderate: patients not in a coma, no seizures, but an initial pH ranging from 7.0 to 7.2 and Severe: patients in a coma, had seizures, or their initial pH was below 7.0. This classification helped in understanding the clinical implications of varying severities of methanol poisoning and guided subsequent interventions and prognosis evaluation.
Patient demographics
A total of 23 patients presented to the ED over the two methanol toxicity outbreaks. The majority of patients were male (19/23, 83%) with a mean age of 29-years-old. Out of the 23 patients, one was pronounced dead on arrival, one died in the ED and the rest were discharged from the ED or were admitted for further management. Table 1 lists the initial presentation of the patients upon arrival to the ED. From the 22 patients who arrived alive to the ED, the most common symptoms were nausea or vomiting (17/22, 74%), altered level of consciousness (10/22, 44%), impaired vision (9/22, 39%) and abdominal pain (7/22, 30%). Only one patient presented asymptomatic with only a history of possible ingestion of methanol and positive methanol serum level. Two patients (9%) were hypotensive upon arrival, eight patients (36%) were initially tachycardic and nine patients were tachypneic (41%). All the patients (100%) had a normal initial temperature. Only eight patients from the total patients (35%) had brain CT and was abnormal in six patients, of which four showed brain edematous changes, and two had no brain perfusion and the rest were normal.
Patient outcomes
Table 2 characterizes those who presented to the ED with methanol poisoning according to severity. The groups were mild, moderate, and severe (3/23; 13%, 11/23; 48%, and 8/23; 35%, respectively). The mean age of the patients was 38 years old in the mild group, 27 years old in the moderate group and 28 years old in the severe group. All patients in the mild and moderate groups were males and only 50% of those in severe group were male. Nausea or vomiting and loss of consciousness were the most common complaints among the moderate group while loss of consciousness predominates in the severe group. Blood pressure readings were normal in the mild and moderate groups but was low (SBP < 100) in 25% of those in the severe group. Tachycardia (> 100 beats/min) among groups were as following: 33% in the mild group, 36% in the moderate group and 37% in the severe group. Tachypnea (> 20 breaths/min) was almost similar in the mild and moderate groups (33% and 27%, respectively). Tachypnea was almost doubled in the severe group (63%). Only 1 patient was having SpO2 < 94% and he was in the severe group. The mild and moderate groups showed an initial mean GCS of 14 and 15, respectively. The severe group, on the other hand, had a mean GCS of 8. VBG results showed a mean PH of 7.2 in the mild group, 7.1 in the moderate group and 6.8 in the severe group. HCO3 concentration had a mean of 15 mmol/l in the mild group, 9 mmol/l in the moderate group, and 14 mmol/l in the severe group. Mean methanol concentration was 136 mg/dl in the severe group, 177 mg/dl in the mild group and 113 mg/dl in the moderate group. White blood cells showed an upward trend among the groups: 9 cells per cubic millimeter in mild group, 14 cells per cubic millimeter in moderate group and 20 cells per cubic millimeter in severe group. In addition, creatinine was 139 µmol/L in the severe group while it was 78 µmol/L and 109 µmol/L in the mild and moderate groups, respectively. The mean anion gap (AGAP) and lactic acid were very high in the severe group (AGAP:25, Lactate:9 mmol/L). While the AGAP in the mild and moderate groups were 25 and 29 respectively and the Lactate were 1.84 mmom/L for mild group and 2.43 for the moderate group. Brain CT showed abnormal changes in certain patients in the severe group. Osmolality was 315 mOsm/kg in the mild group, 336 mOsm/kg in the moderate group and 362 mOsm/kg in the severe group.
The overall mortality rate was (4/23), 17.4%, three patients that died were in the severe group and one patient died up on arrival. Among those who were discharged from the hospital, vision impairment was the most common sequalae of methanol poisoning (7/12 who were assessed by ophthalmology, 58%), four patients (36%) in the moderate group and three patients (38%) in the severe group. Moreover, four patients (63%) in the severe group were diagnosed with brain death or edematous changes. Appendix 1 includes the full data for the patients.
Patient managements
ED management included fomepizole, dialysis, sodium bicarbonate and folate. Almost 91% of the alive cases was started on hemodialysis (20/22). One of those who was not started on dialysis was in mild group and was asymptomatic and the other died in the ED before initiation of the dialysis. For mild group, one case was dialyzed for one time and the other had two sessions of dialysis while in the moderate group, eight cases had only one time of dialysis and three cases needed two sessions. Two cases in the severe group had three sessions of dialysis and two case needed three times of dialysis. The majority of the patients (11/20, 55%), were dialyzed within five hours or less from arrival to the ED. Twenty-two patients (22/22, 100%) in this study were started on fomepizole. All patients in the severe group had to be intubated (8/8, 100%) compared to two from the moderate group (2/11, 18%) and none from the mild group (0/3, 0%).
The multifaceted presentation of methanol poisoning poses a substantial diagnostic challenge, often presenting with a heterogenous constellation of symptoms across patients, potentially delaying suspicion and contributing to its significant morbidity and mortality [ 14 ]. However, prompt recognition and swift therapeutic intervention can dramatically mitigate the severity of sequelae [ 15 ]. Therefore, rapid source identification, coupled with proactive communication and heightened awareness amongst potentially exposed individuals, presents a significant opportunity for improved clinical outcomes. In our healthcare facility, timely diagnosis was achieved on the initial presentation itself, underscoring the critical role of early recognition in combating this potentially devastating toxicologic entity. The initial presenting complaint in this outbreak differed from previous reports. While nausea and vomiting were the most common symptoms observed, consistent with two prior outbreaks [ 14 , 16 ], this contrasts with other studies where visual impairment was the dominant presentation [ 17 , 18 , 19 ]. The potential for ethanol co-ingestion, a less harmful alcohol, might explain this disparity, although further investigation is warranted. Upon emergency department presentation, a comprehensive laboratory evaluation including CBC, electrolytes, VBG, methanol, lactate, and osmolality was conducted based on clinical suspicion. Consistent with established literature [ 14 , 16 , 17 , 18 ], the group with severe presentations exhibited the lowest mean serum pH, alongside the highest mean levels of methanol, potassium, lactate, WBCs, and osmolality. These findings underscore the importance of considering diverse presenting features in methanol poisoning, while highlighting the consistent laboratory profile associated with disease severity. All patients in the severe group, with the exception of the individual who demised before ICU admission, necessitated intensive care support. Notably, the severe group exhibited signs of nephrotoxicity, as evidenced by elevated mean creatinine (139 µmol/L) and blood urea nitrogen (BUN) levels (5.7 mmol/L). This observation aligns with the known nephrotoxic potential of methanol’s direct cytotoxic metabolite. While previous research suggests hypotension as a potential contributor to methanol-induced kidney injury [ 16 ], it is noteworthy that all patients within the hypotensive subgroup in this study also presented with renal impairment. These findings warrant further investigation to elucidate the precise mechanisms underlying and the potential interplay between hypotension and the direct cytotoxic effects of methanol metabolites in the pathogenesis of methanol-associated kidney injury. Upon suspicion of methanol poisoning based on a combination of clinical history, presentation, and metabolic acidosis, immediate therapeutic interventions were initiated as per the established local protocol. This aggressive management employed fomepizole to competitively inhibit methanol metabolism, sodium bicarbonate to rapidly rectify severe acidemia, folate for enhanced formic acid clearance, and hemodialysis for expeditious toxin removal. Notably, the observed mortality rate of 17.4% fell significantly below the average reported in other outbreaks (28-48%). 14,16 This discrepancy can be primarily attributed to the swift diagnosis and prompt initiation of fomepizole and hemodialysis therapy, in contrast to delays or limited availability noted in previous reports. Notably, the majority of patients received fomepizole and dialysis within 3–5 h of emergency department arrival. While a slight delay in fomepizole administration for the initial case occurred, swift recognition of a potential influx of cases triggered a multi-faceted response. This led to operational collaboration and ensured timely fomepizole access for subsequent patients, prompting a comprehensive review of all antidote availability and distribution protocols, detailed elsewhere [ 20 ]. Several prior investigations have established a correlation between the severity of metabolic acidosis and mortality in methanol poisoning, aligning with our observations in this study. Patients who demised in the emergency department exhibited pH values below 7. Notably, four individuals within our cohort presented with similarly low pH (< 7), yet three experienced favorable outcomes and were discharged home, with one leaving against medical advice [ 14 , 16 , 17 , 18 ]. This apparent discrepancy may be attributed to the prompt administration of fomepizole, the swift initiation of hemodialysis, and the number of dialysis sessions undergone. These findings suggest that an aggressive combined therapeutic approach, targeting both metabolic acidosis correction and toxin elimination, may mitigate the adverse prognostic implications associated with severe acidosis in methanol poisoning. Further research is warranted to elucidate the precise interplay between acidosis severity, early intervention, and ultimate prognosis in this complex clinical entity.
Early fomepizole administration can be crucial in preventing death and disability from methanol poisoning, as highlighted in a previous case series from our region with nine cases [ 21 ]. This is particularly important in Saudi Arabia, where alcohol consumption is prohibited due to religious and health reasons. However, there have been multiple outbreaks of methanol poisoning, especially among young people, during the COVID-19 pandemic. The pandemic likely played a role in these outbreaks by disrupting access to regulated alcoholic beverages, potentially leading to increased consumption of unregulated and often methanol-contaminated alternatives. For healthcare systems, this emphasizes the importance of having readily available stocks of essential antidotes like fomepizole and hemodialysis equipment, which can be lifesaving in such cases. Additionally, ongoing education for healthcare providers on the clinical management of toxic alcohol ingestions and the potential for outbreaks, particularly during public health crises, is crucial. By taking these steps, we can be better prepared to respond to future methanol poisoning outbreaks and improve patient outcomes.
This study demonstrates the diverse clinical presentation of methanol poisoning, encompassing a spectrum of gastrointestinal, ophthalmic, and central nervous system manifestations. Notably, the observed low mortality and morbidity rate can be primarily attributed to the prompt diagnostic approach, swift initiation of fomepizole therapy, and rapid deployment of hemodialysis. These findings underscore the paramount importance of prioritizing early recognition and intervention in emergency departments during suspected methanol poisoning outbreaks. Establishing standardized protocols for expedited clinical assessment and laboratory testing, particularly in regions with a higher prevalence of unregulated alcohol consumption, holds crucial value in mitigating the potential morbidity and mortality associated with this toxicological entity.
Data availability
The datasets generated during the current study are available.
Pressman P, Clemens R, Sahu S, Hayes AW. A review of methanol poisoning: a crisis beyond ocular toxicology. 2020;39:173–9. https://doi.org/10.1080/15569527.2020.1768402 .
CAS Google Scholar
Korabathina K. Methanol Toxicity . 2015.
Barceloux DG, Krenzelok EP, Olson K, Watson W, Miller H. American academy of clinical toxicology practice guidelines on the treatment of ethylene glycol poisoning. J Toxicol - Clin Toxicol. 1999;37:537.
Article CAS PubMed Google Scholar
Kruse JA. Methanol and Ethylene Glycol Intoxication. Crit Care Clin. 2012;28:661–711.
Article PubMed Google Scholar
Aisa TM, Ballut OM. Methanol intoxication with cerebral hemorrhage. Neurosciences. 2016;21:275–7.
Article PubMed PubMed Central Google Scholar
Phang PT, Passerini L, Mielke B, Berendt R, King EG. Brain hemorrhage associated with methanol poisoning. Crit Care Med. 1988;16:137–40.
Ekins BR, Rollins DE, Duffy DP, Gregory MC. Standardized treatment of severe methanol poisoning with ethanol and hemodialysis. West J Med. 1985;142:337–40.
CAS PubMed PubMed Central Google Scholar
Chan APL, Chan TYK. Methanol as an unlisted ingredient in supposedly alcohol-based hand rub can pose serious health risk. Int J Environ Res Public Health. 2018;15. https://doi.org/10.3390/ijerph15071440 .
Ahmed F, Khan NU, Ali N, Feroze A. Methanol poisoning: 27 years’ experience at a tertiary care hospital. J Pak Med Assoc. 2017;67:1751–2.
PubMed Google Scholar
Becker CE. Methanol poisoning. J Emerg Med. 1983;1:51–8.
Effrey J, Rent B, Enneth MCM, Artin K, Cott S, Hillips P, Aron YA et al. The New Eng land Jour nal of Medicine FOMEPIZOLE FOR THE TREATMENT OF METHANOL POISONING Background Methanol poisoning may result in. 2001.
Sefidbakht S, Lotfi M, Jalli R, Moghadami M, Sabetian G, Iranpour P. Methanol toxicity outbreak: when fear of COVID-19 goes viral. Emerg Med J. 2020;37:416.
About Saudi - Visit Saudi Official Website. https://www.visitsaudi.com/en/understand (accessed 20 Nov2022).
Md Noor J, Hawari R, Mokhtar MF, Yussof SJ, Chew N, Norzan NA, et al. Methanol outbreak: a Malaysian tertiary hospital experience. Int J Emerg Med. 2020;13:1–7.
Article Google Scholar
Collister D, Duff G, Palatnick W, Komenda P, Tangri N, Hingwala J. A methanol intoxication outbreak from recreational ingestion of Fracking Fluid. Am J Kidney Dis. 2017;69:696–700.
Paasma R, Hovda KE, Tikkerberi A, Jacobsen D. Methanol mass poisoning in Estonia: outbreak in 154 patients. Clin Toxicol. 2007;45:152–7.
Article CAS Google Scholar
Liu JJ, Daya MR, Carrasquillo O, Kales SN. Prognostic factors in patients with methanol poisoning. J Toxicol Clin Toxicol. 1998;36:175–81.
Hovda KE, Hunderi OH, Tafjord AB, Dunlop O, Rudberg N, Jacobsen D. Methanol outbreak in Norway 2002–2004: epidemiology, clinical features and prognostic signs. J Intern Med. 2005;258:181–90.
Naraqi S, Dethlefs RF, Slobodniuk RA, Sairere JS. An outbreak of acute methyl alcohol intoxication. Aust N Z J Med. 1979;9:65–8.
Abu Esba LC, Mardawi G, Al Deeb M. Can’t find the antidote: a root cause analysis. Front Pharmacol. 2022;13. https://doi.org/10.3389/FPHAR.2022.895841 .
Eskandrani R, Almulhim K, Altamimi A, Alhaj A, Alnasser S, Alawi L, et al. Methanol poisoning outbreak in Saudi Arabia: a case series. J Med Case Rep. 2022;16:1–7.
Download references
Acknowledgements
We wholeheartedly acknowledge the invaluable contributions of King Abdulaziz Medical City (KAMC) and King Abdullah International Medical Research Center (KAIMRC) in the successful completion of this study. KAMC provided unwavering support on multiple fronts. By granting access to patient electronic records and fostering a conducive clinical environment for data collection, they laid the cornerstone for our research. Notably, KAMC’s emergency department served as the focal point for both patient presentation and management of the methanol poisoning cases, granting us an unparalleled opportunity for thorough retrospective analysis of the events.
Not applicable.
Author information
Authors and affiliations.
Emergency Medicine Department, Ministry of the National Guard - Health Affairs, Riyadh, Saudi Arabia
Faisal Alhusain, Mohammed Alshalhoub & Mohammad Al Deeb
King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
Faisal Alhusain, Mohammed Alshalhoub, Laila Carolina Abu Esba, Mohammad Alghafees & Mohammad Al Deeb
Emergency Medicine Department, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia
Moath Bin Homaid
Pharmaceutical Care Services, Ministry of the National Guard– Health Affairs, Riyadh, Saudi Arabia
Laila Carolina Abu Esba
Surgery Department, Ministry of the National Guard - Health Affairs, Riyadh, Saudi Arabia
Mohammad Alghafees
You can also search for this author in PubMed Google Scholar
Contributions
Faisal Alhusain: Literature review and manuscript writing Mohammed Alshalhoub: Literature review and manuscript writing Moath Bin Homaid: Literature review, data collection and manuscript review Laila Carolina Abu Esba: Literature review, data collection and data analysisMohammad Alghafees: Literature review and data collection Mohammad Al Deeb: Literature review, manuscript review and work supervision.
Corresponding author
Correspondence to Faisal Alhusain .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was granted by Institutional Review Board King Abdullah International Medical Research Centre via reference number NRC22R/348/07. The informed consent was waived by the same abovementioned ethics committee that approved the study.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Alhusain, F., Alshalhoub, M., Homaid, M.B. et al. Clinical presentation and management of methanol poisoning outbreaks in Riyadh, Saudi Arabia: a retrospective analysis. BMC Emerg Med 24 , 64 (2024). https://doi.org/10.1186/s12873-024-00976-1
Download citation
Received : 17 January 2023
Accepted : 27 March 2024
Published : 16 April 2024
DOI : https://doi.org/10.1186/s12873-024-00976-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Methanol toxicity
- Methanol poisoning outbreak
- Saudi Arabia
BMC Emergency Medicine
ISSN: 1471-227X
- General enquiries: [email protected]
Evidence Review of the Adverse Effects of COVID-19 Vaccination and Intramuscular Vaccine Administration
Vaccines are a public health success story, as they have prevented or lessened the effects of many infectious diseases. To address concerns around potential vaccine injuries, the Health Resources and Services Administration (HRSA) administers the Vaccine Injury Compensation Program (VICP) and the Countermeasures Injury Compensation Program (CICP), which provide compensation to those who assert that they were injured by routine vaccines or medical countermeasures, respectively. The National Academies of Sciences, Engineering, and Medicine have contributed to the scientific basis for VICP compensation decisions for decades.
HRSA asked the National Academies to convene an expert committee to review the epidemiological, clinical, and biological evidence about the relationship between COVID-19 vaccines and specific adverse events, as well as intramuscular administration of vaccines and shoulder injuries. This report outlines the committee findings and conclusions.
Read Full Description
- Digital Resource: Evidence Review of the Adverse Effects of COVID-19 Vaccination
- Digital Resource: Evidence Review of Shoulder Injuries from Intramuscular Administration of Vaccines
- Press Release
Recent News
The Challenge of Predicting Climate Migration
Celebrating Earth Day with the National Academies
Rohr Named U.S. Winner of Frontiers Planet Prize
NAS Launches Science and Innovation Fund for Ukraine
- Load More...

IMAGES
VIDEO
COMMENTS
While I will focus on internal medicine inpatients, the following framework can be applied to patients in any setting with slight modifications. Style. Oral case presentations are generally made to a medical care team, which can be composed of medical and pharmacy students, residents, pharmacists, medical attendings, and others.
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence.1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
Summarize the major points of the case. Provide a limited number (e.g. 3) of takeaway points for the audience. Tailor summary and takeaway points to your audience. Critical Thinking Skills. Successful patient case presentations: Integrate disease and drug knowledge, clinical evidence, and patient factors.
Key elements of each presentation type are described below. Examples of how these would be applied to most situations are provided in italics. The formats are typical of presentations done for internal medicine services and clinics. Note that there is an acceptable range of how oral presentations can be delivered.
A case presentation should be memorized as much as possible by your 3rd year rotations. You can refer to notes, but should not read your presentation. Length - this will vary depending on your service. A full medicine presentation in attending rounds should be under 5 minutes.
4. Remember, this is an iterative process; your decisions are not final. 5. Review the outline with your mentor or interested colleagues, and listen to their decisions. Use the Preparing the Clinical Vignette Presentation Checklist to assist you in preparing the topic outline. If you are scheduled to make a presentation of a clinical vignette ...
7 Ingredients for a Patient Case Presentation Template. 1. The One-Liner. The one-liner is a succinct sentence that primes your listeners to the patient. A typical format is: " [Patient name] is a [age] year-old [gender] with past medical history of [X] presenting with [Y]. 2.
Writing up. Write up the case emphasising the interesting points of the presentation, investigations leading to diagnosis, and management of the disease/pathology. Get input on the case from all members of the team, highlighting their involvement. Also include the prognosis of the patient, if known, as the reader will want to know the outcome.
CLINICAL CASE PRESENTATION - GUIDELINES 'He who studies medicine without books sails an uncharted sea, but he who studies medicine without patients does not go to sea at all' William Osler - the Father of Modern Medicine Guidelines prepared by Dr Danielle Freedman,
Presenting a patient is an essential skill that is rarely taught Clinical presenting is the language that doctors use to communicate with each other every day of their working lives. Effective communication between doctors is crucial, considering the collaborative nature of medicine. As a medical student and later as a doctor you will be expected to present cases to peers and senior colleagues ...
Oral Case Presentation Guidelines for 3rd year Medicine Clerkship. A. Purpose of case presentation - to concisely summarize 4 parts of your patient's presentation: (1) history, (2) physical examination, (3) laboratory results, and (4) your understanding of these findings (i.e., clinical reasoning). The oral case presentation is a story that ...
1. SET THE STAGE. Prepare the audience for what is to come. If the audience is composed of people of mixed expertise, spend a few minutes forming them into small mixed groups of novices and experts. Explain that this is an opportunity for the more junior to learn from the more senior people. Tell them that the case to be presented is extremely ...
Case presentation is either poorly taught or not taught at all in the first two years of medical school. As a result, students are thrust into the spotlight with only sketchy ideas about how to present, prioritize, edit, and focus their case presentations. ... Professor of Medicinem, Department of Medicine, Case Western Reserve University ...
Basic written and oral case presentation skills, obtained in physical diagnosis courses. Specific Learning Objectives. Knowledge: Each student should be able to describe: ... Division of General Medicine 5034 Old Clinic Bldg. CB#7110 Chapel Hill, NC 27599 Phone: (919) 966-7776 Fax: (919) 966-2274 . SOM General Policies
The purpose of the oral case presentation is: To concisely communicate the findings of your history and exam to other members of your team. To formulate and address the clinical questions that are important to your patient's care. On completion of Foundations of Clinical Medicine, students should be able to perform an accurate, complete and ...
Osmosis's Chief Medical Officer, Dr. Rishi Desai, explains 3 helpful tips on how to give an effective oral presentation. Find our full video library only on ...
Oral case presentation is an essential skill in clinical practice that is decidedly varied and understudied in teaching curricula. Methods: We developed a curriculum to improve oral case presentation skills in medical students. Results: As part of an internal medicine clerkship, students receive instruction in the elements of a good oral case ...
A case report is a detailed report of the symptoms, signs, diagnosis, treatment, and follow-up of an individual patient. Case reports usually describe an unusual or novel occurrence and as such, remain one of the cornerstones of medical progress and provide many new ideas in medicine. Some reports contain an extensive review of the relevant ...
The Clinical Case Study PowerPoint template has a clean and minimalistic style that makes your work stand out in high-level professional slides. You'll find medical icons on every PowerPoint slide. Use them to organize your information and direct your audience's attention exactly where you want it to be.
The authors found that assessment-oriented oral case presentations were about 40% faster than traditional presentations without significant differences in case presentation effectiveness. Prior to our study, the nature of the format for inpatient medicine oral case presentations had thus far escaped scrutiny.
Template 4: AIoT Healthcare Applications in Medical Imaging. AIoT is making the medical sector smarter and wiser to improve data management and human-machine interaction. When AIoT is applied to healthcare, enables virtual monitoring and accurate diagnosis of patients to develop a personalized patient experience.
The 3-Minute Emergency Medicine Medical Student Presentation: A Variation on a Theme. This paper is the key resource for mastering case presentations. It goes over the differences between emergency medicine and other specialties, and how these differences impact the best way to present a case.
Download the "Maternal Stroke Clinical Case" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. ... Neurology is one of the most complex branches there is in the field of medicine. Dealing with ...
CASE PRESENTATION Case 1. A 77-year-old man was admitted to our intensive care unit (ICU) because of multiple trauma, including small bilateral hemothorax and multiple rib fractures. Although his general condition was stable after initial resuscitation, a venous thromboembolism was diagnosed on Day 15 of hospitalization.
Case presentations -Discuss the diagnosis and management of orthopedic oncology cases by presenting patient symptoms, medical history, radiologic findings, medical/surgical intervention, and pathologic findings -Facilitate discussion between attend. ... The School of Medicine, State University of New York at Stony Brook, is accredited by the ...
Submit a Case StudyPresentation. A 71-year-old male develops acute respiratory distress 4 weeks after a bone marrow transplant. The patient experiences fever, tachycardia and worsening mentation. Blood and respiratory cultures reveal a gram-negative bacillus, which was not identified by rapid respiratory and blood culture molecular panels. The ...
This was a retrospective case series of methanol poisoning cases which presented to the adult emergency department (ED) at King Abdulaziz Medical City (KAMC) in Riyadh, Saudi Arabia. There were two separate outbreaks in the city, the first one was from September 1 to September 10, 2020 and the second one was from May 14 to May 20, 2021.
WASHINGTON — A new report from the National Academies of Sciences, Engineering, and Medicine reviews evidence for 19 potential harms of the COVID-19 vaccines, and for nine potential shoulder injuries from intramuscular administration of vaccines more broadly. The committee that conducted the review identified sufficient evidence to draw 20 conclusions about whether these vaccines could cause ...