This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search

Search menu
Effective decision-making: applying the theories to nursing practice.
Samantha Watkins
Emergency Department Staff Nurse, Frimley Health NHS Foundation Trust, Frimley
View articles · Email Samantha
Many theories have been proposed for the decision-making conducted by nurses across all practices and disciplines. These theories are fundamental to consider when reflecting on our decision-making processes to inform future practice. In this article three of these theories are juxtaposed with a case study of a patient presenting with an ST-segment elevation myocardial infarction (STEMI). These theories are descriptive, normative and prescriptive, and will be used to analyse and interpret the process of decision-making within the context of patient assessment.
Decision-making is a fundamental concept of nursing practice that conforms to a systematic trajectory involving the assessment, interpretation, evaluation and management of patient-specific situations ( Dougherty et al, 2015 ). Shared decision-making is vital to consider in terms of patient autonomy and professional duty of care as set out in the Nursing and Midwifery Council (NMC) (2018) Code, which underpins nursing practice. Consequently, the following assessment and decision-making processes were conducted within the remits of practice as a student nurse. Decision-making is a dynamic process in nursing practice, and the theories emphasise the importance of adaptability and reflective practice to identify factors that impact on patient care ( Pearson, 2013 ). Three decision-making theories will be explored within the context of a decision made in practice. To abide by confidentiality requirements, the pseudonym ‘Linda’ will be used throughout. Patient consent was obtained prior to writing.
Linda was a 71-year-old who had been admitted to the cardiac ward following an episode of unstable angina. She was on continuous cardiac monitoring as recommended by the National Institute for Health and Care Excellence (NICE) (2016) guideline for chest pain of recent onset. During her stay on the ward, the tracing on the cardiac monitor indicated possible ST-segment elevation ( Thygesen et al, 2018 ). It was initially hypothesised that she might be experiencing an ACS ( Box 1 ) and could be haemodynamically unstable.
Box 1. Acute coronary syndrome
- Acute coronary syndrome is an umbrella term that includes three cardiac conditions that result from a reduction of oxygenated blood through the coronary arteries, causing myocardial ischaemia. An ST-segment elevation myocardial infarction (STEMI) connotes the complete occlusion of one or more of the coronary arteries, which is demonstrated by patient symptoms and ST-segment elevation seen on an electrocardiogram (ECG)
- A non-ST-segment elevation myocardial infarction (NSTEMI) results from a partial occlusion of a coronary artery. Patient symptoms often present alongside dynamic ST-segment depression, T-wave inversion or a normal ECG
- Unstable angina is a result of a transient occlusion of the coronary arteries causing symptoms at rest or on minimal exertion, which may be eased/resolved with rest with or without glyceryl trinitrate (GTN)
- Signs and symptoms of ischaemia experienced by patient include: chest pain with or without radiation to jaw, neck, back, shoulders or arms, which is described as squeezing or crushing. Associated symptoms of lethargy, syncope, pre-syncopal episodes, diaphoresis, dyspnoea, nausea or vomiting, anxiety or a feeling of impending doom often also prevail
Source: Deen, 2018
The possibility that Linda was experiencing ST-segment elevation myocardial infarction (STEMI) meant that she needed rapid assessment of her condition. Stephens (2019) recommended the use of the ABCDE assessment as a timely and effective tool to identify physiological deterioration in patients with chest pain. The student nurse's ABCDE assessment of Linda is shown in Box 2 .
Box 2. ABCDE assessment * of ‘Linda’
- Airway: patent, no audible sounds of obstruction; however, unable to speak in full sentences due to dyspnoea
- Breathing: dyspnoeic, respiratory rate of 27, saturations of 85% on room air—with guidance from the senior charge nurse, 80% oxygen via non-rebreathe mask was administered ( O'Driscoll et al, 2017 )
- Circulation: tachycardia of 112 beats per minute, hypotensive at 92/50 mmHg, oliguric, diaphoretic, and with cool peripherals and a thready radial pulse
- Disability: She was alert on the AVPU scale, but anxious and feeling lethargic. Blood glucose was 5.7 mmol/litre
- Exposure: no erythema or wounds noted. She stated she had central chest pain, which was radiating to her jaw and back, described as ‘pressure’, and rated as a seven out of ten
* in line with Resuscitation Council (2015)
NICE (2016) recommends that the first investigation for patients with chest pain is to conduct an ECG as a rapid and non-invasive assessment for a cardiac cause of the pain. This was carried out and 2 mm ST-segment elevation in the precordial leads V1-V3 was noted, indicating a possible anterior STEMI ( Amsterdam et al, 2014 ). The student nurse had had basic ECG interpretation training as part of the nursing degree undertaken, but had also received informal teaching from registered nursing staff in cardiology. The ECG findings were confirmed by the senior charge nurse after they were alerted to Linda's condition, symptoms, and National Early Warning Score 2 (NEWS 2) ( Royal College of Physicians, 2017 ). The senior charge nurse escalated her care to the cardiology team. A diagnosis of STEMI was made by the cardiology team using the ECG findings and her physiological signs of deterioration from their assessment, within the context of her initial presentation to hospital for unstable angina. This diagnosis, coupled with the deterioration in her condition, meant that she required primary percutaneous coronary intervention (PCI). The NICE (2014) quality standard for acute coronary syndromes and the clinical guideline on STEMI ( NICE, 2013a ) recommend that primary PCI is initiated within 120 minutes to reperfuse the myocardium and prevent further myocardial cellular necrosis. This improves long-term patient outcomes ( Thygesen et al, 2018 ).
Decision-making theories
The recognition of an evolving STEMI on the cardiac monitor corresponds with the model of hypothetico-deductive reasoning ( Pearson, 2013 ) within the descriptive and normative theories ( Box 3 ). Thompson and Dowding (2009) highlighted that this model recognises that decision-making comprises four stages, beginning with cue acquisition. The specific pre-counter cues can be identified as the recognition of the abnormal tracing on the cardiac monitor ( Pearson, 2013 ), suggestive of ST-segment elevation, that indicated Linda might be experiencing haemodynamic deterioration with a cardiac cause. Subsequently, the decision to assess Linda formed the hypothesis generation phase of the decision and the recognition of the clinical signs as indicating STEMI ( Nickerson, 1998 ; Johansen and O'Brien, 2016 ). This hypothesis focused the assessment to identify and examine pertinent factors that supported this conjecture ( Pearson, 2013 ). However, the student nurse required more data to formulate a robust hypothesis thereby initiating the cue interpretation phase by conducting an ABCDE systematic assessment, including ECG. Lindsey (2013) argued that during cue interpretation, the health professional uses prescriptive guidelines to direct the assessment process and provide a rationale.
Box 3. Decision-making theories considered
- Descriptive theory: is concerned with each individuals’ moral beliefs regarding a particular decision
- Normative theory: connotes what decisions individuals should make logically
- Prescriptive theory: encompasses the policies that govern the remits of a decision within the evidence base that informs practice
Source: Pearson, 2013
Arguably, however, clinical knowledge of the pathophysiology of ACS is fundamental to effective cue interpretation, not simply the individual's knowledge of the NICE guidance ( NICE, 2013a ; 2013b ; 2014 ; 2016 ). The student nurse's existing knowledge of the symptoms of ACS supported the cue interpretation with assessing Linda's condition and possible diagnosis of ACS. This knowledge enriched the student nurse's understanding of the guidance, which could then effectively be applied as the central aspect of cue interpretation ( Deen, 2018 ).
Elstein and Schwartz (2002) conceded that the prescriptive theory knowledge synthesised for the decision must be accurate and evidence-based for hypothetico-deductive reasoning to be effective. Courtney and McCutcheon (2009) argued that reliance solely on clinical guidelines can limit decision-making and result in erroneous outcomes and should consequently be used in collaboration with the evidence base. By combining normative theory with prescriptive guidance, clinical decisions can be enriched and validated. Stevens (2013) highlighted that it is vital that the guidance used in corroboration with decision-making models is valid and reliable and therefore prescriptive theory must be critically evaluated against the evidence-base. The guidance published by NICE (2013a) is supported by the American College of Cardiology ( O'Gara et al, 2013 ), European Resuscitation Council ( Nikolaou et al, 2015 ), European Society of Cardiology ( Steg et al, 2012 ) and Cardiac Society of Australia and New Zealand ( Chew et al, 2016 ). Accordingly, these guidelines highlight the clinical signs of STEMI and the diagnostic investigations pertinent to this condition. Within the remits of practice as a student nurse, this evidence supported the decision to escalate Linda's condition.
Antithetically, during cue interpretation and the hypothesis generation phases, Pearson (2013) emphasised the importance of considering multiple hypotheses extrapolated from the clinical data, resulting in the selection of the most appropriate hypothesis when more data are obtained. Despite this, during the interpretation of the cues for the hypothesis, the student nurse failed to consider differential diagnoses, such as pneumothorax or pulmonary embolism, which have similar presentations to STEMI ( Deen, 2018 ). Consequently, this hypothesis generation had an element of uncertainty ( Bjørk and Hamilton, 2011 ), which could have impeded Linda's care by erroneously considering only one potential diagnosis and therefore focusing the assessment on that diagnosis. Student nurses can be considered ‘novice’ health professionals, demonstrating limitations in knowledge regarding differential diagnoses and therefore in potential hypotheses. Pearson (2013) argued that this is because student nurses lack the requisite experience to cluster information as effectively as an ‘expert’ health professional. Consequently, the presentation of one hypothesis is permissible within the remits of practice as a student nurse.
Assessment tools such as ABCDE ( Resuscitation Council UK, 2015 ) ensure that all factors indicative of deterioration are recognised. Consequently, by using a systematic assessment, any potential erroneous hypothesis can be precluded. Therefore, as Carayon and Wood (2010) state, the assessment tool was a barrier to active failure to recognise alternative diagnoses thus circumventing any serious consequences, highlighting the importance of comprehensive assessment to avoid error and safeguard the ethical principle of non-maleficence ( Beauchamp and Childress, 2013 ) fundamental to nursing. Antithetically, Benner et al (2008) argued that even the novice nurse should be able to consider multiple hypotheses within a situation, although they may not be able to reflect on these decisions within the moment. However, as Keller (2009) noted, the hypothetico-deductive model is based on presuppositions recognised by the health professional, such as the evolving cardiac tracing and history of pain, indicating that STEMI was the higher probable cause ( Deen, 2018 ). Consequently, a limitation of hypothetico-deductive reasoning is sufficient experience to aid in generating hypotheses.
Thereafter, in the hypothesis generation phase, the decision-making process evolved to include elements of pattern recognition theory ( Croskerry, 2002 ). The clinical decision that focuses on a single hypothesis can be compared to the use of pattern recognition ( Pearson, 2013 ) where existing knowledge is used to establish the hypothesis. Pearson (2013) commented that hypothetico-deductive reasoning is based on the synthesising and analysing of information whereas the formulation of one hypothesis is suggestive of pattern recognition, where the nurse uses previous experience to evaluate the situation. Consequently, the student nurse's previous experience of assessing a patient in acute STEMI may have guided practice to recognise ST-segment elevation on the telemetry, and then subsequently to conduct an ECG, and to recognise the associated clinical signs of STEMI and to gather a history of the pain using NICE (2013b) guidance on unstable angina, in line with Linda's initial presentation. Croskerry (2002) identified that health professionals who rely on pattern recognition initially recognise visual cues that are then supplemented with more in-depth data, often using assessment tools such as NEWS (and now NEWS 2) and ABCDE. Arguably, the recognition of similarities in clinical presentation, past medical history, and cardiac monitoring tracing of Linda's case to the previous case and use of ABCDE and NEWS 2 to further assess her condition and extrapolate data, identifies that previous experience can facilitate decision-making outcomes.
Finally, in the last phase of the decision-making in the hypothetico-deductive model, the student nurse evaluated the hypothesis and by using the merits from the cues ( Banning, 2008 ) established that STEMI was the most probable cause of Linda's deterioration and could escalate her care appropriately using the prescriptive theory tools described above.
Arguably, by using previous experience to guide practice, an element of confirmation bias may have affected the selection of data ( Thompson and Dowding, 2009 ) and consequently the student may have neglected other important data ( Croskerry, 2003 ). For instance, student nurses are inexperienced with chest auscultation and consequently could not have ruled out differential respiratory diagnoses. Stanovich et al (2013) acknowledged that confirmation bias can be circumvented when evidence is assimilated with hypothesis generation. The consideration that Linda may have been at an increased risk of myocardial infarction due to her age, history of smoking and admission to hospital for unstable angina ( Piepoli et al, 2016 ), indicated that the cause of her deterioration would most likely be cardiac. Thus, an evidence-based approach could inform practice and consequently, any limitations as a ‘novice’ would be minimised through rationalisation and critical thinking. Indeed, Stanovich et al (2013) argued that rationalising and critical thinking are markedly more important than existing knowledge. This is because even an ‘expert’ in a specific field does not have completely comprehensive knowledge, and therefore relies on a critical thought process to make rational decisions.
Conclusively, health professionals must be able to rationalise their decisions ( Johansen and O'Brien, 2016 ) and justify these decisions within the context of each presentation as a central concept of nursing ( NMC, 2018 ).
Communication is vital to establishing consent to treatment where the patient is regarded as having capacity under the Mental Capacity Act 2005. This is particularly significant when conducting investigations and escalating care to ensure that the patient's wishes are respected, and that the patient is empowered with knowledge regarding their condition and care ( Coultier and Collins, 2011 ). Linda was informed that her care required escalation to the appropriate clinical team, and then subsequently recommended to have PCI intervention as the most effective treatment for STEMI ( NICE, 2013a ; 2014 ). Presenting a default decision and using choice architecture can be construed as methods of liberal paternalism used to avoid impeded decision-making from choice overload ( Rosenbaum, 2015 ) or irrational decision bias ( Marewski and Gigerenzer, 2012 ). To escalate Linda's care within the recommended timeframe ( NICE, 2013a ; 2014 ), it was important to use elements of liberal paternalism ( Beauchamp and Childress, 2013 ) while preserving Linda's autonomy of choice ( Kemmerer et al, 2017 ). Linda had a right to make a decision against medical advice as per Re B (Adult, refusal of medical treatment) [2002] and these choices were presented to her by the cardiology team. As a health professional, a duty of care was owed to the patient to escalate concerns regarding her condition under the Code ( NMC, 2018 ).
Conclusively, all three theories of decision-making pertained to this patient's effective care. Nurses must be accountable for their decisions and act within the remits of the NMC (2018) Code. Patient care must consequently be effective, evidence-based and patient-centred. Accountability requires the health professional to act within the remits of their role to ensure safe care is delivered to the patient. This is a fundamental aspect of patient-centric care and principal to effective decision making. Demonstrably, the use of descriptive and normative theories can be interchangeable, however, the use of prescriptive theory is pivotal to validate clinical decision-making. The decision-making process can be further facilitated by use of structured assessment tools to reduce margin of error and improve outcome. Collaborative decision making is pivotal to advancing patient autonomy and empowerment but certain decisions require elements of paternalism to improve the process and uphold the ethical principles of beneficence and non-maleficence. Nevertheless, health professionals have a duty of care to adhere to decisions made by patients established to have capacity to give informed consent, irrespective of the personal beliefs of the professional.
- This article is a reflection on a case scenario where decisions were made in the care of a patient admitted for cardiac monitoring
- Nursing decision making is complex and involves a multitude of processes based on experience, knowledge and skill.
- Understanding the importance of decision-making theory and how these theories apply to practice can be effective in reflecting on practice, and the application of theory to practice can inform patient care
CPD reflective questions
- Consider the three different theories of decision making outlined here—which theory do you deem the most important to your practice? How does this affect your practice?
- Consider how reflecting on your own decision making can improve practice
- What can you do to enrich your own knowledge regarding patients with chest pain?
The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Making Decisions and Solving Problems
CHAPTER 6 Making Decisions and Solving Problems Rose Aguilar Welch This chapter describes the key concepts related to problem solving and decision making. The primary steps of the problem-solving and decision-making processes, as well as analytical tools used for these processes, are explored. Moreover, strategies for individual or group problem solving and decision making are presented. Objectives • Apply a decision-making format to list options to solve a problem, identify the pros and cons of each option, rank the options, and select the best option. • Evaluate the effect of faulty information gathering on a decision-making experience. • Analyze the decision-making style of a nurse leader/manager. • Critique resources on the Internet that focus on critical thinking, problem solving, and decision making. Terms to Know autocratic creativity critical thinking decision making democratic optimizing decision participative problem solving satisficing decision The Challenge Vickie Lemmon RN, MSN Director of Clinical Strategies and Operations, WellPoint, Inc., Ventura, California Healthcare managers today are faced with numerous and complex issues that pertain to providing quality services for patients within a resource-scarce environment. Stress levels among staff can escalate when problems are not resolved, leading to a decrease in morale, productivity, and quality service. This was the situation I encountered in my previous job as administrator for California Children Services (CCS). When I began my tenure as the new CCS administrator, staff expressed frustration and dissatisfaction with staffing, workload, and team communications. This was evidenced by high staff turnover, lack of teamwork, customer complaints, unmet deadlines for referral and enrollment cycle times, and poor documentation. The team was in crisis, characterized by in-fighting, blaming, lack of respectful communication, and lack of commitment to program goals and objectives. I had not worked as a case manager in this program. It was hard for me to determine how to address the problems the staff presented to me. I wanted to be fair but thought that I did not have enough information to make immediate changes. My challenge was to lead this team to greater compliance with state-mandated performance measures. What do you think you would do if you were this nurse? Introduction Problem solving and decision making are essential skills for effective nursing practice. Carol Huston (2008) identified “expert decision-making skills” as one of the eight vital leadership competencies for 2020. These processes not only are involved in managing and delivering care but also are essential for engaging in planned change. Myriad technologic, social, political, and economic changes have dramatically affected health care and nursing. Increased patient acuity, shorter hospital stays, shortage of healthcare providers, increased technology, greater emphasis on quality and patient safety, and the continuing shift from inpatient to ambulatory and home health care are some of the changes that require nurses to make rational and valid decisions. Moreover, increased diversity in patient populations, employment settings, and types of healthcare providers demands efficient and effective decision making and problem solving. More emphasis is now placed on involving patients in decision making and problem solving and using multidisciplinary teams to achieve results. Nurses must possess the basic knowledge and skills required for effective problem solving and decision making. These competencies are especially important for nurses with leadership and management responsibilities. Definitions Problem solving and decision making are not synonymous terms. However, the processes for engaging in both processes are similar. Both skills require critical thinking, which is a high-level cognitive process, and both can be improved with practice. Decision making is a purposeful and goal-directed effort that uses a systematic process to choose among options. Not all decision making begins with a problem situation. Instead, the hallmark of decision making is the identification and selection of options or alternatives. Problem solving, which includes a decision-making step, is focused on trying to solve an immediate problem, which can be viewed as a gap between “what is” and “what should be.” Effective problem solving and decision making are predicated on an individual’s ability to think critically. Although critical thinking has been defined in numerous ways, Scriven and Paul (2007) refer to it as “ the intellectually disciplined process of actively and skillfully conceptualizing, applying, analyzing, synthesizing, and/or evaluating information gathered from, or generated by, observation, experience, reflection, reasoning, or communication, as a guide to belief and action.” Effective critical thinkers are self-aware individuals who strive to improve their reasoning abilities by asking “why,” “what,” or “how.” A nurse who questions why a patient is restless is thinking critically. Compare the analytical abilities of a nurse who assumes a patient is restless because of anxiety related to an upcoming procedure with those of a nurse who asks if there could be another explanation and proceeds to investigate possible causes. It is important for nurse leaders and managers to assess staff members’ ability to think critically and enhance their knowledge and skills through staff-development programs, coaching, and role modeling. Establishing a positive and motivating work environment can enhance attitudes and dispositions to think critically. Creativity is essential for the generation of options or solutions. Creative individuals can conceptualize new and innovative approaches to a problem or issue by being more flexible and independent in their thinking. It takes just one person to plant a seed for new ideas to generate . The model depicted in Figure 6-1 demonstrates the relationship among related concepts such as professional judgment, decision making, problem solving, creativity, and critical thinking. Sound clinical judgment requires critical or reflective thinking. Critical thinking is the concept that interweaves and links the others. An individual, through the application of critical-thinking skills, engages in problem solving and decision making in an environment that can promote or inhibit these skills. It is the nurse leader’s and manager’s task to model these skills and promote them in others. FiGURE 6-1 Problem-solving and decision-making model. Decision Making This section presents an overview of concepts related to decision models, decision-making styles, factors affecting decision making, group decision making (advantages and challenges), and strategies and tools. The phases of the decision-making process include defining objectives, generating options, identifying advantages and disadvantages of each option, ranking the options, selecting the option most likely to achieve the predefined objectives, implementing the option, and evaluating the result. Box 6-1 contains a form that can be used to complete these steps. BOX 6-1 Decision-Making Format Objective: _____________________________________ Options Advantages Disadvantages Ranking Add more rows as necessary. Rank priority of options, with “1” being most preferred. Select the best option. Implementation plan: ______________________________________________________________________________ Evaluation plan: __________________________________________________________________________________ A poor-quality decision is likely if the objectives are not clearly identified or if they are inconsistent with the values of the individual or organization. Lewis Carroll illustrates the essential step of defining the goal, purpose, or objectives in the following excerpt from Alice’s Adventures in Wonderland: One day Alice came to a fork in the road and saw a Cheshire Cat in a tree. “Which road do I take?” she asked. His response was a question: “Where do you want to go?” “I don’t know,” Alice answered. “Then,” said the cat, “it doesn’t matter.” Decision Models The decision model that a nurse uses depends on the circumstances. Is the situation routine and predictable or complex and uncertain? Is the goal of the decision to make a decision conservatively that is just good enough or one that is optimal? If the situation is fairly routine, nurse leaders and managers can use a normative or prescriptive approach. Agency policy, standard procedures, and analytical tools can be applied to situations that are structured and in which options are known. If the situation is subjective, non-routine, and unstructured or if outcomes are unknown or unpredictable, the nurse leader and manager may need to take a different approach. In this case, a descriptive or behavioral approach is required. More information will need to be gathered to address the situation effectively. Creativity, experience, and group process are useful in dealing with the unknown. In the business world, Camillus described complex problems that are difficult to describe or resolve as “wicked” (as cited in Huston, 2008 ). This term is apt in describing the issues that nurse leaders face. In these situations, it is especially important for nurse leaders to seek expert opinion and involve key stakeholders. Another strategy is satisficing. In this approach, the decision maker selects the solution that minimally meets the objective or standard for a decision. It allows for quick decisions and may be the most appropriate when time is an issue. Optimizing is a decision style in which the decision maker selects the option that is best, based on an analysis of the pros and cons associated with each option. A better decision is more likely using this approach, although it does take longer to arrive at a decision. For example, a nursing student approaching graduation is contemplating seeking employment in one of three acute care hospitals located within a 40-mile radius of home. The choices are a medium-size, not-for-profit community hospital; a large, corporate-owned hospital; and a county facility. A satisficing decision might result if the student nurse picked the hospital that offered a decent salary and benefit packet or the one closest to home. However, an optimizing decision is more likely to occur if the student nurse lists the pros and cons of each acute care hospital being considered such as salary, benefits, opportunities for advancement, staff development, and mentorship programs. Decision-Making Styles The decision-making style of a nurse manager is similar to the leadership style that the manager is likely to use. A manager who leans toward an autocratic style may choose to make decisions independent of the input or participation of others. This has been referred to as the “decide and announce” approach, an authoritative style. On the other hand, a manager who uses a democratic or participative approach to management involves the appropriate personnel in the decision-making process. It is imperative for managers to involve nursing personnel in making decisions that affect patient care. One mechanism for doing so is by seeking nursing representation on various committees or task forces. Participative management has been shown to increase work performance and productivity, decrease employee turnover, and enhance employee satisfaction. Any decision style can be used appropriately or inappropriately. Like the tenets of situational leadership theory, the situation and circumstances should dictate which decision-making style is most appropriate. A Code Blue is not the time for managers to democratically solicit volunteers for chest compressions! The autocratic method results in more rapid decision making and is appropriate in crisis situations or when groups are likely to accept this type of decision style. However, followers are generally more supportive of consultative and group approaches. Although these approaches take more time, they are more appropriate when conflict is likely to occur, when the problem is unstructured, or when the manager does not have the knowledge or skills to solve the problem. Exercise 6-1 Interview colleagues about their most preferred decision-making model and style. What barriers or obstacles to effective decision making have your colleagues encountered? What strategies are used to increase the effectiveness of the decisions made? Based on your interview, is the style effective? Why or why not? Factors Affecting Decision Making Numerous factors affect individuals and groups in the decision-making process. Tanner (2006) conducted an extensive review of the literature to develop a Clinical Judgment Model. Out of the research, she concluded that five principle factors influence decision making. (See the Literature Perspective below.) Literature Perspective Resource: Tanner, C. A. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45 (6), 204-211. Tanner engaged in an extensive review of 200 studies focusing on clinical judgment and clinical decision making to derive a model of clinical judgment that can be used as a framework for instruction. The first review summarized 120 articles and was published in 1998. The 2006 article reviewed an additional 71 studies published since 1998. Based on an analysis of the entire set of articles, Tanner proposed five conclusions which are listed below. The reader is referred to the article for detailed explanation of each of the five conclusions. The author considers clinical judgment as a “problem-solving activity.” She notes that the terms “clinical judgment,” “problem solving,” “decision making,” and “critical thinking” are often used interchangeably. For the purpose of aiding in the development of the model, Tanner defined clinical judgment as actions taken based on the assessment of the patient’s needs. Clinical reasoning is the process by which nurses make their judgments (e.g., the decision-making process of selecting the most appropriate option) ( Tanner, 2006 , p. 204): 1. Clinical judgments are more influenced by what nurses bring to the situation than the objective data about the situation at hand. 2. Sound clinical judgment rests to some degree on knowing the patient and his or her typical pattern of responses, as well as an engagement with the patient and his or her concerns. 3. Clinical judgments are influenced by the context in which the situation occurs and the culture of the nursing care unit. 4. Nurses use a variety of reasoning patterns alone or in combination. 5. Reflection on practice is often triggered by a breakdown in clinical judgment and is critical for the development of clinical knowledge and improvement in clinical reasoning. The Clinical Judgment Model developed through the review of the literature involves four steps that are similar to problem-solving and decision-making steps described in this chapter. The model starts with a phase called “Noticing.” In this phase, the nurse comes to expect certain responses resulting from knowledge gleaned from similar patient situations, experiences, and knowledge. External factors influence nurses in this phase such as the complexity of the environment and values and typical practices within the unit culture. The second phase of the model is “Interpreting,” during which the nurse understands the situation that requires a response. The nurse employs various reasoning patterns to make sense of the issue and to derive an appropriate action plan. The third phase is “Responding,” during which the nurse decides on the best option for handling the situation. This is followed by the fourth phase, “Reflecting,” during which the nurse assesses the patient’s responses to the actions taken. Tanner emphasized that “reflection-in-action” and “reflection-on-action” are major processes required in the model. Reflection-in-action is real-time reflection on the patient’s responses to nursing action with modifications to the plan based on the ongoing assessment. On the other hand, reflection-on-action is a review of the experience, which promotes learning for future similar experiences. Nurse educators and managers can employ this model with new and experienced nurses to aid in understanding thought processes involved in decision making. As Tanner (2006) so eloquently concludes, “If we, as nurse educators, help our students understand and develop as moral agents, advance their clinical knowledge through expert guidance and coaching, and become habitual in reflection-on-practice, they will have learned to think like a nurse” ( p. 210 ). Implications for Practice Nurse educators and managers can employ this model with new and experienced nurses to aid in understanding thought processes involved in decision making. For example, students and practicing nurses can be encouraged to maintain reflective journals to record observations and impressions from clinical experiences. In clinical post-conferences or staff development meetings, the nurse educator and manager can engage them in applying to their lived experiences the five conclusions Tanner proposed. The ultimate goal of analyzing their decisions and decision-making processes is to improve clinical judgment, problem-solving, decision-making, and critical-thinking skills. Internal and external factors can influence how the situation is perceived. Internal factors include variables such as the decision maker’s physical and emotional state, personal philosophy, biases, values, interests, experience, knowledge, attitudes, and risk-seeking or risk-avoiding behaviors. External factors include environmental conditions, time, and resources. Decision-making options are externally limited when time is short or when the environment is characterized by a “we’ve always done it this way” attitude. Values affect all aspects of decision making, from the statement of the problem/issue through the evaluation. Values, determined by one’s cultural, social, and philosophical background, provide the foundation for one’s ethical stance. The steps for engaging in ethical decision making are similar to the steps described earlier; however, alternatives or options identified in the decision-making process are evaluated with the use of ethical resources. Resources that can facilitate ethical decision making include institutional policy; principles such as autonomy, nonmaleficence, beneficence, veracity, paternalism, respect, justice, and fidelity; personal judgment; trusted co-workers; institutional ethics committees; and legal precedent. Certain personality factors, such as self-esteem and self-confidence, affect whether one is willing to take risks in solving problems or making decisions. Keynes (2008) asserts that individuals may be influenced based on social pressures. For example, are you inclined to make decisions to satisfy people to whom you are accountable or from whom you feel social pressure? Characteristics of an effective decision maker include courage, a willingness to take risks, self-awareness, energy, creativity, sensitivity, and flexibility. Ask yourself, “Do I prefer to let others make the decisions? Am I more comfortable in the role of ‘follower’ than leader? If so, why?” Exercise 6-2 Identify a current or past situation that involved resource allocation, end-of-life issues, conflict among healthcare providers or patient/family/significant others, or some other ethical dilemma. Describe how the internal and external factors previously described influenced the decision options, the option selected, and the outcome. Group Decision Making There are two primary criteria for effective decision making. First, the decision must be of a high quality; that is, it achieves the predefined goals, objectives, and outcomes. Second, those who are responsible for its implementation must accept the decision. Higher-quality decisions are more likely to result if groups are involved in the problem-solving and decision-making process. In reality, with the increased focus on quality and safety, decisions cannot be made alone. When individuals are allowed input into the process, they tend to function more productively and the quality of the decision is generally superior. Taking ownership of the process and outcome provides a smoother transition. Multidisciplinary teams should be used in the decision-making process, especially if the issue, options, or outcome involves other disciplines. Research findings suggest that groups are more likely to be effective if members are actively involved, the group is cohesive, communication is encouraged, and members demonstrate some understanding of the group process. In deciding to use the group process for decision making, it is important to consider group size and composition. If the group is too small, a limited number of options will be generated and fewer points of view expressed. Conversely, if the group is too large, it may lack structure, and consensus becomes more difficult. Homogeneous groups may be more compatible; however, heterogeneous groups may be more successful in problem solving. Research has demonstrated that the most productive groups are those that are moderately cohesive. In other words, divergent thinking is useful to create the best decision. For groups to be able to work effectively, the group facilitator or leader should carefully select members on the basis of their knowledge and skills in decision making and problem solving. Individuals who are aggressive, are authoritarian, or manifest self-oriented behaviors tend to decrease the effectiveness of groups. The nurse leader or manager should provide a nonthreatening and positive environment in which group members are encouraged to participate actively. Using tact and diplomacy, the facilitator can control aggressive individuals who tend to monopolize the discussion and can encourage more passive individuals to contribute by asking direct, open-ended questions. Providing positive feedback such as “You raised a good point,” protecting members and their suggestions from attack, and keeping the group focused on the task are strategies that create an environment conducive to problem solving. Advantages of Group Decision Making The advantages of group decision making are numerous. The adage “two heads are better than one” illustrates that when individuals with different knowledge, skills, and resources collaborate to solve a problem or make a decision, the likelihood of a quality outcome is increased. More ideas can be generated by groups than by individuals functioning alone. In addition, when followers are directly involved in this process, they are more apt to accept the decision, because they have an increased sense of ownership or commitment to the decision. Implementing solutions becomes easier when individuals have been actively involved in the decision-making process. Involvement can be enhanced by making information readily available to the appropriate personnel, requesting input, establishing committees and task forces with broad representation, and using group decision-making techniques. The group leader must establish with the participants what decision rule will be followed. Will the group strive to achieve consensus, or will the majority rule? In determining which decision rule to use, the group leader should consider the necessity for quality and acceptance of the decision. Achieving both a high-quality and an acceptable decision is possible, but it requires more involvement and approval from individuals affected by the decision. Groups will be more committed to an idea if it is derived by consensus rather than as an outcome of individual decision making or majority rule. Consensus requires that all participants agree to go along with the decision. Although achieving consensus requires considerable time, it results in both high-quality and high-acceptance decisions and reduces the risk of sabotage. Majority rule can be used to compromise when 100% agreement cannot be achieved. This method saves time, but the solution may only partially achieve the goals of quality and acceptance. In addition, majority rule carries certain risks. First, if the informal group leaders happen to fall in the minority opinion, they may not support the decision of the majority. Certain members may go so far as to build coalitions to gain support for their position and block the majority choice. After all, the majority may represent only 51% of the group. In addition, group members may support the position of the formal leader, although they do not agree with the decision, because they fear reprisal or they wish to obtain the leader’s approval. In general, as the importance of the decision increases, so does the percentage of group members required to approve it. To secure the support of the group, the leader should maintain open communication with those affected by the decision and be honest about the advantages and disadvantages of the decision. The leader should also demonstrate how the advantages outweigh the disadvantages, suggest ways the unwanted outcomes can be minimized, and be available to assist when necessary.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Patient Safety
- Developing the Role of Manager
- Care Delivery Strategies
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

- ACN FOUNDATION
- SIGNATURE EVENTS
- SCHOLARSHIPS
- POLICY & ADVOCACY
- ACN MERCHANDISE
- MYACN LOGIN
- THE BUZZ LOGIN
- STUDENT LOGIN

- ACN governance and structure
- Work at ACN
- Contact ACN
- NurseClick – ACN’s blog
- Media releases
- Publications
- ACN podcast
- Men in Nursing
- NurseStrong
- Recognition of Service
- Free eNewsletter
- Areas of study
- Graduate Certificates
- Nursing (Re-entry)
- Preparation for Objective Structured Clinical Examination (OSCE)
- Continuing Professional Development
- Immunisation courses
- Single units of study
- Transition to Practice Program
- Refresher programs
- Principles of Emergency Care
- Medicines Management Course
- Professional Practice Course
- Endorsements
- Student support
- Student policies
- Clinical placements
- Career mentoring
- Indemnity insurance
- Legal advice
- ACN representation
- Affiliate membership
- Undergraduate membership
- Retired membership
- States and Territories
- ACN Fellowship
- Referral discount
- Health Minister’s Award for Nursing Trailblazers
- Emerging Nurse Leader program
- Emerging Policy Leader Program
- Emerging Research Leader Program
- Nurse Unit Manager Leadership Program
- Nurse Director Leadership Program
- Nurse Executive Leadership Program
- The Leader’s Series
- Nurse Executive Capability Framework
- Thought leadership
- Other leadership courses
- National Nurses Breakfast
- National Nursing Forum
- History Faculty Conference
- Next Generation Faculty Summit
- Let’s Talk Leadership
- Virtual Open Day
- National Nursing Roadshow
- Policy Summit
- Nursing & Health Expo
- Event and webinar calendar
- Grants and awards
- First Nations health scholarships
- External nursing scholarships
- Assessor’s login
- ACN Advocacy and Policy
- Position Statements
- Submissions
- White Papers
- Aged Care Solutions Expert Advisory Group
- Nurses and Violence Taskforce
- Parliamentary Friends of Nursing
- Aged Care Transition to Practice Program
- Our affiliates
- Immunisation
- Join as an Affiliated Organisation
- Our Affiliates
- Our Corporate Partners
- Events sponsorship
- Advertise with us
- Career Hub resources
- Critical Thinking
Q&A: What is critical thinking and when would you use critical thinking in the clinical setting?
(Write 2-3 paragraphs)
In literature ‘critical thinking’ is often used, and perhaps confused, with problem-solving and clinical decision-making skills and clinical reasoning. In practice, problem-solving tends to focus on the identification and resolution of a problem, whilst critical thinking goes beyond this to incorporate asking skilled questions and critiquing solutions.
Critical thinking has been defined in many ways, but is essentially the process of deliberate, systematic and logical thinking, while considering bias or assumptions that may affect your thinking or assessment of a situation. In healthcare, the clinical setting whether acute care sector or aged care critical thinking has generally been defined as reasoned, reflective thinking which can evaluate the given evidence and its significance to the patient’s situation. Critical thinking occasionally involves suspension of one’s immediate judgment to adequately evaluate and appraise a situation, including questioning whether the current practice is evidence-based. Skills such as interpretation, analysis, evaluation, inference, explanation, and self-regulation are required to interpret thinking and the situation. A lack of critical thinking may manifest as a failure to anticipate the consequences of one’s actions.
Critical thinking is that mode of thinking – about any subject, content, or problem — in which the thinker improves the quality of his or her thinking by skillfully taking charge of the structures inherent in thinking and imposing intellectual standards upon them.
The Paul-Elder framework has three components:
- The elements of thought (reasoning)
- The intellectual standards that should be applied to the elements of reasoning
- The intellectual traits associated with a cultivated critical thinker that result from the consistent and disciplined application of the intellectual standards to the elements of thought.
Critical thinking can be defined as, “the art of analysing and evaluating thinking with a view to improving it”. The eight Parts or Elements of Thinking involved in critical thinking:
- All reasoning has a purpose (goals, objectives).
- All reasoning is an attempt to figure something out, to settle some question, to solve some problem .
- All reasoning is based on assumptions (line of reasoning, information taken for granted).
- All reasoning is done from some point of view.
- All reasoning is based on data, information and evidence .
- All reasoning is expressed through, and shaped by, concepts and ideas .
- All reasoning contains inferences or interpretations by which we draw conclusions and give meaning to data.
- All reasoning leads somewhere or has implications and consequence.
Q&A: To become a nurse requires that you learn to think like a nurse. What makes the thinking of a nurse different from a doctor, a dentist or an engineer?
It is how we view the health care consumer or aged care consumer, and the type of problems nurses deal with in clinical practice when we engage in health care patient centred care. To think like a nurse requires that we learn the content of nursing; the ideas, concepts, ethics and theories of nursing and develop our intellectual capacities and skills so that we become disciplined, self-directed, critical thinkers.
As a nurse you are required to think about the entire patient/s and what you have learnt as a nurse including; ideas, theories, and concepts in nursing. It is important that we develop our skills so that we become highly proficient critical thinkers in nursing.
In nursing, critical thinkers need to be:
Nurses need to use language that will clearly communicate a lot of information that is key to good nursing care, for handover and escalation of care for improving patient safety and reducing adverse outcomes, some organisations use the iSoBAR (identify–situation–observations–background–agreed plan–read back) format. Firstly, the “i”, for “identify yourself and the patient”, placed the patient’s identity, rather than the diagnosis, in primary position and provided a method of introduction. (This is particularly important when teams are widely spread geographically.) The prompt, “S” (“situation”) “o” for “observations”, was included to provide an adequate baseline of factual information on which to devise a plan of care. and “B” (“background”), “A” “agreed plan” and “R” “read back” to reinforce the transfer of information and accountability.
In clinical practice experienced nurses engage in multiple clinical reasoning episodes for each patient in their care. An experienced nurse may enter a patient’s room and immediately observe significant data, draw conclusions about the patient and initiate appropriate care. Because of their knowledge, skill and experience the expert nurse may appear to perform these processes in a way that seems automatic or instinctive. However, clinical reasoning is a learnt skill.
Key critical thinking skills – the clinical reasoning cycle / critical thinking process
To support nursing students in the clinical setting, breakdown the critical thinking process into phases;
- Decide/identify
This is a dynamic process and nurses often combine one or more of the phases, move back and forth between them before reaching a decision, reaching outcomes and then evaluating outcomes.
For nursing students to learn to manage complex clinical scenarios effectively, it is essential to understand the process and steps of clinical reasoning. Nursing students need to learn rules that determine how cues shape clinical decisions and the connections between cues and outcomes.
Start with the Patient – what is the issue? Holistic approach – describe or list the facts, people.
Collect information – Handover report, medical and nursing, allied health notes. Results, patient history and medications.
- New information – patient assessment
Process Information – Interpret- data, signs and symptoms, normal and abnormal.
- Analyse – relevant from non-relevant information, narrow down the information
- Evaluate – deductions or form opinions and outcomes
Identify Problems – Analyse the facts and interferences to make a definitive diagnosis of the patients’ problem.
Establish Goals – Describe what you want to happen, desired outcomes and timeframe.
Take action – Select a course of action between alternatives available.
Evaluate Outcomes – The effectiveness of the actions and outcomes. Has the situation changed or improved?
Reflect on process and new learning – What have you learnt and what would you do differently next time.
Scenario: Apply the clinical reasoning cycle, see below, to a scenario that occurred with a patient in your clinical practice setting. This could be the doctor’s orders, the patient’s vital signs or a change in the patient’s condition.
(Write 3-5 paragraphs)

Important skills for critical thinking
Some skills are more important than others when it comes to critical thinking. The skills that are most important are:
- Interpreting – Understanding and explaining the meaning of information, or a particular event.
- Analysing – Investigating a course of action, that is based upon data that is objective and subjective.
- Evaluating – This is how you assess the value of the information that you have. Is the information relevant, reliable and credible?
This skill is also needed to determine if outcomes have been fully reached.
Based upon those three skills, you can use clinical reasoning to determine what the problem is.
These decisions have to be based upon sound reasoning:
- Explaining – Clearly and concisely explaining your conclusions. The nurse needs to be able to give a sound rationale for their answers.
- Self-regulating – You have to monitor your own thought processes. This means that you must reflect on the process that lead to the conclusion. Be on alert for bias and improper assumptions.
Critical thinking pitfalls
Errors that occur in critical thinking in nursing can cause incorrect conclusions. This is particularly dangerous in nursing because an incorrect conclusion can lead to incorrect clinical actions.
Illogical Processes
A common illogical thought process is known as “appeal to tradition”. This is what people are doing when they say it’s always been done like this. Creative, new approaches are not tried because of tradition.
All people have biases. Critical thinkers are able to look at their biases and not let them compromise their thinking processes.
Biases can complicate decision making, communication and ultimately effect patient care.
Closed Minded
Being closed-minded in nursing is dangerous because it ignores other team members points of view. Essential input from other experts, as well as patients and their families are also ignored which ultimately impacts on patient care. This means that fewer clinical options are explored, and fewer innovative ideas are used for critical thinking to guide decision making.
So, no matter if you are an intensive care nurse, community health nurse or a nurse practitioner, you should always keep in mind the importance of critical thinking in the nursing clinical setting.
It is essential for nurses to develop this skill: not only to have knowledge but to be able to apply knowledge in anticipation of patients’ needs using evidence-based care guidelines.
American Management Association (2012). ‘AMA 2012 Critical Skills Survey: Executive Summary’. (2012). American Management Association. http://playbook.amanet.org/wp-content/uploads/2013/03/2012-Critical-Skills-Survey-pdf.pdf Accessed 5 May 2020.
Korn, M. (2014). ‘Bosses Seek ‘Critical Thinking,’ but What Is That?,’ The Wall Street Journal . https://www.wsj.com/articles/bosses-seek-critical-thinking-but-what-is-that-1413923730?tesla=y&mg=reno64-wsj&url=http://online.wsj.com/article/SB12483389912594473586204580228373641221834.html#livefyre-comment Accessed 5 May 2020.
School of Nursing and Midwifery Faculty of Health, University of Newcastle. (2009). Clinical reasoning. Instructors resources. https://www.newcastle.edu.au/__data/assets/pdf_file/0010/86536/Clinical-Reasoning-Instructor-Resources.pdf Accessed 11 May 2020
The Value of Critical Thinking in Nursing + Examples. Nurse Journal social community for nurses worldwide. 2020. https://nursejournal.org/community/the-value-of-critical-thinking-in-nursing/ Accessed 8 May 2020.
Paul And Elder (2009) Have Defined Critical Thinking As: The Art of Analysing And Evaluating …
https://www.chegg.com/homework-help/questions-and-answers/paul-elder-2009-defined-critical-thinking-art-analyzing-evaluating-thinking-view-improving-q23582096 Accessed 8 May 2020 .
Cody, W.K. (2002). Critical thinking and nursing science: judgment, or vision? Nursing Science Quarterly, 15(3), 184-189.
Facione, P. (2011). Critical thinking: What it is and why it counts. Insight Assessment , ISBN 13: 978-1-891557-07-1.
McGrath, J. (2005). Critical thinking and evidence- based practice. Journal of Professional Nursing, 21(6), 364-371.
Porteous, J., Stewart-Wynne, G., Connolly, M. and Crommelin, P. (2009). iSoBAR — a concept and handover checklist: the National Clinical Handover Initiative. Med J Aust 2009; 190 (11): S152.
Related posts
Planning your career 5 November 2021

Active Listening 4 November 2021
Ethical Leadership 4 November 2021
Problem solving in clinical nursing practice
Affiliation.
- 1 School of Nursing, Deakin University, Victoria, Australia.
- PMID: 9292367
- DOI: 10.1046/j.1365-2648.1997.1997026329.x
Problem solving in clinical nursing practice is the essence of good care delivery. This paper gives an overview of a research study which identified the cognitive problem solving process nurses use while delivering care. The study was conducted in the clinical setting and used a qualitative research methodology of observation, followed by in-depth semi-structured interview. The analysis of the study revealed diagnostic reasoning is the process used by clinicians. Information regarding the differences between novices and experts is offered as topics for discussion throughout the paper, and recommendations for changes to educational processes are made.
- Clinical Competence*
- Nurse-Patient Relations
- Nursing Care / methods*
- Nursing Methodology Research
- Nursing Process*
- Nursing Staff, Hospital / psychology*
- Problem Solving*
- Socialization
- Surveys and Questionnaires
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Florence Nightingale J Nurs
- v.29(3); 2021 Oct

Creativity in Nursing Care: A Concept Analysis
Mohammad ali cheraghi.
1 Department of Critical Care and Nursing Management; School of Nursing and Midwifery, Tehran University of Medical Sciences; Health Sciences Phenomenology Association; Ministry of Health and Medical Education, Tehran, Iran
Shahzad Pashaeypoor
2 Department of Community Health Nursing & Geriatric Nursing, School of Nursing & Midwifery, Tehran University of Medical Sciences, Tehran, Iran
Leila Mardanian Dehkordi
3 Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran
Sahar Khoshkesht
4 Department of Medical-Surgical Nursing, School of Nursing & Midwifery, Tehran University of Medical Sciences, Tehran, Iran

The aim of this study was to present the concept analysis of creativity in nursing care using the Walker and Avant (2019) approach. In this regard, the keywords “creativity” and “nursing care” were searched through PubMed, Ovid, Scopus, EMBASE, Google Scholar, SID, and Web of Science between the years 2000 and 2018 along with hand searching of reference lists extracted from more than 342 articles. Finally, 37 articles that had inclusion criteria were examined based on the eight stages mentioned in Walker and Avant’s concept analysis approach. Results revealed that creativity in nursing care includes fluidity of mind and the creation and acceptance of new ideas for patient care in such a way that the new methods are simple, useful, efficient, affordable, and safe. This requires a creative vision, creative sensitivity, and creative thinking. If there is a supportive environment, motivation, sensitivity, and divergent thinking skills, individuals can demonstrate their creativity. This may result in successful decision-making in the clinical setting and therefore contribute to increasing the organization’s effectiveness and the quality of care. All nurses can act as agents encouraging change by the use of creativity to improve the quality of care. It is an educational guide for future nurses to implement creativity in practice. Also, this finding can be used for future research and the development of specific tools. Finally, it is suggested to consider creativity in the other aspects of clinical practice as well.
Introduction
With the development of science and technology, society needs people who can take steps in the direction of change and development ( Mosakhani et al. , 2010 ). One of the important capabilities of organizations for their survival, success, and excellence in the globalization age is creativity (Rangaraju & Kennedy, 2012). Health care organizations must provide creative responses in order to deal with all the emerging needs and different circumstances ( Denhardt et al. , 2018 ). The creativity of any social system is based on the creativity of the people of that system. In such a situation, the presence of knowledgeable and creative employees in the organization is very helpful (Tayebi Shirmard & Mirzaei, 2017). Also, nurses often face unpredictable situations, for which they have not been trained before. Their education no longer meets the needs of the 21 st century. To deal with these new and complex situations, nurses need a higher level of competence and attitude and must be able to respond in a timely, effective, creative, and flexible manner (Institute of Medicine, 2010).
First time in 1973, Myra Levine used the metaphor “Linking the art and nursing science” to describe creativity and introduced it as a daily event that was essential for nursing interactions ( Ma et al. , 2018 ). Creativity is an important skill to solve the problem and create a new idea. Nurses should use their creativity to conceive of their potential problems and its subsequent outcomes and prepare themselves for the future. They should also use it for decision-making and problem-solving (Bunkers, 2011).
Nursing creativity can be executed in a variety of areas, including education, research, management, and clinical practice. Obviously, these areas interact with each other. However, creativity in nursing care is a new concept which perceived less than others, and for this reason, the art of nursing care is not publicly visible and remains hidden in the profession.
As new technology and genetic knowledge have changed medical and nursing care (Toole, 2012), there is a need for simple, cost-effective, and low-risk alternatives that embrace nursing creativity. The health system requires new ideas and creative problem-solving methods in the face of future changes ( Cresswell et al. , 2016 ). The authors of Individualized care emphasize the attitude toward patients as unique individuals and the obligation to care for them according to their conditions. Efforts to provide patient-centered care, such as evidence-based medicine, emphasize changes in infrastructures. Therefore, nurses should try to work with other healthcare disciplines to create a creative care model that meets the new needs of patients. Obviously, to improve the quality of patient care in a modern healthcare system, it is crucial to use creativity for harmonizing arts and nursing science ( Hewitt-Taylor, 2015 ).
Although previous studies have shown the importance of creative thinking and creativity in nursing, due to the complexity of the psychological and social forces involved in the formation of creativity, individuals face challenges in understanding and managing the creativity (Sadeghi Mal Amiri, 2015; Ma et al., 2018; Zuber & Moody, 2018).
In the 21st century, there is a growing tendency in health systems toward the concept of creativity and innovation to overcome the challenges of the health system, improve quality of care, increase fair access to care services, and reduce subsequent costs. This is not possible without understanding the concept of creativity. Many studies have been conducted in this field, especially in the humanities ( Fox, 2013 ; Khessina et al. , 2018 ; Nembhard & Lee, 2017; Vermeir et al. , 2018 ; Zuber & Moody, 2018). However, there has been no study emphasizing the dimensions of creativity in nursing care. Therefore, it seems necessary to recognize its features through the process of conceptual analysis and to explain its role in the clinical nursing setting.
Concept analysis is a strategy for examining the semantic structure of a concept. For a concept to be solid in theory and practice, it must be clearly defined and analyzed. Concept analysis helps us to distinguish that concept from others that may be similar but not the same as that concept. Concept analysis can be useful in refining ambiguous concepts and clarifying overused concepts for arriving at precise definitions. Additionally, it can be useful in tool development and language development in nursing. There are several methods for conducting concept analysis; in all of the methods, the analysis of a concept includes the analysis of the descriptive word and its usage. Therefore, a concept analysis of creativity in nursing care can help us to distinguish the concept from other similar borderline concepts, describe it in the nursing care domain, and provide a foundation for further research (Walker & Avant, 2019). Therefore, this study aimed to clarify the concept of creativity in nursing care based on Walker and Avant’s concept analysis approach.
Research Questions
- What is the concept of creativity in patient care?
- What is the manifestation of creativity in patient care?
- What kind of attitude and behavior in the field of patient care reflects the creativity of nursing care?
Walker and Avant’s (2019) approach was used as the framework for this concept analysis. Walker and Avant’s approach is a simplified approach to Wilson’s 11-step systematic process that simplifies the concept by creating a clearer understanding of it. This approach provides a pragmatic framework that emphasizes the conceptual aspect of the concepts ( Chinn & Kramer, 2004 ). Walker and Avant’s (2019) concept analysis process includes eight stages that are described in Table 1 .
Walker and Avant’s Concept Analysis Stages
The concept was searched using keywords “Creativity” and “Nursing care” in credible databases such as PubMed, Ovid, Scopus, EMBASE, Google Scholar, SID, and Web of Science during 2000–2018, with hand searches of reference lists, and the search process was completed using the dictionary.
More than 342 articles were extracted. After removing duplicate items (36 items), examining the relevancy of titles (removing 231 items), reviewing the relevancy of the subject, and the validity of the source, the remaining 37 articles were examined. Exclusion criteria included irrelevant, duplicated articles and lack of access to the article in English. A total of 37 extracted articles were independently reviewed by two researchers S K and L M D who have a brilliant background in teaching nursing theories and concept analysis for nursing students and have written numerous articles in this field. Usually, in analyzing the concept, the quality of studies is not examined using common tools. However, an attempt was made to select the closest and the most authoritative studies in terms of methodological quality from reputable journals and peers review. Finally, the required data were extracted from the initial studies.
Select a Concept
The increase in emerging needs, the emergence of individualized care, and departure of the care from conventional academic stereotypes calls for evidence-based thinking and effective clinical reasoning. All this requires a fluid and creative mind while providing individualized care, which this concept has not been clarified yet. Price (2006) believes that if creativity is described in a complex and inapplicable manner or is not well-defined, it is unlikely to go beyond the conceptual stage.
In this study, after reviewing the literature and based on the researcher’s interest and the increasing role of creativity in clinical nursing, the concept of creativity in nursing care was selected. It should be noted that researchers have paid little attention to this concept in the field of patient care. Therefore, this analysis will help us to achieve a better understanding of this concept in this field.

Purposes of Analysis
The aim of this study was to present the concept analysis of creativity in nursing care and identify attributes, antecedents, and consequences.
Attributes of the Concept
Defining attributes of the concept include descriptive attributes that are used frequently while discussing the concept and play a major role in differentiating between concepts (Walker & Avant, 2019). Creativity can be defined in a variety of ways, including cognitive processes, personality traits, environmental variables, and interactions of these components. Nevertheless, there is a need to combine the concept in a clinical setting.
Creativity comes from the Latin word “creare” which means to create. Oxford dictionary defines creativity as “to use imagination or original ideas to create something” (Medical Dictionary, 2018). Creativity has an extensive definition. Lau (2011) points to three principles in the concept of creativity: (1) the new reconstruction of old ideas; (2) the selection of useful ideas; and (3) the examination of the relationship between ideas. New forms beyond the common rules can be created by creativity. Although , these three principles are not mostly related to nursing education, human simulations and other creative learning methods can join theory to practice so that nursing students can use different forms of creativity in care for patients and successful decision-making in the clinical setting (Marquis & Huston, 2009).
Based on the main purpose, in this study defined nursing care and then analyzed and developed the concept of creativity in nursing care. The medical dictionary considers nursing care as a general term, which refers to procedures and measures that are solely or primarily intended to reduce the pain, symptoms, and discomfort of the patient (Medical Dictionary, 2018). Therefore, any nursing practice that is carried out based on the above aim is called nursing care. Based on the literature review, definitions, and general conclusions, it can be concluded that the concept of creativity in clinical nursing can include three attributes:
- The reconstruction of old ideas or choice of a new way of providing patient care that has more advantages than the usual method.
- The selection of simple, useful, affordable, efficient, and safe ideas.
- The examination of the relationship between ideas and successful decision-making in a clinical setting.
In the other words, creative nursing care is fulfilling new ideas in the face of intricate clinical interactions and practices by nurses utilizing their fluid minds and old ideas and facilities. That is, such creative nursing care is not only new and simple but also affordable, efficient, useful, and safe. In other words, creativity in nursing care means using new thinking to produce a new idea and apply it to nursing care that must necessarily be more useful, efficient, and safer compared to older methods. This can be defined as a new way of providing patient care and may result in successful decision-making in the clinical setting.
Uses of the Concept
Although this concept is not well-clarified, creativity in nursing care has led to the creation of devices that facilitate the work, save time, increase the quality of care, and reduce the nursing workload. It also leads to self-belief, growth and prosperity, social status, and self-confidence in nursing staff. Other benefits of creativity include increased satisfaction, self-efficacy, and pleasure of discovery, lower workload and achieving reputation, social respect, and changing attitudes of authorities, universities, and society toward nursing society (Shahsavari et al., 2015 a).
A model case is a specific example of the intended concept that should have all the features of that concept (Walker & Avant, 2019). Such a model case is discussed below:
“Ms. X, due to her interest in nursing and assisting humankind, chose to be a nurse 20 years ago and graduated from one of the best universities. She has been enthusiastically working in the orthopedic ward for years. Besides other tasks defined for her, she has to change 10–12 wound dressings quickly and with the utmost precision every day. She sees that the risk of surgical site infection and the re-admission of patients after surgery are elevated, which imposes a lot of costs on the patients, system, and nurses. She also observes that her co-workers change the dressing less accurately due to lack of time and high workload. Due to the lack of items needed for changing dressing in the department, shortage of nursing staffs, and a large number of patients, as well as the impossibility of transferring all patients to the only available dressing room due to immobility of some of the orthopedic patients, nurses should use one dressing trolley for all patients, which itself increases the risk of transmission of infection. She always thinks about how to change the dressing of patients quickly and accurately without using hands according to sterile points in a way that the waste material is automatically removed after changing the dressing, and there is no risk of infection for the environment, patient, and nurse. She discusses the issue with the head nurse. The head nurse welcomes her idea and informs the authorities of the hospital. Finally, engineer Y is introduced to them to help change the old trolley’s use to design an automatic wound washing machine with the possibility of waste storage in a closed chamber and automatic waste disposal with the help of Ms. X’s idea.”
Achieving a profound understanding of the problem investigated by Ms. X and her interest to resolve such problem in addition to the supportive environment and the existence of intrinsic (interest in nursing, diligence, and purposefulness) and external motivations (work pressure and lack of time) are the motivating factors for proposing the idea of making this device by the aforementioned nurse. The aforementioned example is a model of creativity in nursing care in which woman X showed sensitivity to the problem, and with her fluid mind and putting aside old ideas proposed the idea of making an automatic wound washing machine. She then designed and built the machine with the help of an expert.
Borderline and Contrary Cases
Borderline cases include some of the attributes embracing the concept that are often mistakenly used instead of the concept (Walker & Avant, 2019). Innovation is one of the borderline cases of creativity. Innovation and creativity are two independent but interrelated concepts that sometimes lead to confusion for readers. Creativity is the process of thought, and innovation is a product obtained through the implementation of that creative thinking ( Sarooghi et al. , 2015 ). Innovation is, in fact, the use of creativity or problem-solving skills that results in a product, strategy, or service that meets needs in a new and different way ( Kaya et al. , 2016 ). In other words, applied creativity should always lead to innovation. Here’s an example of an innovation case:
“Ms. Z is a nurse in the department of surgery. She observes that many patients need self-care counseling after discharge. Although discharge training is practiced, many still need access to a physician and nurse. Therefore, surgical nurses are required to answer the patient’s questions besides their plenty of tasks. She thinks that it is better to establish a telenursing center equipped with a referral system at the hospital’s nursing office in order to save time and money and help the patient have better access to experts. The idea of implementing such a method is given to the hospital manager. Eventually, after examining different aspects, a center was established at the hospital.” This is a nursing innovation aimed at improving quality, saving time, and providing safe services. Though this idea has already existed, in this example, the nurse has used her creative thinking to establish a telenursing center presenting a new method that addresses the needs in a different way. Such thinking provides a coherent approach to define challenges. This helps to identify problems and to proceed according to previous ideas or according to existing guidelines.
If in the previous example, Ms. X only did the dressing process step-by-step according to the existing guidelines, her care lacked creativity. Therefore, routine care can introduce as a contrary case in creative nursing care, patient’s conditions, facilities, environment, and existing problems, as well as characteristics of creativity in nursing care must be considered.
Antecedents and Consequences
Antecedents: Antecedents are situations, events, or phenomena that precede the occurrence of a phenomenon and the main concept occurs due to their presence. It helps to refine the concept (Walker & Avant, 2019). There are six factors that affect people’s creativity: (1) having knowledge and experience; (2) being able to mentally present creative ideas and create new relationships in issues; (3) adopting a creative thinking style and confronting a routine life; (4) motivation; (5) resilient personality, and (6) supportive environment (Jokari & Jorfi, 2012). Participants in Chan’s study (2013) had different opinions about the experience factor. Some believed that laws and experience prevented the emergence of new thinking, while some emphasized the inspirational nature of the experience to create creative ideas. In the case of lack of time and work-related stress, the results are contradictory. Occasionally, work-related stress prevents the emergence of creative ideas, and sometimes the nurses move toward innovative ideas to overcome them. In other words, shortages of time lead to creativity and severe time shortage prevents it. However, there would be different perceptions depending on one’s perception of the problem and the nature of the task ( Denhardt et al. , 2018 ). Shahsavari et al. (2015b) classified the factors influencing creativity in clinical nurses into five groups. The intrinsic motivators include having an interest and love for nursing and doing the duties, positive emotions such as the sense of satisfaction, happiness, self-esteem, and self-belief. External motivators include workplace problems, workload and time pressure, success, and failure. Both of these motivators influence the behavior of nurses in different ways. The third group of motivators includes diligence, purposefulness, etc., and it shows why some people are more successful than others. The fourth group includes related motivators that lead individuals to help people and to be creative by inducing a profound understanding of the clinical issues along with a sense of altruism and empathy. Ultimately, spiritual motivators and religious beliefs also stimulate creativity in clinical nurses. In addition, a review study, which examined ways to develop and measure creativity in nursing, has referred to self-directed learning and teamwork as effective factors in increasing creativity in nursing learning and practice ( Ma et al. , 2018 ). Karpova et al. (2011) claim that the most important factors in increasing creativity include the creation of opportunities for creating ideas (problem-solving, designing and combining experience and knowledge), and being aware of the surroundings (exploring and asking the question), and programs that stimulate motivation and curiosity to raise questions, explore answers, and have diverse and creative thinking. Therefore, while personal characteristics and intrinsic motivations are the most important factors in stimulating creativity, the creation of a supportive environment by managers and authorities that also affects an individual’s motivation plays an indirect role in its emergence ( Tsai et al. , 2013 ).
Consequences: Consequences are caused following the occurrence of a phenomenon. Creativity means offering new thinking to improve quality. The researchers have interpreted the consequences of creativity in different ways. Shahsavari et al. (2015c) concluded in their data analysis phase that creativity is effective at both individual and organizational levels. At the individual level, it improves self-esteem and self-confidence. The pleasure of discovering is also considered as one of the creativity-related positive emotions. Creativity is also the result of positive emotions and physical and mental health. At the organizational level, creativity leads to simplification of the task, increased quality of care, reduced financial burden, safety, and comfort of patients, nurses, and other nursing personnel. Creativity improves organizational effectiveness, motivation, and teamwork. In other words, from an organizational perspective, increased productivity, lower costs, higher quality services are among the consequences of organizational creativity.
Empirical Referents
Empirical referents are recognizable attributes of the concept whose emergence signifies the existence of the concept. Empirical referents are more important, especially when concepts are abstract and difficult to measure. It aims to identify the concept and facilitate its measurement (Walker & Avant, 2011). Here, several empirical examples put forward by the professional panel of the American Nursing Association (ANA) are presented. The predictive care model which enables the health system to anticipate and take special action to prevent disease, design an inspired infant wear, establish a direct caregiver connection for the elderly at the end of life, create safety campaigns for healthcare professionals, collaborative care clinics or professional international clinics, create hospital innovation units with new nursing roles, create units and motivational tools for patients, etc. through obtaining information from electronic medical records are among the creativities of American nurses (Hall & Wood, 2013).
Various tools and software have been developed to improve the quality and efficiency of the health system worldwide. For example, Robea is a nurse robot, the idea for the construction of which has been given by RIKEN-SRK in Japan to help older patients become more independent. New ideas for the construction of surgeon, scrub robots, and etc. are also becoming a reality ( Eriksson & Salzmann-Erikson, 2017 ). Shahsavari et al. (2015c) in Iran interviewed several creative nurses and examples of nursing creativities, including a wound washing machine for orthopedic patients, automatic washing of the dressing, a C-ARM desk (C-shaped arm is an imaging scanner intensifier), a robot that stretches out the patien’s leg during surgery, electronic tourniquet machine, optic laparoscope that is placed under a surgeon’s microscope to help students see eye surgeries better on a monitor.
As aforementioned, creativity in clinical nursing is not limited to the creation of useful devices. Many new creations may be new ways of taking care of or meeting the needs of patients ( Price, 2006 ). The development of useful and practical questionnaires, such as patient assessment forms, shortening forms, creation of online or cellphone-based online content by nurses, creation of international clinics are among different examples of creativity in clinical nursing. However, there is still a long way ahead in the field of creativity in nursing care. Various tools and questionnaires are also explained in the field of nursing creativity which measure different aspects of creativity such as Torrance tests of creative thinking (TTCT) (Torrance, 1990), Spanish creative intelligence test (CREA) (Almansa et al., 2013), and Rendcip’s standardized creativity questionnaire ( Nikbakht et al. , 2014 ). However, only one of them measures creativity in the nursing field. In fact, there is a need for an appropriate tool with satisfactory psychometrics to measure nursing creativity (Ma et al., 2017).
Conclusion and Recommendations
Creativity in nursing care is a complex concept, which has been discussed more frequently in theory than in practice. Therefore, there is a need for extensive studies on concept explanation. The aim of this study was to analyze the concept of creativity in nursing care. Creativity has various meanings, such as creating, making, producing designs, product relationships and attributes, a new and useful set of operations, reconstruction of old ideas, and a problem-solving method. However, the implementation of creativity in nursing clinical settings is of particular importance. Factors such as the existence of a supportive clinical environment, having some personality traits such as motivation, sensitivity to surrounding issues, divergent thinking skills, resistance, and having sufficient knowledge and experience can affect creativity in the clinical setting.
The results of this study revealed that creativity in nursing care includes the mind fluidity and creation of new ideas for patient care in the field of nursing practice in a way that the new method of patient care is simple, useful, effective, cost-effective, and safe. This requires a creative vision, creative sensitivity, and creative thinking in a way that the sensitivity to the problem, the ability to generate new ideas or reconstruction of old ideas, and connecting ideas to select new ways of care result in successful decision-making in the clinical setting.
As noted, creativity in nursing care simplifies tasks, saves time, and improves quality. Therefore, nurses’ perceptions about the concept of creativity in nursing care and the importance of its application in practice will be enhanced if such concept is clarified, and they thus will be able to successfully implement their creative thinking in providing patient care in today’s complex world. It is worth noting that our goal in this article is to refer to creativity in nursing care, which provides a platform for further discussion. There is a need to clarify the concept of creativity in nursing as a profession and other related areas. These include creativity in monitoring, management, budgeting, organizational charter, and human resources, accreditation, quality assurance, payment system, nursing shifts program, personnel charting based on the type of care, and indirect nursing care including nursing report, counseling, follow up, etc. The emergence of creativity in each of the above areas requires us to recognize it and create a way for the emergence of the context at the individual and organizational levels.
The concept of creativity is very complex and abstract. Therefore, clarification of this concept is very difficult. Also, this analysis was carried out relying on the available evidence that we could find, therefore, it is suggested that the results of our finding are combined with other new and unavailable evidence to clarify this concept.
All nurses can act as agents encouraging the change in processes and policies and the use of technology to improve better and cheaper care for patients and society. Nursing creativity leads to the development of better healthcare policies and practices, improvement of the quality of care, and advancement of health information technology. By considering creativity and its roles in patient care, this study was aimed attain these goals. It is an educational guide for future nurses to implement creativity in practice. Also, this finding is basic for further research in the field of creativity and can be used for the development of specific tools.
Author Contributions
Concept – S.K., S.P., L.M.D., M.A.C.; Design – S.K., S.P., L.M.D., M.A.C.; Supervision – S.K., S.P., L.M.D., M.A.C.; Resources – S.K., S.P., L.M.D., M.A.C.; Writing Manuscript – S.K.
Funding Statement
The authors declared that this study has received no financial support.
Peer-review: Externally peer-reviewed.
Conflict of Interest: The authors have no conflicts of interest to declare.
- Almansa P., López-Martínez O., Corbalán J., Limiñana-Gras R. M. (2013). Thinking styles and creativity preferences in nursing . Creative Nursing , 19 , 91–100. 10.1891/1078-4535.19.2.91 Bunkers S. S.2011). What is not yet: Cultivating the imagination . Nursing Science Quarterly , 24 , 324–328. 10.1177/0894318411419219 [ PubMed ] [ Google Scholar ]
- Chan Z. C.2013). Critical thinking and creativity in nursing: learners’ perspectives . Nurse Education Today , 33 , 558–563. 10.1016/j.nedt.2012.09.007 [ PubMed ] [ Google Scholar ]
- Chinn P. L., Kramer M. K. (2004). Integrated knowledge development in nursing . St. Louis, MO: Mosby. (ISBN-13: 978-0323023412; ISBN-10: 032302341X). [ Google Scholar ]
- Cresswell K. M., Cunningham-Burley S., Sheikh A. (2016). Creating a climate that catalyses healthcare innovation in the United Kingdom–learning lessons from international innovators . BMJ Health and Care Informatics , 23 . 10.1016/j.nedt.2012.09.007 [ PubMed ] [ Google Scholar ]
- Denhardt R. B., Denhardt J. V., Aristigueta M. P., Rawlings K. C. (2018). Managing human behavior in public and nonprofit organizations . CQ Press (ISBN-13: 978-1506382661; ISBN-10: 1506382665). [ Google Scholar ]
- Eriksson H., Salzmann‐Erikson M. (2017). The digital generation and nursing robotics: A ethnographic study about nursing care robots posted on social media . Nursing Inquiry , 24 , e12165. 10.1111/nin.12165 [ PubMed ] [ Google Scholar ]
- Fox N. J.2013). Creativity and health: An anti-humanist reflection . Health , 17 , 495–511. 10.1177/1363459312464074 [ PubMed ] [ Google Scholar ]
- Hall J., Wood D. (2013). RNs Putting innovative ideas to work . AMN healthcare . Retrieved from https://www.rn.com/nursing-news/rns-putting-innovative-ideas-to-work/ , 2011 [ Google Scholar ]
- Hewitt-Taylor J.2015). Developing person-centred practice: A practical approach to quality healthcare . London: Macmillan International Higher Education. [ Google Scholar ]
- Joint Commission, & Robert Wood Johnson Foundation initiative on the future of nursing (2010). At the Institute of Medicine. The future of nursing: leading change, advancing health . Washington, DC: The National Academies Press. [ Google Scholar ]
- Jokari M., Jorfi H. (2012). Study the effect of creativity and innovation on nurses productivity in Taleghani hospital (case study in Abadan of Iran) . Interdisciplinary Journal of Contemporary Research in Business , 4 , 1055-1076. Retrived from: https://www.researchgate.net/publication/311104061_Study_the_Effect_of_Creativity_and_Innovation_on_Nurses’_Productivity_in_Taleghani_Hospital_Case_Study_in_Abadan_of_Iran [ Google Scholar ]
- Karpova E., Marcketti S. B., Barker J. (2011). The efficacy of teaching creativity: Assessment of student creative thinking before and after exercises . Clothing and Textiles Research Journal , 29 , 52–66. 10.1177/0887302X11400065 [ Google Scholar ]
- Kaya N., Turan N., Aydın G. Ö. (2016). Innovation in nursing: A concept analysis . Journal of Community and Public Health Nursing , 2 , 2–4. 10.4172/2471-9846.1000108 [ Google Scholar ]
- Khessina O. M., Goncalo J. A., Krause V. (2018). It’s time to sober up: The direct costs, side effects and long-term consequences of creativity and innovation . Research in Organizational Behavior , 38 , 107–135. 10.1016/j.riob.2018.11.003 [ Google Scholar ]
- Lau J. Y.2011). An introduction to critical thinking and creativity: Think more, think better . Chichester: John Wiley & Sons (ISBN-13: 978-0470195093; ISBN-10: 0470195096). [ Google Scholar ]
- Ma X., Yang Y., Wang X., Zang Y. (2018). An integrative review: Developing and measuring creativity in nursing . Nurse Education Today , 62 , 1–8. 10.1016/j.nedt.2017.12.011 [ PubMed ] [ Google Scholar ]
- Marquis B. L., Huston C. J. (2009). Leadership roles and management functions in nursing: Theory and application . Philadelphia: Lippincott Williams & Wilkins (ISBN-13: 978-1496349798; ISBN-10: 1496349792). [ Google Scholar ]
- Medical Dictionary . (2018). Retrieved from https://medical dictionary.thefreedictionary.com/nursing+care [ Google Scholar ]
- Mosakhani M., Ajli Ghashlajughi M., Safavi Mir Mahale R. (2010). Model presentation for assessment rate of organization preparation in knowledge management . Management Researches in Iran , 14 , 221–243. [ Google Scholar ]
- Nembhard I. M., Lee Y. S. H. (2017). Time for more creativity in health care management research and practice . Health Care Management Review , 42 , 191. 10.1097/HMR.0000000000000171 [ PubMed ] [ Google Scholar ]
- Nikbakht A., Salehi S., Naji S. A. (2014). A study of the relationship between knowledge management and creativity in some selected hospitals in Isfahan . Modern Care Journal , 11 (4), 339–344. Retrived from: http://sid.bums.ac.ir/dspace/handle/bums/5020 . [ Google Scholar ]
- Oxford Dictionary (2018). Definition of Creativity in English . Retrieved from https://en.oxforddictionaries.com/definition/creativity [ Google Scholar ]
- Price B.2006). Strategies to explore innovation in nursing practice . Nursing Standard , 21 , 48–55. 10.7748/ns2006.11.21.9.48.c6410 [ PubMed ] [ Google Scholar ]
- Rangaraju M. S., Kennedy S. H. (Eds.) (2012). Innovation in management challenges and opportunities in the next decade . Allied Publishers. [ Google Scholar ]
- Sadeghi Mal Amiri, M.2015). System theory of creativity in the organization . Journal of Innovation and Creativity in Human Science , 4 (4), 163-207. [ Google Scholar ]
- Sarooghi H., Libaers D., Burkemper A. (2015). Examining the relationship between creativity and innovation: A meta-analysis of organizational, cultural, and environmental factors . Journal of Business Venturing , 30 , 714–731. 10.1016/j.jbusvent.2014.12.003 [ Google Scholar ]
- Shahsavari Isfahani S., Hosseini M. A., Fallahi Khoshknab M., Peyrovi H., Khanke H. R. (2015. a). Nurses’ creativity: Advantage or disadvantage . Iranian Red Crescent Medical Journal , 17 , e20895. 10.5812/ircmj.20895 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shahsavari Isfahani S., Hosseini M. A., Fallahi Khoshknab M., Peyrovi H., Khanke H. R. (2015. b). Exploring nurses’ creativity consequences in clinical settings: A qualitative study . Journal of Health Promotion Management , 4 , 59–71. Retrived from: http://jhpm.ir/files/site1/user_files_5cd8d5/eng/shahsavari-A-10-471-2-5377064.pdf . [ Google Scholar ]
- Shahsavari Isfahani S., Hosseini M. A., Fallahi Khoshknab M., Peyrovi H., Khanke H. R. (2015. c). What really motivates Iranian nurses to be creative in clinical settings?: A qualitative study . Global Journal of Health Science , 7 , 132–142. 10.5539/gjhs.v7n5p132 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tayebi Shirmard M., Mirzaei N. (2017). Relationship between creativity and establishment of knowledge management (case study: Social Security Organization) . Public Policy in Administration , 8 , 85–92. [ Google Scholar ]
- Toole B.2013). The creative destruction of medicine: How the digital revolution will create better health care . E. Topol . New York, NY: Basic Books (ISBN-13: 978-0465061839; ISBN-10: 0465061834). [ Google Scholar ]
- Torrance E. R.1990). The Torrance tests of creative thinking . Norms-technical mannual . [ Google Scholar ]
- Tsai H. M., Liou S. R., Hsiao Y. C., Cheng C. Y. (2013). The relationship of individual characteristics, perceived worksite support and perceived creativity to clinical nurses’ innovative outcome . Journal of Clinical Nursing , 22 , 2648–2657. 10.1111/jocn.12269 [ PubMed ] [ Google Scholar ]
- Vermeir P., Degroote S., Mariman A., Tobback E., Peleman R., Verhaeghe R., Vandijck D. (2018). Creativity and innovation to improve quality and safety in healthcare. Retrieved from: https://biblio.ugent.be/publication/8559357. [ Google Scholar ]
- Walker L. O., Avant K. C. (2019). Strategies for theory construction in nursing (6th ed). Boston: Prentice (ISBN-13: 978-0134754079; ISBN-10: 0134754077). [ Google Scholar ]
- Zuber C. D., Moody L. (2018). Creativity and innovation in health care: Tapping into organizational enablers through human-centered design . Nursing Administration Quarterly , 42 , 62–75. 10.1097/NAQ.0000000000000267 [ PubMed ] [ Google Scholar ]
- Open access
- Published: 24 April 2024
Clinical decision making: validation of the nursing anxiety and self-confidence with clinical decision making scale (NASC-CDM ©) into Spanish and comparative cross-sectional study in nursing students
- Daniel Medel ORCID: orcid.org/0009-0007-5883-295X 1 ,
- Tania Cemeli ORCID: orcid.org/0000-0002-6683-3756 1 ,
- Krista White ORCID: orcid.org/0000-0003-4179-5383 2 ,
- Williams Contreras-Higuera ORCID: orcid.org/0000-0002-4872-1590 3 ,
- Maria Jimenez Herrera ORCID: orcid.org/0000-0003-2599-3742 4 ,
- Alba Torné-Ruiz ORCID: orcid.org/0000-0002-8072-1953 1 , 5 ,
- Aïda Bonet ORCID: orcid.org/0000-0001-7382-114X 1 , 6 &
- Judith Roca ORCID: orcid.org/0000-0002-0645-1668 1 , 6
BMC Nursing volume 23 , Article number: 265 ( 2024 ) Cite this article
151 Accesses
1 Altmetric
Metrics details
Decision making is a pivotal component of nursing education worldwide. This study aimed to accomplish objectives: (1) Cross-cultural adaptation and psychometric validation of the Nursing Anxiety and Self-Confidence with Clinical Decision Making (NASC-CDM©) scale from English to Spanish; (2) Comparison of nursing student groups by academic years; and (3) Analysis of the impact of work experience on decision making.
Cross-sectional comparative study. A convenience sample comprising 301 nursing students was included. Cultural adaptation and validation involved a rigorous process encompassing translation, back-translation, expert consultation, pilot testing, and psychometric evaluation of reliability and statistical validity. The NASC-CDM© scale consists of two subscales: self-confidence and anxiety, and 3 dimensions: D1 (Using resources to gather information and listening fully), D2 (Using information to see the big picture), and D3 (Knowing and acting). To assess variations in self-confidence and anxiety among students, the study employed the following tests: Analysis of Variance tests, homogeneity of variance, and Levene’s correction with Tukey’s post hoc analysis.
Validation showed high internal consistency reliability for both scales: Cronbach’s α = 0.920 and Guttman’s λ2 = 0.923 (M = 111.32, SD = 17.07) for self-confidence, and α = 0.940 and λ2 = 0.942 (M = 80.44, SD = 21.67) for anxiety; and comparative fit index (CFI) of: 0.981 for self-confidence and 0.997 for anxiety. The results revealed a significant and gradual increase in students’ self-confidence ( p =.049) as they progressed through the courses, particularly in D2 and D3. Conversely, anxiety was high in the 1st year (M = 81.71, SD = 18.90) and increased in the 3rd year (M = 86.32, SD = 26.38), and significantly decreased only in D3. Work experience positively influenced self-confidence in D2 and D3 but had no effect on anxiety.
The Spanish version (NASC-CDM-S©) was confirmed as a valid, sensitive, and reliable instrument, maintaining structural equivalence with the original English version. While the students’ self-confidence increased throughout their training, their levels of anxiety varied. Nevertheless, these findings underscored shortcomings in assessing and identifying patient problems.
Peer Review reports
Decision making in nursing is a critical process that all nurses around the world use in their daily practice, involving the assessment of information, the identification of health issues, the establishment of care objectives, and the selection of appropriate interventions to address the patient’s health problems [ 1 , 2 ]. Nursing professionals must effectively apply their knowledge, skills, and clinical judgment to ensure the delivery of safe and high-quality care within the context of complex and ever-evolving situations [ 3 ]. For nearly 25 years, clinical decision-making has been highlighted as one of the key aspects of nursing practice [ 2 , 4 ].
Decision making in nursing does not follow a linear relationship that culminates in the decision made; instead, it has a circular nature that repeats through data collection, alternative selection, reasoning, synthesis, and testing [ 5 ]. Expert nurses, moreover, possess the ability to discern patterns and trends within clinical situations, providing them with a general overview of patient issues and facilitating decision making [ 6 ]. In this iterative and dynamic process, a solid knowledge base, clinical experience, reliable information, and a supportive environment are crucial pillars underpinning clinical decisions [ 7 ]. Therefore, nursing students, during their educational journey, require the support of others in decision making [ 4 ] and adequate training that optimizes their learning opportunities [ 8 ]. Clinical decision-making forms the cornerstone of professional nursing practice [ 9 ].
The process of decision making regarding patient care integrates theoretical knowledge with hands-on experience [ 10 ]. This practical experience has been instrumental in augmenting analytical skills, intuition, and cognitive strategies essential for determining sound judgment and decision-making in complex situations [ 11 ]. Although students’ clinical experience is limited, some of them work as nursing assistants or in support roles. This profile of nursing student is quite common [ 12 ]. Hence, prior work experience in healthcare should be considered in nursing students.
Additionally, it has been suggested that emotional factors, such as heightened levels of anxiety and low self-confidence, may influence clinical decision-making processes [ 13 ]. The Nursing Anxiety and Self-Confidence with Clinical Decision Making (NASC-CDM©) scale is used to make a self-report of how they feel about students’ self-confidence and anxiety levels during clinical decision-making [ 14 ] On one hand, nursing students frequently grapple with elevated stress and anxiety, which adversely affect their learning process [ 15 ]. Conversely, self-confidence is defined as a person’s self-recognition of their abilities and capacity to recognize and manage their emotions [ 16 ]. Self-confidence can foster well-being by strengthening positive emotions among nursing students [ 17 ]. In this regard, one of the leading authors in the study of self-confidence is Albert Bandura (1977) [ 18 ]. He employs the term self-efficacy to describe the belief that one holds in being capable of successfully performing a specific task to achieve a given outcome. Consequently, it can be considered a situationally specific self-confidence [ 19 ]; however, these terms are related to potential emotional barriers in decision making [ 20 ].
In line with the aforementioned, and as a rationale for this study, it should be noted that the NASC-CDM© scale offers significant contributions. Firstly, it highlights the ability to address self-reported levels of self-confidence and anxiety, both independently and interrelatedly, as these two are two distinct constructs with relevant effects on clinical decision making. This separation allows for a more comprehensive and precise understanding of the context [ 21 ]. Secondly, it is worth noting that the scale can be administered to both students and professionals [ 22 ]. The results obtained through this scale enable the identification of areas in which students need improvement and provide nursing educators the opportunity to develop strategies to strengthen students’ clinical decision-making skills [ 14 ].
The absence of a validated Spanish version of the Nursing Anxiety and Self-Confidence with Clinical Decision Making (NASC-CDM©) scale poses a significant challenge for researchers and educators. This limitation hinders the accurate assessment of self-confidence and anxiety levels among Spanish-speaking nursing students and professionals in both clinical decision-making both academic and healthcare settings. In heath research, the availability of reliable measurement tools is crucial to ensure accuracy and comparability across cultural and linguistic contexts [ 23 ]. Moreover, it is noteworthy that the NASC-CDM© scale is not only accessible in English [ 14 ] but also in other languages such as Turkish [ 24 ] and Korean [ 22 ], Therefore, its availability in Spanish presents numerous opportunities for cross-cultural comparisons in academic and healthcare settings, as well as between academic and clinical researchers.
Hence, this study aims to address two deficits in the Spanish context: first, to validate the NASC-CDM© scale in Spanish, and second, to employ it to assess self-confidence and anxiety levels in decision making among nursing students by academic year and the influence of prior work experience. By achieving these objectives, the study seeks to provide educators with essential insights to enhance the teaching and learning process in both academic and environments. Additionally, it aims to offer support students in enhancing their decision-making skills, ultimately fostering the development of proficient healthcare professionals capable of delivering care. Therefore, this study was designed to achieve three primary objectives: (1) To perform a cross-cultural and psychometric validation of the Nursing Anxiety and Self-Confidence scale with the Clinical Decision Making (NASC-CDM©) from English to Spanish Nursing Anxiety and Self-Confidence with Clinical Decision Making– Spanish (NASC-CDM-S©) scale.; (2) To compare groups of nursing students from their first to fourth academic year in terms of anxiety and self-confidence in their decision-making processes; and (3) To Investigate the potential impact of the participants’ work experience on their decision-making abilities. Hence, concerning objectives 2 and 3, the following hypothesis was posited: participants in higher academic years and participants with work experience have higher levels of self-confidence and lower levels of anxiety in their decision-making processes.
This study adopted a quantitative cross-sectional and analytical approach.
Setting and sampling
The study population comprised nursing students from the Faculty of Nursing and Physiotherapy, University of Lleida (Spain). The nursing degree program in Spain consists of 240 European Credit Transfer System (ECTS) credits, approximately equivalent to 6000 h, distributed across 4 academic years (60 ECTS per year, totaling 1500 h per year). One ECTS credit corresponds to 25–30 study hours (Royal Decree 1125/2003). The first year primarily focuses on theoretical training in basic sciences, with more specific nursing sciences covered in higher years. Clinical practices gradually increase, with the fourth year being predominantly practical (1st year 6 ECTS, 2nd year 12 ECTS, 3rd year 24 ECTS, and 4th year 39 ECTS).
A convenience sample of 301 participants was used, representing a non-probability sampling method [ 25 ]. The sample size aligns with the recommended person-item ratio, with a minimum of 10 subjects per item for general psychometric approaches and 300–500 for confirmatory factor analysis (CFA) or conducting propriety analysis [ 23 ]. The NASC-CDM© scale contains 27 items. Inclusion criteria were nursing students from all four academic years who were willing to participate, and no exclusion criteria were specified. Participants received no compensation, and their participation was voluntary.
Instrument and variables
The original version of the NASC-CDM© tool was developed by White [ 14 , 21 ]. The use of this tool for the study was authorized in May 2022 through email communication with the instrument’s creator.
Regarding the original instrument, it is noteworthy that it was validated through an exploratory factor analysis (EFA) with 545 pre-licensure nursing students in the United States. The analysis revealed moderate convergent validity and significant correlations between the self-confidence and anxiety variables that constitute two separate sub-scales within the same instrument. The instrument achieved a Cronbach’s α of 0.98 for self-confidence and 0.94 for anxiety [ 14 , 21 ]. This instrument comprises 27 items and uses a 6-point Likert scale for responses (1 = Not at all; 2 = Only a little; 3 = Somewhat; 4 = Mostly; 5 = Almost completely; 6 = Completely). Scores range from 27 to 162 points. The EFA results confirmed a scale with three dimensions (D1, D2, and D3):
D1 (Using resources to gather information and listening fully) includes statements about recognizing clues or issues and assessing their clinical significance. This dimension comprises 13 items, with a minimum score of 13 and a maximum of 78.
D2 (Using information to see the big picture) includes statements about determining the patient’s primary problem. This dimension contains 7 items, with a minimum score of 7 and a maximum of 42.
D3 (Knowing and acting) includes statements about performing interventions to address the patient’s problem. This dimension consists of 7 items, with a minimum score of 7 and a maximum of 42.
Based on the original tool, the questionnaire used in this study consisted of two parts. It included the following variables: (a) sociodemographic data such as age (numeric), gender (male, female, non-binary), academic year (1st, 2nd, 3rd, 4th), university entrance pathway (secondary school, training courses, other university degrees, over 25–45 years old), and participants’ work experience in healthcare (Yes or No); and (b) 27 paired statements about students’ perceptions of their level of self-confidence and anxiety (dependent variable) in decision making as per the translated NASC-CDM©. Regarding work experience, it should be noted that some nursing students work in healthcare facilities as nursing assistants or in support roles during their nursing studies.
Instrument validation
The tool presented by White [ 14 ] underwent translation and adaptation, following the guidance provided by Sousa & Rojjanasrirat [ 23 ] and Kalfoss [ 26 ]. In the forward-translation (English to Spanish) and back-translation phases, two independent bilingual translators participated, who were not part of the research team and who usually work with health-related translations. The back-translated version of the scale was reviewed and approved by the tool’s creator (Dr. White). These steps ensured content validity.
In the expert panel phase, 5 expert nurse educators from our university who were not part of the research team, with a doctoral degree and more than 5 years of teaching experience, assessed content relevancy. The scale proposed by Sousa & Rojjanasrirat [ 23 ] (1 = not relevant, 2 = unable to assess relevance, 3 = relevant but needs minor alteration, 4 = very relevant and succinct), along with the Kappa index were used to assess agreement. The educators rated the 27 items between 3 and 4. The concordance analysis yielded a score of 0.850, which, as per Landis & Koch [ 27 ], is considered nearly perfect. Only some expressions were modified for better cultural adaptation while retaining the original meaning of the statements. Finally, a pilot test was conducted during the pre-testing phase, involving 20 students, to assess comprehension and completion time. The students encountered no comprehension difficulties, and the average response time was 13 min. Therefore, it was concluded that the questionnaire was feasible in terms of time required taken and clarity of the questions/answers [ 28 ].
This validation process concludes with the psychometric testing of the prefinal version of the translated instrument. During this phase, the psychometric properties are established using a sample from the target population, in this case, nursing students [ 23 ]. The psychometric characteristics examined include: (1) the reliability of internal consistency (Cronbach’s Alpha coefficient (α) and Guttman split-half coefficients (λ2); (2) criterion validity, where the concurrent validity of the new version of the instrument was assessed against the original version via confirmatory factor analysis (CFA), and (3) for construct and structural validity, exploratory factor analysis (EFA) and CFA were conducted to demonstrate the discriminant validity of the instrument by comparing groups within the sample.
Data collection
Data collection took place between May 2022 and June 2023. The lead researcher in a classroom administered the questionnaire in a paper format. Response times ranged from 10 to 15 min.
Data analysis
A descriptive statistical analysis of the participants’ study variables was conducted. Reliability was determined using Cronbach’s Alpha coefficient (α) and Guttman split-half coefficients (λ2) for both sub-scales (self-confidence and anxiety) and their respective dimensions (D1, D2, D3). Cronbach’s provides a measure of item internal consistency, while Guttman split-half coefficient assesses the extent to which observed response patterns align with those expected from a perfect scale [ 29 ]. Item correspondence was reviewed by repeating the exploratory factor analysis (EFA) using the extraction and rotation methods outlined by the tool’s creator [ 14 , 21 ]. Factor validity was confirmed through confirmatory factor analysis (CFA), where a value ≥ 0.9 of the fit indices (comparative fit index (CFI), Tucker-Lewis Index (TLI), Bentler-Bonett Non-normed Fit Index (NNFI), and Bollen’s Incremental Fit Index (IFI) indicate reasonable fit [ 30 ]. The root mean square error of approximation (RMSEA) and the unweighted least square (ULS) estimator was used Likert ordinal data [ 31 ]. Sample adequacy was also reviewed using Kaiser-Meyer-Olkin (KMO), Bartlett’s sphericity test, and average variance extracted (AVE).
Normality tests for self-confidence and anxiety data distribution ( N = 301) were performed using Kolmogorov-Smirnov test (K-S = 0.043 and 0.41; p >.05) and multivariable normality (Shapiro-Wilk = 0.993 and 994; p >.05). The results indicated that all dimensions followed a normal distribution. Consequently, parametric tests such as Pearson’s correlation coefficient (r) and group comparison tests (t-Student) were employed. To analyze differences in self-confidence and anxiety among students by academic year (1st, 2nd, 3rd, 4th), the following tests were conducted: analysis of variance (ANOVA) tests, homogeneity of variance tests, and Levene’s test applying Tukey’s post hoc correction to p -values for combined groups correction for combined groups. Effect sizes were determined using Cohen’s d for t-student tests and eta-squared (η²) for ANOVA tests.
Data were analyzed using IBM SPSS Statistics 24 and JASP 0.18.1. A significance level was set at p <.05 for all analyses.
The results are presented in 4 sections: (1) Descriptive data of the participants, (2) Psychometric validation study of the NASC-CDM© questionnaire in Spanish (NASC-CDM-S©), (3) Comparative analysis of self-confidence and anxiety in decision making by academic year, and (4) The impact of students’ work experience on their decision-making processes.
Descriptive data of the participants
The nursing study involved 301 participants, mostly women who entered through high school. The sample comprised students from the 1st year of the degree (28.57%, with an average age of 20.43 years), 2nd year (38.54%, with an average age of 21.10 years), 3rd year (3.29%, with an average age of 23.90 years), and 4th year (19.60%, with an average age of 22.92 years). Nearly 2/3 of the participants entered the nursing program from secondary school, and just over 50% had work experience in healthcare. See Table 1 for Sample Characteristics.
Psychometric validation study of the NASC-CDM© questionnaire in Spanish
The set of items showed high internal consistency reliability in both sub-scales. In self-confidence, Cronbach’s α = 0.920, and Guttman’s λ2 = 0.923 (M = 111.32, SD = 17.07) and in anxiety the values were α = 0.940 and λ2 = 0.942 (M = 80.44, SD = 21.67). The KMO adequacy measure was 0.921 for self-confidence and 0.946 for anxiety, and Bartlett’s sphericity was highly significant, resulting in a p -value not exceeding 0.05, indicating a significantly different item correlation matrix (self-confidence χ2 = 4250.632, p <.001; anxiety χ2 = 5612.051, p <.001). In addition, the average variance extracted (AVE) index exceeded 0.50, confirming the suitability of the original variables in both sub-scales for structure detection.
To confirm the validity of the factors, agreement of item alignment with the dimensions of the original tool was first examined through EFA (factor loading > 0.4), followed by a confirmatory analysis of the entire scale using CFA. Repeating the EFA, as conducted by White (2011) using alpha factoring extraction and Promax rotation with 3 factors (no eigenvalue), the total variance explained in both scales was 48.30% in self-confidence and 55.30% in anxiety, with an average of 51.80%. The agreement between the items in the resulting factor structure matrix from the EFA and the original matrix were very similar for the anxiety sub-scale (89.90%) but only moderately similar for the self-confidence sub-scale (59.30%), where items did not fall within the same dimensions.
Given the low result, a CFA was conducted based on the dimensions proposed by White (2011). The goodness-of-fit indicators of the model were: (CFI, IFI = 0.981, TLI, NNFI = 0.979, and RMSEA = 0.052) for self-confidence and (CFI, TLI, NNFI, IFI = 0.997 and RMSEA = 0.024) for anxiety. This indicates that the three-factor model retains the description with the original items.
Table 2 shows the estimated factor loadings by dimension and item, illustrating the robust composition of the dimensions with no item elimination. Although items Q5, Q27 and Q11 had factor loadings below 0.60, their KMO values were ≥ 0.80, indicating adequate sampling.
Highly significant correlations were found regarding criterion validity and relevance ( p <.001). Correlations within the dimensions within the same scale (D1, D2, D3) were positive, whereas the paired correlations between self-confidence and anxiety were inversely correlated, as increased confidence was associated with decreased anxiety: (D1 r = −.500), (D2 r = −.500) and (D3 r = −.532).
Comparative analysis of self-confidence and anxiety in decision making by academic year
The overall results for self-confidence and anxiety by academic year indicated that students significantly and gradually increased their self-confidence ( p =.049) as they progressed from the 1st year (M = 108.22, SD = 14.96) to the 4th year (M = 115.54, SD = 16.28). However, anxiety was higher in the 1st year (M = 81.71, SD = 18.90) and increased in the 3rd year (M = 86.32, SD = 26.38) (Table 3 ).
Table 4 shows statistically significant differences in dimensions D2 and D3 for self-confidence and D3 for anxiety.
Dimension D1 - using resources to collect information and listening carefully
The post hoc Tukey test results indicate no statistically significant differences between academic years in dimension D1 (Table 4 ). Students in higher academic years did not obtain significantly higher self-confidence or lower anxiety scores (Fig. 1 a). The self-confidence means were similar across all 4 groups, while the anxiety mean had varying values. The highest anxiety was observed in the 3rd year (M = 37.67; SD = 14.63), and the lowest was in the 4th year (M = 31.76; SD = 10.82), although the differences were not statistically significant ( p =.178).
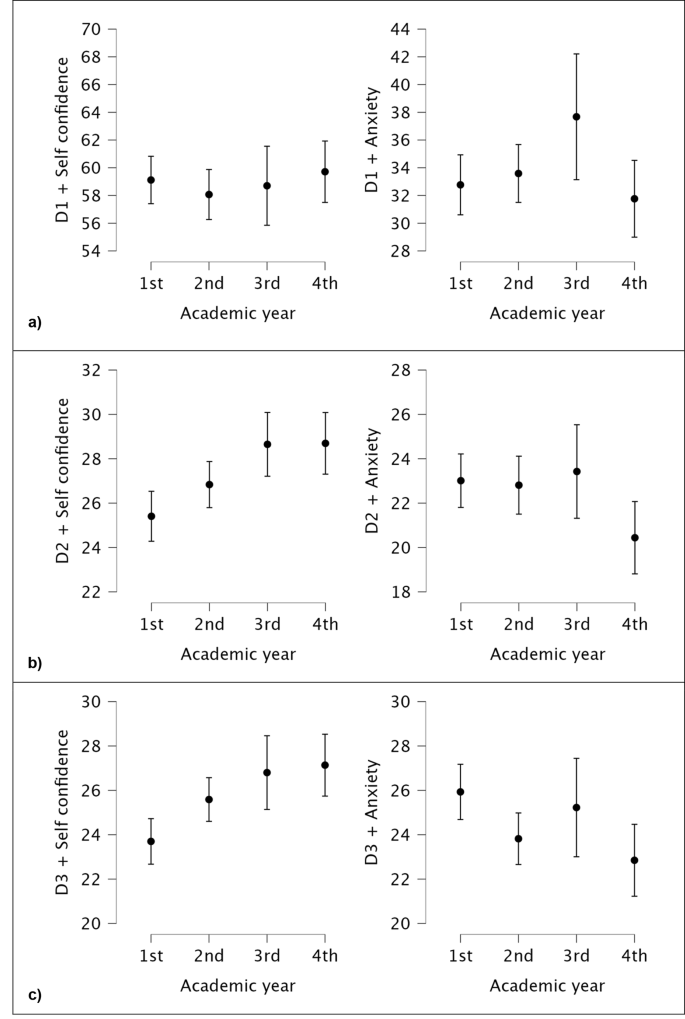
Comparison graphics of different dimensions of different Academic years ( a ) D1. Using resources to collect information and listening carefully: Post Hoc Comparisons Academic year (1st, 2nd, 3rd, 4th) ( b ) D2. Using information to see the big picture: Post Hoc Comparisons Academic year (1st, 2nd, 3rd, 4th). ( c ) D3. Knowing and acting: Post Hoc Comparisons Academic year (1st, 2nd, 3rd, 4th)
Dimension D2 - using information to see the big picture
Students in the higher academic years (3rd and 4th) obtained significantly higher self-confidence scores (M = 28.69; SD = 5.44) compared to the lowest, which is from the 1st year (M = 25.40; SD = 5.33) (Table 4 ; Fig. 1 b). There was a downward trend in anxiety in the later years, but it was not significant. Once again, the highest mean anxiety was observed in the 3rd year (M = 23.42; SD = 6.80) and the lowest in the 4th year (M = 20.44; DS = 6.39).
Dimension D3 - knowing and acting
This is the only dimension where a balance was maintained: self-confidence increased with academic years, while anxiety decreased. Significant differences in self-confidence scores were observed between the 1st year (M = 23.70; SD = 4.85) and the 4th year (M = 27.13; SD = 5.47). At the same time, anxiety significantly decreased between the 1st year (M = 25.93; SD = 5.90) and the 4th year (M = 22.85; SD = 6.36) (Table 4 ; Fig. 1 c).
Effect of students’ work experience on their decision-making processes
A comparative test was conducted between groups based on work experience to identify explanatory variables regarding the extent of self-confidence and anxiety (Table 5 ). Two significant differences were found, indicating that students with work experience, as opposed to students without experience, had higher self-confidence in D2 (M = 27.66, SD = 5.43 vs. M = 26.63, SD = 5.61) and D3 (M = 26.24, SD = 5.52 vs. M = 24.58, SD = 5.10). Meanwhile, the level of anxiety was similar in both groups.
Furthermore, when contrasting individual items, 7 specific items showed significant differences in self-confidence and 2 in anxiety based on students’ work experience (Table 6 ).
Two items belong to D2- Using information to see the big picture, where experienced students exhibited greater self-confidence in detecting important patient information patterns in I1 (M = 4.10 vs. M = 3.98) and experienced less anxiety (M = 2.96 vs. M = 3.30), and simultaneously evaluated their decisions better with patient laboratory results in I7 (M = 4.00 vs. M = 3.67).
The other five items correspond to D3- Knowing and acting, where nursing students with prior nursing experience felt more self-confidence when deciding the best priority alternative for the patient’s problem in I5 (M = 3.53 vs. M = 3.30), more confidence in implementing an intuition-based intervention in I14 (M = 3.95 vs. M = 3.59) with less anxiety (M = 3.38 vs. M = 3.69), more confidence in analyzing the risks associated with interventions I15 (M = 4.10 vs. M = 3.86) a better ability to make autonomous clinical decisions in I17 (M = 3.71 vs. M = 3.42), and to implement a specific intervention in an emergency in I20 (M = 3.79 vs. M = 3.47).
Given the objectives and results of this study, the discussion is subdivided into two sections: (1) Study of the Nursing Anxiety and Self-Confidence with Clinical Decision Making (NASC-CDM©) scale from English to Spanish, and (2) Assessment of self-confidence and anxiety in nursing students.
Study of the nursing anxiety and self-confidence with clinical decision making (NASC-CDM©) tool
The findings of this study highlight the successful adaptation and validation of the NASC-CDM© scale, originally developed by White [ 14 , 21 ], into Spanish (NASC-CDM-S©). This adaptation process demonstrated high reliability in both self-confidence and anxiety scales. The psychometric study conducted confirmed the validity of the three original dimensions. This result was achieved by examining item concordance with the dimensions of the original scale, followed by CFA of the entire scale. This resulted in a total variance exceeding 40% for both scales and across dimensions, confirming construct validity. The Spanish version effectively maintains the three- dimension groupings (D1, D2 and D3), which also preserves the item descriptions. Consequently, the obtained results align closely with White’s original study [ 14 ] and the Turkish version [ 24 ]. Regarding the loading factor, only one item, I5, “Make a decision on the ‘best’ prioritized alternative for the user’s problem,” had a loading value below 0.30 [ 32 ]. While its factor loading was 0.23 and exhibited a low correlation with the other items ( r =.22), its KMO ratio was ≥ 0.80, suggesting potential influence by underlying factors such as age or work experience. Therefore, the decision was made to retain it. However, these findings were not replicated in the translation of the NASC-CDM into Korean (KNASC-CDM) (KNASC-CDM) [ 22 ]. The Korean version comprises 23 items grouped into 4 groupings: (i) Listening fully and using resources to gather information; (ii) Using information to see the big picture; (iii) Knowing and acting; and (iv) Seeking information from clinical instructors.
The observed correlations between the dimensions of self-confidence and anxiety provide valuable and interesting insight. The results indicate an inverse relationship between the two, suggesting that strengthening self-confidence can have a positive impact on reducing anxiety. This aspect was corroborated by the original study by White [ 21 ] and Bektas et al. [ 13 ], demonstrating that metacognitive awareness increases nursing students’ self-confidence in clinical decision-making and reduces anxiety.
Furthermore, it is worth noting that the NASC-CDM© scale has been employed in numerous research studies related to nursing education. Therefore, its potential for educational purposes in both academic and clinical settings as a scale for measuring the enhancement of clinical decision-making skills is acknowledged. Several studies [ 33 , 34 , 35 ] suggest the effectiveness of in-person or virtual simulation in enhancing skills related to self-confidence in clinical decision-making, situational awareness, and communication effectiveness among students. Comparing the outcomes of this study with others utilizing the NASC-CDM© scale to gauge self-confidence and anxiety [ 33 , 36 ], it was noted that self-confidence levels increase with diverse teaching strategies, while anxiety levels are not negatively impacted. Overall, these findings underscore the importance of the NASC-CDM© scale in assessing students’ readiness for decision-making, highlighting the necessity to address emotional factors such as anxiety and the need to bolster self-confidence to enhance the education and preparation of future nursing professionals for challenging clinical scenarios.
Assessment of self-confidence and anxiety in nursing students
The results of the comparative study among nursing students across different academic years reveal an intriguing dynamic between self-confidence and anxiety throughout their academic progression. While self-confidence increases as students advance through their courses due to the acquisition of knowledge and skills, anxiety shows variations over time. Regarding confidence perception, some authors [ 37 ] claim that confident students learn better and that this self-confidence increases with experience, leading to improved knowledge [ 13 ].
One factor that might explain the difference in anxiety levels is that in the initial academic years (first and second), clinical practices are conducted in a more guided and supervised manner. In the third, and especially in the fourth year, clinical practices increase in terms of hours and complexity, requiring students to take on more responsibility and autonomy. This factor might account for the higher levels of anxiety in the third year, when students begin to engage in more autonomous practices and specialized units [ 38 , 39 ]. This stage could induce anxiety due to the increased responsibility and potential consequences in patient care. In other words, even though students become more secure in their skills, they may also experience anxiety due to the weight of their clinical practice decisions in the knowledge that they will soon be certified professional nurses caring for patients. This duality is understandable in a context where decision-making has direct implications for patient health and the potential consequences of their actions in patient care. However, this situation is rectified in the fourth or final year, when anxiety decreases, and self-confidence increases. Clinical experience helps students develop skills and self-confidence, which, in turn, reduces anxiety [ 15 , 40 ]. Just as in the case of nurses, the benefits of experience in decision-making are evident in students [ 3 ]. However, some researchers [ 41 ] emphasize the need to reinforce training in aspects such as situational awareness and cognitive apprenticeship to develop decision-making skills in senior students. There is evidence linking emotion and cognition to clinical decision-making [ 42 ].
Results from this study allow for a more detailed analysis by dimensions (D1, D2, D3) across academic years. Dimension 1 - Using resources to gather information and listening fully (D1) is the only dimension that does not show significant differences by year in either self-confidence or anxiety. This dimension includes fundamental aspects of assessment and information gathering (verbal and non-verbal communication, the ability to review the literature, and information provided by others, among others) [ 14 ]. In Dimension 2 - Using information to see the big picture (D2), self-confidence significantly increases, and anxiety decreases, although the latter is not statistically significant. This dimension encompasses aspects related to interpreting information to identify the patient’s actual problem, filtering out irrelevant information, and applying knowledge to the detected problem [ 14 ]. Finally, Dimension 2 - Knowing and acting (D3) - is the only dimension that behaves as hypothesized, with increasing self-confidence and decreasing anxiety. This dimension includes aspects related to training in addressing the problem and detecting the repercussions of the interventions performed, as well as the student’s autonomous ability to address the detected problem [ 14 ].
The results indicate that although students demonstrate skills in applying knowledge and performing interventions (D2 and D3), there appears to be a lack of training proficiency in the comprehensive assessment of the patient as an individual with specific needs (D1). This shortcoming is likely caused by various factors, including lack of experience, inadequate training skills, and the complexity of the assessment process. Understanding the patient is a complex task, as nurses must consider not only physiological indicators. Therefore, this requires time and experience [ 3 ] This implies that students tend to focus more on pathology and standardized care rather than on the patient as a unique individual with specific needs and characteristics.
In contrast, in the case of nurses, when patients do not align with their prior experience, nurses are more motivated to assess the patient and facilitate decision making [ 3 ]. The need for a proper and personalized patient assessment emerges as a crucial point for improvement in the education of nursing students [ 43 ]. Therefore, an educational intervention focused on strengthening the skill of patient assessment throughout the nursing degree program could favor the development of nursing students as future professionals. Such an intervention could include the implementation of more effective assessment tools and the promotion of careful observation of all aspects of the patient. It should extend beyond nursing-specific procedures involving the development of cognitive skills [ 44 ]. Importantly, it should be implemented not only in the academic context but also in the clinical setting. Given that education alone is not an ideal measure [ 3 ], this clinical involvement is essential based on patient-centered health care ( [ 45 ].
Finally, in relation to students with work experience, those who work as nursing assistants during their nursing education exhibit more self-confidence and less anxiety in various items: seeing patterns in patient information (I1) and implementing interventions based on gut feeling or intuition (I14). They also demonstrate higher self-confidence when making a decision about the ‘best’ priority decision option for the patient’s problem (I5), evaluating whether their clinical decision improved the patient’s laboratory results (I7), analyzing the risks of the interventions (I15), making independent clinical decisions to solve the patient’s problem (I17), and implementing a specific intervention in case of an urgent problem (I20). It can be affirmed that experienced students show more self-confidence in having a holistic view of the patient (D2) and in their knowledge and patient-related actions (D3). Other studies [ 46 ] detail the benefits of work experience in emotional control and stress reduction among students. Moreover, students’ prior work experience contributes to decision making, as it provides them with a more realistic understanding of the role and responsibilities of the nursing profession [ 47 ].
Limitations
Due to its cross-sectional design, this study prevents the establishment of causal relationships between self-confidence and anxiety. The study sample was limited to a specific group of students from a single Spanish-speaking university. Similar to the study by Bektas [ 24 ] only voluntary students participated in this study. It is pertinent to acknowledge potential biases in interpreting differences by academic year, as the sample is disproportional in one of the strata (with 9% margin of error), attributed to the absence of third-year students engaged in mobility programs and clinical practices. Moreover, the present study did not evaluate organizational and nursing practice factors, which could explore nursing students’ perceptions regarding clinical decision-making. Finally, even though the availability of the SNASC-CDM will facilitate its use in other Spanish-speaking countries, it is advisable to conduct specific studies to ensure its validity in a cultural context different from Spain.
Implications for nursing education
Nursing degree programs should prioritize the development of students’ self-confidence and the management of their anxiety. This could involve implementing educational interventions, including clinical simulation and reflective teaching that incorporate elements of metacognition. Collaboration across different subjects is essential to foster the integration of skills and knowledge. It is also vital that nursing programs provide students with opportunities to develop their clinical and communication skills. This will help students feel more secure in their abilities and reduce anxiety in challenging clinical settings.
The findings of this study suggest that nursing students face challenges in assessing patients, which can be attributed to various factors, including lack of time, insufficient training, and limited experience. To address this issue, an educational intervention is proposed for nursing students. This intervention would focus on conducting a comprehensive and holistic patient assessment with the support of practicing nurses and involving the patients themselves in identifying problems and needs. Such an intervention should include discussing the significance of considering the patient’s physical, emotional, spiritual, and social needs. It should also emphasize the importance of building a trusting relationship with the patient.
Conclusions
The Spanish version of the NASC-CDM (NASC-CDM-S©) allows for the identification of self-confidence and anxiety in clinical decision-making in Spanish-speaking nursing students. Moreover, it retains the same structure as the original English version. The availability of the NASC-CDM-S© will facilitate its use in other Spanish-speaking countries, thus enhancing the education and preparation of future nursing professionals in clinical situations.
Self-confidence increases as students progress through their academic years due to knowledge and skills acquisition, while anxiety shows variations over time. Specifically, anxiety tends to increase in the third year, when students transition to more autonomous practices and specialized health care units. However, diverse perceptions are identified depending on the dimension. The only dimension that achieves a positive balance in self-confidence and anxiety is D3 (Knowing and acting). Nevertheless, the findings reveal deficiencies in D1 ( Using resources to gather information and listening fully) regarding assessing and detecting problems.
Students with prior work experience show improved self-confidence in D2 and D3, but the level of anxiety does not differ between students with and without work experience. Therefore, targeted interventions addressing emotional and cognitive aspects are needed to enhance clinical decision-making and provide better patient care. Considering these aspects, future lines of research could explore the impact of teaching interventions, as well as conduct further studies on the NASC-CDM-S©, validating it in different Spanish-speaking countries, and applying it in clinical settings with healthcare professionals.
Data availability
No datasets were generated or analysed during the current study.
Krishnan P. A philosophical analysis of clinical decision making in nursing. J Nurs Educ. 2018;57:73–8. https://doi.org/10.3928/01484834-20180123-03
Article PubMed Google Scholar
Wang Y, Chien WT, Twinn S. An exploratory study on baccalaureate-prepared nurses’ perceptions regarding clinical decision-making in mainland China. J Clin Nurs. 2012;21:1706–15. https://doi.org/10.1111/J.1365-2702.2011.03925.X
Nibbelink CW, Brewer BB. Decision-making in nursing practice: an integrative literature review. J Clin Nurs. 2018;27:917–28. https://doi.org/10.1111/JOCN.14151
Article PubMed PubMed Central Google Scholar
Baxter PE, Boblin S. Decision making by baccalaureate nursing students in the clinical setting. J Nurs Educ. 2008;47:345–50. https://doi.org/10.3928/01484834-20080801-02
Hoffman KA, Aitken LM, Duffield C. A comparison of novice and expert nurses’ cue collection during clinical decision-making: verbal protocol analysis. Int J Nurs Stud. 2009;46:1335–44. https://doi.org/10.1016/J.IJNURSTU.2009.04.001
O’Neill ES, Dluhy NM, Chin E. Modelling novice clinical reasoning for a computerized decision support system. J Adv Nurs. 2005;49:68–77. https://doi.org/10.1111/J.1365-2648.2004.03265.X
Article Google Scholar
Johansen ML, O’Brien JL. Decision making in nursing practice: a concept analysis nurs forum. 2016;51(1):40–8. https://doi.org/10.1111/nuf.12119
de Marques M. Decision making from the perspective of nursing students. Rev Bras Enferm. 2019;72:1102–8. https://doi.org/10.1590/0034-7167-2018-0311
İlaslan E, Adıbelli D, Teskereci G, Üzen Cura Ş. Development of nursing students’ critical thinking and clinical decision-making skills. Teach Learn Nurs. 2023;18:152–9. https://doi.org/10.1016/J.TELN.2022.07.004
Roche JP. A pilot study of teaching clinical decision making with the clinical educator model. J Nurs Educ. 2002;41:365–7. https://doi.org/10.3928/0148-4834-20020801-12
Pretz JE, Folse VN. Nursing experience and preference for intuition in decision making. J Clin Nurs. 2011;20:2878–89. https://doi.org/10.1111/J.1365-2702.2011.03705.X
Giai M, Franco ED. Relation of the profile of the nursing student ofMendoza, Argentina and his academic performance. Revista En La Mira. La educación Superior en Debate. 2023;4(7):1–13.
Google Scholar
Bektas I, Bektas M, Ayar D, Akdeniz Kudubes A, Sal S, Selekoglu OKY, et al. The predict of metacognitive awareness of nursing students on self-confidence and anxiety in clinical decision-making. Perspect Psychiatr Care. 2021;57:747–52. https://doi.org/10.1111/PPC.12609
White KA. Development and validation of a tool to measure self-confidence and anxiety in nursing students during clinical decision making. J Nurs Educ. 2014;53:14–22. https://doi.org/10.3928/01484834-20131118-05
Turner K, McCarthy VL. Stress and anxiety among nursing students: a review of intervention strategies in literature between 2009 and 2015. Nurse Educ Pract. 2017;22:21–9. https://doi.org/10.1016/J.NEPR.2016.11.002
Bayat B, Akbarisomar N, Tori NA, Salehiniya H. The relation between self-confidence and risk-taking among the students. Educ Health Promot. 2019;8:27. https://doi.org/10.4103/jehp.jehp_174_18
Kukulu K, Korukcu O, Ozdemir Y, Bezci A, Calik C. Self-confidence, gender and academic achievement of undergraduate nursing students. J Psychiatr Ment Health Nurs. 2013;20:330–5. https://doi.org/10.1111/J.1365-2850.2012.01924.X
Article CAS PubMed Google Scholar
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. https://doi.org/10.1037/0033-295X.84.2.191
Druckman D, Bjork RA, editors. Learning, remembering, believing: enhancing human performance. National Academy; 1994. https://doi.org/10.17226/2303
Wood R, Bandura A. Impact of conceptions of ability on self-regulatory mechanisms and complex decision making. 1989;56(3):407–15. https://doi.org/10.1037//0022-3514.56.3.407
White KA. The development and validation of a tool to measure self-confidence and anxiety in nursing students while making clinical decisions [Doctoral thesis]. Las Vegas: University of Nevada; 2011. https://doi.org/10.34917/3276068
Yu M, Eun Y, White KA, Kang K. Reliability and validity of Korean version of nursing students’ anxiety and self-confidence with clinical decision making scale. J Korean Acad Nurs. 2019;49:411–22. https://doi.org/10.4040/JKAN.2019.49.4.411
Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: a clear and user-friendly guideline. J Eval Clin Pract. 2011;17:268–74. https://doi.org/10.1111/J.1365-2753.2010.01434.X
Bektas I, Yardimci F, Bektas M, White KA. Psychometric properties of the Turkish version of nursing anxiety and self-confidence with clinical decision making scale (NASC-CDM-T). DEUHFED, 10(2):83–92.
Stratton SJ. Population research: convenience sampling strategies. Prehosp Disaster Med. 2021;36:373–4. https://doi.org/10.1017/S1049023X21000649
Kalfoss M. Translation and adaption of questionnaires: a nursing challenge. SAGE Open Nurs. 2019. https://doi.org/10.1177/2377960818816810/FORMAT/EPUB . 5.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159. https://doi.org/10.2307/2529310
García de Yébenes Prous MJ, Rodríguez Salvanés F, Carmona Ortells L. Validación De Cuestionarios. Reumatol Clin. 2009;5:171–7. https://doi.org/10.1016/J.REUMA.2008.09.007
Callender JC, Osburn HG. An empirical comparison of coefficient alpha, guttman’s lambda– 2, and msplit maximized split-half reliability estimates. J Educ Meas. 1979;16:89–99. https://doi.org/10.1111/J.1745-3984.1979.TB00090.X
Hu LT, Bentler PM. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol Methods. 1998;3:424–53. https://doi.org/10.1037/1082-989X.3.4.424
Morata-Ramirez MÁ, Holgado Tello FP, Barbero-García MI, Mendez G. Análisis factorial confirmatorio. Recomendaciones sobre mínimos cuadrados no ponderados en función del error Tipo I De Ji-Cuadrado Y RMSEA. Acción Psicológica. 2015;12:79–90. https://doi.org/10.5944/ap.12.1.14362
Terwee CB, Bot SDM, de Boer MR, van der Windt DAWM, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42. https://doi.org/10.1016/J.JCLINEPI.2006.03.012
Cobbett S, Snelgrove-Clarke E. Virtual versus face-to-face clinical simulation in relation to student knowledge, anxiety, and self-confidence in maternal-newborn nursing: a randomized controlled trial. Nurse Educ Today. 2016;45:179–84. https://doi.org/10.1016/J.NEDT.2016.08.004
Gandhi S, Yeager J, Glaman R. Implementation and evaluation of a pandemic simulation exercise among undergraduate public health and nursing students: a mixed-methods study. Nurse Educ Today. 2021;98. https://doi.org/10.1016/J.NEDT.2020.104654
Ross JG, Meakim CH, Latz E, Arcamone A, Furman G, Prieto P, et al. Effect of multiple-patient simulation on baccalaureate nursing students’ anxiety and self-confidence: a pilot study. Nurse Educ. 2023;48:162–7. https://doi.org/10.1097/NNE.0000000000001336
Daly S, Roberts S, Winn S, Greene L. Implementation and evaluation of an end-of-life standardized participant simulation in an adult/gerontology acute care nurse practitioner program. Nurs Educ Perspect. 2023. https://doi.org/10.1097/01.NEP.0000000000001167
Zieber M, Sedgewick M. Competence, confidence and knowledge retention in undergraduate nursing students-A mixed method. Nurse Educ Today. 2018;62:16–21. https://doi.org/10.1016/j.nedt.2017.12.008
Inayat S, Younas A, Sundus A, Khan FH. Nursing students’ preparedness and practice in critical care settings: a scoping review. J Prof Nurs. 2021;37:122–34. https://doi.org/10.1016/j.profnurs.2020.06.007
Hernández Oraquel. González Pascual Juan Luis, Fernández Araque AM. Estrés y ansiedad al comienzo de las prácticas clínicas en estudiantes de Enfermería. Metas Enferm. 2020;23:50–8. https://doi.org/10.35667/METASENF.2019.23.1003081613
Kimhi E, Reishtein JL, Cohen M, Friger M, Hurvitz N, Avraham R. Impact of simulation and clinical experience on self-efficacy in nursing students: intervention study. Nurse Educ. 2016;41:E1–4. https://doi.org/10.1097/NNE.0000000000000194
Tower M, Watson B, Bourke A, Tyers E, Tin A. Situation awareness and the decision-making processes of final-year nursing students. J Clin Nurs. 2019;28:3923–34. https://doi.org/10.1111/jocn.14988
Kozlowski D, Hutchinson M, Hurley J, Rowley J, Sutherland J. The role of emotion in clinical decision making: an integrative literature review. BMC Med Educ. 2017;17. https://doi.org/10.1186/S12909-017-1089-7
Smith G, Morais N, Fátima S, Da Costa G, Dias Fontes W, Carneiro AD. Communication as a basic instrument in providing humanized nursing care for the hospitalized patient. Acta Paul Enferm. 2019;22(3). https://doi.org/10.1590/S0103-21002009000300014
Canova C, Brogiato G, Roveron G, Zanotti R. Changes in decision-making among Italian nurses and nursing students over the last 15 years. J Clin Nurs. 2016;25:811–8. https://doi.org/10.1111/JOCN.13101
Cantaert GR, Van Hecke A, Smolderen K. Perceptions of physicians, medical and nursing students concerning shared decision-making: a cross-sectional study. Acta Clin Belg. 2021;76:1–9. https://doi.org/10.1080/17843286.2019.1637487
López F, López J. Situations that generate stress in nursing students in clinical practice. Ciencia Y enfermería. 2011;17(2):47–54.
Wilson A, Chur-Hansen A, Marshall A, Air T. Should nursing-related work experience be a prerequisite for acceptance into a nursing programme? A study of students’ reasons for withdrawing from undergraduate nursing at an Australian university. Nurse Educ Today. 2011;31:456–60. https://doi.org/10.1016/J.NEDT.2010.09.005
Download references
Acknowledgements
The authors wish to acknowledge the students and experts who assisted us in the validation process. We also wish to acknowledge the translator of this article, Mark Lodge.
No funding source.
Author information
Authors and affiliations.
Department of Nursing and Physiotherapy, University of Lleida, 2 Montserrat Roig, St., 25198, Lleida, Spain
Daniel Medel, Tania Cemeli, Alba Torné-Ruiz, Aïda Bonet & Judith Roca
School of Nursing, Georgetown University, Washington, DC, USA
Krista White
Open University of Catalonia (UOC), Barcelona, Spain
Williams Contreras-Higuera
Department of Nursing, University Rovira Virgili, Tarragona, Spain
Maria Jimenez Herrera
Xarxa Assistencial Universitària de Manresa, Hospital Fundació Althaia, Manresa, Spain
Alba Torné-Ruiz
Health Education, Nursing, Sustainability and Innovation Research Group (GREISI), Lleida, Spain
Aïda Bonet & Judith Roca
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: D.M and J.R.; methodology: D.M, T.C, M J-H. and J.R.; software: W. C-H. and J.R.; validation: J.R.; formal analysis: W. C-H, A T-R, J.R. and A.B; resources: J.R and D.M; data curation: W.C-H., AT-R. and J.R.; writing—original draft preparation: DM, TC, WK, AB, A T-R, J.R.; writing—review and editing: D.M., T.C., K.W., W. C-H. and J.R. and supervision: M. J-H. and J.R. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Tania Cemeli .
Ethics declarations
Ethics approval and consent to participate.
This study received authorization from the Research Commission of the Faculty of Nursing and Physiotherapy (FIF) of the University of Lleida (UdL). It was approved by the Research and Transfer Ethics Committee (CERT) of the University of Lleida (nº CERT13_31052023) and the data protection officer of the UdL Data Protection Delegate. Data were collected anonymously. Participants were duly informed about the study, and their written consent was obtained before they completed the questionnaire. Participation was voluntary, and the lead researcher of the study securely held the data. Students were informed that their participation or non-participation would have no impact on the course grade or standing at the university. The study conformed to the standards of the Declaration of Helsinki, the Spanish Biomedical Research Act 14/2007 and data processing was covered by EU Regulation 2016/679.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Medel, D., Cemeli, T., White, K. et al. Clinical decision making: validation of the nursing anxiety and self-confidence with clinical decision making scale (NASC-CDM ©) into Spanish and comparative cross-sectional study in nursing students. BMC Nurs 23 , 265 (2024). https://doi.org/10.1186/s12912-024-01917-w
Download citation
Received : 22 December 2023
Accepted : 05 April 2024
Published : 24 April 2024
DOI : https://doi.org/10.1186/s12912-024-01917-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical decision-making
- Nursing students
- Self confidence
- Reliability
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Contributors
- Privacy Policy
- Sign Up Here!
- Diagnostic frameworks
- Illness scripts
- The IMG Journey
- US Residency Programs VMR
- Inspirational Stories
- Gabriel Talledo’s Scholarship
- Publications
Episode 331: Neurology VMR – Headaches and loss of sensation in the left leg
- by leabischof
- April 24, 2024 April 24, 2024

We continue our campaign to #EndNeurophobia, with the help of Dr. Aaron Berkowitz. This time, Hans presents a case of headaches and loss of sensation in the left leg to Andrew and Maria.
Neurology DDx Schema
Hans Kaus
Hans Kaus received his MD from Ross University School of Medicine. He completed his undergraduate education in Pharmacy at the University of Tübingen, Germany. Driven by a deep desire to understand patient concerns, Hans wanted to go beyond pharmaceutical care. While in medical school, the virtual morning reports, Clinical Problem Solvers, unleashed his passion for solving complex patient cases. The blend of medicine and pharmacy will markedly benefit patients. In his spare time, Hans enjoys embarking on long bicycle rides.
Andrew Sanchez
@ASanchez_PS
Andrew Sanchez is an exiting PGY-3 in internal medicine at Yale New Haven Hospital: he will soon be starting a career in academic hospital medicine at Beth Israel Deaconess Medical Center, Boston. Meeting hospitalized patients and working with them to achieve diagnostic clarity is his primary clinical passion. His interest in diagnosing the undifferentiated patient is the driving force behind deep interest in learning and teaching diagnostic reasoning. On X/Twitter – which he considers the centerpiece of his teaching portfolio – he is known for creating and sharing schemas for both common and uncommon clinical dilemmas, which are frequently accompanied by “Tweetorial” commentary, as well as diagnostic case challenges.
María Jimena Alemán
@MariaMjaleman
María Jimena Alemán was born and raised in Guatemala. After suffering from long-standing neurophobia, she has embraced her love for neurology and will soon be starting her neurology residency at the University of California San Francisco. She looks forward to dedicating her life to improving neurological care and education around the globe. Maria loves art and culture and is currently obsessed with textiles and flowers
Download CPSolvers App here
RLRCPSOLVERS
To join us live on virtual morning report, sign up here
Discover more from The Clinical Problem Solvers
Subscribe now to keep reading and get access to the full archive.
Type your email…
Continue reading

IMAGES
VIDEO
COMMENTS
Abstract. This paper reviews the literature surrounding the research on how individuals solve problems. The purpose of the review is to heighten awareness amongst nurses in general, and nurse academics in particular about the theories developed, approaches taken and conclusions reached on how clinicians problem-solve.
Conclusion. The influencing factors of clinical nurses' problem-solving dilemma are diverse. Hospital managers and nursing educators should pay attention to the problem-solving of clinical nurses, carry out a series of training and counselling of nurses by using the method of situational simulation, optimize the nursing management mode, learn to use new media technology to improve the ...
We found clinical nurses' problem-solving ability to have no positive effect on their perception of professionalism. This contrasts with previous studies, which reported that problem-solving ability is helpful for such perception of professionalism . We also found that problem-solving ability does not affect nursing professional perception ...
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses' continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
clinical problem that needs immediate attention and one that is less acute (del Bueno, 1994); and a tendency to make errors in time sensitive situations where there is a large amount of complex data to process (O‟Neill, 1994). In clinical practice experienced nurses engage in multiple clinical reasoning episodes for each patient in their care.
This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in nurse education curricula Further, it has attracted limited ...
The multi-point nursing strategy using a clinical problem-solving framework provided evidence that it shortened the length of stay, reduce hospitalization costs, improve psychological status ...
Entering any situation with curiosity and engagement that follows the nursing process is EBP for nursing. Identifying the problem is the first of the five steps of EBP and may be the only step required in a particular situation. More often than not, however, thorny clinical issues and problems require greater attention and typically implicate ...
Purpose: Problem solving has been defined as "a goal-directed sequence of cognitive and affective operations as well as behavioural responses to adapting to internal or external demands or challenges. Studies have shown that some nurses lack rational thinking and decision-making ability to identify patients' health problems and make clinical judgements, and have poor cognition and response to ...
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills. ... Clinical judgment. Prioritize a patient's care needs and make adjustments as changes occur. Gather the necessary information and determine what nursing ...
Problem-solving The same basic processes of decision-making are used—or should be— by the individual healthcare provider on a daily basis when solving clinical problems even though the processes are less formal. High benefit, low cost/effort •Ensure handwashing compliance •Use surgical/procedure checklists High benefit, high cost/effort
Abstract. This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills. It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in ...
Overall, efforts to improve decisions in clinical nursing practice must facilitate the incorporation of evidence in nursing decision-making. ... Butler J. Contextualising the trajectory of experience of expert, competent and novice nurses in making decisions and solving problems. Collegian. 2004; 11 (1):21-27.
Clinical problem‐solving in nursing: insights from the literature. This paper reviews the literature surrounding the research on how individuals solve problems. The purpose of the review is to heighten awareness amongst nurses in general, and nurse academics in particular about the theories developed, approaches taken and conclusions reached ...
Clinical problem-solving in nursing: insights from the literature. This paper reviews the literature surrounding the research on how individuals solve problems. The purpose of the review is to heighten awareness amongst nurses in general, and nurse academics in particular about the theories developed, approaches taken and conclusions reached on ...
another: critical thinking, clinical reasoning, clinical judgment, decision-making, problem-solving, and nursing process. 4. Identify four principles of the scientifi c method that are evident in CT. 5. Compare and contrast the terms problem-focused thinking and outcome-focused thinking. 6. Clarify the term critical thinking indicator (CTI). 7.
Decision-making is a fundamental concept of nursing practice that conforms to a systematic trajectory involving the assessment, interpretation, evaluation and management of patient-specific situations (Dougherty et al, 2015).Shared decision-making is vital to consider in terms of patient autonomy and professional duty of care as set out in the Nursing and Midwifery Council (NMC) (2018)Code ...
He defines critical thinking as "necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation." ... Administrative and clinical nursing leaders are required to have strong critical thinking skills to be ...
Conclusion . The influencing factors of clinical nurses' problem-solving dilemma are diverse. Hospital managers and nursing educators should pay attention to the problem-solving of clinical nurses, carry out a series of training and counselling of nurses by using the method of situational simulation, optimize the nursing management mode, learn to use new media technology to improve the ...
Definitions. Problem solving and decision making are not synonymous terms. However, the processes for engaging in both processes are similar. Both skills require critical thinking, which is a high-level cognitive process, and both can be improved with practice.. Decision making is a purposeful and goal-directed effort that uses a systematic process to choose among options.
In literature 'critical thinking' is often used, and perhaps confused, with problem-solving and clinical decision-making skills and clinical reasoning. In practice, problem-solving tends to focus on the identification and resolution of a problem, whilst critical thinking goes beyond this to incorporate asking skilled questions and ...
Problem solving in clinical nursing practice is the essence of good care delivery. This paper gives an overview of a research study which identified the cognitive problem solving process nurses use while delivering care. The study was conducted in the clinical setting and used a qualitative research methodology of observation, followed by in ...
Creativity has various meanings, such as creating, making, producing designs, product relationships and attributes, a new and useful set of operations, reconstruction of old ideas, and a problem-solving method. However, the implementation of creativity in nursing clinical settings is of particular importance.
Decision making in nursing is a critical process that all nurses around the world use in their daily practice, involving the assessment of information, the identification of health issues, the establishment of care objectives, and the selection of appropriate interventions to address the patient's health problems [1, 2].Nursing professionals must effectively apply their knowledge, skills ...
He completed his undergraduate education in Pharmacy at the University of Tübingen, Germany. Driven by a deep desire to understand patient concerns, Hans wanted to go beyond pharmaceutical care. While in medical school, the virtual morning reports, Clinical Problem Solvers, unleashed his passion for solving complex patient cases.