- Case report
- Open access
- Published: 24 April 2021

Cesarean myomectomy: a case report and review of the literature
- Priyanka Garg ORCID: orcid.org/0000-0003-0336-4750 1 , 2 &
- Romi Bansal 2
Journal of Medical Case Reports volume 15 , Article number: 193 ( 2021 ) Cite this article
5210 Accesses
7 Citations
1 Altmetric
Metrics details
Routine myomectomy at the time of cesarean section has been condemned in the past due to fear of uncontrolled hemorrhage and peripartum hysterectomy. It is still a topic of debate worldwide. However, in recent years, many case studies of cesarean myomectomy have been published validating its safety without any significant complications.
Case presentation
We describe the case of a 27-year-old gravida 2 para 1 live birth 1 North Indian woman with one previous lower segment caesarean section (LSCS) at 35 weeks with labor pains and scar tenderness. Her recent ultrasound (USG) report suggested a single live intrauterine pregnancy with an intramural fibroid of 8.6 × 6.5 cm located in the left anterolateral wall of the lower uterine segment. The patient was taken up for emergency cesarean section along with successful removal of the myoma, which was bulging into the incision line, causing difficulty in closure of the uterine wound. Prophylactically, oxytocin infusion, bilateral ligation of uterine arteries, and injection vasopressin (diluted) was administered to decrease the blood loss. The patient was discharged after 7 days without any complications.
Conclusions
Routine myomectomy at the time of cesarean section is not a standard procedure and is not accepted worldwide. However, it may be considered a safe option in carefully selected cases in the hands of an experienced obstetrician with appropriate hemostatic technique. Large multicenter randomized controlled trials should be conducted to evaluate the best practice guidelines for cesarean myomectomy.
Peer Review reports
Leiomyomas are the most common benign tumors of the reproductive tract in women of childbearing age. Their exact incidence in pregnancy is hard to estimate. However, literature reports a prevalence of 2–4% [ 1 ]. The incidence is rising due to delayed childbearing and a rapid increase in the number of cesarean sections over the last few years. The majority of the patients are either asymptomatic or have mild symptoms and need conservative management only. Myomectomy during cesarean section is routinely avoided due to increased vascularity of the gravid uterus leading to massive hemorrhage, unnecessary obstetric hysterectomy, and increased perioperative morbidity and mortality. However, in modern obstetrics, with advancements in anesthesia, adequate availability of blood products, selective devascularization techniques, and a multidisciplinary approach, obstetricians are increasingly choosing to perform myomectomy during cesarean section, thus saving the patient from future morbidity due to multiple surgeries, anesthetic complications, and out-of-pocket expenditure [ 2 ]. Here, we report the case of a successful myomectomy done during an emergency cesarean section without any complications. We intend to break the traditional thumb rule of avoiding myomectomy at the time of cesarean section, and be open to the procedure after careful case selection.
A 27-year-old gravida 2 para 1 live birth 1 North Indian woman with one previous lower segment caesarean section (LSCS) presented to our outpatient department (OPD) at 35 weeks with complaints of intermittent pain in the lower abdomen that was radiating to her back for the last 5 hours. There was no associated complaint of leaking or bleeding per vaginum . Her antenatal period was uneventful. However, she was diagnosed as having a fibroid on the left side of the uterus but reported no complications that could be attributed to it. Her general and systemic examination was unremarkable. All the antenatal investigations were normal. Her recent ultrasound (USG) report suggested a single live intrauterine pregnancy with an intramural fibroid measuring 8.6 × 6.5 cm located in the left anterolateral wall of the lower uterine segment.
On admission, her heart rate was 96 beats per minute, blood pressure was 110/70 mmHg, and mild pallor was present. Abdominal examination revealed a term size uterus with longitudinal lie. Mild uterine contractions were present with positive scar tenderness. On auscultation, fetal heart rate was 142 beats/minute. Vaginal examination depicted a 2 cm dilated cervix, which was 20–30% effaced, presenting part at −3 station with intact membranes. She was taken up for emergency LSCS given previous cesarean section with preterm labor and scar tenderness. Her preoperative hemoglobin was 12.1 gm%, hematocrit was 34.5%, and blood group was O positive. Adequate blood products were arranged and informed written consent was obtained from the patient and her relatives after explaining to them about the risk of excessive bleeding, need for blood transfusion, and peripartum hysterectomy. During surgery, the abdomen was opened by an infra-umbilical vertical incision for adequate access. There was a single large intramural fibroid occupying most of the lower uterine segment. The previous scar was intact but thinned out, possibly because of the stretching effect of the fibroid. A lower segment transverse incision was made below the inferior margin of the fibroid, and a 2.54 kg female baby was delivered, with an APGAR score of 9 at 1 minute. As the fibroid was bulging into the incision line and causing difficulty in closure of the uterine wound, the decision of myomectomy was taken (Fig. 1 ). Prophylactically, oxytocin infusion, bilateral ligation of uterine arteries, and injection of vasopressin (diluted) was injected to decrease the blood loss. The fibroid was then enucleated and the myoma bed closed with delayed absorbable sutures followed by closure of the uterine wound. A complete hemostasis was achieved. The total duration of the surgery was approximately 50 minutes and the amount of blood lost around 1100 mL, which is almost comparable to other cesarean sections. Broad-spectrum antibiotics and analgesics were administered in the postoperative period. Her post-surgery hemoglobin was 11.4 gm% and hematocrit was 33%, thus not requiring any blood transfusion. The patient was discharged on the seventh postoperative day with a normal involuting uterus. On follow-up at 6 weeks, the uterus was completely involuted, and repeat USG did not show any fibroid. On further follow-up to 6 months, she was asymptomatic and had an uneventful course.
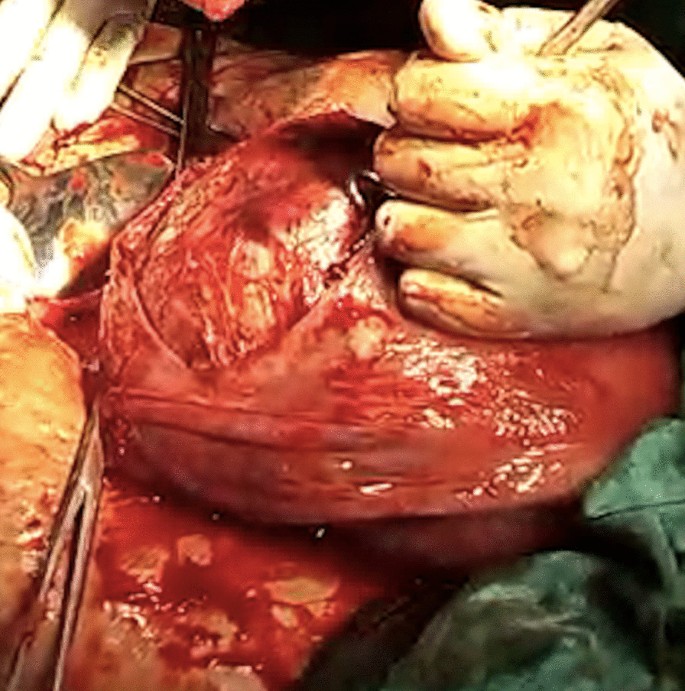
Intraoperative image depicting the fibroid bulging into the incision line
We report a case of successful myomectomy performed at the time of an emergency cesarean section, with an intent to disintegrate the long-established belief of avoiding it due to fear of complications. Pregnancy with fibroid is a high-risk situation. Although the majority of such cases are asymptomatic or have mild symptoms, 10–40% of cases can present with antenatal complications in the form of pregnancy loss, degenerative changes, malpresentation, abruption placenta, preterm labor, dysfunctional labor or uterine inertia, and increased chances of operative delivery, thus increasing maternal and fetal morbidity and mortality [ 3 ]. Treatment is usually conservative during the antenatal period in the form of bed rest, adequate hydration, and analgesics. Myomectomy is rarely required in the case of intractable abdominal pain due to twisting of pedunculated sub-serosal fibroid, red degeneration unresponsive to conservative treatment, or massively enlarged myoma causing abdominal discomfort to the patient [ 1 ]. In a recent study, a successful myomectomy was performed during the first trimester at 11 weeks for a large myoma of 14 cm that was a cause of severe discomfort to the patient [ 4 ]. The patient continued with pregnancy to term and delivered a healthy baby. Another uneventful myomectomy was performed in the second trimester by Bhatla et al . without any adverse impact on pregnancy [ 5 ]. Myomectomy during cesarean section is still a topic of debate in the modern era. Until the last decade, it was considered a dreadful surgery except for pedunculated sub-serosal fibroids. However, many researches have concluded that the procedure is not dangerous and does not lead to complications in the hands of an experienced obstetrician [ 6 ]. Kwawukume performed cesarean myomectomies on 12 patients and reported that enucleation was much easier in pregnancy due to increased softness of the tissue [ 7 ]. A retrospective case–control study, comparing 40 women with fibroids who underwent cesarean myomectomy with 80 women with fibroids forming the control group who underwent cesarean section alone, reported no significant difference in the incidence of hemorrhage between the two groups (12.5% and 11.3%, respectively) [ 8 ]. Similar findings were reported in another study, with no significant differences in hemoglobin levels, incidence of blood transfusions, or postoperative pyrexia. However, not all myomas need to be removed, but only those causing difficulty in delivery of the fetus or wound closure and sub-serosal fibroids. In our case, myomectomy was inevitable as the myoma was in the incision line, making wound closure impossible. Every possible effort should be made to reduce the blood loss. Bilateral ligation of uterine arteries immediately after delivery of the fetus significantly reduces both intraoperative and postoperative blood loss and risk of peripartum hysterectomy [ 9 ]. It also reduces the recurrence of myomas and minimizes the need for future surgery, with no apparent effect on fertility [ 10 ]. This was a key step in our case which prevented the dreaded complications. Also, the postpartum uterus is better adapted physiologically to control bleeding than in any other phase of a woman’s lifetime. The patient and relatives should be properly counseled and informed that removal of myoma is possible, and a final decision can be taken at the time of cesarean based upon the size, number, and location of the fibroid.
The idea of performing myomectomy at the time of cesarean section appears winsome in a low-resource country like India, where fibroids are common. If performed safely, it can avoid the additional morbidity of a future surgery, thus justifying the cost-effectiveness of the procedure. However, the importance of an expert obstetrician, equipped center with adequate manpower and blood products, and careful case selection cannot be ignored.
Availability of data and materials
Not applicable.
Ardovino M, Ardovino I, Castaldi MA, Monteverde A, Colacurci N, Cobellis L. Laparoscopic myomectomy of a subserous pedunculated fibroid at 14 weeks of pregnancy: a case report. J Med Case Rep. 2011;5:2–6.
Article Google Scholar
Kathpalia SK, Arora D, Vasudeva S, Singh S. Myomectomy at cesarean section: a safe option. Med J Armed Forces India. 2016;72:S161–3.
Article CAS Google Scholar
Ma PC, Juan YC, De WI, Chen CH, Liu WM, Jeng CJ. A huge leiomyoma subjected to a myomectomy during a cesarean section. Taiwan J Obstet Gynecol. 2010;49(2):220–2.
Leach K, Khatain L, Tocce K. First trimester myomectomy as an alternative to termination of pregnancy in a woman with a symptomatic uterine leiomyoma: a case report. J Med Case Rep. 2011;5:2–5.
Bhatla N, Dash BB, Kriplani A, Agarwal N. Myomectomy during pregnancy: a feasible option. J Obstet Gynaecol Res. 2009;35(1):173–5.
Guler AE, Guler ZÇD, Kinci MF, Mungan MT. Myomectomy during cesarean section: why do we abstain from? J Obstet Gynecol India. 2020. https://doi.org/10.1007/s13224-019-01303-6 .
Kwawukume E. Myomectomy during cesarean section. Int J Gynecol Obstet. 2002;76(2):183–4.
Kaymak O, Ustunyurt E, Okyay RE, Kalyoncu S, Mollamahmutoglu L. Myomectomy during cesarean section. Int J Gynecol Obstet. 2005;89(2):90–3.
Murmu S. successful myomectomy during caesarean section: a case report. Int J Contemp Med Res [IJCMR]. 2019;6(9):44–5.
Liu WM, Wang PH, Tang WL, Te WI, Tzeng CR. Uterine artery ligation for treatment of pregnant women with uterine leiomyomas who are undergoing cesarean section. Fertil Steril. 2006;86(2):423–8.
Download references
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Obstetric and Gynecology, All India Institute of Medical Sciences, Bathinda, 151505, India
Priyanka Garg
Department of Obstetric and Gynecology, Adesh institute of Medical Sciences and Research, Bathinda, Punjab, India
Priyanka Garg & Romi Bansal
You can also search for this author in PubMed Google Scholar
Contributions
PG and RB treated the patient. PG wrote the manuscript. RB revised and edited the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Priyanka Garg .
Ethics declarations
Ethics approval and consent to participate.
This study did not conduct any experiments on animals or humans. The patient consented to the use of her personal data for the purpose of this case report.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests. The authors have no association with financial or nonfinancial organizations.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Garg, P., Bansal, R. Cesarean myomectomy: a case report and review of the literature. J Med Case Reports 15 , 193 (2021). https://doi.org/10.1186/s13256-021-02785-7
Download citation
Received : 29 January 2021
Accepted : 12 March 2021
Published : 24 April 2021
DOI : https://doi.org/10.1186/s13256-021-02785-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Postpartum hemorrhage
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Decreased Length of Stay for C-section Case Study

Executive Summary
Local problem.
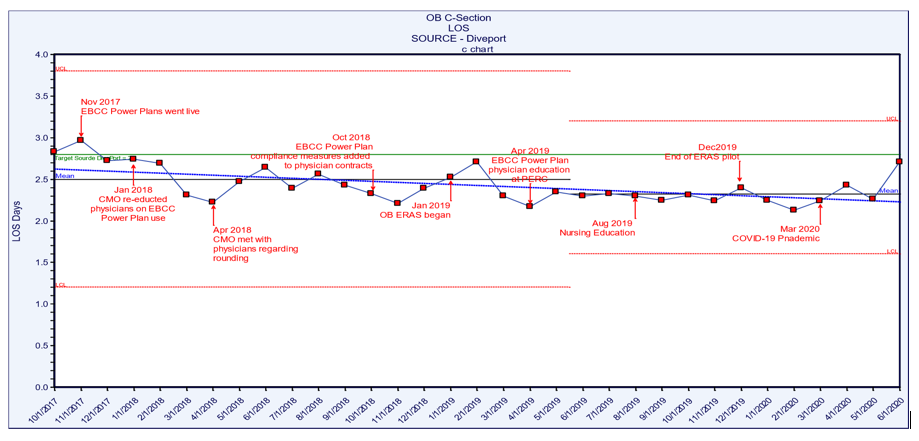
To decrease the variability in care delivery to improve the standard of care and the outcomes of the patients undergoing a cesarean section (C-section) procedure. Baptist Health South Florida’s (BHSF) Homestead Hospital implemented electronic order sets (PowerPlans ™) in 2017 for the patient population, and over time has improved the length of stay (LOS) and maintained zero maternal deaths and zero venous thromboembolisms (VTEs). Homestead also initiated an enhanced recovery after surgery (ERAS) pilot for the cesarean section population. The goal of the ERAS c-Section pilot was to serve as an adjunct to current practices geared to deliver a multidisciplinary approach to care with a defined multimodal perioperative care pathway designed to reduce the stress response to surgery and accelerate the patient’s recovery. This encompassed people, process and technology as change management impacted the way Homestead Hospital delivered care along with the build and design of the electronic healthcare record (EHR) requirements. The ERAS pilot will be discussed in more detail under the Clinical Transformation section as an example of pending development and redesign. Analytics measuring the utilization of the PowerPlans supported the measurement of adherence to the standard of care compliance and improved outcomes with a decrease in LOS. The overall LOS for the patient population with the implementation of the PowerPlan decreased from 3.0 days in FY 2017 to 2.30 days in 2020 pre-COVID-19. There is a slight increase noted in LOS in Q1 2020.
Key Stakeholders
Physicians, nursing, pharmacy, lactation team, discharge planning, informatics and patients/family.
EHR data , clinical decision support alerts (e.g., allergies, sepsis, VTE prevention and fetal demise), PowerPlans for bundle compliance, device integration for vital signs and fetal monitoring, bedside specimen collection and scanning, human milk and formula management and analytics for process and outcomes measurement.
People and Process
Physician and staff buy-in, patient counseling, education and commitment pre-op and post-op; ongoing care team education and commitment to care redesign; neonatal bonding, comfort, feeding, safety and discharge follow-up plan.
Lessons Learned
- Buy-in is key for both the care team and the patient and family
- Education of the PowerPlans and ERAS Pathway is a huge key to success
- Sharing analytics to high-light improvements will help keep the process successful
- The build and design of the EHR tools to support the workflow will assist with compliance
- Neonatal components including safety and comfort will help decrease stress of the mother and support a reduced stress response
Define the Clinical Problem and Pre-Implementation Performance
Childbirth is one of the leading causes of hospital admission in the United States and there is documented evidence of variation in C-section rates, costs and outcomes due to variation in care delivery models. BHSF partnered with Navigant on the T2020 initiative which includes redesigning care for select diagnosis related groups. Navigant and the organization decided upon a structure of an OB/GYN Steering Committee as well as a design team. Both teams included representation from the facilities that provide obstetrical care throughout the health system.
The Steering Committee elected to focus on the cesarean section population to improve overall outcomes, including decreased LOS and bundle compliance. The design team collaborated on creating clinical specifications to ensure every obstetric patient get the same care, every time. Initiatives included a decrease in the LOS and overall improved standardization of care. This case study will focus on the implementation of the PowerPlan and compliance in the utilization.
Perinatal Services also participated in the ERAS pilot for elective C-section patients, which decreased the average LOS, reduced the use of opioids for pain among patients and an improved the infection rate. LOS for ERAS patients as compared to non-ERAS was 1.98 vs. 2.29 for the study period. Non-Opioid use in ERAS patients was 80% and use of non-opioids in non-ERAS patients was 37.74%. The surgical infection rate for the ERAS patients was 0% and non-ERAS was as high as 6.25%. Pain control was also 17% better for the ERAS patients. These indicators show evidence that support the improvements made in the pilot study for the cesarean section ERAS patients and will be the subject of the next phase of work.
The overall LOS for the C-section population with improved bundle compliance decreased from 3.0 days in FY 2017 to 2.30 days in FY 2019 and prior to COVID-19 in Q1 2020. Perinatal Care Quality Measures also include standardization practices such as prophylactic antibiotics, VTE prevention and pain control.
The numerators in this case study are the clinical practice being measured for compliance (PowerPlans) and the LOS for the population. The denominator is the patient population which meets the Medicare Severity Diagnosis Related Groups (MS-DRG) definition for C-section cases. Exclusions include hospice, rehab and expired patients. The organization follows the guidelines and recommendations of The American College of Obstetricians and Gynecology (ACOG), CMS, MS-DRG and benchmarks against Premier. Targeted performance (Premier benchmark) is cesarean section LOS of 2.81, Premier bundle compliance of 80% and zero serious safety evens.
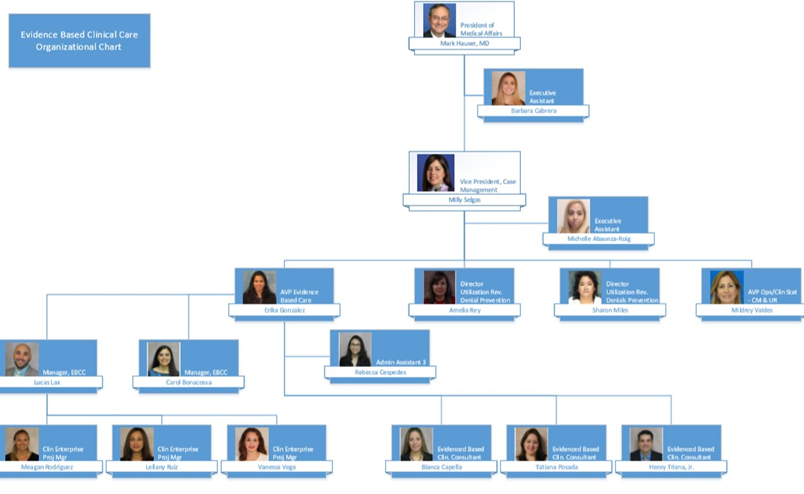
Design and Implementation Model Practices and Governance
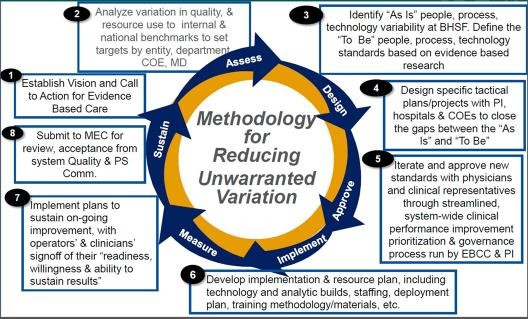
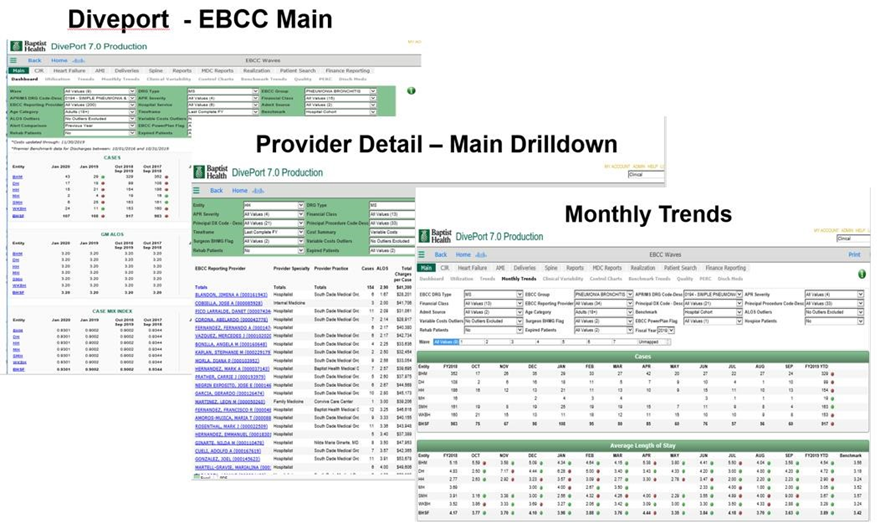
BHSF’s evidence-based clinical care (EBCC) initiative is a strategic system-wide standardization effort to reduce variation and unnecessary costs while focusing on evidence-based, quality care. The process is driven by key stakeholders and is supported by real-time, statistically supported benchmarked data. The charter was signed in 2016 and provides the foundation for a methodical approach to improve patient outcomes (Figure 1).
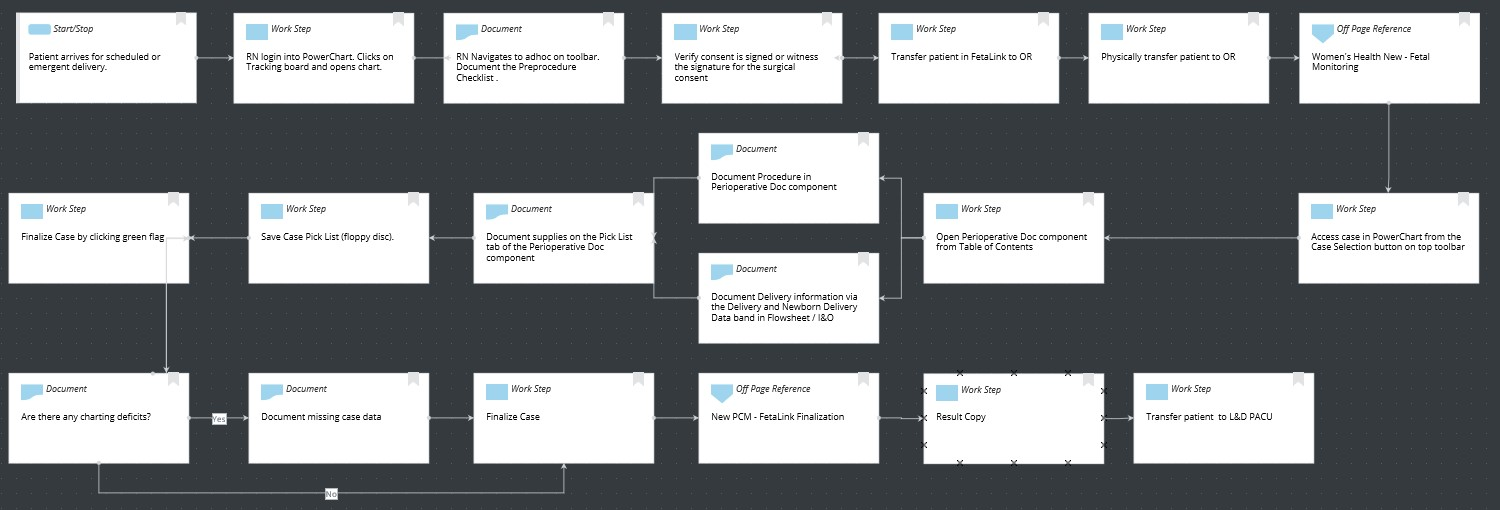
The methodology begins with a call to action to for an evidenced based care assessment of current and future state, design plan, team approval, development of an implementation plan, measurement and sustainment plans (Figure 2).
Each specific project is supported by a sub-group who are experts in on the focus topic. The Service Line Collaborative includes:
- Cardiac and Vascular
- Critical Care
- Emergency Department
- Gastrointestinal
- Infectious Disease
- Neonatology
- Neuroscience
- Orthopedics
- Surgery/PEI/ERAS/NSQIP
The organization has partnered with Navigant on the T2020 initiative which includes redesigning care for select diagnosis related groups. They decided upon a structure of an OB/GYN Steering Committee as well as a design team. Both steering and design teams included member representation from the facilities that provide obstetrical care throughout the system. The steering committee elected to focus on the primary patient population having the largest impact in reducing the overall C-section rate at BHSF. The design team collaborated on creating clinical specifications to ensure obstetric patients get the same care every patient, every time. While the work is still underway to decrease the overall cesarean section rate, the team has successfully decreased the overall LOS for the patient population and instituted a pilot for the utilization of Enhanced Recovery after Surgery (ERAS).
Technologies include EHR data, CDS–alerts such as allergies, sepsis and fetal demise, PowerPlans for bundle compliance, device integration for vital signs and fetal monitoring, bedside specimen collection and scanning, human milk and formula management and analytics for process and outcomes measurement. The PowerPlans were rolled out in 2017 and followed the recommendations from ACOG.
Education was completed via lunch and learns with classroom time, on-line formats on the EBCC website via the intranet and on the Baptist Health South Florida website which is available in the public domain. PowerPlan education is a consistent part of physician education and CME education is available with every MS-DRG or pathway as it rolls out. The education for the ERAS C-section pilot began in December 2018 and the first ERAS patient plan of care was started in January 2019. Other facilities along with BHSF followed the piloted plan of care and additional rollouts are expected. As a recommendation of The Joint Commission, the organization also will begin SIM training for maternal hemorrhage and hypertensive crisis.
The vaginal and C-section delivery steering committee meets monthly and consists of representatives from the EBCC, physicians (CMO), nursing leadership, L&D, HIT, AVP neonatal services, perinatal services and clinical education.
Clinical Transformation enabled through Information and Technology
In November 2017, BHSF implemented the PowerPlans to decrease variation in the care of the C-section patient population. Three key areas of focus for decreasing the LOS in the cesarean section population for Homestead Hospital include the prevention of infection, the prevention of deep vein thrombosis and adequate pain control. Evidence based care practices support the implementation of these key elements as part of the standardized process of care to decrease the overall LOS. In addition to the PowerPlans to minimize the variation in care delivery order sets, the team also focused on education of the PowerPlans early rounding to assess the day before expected discharge and accountability, and in January of 2019, Homestead Hospital initiated a pilot for ERAS in a subset of cesarean section patients. The change in care delivery regarding ERAS and those outcomes will drive the next phase of care delivery and expand to a broader base. Once COVID-19 initiatives begin to fall into place, resources can shift back to these types of projects.
PowerPlans that currently exist for C-section include (Figure 3):
- EBCC anesthesia pre-cesarean
- EBCC anesthesia post-cesarean
- EBCC OB L&D cesarean delivery pre-operative
- EBCC OB postpartum cesarean delivery admission
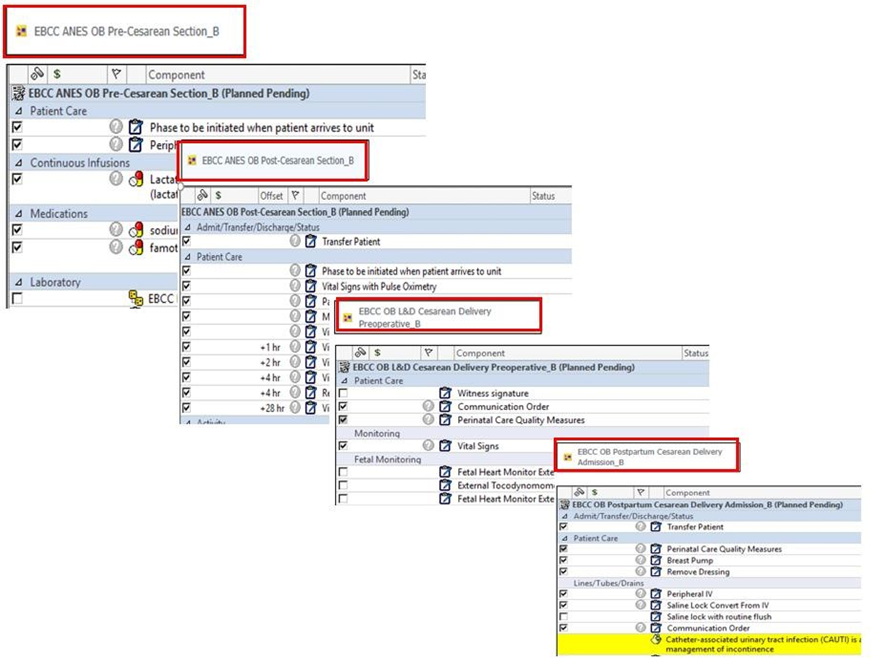
PowerForms™ are used by providers to document the data of the cesarean section delivery. This is extractable data and is pulled into the provider’s note which improves the communication of care for the care team (figure 4).
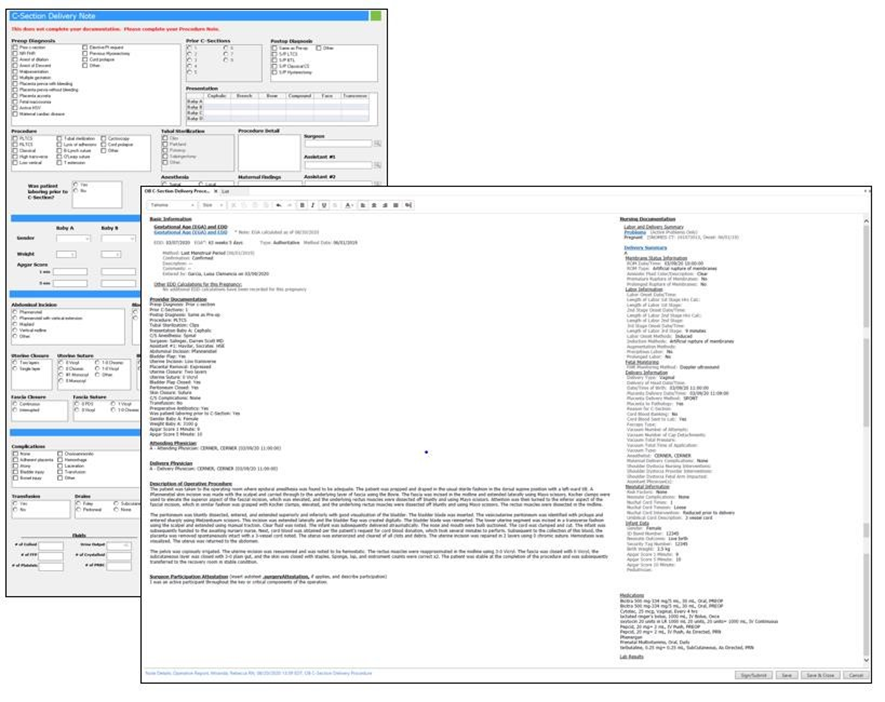
Integration remains seamless, as while in the OR patients are associated to the anesthesia vital sign monitors and vital signs interface into the surgical anesthesia module. All documentation takes place in the anesthesia module and once saved creates a document which is visible within the EHR. All medications and fluids administered while in the OR also display in the patient’s eMAR (Figure 5).
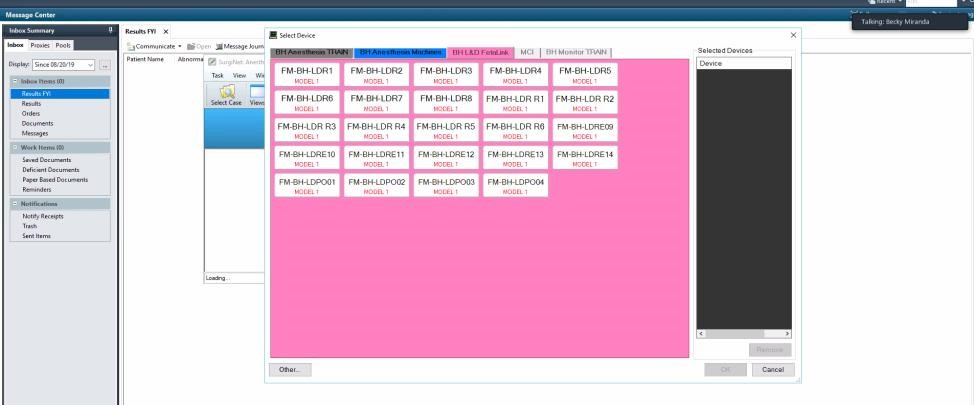
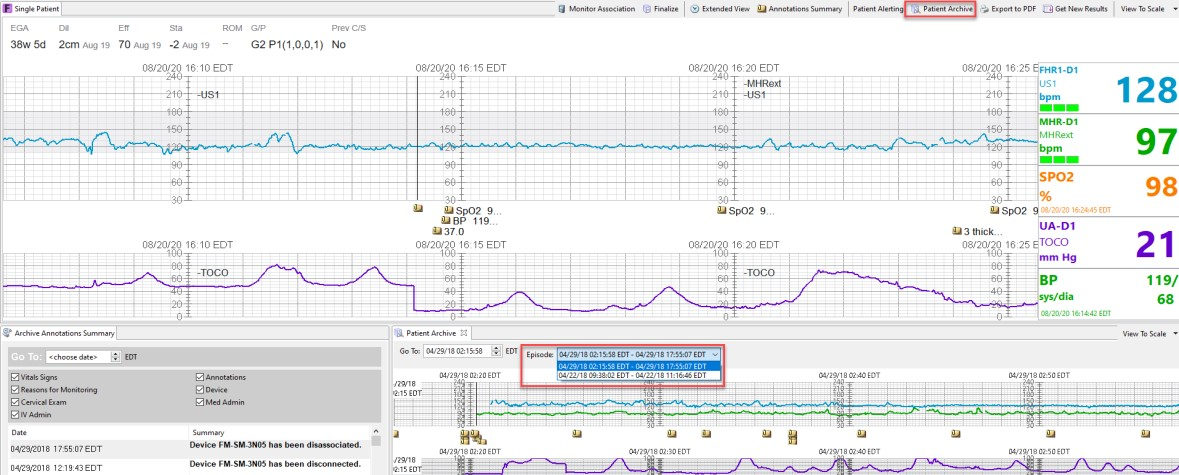
Other safety aspects include the integration with fetal monitoring. Patients are associated to fetal monitors using the Fetalink™ application. Maternal vital signs interface into PowerChart IView™ in addition to all annotations documented within the Fetalink application. Once the patient is in Post-Anesthesia Care Unit (PACU) the patient is then associated to the bedside vital sign monitors using the associate device function in IView™ where vital signs are also interfaced. Maternal previous C-section history status displays within the Fetalink application in addition to gravida and para counts. Providers are also able to view fetal strips remotely using the Fetalink mobile app, Fetalink+. Any previously saved fetal strips archived throughout patient's pregnancy and can be viewed straight from the Fetalink application as well as within the Women's Health Overview component (Figure 6).
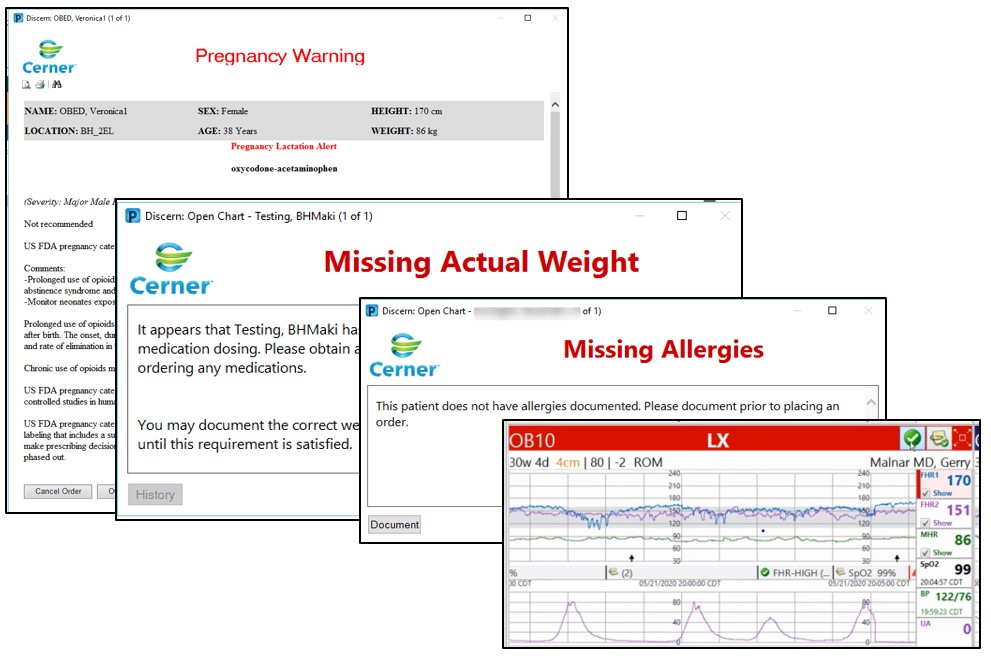
Alerts are visible on monitors, dashboards and within the EHR. CDS alerts such as sepsis with the St. John’s sepsis algorithm, allergies, contraindicated medications, weights and even fetal demise are examples of the alerts firing in real-time to keep mother and baby safe (Figure 7).
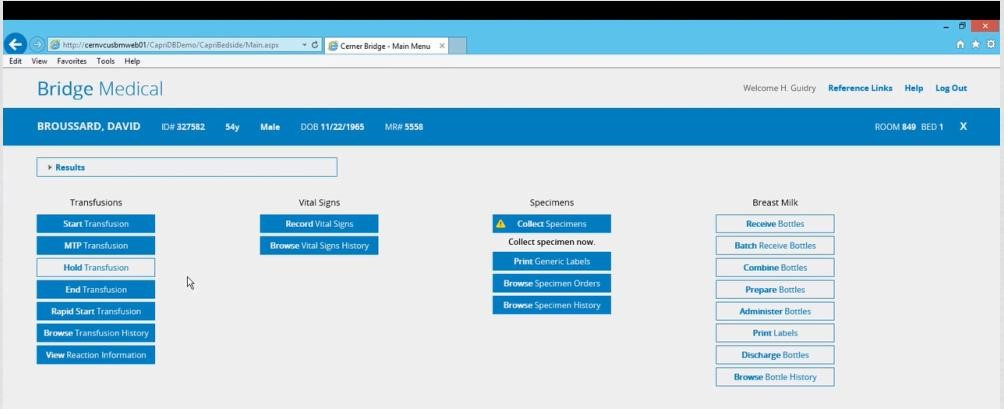
Rounding out the technologies is the capability for bedside scanning for blood, human milk and specimen collection (Figure 8).
People, processes and technology are all important factors in maintaining the safest level of care in the maternal health space. There are many moving pieces and parts, so a fully integrated EHR system increases the ease of use, adoption and standardization of care. The use of evidence based clinical care, tracked with near-real-time analytics helps to ensure improved outcomes such as decreased LOS and decreased safety events such as VTEs and maternal mortalities.
Workflows are mapped out by the interdisciplinary teams and changes are addressed as needed. Clinical decisions and updates to the evidence follow the charter for the EBCC (Figure 9).
Improving Adherence to the Standard of Care
Homestead Hospital, as part of the BHSF care initiatives instituted Power Plans™ to drive the utilization of C-section care bundles to decrease variation of care delivery and improve outcomes for the patient population. Targeting LOS was one of the focus areas with most documented resources support the average hospital LOS post cesarean section to be 2– 4 days. The standardized approach for the PowerPlan rollout, the established educational process and the existing commitment to standardized care via the EBCC structure led to the success of the rollout from the beginning.
The numerator in their care bundle utilization is the clinical practice being measured for compliance (PowerPlan utilization) and the patient population is the denominator which meets the MS-DRG definition for cesarean section cases. BHSF and Homestead Hospital follow the guidelines and recommendations of ACOG, CMS, MS-DRG and benchmarks against Premier. Targeted performance LOS of 2.30 days and bundle compliance of 80% (Figure 10).

Improving Patient Outcomes
The overall LOS for the C-section population with the implementation of the PowerPlan decreased from 3.0 days in FY 2017 to 2.30 days in 2020 pre-COVID-19. The Premier benchmark is 2.81 days. There is a slight increase noted in LOS in Q1 2020. There also were no reported VTEs or maternal deaths within the population (Figure 11).
Of note is also the work done for the C-section ERAS pilot. This work began in January of 2019 and concluded in August of 2019 with a total of 30 patients. The outcomes for those patients included: LOS for ERAS patients as compared to non-ERAS was 1.98 vs. 2.29 for the study period. Non-Opioid use in ERAS patients was 80% and use of non-opioids in non-ERAS patients was 37.74%. The surgical infection rate for the ERAS patients was 0% and for the non-ERAS was as high as 6.25%. Pain control was also 17% better for the ERAS patients. These indicators support the evidence by showing improvements in the ERAS patients in the study. Additional utilization and process redesign will continue with ERAS projects once the impact of COVID-19 stabilizes for the organization.
Accountability and Driving Resilient Care Redesign
Creating a strong governance, incorporating evidence based clinical care and having access to a strong analytic system are all key factors in improving clinical outcomes. The data must be easily captured, readily available, meaningful to key stakeholders and the quality of the data must be trusted. BSFH has created an analytics system that is both successful and sustainable.
The EBCC is the governing body that drives the focus on reducing unnecessary cost and clinical variation through the implementation of evidence-based clinical standards integration, with real-time availability of clinical information and analytics. EBCC monitoring data is housed in DivePort 7.0 (Figure 12).
The implementation of the cesarean section ERAS project is a great example of how data was leveraged to trigger care and process redesign. An ERAS program consists of a multidisciplinary approach to care with a defined multimodal perioperative care pathway designed to reduce the stress response to surgery and accelerate the patient’s recovery. Successful implementation has been shown to decrease variability between patients, resulting in earlier return of gastrointestinal function and reductions in hospital length of stay, complications and total cost.
The goal of the Homestead Hospital ERAS pilot was to have 30 patients in the evaluation. This pilot study was started in January 2019 and completed August 30, 2019, with a total of 30 patients. The outcomes included a reduction in LOS, decreased utilization of opioids with an increased pain management satisfaction score and a zero surgical site infection rate, The success of the C-section ERAS pilot has led to care redesign decisions for other surgical populations. Post COVID-19 turn-around, these initiatives will be implemented on a broader scale.
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
HIMSS Davies Awards
The HIMSS Davies Award showcases the thoughtful application of health information and technology to substantially improve clinical care delivery, patient outcomes and population health.
Begin Your Path to a Davies Award

Breastfeeding rate in the first hour of life according to type of delivery and year of occurrence. CS = cesarean sections, VB = vaginal birth
Regarding the NICU admission rate, it is noticed that neonates born by C-section are more likely to need this type of support than those born by vaginal delivery (6.7% vs 4.5%, p = 0.0078, as shown in Fig. 2 ).
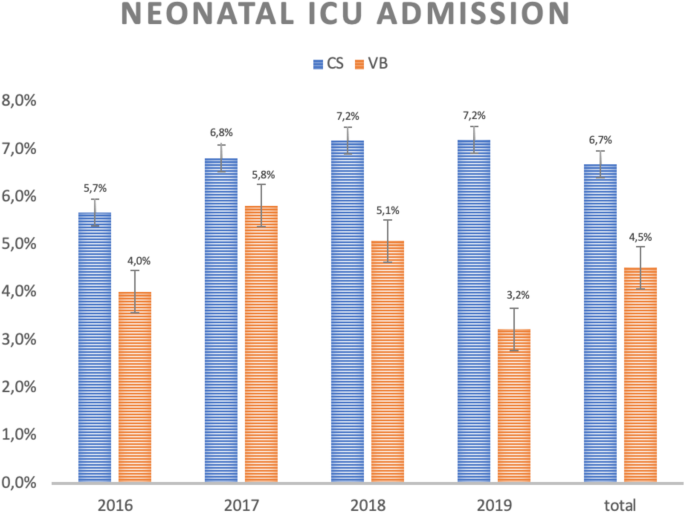
Neonatal ICU admission rate according to type of delivery and year of birth. CS = cesarean sections, VB = vaginal birth
The quantitative analysis of NICU admissions in C-sections also reveals that in less than 5% of cases the cesarean was due to an emergency related to intrapartum fetal distress, so this condition seems not to contribute to the final result.
As with their babies, low-risk parturient who underwent C-sections had higher admission rates to the ICU than those who underwent vaginal delivery (0,8% vs 0,3%, p = 0.001), as shown in Fig. 3 .
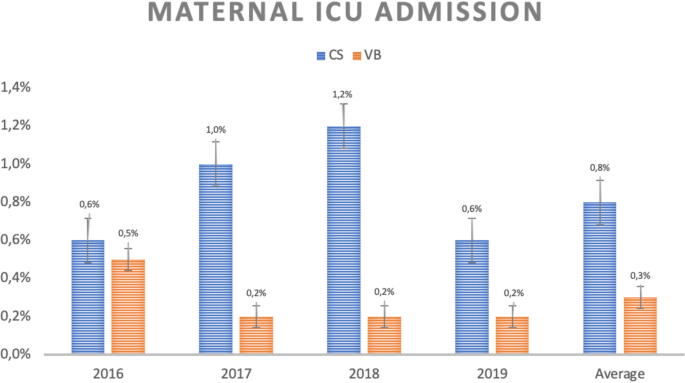
Maternal ICU admission rate according to type of delivery and year of occurrence. CS = C-sections, VB = vaginal birth
The rates of hospital readmission within 30 days from delivery are also higher in those patients submitted to C-sections than to vaginal delivery, although without statistical significance (Fig. 4 ).
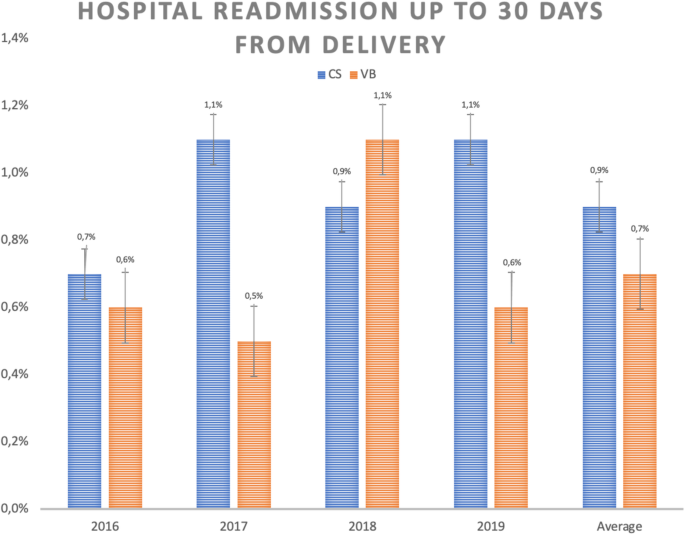
Hospital readmission rate up to 30 days from delivery according to type of delivery and year of occurrence. CS = C-sections, VB = vaginal birth
Finally, considering the average costs (calculated in Brazilian Reais – R$) of hospital stay for mother-baby binomial in low-risk pregnancies, it can be noted that cesarean deliveries cost R$14,0342.04 while vaginal deliveries cost R$12,230.03 (Fig. 5 ).
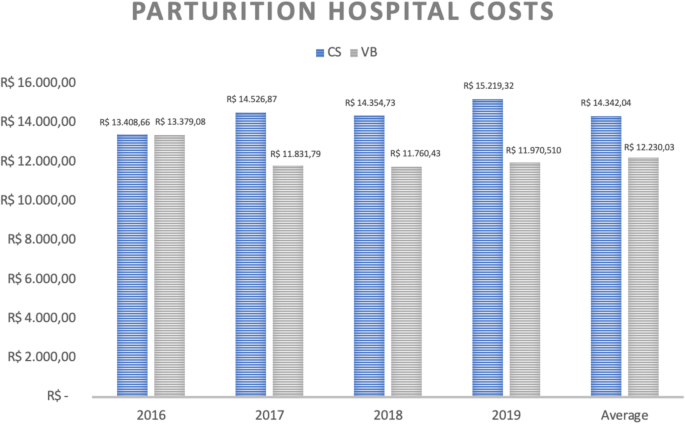
Average of parturition costs (in real) of hospitalization of the parturient-newborn binomial according to type of delivery and year of occurrence. CS = C-section, VB = Vaginal Birth
When analyzing maternal and neonatal hospital costs separately, we observed that C-sections present higher expenses for both settings, as demonstrated in Figs. 6 and 7 .
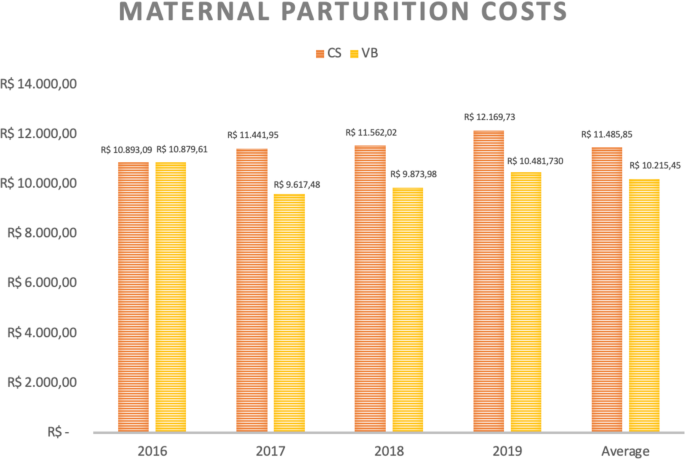
Average costs (in real) of maternal hospitalization for delivery according to type of delivery and year of occurrence. CS = C-section, VB = Vaginal birth

Average costs (in real) of hospitalization of the newborn due to delivery according to type of delivery and year of occurrence. CS = C-sections, VB = Vaginal birth
Vaginal births have lower hospital costs than cesarean sections in low-risk pregnancies. Although C-section has been related to worse results [ 11 ], this study shows which kind of results are better in vaginal delivery, and includes only low risk pregnancies, in which C-sections should be less frequent.
The mothers’ results are better in vaginal birth considering ICU admission rates. The neonatal results are also more favorable in vaginal birth especially considering NICU admission and breastfeeding in the first hour after delivery. This study showed that vaginal births are associated with better healthcare value delivery.
Despite the absence of statistical significance, the maternal rates of hospital readmission within 30 days from delivery were higher in those patients undergoing C-sections than vaginal deliveries. This finding does not allow us to conclude that this is a worse clinical outcome, but it is still contributing for the analysis of medical expenses with C-sections.
Data analysis shows homogeneity between groups and this allows more substantial conclusions. The first item that draws attention is the comparison between the costs of cesarean and vaginal deliveries. Considering the overall hospital costs per patient (mother-baby binomial), cesarean deliveries are almost 15% more expensive than vaginal deliveries in low-risk pregnancies (R$14,0342.04 versus R$12,230.03). As the results showed, the C-sections higher costs must be related to the higher rate of maternal and neonatal ICU admission. Besides that, they may be related to the team needed to provide assistance for a C-section and increased use of medications in this kind of delivery.
Considering a scenario where C-section rates would represent 20% of cases for low risk pregnancies, and therefore still exceeding the 15–18% described as ideal and safe in the literature, the savings in the analyzed period would reach almost R$7million [ 7 ].
To imagine that such a rate is unattainable shows pessimism since the group studied was comprised exclusively by singleton pregnancies of low risk, with cephalic presentation and without previous C-section. In the available literature, low and high-risk pregnancies appear in the same universe of analysis. However, it is precisely the elective C-sections in low-risk groups that seem to promote the highest rate of preventable hospitalization in the NICU. Considering low risk as singleton pregnancies at term with cephalic presentation without previous C-section (Robson groups 1 to 4), which represents around 80% of births in the world, probably the action on these groups should translate in value results: lower costs and better outcomes [ 27 ].
There are already several attempts to reduce the number of caesareans worldwide, especially in Brazil, where these rates are incredibly high [ 28 , 29 ].
The total cost of hospitalization for cesarean delivery is more expensive due to higher maternal and neonatal costs. Literature has shown that newborns of elective cesareans are more likely to have respiratory distress compared with those whose mothers went through labor [ 30 ]. Considering that such discomfort is the main cause of hospitalization in the NICU, greater use of this expensive resource in babies born by C- section was already expected [ 31 ]. Therefore, it is not surprising that there is a difference of almost 30% between hospital costs related to newborns undergoing cesarean delivery and those of vaginal delivery. Besides that, while only 4.5% of the babies born by vaginal delivery were admitted to NICU in this series, more than 6.7% of those born by C-section had the same outcome, which means a difference of approximately 160 admissions in this unit during the analyzed period. It is important to point out that intrapartum emergency C-sections only took place in exceptional conditions, such as fetal distress diagnosed by intrapartum cardiotocography category III and placental abruption.
From the maternal point of view, the results are also unfavorable for C-sections. The analysis of hospital readmission rate in the first 30 days after birth is one of the indicators proposed by the Health Care Payment Learning & Action Network working group. It reveals that it is more than 20% higher in cases of cesarean delivery than in vaginal delivery for the studied groups, although without statistical significance [ 26 ]. Maternal ICU admission rate also denotes a disadvantage for C-sections. Again, the causes are multifactorial but obviously closely related to the complications of the procedure. A retrospective study involving more than 14 thousand cases already exposed a higher rate of hospital readmission. These are mainly related to surgical wound infection in post-cesarean patients and that corroborates the data found in this series [ 32 ].
As proposed by the CQMC (Core Quality Measures Collaborative), breastfeeding in the first hour of life was considered as a value delivery [ 25 ]. Once again, the difference is in favor of vaginal delivery with an average adherence of 92% of cases versus 88% in C-sections. Factors such as postpartum position, anesthetic condition and surgical environment must have contributed to these results [ 33 , 34 ] .
The remaining question is related to the continuity of a potentially harmful practice in relation to the other whose value delivery is shown to be greater. The answer to these questions is complex and involves several factors that generated the preference for C-section. They range from the model of remuneration for childbirth care to the judicialization of health, patient’s apprehension about a painful process, reduction of training in vaginal deliveries, cultural issues (such as fear of a painful process), and lack of active nursing support during labor [ 14 ].
Evidently, particularities about the assistance model of each country must be taken into account. In countries such as Brazil, where private assistance to labor is personalized, the assistance by a team in a shift and dichotomization between prenatal care and delivery may be plausible solutions when requiring more predictable availability from the assistance team. In other countries where this practice is already in vogue, the payment of bonus linked to outcomes could also bring benefits. Furthermore, cultural issues in countries that perceive C-section as the safer mode of delivery may also be addressed in educational campaigns.
Based on the above, it becomes clear that changes in the current form of obstetric care adapted to each economic model are urgent. Adjustments in the remuneration model may be important in countries with personalized and doctor-centered obstetric care. It is difficult to establish the ideal model, especially considering the differences between public and private systems.
However, ideas such as the use of the Global Budget defined by the average diagnosis-related-groups (DRG) of the target population and the payment of salaries to doctors have been used to manage hospitals. In this case, the hospital receives a fixed amount (monthly or yearly) to offer its services, regardless of the volume of resources it uses. With some nuances, as goals to be met and additional compensation by special procedures or accreditations, this model is used in some Social Health Organizations (OSS) in Brazil, in which non-profit companies manage government hospitals by fixed monthly values [ 35 ]. Also, a better structure of a bonus policy for professionals related to value delivery, besides the payment of salaries, could also be considered.
Finally, it is also necessary to build a better health system and medical teaching process to allow improvement in vaginal delivery rate, and consequently achieve better results and low costs regarding the delivery.
Strengths and limitations
The strengths of this study are the detailed analysis of the causes for higher costs of cesarean sections and the description of worse results related to it. One clear advantage was the exclusion of high-risk cases that could cause an interpretation bias.
This study included a specific population and considered only low-risk pregnancies from a Brazilian private hospital. For that reason, it is essential to understand the reality of other medical institutions, both in clinical and cost-related terms. This is because vaginal delivery assistance can vary substantially in quality.
Besides that, the allocation of fixed and variable costs between different institutions may also differ. It is also necessary to understand whether the data can be replicated when the high-risk pregnancies are considered.
Finally, it could be stated that it is common to perform elective cesarean sections due to the maternal desire in the analyzed hospital, a reality that is not always present in every service and that could affect our results.
Data from a national hospital-based cohort with 23,940 postpartum women, held in 2011–2012, showed an initial preference for cesarean delivery of 27.6%, ranging from 15.4% (primiparous public sector) to 73.2% (multiparous women with previous cesarean private sector). The main reason for the choice of vaginal delivery was the best recovery of this type of delivery (68.5%) and for the choice of cesarean, the fear of pain (46.6%). Women from private sector presented 87.5% caesarean, with increased decision for cesarean birth in end of gestation, independent of diagnosis of complications. In both sectors, the proportion of caesarean section was much higher than desired by women [ 36 ].
Cesarean deliveries in low-risk pregnancies were associated with a lower value delivery because, in addition to being more expensive, they had worse perinatal outcomes. Reviewing the financing model as well as the practice itself is essential to deliver more value-based healthcare in obstetrics.
Availability of data and materials
The data of this article are available with the corresponding author, by email [email protected] .
Xu K, Soucat A, Kutzin J, et al. Public spending on health: a closer look at global trends: World Health Organization (WHO); 2018.
Google Scholar
Silveira D. 2019. Available at https://g1.globo.com/economia/noticia/2019/12/20/gasto-de-brasileiros-com-saude-privada-em-relacao-ao-pib-e-mais-que-dobro-da-media-dos-paises-da-ocde-diz-ibge.ghtml ; Accessed Dec 2019.
Barros A in IBGE News. 2019. Available at https://agenciadenoticias.ibge.gov.br/agencia-noticias/2012-agencia-de-noticias/noticias/26444-despesas-com-saude-ficam-em-9-2-do-pib-e-somam-r-608-3-bilhoes-em-2017 ; Accessed Dec 2019.
Ribeiro A, et al. Observatório 2019: ANHAP - Associação Nacional dos Hospitais Privados; 2019.
Médici A, Ribeiro A, et al. Observatório 2020: ANHAP - Associação Nacional dos Hospitais Privados; 2020.
Agency for Healthcare Research and Quality. HCUP Facts and figures: statistics on hospital based care in the United States, 2009. 2011. Available at (last accessed in April, 2020): http://www.hcup-us.ahrq.gov/reports/factsandfigures/2009/pdfs/FF_report_2009.pdf .
Healthcare Cost and Utilization Project. Statistical brief: cost of childbirth. Rockville: Agency for Healthcare Research and Quality; 2008. Available at (last accessed in April, 2020): https://www.hcup-us.ahrq.gov/reports/statbriefs/sb107.pdf . Jan 2019.
Agency for Healthcare Research and Quality. HCUPNet, healthcare cost & utilization project. complications of pregnancy, childbirth, and the puerperium. 2003. Available at (last accessed in April, 2020): http://hcupnet.ahrq.gov
Agency for Healthcare Research and Quality. HCUPNet, healthcare cost & utilization project. certain conditions originating in the perinatal period. 2013. Available at (last accessed in April, 2020): http://hcupnet.ahrq.gov
Global Date. Forthcoming report about preterm births 2015.
American College of Obstetricians and Gynecologists (College); Society for Maternal-Fetal Medicine, Caughey AB, Cahill AG, Guise JM, Rouse DJ. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210(3):179–93. https://doi.org/10.1016/j.ajog.2014.01.026 .
Article Google Scholar
Leite AC, Araujo Júnior E, Helfer TM, Marcolino LA, Vasques FA, Sá RA. Comparative analysis of perinatal outcomes among different typesof deliveries in term pregnancies in a reference maternity of Southeast Brazil. Ceska Gynekol. 2016;81(1):54–7.
CAS PubMed Google Scholar
Etringer AP, Pinto MFT, Gomes MASM. Análise de custos da atenção hospitalar ao parto vaginal e à cesariana eletiva para gestantes de risco habitual no Sistema Único de Saúde. Cien Saude Colet. 2019;24(4).
Truven Health Analytics. The cost of having a baby in the United States. 2013. Available at (last accessed in April, 2020): http://transform.childbirthconnection.org/wp-content/uploads/2013/01/Cost-of-Having-aBaby-Executive-Summary.pdf
Molina G, Weiser TG, Stuart R, et al. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA. 2015;314(21):2263–70. https://doi.org/10.1001/jama.2015.15553 .
Article CAS PubMed Google Scholar
SINASC/DATASUS. Available at (last accessed in April, 2020): http://www2.datasus.gov.br/DATASUS/index.php?area=060702 .
Vogt SE, Silva KS, Dias MAB. Comparison of childbirth care models in public hospitals, Brazil. Rev Saude Publica. 2014;48(2):304–13. https://doi.org/10.1590/S0034-8910.2014048004633 .
Article PubMed PubMed Central Google Scholar
Brown MM, Brown GC, Brown HC, Irwin B, Brown KS. The comparative effectiveness and cost-effectiveness of vitreoretinal interventions. Curr Opin Ophthalmol. 2008;19(3):202–7. https://doi.org/10.1097/ICU.0b013e3282fc9c35 .
Article PubMed Google Scholar
Bae J. Value-based medicine. Epidemiol Health. 2015;37:e2015014. https://doi.org/10.4178/epih/e2015014 .
Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477–81. https://doi.org/10.1056/NEJMp1011024 .
Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington: National Academies Press; 2001.
Institute for Healthcare Improvement. QCV100: an introduction to quality, cost, and value in health care. 2016. http://app.ihi.org/lms/home.aspx .
Quinn K. The 8 basic payment methods in health care. Ann Intern Med. 2015;163(4):300–6. https://doi.org/10.7326/M14-2784 .
OCDE Focus on. Better ways to pay for health care. Available at (last accessed in Apr 2020): https://www.oecd.org/els/health-systems/Better-ways-to-pay-for-health-care-FOCUS.pdf . Jun 201.
U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services. Core measures: Disponível em; 2016. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityMeasures/Core-Measures.html .
Healthcare Payment Learning and Action Network. Accelerating and aligning clinical episode payment models. McLean: The MITRE Corporation; 2018. Available at (last accessed in Apr 2020): http://hcp-lan.org/workproducts/cep-whitepaper-final.pdf .
Vogel JP, Betrán AP, Vindevoghel N, Souza JP, Torloni MR, Zhang J, et al. Use of the Robson classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. Lancet Glob Health. 2015;3(5):e260–70. https://doi.org/10.1016/S2214-109X(15)70094-X .
Negrini R, Ferreira RDDS, Albino RS, Daltro CAT. Reducing caesarean rates in a public maternity hospital by implementing a plan of action: a quality improvement report. BMJ Open Qual. 2020;9(2).
Borem P, de Cássia SR, Torres J, et al. A quality improvement initiative to increase the frequency of vaginal delivery in Brazilian hospitals. Obstet Gynecol. 2020;135(2):415–25. https://doi.org/10.1097/AOG.0000000000003619 .
Curet LB, Zachman RD, Rao AV, Poole WK, Morrison J, Burkett G. Effect of mode of delivery on incidence of respiratory distress syndrome. Int J Gynecol Obstet. 1988;27(2):165–70. https://doi.org/10.1016/0020-7292(88)90002-1 .
Article CAS Google Scholar
Yee W, Amin H, Wood S. Elective cesarean delivery, neonatal intensive care unit admission, and neonatal respiratory distress. Obstet Gynecol. 2008;111(4):823–8. https://doi.org/10.1097/AOG.0b013e31816736e7 .
Ergen EB, Ozkaya E, Eser A, et al. Comparison of readmission rates between groups with early versus late discharge after vaginal or cesarean delivery: a retrospective analyzes of 14,460 cases. J Matern Fetal Neonatal Med. 2018;31(10):1318–22. https://doi.org/10.1080/14767058.2017.1315661 .
Brown A, Jordan S. Impact of birth complications on breastfeeding duration: an internet survey. J Adv Nurs. 2013;69(4):828–39. https://doi.org/10.1111/j.1365-2648.2012.06067.x Epub 2012 Jul 5. PMID: 22765355.
Zanardo V, Svegliado G, Cavallin F, Giustardi A, Cosmi E, Litta P, et al. Elective cesarean delivery: does it have a negative effect on breastfeeding? Birth. 2010;37(4):275–9. https://doi.org/10.1111/j.1523-536X.2010.00421.x PMID: 21083718.
Morais HMM, Albuquerque MSV, Oliveira RS, Cazuzu AKI, Silva NAFD. Social healthcare organizations: a phenomenological expression of healthcare privatization in Brazil. Cad Saúde Pública. 2018;34(1):e00194916. https://doi.org/10.1590/0102-311X00194916 .
Domingues RMSM, Dias MAB, Nakamura-Pereira M, et al. Process of decision-making regarding the mode of birth in Brazil: from the initial preference of women to the final mode of birth. Cad Saúde Pública. 2014;30(Suppl 1):S101–16 [cited 2021 Feb 28]. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2014001300017&lng=en . https://doi.org/10.1590/0102-311X00105113 .
Download references
Acknowledgements
Not applicable.
The authors received no financial support for the research, authorship and publication of this article.
The data was obtained by the hospital’s medical records system with no cost involved.
Author information
Authors and affiliations.
Maternal and Child Department, Hospital Israelita Albert Einstein, Av. Albert Einstein, 627 - Jardim Leonor, São Paulo, SP, 05652-900, Brazil
Romulo Negrini, Raquel Domingues da Silva Ferreira & Daniela Zaros Guimarães
You can also search for this author in PubMed Google Scholar
Contributions
Romulo Negrini: Conceptualization, Methodology, Software, Formal analysis, Writing- Original draft preparation. Raquel D S Ferreira: Validation, Data curation, Writing- Reviewing and Editing, Visualization . Daniela Z Guimarães: Writing- Reviewing and Editing. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Romulo Negrini .
Ethics declarations
Ethics approval and consent to participate.
The study obtained ethical clearance from the Sociedade Israelita Brasileira - Hospital Albert Einstein – SP - Brazil ethical committee (protocol number 31362720.2.0000.0071 / 2020).
The informed consent was waived by this cited ethical committee (Sociedade Israelita Brasileira - Hospital Albert Einstein – SP - Brazil) considering the study used only a hospital database, not collecting information from specific patients or even conducting clinical interventions (opinion of ethic committee number 4.803.450).
All author declares that all procedure in this study were conducted in accordance with the international and institutional (Sociedade Israelita Brasileira - Hospital Albert Einstein) relevant guidelines and regulations.
Consent for publication
Competing interests.
There are no competing interests in this publication.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Negrini, R., da Silva Ferreira, R.D. & Guimarães, D.Z. Value-based care in obstetrics: comparison between vaginal birth and caesarean section. BMC Pregnancy Childbirth 21 , 333 (2021). https://doi.org/10.1186/s12884-021-03798-2
Download citation
Received : 01 December 2020
Accepted : 08 April 2021
Published : 26 April 2021
DOI : https://doi.org/10.1186/s12884-021-03798-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Healthcare cost
- Delivery of healthcare
- Quality of healthcare
- Birth setting
- Obstetric delivery
- Cesarean section
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 07 April 2020
Prevalence, indications, and outcomes of caesarean section deliveries in Ethiopia: a systematic review and meta-analysis
- Getnet Gedefaw 1 ,
- Asmamaw Demis 2 ,
- Birhan Alemnew 3 ,
- Adam Wondmieneh 2 ,
- Addisu Getie 2 &
- Fikadu Waltengus 4
Patient Safety in Surgery volume 14 , Article number: 11 ( 2020 ) Cite this article
18k Accesses
38 Citations
1 Altmetric
Metrics details
Caesarean section rates have increased worldwide in recent decades. Caesarean section is an essential maternal healthcare service. However, it has both maternal and neonatal adverse outcomes. Therefore this systematic review and meta-analysis aimed to estimate the prevalence, indication, and outcomes of caesarean section in Ethiopia.
Twenty three cross-sectional studies with a total population of 36,705 were included. Online databases (PubMed/Medline, Hinari, Web of Science, and Google Scholar) and online university repository was used. All the included papers were extracted and appraised using the standard extraction sheet format and Joanna Briggs Institute respectively. The pooled prevalence of the caesarean section, indications, and outcomes was calculated using the random-effect model.
The overall pooled prevalence of Caesarean section was 29.55% (95% CI: 25.46–33.65). Caesarean section is associated with both maternal and neonatal complications. Cephalopelvic disproportion [18.13%(95%CI: 12.72–23.53] was the most common indication of Caesarean section followed by non-reassuring fetal heart rate pattern [19.57% (95%CI: 16.06–23.08]. The common neonatal complications following Caesarean section included low APGAR score, perinatal asphyxia, neonatal sepsis, meconium aspiration syndrome, early neonatal death, stillbirth, and prematurity whereas febrile morbidity, surgical site infection, maternal mortality, severe anemia, and postpartum hemorrhage were the most common maternal complications following Caesarean section.
In this systematic review and meta-analysis, the rate of Cesarean section was high. Cephalopelvic disproportion, low Apgar score, and febrile morbidity were the most common indication of Caesarean section, neonatal outcome and maternal morbidity following Caesarean section respectively. Increasing unjustified Caesarean section deliveries as a way to increase different neonatal and maternal complications, then several interventions needed to target both the education of professionals and the public.
Caesarean section is the commonest operative delivery technique in the world. Caesarean section is the delivery of the fetus, membrane, and placenta through abdominal and uterine incision after fetal viability [ 1 ].
The rate of Caesarean section is different across countries even between urban and rural areas, due to different socio-economic statuses, and opportunities to access public and private health care services [ 2 ].
According to American College of Obstetricians and Gynecologist (ACOG) report, Caesarean delivery significantly increased woman’s risk vulnerability of pregnancy-related morbidity and mortality which accounts (35.9 deaths per 100,000 live deliveries) as compared to a women posses vaginal delivery (9.2 deaths per 100,000 live births) [ 3 ].
Despite Caesarean section a life saving medical intervention and procedures to the decrease adverse birth outcome, controlling different postoperative neonatal and maternal complications are challenging in terms of patient safety, long duration of hospital stay, cost and psychological trauma. Maternal outcomes of Caesarean section included: postpartum fever, surgical site infection, puerperal sepsis, maternal mortality whereas neonatal sepsis, early neonatal death, stillbirth, perinatal asphyxia, low Apgar score, and prematurity were the most common complication of the newborn [ 4 , 5 , 6 ].
Despite World Health Organization (WHO) recommended the optimal rate of Caesarean section should be lie between 5 and 15%, it is significantly increasing even if the reasons for the continued increase in the Caesarean rates are not completely understood: women are having fewer children, maternal age is rising, use of electronic fetal monitoring is widespread, malpresentation especially breech presentation, frequency of forceps and vacuum delivery is decreased, rate of labor induction increases, obesity dramatically rises and Vaginal birth after Caesarean decreased are some of the possible explanations [ 7 ].
Previous Caesarean scar, malpresentation and malposition, antepartum hemorrhage, obstructed labor, cephalopelvic disproportion, non-reassuring fetal heart rate pattern, and multiple pregnancies are the most common indications of Caesarean section [ 4 , 5 , 6 , 8 ].
According to the 2016 Ethiopia Demographic and Health Survey, the rate of C-section (21.4%) in Addis Ababa was far more than the 10–15% rate recommended by the world health organization. EDHS (2016) report showed there is an absolute difference rate of Caesarean section across different regions in Ethiopia which accounts Amhara (2.3%), Oromia (0.9%), SNNPR(1.9%), Afar (0.7%), Tigray (2%), Somali(0.4%), Benishangul Gumuz (1%) too far from the lowest 5% WHO recommendation of Caesarean section deliveries. This review helps to see C-section rates beyond 15% and below 5% is considered medically unjustified or unnecessary, with negligible benefits for most mothers, and yet costly and unequally distributed throughout the population [ 9 , 10 ].
Ethiopia is a good case study to assess Caesarean prevalence, indications, and outcomes because, like other countries in sub-Saharan Africa, maternal mortality and neonatal mortality did not decline sufficiently to meet the Sustainable Development Goal for maternal health and child, and was estimated at 412 maternal deaths and 29 neonatal deaths per 100,000 live births in 2016 [ 9 ].
Despite a few single studies stated different maternal and fetal outcomes of Caesarean section, there is a lack of data to show the distribution and outcome of Caesarean section in different regions where they are provided.
This systematic review and meta-analysis aimed to estimate the pooled prevalence of Caesarean section deliveries and to determine the indications and outcomes of Caesarean section deliveries in Ethiopia.
This systematic review and meta-analysis have been conducted to estimate the pooled prevalence of Caesarean section, indications, maternal and neonatal outcomes in Ethiopia via the standard PRISMA checklist guideline.
Search strategy
International databases (PubMed, Google Scholar, Web of science and HINARI), different gray works of literature and articles in the university repository were included. The searching engine terms were used using PICO formulating questions. These are: “newborn”, “neonatal”, “birth outcome”, “stillbirth”, perinatal asphyxia””, “neonatal sepsis”, “prematurity”, “early neonatal death”, “low Apgar score”, “preterm”, “maternal mortality”, “wound infection”, “surgical site infection”, “febrile morbidity”,” puerperal sepsis”, “puerperal fever”, postpartum hemorrhage”, “blood loss”, “anemia”, “leading factors of Caesarean section”, “indications of Caesarean section”, “Ethiopia”. The following search engine terms were used: neonate OR newborn OR women OR infant OR fetal OR children AND “neonatal sepsis” OR “perinatal asphyxia” OR “low Apgar score” OR “stillbirth” OR “prematurity” OR “preterm birth” OR “early neonatal death” OR “perinatal” OR “neonatal death” OR “preterm “puerperal sepsis” OR “puerperal fever” OR “wound infection” OR “surgical site infection” OR “postpartum hemorrhage” OR “anemia” OR “maternal mortality” OR “maternal death” OR “blood loss” OR “indication of Caesarean section, ‘factors of Caesarean section”, “leading factors of Caesarean section”, “fetal indication of CS”, “Maternal indication of CS”AND Ethiopia and related terms.
Inclusion and exclusion criteria
Twenty three (23) cross-sectional studies were included. Articles reported prevalence or/and an indication, or/and neonatal outcomes or/and maternal outcomes were incorporated. Only English language literature and research articles were included. Studies published till October 2019 were reviewed, screened and appraised for this study. Whereas, articles without full abstracts or texts and articles reported out of the scope of the outcome interest were excluded.
Quality assessment
GG, AD & AW independently evaluated the quality of each study using the Joanna Briggs Institute (JBI) quality appraisal checklist [ 11 ]. Any disagreement was resolved by the hindrance of the third reviewer (FW, BA &AG). The following JBI items used to appraise cross-sectional studies were: [ 1 ] inclusion criteria, [ 2 ] description of study subject and setting, [ 3 ] valid and reliable measurement of exposure, [ 7 ] objective and standard criteria used, [ 9 ] identification of confounder, [ 10 ] strategies to handle confounder, [ 12 ] outcome measurement, and [ 13 ] appropriate statistical analysis. Hence, studies considered with the JBI checklist value of 50% and above of the quality assessment indicators as low risk and good to be included for the analysis.
Data extraction
All the datasets are exported to Endnote version X8 software, and then we transferred to the Microsoft Excel spreadsheet to remove duplicate data in the review. Three authors (GG, AD, and AG) independently extracted all the important data using a standardized JBI data extraction format. Any disagreement between reviewers was resolved by the second team reviewers (FW, BA & AW). The consensus was declared through critical discussion and evaluation of the articles by the independent group reviewers. The name of the author, sample size, publication year, study area, response rate, region, study design, the prevalence of specific maternal outcomes, the prevalence of neonatal outcomes, indications of Caesarean section, and prevalence of Caesarean section with 95%CI were extracted.
Outcome of measurements
Neonatal outcomes.
Any neonatal outcomes reported following C-section (Stillbirth, prematurity, neonatal sepsis, perinatal asphyxia, low Apgar score, and early neonatal death) were included.
Maternal outcomes
Any maternal complications identified after C-section were included puerperal sepsis, wound infection (surgical site infection), febrile morbidity (puerperal fever), postpartum hemorrhage, severe anemia, and maternal mortality.
Indications of caesarean section
Both maternal and fetal indications (obstructed labor, cephalo pelvic disproportion, NRFHRP (Non-reassuring fetal heart rate pattern), multiple gestations, failed induction, malpresentation, malposition, and antepartum hemorrhage) were included.
Data analysis
A Funnel plot and Eggers regression test was used to check publication bias [ 14 ]. Cochrane Q-test and I-squared statistics were computed to check the heterogeneity of studies [ 15 , 16 ]. Pooled analysis was conducted using a weighted inverse variance random-effects model [ 17 ]. Subgroup analysis was done by study region (area), and sample size. STATA version 11 statistical software was used to compute the analysis. Forest plot format was used to present the pooled point prevalence, indications and outcomes of C-section with 95%Cl.
Characteristics of the included studies
Four hundred twenty-three studies were retrieved at PubMed, Google Scholar, Science Direct, web of science, HINARI and other gray and online repository accessed articles regarding prevalence, indications, and the maternal and fetal outcome of Caesarean section in Ethiopia. After duplicates were expunged, 278 studies remained.
Out of 278 remained articles, 176 articles were excluded after review of their titles and abstracts. Therefore, 102 full-text articles were accessed and assessed for inclusion criteria, which resulted in the further exclusion of 79 articles primarily due to reason. As a result, 23 studies were met the inclusion criteria to undergo the final systematic review and meta-analysis (Fig. 1 ) (Table 1 ).
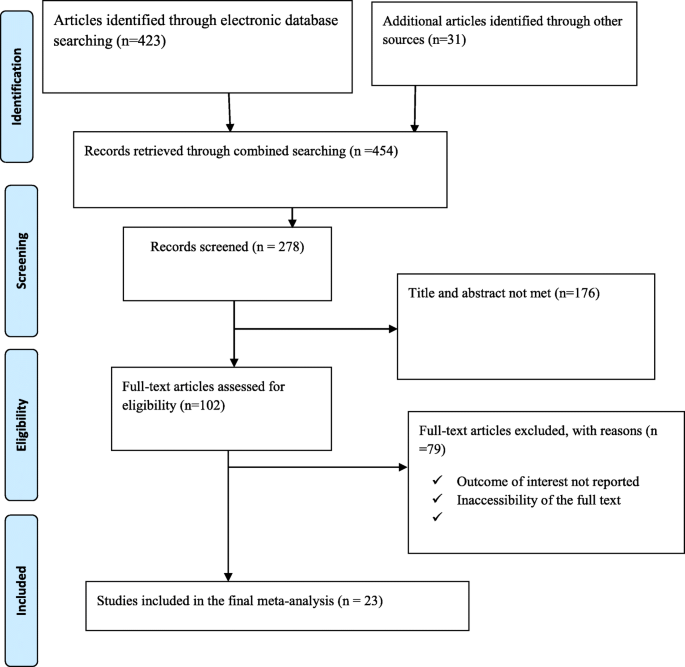
Flow chart of study selection for systematic review and meta-analysis of indications, maternal and fetal outcomes of cesarean section in Ethiopia
Prevalence of caesarean section in Ethiopia
The overall pooled prevalence of Caesarean section is presented with a forest plot ( Fig. 2 ). Therefore, the pooled estimated prevalence of Caesarean section in Ethiopia was 29.55% (95% CI; 25.46–33.65; I2 = 98.7%, P < 0.001).
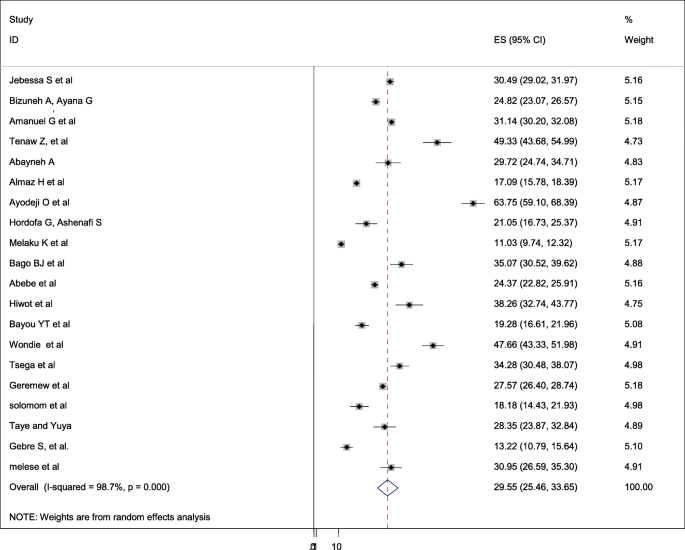
Forest plot of the pooled prevalence of cesarean section in Ethiopia
Publication bias
A funnel plot was assessed for the asymmetry distribution of the Caesarean section using visual inspection of the forest plot ( Fig. 3 ). Egger’s regression test showed with a p -value of 0.251 indicated the absence of publication bias.

Funnel plot with 95% confidence limits of the pooled prevalence of cesarean section in Ethiopia
Subgroup analysis
Subgroup analysis was computed with the evidence of heterogeneity. Hence the Cochrane I 2 statistic =98.7%, P < 0.001) showed the presence of marked heterogeneity in this study. Therefore subgroup analysis was implemented using the study area (region) and sample size using random model effect analysis. Regarding the study area (region), the prevalence of Caesarean section was highest in Addis Ababa, accounted for 40.39% (95%CI: 12.35, 68.43) whereas the rate of Caesarean section was higher among studies of having sample size less than 500, accounted for 34.91% (95%CI: 25.48–44.34) ( Fig. 4 - 5 ).

Forest plot of the subgroup analysis based on region (area) of the study

Forest plot of the subgroup analysis based on the sample size of the study

Indication of caesarean section
In this systematic review and meta-analysis; obstructed labor, cephalopelvic disproportion, multiple pregnancies, non-reassuring fetal heart rate pattern (NRFHRP), failed induction and augmentation, malpresentation and malposition, and antepartum hemorrhage are the most common indications of Caesarean section. In this systematic review and meta-analysis, cephalopelvic disproportion (CPD) is the most common indication of Caesarean section followed by non-reassuring fetal heart rate pattern (NRFHRP), and obstructed labor in Ethiopia ( Table 2 ).
Neonatal complication following caesarean section in Ethiopia
Among women who underwent Caesarean section; neonatal sepsis, early neonatal death, stillbirth, low Apgar score, perinatal asphyxia (PNA), meconium aspiration syndrome, and prematurity were the reported neonatal complications in this study. Among neonatal complications, low Apgar score was the most common adverse complication of the newborn followed by perinatal asphyxia and neonatal sepsis respectively in Ethiopia (Table 3 ).
Maternal complications following caesarean section in Ethiopia
Following Caesarean section different adverse maternal complications were reported. Febrile morbidity, puerperal sepsis, postpartum hemorrhage, surgical site infection, maternal mortality, and severe anemia were the most common adverse maternal complications following Caesarean section. Puerperal fever or febrile morbidity was the leading cause of maternal morbidity following Caesarean section followed by postpartum hemorrhage in Ethiopia (Table 4 ).
Despite Caesarean section is an essential component of comprehensive obstetric and newborn care for reducing maternal and neonatal mortality, there is a lack of data regarding Caesarean section rates, its indications and outcomes in Ethiopia. Studies showed negative or no complications of Caesarean on neonatal mortality in low and middle-income countries where the Caesarean rates are high. Cesarean section is very crucial in settings where the Caesarean rates are very low, due to the unavailability of Caesarean [ 39 ].
Caesarean sections can cause significant and sometimes permanent complications, disability or death particularly in settings that lack the facilities and/or capacity to properly conduct safe surgery and treat surgical complications [ 40 ].
Low- and middle-income countries, wealthy women have more than five times higher C-section use than poor women. In the United States, 32% of births were by C-section in 2015, an increase from 23% in 2000, as the data showed, and in the United Kingdom, 26.2% of births were by C-section in 2015, up from 19.7% in 2000. According to the World Health Organization report, the country with the lowest C-section rate, at 0.6% in 2010, was South Sudan and the country with the highest, at 58.1% in 2014, was the Dominican Republic. Whereas, some countries where more than half of births were by C-section were Brazil, at 55.5% in 2015; Egypt, at 55.5% in 2014; Turkey, at 53.1% in 2015; and Venezuela, at 52.4% in 2013 [ 41 ].
The overall prevalence of Caesarean section in Ethiopia was 29.55% (95% CI: 25.46–33.65). This report is higher than the study done in Saudi Arabia [ 42 ], Nigeria [ 43 ], Pakistan [ 44 ], India [ 5 ], Brazil [ 45 ] and low and middle-income countries analysis [ 46 ]. This discrepancy might be due to the age of the mother elapses the ideal birth time, significantly increasing, non-communicable disease, increasing electronic fetal monitoring availability and accessibility in referral and general hospitals. This study finding is lower than the study done in Nepal, North America and Western Europe, Latin America and the Caribbean [ 47 ]. This difference might be due to countries with a rich wealth index that may have the capacity to have modern operative obstetrics management as compared to low and middle countries. Hence, low and middle-income countries have resource limitation and c-section is resource-constrained, may have low comprehensive obstetric health care services.
Antepartum hemorrhage, non-reassuring fetal heart rate pattern, malpresentation, and malposition, failed induction, obstructed labor, multiple gestations, cephalopelvic disproportion were the most common indications of Caesarean section in Ethiopia. This study finding is supported by the study done in low and middle-income countries [ 46 ], Saudi Arabia [ 42 ], Ghana [ 6 , 8 ], Jordan [ 4 ] and India [ 5 ].
Neonatal sepsis, stillbirth, prematurity, perinatal asphyxia, low Apgar score, and meconium aspiration syndrome were the most common neonatal complications following the Caesarean section in Ethiopia. This study finding is supported by the study done in India [ 5 ], Jordan [ 4 ], and Ghana [ 6 ].
Postpartum hemorrhage, surgical site infection, puerperal fever, anemia, and maternal mortality were the most common neonatal adverse outcome of Caesarean section in Ethiopia. The finding of this study is supported by the study done in India [ 5 ], Jordan [ 4 ], and African countries [ 48 ].
In this study, the overall pooled prevalence of Caesarean section in Ethiopia was high. Non-reassuring fetal heart rate patterns, cephalopelvic disproportion, and obstructed labor were the most common indication of Caesarean section. Low Apgar score, perinatal asphyxia, and neonatal sepsis were the most common complication of neonates whereas postpartum hemorrhage and febrile morbidity were the common maternal complications following the Caesarean section in Ethiopia. Therefore, based on the study findings, the authors recommend a particular emphasis to follow the WHO recommendations and guidelines. Avoiding unjustified and unnecessary indications for Caesarean sections has a significantly higher impact to prevent poor maternal and fetal outcomes.
Availability of data and materials
All related data has been presented within the manuscript. The dataset supporting the conclusions of this article is available from the corresponding author on request.
Abbreviations
- Caesarean section
Postpartum hemorrhage,
Obstructed labor
Cephalopelvic disproportion
Antepartum hemorrhage
South Nation Nationalities and Peoples region
Confidence Interval
Lyell DJ, Power M, Murtough K, Ness A, Anderson B, Erickson K, Schulkin J. Surgical techniques at cesarean delivery: a US survey. Surg J. 2016;2(04):e119–25.
Article Google Scholar
Strom S. Rates, Trends, and Determinants of Cesarean Section Deliveries in El Salvador: 1998 to 2008 (doctoral dissertation); 2013.
Google Scholar
Rayburn WF, Strunk AL. Profiles about practice settings of American College of Obstetricians and Gynecologists fellows. Obstet Gynecol. 2013;122(6):1295–8.
BĂƟĞŚĂ AM, Al-Daradkah SA, Khader YS, Basha A, Sabet F, et al. Cesarean ^ĞcƟŽn͗ incidence, causes, associated factors and outcomes: a NĂƟŽnĂů WrŽƐƉĞcƟǀĞ study from Jordan. Gynecol Obstet Case Rep. 2017;3(3):5.
Desai G, Anand A, Modi D, Shah S, Shah K, Shah A, et al. Rates, indications, and outcomes of caesarean section deliveries: a comparison of tribal and non-tribal women in Gujarat, India. PLoS One. 2017;12(12):e0189260. https://doi.org/10.1371/journal.pone.0189260 .
Article CAS PubMed PubMed Central Google Scholar
Gulati D, Hjelde GI. Indications for Cesarean Sections at Korle Bu Teaching Hospital. Ghana (Master's thesis); 2012.
Betrán AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, Van Look P, Wagner M. Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol. 2007;21(2):98–113.
Faith A, et al. Indication and predictors for caesarean sections in Ghana and the birth outcomes. Euro J Obstetrics Gynecology Reprod Biology. 2019;234:e1–e131.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia demographic and health survey 2016: Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016. available at: https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf , accessed Mar 2020.
Bailey P, Lobis S, Maine D, Fortney JA. Monitoring emergency obstetric care: a handbook: World Health Organization; 2009..
Peters M, Godfrey C, McInerney P, Soares C, Hanan K, Parker D. The Joanna Briggs institute Reviewers' manual 2015: methodology for JBI scoping reviews; 2015.
Akki JS, Gemeda DH, Akessa GM. A review of caesarean delivery in Southwest Ethiopia: incidence, indications, and outcomes. Afr J Midwifery Womens Health. 2015;9(3):106–11.
Ayano B, Guto A. Indications and outcomes of emergency caesarean section at St Paul's hospital medical college, Addis Ababa, Ethiopia 2017:(afoul month retrospective cohort study). Gynecol Reprod Health. 2018;2(5):1–12.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):62934.
Ioannidis J. Interpretation of tests of heterogeneity and bias in metaanalysis. J Eval Clin Pract. 2008;14(5):951–7.
Higgins J, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111.
Tadesse H, Gessessew A, Medhanyie AA. Trends and outcomes of cesarean delivery in Ayder comprehensive specialized hospital, Mekelle City, northern Ethiopia. East Afr J Health Sci. 2019;1(1):62–77.
Tesfaye T, Hailu D, Mekonnen N, Tesfaye R. Magnitude of maternal complication and associated factors among mothers undergone cesarean section at Yirgalem general hospital, SNNPR, Ethiopia. Risk. 2017;100:11.
Tenaw Z, Kassa ZY, Kassahun G, Ayenew A. Maternal Preference, Mode of Delivery and Associated Factors among Women Who Gave Birth at Public and Private Hospitals in Hawassa City, Southern Ethiopia. Ann Global Health. 2019;85(1):1–7. 115. https://doi.org/10.5334/aogh.2578 .
Solomon AA. Prevalence of Ceserean Section and Associated Factors in University of Gondar Comprehensive Referal Hospital, North West Ethiopia. BMC Res Notes Rev. 2019. https://doi.org/10.21203/rs.2.13345/v1 .
Hailu A. Assessment of leading indication and outcome of cesarean delivery in Arba Minch general hospital- a Cross-Sectional Study (MSc dissertation, Arba Minch Universty); 2016.
Olanipekun A. Prevalence of caesarean section and the associated factors in private hospitals in Addis Ababa-a cross-sectional study (Doctoral dissertation, Addis Abeba Universty); 2017.
Gutema H, Shimye A. Cesarean section and associated factors at mizan aman general hospital, Southwest Ethiopia. J Gynecol Obstet. 2014;2(3):37–41.
Yenit MK, Gezahegn T, Adefires M, Shiferaw AM. Cesarean section rate, maternal and fetal outcome of birth following cesarean section at Finoteselam hospital, Northwest Ethiopia: A Descriptive Retrospective Data. Glob J Med Res. 2016.
Bago BJ. Prevalence and its associated factors among women undergone operative delivery at Hawassa University comprehensive specialized hospital, southern Ethiopia, 2017. Gynecol Obstet. 2018;8:461. https://doi.org/10.4172/2161-0932.100046 .
Abebe FE, et al. Factors leading to cesarean section delivery at Felegehiwot referral hospital, Northwest Ethiopia: a retrospective record review. Reprod Health. 2016;13:6. https://doi.org/10.1186/s12978-015-0114-8 .
Article PubMed PubMed Central Google Scholar
Tsegaye H. Prevalence of caesarean section and associated factors in Addis Ababa hospitals, Addis Ababa, Ethiopia, 2017 (Doctoral dissertation, Addis Ababa University); 2017.
Getahun A. Outcome of cesarean section and the associated factors at jugel hospital, harari region, eastern Ethiopia. 2015(doctoral dissertation, Haramaya University); 2015.
Bayou YT, Mashalla YJ, Thupayagale-Tshweneagae G. Patterns of caesarean-section delivery in Addis Ababa, Ethiopia. Afr J Primary Health Care Fam Med. 2016;8(2):1–6.
Wondie AG, Zeleke AA, Yenus H, Tessema GA. Cesarean delivery among women who gave birth in Dessie town hospitals, Northeast Ethiopia. PLoS One. 2019;14(5):e0216344.
Tsega F, Mengistie B, Dessie Y, Mengesha M. Prevalence of cesarean section in urban health facilities and associated factors in eastern Ethiopia: hospital based cross sectional study. J Preg Child Health. 2015;2(3):169–73.
Geremew A, et al. Prevalence and Outcome of Caesarean Section in Attat Hospital, Gurage Zone, SNNPR, Ethiopia. Arch Med. 2015;7(4):8.
Worku S. Rate and associated factors of caesarean section at chirozonal hospital,west harergae, oromia regional state, eastern Ethiopia. (MSc dissertation, Haramaya University); 2016.
Taye A, Yuya M. One year retrospective analysis of prevalence of caesarean section in Jimma University specialized hospital, South Western Ethiopia. J Preg Child Health. 2015;2:172. https://doi.org/10.4172/2376-127X.1000172 .
Mengesha MB, et al. Maternal and fetal outcomes of cesarean delivery and factors associated with its unfavorable management outcomes; in Ayder Specialized Comprehensive Hospital, Mekelle, Tigray, Ethiopia. 2017 BMC Res Notes. 2019;12:650. https://doi.org/10.1186/s13104-019-4690-5 .
Article PubMed Google Scholar
Gebre S, Negasi A, Hailu A. Criteria based clinical audit of cesarean section in a general Hospital in West Tigray, Ethiopia. J Women's Health Care. 2017;6:410. https://doi.org/10.4172/2167-0420.1000410 .
Melese A. Magnitude of cesarean section delivery and its associated factors among mothers who gave birth at public hospitals in north wollo zone, northern Ethiopia. (Msc dissertation, Haramaya University); 2019.
Kyu HH, Shannon HS, Georgiades K, Boyle MH. Caesarean delivery and neonatal mortality rates in 46 low-and middle-income countries: a propensity-score matching and meta-analysis of demographic and health survey data. Int J Epidemiol. 2013;42(3):781–91.
Souza JP, Gulmezoglu A, Lumbiganon P, Laopaiboon M, Carroli G, Fawole B, et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004-2008 WHO global survey on maternal and perinatal health. BMC Med. 2010;8:71.
Article CAS Google Scholar
Boerma T, Ronsmans C, Melesse DY, Barros AJ, Barros FC, Juan L, Moller AB, Say L, Hosseinpoor AR, Yi M, Neto DDLR. Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018;392(10155):1341–8.
Zakai Ghadeer H, Alrowithi Abdullah S, Buhlaigah Afnan M, Alharbi Abdullah A, Hakami Abrar H, Alqahtani Hanoof A. Prevalence of caesarean section and its indicating factors among pregnant women attending delivery at king Abdulaziz University hospital, Jeddah city during 2016. EC Gynaecol. 2018;7(2):43–51.
Adewuyi EO, Auta A, Khanal V, et al. Cesarean delivery in Nigeria: prevalence and associated factors—a population-based crosssectional study. BMJ Open. 2019;9:e027273. https://doi.org/10.1136/bmjopen-2018-027273 .
Amjad A, Amjad U, Zakar R, Usman A, Zakar MZ, Fischer F. Factors associated with caesarean deliveries among child-bearing women in Pakistan: secondary analysis of data from the demographic and health survey, 2012–13. BMC Pregnancy Childbirth. 2018 Dec;18(1):113.
Almeida SD, Bettiol H, Barbieri MA, Silva AA, Ribeiro VS. Significant differences in cesarean section rates between a private and a public hospital in Brazil. Cadernos de saude publica. 2008;24:2909–18.
Ojo VA, Okwerekwu FO. A critical analysis of the rates and indications for caesarean section in a developing country. Asia-Oceania J Obstetrics Gynaecology. 1988 Jun;14(2):185–93.
C-section deliveries nearly doubled worldwide since 2000, study finds. https://edition.cnn.com › c-section-rates-study-parenting-without-borders-intl .
Esterhuizen TM, et al. Maternal and neonatal outcomes after caesarean delivery in the African surgical outcomes study: a 7-day prospective observational cohort study. Lancet Glob Health. 2019;7:e513–22.
Download references
Acknowledgments
Not applicable.
Author information
Authors and affiliations.
Department of Midwifery, College of Health Sciences, Woldia University, P.O.Box:400, Woldia, Ethiopia
Getnet Gedefaw
Department of Nursing, College of Health Sciences, Woldia University, P.O.Box:400, Woldia, Ethiopia
Asmamaw Demis, Adam Wondmieneh & Addisu Getie
Department of Medical Laboratory Sciences, College of Health Sciences, Woldia University, P.O.Box:400, Woldia, Ethiopia
Birhan Alemnew
Department of Midwifery, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Fikadu Waltengus
You can also search for this author in PubMed Google Scholar
Contributions
All authors (GG,AD, BA, AW, AG & FW,) critically reviewed, provided substantive feedback and contributed to the intellectual content of this paper and made substantial contributions to the conception, conceptualization and manuscript preparation of this systematic review. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Getnet Gedefaw .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declared that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gedefaw, G., Demis, A., Alemnew, B. et al. Prevalence, indications, and outcomes of caesarean section deliveries in Ethiopia: a systematic review and meta-analysis. Patient Saf Surg 14 , 11 (2020). https://doi.org/10.1186/s13037-020-00236-8
Download citation
Received : 22 November 2019
Accepted : 30 March 2020
Published : 07 April 2020
DOI : https://doi.org/10.1186/s13037-020-00236-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Maternal complications
- Meta-analysis
- Neonatal complications
Patient Safety in Surgery
ISSN: 1754-9493
- Submission enquiries: [email protected]
- General enquiries: [email protected]
SYSTEMATIC REVIEW article
Meta-analysis of association between caesarean section and postpartum depression risk.

- 1 Nursing College, Guangxi Medical University, Nanning, China
- 2 Department of Neonatology, The First Affiliated Hospital of Guangxi Medical University, Nanning, China
Background: The association of caesarean section (CS) for postpartum depression (PPD) remains controversial. This study aims to explore the relationship between CS and the risk of PPD, in order to provide a basis for preventing PPD.
Material and methods: We searched PubMed, Web of Science, Cochrane Library, and EMBASE databases for literature about the correlation between CS and PPD published as of February 2024. The combined odds ratios (ORs) and 95% confidence intervals (Cls) were obtained by flexible use of fixed-effects models or random-effects models.
Results: A total of 18 publications were ultimately included in the analysis. Among these, 14 were cohort studies and 4 were case-control reports, encompassing 844,328 total cases. All of the included studies were deemed to be of moderate or higher quality. The meta-analysis indicated that the prevalence of PPD among parturients undergoing CS was 13.4% (95% CI: 6.5%-25.5%).The adjusted odds ratio (OR) for the association between CS and PPD was 1.12 (95% CI: 1.04-1.20) compared to the natural vaginal delivery (NVD) group. Specifically, the adjusted OR for the association between CS and PPD was 1.29 (95% CI: 1.18-1.40) during the first 1-6 months postpartum, and 1.23 (95% CI: 1.14-1.33) after 6 months postpartum. Furthermore, in comparison to the NVD group, the adjusted OR for elective caesarean section (ELCS) and emergency caesarean section (EMCS) were 0.96 (0.83, 1.10) and 1.20 (1.08, 1.34), respectively.
Conclusion: Our findings suggest that PPD risk may rise in the presence of CS. In particular, the risk was increased by 20% in the EMCS group, and the risk of PPD within one to six months postpartum after CS increases by 6% compared to that at six months postpartum. In the future, more rational designs and in-depth studies are needed to obtain more accurate information.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/#recordDetails , identifier CRD42023389265.
1 Introduction
Postpartum depression (PPD) is one of the most common mental health issues affecting mothers after childbirth. Statistics indicate that the global incidence of PPD is as high as 10-20% ( 1 ). Typical symptoms include mood swings, sleep disturbances, loss of appetite, weight loss, apathy, and cognitive impairment. In severe cases, suicidal thoughts may also arise ( 2 ), posing a significant risk to the mother. Research has revealed that suicide accounts for nearly 20% of maternal deaths following childbirth ( 3 ). Furthermore, the negative impact of PPD can extend to the well-being of both the mother and the infant, affecting the mother’s physical and mental health, the mother-infant relationship, and marital bonds, while also increasing their risk of experiencing depressive episodes over the next 5 years ( 4 , 5 ). Studies conducted in China and abroad have indicated that identifying risk factors early and implementing preventive interventions can effectively delay the onset and progression of PPD, thereby promoting the overall health and well-being of both the mother and the infant ( 6 , 7 ).
Over the past few decades, the prevalence of caesarean section (CS) has significantly increased among women in both developed and developing countries, leading to heightened interest among public health researchers. These researchers have investigated the potential correlation between CS and PPD, although the nature of this correlation and whether it represents a direct link remain subjects of debate. Some researchers ( 8 – 11 ) have noted that the mode of delivery and the severity of PPD may not be related. Specifically, some researchers ( 8 – 10 ) have reported no discernible correlation between CS and PPD. A particular study ( 11 ) concluded that elective caesarean section (ELCS) showed no association with PPD, while emergent caesarean section (EMCS) was found to be significantly linked to PPD. This implies that unforeseen outcomes could impact the risk of PPD. An earlier report ( 12 ) suggested that women who underwent natural vaginal delivery (NVD) displayed more symptoms of PPD compared to those who had CS. At that time, the women in the study area harbored fear and anxiety regarding the painful experience of NVD. Nonetheless, a consensus has yet to be reached on this matter. Recent studies ( 11 , 13 – 15 ) demonstrated a disparity in the incidence of PPD between CS and NVD, confirming that the occurrence of PPD was notably higher among women who underwent CS (especially EMCS), potentially due to biological or sociological factors. Furthermore, three meta-analysis studies ( 16 – 18 ) identified both types of CS as risk factors for PPD. However, one of these studies ( 17 ) did not find a statistically significant correlation between ElCS and the risk of PPD. This may be because the authors of the study only included data from 6 articles that included ELCS, and the study included information from 2016, which is somewhat outdated. Furthermore, one study ( 16 ) incorporated 25% of studies of inferior quality, whereas a different study ( 18 ) predominantly presented unadjusted results with a slightly reduced count of studies for effect sizes following consolidated adjustment, potentially resulting in a conclusion that lacks a certain degree of accuracy.
Therefore, this study conducted a meta-analysis on recent medium- to high-quality cohort and case-control studies. Women with different delivery types were grouped according to follow-up time in order to investigate the association between CS and PPD. The aim was to provide updated evidence-based information for early identification and effective prevention of maternal PPD for clinical health care providers. Additionally, subgroup analyses were performed to assess the correlation between other factors and CS or PPD.
This meta-analysis was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) ( Supplementary Table S1 ) ( 19 ). This study has been registered on PROSPERO, and the registration number was CRD42023389265.
2.1 Search strategy
Literature related to the correlation between CS and PPD published prior to December 2022 was systematically gathered from databases such as PubMed, Web of Science, Cochrane Library, and EMBASE. To ensure that the latest research was not overlooked, an additional search and update was performed on February 27, 2024. The literature review involved a combination of subject terms and free-text keywords, with citations being followed to encompass a comprehensive scope. The subject terms utilized were “Caesarean section” and “postpartum depression”, and no restrictions were applied regarding language or publication date. Detailed strategies for the literature search can be found in Supplementary Table S2 .
2.2 Inclusion and exclusion criteria
The inclusion and exclusion criteria for this study were strictly established based on the PICOS principles:
Participants: The subjects included in this study were parturients with PPD, regardless of race, region, whether they were primiparae and multiparae, or history of depression.
Intervention measures exposed by this study: parturient undergoing CS (including ELCS and EMCS). Studies in which PPD was managed using alternative therapies or treatments, such as diet, behavioral therapy, or antidepressants, were excluded.
Comparison group: parturients undergoing vaginal delivery (including NVD and assisted vaginal delivery (AVD).
Outcome: In the follow-up assessment, PPD scores of parturients were measured using self-report or clinician-administered measures. The number and probability of PPD in parturients with different modes of delivery were then calculated.
Type of study: cohort study and case-control study. Excluded were meta-analyses, clinical trials, reviews, editorials, preprints, animal studies, and other types of literature; Studies with ambiguous or incomplete data, which were not obtainable after contacting the authors, or studies in which data could not be transformed or combined, were excluded; Studies with a quality assessment score of ≤ 4 on the Newcastle-Ottawa Scale (NOS, Supplementary Table S3 ) ( 20 ) were also excluded.
2.3 Data extraction
The databases were independently searched by two researchers. They then proceeded to screen the titles and abstracts of the literature according to the predetermined inclusion and exclusion criteria. Subsequently, the full texts of the initially eligible literature were thoroughly examined. In cases of discrepancies, a third researcher was consulted for a final decision. Information extracted from the ultimately included literature encompassed the following: the first author’s name, year of publication, type and country of study, study duration, mode of delivery, proportion of CS deliveries, mother’s educational background, feeding method, sample size and age, tools used for depression measurement, outcome and duration of PPD, original odds ratio, adjusted odds ratio, and 95% confidence interval.
2.4 Quality evaluation of included literature
The quality of the included studies was assessed using the NOS, which comprised three dimensions and eight entries. These included research subject selection (4 entries, 4 scores), comparability between groups (1 entry, 2 scores), and outcome measurement or exposure factor measurement (3 entries, 3 points.) The total NOS score was 9. Studies with scores ≤4 were considered low-quality, those with scores of 5 to 6 were categorized as moderate-quality, and those with scores ≥7 were deemed high-quality. The quality evaluations were independently conducted by two researchers. In case of any disagreement, a third researcher intervened for discussion and resolution.
2.5 Publication bias
If the meta-analysis of the primary outcome (number of women with PPD by different modes of delivery) included 10 or more studies, funnel plots were adopted to seek possible publication bias and we visually observed whether there were any significant asymmetries. We planned to use the funnel plots to assess publication bias in the included literature.
2.6 Statistical analysis
Statistical analysis and meta-analysis were conducted using Stata v16.0, RevMan v5.3, and R v4.3.1. The correlation between CS and PPD was determined using OR (odds ratio) and a 95% confidence interval (CI) as the effect size, which were combined using the inverse variance method. The combined incidence and its corresponding 95% CI were utilized to analyze the occurrence of depression in the population. Heterogeneity was assessed using the I 2 test. If I 2 was less than 50%, the heterogeneity was deemed insignificant ( 16 – 18 ), and a fixed-effects model was employed. Conversely, a random-effects model was used. In cases of heterogeneity, sensitivity analysis and subgroup analysis were carried out to identify the sources of heterogeneity. Additionally, the publication bias of the included literature was examined using a funnel plot. A probability of less than 0.05 indicated statistical significance.
3.1 Literature search results
The most recent search results have been selected and evaluated. Following the search process, a total of 541 articles from PubMed, 352 articles from Cochrane, 2,279 articles from EMBASE, and 942 articles from Web of Science were identified. Subsequently, 1,519 duplicate articles were excluded, leaving 2,595 unique articles for initial screening based on their titles and/or abstracts. Following this, the full texts of 1,323 studies were carefully reviewed and evaluated. After a further round of screening, 18 articles were deemed suitable for inclusion in the meta-analysis. A detailed depiction of the database search process is illustrated in Figure 1 .
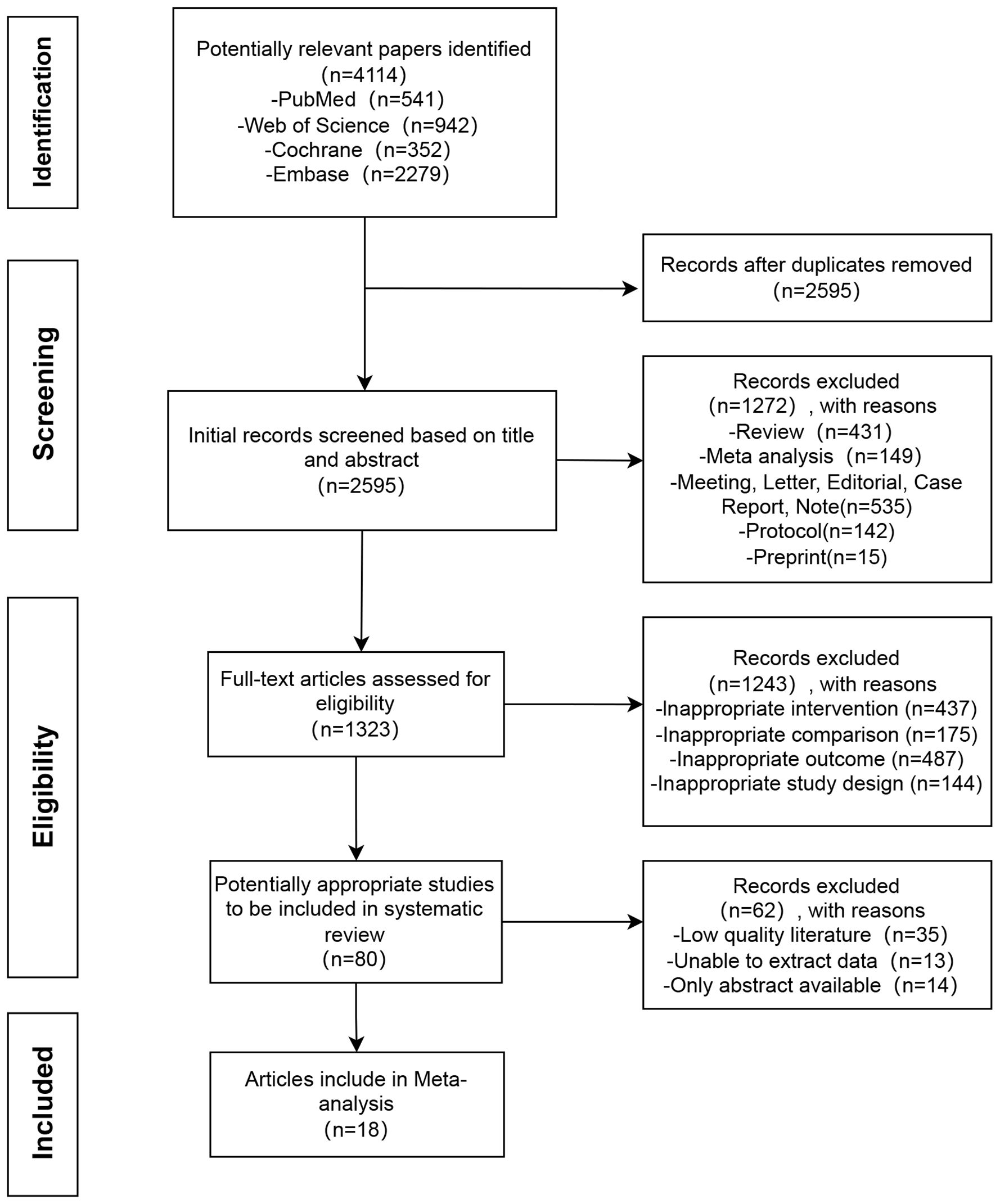
Figure 1 Flow chart of literature search.
3.2 Basic features of included literature
A total of 18 studies ( 11 , 21 – 37 ) were analyzed, involving 844,328 participants. The basic characteristics of the 18 included articles are listed in Table 1 . Among these, seven studies were of moderate quality, while eleven were of high quality, as indicated in Table 2 , which provides detailed evaluations of the literature’s quality. All 18 studies provided sufficient data to assess the correlation between CS and PPD. Among them, 8 studies ( 22 – 25 , 33 , 35 – 37 ) were adjusted for confounding factors. There were 14 cohort studies and 4 case-control studies, with the sample size ranging from 60 to 511,422 participants. Specifically, eleven studies ( 11 , 24 , 26 – 30 , 32 , 35 – 37 ) had <10,000 participants, while the remaining seven studies ( 21 – 23 , 25 , 31 , 33 , 34 ) had >10,000 participants. Furthermore, ten studies ( 21 , 23 , 26 , 28 – 31 , 34 , 36 , 37 ) were conducted in Asia, whereas seven studies ( 22 , 24 , 25 , 27 , 32 , 33 , 35 ) were carried out in Europe, one studies ( 11 ) were conducted in North America. Additionally, ten studies ( 11 , 23 , 24 , 27 – 30 , 34 , 35 , 37 ) utilized the Edinburgh Postnatal Depression Scale (EPDS) to measure PPD levels, two studies ( 22 , 25 ) deployed the SCL-90, two studies ( 21 , 31 ) adopted the 2010 LNHID, one study ( 26 ) used the CES-D, one study ( 36 ) employed the NHIS-NSC, one study ( 32 ) utilized the BDI, and one study ( 33 ) incorporated the HDR. The interventions varied in duration and length across the trials, and the assessment of PPD was conducted between 3 days and 12 months after delivery.
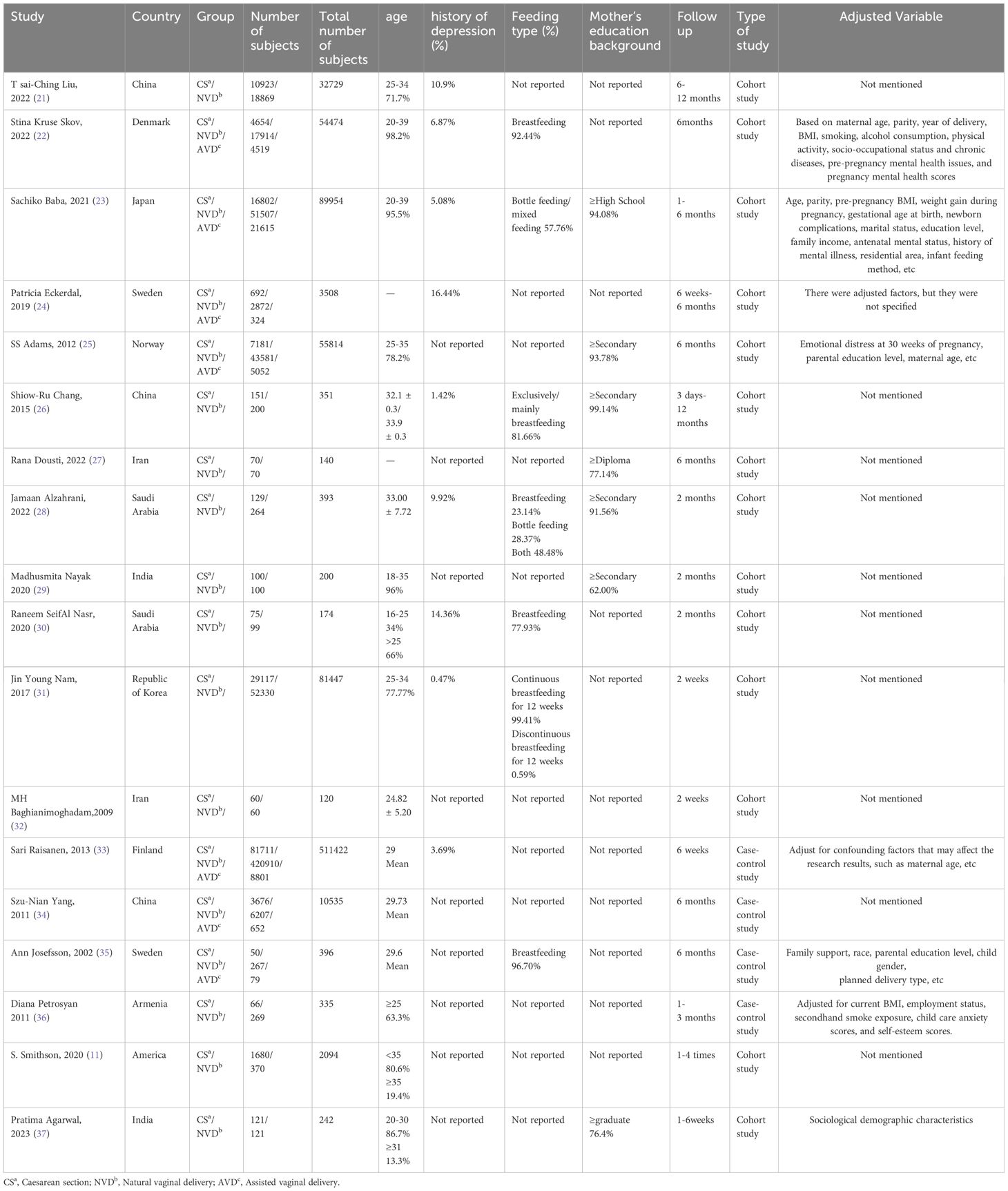
Table 1 Basic features of included studies.
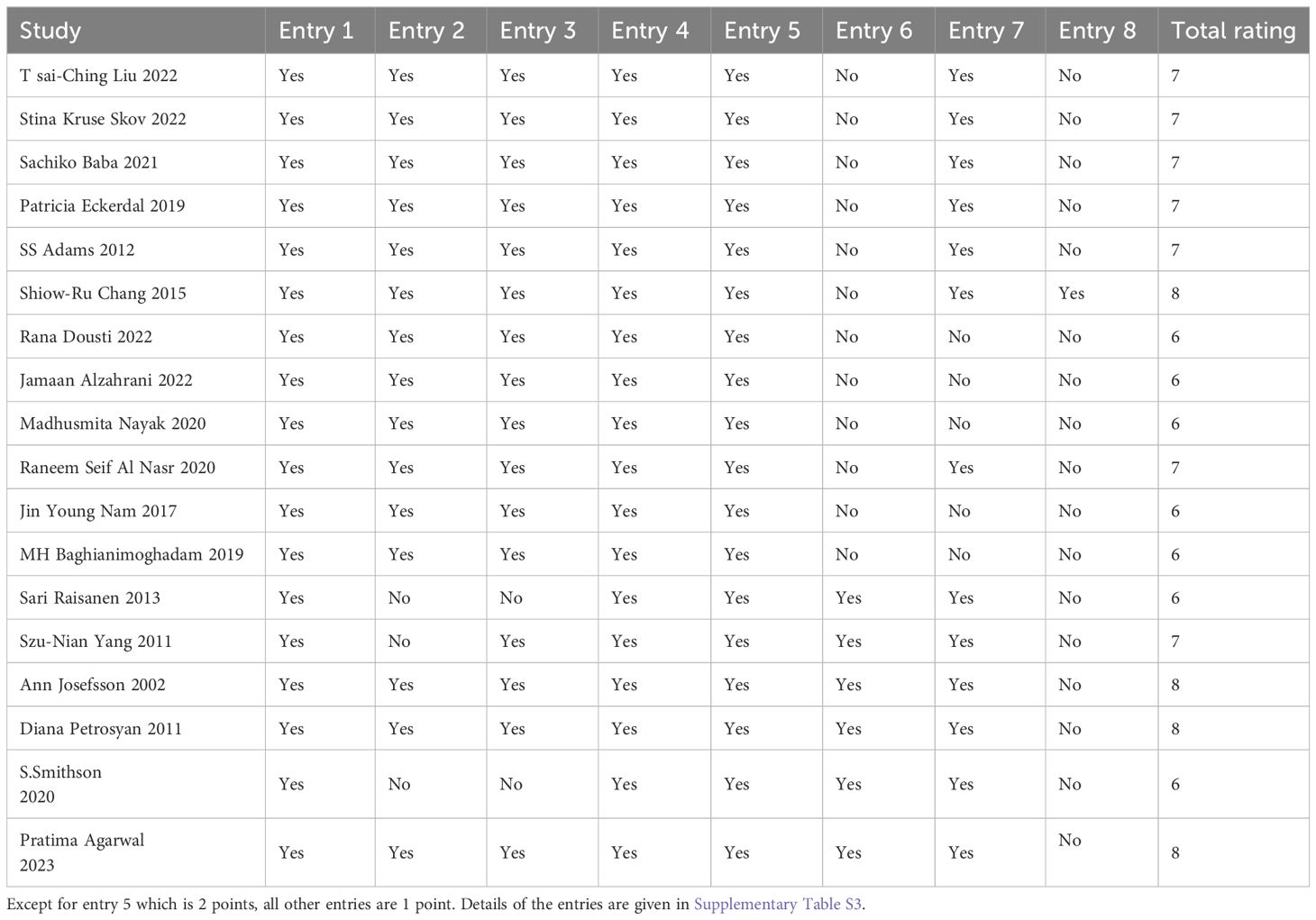
Table 2 Literature quality evaluation.
3.3 Meta-analysis results
3.3.1 incidence of ppd.
We also constructed a forest plot to present the findings regarding the prevalence of PPD in the study population. The prevalence of PPD among the general parturient population was 11.7% (95% CI: 5.5%-23.3%, Supplementary Figure 1 ). The prevalence of PPD among parturients undergoing CS was 13.4% (95% CI: 6.5%-25.5%, Supplementary Figure 2 ), while the prevalence among those undergoing normal vaginal delivery was 10.4% (95% CI: 4.7%-21.2%, Supplementary Figure 3 ).
3.3.2 Association between CS and PPD
Eighteen eligible papers were included in the meta-analysis comparing CS and NVD. A fixed effects model was utilized to analyze the data. The findings indicated that the adjusted odds ratio for the association between CS and PPD was 1.12, with a 95% confidence interval of 1.04-1.20. See Figure 2 for more details. All the studies included were of moderate to high quality, and there was no significant heterogeneity among them (I 2 = 47%). Additionally, subgroup analysis was conducted to further compare based on clinical differences within the NVD group. This analysis considered factors such as the time dimension, different types of CS, race, region, primiparae and multiparae undergoing CS, and population size.
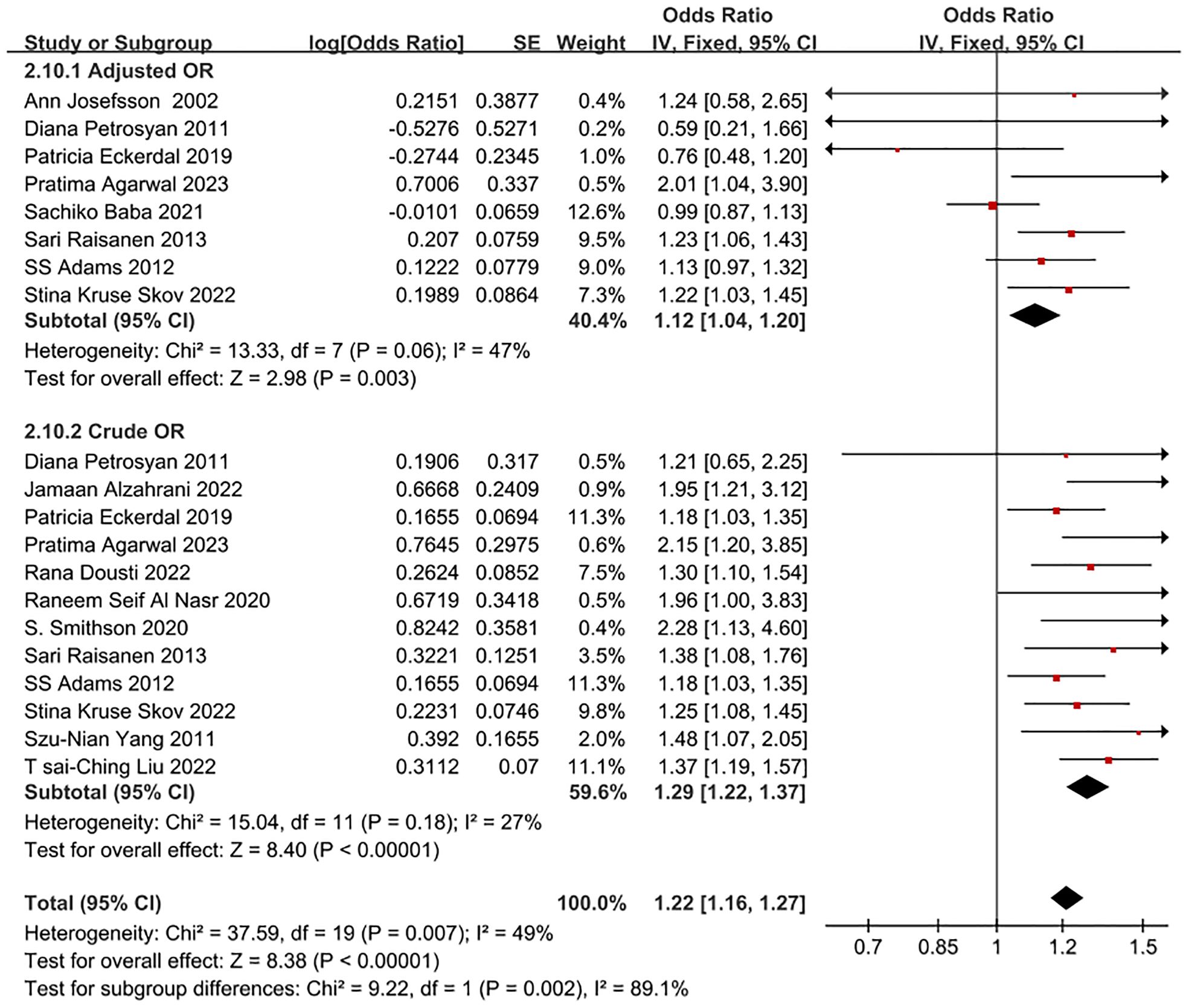
Figure 2 Forest plot of crude OR and adjusted OR for CS and NVD in PPD patients.
3.3.2.1 Subgroup analysis by time dimension
In some studies ( 24 ), we discovered that the association between CS and the increased risk of PPD after one month was minimal compared to normal vaginal delivery (NVD). However, after adjusting for demographic factors, there was no discernible increase in PPD risk after six months postpartum. Therefore, we conducted a subgroup analysis, using postpartum six months as the time node. A total of 10 studies were included in this subgroup analysis by time dimension. The adjusted odds ratio (OR) for the association between CS and PPD within one to six months postpartum was 1.29 (95% CI: 1.18-1.40); after six months postpartum, the adjusted OR was 1.23 (95% CI: 1.14-1.33), as detailed in Figure 3 . The data included in this subgroup analysis were all adjusted OR.
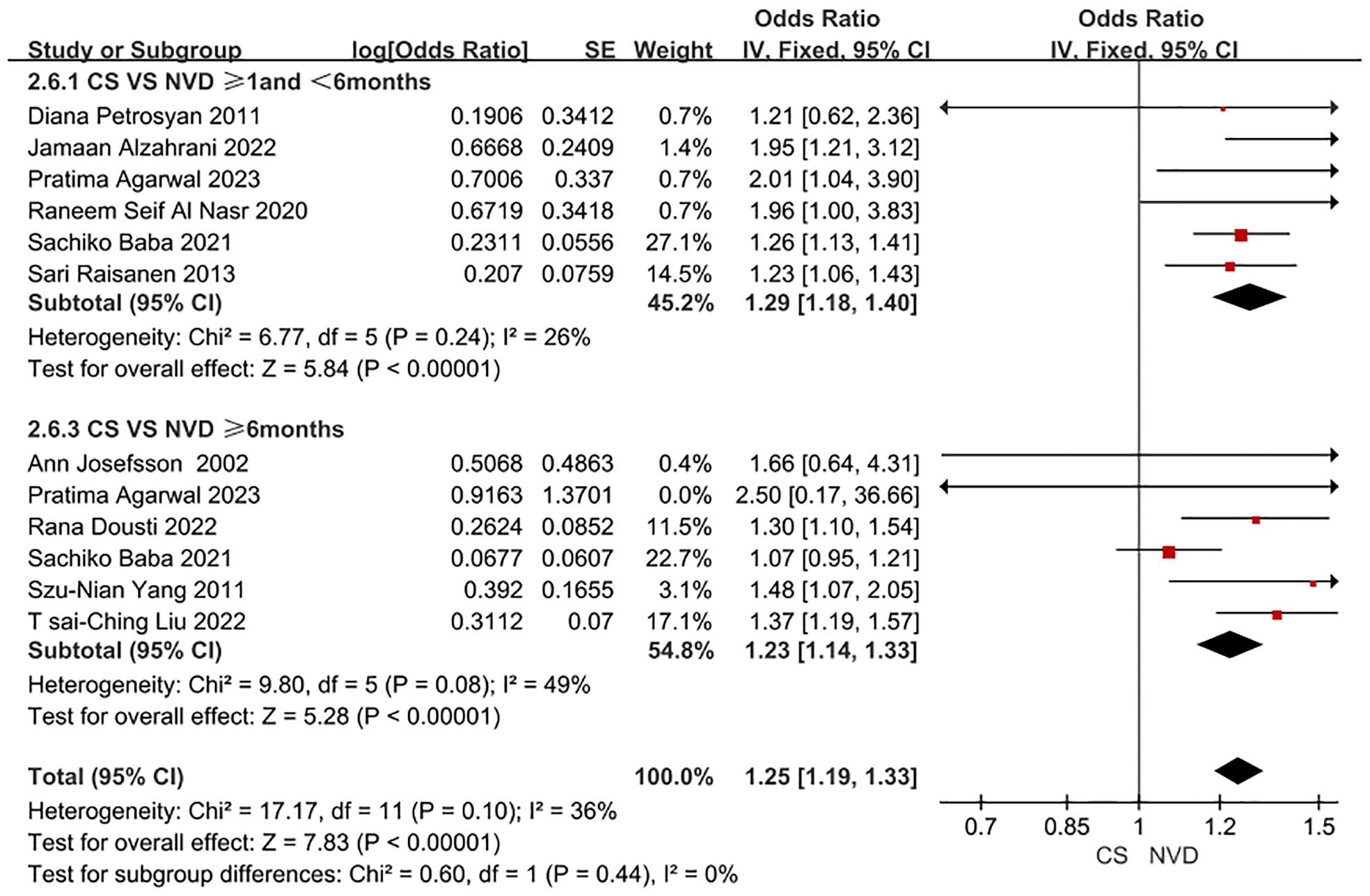
Figure 3 Forest plot of subgroup for PPD patient undergoing CS and NVD in time dimension.
3.3.2.2 Subgroup analysis by CS types
In this subgroup analysis by CS type, a total of 4 studies were included. The adjusted OR for the association between ELCS and PPD was 0.96 (0.83, 1.10), and the adjusted OR for the association between EMCS and PPD was 1.20 (1.08, 1.34). as detailed in Figure 4 . The data included in this subgroup analysis were all adjusted OR.
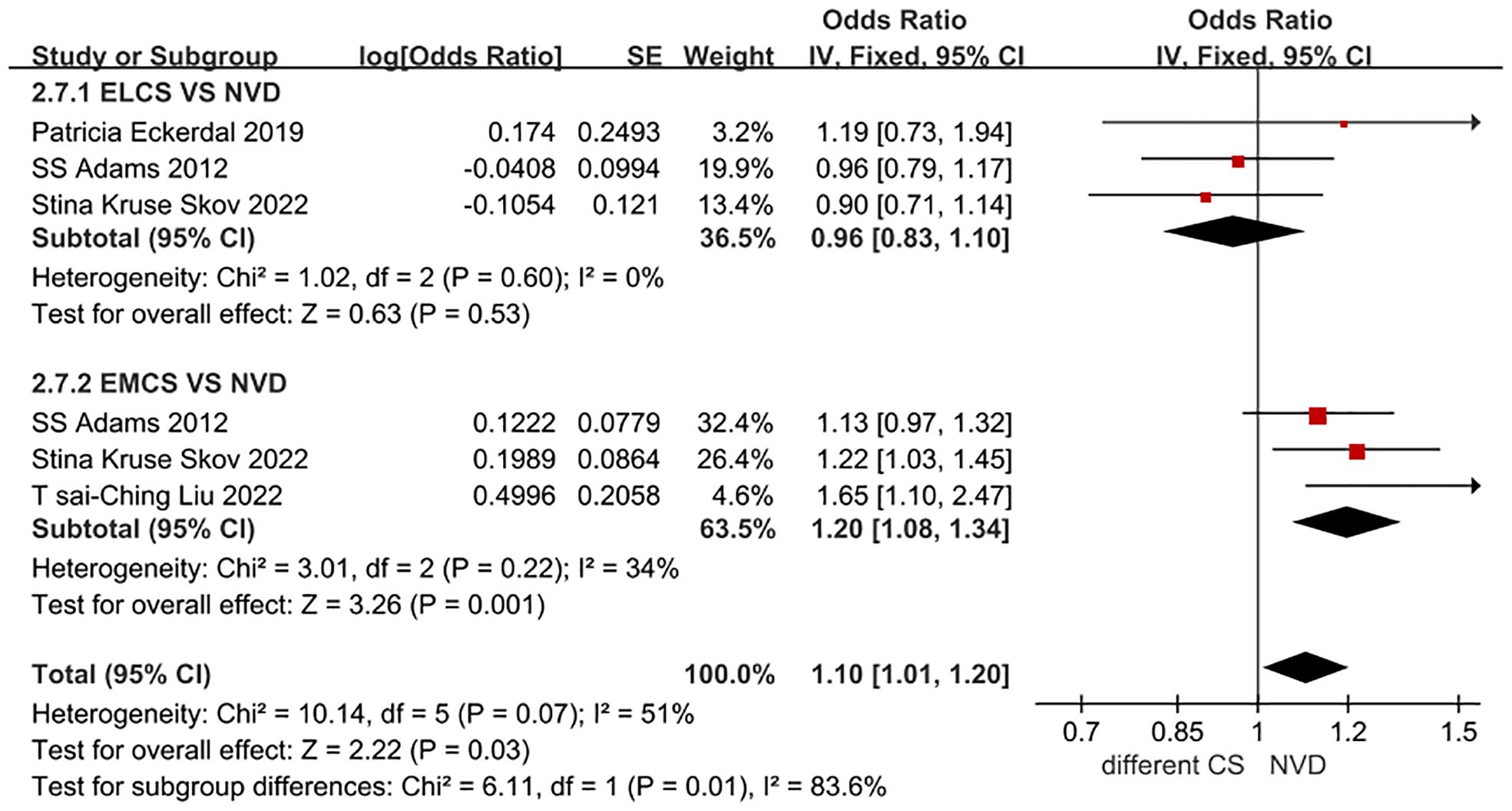
Figure 4 Forest plot for ELCS, EMCS and NVD in PPD patients.
3.3.2.3 Other subgroups
Although there was a high correlation between CS and PPD risk in all populations, we observed a stronger correlation in the Asian population (OR = 1.35, 95% CI: 1.17-1.57, I 2 = 58%, P < 0.001). However, there was significant heterogeneity. In European populations (OR=1.17, 95% CI: 1.06-1.30, I 2 = 16%, P = 0.002), the association was relatively weak, but the heterogeneity was not significant ( Table 3 ). The data included in this subgroup analysis all consisted of adjusted OR.
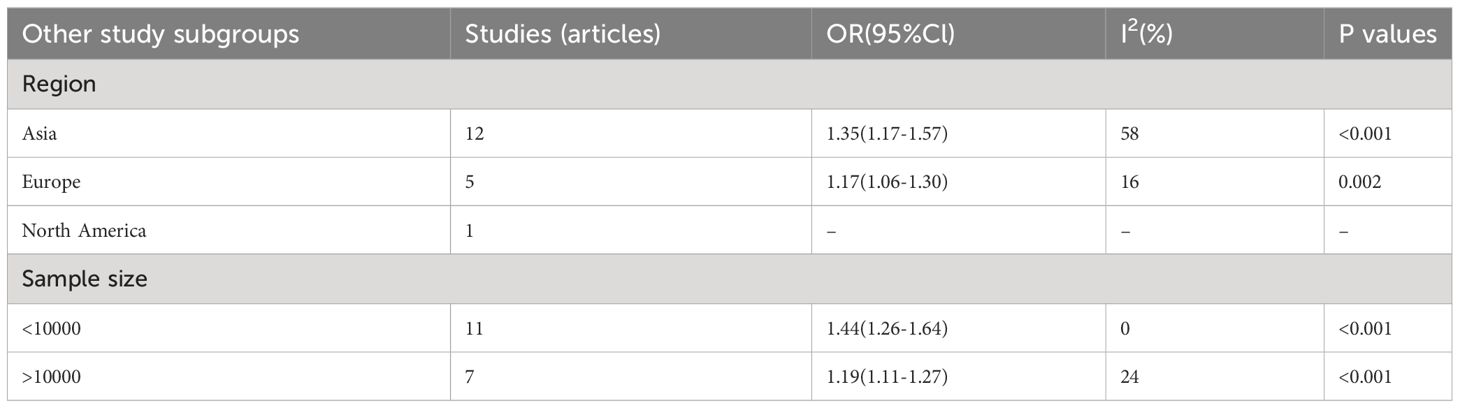
Table 3 Additional subgroup analyses of PPD risk based on the features of included studies.
Eight studies ( 11 , 22 , 24 , 25 , 28 , 31 , 35 , 37 ) were included in the analysis, reporting the adjusted odds ratio (OR) for the incidence of PPD in primiparous women undergoing CS compared to multiparous women and those undergoing normal vaginal delivery (NVD). The OR for the occurrence of PPD in primiparous women undergoing CS was 0.75 (95% CI: 0.25-2.26, I 2 = 92%, P = 0.61), while the OR for the occurrence of PPD in multiparous women undergoing CS was 1.01 (95% CI: 0.57-1.79, I 2 = 84%, P = 0.98), as outlined in Figure 5 . It’s important to note that the data included in this subgroup analysis were all adjusted OR.
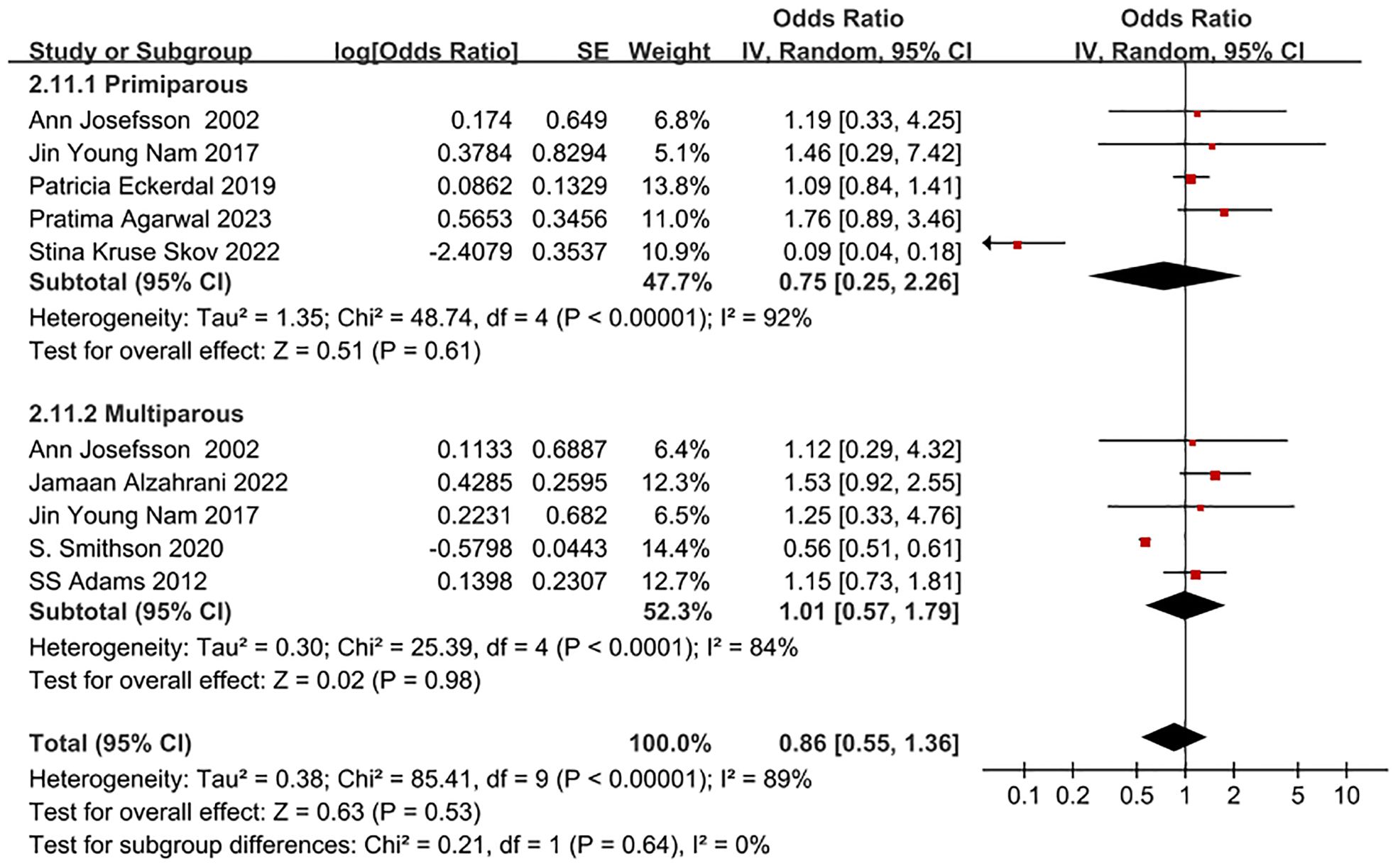
Figure 5 Forest plot of subgroup for whether PPD patient undergoing CS and NVD is primiparae.
The analysis of both CS and PPD in each of the seven largest studies ( 21 – 23 , 25 , 31 , 33 , 34 ) revealed that they accounted for more than 99% of the total cases in this meta-analysis, with a sample size exceeding 10,000. A weaker correlation (OR=1.19, 95% CI: 1.11-1.27, I 2 = 24%, P<0.001) was observed between CS and PPD for the group with over 10,000 participants, compared to the group with fewer than 10,000 participants (OR=1.44, 95% CI: 1.26-1.64, I 2 = 0%, P<0.001) ( Table 3 ). Consequently, it can be inferred that the correlation between CS and PPD gradually diminished as the sample size increased.
3.4 Sensitivity analysis
The meta-analysis was performed again after excluding individual studies one by one, and the combined results revealed there were no significant changes, proving that the combined model was robust and reliable.
3.5 Publication bias
Based on the number of mothers who eventually developed PPD in each group of the 18 included studies, a test for publication bias was performed, and the funnel plot showed that both sides were largely symmetrical, as shown in Figure 6 . At the same time, based on the Egger bias test of this figure, p=0.820 was obtained. indicating no risk of publication bias.
Figure 6 Funnel plot of publication bias for the correlation between CS and PPD.
4 Discussions
The research focused on examining the relationship between CS and PPD. This meta-analysis involved the gathering of data on the correlation between various delivery methods and different modes of CS in relation to PPD. It encompassed eighteen studies, involving 844,328 women from eleven different countries. A comprehensive search strategy utilizing subject terms in combination with free words across multiple databases was employed to encompass all available and eligible studies to date. Furthermore, the included studies comprised cohort and case-control studies of moderate quality and above, with the majority being published within the last five years. Additionally, the study categorized women with different delivery types based on PPD follow-up time and conducted various subgroup analyses to elucidate the association between CS and PPD. These approaches collectively strengthened the credibility of the study’s results.
Our study found that the incidence of PPD was 13.4% in parturients undergoing CS and 10.4% in those undergoing normal vaginal delivery (NVD). This indicates that CS represents a risk factor for PPD in parturients. It is well established that levels of steroid hormones, such as estradiol, progesterone, and cortisol, decrease significantly after delivery ( 38 ), irrespective of the mode of delivery. However, there has been a debate regarding the influence of steroid hormones on depression and PPD ( 39 ). Additionally, CS is linked to various maternal biological changes, including reduced prolactin levels and increased interleukin-6 levels, all of which are PPD risk factors ( 40 ). Furthermore, CS is associated with an increased risk of bleeding, which in turn elevates the likelihood of developing PPD ( 41 ). Societal perceptions and cultural beliefs associating “vaginal delivery” with “normal delivery” have also been reported to impact the psychological state of women undergoing CS, further contributing to the increased likelihood of PPD ( 42 ). These biological and psychological factors help explain why women who opt for CS are at a higher risk of experiencing PPD, thereby supporting the findings of our study. However, it should be noted that residual confounders were present in the pooled estimates due to some studies failing to adjust for confounding factors such as socioeconomic status and social support. While four high-quality studies reported that adjusted odds ratios reduced the risk of PPD in CS mothers by 17%, they had no impact on the overall outcome. This suggests that the adjustment of odds ratios did not affect the correlation between CS and PPD. Psychologically, many women may experience negative emotions such as low self-esteem, feelings of failure, loss of control, or disappointment following CS ( 22 – 25 ). The impact of wound care, slow postpartum recovery, and potential complications may further increase the risk of PPD. Additionally, women undergoing CS may lack confidence due to the inability to give birth naturally, even under necessary circumstances, which can create pressure in raising children. Furthermore, the physical pain and lifestyle changes after delivery can contribute to mental disorders, which may subsequently lead to PPD.
The study also examined the impact of CS mode, time dimension, primiparae and multiparae, and region on PPD risk. The subgroup analysis revealed that PPD risk increased by 20% in parturients undergoing EMCS, while it decreased in parturients undergoing ELCS. This difference may be attributed to the use of different types of anesthesia. Studies ( 43 – 47 ) have shown that women who undergo EMCS often receive general anesthesia, while those who undergo ELCS typically receive spinal anesthesia. General anesthesia has been associated with various biochemical mechanisms that could lead to the occurrence of PPD, such as inhibiting 5-HT uptake, reducing synaptic transmission of serotonin, dopamine, and norepinephrine, and interfering with the synthesis of S-adenosylmethionine. Additionally, women who deliver by EMCS may experience physical fatigue, along with the psychological burden and subjective feeling of being unable to give birth due to NVD failure. These factors can contribute to a negative delivery experience and potentially lead to depression. However, the results for the ELCS group were not statistically significant (P=0.55), possibly due to the limited number of study subjects (only 14,869 pregnant women who chose ELCS). Therefore, more rational designs and in-depth studies focusing on the effect of ElCS and EMCS on PPD risk should be conducted in the future. Our study does not report the original OR and adjusted OR data for the risk of PPD in women on AVD versus CS, which is one of our limitations. It is important to conduct more rational designs and in-depth studies in the future to confirm this conclusion.
Our subgroup analysis involved grouping by time dimension, using 6 months as the designated time node. This choice was made in order to provide a basis for further explanation. The findings of studies ( 24 ) indicated that the association between CS and the risk of PPD was minimal within the first month after delivery, as compared to normal vaginal delivery (NVD). However, upon adjusting for physical, socioeconomic, and psychological factors prior to delivery, the risk of PPD after 6 months postpartum was no longer significant. Additionally, studies ( 48 , 49 ) have shown that women in Western countries, such as Ireland and Sweden, are entitled to at least 26 weeks (6 months) of maternity leave. Upon returning to work or taking care of their children, these women may face increased susceptibility to viral infections, which could contribute to elevated reports of anxiety and depression symptoms at 6 months. As a result, our studies utilized the time period of 6 months postpartum as the threshold for conducting subgroup analysis. Our study highlighted the potential for CS to elevate the occurrence of PPD within the first 1-6 months postpartum, indicating that the choice of CS may carry adverse emotional consequences for many women during the initial 6 months after delivery. Therefore, it is essential for healthcare professionals to recognize the need to impose certain limitations on the preference for CS, bearing in mind the subjective preferences of pregnant women and their clinical requirements.
Our study also revealed that compared to parturients undergoing vaginal delivery (NVD), the risk of PPD in parturients undergoing repeat CS was higher than that in parturients undergoing CS for the first time. A study ( 50 ) has shown that, in addition to considering other biopsychosocial factors, repeat CS is associated with greater pain severity, leading to an increased risk of PPD in parturients undergoing repeat CS, which corroborates the findings of the study we included ( 26 ). Studies ( 51 , 52 ) have also indicated that the fear of pain and the delivery process may contribute to the occurrence of PPD in parturients undergoing repeat CS. During the early postpartum period, abdominal pain and incision scars from CS may result in dissatisfaction with their bodies, further increasing the risk of PPD in parturients undergoing repeat CS. Conversely, a study ( 53 ) has shown that the experience of the primary CS can alleviate the fear of pain in parturients, leading to lower pain scores for parturients undergoing repeat CS and thus reducing the occurrence of PPD. Early identification of the emotional changes of parturients in clinical practice and proactive management of their pain expectations may be beneficial.
In our subgroup analysis, we conducted a comparison between the European and Asian populations. It was found that the risk of PPD in Asian women undergoing CS is 18% higher than that in European women, when compared to NVD. This difference may be partly attributed to the practice of postpartum confinement, which is prevalent in many Asian communities, particularly in inland China and Taiwan, China. During postpartum confinement, mothers adhere to a high-protein diet and prolonged sitting, which can lead to negative body image issues. In contrast, countries like Europe and the United States do not observe the tradition of postpartum confinement ( 52 ). A previous study ( 54 ) has indicated that maintaining a positive body image can help prevent PPD. Similarly, Riquin et al. ( 55 ) have highlighted that dissatisfaction with body image during the perinatal period is linked to a higher risk of depression in mothers. Therefore, healthcare professionals should promote regular postpartum exercise to women, as this can help reduce postpartum weight retention and enhance body satisfaction, consequently lowering the incidence of PPD.
It is important to note that in this study, the Edinburgh Postnatal Depression Scale (EPDS) was used in 10 studies to assess the severity of PPD, while SCL-90 was used in 2 studies, LNHID from 2010 in 2 studies, CES-D in 1 study, NHIS-NSC in 1 study, BDI in 1 study, and HDR in 1 study. For more details, please refer to Supplementary Figure 4 . The findings indicated that there were mostly no significant differences in the summarized results of groups that utilized different scales. We individually discussed each type of scale simultaneously. Notably, LNHID from 2010, NHIS-NSC, and HDR are all national health information databases, and the definition and diagnosis of PPD in parturients have been based on the content of “The Diagnostic and Statistical Manual of Mental Disorders” (DSM) from the American Psychiatric Association, which suggests that the screened data for PPD are similar. In a study ( 56 ) involving 1,831 pregnant women, the sROC curve for EPDS was found to be 0.90. The sROC curve for BDI was 0.91, indicating similarity to that of EPDS. Additionally, a separate study ( 57 ) revealed that the Cronbach’s α of CES-D was 0.84 and the Cronbach’s α of EPDS was 0.80, suggesting that the scales exhibited adequate reliability. Furthermore, the results of CFA in the same study indicated that the theoretical factorial structure of EPDS and CES-D can be sufficiently replicated. The three-factor structure of CES-D (“somatic symptom”, “negative impact”, and “anxiety”) and the three-factor structure of EPDS, including lack of enjoyment, anxiety, and depression, were also found to be replicable. In the case of SCL-90, a study ( 58 ) compared it with EPDS and indicated that their structures for evaluating depression were essentially similar. Research has shown that the results obtained from the various scales included in this study are similar, further indicating that the choice of PPD scale will not significantly impact the results. Thus, in this study, the merging of data from different scales is deemed reasonable and dependable. In future research, we will thoroughly consider the characteristics of the scales included in the study and endeavor to incorporate more data from the same scale for analysis.
4.1 Merits and limitations
This study provides comprehensive postpartum statistical data concerning pregnant women who have undergone various modes of delivery. The data includes the duration of PPD follow-up, demographic characteristics, and the tools used to measure PPD. A notable strength of this study is the large number of participants involved in the meta-analysis, totaling 844,328. This significantly enhances the statistical credibility and persuasiveness of the study, making it more likely to produce consistent results. These studies encompass extensive data on geographically diverse demographic factors and educational levels. The benefit of such a large participant pool is the ability to draw generalizable and consistent assessment results from a wide range of settings, populations, and behaviors ( 34 ). Furthermore, the studies included in this analysis consist primarily of cohort studies and case-control studies that are of moderate quality or higher. Most of these studies were published within the last five years. The majority of their findings have been adjusted to account for potential confounding variables, thereby strengthening the validity of the conclusions derived from the data.
The study has several limitations that need to be addressed. Firstly, by exclusively focusing on English literature, the study may introduce publication bias due to inadequate representation of literature. Secondly, following subgroup analysis, the study found small sample sizes and outcome indicators in each subgroup, necessitating further validation of the findings. Thirdly, the variation in evaluation criteria among different PPD assessment scales could potentially impact the analysis results. Additionally, maternal PPD may be influenced by factors such as duration, maternal age, and mode of CS, highlighting the need for further research. Lastly, the study’s inclusion of a limited number of individuals on AVD may affect the overall conclusions. Therefore, it is recommended that future prospective cohort studies or clinical trials with larger samples and higher quality be conducted to thoroughly examine the relationship between maternal CS and PPD and provide more robust evidence to support PPD prevention efforts. Given the limited quality of the statistical methods used in this study, its conclusions should be considered inconclusive.
5 Conclusion
The results of our study indicate a connection between CSs (especially EMCS) and the risk of developing PPD. It is evident that the risk of PPD in women undergoing CS is higher than in those undergoing Vaginal Delivery (NVD), and the risk of PPD within one to six months postpartum after CS increases by 6% compared to that at six months postpartum. Therefore, it is recommended that pregnant women make careful decisions regarding their mode of delivery and, when appropriate, seek the informed opinion of their healthcare provider. Moving forward, it is essential to carry out more systematic and comprehensive research in order to gain more precise insights.
Data availability statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.
Author contributions
JN: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Writing – original draft. JD: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Writing – original draft. SL: Conceptualization, Data curation, Formal analysis, Investigation, Validation, Writing – review & editing. CL: Data curation, Investigation, Methodology, Writing – review & editing. PZ: Conceptualization, Methodology, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Innovation Project of Guangxi Graduate Education (JYG2023082) and the Study on the construction and ability improvement of the Integrated Eldercare Services with Medical Care in Nanning from the perspective of supply side (RH2300019361).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1361604/full#supplementary-material
Supplementary Figure 1 | Forest plot of the incidence of PPD for parturient in the general population.
Supplementary Figure 2 | Forest plot of incidence of PPD for parturient in the population undergoing CS.
Supplementary Figure 3 | Forest plot of incidence of PPD for parturient in the population undergoing NVD.
Supplementary Figure 4 | Forest plot of subgroup for PPD patient undergoing CS and NVD in different scales.
Supplementary Table 1 | Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Supplementary Table 2 | Database search strategy.
Supplementary Table 3 | Newcastle-Ottawa Scale (NOS).
1. Meltzer-Brody S, Colquhoun H, Riesenberg R, Epperson CN, Deligiannidis KM, Rubinow DR, et al. Brexanolone injection in post-partum depression: two multicenter, double-blind, randomized, placebo-controlled, phase 3 trials. Lancet (London England) . (2018) 392:1058–70. doi: 10.1016/s0140-6736(18)31551-4
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Fancourt D, Perkins R. Could listening to music during pregnancy be protective against postnatal depression and poor wellbeing post birth? Longitudinal associations from a preliminary prospective cohort study. BMJ Open . (2018) 8:e021251. doi: 10.1136/bmjopen-2017-021251
3. Payne JL, Maguire J. Pathophysiological mechanisms implicated in postpartum depression. Front Neuroendocrinol . (2019) 52:165–80. doi: 10.1016/j.yfrne.2018.12.001
4. Logsdon MC, Wisner KL, Pinto-Foltz MD. The impact of postpartum depression on mothering. J obstet gynecol neonatal Nurs JOGNN . (2006) 35:652–8. doi: 10.1111/j.1552-6909.2006.00087.x
CrossRef Full Text | Google Scholar
5. Glasser S, Levinson D, Gordon ES, Braun T, Haklai Z, Goldberger N. The tip of the iceberg: postpartum suicidality in Israel. Israel J Health Policy Res . (2018) 7:34. doi: 10.1186/s13584-018-0228-x
6. Li Y. Review of risk factors screening of postpartum depression and its interventions. Chin Gen Pract . (2020) 23:266–71. doi: 10.12114/j.issn.1007-9572.2019.00.773
7. Alharbi AA, Abdulghani HM. Risk factors associated with postpartum depression in the Saudi population. Neuropsychiatr Dis Treat . (2014) 10:311–6. doi: 10.2147/ndt.S57556
8. Patel RR, Murphy DJ, Peters TJ. Operative delivery and postnatal depression: A cohort study. BMJ (Clinical Res ed) . (2005) 330:879. doi: 10.1136/bmj.38376.603426.D3
9. Eisenach JC, Pan PH, Smiley R, Lavand'homme P, Landau R, Houle TT. Severity of Acute Pain after Childbirth, but Not Type of Delivery, Predicts Persistent Pain and Postpartum Depression. Pain . (2008) 140:87–94. doi: 10.1016/j.pain.2008.07.011
10. Sadat Z, Kafaei Atrian M, Masoudi Alavi N, Abbaszadeh F, Karimian Z, Taherian A. Effect of mode of delivery on postpartum depression in Iranian women. J obstet gynecol Res . (2014) 40:172–7. doi: 10.1111/jog.12150
11. Smithson S, Mirocha J, Horgan R, Graebe R, Massaro R, Accortt E. Unplanned cesarean delivery is associated with risk for postpartum depressive symptoms in the immediate postpartum period. J maternal-fetal neonatal Med . (2022) 35:3860–6. doi: 10.1080/14767058.2020.1841163
12. Chaaya M, Campbell OM, El Kak F, Shaar D, Harb H, Kaddour A. Postpartum depression: prevalence and determinants in Lebanon. Arch women's Ment Health . (2002) 5:65–72. doi: 10.1007/s00737-002-0140-8
13. Silverman ME, Reichenberg A, Savitz DA, Cnattingius S, Lichtenstein P, Hultman CM, et al. The risk factors for postpartum depression: A population-based study. Depression Anxiety . (2017) 34:178–87. doi: 10.1002/da.22597
14. Doke PP, Vaidya VM, Narula APS, Datar MC, Patil AV, Panchanadikar TM, et al. Assessment of Difference in Postpartum Depression among Caesarean and Vaginally Delivered Women at 6-Week Follow-up in Hospitals in Pune District, India: An Observational Cohort Study. BMJ Open . (2021) 11:e052008. doi: 10.1136/bmjopen-2021-052008
15. Ilska M, Banaś E, Gregor K, Brandt-Salmeri A, Ilski A, Cnota W. Vaginal delivery or caesarean section - severity of early symptoms of postpartum depression and assessment of pain in Polish women in the early puerperium. Midwifery . (2020) 87:102731. doi: 10.1016/j.midw.2020.102731
16. Moameri H, Ostadghaderi M, Khatooni E, Doosti-Irani A. Association of postpartum depression and cesarean section: A systematic review and meta-analysis. Clin Epidemiol Global Health . (2019) 7:471–80. doi: 10.1016/j.cegh.2019.02.009
17. Xu H, Ding Y, Ma Y, Xin X, Zhang D. Cesarean section and risk of postpartum depression: A meta-analysis. J psychosom Res . (2017) 97:118–26. doi: 10.1016/j.jpsychores.2017.04.016
18. Sun L, Wang S, Li XQ. Association between mode of delivery and postpartum depression: A systematic review and network meta-analysis. Aust New Z J Psychiatry . (2021) 55:588–601. doi: 10.1177/0004867420954284
19. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The prisma 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical Res ed) . (2021) 372:n71. doi: 10.1136/bmj.n71
20. Stang A. Critical evaluation of the newcastle-ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol . (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
21. Liu TC, Peng HC, Chen C, Chen CS. Mode of delivery is associated with postpartum depression: do women with and without depression history exhibit a difference? Healthc (Basel Switzerland) . (2022) 10(7):1308. doi: 10.3390/healthcare10071308
22. Skov SK, Hjorth S, Kirkegaard H, Olsen J, Nohr EA. Mode of delivery and short-term maternal mental health: A follow-up study in the Danish national birth cohort. Int J gynaecol obstet . (2022) 159:457–65. doi: 10.1002/ijgo.14155
23. Baba S, Ikehara S, Eshak ES, Ueda K, Kimura T, Iso H. Association between mode of delivery and postpartum depression: the Japan environment and children's study (Jecs): A prospective cohort study. J Epidemiol . (2021) 33(5):209–16. doi: 10.2188/jea.JE20210117
24. Eckerdal P, Georgakis MK, Kollia N, Wikström AK, Högberg U, Skalkidou A. Delineating the association between mode of delivery and postpartum depression symptoms: A longitudinal study. Acta obstet gynecol Scandinavica . (2018) 97:301–11. doi: 10.1111/aogs.13275
25. Adams SS, Eberhard-Gran M, Sandvik ÅR, Eskild A. Mode of delivery and postpartum emotional distress: A cohort study of 55,814 women. BJOG . (2012) 119:298–305. doi: 10.1111/j.1471-0528.2011.03188.x
26. Chang SR, Chen KH, Ho HN, Lai YH, Lin MI, Lee CN, et al. Depressive symptoms, pain, and sexual dysfunction over the first year following vaginal or cesarean delivery: A prospective longitudinal study. Int J Nurs Stud . (2015) 52:1433–44. doi: 10.1016/j.ijnurstu.2015.04.019
27. Dousti R, Hakimi S, Pourfathi H, Nourizadeh R, Sattarzadeh N. Cesarean section can be related with postpartum depression: A cross-sectional study. Int J Women’s Health Reprod Sci . (2022) 10:219–24. doi: 10.15296/ijwhr.2022.37
28. Alzahrani J, Al-Ghamdi S, Aldossari K, Al-Ajmi M, Al-Ajmi D, Alanazi F, et al. Postpartum depression prevalence and associated factors: an observational study in Saudi Arabia. Med (Kaunas Lithuania) . (2022) 58(11):1595. doi: 10.3390/medicina58111595
29. Nayak M. Prevalence & Related factors to postnatal depression: A comparison between nvd & Lscs mothers. Int J Res Pharm Sci . (2020) 11:2228–33. doi: 10.26452/ijrps.v11i2.2175
30. Al Nasr RS, Altharwi K, Derbah MS, Gharibo SO, Fallatah SA, Alotaibi SG, et al. Prevalence and predictors of postpartum depression in riyadh, Saudi Arabia: A cross sectional study. PloS One . (2020) 15:e0228666. doi: 10.1371/journal.pone.0228666
31. Nam JY, Choi Y, Kim J, Cho KH, Park EC. The synergistic effect of breastfeeding discontinuation and cesarean section delivery on postpartum depression: A nationwide population-based cohort study in Korea. J Affect Disord . (2017) 218:53–8. doi: 10.1016/j.jad.2017.04.048
32. Baghiani Mm, Shojaeizadeh D, Aminian A. Caesarean section, vaginal delivery and post natal depression. Iranian J Publ Health . (2009) 38:118–22. Available at: https://api.semanticscholar.org/CorpusID:72947585 .
Google Scholar
33. Räisänen S, Lehto SM, Nielsen HS, Gissler M, Kramer MR, Heinonen S. Fear of childbirth predicts postpartum depression: A population-based analysis of 511 422 singleton births in Finland. BMJ Open . (2013) 3:e004047. doi: 10.1136/bmjopen-2013-004047
34. Yang SN, Shen LJ, Ping T, Wang YC, Chien CW. The delivery mode and seasonal variation are associated with the development of postpartum depression. J Affect Disord . (2011) 132:158–64. doi: 10.1016/j.jad.2011.02.009
35. Josefsson A, Angelsiöö L, Berg G, Ekström CM, Gunnervik C, Nordin C, et al. Obstetric, somatic, and demographic risk factors for postpartum depressive symptoms. Obstet gynecol . (2002) 99:223–8. doi: 10.1016/s0029-7844(01)01722-7
36. Petrosyan D, Armenian HK, Arzoumanian K. Interaction of maternal age and mode of delivery in the development of postpartum depression in Yerevan, Armenia. J Affect Disord . (2011) 135:77–81. doi: 10.1016/j.jad.2011.06.061
37. Agarwal P, Dasari P, Sarkar S. Mode of delivery and postpartum depression: A cohort study. J Obstet Gynaecol India . (2023) 73:88–96. doi: 10.1007/s13224-023-01810-7
38. Dipietro JA, Costigan KA, Sipsma HL. Continuity in self-report measures of maternal anxiety, stress, and depressive symptoms from pregnancy through two years postpartum. J psychosom obstet gynaecol . (2008) 29:115–24. doi: 10.1080/01674820701701546
39. O'Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol . (2013) 9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612
40. Seth S, Lewis AJ, Galbally M. Perinatal maternal depression and cortisol function in pregnancy and the postpartum period: A systematic literature review. BMC pregnancy childbirth . (2016) 16:124. doi: 10.1186/s12884-016-0915-y
41. Hebisch G, Neumaier-Wagner PM, Huch R, von Mandach U. Maternal serum interleukin-1 beta, -6 and -8 levels and potential determinants in pregnancy and peripartum. J perinatal Med . (2004) 32:475–80. doi: 10.1515/jpm.2004.131
42. Triebel J, Martínez de la Escalera G, Clapp C, Bertsch T. Vasoinhibins may contribute to postpartum depression. Front Psychiatry . (2017) 8:167. doi: 10.3389/fpsyt.2017.00167
43. Eckerdal P, Kollia N, Löfblad J, Hellgren C, Karlsson L, Högberg U, et al. Delineating the association between heavy postpartum hemorrhage and postpartum depression. PloS One . (2016) 11:e0144274. doi: 10.1371/journal.pone.0144274
44. Sword W, Landy CK, Thabane L, Watt S, Krueger P, Farine D, et al. Is mode of delivery associated with postpartum depression at 6 weeks: A prospective cohort study. BJOG . (2011) 118:966–77. doi: 10.1111/bjo.2011.118.issue-8
45. Meky HK, Shaaban MM, Ahmed MR, Mohammed TY. Prevalence of postpartum depression regarding mode of delivery: A cross-sectional study. J maternal-fetal neonatal Med . (2020) 33:3300–7. doi: 10.1080/14767058.2019.1571572
46. Jansen AJ, Duvekot JJ, Hop WC, Essink-Bot ML, Beckers EA, Karsdorp VH, et al. New Insights into Fatigue and Health-Related Quality of Life after Delivery. Acta obstet gynecol Scandinavica . (2007) 86:579–84. doi: 10.1080/00016340701275424
47. Bergholt T, Stenderup JK, Vedsted-Jakobsen A, Helm P, Lenstrup C. Intraoperative surgical complication during cesarean section: an observational study of the incidence and risk factors. Acta obstet gynecol Scandinavica . (2003) 82:251–6. doi: 10.1080/j.1600-0412.2003.00095.x
48. Hannon S, Gartland D, Higgins A, Brown SJ, Carroll M, Begley C, et al. Physical health and comorbid anxiety and depression across the first year postpartum in Ireland (Mammi study): A longitudinal population-based study. J Affect Disord . (2023) 328:228–37. doi: 10.1016/j.jad.2023.02.056
49. Schramm SH, Moebus S, Lehmann N, Galli U, Obermann M, Bock E, et al. The association between stress and headache: A longitudinal population-based study. Cephalalgia . (2015) 35:853–63. doi: 10.1177/0333102414563087
50. Wilson JM, He J, Flowers KM, Kovacheva V, Soens M, Schreiber KL. Pain severity and pain interference in late pregnancy: an analysis of biopsychosocial factors among women scheduled for cesarean delivery. Pain Med . (2023) 24:652–60. doi: 10.1093/pm/pnac171
51. Dehghani M, Sharpe L, Khatibi A. Catastrophizing mediates the relationship between fear of pain and preference for elective caesarean section. Eur J Pain . (2014) 18:582–9. doi: 10.1002/j.1532-2149.2013.00404.x
52. Chen ML, Chang SR. The relationship between body dissatisfaction and postpartum depressive symptoms: A cross-sectional study. J Affect Disord . (2023) 324:418–23. doi: 10.1016/j.jad.2022.12.102
53. Tan HS, Yeo KA, Tan CW, Chan JJI, Cheng S-M, Sultana R, et al. Pre-operative pain and psychological vulnerability factors associated with primary cesarean delivery: an observational study. Bali J Anesthesiol . (2023) 7:94 – 8. doi: 10.4103/bjoa.bjoa_53_23
54. Han SY, Brewis AA, Wutich A. Body image mediates the depressive effects of weight gain in new mothers, particularly for women already obese: evidence from the Norwegian mother and child cohort study. BMC Public Health . (2016) 16:664. doi: 10.1186/s12889-016-3363-8
55. Riquin E, Lamas C, Nicolas I, Dugre Lebigre C, Curt F, Cohen H, et al. A key for perinatal depression early diagnosis: the body dissatisfaction. J Affect Disord . (2019) 245:340–7. doi: 10.1016/j.jad.2018.11.032
56. Park SH, Kim JI. Predictive validity of the edinburgh postnatal depression scale and other tools for screening depression in pregnant and postpartum women: A systematic review and meta-analysis. Arch Gynecol Obstet . (2023) 307:1331–45. doi: 10.1007/s00404-022-06525-0
57. Heller HM, Draisma S, Honig A. Construct validity and responsiveness of instruments measuring depression and anxiety in pregnancy: A comparison of epds, hads-a and ces-D. Int J Environ Res Public Health . (2022) 19(13):7563. doi: 10.3390/ijerph19137563
58. Korja R, Nolvi S, Scheinin NM, Tervahartiala K, Carter A, Karlsson H, et al. Trajectories of maternal depressive and anxiety symptoms and child's socio-emotional outcome during early childhood. J Affect Disord . (2024) 349:625–34. doi: 10.1016/j.jad.2023.12.076
Keywords: caesarean section, postpartum depression, emergency caesarean section, meta-analysis, systematic review
Citation: Ning J, Deng J, Li S, Lu C and Zeng P (2024) Meta-analysis of association between caesarean section and postpartum depression risk. Front. Psychiatry 15:1361604. doi: 10.3389/fpsyt.2024.1361604
Received: 26 December 2023; Accepted: 19 March 2024; Published: 28 March 2024.
Reviewed by:
Copyright © 2024 Ning, Deng, Li, Lu and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pingping Zeng, [email protected]
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Caesarean section: a case study
- PMID: 3217062
Publication types
- Case Reports
- Cesarean Section / nursing*
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Health Reporting in the States
Standard pregnancy care is now dangerously disrupted in louisiana, report reveals.
Rosemary Westwood

Under Louisiana's abortion ban, doctors face penalties of up to 15 years in prison, $200,000 in fines and loss of their medical license. Dr. Neelima Sukhavasi, a Baton Rouge OB-GYN, says that doctors are scared. Here, Dr. Sukhavasi poses for a portrait in Baton Rouge, La., on Monday, March 18, 2024. Christiana Botic hide caption
Under Louisiana's abortion ban, doctors face penalties of up to 15 years in prison, $200,000 in fines and loss of their medical license. Dr. Neelima Sukhavasi, a Baton Rouge OB-GYN, says that doctors are scared. Here, Dr. Sukhavasi poses for a portrait in Baton Rouge, La., on Monday, March 18, 2024.
In the wake of Louisiana's abortion ban, pregnant women have been given risky, unnecessary surgeries, denied swift treatment for miscarriages and ectopic pregnancies, and forced to wait until their life is at risk before getting an abortion, according to a new report first made available to NPR.
It found doctors are using extreme caution to avoid even the appearance of providing an abortion procedure.
"We were stunned by just how much regular medical practice for pregnant people has been disrupted," said Michele Heisler, the medical director of Physicians for Human Rights and one of the report's authors.
The report is titled " Criminalized Care: How Louisiana's Abortion Bans Endanger Patients and Clinicians ."
It draws on interviews with 30 health care providers and 13 patients conducted in 2023, and was jointly supported by four groups that support abortion access: Physicians for Human Rights, the Center for Reproductive Rights , Lift Louisiana and Reproductive Health Impact .
It's among the most comprehensive research to date showing abortion bans are changing pregnancy care and worsening maternal health. It concludes that Louisiana's ban is impeding a federal law that regulates the provision of emergency health care, and is infringing on reproductive and human rights.
"There are going to be deaths that didn't have to happen. There are going to be severe complications that didn't have to happen," said Dr. Nicole Freehill, a New Orleans OB-GYN interviewed for the report.
Unnecessary C-sections raise alarms
In one of the most extreme examples of how pregnancy care has changed, doctors described cases of women who experienced preterm premature rupture of membranes (when the "water breaks" early in pregnancy, before the fetus is viable). Some of these women were forced to undergo Cesarean section surgeries to empty their uterus and avoid infection, instead of receiving an abortion procedure or medication.
"Which is ludicrous, absolutely ludicrous," said Freehill. "The least safe thing that we do, no matter if it's early in pregnancy or full-term at your due date, is a C-section."
Describing one of these cases, Dr. Michele Heisler with Physicians for Human Rights explained that the C-section was done "to preserve the appearance of not doing an abortion."
The patient wasn't given a choice, she added.
A C-section is major abdominal surgery. NPR consulted three OB-GYNs who were not interviewed for the report, all of whom said a C-section in a case like this is not standard care. Compared to an abortion procedure or an induction, it carries far greater risks for increased hemorrhaging, compromised future fertility, and other complications.
The doctors also added that patients undergoing a C-section in that circumstance would be told that in future pregnancies they couldn't deliver vaginally and risked a ruptured uterus.
"I want to emphasize that this is not what's in the best interest of the patient," said one New Orleans OB-GYN who didn't want her name used because she feared talking publicly could cause her trouble with her employer. "This is what's in the best interest of...the physician in protecting themselves from criminal prosecution."
Doctors face penalties under Louisiana's abortion ban of up to 15 years in prison and $200,000 in fines.
Prenatal care appointments pushed back
In what doctors described as another serious deviation from standard medical practice, OB-GYNs in Louisiana are now delaying routine prenatal care until patients reach 12 weeks of pregnancy — the point at which the risk of miscarriage drops significantly .
One patient interviewed in the report said several different doctors' offices wouldn't see her before 12 weeks. One office told her the abortion ban was "something that's new" and that doctors wanted "to eliminate some of the spontaneous abortions, or miscarriages, that may happen up until that 12-week mark," the patient recounted.

Pins on Dr. Neelima Sukhavasi's coat pocket show her support for women's reproductive health, Baton Rouge, La., on Monday, March 18, 2024. Christiana Botic hide caption
Pins on Dr. Neelima Sukhavasi's coat pocket show her support for women's reproductive health, Baton Rouge, La., on Monday, March 18, 2024.
"I think physicians are scared, and so what can we do to decrease our risk that the attorney general is going to come after us?" said Dr. Neelima Sukhavasi, a Baton Rouge OB-GYN interviewed in the report. "And that is probably one of the things that they saw would be easiest."
Delaying pregnancy care into the second trimester can be dangerous for people who might have complications, such as a history of blood clots or an ectopic pregnancy that goes undiagnosed, doctors told NPR. Without treatment, some pregnancy-related problems can lead to birth defects, stroke, heart attack, or even death.
Delays, transfers, waits for illness to get worse
Physicians are also delaying treatment of miscarriage and ectopic pregnancy out of fear of breaking the law, the report found — as previously reported in news stories from states operating under abortion bans. Ectopic pregnancies — when the embryo implants outside of the uterus — are never viable, and they can even be deadly.
One patient with an ectopic pregnancy said her care was delayed so long that her fallopian tubes ruptured.
"I could have died," she said in the report. "I really could have died."
In another case, Sukhavasi had a patient in her first trimester who came to the hospital bleeding and in pain. The patient wanted an abortion procedure called dilation and curettage, or D&C, which uses suction to empty the contents of the uterus and stop the pain and bleeding.
"I know this pregnancy is not going to make it anywhere near survival. And I was stopped from taking her to the operating room," Sukhavasi said.
The woman waited for hours while hospital officials decided if her abortion was allowed. Sukahavasi said it all goes back to fear.
"Institutions don't want the government coming down on them, accusing us of doing something wrong when what we're doing is just providing essential health care that people are coming to us for," she said.

Sukhavasi, photographed in Baton Rouge, La. Monday, March 18, 2024, had a patient in her first trimester who came to the hospital bleeding and in pain. The patient wanted an abortion procedure called dilation and curettage, or D&C. "I know this pregnancy is not going to make it anywhere near survival. And I was stopped from taking her to the operating room," Sukhavasi said. Christiana Botic hide caption
Sukhavasi, photographed in Baton Rouge, La. Monday, March 18, 2024, had a patient in her first trimester who came to the hospital bleeding and in pain. The patient wanted an abortion procedure called dilation and curettage, or D&C. "I know this pregnancy is not going to make it anywhere near survival. And I was stopped from taking her to the operating room," Sukhavasi said.
When miscarrying women arrive at ERs in rural areas, those rural hospitals are increasingly transferring patients to urban, specialty hospitals, the report found, to avoid having to treat those patients altogether. But refusing miscarriage treatment could be a violation of the Emergency Medical Treatment and Labor Act , or EMTALA — a federal law requiring emergency medical care.
The doctors described numerous cases in the report in which seriously ill patients were denied abortions until they became so sick that their lives were irrefutably at risk.
These included pregnant women with cancer; patients with heart problems and kidney failure, who were on dialysis and hospitalized; and women who'd experienced life-threatening complications from previous pregnancies and found themselves pregnant again.
In one case, an OB-GYN treating a patient with severe heart failure was first required to prescribe multiple cardiac medicines before being allowed to offer an abortion.
"And I'm thinking, but what if she doesn't want to wait that long because she could have a heart attack and die?" the OB-GYN said. "At what point can you act? How many cardiac meds have to fail?"
Another physician in the report couldn't get their colleagues to agree to an abortion for a patient with a history of multiple C-sections, hemorrhaging and infections in past pregnancies.
"It was a risk" to require the patient to stay pregnant, the physician said, but the woman wasn't yet "at the brink of death."
Some hospitals have even told physicians that they can't give patients any information on how to get an abortion outside of Louisiana — because that advice could be construed as "providing" an abortion.
Louisiana's ban allows for abortion in cases of severe fetal anomalies – but only if those anomalies are on a list of conditions published by the state's health department . Women whose fetuses are diagnosed with severe and even fatal conditions that don't appear on that list are also being told they can't get an abortion, the report found. Doctors said patients who can afford to are traveling out of state for abortions, while those who can't remain pregnant.
Louisiana's maternal health outcomes might get worse
Physicians interviewed in the report and those interviewed separately by NPR agreed that women's health and their lives were being put at risk because of the abortion ban, especially Black and low-income women.
Louisiana already suffers from some of the highest rates of maternal mortality and morbidity in the nation. Black women in the state are more than twice as likely to die as a result of their pregnancy as white women .
Nearly two-thirds of maternal deaths in Louisiana are among low-income women on Medicaid.
Some doctors in the report said they have considered leaving Louisiana. Others warned that a possible exodus of OB-GYNs would exacerbate the state's existing shortage of obstetricians.
Louisiana Right to Life , which helped author Louisiana's ban, declined to comment on the report's conclusions, without being able to read it before its public release on Tuesday afternoon
Its executive director, Benjamin Clapper, told NPR that the law clearly allows for the treatment of miscarriages and that OB-GYNs contacted by his organization have seen no change in miscarriage care as a result of the ban.
Clapper has said previously , in response to claims that the law is harming women's health, that these concerns have been "manufactured" by abortion rights supporters.
The report's authors said they have simply documented the facts on the ground.
" The anti-abortion movement in Louisiana has for decades created a culture of harassment and intimidation of people providing abortion care," said Michelle Erenberg , the executive director of Lift Louisiana. "And so for folks in that movement to now say, well, providers are just overcomplying with the law, or they're misunderstanding the law, no. They are terrified."
Beyond going to prison, she said, doctors fear being harassed or ostracized from the institutions where they work, and the communities in which they live.
"And all of that is a legitimate fear," she said.
Clarification March 19, 2024
A previous version of this web story did not explain that Benjamin Clapper declined to comment on some of the findings in the report because it had not yet been publicly released and he had not read it himself.
- miscarriage care
- Lousiana abortion ban
- maternal mortality
- Center for Reproductive Rights
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Pan Afr Med J
A case-control study of factors associated with caesarean sections at health facilities in Kabarole District, Western Uganda, 2016
Jacinta dusabe.
1 Department of Health Policy, Planning and Management, Makerere University College of Health Sciences School of Public Health, P.O Box 7072, Kampala, Uganda
Joseph Akuze
Angela nakanwagi kisakye, benon kwesiga, peter nsubuga, elizabeth ekirapa, introduction.
World Health Organization estimates that the appropriate caesarean section rates should range from 10% to 15% at the population level. There is limited access and utilisation of caesarean section services in Uganda. This case-control study explored factors associated with caesarean section delivery, focusing on service-related and individual level factors.
we interviewed 134 cases that had a caesarean section and 134 controls that had a “normal” vaginal delivery. The study was conducted at health facilities in Kabarole district during March to May 2016. Multivariable logistic regression was used to determine individual factors associated with caesarean sections, at a significance level of p < 0.05. Key Informant (KI) data obtained from health workers was analysed using MAXQDA (version 12) software to determine health service factors affecting caesarean section service delivery.
the mean age of the overall sample was 26 years (SD ± 6.5 years). Cases had 5% more women who belonged to the eldest age group (> 35 years) compared to the controls. The factors associated with caesarean section delivery were: having a previous caesarean section delivery (adjusted odds ratio (AOR): 4.5 CI: 2.22-9.0), attendance of four or more ANC visits (AOR: 2.0 CI: 1.04-3.83). Inadequate human resource, medicines and supplies affected access to the service. Misconceptions such as negative branding of women that have caesarean section deliveries as “lazy” reduced its acceptance thus low utilisation of the service.
health system inadequacies and misconceptions about caesarean section delivery contributed to the low access and utilisation of the service.
Caesarean section is one of the most performed surgeries in obstetric practice globally. The World Health Organization (WHO) estimates that the appropriate caesarean section rate should range from 10% to 15% at the population level [ 1 , 2 ]. Globally, 6.2 million unnecessary caesarean sections are performed and yet 3.18 million additional caesarean sections are needed [ 1 ]. There are inadequate caesarean section rates in most developing countries due to limited access to the service and health systems inadequacies while there is adequate or even unnecessary caesarean section use in middle and high-income settings [ 3 , 4 ]. Studies show that women who have a high level of education and are wealthy were more likely to have a caesarean section [ 5 - 7 ]. However, medical indications account for 77% of caesarean section [ 3 ]. Women who have had one birth by caesarean section usually give birth the same way to reduce the risk of uterine rupture; however, a number of studies, show that vaginal births to women with previous deliveries by caesarean section can be performed safely [ 2 , 3 , 8 , 9 ]. Older maternal age has also been associated with increased co-morbidities and increased perceived need for caesarean section delivery [ 4 , 5 , 10 ]. Optimum provision of caesarean section services is however hampered by weak delivery systems characterized by inadequate human resource, drugs, supplies and poor infrastructure development [ 11 - 16 ]. Furthermore, there is evidence that misconceptions about health services influence perceptions and attitudes of people in communities to utilise the services [ 17 , 18 ]. There are few studies and scanty information on factors influencing access and utilisation of caesarean section services in Uganda. The study area has a caesarean section rate of 5.3% [ 19 ] at the population level this is low compared to WHO recommended rates [ 1 ]. This is an indication of low access and utilisation of the service in the district. This study explored factors associated with caesarean section delivery at health facilities in Kabarole district, Western Uganda. Such knowledge can help planners to set priorities and make appropriate support and resources required to provide caesarean sections available.
Study design and setting: We conducted a case-control study at health facilities in Kabarole district, Western Uganda, during a 3 month period from March through May 2016. Caesarean section services in the district are offered only at the regional referral hospital and at two health centres in the public sector. While in the private sector, the service is offered at three hospitals. In our study, we included all the three public health facilities that provide caesarean section service and two randomly selected private facilities.
Case-control definition: We defined a case as having a caesarean section delivery at the selected health facilities during March, April and May 2016. Controls were women that had a “normal” vaginal delivery at the same health facilities as the cases during the study period. A normal delivery was defined as a spontaneous vaginal delivery without the aid of instrument such as forceps or vacuum extraction. We excluded individuals who had been referred from neighbouring districts in both the case group and control group to avoid selection bias.
Sample size calculation and sample selection: A two-stage sampling method was used in this study. At the first stage, we determined the sample size using James Schlesselman's formula for unmatched case-control [ 20 ]. The odds ratio associated with exposure that would have sufficient public health importance was hypothesized at 2, using 95% confidence interval and power of 80% a sample size of 134 in the case group and 134 in the control group calculated. At the second stage of sampling, we purposefully included all the three public health facilities that provide caesarean section service in the district and also randomly sampled two private health facilities. We used probability proportionate to sample size sampling (PPS), to distribute the total sample size of 268 amongst the five-selected health facilities. Using the admission list in the maternity wards, study participants that met the inclusion criteria were consecutively sampled. For every case that was selected, a control was recruited.
Key informant selection: We also conducted qualitative in-depth interviews with seven purposively selected key informants. These included doctors, midwives and nurses that provide delivery services at the health facilities visited. District health office leaders that included the District Health Officer (DHO) and district in-charge for maternal and child health were also interviewed.
Variables: We assessed individual, maternal and health service related factors. Socio-demographic factors included maternal age, education level, marital status, employment status and socio-economic status. Factors related to maternal obstetric and health conditions were parity, multiple births, pre-existing medical conditions and previous caesarean section. Health services related factors were the distance to health facilities measured using geographical distance in kilometres from a place of residence to a health facility, prenatal care consultations (ANC), availability of health infrastructure, human resources, drugs and supplies.
Data sources, measurement and quality control: Data were collected in the same way for individuals in the case and control groups. Socio-demographic and maternal information was obtained using face-to-face interviews aided by pre-coded, structured pre-tested questionnaires. Key informant (KI) interviews were also conducted on selected health workers aided by KI guides. The research team made daily visits to the hospitals and health centres to identify women that met the inclusion criteria. The interviews were conducted by trained research assistants with a medical background and fluent in the local languages spoken in the study area. Transcribed interviews were compared against recorded interviews to ensure the quality of qualitative data analysed.
Data analysis: After descriptive statistical analysis, bivariable and multivariable analyses were conducted using logistic regression at a significance level of 0.05. We conducted the analysis using STATA statistical package version 12. Crude odds ratios (COR) and adjusted odds ratios (AOR) were obtained with their respective 95% confidence intervals (CI). Covariates that were significant at the bivariable level, with a p-value of less than 0.2 and those determined from literature to be associated with caesarean section were entered in the multivariable stepwise (backward and forward) logistic regression model. Hosmer and Lemeshow's goodness of fit was applied to test the quality model. Previous caesarean section was the most significant variable in the model and was hence taken as the main predictor of caesarean section delivery. Interaction and confounding were tested with the main predictor (i.e. previous caesarean section) using stratified analysis. Confounding was further assessed by comparing the crude odds ratio with the adjusted odds ratio obtained using the Mantel Haenszel. A difference between crude and adjusted odds ratios greater than 10% showed a presence of confounding. Key informant recordings were transcribed and transcripts were uploaded into the qualitative analysis software MAXQDA version 12 and we analysed the data following the six steps of the thematic approach developed by Braun and Clarke [ 21 ].
Ethical approval: We sought ethical approval from the higher degrees research and ethics committee of the Makerere university school of public health, the District Health Officer (DHO) as well as managers of the respective health facilities where the research was conducted. Interviews were conducted after a written informed consent was obtained from the study participants.
Quantitative results: The mean age of the overall sample was 26 years (standard deviation ± 6.5). Women in the case group were relatively older (> 35 years) compared to those in the control group (i.e. 14% of cases and 9% of controls). Women in the case group had a higher level of education compared to those in the control group (i.e. 52% of cases and 48% of controls had attained primary education) ( Table 1 ).
Distribution of descriptive characteristics of women studied to assess factors associated with caesarean section at selected health facilities in Kabarole district, Western Uganda (2016)
Bivariable, stratified analysis and multivariable factors associated with caesarean section: At bivariable analysis, women that had a previous caesarean section were more likely to have a subsequent caesarean section compared to those that did not have a previous caesarean section (COR: 5.6 95% CI: 2.97-10.65). Women that were unemployed were 50% less likely to have a caesarean section compared to those that were employed (COR: 0.5 95%CI: 0.30-0.89) ( Table 2 ). Having a pre-existing medical condition was a confounder thus this variable was included in the final model (Mantel Haenszel AOR: 25.4 CI: 8.33- 77.21). There was no interaction due to age and pre-existing medical condition ( Table 3 ). At multivariable analysis, having a primary caesarean section remained statistically associated with caesarean section (AOR: 4.5 CI: 2.22-9.00). Similarly, women that had four or more prenatal consultations were more likely to have a caesarean section compared to those that had less than four consultations (AOR: 2.0 CI: 1.04-3.83) ( Table 4 ).
Stratified analysis to assess interaction and confounding of exposure factors associated with caesarean section at health facilities in Kabarole district, western Uganda (2016)
Bivariable model (logistic regression) of factors associated with caesarean section at health facilities in Kabarole district, western Uganda (2016)
COR a Crude Odds Ratios
Multivariable model (logistic regression) of factors associated with caesarean section at health facilities, western Uganda (2016)
Qualitative results
Health service factors associated with caesarean section delivery: Several health service factors perceived to affect caesarean section rates were identified from this study. The key themes that emerged ranged from infrastructure, human resource, drugs and supplies as well as misconceptions about caesarean section delivery.
Positive factors
Infrastructure improvements: Health infrastructure improvements were achieved following an intervention (i.e. Saving Mothers Giving Life) implemented by one of the development partners working in the area. The intervention helped the district refurbish as well as construct functional theatres at lower level health facilities. This was highlighted by one of the health mangers at a lower level health facility who commented: "The theatre was refurbished by Baylor and equipped with appropriate equipment and we are now able to cater for many mothers" (KI 2) .
Human resource recruitment: A key informant also highlighted that critical health workers were recruited following the same intervention and this increased the capacity to conduct caesarean section at some of the health facilities. This health facility manager talked about the different cadres of health workers that had been recruited at the facility, he asserted: "A number of doctors, midwives and anaesthetist were recruited this has reduced the work load since we attend to many women daily and have been very few and working in shifts" (KI 4) .
Negative factors
Lack of accommodation for human resource: Lack of accommodation for critical staff involved in caesarean section service provision and absenteeism of staff at health facilities were some of the problems cited in maintaining adequate human resource capacity as noted by a key informant who said: "Lack of accommodation for critical staff is the biggest challenges...most of these facilities are in rural areas and health workers spend a lot of time travelling to the work place and are not available during night time to cater for mothers that may need the service" (KI 7) .
Inadequate medicines and supplies: Inadequate medicines and supplies such as anaesthesia, gloves, blood for transfusion, oxygen cylinders were mentioned to be one of the factors affecting provision of caesarean section services. This was raised by one of the health workers who stated: "Blood sometimes is not available in the facility. We had a mother that got APH(antepartum haemorrhage) so we had to send for blood from the blood bank at the regional referral by the time it got here it was already too late" (KI 1) . Several other health workers who participated in the study confirmed this view, as the following two quotes illustrate: "We haven't had oxygen cylinders for some days so haven't been able to carry out Caesarean Section in a while" (KI 3) . "Mothers sometimes have to buy gloves as well as IV fluids which is a big challenge since some mothers cannot afford and have to be referred"(KI 6) .
Misconceptions about caesarean section: Misconceptions about caesarean section delivery were reported to create fear among women leading to home deliveries and delays in seeking care. Some of the misconceptions reported by the key informants included disregard of caesarean section as mode of delivery, negative branding of women who have a caesarean section as being lazy. This is reflected in the two quotes below: "Some women do not know that caesarean section is a mode of delivery and they think failing to deliver normally is a crime" (KI 5) . "Women that deliver by caesarean section are branded lazy or unlucky by some of their peers and community members" (KI 3) .
We assessed factors associated with caesarean section delivery at health facilities in western Uganda and found that having a previous caesarean section delivery, ANC attendance for atleast four times were statistically associated with caesarean section delivery. Inadequate drugs and supplies, inadequate human resource provision, lack of accommodation for critical human resource, misconceptions about caesarean section among women also affected access and utilisation of the service. Infrastrcture improvements and human resource recruitment enhanced caesarean section delivery service provision. Previous caesarean section was statistically significantly associated with current caesarean section delivery. This is similar to findings in other studies in developing countries that found a previous caesarean section to be a very significant predictor for progressive caesarean section deliveries [ 2 , 10 , 22 ]. Women who have had one birth by caesarean section may be given a trial of labour that is carefully monitored. However due to poor monitoring of trial of labour especially at lower level facilities women who had a previous caesarean section subsequently give birth the same way. The risk of uterine rupture and preference for caesarean section among urban women of a high socio-economic status also lead to subsquent caesarean sections [ 4 , 8 , 17 ]. Women that had attended more than four antenatal care consultations were more likely to have a caesarean section delivery than those that attended less than four consultations. This finding is similar to what was observed in earlier studies conducted at health facilities in Brazil and Cameroon respectively that found high numbers of prenatal consultations among women that delivered by caesarean section [ 4 , 23 ]. Antenatal care is the time when a set of practices and attitudes seeking to promote healthy delivery are applied. Women that have many ANC consultations have been identified as “high-risk” pregnant women so are in constant consultation with the doctors to monitor and prevent adverse outcomes. Prenatal consultations provide an opportunity to assess high-risk pregnant women and to provide counselling related to the mode of delivery [ 24 - 26 ]. However, during this period, health providers can potentially influence decision to implement caesarean section due to the cost benefits of the procedure and fear of legal liabilities in cases of perceived obstetric risks to mother or baby that may result during vaginal delivery. This can lead to unnecessary caesarean sections that are a burden to health systems that work with limited budgets [ 1 , 4 ].
Maternal age was not found to be significantly associated with caesarean section. This is in contrast to other studies that showed that increase in maternal age was associated with caesarean section delivery due to increased co-morbidities such as hypertensive disorders, diabetes and heart disease among others that increase the risk of caesarean section [ 4 , 22 , 23 ]. This might have been due to the relatively younger age distribution in this study where slightly more than half of the respondents were aged 15 to 24 years with fewer women aged above 35 year. There was inadequate human resource capacity to provide caesarean section service mainly at health centre IV level with only two doctors available, when one was sick or on a leave of absence from work the other was left with a heavy workload. Absenteeism of health workers and lack of accommodation for critical staff were the main factors contributing to the inadequate human resource. Studies carried out in African countries have reported human resource crisis characterised by low motivation, absenteeism and shortages at all levels [ 11 - 13 ]. The Saving Mothers Giving Life intervention, which was a current intervention in the district made improvements in infrastructure development, transport referral and human resource improvements however further improvements and sustainability of such interventions are required for long term impacts on health services provision specifically caesarean section in the area [ 19 , 27 ]. The findings from our study also showed inadequate medicines and supplies for caesarean section service provision especially at lower level health facilities. This was due to supply chain challenges such as poor forecasting, distribution and misuse of drugs and supplies. Other studies also found that poor distribution and misuse of drugs by health workers in developing countries contributed to stock-outs at health facilities [ 14 - 16 ]. Misconceptions about caesarean section delivery among women in the community affected utilization of the service. Some women thought that failure to deliver normally would make one less of a woman and such women were branded as lazy. Such misconceptions create fear among these women, delay seeking care and subsequently led to low utilization of caesarean section services. This is similar to findings in studies conducted in Western Uganda and Nigeria that found low utilization of maternal services due to traditional beliefs and poor perceptions in the community [ 17 , 18 ]. Our study was conducted at health facilities thus the case group and control group may not have been very representative of the general population because not all women give birth from health facilities in the area. This may have compromised external validity however all possible measures were undertaken to maintain the internal validity of the study. We recommend that further studies should be carried out in the community.
Health system inadequacies such as drugs and supplies shortages, human resource inadequacies and misconceptions about caesarean section were the main hindrances to access and utilisation of caesarean section services. Previous caesarean section delivery and attendance of at least four antenatal care sessions were the major predictors for caesarean section delivery. Further investments in providing adequate health workers, ensuring adequate provision of drugs and supplies for caesarean section service are required. In addition, measures to improve the productivity of health workers at health facilities should be put in place such as monitoring and supervision by the health authorities. Women should be encouraged to attend at least four prenatal care visits so that women with predictive factors for a caesarean section can be identified, given counselling to facilitate acceptance of caesarean section and ensure delivery in facilities that can provide caesarean sections or that can give an immediate referral.
What is known about this topic
- Medical indications for caesarean section such as obstructed labour, cephalopelvic disproportion, malpresentation, fetal conditions among others have widely been studied and are known on this topic.
What this study adds
- The study assesses individual and health service factors that affect access and utilisation of caesarean section.
Acknowledgments
The authors thank the study respondents for accepting to participate in the study. Special acknowledgement also goes to Kabarole District Health Team for its support in conducting the study.
Competing interests
The authors declare no competing interest.
Authors’ contributions
Jacinta Dusabe Participated in the designing the study and obtaining ethical approval. She supervised field data collection as well as data analysis. She led in writing of drafts of the manuscript and revised the paper for substantial intellectual content. Joseph Akuze and Elizabeth Ekirapa: participated in designing the study, data analysis and revision of draft manuscript for substantial intellectual content. Benon Kwesiga, Angela Nakanwagi Kisakye and Peter Nsubuga: critically reviewed draft manuscript for substantial intellectual content. All the authors have read and agreed to the final manuscript.

IMAGES
VIDEO
COMMENTS
Cesarean section is a fetal delivery through an open abdominal incision (laparotomy) and an incision in the uterus (hysterotomy). ... Di Iorio R. Cesarean section in the absence of labor and risk of respiratory complications in newborns: a case-control study. J Matern Fetal Neonatal Med. 2019 Apr; 32 (7):1160-1166.
Routine myomectomy at the time of cesarean section has been condemned in the past due to fear of uncontrolled hemorrhage and peripartum hysterectomy. It is still a topic of debate worldwide. However, in recent years, many case studies of cesarean myomectomy have been published validating its safety without any significant complications. We describe the case of a 27-year-old gravida 2 para ...
Abstract. Caesarean section as a means of delivering babies has been around for centuries with numerous references to the procedure appearing in ancient writings (Simm & Matthew 2008). It is now the most common major surgical intervention carried out on women in the world, with between 23% and 30% of deliveries in the UK performed by caesarean ...
A retrospective case control study was undertaken at Monmouth Medical Center in New Jersey from January 1, 2008 to December 31, 2018 inclusive. ... The indications for a repeat cesarean section in the TOLA2C group were arrest of dilation (n = 12), nonreassuring fetal heart tracing (n = 11), arrest of descent (n = 1), uterine rupture (n = 1).
Risk factors for surgical site infection following cesarean section in a Brazilian Women's Hospital: A case-control study. Brazilian J Infect Dis [Internet]. ... Johns N, Duggal S, Hewston R, Gale N. Improving the care pathway for women who request Caesarean section: An experience-based co-design study. BMC pregnancy childbirth [internet ...
are performed by cesarean section. CASE STUDY: REPEAT CESAREAN SECTION The patient is a 26-year-old female, gravida 4, para 3 with 41 weeks of high-risk pregnancy, and late prenatal care. According to the patient's medical chart, she has reported abdominal pain, edema in the feet and legs, and no contraception use prior to conception.
Metaanalyses, systematic reviews, randomized controlled studies, nonrandomized controlled studies, reviews, and case series were considered for each individual topic. ... Post-operative urinary tract infection and wound infection in women undergoing cesarean section: a comparison of two study periods in 1985 and 1987. J Hosp Infect. 1989; 13: ...
This rate is all the more surprising when one considers that caesarean section accounted for just 5.3% of UK births in 1973 (Kitzinger 1998). This rising rate has many implications for both clinical practice and the NHS. An Audit Commission report (1997) suggested that each 1% rise in the caesarean section rate would cost the NHS five million ...
These indicators show evidence that support the improvements made in the pilot study for the cesarean section ERAS patients and will be the subject of the next phase of work. The overall LOS for the C-section population with improved bundle compliance decreased from 3.0 days in FY 2017 to 2.30 days in FY 2019 and prior to COVID-19 in Q1 2020.
A case study of caesarean sections in referred cases ... (23.8%).Conclusions: Cesarean section is one of the quickest and most efficient method in the delivery of the baby and thus should in ...
Vaginal births have lower hospital costs than cesarean sections in low-risk pregnancies. Although C-section has been related to worse results [], this study shows which kind of results are better in vaginal delivery, and includes only low risk pregnancies, in which C-sections should be less frequent.The mothers' results are better in vaginal birth considering ICU admission rates.
Caesarean section rates have increased worldwide in recent decades. Caesarean section is an essential maternal healthcare service. However, it has both maternal and neonatal adverse outcomes. Therefore this systematic review and meta-analysis aimed to estimate the prevalence, indication, and outcomes of caesarean section in Ethiopia. Twenty three cross-sectional studies with a total population ...
The following case study highlights Oklahoma Medicaid's innovative and effective Cesarean Section Quality Initiative. This case study is a companion to two other case studies of Tennessee and Wiscon-sin and a 50-state environmental scan of state Medicaid performance measures, improvement projects and incentives promoting women's health ...
Elective Caesarean Section: A Case Study. Zoe Edwards, K. McColgan. Published in Journal of Perioperative… 1 February 2011. Medicine. TLDR. It is suggested that each 1% rise in the caesarean section rate would cost the NHS five million pounds per year and has clinical implications, with some studies suggesting that maternal mortality is three ...
1 Nursing College, Guangxi Medical University, Nanning, China; 2 Department of Neonatology, The First Affiliated Hospital of Guangxi Medical University, Nanning, China; Background: The association of caesarean section (CS) for postpartum depression (PPD) remains controversial. This study aims to explore the relationship between CS and the risk of PPD, in order to provide a basis for preventing ...
A retrospective case-control study, comparing 40 women with fibroids who underwent cesarean myomectomy with 80 women with fibroids forming the control group who underwent cesarean section alone, reported no significant difference in the incidence of hemorrhage between the two groups (12.5% and 11.3%, respectively) . Similar findings were ...
Introduction: Despite known benefits of breastfeeding, including prevention against infections for infants, in the presence of numerous barriers, less than half of infants in high-income countries breastfeed for 6 months. One potential barrier to breastfeeding is birth by cesarean section (C-Section), which can invoke long-term difficulties. However, our structured literature review found that ...
Caesarean section: a case study. Caesarean section: a case study N Z Nurs J. 1988 Sep;81(9):31-2. Author G Erasmus. PMID: 3217062 No abstract available. Publication types Case Reports MeSH terms Adolescent Cesarean Section / nursing* Female Humans Pregnancy ...
A troubling new report from Louisiana shows how the state's abortion ban from 2022 is forcing doctors to delay or withhold medical care in ways that make pregnancy more dangerous.
Study design and setting: We conducted a case-control study at health facilities in Kabarole district, Western Uganda, during a 3 month period from March through May 2016. Caesarean section services in the district are offered only at the regional referral hospital and at two health centres in the public sector.