
Cholangiocarcinoma: Pictorial essay of CT and cholangiographic findings
- Boramae Radiology
- SNUCM Radiology
- SNUBH Radiology
- SNUCM Surgery
Research output : Contribution to journal › Article › peer-review
Cholangiocarcinomas that involve areas from the peripheral intrahepatic duct to the distal common duct have similar morphologic features, and traditional classification schemes based on the location of the involved ducts sometimes overlap. Nevertheless, cholangiocarcinoma is usually classified as either intrahepatic or extrahepatic, and intrahepatic cholangiocarcinoma is further classified as either peripheral or hilar. However, the distinction between peripheral intrahepatic cholangiocarcinoma and hilar cholangiocarcinoma is largely based on the site of origin. Therefore, in some tumors that arise peripheral to the secondary bifurcation of one of the hepatic ducts, clear differentiation between the two types of cholangiocarcinoma is not always possible. In addition, the distinction between hilar cholangiocarcinoma and extrahepatic cholangiocarcinoma is not clearly defined. The different biologic behaviors of the tumors seem to be caused by their varying locations and their size at the time of diagnosis. Further molecular or biochemical investigation is needed to support the "field theory," which states that all cholangiocarcinomas are biologically the same tumor originating from the same biliary epithelium.
- Bile duct radiography, 76.122
- Bile ducts, CT, 76.1211
- Bile ducts, neoplasms, 76.321
- Bile ducts, stenosis or obstruction
Access to Document
- 10.1148/radiographics.22.1.g02ja15173
Other files and links
- Link to publication in Scopus
T1 - Cholangiocarcinoma
T2 - Pictorial essay of CT and cholangiographic findings
AU - Han, Joon Koo
AU - Choi, Byung Ihn
AU - Kim, Ah Young
AU - An, Su Kyung
AU - Lee, Joon Woo
AU - Kim, Tae Kyung
AU - Kim, Sun Whe
N2 - Cholangiocarcinomas that involve areas from the peripheral intrahepatic duct to the distal common duct have similar morphologic features, and traditional classification schemes based on the location of the involved ducts sometimes overlap. Nevertheless, cholangiocarcinoma is usually classified as either intrahepatic or extrahepatic, and intrahepatic cholangiocarcinoma is further classified as either peripheral or hilar. However, the distinction between peripheral intrahepatic cholangiocarcinoma and hilar cholangiocarcinoma is largely based on the site of origin. Therefore, in some tumors that arise peripheral to the secondary bifurcation of one of the hepatic ducts, clear differentiation between the two types of cholangiocarcinoma is not always possible. In addition, the distinction between hilar cholangiocarcinoma and extrahepatic cholangiocarcinoma is not clearly defined. The different biologic behaviors of the tumors seem to be caused by their varying locations and their size at the time of diagnosis. Further molecular or biochemical investigation is needed to support the "field theory," which states that all cholangiocarcinomas are biologically the same tumor originating from the same biliary epithelium.
AB - Cholangiocarcinomas that involve areas from the peripheral intrahepatic duct to the distal common duct have similar morphologic features, and traditional classification schemes based on the location of the involved ducts sometimes overlap. Nevertheless, cholangiocarcinoma is usually classified as either intrahepatic or extrahepatic, and intrahepatic cholangiocarcinoma is further classified as either peripheral or hilar. However, the distinction between peripheral intrahepatic cholangiocarcinoma and hilar cholangiocarcinoma is largely based on the site of origin. Therefore, in some tumors that arise peripheral to the secondary bifurcation of one of the hepatic ducts, clear differentiation between the two types of cholangiocarcinoma is not always possible. In addition, the distinction between hilar cholangiocarcinoma and extrahepatic cholangiocarcinoma is not clearly defined. The different biologic behaviors of the tumors seem to be caused by their varying locations and their size at the time of diagnosis. Further molecular or biochemical investigation is needed to support the "field theory," which states that all cholangiocarcinomas are biologically the same tumor originating from the same biliary epithelium.
KW - Bile duct radiography, 76.122
KW - Bile ducts, CT, 76.1211
KW - Bile ducts, neoplasms, 76.321
KW - Bile ducts, stenosis or obstruction
UR - http://www.scopus.com/inward/record.url?scp=0036370243&partnerID=8YFLogxK
U2 - 10.1148/radiographics.22.1.g02ja15173
DO - 10.1148/radiographics.22.1.g02ja15173
M3 - Article
C2 - 11796906
AN - SCOPUS:0036370243
SN - 0271-5333
JO - Radiographics
JF - Radiographics
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (43,954,836 articles, preprints and more)
- Available from publisher site using DOI. A subscription may be required. Full text
- Citations & impact
- Similar Articles
Cholangiocarcinoma: pictorial essay of CT and cholangiographic findings.
Author information, affiliations, orcids linked to this article.
- Kim TK | 0000-0001-5193-1428
- Lee JW | 0000-0002-7106-5229
Radiographics : a Review Publication of the Radiological Society of North America, Inc , 01 Jan 2002 , 22(1): 173-187 https://doi.org/10.1148/radiographics.22.1.g02ja15173 PMID: 11796906
Abstract
Full text links .
Read article at publisher's site: https://doi.org/10.1148/radiographics.22.1.g02ja15173
References
Articles referenced by this article (12)
Sherlock S, Dooley J.10th ed. London, England: Blackwell, 1997; 642-649.
Tomkins rk, saunders kd, roslyn jj, et al.1990; 211:614-621., intrahepatic peripheral cholangiocarcinoma: comparison of dynamic ct and dynamic mri..
Zhang Y , Uchida M , Abe T , Nishimura H , Hayabuchi N , Nakashima Y
J Comput Assist Tomogr, (5):670-677 1999
MED: 10524843
MR cholangiopancreatography in malignant biliary obstruction.
Pavone P , Laghi A , Passariello R
Semin Ultrasound CT MR, (5):317-323 1999
MED: 10527137
Performance characteristics of magnetic resonance cholangiography in the staging of malignant hilar strictures.
Zidi SH , Prat F , Le Guen O , Rondeau Y , Pelletier G
Gut, (1):103-106 2000
MED: 10601064
Choi BI, Han JK, Kim TK.In: Gazelle SG, eds.New York, NY: Thieme, 1998; 630-676.
Choi bi, han jk, kim tk.in: meyers ma, eds.philadelphia, pa: lippincott-raven, 1998; 503-516., liver cancer study group of japan.tokyo, japan: kanehara, 1997; 6-8., peripheral cholangiocarcinoma of the liver: two-phase spiral ct findings..
Kim TK , Choi BI , Han JK , Jang HJ , Cho SG , Han MC
Radiology, (2):539-543 1997
MED: 9240550
Clonorchiasis: sonographic findings in 59 proved cases.
Lim JH , Ko YT , Lee DH , Kim SY
AJR Am J Roentgenol, (4):761-764 1989
MED: 2646867
Citations & impact
Impact metrics, citations of article over time, article citations, updates in diagnosis and endoscopic management of cholangiocarcinoma..
Caragut RL , Ilie M , Cabel T , Günșahin D , Panaitescu A , Pavel C , Plotogea OM , Rînja EM , Constantinescu G , Sandru V
Diagnostics (Basel) , 14(5):490, 24 Feb 2024
Cited by: 0 articles | PMID: 38472961 | PMCID: PMC10931405
Degradation of AZGP1 suppresses apoptosis and facilitates cholangiocarcinoma tumorigenesis via TRIM25.
Yun H , Jeong HR , Kim DY , You JE , Lee JU , Kang DH , Koh DI , Ryu YS , Bae S , Jin DH
J Cell Mol Med , 28(3):e18104, 06 Jan 2024
Cited by: 1 article | PMID: 38183356 | PMCID: PMC10844717
Three-dimensional visualization and evaluation of hilar cholangiocarcinoma resectability and proposal of a new classification.
Zhang JZ , Yang CX , Gao S , Bu JF , Li QQ , Wang HL , Yang KN , Tong SS , Qian LJ , Zhang J , Hua R , Sun YW , Yan JY , Chen W
World J Surg Oncol , 21(1):239, 05 Aug 2023
Cited by: 1 article | PMID: 37542314 | PMCID: PMC10403901
Algorithm-based approach to focal liver lesions in contrast-enhanced ultrasound.
Leow KS , Kwok CY , Low HM , Lohan R , Lim TC , Low SCA , Tan CH
Australas J Ultrasound Med , 25(3):142-153, 04 Jul 2022
Cited by: 0 articles | PMID: 35978727 | PMCID: PMC9351431
Free full text in Europe PMC
Imaging Spectrum of Intrahepatic Mass-Forming Cholangiocarcinoma and Its Mimickers: How to Differentiate Them Using MRI.
Kovač JD , Janković A , Đikić-Rom A , Grubor N , Antić A , Dugalić V
Curr Oncol , 29(2):698-723, 30 Jan 2022
Cited by: 5 articles | PMID: 35200560 | PMCID: PMC8870737
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Hilar cholangiocarcinoma: thin-section spiral CT findings with cholangiographic correlation.
Han JK , Choi BI , Kim TK , Kim SW , Han MC , Yeon KM
Radiographics , 17(6):1475-1485, 01 Nov 1997
Cited by: 32 articles | PMID: 9397459
Imaging of intrahepatic cholangiocarcinoma: 1. Peripheral cholangiocarcinoma.
Soyer P , Bluemke DA , Reichle R , Calhoun PS , Bliss DF , Scherrer A , Fishman EK
AJR Am J Roentgenol , 165(6):1427-1431, 01 Dec 1995
Cited by: 43 articles | PMID: 7484579
Cholangiocarcinoma: morphologic classification according to growth pattern and imaging findings.
AJR Am J Roentgenol , 181(3):819-827, 01 Sep 2003
Cited by: 158 articles | PMID: 12933488
Helical CT assessment in hilar cholangiocarcinoma: correlation with surgical and pathologic findings.
Feydy A , Vilgrain V , Denys A , Sibert A , Belghiti J , Vullierme MP , Menu Y
AJR Am J Roentgenol , 172(1):73-77, 01 Jan 1999
Cited by: 55 articles | PMID: 9888743
Imaging of intrahepatic and hilar cholangiocarcinoma.
Choi BI , Lee JM , Han JK
Abdom Imaging , 29(5):548-557, 08 Jun 2004
Cited by: 52 articles | PMID: 15185025
Europe PMC is part of the ELIXIR infrastructure
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.32(6); 2016 Dec

Imaging of Cholangiocarcinoma
Cholangiocarcinoma (CC) is the second most common primary hepatobiliary tumour, and it is increasing in incidence. Imaging characteristics, behaviour, and therapeutic strategies in CC differ significantly, depending on the morphology and location of the tumour. In cross-sectional imaging, CCs can be classified according to the growth pattern (mass-forming, periductal infiltrating, intraductal) and the location (intrahepatic, perihilar, extrahepatic/distal). The prognosis of CC is unfavourable and surgical resection is the only curative treatment option; thus, early diagnosis (also in recurrent disease) and accurate staging including the evaluation of lymph node involvement and vascular infiltration is crucial. However, the diagnostic evaluation of CC is challenging due to the heterogeneous nature of the tumour. Diagnostic modalities used in the imaging of CC include transabdominal ultrasound, endosonography, computed tomography, magnetic resonance imaging with cholangiopancreatography, and hybrid imaging such as positron emission tomography/computed tomography. In this review, the potential of cross-sectional imaging modalities in primary staging, treatment monitoring, and detection of recurrent disease will be discussed.
Introduction
Cholangiocarcinoma (CC) is the most frequent malignant tumour of the biliary tract, accounting for 10-20% of all primary liver tumours [ 1 , 2 ]. The vast majority (95%) of CC are adenocarcinomas with a high proportion of fibrous stroma [ 3 , 4 ]. The prevalence of CC shows geographic variations, with the highest prevalence being found in Southeast Asia [ 2 ]. In the US, the incidence of CC has been steadily increasing over the past decades, varying from 0.72 to 0.88 per 100,000 [ 5 ]. Despite recent advances in patient care, surgical resection of the tumour remains the only potentially curable therapy, leading to a 5-year survival of 30-35% [ 6 ]. CC may occur at any segment of the bile duct, i.e. from the terminal ductules to the ampulla of Vater. Therefore, intrahepatic (iCC) and extrahepatic (eCC) tumour localizations are differentiated, and the iCC is subdivided into peripheral and perihilar CC (pCC), the latter also being called Klatskin tumour. In detail, 6-8% of CC are localized peripherally, 50-67% perihilar, and 27-42% occur extrahepatically [ 7 ]. Up to now, the aetiology of CC is not fully understood, but several risk factors like primary sclerosing cholangitis (PSC), liver fluke infestations ( Opisthorchis viverrini , Clonorchis sinensis ), hepatolithiasis, Thorotrast exposure, and choledochal cysts have been identified [ 8 ]. In accordance with the morphologic classification system proposed by the Liver Cancer Study Group of Japan [ 9 ], iCC can be classified into three types based on the dominating morphologic feature: mass-forming (the most common), periductal infiltrating, and intraductal growth (fig. (fig.1). 1 ). Additionally, the growth pattern of eCC is commonly classified as nodular, sclerosing, or papillary [ 10 ]. Imaging modalities like ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI), and also positron emission tomography/computer tomography (PET/CT) are of particular importance in the diagnosis, primary staging, and restaging of CC.

Schematic illustration of the three most common morphologic features of iCC according to the Liver Cancer Study Group of Japan [ 13 ].
When clinical and laboratory findings are suggestive of CC, transabdominal US is commonly used in the initial phase of CC diagnostics. The technique is helpful to investigate the cause of bile duct obstruction and to characterize liver lesions. Recent technical advances, including transabdominal and endoscopic US applications, and also the use of contrast-enhanced US indicate great potential for the evaluation of both luminal and extraluminal masses in CC diagnosis. A detailed discussion of the role of US in the diagnosis of CC, however, is beyond the scope of this review as it is mainly focusing on the cross-sectional imaging techniques CT, MRI, and PET/CT. When CC is suspected in US due to dilatation of the intrahepatic biliary or an intrahepatic mass, further investigations are generally performed with a second-level imaging modality such as CT or MRI.
Computed Tomography
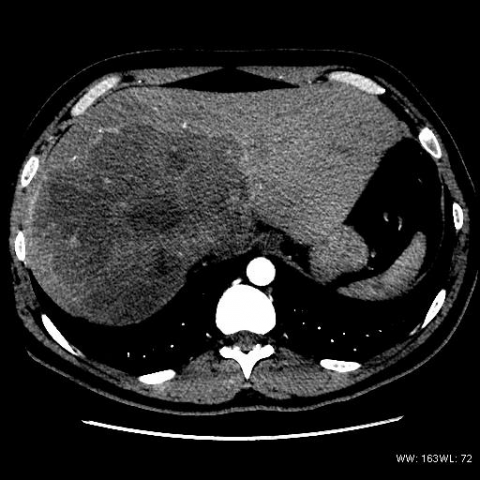
CT is performed in up to 90% of suspected CC, offering the opportunity of assessing the full extension of the tumour and determining potential surgical resectability. Additionally, pathological details, such as vascular infiltration and the presence of lymph node metastasis, can be estimated. In primary staging of CC, multiphase CT scanning protocols are recommended. By means of pre-contrast scanning (fig. (fig.2A), 2A ), intraductal stones (as one of the risk factors of CC) can be identified [ 11 , 12 ]. In the arterial phase, the exact arterial anatomy of the liver and surrounding structures can be displayed, allowing for planning the surgical method in detail (fig. (fig.2B). 2B ). In the portal venous phase (fig. (fig.2C), 2C ), CC mainly show incomplete rim-like contrast enhancement at the tumour periphery and low intratumoural attenuation, increasing the precision in estimating the tumour size and the detection of satellite nodules [ 13 ]. In late-phase scans (5-10 min after contrast injection), a late enhancement of the tumour can be observed, representing the amount of fibrous stroma. In case of tumour necrosis and/or mucin-containing cells, the delayed enhancement may disappear [ 14 ]. Due to the volumetric scanning technique, CT images can be used in preoperative management to estimate the liver volume and potential liver remnants, avoiding postoperative small-for-size-syndrome [ 15 , 16 ]. Based on this information, alternative surgical procedures like ‘associating liver partition and portal vein ligation for staged hepatectomy’ (ALPPS) can be considered [ 17 ]. As already described, the main morphologic pattern of iCC can be characterized as mass-forming, periductal infiltrating, and intraductal growth which can be visualized using CT imaging.

CT images of an iCC. A In non-contrast enhanced images, a hypodense area is present in liver segment V-VI/VII-VIII. B Tumour vascularity can be visualized in major intensity projections of arterial-phase images. C The exact tumour size with peripheral enhancement and typical hypodense areas in the lesion centre are shown in portal-venous phase CT images.
Mass-forming iCC usually appears as a homogeneous low-attenuating mass on non-contrast-enhanced scans. After contrast media injection, an irregular peripheral enhancement with only minor enhancement in the centre of the tumour can be observed [ 13 ]. The degree of central contrast enhancement is increasing from arterial- to late-phase images and depends on the amount of central tumour fibrosis. Additional findings like capsular retraction and dilatation of bile ducts distal to the mass are typical. Narrowing of portal or hepatic veins is observed less frequently. Vascular invasion typically leads to lobar or segmental atrophy of the liver [ 18 ]. Periductal infiltrating iCC is characterized by a growth pattern along the bile duct without mass formation. The involved bile ducts can be dilated or narrowed but show diffuse periductal thickening with increased enhancement from arterial- to delayed-phase CT. Usually, a dilatation of the distal bile ducts is present [ 13 ]. Intraductal growth of iCC is primarily characterized by an irregular duct calibre. Usually, focal duct ectasia with or without a visible intraductal mass can be detected. In case of intraductal mass, a hypoattenuation with irregular margins can be observed on pre-contrast imaging, showing increasing contrast enhancement in portal venous- and delayed-phase images [ 13 ]. Imaging-based preoperative differentiation of growth pattern of eCC into nodular, sclerosing, and papillary remains challenging and does not seem to be of primary importance concerning the surgical strategy [ 19 ].
Primary Staging of Intrahepatic Cholangiocarcinoma
The literature on staging iCC by CT is poor. Prognosis of iCC depends on the tumour size, lymph node metastasis, quantity of hepatic tumours or intrahepatic metastasis, and vascular invasion. In comparison with MRI, CT seems to be more sensitive in detecting vascular involvement and extrahepatic invasion; therefore, it may be advantageous in the primary staging of iCC [ 20 ]. Additionally, CT might be more accurate than MRI in predicting the resectability of iCC, with an accuracy of up to 88% and a negative predictive value of 85-100% [ 21 ].
Primary Staging of Perihilar Cholangiocarcinoma
Based on 16 articles, a meta-analysis from 2012 estimated the accuracy of CT in staging pCC [ 22 ]. When judging the ductal extent of the tumour, CT showed an overall diagnostic accuracy of 86% (95% confidence interval (CI): 77-92%). Portal vein involvement was detected by CT with a sensitivity of 89% (95% CI: 80-94%) and a specificity of 92% (95% CI: 85-96%). CT diagnosis of hepatic artery involvement showed a sensitivity of 84% (95% CI: 63-94%) and a specificity of 93% (95% CI: 69-99%). The accuracy of CT in detecting lymph node metastasis seems to be limited, with a reported sensitivity of 61% (95% CI: 28-86%) and a specificity of 88% (95% CI: 74-95%). Concerning the evaluation of distant metastasis, CT showed a sensitivity of 67% and a specificity of 94%. So far, there are only a few studies which directly compare the accuracy of CT and MRI in the staging of pCC with controversial findings. In one study, the accuracy of estimating the intraductal tumour size was a little higher for MRI (71%) than for CT (64%) [ 23 ]. A second study favoured CT with an accuracy of 80% (MRI 75%) for the estimation of the intraductal tumour size [ 24 ].

Primary Staging of Extrahepatic Cholangiocarcinoma
In the staging of eCC, determining the exact tumour localization and its longitudinal and lateral expansion is of primary importance as the surgical resection method and the patient's prognosis both depend on these factors. Tumour localization is commonly described by using the modified Bismuth-Corlette classification (type I involves the common hepatic duct, type II involves the hepatic duct bifurcation, types IIIA and IIIB involve the right and left hepatic ducts, respectively, and type IV involves both the right and left hepatic ducts) [ 25 ]. Following the current T staging based on the seventh edition of the American Joint Committee on Cancer (AJCC) staging system [ 26 ], proximal and distal eCC are differentiated and T1 tumours are limited to the bile duct, whereas T2 tumours extend beyond the wall of the bile duct. With imaging (CT, MRI) and even in histopathology, the exact determination of the border of the bile duct is difficult [ 27 ]. Therefore, an accurate preoperative distinction of T1 and T2 tumours does not seem to be possible. Up to now, little is known about the exact accuracy of CT in the staging of eCC. The main issue constitutes the determination of tumour spread outside the wall of the bile duct, potentially affecting adjacent structures like the portal vein and hepatic artery, the hepatoduodenal ligament, and the head of the pancreas in T3 and T4 tumours. Preoperative CT-based three-dimensional space (3D) angiography and multiphase fusion imaging technique may be helpful in planning the surgical intervention, potentially minimizing operating time, the extent of surgical resection, and blood loss [ 28 ].
In mass-forming iCC, the degree of enhancement on delayed-phase CT scans seems to be a potential prognostic indicator. Asayama et al. [ 29 ] postulated a worse prognosis for patients with an intratumoural enhancement greater than two thirds on the delayed images. Two studies including 42 and 70 patients with iCC and operative resection showed strong correlations between augmented arterial tumour enhancement in preoperative CT, histopathological vascularity, and higher survival rate. Histological examination of these tumours demonstrated a smaller amount of fibrotic tissue and necrosis but a higher cellularity [ 30 , 31 ]. The estimated overall accuracy of CT in evaluating tumour resectability ranges between 60 and 75% [ 32 , 33 ].
Recurrent Disease
The probability of local recurrence and distant metastasis in iCC is high. Hyder et al. [ 34 ] analysed recurrence patterns of 301 patients who underwent surgical resection of iCC between 1990 and 2011. During the follow-up of 31 months, 53.5% patients developed recurrent, 60.9% intrahepatic, 21% extrahepatic, and 18.6% simultaneous intra- and extrahepatic disease [ 34 ]. Most frequently, metastases are found in the lungs (24%), peritoneum (18%), and bones (14%) [ 35 ]. Therefore, follow-up restaging CT in CC patients has to cover the thorax and main part of the skeletal system.
Novel Computed Tomography Techniques
Contrast-enhanced dual-energy CT (DECT) offers the opportunity of calculating virtual non-enhanced images, thus allowing the detection of bile duct stones without pre-contrast scanning [ 36 ]. Additionally, hepatic calcifications can be accurately diagnosed when using this technique. Due to the utilization of iodine mapping and monoenergetic extrapolation, the detectability of vascularity of the liver and thrombosis can be improved [ 37 , 38 ]. Marin et al. [ 39 ] showed a significant improvement of the conspicuity of hypervascular liver tumours by using low-keV (kilo electron volt) monoenergetic reconstructions. Analysing the virtual spectral curves from monoenergetic reconstructions of focal liver lesions might be helpful in differentiating benign from malign liver tumours [ 40 ]. Potential risk factors of CC like steatosis and iron overload can be estimated by employing dedicated DECT post-processing techniques [ 41 , 42 ]. Functional imaging of volume perfusion CT (VPCT) can help to assess the exact vascularization of the tumour in CC. Compared with the normal parenchyma, CC usually shows increased hepatic arterial perfusion, increased blood volume, and decreased portal perfusion [ 43 , 44 ]. Due to novel treatment regimens such as anti-angiogenetic drugs or targeted therapies, VPCT might be a helpful monitoring tool for judging treatment response by revealing changes in tumour vascularization in the absence of significant changes in tumour size [ 18 ]. Novel techniques in CT post-processing like frequency-selective non-linear blending may offer additional benefits in the diagnosis of CC [ 45 ].
Magnetic Resonance Imaging
In recent years, the field of abdominal MRI experienced a tremendous development, resulting in more reliable imaging sequences and increased image quality, which in turn led to improved tumour detectability, for instance in the case of liver tumours [ 46 ]. In comparison to other imaging techniques, MRI enables higher tissue contrast. According to current guidelines, MRI is the modality of choice for the diagnosis and staging of CC [ 47 ].
For the assessment of CC, comprehensive imaging protocols not only including the liver but also covering the biliary tract and pancreas should be applied in order to rule out other malignancies such as pancreatic head adenocarcinoma. A typical MRI protocol for the assessment of CC encompasses magnetic resonance cholangiopancreatography (MRCP), conventional T1- and T2-weighted sequences, as well as diffusion-weighted imaging (DWI) and dynamic contrast-enhanced (DCE) MRI [ 48 ]. Furthermore, MRI with hepatocyte-specific contrast agents is often performed for the assessment of CC [ 49 ].
MRCP is a non-contrast MRI technique for assessing the biliary system [ 50 ]. In fact, MRCP is the most accurate non-invasive imaging technique for the assessment of the biliary system [ 51 ]. It allows accurate tumour assessment in both proximal and distal bile ducts [ 51 ]. For appropriate depiction of the biliary system in MRCP, heavily T2-weighted sequences with very long echo time are obtained, resulting in high (i.e. hyperintense) fluid signal in the bile ducts and low (i.e. suppressed) background signal [ 48 ]. MRCP sequences are usually acquired using a combination of thick-slab radial T2 sequences and thin 3D T2 sequences. The thick-slab sequences provide a good overview of the biliary system with a good suppression of the surrounding tissue, whereas the thin 3D T2 sequences provide high spatial resolution and allow for the detection of small abnormalities in the bile ducts such as small masses and/or strictures [ 48 ].
In addition to MRCP, which is useful for depicting intraductal CC tumour growth, DWI, DCE-MRI, and late-phase sequences with hepatocyte-specific contrast agents are helpful in the assessment of extraductal tumour growth as well as in the depiction of tumour masses within dilated bile ducts [ 48 , 52 ].
MRI, especially in combination with MRCP, has a high diagnostic accuracy for the assessment of CC. Park et al. [ 53 ] showed that MRCP and MRI revealed a comparable diagnostic accuracy with invasive cholangiography combined with CT imaging for the detection of CC.
Preoperative MRI is commonly performed in patients with CC in order to assess the extent, resectability, and vascular involvement of the tumour. It is also employed for road mapping of the hepatic vessels and for visualization of vascular anatomic variants. Accurate preoperative assessment of liver vasculature has been shown to significantly affect the surgical outcome in patients with CC [ 54 ].
Besides the preoperative staging and follow-up imaging of CC, MRI and MRCP play a central role in the surveillance of patients with an increased risk of CC, e.g. those with PSC. The lifetime incidence of CC in patients with PSC ranges from 5 to 10% [ 48 ]. According to recent recommendations, MRI including MRCP is appropriate for the surveillance of those patients [ 55 ].
Magnetic Resonance Imaging of Mass-Forming Cholangiocarcinoma
Mass-forming CC are often seen in iCC and usually appear as T1 iso- or hypointense as well as T2 hyperintense [ 56 ]. Contrast enhancement of mass-forming iCC is variable. The most frequent pattern is peripheral enhancement on early images, which progresses on late images [ 57 ] (fig. (fig.3). 3 ). Contrast enhancement patterns depend on the tumour size, structure, and composition; small tumours with less fibrotic tissue may show homogeneous enhancement, whereas large fibrotic tumours may only enhance in late images.

MRI of a 64-year-old female patient with mass-forming CC of the right liver lobe. The CC appears hyperintense on T2-weighted images with diffusion restriction on DWI and shows a typical contrast enhancement pattern on the DCE-MRI.
When using hepatocyte-specific contrast agent, mass-forming iCC often has a cloud-like appearance with a central hyperintense area and a rim with lower signal intensity [ 58 ].
Extrahepatic ductal CC can also appear as a mass mimicking pancreatic adenocarcinoma. In these cases, assessment of the pancreatic duct on MRCP can help to differentiate both tumour entities.
Magnetic Resonance Imaging of Periductal Cholangiocarcinoma
Periductal growth is usually seen in pCC and eCC [ 59 ]. Periductal CC grows alongside the wall of the bile duct, resulting in wall thickening and narrowing of the affected segment and dilation of the proximal intrahepatic bile ducts as seen on T2-weighted images and MRCP (fig. (fig.4) 4 ) [ 60 ]. Periductal CC usually shows slow contrast enhancement, which is best seen in late contrast-enhanced images [ 59 ].

A Coronal T2-weighted image and B MRCP of a 75-year-old female patient with periductal CC. The MRCP shows narrowing of the proximal biliary ducts (arrow) and dilation of the intrahepatic ducts.
Magnetic Resonance Imaging of Intraductal Cholangiocarcinoma
Similar to mass-forming CC, intraductal CC begins to enhance on early post-contrast images, with peak enhancement on late post-contrast images [ 18 ]. MRCP is very suitable for the detection of intraductal CC, with a higher diagnostic accuracy when compared to CT [ 18 , 48 ].
Positron Emission Tomography/ Computed Tomography
Primary staging.
PET/CT is increasingly being recognized as a diagnostic tool in order to provide valuable information for the evaluation of CC. Regarding primary tumour detection in PET/CT, a meta-analysis of 1,232 patients in 23 studies provided high sensitivities of 95% and specificities of 83% for iCC [ 61 ], with a decrease to 84% and 76% in sensitivity and to 95% and 74% in specificity being found when evaluating pCC and eCC, respectively. This indicates a dependency of primary tumour evaluation on tumour localization. Other studies provide even lower sensitivities of 55% for primary staging of pCC in 18 F-FDG ( 18 F-fluorodeoxyglucose) PET/CT [ 62 ]. Other false-negative issues include infiltrative growth, periductal sclerosing, and tumours with a high fraction of mucin [ 63 ]. The diagnostic performance of 18 F-FDG PET/CT in primary tumour evaluation of CC, however, depends on several aspects. First of all, there may be false-positive results due to concomitant inflammatory changes of the bile ducts, caused either by tumour-induced bile retention or chemotherapy or following invasive procedures such as implantation of intraluminal bile duct stents. Furthermore, 18 F-FDG PET/CT is limited in detecting small tumours, as only tumours > 1 cm in diameter are eligible for confident detection by this method [ 64 , 65 ]. Additionally, the different histopathological subtypes and the anatomical location of the tumour need to be considered when performing 18 F-FDG PET/CT.
Several studies indicate that in eCC especially, late 18 F-FDG PET imaging (image acquisition after injection 120 min and longer) could be helpful in differentiating benign bile duct strictures from malignant tumours. This theory is based on the continuous uptake of 18 F-FDG in malignant cells over 3 h, whereas benign diseases tend to show a decline in 18 F-FDG uptake over time. This approach might be a helpful tool when using semiquantitative [ 66 ] or visual assessment [ 67 ], with a small increase in diagnostic sensitivity (76 vs. 79%) and accuracy (76 vs. 80%) being found, whereas specificity remained the same (80%) in 39 patients, thereof 34 patients with CC [ 66 ]. Although some studies indicate a correlation between tumour-to-normal liver ratio (TNR) and standardized uptake values (SUV) in 18 F-FDG PET/CT (65 patients, thereof 47 CC patients) [ 68 ], other studies could not confirm this finding and did not find any correlation between tumour marker levels and SUV values (65 patients with ICC) [ 69 ]. However, it is worth noting that 18 F-FDG PET/CT-induced therapy regimens have been reported in 17-24% [ 69 ], indicating a substantial merit of this hybrid technique regarding the correct evaluation of N and M staging. Determination of N staging is crucial because it correlates with the 5-year survival rates which vary from 27% for N1 (regional lymph nodes in the hepatoduodenal ligament) to 50% for N0 [ 70 ]. Special emphasis lies on the detection of the N2 stage (lymph nodes periaortic, pericaval, or adjacent to the mesenteric or celiac artery), as these are being considered as a contraindication for tumour resection [ 70 ]. 18 F-FDG PET/CT showed a significantly higher specificity (88.2 vs. 64.7%) and accuracy (75.9 vs. 60.9%) for N staging in comparison to CT alone (sensitivity: PET/CT 80% vs. CT 20%; specificity: 92.3 vs. 86.4%, respectively) [ 63 , 71 ]. However, Kluge et al. [ 72 ] examined the role of PET in the diagnosis and staging of CC and did not confirm a positive N staging in their collective of 26 patients; they did mention the significant influence of 18 F-FDG PET on M staging (metastases in liver, peritoneal cavity, distant lymph nodes, lung, bones, and brain), though. As advanced biliary cancer shows huge metabolic differences between the tumours [ 73 ] and detection of peritoneal carcinomatosis is difficult even in 18 F-FDG PET/CT imaging, the additional information of 18 F-FDG PET/CT regarding primary staging of CC in general was relatively low in comparison to conventional imaging including diagnostic laparoscopy [ 22 ]. However, the usefulness of preoperative 18 F-FDG PET/CT in CC for N and M staging is stated in the National Comprehensive Cancer Network (NCCN) guidelines [ 74 ].
In conclusion, the evaluation of tumour resectability by means of different imaging methods reveals that CT imaging is the standard, with high reported sensitivities and specificities (for pCC: sensitivity 91-97%, specificity 63-75%) but with limitations in small hepatic lesions and small lymph node metastasis, where PET/CT seems a promising diagnostic tool. MRI provides comparable results (sensitivity 90-97%, specificity 60-81%), with limitations concerning the evaluation of the vessel involvement with a decreased sensitivity of 73% [ 75 ].
Even in the 30% of patients with apparently primarily resectable tumours according to imaging, tumour recurrence occurs in up to 60-80% in the following 5 years [ 76 ]. The localization of tumour recurrence is mainly next to the resection zone and the hilum including locoregional lymph nodes [ 77 ]. Standardized imaging follow-up includes conventional imaging with CT or MRI [ 78 ]. In case of elevated tumour markers but negative conventional imaging, 18 F-FDG PET is helpful in the detection of recurrence (sensitivity 89%, specificity 100%; study with 33 patients) [ 79 ], with even higher values in 18 F-FDG PET/CT ( 18 F-FDG PET/CT sensitivity 94%, specificity 100% vs. CT sensitivity 82%, specificity 43%; study with 16 patients). Seo et al. [ 65 ] suggested that PET/CT may also provide prognostic information as tumour recurrence could be predicted by 18 F-FDG PET/CT. This hypothesis is based on a study that found a lower disease-free survival if the primary tumour showed high metabolic activity with a cut-off value of SUV mean 8.5 (study based on 27 patients with iCC). Another study (25 patients) with distal bile duct adenocarcinoma revealed total lesion glycolysis (TLG) as a better prognostic marker in primarily resected patients than SUV max [ 80 ]. Onal et al. [ 81 ] reported that 18 F-FDG PET/CT may be useful for radiation planning, with a possible dose reduction for adjacent organs at risk of 17% (right kidney, liver; study in 15 patients with eCC).
In conclusion, 18 F-FDG PET/CT seems to be a promising diagnostic tool in the primary staging of CC regarding N and M status. 18 F-FDG PET/CT plays a major role in the detection of tumour recurrence where this hybrid modality has great potential for differentiating between post-therapeutic changes (including fibroses due to radiotherapy) and tumour recurrence (fig. (fig.5) 5 ) [ 82 ]. Moreover, PET/CT may be useful for the monitoring of treatment response, as metabolic changes may precede the anatomical ones [ 83 , 84 ] (fig. (fig.6, 6 , ,7 7 ).

18 F-FDG-PET/CT for restaging of a 46-year-old male patient with iCC after chemotherapy. Hypodense iCC ( A ) with high tracer uptake indicating high metabolism of the lesion ( B ). After systemic therapy, central necrosis occurred ( C ) which cannot be visualized in CT alone ( D ).

45-year-old male patient. Status post hemihepatectomy for pCC 3 years ago. In CT, a small hypodense liver lesion adjacent to surgical clips is seen ( A ) with elevated 18 F-FDG uptake ( B ) indicative for tumour recurrence. In addition to the local recurrence, two paracardial lymph nodes ( C ) show high FDG uptake in PET, which is suspicious for lymph node metastases ( D ).

49-year-old female patient after resection of pCC. In follow-up imaging, post-therapeutic changes were noticed at the resection margin (slight hyperintensity in the T2-weighted images of MRI; arrow). A Adjacent to surgical clips which are visible in CT ( B ). However, differentiation between local fibrotic changes and tumour recurrence was not possible based on the morphologic appearance in CT and MRI alone. In the fused 18 F-FDG-PET/CT, focal 18 F-FDG uptake was found in the corresponding area indicating tumour recurrence at the resection margin ( C ).
Disclosure Statement
The authors declare that no conflicts of interest exist.

- Mass-forming intrahepatic cholangiocarcinoma
- Report problem with article
- View revision history
Citation, DOI, disclosures and article data
At the time the article was created Bruno Di Muzio had no recorded disclosures.
At the time the article was last revised Joshua Yap had no financial relationships to ineligible companies to disclose.
- Peripheral cholangiocarcinomas
- Intrahepatic mass-forming cholangiocarcinoma
Mass-forming intrahepatic cholangiocarcinomas (MF-ICC) , also referred as peripheral cholangiocarcinomas , comprise one of the three recognized growth patterns of intrahepatic cholangiocarcinomas .
On imaging, these tumors usually present as large and relatively well-defined hepatic masses with lobulated margins and showing peripheral rim enhancement. They are often associated with peripheral biliary dilatation .
On this page:
Epidemiology, clinical presentation, radiographic features, differential diagnosis.
- Related articles
- Cases and figures
Mass-forming intrahepatic cholangiocarcinomas are associated with chronic liver diseases , including viral hepatitis 5 .
These tumors tend to present late as larger masses as they rarely cause symptoms when smaller, early in their natural history 4 .
The mass-forming subtype is the most common among the intrahepatic cholangiocarcinomas 4 .
Mass-forming tumors mostly originate from cholangiocarcinomas in the peripheral small bile ducts and, rarely, from a mixed presentation of large duct cholangiocarcinomas with both periductal and mass-forming lesions 5 .
Macroscopic appearance
Peripheral cholangiocarcinomas are commonly large white tumors with dense fibrosis 4 .
Reported mutations associated with mass-forming cholangiocarcinoma include KRAS, TP53, DH1/2, FGFR2 fusions, BAP1, BRAF, ARID1A, SMAD4, and IDH1 8 .
General morphological features that commonly guide radiologists to the diagnosis of mass-forming intrahepatic cholangiocarcinoma are the associated capsular retraction and distal bile duct dilatation.
The enhancement pattern seen on post-contrast dynamic images can be quite variable, depending on tumor size and degree of differentiation. Be aware that enhancement features of mass-forming intrahepatic cholangiocarcinoma and hepatocellular carcinomas can overlap when tumors are smaller than 3 cm and in cirrhotic livers 7 .
These tumors present as a homogeneous and well-delineated liver mass, which commonly has intermediate echogenicity and irregular contours. Other features may include:
- peripheral hypoechoic halo of compressed liver parenchyma
- often associated with capsular retraction 1
- dilated bile ducts distal to the mass
Mass-forming cholangiocarcinomas are relatively well-defined and markedly hypodense on the non-contrast studies. On dynamic post-contrast scans:
- arterial enhancement has been associated with better prognosis 6
- the central part of the tumor usually does not enhance during the early phases, but frequently show gradual centripetal prolonged enhancement at delayed-phases 1,2,4
- rate and extent of enhancement depend on the degree of central fibrosis 1
The bile ducts distal to the mass are typically dilated.
Again, capsular retraction may be evident and is highly suggestive of this etiology. Lobar or segmental hepatic atrophy is usually associated with vascular invasion 3 .
Although narrowing of the portal veins (or less frequently, hepatic veins) is seen, unlike hepatocellular carcinoma, cholangiocarcinoma only rarely forms a tumor thrombus 1 .
- T1: hypointense 7
- T2: hyperintense 7
- central dark area on DWI may represent fibrosis and necrosis 7
- this appearance, although not specific and only seen in less than 50% of cases, helps in distinguishing the mass from a hepatocellular carcinoma
- hypoenhancement reflects poor differentiation
- rim enhancement reflects intermediate differentiation
- diffuse enhancement reflects a well-differentiated tumor
For a mass-forming intrahepatic cholangiocarcinoma consider:
- may appear very similar, particularly in tumors smaller than 3 cm and in a cirrhotic liver 7
- intralesional fat
- diffuse hyperintensity on unenhanced T1 weighted imaging
- nodule-in-nodule appearance
- capsular enhancement in the portal and delayed phases
- tumor thrombus
- capsular retraction is uncommon
- central necrosis (high T2 signal) is more common
- multiplicity is more common
- other primary liver tumors
- 1. Chung YE, Kim MJ, Park YN et-al. Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics. 29 (3): 683-700. doi:10.1148/rg.293085729 - Pubmed citation
- 2. Han JK, Choi BI, Kim AY et-al. Cholangiocarcinoma: pictorial essay of CT and cholangiographic findings. Radiographics. 22 (1): 173-87. Radiographics (full text) - Pubmed citation
- 3. Vilgrain V. Staging cholangiocarcinoma by imaging studies. HPB (Oxford). 2008;10 (2): 106-9. doi:10.1080/13651820801992617 - Free text at pubmed - Pubmed citation
- 4. Joon Koo Han, Byung Ihn Choi, Ah Young Kim, Su Kyung An, Joon Woo Lee, Tae Kyung Kim, Sun-Whe Kim. Cholangiocarcinoma: Pictorial Essay of CT and Cholangiographic Findings1. (2002) RadioGraphics. 22 (1): 173-87. doi:10.1148/radiographics.22.1.g02ja15173 - Pubmed
- 5. Hyungjin Rhee, Myeong-Jin Kim, Young Nyun Park, Chansik An. A proposal of imaging classification of intrahepatic mass-forming cholangiocarcinoma into ductal and parenchymal types: clinicopathologic significance. (2019) European Radiology. 29 (6): 3111. doi:10.1007/s00330-018-5898-9 - Pubmed
- 6. Ji Hye Min, Young Kon Kim, Seo-Youn Choi, Tae Wook Kang, Soon Jin Lee, Jong Man Kim, Soohyun Ahn, Hyun Cho. Intrahepatic Mass-forming Cholangiocarcinoma: Arterial Enhancement Patterns at MRI and Prognosis. (2019) Radiology. 290 (3): 691-699. doi:10.1148/radiol.2018181485 - Pubmed
- 7. Nieun Seo, Do Young Kim, Jin-Young Choi. Cross-Sectional Imaging of Intrahepatic Cholangiocarcinoma: Development, Growth, Spread, and Prognosis. (2017) American Journal of Roentgenology. 209 (2): W64-W75. doi:10.2214/AJR.16.16923 - Pubmed
- 8. Jesus M. Banales, Jose J. G. Marin, Angela Lamarca, Pedro M. Rodrigues, Shahid A. Khan, Lewis R. Roberts, Vincenzo Cardinale, Guido Carpino, Jesper B. Andersen, Chiara Braconi, Diego F. Calvisi, Maria J. Perugorria, Luca Fabris, Luke Boulter, Rocio I. R. Macias, Eugenio Gaudio, Domenico Alvaro, Sergio A. Gradilone, Mario Strazzabosco, Marco Marzioni, Cédric Coulouarn, Laura Fouassier, Chiara Raggi, Pietro Invernizzi, Joachim C. Mertens, Anja Moncsek, Sumera Rizvi, Julie Heimbach, Bas Groot Koerkamp, Jordi Bruix, Alejandro Forner, John Bridgewater, Juan W. Valle, Gregory J. Gores. Cholangiocarcinoma 2020: the next horizon in mechanisms and management. (2020) Nature Reviews Gastroenterology & Hepatology. 17 (9): 557. doi:10.1038/s41575-020-0310-z - Pubmed
Incoming Links
- Target sign (disambiguation)
- Target sign (cholangiocarcinoma)
- Metastatic skull and right orbital masses
- Mass forming cholangiocarcinoma
Related articles: Pathology: Hepato-Pancreato-Biliary
- hepatic amyloidosis
- hepatic hemosiderosis
- Wilson disease
- liver abscess
- alveolar echinococcosis
- intrabiliary rupture
- World Health Organization 2001 classification of hepatic hydatid cysts
- Child-Pugh grading system
- portal hypertension
- regenerative nodule
- acute hepatitis
- autoimmune hepatitis
- lupoid hepatitis
- non-alcoholic steatohepatitis
- hepatitis A virus
- hepatitis B virus
- hepatitis C virus
- hepatitis D virus
- hepatitis E virus
- acute acalculous cholecystitis
- gangrenous cholecystitis
- gallbladder empyema
- sonographic Murphy's sign
- chronic cholecystitis
- primary sclerosing cholangitis
- chemotherapy-induced cholangitis
- eosinophilic cholangitis
- EBV cholangitis
- ascending cholangitis
- recurrent pyogenic (Oriental) cholangitis
- hepatic regenerative nodule
- focal nodular hyperplasia
- inflammatory hepatic adenoma
- HNF 1 alpha mutated hepatic adenoma
- beta-catenin mutated hepatic adenoma
- unclassified hepatic adenoma
- hepatic adenomatosis
- simple hepatic cysts
- ciliated hepatic foregut cyst
- polycystic liver disease
- intrahepatic bile duct adenoma
- intrahepatic bile duct cystadenoma
- hepatic angiomyolipoma
- hepatic lymphangioma and hepatic lymphangiomatosis
- infantile hemangioendothelioma
- hepatic leiomyoma
- hepatocellular carcinoma
- fibrolamellar hepatocellular carcinoma
- spindle cell hepatocellular carcinoma
- hepatic carcinosarcoma
- mass-forming type
- periductal infiltrating type - Klatskin tumors
- intraductal growing type
- extra-hepatic/large duct type
- biliary cystadenocarcinoma
- combined hepatocellular and cholangiocarcinoma
- hepatoblastoma
- undifferentiated carcinoma
- epithelioid hemangioendothelioma
- hepatic angiosarcoma
- hepatic embryonal sarcoma
- hepatic rhabdomyosarcoma
- hepatic leiomyosarcoma
- malignant schwannoma
- hepatic fibrosarcoma
- malignant fibrous histiocytoma
- osteosarcoma
- primary hepatic lymphoma
- hepatic myeloid sarcoma (hepatic chloroma)
- cystic hepatic metastases
- pseudocirrhosis
- adrenal rest tumors
- hepatic fibroma
- hepatic hemangioma
- hepatic Kaposi sarcoma
- pseudolipoma of the Glisson capsule
- hepatic mesenchymal hamartoma
- hepatic myxoma
- hepatic rhabdoid tumor
- hepatic solitary fibrous tumor
- hepatic teratoma
- hepatic yolk sac tumor
- inflammatory myofibroblastic tumor (inflammatory pseudotumor)
- nodular regenerative hyperplasia
- pancreatic rest tumors
- primary hepatic carcinoid
- acute fatty liver of pregnancy
- grading of diffuse hepatic steatosis
- focal hepatic steatosis
- nonalcoholic fatty liver disease
- grading liver trauma
- gallbladder trauma
- cavernous transformation of the portal vein
- extra-hepatic portal vein obstruction
- congenital extrahepatic portosystemic shunt classification
- portal vein calcification
- portal venous aneurysm
- portal venous gas
- Abernethy malformation
- congenital intrahepatic portosystemic shunt classification
- transjugular intrahepatic portosystemic shunt (TIPS)
- porto-portal shunt
- variant hepatic arterial anatomy
- hepatic artery occlusion
- arterioportal shunt
- arteriosystemic venous shunt
- transient hepatic attenuation differences (THAD)
- transient hepatic intensity differences (THID)
- venous-venous shunts
- hepatic sinusoidal dilatation
- sinusoidal obstruction syndrome
- nutmeg liver
- peliosis hepatis
- inferior vena cava web
- inferior vena cava thrombosis
- focal fatty sparing of the liver
- liver thrombotic angiitis
- infra diaphragmatic total anomalous pulmonary venous return (TAPVR)
- hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease)
- Tanaka criteria
- mucinous cystadenoma of pancreas
- mucinous cystadenocarcinoma of pancreas
- serous cystadenoma
- pancreatic intraepithelial neoplasia
- solid pseudopapillary tumor of pancreas
- Whipple triad
- Zollinger-Ellison syndrome
- gastrinoma triangle
- glucagonoma
- somatostatinoma
- non-syndromic
- pancreatic neurofibroma
- pancreatic schwannoma
- pancreatic ganglioneuroma
- pancreatic desmoid tumor
- pancreatic lipoma
- pancreatic perivascular epithelioid cell tumor (PEComa)
- pancreatic mature cystic teratoma (dermoid)
- pancreatic lymphangioma
- pancreatic lymphoma
- pancreatoblastoma
- pancreatic metastases
- simple pancreatic cyst
- gallstone pancreatitis
- interstitial edematous pancreatitis
- necrotizing pancreatitis
- hemorrhagic pancreatitis
- walled-off necrosis (WON)
- CT severity index
- Balthazar score
- Ranson criteria
- APACHE score
- mass-forming chronic pancreatitis
- Ascaris -induced pancreatitis
- tropical pancreatitis
- diagnostic criteria
- emphysematous pancreatitis
- hypertriglyceridemia-induced pancreatitis
- hereditary pancreatitis
- pancreatitis associated with cystic fibrosis
- pancreaticopleural fistula
- paraduodenal pancreatitis
- pancreatic atrophy
- pancreatic lipomatosis
- grading of pancreatic trauma
- pseudopancreatitis
- pancreatic transplant
- gallbladder phrygian cap
- gallbladder agenesis
- gallbladder duplication
- septate gallbladder
- Caroli disease
- hepatisation of the gallbladder
- limy bile/milk of calcium bile
- Mirizzi syndrome
- choledocholithiasis
- low phospholipid-associated cholelithiasis syndrome
- twinkling artefact
- wall-echo-shadow sign
- rolling stone sign
- Mercedes-Benz sign
- emphysematous cholecystitis
- acalculous cholecystitis
- perforated gallbladder
- hemorrhagic cholecystitis
- xanthogranulomatous cholecystitis
- primary biliary cholangitis
- diffuse gallbladder wall thickening (differential)
- focal gallbladder wall thickening (differential)
- adenomyomatosis
- strawberry gallbladder
- porcelain gallbladder
- cholesterol polyps
- inflammatory polyps
- benign gallbladder tumors
- benign vs malignant features
- gallbladder carcinoma
- gallbladder metastases
- gallbladder sarcoma
- gallbladder lymphoma
- ceftriaxone-associated gallbladder pseudolithiasis
- gallbladder volvulus/torsion
- gallbladder dysfunction
- vicarious contrast material excretion
- bile duct dilatation (differential)
- bile duct wall thickening (differential)
- biliary intraepithelial neoplasia (BilIN)
- intraductal papillary neoplasm of the bile duct (IPNB)
- intraductal tubulopapillary neoplasm (ITPN) of the bile duct
- biliary cystadenoma
- multiple biliary hamartomas (von Meyenburg complexes)
- cholangiocarcinoma
Promoted articles (advertising)
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers

Imaging of intrahepatic and hilar cholangiocarcinoma
- Original article
- Published: 08 June 2004
- Volume 29 , pages 548–557, ( 2004 )
Cite this article

- B. I. Choi 1 ,
- J. M. Lee 1 &
- J. K. Han 1
658 Accesses
67 Citations
Explore all metrics
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
PR Ros JL Buck ZD Goodman et al. (1988) ArticleTitle Intrahepatic cholangiocarcinoma: radiologic-pathologic correlation Radiology 67 689–693
Google Scholar
T Nakajima Y Kondo M Miyazaki K Okui (1988) ArticleTitle A histopathologic study of 102 cases of intrahepatic cholangiocarcinoma: histologic classification and mode of spreading Hum Pathol 19 1228–1234 Occurrence Handle 1:STN:280:BiaD3cnmtlA%3D Occurrence Handle 2844646
CAS PubMed Google Scholar
Y Nakanuma H Minato T Kida T Terada (1994) Pathology of cholangiocellular carcinoma T Tobe H Kameda M Okudaira M Ohto (Eds) Primary liver cancer in Japan Springer-Verlag Tokyo 39–50
AR Clemett (1985) ArticleTitle Carcinoma of the major bile ducts Radiology 84 894–903
WJ Lee HK Lim KM Jang et al. (2001) ArticleTitle Radiologic spectrum of cholangiocarcinoma: emphasis on unusual manifestations and differential diagnosis Radiographics 21 97–116
JK Han BI Choi AY Kim et al. (2002) ArticleTitle Cholangiocarcinoma: pictorial essay of CT and cholangiographic findings Radiographics 22 173–187 Occurrence Handle 11796906
PubMed Google Scholar
Y Zhang M Uchida T Abe et al. (1999) ArticleTitle Intrahepatic peripheral cholangiocarcinoma: comparison of dynamic CT and dynamic MRI J Comput Assist Tomogr 23 670–677 Occurrence Handle 10.1097/00004728-199909000-00004 Occurrence Handle 1:STN:280:DyaK1Mvlt1Cktg%3D%3D Occurrence Handle 10524843
Article CAS PubMed Google Scholar
P Pavon A Laghi R Passariello (1999) ArticleTitle MR cholangiopancreatography in malignant biliary obstruction Semin Ultrasound CT MR 20 317–323 Occurrence Handle 10.1016/S0887-2171(99)90063-X Occurrence Handle 10527137
Article PubMed Google Scholar
SH Zidi F Prat O Le Guen et al. (2000) ArticleTitle Performance characteristics of magnetic resonance cholangiography in the staging of malignant hilar strictures Gut 46 103–106 Occurrence Handle 10.1136/gut.46.1.103 Occurrence Handle 1:STN:280:DC%2BD3c%2FmvFGjuw%3D%3D Occurrence Handle 10601064
InstitutionalAuthorName Liver Cancer Study Group of Japan (2000) The general rules for the clinical and pathological study of primary liver cancer, 4th ed Kanehara Tokyo
A Sasaki M Aramaki K Kawano et al. (1998) ArticleTitle Intrahepatic peripheral cholangiocarcinoma: mode of spread and choice of surgical treatment Br J Surg 85 1206–1209 Occurrence Handle 10.1046/j.1365-2168.1998.00815.x Occurrence Handle 1:STN:280:DyaK1cvitlOrsA%3D%3D Occurrence Handle 9752860
M Yamamoto K Takasaki T Yoshikawa et al. (1998) ArticleTitle Does gross appearance indicate prognosis in intrahepatic cholangiocarcinoma J Surg Oncol 69 162–167 Occurrence Handle 10.1002/(SICI)1096-9098(199811)69:3<162::AID-JSO8>3.0.CO;2-L Occurrence Handle 1:STN:280:DyaK1M%2FmtV2gtQ%3D%3D Occurrence Handle 9846503
S Isaji Y Kawarada H Taoka et al. (1999) ArticleTitle Clinicopathological features and outcome of hepatic resection for intrahepatic cholangiocarcinoma in Japan J Hepatobil Pancreat Surg 6 108–116 Occurrence Handle 10.1007/s005340050092 Occurrence Handle 1:STN:280:DyaK1MzivFemuw%3D%3D
Article CAS Google Scholar
JH Lim (2003) ArticleTitle Cholangiocarcinoma: morphologic classification according to growth pattern and imaging findings AJR 181 819–827 Occurrence Handle 12933488
BI Choi JH Park YI Kim et al. (1988) ArticleTitle Peripheral cholangiocarcinoma and clonorchiasis: CT findings Radiology 169 149–153 Occurrence Handle 1:STN:280:BieA3snktlQ%3D Occurrence Handle 2843940
TK Kim BI Choi JK Han et al. (1997) ArticleTitle Peripheral cholangiocarcinoma of the liver: two-phase helical CT findings Radiology 204 539–543 Occurrence Handle 1:STN:280:ByiA1c3lsVI%3D Occurrence Handle 9240550
BI Choi JK Han TK Kim (1998) Diagnosis and staging of cholangiocarcinoma by computed tomography MA Meyers (Eds) Neoplasms of the digestive tract: imaging, staging and management Lippincott-Raven Philadelphia 503–516
BI Choi JK Han YM Shin et al. (1995) ArticleTitle Peripheral cholangiocarcinoma: comparison of MRI with CT Abdom Imaging 20 357–360 Occurrence Handle 1:STN:280:BymD2crgsVY%3D Occurrence Handle 7549743
MF Fan Y Yamashita M Harada et al. (1993) ArticleTitle Intrahepatic cholangiocarcinoma: spin-echo and contrast-enhanced dynamic MR imaging AJR 161 313–317 Occurrence Handle 1:STN:280:ByyA38rltFA%3D Occurrence Handle 8392787
JE Hamrick-Turner PL Abbitt PR Ros (1992) ArticleTitle Intrahepatic cholangiocarcinoma: MR appearance AJR 158 77–79 Occurrence Handle 1:STN:280:By2D1c7lsFc%3D Occurrence Handle 1309221
H Honda H Onitsuka K Yasumori et al. (1993) ArticleTitle Intrahepatic peripheral cholangiocarcinoma: two-phased dynamic incremental CT and pathological correlation J Comput Assist Tomogr 17 397–402 Occurrence Handle 1:STN:280:ByyB28%2Fhs1Y%3D Occurrence Handle 8388005
JM Lacomis RL Baron JH, III Oliver et al. (1997) ArticleTitle Cholangiocarcinoma: delayed CT contrast enhancement patterns Radiology 203 98–104 Occurrence Handle 1:STN:280:ByiB3s3ktVI%3D Occurrence Handle 9122423
BI Choi JK Han JM Cho et al. (1995) ArticleTitle Characterization of focal hepatic tumors: value of two-phase scanning with spiral computed tomography Cancer 76 2434–2442 Occurrence Handle 1:STN:280:BymB38zjtVc%3D Occurrence Handle 8625068
P Soyer DA Bluemke C Vissuzaine et al. (1994) ArticleTitle CT of hepatic tumors: prevalence and specificity of retraction of the adjacent capsule AJR 162 1119–1122 Occurrence Handle 1:STN:280:ByuB3MbjtFU%3D Occurrence Handle 8165994
HA Edmondson PE Steiner (1954) ArticleTitle Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies Cancer 7 462–503 Occurrence Handle 13160935
K Okuda Y Kubo N Okazaki et al. (1977) ArticleTitle Clinical aspects of intrahepatic bile duct carcinoma including hilar carcinoma: a study of 7 autopsy proven cases Cancer 39 232–246 Occurrence Handle 1:STN:280:CSiD1cbit1M%3D Occurrence Handle 64293
AC Friedman S Frazier TM Hendrix PR Ros (1994) Focal disease. Part I. The liver AC Friedman AH Dachman (Eds) Radiology of the liver, biliary tract, and pancreas Mosby St Louis 169–327
P Soyer DA Bluemke R Reichle et al. (1995) ArticleTitle Imaging of intrahepatic cholangiocarcinoma. 2. Hilar cholangiocarcinoma AJR 165 1433–1436 Occurrence Handle 1:STN:280:BymD2s3mvFY%3D Occurrence Handle 7484580
JH Lim C Yi HK Lim et al. (2002) ArticleTitle Radiological spectrum of intraductal papillary tumors of the bile ducts Korean J Radiol 3 57–63 Occurrence Handle 11919480
JW Lee JK Han TK Kim et al. (2000) ArticleTitle CT features of intraductal intrahepatic cholangiocarcinoma AJR 175 721–725 Occurrence Handle 1:STN:280:DC%2BD3cvnsFaruw%3D%3D Occurrence Handle 10954456
YS Kim ST Myung SY Kim et al. (1998) ArticleTitle Biliary papillomatosis: clinical, cholangiographic and cholangioscopic findings Endoscopy 30 763–767 Occurrence Handle 1:STN:280:DyaK1M7ivFGgtw%3D%3D Occurrence Handle 9932755
KH Yoon HK Han CG Kim et al. (2000) ArticleTitle Malignant papillary neoplasms of intrahepatic bile ducts: CT and histopathologic features AJR 175 1135–1139 Occurrence Handle 1:STN:280:DC%2BD3cvpvVyqsw%3D%3D Occurrence Handle 11000178
JH Lim MH Kim TK Kim et al. (2003) ArticleTitle Papillary neoplasms of the bile duct that mimic biliary stone disease Radiographics 23 447–455 Occurrence Handle 12640158
JK Han BI Choi TK Kim et al. (1997) ArticleTitle Hilar cholangiocarcinoma: thin-section spiral CT findings with cholangiographic correlation Radiographics 17 1475–1485 Occurrence Handle 1:STN:280:DyaK1c%2FlvFynug%3D%3D Occurrence Handle 9397459
BI Choi JK Han TK Kim (1998) Benign and malignant tumors of the biliary tree SG Gazelle (Eds) Hepatobiliary and pancreatic radiology Thieme New York 630–676
LA Wetter EJ Ring CA Pellegrini LW Way (1991) ArticleTitle Differential diagnosis of sclerosing cholangiocarcinoma of the common hepatic ducts (Klatskin tumors) Am J Surg 161 57–63 Occurrence Handle 10.1016/0002-9610(91)90361-G Occurrence Handle 1:STN:280:By6C3czjvFw%3D Occurrence Handle 1846276
LE Hann KV Greatrex AM Bach et al. (1997) ArticleTitle Cholangiocarcinoma at the hepatic hilus: sonographic findings AJR 168 985–989 Occurrence Handle 1:STN:280:ByiB2czjt1U%3D Occurrence Handle 9124155
JT Ferrucci (1994) ArticleTitle Liver tumor imaging: current concepts Radiol Clin North Am 32 39–54 Occurrence Handle 1:STN:280:ByuC3M3hvVU%3D Occurrence Handle 8284360
SC Stain HU Baer AR Dennison LH Blumgart (1992) ArticleTitle Current management of hilar cholangiocarcinoma Surg Gynecol Obstet 175 579–588 Occurrence Handle 1:STN:280:ByyD2sbmtlA%3D Occurrence Handle 1280374
H Honda Y Matsuura H Onitsuka et al. (1992) ArticleTitle Differential diagnosis of hepatic tumors (hepatoma, hemangioma, and metastasis) with CT: value of two-phase incremental imaging AJR 159 735–740 Occurrence Handle 1:STN:280:By2H3M7gs1U%3D Occurrence Handle 1326884
A Adam IS Benjamin (1992) ArticleTitle The staging of cholangiocarcinoma Clin Radiol 46 299–303 Occurrence Handle 1:STN:280:ByyD1MbntF0%3D Occurrence Handle 1334451
Download references
Author information
Authors and affiliations.
Department of Radiology and Institute of Radiation Medicine, Seoul National University, College of Medicine, 28, Yongon-Dong, Chongno-Gu, Seoul 110-744, Korea
B. I. Choi, J. M. Lee & J. K. Han
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
About this article
Choi, B., Lee, J. & Han, J. Imaging of intrahepatic and hilar cholangiocarcinoma. Abdom Imaging 29 , 548–557 (2004). https://doi.org/10.1007/s00261-004-0188-1
Download citation
Published : 08 June 2004
Issue Date : September 2004
DOI : https://doi.org/10.1007/s00261-004-0188-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cholangiocarcinoma
- Hilar Cholangiocarcinoma
- Intrahepatic Cholangiocarcinoma
- Clonorchiasis
- Find a journal
- Publish with us
- Track your research

- Advanced Search
- Teaching Cases
- Submit a Case
Cholangiocarcinoma: a casual diagnosis in a young man
Abdominal imaging
Clinical Cases
Gabelloni M, Fiorini S, Cervelli R, Lorenzoni G, Angeli S, Faggioni L, Bartolozzi C.

39 years, male
[1] Anderson CD, Pinson W, Berlin J, Chari RS (2004) Diagnosis and treatment of cholangiocarcinoma. The oncologist 9: 43-57 (PMID: 14755014 )
[2] Han K, Choi BI, Kim AY, An SK, Lee W, Kim TK, Kim SW (2002) Cholangiocarcinoma: pictorial essay of CT and cholangiographic findings. Radiographics 22: 173-187 (PMID: 11796906 )
[3] Sainani NI, Catalano OA, Holalkere NS, Zhu AX, Hahn PF, Sahani DV. (2008) Cholangiocarcinoma: current and novel imaging techniques. Radiographics 28:1263-1287 (PMID: 18794305 )
[4] Chung YE, Kim MJ, Park YN, Choi JY, Pyo JY, Kim YC, Cho HJ, Kim KA, Choi SY. (2009) Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics 29:683-700 (PMID: 19448110 )
[5] Menias CO, Surabhi VR, Prasad SR, Wang HL, Narra VR, Chintapalli KN. (2008) Mimics of cholangiocarcinoma: spectrum of disease. Radiographics 28:1115-1129 (PMID: 18635632 )
Abdominal ultrasonography

Imaging findings on multiphase MDCT
CT angiography and biliography


IMAGES
VIDEO
COMMENTS
Abstract. Cholangiocarcinomas that involve areas from the peripheral intrahepatic duct to the distal common duct have similar morphologic features, and traditional classification schemes based on the location of the involved ducts sometimes overlap. Nevertheless, cholangiocarcinoma is usually classified as either intrahepatic or extrahepatic ...
Intrahepatic cholangiocarcinoma is the second most common primary malignancy of the liver (10% to 15% of primary liver tumors). It is more common in males, after 70 years [5] [6] . Its main risk ...
However, the distinction between peripheral intrahepatic cholangiocarcinoma and hilar cholangiocarcinoma is largely based on the site of origin. Therefore, in some tumors that arise peripheral to the secondary bifurcation of one of the hepatic ducts, clear differentiation between the two types of cholangiocarcinoma is not always possible.
Request PDF | Cholangiocarcinoma: Pictorial Essay of CT and Cholangiographic Findings1 | Cholangiocarcinomas that involve areas from the peripheral intrahepatic duct to the distal common duct have ...
Further molecular or biochemical investigation is needed to support the "field theory," which states that all cholangiocarcinomas are biologically the same tumor originating from the same biliary epithelium. Cholangiocarcinomas that involve areas from the peripheral intrahepatic duct to the distal common duct have similar morphologic features, and traditional classification schemes based on ...
Search worldwide, life-sciences literature Search. Advanced Search Coronavirus articles and preprints Search examples: "breast cancer" Smith J
The radiologic manifestations of cholangiocarcinomas are extremely diverse, since these tumors vary greatly in location, growth pattern, and histologic type. Familiarity with the imaging manifestations of cholangiocarcinomas is important for accurate detection and characterization of these tumors and assessment of resectability. Advances in imaging techniques have led to the availability of an ...
Cholangiocarcinoma (CCA) is the second most common primary hepatobiliary malignancy and presents as three separate morphological subtypes; namely mass-forming, periductal-infiltrating, and intraductal-growing patterns. Each of these subtypes have distinct imaging characteristics, as well as a variety of benign and malignant mimics, making accurate diagnosis of CCA on imaging challenging ...
Cholangiocarcinoma is the second most common primary hepatic malignancy and is a heterogeneous tumor of biliary epithelium. We discuss the risk factors, anatomic classification of cholangiocarcinoma (CC) as well as the different morphologic subtypes of CC. Imaging findings of CC on different modalities are described, focusing on intrahepatic CC.
Cholangiocarcinoma: Pictorial essay of CT and cholangiographic findings. Han J; Choi B; Kim A; et al. See more; ... In addition, the distinction between hilar cholangiocarcinoma and extrahepatic cholangiocarcinoma is not clearly defined. The different biologic behaviors of the tumors seem to be caused by their varying locations and their size ...
Cholangiocarcinoma is a malignant tumor arising from the epithelium of the bile ducts. ... imaging findings of intrahepatic and extrahepatic intraductal papillary cholangiocarcinoma are described separately. ... pictorial essay of CT and cholangiographic findings Radiographics 22 173-187 Occurrence Handle 11796906 ...
Cholangiocarcinoma: pictorial essay of CT and cholangiographic findings. RadioGraphics 2002;22(1):173-187. Link, Google Scholar; 11 Kim TK, Choi BI, Han JK, Jang HJ, Cho SG, Han MC. Peripheral cholangiocarcinoma of the liver: two-phase spiral CT findings. Radiology 1997;204(2):539-543. Link, Google Scholar
Citation, DOI, disclosures and article data. Cholangiocarcinomas (commonest type of bile duct cancers) are malignant epithelial tumors arising from the biliary tree, excluding the gallbladder or ampulla of Vater. Cholangiocarcinoma is the third most common primary hepatobiliary malignancy after hepatocellular carcinoma (HCC) and gallbladder ...
Cholangiocarcinoma, a tumor of biliary epithelium, is increasing in incidence. The imaging appearance, behavior, and treatment of cholangiocarcinoma differ according to its location and morphology. Cholangiocarcinoma is usually classified as intrahepatic, perihilar, or distal. The three morphologies are mass-forming, periductal sclerosing, and intraductal growing. As surgical resection is the ...
Introduction. Cholangiocarcinoma (CC) is the most frequent malignant tumour of the biliary tract, accounting for 10-20% of all primary liver tumours [1,2].The vast majority (95%) of CC are adenocarcinomas with a high proportion of fibrous stroma [3,4].The prevalence of CC shows geographic variations, with the highest prevalence being found in Southeast Asia [].
Cholangiocarcinomas that involve areas from the peripheral intrahepatic duct to the distal common duct have similar morphologic features, and traditional classification schemes based on the location of the involved ducts sometimes overlap. Nevertheless, cholangiocarcinoma is usually classified as either intrahepatic or extrahepatic, and intrahepatic cholangiocarcinoma is further classified as ...
Cholangiocarcinoma is the second most common primary malignant hepatobiliary neoplasm, accounting for approximately 15% of liver cancers. ... et al. Cholangiocarcinoma: pictorial essay of CT and cholangiographic findings. RadioGraphics 2002;22:173-187. ... Villacorta J. CT findings in Mirizzi syndrome. J Comput Assist Tomogr 1983;7:419-425 ...
Mass-forming intrahepatic cholangiocarcinomas (MF-ICC), also referred as peripheral cholangiocarcinomas, comprise one of the three recognized growth patterns of intrahepatic cholangiocarcinomas . On imaging, these tumors usually present as large and relatively well-defined hepatic masses with lobulated margins and showing peripheral rim ...
On CT, the typical appearance of peripheral cholangiocarcinoma is a large, irregular, hypoattenuating mass that demonstrates minimal contrast enhancement at the periphery, with focal intrahepatic bile ductal dilation around the tumor (Fig. 1) [15, 16].Satellite or daughter nodules are frequent and vary in size (Fig. 2).Additional ancillary CT findings are slightly high-attenuation areas within ...
OBJECTIVE. The purpose of this article is to review imaging workup of perihilar cholangiocarcinoma, including MDCT and MRI protocols, imaging findings, differential diagnosis, and staging. A reporting template is included. CONCLUSION. Imaging plays a central role in the detection, differential diagnosis, and staging of perihilar cholangiocarcinoma.
CT findings were indicative of cholangiocarcinoma, mass-forming type. ... Lee W, Kim TK, Kim SW (2002) Cholangiocarcinoma: pictorial essay of CT and cholangiographic findings. Radiographics 22: 173-187 (PMID: 11796906) [3] Sainani NI, Catalano OA, Holalkere NS, Zhu AX, Hahn PF, Sahani DV. (2008) Cholangiocarcinoma: current and novel imaging ...
Intrahepatic cholangiocarcinoma is the second most common primary hepatic tumor. Various risk factors have been reported for intrahepatic cholangiocarcinoma, and the radiologic and pathologic findings of this disease entity may differ depending on the underlying risk factors. Intrahepatic cholangiocarcinoma can be classified into three types on the basis of gross morphologic features: mass ...
Cholangiocarcinoma (CCA), intrahepatic cholangiocarcinoma (ICC, ICCA) Synonyms. Cholangiocellular carcinoma or bile duct adenocarcinoma. Definitions. Malignancy that arises from intrahepatic bile duct (IHBD) or extrahepatic bile duct epithelium.