Population Data Centre Profile: The Manitoba Centre for Health Policy
Affiliation.
- 1 Manitoba Centre for Health Policy, Rady Faculty of Health Sciences, University of Manitoba, 408-727 McDermot Ave, Winnipeg, Manitoba, Canada R3E 3P5.
- PMID: 32935035
- PMCID: PMC7473284
- DOI: 10.23889/ijpds.v5i1.1131
Objective: To profile the Manitoba Centre for Health Policy (MCHP), a population health data centre located at the University of Manitoba in Winnipeg, Canada.
Approach: We describe how MCHP was established and funded, and how it continues to operate based on a foundation of trust and respect between researchers at the University of Manitoba and stakeholders in the Manitoba Government's Department of Health. MCHP's research priorities are jointly determined by its scientists' own research interests and by questions put forward from Manitoba government ministries. Data governance, data privacy, data linkage processes and data access are discussed in detail. We also provide three illustrative examples of the MCHP Data Repository in action, demonstrating how studies using a variety of Repository datasets have had an impact on health and social policies and programs in Manitoba.
Discussion: MCHP has experienced tremendous growth over the last three decades. We discuss emerging research directions as the capacity for innovation at MCHP continues to expand, including a focus on natural language processing and other applications of artificial intelligence techniques, a leadership role in the new SPOR Canadian Data Platform, and a foray into social policy evaluation and analysis. With these and other exciting opportunities on the horizon, the future at MCHP looks exceptionally bright.

IJPDS International Journal of Population Data Science

Population Data Centre Profile: The Manitoba Centre for Health Policy
Main article content.
Objective To profile the Manitoba Centre for Health Policy (MCHP), a population health data centre located at the University of Manitoba in Winnipeg, Canada.
Approach We describe how MCHP was established and funded, and how it continues to operate based on a foundation of trust and respect between researchers at the University of Manitoba and stakeholders in the Manitoba Government’s Department of Health. MCHP’s research priorities are jointly determined by its scientists’ own research interests and by questions put forward from Manitoba government ministries. Data governance, data privacy, data linkage processes and data access are discussed in detail. We also provide three illustrative examples of the MCHP Data Repository in action, demonstrating how studies using a variety of Repository datasets have had an impact on health and social policies and programs in Manitoba.
Discussion MCHP has experienced tremendous growth over the last three decades. We discuss emerging research directions as the capacity for innovation at MCHP continues to expand, including a focus on natural language processing and other applications of artificial intelligence techniques, a leadership role in the new SPOR Canadian Data Platform, and a foray into social policy evaluation and analysis. With these and other exciting opportunities on the horizon, the future at MCHP looks exceptionally bright.
A Brief History of the Manitoba Centre for Health Policy
The Manitoba Centre for Health Policy ( MCHP ) is a population health data centre located at the University of Manitoba 1 in Winnipeg, Canada. It was formally established in 1991, but the story of how it came to be extends back two more decades, when the two researchers who would later become its co-founders first arrived in Manitoba [1].
In 1973, Les and Noralou Roos were working in the business school at the University of Manitoba, having recently completed doctoral degrees in political science at the Massachusetts Institute of Technology. The Dean of Medicine, having decided that aligning the faculty’s research programs with the new universal health care system was an important priority, arranged a meeting between the Rooses and the lead physician at the Manitoba Health Services Commission. The province’s practice of routinely recording hospital and physician contacts for the whole population of Manitoba opened the door to new research opportunities using anonymized provincial health data [1]. These early studies [2,3] were funded by external agencies based on topics of interest to the Department of Manitoba Health, Seniors & Active Living (shortened here to ‘Manitoba Health’) and clinical experts, and resulted in collaborations with researchers based at Dartmouth College in the U.S.
As their grant funding and publication records grew, Les and Noralou Roos gained national and international recognition for their work. The Canadian Institute for Advanced Research, which was focusing on the role of socioeconomic status and education as health determinants, convinced the Minister of Health that investing in the Roos research capabilities made sense; a three-year contract to establish and launch the Manitoba Centre for Health Policy and Evaluation (as it was then called) was signed in 1991 [1]. A Canadian Foundation for Innovation ( CFI ) grant received in 1999 was used to fund new office space and to bring the Department of Education and the Department of Family Services datasets into MCHP. In 2001, MCHP was awarded the Health Services Research Advancement Award by the Canadian Health Services Research Foundation.
Since 1991, the funding model has been a contract between the provincial government and MCHP for research ‘deliverables’. The focus for these projects is determined by interests of and issues facing the Department of Health in periodic meetings between MCHP and the Deputy Minister of Health. In addition, many MCHP researchers and affiliated scientists hold faculty positions at the University of Manitoba [4] and lead independent research programs supported by research grants from the Canadian Tri-Council agencies and other funding bodies.
The Manitoba Centre for Health Policy: Governance and Research Priorities
The MCHP Director is appointed by the Department of Community Health Sciences, and reports through the Department Head to the Dean of the College of Medicine at the University of Manitoba. The Director leads an executive team comprising four Associate Directors (in the areas of Research, Repository and Deliverables, Data Access and Use, and Planning and Development), whose collective role is to guide MCHP in achieving its strategic priorities [5]. MCHP also operates under the guidance of an advisory board comprising both government and university appointees [6]. The board currently includes deputy ministers from government departments, senior university administrators and public representatives.
MCHP has had an ongoing contract with the Manitoba Government’s Department of Health for completing arm’s-length research projects since 1991. Proposed project topics are submitted by MCHP researchers, from within government departments, and by the provincial health region leads. Five topics are chosen annually by Manitoba Health, including at least one project on child health selected by the Healthy Child Committee of Cabinet. MCHP employs approximately 60 staff, including researchers, data analysts, research project coordinators, and support staff.
Operating Model
MCHP acts as the steward of data routinely collected during the delivery of public services in Manitoba. The data are derived primarily from Manitoba Government departments, including Manitoba Health, Manitoba Families, Manitoba Education & Training, Manitoba Justice, and several other cross-departmental government agencies. Other data come from provincial laboratories, clinical programs, community and social outreach organizations, and Indigenous governance bodies. The 90+ datasets are held in the centralized Manitoba Population Research Data Repository (shortened here to ‘the Repository’) at MCHP. See Supplementary File 1 for a sample of Repository datasets.
Population & Setting
The Repository contains information on nearly all residents of the province of Manitoba, with coverage for some datasets extending as far back as 1970 [7]. Manitoba is a central Canadian province with a universal healthcare system and a population of about 1.3M people [8]. About 57% of the population resides in the major urban centre, Winnipeg [9]. The remainder live in rural settings, mainly in the southern part of the province. The age distribution of Manitoba is similar to the rest of Canada, with residents age 0-14 making up 19%, age 15-64 making up 65%, and age 65+ making up the remaining 16% of the total population [8].
While the Repository data cover the vast majority of Manitoba residents, a few groups are not well represented. Military personnel and individuals incarcerated in federal prisons are federally insured and are therefore not part of the provincial health insurance registry. This means that although they are included in the Repository, their records are incomplete in select datasets. Indigenous populations in Manitoba (First Nations, Metis, and Inuit peoples) may not be completely identified in some datasets, as some data are not collected in reserve communities.
Data Governance & Legislation
The Manitoba Government and other data providers listed in the section above are the trustees of the data in the Repository. As the custodian of this sensitive information, MCHP adheres to the rules for privacy and protection of personal information outlined in the province’s Personal Health Information Act ( PHIA ) [10] and the Freedom of Information and Protection of Privacy Act ( FIPPA ) [11] of Manitoba. Depending on the data source and use, requirements for data disclosure and use at MCHP might also be influenced by the Mental Health Act of Manitoba, [12] the Youth Criminal Justice Act of Canada, [13] the Child and Family Services Act of Manitoba, [14] the Statistics Act of Canada, [15] and the Privacy Act of Canada, [16] and others.
Consent Model
Ensuring the privacy and confidentiality of individual Manitoban’s personal information is a priority for MCHP. In Manitoba, PHIA grants individuals the right to access to their own medical records, and the right to privacy, which ensures that their personal health information will be protected from unauthorized collection, use, disclosure, retention and destruction [10]. PHIA upholds these rights by placing limits on how trustees can handle a person’s medical records. Meanwhile, FIPPA provides individuals the right to access information in records (other than health records) held by public bodies [11]. Under this provincial legislation, individual patients or participants must give consent for disclosure and use of their data in research when direct contact with these individuals is anticipated.
However, for projects involving MCHP Repository data, the Manitoba Health Information Privacy Committee ( HIPC ) and the University of Manitoba Health Research Ethics Review Board ( UM-HREB ) typically waive this requirement for individual consent, for several reasons: first, research projects using the Repository data are a secondary use of data, and therefore there is no direct contact with patients or participants; second, the ‘greater good’ of the research outweighs the risk of intrusion on Manitobans’ privacy, and it is impractical to obtain consent; and third, measures (such as de-identification and limited access to the Repository data) have been taken to protect individual privacy. While it is technically possible to 'opt out’ of some Manitoba Health administrative data systems, fewer than 0.1% of individuals have ever done so. Privacy measures at MCHP are described in more detail in the sections below.
Data Linkage
MCHP uses a trusted third-party system to ensure that newly acquired datasets and data updates being brought into the Repository have been stripped of any directly identifying information [17]. Briefly, the data provider sends any demographic data that could be used to identify an individual (e.g., names, address, phone numbers) and an internal reference number to the Information Management and Analytics Unit of Manitoba Health. There, the identifying information is used to match each individual to their existing 9-digit Personal Health Identification Number ( PHIN ) using a custom-developed software package called LINKPRO. The process starts with deterministic approach, with probabilistic follow-up on non-matched individuals; several passes through the data using different combinations of variables helps to ensure this match is as certain as possible. Next, the directly identifying details are removed from the records, and a scrambled (encrypted) version of the PHIN is attached. The scrambled PHIN is generated using a consistent, standard algorithm and is permanently stored in each record. The number is scrambled the same way for each individual’s records. This ensures that the records can be linked together at a later date, but protects the person’s identity.
At the same time that the data are being de-identified by Manitoba Health, the data provider also sends the internal reference numbers and program data (e.g., clinical test results or other public service use information) to MCHP. The de-identified records are sent electronically to MCHP and kept separate from the Repository until approvals from the data provider are in place. The program data are linked to the scrambled PHINs by the internal reference number. The data within the Repository are then linked on a project-by-project basis using the scrambled PHIN.
It is important to note that at no point in the data linkage process does any party have possession of all of the pieces of the linkage puzzle: the data provider does not have access to the scrambled PHIN, Manitoba Health does not have access to the program data, and MCHP does not have access to the identifying information. This system safeguards the privacy and security of the data. This third party approach has been very successful in building trust between partners, allowing the work that MCHP does to proceed with confidence.
Data Architecture & Information Technology
The Repository data are stored in a SAS-based SQL server providing user and project level access controls. Analytic systems are supported on Microsoft Windows 2012 servers, providing ETL/Acquisition, MCHP internal analytics, and remote access within Manitoba (as stipulated by the agreement between Manitoba Health and MCHP). Remote access is supported from Microsoft Windows-based computers and requires unique individual accounts with two factor authentication assigned by MCHP. The platform supports SAS as the default analytic environment, although STATA and R software are also available.
Data Quality
MCHP follows a data quality framework providing a comprehensive and consistent evaluation of every database and update received [17,18]. Assessing data quality is particularly important for secondary use of information, as MCHP rarely has control over the data collection and maintenance processes. The data quality framework was developed from a review of quality assessment practices in other Canadian and international population data centres, and includes as core components the concepts of accuracy (e.g., completeness, correctness), internal and external validity, timeliness and interpretability.
Privacy by Design
Several layers of protections are in place to ensure data privacy for individuals whose information is included in the Repository. These privacy measures include:
- All research projects must be reviewed for privacy, ethics, and impact by individual data providers, HIPC and UM-HREB to ensure the data are being used appropriately.
- Before accessing the Repository, individuals with access to an MCHP computer system and all principal investigators on MCHP projects complete an accreditation session, which provides an overview of the data access and use process. They are required to sign a pledge of confidentiality and an agreement that the analyses will be conducted in alignment with MCHP’s research processes and the Government of Manitoba’s requirements.
- System and data access are tracked, and individuals using the analytic systems at MCHP must log in using their unique ‘userID’ with two-factor authentication.
- Data access is provided to individual users based on the level of permissions they have obtained for their research projects. Access is provided only to individuals who have been identified as having ‘line level access’ on approved projects.
- Data extracted for non-MCHP researchers or analysts is the minimum level required to complete the outlined research project(s).
- The Repository contains no directly identifying information such as names or addresses.
- Information taken off of the MCHP analytic systems must be aggregate or statistical in nature with no strata representing an identifiable individual. This is implemented by requiring all aggregate data to represent at least 6 individuals or events, and any suppressed information (1-5 individuals or events) cannot be recreated through the use of simple math. Information taken off of the analytic system is manually reviewed for project association and small numbers.
- Prior to presenting or publishing data, the material must be reviewed by the data providers to ensure appropriate use within the scope of the project, flag any chance of re-identifying individuals, and confirm suitable representation of associated programs or departments. This review must be conducted at least 10 days prior to presentations and 30 days prior to publication.
Data Access and Publication
Access to Repository data must follow the requirements established by MCHP and individual data providers. This process is outlined on the MCHP website [19], and described briefly below. Research project set-up steps include:
- Complete MCHP Accreditation Session.
- Submit MCHP Feasibility Request (estimate letter and approvals required by the MCHP Data Access Unit).
- Obtain approvals from UM-HREB, HIPC and data providers; requires proof of funding for the research project.
- Complete a signed Research Agreement between the data provider and the researcher or research institution.
- Initiate data system set-up and data extraction, and review project requirements with MCHP analyst.
- If remote access to the Repository is required, an MCHP computer account will need to be configured.
Completing steps 1-4 typically takes an average of 3-4 months, but this can vary considerably depending on whether the research is privately or publically funded, whether the researcher has sought approvals before requesting a feasibility review, and whether the request is well-defined. The time required for step 5 depends on the complexity of the project (e.g., number of datasets and fields to be extracted), but with as many as 20 analysts available at MCHP, completing this step usually takes days or weeks (not months). Step 6 can be completed in a day or two.
Other Considerations
Access to datasets must occur through MCHP-based systems. Remote access from physically secure locations and with appropriate approvals can be arranged. Researchers preparing to publish findings using the Repository data must submit a draft of the publication ahead of public release to the data providers for review and feedback. The final version of a presentation or publication must be provided to HIPC once the presentation is complete or the publication is accepted.
Noteworthy Outputs
In this section, we describe three studies that used data from a variety of Repository sources to make an impact on health and social policies and programs in Manitoba.
(1) Enhancing Academic Programming for Students from Low-Income Families
Our report on Manitoba children’s educational outcomes included an analysis of Grade 12 standardized test scores by socioeconomic status [20]. The left-hand panel of Figure 1 illustrates a mild income gradient, with students from the poorest families having an average passing rate of 75% on the test, while students from the highest income areas had an average passing rate of 95%. However, this panel only shows results for students who wrote the test. The right-hand panel shows the results for both students who wrote the test and students who should have written the test had they progressed through the school system as expected. This latter group includes students who were held back a year or dropped out of school. The income gradient in this population-based analysis is much steeper, with passing rates at only 16% for the lowest income students and 80% for the highest income students.

Performance of Grade 12 Students in Manitoba by Socioeconomic Status.
These findings, together with other analyses presented in our 2001 Child Health Atlas [21], led to the development of the Community School Investigators (CSI) program [22], which provides services to enrich and enhance the academic achievement of children in inner-city low-income neighbourhoods.
(2) Establishing the Positive Impacts of an Unconditional Prenatal Benefit
In 2001, Manitoba introduced the Healthy Baby Prenatal Benefit (HBPB) to improve prenatal health and birth outcomes in families with a documented annual income of less than CAN $32,000. The program provides eligible women with an unconditional income supplement of up to $81.41/month during their second and third trimester of pregnancy. In addition, pamphlets with information about prenatal and postnatal care (e.g., the importance of prenatal nutrition and information about breastfeeding) are included with the monthly payment [23].
In 2010, MCHP evaluated the impacts of the HBPB on the birth outcomes of recipients [24]. Using a quasi-experimental retrospective cohort design, we examined all births (2003-2010) to Manitoba women who were receiving income assistance and either did or did not receive the HBPB. The two groups had comparable low mean annual incomes at $9,941 and $9,972, respectively. Thus, for women who received the HBPB, the benefit represented an increase in their monthly incomes of almost 10%.
Remarkably, receiving the HBPB was significantly associated with a reduction in low birth weight births and preterm births, and an increase in breastfeeding initiation. Population-preventable fractions for low birth weight and pre term births were decreases of 21% and 17.5%, respectively, and the population-attributable fraction for breastfeeding was a 4% increase. These findings were subsequently published in Pediatrics [25], and together with a follow-up study demonstrating that receipt of HBPB was associated with increased population-level health equity [26], attracted the attention of news media in Canada [27] and the US [28,29]. This evidence of the effectiveness of the HBPB has also contributed to its longevity (nearly 20 years) as a Manitoba government program.
(3) Projecting Personal Care Home Bed Needs in Manitoba
Modern industrial societies are facing new challenges due to an increasing older adult population. Both the ‘baby boom’ and improved health and longevity of older populations have contributed to this phenomenon. In 2011, an MCHP report pointed to dramatic increases in the number of individuals over age 65 in Manitoba; this number is projected to rise from 14% of the population in 2009 to more than 18% in 2036 [30]. This creates potential challenges for governments planning for the needs of older adults in supportive housing, nursing homes (known as personal care homes in Manitoba), and long-term care facilities.
In 2012, MCHP released a second report examining to what extent Manitoba’s need for personal care home (PCH) beds, or alternatives such as supportive housing and extended home care, was expected to grow over the next several decades [31]. Figure 2 shows the actual and projected population numbers for three age groups: age 65-74 (top line), age 75-84 (middle line), and age 85+ (lower line). Note how the slope of each line changes at a different rate as the baby boom generation grows older.

Actual and Projected Number of Older Adults Living in Manitoba, by Age Group.
The PCH bed projection study generated a number of important findings. First, the proportion of older adults using PCHs has been shrinking since 1985. This trend was attributed to a healthier population of older adults and increased use of supportive housing and home care services. Second, since most PCH residents are age 85 or older, when baby boomers reach the age of 85 (starting in 2031), we would expect the number of days Manitobans spend in PCH facilities to rise dramatically. The study predicted that between 5,100 and 6,300 additional beds will be needed in personal care homes, supportive housing or expanded home care services – an increase of 55-70% more than current capacity. Third, researchers found that older adults who were married or had children were less likely to be residents of personal care homes. The findings of this report and related work by MCHP continue to serve as the basis for long-term healthcare planning by the Manitoba government and other agencies [32,33].
Since its inception, MCHP has been one of the central drivers of data linkage science and population health research in Canada and worldwide. The Manitoba Population Research Data Repository was initially known as the Population Health Data Repository. As the data centre has grown from maintaining 12 health service delivery datasets in 1991 to more than 90 datasets in 2019, the breadth of non-healthcare data led to the change to a more inclusive name. And while these data serve as a tremendous resource for researchers, clinicians and decision makers to better understand the Manitoba population’s health and social well-being, there are still many opportunities for growth and advancement.
For example, while many of the 90+ datasets in the Repository are regularly updated, the time lag from when the data are collected to when they are transferred to the Repository sometimes hinders researchers from providing up-to-date answers to time-sensitive questions. MCHP is dependent on data providers to make regular updates to datasets available, and negotiating more timely access to these records is part of ongoing discussions with Manitoba Health in regards to the impact of MCHP’s research deliverables.
There is work underway to acquire more clinical data into the Repository. Over the past several years, clinician-led projects have increased significantly but relatively few clinicians have recognized the potential the Repository holds to answer their research questions. MCHP continues to emphasize the value-add of linking clinical data to administrative health and social data, which together can provide greater context to clinical queries and bring innovative solutions into focus.
MCHP continues to grow our capacity to access and understand complex ‘free-text’ or ‘unstructured’ data in existing Repository datasets, such as clinician notes in electronic medical records, and case notes from social services files. These free-text data often contain unique types of identifiers, and entail additional processes for de-identification. Analyses of free-text require sophisticated language processing methods that have not yet become widely available in the health sector [34]. However, MCHP is currently working to adapt and apply machine-learning techniques and deep neural learning approaches used in the field of computer science, with the ultimate goal of addressing knowledge gaps and challenges in the health system and social sector.
MCHP continues to develop and build an innovative knowledge translation strategy that will integrate knowledge users into our research process and ensure that our research is policy-relevant. This strategy is based on MCHP’s long history of integrated knowledge exchange, including the work of a national award-winning research collaborative called the Need to Know Team [35–37], which facilitates knowledge sharing among university-based researchers, high-level planners from the health regions in Manitoba, and policy-makers from Manitoba Health. Established in 2001, this team has revolutionized how administrative data sources can be used to inform health and social policy issues.
Finally, MCHP recognizes that many of our strengths in advancing our work are the product of the fruitful partnerships formed with stakeholders, community organizations and decision makers. Our long-standing relationship with Manitoba Health has for many years been the foundation of MCHP and the research we do. More recently, we have formed partnerships with Indigenous groups in Manitoba through our work on health equity [38], primary care [39], and two soon-to-be-released reports on First Nations health status and access to healthcare. As well, MCHP plays a key role in the recently-announced Strategy for Patient-Oriented Research (SPOR) Canadian Data Platform, a national initiative to harmonize administrative health data across the provinces and territories [40].
Lessons Learned
Throughout MCHP’s rich history, the many lessons we learned have proved invaluable for building and maintaining an enduring research enterprise. First, we have learned that building trust with stakeholders is absolutely essential to maintaining and expanding the Repository. Our commitment to ensuring that the Repository data and secure are de-identified means that the possibility of individuals in our studies being identified is extremely remote. This instills confidence amongst our stakeholders, and smooths the way for further interactions.
Second, we have come to appreciate how important it is to work closely with our partners throughout the research process (from beginning to end) to ensure we are interpreting their data correctly, and that we all understand both the context and limitations that accompany any data collection processes and analyses. Providing our partners a first look at results allows them to prepare for any possible policy implications that might arise. Typically, our agreements stipulate that data providers receive a 60-day review period prior to any research findings being publically released. However, this review does not allow for suppression or reinterpretation of findings unless gross errors have been made.
Third, we realized early on that keeping track of research methodology (how we measure things) was going to be critical for constancy of interpretation over time. In response, we developed the Concept Dictionary and Glossary, available to the public on MCHP’s website. The Concept Dictionary has been a vital resource over the years, not only in enhancing consistency in how we interpret our findings, but also in reducing the time and effort required to complete subsequent research projects.
Finally, whenever possible, we take the research interests of the data providers into account when we initiate new projects. In many cases, they serve as project co-investigators, allowing them to enhance their research acumen, provide important contextual information regarding the data or the findings, and initiate the knowledge translation process. It remains essential, however, that the principal investigator retains the right to report any findings that arise, and that the partnership agreement is supported by the rights and freedoms granted to academic researchers working at a Canadian university.
Conclusions
MCHP continues to lead in developing innovative research resources based on routinely collected administrative data, forging new techniques in cross-jurisdictional analysis, and building lasting relationships with policy makers and Indigenous partners. The announcement of substantial new funding in the form of the SPOR Canadian Data Platform promises ongoing opportunities to continue our trail-blazing role in using administrative data to answer policy-relevant questions. Healthcare delivery is evolving rapidly as new technology enters the clinical environment and system planners endeavor to bend the cost curve, making the availability of data to support health system change even more critical than before. These data need to be amenable to new Artificial Intelligence techniques and the data architecture able to support the greater computing power necessary to exploit these opportunities.
The combination of real-time clinical data and administrative claims data has huge appeal, due to the synergy between these different data types and the potential for capitalizing on the new knowledge they can generate. While our capacity to achieve this goal is still to be realized, planning of future hardware and data architecture requirements should include consideration of these future developments. To date, the dramatic improvements in computing power that will facilitate these types of change have not been matched with advances in privacy protection, and other challenges in benefiting from these advances still exist.
MCHP has been a leader in acquiring and using social data in analyses that incorporate and take into account the social determinants of health. Although the Repository has not yet contributed to social research in a significant way, new funding from the Social Sciences & Humanities Research Council has been used to establish a multi-sector partnership to conduct S ocial P olicy E valuation C ollaborative T eam R esearch at the U niversities in M anitoba ( SPECTRUM ) 2 . Through SPECTRUM, MCHP is conducting applied research and evaluation on existing social services, programs and policies in Manitoba, melding the expertise of knowledge creators, mobilizers and users to address real-world policy questions through use of the Repository at MCHP.
With these and other exciting opportunities on the horizon, the future at MCHP looks exceptionally bright.
Acknowledgments
Many thanks to Les Roos, Noralou Roos and Marni Brownell for their careful review of this paper.
Ethics Statement
This work did not require ethical approval as it was descriptive and not a research study involving human participants.
Abbreviations
Statement on conflicts of interest.
The authors declare that they have no competing interests relevant to the content of this article.
For more information on the Manitoba Centre for Health Policy, visit our homepage at http://umanitoba.ca/faculties/health_sciences/medicine/units/chs/departmental_units/mchp/
More information on SPECTRUM is available at www.spectrum-mb.ca .
Marchessault G. The Manitoba Centre for Health Policy: A Case Study. Healthc Policy. 2011;6(Spec Issue):29–43. 10.12927/hcpol.2011.22117
Roos N, Henteleff P, Roos L. A new audit procedure applied to an old question: Is the frequency of T&A justified? Med Care. 1977;15:1–8. 10.1097/00005650-197701000-00001
Roos N, Roos L, Henteleff P. Elective surgical rates - Do high rates mean lower standards? Tonsillectomy and adenoidectomy in Manitoba. N Engl J Med. 1977;297(360–65). 10.1056/nejm197708182970705
Manitoba Centre for Health Policy. MCHP Faculty and Staff [Internet]. 2019 [cited 2019 May 23]. Available from: http://umanitoba.ca/faculties/health_sciences/medicine/units/chs/departmental_units/mchp/aboutPeople.html
Manitoba Centre for Health Policy. Mission and Values [Internet]. 2019 [cited 2019 May 23]. Available from: http://umanitoba.ca/faculties/health_sciences/medicine/units/chs/departmental_units/mchp/mission.html
Manitoba Centre for Health Policy. MCHP Advisory Board [Internet]. 2019 [cited 2019 May 23]. Available from: http://umanitoba.ca/faculties/health_sciences/medicine/units/chs/departmental_units/mchp/aboutAdvisoryBoard.html
Manitoba Centre for Health Policy. Population Estimates and Comparison of Data Sources [Internet]. 2009 [cited 2019 May 23]. Available from: http://mchp-appserv.cpe.umanitoba.ca/viewConcept.php?conceptID=1203
Statistics Canada. Census Profile - Manitoba [Internet]. 2016 Census. 2019 [cited 2019 May 23]. Available from: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang=E&Geo1=PR&Code1=46&Geo2=PR&Code2=01&Data=Count&SearchText=46&SearchType=Begins&SearchPR=01&B1=All&Custom=&TABID=3
Fransoo R, Martens P, The Need to Know Team, Prior H, Burchill C, Koseva I, et al. The 2013 RHA Indicators Atlas. Winnipeg, Canada: Manitoba Centre for Health Policy; 2013.
Legislative Assembly of Manitoba. The Personal Health Information Act C.C.S.M. c. P33.5 [Internet]. Canada: May 21; 2017. Available from: http://web2.gov.mb.ca/laws/statutes/ccsm/p033-5e.php
Legislative Assembly of Manitoba. The Freedom of Information and Protection of Privacy Act C.C.S.M. c. F175 [Internet]. Canada: March 15; 2018. Available from: https://web2.gov.mb.ca/laws/statutes/ccsm/f175e.php
Legislative Assembly of Manitoba. The Mental Health Act C.C.S.M. c. M110 [Internet]. Canada: January 1; 2019. Available from: http://web2.gov.mb.ca/laws/statutes/ccsm/m110e.php
Legislative Assembly of Manitoba. Youth Criminal Justice Act [Internet]. S.C. c. 1. Canada; 2002. Available from: https://laws-lois.justice.gc.ca/PDF/2002_1.pdf
Legislative Assembly of Manitoba. The Child and Family Services Act [Internet]. C.C.S.M. c. C80. Canada; 2019. Available from: https://web2.gov.mb.ca/laws/statutes/ccsm/_pdf.php?cap=c80
Government of Canada. Statistics Act of Canada R.S.C., 1985, c. S-19 [Internet]. Canada: December 12; 2017. Available from: https://laws-lois.justice.gc.ca/eng/acts/S-19/
Government of Canada. Privacy Act of Canada R.S.C., 1985, c. P-21 [Internet]. Canada: December 13; 2018. Available from: https://laws-lois.justice.gc.ca/eng/acts/P-21/page-1.html#h-397172
Smith M, Roos L, Burchill C, Turner K, Towns D, Hong S, et al. Health services data: Managing the data warehouse: 25 years of experience at the Manitoba Centre for Health Policy. In: Sobolev B, Levy A, Goring S, editors. Data and Measures in Health Services Research. Boston, MA: Springer; 2015. p. 1–26. 10.1007/978-1-4939-8715-3_3
Smith M, Lix LM, Azimaee M, Enns JE, Orr J, Hong S, et al. Assessing the quality of administrative data for research: a framework from the Manitoba Centre for Health Policy. JAMIA. 2017. 10.1093/jamia/ocx078
Manitoba Centre for Health Policy University of Manitoba. Applying for Access [Internet]. 2018 [cited 2019 May 24]. Available from: http://umanitoba.ca/faculties/health_sciences/medicine/units/chs/departmental_units/mchp/resources/access.html
Brownell M, Roos NP, Fransoo R, Guevremont A, MacWilliam L, Derksen S, et al. How do educational outcomes vary with socioeconomic status? Key findings from the Manitoba Child Health Atlas 2004. Winnipeg, Canada: Manitoba Centre for Health Policy; 2004.
Brownell M, Martens P, Kozyrskyj A, Fergusson P, Lerfald J, Mayer T, et al. Assessing the health of children in Manitoba: A population-based study. Winnipeg, Canada: Manitoba Centre for Health Policy; 2001.
Boys & Girls Clubs of Winnipeg. CSI Report: A program of Boys and Girls Clubs of Winnipeg [Internet]. Winnipeg, MB; 2012. Available from: http://www.bgcwinnipeg.ca/system/resources/W1siZiIsIjIwMTQvMDEvMTYvMTgvMDQvMzUvNDE3L0NTSV9SZXBvcnRfMjAxMi5wZGYiXV0/CSI Report 2012.pdf
Healthy Child Manitoba. Healthy Baby [Internet]. 2018 [cited 2018 Jan 5]. Available from: https://www.gov.mb.ca/healthychild/healthybaby/index.html
Brownell Marni, Chartier M, Au W, Schultz J. Evaluation of the Healthy Baby Program. Winnipeg, Canada: Manitoba Centre for Health Policy; 2010.
Brownell M, Chartier M, Nickel N, Chateau D, Martens P, Sarkar J, et al. Unconditional prenatal income supplement and birth outcomes. Pediatr. 2016;137(6):e20152992. 10.1542/peds.2015-2992
Brownell M, Nickel N, Chartier M, Enns J, Chateau D, Sarkar J, et al. An unconditional prenatal income supplement reduces population inequities in birth outcomes. Health Aff. 2018;37(3). 10.1097/01.ogx.0000499837.81731.90
Zafar A, Birak C. $81 a month buys a healthier baby. CBC News [Internet]. 2016 May 12; Available from: https://www.cbc.ca/news/health/healthy-baby-prenatal-income-benefit-1.3578029
Brownell M. Income Supplements for Pregnant Women: What will it take to spread the model? [Internet]. Health Affairs Blog. 2018 [cited 2019 May 24]. Available from: https://www.healthaffairs.org/do/10.1377/hblog20180816.109979/full/
Galvin G. Motherhood in Manitoba. US News & World Report [Internet]. 2018 Oct 16; Available from: https://www.usnews.com/news/best-countries/articles/2018-10-16/canadian-program-aims-to-boost-birth-outcomes-for-low-income-women
Doupe M, Fransoo R, Chateau D, Dik N, Burchill C, Soodeen R-A, et al. Population Aging and the Continuum of Older Adult Care in Manitoba. Winnipeg, Canada: Manitoba Centre for Health Policy; 2011.
Chateau D, Doupe M, Walld R, Soodeen R-A, Ouelette C, Rajotte L. Projecting Personal Care Home Bed Equivalent Needs in Manitoba Through 2036. Winnipeg, Canada: Manitoba Centre for Health Policy; 2012.
Manitoba Nurses Union. The Future of Long-Term Care is Now: Addressing nursing care needs in Manitoba’s Personal Care Homes. Winnipeg, Canada; 2018. Available from: https://manitobanurses.ca/system/files/MNU-Long Term Care Report 2018.pdf
CUPE Manitoba. For the Care We All Deserve: The impact of working short on Manitoba personal care home workers. Winnipeg, Canada; 2015. Available from: https://cupe.mb.ca/files/2013/07/LTC-Report-for-web.pdf
Hearst M. Untangling Text Data Mining. In: Proceedings of the 37th Annual Meeting of the Association for Computational Linguistics. 1999. 10.3115/1034678.1034679
Bowen S, Martens P, The Need to Know Team. Demystifying knowledge translation: learning from the community. J Heal Serv Res Policy. 2005;10(4):203–11. 10.1258/135581905774414213
Bowen S, Erickson T, Martens P, Crockett S. More than “using research”: the real challenges in promoting evidence-informed decision-making. Heal Policy. 2009;4(3):87–102. 10.12927/hcpol.2009.20538
Bowen S, Martens P. A model for collaborative evaluation of university-community partnerships. J Epidemiol Community Heal. 2006;60(10):902–7. 10.1136/jech.2005.040881
Brownell MD, Nickel NC, Enns JE, Chartier M, Campbell R, Phillips-Beck W, et al. Association between home visiting interventions and First Nations families’ health and social outcomes in Manitoba, Canada: protocol for a study of linked population-based administrative data. BMJ Open. 2017;7(10):e017626. 10.1136/bmjopen-2017-017626
Kyoon-Achan G, Lavoie J, Avery Kinew K, Phillips-Beck W, Ibrahim N, Sinclair S, et al. Innovating for transformation in First Nations health using community-based participatory research. Qual Heal Res. 2018;28(7):1036–49. 10.1177/1049732318756056
Government of Canada. Minister of Health announces $81M initiative to increase access to health research data [news release] [Internet]. 2019 [cited 2019 May 24]. Available from: https://www.canada.ca/en/institutes-health-research/news/2019/04/minister-of-health-announces-81m-initiative-to-increase-access-to-health-research-data.html
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License .
Article Sidebar
Most read articles by the same author(s).
- Kim McGrail, Ros Moran, Christine O'Keefe, David Preen, Hude Quan, Claudia Sanmartin, Michael Schull, Mark Smith, Christine Williams, Tyler Williamson, Grant Wyper, Rachael Moorin, Hye-Chung Kum, Kerina Jones, Ashley Akbari, Tell Bennett, Andrew Boyd, Fabrizio Carinci, Xinjie Cui, Spiros Denaxas, Nadine Dougall, David Ford, Russell S Kirby, Milton Kotelchuck, A Position Statement on Population Data Science: , International Journal of Population Data Science: Vol. 3 No. 1 (2018): IJPDS Standard Issue
- Lisa Lix, Rolf Puchtinger, Kim Reimer, Cynthia Robitaille, Mark Smith, Lawrence Svenson, Karen Tu, Linda VanTil, Sean Waits, Louise Pelletier, Karen Phillips, Catherine Pelletier, J. Michael Paterson, James Ayles, Sharon Bartholomew, Charmaine Cooke, Joellyn Ellison, Valerie Emond, Naomi Hamm, Heather Hannah, Sonia Jean, Shannon LeBlanc, Siobhan O'Donnel, The Canadian Chronic Disease Surveillance System: A model for collaborative surveillance , International Journal of Population Data Science: Vol. 3 No. 3 (2018): IJPDS Special Issue: Cross-Centre Working
- Alan Katz, Jennifer Enns, Sabrina T Wong, Tyler Williamson, Alexander Singer, Kimberlyn McGrail, Jeffery A Bakal, Carole Taylor, Sandra Peterson, Challenges Associated with Cross-Jurisdictional Analyses using Administrative Health Data and Primary Care Electronic Medical Records in Canada , International Journal of Population Data Science: Vol. 3 No. 3 (2018): IJPDS Special Issue: Cross-Centre Working
- Magdalena Janus, Nazeem Muhajarine, Marni Brownell, Eric Duku, Simon Webb, Ashley Gaskin, Rob Raos, Barry Forer, Jennifer Enns, Martin Guhn, A Pan-Canadian Data Resource for Monitoring Child Developmental Health: The Canadian Neighbourhoods Early Child Development (CanNECD) Database , International Journal of Population Data Science: Vol. 3 No. 3 (2018): IJPDS Special Issue: Cross-Centre Working
- Sylvia Aponte-Hao, Sabrina T. Wong, Manpreet Thandi, Paul Ronksley, Kerry McBrien, Joon Lee, Mathew Grandy, Dee Mangin, Alan Katz, Alexander Singer, Donna Manca, Tyler Williamson, Machine learning for identification of frailty in Canadian primary care practices , International Journal of Population Data Science: Vol. 6 No. 1 (2021): IJPDS Standard Issue
- Lindsey Todd Dahl, Jennifer D Walker, Michael Schull, P. Alison Paprica, James Ted McDonald, Frank Gavin, Jean-Francois Ethier, Brent Diverty, Kimberlyn McGrail, Alan Katz, Juliana Wu, The SPOR-Canadian Data Platform: a national initiative to facilitate data rich multi-jurisdictional research , International Journal of Population Data Science: Vol. 5 No. 1 (2020): IJPDS Standard Issue
- Mark Smith, Ken Turner, Ruth Bond, Tiva Kawakami, Leslie Leon Roos, The Concept Dictionary and Glossary at MCHP , International Journal of Population Data Science: Vol. 4 No. 1 (2019): IJPDS Standard Issue
- Tyler Williamson, PhD, Sylvia Aponte-Hao, BSc, Bria Mele, MSc, Brendan Cord Lethebe, MSc, Charles Leduc, MD, MSc, Manpreet Thandi, RN, MSN, MPH, Alan Katz, MBChB, MSc, CCFP, Sabrina Wong, RN, PhD, Developing and validating a primary care EMR-based frailty definition using machine learning , International Journal of Population Data Science: Vol. 5 No. 1 (2020): IJPDS Standard Issue
- Alan Katz, Kathi Avery Kinew, Leona Star, Ethical Data Linkage with Indigenous Communities: The Manitoba Experience , International Journal of Population Data Science: Vol. 5 No. 5 (2020): Conference Proceedings for International Population Data Linkage Conference 2020
- Marcello Nesca, Alan Katz, Carson Leung, Lisa Lix, A scoping review of preprocessing methods for unstructured text data to assess data quality , International Journal of Population Data Science: Vol. 7 No. 1 (2022): IJPDS Standard Issue
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Population Study Article
- Published: 14 January 2020
Assessing childhood health outcome inequalities with area-based socioeconomic measures: a retrospective cross-sectional study using Manitoba population data
- Atul K. Sharma 1 ,
- Kristine Kroeker 2 ,
- Dan Chateau 3 ,
- Marni Brownell 3 &
- Celia J. Rodd 1
Pediatric Research volume 88 , pages 496–502 ( 2020 ) Cite this article
846 Accesses
7 Citations
12 Altmetric
Metrics details
Socioeconomic gradients in health exist in Canada. Although multiple Canadian area-based socioeconomic measures (ABSM) have been developed, none have been specifically validated against pediatric outcomes. Our objective was to compare the strength of association between key pediatric health outcomes and a number of ABSM, including income quintile.
This was a retrospective cross-sectional assessment of the association between socioeconomic status (SES) measured by ABSM and 20 specific pediatric health outcomes. Data from the Manitoba Population Research Data Repository were used for residents aged 0–19 years from 2010 to 2015. Outcomes included birth-related events (e.g. mortality), vaccination uptake, hospitalizations, and teen pregnancy. Regression goodness of fit was used to assess the strength of individual associations. Inequality was measured by slope index of inequality (SII) and relative index of inequality (RII).
Overall, 19 of 20 outcomes had socioeconomic gradients identified by SII and RII. The multidimensional CAN-Marg indices had the best explanatory power in standard regression models. The simplest ABSM—income quintile—detected 16 of 19 confirmed inequalities, more than any other single measure.
Conclusions
At all ages, many pediatric health outcomes in Manitoba were associated with significant socioeconomic inequalities; while income quintile detected most, CAN-Marg composite indices had the best explanatory power.
You have full access to this article via your institution.
Similar content being viewed by others
Integrating social vulnerability into high-resolution global flood risk mapping

The WHO estimates of excess mortality associated with the COVID-19 pandemic
Social capital I: measurement and associations with economic mobility
Introduction.
The existence of socioeconomic gradients in health is a well-established fact in Canada and elsewhere, 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 with many health outcomes improving with increasing socioeconomic status (SES). Since the collection of individual-level SES data is costly and intrusive, policymakers and governments rely on area-based socioeconomic measures (ABSM), typically derived from the rich data available in the national census. 11 , 12 , 13 There are a number of ABSM available in Canada e.g. Raymond−Pampalon material and social deprivation indices developed at the Institut National de Santé Publique du Québec (INSPQ), Manitoba’s Socio-Economic Factor Index-2 (SEFI 2 ,) and the Canadian Marginalization Index (CAN-Marg); 12 , 14 , 15 although extensively used for assessing health outcomes in adults, there are fewer studies using these ABSM to study health outcomes of specific importance in pediatrics. 1 , 2 , 4 , 6 , 16 , 17
Since ABSM quantify community characteristics, they are not necessarily interchangeable with individual SES, particularly if individual rather than community characteristics are the primary concern. 18 , 19 Moreover, ABSM capture different dimensions of social inequality. Townsend’s seminal work distinguished two forms of deprivation: Material deprivation reflected lack of access to health-related goods and services, including health information. Social deprivation reflected social capital and the impact of isolation, mutual assistance, and trust. 11 , 12 In Canada for example, the proportion of single-parent families has consistently been identified as a relevant measure on both theoretical and empiric grounds. 12 , 15 More recently, the Canadian Marginalization Index introduced four distinct dimensions, each potentially related to disease-specific pathways e.g. residential instability was strongly associated with binge drinking in adults. 14 Nevertheless, a recent pediatric scoping review concluded that pediatric studies generally rely on a variety of different SES measures, often selected “without an evidence-based rationale”. 16
Importantly, ABSM using “small” regions or census dissemination areas (DA; by definition, 400–700 people) may be as effective as SES obtained at the individual level. 13 , 20 Compared to individual measures, small area ABSM are easier to obtain from geocoded postal codes and census data. Moreover, ASBM may be more effective for assessing “neighborhood context”, including factors like the availability of health-related services or socio-environmental stressors. 21
One of the key rationales for obtaining information about SES using ABSM is to inform policymakers and governments about health inequalities so that they can more easily target high-risk populations to improve health at regional levels. Despite a variety of nuanced and multidimensional ABSM to assess health inequalities in adults, many governments—including the Manitoba Ministry of Health—rely specifically on average household income or income quintile. 2 For policymakers, this may facilitate the interpretation of associations between SES and health; as a result our study was in part motivated by the hypothesis that income alone would fail to capture important dimensions of inequality, making it an unsuitable surrogate for general health planning. Moreover, income data may be suppressed from small DA or vary for idiosyncratic reasons e.g. high-income laborers in remote northern communities. 22
In Manitoba, we have 11 different ABSM indices available in addition to income quintile (see Methods for details): Two national Raymond–Pampalon (INSPQ) indices measuring material and social deprivation; two regional INSPQ indices; two geographic INSPQ indices; SEFI 2 , a Manitoba-specific index similar to INSPQ material deprivation; and four CAN-Marg indices. All can be used to identify SES gradients in health outcomes. 12 , 14 , 22
Our primary objective was to examine the strength of the association between all available ABSM and key pediatric health outcomes using retrospective, provincial and cross-sectional data. Although generally underappreciated, it has recently been reported that existing ABSM do not capture sex-specific discrepancies in Canadian adults. 23 Secondarily, we therefore sought to identify interactions between the effects of sex and ABSM on health outcome rates in children. Lastly, we sought to compare income quintile with more nuanced alternatives to detect SES gradients in key childhood outcomes using standard measures, such as slope index of inequality (SII), relative mean index of inequality (RII mean ), and relative ratio index of inequality (RII ratio ). 9 , 24
Data source
The Manitoba Population Research Data Repository (the Repository), held at the Manitoba Centre for Health Policy (MCHP), is a collection of deidentified administrative, survey, clinical, and registry datasets linked together for research purposes. 25 The Population Registry represents all residents in Manitoba who are registered to receive healthcare and contains scrambled personal health identification numbers. The Population Registry also has date of birth, sex, date of death and reason for leaving the Registry (e.g., moved away from the province). Population Registry data were linked to Canadian census data by a six-digit postal code. Repository databases used in this study were health insurance registry, hospital discharge abstracts, medical services database, midwifery summary reports and immunizations.
The period of interest was 2010/2011 to 2014/2015. All outcomes were averaged over a 5-year period to avoid spurious annual variations.
Health outcomes
Twenty pediatric outcomes were categorized into four groups: infant, vaccination, adolescent, and hospitalizations (see Table 1 for outcomes and their overall rates). Thirteen infant outcomes were defined at birth or within the first year of life. For rates, the denominator was taken as the number of live births. Individuals were excluded if gestational age was less than 20 weeks or missing, weight less than 0.5 kg or missing, or stillborn. 2 For small-for-gestational age (SGA) and large-for-gestational age (LGA) outcomes, multiple births were excluded. Gestational ages were extracted from newborn hospital and midwifery records for all live births in Manitoba and categorized as follows: Preterm <37 weeks; early preterm <34 weeks; late preterm 34 weeks to ≤36 weeks; early term 37 weeks to ≤38 weeks; term 37 weeks to ≤41 weeks; post-term ≥42 weeks. When both hospital and midwifery records were available, the former were used preferentially.
Apgar scores at 5 min were divided into two groups: ≤7 vs. 8–10, with the former treated as an adverse outcome. Individuals with missing Apgar scores were excluded. For breastfeeding rates, either the hospital separation date or the birth date from the midwife record had to fall within the study period, with breastfeeding initiation if breastfeeding was reported at least once in hospital or midwifery records, excluding cases with missing breastfeeding information.
Newborn hospital and midwifery records for all live births in Manitoba were used to categorize SGA and LGA newborns, based on the 10th and 90th percentiles for sex, gestational age, and birth weight from Fenton and Kim. 26
Infant mortality was defined for all individuals born between April 1, 2009 and March 31, 2015 with a death date within 0 and 364 days. Death was identified by the reason for end of health coverage, and time to death was calculated from the birth and end of coverage dates. Neonatal mortality occurred within 0–27 days of age, and post-neonatal mortality at 28–364 days, and the denominator was the number of live births in each fiscal year. Individuals were excluded if gestational age was less than 20 weeks or missing, weight less than 0.5 kg or missing, stillborn, or missing cancellation code.
Vaccination completion rates were defined using the registry and Manitoba Immunization Monitoring System (MIMS) data. Individuals born between April 1, 2008 and March 31, 2013 with 24 months of continuous healthcare coverage that ended in the study period were included. To be considered “complete”, children had to receive the contemporaneous 18-month vaccine schedule recommended by Manitoba Health by age 24 months.
Hospital utilization was defined using hospital and registry records as any inpatient hospital visit with admission date in the study period for individuals less than 17 years of age. Newborn admissions were excluded. The denominator was defined using person-years at risk.
Teen pregnancy and teen live births for individuals between 13 and 19 years were counted. All pregnancies were counted for individuals with multiple pregnancies during the study. The denominator was the number of person-years of coverage for 13–19-year-old females.
Adolescent mood and anxiety disorders were defined based on records from hospitalization admissions, physician visits, and relevant drug dispensations identified through the Anatomical Therapeutic Chemical Classification System for children aged 12–18 years. The denominator was the number of person-years of coverage for this age group. 2
ABSM and income quintile
The first national Canadian ABSM was the Raymond−Pampalon ABSM; this was modeled after the Townsend Deprivation Index and developed by the INSPQ. 12 It was validated nationally using the 2001 census; it has been subsequently updated for the 2006 and 2011 censuses and was recently re-validated in adults in Quebec. 27
Using principal component or factor analysis (PCA), INSPQ created composite measures for both material and social deprivation, each based on multiple census measures for each DA and uncorrelated with each other by design. Material deprivation is based on average income, employment/population ratio of people aged 15 years and older, and proportion of adults with a high-school diploma. Social deprivation is based on the proportion of adults living alone; proportion of single-parent families; and proportion of marriages that were separated, divorced, or widowed.
The two national INSPQ indices (material and social) are available as both continuous (centiles) and categorical (quintiles) indices while their alternate forms (Prairie-Geographic and Prairie-Regional) are only available as quintiles. 27 INSPQ and Statistics Canada divide Canada into five regions. Since the Prairie provinces, including Manitoba, are culturally and economically similar, the regional indices are based on PCA applied to the region as a whole; in contrast, the geographic indices are based on comparisons within four zones defined by census metropolitan area population numbers, ranging from rural communities to large urban centers. In both cases, the Prairie indices are intended for comparisons only within the Prairie region.
The Canadian Marginalization Index (CAN-Marg) reflects four dimensions of inequality/marginalization associated with the following neighborhood census characteristics 14 : Material Deprivation (proportion of 25+ without certificate, diploma or degree; proportion of lone-parent families; proportion government transfer payments; proportion 15+ unemployment; proportion below low-income cut-off; proportion of homes needing major repairs). Residential Instability (proportion living alone; proportion of youth population aged 5–15 years; crowding = average number of persons per dwelling; proportion multiunit housing; proportion of the population married/common-law; proportion of dwellings that are owned; proportion of residential mobility i.e. not in the same house as 5 years ago). Ethnic Concentration (proportion of immigrants in the past 5 years; proportion of visible minorities). Dependency (proportion of seniors 65+; dependency ratio = ([0 − 14 + 65+]/[15–64]; labor force participation 15+). They were also created by factor analysis using DA level data from the 2006 and 2011 censuses and are suitable for use in rural or urban settings. In adults, each of the four components demonstrated strong associations with selected health outcomes. 14 Again, each index is reported as either a centile or quintile, where quintile 5 represents the most disadvantaged.
Manitoba has long been a leader in the field of ABSM and several specific provincial measures have been developed here, including the SERI and its successor, the Socio-Economic Factor Index-2 (SEFI 2 ). 22 The latter evolved from the original SEFI (based on high-school completion, unemployment rates, and the proportion of single-parent households in each census enumeration area). SEFI 2 exploits smaller census DA and adds average household income, which had previously been suppressed. 15 It is a continuous z -score with a mean of zero and a negative score identifying more affluent DAs. It is categorized by SD-score i.e. SEFI 2 > 1, 0 < SEFI 2 < 1, −1 ≤ SEFI 2 ≤ 0, and SEFI 2 < −1. 22
Given the expected variations in both income and living costs, it should be noted that DA income quintiles did not rely on national cut-points, but were calculated separately for rural and urban areas using Manitoba-specific census data. 22 For these analyses, the populations of Brandon and Winnipeg were designated urban, representing more than 60% of the provincial population of 1.3 million. To ensure consistent interpretation, regression models for income quintile were also ordered from least to most disadvantaged (e.g. from highest to lowest income).
For consistency, all ABSM indices and income quintile were based on the 2006 Canadian census. Postal codes were extracted at 24 months for vaccinations, study period entrance for hospital utilization and teen pregnancy, and at birth for the remaining pediatric outcomes. Seven ABSMs were measured as continuous and categorical including: SEFI 2 , CAN-Marg residential instability, CAN-Marg material deprivation, CAN-Marg dependency, CAN-Marg ethnic concentration, INSPQ National material deprivation, and INSPQ National social deprivation. The remaining five ABSMs were only available as quintiles, including: INSPQ Prairie Geographic material deprivation, INSPQ Prairie Geographic social deprivation, INSPQ Prairie Regional material deprivation, INSPQ Prairie Regional social deprivation, and income quintile.
Associations between ABSM and pediatric outcomes
For continuous outcome (i.e. birth weight), a gaussian general linear model (GLM) was applied to each continuous index (seven continuous ABSM) plus income quintile. These analyses were repeated using the categorical versions of all ABSMs. For each pediatric outcome, the best model was assessed by standard goodness of fit (AIC, with a smaller AIC reflecting a better fit). To compare across ABSM, %AIC compares model fit to the AIC for the corresponding model with income quintile.
For categorical outcomes (e.g. small/large for gestational age), the association between outcome rates and ABSM was assessed in either logistic regression or negative binomial count regression models. In some cases, offsets were required for differing exposure time in the at-risk cohort: In the negative binomial count models used for rates of hospital utilization, injury hospitalization, and unintentional injury hospitalization, a log-offset was applied for person-years at risk. In the logistic regression models for live births, teen-pregnancy, and mood-anxiety disorders, a complementary log−log link was used with a log-offset for individual years at risk. 28 Other categorical outcomes were analyzed using a logistic regression model with a standard logit link.
For each outcome, standard goodness of fit measures were used to compare individual models i.e. AIC and the likelihood ratio test (LRT). For each outcome, except teen pregnancy and teen live births, two additional models were run, one with sex as a main effect (sex+) and one with both sex as a main effect and a sex:ABSM interaction term (sex*). The Wald test for the interaction term was used to assess modification of the relationship between the outcome and ABSM by child sex.
Degree of social inequality
The degree of inequality in each pediatric outcome was measured using the slope index of inequality (SII), relative mean index of inequality (RII mean ), and the relative ratio index of inequality (RII ratio ). Regression slopes are calculated by GLM without adjustment for other covariates. 9 , 24 , 29 SII is an absolute measure of inequality, which represents the slope of the regression comparing mean outcome rates ( y- axis, rate as % of number at risk) to the cumulative percent of the Manitoba population ( x -axis) ranked from most deprived to least deprived. For comparisons across outcomes, RII is a relative measure of inequality, where RII mean divides the SII by the mean rate in the population. For both, a negative slope reflects higher rates in more disadvantaged communities. RII ratio is also a relative measure, which divides the predicted outcome rate in the least deprived group by the predicted rate in the most deprived, and values <1 reflect increased rates in lower SES categories. To reflect statistically significant inequality, both slope and ratio indices required p values < 0.05.
Statistical analyses
Rates for pediatric health outcomes were calculated over the study period (Table 1 ). We used p < 0.05 to denote statistical significance. For unsampled population data, no sample size restriction was required.
Ethics approval was obtained from the University of Manitoba Health Research Ethics Board (HREB), Bannatyne Campus. Permission was obtained from the Manitoba Health Information Privacy Committee (HIPC No. 2016/2017-20) to use the Manitoba Health administration data.
Table 1 depicts rates per 1000 or per 1000 person-years for the 20 pediatric health outcomes averaged over a 5-year period in Manitoba. Of note, term births accounted for 91.1% of all live births while 7.5% were preterm and 1.3% were post-term. Breastfeeding initiation was high at 83.5%; infant mortality rate was 0.4%. Only 64.4% of all children aged 24 mo received their full complement of 18-month vaccinations.
Supplementary Table S1 summarizes model fit for the outcome vs. ABSM GLM. Both absolute AIC and %AIC are compared to the same model with income quintile. When available, both continuous and categorical versions of ABSM are reported.
CAN-Marg indices generally outperformed other ABSM, with AICs up to 25% lower than for income quintile. Based on model fit, performance of SEF1 2 and INSPQ ABSM was similar to income quintile. Despite some significant differences between categorical and continuous versions of the same index, there did not appear to be a consistent pattern favoring one over the other. While sex often affected outcome rates, the sex:ABSM interaction term speaks to sex as a modifier of the relationship between outcomes and ABSM i.e. sex-specific patterns of inequality. Although there were some striking examples (e.g. injury hospitalization, unintentional injury hospitalization, mood and anxiety), results were often inconsistent for different ABSM even within the same outcome. Overall, sex:ABSM interactions were noted for 10 of 18 outcomes (excluding teen live pregnancies and teen live births).
To illustrate some of these results graphically, Fig. 1 displays infant mortality and injury hospitalization rates. Model fit (explanatory power) is depicted as %AIC i.e. the percentage of the corresponding model using income quintile. CAN-Marg generally performed better with either continuous or categorical predictors.
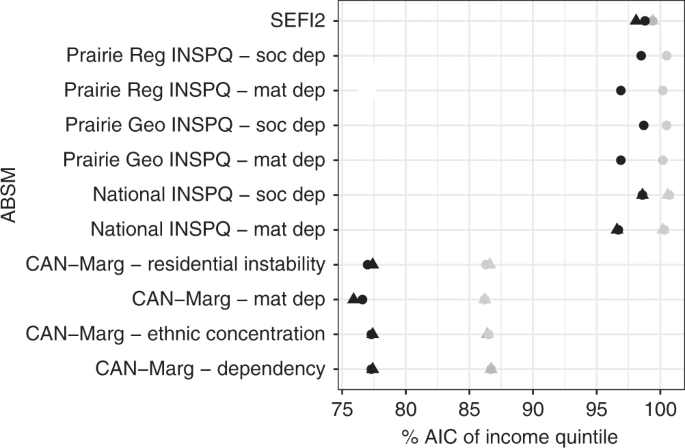
Model fit results are illustrated here for rates of infant mortality (gray) and injury hospitalization (black). As in Supplementary Table S1 , %AIC is the percentage of the values in the corresponding model using income quintile. ABSM were treated as categorical (e.g. quintiles, marked by circles) or continuous (e.g. centiles, marked by triangles) predictors, with only small differences in explanatory power. In contrast, %AIC for CAN-Marg indices were up to 25% lower than for income quintile.
To investigate SES inequalities associated with specific pediatric outcomes, Supplementary Table S2 summarizes SII, RII mean and RII ratio for each outcome. Inequality was deemed present if all slope and ratio indices were significantly different ( p < 0.05) compared to the null hypothesis (slope = 0 for the SII and RII mean and RII ratio = 1). All but one health outcome (neonatal mortality) demonstrated gradients for at least one ABSM. Figure 2a provides SII graphs for infant mortality based on three different ABSM: SEFI 2 , CAN-Marg material deprivation, and income quintile. Figure 2b presents similar results for injury hospitalization. In both, deprived strata did less well, which was a consistent finding across all 19 outcomes with confirmed inequality.
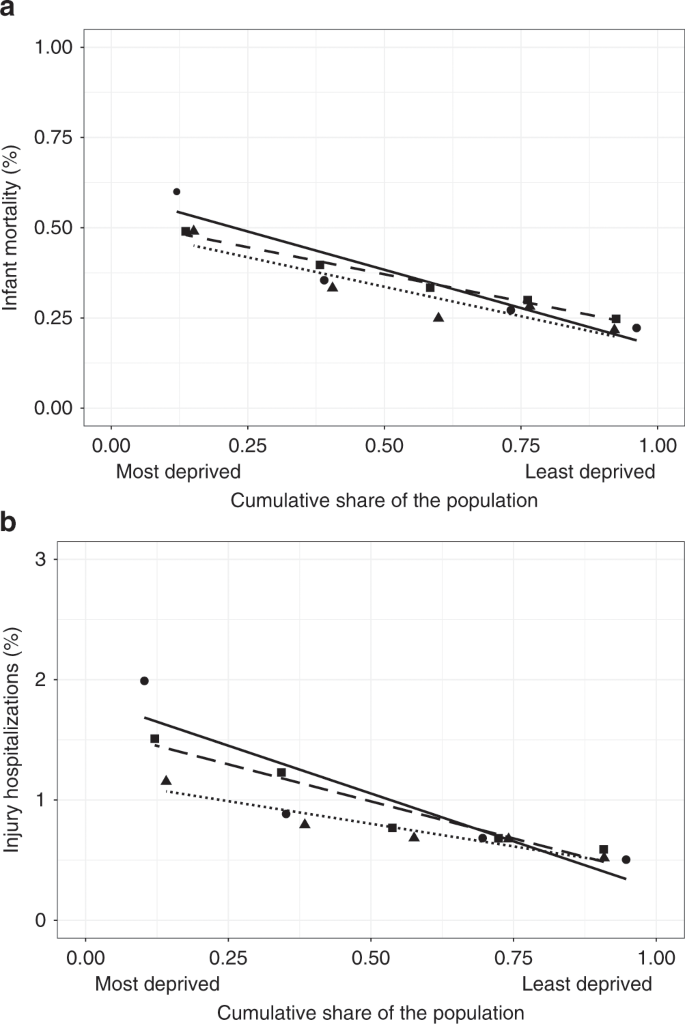
As in Supplementary Table S2 , the slope index of inequality (SII) is an absolute measure of inequality, which represents the slope of the regression comparing mean outcome rates ( y- axis, rate as % of numbers at risk—see Table 1 ) to the cumulative percent of the Manitoba population ( x- axis) ranked from most deprived to least deprived for each ABSM. Negative slopes reflect higher rates in more disadvantaged communities. In panels a infant mortality and b injury hospitalization, we compare SEFI 2 (circle, solid line), income quintile (square, dashed line), and CAN-Marg material deprivation (triangle, dotted line).
Lastly, Fig. 3 summarizes the number of health inequalities detected by each ABSM, including income quintile. There were 20 potential inequalities, grouped here by type of outcome: infant ( N = 13), vaccination ( N = 1), adolescent ( N = 3), or hospitalizations ( N = 3). Income quintile alone detected 16 of 19; the next best single measure was CAN-Marg material deprivation, detecting 11. In combination with CAN-Marg ethnic concentration, an additional five infant outcomes were detected. As a result, the combination of two CAN-Marg indices (material deprivation and ethnic concentration) was comparable to income quintile in detecting 16 of 19 cases, although there were some differences: Income quintile detected 9 of 12 inequalities in infant outcomes, but did not detect those in Apgar, early term births, and SGA. The CAN-Marg pair detected 10/12 infant inequalities, but missed early and post-term births; in older children, the pair also missed adolescent mood and anxiety disorders. All other ABSM performed less well.
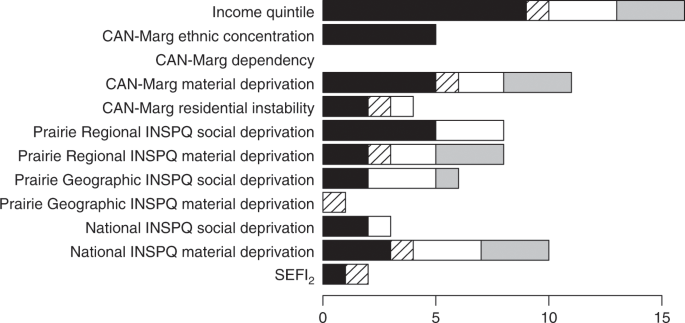
The bar chart displays the number of inequalities detected by each ABSM. ABSM are grouped by type: solid black = infant, 13 diagonal hatch = vaccination, 1 white = adolescent, 3 gray = hospitalizations. 3
We found inequalities in all but 1 of our 20 pediatric outcomes in Manitoba (the exception being neonatal mortality). These outcomes had been selected because they covered a broad spectrum in terms of both age and disorders. Income quintile alone identified the vast majority of these inequalities (16/19) compared to all other ABSM; the four CAN-Marg indices generally had better explanatory power (measured by AIC) than either income quintile or other well-known Canadian ABSM. The CAN-Marg indices even outperformed the Manitoba-specific ABSM (SEFI 2 ), which is generally regarded as the preferred measure for adult outcomes in Manitoba. 15 As previously reported in adults, 23 child sex was seen to modify inequalities for roughly half of outcomes.
Moving forward, our results support the continued use of income quintile as a measure of pediatric social inequality in regional health planning. In this study, income quintile was consistently able to detect inequalities across the pediatric age range, where it identified 9 of 12 inequalities in infancy and all others in older children. No other single measure performed as well for either infant or non-infant outcomes. The sensitivity of this relatively simple measure is somewhat surprising. In both a Canadian and international context, there is general consensus that more nuanced and perhaps multidimensional indices are needed to capture the relationships between SES and health outcomes, at least in adults. 22 , 30 , 31 , 32 In contrast, for both childhood lead poisoning and SGA births, children showed larger gradients in economic poverty (i.e. median household income or poverty categories) compared to indices based on education, occupation, or wealth. 33 It may simply be that for children, income disparity is a more important driver of health outcomes, by limiting access to health-related goods and services, including health information. 11 This may also be true in younger adults. 34
Although the choice of index is frequently driven by data availability or comparability with estimates from other countries, income quintiles are easily calculated, understood, and communicated, particularly for nonexperts or policymakers considering programs like income redistribution or subsidies. For interpretation purposes, the reader should note that all deprivation quintiles, including income, were ordered from most- to least deprived. Of the three measures of inequality, gradients are most easily described in terms of RII ratio , which measures the ratio of the predicted rate in the least deprived group to the predicted rate in the most deprived. As a result, values <1 will reflect higher rates in more disadvantaged communities. Taking income quintile as an example, the RII ratio for infant mortality was 0.43 (95% CI 0.38–0.49). Similarly, the teen-pregnancy RII ratio was 0.093 (0.05–0.16). For breastfeeding initiation, RII ratio was 1.37 (1.12–1.70) (Supplementary Table S2 and Fig. 2 ). In our experience, framing disparities in these terms facilitates discussions with policymakers and the general public.
As described above, the combination of CAN-Marg material deprivation with CAN-Marg ethnic concentration also managed to detect 16 of 19 inequalities, missing two infant outcomes (early term and post-term birth) and mood and anxiety disorders. Ethnic concentration was particularly effective in the infant age group. Ethnic concentration reflects the proportion of visible minorities or immigrants; in Manitoba this may reflect high proportion of indigenous children and the fact that Winnipeg is the second most important urban destination for new immigrants to Canada in terms of the percentage of recent immigrants in the general population (2011–2016). 35 , 36 Unlike income quintile, CAN-Marg material deprivation measures income inequality through the proportion of families below the low-income cut-off. In addition, it incorporates data pertaining to educational attainment, single-parent families, intergovernmental equalization transfers, unemployment rates, and homes in need of major repairs (see Methods). It clearly provides a more detailed measure of SES that reflects neighborhood context. 14 The additional information gleaned when combing CAN-Marg dimensions may therefore provide a more nuanced picture of risk factors other than just income.
As noted in the introduction, ABSM may also be interpreted in terms of potential disease pathways. We observe that residential instability was associated with vaccine uptake, SGA births, and early term deliveries. This may plausibly reflect disruption in the provision of routine well-child or prenatal care. The lack of association between the CAN-Marg dependency index and any single outcome is more difficult to explain: Given a relatively young population in Manitoba, 2 dependency relationships may be more related to young children in the household than to elder-care, with different burdens and implications. CAN-Marg ethnic concentration may speak to both material deprivation among indigenous and immigrant communities and access to health information in an appropriate language. The fact that income quintile and related measures of material deprivation were consistently associated with a wide variety of specific diseases at all ages may also be informative, suggesting that lack of access to health-related goods and services may be driving poorer outcomes in more disadvantaged neighborhoods. As noted by Townsend and others, material deprivation is not the same as poverty, though both effect access to necessary goods and services. 11 , 12 Further research is needed to clarify these relationships, with obvious implications for mitigation strategies.
We were particularly intrigued to note that our Manitoba-specific ABSM (SEFI 2 ) did not perform well, failing to identify 17 of 19 pediatric outcome inequalities, with a weaker fit by AIC. Based on PCA analysis of province-wide Manitoba data and validated for key adult health outcomes, the underlying census measures are in fact shared by a number of other indices, including INSPQ material deprivation. Nevertheless, factor loadings differ, 15 which may contribute to relatively poor performance of the weighted composite measure in children. Care must clearly be used when applying established measures in a pediatric context without prior validation.
Our results suggest that the continuous and categorical forms of ABSM may be used interchangeably. Recent reports of sex differences in ABSM applied to adults in a number of Canadian cities (including Winnipeg) 23 prompted us to examine whether child sex can modify health inequalities. Perhaps surprisingly, this often appears to be the case, though not consistently noted for every outcome or index. Given the ease with which sex:ABSM interactions can be tested, we are inclined to recommend routine inclusion in such studies.
The AIC is a likelihood-based measure of model fit with a penalty for model complexity (number of fitted parameters). When applied to common response data, even non-nested models may be compared in terms of explanatory power, analogous to the mean squared error in ordinary linear regression. Of note, the four CAN-Marg indices generally had lower AICs than other ABSM. Compared to income quintile, they provide more explanatory power, and as composite indices, they may be particularly useful when needing to account for multiple confounders and covariates.
The various INSPQ indices—national, regional, and geographic—did not consistently detect inequalities. While the national material deprivation index detected 10 of 19 inequalities, AIC was similar to income quintile. Interestingly, the National INSPQ has been validated in several pediatric studies, mostly in Quebec. 37 Perhaps there are regional differences in outcomes, differences in the outcomes studied, differences in ethnic blend, or differences in poverty rates that account for its suboptimal performance in Manitoba. Jurisdictions may also vary in the nature and consequences of inequality or in the availability of additional supports, particularly for children. Unlike most other provinces in Canada, Manitoba has one of the largest Indigenous pediatric populations; these children often live on reservations, have much lower SES, and are more likely to have poorer health outcomes. 36 , 38
The application of ABSM is often driven by data availability and the lack of individual-level SES data in medical charts or administrative records. In recent Canadian studies, both types of measures effectively identified inequalities in adult outcomes, but individual-level data revealed larger inequalities or stronger associations. 30 , 39 In Mather et al., the discrepancy was particularly marked in younger adults (45–64 years). 34 In other adult studies, the inequalities were similar whether based on individual or area-based population measures. 32 , 40 Although comparable studies in children are rare, results are conflicting: In Italy, asthma severity and hospitalization rates seem to be more strongly associated with individual-level measures than ABSM. 18 In Olmsted County MN, self-reported individual-level income was more strongly associated with three childhood health outcomes. 19 Significant disagreement rates of 22–31% were reported, with weighted Cohen’s kappa between 0.15 and 0.22, suggesting poor agreement between individual-level and ABSM. In contrast in Massachusetts and Rhode Island, pediatric lead poisoning and SGA births showed similar effect sizes for individual and area-based measures, as did a study of low birth weight in Massachusetts. 21 , 33 Clearly, this question remains unresolved, and area-level SES may be an unsuitable proxy when individual rather than community characteristics are of primary concern. Nevertheless, in both adults and children, the two types of indices appear to be independently and additively associated with outcomes, suggesting that they provide complementary information. Inclusion of neighborhood ABSM may therefore be important even when individual data are available, a practice which we are inclined to recommend.
Differences in effectiveness may also be related to the granularity of the data used to create the ASBM. 13 , 33 In Canada, the census DA for all of the ABSM were designed to be socially homogenous with a total population of 400–700. In contrast, US zip code target areas are based on populations in the tens of thousands. In their study of pediatric lead poisoning and SGA births, Krieger et al. showed that ABSM based on smaller census block groups (population mean ± SD 1085 ± 655) or census tracts (4572 ± 2080) led to stronger gradients than those based on zip codes (12,720 ± 12,244). 33
Our study has several strengths including the use of a rich, well-characterized, population data set. Our analyses covered a broad spectrum of pediatric ages and outcomes. However, our findings may not be generalizable to other jurisdictions, and similar studies may need to be performed elsewhere using a comparable range of diseases and indices. Inevitably, there are limitations inherent in the use of administrative data, including misclassification errors and selection biases. For example, diagnosis of mood and anxiety disorders may be biased by reliance on medication prescription records in addition to hospitalization admissions and physician visits. Even when based on specific billing codes, diagnoses may be imprecise or require arbitrary definitions e.g. for vaccine uptake, where children were allowed 2 years for completion of their 18-month schedules.
For health policy planning, area-based income quintiles may be sufficient for identifying inequalities in a broad range of pediatric health outcomes. However, quantitative analyses using regression models to assess the impact of SES likely favor the multidimensional CAN-Marg indices, which consistently demonstrated greater explanatory power by AIC and may provide important insights as to underlying disease mechanisms. Investigators applying CAN-Marg to their own populations have a choice of four distinct dimensions (ethnic concentration, material deprivation, residential instability, and dependency) and may prefer to study more than one index based on our findings. Given the relatively poor performance of SEFI 2 , which was developed and validated for adults in Manitoba, we would hope that other jurisdictions will be prompted by our results to conduct similar detailed studies before assuming that adult ABSM can be applied directly in studies of pediatric health. Given the observed impact of child sex with many health inequalities, we believe that the effects of sex should also be considered in such studies.
Bambang, S., Spencer, N. J., Logan, S. & Gill, L. Cause-specific perinatal death rates, birth weight and deprivation in the West Midlands, 1991–93. Child Care Health Dev. 26 , 73–82 (2000).
Article CAS Google Scholar
Brownell, M. et al. How Are Manitoba’s Children Doing? (Manitoba Centre for Health Policy, Winnipeg, Manitoba, 2012).
Corbett, S. S., Drewett, R. F., Durham, M., Tymms, P. & Wright, C. M. The relationship between birthweight, weight gain in infancy, and educational attainment in childhood. Paediatr. Perinat. Epidemiol. 21 , 57–64 (2007).
Article Google Scholar
El-Sayed, A. M., Scarborough, P. & Galea, S. Socioeconomic inequalities in childhood obesity in the United Kingdom: a systematic review of the literature. Obes. Facts 5 , 671–692 (2012).
Krieger, N., Chen, J. T., Waterman, P. D., Rehkopf, D. H. & Subramanian, S. V. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures-the public health disparities geocoding project. Am. J. Public Health 93 , 1655–1671 (2003).
Martens, P. J., Mayer, T. & Derksen, S. Factors affecting adolescent reproductive health in Manitoba. Can. J. Public Health Rev. Can. Sante Publique 93 (Suppl 2), S39–S43 (2002).
McNally, R. J. Q., Alston, R. D., Cairns, D. P., Eden, O. B. & Birch, J. M. Geographical and ecological analyses of childhood acute leukaemias and lymphomas in north-west England. Br. J. Haematol. 123 , 60–65 (2003).
Morris, R. & Carstairs, V. Which deprivation? A comparison of selected deprivation indexes. J. Public Health Med. 13 , 318–326 (1991).
CAS PubMed Google Scholar
Regidor, E. Measures of health inequalities: part 1. J. Epidemiol. Community Health 58 , 858–861 (2004).
Regidor, E., Banegas, J. R., Gutiérrez-Fisac, J. L., Domínguez, V. & Rodríguez-Artalejo, F. Socioeconomic position in childhood and cardiovascular risk factors in older Spanish people. Int. J. Epidemiol. 33 , 723–730 (2004).
Townsend, P. Deprivation. J. Soc. Policy 16 , 125–146 (1987).
Pampalon, R. & Raymond, G. A deprivation index for health and welfare planning in Quebec. Chronic Dis. Can. 21 , 104–113 (2000).
Adams, J., Ryan, V. & White, M. How accurate are Townsend Deprivation Scores as predictors of self-reported health? A comparison with individual level data. J. Public Health 27 , 101–106 (2005).
Matheson, F. I., Dunn, J. R., Smith, K. L. W., Moineddin, R. & Glazier, R. H. Development of the Canadian Marginalization Index: a new tool for the study of inequality. Can. J. Public Health Rev. Can. Sante Publique 103 , S12–S16 (2012).
Chateau, D., Metge, C., Prior, H. & Soodeen, R.-A. Learning from the census: the Socio-economic Factor Index (SEFI) and health outcomes in Manitoba. Can. J. Public Health Rev. Can. Sante Publique 103 , S23–S27 (2012).
Kachmar, A. G., Connolly, C. A., Wolf, S. & Curley, M. A. Q. Socioeconomic status in pediatric health research: a scoping review. J. Pediatr. 213 , 163–170 (2019).
Martens, P. J., Derksen, S. & Gupta, S. Predictors of hospital readmission of Manitoba newborns within six weeks postbirth discharge: a population-based study. Pediatrics 114 , 708–713 (2004).
Cesaroni, G., Farchi, S., Davoli, M., Forastiere, F. & Perucci, C. A. Individual and area-based indicators of socioeconomic status and childhood asthma. Eur. Respir. J. 22 , 619–624 (2003).
Pardo-Crespo, M. R. et al. Comparison of individual-level versus area-level socioeconomic measures in assessing health outcomes of children in Olmsted County, Minnesota. J. Epidemiol. Community Health 67 , 305–310 (2013).
Mustard, C. A., Derksen, S., Berthelot, J. M. & Wolfson, M. Assessing ecologic proxies for household income: a comparison of household and neighbourhood level income measures in the study of population health status. Health Place 5 , 157–171 (1999).
Subramanian, S. V., Chen, J. T., Rehkopf, D. H., Waterman, P. D. & Krieger, N. Comparing individual- and area-based socioeconomic measures for the surveillance of health disparities: a multilevel analysis of Massachusetts births, 1989−1991. Am. J. Epidemiol. 164 , 823–834 (2006).
Martens, P. J., Frohlich, N., Carriere, K. C., Derksen, S. & Brownell, M. Embedding child health within a framework of regional health: population health status and sociodemographic indicators. Can. J. Public Health Rev. Can. Sante Publique 93 (Suppl 2), S15–S20 (2002).
Haworth-Brockman, M. J. Gender, Deprivation and Health in Winnipeg . Thesis submitted to the Faculty of Graduate Studies of The University of Manitoba. https://mspace.lib.umanitoba.ca/bitstream/handle/1993/18333/Haworth_Brockman_Margaret.pdf?sequence=1 (2013).
Ontario Agency for Health Protection and Promotion (Public Health Ontario). Summary Measures of Socioeconomic Inequalities in Health (Ontario Agency for Health Protection and Promotion (Public Health Ontario), Toronto, ON, 2013).
Manitoba Centre for Health Policy, Department of Community Health Sciences, Rady Faculty of Health Sciences [Internet]. http://umanitoba.ca/faculties/health_sciences/medicine/units/chs/departmental_units/mchp/ (2019).
Fenton, T. R. & Kim, J. H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 13 , 59 (2013).
Institut national de santé publique du Québec; INSPQ [Internet]. https://www.inspq.qc.ca/en/information-management-and-analysis/deprivation-index (2019).
SAS Institute Inc. SAS/STAT® 9.2 User’s Guide , 2nd edn. (SAS Institute Inc., Cary, NC, 2009).
Regidor, E. Measures of health inequalities: part 2. J. Epidemiol. Community Health 58 , 900–903 (2004).
Pampalon, R., Hamel, D. & Gamache, P. A comparison of individual and area-based socio-economic data for monitoring social inequalities in health. Health Rep. 20 , 85–94 (2009).
PubMed Google Scholar
Blakely, T., Hales, S. & Woodward, A. Poverty: assessing the distribution of health risks by socioeconomic position at national and local levels. (World Health Organization Protection of the Human Environment Geneva; 2004).
Galobardes, B. et al. Indicators of socioeconomic position (part 1). J. Epidemiol. Community Health 60 , 7–12 (2006).
Krieger, N. et al. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: the Public Health Disparities Geocoding Project (US). J. Epidemiol. Community Health 57 , 186–199 (2003).
Mather, T. et al. Variation in health inequalities according to measures of socioeconomic status and age. Aust. N. Z. J. Public Health 38 , 436–440 (2014).
Government of Canada Statisitics Canada. Geographic distribution of immigrants and recent immigrants and their proportion within the population of census metropolitan areas, Canada, 2016 [Internet]. https://www150.statcan.gc.ca/n1/daily-quotidien/171025/t001b-eng.htm#fn02 (2017).
Government of Canada SC. Aboriginal peoples: fact sheet for Manitoba [Internet]. https://www150.statcan.gc.ca/n1/pub/89-656-x/89-656-x2016008-eng.htm (2016).
Pampalon, R. et al. An area-based material and social deprivation index for public health in Québec and Canada. Can. J. Public Health Rev. Can. Sante Publique 103 , S17–S22 (2012).
Greenwood, M. L. & de Leeuw, S. N. Social determinants of health and the future well-being of Aboriginal children in Canada. Paediatr. Child Health 17 , 381–384 (2012).
PubMed PubMed Central Google Scholar
Fuller, D. et al. Individual- and area-level socioeconomic inequalities in diabetes mellitus in Saskatchewan between 2007 and 2012: a cross-sectional analysis. CMAJ Open 7 , E33–E39 (2019).
Rehkopf, D. H. et al. Monitoring socioeconomic disparities in death: comparing individual-level education and area-based socioeconomic measures. Am. J. Public Health 96 , 2135–2138 (2006).
Download references
Acknowledgements
We acknowledge generous funding for an operating grant from the Children’s Hospital Research Institute of Manitoba (CHRIM) and the Children’s Hospital Foundation of Manitoba. Additionally, we acknowledge the Institute’s support of the research environment. The authors acknowledge the Manitoba Centre for Health Policy for use of data contained in the Manitoba Population Research Data Repository under HIPC No. 2016/2017-20. The results and conclusions are those of the authors and no official endorsement by the Manitoba Centre for Health Policy, Manitoba Health, or other data providers is intended or should be inferred. Data used in this study are from the Manitoba Population Research Data Repository housed at the Manitoba Centre for Health Policy, University of Manitoba and were derived from data provided by Manitoba Health and other data providers.
Author information
Authors and affiliations.
Department of Pediatrics and Child Health, University of Manitoba, Winnipeg, MB, Canada
Atul K. Sharma & Celia J. Rodd
Centre for Healthcare Innovation, University of Manitoba, Winnipeg, MB, Canada
Kristine Kroeker
Manitoba Centre for Health Policy and Department of Community Health Sciences, University of Manitoba, Winnipeg, MB, Canada
Dan Chateau & Marni Brownell
You can also search for this author in PubMed Google Scholar
Contributions
All authors met the Pediatric Research authorship requirements including substantial contributions to conception, design and acquisition of data or analysis and interpretation. Additionally, all assisted with drafting, revising the manuscript and provided final approval for this last version to be published.
Corresponding author
Correspondence to Celia J. Rodd .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary table 1, supplementary table 2, rights and permissions.
Reprints and permissions
About this article
Cite this article.
Sharma, A.K., Kroeker, K., Chateau, D. et al. Assessing childhood health outcome inequalities with area-based socioeconomic measures: a retrospective cross-sectional study using Manitoba population data. Pediatr Res 88 , 496–502 (2020). https://doi.org/10.1038/s41390-020-0755-3
Download citation
Received : 18 September 2019
Revised : 18 December 2019
Accepted : 21 December 2019
Published : 14 January 2020
Issue Date : September 2020
DOI : https://doi.org/10.1038/s41390-020-0755-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Lower socioeconomic status is associated with an increased incidence and spectrum of major congenital heart disease and associated extracardiac pathology.
- Christopher Smith
- Oluwayomi Olugbuyi
- Lisa K. Hornberger
Pediatric Cardiology (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Manitoba Centre for Health Policy Data Repository
- Reference work entry
- First Online: 01 January 2024
- pp 4072–4076
- Cite this reference work entry
- Tyler Ostapyk 2
The Population Health Research Data Repository (repository) is a comprehensive world-class collection of data files housed at the Manitoba Centre for Health Policy (MCHP) , a research unit within the Faculty of Medicine, Department of Community Health Sciences, University of Manitoba. The repository contains administrative, registry, survey, and other types of data primarily relating to residents in the province of Manitoba. All data files are de-identified: names, addresses, phone numbers, and real PHINs (personal health identification numbers) are removed before transfer to MCHP by the data provider. The data repository was developed to describe and explain patterns of health care and profiles of health and illness, facilitating intersectoral research in areas such as health, education , and social services within legislative privacy regulations and ethical frameworks.
Description
Unique in terms of its comprehensiveness, degree of integration, and orientation around a...
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Atherton, K., Fuller, E., Shepherd, P., Strachan, D. P., & Power, C. (2008). Loss and representativeness in a biomedical survey at age 45 years, 1958 British birth cohort. Journal of Epidemiology and Community Health, 62 (3), 216–223.
Article Google Scholar
Black, C., & Roos, N. P. (1998). Administrative data: Baby or bathwater? Medical Care, 36 (1), 3–5.
Huston, P., & Naylor, C. D. (1996). Health services research: Reporting on studies using secondary data sources. Canadian Medical Association Journal, 155 (12), 1697–1702.
Google Scholar
Leslie, L. L., Brownell, M., Lix, L., Roos, N. P., Walld, R., & Macwilliam, L. (2008). From health research to social research: Privacy, methods, approaches. Social Science & Medicine, 66 (1), 117–129.
Lix, L. M., Smith, M., Azimaee, M., Dahl, M., Nicol, P., Burchill, C., et al. (2012). A systematic investigation of Manitoba’s Laboratory Data . Winnipeg: Manitoba Centre for Health Policy.
Robinson, J. R., Young, T. K., Roos, L. L., & Gelskey, D. E. (1997). Estimating the burden of disease: Comparing administrative data and self-reports. Medical Care, 35 , 932–947.
Roos, L. L., & Nicol, J. P. (1999). A research registry: Uses, development, and accuracy. Journal of Clinical Epidemiology, 52 (1), 39–47.
Roos, N. P., & Shapiro, E. (1995). Medical care: Health and health care: Experience with a population-based health information system. Medical Care, 33 (Suppl 12), DS1–DS146.
Roos, L. L., Roos, N. P., Cageorge, S. M., & Nicol, J. P. (1982). How good are the data: Reliability of one health care data bank. Medical Care, 20 , 266–276.
Roos, L. L., Sharp, S. M., & Wajda, A. (1989). Assessing data quality: A computerized approach. Social Science & Medicine, 28 (2), 175–182.
Roos, L. L., Walld, R., Wajda, A., Bond, R., & Hartford, K. (1996). Record linkage strategies, outpatient procedures and administrative data. Medical Care, 34 (6), 570–582.
Roos, L. L., Romano, P. S., & Fergusson, P. (1998). Administrative data bases. In P. Armitage & T. Colton (Eds.), Encyclopedia of biostatistics (pp. 62–73). Chichester: Wiley.
Roos, L. L., Gupta, S., Soodeen, R. A., & Jebamani, L. (2005). Data quality in an information-rich environment: Canada as an example. Canadian Journal on Aging, 24 (Suppl 1), 153–170.
Download references
Author information
Authors and affiliations.
Manitoba Centre For Health Policy, Department of Community Health Sciences, University of Manitoba, Winnipeg, MB, Canada
Tyler Ostapyk
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Tyler Ostapyk .
Editor information
Editors and affiliations.
Dipartimento di Scienze Statistiche, Sapienza Università di Roma, Roma, Roma, Italy
Filomena Maggino
Section Editor information
Department of Political Science, University of Naples Federico II, Naples, Italy
Mara Tognetti
Rights and permissions
Reprints and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this entry
Cite this entry.
Ostapyk, T. (2023). Manitoba Centre for Health Policy Data Repository. In: Maggino, F. (eds) Encyclopedia of Quality of Life and Well-Being Research. Springer, Cham. https://doi.org/10.1007/978-3-031-17299-1_3483
Download citation
DOI : https://doi.org/10.1007/978-3-031-17299-1_3483
Published : 11 February 2024
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-17298-4
Online ISBN : 978-3-031-17299-1
eBook Packages : Social Sciences Reference Module Humanities and Social Sciences Reference Module Business, Economics and Social Sciences
Share this entry
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.7(10); 2017

Protocol for establishing an infant feeding database linkable with population-based administrative data: a prospective cohort study in Manitoba, Canada
Nathan christopher nickel.
1 Department of Community Health Sciences, Max Rady College of Medicine, Rady Faculty of Health Sciences, Universityof Manitoba, Winnipeg, Manitoba, Canada
2 Manitoba Centre for Health Policy, University of Manitoba, Winnipeg, Manitoba, Canada
Lynne Warda
3 Department of Pediatrics and Child Health, Max Rady College of Medicine, Rady Faculty of Health Sciences, Universityof Manitoba, Winnipeg, Manitoba, Canada
4 Injury Prevention and Child Health, Public Health Program, Winnipeg Regional Health Authority, Winnipeg, Manitoba, Canada
Leslie Kummer
5 Academic General Pediatrics, Division of General Pediatrics and Adolescent Health, University of Minnesota, Minneapolis, Minnesota, USA
Joanne Chateau
Maureen heaman.
6 College of Nursing, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, Manitoba, Canada
Chris Green
7 Population & Public Health, Winnipeg Regional Health Authority, Winnipeg, Manitoba, Canada
8 Department of Family Medicine, Max Rady College of Medicine, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, Manitoba, Canada
9 Field Services Training Unit, Health Security Infrastructure Branch, Public Health Agency of Canada, Ottawa, Ontario, Canada
Carolyn Perchuk
Darlene girard, lorraine larocque.
10 Department of Public Health, Northern Health Region, Thompson, Manitoba, Canada
Jennifer Emily Enns
Souradet shaw.
11 Department of Surveillance and Epidemiology, Winnipeg Regional Health Authority, Winnipeg, Manitoba, Canada
Associated Data
bmjopen-2017-017981supp001.pdf
Introduction
Breast feeding is associated with many health benefits for mothers and infants. But despite extensive public health efforts to promote breast feeding, many mothers do not achieve their own breastfeeding goals; and, inequities in breastfeeding rates persist between high and low-income mother–infant dyads. Developing targeted programme to support breastfeeding dyads and reduce inequities between mothers of different socioeconomic status are a priority for public health practitioners and health policy decision-makers; however, many jurisdictions lack the timely and comprehensive population-level data on infant-feeding practices required to monitor trends in breastfeeding initiation and duration. This protocol describes the establishment of a population-based infant-feeding database in the Canadian province of Manitoba, providing opportunities to develop and evaluate breastfeeding support programme.
Methods and analysis
Routinely collected administrative health data on mothers’ infant-feeding practices will be captured during regular vaccination visits using the Teleform fax tool, which converts handwritten information to an electronic format. The infant-feeding data will be linked to the Manitoba Population Research Data Repository, a comprehensive collection of population-based information spanning health, education and social services domains. The linkage will allow us to answer research questions about infant-feeding practices and to evaluate how effective current initiatives promoting breast feeding are.
Ethics and dissemination
Approvals have been granted by the Health Research Ethics Board at the University of Manitoba. Our integrative knowledge translation approach will involve disseminating findings through government and community briefings, presenting at academic conferences and publishing in scientific journals.
Strengths and limitations of this study
- This study is among the first to establish a mechanism for collecting infant-feeding data at a population level in Canada, providing longitudinal data to study the impact of policy, programme and services on infant-feeding practices.
- Our ability to link the infant-feeding database with a large repository of administrative data spanning several domains increases the number of confounding characteristics we can adjust for in our analyses.
- Using linked whole population data means there will be minimal loss to follow-up and allows us to compare individuals captured in the infant-feeding database with individuals who were not.
- Using vaccination visits as the point of contact for data collection means some individuals will be missed (although more than 90% of infants receive the recommended vaccinations at 2 months of age).
- Collecting data on infant feeding routinely relies on maternal report, which can be subject to social desirability bias.
Breast feeding is associated with numerous health benefits for mothers and their infants. 1–7 The WHO, Unicef and other health authorities recommend exclusive breast feeding for the first 6 months of life, followed by continued feeding of breast milk along with complementary foods for 2 years and beyond. 8–12 However, in spite of extensive public health efforts to support breast feeding, two challenges remain: (1) many mothers do not achieve their own breastfeeding goals and (2) inequities in breastfeeding outcomes persist between mother–baby dyads living in marginalised circumstances and their more advantaged counterparts. 13–15 Findings from the Canadian Maternity Experiences Survey showed that although breastfeeding initiation rates were relatively high in Canada, exclusive breastfeeding duration fell short of globally recommended standards, with only 14.4% of mother–baby dyads breast feeding exclusively at 6 months after birth. 16 Based on these figures, developing targeted programme and interventions to support breastfeeding dyads and reduce breastfeeding inequities have become a priority for public health practitioners and health policy decision-makers. 17 18 However, many jurisdictions lack the timely and comprehensive population-level data on infant-feeding practices required to monitor trends in breastfeeding initiation and duration.
Current state of infant-feeding surveillance
In North America, much of the data on infant-feeding practices are collected through primary data collection methods such as cross-sectional surveys and cohort studies. Most global surveillance of longitudinal infant feeding is accomplished through periodic surveys of populations, often at the time of hospital discharge or in the postpartum period. 19–22 These methods of epidemiological surveillance have some important limitations 23–27 :
- Significant resources are required to design and implement novel high-quality cohort studies;
- Families living in disadvantaged social and economic circumstances—such as low-income households and families with high residential mobility—may be under-represented in survey research;
- Lack of whole population data makes generalisability challenging and limits planners’ ability to conduct small area-level analyses;
- Relying on survey data collected for a single purpose makes it difficult to track outcomes across the life span.
In light of these and other limitations, researchers are turning to routinely collected administrative health data to conduct a wide variety of epidemiological research studies. 27
How can administrative health and social data help address evidence gaps?
Contacts with the health and social services systems generate data in the form of administrative records. Linking these routinely collected records across sectors is a powerful tool for conducting large-scale, longitudinal epidemiological research. 23 25–28 For example, researchers in Europe and Australia have been using linked administrative health data to monitor breastfeeding initiation and duration rates for the last two decades. 29–32 In Canada, studies have used breastfeeding initiation data obtained from the birth hospital discharge abstracts to track trends and inequities in breastfeeding initiation and examine outcomes associated with initiating breast feeding during the first days of life. 13 33 Although providers routinely ask questions about infant-feeding practices during well-baby visits throughout the first year of life, including questions about breastfeeding duration, this information is seldom integrated into a centralised database. Thus, researchers and programme planners lack comprehensive data on infant-feeding practices once the mother–baby dyad is discharged from the birth hospital stay. Therefore, there is a critical need to identify a mechanism whereby infant-feeding information that is routinely collected during well-baby visits can be consolidated in a whole population database.
Research objective
The objective of this work is to establish a mechanism for collecting infant-feeding information during routine contacts with the healthcare system, which can then be linked with a centralised data repository of administrative health data. Specifically, it will evaluate whether a Teleform fax system is a viable mechanism for (1) collecting infant-feeding data when infants receive their 2, 4 and 6-month vaccinations and (2) automatically depositing that information into the new Manitoba Infant Feeding Database (MIFD) and linking it at the individual level with the Manitoba Population Research Data Repository, an established repository of administrative health and social data.
We will address the following research questions:
- What per cent of data collected using the Teleform have transcription errors when automatically read into an electronic format, requiring manual verification and edits?
- What are the patterns of missing data in the Manitoba Infant Feeding Database?
- What per cent of infants are captured at the 2, 4 and 6-month vaccination visits?
- Do data capture rates differ by rural/urban status of the study sites?
- What maternal characteristics (maternal age, income, residential mobility) and infant characteristics (sex, small for gestational age, large for gestational age, Apgar score) are associated with data captured at the 2, 4 and 6-month vaccination visits?
The study funding period began in October 2014 and ends in August 2018. The study takes place in Manitoba, a central Canadian province with approximately 1.3 million residents. For the past 4 years, the annual number of births in the province has ranged between 15 000 and 17 000 births. Just over 80% of mother–infant dyads initiate breast feeding during the birth hospital stay; however, initiation rates follow a socioeconomic gradient where low-income dyads are less likely to initiate breast feeding compared with their higher income counterparts. 13–15
A unique and advantageous feature of establishing an infant-feeding database in Manitoba is our ability to link the new Manitoba Infant Feeding Database to the established Manitoba Population Research Data Repository. 34 35 The Repository contains more than 30 years of population-based, individual-level information on all Manitobans who are registered with the province of Manitoba’s universal health insurance programme; thus, the Repository contains information on 99.9% of Manitobans residents. Each time a Manitoba resident is in contact with the healthcare system, the information from that contact is recorded and held in the repository. The repository data are deidentified using strict protocols to preserve residents’ anonymity but can be linked longitudinally and across sectors using a scrambled personal identification number. 23 25 27 Besides health information, the repository includes administrative records from social services and government programme, children’s education records and contacts with the criminal justice system. 23 25 The repository data have been validated and used extensively for maternal and child health research studies. 36–40
Identifying opportunities for data collection at routine vaccination visits
We began by identifying infant vaccination visits as a consistent and opportune routine point of contact with the healthcare system, whereby population-based information on infant feeding could be collected. In Manitoba, more than 90% of infants complete their 2-month vaccination schedules and 78% complete their 1 year vaccination schedules. 41 Thus, using this point of contact, infant-feeding information could be collected from nearly every mother–baby dyad in the province. With consideration for the funding timeline, we selected the 2, 4 and 6-month vaccination visits as infant-feeding data collection time points.
Selecting and optimising a tool for data collection: the teleform fax tool
It was important to choose a tool that falls within the requirements of the personal health information legislation in Manitoba and that could be widely applied across the province. Manitoba does not currently have an online system that complies with privacy legislation for personal health information sharing; online data collection and sharing would also not be feasible in many of Manitoba’s rural and remote communities where internet connectivity is poor or non-existent. We selected the Teleform Fax Tool 42 since it is compliant with Manitoba’s personal health information legislation and can be used without internet access. Fax technology is also routinely used to collect health information in jurisdictions across Canada, 43–46 and as such, is an accepted tool for collecting survey data.
To place a minimum burden on mothers and healthcare workers, ensure that the Teleform questions could be answered quickly and easily and maximise the possibility that such a system could be routinely implemented across the province, we conducted a literature search to identify a short set of questions that would yield rich data on infant-feeding practices posthospital discharge. 47 During the summer of 2015, we piloted a draft version of the questions ( box ) by conducting three focus groups with new mothers: one urban group comprising 8 mothers, one group of 9 mothers in a rural agricultural community and one group of 12 mothers from a remote rural community.
Infant Feeding Questions Pilot Tested with Manitoba Mothers
- Only Breastmilk. (End of questions)
- Only formula/other food. (End of questions)
- Breastmilk and formula/other food. (Go to question 2)
- Breastmilk only. (Go to question 3)
- Breastmilk and formula/other food. (Go to question 4)
- Only formula/other food. (Go to question 5)
- Yes, my baby was only supplemented in the hospital. Otherwise I have only breastfed (End of questions)
- No, my baby was supplemented in the hospital and at home. (Go to question 4)
- How many weeks old was your baby when you first fed formula/other food?
- How many weeks old was your baby when you completely stopped breastfeeding?
During the focus groups, the mothers each answered the questions on infant-feeding practices and then discussed as a group how they interpreted each question. They provided feedback on question structure and order to improve the clarity of questions and reduce response burden. The final set of questions included in the Teleform to measure infant-feeding practices were selected based on the focus group feedback; these are based on questions used in other prospective studies that follow mother–infant dyads from birth through the first year of life, aimed at measuring breastfeeding duration. 48 49 As well, these questions will capture data that will allow us to construct variables on infant feeding in alignment with the WHO’s definitions of breast feeding. 50–53
Our questions ask mothers to report duration of exclusive breast feeding and complementary breastfeeding. Research has shown maternal recall of breastfeeding duration is high when the recall period is less than 1 year. 54 The Teleform does not rely exclusively on 24 hours recall to measure infant-feeding practices since some studies have shown that 24 hours recall may overestimate prevalence of exclusive breast feeding and thus recommend that infant feeding be prospectively measured with a combination of current status and recall since birth. 55–60
The Teleform also collects data for linkage purposes, including: (1) the mother’s and infant’s personal health identification numbers (PHINs; unique, person-level identifiers held in the repository); (2) the infant’s birth date; (3) the infant’s sex and (4) the mother’s postal code. The final version of the Teleform is presented in see online supplementary file 1 .
Supplementary file 1
Recruitment and data collection.
Recruitment and data collection began in September 2015 and will continue until December 2017. Six study sites are enrolled: one urban clinic where 75% of all urban-dwelling children in Manitoba receive their vaccinations, two rural public health offices located in agricultural communities and three rural public health offices located in rural remote settings. Over the past 3 years, the annual number of children vaccinated across all six sites ranged between 1500 and 2000 children.
Mothers who bring their infants to study site clinics for vaccination visits are asked by clinic staff members to participate in the study. Clinic staff provide them with documents describing the study and its purpose, along with informed consent documentation. Mothers who review the documents and give written informed consent are enrolled in the study. Study participants are asked to complete the Teleform at their infants’ 2, 4 and 6-month vaccination visits. Mothers fill out the Teleform during the visit and then return it to staff before leaving the clinic. Data collected with the Teleform are faxed by the clinic staff to the research study office located within a government agency. There, the data are automatically extracted from the faxed form and an image of the form is placed on a password-protected network in a secure data environment with restricted card access. Data quality checks are run manually to identify transcription errors and missing data. For each data field, we are documenting the percentage with transcription errors, requiring manual verification and needing manual edits to address research question 1.
Table 1 presents preliminary summary enrolment figures and vaccination rates of infants at each study site (September 2015 to December 2016). During this period, approximately 75% of mothers consented to provide feeding data for the study. At the end of the data collection phase, we will conduct descriptive summary statistics to identify patterns of transcription errors and missing data to answer our first two research questions.
Numbers of mother–infant dyads with infant-feeding data captured in the Manitoba Infant Feeding Database at each vaccination visit, per year
*Estimated number of children seen at each study site during a 1-year period based on information provided by clinic administrators. Precise numbers of children seen at each clinic will be determined once the MIFD is linked with the Manitoba Population Research Data Repository.
†Vaccination rates estimated for the first year of the study period from previous years’ administrative health data held in the Manitoba Population Research Data Repository.
‡All mother–infant dyads who attend a vaccination visit will be invited to participate in the study. Between 1 September 2015 and 31 December 2016, roughly 75% of them enrolled in the study. This column presents the number of mother–infant dyads who have consented to participate in the study and whose infant-feeding data was captured in the Manitoba Infant Feeding Database.
§Based on current enrolment rates (75%) and vaccination rates, this column represents the anticipated number of mother–infant dyads whose data will be captured at the 4 and 6-month vaccination visits.
MIFD, Manitoba Infant Feeding Database.
Linking infant-feeding data with the Manitoba population research data repository
The MIFD is composed of two datasets: (1) the Infant Feeding Dataset consisting of infant-feeding data and individuals’ unique study identification (ID) and (2) the Identifying Dataset comprising mothers’ and infants’ PHINs, infant’s date of birth, infant’s sex, mother’s postal code and infant’s unique study ID. Table 2 depicts the information held in the two datasets. Figure 1 shows the data flow process from point of data collection to acquisition into the Manitoba Population Research Data Repository for data analyses.
Datasets in the Manitoba Infant Feeding Database
ID, identification; PHIN, personal health identification number.

Manitoba Infant Feeding Database data flow diagram. ID, identification; PHIN, Personal Health Identification Number. Data are collected at vaccination visits using the Teleform and faxed to a central office. The identifiable data file contains two datasets: (1) Infant Feeding Data (a dataset that includes infant-feeding information and study ID) and (2) Identifying Data (a dataset that includes identifying information and study ID). The Identifying Data are sent to Manitoba Health for deidentification and attachment of scrambled PHIN. Manitoba Health generates a cross-walk file with instructions for data lnkage. The Infant Feeding Data are sent to the Manitoba Population Research Data Repository. The Scrambled PHIN, study ID and cross-walk file are used to link infant-feeding data with the rest of the administrative data held in the repository. The linked databases form the analytical data for the study.
The MIFD will be held in and linked to the Manitoba Population Research Data Repository. The Repository is a collection of over 70 databases containing information on health, education, receipt of social services and interactions with the justice system. The Manitoba Health Insurance Registry includes individuals’ unique scrambled PHINs and a family registration number, which allows linkages between mothers and their infants. Using scrambled PHINs and cross-walk files generated by Manitoba Health, individual-level data can be linked across all datasets held in the repository in a deidentified way.
Study cohort development
We will construct the study cohort using the whole population data held in the repository. The cross-walk file generated by Manitoba Health will be used to link mothers and infants and to link infants’ feeding data with their health records in the repository. Specifically, infant-feeding data will be linked with the following administrative health data: (1) the dyad’s birth hospital discharge data, (2) the infant’s vaccination records held in the Manitoba Immunisation Monitoring System, (3) medical billing records associated with the infant’s primary care visits held in the Medical Services dataset and (4) the mother’s postal code of residence held in the Manitoba Health Insurance Registry. The cohort will include all mothers and infants who had at least one vaccination visit at one of the study sites between 1 September 2015 and 31 December 2017; thus it, will include infants with and without feeding data. For those without feeding data, the relevant data fields in the Manitoba Infant Feeding Database will read ‘missing’. We will use multivariable logistic regression models to identify characteristics associated with having missing data in the MIFD.
Variable construction
Using the study cohort, we will develop variables to address research questions 3–5. Table 3 presents each of the outcome variables we will examine in these analyses. Because the data include all contacts with the healthcare system, we will be able to follow infants as they access healthcare services across the province; we will be able to track all vaccinations for infants in the study, regardless of whether or not that vaccination was given at one of the study sites. We will construct a set of three variables—one for each vaccination visit—to describe whether we captured infant feeding data from the dyad. For each visit, the variable will tell us (1) if feeding data were recorded, (2) if a vaccination visit was recorded at a study site but feeding data are missing, (3) if a vaccination visit was recorded at a non-study site and (4) whether an infant has a vaccination recorded for that time point.
Outcome variables for analyses
A feeding history for each infant will be constructed using data from the hospital discharge abstract and feeding data collected at each vaccination visit. The feeding history will indicate whether an infant is exclusively breast feeding, complementary breast feeding or exclusively formula feeding at four contacts with the healthcare system: birth hospital discharge, 2, 4 and 6-month vaccination visits (definitions presented in table 2 ). We use the WHO definitions for infant-feeding status at each time point:
- Exclusive breast feeding—an infant is only fed breast milk (including milk expressed or from a wet nurse) and not fed anything else and
- Complementary Feeding—an infant is fed breast milk (including milk expressed or from a wet nurse) and solid or semi-solid foods, allowing for any food or liquid including non-human milk and formula. 50–53
The data collected on the Teleform will also be used to determine (1) the infant’s age when a food other than human milk was first introduced (cessation of exclusive breast feeding) and (2) the infant’s age when the dyad stopped breast feeding entirely (breastfeeding cessation). Taken together, this information can be used to identify each infant’s duration of exclusive and complementary breast feeding.
In addition to infant feeding status, we will construct a dichotomous variable that describes infant feeding history. An infant feeding history can be constructed from the available data for each infant if (a) the date of exclusive and breastfeeding cessation are both recorded, (b) the infant had all age-appropriate vaccination visits and was still breast feeding at the last recorded visit (in this instance, the data are right censored) or (c) feeding data are recorded for each visit, regardless of feeding practice. Because we will have data on every infant, we will be able describe how those with missing feeding data or those whose data were not captured in the database differ from infants with feeding data recorded at each contact with the healthcare system. Table 4 presents the explanatory variables that we will use in these analyses. Explanatory variables will be developed using repository data from the mother and/or infant.
Explanatory variables
Data analysis plan
We will generate descriptive statistics to identify the percentage of infants in the cohort with feeding data at 2, 4 and 6-month vaccination visits and test whether data capture rates differ across time (research question 3). We will also test whether the percentage of infants with captured data differs by urban/rural status of the study site where they were vaccinated (research question 4). For each time point, we will calculate the socioeconomic distribution of infants across four categories: (1) infant has feeding data; (2) infant has vaccination recorded at a study site but does not have feeding data; (3) infant has a vaccination recorded at a non-study site and (4) infant does not have a vaccination recorded.
We will calculate the percentage of infant feeding data that are missing due to the infant receiving one or two vaccinations at a non-study site. Identifying the frequency with which this occurs will provide an estimate of the percentage of infants that could have complete infant-feeding data if Manitoba had a universal system that captured infant-feeding information.
Characteristics associated with having infant-feeding data captured in the database will be examined using logistic regression models for the 2, 4 and 6-month visits (research question 5). The outcome will be a dichotomous variable identifying whether or not a mother–infant dyad’s infant-feeding information is captured in the database. Models will include the variables listed in table 4 . Each model will include a subcohort of age-appropriate infants; for example, analyses examining data collected at the 4-month vaccination visit will exclude anyone ≥4 months of age. Results from these analyses will indicate whether mother–infant dyads captured by this strategy differ systematically from those who have missing data.
Finally, we will examine characteristics associated with whether or not we can construct an age-appropriate infant-feeding history using data held in the Manitoba Infant Feeding Database. The outcome variable will describe whether or not a complete infant-feeding history can be constructed based on available data. Explanatory variables will include those listed in table 4 .
Ethical considerations
The research team has completed the Tri-Council Course on Research Ethics. We have obtained approvals from the Health Research Ethics Board at the University of Manitoba, the Health Information Privacy Committee of Manitoba Health and the ethics committees in participating regional health authorities. Participation in the study is voluntary. Study participants are informed of the purpose of the study, potential risks associated with participation (compromise of data), their rights and obligations as participants and their ultimate right to withdraw at any point without negative consequences. We ask study participants for consent to link their data with the repository. Participants are informed that they will not be identifiable in any reports or publications. Informed consent is obtained from participants prior to data collection. Identified data are housed on a password-protected server in a secure data environment at the research office. The data are sent to Manitoba Health for deidentification and encryption. Only the data analysts have access to the deidentified data. Analyses using the deidentified data will be conducted in the secure data environment at the Manitoba Centre for Health Policy.
Integrated knowledge translation and dissemination of findings
The research team has adopted an integrative knowledge translation approach. In addition to academic researchers, the broader team comprises an interdisciplinary group of stakeholders from government departments, public health offices and regional health authorities. Over a 6-month prefunding planning period, the team worked together to develop a research plan and to secure peer-reviewed funding through a Research Manitoba New Investigator Operating Grant. While the core research team leads the study, the stakeholders are serving as advisory group members to ensure that findings can be applied to the population-based infant-feeding data collection strategy. The advisory group also strategises with the core research team on methods for disseminating findings to healthcare workers and other stakeholders in and outside of Manitoba.
Even at this early stage, there has been great interest in the study from stakeholders in government and public health. To date, we have presented the research plan and preliminary findings to public health officers in each regional health authority active in the study, and we have participated in two provincial meetings on breastfeeding practices. We have also widely disseminated the study aims and early findings in the academic community at the University of Manitoba. Near the end of the funding period, the team will host a province-wide workshop that will bring together public health nurses, clinic staff members and stakeholders to discuss the study findings and experiences with implementing the data collection mechanism. Two advisory group members are actively involved with the Breastfeeding Committee for Canada and will arrange for webinars to disseminate findings through this organisation. Findings will be presented at national and/or international conference(s) and will be submitted for peer-review publication to inform further research around infant-feeding data collection and provide evidence for building new population-based data collection systems.
Supplementary Material
Acknowledgments.
This study was part of a program of research conducted by the Manitoba Infant Feeding Database Development Team. The authors thank the clinic staff and public health nurses who collaborated with us on this project. The authors express their gratitude to the Developmental Origins of Chronic Disease in Children Network (DEVOTION) and the Lawson Foundation for their partnership. The authors also acknowledge the Manitoba Centre for Health Policy (MCHP) for use of the data in the Population Health Research Data Repository under project (HIPC No. 2014/2015-37). Data used in this study are from the Population Health Research Data Repository and were derived from data provided by Manitoba Health, Seniors and Active Living. The results and conclusions are those of the authors and no official endorsement by MCHP, Manitoba Health, Seniors and Active Living is intended or should be inferred.
Contributors: The study was conceived by NCN, the principal investigator on the original funded grant. NCN, LW, MH, AK and CG participated in designing the study and were listed as collaborators on the grant. NCN, JC and LW were involved in recruiting participating study sites, and NCN and JC are working with study sites on data collection processes. JC and JP are involved in data cleaning and verification. NCN, LK and JEE drafted the manuscript. All authors contributed to critically revising the manuscript for important intellectual content, gave their final approval and agreed to be accountable for all aspects of the work, and they will participate in future interpretation of the data and drafting of further manuscripts arising from this work.
Funding: This work was supported by a New Investigator Operating Grant from Research Manitoba (Formerly Manitoba Health Research Council) - New Investigator Operating Grant Number 796. It is part of the Developmental Origins of Chronic Disease in Children Network (DEVOTION) and was supported in part by the Lawson Foundation (GRT2015-6).
Competing interests: None declared.
Ethics approval: Health Ethics Research Board at the University of Manitoba.
Provenance and peer review: Not commissioned; externally peer reviewed.
Collaborators: The Manitoba Infant Feeding Database Development Team: Joanne Chateau, Lawrence Elliott, Darlene Girard, Janet Grabowski, Christopher Green, Maureen Heaman, Alan Katz, Lisa Labine, Lorraine Larocque, Janice Loe, Eunice Lunsted, Teresa Mayer, Nathan C Nickel, Pam Noseworthy, Julia Paul, Carolyn Perchuk, Dawn Ridd, Elske Hildes Ripstein, Linda Romphf, Rob Santos, Geert t’Jong, Lynne Warda.
The University of Manitoba campuses are located on original lands of Anishinaabeg, Cree, Oji-Cree, Dakota, and Dene peoples, and on the homeland of the Métis Nation. More
Max Rady College of Medicine
- Why UM: Explore our viewbook
- Undergraduate admissions
- Graduate admissions
- Extended Education
- Indigenous students
- Financial Aid and Awards
- Apply to UM
- Faculties, colleges and schools
- Academic Calendar
- Registrar's Office
- Undergraduate programs
- Graduate programs
- Extended Education programs
- TeachingLIFE
- Opportunities and support
- Research Chairs
- Centres and institutes
- Partnerships and Innovation
- Awards and recognition
- International Centre
- ResearchLIFE
- Academic supports
- Accessibility
- Career Services
- Get involved
- Health and wellness
- Respectful conduct
- Sexual violence
- Student services at Bannatyne campus
- Indigenous community
- Sport and Recreation
- Mini U Programs
- Faculty, staff and retirees giving campaign
University of Manitoba Winnipeg, Manitoba Canada, R3T 2N2
Term: Manitoba Population Research Data Repository (Repository)
Printer friendly
Glossary Definition
Last Updated : 2021-11-19 Last Reviewed : 2009-08-27 -->
Definition:
- what the Data Repository is for,
- the Repository Data List and Data Descriptions resource tools and links to these tools,
- the Applying for access and use process for doing research with the Repository,
- a description of the MCHP Concept Dictionary and Glossary resource,
- a description of the Data Quality (DQ) process used at MCHP, with links to DQ-related SAS programs, and
- more information about the Data Repository, including study design and methods considerations, and acknowledgements and disclaimers when using the data.
Related concepts
- Calculating Costs/Expenditures for Pharmaceuticals
- International Classification of Disease (ICD) Coding in MCHP Data
- Manitoba Immunization Monitoring System (MIMS)
- Manitoba Population Research Data Repository (Repository)
- Record Linkage in Manitoba
Related terms
- Administrative Data
- Administrative Health Data
- Data Management Process
- Data Quality Framework
- Drug Program Information Network (DPIN) Data
- Francophone
- Geographic Mobility in Manitoba
- Health Survey
- Hospital Abstracts Data
- Interprovincial Migration
- Manitoba Centre for Health Policy (MCHP)
- Manitoba First Nations Research File (MFNRF)
- Manitoba Health
- Manitoba Health Insurance Registry Data
- MCHP Research Registry
- Metadata Repository
- Physician Claims
- Physician Resource Database
- Population-Based Health Information System (POPULIS)
- Survey Data Used at MCHP
- Vital Statistics Mortality Registry Data
Links
- Manitoba Population Research Data Repository web page
References
- Finlayson G, Reimer J, Dahl M, Stargardter M, McGowan K. The Direct Cost of Hospitalizations in Manitoba, 2005/06 . Winnipeg, MB: Manitoba Centre for Health Policy, 2009. [ Report ] [ Summary ] [ Additional Materials ] ( View )
Term used in
- Brownell M, Chartier M, Au W, Schultz J. Evaluation of the Healthy Baby Program . Winnipeg, MB: Manitoba Centre for Health Policy, 2010. [ Report ] [ Summary ] ( View )
- Brownell M, Chartier M, Santos R, Ekuma O, Au W, Sarkar J, MacWilliam L, Burland E, Koseva I, Guenette W. How are Manitoba's Children Doing? Winnipeg, MB: Manitoba Centre for Health Policy, 2012. [ Report ] [ Summary ] [ Updates and Errata ] [ Additional Materials ] ( View )
- Brownell M, De Coster C, Penfold R, Derksen S, Au W, Schultz J, Dahl M. Manitoba Child Health Atlas Update . Winnipeg, MB: Manitoba Centre for Health Policy, 2008. [ Report ] [ Summary ] [ Additional Materials ] ( View )
- Brownell M, Santos R, Kozyrskyj A, Roos N, Au W, Dik N, Chartier M, Girard D, Ekuma O, Sirski M, Tonn N, Schultz J. Next Steps in the Provincial Evaluation of the BabyFirst Program: Measuring Early Impacts on Outcomes Associated with Child Maltreatment . Winnipeg, MB: Manitoba Centre for Health Policy, 2007. [ Report ] [ Summary ] ( View )
- Chartier M, Finlayson G, Prior H, McGowan K, Chen H, de Rocquigny J, Walld R, Gousseau M. Health and Healthcare Utilization of Francophones in Manitoba . Winnipeg, MB: Manitoba Centre for Health Policy, 2012. [ Report ] [ Summary ] ( View )
- Chateau D, Enns M, Ekuma O, Koseva I, McDougall C, Kulbaba C, Allegro E. Evaluation of the Manitoba IMPRxOVE Program . Winnipeg, MB: Manitoba Centre for Health Policy, 2015. [ Report ] [ Summary ] ( View )
- Chateau D, Doupe M, Walld R, Soodeen R, Ouelette C, Rajotte L. Projecting Personal Care Home Bed Equivalent Needs in Manitoba Through 2036 . Manitoba Centre for Health Policy, 2012. [ Report ] [ Summary ] [ Updates and Errata ] ( View )
- Doupe M, Kozyrskyj A, Soodeen R, Derksen S, Burchill C, Huq S. An Initial Analysis of Emergency Departments and Urgent Care in Winnipeg . Winnipeg, MB: Manitoba Centre for Health Policy, 2008. [ Report ] [ Summary ] [ Additional Materials ] ( View )
- Doupe M, Finlayson G, Khan S, Yogendran M, Schultz J, McDougall C, Kulbaba C. Supportive Housing for Seniors: Reform Implications for Manitoba's Older Adult Continuum of Care . Winnipeg, MB: Manitoba Centre for Health Policy, 2016. [ Report ] [ Summary ] [ Additional Materials ] ( View )
- Finlayson G, Leslie WD, MacWilliam L. Diagnostic Imaging Data in Manitoba: Assessment and Applications . Winnipeg, MB: Manitoba Centre for Health Policy, 2004. [ Report ] [ Summary ] ( View )
- Finlayson G, Smith M, Burchill C, Towns D, Peeler W, Soodeen RA, Prior H, Huq S, Guenette W. Social Housing in Manitoba. Part I: Manitoba Social Housing Data . Winnipeg, MB: Manitoba Centre for Health Policy, 2013. [ Report ] [ Summary ] ( View )
- Finlayson G, Ekuma O, Yogendran M, Burland E, Forget E. The Additional Cost of Chronic Disease in Manitoba . Winnipeg, MB: Manitoba Centre for Health Policy, 2010. [ Report ] [ Summary ] ( View )
- Fransoo R, Martens P, Prior H, Chateau D, McDougall C, Schultz J, McGowan K, Soodeen R, Bailly A. Adult Obesity in Manitoba: Prevalence, Associations, and Outcomes . Winnipeg, MB: Manitoba Centre for Health Policy, 2011. [ Report ] [ Summary ] ( View )
- Fransoo R, Martens P, The Need to Know Team, Prior H, Burchill C, Koseva I, Bailly A, Allegro E. The 2013 RHA Indicators Atlas . Winnipeg, MB: Manitoba Centre for Health Policy, 2013. [ Report ] [ Summary ] [ Additional Materials ] ( View )
- Fransoo R, Martens P, The Need to Know Team, Prior H, Burchill C, Koseva I, Rajotte L. Who is in our Hospitals.and why? Winnipeg, MB: Manitoba Centre for Health Policy, 2013. [ Report ] [ Summary ] [ Additional Materials ] ( View )
- Garland A, Fransoo R, Olafson K, Ramsey C, Yogendran M, Chateau D, McGowan K. The Epidemiology and Outcomes of Critical Illness in Manitoba . Winnipeg, MB: Manitoba Centre for Health Policy, 2012. [ Report ] [ Summary ] ( View )
- Heaman M, Kingston D, Helewa M, Brownell M, Derksen S, Bogdanovic B, McGowan K, Bailly A. Perinatal Services and Outcomes in Manitoba . Winnipeg, MB: Manitoba Centre for Health Policy, 2012. [ Report ] [ Summary ] [ Updates and Errata ] ( View )
- Hilderman T, Katz A, Derksen S, McGowan K, Chateau D, Kurbis C, Allison S, Reimer JN. Manitoba Immunization Study . Winnipeg, MB: Manitoba Centre for Health Policy, 2011. [ Report ] [ Summary ] ( View )
- Katz A, Bogdanovic B, Soodeen R. Physician Integrated Network Baseline Evaluation: Linking Electronic Medical Records and Administrative Data . Winnipeg, MB: Manitoba Centre for Health Policy, 2010. [ Report ] [ Summary ] ( View )
- Katz A, Chateau D, Bogdanovic B, Taylor C, McGowan K-L, Rajotte L, Dziadek J. Physician Integrated Network: A Second Look . Winnipeg, MB: Manitoba Centre for Health Policy, 2014. [ Report ] [ Summary ] [ Updates and Errata ] ( View )
- Katz A, Bogdanovic B, Ekuma O, Soodeen RA, Chateau D, Burnett C. Physician Resource Projection Models . Winnipeg, MB: Manitoba Centre for Health Policy, 2009. [ Report ] [ Summary ] ( View )
- Katz A, Avery Kinew K, Star L, Taylor C, Koseva I, Lavoie J, Burchill C, Urquia M, Basham A, Rajotte L, Ramayanam V, Jarmasz J, Burchill S. The Health Status of and Access to Healthcare by Registered First Nation Peoples in Manitoba . Winnipeg, MB: Manitoba Centre for Health Policy, 2019. [ Report ] [ Summary ] [ Updates and Errata ] [ Additional Materials ] ( View )
- Katz A, Martens P, Chateau D, Bogdanovic B, Koseva I, McDougall C, Boriskewich E. Understanding the Health System Use of Ambulatory Care Patients . Winnipeg, MB: Manitoba Centre for Health Policy, 2013. [ Report ] [ Summary ] ( View )
- Kozyrskyj A, Raymond C, Dahl M, Ekuma O, Schultz J, Sklepowich M, Bond R. Effects of Manitoba Pharmacare Formulary Policy on Utilization of Prescription Medications . Winnipeg, MB: Manitoba Centre for Health Policy, 2009. [ Report ] [ Summary ] ( View )
- Lix L, Smith M, Azimaee M, Dahl M, Nicol P, Burchill C, Burland E, Goh C, Schultz J, Bailly A. A Systematic Investigation of Manitoba's Provincial Laboratory Data . Winnipeg, MB: Manitoba Centre for Health Policy, 2012. [ Report ] [ Summary ] ( View )
- Martens P, Nickel N, Forget E, Lix L, Turner D, Prior H, Walld R, Soodeen RA, Rajotte L, Ekuma O. The Cost of Smoking: A Manitoba Study . Winnipeg, MB: Manitoba Centre for Health Policy, 2015. [ Report ] [ Summary ] [ Updates and Errata ] [ Additional Materials ] ( View )
- Martens P, Fransoo R, The Need to Know Team, Burland E, Prior H, Burchill C, Romphf L, Chateau D, Bailly A, Ouelette C. What Works? A First Look at Evaluating Manitoba's Regional Health Programs and Policies at the Population Level . Winnipeg, MB: Manitoba Centre for Health Policy, 2008. [ Report ] [ Summary ] [ Additional Materials ] ( View )
- Menec V, Lix L, Steinbach C, Ekuma O, Sirski M, Dahl M, Soodeen R. Patterns of Health Care Use and Cost at the End of Life . Winnipeg, MB: Manitoba Centre for Health Policy, 2004. [ Report ] [ Summary ] ( View )
- Metge C, Chateau D, Prior H, Soodeen R, De Coster C, Barre L. Composite Measures/Indices of Health and Health System Performance . Winnipeg, MB: Manitoba Centre for Health Policy, 2009. [ Report ] [ Summary ] ( View )
- Raymond C, Metge C, Alessi-Severini S, Dahl M, Schultz J, Guenette W. Pharmaceutical Use in Manitoba: Opportunities to Optimize Use . Winnipeg, MB: Manitoba Centre for Health Policy, 2010. [ Report ] [ Summary ] ( View )
- Santos R, Brownell M, Ekuma O, Mayer T, Soodeen R-A. The Early Development Instrument (EDI) in Manitoba: Linking Socioeconomic Adversity and Biological Vulnerability at Birth to Children's Outcomes at Age 5 . Winnipeg, MB: Manitoba Centre for Health Policy, 2012. [ Report ] [ Summary ] ( View )
- Smith M, Finlayson G, Martens P, Dunn J, Prior H, Taylor C, Soodeen RA, Burchill C, Guenette W, Hinds A. Social Housing in Manitoba. Part II: Social Housing and Health in Manitoba: A First Look . Winnipeg, MB: Manitoba Centre for Health Policy, 2013. [ Report ] [ Summary ] ( View )
Request information in an accessible format
If you require access to our resources in a different format, please contact us:
- by phone at 204-789-3819
- by email at [email protected]
We strive to provide accommodations upon request in a reasonable timeframe.
Manitoba Centre for Health Policy Community Health Sciences, Max Rady College of Medicine, Rady Faculty of Health Sciences, Room 408-727 McDermot Ave. University of Manitoba Winnipeg, MB R3E 3P5 Canada

IMAGES
COMMENTS
The Manitoba Population Research Data Repository is a comprehensive collection of administrative, registry, survey, and other data primarily relating to residents of Manitoba. It was developed to describe and explain patterns of health care and profiles of health and illness, facilitating interdisciplinary research in areas such as health care, education, social services and justice.
The University of Manitoba campuses are located on original lands of Anishinaabeg, Cree, Oji-Cree, Dakota, and Dene peoples, and on the homeland of the Métis Nation. More. University of Manitoba Winnipeg, Manitoba Canada, R3T 2N2 Maps and directions 1-800-432-1960 (North America) Emergency: 204-474-9341 Emergency Information. Careers
The Manitoba Population Research Data Repository was initially known as the Population Health Data Repository. As the data centre has grown from maintaining 12 health service delivery datasets in 1991 to more than 90 datasets in 2019, the breadth of non-healthcare data led to the change to a more inclusive name. ...
The Manitoba Population Research Data Repository is a comprehensive collection of administrative, registry, survey, and other data primarily relating to residents of Manitoba. ... The term Population Health Research Data Repository. was used to describe the Repository in MCHP research from September 2000 to November 2016. The new name, Manitoba ...
The Manitoba Centre for Health Policy (MCHP) is a centre of research excellence that conducts world-class population-based research on health and the social determinants of health. We develop and maintain a comprehensive population-based data repository on behalf of our province for use by the local, national and international research community.
The Manitoba Multigenerational Cohort (MMC) has been developed using routinely collected and de-identified administrative healthcare data to facilitate health and social research using family-based designs. The MMC is a population-based cohort of individuals born in the province of Manitoba, Canada, from 1974 to 2019 ( n = 744 265) with ...
COVID-19 and Repository data. The Manitoba Population Research Data Repository has three, specific COVID-19 datasets available for research, and some of the regular repository data with relevance to COVID-19 research is being updated on a monthly/quarterly basis.
The Population Health Research Data Repository (repository) is a comprehensive world-class collection of data files housed at the Manitoba Centre for Health Policy (MCHP), a research unit within the Faculty of Medicine, Department of Community Health Sciences, University of Manitoba.The repository contains administrative, registry, survey, and other types of data primarily relating to ...
Objective: To profile the Manitoba Centre for Health Policy (MCHP), a population health data centre located at the University of Manitoba in Winnipeg, Canada. Approach: We describe how MCHP was established and funded, and how it continues to operate based on a foundation of trust and respect between researchers at the University of Manitoba and stakeholders in the Manitoba Government's ...
Population Data Centre Profile: The Manitoba Centre for Health P olicy Katz, A 1* , Enns, J 1 , Smith, M 1 , Burchill, C 1 , Turner, K 1 , and T owns, D 1 Submission History
The Population Health Research Data Repository housed at MCHP is a comprehensive collection of administrative, registry, survey, and other data primarily relating to residents of Manitoba. It was developed to describe and explain patterns of health care and profiles of health and illness, facilitating inter-sectoral research in areas such as ...
The Manitoba Population Research Data Repository is a comprehensive collection of administrative, registry, survey and other data primarily comprised of residents of Manitoba. This repository is housed at the Manitoba Centre for Health Policy (MCHP). It was developed to describe and explain patterns of health care and profiles of health and ...
MCHP researchers rely upon the unique Manitoba Population Research Data Repository (Repository) to describe and explain patterns of care and profiles of illness and explore other factors that influence health, including income, education, employment, and social status. The repository is unique in terms of its comprehensiveness, degree of ...
The Social Determinants of Health Digital Library (SDOH-DL) is an ongoing initiative aimed at expanding and systematizing data in the Manitoba Population Research Data Repository to better study the social determinants of health (SDOH). This project is led by Dr. Marcelo Urquia and is supported by the Canada Foundation for Innovation, Research Manitoba, and MCHP.
The term Population Health Research Data Repository. was used to describe the Repository in MCHP research from September 2000 to November 2016. The new name, Manitoba Population Research Data Repository, reflects the expansion of research into areas beyond health care. MCHP Data Repository Domains. The MCHP Data Repository currently consists of ...
The Manitoba Population Research Data Repository was initially known as the Population Health Data Repository. As the data centre has grown from maintaining 12 health service delivery datasets in 1991 to more than 90 datasets in 2019, the breadth of non-healthcare data led to the change to a more inclusive name. ...
The Manitoba Population Research Data Repository (the Repository), held at the Manitoba Centre for Health Policy (MCHP), is a collection of deidentified administrative, survey, clinical, and ...
The CPTP is Canada's largest population health research platform, containing personal health, lifestyle and environmental data from more than 300,000 Canadians between the ages of 35 to 69. ... The MCHP houses the Population Health Research Data Repository which is a collection of over 20 Manitoba-based administrative, registry and survey data ...
This document provides information regarding the inclusion of data in the Manitoba Centre for Health Policy (MCHP) Manitoba Population Research Data Repository. There are three groups of data housed at MCHP: Repository data, Inactive Repository data, and Project Specific data. ... • Manitoba Population Research Data Repository - Overview Data ...
The Manitoba Population Research Data Repository The Repository is a comprehensive collection of administrative, registry, survey and other databases primarily relating to residents of Manitoba. It was developed to describe and explain patterns of health care and profiles of health and illness, facilitating intersectoral research in areas such ...
The Population Health Research Data Repository (repository) is a comprehensive world-class collection of data files housed at the Manitoba Centre for Health Policy (MCHP), a research unit within the Faculty of Medicine, Department of Community Health Sciences, University of Manitoba.The repository contains administrative, registry, survey, and other types of data primarily relating to ...
The authors also acknowledge the Manitoba Centre for Health Policy (MCHP) for use of the data in the Population Health Research Data Repository under project (HIPC No. 2014/2015-37). Data used in this study are from the Population Health Research Data Repository and were derived from data provided by Manitoba Health, Seniors and Active Living.
The Manitoba Population Research Data Repository is a comprehensive collection of administrative, registry, survey and other data primarily comprised of residents of Manitoba. ... The term Population Health Research Data Repository was used to describe the Repository in MCHP research from September 2000 to November 2016. The new name, Manitoba ...