Health Education Workforce: Opportunities and Challenges
ESSAY — Volume 15 — June 28, 2018

Rebecca A. Bruening, MPH 1 ; Fátima Coronado, MD, MPH 2 ; M. Elaine Auld, MPH, MCHES 3 ; Gabrielle Benenson, MPH 2 ; Patricia M. Simone, MD 2 ( View author affiliations )
Suggested citation for this article: Bruening RA, Coronado F, Auld ME, Benenson G, Simone PM. Health Education Workforce: Opportunities and Challenges. Prev Chronic Dis 2018;15:180045. DOI: http://dx.doi.org/10.5888/pcd15.180045 external icon .
Skill Sets of Health Educators to Meet Public Health Needs
Health educator employment data, call to action, acknowledgments, author information.
Public health is facing unprecedented opportunities and challenges. Health departments face shifts from less clinical service delivery to increased population-based services to address the growing burden of chronic diseases (eg, obesity prevention, tobacco and drug use prevention) and new responsibilities to collaborate with other sectors in conducting community needs assessments and data sharing (1–3). State and local health departments continue to be challenged by health policy changes, reduced budgets, and difficulty recruiting and retaining staff (2). These challenges need to be met with a public health workforce of adequate size, composition, distribution, and skills. Formally trained health educators are an important but often underutilized part of the workforce needed to meet such challenges. Although various health workers inform the public, many employers are unaware of the professional training and roles of health educators (4). Health educators (also referred to as health education specialists) address chronic and other conditions by applying their competencies to the design and execution of behavioral health and policy or systems interventions (4). This essay highlights how the skill sets of health educators can address current and future public health challenges, the need for improved health educator workforce data, and a call to action for various stakeholders to optimally deploy health educators to improve the public’s health.
Health educators are uniquely positioned to address public health needs by deploying their training and competencies in the application of behavioral theories across a wide range of interventions designed to improve population health. Health educators use a holistic approach to changing health behaviors, implementing evidence-based interventions and adapting to changing population needs. For example, health educators can help multicultural populations with access to and use of the health system by improving their health insurance literacy and understanding of enrollment options and can conduct community health needs assessments required for nonprofit hospitals, modify policies or systems to improve access to preventive health services, and strengthen clinical and community linkages (5). In addition, health educators can develop and implement training programs for professionals and consumers, market health programs and services, conduct evaluation research, analyze data and educate populations about wellness behaviors (eg, vaccination campaigns, opioid abuse prevention programs), provide consultation to health agencies about different topics (eg, smoking prevention and cessation efforts), and apply their skills in cross-cultural communication and community organizing (eg, prenatal programs for expectant mothers in diverse communities) (5).
A health educator has training in public health, health promotion, or community health at the bachelor’s, master’s, or doctoral levels. To maintain the highest level of competence in the health education workforce, health educators can obtain additional certifications such as the Certified Health Education Specialist (CHES) and Master Certified Health Education Specialist (MCHES), both awarded through the National Commission for Health Education Credentialing to people who have met academic preparation and examination qualifications, which requires that the person remains up to date with education requisites, acquiring at least 75 continuing education contact hours every 5 years.
Although many people are professionally prepared as health educators, available data are limited about where they work, how they contribute, or how they can be better deployed to serve public health needs. Despite the US Department of Labor’s Standard Occupational Classification of health educators, the definition is not widely embraced throughout the government public health system. Because job descriptions often include functions of other health workers, including health communicators and community health workers, some employers might have difficulty distinguishing health educators from other professionals. Furthermore, professional identification and occupational classifications can differ substantially among health educators. Employers often use other titles to classify positions for health educators, likely underestimating the number of health educators working under alternative job titles and complicating efforts to collect and interpret workforce data (4).
Describing the health educator workforce is further challenged by limited employment data available across all industries, a concern common to many public health professions (6). Health educators work in diverse settings, including governmental public health agencies, health care organizations, schools and colleges, community organizations, and corporations. In 2015, the US Bureau of Labor Statistics reported that 57,750 people were employed as health educators, compared with 63,320 in 2006; the industries with the highest levels of health educator employment were government (22%), hospitals (21%), and ambulatory health care services (16%) (7). However, it is possible that this trend could be because these industries might have a similar approach to job classifications, as noted earlier.
In a 2016 survey of local health departments, 53% of respondents indicated that health education is a high-priority occupation in their agencies, and 76% reported the need for more health educator positions (8). Although the US Department of Labor predicted growth in the number of health educators attributable to increased focus on prevention driven by changes in health care systems and insurance coverage (7), from 2010 to 2013 the numbers remained the same at the local government level and dropped in state health departments (9). Part of the reason might be ambiguity regarding the competencies of health educators and community health workers. The 2 occupations have distinct standard occupational classifications, but their descriptions are combined in the US Department of Labor Occupational Handbook. Although the two have complementary roles in addressing community and individual health needs, their training and skill levels differ.
Health educators play a vital role in addressing public health concerns, but opportunities exist for even greater contributions. As the nation develops Healthy People 2030 objectives, improvements are needed in educating employers about health educator competencies, collecting and analyzing health educator workforce data, and strengthening health educator professional preparation and in-service training. We propose a set of actions for the health education community and other stakeholders in schools and programs of public health, government public health agencies, health systems, and professional associations, to help address these challenges.
Skills . The health educator profession should continue to incorporate broad-based skills that match current public health needs into professional preparation and continuing education. To keep pace with emerging public health challenges, government public health workers, including health educators, increasingly require more strategic skills that address the social, community-based, and economic determinants of health (10). Training needs include understanding systems thinking and identifying high-impact interventions, changing management approaches to scale programs in response to evolving environments, using data for decision making, identifying and solving problems and evaluating results, engaging underrepresented populations, acquiring human and fiscal resource management knowledge, and addressing public health concerns while engaging a broader audience of policy and decision makers (10).
Advocacy . The health educator community can be effective advocates for their own profession, educating their human resource departments about expected competencies of professionally trained health educators, the differences between health educators and community health workers, certifications, recruitment avenues, and the contributions of health educators to the bottom line (5). They can help others in the public health community recognize the value of health education by promoting certification as a quality assurance mechanism for the field, disseminating results about health educators’ contributions to health outcomes, and regularly assessing competencies needed for health educators to meet contemporary public health challenges. Similarly, they can help inform grant funders as well as public and private employers on how the use of contemporary health educator skills can help them achieve their population health goals.
Data . Data from health educator-related academic programs regarding the employment outcomes of their graduates can help assess the quality of professional preparation in terms of employment job duties. To complement data from academic programs, public and private workforce surveys should include questions about professional training and link to occupational classifications by using an established taxonomy (6). Such data are crucial to determine whether the supply of professionally prepared health educators is sufficient to meet demand and to guide decision makers and researchers to identify workforce gaps, improve workforce development, and recruit and retain health educators in sectors where they are most needed. Because the challenges of describing the health education workforce are similar to those of the larger public health workforce, health education stakeholders should engage with other public health partners on innovative, cross-cutting solutions for shared workforce priorities, addressing them in a coordinated approach.
With shrinking resources and mounting public health demands, public health agencies and organizations must collaborate to deploy the capabilities of all public health workers, including health educators, at their highest levels of competence. Trained health educators are vital to addressing public health needs and contributing to healthy communities. By incorporating broad-based competencies into professional preparation, promoting health educator skills and competencies to employers, and improving enumeration and tracking of health educators and other public health professions in the public health workforce, we will be poised to achieve Healthy People 2030 objectives, for the nation and beyond.
The work of the first author was supported by cooperative agreement no. NU36OE000006 from the Centers for Disease Control and Prevention and the Association of Schools and Programs of Public Health. The other authors received no financial support for this work. This work contains no copyrighted materials. The ideas expressed in this article are those of the authors and do not necessarily reflect the official position of Centers for Disease Control and Prevention.
Corresponding Author: Fátima Coronado, MD, MPH, Deputy Associate Director for Science, Division of Scientific Education and Professional Development, Center for Surveillance, Epidemiology and Laboratory Services, Centers for Disease Control and Prevention, 1600 Clifton Rd, MS E-96, Atlanta GA 30329. Telephone: 404-498-6551. Email: [email protected] .
Author Affiliations: 1 Association of Schools & Programs of Public Health Fellow, Division of Scientific Education and Professional Development, Centers for Disease Control and Prevention, Atlanta, Georgia. 2 Division of Scientific Education and Professional Development, Centers for Disease Control and Prevention, Atlanta, Georgia. 3 Society for Public Health Education, Washington, District of Columbia.
- Anderson G. Chronic Care: Making the Case for Ongoing Care. Princeton (NJ): Robert Wood Johnson Foundation; 2010. https://www.rwjf.org/en/library/research/2010/01/chronic-care.html. Accessed January 25, 2018.
- National Association of County and City Health Officials. The changing public health landscape: findings of the 2015 Forces of Change Survey. http://nacchoprofilestudy.org/forces-of-change/2015-forces-of-change/. Accessed January 25, 2018.
- DeSalvo KB, Wang YC, Harris A, Auerbach J, Koo D, O’Carroll P. Public health 3.0: a call to action for public health to meet the challenges of the 21st century. Prev Chronic Dis 2017;14:E78. CrossRef external icon PubMed external icon
- Gambescia SF, Cottrell RR, Capwell E, Auld ME, Mullen Conley K, Lysoby L, et al. Marketing health educators to employers: survey findings, interpretations, and considerations for the profession. Health Promot Pract 2009;10(4):495–504. CrossRef external icon PubMed external icon
- Auld ME. Health education careers in a post-health reform era. Health Promot Pract 2017;18(5):629–35. CrossRef external icon PubMed external icon
- Beck AJ, Coronado F, Boulton ML, Merrill JA; Public Health Enumeration Working Group. The public health workforce taxonomy: revisions and recommendations for implementation. J Public Health Manag Pract 2017. Epub 2017 November 2. CrossRef external icon PubMed external icon
- US Department of Labor. Occupational outlook handbook. Washington (DC): US Bureau of Labor Statistics; 2017. https://www.bls.gov/ooh/community-and-social-service/health-educators.htm. Accessed January 25, 2017.
- Beck AJ, Leider JP, Coronado F, Harper E. State health agency and local health department workforce: identifying top development needs. Am J Public Health 2017;107(9):1418–24. CrossRef external icon PubMed external icon
- Beck AJ, Boulton ML. Trends and characteristics of the state and local public health workforce, 2010–2013. Am J Public Health 2015;105(Suppl 2):S303–10. CrossRef external icon PubMed external icon
- deBeaumont Foundation. National consortium for public health workforce development report: a call to action. http://www.debeaumont.org/consortiumreport/. Accessed January 25, 2018.
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
AI in Medical Education: Global situation, effects and challenges
- Published: 10 July 2023
- Volume 29 , pages 4611–4633, ( 2024 )
Cite this article
- Wei Zhang 1 ,
- Mingxuan Cai 1 ,
- Hong Joo Lee 2 ,
- Richard Evans 3 ,
- Chengyan Zhu 4 &
- Chenghan Ming 5
1752 Accesses
4 Citations
Explore all metrics
Artificial Intelligence (AI) is transforming healthcare and shows considerable promise for the delivery of medical education. This systematic review provides a comprehensive analysis of the global situation, effects, and challenges associated with applying AI at the different stages of medical education.
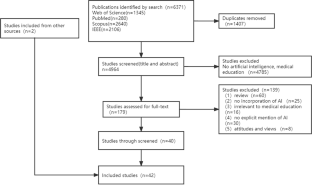
This review followed the PRISMA guidelines, and retrieved studies published on Web of Science, PubMed, Scopus, and IEEE Xplore, from 1990 to 2022. After duplicates were removed (n = 1407) from the 6371 identified records, the full text of 179 records were screened. In total, 42 records were eligible.
It revealed three teaching stages where AI can be applied in medical education (n = 39), including teaching implementation (n = 24), teaching evaluation (n = 10), and teaching feedback (n = 5). Many studies explored the effectiveness of AI adoption with questionnaire survey and control experiment. The challenges are performance improvement, effectiveness verification, AI training data sample and AI algorithms.
Conclusions
AI provides real-time feedback and accurate evaluation, and can be used to monitor teaching quality. A possible reason why AI has not yet been applied widely to practical teaching may be the disciplinary gap between developers and end-user, it is necessary to strengthen the theoretical guidance of medical education that synchronizes with the rapid development of AI. Medical educators are expected to maintain a balance between AI and teacher-led teaching, and medical students need to think independently and critically. It is also highly demanded for research teams with a wide range of disciplines to ensure the applicability of AI in medical education.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

AIM in Medical Education

Systematic review of research on artificial intelligence applications in higher education – where are the educators?
Olaf Zawacki-Richter, Victoria I. Marín, … Franziska Gouverneur
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Aldeman, N. L. S., de SáUrtigaAita, K. M., Machado, V. P., da Mata Sousa, L. C. D., Coelho, A. G. B., da Silva, A. S., Silva Mendes, A. P., de Oliveira Neres, F. J., & do Monte, S. J. H. (2021). Smartpathk: A platform for teaching glomerulopathies using machine learning. BMC Medical Education, 21 (1), 248. https://doi.org/10.1186/s12909-021-02680-1
Article PubMed PubMed Central Google Scholar
Alonso-Silverio, G. A., Pérez-Escamirosa, F., Bruno-Sanchez, R., Ortiz-Simon, J. L., Muñoz-Guerrero, R., Minor-Martinez, A., & Alarcón-Paredes, A. (2018). Development of a Laparoscopic Box Trainer Based on Open Source Hardware and Artificial Intelligence for Objective Assessment of Surgical Psychomotor Skills. Surgical Innovation, 25 (4), 380–388. https://doi.org/10.1177/1553350618777045
Article PubMed Google Scholar
Baloul, M. S., Yeh, V.J.-H., Mukhtar, F., Ramachandran, D., Traynor, M. D., Shaikh, N., Rivera, M., & Farley, D. R. (2022). Video Commentary & Machine Learning: Tell Me What You See, I Tell You Who You Are. Journal of Surgical Education, 79 (6), e263–e272. https://doi.org/10.1016/j.jsurg.2020.09.022
Bienstock, J. L., Katz, N. T., Cox, S. M., Hueppchen, N., Erickson, S., & Puscheck, E. E. (2007). To the point: Medical education reviews—providing feedback. American Journal of Obstetrics and Gynecology, 196 (6), 508–513. https://doi.org/10.1016/j.ajog.2006.08.021
Bing-You, R., Hayes, V., Varaklis, K., Trowbridge, R., Kemp, H., & McKelvy, D. (2017). Feedback for Learners in Medical Education: What Is Known? A Scoping Review . Wolters Kluwer. https://doi.org/10.1097/ACM.0000000000001578
Bissonnette, V., Mirchi, N., Ledwos, N., Alsidieri, G., Winkler-Schwartz, A., Del Maestro, R. F., Yilmaz, R., Siyar, S., Azarnoush, H., Karlik, B., Sawaya, R., Alotaibi, F. E., Bugdadi, A., Bajunaid, K., Ouellet, J., & Berry, G. (2019). Artificial Intelligence Distinguishes Surgical Training Levels in a Virtual Reality Spinal Task. Journal of Bone and Joint Surgery-American, 101 (23), e127. https://doi.org/10.2106/JBJS.18.01197
Article Google Scholar
Borakati, A. (2021). Evaluation of an international medical E-learning course with natural language processing and machine learning. BMC Medical Education, 21 (1), 181. https://doi.org/10.1186/s12909-021-02609-8
Chan, H.-P., Samala, R. K., Hadjiiski, L. M., & Zhou, C. (2020). Deep Learning in Medical Image Analysis. In G. Lee & H. Fujita ( Ed.), Deep Learning in Medical Image Analysis: Challenges and Applications (pp. 3–21). Springer International Publishing. https://doi.org/10.1007/978-3-030-33128-3_1
Chan, K. S., & Zary, N. (2019). Applications and Challenges of Implementing Artificial Intelligence in Medical Education: Integrative Review. JMIR Medical Education, 5 (1), e13930. https://doi.org/10.2196/13930
Chen, C.-K. (2010). Curriculum Assessment Using Artificial Neural Network and Support Vector Machine Modeling Approaches: A Case Study. IR Applications. Volume 29. In Association for Institutional Research (NJ1) . Association for Institutional Research. https://eric.ed.gov/?id=ED524832
Chen, L., Chen, P., & Lin, Z. (2020). Artificial Intelligence in Education: A Review. Ieee Access, 8 , 75264–75278. https://doi.org/10.1109/ACCESS.2020.2988510
Cheng, C.-T., Chen, C.-C., Fu, C.-Y., Chaou, C.-H., Wu, Y.-T., Hsu, C.-P., Chang, C.-C., Chung, I.-F., Hsieh, C.-H., Hsieh, M.-J., & Liao, C.-H. (2020). Artificial intelligence-based education assists medical students’ interpretation of hip fracture. Insights into Imaging, 11 (1), 119. https://doi.org/10.1186/s13244-020-00932-0
de Lima, R. M., de Medeiros Santos, A., Mendes Neto, F. M., de Sousa, F., Neto, A., Leão, F. C. P., de Macedo, F. T., & de Paula Canuto, A. M. (2016). A 3D serious game for medical students training in clinical cases. IEEE International Conference on Serious Games and Applications for Health (SeGAH), 2016 , 1–9. https://doi.org/10.1109/SeGAH.2016.7586255
Dharmasaroja, P., & Kingkaew, N. (2016). Application of artificial neural networks for prediction of learning performances. 2016 12th International Conference on Natural Computation, Fuzzy Systems and Knowledge Discovery (ICNC-FSKD) , 745–751. https://doi.org/10.1109/FSKD.2016.7603268
Estai, M., & Bunt, S. (2016). Best teaching practices in anatomy education: A critical review. Annals of Anatomy - Anatomischer Anzeiger, 208 , 151–157. https://doi.org/10.1016/j.aanat.2016.02.010
Fajrianti, E. D., Sukaridhoto, S., Rasyid, M. U. H. A., Suwito, B. E., Budiarti, R. P. N., Hafidz, I. A. A., Satrio, N. A., & Haz, A. L. (2022). Application of Augmented Intelligence Technology with Human Body Tracking for Human Anatomy Education. IJIET: International Journal of Information and Education Technology , 12 (6), Article 6.
Fang, Z., Xu, Z., He, X., & Han, W. (2022).Artificial intelligence-based pathologic myopia identification system in the ophthalmology residency training program. Frontiers in Cell and Developmental Biology , 10 . https://doi.org/10.3389/fcell.2022.1053079
Fazlollahi, A. M., Bakhaidar, M., Alsayegh, A., Yilmaz, R., Winkler-Schwartz, A., Mirchi, N., Langleben, I., Ledwos, N., Sabbagh, A. J., Bajunaid, K., Harley, J. M., & Del Maestro, R. F. (2022). Effect of Artificial Intelligence Tutoring vs Expert Instruction on Learning Simulated Surgical Skills Among Medical Students: A Randomized Clinical Trial. JAMA Network Open, 5 (2), e2149008. https://doi.org/10.1001/jamanetworkopen.2021.49008
Fernández-Alemán, J. L., López-González, L., González-Sequeros, O., Jayne, C., López-Jiménez, J. J., & Toval, A. (2016). The evaluation of i-SIDRA – a tool for intelligent feedback – in a course on the anatomy of the locomotor system. International Journal of Medical Informatics, 94 , 172–181. https://doi.org/10.1016/j.ijmedinf.2016.07.008
Foss, C. L. (1987). Learning from errors in ALGEBRALAND . Institute for Research on Learning.
Furlan, R., Gatti, M., Menè, R., Shiffer, D., Marchiori, C., Levra, A. G., Saturnino, V., Brunetta, E., & Dipaola, F. (2021). A Natural Language Processing-Based Virtual Patient Simulator and Intelligent Tutoring System for the Clinical Diagnostic Process: Simulator Development and Case Study. JMIR Medical Informatics, 9 (4), e24073. https://doi.org/10.2196/24073
Gendia, A. (2022). Cloud Based AI-Driven Video Analytics (CAVs) in Laparoscopic Surgery: A Step Closer to a Virtual Portfolio. Cureus , 14 (9). https://doi.org/10.7759/cureus.29087
Gil, D. H., Heins, M., & Jones, P. B. (1984). Perceptions of medical school faculty members and students on clinical clerkship feedback. Academic Medicine, 59 (11), 856.
Article CAS Google Scholar
Goh, P. S. (2021). The vision of transformation in medical education after the COVID-19 pandemic. Korean Journal of Medical Education, 33 (3), 171–174. https://doi.org/10.3946/kjme.2021.197
Article MathSciNet PubMed PubMed Central Google Scholar
Gorospe-Sarasúa, L., Munoz-Olmedo, J. M., Sendra-Portero, F., & de Luis-García, R. (2022a). Challenges of Radiology education in the era of artificial intelligence . 6.
Gorospe-Sarasúa, L., Muñoz-Olmedo, J. M., Sendra-Portero, F., & de Luis-García, R. (2022b). Challenges of Radiology education in the era of artificial intelligence. Radiología (english Edition), 64 (1), 54–59. https://doi.org/10.1016/j.rxeng.2020.10.012
Han, R., Yu, W., Chen, H., & Chen, Y. (2022). Using artificial intelligence reading label system in diabetic retinopathy grading training of junior ophthalmology residents and medical students. BMC Medical Education , 22 (1), Article 1. https://doi.org/10.1186/s12909-022-03272-3
Hattie, J., & Timperley, H. (2007). The power of feedback. Review of educational research, 77 (1), 81–112. https://doi.org/10.3102/003465430298487
Hedderich, D. M., Keicher, M., Wiestler, B., Gruber, M. J., Burwinkel, H., Hinterwimmer, F., Czempiel, T., Spiro, J. E., Pinto dos Santos, D., Heim, D., Zimmer, C., Rückert, D., Kirschke, J. S., & Navab, N. (2021). AI for Doctors—A Course to Educate Medical Professionals in Artificial Intelligence for Medical Imaging. Healthcare , 9 (10), Article 10. https://doi.org/10.3390/healthcare9101278
Hewson, M. G., & Little, M. L. (1998). Giving Feedback in Medical Education. Journal of General Internal Medicine, 13 (2), 111–116. https://doi.org/10.1046/j.1525-1497.1998.00027.x
Article CAS PubMed PubMed Central Google Scholar
Hisan, U. K., & Amri, M. M. (2023). ChatGPT and Medical Education: A Double-Edged Sword. Journal of Pedagogy and Education Science , 2 (01), Article 01. https://doi.org/10.56741/jpes.v2i01.302
Hisey, R., Camire, D., Erb, J., Howes, D., Fichtinger, G., & Ungi, T. (2022). System for Central Venous Catheterization Training Using Computer Vision-Based Workflow Feedback. IEEE Transactions on Biomedical Engineering, 69 (5), 1630–1638. https://doi.org/10.1109/TBME.2021.3124422
Hosny, A., Parmar, C., Quackenbush, J., Schwartz, L. H., & Aerts, H. J. W. L. (2018). Artificial intelligence in radiology. Nature Reviews Cancer , 18 (8), Article 8. https://doi.org/10.1038/s41568-018-0016-5
Hu, H., Li, J., Lei, X., Qin, P., & Chen, Q. (2019). Design of health statistics intelligent education system based on Internet +. Journal of Physics: Conference Series, 1168 (6), 062003. https://doi.org/10.1088/1742-6596/1168/6/062003
Hwang, G.-J., Xie, H., Wah, B. W., & Gašević, D. (2020). Vision, challenges, roles and research issues of Artificial Intelligence in Education. Computers and Education: Artificial Intelligence, 1 , 100001. https://doi.org/10.1016/j.caeai.2020.100001
Islam, G., Kahol, K., Li, B., Smith, M., & Patel, V. L. (2016). Affordable, web-based surgical skill training and evaluation tool. Journal of Biomedical Informatics, 59 , 102–114. https://doi.org/10.1016/j.jbi.2015.11.002
Karambakhsh, A., Kamel, A., Sheng, B., Li, P., Yang, P., & Feng, D. D. (2019). Deep gesture interaction for augmented anatomy learning. International Journal of Information Management, 45 , 328–336. https://doi.org/10.1016/j.ijinfomgt.2018.03.004
Kirubarajan, A., Young, D., Khan, S., Crasto, N., Sobel, M., & Sussman, D. (2022). Artificial Intelligence and Surgical Education: A Systematic Scoping Review of Interventions. Journal of Surgical Education, 79 (2), 500–515. https://doi.org/10.1016/j.jsurg.2021.09.012
Klar, R., & Bayer, U. (1990). Computer-assisted teaching and learning in medicine. International Journal of Bio-Medical Computing, 26 (1–2), 7–27. https://doi.org/10.1016/0020-7101(90)90016-N
Article CAS PubMed Google Scholar
Kurniawan, M. H., Suharjito, Diana, & Witjaksono, G. (2018). Human Anatomy Learning Systems Using Augmented Reality on Mobile Application . 135 , 80–88. https://doi.org/10.1016/j.procs.2018.08.152
Lam, A., Lam, L., Blacketer, C., Parnis, R., Franke, K., Wagner, M., Wang, D., Tan, Y., Oakden-Rayner, L., Gallagher, S., Perry, S. W., Licinio, J., Symonds, I., Thomas, J., Duggan, P., & Bacchi, S. (2022a). Professionalism and clinical short answer question marking with machine learning. Internal Medicine Journal, 52 (7), 1268–1271. https://doi.org/10.1111/imj.15839
Lam, K., Chen, J., Wang, Z., Iqbal, F. M., Darzi, A., Lo, B., Purkayastha, S., & Kinross, J. M. (2022b). Machine learning for technical skill assessment in surgery: A systematic review. Npj Digital Medicine , 5(1), Article 1. https://doi.org/10.1038/s41746-022-00566-0
Lazarus, M. D., Truong, M., Douglas, P., & Selwyn, N. (2022). Artificial intelligence and clinical anatomical education: Promises and perils. Anatomical Sciences Education , n/a (n/a). https://doi.org/10.1002/ase.2221
Lee, J., Wu, A. S., Li, D., Kulasegaram, K., & (Mahan). (2021). Artificial Intelligence in Undergraduate Medical Education: A Scoping Review. Academic Medicine, 96 (11S), S62. https://doi.org/10.1097/ACM.0000000000004291
Lee, L. S., Aluwee, S. A. Z. S., Meng, G. C., Palanisamy, P., & Subramaniam, R. (2020). Interactive Tool Using Augmented Reality (AR) for Learning Knee and Foot Anatomy Based on CT Images 3D Reconstruction. 2020 International Conference on Computational Intelligence (ICCI) , 281–286. https://doi.org/10.1109/ICCI51257.2020.9247820
Li, Y., Bai, C., & Reddy, C. K. (2016). A distributed ensemble approach for mining healthcare data under privacy constraints. Information Sciences, 330 , 245–259. https://doi.org/10.1016/j.ins.2015.10.011
Li, Y. S., Lam, C. S. N., & See, C. (2021). Using a Machine Learning Architecture to Create an AI-Powered Chatbot for Anatomy Education. Medical Science Educator, 31 (6), 1729–1730. https://doi.org/10.1007/s40670-021-01405-9
Luan, H., Geczy, P., Lai, H., Gobert, J., Yang, S. J. H., Ogata, H., Baltes, J., Guerra, R., Li, P., & Tsai, C.-C. (2020). Challenges and Future Directions of Big Data and Artificial Intelligence in Education. Frontiers in Psychology , 11 . https://doi.org/10.3389/fpsyg.2020.580820
Martin, J. A., Regehr, G., Reznick, R., Macrae, H., Murnaghan, J., Hutchison, C., & Brown, M. (1997). Objective structured assessment of technical skill (OSATS) for surgical residents. BJS (british Journal of Surgery), 84 (2), 273–278. https://doi.org/10.1046/j.1365-2168.1997.02502.x
Mirchi, N., Bissonnette, V., Yilmaz, R., Ledwos, N., Winkler-Schwartz, A., & Del Maestro, R. F. (2020). The Virtual Operative Assistant: An explainable artificial intelligence tool for simulation-based training in surgery and medicine. Plos One, 15 (2), e0229596. https://doi.org/10.1371/journal.pone.0229596
Muller, S. (1984). Physicians for the twenty-first century: Report of the project panel on the general professional education of the physician and college preparation for medicine. Journal of Medical Education, 59 , 1–208.
Google Scholar
Nagaraj, M. B., Namazi, B., Sankaranarayanan, G., & Scott, D. J. (2023). Developing artificial intelligence models for medical student suturing and knot-tying video-based assessment and coaching. Surgical Endoscopy, 37 (1), 402–411. https://doi.org/10.1007/s00464-022-09509-y
Nakawala, H., Ferrigno, G., & De Momi, E. (2018). Development of an intelligent surgical training system for Thoracentesis. Artificial Intelligence in Medicine, 84 , 50–63. https://doi.org/10.1016/j.artmed.2017.10.004
Neves, S. E., Chen, M. J., Ku, C. M., Karan, S., DiLorenzo, A. N., Schell, R. M., Lee, D. E., Diachun, C. A. B., Jones, S. B., & Mitchell, J. D. (2021). Using Machine Learning to Evaluate Attending Feedback on Resident Performance. Anesthesia & Analgesia, 132 (2), 545–555. https://doi.org/10.1213/ANE.0000000000005265
Niitsu, H., Hirabayashi, N., Yoshimitsu, M., Mimura, T., Taomoto, J., Sugiyama, Y., Murakami, S., Saeki, S., Mukaida, H., & Takiyama, W. (2013). Using the Objective Structured Assessment of Technical Skills (OSATS) global rating scale to evaluate the skills of surgical trainees in the operating room. Surgery Today, 43 (3), 271–275. https://doi.org/10.1007/s00595-012-0313-7
Ötles, E., Kendrick, D. E., Solano, Q. P., Schuller, M., Ahle, S. L., Eskender, M. H., Carnes, E., & George, B. C. (2021). Using Natural Language Processing to Automatically Assess Feedback Quality: Findings From 3 Surgical Residencies. Academic Medicine, 96 (10), 1457. https://doi.org/10.1097/ACM.0000000000004153
Ouyang, F., Zheng, L., & Jiao, P. (2022). Artificial intelligence in online higher education: A systematic review of empirical research from 2011 to 2020. Education and Information Technologies . https://doi.org/10.1007/s10639-022-10925-9
Peter, H., & Goodridge, W. (2004). Integrating Two Artificial Intelligence Theories in a Medical Diagnosis Application. In M. Bramer & V. Devedzic ( Ed.), Artificial Intelligence Applications and Innovations (pp. 11–23). Springer US. https://doi.org/10.1007/1-4020-8151-0_2
Qian, X., Jingying, H., Xian, S., Yuqing, Z., Lili, W., Baorui, C., Wei, G., Yefeng, Z., Qiang, Z., Chunyan, C., Cheng, B., Kai, M., & Yi, Q. (2022). The effectiveness of artificial intelligence-based automated grading and training system in education of manual detection of diabetic retinopathy. Frontiers in Public Health, 10 , 1025271. https://doi.org/10.3389/fpubh.2022.1025271
Razzak, M. I., Naz, S., & Zaib, A. (2018). Deep Learning for Medical Image Processing: Overview, Challenges and the Future. In N. Dey, A. S. Ashour, & S. Borra ( Ed.), Classification in BioApps: Automation of Decision Making (pp. 323–350). Springer International Publishing. https://doi.org/10.1007/978-3-319-65981-7_12
Sadeghi Esfahlani, S., Izsof, V., Minter, S., Kordzadeh, A., Shirvani, H., & Esfahlani, K. S. (2020). Development of an Interactive Virtual Reality for Medical Skills Training Supervised by Artificial Neural Network. In Y. Bi, R. Bhatia, & S. Kapoor ( Ed.), Intelligent Systems and Applications (pp. 473–482). Springer International Publishing. https://doi.org/10.1007/978-3-030-29513-4_34
Shiang, T., Garwood, E., & Debenedectis, C. M. (2022). Artificial intelligence-based decision support system (AI-DSS) implementation in radiology residency: Introducing residents to AI in the clinical setting. Clinical Imaging, 92 , 32–37. https://doi.org/10.1016/j.clinimag.2022.09.003
Siyar, S., Azarnoush, H., Rashidi, S., Winkler-Schwartz, A., Bissonnette, V., Ponnudurai, N., & Del Maestro, R. F. (2020). Machine learning distinguishes neurosurgical skill levels in a virtual reality tumor resection task. Medical and Biological Engineering and Computing, 58 (6), 1357–1367. https://doi.org/10.1007/s11517-020-02155-3
Solano, Q. P., Hayward, L., Chopra, Z., Quanstrom, K., Kendrick, D., Abbott, K. L., Kunzmann, M., Ahle, S., Schuller, M., Ötleş, E., & George, B. C. (2021). Natural Language Processing and Assessment of Resident Feedback Quality. Journal of Surgical Education, 78 (6), e72–e77. https://doi.org/10.1016/j.jsurg.2021.05.012
Stephens, G. C., Rees, C. E., & Lazarus, M. D. (2021). Exploring the impact of education on preclinical medical students’ tolerance of uncertainty: A qualitative longitudinal study. Advances in Health Sciences Education, 26 (1), 53–77. https://doi.org/10.1007/s10459-020-09971-0
Sqalli, M. T., Al-Thani, D., Elshazly, M. B., & Al-Hijji, M. (2022). A Blueprint for an AI & AR-Based Eye Tracking System to Train Cardiology Professionals Better Interpret Electrocardiograms. In N. Baghaei, J. Vassileva, R. Ali, & K. Oyibo ( Ed.), Persuasive Technology (pp. 221–229). Springer International Publishing. https://doi.org/10.1007/978-3-030-98438-0_17
Szasz, P., Louridas, M., Harris, K. A., Aggarwal, R., & Grantcharov, T. P. (2015). Assessing Technical Competence in Surgical Trainees: A Systematic Review. Annals of Surgery, 261 (6), 1046. https://doi.org/10.1097/SLA.0000000000000866
Torre, D. M., Sebastian, J. L., & Simpson, D. E. (2003). Learning Activities and High-Quality Teaching: Perceptions of Third-Year IM Clerkship Students. Academic Medicine, 78 (8), 812.
Vayena, E., & Blasimme, A. (2017). Biomedical Big Data: New Models of Control Over Access, Use and Governance. Journal of Bioethical Inquiry, 14 (4), 501–513. https://doi.org/10.1007/s11673-017-9809-6
Voss, G., Bockholt, U., Los Arcos, J. L., Müller, W., Oppelt, P., & Stähler, J. (2000). Lahystotrain. Studies in Health Technology and Informatics, 70 , 359–364. https://doi.org/10.3233/978-1-60750-914-1-359
Wang, M., Sun, Z., Jia, M., Wang, Y., Wang, H., Zhu, X., Chen, L., & Ji, H. (2022). Intelligent virtual case learning system based on real medical records and natural language processing. BMC Medical Informatics and Decision Making, 22 (1), 60. https://doi.org/10.1186/s12911-022-01797-7
Willan, P. L. T., & Humpherson, J. R. (1999). Concepts of variation and normality in morphology: Important issues at risk of neglect in modern undergraduate medical courses. Clinical Anatomy, 12 (3), 186–190. https://doi.org/10.1002/(SICI)1098-2353(1999)12:3%3c186::AID-CA7%3e3.0.CO;2-6
Wolverton, S. E., & Bosworth, M. F. (1985). A survey of resident perceptions of effective teaching behaviors. Family Medicine, 17 (3), 106–108.
CAS PubMed Google Scholar
Wood, B. P. (2000). Feedback: A Key Feature of Medical Training. Radiology, 215 (1), 17–19. https://doi.org/10.1148/radiology.215.1.r00ap5917
Article MathSciNet CAS PubMed Google Scholar
Yang, W., Hebert, D., Kim, S., & Kang, B. (2019). MCRDR Knowledge-Based 3D Dialogue Simulation in Clinical Training and Assessment. Journal of Medical Systems, 43 (7), 200. https://doi.org/10.1007/s10916-019-1262-0
Yilmaz, Y., Nunez, A. J., Ariaeinejad, A., Lee, M., Sherbino, J., & Chan, T. M. (2022). Harnessing Natural Language Processing to Support Decisions Around Workplace-Based Assessment: Machine Learning Study of Competency-Based Medical Education. JMIR Medical Education, 8 (2), e30537. https://doi.org/10.2196/30537
Yilmaz-Recai, Winkler-Schwartz, A., Mirchi, N., Reich, A., Christie, S., Tran, D. H., Ledwos, N., Fazlollahi, A. M., Santaguida, C., Sabbagh, A. J., Bajunaid, K., & Del Maestro, R. (2022). Continuous monitoring of surgical bimanual expertise using deep neural networks in virtual reality simulation. Npj Digital Medicine , 5 (1), Article 1. https://doi.org/10.1038/s41746-022-00596-8
Zahiri, M., Booton, R., Siu, K.-C., & Nelson, C. A. (2016). Design and Evaluation of a Portable Laparoscopic Training System Using Virtual Reality. Journal of Medical Devices , 11(1). https://doi.org/10.1115/1.4034881
Zhao, S., Zhang, X., Jin, F., & Hahn, J. (2021). An Auxiliary Tasks Based Framework for Automated Medical Skill Assessment with Limited Data. 2021 43rd Annual International Conference of the IEEE Engineering in Medicine Biology Society (EMBC) , 1613–1617. https://doi.org/10.1109/EMBC46164.2021.9630498
Download references
This paper is supported by National Natural Science Foundation of China (Project No. 72104087, 72004070) and University-Industry Collaborative Education Program supported by Ministry of Education in China (220505084312449).
Author information
Authors and affiliations.
School of Medicine and Health Management, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Wei Zhang & Mingxuan Cai
Department of Business Administration, The Catholic University of Korea, Seoul, Korea
Hong Joo Lee
Faulty of Computer Science, Dalhousie University, Halifax, Canada
Richard Evans
School of Political Science and Public Administration, Wuhan University, Wuhan, China
Chengyan Zhu
College of Public Administration and Law, Hunan Agricultural University, Changsha, China
Chenghan Ming
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Chengyan Zhu .
Ethics declarations
Conflict of interest, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 13 KB)
Supplementary file2 (docx 60 kb), rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Zhang, W., Cai, M., Lee, H.J. et al. AI in Medical Education: Global situation, effects and challenges. Educ Inf Technol 29 , 4611–4633 (2024). https://doi.org/10.1007/s10639-023-12009-8
Download citation
Received : 11 March 2023
Accepted : 26 June 2023
Published : 10 July 2023
Issue Date : March 2024
DOI : https://doi.org/10.1007/s10639-023-12009-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Artificial intelligence
- Applications of AIMED
- Effectiveness of AIMED
- Challenges of AIMED
- Find a journal
- Publish with us
- Track your research
Challenges in healthcare education: a correlational study of outcomes using two learning techniques
Affiliation.
- 1 Clinical Education Services, St. Luke's Regional Medical Center, Boise, Idaho 83712, USA. [email protected]
- PMID: 20354404
- DOI: 10.1097/NND.0b013e3181d4782c
Electronic learning has become an important tool in today's changing healthcare environment. Institutions confronted with limited resources, in the face of increased demands for education and a shortage of educators, have found electronically based education a significant resource. This study compares electronic-blended instruction technique with instructor-led delivery of the same content and examines the correlation of learning effectiveness to each delivery method.
Publication types
- Comparative Study
- Evaluation Study
- Academic Medical Centers
- Attitude of Health Personnel
- Clinical Competence
- Computer-Assisted Instruction / methods*
- Education, Nursing, Continuing / methods*
- Educational Measurement
- Electrocardiography / nursing*
- Northwestern United States
- Nursing Education Research
- Nursing Staff, Hospital / education*
- Nursing Staff, Hospital / psychology
- Pilot Projects
- Program Evaluation
- Self Efficacy
- Teaching / methods*
- Open access
- Published: 29 March 2024
Validation of clinical simulation scenarios for the teaching of soft skills in child-centered care
- Vivianne Izabelle de Araújo Baptista 1 , 2 ,
- Liliane Pereira Braga 1 ,
- Ádala Nayana de Sousa Mata 1 ,
- Bruno Oliveira Carreiro 1 ,
- Luiz Paulo Gomes dos Santos Rosa 1 ,
- Hécio Henrique Araújo de Morais 3 ,
- George Dantas de Azevedo 1 &
- Simone Appenzeller 2 , 4
BMC Medical Education volume 24 , Article number: 355 ( 2024 ) Cite this article
Metrics details
Consultations with children and their families are complex and require soft skills. However, there is a gap in the medical curriculum concerning these skills, especially as encounter training is often adult-centered. We developed, validated, and applied simulation scenarios that prioritize active participation of children to train soft skills in child-centered care for undergraduate medical students. This is a methodological study to develop three scenarios and a checklist of what is expected. The content was validated by 18 experts. A pre-test was carried out for adjustments. Then, the simulations were applied and evaluated by 18 medical undergraduate students. They included the participation of 6 pediatric simulated patients aged 9–12 years trained by a drama teacher. According to the results, the scenarios and checklist proved to be valid instruments in content terms (ICV-I > 0.8). The scripts were followed by the simulated pediatric patients, but they had difficulty mimicking a hypoactive state. Some were anxious, but everyone enjoyed participating in the feedback. The simulated parents had difficulty participating and giving space to the child's speech. Participants assessed that the simulations performed as they were proposed and, after experimenting them, felt more prepared. The simulations provided an opportunity for students to practice soft skills by interacting with children in a safe environment. Using children as simulated patients is feasible but presents some challenges. Our study has expanded the ways in which children's health content can be taught. We are investigating whether this training leads to better patient outcomes in real clinical settings.
Peer Review reports
Children are often marginalized in appointments or excluded from decisions involving their own health. Especially, because they are vulnerable, and the appointments involve the complex triadic relationship patients-parents-physician [ 1 ]. However, active participation of children is associated with significant improvements in understanding the health-disease process, adherence to treatment, and emotional health [ 2 ]. To medical care effectively, soft skills are essential. In particular, communication, interpersonal skills, rapport and resilience [ 3 ].
The national guidelines to medical training emphatically guide a person-centered medical practice [ 4 ]. However, interactions with children are often observational [ 5 ], while soft skills training is aimed at parents and caregivers [ 6 , 7 , 8 ]. This standard differs from the recommended one regarding the autonomy, dignity, and safety of children [ 9 ]. In addition, students' first experiences with pediatric patients occur without them being adequately prepared. Therefore, there is a gap to be bridged in medical education [ 10 ].
Clinical simulation is a method that allows the creation of credible scenarios for care in a safe environment [ 11 , 12 ]. In this environment, it is possible to insert pediatric simulated patients, which consist of children trained to consistently portray health conditions [ 13 ]. But soft skills scenarios in pediatrics often use adults as simulated patients [ 6 , 8 , 14 , 15 , 16 , 17 ]. This is due to many ethical issues involved regarding the risk of maleficence, as well as the challenging logistics for the development of strategies that ensure children are supported and receive adequate training [ 18 ].
Physicians also need to develop soft skills to provide care that is focused on the child as part of a family context and to ensure the child's right to be a protagonist in his or her health care [ 19 ]. In this context, this study developed, validated, and applied clinical simulation scenarios that promoted the active participation of children. The goal of the study was to teach soft skills in child-centered care to undergraduate medical students. Recommendations for improving simulation scenarios involving simulated pediatric patients were also presented.
This is a methodological study to develop three scenarios and a checklist. It was carried out between 18th of July and 10th of November, 2022, during the application of the Child’s Health Module of the Multicampi School of Medical Sciences (EMCM) of the Federal University of Rio Grande do Norte – UFRN, Caicó – Brazil. This module is offered to third-year medical undergraduate students and aims to develop skills to perform clinical examination, diagnosis, and therapeutic management in pediatrics.
Study protocol
Construction of simulation scenarios and evaluator’s checklist.
A directed search was conducted with the aim to find materials. Search terms used were: Pediatric medical education AND soft skills OR communication OR interpersonal skills AND simulated patient OR patient simulation AND child OR children. The databases used were Medline/PubMed and Scielo. Books, regulations, articles in English and Portuguese, guides and checklists were considered. But we had trouble finding articles on the subject. So, we did a manual search, contacting some authors for materials.
Based on book chapters [ 20 , 21 ], EMCM medical course regulations [ 22 ] and national guidelines for medical training [ 4 ] a preliminary version of the scenarios and checklist was structured. This version was improved based on the Calgary-Cambridge Guide validated in Brazil [ 23 ] and with support of a multidisciplinary group composed by 2 physicians with trained in family medicine, 2 psychologists with expertise in health communication and 1 nurse with trained in clinical simulation. They were all professors at EMCM.
The textual elaboration of the scenario followed a pre-established theoretical-practical model from Fabri et al. [ 24 ]. The group discussed aspects of soft skills in child-centered care from different professional perspectives. In addition, the psychologists acted to minimize possible harm to the participating children. The same group also participated in the pre-testing phase described below.
Validation by judges
The committee was composed of 18 judges, 6 for each scenario. The selection of judges was by convenience. Then, the snowball sampling technique was used, so the professionals who received the instrument acted as key informants, providing the electronic address of three other professionals and so on.
Health professionals with experience in child health, health communication and/or clinical simulation were selected. The criteria for selection of judges were adapted from those proposed by Fehring [ 25 ]: master’s degree = 4; master’s degree in one of the cited areas = 1; articles published on the topics = 2; PhD in one of the study areas = 1; clinical experience = 2; teaching experience = 2. A minimum score of 5 points was used.
The judges received a letter of invitation via email, the constructed materials and the validity form via Google Forms®. Each scenario was evaluated regarding comprehensiveness and then item by item concerning clarity and representativeness of the psychometry. For this purpose, a 4-point Likert-type scale was used, as follows: 1 – item not clear or not representative; 2 – item unclear or requiring major revision to be representative; 3 – item quite clear or requiring minor revision to be representative; and 4 – item very clear or representative. There were also spaces throughout the instrument for suggestions and criticism.
To systematize the opinion of experts, the Delphi method was used [ 26 ].
Nine students from the EMCM/UFRN medicine course participated, selected by purposive sampling. They were regularly enrolled in the course and had already completed the child’s health module. Scenarios were tested and then a session of brainstorm was carried out for semantic evaluation, achievement of objectives, and factors that facilitated or prevented implementation.
The multidisciplinary group of teachers also participated. They made a qualitative analysis of the checklist.
Application and validation by medical undergraduate students
Eighteen third-year medical students from the EMCM/UFRN who were taking the child health module participated. Exclusion criteria were having already taken the child health module; having already taken more advanced modules of the course; having less than 75% participation in the activities offered; refusal to sign the informed consent form.
They were selected by random sampling. They were then divided into two smaller groups ( n = 9, each) to experience the simulations. The three scenarios were developed for three consecutive weeks and were applied twice on each application day. Each time, a different student volunteered to realize the appointment, while the others watched the performance in the auditorium via live transmission.
The simulations were designed to last 1 h, intended for: 15 min – briefing; 15 min – scenario; and 30 min—debriefing. The purpose and general objective of the scenarios, the type of simulation, and the sequence of steps until the debriefing were informed in the briefing. Additionally, a fictional contract was established for students to suspend disbelief and acknowledge the scenario.
After simulations, the students anonymously evaluated the experience using a 10-question questionnaire. A Likert-type scale was used, with classification ranging from 1 to 5 in the order of the following concepts: 1 – Totally disagree; 2 – Partially disagree; 3 – Neither agree nor disagree (indifferent); 4 – Partially agree; 5 – Totally agree.
Three professors participated: a psychologist, a physician, and a nurse with training in clinical simulation who led the simulations. There were also the participation of a laboratory technician and a cameraman. The professors received guidance on the objectives and skills to be worked on scenarios, the use of the evaluation instrument, and the debriefing in PEARLS model [ 27 ]. They watched the simulations in the control room, which had one-way mirrored glass.
Furthermore, all students involved in the research received study materials, which contained book chapters [ 20 , 21 ] and videos with examples of communication with children and their families [ 28 , 29 ]. Then they had expository-dialogued classes on bioethics and pediatrics and soft skills in child-centered care according to development stages.
Six children aged 9–12 years old, who had been previously trained, participated as pediatric simulated patients in both the pre-test and the application. Of these, 2 were boys, 4 were girls, 1 was black and the rest were white. They all belonged to the upper middle class. Each child acted in a single scenario. In turn, two mothers and one father took turns in the roles of simulated parents. All of them were trained by a drama teacher. Simulation facilitator also participated in the training.
Data analysis
The content validity Index (CVI) was calculated using two mathematical equations: I-CVI (item-level content validity index) and S-CVI/Ave (scale-level content validity index). The I-CVI was used to evaluate the agreement of each item evaluated. It was calculated by adding the number of “3” and “4” responses from the judges or “4” and “5” from the target audience divided by the sum of the total number of responses. The S-CVI/Ave was used to evaluate the mean of the I-CVIs in each domain. It was calculated by summing the I-CVI of all items, dividing by the total number of items evaluated per domain. The I-CVI ≥ 0.8 and S-CVI / ≥ 0.9 were considered desirable for validation [ 30 ]. When necessary, the Modified Kappa Coefficient (MKC) was also calculated to assess the possibility of random agreement. An MKC ≥ 0.74 was considered desirable [ 31 ].
Each scenario was composed by four domains: 1 – Context and Previous Components; 2 – Scenario Preparation; 3 – Design; and 4 – Final Components. Domains 1, 2, and 4 were identical to three scenarios, while domain 3 addressed the simulated case and specific scripts of each scenario.
The purpose of the scenarios was to teach. Therefore, they were structured with common clinical situations in pediatrics: sore throat and fever, vomiting, and asthma attacks. In addition, the scenarios were organized in increasing levels of complexity and required the performance of different actions to solve the problems (Table 1 ). The simulations were of the scenic type, set in a medical office for pediatrics, with simulated pediatric patients accompanied by their simulated parents.
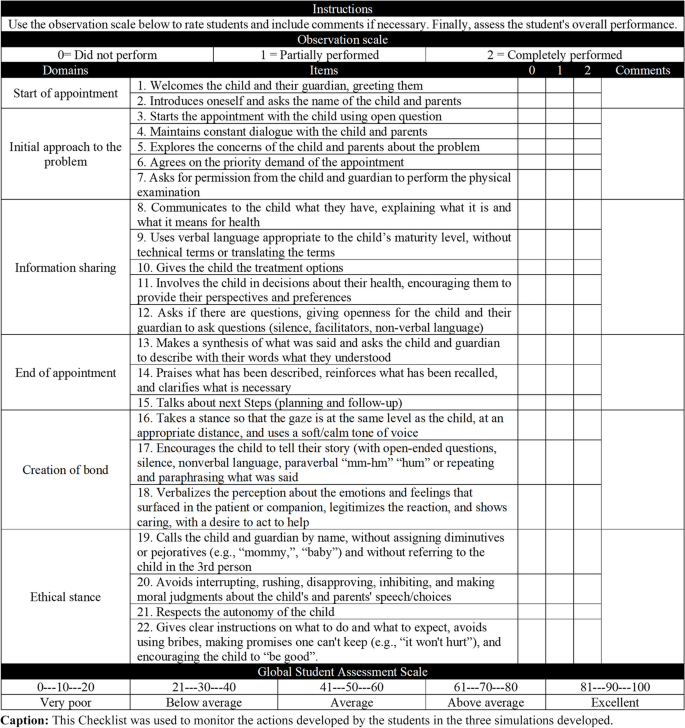
In order to monitor the actions developed by the students, a checklist with 22 items divided into six domains was created (Fig. 1 ). Professors could record whether the candidate "did not perform (0 points), partially performed (1 point), and completely performed (2 points)" the actions, with spaces for comments on each item. There was also a global student rating scale at the end of the checklist.
Checklist after content validation and pre-test
Judges from thirteen different higher education institutions served on the panel. They were predominantly women (16; 89%) and had a mean age of 47 (± 6.8) years old. All of them had at least 10 years of training, teaching experience, and scientific publications in the areas of study. Most had degrees in medicine (8; 44%) and nursing (7; 39%); PhD (16; 89%); theses in the areas of health communication and/or child health and/or clinical simulation (10; 56%); care experience in the areas involved (17; 94%); had as their main activity research, teaching, and extension (16; 89%); and had already given training involving the themes mentioned (17; 94%).
Consensus was reached in the first round of evaluation. Respondents unanimously agreed on the scope of the four domains that make up each scenario (I-CVI = 1.00). It was considered the judgment of the 18 judges for the evaluation of the items identical of the three scenarios (domains 1, 2 and 4) and of the 6 judges for the specific items (domain 3). The I-CVI concerning clarity and representativeness of the items identical to the scenarios exceeded ≥ 0.8 and the CVI/Ave of each domain exceeded ≥ 0.9 (Table 2 ). In specific items, since there were 6 evaluators, in addition to the CVI, the MKC was also calculated to assess the possibility of random agreement. The respondents were also unanimous (I-CVI and CVI/Ave = 1.00; MKC = 1.00).
The judges made suggestions involving elements of writing, structure, and organization of the materials which were accepted. Some comments also raised concerns about the performance of children as simulated pediatric patients, especially regarding their ability to memorize the lines of the scripts. Furthermore, they pointed out the presence of parents in the scenarios could be a distraction since doctors tend to only communicate with them.
So, general guidelines were inserted with the reasons for simulated pediatric patients and simulated parents speaking or not the information. In the scripts, possible dialogues and their outcomes were inserted, facilitating the orientation of the children. It was explained to the simulated parents that the simulation should prioritize the active participation of the children. Therefore, they should only answer questions directed to them and help the children if they forgot something or asked for help. If for any reason a child felt uncomfortable participating in the simulation, they could ask to go to the restroom and leave the scene (Additional file 1 ).
Furthermore, the training was structured in a more playful and longer format, with weekly meetings for 2 months. Additional sessions could be scheduled according to the children's needs. The children needed to feel safe and comfortable with the scenarios, the simulation facilitator, and the simulated parents.
All participants considered the scenarios relevant, well written, capable of achieving the proposed objectives and with adequate time available. Regarding the performance of the simulated patients, it was suggested that the simulated parents should talk and gesture more to denote concern. It was also suggested that the simulated pediatric patients should perform more realistically when using the spray medication during scenario 3 (Additional file 1 ). Thus, these aspects were reinforced to parents during training, as well as a seal was developed for the spray applicator to prevent children from coming into contact with the medicine when simulating its use.
The evaluators suggested modifying the order of the domains of the checklist (Fig. 1 ) from “beginning of the appointment, initial approach to the problem, creation of bond, information sharing, ethical stance, and end of the consultation” to “initial approach to the problem, information sharing, end of the consultation, creation of bond, and ethical stance” in order to facilitate filling. In the ethical stance section, they advised modifying the item “respects the autonomy of the child, but recognizes that the parents are responsible for the final decisions of the treatment and involvement of the child” to “respects the autonomy of the child,” since the first option suggests a treatment without partnership.
All child actors participated in the pre-test to experience the simulation process. Some were apprehensive but were reassured by the psychologists and none refused to participate. During the feedback, the children were happy to be involved in medical consultations and to be able to express their preferences.
The development of the three scenarios occurred according to the scripts, except in Scenario 2. This scenario did not present the expected challenge (Table 1 ), because the simulated pediatric patients did not present in accordance with the described condition (Additional file 1 ). They showed a regular general condition that was not consistent with a general state of hypoactivity described in the physical examination. Therefore, the lines associated with the distractor were removed from the script, as well as the information characterizing this condition. The scenario was rerun, and the expected result was verified.
Each of the three scenarios was applied twice and each child acted in a single scenario. In this way, the six actors alternated their participation, so as not to overload each other. The simulated sessions included the direct observation and debriefing. The debriefings sessions were used to discuss positive points and opportunities for improvement. The checklist was used to monitor the actions performed and to work on the students’ self-assessment. The facilitator observed and guided the students' speech, inviting experts and simulated patients to give feedback.
The students evaluated the simulated experiences (Table 3 ). In all items there was total or partial agreement with the statements, obtaining values ≥ 0.94 (I-CVI) and ≥ 0.98 (S-CVI/Ave). All students (18; 100%) agreed that the simulation was in line with the proposed topic, that a safe and respectful environment was created, that the didactic resources used were appropriate, and that the objectives and goals were explained. They also considered the feedback they received to be positive and stated that they felt more prepared for professional practice after participating in the sessions. Lower proportions of students fully agreed that prior knowledge from previous modules helped them understand the scenarios (11; 61%), felt motivated to participate in the sessions (10; 55.5%), and indicated that the theoretical framework was sufficient to support the solution of the scenarios (9; 50%).
Physicians’ lack of soft skills for child-centered care is a global challenge [ 32 ]. About that, the quality of child health care is compromised [ 33 ]. We developed, validated, and applied three scenarios adapted to the active participation of the child. The results showed that our scenarios and checklist are valid tools in terms of content. The simulated pediatric patients acted according to the scripts but had difficulty simulating a hypoactive state. Some were anxious and all enjoyed participating in the feedback. The simulated parents had difficulty participating and giving space to the child's speech. Participants felt that the simulations accomplished what they had proposed, and that they felt more prepared after experiencing them.
Similar scenarios were found in the studies by Frost et al. [ 6 ] and Kindratt et al. [ 8 ]. However, they focused on parent-centered care. As noted by Wissow et al. [ 34 ] and according to the judges who validated the scenarios, physicians tend to show a higher degree of centrality on parents during triadic consultation. Therefore, it is important to have clinical simulation scenarios to teach soft skills in child-centered care to physicians. They need to be validated to verify that they are achieving their intended goals [ 35 ] and that there are no elements that could compromise their effectiveness [ 36 ].
Content validation followed the previous recommendation of the minimum number of judges [ 37 ] and widely used measures were applied to verify agreement [ 31 ]. However, our sample was very specialized, with few non-experts, who are also important for evaluating the form, overall impression and categorization of the degree of difficulty [ 38 ]. A limiting point was the difficulty of receiving responses in a timely manner.
Judges were also concerned about the use of children as simulated pediatric patients. However, it should be noted that learning soft skills requires the participation of the "other" and cannot be taught using pediatric mannequins [ 39 ]. Furthermore, practice with real patients is not recommended, as it disregards patient safety and can cause harmful effects [ 5 ]. Therefore, there are important ethical considerations that must be followed. The age of the child (older children have greater autonomy), the role they will play, the duration of the activity, the opportunity for feedback, and a team committed to defending the rights of the child are some of them. Family involvement is essential. Educators must also be sensitive to the child's objection and consent [ 10 , 13 , 18 ].
In the pre-test stage and application stages adjustments were made to actors’ scripts. So, one can note that validation goes beyond the mere evaluation of an instrument and is materialized in practice, with the dynamic interaction of the participants [ 40 ]. Moreover, the child actors showed difficulty in maintaining, throughout the scenario 2, a general state of hypoactivity. This aspect had already been pointed out by Khoo et al. [ 18 ] and may suggest that children have difficulty staging more specific behaviors. So, it is recommended to work on milder health conditions, as we did, or to include elements in the scenarios that reinforce the seriousness of the situation. For example, placing the child lying on a stretcher, using moulage to simulate some signal, and reinforcing the parents to be more stressed.
Working with simulated pediatric patients presents some potential challenges. The lines in the scripts must be planned, unlike adult simulations, which only require a story line. The simulated parents need to be well oriented so as not to replace the child's speech, but not so rigid that they fail to convey the realism of the situation being experienced. Children need to be familiar with the health conditions covered, as they may feel anxious. A good relationship between the child, the simulated parent and the simulation facilitator is also crucial. Hence the importance of lengthy training and the presence of psychologists on the team.
Our study considered all ethical norms and guidelines recommended for the use of children as simulated patients. The terms of consent and assent were signed; children were over 8 years old; simulations were short; the roles involved everyday situations, which most of them had already experienced; actors were rotated at each simulated session; children could leave the scene if they felt uncomfortable and provide feedback during debriefing.
In addition, among the evaluators there was a psychologist to intervene in possible damage, and all were aligned with the scenario proposal and trained for the debriefing. The debriefing is the most important part of the simulation. It is the basis for fixing and correcting behaviors. It occurs immediately after the simulated experience and is conducted by the students themselves, who analyze the situation and critically reflect on the performance, while the facilitator observes and directs the actions [ 41 ].
All students partially or fully agree that the feedback they received after the simulations was positive. They also felt prepared for their professional practice after the experience. This suggests a positive evaluation. Lower proportions of totally agree were obtained about the motivation to participate in the simulations (10; 55.5%) and the theoretical framework being sufficient to support the solution of the scenarios (9; 50%). This can be explained by the fact that our simulations were not focused on highly valued technical skills (hard skills), but on the soft skills that students tend to consider less important [ 3 ]. It is noteworthy that the students were at an intermediate level and clinical management of issues was discussed throughout the child’s health module.
It is important to emphasize what may limit the applicability of the research results. Only 6 pediatric patients with similar characteristics participated in the study. The lack of availability of mothers/fathers to participate in the scenarios. The need for teachers with differentiated knowledge and more time to train the children. Regarding the validation process, we did not conduct a new round of validation after incorporating the judges' suggestions.
Our scenarios and checklist provided an opportunity for medical students to practice soft skills by interacting with children in a safe environment. Using children as simulated patients was feasible, but not without challenges. We recommend working with lighter health situations, including dialogues and possible outcomes in the scripts, allowing more training time and involving the simulation facilitator, familiarizing the child with the simulation process, including psychologists in the team, and valuing the child's feedback in the debriefing.
Despite this, there is a gap in medical education that needs to be discussed. Our study has expanded the ways in which children's health content can be taught in medical curricula. We are now investigating whether this training translates into better patient outcomes in real clinical settings. This research could strengthen the overall robustness and applicability of the study's conclusions.
Availability of data and materials
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
Coyne I. Children’s participation in consultations and decision-making at health service level: A review of the literature. Int J Nurs Stud. 2008;45:1682–9.
Article Google Scholar
Carlsson IM, Arvidsson S, Svedberg P, Nygren JM, Viklund Å, Birkeland AL, et al. Creating a communication space in the healthcare context: Children’s perspective of using the eHealth service. Sisom Journal of Child Health Care. 2021;25:31–43.
Iorio S, Cilione M, Martini M, Tofani M, Gazzaniga V. Soft Skills Are Hard Skills—A Historical Perspective. Medicina (Lithuania). 2022;58(8):1044.
Google Scholar
Ministério da Educação (BR). Conselho Nacional de Educação. Curso de Educação Superior. (2014) Resolução CNE/CES no 3, de 20 de junho de 2014. [accessed 2023 May 1] http://portal.mec.gov.br/index.php?option=com_docman&view=download&alias=15874-rces003-14&category_slug=junho-2014-pdf&Itemid=30192
Sullivan C, Condron C, Mulhall C, Almulla M, Kelly M, O’Leary D, et al. Preparing for Pediatrics: Experiential Learning Helps Medical Students Prepare for Their Clinical Placement. Front Pediatr. 2022;10:834825.
Frost KA, Metcalf EP, Brooks R, Kinnersley P, Greenwood SR, Powell CVE. Teaching pediatric communication skills to medical students. Adv Med Educ Pract. 2015;6:35–43.
Harahsheh AS, Ottolini M, Lewis K, Blatt B, Mitchell S, Greenberg L. An Innovative Pilot Curriculum Training Pediatric Residents in Referral and Communication Skills on a Cardiology Rotation. Acad Pediatr. 2016;16(7):700–2. https://doi.org/10.1016/j.acap.2016.05.146 .
Kindratt T, Bernard B, Webb J, Pagels P. Parent-provider paediatric literacy communication: A curriculum for future primary care providers. Perspect Med Educ. 2019;8:110–7.
United Nations Children's Fund. 1989. Convention on the Rights of the Child text | UNICEF. [cited 1 May 2023]. Available: https://www.unicef.org/child-rights-convention/convention-text
Gamble A, Bearman M, Nestel D. A systematic review: Children & Adolescents as simulated patients in health professional education. Adv Simul. 2016;1:1. https://doi.org/10.1186/s41077-015-0003-9.1 .
de Oliveira Costa RR, de Medeiros SM, Martins JCA, Coutinho VRD. Simulation in training nurses: Reflections and justifications based on bioethics and human rights approaches. Acta Bioeth. 2018;24:31–8.
So HY, Chen PP, Kwok G, Wong C, Tung T, Chan N. Simulation in medical education. J R Coll Physicians Edinb. 2019;49:52–7.
Tsai TC. Using children as standardised patients for assessing clinical competence in paediatrics. Arch Dis Child. 2004;89:1117–20.
Nikendei C, Bosse HM, Hoffmann K, Möltner A, Hancke R, Conrad C, et al. Outcome of parent-physician communication skills training for pediatric residents. Patient Educ Couns. 2011;82:94–9.
Woods JL, Pasold TL, Boateng BA, Hensel DJ. Adolescent health care and the trainee: Roles of self-efficacy, standardized patients, and an adolescent medicine rotation. Simulation in Healthcare. 2013;8:359–67.
Woods JL, Pasold TL, Boateng BA, Hense DJ. Medical student self-efficacy, knowledge and communication in adolescent medicine. Int J Med Educ. 2014;5:165–72.
Teles MG, Mendes-Castillo AMC, Souza Oliveira-Kumakura AR, Silva JLG. Clinical simulation in teaching Pediatric Nursing: students’ perception. Rev Bras Enferm. 2020;73:e20180720.
Khoo EJ, Schremmer RD, Diekema DS, Lantos JD. Ethics rounds: Ethical concerns when minors act as standardised patients. Pediatrics. 2017;139:e20162795.
Ford K, Campbell S, Carter B, Earwaker L. The concept of child-centered care in healthcare: a scoping review protocol. JBI Database System Rev Implement Rep. 2018;16(4):845–51. https://doi.org/10.11124/JBISRIR-2017-003464 .
Alves R, Grosseman S. Aspectos éticos em pediatria: a consulta, o prontuário e as mídias sociais. In: Leone C, Cabral SA, editors. PROPED Programa de Atualização em Terapêutica Pediátrica. Brasil: Artmed; 2020. p. 51–84.
Grosseman S, Alves R, Funk TB. Comunicação com crianças e suas famílias antes da adolescência. In: Dohms M, Gusso G, editors. Comunicação Clínica: aperfeiçoando os encontros em saúde. 1st ed. Brasil: Artmed; 2021. p. 151–67.
Universidade Federal do Rio Grande do Norte. Projeto Pedagógico do Curso de Medicina CERES-FACISA/UFRN. 2014 p. 101. [cited 1 May 2023] Available: https://arquivos.info.ufrn.br/arquivos/20130470880f521533387821e2acdd64a/Projeto_Pedaggico_-_Medicina_-_CERES_-_FACISA.pdf .
Dohms MC, Collares CF, Tiberio IC. Brazilian version of calgary-cambridge observation guide 28-item version: Cross-cultural adaptation and psychometric properties. Clinics. 2021;76:e1706.
Fabri RP, Mazzo A, Martins JCA, da Silva Fonseca A, Pedersoli CE, Miranda FBG, et al. Development of a theoretical-practical script for clinical simulation. Revista da Escola de Enfermagem. 2017;51:e03218.
Fehring RJ. Methods to validate nursing diagnoses. Heart Lung. 1987;16(6 Pt 1):625–9.
Dalkey N. An experimental study of group opinion: The Delphi method. Futures. 1969;1:408–26.
Eppich W, Cheng A. Promoting excellence and reflective learning in simulation (PEARLS): Development and rationale for a blended approach to health care simulation debriefing. Simulation in Healthcare. 2015;10:106–15.
University of Nottingham. 2013, November 14a. (310) Clinical communication skills - communication with child patients version 1 - YouTube. [cited 1 May 2023]. Available: https://www.youtube.com/watch?v=BZfOYvPmcjo
University of Nottingham. 2013, November 14b. (310) Clinical communication skills - communication with child patients version 2 - YouTube. [cited 1 May 2023]. Available: https://www.youtube.com/watch?v=I7QiPXqL9pY
Polit DF, Beck CT. The content validity index: Are you sure you know what’s being reported? Critique and recommendations Res Nurs Health. 2006;29:489–97.
Polit DF, Beck CT, Owen SV. Focus on research methods: Is the CVI an acceptable indicator of content validity? Appraisal and recommendations Res Nurs Health. 2007;30:459–67.
Quaye AA, Castor C, Coyne I, Söderbäck M, Hallström IK. How are children’s best interests expressed during their hospital visit?-An observational study. J Clin Nurs. 2021;30(23–24):3644–56. https://doi.org/10.1111/jocn.15886 .
Mǎrginean CO, Meliţ LE, Chinceşan M, Mureşan S, Georgescu AM, Suciu N, et al. Communication skills in pediatrics - The relationship between pediatrician and child. Medicine (United States). 2017;96:e8399.
Wissow L, Gadomski A, Roter D, Larson S, Lewis B, Brown J. Aspects of mental health communication skills training that predict parent and child outcomes in pediatric primary care. Patient Educ Couns. 2011;82:226–32.
de Almeida AO, Dantas SRPE, de Paula MAB, Silva JLG, Franck EM, de Souza Oliveira-Kumakura AR. Development, validation and application of clinical simulation scenarios for assessment of stomatherapy specialists. Rev Bras Enferm. 2021;74:e20200360.
de Carvalho LR, Zem-Mascarenhas SH. Construction and validation of a sepsis simulation scenario: a methodological study*. Revista da Escola de Enfermagem. 2020;54:1–9.
Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35(6):382–5.
Franco RS, Franco CAGS. Avaliação com o uso de Checklists e Escalas de Avaliação Global. In: Pereira Júnior GA, Guedes HTV, editores. Simulação em saúde para ensino e avaliação. 1th ed. Brasil: editora cubo; 2021.p. 205–220. https://doi.org/10.4322/978-65-86819-11-3 .
Bhatti A, Ahmed M. How should pediatric communication skills be taught? The medical student perspective. Adv Med Educ Pract. 2017;8:167–8.
de Oliveira Nascimento Andrade P, de Oliveira SC, Morais SCRV, Guedes TG, de Melo GP, Linhares FMP. Validation of a clinical simulation setting in the management of postpartum haemorrhage. Rev Bras Enferm. 2019;72:624–31.
Franco RS, Franco CAGS. O uso do feedback e debriefing na simulação. In: Pereira Júnior GA, Guedes HTV, editores. Simulação em saúde para ensino e avaliação. 1th ed. Brasil: editora cubo; 2021.p. 205–220. https://doi.org/10.4322/978-65-86819-11-3 .
Download references
Acknowledgements
We would like to thank all participants for their availability and collaboration. We would also like to thank too Espaço da Escrita – Pró-Reitoria de Pesquisa – UNICAMP – for the language services provided.
This work was partly financed by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001 and Conselho Nacional de Desenvolvimento Científico e Tecnológico- Brasil CNPq (305981/2023-4).
Author information
Authors and affiliations.
Multicampi School of Medical Sciences of Rio Grande Do Norte, Federal University of Rio Grande Do Norte, Rio Grande Do Norte, Caicó, Brazil
Vivianne Izabelle de Araújo Baptista, Liliane Pereira Braga, Ádala Nayana de Sousa Mata, Bruno Oliveira Carreiro, Luiz Paulo Gomes dos Santos Rosa & George Dantas de Azevedo
Graduate Program in Child and Adolescent Health, School of Medical Sciences, University of Campinas, Campinas, São Paulo, Brazil
Vivianne Izabelle de Araújo Baptista & Simone Appenzeller
State University of Rio Grande Do Norte, Rio Grande Do Norte, Caicó, Brazil
Hécio Henrique Araújo de Morais
Department of Orthopedics, Rheumatology and Traumatology, School of Medical Sciences, University of Campinas, Campinas, São Paulo, Brazil
Simone Appenzeller
You can also search for this author in PubMed Google Scholar
Contributions
VIAB: Conceptualization (lead), Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft preparation, Writing review & editing. LPB: Conceptualization (supporting), Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. ANSM: Formal analysis, Methodology, Validation, Writing – review & editing. BOC: Investigation. LPGSR: Investigation. HHAM: Investigation. GDA: Conceptualization (supporting), Methodology. SA: Conceptualization (supporting), Methodology, Project Administration, Writing – review & editing.
Corresponding author
Correspondence to Vivianne Izabelle de Araújo Baptista .
Ethics declarations
Ethics approval and consent to participate.
The research was reviewed and approved by the Ethic Committee of the Federal University of Rio Grande do Norte, UFRN, under the opinion number 5.411.233, 16/05/2022, CAAE: 48272921.3.0000.5568. Written informed consent was obtained from all participants before the search. About children, parents provided written informed consent and children provided assent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
de Araújo Baptista, V.I., Braga, L.P., de Sousa Mata, Á.N. et al. Validation of clinical simulation scenarios for the teaching of soft skills in child-centered care. BMC Med Educ 24 , 355 (2024). https://doi.org/10.1186/s12909-024-05284-7
Download citation
Received : 17 November 2023
Accepted : 11 March 2024
Published : 29 March 2024
DOI : https://doi.org/10.1186/s12909-024-05284-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Validation study
- Simulation training
- Clinical competence
- Child health
- Undergraduate
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Student hackers forge health care solutions at 1819 Innovation Hub
Revuc hackathon inspires students to think about transformative technologies.

The University of Cincinnati's 1819 Innovation Hub hosted the 13th annual RevolutionUC Hackathon.
Three standout teams emerged victorious, showcasing groundbreaking solutions to pressing challenges, including health care. The event was a testament to the power of innovation and compassion.
As one of Ohio's oldest and largest student-run hackathons, RevolutionUC is organized by the Association for Computing Machinery at UC and supported by the UC Center for Entrepreneurship . It is open to all college and high school students across the region, regardless of major or programming background.
Student hackathons are fertile grounds for innovation, fostering collaboration, creativity and problem-solving skills among aspiring entrepreneurs and technologists.
RevUC offers UC students of all majors and technical backgrounds the opportunity to experiment and test their innovative ideas in a fun and supportive environment while also taking advantage of the mentorship from leading industry partners who were on-site exposing students to the latest technology that corporate America offers.
Kate Harmon Assistant vice president of the 1819 Innovation Hub, executive director of the UC Center for Entrepreneurship
"RevUC offers UC students of all majors and technical backgrounds the opportunity to experiment and test their innovative ideas in a fun and supportive environment while also taking advantage of the mentorship from leading industry partners who were on-site exposing students to the latest technology that corporate America offers," said Kate Harmon, assistant vice president in the 1819 Innovation Hub and executive director of the UC Center for Entrepreneurship.
Judges scored projects based on creativity, technical depth, challenge of the work and usefulness in the real world.
The following three student teams captivated RevolutionUC judges and spectators alike with their transformative projects aimed at revolutionizing medical care:
- CHAAP: A Chrome extension that can communicate with any webpage
- PhizzIO: Empowers patients through interactive physiotherapy
- Memento Assistant: Pioneering solution for patients with cognitive decline
With analytical thinking and problem-solving among the most in-demand job skills today, hackathons give students a jumpstart into their future success. Participants are encouraged to push the boundaries of traditional thinking, igniting a spirit of ingenuity that can yield transformative solutions.
Hackathons are a crash course in solving problems quickly. Nowhere is this potential more evident than in health care.
With their pioneering solutions, the following student innovations pave the way for a brighter, more inclusive future. Each team harnessed their diverse perspectives and collaborative talents to maximize the use of artificial intelligence to improve the lives of others.
Team CHAAP: Jack McKain, Bek Dukenbaev, Arnav Chandra Komaragiri and Andrew Gerstenslager. Photo/RevUC
CHAAP co-founders: Jack McKain, Bek Dukenbaev, Arnav Chandra Komaragiri and Andrew Gerstenslager
- Winner: First place overall
- Winner: Best use of AWS
- Winner: Best data science and analytics hack (fortified data)
Rooted in a profound understanding of data constraints, Chat With Any Anonymous Page (CHAAP) seamlessly interacts with any webpage and employs sophisticated reasoning capabilities. Motivated by a dedication to maintaining stringent privacy standards while optimizing functionality, the solution was conceived and executed as a Chrome extension with an innovative and proprietary HEMLock algorithm to safeguard user data and privacy.
The hallmark of CHAAP lies in its versatility, facilitating conversations with countless language model systems, from AWS to OLLaMA to GPT, transcending the boundaries of conventional chatbot functionalities.
Team CHAAP integrates diverse technologies, leveraging frameworks like Tembo for RAG, AWS for LLM inference and HuggingFace alongside Presidio for robust anonymization.
Looking ahead, Team CHAAP envisions a future brimming with possibilities. It plans to integrate image capabilities, fortify anonymization measures and explore the potential of a decentralized protocol for language model routing.
Team PhizzIO: Joe Kuncheria Panjikaran and Aniruddhan Ramesh. Photo/RevUC
PhizzIO co-founders: Joe Kuncheria Panjikaran and Aniruddhan Ramesh
- Winner: Second place overall
- Winner: Parkinson's Together Synapse Sprint
For Team PhizzIO, the catalyst for bridging the communication gap between patients and physiotherapists arose from Panjikaran's struggle with recovery after tearing his ACL. The solution was to create an interactive platform that guides, monitors and motivates patients throughout their rehabilitation journey.
PhizzIO honed their expertise for their startup as cohorts of the UC Venture Lab program located inside the 1819 Innovation Hub. Their innovative patient analytics dashboard features an advanced "proper body form" guide to accurately screen and track patients' movements, delivering real-time feedback aligned with personalized treatment goals. The technology empowers individuals to confidently adhere to and perform exercises, eliminating barriers such as wait times and geographical constraints.
PhizzIO remains committed to enhancing the quality of care for patients undergoing rehabilitation. It plans to integrate AI chatbots and expand its dataset of physiotherapy exercises in the future.
Memento Assistant
Team Memento Assistant: Grant E. Kilgard, Raihan Rafeek, Kaaustaaub Shankar and Arya Garg. Photo/RevUC
Memento Assistant co-founders: Grant E. Kilgard, Raihan Rafeek, Kaaustaaub Shankar and Arya Garg
- Winner: Third place overall
- Winner: Best social impact hack
- Winner: Best digital solution to improve the clinical trial process (Medpace)
- Winner: Best use of Postgres (Tembo)
The journey toward victory was deeply personal for Team Memento. Inspired by Kilgard's familial experience with Alzheimer's disease, the team embarked on a mission to address the unmet needs of patients and caregivers. Their brainchild, Memento, is an app-based integration for patients and caregivers designed to serve as a digital journal for individuals grappling with degenerative cognitive diseases.
Memento's intuitive interface and AI-powered assistant seamlessly integrate journal entries, images, audio recordings and geographic locations, creating a comprehensive repository of memories. This innovative platform fosters patient independence and structure and facilitates communication between caregivers and health care providers. Leveraging AI algorithms, Memento delivers personalized responses and insights, enriching the lives of those affected by Alzheimer's.
Looking ahead, the team envisions expanding Memento's capabilities, integrating support for additional data types and sensory stimuli. With aspirations to create an iOS version and enhance collaboration with health care providers, Team Memento remains at the forefront of innovation in Alzheimer's care.
The accomplishments of CHAAP, PhizzIO and Memento at the RevUC Hackathon stand as a testament to the transformative potential of technology in health care and beyond.
Featured image at top: UC hosted the 13th annual RevolutionUC Hackathon. Photo/provided

Next Lives Here
The University of Cincinnati is leading public urban universities into a new era of innovation and impact. Our faculty, staff and students are saving lives, changing outcomes and bending the future in our city's direction. Next Lives Here.
- Center for Entrepreneurship & Commercialization
- Office of Innovation
- 1819 Innovation Hub
- Innovation Agenda
- Cincinnati Innovation District
Related Stories
Uc venture lab next summer program paves way for student startup success.
March 21, 2024
Young founders with an idea or technology they want to develop into a business while still in school have an increasing number of resources to tap into at the University of Cincinnati. Venture Lab NEXT is a student accelerator program designed to offer tailored resources and guidance to student teams who have already gained traction and are seeking specialized mentorship aligned with their industry domain or stage of development.
March 29, 2024
The University of Cincinnati's 1819 Innovation Hub hosted the 13th annual RevolutionUC Hackathon. Three standout teams emerged victorious, showcasing groundbreaking solutions to pressing challenges, including health care. The event was a testament to the power of innovation and compassion.
UC grad harnesses education to support women entrepreneurs
July 17, 2023
Most small business owners struggle to navigate the long and winding road to success, especially entrepreneurs from underrepresented communities. Yet, while an increasing number of banks and nonprofits are creating small business assistance programs, they need help identifying the professionals who could use their support.

Nursing Home Basics: Who Qualifies, Who Pays, and Other Helpful Facts
Why it matters.
Understanding how nursing homes work can be confusing because standards for eligibility, insurance coverage, etc. vary from state to state in the US.
In this second article in our series on nursing homes ( read Part I here ), we answer some commonly asked questions about nursing home structures and functions.
Who Is Eligible to Enter a Nursing Home?
People qualify for nursing home/facility level of care (NFLOC) if they are unable to live alone safely in the community. There is no federal definition of NFLOC and the exact rules governing level of care vary from state to state. Despite this lack of consistency, the following four areas are commonly considered when a state determines a person’s level of care need: physical functional ability; health issues/medical needs; cognitive impairment; and behavioral issues. In many states, there has been significant rebalancing toward home and community-based services and away from nursing home care. Check state websites for updated information on specific eligibility requirements.
Who Pays for Nursing Home Care?
Medicare is the federal health insurance program for people in the US who are 65 or older, some younger people with disabilities, people with End-Stage Renal Disease. A common misconception is that Medicare will pay for all nursing home costs. This is not true.
Post-acute care (PAC) or skilled nursing facility (SNF) care is usually covered by Medicare or private insurance up to 100 days (100 percent for 20 days and then 80 percent for 80 days based on certain criteria). Long-term care (meals, room and board, and basic health services) is often paid for privately until funds are spent down. A “ spend down ” is how someone with Medicare may qualify for Medicaid — a joint federal and state program that provides health coverage to some people with limited income and resources — even if their income is higher than a state's Medicaid limit. Under a spend down, a state lets the person subtract their non-covered medical expenses and cost sharing (like Medicare premiums and deductibles) from their available income. Each state’s Medicaid program covers approximately 70 percent of nursing home care. Long-term care insurance can also pay for nursing home care, but relatively few people have it.
The average cost of a nursing home is over $90,000 per year but this varies state to state. Multiple organizations provide information about nursing home costs and Medicaid daily rates online, including the American Council on Aging .
Who Oversees and Regulates Nursing Home Quality and Safety?
The Centers for Medicare and Medicaid Services (CMS) oversees nursing home quality and safety at the federal level. Several divisions have regulations that pertain to nursing homes.
The CMS Division of Nursing Homes develops and oversees most nursing home regulations. CMS delegates nursing home surveys and inspections to a designated organization in each state, usually the State Survey Agency (SSA). SSAs conduct annual, recertification, and complaint surveys and assess compliance with regulations. There is also a Special Focus Facility program for a small number of low-performing nursing homes that receive more intensive oversight and guidance on quality improvement in each state.
How Do We Measure Nursing Home Quality?
Because definitions of quality may vary, there are different methods used by federal, state, or private organizations to collect and analyze quality data. Here are a few examples:
- Minimum Data Set (MDS) is a standardized assessment tool required by CMS that measures health status in nursing home residents. All nursing homes that accept Medicare or Medicaid must submit the MDS regularly for each resident to receive payment.
- National Healthcare Safety Network is an electronic system for infection reporting, including COVID and other data that goes to CDC.
- CMS Five Star Quality Rating System gathers information from inspections (surveys), quality measures, and staffing from each nursing home and makes this information publicly available on the CMS website.
- Medicare’s Care Compare allows users to locate and compare data from nursing homes.
What are Quality Innovation Networks-Quality Improvement Organizations (QIN-QIOs)?
QIN-QIOs focus on working with nursing homes, states, and regions to improve quality of life and quality of care across settings, including nursing homes. QIN-QIOs have their own separate line item in the US federal budget to support the national program which covers all 50 states and US territories . QIN-QIOs are not part of state survey agencies or the survey process. Their focus is on quality improvement, support, education, and training, which are often provided free or at very low cost.
Who Works in Nursing Homes?
Women make up most of the nursing home workforce, particularly direct care workers such as certified nursing assistants (CNAs). ( Almost 90 percent of nursing assistants are female). Many are single parents. People of color comprise most of the US nursing assistant workforce.
Most nursing assistants are low-income wage earners. Many live at or near the federal poverty level and almost half receive some type of public assistance. Nursing homes typically pay CNAs the minimum wage, but this is not necessarily a livable wage depending on where they live. For this reason, CNAs often work in multiple settings and have multiple jobs. For many CNAs, English is not their first language, and they may have limited English proficiency. Many are immigrants.
What Are Some Challenges Faced by the Nursing Home Workforce?
There are many issues facing nursing home CNAs today and some new opportunities. The National Association of Health Care Assistants (NAHCA) conducted a survey of 1,420 CNAs in July 2023. When asked about their jobs, many CNAs reported that low wages and benefits would be the primary reasons they intend to seek another type of employment. They also cited unstable or inadequate hours, lack of supervisor’s/manager’s support, lack of career advancement or professional development, and feeling under-valued.
High rates of turnover (in some cases over 100 percent in a year) and the need for stronger, stable leadership are important reasons to better support CNAs and other direct care workers. Creating and testing standardized career ladders or lattices and providing more training and education on topics of interest to CNAs represent opportunities to promote better retention and reduce turnover. Another way to respond to CNA concerns is by becoming an Age-Friendly Health Systems Nursing Home .
Alice Bonner, PhD, RN, is IHI’s Senior Advisor for Aging. Amanda Meier, BSW, MA, is IHI’s Project Manager, Age-Friendly Health Systems. If you have any questions or ideas about nursing homes or related policy issues, please feel free to reach out to Alice Bonner ( [email protected] ) or Amanda Meier ( [email protected] ).
You may also be interested in:
The Basics We (and Policymakers) Should Know about Nursing Homes
Centering What Matters: The Core of Age-Friendly Care
Related Insights
ORIGINAL RESEARCH article
This article is part of the research topic.
Co-designing and Evaluating Oral Health Promotion Interventions for Vulnerable Groups
Adolescents' Views on Oral Health Care and Promotion in Norway: Everyday Practices, Recommendations, and Future Visions Provisionally Accepted

- 1 Norwegian University of Science and Technology, Norway
- 2 SINTEF, Norway
The final, formatted version of the article will be published soon.
In this study, we aimed to understand adolescents' perspectives on oral health care and promotion. 9Our research was conducted in the context of Norway's oral health care system, where societal 10 factors like income and education influence health disparities. Despite free public dental care for all 11 residents younger than 19 years, challenges persist in promoting oral health among adolescents, a 12 group whose oral health behavior and literacy remain largely unexplored. A thematic analysis of an 13 anonymized dataset from around 80 adolescents aged 12-20 years, led to the recognition of five 14 central themes: (1) Feeling fresh vs. feeling indifferent: A broad spectrum of attitudes; (2) Bridging 15 gaps, building habits: Collaborative efforts in oral care; (3) "Create good experiences at the dentist so 16 people come back again"; (4) Requested qualities in oral health promoting solutions; (5) Reminder 17 tools for everyday use. Taken together, these themes highlight adolescents' oral health practices and 18 resources, recommendations for dental clinics, and visions for future oral health promotion. The 19 results emphasize the importance of tailored oral health promotion for adolescents. Some reflections 20 on the theme of social inequalities are provided.
Keywords: adolescents, oral health promotion, social inequalities, qualitative methods Font: (Default) Times New Roman, 12 pt Font: (Default) Times New Roman, 12 pt Formatted ... [2] Formatted: Font: (Default) Times New Roman, 12 pt Formatted: Font: (Default) Times New Roman, 12 pt Font colour: Black
Received: 07 Sep 2023; Accepted: 27 Mar 2024.
Copyright: © 2024 Høiseth and Jasbi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Dr. Marikken Høiseth, Norwegian University of Science and Technology, Trondheim, Norway
People also looked at
Biomedical Engineering Education in Nigeria
Emergence, challenges, prospects and areas for development.
- Ayodele James Oyejide Afe Babalola University
In the past five decades, Nigeria has witnessed a range of Biomedical Engineering (BME) and technology activities within private and public hospitals, research institutions, and a limited number of universities. These have mainly centred on the procurement, installation, and maintenance of medical equipment and devices. Trained technologists and technicians, equipped with relevant skills and certification, have primarily spearheaded these efforts. Consequently, the country has made a minimal contribution to the global knowledge base in BME research. However, academic programmes leading to degrees and dedicated research in BME have recently emerged within Nigerian universities. This article assesses the current state of BME education in the country, including the milestones achieved, ongoing challenges, and prospects for future development. It draws on a critical analysis of the existing literature on BME practices and education in Nigeria as well as the author’s informed perspective. The findings highlight that BME education in Nigeria is yet to match international standards. To further develop these programmes, it recommends that attention focus on seven key areas that have proven instrumental in the development of similar university programmes in developed nations. Strategies are also proposed to foster collaboration among universities, researchers, the health sector, and government entities that would promote interdisciplinary BME education, ultimately enhancing the healthcare delivery system, and research and development (R&D) in Nigeria.
How to Cite
- Endnote/Zotero/Mendeley (RIS)
Copyright (c) 2024 International Journal of African Higher Education

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License .
Developed By
Information.
- For Readers
- For Authors
- For Librarians
Make a Submission
Blog The Education Hub
https://educationhub.blog.gov.uk/2024/03/14/how-supporting-university-students-mental-health/
How we’re supporting university students with their mental health

Going to university is a fun and exciting time for most students – but it comes with unique challenges and stresses. We believe that all students’ mental health and wellbeing should be properly supported during their time at university.
There is a range of mental health support available to students, from online mental health and wellbeing platform Student Space to counselling and one-to-one support. Here’s what you need to know.
What action are you taking to support students’ mental health?
Students struggling with their mental health can access Student Space , a mental health and wellbeing hub supporting students.
Funded by £3.6 million from the Office for Students (OfS), Student Space provides dedicated one-to-one text and web chat support services. It’s also an online platform providing vital mental health and wellbeing resources.
This service is part of the £15 million we have asked the OfS to allocate towards student mental health in 2023/2024. This funding will also be used to give additional support for those making the transition from school or college to university, in particular through counselling services.
It will also be used to address any challenges that students may face in accessing local support services through their university, by establishing better partnerships between universities and local NHS services.
To ensure all the information is readily available for students and young people, we have put together some useful links and sources of mental health support so that everyone can get the advice and help they need. This information is available here .
We are also asking universities to take a whole university approach to mental health by setting a target for all universities to sign up to the University Mental Health Charter Programme by September 2024.
To support this target t he Office for Students ( OfS ) is providing £400,000 additional funding to Student Minds to support expansion of the Programme . You can read more about it on the OfS website .
What is the University Mental Health Charter Programme?
Universities that are part of the University Mental Health Charter programme will be supported to make cultural change so that all aspects of university life promote and support mental health.
Both students and staff will benefit from better support for their mental health and wellbeing as a result.
The Charter Award is given to the universities that are part of the Programme members which demonstrate excellent practice in supporting student mental health.
What is the Department doing to reduce suicides at universities?
Every student death is a tragedy and preventing suicide and self-harm in our student populations is a key priority.
So that students are better protected we have asked universities to fully implement best practice including the Suicide Safer Universities guidance, led by Universities UUK and Papyrus.
This includes guidance for universities on sharing information with family and friends in the event of a mental health crisis and practical advice on compassionate, confident, and timely support when a tragedy occurs.
Understanding student suicide data and risk factors is central to informing preventative action, which is why we have worked with the Office for National Statistics, which has published updated data and analysis .
We appointed Professor Edward Peck as Higher Education Student Support Champion in May 2022 for a two-year term and extended the appointment for another year until 31 May 2025 . Professor Peck has been speaking to bereaved parents to understand where improvements can be made.
To deliver better practice in mental health support across the higher education sector Professor Peck is chairing a Higher Education Mental Health Implementation Taskforce, which will include bereaved parents, students, mental health experts, charities and sector representatives.
It has been asked to deliver a report with a plan for better early identification of students at risk, a University Student Commitment on dealing with students sensitively on disciplinary issues, and a set of clear targets for improvements in practice by providers.
Its first stage report has been published outlining progress so far and setting out new areas of focus, including improving join up between higher education and NHS mental health services. It is due to publish a second stage report by July 2024.
We have also appointed the National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH) to carry out a National Review of Higher Education Suicides.
This will ensure that valuable lessons from past tragedies can be learnt to help us better protect students in future. Its findings report will be published by Spring 2025 outlining good practice and areas for improvement around suicide prevention in higher education.
Providers’ participation in the National Review of HE Suicides will be supported by the additional one-off £10m funding we have asked the OfS to allocate on mental health and hardship, which comes top of the £15 million already distributed this year on HE student mental health.
What should I do if I’m worried about a friend or family member at university?
We understand that helping a friend or family member with mental health issues can be difficult. It is important that students feel supported at this difficult time. There is support in place and people who are available to listen.
If for any reason you have cause to believe that someone you know is struggling with mental health and wellbeing issues at university, we recommend following NHS guidance .
Universities have support services in place for their students which can be accessed via their website, or by looking up your university on the Student Space support pages .
You may also be interested in:
- Mental health resources for children, students, parents, carers and school/college staff
- What we are doing to improve the mental health of children and young people
- Five things you didn’t know about mental health support in schools
Tags: Mental health , mental health resources , Office for Students , Pupil mental health , Universities UK , University , Wellbeing
Sharing and comments
Share this page, related content and links, about the education hub.
The Education Hub is a site for parents, pupils, education professionals and the media that captures all you need to know about the education system. You’ll find accessible, straightforward information on popular topics, Q&As, interviews, case studies, and more.
Please note that for media enquiries, journalists should call our central Newsdesk on 020 7783 8300. This media-only line operates from Monday to Friday, 8am to 7pm. Outside of these hours the number will divert to the duty media officer.
Members of the public should call our general enquiries line on 0370 000 2288.
Sign up and manage updates
Follow us on social media, search by date, comments and moderation policy.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Public Health
Grand Challenges for Public Health Education and Promotion
Christiane stock.
1 Institute of Health and Nursing Science, Charité–Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany
2 Unit for Health Promotion Research, University of Southern Denmark, Esbjerg, Denmark
Introduction
The Section Public Health Education and Promotion aims to advance the scientific basis of knowledge and action for current and future health education and promotion researchers and professionals, including those working with lay audiences. The section seeks to foster research on a broad range of health education, health promotion and disease prevention approaches operating at individual, organizational, community and society level. The Ottawa Charter ( 1 ) has provided a basis for addressing public health challenges in fundamentally new ways with building public policy, creating supportive environments for health, strengthening community action, developing personal skills and reorienting health services. However since the Charter has been launched many social and economic changes have occurred and globalization as well as digitization have had strong impacts on systems, governance structures, economies and therewith on the daily lives of people. Therefore, the conference on health promotion in 2016 has released the Shanghai Declaration on promoting health in the 2030 Agenda for Sustainable Development ( 2 ), which suggests that health promotion methods and strategies play a key role to achieve the UN Sustainable Development Goals (SDGs) ( 3 ) and the Declaration puts Healthy Cities, improved governance for health and health literacy in the focus of actions. More recently, the COVID-19 pandemic has reminded us that health is multi-faceted and that there are multiple and interacting impacts of the pandemic in the settings of our everyday lives ( 4 ). Therefore, the Section Public Health Education and Promotion aims to foster innovative research, education and practice that can help individuals to better deal with the challenges of rapidly changing environments and make better personal health choices, health education and promotion professionals more effectively engage in evidence-based practices, and societies enhance programmatic efforts and policy initiatives to protect and promote population health. In order to support the goals of the Ottawa Charter and the Shanghai Declaration, the following eight topics and themes should be addressed in future research to create better evidence for tackling the present and future public health challenges effectively.
Health Promotion in Settings
The importance of settings as “.. a place or context in which people engage in daily activities in which environmental, organizational and personal factors interact to affect health and wellbeing” ( 5 ) for sustainable health and wellbeing has been expressed in many different WHO documents since the Ottawa Charter has shed the light on the settings-based approach to health promotion in 1986. The importance of settings is presently re-affirmed, because the recovery from COVID-19 will to a large extent be determined by and experienced in the settings in which we live our lives, and a settings approach is thus needed to mitigate the negative impacts of COVID-19 ( 6 ). Whitelaw et al. ( 7 ) have distinguished different types of setting based approaches and provided a better understanding of how setting-based health promotion is implemented in current practice. The types range from the passive model, where the setting provides access to population groups or individuals to address health behavior change and development of personal skills, to the organic model requiring active engagement of the community and the comprehensive model, where health promotion is the central component of the setting development. In the settings-based approach to health promotion participation and empowerment of both individuals and communities is key. However, more research is needed to investigate the effectiveness of the different types of health promotion within settings on health and wellbeing of the members of the setting and the wider communities with which settings are deeply interconnected ( 8 ).
Health Literacy With Focus on the Health Literacy Environment
The last two decades have seen an extraordinary increase in published papers on the subject of health literacy showing the growth in interest in this topic. Health literacy has been described as the ability to assess, understand, appraise and apply health-related information in the domains of health promotion, prevention and health care ( 9 ). There is a body of research showing that health literacy has influence on behavioral choices and the use of health services, which in turn creates an impact on health outcomes and health service costs ( 10 – 12 ). Given the relevance of health literacy to improve population health there is still a lack of research both in terms of measuring the level of health literacy as well as to improve health literacy in diverse populations. The focus of the majority of studies has been on interventions providing information, effective communications and structured education in clinical settings and directed toward improving functional health literacy, while implementation of national policies and programs still seems to be lacking behind ( 13 ). In addition, more research is needed on health literacy environment approaches encompassing programmes, interventions and policies to make health services more user-friendly and to reduce communication barriers.
Digital Health Education and Promotion
Since technology is shaping nearly every aspect of our lives in information societies health education and health promotion is also transitioning into a new technological and digital era and digital health promotion is evolving ( 14 , 15 ). While the technology is rapidly developing and improving and the connectivity and adoption of devices is increasing world-wide, there are many new options to reach out to hard-to-access populations and communities in better and more affordable ways. Another advantage is the potential use of new ways to communicate digitally with tailored and even individually personalized health information and messages, health promotion services. With the decreasing costs of digital technologies reaching out to large populations with digital health promotion seems to be possible even in low- and middle income countries. However, successful digital health promotion needs to take some environmental factors into account that are minimizing still existing digital divides in terms of access, the need to develop applications that are easy to use across generations and age groups, to incorporate interactivity and gamification elements, to deliver incentives for use in real time and to establish trust in terms of high standards of data protection ( 15 ). A scoping review has shown that digital health promotion uses a variety of technologies ranging from computer- and web-based programs to mobile devices/smartphone apps and telemonitoring in form of sensors ( 14 ). However, the authors also conclude that there is still a lack of research of environmental and structural approaches in the field of digital health promotion and that most applications and programs operating with digital technologies focus on individual behavior change ( 15 ). In addition, more research is needed to address key challenges of digital health promotion and education in terms of privacy control, appropriate use of data including secondary usage beyond the original intention and the appropriate limits of nudging vs. the free choice ( 15 ).
Co-Creation in Intervention Development and Stakeholder Engagement
It is widely accepted that co-creation of new interventions and stakeholder involvement has the potential to develop more effective interventions with strong and enduring impact on health outcomes ( 16 ) and to speed up the application in practice ( 17 ). Co-creation has emerged from the participatory design paradigm ( 18 ) and ensures that programs are designed with those that are ultimately the recipients of a health intervention ( 19 ). While Co-creation has been initially used in developing health care services ( 20 ) it may also be a promising strategy to adopt to address other complex health behaviors ( 19 ). Interventions and programmes developed in co-creation with stakeholders, users and recipients of programmes have thus demonstrated value for researchers, users and society at large ( 21 ). In addition, the need to include wider stakeholder groups during the intervention development process has been identified more recently in order to ensure that user generated ideas are feasible and applicable in practice ( 22 ). Co-creation processes ensure that emphasis is placed on empowering participants and that all solutions emerging from co-design are user centered and stakeholder supported. The participation and engagement of stakeholders and/or programme recipients in various stages of the intervention development process, has different origins but shares important assumptions and operating principals ( 16 , 23 ). While collaboration and engagement with users and stakeholders during intervention development processes are considered vital, clear articulation of procedures and considerations for various co-creation methodologies warrants further research attention ( 19 ).
Social Marketing Approaches
Health education and health promotion build to a large extent on research and approaches developed within social marketing. Co-creation e.g., has its roots in participatory action research, but also in co- design originating from service design thinking in marketing ( 19 ). Moreover, social norms approaches are widely used to shift risk-taking behavior toward more responsible health behavior, which have their origin in social marketing. While social marketing approaches and techniques are of high value and relevance for health promotion practitioners and researchers, the sharing of knowledge and practices between these fields of science should be intensified. Thus, more social marketing research should be published in the Section Public Health Education and Promotion in order to make innovative social marketing approaches more visible for public health scientists and practitioners.
Health Communication and Risk Communication
Significant communication components are involved in the management of public health issues. This became even more urgent during the COVID-19 pandemic. Communication strategies are needed to effectively prompt warnings about risks, increase self-efficacy of individuals for behavioral change, and inform about symptomatology and medical treatment. Risk communication is a science-based approach for communicating effectively in such high concern situations than in a pandemic, and it is based on a multi-level process of interactive exchange of information between public government and citizens ( 24 ). More research is needed to fully understand how multiple messages about the nature of the risk and about the legal and the institutional arrangements for risk management can be effectively communicated to broad and diverse audiences in times of fake news and misinformation.
New Ways to Evaluate Health Education and Promotion Programmes
The last decades have seen an increasing emphasis on evidence-based programmes and actions in the field of health promotion and prevention. However, developing such evidence is still a challenge given the complex nature of many of the community or settings-based interventions with multiple intervention strategies and the diversity of the outcomes on both behavioral and structural level. Since the randomized-controlled trial (RCT) as the gold standard in intervention evaluation is often too restrictive to fit to the diverse types of interventions, the research methods to evaluate their success need to vary according to the type of intervention including qualitative, quantitative, economic and participative methods ( 25 ). In addition, new ways to evaluate the effectiveness of digital health tools are needed that allow for capturing dynamic changes of digital health interventions over time ( 26 ). Additionally, more research is needed in developing evaluation strategies to tackle the lengthy and costly nature of RCTs.
Innovative Teaching and Learning in Health Education and Promotion
The multiple and rapid societal end environmental changes in the context of globalization and digitisation require also adaptations and responses in how we teach and learn in the field of health education and promotion. Moreover, the COVID-19 pandemic has changed the way we teach and learn fundamentally with the rapid enforcement of online teaching in many countries. Research addressing the short-, mid- and long-term consequences of distance learning practices on learning outcomes and social interaction among peers and between educators and students are needed. In addition, research about new ways to teach and learn interactively via distance, hybrid or classroom teaching is also warranted.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
I thank Kristoffer Drue Knudsen for support in managing the reference list.

COMMENTS
The education of health professionals substantially changed before, during, and after the COVID-19 pandemic. A 2010 Lancet Commission examined the 100-year history of health-professional education, beginning with the 1910 Flexner report. Since the publication of the Lancet Commission, several transformative developments have happened, including in competency-based education, interprofessional ...
The Health Policy paper by Julio Frenk and colleagues1 in The Lancet on educating health professionals after the COVID-19 pandemic highlights the post-pandemic learning environment, use of technology to improve learning, interprofessional education (IPE), and lifelong continuing education and training for the health professions. The perpetual shortage and maldistribution of health ...
These challenges need to be met with a public health workforce of adequate size, composition, distribution, and skills. Formally trained health educators are an important but often underutilized part of the workforce needed to meet such challenges. Although various health workers inform the public, many employers are unaware of the professional ...
Major challenges face today's health care system for which health professionals have to be prepared. This chapter describes these challenges—incorporating related evidence and the views expressed by participants in the Health Professions Education Summit—and examines the resulting implications for the education of health professionals and its reform.
The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity report (NASEM, 2021) provides a comprehensive plan to improve the quality of health care and candidly acknowledges historical and contemporary issues that have stalled previous efforts to dismantle health care disparities. This article spotlights the role that nursing education, nurse leaders, and faculty play in ...
It is, of course, impossible to predict today the long‐term effects of the disruption we are now experiencing from the COVID‐19 pandemic. That disruption has profoundly affected the health of the public with corollary challenges to the health‐care delivery system and health professions education.
Medical education and the health professions are facing multiple global challenges that are context specific yet are patterned across contexts. These challenges have been described as wicked issues that defy known solutions and are viewed differently by different people. Three simple approaches, inquiry, pattern recognition, and Adaptive Action, are presented as a way forward to tame wicked ...
Medical education and the health professions are facing multiple global challenges that are context specific yet are patterned across contexts. These challenges have been described as wicked issues that defy known solutions and are viewed differently by different people. ... Conflict between individuals and groups is a constant challenge in ...
Health education has changed in many ways since Health Education Journal was first published, with developments moving the discipline forward in ways not envisaged 75 years ago. While there have been recent concerns about the decline in status of health promotion and linked worries about health education, the contemporary evidence base has grown to support the delivery of good quality health ...
Edwards H, Higgs J (1999) Challenges, cooperation and choice: Creating the future of health professional education. In: Higgs J, Edwards H, eds. Educating beginning practitioners: Challenges for health professional education. Oxford: Butterworth-Heinemann, 289-96.
Medical education faces challenges in keeping pace with the rapidly changing healthcare needs of populations worldwide. [1][2][3] Traditional curricula, inadequate funding, and weak quality assurance and accreditation practices contribute to the production of under-equipped graduates. 4 To effectively address the health problems of the 21st century, there is a need for new, more efficient, and ...
reviews health education theories and definitions, identifies the components of evidence-based health education and outlines the abilities necessary to engage in effective practice. Much has been written over the years about the relationship and overlap between health education, health promotion and other concepts, such as health literacy.
9 challenges medical educators want to solve right now. Oct 8, 2015 . 7 MIN READ. By. Staff News Writer. Faculty and students from more than 110 medical institutions discussed the future of physician education last week at the AMA's CHANGEMEDED conference. The three-day event culminated in an "unconference," a special session in which ...
Leading educators and health professionals have long documented the interdependent relationship between health and education (Basch, 2011; Institute of Medicine, 1997; Kolbe, 2019).School-age children and adolescents experiencing health issues such as stress, physical and emotional abuse, hunger, safety concerns, vision, hearing or dental problems, asthma, or other chronic illnesses have ...
Purpose Artificial Intelligence (AI) is transforming healthcare and shows considerable promise for the delivery of medical education. This systematic review provides a comprehensive analysis of the global situation, effects, and challenges associated with applying AI at the different stages of medical education. Methods This review followed the PRISMA guidelines, and retrieved studies ...
The review articles encompass a wide range of topics, each offering unique perspectives on key aspects of healthcare. One article (Lyu & Li 2023) explores the challenges of translating evidence into practice and the role of clinical practice guidelines in guiding healthcare decisions. It emphasizes the importance of evidence-based practices in improving patient outcomes while highlighting the ...
Challenge 3: Consumerization of healthcare. The last challenge that healthcare organizations need to consider is the shift to a consumer focus. We need to meet our patients where they're at—not only from a linguistic and reading level perspective but also from a technology perspective. Patients like visually appealing content.
The perceived usefulness of specific features of each were highlighted. In closing, a multi-modal model of epistemology, axiology and ontology in healthcare technology, digital health and medical education - including content, skills, technology development and challenges/constraints - is presented.
I NTRODUCTION. The domain of cultural competency in medical education deals with the varied cultural backgrounds and specific needs of different patients who are accessing health-care delivery services. [] In simple words, cultural competence refers to the ability of health-care professionals, including medical students to acknowledge, comprehend, and effectively communicate with patients from ...
Institutions confronted with limited resources, in the face of increased demands for education and a shortage of educators, have found electronically based education a significant resource. ... Challenges in healthcare education: a correlational study of outcomes using two learning techniques J Nurses Staff Dev. 2010 Mar-Apr;26(2) :49-53 ...
Approximately 80% of clinical education occurs in inpatient settings, yet 80-90% of medicine is practiced in the outpatient arena. The least experienced learners begin their in-depth clinical exposure in the most complicated, fastest paced, environments of health-care delivery. In these arenas, novice students are increasingly displaced by ...
Consultations with children and their families are complex and require soft skills. However, there is a gap in the medical curriculum concerning these skills, especially as encounter training is often adult-centered. We developed, validated, and applied simulation scenarios that prioritize active participation of children to train soft skills in child-centered care for undergraduate medical ...
The University of Cincinnati's 1819 Innovation Hub hosted the 13th annual RevolutionUC Hackathon. Three standout teams emerged victorious, showcasing groundbreaking solutions to pressing challenges, including health care. The event was a testament to the power of innovation and compassion.
Despite this lack of consistency, the following four areas are commonly considered when a state determines a person's level of care need: physical functional ability; health issues/medical needs; cognitive impairment; and behavioral issues. In many states, there has been significant rebalancing toward home and community-based services and ...
While increasing organs available in the donor pool, important challenges merit consideration and ongoing education and research are needed. The Canadian HIV Trial Network (CTN) is a Canada-wide partnership of researchers, People with HIV, their caregivers, and health advocates committed to generating knowledge and maximizing the impact of ...
In this study, we aimed to understand adolescents' perspectives on oral health care and promotion. 9Our research was conducted in the context of Norway's oral health care system, where societal 10 factors like income and education influence health disparities. Despite free public dental care for all 11 residents younger than 19 years, challenges persist in promoting oral health among ...
This article assesses the current state of BME education in the country, including the milestones achieved, ongoing challenges, and prospects for future development. ... the health sector, and government entities that would promote interdisciplinary BME education, ultimately enhancing the healthcare delivery system, and research and development ...
Going to university is a fun and exciting time for most students - but it comes with unique challenges and stresses. We believe that all students' mental health and wellbeing should be properly supported during their time at university. There is a range of mental health support available to students, from online mental health and wellbeing platform Student Space to counselling and one-to ...
The study method entails two main factors, purpose and the research synthesis process of the study. This study aims to explore the understanding and awareness of the teachers and students about STEM education; the challenges faced by them and their solutions in the light of literature review and research amalgamation and the abilities and skills to overcome these challenges.
The Section Public Health Education and Promotion aims to advance the scientific basis of knowledge and action for current and future health education and promotion researchers and professionals, including those working with lay audiences. The section seeks to foster research on a broad range of health education, health promotion and disease ...