Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character

Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
- Ned H. Kalin , M.D.
Search for more papers by this author
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health ( 1 ) suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol. When considering other substances, the report estimated that 4.4 million individuals had a marijuana use disorder and that 2 million people suffered from an opiate use disorder. It is well known that stress is associated with an increase in the use of alcohol and other substances, and this is particularly relevant today in relation to the chronic uncertainty and distress associated with the COVID-19 pandemic along with the traumatic effects of racism and social injustice. In part related to stress, substance use disorders are highly comorbid with other psychiatric illnesses: 9.2 million adults were estimated to have a 1-year prevalence of both a mental illness and at least one substance use disorder. Although they may not necessarily meet criteria for a substance use disorder, it is well known that psychiatric patients have increased usage of alcohol, cigarettes, and other illicit substances. As an example, the survey estimated that over the preceding month, 37.2% of individuals with serious mental illnesses were cigarette smokers, compared with 16.3% of individuals without mental illnesses. Substance use frequently accompanies suicide and suicide attempts, and substance use disorders are associated with a long-term increased risk of suicide.
Addiction is the key process that underlies substance use disorders, and research using animal models and humans has revealed important insights into the neural circuits and molecules that mediate addiction. More specifically, research has shed light onto mechanisms underlying the critical components of addiction and relapse: reinforcement and reward, tolerance, withdrawal, negative affect, craving, and stress sensitization. In addition, clinical research has been instrumental in developing an evidence base for the use of pharmacological agents in the treatment of substance use disorders, which, in combination with psychosocial approaches, can provide effective treatments. However, despite the existence of therapeutic tools, relapse is common, and substance use disorders remain grossly undertreated. For example, whether at an inpatient hospital treatment facility or at a drug or alcohol rehabilitation program, it was estimated that only 11% of individuals needing treatment for substance use received appropriate care in 2018. Additionally, it is worth emphasizing that current practice frequently does not effectively integrate dual diagnosis treatment approaches, which is important because psychiatric and substance use disorders are highly comorbid. The barriers to receiving treatment are numerous and directly interact with existing health care inequities. It is imperative that as a field we overcome the obstacles to treatment, including the lack of resources at the individual level, a dearth of trained providers and appropriate treatment facilities, racial biases, and the marked stigmatization that is focused on individuals with addictions.
This issue of the Journal is focused on understanding factors contributing to substance use disorders and their comorbidity with psychiatric disorders, the effects of prenatal alcohol use on preadolescents, and brain mechanisms that are associated with addiction and relapse. An important theme that emerges from this issue is the necessity for understanding maladaptive substance use and its treatment in relation to health care inequities. This highlights the imperative to focus resources and treatment efforts on underprivileged and marginalized populations. The centerpiece of this issue is an overview on addiction written by Dr. George Koob, the director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and coauthors Drs. Patricia Powell (NIAAA deputy director) and Aaron White ( 2 ). This outstanding article will serve as a foundational knowledge base for those interested in understanding the complex factors that mediate drug addiction. Of particular interest to the practice of psychiatry is the emphasis on the negative affect state “hyperkatifeia” as a major driver of addictive behavior and relapse. This places the dysphoria and psychological distress that are associated with prolonged withdrawal at the heart of treatment and underscores the importance of treating not only maladaptive drug-related behaviors but also the prolonged dysphoria and negative affect associated with addiction. It also speaks to why it is crucial to concurrently treat psychiatric comorbidities that commonly accompany substance use disorders.
Insights Into Mechanisms Related to Cocaine Addiction Using a Novel Imaging Method for Dopamine Neurons
Cassidy et al. ( 3 ) introduce a relatively new imaging technique that allows for an estimation of dopamine integrity and function in the substantia nigra, the site of origin of dopamine neurons that project to the striatum. Capitalizing on the high levels of neuromelanin that are found in substantia nigra dopamine neurons and the interaction between neuromelanin and intracellular iron, this MRI technique, termed neuromelanin-sensitive MRI (NM-MRI), shows promise in studying the involvement of substantia nigra dopamine neurons in neurodegenerative diseases and psychiatric illnesses. The authors used this technique to assess dopamine function in active cocaine users with the aim of exploring the hypothesis that cocaine use disorder is associated with blunted presynaptic striatal dopamine function that would be reflected in decreased “integrity” of the substantia nigra dopamine system. Surprisingly, NM-MRI revealed evidence for increased dopamine in the substantia nigra of individuals using cocaine. The authors suggest that this finding, in conjunction with prior work suggesting a blunted dopamine response, points to the possibility that cocaine use is associated with an altered intracellular distribution of dopamine. Specifically, the idea is that dopamine is shifted from being concentrated in releasable, functional vesicles at the synapse to a nonreleasable cytosolic pool. In addition to providing an intriguing alternative hypothesis underlying the cocaine-related alterations observed in substantia nigra dopamine function, this article highlights an innovative imaging method that can be used in further investigations involving the role of substantia nigra dopamine systems in neuropsychiatric disorders. Dr. Charles Bradberry, chief of the Preclinical Pharmacology Section at the National Institute on Drug Abuse, contributes an editorial that further explains the use of NM-MRI and discusses the theoretical implications of these unexpected findings in relation to cocaine use ( 4 ).
Treatment Implications of Understanding Brain Function During Early Abstinence in Patients With Alcohol Use Disorder
Developing a better understanding of the neural processes that are associated with substance use disorders is critical for conceptualizing improved treatment approaches. Blaine et al. ( 5 ) present neuroimaging data collected during early abstinence in patients with alcohol use disorder and link these data to relapses occurring during treatment. Of note, the findings from this study dovetail with the neural circuit schema Koob et al. provide in this issue’s overview on addiction ( 2 ). The first study in the Blaine et al. article uses 44 patients and 43 control subjects to demonstrate that patients with alcohol use disorder have a blunted neural response to the presentation of stress- and alcohol-related cues. This blunting was observed mainly in the ventromedial prefrontal cortex, a key prefrontal regulatory region, as well as in subcortical regions associated with reward processing, specifically the ventral striatum. Importantly, this finding was replicated in a second study in which 69 patients were studied in relation to their length of abstinence prior to treatment and treatment outcomes. The results demonstrated that individuals with the shortest abstinence times had greater alterations in neural responses to stress and alcohol cues. The authors also found that an individual’s length of abstinence prior to treatment, independent of the number of days of abstinence, was a predictor of relapse and that the magnitude of an individual’s neural alterations predicted the amount of heavy drinking occurring early in treatment. Although relapse is an all too common outcome in patients with substance use disorders, this study highlights an approach that has the potential to refine and develop new treatments that are based on addiction- and abstinence-related brain changes. In her thoughtful editorial, Dr. Edith Sullivan from Stanford University comments on the details of the study, the value of studying patients during early abstinence, and the implications of these findings for new treatment development ( 6 ).
Relatively Low Amounts of Alcohol Intake During Pregnancy Are Associated With Subtle Neurodevelopmental Effects in Preadolescent Offspring
Excessive substance use not only affects the user and their immediate family but also has transgenerational effects that can be mediated in utero. Lees et al. ( 7 ) present data suggesting that even the consumption of relatively low amounts of alcohol by expectant mothers can affect brain development, cognition, and emotion in their offspring. The researchers used data from the Adolescent Brain Cognitive Development Study, a large national community-based study, which allowed them to assess brain structure and function as well as behavioral, cognitive, and psychological outcomes in 9,719 preadolescents. The mothers of 2,518 of the subjects in this study reported some alcohol use during pregnancy, albeit at relatively low levels (0 to 80 drinks throughout pregnancy). Interestingly, and opposite of that expected in relation to data from individuals with fetal alcohol spectrum disorders, increases in brain volume and surface area were found in offspring of mothers who consumed the relatively low amounts of alcohol. Notably, any prenatal alcohol exposure was associated with small but significant increases in psychological problems that included increases in separation anxiety disorder and oppositional defiant disorder. Additionally, a dose-response effect was found for internalizing psychopathology, somatic complaints, and attentional deficits. While subtle, these findings point to neurodevelopmental alterations that may be mediated by even small amounts of prenatal alcohol consumption. Drs. Clare McCormack and Catherine Monk from Columbia University contribute an editorial that provides an in-depth assessment of these findings in relation to other studies, including those assessing severe deficits in individuals with fetal alcohol syndrome ( 8 ). McCormack and Monk emphasize that the behavioral and psychological effects reported in the Lees et al. article would not be clinically meaningful. However, it is feasible that the influences of these low amounts of alcohol could interact with other predisposing factors that might lead to more substantial negative outcomes.
Increased Comorbidity Between Substance Use and Psychiatric Disorders in Sexual Identity Minorities
There is no question that victims of societal marginalization experience disproportionate adversity and stress. Evans-Polce et al. ( 9 ) focus on this concern in relation to individuals who identify as sexual minorities by comparing their incidence of comorbid substance use and psychiatric disorders with that of individuals who identify as heterosexual. By using 2012−2013 data from 36,309 participants in the National Epidemiologic Study on Alcohol and Related Conditions–III, the authors examine the incidence of comorbid alcohol and tobacco use disorders with anxiety, mood disorders, and posttraumatic stress disorder (PTSD). The findings demonstrate increased incidences of substance use and psychiatric disorders in individuals who identified as bisexual or as gay or lesbian compared with those who identified as heterosexual. For example, a fourfold increase in the prevalence of PTSD was found in bisexual individuals compared with heterosexual individuals. In addition, the authors found an increased prevalence of substance use and psychiatric comorbidities in individuals who identified as bisexual and as gay or lesbian compared with individuals who identified as heterosexual. This was most prominent in women who identified as bisexual. For example, of the bisexual women who had an alcohol use disorder, 60.5% also had a psychiatric comorbidity, compared with 44.6% of heterosexual women. Additionally, the amount of reported sexual orientation discrimination and number of lifetime stressful events were associated with a greater likelihood of having comorbid substance use and psychiatric disorders. These findings are important but not surprising, as sexual minority individuals have a history of increased early-life trauma and throughout their lives may experience the painful and unwarranted consequences of bias and denigration. Nonetheless, these findings underscore the strong negative societal impacts experienced by minority groups and should sensitize providers to the additional needs of these individuals.
Trends in Nicotine Use and Dependence From 2001–2002 to 2012–2013
Although considerable efforts over earlier years have curbed the use of tobacco and nicotine, the use of these substances continues to be a significant public health problem. As noted above, individuals with psychiatric disorders are particularly vulnerable. Grant et al. ( 10 ) use data from the National Epidemiologic Survey on Alcohol and Related Conditions collected from a very large cohort to characterize trends in nicotine use and dependence over time. Results from their analysis support the so-called hardening hypothesis, which posits that although intervention-related reductions in nicotine use may have occurred over time, the impact of these interventions is less potent in individuals with more severe addictive behavior (i.e., nicotine dependence). When adjusted for sociodemographic factors, the results demonstrated a small but significant increase in nicotine use from 2001–2002 to 2012–2013. However, a much greater increase in nicotine dependence (46.1% to 52%) was observed over this time frame in individuals who had used nicotine during the preceding 12 months. The increases in nicotine use and dependence were associated with factors related to socioeconomic status, such as lower income and lower educational attainment. The authors interpret these findings as evidence for the hardening hypothesis, suggesting that despite the impression that nicotine use has plateaued, there is a growing number of highly dependent nicotine users who would benefit from nicotine dependence intervention programs. Dr. Kathleen Brady, from the Medical University of South Carolina, provides an editorial ( 11 ) that reviews the consequences of tobacco use and the history of the public measures that were initially taken to combat its use. Importantly, her editorial emphasizes the need to address health care inequity issues that affect individuals of lower socioeconomic status by devoting resources to develop and deploy effective smoking cessation interventions for at-risk and underresourced populations.
Conclusions
Maladaptive substance use and substance use disorders are highly prevalent and are among the most significant public health problems. Substance use is commonly comorbid with psychiatric disorders, and treatment efforts need to concurrently address both. The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to better serve those afflicted with addictions. While treatments exist, the need for more effective treatments is clear, especially those focused on decreasing relapse rates. The negative affective state, hyperkatifeia, that accompanies longer-term abstinence is an important treatment target that should be emphasized in current practice as well as in new treatment development. In addition to developing a better understanding of the neurobiology of addictions and abstinence, it is necessary to ensure that there is equitable access to currently available treatments and treatment programs. Additional resources must be allocated to this cause. This depends on the recognition that health care inequities and societal barriers are major contributors to the continued high prevalence of substance use disorders, the individual suffering they inflict, and the huge toll that they incur at a societal level.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 US Department of Health and Human Services: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2018. Rockville, Md, SAMHSA, 2019 ( https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2018-NSDUH ) Google Scholar
2 Koob GF, Powell P, White A : Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19 . Am J Psychiatry 2020 ; 177:1031–1037 Link , Google Scholar
3 Cassidy CM, Carpenter KM, Konova AB, et al. : Evidence for dopamine abnormalities in the substantia nigra in cocaine addiction revealed by neuromelanin-sensitive MRI . Am J Psychiatry 2020 ; 177:1038–1047 Link , Google Scholar
4 Bradberry CW : Neuromelanin MRI: dark substance shines a light on dopamine dysfunction and cocaine use (editorial). Am J Psychiatry 2020 ; 177:1019–1021 Abstract , Google Scholar
5 Blaine SK, Wemm S, Fogelman N, et al. : Association of prefrontal-striatal functional pathology with alcohol abstinence days at treatment initiation and heavy drinking after treatment initiation . Am J Psychiatry 2020 ; 177:1048–1059 Link , Google Scholar
6 Sullivan EV : Why timing matters in alcohol use disorder recovery (editorial). Am J Psychiatry 2020 ; 177:1022–1024 Abstract , Google Scholar
7 Lees B, Mewton L, Jacobus J, et al. : Association of prenatal alcohol exposure with psychological, behavioral, and neurodevelopmental outcomes in children from the Adolescent Brain Cognitive Development Study . Am J Psychiatry 2020 ; 177:1060–1072 Link , Google Scholar
8 McCormack C, Monk C : Considering prenatal alcohol exposure in a developmental origins of health and disease framework (editorial). Am J Psychiatry 2020 ; 177:1025–1028 Abstract , Google Scholar
9 Evans-Polce RJ, Kcomt L, Veliz PT, et al. : Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates . Am J Psychiatry 2020 ; 177:1073–1081 Abstract , Google Scholar
10 Grant BF, Shmulewitz D, Compton WM : Nicotine use and DSM-IV nicotine dependence in the United States, 2001–2002 and 2012–2013 . Am J Psychiatry 2020 ; 177:1082–1090 Link , Google Scholar
11 Brady KT : Social determinants of health and smoking cessation: a challenge (editorial). Am J Psychiatry 2020 ; 177:1029–1030 Abstract , Google Scholar
- Cited by None
- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues
- Open access
- Published: 21 June 2021
A review of research-supported group treatments for drug use disorders
- Gabriela López 1 ,
- Lindsay M. Orchowski ORCID: orcid.org/0000-0001-9048-3576 2 ,
- Madhavi K. Reddy 3 ,
- Jessica Nargiso 4 &
- Jennifer E. Johnson 5
Substance Abuse Treatment, Prevention, and Policy volume 16 , Article number: 51 ( 2021 ) Cite this article
27k Accesses
7 Citations
3 Altmetric
Metrics details
This paper reviews methodologically rigorous studies examining group treatments for interview-diagnosed drug use disorders. A total of 50 studies reporting on the efficacy of group drug use disorder treatments for adults met inclusion criteria. Studies examining group treatment for cocaine, methamphetamine, marijuana, opioid, mixed substance, and substance use disorder with co-occurring psychiatric conditions are discussed. The current review showed that cognitive behavioral therapy (CBT) group therapy and contingency management (CM) groups appear to be more effective at reducing cocaine use than treatment as usual (TAU) groups. CM also appeared to be effective at reducing methamphetamine use relative to standard group treatment. Relapse prevention support groups, motivational interviewing, and social support groups were all effective at reducing marijuana use relative to a delayed treatment control. Group therapy or group CBT plus pharmacotherapy are more effective at decreasing opioid use than pharmacotherapy alone. An HIV harm reduction program has also been shown to be effective for reducing illicit opioid use. Effective treatments for mixed substance use disorder include group CBT, CM, and women’s recovery group. Behavioral skills group, group behavioral therapy plus CM, Seeking Safety, Dialectical behavior therapy groups, and CM were more effective at decreasing substance use and psychiatric symptoms relative to TAU, but group psychoeducation and group CBT were not. Given how often group formats are utilized to treat drug use disorders, the present review underscores the need to understand the extent to which evidence-based group therapies for drug use disorders are applied in treatment settings.
Drug use disorders are a significant public health concern in the United States. According to the National Epidemiologic Survey of Alcohol and Related Conditions-III, the lifetime prevalence rate of DSM-5 drug use disorders is 9.9%, which includes amphetamine, cannabis, club drug, cocaine, hallucinogen, heroin, opioid, sedative/tranquilizer, and solvent/inhalant use disorders [ 1 ]. Drug use disorders are defined in terms of eleven criteria including physiological, behavioral and cognitive symptoms, as well as consequences of criteria, any two of which qualify for a diagnosis [ 2 , 3 ]. The individual and community costs of drug use are estimated at over $193 billion [ 4 , 5 ] and approximately $78.5 billion [ 6 ] for opioids alone. Consequences include overdose [ 7 ], mental health problems [ 8 ], and a range of medical consequences such as human immunodeficiency virus [ 9 , 10 ], hepatitis C virus [ 9 ], and other viral and bacterial infections [ 11 ].
Evidence-based practice was formally defined by Sackett et al. [ 12 ] in 1996 to refer to the “conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients” (p. 71). In 2006, the American Psychological Association [ 13 ] developed a policy on evidence-based practice (EBP) of psychotherapy, which emphasized the integration of best research evidence (i.e., data from meta-analyses, randomized controlled trials, effectiveness trials, and other forms of systematic case studies and reviews) with clinical expertise and judgment to deliver treatment in the context of a patient’s individual needs, preferences and culture. The shift towards EBP for substance use disorders has multiple benefits for practitioners and patients, including an increased focus on the implementation of treatments that are safe and cost-effective [ 14 ]. A recent survey of clinicians’ practices with substance use treatment found that clinicians often conducted therapy in groups [ 15 ]. While most clinicians who completed the survey reported use of evidence-based treatment practices (EBT) some also reported the use of non-EBT practices [ 15 ]. Ensuring that clinicians can readily access information regarding the current state of evidence regarding group-based therapies for substance use disorders is critical for fostering increased use of EBTs.
Although any effort to summarize a literature as large and complex as the psychological treatment literature is useful, there are several limitations. With few exceptions, research-supported treatment lists categorize treatments by formal change theory (e.g., cognitive-behavioral, interpersonal) and describe little about the context, format, or setting in which treatments were conducted and tested [ 16 ]. As a result, it is often difficult to ascertain from existing resources whether research supported treatments were conducted in group or individual format. A group format is often used in substance use treatment [ 17 ] and aftercare programs [ 18 , 19 , 20 , 21 , 22 ] . The discrepancy between the wide-spread use of group therapy in clinical practice and the relative paucity of research on the efficacy of group treatments has been noted by treatment researchers [ 23 ] and clinicians [ 24 ]. According to Lundahl’s [ 25 ] 2010 meta-analysis of studies evaluating the efficacy of motivational interviewing (MI), a commonly used treatment for substance use disorders, examination of the 119 studies concluded that studies of MI in a group format were too rare to draw solid conclusions about the efficacy of group MI. Also, it is possible that efficacy of treatments developed for individual delivery will be altered when delivered in a group format and vice versa. Given the limited empirical inquiry on group treatments for substance use, a framework organizing the literature on the efficacy of group therapy to treat substance use disorders would be useful. There is also a need for a more recent rigorous review of the empirical evidence to support group-based treatments for substance use disorders. Over 15 years ago, Weiss and colleagues conducted a review of 24 treatment outcome studies within the substance use disorder intervention literature comparing group therapy to other treatments conditions (i.e., no group therapy, individual therapy, group therapy plus individual therapy), and found no differences between group and individual therapy [ 26 ].
Given the importance of understanding the current evidence base for group-delivered treatments for substance use disorders, the present review sought to provide a summary of the literature on the benefits of group treatments for drug use disorders. Group treatments are potentially cost-effective, widely disseminable, and adaptable to a variety of populations but are lagging individual treatments in terms of research attention. Thus, highlighting characteristics of group treatments that are potentially efficacious is of import to stimulate further empirical inquiry. The review is organized by drug type (cocaine, methamphetamine, marijuana, opiate, mixed substance use disorders; SUD) and co-occurring SUD and psychiatric problems. We excluded studies focused on alcohol use disorder alone as this literature is summarized elsewhere (see Orchowski & Johnson, 2012). Given research suggesting that several factors impact outcomes of group treatments, including formal change theory driving the treatment approach (i.e., cognitive-behavioral, motivational interviewing), as well as patient factors [ 27 ], the review begins by first reviewing each theory of change (i.e., type of treatment), and then concludes by summarizing the research examining the extent to which patient factors influence the efficacy of group treatments for SUD.
To locate studies that evaluated a group treatment for SUD that met review inclusion criteria, the authors conducted a comprehensive literature search of PsycINFO and MedLine through 2020. Three individuals then examined abstracts of the articles for relevance. In addition, the authors utilized the reference lists of review studies and meta-analyses of SUD- treatments to locate additional studies that might meet the review inclusion criteria. The authors and a research assistant then reviewed full articles with relevance to the current study and excluded any studies that did not meet the review inclusion criteria (see Fig. 1 ).
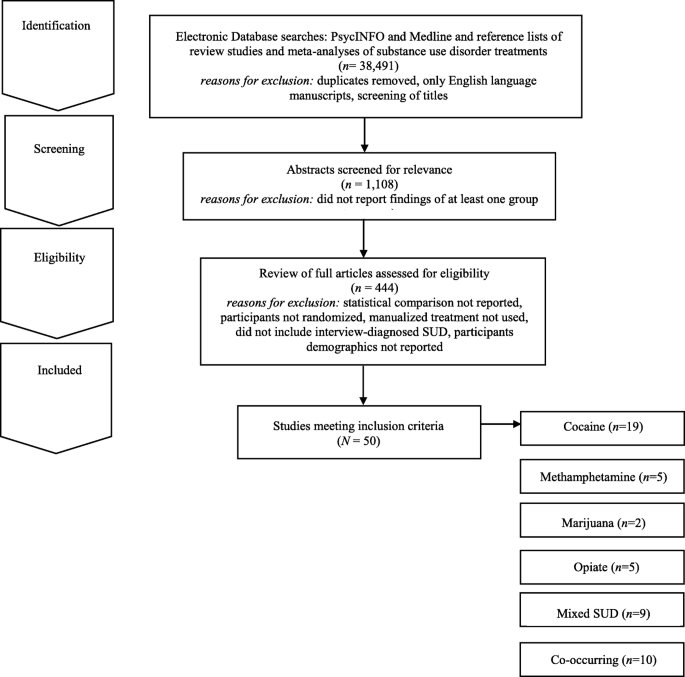
Electronic Search Strategy Flowchart
For inclusion in the review, studies needed to meet the following criteria: 1) report the findings of at least one group treatment; 2) provide at least one statistical comparison between the group treatment and a control condition; 3) randomize participants between the group treatment and control condition; 4) utilize a manualized treatment; 5) include patients with an interview-diagnosed SUD; and 6) provide information regarding the demographic characteristics of the participants in the study. Studies’ methods and results were used for data extraction. Studies which maintained a primary focus on the treatment of SUD, but also included treatment of a co-occurring psychiatric condition, were included in the review. Studies which included alcohol use as a comorbid diagnosis along another substance use were included. Studies examining the efficacy of group treatment for only alcohol use were excluded. The final set of articles included were 50 research studies that utilized a group treatment modality for the treatment of SUD, including separately examining cocaine, methamphetamine, marijuana, opioid, mixed substance, or SUD with comorbid psychiatric problems in adults.
It should be noted that several studies that met inclusion criteria were not reported in the present review because they did not report the use of a specific screening instrument for SUD as a part of the study inclusion/exclusion criteria. These studies are as follows and include these comparisons: group-based relational therapy [ 28 ] two studies by Guydish et al. [ 29 , 30 ] comparing a day treatment program to residential treatment (RT) program, a day treatment program to a coping skills group [ 31 ], standard care to a harm reduction group [ 32 ], 12 step group to a CBT group [ 33 ], medical management treatment (MMT) with CBT group to an MMT plus treatment reinforcement plan [ 34 ], treatment as usual to contingency management (CM) [ 35 ], professionally led recovery training group to treatment as usual (TAU) [ 36 ], two 4 month residential treatment programs [ 37 ], varying lengths of therapeutic community program (TPC) with and without relapse prevention [ 38 ], and Information and Referral plus peer advocacy to a Motivational group with CBT group [ 39 ].
Review of evidence-based theories of change
The 50 research studies meeting inclusion criteria tested the following group treatment modalities: contingency management (CM), motivational interviewing (MI), relapse prevention (RP), social support (SS), cognitive-behavioral (CBT), coping skills (CS), harm reduction (HR), cognitive therapy (CT), drug counseling (DC), recovery training (RT), standard group therapy (SGT), family therapy (FT), intensive group therapy (IGT), 12 step facilitation group therapy (12SG), relational psychotherapy mothers’ group (RPMG), psychoeducational therapy group (PET), behavioral skills (BS), and seeking safety (SS). Below, we briefly review the theory of change that drives each of these treatments.
Several treatment approaches are grounded in behavioral therapies and/or cognitive therapies. Broadly, cognitive therapy is an approach that focuses exclusively on targeting thoughts that are identified as part of a diagnosis or behavioral problem [ 28 ]. Cognitive-behavioral (CBT) therapy is an approach that targets specific symptoms, thoughts, and behaviors that are identified as part of a diagnosis or presenting problem [ 28 ]. Under the umbrella of CBT several other treatment modalities exist. For example, relapse prevention is a CBT treatment that hypothesizes that there are cognitive, behavioral, and affective mechanism that underlie the process of relapse [ 40 ]. Recovery training is a more specific form of relapse prevention, including education on addiction and recovery and reinforcing relapse prevention skills (e.g., understanding triggers, coping with cravings etc.) [ 41 , 42 ]. Other treatments focus on coping skills more broadly. For example, coping skills treatments include a focus on components of adaptability in interpersonal relationships, thinking and feeling, as well as approaches to self and life [ 28 ]. Some treatment approaches also recognize that individuals may not be ready to change their substance use. For example, motivational interviewing is often described as a therapy guiding technique in which the therapist is a helper in the behavior change process and expressed acceptance of the patient [ 43 ]. Standard group therapy includes 90 min sessions approximately twice a week in a group setting, [ 44 ] whereas intensive group therapy is a heavier dose of standard group therapy that includes 120-min sessions up to five times a week [ 44 ]. Psychoeducational therapy group focused on providing information on the immediate and delayed problems of substance use disorders to patients [ 45 ]. Lastly, dialectical behavior therapy (DBT) is a type of CBT therapy that focuses on helping regulate intense emotional states and provides skills to reduce arousal levels, and increase mindfulness, emotional regulation, and interpersonal skills [ 46 ].
Grounded within behavioral therapies, are behavioral skills training which focused on developing behaviors that are adaptive [ 28 ]. Contingency management is a type of behavioral therapy in which patients are reinforced or rewarded for positive behavioral change [ 47 ]. Harm reduction is a term for interventions aiming to reduce the problematic effects of behaviors [ 48 ]. Several treatment approaches also focus on interpersonal networks and building interpersonal skills. For example, social support is any psychological resources provided by a social network to help patients cope with stress [ 49 ]. Twelve-step facilitation group therapy is a more specific form of social support, which focuses on introducing patients to the 12 steps of alcoholics anonymous or related groups (i.e., cocaine or narcotics anonymous) to encourage 12-step meeting attendance in their community [ 33 , 50 ]. Seeking Safety is a present-focused and empowerment-based intervention focused on coping skills that emphasizes the importance of safety within interpersonal relationships [ 51 ]. Drug counseling describes treatment that aims to facilitate abstinence, encourage mutual support, and provide coping skills [ 52 ]. Finally, family therapy is a family-based intervention that aims to change, parenting behaviors and family interactions [ 53 ]. Overall, there are many overlapping components and skill sets in the models discussed above (See Table 1 ).
Group-based cocaine use treatments for adults
Nineteen studies were identified that targeted cocaine use and utilized some form of group therapy, the most of any drug in this review (see Table 2 ). Overall, the studies showed that all of the group therapy modalities included in this review generally reduced cocaine use when compared to treatment as usual (TAU), including day hospital groups [ 54 ]. Two studies, Magura et al. (1994) and Magura et al. (2002) did not find group differences between 8 months CBT and 8 months of TAU that consisted of methadone maintenance therapy among 141 patients with cocaine disorder [ 60 , 69 ]. When compared directly, individuals in CBT groups achieved longer abstinence than individuals in 12 step facilitation groups [ 33 ] or low intensity groups [ 64 , 65 ]. However, in another study, individuals with cocaine dependence receiving 12-step based Group Drug Counseling (GDC; similar to 12-step facilitation) had similar cocaine abstinence outcomes with or without additional individual CBT [ 41 ]. This may suggest that group 12-step facilitation is an effective intervention for cocaine dependence. Two studies demonstrated the superiority of CM groups for reducing cocaine use as compared to CBT [ 62 ] or TAU groups [ 61 , 62 ] at 12 weeks [ 54 ], 17 weeks [ 53 ], 26 weeks [ 53 ] and 52 weeks follow up [ 51 ]. Therefore, CBT group therapy and contingency management groups appear to be more effective at reducing cocaine use than TAU groups.
Group-based methamphetamine use treatments for adults
Only five treatment studies were identified that examined group treatments for methamphetamine use (see Table 3 ). Three studies found longer periods of abstinence for the group treatment (CM or drug+CM) than for TAU or non-CM conditions. The first study conducted by Rawson and colleagues compared matrix model (MM) with TAU in eight community outpatient settings [ 71 ]. The MM consisted of CBT groups, family education groups, social support groups, and individual counseling sessions along with weekly urine screens for 16 weeks. Participants in the MM condition attended more sessions, stayed in treatment longer, had more than twice as many contacts, evidence longer abstinence and greater self-reported psychosocial functioning relative to the TAU group. However, these significant differences did not persist 6 months later at follow-up.
Shoptaw et al. (2006) [ 73 ] compared four groups for treating methamphetamine dependence sertraline + CM, sertraline only, placebo + CM, and placebo [ 73 ]. Additionally, all participants attended a relapse prevention group conducted three times a week over a 14-week period. Findings provided support for the efficacy of CM for amphetamine use disorders. Group treatment (CM or drug + CM) was more effective for sustaining longer periods of abstinence relative to TAU or non-CM conditions. Roll et al. [ 72 ] found that effects of CM relative to TAU became larger as the duration of CM increased. Jaffe et al. [ 70 ] evaluated a culturally tailored intervention for 145 methamphetamine dependent gay and bisexual males. Participants in the Gay Specific CBT condition reported the most rapid decline in levels of methamphetamine use relative to standard CBT, CBT + CM, suggesting benefits for culturally appropriate group methamphetamine interventions.
Group-based marijuana use treatments for adults
Two studies examining group treatments for adults with marijuana use disorders were identified (see Table 4 ). Both studies were conducted by the same research group, utilizing the same inclusion criteria for marijuana use (50 times in 90 days). The studies examined group relapse prevention (RP) [ 76 ], specifically designed for adult marijuana users. The first trial [ 75 ] ( n = 212) comparing relapse prevention to a social support group found participants in both group treatment conditions did well overall, with two-thirds (65%) reporting abstinence of marijuana use for 2 weeks after session 4 or the quit date and 63% reporting abstinence during the last 2 weeks of treatment. Gender differences emerged; no differences between group treatments were found for women, but men in the relapse prevention group reported reduced marijuana use at the 3-month follow-up compared to men in the social support group.
A second trial [ 74 ] randomized participants to 14 sessions of group RP enhanced with cognitive behavioral skills training, two sessions of motivational interviewing (MI) with feedback and advice on cognitive behavioral skills (modeled after the Drinkers Check-up) [ 77 ], or a 4-month delayed treatment control (DTC) group which consisted of the RP group or individual MI treatment of the participants choosing. Compared to individuals randomly assigned to the DTC condition, participants in the group RP and individual MI conditions evidenced a significantly greater reduction in marijuana use and related problems over 16-month follow-up. However, examination of participants’ reactions to DTC assignment indicated that participants who felt that changing their marijuana use was their own responsibility were more likely than those who did not to change their use patterns without treatment engagement.
Group-based opiate use treatments for adults
Five group treatment studies for opioid use were identified (see Table 5 ). Two studies compared the effectiveness of pharmacotherapy plus group therapies [ 79 , 80 , 81 ] to pharmacotherapy alone in samples of opioid dependent persons, and both found that adding group treatment improved outcomes. The first study compared Naltrexone with monthly medical monitoring visits to an enhanced group condition (EN) consisting of Naltrexone plus a Matrix Method (MM) [ 79 ]. MM consisted of hourly individual sessions, 90-min CBT group, and 60 min of cue-exposure weekly for weeks 1–12; hourly individual sessions and CBT group sessions for weeks 13–26; and 90-min social support group sessions for weeks 27–52. Results found that EN participants took more study medication, were retained in treatment longer, used less opioids while in treatment, and showed greater improvement on psychological and affective dimensions than Naltrexone only participants. No difference by treatment condition was found at 6- and 12-month follow-ups. Similarly, Scherbaum et al. [ 80 ] compared routine Methadone Maintenance Therapy (MMT) with routine MMT plus group CBT psychotherapy (20 90-min sessions for 20 weeks). MMT plus group CBT participants showed less drug use than participants in the MMT group (i.e., control group). In contrast, a higher dose of group therapy provided without methadone maintenance was less effective for heroin use than was a lower dose of group therapy with methadone maintenance (Sees et al. [ 81 ]. This suggests that the combination of pharmacotherapy and group therapy for opioid use is optimal.
Shaffer et al. [ 22 ] compared psychodynamic group therapy with a hatha yoga group. All participants received methadone maintenance and individual therapy. No differences between two treatment conditions were found. For all participants, longer participation in treatment was associated with reduction in drug use and criminal activity. Lastly, Des Jarlais et al. [ 78 ] compared a group social learning AIDS/drug injection treatment program (4 sessions, 60–90 min, over 2 weeks) to a control condition. All participants received information about AIDS and HIV antibody test counseling. Compared to control participants, intervention participants reported lower rates of drug injection over time.
Group treatments for mixed SUD for adults
Nine treatment studies were identified that targeted mixed substance use with group treatments (see Table 6 ). Three involved CBT. Downey et al. [ 82 ] compared group CBT plus individual CBT to group CBT plus vouchers in a sample of 14 polysubstance users (cocaine and heroin) maintained on buprenorphine. The study was significantly underpowered and they found no significant differences on treatment outcomes. Marques and Formiogioni [ 84 ] compared individual CBT to group CBT in a sample of 155 participants with alcohol and/or drug dependence. They found that both formats resulted in similar outcomes, with higher compliance in the group CBT participants (66.7% compliance with treatment). Rawson et al. [ 87 ] compared three 16-week treatments: CM, group CBT, and CM plus group CBT, among 171 participants with cocaine disorder or methamphetamine abuse. They found that CM produced better retention and lower rates of stimulant use than CBT during treatment, but CBT produced comparable longer-term outcomes.
Two studies involved Group Drug Counseling (GDC). Greenfield et al. [ 52 ] compared a group drug counseling (GDC) (mixed gender) to a women’s recovery group (WRG) that both met weekly, for 12 weeks, for 90-min sessions among 44 participants that had a substance use disorder other than nicotine. WRG evidenced significantly greater reductions in drug and alcohol use over the follow up compared with GDC. Schottenfeld et al. [ 88 ] compared GDC (weekly, 1-h group sessions) to a community reinforcement approach (CRA; twice weekly sessions for the first 12 weeks and then weekly the following 12 weeks) among 117 patients with an opioid and cocaine use disorder. There were no differences in retention or drug use.
Remaining studies examined other interventions. Margolin et al. [ 83 ] compared an HIV Harm reduction program (HHRP) that met twice weekly for 2 h to an active control group that met six times in a sample of 90 HIV-seropositive methadone-maintained injection drug users with opioid dependence, and abuse or dependence on cocaine. At follow up, they had lower addiction severity scores and were less likely to have engaged in high risk behaviors compared to control. McKay et al. [ 85 ] compared weekly phone monitoring and counseling plus a support group in the first 4 weeks (TEL), twice-weekly individualized relapse prevention, and twice-weekly standard group counseling (STND) among 259 referred participants with alcohol use disorder or cocaine disorder. STND resulted in more days abstinent than TEL. Nemes et al. [ 86 ] compared a 12-month group program (10 months inpatient and 2 months outpatient) to an abbreviated group program (6 months inpatient, 6 months outpatient) among 412 patients with multiple drug/alcohol use disorders. Results indicated that both groups had reduction in arrests and drug use. There were no significant difference between groups. Lastly, Smith et al. [ 89 ] compared a standard treatment program (STP, daily group counseling, family outreach, 12-step program introduction, four 2 h sessions for family) to an enhanced treatment program (ETP; twice weekly group on relapse prevention and interpersonal violence in additional to all STP components) among 383 inpatient veterans meeting for an alcohol, cocaine, or amphetamine use disorder. Results indicated that ETP had enhanced abstinence rates at 3-month and 12-month follow up compared to STP, regardless of type of drug use.
Group Treatments for SUD and Co-Occurring Psychiatric Problems
Individuals with psychiatric distress are at high risk for comorbid SUD [ 90 ]. Ten randomized controlled studies meeting our inclusion criteria examined the efficacy of group therapy for SUD and co-occurring psychiatric problems (see Table 7 ). Three studies described group treatment of SUD and co-occurring DSM-IV Axis II disorders [ 18 , 91 , 96 ], three studies examined group treatment of drug abuse and co-occurring DSM-IV classified Axis I disorders [ 92 , 93 , 99 ], one study explored group drug abuse treatment and co-occurring psychiatric problems among homeless individuals without limiting to DSM-IV Axis I or Axis II diagnoses [ 97 ], and one study focused on group drug treatment among individuals testing positive for HIV [ 98 ]. Within this diverse set of RCTs, participants generally included individuals diagnosed with any form of SUD; however, some studies focused specifically on individuals using cocaine [ 91 , 97 ] or cocaine/opioids [ 98 ].
A range of group treatment approaches are represented, including group psychoeducational therapy, group CBT approaches, group DBT, Seeking Safety and CM. DiNitto and colleagues [ 92 ] evaluated the efficacy of adding a group-based psychoeducational program entitled “Good Chemistry Groups” to standard inpatient SUD treatment services among 97 individuals with a dual diagnosis of SUD and a DSM-IV Axis I psychological disorder. The nine 60-min Good Chemistry Group sessions were offered 3 times per week for 3 weeks. When compared to standard inpatient treatment, the addition of the psychoeducational group was not associated with any changes in medical, legal, alcohol, drug, psychiatric or family/social problems among participants.
The efficacy of adding a psychoeducational group treatment to standard individual therapy to address HIV risk among cocaine users has also been examined [ 91 ]. Participants were randomly assigned to complete the following: 1) individually-administered Standard Intervention developed by the NIDA Cooperative Agreement Final Cohort sites [ 100 ] including HIV testing, and pre- and post-HIV testing counseling on risks relating to cocaine use, transmission of STDs/HIV, condom use, cleaning injection equipment, and the benefits of treatment; or) Standard Intervention plus four 2-h peer-delivered psychoeducational groups addressing stress management, drug awareness, risk reduction strategies, HIV education and AIDS. Among the sample of 966 individuals completing the 3-month follow-up, the group psychoeducational treatment was not differentially effective in reducing drug use and HIV risk behavior in comparison to standard treatment alone at 3-months post-baseline, regardless of treatment type, individuals with antisocial personality disorder (ASPD) demonstrated less improvement in crack cocaine use compared to individuals without ASPD or depression.
The following types of group CBT have sustained research evaluation meeting our inclusion criteria to address co-occurring SUD and Axis I or Axis II disorders: 1) group behavioral skills training; 2) group cognitive behavioral therapy; 3) group-based Seeking Safety [ 51 ], and 4) group dialectical behavioral therapy. Specifically, Jerrell and Ridgely [ 93 ] examined the efficacy of group behavioral skills (BS) training, group-based 12-step facilitation (TS) treatment, and intensive case management among 132 individuals with a dual diagnosis of SUD and another Axis I psychiatric problem over the course of 24-months. Based on the Social and Independent Living Skills program [ 101 ], the BS group included one group per week addressing self-management skills designed to enhance abstinence, including medication management, relapse prevention, social skills, leisure activities and symptom monitoring. Relative to participants in TS groups, participants in the BS groups evidenced increased psychosocial functioning and decreased psychiatric symptoms (i.e., schizophrenia, depressive symptoms, mania, drug use and alcohol use) across the 6-, 12- and 18-month follow-up assessments after treatment entry.
Lehman and colleagues’ [ 95 ] examination of the efficacy of group CBT for substance abuse compared to TAU among 54 individuals with SUD and either schizophrenia or a major affective disorder revealed no differences between treatment groups over the course of a 1-year follow-up period. More promising findings were reported in Fisher and Bentley’s [ 18 ] evaluation of a group CBT and group therapy based in the disease and recovery model (DRM) among 38 individuals with dual diagnosis of SUD and a personality disorder. Groups met three times per week for 12 weeks and were compared to TAU. Individuals in group CBT and group DRM indicated improved social and family functioning compared to TAU, and among those who completed the group in an outpatient setting, CBT was more effective in reducing alcohol use, enhancing psychological functioning and improving social and family functioning compared to DRM and TAU.
Group behavioral therapy plus abstinence contingent housing and work administered in the context of a day treatment program was compared to behavioral group treatment alone among individuals with cocaine abuse/dependence, non-psychotic psychiatric conditions, and homelessness [ 97 , 102 ]. The group behavioral therapy included 8 weeks of daily treatment (4 h and 50 min per day) of groups addressing relapse prevention training, assertiveness training, AIDS education, 12-step facilitation, relaxation, recreation development, goal setting, and goal planning. Participants also engaged in a process-oriented group as well as individual counseling and urine monitoring and engaged in a weekly 90 min psychoeducational group therapy during months 3–6 following treatment enrollment. Individuals who received contingency-based work and housing were provided with rent-free housing and employment in construction or food service industries after 2 consecutive weeks of abstinence [ 103 ]. Relative to BS groups alone, group behavioral day treatment plus contingency management was associated with greater abstinence at 2- and 6-month follow-ups [ 102 ] and were less likely to relapse [ 97 ], although gains were not maintained at 12-months [ 104 ]. Both groups evidenced positive changes in drug use overtime compared to baseline [ 104 ].
Zlotnick, Johnston and Najavits [ 99 ] evaluated the efficacy of Seeking Safety (SS), in comparison to treatment as usual (TAU) among 49 incarcerated women with substance use disorder (SUD) and full or subthreshold posttraumatic stress disorder (PTSD). SS aims to decrease PTSD and SUD through psychoeducational and present-focused and empowerment-based instruction on coping skills that emphasize abstinence and safety [ 51 ]. The SS group treatment included 90-min group sessions held three times per week, that were completed in addition to the 180 to 240 h of group and individual therapy provided in TAU. All participants showed similar improvement on assessments of PSTD, SUD, legal problems and other psychiatric concerns at 12-week, 3- and 6-month follow-ups following prison release. Nonetheless, there was a trend for improved PTSD and continued improvements in psychiatric symptoms at follow-up among participants completing SS compared to TAU. Greater completion of SS sessions was associated with increased improvement in PTSD as well as drug use among women [ 99 ].
Dialectical behavioral group therapy (DBT), a CBT-focused treatment for individuals with borderline personality disorder (BPD), has also been evaluated in comparison to TAU among individuals with BPD and co-occurring SUD [ 96 ]. Core elements of DBT are manualized [ 105 ], and have been evaluated in prior research [ 106 , 107 , 108 ]. Techniques center on providing the participant with acceptance and validation while maintaining a continual focus on behavior change, and include the following: mindfulness skills training, behavioral analysis of dysfunctional behavior, cognitive restructuring, coping skills training, exposure-based strategies addressing maladaptive emotions, and behavioral management skills training. DBT was administered through 2 ¼ hour weekly group sessions administered in combination with 60 min of weekly individual therapy and the opportunity for skills-coaching phone calls. Relative to TAU, participants randomly assigned to DBT demonstrated greater reductions in drug use during the 12-month treatment and at the 16-month follow-up assessment, as well as greater gains in adjustment at the 16-month follow-up assessment.
Although contingency management is commonly administered individually, Petry and colleagues [ 98 ] examined the efficacy of weekly 60-min group-based contingency management (CM) for reinforcing health behaviors and HIV-positive individuals with cocaine or opioid disorders ( N = 170) in comparison to 12-step facilitation (TS) over the course of a 24-week period. Overall, participants in CM were more likely than those in TS to submit consecutive drug-free urine specimens, although the overall proportion of drug-free specimens did not vary between groups during treatment or over the follow-up period. Notably, during treatment, group CM was associated with greater reductions in HIV-risk behaviors as well as overall viral load compared to TS; although effects were not maintained over the follow-up period.
Across these studies, many trials showed positive gains for both group treatments examined [ 18 , 97 , 98 ], or no difference between groups when examining the benefit of adding group treatment to existing TAU [ 91 , 92 , 95 , 99 ]. However, one study demonstrated greater reductions in drug use among individuals with BPD and SUD who completed group DBT in comparison to TAU [ 96 ]. Further, BS groups were more effective than TS groups in improving psychosocial functioning and decreasing substance use [ 93 ]. Finally, CBT was more effective than DRM in reducing alcohol use, enhancing psychological functioning and improving social and family functioning compared to DRM and TAU among individuals dually diagnosed with SUD and a personality disorder [ 18 ].
Factors associated with treatment efficacy
Gender and treatment efficacy.
Five of the studies included in the present review examined whether treatment was differentially effective for men and women. Although Jarrell and Ridgely’s [ 93 ] evaluation of group BS, group TS and individual case management for individuals with SUD and co-occurring Axis I disorders did not examine whether group treatment types were differentially effective for men and women, data indicated that women—regardless of treatment group—reported higher role functioning (i.e.., independent living, work productivity, as well as immediate and extended social relationships), increased psychiatric symptomatology (depression, mania, drug use, alcohol use) across the follow-up periods compared to men.
Race and ethnicity and treatment efficacy
Among the studies included in the present review, only three examined whether treatment efficacy varied as a function of race and ethnicity. A secondary examination of the efficacy of group BS in comparison to group TS and individual case management [ 93 ] suggested that outcomes in each group treatment among ethnic and racial minority clients were equivalent to White participants during the 6-month follow [ 94 ]. The initial evaluation indicated that—regardless of group treatment type—racial/ethnic minority participants reported lower scores in personal well-being, lower life satisfaction (i.e., satisfaction with living), worse role functioning (i.e., independent living, work productivity, immediate and extended social relationships) over the follow-up periods compared to White participants [ 93 ].
Conclusions
In general, participants in group treatment for drug use disorders exhibit more improvement on typical measures of outcome (e.g., abstinence & use rates, objective measures, urinalysis) when compared to standard care without group [ 18 , 109 ] and those who refuse or drop out of treatment [ 110 ]. Specifically, CBT and CM appear to be more effective at reducing cocaine use than TAU groups. CM is effective in increasing periods of abstinence among users of methamphetamine. Both relapse prevention and social support group therapy were effective for marijuana use although relapse prevention was more helpful for men than for women. Brief MI and relapse prevention were both effective at reducing marijuana use. CBT and CBT-related treatments (including the matrix model) when added to pharmacotherapy were more effective for opioid use disorder than pharmacotherapy alone. Effective treatments for Mixed SUD include group CBT, CM, and women’s recovery group. Longer relapse prevention periods appear to be more helpful in reducing mixed SUD. Behavioral skills and behavioral skills plus contingency management helped decreased psychiatric symptoms and drug use behaviors. Psychoeducation groups alone, a commonly used intervention, were not effective at addressing SUD and co-occurring psychiatric problems. Additionally, it is important to note that there is potential for risk of bias in the studies included across four domains: participants, predictors, outcome, and analysis [ 111 ]. The current study did not comprehensively assess for risk of bias and this is a study limitation. Future research could assess for risk of bias by following the guidelines suggested by the Cochrane Handbook [ 112 ].
The current literature offers a wide variety of group treatments with varying goals and based on varying formal change theories. Overall, studies that reported between-group effect size ( n = 7) reported small to medium effect sizes potentially suggesting differences were moderate but of potential theoretical interest. Of those seven studies, only two studies reported large effect sizes (both comparing an active treatment to a delayed treatment/untreated condition). In order to better characterize magnitude of intervention effects, future studies should report effect sizes and their confidence intervals [ 113 , 114 ]. Moreover, groups based on cognitive-behavioral theory [ 35 ], motivational enhancement theory [ 43 ], stages of change theory [ 115 ], 12-step theory [ 41 ] and psychoeducational group models [ 116 ] have all been the subject of recent studies. Steps of treatment have also been used to classify groups for acutely ill individuals with SUD versus middle stage (recovering) or after care groups, with the latter mainly focusing on relapse prevention. Group therapy is provided – at least as an augment to multimodal interventions – in most of the outpatient and inpatient programs in English speaking and European countries [ 17 , 117 ]. Therefore, continued efforts to implement and scale up group-based treatments for SUD known to be effective are needed. CM appears to be effective at addressing various drug use problems and further research should evaluate whether it would also be useful for marijuana use.
Future Research Questions
Studies of other group treatments for SUD that use rigorous, interview-based diagnosis, use control groups, randomly assign participants to condition, report the ethnic and racial composition of the sample, are adequately powered, implement a treatment manual, and compare outcomes to individual treatment as well are necessary.
Little is known regarding the possible mediators and moderators of treatment outcome in group interventions for SUD
Key Learning Objectives
Group treatment approaches are widely utilized and are often less costly to implement than individual treatments, currently we know very little whether one group approach is superior to another in the treatment of SUD.
Group treatment approaches seem to be more effective at improving positive outcomes (e.g., abstinence, use rates, objective measures, urinalysis) when compared to standard care without group [ 18 , 109 ], and those who refuse and drop out of treatment
More thorough randomized controlled trials of group SUD treatments are needed [ 110 ].
Availability of data and materials
Not applicable. The present study does not include original data. However, the authors of the study have listed all articles reviewed in this study in the reference section.
Abbreviations
Twelve Step Facilitation Group Therapy
Alcohol Dependence
Acquired Immunodeficiency Syndrome
Addiction Severity Index
Antisocial Personality Disorder
Abbreviated Program
Behavioral Skills
Borderline Personality Disorder
Cognitive Behavioral Therapy
Cocaine Dependence
Composite Diagnostic Interview Schedule
Contingency Management
Community Reinforcement Approach
Coping Skills
Cognitive Therapy
Dialectical Behavioral Therapy
Day Treatment
Drug Counseling
Diagnostic Interview Schedule
Diagnostic and Statistical Manual
Disease and Recovery Model
Delayed to Control
Evidence-Based Practice
Evidence-Based Treatment Practice
Enhanced Group Condition
Enhanced Treatment Program
Family Therapy
Group Drug Counseling
Human Immunodeficiency Virus
HIV Harm Reduction
Harm Reduction
Intensive Group Therapy
Individual Therapy
Motivational Interviewing
Matrix Model
Methadone Maintenance Therapy
National Institute of Drug Abuse
Psychoeducational Therapy Group
Pre-Post with Comparison Group (matched or otherwise)
Post Traumatic Stress Disorder
Random Assignment with Control
Relapse Prevention
Recovery Training
Random Assignment to Active Treatment
Relational Psychotherapy Mothers’ Group
Structured Clinical Interview for Diagnosis
Social Support
Standard Group Therapy
Substance Use Disorder
Seeking Safety
Standard Group Counseling
Standard Treatment Program
Treatment as Usual
Phone Monitoring and Counseling, with Support Group
Therapeutic Community Program
Twelve Step
Women’s Recovery Group
Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, et al. Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on alcohol and related conditions-III. JAMA Psychiatry. 2016;73(1):39–47.
Article PubMed PubMed Central Google Scholar
Edition F. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed; 2013.
Google Scholar
Rehm J, Marmet S, Anderson P, Gual A, Kraus L, Nutt DJ, et al. Defining substance use disorders: do we really need more than heavy use? Alcohol Alcohol. 2013;48(6):633–40.
Article CAS PubMed Google Scholar
Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011;12(4):657–67.
Article PubMed Google Scholar
Center NDI. National Drug Threat Assessment. Washington: United States Department of Justice; 2011.
Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54(10):901–6.
Kamal R, Cox C, Rousseau D, Foundation ftKF. Costs and outcomes of mental health and substance use disorders in the US. JAMA. 2017;318(5):415.
Hall WD, Patton G, Stockings E, Weier M, Lynskey M, Morley KI, et al. Why young people's substance use matters for global health. Lancet Psychiatry. 2016;3(3):265–79.
Khalsa JH, Treisman G, McCance-Katz E, Tedaldi E. Medical consequences of drug abuse and co-occurring infections: research at the National Institute on Drug Abuse. Subst Abus. 2008;29(3):5–16.
McCoy CB, Lai S, Metsch LR, Messiah SE, Zhao W. Injection drug use and crack cocaine smoking: independent and dual risk behaviors for HIV infection. Ann Epidemiol. 2004;14(8):535–42.
Contoreggi, md C, Rexroad, rph VE, Lange, md, et al. Current Management of Infectious Complications in the injecting drug user. J Subst Abus Treat. 1998;15(2):95–106.
Article Google Scholar
Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312(7023):71–2.
Article CAS PubMed PubMed Central Google Scholar
American Psychological Association PTFoE-BP. Evidence-based practice in psychology. Am Psychol. 2006;61:271–85.
Pope C. Resisting evidence: the study of evidence-based medicine as a contemporary social movement. Health. 2003;7(3):267–82.
Wendt D. Group therapy for substance use disorders: a survey of clinician practices. J Groups Addict Recover. 2017;12(4):243 EOA.
Johnson J. Using research-supported group treatments. J Clin Psychol In Session. 2008;64(11):1206–24.
Stinchfield RD, Owen P, Winters K. Group therapy for substance abuse: A review of the empirical research. In: Burlingame AFG, editor. Handbook of group psychotherapy. New York: Wiley; 1994. p. 458–88.
Fisher MS Sr, Bentley KJ. Two group therapy models for clients with a dual diagnosis of substance abuse and personality disorder. Psychiatr Serv. 1996;47(11):1244–50.
Kaminer Y, Burleson JA, Blitz C, Sussman J, Rounsaville BJ. Psychotherapies for adolescent substance abusers: a pilot study. J Nerv Ment Dis. 1998;186(11):684–90.
McKay JR, Alterman AI, Cacciola JS, O'Brien CP, Koppenhaver JM, Shepard DS. Continuing care for cocaine dependence: comprehensive 2-year outcomes. J Consult Clin Psychol. 1999;67(3):420–7.
McKay JR, Alterman AI, Cacciola JS, Rutherford MJ, O'Brien CP, Koppenhaver J. Group counseling versus individualized relapse prevention aftercare following intensive outpatient treatment for cocaine dependence: initial results. J Consult Clin Psychol. 1997;65(5):778–88.
Shaffer HJ, LaSalvia TA, Stein JP. Comparing hatha yoga with dynamic group psychotherapy for enhancing methadone maintenance treatment: a randomized clinical trial. Altern Ther Health Med. 1997;3(4):57–66.
CAS PubMed Google Scholar
Morgan-Lopez AA, Fals-Stewart W. Analytic methods for modeling longitudinal data from rolling therapy groups with membership turnover. J Consult Clin Psychol. 2007;75(4):580–93.
Weiss RD. Treating patients with bipolar disorder and substance dependence: lessons learned. J Subst Abus Treat. 2004;27(4):307–12.
Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A meta-analysis of motivational interviewing: twenty-five years of empirical studies. Res Soc Work Pract. 2010;20(2):137–60.
Weiss RD, Jaffee WB, de Menil VP, Cogley CB. Group therapy for substance use disorders: what do we know? Harvard Rev Psychiatry. 2004;12(6):339–50.
Burlingame GM, MacKenzie KR, Strauss B. Bergin & Garfields Handbook Of Psychotherapy And Behavior Change. Small group treatment: Evidence for effectiveness and mechanisms of change. In: Lambert M, editor. Handbook of psychotherapy and behavior change. 5th ed. New York: Wiley; 2003. p. 647–96.
Beck AT. Cognitive therapy: nature and relation to behavior therapy. Behav Ther. 1970;1(2):184–200.
Guydish J, Sorensen JL, Chan M, Werdegar D, Bostrom A, Acampora A. A randomized trial comparing day and residential drug abuse treatment: 18-month outcomes. J Consult Clin Psychol. 1999;67(3):428–34.
Guydish J, Werdegar D, Sorensen JL, Clark W, Acampora A. Drug abuse day treatment: a randomized clinical trial comparing day and residential treatment programs. J Consult Clin Psychol. 1998;66(2):280–9.
Avants SK, Margolin A, Sindelar JL, Rounsaville BJ, Schottenfeld R, Stine S, et al. Day treatment versus enhanced standard methadone services for opioid-dependent patients: a comparison of clinical efficacy and cost. Am J Psychiatry. 1999;156(1):27–33.
Avants SK, Margolin A, Usubiaga MH, Doebrick C. Targeting HIV-related outcomes with intravenous drug users maintained on methadone: a randomized clinical trial of a harm reduction group therapy. J Subst Abus Treat. 2004;26(2):67–78.
Maude-Griffin PM, Hohenstein JM, Humfleet GL, Reilly PM, Tusel DJ, Hall SM. Superior efficacy of cognitive-behavioral therapy for urban crack cocaine abusers: main and matching effects. J Consult Clin Psychol. 1998;66(5):832–7.
Rohsenow DJ, Monti PM, Martin RA, Michalec E, Abrams DB. Brief coping skills treatment for cocaine abuse: 12-month substance use outcomes. J Consult Clin Psychol. 2000;68(3):515–20.
Beck ATW, F. D.; Newman, C. F.; Liese, B. S. Cognitive therapy of substance abuse. New York: Guilford; 1993.
McAuliffe WE. A randomized controlled trial of recovery training and self-help for opioid addicts in New England and Hong Kong. J Psychoactive Drugs. 1990;22(2):197–209.
Czuchry M, Dansereau DF. Node-link mapping and psychological problems. Perceptions of a residential drug abuse treatment program for probationers. J Subst Abus Treat. 1999;17(4):321–9.
Article CAS Google Scholar
McCusker J, Bigelow C, Frost R, Garfield F, Hindin R, Vickers-Lahti M, et al. The effects of planned duration of residential drug abuse treatment on recovery and HIV risk behavior. Am J Public Health. 1997;87(10):1637–44.
Rosenblum A, Magura S, Kayman DJ, Fong C. Motivationally enhanced group counseling for substance users in a soup kitchen: a randomized clinical trial. Drug Alcohol Depend. 2005;80(1):91–103.
Marlatt GA, Donovan DM. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. 2nd ed. New York: The Guilford Press; 2005. p. xiv, 416-xiv
Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken LS, et al. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse collaborative cocaine treatment study. Arch Gen Psychiatry. 1999;56(6):493–502.
Luthar SSS, N.E.; Altomare, M. Relational psychotherapy Mother’s group: A randomized clinical trial for substance abusing mothers. Dev Psychopathol. 2007;19:243–61.
Miller WRR, S. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford Press; 1991.
Hoffman JA, Caudill BD, Koman JJ 3rd, Luckey JW, Flynn PM, Mayo DW. Psychosocial treatments for cocaine abuse. 12-month treatment outcomes. J Subst Abus Treat. 1996;13(1):3–11.
Kaminer Y, Burleson JA, Goldberger R. Cognitive-behavioral coping skills and psychoeducation therapies for adolescent substance abuse. J Nerv Ment Dis. 2002;190(11):737–45.
Linehan M. DBT skills training manual. 2nd ed. London: The Guilford Press; 2015.
Petry NM. Contingency management: what it is and why psychiatrists should want to use it. Psychiatrist. 2011;35(5):161–3.
Logan DE, Marlatt GA. Harm reduction therapy: a practice-friendly review of research. J Clin Psychol. 2010;66(2):201–14.
PubMed PubMed Central Google Scholar
Ellis B, Bernichon T, Yu P, Roberts T, Herrell JM. Effect of social support on substance abuse relapse in a residential treatment setting for women. Eval Program Plan. 2004;27(2):213–21.
Nowinski J, Baker S. The twelve-step facilitation handbook: A systematic approach to early recovery from alcoholism and addiction. San Francisco: Jossey-Bass; 1992. p. xxii. 215-xxii
Najavits LM. Seeking safety: a treatment manual for PTSD and substance abuse. New York: Guilford; 2002.
Greenfield SF, Trucco EM, McHugh RK, Lincoln M, Gallop RJ. The Women's recovery group study: a stage I trial of women-focused group therapy for substance use disorders versus mixed-gender group drug counseling. Drug Alcohol Depend. 2007;90(1):39–47.
Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, Tejeda M. Multidimensional family therapy for adolescent drug abuse: results of a randomized clinical trial. Am J Drug Alcohol Abuse. 2001;27(4):651–88.
Coviello DM, Alterman AI, Rutherford MJ, Cacciola JS, McKay JR, Zanis DA. The effectiveness of two intensities of psychosocial treatment for cocaine dependence. Drug Alcohol Depend. 2001;61(2):145–54.
Crits-Christoph P, Siqueland L, McCalmont E, Weiss RD, Gastfriend DR, Frank A, et al. Impact of psychosocial treatments on associated problems of cocaine-dependent patients. J Consult Clin Psychol. 2001;69(5):825–30.
Siqueland L, Crits-Christoph P, Gallop R, Barber JP, Griffin ML, Thase ME, et al. Retention in psychosocial treatment of cocaine dependence: predictors and impact on outcome. Am J Addict. 2002;11(1):24–40.
Mercer D, Carpenter G, Daley D. The adherence and competence scale for group addiction counseling for TCACS: Center for Psychotherapy Research, Department of Psychiatry, University of Pennsylvania Medical School; 1994.
Luborsky L. Principles of psychoanalytic psychotherapy a manual for supportive-expressive treatment; 1984.
Epstein DH, Hawkins WE, Covi L, Umbricht A, Preston KL. Cognitive-behavioral therapy plus contingency management for cocaine use: findings during treatment and across 12-month follow-up. Psychol Addict Behav. 2003;17(1):73–82.
Magura S, Rosenblum A, Lovejoy M, Handelsman L, Foote J, Stimmel B. Neurobehavioral treatment for cocaine-using methadone patients: a preliminary report. J Addict Dis. 1994;13(4):143–60.
Petry NM, Alessi SM, Hanson T. Contingency management improves abstinence and quality of life in cocaine abusers. J Consult Clin Psychol. 2007;75(2):307–15.
Rawson RA, Huber A, McCann M, Shoptaw S, Farabee D, Reiber C, et al. A comparison of contingency management and cognitive-behavioral approaches during methadone maintenance treatment for cocaine dependence. Arch Gen Psychiatry. 2002;59(9):817–24.
Rohsenow DJ, Monti PM, Rubonis AV, Gulliver SB, Colby SM, Binkoff JA, et al. Cue exposure with coping skills training and communication skills training for alcohol dependence: 6- and 12-month outcomes. Addiction. 2001;96(8):1161–74.
Rosenblum A, Magura S, Foote J, Palij M, Handelsman L, Lovejoy M, et al. Treatment intensity and reduction in drug use for cocaine-dependent methadone patients: a dose-response relationship. J Psychoactive Drugs. 1995;27(2):151–9.
Rosenblum A, Magura S, Palij M, Foote J, Handelsman L, Stimmel B. Enhanced treatment outcomes for cocaine-using methadone patients. Drug Alcohol Depend. 1999;54(3):207–18.
Volpicelli JR, Markman I, Monterosso J, Filing J, O'Brien CP. Psychosocially enhanced treatment for cocaine-dependent mothers: evidence of efficacy. J Subst Abus Treat. 2000;18(1):41–9.
Weinstein SP, Gottheil E, Sterling RC. Randomized comparison of intensive outpatient vs. individual therapy for cocaine abusers. J Addict Dis. 1997;16(2):41–56.
Gottheil E, Weinstein SP, Sterling RC, Lundy A, Serota RD. A randomized controlled study of the effectiveness of intensive outpatient treatment for cocaine dependence. Psychiatr Serv. 1998;49(6):782–7.
Magura S, Rosenblum A, Fong C, Villano C, Richman B. Treating cocaine-using methadone patients: predictors of outcomes in a psychosocial clinical trial. Subst Use Misuse. 2002;37(14):1927–55.
Jaffe A, Shoptaw S, Stein J, Reback CJ, Rotheram-Fuller E. Depression ratings, reported sexual risk behaviors, and methamphetamine use: latent growth curve models of positive change among gay and bisexual men in an outpatient treatment program. Exp Clin Psychopharmacol. 2007;15(3):301–7.
Rawson RA, Marinelli-Casey P, Anglin MD, Dickow A, Frazier Y, Gallagher C, et al. A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction. 2004;99(6):708–17.
Roll JM, Chudzynski J, Cameron JM, Howell DN, McPherson S. Duration effects in contingency management treatment of methamphetamine disorders. Addict Behav. 2013;38(9):2455–62.
Shoptaw S, Huber A, Peck J, Yang X, Liu J, Jeff D, et al. Randomized, placebo-controlled trial of sertraline and contingency management for the treatment of methamphetamine dependence. Drug Alcohol Depend. 2006;85(1):12–8.
Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000;68(5):898–908.
Stephens RS, Roffman RA, Simpson EE. Treating adult marijuana dependence: a test of the relapse prevention model. J Consult Clin Psychol. 1994;62(1):92–9.
Marlatt GAG, J.R. Relapse prevention (unpublished manuscript). In: Luther SSS, Boltas D, editors. Relational parenting Mother’s group: A therapist’s manual. New York: Guilford Press; 1985.
Miller WR, Benefield RG, Tonigan JS. Enhancing motivation for change in problem drinking: a controlled comparison of two therapist styles. J Consult Clin Psychol. 1993;61(3):455–61.
Des Jarlais DC, Casriel C, Friedman SR, Rosenblum A. AIDS and the transition to illicit drug injection--results of a randomized trial prevention program. Br J Addict. 1992;87(3):493–8.
Rawson RA, McCann MJ, Shoptaw SJ, Miotto KA, Frosch DL, Obert JL, et al. Naltrexone for opioid dependence: evaluation of a manualized psychosocial protocol to enhance treatment response. Drug Alcohol Rev. 2001;20(1):67–78.
Scherbaum N, Kluwig J, Specka M, Krause D, Merget B, Finkbeiner T, et al. Group psychotherapy for opiate addicts in methadone maintenance treatment--a controlled trial. Eur Addict Res. 2005;11(4):163–71.
Sees KL, Delucchi KL, Masson C, Rosen A, Clark HW, Robillard H, et al. Methadone maintenance vs 180-day psychosocially enriched detoxification for treatment of opioid dependence: a randomized controlled trial. JAMA. 2000;283(10):1303–10.
Downey KK, Helmus TC, Schuster CR. Treatment of heroin-dependent poly-drug abusers with contingency management and buprenorphine maintenance. Exp Clin Psychopharmacol. 2000;8(2):176–84.
Margolin A, Avants SK, Warburton LA, Hawkins KA, Shi J. A randomized clinical trial of a manual-guided risk reduction intervention for HIV-positive injection drug users. Health Psychol. 2003;22(2):223–8.
Marques AC, Formigoni ML. Comparison of individual and group cognitive-behavioral therapy for alcohol and/or drug-dependent patients. Addiction. 2001;96(6):835–46.
McKay JR, Lynch KG, Shepard DS, Morgenstern J, Forman RF, Pettinati HM. Do patient characteristics and initial progress in treatment moderate the effectiveness of telephone-based continuing care for substance use disorders? Addiction. 2005;100(2):216–26.
Nemes S, Wish ED, Messina N. Comparing the impact of standard and abbreviated treatment in a therapeutic community. Findings from the district of Columbia treatment initiative experiment. J Subst Abus Treat. 1999;17(4):339–47.
Rawson RA, McCann MJ, Flammino F, Shoptaw S, Miotto K, Reiber C, et al. A comparison of contingency management and cognitive-behavioral approaches for stimulant-dependent individuals. Addiction. 2006;101(2):267–74.
Schottenfeld RS, Pantalon MV, Chawarski MC, Pakes J. Community reinforcement approach for combined opioid and cocaine dependence. Patterns of engagement in alternate activities. J Subst Abus Treat. 2000;18(3):255–61.
Smith TL, Volpe FR, Hashima JN, Schuckit MA. Impact of a stimulant-focused enhanced program on the outcome of alcohol- and/or stimulant-dependent men. Alcohol Clin Exp Res. 1999;23(11):1772–9.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the epidemiologic catchment area (ECA) study. JAMA. 1990;264(19):2511–8.
Compton WM, Cottler LB, Ben-Abdallah A, Cunningham-Williams R, Spitznagel EL. The effects of psychiatric comorbidity on response to an HIV prevention intervention. Drug Alcohol Depend. 2000;58(3):247–57.
DiNitto DM, Webb DK, Rubin A. Gender differences in dually-diagnosed clients receiving chemical dependency treatment. J Psychoactive Drugs. 2002;34(1):105–17.
Jerrell JM, Ridgely MS. Comparative effectiveness of three approaches to serving people with severe mental illness and substance abuse disorders. J Nerv Ment Dis. 1995;183(9):566–76.
Jerrell JM, Wilson JL. Ethnic differences in the treatment of dual mental and substance disorders. A preliminary analysis. J Subst Abus Treat. 1997;14(2):133–40.
Lehman AF, Herron JD, Schwartz RP, Myers CP. Rehabilitation for adults with severe mental illness and substance use disorders. A clinical trial. J Nerv Ment Dis. 1993;181(2):86–90.
Linehan MM, Schmidt H 3rd, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. Am J Addict. 1999;8(4):279–92.
Milby JB, Schumacher JE, Vuchinich RE, Wallace D, Plant MA, Freedman MJ, et al. Transitions during effective treatment for cocaine-abusing homeless persons: establishing abstinence, lapse, and relapse, and reestablishing abstinence. Psychol Addict Behav. 2004;18(3):250–6.
Petry NM, Weinstock J, Alessi SM, Lewis MW, Dieckhaus K. Group-based randomized trial of contingencies for health and abstinence in HIV patients. J Consult Clin Psychol. 2010;78(1):89–97.
Zlotnick C, Johnson J, Najavits LM. Randomized controlled pilot study of cognitive-behavioral therapy in a sample of incarcerated women with substance use disorder and PTSD. Behav Ther. 2009;40(4):325–36.
Wechsberg WM, MacDonald BR, Dennis ML, Inciardi JA, Surratt HL, Leukefeld CG, et al. The standard intervention for reduction in HIV risk behavior; protocol changes suggested by the continuing HIV/AIDS epidemic. Bloomington: Lighthouse Institute; 1997.
Liberman RP, Massel HK, Mosk MD, Wong SE. Social skills training for chronic mental patients. Hosp Community Psychiatry. 1985;36(4):396–403.
Milby JB, Schumacher JE, McNamara C, Wallace D, Usdan S, McGill T, et al. Initiating abstinence in cocaine abusing dually diagnosed homeless persons. Drug Alcohol Depend. 2000;60(1):55–67.
Milby JB, Schumacher JE, Raczynski JM, Caldwell E, Engle M, Michael M, et al. Sufficient conditions for effective treatment of substance abusing homeless persons. Drug Alcohol Depend. 1996;43(1–2):39–47.
Milby JB, Schumacher JE, Wallace D, Frison S, McNamara C, Usdan S, et al. Day treatment with contingency management for cocaine abuse in homeless persons: 12-month follow-up. J Consult Clin Psychol. 2003;71(3):619–21.
Linehan MMD, L.A. Dialectical behavior therapy manual of treatment interventions for drug abusers with borderline personality disorder. Seattle: University of Washington; 1997.
Linehan MM, Heard HL, Armstrong HE. Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1993;50(12):971–4.
Linehan MM, Tutek DA, Heard HL, Armstrong HE. Interpersonal outcome of cognitive behavioral treatment for chronically suicidal borderline patients. Am J Psychiatry. 1994;151(12):1771–6.
Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48(12):1060–4.
Burtscheidt W, Schwarz R, Redner C, Gaebel W. Behavioral therapeutic methods in ambulatory treatment of alcoholism. Early results of an experimental study. Fortschr Neurol Psychiatr. 1999;67(6):274–80.
Sandahl C, Herlitz K, Ahlin G, Rönnberg S. Time-limited group psychotherapy for moderately alcohol dependent patients: A randomized controlled clinical trial. Psychother Res. 1998;8(4):361–78.
Wolff RF, Moons KG, Riley RD, Whiting PF, Westwood M, Collins GS, et al. PROBAST: a tool to assess the risk of bias and applicability of prediction model studies. Ann Intern Med. 2019;170(1):51–8.
Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. In: Cochrane handbook for systematic reviews of interventions; 2019. p. 205–28.
Chapter Google Scholar
Diener MJ. The Corsini Encyclopedia of Psychology; 2010. p. 1.
Book Google Scholar
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Trials. 2010;11(1):1–8.
Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviors. Prog Behav Modif. 1992;28:183–218.
Drake RE, McLaughlin P, Pepper B, Minkoff K. Dual diagnosis of major mental illness and substance disorder: an overview. New Dir Ment Health Serv. 1991;1991(50):3–12.
Kunzke D, Strauss B, Burtscheidt W. The effectiveness of psychodynamic group therapy in the treatment of alcohol abuse. A review. Gruppenpsychotherapie und Gruppendynamik. 2002;38:53–70.
Download references
Acknowledgements
The authors have no acknowledgements.
The study is not supported through funding.
Author information
Authors and affiliations.
Center for Alcohol and Addiction Studies, Brown University, Providence, RI, 02912, USA
Gabriela López
Alpert Medical School of Brown University, Department of Psychiatry and Human Behavior, Providence, RI, 02904, USA
Lindsay M. Orchowski
Walter Reed Army Institute of Research, Silver Spring, MD, 20910, USA
Madhavi K. Reddy
Massachusetts General Hospital, Harvard Medical School, Boston, MA, 02115, USA
Jessica Nargiso
Division of Public Health, Michigan State University, Flint, MI, 48502, USA
Jennifer E. Johnson
You can also search for this author in PubMed Google Scholar
Contributions
All authors participated in the review of manuscripts included in the study, writing of sections of the manuscript, as well as final editing of the paper. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Lindsay M. Orchowski .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
López, G., Orchowski, L.M., Reddy, M.K. et al. A review of research-supported group treatments for drug use disorders. Subst Abuse Treat Prev Policy 16 , 51 (2021). https://doi.org/10.1186/s13011-021-00371-0
Download citation
Accepted : 03 April 2021
Published : 21 June 2021
DOI : https://doi.org/10.1186/s13011-021-00371-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Substance use disorders
- Group therapy
Substance Abuse Treatment, Prevention, and Policy
ISSN: 1747-597X
- General enquiries: [email protected]
Insight in substance use disorder: A systematic review of the literature
Affiliations.
- 1 School of Psychology, University of Wollongong, Wollongong, Australia; Illawarra Health and Medical Research Institute, University of Wollongong, NSW, Australia. Electronic address: [email protected].
- 2 School of Psychology, University of Wollongong, Wollongong, Australia; Illawarra Health and Medical Research Institute, University of Wollongong, NSW, Australia.
- 3 School of Medicine and Public Health, University of Newcastle, Callaghan, Australia.
- 4 Eastern Health Clinical School, Faculty of Medicine, Nursing & Health Sciences, Monash University, Melbourne, Australia; Turning Point, Eastern Health, Melbourne, Australia.
- 5 School of Medicine and Public Health, University of Newcastle, Callaghan, Australia; Centre for Innovation in Mental and Physical Health and Clinical Treatment Strategic Research Centre, School of Medicine, Deakin University, Geelong, Australia.
- 6 Centre for Innovation in Mental and Physical Health and Clinical Treatment Strategic Research Centre, School of Medicine, Deakin University, Geelong, Australia; Florey Institute for Neuroscience and Mental Health, University of Melbourne, Melbourne, Australia.
- 7 Illawarra Drug and Alcohol Service, Illawarra Shoalhaven Local Health District, Wollongong, Australia.
- 8 National Drug and Alcohol Research Centre, University of New South Wales, Sydney, Australia.
- PMID: 32731008
- DOI: 10.1016/j.addbeh.2020.106549
Insight refers to a person's understanding of themselves and the world around them. Recent literature has explored people's insight into their substance use disorder (SUD) and how this is linked to treatment adherence, abstinence rates, and comorbid mental health symptoms. The aim of this systematic review was to synthesise and critically examine the existing literature on insight in SUD. Five academic databases (Medline, PsychINFO, SCOPUS, CINAHL, Web of Science) were searched for key terms related to insight and substance use. Included studies were on humans aged 18 years or over with SUD that examined the relationship between substance use and insight using a quantifiable measure of insight. Of 10,067 identified papers, 20 met the inclusion criteria, employing 13 different measures of insight. The most commonly used measure was the Hanil Alcohol Insight Scale (HAIS) which was the only measure designed for a substance use population and was specific to alcohol use. Based on a pooled sample from five studies (n = 585), 57% of participants had poor insight, 36% had fair insight, and 7% had good insight on the HAIS. Better insight was generally related to negative consequences from substance use, better treatment adherence and maintaining abstinence. Insight appears to be an important factor to consider within SUD. Exploring the most appropriate way to measure insight and assess its role in SUD has implications for intervention design, and engaging and maintaining people with SUD in treatment.
Keywords: Addiction; Insight; Substance use disorder.
Copyright © 2020 Elsevier Ltd. All rights reserved.
Publication types
- Research Support, Non-U.S. Gov't
- Systematic Review
- Mental Health
- Substance-Related Disorders* / epidemiology
A Systematic Literature Review of Strengths-Based Approaches to Drug Use Management and Treatment
- Original Paper
- Published: 08 May 2023
- Volume 51 , pages 294–305, ( 2023 )
Cite this article

- Jerel M. Ezell ORCID: orcid.org/0000-0002-9884-7909 1 , 2 ,
- Mai Pho 3 ,
- Jessica Jaiswal 4 ,
- Babatunde Patrick Ajayi 1 , 5 ,
- Natalie Gosnell 1 , 5 ,
- Emma Kay 6 ,
- Ellen Eaton 4 &
- Ricky Bluthenthal 7
1151 Accesses
7 Altmetric
Explore all metrics
A Correction to this article was published on 30 May 2023
This article has been updated
Strengths-based theory, a pillar of clinical social work practice, emphasizes the importance of recognizing the inherent and learned skills and abilities that people possess and can leverage toward self-actualization and wellness. However, strengths-based approaches are under-investigated in the field of drug use management and treatment, foreclosing a richer view into how to better understand, engage, and support people who nonmedically use drugs (PWUD) through practice and research. Focusing on interventions conducted with PWUD, we conducted a systematic literature review to identify, classify, and characterize existing strengths-based paradigms and approaches to drug use management and treatment. Using these findings, we formulate and describe a holistic conceptual model for advancing training, practice, and research in this space. The following domains emerged and were contextualized for their strengths-based dimensions: (1) Harm Reduction Services; (2) Strengths-Based Case Management; (3) Trauma-Informed Practice; and (4) Collectivist Racial, Ethnic, Gender, Sexual, and Intersectional Identity-Focused Interventions. These bodies of literature showed limited connectivity as a comprehensive clinical modality, which we proposed to address through the Integrated Strengths-Based Engagement Framework (ISBEF). To this end, a complex array of strengths-based paradigms have been developed and implemented to support the well-being of PWUD. However, there is a need for more rigorous and uniform approaches for the implementation and measurement of strengths-based approaches, particularly in work with racial, ethnic, gender, and sexual minority populations, which the ISBEF provides a structure for.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
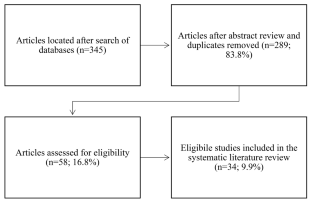
Similar content being viewed by others

Why do children and adolescents (not) seek and access professional help for their mental health problems? A systematic review of quantitative and qualitative studies
Jerica Radez, Tessa Reardon, … Polly Waite

The Biopsychosocial Approach: Towards Holistic, Person-Centred Psychiatric/Mental Health Nursing Practice

Person-Centred Approaches to Social Work Practice
Change history, 30 may 2023.
A Correction to this paper has been published: https://doi.org/10.1007/s10615-023-00875-1
Abbreviations
Hepatitis C
Medication-assisted treatment
Medication for opioid use disorder
Opioid use disorder
People who nonmedically use drugs
Syringe Services Program
Strengths-Based Case Management
Trauma-informed Practice
Anderson, J. (1988). for Social Work Practice. Paradigms of Clinical Social Work: Emphasis on Diversity, 3 , 19.
Bartholomew, T. S., Andraka-Cristou, B., Totaram, R. K., Harris, S., Doblecki-Lewis, S., Ostrer, L., & Tookes, H. E. (2022). “We want everything in a one-stop shop”: acceptability and feasibility of PrEP and buprenorphine implementation with mobile syringe services for Black people who inject drugs. Harm Reduction Journal, 19 (1), 133.
Bluthenthal, R. N., Kral, A. H., Gee, L., Erringer, E. A., & Edlin, B. R. (2000). The effect of syringe exchange use on high-risk injection drug users: a cohort study. Aids, 14 (5), 605–611.
Bobashev, G. V., & Warren, L. K. (2022). National polydrug use patterns among people who misuse prescription opioids and people who use heroin. Results from the National Household Survey on Drug Use and Health. Drug and alcohol dependence,238 , 109553.
Brook, J. S., Whiteman, M., Balka, E. B., Win, P. T., & Gursen, M. D. (1998). Drug use among puerto ricans: Ethnic identity as a protective factor. Hispanic Journal of Behavioral Sciences, 20 (2), 241–254.
Article Google Scholar
Brown, V. B., Harris, M., & Fallot, R. (2013). Moving toward trauma-informed practice in addiction treatment: A collaborative model of agency assessment. Journal of Psychoactive Drugs, 45 (5), 386–393.
Article PubMed Google Scholar
Brun, C., & Rapp, R. C. (2001). Strengths-based case management: Individuals’ perspectives on strengths and the case manager relationship. Social Work, 46 (3), 278–288.
Buning, E., Drucker, E., Matthews, A., Newcombe, R., & O’Hare, P. (2013). The reduction of drug-related harm: A conceptual framework for theory, practice and research. Routledge.
Butsashvili, M., Kamkamidze, G., Kajaia, M., Gvinjilia, L., Kuchuloria, T., Khonelidze, I., & Averhoff, F. (2020). Integration of hepatitis C treatment at harm reduction centers in Georgia—Findings from a patient satisfaction survey. International Journal of Drug Policy, 84 , 102893.
Cano, M. (2020). Racial/ethnic differences in US drug overdose mortality, 2017–2018. Addictive Behaviors, 112 , 106625.
Cochran, G., Chen, Q., Field, C., Seybert, A. L., Hruschak, V., Jaber, A., Gordon, A. J., & Tarter, R. (2019a). A community pharmacy-led intervention for opioid medication misuse: A small-scale randomized clinical trial. Drug and Alcohol Dependence, 205, 107570. https://doi.org/10.1016/j.drugalcdep.2019a.107570
Article PubMed PubMed Central Google Scholar
Cochran, G., Smid, M. C., Krans, E. E., Bryan, M. A., Gordon, A. J., Lundahl, B., Silipigni, J., Haaland, B., & Tarter, R. (2019b). A pilot multisite study of patient navigation for pregnant women with opioid use disorder. Contemporary Clinical Trials, 87, 105888.
Collins, A. B., Boyd, J., Cooper, H. L. F., & McNeil, R. (2019). The intersectional risk environment of people who use drugs. Social Science & Medicine, 234 , 112384.
Colpitts, E., & Gahagan, J. (2016). The utility of resilience as a conceptual framework for understanding and measuring LGBTQ health. International journal for equity in health, 15 (1), 1–8.
Crocq, M.-A. (2022). Historical and cultural aspects of man’s relationship with addictive drugs. Dialogues in Clinical Neuroscience .
Curran, L., Arthur-Jordan, B., Rice, J., & Tan, T. (2021). The risk of child removal by child protective services among pregnant women in medication-assisted treatment for opioid use disorder. Journal of Social Work Practice in the Addictions, 1–15.
D’Onofrio, G., Chawarski, M. C., O’Connor, P. G., Pantalon, M. V., Busch, S. H., Owens, P. H., & Fiellin, D. A. (2017). Emergency department-initiated buprenorphine for opioid dependence with continuation in primary care: Outcomes during and after intervention. Journal of General Internal Medicine, 32 , 660–666.
Doorn, N., Gardoni, P., & Murphy, C. (2019). A multidisciplinary definition and evaluation of resilience: The role of social justice in defining resilience. Sustainable and Resilient Infrastructure, 4 (3), 112–123.
El-Bassel, N., & Shoptaw, S. (2021). Addressing long overdue social and structural determinants of the opioid epidemic .
Eversman, M. H. (2015). “We want a living Solution”: Views of Harm Reduction Programs in Black US Communities. Journal of Ethnicity in Substance Abuse, 14 (2), 187–207.
Ezell, J. M., Olson, B., Walters, S. M., Friedman, S. R., Ouellet, L., & Pho, M. T. (2022). A Sociology of Empathy and Shared Understandings: Contextualizing Beliefs and Attitudes on Why People Use Opioids. Rural Sociology, 87 (3), 1053–1087.
Fagan, J., & Wexler, S. (1988). Explanations of sexual assault among violent delinquents. Journal of Adolescent research, 3 (3–4), 363–385.
Farmer, T. W., Clemmer, J. T., Leung, M. C., Goforth, J. B., Thompson, J. H., Keagy, K., & Boucher, S. (2005). Strength-based assessment of rural African American early adolescents: Characteristics of students in high and low groups on the behavioral and emotional rating scale. Journal of Child and Family Studies, 14 , 57–69.
Fatkin, T., Moore, S. K., Okst, K., Creedon, T., Samawi, F., Fredericksen, A. K., Roll, D., Oxnard, A., Cook, B., & Schuman-Olivier, Z. (2021). Feasibility and acceptability of mindful recovery opioid use care continuum (M-ROCC): A concurrent mixed methods study. Journal of Substance Abuse Treatment, 108415.
Faulkner-Gurstein, R. (2017). The social logic of naloxone: Peer administration, harm reduction, and the transformation of social policy. Social Science & Medicine, 180 , 20–27.
Fox, A. D., Sohler, N. L., Frost, T., Lopez, C., & Cunningham, C. O. (2017). Development and evaluation of a community-based buprenorphine treatment intervention. Harm Reduction Journal, 14 (1), 1–7.
Fusco, R. A. (2019). Perceptions of Strengths-Based Child Welfare Practices among Mothers with Drug Use Histories. Journal of Family Issues, 40 (17), 2478–2498. https://doi.org/10.1177/0192513X19859392
Geronimus, A. T. (1992). The weathering hypothesis and the health of african-american women and infants: Evidence and speculations. Ethnicity & Disease, 2 (3), 207–221.
Google Scholar
Goodman, D. J., Saunders, E. C., & Wolff, K. B. (2020). In their own words: A qualitative study of factors promoting resilience and recovery among postpartum women with opioid use disorders. BMC Pregnancy and Childbirth, 20 (1), 178. https://doi.org/10.1186/s12884-020-02872-5
Grella, C. E., Hser, Y.-I., & Huang, Y.-C. (2006). Mothers in substance abuse treatment: Differences in characteristics based on involvement with child welfare services. Child Abuse & Neglect, 30 (1), 55–73.
Han, J. K., Hill, L. G., Koenig, M. E., & Das, N. (2017). Naloxone Counseling for Harm Reduction and Patient Engagement. Family medicine, 49 (9), 730–733.
Hanson, B. L., Porter, R. R., Zöld, A. L., & Terhorst-Miller, H. (2020). Preventing opioid overdose with peer-administered naloxone: Findings from a rural state. Harm Reduction Journal, 17 (1), 1–9.
Havens, J. R., Cornelius, L. J., Ricketts, E. P., Latkin, C. A., Bishai, D., Lloyd, J. J., Huettner, S., & Strathdee, S. A. (2007). The effect of a case management intervention on drug treatment entry among treatment-seeking injection drug users with and without comorbid antisocial personality disorder. Journal of Urban Health, 84 (2), 267–271.
Israel, B. A., Eng, E., Schulz, A. J., & Parker, E. A. (2012). Methods for community-based participatory research for health . John Wiley & Sons.
Jacka, B. P., Goldman, J. E., Yedinak, J. L., Bernstein, E., Hadland, S. E., Buxton, J. A., Sherman, S. G., Biello, K. B., & Marshall, B. D. (2020). A randomized clinical trial of a theory-based fentanyl overdose education and fentanyl test strip distribution intervention to reduce rates of opioid overdose: Study protocol for a randomized controlled trial. Trials, 21 (1), 1–10.
Ja’nina, J., & Longmire-Avital, B. (2018). Resilience and depression: The roles of racial identity, sexual identity, and social support on well-being for Black LGB emerging adults. Journal of Black Sexuality and Relationships, 4 (4), 1–15.
Jenson, J. M., & Fraser, M. W. (2006). Toward the Integration of Child, Youth, and Family Policy. Social Policy for Children and Families: A Risk and Resilience Perspective , 265.
Kirkinis, K., Pieterse, A. L., Martin, C., Agiliga, A., & Brownell, A. (2021). Racism, racial discrimination, and trauma: A systematic review of the social science literature. Ethnicity & Health, 26 (3), 392–412.
Knaak, S., Christie, R., Mercer, S., & Stuart, H. (2019). Harm reduction, stigma and the problem of low compassion satisfaction. Journal of Mental Health and Addiction Nursing, 3 (1), e8–e21.
Kral, A. H., Lambdin, B. H., Comfort, M., Powers, C., Cheng, H., Lopez, A. M., Murdoch, R. O., Neilands, T. B., & Lorvick, J. (2018). A Strengths-Based Case Management intervention to reduce HIV viral load among people who use drugs. AIDS and Behavior, 22 (1), 146–153. https://doi.org/10.1007/s10461-017-1903-6
Kral, A. H., Lambdin, B. H., Wenger, L. D., & Davidson, P. J. (2020). Evaluation of an unsanctioned safe consumption site in the United States. New England Journal of Medicine, 383 (6), 589–590.
Kulesza, M., Matsuda, M., Ramirez, J. J., Werntz, A. J., Teachman, B. A., & Lindgren, K. P. (2016). Towards greater understanding of addiction stigma: Intersectionality with race/ethnicity and gender. Drug and alcohol dependence , 169, 85–91.
Kurtz, S. P., Pagano, M. E., Buttram, M. E., & Ungar, M. (2019). Brief interventions for young adults who use drugs: The moderating effects of resilience and trauma. Journal of Substance Abuse Treatment, 101 , 18–24. https://doi.org/10.1016/j.jsat.2019.03.009
Lean, R. E., Pritchard, V. E., & Woodward, L. J. (2013). Child protection and out-of-home placement experiences of preschool children born to mothers enrolled in methadone maintenance treatment during pregnancy. Children and Youth Services Review, 35 (11), 1878–1885.
Lewis, D. A., Park, J. N., Vail, L., Sine, M., Welsh, C., & Sherman, S. G. (2016). Evaluation of the overdose education and naloxone distribution program of the Baltimore Student Harm Reduction Coalition. American journal of public health, 106 (7), 1243–1246.
Liu, R. T., Sheehan, A. E., Walsh, R. F., Sanzari, C. M., Cheek, S. M., & Hernandez, E. M. (2019). Prevalence and correlates of non-suicidal self-injury among lesbian, gay, bisexual, and transgender individuals: A systematic review and meta-analysis. Clinical psychology review, 74 , 101783.
López-Castro, T., Hu, M., Papini, S., Ruglass, L. M., & Hien, D. A. (2015). Pathways to change: Use trajectories following trauma‐informed treatment of women with co‐occurring post‐traumatic stress disorder and substance use disorders. Drug and Alcohol Review, 34 (3), 242–251.
Lunze, K., Kiriazova, T., Blokhina, E., Bushara, N., Bridden, C., Gnatienko, N., Bendiks, S., Quinn, E., Krupitsky, E., Raj, A., & Samet, J. H. (2020). Linking HIV-positive people in addiction care to HIV services in St. Petersburg, Russia – mixed-methods implementation study of strengths-based case management. Global Public Health, 1–13. https://doi.org/10.1080/17441692.2020.1834599
Maclin-Akinyemi, C., Thurston, I. B., Howell, K. H., Jamison, L. E., & Anderson, M. B. (2019). The protective roles of ethnic identity and community cohesion on substance use among black women experiencing adversity. Journal of Ethnicity in Substance Abuse, 1–16. https://doi.org/10.1080/15332640.2019.1622477
Madden, E. F. (2019). Intervention stigma: How medication-assisted treatment marginalizes patients and providers. Social Science & Medicine, 232 , 324–331.
Maidman, F., & Kirsch, S. (1984). Child Welfare Problems and Practice: An Ecological Approach. Child Welfare: A Source Book of Knowledge and Practice , 1–14.
Marcellus, L. (2014). Supporting women with substance use issues: Trauma-informed care as a foundation for practice in the NICU. Neonatal Network, 33 (6), 307–314.
Meichenbaum, D. (1985). Stress inoculation training. New York, 304.
Meinhofer, A., Onuoha, E., Angleró-Díaz, Y., & Keyes, K. M. (2020). Parental drug use and racial and ethnic disproportionality in the U.S. foster care system. Children and Youth Services Review, 118 , 105336. https://doi.org/10.1016/j.childyouth.2020.105336
Merrick, M. T., Ford, D. C., Haegerich, T. M., & Simon, T. (2020). Adverse childhood experiences increase risk for prescription opioid misuse. The Journal of Primary Prevention, 41 (2), 139–152.
Morgan, A. A., Thomas, M. E., & Brossoie, N. (2020). Trauma-informed care (TIC) as a framework for addressing the opioid epidemic in Appalachia: An exploratory interpretative phenomenological analysis. Journal of Rural Mental Health, 44 (3), 156.
Muncan, B., Walters, S. M., Ezell, J., & Ompad, D. C. (2020). “They look at us like junkies”: Influences of drug use stigma on the healthcare engagement of people who inject drugs in New York City. Harm Reduction Journal, 17 (1), 1–9.
Murray, J., Farrington, D. P., & Sekol, I. (2012). Children's antisocial behavior, mental health, drug use, and educationalperformance after parental incarceration: a systematic review and meta-analysis. Psychological Bulletin, 138 (2), 175.
NASW Standards for Social Work Case Management. (2013). National Association of Social Workers. https://www.socialworkers.org/LinkClick.aspx?fileticket=acrzqmEfhlo%3D&portalid=0
Oh, H., Kim, K., Miller, D., Veloso, D., Lin, J., & McFarland, W. (2020). Fentanyl self-testing in a community-based sample of people who inject drugs, San Francisco. International Journal of Drug Policy, 82 , 102787.
O’Rourke, A., White, R. H., Park, J. N., Rodriguez, K., Kilkenny, M. E., Sherman, S. G., & Allen, S. T. (2019). Acceptability of safe drug consumption spaces among people who inject drugs in rural West Virginia. Harm Reduction Journal, 16 (1), 51. https://doi.org/10.1186/s12954-019-0320-8
Paschen-Wolff, M. M., Kidd, J. D., & Paine, E. A. (2023). The State of the Research on Opioid Outcomes Among Lesbian, Gay, Bisexual, Transgender, Queer, and Other Sexuality-and Gender-Diverse Populations: A Scoping Review. LGBT health, 10 (1), 1–17.
Peacock-Chambers, E., Feinberg, E., Senn-McNally, M., Clark, M. C., Jurkowski, B., Suchman, N. E., Byatt, N., & Friedmann, P. D. (2020). Engagement in early intervention services among mothers in Recovery from Opioid Use Disorders. Pediatrics, 145 (2), e20191957. https://doi.org/10.1542/peds.2019-1957
Rapp, R. C., Kelliher, C. W., Fisher, J. H., & Hall, F. J. (1994). Strengths-based case management. A role in addressing denial in substance abuse treatment. Journal of Case Management, 3 (4), 139–144.
Redko, C., Rapp, R. C., Elms, C., Snyder, M., & Carlson, R. G. (2007). Understanding the Working Alliance between persons with substance abuse problems and Strengths-Based case managers. Journal of Psychoactive Drugs, 39 (3), 241–250. https://doi.org/10.1080/02791072.2007.10400610
Regis, A., Meyers-Ohki, S. E., Mennenga, S. E., Greco, P. P., Glisker, R., Kolaric, R., McCormack, R. P., Rapp, R. C., & Bogenschutz, M. P. (2020). Implementation of strength-based case management for opioid-dependent patients presenting in medical emergency departments: Rationale and study design of a randomized trial. Trials, 21 (1), 1–14.
Resnicow, K., Soler, R., Braithwaite, R. L., Ahluwalia, J. S., & Butler, J. (2000). Cultural sensitivity in substance use prevention. Journal of Community Psychology, 28 (3), 271–290.
Roth, A. M., Mitchell, A. K., Mukherjee, R., Scheim, A. I., Ward, K. M., & Lankenau, S. E. (2021). Prevalence and correlates of syringe disposal box use in a Philadelphia neighborhood with high levels of public drug injection. Substance Use & Misuse, 56 (5), 668–673.
Rowe, C., Santos, G. M., Vittinghoff, E., Wheeler, E., Davidson, P., & Coffin, P. O. (2015). Predictors of participant engagement and naloxone utilization in a community-based naloxone distribution program. Addiction, 110 (8), 1301–1310.
Rowlands, A. (2001). Ability or disability? Strengths-based practice in the area of traumatic brain injury. Families in Society, 82 (3), 273–286.
Samet, J. H., Blokhina, E., Cheng, D. M., Walley, A. Y., Lioznov, D., Gnatienko, N., Quinn, E. K., Bridden, C., Chaisson, C. E., & Toussova, O. (2019). A strengths-based case management intervention to link HIV-positive people who inject drugs in Russia to HIV care. AIDS (London, England), 33 (9), 1467.
SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach . (2014). Substance Abuse and Mental Health Services Administration. https://ncsacw.samhsa.gov/userfiles/files/SAMHSA_Trauma.pdf
Schorr, M. T., Tietbohl-Santos, B., de Oliveira, L. M., Terra, L., de Borba Telles, L. E., &Hauck, S. (2020). Association between different types of childhood trauma and parental bonding with antisocial traits inadulthood: A systematic review. Child Abuse & Neglect, 107 , 104621.
Selekman, M. D. (2006). Working with self-harming adolescents: A collaborative, strengths-based therapy approach . WW Norton & Co.
Sherman, S. G., Schneider, K. E., Park, J. N., Allen, S. T., Hunt, D., Chaulk, C. P., & Weir, B. W. (2019). PrEP awareness, eligibility, and interest among people who inject drugs in Baltimore, Maryland. Drug and alcohol dependence, 195 , 148–155.
Skinner-Osei, P., & Levenson, J. S. (2018). Trauma-informed services for children with incarcerated parents. Journal of Family Social Work, 21 (4-5), 421–437.
Sperlich, M. I., Bascug, E. W., Green, S. A., Koury, S., Hales, T., & Nochajski, T. H. (2021). Trauma-informed parenting education support groups for mothers in substance abuse recovery. Research on Social Work Practice, 10497315211007568.
Steel, D., Marchand, K., & Oviedo-Joekes, E. (2017). Our life depends on this drug: Competence, inequity, and voluntary consent in clinical trials on supervised injectable opioid assisted treatment. The American Journal of Bioethics, 17 (12), 32–40.
Stevens-Watkins, D., Perry, B., Harp, K. L., & Oser, C. B. (2012). Racism and illicit drug use among african american women: The protective effects of ethnic identity, affirmation, and behavior. Journal of Black Psychology, 38 (4), 471–496.
Strathdee, S. A., Ricketts, E. P., Huettner, S., Cornelius, L., Bishai, D., Havens, J. R., Beilenson, P., Rapp, C., Lloyd, J. J., & Latkin, C. A. (2006). Facilitating entry into drug treatment among injection drug users referred from a needle exchange program: Results from a community-based behavioral intervention trial. Drug and Alcohol Dependence, 83 (3), 225–232.
Sweeney, D. S. (1988). Across the Life Span. Paradigms of Clinical Social Work: Emphasis on Diversity , 3, 105.
Taplin, C., Saddichha, S., Li, K., & Krausz, M. R. (2014). Family history of alcohol and drug abuse, childhood trauma, and age of first drug injection. Substance Use & Misuse, 49 (10), 1311–1316.
Tedmanson, D., & Guerin, P. (2011). Enterprising social wellbeing: Social entrepreneurial and strengths based approaches to mental health and wellbeing in “remote” indigenous community contexts. Australasian Psychiatry, 19 (1_suppl), S30–S33.
Tervalon, M., & Murray-Garcia, J. (1998). Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. Journal of health care for the poor and underserved, 9 (2), 117–125.
Thompson, J. R., Shogren, K. A., & Wehmeyer, M. L. (2016). Supports and support needs in strengths-based models of intellectual disability. In Handbook of research-based practices for educating students with intellectual disability (pp. 39–57). Routledge.
Wallace, J. M. (1998). Explaining race differences in adolescent and young adult drug use: The role of racialized social systems. Drugs & Society, 14 (1–2), 21–36. https://doi.org/10.1300/J023v14n01_03
Wehmeyer, M. L. (2019). Strengths-based approaches to educating all learners with disabilities: Beyond special education . Teachers College Press.
Wilson, D., Donald, B., Shattock, A. J., Wilson, D., & Fraser-Hurt, N. (2015). The cost-effectiveness of harm reduction. International Journal of Drug Policy, 26 , S5–S11.
Wood, E., & Elliott, M. (2020). Opioid addiction stigma: the intersection of race, social class, and gender. Substance Use & Misuse, 55 (5), 818–827.
Xie, H. (2013). Strengths-based approach for mental health recovery. Iranian Journal of Psychiatry and Behavioral Sciences, 7 (2), 5.
PubMed PubMed Central Google Scholar
Yang, Y. T., & Beletsky, L. (2020). United States vs Safehouse: The implications of the Philadelphia supervised consumption facility ruling for law and social stigma. Preventive Medicine, 135 , 106070.
Download references
This research was funded by the National Institute on Drug Abuse (4UH3DA044829-03).
Author information
Authors and affiliations.
Division of General Internal Medicine, Weill Cornell Medicine, 420 East 70th Street, 3rd Floor, New York, NY, 10021, USA
Jerel M. Ezell, Babatunde Patrick Ajayi & Natalie Gosnell
Center for Cultural Humility, Cornell University, Ithaca, NY, USA
Jerel M. Ezell
Department of Medicine, Section of Infectious Diseases and Global Health, University of Chicago Medicine, Chicago, IL, USA
Department of Medicine, University of Alabama – Birmingham, Birmingham, AL, USA
Jessica Jaiswal & Ellen Eaton
Biological Sciences, Cornell University, Ithaca, NY, USA
Babatunde Patrick Ajayi & Natalie Gosnell
Magic City Research Institute, Birmingham AIDS Outreach, Birmingham, AL, USA
Department of Population and Public Health Sciences, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Ricky Bluthenthal
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jerel M. Ezell .
Ethics declarations
Competing interests.
The authors have no conflicts of interest, financial or otherwise, to report.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: the spelling of author name Ricky Bluthenthal and the first affiliation has been corrected.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Ezell, J.M., Pho, M., Jaiswal, J. et al. A Systematic Literature Review of Strengths-Based Approaches to Drug Use Management and Treatment. Clin Soc Work J 51 , 294–305 (2023). https://doi.org/10.1007/s10615-023-00874-2
Download citation
Accepted : 20 April 2023
Published : 08 May 2023
Issue Date : September 2023
DOI : https://doi.org/10.1007/s10615-023-00874-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Drug injection
- Harm reduction
- Positive psychology
- Strengths-based
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 20 April 2024
“Everything is kind of the same except my mind is with me”: exploring cannabis substitution in a sample of adults in early recovery from an opioid or stimulant addiction
- Corinne A. Beaugard 1 , 3 ,
- Alexander Y. Walley 2 &
- Maryann Amodeo 1
Harm Reduction Journal volume 21 , Article number: 83 ( 2024 ) Cite this article
179 Accesses
1 Altmetric
Metrics details
Recovery from addiction is frequently equated with abstinence. However, some individuals who resolve an addiction continue to use substances, including via substitution (i.e., increased use of one substance after eliminating/ reducing another). Substitution may play a distinct role during early recovery (≤ 1 year), as this period is marked by dramatic change and adjustment. Cannabis is one of the most used substances and is legal for medical and recreational use in an increasing number of states. Consequently, cannabis an increasingly accessible substitute for substances, like fentanyl, heroin, cocaine and methamphetamine, with higher risk profiles (e.g., associated with risk for withdrawal, overdose, and incarceration).
Fourteen participants reported that they had resolved a primary opioid or stimulant addiction and subsequently increased their cannabis use within the previous 12 months. Using grounded theory, the interviewer explored their experiences of cannabis use during early recovery. Data were analyzed in three stages: line by line coding for all text related to cannabis use and recovery, focused coding, and axial coding to generate a theory about recovery with cannabis substitution. The motivational model of substance use provided sensitizing concepts.
Results & discussion
The final sample included eight men and six women ranging in age from 20 to 50 years old. Three participants resolved an addiction to methamphetamine and the remaining 11, an addiction to opioids. Participants explained that cannabis was appealing because of its less harmful profile (e.g., no overdose risk, safe supply, few side effects). Participants’ primary motives for cannabis use included mitigation of psychiatric symptoms, withdrawal/ cravings, and boredom. While cannabis was effective toward these ends, participants also reported some negative side effects (e.g., decreased productivity, social anxiety). All participants described typical benefits of recovery (e.g., improved self-concept, better relationships) while continuing to use cannabis. Their experiences with and beliefs about substitution suggest it can be an effective strategy for some individuals during early recovery.
Conclusions
Cannabis use may benefit some adults who are reducing their opioid or stimulant use, especially during early recovery. The addiction field’s focus on abstinence has limited our knowledge about non-abstinent recovery. Longitudinal studies are needed to understand the nature of substitution and its impact on recovery over time.
Most addiction treatment settings, mutual aid groups, and research on recovery posit that recovery is built upon a foundation of abstinence from psychoactive drugs, excluding nicotine and prescription medication [ 1 , 2 ]. This operationalization of recovery aligns with the Substance Abuse and Mental Health Services Administration (SAMHSA)’ definition which states, “[Recovery is] a process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential” [ 3 ]. And while this definition suggests that recovery incorporates holistic growth, the SAMHSA text later specifies that “abstinence from the use of alcohol, illicit drugs, and non-prescribed medications is the goal for those with addictions” [ 3 ]. This standard orientation toward recovery excludes individuals who resolved their addictions without abstinence, thus limiting the field’s capacity to understand and support this potentially large and heterogenous population. Among individuals who are in non-abstinence recovery, a subset “substitute,” or increase use of one substance following the decreased use or cessation of another. Motives for substitution vary and include the relative availability or cost, side effects, and risks of the original and substitute substances [ 4 , 5 , 6 , 7 , 8 , 9 , 10 ].
Second to alcohol and tobacco, cannabis is the most frequently used substance [ 3 ]. Cannabis is perceived to be less harmful than other substances, and consequent to its increasing legalization for medical and recreational purposes, has been viewed more favorably by the public [ 11 , 12 , 13 ]. Research on cannabis substitution suggests it can be an effective strategy to decrease more harmful substance use (e.g., crack cocaine, opioids, alcohol, or prescription drugs) in part because it has less adverse side effects and less withdrawal potential than other drugs [ 7 , 9 , 14 ]. Paradoxically, in clinical samples, cannabis use clustered with more active and severe use of other substances. For example, in one study cannabis substitution was associated with a 27% reduction in odds of abstinence from other drugs or alcohol [ 15 ]. In another, cannabis use was three times higher amongst those who returned to cocaine use; however, cannabis use was not associated with a return to heroin use [ 16 ].
There is little research on cannabis substitution amongst individuals in recovery– likely due to the addiction field’s normative conflation of abstinence and recovery [ 1 , 17 , 18 , 19 , 20 ]. Substitution during recovery, or after resolving an addiction, may function similarly to substitution during an addiction; however, there is no research that examines the experience and function of substitution during recovery. Early recovery, often defined as one year [ 19 , 21 ], is a unique period marked by dramatic change in behavior and lifestyle, and experiences during this period are associated with future recovery outcomes [ 22 , 23 , 24 ]. Because early recovery is distinct in the magnitude of change that occurs across many domains (e.g., professional, family, community, physical and mental health), substitution might be more common or have specific functions during this period [ 19 ].
This study was designed to address the gap in research on substitution among people in recovery. Exploring how people in early recovery from an opioid or stimulant addiction experience cannabis substitution can provide insight on whether increased use of one substance supports recovery from another. The primary aims of this study were: (1) to identify individuals’ motives for cannabis use after resolving an opioid or stimulant addiction (2), to describe individuals’ experiences using cannabis, and (3) to understand whether cannabis substitution and addiction resolution are compatible.
Participants and recruitment
Data for this study were collected from a community sample of people who resolved a stimulant or opioid addiction in the previous 12 months and subsequently increased their cannabis use. Additional eligibility requirements included being at least 18 years old, English language fluency, US residence, and the ability to consent.
For the purposes of recruitment and clarity of construct, “resolved an addiction” was chosen instead of “recovery” so that potential participants did not exclude themselves based on an association between recovery and abstinence. The term “addiction” was used rather than “substance use disorder” so that people could identify with this more common phrase rather than a formal diagnostic term. The authors posted recruitment materials on Facebook and Reddit pages related to addiction and recovery. The materials opened with, “Are you in the first 12 months of resolving an opioid or stimulant addiction?” and stated that the study was designed to, “understand more about non-abstinence recovery for people who resolved an opioid or stimulant addiction and currently use cannabis.” Most participants described themselves as in “recovery,” which is how they will be described in the results. During the phone screening, participants stated which addiction they resolved, their current substance use, and whether their cannabis use increased, decreased, or stayed the same after resolving their addiction (see Fig. 1 ).
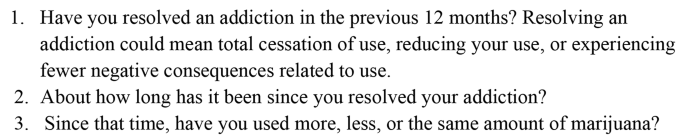
Interview Screening Questions
The first author interviewed 14 participants over Zoom. Participants resided across the US, in the Northeast, Southeast, Midwest, and Pacific Northwest regions. The authors did not collect any identifying information about participants and chose participant pseudonyms that reflected each participant’s self-reported racial and ethnic identities. Before the interview, the first author reviewed the consent document with each participant and received verbal consent. Interviews lasted approximately 1 h, and participants received a $30 Amazon electronic gift card upon completion. The Boston University Charles River Campus IRB approved this study.
The interview guide included questions about participants’ substance use routines, experiences that prompted cannabis use, and the effect of cannabis on their recovery. The interview opened with the question, “Since you’ve been in recovery, what substances have you used?” In many cases, participants described their substance use and provided context for this use. Building on their context, probes included questions such as, “What types of things make you want to use cannabis?” or, in response to a specific example of cannabis use, “Can you describe what was going on before you used cannabis?” After participants thoroughly described motives for cannabis use, follow up prompts aimed to understand their experience using cannabis, for example, “How did you feel after you used cannabis?” Of note, prompts reflected the participants’ language about cannabis and their mechanisms of use, such that the phrasing was modified for each participant (e.g., “Can you describe what was going on before you smoked pot?”).
Constructivist grounded theory and the motivational model of substance use
The intent of constructivist grounded theory is to create new theory with the acknowledgment that research is inevitably influenced by researchers’ knowledge about the world and pre-existing theories. Thus, theories can be integrated into this methodology for the purpose of “sensitizing concepts,” which inform the research, rather than direct it. Sensitizing concepts help the researcher find “a place to start inquiry, not to end it” (p. 31) [ 25 ].
The motivational model of substance use is a framework that proposes reasons that people use substances and includes four primary motives: to cope with psychological discomfort (e.g., affect regulation), to be comfortable in social situations, to experience enhancement (e.g., to increase pleasure), and to conform (e.g., to align with peer expectations) [ 26 ]. Coping and enhancement motives are generally associated with more frequent substance use, as well as more severe substance-related problems [ 27 , 28 , 29 ]. During analysis, this theoretical model was used to suggest sensitizing concepts related to substitution motives.
Data analysis: grounded theory
Interviews were recorded and transcribed. In traditional grounded theory research, interviews are conducted and analyzed simultaneously [ 25 ]. This study took a modified grounded theory approach. The first author conducted and analyzed three interviews simultaneously and drafted an initial codebook from these interviews; they analyzed the remaining 11 interviews together. A second coder [MA] independently coded 11 transcripts using the codebook. The two coders discussed discrepancies until consensus was reached.
Following a grounded theory approach, authors coded the interviews in three stages [ 25 ]. The first stage involved line-by-line coding for all text related to participants’ substance use after resolving a primary addiction, experiences using cannabis, and beliefs about the effects of cannabis on their recovery. During initial coding, the motivational model provided sensitizing concepts (i.e., the four motives for substance use) [ 30 ]. During focused coding, the authors identified the salient processes and actions that explained motives for cannabis use, the physical and psychological effects of cannabis, and the role of cannabis use in participants’ lives. Finally, during axial coding, authors identified the relationships across themes to build an explanatory model for cannabis substitution.

Methodological integrity
The interviewer [CAB] had worked in addiction settings, was trained in qualitative methods, and had conducted previous interviews with people in recovery, as well as people with current addictions. During this study, a qualitative scholar provided methodological supervision related to study design, interviewing, and data analysis. Co-authors [AYW and MA], both experts in addiction treatment, offered guidance on the inclusion criteria, recruitment strategies, the interview protocol, and analysis.
Authors engaged with reflexivity by writing memos after each interview and meeting to discuss the interviews and coding to mitigate bias during analysis. Writing after each interview allowed authors to disentangle participants’ construction of the concepts from their impressions and anticipated responses [ 31 ]. As the interviews and analyses progressed, it became apparent that the experience of non-abstinence recovery with cannabis substitution was different from what had been expected. This realization affirmed the importance of this methodology; a different approach (e.g., surveys or more structured interviews), would have limited participants’ ability to shape the preliminary theory of non-abstinence recovery with substitution.
Participants described their experiences of increasing cannabis use after resolving a primary opioid or stimulant addiction (See Table 1 ). Most participants were non-Hispanic White [ 11 ], two participants were Hispanic, and one participant was Black Somali. The sample included eight men and six women ranging in age from 20 to 50 years old. Three participants resolved an addiction to methamphetamine and the remaining 11, an addiction to opioids (primarily fentanyl, reflecting the current drug supply). None of the participants reported their cannabis use was exclusively for medical purposes and only one participant reported access to medical cannabis. The major themes and processes that emerged from interviews included: (1) cannabis is a better alternative: relatively safe, legally accessible, & socially acceptable; (2) cannabis use is motive driven; (3) negative effects of cannabis; and (4) benefits of recovery while using cannabis.
A better alternative: relatively safe, legally accessible, & socially acceptable
All participants believed cannabis was a safe alternative to other drugs. Maya explained that cannabis, even when illicitly procured, was unlikely to be contaminated, making it safter and more reliable than methamphetamine: “Cannabis is pretty safe like as far as adulteration and you know illicit drug use, or whatever. Like, I know what I’m actually putting into my body when I use it, which is a big deal.” Many participants pointed to the relatively lower risk profile of cannabis as one reason for substitution. Sam had previously used synthetic opioids and research chemicals (i.e., unclassified drugs with unpredictable effects) that he purchased online: “All the other drugs, I was doing had serious consequences, and could absolutely kill you during your use. So, I think it was kind of a relief to do something that was safe and kind of fun.” Sam said he, “couldn’t afford to screw up [his] life anymore,” and was relieved that cannabis offered a safer alternative.
Unlike opioids or stimulants, many participants procured cannabis legally. Jessica purchased cannabis from a medical dispensary: “Weed isn’t like a drug. Not like that. I have my prescription card, my medical marijuana card. I went to a doctor about it.” Using cannabis for medical purposes differentiated it from her previous injection opioid use. Terry lived in a state with recreational cannabis and she purchased it from dispensaries: “And marijuana is legal. You know? So, it’s like I consider myself sober as long as I’m not on any illicit street drugs.” Acquiring cannabis legally informed participants’ conceptualization of cannabis as materially different from their previous substance use.
A few participants attributed their beliefs about cannabis to their family of origin’s beliefs about the substance. Russell stated, “Weed was never presented as like a drug to me. People have always smoked weed. My family smoked…It’s not, it’s not looked at like alcohol or even cigarettes.” Terry and Kelly shared similar stories about their families’ beliefs about cannabis. Familial endorsement differentiated it from illicit street drugs, and even from alcohol, as a safe, non-addictive drug that did not interfere with their recovery.
Cannabis use is motive driven
Replacing other drugs.
All participants reported that cannabis helped them avoid using opioids or stimulants. They described this replacement as taking at least three forms: 1) to cope with the cravings for another drug, b) to mimic the effects of another drug, and c) to replace the ritualistic features of other drug use.
Russell explained that cannabis did not prevent cravings, but muted their intensity:
[The cravings are] not completely gone, but they’re tolerable, and I can deal with them… [Using opioids] just doesn’t sound like as good an idea anymore. You know it doesn’t seem like it’s a, it seems like more of a want than a need. You know, like that would be nice if I had some drugs, but I just don’t really feel like going to do that, right now. You know, rather than I need to go get some drugs.
Omar had a similar experience: “Yeah, I’ve pretty much had [cravings] daily and then after [I use] the cannabis, the optimistic sense kind of hits me, and it has been like, ‘Oh I don’t actually need [the opioids].’” Cannabis improved his mood enough so that he could reevaluate his desire to use opioids.
When Jimmy experienced cravings for methamphetamine and used cannabis instead, his cravings were entirely relieved: “It’s good for, for curing cravings. I don’t think about, I honestly, after that initial getting stoned, I don’t think about speed. That’s, that’s a big thing. Like I don’t think, ‘God, I really need to hit right now.’” His infrequent cannabis use meant that he experienced its intoxicating effects more acutely, likely helping him pass through the initial cravings. Jessica used cannabis frequently and believed it prevented the onset of opioid cravings:
It pretty much took [the cravings for opioids] away because I would, I would get high [on cannabis], and I would be relaxed. And I get hungry and [am] able to sleep. And as long as I could do all those things, I’m fine.
The physical effects of cannabis mimicked some of the desired effects of opioids (e.g., relaxation, sleepiness), thus reducing her need to use opioids. Like Jessica, Terry described cannabis as a replacement: “The marijuana feeling is mostly a downer feeling, like benzos and heroin and stuff. It’s basically taken place of other drugs. Know what I mean? It’s like a substitution thing.” Cannabis satisfied her desire for the effects of opioids and benzodiazepines well enough so that she could avoid using those substances.
The final way cannabis helped participants avoid using their primary substance was through behavioral rituals. Ava reflected that ritualizing cannabis use served some of the same purposes of her opioid use:
I would say it helped [my recovery]. Because it was something that I could still kind of ritualize, which was like I said a big part of my opiate use. So, it was something that I could still kind of find a ritual in, which is very calming to me.
Replacing opioid-related rituals with cannabis rituals decreased her desire to use them. Simon also ritualized cannabis use. He typically used opioids before and after his evening shift, which he identified as his two “trigger points:”
[Buying cannabis after work] made it easy. Because there was already that concept of like picking up something at night, which I think a lot of drug addiction at some points is…just like the ritual surrounding it…like exchanging money for goods and services. That little monkey part of my brain was like, ‘Alright, cool. We’re satisfied.’
Simon believed that continuing some of the same drug-related behaviors (e.g., procurement after work, using as a reward at the end of the day), helped him avoid using opioids.
Regulating affect
All but one participant explained that cannabis use helped regulate their mood. Many described disabling anxiety and attempting to manage the symptoms with cannabis. Jimmy was in the first few weeks of recovery from methamphetamine addiction and described emotional lability, extreme fatigue, and disrupted sleep. He smoked cannabis to soften the moments that were “very prickly, like sharp and hard to deal with”:
I do think the weed helps me at least relax my mind enough to say, ‘You know what yeah, okay, this is something we need to take care of. You’re okay, right now, nothing is crashing down on you because of this.’
Many participants shared this desire - to reduce perseveration and anxiety. Ava was diagnosed with bipolar disorder and did not believe her medication reduced her symptoms to a tolerable level. Cannabis dampened some of the remaining symptoms: “My brain is just always very loud. I usually have a lot of thoughts going on at one time, so [cannabis] kind of just slows everything down, makes everything a little bit more manageable for me.” The motivation to reduce psychiatric symptoms with cannabis could be described as self-medication. For example, Maya explained that her anxiety and social phobias prohibited her from going to the grocery store; but when she used cannabis beforehand, she could complete her tasks with less worry:
It’s easier to be in the moment I guess instead of [wondering]… ‘What do [the staff at the grocery store] think? What am I doing this wrong?’ This that, like all these, like freaking out in every direction about how others are perceiving me.
In this case, Maya was describing using cannabis instead of benzodiazepines to manage anxiety; she did so because cannabis had fewer negative consequences. She acknowledged that some of her anxiety and paranoia were due to her continued methamphetamine use: “I mean, yeah, like literally [this panic has] happened, regardless of whether or not I’m on speed. It usually does if I’m on speed.” She also described similar experiences without using methamphetamine. Participants were not always clear whether symptoms were negative drug-induced side effects or endogenous psychiatric conditions. Regardless, they reported that cannabis use mitigated their anxiety and improved their functioning.
Work was a frequent external stressor that provoked anxiety and led to cannabis use. Eric recently started a new job canvassing and found the work challenging. Smoking after work helped him calm down: “[Cannabis] makes me a little bit less crazy. It makes the anxiety and like racing thoughts like drift away and I’m like - it just helps me like relax after like a long like f-cking stressful day.” Jessica recently quit a telemarketing job due to the stress, however while still employed, she reported using cannabis throughout the day to ease her discomfort: “You’re getting yelled at constantly, getting hung up on… It feels much better when you get to go to the car and smoke a bowl. You know, and then you’re a lot more relaxed and it’s easier to deal with the 200 phone calls.” Omar was frequently responsible for family tasks and stated that completing errands for his mother was a major stressor.
And [my mom] can get angry and be very vocal if I make any mistakes. So sometimes I’ll be nervous to complete the job and make sure I don’t make any mistakes. But if I smoke first then I’ll kind of be more into the flow and end up making less mistakes. So, it’s like yeah, this sense of optimism is - comes from a sense of less anxiety. Omar believed that by reducing his anxiety, cannabis allowed him to complete tasks effectively with less distraction.
Avoiding boredom
Participants consumed cannabis when they wanted distraction from boredom or were completing uninteresting tasks. Russell described this as a long-term strategy to motivate him through monotonous tasks: “[I smoke more] if I’m like doing yard work and sh-t like that, or monotonous like physical labor. There’s nothing like being high and having to like clean the house or do the dishes, like it makes it so much easier.” Participants struggled to manage boredom, whether limited to specific tasks or more generalized boredom. Kathryn attended an intensive outpatient program each morning but had few other obligations; she described her discomfort with managing unstructured time: “Smoking [cannabis] helps with that. It makes it not so hard because, just like my brain is so much more clear than it was before that it’s hard to just do like mundane things. So, sitting around and doing nothing is like hard.” Kathryn stated she was offered a job and believed working would lead to reduced cannabis use.
Negative effects of cannabis
Though all participants believed cannabis positively impacted their recovery, many also reported negative side effects. Whereas several people reported cannabis minimized their anxiety, increased social anxiety was the most common negative side effect. Eric explained, “It does kind of take me out of it and make it a little harder for me to connect with people, I think. Like puts you on a different plane of understanding and you get a little anxiety accompanying that.” Sam also experienced increased social anxiety: “With cannabis, the bad effects are, for me, mainly my social anxiety becomes worse. I get too caught up in my own thoughts. Like trains of thought will run on when I don’t want them to.” To prevent this, Sam rarely used cannabis in social situations unless he was with close friends.
Some participants said that cannabis increased their focus and helped them accomplish mundane or monotonous tasks, however others explained it decreased their motivation and productivity. Decreased focus and energy helped some pass the time, but others experienced these effects as counterproductive. Kathryn stated, “And when I’m high I just think, like, I’m not really on my A game. I’m not thinking as like clearly…. And I just feel like I don’t get much done.” She indicated that cannabis’ dulling effects positively affected her recovery because it helped her manage her spare time, simultaneously it negatively affected her recovery because it limited her clarity of mind. The complex, and at times conflicting, side effects of cannabis made its effect unpredictable.
Using cannabis to replace primary drugs was a common reason that participants increased their use during recovery. A few people explained, though, that using cannabis in response to an opioid craving increased their desire to feel the effects of opioids. Eva compared it to ineffectively scratching an itch:
That feeling of I have an itch but it’s not really being scratched. Because it, you know, obviously doesn’t have the same effects as, like an opiate or something like that. But it’s like just barely enough to keep you like from wanting to do anything else, but then that can also be frustrating.
In Marco’s case, this strategy led to opioid use: “One of the times I did relapse was because I thought I was going to feel better, I took a hit [of cannabis], right. And what it actually did was intensified my thinking to where I was like, ‘Oh now I need to calm down, right.’” Marco was the only participant who shared that he used opioids in response to cannabis use. While not common in this sample, return to use is one substantial risk of cannabis substitution.
Benefits of recovery while using cannabis
Despite ongoing challenges related to psychiatric conditions and continued substance use, every participant reported meaningful improvements after resolving their primary addiction and increasing their cannabis use. Many had better, more honest relationships with their families. Ava said that she was able, “to be myself in front of my family and friends, because I’m not hiding anything anymore.” Prior to resolving her addiction, Ava concealed her opioid use. However, her family used cannabis together, and she could join them now without having to hide other substance use. In other cases, participants did not describe using cannabis with their families, but had improved relationships with their families because they were less impaired. Terry was happy to spend more time with her family, “And they want to connect with me more too because I’m not fu-ked up.” Ian echoed a similar experience, “I got to get closer to my mom. And my mother-in-law. So that’s been nice.” Strengthening family intimacy was just one of the benefits of their recovery, even while using cannabis.
Participants also reported relief from the elimination of opioid and stimulant-related consequences. Freeing herself from the powerful hold that opioids had over her, Jessica regained her autonomy:
If I’m going to be dope sick, then I’m not coming. You know what I’m saying? Or I’m going and getting that first. Or, or if I get there, and I have to go get it, I’m going to leave in the middle of family dinner. I’m gonna [sic] go get my drugs… Nothing’s going to stand in the way of me getting, of getting right…the opiates they completely control[ed] my life.
Without urgency to acquire money or drugs, she was more accountable to herself and her family. Kelly shared similar relief that she was rid of the effects of methamphetamine addiction:
[Methamphetamine] just takes over your freakin [sic] life, you forget to eat, you forget to sleep. I’ll be like three days in and not realize I haven’t slept yet, and then you know you start seeing things in the corner of your eyes, because you’re sleep deprived and you’re on this major drug. So yeah, it’s a big difference.
Kelly continued to struggle with her mental health and to moderate her alcohol use. Even so, she was relieved to be rid of methamphetamine-induced deprivation and psychosis: “Everything is kind of the same, except my mind is with me.” The relief from consequences related to opioid and stimulant use was described consistently as impactful to participants’ recovery. Maya was proud of her self-directed change:
I don’t feel any shame whatsoever. I’m actually really proud… I rose to the occasion. Like I made choices, like intentional choices. And followed through on those choices to ensure that I can be responsible and trustworthy.
Maya continued to use methamphetamine, but at a decreased frequency and quantity (i.e., a small amount in the morning), and reaped profound benefits related to improved self-concept and stable employment. Kathryn summarized her growth over the past few months, touching upon many of the themes identified above:
I wake up in the morning and like let my dog out, feed my animals and stuff I could not do before, because I was sick all the time… I read three books which I haven’t read any books and, like the last few years. I made friends, which I didn’t have before. I answer my phone. Less fighting with my husband because I’m not trying to sneak out and go get high. A lot of good things, a lot of little things. I got on depression medication, finally, because I went to the doctor.
For some, cannabis use was directly linked to recovery experiences (e.g., Ava spent time with her family, which involved cannabis use). For the most part, though, cannabis use benefitted participants’ recovery indirectly. They explained that cannabis use helped them reduce or eliminate their primary substance and tolerate experiences without those substances, via replacement, affect regulation, and avoiding boredom; this elimination or reduction facilitated their myriad positive outcomes.
This study identified participants’ motives for, experiences with, and reflections on cannabis use after resolving a primary opioid or stimulant addiction. Participants illustrated cannabis’ host of functional roles. They assessed the risks of cannabis use in comparison to the risks of their previous opioid and methamphetamine use and reasonably concluded that cannabis substitution was substantially less harmful and facilitated progress in their recovery.
Relative risk
In the absence of a safe drug supply, universal healthcare, and access to safe use supplies, individuals with addictions to opioids and/or stimulants face some of the greatest risks for health and social harms related to drug use, risks that are not attributable to cannabis use [ 32 ]. Chronic opioid and methamphetamine use are associated with severe health consequences, including impaired memory and cognition; structural brain changes; increased impulsivity and violent behavior; anxiety, delusions, hallucinations, and psychosis; heart attacks, seizures, liver and kidney damage, and death [ 33 , 34 ]. Some of these changes are permanent, or persist into a period of abstinence [ 35 ]. Additionally, opioid use continues to be a leading cause of drug-related deaths in the U.S., thus, any decrease in opioid use increases survival likelihood [ 36 ].
While cannabis substitution may reduce mortality and morbidity related to opioid or stimulant use, cannabis use is not without acute and long-term risk, especially for youth or pregnant people [ 37 , 38 ]. Acute side-effects include impaired non-verbal learning and memory, attentional control, and motor inhibition, however these side effects generally subside after a period of abstinence [ 37 , 38 ]. However, the changing drug supply may challenge the validity of these findings, as the average THC concentration has increased annually since 1970 [ 39 ]. While research on high potency THC products is nascent, some has found a correlation between high THC and increased likelihood of cannabis use disorder (CUD), increased “dependence,” and increased side effects including memory impairment and paranoia [ 40 , 41 ].
Motivational model and cannabis substitution during recovery
The motivational model was an informative framework in examining participants’ cannabis use. Of the motivational model’s extant motives, “to cope” was the most salient motive for cannabis use during recovery. Cannabis use during recovery supported two types of coping: [ 1 ] to regulate affect; and [ 2 ] to avoid boredom or negative thought patterns. Notably, using cannabis for pleasure or for social purposes was uncommon in this study. Even more than these motives, participants emphasized that cannabis helped them avoid using opioids or methamphetamine. The motivational model does not include a substitution motive and this study suggests that, while similar to the coping motive, substitution is likely a distinct construct. The motivational model’s “to cope” has typically referred to psychological coping with distress of any kind; in contrast, substitution involves physical and psychological dimensions and is exclusively driven by reduced substance use. Additional research may be helpful to determine whether these are different factors.
Motives for use
Substitution.
In line with previous research, participants believed that cannabis use protected them from returning to their primary substance or former pattern of use, in part because cannabis helped them manage cravings [ 32 ]. In studies on the effect of cannabis use on the return to opioid use by individuals taking medication for opioid use disorder (MOUD), cannabis was associated with decreased likelihood of opioid, alcohol, or cocaine use [ 42 , 43 ]. In one study, experiencing euphoria or being “high” was associated with decreased likelihood of any opioid use. In the current study, cannabis intoxication did not change participants’ assessment of cannabis’ effectiveness as a deterrent to opioid or methamphetamine use. For example, some participants benefitted from their cannabis use rituals, which were unrelated to its psychoactive effects.
Affect regulation
Reducing anxiety was the most reported mood-related motive for cannabis use, suggesting some degree of self-medication [ 44 , 45 ]. Many participants in this study reported complex psychiatric disorders and previous trauma, which they aimed to treat with cannabis. In many cases participants described high frequency of use to mitigate these symptoms. Further exploration of self-medication with cannabis use is warranted to discern whether it can be exclusively therapeutic, or whether there are always ancillary motives and/or effects. Other participants experienced increased anxiety, especially social anxiety, after using cannabis. Research on cannabis and anxiety reflects these mixed outcomes. A review on this topic found some evidence that cannabis has anxiolytic effects, though many studies had inverse or null results [ 46 ]. While cannabis is likely to be inadequate to treat patients’ anxiety without additional mental health intervention, many participants in this study indicated skillful use of cannabis by moderating use according to its effects (e.g., only using cannabis with close friends to avoid increased social anxiety).
Boredom, the aversive state due to a monotonous environment and difficulty remaining engaged with the environment, is a natural part of early recovery. Boredom and even the anticipation of boredom are known barriers to entering or staying in recovery [ 47 , 48 , 49 ]. In the general population, people use cannabis to mitigate boredom [ 50 , 51 ] yet there is little research on the relationship between boredom and recovery and how cannabis use interacts with these states. In the present study, participants described the connection between cannabis use and boredom in three ways: first, cannabis helped them accomplish tasks in which they had little interest; second, it ameliorated negative emotional experiences prompted by boredom; and third, it helped them tolerate boredom produced by unstructured time, in many cases due to unemployment.
Unemployment is common in early recovery and increased participation in the workforce often occurs over time in recovery [ 52 , 53 ]. For those in early recovery, engagement with community, work, or hobbies increases recovery capital and diminishes boredom [ 54 ]. Employment interventions in abstinence-based treatment settings have been associated with positive substance use outcomes [ 55 ]. However, many individuals like those in this study do not have clear pathways to access employment, nor are they embedded in peer support communities, which often help people re-enter the workforce. This barrier to services and recovery capital points toward an important area for future intervention development.
Implications for conceptions of recovery
Research increasingly acknowledges that recovery includes both abstinent and non-abstinent paths, paths which may vary by addiction and psychiatric severity, complexity, and chronicity [ 2 , 20 , 56 ]. Yet, there are few treatment or mutual aid settings where non-abstinent individuals can access the recovery resources available to their abstinence-seeking peers, as such settings view cannabis use as incompatible with recovery.
Due to potential medical use, cannabis use may or may not violate the principle of abstinence from non-prescribed psychoactive substances. Taking cannabis to treat a condition (e.g., chronic pain, posttraumatic stress disorder, chemotherapy-induced nausea) may be categorically closer to taking a prescription stimulant for Attention-deficit/hyperactivity disorder (ADHD) than to using cannabis recreationally. However, unlike medication for ADHD, there are no dosing guidelines or maximum dosing thresholds [ 57 ]. Without parameters for use, it remains challenging to classify cannabis use as strictly medical. Further study on the role of medical cannabis use in recovery is warranted to understand whether its use is compatible with the construct of abstinence.
Many participants reported previous treatment or 12-step participation, noting that these settings viewed their goals as incompatible with the settings’ conceptualization of successful recovery [ 56 ]. Upholding the belief that abstinence is the foundation of recovery, as many treatment and mutual aid settings do, discounts the substantial growth and improvement of people who, despite non-abstinence, recover from their addictions [ 2 ]. Equating abstinence with recovery reinforces stigmatizing conceptualizations of this population by differentiating between those who have and have not changed their substance consumption “enough,” or those who do and do not count as “recovered” [ 58 , 59 ]. Without embracing a more inclusive recovery paradigm, individuals like the participants in this study will continue to be perceived as “less well” and will continue to have fewer options for medical and mental health support compared to their abstinence-seeking peers [ 60 ].
Study limitations
Findings should be interpreted in the context of these limitations. First, this preliminary study on cannabis substitution was conducted with a small sample, which may mean that conceptual categories integral to non-abstinence recovery with substitution were missed [ 25 ]. Future qualitative studies on this topic should aim for larger samples and could consider the addition of quantitative measures. Recruiting via social media sites was effective in accessing a hard-to-reach population, but the resultant sample was limited to individuals who were aware of and engaged with these sites. The sample was predominantly White, which possibly reflects the demographics of individuals using Reddit, the recruitment site for most participants. Clinical settings, including primary care and addiction specific clinics, may be useful settings for recruitment in future studies. The interview did not explicitly ask about mental health history and likely missed some participants’ diagnoses and psychiatric medication. Although participants described their substance use history, they did not complete a clinical intake and thus their drug-use severity is unknown. In future work, researchers should collect precise data about mental health and addiction history to improve the understanding of who substitutes with cannabis and under what circumstances. Finally, this study was a single point in time and longitudinal studies are critical to understanding whether substitution and its effects change over time.
This study increases our insight about cannabis substitution in early recovery, documenting its potential roles during this period. At this time, cannabis’ relatively lower- risk profile makes it an effective harm reduction strategy for those in early recovery from an opioid or stimulant addiction [ 7 , 32 ]. Future studies are needed to assess the degree to which this substitution strategy is sustainable over time, as well as the later risks for primary addiction recurrence or development of a cannabis use disorder. Taking a harm reduction approach to drug use and addiction recovery has the potential to positively transform this population’s recovery experiences and willingness to seek support [ 61 , 62 ].
Data availability
No datasets were generated or analysed during the current study.
Bartram M. It’s really about wellbeing’: a Canadian investigation of harm reduction as a bridge between mental health and addiction recovery. Int J Ment Health Addict. 2021;19(5):1497–510.
Article PubMed Google Scholar
Paquette CE, Daughters SB, Witkiewitz K. Expanding the continuum of substance use disorder treatment: nonabstinence approaches. Clin Psychol Rev. 2022;91:102110.
Substance Abuse and Mental Health Services Administration. SAMHSA’s working definition of recovery: 10 guiding principles of recovery. [Internet]. 2012 [cited 2023 Jun 1]. https://store.samhsa.gov/sites/default/files/d7/priv/pep12-recdef.pdf .
Kim HS, Hodgins DC, Garcia X, Ritchie EV, Musani I, McGrath DS, et al. A systematic review of addiction substitution in recovery: clinical lore or empirically-based? Clin Psychol Rev. 2021;89:102083.
Lake S, Nosova E, Buxton J, Walsh Z, Socías ME, Hayashi K, et al. Characterizing motivations for cannabis use in a cohort of people who use illicit drugs: a latent class analysis. PLoS ONE. 2020;15(5):e0233463.
Article CAS PubMed PubMed Central Google Scholar
Lucas P, Baron EP, Jikomes N. Medical cannabis patterns of use and substitution for opioids & other pharmaceutical drugs, alcohol, tobacco, and illicit substances: results from a cross-sectional survey of authorized patients. Harm Reduct J. 2019;16(1):9.
Article PubMed PubMed Central Google Scholar
Reiman A. Cannabis as a substitute for alcohol and other drugs. Harm Reduct J. 2009;6(1):35.
Shapira B, Rosca P, Berkovitz R, Gorjaltsan I, Neumark Y. The switch from one substance-of-abuse to another: illicit drug substitution behaviors in a sample of high-risk drug users. PeerJ. 2020;8:e9461.
Siklos-Whillans J, Bacchus A, Manwell LA. A scoping review of the use of cannabis and its extracts as potential harm reduction strategies: insights from preclinical and clinical research. Int J Ment Health Addict. 2021;19(5):1527–50.
Article Google Scholar
Socías ME, Kerr T, Wood E, Dong H, Lake S, Hayashi K, et al. Intentional cannabis use to reduce crack cocaine use in a Canadian setting: a longitudinal analysis. Addict Behav. 2017;72:138–43.
Boucher LM, Marshall Z, Martin A, Larose-Hébert K, Flynn JV, Lalonde C, et al. Expanding conceptualizations of harm reduction: results from a qualitative community-based participatory research study with people who inject drugs. Harm Reduct J. 2017;14(1):18.
Pacek LR, Mauro PM, Martins SS. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend. 2015;149:232–44.
Smart R, Pacula RL. Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: findings from state policy evaluations. Am J Drug Alcohol Abuse. 2019;45(6):644–63.
Mok J, Milloy MJ, Grant C, Lake S, DeBeck K, Hayashi K, et al. Use of Cannabis as a harm reduction strategy among people who use drugs: a cohort study. Cannabis Cannabinoid Res. 2023;8(4):670–8.
Article CAS PubMed Google Scholar
Mojarrad M, Samet JH, Cheng DM, Winter MR, Saitz R. Marijuana use and achievement of abstinence from alcohol and other drugs among people with substance dependence: a prospective cohort study. Drug Alcohol Depend. 2014;142:91–7.
Aharonovich E, Liu X, Samet S, Nunes E, Waxman R, Hasin D. Postdischarge Cannabis use and its relationship to cocaine, alcohol, and heroin use: a prospective study. Am J Psychiatry. 2005;162(8):1507–14.
Donovan DM, Ingalsbe MH, Benbow J, Daley DC. 12-Step interventions and mutual support programs for substance use disorders: an overview. Soc Work Public Health. 2013;28(3–4):313–32.
Kaskutas LA, Witbrodt J, Grella CE. Recovery definitions: do they change? Drug Alcohol Depend. 2015;154:85–92.
Martinelli TF, Nagelhout GE, Bellaert L, Best D, Vanderplasschen W, van de Mheen D. Comparing three stages of addiction recovery: long-term recovery and its relation to housing problems, crime, occupation situation, and substance use. Drugs Educ Prev Policy. 2020;27(5):387–96.
Witkiewitz K, Tucker JA. Abstinence not required: expanding the definition of recovery from Alcohol Use Disorder. Alcohol Clin Exp Res. 2020;44(1):36–40.
Betty Ford Institute Consensus Panel. What is recovery? A working definition from the Betty Ford Institute. J Subst Abuse Treat. 2007;33(3):221–8.
Kelly JF, Abry AW, Milligan CM, Bergman BG, Hoeppner BB. On being in recovery: a national study of prevalence and correlates of adopting or not adopting a recovery identity among individuals resolving drug and alcohol problems. Psychol Addict Behav. 2018;32(6):595–604.
Laudet AB. The case for considering quality of life in addiction research and clinical practice. Addict Sci Clin Pract. 2011;6(1):44–55.
PubMed PubMed Central Google Scholar
Shumway ST, Bradshaw SD, Harris KS, Baker AK. Important factors of early addiction recovery and inpatient treatment. Alcohol Treat Q. 2013;31(1):3–24.
Charmaz K. Constructing grounded theory. 2nd edition. London; Thousand Oaks, Calif: Sage; 2014. 388 p. (Introducing qualitative methods).
Adams ZW, Kaiser AJ, Lynam DR, Charnigo RJ, Milich R. Drinking motives as mediators of the impulsivity-substance use relation: pathways for negative urgency, lack of premeditation, and sensation seeking. Addict Behav. 2012;37(7):848–55.
Gilson KM, Bryant C, Bei B, Komiti A, Jackson H, Judd F. Validation of the drinking motives Questionnaire (DMQ) in older adults. Addict Behav. 2013;38(5):2196–202.
Grant VV, Stewart SH, Mohr CD. Coping-anxiety and coping-depression motives predict different daily mood-drinking relationships. Psychol Addict Behav. 2009;23(2):226–37.
Charmaz K. With constructivist grounded theory you can’t hide: Social Justice research and critical inquiry in the public sphere. Qual Inq. 2020;26(2):165–76.
Cooper ML, Kuntsche E, Levitt A, Barber LL, Wolf S. Motivational models of substance use: A review of theory and research on motives for using alcohol, marijuana, and tobacco. In: Sher KJ, editor. The Oxford Handbook of Substance Use and Substance Use Disorders: Volume 1 [Internet]. Oxford University Press; 2016 [cited 2023 Oct 2]. p. 0. https://doi.org/10.1093/oxfordhb/9780199381678.013.017 .
Charmaz K, Thornberg R. The pursuit of quality in grounded theory. Qual Res Psychol. 2021;18(3):305–27.
Reddon H, Lake S, Socias ME, Hayashi K, DeBeck K, Walsh Z, et al. Cannabis use to manage opioid cravings among people who use unregulated opioids during a drug toxicity crisis. Int J Drug Policy. 2023;119:104113.
Baldacchino A, Balfour DJK, Passetti F, Humphris G, Matthews K. Neuropsychological consequences of chronic opioid use: a quantitative review and meta-analysis. Neurosci Biobehav Rev. 2012;36(9):2056–68.
Darke S, Kaye S, McKETIN R, Duflou J. Major physical and psychological harms of methamphetamine use. Drug Alcohol Rev. 2008;27(3):253–62.
van Holst RJ, Schilt T. Drug-related decrease in neuropsychological functions of abstinent drug users. Curr Drug Abuse Rev 4(1):42–56.
Mattson CL. Trends and geographic patterns in drug and synthetic opioid overdose deaths — United States, 2013–2019. MMWR Morb Mortal Wkly Rep [Internet]. 2021 [cited 2023 Oct 2];70. https://www.cdc.gov/mmwr/volumes/70/wr/mm7006a4.htm .
Hasin DS. US Epidemiology of Cannabis Use and Associated problems. Neuropsychopharmacology. 2018;43(1):195–212.
Kroon E, Kuhns L, Cousijn J. The short-term and long-term effects of cannabis on cognition: recent advances in the field. Curr Opin Psychol. 2021;38:49–55.
Freeman TP, Craft S, Wilson J, Stylianou S, ElSohly M, Di Forti M, et al. Changes in delta-9‐tetrahydrocannabinol (THC) and cannabidiol (CBD) concentrations in cannabis over time: systematic review and meta‐analysis. Addiction. 2021;116(5):1000–10.
Arterberry BJ, Treloar Padovano H, Foster KT, Zucker RA, Hicks BM. Higher average potency across the United States is associated with progression to first cannabis use disorder symptom. Drug Alcohol Depend. 2019;195:186–92.
Freeman TP, Winstock AR. Examining the profile of high-potency cannabis and its association with severity of cannabis dependence. Psychol Med. 2015;45(15):3181–9.
Best D, Gossop M, Greenwood J, Marsden J, Lehmann P, Strang J. Cannabis use in relation to illicit drug use and health problems among opiate misusers in treatment. Drug Alcohol Rev. 1999;18(1):31–8.
Rosic T, Kapoor R, Panesar B, Naji L, Chai DB, Sanger N, et al. The association between cannabis use and outcome in pharmacological treatment for opioid use disorder. Harm Reduct J. 2021;18(1):24.
Asselin A, Lamarre OB, Chamberland R, McNeil SJ, Demers E, Zongo A. A description of self-medication with cannabis among adults with legal access to cannabis in Quebec, Canada. J Cannabis Res. 2022;4(1):26.
Turner S, Mota N, Bolton J, Sareen J. Self-medication with alcohol or drugs for mood and anxiety disorders: a narrative review of the epidemiological literature. Depress Anxiety. 2018;35(9):851–60.
van Ameringen M, Zhang J, Patterson B, Turna J. The role of cannabis in treating anxiety: an update. Curr Opin Psychiatry. 2020;33(1):1.
Bonny-Noach H, Gold D. Addictive behaviors and craving during the COVID-19 pandemic of people who have recovered from substance use disorder. J Addict Dis. 2021;39(2):257–64.
Levy MS. Listening to our clients: the prevention of relapse. J Psychoact Drugs. 2008;40(2):167–72.
McKay JR, Franklin TR, Patapis N, Lynch KG. Conceptual, methodological, and analytical issues in the study of relapse. Clin Psychol Rev. 2006;26(2):109–27.
Fahlman SA, Mercer KB, Gaskovski P, Eastwood AE, Eastwood JD. Does a lack of life meaning cause boredom? Results from psychometric, longitudinal, and experimental analyses. J Soc Clin Psychol. 2009;28(3):307–40.
LaPera N. Relationships between boredom proneness, mindfulness, anxiety, depression, and substance use. New Sch Psychol Bull. 2011;8(2):15–25.
Google Scholar
Dennis ML, Foss MA, Scott CK. An eight-year perspective on the relationship between the duration of abstinence and other aspects of recovery. Eval Rev. 2007;31(6):585–612.
Laudet AB. Rate and predictors of employment among formerly polysubstance dependent urban individuals in recovery. J Addict Dis. 2012;31(3):288–302.
O’Sullivan D, Xiao Y, Watts JR. Recovery capital and quality of life in stable recovery from addiction. Rehabil Couns Bull. 2019;62(4):209–21.
Walton MT, Hall MT. The effects of employment interventions on addiction treatment outcomes: a review of the literature. J Soc Work Pract Addict. 2016;16(4):358–84.
Slawek D, Arnsten JH. Medical use of cannabis and cannabinoids in adults. 2023 Nov.
Rosenberg H, Grant J, Davis AK. Acceptance of non-abstinence as an outcome goal for individuals diagnosed with substance use disorders: a narrative review of published research. J Stud Alcohol Drugs. 2020;81(4):405–15.
Neale J, Nettleton S, Pickering L. Recovery from problem drug use: what can we learn from the sociologist Erving Goffman? Drugs Educ Prev Policy. 2011;18(1):3–9.
Sussman S, Commentary. Addiction, stigma, and neurodiversity. Eval Health Prof. 2021;44(2):186–91.
Proctor SL, Lipsey J, Rigg KK. The insanity of addiction treatment in America. Addict Res Theory. 2022;30(4):231–6.
Biancarelli DL, Biello KB, Childs E, Drainoni M, Salhaney P, Edeza A, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–6.
Hawk M, Coulter RWS, Egan JE, Fisk S, Reuel Friedman M, Tula M, et al. Harm reduction principles for healthcare settings. Harm Reduct J. 2017;14(1):70.
Download references
Acknowledgements
I would like to thank Renée Spencer, EDD, MSSW for her methodological training and consistent support, which made this study possible.
Funding for this work was provided by the Boston University School of Social Work grant for doctoral dissertations.
Author information
Authors and affiliations.
Boston University School of Social Work, 264 Bay State Road, Boston, MA, 02215, USA
Corinne A. Beaugard & Maryann Amodeo
Boston Medical Center, Grayken Center for Addiction, Clinical Addiction Research and Education Unit, Section of General Internal Medicine, Department of Medicine, Boston University Chobanian & Avedisian School of Medicine, 801 Massachusetts Ave, 2nd Floor, Boston, MA, 02118, USA
Alexander Y. Walley
Department of Psychiatry, Boston Medical Center Crosstown Center, 4th Floor 801 Massachusetts Avenue, 02118, Boston, MA, USA
Corinne A. Beaugard
You can also search for this author in PubMed Google Scholar
Contributions
CAB: conceptualization, methodology, formal analysis, writing- original draft.MA and AYW: writing- review and editing, supervision .
Corresponding author
Correspondence to Corinne A. Beaugard .
Ethics declarations
Ethics approval and consent to participate.
The Boston University Charles River Campus Institutional Review Board approved this study.
Consent to participate
All participants provided verbal consent for participation.
Consent to publish
All authors provided consent for this publication.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Beaugard, C.A., Walley, A.Y. & Amodeo, M. “Everything is kind of the same except my mind is with me”: exploring cannabis substitution in a sample of adults in early recovery from an opioid or stimulant addiction. Harm Reduct J 21 , 83 (2024). https://doi.org/10.1186/s12954-024-01002-0
Download citation
Received : 22 December 2023
Accepted : 06 April 2024
Published : 20 April 2024
DOI : https://doi.org/10.1186/s12954-024-01002-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Harm Reduction Journal
ISSN: 1477-7517
- Submission enquiries: [email protected]

An official website of the United States government, Department of Justice.
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Substance Use Treatment Programs
Youth substance use treatment programs aim to reduce alcohol and illicit drug use, and the misuse of licit drugs, in youths who have been clinically diagnosed with a substance use problem. These programs differ from prevention programs, which aim to promote abstinence in youths to prevent their initial or escalating use. [1] Treatment programs can take a multitude of approaches, such as court-based, residential-based, and family-inclusive programs to help youth develop skills and knowledge to reduce substance use (Drake, 2012; Van Ryzin et al., 2016; Winters, Botzet, and Fahnhorst, 2011).
Substance use disorder in youth is a prevalent problem. An estimated 2.8 percent (712,000) of youths ages 12 to 17 experienced an alcohol use disorder in the past year, and 6.3 percent (1.6 million) of youths ages 12 to 17 experienced a substance use disorder in the past year (SAMSHA, 2021). However, the rate of utilization of substance use treatment programs is low. According to a study by Haughwout and colleagues (2016), fewer than 12 percent of youths who have a substance use disorder participate in treatment.
This literature review focuses on substance use disorder among youths under 18 and on the utilization of substance use treatment programs. The review describes the scope of substance use among youth, the theoretical base of substance-use treatment programs, risk factors that can lead to substance use disorders, protective factors that can buffer against substance use disorders, various types of treatment programs and outcome evidence, limitations to treatment programs, and the research currently available.
[1] For more information, see the Model Programs Guide literature review on Substance Use Prevention Programs .
Scope of the Problem
Overview of substance use disorders.
Among youth in the United States, it is estimated that 8 percent will experience an alcohol use disorder, and 2 percent to 3 percent will experience an illicit drug use disorder before turning 18 Merikangas et al., 2010; Swendsen et al., 2012; SAMSHA, 2011). Several surveys collect information on youths' self-reported use of alcohol and their use of illicit [1] and licit [2] drugs. These self-reported data are then used to calculate the prevalence rates of youth substance use (such as 30-day prevalence in alcohol use or past-year use of narcotics). However, few surveys collect information specifically regarding the prevalence of substance use disorders in youth. Substance use disorder is a diagnosable condition of ongoing and habitual use, and is distinct from substance use, which refers to episodes of occasional use. Most of the information provided below on prevalence rates of youth substance use disorders (and specific disorders such as alcohol use disorder) come from one survey, the National Survey on Drug Use and Health ( NSDUH ), which is the most comprehensive and up-to-date federal survey.
The NSDUH is administered by the Substance Abuse and Mental Health Services Administration (SAMHSA) and collects national and state-level data annually from all 50 states and the District of Columbia. In 2020, more than 36,000 people ages 12 and older were surveyed, including 6,337 interviews conducted with youths ages 12 to 17. Findings pertaining to substance use disorders—including alcohol use disorder, illicit drug use disorder, and more-specific disorders resulting from marijuana, cocaine, heroin, prescription pain reliever, or opioid use—are presented in an annual report.
In general, rates of substance use disorder among youth have declined and leveled off since the first decade of the 2000s. Specifically, among 12- to 17-year-olds, past-year alcohol use disorder declined from 5.9 percent (or 1.5 million youths) in 2002 to 1.7 percent (or 414,000 youths) in 2019. Within the same age group, 3.4 percent (or 894,000 youths) had a past-year illicit drug use disorder in 2019, which was higher than estimates in 2017 and 2018, but similar to estimates in 2015 and 2016. [3
In 2020 the NSDUH used the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition ( DSM–5 ) criteria to assess substance use disorder. The DSM-5 is the most current diagnostic tool published by the American Psychiatric Association (APA), and it serves as the principal authority for psychiatric diagnoses. Previous surveys used the DSM–4 criteria, meaning that the 2020 findings cannot be easily compared with previous years. In 2020, respondents were identified as having a substance use disorder if they met two or more of the following criteria in a 12-month period:
- Consuming the substance in larger amounts or over a longer period of time than intended.
- Desiring to cut back on or stop use of the substance but being unsuccessful in these attempts.
- Spending a significant amount of time obtaining, using, or recovering from using the substance.
- Experiencing cravings and urges to use the substance.
- Failing to meet school, home, or work obligations because of substance use.
- Continuing to use the substance despite problems it has caused.
- Giving up important social, occupational, or recreational activities because of substance use.
- Continuing to use substances, even in situations where it is physically dangerous.
- Continuing to use substances, despite having physical or psychological problems that may have been caused or made worse by the substance.
- Needing more of the substance to achieve the desired effect (increased tolerance).
- Development of withdrawal symptoms, which can be relieved by taking more of the substance.
Using these criteria, it was estimated that 6.3 percent (1.6 million) of youths ages 12 to 17 experienced a substance use disorder in the past year (SAMHSA, 2021).
Alcohol Use Disorder
Alcohol is the most commonly used drug among youth (NIAAA, 2022). According to the 2020 NSDUH, 8.2 percent of youths reported using alcohol in the past month, 4.1 percent reported binge alcohol use, and 0.6 percent reported heavy alcohol use [4] in the past month (SAMHSA, 2021). However, while any alcohol use by youths is problematic, not all youths who drink alcohol meet the criteria for an alcohol use disorder.
The NSDUH identified respondents as having alcohol use disorder if they had used alcohol on 6 or more days in the past 12 months and if they also met two or more of the DSM–5 criteria for alcohol use disorder. The criteria for alcohol use disorder are as follows:
- Used alcohol in larger amounts or for a longer time period than intended.
- Had a persistent desire or made unsuccessful attempts to cut down on alcohol use.
- Spent a great deal of time in activities to obtain, use, or recover from alcohol use.
- Felt a craving or strong desire to use alcohol.
- Engaged in recurrent alcohol use resulting in failure to fulfill major role obligations at work, school, or home.
- Continued to use alcohol despite social or interpersonal problems caused by the effects of alcohol.
- Gave up or reduced important social, occupational, or recreational activities because of alcohol use.
- Continued to use alcohol in physically hazardous situations.
- Continued to use alcohol despite physical or psychological problems caused by alcohol use.
- Developed tolerance (i.e., needed to use alcohol more than before to get desired effects or noticing that the same amount of alcohol had less effect than before.
- Experienced a required number of withdrawal symptoms after cutting back or stopping alcohol use.
Based on these requirements, the NSDUH estimated that 2.8 percent (712,000) of youths ages 12 to 17 experienced alcohol use disorder in the past year.
Illicit Drug Use Disorder
Many youths experiment with illicit drugs, in addition to alcohol. In 2020, 13.8 percent of youths who responded to the NSDUH indicated past-year illicit drug use (SAMHSA, 2021). However, not all youths who engage in illicit drug use will meet the criteria for an illicit drug use disorder.
The NSDUH identified respondents as having an illicit drug use disorder if they met the DSM–5 substance use disorder criteria (described above under Overview of Substance Use Disorders) for one or more of the following illicit drugs: marijuana, cocaine, heroin, hallucinogens, inhalants, methamphetamine, or prescription psychotherapeutic drugs (stimulants, tranquilizers or sedatives, and pain relievers). For respondents whose drug use concentrated on a certain substance, specific disorders (such as marijuana use disorder, opioid use disorder, prescription pain reliever use disorder, cocaine use disorder, and heroin use disorder) were included.
In 2020, using past-year use rates among 12- to 17-year-olds, the NSDUH (SAMHSA, 2021) estimated that 4.9 percent (1.4 million youths) met criteria for at least one illicit drug use disorder. Specifically:
- 4.1 percent (1 million youths) met criteria for marijuana use disorder.
- 0.3 percent (80,000 youths) met criteria for opioid use disorder.
- 0.3 percent (80,000 youths) met criteria for prescription pain reliever use disorder.
- 0.1 percent (28,000 youths) met criteria for cocaine use disorder.
- Estimates for heroin use disorder could not be calculated with sufficient precision.
Co-Occurring Mental Health Disorders and Substance Use Disorders Among Youth
Youth substance use and mental health problems are commonly experienced simultaneously; an estimated 60 percent to 75 percent of youths with substance use disorders also have a co-occurring mental health disorder (Torrens et al., 2012; Burkstein and Horner, 2010; Chan, Dennis, and Funk, 2008; Turner et al., 2004; Hoffman et al., 2004). Common co-occurring mental health problems include conduct disorder, Attention Deficit Hyperactivity Disorder (ADHD), mood disorders, and trauma-related disorders (Burkstein and Horner, 2010).
Youths may turn to alcohol or drugs to help alleviate symptoms associated with mental health disorders, such as hopelessness, anxiety, irritability, or negative thoughts. However, substance use can have the opposite effect, which can lead to exacerbating and/or worsening these symptoms (Ramo et al., 2005). As a result, co-occurring disorders are associated with more-severe substance use disorder symptoms (Chan, Dennis, and Funk, 2008; Wise, Cuffe, and Fischer, 2001).
Research on co-occurring substance use disorder and mental health disorders in youth has largely focused on mood disorders, or mental health disorders that largely affect one’s emotional state such as depression and anxiety. Youths who have experienced a major depressive episode (MDE) are twice as likely to engage in alcohol or illicit drug use, compared with youths who have not experienced one (SAMHSA, 2021). Using DSM–5 criteria, youths were identified as having experienced an MDE if in the past year if 1) they had at least one period of 2 weeks or longer when, for most of the day nearly every day, they felt depressed or lost interest or pleasure in daily activities, and 2) they also had problems with sleeping, eating, energy, concentration, or self-worth or had recurrent thoughts of death or recurrent suicidal ideation. In 2020, 2.7 percent of adolescents surveyed (644,000 people) experienced a substance use disorder and a major depressive episode in the same year (SAMHSA, 2021). The 2020 NSDUH examined rates of substance use disorder in youths who experienced MDE in the past year. Based on these criteria, an estimated 2.7 percent (644,000) of youths ages 12 to 17 experienced both MDE and substance use disorder in the past year (SAMHSA, 2021).
Overall Key Findings
Findings from the NSDUH showed that 2.8 percent of youths ages 12 to 17 met the criteria for alcohol use disorder and 4.9 percent met the criteria for at least one illicit drug use disorder. T he most common type of illicit drug use disorder was marijuana use disorder (4.1 percent), with well under 1 percent of youths experiencing opioid, prescription pain reliever, or cocaine use disorder. The NSDUH also found that 2.7 percent of youths experienced both a substance use disorder and a major depressive episode. Yet, substance use treatment use remained low among youths who met the criteria for substance use disorder and therefore demonstrated a need for treatment (SAMHSA, 2021).
Differences in Substance Use Disorder by Gender
While many studies have described the differences between adult men and women in the prevalence of substance use disorders (e.g., Vasilenko, Evans–Polce, and Lanza, 2017), and some research have focused on the differences between adolescent boys and girls in substance use and initiation (e.g., Johnston et al., 2020), there is limited research on the difference in the prevalence of substance use disorders between adolescent boys and girls (Aarons et al., 2001; Gau et al., 2007; McHugh et al., 2018). For example, a study of prevalence of adolescent substance use disorders among youth ages 13 to 18 across five sectors of care (e.g., juvenile justice system, mental health system, child welfare) found that rates of substance use disorder were higher among males (Aarons et al., 2001). Also, a study from Taiwan found that boys were more likely than girls to develop substance use disorders in adolescence (Gau et al., 2007). Studies of older youth (ages 16 to 25) have found that documented opioid use disorder was higher for males than females (Bagley et al., 2021). However, several sources find that there is more gender parity in problematic substance use in adolescence than in adulthood (e.g., Young et al., 2002; McHugh et al., 2018) and that the differences by gender that had existed in the past have been getting smaller.
[1] Illicit drugs include marijuana (in 40 states), opioids (e.g., heroin), certain stimulants (e.g., methamphetamine, cocaine), hallucinogens (e.g., LSD), and dissociative drugs (e.g., PCP) [NIDA, 2020].
[2] Licit drugs include alcohol, nicotine (e.g., cigarettes), marijuana (as of 2022, in Alaska, California, Colorado, the District of Columbia, Maine, Massachusetts, Michigan, Nevada, Oregon, and Washington), certain stimulants (e.g., coffee), medicines used for illnesses, over-the-counter drugs used as directed, and prescription medicines used by the person to whom the drugs were prescribed (NIDA, 2020).
[3] The 2015 NSDUH was the first year during which estimates were provided for any illicit drug use disorder among youths. Previous years collected data on specific illicit drug use disorders only (e.g., marijuana, cocaine, and heroin use disorders).
[4] The NSDUH defines binge drinking for males as having 5 or more drinks on the same occasion at least 1 day in the past 30 days. Binge drinking for females is defined as having 4 or more drinks on the same occasion at least 1 day in the past 30. Heavy alcohol use is defined as binge drinking on 5 or more days in the past 30 days based on the thresholds described (SAMHSA, 2021).
Theoretical Background
The various treatment approaches for youths experiencing substance use disorders are grounded in numerous theories. These theories inform treatment programming that works to encourage behavioral change and improve youths’ interpersonal relationships (Liddle et al., 2018, Slesnick and Prestopnik, 2009, Akers et al., 1979). Prevalent theories underlying substance use disorder treatment programs for youth include various learning theories (i.e., cognitive–behavioral), family-based theories, and therapeutic justice. Also, several authors use self-determination theory to examine the influence of motivation in treatment engagement among youths (Bowers et al., 2017; Cleverley, Grenville, and Henderson, 2018).
Learning Theories. Classical, operant, and social learning theories have been applied to understand youths' substance use behavior and to inform treatment programming. Within these theories, substance use is viewed as behavior that is learned in the context of social interactions (e.g., observing parents, siblings, or peers) and that persists depending on whether there are rewards or punishments for the behavior (Akers et al., 1979). These theories inform behavior or cognitive–behavioral models that conceptualize adolescent substance use as learned behaviors initiated and maintained in the context of environmental factors (Waldron and Kaminer, 2004) and that can be changed by modifying thought processes or reinforcing new behaviors (Winters et al., 2018). With this, the majority of individual and group-based cognitive–behavioral treatments have involved multicomponent approaches of cognitive strategies, such as identifying distorted thinking patterns, combined with behavioral strategies, such as problem-solving, coping with cravings, and substance refusal skills training, which teach strategies for avoiding high-risk drug use situations (Waldron and Turner, 2008). These treatments help build youths' motivation to change by providing incentives for abstinence (Winters et al., 2018). Often, cognitive–behavioral therapy for substance use will include components such as self-monitoring, avoidance of stimulus cues, altering reinforcement contingencies, and coping-skills training to manage and resist urges to use. The use of modeling, behavior rehearsal, feedback, and homework assignments are characteristic during treatment sessions (Waldron and Kaminer, 2004).
Self-Determination Theory. This is a theory of human motivation based on three basic psychological needs: 1) autonomy, 2) competence, and 3) relatedness (Deci and Ryan, 2012; Ryan and Deci, 2000). It has been applied in many life domains, including substance use treatment engagement (Bowers et al., 2017; Groshkova, 2010). The theory proposes that there are several types of external motivation and that levels of engagement in treatment are determined by how individuals subjectively perceive these external pressures (Cleverley, Grenville, and Henderson, 2018; Deci and Ryan, 1985; Wild and Enzle, 2002). For example, youths often are extrinsically motivated by their parents to enter treatment. This could result in youths’ resentfully complying out of fear of consequences or, by contrast, understanding and accepting that substance use is an instrumental step toward a better future. These differing patient perceptions lead to different treatment experiences (Cleverley, Grenville, and Henderson, 2018; Ryan and Deci, 2000).
Family Systems Theory . General systems theory, which focuses on how the parts of a system interact with one another, helped inform development of family systems theory, which was developed in the late 1960s and early 1970s. Key concepts in family systems theory are feedback, homeostasis, and boundaries (Lander, Howsare, and Byrne, 2013). Homeostasis refers to the idea that it is the tendency of a system to seek stability and equilibrium (Brown and Christensen, 1986), and in family systems theory this means that each family member tends to function in such a way that keeps the whole system in balance, even if it is not healthy for specific individuals (Lander, Howsare, and Byrne, 2013). Feedback refers to the circular way in which parts of the family system communicate with one another. Finally, boundaries regulate interpersonal contact, either in a healthy way (e.g., boundaries define healthy adult and child roles in the family) or an unhealthy way (e.g., maintaining secrets) [Lander, Howsare, and Byrne, 2013].
Multiple models of family therapy have been developed using the family systems theory and focusing on improving family functioning and social relationships (Waldron and Turner, 2008; Liddle et al., 2009; Liddle et al., 2018), including the multisystemic family systems therapy model. Some treatment programs incorporate concepts from the crisis intervention theory , which contends that families are more amenable to counseling and open to change during a crisis (e.g., youth running away, youth using alcohol or drugs) [Slesnick and Prestopnik, 2009]. Therefore, these programs start by bringing the family together to address the immediate issues the youth is experiencing. In general, approaches that involve family are based on the therapeutic premise that the family has the most significant and long-lasting influence on adolescent development (Winters et al., 2018).
Although family is an important part of a young person's social environment and often is essential to resolving a young person's substance use problems, interventions at the family system level alone may not be sufficient depending on the individual's situation (Liddle, 1999). Therefore, many family and individual treatment approaches address the multiple systems that maintain youths' substance use, including individual, familial, and extrafamilial systems (Liddle, 1999). Many substance-use-treatment programs for youth integrate multiple therapeutic strategies within their treatment service framework, incorporating elements from family-based treatment, group and individual cognitive–behavioral therapy, motivational approaches, among others to enhance outcomes (Gray and Squeglia, 2018). Common components among them are teaching skills to resist the triggers associated with a youth's substance use, addressing life functioning issues that may have contributed to both the onset and maintenance of the substance use (including mental health and family issues), and identifying and building on a young person's strengths (Winters et al., 2018).
Therapeutic Jurisprudence. In addition, courts-based treatment programs for youth are often grounded in the theoretical perspective of therapeutic jurisprudence, which integrates knowledge of mental health and behavioral change with the implementation of law (Wilson, Olaghere, and Kimbrell, 2019). Under therapeutic jurisprudence, it is argued that legal rules and procedures can be used to improve the mental and physical well-being of youths (that is, justice-involved juveniles often with drug-involved offenses) within the court system. The emphasis under this model is on the selection of a therapeutic option that promotes health but does not conflict with the normative values of the justice system, such as due process (Rottman and Casey, 1999). Principles of therapeutic justice include close monitoring of a youth's behavior, multidisciplinary involvement, and collaboration with community-based and governmental organizations (Wilson, Olaghere, and Kimbrell, 2019). Drug courts are a primary example of court-based programs that use the principles of therapeutic jurisprudence (BJA, 2003).
Risk Factors for Substance Use Disorder
Risk factors [1] consist of personal traits, characteristics of the environment, and conditions in the family, school, and community that are linked to a youth's likelihood of engaging in delinquency and other problem behaviors such as substance use (Murray and Farrington, 2010). These risk factors can exist at the individual, peer, school, family, and community levels. Research on risk factors that can affect youths' likelihood of success in substance use treatment programs is largely limited; therefore, the research discussed below focuses on risk factors that are linked to a youth's likelihood of developing a substance use disorder. However, this research is limited, as many studies focus on risk factors of substance use initiation rather than on specific disorders (Bacio et al., 2015). Additional information on substance use initiation can be found in the Substance Use Prevention Programs Literature Review .
Individual . These risk factors include any characteristic directly related to or within a youth that affect the likelihood of their engaging in a specific behavior, such as substance use. These risk factors can stem from genetics, early moral development, personality traits, temperament, and negative life events (Development Services Group, 2015; Wong, Slotboom, and Bijleveld, 2010; Dick et al., 2013; Hodgins, Kratzer, and McNeil, 2001). For example, research has found that genetics play a role in the development of a substance use disorder in youth, and some biobehavioral traits attributed to predisposition for substance use disorders are influenced by genetics (Dick et al., 2013). However, studies emphasize that parenting and environmental factors affect risk factors related to genetics (Hines et al., 2015; Sloboda, Glantz, and Tarter, 2012; Prom–Wormley et al., 2017); this is seen especially in studies involving twins (Dick et al., 2013).
Other researchers have examined the effect of personality profiles on youth substance use disorders. One study found that youths with substance use disorders had greater levels of neuroticism, lower agreeableness, and lower conscientiousness than siblings of similar ages without substance use disorders (Anderson et al., 2007; Kotov et al., 2010).
As previously mentioned, various mental health disorders, such as Attention Deficit Hyperactivity Disorder (ADHD), conduct disorders, and mood disorders, are associated with substance use disorders (Lee et al., 2011; Mason et al., 2019; Torrens et al., 2012; Wilens et al., 2011). A 3-year longitudinal study of adolescents in Taiwan found that conduct disorder and ADHD were two of the most significant predictive factors for adolescent substance use disorder (Gau et al., 2007). In addition, a meta-analysis of 37 longitudinal studies with more than 750,000 participants examining the relationship between childhood psychiatric disorders and subsequent substance abuse found that childhood ADHD, oppositional defiant disorder, conduct disorder, and depression increased the risk of developing substance-related disorders (Groenman, Janssen, and Oosterlaan, 2017). However, researchers in several different studies have emphasized that the relationship between mental health disorders and substance use disorders can be multidirectional, which means causation cannot necessarily be established (Wilens et al., 2004; Winters et al., 2014). In other words, it is difficult to determine whether the mental health disorder preceded the substance use disorder, or the other way around.
Peer. Research on peer influences and substance use disorder is limited. However, available research indicates many findings of the impact of peer influences on youth substance use and initiation. Peer risk factors for substance use include having friends who engage in delinquent behavior, having friends who use substances, and gang membership. Research demonstrates that an association with peers who engage in deviant behavior and use substances is one of the strongest risk factors for youth substance use and initiation (Coffman, Melde, and Esbensen, 2015; Ferguson and Meehan, 2011; Handren, Donaldson, and Crano, 2016; Whitesell et al., 2013). For example, a study of youths in Ohio found that association with delinquent peers was the strongest correlate to substance use, even when other relevant factors (such as family and neighborhood) were controlled for (Ferguson and Meehan, 2011). Peer influences also appear to affect frequency of substance use among youth. A study of 16- to 21-year-olds found that the perceived extent of peer substance involvement was statistically significantly correlated with frequency and intensity of cannabis use, and frequency of drinking alcohol (Boys et al., 1999).
As with studies on individual risk factors, research has shown that the causal pathway between peers and substance use is multidirectional (Winters et al., 2014). Youths choose their peers based on shared interests and behaviors, but interests and behaviors are shaped by peers. Evidence shows that youths who use substances seek friendships with other youths who use substances (Light et al., 2013, Osgood et al., 2013; Young and Rees, 2013). However, there is limited research on the development of youth substance use disorders and peer relationships, compared with the available research on the impact of peer relationships on substance use in general.
School. School risk factors can also affect the risk of developing a future substance use disorder. Poor performance in school, such as low grades and low academic motivation, is linked to initiation of substance use and substance use disorders in youth (Bugbee et al., 2019; Patte, Qian, and Leatherdale, 2017; Weinberg, 2001). Other school factors, such as truancy and suspension, also are associated with substance use disorders (Henry, Knight, and Thornberry, 2012; Flaherty, Sutphen, and Ely; 2012). A longitudinal study of 1,241 girls found that many school behaviors in youth were associated with later substance use disorders, such as low seventh and eighth grade standardized math scores, suspension from school, truancy, and not having a high school diploma (Fothergill et al., 2008). However, this is yet another area where the direction of association is unclear. Whether academic failure leads to substance use disorders or substance use disorders lead to academic failure cannot be determined clearly (Cooley–Strickland et al., 2009; Weinberg, 2001).
Family. Family-level risk factors, such as parental behaviors and family structure, can also affect a youth’s likelihood of developing a substance use disorder. Research has shown that neglect and abuse can make a strong impact on substance use and disorder on a youth. A study of more than 34,000 people found that physical abuse, sexual abuse, emotional abuse, physical neglect, and emotional neglect in youth were all associated with various substance use disorders later in life (Danielson, 2016; Afifi et al., 2012). While research has found that substance use disorders in parents also make a strong impact on youth substance use, there is little research on how parents' substance disorders influence disorders in their children (Biederman et al., 2000; Lucenko et al., 2015, Whitten et al., 2019). Some research indicates that family risk factors may differ by gender. For example, a study of 1,421 youths ages 10 to 16 found that family conflict was significantly associated with substance use disorder for girls but not for boys (Skeer et al., 2011).
Community. Community-level risk factors are another area where there is much research on youth substance use and initiation, but not a lot of research focused on the impact on youth substance use disorders. One study, using data from 38,115 youths ages 11 to 17, found that higher self-reported neighborhood disorganization (defined by the study as perceived levels of safety and crime) was associated with higher levels of substance use dependence as defined by the DSM–4, even after controlling for individual- and family-level risk factors. Youths who reported both medium and high levels of neighborhood disorganization had higher odds of both substance use and dependence, compared with youths who reported low levels of neighborhood disorganization (Winstanley et al., 2008).
[1] For more information, see the Model Programs Guide literature review on Risk Factors for Delinquency .
Protective Factors Against Substance Use Disorders
Protective factors [1] are factors in a youth's life that can prevent or mitigate the likelihood of substance use disorder. These factors are aspects of a youth's life that act as a buffer to reduce negative effects of adversity (Vanderbilt–Adriance and Shaw, 2008). Compared with risk factors, there is less research on protective factors regarding substance use. There is even less research focused on protective factors and substance use disorders or protective factors that increase the likelihood of success in substance use treatment programs (Cleveland et al., 2008).
Similar to risk factors, protective factors can occur on the individual, peer, school, family, and community level. As previously stated, protective factors mitigate the effect of adversity and other risk factors. For example, prosocial peers serve as a protective factor against many forms of deviant behavior, and against substance use and initiation (Osgood et al., 2013). The presence of close peers can also mitigate the effect that metal health disorders, such as depression, have on the likelihood of developing a substance use disorder (Mason et al., 2019).
Additionally, early-sustained abstinence following residential substance use treatment has been shown to be predictive of long-term abstinence, suggesting that even a short period of continuing-care posttreatment can significantly improve long-term abstinence rates (Godley et al., 2007).
Though research on community-level factors often focuses on substance use and initiation, it has been found also to make an impact on a youth’s likelihood of developing a substance use disorder. One study found that higher levels of social capital, defined as community engagement and involvement in various volunteering programs, decreased the likelihood of a youth’s using substances or developing a substance dependence as defined by the DSM–4 (Winstanley et al., 2008). Researchers have also found that family factors, such as living in a household with two parents (Gau et al., 2007), and school factors, such as good academic performance (Gau et al., 2007), can protect against developing a substance use disorder.
For youths with certain mental health disorders, there also is some research on the effect of treatments that use medications on later substance use. For example, some research on treatment for ADHD found that the use of medication as part of treatment reduced later substance use problems in adolescence (Hammerness et al., 2017; Wilens et al., 2003), though other researchers have found that this treatment did not influence substance use outcomes (Wise, Cuffe, and Fischer, 2001; Humphreys, Engs, and Lee, 2013).
[1] For more information, see the Model Programs Guide literature review on Protective Factors Against Delinquency .
Substance Use Treatment Utilization
Research indicates that treatment initiation, engagement, and completion among youths with substance use disorders is low—significantly lower than among adults (Alinsky et al., 2020; Brorson et al., 2013; Cummings et al., 2011; Merikangas et al., 2010). Because engagement and retention in treatment is one of the strongest predictors of improved outcomes among adolescents (Acevedo et al., 2020), examining utilization is important.
The NSDUH asks respondents who have used alcohol or illicit drugs in their lifetime whether they ever have received substance use treatment, and for those who have received treatment whether this treatment was received in the 12 months before completing the survey. Treatment includes care received at any location, such as a hospital (inpatient), a rehabilitation facility (inpatient or outpatient), a mental health center, an emergency room, a private doctor's office, prison or jail, or a self-help group (e.g., Alcoholics or Narcotics Anonymous). In acknowledgment of the COVID–19 pandemic, the NSDUH also asked respondents whether they had received professional counseling, medication, or treatment through virtual or telehealth services. The 2020 NSDUH additionally collected information on treatment received at specialty facilities, which was defined as treatment received at a hospital (inpatient only), a drug or alcohol rehabilitation facility (inpatient or outpatient), or a mental health center. Specialty facilities did not include any services received virtually (SAMHSA, 2021).
In 2020, 6.4 percent (1.6 million) of youths ages 12 to 17 demonstrated a need for substance use treatment (regardless of whether they met criteria for substance use disorder). This is defined by the NSDUH as if respondents indicated they felt they needed treatment. Among these youths, 3.5 percent previously received substance use treatment in a specialty facility. Among youths ages 12 to 17 who met the criteria for a substance use disorder, 7.6 percent received any kind of substance use treatment within the past year. The 2020 NSDUH found that 98.4 percent of youths ages 12 to 17 who did not receive treatment at a specialty facility cited that they did not feel they needed treatment (SAMHSA, 2021).
Among the 644,000 youths ages 12 to 17 in 2020 with a co-occurring substance use disorder and a major depressive episode in the past year, 69 percent (438,000 youths) received either substance use treatment at a specialty facility or mental health services in the past year, 66.8 percent (424,000 youths) received only mental health services, and 0.9 percent (6,000 youths) received both substance use treatment at a specialty facility and mental health services (SAMHSA, 2021).
Factors That Influence Participation in Treatment
Several factors influence participation in treatment programs. A small body of literature evaluates these factors, which include motivation, preexisting mental health disorders, diagnoses, family support, and demographic variables such as gender, race, ethnicity, and age (Haughwout et al., 2016; Settipani et al., 2018; Groshkova, 2010; McHugh et al., 2018). Studies examine various aspects of participation, including program initiation, program engagement, and program completion (Bowers, 2021; Haughwout et al., 2016; Becan et al., 2015).
Severity of the problem. Haughwout and colleagues (2016) used NSDUH findings from 2002 through 2013 to examine treatment-seeking behaviors among youth. They found that treatment utilization was higher among those youths who met criteria for a substance use disorder, compared with those youths who used substances but did not meet criteria for substance use disorder. Treatment engagement was greater for youths with illicit drug use disorders, such as marijuana dependence, compared with alcohol use disorder. Overall, findings indicated that, among youths with a substance use disorder, the severity of the problems caused by substance use (e.g., involvement in the criminal justice system) and the perceived need for treatment were associated with higher treatment utilization. Additionally, youths with illicit drug use disorders using more than one substance had an increased treatment utilization rate (Haughwout et al., 2016).
Family influence. Some studies examine family factors such as parental discipline styles, expectations, support, and socioeconomic status (e.g., Berridge et al., 2017; Dakof, Tejeda, and Liddle, 2001; Haughwout et al., 2016; Santisteban et al., 2015; Settipani et al., 2018). For example, a study of 224 youths ages 12 to 17 who were referred to drug treatment found that youths who had parents with higher expectations for their children’s educational attainment were more likely to participate in at least four drug abuse treatment sessions than youths who did not have parents with these high expectations (Dakof, Tejeda, and Liddle, 2001). Also, analysis of NSDUH data from 2002 through 2013 found that talking with parents about the need for treatment increased treatment utilization (Haughwout et al., 2016). A qualitative study of 31 youths and young adults ages 17 to 25 found that those who entered treatment indicated that pressure from parents to enter treatment, and parental support such as making appointments, providing financial support, and ensuring medication adherence were significant motivations for entering treatment (Cleverley, Grenville, and Henderson, 2018). A study of 110 Hispanic substance-misusing adolescents assessed parenting practices in five dimensions: 1) positive parenting, 2) discipline effectiveness, 3) discipline avoidance, 4) rules on having a set time to be home, and 5) extent of involvement. They found that youths who had parents with better discipline strategies and who felt effective and competent in their parenting were more likely to seek residential or outpatient treatment services (Santisteban et al., 2015). This study also found that youths with parents who had spent more years in the United States were more likely to use outpatient services (as compared with no services), and youths with parents who had lower parenting stress were more likely to use residential treatment services (compared with no services).
Finally, some studies have found that family financial and educational situations can influence treatment seeking behaviors. In a study of 189 youths seeking treatment for substance use concerns, 70 percent reported that they expected their finances to have an impact on their treatment (Settipani et al., 2018). Additionally, a longitudinal study of 358 adolescents in outpatient programs found that parental education was significantly associated with attendance at 12-step programs, meaning that adolescents whose parents had higher levels of education were more likely to attend the treatment program than those with parents with lower levels of education (Lui et al., 2017). However, the same study found no socioeconomic differences in treatment initiation or treatment retention. This may be due to everyone in the sample's having health insurance and to the near-full employment status of the adolescents' parents.
Other mental health diagnoses. Externalizing disorders have been identified as risk factors for not participating in or not successfully completing substance use treatment (Santisteban et al., 2015; Wise, Cuffe, and Fischer, 2001), while internalizing disorders have been identified as predictors of participating in treatment (Bowers, 2021). A study of 91 adolescents in a residential substance abuse treatment program examined factors associated with successful treatment, as defined by the treatment team at the time of discharge in terms of attendance, positive interactions in groups, level of denial, quality of projects, interactions with peers and staff, and meeting individualized treatment plan goals (Wise, Cuffe, and Fischer, 2001). They found that participants with Attention Deficit Hyperactivity Disorder (ADHD) or Conduct Disorder were less likely to participate successfully in treatment than those without ADHD or Conduct Disorder. Another study of more than 300 youths and young people ages 14 to 24 who were receiving outpatient services for concurrent disorders found that the strongest predictor of attending five or more sessions was having an internalizing problem (Bowers, 2021). In other words, individuals with higher levels of internalizing problems (such as depression) were more engaged in treatment than those with lower levels of internalizing problems.
Motivation. Motivation is considered a key factor in successfully engaging in substance use treatment (DiClemente, 1999; Groshkova, 2010). The role of motivation is particularly relevant to youth, since many enter treatment because it has been mandated or recommended, as opposed to self-referring (Bowers et al., 2017; Cleverley, Grenville, and Henderson, 2018; Knight et al., 2016). Several studies have examined the influence of motivation on participation in substance use treatment. A study of 547 youths from multiple substance use treatment programs found that participants with higher pretreatment motivation were more likely to have stronger relationships with program counselors, which predicted more successful outcomes after leaving the programs (Joe et al., 2014). Motivation also predicted stronger relationships with peers in the treatment program. A small qualitative study of 31 youths ages 17 to 25 in mental health treatment found that internal factors, such as wanting to better their academic, social, or financial situation, and external factors, such as familial pressure, were identified as motivating these young people to seek treatment (Bowers et al., 2017). Several interventions have been designed to increase youths' motivation to engage in treatment (Becan et al., 2015; Knight et al., 2016).
Gender. There is limited information on gender differences in treatment engagement for substance use disorders. Some research has found that adolescent girls are more likely than adolescent boys to receive treatment for alcohol use disorder, while boys are more likely than girls to receive treatment for marijuana use disorder, or for any type of illicit substance treatment overall (Haughwout et al., 2016; McHugh et al., 2018). Other studies have found no difference in treatment initiation or retention by gender (e.g., Lui et al., 2017). Several studies have found that girls have a higher comorbidity between substance use disorder and mental health disorders and greater histories of trauma than boys (e.g., Fernández-Artamendi, Martínez-Loredo, and López-Núñez, 2021; Yildiz, Ciftci, and Yalcin, 2020), which can affect engagement and success in treatment interventions. Once youths are in a treatment program, some studies have found that girls are more likely than boys to engage, succeed, and complete the program. For example, a study of 91 adolescents in a residential substance abuse treatment program (Wise, Cuffe, and Fischer, 2001, mentioned above) found that girls were more likely than boys to successfully participate in treatment.
Race and ethnicity. Several studies have examined racial and ethnic disparities among substance use treatment utilization. In their analyses of more than 140,000 adolescents from the NSDUH , Cummings and colleagues (2011) found that among youths with substance use disorders Black and Hispanic adolescents were less likely than white adolescents to receive treatment. A literature review of behavioral health services for youths of racial and ethnic minority groups found that, compared with non-Latino white adolescents with a substance use disorder, Black adolescents with a substance use disorder reported receiving less specialty and informal care, while Latinos with a substance use disorder reported receiving fewer informal services (Alegria et al., 2011). Several studies of youth in the juvenile justice system have found similar racial and ethnic disparities (e.g., Farenthold, 2010; Mansion and Chassin, 2016). A systematic literature review of studies examining juvenile justice system processing found that most studies examining referral to mental health or substance misuse treatment from within the juvenile justice system found at least some race effects disadvantaging youths of color (Spinney et al., 2016). For example, a study of about 600 juveniles on probation in New York found that, relative to white juveniles, Black and Hispanic juveniles who were screened and referred for mental health or substance use services were significantly less likely to access them (Wasserman et al., 2009). The study also found that Black juveniles were significantly less likely than others to participate in the initial screening. However, racial and ethnic disparities in referral to and utilization of substance use treatment are not always found (e.g., Mulvey, Schubert, and Chung, 2007; Yan and Dannerbeck, 2011).
Types of Substance Use Treatment Programs and Outcome Evidence
Treatment programs primarily focus on helping youths with existing substance use issues who have been clinically diagnosed with a substance use disorder by the Diagnostic and Statistical Manual for Mental Disorders criteria. However, some treatment programs serve youths without a formal diagnosis who exhibit or report risky substance use behavior or have come into contact with the justice system.
For youths currently experiencing substance use disorders, particularly youths involved in the juvenile justice system, more intensive services may be needed, compared with the programming youths may receive in prevention interventions. Treatment services typically are more comprehensive than prevention programs, owing to their retroactive (rather than proactive) focus. Specifically, treatment programs include components related to prosocial development as a means to address existing antisocial behaviors, negative peer relations, and poor family functioning (Development Services Group, 2015).
It is important to recognize that programs that have been shown to reduce adult substance use may not translate as well for youth. Substance-using youths seldom are dependent on substances in the traditional sense that adults experience addiction. Youths and adults may misuse drugs for different reasons, and there are differences in the psychology of juvenile and adult substance use disorders (Bureau of Justice Assistance, 2003). Adolescence is an important development phase that involves changes in cognitive, emotional, behavioral, and social skills necessary for a productive life that are influenced by important relationships, such as those with family, friends/peers, school, and the community (Development Services Group, 2015; Gray and Squeglia, 2018).
Various types of youth substance use treatment programs, including those featured in the Model Programs Guide, are discussed below.
Motivational Interviewing
Motivational interviewing (MI) is a counseling method that can be implemented as a standalone program or can be incorporated as an element of a larger program. MI uses collaborative, client-centered, goal-oriented communication to address hesitancy toward behavioral change by encouraging and evoking personal desires for transformation (Stein et al., 2006b, Naar–King, 2011). MI aims to increase an individual's perspective on the importance of change. When provided to youths with substance use issues, the long-term goal is to help them reduce or stop using drugs and alcohol. A youth's subtle desires for change are uncovered through a series of selective interviews guiding the youth to concentrate on their behaviors and explore overarching goals in regard to personal motivations, values, and opinions and reasons to change (Stein et al., 2006b; D’Amico et al., 2013).
Stein and colleagues (2006b) examined the effects of a standalone MI program for substance abuse issues of juveniles in a state facility . The program focused on youth engagement with substance use therapy and targeted youths who reported regular or binge marijuana or alcohol use or who were sentenced to a post-adjudication facility. For this program, motivational interviewing was designed to be modified as appropriate to be meaningful for each youth and their desire to change. This MI program was delivered by research counselors and consisted of four components: 1) establishing rapport, 2) assessing the youth’s motivation for change, 3) motivational enhancement, and 4) establishing goals for change. The study authors compared youths receiving MI with a control group of youths who did not receive MI. They found that the control group experienced statistically significantly more negative engagement with substance use therapy than the MI treatment group, meaning that youths who received MI were more likely than youth in the control group to take treatment seriously (Stein et al., 2006b). However, there was no statistically significant impact on positive treatment engagement, meaning juveniles who received MI were no more likely to actively participate in treatment sessions, compared with youths in the control group. Another study by Stein and colleagues (2006a), which examined the same sample of youths 3 months later, found the effectiveness of MI treatment appeared to be mediated by depressive symptoms. The authors found that, compared with the control group, the MI treatment group had statistically significantly lower self-reported measures of risky driving behavior (such as driving under the influence of alcohol and marijuana), but only for youths with low depressive symptoms. When examining youths with high depressive symptoms, researchers found the control group had statistically significantly lower self-reported measures of risky driving behavior, compared with the MI treatment group. The entire treatment group was statistically significantly less likely to report driving solo under the influence of alcohol, compared with the control group, but there were no statistically significant differences between the groups in driving alone under the influence of marijuana or being a passenger in a car operated by a driver under the influence of alcohol or marijuana (Stein et al., 2006b).
Juvenile Drug Courts/Court-Based Programs
Juvenile drug courts (JDCs)are specialized juvenile court dockets for youths with substance use problems and substance use disorders in need of specialized treatment services, allowing for intensive judicial supervision that is not ordinarily available in traditional juvenile courts (Latimer, Morton–Bourgon, and Chrétien, 2006; Mitchell et al., 2012; Shaffer, 2006; Drake, 2012). JDCs work conjointly with treatment providers, social services, school and vocational programs, law enforcement, probation, and other agencies (Latimer, Morton–Bourgon, and Chrétien, 2006; Mitchell et al., 2012; Shaffer, 2006; Drake, 2012). Core elements of JDCs include drug testing and treatment services, regular judicial contact, and meetings with a case manager and/or a probation officer. Additionally, most JDCs make referrals for educational programs, job training, and mental health services. [1]
Evaluations of programs have found mixed results with regard to the effectiveness of JDCs in both substance use and recidivism outcomes. For example, Juvenile Drug Courts in Utah operate with basic drug court components, including screening and assessment, individualized treatment plans, judicial supervision, community-based treatment, regular court hearings, accountability and compliance monitoring, comprehensive services, and a nonadversarial team approach (Hickert et al., 2011). An evaluation of the four largest JDCs in Utah by Hickert and colleagues (2011) found no statistically significant difference between youths who participated in the JDCs and youths in the probation comparison group for alcohol and other drug recidivism after 30 months. However, they did find that youths in the JDCs had statistically significantly fewer subsequent criminal offenses (i.e., recidivism of any offense), compared with youths in the comparison group. Other evaluations have shown more positive results. The Baltimore County (Md.) Juvenile Drug Court targets 13- to 17-year-olds who admit to drug or alcohol abuse. The program has four phases, each of which focuses on different aspects of treatment and services. The first two phases are highly structured and include frequent treatment sessions, supervision meetings, and drug testing. The last two phases are designed as aftercare phases, which involve decreasing supervision and treatment sessions and focus on relapse prevention. An evaluation by Mackin and colleagues (2010) showed youths in the program had statistically significantly lower average numbers of re-arrests for drug charges and total re-arrests (for any charge), compared with youths in the comparison group, at the 2-year follow-up.
Numerous meta-analyses examining the effectiveness of juvenile drug courts have also found mixed effects. When examining measures of general recidivism, Drake (2012) and Shaffer (2006) found small, statistically significant decreases in the recidivism of JDC participants, compared with nonparticipants. Conversely, Latimer and colleagues (2006) did not find a statistically significant impact of JDCs on recidivism measures. With regard to other outcomes, Mitchell and colleagues (2012) reviewed four studies that examined the effect of JDCs on drug use and found no statistically significant effect. Tanner–Smith and colleagues (2016) reviewed eight studies and also found an overall non–statistically significant effect on drug use, suggesting that JDCs have not been found to have a consistent effect on drug use.
An example of a court-based program is the Juvenile Breaking the Cycle (JBTC) Program in Lane County, Oregon . The program was a post-arrest effort designed to help substance-using youth, using a comprehensive approach. The primary goals of the program were to increase access to treatment, reduce substance use, and reduce delinquency among high-risk, antisocial youths through intensive case-management services. Youths ages 9 to 18 with alcohol or other drug problems and assessed as high risk for involvement in serious and chronic offenses were eligible for JBTC. Components of the model included substance abuse treatment, mental health services, judicial oversight (incorporating drug court for some participants), and case management that consisted of supervision by a probation counselor and service coordination by a service coordinator (along with urinalysis). Lattimore and colleagues (2004) found that participation in the JBTC program had no statistically significant effect on whether youths reported using alcohol or illicit drugs (other than marijuana), at the follow-up period. However, participation in the JBTC program was associated with a statistically significant reduction in marijuana use. Regarding recidivism outcomes, JBTC youths were statistically significantly less likely to be re-arrested, and participation in the JBTC program was associated with a statistically significant decrease in the number of re-arrests after 12 months (Lattimore et al., 2004).
Family-Inclusive Therapy
As previously discussed, research has shown that family dynamics often contribute to the development of youths' substance use disorders (Van Ryzin et al., 2016). The importance of family involvement and familial relationships in the recovery of substance-using youths is regularly reiterated throughout evaluation research of treatment programs (Christie, Cheetham, and Lubman, 2020). Other studies have shown family-based treatments to have higher retention rates, which may be related to positive treatment outcomes (Rowe and Liddle, 2003; Liddle et al., 2018). Further, intensive family-based treatments have been shown to reduce family and community environmental risk factors (such as familial conflict or association with negative peer groups) that contribute to adolescent substance use problems and disorders (Liddle et al., 2009; Liddle et al., 2018; Horigian, Anderson, and Szapocznik, 2016).
In general, family-based interventions can include a wide range of programs that are designed to decrease youths’ problem and antisocial behaviors, including substance use, by making positive changes in their familial and social environments (Dopp et al., 2017). Specifically, these interventions focus on establishing better communication and reducing conflict between parents and youths, improving parenting skills, and helping youths better engage with their families and in their school environment (Baldwin et al., 2012). Various therapies inform the specific treatment techniques used, including behavioral and cognitive–behavioral therapies. Dopp and colleagues (2017) conducted a meta-analysis of 24 effect sizes from 10 studies and found that family-based treatment had statistically significant positive effects on substance use for treatment group youths, compared with control group youths.
Numerous specific therapeutic models concentrate on including the family in treatment services for youth. Multidimensional Family Therapy (MDFT) is a well-established approach for youth substance use treatment (Liddle et al., 2001; Waldron and Turner, 2008; Rigter et al., 2013; van der Pol et al., 2018) that promotes communication among family members, targeting social competence and parental involvement/relationships. The MDFT approach is individualized, family based, and comprehensive, requiring collaboration across many social systems (Liddle et al., 2009). Using a multidimensional approach, the MDFT intervention emphasizes improving four major domains for youth, which are seen as contributing factors to the rise and decline of behavioral problems in a youth's life: 1) the youth, 2) parents, 3) family, and 4) the community (that is, peers, school, and so forth) [Liddle et al., 2018; Rigter et al., 2013; van der Pol, 2018]. Overall, the goal of the program is to improve individual and family functioning to reduce substance misuse and related problem behaviors (such as committing crimes). There have been numerous evaluations of MDFT. Rigter and colleagues (2013) evaluated the efficacy of MDFT on substance use and dependence among Western European youths ages 13 to 18 from five outpatient treatment sites. Eligible youths were diagnosed with a cannabis-use disorder by the DSM–4 guidelines and had at least one parent willing to participate. However, at the 12-month follow-up, there were no statistically significant differences in the prevalence of diagnosis of cannabis use disorder between youths in the MDFT intervention group and youths in the treatment-as-usual comparison group. Conversely, Liddle and colleagues (2018) evaluated the efficacy of MDFT in a sample of youths in the United States diagnosed with a substance use disorder and at least one comorbid psychiatric disorder. At the 18-month follow-up, youths in the MDFT intervention group reported a statistically significant decrease in substance use problems, compared with youths in the treatment-as-usual group.
Another example of an intervention that incorporates family into programming services is the Multisystemic Therapy | Family Integrated Transitions (MST–FIT) program, which provides integrated and family services to youths in a residential facility who have committed offenses and have co-occurring mental health and chemical dependency disorders (Trupin et al., 2011). Services are provided during a youth's transition from incarceration back into the community. The overall goal of MST–FIT is to provide necessary treatment to youths to reduce recidivism. The program also seeks to connect youths and families to appropriate community supports, increase youths' abstinence from alcohol and drugs, improve youths' mental health, and increase youths' prosocial behavior. Trupin and colleagues (2011) found that the MST–FIT program statistically significantly reduced felony recidivism at 36 months postrelease; however, the program did not have a statistically significant effect on measures of overall recidivism (i.e., felony and misdemeanors combined), misdemeanor recidivism, or violent felony recidivism. In addition, the program evaluation did not examine the impact on youths' substance use.
Multisystemic Therapy | Substance Abuse (MST for substance use) is a version of multisystemic therapy (MST) for youths with substance abuse and dependency issues who are diagnosed using the DSM–4 . Although the emphasis is on youths, MST operates by incorporating the youths' family and friends and addressing all potential spheres of behavioral influence. It aims to enhance a family's capacity to keep track of adolescent behavior and instill clear rewards and punishments for positive and negative/irresponsible behavior. Henggeler and colleagues (2002) found that youths who received MST for substance abuse showed statistically significantly higher rates of abstinence from marijuana, compared with control group youths who did not receive MST, at the 4-year follow-up. However, there were no statistically significant differences between groups on cocaine use. Another study by Henggeler and colleagues (2006) found no statistically significant difference in alcohol use between youths who participated in a drug court program and received MST for substance abuse and youths in the control group who received no services, at the 12-month follow-up. However, youths who received MST in a drug court program showed statistically significant reductions in heavy alcohol use, marijuana use, and multiple-/poly-drug use, compared with control group youths.
Some interventions specifically aim to treat youths' substance abuse after a family crisis. Ecologically Based Family Therapy (EBFT) is a home-based, family preservation model for families in crisis because a youth has run away from home. The model targets 12- to 17-year-olds who are staying in a runaway shelter and dealing with substance use issues. Treatment begins by preparing the youth and the family members, in individual sessions, to come together and talk about the issues that led to the runaway episode. After the individual sessions, the family and youth are brought together to address the issues associated with the dysfunctional interactions between family members and the continuation of problem behaviors. An evaluation by Slesnick and Prestopnik (2009) found that treatment group youths who participated in EBFT reported a statistically significant reduction in the percentage of days they used alcohol or drugs, compared with control group youths who received services as usual, at the 15-month follow-up.
Residential-Based Treatment
Youths may receive treatment while they are placed in a residential facility. The period of residential placement offers an opportunity to intervene in the cycle of youths' drug or alcohol use. Different types of residential-based substance use treatment programs are available, including therapeutic communities or group counseling (Mitchell, Wilson, and MacKenzie, 2012). Residential treatment is an important option for youths at high risk of overdose or suicide, those who present a public safety risk, or are without family members who can be involved in treatment (Liddle et al., 2018).
Incarceration-Based Therapeutic Communities (TC) for Juveniles employ a comprehensive, residential drug-treatment program model for substance-using youths who have committed offenses. The programs are designed to foster changes in attitudes, perceptions, and behaviors related to youth substance use. The TC for juveniles uses a developmentally appropriate comprehensive approach to a) address substance use and mental health issues and b) promote healthy development. Mitchell, Wilson, and MacKenzie (2012) synthesized four studies looking at the effectiveness of incarceration-based TCs for youths in reducing recidivism and found no statistically significant difference between treatment group and comparison group youths on recidivism postrelease. Drake (2012) analyzed the effect sizes from three studies on the efficacy of incarceration-based TCs for juveniles on recidivism and also found no statistically significant difference between treatment group and comparison group youths on recidivism postrelease. However, the results from both meta-analyses should be interpreted with caution, given the limited number of studies included. Further, neither meta-analysis examined the effectiveness of incarceration-based TCs in reducing substance use.
Brief Interventions
Brief interventions designed to address substance use in youth vary in terms of length and structure and can be delivered in an electronic format, in-person by a service provider (such as a counselor, physician, or nurse), or even self-administered by youth. In general, these are concise, convenient, and cost-effective interventions designed to motivate and provide resources to participants to help them change their alcohol or drug consumption behavior, and to seek more intensive treatment if needed (Tanner–Smith and Lipsey, 2015). However, one limitation to this type of program is that it usually is not targeted specifically toward substance use disorder, and therefore substance use disorder is not typically an outcome of interest. This is an area where more research is required (Smedslund et al., 2017).
Computerized Brief Interventions for Youth Alcohol Use are designed to appeal to younger generations who have grown up in the digital media age (Smedslund et al., 2017). Specifically, these interventions target individuals ages 15 to 25, who are high or risky consumers of alcohol but motivated to change. Risky consumption of alcohol is defined as consuming 1) at least 5 beverages during any one drinking session or more than 14 alcoholic beverages a week for males and 2) 4 beverages during any one drinking session or more than 7 alcoholic beverages a week for females. Computerized brief interventions usually consist of three components: 1) assessment, 2) feedback, and 3) decisionmaking. The assessment component classifies users as low-risk, medium-risk, high-risk, or very high-risk alcohol drinkers and provides the individuals with a recommendation on whether they would benefit from a more formalized treatment program than the computerized brief intervention. The feedback component provides the users with information on their scores after each assessment and responds to their reactions to their assessment. Finally, the decisionmaking component asks users to specify their motivation for behavioral change. Smedslund and colleagues (2017) aggregated the results of 15 studies (those that included both assessment and feedback components, but no decisionmaking component) and found that computerized brief interventions statistically significantly reduced short-term alcohol consumption for youths who participated, compared with youths who received no interventions.
Targeted Brief Alcohol Interventions (BAI) for Alcohol Use for Adolescents and Young Adults seek to reduce alcohol use or alcohol-related problems for youths and young adults using a short-term intervention (one to five sessions). BAIs can be delivered in a variety of settings such as primary care/student health centers, schools/universities, and emergency rooms; for youths, they can also be self-administered by participants. They typically include at least one of the following components: a discussion of alcohol consumption, feedback on risk or levels of alcohol use, comparisons with local or national norms, information on potential harms, or coping strategies and goal-setting plans for dealing with drinking situations. Tanner–Smith and Lipsey (2015) reviewed 24 studies that included adolescent samples (ages 11 to 17) and found that youths who participated in BAIs reported statistically significant reductions in levels of alcohol consumption and levels of alcohol-related problems, compared with control group youths.
Prevention Programming
Prevention programs are typically designed to deter adolescents from initial substance use. However, some early prevention programs are designed specifically with the goal of making a long-term impact on substance use disorders. These programs have a theoretical framework surrounding the goal of reducing early risk factors that can lead to later problem behaviors such as substance use disorders (Kellman et al., 2008).
Good Behavior Game is one such program. It is a classroom management strategy designed to reduce aggressive and disruptive classroom behavior. By preventing these early risk factors, it seeks to reduce future problem behaviors such as criminal activity and substance use. Good Behavior Game is a group-contingent reinforcement game, in which students work in teams and are rewarded as a team for following classroom rules. This creates an incentive for students to manage their own behavior through group reinforcement and mutual self-interest. Kellman and colleagues (2008) conducted a randomized controlled trial to examine the impact of Good Behavior Game on lifetime alcohol abuse or dependence disorders. The participants were ages 5 to 10 during the program and were surveyed 14 years after the program ended. The study authors found that treatment group participants had lower rates for lifetime alcohol abuse or dependence disorders, compared with the control group, at the 14-year follow-up. This difference was statistically significant.
[1] For more information, see the MPG literature review on Juvenile Drug Courts .
Limitations of Research on Treatment Programs
Although there is research on how well treatment programs can (or cannot) reduce youth substance use and/or improve substance use disorders, it has some limitations. Most substance use treatment programs evaluated within the juvenile justice system typically examine recidivism-based outcomes and often neglect to examine substance use outcomes fully (Trupin et al., 2011; Anspach and Ferguson, 2005; Hickert et al., 2011). In addition, because these programs are so closely linked with the juvenile justice system, they usually rely on one measure of substance use, such as one or more positive drug screen results (Anspach and Ferguson, 2005; Hickert et al., 2011). While instances of positive drug screens may be one way to measure substance use, this measure fails to incorporate self-reported drug or alcohol use, or substance use identified through other screening methods administered by service professionals.
Further, with research of youth substance use disorders and treatment programs, there often are barriers to conducting research with young people. It can be particularly challenging to follow up with youths who struggle to access services because of their inaccessibility, and there are ethical considerations related to consent in youth participants (Christie, Cheetham, and Lubman, 2020).
Other limitations exist when attempting to examine the specific components that make a program effective, particularly with regard to different types of illicit or licit substance use. If different family, courts-based, or residential-based programs incorporate similar elements, it is difficult to discern which specific program components successfully affect substance use (Trupin et al., 2011; Henggeler et al., 2006). For example, motivational interviewing can be implemented as a standalone program (Stein et al., 2006a; Stein et al., 2006b) or it may be included as a specific component in a juvenile drug court or as part of a specific program, such as Multidimensional Family Therapy. MDFT and juvenile drug court programs both incorporate some kind of family-based treatment (Waldron and Turner, 2008; Liddle et al., 2018; Liddle et al., 2009; Hickert et al., 2011; Anspach and Ferguson, 2005). Additionally, there is limited research into which types of programs are the most effective for different types of substances (McGovern and Carroll, 2013).
Further, there is little research on pharmacotherapy for youth licit and illicit substance use (Squeglia et al., 2019; Winters et al., 2018). Although research on adults with substance use disorders has shown positive results with treatments such as Methadone Maintenance Therapy and Buprenorphine Maintenance Therapy , especially when addressing opioid use disorders/dependence (Mattick et al., 2009; Mattick et al., 2014), this research has not be conducted much with youth, in part because a) federal regulations restrict methadone access for adolescents, b) training and U.S. Food and Drug Administration approval are required for prescribing buprenorphine, and c) there is stigma regarding medications for opioid use disorder (Chatterjee et al., 2019). However, there is some evidence that reception of medication-assisted treatments influences treatment duration among youths. Researchers examining a sample of more than 4,500 youths ages 13 to 22 found that youths who received opioid use disorder medication (e.g., buprenorphine, naltrexone) within 3 months of diagnosis with an opioid use disorder stayed in treatment longer than those who did not receive the medication (150 days of treatment, compared with 67 days of treatment) [Hadland et al., 2018]. Research indicates that the effect of pharmacotherapy for youth is unclear.
Additionally, most youths who participate in substance use treatment programs are not able to sustain long-term substance use reduction or cessation; some interventions do not see results related to continued substance use lasting more than 1 year posttreatment, including some of the programs discussed in the previous section (Tanner–Smith and Lipsey, 2015; Gray and Squeglia, 2018; Dennis et al., 2004). This has encouraged the development of aftercare or continuing care programs (Godley et al., 2007; Godley et al., 2014), usually after residential treatment or drug court participation. As stated previously, research shows that early-sustained abstinence is predictive of long-term abstinence (Godley et al., 2007). However, many substance use treatment programs for youth still lack this component, with youths returning to the community without the continued support needed to promote continued abstinence (Godley et al., 2007). Further research is needed regarding the effectiveness of aftercare or continuing care for youth following both outpatient and residential treatment, and on the best approaches for implementation (Kaminer, Burleson, and Burke, 2008; Godley et al., 2014; Gonzales et al., 2014).
Conclusions
Though rates of substance use disorder among youth have declined and leveled off since the first decade of the 2000s, it remains a prevalent issue, and research demonstrates a clear need for treatment programs directed toward adolescents (Chatterjee et al., 2019; SAMSHA, 2021).
There are a wide range of substance use treatment programs for adolescents, depending on their needs and situation. Family-inclusive therapies, for example, are common substance-use-disorder treatment programs, because family dynamics often make a strong impact on the development of substance use disorders (Van Ryzin et al., 2016). Residential-based treatment programs are also important in the field, as they are beneficial for youths with a substance use disorder who may not have family able to become involved with their treatment (Liddle et al., 2018).
Though 2.8 percent of youths ages 12 to 17 experienced alcohol use disorder in the past year, and 4.9 percent of 12- to 17-year-olds met criteria for at least one illicit drug use disorder, there is still limited research regarding specific risk factors, protective factors, and treatment options for youths diagnosed with a substance use disorder, according to DSM–4 criteria (Bacio et al., 2015; Cleveland et al., 2008; SAMSHA, 2021). Further research could overcome current limitations, such as examining substance use–related outcomes outside of the juvenile justice system, conducting studies on pharmacotherapy for youths' licit and illicit substance use, and exploring risk and protective factors specifically surrounding substance use disorders in youths.
Aarons, G.A., Brown, S.A., Hough, R.L., Garland, A.F., and Wood, P.A. 2001. Prevalence of adolescent substance use disorders across five sectors of care. Journal of the American Academy of Child & Adolescent Psychiatry 40(4):419–426.
Acevedo, A., Harvey, N, Kamanu, M., Tendulkar, S., and Fleary, S. 2020. Barriers, facilitators, and disparities in retention for adolescents in treatment for substance use disorders: A qualitative study with treatment providers. Substance Abuse Treatment, Prevention and Policy 15(42):1–13.
Afifi, T.O., Henriksen, C.A., Asmundson, G.J.G., and Sareen, J. 2012. Childhood maltreatment and substance use disorders among men and women in a nationally representative sample. Canadian Journal of Psychiatry 57(11):677–686.
Akers, R.L., Krohn, M.D., Lanza–Kaduce, L., and Radosevich, M. 1979. Social learning and deviant behavior: A specific test of a general theory. American Sociological Review 44(August):636–655.
Alegria, M., Carson, N.J., Goncalves, M., and Keefe, K. 2011. Disparities in treatment for substance use disorders and co-occurring disorders for ethnic/racial minority youth. Journal of the American Academy of Child and Adolescent Psychiatry 50(1):22–31.
Alinksy, R.H., Zima, B.T., Rodean, J., Matson, P.A., Larochelle, M.R., Adger, H, Bagley, S.M., and Hadland, S.E. 2020. Receipt of addiction treatment after opioid overdose among Medicaid-enrolled adolescents and young adults. Journal of the American Medical Association Pediatrics 174(3):1–10.
Anderson, K.G., Tapert, S.F., Moadab, I., Crowley, T.J., and Brown, S.A. 2007. Personality risk profile for conduct disorder and substance use disorders in youth. Addictive Behaviors, 32(10):2377–2382.
Anspach, D.F., and Ferguson, A.S. 2005. Part II: Outcome Evaluation of Main’s Statewide Juvenile Drug Treatment Court Program. Augusta, ME: University of Southern Maine.
Bacio, G.A., Estrada, Y., Huang, S., Martínez, M., Sardinas, K., and Prado, G. 2015. Ecodevelopmental predictors of early initiation of alcohol, tobacco, and drug use among Hispanic adolescents. Journal of School Psychology 53(3):195–208.
Bagley, S.M., Chavez, L., Braciszewski, J.M., Akolsile, M., Boudreau, D.M., Lapham, G., Campbell, C.I., Bart, G., Yarborough, B.J.H., Samet, J.H., Saxon, A.J., Rossom, R.C., Binswanger, I.A., Murphy, M.T., Glass, J.E., and Bradley, K.A. 2021. Receipt of medications for opioid use disorder among youth engaged in primary care: Data from six health systems. Addiction Science & Clinical Practice 16(1):1 – 18.
Baldwin, S.A., Christian, S., Berkeljon, A., Shadish, W.R., and Bean, R. 2012. The effects of family therapies for adolescent delinquency and substance abuse: A meta-analysis. Journal of Marital and Family Therapy 38(1):281–304.
Becan, J.E., Knight, D.K., Crawley, R.D., Joe, G.W., and Flynn, P.M. 2015. Effectiveness of the Treatment Readiness and Induction Program for increasing adolescent motivation for change. Journal of Substance Abuse Treatment 50:38 – 49.
Berridge, J., McCann, T.V., Lubman, D.I., and Cheetham, A. Perceived barriers and enablers of help-seeking for substance use problems during adolescence. SAGE Journals 19(1).
Biederman, J., Faraone, S.V., Monuteaux, M.C., and Feighner, J.A. 2000. Patterns of alcohol and drug use in adolescents can be predicted by parental substance use disorders. Pediatrics 106(4):792–797.
(BJA) Bureau of Justice Assistance. 2003. Juvenile Drug Court: Strategies in Practice. Washington, DC: U.S. Department of Justice (DOJ), Office of Justice Programs (OJP), BJA.
Bowers, A. 2021. Factors Influencing Service Engagement of Youth in Services for Concurrent Disorders: A Mixed-Methods Approach. Doctoral dissertation. Toronto, Ontario: University of Toronto.
Bowers, A., Cleverley, K., Di Clemente, C., and Henderson, J. 2017. Transitional-aged youth perceptions of influential factors for substance-use change and treatment seeking. Patient Preference and Adherence 11:1939–1948.
Boys, A., Marsden, J., Griffiths, P., Fountain, J., Stillwell, G., and Strang, J. 1999. Substance use among young people: The relationship between perceived functions and intentions. Addiction 94(7):1043–1050.
Brorson, H.H., Arnevik, E.A., Rand–Hendriksen, K., and Duckert, F. 2013. Dropout from addiction treatment: A systematic review of risk factors. Clinical Psychology Review 33:1010–1024.
Brown, J., and Christensen, D. 1986. Family Therapy Theory and Practice. Monterey, CA: Brooks/Cole.
Bugbee, B.A., Beck, K.H., Fryer, C.S., and Arria, A.M. 2019. Substance use, academic performance, and academic engagement among high school seniors. Journal of School Health 89(2):145–156.
Bukstein, O.G., and Horner, M.S. 2010. Management of the adolescent with substance use disorders and comorbid psychopathology. Child and Adolescent Psychiatric Clinics of North America 19(3):609–623.
Chan, Y.F., Dennis, M.L., and Funk, R.R. 2008. Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. Journal of Substance Abuse Treatment 34(1):14–24.
Chatterjee, A., Larochelle, M. R., Xuan, Z., Wang, N., Bernson, D., Silverstein, M., and Bagley, S.M. 2019. Nonfatal opioid-related overdoses among adolescents in Massachusetts 2012–14. Drug and Alcohol Dependence 194:28–31.
Christie, G.I.G., Cheetham, A., and Lubman, D.I. 2020. Interventions for alcohol and drug use disorders in young people: Ten key evidence-based approaches to inform service delivery. Current Addiction Reports 7:464–474.
Cleveland, M.J., Feinberg, M., Bontempo, D., and Greenberg, M. 2008. The role of risk and protective factors in substance use across adolescence. Journal of Adolescent Health 43(2):157–164.
Cleverley, K., Grenville, M., and Henderson, J. 2018. Youths perceived parental influence on substance use changes and motivation to seek treatment. Journal of Behavioral Health Services & Research. doi: 10.1007/s11414–018–9590–2
Coffman, D., Melde, C., and Esbensen, F.–A. 2015. Gang membership and substance use: Guilt as a gendered causal pathway. Journal of Experimental Criminology 11(1):71–95.
Cooley–Strickland, M., Quille, T.J., Griffin, R.S., Stuart, E.A., Bradshaw, C.P., and Furr–Holden, D. 2009. Community violence and youth: Affect, behavior, substance use, and academics. Clinical Child and Family Psychology Review 12(2):127–156.
Cummings, J.R., Wen, H., and Druss, B.G. 2011. Racial/ethnic differences in treatment for substance use disorders among U.S. adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 50(12):1265–1274.
Dakof, G.A., Tejeda, M., and Liddle, H.A. 2001. Predictors of engagement in adolescent drug abuse treatment. Journal of the American Academy of Child & Adolescent Psychiatry 40(3):274–281.
D’Amico, E.J., Hunter, S.B., Miles, J., Ewing, B.A., and Osilla, K.C. 2013. A randomized controlled trial of a group motivational interviewing intervention for adolescents with a first-time alcohol or drug offense. Journal of Substance Abuse Treatment 45(5):1–21.
Danielson, C. 2016. Reducing risk for substance use problems among adolescents with a child maltreatment history. Journal of the American Academy of Child and Adolescent Psychiatry 55(10):S293.
Deci, E.L., and Ryan, R.M. 1985. The general causality orientations scale: Self-determination in personality. Journal of Research in Personality 19(2):109–134.
Deci, E.L., and Ryan, R.M. 2012. Self-determination theory. In Handbook of Theories of Social Psychology, edited by P.A.M. Van Lange, A.W. Kruglanski, and E.T. Higgins. Newbury Park, CA: SAGE Publications Ltd., pp. 416–436.
Dennis, M., Godley, S.H., Diamond, G., Tims, F.M. , Babor, T., Donaldson, J., and Liddle, H. 2004. The Cannabis Youth Treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment 27:197–213.
Development Services Group, Inc. 2015. Protective Factors for Delinquency. Literature review. Washington, DC: DOJ, OJP, Office of Juvenile Justice and Delinquency Prevention (OJJDP). https://ojjdp.ojp.gov/model-programs-guide/literature-reviews/protective_factors.pdf
Dick, D.M., Aliev, F., Latendresse, S.J., Hickman, M., Heron, J., Macleod, J., Joinson, C., Maughan, B., Lewis, G., and Kendler, K.S. 2013. Adolescent alcohol use is predicted by childhood temperament factors before age 5, with mediation through personality and peers. Alcoholism: Clinical and Experimental Research 37:2108–2117.
DiClemente, C.C. 1999. Motivation for change: Implications for substance abuse treatment. Psychological Science 10(3):209–213.
Dopp, A.R., Borduin, C.M., White, M.H., and Kuppens, S. 2017. Family-based treatments for serious juvenile offenders: A multilevel meta-analysis. Journal of Consulting and Clinical Psychology 85(4):335–354.
Drake, E. 2012. Chemical Dependency Treatment for Offenders: A Review of the Evidence and Benefit–Cost Findings . Olympia, WA: Washington State Institute for Public Policy.
Farenthold, E.C. 2010. The Effect on Juvenile Re-Offending of Confining and Treating Juveniles With Substance Use Disorders in Harris County . Doctoral dissertation. Ann Arbor, MI: UMI Dissertation Publishing.
Ferguson, C.J., and Meehan, D.C. 2011. With friends like these…: Peer delinquency influences across age cohorts on smoking, alcohol, and illegal substance use. European Psychiatry 26(1):6–12.
Fernández–Artamendi, S., Martínez–Loredo, V., & López–Núñez, C. 2021. Sex differences in comorbidity between substance use and mental health in adolescents: Two sides of the same coin. Psicothema 33(1):36–43.
Flaherty, C.W., Sutphen, R.D., and Ely, G.E. 2012. Examining substance abuse in truant youths and their caregivers: Implications for truancy intervention. Children and Schools 34(4):201–211.
Fothergill, K.E., Ensminger, M.E., Green, K.M., Crum, R.M., Robertson, J., and Juon, H.–S. 2008. The impact of early school behavior and educational achievement on adult drug use disorders: A prospective study. Drug and Alcohol Dependence 92:191–199.
Gau, S.S.F., Chong, M.–Y., Yang, P., Yen, C.–F., Liang, K.–Y., and Cheng, A.T.A. 2007. Psychiatric and psychosocial predictors of substance use disorders among adolescents. British Journal of Psychiatry 190:42–48.
Godley, M.D., Godley, S.H., Dennis, M.L., Funk, R.R., and Passetti, L.L. 2007. The effect of assertive continuing care (ACC) on continuing care linkage, adherence, and abstinence following residential treatment for adolescents. Addiction 102:81–93.
Godley, M.D., Godley, S.H., Dennis, M.L., Funk, R.R., and Passetti, L.L. 2014. A randomized trial of assertive continuing care and contingency management for adolescents with substance use disorders. Journal of Consulting and Clinical Psychology 82(1):40–51.
Gonzales, R., Ang, A., Murphy, D.A., Glik, D.C., and Anglin, M.D. 2014. Substance use recovery outcomes among a cohort of youth participating in a mobile-based texting aftercare pilot program. Journal of Substance Abuse Treatment 47(1):20–26.
Gray, K.M., and Squeglia, L.M. 2018. Research review: What have we learned about adolescent substance use? Journal of Child Psychology and Psychiatry 59(6):618–627.
Groenman, A.P., Janssen, T.W.P., and Oosterlaan, J. 2017. Childhood psychiatric disorders as risk factor for subsequent substance abuse: A meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry 56(7):556–569.
Groshkova, T. 2010. Motivation in substance misuse treatment. Addiction Research & Theory 18(5):494–510.
Hadland, S.E., Bagley, S. M., Rodean, J., Silverstein, M., Levy, S., Larochelle, M.R., and Zima, B.T. 2018. Receipt of timely addiction treatment and association of early medication treatment with retention in care among youths with opioid use disorder. Journal of the American Medical Association Pediatrics 172(11):1029–1037.
Hammerness, P., Petty, C., Faraone, S.V., and Biederman, J. 2017. Do stimulants reduce the risk for alcohol and substance use in youth with ADHD? A secondary analysis of a prospective, 24-month open-label study of osmotic-release methylphenidate. Journal of Attention Disorders 21(1):71–77.
Handren, L.M., Donaldson, C.D., and Crano, W.D. 2016. Adolescent alcohol use: Protective and predictive parent, peer, and self-related factors. Prevention Science 17(7):862–871.
Haughwout, S.P., Harford, T.C., Castle, I.J.P., and Grant, B.F. 2016. Treatment utilization among adolescent substance users: Findings from the 2002 to 2013 National Survey on Drug Use and Health. Alcoholism: Clinical and Experimental Research 40(8):1717–1727.
Henggeler, S.W., Flingempeel, W.G., Brondino, M.J., and Pickrel, S.G. 2002. Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. Journal of the American Academy of Child and Adolescent Psychiatry 41:868–874.
Henggeler, S.W., Halliday–Boykins, C.A., Cunningham, P.B., Randall, J., Shapiro, S.B., and Chapman, J.E. 2006. Juvenile drug court: Enhancing outcomes by integrating evidence-based treatments. Journal of Consulting and Clinical Psychology 74:42–54.
Henry, K.L., Knight, K., and Thornberry, T. 2012. School disengagement as a predictor of dropout, delinquency, and problem substance use during adolescence and early adulthood. Journal of Youth and Adolescence 41(2):156–166.
Hickert, A., Becker, E., Prospero, M., and Moleni, K. 2011. Impact of juvenile drug courts on drug use and criminal behavior. OJJDP Journal of Juvenile Justice 1(1):60–77.
Hines, L.A., Morley, K.I., Mackie, C., and Lynskey, M. 2015. Genetic and environmental interplay in adolescent substance use disorders. Current Addiction Reports 2:122–129.
Hodgins, S., Kratzer, L., and McNeil, T.F. 2001. Obstetric complications, parenting, and risk of criminal behavior. Archives of General Psychiatry 58(8):746–752.
Horigian, V.E., Anderson, A.R., and Szapocznik, J. 2016. Family-based treatments for adolescent substance use. Child and Adolescent Psychiatric Clinics of North America 25(4):603–628.
Humphreys, K. L., Eng, T., and Lee, S. S. 2013. Stimulant medication and substance use outcomes: A meta-analysis. Journal of the American Medical Association Psychiatry 70(7):740–749.
Joe, G.W., Knight, D.K., Becan, J.E., and Flynn, P.M. 2014. Recovery among adolescents: Models for posttreatment gains in drug abuse treatments. Journal of Substance Abuse Treatment 46(3):362–373.
Johnston, L.D., Miech, R.A., O’Malley, P.M., Bachman, J.G., Schulenberg, J.E., and Patrick, M.E. 2020. Monitoring the Future National Survey Results on Drug Use 1975–2019: 2019 Overview, Key Findings on Adolescent Drug Use. Ann Arbor, MI: University of Michigan, Institute for Social Research.
Kaminer, Y., Burleson, J.A., and Burke, R.H. 2008. The efficacy of aftercare for adolescents with alcohol-use disorders: A randomized controlled study. Journal of the American Academy of Child and Adolescent Psychiatry 47(12):1405–1412.
Kellman, S.G., Hendricks Brown, C., Poduska, J.M., Ialongo, N.S., Wang, W., Toyinbo, P., Petras, H., Ford, C., Windham, A., and Wilcox, H.C. 2008. Effects of a universal classroom behavior management program in first and second grades on young adult behavioral, psychiatric, and social outcomes. Drug and Alcohol Dependence 95 (Supplement 1):S5–S28.
Knight, D.K., Joe, G.W., Crawley, R.D., Becan, J.E., Dansereau, D.F., and Flynn, P.M. 2016. The effectiveness of the Treatment Readiness and Induction Program (TRIP) for improving during-treatment outcomes. Journal of Substance Abuse Treatment 62:20–27.
Kotov, R., Gamex, W., Schmidt, F., and Watson, D. 2010. Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin, 136(5):768–821.
Lander, L., Howsare, J, and Byrne, M. 2013. The impact of substance use disorders on families and children: From theory to practice. Social Work and Public Health 28(0):194–205.
Latimer, J., Morton–Bourgon, K., and Chretien, J.–A. 2006. A meta-analytic examination of drug treatment courts: Do they reduce recidivism? Ottawa, Ontario: Department of Justice Canada.
Lattimore, P.K., Krebs, C.P., Graham, P., and Cowell, A.J. 2004. Evaluation of the Juvenile Breaking the Cycle Program. Research Triangle Park, NC: RTI International.
Lee, S.S., Humphreys, K.L., Flory, K., Liu, R., and Glass, K. 2011. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review. Clinical Psychology Review 31(3):328–341.
Liddle, H.A. 1999. Theory development in a family-based therapy for adolescent drug abuse. Journal of Clinical and Child Psychology 28(4):521–532.
Liddle, H.A., Dakof, G.A., Parker, K., Diamond, G.S., Barrett, K., and Tejeda, M. 2001. Multidimensional Family Therapy for adolescent drug abuse: Results of a randomized clinical trial. American Journal of Drug and Alcohol Abuse 27(4):651–688.
Liddle, H.A., Dakof, G.A., Rowe, C.L., Henderson, C.E., Greenbaum, P., Wang, W., and Alberga, L. 2018. Multidimensional family therapy as a community-based alternative to residential treatment for adolescents with substance use and co-occurring mental health disorders. Journal of Substance Abuse Treatment 90:47–56.
Liddle, H.A., Rowe, C.L., Dakof, G.A., Henderson, C.E., and Greenbaum, P.E. 2009. Multidimensional Family Therapy for young adolescent substance abuse: Twelve-month outcomes of a randomized controlled trial. Journal of Consulting and Clinical Psychology 77(1):12–25.
Light J.M., Greenan, C.C., Rusby, J.C., Nies, K.M., and Snijders, T.A.B. 2013. Onset to first alcohol use in early adolescence: A network diffusion model . Journal of Adolescent Research 23:48–49.
Lucenko, B.A., Sharkova, I.V., Huber, A., Jemelka, R., and Mancuso, D. 2015. Childhood adversity and behavioral health outcomes for youth: An investigation using state administrative data. Child Abuse and Neglect 47:48–58.
Lui, C.K., Sterling, S.A., Chi, F. W., Lu, Y., and Campbell, C.I. 2017. Socioeconomic differences in adolescent substance abuse treatment participation and long-term outcomes. Addictive Behaviors 68:45–51.
Mackin, J.R., Lucas, L.M., Lambarth, C.H., Herrera, T.A., Wallter, M.S., Carey, S.M., and Finigan, M.W. 2010. Baltimore County Juvenile Drug Court Outcome and Cost Evaluation. Portland, OR: NPC Research.
Mansion, A.D., and Chassin, L.A. 2016. The effect of race/ethnicity on the relation between substance use disorder diagnosis and substance use treatment receipt among male serious adolescent offenders. Children and Youth Services Review 61:237–244.
Mason, M., Mennis, J., Russell, M., Moore, M., and Brown, A. 2019. Adolescent depression and substance use: The protective role of prosocial peer behavior. Journal of Abnormal Child Psychology 47:1065–1074.
Mattick, R.P., Breen, C., Kimber, J., and Davoli, M. 2009. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews (3):CD002209.
Mattick, R.P., Breen, C., Kimber, J., and Davoli, M. 2014. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database of Systematic Review (2):CD002207.
McGovern, M.P., and Carroll, K.M. 2013. Evidence-based practices for substance use disorders. Psychiatric Clinics of North America 26(4):991–1010.
McHugh, R.K., Votaw, V.R., Sugarman, D.E., and Greenfield, S.F. 2018. Sex and gender differences in substance use disorders. Clinical Psychology Review 66(December):12–23.
Merikangas, K.R., He, J.P., Burstein, M., Swanson, S.A., Avenevoli, S., Cui, L., Benjet, C., Georgiades, K., and Swendsen, J. 2010. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication | Adolescent Supplement. Journal of the American Academy of Child and Adolescent Psychiatry 49(10):980–989.
Mitchell, O., Wilson, D., Eggers, A., and Mackenzie, D. 2012. Drug courts’ effects on criminal offending for juveniles and adults. Campbell Systematic Reviews 4.
Mulvey, E.P., Schubert, C.A., and Chung, H.L. 2007. Service use after court involvement in a sample of serious adolescent offenders. Children and Youth Services Review 29 (4):518–544.
Murray, J., and Farrington, D.P. 2010. Risk factors for conduct disorder and delinquency: Key findings from longitudinal studies. Canadian Journal of Psychiatry 55(10):633–642.
Naar–King, S. 2011. Motivational interviewing in adolescent treatment. Canadian Journal of Psychiatry 56(11):651–657.
NIAAA (National Institute on Alcohol Abuse and Alcoholism). 2022, October. Underage Drinking . Bethesda, MD: National Institutes of Health, NIAAA. Retrieved January 3, 2023, from the web: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/underage-drinking#:~:text=Underage%20drinking%20is%20a%20serious,enormous%20health%20and%20safety%20risks
NIDA (National Institute on Drug Abuse). 2014, January. Principles of Adolescent Substance Use Disorder Treatment: A Research-Based Guide . Bethesda, MD: National Institutes of Health, NIDA. Retrieved January 5, 2023, from the web: https://nida.nih.gov/publications/principles-adolescent-substance-use-disorder-treatment-research-based-guide/director
Osgood, D.W., Ragan, D.T., Wallace, L., Gest, S.D., Feinberg, M.E., and Moody, J. 2013. Peers and the emergence of alcohol use: Influence and selection processes in adolescent friendship networks. Journal of Research on Adolescence 23:500–512.
Patte, K.A., Qian, W., and Leatherdale, S.T. 2017. Marijuana and alcohol use as predictors of academic achievement: A longitudinal analysis among youth in the COMPASS study. Journal of School Health 87(5):310–318.
Prom–Wormley, E.C., Ebejer, J., Dick, D.M., and Bowers, M.S. 2017. The genetic epidemiology of substance use disorder: A review. Drug and Alcohol Dependence 180:241–259.
Ramo, D.E., Anderson, K.G., Tate, S.R., and Brown, S.A. 2005. Characteristics of relapse to substance use in comorbid adolescents. Addictive Behaviors 30:1811–1823.
Rigter, H., Henderson, C.E., Pelc, I., Tossmann, P., Phan, O., Hendrinks, V., Schaub, M., and Rowe, C.L. 2013. Multidimensional family therapy lowers the rate of cannabis dependence in adolescents: A randomized controlled trial in western European outpatient settings. Drug and Alcohol Dependence 130(1–3):85–93.
Rottman, D., and Casey, P. 1999. Therapeutic jurisprudence and the emergence of problem-solving courts. National Institute of Justice :12–19.
Rowe, C.L., and Liddle, H.A. 2003. Substance abuse. Journal of Marital and Family Therapy 29(1):97–120.
Ryan, R.M., and Deci, E.L. 2000a. Intrinsic and extrinsic motivations: Class definitions and new directions. Contemporary Education Psychology 25(1):54–67.
Ryan, R.M., and Deci, E.L. 2000b. Self-determination theory: Basic psychological needs in motivation, development, and wellness. American Psychologist 55(1):68–78.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2011. Results From the 2010 National Survey on Drug Use and Health: Summary of National Findings. NSDUH Series H–41, HHS Publication No. (SMA) 11–4658. Rockville, MD: U.S. Department of Health and Human Services (HHS), SAMHSA.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2021. Key Substance Use and Mental Health Indicators in the United States: Results From the 2020 National Survey on Drug Use and Health. Publication No. PEP21–07–01–003. Rockville, MD: HHS, SAMHSA.
Santisteban, D. A., Mena, M. P., Muir, J., McCabe, B. E., Abalo, C., & Cummings, A. M. 2015. The efficacy of two adolescent substance abuse treatments and the impact of comorbid depression: Results of a small randomized controlled trial. Psychiatric Rehabilitation Journal 38(1):55–64.
Settipani, C.A., Hawke, L.D., Virdo, G., Yorke, E., Mehra, K., and Henderson, J. 2018. Social determinants of health among youth seeking substance use and mental health treatment. Journal of the Canadian Academy of Child and Adolescent Psychiatry 27(4):213–221.
Shaffer, D. 2006. Reconsidering Drug Court Effectiveness: A Meta-Analytic Review. Las Vegas, NV: University of Las Vegas Department of Criminal Justice.
Skeer, M.R., McCormick, M.C., Normand, S.–L. T., Mimiaga, M.J., Buka, S.L., and Gilman, S.E. 2011. Gender differences in the association between family conflict and adolescent substance use disorders. Journal of Adolescent Health 49(2):187–192.
Slesnick, N., and Prestopnik, J. 2009. Comparison of family therapy outcome with alcohol abusing, runaway adolescents. Journal of Marital and Family Therapy 35(3):255–277.
Sloboda, Z., Glantz, M.D., and Tarter, R.E. 2012. Revisiting the concepts of risk and protective factors for understanding the etiology and development of substance use and substance use disorders: Implications for prevention. Substance Use and Misuse 47:944–962.
Smedslund, G., Wollscheid, S., Fang, L., Nilsen, W., Steiro, A., and Larun, L. 2017. Effects of early, computerized brief interventions on risky alcohol use and risky cannabis use among young people. Campbell Collaboration 6.
Spinney, E., Yeide, M., Feyerherm, W., Cohen, M., Stephenson, R., and Thomas, C. 2016. Racial disparities in referrals to mental health and substance abuse services from the juvenile justice system: A review of the literature. Journal of Crime and Justice 39(1):153–573.
Squeglia, L.M., M.C., Fadus, McClure, E.A., Tomko, R.L., and Gray, K.M. 2019. Pharmacological treatment of youth substance use disorders. Journal of Child and Adolescent Psychopharmacology 29(7):559–572.
Stein, L.A.R., Colby, S.M., Barnett, N.P., Monti, P.M., Golembeske, C., and Lebeau–Craven, R. 2006a. Effects of motivational interviewing for incarcerated adolescents on driving under the influence after release. American Journal on Addictions 15:50–57.
Stein, L.A.R., Colby, S.M., Barnett, N.P., Monti, P.M., Golembeske, C., Lebeau–Craven, R., and Miranda, R. 2006b. Enhancing substance abuse treatment engagement in incarcerated adolescents. Psychological Services 3(1):25–34.
Swendsen, J., Burstein, M., Case, B., Conway, K., Dierker, L., He, J., and Merikangas, K.R. 2012. The use and abuse of alcohol and illicit drugs in U.S. adolescents: Results from the National Comorbidity Survey | Adolescent Supplement. Archives of General Psychiatry 69(4):390–398.
Tanner–Smith, E.E., and Lipsey, M.W. 2015. Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment 51:1–18.
Tanner–Smith, E.E., Lipsey, M.W., and Wilson, D.B. 2016. Juvenile drug court effects on recidivism and drug use: A systematic review and meta-analysis. Journal of Experimental Criminology 12(4):477–513.
Torrens, M., Rossi, P.C., Martinez–Riera, R., Martinez–Sanvisens, D., and Bulbena, A. 2012. Psychiatric co-morbidity and Substance Use Disorders: Treatment in parallel systems or in one integrated system? Substance Use and Misuse 47(8–9):1005–1014.
Trupin, E.J., Kerns, S.E.U., Cusworth Walker, S., DeRobertis, M.T., and Steward, D.G. 2011. Family integrated transitions: A promising program for juvenile offenders with co-occurring disorders. Journal of Child and Adolescent Substance Abuse 20:421–436.
Turner, W.C., Muck, R.D., Muck, R.J., Stephens, R.L., and Sukumar, B. 2004. Co-occurring disorders in the adolescent mental health and substance abuse treatment systems. Journal of Psychoactive Drugs. 36(4):455–462.
Vanderbilt–Adriance, E., and Shaw, D. 2008. Conceptualizing and reevaluating resilience across levels of risk, time, and domains of competence. Clinical Child and Family Psychology Review 11(1–2):30–58.
van der Pol, T.M., Henderson, C.E., Hendriks, V., Schaud, M.P., and Rigter, H. 2018. Multidimensional family therapy reduces self-reported criminality among adolescents with a cannabis use disorder. International Journal of Offender Therapy and Comparative Criminology 62(6):1573–1588.
Van Ryzin, M.J., Roseth, C.J., Fosco, G.M., Lee, Y., and Che, I. 2016. A component-centered meta-analysis of family-based prevention programs for adolescent substance use. Clinical Psychology Review 45:72–80.
Vasilenko, S.A., Evans–Polce, R.J., and Lanza, S.T. 2017. Age trends in rates of substance use disorders across ages 18–90: Differences by gender and race/ethnicity. Drug and Alcohol Dependence 180:260–264.
Waldron, H.B., and Kaminer, Y. 2004. On the learning curve: The emerging evidence supporting cognitive–behavioral therapies for adolescent substance abuse. Addiction 99(Suppl 2):93–105.
Waldron, H.B., and Turner, C.W. 2008. Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical Child and Adolescent Psychology 37(1):238–261.
Wasserman, G.A., McReynolds, L.S., Musabegovic, H., Whited, A.L., Keating, J.M., and Huo, Y. 2009. Evaluating project connect: Improving juvenile probationers’ mental health and substance use service access. Administration and Policy in Mental Health and Mental Health Services Research 36(6):393–405.
Weibnerg, N.Z. 2001. Risk factors for adolescent substance abuse. Journal of Learning Disabilities 34(4):343–351.
Whitesell, M., Bachand, A., Peel, J., and Brown, M. 2013. Familial, social, and individual factors contributing to risk for adolescent substance use. Journal of Addiction. doi: 10.1155/2013/579310
Whitten, T., Burton, M., Tzoumakis, S., and Dean, K. 2019. Parental offending and child physical health, mental health, and drug use outcomes: A systematic literature review. Journal of Child and Family Studies 28(5):1155–1168.
Wild, T.C., and Enzle, M.E. 2002. Social contagion of motivational orientations. In Handbook of Self-Determination, edited by E.L. Deci and R.M. Ryan. Rochester, NY: University of Rochester Press, pp. 141–157.
Wilens, T.E., Biederman, J., Kwon, A., Ditterline, J., Forkner, P., Moore, H., Swezey, A., Snyder, L., Henin, A., Wozniak, J. and Faraone, S.V. 2004. Risk of substance use disorders in adolescents with bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 43(11):1380–1386.
Wilens, T.E., Faracone, S., Biedermann, J., and Gunawardene, S. 2003. Does stimulant therapy of ADHD beget later substance abuse: A meta analytic review of the literature. Pediatrics 11:179–185.
Wilens, T.E., Martelon, M., Joshi, G., Bateman, C., Fried, R., Petty, C., and Biederman, J. 2011. Does ADHD predict substance use disorders? A 10-year follow-up study of young adults with ADHD. Journal of the American Academy of Child and Adolescent Psychiatry 50(6):543–553.
Wilson, D.B., Olaghere, A., and Kimbrell, C.S. 2019. Implementing juvenile drug treatment courts: A meta-aggregation of process evaluations. Journal of Research in Crime and Delinquency 56(4).
Winstanley, E., Steinwachs, D., Ensminger, M., Latkin, C., Stitzer, M., and Olsen, Y. 2008. The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug and Alcohol Dependence 92(1–3):173–182.
Winters, K.C., Botzet, A.M., and Fahnhorst, T. 2011. Advances in adolescent substance abuse treatment. Current Psychiatry Reports 13(5):416–421.
Winters, K.C., Botzet, A.M., Stinchfield, R., Gonzales–Castaneda, R., Finch, A.J., Piehler, T.F., Ausherbauer, K., Chalmers, K., and Hemze, A. 2018. Adolescent substance abuse treatment: A review of evidence-based research. In Adolescent Substance Abuse: Issues in Children’s and Families’ Lives, edited by C. Leukefeld and T. Gullotta. New York, NY: Springer.
Winters, K.C., Tanner–Smith, E.E., Bresani, E., and Meyers, K. 2014. Current advances in the treatment of adolescent drug use. Adolescent Health, Medicine, and Therapeutics 5:199–210.
Wise, B.K., Cuffe, S.P., and Fischer, T. 2001. Dual diagnosis and successful participation of adolescents in substance abuse treatment. Journal of Substance Abuse Treatment 21(3):161–165.
Wong, T., Slotboom, A.M., and Bijeveld, C. 2010. Risk factors for delinquency in adolescent and young adult females: A European review. European Journal of Criminology 7:266–284.
Yan, J., and Dannerbeck A. 2011. Exploring the relationship between gender, mental health needs, and treatment orders in a metropolitan juvenile court. Journal of Child & Family Studies 20(1):9–22.
Yildiz, D., Ciftci, A., and Yalcin, O. 2020. The association between trauma history, trauma-related psychopathology, and treatment completion at an adolescent inpatient substance abuse treatment center in turkey. Journal of Child & Adolescent Substance Abuse 29(1):58–67.
Young, S.E., Corley, R.P., Stallings, M.C., Rhee, S.H., Crowley, T.J., and Hewitt, J.K. 2002. Substance use, abuse and dependence in adolescence: Prevalence, symptom profiles and correlates. Drug and Alcohol Dependence 68:309–322.
Young, J.T., and Rees, C. 2013. Social networks and delinquency in adolescence: Implications for life-course criminology. In Handbook of Life-Course Criminology, edited by C.L. Gibson and M.D. Krohn. New York, NY: Springer, pp. 159–180.
About this Literature Review
Suggested Reference: Development Services Group, Inc. January 2023. "Substance Use Treatment Programs." Literature review. Washington, DC: Office of Juvenile Justice and Delinquency Prevention. https://ojjdp.ojp.gov/model-programs-guide/literature-reviews/Substance-Use-Treatment-Programs
Prepared by Development Services Group, Inc., under Contract Number: 47QRAA20D002V.
Last Update: January 2023
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Med Libr Assoc
- v.101(2); 2013 Apr
Mapping the literature of addictions treatment
Associated data, objectives:.
This study analyzes and describes the literature of addictions treatment and indexing coverage for core journals in the field.
Citations from three source journals for the years 2008 through 2010 were analyzed using the 2010 Mapping the Literature of Nursing and Allied Health Professions Project Protocol. The distribution of cited journals was analyzed by applying Bradford's Law of Scattering.
More than 40,000 citations were analyzed. Journals (2,655 unique titles) were the most frequently cited form of literature, with 10 journals providing one-third of the cited journal references. Drug and Alcohol Dependence was the most frequently cited journal. The frequency of cited addictions journals, formats cited, age of citations, and indexing coverage is identified.
Conclusions:
Addictions treatment literature is widely dispersed among multidisciplinary publications with relatively few publications providing most of the citations. Results of this study will help researchers, students, clinicians, and librarians identify the most important journals and bibliographic indexes in this field, as well as publishing opportunities.
- Counseling literature is underrepresented in the core literature of addictions treatment.
- As in other mapping studies, journals were most frequently cited, followed by books.
- Addictions treatment literature draws most frequently from the literature of drug and alcohol abuse, medicine, psychiatry, psychology, public health, pharmacology, neurology, and brain science, among others.
Implications
- Librarians, educators, and researchers should assess their collections and research tools and revise instruction strategies accordingly.
- Both the National Library of Medicine's MEDLINE and the American Psychological Association's PsycINFO databases should be searched for comprehensive searches of the addictions treatment literature.
INTRODUCTION
This study uses the research methodology devised by the Task Force on Bibliographic Access for the Allied Health Literature, Nursing and Allied Health Resources Section (NAHRS) of the Medical Library Association (MLA) 1 . This NAHRS task force was formed in 1993 to study the literature of allied health fields in order to identify core journals in a discipline, “core” being defined as those journals that are most significant and important for scholarly communication in a subject and valuable for a library's research collection. Additional goals were to analyze the formats and features of cited materials and provide quantitative evidence for collection development for librarians. Schloman described the project's original rationale:
Because bibliographic references that appear in journal articles provide a measurable path of information transfer occurring within a field, it is possible to assess quantitatively the characteristics of the literature of that field: the type of literature used, its currency, the core journals, and the extent of dispersion of the journal literature. 2
As of October 2012, more than thirty-four studies of the literature of nursing, nursing subspecialties, and allied health disciplines have been published in the Journal of the Medical Library Association (JMLA) and its predecessor title, the Bulletin of the Medical Library Association (BMLA) .
The Public Policy Statement on Treatment for Alcohol and Other Drug Addiction issued by the American Society of Addiction Medicine (ASAM) in 2010 defines treatment as:
the use of any planned, intentional intervention in the health, behavior, personal and/or family life of an individual suffering from alcoholism or from another drug addiction, and which is designed to enable the affected individual to achieve and maintain sobriety, physical, spiritual and mental health, and a maximum functional ability. 3
The ASAM Patient Placement Criteria for the Treatment of Substance-Related Disorders are the officially recognized criteria adopted in thirty states to appropriately place persons with addictions and any co-occurring disorders into the treatment system 4 .
Overview of and trends in addictions treatment in the United States
The definition of addiction and what to do about it have been in dispute throughout history. Miller and Carroll noted that “the names used to describe phenomena affect the ways in which one thinks about a problem and what to do about it” 5 . Prior to the 1960s, alcoholism and drug addiction were often understood as either a problem originating in choice, character flaws, or a moral failing. The present addictions treatment field emerged in the 1960s and 1970s, with the development of medical approaches that were very different from the self-help and religious approaches prominent in the United States 6 . By then, the American Medical Association (AMA) and other medical groups officially recognized alcoholism as a physical disease process, although this view was met with stiff opposition from recovery communities such as Alcoholics Anonymous 5 . Today, modern medicine widely upholds the AMA view, paving the way for establishing addiction medicine as a medical specialty. In 2011, ASAM adopted a statement that expanded on the findings of recent neuroimaging research, stating that not only the brain's reward circuitry, but also memory, motivation, and other neurological phenomena are involved in addiction 7 . The ASAM definition is likely to have broad implications for the criminal justice system and law, primary care and specialized medical practice, public policy, and public health, as well as the addictions treatment and counseling fields 8 . However, the inclusion of sex, gambling, and Internet addictions as true addictions continues to be in dispute, especially between the fields of medicine, psychology, and counseling.
The problem of who can help and how an addict or alcoholic can be helped is also somewhat controversial. Self-help communities of recovery such as Alcoholics Anonymous have helped many, but medical interventions now offer new hope based on research.
Treatment settings
Hospital-based addiction treatment programs proliferated in the 1980s due to the willingness of private health insurance plans to pay for in-patient detoxification stays but were drastically reduced and shifted to outpatient treatment in the 1990s under managed care programs. Now the pendulum is swinging back to reestablish addiction treatment coverage in health plans and in medical settings. The Mental Health Parity and Addiction Equity Act of 2008 and the Patient Protection and Affordable Care Act and the Health Care and Education Reconciliation Act of 2010 propelled the addiction treatment system to undergo major and rapid changes in anticipation of increased demand for services 9 . Under recent health reform, insurers are required to provide coverage for substance abuse and mental health services on a par with other covered medical conditions with the same financial requirements and benefits limitations in their plans. Also, behavioral health treatment services are subject to the same standards for qualifications for payment by insurers as primary health care services 9 . These recent reforms enable more people who need and desire treatment to receive treatment because many more will have insurance, and those with insurance will have coverage for addiction treatment.
Currently, treatment primarily takes place in specialized treatment facilities (68%) or mental health facilities (5%), according to a 2010 Substance Abuse and Mental Health Services Administration (SAMHSA) survey of 15,390 eligible treatment facilities 10 . Most treatment takes place on an outpatient basis (90%). Only a fraction of treatment takes place in hospital settings (less than 1%), while 9% takes place in residential settings, but this is anticipated to change.
Staffing of treatment facilities varies, depending on state and local law and diagnosis of any co-occurring mental disorders or physical findings 21 . Professionals from counseling, rehabilitation, social work, medicine, criminal justice, nursing, and psychology disciplines are most commonly involved in treatment, and most of these fields have credentialing programs 22 , 23 ( Table 1 ). The typical addiction treatment program in the United States employs mostly counselors, each treating a caseload of 60 to 80 clients; very few other professional disciplines are represented in most programs 24 . The Bureau of Labor Statistics (BLS) reported 86,100 addictions counselors were employed in 2008, and that number was expected to grow “much faster than average” for other occupations 14 . Over 18,000 additional counselors are forecasted to be added to the system, for a projected employment of 104,200 by the year 2018.
Professional credentials for addiction treatment workers

Other professionals such as pastoral counselors and marital and family therapists may also work in the treatment field, providing a variety of skills and perspectives in treatment and support of recovery. The master's degree is considered the professional level of practice in the treatment field, although counselor certification also exists for high school diploma and bachelor's degree–prepared professionals who work under supervision 9 , 10 , 15 . A combination of education hours or degrees and clinical practice hours is required for certification. Not all professional credentials are accepted nationally, though many state certifications for counselors are reciprocal with other states. Continuing education activities, including reading the professional literature, are an important part of keeping credentials current.
Literature review
Although various directories of journals, newsletters, and magazines in the field are available, no study describing a core collection of addictions treatment journals has been conducted. Howard and Howard's investigation in 1992 examined the citation rates of 541 selected articles in 12 drug and alcohol journals indexed in the Social Science Citation Index for the 5-year period of 1984–1988 25 . They noted the need for increased research on addiction literature using bibliometric methods and recognized the difficulties of using citation counts where the intended audiences of particular journals and articles were not scientists.
Weiner and White studied addiction periodical literature from 1776–2001 in relation to its origins in social movements and medical and mutual aid societies 26 . West and McIlwaine's 2002 study of citation counts to research published in the journal Addiction found no link between citation counts and peer ratings of quality 27 . Another citation study of Addiction by Valderrama Zurian found most citations were to journal articles (76.00%) and books and chapters (23.25%) 28 . A small number of citations to conference proceedings, doctoral theses, and other gray literature or Internet sites was noted. Other studies looked at topics, authors, and submission patterns 29 – 31 . Carbonnell's 2009 study, published in the JMLA, described publication characteristics of research on addictions to Internet, video games, and cell phones over a 10-year period and found 179 articles widely dispersed among 96 journals 32 .
As stated in the introduction, this study used a protocol developed by the NAHRS Task Force on Bibliographic Access for the Allied Health Literature, revised in 2010. The selection of source journals is the most critical step of the 2010 mapping study protocol 1 . According to the protocol, source journals should provide coverage of the literature of the profession comprehensively, rather than narrow aspects. In the mapping studies, source journals most often originate in the United States and are US focused. A review of directories of alcohol and drug abuse literature produced numerous magazines as well as scholarly journals. The decision was made to focus on the literature of patient care and client care, rather than the genre of alcohol and addiction in general. Only peer-reviewed, scholarly journals focused on treatment and published in English primarily, for a US audience, were considered for this study. Journals were reviewed for their intended audience of clinicians and students, but locating candidates for source journals proved difficult.
Suggestions for a list of “Top 5” addictions treatment journals were solicited from Governors State University faculty and external librarian colleagues via email, resulting in a variety of candidates, most which did not meet the inclusion criteria. Title searches in Ulrich's Periodicals Directory 33 and the Substance Abuse Librarians & Information Specialists (SALIS) directory of journals 34 were reviewed, as well as journal websites, noting scope notes and reviews. NAHRS mapping studies often look to professional society journals as source journals, but the most likely candidate, Counselor: The Magazine for Addictions Professionals, did not meet the “scholarly” criteria. Due to the fact that most of the professionals in treatment settings are counselors, the inclusion of an addiction counseling journal was important. The British journal Addiction was considered but was rejected in favor of Drug and Alcohol Dependence , a US journal. The following journals were selected:
- Drug and Alcohol Dependence is the journal of the College on Problems of Drug Dependence, the oldest society in the United States concerned with drug dependence research. The journal is published by Elsevier. The purpose of the journal is “to promote mutual understanding of the many facets of drug abuse to the benefit of all investigators involved in drug and alcohol research, and to facilitate the transfer of scientific findings to successful treatment and prevention practices” 35 .
- The Journal of Addictions and Offender Counseling, published by Wiley-Blackwell, is the official journal of the International Association of Addiction and Offenders Counselors, a division of the American Counseling Association. The journal “contains articles of interest to professionals in the fields of addictions and offender counseling and focuses on descriptions of prevention and treatment programs, theoretical and philosophical rationales for programs with juvenile and adult offenders, and descriptions of research conducted on rehabilitation programs with offenders and public offender counselors. It is also open to literature focusing on the attitudes and behaviors of addictions and offender counselors” 36 . Despite the inclusion of offenders in its scope, only a few non-addiction articles were published during the study period.
- The Journal of Substance Abuse Treatment “values high quality empirical research that is relevant for translation by treatment practitioners from all disciplines and across any setting where persons with substance use problems are encountered” 37 . Also published by Elsevier, this journal seemed to most effectively meet the inclusion criteria.
Following the protocol, full-length journal articles for the three-year period of 2008, 2009, and 2010 were studied. Letters to the editor, brief communications, editorials, special issues, and book and media reviews were excluded. A database was created consisting of all cited references from all full-length articles published in the three source journals in the study period, using an Excel spreadsheet and manual data entry because exporting citations from sources proved unworkable and there were problems with the accuracy and completeness of citations in secondary sources.
Key elements from each cited reference were entered into the following columns: accession number, source journal, source year, volume/issue, publication type or title of the cited journal, citation year, and notes. Each citation was categorized as a “Book,” “Journal,” Government Document,” “Internet,” or “Miscellaneous”; the latter category included gray literature such as psychological tests and assessments, theses, software, scholarly presentations, and unpublished manuscripts. Books, journals, and US government publications were counted as those material types, regardless of whether the publication was digital or in print or what the material type was. Journals and books would be counted as government publications if that designation were obvious. Non-US government publications were categorized as “Miscellaneous.” Only websites that did not fall into other categories were placed in the “Internet” category.
Upon completion of data entry, the researcher collapsed variations in journal titles due to name changes and recorded the journals under the most recent journal titles. Errors in journal title abbreviations were corrected. The National Library of Medicine (NLM) abbreviation was chosen for uniformity, using the NLM Journals Database 38 and Ulrich's Periodicals Directory 33 .
Using the Excel pivot table function, journal titles and material formats were counted and sorted by the most to the least frequently cited, and Bradford's Law of Scattering was applied. Bradford's Law of Scattering states that in any given subject area: “there are a few very productive periodicals, a larger number of more moderate producers, and still larger number of constantly diminishing productivity” 39 . The cited journals were divided into three approximately equal portions or “zones,” based on their total counts of cited references. Zone 1, the most frequently cited journal titles, could be considered the most important in the field and therefore of highest interest to librarians, researchers, publishers, indexers, and professionals in the field. Zone 2 is the middle ground of less frequently cited journals, which are possibly of decreasing importance in consideration for a core bibliography for the field. Zone 3 lists those journals that are infrequently cited and thus would be of least importance to the literature of addictions treatment.
Also using the pivot table function, the researcher sorted citations by format types and organized them by publication year in order to analyze age of citations. Manuscripts, in-process, or journal citations without dates were counted as published in 2010.
The final step was to investigate the availability of indexing of Zone 1 and Zone 2 journals in standard indexing tools. CINAHL Plus with Full Text was selected for database comparison, along with MEDLINE and PsycINFO. Although not widely available in health sciences libraries, the Science Citation Index (SCI), Social Science Citation Index (SSCI), Science Citation Index Expanded (SCI Exp), and BIOSIS Previews databases were also reviewed due to their comprehensive coverage of high-quality physical, life, and social science literature. Each Zone 1 and Zone 2 journal was checked against the CINAHL Plus with Full Text coverage list 40 , the Thomson Reuters Master Journals List (for SCI, BIOSIS, SSCI, and SCI Exp) 41 , the NLM Journals Database for MEDLINE indexing 38 , and the List of Journals Indexed for PsycINFO 42 . The availability of indexing was noted for all indexes, and coverage years were noted for MEDLINE, CINAHL, and PsycINFO.
Drug and Alcohol Dependence proved the most productive journal, providing 25,335 cited references, almost double the number from the Journal of Substance Abuse Treatment, which supplied 14,747 cited references ( Table 2 ). Both source journals overshadowed the Journal of Addictions and Offender Counseling, which provided only 875 citations. Citations to journals made up the large majority of citations, with more than 82% of the total. Books were cited the next most frequently, with more than 8% of total citations. The miscellaneous category—citations to assessments, gray literature, theses, conference presentations, non-US government publications, and so on—constituted 4.9% of citations, while government documents were cited slightly less frequently at 3.9%. Internet sites not falling into other categories were cited infrequently. The Journal of Addictions and Offender Counseling cited books more frequently (24.7%) than the other 2 source journals (7.0%, 9.0%), while citing journals less frequently than the others for the study period.
Format types by source journal and citation frequency

The review of the publication date ranges of the cited references in Table 3 shows that the majority of references from 2008, 2009, and 2010 articles (58%) were published in the decade of 2001–2010, while articles from the years 2001–2005 were cited the most frequently (35%). Citations for older 5-year segments diminished about 50% for each 5-year period.
Cited format types by publication year periods

Table 4 shows the scattering predicted by Bradford's law. Less than 0.5% of the 2,655 total journals cited are Zone 1 journals, with a very heavy concentration of citations in just 10 journals in this subject area. Zone 2 contains 80 journals, accounting for almost 3% of the total number of journals. More than 2,565 journals fall in the long tail, as predicted by Bradford et al., making up almost 97% of the journal titles cited. One-thousand three hundred fifty-two of these journals were cited only once.
Distribution of cited journals and references by zone

Table 5 provides a listing of Zone 1, with the results of the investigation of indexing coverage. (For a complete list of Zone 1 and Zone 2 titles and coverage, see Table 6, online only.) In addition to serving as a prolific source of articles, Drug and Alcohol Dependence, not surprisingly, was cited the most often in this study with 2,224 citations. Addiction and Journal of Substance Abuse Treatment are close behind in concentration of cited references with 1,996 and 1,655 cited articles, respectively. A very thin line of 1 citation separates Zone 1 from Zone 2, but the decision was made to keep Psychopharmacology (Berlin) in Zone 2 in order to most closely adhere to the protocol's directive to identify 3 equal zones.
Distribution and indexing coverage of Zone 1 for 2010 * †

MEDLINE provided the most comprehensive coverage of Zone 1 and Zone 2 journals, with two additional journals having PubMed citations, but not indexed in MEDLINE. PubMed includes the MEDLINE database as well as non-reviewed prepublication and historical citations supplied by publishers and other sources. BIOSIS and the Science Citation Indexes provided less coverage of Zone 1 and Zone 2 journals, while PsycINFO provided the next best comprehensive coverage after MEDLINE.
This study sets a record of 40,957 citations studied; the previous record of 29,305 citations was set by Taylor et al. in their 2007 study of the health care management literature from 5 source journals 43 . In the NAHRS mapping study series, this study is perhaps most similar to Taylor's in describing the literature of a professional field with diverse stakeholders. However, the number of Zone 1 and 2 journals in the current study (90) is much greater than that of the health care management literature study (58), showing that the literature is more widely distributed 43 . Zone 3, those journals that are more peripheral to the field, is twice the size in addiction treatment literature, containing 2,565 journals compared to 1,766 Zone 3 journals in the health care management study. This difference may indicate that librarians developing collections that support treatment professionals—especially in psychology, medicine, psychiatry, and addiction medicine—may need to consider a larger number of journals than for other disciplines.
As with other NAHRS mapping studies, journals were the most frequently cited format of literature, followed by books, miscellaneous/gray literature, government documents, and Internet. This study found similar results to Valderrama Zurian's study of five years of Addiction citations, finding that journal articles and books were cited most frequently 28 .
This study is also the first known in the mapping series where the selected source journal did not appear in Zone 1 or Zone 2. The Journal of Addictions and Offender Counseling ranked number 240 in this study. The appearance of JAMA as one of the Zone 1 journals in this study is surprising but also not totally unexpected, given its leading role in health sciences literature. Other Zone 1 journals, the American Journal of Psychiatry and Archives of General Psychiatry, are available in many general health sciences library collections. Surprisingly, Alcoholism Treatment Quarterly is the only counseling journal in Zones 1 and 2, contrasting with the predominance of counselors in the treatment workforce. The literature of addiction treatment is widely dispersed among the disciplines of drug and alcohol abuse, psychology, medicine, psychiatry, pharmacology and therapeutics, psychopharmacology, public health, epidemiology, neurology and brain science, and infectious disease, among others.
US government–related journals, such as Alcohol Research and Health at number 40 and Public Health Reports at number 86, were not counted as government documents but accounted for 201 citations. If these journals were added to the government documents total, government documents would be cited nearly as frequently (973) as miscellaneous (976). Internet websites not falling into other categories were cited infrequently, but there was a large difference between Drug and Alcohol Dependence and the other source journals.
NLM's MEDLINE was found to provide the best indexing coverage for addiction treatment journals. All but two of the top ninety most cited journals in this study (Zones 1 and 2) are indexed in MEDLINE. Even though Alcoholism Treatment Quarterly is not currently indexed for MEDLINE, citations to selected articles can be located in PubMed with links to the full text in PubMed Central. Five citations were found in MEDLINE for the Journal of Drug Issues , but it is currently not indexed. PubMed included another sixty-one non-indexed citations from this title with links to full text in PubMed Central. PsycINFO provided excellent coverage of Zone 1 and Zone 2 journals but did not include as many titles as MEDLINE. PsycINFO often provides earlier coverage than MEDLINE, but MEDLINE indexes public health, internal medicine, and health services titles not covered in PsycINFO. CINAHL expanded coverage of addictions literature beginning with 2006, and this database should be considered by the searcher working on topics related to care that the nursing and allied health care team provides.
The Thompson Reuters SCI, SSCI, SCI Exp, and BIOSIS indexes may prove useful to researchers for indexing coverage because some titles extend to the early 1900s, but given the coverage of more widely available indexes, the use of these indexes may not be normally required.
Some of the results in the NAHRS mapping series have been used to advocate to publishers of indexes to expand coverage in a discipline, but this study shows that indexes available through most academic and health sciences libraries and for free on the Internet already provide excellent indexing coverage.
Limitations
The use of professional knowledge and judgment in selecting study journals is both a strength and the greatest limitation of this methodology. In retrospect, Drug and Alcohol Dependence could have been used as a single source of study citations because it supplied 25,355 citations and would have produced similar results in terms of types of materials cited. The disparity in journal output between the 3 source journals likely skewed the results in favor of the influence of citations in Drug and Alcohol Dependence .
Zone 1 journals could be considered a core list, but this list should be balanced with knowledge of local needs and requirements. Neurology and pharmacology research literature might not be useful for a community college library supporting an addictions studies program, for example. The distinctions between zones are somewhat arbitrary; there is a difference of only a few citation counts between journals at the margins. As Corby stated in regard to defining a core journal list, “no study is ever definitive” 44 .
CONCLUSIONS
Librarians should note that training of addictions counselors and other professionals is likely to increase to meet the demand created by health care reform. The new medical specialty of addiction medicine, a residency program recently established by the American Board of Addiction Medicine, indicates new recognition of the importance of addiction treatment, and this may influence medical school and nursing and allied health curricula. Librarians can use Zone 1 and Zone 2 journal titles to assist in making collection development decisions to support academic programs and clinicians' information needs. Instructors and authors may find the results useful for guiding students in the field and identifying publishing opportunities.
MEDLINE provides the most comprehensive coverage of addiction treatment literature, but PsycINFO should also be searched for comprehensive searches. CINAHL indexing coverage has increased in Zone 1 and Zone 2 journals since 2006 and should also be searched for nursing, allied health, and rehabilitation-related topics.
This study identifies a gap between the professions working in the field and the scholarly literature of addictions treatment. Only one counseling journal was identified in Zones 1 and 2, and no nursing, social work, or criminal justice journals were identified, possibly identifying a gap in translating research into practice, but more needs to be known about the clinician's actual usage of the literature including monographs and government documents. This study contributes to the body of research on the literature of addictions, but more research is needed. The NAHRS mapping protocol could also be used to study subspecialty areas such as addictions counseling, addictions medicine, prevention, addictions nursing, and social work in the addictions.
Electronic Content
Acknowledgments.
The author expresses thanks to Lynn DiMaggio for her invaluable assistance with the data collection portion of this study, Judy Hanacek for her assistance, and Stacey Knight Davis for her assistance. Thanks also to Laura Sklansky for introducing me to SALIS and for providing early support for conducting this research. I am especially grateful to Frances Delwiche for her guidance and support throughout this project.
EC Supplemental Table 6 is available with the online version of this journal.

IMAGES
VIDEO
COMMENTS
Substance or Drug abuse is a serious public health problem affecting usually adolescents and young adults. It affects both males and females and it is. the major source of crimes in youth and ...
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
This paper reviews methodologically rigorous studies examining group treatments for interview-diagnosed drug use disorders. A total of 50 studies reporting on the efficacy of group drug use disorder treatments for adults met inclusion criteria. Studies examining group treatment for cocaine, methamphetamine, marijuana, opioid, mixed substance, and substance use disorder with co-occurring ...
Our study contributes to the expanding recovery literature by providing insights into how people with drug addiction experience recovery over time. Because our sample is highly heterogenous and recruited from a variety of settings, our findings provide recovery experiences that supersede those of studies performed in a particular treatment setting.
Substance-Related Disorders* / epidemiology. Insight refers to a person's understanding of themselves and the world around them. Recent literature has explored people's insight into their substance use disorder (SUD) and how this is linked to treatment adherence, abstinence rates, and comorbid mental health symptoms. The aim of this systematic ….
Drug addiction is a chronic, relapsing disorder in which compulsive drug-seeking and drug-taking behavior persists despite serious negative consequences. Addictive substances induce pleasant ...
David Best. Addiction recovery is a complex, dynamic and non-linear process of change on multiple life domains, and in substance use patterns in particular (Dekkers et al., 2020; White, 2007 ). While early definitions equated recovery with 'remission', 'abstinence' or absence of symptoms of dependence, later conceptualisations have also ...
Insight refers to a person's understanding of themselves and the world around them. Recent literature has explored people's insight into their substance use disorder (SUD) and how this is linked to treatment adherence, abstinence rates, and comorbid mental health symptoms. The aim of this systematic review was to synthesise and critically ...
In this section, the findings from the literature review are discussed in 4 parts: definition of concept, attributes, antecedents, consequences, and method of measurement of the concept. ... The consequences of recovery from drug addiction are as follow: Sustained control over substance use: Sustained abstinence is an important consequence of ...
Following a process informed by literature located using the aforementioned keywords, we developed tentative operative and analytic categories for strengths-based practice based on correspondence to recognized values of strengths-based philosophy, namely a focus on client agency, autonomy, and self-determination in changing or maintaining one's drug use patterns (NASW Standards for Social ...
Alcohol is the most commonly used substance among adolescents, with 64% of 18 year olds endorsing lifetime alcohol use, followed by marijuana (45%) and cigarette use (31%) ( Johnston et al., 2017 ). Overall, rates of adolescent substance use have remained relatively stable over the past several years, with a few notable exceptions.
Most addiction treatment settings, mutual aid groups, and research on recovery posit that recovery is built upon a foundation of abstinence from psychoactive drugs, excluding nicotine and prescription medication [1, 2].This operationalization of recovery aligns with the Substance Abuse and Mental Health Services Administration (SAMHSA)' definition which states, "[Recovery is] a process of ...
Introduction and background. Drug misuse is a widespread issue; in 2016, 5.6% of people aged 15 to 26 reported using drugs at least once [].Because alcohol and illegal drugs represent significant issues for public health and urgent care, children and adolescents frequently visit emergency rooms [].It is well known that younger people take drugs more often than older adults for most drugs.
Substance abuse during adolescence. The use of substances by youth is described primarily as intermittent or intensive (binge) drinking and characterized by experimentation and expediency (Degenhardt et al., Citation 2016; Morojele & Ramsoomar, Citation 2016; Romo-Avilés et al., Citation 2016).Intermittent or intensive substance use is linked to the adolescent's need for activities that ...
Literature Review Drug Addiction in Prison. The epidemiology of drug addiction is complicated and the direction of causality can be difficult to tease out, but substance use disorder is statistically correlated with social disadvantage and exclusion (McPhee et al., 2019a).
Drug abuse is a serious public health problem that affects almost every community and family in some way. Each year drug abuse causes millions of serious illnesses or injuries among Americans. ... The review of the research literature below outlines the association between substance use disorders (SUD) and the various systems it affects. From ...
This literature review focuses on substance use disorder among youths under 18 and on the utilization of substance use treatment programs. ... Parker, K., Diamond, G.S., Barrett, K., and Tejeda, M. 2001. Multidimensional Family Therapy for adolescent drug abuse: Results of a randomized clinical trial. American Journal of Drug and Alcohol Abuse ...
INTRODUCTION. Substance abuse is a common phenomenon in the world and has invaded the human society as the most important social damage.[1,2] Substance abuse is a nonadaptive model of drug use, which results in adverse problems and consequences, and includes a set of cognitive, behavioral, and psychological symptoms.[]Iran also, due to its specific human and geographic features, has a ...
Indirect costs such as lost workdays. Single (1998) estimates that the law enforcement costs are 29 percent of the total of all costs incurred due to drug and alcohol abuse. Illicit drug use accounts for approximately 7.4 percent of this cost (40.8 percent due to alcohol and 51.8 percent due to tobacco).
The criminal history of the addict is used as an organizing principle for a literature review. Issues covered include the temporal relationship between crime and addiction, the criminal behavior of addicts, and the impact of treatment on this behavior. The types of crime most closely associated with addiction, and changes in criminality patterns after addiction, are discussed, and 5 general ...
This study aims to fill this gap in the literature and inform programs aimed at reducing substance use among LGB youth: Cross-sectional: Marijuana, inhalants, prescription pain medication, and other illegal drugs ... this review focused on worldwide drug abuse studies, rather than the broader context of substance abuse including alcohol and ...
2. REVIEW OF LITERATURE. Alcohol, opium and cannabis have been the traditional drugs of use in India with moderate consumption being ritualised in social gatherings. Associated major health or social problems are not obvious since several informal social controls against abuse are in place. Traditional use continues today (Ganguly et al 1995).
Our literature review synthesises two major analytical approaches explaining the drug war: as penal populism and as moral politics. Scholars describe the War on Drugs as a way of governing society through violence and with impunity for extrajudicial killings and human rights abuses, using legitimising moral discourses.
A review of directories of alcohol and drug abuse literature produced numerous magazines as well as scholarly journals. The decision was made to focus on the literature of patient care and client care, rather than the genre of alcohol and addiction in general. ... The review of the publication date ranges of the cited references in Table 3 ...