- ASH Foundation
- Log in or create an account
- Publications
- Diversity Equity and Inclusion
- Global Initiatives
- American Society of Hematology
- Resources for Hematology Fellows

Hematopoiesis Case Studies
- Agenda for Nematology Research
- Precision Medicine
- Genome Editing and Gene Therapy
- Immunologic Treatment
- Research Support and Funding
Case studies are board-style questions with explanations and links to related articles featured in Hematopoiesis , an e-newsletter that is sent to hematology trainees on a quarterly basis.
- A 73-Year-Old Man With Extensive Bruising
- A 2.5-Year-Old Girl With Fever and Pancytopenia
- 21-Year-Old With Duodenal Adenocarcinoma and a History of T- cell Lymphoma
- 78-Year-Old Woman with Thrombocytopenia and Splenomegaly
- 48-Year-Old Woman With Weight Loss, Hepatomegaly, and Splenomegaly
- Diagnosis of a 64-Year-Old Man With Anemia and Thrombocytopenia
- Prenatal Management of 21-Year-Old Woman to Reduce Risk of Severe Thrombocytopenia and Intracranial Hemorrhage
- Three-year-old Boy With Pancytopenia
- COVID-19 Management in Patients With Hematologic Malignancies
- 25-Year-Old Woman Referred to Clinic for Erythrocytosis
- 60-Year-Old Woman With Headache and Blurred Vision
- Chronic Immune Thrombocytopenia Purpura
- New Therapies for Acute Myeloid Leukemia
- Sickle Cell Disease – A 25-Year-Old in Transition
- Supportive Care in Multiple Myeloma
- Managing Toxicities in CAR T Cell Therapy
- Bicytopenia and Syndromic Features in a Four-Year-Old Child
- Emerging Therapies in Hemophilia
- 47-Year-Old Woman With New-Onset AML and Leukostasis
- The Smart Choice for Prevention of Recurrent Venous Thromboembolism
- 36-Year-Old Man with Severe Low Back Pain and BCP-ALL
- 52 Year-Old Woman with Fatigue and Neuropathy
- 29-Year-Old Woman with Postpartum Hemorrhage
- 30 Year-Old Female with Pancytopenia and Fatigue
- Progressive Fatigue and Cytopenias in a 70-Year-Old Man
- 32-year old man with neurologic changes and cytopenias
- 44-Year-Old Man with Fever, Abdominal Pain, and Pancytopenia
- Unexplained Thrombocytopenia in a Child
- Neutropenia in a Patient with Rheumatoid Arthritis
- 50-Year-Old Woman with Fibrous Capsule after Breast Augmentation
- 32-Year-Old Female with Multiple Ecchymoses
- 32-Year-Old Female with Anemia and Confusion
- GI Bleed in a Patient with Amyloidosis
- 32-Year-Old Man Admitted to Hospital With Diffuse Lymphadenopathy
- Image Challenge: 54-Year-Old Man With Abnormal Circulating Lymphocytes
- Image Challenge: Hematology Consult - Middle-Age Woman With Neutropenia and Splenomegaly
- Image Challenge: Hematology Consult - Middle-Age Man With Neuropathy and Splenomegaly
- Image Challenge: Bone Marrow Aspirate (August 2012)
- 65-Year-Old with History of Waldenström Macroglobulinemia (May 2012)
- Cervical Adenopathy, Weight Loss, and Night Sweats (February 2012)
- 12-Year-Old Boy With Normocytic Anemia and Bone Pain (August 2011)
- Putting Two and Two Together (May 2011)
- Four-Year-Old Male with Red Urine and Fever (February 2011)
- Intermittent Epistaxis in a Young Boy
- Prognostic Factors in Acute Lymphocytic Leukemia
- 55-Year-Old Male With Multiple Myeloma and Prognosis of Undetermined Significance
- 24-Year-Old Woman With Dark-Colored Urine
- Personalizing Anticoagulation: Determination of Warfarin Dosing
- Microcytic Anemia Refractory to Oral Iron Supplementation
- ITP is Also a Platelet Production Problem
- A 26-Year-Old Man With History of Fatigue, Fevers, and Gingival Bleeding
- Finding the Best Prognostic Outcome in a Patient With AML
- Bcl-6 and Its Relationship to Diffuse Large B-Cell Lymphoma
- A 78-Year-Old Man With Elevated Leukocytes and Anemia
- Flow Cytometry Pattern in APL
- Identifying One of the 5q- Syndrome Genes
- Do You Know JAK?
Table of Contents
Explore the latest case studies and articles from Hematopoiesis .
- Announcing Hematopoiesis, Our New ASH Trainee Council Newsletter by Trainees and for Trainees
- A Primer on Advocacy for the Hematology Trainee
- Blood Smear: The Fifth Vital Sign in Hematology
- Chimeric Antigen Receptor T-cell Therapy: What Fellows Need to Know
- The Blood Sisters Project
- Case Study: A 73-Year-Old Man With Extensive Bruising
- Case Study: A 2.5-Year-Old Girl With Fever and Pancytopenia
- Privacy Policy
- Clinical Microscopy
- Clinical Pathology
- Cytopathology
- Hematopathology
- Histotechnology
- Informatics
- Laboratory Medicine
- Surgical Pathology
Case Studies in Hematology and Coagulation

- Product Description
This compendium of 200 case studies is the result of a unique collaboration of leading hematologists, hematopathologists, and oncologists. It serves as both a case-based guide to the diagnosis and management of patients suffering from hematologic conditions and a valuable teaching tool.
The editors have compiled an invaluable collection of cases covering common and rare entities—from anemias and acute leukemias to plasma cell, platelet and coagulation disorders. Cases are presented in an easy-to-follow format, grouped by related conditions. The final two sections present 27 self-study challenge cases that include answers (with images) provided by the authors of each case.
A broad range of topics in hematology and coagulation are covered in this CaseSet, including:
- Myeloproliferative Disorders
- Myelodysplastic Syndromes
- Lymphoproliferative Disorders
- Lymphomas and Their Mimicks
- Plasma Cell Disorders
- Platelet Disorders
- Hematologic Infectious Diseases
- Other Hematologic Disorders
- Bleeding Disorders
- Thrombophilias
- Other Hemostasis Disorders
Home | About Us | Contact Us
© Copyright 2024 Created on iPublishCentral
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.14(4); 2022 Apr

The Case Report of a 97-Year-Old Patient With Chronic Anemia and Hemoglobin Value of 1.7 g/dl and Review of the Literature
Andreas kyvetos.
1 2nd Department of Internal Medicine, General and Oncology Hospital of Kifissia “Agioi Anargyroi”, Athens, GRC
Stefani Panayiotou
Panagiota voukelatou, ioannis vrettos, georgios boulmetis.
Although hemoglobin levels beneath 6.5 g/dl are considered to be life-threatening and the patients theoretically suffer from a cluster of symptoms, few cases of patients who seek medical assistance when their hemoglobin levels had fallen beneath 3 g/dl have been reported in the literature. Here, we describe the case of a 97-year-old patient who was transferred to the emergency department with dyspnea and the initial screening tests showed a hemoglobin level of 1.7 g/dl, due to iron deficiency. The patient was hemodynamically stable, and no ischemic lesions were seen on the electrocardiogram. His dyspnea was due to a lower respiratory tract infection and bilateral pleural effusion. He was bedridden for two years. His absence of physical activity in combination with the slow onset of anemia and the absence of severe underlying pulmonary and cardiovascular diseases could hide the symptoms until additional stressful events, such as the respiratory tract infection and the deterioration of heart function, occurred. So, we must keep in mind that in elderly patients with reduced physical activity and without severe pulmonary and cardiovascular comorbidities, the symptoms of severe anemia may go unnoticed until hemoglobin reaches life-threatening levels.
Introduction
The symptoms of anemia like dyspnea, tachypnea, palpitations, cold skin, heart failure, cognitive dysfunction, etc. depend, inter alia, on the severity of anemia, the rapidity of its onset, the age, and the physiological status of the patient. Various adaptive mechanisms are mobilized by the human body in order to counterbalance the effects of anemia, although almost every organ system is finally affected [ 1 ]. The most significant adaptive responses involve the cardiovascular system. These adaptive responses include increased cardiac output and redistribution of blood flow toward the heart and central nervous system and away from the splanchnic vascular beds [ 2 ].
In cases of chronic anemia, it has been postulated that the hyperkinetic response in patients at rest, occurs only when hemoglobin level falls beneath 7 g/dl [ 3 ]. Moreover, in hemoglobin levels beneath 7.5 g/dl, 100 ml of arterial blood contains 10 ml of oxygen instead of 20 ml in healthy subjects [ 1 ]. Nevertheless, certain symptoms or complications experienced by a patient cannot be determined with the accuracy of hemoglobin levels alone [ 4 ]. Heart, lung, and cerebrovascular diseases, as well as age, may limit the adaptive responses to anemia [ 2 ]. On the other hand, in young and otherwise healthy persons, chronic anemia may remain unnoticed until hemoglobin level falls beneath a critical level or episodes of exertional stress occur [ 1 ].
According to several grading systems for anemia, hemoglobin levels beneath 6.5 g/dl are considered life-threatening [ 5 ], and the patient theoretically suffers from a cluster of symptoms. However, a few cases of patients have been reported in the literature [ 6 - 12 ] who seek medical assistance when their hemoglobin levels had fallen beneath 3 g/dl and therefore their hematocrit levels were beneath 10%.
In this report, we describe the case of a “too hard to die” 97-year-old patient who was transferred to the emergency department with dyspnea and the initial screening tests showed a hemoglobin level of 1.7 g/dl, and we review and discuss the reported cases of other “too hard to die” patients with hemoglobin concentrations beneath 3.0 g/dl due to chronic anemia. This paper is an extended version of a work presented at the 24ο Panhellenic Congress of Internal Medicine, Athens, Greece, on 3-6 November 2021.
Case presentation
A 97-year-old patient was admitted to the emergency department due to shortness of breath for one week, without other symptoms. According to his medical history, the patient suffered from anemia, treated with 247.25 mg ferrous sulfate, 5 mg folic acid daily, and hypothyroidism treated with levothyroxine sodium 75 mcg. His relatives were aware of his anemia but they preferred to treat it with per-os medication without investigating the cause of the anemia. They reported that the patient’s stools for several days were tarry but they believed it to be due to the iron he was receiving. Six months ago, he was diagnosed with pulmonary embolism which was effectively managed with apixaban 110 mg twice daily and two years ago he had an ischemic stroke that left him bedridden.
At the time of presentation, he appeared pale and lethargic (Glasgow Coma Scale 7/15) with tachypnea (30 breaths/min). Bilateral crepitations and rhonchi were present in lung auscultation. There was a systolic murmur throughout the precordium. A digital rectal examination was performed and it was negative for melena. His blood pressure was 120/60 mmHg with a regular pulse rate of 90 beats/min. Other findings from the physical examination were unremarkable. The laboratory test revealed hypochromic microcytic anemia, with hemoglobin value of 1.7 g/dl (normal range: 12-16 g/dl), hematocrit 6.9% (normal range: 37-48%), red blood cell count of 1.53 Μ/ml (normal range: 4.5-6.3 Μ/ml), mean corpuscular volume of 75 fl (normal range: 80-96 fl), and mean corpuscular hemoglobin of 23.8 pg (normal range: 27-34 pg). The complete blood count was examined twice in order to avoid a laboratory error in measurement. Other laboratory results showed: white blood cells 6.47 K/μl (normal range: 4.0-11.0 Κ/μl), platelets 121 Κ/μl (normal range: 150-400 Κ/μl), C-reactive protein 3.56 mg/dl (normal range: <0.5 mg/dl), creatinine 1.7 mg/dl (normal range: 0.6-1.4 mg/dl), urea 135 mg/dl (normal range: 10-50 mg/dl), total bilirubin 0.7 mg/dl (normal range: 0.2-1 mg/dl), ferritin 20 ng/ml (normal range: 11-204 ng/ml), folicid acid >40 ng/ml (normal range: 3.1-20 ng/ml), cobalamin 700 pg/ml (normal range: 187-883 pg/ml), erythrocyte sedimentation rate 10 mm/h (normal range: 2-20 mm/h), direct Coombs test negative, a normal urinalysis test, high sensitivity troponin I (HS-TnI) 34 pg/ml (normal range: <11.6 pg/ml), and brain natriuretic peptide (BNP) 804.30 pg/ml (normal range: <100 pg/ml). No ischemic lesions were seen on the electrocardiogram (Figure 1 ) and the second sample of HS-TnI was within the normal range. Hematological consultation was requested and the blood smear revealed normal platelets count of 199 Κ/μl and microcytic red blood cells with hypochromia. Erythropoietin levels and total iron-binding capacity were not performed due to the lack of these laboratory tests in our hospital.

Cardiac echocardiography was performed that showed signs of heart failure with preserved ejection fraction and grade I diastolic dysfunction. A chest CT scan revealed a lower respiratory tract infection and a bilateral pleural effusion (Figure 2 ) compatible with his heart failure. An abdominal CT scan was performed that did not reveal any pathology.

It revealed a lower respiratory tract infection (blue arrows) and bilateral pleural effusion (red arrows).
The patient was treated with furosemide, ceftriaxone 2 g once daily and clindamycin 600 mg three times daily. A total of 5 units of packed RBCs were transfused resulting in a hemoglobin value of 8.7 g/dl. The renal function at the admission was impaired but gradually it was improved and the discharge creatinine was 0.8 mg/dl. Gastroscopy and colonoscopy were scheduled but his relatives refused any further investigation to identify the cause of anemia. Although the investigation for the cause of anemia was inadequate, the history of tarry stools in a patient receiving anticoagulant, in combination with a ferritin value of 20 ng/ml made us assume that the main cause of his anemia was chronic bleeding from the gastrointestinal tract. So, he received 1 g of intravenous iron. The patient had a remarkable recovery to his preadmission state and he was discharged home 11 days after.
Our patient had one of the lowest hemoglobin levels that have ever been reported. To our knowledge, the lowest hemoglobin concentration that has ever been reported in a non-trauma patient is 1.2 g/dl (hematocrit of 3.0%) due to paroxysmal nocturnal hemoglobinuria. The 21-year-old male patient was presented with profound weakness and abdominal pain, although hemodynamically stable [ 6 ]. The second-lowest reported hemoglobin was 1.3 g/dl (hematocrit of 4.7%) and it was due to iron deficiency, because of chronic uterine bleeding [ 7 ]. The patient was a 44-year-old woman with weakness and dyspnea at rest. She had regular pulses, normal arterial pressure, and 25 breaths per minute. She had severe lactic acidosis and inverted T waves in leads III, aVF in her ECG.
Likewise, an extremely low hemoglobin level, in a patient with chronic anemia, has been reported by Jost et al. They presented a 29-year-old woman with celiac disease, bulimia nervosa, and iron-deficiency anemia. She had a hemoglobin level of 1.7 g/dl. She was malnourished and she reported exhaustion, fatigue, and abdominal pain but no critical symptoms [ 8 ]. On the other hand, a 76-year-old woman had critical symptoms with hemoglobin 2.4 g/dl due to gastric adenocarcinoma. She was hemodynamically unstable and reported increased fatigue, reduced activity, intermittent nausea or vomiting, and melena. Clarke and Weston-Smith reported a case of folate deficiency in a 50-year-old woman with hemoglobin of 2.6 g/dl. They reported that the patient was stable, alert, and keen to avoid admission. She had a soft ejection systolic murmur and her ECG was in normal sinus rhythm of 90 beats per minute with ST-segment depression in lateral leads [ 10 ].
Another case that was presented by Reibke et al. was a 32-year-old male with hemoglobin 2.9 g/dl due to B12 deficiency and minor beta-thalassemia [ 11 ]. Finally, extremely low hemoglobin levels have been reported by Bhatia et al., who performed coronary hemodynamic studies on 14 patients with chronic anemia. They reported three patients with hemoglobin levels ≤3.0 mg/dl; they had hemoglobin levels of 1.6 mg/dl, 2.4 mg/dl, and 3.0 mg/dl, and all of them were between 23 to 25 years old. Two of them had iron-deficiency anemia due to ankylostomiasis and the third had B12 deficiency [ 12 ].
All of these patients had no underlying pulmonary and cardiovascular diseases and they developed gradually severe anemia. This gradual onset allowed the compensatory mechanisms to take place and so, the patients arrived at the emergency departments with hemoglobin levels much lower than that considered to be life-threatening. The difference with our patients is that almost all, with one exception [ 9 ], were less than 50 years old and so, theoretically, they had satisfactory adaptive responses to anemia. The exception [ 9 ] was referred to as a 76-year-old woman with gastric adenocarcinoma that arrived at the emergency department with hypotension and tachycardia. This woman had symptoms compatible with anemia for several weeks.
In contrast, our patient was hemodynamically stable, and he had no profound symptoms until the time dyspnea was developed due to both the lower respiratory tract infection and also the deterioration of cardiac function which was triggered probably both by anemia and the respiratory tract infection. What hid the patient’s symptoms from his relatives, according to our opinion, was the non-existent, even the minimal, physical activity of this elderly. His absence of physical activity in combination with the slow onset of anemia and the absence of severe underlying pulmonary and cardiovascular diseases could hide the symptoms until the time of additional stressful events, such as the respiratory tract infection and the deterioration of heart function, occurred.
Conclusions
Symptomatic anemia is a common finding in elderly patients. Whereas, in elderly patients with reduced physical activity and without severe pulmonary and cardiovascular comorbidities, the symptoms of severe anemia may go unnoticed until hemoglobin reaches life-threatening levels. Careful surveillance of these patients is mandatory with regular clinical examination and laboratory blood tests, especially for those who are receiving anticoagulant therapy.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
- IN THIS TOPIC
Lablogatory
A blog for medical laboratory professionals

Hematology Case Study: 75 Year Old Man with Leukopenia
A 75 year old male first presented earlier this year with abnormal CBC results. The patient has a history of Type 2 diabetes, high blood pressure and atrial fibrillation. He was diagnosed with non-small-cell lung cancer (NSCLC) 6 years ago. His stage II NSCLC was completely removed with surgery. Surgery was followed up with adjuvant cisplatin-based chemotherapy to reduce the chance that the cancer would return. In June, he was referred to the hematology oncology department following consecutive CBCs that revealed leukopenia and thrombocytopenia. The CBC results from these specimens are shown below in Table 1.
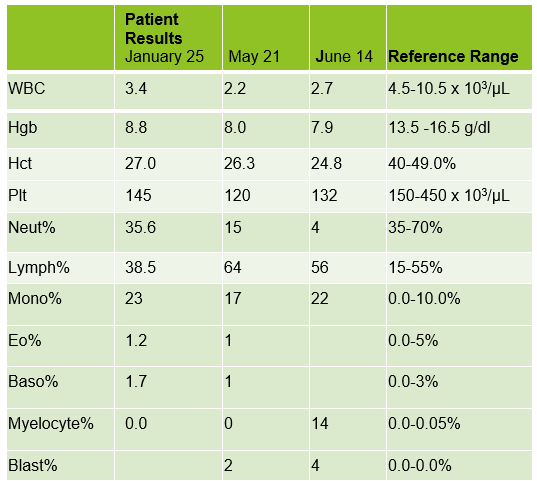
The peripheral blood sample from June was sent for flow cytometry. A leukemia/lymphoma phenotype was performed. Result comments noted proportionately decreased granulocytes with a left shift and 4% blasts. The blasts were CD34+, CD117+, HLA-DR+, CD13+ and CD33+ and were identified as myeloblasts. There were proportionately increased atypical monocytes with CD23 expression. Lymphocytes were also proportionately increased and included an increased population of CD57+, CD3+ T cells consistent with T-cell large granular (LGL) expansion. Immunophenotypic findings raised a concern for a myelodysplastic process. The hematologist discussed the findings with the patient and the patient was scheduled for a bone marrow biopsy. The procedure was performed 3 weeks later. CBC results on the day of the procedure are shown below in Table 2.
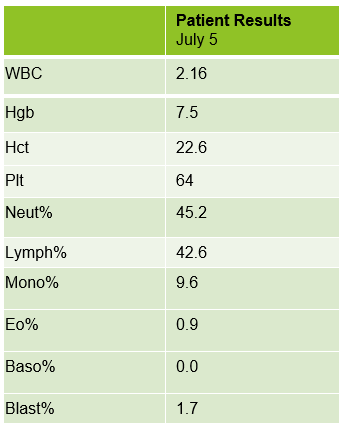
Bone marrow aspirate showed markedly increased myeloblasts (55%), consistent with acute myeloid leukemia (AML), nonacute promyelocytic leukemia (APL) type. The phenotype of the blasts was CD13+, CD33+, CD117+ and HLA-DR+. Blasts were negative for CD34. Several genomic variations were found in the specimen. These included variations in IDH2, SRSF2, STAG2 and ASXL1. Diagnosis: Increase in myeloblasts consistent with AML, nonAPL type.
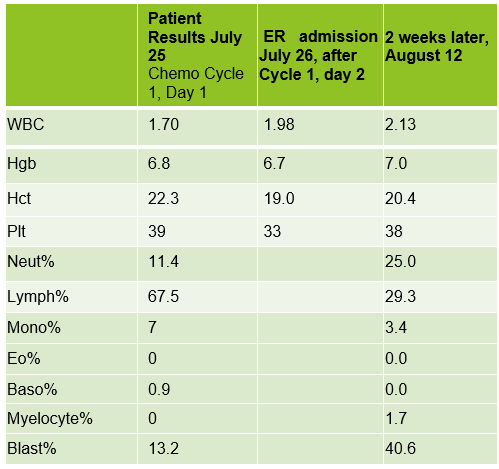
In July, 20 days after the bone marrow procedure and AML diagnosis, the patient was scheduled to begin his first cycle of Azacitidine (Vidaza). Based on his critical hemoglobin, the patient received 1 unit of packed RBCs followed by his first Vidaza injections. This Cycle 1, Day 1 chemotherapy was well tolerated, and he returned home. The following day he returned for his second treatment. His CBC showed good response to the previous day’s transfusion and his Cycle 1, Day 2 Vidaza was administered without incident. However, that evening the patient presented to the ER with nausea, vomiting and nose bleeds. The patient was admitted to the hospital and received another RBC transfusion. For the next several days the patient continued to do poorly, requiring additional RBC transfusions, and the Vidaza treatments were deferred, then discontinued. The patient had several ER visits and hospital admissions with transfusions over the next 2 weeks. During this time, we saw his blast% on his differential peak at over 60%. The patient was transferred to the palliative care team with care and comfort measures. CBC results from Cycle 1, Day 1 and subsequent CBC results are shown below. Note the sharp increase in blasts over a 2-week period.
AML is the most common acute leukemia in adults. In AML with minimal differentiation, evidence of bone marrow failure is characterized by anemia, neutropenia, and thrombocytopenia. The median age for patients with AML in the US is 66-67, and those who are older than 55-65 at diagnosis often have challenges and lower odds for long term survival. These older patients tend to have poor tolerance to traditional aggressive chemotherapy because of other health issues. This patient was likely not a good candidate for strong chemotherapy because of his age and health history. In these more fragile patients, Vidaza may be used. Vidaza is a class of drug called a hypomethylating agent that works by switching off DNA methyltransferase. This switches on genes that stop the cancer cells growing and dividing. The goal is to reduce the number of abnormal blood cells and to control cell growth.
As you can see from the CBC results, the onset of this patient’s AML was very abrupt, and the disease progressed rapidly. He has several risk factors that made him more likely to be diagnosed with AML. Older age is a risk factor for AML, and AML is more common in males than females. He has a history of smoking which is a behavioral risk factor associated with AML. Additionally, patients with cancer who are treated with certain chemotherapy drugs are more likely to develop AML in the years following treatment. This patient was treated with cisplatin following lung cancer surgery. Cisplatin is an alkylating agent which has been linked to an increased risk of AML.
Also interesting is the note on the peripheral blood phenotype interpretation that a T-cell large granular lymphocyte (LGL) expansion was present. These are an increased population of CD57+, CD3+ T cells. LGL clones have been described in AML and a hallmark of this association is cytopenia, as is observed in this patient. The patient’s poor prognosis can partly be attributed to the p.Gly646TrfsTer12 alteration in the ASXL1 gene, identified in the bone marrow interpretation. This alteration is associated with decreased overall survival and poor prognosis which was observed in this patient.
I work in a hospital with a large hematology/oncology practice, and we see a lot of adult leukemia patients. Many of the patients we see regularly have Chronic Lymphocytic Leukemia (CLL). We feel like we get to know these patients, because even though we never see them, we see their CBCs every week, sometimes for many years. This was an interesting case because it reminded me of the sudden onset and rapid progression of AML. It was amazing to see the differentials change so dramatically in a matter of weeks. This patient is currently receiving care and comfort end of life measures.
Fattizzo, B, Bellani, V, et al. Large Granular Lymphocyte Expansion in Myeloid Diseases and Bone Marrow Failure Syndromes: Whoever Seeks Finds. Front. Oncol., Sec. Cancer Immunity and Immunotherapy. 01 October 2021.
Pratcorona M, Abbas S, Sanders MA, Koenders JE, et al.Acquired mutations in ASXL1 in acute myeloid leukemia: prevalence and prognostic value. Haematologica. 2012 Mar;97(3):388-92. doi: 10.3324/haematol.2011.051532. Epub 2011 Nov 4. PMID: 22058207; PMCID: PMC3291593.
https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/types-treatment
Thomas XG, Dmoszynska A, Wierzbowska, et al. Results from a randomized phase III trial of decitabine versus supportive care or low-dose cytarabine for the treatment of older patients with newly diagnosed AML. Journal of Clinical Oncology 29:2011
Turgeon, Mary Louis. Clinical Hematology Theory and Procedures, 6 th ed, Jones and Bartlett Learning, 2017.

-Becky Socha, MS, MLS(ASCP) CM BB CM graduated from Merrimack College in N. Andover, Massachusetts with a BS in Medical Technology and completed her MS in Clinical Laboratory Sciences at the University of Massachusetts, Lowell. She has worked as a Medical Technologist for over 40 years and has taught as an adjunct faculty member at Merrimack College, UMass Lowell and Stevenson University for over 20 years. She has worked in all areas of the clinical laboratory, but has a special interest in Hematology and Blood Banking. She currently works at Mercy Medical Center in Baltimore, Md. When she’s not busy being a mad scientist, she can be found outside riding her bicycle.
Share this:
One thought on “hematology case study: 75 year old man with leukopenia”.
clinical data of fever, recent illness, history of drug intake, differential leucocytic count and white blood cells morpholog is needed
Leave a comment Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .

- Already have a WordPress.com account? Log in now.
- Subscribe Subscribed
- Copy shortlink
- Report this content
- View post in Reader
- Manage subscriptions
- Collapse this bar
- Current Issue
- Supplements
Category: Clinical Case Study
Metastatic pancreatic poorly differentiated neuroendocrine carcinoma: current treatment considerations.
Clinical Advances in Hematology & Oncology December 2013, Volume 11, Issue 12 Metastatic Pancreatic Poorly Differentiated Neuroendocrine Carcinoma: Current Treatment Considerations Steven Sorscher, MD, Department of Internal Medicine, […]
Periorbital Necrobiotic Xanthogranuloma Treated Successfully With Novel Multiple Myeloma Therapy
Clinical Advances in Hematology & Oncology October 2013, Volume 11, Issue 10 Periorbital Necrobiotic Xanthogranuloma Treated Successfully With Novel Multiple Myeloma Therapy Sofia Ghani, MD1 Omar Al […]
Myocardial Infarction in a Young Man Receiving Chemotherapy for Acute Lymphoblastic Leukemia
Clinical Advances in Hematology & Oncology October 2013, Volume 11, Issue 10 Myocardial Infarction in a Young Man Receiving Chemotherapy for Acute Lymphoblastic Leukemia Wei Yang, MD1 […]
Pulmonary Langerhans Cell Histiocytosis Masquerading as Adenocarcinoma of the Lung
Clinical Advances in Hematology & Oncology September 2013, Volume 11, Issue 9 Muhammad Rizwan Khawaja, MD, MPH1 Thomas M. Ulbright, MD2 Shadia Jalal, MD1 1Division […]
Carfilzomib-Related Acute Kidney Injury
Clinical Advances in Hematology & Oncology September 2013, Volume 11, Issue 9 Kenar D. Jhaveri, MD1,4 Shailaja Chidella, MD1,4 Jeny Varghese, MD4 Lionel Mailloux, MD1,4 […]
Hodgkin Lymphoma in Pregnancy: A Case Report
Clinical Advances in Hematology & Oncology August 2013, Volume 11, Issue 8 Magdalena Sanchez, MD1 Begoña Pellicer, MD2 Maria del Puig Cozar, MD3 Vicente Martínez-Sanjuan, […]
A Case Report of Hairy Cell Leukemia and Breast Cancer
Clinical Advances in Hematology & Oncology July 2013, Volume 11, Issue 7 Evgeny Mikler, PA-C1 Bruce Petersen, MD2 John Mascarenhas, MD1 1Division of Hematology and […]
Ataxia in a Patient With Urothelial Carcinoma: Pathologic Confirmation, Recovery, and Improved Survival
Clinical Advances in Hematology & Oncology July 2013, Volume 11, Issue 7 Faithlore P. Gardner, MD and Winston W. Tan, MD Department of Hematology/Oncology, Mayo Clinic, […]
Unusual Presentation of Bladder Myeloid Sarcoma Causing Acute Renal Failure: Case Report and Review of the Literature
Clinical Advances in Hematology & Oncology June 2013, Volume 11, Issue 6 Sonia John, MD1 Hussein Ali Ahmad, MD2 Terence Dunn, PhD3 William Kern, MD3 […]
Complete Response to Brentuximab Vedotin in a Transplant-Naive Patient With Relapsed CD30-Positive Nodular Lymphocyte-Predominant Hodgkin Lymphoma
Clinical Advances in Hematology & Oncology June 2013, Volume 11, Issue 6 Ciara C. O’Sullivan, MD1 Metin Ozdemirli, MD, PhD2 Michael Bazylewicz, MD3 Bruce D. […]
Hypereosinophilic Syndrome Presenting As an Unusual Triad of Eosinophilia, Severe Thrombocytopenia, and Diffuse Arterial Thromboses, With Good Response to Mepolizumab
Clinical Advances in Hematology & Oncology May 2013, Volume 11, Issue 5 Roberto A. Leon-Ferre, MD1 Catherine R. Weiler, MD, PhD2 Thorvardur R. Halfdanarson, MD3 […]
Reduced-Dose Carboxypeptidase-G2 Successfully Lowers Elevated Methotrexate Levels in an Adult With Acute Methotrexate-Induced Renal Failure
Clinical Advances in Hematology & Oncology May 2013, Volume 11, Issue 5 Steven Trifilio, RPh Shuo Ma, MD, PhD Adam Petrich, MD Division of Hematology-Oncology, […]
Acute Lymphoblastic Leukemia During Enzyme Replacement Therapy in Type 1 Gaucher’s Disease
Clinical Advances in Hematology & Oncology April 2013, Volume 11, Issue 4 Sinem Civriz Bozdag, MD1 Pervin Topcuoglu, MD2 Isinsu Kuzu, MD3 Mutlu Arat, MD4 1Hematology […]
Safe and Effective Treatment of Aggressive Non-Hodgkin Lymphoma With Rituximab and Bendamustine in Patients With Severe Liver Impairment
Clinical Advances in Hematology & Oncology March 2013, Volume 11, Issue 3 James K. McCloskey, MD, Catherine M. Broome, MD, and Bruce D. Cheson, MD Division of […]
Successful Treatment of Hepatosplenic T-Cell Lymphoma With ESHAP Followed by Autologous Stem Cell Transplant
Clinical Advances in Hematology & Oncology February 2013, Volume 11, Issue 2 Anna W. Chalmers, MD1 Deborah A. Katz, MD2 Ira J. Miller, MD, PhD3 […]
CA 19-9 Tumor Marker: Is It Reliable? A Case Report in a Patient With Pancreatic Cancer
Clinical Advances in Hematology & Oncology January 2013, Volume 11, Issue 1 Zheng Wu, MD, PhD1 Anne I. Kuntz, RN, OCN2 Robert G. Wadleigh, MD2 […]
Malignant Paraganglioma of the Urinary Bladder in a 45-Year-Old Woman
Clinical Advances in Hematology & Oncology December 2012, Volume 10, Issue 12 Amruth R. Palla, MD, MPH1 Thomas Hogan, MD2 Sindhu Singh, MD2 1Department of Internal […]

Spontaneous Regression of Classical Hodgkin Lymphoma: A Case Report and Review of the Literature
Clinical Advances in Hematology & Oncology November 2012, Volume 10, Issue 11 Amr Mohsen, MD Hady Ghanem, MD Jehan El-Bayoumi, MD, FACP Imad Tabbara, MD George […]
Chronic Lymphocytic Leukemia With Essential Thrombocythemia: Asbestos Exposure Association?
Clinical Advances in Hematology & Oncology November 2012, Volume 10, Issue 11 Rangaswamy Chintapatla, MD1 Ramakrishna Battini, MD2 Peter H. Wiernik, MD1 1Continuum Cancer Centers of […]
Autoimmune Pancreatitis in the Setting of Multifocal Castleman Disease in an HIV-Negative, HHV-8–Negative, 70-Year-Old Man
Margaret E. Gatti-Mays, MD, MPH, David Kardon, MD, Ton That Chieu, MD, and Kashif Firozvi, MD 1Georgetown University Hospital, Department of Medicine, Washington, DC; 2George Washington […]
Advertisement
Case Report: A 19-Years Old Patient with Haemophilia a with High Response Inhibitor Screening and Quantitation and the Bethesda Method
- Split-Screen
- Request Permissions
- Cite Icon Cite
- Search Site
Marianela Trejos Herrera , Alicia Lopez Campos; Case Report: A 19-Years Old Patient with Haemophilia a with High Response Inhibitor Screening and Quantitation and the Bethesda Method. Blood 2016; 128 (22): 4956. doi: https://doi.org/10.1182/blood.V128.22.4956.4956
Download citation file:
- Ris (Zotero)
- Reference Manager
A severe haemophiliac patient, high response inhibitors, 19 years, who was diagnosed at 8 months old and since then he begins to administer factor VIII concentrates. However, a year later after the start of treatment, they were detected inhibitors that behave as high response inhibitors from the start.
He discontinues treatment with Factor VIII concentrate and instead he begins to administer Factor IX concentrate and prothrombin complex as an alternative treatment.
Through his illness, the patient has made significant bleeding at the level of joint and other muscles such as the psoas. It is a bleeding patient at rest up for what is currently administered prophylactically Prothrombin Concentrate 3 times a week.
This case, the comment will be directed towards laboratory diagnosis and its evolution since he was diagnosed in 1994 to date.
From 2013, screening protocols and quantification of both factors and inhibitors were modified in the Specialized Hematology laboratory of Hospital México, due to problems in the sensitivity and specificity of the method and reagents we were using. The results from these patient specific inhibitors are described in the following paragraphs.
Observations
With the experience and current knowledge of the following it is concluded, according to a literature review that was performed (see Table 1):
1) This time period has persisted inhibitor high title, which is evidenced of the study of mixtures which do not clearly show a potentiation by incubating 2 hours at 37 ° C, since the values of the Control Mix and patient give very similar high values.
2) We were shown only on the date of 14.02.2013, there was a real interference Lupic Anticoagulant (LA), which is confirmed by the method of Russel viper venom.
3) The dates high titer inhibitors were reported against factor VIII (from 6 November 2013 to date), both screening and for the Bethesda, aPTT reagent was used with Kaolin activator which is low sensitivity to LA.
4) On November 20, 2015 there was an error in the interpretation and anti factor VIII inhibitors as negative were reported as potentiation at 37 ° C is not evidenced, but rather was interpreted as interference of an LA, which was communicated to the medical and preventive measures cited in paragraph corrections were made.
5) The last date that the sample was processed, on February 1, 2016, the inhibitor against factor VIII did not affect dilution of silica APTT, so the index ROSNER was not affected (<12) and it was not necessary to mount the LA test, according to the request in identifying protocols inhibitors.
6) Factor VIII deficient plasma is currently being used, which contains von Willebrand factor, as recommended by international guidelines quantization factors.
Conclusions
According to an experience as support center Reference Center in our country, we conclude and recommend the following:
1) Registration of haemophiliac patients with high antibody titer is essential as the description of the protocol to be followed in these patients.
2) The behavior of this inhibitor in the screening test of time and temperature dependence, it was decided to directly mount the Bethesda assay, following the recommendations of the literature on when the use of a reagent with low sensitivity to lupus inhibitor.
3) Within the protocol and as far as we can, we will process the purchase for quantification of factor VIII chromogenic by ELISA methodology, as a confirmatory method.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.
This feature is available to Subscribers Only
- Previous Article
- Next Article
Email alerts
Affiliations.
- Current Issue
- First edition
- Collections
- Submit to Blood
- About Blood
- Subscriptions
- Public Access
- Permissions
- Blood Classifieds
- Advertising in Blood
- Terms and Conditions
American Society of Hematology
- 2021 L Street NW, Suite 900
- Washington, DC 20036
- TEL +1 202-776-0544
- FAX +1 202-776-0545
ASH Publications
- Blood Advances
- Hematology, ASH Education Program
- ASH Clinical News
- The Hematologist
- Publications
- Privacy Policy
- Cookie Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Case report
Journal of Hematology & Oncology welcomes well-described reports of cases that include the following:
- Unreported or unusual side effects or adverse interactions involving medications
- Unexpected or unusual presentations of a disease
- New associations or variations in disease processes
- Presentations, diagnoses and/or management of new and emerging diseases
- An unexpected association between diseases or symptoms
- An unexpected event in the course of observing or treating a patient
- Findings that shed new light on the possible pathogenesis of a disease or an adverse effect
Case reports submitted to Journal of Hematology & Oncology should make a contribution to medical knowledge and must have educational value or highlight the need for a change in clinical practice or diagnostic/prognostic approaches. The journal will not consider case reports describing preventive or therapeutic interventions, as these generally require stronger evidence.
Authors are encouraged to describe how the case report is rare or unusual as well as its educational and/or scientific merits in the covering letter that accompanies the submission of the manuscript.
For case reports, Journal of Hematology & Oncology requires authors to follow the CARE guidelines . The CARE checklist should be provided as an additional file. Submissions received without these elements will be returned to the authors as incomplete.
Preparing your manuscript
The information below details the section headings that you should include in your manuscript and what information should be within each section.
Please note that your manuscript must include a 'Declarations' section including all of the subheadings (please see below for more information).
Title page
The title page should:
- "A versus B in the treatment of C: a randomized controlled trial", "X is a risk factor for Y: a case control study", "What is the impact of factor X on subject Y: A systematic review, A case report etc."
- or, for non-clinical or non-research studies: a description of what the article reports
- if a collaboration group should be listed as an author, please list the Group name as an author. If you would like the names of the individual members of the Group to be searchable through their individual PubMed records, please include this information in the “Acknowledgements” section in accordance with the instructions below
- Large Language Models (LLMs), such as ChatGPT , do not currently satisfy our authorship criteria . Notably an attribution of authorship carries with it accountability for the work, which cannot be effectively applied to LLMs. Use of an LLM should be properly documented in the Methods section (and if a Methods section is not available, in a suitable alternative part) of the manuscript
- indicate the corresponding author
The Abstract should not exceed 350 words. Please minimize the use of abbreviations and do not cite references in the abstract. The abstract must include the following separate sections:
- Background: why the case should be reported and its novelty
- Case presentation: a brief description of the patient’s clinical and demographic details, the diagnosis, any interventions and the outcomes
- Conclusions: a brief summary of the clinical impact or potential implications of the case report
Keywords
Three to ten keywords representing the main content of the article.
The Background section should explain the background to the case report or study, its aims, a summary of the existing literature.
Case presentation
This section should include a description of the patient’s relevant demographic details, medical history, symptoms and signs, treatment or intervention, outcomes and any other significant details.
Discussion and Conclusions
This should discuss the relevant existing literature and should state clearly the main conclusions, including an explanation of their relevance or importance to the field.
List of abbreviations
If abbreviations are used in the text they should be defined in the text at first use, and a list of abbreviations should be provided.
Declarations
All manuscripts must contain the following sections under the heading 'Declarations':
Ethics approval and consent to participate
Consent for publication, availability of data and materials, competing interests, authors' contributions, acknowledgements.
- Authors' information (optional)
Please see below for details on the information to be included in these sections.
If any of the sections are not relevant to your manuscript, please include the heading and write 'Not applicable' for that section.
Manuscripts reporting studies involving human participants, human data or human tissue must:
- include a statement on ethics approval and consent (even where the need for approval was waived)
- include the name of the ethics committee that approved the study and the committee’s reference number if appropriate
Studies involving animals must include a statement on ethics approval and for experimental studies involving client-owned animals, authors must also include a statement on informed consent from the client or owner.
See our editorial policies for more information.
If your manuscript does not report on or involve the use of any animal or human data or tissue, please state “Not applicable” in this section.
If your manuscript contains any individual person’s data in any form (including any individual details, images or videos), consent for publication must be obtained from that person, or in the case of children, their parent or legal guardian. All presentations of case reports must have consent for publication.
You can use your institutional consent form or our consent form if you prefer. You should not send the form to us on submission, but we may request to see a copy at any stage (including after publication).
See our editorial policies for more information on consent for publication.
If your manuscript does not contain data from any individual person, please state “Not applicable” in this section.
All manuscripts must include an ‘Availability of data and materials’ statement. Data availability statements should include information on where data supporting the results reported in the article can be found including, where applicable, hyperlinks to publicly archived datasets analysed or generated during the study. By data we mean the minimal dataset that would be necessary to interpret, replicate and build upon the findings reported in the article. We recognise it is not always possible to share research data publicly, for instance when individual privacy could be compromised, and in such instances data availability should still be stated in the manuscript along with any conditions for access.
Authors are also encouraged to preserve search strings on searchRxiv https://searchrxiv.org/ , an archive to support researchers to report, store and share their searches consistently and to enable them to review and re-use existing searches. searchRxiv enables researchers to obtain a digital object identifier (DOI) for their search, allowing it to be cited.
Data availability statements can take one of the following forms (or a combination of more than one if required for multiple datasets):
- The datasets generated and/or analysed during the current study are available in the [NAME] repository, [PERSISTENT WEB LINK TO DATASETS]
- The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
- All data generated or analysed during this study are included in this published article [and its supplementary information files].
- The datasets generated and/or analysed during the current study are not publicly available due [REASON WHY DATA ARE NOT PUBLIC] but are available from the corresponding author on reasonable request.
- Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
- The data that support the findings of this study are available from [third party name] but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of [third party name].
- Not applicable. If your manuscript does not contain any data, please state 'Not applicable' in this section.
More examples of template data availability statements, which include examples of openly available and restricted access datasets, are available here .
BioMed Central strongly encourages the citation of any publicly available data on which the conclusions of the paper rely in the manuscript. Data citations should include a persistent identifier (such as a DOI) and should ideally be included in the reference list. Citations of datasets, when they appear in the reference list, should include the minimum information recommended by DataCite and follow journal style. Dataset identifiers including DOIs should be expressed as full URLs. For example:
Hao Z, AghaKouchak A, Nakhjiri N, Farahmand A. Global integrated drought monitoring and prediction system (GIDMaPS) data sets. figshare. 2014. http://dx.doi.org/10.6084/m9.figshare.853801
With the corresponding text in the Availability of data and materials statement:
The datasets generated during and/or analysed during the current study are available in the [NAME] repository, [PERSISTENT WEB LINK TO DATASETS]. [Reference number]
If you wish to co-submit a data note describing your data to be published in BMC Research Notes , you can do so by visiting our submission portal . Data notes support open data and help authors to comply with funder policies on data sharing. Co-published data notes will be linked to the research article the data support ( example ).
All financial and non-financial competing interests must be declared in this section.
See our editorial policies for a full explanation of competing interests. If you are unsure whether you or any of your co-authors have a competing interest please contact the editorial office.
Please use the authors initials to refer to each authors' competing interests in this section.
If you do not have any competing interests, please state "The authors declare that they have no competing interests" in this section.
All sources of funding for the research reported should be declared. If the funder has a specific role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript, this should be declared.
The individual contributions of authors to the manuscript should be specified in this section. Guidance and criteria for authorship can be found in our editorial policies .
Please use initials to refer to each author's contribution in this section, for example: "FC analyzed and interpreted the patient data regarding the hematological disease and the transplant. RH performed the histological examination of the kidney, and was a major contributor in writing the manuscript. All authors read and approved the final manuscript."
Please acknowledge anyone who contributed towards the article who does not meet the criteria for authorship including anyone who provided professional writing services or materials.
Authors should obtain permission to acknowledge from all those mentioned in the Acknowledgements section.
See our editorial policies for a full explanation of acknowledgements and authorship criteria.
If you do not have anyone to acknowledge, please write "Not applicable" in this section.
Group authorship (for manuscripts involving a collaboration group): if you would like the names of the individual members of a collaboration Group to be searchable through their individual PubMed records, please ensure that the title of the collaboration Group is included on the title page and in the submission system and also include collaborating author names as the last paragraph of the “Acknowledgements” section. Please add authors in the format First Name, Middle initial(s) (optional), Last Name. You can add institution or country information for each author if you wish, but this should be consistent across all authors.
Please note that individual names may not be present in the PubMed record at the time a published article is initially included in PubMed as it takes PubMed additional time to code this information.
Authors' information
This section is optional.
You may choose to use this section to include any relevant information about the author(s) that may aid the reader's interpretation of the article, and understand the standpoint of the author(s). This may include details about the authors' qualifications, current positions they hold at institutions or societies, or any other relevant background information. Please refer to authors using their initials. Note this section should not be used to describe any competing interests.
Footnotes can be used to give additional information, which may include the citation of a reference included in the reference list. They should not consist solely of a reference citation, and they should never include the bibliographic details of a reference. They should also not contain any figures or tables.
Footnotes to the text are numbered consecutively; those to tables should be indicated by superscript lower-case letters (or asterisks for significance values and other statistical data). Footnotes to the title or the authors of the article are not given reference symbols.
Always use footnotes instead of endnotes.
Examples of the Vancouver reference style are shown below.
See our editorial policies for author guidance on good citation practice
Web links and URLs: All web links and URLs, including links to the authors' own websites, should be given a reference number and included in the reference list rather than within the text of the manuscript. They should be provided in full, including both the title of the site and the URL, as well as the date the site was accessed, in the following format: The Mouse Tumor Biology Database. http://tumor.informatics.jax.org/mtbwi/index.do . Accessed 20 May 2013. If an author or group of authors can clearly be associated with a web link, such as for weblogs, then they should be included in the reference.
Example reference style:
Article within a journal
Smith JJ. The world of science. Am J Sci. 1999;36:234-5.
Article within a journal (no page numbers)
Rohrmann S, Overvad K, Bueno-de-Mesquita HB, Jakobsen MU, Egeberg R, Tjønneland A, et al. Meat consumption and mortality - results from the European Prospective Investigation into Cancer and Nutrition. BMC Medicine. 2013;11:63.
Article within a journal by DOI
Slifka MK, Whitton JL. Clinical implications of dysregulated cytokine production. Dig J Mol Med. 2000; doi:10.1007/s801090000086.
Article within a journal supplement
Frumin AM, Nussbaum J, Esposito M. Functional asplenia: demonstration of splenic activity by bone marrow scan. Blood 1979;59 Suppl 1:26-32.
Book chapter, or an article within a book
Wyllie AH, Kerr JFR, Currie AR. Cell death: the significance of apoptosis. In: Bourne GH, Danielli JF, Jeon KW, editors. International review of cytology. London: Academic; 1980. p. 251-306.
OnlineFirst chapter in a series (without a volume designation but with a DOI)
Saito Y, Hyuga H. Rate equation approaches to amplification of enantiomeric excess and chiral symmetry breaking. Top Curr Chem. 2007. doi:10.1007/128_2006_108.
Complete book, authored
Blenkinsopp A, Paxton P. Symptoms in the pharmacy: a guide to the management of common illness. 3rd ed. Oxford: Blackwell Science; 1998.
Online document
Doe J. Title of subordinate document. In: The dictionary of substances and their effects. Royal Society of Chemistry. 1999. http://www.rsc.org/dose/title of subordinate document. Accessed 15 Jan 1999.
Online database
Healthwise Knowledgebase. US Pharmacopeia, Rockville. 1998. http://www.healthwise.org. Accessed 21 Sept 1998.
Supplementary material/private homepage
Doe J. Title of supplementary material. 2000. http://www.privatehomepage.com. Accessed 22 Feb 2000.
University site
Doe, J: Title of preprint. http://www.uni-heidelberg.de/mydata.html (1999). Accessed 25 Dec 1999.
Doe, J: Trivial HTTP, RFC2169. ftp://ftp.isi.edu/in-notes/rfc2169.txt (1999). Accessed 12 Nov 1999.
Organization site
ISSN International Centre: The ISSN register. http://www.issn.org (2006). Accessed 20 Feb 2007.
Dataset with persistent identifier
Zheng L-Y, Guo X-S, He B, Sun L-J, Peng Y, Dong S-S, et al. Genome data from sweet and grain sorghum (Sorghum bicolor). GigaScience Database. 2011. http://dx.doi.org/10.5524/100012 .
Figures, tables and additional files
See General formatting guidelines for information on how to format figures, tables and additional files.
Submit manuscript
Official journal of

Journal of Hematology & Oncology is the official journal of the Chinese American Hematologist and Oncologist Network .
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- Instructions for authors
- Sign up for article alerts and news from this journal
- Follow us on Twitter
Annual Journal Metrics
2022 Citation Impact 28.5 - 2-year Impact Factor 23.1 - 5-year Impact Factor 4.045 - SNIP (Source Normalized Impact per Paper) 6.046 - SJR (SCImago Journal Rank)
2023 Speed 5 days submission to first editorial decision for all manuscripts (Median) 59 days submission to accept (Median)
2023 Usage 3,173,795 downloads 2,671 Altmetric mentions
- More about our metrics
On the blog

PEAR-TREE: Understanding the usefulness of the PEAR-BIO platform in patients with kidney cancer
08 January 2024

Winners of the 2022 Cardio-Oncology Journal Prize
06 April 2023

Brain Tumor Awareness Month: Can proton beam therapy improve the long-term quality of life of patients with oligodendroglioma brain tumors?
22 March 2023
Institutional membership

IMAGES
VIDEO
COMMENTS
3 min. Case studies are board-style questions with explanations and links to related articles featured in Hematopoiesis, an e-newsletter that is sent to hematology trainees on a quarterly basis. A 73-Year-Old Man With Extensive Bruising. A 2.5-Year-Old Girl With Fever and Pancytopenia. 21-Year-Old With Duodenal Adenocarcinoma and a History of T ...
Case Study: Hematology. Pediatric case of Plasmodia Falciparum (Malaria) A 13 year-old previously healthy girl who is one of Jehovah's Witnesses, with a history of malaria 4 years ago, presented with fever, headache, nausea, vomiting and abdominal pain after a recent trip to Liberia to visit family. During her visit, she was taking ...
Case History. A 20 year old Black male with a known history of HbS trait went to the primary care office for a pre-surgical evaluation for elective laparoscopic cholecystectomy for symptomatic cholelithiasis. All physical exam findings were negative. The patient had blood work completed and was found to have mild anemia with microcytosis.
The Atlas is a collection of classic hematology cases, representing both adult and pediatric conditions. Each case in the Atlas consists of a concise patient history, corresponding CBC findings and other pertinent laboratory data, as well as digitized slide(s) of peripheral blood smears, bone marrow aspirates/biopsies, lymph node biopsies, and ...
Case Studies in Hematology and Coagulation. This compendium of 200 case studies is the result of a unique collaboration of leading hematologists, hematopathologists, and oncologists. It serves as both a case-based guide to the diagnosis and management of patients suffering from hematologic conditions and a valuable teaching tool.
Case Reports in Hematology publishes case reports and case series in all areas of hematology, including general hematology, pathology, and oncology, with a specific focus on lymphomas and leukemias. ... 2014). Despite knowing the increased incidence of VTEs in cancer patients, there are few studies to date that analyze the composition of ...
Many studies address the lack of long-lived specific antibody responses, whereas other studies have investigated the reasons for and deficits produced by abnormal cellular immune pathways. The incidence of CVID is estimated to be between 1:25 000 and 1:50 000 in white individuals, but it is apparently less common in Asian and African American ...
Finally, extremely low hemoglobin levels have been reported by Bhatia et al., who performed coronary hemodynamic studies on 14 patients with chronic anemia. They reported three patients with hemoglobin levels ≤3.0 mg/dl; they had hemoglobin levels of 1.6 mg/dl, 2.4 mg/dl, and 3.0 mg/dl, and all of them were between 23 to 25 years old.
Case Studies /. Anemia in a 42-year-old woman. Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada) — dedicated to using leading-edge science to save and improve lives around the world. Learn more about the MSD Manuals and our commitment to Global Medical Knowledge.
Hematology Case Study: 75 Year Old Man with Leukopenia. A 75 year old male first presented earlier this year with abnormal CBC results. The patient has a history of Type 2 diabetes, high blood pressure and atrial fibrillation. He was diagnosed with non-small-cell lung cancer (NSCLC) 6 years ago. His stage II NSCLC was completely removed with ...
Hematology Case Studies with Blood Cell Morphology and Pathophysiology compiles specialized case studies with specific information on various hematological disorders with Full Blood Examination (FBE or CBC), blood film images and pathophysiology of each condition. In addition, it provides basic information on how to recognize and diagnose ...
Sequential coagulation studies in purpura fulminans. N Engl J Med 1967;276:1287-1290. Crossref. PubMed. ISI. ... Hematology/Oncology General; Infectious Disease General; Pediatrics General; Shock;
Laboratory studies in the ED (Table 125-1) reveal a significant microcytic anemia and a prolonged activated partial thromboplastin time (aPTT). Four units of packed red blood cells and two units of fresh-frozen plasma are ordered. Hematology is consulted, and additional coagulation studies are sent to an out-of-state reference laboratory.
Safe and Effective Treatment of Aggressive Non-Hodgkin Lymphoma With Rituximab and Bendamustine in Patients With Severe Liver Impairment. Clinical Advances in Hematology & Oncology March 2013, Volume 11, Issue 3 James K. McCloskey, MD, Catherine M. Broome, MD, and Bruce D. Cheson, MD Division of […]
Case Studies in Hematology - Nonmalignant WBC Disorders. (Online CE Course) (based on 721 customer ratings) Margaret Reinhart, MS, MT (ASCP) Reviewer: Kyle Magee, MLS (ASCP) CM and Rory Huschka, M.Ed., MT (ASCP) This course presents case studies pertaining to both non-malignant white blood cell disorders and malignant/neoplastic disorders.
From 2013, screening protocols and quantification of both factors and inhibitors were modified in the Specialized Hematology laboratory of Hospital México, due to problems in the sensitivity and specificity of the method and reagents we were using. The results from these patient specific inhibitors are described in the following paragraphs.
Hematology is the study of blood in relation to health and disease. Problems with the blood can affect several of the body's systems, such as the lymphatic system, a network of tissues and ...
Journal of Hematology & Oncology welcomes well-described reports of cases that include the following: Unreported or unusual side effects or adverse interactions involving medications. Unexpected or unusual presentations of a disease. New associations or variations in disease processes. Presentations, diagnoses and/or management of new and ...