- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
- Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
- Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring

Consumer Health Information, Essay Example
Pages: 3
Words: 690
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
Introduction
Consumer health literacy is an important component of modern healthcare practice because it enables patients to be proactive in understanding the issues that impact their health, as well as in recognizing how to best overcome personal health concerns that influence their own perspectives regarding health. It is important to recognize that many consumers who are tech-savvy may have a tendency to self-diagnose using various websites; however, this does not replace truthful and unbiased healthcare information comprised of the facts that is available from reputable sources. It is necessary for consumers to properly decipher and interpret health information effectively in order to identify areas where health information is lacking or is inappropriate in meeting patient needs.
Interpreting health information in the appropriate manner requires a high level of focus and an understanding of the different expectations that consumers have regarding information that is easily accessible on the web and in other locations (Goldberg et.al, 2011). In this context, consumers must be able to obtain health information that is accurate and timely, rather than to rely on information that is untruthful and outdated (Goldberg et.al, 2011). Health information must be properly evaluated and provide useful insight regarding health issues of concern that impact many consumers (Goldberg et.al, 2011). Consumers must also be receptive and willing to learn about health issues through skill development and literacy strategies to improve confidence in health information and in the experts who provide this information to the masses (Car et.al, 2011). These practices require expert knowledge and guidance in advancing health and in supporting preventative and proactive strategies to protect health through improved knowledge and awareness (Car et.al, 2011).
Patients must be adequately prepared to improve their health literacy and to seek out information freely regarding health topics; however, this practice must also take other factors into consideration, such as preventative education that is used to address primary health concerns (Car et.al, 2011). Health literacy is a lifelong phenomenon that requires an effective understanding of the different elements that attract consumers to this practice, such as information that is truthful yet relatively easy to understand (Schnitzer et.al, 2011). These practices require individuals to take the steps that are required to ensure they are health literate and possess knowledge of a variety of health topics from a honest and truthful perspective so that they are able to better understand their own issues more effectively (Schnitzer et.al, 2011). At the same time, it is important for consumers to develop an effective understanding of their needs and to be proactive in recognizing that health literacy is a critical factor in their own growth and maturity (Sheridan et.al, 2011). These factors require experts to educate others regarding health literacy and to be cognizant of the issues that may emerge that impact health knowledge in different ways (Sheridan et.al, 2011).
Consumers must be able to receive and comprehend health information in an effective manner, as this provides a greater sense of accomplishment and an understanding of the different elements that impact their own wellbeing. Health literacy is a lifelong process that requires health knowledge to be accurate and appropriate for consumers so that they are able to identify specific factors related to their own health. This practice also requires a long-term commitment to educating individuals across different age groups so that they are able to actively participate in making decisions regarding their own health that will have a positive impact on their lives throughout the life span.
Car, J., Lang, B., Colledge, A., Ung, C., & Majeed, A. (2011). Interventions for enhancing consumers’ online health literacy. Cochrane Database Syst Rev , 6 .
Goldberg, L., Lide, B., Lowry, S., Massett, H. A., O’Connell, T., Preece, J., … & Shneiderman, (2011). Usability and accessibility in consumer health informatics: current trends and future challenges. American journal of preventive medicine , 40 (5), S187-S197.
Schnitzer, A. E., Rosenzweig, M., & Harris, B. (2011). Health literacy: A survey of the issues and solutions. Journal of Consumer Health on the Internet , 15 (2), 164-179.
Sheridan, S. L., Halpern, D. J., Viera, A. J., Berkman, N. D., Donahue, K. E., & Crotty, K. (2011). Interventions for individuals with low health literacy: a systematic review. Journal of Health Communication , 16 (sup3), 30-54.
Stuck with your Essay?
Get in touch with one of our experts for instant help!
Death of a Sales Man, Movie Review Example
Tips for Online Students, Research Paper Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Voting as a civic responsibility, essay example.
Pages: 1
Words: 287
Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Pages: 2
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Pages: 4
Words: 999
The Term “Social Construction of Reality”, Essay Example
Words: 371
Loading metrics
Open Access
Essays are opinion pieces on a topic of broad interest to a general medical audience.
See all article types »
The Rise of Consumer Health Wearables: Promises and Barriers
* E-mail: [email protected]
Affiliation School of Management, University of Bath, Bath, United Kingdom
Affiliation Department of Psychology, Lancaster University, Lancaster, United Kingdom
Affiliation Division of Psychology, Nottingham Trent University, Nottingham, United Kingdom
- Lukasz Piwek,
- David A. Ellis,
- Sally Andrews,
- Adam Joinson

Published: February 2, 2016
- https://doi.org/10.1371/journal.pmed.1001953
- Reader Comments
Citation: Piwek L, Ellis DA, Andrews S, Joinson A (2016) The Rise of Consumer Health Wearables: Promises and Barriers. PLoS Med 13(2): e1001953. https://doi.org/10.1371/journal.pmed.1001953
Copyright: © 2016 Piwek et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: No funding bodies had any role in study design, data collection and analysis, and decision to publish. A Research Investment Grant (RIF2014–31) from The University of Lincoln supported the preparation of this manuscript.
Competing interests: The authors have declared that no competing interests exist.
Abbreviations: ECG, electrocardiogram; EEG, electroencephalogram; GPS, Global Positioning System; IoT, Internet of Things; PTSD, post-traumatic stress disorder; QS, Quantified Self
Provenance: Not commissioned; externally peer-reviewed
Summary Points
- Consumer wearables can provide patients with personalized health data, which could assist with self-diagnosis and behaviour change interventions.
- There are a number of concerns about the safety, reliability, and security of using consumer wearables in health care.
- Practitioners and researchers should consider how these technological advances may impact health care in the 21st century.
Will consumer wearable technology ever be adopted or accepted by the medical community? Patients and practitioners regularly use digital technology (e.g., thermometers and glucose monitors) to identify and discuss symptoms. In addition, a third of general practitioners in the United Kingdom report that patients arrive with suggestions for treatment based on online search results [ 1 ]. However, consumer health wearables are predicted to become the next “Dr Google.” One in six (15%) consumers in the United States currently uses wearable technology, including smartwatches or fitness bands. While 19 million fitness devices are likely to be sold this year, that number is predicted to grow to 110 million in 2018 [ 2 ]. As the line between consumer health wearables and medical devices begins to blur, it is now possible for a single wearable device to monitor a range of medical risk factors ( Fig 1 ). Potentially, these devices could give patients direct access to personal analytics that can contribute to their health, facilitate preventive care, and aid in the management of ongoing illness. However, how this new wearable technology might best serve medicine remains unclear.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Heart rate can be measured with an oximeter built into a ring [ 3 ], muscle activity with an electromyographic sensor embedded into clothing [ 4 ], stress with an electodermal sensor incorporated into a wristband [ 5 ], and physical activity or sleep patterns via an accelerometer in a watch [ 6 , 7 ]. In addition, a female’s most fertile period can be identified with detailed body temperature tracking [ 8 ], while levels of mental attention can be monitored with a small number of non-gelled electroencephalogram (EEG) electrodes [ 9 ]. Levels of social interaction (also known to affect general well-being) can be monitored using proximity detections to others with Bluetooth- or Wi-Fi-enabled devices [ 10 ]. Consumer wearables can deliver personalised, immediate, and goal-oriented feedback based on specific tracking data obtained via sensors and provide long lasting functionality without requiring continual recharging. Their small form factor makes them easier to wear continuously. While smartphones are still required to process the incoming data for most consumer wearables, it is conceivable that in the near future all processing functionality will be self contained.
https://doi.org/10.1371/journal.pmed.1001953.g001
Do Wearables Affect Behaviour?
Healthy individuals.
At present, wearables are more likely to be purchased by individuals who already lead a healthy lifestyle and want to quantify their progress [ 2 ]. The majority of wearable manufacturers (e.g., Fitbit, Jawbone, and Nike) stress the potential of their devices to become an “all-in-one" platform for improving physical performance and positive habit formation. Wearable manufacturers utilise a range of digital persuasive techniques and social influence strategies to increase user engagement, including the gamification of activity with competitions and challenges, publication of visible feedback on performance utilising social influence principles, or reinforcements in the form of virtual rewards for achievements. There is also a small, but growing, population of wearable users specifically interested in the concept of self-discovery via personal analytics—the Quantified Self (QS) movement [ 11 ]. A number of scientific and popular publications describe methods and techniques for using consumer wearables as “self-hacking” devices—to improve sleep, manage stress, or increase productivity [ 12 ]. But do these interventions make people healthier?
Current empirical evidence is not supportive. Evidence for the effectiveness of QS methods comes from single-subject reports of users describing their experiences. Subjective reports like these cannot be treated as reliable scientific evidence. Very few longitudinal, randomised controlled studies focus on the impact of wearable technology on healthy users’ behaviour. One exception found that pedometers (and consultations) increased physical activity among older people [ 13 ]. It remains unclear how similar interventions may benefit younger adults who are regularly exposed to wearables that provide an ever-increasing stream of behavioural and physiological feedback. Additionally, recent surveys showed that 32% of users stop wearing these devices after six months, and 50% after one year [ 14 ]. Many wearables suffer from being a “solution in search of a problem." In other words, they don’t add functional value that is already expected from personal technology of that type, and they require too much effort, which breaks the seamless user experience [ 15 ]. Poor implementation of user experience principles [ 16 ] alongside the ad hoc design of user interfaces stems in part from the rapid nature of development, which may also explain the lack of randomised trials. Those who market and develop consumer level devices may underestimate the distance between designing a product that appears to be associated with a healthy lifestyle and providing evidence to support this underlying assumption. This is not merely a bureaucratic limitation, as even the best experts are often unable to predict which novel interventions will show benefits when considered as part of a randomised trial [ 17 ].
Patients with a Defined Illness or Comorbidity
How useful are consumer wearables as a patient-driven, “secondary" diagnostic tool? For chronic conditions, wearables could effortlessly provide detailed longitudinal data in order to monitor patients’ progress without involving more sophisticated, uncomfortable, and expensive alternatives. For instance, it is possible to identify the severity of depressive symptoms based on the number of conversations, amount of physical activity, and sleep duration using a wearable wristband and smartphone app [ 18 , 19 ]. Sleep apnoea could be quickly diagnosed, and sleep quality improved, with a lightweight wearable that measures heart rate, breathing volume, and snoring (through tissue vibration) instead of a heavy polysomnograph [ 20 ]. Wearables could also feed into a broader system of “predictive preventive diagnosis." For example, a microanalysis of body movement data can be used to detect early symptoms of Parkinson disease [ 21 ]. Wearables could provide a platform for at-home management of long-term chronic conditions. Stationary computerised solutions such as web-based services, electronic self-reports, and feedback via emails already facilitate positive behaviour change for such medical issues as obesity [ 22 ], anxiety [ 23 ], panic disorders [ 24 ], post-traumatic stress disorder (PTSD) [ 25 ], and asthma [ 26 ]. However, those stationary computerised solutions already appear out of date and are almost impossible to use by patients when they are away from their home computer. Despite their widespread use, these solutions result in a high level of patient attrition [ 27 ], which might be a result of requiring patients to delay self-report until they are next able to use their home computer [ 28 ]. Wearables could address some of the limitations of other interventions by providing instant feedback and offer an individualistic approach while remaining practical [ 11 , 15 ].
In spite of these promises, the actual use of consumer wearables within a clinical population remains limited. The potential applications described above are still in the early stages of development, have not been approved for medical use, and have so far been explored predominantly within an academic research rather than a real-world context. Clinical studies to date that have a closer resemblance to consumer wearables involve (1) pedometers and smartphone apps to tackle a sedentary lifestyle and obesity and (2) home telemonitoring solutions for patients with pulmonary conditions, diabetes, hypertension, and cardiovascular diseases.
The use of pedometers has been associated with significant increases in physical activity and significant decreases in body mass index and blood pressure [ 29 ]. Smartphone apps have been shown to complement interventions supporting weight loss [ 28 , 30 ] and increase physical activity [ 31 ]. However, interventions involving pedometers and smartphone apps across clinical populations show no evidence of continued behavioural change beyond the duration of the original intervention [ 29 ]. There are also inconclusive results regarding home telemonitoring. Reviews illustrating the effects of telemonitoring on clinical outcomes (e.g., a decrease in emergency visits, hospital admissions, and average hospital stay) are more favourable in pulmonary and cardiac patients than in those suffering from diabetes and hypertension [ 32 , 33 ]. However, a number of trials report no beneficial effect of self-monitoring on blood glucose [ 34 ], and several demonstrate negative outcomes, including elevated levels of depression [ 35 ]. Aspects such as quality of life, acceptability, and cost benefits are infrequently or incompletely reported in telemonitoring trials [ 33 , 36 ], and existing reviews of remote monitoring have frequently been criticised for their poor methodology [ 37 ].
Into the Cloud: Is Wearable-Generated Data Safe, Reliable, and Secured?
This new technology raises additional questions concerning the impact on users’ health and well-being. Currently, wearables exist within a “grey area” regarding user safety. The potential issue of harm is largely absent from the current literature, but it is conceivable that people may become over-reliant on automated systems that provide a false sense of security or fuel a self-driven misdiagnosis [ 38 , 39 ]. Patients could also suffer from negative consequences of excessive self-monitoring by finding it uncomfortable, intrusive, and unpleasant. For instance, several studies have observed that type 2 diabetics who self-monitored their own blood glucose concentration did not benefit from increased glycaemic control but rather found their disease more intrusive [ 35 ]. The interaction between a wearable device and a patient is likely to be complex, and further research needs to consider these in more detail. For example, an individual’s personality is likely to play a key role in determining the perceived usefulness of a given device [ 40 ].
The reliability and validity of wearable devices is also concerning. Devices are marketed under the premise that they will help improve general health and fitness, but the majority of manufactures provide no empirical evidence to support the effectiveness of their products. Recent comparisons between various wearables for tracking physical activity showed large variations in accuracy between different devices—with error margins of up to 25% [ 41 , 42 ]. This is a serious discrepancy, and it echoes problems witnessed in the medical apps market. For instance, a review in JAMA Dermatology showed that smartphone apps for melanoma detection have a 30% failure rate [ 43 ]. Lack of reliability is a serious obstacle that needs to be addressed long before a device could be considered for any medical application.
Finally, for patients and medical practitioners, the privacy and security of personal data generated by consumer wearables remains problematic. Users who buy wearable devices today often do not “own” their data. Instead, data may be collected and stored by the manufacturer who sells the device. Being provided with only a summary of results extracted from these data creates a rather odd paradox for the user—they own the device, but not the resulting data. Some manufacturers charge users a monthly fee for access to their own raw data, which is regularly sold to third-party agencies. Other companies are also willing to share a users’ location, age, sex, email, height, weight, or “anonymised” Global Positioning System (GPS)-tracked activities [ 44 , 45 ]. However, “anonymising” data via a simple distortion or removal of identifying features does not provide adequate levels of anonymity and is not sufficient to prevent identity fraud. Sophisticated algorithms can now cross-reference wearable-generated biometric data with other “digital traces” of users’ behaviour. “Digital traces” of behaviour such as time of activity and user location can reveal a person’s identity [ 46 ]. Research on “digital traces” from other sources (e.g., social media) demonstrates that these can be alarmingly accurate when it comes to predicting personality [ 47 ] and risk-taking behaviours [ 48 ], two very individual and personal traits. Furthermore, some wearable devices are easy to hack as a result of various communication technologies that aid the transfer of data between wearables and smartphones [ 49 ]. This resonates with similar problems observed in wireless digital pacemakers and glucose pumps, which were vulnerable to cyber-attacks in the past [ 50 , 51 ]. While the consequences of hacks are reduced for noninvasive wearables, a well-coordinated cyber-attack could lead to patient health data being compromised, lost, or distorted.
Moving Forward: What’s to Come for Wearables in Health Care?
What can make affordable, wearable technology a real asset for health care? One option is to create a simple regulatory framework that doesn’t suppress innovation but helps wearable devices become validated in the context of their health-oriented value. Such an approach was recently discussed in The New England Journal of Medicine , but in relation to smartphone health apps’ regulatory status in the US [ 52 ]. Authors pointed towards a risk-based classification (e.g., administrative apps, health management apps, and medical apps) that “promotes innovation, protects patient safety, and avoids regulatory duplication" (p. 375 of [ 52 ]). As part of this model, the US Food and Drug Administration jurisdiction covers higher-risk medical apps. The National Health Service in the UK adopts a similar pathway with their regulatory framework for mobile apps, which can be classified as “medical devices” by the Medicines and Healthcare Products Regulatory Agency [ 53 ]. Applied to a health-oriented wearable device, such a solution could persuade the private sector to provide open access to their data collection practices, analysis methodologies, and measurement concerns. This would address not only the issue of wearables reliability but also secondary concerns relating to data storage and privacy. Apple has recently announced a development of a ResearchKit—an open-source software framework to create smartphone apps and to use wearables for medical research [ 54 ]. This is widely perceived as an attempt to accelerate and standardise procedures for regulating Apple’ s apps alongside wearables as they apply to medical research. We envision that other smartphone and wearable manufacturers will mirror this approach, therefore making it easier for medical researchers to address issues of reliability, safety, and security of patient data. Combining such standardised solutions created by manufacturers with the correct regulatory framework has the potential to accelerate high-quality, large-scale randomised controlled trials in order to deconstruct complex causal interactions and better understand how to make wearables safer and more useful if they are to be adopted in health care.
Another way to address data reliability and behavioural usability issues is to reach the next level in decoding “big data” from wearable devices. Right now, feedback systems built around consumer health wearables are based on simple descriptive statistics—for example, average weekly heart rate and level of activity. Simple summary statistics appear almost trivial given the complex nature of the data that most wearables collect. The same criticism can also be applied to the sociodemographic information recorded by users. The next step will be to move from unsophisticated exploratory feedback to intelligent and personalised explanatory feedback [ 55 ]. Interactive computing systems that already exist in smartphones such as Google Now, Apple Siri, and Microsoft Cortana could be used to improve user experience and interaction with wearable technology by making rich data outcomes and feedback more accessible and intelligible [ 56 ]. Such systems will be further empowered by the “Internet of Things” (IoT)—a pervasive network of interconnected sensors embedded in everyday spaces and objects that communicate with wearable technology and provide an additional layer of information for users or patients [ 57 ]. For example, the Withings system links multiple devices together, including a wearable fitness tracker and sleep sensor placed under the mattress. A smart weight scale also records heart rate, body fat, and air quality, providing even more information about a user’s daily health habits [ 58 ]. However, successful applications of “intelligent” computing and the use of multiple consumer sensors requires a truly interdisciplinary approach in order to decode “individual big data.” Computer and data scientists, who write such computational algorithms, have to work closely with clinicians to accurately quantify various health conditions and risk factors. Behavioural scientists and interface designers have to be on board to facilitate and develop more personalised, intuitive, and user-friendly systems of behavioural engagement and feedback. Those whose expertise lies in the design, manufacture, and marketing of consumer wearables should be mindful of the limitations that have plagued previous medical and psychological interventions—specifically, the assumption that the impact of a seemingly positive intervention can be assessed without randomised controlled trials.
While many champion wearables as data-rich devices that will revolutionise 21st century medicine, it remains highly probable that, like many technological trends, these mass-marketed gadgets will drift into obscurity. However, given their continued popularity, particularly amongst those who already maintain a watchful eye over their lifestyle, health practitioners may need to prepare themselves for an increase in patients who bring wearable data to their next consultation. This may generate additional confusion and anxiety for both practitioner and patient. More worryingly, the margin of error can be high when patients without medical training attempt to attribute symptoms to a specific stream of data from devices that may themselves be unreliable. Drawing a parallel with patient-obtained diagnoses via Google, less than 5% of surveyed health care providers felt that any Internet self-diagnosis was helpful [ 1 ]. Alternatively, if frameworks are in place allowing wearable devices to be integrated into health care systems, this could, in turn, kick-start the development of validation programmes that would sit alongside appropriate training for health care professionals. This knowledge and understanding could then be disseminated to patients as validated devices become standardised, providing both individual and aggregated data for patients, governments, and health care providers. Moving forward, practitioners and researchers should try to work together and open a constructive dialogue on how to approach and accommodate these technological advances in a way that ensures wearable technology can become a valuable asset for health care in the 21st century.
Author Contributions
Wrote the first draft of the manuscript: LP DAE. Contributed to the writing of the manuscript: LP DAE SA AJ. Agree with the manuscript's results and conclusions: LP DAE SA AJ. All authors have read, and confirm that they meet, ICMJE criteria for authorship.
- 1. Cello Health Insight. The Digital Health Debate; 2014. http://cellohealthinsight.com/digital-health-debate/ [cited 04 Nov 2014].
- 2. Juniper Research. Smart Wearable Devices. Fitness, Healthcare, Entertainment & Enterprise 2013–2018.; 2013. http://www.juniperresearch.com/reports/Smart_Wearable_Devices [cited 30 Oct 2014].
- View Article
- Google Scholar
- PubMed/NCBI
- 5. Sandulescu V, Andrews S, Ellis D, Bellotto N, Mozos O. Stress Detection Using Wearable Physiological Sensors. In: Ferrández Vicente JM, Álvarez Sánchez JR, de la Paz López F, Toledo-Moreo FJ, Adeli H, editors. Artificial Computation in Biology and Medicine. vol. 9107 of Lecture Notes in Computer Science. Springer International Publishing; 2015. p. 526–532.
- 9. Poltavski DV. The Use of Single-Electrode Wireless EEG in Biobehavioral Investigations. In: Rasooly A, Herold KE, editors. Mobile Health Technologies: Methods in Molecular Biology. Springer New York; 2015. p. 375–390.
- 14. Ledger D, Partners E, Scientist B, Manager P. Inside Wearables. How the Science of Human Behavior Change. Endevour Partners; 2014. http://endeavourpartners.net/white-papers/ .
- 16. Norman D. The Design of Everyday Things (revised and expanded edition). MIT Press; 2013.
- 18. Chen Z, Chen Y, Hu L, Wang S, Jiang X, Ma X, et al. ContextSense: unobtrusive discovery of incremental social context using dynamic bluetooth data. In: Proceedings of the 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing Adjunct Publication—UbiComp ‘14 Adjunct. Seattle, USA: ACM Press; 2014. p. 23–26.
- 21. Arora S, Venkataraman V, Donohue S, Biglan KM, Dorsey ER, Little MA. High accuracy discrimination of Parkinson’s disease participants from healthy controls using smartphones. In: 2014 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP). Florence, Italy: IEEE; 2014. p. 3641–3644.
- 45. Strava Labs [homepage on the Internet]; c2009-14 [cited 30 Oct 2014]. http://labs.strava.com .
- 47. Lambiotte BR, Kosinski M. Tracking the Digital Footprints of Personality. In: Proceedings of the IEEE. vol. 102; 2015. p. 1934–1939.
- 54. Apple ResearchKit [homepage on the Internet]; c2015 [cited 23 Mar 2015]. https://www.apple.com/researchkit/ .
- 58. Withings [homepage on the Internet]; c2008-15 [cited 8 Jul 2015]. http://www.withings.com/uk/ .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Consumer engagement in health care policy, research and services: A systematic review and meta-analysis of methods and effects
Louise k. wiles.
1 Allied Health and Human Performance, University of South Australia, Adelaide, South Australia, Australia
2 Centre for Healthcare Resilience and Implementation Science, Australian Institute of Health Innovation, Macquarie University, North Ryde, New South Wales, Australia
3 South Australian Health and Medical Research Institute (SAHMRI), Adelaide, South Australia, Australia
4 Health Consumer Advocate/Representative, Adelaide, South Australia, Australia
Julie A. Luker
Anthea worley, jane austin.
5 Health Performance Council, Adelaide, South Australia, Australia
6 National Disability Insurance Agency, Adelaide, South Australia, Australia
Michael Cousins
7 Carers SA, Seaton, South Australia, Australia
Sarah Dalton
8 The Children’s Hospital at Westmead, Westmead, New South Wales, Australia
9 Agency for Clinical Innovation, St Leonards, New South Wales, Australia
Ellie Hodges
10 Lived Experience Representative, Adelaide, South Australia, Australia
Lidia Horvat
11 Safer Care Victoria, Melbourne, Victoria, Australia
Ellen Kerrins
12 SAHMRI Community Advisory Group, Adelaide, South Australia, Australia
Julie Marker
Michele mckinnon.
13 SA Health, Adelaide, South Australia, Australia
Penelope McMillan
Maria alejandra pinero de plaza.
14 Caring Futures Institute, College of Nursing and Health Sciences, Flinders University, Bedford Park, South Australia, Australia
15 National Health and Medical Research Council Transdisciplinary Centre of Research Excellence in Frailty Research to Achieve Healthy Ageing, Adelaide, South Australia, Australia
16 Royal District Nursing Service, Keswick, South Australia, Australia
David Yeung
17 Royal Adelaide Hospital, Adelaide, South Australia, Australia
18 SA Pathology, Adelaide, South Australia, Australia
Susan L. Hillier
Associated data.
All relevant data are within the paper and its Supporting Information files.
To assess the effects of consumer engagement in health care policy, research and services. We updated a review published in 2006 and 2009 and revised the previous search strategies for key databases (The Cochrane Central Register of Controlled Trials; MEDLINE; EMBASE; PsycINFO; CINAHL; Web of Science) up to February 2020. Selection criteria included randomised controlled trials assessing consumer engagement in developing health care policy, research, or health services. The International Association for Public Participation, Spectrum of Public Participation was used to identify, describe, compare and analyse consumer engagement. Outcome measures were effects on people; effects on the policy/research/health care services; or process outcomes. We included 23 randomised controlled trials with a moderate or high risk of bias, involving 136,265 participants. Most consumer engagement strategies adopted a consultative approach during the development phase of interventions, targeted to health services . Based on four large cluster-randomised controlled trials, there is evidence that consumer engagement in the development and delivery of health services to enhance the care of pregnant women results in a reduction in neonatal, but not maternal, mortality. From other trials, there is evidence that involving consumers in developing patient information material results in material that is more relevant, readable and understandable for patients, and can improve knowledge. Mixed effects are reported of consumer-engagement on the development and/or implementation of health professional training. There is some evidence that using consumer interviewers instead of staff in satisfaction surveys can have a small influence on the results. There is some evidence that consumers may have a role in identifying a broader range of health care priorities that are complementary to those from professionals. There is some evidence that consumer engagement in monitoring and evaluating health services may impact perceptions of patient safety or quality of life. There is growing evidence from randomised controlled trials of the effects of consumer engagement on the relevance and positive outcomes of health policy, research and services. Health care consumers, providers, researchers and funders should continue to employ evidence-informed consumer engagement in their jurisdictions, with embedded evaluation.
Systematic review registration: PROSPERO CRD42018102595 .
Introduction
Engaging consumers in health care decisions is widely recognised as being important in health care policy, research and services. Consumer participation can be viewed as a goal in itself, by encouraging participative democracy, public accountability and transparency. Consumers may offer different and complementary perspectives and priorities to those of professionals; furthermore, they may not have the same conflicts of interest and loyalties as professionals. The concept of consumer engagement is founded on the principle that health care policy, research and health services are in the public interest [ 1 ] and people have the right to be engaged with and contribute to decisions which will affect them [ 1 , 2 ]. In their review, Degeling et al [ 3 ] found the purpose for involving consumers in health policy processes is to capture the plethora of community perspectives, to enable consumer responsibility, and to examine acceptability of approaches to generate evidence for policymaking [ 3 ]. In health research, evidence supports the notion that consumer engagement leads to research of greater quality and clinical relevance [ 4 ] and application of findings [ 5 ]. There is also some evidence that input from consumers in planning health care can lead to more accessible and acceptable health services [ 6 ]. That said, there is a lack of contemporary research that reliably or systematically investigates whether consumer engagement achieves these intended benefits and if so, which methods of consumer engagement are most effective, and how these effects might be measured.
Despite the development of policy to support consumer engagement, there is evidence of widespread national and international variation in the extent to and the manner in which consumers are engaged. For example, membership of peak grant committees has been found to be dominated by academics and clinicians in over 70% of eleven nationally-based research funding organisations recently surveyed, and only one organisation provided public access to full protocols for completed or ongoing research [ 7 ]. Furthermore, and notwithstanding the availability of well-established standards for consumer (stakeholder) engagement in creating clinical practice guidelines [ 8 – 10 ], there are considerable inconsistencies and gaps in practice [ 11 – 13 ]. Conversely, several consumer engagement strategies have led to tangible improvements across a range of metrics. The Guidelines International Network sought to operationalise their published standards for guideline development [ 9 ] as a toolkit [ 14 ] employing a mixed approach of literature reviews and stakeholder panels, they specifically focused on ways to meaningfully involve patients and members of the public in developing guidelines. In addition, a number of initiatives have been implemented by organisations such as Planetree International (e.g. consulting and training programs), The King’s Fund (e.g. involving patients and carers in research, conference planning and collaborative leadership) [ 15 ], and the UK National Health Service project aimed at exploring how patients and carers can act as leaders, provide feedback and improve the experience of healthcare (e.g. ‘patients as leaders’ which resulted in the generation of building blocks for success and identification of key roles across systems) [ 16 ].
Many health professionals, consumers and organisations are calling for hard evidence and robust evaluations of many factors around consumer engagement including impact, how it leads to benefits, the best method for translation and implementation and even how it should be conceptualized [ 17 – 22 ]. Not all of these gaps in knowledge and application can be addressed by this review. However, we can aim to identify good practice to support and advise uptake in areas that are currently active, as well as provide evidence to support engagement in settings where it is not as common. A review was first published on this topic in 2006 and updated in 2009 [ 23 ]. Since 2009 there have been numerous developments regarding consumer engagement (sometimes termed ‘patient and public involvement’) in health care services, policy and research. This has been accompanied by considerable growth in people and organisations undertaking consumer engagement [ 24 , 25 ], shifts in terminology [ 26 ], and new conceptual models and frameworks to explore, explain and evaluate consumer engagement in health [ 27 – 30 ]. In our review which updates the 2009 review [ 23 ], we aim to report on: (a) the methods of consumer engagement strategies used in societal decisions on health care policy, research and services (according to the IAP2 Public Participation Spectrum); and, (b) their effects on the people involved in the engagement, on the research/policy/health care service, as well as process outcomes.
The primary objective of the review was to assess the effects of consumer engagement on health care policy, research and services [ 23 ]. Secondary objectives were to explore whether differences between studies might explain any differences between the effects [ 23 ]. We were specifically interested in differences in the:
- methods (levels) of consumer engagement (e.g. fact sheets, focus groups, patient advisory committees representing the levels of inform, consult, involve, collaborate or empower) [ 23 ];
- stages (i.e. development, implementation, monitoring, evaluation) of health care policy, research and services in which consumers are engaged [ 23 ]; and
- characteristics of consumer or professional participants (e.g. background, experience or training in consumer engagement) [ 23 ].
Human Research Ethics Committee approval was granted from the University of South Australia (protocol number 0000036486) and La Trobe University (approval number S17-013). Written and oral consent was obtained.
Patient and public involvement statement
A new author team was formed to undertake an update on the 2009 review [ 23 ] that included researchers and a consumer representative. In addition, we elected to partner with a stakeholder advisory group (including ten consumers) to enhance the relevance and currency of the review to potential readers and users. Further details of the stakeholder group members and the engagement process are included in S1 Appendix. Given the significant developments since the last review, the author team as advised by the stakeholder group, deemed the publication of a new review protocol and results to be relevant and necessary [ 31 ]. At key stages of the systematic review process, stakeholders were invited to provide perspectives and feedback which were used to: craft and refine the research question(s) and definitions for the population, intervention, comparator/control, outcome [PICO] criteria; contextualize initial analyses of results from included studies; and ensure the appropriateness of interpretations from the study findings in the draft final review report.
Criteria for considering studies for this review
Our review protocol was published a priori in PROSPERO [ 31 ]; for further details of our methods please refer to this listing. For our working definitions of consumer engagement, health care consumer, health care professional/researcher/policy-maker, health care policy, health care services, health care research and further descriptors of potential outcomes, S2 Appendix.
Our definition of health care consumer
We used the following definition of health care consumer: patients and potential patients, carers, and people who use health care services. Collectively, ‘consumers’ and ‘community members’ may be referred to as ‘the public’ [ 32 ]. However, given the variations in terminology within different contexts, we included any of the following terms for health care consumers: patients; unpaid carers (current or former); parents/ guardians/family; users and potential users of health care services; people with lived experience; peer workforce; people with disability; members of the public who are the potential recipients of health promotion/public health programmes; groups asking for research because they believe they have been exposed to potentially harmful circumstances, products or services; groups asking for research because they believe they have been denied products or services from which they believe they could have benefited; and organisations that represent service users and carers [ 23 ]. Depending on the context, they could be described with any of the following terms: ’lay’, ’service user’, ’survivor’, ‘patient and public involvement’ or ‘member of the general public’ [ 23 ]. We acknowledge that our broad definition means that every individual would be included as a health care consumer. As such, we focused on the role played; that is, only included participants as health care consumers when they had been engaged in health care services, policy or research with the identifiable purpose of bringing a consumer perspective.
Our definition of health care professional, researcher or policy maker
We used the following definition of a health care professional, researcher or policy maker: people who are employed in health care services, research institutions or government health departments or related agencies as health care professionals (in any professional discipline), health care service managers, researchers, and policy-makers who participate in the included study according to one (or more) of these roles [ 23 ].
Our definition of ’consumer engagement’
We used the following definition of consumer engagement: “an informed dialogue between an organisation and consumers, carers and the community which encourages participants to share ideas or options and undertake collaborative decision making, sometimes as partners" [ 33 ].
As discussed, we have chosen to use the IAP2 Public Participation Spectrum to help us determine what should be included as a consumer engagement study [ 34 ]. Examples of methods of engagement (for each IAP2 participation level) include: mass media and fact sheets (inform), focus groups and patient surveys (consult), patient advisory committees and Delphi processes (collaborate), and citizen panels or consumer managed projects and services (empower) [ 35 ]. As such, we included studies that described a consumer engagement activity that met the criteria for consult, involve, collaborate or empower (i.e. all items with the exception of ‘inform’ as it does not fit with our definition of consumer engagement being a two-way ’informed dialogue’). This is also consistent with the way in which the UK’s NIHR INVOLVE [ 26 ] defines what they term ‘public involvement’ in research, clarifying it does not include ‘researchers raising awareness of research, sharing knowledge or engaging and creating a dialogue with the public’.
Given the different terminology used to describe consumer engagement, we accepted any terminology used in the studies (i.e. participation, involvement, co-production, co-design), as long as the description about what was involved met our criteria for engagement.
Our definition of health care policy
We defined health care policy as "decisions, plans, and actions that are undertaken to achieve specific health care goals within a society. An explicit health policy can achieve several things: it defines a vision for the future which in turn helps to establish targets and points of reference for the short and medium term. It outlines priorities and the expected roles of different groups; and it builds consensus and informs people" [ 36 ]. Common outputs of health care policy include standards, practice guidelines or position statements. We included studies in health care policy undertaken by any health care organisations, e.g. national, state and local governments, non-government organisations, health care services, private organisations or consumer groups, and at any stage of the policy-making cycle (commonly described as agenda setting, formulation, adoption, implementation, and evaluation).
Our definition of health care services
We defined health care as “services provided to individuals or communities by health service providers for the purpose of promoting, maintaining, monitoring or restoring health” [ 37 ]. Health care services providing direct care to patients in primary, secondary or tertiary settings were included in this review. Within this context, consumers might be involved in activities like health care service governance, health care service redesign, developing patient information for informed decision-making/consent, among others. An important distinction is that we did not include studies where the aim was to engage consumers in their own individual care, but rather they are involved in broader activities of the health care service.
Our definition of health care research
We defined health care research as clinical research, epidemiological research and health care services research (investigating need, demand, supply, use, and outcome of health care services) [ 38 ]. This also included public health and health promotion research. Within this context, consumers might be involved in research funding decisions, setting research priorities, and planning, undertaking or disseminating research, among others. This does not include studies where the only role consumers have is as a participant of the study.
Types of studies
Randomised controlled trials (RCTs), cluster-RCTs and quasi-RCTs (as defined by the Cochrane Collaboration Handbook) [ 39 ].
Types of participants
We included studies investigating the effects of consumer engagement on health care services, policy or research. There are two layers of participants in this review: (1) ’Engagement participants’ who are involved in the engagement process and (2) ’Intended recipient participants’ of the health care policy, research or services that have been developed, implemented, monitored, and/or evaluated using the consumer engagement strategy. ’Engagement participants’ are health care consumers and professionals (meaning health care practitioners, researchers or policymakers).
Types of interventions
We defined consumer engagement as “an informed dialogue between an organisation and consumers, carers and the community which encourages participants to share ideas or options and undertake collaborative decision making, sometimes as partners" [ 33 ], and used the IAP2 Public Participation Spectrum to help us determine what should be included as a consumer engagement study [ 28 ]. We included studies which compared consumer engagement to no consumer engagement or compared one method of consumer engagement to another method of consumer engagement, in the context of health care policy, research or services, where that engagement met the criteria for consult, involve, collaborate or empower (i.e. all items with the exception of ‘inform’ as it does not fit with our definition of consumer engagement being a two-way ’informed dialogue’).
Types of outcome measures
To be included, a trial must have had a quantitative measure, based on the following three broad outcome categories to describe the range of effects: effects on people; effects on health care policy/research/ services; and process outcomes (S2 Appendix).
Search methods for identification of studies
We revised previous search strategies (S3 Appendix) and searched the following databases without language restriction: The Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, February 2020); MEDLINE (OvidSP) (2009 to February 2020); EMBASE (OvidSP) (2009 to February 2020); PsycINFO (OvidSP) (2009 to February 2020); CINAHL (EbscoNet) (2009 to February 2020); Web of Science (2009 to February 2020).
We searched the following additional sources and places for published and unpublished studies: websites of relevant organisations; clinical trials registries; Google Scholar; reference lists of included studies; and citation tracking of included studies. In addition, we liaised with our stakeholder group and contacted experts in the field directly. We also promoted our review on Twitter and Facebook, inviting people to send us studies. All revised and updated search strategies are available from the principal author.
Data collection and analysis
Two authors (two of LW, AW, JL, SH) independently screened all titles and abstracts identified from searches to determine which met the inclusion criteria, with the assistance of Covidence systematic review software [Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia]. We retrieved in full text any papers identified as potentially relevant. Two review authors independently screened full-text articles for inclusion or exclusion, with discrepancies resolved by discussion and consulting a third author, if necessary, to reach consensus. A pilot screening of 100 papers was conducted to ensure all criteria were being applied consistently across studies by the four authors. All potentially relevant papers excluded from the review at this stage are listed as excluded studies, with reasons available from the authors. We also noted citation details and any available information about ongoing studies and collated and reported details of duplicate publications, so that each study (rather than each report) is the unit of interest in the review. Studies with more than one reference were identified by the year the study was conducted or completed. We report the screening and selection process in an adapted PRISMA flow chart ( Fig 1 ) and checklist (S4 Appendix) [ 40 ].

Data extraction and management
Two review authors (two of LW, JL, SH) extracted data independently from included studies using a standardised data extraction form. Any discrepancies were resolved by discussion until consensus was reached, or through consultation with other authors where necessary. We piloted the data extraction template to ensure sufficient information about the study design, participants, consumer engagement and study methods, and outcomes measured to inform the interpretation of the results. All extracted data were entered into RevMan (RevMan 2012) by two review authors (JL and SH) and were checked for accuracy against the data extraction sheets by a third review author working independently. In addition to data items to be extracted, the author team assessed the extent of the consumer engagement in each included study. To do this, the method of consumer engagement used in included studies was mapped onto one of the four items of the IAP2 Spectrum of Public Participation (i.e. consult, involve, collaborate or empower), and scored (Yes/No/can’t tell) according to the seven principles of the IAP2 quality assurance standard [ 28 ] ( Table 1 ).
Assessment of risk of bias in included studies
We assessed and reported on the methodological risk of bias of included studies in accordance with the Cochrane Handbook [ 39 ], which recommends the explicit reporting of the following individual elements for RCTs: random sequence generation; allocation sequence concealment; blinding (participants, personnel); blinding (outcome assessment); completeness of outcome data; selective outcome reporting; and other sources of bias. Using Covidence systematic review software, two authors (JL, LW) independently assessed the risk of bias of included studies, with any disagreements resolved by discussion with a senior (SH) and consumer author (DK), to reach consensus.
We also contacted study authors for additional information about the included studies when necessary to clarify methods, data or expected completion dates. Studies were categorised as ’awaiting classification’ if additional information was not able to be sought, or ‘ongoing’ if the trial was deemed in progress.
Data synthesis
We decided whether to meta-analyse data based on whether the interventions in the included trials were similar enough in terms of participants, settings, intervention, comparison and outcome measures to ensure meaningful conclusions from a statistically pooled result.
Where we were unable to pool the data statistically using meta-analysis, we had clear reasons for this decision (outlined in the Results section) and presented the data in tables and narratively synthesised results. We have presented the major outcomes and effects, organised by intervention categories according to the major types and/or aims of the identified interventions. Within the data categories, we explored the main comparisons of the review: consumer engagement to no consumer engagement; one method of consumer engagement to another method of consumer engagement.
If studies compared more than one consumer engagement intervention (e.g. two or more interventions and a no-intervention/control group), we would have compared each intervention separately to the no intervention/control group; and with one another.
Measures of treatment effect
For dichotomous outcomes, we analysed data based on the number of events and the number of people assessed in the intervention and comparison groups. We used these to calculate the odds ratio (OR) or risk ratio (RR) and 95% confidence interval (CI). For continuous measures, we analysed data based on the mean, standard deviation (SD) and number of people assessed for both the intervention and comparison groups to calculate the mean difference (MD) and 95% CI. If the MD was reported without individual group data, we used this to report the study effects. If more than one study measured the same outcome using different tools, we would have calculated the standardised mean difference (SMD) and 95% CI using the inverse variance method in RevMan 5.
The range of outcomes considered in this review was developed collaboratively with our stakeholder panel and is substantial. Where studies recorded outcome data at multiple time points, we reported the data from the final follow-up, because longer-term outcomes were considered most important in practice by our stakeholder panel. Therefore, we did not report outcome data recorded at other time points.
Unit of analysis issues
If cluster-RCTs were included, we checked for unit-of-analysis errors. If errors were found, and sufficient information was available, we would have re-analysed the data using the appropriate unit of analysis, by taking account of the intra-cluster correlation (ICC). We planned to obtain estimates of the ICC by contacting authors of included studies or imputing them using estimates from external sources (e.g. similar studies, resources that provide examples of ICCs, or ICC patterns for particular types of cluster or outcome) [ 39 ]. If it was not possible to obtain sufficient information to re-analyse the data we would have reported effect estimates and annotated with a ‘unit-of-analysis error’ message.
Assessment of heterogeneity
Where studies were considered similar enough (based on consideration of the populations, consumer engagement activities, or other factors such as outcomes) [ 42 ] to allow pooling of data using meta-analysis, we assessed the degree of heterogeneity by visual inspection of forest plots and by examining the I 2 test for heterogeneity. We reported our reasons for deciding that studies were similar enough to pool statistically. Heterogeneity was quantified using the I 2 statistic. An I 2 value of 50% or more was considered to represent substantial levels of heterogeneity, but this value was interpreted in light of the size and direction of effects and the strength of the evidence for heterogeneity, based on the p-value from the I 2 test [ 39 ]. Where heterogeneity was present in pooled effect estimates we planned to explore possible reasons for variability by conducting subgroup analysis.
Assessment of reporting biases
We assessed reporting bias qualitatively based on the characteristics of the included studies (e.g. if only small studies that indicate positive findings were identified for inclusion), and if information that we obtained from contacting experts and authors or studies suggested that there were relevant unpublished studies. If we identified sufficient studies (at least 10) for inclusion in the review we planned to construct a funnel plot to investigate small study effects, which may indicate the presence of publication bias. We would formally test for funnel plot asymmetry, with the choice of test made based on advice in Higgins et al [ 39 ], and bearing in mind that there may be several reasons for funnel plot asymmetry when interpreting the effects.
Subgroup analysis and investigation of heterogeneity
Given the nature and quantity of trials, it was unlikely we would be able to conduct a formal sub-group analysis; we therefore explored any potential effect modifiers narratively. We considered whether the differences in any of the following factors might explain any differences in the effects:
- the methods of consumer engagement per IAP2 participation level [ 28 ] (recorded verbatim from included studies; e.g. focus groups and patient surveys, patient advisory committees and Delphi processes, and citizen panels or consumer managed projects and services) [ 23 , 35 ];
- IAP2 Public Participation Spectrum (with the four items: consult, involve, collaborate, and empower) [ 28 ], the stages (i.e. development, implementation, monitoring, evaluation) of health care policy, research and services in which consumers are engaged;
- differences between consumer or professional participants; and
- context (health care policy, research, services).
Sensitivity analysis
Where meta-analysis was possible, we considered a sensitivity analysis to determine the effects of including studies at highest risk of bias. This meant comparing the effects of studies deemed at highest risk of bias (as outlined in Assessment of risk of bias of included studies ) with those rated at lower risk of bias. By default, the highest risk of bias studies would include quasi-RCTs.
Description of included studies
The prior reviews [ 23 ] reported on a total of six included trials. The revised and updated searches for the 2020 version identified an additional 14,540 citations, with full-text copies of 156 articles retrieved for further assessment. Seventeen new trials, described in 41 papers, were then added to the six trials from the original review ( Fig 1 for flow chart of search results). We identified 16 trials through database searches, one from hand searching the reference lists of relevant publications, and three ongoing studies from searches of trial registries (ISRCTN41083256; {"type":"clinical-trial","attrs":{"text":"NCT02319967","term_id":"NCT02319967"}} NCT02319967 ; KT Canada 87776; ACTRN12614000457640).
Twelve inclusions were RCTs, and the remaining 11 were cluster RCTs [ 43 – 53 ]. Six studies included 100 or fewer participants [ 11 , 45 , 52 , 54 – 56 ], nine studies had between 100 and 1,000 participants, and eight had more than 1,000 participants including three studies with over 20,000 participants [ 44 , 47 , 51 ]. Study authors (n = 4) were contacted via email (up to a maximum of three occasions over a two-month period) to clarify: (i) study completion dates (for published study protocols and pilot/foundational studies that indicated the main study was still in progress), and (ii) details of the consumer engagement strategies (especially how they were developed) to determine if they met our eligibility criteria. Author contact for the latter was not especially helpful as methodological ambiguity most often arose from older studies, the authors of which typically did not reply.
Participants and setting
Included studies were conducted in ten countries (USA, UK, Canada, Bangladesh, Norway, Ghana, Japan, Nepal, Vietnam, Belgium), in both urban and rural settings. Nine studies were set in (self-described) low socioeconomic countries and/or within disadvantaged communities [ 43 , 44 , 46 , 47 , 50 , 51 , 53 , 56 , 57 ]. The interventions for most studies took place within outpatient [57–60 or local community health clinics [ 43 , 45 , 49 ], or social support hubs [ 44 , 47 , 50 , 51 ], and two studies were conducted in hospital inpatient settings [ 55 , 61 ], one in a medical school [ 62 ], and one in aged care facilities [ 52 ].
The interventions were directed at people within various diagnostic groupings including mental illness [ 49 , 53 , 56 , 59 , 60 ]; pregnant and birthing women [ 44 , 47 , 50 , 51 ]; and chronic diseases [ 45 , 58 ] including smoking [ 46 ]. Other targeted participants were users of health care services such as participants undertaking hospital procedures [ 55 , 61 ], attending Oncology clinics [ 63 ], or attending Paediatric clinics [ 57 ]. Other participants represented general health care users in their community [ 43 , 54 , 64 ], military veterans [ 48 ], nursing home residents [ 52 ], advocates for patients with Alzheimer’s and their caregivers [ 11 ], and medical students [ 62 ].
Interventions
To describe the interventions involving consumer engagement, we classified trials according to the area (context), level (methods), stage and characteristics of the consumers. Table 2 provides a summary of these features.
Key: CE = consumer engagement; CI = confidence interval; PICOT = Population, Intervention, Comparator, Outcome, Time; QoL = quality of life; OR = odds ratio; PCA = patient controlled analgesia; RR = relative risk; SF-36 = Short Form (36) Health Survey; TCU-HF = Texas Christian University Health Form.
Areas of consumer engagement
The majority of interventions were in the area of health services [ 15 ], predominantly in the development (and/or implementation) of the service itself; although two were more specifically involved in developing patient information material [ 55 , 61 ], two in developing training material for health professionals who deliver health services [ 62 , 63 ]. Four studies engaged consumers in health-related research , spanning development, implementation and monitoring within the research process [ 48 , 49 , 59 , 60 ]. The final four trials employed consumer engagement in the area of health policy , predominantly in developing priorities [ 45 , 53 , 54 , 64 ] but also in the development of a clinical practice guideline [ 11 ].
Levels of consumer engagement
Using the IAP2 descriptors of consumer engagement, five trials were judged to be consulting [ 55 , 57 , 58 , 61 , 63 ], four were involving [ 45 , 48 , 49 , 60 ], nine were collaborating [ 11 , 43 , 46 , 52 – 54 , 59 , 62 , 64 ] and five were empowering [ 44 , 47 , 50 , 51 , 56 ].
Stages of consumer engagement
Consumer engagement occurred mostly at the stage of development (n = 18), with 11 at the stage of implementation , four monitoring and one evaluating . Ten trials engaged with consumers at two or more stages ( Table 2 ).
Characteristics of consumers
In all trials, the consumer engagement participants had the relevant background as the intended recipient participants—whether that was related to a particular cultural or ethnic characteristic, or diagnostic or sociodemographic grouping (e.g. age or community-dwelling or service user). No consumers in the engagement process were reported to have had prior training in engagement, but the majority received relevant training as part of the trial process (13 trials) [ 43 – 47 , 50 – 53 , 56 , 57 , 59 , 60 ] which ranged from an hour or two familiarising the consumers with the task at hand, through to several days spent in training, discussion and development.
Table 2 summarises the outcome measures used across the trials. Twenty-one trials [ 43 – 53 , 55 – 64 ] considered the effects on the intended recipient participants; only one trial [ 48 ] measured the effects of the intervention on the engagement participants themselves; five [ 11 , 45 , 52 , 54 , 57 ] measured the effects on research, policy or health care service itself and nine [ 11 , 43 – 47 , 50 , 51 , 53 ] measured process outcomes.
Excluded studies
Of the 180 full texts excluded in this update, 43 studies used an intervention that did not fit our definitions for consumer engagement, and 58 used the wrong study design (i.e. were not RCTs), nine were conference abstracts, and one did not relate to health research, policy or services (i.e. wrong subject area). The most common reason for exclusion (n = 64 studies) was the use of a design that could not differentiate the effect of consumer engagement intervention from other effects (for a full list please contact authors).
Risk of bias in included studies
Overall the risk of bias in the included studies was high, confounded by poor (unclear) reporting particularly in the earlier studies as noted in the 2006 and 2009 reviews; on average, there were 6.3 items with unclear risk of bias ratings for the 7 studies published between 1997 and 2007), compared with 2.3 items for those (n = 16) from 2008 onwards. Only two studies achieved four criteria as low risk [ 45 , 49 ]; the average number of criteria judged as low risk was only 1.3 per trial. Fig 2 shows individual ratings for each risk category.

Effects of interventions
Twenty-one [ 11 , 43 – 53 , 55 – 63 ] of the 23 included trials were comparisons of consumer engagement versus no consumer engagement. Two trials involved comparisons of different methods or degrees of consumer engagement, all compared with no consumer engagement [ 54 , 64 ]. No trials were identified that only compared one type of engagement with another. Subgroup analyses were not able to be performed with insufficient numbers of trials in any sub-group of interest, as expected.
Consumer engagement versus no consumer engagement in health services (15 included trials)
Health service delivery.
We were able to find four studies [ 44 , 47 , 50 , 51 ] sufficiently similar across the PICO domains to allow meta-analyses. These studies all investigated women giving birth who received a comprehensive health services intervention for healthy birthing that was developed and implemented with consumer engagement at an empowering level, compared to birthing education and support developed and delivered without consumer engagement (across three different countries) [ 44 , 47 , 50 , 51 ]. All four trials used cluster randomisation and all four performed appropriate analyses at both the individual and cluster levels. All stated their intent to account for the cluster design in their protocols and all carried this intention out in the final reports; therefore, no unit of analysis issues were present in the outcome data. For the outcomes of neonatal mortality, we extracted data for 83,925 births, with a total of 1,028 deaths for the intervention group and 1,282 for the control group; this gave a meta odds ratio of 0.8 in favour of the intervention group (95% CI 0.77, 0.91; p<0.0001) ( Fig 3 ) (or Risk Ratio of 0.84; 95% CI 0.77, 0.91; p<0.0001). The heterogeneity (as assessed by the I 2 ) was high at 72% and mostly explained by the large range of frequencies of event. The second outcome (maternal deaths) that afforded meta-analysis returned a non-significant finding from the same four studies [ 44 , 47 , 50 , 51 ] and same number of births with 80 maternal deaths in the intervention group versus 78 in the control (OR of 1.10, 95% CI 0.81,1.51; p = 0.54) ( Fig 4 ). A risk ratio analysis revealed the same results. Again the heterogeneity was high at 83% and this time was predominantly explained by the result of one study [ 44 ] which reported an unforeseen maternal death rate of 63 in the consumer engaged group versus 35 in the control; in addition, heterogeneity by chance may have been exaggerated by the small number of events (maternal deaths). The authors could not explain the reason for this and felt it was not attributable to the intervention as there was no common cause of death. The other three studies [ 47 , 50 , 51 ], in contrast, all reported lower maternal death rates in the intervention groups (two of the three non-significant).

Based on these four trials [ 44 , 47 , 50 , 51 ] there is evidence that consumer engagement in developing and implementing health services , to enhance the care of mothers and their babies, results in a reduction in neonatal, but not maternal, mortality.
Three other trials [ 46 , 57 , 58 ] investigated the effect of consumers in developing health services . Choi et al [ 46 ] collaborated with consumers from a culturally appropriate community group to develop community-based smoking cessation program, finding in favour of increased self-reported quitting for the consumer engagement intervention, but no effect on saliva-based testing for smoking abstinence. Coker et al [ 57 ] consulted parents to develop parent coaches for children from lower-income groups, and reported favourable effects on improved receipt of services and satisfaction with consumer engagement-developed services compared to non-consumer engagement. Early et al [ 58 ] consulted with consumers in the development of respiratory outpatient services but found no difference in outcomes between the services that were consumer-consulted versus not. Based on these findings there is some evidence that some aspects of health service development may be improved by consumer engagement, but the evidence is not clear as to what aspects these may be in any consistent way.
One trial [ 56 ] investigated the effect of consumer engagement on implementation only of health services. Corrigan et al [ 56 ] used an empowerment model with consumers to implement services for people who were both homeless and with mental health issues. They reported that all outcomes were in favour of the consumer engagement-empowered services including health status, quality of life, and rates of homelessness. One trial [ 43 ] collaborated with consumers in the monitoring and evaluation of health services for safety, quality and health staff motivation. They reported that patient safety and staff motivation improved with the consumer-collaboration processes, and no change for quality items. Van Malderen et al [ 52 ] collaborated with residents of an aged care facility to develop, implement, monitor and evaluate several training interventions versus an intervention with no consumer input. They reported no difference between the various interventions except that the consumer-collaboration interventions favoured improved quality of life.
Patient information
Two trials evaluated products (patient information leaflets about endoscopic procedures [ 55 ] and post-operative patient-controlled analgesia (PCA) [ 61 ]) which were developed following consumer consultation. The leaflets were compared with patient information developed without consumer consultation. Based on these two trials [ 55 , 61 ] evidence is equivocal for consumer consultation prior to developing patient information material; while the CE material resulted in better anxiety outcomes for endoscopy patients in one study (no effect for satisfaction) [ 55 ], the other showed that despite the CE material presenting information more clearly and improving patient knowledge of PCA, there was no effect for worry about PCA-use [ 61 ]. Both studies had unclear risk for all biases (i.e. not stated within methodology) except for low risk of selection bias (use of random allocation) [ 61 ], and high risk for attrition (not all outcome data reported, no reasons given) and selective reporting bias [ 61 ] ( Fig 2 ).
Health professional training
Two trials [ 62 , 63 ] engaged consumers in the development of education material for medical practitioners. Fujimori et al [ 63 ] consulted with consumers in the development of communication training with oncologists and reported that consumer-based training led to improved objective performance and confidence in communication by the doctors and possible improvement in patient trust, though there were no differences for patient anxiety or satisfaction. Jha et al [ 62 ] collaborated with consumers to develop and implement training for junior doctors in patient safety and reported no difference in junior doctors’ attitudes to safety but favourable changes in their positive affect. Based on these two trials [ 62 , 63 ] there are mixed effects of consumer-engagement (consultation) on the development and/or implementation of health professional training.
Consumer engagement versus no consumer engagement in health care policy (five included trials)
Two trials [ 45 , 54 ] engaged consumers in priority setting processes for health services. Abelson et al [ 54 ] compared three different methods of consulting consumers, reporting that consumers did have some different perspectives with a greater focus on environmental, local education and employment conditions. Boivin et al [ 45 ] involved consumers in setting priorities for chronic disease prevention and management, finding that consumers and professionals were in broad agreement although differed on specifics; for example, consumers were more focused on community whilst the professionals were more focused on the technical aspects. Carman et al [ 64 ] collaborated with consumers in exploring ethical decision-making in health care—they compared different ways of deliberating with the consumer group via face to face or online options compared to no consumer engagement and reading material only, and found that all options which involved consumer engagement were superior to the control group for knowledge and attitudes towards decision-making, as well as attitudes to hospital use. Based on these studies there is some evidence that consumers may have a role in identifying a broader range of health care priorities that are complementary to those identified by professionals [ 45 , 54 ]. In addition to supporting decision-making processes in health (reflected in public deliberation increasing participants’ knowledge of and attitudes towards the role of medical evidence) [ 64 ], there is also some evidence of consumers contributing positively to identifying need and developing mental health service directions [ 53 ]. The fourth policy-based trial [ 53 ] collaborated with consumers with previous mental health issues in identification, planning, development (and implementation) of community-based services. The services developed with consumer collaboration were superior to services developed with no consumer engagement in all measured items (mental health scores, service use and so forth), except employment and medication use.
The remaining policy-related trial [ 11 ] compared two guideline development groups, one collaborating with consumers and one without, to craft Population, Intervention, Comparator, Outcome, Time (PICOT) questions, and identify key benefits and harms on the topic of using amyloid positron emission tomography in the diagnosis of dementia. “The proposed guideline questions, and benefits and harms, were largely similar between the two groups” [11 p.1]; however, only the group that collaborated with consumers “proposed outcomes around the future development of cognitive impairment at certain time points and proposed rate of progression (rather than considering the development of dementia as a binary [yes/no] outcome) [11 p.9-10]. Armstrong et al [ 11 ] reported that consumer collaboration also influenced the “conduct of guideline development, scope, inclusion of patient-relevant topics, outcome selection, and planned approaches to recommendation development, implementation, and dissemination” [11 p.11].
Consumer engagement versus no consumer engagement in research (four included trials)
Overall four studies investigated consumer engagement in the conduct of research–three of which were in the earlier review by Nilsen et al [ 23 ]. As reported in the first review, two trials compared consumers (former patients) with professionals as data collectors in patient satisfaction surveys in mental health services [ 59 , 60 ], Both studies found that participants reported high levels of satisfaction with mental health outpatient services irrespective of interviewer. However Clark et al [ 59 ] found that consumer interviewers elicited significantly more ’extreme negative’ responses, compared to responses gained by staff interviewers (p = 0.02). Polowczyk et al [ 60 ] also found that the consumer (client) interviewed group on average gave lower satisfaction scores than in the staff interviewed group (0.16 on a scale from 1 to 4, p = 0.05) [ 60 ]. Nilsen et al pooled the results of these two trials [ 59 , 60 ] finding the overall difference was similar (0.14 on a scale from 0 to 4, p = 0.001), ( Fig 5 ) [ 23 ]. Their summary remains appropriate: based on these same two trials there are small differences in satisfaction survey results when consumer interviewers are used instead of staff interviewers.

Two trials [ 48 , 49 ] engaged with heath researchers in other research processes. Guarino et al [ 48 ] (included in the earlier review [ 23 ]) compared an informed consent document developed with consumer involvement (potential trial participants) to a consent document developed by professionals (trial investigators). They found no overall difference in understanding between the two groups. Hughes-Morley et al [ 49 ] (new in this review) involved consumers in recruiting participants for a mental health care trial and found no difference between the number recruited using consumer engagement-based processes versus non-consumer engagement involved methods. Despite the addition of this second trial [ 49 ], there is no change to the results reported in Nilsen et al [ 23 ]: consumer consultation in the development of consent documents or recruitment may have little, if any, impact on trial participant’s self-reported understanding, satisfaction, adherence or recruitment.
Statement of principal findings
The primary objective of this updated review was to assess the effects of consumer engagement on health care policy, research and services. There has been a rapid increase in the number (and, in some instances, quality) of randomised controlled trials investigating the effectiveness of consumer engagement. The most noteworthy rise in the number of trials is in the area of health services (up from 2 to 15), with only a single addition in each of the policy and research domains. Typically, the trials compared a form of engagement with no engagement. The most common objective of the health service trials was to improve patient outcomes and the primary meta-analysis gave evidence that empowering consumers in the development and implementation of community-based services for pregnant women can reduce neonatal mortality, although there was no effect on maternal death rates. Coupled with other single trials, there is emerging evidence that consumer engagement in health service delivery affords benefits (and no evidence of harms to date) and these seem to be particularly evident in community health care settings. It should also be noted that the outcomes of the health services trials were wide ranging beyond health effects on the intended trial participants and included satisfaction, health behaviour adoption, knowledge and service utilisation. There is some evidence that consumers can have a positive role in the training of health professionals and in providing information for patients to inform their decision-making, although there is still no trial evidence for the role of consumers in guideline production.
Investigations into the effect of consumer engagement in health policy were less prevalent but did include some trials demonstrating potential benefits of collaborating with consumers in health priority-setting where they can broaden the perspectives otherwise gained from health professionals alone. There remains a dearth of investigation into the effect of consumer engagement in policy decision-making. The investigations of the effect of consumer engagement in health research remains limited to process indicators like recruitment, adherence, information and satisfaction, with no trials investigating the benefits of consumers being engaged in setting a research agenda or research methodology.
Secondary objectives were to explore whether differences between studies might explain any differences between the effects. We were specifically interested in differences in the:
- methods (levels) of consumer engagement (e.g. fact sheets, focus groups, patient advisory committees);
- stages (i.e. development, implementation, monitoring, evaluation) of health care policy, research and services in which consumers are engaged; and
- characteristics of consumer or professional participants (e.g. background, experience or training in consumer engagement).
Such a broad range of trials did not allow for rigorous investigation of the influence of these differences using sub-group analyses. However, there are patterns that warrant commentary. Firstly the strongest evidence (community-based antenatal care for pregnant women) lay in the method of engagement that lies within the definition of empowerment —using the definitions from the IAP2 of placing "the final decision-making in the hands of the public" and with the tacit understanding "we will implement what you decide" [ 28 ]. The four studies [ 44 , 47 , 50 , 51 ] that provided the evidence for improved neonatal mortality all empowered consumers in this decision-making, with the consumer supported project and sustainable community development. Other key characteristics were that the local community (i.e. women’s groups, community leaders and member, locally recruited facilitators) were embedded in every phase of the CE program; in developing its content, its implementation plan, and its delivery. The majority of the remaining studies used collaborative methods such as advisory groups, special meetings and committees; and smaller numbers using involving methods (via public meetings) or consulting (via focus groups and surveys), Tables Tables1 1 and and2 2 .
The predominant stage of consumer engagement was in development (over 75%), with a third of these [ 44 , 47 , 50 , 51 , 53 , 62 ] (including the four comprehensive health service interventions for healthy birthing) [ 44 , 47 , 50 , 51 ] undertaking engagement in both development AND implementation . This seems a logical paired process and again was most common in the community settings, to ensure buy-in and relevance for service delivery in most examples. Only one trial [ 52 ] collaborated with consumers at all stages from development through to evaluation. However, the numbers are too small to allow a statistical analysis of the import of this factor on effectiveness.
Finally, we considered the characteristics of the consumers in the trials. Again, there was a consistent finding that the consumers were not formally trained in engagement methods prior to the engagement, but the majority received requisite training in the study methodology or intervention to be delivered as part of the engagement process. In three studies [ 52 , 59 , 60 ], health professional participants were reported to receive this same training. Only eight trial consumer cohorts [ 11 , 49 , 54 , 55 , 58 , 61 , 62 , 64 ] received no training before or during the trial—bringing their lived experience as sufficient expertise for the purposes of the evaluation. This is an important finding for future trials—to consider the engagement of all participants–professionals and consumers–in health care stages across policy, research and services.
We found no evidence of adverse effects in engaging with consumers; most trials did not collect data on this aspect. The trials with patient health level data (such as neonatal mortality) [ 44 , 50 ] considered unintended effects in terms of examining the risk ratios for all outcomes between the two groups. None of the included trials addressed possible other adverse effects of consumer engagement, such as tokenism or time and other resource impacts. Seven studies [ 43 , 45 – 47 , 50 , 51 , 53 ] did consider cost-effectiveness, reporting favourably on the cost per life saved and/or cost of years of life saved in the case of the neonatal care studies, or the cost of the intervention itself, but with no benefits or effectiveness analysis [ 53 ].
Strengths and weaknesses of the study
By including a strong stakeholder engagement at key stages in the review process we believe we have mitigated against any major biases.
Our included trials were wide ranging internationally and across diverse health populations. In particular, we were struck by the number of trials engaging with consumers who were most likely to experience disparity or disadvantage in health services. The settings were predominantly in the community—this seems to lend itself to participatory processes. However, there were some examples of consumer engagement in acute and outpatient settings that augur well for ongoing investigations across the health services spectrum. Positive findings across this range suggests that consumer engagement has a role in many settings, however this does not negate the need for consideration to always be paid to these contextual factors when developing, implementing, monitoring and evaluating consumer engagement processes.
Whilst we note the increase in number of more strongly designed (randomised controlled) trials in this important area, most still had a relatively high risk of bias. It should be acknowledged that it can be hard to blind participants–consumers and professionals–in a health care intervention. However, more achievable aspects like adequate randomisation and allocation should be more stringently adhered to, as well as better reporting of outcomes and attrition.
Strengths and weaknesses in relation to other studies
Treweek et al [ 65 ] published a Cochrane review regarding strategies to improve recruitment to randomised trials. Their key results relating to consumer engagement in recruitment are similar to the results we have found with respect to patient information; in that consumer involvement in developing the content, format and appearance of information leaflets for potential research participants resulted in only a 1% absolute improvement in recruitment (95% CI: −1% to 3%) [65 p.2].
Crawford et al [ 6 ] published a systematic review with the aim of examining the effects of involving patients in the planning and development of health care. They reported a low level of studies (mostly case studies) which support the notion that involving patients does contribute to changes across a range of settings, however they found no evidence base for the effects of this involvement on various outcomes such as health, service usage and/or quality.
Meaning of the study: Possible explanations and implications for clinicians and policymakers
Engaging consumers can have a positive effect in health care policy, research and services, however there are no standard metrics to guide and benchmark evaluation of this effect across settings and contexts. The factors that underpin successful consumer engagement can be hypothesised from the included trials as involving consumer empowerment processes, in the development and implementation phases; there is a lack of evidence arising from the trials regarding the effect of other elements of engagement (inform, consult, involve, collaborate and empower) across all phases. Our recommendation is to use a tailored approach to consumer engagement with an IAP2 level that is as high and appropriate to the goals and promises to the public, and embedded evaluation.
The effect of engaging consumers in health care policy, research and services is gaining attention in the literature. The 23 trials included in this review demonstrate that randomised controlled trials of consumer engagement are feasible. Variation in practice reflects the complex nature of consumer engagement and a climate of innovation rather than evidence-based practice. The evidence from this review suggests that the best methods to achieve effective engagement are likely to vary and will need to engage participants (professionals and consumers). It is our contention that more work needs to be done to implement consumer engagement strategies and solutions specific to each problem. For instance, metrics used in assessing effectiveness and overall quality improvements associated with a health care service delivery project may be very different to that of a clinical trial, versus that of a more translational research-based project. The small number of studies available have forced the comparison of methods and outcomes across different contexts and metrics. Trials are needed to evaluate the effects of different methods of:
- identifying participants (health consumers and professionals)
- determining and utilising the elements and phases of engagement
- participant engagement training and support
- distinguishing purposefully between consumers with lived experience versus the community at large (acknowledging that health professionals have a unique and privileged knowledge of the health sector and therefore, while consumers of health policy, research and services, cannot be seen to contribute a consumer voice representative of the wider community)
- timing the engagement (which included studies did not evaluate)
- engaging individuals, groups and organisations
- resourcing engagement including customised models of financial support
- evaluation.
There is growing evidence from randomised controlled trials of the effects of consumer engagement on the relevance and positive outcomes of health policy, research and services; however, there are no standard metrics to guide evaluation of this effect. The factors that underpin successful consumer engagement can be hypothesised from the included trials as involving consumer empowerment processes, in the development and implementation phases. Our recommendation is for health care consumers, providers, researchers and funders to continue to employ evidence-informed consumer engagement in their jurisdictions, using a tailored approach with an IAP2 level that is as high and appropriate to the goals and promises to the public, and embedded evaluation.
Supporting information
S1 appendix, s2 appendix, s3 appendix, s4 appendix, acknowledgments.
The authors would like to thank Ms Anneliese Synnot and Ms Anne Parkhill for their assistance in this systematic review.
The University of South Australia provided salaries for the author SH, and via internal grant funding for LW, JL and AW. We are very grateful for the volunteer work of DK and the stakeholder group.
Funding Statement
The author(s) received no specific funding for this work.

Data Availability
- PLoS One. 2022; 17(1): e0261808.
Decision Letter 0
17 Mar 2021
PONE-D-20-36087
Consumer engagement in health care policy, research and services: methods and effects
Dear Dr. Wiles,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
The reviewer has requested some revisions, in addition to the items raised by the reviewer, please address the following points before more consideration:
Consumer (Or an illustrative term Customer) is a crucial part of any system success, and play a determinant role in policy/ program success and quality. There are a rigorous relationship between customer participation in service delivery and quality improvement.
It appears you needs to a revise your search strategy and search terms to cover all relevant studies. For example we investigate the role of pregnant women in both quality improvement and assessment activities as customer self-audit. There are many relevant studies using Centering Pregnancy® program to participate women in their own maternity services.
• Gholipour K, Tabrizi JS, Jafarabadi MA, Iezadi S, Mardi A. Effects of customer self-audit on the quality of maternity care in Tabriz: A cluster-randomized controlled trial. PloS one. 2018 Oct 11;13(10):e0203255.
• Gholipour K, Tabrizi JS, Asghari Jafarabadi M, Iezadi S, Farshbaf N, Farzam Rahbar F, Afsharniya F. Customer's self-audit to improve the technical quality of maternity care in Tabriz: a community trial. EMHJ-Eastern Mediterranean Health Journal. 2016;22(5):309-17.)
Please submit your revised manuscript by Apr 23 2021 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols
We look forward to receiving your revised manuscript.
Kind regards,
Kamal Gholipour, PhD
Academic Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. Please ensure that you have addressed all items recommended in the PRISMA checklist including identifying the study as a meta-analysis in the title.
3. Thank you for submitting the above manuscript to PLOS ONE. During our internal evaluation of the manuscript, we found significant text overlap between your submission and the following previously published works.
- https://cccrg.cochrane.org/priority-reviews/more-about-our-consumer-engagement-priority-review
- https://doi.org/10.1002/14651858. {"type":"entrez-nucleotide","attrs":{"text":"CD004563","term_id":"30321301"}} CD004563 .pub2
- https://www.who.int/evidence/sure/PatientSafetyfullreport10052014.pdf?ua=1
We would like to make you aware that copying extracts from previous publications, especially outside the methods section, word-for-word is unacceptable, even for works which you authored. In addition, the reproduction of text from published reports has implications for the copyright that may apply to the publications.
Please revise the manuscript to rephrase the duplicated text, cite your sources, and provide details as to how the current manuscript advances on previous work. Please note that further consideration is dependent on the submission of a manuscript that addresses these concerns about the overlap in text with published work.
We will carefully review your manuscript upon resubmission, so please ensure that your revision is thorough.
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Yes
Reviewer #2: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #1: No
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: Please see attachment. Answer to question 2 above--statistical analysis-- relates to the presentation, and possible synthesis of odds ratios. Please see attached review for more specifics.
xxxxxxxxxxx
Reviewer #2: This is a thorough and careful job, and this work will be of interest to everyone who wishes to promote patient engagement in health services, policy and research. I am recommending acceptance because I do not feel that I need to see it again. I do have a couple of comments.
First, it is surprising that the authors report no specific funding for such a substantial effort. Surely somebody must have been paying salaries for this. Also, the idea that you involved patient advocates and other stakeholders in the work without providing any compensation seems contrary to the spirit of the thing. I think readers would want to know how this was resourced.
It is rather odd to see repeated use of the conditional in the methods. If it turned out that the nature of the available publications did not allow you to use a certain method you can just say that.
On the whole, with the exception of neonatal mortality, the evidence for most of the outcomes seems quite weak. This is not only because of risk of bias, but also because in many cases the investigators looked at multiple outcomes and found evidence for some but not others. The positive findings often pertained to intermediate outcomes and not to more downstream outcomes, as well. While you do generally acknowledge the need for more evidence and you are restrained in endorsing conclusions, I still have an overall feeling that you might be overselling the findings just a bit. Maybe that's just me. Anyway I appreciated this and I think it's a worthy contribution.
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #2: Yes:
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Submitted filename: PLoSOne_ConsumerEngagement_Review.pdf
Author response to Decision Letter 0
22 Jul 2021
Please refer to the attached 'Response to reviewers' document (July 21 updated) which contains detailed responses to each feedback item.
Submitted filename: R2R_July 2021 updated.docx
Decision Letter 1
13 Dec 2021
Consumer engagement in health care policy, research and services: A systematic review and meta-analysis of methods and effects.
PONE-D-20-36087R1
Dear Dr. Hillier,
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
Additional Editor Comments (optional):
Acceptance letter
28 Dec 2021
Dear Dr. Hillier:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
If we can help with anything else, please email us at gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Kamal Gholipour
Perspectives on consumer health and wellness
Health | Fitness | Nutrition | Appearance | Sleep | Mindfulness

Hungry and confused: The winding road to conscious eating

Still feeling good: The US wellness market continues to boom

How to thrive in the global wellness market

The Next Normal – The future of wellness
~40–60% of wellness spending.

Are personalized vitamins the future of wellness?

Wellness worldwide: Consumer insights from four countries

Looking ahead in US consumer health: An interview with Scott Melville

At the heart of a crisis: How consumer-health companies can lead in the time of coronavirus

GSK’s Brian McNamara on the business impact of COVID-19

Speeding up to become even more consumer-obsessed: An interview with GSK’s Keith Choy
~10-30% of wellness spending.

Sweating for the fitness consumer
>1/3 of consumers plan to spend more.

Consumers with food allergies: A growing market remains underserved
~65% of consumers.

Taking a good look at the beauty industry
How COVID-19 is changing the world of beauty

Connectivity with the consumer: The Honest Company’s formula for growth
1/2 of consumers want.

Sleep on it: Addressing the sleep-loss epidemic through technology

Investing in the growing sleep-health economy
Mindfulness, >1/2 of consumers say, strong minds, strong futures: behavioral health for the next generation.

Connect with our Consumer Packaged Goods Practice
We review brands to help you make a smarter purchase decision.

Understanding What is Consumer Health and Why it is Important
Table of Contents
- 0.1 Key Takeaways:
- 1.1 Benefits of Consumer Health Information:
- 2 The Evolution of Consumer Health Care
- 3.1 Key Points:
- 4.1 Enhancing Consumer Needs with Targeted Information
- 5.1 Relevance
- 5.2 Comprehensibility
- 5.3 Credible Information Sources
- 6.1 Disease Prevention
- 7 Promoting Wellness at Every Stage of Life
- 8 The Importance and Impact of Consumer Health
- 9.1 What is consumer health?
- 9.2 Why is consumer health important?
- 9.3 What is consumer health information?
- 9.4 What is the role of consumer health librarians?
- 9.5 How has the healthcare landscape shifted towards consumer-directed care?
- 9.6 How has the internet impacted health information seeking?
- 9.7 Why is it important to promote health literacy?
- 9.8 What is the goal of consumer information?
- 9.9 How can consumer health information be made relevant, comprehensible, and credible?
- 9.10 What role do governmental health agencies play in consumer health?
- 9.11 How does consumer health promote wellness at every stage of life?
- 9.12.0.1 Dr. Sam D Granger
- 9.13 Related
Consumer health is a term that refers to the state of well-being achieved by individuals who make informed choices about their health and use products and services that are deemed safe by research. It encompasses physical, social, and mental wellness and aims to prevent illness. In today’s world, consumer health plays a crucial role in our lives, empowering us to take control of our health, make educated decisions, and prevent the spread of diseases.
Consumer health information is provided to the public through various channels, including government agencies, to ensure that individuals have access to accurate and reliable information. By having the right knowledge and understanding, we can make informed decisions about our health and well-being, leading to better overall outcomes.
Now, let’s explore the importance of consumer health and why it matters in our daily lives.

Key Takeaways:
- Consumer health involves making informed choices about our health and using safe products and services.
- It encompasses physical, social, and mental wellness and aims to prevent illness.
- Consumer health empowers individuals to take control of their health and make educated decisions.
- Access to accurate and reliable consumer health information is crucial for making informed choices.
- By prioritizing consumer health, we can improve our overall well-being and prevent the spread of diseases.
The Role of Consumer Health Information
Consumer health information (CHI) plays a vital role in promoting consumer health awareness , education, and responsibility. It provides individuals with the necessary knowledge and resources to make informed decisions about their health and well-being. CHI includes a wide range of information on prevention, self-care, diseases, treatment options, and healthcare services.
Consumer health librarians are key players in the provision of CHI. They specialize in evaluating, selecting, and delivering CHI to library patrons. Their expertise allows them to assess individual information needs, search for reliable sources, and present information in a format that is easily understood by consumers. By collaborating with consumers, these librarians help bridge the gap between complex medical information and the general public.
Consumer health information also empowers individuals to take an active role in their healthcare decisions. By providing access to accurate and reliable information, CHI helps individuals make choices that align with their healthcare needs and preferences. It promotes health literacy, enabling individuals to evaluate the credibility of information sources and make informed decisions about their health. Ultimately, the goal of CHI is to empower individuals to become proactive participants in their own health and well-being.
Benefits of Consumer Health Information:
- Increased consumer awareness of health-related issues
- Improved knowledge about preventive measures and self-care
- Enhanced ability to make informed healthcare decisions
- Promotion of health literacy and critical thinking skills
- Empowerment of individuals to take control of their health
- Facilitation of open and informed communication with healthcare professionals
The Evolution of Consumer Health Care
The healthcare landscape has undergone a significant transformation, shifting from a paternalistic model to a more consumer-centered approach. In the past, healthcare decisions were predominantly made by medical professionals, and patients would typically follow their instructions without questioning. However, societal changes, advancements in medical science, and the availability of online health information have led to the evolution of consumer-directed health care.
With the advent of evolving consumer-directed health care , patients are now expected to actively participate in treatment decision-making. They are encouraged to provide input, voice their concerns, and ask questions about their health. Patients have become more proactive in seeking health information independently, utilizing various resources to educate themselves about their conditions and available treatment options.
This shift towards patient-centered care emphasizes the importance of empowering individuals to become active participants in their own healthcare. By involving patients in the decision-making process, healthcare providers can better understand their unique needs, preferences, and goals. This collaborative approach allows for more personalized care that takes into account the individual’s values and beliefs, ultimately leading to improved health outcomes.
The Impact of Online Health Information
The availability of online health information has revolutionized the way people seek knowledge about their health. With just a few clicks, individuals can access a wealth of information on various health topics, symptoms, treatments, and preventive measures. This easy access to information has empowered individuals to take control of their health and make informed decisions.
However, it is important to note that not all online health information is created equal. The quality and accuracy of the information available on the internet can vary greatly. It is essential for individuals to employ critical thinking skills and evaluate the reliability and credibility of the sources they rely on. By doing so, they can avoid potential misinterpretation and misinformation that may lead to negative health outcomes.
To ensure the quality of online health information , it is crucial for individuals to seek information from reputable sources such as government health agencies, well-established medical websites, and peer-reviewed journals. These sources typically provide evidence-based information that is backed by scientific research and expert opinions. Additionally, it is beneficial to consult healthcare professionals who can provide personalized guidance and validate the information found online.
Key Points:
- Online health information has revolutionized how individuals seek knowledge about their health.
- Not all online health information is accurate and reliable, requiring individuals to evaluate the credibility of sources.
- Reputable sources such as government health agencies and medical websites offer evidence-based information.
- Consulting healthcare professionals can provide personalized guidance and validate online health information.
The Role of Consumer Information in Health Care Decisions
Consumer information plays a crucial role in empowering individuals to actively participate in their health care decisions . By providing valuable and relevant information, consumers can make informed choices that align with their unique needs and preferences. In today’s era of consumer-directed health care, it is important to recognize the significance of consumer information in promoting patient autonomy and improving health outcomes.
Consumer information serves as a tool to meet the information needs of individuals and help them navigate the complexities of the health care system. It provides resources on health plans, quality indicators, and comparative health plan performance data, allowing consumers to compare and select the best options based on cost, benefits, and quality of care. By arming consumers with this information, they are empowered to make decisions that prioritize their health and well-being.
Furthermore, consumer information promotes social marketing , which focuses on creating awareness and influencing behaviors in order to achieve positive health outcomes. It aims to educate individuals about available health care services, preventive measures, and lifestyle choices that can contribute to better health. Social marketing campaigns utilize various channels, such as television, radio, and online platforms, to disseminate relevant information and encourage active consumer participation in health care decisions .
Enhancing Consumer Needs with Targeted Information
- Understanding consumer needs : Effective consumer information is tailored to address the diverse information needs of individuals based on factors such as age, gender, socioeconomic status, and health conditions.
- Engaging with consumers: It is essential to actively involve consumers in the development and dissemination of consumer information, ensuring that their voices and perspectives are heard and incorporated.
- Promoting health literacy: Consumer information should be presented in a way that is comprehensible to all individuals, regardless of their educational background or health literacy levels.
- Supporting shared decision-making: Consumer information should facilitate shared decision-making between patients and healthcare providers, encouraging open communication and collaboration.
In conclusion, the availability of consumer information is instrumental in empowering individuals to make informed decisions about their health care. By promoting active consumer participation , addressing consumer needs , and utilizing social marketing strategies, consumer information plays a vital role in improving overall health outcomes and promoting a patient-centered approach to healthcare.
Ensuring Relevance, Comprehensibility, and Credibility of Consumer Health Information
When it comes to consumer health information, three key factors must be considered: relevance, comprehensibility, and credibility. These factors are essential in providing individuals with the necessary tools to make informed decisions about their health. Let’s take a closer look at each of these aspects.
Consumer health information should be tailored to meet the unique needs of individuals. Different factors such as age, gender, cultural background, and health conditions can influence the relevance of information. By delivering information that is specific to an individual’s circumstances, we can ensure that it addresses their concerns and supports their decision-making process.
Comprehensibility
For consumer health information to be effective, it must be easily understood by the target audience. Complex medical jargon and technical terms can be overwhelming and confusing to individuals seeking guidance. By presenting information in a clear and concise manner, using language that is accessible to the intended audience, we can empower individuals to comprehend and apply the information to their health decisions.
Credible Information Sources
It is paramount to ensure that consumer health information is derived from credible and trustworthy sources. In a world filled with misinformation, it is crucial to rely on evidence-based research, peer-reviewed studies, and reputable healthcare organizations. By providing information from reliable sources, we can establish trust and confidence in individuals seeking consumer health information.
By prioritizing relevance, comprehensibility, and credibility, we can ensure that consumer health information is accurate, meaningful, and beneficial for individuals seeking guidance and making informed decisions about their health.
Protecting Public Health and Safety
When it comes to consumer health, the protection of public health and safety is of utmost importance. Governmental health agencies play a vital role in this endeavor by providing valuable information on food safety , drug safety , and product safety . These agencies work tirelessly to prevent illness and ensure the well-being of consumers.
One crucial aspect of protecting public health is ensuring food safety . Government agencies provide consumers with information about potential foodborne illnesses, contamination outbreaks, and proper food handling practices. By raising awareness and educating the public, these agencies help prevent the spread of diseases and promote safe consumption habits.
Another essential component of safeguarding public well-being is drug safety . Government agencies monitor the safety and efficacy of medications, issuing warnings about potential risks or side effects. By keeping consumers informed about the latest findings, these agencies empower individuals to make informed decisions about their healthcare and prevent adverse reactions to medications.
Disease Prevention
In addition to food and drug safety , government health agencies focus on disease prevention and control. They actively promote vaccines, tests, and therapies to combat infectious diseases and protect the public from outbreaks. By disseminating accurate information and fostering a culture of prevention, these agencies contribute to improved consumer health outcomes and reduce the burden on healthcare systems.
Overall, the efforts made by government health agencies in ensuring public safety and promoting disease prevention are crucial for maintaining consumer health. By raising awareness, providing information, and implementing safety measures, these agencies play a pivotal role in protecting and enhancing the well-being of individuals and communities.
Promoting Wellness at Every Stage of Life
Consumer health organizations play a crucial role in promoting wellness at every stage of life, offering valuable information and advice to individuals of all ages. From prenatal advice for expectant mothers to addressing the health needs of children and adolescents, and providing guidance on maintaining health in adulthood and old age, consumer health information aims to improve overall health outcomes and prevent the onset of illnesses and chronic conditions.
For expectant mothers, prenatal advice is available to help ensure a healthy pregnancy and provide guidance on proper nutrition, exercise, and prenatal care. As children grow, consumer health resources support child health by providing guidance on vaccinations, nutrition, and development milestones, helping parents make informed decisions about their child’s well-being.
During adolescence, consumer health information addresses the specific health needs and challenges of this age group, such as sexual health education, mental health resources, and guidance on healthy lifestyle choices. In adulthood, consumer health information focuses on maintaining and improving health through resources on preventive care, chronic disease management, and healthy lifestyle habits.
Consumer health organizations also provide valuable information for the elderly population, addressing the unique health concerns associated with aging. This includes resources on managing chronic conditions, promoting mobility and independence, and ensuring quality of life in later years. By addressing age-specific health concerns at every stage of life, consumer health information empowers individuals to make informed decisions about their health, leading to improved overall wellness and a higher quality of life.
The Importance and Impact of Consumer Health
Consumer health plays a vital role in promoting well-being and empowering individuals to make informed healthcare decisions. It encompasses physical, social, and mental wellness, enabling individuals to take control of their own health. By having access to accurate and reliable information, individuals can prevent diseases, improve overall wellness, and make choices that align with their healthcare needs and preferences.
One of the key benefits of consumer health is its impact on public health and safety. Through consumer health information, individuals are educated about food safety , drug safety, and product safety , ensuring that they are aware of potential risks and can take necessary precautions. Moreover, consumer health organizations raise awareness about disease prevention and control, promoting vaccines, tests, and therapies to combat infectious diseases.
Consumer health information also has a significant impact on different stages of life. It provides prenatal advice to pregnant women, addresses the health needs of children and adolescents, and offers guidance on maintaining health in adulthood and old age. By addressing age-specific health concerns, consumer health information aims to improve overall health outcomes, prevent illnesses, and promote wellness at every stage of life.
In conclusion, the importance of consumer health cannot be overstated. It empowers individuals to take charge of their own health, make informed choices, and prevent the spread of diseases. By providing access to accurate and reliable information, consumer health information promotes health awareness, education, and responsibility. It not only benefits individuals but also contributes to the overall improvement of public health and safety. It is crucial to continue promoting the relevance, comprehensibility, and credibility of consumer health information to empower individuals and protect their well-being.
What is consumer health?
Consumer health refers to the state of well-being achieved by individuals who make informed choices about their health and use products and services that are deemed safe by research. It encompasses physical, social, and mental wellness and aims to prevent illness.
Why is consumer health important?
Consumer health is important because it empowers individuals to take control of their health, make educated decisions, and prevent the spread of diseases.
What is consumer health information?
Consumer health information (CHI) is information on health and medical topics provided in response to requests from the general public. It is designed to be educational and helps individuals make decisions about health-related behaviors and medical treatments.
What is the role of consumer health librarians?
Consumer health librarians specialize in the selection, evaluation, and provision of CHI. They play a crucial role in assessing individual information needs, searching for reliable sources, acquiring resources, and delivering information in a format easily understood by library patrons.
How has the healthcare landscape shifted towards consumer-directed care?
The healthcare landscape has shifted from a paternalistic model to a more consumer-centered approach, where patients are expected to provide input in treatment decision-making and often seek health information independently.
How has the internet impacted health information seeking?
The internet has significantly changed the way people seek health information. Studies have shown that a large percentage of adults in the United States use the internet to search for health information.
Why is it important to promote health literacy?
It is important to promote health literacy and educate individuals on how to evaluate the reliability and credibility of online health information to mitigate the potential for misinterpretation and misinformation.
What is the goal of consumer information?
The goal of consumer information is to empower consumers to compare and select the best healthcare options based on cost, benefits, and quality of care.
How can consumer health information be made relevant, comprehensible, and credible?
Consumer health information should be relevant, comprehensible, and credible. This includes taking into account individual information needs, presenting information in an easily understood manner, and ensuring it is based on scientific research, accurate, and up-to-date.
What role do governmental health agencies play in consumer health?
Governmental health agencies play a crucial role in protecting public health and safety by providing information on food safety, drug safety, and product safety , as well as focusing on disease prevention and control.
How does consumer health promote wellness at every stage of life?
Consumer health organizations offer information and advice to promote wellness at every stage of life, addressing age-specific health concerns to improve overall health outcomes and prevent the onset of illnesses and chronic conditions.
What is the impact of consumer health in empowering individuals?
Consumer health plays a vital role in empowering individuals to take control of their own health and make informed healthcare decisions, promoting health awareness, education, and responsibility.

Dr. Sam D Granger
Sam D Granger is the creator and cheif editor of CustomerViewReports.com. He is a certified health writer and editor. He graduated from Columbia University, in the City of New York. Sam has written for various publications, covering topics such as health, gardening, lifestyle, and personal development. When he’s not writing, Sam enjoys hiking.
- McMaster University Health Sciences Library
Consumer Health
What is consumer health.
- Evaluating Information: The CRAAP Test
- Aging and Seniors' Health
- Complementary and Alternative Therapies
- Diseases and Conditions
- Drug and Medication Information
- Family and Children's Health
- Indigenous Health
- LGBTQ Health
- Mental Health
- Nutrition and Healthy Eating
- Pregnancy and Childbirth
- Rehabilitation
- Sexuality and Reproductive Health
“Consumer health information is intended for potential or current users of medical services (all of us!). It is designed to be educational, and can help individuals make decisions about health-related behavior and medical treatments. It differs from clinical information—that is, information written by and for medical professionals—in that it is developed with the layperson in mind, involving less technical language and more user-friendly formats. Consumer health information may include resources about prevention, self-care and wellness, diseases and conditions, treatment, health care options, and more.”
Arnott, S. C., & Keselman, A. (2015). Meeting health information needs outside of healthcare : Opportunities and challenges . ProQuest Ebook Central https://ebookcentral.proquest.com
- << Previous: Welcome!
- Next: Evaluating Health Information on the Internet >>
- Last Updated: Feb 29, 2024 12:02 PM
- URL: https://hslmcmaster.libguides.com/consumer

Address Information
McMaster University 1280 Main Street West HSC 2B Hamilton, Ontario Canada L8S 4K1
Consumer Health Informatics: Challenges and Opportunities Report
Consumer health informatics and the challenges of its implementation.
With the rapid development of modern technologies, all the spheres of human life are in demand of new tools to facilitate them, and medicine is no exception to the rule. Both caregivers and their patients need to find ways to make the exchange of information easier and the treatment more efficient. Consumer health informatics or CHI provides new solutions for hospitals to manage their activities and give access to the data to all of the treatment participants. However, as in the case of any new field of research, CHI faces numerous challenges comparable to the opportunities it provides for increasing the health of the population as a whole.
The principal task of consumer health informatics is to enable people without medical education to receive reliable information on managing their health. Providing access to personal health records and making information resources available to the consumers contributes to a better understanding of a patient’s conditions and the possible ways to improve them [3]. With the help of the newest technologies, both patients and nurses would be able to communicate more efficiently and find solutions faster than before.
Being one of the technologies that can help to solve modern problems in medical treatment, consumer health informatics faces some challenges it has to overcome in the future. First of all, the ability of healthcare providers to accept the new tools does not correspond to the strategic plan of the government on its adaptation [2]. The number of doctors who start to use technology is increasing, but it is still not enough to make a significant difference to the system.
There is a need for including the developing technologies into curricula of medical students to make them ready for their use in future practice and making them available to the population regardless of their age, nationality, or social status.
Another challenge is in the fact that the participants’ level of literacy does not allow them to benefit from technology usage. “Computer and technology literacy” is becoming the main factor preventing patients from active participation in its development [2]. Young patients that are already computer literate seem to be the only ones who managed to successfully use it, whereas the older generation faces some problems. That is why the priorities of consumer health informaticians lie in addressing inequalities between the patients and making consumer health informatics available to any medical institution.
As one can see from figure 1 below [4], the amount of US hospitals that provide patients with access to their health records and other medical information is increasing. Nowadays they can view, download and transmit the data anytime it is needed to facilitate communication between medical personnel and patients. These technologies keep spreading rapidly, and there is a need to find a solution to these problems as soon as possible. Thus, to successfully implement the new medical technology, its creators need to eliminate the factors mentioned above by adjusting it to any consumer of any age.
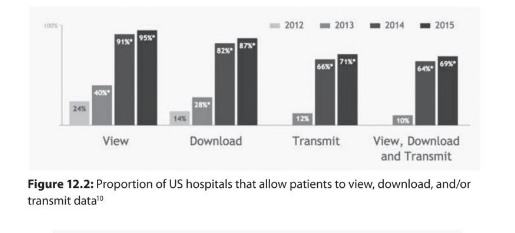
To enable patients to interact directly with the medical personnel and facilitate the data transmission within a medical institution, as well as to create new tools for them, consumer health informaticians are developing strategies in keeping with the realities of countries. One of the examples of such implementations is the peer network strategy in Canada [5]. The Canadian Association of Schools of Nursing created a network of representatives of different regions of the country to integrate the new technologies into the curricula of medical students. Therefore, they can increase the awareness about the latest technologies in nursing care that are going to be a part of their work in the future, and let the students learn about new opportunities in the sphere of digital health.
Students discover new ways to find solutions for their future patients, protect their data, and use electronic health records to facilitate data exchange between them and the patients. This strategy can help to educate the new generation of doctors familiar with the latest technologies and increase the readiness of future specialists to implement them into their practice. An example of these communication tools in Canada is a Moodle website [5]. It provides the medical personnel with numerous resources and the opportunity for their discussion online. Thus, specialists are becoming more knowledgeable and competent in their work and find better solutions for patients.
One of the successful examples of consumer health informatics strategy implementation in Saudi Arabia in the development of a strategic plan for mental illness treatment and improving the quality of services patients receive. The sphere of mental illnesses in the country is still under-researched in comparison to other types of diseases and medical assistance for them, so e-mental health is a relatively new technological area.
The Saudi authorities have several directions of work for implementation of new technologies shown in figure 2 below [1]. The hospitals in Saudi Arabia are starting to use modern health technologies such as mobile applications and SMS therapy for people with anxiety and depression [1]. The goal of the local consumer health informaticians is to make these services accessible and safe for a more significant amount of patients. Even though the new technologies are beneficial in general, they still have some downsides. There is still no mechanism for quality control and distribution among people with severe mental diseases.
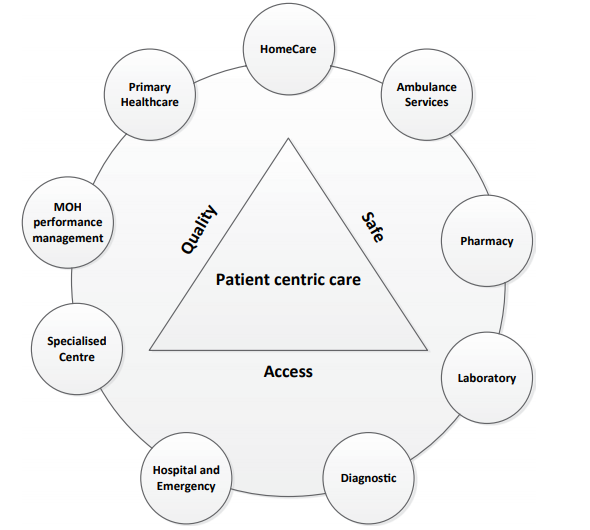
Since there were no technologies used in the sphere of mental illnesses in the Saudi healthcare system, and this opportunity is still unknown to caregivers, consumer health informaticians needed to take an already existing system as an example. They considered the usage of consumer health informatics in Australia as a successful example of modern technology implementation for the needs of the country’s hospitals. As one can see from table 1 below, Australia implemented the tools for such types of mental health services as health promotion, prevention and early intervention, crisis intervention, and suicide prevention, treatment, and recovery [1]. It will take some time to adjust the system like the one used in Australia to the Saudi healthcare system due to the difference in the realities of the two countries.
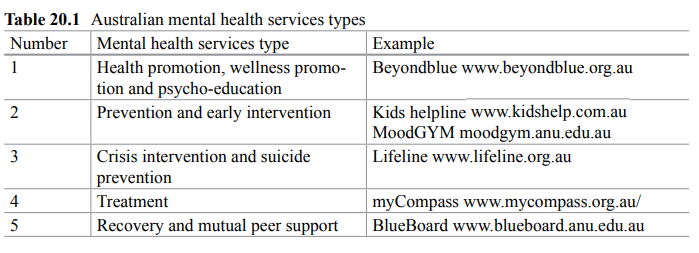
Modern technologies in the sphere of medicine keep developing and spreading by the development of new tools to facilitate human life. The future of society bases on their progress, and both medical personnel and patients will need to adjust to these technologies to use them with the most significant benefit. Consumer health technologies enable to creation a platform for communication and data exchange between the participants. The essential task is to learn how to implement them most efficiently and keep up with the development of new tools intended to facilitate access to health facilities.
- Binhadyan B., Peszynski K., Wickramasinghe N. Using e-Mental Health Services for the Benefit of Consumers in Saudi Arabia. In: Wickramasinghe N., Troshani I., Tan J., editors. Contemporary Consumer Health Informatics. Healthcare Delivery in the Information Age. Springer, Cham. 2016. p.367-377.
- Gibbons C., Shaikh Y. Introduction to consumer health informatics and digital inclusion. In: Edmunds M., Hass C., Holve E., editors. Consumer information and digital health. Solutions for health and health care. 1st ed. Germany: Springer International Publishing, 2019. p. 25-42.
- Gray K., Stephen R., Terrill B., Wilson B., Middleton A., Tytherleigh R., et al. Consumer health informatics aspects of direct-to-consumer personal genomic testing. In: Jaulent M.C., Zhao D., Gundlapalli A.V., editors. MEDINFO 2017: Precision Healthcare through Informatics. 1st ed. Netherlands: IOS Press; 2018. p. 89-93.
- Hersh W.R., Gibbons C., Shaikh Y., Hoyt R.E. Consumer health informatics. In: Hoyt R.E., Hersh W.R., editors. Health informatics. Practical guide. 7th ed. Singapore: Lulu.com, 2018. p. 253-264.
- Nagle LM. Canada’s digital health faculty peer network strategy. The online journal of nursing informatics. 2016.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 21). Consumer Health Informatics: Challenges and Opportunities. https://ivypanda.com/essays/consumer-health-informatics-challenges-and-opportunities/
"Consumer Health Informatics: Challenges and Opportunities." IvyPanda , 21 Feb. 2024, ivypanda.com/essays/consumer-health-informatics-challenges-and-opportunities/.
IvyPanda . (2024) 'Consumer Health Informatics: Challenges and Opportunities'. 21 February.
IvyPanda . 2024. "Consumer Health Informatics: Challenges and Opportunities." February 21, 2024. https://ivypanda.com/essays/consumer-health-informatics-challenges-and-opportunities/.
1. IvyPanda . "Consumer Health Informatics: Challenges and Opportunities." February 21, 2024. https://ivypanda.com/essays/consumer-health-informatics-challenges-and-opportunities/.
Bibliography
IvyPanda . "Consumer Health Informatics: Challenges and Opportunities." February 21, 2024. https://ivypanda.com/essays/consumer-health-informatics-challenges-and-opportunities/.
- Transforming Nursing and Healthcare Through Technology
- Research and Evaluation in Nursing Informatics
- Informatics Nurses, Their Roles and Skills
- Nursing Informatics: Dr. Jude Murphy and Patricia Abbott
- Aspects of Nursing Informatics
- Evidence-Based Practice in Informatics
- Overview of Nursing Informatics
- Organizational Informatics
- Importance of Nursing Informatics
- Health Informatics in the United States
- Stem Cells Therapy of Rheumatoid Arthritis
- Nurse Retention & Mentorship: Translational Research
- The Role of Vaccination Coverage, Individual Behaviors, and the Public Health Response in the Control of Measles Epidemics
- Parental Report of Vaccine Receipt in Children With Autism Spectrum Disorder
- Components of Family-Professional Collaboration in Healthcare
Home — Essay Samples — Law, Crime & Punishment — Consumer Protection — The importance and purpose of consumer health informatics
The Importance and Purpose of Consumer Health Informatics
- Categories: Consumer Protection
About this sample

Words: 643 |
Published: Dec 18, 2018
Words: 643 | Page: 1 | 4 min read
Table of contents
Summary of first article, summary of second article.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof Ernest (PhD)
Verified writer
- Expert in: Law, Crime & Punishment

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 587 words
1 pages / 740 words
1 pages / 484 words
3 pages / 1344 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Consumer Protection
Consumer behaviour is the study of how individual customers, groups or organizations select, buy, use, and dispose ideas, goods, and services to satisfy their needs and wants. It refers to the actions of the consumers in the [...]
The process of development along with the expanding globalization and liberalization process has increased the number of consumer-related issues. Consumer protection has earned an important place in the political, economic and [...]
The Bahamas is a constitutional government identifying Queen Elizabeth II as the head of state. She is exemplified to by a Governor-General selected on the appeal of the government department. The state is a democratic [...]
A written constitution is a formal document defining the nature of the constitutional settlement, the rules that govern the political system and the rights of citizens and governments in a codified form. The UK's constitution [...]
In the United States, it is illegal for anyone under the age of twenty-one to consume alcohol. Strict laws are enforced in order to restrict any individual under twenty-one from having access to these toxins. Serving time in [...]
Significant change of Australian land ownership. The Mabo (No.2) case In 1770, British Captain James Cook arrived and imported all laws from England in Australia. He then had justified the denial of the native’s connection to [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Essay on Health for Students and Children
500+ words essay on health.
Essay on Health: Health was earlier said to be the ability of the body functioning well. However, as time evolved, the definition of health also evolved. It cannot be stressed enough that health is the primary thing after which everything else follows. When you maintain good health , everything else falls into place.

Similarly, maintaining good health is dependent on a lot of factors. It ranges from the air you breathe to the type of people you choose to spend your time with. Health has a lot of components that carry equal importance. If even one of them is missing, a person cannot be completely healthy.
Constituents of Good Health
First, we have our physical health. This means being fit physically and in the absence of any kind of disease or illness . When you have good physical health, you will have a longer life span. One may maintain their physical health by having a balanced diet . Do not miss out on the essential nutrients; take each of them in appropriate quantities.
Secondly, you must exercise daily. It may be for ten minutes only but never miss it. It will help your body maintain physical fitness. Moreover, do not consume junk food all the time. Do not smoke or drink as it has serious harmful consequences. Lastly, try to take adequate sleep regularly instead of using your phone.
Next, we talk about our mental health . Mental health refers to the psychological and emotional well-being of a person. The mental health of a person impacts their feelings and way of handling situations. We must maintain our mental health by being positive and meditating.
Subsequently, social health and cognitive health are equally important for the overall well-being of a person. A person can maintain their social health when they effectively communicate well with others. Moreover, when a person us friendly and attends social gatherings, he will definitely have good social health. Similarly, our cognitive health refers to performing mental processes effectively. To do that well, one must always eat healthily and play brain games like Chess, puzzles and more to sharpen the brain.
Get the huge list of more than 500 Essay Topics and Ideas
Physical Health Alone is Not Everything
There is this stigma that surrounds mental health. People do not take mental illnesses seriously. To be completely fit, one must also be mentally fit. When people completely discredit mental illnesses, it creates a negative impact.
For instance, you never tell a person with cancer to get over it and that it’s all in their head in comparison to someone dealing with depression . Similarly, we should treat mental health the same as physical health.
Parents always take care of their children’s physical needs. They feed them with nutritious foods and always dress up their wounds immediately. However, they fail to notice the deteriorating mental health of their child. Mostly so, because they do not give it that much importance. It is due to a lack of awareness amongst people. Even amongst adults, you never know what a person is going through mentally.
Thus, we need to be able to recognize the signs of mental illnesses . A laughing person does not equal a happy person. We must not consider mental illnesses as a taboo and give it the attention it deserves to save people’s lives.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

- Share full article
Advertisement
Supported by
ESSAY; Moscow's China Card
By William Safire
- Sept. 8, 1986
Every decade or so, China undergoes a political convulsion. In 1948-49, the Communists threw out the Kuomintang; in 1956, Mao's ''Great Leap Forward'' plunged the country into a depression; in 1966, the Cultural Revolution to purify the party brought on a new Dark Ages; in 1976-78, we saw Mao's would-be radical successors, the ''Gang of Four,'' replaced by pragmatic Deng Xiaoping.
Now we are celebrating the 10th anniversary of the death of Mao, and some Pekingologists would have us believe that this decade's upheaval will not come.
Mr. Deng, at 82, has provided for his succession, we are assured: it's all set for Hu Yaobang and Zhao Ziyang to succeed him, with Hu Qili of the next generation right behind. Not to worry, goes the current Edgar Snow-job: China's new era of ''commutalism,'' communism with a capitalist face, will march undisturbed into the next millennium.
I wonder. Maybe the conventional wisdom will prove right for once. But for argument's sake, let's look at what is happening in China through a different set of glasses, seeking truth from facts.
Fact number one is that a wave of materialism is sweeping across the billion people of China. After a generation of repression, good ol' greed is back in the saddle, and an I'm-all right-Deng attitude permeates the new entrepreneurs.
As a longtime expositor of the virtue of greed in powering the engine of social progress, I cannot cluck-cluck at this. But there is a difference between the materialism of the Chinese on Taiwan, who are accustomed to free enterprise, and the lust for the good life of available goods on the mainland, where a terrible thirst has been a-building.
Let us assume that the outburst of materialism in China leads to some reaction: that some spoilsport faction emerges to summon up the ghost of Mao's ideological purity, and that this new gang of fortyish Outs finds its way back in. It is at least a possibility.
I think that shrewd old Deng is well aware of this possibility. That is why, despite his ostentatious rejection of personal cultdom, he is preparing his most dramatic assault on the memory of Mao. That father of the revolution startled the world by breaking with the Soviet Union; Mr. Deng, playing a revisionist Lenin to Mao's Marx, wants to startle the world and overwhelm internal opposition by a rapprochement with Moscow.
Accordingly, fact two: He has abandoned his demand that Russia move back its huge army from the Chinese border, thereby double-crossing his own Army leaders. He has forgotten his requirement that Soviet forces be withdrawn from Afghanistan, thereby double-crossing his Westernish ally, Pakistan.
All Mr. Deng now asks of the Russians is that they try to squeeze their Vietnamese clients to pull out of Cambodia. Of course they'll try - ''best efforts'' is an easy promise - and since the Vietnamese are notoriously independent, Moscow cannot be blamed for not succeeding. Result: Mr. Deng takes the salute from atop the wall in Red Square.
That reestablishes his Communist credentials, defanging hard-left opposition at home. And it is Middle Kingdom orthodoxy; I suspect Chinese agents in the U.S. supply the K.G.B. with intelligence, just as Peking permits our Big Ears on its soil to overhear Kremlin transmissions. Chinese policy has always been to play the barbarians against each other.
This theory would also explain fact three: Mr. Gorbachev's seizure of a U.S. newsman as hostage. It is no coincidence that this particular hostage selection follows China's arrest and expulsion of a reporter for a U.S. newspaper. The Soviet leader, advised by Anatoly Dobrynin, must have known that this slap in the face would jeopardize a summit - and went ahead with his calculated humiliation, similar to Mr. Nixon's mining of Haiphong harbor before his Moscow summit in 1972.
Because the Russians now have the prospect of a pilgrimage to Moscow by Mr. Deng, they can taunt the U.S. President with impunity. As Mr. Dobrynin probably predicted, Mr. Reagan is reduced to begging for the hostage's release, in effect volunteering testimony to a Soviet court, in his eagerness to crown his Presidency with a peacemaking summit.
Now Mr. Gorbachev can hang tough, holding a show trial and thereby delaying negotiations with the U.S. until the Deng visit - or can graciously accede to the Reagan plea, thereby establishing his dominance. And the overconfident Mr. Reagan never suspected, as he sat down to summit poker, that this time the China card was in his opponent's hand.

IMAGES
VIDEO
COMMENTS
Consumer health literacy is an important component of modern healthcare practice because it enables patients to be proactive in understanding the issues that impact their health, as well as in recognizing how to best overcome personal health concerns that influence their own perspectives regarding health. It is important to recognize that many ...
1. INVOLVING CONSUMERS IN IMPROVING THE DELIVERY OF HEALTH CARE IS IMPORTANT. Incorporating consumer opinions and perspectives to inform the development and improvement of health‐care practice is becoming increasingly recognized as essential to the delivery of quality health care. 1 The importance of consumer involvement in shaping health care is widely acknowledged and supported. 2, 3 ...
1 Introduction. Consumer health informatics (CHI) has been defined by Eysenbach 1 as the branch of health informatics that analyses consumers' needs for information studies, implements methods of making information accessible to consumers, and models and integrates consumers' preferences into medical information systems, thereby, making it perhaps the most challenging and rapidly expanding ...
However, consumer health wearables are predicted to become the next "Dr Google.". One in six (15%) consumers in the United States currently uses wearable technology, including smartwatches or fitness bands. While 19 million fitness devices are likely to be sold this year, that number is predicted to grow to 110 million in 2018 [ 2 ].
Engaging consumers in health care decisions is widely recognised as being important in health care policy, research and services. Consumer participation can be viewed as a goal in itself, by encouraging participative democracy, public accountability and transparency. ... All potentially relevant papers excluded from the review at this stage are ...
July 22, 2021 -. The wellness market is booming. Consumers intend to keep spending more on products that improve their health, fitness, nutrition, appearance, sleep, and mindfulness. In this edition, The Next Normal explores the fast-changing, fast-growing wellness industry.
This essay offers two new lenses for studying consumer health. Theories of psycholmmunology and institutional environments bring a wider array of individual, social, cultural, and organizational ...
This essay, "Consumer Health Information Resources" is published exclusively on IvyPanda's free essay examples database. You can use it for research and reference purposes to write your own paper. However, you must cite it accordingly. Donate a paper. Removal Request.
However, the results indicated that the reviewed papers were fairly recent, with all the 32 (100%) included studies published between 2018 and 2023. ... While such consumer health questions ...
Essays on Health Insurance: Public Opinion and Consumer Behavior ABSTRACT In this dissertation, I consider health insurance coverage in the United States from two perspectives. I open with a high-level analysis of trends in public opinion that underpin current political debates around health reform.
Consumer health is a term that refers to the state of well-being achieved by individuals who make informed choices about their health and use products and services that are deemed safe by research. It encompasses physical, social, and mental wellness and aims to prevent illness. In today's world, consumer health plays a crucial role in our ...
What is Consumer Health? "Consumer health information is intended for potential or current users of medical services (all of us!). It is designed to be educational, and can help individuals make decisions about health-related behavior and medical treatments. It differs from clinical information—that is, information written by and for ...
Consumer Health: Making Informed Decisions is a concise, current text with the most up-to-date information about health care reform and insurance. It is devoted to the most important issues relative to consumer health issues, including advertising, dietary supplements, herbal remedies, weight management, and medications. There are in-depth analyses of the American health care system, insurance ...
The buyer's pursuit of better services has been so influential that Business Week has labeled the 1990s the "Decade of the Customer." 2. Changes in customers' expectations are moving into ...
Consumer health informatics or CHI provides new solutions for hospitals to manage their activities and give access to the data to all of the treatment participants. However, as in the case of any new field of research, CHI faces numerous challenges comparable to the opportunities it provides for increasing the health of the population as a whole.
These two articles have shown the importance and purpose of consumer health informatics for every patient. Through these articles, more consumers will be aware of the need to access and become more knowledgeable about them, especially about requesting for access of their health records. Additionally, these findings can help the medical industry ...
Consumer Health Midterm Essay Questions. The three characteristics of quality medical studies include: a. clinical studies, large sample sizes, and triple blind studies. b. randomized controlled trials, triple blind studies, and clinical studies. c. clinical studies, large sample sizes, and control groups.
J Epidemiol Community Health 2005;59:679-84. 11 Farsalinos KE, Romagna G, Tsiapras D, Kyrzopoulos S, Voudris V. Characteristics, perceived side effects and benefits of electronic cigarette use: a worldwide survey of more than 19,000 consumers. Int J Envir Res Pub Health 2014;11:4356-73. 12 Brown J, Beard E, Kotz D, Michie S, West R. Real-world
500+ Words Essay on Health. Essay on Health: Health was earlier said to be the ability of the body functioning well. However, as time evolved, the definition of health also evolved. It cannot be stressed enough that health is the primary thing after which everything else follows. When you maintain good health, everything else falls into place.
Essay "Consumer health it applications" - grade A; Essay "Healthcare quality assurance" - grade A; Essay "Week 6" - grade A; Seminar assignments - Week 5 ; Essay "Managed care issues and trends in america" - grade A; Essay "Case study summary/essay from textbook" - grade A; Related documents.
Sustainability and Climate Change
digital transformation of health systems and increasing digitalization of everyday life mean the availability and ubiquity of health-related information has increased rapidly and substantially over recent decades. So far, school health promotion has only partially tapped the potential and challenges of digital media. We therefore:
See the article in its original context from September 8, 1986, Section A, Page 23 September 8, 1986, Section A, Page 23