All Section
- For Providers
- For Patients
- About SMSNA for Patients
- Sex Health Blog
- Did You Know?
- Find a Provider
- Patient Education Videos

Medicaid Coverage of Transgender Transition-Related Health Care by State
As anyone who has ever tried to navigate health care coverage can attest, it is all too often a frustrating, fruitless endeavor characterized by multiple phone calls, numerous transfers, and invariably long hold times. This cumbersome process creates an obstacle for those seeking medical treatment and may disproportionately affect transgender individuals seeking treatment for gender dysphoria.
A transgender individual is a person whose gender does not align with the sex that they were assigned at birth. This incongruence between gender identity and sex can cause significant psychological distress for a transgender person, which is known as gender dysphoria.
Gender dysphoria can lead to feelings of restlessness, anxiety, and depression. The certainty that one’s true gender is not reflected by one’s body can be an extremely distressing experience that impacts all areas of a person’s life. Transgender individuals may feel disgust towards their genitals and other sex-related physical traits and have a strong desire to be rid of them. This chronic state of stress may lead to thoughts or acts of self-harm, or even suicidality. A 2015 national survey of transgender individuals found that 40% of survey respondents had attempted suicide at least once in their life, with 7% having attempted suicide in the past year.
To compound matters, transgender individuals experience a higher rate of health disparities than the average U.S. citizen. The above-mentioned 2015 survey revealed that 29% of the transgender respondents were living in poverty, and more than half (55%) of those surveyed had been denied coverage for transition-related surgery, while a quarter had been denied coverage for transition-related hormone therapy.
With this information in mind, the authors of a 2020 Journal of Sexual Medicine study set out to determine which U.S. states’ Medicaid programs cover gender-affirming hormone therapy (GAHT) and which cover genital gender-affirming surgery (GAS) for transgender individuals. GAHT and GAS, along with counselling to support transgender people in their transition are the three predominant health services for gender dysphoria at this time.
Results showed that GAHT and GAS are not covered by all state Medicaid programs, and although several states’ Medicaid programs do cover these treatments, the information was often difficult to find, requiring several phone calls and substantial time to track down.
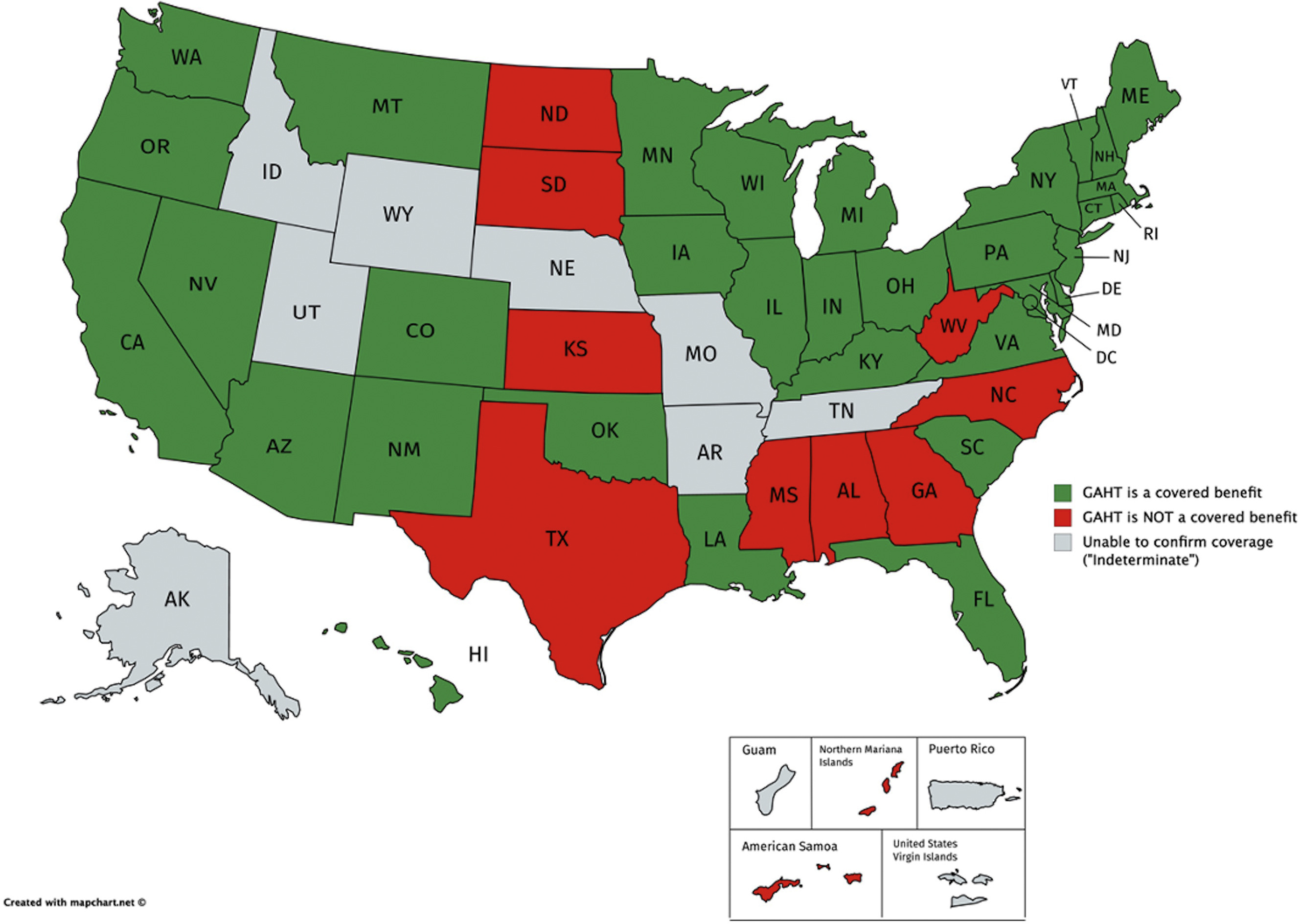
According to this study, GAHT is covered by 34 of 51 state Medicaid programs (including Washington, DC), is not covered by 9 of 51 state programs, and coverage status was deemed “indeterminate” in 8 of 51 states (Figure 1). To find this information, the authors completed an average of 3 phone calls per state (range of 1-10 phone calls) and spent an average of 31.8 minutes on the phone for each unique call (range of 1.5-124.8 minutes).
GAS is even less likely to be covered by Medicaid than GAHT, and it is only covered by 25 of 51 state Medicaid programs. It is not covered by 22 of 51 state programs, and coverage was classified as “indeterminate” in 4 of 51 states (Figure 2). Researchers completed an average of 3.3 phone calls per state to attain this information (range of 1-12 phone calls) and spent an average of 33.2 minutes on the phone during each call (range of 1.5-119.8 minutes).
The authors of this study concluded that several barriers to health care access exist for transgender people and that the process of determining coverage for medical treatments can be very challenging and time-consuming for these patients.
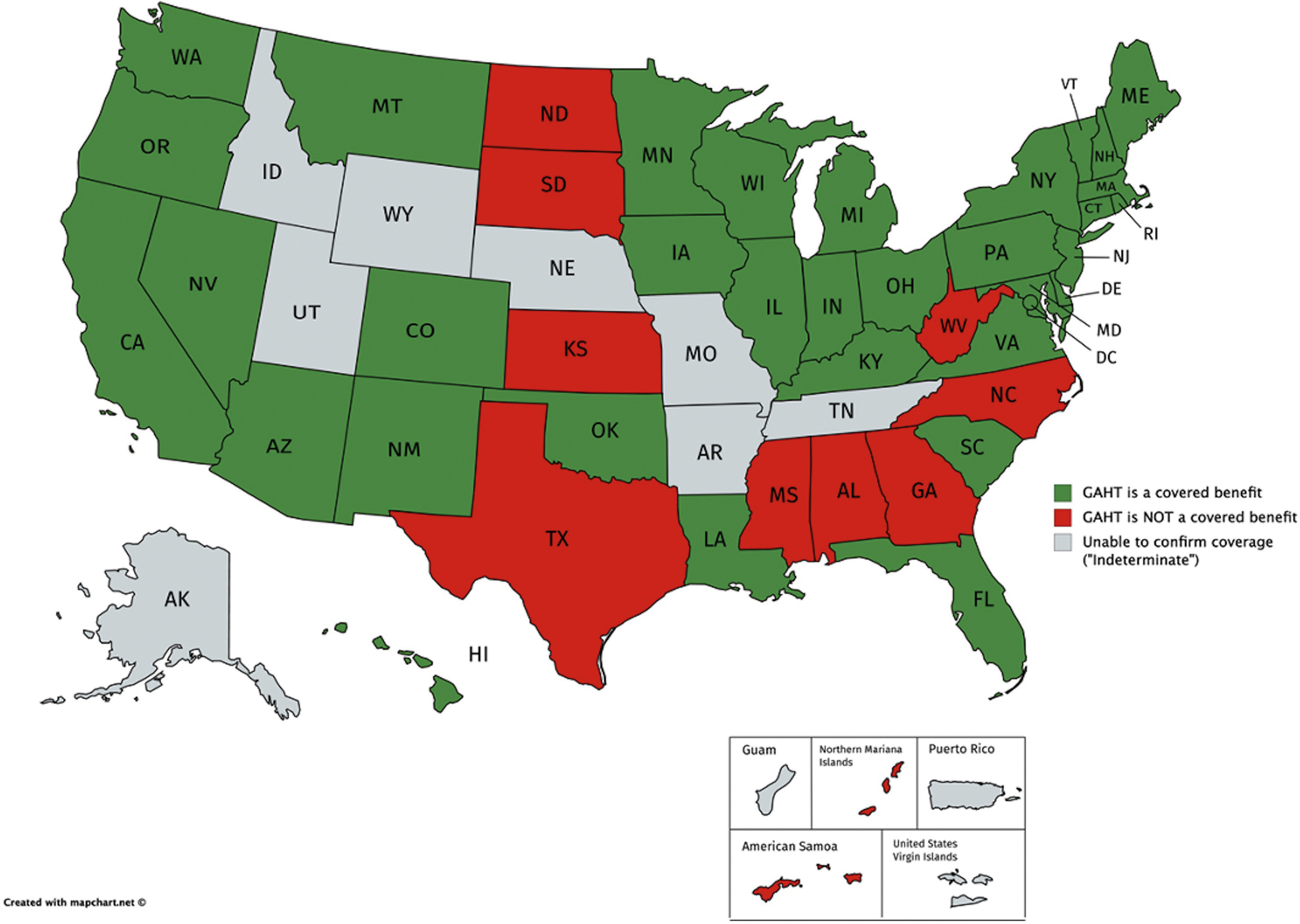
Figure 1. Maps of all 51 U.S. states (includes District of Columbia) and 5 U.S. territories, colored based on whether GAHT is a covered benefit (green), is not a covered benefit (red), or whether coverage remains “indeterminate” (gray). This image was published in The Journal of Sexual Medicine, 18 (2), Zaliznyak, M., Jung, E.E., Bresee, C., & Garcia, M.M., Which U.S. States’ Medicaid Programs Provide Coverage for Gender-Affirming Hormone Therapy and Gender-Affirming Genital Surgery for Transgender Patients?: A State-by-State Review, and a Study Detailing the Patient Experience to Confirm Coverage of Services, p. 415, Copyright Elsevier (2021).
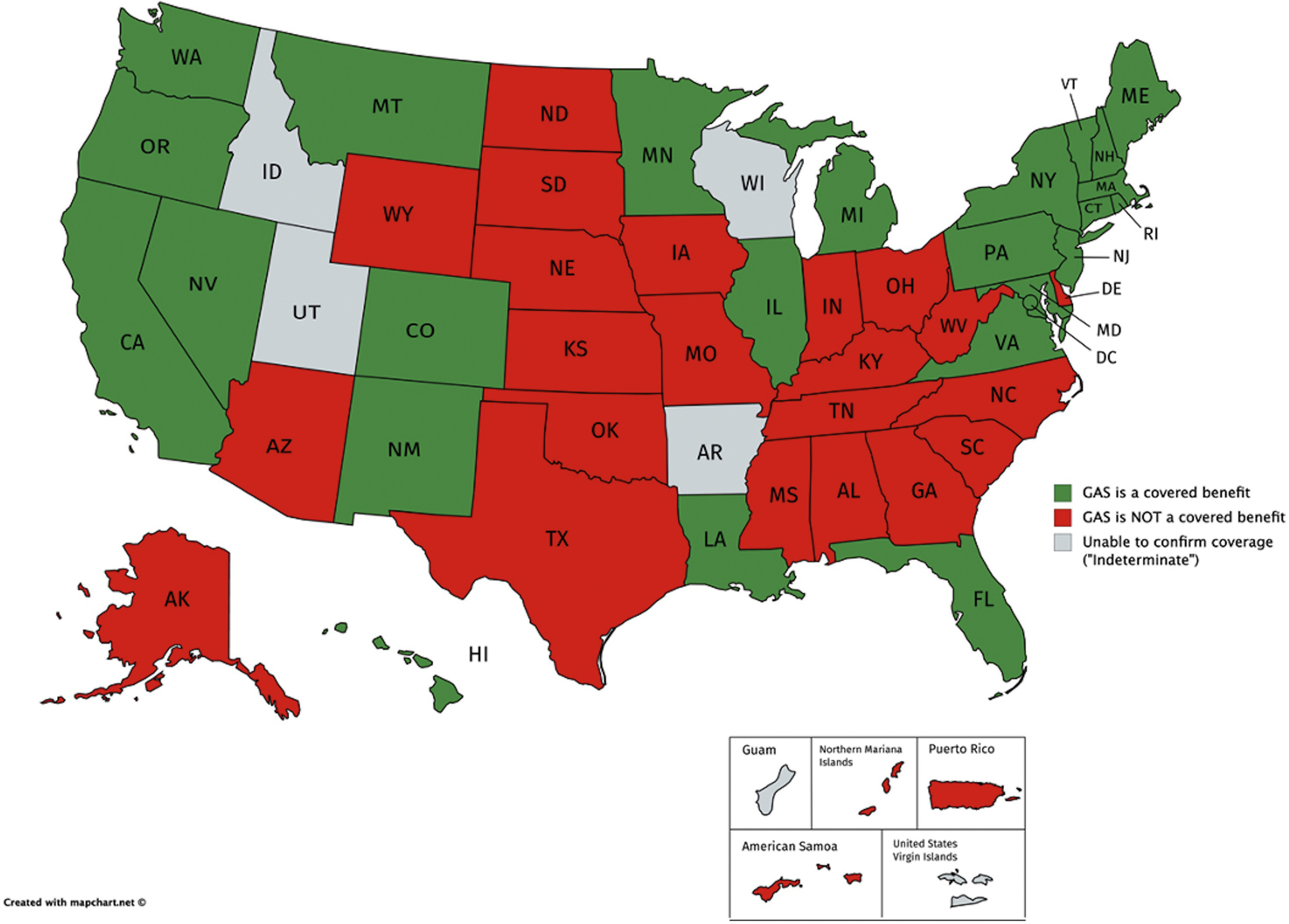
Figure 2. Maps of all 51 U.S. states (includes District of Columbia) and 5 U.S. territories, colored based on whether GAS is a covered benefit (green), is not a covered benefit (red), or whether coverage remains “indeterminate” (gray). This image was published in The Journal of Sexual Medicine, 18 (2), Zaliznyak, M., Jung, E.E., Bresee, C., & Garcia, M.M., Which U.S. States’ Medicaid Programs Provide Coverage for Gender-Affirming Hormone Therapy and Gender-Affirming Genital Surgery for Transgender Patients?: A State-by-State Review, and a Study Detailing the Patient Experience to Confirm Coverage of Services, p. 416, Copyright Elsevier (2021).
Zaliznyak, M., Jung, E.E., Bresee, C., & Garcia, M.M. (2021). Which U.S. States’ Medicaid Programs Provide Coverage for Gender-Affirming Hormone Therapy and Gender-Affirming Genital Surgery for Transgender Patients?: A State-by-State Review, and a Study Detailing the Patient Experience to Confirm Coverage of Services. The Journal of Sexual Medicine, 18 (2), 410-422. https://www.jsm.jsexmed.org/article/S1743-6095(20)31062-6/fulltext
- What You Can Do
- Contributors
- SMSNA Select
- For Institutes
- For Fellows
- Subscribe Now
The independent source for health policy research, polling, and news.
Update on Medicaid Coverage of Gender-Affirming Health Services
Ivette Gomez , Usha Ranji , Alina Salganicoff , Lindsey Dawson , Carrie Rosenzweig, Rebecca Kellenberg, and Kathy Gifford Published: Oct 11, 2022
- Issue Brief
Transgender and nonbinary adults often face challenges and barriers to accessing needed health services and face worse health outcomes than their cisgender peers. Transgender adults are mo re likely than cisgender adults to be uninsured, report poor health, have lower household incomes, and face barriers to care due to cost. Given their lower incomes, Medicaid plays an important role in health coverage for transgender people. A 2019 report by the Williams Institute estimated that among the 1.4 million transgender adults living in the United States, approximately 152,000 had Medicaid coverage.
Medicaid is the country’s health coverage program for low-income people and is jointly funded by the federal government and states. Under Medicaid, states must cover certain mandatory benefits , such as inpatient and outpatient services, home health services, and family planning services. While there are no specific federal requirements regarding coverage or exclusion of gender-affirming health care services as a category of Medicaid benefits, there are rules regarding comparability requiring that services must be equal in amount, duration, and scope for all beneficiaries within an eligibility group.
Medicaid benefits are subject to Section 1557 of the Affordable Care Act (ACA), the law’s major non-discrimination provisions, which prohibit discrimination based on sex. The Biden Administration recently proposed a new rule on Section 1557 that explicitly states that it interprets, and will enforce, sex-based protections to include sexual orientation and gender identity. The administration had already asserted this position in guidance stating that under 1557 protections, “categorically refusing to provide treatment to an individual based on their gender identity is prohibited discrimination” and it returns to a position more closely aligned to that under the Obama administration but walked back under the Trump administration.
Despite these protections, some states have recently moved to implement or consider actions aimed at limiting access to gender-affirming health care, particularly for youth. This has included restrictions on coverage of benefits as well as bans on the provision of gender-affirming care by health care providers. A number of lawsuits are pending.
What gender affirming services do states report covering through Medicaid?
The standards of care for gender-affirming health services set by the World Professional Association for Transgender Health include hormone therapy, surgeries, fertility assistance, voice and communication therapy, primary care, and behavioral health interventions. Additionally, the Endocrine Society supports gender-affirming care in their clinical practice guidelines . Together, these guidelines form the standard of care for treatment of gender dysphoria. Gender-affirming care is highly individualized, and while not all transgender and nonbinary individuals will want or seek any or all of these medically necessary services, limiting access to them can lead to negative and life threating outcomes. Major U.S. medical associations, such as the American Medical Association , the American College of Obstetricians and Gynecologists , the American Academy of Nursing , the American Psychiatric Association , among others , have issued statements underscoring the medical necessity of gender-affirming care.
In a survey of states on coverage of sexual and reproductive health services conducted in Summer 2021, KFF and Health Management Associates (HMA) asked states about coverage of five gender-affirming care services: gender-affirming counseling, hormones, surgery, voice and communication therapy, and fertility assistance for transgender enrollees (Questions presented in Appendix Table 1 ). Because the survey focused on adult access, states were not asked about puberty blocking hormones. States were asked if a service was covered, excluded from coverage, or whether coverage was not addressed in state policy or statute for adults over the age of 21, as of July 1, 2021. Services that are not addressed in state policy or statute may or may not be covered by the state, or coverage may vary by case. The survey instrument was distributed via email to state Medicaid directors and where applicable, Medicaid agency staff working on women’s health and reproductive health issues. Forty-one states and the District of Columbia responded to the survey. Tennessee responded to the survey but did not answer questions related to gender-affirming services. Survey findings are summarized in Figure 1 and Table 1 and highlights are presented below.
Overall coverage of gender-affirming care:
As detailed below, many state Medicaid programs cover aspects of gender-affirming health services. However, only two of the 41 states responding to this survey, Maine and Illinois, reported covering all five services. Two states, Alabama and Texas, reported they do not cover any of these services under Medicaid.
Gender-Affirming Hormone Therapy:
Gender-affirming hormone drugs include estrogen, anti-androgens, and progestins (feminizing hormones), as well as testosterone and other agents (masculinizing hormones). Under federal law, and subject to exceptions for a few drugs or drug classes, state Medicaid programs are required to cover all drugs from manufacturers that have entered into a rebate agreement with the Secretary of Health and Human services under the federal Medicaid Drug Rebate program . Twenty-five states reported covering gender-affirming hormones, and 10 of these states require prior authorization. Thirteen states said coverage was not addressed in state statute or policy, and three states— Alabama , Hawaii , and Texas —exclude coverage of gender-affirming hormone therapy.
Gender Affirming Surgery:
Gender-affirming surgery can include chest surgery, genital surgery, facial surgery, and other surgical procedures aimed at helping a transgender or nonbinary person transition to their self-identified gender. Not all transgender or nonbinary individuals seek or want surgical treatments. Twenty-three of the 41 responding states reported covering gender-affirming surgery for adults through their state Medicaid programs. Nine states reported coverage was not addressed in state statute or policy, and nine states reported that they excluded gender-affirming surgery from coverage. This survey did not ask states to specify what surgical procedures they cover, but some states provided additional details, which can be found in Appendix Table 2 .
Ten of 23 covering states require prior authorization. For example, Colorado requires a clinical diagnosis of gender dysphoria and that the patient has lived in their preferred gender for 12 continuous months. Colorado and Wisconsin also require that the patient has completed 12 continuous months of hormone therapy.
Voice and Communication Therapy
Some transgender people have challenges with developing a voice that matches their gender identity. Voice therapy services can encompass a range of treatments that address pitch, intonation, articulation, pragmatic speech and other aspects of communication.
Thirteen of the 41 responding survey states report that they cover gender-affirming speech or voice therapy services, some requiring prior authorization. Ten of the survey states reported that they exclude coverage for gender-affirming voice therapy services, and 18 states responded that they have not addressed this coverage in their state policy.
Fertility Services:
A broad array of diagnostic and treatment services are available to assist with achieving a pregnancy. Diagnostics typically include lab tests, semen analysis and imaging studies, or procedures of the reproductive organs. Treatment services include medications, reproductive system procedures to allow for pregnancy, and an array of other interventions to help an individual achieve pregnancy, such as intrauterine insemination (IUI) and in-vitro fertilization (IVF). While federal rules require states to cover most prescription medications under Medicaid, there is an exception that allows states to exclude coverage for fertility medications.
Fertility services can be unaffordable without insurance coverage but few states (11) cover services for any beneficiaries, regardless of gender identity. In this survey, just three states ( Illinois , Maryland , and Maine ) reported covering fertility services as part of gender-affirming care. Of these three states, Illinois is the only one that reported covering services for beneficiaries without exceptions. More than half of states (29) reported that they exclude coverage for fertility services for transgender individuals, and nine states responded that they have not addressed this coverage in their state policy ( Table 1 ).
Mental Health Counseling:
Transgender and nonbinary individuals may seek mental health services to address issues related to their gender identity and transition but may also seek care to address issues that are not related to their gender transitions. As noted, in some cases a diagnosis of gender dysphoria is required before gender-affirming services can be accessed.
Twenty-seven states reported covering mental health counseling and services specifically related to gender affirming health services, 11 states reported coverage was not addressed in their state statute or policy, and three states, Alabama , Kansas , and Texas , reported that they exclude this benefit.
Some states reported requiring that transgender and non-binary Medicaid enrollees receive mental health assessments prior to receiving hormone therapy or having gender-affirming surgeries. For example, Delaware requires prior authorization for mental health counseling related to gender-affirming care, and Connecticut reported that depending on the type of service, prior authorization may be required.
The need for coverage of and access to medically necessary gender-affirming care has been recognized by leading medical and health professional organizations. However, some states have enacted laws banning the provision of gender-affirming health services to youth, and coverage for gender-affirming health services is uneven in state Medicaid programs. In most states, there is variation in coverage for specific services and some states do not have policies addressing coverage in their state Medicaid programs, potentially leaving many low-income transgender and nonbinary individuals without access to medically necessary health services.
Since this survey was conducted, the Biden Administration has proposed a new rule on Section 1557, which is consistent with their prior guidance, and proposes that excluding coverage for gender-affirming care constitutes sex discrimination. In addition, beyond what is stated in rulemaking by the current or previous administrations, some courts have found that the statue itself (i.e., sex non-discrimination provisions) protects against health care discrimination based on gender identity and sexual orientation. For example, a federal district court permanently enjoined the Wisconsin Medicaid program from categorically excluding gender-affirming services from coverage, relying on the statute. Similarly, in recent months, federal courts have ruled the Georgia and West Virginia must cover gender-affirming care in their Medicaid programs. Most recently, in June 2022, Florida’s Medicaid agency announced it would ban coverage of gender-affirming health services in the state. The policy went into effect in August and was challenged in court a few weeks later (with the case still pending). States that do not cover components of gender-affirming care may be in violation of Sec. 1557 of the ACA. However, there are a number of pending legal challenges to the Sec. 1557 rule as well as over specific Medicaid state policies related to coverage of gender-affirming services which will be important to watch moving forward to fully understand this evolving landscape.
- Women's Health Policy
news release
- Few State Medicaid Programs Report Covering a Broad Range of Gender-Affirming Health Services for Adults
Also of Interest
- Demographics, Insurance Coverage, and Access to Care Among Transgender Adults
- Health and Access to Care and Coverage for Lesbian, Gay, Bisexual, and Transgender (LGBT) Individuals in the U.S.
- Youth Access to Gender Affirming Care: The Federal and State Policy Landscape
- Recent and Anticipated Actions to Reverse Trump Administration Section 1557 Non-Discrimination Rules

Popular Services
- Patient & Visitor Guide
Committed to improving health and wellness in our Ohio communities.
Health equity, healthy community, classes and events, the world is changing. medicine is changing. we're leading the way., featured initiatives, helpful resources.
- Refer a Patient
Gender-Affirming Surgeries

What is gender-affirming surgery?
Gender-affirming surgeries change the look and function of your assigned sex to more closely match the gender you identify with. Having a gender-affirming surgery may be part of your journey to becoming more of your true self.
Surgical options for gender-affirmation include facial surgery, voice surgery, and top and bottom surgeries. Patients whose assigned sex and gender identity are different may experience gender dysphoria. Gender-affirming surgery is an important part of the management of patients with gender dysphoria.
Top surgery includes procedures to create or remove breasts. Feminizing bottom surgery includes procedures to remove the penis and testicles and create a new vagina, labia and clitoris. Learn more about feminizing bottom surgery .
Masculinizing bottom surgery includes procedures to remove the uterus or add a penis for intercourse and urinating or a small penis to urinate standing up. Learn more about masculinizing bottom surgery .
We follow the World Professional Association for Transgender Health’s standards when performing gender-affirming surgeries. These guidelines are set for safe, effective physical and mental health care for transgender and gender-nonconforming patients. Requirements for each procedure will vary.
Why choose Ohio State for gender-affirming surgery?
The Ohio State Wexner Medical Center is one of only a few academic health centers in the country to offer bottom gender-affirming surgery. We have a dedicated team of medical experts in every field, and through close collaboration aim to serve the LGBTQ population of Columbus and beyond.
Surgical options for gender-affirmation
- Facial surgery options
- Feminization surgery
- Masculinization surgery
- Meet our gender-affirming care surgical team Meet your surgical team
Helpful Links
- LGBTQ+ Employee Resource Group HealthBeat HUB Channel (Internal Access Only)
- Plastic and Reconstructive Surgery Services
- Transgender Primary Care Clinic
- Ear, Nose and Throat Services
- Urology Services
Subscribe. Get just the right amount of health and wellness in your inbox.
Which U.S. States' Medicaid Programs Provide Coverage for Gender-Affirming Hormone Therapy and Gender-Affirming Genital Surgery for Transgender Patients?: A State-by-State Review, and a Study Detailing the Patient Experience to Confirm Coverage of Services
Affiliations.
- 1 Division of Urology, Cedars-Sinai Medical Center, Los Angeles, CA, USA; Cedars-Sinai Transgender Surgery and Health Program, Cedars-Sinai Medical Center, Los Angeles, CA, USA.
- 2 Division of Urology, Cedars-Sinai Medical Center, Los Angeles, CA, USA.
- 3 Biostatistics and Bioinformatics Core, Cedars-Sinai Samuel Oschin Comprehensive Cancer Center, Los Angeles, CA, USA.
- 4 Division of Urology, Cedars-Sinai Medical Center, Los Angeles, CA, USA; Cedars-Sinai Transgender Surgery and Health Program, Cedars-Sinai Medical Center, Los Angeles, CA, USA; Department of Urology, University of California San Francisco San Francisco, CA, USA; Department of Anatomy, University of California San Francisco San Francisco, CA, USA. Electronic address: [email protected].
- PMID: 33422448
- DOI: 10.1016/j.jsxm.2020.11.016
Background: To date, a comprehensive state-by-state assessment of transgender transition-related health care coverage for gender-affirming hormone therapy (GAHT) and genital gender-affirming surgery (GAS) has not been reported.
Aims: The aims of this study were 1) to verify which U.S. states' Medicaid systems do/do not cover GAHT and GAS; 2) to assess the ease/difficulty for patients to determine whether GAHT and GAS are Medicaid-covered benefits; and 3) to understand possible state-related predictors of Medicaid coverage for gender-affirming care.
Methods: We reviewed the official Medicaid Handbook and website for all 51 states (+D.C.) and 5 territories to confirm whether GAHT and GAS are covered benefits. When indeterminate, we called the Medicaid office in each state, and for many, Medicaid managed care organizations (MCOs), and individual in-state providers, to confirm coverage. We recorded our experiences, number of, and duration of phone calls to confirm coverage.
Outcomes: The main outcome was a definitive answer from the state/territory's Medicaid program or MCOs regarding whether GAHT and GAS are/are not covered benefits. Secondary outcome measures included responses we received and the total number/duration of phone calls necessary to confirm coverage.
Results: Only 12 of 51 states and 0 of 5 territories featured their policy regarding coverage for GAHT in their Medicaid Handbook/webpages. We confirmed that 34 of 51 state Medicaid programs do cover GAHT, whereas 9 of 51 states' and 2 of 5 territories' do not. We could not confirm coverage of GAHT in 8 of 51 states and 3 of 5 territories. Only 26 of 51 states and 0 of 5 territories featured their policy regarding coverage for GAS in their Medicaid Handbook/webpages. We confirmed that 25 of 51 state Medicaid programs do cover GAS, whereas 22 of 51 states' and 3 of 5 territories' do not. We could not confirm coverage of GAS in 4 of 51 states and 2 of 5 territories. Up to 12 calls, lasting up to 125 minutes, were required to confirm coverage for GAHT/GAS.
Clinical implications: Our findings indicate that important health care access barriers/disparities exist today and warrant improvement.
Strengths & limitations: To our knowledge, this is the most comprehensive assessment of transgender transition-related health care coverage. Limitations include possible bias, as it could be that we were more persistent than actual patients would be to determine service coverage, and a lack of specificity regarding which specific hormone formulations or procedures are/are not covered.
Conclusion: Our findings show that only 34 of 51 (67%) states' Medicaid programs include GAHT and 25 of 51 (49%) include GAS as covered benefits. Our experience suggests that the process to confirm coverage can be especially time-consuming and frustrating for patients. Zaliznyak M, Jung EE, Bresee C, et al. Which U.S. States' Medicaid Programs Provide Coverage for Gender-Affirming Hormone Therapy and Genital Gender-Affirming Surgery for Transgender Patients?: A State-by-State Review, and a Study Detailing the Patient Experience to Confirm Coverage of Service. J Sex Med 2021;18:410-422.
Keywords: Gender Dysphoria; Gender-Affirming Hormone Therapy (GAHT); Gender-Affirming Surgery (GAS); Medicaid Assistance Program; Sex Reassignment Surgery (SRS); Transgender.
Copyright © 2020 International Society for Sexual Medicine. Published by Elsevier Inc. All rights reserved.
- Patient Outcome Assessment
- Transgender Persons*
- United States


Ohio judge temporarily blocks ban on gender-affirming care for transgender minors
A Franklin County judge on Tuesday temporarily blocked an impending law that would restrict medical care for transgender minors in Ohio.
The decision came weeks after the American Civil Liberties Union filed a lawsuit challenging House Bill 68 on behalf of two transgender girls and their families. The measure prevents doctors from prescribing hormones, puberty blockers or gender reassignment surgery before patients turn 18.
Attorneys contend the law violates the state Constitution , which gives Ohioans the right to choose their health care.
"Today's ruling is a victory for transgender Ohioans and their families," said Harper Seldin, staff attorney for the ACLU. "Ohio's ban is an openly discriminatory breach of the rights of transgender youth and their parents alike and presents a real danger to the same young people it claims to protect."
House Bill 68 was set to take effect April 24 after House and Senate Republicans voted to override Gov. Mike DeWine's veto. Proponents of the bill contend it will protect children, but critics say decisions about transition care should be left to families and their medical providers.
The suit in Ohio mirrors efforts in other states to challenge laws that restrict gender-affirming care for minors. A federal judge struck down a similar policy in Arkansas , arguing it violates the constitutional rights of transgender youth and their families. The state is appealing that decision.
“This is just the first page of the book,” Attorney General Dave Yost said Monday. “We will fight vigorously to defend this properly enacted statute, which protects our children from irrevocable adult decisions. I am confident that this law will be upheld.”
What does House Bill 68 do?
House Bill 68 allows Ohioans younger than 18 who already receiving hormones or puberty blockers to continue, as long as doctors determine stopping the prescription would cause harm. Critics say that's not enough to protect current patients because health care providers could be wary of legal consequences.
The legislation does not ban talk therapy, but it requires mental health providers to get permission from at least one parent or guardian to diagnose and treat gender dysphoria.
The bill also bans transgender girls and women from playing on female sports teams in high school and college. It doesn't specify how schools would verify an athlete's gender if it's called into question. Players and their families can sue if they believe they lost an opportunity because of a transgender athlete.
The lawsuit doesn't specifically challenge the athlete ban. But it argues that House Bill 68 flouts the constitution's single-subject rule, which requires legislation to address only one topic. House Republicans introduced separate bills on gender-affirming care and transgender athletes before combining them into one .
In Tuesday's decision, Franklin County Judge Michael Holbrook indicated that the law could be tossed out because of a single-subject violation.
"It is not lost upon this Court that the General Assembly was unable to pass the (Saving Ohio Adolescents from Experimentation) portion of the Act separately, and it was only upon logrolling in the Saving Women’s Sports provisions that it was able to pass," Holbrook wrote.
Panel clears ban on gender reassignment surgery for minors
Tuesday's decision came one day after a legislative panel cleared the way for an administrative rule that will ban gender reassignment surgery for minors. Ohio health care providers say they do not perform that procedure on patients under 18.
The rule will take effect May 3.
The measure was among several that DeWine proposed to regulate gender-affirming care after he vetoed House Bill 68. In testimony for Monday's meeting, opponents argued that the rules overstep the administration's authority and conflict with federal law.
"The proposed administrative rule changes are based on biased definitions, ignore well-established best practices and restrict countless patients’ access to gender-affirming care," said Mallory Golski, civic engagement and advocacy manager for Kaleidoscope Youth Center.
DeWine's other proposals are still working their way through the rulemaking process. That includes a requirement for transgender minors to undergo at least six months of counseling before further treatment occurs. Another rule would require providers to report non-identifying data on gender dysphoria diagnoses and treatment.
Haley BeMiller is a reporter for the USA TODAY Network Ohio Bureau, which serves the Columbus Dispatch, Cincinnati Enquirer, Akron Beacon Journal and 18 other affiliated news organizations across Ohio.
This article originally appeared on The Columbus Dispatch: Ohio judge temporarily blocks ban on gender-affirming care for transgender minors

House bill would ban gender reassignment surgery and medical treatments in Ohio

A bill that would make it illegal for minors to get puberty blockers or undergo gender reassignment surgeries has been re-introduced in the Ohio House.
Gary Click (R-Vickery) said he’s re-introducing his bill that is being called the "SAFE Act". It received hearings but didn’t pass last year. He said he's bringing it back because it is important to keep doctors in Ohio from doing gender reassignment surgery on or prescribing other gender altering treatments to anyone under 18 years old.
“This bill will save lives and that’s why we are doing this," Click said.
Click stressed this bill does not deny health or psychiatric care to transgender students - only surgeries and medications that could alter their bodies. He said 85-95% of the kids who feel they are trapped in the body of someone of the opposite gender outgrow that feeling as an adult but didn't cite a source for those numbers.
However, Click did invite Scott Newgent of Texas to testify about how he regrets undergoing transition surgery when he was 42 years old. Newgent, the founder of TReVoices, a group of trans educators who oppose allowing minors to undergo these treatments, said the surgeries and treatments have had a lasting effect on him.
"I underwent close to $1 million in surgeries and hormone therapies to change from Kellie to Scott, a trans man and I almost died in the process. And I certainly have cut many, many years off my life," Newgent said.
A Columbus woman, Ronli Moses, said she felt the medical professionals who dealt with her 14 year old son were putting pressure on her to allow transition surgery instead of dealing with the root problem.
"His mental health was ignored in lieu of a quick fix that in reality, fixes nothing on the inside which is where the problem lives," Moses said.
Moses said her son, who is a transgender man, did not end up going through the surgery. She said he is now an adult, going to college.
Click said his bill would also require medical providers to keep anonymous information that would serve as data for determining the future outcomes of the effectiveness of these treatments.
Click said this bill would also prohibit doctors from "aiding and abetting" by sending patients to other states for this treatment, but he was unclear on the details of the limits of that language.
"Basically it says you cannot aid or abet doing this damage to a young person. So anything that you are doing to take a young person, as a medical professional to a place where they are getting illegal hormone blockers, illegal hormones, or illegal surgery is considered aiding and abetting."
Equality Ohio’s Maria Bruno says that language is vague. She says this version of the bill seems even more draconian than the version Click sponsored last year.
"Our understanding is the medical limitations as well as the addition of some very vague language around aiding and abetting someone, which seems to be undefined in the context of the bill, so we have some things to research but this is definitely not a compromise."
The president of the Ohio Children's Hospital Association testified on the earlier version of the bill. And the American Academy of Pediatrics has issued a statement in support of doctors supplying a wide range of care for transgender children, including drug therapies or surgeries.
Click rejects that, saying doctors who oppose this strategy are being pressured to stay quiet. Bruno said doctors need to be able to adhere to the best practices in medicine. She said this bill runs counter to those.
"What's so frustrating here is that medical best practices is directly contradictory to what is prescribed in this legislation which is a perfect example of why politicians should not be pretending to be doctors," Bruno said.
Bruno and Click both said they know young transgender kids often experience bullying. Bruno said this legislation does nothing to address that.
"This bill has the exact opposite impact of deterring bullying. All this does is further spread misinformation about how trans affirming medical care works in the first place and it makes transgender kids and their families feel like they are under attack," Bruno said.
Bruno said some families with transgender kids are now considering whether to move out of state if this bill passes.
The bill has just been introduced. While this bill didn't get hearings last time it was proposed, other bills dealing with trans kids did. So if past is prologue, this bill will likely generate a lot of testimony in future hearings.

TLDEF's Trans Health Project
Gender affirmation surgery.
Policy: Gender Affirmation Surgery Policy Number: HUM-0518-020 Last Update: 2023-09-28
Please ctrl + F to find the correct document titled "gender affirmation surgery" and download the pdf.
Back to top
Updated on Nov 27, 2023
The page could not be loaded. The CMS.gov Web site currently does not fully support browsers with "JavaScript" disabled. Please enable "JavaScript" and revisit this page or proceed with browsing CMS.gov with "JavaScript" disabled. Instructions for enabling "JavaScript" can be found here. Please note that if you choose to continue without enabling "JavaScript" certain functionalities on this website may not be available.

An official website of the United States government
Here's how you know
The .gov means it's official.
Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure.
The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Gender Dysphoria and Gender Reassignment Surgery
Tracking information, description information.
Please Note: This may not be an exhaustive list of all applicable Medicare benefit categories for this item or service.
A. General
Gender reassignment surgery is a general term to describe a surgery or surgeries that affirm a person's gender identity.
B. Nationally Covered Indications
C. Nationally Non-Covered Indications
D. Other
The Centers for Medicare & Medicaid Coverage (CMS) conducted a National Coverage Analysis that focused on the topic of gender reassignment surgery. Effective August 30, 2016, after examining the medical evidence, CMS determined that no national coverage determination (NCD) is appropriate at this time for gender reassignment surgery for Medicare beneficiaries with gender dysphoria. In the absence of an NCD, coverage determinations for gender reassignment surgery, under section 1862(a)(1)(A) of the Social Security Act (the Act) and any other relevant statutory requirements, will continue to be made by the local Medicare Administrative Contractors (MACs) on a case-by-case basis.
(This policy last reviewed August 2016.)
Transmittal Information
03/2017 - Effective Date: 08/30/2016. Implementation Date: 04/04/2017. ( TN 194 ) (CR9981)
National Coverage Analyses (NCAs)
This NCD has been or is currently being reviewed under the National Coverage Determination process. The following are existing associations with NCAs, from the National Coverage Analyses database.
- Original Consideration for Gender Dysphoria and Gender Reassignment Surgery (CAG-00446N)
Coding Analyses for Labs (CALs)
This NCD has been or is currently being reviewed under the National Coverage Determination process. The following are existing associations with CALs, from the Coding Analyses for Labs database.
Additional Information
Email this document to yourself or someone else.
An asterisk ( * ) indicates a required field. This email will be sent from you to the recipient email address(es) you enter. Please do not use this feature to contact CMS. To submit a comment or question to CMS, please use the Feedback/Ask a Question link available at the bottom of every MCD page.
Page Help for NCD - Gender Dysphoria and Gender Reassignment Surgery (140.9)
Introduction.
This page displays your requested National Coverage Determination (NCD). The document is broken into multiple sections. You can use the Contents side panel to help navigate the various sections. National Coverage Determinations (NCDs) are national policy granting, limiting or excluding Medicare coverage for a specific medical item or service.
More information
NCDs are developed and published by CMS and apply to all states. NCDs are made through an evidence-based process, with opportunities for public participation. Medicare coverage is limited to items and services that are considered "reasonable and necessary" for the diagnosis or treatment of an illness or injury (and within the scope of a Medicare benefit category). An NCD sets forth the extent to which Medicare will cover specific services, procedures, or technologies on a national basis. Medicare Administrative Contractors (MACs) are required to follow NCDs. If an NCD does not specifically exclude/limit an indication or circumstance, or if the item or service is not mentioned at all in an NCD or in a Medicare manual, an item or service may be covered at the discretion of the MAC based on a Local Coverage Determination (LCD). LCDs cannot contradict NCDs, but exist to clarify an NCD or address common coverage issues. Prior to implementation of an NCD, CMS must first issue a Manual Transmittal, CMS ruling, or Federal Register Notice giving specific directions to claims-processing contractors. That issuance, which includes an effective date and implementation date, is the NCD. If appropriate, the Agency must also change billing and claims processing systems and issue related instructions to allow for payment. The NCD will be published in the Medicare National Coverage Determinations Manual. An NCD becomes effective as of the date of the decision memorandum.
Printing a Document to PDF
Frequently Asked Questions (FAQs)
Are you a provider and have a question about billing or coding.
Please contact your Medicare Administrative Contractor (MAC). MACs can be found in the MAC Contacts Report .
Do you have questions related to the content of a specific Local Coverage Determination (LCD) or an Article?
Are you a beneficiary and have questions about your coverage, are you looking for codes (e.g., cpt/hcpcs, icd-10), local coverage.
For the most part, codes are no longer included in the LCD (policy). You will find them in the Billing & Coding Articles. Try using the MCD Search to find what you're looking for. Enter the code you're looking for in the "Enter keyword, code, or document ID" box. The list of results will include documents which contain the code you entered.
Please Note: For Durable Medical Equipment (DME) MACs only, CPT/HCPCS codes remain located in LCDs. All other Codes (ICD-10, Bill Type, and Revenue) have moved to Articles for DME MACs, as they have for the other Local Coverage MAC types.
National Coverage
NCDs do not contain claims processing information like diagnosis or procedure codes nor do they give instructions to the provider on how to bill Medicare for the service or item. For this supplementary claims processing information we rely on other CMS publications, namely Change Requests (CR) Transmittals and inclusions in the Medicare Fee-For-Service Claims Processing Manual (CPM).
In order for CMS to change billing and claims processing systems to accommodate the coverage conditions within the NCD, we instruct contractors and system maintainers to modify the claims processing systems at the national or local level through CR Transmittals. CRs are not policy, rather CRs are used to relay instructions regarding the edits of the various claims processing systems in very descriptive, technical language usually employing the codes or code combinations likely to be encountered with claims subject to the policy in question. As clinical or administrative codes change or system or policy requirements dictate, CR instructions are updated to ensure the systems are applying the most appropriate claims processing instructions applicable to the policy.
How do I find out if a specific CPT code is covered in my state?
Enter the CPT/HCPCS code in the MCD Search and select your state from the drop down. (You may have to accept the AMA License Agreement.) Look for a Billing and Coding Article in the results and open it. (Or, for DME MACs only, look for an LCD.) Review the article, in particular the Coding Information section.
If you need more information on coverage, contact the Medicare Administrative Contractor (MAC) who published the document. The contractor information can be found at the top of the document in the Contractor Information section (expand the section to see the details).
If you don’t find the Article you are looking for, contact your MAC .
Did you receive a Medicare coverage denial?
Was your Medicare claim denied? Here are some hints to help you find more information:
1) Check out the Beneficiary card on the MCD Search page.
2) Try using the MCD Search and enter your information in the "Enter keyword, code, or document ID" box. Your information could include a keyword or topic you're interested in; a Local Coverage Determination (LCD) policy or Article ID; or a CPT/HCPCS procedure/billing code or an ICD-10-CM diagnosis code. Try entering any of this type of information provided in your denial letter.
3) Contact your MAC .
4) Visit Medicare.gov or call 1-800-Medicare.
It is Thursday and the weekly MCD data isn’t refreshed?
Are you having technical issues with the medicare coverage database (mcd), mcd session expiration warning.
Your MCD session is currently set to expire in 5 minutes due to inactivity. If your session expires, you will lose all items in your basket and any active searches. If you would like to extend your session, you may select the Continue Button.
Reset MCD Search Data
If you are experiencing any technical issues related to the search, selecting the 'OK' button to reset the search data should resolve your issues.

IMAGES
COMMENTS
intersex surgery, transgender surgery, gender reassignment, and gender ... that are medically necessary, or the coverage of health services related to gender transition, CareSource utilizes neutral standards supported by evidence -based criteri a. ... Gender Affirming Surgery . OHIO MEDICAID . MM-0034 . Effective date: 11/01/2021 . b. Hormones ...
Policy: Gender Dysphoria (Ohio Medicaid) Policy Number: MM-0034. Last Update: 2019-10-01. Issued in: Ohio. This policy applies to Medicaid. Breast Reconstruction: The following are requirements that apply for consideration of sexual reassignment surgery: (List is not meant to represent all requirements) 1. Breast/chest surgery.
that are medically necessary, or the coverage of health services related to gender transition, CareSource utilizes neutral standards supported by evidencebased criteria.- I. Covered Services ... Gender Affirming Surgery . OHIO MEDICAID . MM-0034 . Effective date: 01/01/2021 (8) The behavioral health provider communicates willingness to be ...
GAS is even less likely to be covered by Medicaid than GAHT, and it is only covered by 25 of 51 state Medicaid programs. It is not covered by 22 of 51 state programs, and coverage was classified as "indeterminate" in 4 of 51 states (Figure 2). Researchers completed an average of 3.3 phone calls per state to attain this information (range of ...
Ohio Medicaid has no explicit policy regarding transgender-related health care. Regulations: OH OAC 5160-2-03 (2017; since 2015) ... Gender transformation. Clinical Policies: CareSource - Gender Dysphoria Premier Health Plan - Gender Reassignment Notes: Even though there is an explicit exclusion on the books, both the Washington Post and ...
Overall coverage of gender-affirming care: As detailed below, many state Medicaid programs cover aspects of gender-affirming health services. However, only two of the 41 states responding to this ...
Gender-affirming surgery is an important part of the management of patients with gender dysphoria. Top surgery includes procedures to create or remove breasts. Feminizing bottom surgery includes procedures to remove the penis and testicles and create a new vagina, labia and clitoris. Learn more about feminizing bottom surgery .
SUMMARY: The Gender Dysphoria medical policy outlines information consistent with the most up-to-date evidence-based medical literature related to three common gender dysphoria treatment approaches: psychotherapy, hormonal therapy and sexual reassignment surgery. Policy coverage rationale is outlined according to state and federal guidelines.
Grants for individuals with financial need who want to pursue gender-affirming surgery. Focuses on access to trans-related health care including health insurance tutorials, state health insurance guidelines, provider lists, information on appealing medical necessity denials, and financial support resources for gender-affirming surgery.
Background: To date, a comprehensive state-by-state assessment of transgender transition-related health care coverage for gender-affirming hormone therapy (GAHT) and genital gender-affirming surgery (GAS) has not been reported. Aims: The aims of this study were 1) to verify which U.S. states' Medicaid systems do/do not cover GAHT and GAS; 2) to assess the ease/difficulty for patients to ...
A Leader in Inclusive Care. Four OhioHealth hospitals earned a top score of 100 in the 2019 Human Rights Campaign Foundation's Healthcare Equality Index, achieving designation as LGBTQ+ Healthcare Equality Leaders. OhioHealth provides transgender and LGBT healthcare services to care for patients' health and wellness journeys.
Scenario 1: The insurance plan covers the surgery. If people have a health insurance plan that covers gender affirmation surgery, people will need to take steps to ensure they meet certain ...
Tuesday's decision came one day after a legislative panel cleared the way for an administrative rule that will ban gender reassignment surgery for minors. Ohio health care providers say they do ...
Medicaid coverage of best-practice care for transgender youth, prohibiting private insurers from covering gender-affirming care for minors; allowing private insurers to refuse to cover gender-affirming care for adults; and more. • *In June 2023, a federal judge permanently blocked HB1570, ruling the law unconstitutional.
Gender Dysphoria OHIO MEDICAID MM-0034 Effective date: 10/1/2019 2 A. SUBJECT ... or the coverage of health services related to gender transition, CareSource ... serious limitations in study designs it permits only weak conclusions regarding sex reassignment surgery. No conclusions can be made about the benefits of SRS or about
A previous version of a ban on gender reassignment treatments for minors was considered by the last Ohio General Assembly, but there are some changes in the measure this time. ... He said he's bringing it back because it is important to keep doctors in Ohio from doing gender reassignment surgery on or prescribing other gender altering ...
Medicaid Regulations and Guidance; Gender Centers; Trans Health Care Providers; ... Prev Index Gender Dysphoria/Reassignment [100 of 163] Next. Humana Gender Affirmation Surgery. Policy: Gender Affirmation Surgery Policy Number: HUM-0518-020 Last Update: 2023-09-28 ...
that Medicaid covers gender-affirming care.9 The guidance has been updated and expanded ... or burdens for transgender people seeking care. The guidance was updated most recently in March 2019 to provide for coverage of gender-affirmation surgery intended to refine ... 19 Gender Reassignment Codes 54400 through 54417 and 19318 May be ...
Response: The decisions on whether to cover gender reassignment surgery in a particular case are made on the basis of the statutory language in section 1862 of the Social Security Act that establish exclusions from coverage and would not depend on the cost of the procedure. 2. Coverage with Evidence Development and Research
Ohio Medicaid Policy Name & Number Date Effective Gender Affirming Surgery-OH MCD-MM-0034 11/01/2022-11/30/2023 Policy Type MEDICAL ... Coverage), then the plan contract (i.e., Evidence of Coverage) will be the controlling document used to make the determination.
The standard premium for Medicare Part B in 2020 is $144.60 each month, and there is a $198 annual deductible cost. After a person pays the deductible, Medicare pays 80% of the allowable costs ...
In the absence of an NCD, coverage determinations for gender reassignment surgery, under section 1862 (a) (1) (A) of the Social Security Act (the Act) and any other relevant statutory requirements, will continue to be made by the local Medicare Administrative Contractors (MACs) on a case-by-case basis. (This policy last reviewed August 2016.)
Transfeminine surgery removes a penis and testicles to create a transgender vagina. Until 2014, Original Medicare would not cover gender confirmation surgery due to outdated thinking involving LGBTQ+ healthcare. Today, Original Medicare provides coverage for gender confirmation surgery on a case-by-case basis in the same way it applies such ...