Does your provider accept Medicare as full payment?
You can get the lowest cost if your doctor or other health care provider accepts the Medicare-approved amount as full payment for a covered service. This is called “accepting assignment.” If a provider accepts assignment, it’s for all Medicare-covered Part A and Part B services.

Using a provider that accepts assignment
Most doctors, providers, and suppliers accept assignment, but always check to make sure that yours do.
If your doctor, provider, or supplier accepts assignment:
- Your out-of-pocket costs may be less.
- They agree to charge you only the Medicare deductible and coinsurance amount, and usually wait for Medicare to pay its share before asking you to pay your share.
- They have to submit your claim directly to Medicare and can't charge you for submitting the claim.
How does assignment impact my drug coverage?
Using a provider that doesn't accept Medicare as full payment
Some providers who don’t accept assignment still choose to accept the Medicare-approved amount for services on a case-by-case basis. These providers are called "non-participating."
If your doctor, provider, or supplier doesn't accept assignment:
- You might have to pay the full amount at the time of service.
- They should submit a claim to Medicare for any Medicare-covered services they give you, and they can’t charge you for submitting a claim. If they refuse to submit a Medicare claim, you can submit your own claim to Medicare. Get the Medicare claim form .
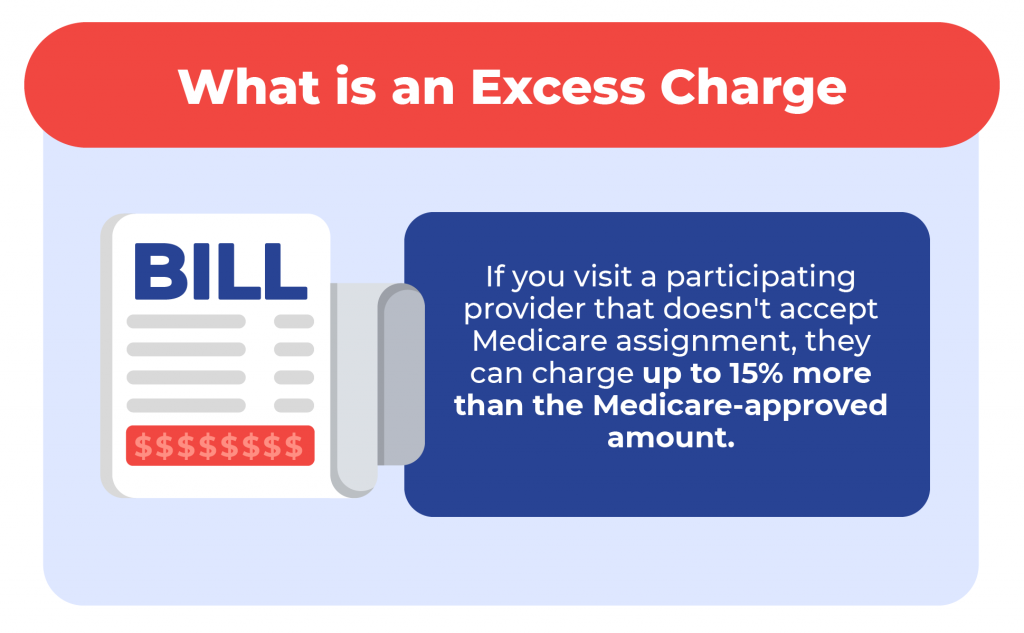
- They can charge up to 15% over the Medicare-approved amount for a service, but no more than that. This is called "the limiting charge."
Does the limiting charge apply to all Medicare-covered services?
Using a provider that "opts-out" of Medicare
- Doctors and other providers who don’t want to work with the Medicare program may "opt out" of Medicare.
- Medicare won’t pay for items or services you get from provider that opts out, except in emergencies.
- Providers opt out for a minimum of 2 years. Every 2 years, the provider can choose to keep their opt-out status, accept Medicare-approved amounts on a case-by-case basis ("non-participating"), or accept assignment.
Find providers that opted out of Medicare.
Private contracts with doctors or providers who opt out
- If you choose to get services from an opt-out doctor or provider you may need to pay upfront, or set up a payment plan with the provider through a private contract.
- Medicare won’t pay for any service you get from this doctor, even if it’s a Medicare-covered service.
What are the rules for private contracts?
You may want to contact your State Health Insurance Assistance Program (SHIP) for help before signing a private contract with any doctor or other health care provider.
What do you want to do next?
- Next step: Get help with costs
- Take action: Find a provider
- Get details: How to get Medicare services
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Medicare Assignment: Everything You Need to Know
Medicare assignment.
- Providers Accepting Assignment
- Providers Who Do Not
- Billing Options
- Assignment of Benefits
- How to Choose
Frequently Asked Questions
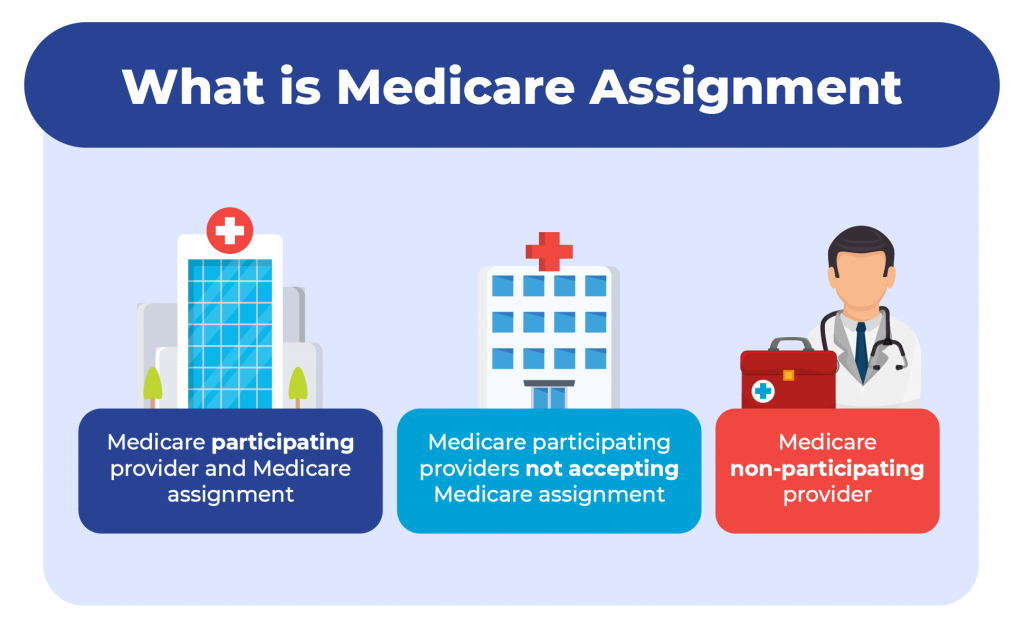
Medicare assignment is an agreement between Medicare and medical providers (doctors, hospitals, medical equipment suppliers, etc.) in which the provider agrees to accept Medicare’s fee schedule as payment in full when Medicare patients are treated.
This article will explain how Medicare assignment works, and what you need to know in order to ensure that you won’t receive unexpected bills.
fizkes / Getty Images
There are 35 million Americans who have Original Medicare. Medicare is a federal program and most medical providers throughout the country accept assignment with Medicare. As a result, these enrollees have a lot more options for medical providers than most of the rest of the population.
They can see any provider who accepts assignment, anywhere in the country. They can be assured that they will only have to pay their expected Medicare cost-sharing (deductible and coinsurance, some or all of which may be paid by a Medigap plan , Medicaid, or supplemental coverage provided by an employer or former employer).
It’s important to note here that the rules are different for the 29 million Americans who have Medicare Advantage plans. These beneficiaries cannot simply use any medical provider who accepts Medicare assignment.
Instead, each Medicare Advantage plan has its own network of providers —much like the health insurance plans that many Americans are accustomed to obtaining from employers or purchasing in the exchange/marketplace .
A provider who accepts assignment with Medicare may or may not be in-network with some or all of the Medicare Advantage plans that offer coverage in a given area. Some Medicare Advantage plans— health maintenance organizations (HMOs) , in particular—will only cover an enrollee’s claims if they use providers who are in the plan's network.
Other Medicare Advantage plans— preferred provider organizations (PPOs) , in particular—will cover out-of-network care but the enrollee will pay more than they would have paid had they seen an in-network provider.
Original Medicare
The bottom line is that Medicare assignment only determines provider accessibility and costs for people who have Original Medicare. People with Medicare Advantage need to understand their own plan’s provider network and coverage rules.
When discussing Medicare assignment and access to providers in this article, keep in mind that it is referring to people who have Original Medicare.
How to Make Sure Your Provider Accepts Assignment
Most doctors, hospitals, and other medical providers in the United States do accept Medicare assignment.
Provider Participation Stats
According to the Centers for Medicare and Medicaid Services, 98% of providers participate in Medicare, which means they accept assignment.
You can ask the provider directly about their participation with Medicare. But Medicare also has a tool that you can use to find participating doctors, hospitals, home health care services, and other providers.
There’s a filter on that tool labeled “Medicare-approved payment.” If you turn on that filter, you will only see providers who accept Medicare assignment. Under each provider’s information, it will say “Charges the Medicare-approved amount (so you pay less out-of-pocket).”
What If Your Provider Doesn’t Accept Assignment?
If your medical provider or equipment supplier doesn’t accept assignment, it means they haven’t agreed to accept Medicare’s approved amounts as payment in full for all of the services.
These providers can still choose to accept assignment on a case-by-case basis. But because they haven’t agreed to accept Medicare assignment for all services, they are considered nonparticipating providers.
Note that "nonparticipating" does not mean that a provider has opted out of Medicare altogether. Medicare will still pay claims for services received from a nonparticipating provider (i.e., one who does not accept Medicare assignment), whereas Medicare does not cover any of the cost of services obtained from a provider who has officially opted out of Medicare.
If a Medicare beneficiary uses a provider who has opted out of Medicare, that person will pay the provider directly and Medicare will not be involved in any way.
Physicians Who Have Opted Out
Only about 1% of all non-pediatric physicians have opted out of Medicare.
For providers who have not opted out of Medicare but who also don’t accept assignment, Medicare will still pay nearly as much as it would have paid if you had used a provider who accepts assignment. Here’s how it works:
- Medicare will pay the provider 95% of the amount they would pay if the provider accepted assignment.
- The provider can charge the person receiving care more than the Medicare-approved amount, but only up to 15% more (some states limit this further). This extra amount, which the patient has to pay out-of-pocket, is known as the limiting charge . But the 15% cap does not apply to medical equipment suppliers; if they do not accept assignment with Medicare, there is no limit on how much they can charge the person receiving care. This is why it’s particularly important to make sure that the supplier accepts Medicare assignment if you need medical equipment.
- The nonparticipating provider may require the person receiving care to pay the entire bill up front and seek reimbursement from Medicare (using Form CMS 1490-S ). Alternatively, they may submit a claim to Medicare on behalf of the person receiving care (using Form CMS-1500 ).
- A nonparticipating provider can choose to accept assignment on a case-by-case basis. They can indicate this on Form CMS-1500 in box 27. The vast majority of nonparticipating providers who bill Medicare choose to accept assignment for the claim being billed.
- Nonparticipating providers do not have to bill your Medigap plan on your behalf.
Billing Options for Providers Who Accept Medicare
When a medical provider accepts assignment with Medicare, part of the agreement is that they will submit bills to Medicare on behalf of the person receiving care. So if you only see providers who accept assignment, you will never need to submit your own bills to Medicare for reimbursement.
If you have a Medigap plan that supplements your Original Medicare coverage, you should present the Medigap coverage information to the provider at the time of service. Medicare will forward the claim information to your Medigap insurer, reducing administrative work on your part.
Depending on the Medigap plan you have, the services that you receive, and the amount you’ve already spent in out-of-pocket costs, the Medigap plan may pay some or all of the out-of-pocket costs that you would otherwise have after Medicare pays its share.
(Note that if you have a type of Medigap plan called Medicare SELECT, you will have to stay within the plan’s network of providers in order to receive benefits. But this is not the case with other Medigap plans.)
After the claim is processed, you’ll be able to see details in your MyMedicare.gov account . Medicare will also send you a Medicare Summary Notice. This is Medicare’s version of an explanation of benefits (EOB) , which is sent out every three months.
If you have a Medigap plan, it should also send you an EOB or something similar, explaining the claim and whether the policy paid any part of it.
What Is Medicare Assignment of Benefits?
For Medicare beneficiaries, assignment of benefits means that the person receiving care agrees to allow a nonparticipating provider to bill Medicare directly (as opposed to having the person receiving care pay the bill up front and seek reimbursement from Medicare). Assignment of benefits is authorized by the person receiving care in Box 13 of Form CMS-1500 .
If the person receiving care refuses to assign benefits, Medicare can only reimburse the person receiving care instead of paying the nonparticipating provider directly.
Things to Consider Before Choosing a Provider
If you’re enrolled in Original Medicare, you have a wide range of options in terms of the providers you can use—far more than most other Americans. In most cases, your preferred doctor and other medical providers will accept assignment with Medicare, keeping your out-of-pocket costs lower than they would otherwise be, and reducing administrative hassle.
There may be circumstances, however, when the best option is a nonparticipating provider or even a provider who has opted out of Medicare altogether. If you choose one of these options, be sure you discuss the details with the provider before proceeding with the treatment.
You’ll want to understand how much is going to be billed and whether the provider will bill Medicare on your behalf if you agree to assign benefits (note that this is not possible if the provider has opted out of Medicare).
If you have supplemental coverage, you’ll also want to check with that plan to see whether it will still pick up some of the cost and, if so, how much you should expect to pay out of your own pocket.
A medical provider who accepts Medicare assignment is considered a participating provider. These providers have agreed to accept Medicare’s fee schedule as payment in full for services they provide to Medicare beneficiaries. Most doctors, hospitals, and other medical providers do accept Medicare assignment.
Nonparticipating providers are those who have not signed an agreement with Medicare to accept Medicare’s rates as payment in full. However, they can agree to accept assignment on a case-by-case basis, as long as they haven’t opted out of Medicare altogether. If they do not accept assignment, they can bill the patient up to 15% more than the Medicare-approved rate.
Providers who opt out of Medicare cannot bill Medicare and Medicare will not pay them or reimburse beneficiaries for their services. But there is no limit on how much they can bill for their services.
A Word From Verywell
It’s in your best interest to choose a provider who accepts Medicare assignment. This will keep your costs as low as possible, streamline the billing and claims process, and ensure that your Medigap plan picks up its share of the costs.
If you feel like you need help navigating the provider options or seeking care from a provider who doesn’t accept assignment, the Medicare State Health Insurance Assistance Program (SHIP) in your state may be able to help.
A doctor who does not accept Medicare assignment has not agreed to accept Medicare’s fee schedule as payment in full for their services. These doctors are considered nonparticipating with Medicare and can bill Medicare beneficiaries up to 15% more than the Medicare-approved amount.
They also have the option to accept assignment (i.e., accept Medicare’s rate as payment in full) on a case-by-case basis.
There are certain circumstances in which a provider is required by law to accept assignment. This includes situations in which the person receiving care has both Medicare and Medicaid. And it also applies to certain medical services, including lab tests, ambulance services, and drugs that are covered under Medicare Part B (as opposed to Part D).
In 2021, 98% of American physicians had participation agreements with Medicare, leaving only about 2% who did not accept assignment (either as a nonparticipating provider, or a provider who had opted out of Medicare altogether).
Accepting assignment is something that the medical provider does, whereas assignment of benefits is something that the patient (the Medicare beneficiary) does. To accept assignment means that the medical provider has agreed to accept Medicare’s approved fee as payment in full for services they provide.
Assignment of benefits means that the person receiving care agrees to allow a medical provider to bill Medicare directly, as opposed to having the person receiving care pay the provider and then seek reimbursement from Medicare.
Centers for Medicare and Medicaid Services. Medicare monthly enrollment .
Centers for Medicare and Medicaid Services. Annual Medicare participation announcement .
Centers for Medicare and Medicaid Services. Lower costs with assignment .
Centers for Medicare and Medicaid Services. Find providers who have opted out of Medicare .
Kaiser Family Foundation. How many physicians have opted-out of the Medicare program ?
Center for Medicare Advocacy. Durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) updates .
Centers for Medicare and Medicaid Services. Check the status of a claim .
Centers for Medicare and Medicaid Services. Medicare claims processing manual. Chapter 26 - completing and processing form CMS-1500 data set .
Centers for Medicare and Medicaid Services. Ambulance fee schedule .
Centers for Medicare and Medicaid Services. Prescription drugs (outpatient) .
By Louise Norris Norris is a licensed health insurance agent, book author, and freelance writer. She graduated magna cum laude from Colorado State University.
Use our RMD calculator to estimate your required withdrawals from tax-deferred retirement plans.
Popular Searches
AARP daily Crossword Puzzle
Hotels with AARP discounts
Life Insurance
AARP Dental Insurance Plans
Suggested Links
AARP MEMBERSHIP — $12 FOR YOUR FIRST YEAR WHEN YOU SIGN UP FOR AUTOMATIC RENEWAL
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
- right_container
Work & Jobs
Social Security
AARP en Español
- Membership & Benefits
AARP Rewards
- AARP Rewards %{points}%
Conditions & Treatments
Drugs & Supplements
Health Care & Coverage
Health Benefits

Staying Fit
Your Personalized Guide to Fitness

AARP Hearing Center
Ways To Improve Your Hearing

Brain Health Resources
Tools and Explainers on Brain Health
How to Save Your Own Life
Scams & Fraud
Personal Finance
Money Benefits

View and Report Scams in Your Area

AARP Foundation Tax-Aide
Free Tax Preparation Assistance

AARP Money Map
Get Your Finances Back on Track

Budget & Savings
Make Your Appliances Last Longer
Small Business
Age Discrimination

Flexible Work
Freelance Jobs You Can Do From Home

AARP Skills Builder
Online Courses to Boost Your Career

31 Great Ways to Boost Your Career

ON-DEMAND WEBINARS
Tips to Enhance Your Job Search

Get More out of Your Benefits

When to Start Taking Social Security

10 Top Social Security FAQs

Social Security Benefits Calculator

Medicare Made Easy
Original vs. Medicare Advantage

Enrollment Guide
Step-by-Step Tool for First-Timers

Prescription Drugs
9 Biggest Changes Under New Rx Law

Medicare FAQs
Quick Answers to Your Top Questions
Care at Home
Financial & Legal
Life Balance

LONG-TERM CARE
Understanding Basics of LTC Insurance

State Guides
Assistance and Services in Your Area

Prepare to Care Guides
How to Develop a Caregiving Plan

End of Life
How to Cope With Grief, Loss
Recently Played
Word & Trivia
Atari® & Retro
Members Only
Staying Sharp
Mobile Apps
More About Games

Right Again! Trivia

Right Again! Trivia – Sports

Atari® Video Games

Throwback Thursday Crossword
Travel Tips
Vacation Ideas
Destinations
Travel Benefits

Beach vacation ideas
Vacations for Sun and Fun

Plan Ahead for Tourist Taxes

AARP City Guide
Discover Seattle

How to Pick the Right Cruise for You
Entertainment & Style
Family & Relationships
Personal Tech
Home & Living
Celebrities
Beauty & Style

TV for Grownups
Best Reality TV Shows for Grownups

Robert De Niro Reflects on His Life
Free Online Novel
Read 'Chase'

Sex & Dating
Spice Up Your Love Life

Navigate All Kinds of Connections

How to Create a Home Gym

Store Medical Records on Your Phone?

Maximize the Life of Your Phone Battery

Virtual Community Center
Join Free Tech Help Events

Create a Hygge Haven

Soups to Comfort Your Soul

AARP Smart Guide
Spring Clean All of Your Spaces
Driver Safety
Maintenance & Safety
Trends & Technology

How to Keep Your Car Running

We Need To Talk
Assess Your Loved One's Driving Skills

AARP Smart Driver Course

Building Resilience in Difficult Times

Tips for Finding Your Calm

Weight Loss After 50 Challenge

Cautionary Tales of Today's Biggest Scams

7 Top Podcasts for Armchair Travelers

Jean Chatzky: ‘Closing the Savings Gap’

Quick Digest of Today's Top News

AARP Top Tips for Navigating Life

Get Moving With Our Workout Series
You are now leaving AARP.org and going to a website that is not operated by AARP. A different privacy policy and terms of service will apply.
Go to Series Main Page
What is Medicare assignment and how does it work?
Kimberly Lankford,
Because Medicare decides how much to pay providers for covered services, if the provider agrees to the Medicare-approved amount, even if it is less than they usually charge, they’re accepting assignment.
A doctor who accepts assignment agrees to charge you no more than the amount Medicare has approved for that service. By comparison, a doctor who participates in Medicare but doesn’t accept assignment can potentially charge you up to 15 percent more than the Medicare-approved amount.
That’s why it’s important to ask if a provider accepts assignment before you receive care, even if they accept Medicare patients. If a doctor doesn’t accept assignment, you will pay more for that physician’s services compared with one who does.

AARP Membership — $12 for your first year when you sign up for Automatic Renewal
How much do I pay if my doctor accepts assignment?
If your doctor accepts assignment, you will usually pay 20 percent of the Medicare-approved amount for the service, called coinsurance, after you’ve paid the annual deductible. Because Medicare Part B covers doctor and outpatient services, your $240 deductible for Part B in 2024 applies before most coverage begins.
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies , without paying a deductible or coinsurance if the provider accepts assignment.
What if my doctor doesn’t accept assignment?
A doctor who takes Medicare but doesn’t accept assignment can still treat Medicare patients but won’t always accept the Medicare-approved amount as payment in full.
This means they can charge you up to a maximum of 15 percent more than Medicare pays for the service you receive, called “balance billing.” In this case, you’re responsible for the additional charge, plus the regular 20 percent coinsurance, as your share of the cost.
How to cover the extra cost? If you have a Medicare supplement policy , better known as Medigap, it may cover the extra 15 percent, called Medicare Part B excess charges.
All Medigap policies cover Part B’s 20 percent coinsurance in full or in part. The F and G policies cover the 15 percent excess charges from doctors who don’t accept assignment, but Plan F is no longer available to new enrollees, only those eligible for Medicare before Jan. 1, 2020, even if they haven’t enrolled in Medicare yet. However, anyone who is enrolled in original Medicare can apply for Plan G.
Remember that Medigap policies only cover excess charges for doctors who accept Medicare but don’t accept assignment, and they won’t cover costs for doctors who opt out of Medicare entirely.
Good to know. A few states limit the amount of excess fees a doctor can charge Medicare patients. For example, Massachusetts and Ohio prohibit balance billing, requiring doctors who accept Medicare to take the Medicare-approved amount. New York limits excess charges to 5 percent over the Medicare-approved amount for most services, rather than 15 percent.

AARP NEWSLETTERS

%{ newsLetterPromoText }%
%{ description }%
Privacy Policy
ARTICLE CONTINUES AFTER ADVERTISEMENT
How do I find doctors who accept assignment?
Before you start working with a new doctor, ask whether he or she accepts assignment. About 98 percent of providers billing Medicare are participating providers, which means they accept assignment on all Medicare claims, according to KFF.
You can get help finding doctors and other providers in your area who accept assignment by zip code using Medicare’s Physician Compare tool .
Those who accept assignment have this note under the name: “Charges the Medicare-approved amount (so you pay less out of pocket).” However, not all doctors who accept assignment are accepting new Medicare patients.
AARP® Vision Plans from VSP™
Exclusive vision insurance plans designed for members and their families
What does it mean if a doctor opts out of Medicare?
Doctors who opt out of Medicare can’t bill Medicare for services you receive. They also aren’t bound by Medicare’s limitations on charges.
In this case, you enter into a private contract with the provider and agree to pay the full bill. Be aware that neither Medicare nor your Medigap plan will reimburse you for these charges.
In 2023, only 1 percent of physicians who aren’t pediatricians opted out of the Medicare program, according to KFF. The percentage is larger for some specialties — 7.7 percent of psychiatrists and 4.2 percent of plastic and reconstructive surgeons have opted out of Medicare.
Keep in mind
These rules apply to original Medicare. Other factors determine costs if you choose to get coverage through a private Medicare Advantage plan . Most Medicare Advantage plans have provider networks, and they may charge more or not cover services from out-of-network providers.
Before choosing a Medicare Advantage plan, find out whether your chosen doctor or provider is covered and identify how much you’ll pay. You can use the Medicare Plan Finder to compare the Medicare Advantage plans and their out-of-pocket costs in your area.
Return to Medicare Q&A main page
Kimberly Lankford is a contributing writer who covers Medicare and personal finance. She wrote about insurance, Medicare, retirement and taxes for more than 20 years at Kiplinger’s Personal Finance and has written for The Washington Post and Boston Globe . She received the personal finance Best in Business award from the Society of American Business Editors and Writers and the New York State Society of CPAs’ excellence in financial journalism award for her guide to Medicare.
Discover AARP Members Only Access
Already a Member? Login

More on Medicare

How Do I Create a Personal Online Medicare Account?
You can do a lot when you decide to look electronically

I Got a Medicare Summary Notice in the Mail. What Is It?
This statement shows what was billed, paid in past 3 months
Understanding Medicare’s Options: Parts A, B, C and D
Making sense of the alphabet soup of health care choices
Recommended for You
AARP Value & Member Benefits

Learn, earn and redeem points for rewards with our free loyalty program

AARP® Dental Insurance Plan administered by Delta Dental Insurance Company
Dental insurance plans for members and their families

The National Hearing Test
Members can take a free hearing test by phone

AARP® Staying Sharp®
Activities, recipes, challenges and more with full access to AARP Staying Sharp®
SAVE MONEY WITH THESE LIMITED-TIME OFFERS
Medicare Interactive Medicare answers at your fingertips -->
Participating, non-participating, and opt-out providers, outpatient provider services.
You must be logged in to bookmark pages.
Email Address * Required
Password * Required
Lost your password?
If you have Original Medicare , your Part B costs once you have met your deductible can vary depending on the type of provider you see. For cost purposes, there are three types of provider, meaning three different relationships a provider can have with Medicare . A provider’s type determines how much you will pay for Part B -covered services.
- These providers are required to submit a bill (file a claim ) to Medicare for care you receive. Medicare will process the bill and pay your provider directly for your care. If your provider does not file a claim for your care, there are troubleshooting steps to help resolve the problem .
- If you see a participating provider , you are responsible for paying a 20% coinsurance for Medicare-covered services.
- Certain providers, such as clinical social workers and physician assistants, must always take assignment if they accept Medicare.
- Non-participating providers can charge up to 15% more than Medicare’s approved amount for the cost of services you receive (known as the limiting charge ). This means you are responsible for up to 35% (20% coinsurance + 15% limiting charge) of Medicare’s approved amount for covered services.
- Some states may restrict the limiting charge when you see non-participating providers. For example, New York State’s limiting charge is set at 5%, instead of 15%, for most services. For more information, contact your State Health Insurance Assistance Program (SHIP) .
- If you pay the full cost of your care up front, your provider should still submit a bill to Medicare. Afterward, you should receive from Medicare a Medicare Summary Notice (MSN) and reimbursement for 80% of the Medicare-approved amount .
- The limiting charge rules do not apply to durable medical equipment (DME) suppliers . Be sure to learn about the different rules that apply when receiving services from a DME supplier .
- Medicare will not pay for care you receive from an opt-out provider (except in emergencies). You are responsible for the entire cost of your care.
- The provider must give you a private contract describing their charges and confirming that you understand you are responsible for the full cost of your care and that Medicare will not reimburse you.
- Opt-out providers do not bill Medicare for services you receive.
- Many psychiatrists opt out of Medicare.
Providers who take assignment should submit a bill to a Medicare Administrative Contractor (MAC) within one calendar year of the date you received care. If your provider misses the filing deadline, they cannot bill Medicare for the care they provided to you. However, they can still charge you a 20% coinsurance and any applicable deductible amount.
Be sure to ask your provider if they are participating, non-participating, or opt-out. You can also check by using Medicare’s Physician Compare tool .
Update your browser to view this website correctly. Update my browser now
What Is Medicare Assignment?
Written by: Rachael Zimlich, RN, BSN
Reviewed by: Eboni Onayo, Licensed Insurance Agent
Key Takeaways
Medicare assignment describes the fee structure that your doctor and Medicare have agreed to use.
If your doctor agrees to accept Medicare assignment, they agree to be paid whatever amount Medicare has approved for a service.
You may still see doctors who don’t accept Medicare assignment, but you may have to pay for your visit up front and submit a claim to Medicare for reimbursement.
You may have to pay more to see doctors who don’t accept Medicare assignment.
How Does Medicare Assignment Work?
What is Medicare assignment ?
Medicare assignment simply means that your provider has agreed to stick to a Medicare fee schedule when it comes to what they charge for tests and services. Medicare regularly updates fee schedules, setting specific limits for what it will cover for things like office visits and lab testing.
When a provider agrees to accept Medicare assignment, they cannot charge more than the Medicare-approved amount. For you, this means your out-of-pocket costs may be lower than if you saw a provider who did not accept Medicare assignment. The provider acknowledges that the amount Medicare set for a particular service is the maximum amount that will be paid.
You may still have to pay a Medicare deductible and coinsurance, but your provider will have to submit a claim to Medicare directly and wait for payment before passing any share of the costs onto you. Doctors who accept Medicare assignment cannot charge you to submit these claims.
Find the Medicare Plan that works for you.
How Do I Know if a Provider Accepts Medicare Assignment?
There are a few levels of commitment when it comes to Medicare assignment.
- Providers who have agreed to accept Medicare assignment sign a contract with Medicare.
- Those who have not signed a contract with Medicare can still accept assignment amounts for services of their choice. They do not have to accept assignment for every service provided. These are called non-participating providers.
- Some providers opt out of Medicare altogether. Doctors who have opted out of Medicare completely or who use private contracts will not be paid anything by Medicare, even if it’s for a covered service within the fee limits. You will have to pay the full cost of any services provided by these doctors yourself.
You can check to see if your provider accepts Medicare assignment on Medicare’s website .
Billing Arrangement Options for Providers Who Accept Medicare
Doctors that take Medicare can sign a contract to accept assignment for all Medicare services, or be a non-participating provider that accepts assignment for some services but not all.
A medical provider that accepts Medicare assignment must submit claims directly to Medicare on your behalf. They will be paid the agreed upon amount by Medicare, and you will pay any copayments or deductibles dictated by your plan.
If your doctor is non-participating, they may accept Medicare assignment for some services but not others. Even if they do agree to accept Medicare’s fee for some services, Medicare will only pay then 95% of the set assignment cost for a particular service.
If your provider does plan to work with Medicare, either the provider or you can submit a claim to Medicare, but you may have to pay the entire cost of the visit up front and wait for reimbursement. They can’t charge you for more than the amount approved by Medicare, but they can charge you above the Medicare-approved amount. This is called the limiting charge, and can be up to 15% more than Medicare-approved amount for non-participating providers.
What Does It Mean When a Provider Does Not Accept Medicare Assignment?
Providers who refuse Medicare assignment can still choose to accept Medicare’s set fees for certain services. These are called non-participating providers.
There are a number of providers who opt out of participating in Medicare altogether; they are referred to as “opt-out doctors”. This means they have signed an opt-out agreement with Medicare and can’t be paid by Medicare at all — even for services normally covered by Medicare. Opt-out contracts last for at least two years. Some of these providers may only offer services to patients who sign contracts.
You do not need to sign a contract with a private provider or use an opt-out provider. There are many options for alternative providers who accept Medicare. If you do choose an opt-out or private contract provider, you will have to pay the full cost of services on your own.
Let’s find your ideal Medicare Advantage plan.
Do providers have to accept Medicare assignment?
No. Providers can choose to accept a full Medicare assignment, or accept assignment rates for some services as a non-participating provider. Doctors can also opt out of participating in Medicare altogether.
How much will I have to pay if my provider doesn't accept Medicare assignment?
Some providers that don’t accept assignment as a whole will accept assignment for some services. These are called non-participating providers. For these providers and providers who have completely opted out of Medicare, you will pay the majority of or the full amount for your care.
How do I submit a claim?
If you need to submit your own claim to Medicare, you can call 1-800-MEDICARE or use Form CMS-1490S .
Can my provider charge to submit a claim?
No. Providers are not allowed to charge to submit a claim to Medicare on your behalf.
Lower Costs with Assignment. Medicare.gov.
Fee Schedules . CMS.gov.
This website is operated by GoHealth, LLC., a licensed health insurance company. The website and its contents are for informational and educational purposes; helping people understand Medicare in a simple way. The purpose of this website is the solicitation of insurance. Contact will be made by a licensed insurance agent/producer or insurance company. Medicare Supplement insurance plans are not connected with or endorsed by the U.S. government or the federal Medicare program. Our mission is to help every American get better health insurance and save money. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
Let's see if you're missing out on Medicare savings.
We just need a few details.
Related Articles

What Is Medicare IRMAA?
What Is an IRMAA in Medicare?

Do All Doctors Accept Medicare?
What Does It Mean for a Doctor to Accept Medicare Assignment?

How to Report Medicare Fraud
Medicare Fraud Examples & How to Report Abuse

How to Change Your Address with Medicare
Reporting a Change of Address to Medicare

Can I Get Medicare if I’ve Never Worked?
Can You Get Medicare if You've Never Worked?

Why Are Some Medicare Advantage Plans Free?
Why Are Some Medicare Advantage Plans Free? $0 Premium Plans Explained

Am I Enrolled in Medicare?

When and How Do I Enroll?
When and How Do I Enroll in Medicare?

Medicare Frequently Asked Questions
Let’s see if you qualify for Medicare savings today!
Medicare Assignment: Understanding How It Works

Medicare assignment is a term used to describe how a healthcare provider agrees to accept the Medicare-approved amount. Depending on how you get your Medicare coverage, it could be essential to understand what it means and how it can affect you.
What is Medicare assignment?
Medicare sets a fixed cost to pay for every benefit they cover. This amount is called Medicare assignment.
You have the largest healthcare provider network with over 800,000 providers nationwide on Original Medicare . You can see any doctor nationwide that accepts Medicare.
Understanding the differences between your cost and the difference between accepting Medicare and accepting Medicare assignment could be worth thousands of dollars.
Doctors that accept Medicare
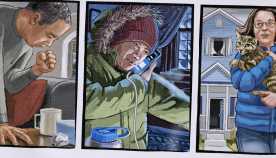
Your healthcare provider can fall into one of three categories:
Medicare participating provider and Medicare assignment
Medicare participating providers not accepting medicare assignment, medicare non-participating provider.
More than 97% of healthcare providers nationwide accept Medicare. Because of this, you can see almost any provider throughout the United States without needing referrals.
Let’s discuss the three categories the healthcare providers fall into.
Participating providers are doctors or healthcare providers who accept assignment. This means they will never charge more than the Medicare-approved amount.
Some non-participating providers accept Medicare but not Medicare assignment. This means you can see them the same way a provider accepts assignment.
You need to understand that since they don’t take the assigned amount, they can charge up to 15% more than the Medicare-approved amount.
Since Medicare will only pay the Medicare-approved amount, you’ll be responsible for these charges. The 15% overcharge is called an excess charge. A few states don’t allow or limit the amount or services of the excess charges. Only about 5% of providers charge excess charges.
Opt-out providers don’t accept Original Medicare, and these healthcare providers are in the minority in the United States. If healthcare providers don’t accept Medicare, they won’t be paid by Medicare.
This means choosing to see a provider that doesn’t accept Medicare will leave you responsible for 100% of what they charge you. These providers may be in-network for a Medicare Advantage plan in some cases.
Avoiding excess charges
Excess charges could be large or small depending on the service and the Medicare-approved amount. Avoiding these is easy. The simplest way is to ask your provider if they accept assignment before service.
If they say yes, they don’t issue excess charges. Or, on Medicare.gov , a provider search tool will allow you to look up your healthcare provider and show if they accept Medicare assignment or not.
Medicare Supplement and Medicare assignment
Medigap plans are additional insurance that helps cover your Medicare cost-share . If you are on specific plans, they’ll pay any extra costs from healthcare providers that accept Medicare but not Medicare assigned amount. Most Medicare Supplement plans don’t cover the excess charges.
The top three Medicare Supplement plans cover excess charges if you use a provider that accepts Medicare but not Medicare assignment.
Medicare Advantage and Medicare assignment
Medicare assignment does not affect Medicare Advantage plans since Medicare Advantage is just another way to receive your Medicare benefits. Since your Medicare Advantage plan handles your healthcare benefits, they set the terms.
Most Medicare Advantage plans require you to use network providers. If you go out of the network, you may pay more. If you’re on an HMO, you’d be responsible for the entire charge of the provider not being in the network.
Do all doctors accept Medicare Supplement plans?
All doctors that accept Original Medicare accept Medicare Supplement plans. Some doctors don’t accept Medicare. In this case, those doctors won’t accept Medicare Supplements.
Where can I find doctors who accept Medicare assignment?
Medicare has a physician finder tool that will show if a healthcare provider participates in Medicare and accepts Medicare assignments. Most doctors nationwide do accept assignment and therefore don’t charge the Part B excess charges.
Why do some doctors not accept Medicare?
Some doctors are called concierge doctors. These doctors don’t accept any insurance and require cash payments.
What is a Medicare assignment?
Accepting Medicare assignment means that the healthcare provider has agreed only to charge the approved amount for procedures and services.
What does it mean if a doctor does not accept Medicare assignment?
The doctor can change more than the Medicare-approved amount for procedures and services. You could be responsible for up to a 15% excess charge.
How many doctors accept Medicare assignment?
About 97% of doctors agree to accept assignment nationwide.
Is accepting Medicare the same as accepting Medicare assignment?
No. If a doctor accepts Medicare and accepts Medicare assigned amount, they’ll take what Medicare approves as payment in full.
If they accept Medicare but not Medicare assignment, they can charge an excess charge of up to 15% above the Medicare-approved amount. You could be responsible for this excess charge.
What is the Medicare-approved amount?
The Medicare-approved amount is Medicare’s charge as the maximum for any given medical service or procedure. Medicare has set forth an approved amount for every covered item or service.
Can doctors balance bill patients?
Yes, if that doctor is a Medicare participating provider not accepting Medicare assigned amount. The provider may bill up to 15% more than the Medicare-approved amount.

What happens if a doctor does not accept Medicare?
Doctors that don’t accept Medicare will require you to pay their full cost when using their services. Since these providers are non-participating, Medicare will not pay or reimburse for any services rendered.
Get help avoiding Medicare Part B excess charges
Whether it’s Medicare assignment, or anything related to Medicare, we have licensed agents that specialize in this field standing by to assist.
Give us a call, or fill out our online request form . We are happy to help answer questions, review options, and guide you through the process.
Related Articles
- What are Medicare Part B Excess Charges?
- How to File a Medicare Reimbursement Claim?
- Medicare Defined Coinsurance: How it Works?
- Welcome to Medicare Visit
- Guide to the Medicare Program

CALL NOW (833) 972-1339
Everything PTs Need to Know About Accepting Medicare Assignment
There's no one-size-fits-all answer as to whether or not a PT should accept Medicare assignment, but you can better understand your options.
There's no one-size-fits-all all answer as to whether or not a PT should accept Medicare assignment, but you can better understand your options.

Get the latest news and tips directly in your inbox by subscribing to our monthly newsletter
Discuss any topic within rehab therapy, and chances are that Medicare will come up at some point. Whether it’s talking about Medicare and direct access or Medicare supervision requirements , it’s hard to avoid discussing the ins and outs of the program, given its prominence in healthcare at large. However, there’s one question that probably doesn't get asked enough: do providers have to participate in Medicare? We’re going to dive into the specifics of what rehab therapists can and can’t do when it comes to accepting Medicare assignment, and the pros and cons of each.
What it means to “accept Medicare assignment”
In short, accepting Medicare assignment means signing a contract to accept whatever Medicare pays for a covered service as full payment. Participating and non-participating status only applies to Medicare Part B; Medicare Advantage plans operate with contracts similar to commercial insurance with in-network and out-of-network providers.
Participating Providers
If you’re accepting Medicare assignment for all covered services, you are considered to be a participating provider under Medicare and may not charge patients above and beyond what Medicare agrees to pay. In this case, you can charge 100% of the Medicare Physician Fee Schedule (MPFS) and are paid at 80% of that rate, minus the Multiple Procedure Payment Reduction (MPPR) and the 2% sequestration adjustment.
You may, however, collect patient deductibles and coinsurances—although, as explained in the Medicare payer guide , these providers typically ask Medicare to pay its share before collecting anything from the patient. Per the same resource, these providers are required to submit claims directly to Medicare for reimbursement and cannot charge patients for the claim submission. As Dr. Jarod Carter, PT, DPT, MTC, writes in Medicare and Cash-Pay PT Services , “This is the most common and best-understood relationship that physical therapists have with Medicare.”
Because Medicare beneficiaries often pay less out-of-pocket costs when receiving care from a provider who accepts assignment, patients may be more willing to work with these providers. Thus, if you accept assignment, you may have access to not only more Medicare patients but also more potential referral partners who only work with assignment-accepting providers.
You must accept whatever Medicare deems appropriate compensation, and as we know, that’s below market value more often than not. Given the recently announced cuts to assistant-provided services and the 8% cut to all physical therapy services , accepting assignment may be increasingly less appealing to physical therapists. That said, if you serve a large Medicare population, the volume of patients you see may make it financially beneficial for you to continue playing by Medicare’s rules.
If you don’t want to accept Medicare assignment, what are your other options?
Non-participating providers.
As Meredith Castin explains in 4 Things to Know About Billing for Cash-Pay PT , Medicare also allows physical therapists to be non-participating providers (a.k.a. non-enrolled providers), which simply means that, while they are still in a contractual relationship with Medicare (and thus, are eligible to provide covered services to Medicare beneficiaries), they have not agreed to accept assignment across the board.
If a non-participating provider opts to accept assignment for a case, they can charge 95%.
If they do not accept assignment but still treat the patient, these providers may charge up to what Medicare calls “the limiting charge” for a service—which is 15% above the Medicare allowed amount. Non-participating providers may choose to accept assignment for some services, but not others —or no services at all. For services that are not under assignment, the provider may collect payment directly from the patient; however, he or she must still bill Medicare, so that Medicare may reimburse the patient.
Non-participating providers are still eligible to serve Medicare beneficiaries, but they maintain some degree of freedom when it comes to pricing their services. In other words, if you are a non-participating provider, you are less beholden to what Medicare deems as appropriate payment than you are as a participating provider.
That said, you do still have to charge within Medicare’s limit, which means your freedom is far from total. Additionally, because patients may have to pay more out of pocket for your services and/or pay and wait for reimbursement from Medicare, you may have to work harder to convince them that you’re worth the financial investment. With the right data and marketing , it’s definitely doable; it may just require more effort.
No Relationship with Medicare
Physicians are eligible to “opt-out” of Medicare, which means that even if they are neither participating nor non-participating providers, they can still see Medicare beneficiaries on a cash-pay basis. Physical therapists do not enjoy the same privilege. So, if you decide not to be a Medicare participating provider or non-participating provider, then you effectively have no relationship with Medicare. Thus, you are not able to provide Medicare-covered services to Medicare beneficiaries.
That said, all physical therapists, regardless of their relationship with Medicare, may provide never-covered services to Medicare beneficiaries, including wellness services. According to Castin, though, providers who go down that route, “need to be very clear about Medicare’s definition of ‘wellness services’ versus ‘physical therapy services.’” According to cash-pay PT Jarod Carter , it’s imperative for your documentation to clearly support that the services were indeed wellness as opposed to therapy.
As a provider with no relationship with Medicare, you’re not required to play by Medicare’s rules when it comes to reporting requirements or (lowball) payments. You’re also not at all affected by Medicare’s most recent cuts, which, quite frankly, is a big bonus.
However, as of 2007 , 15% of the US population was enrolled in Medicare; that’s 44 million people—most of whom could benefit from seeing a physical therapist to improve function and mobility and decrease pain. And that number is projected to grow to 79 million people by 2030. As such, choosing not to play ball with Medicare means you’re walking away from a very large market of patients who need your services.
It’s your decision.
Deciding on accepting Medicare assignment—and what type of relationship you’d like to have with Medicare—is not an easy decision to make, and there are a lot of factors to take into consideration before getting involved or breaking it off with this substantial federal payer. That said, it is important to know that you have options. Have more questions about what it means to accept assignment as a PT? Ask them below, and we’ll do our best to find you an answer.
Related posts

Four Things You Need to Know About OT Salary

Founder Letter: What We Can Learn from Change Healthcare

How to Document and Bill for Home-Based Physical Therapy Services

Medicare and Cash-Pay PT Services, Part 1: The Must-Know Concepts to Avoid Legal Issues and Capitalize on Opportunities

Medicare and Direct Access

The Medicare Maintenance Care Myth

Learn how WebPT’s PXM platform can catapult your practice to new heights.

Sixty-Five Incorporated
Sponsored by interim healthcare ®.
- When Can I Sign Up For Medicare
- i65 Resources
What does ‘accepting assignment’ mean?
Accepting assignment is a real concern for those who have Original Medicare coverage. Physicians (or any other healthcare providers or facilities) who accept assignment agree to take Medicare’s payment for services. They cannot bill a Medicare beneficiary in excess of the Medicare allowance, which is the copayment or coinsurance. While providers who participate in the Medicare program must accept assignment on all Medicare claims, they do not have to accept every Medicare beneficiary as a patient.
There are basically three Medicare options for physicians.
- Physicians may sign a participating agreement and accept Medicare’s allowed charge as payment-in-full for all of their Medicare patients. Use the Physician Compare database to find physicians who accept assignment.
- They may elect to be non-participating, in which case, they make decisions about accepting Medicare assignment on a case-by-case basis. They can bill patients up to 15% more than the Medicare allowance. Some Medigap policies offer a benefit to cover this amount, known as Part B excess charges.
- Or, they may opt out of Medicare entirely and become private contracting physicians. They establish contracts with their patients to bill them directly. Neither the physicians nor the patients would receive any payments from Medicare.
Accepting assignment can also be a concern for beneficiaries with coverage other than Original Medicare, including those:
- in a Medicare Advantage Private Fee-for-service (PFFS) plan who get services outside the network.
- in a Medicare Advantage Medical Savings Account (MSA) plan because this plan does not utilize networks.
Learn the “Lingo” of Medicare Part D
Comparing Medicare Part D drug plans is useless – unless you know the lingo . What is Catastropic Coverage and the Coverage Gap? What are tiers and quantity limits? Find out!
Get the FREE Part D Lingo whitepaper.
Medicare Options
To help ensure that physicians are making informed decisions about their contractual relationships with the Medicare program, the AMA has developed a “Medicare Participation Kit”(www.ama-assn.org) that explains the various participation options that are available to physicians. A summary of those options is presented below. The AAFP is not advising or recommending any of the options. The purpose of sharing this information is merely to ensure that physician decisions about Medicare participation are made with complete information about the available options. Please note that the summary below does not account for any payment adjustments that a participating or non-participating physician may incur through one of the Medicare initiatives, such as the Physician Quality Reporting System. Physicians wishing to change their Medicare participation or non-participation status for a given year are usually required to do so by December 31 of the prior year (e.g., December 31, 2015 for 2016). Participation decisions are effective January 1 of the year in question and are binding for the entire year.
The Three Options
There are basically three Medicare contractual options for physicians. Physicians may sign a participating (PAR) agreement and accept Medicare's allowed charge as payment in full for all of their Medicare patients. They may elect to be a non-PAR physician, which permits them to make assignment decisions on a case-by-case basis and to bill patients for more than the Medicare allowance for unassigned claims. Or they may become a private contracting physician, agreeing to bill patients directly and forego any payments from Medicare to their patients or themselves. Physicians who wish to change their status from PAR to non-PAR or vice versa may do so annually. Once made, the decision is generally binding until the next annual contracting cycle except where the physician's practice situation has changed significantly, such as relocation to a different geographic area or a different group practice. To become a private contractor, physicians must give 30 days notice before the first day of the quarter the contract takes effect. Those considering a change in status should first determine that they are not bound by any contractual arrangements with hospitals, health plans or other entities that require them to be PAR physicians. In addition, some states have enacted laws that prohibit physicians from balance billing their patients.
Participation
PAR physicians agree to take assignment on all Medicare claims, which means that they must accept Medicare's approved amount (which is the 80% that Medicare pays plus the 20% patient copayment) as payment in full for all covered services for the duration of the calendar year. The patient or the patient's secondary insurer is still responsible for the 20% copayment but the physician cannot bill the patient for amounts in excess of the Medicare allowance. While PAR physicians must accept assignment on all Medicare claims, however, Medicare participation agreements do not require physician practices to accept every Medicare patient who seeks treatment from them.
Medicare provides a number of incentives for physicians to participate:
- The Medicare payment amount for PAR physicians is 5% higher than the rate for non-PAR physicians.
- Directories of PAR physicians are provided to senior citizen groups and individuals who request them.
- Medicare administrative contractors (MAC) provide toll-free claims processing lines to PAR physicians and process their claims more quickly.
Non-Participation
Medicare approved amounts for services provided by non-PAR physicians (including the 80% from Medicare plus the 20% copayment) are set at 95% of Medicare approved amounts for PAR physicians, although non-PAR physicians can charge more than the Medicare approved amount.
Limiting charges for non-PAR physicians are set at 115% of the Medicare approved amount for non-PAR physicians. However, because Medicare approved amounts for non-PAR physicians are 95% of the rates for PAR physicians, the 15% limiting charge is effectively only 9.25% above the PAR approved amounts for the services. Therefore, when considering whether to be non-PAR, physicians must determine whether their total revenues from Medicare, patient copayments and balance billing would exceed their total revenues as PAR physicians, particularly in light of collection costs, bad debts and claims for which they do accept assignment. The 95% payment rate is not based on whether physicians accept assignment on the claim, but whether they are PAR physicians; when non-PAR physicians accept assignment for their low-income or other patients, their Medicare approved amounts are still only 95% of the approved amounts paid to PAR physicians for the same service. Non-PAR physicians would need to collect the full limiting charge amount roughly 35% of the time they provided a given service in order for the revenues from the service to equal those of PAR physicians for the same service. If they collect the full limiting charge for more than 35% of the services that they provide, their Medicare revenues will exceed those of PAR physicians.
Assignment acceptance, for either PAR or non-PAR physicians, also means that the MAC pays the physician the 80% Medicare payment. For unassigned claims, even though the physician is required to submit the claim to Medicare, the program pays the patient, and the physician must then collect the entire amount for the service from the patient.
Example: A service for which Medicare fee schedule amount is $100
Private contracting.
Provisions in the Balanced Budget Act of 1997 give physicians and their Medicare patients the freedom to privately contract to provide health care services outside the Medicare system. Private contracting decisions may not be made on a case-by-case or patient-by-patient basis, however. Once physicians have opted out of Medicare, they cannot submit claims to Medicare for any of their patients for a two-year period.
A physician who has not been excluded under sections 1128, 1156 or 1892 of the Social Security Act may, however, order, certify the need for, or refer a beneficiary for Medicare-covered items and services, provided the physician is not paid, directly or indirectly, for such services (except for emergency and urgent care services). For example, if a physician who has opted out of Medicare refers a beneficiary for medically necessary services, such as laboratory, DMEPOS or inpatient hospitalization, those services would be covered by Medicare.
To privately contract with a Medicare beneficiary, a physician must enter into a private contract that meets specific requirements, as set forth in the sample private contract below. In addition to the private contract, the physician must also file an affidavit that meets certain requirements, as contained in the sample affidavit below. To opt out, a physician must file an affidavit that meets the necessary criteria and is received by the MAC at least 30 days before the first day of the next calendar quarter. There is a 90-day period after the effective date of the first opt-out affidavit during which physicians may revoke the opt-out and return to Medicare as if they had never opted out.
Emergency and Urgent Care Services Furnished During the "Opt-Out" Period
Physicians who have opted-out of Medicare under the Medicare private contract provisions may furnish emergency care services or urgent care services to a Medicare beneficiary with whom the physician has previously entered into a private contract so long as the physician and beneficiary entered into the private contract before the onset of the emergency medical condition or urgent medical condition. These services would be furnished under the terms of the private contract.
Physicians who have opted-out of Medicare under the Medicare private contract provisions may continue to furnish emergency or urgent care services to a Medicare beneficiary with whom the physician has not previously entered into a private contract, provided the physician:
- Submits a claim to Medicare in accordance with both 42 CFR part 424 (relating to conditions for Medicare payment) and Medicare instructions (including but not limited to complying with proper coding of emergency or urgent care services furnished by physicians and qualified health care professionals who have opted-out of Medicare).
- Collects no more than the Medicare limiting charge, in the case of a physician (or the deductible and coinsurance, in the case of a qualified health care professional).
Note that a physician who has been excluded from Medicare must comply with Medicare regulations relating to scope and effect of the exclusion (42 C.F.R. § 1001.1901) when the physician furnishes emergency services to beneficiaries, and the physician may not bill and be paid for urgent care services.
Sample Medicare Private Contract and Affidavit
The sample private contract and affidavit below contain the provisions that Medicare requires (unless otherwise noted) to be included in these documents.
Private contracts must meet specific requirements:
- The physician must sign and file an affidavit agreeing to forgo receiving any payment from Medicare for items or services provided to any Medicare beneficiary for the following 2-year period (either directly, on a capitated basis or from an organization that received Medicare reimbursement directly or on a capitated basis).
- Medicare does not pay for the services provided or contracted for. The contract must be in writing and must be signed by the beneficiary before any item or service is provided.
- The contract cannot be entered into at a time when the beneficiary is facing an emergency or an urgent health situation.
In addition, the contract must state unambiguously that by signing the private contract, the beneficiary:
- gives up all Medicare payment for services furnished by the "opt out" physician;
- agrees not to bill Medicare or ask the physician to bill Medicare;
- is liable for all of the physician's charges, without any Medicare balance billing limits;
- acknowledges that Medigap or any other supplemental insurance will not pay toward the services; and acknowledges that he or she has the right to receive services from physicians for whom Medicare coverage and payment would be available.
If you determine that you want to "opt out" of Medicare under a private contract, we recommend that you consult with your attorney to develop a valid contract containing other standard non-Medicare required provisions that generally are included in any standard contract.
Download sample contracts:
- Sample Medicare Private Contract
- Sample Medicare Private Contracts "Opt-Out" Affidavit
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
CMS Newsroom
Search cms.gov.
- Physician Fee Schedule
- Local Coverage Determination
- Medically Unlikely Edits
Provider Assignment
On this page:, provider nomination and the geographic assignment rule.
- Part A and Part B (A/B) and Home Health and Hospice (HH+H)
- Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS)
- Specialty Providers and Demonstrations
- Railroad Retirement Beneficiaries Entitled to Medicare
- Qualified Chains
- Out-of-Jurisdiction Providers (OJP)
Section 911(b) of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA), Public Law 108-173 , repealed the provider nomination provisions formerly found in Section 1816 of the Title XVIII of the Social Security Act and replaced it with the Geographic Assignment Rule. Generally, a provider or supplier will be assigned to the Medicare Administrative Contractor (MAC) that covers the state where the provider or supplier is located. The Center for Medicare & Medicaid Services’ (CMS) has defined the following approach for assigning providers, physicians, and suppliers to MACs.
return to top
Part A/Part B (A/B) and Home Health and Hospice (HH+H) Rule
All A/B and HH+H providers will be assigned to the MAC contracted by CMS to administer A/B and HH+H claims for the geographic locale in which the provider is physically located. Learn more about the current A/B MAC jurisdictions and HH+H areas and view the corresponding maps at Who are the MACs.
Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) Rule
Each DMEPOS supplier submits claims to the DME MAC contracted by CMS to administer DMEPOS claims for the geographic locale in which the beneficiary resides permanently. Learn more about the current DME MAC jurisdictions and view the corresponding map at Who are the MACs.
Specialty Providers and Demonstrations Rule
Specialty providers and providers involved with certain demonstrations will submit claims to a specific MAC designated by CMS. Learn more about a specific A/B MAC or DME MAC and view the corresponding maps at Who are the MACs .
Railroad Retirement Beneficiaries Entitled to Medicare Rule
Physicians and other suppliers (except for DMEPOS suppliers) will continue to enroll with and bill the contractor designated by the Railroad Retirement Board for Part B services furnished to their beneficiaries. Each DMEPOS supplier will submit claims to the DME MAC contracted by CMS to administer DMEPOS claims for the geographic locale in which the beneficiary resides permanently. Learn more about the current DME MAC jurisdictions and view the corresponding map at W ho are the MACs.
Qualified Chains Rule
The Geographic Assignment Rule states that generally, a provider or supplier will be assigned to the MAC that covers the state where the provider or supplier is located. However, it does provide an exception for qualified chains. A qualified chain home office may request that its hospitals and skilled nursing facilities be serviced by the A/B MAC that covers the state where the home office is located. A qualified chain home office may send an inquiry to: CMS [email protected]
Out-of-Jurisdiction Providers (OJP) Rule
An OJP is a provider that is not currently assigned to an A/B MAC in accordance with the geographic assignment rule and the qualified chain exception. For example, a hospital not part of a qualified chain located in Maine, but currently assigned to the A/B MAC in Jurisdiction F would be an OJP.
Each A/B MAC will initially service some OJPs until CMS undertakes the final reassignment of all OJPs to their destination MACs based on the geographic assignment rule and its exceptions.
CMS has not set a timetable for moving OJP’s.
- Newsletters
- FAC Articles

Working from home?
Keep your critical coding and billing tools with you no matter where you work.
Create your Find-A-Code account today!
Find-A-Code Articles, Published 2014, August 1
What does accept assignment mean.
by InstaCode Institute Aug 1st, 2014 - Reviewed/Updated Mar 5th
What does it mean to accept assignment on the CMS 1500 claim form - also called the HCFA 1500 claim form.? Should I accept assignment or not? What are the guidelines for accepting assignment in box 27 of the 1500 claim?
These commonly asked questions should have a simple answer, but the number of court cases indicates that it is not as clear cut as it should be. This issue is documented in the book “Problems in Health Care Law” by Robert Desle Miller. The definition appears to be in the hands of the courts. However, we do have some helpful guidelines for you.
One major area of confusion is the relationship between box 12, box 13 and box 27. These are not interchangeable boxes and they are not necessarily related to each other.
According to the National Uniform Claim Committee (NUCC), the "Accept Assignment" box indicates that the provider agrees to accept assignment. It simply says to enter an X in the correct box. It does NOT define what accepting assignment might or might not mean.
It is important to understand that if you are a participating provider in any insurance plan or program, you must first follow the rules according to the contract that you sign. That contract supersedes any guidelines that are included here.
Medicare Instructions / Guidelines
PARTICIPATING providers MUST accept assignment according to the terms of their contract. The contract itself states:
“Meaning of Assignment - For purposes of this agreement, accepting assignment of the Medicare Part B payment means requesting direct Part B payment from the Medicare program. Under an assignment , the approved charge, determined by the Medicare carrier, shall be the full charge for the service covered under Part B. The participant shall not collect from the beneficiary or other person or organization for covered services more than the applicable deductible and coinsurance.”
By law, the providers or types of services listed below MUST also accept assignment:
- Clinical diagnostic laboratory services;
- Physician services to individuals dually entitled to Medicare and Medicaid;
- Services of physician assistants, nurse practitioners, clinical nurse specialists, nurse midwives, certified registered nurse anesthetists, clinical psychologists, and clinical social workers;
- Ambulatory surgical center services for covered ASC procedures;
- Home dialysis supplies and equipment paid under Method II;
- Ambulance services;
- Drugs and biologicals; and
- Simplified Billing Roster for influenza virus vaccine and pneumococcal vaccine.
NON-PARTICIPATING providers can choose whether to accept assignment or not, unless they or the service they are providing is on the list above.
The official Medicare instructions regarding Boxes 12 and 13 are:
“Item 12 – The patient's signature authorizes release of medical information necessary to process the claim. It also authorizes payments of benefits to the provider of service or supplier when the provider of service or supplier accepts assignment on the claim.” “Item 13 - The patient’s signature or the statement “signature on file” in this item authorizes payment of medical benefits to the physician or supplier. The patient or his/her authorized representative signs this item or the signature must be on file separately with the provider as an authorization. However, note that when payment under the Act can only be made on an assignment-related basis or when payment is for services furnished by a participating physician or supplier, a patient’s signature or a “signature on file” is not required in order for Medicare payment to be made directly to the physician or supplier.”
Regardless of the wording on these instructions stating that it authorizes payments to the physician, this is not enough to ensure that payment will come directly to you instead of the patient.To guarantee payment comes to you, you MUST accept assignment.
Under Medicare rules, PARTICIPATING providers are paid at 80% of the physician fee schedule allowed amount and NON-participating providers are paid at 80% of the allowed amount, which is 5% less than the full Allowed amount for participating providers. Only NON-participating providers may "balance bill" the patient for any amounts not paid by Medicare, however, they are subject to any state laws regarding balance billing.
TIP: If you select YES, you may or may not be subject to a lower fee schedule, but at least you know the payment is supposed to come to you.
NON-MEDICARE Instructions / Guidelines
PARTICIPATING providers MUST abide by the terms of their contract. In most cases, this includes the requirement to accept assignment on submitted claims.
NON-PARTICIPATING providers have the choice to accept or not accept assignment.
YES means that payment should go directly to you instead of the patient. Generally speaking, even if you have an assignment of benefits from the patient (see box 12 & 13), payment is ONLY guaranteed to go to you IF you accept assignment.
NO is appropriate for patients who have paid for their services in full so they may be reimbursed by their insurance. It generally means payment will go to the patient.
What Does Accept Assignment Mean?. (2014, August 1). Find-A-Code Articles. Retrieved from https://www.findacode.com/articles/what-does-accept-assignment-mean-34840.html
Article Tags (click on a tag to see related articles)
Thank you for choosing Find-A-Code, please Sign In to remove ads.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Care Financ Rev
- v.1(3); Winter 1980

Physicians' Charges Under Medicare: Assignment Rates and Beneficiary Liability
Under Medicare's Part B program, the physician decides whether to accept assignment of claims. When assignment is accepted, the physician agrees to accept as full payment Medicare's allowed charge. Physicians' acceptance of assignment is of considerable importance in relieving the beneficiaries of the burden of the costs of medical care services. This factor and the beneficiaries' liabilities for premiums, the annual deductible, and coinsurance are analyzed in considerable detail in this report.
Data from physicians' claims for services in 1975 show that 45.8 percent of the services and 47.2 percent of the charges were assigned for the aged. There were wide variations in the rate of acceptance of assignment by physician specialty, and by age, race, and residence of beneficiaries. Total beneficiary liability from the deductible, coinsurance, and from unassigned claims amounted to 37.7 percent of total physicians' charges due. When the premium which the beneficiary pays for Part B is included, beneficiary liability rises to 69.2 percent of total physicians' charges due.
Medicare's Part B program (Supplementary Medical Insurance) provides basic health insurance coverage to ease the financial burden of health care services for the aged population of the nation, for disabled Social Security beneficiaries, and for persons with end stage renal disease. Although the program was not intended to cover all the costs of medical care, several factors can diminish the protection beneficiaries have against the burden of large medical bills. These factors include the level of physicians' acceptance of assignment and the program's cost-sharing mechanisms.
This paper provides a detailed description of physicians' assignment rates for services rendered in 1975; assignment rates are analyzed by demographic characteristics of the beneficiaries, (that is, persons enrolled in Part B) by geographic area, and by physician specialty. This paper also analyzes total beneficiary outlays (for the premium, the deductible, coinsurance, and liability from unassigned claims) to determine the total burden on beneficiaries and compares that total with program reimbursements.
Physicians' assignment decisions determine to a significant extent the degree to which beneficiaries are protected by Medicare's Part B insurance. Under the Medicare program, the physician decides whether to accept assignment on each Medicare claim. If the claim is assigned, the physician agrees to accept as full payment the amount Medicare determines as reasonable. 1 If the physician does not accept assignment, the Medicare patient is liable for the difference between the amount charged and the amount Medicare allows; if this difference is large, beneficiary liability can be substantial. In such instances, the program is less successful in protecting beneficiaries from the cost of health care. 2
Beginning with 1968, national data are available on the rate of acceptance of assignment based on the total number of claims. In that year, the net assignment rate 3 was 59.0 percent. In 1969, the proportion rose to 61.5 percent, the highest it has ever registered since data have been available. Thereafter, there was a general decline each year in the percent of assigned claims. Comparable data are also available beginning with 1971 on the percent of total charges that were assigned. As may be seen in the following data, the percentage of total charges assigned was lower each year than the percentage of claims assigned. The percent of charges assigned reached a low point in 1976 (47.6 percent), then rose in 1977 and again in 1978.
It should be noted that the data above—as well as the data generated for this study—include claims for Medicare beneficiaries who are also enrolled in Medicaid. For Medicaid beneficiaries, assignment is mandatory. Consequently, if the assignment rate were computed for voluntary assignment only, the rate would be lower.
Sources of Data
The detailed information that follows is derived from a new and continuing data set based on claims for physicians' services in 1975. The data are furnished centrally to HCFA from claims submitted on Medicare “1490” forms and processed by Medicare carriers for a 5 percent sample of Medicare beneficiaries throughout the nation. To facilitate data processing for this study, a subset was used consisting of a 1 percent sample of Medicare beneficiaries. This new data system was designed to provide a greater depth of information about the use of physicians' services than previously available from the ongoing payment record system. Data items available, beginning with 1975 services, include the Medicare identification number of the patient, the physician's total charge, the amount Medicare allowed, the Medicare reimbursement, whether or not the claim was assigned, the speciality of the physician, type of service (that is, medical care, surgery, laboratory service, etc.), and site of service (office, hospital, etc.). Data from the master health insurance enrollment file—which contains the age, sex, race, and residence of the beneficiary—are incorporated into the claims file data to provide information about the characteristics of the users.
Variations in Assignment by Age, Sex, and Race
Table 1 shows the percent of services assigned and the percent of charges assigned based on the new data set.
Among the aged, 45.8 percent of all physicians' services and 47.2 percent of all physicians' charges were assigned. Physicians' acceptance of assignment for services of males versus females showed little difference (45.5 percent and 45.9 percent of services respectively). It is notable that acceptance of assignment was greater with successively older age groups of beneficiaries—42.0 percent of services in the group 65-69 years of age compared to 56.8 percent for persons aged 85 and over. These findings may reflect several factors, including increased willingness on the part of physicians to accept assignment for steady, long-time patients, or for patients who are likely to have diminished income and assets. Also, as age increases there is increased participation in Medicaid—for which there is mandatory assignment.
Services for non-white beneficiaries were assigned at a considerably higher rate than services for white beneficiaries. For non-white beneficiaries 78.4 percent of services were assigned in contrast to 43.4 percent of services for white beneficiaries. Socioeconomic factors (such as poverty or physician behavior toward non-white beneficiaries) may influence the racial variation, but required assignment for Medicare beneficiaries who are also State Medicaid beneficiaries very likely explains much of the difference. 4
The Disabled
Among the disabled, physicians accepted assignment for 59.7 percent of the services provided—a proportion considerably higher than that for the aged. Unlike the aged, assignment of services for the disabled was lower for successively older age groups—77.1 percent for persons under 25 years of age to 56.7 percent for those in the age group 45-64 years. Similar to the aged, the sex of the disabled was not a determining factor. Also similar to the findings on the aged, data on non-whites showed a much higher assignment rate than data on whites—84.5 percent versus 56.1 percent of services respectively. This difference again is very likely explained by the levels of Medicaid entitlement.
Assignment by Geographic Area
Table 2 shows assignment rates by census region, division, and State. 5 Among the census regions, acceptance of assignment for services to the aged ranged from a low in the North Central region of 35.2 percent to a high of 56.8 percent in the Northeast region. Among the census divisions, the lowest percentages of services assigned were in the West North Central (32.4), Mountain (35.8), and East North Central (36.7) divisions while the highest rate was in the New England division (66.3). Similar variations were seen for the disabled population except that the rates for the disabled were consistently higher than those for the aged in all areas, possibly reflecting physicians' perceptions of less favorable economic conditions of the disabled compared with the aged.
There were wide variations in assignment rates among the States, with the figures for the aged ranging from a low of 18.0 percent of services assigned in Oregon to a high of 80.6 percent in Rhode Island. No geographic pattern in rate of assignment was apparent. In fact, adjacent States often had greatly different rates: Pennsylvania—56.9 percent and Ohio—27.3 percent; Connecticut—31.2 percent and Rhode Island—80.6 percent.
It may be noted that in most areas the percent of charges assigned was a little higher than the percent of services assigned, indicating that the average charge for assigned services was generally a little higher than the average charge for unassigned services.
These State data also show the same pattern of higher assignment rates for the disabled compared to the aged with the figures for the disabled ranging from a low of 11.7 percent of services assigned in Montana to a high of 96.5 percent in Vermont.
Assignment by Physician Specialty
Table 3 shows the rate of assignment of services and charges according to the specialties of the physicians. Assignment rates varied considerably among the physician specialties. For the aged, the percentages of services assigned ranged from 32.0 percent for services by licensed chiropractors to 67.1 percent for services by pathologists. For the disabled, the percentages ranged from 39.8 percent for otology/rhinology/laryngology services to 72.0 percent for podiatrists' services. Figure 1 shows the percents of total charges assigned for the five types of physicians that serve the greatest number of beneficiaries. Of these five types of physicians, acceptance of assignment for the aged was highest for Radiologists (55.5) and lowest for Ophthalmologists (44.0). The figure also shows that for each specialty except ophthalmology, the rate of assigned charges for the disabled is approximately 15 percentage points higher than for the aged.

Specialties varied considerably with geography. Table 4 shows the rates of assignment for the four most frequently used specialties by census region.
For the aged, the North Central region consistently had the lowest assignment rate among these four specialties. The Northeast region had the highest rate for internal medicine (55.8 percent), general surgery (60.9 percent), and radiology (72.6 percent). For the disabled, assignment rates were consistently higher in the Northeast compared to the South and North Central regions.
Physicians' Average Charge Per Service by Specialty and by Assignment
Table 5 shows the physicians' average submitted charge per service by specialty and by assignment. For the aged, average submitted charge by specialty ranged from a low of $6.76 per service by pathologists to a high of $50.30 per service by orthopedic surgeons. For the disabled, average charges ranged from $5.07 per service by pathologists to $47.98 per service by orthopedic surgeons.
For most specialties, the average charge per service was higher for assigned services in comparison to unassigned services. For the aged, exceptions to this rule were services by pathologists and radiologists. For the disabled, exceptions were for services by ophthalmologists and radiologists. For the aged, the ratio of average charge per service on assigned claims to average charge per service on unassigned claims reached a high of 1.44 for services by ophthalmologists, and for the disabled, the ratio reached 1.57 for services by otologists/rhinologists/laryngologists.
Average Percent Reduction
Under Medicare's Customary, Prevailing, and Reasonable Charge (CPR) mechanism, physicians' charges are passed through screens to determine the “reasonable” or “allowed” charge for each service. The total charges submitted by all physicians for services in 1975 were reduced 18.4 percent as a result of the CPR mechanism. Table 6 shows average percent reduction of submitted charges to allowed charges by specialty and by assignment. For the aged, the average percent reduction ranged from a low of 13.3 percent for charges by licensed chiropractors to a high of 23.6 percent for charges by anesthesiologists; for the disabled, the range was from 13.9 percent for charges by pathologists to 23.4 percent for charges by anesthesiologists. These differences by specialty in the rate of reduction of submitted charges reflect differences in charge patterns including differences by specialty in the rate of increase of current charges compared to charges submitted the previous calendar year (the period on which the reasonable charge determinations are based).
Examination of percent reduction by specialty according to assigned and unassigned charges shows that the percent reduction was generally a little higher on assigned charges in comparison to unassigned charges. For both the aged and disabled the most notable exceptions to this rule were charges by pathologists and radiologists.
It has been suggested that the size of the bill and the percent reduction on the bill are factors in the physician's decision to accept or reject assignment. In regard to these factors, one hypothesis is that as the size of the bill increases, the rate of assignment increases, because the larger the bill the greater the risk of the patient not being able to pay for it out-of-pocket. Thus, accepting assignment assures payment. Another hypothesis is that as the amount of reduction on the bill increases, the rate of assignment decreases, because refusing assignment allows the physician to recover the total charge from the patient.
Unfortunately, these hypotheses cannot be tested with the Medicare claims payment system. Under Medicare's system, if the beneficiary accumulates several bills from the same physician and submits them together they become one “claim.” Consequently, a $180 unassigned claim can actually represent bills for, say, a $50 service, a $30 service, and five $20 services rendered over a period of a year. Thus, the amount of a Medicare unassigned claim is an artifact of the way beneficiaries submit bills. Similarly, the percent reduction on an unassigned claim is an artifact of the way the beneficiary submits his or her bills, so that a 20 percent reduction on an unassigned claim can be the net effect of, say, a 30 percent reduction on a bill given to the beneficiary in February and a 15 percent reduction on a bill given to the beneficiary in July.
One hypothesis that can be tested is: Do the total charges a beneficiary accumulates from physicians over the year influence whether the charges will be assigned? The results of a special computer tabulation that groups beneficiaries by total annual charges per beneficiary indicates that the percent of charges assigned increases quite steadily as the beneficiaries' total charges increase. Table 7 (for all specialties) shows that for persons with annual charges under $100, only 38.2 percent were assigned. For persons with annual charges of $2,500 or more, 60.8 percent of the charges were assigned. Thus, it appears that the amount of total charges incurred by a beneficiary during the year is a determining factor in assignment decisions. Tabulations for general practice, internal medicine, general surgery, and radiology were also run ( Tables 8 , ,9, 9 , ,10, 10 , and and11). 11 ). The results were similar except for radiology, which exhibited no clear pattern as total charges increased.
Impact of Unassigned Claims on Aged Beneficiaries
Unassigned claims affect a high proportion of the beneficiaries. In 1975, of the total Medicare beneficiaries in the U.S. who received payments for physician services, nearly 70 percent had some liability from unassigned claims, that is, liability for the difference between the physician's charges and the Medicare-allowed charges. Table 12 shows the percentage of users with liability from unassigned claims and the percentage of users with $100 or more of liability. The data show that in the U.S., 9.7 percent of the users were liable for $100 or more from unassigned claims.
It may be observed that there is a wide variation by State in the percentage of beneficiaries affected by unassigned claims. The highest percentage of users with liability was in Oregon where 93.3 percent were affected by unassigned claims. Table 12 also shows that nearly 17 percent of the users in Oregon were liable for $100 or more from unassigned claims.
Beneficiaries' Cost-Sharing
Beneficiary participation or cost-sharing begins with the fixed monthly premium. Additional cost-sharing in outlays for the deductible and coinsurance is a variable expense and depends upon use. Similarly, liability arising from unassigned claims is a variable expense that depends upon the level of use and charges for services.
Deductible, Coinsurance, and Liability on Unassigned Claims
Table 13 provides a breakdown of estimated variable expenses for physicians' services incurred by the aged. The total estimated variable expenses were $1.73 billion in 1975 or $79.17 per beneficiary. Of the total variable expense, the deductible accounted for 35.1 percent, coinsurance accounted for 39.8 percent, and liability from unassigned claims accounted for 25.1 percent. The data indicate that variable liability was higher for successively older age groups—an average of $66.07 per beneficiary for those aged 65-69 years to $92.89 per beneficiary for those aged 80-84 years; as age increased, so did use. Total variable expenses for males were estimated at $81.17 per beneficiary compared to $77.83 per beneficiary for females. A wide difference was seen by race with white beneficiaries averaging $82.52 in variable expenditures and non-white persons averaging $53.09; the difference reflected both lower use and a higher rate of assigned claims for non-white beneficiaries. By census region, expenditures ranged from $71.16 per beneficiary in the North Central region to $85.00 in the Northeast region.
Not all of these expenses are paid out-of-pocket by Medicare beneficiaries. Of the total aged beneficiaries enrolled in Part B, 11.3 percent were included under the Medicaid “buy-in” provision. In addition, more than half of Medicare beneficiaries have private health insurance which supplements Medicare coverage. These policies are quite varied and may cover some or all of the charges not reimbursed by Medicare.
Monthly Premium
The remaining source of beneficiary outlay is the fixed expenditure for the monthly premium. Table 14 shows the fixed premium expenditures as well as the variable expenditures as components of total beneficiary liability. The fixed annual Part B premium shown of $66.01 is a prorated figure based on reimbursements for physicians' services as a percentage of total Part B reimbursement. 6
Overall, total beneficiary liability for physicians' services was estimated at $3.16 billion or $145.18 per beneficiary. Fixed expenditures (the premiums) represented 45.5 percent while variable expenditures made up 54.5 percent—(19.1 percent for the deductible, 21.7 percent for coinsurance, and 13.7 percent for liability on unassigned claims).
Medicare Reimbursements Compared to Beneficiary Liability
By comparing total beneficiary liability with Medicare reimbursements, the degree of insurance protection afforded the aged for physicians' services by the Medicare program can be further assessed. These total estimated expenditures of $4.57 billion or $209.81 per beneficiary are the physicians' charges less the charges above the allowed charges on assigned claims. Overall, the amount channeled through Medicare was $2.8 billion or 62.3 percent for physicians' services, while beneficiaries had liabilities (not including premiums) of $1.73 billion or 37.7 percent of total estimated expenditures for Part B physicians' services ( Table 15 ). Per beneficiary, figures were $130.64 paid by Medicare and $79.17 for which the beneficiary was liable.
Table 16 presents a different perspective by comparing the total liabilities of the beneficiaries (including the premium contributions as well as expenses due to the deductible, coinsurance, and the liability from unassigned claims) with the net Medicare contribution, that is, Medicare reimbursement less beneficiaries' premiums. The data indicate that the net amount contributed by public Medicare funds was $1.41 billion or 30.8 percent compared to $3.16 billion or 69.2 percent paid by or on behalf of the beneficiaries (that is, paid by the beneficiary or for the beneficiary, for example, by Medicaid or other insurance).
Figure 2 provides a comparison of the data in Tables 15 and and16. 16 . The bar on the left represents the channeling of payments for total physicians' charges that are due (from Table 15 ) and the bar on the right represents the sources of the funds for total physicians' charges that are due (from Table 16 ). The figure also suggests the complexity of the mechanism for the funding and for the payment of benefits for physicians' services under Medicare; the large proportion representing “Beneficiary Liability” is paid from several sources including out-of-pocket, by Medicaid, and by Medigap policies (the term given to insurance policies that fill in Medicare gaps in coverage.)

Summary and Conclusions
This cross-sectional analysis shows that assignment rates vary considerably by geographic area and by specialty of the physician. In some areas of the nation, nearly all charges are assigned so that many of the beneficiaries are relieved of the burden of paying the physician any charges beyond those deemed “reasonable.” Additionally, beneficiaries residing in areas where physicians generally accept assignment are relieved of the burden of the paper work involved in submitting claims—which can be difficult and confusing to an older and perhaps ill beneficiary. In contrast, in areas where the assignment rate is low, a vast majority of the beneficiaries have these burdens to contend with.
This analysis shows that of the total physicians' charges (excluding charges above the allowed on assigned claims), the payments channeled through Medicare amounted to 62 percent while payments made by or on behalf of the beneficiaries for the deductible, coinsurance, and for liability on unassigned claims amounted to nearly 38 percent of total physicians' charges. The percentage of payments for which the beneficiaries were liable was very high relative to Medicare's Part A program—where beneficiary liability was less than 10 percent of hospital charges in 1975.
A majority of Medicare beneficiaries carry private insurance to supplement Part B coverage. Of course, for this coverage, beneficiaries must pay additional premiums that generally are set high enough to cover benefits and administrative costs.
This analysis also shows that of the total physicians' charges (excluding charges above the allowed on assigned claims), the net amount contributed by Medicare was 30 percent (excluding prorated premium contributions). The remaining 70 percent of physicians' charges are attributed to liability for premium payments by or on behalf of the beneficiaries and for the deductible, coinsurance, and the amount exceeding the allowed charge on unassigned claims.
Because the percentage increase in Medicare Part B premiums is restricted to no more than the percentage increase in social security beneficiaries' checks, premium payments by or on behalf of beneficiaries—as a percent of total Medicare Part B receipts—has been declining while the general revenue portion of total Medicare receipts has been rising. In 1978 the percent from general revenues reached 69.4 percent while the percent from premium payments by beneficiaries fell to 24.1 percent ( Gibson, 1978 ). Thus, of the total Part B outlays, beneficiary contributions play a smaller role now than when Medicare began (approximately 50-50 contributions) and are likely to continue to decline. However, of the total physicians' charges that are liable for payment, the beneficiary portion may not simultaneously decline. First, the rate of reduction (that is, the difference between what the physicians charge and what Medicare allows) has been increasing (approximately 11 percent reduction in 1971 compared to 19 percent in 1975). Second, the assignment rate has generally been declining. Consequently, these forces may counteract the lower contribution of beneficiaries to Medicare outlays and may tend to keep up the amount of the total physicians' charges for which the beneficiaries are liable.
Technical Note
Reliability of estimates *.
The data used in this paper are estimates based on a 1 percent sample (except for Table 5 which is based on a 5 percent sample) of the beneficiary population and hence are subject to sampling variability. Tables A through throughI I will enable the reader to obtain approximate standard errors for the estimates in this paper. The standard error is primarily a measure of sampling variability—that is, of the variation that occurs by chance because a sample rather than the whole population is used. To calculate the standard errors at a reasonable cost for the wide variety of estimates in this paper, it was necessary to use approximation methods. Thus, these tables should be used only as indicators of the order of magnitude of the standard errors for specific estimates.
The sample estimate and an estimate of its standard error permit us to construct interval estimates with prescribed confidence that the interval includes the average result of all possible samples (for a given sampling rate).
To illustrate, if all possible samples were selected, if each of these were surveyed under essentially the same conditions, and if an estimate and its estimated standard error were calculated from each sample, then:
- Approximately ⅔ of the intervals from one standard error below the estimate to one standard error above the estimate would include the average value of all possible samples. We call an interval from one standard error below the estimate to one standard error above the estimate a ⅔ confidence interval.
- Approximately 9 / 10 of the intervals from 1.6 standard errors below the estimate to 1.6 standard errors above the estimate would include the average value of all possible samples. We call an interval from 1.6 standard errors below the estimate to 1.6 standard errors above the estimate a 90 percent confidence interval.
- Approximately 19 / 20 of the intervals from two standard errors below the estimate to two standard errors above the estimate would include the average value of all possible samples. We call an interval from two standard errors below the estimate to two standard errors above the estimate a 95 percent confidence interval.
- Almost all intervals from three standard errors below the sample estimate to three standard errors above the sample estimate would include the average value of all possible samples.
The average value of all possible samples may or may not be contained in any particular computed interval. But for a particular sample, one can say with specified confidence that the average of all possible samples is included in the constructed interval.
The relative standard error is defined as the standard error of the estimate divided by the value being estimated. In general, estimates for small subgroups, and percentages or means with small bases tend to be relatively unreliable. The reader should be aware that some of the estimates in this paper have high relative standard errors.
The use of Tables A and andB B is straightforward. For example, the standard error of an estimated $100 million reimbursement is found to be $3.5 million. Simple linear interpolation may be used for values not tabled.
Tables C through throughH H are for estimated percentages or means per beneficiary and require knowledge of the number in the base of the estimate. Thee numbers can be found in Tables J through throughO. O . To illustrate their use, Table 13 shows the amount of deductible per beneficiary for age group 65-69 to be $23.06. The following steps, using double linear interpolation, show how to obtain the standard error of this estimate.
- Table J shows the number of beneficiaries in the base to be 7,345,221.
- Standard error for $20.00 and 7 million enrolled—$.60.
- Standard error for $30.00 and 7 million enrolled—$.74.
- The interpolated standard error for $23.06 and 7 million is $.64.
- Standard error for $20.00 and 10 million enrolled—$.50.
- Standard error for $30.00 and 10 million enrolled—$.62.
- The interpolated standard error for $23.06 and 10 million is $.54.
- Interpolating between $.64 and $.54 for the 7,345,221 beneficiaries in the base, we find the standard error of the estimate to be $.63.
Table I contains the relative standard error of dollars per service. (Note that this table is based on a 5 percent sample whereas all other standard error tables are based on a 1 percent sample). To illustrate its use, assume we have an estimate of $18 per service based on 7,000,000 services. The relative standard error is .0089 and the standard error .0089 × $18 = $.16.
Acknowledgments
The authors wish to acknowledge the assistance of Jill M. Hare in coordinating the preparation and typing of this report.
1 The “reasonable” or “allowed” charge is the lowest of (1) the actual charge made by the physician for that service, (2) the physician's customary charge (the physician's 50th percentile) for that service or (3) the prevailing charge (set at the 75th percentile of weighted customaries) in that locality for that service.
2 For example, suppose a beneficiary has met the $60 deductible and is charged $80 for a physician service. If the reasonable charge is determined to be $60 and the physician accepts assignment, the program reimbuses the physician 80 percent or $48. The beneficiary owes the 20 percent coinsurance or $12. If the physician does not accept assignment, the beneficiary owes the $12 coinsurance plus $20, the amount above the reasonable charge.
3 The net assignment rate is the number of assigned claims expressed as a percentage of claims received, omitting claims from hospital-based physicians and group-practice prepayment plans which are considered assigned by definition. Data are from the Bureau of Program Operations, HCFA.
4 Medicare data for the aged for 1975 shows that 11.3 percent of total beneficiaries were included in state “buy-ins” to Medicare. By race, the percent of white persons was 9.3 percent and for non-whites, 35.3 percent. For the disabled, 18.6 percent of Part B beneficiaries were included in State “buy-ins” to Medicare. The percent for white persons was 16.5 and for non-whites, 31.6 percent.
5 Codes submitted for this data base to indicate whether claims were assigned are unreliable for California. Because California's assignment rate significantly affects the rate for the census division and region, data are also omitted for the Pacific division and the Western region. Workload reports generated by the Bureau of Program Operations, HCFA, indicate that 57.6 percent of total claims (aged and disabled combined) and 48.4 percent of total charges processed by California fiscal agents (carriers) in 1975 were assigned.
6 The total annual premium was $80.40; reimbursements for physician services accounted for 82.1 percent of the Part B reimbursement.
* Prepared by James C. Beebe, Statistical and Research Services Branch, Office of Research.
- For a detailed discussion of source of Medicare funds, see Gibson Robert M. National Health Expenditures, 1978. Health Care Financing Review. 1979 Summer; [ PMC free article ] [ PubMed ] [ Google Scholar ]

COMMENTS
If your doctor, provider, or supplier doesn't accept assignment: You might have to pay the full amount at the time of service. They should submit a claim to Medicare for any Medicare-covered services they give you, and they can't charge you for submitting a claim. If they refuse to submit a Medicare claim, you can submit your own claim to ...
A nonparticipating provider can choose to accept assignment on a case-by-case basis. They can indicate this on Form CMS-1500 in box 27. The vast majority of nonparticipating providers who bill Medicare choose to accept assignment for the claim being billed. Nonparticipating providers do not have to bill your Medigap plan on your behalf.
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies, without paying a deductible or coinsurance if the provider accepts assignment.
Medicare assignment is an agreement by your doctor or other healthcare providers to accept the Medicare-approved amount as the full cost for a covered service. Providers who "accept assignment" bill Medicare directly for Part B-covered services and cannot charge you more than the applicable deductible and coinsurance.
Medicare assignment is a fee schedule agreement between the federal government's Medicare program and a doctor or facility. When Medicare assignment is accepted, it means your doctor agrees to the payment terms of Medicare. Doctors that accept Medicare assignment fall under one of three designations: a participating doctor, a non ...
Participating providers accept Medicare and always take assignment. Taking assignment means that the provider accepts Medicare's approved amount for health care services as full payment. These providers are required to submit a bill (file a claim) to Medicare for care you receive. Medicare will process the bill and pay your provider directly ...
Medicare "participation" means you agree to accept claims assignment for all Medicare-covered services to your patients. By accepting assignment, you agree to accept Medicare-allowed amounts as payment in full. You may not collect more from the patient than the Medicare deductible and coinsurance or copayment. Participating Provider or ...
Doctors that take Medicare can sign a contract to accept assignment for all Medicare services, or be a non-participating provider that accepts assignment for some services but not all. A medical provider that accepts Medicare assignment must submit claims directly to Medicare on your behalf. They will be paid the agreed upon amount by Medicare ...
Summary: Medicare Assignment is an agreement between healthcare providers and Medicare, where providers accept the Medicare-approved amount as full payment, preventing them from charging beneficiaries extra. This benefits Medicare beneficiaries by controlling their costs and ensuring they only pay deductibles and copayments.
The Medicare accept assignment definition pertains to physicians, medical suppliers and medical providers that agree to accept Medicare-approved charges as total and full payment for all covered services without adding extra charges. ... Providers who accept Medicare assignment must submit all claims directly to Medicare, so recipients can't be ...
Medicare participation means you agree to accept claims assignment for all covered patient services. By accepting assignment, you agree to accept Medicare-allowed amounts as payment in full. You can't collect more from the patient than the deductible and coinsurance or copayment.The Social Security Act says you must submit patient Medicare claims whether or not you participate.
Non-assignment of Benefits. Non-assigned is the method of reimbursement a physician/supplier has when choosing to not accept assignment of benefits. Under this method, a non-participating provider is the only provider that can file a claim as non-assigned. When the provider does not accept assignment, the Medicare payment will be made directly ...
Nonassignment of Benefits. The second reimbursement method a physician/supplier has is choosing to not accept assignment of benefits. Under this method, a non-participating provider is the only provider that can file a claim as non-assigned. When the provider does not accept assignment, the Medicare payment will be made directly to the beneficiary.
Option 1: Medicare participation. PAR physicians agree to take assignment on all Medicare claims, which means physicians must accept Medicare's approved amount (which is the 80% that Medicare pays plus the 20% patient copayment) as payment in full for all covered services for the duration of the calendar year.
Medicare sets a fixed cost to pay for every benefit they cover. This amount is called Medicare assignment. You have the largest healthcare provider network with over 800,000 providers nationwide on Original Medicare. You can see any doctor nationwide that accepts Medicare. Understanding the differences between your cost and the difference ...
What it means to "accept Medicare assignment". In short, accepting Medicare assignment means signing a contract to accept whatever Medicare pays for a covered service as full payment. Participating and non-participating status only applies to Medicare Part B; Medicare Advantage plans operate with contracts similar to commercial insurance ...
Accepting assignment is a real concern for those who have Original Medicare coverage. Physicians (or any other healthcare providers or facilities) who accept assignment agree to take Medicare's payment for services. They cannot bill a Medicare beneficiary in excess of the Medicare allowance, which is the copayment or coinsurance.
PAR physicians agree to take assignment on all Medicare claims, which means that they must accept Medicare's approved amount (which is the 80% that Medicare pays plus the 20% patient copayment) as ...
A: If your doctor doesn't "accept assignment," (ie, is a non-participating provider) it means he or she might see Medicare patients and accept Medicare reimbursement as partial payment, but wants to be paid more than the amount that Medicare is willing to pay. As a result, you may end up paying the difference between what Medicare will ...
Provider Nomination and the Geographic Assignment Rule. Section 911(b) of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA), Public Law 108-173, repealed the provider nomination provisions formerly found in Section 1816 of the Title XVIII of the Social Security Act and replaced it with the Geographic Assignment ...
According to the National Uniform Claim Committee (NUCC), the "Accept Assignment" box indicates that the provider agrees to accept assignment. It simply says to enter an X in the correct box. It does NOT define what accepting assignment might or might not mean. It is important to understand that if you are a participating provider in any ...
According to the Medicare website: Assignment means that your doctor, provider, or supplier agrees (or is required by law) to accept the Medicare-approved amount as full payment for covered services. This means that for Medicare to cover the entire cost of a covered service, you'll need to go to a service provider who accepts assignment.
Thus, accepting assignment assures payment. Another hypothesis is that as the amount of reduction on the bill increases, the rate of assignment decreases, because refusing assignment allows the physician to recover the total charge from the patient. Unfortunately, these hypotheses cannot be tested with the Medicare claims payment system.