
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To The Science

Framingham Heart Study (FHS)
- At a Glance
- Key Findings
- How It's Conducted
- Related Reading
What is the goal of the FHS?
The NHLBI has a long history of supporting large population and epidemiology studies that have transformed the way the public approaches heart disease. These studies involve studying the health of various populations to uncover patterns, trends, and outcomes that may be applicable to the general population. When it launched in 1948 the original goal of the Framingham Heart Study (FHS) was to identify common factors or characteristics that contribute to cardiovascular disease. Over the years, the FHS has become a successful, multigenerational study that analyzes family patterns of cardiovascular and other diseases, while gathering more genetic information from the two generations that followed the original study participants. The FHS also has expanded to include diverse populations so that risk factors in these different groups can be understood.
AT A GLANCE
- The FHS had over 15,000 people from three generations, including the original participants, their children, and their grandchildren at the start of each cohort.
- FHS findings have informed the understanding of how cardiovascular health affects the rest of the body.
- The study found high blood pressure and high blood cholesterol to be major risk factors for cardiovascular disease.
- In the past half century, the study has produced approximately 6,000 articles in leading medical journals.
- Data and biologic resources from the study are available for researchers to use, which continue to spur new scientific discoveries.
What are the key findings of the FHS?
This research has contributed transformative discoveries related to the treatment of heart disease. Through the FHS, scientists have learned the risk factors for heart disease, and they now know that many of those risks can be changed. It is why, in routine physicals, doctors check for high blood pressure, high cholesterol, unhealthy eating patterns, smoking, physical inactivity, or unhealthy weight. Researchers also know that these conditions can affect people differently depending on a patient’s sex or race. Findings such as these pave the way for new interventions to preempt, prevent, or treat these conditions more effectively.
More Information - Framingham Heart Study (FHS)
In the past half century, the study has produced approximately 3000 articles in leading medical journals. Here are a few of the major findings from the FHS:
- 1960s: Cigarette smoking was found to increase the risk of heart disease, and cholesterol level, blood pressure, and electrocardiogram abnormalities were found to increase the risk of heart disease.
- 1970s: High blood pressure was found to increase the risk of stroke; atrial fibrillation was found to increase stroke risk five-fold; and menopause was found to increase the risk of heart disease.
- 1980s: High levels of HDL cholesterol were found to reduce risk of death.
- 1990s: An enlarged left ventricle, one of two lower chambers of the heart, was shown to increase the risk of stroke.
- 2000s: Prehypertension was associated with an increased risk of cardiovascular disease, emphasizing the need to determine whether lowering high-normal blood pressure can reduce the risk of cardiovascular disease
- 2010s: Sleep apnea was tied to an increased risk of stroke; FHS researchers identified additional genes that may play a role in Alzheimer's disease; study investigators discovered hundreds of genes underlying major heart disease risk factors.
- 2020s: Novel and known candidate genes were found to be associated with coronary artery calcification scores and heart attack using an integrative trans-omics approach; sex-based differences in inter-trait genetic and environmental correlations between cardiac structure and function were identified; atrial fibrillation was reported to be associated not only with clinical stroke but also with impaired cognitive performance and longitudinal cognitive decline.
Since its early days, the FHS has been committed to data sharing. In 1968, the FHS made massive data tables of FHS-collected measures freely available to outside researchers, many of whom lacked computing resources. NHLBI has continued to leverage FHS resources to spur new scientific discovery through data sharing.
- The NHLBI is using FHS data in the TOPMed Program to better understand the genetic and environmental factors contributing to cardiovascular disease.
- Study datasets from the FHS, including cohort examination data from the first 30 clinical exams, are available for request via NHLBI’s Biologic Specimen and Data Repositories Information Coordinating Center (BioLINCC) .
- Researchers also can request FHS genetic data, along with information about major disease risk factors (e.g., systolic blood pressure, cholesterol levels, cigarette use), in the database of Genotypes and Phenotypes (dbGaP) .
How is the FHS conducted?
When the FHS began in 1948, researchers recruited 5,209 men and women between the ages of 30 and 62 from the town of Framingham, Massachusetts. This was for the first round of extensive physical examinations and lifestyle interviews they would later analyze for common patterns related to cardiovascular disease development. Since then, the participants have continued to return to the study approximately every two to six years to give researchers a detailed medical history and to get physical exams and laboratory tests done. In 1971, the study enrolled a second generation—5,124 of the original participants' adult children and their spouses—to participate in similar examinations. In April 2002, the study entered a new phase: the enrollment of a third generation of participants, the grandchildren of the original cohort.
Researchers recognized the need to establish a new study reflecting Framingham’s more diverse communities. In 1994 they enrolled the first Omni Cohort of the Framingham Heart Study—507 men and women of African-American, Hispanic, Asian, Indian, Pacific Islander, and Native American descent. In 2003, a second group of Omni participants was enrolled. Learn more about the cohorts .
The Framingham Heart Study marked its 75th anniversary in 2023. Findings from the study over three generations of participants have changed how Americans and their doctors view heart disease and how to prevent, predict, and treat it. The study has expanded its research activities to other disease domain areas such as stroke, dementia, and impaired cognitive function. More recently, the study has investigated the impact of gut microbes on human health and leveraged new genetic, omics, emerging imaging, and machine learning/artificial intelligence tools to enhance our understanding of cardiovascular physiology through its deeply phenotyped participants and the multitude of mechanistic studies.
Related Scientific Focus Areas
Related health topics.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

The role of cardiac rehabilitation in improving cardiovascular outcomes
Rod s. taylor.
1 MRC/CSO Social and Public Health Sciences Unit & Robertson Centre for Biostatistics, Institute of Health & Well Being, University of Glasgow, Glasgow, UK
2 College of Medicine and Health, University of Exeter, Exeter, UK
Hasnain M. Dalal
3 University of Exeter Medical School (Primary Care), Smeall Building, St Luke’s Campus, Exeter, UK
Sinéad T. J. McDonagh
Cardiac rehabilitation is a complex intervention that seeks to improve the functional capacity, wellbeing and health-related quality of life of patients with heart disease. A substantive evidence base supports cardiac rehabilitation as a clinically effective and cost-effective intervention for patients with acute coronary syndrome or heart failure with reduced ejection fraction and after coronary revascularization. In this Review, we discuss the major contemporary challenges that face cardiac rehabilitation. Despite the strong recommendation in current clinical guidelines for the referral of these patient groups, global access to cardiac rehabilitation remains poor. The COVID-19 pandemic has contributed to a further reduction in access to cardiac rehabilitation. An increasing body of evidence supports home-based and technology-based models of cardiac rehabilitation as alternatives or adjuncts to traditional centre-based programmes, especially in low-income and middle-income countries, in which cardiac rehabilitation services are scarce, and scalable and affordable models are much needed. Future approaches to the delivery of cardiac rehabilitation need to align with the growing multimorbidity of an ageing population and cater to the needs of the increasing numbers of patients with cardiac disease who present with two or more chronic diseases. Future research priorities include strengthening the evidence base for cardiac rehabilitation in other indications, including heart failure with preserved ejection fraction, atrial fibrillation and congenital heart disease and after valve surgery or heart transplantation, and evaluation of the implementation of sustainable and affordable models of delivery that can improve access to cardiac rehabilitation in all income settings.
In this Review, Taylor and colleagues provide a summary of the current evidence base supporting the use of cardiac rehabilitation, an overview of international guidelines for cardiac rehabilitation and a discussion of major contemporary issues facing cardiac rehabilitation delivery around the world.
- Cardiac rehabilitation is a complex, multicomponent intervention that includes exercise training and physical activity promotion, health education, cardiovascular risk management and psychological support, personalized to the individual needs of patients with heart disease.
- Data from randomized, controlled trials support cardiac rehabilitation as a clinically effective and cost-effective intervention for patients with acute coronary syndrome or heart failure with reduced ejection fraction and after coronary revascularization.
- Despite this robust evidence base and strong guideline recommendations, global access to cardiac rehabilitation is persistently poor, with scarce cardiac rehabilitation provision in low-income and middle-income settings.
- Home-based and technology-based models of cardiac rehabilitation with appropriate quality assurance as an alternative or adjunct to traditional, centre-based programmes are needed to improve access to cardiac rehabilitation.
- Cardiac rehabilitation programmes need to cater for and manage the needs of the increasing number of patients with heart disease who present with two or more chronic diseases.
- Further research needs to strengthen the evidence base for cardiac rehabilitation in patients with heart failure with preserved ejection fraction, atrial fibrillation or congenital heart disease and after cardiac valve surgery or heart transplantation.
Introduction
Cardiac rehabilitation is a complex intervention that includes exercise training, physical activity promotion, health education, cardiovascular risk management and psychological support, personalized to the individual needs of patients with diagnosed heart disease 1 (Fig. 1 ). In addition to secondary prevention and improvement in cardiovascular prognosis, a focus of modern cardiac rehabilitation has been the drive to improve patient wellbeing and health-related quality of life 2 – 4 .

A schematic summary of the major components of comprehensive cardiac rehabilitation. Adapted by permission from BMJ Publishing Group Limited. [Advances in rehabilitation for chronic diseases: improving health outcomes and function. Richardson C.R., Franklin B., Moy M.L., Jackson E.A., 365, l2191, 2019].
Introduced in the late 1960s, the recommendation for the provision of cardiac rehabilitation was, at that time, confined to low-risk patients who had survived an acute myocardial infarction (MI). With the development of an evidence base over the past two decades supporting the benefits of cardiac rehabilitation, contemporary clinical guidelines now routinely recommend the referral to comprehensive cardiac rehabilitation across a wider range of cardiac diagnoses, including acute coronary syndrome, heart failure with reduced ejection fraction (HFrEF) and coronary revascularization (percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) surgery).
An important emphasis of contemporary guidelines, including the 2020 position statement from the European Association of Preventive Cardiology (EAPC) 5 , the 2017 guidance from the British Association for Cardiovascular Prevention and Rehabilitation 6 and the 2020 position statement from the Secondary Prevention and Rehabilitation Section of EAPC, is the importance of quality assurance in cardiac rehabilitation delivery 7 (Box 1 ). Key quality assurance elements include the involvement of a multidisciplinary team (including cardiologists, general practitioners and physicians with special interest, nurse specialists, physiotherapists, dietitians and psychologists) trained in the core competencies and effective delivery of the various core elements of a comprehensive cardiac rehabilitation programme (that is, exercise training and promotion, risk factor and self-management education, and psychological support) 1 , 6 , following a detailed initial assessment of the patient. Initially, cardiac rehabilitation was primarily practised as an exercise training intervention alone 8 . Although exercise training remains a central component of cardiac rehabilitation, the comprehensive model of modern cardiac rehabilitation is central to enabling patients to reduce their cardiovascular risk, foster and maintain their health-promotion behavioural patterns, increase their mental wellbeing, reduce their disability and promote an active lifestyle — with the overall aim of improving wellbeing and health-related quality of life. In response to the continuing evolution of cardiac rehabilitation practice and policy, this Review provides a state-of-the-art contemporary overview.
In this Review, we provide a detailed summary of the current evidence base supporting the use of cardiac rehabilitation, an overview of key international guidelines and position statements for cardiac rehabilitation and a synopsis of four key contemporary issues facing cardiac rehabilitation delivery across the globe: improving poor uptake, the effects of the coronavirus disease 2019 (COVID-19) pandemic, managing patient multimorbidity, and the provision of cardiac rehabilitation in low-income and middle-income countries (LMICs). We conclude with our recommendations for future research.
Box 1 Quality assurance standards according to BACPR 6
The British Association of Cardiopulmonary Rehabilitation (BACPR) has six standards for cardiovascular prevention and rehabilitation.
- Standard One. The delivery of six core components by a qualified and competent multidisciplinary team led by a clinical coordinator.
- Standard Two. Prompt identification, referral and recruitment of eligible patient populations.
- Standard Three. Early initial assessment of individual patient needs, which informs the agreed personalized goals, which are reviewed regularly.
- Standard Four. Early provision of a structured cardiovascular prevention and rehabilitation programme, with a defined pathway of care, which meets the individual’s goals and is aligned with patient preference and choice.
- Standard Five. Upon programme completion, a final assessment of individual patient needs and demonstration of sustainable health outcomes.
- Standard Six. Registration and submission of data to the National Audit for Cardiac Rehabilitation and participation in the National Certification Programme.
Box 1 adapted courtesy of British Association for Cardiovascular Prevention and Rehabilitation.
Overview of the evidence base
Our evidence overview is based on Cochrane systematic reviews and meta-analyses of cardiac rehabilitation. Cochrane reviews, with their rigorous methodological requirements and inclusion of only randomized controlled trials (RCTs), are internationally regarded as providing the highest quality of evidence for interventions. We focus on Cochrane reviews that compare the effects of exercise-based cardiac rehabilitation (exercise interventions alone or a comprehensive programme) with a control group (who did not receive cardiac rehabilitation). Key outcome findings (mortality, cardiovascular events, hospitalizations and health-related quality of life) for each indication are presented in Table 1 and summarized below. Researchers used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to summarize the certainty of the evidence for each outcome 9 (Box 2 ).
Evidence for cardiac rehabilitation: summary of Cochrane review findings
All outcomes are pooled outcomes at 6–12 months of follow-up, and quality assessment is based on the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system, unless otherwise stated. CABG, coronary artery bypass graft; CVD, cardiovascular disease; EQ5D VAS, EuroQoL Visual Analogue Scale; HFrEF, heart failure with reduced ejection fraction; MCS, mental component score; MD, mean difference; MI, myocardial infarction; MLwHF, Minnesota Living with Heart Failure questionnaire; NR, not reported; PCI, percutaneous coronary intervention; PCS, physical component score; RR, relative risk; SF, Short-Form; SMD, standardized mean difference. a Serious adverse events defined as any untoward medical occurrence that was life-threatening, resulting in death or that was persistent or leading to substantial disability; any medical event that had jeopardized the patient or required intervention to prevent it; any hospital admission or prolongation of existing hospital admission.
Box 2 The GRADE system
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system 9 is a framework for rating the quality of evidence, applied to each outcome in a Cochrane systematic review, because the quality of evidence often varies between outcomes. GRADE has four levels of evidence (also known as certainty in evidence or quality of evidence).
- Very low: the true effect is probably markedly different from the estimated effect.
- Low: the true effect might be markedly different from the estimated effect.
- Moderate: the authors believe that the true effect is probably close to the estimated effect.
- High: the authors have high confidence that the true effect is similar to the estimated effect.
Evidence from randomized controlled trials starts at high quality. The certainty in the evidence is increased or decreased for several reasons. Reasons why certainty can be rated down:
- Risk of bias: when the results of a study do not represent the truth because of inherent limitations in the design or conduct of a study
- Imprecision: the rating focuses on the 95% confidence interval around the best estimate of the intervention effect
- Inconsistency: assessed by similarity of point estimates and the overlap of their confidence intervals (statistical heterogeneity)
- Indirectness: if the patients or intervention studied are different from those for whom the recommendation applies or the reported outcome is a surrogate for a different outcome
- Publication bias: when the trial outcome influences the decision whether to publish or otherwise distribute the finding
Reasons why certainty can be rated up:
- Large magnitude of effect
- Dose–response gradient
Coronary heart disease
The 2021 update 10 of the 2016 version 11 of the Cochrane review of cardiac rehabilitation for coronary heart disease included 23,172 patients with MI (40 RCTs) or stable angina pectoris (five RCTs), after revascularization (14 RCTs) or in mixed populations. Meta-analysis of trials with outcomes up to 12 months of follow-up showed no effect of cardiac rehabilitation compared with control on all-cause mortality or the risk of revascularization. Participation in cardiac rehabilitation resulted in reductions in the risk of fatal or non-fatal MI and all-cause hospitalization. Although 29 trials collected health-related quality-of-life data, pooling of data was limited owing to variation in the outcome measures. Pooled analysis across three trials showed that cardiac rehabilitation improved generic health-related quality of life, assessed with the Short-Form 36 or 12 (mental component score), but had weak evidence of an improvement in the physical component score. Twenty of the 29 trials reported higher levels of health-related quality of life in one or more subscales with exercise-based cardiac rehabilitation than with control at follow-up. Outcome evidence assessed by GRADE was judged to be of ‘moderate’ certainty, downgraded owing to poor reporting on the randomization process (selection bias), lack of blinding (detection bias) and wide 95% confidence intervals (imprecision). Meta-regression (trial-level) analyses indicated that the benefits of cardiac rehabilitation seemed to be consistent across types and settings of cardiac rehabilitation (home versus centre, exercise-only versus comprehensive cardiac rehabilitation programmes, aerobic versus aerobic plus resistance training, dose of aerobic exercise) and study characteristics (single-centre versus multicentre).
This Cochrane review has been criticized for the inclusion of older RCTs that might not reflect contemporary practice and studies that might not have used robust quality assurance in terms of the delivery of the cardiac rehabilitation intervention — for example, the UK-based, multicentre RAMIT trial 12 , 13 . Given that trials included in the Cochrane review span the period 1974–2020, the authors sought to address this issue by undertaking an assessment of the change in cardiac rehabilitation outcome over time. Interestingly, weak evidence exists of a reduction (slope 1.005, 95% CI 0.0098–1.0118, P = 0.13) in the all-cause mortality effect (log relative risk) of cardiac rehabilitation over time (Fig. 2 ). The authors interpreted this absence of an improvement in the effect of cardiac rehabilitation on all-cause mortality over the past 2–3 decades as reflecting the evolution of usual care and the introduction of life-saving therapies, including thrombolysis and secondary prevention drugs, such as β-blockers and statins. Interestingly, the 2020 meta-analysis of the CROSII study 14 , which included RCTs and prospective and retrospective cohort studies, reported a reduction in mortality with cardiac rehabilitation in patients with acute coronary syndrome or after revascularization, with an index event in 1995 or later. However, with the inclusion of observational evidence, the prognostic benefit reported by the CROSII study is subject to selection bias and confounding.

Meta-regression analysis of the treatment effect of cardiac rehabilitation on all-cause mortality over time in patients with coronary heart disease. The area of each data point is inversely related to the standard error of log relative risk (RR). The absence of an improvement in the effect of cardiac rehabilitation on all-cause mortality over the past 2–3 decades might reflect the evolution of usual care and the introduction of life-saving therapies, including thrombolysis and secondary prevention drugs.
Heart failure
A 2019 Cochrane review of cardiac rehabilitation in heart failure included 44 RCTs in 5,783 participants, predominantly with HFrEF 15 . This meta-analysis showed that participation in cardiac rehabilitation was associated with reduced rates of all-cause and heart-failure-specific hospitalization and improved health-related quality of life compared with control, whereas no significant effect of cardiac rehabilitation on all-cause mortality was detected. Pooled data across the 17 trials reporting the Minnesota Living with Heart Failure questionnaire (a disease-specific, health-related quality-of-life measure) showed not only a significant improvement with cardiac rehabilitation (mean difference –7.1, 95% CI −10.5 to –3.7), but also a magnitude of effect that is deemed ‘clinically important’ (an increase in the score by ≥5 points, compared with control) 16 . Certainty of outcomes was judged to be low to moderate, downgraded primarily owing to selection bias, imprecision (wide 95% confidence intervals or lack of events) and detection bias or placebo effects (health-related quality of life). Meta-regression analyses indicated that the benefits of cardiac rehabilitation for heart failure were consistent, irrespective of the nature of the cardiac rehabilitation or the setting.
Atrial fibrillation
The 2017 Cochrane review of cardiac rehabilitation in atrial fibrillation included six RCTs in 421 patients with various types of atrial fibrillation 17 . Given the small number of trials and reported clinical events, the effect of cardiac rehabilitation in this patient population in terms of the key outcomes of mortality, cardiovascular events, hospitalizations and health-related quality of life are all uncertain, with moderate to very low certainty (downgraded primarily owing to imprecision as a result of the small evidence base). Peak oxygen uptake (aerobic exercise capacity) was, on average, 3.76 ml/kg/min (95% CI 1.37–6.15 ml/kg/min) higher with cardiac rehabilitation than with the control (moderate quality of evidence).
Congenital heart disease
The 2020 Cochrane review focused on physical activity interventions across 15 RCTs in 924 adults and children with various forms of congenital heart disease 18 . Owing to the absence of trials reporting events, the authors concluded that there was no basis to determine the effect of cardiac rehabilitation in terms of either mortality or hospitalizations. In addition, evidence supporting the effect of cardiac rehabilitation on health-related quality of life was uncertain (very low quality of evidence owing to a small evidence base). Small improvements in both peak oxygen uptake (mean difference 1.89 ml/kg/min, 95% CI 0.22–3.99 ml/kg/min; 14 trials, 732 patients) and muscle strength (mean difference 17.1 N/m, 95% CI 3.4–30.8 N/m) were reported with cardiac rehabilitation (both moderate quality of evidence).
After cardioverter–defibrillator implantation
The 2019 Cochrane review included eight RCTs in 1,730 individuals with an implanted cardioverter–defibrillator, primarily for an indication of heart failure 19 . Owing to the small number of trials and reported events, the effect of cardiac rehabilitation on mortality, adverse events and health-related quality of life were all uncertain (low to very low quality of evidence). Low-quality evidence indicated that participating in cardiac rehabilitation resulted in a small increase in exercise capacity (determined by peak oxygen uptake) compared with control (mean difference 0.91 ml/kg/min, 95% CI 0.60–1.21 ml/kg/min; seven trials, 1,485 patients).
After heart transplantation
The 2017 Cochrane review included ten RCTs in 300 individuals after heart transplantation 20 . Cardiac rehabilitation increased peak oxygen uptake compared with the no-exercise control group (mean difference 2.5 ml/kg/min, 95% CI 1.63–3.36 ml/kg/min; nine trials, 284 patients, moderate quality of evidence). Although a meta-analysis was not possible owing to the lack of consistency of outcome reporting, the three individual trials that reported health-related quality of life showed no consistent advantage of cardiac rehabilitation over control. Owing to the small number of trials and reported events, a meta-analysis was not undertaken, and the effect of cardiac rehabilitation on all-cause mortality and hospitalizations was uncertain.
After valve surgery
The 2021 Cochrane review included six RCTs in 364 patients who had received either open or percutaneous heart valve surgery 21 . Owing to the lack of trials and outcome data, the authors were unable to conclude definitively the effect of cardiac rehabilitation in this population in terms of mortality, hospitalization or health-related quality of life (all very low quality of evidence). Cardiac rehabilitation increased peak oxygen uptake for all but the submaximal measures (mean difference 2.38 ml/kg/min, 95% CI 0.36–4.40 ml/kg/min; five trials, 294 patients, moderate quality of evidence) compared with no exercise.
General quality of evidence
Although systematic reviews and meta-analyses of RCTs are the gold standard for establishing the effects of intervention, a consistent limitation identified across the Cochrane reviews was the potential risk of bias and lack of consistency of outcomes reported by RCTs on cardiac rehabilitation to date. Therefore, improvement in the certainty of the evidence base for cardiac rehabilitation in the future depends on the conduct and reporting of high-quality RCTs, including the consistent collection and reporting of outcome measures, such as health-related quality of life (Box 3 ). It is important to recognize the limitations of meta-regression analyses and that this analysis can be subject to ecological fallacy, that is, study-level assessment of the relationships between study characteristics and patient outcomes does not necessarily reflect the true (patient-level) association 22 . For example, both meta-regression analyses reported in the Cochrane reviews on coronary heart disease and heart failure indicate that the benefit of cardiac rehabilitation is not affected by the study-level dose of exercise prescription. However, other (patient-level) data show that the dose of exercise is very important and that cardiac rehabilitation might result in no benefits when the prescription of exercise is too low in intensity or is of insufficient duration 23 , 24 . A more detailed review on this topic was published previously 5 .
Although developing areas for the application of cardiac rehabilitation, such as cardio-oncology and patients with left ventricular assist devices or spontaneous coronary artery dissection, have not been the subject of a Cochrane review, reviews of the evidence base for cardiac rehabilitation in these indications have been reviewed previously 25 – 27 .
Box 3 Future research recommendations
The following key priorities for future cardiac rehabilitation research are drawn from current Cochrane reviews, clinical guidelines and other sources cited in this Review. These priorities apply to the following indications: heart failure with preserved ejection fraction, stable angina pectoris, atrial fibrillation, congenital heart disease and heart transplantation.
- Future evidence collection should take the form of well-reported, large, multicentre, randomized, controlled trials, adequately powered and deemed high in quality and low in risk of bias, and should collect data on key outcomes, including mortality, hospitalization, health-related quality of life, health-care and societal costs and cost-effectiveness.
- Given the current suboptimal uptake of cardiac rehabilitation, future trials of alternative models of cardiac rehabilitation delivery that can improve patient access and adherence are needed, including home-based and mobile, computer and digital technology-assisted programmes, as an alternative to or alongside traditional, centre-based models of delivery, especially for marginalized groups, for example, elderly individuals, women, and those from ethnic minorities and socioeconomically deprived groups. These trials need to consider assessing the patient-level and system-level outcome, including safety, costs and the quality assurance of programme delivery.
- Development and evaluation of rehabilitation programmes that serve the needs of patients with cardiac disease who present with multimorbidity (the presence of two or more long-term conditions).
- Development and evaluation of affordable and sustainable cardiac rehabilitation for patients with cardiac disease in low-income and middle-income countries.
Cost-effectiveness
In addition to clinical efficacy (‘effectiveness’) and safety, with the growing cost pressures on health-care systems across the world, the costs and cost-effectiveness of cardiac rehabilitation need to be considered. A 2018 systematic review of the cost-effectiveness of cardiac rehabilitation identified 19 economic studies 28 . Seven of these studies compared cardiac rehabilitation with no cardiac rehabilitation and the remaining studies compared intervention types within cardiac rehabilitation, for example, home-delivered or digitally delivered versus centre-based programmes. To facilitate comparison across studies, the authors converted all costs into 2016 US$, with the use of the consumer price index and purchasing power parity conversion. Most of the studies concluded that cardiac rehabilitation was cost-effective compared with no cardiac rehabilitation (incremental cost-effectiveness ratios (ICERs) ranged from US$1,065 to US$71,755 per quality-adjusted life-year (QALY)). In the UK, an acceptable level of cost-effectiveness is judged to be intervention with an ICER between £20,000 and £30,000 per QALY or lower, that is, ~US$25,000 to ~US$45,000 per QALY or lower 29 . Although generally cost-effective, the authors of the review concluded that further research was required to determine the most cost-effective design of cardiac rehabilitation, for example, a comparison of the cost-effectiveness of different modes of delivery (centre-based, home-based or using mobile technology) and combinations of interventions.
Clinical guideline recommendations
Reflecting the RCT evidence presented above, current clinical guidelines consistently provide a strong recommendation for cardiac rehabilitation referral for patients with MI or heart failure and after revascularization (CABG surgery or PCI). Table 2 summarizes the guideline statements from the ESC 30 , 31 , AHA/ACC 32 , 33 , National Institute for Health and Care Excellence (NICE) 34 , 35 in the UK, and National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand 36 , 37 .
Cardiac rehabilitation recommendations in international guidelines for CHD and HF
ACS, acute coronary syndrome; CCS, chronic coronary syndrome; CHD, coronary heart disease; CSANZ, Cardiac Society of Australia and New Zealand; HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; HRQOL, health-related quality of life; LVEF, left ventricular ejection fraction; NHFA, National Heart Foundation of Australia; NICE, National Institute for Health and Care Excellence; PCI, percutaneous coronary intervention. a Includes ACS, acute myocardial infraction, post-revascularization, stable angina and PCI. b Unlike other guidelines, evidence informing the UK NICE guidance is assessed based on Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria and the class/level approach is not used. c Includes HFrEF and HFpEF. AHA/ACC guidelines adapted with permission from refs 32 , 33 , Elsevier. NICE guidelines adapted with permission from refs 34 , 35 , NICE. NHFA/CSANZ guidelines adapted with permission from refs 36 , 37 , Wiley.
European, US and Australian/New Zealand guidelines all give cardiac rehabilitation their highest recommendation (class I: evidence and/or general agreement that a given treatment or procedure is beneficial, useful and effective and should be recommended) on the basis of an evidence rating of level A (data derived from multiple RCTs or meta-analyses) or level B (data derived from a single RCT or large non-randomized studies). The NICE recommendations are based on both clinical effectiveness and cost-effectiveness. Although these latter recommendations do not use the class and level approach, a strong recommendation for cardiac rehabilitation is made.
Given the small number of RCTs in patients with stable angina or heart failure with preserved ejection fraction, the European and Australian/New Zealand recommendations focus on HFrEF, and a level B rating is given for angina by the AHA/ACC. These guidelines recommend the need to conduct further research in these indications. The importance of a comprehensive nature of modern cardiac rehabilitation delivery is emphasized by the UK NICE guidance, recommending that programmes comprise physical activity, lifestyle advice, stress management and health education components.
Given the current underuse (referral and uptake) of cardiac rehabilitation services, with only a minority of eligible patients participating in cardiac rehabilitation over the past decade, the clinical guidelines emphasize the importance of alternative models of cardiac rehabilitation delivery to the traditional, centre-based programmes. The Australian/New Zealand, UK and US guidance all include a formal recommendation for consideration of home-based delivery to improve access to cardiac rehabilitation. The 2019 American Association of Cardiovascular and Pulmonary Rehabilitation, AHA and ACC joint scientific statement notes that although home-based cardiac rehabilitation is a common model in Canada and Europe, it is less common in the USA and emphasizes the need for quality assurance for the delivery of home-based cardiac rehabilitation programmes in their country 38 .
Given the more limited RCT evidence, current guidelines for the management of other cardiac indications, such as atrial fibrillation and congenital heart disease, provide no strong recommendation for or against the use of cardiac rehabilitation. Future high-quality RCTs of cardiac rehabilitation in these indications are needed to inform future guideline updates and clinical policy and practice. Although not the focus of this Review, a previous comparison of cardiac rehabilitation guidelines provides details of the differences and consensus in recommendations for exercise testing, prescription and monitoring 39 .
Major contemporary issues
Improving poor uptake.
Despite the evidence for benefits of cardiac rehabilitation and strong guideline recommendations, the uptake of cardiac rehabilitation remains poor. Although the availability of cardiac rehabilitation is virtually absent in some global localities, in many areas, including Europe, North America and Australasia, a fairly small proportion of patients with acute coronary syndrome or HFrEF or who have undergone revascularization are currently referred for cardiac rehabilitation.
The latest data from the 2019 UK National Audit of Cardiac Rehabilitation (NACR) reported that 68,074 out of 135,861 (50%) individuals with a main diagnosis of coronary heart disease received cardiac rehabilitation (MI 29%, PCI 51% and CABG surgery 75%) 40 . For heart failure, the national level of cardiac rehabilitation attendance was <10% 40 . Cardiac rehabilitation participation rates in the USA are very low, ranging from 19% to 34% in national analyses, with large state-by-state geographical variations and differences according to cardiac diagnosis 41 . Consistent with the findings of many national and single-centre studies of cardiac rehabilitation, the 2019 UK NACR data show that certain groups are much less likely to attend cardiac rehabilitation than others, that is, older individuals, women, non-white and ethnic minority groups and patients with multimorbidity (defined as the presence of two or more long-term conditions) 40 .
The basis of suboptimal uptake of cardiac rehabilitation is complex and multilayered and reflects potential barriers at the level of the clinician, the patient and the health service (Table 3 ). At the clinician level, the absence of education on cardiac rehabilitation in their general medical and cardiology training might result in the low rate of referral by physicians 41 – 43 . For patients, a range of factors might influence their individual decision to act on this referral and attend a cardiac rehabilitation programme, such as inconvenience (and costs) of transport to attend a centre-based programme held during the ‘9–5’ working day, especially if these individuals are in employment. At the health service level, barriers can include the capacity and funding of cardiac rehabilitation programmes. For example, the 2019 UK NACR showed that group-based, supervised cardiac rehabilitation was the most common mode of delivery of cardiac rehabilitation, with 75.4% of patients receiving this method of cardiac rehabilitation compared with only 8.8% taking up home-based cardiac rehabilitation 40 . Barriers at these three levels are probably interactive. For example, travelling to centres and a dislike of group-based cardiac rehabilitation sessions are known to be particularly relevant for certain groups of patients, including women, ethnic minorities and people from areas of high deprivation who are elderly, living with complex health conditions or living in rural areas 42 , 43 . Cardiac rehabilitation is a crucial environment to contribute to the optimization of a patient’s cardiovascular risk, with opportunities for screening, education and medical treatment (exercise, nutrition, smoking cessation and medications). Despite these potential benefits of risk-factor reduction, the results from the EUROASPIRE III study 44 indicated the underuse of cardiac rehabilitation, with poor referral and low participation rates and wide variations between European countries. Some of the key proposed solutions to these patient, clinician and health service barriers to accessing cardiac rehabilitation are summarized in Box 4 .
Barriers to accessing CR and potential solutions
CR, cardiac rehabilitation. Adapted from ref. 43 , CC BY 4.0 ( https://creativecommons.org/licenses/by/4.0/ ).
Given that the potential loss to patients of important gains in health-related quality of life and the rise in pressures and costs on health-care systems as a result of increased unplanned hospitalization, poor participation (uptake) of cardiac rehabilitation is an increasingly important policy priority. For example, in the UK, the NHS England Long Term Plan 45 was published in 2019, with the aim to increase the overall national uptake of cardiac rehabilitation to 85% (from the current 50%) of all eligible patients by 2028. In the USA, a road map was proposed to achieve >70% participation in cardiac rehabilitation by 2022, with the aim of saving 25,000 lives and preventing 180,000 hospitalizations per year 46 .
An example of innovative service development is the Rehabilitation Enablement in Chronic Heart Failure (REACH-HF) programme of facilitated cardiac rehabilitation. This comprehensive programme of cardiac rehabilitation for use at home comprises a heart failure manual, a relaxation CD, a choice of exercise (walking programme or a chair-based DVD), a progress tracker for patients, and a family and friends resource for caregivers. A UK-based, multicentre RCT in 216 individuals with HFrEF confirmed that the addition of REACH-HF to usual care compared with usual care alone was effective in improving the primary outcome of health-related quality of life, which was assessed using the Minnesota Living with Heart Failure questionnaire (–5.7 points, 95% CI −10.6 to −0.7 points, P = 0.025) 47 . Subsequent economic modelling on the basis of the results from the trial confirmed the acceptable cost-effectiveness of the REACH-HF programme, with an ICER of £1,720 per QALY 48 . Given its clinical effectiveness and cost-effectiveness, the REACH-HF programme is now being rolled out into routine care across the UK and the Republic of Ireland to improve access to and uptake of cardiac rehabilitation 49 , 50 .
A growing body of research now shows that home-based models of cardiac rehabilitation delivery achieve similar gains in patient efficacy and safety to traditional, centre-based programmes at similar cost-effectiveness and, indeed, might lead to higher levels of patient adherence 51 , 52 . As with many previous trials of cardiac rehabilitation, studies of home-based cardiac rehabilitation have focused on low–moderate risk populations. Several cardiac rehabilitation programmes are now using a hybrid approach to deliver cardiac rehabilitation. For example, this approach initially offers patients centre-based cardiac rehabilitation and then evolves to longer-term maintenance through technology-supported, home-based sessions 53 . The effectiveness of these innovative models is likely to depend on active, ongoing contact between patients and health-care professionals through more traditional methods, such as home visits and telephone consultations, or the use of technology-based solutions, which include web-based video calls and social networking platforms 54 .
Box 4 Strategies to facilitate increased referral to and enrolment and long-term participation in CR programmes
- Achieve strong endorsement of cardiac rehabilitation (CR) by referring clinicians (cardiologists, physicians and health-care professionals) by incorporating it into the hospital discharge plan.
- Automatically refer all eligible patients for CR at the time of hospital discharge — giving patients a choice to attend a centre-based or home-based hybrid programme.
- Provide CR information (printed and web links or videos) and education to inpatients before discharge from hospital.
- Ensure good communication with the patient’s primary care physician or general practitioner so they are sent the discharge details with information on CR programmes — giving the option of centre-based CR or home-based CR (for low-to-moderate-risk patients) or a hybrid programme.
- Schedule CR enrolment appointments via the patient’s preferred communication mode (telephone call, text message, e-mail or post).
- Advise the patient’s primary care physician or general practitioner to refer patients for CR if the patient has not been referred — encouraging enrolment and participation.
- Consider system-level, provider-level and patient-level financial incentives for referral to, enrolment in and completion of CR sessions.
- Target and identify racial and ethnic minorities, women, older adults, and rural and socioeconomically deprived groups who are least likely to enrol in and complete CR.
- Encourage long-term support through trained health-care professionals using face-to-face or web-based applications to track ongoing efforts for cardiovascular risk reduction, including physical activity and fitness, for example, by the primary-care team.
Box 4 adapted with permission from ref. 38 , Elsevier.
Effects of the COVID-19 pandemic
The COVID-19 pandemic has had a major global effect on the use and delivery of health and health-care systems. As we write this Review, the UK has become the first European country to officially record >125,000 deaths associated with COVID-19. Although vaccine rollout has begun, many countries across the world are having to take various public-health measures to suppress virus transmission rates, including lockdown measures, provision of social distancing guidance, track and trace of individuals with COVID-19 and quarantining of travellers between one country and another 55 .
Worse COVID-19 outcomes and increased risk of death are linked to pre-existing cardiovascular disease 56 – 58 , and these individuals are advised to shield or self-isolate at home to minimize the risk of infection 59 . The pandemic has led to the disruption of many hospital services, including non-urgent outpatient appointments and routine ambulatory care, which have been curtailed or minimized. For cardiac rehabilitation, the pandemic has accentuated existing barriers to access discussed above (Table 3 ). In Canada, the USA and Europe, many cardiac rehabilitation centres have been closed, with some countries observing an overall reduction in cardiac rehabilitation participation 60 , 61 . In addition, cardiac rehabilitation capacity has been reduced because rehabilitation staff are being deployed to the ‘front line’ of intensive medical care for COVID-19. The increased risk of infection can lead to patients with diagnosed heart disease being anxious about travelling to centres to undertake rehabilitation. The dramatic effect of the pandemic on access to cardiac rehabilitation is illustrated by the British Heart Foundation NACR 61 , which has observed more than a two-thirds decrease in cardiac rehabilitation attendance in patients with heart failure from the pre-COVID period (4,969 patients in May 2019 to January 2020) to the COVID period (1,474 patients in February 2020 to August 2020). However, this drop in uptake was associated with a substantial increase in the proportion of patients enrolling in home-based cardiac rehabilitation programmes, which increased from 22.2% to 72.4% in the same time frame.
Conventional cardiac rehabilitation services that have relied on patients attending group-based sessions in hospitals or community centres have been difficult to sustain, and renewed calls have been made for alternatives to centre-based cardiac rehabilitation 59 , 60 . Even before the outbreak of COVID-19, the uptake of cardiac rehabilitation in many countries was suboptimal.
As described above, increasing evidence supports the effectiveness and safety of mobile-technology-supported models of delivery 62 – 64 , which are recommended in international guidelines 34 – 54 and receive reimbursement from external agencies 65 . Endorsement of remote delivery of cardiac rehabilitation in the COVID-19 era has come from various international sources 47 , 48 , 54 , 55 , 60 , 61 , 66 , 67 . EAPC has made an emphatic call for cardiac tele-rehabilitation to maintain the delivery of the core components of cardiac rehabilitation and has provided a practical guide for the set-up of a comprehensive cardiac tele-rehabilitation intervention during the COVID-19 pandemic 60 . However, concerns have been raised about equity in the use of technology to maintain access to outpatient care. Lower rates of technology and Internet use and access to these facilities have been documented in elderly individuals, those of lower socioeconomic status and ethnic minorities, mirroring the groups associated with limited enrolment and low levels of participation in cardiac rehabilitation 68 , 69 . In a cohort study of 2,940 patients scheduled to attend cardiology clinics at one centre in the USA in 2020, those individuals with lower income and who were non-English-speaking, female and/or older had more difficulty in engaging in care via telemedicine, suggesting that its rapid adoption exacerbates existing inequities 70 , 71 .
The pandemic has prompted providers of cardiac rehabilitation to seriously consider remote models of delivery, so that patients with heart disease can follow a self-care rehabilitation programme from their own home, which could also include support from their family and friends. A beacon model of innovative, evidence-based service delivery in the UK during the pandemic has been the REACH-HF programme 72 .
Managing multimorbidity
Cardiac rehabilitation has traditionally been commissioned and delivered as a ‘single disease’ service and focuses on the needs of patients with MI or heart failure or who have undergone revascularization. Although referred for cardiac rehabilitation for a specific indication, patients do not typically present with their single index disease alone, but instead have several long-term comorbidities. For example, the large, US-based, multicentre, randomized, controlled HF-ACTION trial 73 of cardiac rehabilitation reported that in addition to an index diagnosis of heart failure, at entry to the study, a substantial proportion of the 2,331 patients with heart failure had several comorbidities, including 59% with hypertension, 21% with atrial fibrillation or flutter and 32% with diabetes mellitus. The 2019 UK NACR reported that approximately 50% of all 6,502 patients referred for cardiac rehabilitation had two or more comorbidities 40 .
The management of multimorbidity is an important challenge facing health-care systems 74 . Levels of multimorbidity are predicted to grow with population demographic changes and improved survival rates resulting in increased numbers of older individuals 75 , 76 . Importantly, patients with multimorbidity are at higher risk of dying prematurely, being admitted to hospital, having longer stays in hospital and having a reduced health-related quality of life 75 , 76 than patients with only one chronic medical condition. The presence of multimorbidity seems to affect the provision of cardiac rehabilitation services. The 2019 UK NACR data set showed that multimorbidity was a strong risk factor for both non-use of cardiac rehabilitation and programme non-completion 40 . For example, a higher proportion of non-completers have symptoms of anxiety (5% higher) and depression (8% higher) than completers 77 .
The increasing burden and complexity of multimorbidity challenge our traditional model of cardiac rehabilitation. Although a core component of cardiac rehabilitation is a detailed patient assessment that includes the assessment of comorbidity, with its focus on single-disease management instead of individualized or personalized care, the delivery of existing programmes of cardiac rehabilitation might be failing to meet the health needs of patients with cardiac disease and multimorbidity. These patients have a high risk of non-referral to a cardiac rehabilitation programme. Furthermore, even if they are referred to rehabilitation, a high risk exists that the programmes will not fully address the needs of patients with multimorbidity. Instead, we need to adapt to the change in population demographics and look to provide a model of personalized multimorbidity rehabilitation that meets the needs of patients, irrespective of their index diagnosis, cardiovascular or otherwise. Arguments for this multimorbidity rehabilitative model approach are summarized in Box 5 .
Although a move to a model of cardiac rehabilitation that more comprehensively addresses the needs of patients with heart disease and their multimorbidity is appealing, the evidence base for innovation remains limited. At present, only two small, developmental studies have specifically focused on multimorbidity rehabilitation. A pilot RCT evaluated the feasibility of 8 weeks of a ‘generic rehabilitation’ programme of supervised exercise and education (based on the principles of cardiac rehabilitation and pulmonary rehabilitation) or no rehabilitation control in 16 patients with multimorbidity at a single centre in Australia 78 . The researchers reported that 71% of patients completed the rehabilitation intervention and had a higher mean improvement in 6-min walking distance than the control population (44 m versus 23 m) 78 .
The Healthy and Active Rehabilitation Programme (HARP) was established in Ayrshire, Scotland, in 2015 (ref. 79 ). The HARP model was developed to focus specifically on deprived and rural communities and those with high unscheduled care demand (that is, cardiac or pulmonary disease, cancer, stroke, diabetes and/or a high risk of falls). Developed from existing models of cardiac rehabilitation and pulmonary rehabilitation, HARP is based on a comprehensive patient assessment followed by a 10-week exercise and education programme. Interviews with patients with multimorbidity indicated that the HARP programme was well received and was perceived to improve confidence and motivation for physical activity and other healthy behaviours.
In the absence of an established evidence base, an urgent need exists for research into the acceptability, efficacy and cost-effectiveness of personalized models of rehabilitation for multimorbidity. Although we should not abandon our existing cardiac rehabilitation practice, there remains the challenge of more comprehensively meeting the needs of patients with cardiac disease and multimorbidity and developing a robust evidence base around these developments. A 2020 editorial identified key research questions around the future evolution of cardiac rehabilitation services for multimorbidity 80 .
Box 5 Adapting the traditional model of cardiac rehabilitation
Advantages of adapting the traditional (single-index) cardiac rehabilitation model for patients with multimorbidity 80 .
Sustainability
In the current financially challenged health service, health-care commissioners and purchasers are likely to consider the expansion of disease-specific rehabilitation services as inefficient and unsustainable. Instead, they would be more attracted to a programme that caters for patients with multimorbidity as a more appropriate and cost-effective model of care.
The failure to consider the effect of multimorbidity on the wellbeing and functionality of the patient and, for example, ‘just rehabilitate their heart failure’ is likely to diminish greatly the potential benefits of rehabilitation. Given that candidate patients for pulmonary and cardiac rehabilitation commonly have multiple chronic conditions, many of the important clinical problems that these patients face are probably not directly related to their cardiac or respiratory disease. We know from qualitative research that treating one condition at a time is inconvenient and unsatisfactory for patients with chronic conditions.
Inclusivity
Personalized multimorbidity rehabilitation presents an opportunity to develop a model by which to extend services to other important long-term conditions that would be amenable to rehabilitation, such as atrial fibrillation. Furthermore, this model could be extended to include other patient groups with, for example, transient ischaemic attack, mild stroke or peripheral vascular disease.
Box 5 adapted with permission from ref. 80 , Oxford University Press.
Improving access in LMICs
It is estimated that by 2030, more than 80% of cardiovascular-related disability and death will occur in the 139 LMICs owing to increasing prevalence of risk factors, such as hypertension, smoking, diabetes and obesity 81 , 82 . Although secondary prevention strategies are vitally important to stemming this growing epidemic, cardiac rehabilitation programmes remain largely non-existent in the LMIC setting compared with high-income economies.
The global inequality in cardiac rehabilitation provision was quantified by the International Council of Cardiovascular Prevention and Rehabilitation (ICCPR) audit 83 . Published in 2019, this ICCPR study revealed that cardiac rehabilitation is available in only half of the countries of the world, and this geographical distribution of cardiac rehabilitation is negatively correlated with the incidence of ischaemic heart disease, according to the Global Burden of Disease study 84 (Fig. 3 ).

a | Age-standardized incidence of ischaemic heart disease. b | Total number of cardiac rehabilitation (CR) programmes per country. CR is available in only approximately half of the countries of the world and, in broad terms, the geographical distribution of CR is negatively correlated with the incidence of ischaemic heart disease. Data from ref. 83 .
This inequality is put into sharp focus by the contrasting densities in cardiac rehabilitation provision of only one cardiac rehabilitation place available for every 66 patients with ischaemic heart disease in LMICs, compared with one place for every 3.4 patients in high-income counties 85 . For example, Bangladesh has only one cardiac rehabilitation programme across the whole country, whereas England has more than 200 cardiac rehabilitation programmes, despite a similar annual incidence of ischaemic heart disease (409,000 versus 318,284, respectively). Although the barriers to the availability of cardiac rehabilitation are complex (Table 3 ), crucial additional economic constraints include limited health-care system budgets plus the consequent need for patient out-of-pocket payment, for which public funding is not available or is limited 43 .
Although the evidence demonstrating the beneficial effects of cardiac rehabilitation to date has mainly been collected in RCTs conducted in high-income settings, there is now a growing body of literature from developing countries. An ongoing systematic review has identified 26 RCTs of cardiac rehabilitation in 6,380 patients (primarily with ischaemic heart disease or heart failure) conducted across eight LMICs (Bangladesh, Brazil, China, Egypt, India, Iran, Nigeria and Pakistan) 86 . Meta-analysis of these trials conducted in LMICs shows that the increase in exercise capacity with cardiac rehabilitation (mean increase in peak oxygen uptake of 3.1 ml/kg/min, 95% CI 2.6–3.6 ml/kg/min) compared with the control population who received no cardiac rehabilitation was similar to figures reported in trials of cardiac rehabilitation conducted in high-income countries (3.3 ml/kg/min, 95% CI 2.6–4.0 ml/kg/min) 87 .
A systematic review of economic evaluations of cardiac rehabilitation in LMICs found no studies from low-income countries 88 . However, five studies in middle-income settings in Latin America indicated that cardiac rehabilitation could be a cost-effective intervention. In Brazil, the mean cost per patient was US$503 for a 3-month cardiac rehabilitation programme, with a mean monthly saving in health-care costs of US$190 for cardiac rehabilitation, compared with an increase of US$48 in the control group receiving no cardiac rehabilitation. Given the limited health-care budgets in many LMICs, the researchers of this study emphasized the need for affordable cardiac rehabilitation models in this setting 89 .
Box 6 provides a case example of the development of cardiac rehabilitation in the LMIC setting of Bangladesh 90 . Expansion of cardiac rehabilitation services is urgently needed to mitigate the epidemic of cardiovascular diseases in LMICs. Unlike high-resource settings, in which cardiac rehabilitation has traditionally been delivered in the hospital setting, often with a team of highly specialist staff, considerations of affordability, scalability and the needs of the local populations and health-care systems demand alternative approaches for the provision of cardiac rehabilitation services in LMICs. This alternative approach includes home-based and community-based programmes supported by accessible digital technology (such as Internet and mobile phone accessibility) and cost-effective training programmes for health-care staff to ensure the quality of delivery of cardiac rehabilitation practice 91 , 92 . An imperative on the global health community is to incorporate novel cardiac rehabilitation delivery models into efforts directed at the secondary prevention of cardiovascular disease, in line with the WHO’s dual strategic targets of reducing mortality from non-communicable diseases by 25% by 2030 and overcoming the ever-increasing unmet need for rehabilitation worldwide, which is particularly profound in LMICs 93 , 94 .
Box 6 Case example: cardiac rehabilitation in Bangladesh
In the past 10 years, Bangladesh has expanded the number of cardiovascular care facilities and improved service quality throughout the country. These facilities are run by public, private and autonomous sectors and include dedicated cardiac institutions and multi-speciality institutions with cardiac care facilities, with most located in the capital, Dhaka. Although the number of acute cardiac care facilities has increased, currently only one hospital-based cardiac rehabilitation programme is available in Bangladesh, based at the Ibrahim Cardiac Hospital & Research Institute (ICHRI).
From 2010, ICHRI introduced an exercise-based and education-based multidisciplinary cardiac rehabilitation programme for patients after cardiac surgery, consisting of a 30-min group exercise programme supported with a leaflet on sternum protection containing advice that can be followed at home. A single-centre, quasi-randomized controlled trial indicated that this cardiac rehabilitation programme was feasible and had potential benefits in terms of coronary heart disease risk factors, health-related quality of life, mental wellbeing and exercise capacity 90 . Following a 12-month clinical fellowship in Denmark and the UK in 2015, Jamal Uddin (a senior physiotherapist) started a comprehensive cardiac rehabilitation programme at the ICHRI. This programme consists of a group exercise programme from the seventh postoperative day, a risk-factor management educational class, dietary advice from dietitians and a manual to allow participants to maintain home-based cardiac rehabilitation. The manual includes upper-limb and lower-limb exercises, breathing exercises and aerobic exercise (a walking programme). The ICHRI also offers a 1-year cardiac rehabilitation follow-up (three follow-up visits within 1 year). During this follow-up, the patient first visits the cardiology unit and then the physiotherapy and cardiac rehabilitation unit for a cardiac fitness test and receives complete instructions for following an exercise programme.
A stakeholder round-table meeting was held in Dhaka on 30 November 2019: researchers, clinicians, health-care professionals and health-care policy-makers met to discuss affordable, flexible and feasible ways to scale up cardiac rehabilitation provision in Bangladesh and South Asia. This round-table meeting called for three key actions: expand and increase the reach of cardiac rehabilitation services through centre-based and home-based cardiac rehabilitation programmes; emphasize the importance of involving more cardiologists and cardiac surgeons to refer patients to cardiac rehabilitation; and offer inclusive, professional development training for health-care providers to promote the establishment of more cardiac rehabilitation programmes in Bangladesh.
Conclusions
Cardiac rehabilitation is a complex, multicomponent intervention that includes exercise training and physical activity promotion, health education, cardiovascular risk management and psychological support, personalized to the individual needs of patients diagnosed with heart disease. First introduced in the 1960s for low-risk patients who survived an acute MI, a growing body of RCT evidence over the past 3–4 decades now supports contemporary clinical guidelines, which recommend routine referral for cardiac rehabilitation across a range of cardiac diagnoses, including acute coronary syndrome, heart failure and after coronary revascularization (PCI or CABG surgery). As discussed in this Review, despite consistent and strong recommendations for cardiac rehabilitation referral in international clinical guidelines, contemporary cardiac rehabilitation practice faces a number of challenges. Global access to cardiac rehabilitation is persistently poor, with only 5–50% of eligible patients with cardiac disease receiving rehabilitation. Sadly, the ongoing COVID-19 pandemic has substantially added to this challenge: existing centre-based programmes have paused their services, with rehabilitation staff being relocated to critical care settings and patients being anxious about travelling to a centre for their rehabilitation. However, out of this ‘access challenge’ has come the opportunity to expedite the switch to (or combine) accessible home-based and technology-based models of cardiac rehabilitation, with appropriate quality assurance for their delivery. The development and provision of innovative models of delivery are likely to be especially important in LMICs, in which cardiac rehabilitation services are scarce, and scalable and affordable models are much needed. Key areas of research to support the future practice of cardiac rehabilitation are summarized in Box 3 .
Acknowledgements
The authors thank J. Uddin (Physiotherapy Unit, Department of Cardiac Surgery Ibrahim Cardiac Hospital & Research Institute, Dhaka, Bangladesh) for drafting the content of Box 6, G. Dibben (MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, UK) for preparing Fig. 2 for initial submission and U. Ahmed (MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, UK) for editorial review of the text.
Author contributions
All the authors researched data for the article, contributed substantially to discussions of its content, wrote the article, and reviewed and/or edited the manuscript before submission.
Competing interests
R.S.T. is a member of the ESC Association of Cardiovascular Nursing and Allied Professions (ACNAP) Science Committee 2020–2022 and lead investigator for the following ongoing funded projects: ‘Implementation of an evidence-based cardiac rehabilitation home programme for heart failure patients and their caregivers in Scotland: SCOT:REACH-HF project’, funded by Heart Research UK; ‘A randomized controlled trial of a facilitated home-based rehabilitation intervention in patients with heart failure with preserved ejection fraction and their caregivers: the REACH-HFpEF Study’, funded by NIHR HTA Programme (NIHR130487). H.M.D. is a co-opted member of the British Association of Cardiovascular Prevention and Rehabilitation (BACPR) and a co-lead for the ongoing funded research projects: ‘D REACH-HF: Digital Rehabilitation Enablement in Chronic Heart Failure’, funded by the British Heart Foundation, Hope for Hearts fund’; ‘Extending the reach and implementation of the successful REACH-HF programme with a digitally delivered training programme’, funded by NIHR Programme Development Grant (NIHR202040). S.J.D.M. is a researcher on the following ongoing funded research projects: ‘D REACH-HF: Digital Rehabilitation Enablement in Chronic Heart Failure’, funded by the British Heart Foundation, Hope for Hearts fund’; ‘Extending the reach and implementation of the successful REACH-HF programme with a digitally delivered training programme’, funded by NIHR Programme Development Grant (NIHR202040).
Peer review information
Nature Reviews Cardiology thanks D. Forman and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Clinical Trials
Heart failure.
Displaying 203 studies
The objectives of this study are to use qualitative methods to characterize patients’ distress, to use qualitative methods to explore how distress can impact healthcare behaviors and caregiver support; specifically, their motivation to sustain critical lifestyle changes and provide assertive communication with caregivers and medical teams, and to use qualitative methodology to explore if themes found in patients with symptomatic heart failure (HF) translate to patients with left ventricular assist devices (LVAD) or if they will be superseded by LVAD-specific themes.
This study is being done to study how well the heart contracts and relaxes during exercise. In addition to traditional measures of heart function, we will use a new computer program that may improve understanding of why people feel shortness of breath or fatigue.
CONNECT-HF is a large-scale, pragmatic, cluster-randomized clinical trial to evaluate the effect of a customized, multifaceted, health system-level quality-improvement (QI) program compared with usual care on heart failure (HF) outcomes and HF quality-of-care metrics.
The purpose of this study is to modify and adapt the algorithm to be usable in a mobile form factor with a limited number of leads. For this, will prospectively test and validate the adapted algorithm in outpatients presenting to the echocardiography laboratory and to test the sensitivity and specificity of a single lead ECG to identify people with decreased left ventricular EF.
The objective of the CAPACITY-HFpEF study is to evaluate the safety and efficacy of 3 dose levels of IW-1973 compared with placebo when administered daily for approximately 12 weeks to patients with HFpEF. The study will evaluate the effect of oral IW-1973 on peak exercise capacity in patients with HFpEF, with or without permanent or persistent atrial fibrillation.
This study will determine what factors are involved in recruiting lung surface area for gas exchange during exercise in HFpEF patients, providing insight into the relationship between lung diffusing capacity and pulmonary vascular pressures.
The purpose of this study is to compare the experienced quality of life of patients who have received both a left ventricular assist device (LVAD), followed by a heart transplant and to measure the results.
The purpose of this study is to determine the benefits and safety of intravenous administration of low dose nesiritide or low dose dopamine in patients with congestive heart failure and kidney dysfunction.
The primary objective is to test the hypothesis that, compared with placebo, therapy with Subcutaneous (SQ) GLP-1 agonist in the post-Acute Heart Failure Syndrome (AHFS) discharge period will be associated with greater clinical stability at six months as assessed by a composite clinical endpoint.
The purpose of this study is to examine that signal processed ECGs can be used to monitor changes in serum concentrations of potassium based on T-wave features.
The goal of this project is to study mechano- and- metaboreceptor function (mechanoreflex and metaboreflex, respectively) associated with exercise in HF. We will measure blood pressure, systemic vascular resistance (SVR), and the slope of the ventilatory equivalent to carbon dioxide output ratio (VE/VCO2) slope responses to stimulation of these pathways. We also aim to determine the influence of changes in blood biochemistry and intra-venous pressure on mechano- and- metaboreflex activation.
Participants in this study will either have heart failure (HF) and are scheduled to undergo cardiac resynchronization therapy pacemaker (CRT-P) or cardiac resynchronization therapy defibrillator (CRT-D) implantation, or have atrioventricular (AV) block and are scheduled to undergo dual chamber pacemaker implantation. In this study additional heart rhythm measurements will be collected during the implant procedure to better understand how His bundle and/or parahisian pacing (HISP) effects electrical conduction in the hearts of patients with HF or AV block. The hypothesis is that His bundle or parahisian pacing (HISP) may normalize atrioventricular (AV) conduction with a narrow combination of the Q ...
The primary objective of the study is to determine whether, in patients with symptomatic, advanced heart failure due to left ventricular systolic dysfunction, treatment with LCZ696 for 24 weeks will improve Pro-B-type Natriuretic Peptide (NT-proBNP) levels, which reflect hemodynamic and clinical status, compared to treatment with valsartan.
The objective of this proposal is to assess blood-plasma volume (TBV-PV) status quantitatively in patients with DHF admitted to hospital for volume management, and to determine how effective standard diuretic therapy is in achieving euvolemia and the impact of their quantitated volume status at the time of hospital discharge on heart failure related morality and re-hospitalizations. Thus, to determine if quantitative blood volume analysis could potentially serve as an effective tool to guide more effective in-hospital diuretic therapy to achieve better outcomes in patients hospitalized with clinically identified volume overload.
The purpose of this GUIDE-HF IDE clinical trial is to demonstrate the effectiveness of the CardioMEMS™ HF System in an expanded patient population including heart failure (HF) patients outside of the present indication, but at risk for future HF events or mortality.
The purpose of this study is to determine how changes in pacemaker rate affect systemic hemodynamics, including blood pressure and cardiac output, in acutely ill patients with cardiac pacemakers.
The purpose of this study is to evaluate the effect of LCZ696 compared to valsartan in the reduction of cardiovascular death and heart failure(HF) hospitalizations in patients who have HF with preserved ejection fraction.
Heart failure with preserved ejection fraction (HFpEF) is a major public health problem that has no proven effective treatment. This study will assess the effects of acute nitrite administration on resting and exercise hemodynamics in patients with HFpEF referred to the catheterization lab.
The main objective of this study to assess the quality of the ECG readings between different filters from both the GE machine and the Smartheart device.
The purpose of this study is to further evaluate the clinical effectiveness of the Corvia Atrial Shunt in symptomatic heart failure patients with a left ventricular ejection fraction (LVEF) ≥ 40%, and elevated left sided filling pressures despite standard GuidelineDirected Medical Therapy (GDMT); and to confirm the treatment effect observed in the responder group of the REDUCE LAP-HF Randomized Trial II.
The most promising chimeric natriuretic peptide designed and studied by our group has been CD-NP which has anti-fibrotic and cardioprotective properties in vivo, vitro and in normal volunteers and human heart failure patients. Since left ventricular assist device (LVAD) can not reverse remodeling of the heart whereas it can improve hemodynamics, CD-NP may be novel anti-fibrotic and anti-remodeling drug as co-therapy during LVAD support.
The purpose of this study is to determine the effect of a single dose of an oral acute MPO inhibitor drug on resting and exercise hemodynamics (arterial blood pressure and cardiac blood flow) in patients with heart failure with preserved ejection fraction (HFpEF).
The purpose of this study is to demonstrate acute effectiveness and safety of minimally-invasive pericardiotomy in patients with Heart Failure (HFpEF).
The objective of this clinical evaluation is to assess the safety and initial effectiveness of catheter-based unilateral ablation of the right greater splanchnic nerve (GSN) in subjects having heart failure with preserved ejection fraction (HFpEF).
The Pilot study is designed to evaluate the overall safety and feasibility of a strategy based on subcutaneous delivery of furosemide. It will be used to inform the subsequent evaluation phase of the study (separate protocol). The primary objective of the study is to determine if a strategy of a novel subcutaneous delivery of furosemide is safe and feasible in patients with acute heart failure.
The purpose of this study is to evaluate initial clinical safety, device functionality and effectiveness of the Edwards Transcatheter Atrial Shunt System.
The purpose of this study is to evaluate the use of Hand-Held Echocardiography (HHE) as a diagnostic tool and extension of physical assessment by trained Advanced Practice Providers (APPs) in patients admitted with congestive heart failure (CHF) in comparison to that of an expert
Compare transapical and transfemoral TAVR as regards clinical outcomes (both beneficial including improvement in heart failure class (NYHA) and reduced number of hospitalizations; and adverse including mortality and MACE.) Also, to compare cardiac mechanics’ outcomes in the short and intermediate follow up and correlate the baseline, percent change and final cardiac mechanics values with the clinical outcomes. So that this all comes down to being able to provide these information to the patients if there appeared to be a correlation between cardiac mechanics and clinical outcomes:
The purpose of this research study is to understand the effects of changes in the capability of the heart on brain function so that we can better predict who will most benefit from cardio-resynchronization therapy (CRT) and how it may enhance brain health.
The pilot study aims to recruit 60 subjects classified as New York Heart Assosciation (NYHA) class 1-2 HF patients (n = 15), NYHA class 2-3 HF patients (n = 15), HF patients admitted to the emergency room for treatment of fluid overload (n = 15), and healthy controls (n = 15). Breath samples will be collected form these patients using a ReCIVA Breath Sampler (Owlstone Medical Ltd.) to determine the levels of exhaled volatile organic compounds (VOCs). Following enrollment and study completion, study staff will access the participants’ clinic records to obtain information about their NYHA classification, blood biomarker levels, excess fluid status, ...
The purpose of this study is to evaluate whether the Temporary Total Artificial Heart can support patients with life-threatening irreversible biventricular heart failure who are not eligible for transplantation.
The main purpose of this research is to determine whether injecting mesenchymal precursor cells (MPC) into the heart during surgery to implant a left ventricular assist device (LVAD) is safe. MPCs are normally present in human bone marrow and have been shown to increase the development of blood vessels and new heart muscle cells in the heart. In addition, this research is being done to test whether injecting the MPCs into the heart is effective in improving heart function.
The primary objective of this study is to determine the efficacy and safety of iron therapy using intravenous (IV) ferric carboxymaltose (FCM), relative to placebo, in the treatment of participants in heart failure with iron deficiency and with a reduced ejection fraction.
To determine biomarker responses to Entresto™in patients with Heart Failure with preserved Ejection Fraction (HFpEF) and who have high or low serum neprilysin (NEP) levels.
This Is a Humanitarian Use Protocol for the Impella RP® System which is indicated for providing circulatory assistance for up to 14 days in pediatric or adult patients with a body surface area ≥ 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, myocardial infarction, heart transplant, or open-heart surgery.
The purpose of this study is to investigate the potential benefits to pulmonary function using a unique respiratory “training mask” during exercise on patients with heart failure.
The purpose of this study is to evaluate the effectiveness and implementation of a new shared decision support tool. Using feedback from patients, caregivers, and clinicians, a paper and video decision aid has been made to help people who are offered DT LVAD (a partial artificial heart—so-called destination therapy left ventricular assist device) make this most difficult of decisions. Although patients may live longer with a DT LVAD, it poses many risks, including stroke, serious infection, and bleeding.Unlike the information that is now available, our decision aid focuses on options, fears, and the needs of caregivers, is balanced, and is paired with ...
This study is being done because the investigators are trying to understand how feedback from the muscles can influence your blood pressure and breathing during exercise, and if the investigators can reduce this response in heart failure patients. The investigators are also trying to determine ways to improve tolerance to exercise in heart failure patients.
Right ventricular (RV) pacemaker dependent patients without left ventricular (LV) systolic or diastolic dysfunction at baseline will demonstrate worse LV diastolic and systolic function and pulmonary gas exchange reserve during exercise stress compared to patients with physiologic pacing.
Thte purpose of this study is to determine the impact of acute interval-style exercise training, with or without essential amino acid ingestion, on markers of muscle turnover and mitochondrial biogenesis. The study also aims to determine the impact of acute interval-style exercise training, with or without essential amino acid ingestion, on skeletal muscle satellite cell and myonuclei content.
The primary hypothesis is that patients with HFREF (heart failure with reduced ejection fraction) will demonstrate a markedly expanded intravascular volume which will correlate with elevated right heart hemodynamics and increased venous capacitance parameters, whereas patients with HFPEF(heart failure with preserved ejection fraction) will demonstrate euvolemia to mild volume expansion and a lack of correlation with hemodynamic and venous compliance parameters.
The primary objective of this study is to determine whether transendocardial delivery of allogeneic human bone marrow-derived MPCs (rexlemestrocel-L) is effective in the treatment of chronic heart failure due to LV systolic dysfunction.
The primary purpose of this study is to collect long-term (2-month duration) data with the ADI CHF Device on patients at home to demonstrate effectiveness of the device in accurately measuring biologically relevant parameters and detecting fluid status as compared to the standard of care (weight scale).
The purpose of the study is to evaluate the safety and effectiveness of the ReliantHeart HeartAssist 5® VAD System in patients listed for heart transplantation and at risk of death from refractory end-stage heart failure.
The Food and Drug Administration (FDA) recognizes the importance of developing patient-centric endpoints that are relevant to patients beyond mortality and hospitalizations. Patients with HF have reduced function capacity and quality of life (QoL) and hence it is imperative to explore interventions that impact endpoints that directly measure how a patient feels or functions on a daily basis. Recently, new mobile health technologies have emerged as clinical tools and offer an opportunity to overcome these challenges in measuring functional capacity and recording symptoms. These technologies are able to capture and integrate data from disparate sources from individual patients reflecting ...
The primary purpose of this study is to evaluate the correlation between Non-Invasive Venous Waveform Analysis (NIVA) score and Total Blood Volume (TBV) in Heart Failure (HF) patients on admission for decompensation and at discharge after diuresis.
This is a prospective, multi-center,single arm study that will evaluate the thoracotomy implant technique in up to 120 subjects implanted via thoracotomy with the HeartWare HVAD® System and enrolled in the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS®) protocol and database. All participating centers will be current INTERMACS® sites in good standing and will follow the INTERMACS® protocol and procedures.
The purpose of this study is to determine whether treatment with Dapagliflozin (DAPA) for 6 months will improve pulmonary capillary wedge pressure (PCWP) during exercise in heart failure/preserved ejection fraction (HFpEF) and improve cardiac metabolism.
The purpose of this study is to evaluate the safety and effectiveness of the WiSE-LV System for Cardiac Re-synchronization Therapy.
Congestive heart failure (CHF) affects nearly 5 million Americans and claims more than 300,000 lives annually. A primary pathophysiologic mechanism in this deadly syndrome is an abnormally enhanced sympathetic nervous system that results in profound peripheral vasoconstriction, attenuated cardiovascular reflexes, higher susceptibility to ventricular arrhythmias, and sudden cardiac death. The reduction in mortality and morbidity in CHF by pharmacologic neurohumoral antagonists such as beta-receptor inhibitor and angiotensin II-converting enzyme (ACE) inhibitor has taught us that regulation of the impaired neurohumoral axis is important for improving clinical outcome. In addition, an emerging nonpharmacologic approach, cardiac resynchronization therapy (CRT), has shown promise ...
The purpose of this study is to understand the experience of heart failure symptoms on the adolescent patient population, including the impact of symptoms on quality of life and wellbeing.
The purpose of this study is to assess the impact of continuous-flow Left Ventricle Assist Device (LVAD) therapy and total artificial heart (TAH) therapy on the alveolar-capillary interface and bronchial circulation of lungs in patients with heart failure (HF).
The purpose of this international study is to evaluate the effect of dapagliflozin 10 mg versus placebo in HFpEF patients, given once daily in addition to background regional standard of care therapy, including treatments to control co-morbidities, in reducing the composite of CV death or heart failure events.
The purpose of this study is to assess the presence and severity of mechanical dyssynchrony in patients with congestive heart failure (CHF) when selecting to CRT in resting and after-exercise echocardiography by multiple echocardiographic techniques, and to evaluate association of exercise-induced mechanical dyssynchrony with acute response to CRT.
The purpose of this study is to address the unmet need of an effective pharmacologic intervention in patients with Heart Failure with Preserved Ejection Fraction (HFpEF) and leverage the favorable cellular underpinnings of rapamycin to improve multiorgan reserve capacity and physical function with reduction in inflammation and cellular senescence (biological aging).
We are currently enrolling both healthy volunteers and people who have been diagnosed with heart failure to participate in our research study. The purpose of this study is to better understand the relationship between exercise, breathing, blood flow and blood pressure. This study includes two study visits if you are a healthy or heart failure volunteer. All testing will be performed at our testing center at St. Mary’s Hospital located in Rochester, MN.
On the first study visit, the research activities will be discussed and all questions will be answered. Once written consent is provided and the ...
Patients admitted for heart failure that are provided discharge medication services by a pharmacist are less likely to be readmitted within 30 days of primary admission.
This study is a pilot study evaluating the feasibility and early efficacy of cardiac rehabilitation to improve frailty and symptoms in patients with advanced heart failure (NYHA class III-IV), who are being considered for LVAD therapy.
The purpose of this study is to examine PRO-HIIT compared with CON-HIIT on effectiveness for improving locomotor muscle mitochondrial function in heart failure (HF) patients.
The purpose of this study is to determine if patiromer treatment of subjects who developed hyperkalemia while receiving RAASi medications will result in continued use of RAASi medications in accordance with heart failure (HF) treatment guidelines and thereby decrease the occurrence of the combined endpoint of cardiovascular (CV) death and CV hospitalization events compared with placebo treatment.
This study assesses the 18-month incidence of inappropriate shocks in subjects implanted with the EMBLEM Subcutaneous Implantable Defibrillator (S-ICD) for primary prevention of sudden cardiac death. Devices are to be programmed with zone cutoffs at 200 bpm and 250 bmp in order to mimic the programming settings for transvenous ICDs in the MADIT RIT study. The incidence of inappropriate S-ICD shocks will be compared to the incidence of inappropriate shocks observed in the MADIT RIT study.
The primary purpose of this study is to provide continuing evaluation and periodic reporting of safety and effectiveness of Medtronic market-released products for their intended use.
The purpose of this study is to assess the effect of inorganic nitrite on aerobic capacity (peak VO2) after four weeks of giving it to patients who have heart failure with a preserved ejection fraction.
The aim of this study is to prospectively validate the novel AI based model in patients undergoing clinically indicated transthoracic echocardiography using a four-chamber view acquired with a hand-held point of care ultrasound.
The purpose of this study is to assess the safety and tolerability profile of JK07, administered intravenously, according to protocol-defined dosing regimen.
Real-world evidence of the clinical course of patient symptoms following initiation of sacubitril/valsartan via PROs with a patient-centered study design will provide important evidence of potentially beneficial outcomes associated with the use of this therapy.
The purpose of this study is to compare the safety and effectiveness of home monitoring of INR (blood clotting factors) to standard of care clinic monitoring for adults with congenital heart disease.
The objective of the study is to evaluate the safety and effectiveness of the HM3 LVAS by demonstrating non-inferiority to the HMII LVAS (HMII) when used for the treatment of advanced, refractory, left ventricular heart failure.
The purpose of this study is to assess how often blood clots form in the FDA-approved HeartMate® II (HM II) Left Ventricular Assist Device (LVAD) and to identify risks related to clotting within the pump.
A randomized, double-blinded, placebo-controlled crossover study to assess effect of isosorbide mononitrate with dose up-titration on activity tolerance as assessed by (hip-worn, tri-axial) accelerometry.
This is a study to evaluate whether macitentan is an effective and safe treatment for patients with heart failure with preserved ejection fraction (HFpEF) and pulmonary vascular disease. The primary objective is to evaluate whether macitentan 10 mg reduces N-terminal pro-brain natriuretic peptide (NT-pro-BNP) as compared to placebo in these patients.
Heart failure with preserved ejection fraction (HFpEF) is a major public health problem that has no proven effective treatment. This study will assess the effects of nebulized inhaled nitrite administration on resting and exercise hemodynamics in patients with HFpEF referred to the catheterization lab.
A randomized, double-blinded, placebo-controlled study of continuous 6-hour IV infusions of CXL-1427 in hospitalized patients with systolic heart failure.
The purpose of this study is to determine the role of blood vessel tissue function in heart failure, and the effect of cardiac resynchronization therapy (CRT) on tissue and heart function.
The primary objective is to determine the efficacy of a strategy of biomarker-guided therapy compared with usual care in high risk patients with left ventricular systolic dysfunction.
The purpose of this study is to gather information to develop and validate a predictive tool for predicting the response to CRT therapy.
The purpose of this study is to assess intravascular volume heterogeneity in relation to neuroendocrine profiles in patients admitted to hospital with decompensated acute on chronic systolic heart failure with serial assessments post-discharge
The purpose of this study is to identify the burden, benefits, or impact of caregiving on the health of the caregiver and patient with heart failure.
The purpose of this study is to compare pulse oximetry performances from different manufacturers and with different anatomical sensor locations during stress tests in heart failure patients, evaluating effectiveness against motion and poor circulation.
The purpose of this study is to characterize the contribution of isolated diastolic heart failure to heart failure using active surveillance to measure the plasma levels of brain natriuretic peptide (BNP) among persons with heart failure and to define the prognostic value of BNP in all cases of heart failure.
The objectives of this study are to collect and store samples and information from participants’ health records for future research about heart failure.
The purpose of this study is to use a noninvasive method of recording together skin sympathetic nerve activity and electrocardiogram (ECG) to assess the sympathetic activity of the heart. The potential use of this is in the prediction of ventricular arrhymia and identifying the response to resynchronization therapy.
The purpose of this study is to evaluate the clinical efficiency and safety of a non-surgical medical device (the IASD System II) in symptomatic heart failure patients.
The purpose of this study is to continue to evaluate the safety and clinical performance of the HeartMate MOMENTUM 3 left ventricle assist system for the treatment of advanced, refractory, left ventricular heart failure following completion of participation in the the MOMENTUM 3 IDE study.
This study is a single centre, randomised, double-blind, sponsor-unblinded, placebo-controlled, 2 by 2 crossover study in adults with heart failure. In blocking the TRPV4 ion channel and reducing pulmonary interstitial fluid, GSK2798745 may improve pulmonary function, respiration, and gas exchange as well as sleep-disordered breathing in patients with heart failure. Therefore, the current study is designed to investigate the effect of repeat administration of GSK2798745 on pulmonary gas exchange and pulmonary function.
A sufficient number of subjects with heart failure will be enrolled so that 12 subjects complete the two study periods and critical assessments. Subjects will be randomised to receive ...
The purpose of this study is to evaluate the ability to determine the first heart sound (S1) and its relationship to aerobic capacity.
The primary purpose of this study is to identify which aspects of treatment are most prevalent and burdensome to patients with advanced heart failure.
Determine the impact of restoring normal heart rate response during exercise and daily activity in patients with heart failure and a preserved ejection fraction (HFpEF) and chronotropic incompetence (CI).
The purpose of this study is to investigate clinical outcomes from two current standard of care pain control procedures performed for patients undergoing pacemaker insertion.
The purpose of this study is to demonstrate the event rate of the primary outcome, defined as failure of DFT at a single shock at 10 Joules below maximal capacity of the device.
Heart failure with reduced ejection (HFrEF) is a major health concern. HFrEF is associated with significant endothelial dysfunction (ED). The purpose of this study is to compare the effects of a Western diet (WD) to a high-carbohydrate, high-fiber diet (HCHF) on endothelial function in patients with HFrEF. the study will look at the distribution of intestinal microbe communities after following the diets as well as explore relationships between gut health and ED in patients with HFrEF.
We propose to address this important gap in the literature with a study design that is responsive to needs in the area of healthcare delivery and ...
The purpose of this study is to identify measures of heart rate and heart rate variability responses to changes in nervous system activity, breathing variability, and lung fluid in HF patients as early as possible in the course of their hospital admission and subsequently just prior to discharge, using a simplified approach, in order to determine if these measures can assess readiness for discharge and more accurately predict likelihood for readmission.
The objective of this proposal is to determine the effect of resistance exercise training on locomotor muscle function, exercise capacity, exertional symptoms, and quality of life in HF patients with preserved ejection fraction (HFpEF).
This study is being done to develop a serum and tissue bank for future research of patients with heart failure, mechanical circulatory support and/or cardiothoracic transplants. This blood/tissue will be used for three principle purposes: (1) laboratory tests which will be available in the future but that are not currently available and which may be of benefit to the patient, (2) review of previous patient laboratory results made necessary by development of a new disease process by the patient, and (3) future unspecified research purposes.
The purpose of this study is to look at the differences in how individuals with HFpEF-CKD and HFpEF-EI’s bodies function using Sacubatril/valsartan (Entresto 97/103 mg), which is FDA approved for the management of HFpEF, and MANP which is an investigational drug.
The purpose of this study is to measure and identify chest fluid volumes associated with heart failure and to determine their impact on lung structure and function, and also assess the effect of body position on shifts in fluid and the effects of this on lung function, mechanics and gas exchange.
The response to therapy with a fixed dose combination of isosorbide dinitrate and hydralazine (FDC I/H) is enhanced in African Americans with heart failure and reduced ejection fraction (HFrEF) when compared to similar white cohorts. This study will seek to confirm the previous genetic sub-study from AHeFT which suggested a functional polymorphism of guanine nucleotide binding protein beta polypeptide 3 subunit (GNB3), C825T in exon 10, influences the therapeutic efficacy of FDC I/H. This study will initiate treatment with FDC I/H in 500 self designated African American subjects with systolic heart failure. They will be followed for up to two ...
Participants with heart failure with preserved ejection fraction will undergo 12 weeks of cardiac rehabilitation for exercise training (ET) and be randomized to either nebulized sodium nitrite inhalation solution or placebo inhalation solution (normal saline) through the training period. Study drug is administered 3 times daily during daytime hours with one of these doses being immediately prior to onset of ET sessions throughout the 12 week trial. The objective is to determine if the inhaled sodium nitrite improves the clinical responses and tolerability of ET.
Primary Objectives: - Assess the safety and tolerability of sotagliflozin in hemodynamically stable patients with worsening of heart failure, compared to placebo. - Estimate the effects of sotagliflozin on plasma volume changes in hemodynamically stable patients with worsening of heart failure, compared to placebo. Secondary Objectives: - Explore the effect of sotagliflozin on erythropoiesis, as assessed by changes in plasma erythropoietin levels, in hemodynamically stable patients with worsening of heart failure, compared to placebo. - Explore the effect of sotagliflozin on changes in plasma NT-proBNP levels, in hemodynamically stable patients with worsening of heart failure, compared to placebo.
The purpose of this study is to determine the long-term outcome of cardiac resynchronization therapy (CRT) recipients with congestive heart failure and any indications for CRT at Mayo Clinic.
The purpose of this study is to understand how feedback from your breathing muscles influence blood flow and blood pressure during exercise and if we can reduce this response in heart failure patients with breathing muscle training.
The purpose of this study is to determine the safety and effectiveness of the HeartWare Ventricular Assist System in patients with chronic Stage D/NYHA Class IIIB/IV left ventricular failure who have received and failed optimal medical therapy, and who are ineligible for cardiac transplantation.
The proposed study will directly examine whether bone mineral density (BMD) and bone microstructure are better preserved among HF patients on chronic β-blockers and account for the reports of decreased fracture.
The purpose of this study is because we are testing the variation in a gene that may influence receptors in your heart, blood vessels and lungs.
INVESTED will test the hypothesis that high dose trivalent influenza vaccine will reduce cardiopulmonary events to a greater extent than standard dose quadrivalent influenza vaccine in high-risk cardiovascular patients with a recent history of myocardial infarction or heart failure. The trial will enroll 9300 participants over one Vanguard (pilot) season and three additional influenza seasons. The primary endpoint will be a composite of all-cause mortality or cardiopulmonary hospitalization.
The purpose of this study is to evaluate the ability of the TYRX Absorbable Antibacterial Envelope to reduce major cardiovascular implantable electronic device infections through 12-months post-procedure following generator replacement, upgrade, revision, or new CRT-D implant.
The purpose of this study is to compare treatment with the CardiAMP cell therapy to a sham treatment. A roll-in phase with a maximum of 10 subjects will precede the randomised phase.
The purpose of this study is to investigate the use of shear wave elastography to assess diastolic heart muscle stiffness for diastolic heart failure patients, and compare the stiffness measurements with the cardiac catheterization (cath lab) results.
The purpose of this study is two-fold. The first purpose is to understand how feedback from your muscles can change ventilation at rest and during exercise in low and high oxygen conditions. The second purpose is to understand how feedback from your muscles can influence muscle fatigue and muscle function in normal and low oxygen conditions. The ventilatory response to exercise and skeletal muscle fatigability in healthy controls and HF patients will advance our understanding of tolerance to exercise in HF patients.
The purpose of this study is to assess barriers to completion of cardiac rehabilitation program and to identify potential ways to improve cardiac rehabilitation completion.
The purpose of this study is to identify clinical demographics of patients initiated on inotropes during a heart failure admission and observe clinical practice surrounding their use as well as compare whether the perception of treatment duration/outcome of the treating clinicians is different to actual clinical outcomes.
The primary objective of this study is to determine whether transendocardial delivery of human bone marrow-derived stem cells (CEP-41750) is effective in the treatment of chronic heart failure due to LV systolic dysfunction.
The purpose of the CardioMEMS HF System post approval study is to evaluate the use of the CardioMEMS HF System in patients with NYHA class III heart failure in a commercial setting.
The purpose of this study is to assess frailty in patients being evaluated in the Congestive Heart Failure Clinic with NYHA class III-IV heart failure and to enroll these patients in cardiac rehabilitation program aimed at improving frailty and functional independence.
We will longitudinally (at enrollment and 6 months after) ascertain patients’ end of life preferences, patient activation and health literacy in prospectively enrolled Southeastern Minnesota residents hospitalized with heart failure (HF).
We will define the relationship between HF patients’ end of life preferences and degree of advance care planning and healthcare resource utilization.
We will measure perceived treatment burden in patients hospitalized with heart failure using a novel questionnaire that has been validated in patients with multimorbidity.
We will evaluate the end to end remote monitoring system in a less controlled environment and concurrently develop the infrastructure to support the back end of the system
RESPOND-HF is a prospective, multi-center, non-significant risk pilot study with cross-over design. The purpose of the study is to investigate if rate adaptive pacing has the potential to provide benefit to HF patients with preserved ejection fraction, referred to as HFpEF patients. Findings from this pilot study may be used to guide subsequent efforts to design and conduct a prospective, randomized, multi-center pivotal trial powered to show improvement in patient outcomes.
To determine if a strategy of early discharge using a novel subcutaneous delivery system for parenteral furosemide can improve clinical outcomes within 30 days of randomization (days alive and outside the hospital) compared to usual care.
The purpose of this study is to determine if epidural spinal cord stimulation can affect blood pressure control and blood vessel resistance during exercise in heart failure patients by intercepting messages of muscle fatigue and shortness of breath.
The purpose of this study is to evaluate the detection performance and safety of an investigational Wearable Cardioverter defibrillator (WCD).
The purpose of this study is to examine whether people without HFpEF display less visceral adipose tissue (VAT) compared to patients with diagnosed HFpEF.
The purpose of this study is to compare microembolic signal detection (MSD) and cerebral vasomotor reactivity (CVR) on transcranial doppler in patients with left ventricular assistance devices.
The objectives of this study are to determine the best method for integration of respiratory muscle training (RMT) into the clinical ventricular assist device (VAD) practice at Mayo, to determine the clinical benefits of using RMT in the VAD population at Mayo Clinic, to gain initial insight on means by which RMT can impact clinical outcomes in the VAD population, and to create an algorithm for integration of perioperative RMT in the VAD and other distinct populations at Mayo Clinic.
Medtronic is sponsoring the Micra Continued Access (CA) study to provide continued access to the Micra System while the marketing application is under review by the Food and Drug Administration (FDA).
The primary objective of this study is to test the hypothesis that high-dose spironolactone will lead to greater proportional reduction in NT-proBNP levels from randomization to 96 hours over standard of care.
The purpose of this study is for evaluating an ultrasound-based technology (similar to standard clinical echocardiography) for measuring the stiffness of your heart muscle and your peripheral arteries. This type of information may prove to be clinically important.
This study evaluates the effectiveness of remote tele-monitoring and health coaching in helping to reduce hospitalizations in heart failure patients. Half of participants will receive tele-monitoring and health coaching, while the other half will receive standard health care provided by their chosen provider.
To comprehensively characterize Left Ventricular (LV) remodeling after Myocardial Infarction (MI) in the community, study the association between patterns of remodeling and biological pathways and examine the association between the predictors of remodeling and heart failure after Myocardial Infarction.
The purpose of this study is to prospectively evaluate a newly-developed screening tool for ALVSD.
The purpose of this research is to find out if an aggressive intervention to lose weight, will improve symptoms in patients with obesity-related cardiomyopathy, which is also known as the obese phenotype of heart failure with preserved ejection fraction (HFpEF).
The purpose of this study is to look at kidney function and hormonal function in patients with a history of heart failure and kidney dysfunction, and to see how the use of a new drug, ANX-042, affects those functions.
The objective of this study is to obtain preliminary data to evaluate the accuracy of non-invasive blood pressure measurement in patients supported by continuous-flow left ventricular assist device (LVAD) using non-invasive supra-systolic methods in highly sensitive experimental blood pressure monitor.
The presence of chronic obstructive pulmonary disease (COPD) would confer increased in-hospital mortality and length of hospital stay in patients with acute decompensated heart failure Assess the (1) prevalence of COPD in patients who are hospitalized for acute decompensated heart failure and (2) the association between COPD and in-hospital mortality or length of stay in this cohort.
The primary purpose of this study is to assess the feasibility of performing lung and kidney and lung ultrasound elastography among patients with critical illness from different etiologies that could be associated with volume overload.
The purpose of this study is to evaluate the effectiveness and safety of intermittent levosimendan compared with placebo in hemodynamic improvement with exercise in PH-HFpEF subjects.
This study is designed to assess the efficacy, safety and tolerability of ixmyelocel-T compared to placebo (vehicle control) when administered via transendocardial catheter-based injections to patients with end stage heart failure due to IDCM, who have no reasonable revascularization options (either surgical or percutaneous interventional) likely to provide clinical benefit.
The purpose of this study is to evaluate the safety and tolerability of 134 days of daily dosing of HU6, to ealuate the effectiveness of HU6 on weight reduction, and to evaluate the effect of HU6 treatment on exercise capacity.
The purposed of this study are to investigate whether structured exercise training improves cardiac and pulmonary haemodynamic function, exercise capacity, and short-term clinical outcomes in heart failure (HF) patients with Pulmonary Hypertension (PH), and to develop a multivariable exercise pulmonary gas exchange ‘score’ that accurately differentiates HF patients with pre- and post-capillary PH (CpcPH) from HF patients with isolated post-capillary PH (IpcPH).
The purpose of this study is to evaluate AG10 800 mg compared to placebo in subjects with symptomatic Transthyretin Amyloid Cardiomyopathy (ATTR-CM).
Patients with a patent foramen ovale in the setting of endocardially placed cardiac implantable electronic devices such as pacemakers, defibrillators, or resynchronization therapies are likely at higher risk for paradoxical embolic events from device lead thrombus. The investigators are conducting this study to determine if the anticoagulant medication Apixaban is more effective at reducing MRI detected brain lesions compared to placebo.
The purpose of this study is to evaluate the effectiveness of MayoExpertAdvisor, a knowledge delivery tool, to improve provider adherence to guidelines of best practice for patients with hyperlipidemia, atrial fibrillation and heart failure.
The purpose of this study is to evaluate the safety, performance, and initial clinical efficacy of the Rivet PVS therapy in patients with symptomatic pulmonary hypertension.
The purpose of this study is to assess the effectiveness and safety of NEOD001 administered intravenously in adults with light chain amyloidosis who have had a hematologic response to previous treatment for their amyloidosis (e.g., chemotherapy, autologous stem cell transplant [ASCT]) and have persistent cardiac dysfunction.
The purpose of this study is to determine if allopurinol is effective in relieving symptoms for patients who have heart failure and high blood uric acid levels.
This is a multicenter, randomized (1:1; oral treprostinil to placebo), double-blind, placebo-controlled study in subjects with World Health Organization (WHO) Group 2 pulmonary hypertension (PH) associated with heart failure with preserved ejection fraction (HFpEF). Once randomized, subjects will take the initial dose of study drug at the study site on the day of randomization. Subjects will return to the study site for visits scheduled at Weeks 6, 12, 18, and 24. The treatment phase of the study will last approximately 24 weeks.
This is an open-label study to evaluate the safety of continued therapy with oral treprostinil in subjects who have completed Study TDE-HF-301. This study will provide long-term, open-label data regarding the effect of continued long-term oral treprostinil therapy for the treatment of pulmonary hypertension (PH) associated with heart failure with preserved ejection fraction (HFpEF). Subject visits will occur at Baseline, Weeks 6, 12, 18, 24, and every 12 weeks thereafter until either oral treprostinil becomes commercially available to treat PH associated with HFpEF or the study is discontinued by the Sponsor.
The enormous and rapidly growing burden of Heart Failure with Preserved Ejection Fraction (HFpEF) has led to a need to understand the pathogenesis and treatment options for this morbid disease. Recent research from the investigator's group and others have shown that pulmonary hypertension (PH) is highly prevalent in HFpEF, and right ventricular (RV) dysfunction is present in both early and advanced stages of HFpEF.
These abnormalities in the RV and pulmonary vasculature are coupled with limitations in pulmonary vasodilation during exercise. There are no therapies directly targeted at the pulmonary vasculature that have been clearly shown to be effective ...
The purpose of this study is to evaluate the effectiveness and safety of sotatercept versus placebo in adults with Cpc-PH due to HFpEF. Effectiveness is measured by change from baseline in pulmonary vascular resistance (PVR, primary endpoint) and 6-minute walk distance (6MWD, key secondary endpoint).
The purpose of this study is to evaluate the data accuracy of the cardiac acoustic biomarkers (CABs) recorded the FDA-approved LifeVest® Wearable Cardioverter Defibrillator (WCD). To show accuracy, these data will be compared with CABs data simultaneously recorded by the AUDICOR® AM device, a FDA cleared, acoustic cardiography recorder.
The purpose of this study is to evaluate for safety and effectiveness weekly, open-label doses of levosimendan over extended use in patients with pulmonary hypertension with heart failure and preserved left ventricular ejection fraction (PH-HFpEF).
The purpose of this study is to attempt to establish the various ranges of proteins that can be assayed from the plasma and urine of patients with all classes of heart failure and MI (myocardial infarction).
The purpose of this study is to study circulating progenitor cells in human subjects with heart failure and before and after LVAD therapy.
This study is a multi-center, prospective, randomized, double blind, placebo-controlled clinical trial. Subjects in the study will be adults with New York Heart Association (NYHA) Class II-IV heart failure (HF) due to left ventricular systolic dysfunction (LVSD), left ventricular ejection fraction (LVEF) <0.40, and secondary pulmonary hypertension (PH). The purpose of the study is to evaluate the safety, effectiveness, and effects of tadalafil compared to placebo on the subjects' functional capacity / quality of life.
This is a prospective, randomized, controlled, unblinded, multi-center evaluation of the stroke incidence in patients implanted with a HeartWare HVAD who receive optimal blood pressure management. The study compares results of stroke incidence in a new cohort of subjects receiving optimal blood pressure management to a reference stroke incidence observed in the original IDE clinical trial (HW004) that did not specify optimal blood pressure management. In addition, a secondary endpoint will evaluate non-inferiority of stroke-free success on the originally implanted device to a control group (i.e. any FDA-approved LVAD for destination therapy). Subjects will be randomized to HeartWare HVAD or ...
The purpose of this study is test the effectiveness and safety of NNC6019-0001 to determine if it can reduce the symptoms of a heart disease due to TTR (Transthyretin ) amyloidosis, such as heart failure.
The purpose of this studyis to determine the effectiveness of an AI-enabled ECG to detect cardiomyopathy and its impact on clinical outcomes in a predominantly Black obstetric population in Nigeria
The purpose of the study is collect specimens for future studies to identify markers circulating in the blood that are associated with the development of further complications of heart disease.
The primary endpoint is to assess the safety and tolerability of CD-NP with the incidence of symptomatic hypotension being one of the key safety variables.
The purpose of this study is to evaluate long-term safety and tolerability data in eligible CLCZ696B2319 (PANORAMA-HF) pediatric patients receiving open-label sacubitril/valsartan.
The purpose of this study is to investigate skin sympathetic nerve activity (SKNA) in correlation with cardiac arrhythmias and/or heart failure.
The purpose of this study is to evaluate different strategies of cardiovascular therapy with Carvedilol, aiming to reduce the incidence of left ventricular ejection fraction (LVEF) decline and heart failure (HF) in patients undergoing curative intent Trastuzumab for breast cancer.
The purpose of this study is to define the effects of decreasing the furosemide (lasix) dose on heart, kidney and biochemical balance, in people with compensated heart failure and kidney dysfunction and also in people with compensated heart failure without kidney dysfunction.
The purpose of this study is to evaluate the baseline presence of plasma levels of biomarkers of renal injury and changes in these biomarkers during the course of in-hospital intravenous diuretic therapy can predict when threshold values that would indicate a clinically significant change in renal function that would warrant a change in diuretic therapy to occur.
A multicenter prospective randomized clinical trial testing the hypothesis that a patient-centered actigraphy intervention will result in increased physical activity for frail older adults increase during the critical first 30 days after a cardiovascular hospitalization.
The purpose of this trial is to identify cancer survivors who are at increased risk of developing late-occurring complications after undergoing treatment for childhood cancer. A patient's genes may affect the risk of developing complications, such as congestive heart failure, heart attack, stroke, and second cancer, years after undergoing cancer treatment. Genetic studies may help doctors identify survivors of childhood cancer who are more likely to develop late complications.
The purposes of this study are to determine: the risk of cardiomyopathy and heart failure, and cardiac structure and function in patients with THA and TKA. This study will also determine the association between serum and/or synovial fluid metal ion levels with cardiac structure and function in 100 prospectively-recruited THA and TJA patients.
The purpose of this 12 week study is to assess the safety of oral IW-1973 when administered to patients with heart failure with preserved ejection fraction (HFpEF) and its effect on peak exercise capacity, both in all patients and in patients without permanent or persistent atrial fibrillation
This study is being done to: (1) develop a simple tool to assess breathing muscle performance; (2) measure the oxygen cost of breathing during exercise; (3) measure the respiratory muscle blood flow requirements of hyperpnea during exercise; and (4) to quantify the energy cost of exercise in relation to disease severity.
The purpose of this study is to learn whether Cardiac Magnetic Resonance Imaging (cMRI) and/or echocardiogram is useful to diagnose patients with unique heart conditions. This research study focuses on evaluating the use of cMRI or echocardiogram as a novel, non-invasive method for evaluating specific heart conditions.
The researchers are doing this study to find out whether there will be less increase in cardiac filling pressure after the surgeon opens the pericardium (the membrane around the heart) than when the pericardium is intact. The researchers want to see whether opening the pericardium is an effective way to reduce the blood filling pressures in the heart.
The primary objective of this study is to determine the prevalence of transthyretin cardiac amyloidosis (TTR-CA) in a community-based cohort of consecutive heart failure with preserved ejection fraction (HFpEF) patients with increased LV wall thickness using 99mTc-PYP single-photon positive emission computed tomography with computed tomography (SPECT/CT). As a secondary (exploratory) objective, we seek to establish and validate novel biomarker assays to screen for TTR-CA using blood and urine samples collected from study participants.
The purpose of this study is to gather information on the safety and effectiveness of cardiac resynchronization therapy (CRT) in patients who have mild heart failure (HF) and left bundle branch block (LBBB).
The purpose of this research study is to see if Atorvastatin(Lipitor) 40 mg by mouth daily decreases the chance of developing heart problems in women who are receiving anthracycline-based chemotherapy for breast cancer.
The primary objective of this study is to determine whether a Mayo-developed, highly miniaturized physiologic monitoring instrument can provide early detection of heart failure (HF) in children with congenital or acquired heart disease at risk for or with evidence of heart failure (HF).
The purpose of this study is to look at how participants' daily life is affected by their heart failure. The study will also look at the change in participants' body weight. This study will compare the effect of semaglutide (a new medicine) compared to "dummy" medicine on body weight and heart failure symptoms. Participants will either get semaglutide or "dummy" medicine, which treatment participants get is decided by chance. Participants will need to take 1 injection once a week.
The purpose of this study is to determine the prevalence of Obstructive Sleep Apnea (OSA) in HFpEF, and its clinical and hemodynamic correlates, and to determine the impact of intervention with CPAP therapy on exercise capacity and quality of life in HFpEF patients with OSA.
The purpose of this study is to better understand how the heart’s health and function is affected by HIV infection and use of active antiretroviral therapy.
The primary purpose of this study is to evaluate the impact of dapagliflozin, as compared with placebo, on heart failure, disease specific biomarkers, symptoms, health status and quality of life in patients with type 2 diabetes or prediabetes and chronic heart failure with preserved systolic function.
The primary purpose of this study is to evaluate the impact of dapagliflozin, as compared with placebo, on heart failure disease-specific biomarkers, symptoms, health status, and quality of life in patients who have type 2 diabetes and chronic heart failure with reduced systolic function.
The purpose of this study is to evaluate comparisons between a hybrid program of center-based CR which incorporates mHealth remote case management technology (CON+) to a traditional center-based program alone (CON) as well as comparisons between home-based mHealth remote case management alone (HOM+) to a traditional center-based program (CON).
The aim of this study is to identify genes shared between humans and rhesus macaque primates who have been diagnosed with hypertrophic cardiomyopathy and have died suddenly.
The purpose of this study is to evaluate different strategies of cardiovascular therapy with carvedilol aiming to reduce the incidence of heart function declines and heart failure in at-risk breast cancer patients while on trastuzumab therapy.
The purpose of this study is to determine the optimal medical therapy to improve left ventricular (LV) function. Improvement in LV function has the potential to reduce the burden of heart failure and improve clinical outcomes in the Tetralogy of Fallot (TOF) population.
The purpose of this study is to develop a registry of patients with clinical cardiogenic shock (CS) in order to allow better definition of several key issues regarding cardiogenic shock.
The purpose of this study to test the feasibility and safety for autologous (from your own body) skin cells that are manufactured into stem cells of cardiac lineage to be delivered into the heart muscle to determine if those stem cells will strengthen the heart muscle and can be used as an additional treatment for the management of congenital heart disease.
The aim of this project is to assess the feasibility and utility of a virtual world-based cardiac rehabilitation (CR) program as an extension of a face-to-face conventional CR program (Destination Rehab).
The objective of this study is to determine the safety and efficacy of transcatheter aortic valve replacement (TAVR) via a transfemoral approach in HF patients with moderate AS as compared with OHFT.
Obstructive Sleep Apnea (OSA) is a condition in which a person stops breathing for several seconds at a time due to relaxation of the throat muscles. This can occur many times during sleep and is known to cause sleepiness and poor concentration during the day. Research indicates that OSA may be a modifiable risk factor for cardiovascular disease due to its association with hypertension, stroke, heart attack and sudden death. The standard therapy for symptomatic OSA is continuous positive airway pressure (CPAP). CPAP has been shown to effectively reduce snoring, obstructive episodes and daytime sleepiness and to modestly reduce blood pressure ...
The purpose of this study is to determine if Brain Natriuretic Peptide (NT-pro-BNP) values increase over time in breast cancer survivors and correlate with cardiac dysfunction. This study will define the average NT-pro-B-natriuretic peptide values in female breast cancer patients 1, 2, 3, 4, and 5 years out from anthracycline-based chemotherapy.
The purpose of this study are to evaluate whether serum sST2 levels increase after RT compared to troponin (as a control), and to correlate serum sST2 and troponin levels at completion of RT with cardiac radiation dosimetry.
The purpose of this study is to evaluate the impact of interventions on important CV biomarkers to provide valuable information on the mechanism linking depression and anxiety to cardiac prognosis resulting in improved quality of life and diagnosis.
This randomized phase IIb trial studies how well low-dose carvedilol works in preventing heart failure in cancer survivors exposed to high dose anthracyclines for management of childhood cancer. Patients who received high-dose anthracycline chemotherapy are at a much greater risk for developing heart failure compared to survivors who didn't get any anthracycline chemotherapy. Heart failure happens when the heart muscle has been weakened and can't pump blood as well as it should. Carvedilol may help lower the risk of cardiovascular complications.
The purpose of this study is to assess the safety and performance of the Caisson Interventional Transcatheter MitralValve Replacement (TMVR) system for the treatment of severe symptomatic MitralValve Regurgitation (MR).
The purpose of the Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation (COAPT) Trial is to confirm the safety and effectiveness of the MitraClip System for the treatment of moderate-to-severe or severe functional mitral regurgitation (FMR) in Symptomatic Heart Failure Subjects who are treated per standard of care and who have been determined by the site's local heart team as not appropriate for mitral valve surgery. This randomized controlled trial will provide the opportunity to strengthen or add labeling claims regarding safety and clinical benefits of the MitraClip System for symptomatic heart ...
The purpose of this study is to characterize TRPC6 risk variants for doxorubicin-related cardiotoxicity in prospectively collected samples from breast cancer patients.
Breast cancer patients are more than three times at risk for developing congestive heart failure (CHF), compared with patients who did not have cancer. The increased risk of HF is observed as early as one year from diagnosis of cancer and overall, 7% of patients develop CHF (median follow-up 8.5 years)
The purpose of this study is t o identify correlates of healthcare-seeking behavior in patients with ACS and CHF and its association with psychosocial and health outcomes.
Hypothesis: We hypothesize that patients from the Family Medicine Department at Mayo Clinic Florida who participate in RPM will have significantly reduced emergency room visits, hospitalizations, and hospital contacts.
Aims, purpose, or objectives: In this study, we will compare the RPM group to a control group that does not receive RPM. The primary objective is to determine if there are significant group differences in emergency room visits, hospitalizations, outpatient primary care visits, outpatient specialty care visits, and hospital contacts (inbound patient portal messages and phone calls). The secondary objective is to determine if there are ...
The purpose of this study is to determine whether short-term treatment with Fisetin reduces the rate of death and long term complications related to COVID-19.
This study (SE2030) will establish a platform of data to build the perfect stress echo test, suitable for all patients, anywhere, anytime, also quantitative and operator independent.
The purpose of this study is to evaluate the effietiveness of remdesivir (RDV) in reducing the rate of of all-cause medically attended visits (MAVs; medical visits attended in person by the participant and a health care professional) or death in non-hospitalized participants with early stage coronavirus disease 2019 (COVID-19) and to evaluate the safety of RDV administered in an outpatient setting.
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
Intermittent Fasting Linked to Higher Risk of Death From Heart Disease, Preliminary Study Finds
New research challenges the idea that restricting eating to a limited time frame is beneficial—though the work has some notable limitations, such as a reliance on self-reported eating habits
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Will-Sullivan-photo.png)
Will Sullivan
Daily Correspondent
:focal(1061x707:1062x708)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer_public/fe/13/fe137a7a-df89-41ab-b1b7-abdcc88a426f/gettyimages-1427582363.jpg)
Intermittent fasting , a dietary plan that involves eating only during certain times, has been gaining popularity in the United States and beyond. But new research, which has not yet been published in a peer-reviewed journal, offers a note of caution. Scientists looked at more than 20,000 adults who had completed a survey about their diets and found that, as of December 2019, people who restricted their eating to eight hours of a day were more likely to have died from cardiovascular disease than people who followed a more regular eating schedule.
The findings were recently presented at an American Heart Association (AHA) scientific conference.
Victor Wenze Zhong , a co-author of the research and epidemiologist at Shanghai Jiao Tong University, tells NBC News ’ Aria Bendix that it’s too early to make recommendations about fasting based on the findings.
“There is nothing here that would suggest I make any clinical recommendations one way or the other,” adds Sean P. Heffron , a cardiologist at NYU Langone Heart who did not contribute to the findings, to Today.com ’s Linda Carroll.
The research only identified a correlation between intermittent fasting and mortality—it did not show the eating pattern causes heart disease deaths—and other factors could be at play in this relationship. But Penny Kris-Etherton , a dietitian and member of the AHA nutrition committee, tells NBC News that people could “maybe consider a pause in intermittent fasting until we have more information or until the results of the study can be better explained.”
Time-restricted eating, a type of intermittent fasting that involves only eating during certain time periods each day, has previously been linked to better blood pressure, blood sugar and cholesterol levels, according to a statement from the AHA. But some of the earliest studies were in mice, and most of the human trials that followed were small and only lasted one to three months, writes the Washington Post ’s Anahad O’Connor.
The new research involved participants who recalled what they ate for two 24-hour periods as part of the National Health and Nutrition Examination Survey between 2003 and 2018. The researchers used the times people recalled eating during these two days to determine whether they were intermittently fasting.
To gather information on participant death, the team used the National Death Index. All participants were at least 20 years old, around half were men, and 73 percent self-identified as non-Hispanic white adults. The researchers followed participants for around eight years on average. People who ate all their food in less than eight hours were 91 percent more likely to die from heart disease during the study period than people who ate throughout a 12- to 16-hour window.
The study did not make conclusions about why this trend appeared. But Zhong tells NBC News that people who ate only during eight-hour periods had lower levels of lean muscle mass, which has been associated with risk of cardiovascular death in a recent study .
Importantly, the findings come with several caveats. Reliance on self-reported eating habits, which both could be remembered incorrectly or may not be representative of participants’ typical eating, is one limitation of the study, per the AHA’s statement.
Dietary recall “is imperfect,” Deepak Bhatt , a cardiologist at Mount Sinai Fuster Heart Hospital who did not contribute to the findings, tells Today.com . “People often don’t recall what they had for breakfast. For this sort of research, you need detailed dietary information gathered in real time.”
Additionally, the amount of data on each participant’s eating habits is small. “It’s a retrospective study looking at two days’ worth of data, and drawing some very big conclusions from a very limited snapshot into a person’s lifestyle habits,” Pam Taub , a cardiologist at the University of California, San Diego, who was not involved in the research, tells NBC News.
Other researchers would like to see more information on what people were eating and what factors may have affected their eating habits. For instance, the participants did not record whether they were trying intermittent fasting as a choice. Some people could have had restricted eating windows because of health conditions or treatments that affected their appetites, Benjamin Horne , an epidemiologist at the Intermountain Heart Institute who was not involved in the research, tells New Scientist ’s Clarissa Brincat.
Christopher Gardner , who studies nutrition at Stanford University and did not contribute to the findings, tells the Washington Post that he would want to look at possible demographic differences between study participants.
“Did they all have the same level of disposable income and the same level of stress?” Gardner tells the publication. “Or is it that the people who ate less than eight hours a day worked three jobs, had very high stress and didn’t have time to eat?”
Get the latest stories in your inbox every weekday.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Will-Sullivan-photo.png)
Will Sullivan | | READ MORE
Will Sullivan is a science writer based in Washington, D.C. His work has appeared in Inside Science and NOVA Next .
- Share full article
Advertisement
Supported by
Is Intermittent Fasting Bad for Your Heart? Here’s What We Know.

By Alice Callahan
You may have seen the headlines: “Intermittent fasting linked to 91 percent increase in risk of death from heart disease”; “The intermittent fasting trend may pose risks to your heart.”
The news came from an abstract presented Monday at an American Heart Association conference in Chicago. The study has not yet been published in a peer-reviewed journal, and experts cautioned that it had many limitations. Here’s what we know.

The Background
Intermittent fasting involves cycling between eating and fasting for specific periods of time. A common approach, for example, is to eat only within an eight-hour window each day, said Krista Varady, a professor of nutrition at the University of Illinois Chicago.
Several short-term trials have suggested that this eating style can lead to some weight loss and may lower blood pressure and improve blood sugar control in certain people, she said.
But the longest intermittent fasting trial lasted only one year , said Victor Wenze Zhong, lead author of the new study and an epidemiologist at Shanghai Jiao Tong University School of Medicine in China. His aim, he said, was to look at longer term health.
The Research
The new study included more than 20,000 adults from the United States. The participants completed two interviews, less than two weeks apart, about what time they ate on the previous day. The researchers then calculated the participants’ average eating windows and assumed it was their typical schedule for the rest of the study, Dr. Zhong said. The participants were followed for an average of eight years.
During that time, the participants who limited their eating to eight hours in a day had a 91 percent greater chance of dying from cardiovascular disease than those who ate over a 12- to 16-hour time frame, the researchers reported.
But there were just 414 people in the eight-hour eating group, Dr. Zhong said. And they tended to be younger and less educated; have lower income and less access to food; and be more likely to smoke than the other participants.
The researchers accounted for these factors in their analysis, Dr. Zhong said. But the study did not show that this style of eating caused deaths from cardiovascular disease, only that the two were linked.

The Limitations
Since the study has not been published or peer-reviewed, it’s challenging to fully evaluate it, Dr. Varady said.
A “major limitation” is that they used just two reports to accurately represent people’s typical eating pattern, Dr. Varady said; and the study did not seem to evaluate what kinds of foods people ate.
Dr. Dariush Mozaffarian, a cardiologist and professor of medicine at Tufts University, called the study “very problematic.” The eight-hour eating group may have included many people who were very busy, or faced other challenges that forced them to miss meals or eat erratically, he said.
The group also could have included people who were already in poor health — those with eating disorders or illness that reduced their appetite, for instance, which may have resulted in them eating during a shorter window, said Satchidananda Panda, a professor at the Salk Institute for Biological Studies in San Diego.
And if intermittent fasting is really harmful, it’s not clear why that might be. Dr. Zhong said that his study was not designed to answer that question.
What’s Next
More research is needed to evaluate the long term health effects of intermittent fasting, Dr. Zhong said.
Intermittent fasting isn’t a good fit for everyone, said Dr. Pam Taub, a cardiologist at the University of California, San Diego. But many of her patients have enjoyed its benefits, like reduced cholesterol levels.
Now, her patients are “confused and scared” by the headlines they’re reading, Dr. Taub said. But she won’t recommend that they change anything based on this study, she said, adding that people should always talk with their doctor before shifting their diet or lifestyle.
An earlier version of this story misrepresented the way researchers collected diet information with the study participants. It was via two interviews, not two questionnaires.
How we handle corrections
Alice Callahan is a Times reporter covering nutrition and health. She has a Ph.D. in nutrition from the University of California, Davis. More about Alice Callahan
A Guide to Better Nutrition
How much salt is too much? Should I cut back ? We asked experts these and other questions about sodium.
Patients were told for years that cutting calories would ease the symptoms of polycystic ovary syndrome. But research suggests dieting may not help at all .
We asked a nutrition expert how she keeps up healthy habits without stressing about food. Here are seven tips she shared for maintaining that balance.
There are many people who want to lose a few pounds for whom weight loss drugs are not the right choice. Is old-fashioned dieting a good option ?
Salmon is good for you, but choosing the right type to eat isn’t so easy. Here are answers to all your questions about this nutritional powerhouse .
Read these books to shift into a healthier way of thinking about food .
Sign up for Well’s Mediterranean diet week : Each day, we’ll send guidance and recipes to help make 2024 your most nourishing year yet.
Secrets of the naked mole-rat: new study reveals how their unique metabolism protects them from heart attacks
This unusual, subterranean mammal with extreme longevity shows genetic adaptations to low oxygen environments which could offer opportunities for advancing other areas of physiological and medical research in humans, including the development of novel therapeutic approaches.
New research from Queen Mary University of London led by Dr Dunja Aksentijevic in the Faculty of Medicine and Dentistry has revealed that that the genome of the naked mole-rat contains specific adaptations that allow them to survive in low-oxygen, and even no oxygen environments in their natural habitat. The findings also show the mammals' distinct cardiometabolic profile helps to avoid damage to their hearts caused by cardiovascular events.
Dr Aksentijevic led the team of scientists from London, Pretoria and Cambridge to sample heart tissue from the naked mole-rat and compared it to samples from other African mole-rat species (Cape, Cape dune, common, Natal, Mahali, highveld and Damaraland mole-rats), as well as evolutionarily divergent mammals (Hottentot golden mole and C57/BL6 mouse).
In this study, they found that the naked mole-rat has a unique expression of genes in heart cells controlling energy generation from sugars resulting in a metabolic profile that is distinct from any of the other mole-rats as well as the other species studied. These unique cardiac metabolic and genetic features of the naked mole-rat heart led to enhanced energy reserves even during blood occlusion and return of blood flow after in vitro simulated heart attack. Collectively, these adaptations result in the naked mole-rat 's tolerance to reduced oxygen and negligible damage to their heart tissue.
Dr Chris Faulkes, Reader (Associate Professor) in Evolutionary Ecology at Queen Mary and Lead Author, said: "Naked mole-rats live in a unique hypoxic and social environment, and we believe these factors have driven the evolution of special adaptations in their hearts that contribute to their exceptional longevity and health span,"
Dr Dunja Aksentijevic, Wellcome Trust Career Re-Entry Fellow, Reader (Associate Professor) in Cardiovascular Physiology and Metabolism at Queen Mary, said: "Unlike humans, who are prone to heart injury by hypoxia and anoxia caused by blood occlusion during heart attacks, NMR hearts have adapted to evade such damage. Thanks to our research, we are now able to understand the metabolic and genetic mechanisms underpinning this unique level of protection."
- Heart Disease
- Personalized Medicine
- Stroke Prevention
- Extreme Survival
- Evolutionary Biology
- Personalized medicine
- Oxygen therapy
- Gene therapy
- Veterinary medicine
- Biopharmaceutical
Story Source:
Materials provided by Queen Mary University of London . Note: Content may be edited for style and length.
Journal Reference :
- Chris G. Faulkes, Thomas R. Eykyn, Jan Lj. Miljkovic, James D. Gilbert, Rebecca L. Charles, Hiran A. Prag, Nikayla Patel, Daniel W. Hart, Michael P. Murphy, Nigel C. Bennett, Dunja Aksentijevic. Naked mole-rats have distinctive cardiometabolic and genetic adaptations to their underground low-oxygen lifestyles . Nature Communications , 2024; 15 (1) DOI: 10.1038/s41467-024-46470-x
Cite This Page :
Explore More
- Illuminating Oxygen's Journey in the Brain
- DNA Study IDs Descendants of George Washington
- Heart Disease Risk: More Than One Drink a Day
- Unlocking Supernova Stardust Secrets
- Why Do Some Memories Become Longterm?
- Cell Division Quality Control 'Stopwatch'
- What Controls Sun's Differential Rotation?
- Robot, Can You Say 'Cheese'?
- Researchers Turn Back the Clock On Cancer Cells
- Making Long-Term Memories: Nerve-Cell Damage
Trending Topics
Strange & offbeat.
We've detected unusual activity from your computer network
To continue, please click the box below to let us know you're not a robot.
Why did this happen?
Please make sure your browser supports JavaScript and cookies and that you are not blocking them from loading. For more information you can review our Terms of Service and Cookie Policy .
For inquiries related to this message please contact our support team and provide the reference ID below.
More than one alcoholic drink a day raises heart disease risk for women
Young to middle-aged women who drink more than one alcoholic beverage a day, on average, were more likely to develop coronary heart disease than people who drink less, according to new research by Kaiser Permanente Northern California.
Women in the study who reported drinking eight or more alcoholic beverages per week were 33 to 51 percent more likely to develop coronary heart disease. And women who binge drink — three alcoholic beverages per day — were 68 percent more likely to develop coronary heart disease than those who drink in moderation, the research showed.
“There has been an increasing prevalence of alcohol use among young and middle-aged women as women may feel they’re protected against heart disease until they’re older, but this study shows that even in that age group, women who drink more than the recommended amount of one drink per day or tend to binge drink, are at risk for coronary heart disease,” Jamal Rana , a cardiologist with the Permanente Medical Group and the study’s lead author, wrote in an email.
The study will be presented at the American College of Cardiology’s Annual Scientific Session in early April. It was funded by the National Institutes of Health (NIH) and the National Institute on Alcohol Abuse and Alcoholism.
Risk is highest for binge drinking
The study used data from 432,265 adults, ages 18 to 65, who received care in the Kaiser Permanente Northern California integrated health organization. The group was composed of about 243,000 men and 189,000 women who filled out routine assessments between 2014 and 2015 in which they reported their alcohol intake. Researchers then looked at the coronary heart disease diagnoses among participants over the four years that followed.
Get Well+Being tips straight to your inbox

Participants were divided into three groups, according to their alcohol intake: low (one to two drinks per week), moderate (three to 14 drinks per week for men and three to seven drinks per week for women), or high (15 or more drinks per week for men and eight or more drinks per week for women).
Participants were also categorized as either engaging in binge drinking or not, with binge drinking being defined for men as having more than four drinks in a single day and for women as having more than three drinks a day, in the prior three months. Those who reported no alcohol use were not included.
During the four-year follow-up period, 3,108 participants were diagnosed with coronary heart disease. Higher levels of alcohol consumption were associated with a higher incidence of coronary heart disease. Both men and women who reported heavy episodic drinking, or binge drinking, had the highest risk.
The link between alcohol and coronary heart disease proved to be especially strong among women, the data showed.
Coronary heart disease, also known as coronary artery disease, is the most common type of heart disease in the United States, according to the Centers for Disease Control and Prevention . The disease develops when the arteries of the heart are unable to deliver enough oxygen-rich blood to the heart because of plaque buildup.
Heart disease is the No. 1 killer of American women , according to the CDC. Symptoms differ, and often there are none until people suffer from a heart attack or other problem, a NIH report said.
“There has long been this idea that alcohol is good for the heart, but more and more evidence is challenging that notion,” Rana wrote.
Alcohol is a risk factor for many health issues
Alcohol is actually a toxin to the heart, said Nieca Goldberg , a clinical associate professor of medicine at NYU Grossman School of Medicine and medical director of Atria New York City. Alcohol raises blood pressure , increases the risk for heart rhythm problems, especially during times of binge drinking, is associated with an enlarged heart and is a toxin to the heart muscle , she said.
“I think this is an important study to do because for a while, people thought that alcohol was protective against the heart because of earlier studies that were done in the past. But in fact, we don’t prescribe alcohol to fight heart disease,” she said.
Alcohol use is rising among women
The link between alcohol and heart disease for women is cause for concern, given that alcohol use among women is on the rise. While men used to drink more, studies over the past several years show that gap is closing.
Approximately 13 percent of adult women report binge drinking , with 25 percent of those women saying they do so at least weekly, on average, and 25 percent saying they consume at least six drinks during a binge drinking occasion, according to the CDC. A study in July in JAMA Network Open showed the number of alcohol-related deaths among women was rising at a faster rate than those among men, particularly for people 65 and older.
“I think this raises an important issue, because oftentimes, we think of heavy drinkers as men only. But we have to have heightened awareness that women may be heavy alcohol drinkers,” Goldberg said.
Occasional binge drinking can affect heart health
But it wasn’t just heavy drinkers who were affected, said Mary Ann McLaughlin , cardiologist at the Mount Sinai Fuster Heart Hospital. The study is interesting because it showed that even occasional drinking, if it reaches the level of binge drinking, can affect heart health, she said.
There are those who thought just drinking on the weekends was not a big deal, because they weren’t drinking every day, she said. “But the fact is, if they have more than four drinks as a woman or more than five drinks as a man on one day, in the past three months, they were at increased risk,” McLaughlin said.
Women are more adversely affected by alcohol
It is not a surprise that alcohol poses a higher risk for women than men when it comes to heart health, said C. Noel Bairey Merz , director of the Barbra Streisand Women’s Heart Center in the Smidt Heart Institute at Cedars-Sinai.
Women are more adversely affected than men by a lot of things such as cigarettes and pharmaceuticals and a bottle of beer or a glass of wine, where the dosage for men and women is the same and yet women are smaller, she said, referring to women being physically smaller, on average. Women also metabolize differently, their blood pressure is different, their liver function is different, they even deposit fat differently, Merz said.
“Women and men are built differently,” she said, noting she wasn’t even referring to the obvious reproductive differences. “It could be that in addition to body surface area … there are just pure biological differences in how the alcohol is metabolized.”
It’s possible to mitigate some of the ill effects of alcohol, the experts said. For instance, when people reduce or stop drinking, their blood pressure can improve and some lose weight as alcohol is a sugar that is no longer being consumed.
But issues such as enlargement of the heart happen with long-term heavy drinking, and even if the person stops, that may not improve, they said.
“If one stops drinking, some of the risk could reverse,” McLaughlin said. “The degree of improvement would depend on the age of the person and number of years of drinking.”
Read more from Well+Being
Well+Being shares news and advice for living well every day. Sign up for our newsletter to get tips directly in your inbox.
Vitamin B12 for fatigue has no proven benefit unless you have a deficiency that causes anemia.
Flashes, shimmers and blind spots: Here’s what migraine aura looks like.
Sparkling water is a better choice for your teeth than most popular beverages.
You can help your brain form healthy habits and break the bad ones.
Our 7 best tips to build an exercise habit .

Heart disease, stroke risk may be higher in certain neighborhoods
By American Heart Association News

People living in neighborhoods with high rates of environmental and socioeconomic problems may face a higher risk for heart disease and double the risk for stroke, new research finds.
The study , published Wednesday in the Journal of the American Heart Association, found the combination of chronic environmental and social issues, including higher rates of pollution and unemployment, contributed to widening disparities in cardiovascular health and that environmental factors alone played a significant role.
"Our study is one of the first to examine the impact of both social and environmental factors in combination and looked at the complex interplay between them," senior author Dr. Sarju Ganatra said in a news release . Ganatra, a cardiologist, is vice chair in the department of medicine for research and director of the Cardio-Oncology Program and South Asian Cardio-Metabolic Program at Lahey Hospital and Medical Center in Burlington, Massachusetts.
Recent studies have shown neighborhoods with greater social and environmental disadvantages have higher rates of cardiovascular disease and its risk factors. In this new study, researchers wanted to explore how much of a role environmental factors played both independently and in combination with socioeconomic factors.
For the study, environmental disadvantages included air and water pollution, the presence of potentially hazardous or toxic sites, few recreational parks and heavy road traffic, along with the presence of railways or airports. Social factors included racial and ethnic minority status, income, education and employment levels, housing status and access to the internet and health care.
The analysis showed residents of the most environmentally and socially vulnerable neighborhoods had 1.68 times the rate of coronary heart disease and more than twice the rate of stroke compared to people in the least vulnerable neighborhoods. People in the most vulnerable areas also had higher rates of Type 2 diabetes, chronic kidney disease, high blood pressure and obesity.
"I was amazed to see the tight links and complex interplay between social and environmental factors on health outcomes," Ganatra said. "We were able to demonstrate their 'dual hit' on health outcomes. And beyond that, we were more amazed by the fact that even after adjusting for socioeconomic factors, environmental factors played a crucial and independent role in determining various heart disease and other related health outcomes."
People living in the most environmentally and socially vulnerable neighborhoods had the highest percentage of Black and Hispanic adults (30% and 48%, respectively), while the least vulnerable neighborhoods had the lowest percentage of racial and ethnic minorities (5% and 11%).
The researchers, Ganatra said, believe reversing the impact of environmental and socioeconomic disadvantages will require a multipronged approach that includes reducing exposure to air pollution and establishing policies to address poverty, urban revitalization, public education, job creation and affordable housing, as well as increased access to quality health care.
"Our aim is to empower the health care community to better inform patients about environmental factors they encounter daily," he said. "Patients, in turn, gain the ability to reduce their exposure to harmful environmental conditions, such as exposure to harmful chemicals and air pollutants to minimize health hazards and mitigate health risks."
American Heart Association News Stories
Copyright is owned or held by the American Heart Association, Inc., and all rights are reserved. Permission is granted, at no cost and without need for further request, for individuals, media outlets, and non-commercial education and awareness efforts to link to, quote, excerpt from or reprint these stories in any medium as long as no text is altered and proper attribution is made to American Heart Association News.
Other uses, including educational products or services sold for profit, must comply with the American Heart Association’s Copyright Permission Guidelines. See full terms of use . These stories may not be used to promote or endorse a commercial product or service.
HEALTH CARE DISCLAIMER: This site and its services do not constitute the practice of medical advice, diagnosis or treatment. Always talk to your health care provider for diagnosis and treatment, including your specific medical needs. If you have or suspect that you have a medical problem or condition, please contact a qualified health care professional immediately. If you are in the United States and experiencing a medical emergency, call 911 or call for emergency medical help immediately.
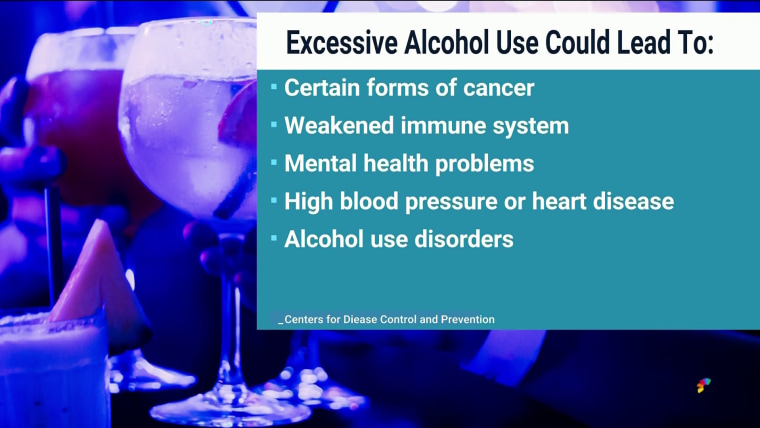
New study shows a link between alcohol and heart disease in women

Teens seeking help for substance abuse turn to drugs and alcohol to de-stress
Hidden cholesterol risk could affect millions of Americans

NBC investigates how HCA hospitals put profits before patients

'Essential eight' behaviors that may slow biological aging

Exploring rarities of cardiac arrest in young athletes after Bronny James' collapse

LeBron James' son Bronny in stable condition after suffering cardiac arrest

How to recognize heart attack symptoms and save a life

Heart attack survivor thanks women who saved her on dance floor

Young cardiac arrest survivor spreads life-saving CPR message

Comedian Phoebe Robinson on walking the runway for a good cause

What if you could take three heart medications in one pill?

3 exercises to improve heart health

What toll has the pandemic taken on heart health?

‘Broken heart syndrome’ spikes during COVID-19: What is it?

Watch: Woman begs for water and medical attention, later dies from heart infection

How a rare condition can cause heart attacks in healthy young women

Meet the couple teaching tai chi to the homeless

Mom who survived 2 heart attacks by age 32 sheds light on heart health

3 products that give back to heart-health organizations
Nbc news now.
A new study from Kaiser Permanente of Northern California is showing a link between alcohol use and heart disease in women. The research found that women who drink more than one drink a day are up to 50% more likely to develop heart disease. NBC News’ Medical Fellow, Dr. Akshay Syal, explains the results of the new study. March 29, 2024
Best of NBC News

Nightly News Netcast
Nightly news full broadcast (march 30th).

Nightly News
Arrests made in connection to women saying they were punched in the face in new york city.
Evictions skyrocket nationwide as housing costs rise

A teen battling a rare disease had her musical dreams come true

OpenAI unveils its Voice Engine tool that can replicate people’s voices
Pope Francis commences Easter weekend amid health concerns

IMAGES
COMMENTS
The Framingham Heart Study marked its 75th anniversary in 2023. Findings from the study over three generations of participants have changed how Americans and their doctors view heart disease and how to prevent, predict, and treat it. The study has expanded its research activities to other disease domain areas such as stroke, dementia, and ...
R.O. Roswell and Others. N Engl J Med 2024;390:1030-1043. A 55-year-old man had an out-of-hospital cardiac arrest. An evaluation showed 2-mm ST-segment elevations in the inferior leads on ...
The remaining lifetime risk of cardiovascular disease fell between 1960-1979 and 2000-2018 - from 36.3% to 26.5% in women, and from 52.5% to 30.1% in men. Researchers also found men and women in the 21st century were having their first cardiovascular disease events later in life. From 2000-2018, the average age of a first cardiovascular event ...
In one study, researchers wanted to see whether restricting dietary sodium could lower the incidence of future adverse clinical events in people with heart failure. The research team randomly assigned 806 people with chronic heart failure from six countries (Australia, Canada, Chile, Colombia, Mexico and New Zealand) to two different regimens.
For example, the large, US-based, multicentre, randomized, controlled HF-ACTION trial 73 of cardiac rehabilitation reported that in addition to an index diagnosis of heart failure, at entry to the study, a substantial proportion of the 2,331 patients with heart failure had several comorbidities, including 59% with hypertension, 21% with atrial ...
The following patients were excluded: patients who did not have a clinical diagnosis of heart failure according to Framingham Heart Study criteria or had a B-type natriuretic peptide level that ...
Since 1949, the American Heart Association has invested more than $5 billion toward scientific research, more than any other non-profit organization outside of the federal government. If you are a researcher, the AHA has resources available for you. Learn more about our varied initiatives, and how you can play a valuable role.
The purpose of this study is to learn whether Cardiac Magnetic Resonance Imaging (cMRI) and/or echocardiogram is useful to diagnose patients with unique heart conditions. This research study focuses on evaluating the use of cMRI or echocardiogram as a novel, non-invasive method for evaluating specific heart conditions.
Research Highlights: A study of over 20,000 adults found that those who followed an 8-hour time-restricted eating schedule, a type of intermittent fasting, had a 91% higher risk of death from cardiovascular disease. People with heart disease or cancer also had an increased risk of cardiovascular death.
The Ruth L. Kirschstein Institutional Research Training Program (T32) is a post-doctoral research fellowship in pathophysiology of myocardial disease. This program provides a broad approach to cardiovascular research, allowing trainees to pursue any area of research. The Johns Hopkins Heart and Vascular Institute welcomes our fellow physicians ...
A cardiovascular research study used social media sites including Facebook, Twitter, ... Dickson et al 55 performed a mixed-methods study with 30 black patients with heart failure to assess cultural beliefs, social support, and beliefs about self-care. In-depth interviews and standardized instruments measuring self-care and social-support were ...
A Study to Assess Emotional Experiences in Patients with Symptomatic Heart Failure and Left Ventricular Assist Devices Rochester, MN . The objectives of this study are to use qualitative methods to characterize patients' distress, to use qualitative methods to explore how distress can impact healthcare behaviors and caregiver support; specifically, their motivation to sustain critical ...
The new study, published Friday in the American Heart Association journal Circulation, examined the nature and extent of the heart damage and inflammation in the sickest people with COVID-19. Researchers looked at 342 COVID-19 patients with high levels of the protein troponin in 25 United Kingdom hospitals between June 2020 and March 2021.
People who ate all their food in less than eight hours were 91 percent more likely to die from heart disease during the study period than people who ate throughout a 12- to 16-hour window.
Subsequent studies by Appelbaum 50 demonstrated that potential participants in research studies had better comprehension when there was a ... an observational population-based study of brain arteriovenous malformations. 70 Similar experience has been reported in studies of ischemic heart disease. 71,72 Annas 73 notes the reality of wide ...
The Research. The new study included more than 20,000 adults from the United States. The participants completed two interviews, less than two weeks apart, about what time they ate on the previous day.
Secrets of the naked mole-rat: new study reveals how their unique metabolism protects them from heart attacks. ScienceDaily . Retrieved March 29, 2024 from www.sciencedaily.com / releases / 2024 ...
Limiting mealtimes to a period of just eight hours a day was linked to a 91% increase in risk of death from heart disease in the study. The safety of intermittent fasting, a popular strategy to ...
Women in the study who reported drinking eight or more alcoholic beverages per week were 33 to 51 percent more likely to develop coronary heart disease. And women who binge drink — three ...
People living in neighborhoods with high rates of environmental and socioeconomic problems may face a higher risk for heart disease and double the risk for stroke, new research finds. The study, published Wednesday in the Journal of the American Heart Association, found the combination of chronic environmental and social issues, including ...
A new study from Kaiser Permanente of Northern California is showing a link between alcohol use and heart disease in women. The research found that women who drink more than one drink a day are up ...
Early research has suggested that if you have heart disease, intermittent fasting may raise the risk of death from heart disease, drawing skepticism from experts and cautions from the researchers ...