

Essay Drug Abuse and Mental Health
- 5 Works Cited
Substance abuse complicates almost every aspect of care for the person with a mental disorder. When drugs enter the brain, they can interrupt the work and actually change how the brain performs its jobs; these changes are what lead to compulsive drug use. Drug abuse plays a major role when concerning mental health. It is very difficult for these individuals to engage in treatment. Diagnosis for a treatment is difficult because it takes time to disengage the interacting effects of substance abuse and the mental illness. It may also be difficult for substance abusers to be accommodated at home and it may not be tolerated in the community of residents of rehabilitation programs. The author states, that they end up losing their support systems …show more content…
According to the American Psychiatric Association chronic drug abuse may occur together with any mental illness that may include some of the following disorders. “Some common serious mental disorders associated with chronic drug abuse include schizophrenia, bipolar disorder, manic depression, attention deficit hyperactivity disorder (ADHD), generalized anxiety disorder, obsessive-compulsive disorder, post-traumatic stress disorder, panic disorder, and antisocial personality disorder” (Center, 2004). Some of these disorders carry with them an increased risk of drug abuse. Another example of a drug that can cause a mental disorder, is MDMA (3, 4-methylenedioxymethamphetamine) which is commonly known as ecstasy. It produces long term deficits in serotonin function in the brain, leading to mental disorders such as depression and anxiety. In addition, chronic drug abuse by teenagers during a time of development it is a particular concern because, it can interfere with normal socialization and cognitive development and thus frequently contributes to the development of mental disorders. Violence has become more prevalent among the diagnosed population of drugs and mental disorders. Domestic violence and suicide attempts are more common of the mentally ill who end up incarcerated; there is
Essay about Mental Health Drugs
- 10 Works Cited
As the second decade of the 21st century progresses, the population approaches seven billion. With so many people, how are people supposed to stand out in job applications, or catch the administrators’ eye as he or she reads applications to highly prestigious colleges and universities? More and more people are asking this question, and more and more people are finding help in a small pill. Originally diagnosed for Alzheimer’s disease and ADHD, these drugs are increasingly used off label in universities and workplaces. In society, people call this form of off label use of neuroenhancing drugs chiefly two different things: smart drugs informally, and nootropics formally. The word nootropic originated from a Romanian Dr. Corneliu E.
Substance Abuse In College Essay
Difficulty meeting academic responsibilities is one of the most common consequences of drug use and abuse. The relationship between drug use/abuse and the academic performance of college students rises every year that causes a critical issue on Colleges and Universities campus. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) Task Force on College Drug reports that about 25 percent of college students report academic problems caused by drug use, such as earning lower grades, doing poorly on exams or papers, missing class dramatically, and falling behind. However, the history of drug abuse has been rooted in the early stages of life. Drug use/abuse has been classified as a major problem of students as early as in the fourth grade. Consequently, it
Benefits Of Dual Diagnosis
Drug addiction and mental illness are two topics that are becoming more popular for discussion in American households. As stated from DrugAbuse.com, “mental illness is common amongst a population suffering from substance abuse and addiction. The relationship is so strong that many people believe the drugs play a causative role in the development of the mental illness. In most instances, this is not the case. In the United States, approximately 8.9 million people have both a mental health and a substance abuse issue”. This overwhelming amount of the United States population is often give as a dual diagnosis making persons suffering
The Effects Of Homeless Conditions, Drug Abuse, And Mental Illness
There are many variables when it comes to talking about substance abuse and addiction. According to (L. Lagoni, 2010), links are present between mental illness and self-medication referred to as the self-medication hypotheses. The research in this peer reviewed article was comprehensive and viewed psychiatric disorders from many different angles. They looked at illicit drug and alcohol users and found that many mental health disorders such as Thought, Depression, Anxiety, Bipolar, PTSD, ADHD, and APD are connected to many societal issues which include homelessness, health issues, unemployment crime, and early deaths.
In our world today there are a very large number of problems that human service client
The National Institute on Drug Addiction reveals substance abuse has been linked to mental health problems, illness and occupational problems. It affects their social life and their ability to function as a healthy individual (The Truth about Drugs pg.21, 22, 35). The complexity of the assistance required from the human service professional depends on the severity of the problem and the state of the client.
Substance Abuse Untreated
The resulting behaviors weaken the person’s ability to control impulses, disregarding the negative consequences (National Institute on Drug Abuse 2). It happens quite frequently that one with a drug addiction has a co-occurring mental illness because often times, one will lead to the other. Many people who are addicted to drugs are also diagnosed with a mental disorder or vice versa. For example, compared with the general population, people with severe mental illnesses were approximately “four times more likely to be heavy alcohol users, 3.5 times more likely to use marijuana regularly and 4.6 times more likely to use other drugs at least ten different times in their lifetime” (National Institutes of Health 7). In addition, people who have a drug addiction are about two times as likely to suffer from a mood or an anxiety disorder (National Institute on Drug Abuse 3). It is clear that drug abuse may show symptoms of mental illnesses. In reverse, mental disorders can lead to drug abuse, commonly as a means of “self-medication.” Drug abuse is a mental illness in itself, and many times it is a sign of additional underlying mental
Is Substance Abuse A Mental Disorder? Essay
Substance abuse disorder, or what is referred to now as substance use disorder, is a condition where reliance to various substances, may it be licit or illicit, continues to permeate the lives of the sufferer, even to the point that this reliance is detrimental to the person’s life. This definition is merely an oversimplification of the said disorder. In reality, the criteria for substance use disorder has been “defined and redefined over the past several decades and these definitions have now achieved international acceptance” (Oxford, 2012). As an evidence, the recently published DSM-5 has made major revisions to the definition of substance use disorder; the revisions are the removal of the relation of substance-use with the law, the addition of craving as one of the criterion, and the elimination of the dependence symptoms (Fitzgerald, 2012, p. 609). Nonetheless, despite these efforts to improve the diagnosis for substance use disorder, several critics argued that the aforementioned syndrome is inappropriate to be classified as a mental health disorder. From this criticism, it is then necessary to define what a mental disorder is and what the criteria are to be classified as such. Upon defining the meaning of mental health disorder, it is now then possible to conclude whether substance abuse is a mental disorder or not.
Drug Abuse On The United States Essay
“In 2014, nearly two million Americans either abused or were dependent on prescription opioid pain relievers (“Injury Prevention and Control: Opioid Overdose,” 2016.)” The CDC is now saying that the United States is in an epidemic. The purpose of this paper is to explore the increasing drug use in the United States over the last decade. The primary focus is on the administration of opioid analgesics and the addicting mechanisms of these medications, and what they are used for. It will talk about the deaths related to these medications and the health effects, and the other types of drugs these medications can lead to, such as heroin. This paper will also talk about the costs related to opioid analgesics in the hospitals and in the community, and what we as health care providers can be doing to help stop this epidemic.
Drug Recovery Essay
Drug treatment centers are far more abundant now than they have been in terms of effectiveness as research and studies have been conducted. In particular THE CAMP Recovery Center is a “Nationally-accredited program run by an expert staff with extensive training” and has had numerous success and recovery stories from struggling addicts that just wanted a way out, including one from a family member of mine. THE CAMP is located in Santa Cruz mountain with an offering a variety of outdoor focused activities to supplement group therapy and other recovery-related programming. The clinic offers a variety of different detoxification options depending on the addiction a person has. The Center offers detox/treatment programs for the following additions:
Mental Illness And Coexisting Disorders
It is well known that there is a growing comorbidity between psychiatric and physical disorders and substance abuse or addiction. The aim of this research article is to explore issues related to substance abuse disorders in individuals with physical disabilities and/or mental disabilities, and the relationship between substance abuse disorders and co-existing disabilities. There are several different terms used to describe the combination of, and connection between, substance abuse or addiction and physical or mental illnesses. The terms most commonly used to reflect the coexistence of substance abuse and psychological or physical disabilities are ‘dual diagnosis’ and ‘comorbidity’. Dual diagnosis literally means being diagnosed with both substance
Substance Abuse Essay
Substance abuse (alcoholism and addiction) and depression are other common factors that lead veterans to become homeless today (Goldstein, Luther, Haas, Appelt, & Gordon, 2010). Many who are dealing with depression or PTSD will turn to alcohol or to another substance drug to try to get relief or an escape from the mental illness they are facing. Veterans that are exposed to high combat while serving are at higher risks in using alcohol or other substances. Veterans have admitted to miss using alcohol from suffering from PTSD or depression or from both disorders (Helternes, Clouser, MacGreogor, Normari, & Galarneau, 2014). Veterans that are dependent on alcohol, who have higher triggers with PTSD, also have a higher desire
Psychological Illness Disorder And Controlled Substance Abuse Essay
Psychological illness, disorder and controlled substance abuse include our mental and emotional health with this the behavior therapy care is the treatment choice (Bissell & Royce, 1994). This cognitive treatment helps client to search inside themselves and help them focus, transforming unhealthy inadequate attitudes, opinions or irrational ideas (My Unique Student Experience. 2017). Clients must understand that an individual thought process typically governs their actions. Clearly explain to the client that their belief system affects his or her performance. Undesirable habit can be temporary, and not repeated. If the client will make the efforts to alter previous negative lifestyles.
Drug Addiction Essay
Many people don't understand why or how other people become addicted to drugs. They may mistakenly think that those who use drugs lack moral principles or willpower and that they could stop their drug use simply by choosing to. In reality, drug addiction is a complex disease, and quitting usually takes more than good intentions or a strong will. Drugs change the brain in ways that make quitting hard, even for those who want to. Fortunately, researchers know more than ever about how drugs affect the brain and have found treatments that can help people recover from drug addiction and lead productive lives.
Drug Abuse Essay
Drugs have killed 2,000,000 people every year for the last decade from overdoses based off the NIDA’s information and graphs.Drugs like Methamphetamine , cocaine,heroin ,tobacco and alcohol,As said from the NIDA “drug abuse kill 500 people every day” .Most people start taking drugs in moments of stress or hard times.People have started to get addicted to the drug thinking that they help release their stress.so people try to pass on their bad choices to others to help them release their stress.side effects in the drugs may cause illnesses,body pains and sometimes death.Many people die because of these drugs without having a care in the world ,all they know is that the drugs help them feel good about themselves.”Tobacco is just as bad it
Drugs and Alcohol Essay
Drugs are heavily used throughout the entire world. However, it is important to understand and not undermine the variability in which drugs are used. It is clear some are for distinct medical treatment and others are for recreational use. In the United States, marijuana has been and continues to be a very controversial drug. Some states have allowed marijuana consumption for medicinal purposes, while others have completely outlawed the drug. Those who are against the legalization and regulation of marijuana suggest the economical and health risk associated with consumption of the drug are too high. Although there is risk involved with the legalization of the marijuana, our country has already been risking too much banning the drug.
Sign Up Now
Get instant access to over 1 million+ study documents
Already registered? click here to login
By creating your account, you agree to our terms of service , privacy policy and student honor code .

- Homework Help
- Essay Examples
- Citation Generator
- Writing Guides
- Essay Title Generator
- Essay Outline Generator
- Flashcard Generator
- Plagiarism Checker
- Paraphrasing Tool
- Conclusion Generator
- Thesis Statement Generator
- Introduction Generator
- Literature Review Generator
- Hypothesis Generator
- Mental Disorder
- Mental Health and Addiction Essay
Mental Health And Addiction Essay
"Recovery requires a twin track approach: enabling and supporting individual recovery journeys, while creating environmental conditions that enable and support a 'social contagion' of recovery, in which recovery is transmitted through supportive social networks and dedicated recovery groups, such as mutual aid" (Best & Lubman, 2012, p. 593). By addicts becoming involved in society, they gain a purpose and build self-esteem. This self-esteem then translates to hope and empowerment. Such transformations from addict to recovered require these key feelings in order to effectively begin and finish the process. It appears that active involvement in the community and having goals apart from the self enables faster recovery among addicts and makes for a strong advantage for the recovery model. As the previous study demonstrated when an addict seeks to make him or herself useful to society, the need for escape subsides. Support perceived to be ineffective emerged in dyads with no operationalized goal, and high emotional availability with low degree of practical support. Support perceived to be effective was signified by the sponsor attending to power imbalance and the addict coming into position to help others and feel useful (Johansen, Brendryen, Darnell, & Wennesland, 2013, p. 1). Although this has shown that people can and will progress towards their goals using the framework from the recovery model, there are some setbacks. For example, some people just cannot find purpose within their community. Community, a support system, all these things involve success human to human interaction. Often times addicts and those that mentally ill cannot achieve this. They may have a horrible family, no friends, and no one there to actively enable their participation in a community. They may have socialization issues and cannot achieve these tasks by themselves. Thus the recovery model cannot work for them. The recovery model is a useful model, but it involves people, not just the person involved. It would take great discipline, courage, and effort in order for the person to do these steps that are part of the model by themselves. This rings especially true for community participation because that involves a coordinated effort. While some critics of the disease model of treatment believe labeling addiction as a disease is not conducive to encouraging recovery among addicts (Hammer et al., 2013), it is something that with new technology, researchers are investigating. "Advances in neuroscience identified addiction as a chronic brain disease with strong genetic, neurodevelopmental, and sociocultural components. Drug-induced impairments are long lasting; thus, interventions designed to mitigate or even reverse them would be beneficial for the treatment of addiction" (Volkow & Morales, 2015, p. 712). This combined with the recovery model can yield benefits that will lead towards progress. The recovery model of treatment asks the afflicted person to feel hope and be empowered to change. However, if that person cannot do so on their own, drug intervention may prove useful. The benefits of the recovery model are that individuals treated in this way gain a sense of control and personal identity that more traditional methods would not yield. In addition, the stigma attached to being mentally ill or being an addict is removed/reduced. When people who have to deal with these personal problems look for and seek help, they do so assuming they will be ostracized as is the norm in society. Because of the recovery model, these people are no longer dehumanized and instead are made to feel like they can reach that level of normalcy they once had or could have should they successfully recover. There is considerable indication of the numerous benefits to the implementation of a recovery-oriented mental health care model. Some of which are reduction in occurrence of violence, decrease in events of self-harm, shorter inpatient stays, as well as reduced need for the use of fetters and most significantly, greater independence and feelings of self-control for the patient (Barker & Buchanan-Barker, 2012). By removing the stigma attached to the patient, it invites the patient to take recovery into his or her own hands. Hope in relation to the recovery model offers the motivating and essential message that there can be a better future. So many that become addicts or mentally ill feel the obstacles and barriers they face cannot be overcome. However, hope brought on by recovery helps them gain the strength to overcome them. Hope can be fostered through providers, peers, friends, and families and often if the catalyst and…
Cite this Document:
"Mental Health And Addiction" (2016, July 24) Retrieved April 3, 2024, from https://www.paperdue.com/essay/mental-health-and-addiction-2161273
"Mental Health And Addiction" 24 July 2016. Web.3 April. 2024. < https://www.paperdue.com/essay/mental-health-and-addiction-2161273 >
"Mental Health And Addiction", 24 July 2016, Accessed.3 April. 2024, https://www.paperdue.com/essay/mental-health-and-addiction-2161273
Related Documents
Mental health care system.
Mental Health Care System The mental healthcare system in the United States is historically fractured. A "silo"-based foundation precludes correlation between varied and integral systems that, collectively, offer a range of services to treat the whole patient. The President's New Freedom Commission on Mental Health roused the debate of the mental health community and rallied them around one goal: providing thorough, coherent, and appropriate treatment to Americans with mental health and
Mental Health the Technological Developments
The attitude of parents which came across as more authoritative, uncompromising, uncooperative and unaffectionate does result in higher levels of depression in the subject. Even though parental authority was required for disciplining the adolescents, it was the accentuated sort of antagonistic authority that resulted in higher levels of depression as well as increased the possibility of clashes and irritation. The fact of the matter is that in most occasions when
Mental Health and Primary Care
It promised to be a very important resource to the primary care setting, but at present, the performance has not been considerable and there have been lack of funds and local consensus, which thwart its implementation (Pidd). Shared Care Between GP Practices and Community Health Teams This initiative aimed at developing cooperative partnership between these teams as well as establishing systems for proactive, structured care at the practice level (Pidd 2004).
Mental Health Problems
Mental health counseling is a field that focuses on helping people to achieve mental and emotional wellness. The treatment plan will typically consist of seeing clients continuously throughout the year. Specific areas of specialization exist in mental health counseling, such as counseling for addiction, trauma, or youth services. If a mental health counselor specializes in youth services, he could work in a variety of different settings, such as a school
Solitary Confinement and Mental Health Issues in Corrections
Functions, Issues, and Objectives in Corrections Introduction The functions of the historical state correctional system have changed since the founding of the nation more than 200 years ago. The Jacksonian Era, the Era of Reconstruction and the Progressive Era on up to the reform of the 1970s all effected different changes to the function—i.e., the goals and activities—of the correctional system. Pennsylvania’s state correctional system was the first to introduce solitary confinement
Mental Health in the U.S. Among African American Men
Abstract:Today, mental health in the U.S. has become the focus of a growing body of scholarship as researchers examine the antecedents to the nation�s current political polarization and increasingly violent responses to the multiple existential threats that confront humanity. The ongoing COVID-19 pandemic, for instance, has not only brought to the forefront the critical importance of public health but has also exposed the vulnerabilities in the nation's mental health infrastructure.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
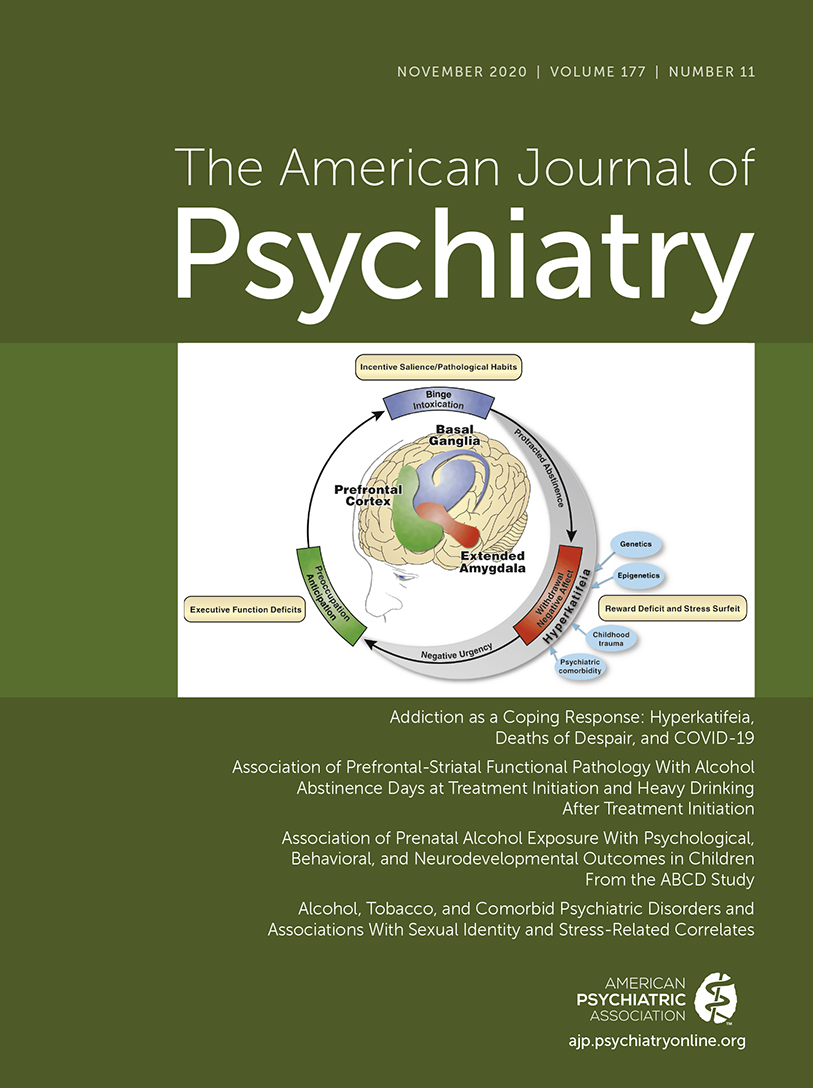
Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
- Ned H. Kalin , M.D.
Search for more papers by this author
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health ( 1 ) suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol. When considering other substances, the report estimated that 4.4 million individuals had a marijuana use disorder and that 2 million people suffered from an opiate use disorder. It is well known that stress is associated with an increase in the use of alcohol and other substances, and this is particularly relevant today in relation to the chronic uncertainty and distress associated with the COVID-19 pandemic along with the traumatic effects of racism and social injustice. In part related to stress, substance use disorders are highly comorbid with other psychiatric illnesses: 9.2 million adults were estimated to have a 1-year prevalence of both a mental illness and at least one substance use disorder. Although they may not necessarily meet criteria for a substance use disorder, it is well known that psychiatric patients have increased usage of alcohol, cigarettes, and other illicit substances. As an example, the survey estimated that over the preceding month, 37.2% of individuals with serious mental illnesses were cigarette smokers, compared with 16.3% of individuals without mental illnesses. Substance use frequently accompanies suicide and suicide attempts, and substance use disorders are associated with a long-term increased risk of suicide.
Addiction is the key process that underlies substance use disorders, and research using animal models and humans has revealed important insights into the neural circuits and molecules that mediate addiction. More specifically, research has shed light onto mechanisms underlying the critical components of addiction and relapse: reinforcement and reward, tolerance, withdrawal, negative affect, craving, and stress sensitization. In addition, clinical research has been instrumental in developing an evidence base for the use of pharmacological agents in the treatment of substance use disorders, which, in combination with psychosocial approaches, can provide effective treatments. However, despite the existence of therapeutic tools, relapse is common, and substance use disorders remain grossly undertreated. For example, whether at an inpatient hospital treatment facility or at a drug or alcohol rehabilitation program, it was estimated that only 11% of individuals needing treatment for substance use received appropriate care in 2018. Additionally, it is worth emphasizing that current practice frequently does not effectively integrate dual diagnosis treatment approaches, which is important because psychiatric and substance use disorders are highly comorbid. The barriers to receiving treatment are numerous and directly interact with existing health care inequities. It is imperative that as a field we overcome the obstacles to treatment, including the lack of resources at the individual level, a dearth of trained providers and appropriate treatment facilities, racial biases, and the marked stigmatization that is focused on individuals with addictions.
This issue of the Journal is focused on understanding factors contributing to substance use disorders and their comorbidity with psychiatric disorders, the effects of prenatal alcohol use on preadolescents, and brain mechanisms that are associated with addiction and relapse. An important theme that emerges from this issue is the necessity for understanding maladaptive substance use and its treatment in relation to health care inequities. This highlights the imperative to focus resources and treatment efforts on underprivileged and marginalized populations. The centerpiece of this issue is an overview on addiction written by Dr. George Koob, the director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and coauthors Drs. Patricia Powell (NIAAA deputy director) and Aaron White ( 2 ). This outstanding article will serve as a foundational knowledge base for those interested in understanding the complex factors that mediate drug addiction. Of particular interest to the practice of psychiatry is the emphasis on the negative affect state “hyperkatifeia” as a major driver of addictive behavior and relapse. This places the dysphoria and psychological distress that are associated with prolonged withdrawal at the heart of treatment and underscores the importance of treating not only maladaptive drug-related behaviors but also the prolonged dysphoria and negative affect associated with addiction. It also speaks to why it is crucial to concurrently treat psychiatric comorbidities that commonly accompany substance use disorders.
Insights Into Mechanisms Related to Cocaine Addiction Using a Novel Imaging Method for Dopamine Neurons
Cassidy et al. ( 3 ) introduce a relatively new imaging technique that allows for an estimation of dopamine integrity and function in the substantia nigra, the site of origin of dopamine neurons that project to the striatum. Capitalizing on the high levels of neuromelanin that are found in substantia nigra dopamine neurons and the interaction between neuromelanin and intracellular iron, this MRI technique, termed neuromelanin-sensitive MRI (NM-MRI), shows promise in studying the involvement of substantia nigra dopamine neurons in neurodegenerative diseases and psychiatric illnesses. The authors used this technique to assess dopamine function in active cocaine users with the aim of exploring the hypothesis that cocaine use disorder is associated with blunted presynaptic striatal dopamine function that would be reflected in decreased “integrity” of the substantia nigra dopamine system. Surprisingly, NM-MRI revealed evidence for increased dopamine in the substantia nigra of individuals using cocaine. The authors suggest that this finding, in conjunction with prior work suggesting a blunted dopamine response, points to the possibility that cocaine use is associated with an altered intracellular distribution of dopamine. Specifically, the idea is that dopamine is shifted from being concentrated in releasable, functional vesicles at the synapse to a nonreleasable cytosolic pool. In addition to providing an intriguing alternative hypothesis underlying the cocaine-related alterations observed in substantia nigra dopamine function, this article highlights an innovative imaging method that can be used in further investigations involving the role of substantia nigra dopamine systems in neuropsychiatric disorders. Dr. Charles Bradberry, chief of the Preclinical Pharmacology Section at the National Institute on Drug Abuse, contributes an editorial that further explains the use of NM-MRI and discusses the theoretical implications of these unexpected findings in relation to cocaine use ( 4 ).
Treatment Implications of Understanding Brain Function During Early Abstinence in Patients With Alcohol Use Disorder
Developing a better understanding of the neural processes that are associated with substance use disorders is critical for conceptualizing improved treatment approaches. Blaine et al. ( 5 ) present neuroimaging data collected during early abstinence in patients with alcohol use disorder and link these data to relapses occurring during treatment. Of note, the findings from this study dovetail with the neural circuit schema Koob et al. provide in this issue’s overview on addiction ( 2 ). The first study in the Blaine et al. article uses 44 patients and 43 control subjects to demonstrate that patients with alcohol use disorder have a blunted neural response to the presentation of stress- and alcohol-related cues. This blunting was observed mainly in the ventromedial prefrontal cortex, a key prefrontal regulatory region, as well as in subcortical regions associated with reward processing, specifically the ventral striatum. Importantly, this finding was replicated in a second study in which 69 patients were studied in relation to their length of abstinence prior to treatment and treatment outcomes. The results demonstrated that individuals with the shortest abstinence times had greater alterations in neural responses to stress and alcohol cues. The authors also found that an individual’s length of abstinence prior to treatment, independent of the number of days of abstinence, was a predictor of relapse and that the magnitude of an individual’s neural alterations predicted the amount of heavy drinking occurring early in treatment. Although relapse is an all too common outcome in patients with substance use disorders, this study highlights an approach that has the potential to refine and develop new treatments that are based on addiction- and abstinence-related brain changes. In her thoughtful editorial, Dr. Edith Sullivan from Stanford University comments on the details of the study, the value of studying patients during early abstinence, and the implications of these findings for new treatment development ( 6 ).
Relatively Low Amounts of Alcohol Intake During Pregnancy Are Associated With Subtle Neurodevelopmental Effects in Preadolescent Offspring
Excessive substance use not only affects the user and their immediate family but also has transgenerational effects that can be mediated in utero. Lees et al. ( 7 ) present data suggesting that even the consumption of relatively low amounts of alcohol by expectant mothers can affect brain development, cognition, and emotion in their offspring. The researchers used data from the Adolescent Brain Cognitive Development Study, a large national community-based study, which allowed them to assess brain structure and function as well as behavioral, cognitive, and psychological outcomes in 9,719 preadolescents. The mothers of 2,518 of the subjects in this study reported some alcohol use during pregnancy, albeit at relatively low levels (0 to 80 drinks throughout pregnancy). Interestingly, and opposite of that expected in relation to data from individuals with fetal alcohol spectrum disorders, increases in brain volume and surface area were found in offspring of mothers who consumed the relatively low amounts of alcohol. Notably, any prenatal alcohol exposure was associated with small but significant increases in psychological problems that included increases in separation anxiety disorder and oppositional defiant disorder. Additionally, a dose-response effect was found for internalizing psychopathology, somatic complaints, and attentional deficits. While subtle, these findings point to neurodevelopmental alterations that may be mediated by even small amounts of prenatal alcohol consumption. Drs. Clare McCormack and Catherine Monk from Columbia University contribute an editorial that provides an in-depth assessment of these findings in relation to other studies, including those assessing severe deficits in individuals with fetal alcohol syndrome ( 8 ). McCormack and Monk emphasize that the behavioral and psychological effects reported in the Lees et al. article would not be clinically meaningful. However, it is feasible that the influences of these low amounts of alcohol could interact with other predisposing factors that might lead to more substantial negative outcomes.
Increased Comorbidity Between Substance Use and Psychiatric Disorders in Sexual Identity Minorities
There is no question that victims of societal marginalization experience disproportionate adversity and stress. Evans-Polce et al. ( 9 ) focus on this concern in relation to individuals who identify as sexual minorities by comparing their incidence of comorbid substance use and psychiatric disorders with that of individuals who identify as heterosexual. By using 2012−2013 data from 36,309 participants in the National Epidemiologic Study on Alcohol and Related Conditions–III, the authors examine the incidence of comorbid alcohol and tobacco use disorders with anxiety, mood disorders, and posttraumatic stress disorder (PTSD). The findings demonstrate increased incidences of substance use and psychiatric disorders in individuals who identified as bisexual or as gay or lesbian compared with those who identified as heterosexual. For example, a fourfold increase in the prevalence of PTSD was found in bisexual individuals compared with heterosexual individuals. In addition, the authors found an increased prevalence of substance use and psychiatric comorbidities in individuals who identified as bisexual and as gay or lesbian compared with individuals who identified as heterosexual. This was most prominent in women who identified as bisexual. For example, of the bisexual women who had an alcohol use disorder, 60.5% also had a psychiatric comorbidity, compared with 44.6% of heterosexual women. Additionally, the amount of reported sexual orientation discrimination and number of lifetime stressful events were associated with a greater likelihood of having comorbid substance use and psychiatric disorders. These findings are important but not surprising, as sexual minority individuals have a history of increased early-life trauma and throughout their lives may experience the painful and unwarranted consequences of bias and denigration. Nonetheless, these findings underscore the strong negative societal impacts experienced by minority groups and should sensitize providers to the additional needs of these individuals.
Trends in Nicotine Use and Dependence From 2001–2002 to 2012–2013
Although considerable efforts over earlier years have curbed the use of tobacco and nicotine, the use of these substances continues to be a significant public health problem. As noted above, individuals with psychiatric disorders are particularly vulnerable. Grant et al. ( 10 ) use data from the National Epidemiologic Survey on Alcohol and Related Conditions collected from a very large cohort to characterize trends in nicotine use and dependence over time. Results from their analysis support the so-called hardening hypothesis, which posits that although intervention-related reductions in nicotine use may have occurred over time, the impact of these interventions is less potent in individuals with more severe addictive behavior (i.e., nicotine dependence). When adjusted for sociodemographic factors, the results demonstrated a small but significant increase in nicotine use from 2001–2002 to 2012–2013. However, a much greater increase in nicotine dependence (46.1% to 52%) was observed over this time frame in individuals who had used nicotine during the preceding 12 months. The increases in nicotine use and dependence were associated with factors related to socioeconomic status, such as lower income and lower educational attainment. The authors interpret these findings as evidence for the hardening hypothesis, suggesting that despite the impression that nicotine use has plateaued, there is a growing number of highly dependent nicotine users who would benefit from nicotine dependence intervention programs. Dr. Kathleen Brady, from the Medical University of South Carolina, provides an editorial ( 11 ) that reviews the consequences of tobacco use and the history of the public measures that were initially taken to combat its use. Importantly, her editorial emphasizes the need to address health care inequity issues that affect individuals of lower socioeconomic status by devoting resources to develop and deploy effective smoking cessation interventions for at-risk and underresourced populations.
Conclusions
Maladaptive substance use and substance use disorders are highly prevalent and are among the most significant public health problems. Substance use is commonly comorbid with psychiatric disorders, and treatment efforts need to concurrently address both. The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to better serve those afflicted with addictions. While treatments exist, the need for more effective treatments is clear, especially those focused on decreasing relapse rates. The negative affective state, hyperkatifeia, that accompanies longer-term abstinence is an important treatment target that should be emphasized in current practice as well as in new treatment development. In addition to developing a better understanding of the neurobiology of addictions and abstinence, it is necessary to ensure that there is equitable access to currently available treatments and treatment programs. Additional resources must be allocated to this cause. This depends on the recognition that health care inequities and societal barriers are major contributors to the continued high prevalence of substance use disorders, the individual suffering they inflict, and the huge toll that they incur at a societal level.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 US Department of Health and Human Services: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2018. Rockville, Md, SAMHSA, 2019 ( https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2018-NSDUH ) Google Scholar
2 Koob GF, Powell P, White A : Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19 . Am J Psychiatry 2020 ; 177:1031–1037 Link , Google Scholar
3 Cassidy CM, Carpenter KM, Konova AB, et al. : Evidence for dopamine abnormalities in the substantia nigra in cocaine addiction revealed by neuromelanin-sensitive MRI . Am J Psychiatry 2020 ; 177:1038–1047 Link , Google Scholar
4 Bradberry CW : Neuromelanin MRI: dark substance shines a light on dopamine dysfunction and cocaine use (editorial). Am J Psychiatry 2020 ; 177:1019–1021 Abstract , Google Scholar
5 Blaine SK, Wemm S, Fogelman N, et al. : Association of prefrontal-striatal functional pathology with alcohol abstinence days at treatment initiation and heavy drinking after treatment initiation . Am J Psychiatry 2020 ; 177:1048–1059 Abstract , Google Scholar
6 Sullivan EV : Why timing matters in alcohol use disorder recovery (editorial). Am J Psychiatry 2020 ; 177:1022–1024 Abstract , Google Scholar
7 Lees B, Mewton L, Jacobus J, et al. : Association of prenatal alcohol exposure with psychological, behavioral, and neurodevelopmental outcomes in children from the Adolescent Brain Cognitive Development Study . Am J Psychiatry 2020 ; 177:1060–1072 Link , Google Scholar
8 McCormack C, Monk C : Considering prenatal alcohol exposure in a developmental origins of health and disease framework (editorial). Am J Psychiatry 2020 ; 177:1025–1028 Abstract , Google Scholar
9 Evans-Polce RJ, Kcomt L, Veliz PT, et al. : Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates . Am J Psychiatry 2020 ; 177:1073–1081 Abstract , Google Scholar
10 Grant BF, Shmulewitz D, Compton WM : Nicotine use and DSM-IV nicotine dependence in the United States, 2001–2002 and 2012–2013 . Am J Psychiatry 2020 ; 177:1082–1090 Link , Google Scholar
11 Brady KT : Social determinants of health and smoking cessation: a challenge (editorial). Am J Psychiatry 2020 ; 177:1029–1030 Abstract , Google Scholar
- Cited by None
- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues
- Open access
- Published: 24 June 2020
Mental health problems among young people in substance abuse treatment in Sweden
- Torkel Richert ORCID: orcid.org/0000-0003-0653-0849 1 ,
- Mats Anderberg 2 &
- Mikael Dahlberg 2
Substance Abuse Treatment, Prevention, and Policy volume 15 , Article number: 43 ( 2020 ) Cite this article
29k Accesses
25 Citations
15 Altmetric
Metrics details
Young people with substance use problems face a high risk of co-occurring mental health problems, something that may involve a more difficult life situation, social problems as well as worse treatment outcomes. The aim of this study is to analyse self-reported mental health problems among young people receiving outpatient treatment for substance use problems in Sweden. We explore what types of mental health problems are more or less predominant, and whether there are significant differences between boys and girls. In addition, we analyse how various mental health problems covary with indicators of substance abuse severity.
The study is based on structured interviews with 1970 young people enrolled at outpatient clinics in 11 Swedish cities. The data was analysed through frequency- and averages-calculations, Chi-square tests and multivariate logistic regression analyses.
Self-reported mental health problems were common among the young people in the study. A relatively large percentage of the total group (34–54%) reported problems such as concentration difficulties, sleeping difficulties, anxiety and depression. At the same time, many of the young people did not report any symptoms and only a small group, about 20%, reported diagnosed mental health disorders. The results show substantial gender differences, with girls reporting significantly higher levels of mental health problems.
Multivariate logistic regression analyses demonstrated significant associations between severity of drug use problems and anxiety, concentration difficulties, aggression, hallucinations and mental stress caused by experiences of trauma.
Conclusions
Treatment needs are diverse within this group of young people who use drugs. Since girls report higher levels of all mental health problems, and a larger burden of psychosocial risk factors than boys, they are likely to require more comprehensive treatment interventions. The link between more severe drug problems and mental health problems points to the importance of exploring this relationship in treatment. A multidisciplinary approach, in which co-occurring problems can be addressed simultaneously, may be the best treatment form for many young people with drug problems.
Introduction
The majority of young people with drug and alcohol problems suffer from concurrent mental health problems, referred to as co-occurring disorders or comorbidity [ 1 , 2 , 3 , 4 ]. Externalizing disorders such as Conduct Disorder (CD) and Attention Deficit Hyperactivity Disorder (ADHD) appear to be the most common mental health problems, but internalizing disorders such as depression, dysthymia and anxiety also commonly occur [ 5 ]. Boys are usually over-represented with respect to externalizing disorders, while the opposite holds true for internalizing disorders [ 6 , 7 ], even though some studies report equal gender distribution [ 1 , 5 ].
Most studies show that young people with co-occurring problems have more extensive drug problems, higher levels of social problems and criminality, as well as worse treatment outcomes and greater risk of relapse, compared with young people with substance use problems alone [ 1 , 2 , 3 , 4 , 8 , 9 , 10 , 11 , 12 ].
On the other hand, there are also studies demonstrating that a relatively large proportion of adolescents with substance use problems do not report any mental disorders or symptoms at initiation of treatment [ 10 , 13 , 14 ], and studies showing minor differences between young people with and without mental health problems with respect to treatment involvement, dropout rate and treatment outcome [ 15 , 16 , 17 , 18 , 19 ].
Few Swedish studies have addressed the association between drug use and mental health problems among young people. This despite a recent trend with an increased prevalence of mental health problems among young people, and a development with a growing number of young people being diagnosed with, and treated for drug use problems [ 20 , 21 ].
The Swedish studies that have been conducted – mainly based on adolescents in inpatient or emergency care – show that the vast majority of young people have mental health problems prior to onset of drug use, and that as many as 90% demonstrate co-occurring disorders [ 22 ]. There is little knowledge regarding mental health problems among broader groups of young people who use drugs in Sweden. There is also a lack of research on how different types of mental health problems may be linked to drug use severity among young people – this applies to Swedish research as well as to research on young people in general.
The aim of this article is to study self-reported occurrence of mental health problems among young people receiving outpatient treatment for substance use problems. We explore what types of mental health problems and social problems are more or less predominant, and whether there are significant differences in prevalence between boys and girls. In addition, we analyse how various mental health problems covary with indicators of substance abuse severity such as early onset of use, high frequency of use and poly drug use.
Occurrence of mental health problems among young people in substance abuse treatment
As stated earlier, co-occurring mental health problems are relatively common among young people with drug and alcohol problems, even though such occurrence may demonstrate large variations [ 23 , 24 ]. For example, several research reviews state that 50% to 90% of young people with drug and alcohol problems also have extensive mental health problems [ 1 , 2 , 3 , 5 , 12 , 23 , 24 , 25 , 26 ].
Studies involving inpatient subjects generally demonstrate higher prevalence of mental health problems compared with studies on young people treated in outpatient or community-based programmes [ 1 , 5 , 7 , 11 , 27 , 28 ]. In one Swedish study on young people enrolled at an emergency care center, 90% of girls and 81% of boys met the criteria for at least one psychiatric disorder in addition to their substance use problems [ 23 ]. Another Swedish study of young people receiving outpatient care for drug problems showed that 64% met the criteria for a psychiatric diagnosis [ 29 ]. An Australian study with a broad selection of young people in different types of treatment for substance use problems found that only one third had co-occurring mental health problems [ 14 ].
A research review by Couwenbergh and colleagues [ 5 ] concluded that externalizing disorders such as CD and ADHD are the most frequently found co-occurring psychiatric disorders among young people with substance use problems, followed by internalizing disorders such as depression or dysthymia and anxiety. However, the rate of various disorders varies greatly between different studies: 24% to 82% for CD, 3% to 48% for depression/dysthymia, 1% to 38% for anxiety disorders, 3% to 38% for ADHD and 10% to 12% for post-traumatic stress disorder (PTSD).
Several studies suggests that it is common for young people with drug and alcohol problems to have multiple co-occurring psychiatric diagnoses when in treatment [ 9 , 11 , 18 , 30 ], and that the occurrence of problems varies with age, co-occurring problems being more common among people in their late teens or early adulthood [ 19 , 31 ].
In summary, prior research points to great variation in levels of co-occurring mental health problems among young people in treatment for drug and alcohol problems, as well as what types of mental disorders occur most frequently. The variation found in the different studies may have several explanations. These include differences in selection criteria, types of care, assessment methodology, diagnostic tools, diagnostic systems and timeframes during which the conditions occur (e.g., the past month, past year, any time in life), which collectively make comparisons between different studies and contexts difficult.
Associations between psychiatric disorders and severity of substance use problems
Only a few studies have investigated associations between various psychiatric disorders and indicators of severity of drug use problems among young people.
A study from Australia found that weakly or more frequent cannabis use in teenagers predicted an approximately twofold increase in risk for later depression and anxiety. In contrast, depression and anxiety in teenagers predicted neither later weekly nor daily cannabis use. Daily use in young women was associated with an over fivefold increase in the odds of reporting a state of depression and anxiety after adjustment for intercurrent use of other substances [ 32 ]. Similarly, a study on undergraduate students in the US found frequent marijuana use to be associated with depression and other substance use and alcohol-related negative outcomes [ 33 ].
Early onset of cannabis use has been associated with higher rates of later substance use, juvenile offending, mental health problems, unemployment and school dropout [ 34 ].
Results from a longitudinal study from substance use treatment facilities in Norway showed a co-occurrence between poly-drug use and mental distress. Mental distress increased both in magnitude and over time with the number of drugs used. The authors conclude that use of multiple drugs and mental distress appears strongly co-related over time [ 35 ].
There are various theories about the causal relationship between mental health problems and drug problems. According to several researchers, psychiatric problems usually precede drug and alcohol problems [ 12 , 36 , 37 , 38 ]. This can for instance be explained by the drugs serving as a self-medicating function by alleviating stress and other unpleasant emotions [ 39 ]. However, the link between mental health problems and drug use cannot be explained solely on the basis of self-medication, since young people primarily state other reasons for using drugs [ 40 , 41 , 42 ]. The relationship between the two conditions can also be reversed, where drug and alcohol use increase the risk of mental health problems [ 32 , 43 , 44 ] . Another possible explanation is that underlying factors, such as difficult childhood circumstances or family problems may be the cause of both [ 4 , 45 , 46 ]. Mental health problems and substance abuse problems may also be intertwined and develop simultaneously over time. Finally, substance abuse and mental health problems may be mutually exclusive and coexist without any link [ 3 , 32 , 40 ]. It can be concluded that the association between drug and alcohol use problems and mental disorders is strong but extremely complex [ 25 ].
Materials and methods
Setting and sample.
The study is based on structured interviews with young people receiving treatment for drug and alcohol problems. Data were gathered from specialized outpatient clinics for young people (13–21 years of age) with substance use problems in 11 Swedish cities. The participating cities are part of a researcher-practitioner collaboration network focusing on knowledge development in outpatient treatment for the present target group. The participating clinics represent Sweden’s three largest cities and eight additional cities around the country. The basic characteristics of the current sample are consistent with previous Swedish studies on the target group in outpatient treatment [ 13 ]. The centers, usually referred to as Maria clinics, are carried out as a collaboration between the social services and the healthcare system. All of the clinics offer various types of treatment for substance use problems, as well as counselling and support for young people and their families. Average length of care is 4–6 months. Services offered by all clinics include psychosocial and medical assessment with a focus on substance use problems, drug testing, individual or family counselling, and manual-based treatment programmes. Personnel include social workers, nurses, psychologists and doctors [ 13 ].
Between 2014 and 2016, 2099 young people begun outpatient treatment for substance abuse problems at the participating Maria clinics. All young people initiating treatment are asked to participate in an enrolment interview that is used for both treatment and research purposes. Of the total group, 129 individuals were excluded in the study because they did not want to participate or because the information gathered was incomplete. The study is based on a total of 1970 young people, of whom 27% were girls and 73% boys. The average age was 17.6 years for both boys and girls. 28% of the young people were either born outside of Sweden or have two parents born outside Sweden. This means that the sample, in this respect, is representative for young people in Sweden’s larger cities.
Instruments and materials
UngDOK is a structured interview that was developed specifically for young people with various types of drug and alcohol problems. The primary purpose of the interview is to identify the problems, needs and current social situation of young people in order to arrive at the appropriate assessment, plan and implementation of treatment. The information gathered can also serve as a basis for follow-up and evaluation of the interventions and outcomes of the various local clinics. In a reliability and validation study, the quality of the UngDOK interview method was found to be satisfactory [ 47 ].
The interviews were conducted by the therapists at the time of admission. It contains a total of 75 questions covering the following ten aspects of life: housing and financial support, occupation, treatment history, criminality, childhood environment, exposure to violence, family and relationships, physical health, mental health, as well as alcohol and drug use.
The analysed variables describe individual characteristics regarding: social situation, drug and alcohol use, and mental health. The study only uses anonymized data, and permission for storage and processing of data for research purposes has been obtained from the research ethics committee at the National Board of Health and Welfare.
Variables and statistical analysis
Initially, the study group was categorized by gender and the variables included in the study regarding mental health problems were analysed for gender differences. The data was processed and analysed by SPSS Statistics 24 software and Chi 2 and t-tests were used for analysing levels of significance. To investigate the relationship between various mental health problems and drug use, multivariate logistic regression analysis with three models was carried out. As dependent variables, we used the following dichotomized variables that indicate severity of drug use: high frequency of use, i.e. two–three days a week or more for the primary drug (model 1), early onset of substance use, i.e. age 12 or younger for alcohol intoxication and age 13 or younger for drugs use (model 2), and presence of poly drug use, i.e. regular use of two or more drugs during the last three months (model 3). The independent variables in all three analysis models include age and gender, as well as self-reported mental health problems over the past 30 days: depression, anxiety, concentration difficulties, aggressive behaviour, suicidal thoughts, hallucinations, eating disorders, self-harming behaviour, and psychological stress from traumatic events (e.g. witnessed or being subjected to violence or sexual abuse). The results of these analyses are reported using odds ratios and significance levels. The explained variance for each model is presented using Cox & Snell and Nagelkerke.
Table 1 shows the childhood environment and social situation of the young people, as well as their self-reported drug and alcohol use at treatment initiation.
The majority of the young people live with their parents, are engaged in studies, traineeship, or work. However, most have or have had extensive difficulties in school that have impacted their attendance, satisfaction and performance. The percentage of girls with school problems is significantly greater than the percentages of boys.
About one third of the young people have grown up under difficult circumstances. Here too significant gender differences are found, where girls, to a much greater degree than boys, have experienced financial constraints, substance use problems, mental health problems and violence in their childhood environment.
A significant higher proportion of boys have been arrested by police or convicted of various crimes. Girls, however, report that they have been subjected to physical, mental and sexual violence or assault to a greater degree. An estimated two thirds of both boys and girls associate with friends who commit crimes or use drugs.
A number of gender differences were found regarding drug and alcohol use. For both genders, cannabis is the drug that causes the greatest problem or is the underlying reason for initiation of care, even though the percentage of boys that report this is significantly larger than the percentage of girls. The opposite gender pattern is seen with alcohol and other drugs. Girls initiate their primary drug somewhat earlier than boys and they also use that drug more often than boys. Gender differences are also reflected in alcohol use, where girls to a significant higher extent report risky alcohol consumption according to their AUDIT-C scores [ 48 ].
Table 2 shows that the most common self-reported mental health problems or disorders among young people over the past month are concentration difficulties, followed by sleeping difficulties, anxiety, depression, traumatic life events and problems controlling aggressive behaviour. The ranking is essentially similar for both boys and girls, although girls consistently report significantly higher levels.
Mental health problems such as suicidal thoughts, suicide attempts, hallucinations, eating disorders and self-harming behaviour are much less commonly reported (10% or less for the total group). These problems are however two to three times more common among the girls.
Almost half of the girls and a quarter of the boys have experienced a serious traumatic event or accident from which they have not yet psychologically recovered.
One-fifth of the young people state that they have an ongoing contact with psychiatry. About the same proportion state that they have received prescription medication for a psychiatric disorder or functional impairment and that they have a neuropsychiatric diagnosis. Girls report being in contact with psychiatric care or taking medication to a significantly larger extent, while no significant gender differences was found with respect to neuropsychiatric diagnosis.
Table 3 shows how frequency of drug use, age at onset of drug use, and occurrence of poly drug use covary with nine self-perceived mental health problems, as well as with age and gender.
Young people with a high frequency of drug use (two–three days a week or more) were significantly more likely to report anxiety (OR = 1.719), concentration difficulties (OR = 1.408), and difficulty in controlling aggressive behaviour (OR = 1.381), in comparison with young people with a low frequency of drug use. High frequent users were also significantly more likely to be older (OR = 1.264).
Young people with early onset of drug use were significantly more likely to report concentration difficulties (OR = 1.555), and difficulty in controlling aggressive behaviour (OR = 1.576), in comparison with those not reporting early onset of drug use. People with an early onset of drug use were significantly less likely to be older (OR = 0.857).
Young people with poly drug use were significantly more likely to report anxiety (OR = 1.358), concentration difficulties (OR = 1.434), hallucinations (OR = 1.652) and traumatic life events (OR = 1.302) in comparison with those not reporting poly drug use. People with poly drug use were also significantly more likely to be older (OR = 1.296).
The aim of this study was to analyse self-reported mental health problems among young people receiving outpatient treatment for substance use problems in Sweden. We explore what types of mental health problems are more or less predominant, how various mental health problems covary with indicators of substance abuse severity, as well as gender differences related to drug use and mental health problems.
The study shows that the young people who initiate outpatient treatment at Maria clinics for drug and alcohol problems are characterized by both heterogeneity and pronounced differences between boys and girls. Overall, the most common self-reported mental health problems among the young people are concentration difficulties, followed by sleep disturbances, anxiety, depression, traumatic experiences and difficulties managing anger and violent behaviour. This ranking is largely in line with many other studies [ 5 ]. Although the list of problems is ranked similarly by gender, the percentage of girls with various mental health problems is consistently higher than boys, sometimes many times higher.
A relatively large percentage (34–54%) of the total group report self-assessed problems such as depression, anxiety and concentration difficulties. These findings are in line with current descriptions of health among Swedish young people in general, where a growing number of boys and girls report psychosomatic symptoms and stress-related mental health problems [ 20 ]. The increase in mental health problems encompasses broad groups of young people in Sweden, which indicate that the underlying causes are located in living conditions and environments that are common to most young people. The Public Health Agency of Sweden [ 20 ] has highlighted inadequacies in the school system and the increasing demands for performance that many young people experience, as well as concerns about entering into adult life and the future demands of the labor market as the primary factors underlying this trend. The fact that young people spend more time on social media has also been highlighted as a possible risk factor. Another possible explanation is that the social stigma of mental illness has decreased, something that can lead to more young people reflecting on and reporting mental health problems, as well as seeking help for these problems to a higher extent [ 20 ]. Social norms that place a premium on success and perfection, when combined with a weak social position in relation to peers, has also been shown to generate stress-related mental health problems among young people in upper secondary school [ 49 ].
A smaller but still significant group of the young people (about 20–30%), report problems that may indicate more serious mental health and drug use problems. These include, among other things, being exposed to a serious traumatic event, having a diagnosed neuropsychiatric disorder, being in psychiatric treatment, taking prescription medications for specific mental health problems, having a poly drug use, and prior experience of substance abuse treatment. A small percentage of the young people (2–10%) reported problems such as hallucinations, eating disorders, self-harming behaviour, suicidal thoughts and suicide attempts, which may indicate severe or long-lasting psychiatric conditions.
However, the majority of the young people (about 70–80%) do not show signs of having severe mental health problems. Many of these young people are from relatively stable home environments and are well-integrated in society with a satisfactory school career, regular leisure activities and positive relationships with their parents [ 13 ]. They have less severe alcohol and drug problems which likely stem from more experimental or social drug use motivated by curiosity or sporadic use with friends [ 50 ]. The findings of this study, in this respect, contradict several earlier studies that concluded that it is the rule rather than the exception that young people with drug and alcohol problems have co-occurring mental health problems [ 1 , 2 , 3 , 5 , 12 , 22 ]. This difference can be explained in part by the different target groups that have been studied: young people in outpatient care tend to be a more heterogeneous group, while those recruited from inpatient care or emergency care usually have more extensive social and mental health problems [ 1 , 5 , 7 , 11 , 27 ].
What specific mental health problems are related to more severe substance use problems? The study results suggest a strong link between concentration difficulties and severity of drug use problems. High frequency of use, early onset of drug use, as well as poly drug use, were associated with higher likelihood of reporting concentration difficulties. Concentration difficulties may be a cause of early onset of drug use for some adolescents and a consequence of extensive drug use for others. According to our findings, anxiety problems appear to be clearly linked with poly drug use and frequent drug use, but not to early onset of use. Anxiety problems in adolescence have been shown to predict alcohol use problems in young adulthood [ 46 ]. Regarding cannabis, the opposite appears to be true: cannabis use in adolescence can increase the risk of anxiety and depression later in life [ 32 , 46 , 51 ]. Aggressive behaviour, which may be linked to the condition often referred to as conduct disorder, was mainly associated with early onset of drug use. An association also suggested by several other studies [ 5 , 22 , 45 ]. In our study, hallucinations and psychological stress from traumatic events – which may be indications of more severe mental health problems – are only linked to poly drug use. According to a study by Harrison, Fulkerson & Beebe [ 52 ], young people with experiences of physical and sexual abuse reported high rates of poly drug use, initiated substance use earlier than their peers and gave more reasons for using, including use to cope with painful emotions. PTSD (post-traumatic stress disorder), which can be a result of traumatic experiences such as abuse, has also been shown to increase the risk of developing substance use problems [ 46 , 53 ]. Furthermore, results from a longitudinal growth research study from substance use treatment facilities in Norway show that use of multiple drugs and mental distress are strongly co-related over time [ 35 ].
Several mental health problems such as depression, suicidal thoughts, eating disorders and self-harming behaviour did not show significant associations with either high frequency of use, early onset of drug use, or poly drug use. This finding suggests that young people with substance use problems may have co-occurring mental health problems without any clear link between the two [ 25 ]. However, these mental health problems are more common in the study group compared with young people in general [ 20 ]. This may in part be explained by the fact that the young people in the study, compared with young people in the general population at large, have more difficult childhood circumstances and a greater social vulnerability.
The explained variance in the three analysed models (Table 3 ) is relatively low (according to Cox & Snell and Nagelkerke), which suggests that a number of other factors are in play. One possible explanation is that a large number of social factors that could affect the relation between drug use and mental health are not included in the model, such as social relationships, social norms, peer pressure, school problems, and access to drugs.
The study findings show substantial gender differences, with a larger percentage of girls reporting both mental health problems and receiving psychiatric care and prescription medications for psychiatric disorders. The gender differences – with the exception of neuropsychiatric diagnoses – are significant for all reported conditions. The results are in line with several other studies on young drug users [ 14 , 54 , 55 , 56 ]. Clear gender differences in mental health problems are also found in Swedish young people in general. The proportion of young people reporting symptoms of mental health problems in Sweden has doubled over the past two decades. This trend is true for both boys and girls, but the prevalence is about twice as high for young girls [ 20 ]. Regarding drug problems, the differences between girls and boys have decreased in Sweden in recent decades. However, gender differences remain as the proportion of girls with drug problems is smaller than the proportion of boys, while girls generally report more severe drug problems [ 13 ].
Experiences of traumatic events, violence and physical abuse, which are more common among the girls in the study, can be one explanation for their higher level of mental health problems. It is also probable that some girls begin to use drugs or alcohol to alleviate or manage such painful experiences and the stress that they cause [ 57 , 58 , 59 , 60 ]. The girls in the study generally show somewhat earlier onset of drug use and more frequent use. However, the multivariate analyses did not point to any distinct gender differences, suggesting that the link between severity of substance use problems and various mental health problems holds regardless of gender.
There are some limitations to the study. The empirical material is based on self-reported data gathered from interviews at initiation of treatment. It is difficult to draw conclusions about causal relationships between mental health problems and substance use problems with this type of cross-sectional data. Consequently, the study is not based on established psychiatric diagnoses. However, the reliability of the screening instruments and assessment methodology in identifying and assessing mental health problems in children and young people is also generally weak, which may result in both under-reporting [ 4 ], and over-reporting of mental health problems [ 61 ]. Diagnoses are often re-classified, their criteria and boundaries change over time, and they are affected by societal developments [ 40 , 62 ].
Implications
Studying self-reported mental health problems in young people with drug and alcohol problems can yield important new knowledge. Greater knowledge of how various mental health, drug-related and social problems covary, can be of general value and may also be instrumental in developing and organising treatment interventions for the target group. Staff and managers at the Maria clinics can benefit from data about their target group at an aggregated level. This can provide guidance on which problems and combinations of problems are more or less common and thus what types of treatment efforts may need to be strengthened or prioritized. It is not unusual for individuals with both mental health problems and drug and alcohol problems to be passed from one care provider to the next without receiving relevant help for their co-occurring problems [ 5 ]. A multidisciplinary approach is far preferable, in which both conditions are addressed and concomitant treatment goals are formulated together with the young person. Integrated treatment for co-occurring problems has strong scientific support [ 2 ]. In this regard the Maria clinics represent a positive example of working with the target group, in which treatment for both conditions can be provided within one and the same service, such as psychosocial treatment combined with medication [ 25 ]. However, there is a risk that an increased focus on medical conditions may contribute to a psychiatrization and medicalization leading to the subordination of social issues in substance abuse treatment [ 63 ]. It is of great importance that these young people are also provided with the opportunity for social inclusion and support for meaningful employment and recreational activities to help them address both their drug use problems and mental health issues. This is obvious given that the majority of young people in the study have school problems and socialize with friends who commit crimes or use drugs.
Early onset of drug, frequent use and poly drug use were all significantly associated with increased likelihood of reporting various mental health problems, in particular anxiety, concentration difficulties and problems controlling aggressive behaviour. Poly drug use was also linked to experiences of hallucinations and traumatic life events. This points to the importance of screening for mental health problems when treating young people with drug use problems. It also points to the importance of exploring the specific roles or functions that drug use have for young people, especially how these functions may relate to traumatic events and different mental health problems.
Since girls have a larger burden of psychosocial risk factors than boys, they are also more likely to require more comprehensive and multidimensional treatment interventions that extend over a longer period [ 28 , 56 ]. It is especially important to consider difficult home environments and reported severe psychological problems from which many young people suffer. Past traumatic experiences also need to be considered and addressed in treatment, especially among girls, who are more likely to have had such experiences [ 56 , 64 , 65 ]. Since a large proportion of girls have previously been in psychiatric care, it should also be possible to identify such girls in order to offer more relevant support at an earlier stage.
In summary, the study shows that various forms of self-reported mental health problems are common among young people with drug and alcohol problems who begin outpatient treatment in Sweden. At the same time, many young people report that they do not have any symptoms and only a small percentage report documented psychiatric conditions. The need for support or treatment for mental health problems within this group is thus highly diverse, but should be analysed and assessed on a case-by-case basis. Since girls report higher levels of all mental health problems, and a larger burden of psychosocial risk factors than boys, they are likely to require more comprehensive treatment interventions. The link between the severity of drug problems and mental health problems points to the importance of highlighting and exploring this relationship when treating young people and specifically the role played by the drug use. A multidisciplinary approach, in which co-occurring problems can be addressed simultaneously may be the best treatment form for many young people with drug problems.
Additional studies are needed in this field. There is a need for studies that investigate different causal relationships between mental health problems and the severity of drug use problems. There is also a need for qualitative studies that focus on young people’s different motives for and experiences of drug use, and how these relate to mental health problems.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
Attention Deficit Hyperactivity Disorder
The Alcohol Use Disorders Identification Test – Consumption
Conduct Disorder
Post-traumatic stress disorder
Statistical Package for the Social Sciences
Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psychol. 2002;70(6):1224–39.
PubMed Google Scholar
Bender K, Springer DW, Kim JS. Treatment effectiveness with dually diagnosed adolescents: a systematic review. Brief Treat Crisis Interv. 2006;6(3):177–205.
Google Scholar
Deas D. Adolescent substance abuse and psychiatric comorbidities. J Clin Psychiatry. 2006;67(Suppl 7):18–23.
Hawkins EH. A tale of two systems: co-occurring mental health and substance abuse disorders treatment for adolescents. Annu Rev Psychol. 2009;60:197–227.
Couwenbergh C, van den Brink W, Zwart K, Vreugdenhil C, van Wijngaarden-Cremers P, van der Gaag RJ. Cormobid psychopathology in adolescents and young adults treated for substance use disorders. Eur Child Adolescent Psychiatry. 2006;15(6):319–28.
Dakof GA. Understanding gender differences in adolescent drug abuse: issues of comorbidity and family functioning. J Psychoactive Drugs. 2000;32(1):25–32.
CAS PubMed Google Scholar
O’Neil KA, Conner BT, Kendall PC. Internalizing disorders and substance use disorders in youth: Cormobidity, risk, temporal order, and implications for intervention. Clin Psychol Rev. 2011;31(1):104–12.
Babor TF, Webb C, Burleson JA, Kaminer Y. Subtypes for classifying adolescents with marijuana use disorders: construct validity and clinical implication. Addiction. 2002;97(Suppl 1):58–69.
Diamond G, Panichelli-Mindel SM, Shera D, Dennis M, Tims F, Ungemack J. Psychiatric syndromes in adolescents with marijuana abuse and dependency in outpatient Treatement. J Child Adolesc Subst Abuse. 2006;15(4):37–54.
Godley SH, Hunter BD, Fernández-Artamendi S, Smith JE, Meyers RJ, Godley MD. A comparison of treatment outcomes for adolescent community reinforcement approach participants with and without co-occurring problems. J Subst Abus Treat. 2014;46(4):463–71.
Grella CE, Hser Y-I, Joshi V, Rounds-Bryant J. Drug treatment outcomes for adolescents with Cormobid mental and substance use disorders. J Nerv Ment Dis. 2001;189(6):384–92.
Jakobsson J, Richter C, Tengström A & Borg S. Ungdomar och missbruk – kunskap och praktik. Rapport för Missbruksutredningen (SOU 2008:4). [Young people and addiction - knowledge and practice. Report for the Abuse Study] Stockholm: Beroendecentrum; 2011.
Anderberg M, Dahlberg M. Gender differences among adolescents with substance abuse problems at Maria clinics in Sweden. Nordic Stud Alcohol Drugs. 2018;35(1):24–38.
Mitchell PF, Kutin JJ, Daley K, Best D, Bruun AJ. Gender differences in psychosocial complexity for a cohort of adolescents attending youth-specific substance abuse services. Child Youth Serv Rev. 2016;68:34–43.
Battjes DSW, Gordon MS, O’Grady KE, Kinlock TW, Carswell MA. Factors that predict adolescent motivation form substance abuse treatment. J Subst Abus Treat. 2003;24(3):221–32.
Bertrand K, Brunelle N, Richer I, Beaudoin I, Lemieux A, Ménard J-M. Assessing covariates of drug use trajectories among adolescents admitted to a drug addiction center: mental health problems, therapeutic Alliance, and treatment persistence. Substance Use Misuse. 2013;48(1–2):117–28.
Pagey B, Deering D, Sellman D. Retention of adolescents with substance dependence and coexisting mental health disorders in outpatient alcohol and drug group therapy. Int J Ment Health Nurs. 2010;19(6):437–44.
Rowe CL, Liddle HA, Greenbaum PE, Henderson CE. Impact of psychiatric cormobidity on treatment of adolescent drug abusers. J Subst Abus Treat. 2004;26(2):129–40.
Tanner-Smith EE, Wilson SJ, Lipsey MW. The comparative effectiveness of outpatient treatment for adolescent substance abuse: a meta-analysis. J Subst Abus Treat. 2013;44(2):145–58.
Folkhälsomyndigheten. Varför har den psykiska ohälsan ökat bland barn och unga i Sverige? Utvecklingen under perioden 1985-2014. [Why has mental illness increased among children and young people in Sweden? Developments during the period 1985–2014]. Östersund: Folkhälsomyndigheten; 2018.
Socialstyrelsen. Utvecklingen av psykisk ohälsa bland barn och unga vuxna. Till och med 2016. [The development of mental health problems among children and young adults. Up until 2016]. Stockholm: Socialstyrelsen; 2017.
Hodgins S, Tengström A, Bylin S, Göransson M, Hagen L, Jansson M, et al. Consulting for substance abuse: mental disorders among adolescents and their parents. Nordic J Psychiatry. 2007;61(5):379–86.
CAS Google Scholar
Stone AL, Becker LG, Huber AM, Catalano RF. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addict Behav. 2012;37(7):747–75.
Turner WC, Muck RD, Stephens RL, Sukumar B. Co-occurring disorders in the adolescent mental health and substance abuse treatment systems. J Psychoactive Drugs. 2004;36(4):455–62.
Morisano D, Babor TF, Robaina KA. Co-occurrence of substance disorders with other psychiatric disorders: implications for treatment services. Nordic Stud Alcohol Drugs. 2014;31(1):5–25.
Riggs PD. Treating adolescents for substance abuse and Cormobid psychiatric disorders. Sci Practice Perspectives. 2003;2(1):18–29.
Hser Y-I, Grella CE, Hubbard RL, Hsieh S-C, Fletcher BW, Brown BS, Anglin MD. An evaluation of drug treatments for adolescents in 4 US cities. Arch Gen Psychiatry. 2001;58(7):689–93.
Stevens SJ, Estrada B, Murphy BS, McKnight KM, Tims F. Gender differences in substance use, mental health, and criminal justice involvement of adolescents at treatment entry and at three, six, twelve and Firthy month follow-up. J Psychoactive Drugs. 2004;36(1):13–25.
Olsson M. Problematic substance use and co-occurring psychiatric problems in young clinical patients and in criminal justice clients. Stuides of mortality, measurements and intervention. Lund: Lund University, Faculty of Medicine; 2017.
Tims FM, Dennis ML, Hamilton N, Buchan BJ, Diamond G, Funk R, Brantley LB. Characteristics and problems of 600 adolescent cannabis abusers in outpatient treatment. Addiction. 2002;97(Suppl 1):46–57.
Chan YF, Dennis ML, Funk RR. Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. J Subst Abus Treat. 2006;34(1):14–24.
Patton GC, Coffey C, Carlin JB, Degenhardt L, Lynskey M, Hall W. Cannabis use and mental health in young people: cohort study. BMJ. 2002;325(7374):1195–8.
PubMed PubMed Central Google Scholar
Keith DR, Hart CL, McNeil MP, Silver R, Goodwin RD. Frequent marijuana use, binge drinking and mental health problems among undergraduates. Am J Addict. 2015;24:499–506.
Fergusson DM, Horwood LJ. Early onset cannabis use and psychosocial adjustment in young adults. Addiction. 2006. https://doi.org/10.1111/j.1360-0443.1997.tb03198.x .
Burdzovic J, Lauritzen AG, Nordfjærn T. Co-occurrence between mental distress and poly-drug use: a ten year prospective study of patients from substance abuse treatment. Addict Behav. 2015;48:71–8.
Conway KP, Swendsen J, Husky MM, He JP, Merikangas KR. Association of Lifetime Mental Disorders and Subsequent Alcohol and illicit drug use: results from the National Comorbidity Survey-Adolescent Supplement. J Am Acad Child Adolesc Psychiatry. 2017;55(4):280–8.
Hussong AM, Ennet ST, Cox MJ, Haroon M. A systematic review of the unique prospective association of negative affect symptoms and adolescent substance use controlling for externalizing symptoms. Psychol Addict Behav. 2017;31(2):137–47.
Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Study-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–9.
Maniglio R. Association between peer victimization in adolescence and cannabis use: a systematic review. Aggress Violent Behav. 2015;25:252–8.
Lembke A. Time to abandon the self-medication hypothesis in patients with psychiatric disorders. Am J Drug Alcohol Abuse. 2012;38(6):524–9.
Patrick ME, Schulenberg JE, O’Malley PM, Jonhston LD, Bachman JG. Adolescents’ reported reasons for alcohol and marijuana use as predictors of substance use and problems in adulthood. J Studies Alcohol Drugs. 2011;72(1):106–16.
Wilens TE, Adamson J, Sgambati S, Whitley J, Santry A, Monuteaux MC, Biederman J. Do individuals with ADHD self-medicate with cigarettes and substances of abuse? Results from a controlled family study of ADHD. Am J Addict. 2007;16(suppl 1):14–23.
Coffey C, Patton GC. Cannabis use in adolescence and young adulthood: a review of findings from the Victorian adolescent health cohort study. Can J Psychiatry. 2016;61(6):318–27.
Duperrouzel J, Hawes SW, Lopez-Quintero C, Pacheco-Colón I, Comer J, Gonzalez R. The association between adolescent cannabis use and anxiety: a parallel process analysis. Addict Behav. 2018;78:107–13.
Griffith-Lendering MFH, Huijbregts SCJ, Mooijart A, Vollebergh WAM, Swaab H. Cannabis use and development of externalizing and internalizing behavior problems in early adolescence: a TRAILS study. Drug Alcohol Depend. 2011;116(1–3):11–7.
Wolitzky-Taylor K, Bobova L, Zinbarg RE, Meneka S, Craske M. Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice verca. Addict Behav. 2012;37(8):982–5.
Dahlberg M, Anderberg M, Wennberg P. Psychometric properties of the UngDOK – a structured interview for adolescents with substance use problems. Nordic Stud Alcohol Drugs. 2017;34(1):160–72.
Reinert DF, Allen JP. The alcohol use disorders identification test: an update of research findings. Alcohol Clin Exp Res. 2007;31(2):185–99.
Hiltunen L. Lagom perfekt. Erfarenheter av ohälsa bland unga tjejer och killar. [Moderately perfect. Experiences of ill-health among young girls and boys.] Lund: Arkiv förlag; 2017.
Mirza KAH, Mirza S. Adolescent substance misuse. Psychiatry. 2008;7(8):357–62.
Degenhardt L, Hall W, Lynskey M. Exploring the association between cannabis use and depression. Addiction. 2003;98(11):1493–504.
Harrison PA, Fulkerson JA, Beebe TJ. Multiple substance use among adolescent physical and sexual abuse victims. Child Abuse Negl. 1997;21(6):529–39.
Clark DB, De Bellis MD, Lynch KG, Cornelius JR, Martin CS. Physical and sexual abuse, depression and alcohol use disorders in adolescents: onsets and outcomes. Drug Alcohol Depend. 2003;69(1):51–60.
Brunelle N, Tremblay J, Blanchette-Martin N, Gendron A, Tessier M. Relationship between drugs and delinquency in adolescence: influence of gender and victimization experiences. J Child Adolesc Subst Abuse. 2014;23(1):19–28.
James PD, Smyth BP, Apantaku-Olajide T. Substance use and psychiatric disorders in Irish adolescents: a cross-sectional study of patients attending substance abuse treatment service. Ment Health Subst Use. 2013;6(2):124–32.
Kloos A, Weller RA, Chan R, Weller EB. Gender differences in adolescent substance abuse. Curr Psychiatry Rep. 2009;11(2):120–6.
Danielson CK, Amstadter AB, Dangelmaier RE, Resnick HS, Saunders BE, Kilpatrick DG. Trauma-related risk factors for substance abuse among male versus female young adults. Addict Behav. 2009;34(4):395–9.
Pinchevsky GM, Fagan AA, Wright EM. Victimization experiences and adolescent substance use: does the type and degree of victimization matter? J Inpersonal Violence. 2014;29(2):299–319.
Sabri B. Severity of victimization and co-occurring mental health disorders among substance using adolescents. Child Youth Care Forum. 2012;41(1):37–55.
Simpson TL, Miller WR. Concomitance between childhood sexual and physical abuse and substance use problems. Clin Psychol Rev. 2002;22(1):27–77.
Roseman M, Kloda LA, Saadat N, Riem KE, Ickowicz A, Baltzer F, et al. Accuracy of depression screening tools to detect major depression in children and adolescents: a systematic review. Can J Psychiatry. 2016;61(12):746–57.
Frances A. Saving normal. An Insider's revolt against out-of-control psychiatric diagnosis, DSM-5, big Pharma, and the medicalization of ordinary life. New York: William Morrow and co; 2014.
Stenius K. Public health is not an innocent concept. Nordic Stud Alcohol Drugs. 2018;35(2):100–3.
Anderberg M, Dahlberg M. Experiences of victimization among adolescents with substance abuse disorders in Sweden. Scand J Child Adolescent Psychiatry Psychol. 2016;4(3):123–31.
Torchalla I, Nosen L, Rostam H, Allen P. Integrated treatment programs for individuals with concurrent substance use disorders and trauma experiences: a systematic review and meta-analysis. J Subst Abus Treat. 2012;42(1):65–77.
Download references
Acknowledgements
Not applicable.
Open access funding provided by Malmö University.
Author information
Authors and affiliations.
Department of Social Work, Malmö University, Citadellsvägen 7, 211 18, Malmö, Sweden
Torkel Richert
Department of Pedagogy and Learning, Linnaeus University, Växjö, Sweden
Mats Anderberg & Mikael Dahlberg
You can also search for this author in PubMed Google Scholar
Contributions
All three authors, MA, MD and TR, have made substantial contributions to all phases of the paper. All authors were involved in study design, review of previous research, analyses and discussion. TR prepared the final draft, which was discussed, edited and approved by all authors.
Corresponding author
Correspondence to Torkel Richert .
Ethics declarations
Ethics approval and consent to participate.
This study only uses anonymized data, and permission for storage and processing of data for research purposes has been obtained from the research ethics committee at the National Board of Health and Welfare.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Richert, T., Anderberg, M. & Dahlberg, M. Mental health problems among young people in substance abuse treatment in Sweden. Subst Abuse Treat Prev Policy 15 , 43 (2020). https://doi.org/10.1186/s13011-020-00282-6
Download citation
Received : 14 February 2020
Accepted : 06 June 2020
Published : 24 June 2020
DOI : https://doi.org/10.1186/s13011-020-00282-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Young people
- Adolescents
- Mental health problems
- Drug use problems
- Substance abuse treatment
- Gender differences
Substance Abuse Treatment, Prevention, and Policy
ISSN: 1747-597X
- General enquiries: [email protected]
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
The Effects of Drug Addiction on the Brain and Body
Signs of drug addiction, effects of drug addiction.
Drug addiction is a treatable, chronic medical disease that involves complex interactions between a person’s environment, brain circuits, genetics, and life experiences.
People with drug addictions continue to use drugs compulsively, despite the negative effects.
Substance abuse has many potential consequences, including overdose and death. Learn about the effects of drug addiction on the mind and body and treatment options that can help.
Verywell / Theresa Chiechi
Drug Abuse vs. Drug Addiction
While the terms “drug abuse” and “drug addiction” are often used interchangeably, they're different. Someone who abuses drugs uses a substance too much, too frequently, or in otherwise unhealthy ways. However, they ultimately have control over their substance use.
Someone with a drug addiction uses drugs in a way that affects many parts of their life and causes major disruptions. They can't stop using drugs, even if they want to.
The signs of drug abuse and addiction include changes in behavior, personality, and physical appearance. If you’re concerned about a loved one’s substance use, here are some of the red flags to watch out for:
- Changes in school or work performance
- Secretiveness
- Relationship problems
- Risk-taking behavior
- Legal problems
- Aggression
- Mood swings
- Changes in hobbies or friends
- Sudden weight loss or gain
- Unexplained odors on the body or clothing
Drug Addiction in Men and Women
Men and women are equally likely to develop drug addictions. However, men are more likely than women to use illicit drugs, die from a drug overdose, and visit an emergency room for addiction-related health reasons. Women are more susceptible to intense cravings and repeated relapses.
People can become addicted to any psychoactive ("mind-altering") substance. Common addictive substances include alcohol , tobacco ( nicotine ), stimulants, hallucinogens, and opioids .
Many of the effects of drug addiction are similar, no matter what substance someone uses. The following are some of the most common effects of drug addiction.
Effects of Drug Addiction on the Body
Drug addiction can lead to a variety of physical consequences ranging in seriousness from drowsiness to organ damage and death:
- Shallow breathing
- Elevated body temperature
- Rapid heart rate
- Increased blood pressure
- Impaired coordination and slurred speech
- Decreased or increased appetite
- Tooth decay
- Skin damage
- Sexual dysfunction
- Infertility
- Kidney damage
- Liver damage and cirrhosis
- Various forms of cancer
- Cardiovascular problems
- Lung problems
- Overdose and death
If left untreated drug addiction can lead to serious, life-altering effects on the body.
Dependence and withdrawal also affect the body:
- Physical dependence : Refers to the reliance on a substance to function day to day. People can become physically dependent on a substance fairly quickly. Dependence does not always mean someone is addicted, but the longer someone uses drugs, the more likely their dependency is to become an addiction.
- Withdrawal : When someone with a dependence stops using a drug, they can experience withdrawal symptoms like excessive sweating, tremors, panic, difficulty breathing, fatigue , irritability, and flu-like symptoms.
Overdose Deaths in the United States
According to the Centers for Disease Control and Prevention (CDC), over 100,000 people in the U.S. died from a drug overdose in 2021.
Effects of Drug Addiction on the Brain
All basic functions in the body are regulated by the brain. But, more than that, your brain is who you are. It controls how you interpret and respond to life experiences and the ways you behave as a result of undergoing those experiences.
Drugs alter important areas of the brain. When someone continues to use drugs, their health can deteriorate both psychologically and neurologically.
Some of the most common mental effects of drug addiction are:
- Cognitive decline
- Memory loss
- Mood changes and paranoia
- Poor self/impulse control
- Disruption to areas of the brain controlling basic functions (heart rate, breathing, sleep, etc.)
Effects of Drug Addiction on Behavior
Psychoactive substances affect the parts of the brain that involve reward, pleasure, and risk. They produce a sense of euphoria and well-being by flooding the brain with dopamine .
This leads people to compulsively use drugs in search of another euphoric “high.” The consequences of these neurological changes can be either temporary or permanent.
- Difficulty concentrating
- Irritability
- Angry outbursts
- Lack of inhibition
- Decreased pleasure/enjoyment in daily life (e.g., eating, socializing, and sex)
- Hallucinations
Help Someone With Drug Addiction
If you suspect that a loved one is experiencing drug addiction, address your concerns honestly, non-confrontationally, and without judgment. Focus on building trust and maintaining an open line of communication while setting healthy boundaries to keep yourself and others safe. If you need help, contact the SAMHSA National Helpline at 1-800-662-4357.
Effects of Drug Addiction on an Unborn Child
Drug addiction during pregnancy can cause serious negative outcomes for both mother and child, including:
- Preterm birth
- Maternal mortality
Drug addiction during pregnancy can lead to neonatal abstinence syndrome (NAS) . Essentially, the baby goes into withdrawal after birth. Symptoms of NAS differ depending on which drug has been used but can include:
- Excessive crying
- Sleeping and feeding issues
Children exposed to drugs before birth may go on to develop issues with behavior, attention, and thinking. It's unclear whether prenatal drug exposure continues to affect behavior and the brain beyond adolescence.
While there is no single “cure” for drug addiction, there are ways to treat it. Treatment can help you control your addiction and stay drug-free. The primary methods of treating drug addiction include:
- Psychotherapy : Psychotherapy, such as cognitive behavioral therapy (CBT) or family therapy , can help someone with a drug addiction develop healthier ways of thinking and behaving.
- Behavioral therapy : Common behavioral therapies for drug addiction include motivational enhancement therapy (MET) and contingency management (CM). These therapy approaches build coping skills and provide positive reinforcement.
- Medication : Certain prescribed medications help to ease withdrawal symptoms. Some examples are naltrexone (for alcohol), bupropion (for nicotine), and methadone (for opioids).
- Hospitalization : Some people with drug addiction might need to be hospitalized to detox from a substance before beginning long-term treatment.
- Support groups : Peer support and self-help groups, such as 12-step programs like Alcoholics Anonymous, can help people with drug addictions find support, resources, and accountability.
A combination of medication and behavioral therapy has been found to have the highest success rates in preventing relapse and promoting recovery. Forming an individualized treatment plan with your healthcare provider's help is likely to be the most effective approach.
Drug addiction is a complex, chronic medical disease that causes someone to compulsively use psychoactive substances despite the negative consequences.
Some effects of drug abuse and addiction include changes in appetite, mood, and sleep patterns. More serious health issues such as cognitive decline, major organ damage, overdose, and death are also risks. Addiction to drugs while pregnant can lead to serious outcomes for both mother and child.
Treatment for drug addiction may involve psychotherapy , medication, hospitalization, support groups, or a combination.
If you or someone you know is experiencing substance abuse or addiction, contact the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-4357.
American Society of Addiction Medicine. Definition of addiction .
HelpGuide.org. Drug Abuse and Addiction .
Tennessee Department of Mental Health & Substance Abuse Services. Warning signs of drug abuse .
National Institute on Drug Abuse. Sex and gender differences in substance use .
Cleveland Clinic. Drug addiction .
National Institute on Drug Abuse. Drugs, Brains, and Behavior: The Science of Addiction Drugs and the Brain .
American Heart Association. Illegal Drugs and Heart Disease .
American Addiction Centers. Get the facts on substance abuse .
Szalavitz M, Rigg KK, Wakeman SE. Drug dependence is not addiction-and it matters . Ann Med . 2021;53(1):1989-1992. doi:10.1080/07853890.2021.1995623
Centers for Disease Control and Prevention. Drug overdose deaths in the U.S. top 100,000 annually .
American Psychological Association. Cognition is central to drug addiction .
National Institute on Drug Abuse. Understanding Drug Use and Addiction DrugFacts .
MedlinePlus. Neonatal abstinence syndrome .
National Institute on Drug Abuse. Treatment and recovery .
Grella CE, Stein JA. Remission from substance dependence: differences between individuals in a general population longitudinal survey who do and do not seek help . Drug and Alcohol Dependence. 2013;133(1):146-153. doi:10.1016/j.drugalcdep.2013.05.019
By Laura Dorwart Dr. Dorwart has a Ph.D. from UC San Diego and is a health journalist interested in mental health, pregnancy, and disability rights.

For people with mental illness, drugs and alcohol can be a key survival strategy. I’ve learned they shouldn’t have to ‘get clean’ to get treatment
Mental Health Social Worker and PhD Candidate, Staffordshire University
Disclosure statement
Simon Bratt does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Staffordshire University provides funding as a member of The Conversation UK.
View all partners
A decade ago, while working in a women’s prison, I met a young woman whose story would leave an indelible mark on me. She had endured severe abuse at the hands of men, and I was initially concerned that, as a male social worker, my presence might rekindle her trauma. Yet, through careful and considered engagement, we were able to forge a relationship of trust.
Jenny* confided in me that heroin had become her refuge – the only respite that quieted the relentless storm of her thoughts. But her dependency had brought dire consequences: the removal of her children and her subsequent imprisonment for possession with intent to supply. Even so, Jenny told me that before she was imprisoned: “Heroin was the only thing that helped me to cope.”
While inside, she experienced regular flashbacks and profound anxiety. Her treatment regime included antipsychotic medication Seroquel and heroin replacement Subutex – but Jenny didn’t use them conventionally. “The only way they help is if I grind them together and snort them,” she explained. This method provided her a fleeting, euphoric respite from her psychological torment.

Across the world, we’re seeing unprecedented levels of mental illness at all ages, from children to the very old – with huge costs to families, communities and economies. In this series , we investigate what’s causing this crisis, and report on the latest research to improve people’s mental health at all stages of life.
It wasn’t Jenny’s drug revelation that struck me most profoundly, but the reaction of some of my prison colleagues. Her unconventional use of the medication was labelled substance abuse, leading to her being ostracised by the prison’s mental health service, which refused to work with her until she “sorted out” her drug issues.
Even though I had known Jenny for a year, it was only when she was about to be released from prison that I really understood how serious her situation was. I was shocked to see her breaking the prison’s rules on purpose because she didn’t want to leave. She started smoking in places she shouldn’t, damaged her own cell and areas everyone used, attacked another prisoner, which was not like her at all, and started using spice and hooch.
Jenny preferred staying in jail over facing life outside, but she was let out all the same. A week after her release, I received news that she had died from a heroin overdose.
My search for answers
Mental health problems are experienced by the majority of drug and alcohol users in community substance use treatment. Death by suicide is also common, with a history of alcohol or drug use being recorded in 54% of all suicides in people experiencing mental health problems. ( Public Health England guide , 2017.)
Jenny’s tragic story left me with many questions – what were the underlying causes of mental illness? What spurred the spiral into addiction? Why did individuals turn to substance use? – that, even after six years as a mental health social worker working in prisons and psychiatric hospitals, I had neither the knowledge nor experience to answer. Talking to colleagues did not resolve them, so I sought answers by returning to academia alongside my day job.
A postgraduate diploma helped me better understand the theories of mental health from neuroscientific, psychiatric and pharmacological perspectives. But above all, I realised that many of the people I was now encountering in my new role, working in a crisis home treatment team (a community-based team set up to support people experiencing severe mental health issues), would never get better. Rather, they would just keep coming back with a new crisis.
And for a large majority of them (around four in five), substances ranging from highly addictive narcotics to potent, mind-altering chemicals would be a key part of their daily lives in addition to, or as an alternative for, their prescribed psychiatric medication.

This article is part of Conversation Insights The Insights team generates long-form journalism derived from interdisciplinary research. The team is working with academics from different backgrounds who have been engaged in projects aimed at tackling societal and scientific challenges.
Roger was one of many people I met who relied on Spice , a synthetic cannabinoid designed to mimic the effects of naturally occurring THC . (In addition to consumption by smoking, there are increasing reports of synthetic cannabinoids being used in e-cigarettes or vapes .)
Nonetheless, Roger told me Spice was the “only thing that would help sort my head out”. And, after listening to a lecture from me about the dangers of these substances, he responded:
I know how much to take – I know when I’ve taken too much or not enough. I use it in doses now. Why would I stop if it’s the only thing that works?
It was clear that Roger knew much more about the effects of Spice than I did. Interactions like this ignited a desire in me for deeper knowledge – not from books or universities, but directly from people with co-existing mental health and addiction problems.
Perhaps surprisingly, in the UK we don’t know how many people are living in this combined state. Estimates have tended to focus only on people with severe mental health problems and problematic substance use. For example, a 2002 Department of Health guide suggested that 8-15% of its patients had a dual diagnosis – while acknowledging that it is difficult to assess exact levels of substance use, both in the general population and among those with mental health problems.
A decade earlier, US research had identified that for people with schizophrenia , substance use (non-prescribed drugs) was a significant problem relative to the general population. More recently, a 2023 global review of evidence identified that the prevalence of co-existing mental health and substance use among children and adolescents treated for psychiatric conditions ranged between 18.3% and 54%.

But what I found particularly interesting was an analysis of the writings of Thomas De Quincey from more than 200 years ago. In his 2009 article Lessons From an English Opium Eater: Thomas De Quincey Reconsidered , leading clinical academic, John Strang, highlighted that issues raised by De Quincey in 1821 remain causes for concern some two centuries later.
De Quincey was arguably the first person to document his own use of substances, in particular opium. His writing shows that he self-medicated to manage pain, including “excruciating rheumatic pains of the head and face”:
It was not for the purpose of creating pleasure, but of mitigating pain in the severest degree, that I first began to use opium as an article of daily diet … In an hour, oh Heavens! What an upheaving, from its lowest depths, of the inner spirit!
De Quincey’s use of non-prescribed drugs mirrors that of John, Jenny, Roger and so many other people I have met as a social worker. Clearly, we’ve known about the close relationship between mental illness and substance abuse for hundreds of years, yet are still wrestling with how best to respond.
Read more: Guide to the classics: Confessions of an English Opium Eater by Thomas De Quincey – a dense, strange journey through addiction
Official guidance almost always advocates for a “no wrong door” policy , meaning that those with dual addiction and mental health issues will get help whichever service encounters them first. But from what people with lived experience were telling me, this was not the case.
I sent freedom of information requests to 54 mental health trusts across England, to try to discern any patterns of variation in the way their patients were being measured and treated. Some 90% of the trusts responded, of which a majority (58%) recognised the dual occurrence of mental illness and substance use. However, the estimated prevalence of this dual diagnosis varied widely – from only nine to around 1,200 patients per trust.
What I found most alarming was that less than 30% of the mental health trusts said they have a specialised service for addiction which accepts referrals for dual diagnosis patients. In other words, throughout England, a lot of these patients are not being appropriately supported.

‘When I say I use heroin, people change’
I started using when I was around 18. Things weren’t good in my life at the time, and I got in with a crowd who offered me heroin. It was the most amazing experience; all my worries disappeared better than the antidepressants I had been taking. But the more I used, the more I needed it. Now I use it in stages, just before I go to work and at night.
Carl had been using heroin for more than ten years when I interviewed him. When I asked if he wanted to stop, he shrugged and said no, explaining:
I’ve tried so many times – I’ve been on methadone but that was worse, especially coming off it. I know how much to take, and no one knows I use gear – so, no. But, as soon as you tell a professional you take heroin, their whole attitude changes. I’ve seen it many times. I dress quite well and I have a job, but as soon as I say I use heroin, they change. It’s almost as if they don’t see the same person any more.
Talking to Carl underlined that many users know far more than me about the substances they take and why they take them. Yet as soon as a professional (typically a nurse, social worker or doctor) hears they are taking an illegal substance, or are misusing a legal substance such as alcohol, they are stigmatised and often ostracised from service provision.
Suzanne was homeless and also using heroin, but for different reasons to Carl. I asked why she started using it:
I’ve had a shit life – it numbs all of that. Now being homeless, it helps me to sleep and keeps me warm, but I only use it in the winter because I need to sleep.
In summer, Suzanne explained, she would switch to taking “phet” – amphetamines. I asked her why:
You need to be awake – there are lots of dickheads around. I’ve been beaten and raped in the summer when I was asleep, so you need to be awake more.
Hearing the stories of people fighting their personal battles with mental health and substance use issues was at once haunting and cathartic for me. It was deeply moving to hear them, time and again, struggling with the most difficult aspect of their condition: the simple decision to ask for help. And sadly, far too often, when they did summon the courage, their requests would go unheard, unheeded, or they would be engulfed by a sprawling system that seemed unable to help.
Dave had been using alcohol for many years and had asked for support on several occasions – only to be passed from service to service:
I was made redundant and, at 50, was finding it hard to get another job. I wasn’t drinking all of the time then. But as I started to get into more debt and the bailiffs were knocking on the door, I needed a drink to get me through it. It was not until I was charged with drunk driving that I knew I had a problem.
Dave said he wasn’t shy about asking for help – at least, for a while. But he found himself caught in a downward spiral that led to more drinking, more suffering, and less support:
So many times I’d stop drinking, but I couldn’t deal with the voices in my head. I’d ask for support, but the waiting lists were so long. The medication the doctor gave me did nothing, so I’d start drinking again, and because I’d start to drink again, mental health services wouldn’t touch me. All they kept saying was: ‘You should stop drinking first.’

The biggest barrier to getting support
To expand my understanding, I also sought the perspectives of a dozen people working on the frontline of mental healthcare – from professionals in NHS mental health and substance use teams, to people working for charitable support groups. Their insights revealed a frayed and fragmented network of services , with the holes and inefficiencies obvious and crying out for attention and repair. As one nurse explained:
The stress of trying to get services to help is unbelievable. You’ve got pressure from the person’s family because they are afraid they’ll end up dead. You’ve got pressure from managers to discharge the person. All I’d get is criticism which far outweighed encouragement or support. The stress made me so anxious that I almost gave it all up – and even considered suicide myself.
Over 80% of the professionals I spoke to called for an integration of mental health and substance use teams, in part because of the huge cuts nationwide in funding to substance use services. One social worker in a substance use service explained the current situation:
If you get someone with an alcohol addiction, it becomes quite apparent that they use drink as a way of coping with their mental health. But, because of massive waiting lists within mental health services or because they are told they need to stop drinking before [they can be treated], mental health support can’t be offered. So, the person just keeps drinking and eventually disengages from our services as there is no hope for them. We shouldn’t expect someone to stop using a substance that they perceive is helping without offering an alternative treatment.
For all the professionals I interviewed, the most significant barrier to getting support for someone’s mental health issues was that they used substances and would not receive any treatment until they addressed this. As one mental health nurse told me:
I had one chap who was using cocaine, mainly due to social anxiety. Initially, he’d use it when socialising with friends. But because it gave him confidence and he could talk to people, he started to use it all the time and got himself in debt. I wanted to address the root cause, the social anxiety, so I referred him to our Improving Access to Psychological Therapy service. But I was told he needed to be abstinent from cocaine for three months before they’d accept him. He eventually disengaged, and I haven’t seen him since.
A seismic shift is needed
In the shadows of our society, hidden behind the walls of our prisons and in the dark corners of our streets, the experiences of Jenny and countless others bear witness to the profound failings of our healthcare system to address co-existing mental health and substance use issues. For those caught in the merciless cycle of addiction and illness, these systemic inefficiencies and administrative blockades do much to intensify their torment.
Their often brutally honest accounts (and the insights of those who try to support them) draw a portrait of a split and underfunded service, collapsing under the weight of its contradictions. The loud calls for integrated mental health and substance addiction treatment become muffled amid the bureaucratic din of funding cuts, lengthy waiting lists and policy neglect.
The evidence overwhelmingly confirms the need for a model of care that is holistic and integrated – one that shifts the narrative from stigma and isolation to awareness and support.
The economic case for reshaping investment in our mental health and substance misuse services is powerful. The annual cost of mental health problems to the UK economy is a staggering £117.9 billion – equivalent to 5% of its annual GDP – with substance misuse adding a further £20 billion .
However, these figures tell only part of the tale. While we know that 70% of people in treatment for drug misuse and 86% of people in treatment for alcohol misuse have a mental health diagnosis, the full financial impact of people with these co-occurring disorders is probably far greater.
This also includes people who often plough through a punitive and bewildering series of services as they navigate their intersecting problems, encountering barriers at every turn that fail to address their acute health and social care needs. As their distress is amplified, the costs to wider society escalate too – as one social worker explained to me:
I am currently supporting a woman who is struggling with alcohol dependency, a condition that began after she endured significant domestic abuse. The cycle is devastating: her trauma cannot be effectively addressed because of her dependency on alcohol, and she cannot abandon alcohol because it’s the only solace she finds from her emotional torment. Despite several attempts at rehabilitation, none of the programmes have sufficiently tackled the mental health aspects of her trauma. Now, with cirrhosis of the liver, her health is in critical decline. It’s a heart-wrenching situation – a stark reminder of the desperate need for integrated treatment approaches that address both substance dependency and the underlying psychological trauma.

‘I might as well be dead’
In the quiet confines of a West Midlands mental health crisis centre, I’m preparing to meet someone whose story I know only from the clinical notes on my screen. The phrase “is alcohol dependent” is highlighted in bold. Behind those words is another person whose life is unravelling in the silence of a battle fought alone.
John walks into the room, a man living in the grip of two relentless forces – addiction and mental illness. “It was just to stop the noises,” he says of the whisky he uses as medication for his inner turmoil. His hands are trembling. This is the moment of truth – his story is no longer trapped within the clinical pages of a case file.
“I’ve lost everything,” he tells me. “I might as well be dead.”
Then John explains why he’s given up hope:
I’ve asked for help so many times, but all I get told is that I need to stop drinking before my mental health can be treated. However, alcohol is the only thing that works for me. I’ve gone through detox, but then I had to wait months for counselling. I just can’t cope that long without any support – antidepressants don’t do anything for me. What’s the point?
Over the past 15 years, I have met countless “Johns”, both during my day job as a mental health social worker and, latterly, in my academic research. This has led me to conclude that the health and social care system in which I work falls catastrophically short.
This is no mere professional critique. It is an impassioned plea for society to rediscover its collective heart; to explore the human stories that lie hidden in statistics such as that, between 2009 and 2019, 53% of UK suicides were among people with comorbid diagnoses of mental health and substance use.
Instead of viewing people through the limiting lens of labels, we should endeavour to see their humanity. Engaging in conversation, extending empathy and showing compassion are powerful actions. A kind word, an understanding nod or a gesture of support can affirm their dignity and spark a connection that resonates with their innate human spirit. Or as John, whose journey I’ve had the privilege to witness, puts it:
It’s not about the help offered but the meaning behind it. Knowing you’re seen as a person, not just a problem to be solved – that’s what sticks with you.
*All names in this article have been changed to protect the anonymity of the interviewees.
If you or anyone you know require expert advice about the issues raised in this article, the NHS provides this list of local helplines and support organisations .

For you: more from our Insights series :
Insomnia: how chronic sleep problems can lead to a spiralling decline in mental health
Existential crisis: how long COVID patients helped us understand what it’s like to lose your sense of identity and purpose in life
OCD is so much more than handwashing or tidying. As a historian with the disorder, here’s what I’ve learned
How music heals us, even when it’s sad – by a neuroscientist leading a new study of musical therapy
To hear about new Insights articles, join the hundreds of thousands of people who value The Conversation’s evidence-based news. Subscribe to our newsletter .
- Mental health
- Mental illness
- Mental illness cost
- Drug addiction
- Heroin dependence
- Social worker
- Insights series
- Tackling the mental health crisis

Events Officer

Lecturer (Hindi-Urdu)

Director, Defence and Security

Opportunities with the new CIEHF

School of Social Sciences – Public Policy and International Relations opportunities

Essay on Drug/ Substance Abuse
Drug and substance abuse remains one of the most challenging and destructive problems facing societies worldwide. It refers to the harmful or hazardous use of psychoactive substances, including alcohol and illicit drugs. This essay aims to delve into the complexities of drug and substance abuse, examining its causes, effects, and the crucial steps needed to address this epidemic.
Drug and Substance Abuse
Drug and Substance Abuse involves the recurrent use of drugs or substances leading to significant impairment, including health problems, disability, and failure to meet responsibilities at work, school, or home. This includes the misuse of legal substances like alcohol and prescription medications, as well as illegal substances like heroin, cocaine, and methamphetamines.
Causes of Drug and Substance Abuse
The reasons behind drug and substance abuse are multifaceted and can vary from individual to individual:
- Genetic Predisposition : Research indicates a genetic component to the susceptibility to substance abuse.
- Mental Health Disorders : Many individuals with mental health disorders such as depression, anxiety, or PTSD turn to substances as a form of self-medication.
- Peer Pressure : Particularly among adolescents and young adults, peer pressure can significantly influence substance use.
- Stressful Life Events : Traumatic experiences, chronic stress, or life-changing events can lead to substance abuse as a coping mechanism.
- Curiosity and Experimentation : Often, particularly in young individuals, there’s a desire to experiment, which can lead to misuse and addiction.
Effects of Drug and Substance Abuse
Drug and substance abuse, a major public health challenge, affects individuals, families, and communities across the globe. This essay explores the multifaceted effects of drug and substance abuse, including physical health, mental well-being, social relationships, and broader societal impacts.
Physical Health Effects
Immediate physical effects.
- Altered State of Consciousness : Substances like alcohol, marijuana, and hallucinogens alter perception, mood, and consciousness.
- Overdose Risk : Excessive consumption of drugs can lead to overdose, potentially resulting in coma or death.
- Infectious Diseases : Intravenous drug use increases the risk of diseases like HIV and Hepatitis B and C due to needle sharing.
Long-Term Health Effects
- Organ Damage : Chronic substance abuse can lead to severe damage to vital organs like the liver (cirrhosis), heart, and brain.
- Neurological Impact : Long-term effects on the brain can include memory loss, cognitive decline, and mental health disorders.
- Physical Dependency : Prolonged use leads to dependency, where the body requires the substance to function normally.
Mental Health and Psychological Effects
- Mental Health Disorders : Substance abuse can trigger or exacerbate mental health conditions like depression, anxiety, and psychosis.
- Behavioral Changes : Changes in behavior, such as increased aggression or impulsivity, are common.
- Cognitive Impairments : Drugs can impair decision-making abilities, judgment, and other cognitive functions.
Social and Relationship Impacts
- Family Dynamics : Drug abuse can strain family relationships, leading to conflict, mistrust, and breakdown of family structures.
- Workplace Issues : It affects job performance, leading to decreased productivity, absenteeism, and higher risk of accidents.
- Legal Problems : Substance abuse can result in legal issues, including arrests for possession, driving under the influence, or engaging in illegal activities to support the addiction.
Societal and Economic Impacts
- Healthcare Costs : Treating drug-related health complications burdens healthcare systems.
- Crime and Safety : There’s a correlation between substance abuse and increased crime rates, impacting community safety.
- Economic Burden : The economic impact includes loss of productivity, healthcare expenses, and law enforcement costs.
Prevention and Treatment
- Education and Awareness : Programs aimed at educating individuals about the risks of drug use are crucial.
- Rehabilitation Programs : Effective treatment programs, including therapy and medication-assisted treatment, help individuals recover.
- Support Systems : Family, community, and peer support are vital in the recovery process.
Addressing Drug and Substance Abuse
- Prevention Programs : Education and awareness programs, particularly targeting young people, are crucial in preventing substance abuse.
- Treatment and Rehabilitation : Access to effective treatment, including counseling, medication, and support groups, is vital for recovery.
- Policy and Regulation : Government policies to regulate the availability of substances, and laws to address drug trafficking and misuse, play a critical role.
- Community Support : Community-based efforts, including support from families, schools, and religious organizations, are essential in supporting those affected.

The Role of Society and Individuals
- Destigmatization : Removing the stigma around substance abuse and addiction encourages individuals to seek help.
- Educational Initiatives : Schools and universities should have programs to educate students about the dangers of substance abuse.
- Role Models : Influential figures and celebrities should promote healthy lifestyles and speak out against substance abuse.
- Supportive Environment : Creating an environment that fosters open discussion and support for those struggling with substance abuse.
In conclusion, Drug and substance abuse is a complex issue requiring a multifaceted approach. It is not just a personal problem but a societal challenge that calls for comprehensive prevention strategies, effective treatment programs, supportive policies, and community involvement. Understanding and addressing the root causes, along with providing support and care for those affected, is crucial in mitigating the impact of this global issue. For students participating in essay competitions, exploring this topic provides an opportunity to contribute to a critical dialogue, advocating for change and supporting those in need.

Essay Generator
Text prompt
- Instructive
- Professional
Generate an essay on the importance of extracurricular activities for student development
Write an essay discussing the role of technology in modern education.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Substance Abuse and Public Health: A Multilevel Perspective and Multiple Responses
Substance abuse has been a thorny public health concern throughout human history. Manifestly, prevention and treatment are the two main strategies commonly adopted to tackle the problem of substance abuse. They are in fact cross-disciplinary, and they relate to the various domains of heredity, biology, psychology, cognitive science, family, social development and cultural structures. This special issue, “Substance Abuse, Environment and Public Health,” has published empirical studies from different regions and countries globally to enhance the international exchange of latest views and findings on the etiology, processes and influences of substance abuse across different domains, through which a multilevel perspective is considered more helpful for analyzing its complex nature, courses and consequences. This in turn suggests the possible need to employ multiple responses dynamically and integratively in the prevention and treatment of substance abuse.
1. Introduction
It is apparent that substance abuse is a cross-disciplinary topic of research and concern [ 1 , 2 ], which involves the need to employ concomitantly various theoretical explications and empirical evidence in collaborative efforts to strive for more optimal solutions to limit its contagiousness, and to curb any direct and indirect harm [ 3 , 4 ]. Substance abuse has been described as a “chronic relapsing disease”, with extremely high relapse rates that range from 56.8% to 81.8% [ 5 , 6 ]. Recently, the United Nations reported that “(i)n 2017, an estimated 271 million people, or 5.5 per cent of the global population aged 15–64, had used substances in the previous year” ([ 7 ], p.7). This is 11.5% higher than the estimated number of substance-using people in 2012 [ 8 ]. Due to the nature of recurrence and the rising number of substance users globally, a continuing upsurge in human, social, health and economic costs in the form of substance-related violence, criminal acts, health care needs, legal orders, rehabilitative services, reduced labor productivity and judicial expenditure is evident [ 4 , 6 , 9 ]. Undoubtedly, prevention and treatment are two main intervention approaches that have been commonly adopted to tackle substance abuse [ 2 , 10 ], in which the former focuses primarily on enhancing public awareness of the dangers of substance misuse and addiction, and the latter mainly emphasizes helping substance abusers to attain complete abstinence and avoid relapse. Both prevention and treatment of substance abuse are pertinent to public health, as the two approaches need to employ a multilevel perspective to conceptualize and solve fallout generated from drug trafficking, misuse and harm [ 11 , 12 ]. This points to the need to investigate human hereditary, biological, and psychological needs, cognitive and mental conditions, social development and cultural structures simultaneously and interactively.
For a comprehensive understanding of the nature, processes and impact of substance abuse on human individuals and societies as a whole, an international exchange of the latest scholarly views and empirical research findings is needed. This special issue, “Substance Abuse, Environment and Public Health,” aims to promote international exchange of empirical academic works on substance abuse and its related concerns. It includes 14 empirical research articles and one intervention paper from Bosnia, Croatia, Hong Kong, Italy, mainland China, Norway, Poland, Singapore, South Korea, Spain, Slovenia, Sweden and the United States, and covers the topics of substance misuse and addiction amongst various social groups, different types and forms of illicit and legally approved substances and multiple research methods and designs. Importantly, the scholarly works published in this special issue are expected to present an opportunity to enhance the international exchange of cross-disciplinary research and academic inquiries in the prevention and treatment of substance abuse.
2. Substance Abuse and Different Social Groups
When researching substance abuse and its harmful effects, researchers predominantly focus on certain social groups with a higher tendency towards substance taking and misuse, such as adolescents and male adults [ 13 , 14 , 15 , 16 , 17 , 18 ]. This is valid, as they may encounter various demanding life and social challenges, expectations, interpersonal alienation and biological impulses, all of which are relevant to the triggering of their initiation into drug experimentation as a form of self-medication. Substances may also act as a comforting “soul mate” to help users evade hard realities [ 19 , 20 ]. In this special issue, Zubak et al. [ 21 ] examined the effects of scholastic factors—for example, grade point averages, school and other unexcused absences and poor behavior—in relation to illicit drug misuse (IDM) and its initiation among adolescents in Bosnia and Herzegovina. Jee et al. [ 22 ] investigated the trajectories of different smoking groups of young South Korean male adults and the implication of the habit in their atherosclerotic cardiovascular disease (ASCVD) in middle age. However, substance takers are never restricted to any specific social groups; they can be found in communities of professionals, social talents, elders and university students. Devcic et al. [ 23 ] examined socio-demographics, sports-related factors, factors of hesitation, doping-related factors, consumption of dietary supplements, knowledge of doping and predictors of doping behavior in terms of misusing performance-enhancing substances among high-level competitive swimmers in Slovenia. Wang et al. [ 24 ] investigated how gender, residential areas and study majors were related to misconceptions about antibiotic use among Chinese university students, which in turn linked to their antibiotic misuse behavior. Through the use of a community-based participatory research design, Walter et al. [ 25 ] inquired how work-related musculoskeletal disorders (MSDs) and injuries among US fishing industry workers affected their use of prescription opioids to treat their pain, which in turn exposed them to increased risk of developing substance disorders. Apparently, different social groups are equally susceptible to the risk of substance abuse and addiction [ 3 , 4 , 12 ], and this is likely to be affected by their specific personal characteristics and environmental conditions. Hence, there is a need for researchers to discover both common and unique precursors germane to different social groups which lead to their substance using behavior.
3. Substance Abuse and Its Types and Forms
Substances that are misused or abused can be categorized into two forms. These include illicit and legally approved substances of various types. The most common illicit types of substances include cannabis, amphetamines, ketamine, methamphetamines, cocaine, ecstasy and heroin [ 2 , 6 ], which are largely banned in most countries. However, marijuana products have recently been legalized and commercialized in some northern American and Western states and regions under the umbrella of “control of reasonable use,” which casts a contemplative doubt over the original intent of reducing cannabis-related criminality and public health problems; hence, more research is needed on this subject [ 26 , 27 , 28 ]. Tobacco and alcohol are two legally approved types of substances that have been widely used by different social groups across different societies and cultures [ 6 , 11 , 29 ]. Some legally prescribed drugs, such as cough medications and the antibiotics mentioned above, can also be easily misused and abused by the general public, and these too merit the further attention of researchers [ 2 , 30 ].
In this special issue, Lo et al. [ 31 ] explored how far using illicit drugs, smoking cigarettes and drinking alcohol predicted sexual misconduct among Macau youths, while simultaneously adjusting for the effects of susceptibility to peer influence and school attachment/commitment. Assari et al. [ 32 ] attempted to assess the impact of subjective and objective socioeconomic status on the cigarette smoking and alcohol use of older African Americans by controlling the effects of pertinent covariates, which included demographic factors (age and gender), living arrangement and family type, health insurance status, chronic medical conditions, self-rated health, sick days, depression and chronic pain. Muller et al. [ 33 ] investigated changes in exercise and nicotine use among 1464 Norwegian prison inmates by classifying them into harmful and non-harmful substance use pre-incarceration groups, according to the Drug Use Disorders Identification Test (DUDIT) and the Alcohol Use Disorders Identification Test (AUDIT), both of which are commonly used by healthcare practitioners and researchers to assess the severity of illicit drug and intoxicant use. Wang et al. [ 34 ] analyzed the sources of antibiotics leftovers in the home and the risk factors of keeping them in relation to antibiotic self-medication among Chinese university students. Taken together, the relationships between the use of illicit drugs and legally approved substances are complex and intertwined or mutually reinforcing [ 35 , 36 ]. They may be affected by the personal circumstances and environmental conditions of the abusers, and may cause other forms of behavioral maladjustment [ 17 , 37 , 38 ]. Nevertheless, our current understanding of this complicated phenomenon of substance abuse is limited, and so more cross-disciplinary research is again recommended.
4. Researching Substance Abuse: Methods and Designs
As has been mentioned, substance abuse is a public health concern that involves human biological and physical needs, psychosocial demands, cognitive and spiritual fulfillment, and environmental formulations. Therefore, cross-disciplinary research using different methodologies and designs is much needed to scrutinize substance abuse in respect of etiology, maintenance, consequences, abstinence and relapse. Generally speaking, empirical studies using quantitative methods are more common than research involving qualitative inquiry, analysis of secondary data and/or documentary inspection [ 16 , 39 , 40 ]. In fact, research based on a range of methods and designs is useful in enhancing our comprehension of the nature and impact of substance abuse from different perspectives. This special issue incorporates empirical studies conducted by quantitative, qualitative and documentary methods. For quantitative research designs, study findings based on a representative sample or any of the random sampling procedures are desirable, and can strengthen empirical evidence and provide greater external validity [ 41 ]. For example, Oh et al. [ 42 ] investigated whether those who had current or previous experience of facial flushing would drink for different primary reasons, compared with those who had no experience of facial flushing. The sample comprised 4590 college students who were recruited by stratified random sampling procedures proportionately in 82 colleges in South Korea. There are other empirical studies in this special issue that similarly used a representative sample [ 21 , 24 , 31 , 34 ]. However, using quantitative methods to survey empirically the attitudes and behaviors of certain health and human service professional groups is less likely to require a representative sample, and so it is necessary to use non-probabilistic sampling procedures such as quota, purposive or snowballing sampling designs. Molina-Mula et al. [ 43 ] analyzed the attitudes and perceptions of emergency and mental health nurses with regard to alcoholics. Their findings will hopefully help to develop appropriate professional and clinical responses to substance abuse.
Qualitative research methods can help reveal in-depth and formative information related to the processes and development of substance abuse. For their qualitative study, Chan et al. [ 44 ] interviewed 67 drug abusers to explore how their psychological experiences—with special emphasis on interpersonal relatedness—affected their drug taking and relapse behaviors. Walter et al. [ 25 ] used qualitative interviewing to examine knowledge of and attitudes towards opioid use among 21 fishing industry workers in the US. In addition, use of secondary data or documentary information can efficiently and objectively assist in the transition processes of substance users. For example, Asharani et al. [ 45 ] employed and analyzed recorded data from the Registry of Birth and Death, Immigration and Checkpoint Authority of Singapore to investigate the unnatural deaths of 42 treatment seekers of substance addiction between 2011–2015. Their findings provide evidence of the lethal consequences of substance abuse in an unobtrusive manner. Moreover, Chmielowiec et al. [ 46 ] examined the relationship between the mesolimbic dopamine system and addiction in a group of 299 addicted subjects and another group of 301 non-addict controls by analyzing two polymorphisms in their genes (a variable number of tandem repeats in DRD4 and DAT1), which are mainly responsible for dopaminergic transmission, representing a human reward system that is closely related to substance abuse and misuse. It is clear that research using different methods and designs is useful in fortifying and enhancing currently established concepts and knowledge of substance abuse. Therefore, more novel research methods and designs should be encouraged, so that patterns of substance abuse can be more efficiently dissected.
5. Conclusions
Substance abuse has been an issue of public health for hundreds of years [ 47 ]. Nevertheless, professionals and researchers of different domains tend to adopt a one-dimensional view based on their particular expertise when examining, explaining and trying to find solutions to this complex problem [ 10 , 48 , 49 ]. Thus, various and often competing perspectives rooted in the paradigms of heredity, biology, psychology, cognitive science, family, social development and cultural structures can exist simultaneously, thereby unwittingly compounding the problem [ 1 , 2 , 39 , 50 ]. However, as substance abuse is composed of layers of individual development, family and social influences, cultural values and environmental conditions, a multilevel perspective is needed to analyze its etiology, maintenance and consequences. Various theories and models from different scholarly paradigms at different levels of social systems should be employed concomitantly to help examine and resolve the issues as part of a dynamic and comprehensive process [ 2 , 3 , 12 ]. Employing such a multilevel perspective requires researchers and practitioners to explore the interaction of hereditary, physical, psychological, cognitive, mental, family, social, cultural and environmental factors, and to show exactly how such synergy leads to and/or maintains substance use and addiction. Doing so will help in the design of improved multiple responses to the fallout from substance abuse.
As substance abuse is never limited to particular social groups in human societies, it is essential to understand the unique psychological, personality, cognitive, socioeconomic, familial and cultural differences of various social groups, and to explore what common and unique characteristics they hold in terms of the initiation, processes and consequences of substance abuse [ 4 , 6 ]. If researchers, service practitioners, educators and policy makers were able to understand the common and unique etiological causes and stimulants that incur experimentation and the subsequent maintenance of substance abuse, more effective prevention and treatment strategies and programs could be introduced. Furthermore, because each society or nation is comprised of multiple differing social groups, a knowledge and understanding of their unique cultural and ethnic structures would be empirically useful for researchers trying to unearth the common and distinct etiological causes and stimulants of substance use and abuse. This is a largely unchartered area of research.
The abuse of different types and forms of substances may generate different levels of addiction and harm [ 2 , 51 ], which in turn may trigger distinct social maladjustment and craving behaviors [ 12 , 52 ]. Therefore, future research should discern and clarify the effects of different types and forms of substances on the progress, abstinence and relapse of addicts; this would lead to a better comprehension of the nature and impact of substance abuse. Quantitative methods and designs should be adopted to this end, in addition to other methods and designs that will broaden our perspectives on the topic. In other words, future addiction research should consider the employment of mixed-method designs to investigate the nature of different types and forms of substances and their effects on different social groups. Furthermore, the interaction between the biological, individual, family, social and cultural factors that lead to substance abuse is worthy of research, but will require more advanced methodological designs and mathematical and statistical procedures.
The processes and consequences of substance abuse can be seen to evolve in step with social, technological and cultural developments [ 4 , 39 ]. The patterns and forms of substance abuse can vary according to different social groups. Therefore, comparative and longitudinal research is more useful and insightful in helping to reveal its precarious and dynamic influences. In fact, polysubstance abuse—in which substance addicts expect to achieve higher substance-synergy effects of enjoyability by simultaneously abusing multiple types of drugs and substances—has become more common in the past decade [ 53 , 54 ]. This apparently presents an even greater challenge to treatment and healthcare services. In the face of this new phenomenon, the role of empirical research becomes more pivotal in helping to configure effective approaches and solutions.
In conclusion, substance abuse has long been a thorny public health problem, and it continues to evolve. Multiple responses supported by the employment of a multilevel research perspective are needed. Cross-disciplinary collaboration and concerted research are urgently required if we are to optimize our current strategies and remediation.
Author Contributions
T.W.L., J.W.K.Y., and C.H.L.T. conceived the topic for the Special Issue and were the guest editors. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
108 Drug Abuse Essay Topic Ideas & Examples
🏆 best drug abuse topic ideas & essay examples, 👍 good essay topics on drug abuse, 💡 most interesting drug abuse topics to write about, ❓ drug abuse research questions.
Drug abuse essays are an excellent way to learn about the issue and its influence on various groups and populations while demonstrating your understanding.
Various substances, including alcohol, narcotics, and other mind-altering products, are a popular method for recreation in some communities.
However, they are prone to result in addiction, psychological as well as mental, and lead the person to pursue another dose before anything else.
In doing so, he or she can eventually ruin his or her life, which is why most drugs are currently banned around the world. This article will offer you some tips that will help you write an excellent essay and receive the top grade.
Youth is a major demographic that is affected by addiction issues due to drug consumption. Young people are impressionable and prone to search for new sensations. Drugs can offer a sense of novelty and provide an experience they have not had before, leading to considerable appeal.
Considering that young people are generally not wealthy and have to focus on work to succeed in life, essays on drug among youth can use a variety of excellent topics. You can offer your ideas on the reason for the phenomenon’s existence and ways in which it can be prevented.
However, remember that the purpose of the programs should be to help the people who are at risk.
There are many other drug abuse essay topics that you can explore, with poverty being a prominent example. Despite their conditions, many people turn to substance abuse to try and escape the unpleasant aspects of their life.
These population segments are more likely to suffer after acquiring a drug habit than young people because they generally receive less attention.
Furthermore, poor neighborhoods with relatively low amounts of surveillance by law enforcement are likely to house drug dealers who prey on vulnerable people.
You can discuss this topic or discuss a variety of other ones, as the relationship between poverty and poor outcomes has been researched deeply.
Here are some additional tips for your essay:
- Try to use examples to illustrate your points about various aspects of the issue. Drug addiction essay quotations from people who are affected by the condition or have overcome it can offer valuable insights. They also legitimize your findings by providing parallels with the real world.
- Alcohol essays are an excellent choice, as the substance is legal and available to everyone without much difficulty. Nevertheless, its effects can be devastating, especially if a person’s consumption is chronic.
- Try to write a drug abuse essay outline before starting work, as it will help you to organize the essay. Select some prominent ideas that you want to discuss and organize them in a manner that represents a logical progression. You do not have to discard all of the other concepts, as you can make them sub-headings under your main titles.
- Be sure to include a drug abuse essay introduction and conclusion in your work. They will help you provide a structure to the essay and make it easier for the reader to understand your ideas. The introduction should describe the topic and provide the thesis, and the conclusion should restate your main points.
Visit IvyPanda for drug abuse essay titles, and other useful samples on various subjects to help you with your writing work!
- Drug Trafficking and Drug Abuse Drug trafficking contributes to drug abuse in the society. Drug trafficking also contributes to increased criminal activities that affect the security of citizens.
- Drug Abuse and Current Generation Drug abuse also breeds an array of behavioral problems among young people, which may affect their suitability to fit in the society.
- Drug and Alcohol Abuse For along time now, drug and alcohol abuse in the society has been a problem that affects the youth and the society at large. This paper highlights the problems of drug abuse and alcohol drinking […]
- Consequences of Drug Abuse The endless stream of drugs, obtainable to the individuals with little or no restrictions, poses a serious inquiry. When assessing the advantages of using pharmaceutical drugs, it is essential to consider the severity of health […]
- Drug Abuse & Its Effects on Families Focusing on the family seems to be by far, the most known and effective way of finding a solution with regards to the “war on drugs” since it more promising to end the vicious cycle […]
- Merton’s Argument of Deviance: The Case of Drug Abuse The most prominent example in support of Merton’s argument in relation to drug abuse is that cultural and social circumstances play a crucial role in defining people’s desire to engage in drug use.
- Social Media Impact on Drug Abuse Thus, social media platforms definitely contribute to the misuse of various drugs by romanticizing their consumption and making “social drug use” acceptable among users.
- Reasons Behind Youth’s Engagement to Drug Abuse in the 21st Century Although youths in the 21st century engage in drug abuse due to several factors, it suffices to declare factors such as the rising unemployment status, peer pressure, and their hiked tendency to copy their parents’ […]
- Drug and Substance Abuse Many experts consider addiction as a disease as it affects a specific part of the brain; the limbic system commonly referred to as the pleasure center.
- Drug Abuse: Age, Gender and Addictive Susceptibility This incorporates the aspects of gender where males and females possess varying biological constitutions that might affect the prescribed treatments in the realms of addiction. It is important to consider the rapidity and susceptibility of […]
- Drug Abuse. “Nine Years Under” Book by Sheri Booker The book is thought provoking and important because it allows representing the difficult social situation and the problems of gang violence and drugs in the United States from the personal point of view.
- Drug Abuse in High School and College With respect to social work and the problem of substance abuse, research has been carried out in terms of investigating the relationship between drug abuse and poverty, the effects of drug abuse on the society.
- Drug Abuse as an Ethical Issue On the side of duties and obligations, the societal norms stipulate that individuals should be caring to other members of the society especially the children and the old.
- Alcoholism, Domestic Violence and Drug Abuse Kaur and Ajinkya researched to investigate the “psychological impact of adult alcoholism on spouses and children”. The work of Kaur and Ajinkya, reveals a link between chronic alcoholism and emotional problems on the spouse and […]
- Drug Abuse and Its Psychological Effects The purpose of this paper is to explore in more depth the psychological effects of addiction on the family and inner circle of the addict.
- Drug Abuse, Aggression and Antisocial Behavior The use of abusive drugs can cause anger in people because of the effect they have on the brain. An example of how alcohol can cause aggression in a person is that it impairs an […]
- Policies for Pregnant Women With Drug Abuse Thus, out of all the offered policies, financial support for therapy is the best one, as it motivates prevention and treatment, which, in turn, causes the improvement of this situation.
- The Formative Evaluation: Program of Addressing Drug Abuse in Schools The proposed program sought to educate students about the challenges of drug abuse, its impacts on academic performance, and the best techniques to avoid the vice.
- Alcohol and Drug Abuse in Canada Therefore, it contributes as a central factor in the essence of the character, and it is crucial to understand the core definition and the elements that foster the ideology.
- Mitigating Drug Abuse in Pine View School The inclusion of professionals in the fields of health care, counseling, and drugs is expected to promote the delivery of desirable results.
- Drug Abuse and Its Negative Effects This paper aims to highlight what the field of psychology says about the negative effects of drugs and why people continue using despite the consequences. The main effect is that it creates a memory of […]
- Prevention Programs: Drug Abuse Resistance Education This program focuses on handling peer pressure among youths, a crucial cause of drug abuse in the country. The program is also grounded on sound research, which offers the critical elements vital to handling the […]
- Drug Abuse in Lake County, California The topic of drug abuse is essential for discussion due to the need to develop strategies to prevent and minimize the dangerous consequences of drug abuse in different regions.
- Drug Abuse Among Homeless Young Adults in New Jersey The reason why young adults in New Jersey get involved in drugs and alcohol after becoming homeless is to manage their situations in an attempt to attain the tentative pleasure of life despite their problems. […]
- Community Intervention Practices Against Drug Abuse The key features that result in successful community-based intervention on drug abuse are integrated for effectiveness and efficiency. On the other hand, drug abuse refers to the consumption of substances that elicit particular feelings and […]
- Teenage Drug Abuse in the United States The problem of teenage drug abuse inflicts a threat to the future society and health state of the overall population in the United States.
- Drug Abuse Effects on Health and Nervous System These numerous damages severely affect the quality of the brains work and the health of the nervous system. While discussing the effects of drug addiction, it is essential to notice that it has a devastating […]
- Early Substance Abuse Education Prevents Future Drug Abuse Still, this desire to get away from problems by means of substances instead of making effort to improve an individual’s environment contributed to the evolution of the challenge of substance abuse into a real public […]
- Drug Abuse Survey Analysis National survey results on drug use obtained by Monitoring the Future have a significant value to the development of various approaches with regard to the prevention of drug abuse.
- The Health Issues Associated With Drug Abuse It is therefore imperative to develop strategies for health promotion to reduce the number of teenagers, the most at-risk family member when it comes to drug abuse.
- Fentanyl – Drug Profile and Specific and Drug Abuse The drug has the effect of depressing the respiratory center, constricting the pupils, as well as depressing the cough reflex. The remainder 75% of fentanyl is swallowed and absorbed in G-tract.
- Cases of Drug Abuse Amongst Nursing Professionals It is noteworthy that at the top of the information, the date posted is Monday, February 14, 2011, yet against the information, the date is February 11, 2011.
- The Treatment of Drug Abuse Any medical practitioner treating a drug abuse patient has to be careful in many aspects, like: He has to be careful on the issue that if the addiction has effected the brain of the patient.
- Workplace Drug Abuse Over the past years, the issue of drug abuse in the workplace, whether the issue concerns the employees or their families, has become quite significant in the global context.
- Drug Abuse: Drug Court and Detoxification However, since 1989, the US federal system has been providing the majority of drug abusers with proper treatment or education with the help of a drug court option.
- Drug Abuse and Prevention Strategies When specialists deal with preventative factors, they pay attention to both mental and physical ways to resist the drug. The symbiosis of these procedures is exceptionally efficient in terms of the drug rehabilitation process when […]
- Drug Abuse – A Public Health Menace in Adolescents Between 15-19 Years In addition, the objectives of the paper are as follows: the first aim is to analyze the collected data and produce a review of the information.
- Drug Abuse in Adolescents and Its Causes Scientific research shows that the development factors for adolescent drug abuse are not limited to a set of three to five causes, but are usually linked to the integration of destructive environmental conditions.
- Drug Abuse and Addiction Holimon has succeeded in reviving some of her family relations, and she is still putting a lot of effort to get ahead in this area to the fullest extent possible.
- Drug Abuse and Sporting Activities His comments made me realize that it would be unwise by the end of the day for any parent to leave their children under the mercy of the media where they learned that doing drugs […]
- Intervention Techniques Focusing Drug Abuse and Alcoholism A technique of Family Intervention needs the concern, care and supremacy of love to penetrate the denial and start the treatment.
- Critical Issues in Education: Drug Abuse and Alcoholism For this case, the ministry concerned has a very hard task of ensuring there are no critical issues that are left unsolved that relate to education, failure to which will affect the performance of students […]
- Drug Abuse Resistance Education and Its Outcomes While evaluating the effectiveness of the DARE program analysis in accordance with the methodologies and evaluation criteria used, the given assessments refer to various methods of the analysis of participants, as well as various data […]
- Drug Abuse and Depression Treatment She states that her father was the main person who was able to give the right pieces of advice and she was not afraid of making the wrong decision.
- Drug Abuse Diagnostics in Counseling If either the client or the professional wishes to determine the extent to which an individual is dependent on drugs, the only thing he or she would have to do is read the individual’s behavior.
- Biopsychosocial Experience in Drug Abuse Treatment There has to be a preventive strategy in every intervention procedure to avoid the occurrence of a disease. I find the course of treatment in this intervention beneficial for the creation of the needed preventive […]
- Addictive Behavior Programs and Drug Abuse Trends The involvement of stakeholders is an essential condition for the effectiveness of this model of work and its results, and all the roles should be allocated in accordance with the capabilities of the program’s participants.
- Drug Abuse Among Young People in the US The paper analyzes studies regarding some of the most widespread types of substances, as well as discusses the role of the rap culture in the growing number of young addicts in the U.S.
- Social Behaviour as a Science: Drug Abuse in Youth Thus, the application of social psychology to the phenomenon of youth drug abuse helps to explain how social factors impact the prevalence of and risk for drug abuse.
- ACTIQ Prescription Drug Abuse The fast-acting characteristic of ACTIQ is a result of being absorbed in the mucosal lining of the mouth. ACTIQ is a synthetic drug that is available as lozenges/lollipops, which are designed to be sucked in […]
- Prescription Drug Abuse and Lebanon Students The first two authors are the representatives of the Department of Epidemiology and Population Health at the American University of Beirut, and Martins is from the Department of Mental Health, the John Hopkins University.
- Drug Abuse Decreasing: Financial Plan Therefore, the first preferred sources for the program are the County Commission and the Alabama Department of Corrections. The program can be financed by the Montgomery County Commission in the short term and Alabama Department […]
- Addressing the Drug Abuse in Parolees and Probationers The aim of the program is to address the drug abuse in parolees and probationers during their probations and decrease the use of drugs in them.
- Problem of Drug Abuse in Schools The research worked on the hypothesis that the treatment would reduce or result in the total cessation of drug use, and better relations with family and friends.
- Youth Drug Abuse Among, Education, and Policies Although drug abuse encompasses improper use of drugs disregarding the prescriptions of medical practitioners, the principal challenges of drug abuse occasion from abuse of drugs such as cocaine, heroin, and marijuana.
- Prescription Drug Abuse in the United States The combination of Ibuprofen and acetaminophen are effective for the patients, who want to reduce and control the level of pain.
- Drug Abuse Prevention in Probationers To reduce drug use in probationers and the probability of a new crime, the approach to drug testing needs to be changed.
- Drug Abuse and Medicaid Program The emergence of alcohol and drug abuse as a problem and the intensification of people with mental health problems, have exposed the society to the likelihood of involvement of the population in substance abuse.
- Drug Abuse Among the Youth Essentially, this case study will allow the evaluation of the prevailing cases of drug abuse among the youth. In this regard, the pain and peer pleasure cannot be persevered to allow an explicit cure of […]
- Impact of Drug Abuse on Adolescent Development Therefore, it is important for counselors to consider these stages to help them address the issue of substance abuse among adolescents. In the habitual stage, most adolescents take drugs to help them modify their moods.
- Prevention Research: The Fight Against Drug Abuse It is agreeable that US’s ‘War on Drugs’ has been an effective substance abuse prevention plan despite the hiccups that the program faces and its inability to attain some of its designated mandates within the […]
- Drug Abuse Prevention Programs Additionally, it is possible to prospect the success of the program in case the required readiness from the community can be unveiled prior to the program execution.
- The Cultural Context and Ethics of Prevention of Drug Abuse The first prevention strategy outlined in the document is the involvement of young people in all levels of the prevention program establishment. Concurrently, it is crucial to relate this technique with the subject of culture […]
- Use of Psychotropic Medications in the Treatment of Drug Abuse This is because the mental illness is, literally, the one that sustains the abuse of drugs and thus after it is healed; the patient will have no reason to continue abusing the drugs.
- Drug Abuse: Awareness Amongst the Youths This project is going to carry out a public awareness campaign with the aim of educating the young people on the hazards related to the vice of drug and substance abuse. The awareness campaign is […]
- A New Alcohol and Drug-Abuse Rehabilitation Center in Liverpool Hospital, Sydney The hospital, in response to this distress, has decided to bring help closer to the people of Liverpool by the construction of the annex facility.
- Spirituality Effect on Drug Abuse Treatment Programs The hypothesis of the study was that spirituality is appropriate in the formal treatment of addiction; the study confirmed this hypothesis.
- Drug Abuse and Religious Spirituality Concept Particularly, this high rate of relapses was determined by Olmstead et al.as a direct result of a degree of failure on the part of drug abuse treatment programs to sufficiently address the primary reason why […]
- Drug Abuse and Harmful Health Effects The principle recognizes the importance of helping drug addicts out of the activity but also sees the importance of protecting their rights to health matters if the country is to realize economic development.
- The Extent of Drug Abuse Among People in America Toronto Mayor Rob Ford Said He Lied about Crack Cocaine Use Because He Was Embarrassed Mayor lied about the use of crack cocaine The article titled “Toronto Mayor Rob Ford said he lied about crack […]
- Drug Use and Abuse in America: Historical Analysis The new law was similar to the Boggs Act of 1951 in that it employed the same formula of using perceived increase in drug use in the country.
- “Cocaine: Abuse and Addiction” by National Institute on Drug Abuse The literature provides us with a report of a research that has been conducted in the US regarding the topic of cocaine and drug abuse.
- Drug Abuse and Society Regardless of the many intervention measures that can be adopted to solve this problem of drug abuse, the most effective intervention measure is to create awareness to youths to enable them change their behaviors and […]
- Prescription Painkillers, the New Drug Abuse of Choice Studies attribute the recent increase in the misuse of prescription drugs to an increase in the use of the Internet, which facilitates the growth of illegitimate online drug stores and uncontrolled online prescription drug sales.
- Music Analysis: Drug Abuse in Music So in this song the artist is also lamenting the dangers of drugs and the theme of the music is one that advocates against tackling the problem with issues of drug abuse by arguing the […]
- Drug Abuse: Comprehensive Review The effects associated with drug abuse tend to vary depending on an individual’s age and the phase of drug abuse that the person is in.
- Drug Abuse as a Social Problem This poses as problem to the society because many of the people who are unemployed will resort to different ways of seeking money and pleasure.
- Adolescent’s Drug Abuse and Therapy Success When one accepts to put up with negative peer pressure, they end up giving up the personal trusts and values thus the pressure becomes a form of a negative force.”Does peer pressure affect the decision […]
- What Are Influences That Cause Drug Abuse on Youth?
- What Are Some Solutions to Drug Abuse?
- What Are the Primary Causes and Effects of Alcoholism and Drug Abuse Among Young People?
- What Causes Teenage Drug Abuse?
- What Does Drug Abuse Truly?
- Why Do Children Need to Be Educated About Drug Abuse?
- Why Has the American Government Not Managed to Stop Drug Abuse All These Years?
- How Does Drug Abuse Affect Personal Development of Hong Kong Teenagers?
- How Does Pericarditis Form Due to Drug Abuse?
- How Drug Abuse Ruins Families and Destroys Relationships?
- How Does Prescription Drug Abuse Affect Teens?
- Does the Drug Abuse Resistance Education Program Work?
- What Is the Drug of Abuse?
- What Are the Four Types of Drugs Abused?
- Which Is an Example of Drug Abuse?
- What Is the Leading Cause of Drug Abuse?
- What Are the Causes and Effects of Drug Abuse?
- What Are the Main Consequences of Drug Abuse?
- How Does Drug Abuse Affect Our Society?
- How Can We Prevent Drug Abuse?
- Why Is It Essential to Prevent Drugs?
- What Are the Ten Most Abused Drugs?
- How Do Drugs Affect Mental Health?
- What Are the Effects of Drug Abuse on Youths?
- What Is the Connection Between Adolescents From Divorced Families and Drug Abuse?
- Are Alcohol and Drug Abuse the Most Common Issues of Today?
- What Is Athletes’ Motivation for Performance-Enhancement Drug Abuse?
- What Is the Correlation Between Parietal and Adolescent Drug Abuse?
- How Is Dealing With Teenage Drug Abuse?
- What Is the Difference Between Drug Use and Drug Abuse?
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 26). 108 Drug Abuse Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/drug-abuse-essay-examples/
"108 Drug Abuse Essay Topic Ideas & Examples." IvyPanda , 26 Feb. 2024, ivypanda.com/essays/topic/drug-abuse-essay-examples/.
IvyPanda . (2024) '108 Drug Abuse Essay Topic Ideas & Examples'. 26 February.
IvyPanda . 2024. "108 Drug Abuse Essay Topic Ideas & Examples." February 26, 2024. https://ivypanda.com/essays/topic/drug-abuse-essay-examples/.
1. IvyPanda . "108 Drug Abuse Essay Topic Ideas & Examples." February 26, 2024. https://ivypanda.com/essays/topic/drug-abuse-essay-examples/.
Bibliography
IvyPanda . "108 Drug Abuse Essay Topic Ideas & Examples." February 26, 2024. https://ivypanda.com/essays/topic/drug-abuse-essay-examples/.
- Drugs Titles
- Opioids Research Topics
- Cannabis Essay Titles
- Drug Trafficking Research Topics
- Addiction Essay Topics
- War on Drugs Questions
- Mental Disorder Essay Topics
- Crime Ideas
- Alcohol Abuse Paper Topics
- Mental Health Essay Ideas
- Human Behavior Research Topics
- Mental Illness Research Topics
- AIDS Titles
- Criminal Behavior Essay Topics
- Juvenile Delinquency Essay Titles
Making Addiction Treatment More Realistic and Pragmatic: The Perfect Should Not be the Enemy of the Good

This essay was also published by Health Affairs on January 3, 2022.
Last year saw drug overdose deaths in the U.S. surpass an unthinkable milestone: 100,000 deaths in a year. This is the highest number of drug overdoses in our country’s history, and the numbers are climbing every month.
There is an urgent need for a nationwide, coordinated response that a tragedy of this magnitude demands. Recent data from 2020 shows that only 13 percent of people with drug use disorders receive any treatment. Only 11 percent of people with opioid use disorder receive one of the three safe and effective medications that could help them quit and stay in recovery.
The magnitude of this crisis demands out-of-the-box thinking and willingness to jettison old, unhelpful, and unsupported assumptions about what treatment and recovery need to look like. Among them is the traditional view that abstinence is the sole aim and only valid outcome of addiction treatment.
While not using any drugs or alcohol poses the fewest health risks and is often necessary for sustained recovery, different people may need different options. Temporary returns to use after periods of abstinence are part of many recovery journeys, and it shouldn’t be ruled out that some substance use or ongoing use of other substances even during treatment and recovery might be a way forward for some subset of individuals.
Reduced number of heavy drinking days is already recognized as a meaningful clinical outcome in research and medication development for alcohol addiction. Clinical endpoints other than abstinence , such as reduced use, are now being considered in medication trials for drug use disorders. This could facilitate the approval of a wider range of medications to treat addiction, as well as open the door to medications that address symptoms associated with it, such as sleep disorders and anxiety. The existing medications methadone, buprenorphine, and naltrexone have proven to be effective at reducing relapse risk and improving other outcomes in patients with opioid use disorder, but more options could benefit more patients. And medications to treat other drug use disorders are needed.
Temporary returns to drug use are so common and expected during treatment and recovery that addiction is described as a chronic relapsing condition, like some autoimmune diseases. Yet these setbacks may still be regarded by family, friends, communities, and even physicians as failures, resetting the clock of recovery to zero. Patients in some drug addiction treatment programs are even expelled if they produce positive urine samples.
Healthcare and society must move beyond this dichotomous, moralistic view of drug use and abstinence and the judgmental attitudes and practices that go with it.
There are still many unknowns about the different trajectories that recovery may take, but stereotypes should not guide us in the absence of knowledge. Research in the field of nicotine addiction shows that a person’s first cigarette after a period of abstinence raises the risk of returning to their pre-treatment use pattern but does not always have that outcome. Research on the consequences of returning to opioid, stimulant, or cannabis use after a period of non-use is still needed, but there is little evidence to support the assumption—reinforced in movies and TV shows—that a single return to drug use following on a one-time loss of resolve will automatically lead the individual straight back to their former compulsive consumption.
Medicine can perhaps learn from the recovery world, where a distinction is increasingly made between a one-time return to drug use, a “slip” or “lapse,” and a return to the heavy and compulsive use pattern of an individual’s active addiction—the more stereotypical understanding of relapse. The distinction is meant to acknowledge that a person’s resolve to recover may even be strengthened by such lapses and that they need not be catastrophic for the individual’s recovery.
A return to substance use after a period of abstinence may also, in some cases, lead to less frequent use than before treatment. Such a trajectory has been identified in research on drug and alcohol treatment outcomes in adolescents . For some drugs, any reduced use is likely beneficial : Less frequent illicit substance use means less frequent need to obtain an illicit substance and fewer opportunities for infectious disease transmission or fatal overdose. It may also increase the likelihood that a person can be a supportive family member, hold a job, and make other healthy choices in their life.
But as long as treatment is only regarded as successful if it produces abstinence, then even one-time lapses can trigger unnecessary guilt, shame, and hopelessness. If an individual feels like they are bad, weak, or wrong for taking a drink or drug after a period in recovery, it could potentially make it more likely for those slips to become more serious relapses. As it now stands, even a slip can produce a positive urine sample or force the honest patient to self-report a return to drug use, which can then trigger the judgment and punitive policies of their treatment program or the law as well as trigger the personal sense that they have failed again and there is no hope for their recovery.
Another deleterious effect of equating treatment success with abstinence and drug use with treatment failure is that some people with SUDs are unready to give up substances completely. In fact, this is one of the main reasons people who could benefit from addiction treatment do not seek it. Although it may not be ideal or optimal, treating an opioid or methamphetamine use disorder even while a person continues to use cannabis or alcohol would be a net individual and public health benefit.
Realistically and pragmatically addressing addiction requires that we not let the perfect be the enemy of the good. Right now, we need all the good we can get. It also means offering supports for people with SUD that protect against the worst consequences of drug use. Syringe-services programs reduce HIV transmission and offer people an entry point into treatment; naloxone distribution to people who use opioids and their families reduces overdose fatalities. Neither of these measures increase drug use in communities that implement them, as critics often worry.
Other harm-reduction modalities being studied include personal drug-testing equipment like fentanyl test strips, as well as overdose prevention centers—places where people can use drugs under medical supervision, which are in operation in other countries and, as of late November, are available in New York City. Such services could potentially help mitigate some of the risks associated with lapses and relapses, such as heightened risk of overdose due to lost tolerance. The latter currently accounts for many fatal overdoses after people with an untreated opioid use disorder are released from prison, for example.
Drug addiction is a chronic but treatable disorder with well-understood genetic and social contributors. It is not a sign of a person’s weakness or bad character. Continued or intermittent use of drugs, even by people who know they have a disorder and are trying hard to recover from it, must be acknowledged as part of the reality of the disorder for many who struggle with it. Just as we must stop stigmatizing addiction, we must also stop stigmatizing people who use drugs as being bad or weak, and instead offer them support to help prevent addiction’s most adverse consequences.

Dr. Nora Volkow, Director
Here I highlight important work being done at NIDA and other news related to the science of drug use and addiction.
Recent Blog Posts
50 years after founding, NIDA urges following science to move beyond stigma

The power of protective layers: Employers advancing whole-person health

Innovative projects answer NIDA’s challenge to implement substance use prevention in primary care
Social Trends
Never stop moving.
Understanding the Impact of Drug Use on Health

Exploring the vast landscape of drug use and its implications on health unfolds an intricate tableau that is as complex as it is fascinating. It’s a topic that wades through the muddy waters of scientific research, societal norms, and personal choices. In this discourse, we aim to dissect the myriad ways in which drugs – be they prescribed, over-the-counter, or illicit – play a role in shaping our health landscape. Let’s dive into this nuanced exploration with an open mind and a touch of curiosity.
The Role of Community in Recovery and Prevention
To begin, it seems pertinent to highlight that community resources and support networks play an indispensable role in both the prevention of drug misuse and the recovery process. Broader access to healthcare can help connect community members to unknown substance drug testing , treatment, recovery centers, and more. From there, resources like peer support groups and community education programs offer a framework for shared experiences and collective healing. Engaging with community initiatives can bolster individual resilience, reduce stigma, and promote a culture of health and well-being.
Navigating the World of Over-the-Counter Drugs
Over-the-counter (OTC) drugs, accessible and ubiquitous, offer both convenience and challenge. Their availability empowers individuals to manage minor health issues independently, fostering an environment of proactive self-care. However, the ease of access to OTC drugs can also lead to underestimated risks, including misuse and interactions with other medications . Enlightening ourselves about these potential pitfalls is key to maximizing their benefits while minimizing harm.
The Double-Edged Sword of Prescription Medications
Prescription medications, while a cornerstone of modern medicine, wield immense power over our health. These meticulously crafted compounds, when utilized with precision, can be life-saving. Yet, their misuse or overuse heralds a different tale – one of dependency, adverse reactions, and a cascading series of health complications. Unraveling the delicate balance between benefit and harm uncovers the critical importance of informed usage and healthcare guidance.
Advancements in Medical Treatments for Addiction
The field of addiction medicine has seen remarkable advancements in recent years, with new medications and therapies offering hope to those struggling with drug dependence. These medical interventions, when coupled with supportive psychotherapy and holistic care, can significantly improve outcomes for individuals. It’s an exciting time in the realm of substance use treatment, as researchers and clinicians continue to push the boundaries of what’s possible.
The Physical Body on Drugs: A Biological Perspective
At their core, drugs interact with the body’s biological systems in profound ways. This interaction, depending on the substance and the context, can either reinforce health or ravage it. This segment delves into the mechanics of how various drugs affect the body, highlighting the sometimes astonishing, sometimes alarming physiological changes that ensue.
The Ripple Effect of Illicit Drug Use
The realm of illicit drugs is fraught with danger, not solely because of legal implications but due to the profound and often irreversible impact they have on health. From the immediate high to the long-term degradation of mental and physical well-being , the ripple effects are wide-reaching. This section explores the intricate web of consequences that illicit drug use weaves, shedding light on the broader societal and individual health ramifications.
Prevention and Recovery: Navigating the Path to Health
While the landscape of drug use is undoubtedly complex, there lies hope in prevention, treatment, and recovery. The journey towards health, for those touched by drug use, is both personal and collective. Society’s role in supporting prevention efforts and recovery paths underscores the importance of compassion, understanding, and comprehensive health strategies.
Psychological Thrills and Spills: The Mental Health Equation
Drug use does not exist in a vacuum; its influence on mental health is significant and multifaceted. From temporary euphoria to the depths of depression, the psychological roller-coaster associated with drug use can be as compelling as it is catastrophic. Understanding the complex interplay between drugs and our mental state offers insights into the broader discussion of substance use and mental health care.
Exploring Holistic Approaches to Drug Recovery
In recent years, the move towards holistic care paradigms has been gathering momentum. This approach emphasizes the interconnectedness of physical, psychological, and social health, advocating for strategies that encompass all aspects of a person’s life. By integrating traditional medical treatments with complementary therapies such as meditation, exercise, and nutritional counseling, individuals are finding new paths to recovery that are both empowering and sustainable.
Delving into the impact of drug use on health reveals a tapestry rich with challenges, lessons, and opportunities. As we navigate this intricate terrain, the importance of informed choices, supportive networks, and resilient health systems becomes glaringly apparent. It’s a journey that demands our attention, empathy, and action. Let’s tread this path with awareness and an eagerness to understand the vast spectrum of human health in the context of drug use.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

25,000+ students realised their study abroad dream with us. Take the first step today
Meet top uk universities from the comfort of your home, here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- School Education /
Essay on Drug Abuse in 250 and 500 Words in English for Students
- Updated on
- Apr 2, 2024

Drug abuse refers to the excessive and frequent consumption of drugs. Drug abuse can have several harmful effects on our mental and physical health. Ronald Reagan, the 40th President of the USA, passed the Anti-Drug Abuse Act of 1986 and initiated the War on Drugs . He said, ‘Let us not forget who we are. Drug abuse is a repudiation of everything America is.’
Consuming drugs not only harms the individual himself but also affects society as a whole. Studies have shown that people who consume drugs become addicted to it. This addiction turns into substance abuse, resulting in self-damage, behaviour changes, mood swings, unnecessary weight loss, and several other health problems. Let’s understand what drug abuse is and how to fight it.
This Blog Includes:
Essay on drug abuse in 250 words, why do people consume drugs, why is drug abuse bad, laws in india against drug consumption, steps to prevent drug addiction, 10 lines essay on drug abuse.
Quick Read: Essay on CAA (Citizenship Amendment Act)
‘When people consume drugs regularly and become addicted to it, it is known as drug abuse. In medical terminology, drugs means medicines. However, the consumption of drugs is for non-medical purposes. It involves the consumption of substances in illegal and harmful ways, such as swallowing, inhaling, or injecting. When drugs are consumed, they are mixed into our bloodstream, affecting our neural system and brain functioning.
The Indian government has taken significant steps to help reduce the consumption of drugs. In 1985, the Narcotics Drugs and Psychotropic Substances Act came into force. This act replaced the Opium Act of 1857, the Opium Act of 1878, and the Dangerous Drugs Act of 1930.
Drug abuse can lead to addiction, where a person becomes physically or psychologically dependent on the substance and experiences withdrawal symptoms when attempting to stop using it.
Drug abuse can have serious consequences for the individual and society as a whole. On an individual level, drugs can damage physical health, including organ damage, infectious diseases, and overdose fatalities. Not only this, a person already suffering from mental health disorders will face more harmful aftereffects. Addiction disrupts our cognitive functioning and impairs our decision-making abilities.
To fight drug abuse, we need collective action from all sections of society. Medical professionals say that early intervention and screening programmes can identify individuals at risk of substance misuse and provide them with the necessary support services. Educating people, especially those who are at-risk, about drug abuse and its harmful effects can significantly help reduce their consumption.
Drug abuse is serious and it must be addressed. Drug abuse is killing youth and society. Therefore, it is an urgent topic to address, and only through sustainable and collective efforts can we address this problem.
Quick Read: Success in Life Speech
Essay on Drug Abuse in 500 Words
Drug abuse is known as frequent consumption. In time, these people become dependent on drugs for several reasons. Curiosity drives adolescents and teenagers, who are among the most susceptible groups in our society. Cocaine, marijuana, methamphetamine, heroin, etc. are some of the popular drugs consumed.
The very first question about drugs is: why do people consume drugs? Studies have shown that more than 50% of drug addicts consider drugs as a coping mechanism to alleviate emotional or psychological distress. In the beginning, drugs temporarily relieve feelings of anxiety, depression, or trauma, providing a temporary escape from difficult emotions or life circumstances.
Some consume drugs out of curiosity, some under peer pressure, and some want to escape the painful experiences. Some people enjoy the effects drugs produce, such as euphoria, relaxation, and altered perceptions. Recreational drug use may occur in social settings or as a form of self-medication for stress relief or relaxation.
The National Institute on Drug Abuse states that drugs can worsen our eyesight and body movement, our physical growth, etc. Marijuana, one of the most popular drugs, can slow down our reaction time, affecting our time and distance judgement and decreasing coordination. Cocaine and Methamphetamine can make the consumer aggressive and careless.
Our brain is the first victim of drugs. Drugs can disorder our body in several ways, from damaging organs to messing with our brains. Drugs easily get mixed into our bloodstream, and affect our neural system. Prolonged and excessive consumption of drugs significantly harms our brain functioning.
The next target of drug abuse is our physical health and relationships. Drugs can damage our vital organs, such as the liver, heart, lungs, and brain. For example, heavy alcohol use can lead to cirrhosis of the liver, while cocaine use can increase the risk of heart attack and stroke.
Here is an interesting thing; the USA has the highest number of drug addicts and also has strict laws against drug consumption. According to a report by the Narcotics Control Bureau, around 9 million people in India consume different types of drugs. The Indian government has implemented certain laws against drug consumption and production.
The Narcotic Drugs and Psychotropic Substances Act, 1985 (NDPS), prohibits the production, sale, purchase, and consumption of narcotics and other illegal substances, except for scientific and medical purposes.
Also, Article 47 of the Indian Constitution states that ‘ The State shall endeavour to bring about prohibition of the consumption, except for medicinal purposes, of intoxicating drinks and drugs which are injurious to health.’
Quick Read: Essay on Indian Festivals in 500 Words
Several steps can be taken to prevent drug addiction. But before we start our ‘War on Drugs’ , it is crucial to understand the trigger point. Our social environment, mental health issues and sometimes genetic factors can play a role in drug abuse.
- Education and awareness are the primary weapons in the fight against drugs.
- Keeping distance from people and places addicted to drugs.
- Encourage a healthy and active lifestyle and indulge in physical workouts.
- Watch motivating videos and listen to sound music.
- Self-motivate yourself to stop consuming drugs.
- Talk to a medical professional or a psychiatrist, who will guide you to the right path.
Drug abuse is a serious problem. The excessive and frequent consumption of drugs not only harms the individual but also affects society as a whole. Only a collective approach from lawmakers, healthcare professionals, educators, community leaders, and individuals themselves can combat drug abuse effectively.
Quick Read: Speech About Life
Here is a 10-line essay on drug abuse.
- Drug abuse can significantly affect our physical growth
- Drug abuse can affect our mental functioning.
- Drug abuse may provide instant pleasure, but inside, it weakens our willpower and physical strength.
- Educating people, especially those who are at-risk, about drug abuse and its harmful effects can significantly help reduce their consumption.
- Drugs easily get mixed into our bloodstream, and affect our neural system.
- Prolonged and excessive consumption of drugs significantly harms our brain functioning.
- In 1985, the Narcotics Drugs and Psychotropic Substances Act came into force.
- The USA has the highest number of drug addicts and also has strict laws against drug consumption.
- Drug addicts consider drugs as a coping mechanism to alleviate emotional or psychological distress.
- Adolescents and teenagers are the most vulnerable section of our society and are driven by curiosity.
Ans: Drug abuse refers to the excessive and frequent consumption of drugs. Drug abuse can have several harmful effects on our mental and physical health.
Ans: ‘When people consume drugs regularly and become addicted to it, it is known as drug abuse. In medical terminology, drugs means medicines. However, the consumption of drugs is for non-medical purposes. It involves the consumption of substances in illegal and harmful ways, such as swallowing, inhaling, or injecting. When drugs are consumed, they are mixed into our bloodstream, affecting our neural system and brain functioning.
Ans: Drug abuse is known as frequent consumption. In time, these people become dependent on drugs for several reasons. Adolescents and teenagers are the most vulnerable section of our society who are driven by curiosity. Cocaine, marijuana, methamphetamine, heroin, etc. are some of the popular drugs consumed. The Narcotic Drugs and Psychotropic Substances Act, 1985 (NDPS), prohibits the production, sale, purchase, and consumption of narcotics and other illegal substances, except for scientific and medical purposes.
Popular Essay Topics for Students
For more information on such interesting topics, visit our essay writing page and follow Leverage Edu.
Shiva Tyagi
With an experience of over a year, I've developed a passion for writing blogs on wide range of topics. I am mostly inspired from topics related to social and environmental fields, where you come up with a positive outcome.
Leave a Reply Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Contact no. *

Connect With Us
25,000+ students realised their study abroad dream with us. Take the first step today.

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
January 2024
September 2024
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
Have something on your mind?

Make your study abroad dream a reality in January 2022 with
India's Biggest Virtual University Fair

Essex Direct Admission Day
Why attend .

Don't Miss Out

Essay on Addiction
Students are often asked to write an essay on Addiction in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Addiction
Understanding addiction.
Addiction is a strong desire to do something repeatedly, even if it’s harmful. It’s like a brain disease. People can get addicted to different things like drugs, alcohol, or even activities like gambling.
Why People Get Addicted
People can get addicted for many reasons. Some may feel good when they do something, so they repeat it. Others may want to escape from problems or stress. Sometimes, it’s because of peer pressure or trying to fit in.
Effects of Addiction
Addiction can harm a person’s health. It can lead to diseases, mental problems, and even death. It can also ruin relationships and cause problems at work or school.
Overcoming Addiction
Overcoming addiction is hard, but possible. It needs strong willpower and often help from doctors or therapists. Support from family and friends is also important. Remember, it’s okay to ask for help.
Preventing Addiction
To avoid addiction, we should learn about its dangers. It’s also important to make good friends and have healthy habits. Always remember, it’s okay to say no if something doesn’t feel right.
250 Words Essay on Addiction
What is addiction.
Addiction is when a person can’t stop doing something, even if it’s harmful. It can be about drugs, alcohol, games, or even food. The person knows it’s bad but can’t stop. It’s like a strong pull that keeps them going back.
How Does it Start?
Addiction often starts with trying something new. This could be a friend offering a cigarette, or playing a new video game. At first, it seems fun and exciting. But over time, the person starts needing it more and more. It becomes a need, not just a want.
The Impact of Addiction
Addiction can hurt a person in many ways. It can make them sick, or cause problems at school or work. It can also hurt their relationships with family and friends. They may lie or steal to keep doing what they’re addicted to. This can lead to feelings of guilt and shame.
Fighting Addiction
Fighting addiction is hard, but not impossible. It starts with admitting there’s a problem. Then, the person needs help from professionals like doctors or counselors. They can give advice, medicine, or therapy to help the person quit. Support from family and friends is also important.
Remember, it’s okay to ask for help. Everyone struggles with something at some point. With the right help and support, anyone can overcome addiction.
Addiction is a serious problem that can harm a person’s health, work, and relationships. But with help and support, it can be overcome. It’s important to understand addiction so we can help others or ourselves if needed.
500 Words Essay on Addiction
Addiction is a serious issue that affects many people around the world. It is a state where a person cannot stop using a substance or engaging in a behavior, even if it is harmful. The person becomes dependent on the substance or the activity to feel good or normal.
Types of Addiction
Addiction can be of two types: substance addiction and behavioral addiction. Substance addiction involves drugs, alcohol, nicotine, or other substances. Behavioral addiction involves activities like gambling, eating, or using the internet.
Causes of Addiction
There is no single reason why someone becomes addicted. It can be due to a mix of genetic, environmental, and psychological factors. Some people may be more prone to addiction because of their genes. Others may turn to addictive substances or behaviors to cope with stress or emotional issues.
Addiction has a negative impact on a person’s health, relationships, and daily life. It can lead to physical health problems like heart disease or mental health issues like depression. Addiction can also strain relationships with family and friends and make it hard for the person to perform well at school or work.
Overcoming addiction is not easy, but it is possible with the right help and support. This can include professional treatment like therapy or medication, as well as support from loved ones. It is important for the person to learn healthy ways to cope with stress and other triggers that may lead to addictive behavior.
Prevention is key in the fight against addiction. This can involve teaching young people about the dangers of substance use and addictive behaviors. It also means creating supportive environments where people can talk about their struggles and seek help if they need it.
In conclusion, addiction is a complex issue that requires understanding, support, and prevention efforts. It is important for everyone to be aware of the signs of addiction and to seek help if they or someone they know is struggling. Remember, overcoming addiction is possible with the right help and support.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Actual Self
- Essay on Things To Argue
- Essay on Things That Matter
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

Medicalization and the Philosophy of Addiction
Addiction medicine has brought great benefits. but it is not without limits..
Updated March 29, 2024 | Reviewed by Gary Drevitch
- What Is Addiction?
- Find a therapist to overcome addiction
The term "medicalization" was popularized by the Catholic philosopher and social critic Ivan Illich. Illich was troubled by the way in which what was formerly regarded as deviant behavior had come to be the province of medicine, as well as with the prevalence of those harms he deemed "iatrogenic"—that is, caused by medical treatment itself—in another term popularized by Illich.
Illich's major work on this topic, Medical Nemesis , was published in 1975, and is not nearly as widely discussed as it once was. (He used to be discussed regularly in American mass media, such as Time magazine, but I find that many philosophers and social workers today don't know his name). As it happens, this was around the same moment that the field of "addiction medicine" as we now know it was born. The National Institute of Drug Abuse was founded in 1974, and the American Academy of Addictionology (a precursor to the American Society of Addiction Medicine) was founded by physician G. Douglas Talbott shortly afterward.
Now, roughly 50 years later, addiction medicine has expanded vastly while Illich's work has become, as I have said, obscure. Nonetheless, it is worth reconsidering the achievements of addiction medicine from the point of view of Illich's work, or from the point of view of what Illich might have called the "medicalization of addiction."

The achievements of addiction medicine are many and probably not celebrated frequently enough: the management of alcohol withdrawal (which can be fatal when untreated), the development and deployment of nicotine replacement therapy for tobacco addiction, and, perhaps most prominent in recent discussions, the deployment of medicines (such as Suboxone) for the management of opioid use disorder, as well as of medicines (Naloxone) that reverse opiate overdoses. These medical interventions have simply been life-saving for many people.
Yet the specter of "medicalization" still looms. It is perhaps most clear when we consider addictions whose relationship to substances, and so to the traditional provinces of medicine, are more remote.
In a 2011 article, the British physician Andrew Moscrop argued that "problem gambling" has increasingly come to be seen as a medical issue, with primary care physicians expected to serve as the first line for intervention with gamblers. Moscrop's hypothesis is that our traditional tendencies to scorn those who are profligate or wasteful has been transmuted, in an era of medicalization, to see "problem gambling" as a medical issue, and to see "problem gamblers" as individuals in need of treatment. Among other things, this framing has the advantage of allowing us to understand gambling challenges in individual-level terms, rather than as understanding them as consequences of larger social and economic inequities.
Moscrop therefore proposes that, for at least some addictions, we should exercise some caution in understanding them in medical terms. This does not require us to be Illichian skeptics about much of medicine, but it does call for a certain degree of humility about the medical enterprise. He writes: "Our patients present problems that are frequently neither physical nor psychological, but social or even spiritual . For their sake and ours it is imperative that we possess a secure sense of what problems we might address usefully and which ones we risk medicalising with admirably-intentioned, but ultimately unhelpful, interventions."
Despite the reservations voiced by Moscrop and some other physicians, many people continue to take a medicalized view of addiction – even in addictions, such as gambling, that tend to take place outside the purview of the traditional provinces of medicine. This is true not only of physicians themselves, who may in fact be more sensitive than most to the limits of medical interventions, but of the broader culture. Why is this?
One reason, I believe, is a limited sense of the available alternatives. Medical approaches to addiction have displaced more legal and indeed criminal approaches to the treatment of addiction, though this process is still incomplete in many places. And if our only alternative to a medical approach to addiction is a criminal one, then we should take it. Even if a hospital or a primary care office is not the ideal setting for the treatment of a gambling addiction, it is certainly much better than a jail.
But these are not our only alternatives. I argue that addiction is a disability , and – like disabilities generally – it should not be presumed to be a defect that needs to be treated or managed by physicians, though disabilities have often been seen that way in the past, and in many places still are. Rather, people with disabilities are different, and may want to avail themselves of medical interventions, but may also rationally choose to decline them. So too, I want to say, for addiction.

This does not mean addiction should be treated criminally, any more that we think disabilities call for criminal sanction (which, of course, they do not). Rather, it calls us to articulate a third alternative, on which addiction is to be approached neither through the criminal law, nor primarily through medicine, but through politics . People with addictions are a class of people, with certain interests, and what is needed, I think, is that their interests be fairly represented in the political process. Physicians will have a role in this process, but not an authoritative one. Rather, it is addicted people themselves who must have the final say.
A. Moscrop (2011), "Medicalisation, morality, and addiction: why we should be wary of problem gamblers in primary care," British Journal of General Practice 61: 836-838.

John T. Maier, Ph.D., MSW , is a psychotherapist in private practice in Cambridge, Massachusetts.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- Engineering
- Write For Us
- Privacy Policy

Essay on Drug Abuse

Here we have shared the Essay on Drug Abuse in detail so you can use it in your exam or assignment of 150, 250, 400, 500, or 1000 words.
You can use this Essay on Drug Abuse in any assignment or project whether you are in school (class 10th or 12th), college, or preparing for answer writing in competitive exams.
Topics covered in this article.
Essay on Drug Abuse in 150 words
Essay on drug abuse in 250-300 words, essay on drug abuse in 500-1000 words.
Drug abuse is a global issue that poses serious risks to individuals and society. It involves the harmful and excessive use of drugs, leading to physical and mental health problems. Drug abuse can result in addiction, organ damage, cognitive impairment, and social and economic difficulties. Prevention efforts should focus on education, raising awareness about the dangers of drug abuse, and promoting healthy lifestyles. Access to quality healthcare and addiction treatment services is crucial for recovery. Strengthening law enforcement measures against drug trafficking is necessary to address the supply side of the problem. Creating supportive environments and opportunities for positive engagement can help prevent drug abuse. By taking collective action, we can combat drug abuse and build healthier communities.
Drug abuse is a growing global concern that poses significant risks to individuals, families, and communities. It refers to the excessive and harmful use of drugs, both legal and illegal, that have negative effects on physical and mental health.
Drug abuse has severe consequences for individuals and society. Physically, drug abuse can lead to addiction, damage vital organs, and increase the risk of overdose. Mentally, it can cause cognitive impairment, and psychological disorders, and deteriorate overall well-being. Additionally, drug abuse often leads to social and economic problems, such as strained relationships, loss of employment, and criminal activities.
Preventing drug abuse requires a multi-faceted approach. Education and awareness programs play a crucial role in informing individuals about the dangers of drug abuse and promoting healthy lifestyle choices. Access to quality healthcare and addiction treatment services is vital to help individuals recover from substance abuse. Strengthening law enforcement efforts to curb drug trafficking and promoting international cooperation is also essential to address the supply side of the issue.
Community support and a nurturing environment are critical in preventing drug abuse. Creating opportunities for individuals, especially young people, to engage in positive activities and providing social support systems can serve as protective factors against drug abuse.
In conclusion, drug abuse is a significant societal problem with detrimental effects on individuals and communities. It requires a comprehensive approach involving education, prevention, treatment, and enforcement. By addressing the root causes, raising awareness, and providing support to those affected, we can combat drug abuse and create a healthier and safer society for all.
Title: Drug Abuse – A Global Crisis Demanding Urgent Action
Introduction :
Drug abuse is a pressing global issue that poses significant risks to individuals, families, and communities. It refers to the excessive and harmful use of drugs, both legal and illegal, that have detrimental effects on physical and mental health. This essay explores the causes and consequences of drug abuse, the social and economic impact, prevention and treatment strategies, and the importance of raising awareness and fostering supportive communities in addressing this crisis.
Causes and Factors Contributing to Drug Abuse
Several factors contribute to drug abuse. Genetic predisposition, peer pressure, stress, trauma, and environmental influences play a role in initiating substance use. The availability and accessibility of drugs, as well as societal norms and cultural acceptance, also influence drug abuse patterns. Additionally, underlying mental health issues and co-occurring disorders can drive individuals to self-medicate with drugs.
Consequences of Drug Abuse
Drug abuse has devastating consequences on individuals and society. Physically, drug abuse can lead to addiction, tolerance, and withdrawal symptoms. Substance abuse affects vital organs, impairs cognitive function, and increases the risk of accidents and injuries. Mental health disorders, such as depression, anxiety, and psychosis, are often associated with drug abuse. Substance abuse also takes a toll on relationships, leading to strained family dynamics, social isolation, and financial instability. The social and economic costs of drug abuse include increased healthcare expenses, decreased productivity, and the burden on criminal justice systems.
Prevention and Education
Preventing drug abuse requires a comprehensive and multi-faceted approach. Education and awareness programs are essential in schools, communities, and the media to inform individuals about the risks and consequences of drug abuse. Promoting healthy coping mechanisms, stress management skills, and decision-making abilities can empower individuals to resist peer pressure and make informed choices. Early intervention programs that identify at-risk individuals and provide support and resources are crucial in preventing substance abuse.
Treatment and Recovery
Access to quality healthcare and evidence-based addiction treatment is vital in addressing drug abuse. Treatment options include detoxification, counseling, behavioral therapies, and medication-assisted treatments. Rehabilitation centers, support groups, and outpatient programs provide a continuum of care for individuals seeking recovery. Holistic approaches, such as addressing co-occurring mental health disorders and promoting healthy lifestyles, contribute to successful long-term recovery. Support from family, friends, and communities plays a significant role in sustaining recovery and preventing relapse.
Law Enforcement and Drug Policies
Effective law enforcement efforts are necessary to disrupt drug trafficking and dismantle illicit drug networks. International cooperation and collaboration are crucial in combating the global drug trade. Additionally, drug policies should focus on a balanced approach that combines law enforcement with prevention, treatment, and harm reduction strategies. Shifting the emphasis from punitive measures toward prevention and rehabilitation can lead to more effective outcomes.
Creating Supportive Communities:
Fostering supportive communities is vital in addressing drug abuse. Communities should provide resources, social support networks, and opportunities for positive engagement. This includes promoting healthy recreational activities, providing vocational training, and creating safe spaces for individuals in recovery. Reducing the stigma associated with drug abuse and encouraging empathy and understanding are crucial to building a compassionate and supportive environment.
Conclusion :
Drug abuse remains a complex and multifaceted issue with far-reaching consequences. By addressing the causes, raising awareness, implementing preventive measures, providing quality treatment and support services, and fostering supportive communities, we can combat drug abuse and alleviate its impact. It requires collaboration and a collective effort from individuals, communities, governments, and organizations to build a society that is resilient against the scourge of drug abuse. Through education, prevention, treatment, and compassion, we can pave the way toward a healthier and drug-free future.
The Global Prevalence of Problem and Pathological Gambling and Its Associated Factors Among Individuals with Substance Use Disorders: A Meta-analysis
- Original Article
- Published: 12 October 2023
Cite this article
- Bahram Armoon ORCID: orcid.org/0000-0001-5467-9889 1 ,
- Mark D. Griffiths 2 ,
- Marie-Josée Fleury 3 , 4 ,
- Rasool Mohammadi 5 &
- Amir-Hossien Bayat 6 , 1
376 Accesses
Explore all metrics
The present systematic review and meta-analysis assessed the prevalence, sociodemographic factors, mental health disorders, and type of drug use disorders associated with problem/pathological gambling among individuals with substance use disorders (SUDs). Published studies before January 1, 2023, were reviewed. Out of 8351 papers initially identified, 61 studies remained for meta-analysis. The findings indicated that among individuals with SUDs there was a lifetime pooled prevalence rate of 23% for at-risk gambling disorder (GD), 19% for problem gambling, and 17% for pathological gambling. The pooled lifetime prevalence of SUDs among individuals with problem/pathological gambling was 18%. The findings indicated that individuals with SUDs who were male, had depressive and mood disorders, and had alcohol, tobacco, and cannabis use disorders were more likely to report problem and/or pathological gambling. Consideration of type of substance use and individuals’ mental health disorders during primary treatment could be useful for reducing GD among individuals with SUDs.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
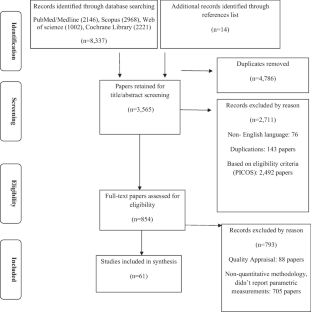
Similar content being viewed by others

Risk and protective factors of drug abuse among adolescents: a systematic review
Azmawati Mohammed Nawi, Rozmi Ismail, … Nurul Shafini Shafurdin

An update on the prevalence of eating disorders in the general population: a systematic review and meta-analysis
Jie Qian, Ying Wu, … Dehua Yu

Stability of Drinking Reductions and Long-term Functioning Among Patients with Alcohol Use Disorder
Katie Witkiewitz, Henry R. Kranzler, … Raymond F. Anton
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Confidence intervals
Gambling disorder
Problem Gambling Severity Index
Medical Subject Headings
Newcastle-Ottawa Scale
Odds ratios
Population, exposures, comparison, outcome, and study design
Protocols of Systematic Reviews and Meta-Analyses
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders
The National Opinion Research Center DSM Screen for Gambling Problems
The South Oaks Gambling Screen
Substance use disorders (SUDs)
References with an asterisk denote the studies that were included in the meta-analysis
Abdollahnejad, R., Delfabbro P., & Denson, L. (2014). Understanding the relationship between pathological gambling and gambling-related cognition scores: The role of alcohol use disorder and delusion proneness. International Gambling Studies, 14 (2), 183–195. https://doi.org/10.1080/14459795.2014.886711
*Adamson, S. J., Todd, F. C., Douglas Sellman J., Huriwai, T., & Porter, J. (2006). Coexisting psychiatric disorders in a New Zealand outpatient alcohol and other drug clinical population. Australian & New Zealand Journal of Psychiatry, 40 (2), 164–170. https://doi.org/10.1080/j.1440-1614.2006.01764.x
Alcaro, A., Brennan, A., & Conversi, D. (2021). The seeking drive and its fixation: A neuro-psycho-evolutionary approach to the pathology of addiction. Frontiers in Human Neuroscience, 15 , 635932. https://doi.org/10.3389/fnhum.2021.635932
Article CAS PubMed PubMed Central Google Scholar
Alessi, M. C., Martinotti, G., De Berardis, D., Sociali, A., Di Natale, C., Sepede, G., Cheffo, D. P. R., Monti, L., Casella, P., & Pettorruso, M. (2022). Craving variations in patients with substance use disorder and gambling during COVID-19 lockdown: The Italian experience. World Journal of Clinical Cases, 10 (3), 882. https://doi.org/10.12998/wjcc.v10.i3.882
Article PubMed PubMed Central Google Scholar
Algren, M. H., Ekholm, O., Davidsen, M., Larsen, C. V. L., & Juel, K. (2015). Health behaviour and body mass index among problem gamblers: Results from a nationwide survey. Journal of Gambling Studies, 31 (2), 547–556. https://doi.org/10.1007/s10899-013-9437-y
Article PubMed Google Scholar
*Anpaa Nalpas, B., Yguel, J., Fleury, B., Martin, S., Jarraud, D., & Craplet, M. (2011). Pathological gambling in treatment-seeking alcoholics: A national survey in France. Alcohol and Alcoholism, 46 (2), 156–160. https://doi.org/10.1093/alcalc/agq099
American Psychiatric Association [APA]. (2013). Diagnostic and statistical manual of mental disorders : DSM-5 . Arlington , VA : American Psychiatric Association.
*Baldo V., Cristofoletti M., Majori S., Cibin M., Peron C., Dal Zotto A., Zampieri N., Saia M., & Trivello, R. (2006). Relationship between pathological gambling, alcoholism and drug addiction. Annals of Hygiene, 18 (2), 147–153.
Balodis, I. M., & Potenza, M. N. (2020). Common neurobiological and psychological underpinnings of gambling and substance-use disorders. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 99 , 109847. https://doi.org/10.1016/j.pnpbp.2019.109847
*Barnes G. M., Welte J. W., Tidwell M. C. O., & Hoffman, J. H. (2015). Gambling and substance use: Co-occurrence among adults in a recent general population study in the United States. International Gambling Studies, 15 (1), 55–71. https://doi.org/10.1080/14459795.2014.990396
Betancourt, L. M., Brodsky, N. L., Brown, C. A., McKenna, K. A., Giannetta, J. M., Yang, W., Romer, D., & Hurt, H. (2012). Is executive cognitive function associated with youth gambling? Journal of Gambling Studies, 28 (2), 225–238. https://doi.org/10.1007/s10899-011-9256-y
*Bonnaire, C., Kovess-Masfety, V., Guignard, R., Richard, J. B., du Roscoät, E. & Beck, F. (2017). Gambling type, substance abuse, health and psychosocial correlates of male and female problem gamblers in a nationally representative French sample. Journal of Gambling Studies, 33 (2), 343–369. https://doi.org/10.1007/s10899-016-9628-4
Borenstein, M., Higgins, J. P. T., Hedges, L. V., & Rothstein, H. R. (2017). Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Research Synthesis Methods, 8 (1), 5–18. https://doi.org/10.1002/jrsm.1230
*Brewer, J. A., Potenza, M. N., & Desai, R. A. (2014). Differential associations between problem and pathological gambling and psychiatric disorders in individuals with and without alcohol abuse or dependence. CNS Spectrums, 15 (1), 33–44. https://doi.org/10.1017/S1092852900000286
*Bussu A., & Detotto, C. (2015). The bidirectional relationship between gambling and addictive substances. International Gambling Studies, 15 (2), 285–308. https://doi.org/10.1080/14459795.2015.1042493
Caldeira, K. M., Arria, A. M., O’Grady, K. E., Vincent, K. B., Robertson, C., & Welsh, C. J. (2017). Risk factors for gambling and substance use among recent college students. Drug and Alcohol Dependence, 179 , 280–290. https://doi.org/10.1016/j.drugalcdep.2017.06.024
Campbell-Meiklejohn, D., Wakeley, J., Herbert, V., Cook, J., Scollo, P., Ray, M. K., Selvaraj, S., Passingham, R. E., Cowen, P., & Rogers, R. D. (2011). Serotonin and dopamine play complementary roles in gambling to recover losses. Neuropsychopharmacology, 36 (2), 402–410. https://doi.org/10.1038/npp.2010.170
Article CAS PubMed Google Scholar
*Cardone S. S., Anderson, C., Sedlacek , J., Fazio, P. (1997). The design and implementation of a gambling addiction program within a substance abuse agency. Psychiatric Rehabilitation Skills, 2 (1), 49–66. https://doi.org/10.1080/10973435.1997.10387551
Carlbring, P., & Smit, F. (2008). Randomized trial of internet-delivered self-help with telephone support for pathological gamblers. Journal of Consulting and Clinical Psychology, 76 , 1090–1094. https://doi.org/10.1037/a0013603
*de Carvalho, S. V., Collakis, S. T., de Oliveira, M. P., & da Silveira, D. X. (2005). [Frequency of pathological gambling among substance abusers under treatment]. Revista de Saúde Pública, 39 (2), 217–222. https://doi.org/10.1590/s0034-89102005000200012
*Castrén, S., Salonen, A. H., Alho, H., Lahti, T., & Simojoki, K. (2015). Past-year gambling behaviour among patients receiving opioid substitution treatment. Substance Abuse Treatment Prevention and Policy, 10 (1), 4. https://doi.org/10.1186/1747-597X-10-4
Chambers, R. A., & Potenza, M. N. (2003). Neurodevelopment, impulsivity, and adolescent gambling. Journal of Gambling Studies, 19 (1), 53–84. https://doi.org/10.1023/A:1021275130071
Cheung, N. W. T. (2014). Low self-control and co-occurrence of gambling with substance use and delinquency among Chinese adolescents. Journal of Gambling Studies, 30 (1), 105–124. https://doi.org/10.1007/s10899-012-9351-8
*Chou, K. L, & Afifi, T. O. (2011). Disordered (pathologic or problem) gambling and axis I psychiatric disorders: Results from the national epidemiologic survey on alcohol and related conditions. American Journal of Epidemiology, 173 (11), 1289–1297. https://doi.org/10.1093/aje/kwr017
*Ciarrocchi, J. W. (1993). Rates of pathological gambling in publicly funded outpatient substance abuse treatment. Journal of Gambling Studies, 9 (3), 289–293. https://doi.org/10.1007/BF01015924
Cowlishaw, S., Merkouris, S., Chapman, A., & Radermacher, H. (2014). Pathological and problem gambling in substance use treatment: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 46 (2), 98–105. https://doi.org/10.1016/j.jsat.2013.08.019
Cowlishaw, S., Merkouris, S., Dowling, N., Anderson, C., Jackson, A., & Thomas, S. (2012). Psychological therapies for pathological and problem gambling. Cochrane Database of Systematic Reviews, 11, CD008937. https://doi.org/10.1002/14651858.CD008937.pub2
*Cunningham-Williams, R. M., Cottler, L. B., Compton, W. M, Spitznagel, E. L, & Ben-Abdallah, A. (2000). Problem gambling and comorbid psychiatric and substance use disorders among drug users recruited from drug treatment and community settings. Journal of Gambling Studies, 16 (4), 347–376. https://doi.org/10.1023/A:1009428122460
*Daghestani, A. N., Elenz, E., & Crayton, J. W. (1996). Pathological gambling in hospitalized substance abusing veterans. Journal of Clinical Psychiatry, 57 (8), 360–363.
Delfabbro, P., Lahn, J., & Grabosky, P. (2006). It’s not what you know, but how you use it: Statistical knowledge and adolescent problem gambling. Journal of Gambling Studies, 22 (2), 179–193. https://doi.org/10.1007/s10899-006-9009-5
Dowling, N. A., Cowlishaw, S., Jackson, A. C., Merkouris, S. S., Francis, K. L., & Christensen, D. R. (2015). Prevalence of psychiatric co-morbidity in treatment-seeking problem gamblers: A systematic review and meta-analysis. Australian & New Zealand Journal of Psychiatry, 49 (6), 519–539. https://doi.org/10.1177/0004867415575774
Article Google Scholar
*Dufour, M., Nguyen, N., Bertrand, K., Perreault, M., Jutras-Aswad, D., Morvannou, A., Bruneau, J., Berbiche, D., & Roy, É. (2016). Gambling problems among community cocaine users. Journal of Gambling Studies, 32 (3), 1039–1053. https://doi.org/10.1007/s10899-016-9594-x
*Duhig, A. M., Maciejewski, P. K., Desai, R. A., Krishnan-Sarin, S., & Potenza, M. N. (2007). Characteristics of adolescent past-year gamblers and non-gamblers in relation to alcohol drinking. Addictive Behaviors, 32 (1), 80–89. https://doi.org/10.1016/j.addbeh.2006.03.021
*Elia, C., & Jacobs, D. F. (1993). The incidence of pathological gambling among native Americans treated for alcohol dependence. International Journal of the Addictions, 28 (7), 659–666. https://doi.org/10.3109/10826089309039654
Estévez, A., Momeñe, J., Jauregui, P., & Etxaburu, N. (2022). Shame and blame in gambling: Relationship with emotion regulation and gambling motives. International Journal of Mental Health and Addiction . https://doi.org/10.1007/s11469-022-00970-3
*Feigelman, W., Kleinman, P. H., Lesieur, H. R., Millman, R. B., & Lesser, M. L. (1995). Pathological gambling among methadone patients. Drug and Alcohol Dependence, 39 (2), 75–81. https://doi.org/10.1016/0376-8716(95)01141-K
Field, M., Wiers, R. W., Christiansen, P., Fillmore, M. T., & Verster, J. C. (2010). Acute alcohol effects on inhibitory control and implicit cognition Implications for loss of control over drinking. Alcohol and Clinical Experimental Research, 34 (8), 1346–1352. https://doi.org/10.1111/j.1530-0277.2010.01218.x
Article CAS Google Scholar
*Ford, M., & Håkansson, A. (2020). Problem gambling, associations with comorbid health conditions, substance use, and behavioural addictions: Opportunities for pathways to treatment. PloS One, 15 (1), e0227644. https://doi.org/10.1371/journal.pone.0227644
*Gambino, B., Fitzgerald, R., Shaffer, H. J., Renner, J., & Courtnage, P. (1993). Perceived family history of problem gambling and scores on SOGS. Journal of Gambling Studies, 9, 169–184. https://doi.org/10.1007/BF01014866
*Geisner, I. M., Huh, D., Cronce, J. M., Lostutter, T. W., Kilmer, J., & Larimer, M. E. (2016). Exploring the relationship between stimulant use and gambling in college students. Journal of Gambling Studies, 32 (3), 1001–1016. https://doi.org/10.1007/s10899-015-9586-2
Genauck, A., Quester, S., Wüstenberg, T., Mörsen, C., Heinz, A., & Romanczuk-Seiferth, N. (2017). Reduced loss aversion in pathological gambling and alcohol dependence is associated with differential alterations in amygdala and prefrontal functioning. Scientific Reports, 7 (1), 16306. https://doi.org/10.1038/s41598-017-16433-y
Goudriaan, A. E., Oosterlaan, J., De Beurs, E., & Van Den Brink, W. (2006). Neurocognitive functions in pathological gambling: A comparison with alcohol dependence. Tourette Syndrome and Normal Controls. Addiction, 101 (4), 534–547. https://doi.org/10.1111/j.1360-0443.2006.01380.x
Grant, J. E., & Chamberlain, S. R. (2014). Impulsive action and impulsive choice across substance and behavioral addictions: Cause or consequence? Addictive Behaviors, 39 (11), 1632–1639. https://doi.org/10.1016/j.addbeh.2014.04.022
Grant, J. E., Kushner, M. G., & Kim, S. W. (2002). Pathological gambling and alcohol use disorder. Alcohol Research and Health, 26 (2), 143–150.
PubMed Central Google Scholar
Green, J. M., Sundman, M. H., & Chou, Y.-H. (2022). Opioid-induced microglia reactivity modulates opioid reward, analgesia, and behavior. Neuroscience & Biobehavioral Reviews, 135 , 104544. https://doi.org/10.1016/j.neubiorev.2022.104544
Griffiths, M. D., & Calado, F. (2022). Gambling disorder. In H. M. Pontes (Ed.), Behavioral addictions: Conceptual, clinical, assessment, and treatment approaches (pp. 1–29). Springer International Publishing.
Google Scholar
*Griffiths, M.D., Wardle, H., Orford, J., Sproston, K,, & Erens, B. (2010). Gambling, alcohol, consumption, cigarette smoking and health: Findings from the 2007 British Gambling Prevalence Survey. Addiction Research & Theory, 18 (2), 208–223. https://doi.org/10.3109/16066350902928569
*Griffiths, M. D. (1994). An exploratory study of gambling cross addictions. Journal of Gambling Studies, 10 (4), 371–384. https://doi.org/10.1007/BF02104903
*Håkansson, A., & Ek, J. (2018). Pilot study of problem gambling in specialized substance use disorder treatment—high lifetime prevalence of problem gambling in opioid maintenance treatment patients. Open Journal of Psychiatry, 8 (3), 233–243. https://doi.org/10.4236/ojpsych.2018.83020
Hartmann, M., & Blaszczynski, A. (2018). The longitudinal relationships between psychiatric disorders and gambling disorders. International Journal of Mental Health and Addiction, 16 (1), 16–44. https://doi.org/10.1007/s11469-016-9705-z
Hodgins, D. C., Peden, N., & Cassidy, E. (2005). The association between comorbidity and outcome in pathological gambling: A prospective follow-up of recent quitters. Journal of Gambling Studies, 21 (3), 255–271. https://doi.org/10.1007/s10899-005-3099-3
Hodgins, D. C., Currie, S. R., Currie, G., & Fick, G. H. (2009). Randomized trial of brief motivational treatments for pathological gamblers: More is not necessarily better. Journal of Consulting and Clinical Psychology, 77 , 950–960. https://doi.org/10.1037/a0016318
Jazaeri, S. A., & Habil, M. H. B. (2012). Reviewing two types of addiction − pathological gambling and substance use. Indian Journal of Psychological Medicine, 34 (1), 5–11. https://doi.org/10.4103/0253-7176.96147
*Jun, H.-J., Sacco, P., & Cunningham-Williams, R. M. (2021). Gambling in emerging adulthood: The role of adolescent depressive symptoms, antisocial behaviors, and alcohol use. International Journal of Mental Health and Addiction, 19 (2), 494–507. https://doi.org/10.1007/s11469-019-00087-0
Joukhador, J., Maccallum, F., & Blaszczynski, A. (2003). Differences in cognitive distortions between problem and social gamblers. Psychological Reports, 92 (3), 1203–1214. https://doi.org/10.2466/pr0.2003.92.3c.1203
Karaca, S., Saleh, A., Canan, F., & Potenza, M. N. (2017). Comorbidity between behavioral addictions and attention deficit/hyperactivity disorder: A systematic review. International Journal of Mental Health and Addiction, 15 (3), 701–724. https://doi.org/10.1007/s11469-016-9660-8
Kim, S. W., Grant, J. E., Eckert, E. D., Faris, P. L., & Hartman, B. K. (2006). Pathological gambling and mood disorders: Clinical associations and treatment implications. Journal of Affective Disorders, 92 (1), 109–116. https://doi.org/10.1016/j.jad.2005.12.040
*Knaebe, B,, Rodda, S. N., Hodgins, D. C, & Lubman, D. I. (2019). Behaviour change strategies endorsed by gamblers subtyped by psychological distress, risky alcohol use, and impulsivity. Journal of Gambling Studies, 35 (1), 275–292. https://doi.org/10.1007/s10899-018-9803-x
Koob, G. F., & Volkow, N. D. (2016). Neurobiology of addiction: A neurocircuitry analysis. The Lancet Psychiatry, 3 (8), 760–773. https://doi.org/10.1016/S2215-0366(16)00104-8
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33 (1), 159–174. https://doi.org/10.2307/2529310
*Langenbucher, J., Bavly, L., Labouvie, E., Sanjuan, P. M., & Martin, C. S. (2001). Clinical features of pathological gambling in an addictions treatment cohort. Psychology of Addictive Behaviors, 15 , 77–79. https://doi.org/10.1037/0893-164X.15.1.77
*Lawrence, A. J., Luty, J., Bogdan, N. A., Sahakian, B. J., & Clark, L. (2009). Problem gamblers share deficits in impulsive decision-making with alcohol-dependent individuals. Addiction, 104 (6), 1006–1015. https://doi.org/10.1111/j.1360-0443.2009.02533.x
Leavens, E., Marotta, J., & Weinstock, J. (2014). Disordered gambling in residential substance use treatment centers: An unmet need. Journal of Addictive Diseases, 33 (2), 163–173. https://doi.org/10.1080/10550887.2014.909697
*Ledgerwood, D. M., & Downey, K. K. (2002). Relationship between problem gambling and substance use in a methadone maintenance population. Addictive Behaviors, 27 (4), 483–491. https://doi.org/10.1016/S0306-4603(01)00187-3
Leino, T., Molde, H., Griffiths, M. D., Mentzoni, R. A., Sagoe, D., & Pallesen, S. (2017). Gambling behavior in alcohol-serving and non-alcohol-serving-venues: A study of electronic gaming machine players using account records. Addiction Research & Theory, 25 (3), 201–207. https://doi.org/10.1080/16066359.2017.1288806
*Leino, T., Torsheim, T., Griffiths, M. D., & Pallesen, S. (2021). The relationship between substance use disorder and gambling disorder: A nationwide longitudinal health registry study. Scandinavian Journal of Public Health, 51 (1), 28–34. https://doi.org/10.1177/14034948211042249
*Lejoyeux, M., Feuché, N., Loi, S., Solomon, J., & Adès, J. (1999). Study of impulse-control disorders among alcohol-dependent patients. Journal of Clinical Psychiatry, 60 (5), 302–305. https://doi.org/10.4088/jcp.v60n0506
Lesieur, H. R., Blume, S. B., & Zoppa, R. M. (1986). Alcoholism, drug abuse, and gambling. Alcohol Clinical and Experimental Research, 10 (1), 33–38. https://doi.org/10.1111/j.1530-0277.1986.tb05610.x
*Lesieur, H. R., & Heineman, M. (1988). Pathological gambling among youthful multiple substance abusers in a therapeutic community. British Journal of Addiction, 83 (7), 765–771. https://doi.org/10.1111/j.1360-0443.1988.tb00509.x
*Lind, K., Salonen, A. H., Järvinen-Tassopoulos, J., Alho, H., & Castrén, S. (2019). Problem gambling and support preferences among finnish prisoners: A pilot study in an adult correctional population. International Journal of Prisoner Health, 15 (4), 316–331. https://doi.org/10.1108/IJPH-07-2018-0041
*Lopes, C. S., Lewis, G., & Mann, A. (1996). Psychiatric and alcohol disorders as risk factors for drug abuse. Social Psychiatry and Psychiatric Epidemiology, 31 (6), 355–363. https://doi.org/10.1007/BF00783425
Lorains, F. K., Cowlishaw, S., & Thomas, S. A. (2011). Prevalence of comorbid disorders in problem and pathological gambling: Systematic review and meta-analysis of population surveys. Addiction, 106 (3), 490–498. https://doi.org/10.1111/j.1360-0443.2010.03300.x
*Manning, V., Dowling, N. A., Lee, S, Rodda, S., Garfield, J. B. B, Volberg, R., Kulkarni, J., & Lubman, D. I. (2017). Problem gambling and substance use in patients attending community mental health services. Journal of Behavioral Addictions, 6 (4), 678–688. https://doi.org/10.1556/2006.6.2017.077
*Martínez-Loredo, V., Grande-Gosende, A., Fernández-Artamendi, S., Secades-Villa, R., & Fernández-Hermida, J. R. (2019). Substance use and gambling patterns among adolescents: Differences according to gender and impulsivity. Journal of Gambling Studies, 35 (1), 63–78. https://doi.org/10.1007/s10899-018-09824-x
*Mathias, A. C. R., Vargens, R. W., Kessler, F. H., & Cruz, M. S. (2009). Differences in addiction severity between social and probable pathological gamblers among substance abusers in treatment in Rio de Janeiro. International Journal of Mental Health and Addiction, 7 (1), 239–249. https://doi.org/10.1007/s11469-008-9183-z
*McCormick, R. A. (1993). Disinhibition and negative affectivity in substance abusers with and without a gambling problem. Addictive Behaviors, 18 (3), 331–336. https://doi.org/10.1016/0306-4603(93)90034-7
Menninger, J. A. (2002). Assessment and treatment of alcoholism and substance-related disorders in the elderly. Bulletin of the Menninger Clinic, 66 (2), 166–183. https://doi.org/10.1521/bumc.66.2.166.23364
Mick, I., Myers, J., Ramos, A. C., Stokes, P. R. A., Erritzoe, D., Colasanti, A., Gunn, R. N., Rabiner, E. A., Searle, G. E., Waldman, A. D., Parkin, M. C., Brailsford, A. D., Galduróz, J. C. F., Bowden-Jones, H., Clark, L., Nutt, D. J., & Lingford-Hughes, A. R. (2016). Blunted endogenous opioid release following an oral amphetamine challenge in pathological gamblers. Neuropsychopharmacology, 41 (7), 1742–1750. https://doi.org/10.1038/npp.2015.340
Mide, M., Arvidson, E., & Gordh, A. S. (2023). Clinical differences of mild, moderate, and severe gambling disorder in a sample of treatment seeking pathological gamblers in Sweden. Journal of Gambling Studies . Advance Online Publication. https://doi.org/10.1007/s10899-022-10183-x
*Mills, D. J., Marchica, L., Keough, M. T., & Derevensky, J. L. (2020). Exploring differences in substance use among emerging adults at-risk for problem gambling, and/or problem video gaming. International Gambling Studies, 20 (3), 539–555. https://doi.org/10.1080/14459795.2020.1752768
*Nelson, K. G., & Oehlert, M. E. (2008). Evaluation of a shortened South Oaks Gambling Screen in veterans with addictions. Psychology of Addictive Behaviors, 22, 309–312. https://doi.org/10.1037/0893-164X.22.2.309
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372 , n71. https://doi.org/10.1136/bmj.n71
Peles, E., Schreiber, S., & Adelson, M. (2009). Pathological gambling and obsessive compulsive disorder among methadone maintenance treatment patients. Journal of Addictive Diseases, 28 (3), 199–207. https://doi.org/10.1080/10550880903014106
*Peles, E., Schreiber, S., Linzy, S., & Adelson, M. (2010). Pathological gambling in methadone maintenance clinics where gambling is legal versus illegal. American Journal of Orthopsychiatry, 80, 311–316. https://doi.org/10.1111/j.1939-0025.2010.01034.x
Peterson, J., Welch, V., Losos, M., & Tugwell, P. (2011). The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses . Ottawa Hospital Research Institute.
*Petry, N. M., Stinson, F. S., & Grant, B. F. (2005). Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry, 66 (5), 564–574. https://doi.org/10.4088/jcp.v66n0504
Philippe, F., & Vallerand, R. J. (2007). Prevalence rates of gambling problems in Montreal, Canada: A look at old adults and the role of passion. Journal of Gambling Studies, 23 (3), 275–283. https://doi.org/10.1007/s10899-006-9038-0
Potenza, M. N. (2013). Neurobiology of gambling behaviors. Current Opinion in Neurobiology, 23 (4), 660–667. https://doi.org/10.1016/j.conb.2013.03.004
Potenza, M. N., Balodis, I. M., Derevensky, J., Grant, J. E., Petry, N. M., Verdejo-Garcia, A., & Yip, S. W. (2019). Gambling Disorder. Nature Reviews Disease Primers, 5 (1), 51. https://doi.org/10.1038/s41572-019-0099-7
Rash, C. J., Weinstock, J., & Van Patten, R. (2016). A review of gambling disorder and substance use disorders. Substance Abuse and Rehabilitation, 7 , 3–13. https://doi.org/10.2147/sar.s83460
*Rodriguez-Monguio, R., Errea, M., & Volberg, R. (2017). Comorbid pathological gambling, mental health, and substance use disorders: Health-care services provision by clinician specialty. Journal of Behavioral Addictions, 6 (3), 406–415. https://doi.org/10.1556/2006.6.2017.054
Roy, A., Adinoff, B., Roehrich, L., Lamparski, D., Custer, R., Lorenz, V., Barbaccia, M., Guidotti, A., Costa, E., & Linnoila, M. (1988). Pathological gambling: A psychobiological study. Archives of General Psychiatry, 45 (4), 369–373. https://doi.org/10.1001/archpsyc.1988.01800280085011
*Rudd, C., & Thomas, S. D. M. (2016). The prevalence, mental health and criminal characteristics of potential problem gamblers in a substance using treatment seeking population. International Journal of Mental Health and Addiction, 14 (5), 700–714. https://doi.org/10.1007/s11469-015-9604-8
*Rupcich, N., Frisch G. R., & Govoni, R. (1997). Comorbidity of pathological gambling in addiction treatment facilities. Journal of Substance Abuse Treatment, 14 (6), 573–574. https://doi.org/10.1016/s0740-5472(97)00015-9
*Rush, B. R., Bassani, D. G., Urbanoski, K. A., & Castel, S. (2008). Influence of co-occurring mental and substance use disorders on the prevalence of problem gambling in Canada. Addiction, 103 (11), 1847–1856. https://doi.org/10.1111/j.1360-0443.2008.02338.x
Russell, A. M. T., Browne, M., Hing, N., Visintin, T., Begg, S., Rawat, V., & Rockloff, M. (2022). Stressful life events precede gambling problems, and continued gambling problems exacerbate stressful life events; A life course calendar study. Journal of Gambling Studies, 38 (4), 1405–1430. https://doi.org/10.1007/s10899-021-10090-7
*Sarkar, S., Singh-Balhara, Y. P., Parmar, A., & Rajhans, P. (2018). A study of pathological gambling and its correlates among patients seeking treatment for substance use disorders in North India. Journal of Substance Use, 23 (2), 193–198. https://doi.org/10.1080/14659891.2017.1378742
Schluter, M. G., Kim, H. S., Poole, J. C., Hodgins, D. C., McGrath, D. S., Dobson, K. S., & Taveres, H. (2019). Gambling-related cognitive distortions mediate the relationship between depression and disordered gambling severity. Addictive Behaviors, 90 , 318–323. https://doi.org/10.1016/j.addbeh.2018.11.038
Shaffer, H. J., LaPlante, D. A., LaBrie, R. A., Kidman, R. C., Donato, A. N., & Stanton, M. V. (2004). Toward a syndrome model of addiction: Multiple expressions, common etiology. Harvard Review of Psychiatry, 12 (6), 367–374. https://doi.org/10.1080/10673220490905705
*Shaffer, H. J., Freed, C. R., & Healea, D. (2002). Gambling disorders among homeless persons with substance use disorders seeking treatment at a community center. Psychiatric Services, 53 (9), 1112–1117. https://doi.org/10.1176/appi.ps.53.9.1112
*Shepherd, R. M. (1996). Clinical obstacles in administrating the South Oaks Gambling Screen in a methadone and alcohol clinic. Journal of Gambling Studies, 12 (1), 21–32. https://doi.org/10.1007/BF01533187
*Sherba, R. T., & Martt, N. J. (2015). Overall gambling behaviors and gambling treatment needs among a statewide sample of drug treatment clients in Ohio. Journal of Gambling Studies, 31 (1), 281–293. https://doi.org/10.1007/s10899-013-9406-5
Slutske, W. S. (2006). Natural recovery and treatment-seeking in pathological gambling: Results of two U.S. national surveys. American Journal of Psychiatry, 163 (2), 297–302. https://doi.org/10.1176/appi.ajp.163.2.297
Slutske, W. S., Caspi, A., Moffitt, T. E., & Poulton, R. (2005). Personality and problem gambling: A prospective study of a birth cohort of young adults. Archives of General Psychiatry, 62 (7), 769–775. https://doi.org/10.1001/archpsyc.62.7.769
*Slutske, W. S., Eisen, S., True, W. R., Lyons, M. J., Goldberg, J., & Tsuang, M. (2000). Common genetic vulnerability for pathological gambling and alcohol dependence in men. Archives of General Psychiatry, 57 (7), 666–673. https://doi.org/10.1001/archpsyc.57.7.666
Southwell, J., Boreham, P., & Laffan, W. (2008). Problem gambling and the circumstances facing older people. Journal of Gambling Studies, 24 (2), 151–174. https://doi.org/10.1007/s10899-007-9079-z
*Spunt, B., Lesieur, H., Liberty, H. J,. & Hunt, D. (1996). Pathological gamblers in methadone treatment: A comparison between men and women. Journal of Gambling Studies, 12 (4), 431–449. https://doi.org/10.1007/BF01539187
Steinberg, L., & Tremblay, A. M. (2009). The effects of stress and placebo alcohol on cognitive activation and inhibitory control in male problem gamblers and problem gamblers with alcohol use disorder. (Master of Science) University of Toronto Toronto Canada.
Svensson, J., Romild, U., Nordenmark, M., & Månsdotter, A. (2011). Gendered gambling domains and changes in Sweden. International Gambling Studies, 11 (2), 193–211. https://doi.org/10.1080/14459795.2011.581676
*Tómasson, K., & Vaglum, P. (1995). A nationwide representative sample of treatment-seeking alcoholics: A study of psychiatric comorbidity. Acta Psychiatrica Scandinavica, 92 (5), 378–385. https://doi.org/10.1111/j.1600-0447.1995.tb09600.x
Toneatto, T., Ferguson, D., & Brennan, J. (2003). Effect of a new casino on problem gambling in treatment-seeking substance abusers. Canadian Journal of Psychiatry, 48 (1), 40–44. https://doi.org/10.1177/070674370304800108
Tse, S., Hong, S.-I., Wang, C.-W., & Cunningham-Williams, R. M. (2012). Gambling behavior and problems among older adults: A systematic review of empirical studies. The Journals of Gerontology: Series B, 67 (5), 639–652. https://doi.org/10.1093/geronb/gbs068
von Hippel, W., Ng, L., Abbot, L., Caldwell, S., Gill, G., & Powell, K. (2009). Executive functioning and gambling: Performance on the trail making test is associated with gambling problems in older adult gamblers. Aging, Neuropsychology, and Cognition, 16 (6), 654–670. https://doi.org/10.1080/13825580902871018
Walther, B., Morgenstern, M., & Hanewinkel, R. (2012). Co-occurrence of addictive behaviours: Personality factors related to substance use, gambling and computer gaming. European Addiction Research, 18 (4), 167–174. https://doi.org/10.1159/000335662
*Weinstock, J., Blanco, C., & Petry, N. M. (2006). Health correlates of pathological gambling in a methadone maintenance clinic. Experimental and Clinical Psychopharmacology, 14, 87–93. https://doi.org/10.1037/1064-1297.14.1.87
*Welte, J., Barnes, G., Wieczorek, W., Tidwell, M. C., & Parker, J. (2001). Alcohol and gambling pathology among U.S. adults: Prevalence, demographic patterns and comorbidity. Journal of Studies on Alcohol, 62 (5), 706–712. https://doi.org/10.15288/jsa.2001.62.706
*Wickwire, Jr, E. M., Burke, R. S., Brown, S. A., Parker, J. D., & May, R. K. (2008). Psychometric evaluation of the national opinion research center DSM-IV screen for gambling problems (NODS). American Journal on Addictions, 17 (5), 392–395. https://doi.org/10.1080/10550490802268934
*Widinghoff, C., Berge, J., Wallinius, M., Billstedt, E., Hofvander, B., & Håkansson, A. (2019). Gambling disorder in male violent offenders in the prison system: Psychiatric and substance-related comorbidity. Journal of Gambling Studies, 35 (2), 485–500. https://doi.org/10.1007/s10899-018-9785-8
Wong, G., Zane, N., Saw, A., & Chan, A. K. K. (2013). Examining gender differences for gambling engagement and gambling problems among emerging adults. Journal of Gambling Studies, 29 , 171–189. https://doi.org/10.1007/s10899-012-9305-1
*Xian, H., Giddens, J. L., Scherrer, J. F., Eisen, S. A., & Potenza, M. N. (2014). Environmental factors selectively impact co-occurrence of problem/pathological gambling with specific drug-use disorders in male twins. Addiction, 109(4), 635–644. https://doi.org/10.1111/add.12407
Zaranek, R. R., & Chapleski, E. E. (2005). Casino gambling among urban elders: Just another social activity? The Journals of Gerontology: Series B, 60 (2), S74–S81. https://doi.org/10.1093/geronb/60.2.S74
Zhai, Z. W., Duenas, G. L., Wampler, J., & Potenza, M. N. (2020). Gambling, substance use and violence in male and female adolescents. Journal of Gambling Studies, 36 (4), 1301–1324. https://doi.org/10.1007/s10899-020-09931-8
Download references
Author information
Authors and affiliations.
Social Determinants of Health Research Center, Saveh University of Medical Sciences, Saveh, Iran
Bahram Armoon & Amir-Hossien Bayat
International Gaming Research Unit, Psychology Department, Nottingham Trent University, Nottingham, UK
Mark D. Griffiths
Douglas Hospital Research Centre, Douglas Mental Health University Institute, Montreal, QC, Canada
Marie-Josée Fleury
Department of Psychiatry, McGill University, Montreal, QC, Canada
Social Determinants of Health Research Center, School of Health and Nutrition, Lorestan University of Medical Sciences, Khorramabad, Iran
Rasool Mohammadi
Department of Neuroscience, School of Sciences and Advanced Technology in Medicine, Hamadan University of Medical Science, Hamadan, Iran
Amir-Hossien Bayat
You can also search for this author in PubMed Google Scholar
Contributions
BA conceived the study. BA collected all data. RM and BA analyzed and interpreted the data. BA and AHB drafted the manuscript. BA, MJF, and MDG contributed to the revised paper, and MDG was responsible for all final editing. All authors commented on the drafts of the manuscript and approved the final copy of the paper for submission.
Corresponding author
Correspondence to Bahram Armoon .
Ethics declarations
Ethics approval.
The present study was an analysis of preexisting literature and did not use human participants.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare that there are no conflicts of interest except MDG. MDG has received research funding from Norsk Tipping (the gambling operator owned by the Norwegian government). MDG has received funding for a number of research projects in the area of gambling education for young people, social responsibility in gambling, and gambling treatment from GambleAware (formerly the Responsibility in Gambling Trust ), a charitable body which funds its research program based on donations from the gambling industry. MDG undertakes consultancy for various gambling companies in the area of social responsibility in gambling.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 16 KB)
Supplementary file2 (docx 21 kb), supplementary file3 (pdf 6 kb), supplementary file4 (pdf 7 kb), supplementary file5 (pdf 6 kb), supplementary file6 (pdf 6 kb), supplementary file7 (pdf 7 kb), supplementary file8 (pdf 8 kb), supplementary file9 (pdf 7 kb), supplementary file10 (pdf 7 kb), supplementary file11 (pdf 48 kb), supplementary file12 (pdf 29 kb), supplementary file13 (pdf 83 kb), supplementary file14 (pdf 49 kb), supplementary file15 (pdf 52 kb), supplementary file16 (pdf 52 kb), supplementary file17 (pdf 42 kb), supplementary file18 (pdf 45 kb), supplementary file19 (pdf 41 kb), supplementary file20 (pdf 35 kb), supplementary file21 (pdf 43 kb), supplementary file22 (pdf 51 kb), supplementary file23 (pdf 46 kb), supplementary file24 (pdf 40 kb), supplementary file25 (pdf 32 kb), supplementary file26 (pdf 27 kb), supplementary file27 (docx 14 kb), supplementary file28 (docx 13 kb), supplementary file29 (docx 12 kb), supplementary file30 (docx 13 kb), supplementary file31 (docx 13 kb), rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Armoon, B., Griffiths, M.D., Fleury, MJ. et al. The Global Prevalence of Problem and Pathological Gambling and Its Associated Factors Among Individuals with Substance Use Disorders: A Meta-analysis. Int J Ment Health Addiction (2023). https://doi.org/10.1007/s11469-023-01167-y
Download citation
Accepted : 17 September 2023
Published : 12 October 2023
DOI : https://doi.org/10.1007/s11469-023-01167-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Problem gambling
- Pathological gambling
- Alcohol use disorders
- Opioid use disorders
- Substance use disorders
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Essay Drug Abuse and Mental Health. Substance abuse complicates almost every aspect of care for the person with a mental disorder. When drugs enter the brain, they can interrupt the work and actually change how the brain performs its jobs; these changes are what lead to compulsive drug use. Drug abuse plays a major role when concerning mental ...
The Impact of Drug Abuse on Mental Health. Drug abuse can exacerbate existing mental health disorders and lead to the development of substance-induced mental disorders. This often results in a dual diagnosis, where individuals struggle with both a mental health disorder and substance abuse simultaneously, making treatment more challenging.
1 Introduction. The risk of morbidity and mortality of mental disorders increases with substance misuse. Positive comorbidity has also been observed between psychiatric and substance use among men (48%) and women (47%), having an antisocial personality disorder (25.1%), and major depression (15.8%), respectively. A recent national-wide cross-sectional study identified the prevalence of ...
Mental Health And Addiction Essay. Recovery can be a difficult journey for many. The reality of having to change old habits for new ones can take a lifetime. The recovery approach/model realizes the struggle of change and transformation and makes it so that way emphasis is not placed on the destination, but rather the journey.
Addiction and Health ... z Parents' drug abuse often means chaotic, stress-filled homes, as well as child abuse and neglect. Such conditions harm the well- ... exposure to physical or sexual abuse, genetic susceptibility, or mental illness. Still, the fact remains that early use is a strong indicator of problems ahead, including addiction.
Substance abuse and mental health are two interrelated issues that have profound implications for individuals, families, and society as a whole. This essay explores the intricate relationship between substance abuse and mental health, shedding light on how they intersect and impact one another. Substance abuse encompasses the harmful or ...
The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to better serve those afflicted with addictions. ... Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2018. Rockville ...
Many individuals who develop substance use disorders (SUD) are also diagnosed with mental disorders, and vice versa.2,3 Although there are fewer studies on comorbidity among youth, research suggests that adolescents with substance use disorders also have high rates of co-occurring mental illness; over 60 percent of adolescents in community-based substance use disorder treatment programs also ...
Khantzian examines both sides of my topic through his solidarity efforts in this article. As the title suggests, many addicts choose substances to help mask their pain and depression. He also states, that many of these drugs such as heroin and cocaine can bring upon many mental disorders as well. As we have learned from the book, heroin can ...
The majority of young people with drug and alcohol problems suffer from concurrent mental health problems, referred to as co-occurring disorders or comorbidity [1,2,3,4].Externalizing disorders such as Conduct Disorder (CD) and Attention Deficit Hyperactivity Disorder (ADHD) appear to be the most common mental health problems, but internalizing disorders such as depression, dysthymia and ...
Effects of Drug Addiction on Behavior. Psychoactive substances affect the parts of the brain that involve reward, pleasure, and risk. They produce a sense of euphoria and well-being by flooding the brain with dopamine. This leads people to compulsively use drugs in search of another euphoric "high.".
The present research paper explored the impact of drug addiction on mental health. Method:The present study consists of 60 subjects randomly selected among which 30 were adolescents (15 males and ...
Official guidance almost always advocates for a "no wrong door" policy, meaning that those with dual addiction and mental health issues will get help whichever service encounters them first ...
Mental Health Disorders: Substance abuse can trigger or exacerbate mental health conditions like depression, anxiety, and psychosis. Behavioral Changes: Changes in behavior, such as increased aggression or impulsivity, are common. Cognitive Impairments: Drugs can impair decision-making abilities, judgment, and other cognitive functions.
2. Substance Abuse and Different Social Groups. When researching substance abuse and its harmful effects, researchers predominantly focus on certain social groups with a higher tendency towards substance taking and misuse, such as adolescents and male adults [13,14,15,16,17,18].This is valid, as they may encounter various demanding life and social challenges, expectations, interpersonal ...
Fentanyl - Drug Profile and Specific and Drug Abuse. The drug has the effect of depressing the respiratory center, constricting the pupils, as well as depressing the cough reflex. The remainder 75% of fentanyl is swallowed and absorbed in G-tract. Cases of Drug Abuse Amongst Nursing Professionals.
This essay was also published by Health Affairs on January 3, 2022. ... Drug addiction is a chronic but treatable disorder with well-understood genetic and social contributors. It is not a sign of a person's weakness or bad character. Continued or intermittent use of drugs, even by people who know they have a disorder and are trying hard to ...
Substance abuse during adolescence. The use of substances by youth is described primarily as intermittent or intensive (binge) drinking and characterized by experimentation and expediency (Degenhardt et al., Citation 2016; Morojele & Ramsoomar, Citation 2016; Romo-Avilés et al., Citation 2016).Intermittent or intensive substance use is linked to the adolescent's need for activities that ...
Drug use does not exist in a vacuum; its influence on mental health is significant and multifaceted. From temporary euphoria to the depths of depression, the psychological roller-coaster associated with drug use can be as compelling as it is catastrophic. Understanding the complex interplay between drugs and our mental state offers insights ...
Essay on Drug Abuse in 250 Words. 'When people consume drugs regularly and become addicted to it, it is known as drug abuse. In medical terminology, drugs means medicines. However, the consumption of drugs is for non-medical purposes. It involves the consumption of substances in illegal and harmful ways, such as swallowing, inhaling, or ...
Essay on Drug Addiction: Addiction refers to the harmful need to consume substances that have damaging consequences on the user. Addiction affects not just the body but also on the person's mental health and soundness of mind. Addiction is one of the most severe health problems faced around the world and is termed as a chronic disease.
How to prevent Drug addiction (essay) ... Substance Abuse and Mental Health Services Administration. (2021). Treatment for substance use disorders. United Nations Office on Drugs and Crime. (2021). World drug report 2021. Volkow, N. D., Koob, G. F., & McLellan, A. T. (2016). Neurobiologic advances from the brain disease model of addiction.
250 Words Essay on Addiction ... Addiction can be of two types: substance addiction and behavioral addiction. Substance addiction involves drugs, alcohol, nicotine, or other substances. ... It can lead to physical health problems like heart disease or mental health issues like depression. Addiction can also strain relationships with family and ...
The achievements of addiction medicine are many and probably not celebrated frequently enough: the management of alcohol withdrawal (which can be fatal when untreated), the development and ...
persuasive essay draft drug abuse plays significant role when it comes to mental health. when the body becomes intoxicated drugs it effects the brain and how. ... There is a direct connection between substance abuse and mental disorders, whether it be from the prolonged use of drugs or in some cases there is an underlying mental disorder that ...
Essay on Drug Abuse in 250-300 words. Drug abuse is a growing global concern that poses significant risks to individuals, families, and communities. It refers to the excessive and harmful use of drugs, both legal and illegal, that have negative effects on physical and mental health. Drug abuse has severe consequences for individuals and society.
Impact of Drug Addiction on Society. Drug addiction has been a significant issue worldwide for many decades, impacting not only individuals addicted to illegal substances but also the society surrounding them. This essay aims to explore the influence of drug addiction on society at the local, national, and global scale.
The present systematic review and meta-analysis assessed the prevalence, sociodemographic factors, mental health disorders, and type of drug use disorders associated with problem/pathological gambling among individuals with substance use disorders (SUDs). Published studies before January 1, 2023, were reviewed. Out of 8351 papers initially identified, 61 studies remained for meta-analysis. The ...