- Open access
- Published: 18 September 2021

Implementation of active learning methods by nurse educators in undergraduate nursing students’ programs – a group interview
- Sanela Pivač 1 ,
- Brigita Skela-Savič 1 ,
- Duška Jović 2 ,
- Mediha Avdić 3 &
- Sedina Kalender-Smajlović 1
BMC Nursing volume 20 , Article number: 173 ( 2021 ) Cite this article
19k Accesses
6 Citations
1 Altmetric
Metrics details
Modern and active learning methods form an important part in the education of Nursing students. They encourage the development of communication and critical thinking skills, and ensure the safe health care of patients. Our aim was to obtain naturalistic data from nurse educators regarding want the use and effects of implementing active learning methods (Peyton’s Four-Step Approach, Mind Mapping, Debriefing and Objective Structured Clinical Examination methods) in the study process of students of Nursing after a completed education module, Clinical skills of mentors , as part of the Strengthening Nursing in Bosnia and Herzegovina Project. We wish to learn about the perception of nurse educators regarding the use of active learning methods in the study process of Nursing in the future.
Qualitative research was conducted and a group interview technique was used for data collection. Beforehand, research participants were included in a two-day education module, Clinical skills of mentors , as part of the Strengthening Nursing in Bosnia and Herzegovina Project. Content analysis of the discussion transcriptions was conducted.
Fourteen nurse educators participated. Group interviews were conducted in September 2019. The obtained categories form four topics: (1) positive effect on the development of students’ communication skills (2) positive effect of learning methods on the development of students’ critical thinking skills (3) ensuring a safe learning environment (4) implementation of active learning methods.
Conclusions
The use of various active learning methods in simulation settings improves the Nursing students’ critical thinking and communication skills. Therefore, we believe that Peyton’s Four-Step Approach, Mind Mapping and Debriefing methods should be included as tools for effective student learning and as preparation for directly performing safe nursing interventions with a patient. Effective approaches to the assessment of Nursing students may ensure quality patient health care in accordance with the vision of the nursing profession.
Peer Review reports
Introduction
Education of nurses in Bosnia and Herzegovina (BiH) has been undergoing rapid development. In BiH, the emphasis of the health care system and the education of health professionals is mainly on curative care and medical services. This might limit the potential of the nursing staff to react to the population’s present and future health needs. To avoid the negative consequences of reduced competencies and practice, nurses developed a project that would strengthen nursing in BiH [ 1 ].
Several nursing-related challenges that currently have a negative effect on the nursing profession and which, therefore, hinder health outcomes in BiH, were identified in collaboration with major stakeholders in BiH, including faculties of nursing and other important organizations [ 2 ]. As stated by Francis and O’Brien [ 3 ], teaching clinical skills is an important part in educating students of Nursing in an increasingly more complex health care and social environment. As a method of teaching, skills-lab training is viewed as a key component of curricula in the majority of our faculties that offer health-related study programs as it enables a protected training environment where students are permitted to make mistakes and where they can practice their skills on mannequins before working on real patients [ 4 ].
In BiH, mentorship at faculties of Nursing is conducted by graduate nurses who are teaching assistants or senior teaching assistants rather than mentors, and are employed full-time or are outsourced. In BiH, there are no additional training options that would equip nurses to work as mentors, either full time or part time, so they only need to meet the general and specific criteria for an associate/teacher position [ 5 ]. That is why in 2017, the Strengthening Nursing in BiH Project developed a training program for BiH clinical skills mentors that comprised seven modules (34 h in total) and was focused on different aspects of adult education, and teaching tools and methods. In BiH, the faculties offering Nursing courses have been faced with challenges regarding the organization of additional training for clinical skills mentors. In order for mentors to be prepared for this role as best as they can, they use professional literature, the internet and engage in team meetings [ 6 ].
In order to improve nursing education, various teaching methods have been introduced to assist students in gaining knowledge, skills and attitudes that are relevant for nursing practice.
The implementation of active learning methods into the study process might result in students’ improved motivation for learning, encourage their critical thinking skills and independent learning [ 7 ]. Rather than continuing with employing traditional teacher-centered educational approaches, faculties should introduce an active student-centered learning environment since creating learning experiences that encourage reflection, knowledge building, problem-solving, inquiry, and critical thinking are highly significant [ 8 ]. Authors [ 9 , 10 ] state that active learning methods in nursing education are highly significant with an aim to eliminate passive listening and transition to assuming an active role in the educational process and obtain the ability to apply information from lectures in a meaningful way. The development of the pedagogical skills occurs according to the actual situation in the process of the nurse’s practical work [ 11 ].
The use of simulation-based learning contributes to the development of students’ sense of safety when they perform various tasks [ 12 ]. The skill laboratory functions as a transitional setting between a classroom and clinical venues [ 13 ].
Peyton’s Four-Step Approach is a learning method that comprises four steps and is highly effective in the learning process of nursing interventions. The first step is demonstration , in which the teacher demonstrates the intervention at their normal pace without giving any additional verbal explanations. The second step is deconstruction , in which the teacher performs the intervention by giving detailed descriptions of all the phases of the intervention. In the third step referred to as comprehension , the teacher performs the intervention according to the student’s instructions of each step of the intervention. In the final, fourth step called intervention , students perform the intervention by themselves without the help of the teacher [ 14 ]. In the research on the effectiveness of the method, the authors found that the Peyton’s Four-Step Approach method enables students’ active involvement in the process of learning about nursing intervention [ 15 ]. The process of self-explanation, which Peyton’s Four-Step Approach contains when a student is thinking aloud, enables an improved learning process and the development of critical thinking skills [ 16 ].
The Mind Mapping method is an excellent pedagogical tool used to help students achieve positive learning outcomes [ 17 ] that may be successfully implemented in the education process as it ensures a creative environment and is an effective tool for teachers, mentors, students and researchers [ 18 ]. The Mind Mapping method encourages students to obtain relevant information and develops critical thinking skills, which in turn, has positive effects on the provision of safe health care for patients [ 19 ]. There are several reasons why using the Mind Mapping method in learning and teaching is recommended. Firstly, there is no long text. Also, it enables learning through synthesizing, as well as clarification and better reorganization of ideas. Furthermore, it assists with revision, encourages visualization of the content that had been learnt before, enables cooperation via studying in groups, which has positive consequences for everybody involved, and finally, mind maps that are submitted to the group result in a better experience because more participants are involved, which produces more ideas and stimulates the use of critical thinking skills [ 20 , 21 , 22 ].
A guided discussion is also quite significant in teaching Nursing students as it enables very authentic simulations of reality since a mentor asks students to critically evaluate their knowledge and skills that they had demonstrated while performing the scenario. Despite much research conducted on educating with simulation, the guided discussion has not yet been sufficiently defined [ 23 ]. The use of scenarios with debriefing constitutes a strategy facilitating the teaching-learning process in the undergraduate nursing course [ 24 ].
The assessment of clinical skills is also highly significant in nursing education. Therefore, the Objective Structured Clinical Examination (OSCE) may be considered to be a sound assessment tool whose objective is the assessment of nursing students’ clinical competences in a safe and controlled environment, which enables simple assessment of the knowledge and performance of clinical skills that are important in nursing practice. Also, the assessment tool may serve to better prepare students for their profession [ 25 , 12 ].
A higher education teacher is one of the key factors for a nursing student to be successful in their studies [ 26 ], so teachers should be familiar with effective teaching methods [ 27 ]. A teacher’s primary task is to ensure a creative environment and a learning path that engages a student [ 28 ]. A suitable learning method may encourage nursing students to learn, improve students’ communication, and motivate and inform them about effective learning [ 29 ].
Aim of the study
After conducting the educational module Clinical skills of mentors as part of the Strengthening Nursing in BiH Project, our aim was to obtain naturalistic data from nurse educators regarding the use and effects of introducing active learning methods (Peyton’s Four-Step Approach, Mind Mapping, Debriefing and Objective Structured Clinical Examination methods) in the study process of Nursing students. Nurse educators in BiH have not yet developed knowledge in the field of active and contemporary learning methods or competencies to transition to modern teaching methods from more traditional ones. That is why we conducted the research to learn about the perception of nurse educators about the use of active learning methods in the study process of Nursing in the future.
Our research question was
What is the perception of nurse educators on the use and effects of active learning methods in nursing undergraduate study programs?
The qualitative descriptive study of a formal group interview was used [ 30 ]. The group interview was conducted in pre-existing “natural” groups of nursing educators in a region of BiH. Invited participants attended a two-day education module: Clinical skills of mentors as part of the Strengthening Nursing in BiH Project that was hosted by two higher education senior lecturers of Nursing from Slovenia, where higher education and clinical mentorship in Nursing is developed in accordance with international [ 31 , 32 ] and national guidelines for Nursing education [ 33 ].
A group interview allows group members to influence each other with their comments and experience, and to form an opinion regarding the issue currently discussed after reflecting on it as a group [ 34 ], which results in obtaining more information than with face-to-face interviews [ 35 ].
Setting and participants
The environment in which the research was conducted impacted the format of the group [ 27 ] that was invited to participate for research purposes. 14 nurse educators that are employed at the faculty (n = 6) and/or in a clinical setting (n = 8) participated in a group interview. 12 women and two men participated, the average age of the participants was 35.7 years (SD = 0.7), the average length of service was 15.1 years (SD = 11.1). One participant had completed doctoral studies, nine held master’s degrees in Nursing and four held bachelor degree in Nursing.
Semi-structured guiding questions that were being updated throughout the discussion were used in the group interview. The semi-structured interview contained eight basic questions:
What is your opinion regarding the significance of the qualifications of nurse educators to work with Nursing students?
What skills should nurse educators have in order to teach students of Nursing effectively?
How useful do you think the Peyton’s Four-Step Approach method is for teaching Nursing students?
What is your opinion on the usefulness of the OSCE stations as a method of assessing Nursing students?
How do you assess the usefulness of the Mind Mapping method in the learning process?
What is your attitude towards using and implementing the Debriefing method in the process?
Which presented method do you think is most suitable for teaching the students of Nursing?
What is your attitude towards the impact of the presented learning methods and assessment on the development of critical thinking skills of Nursing students?
The reliability of the research was ensured by considering the homogeneity of the group, an appropriate number of participants in the interview, by giving instructions before the start of the interview emphasizing that everyone has the possibility to participate in the discussion and by encouraging them with questions when guiding the group interview [ 36 ]. The reliability check was ensured by digitally recording the conversations in the group interview. We then transcribed the recording and checked that the transcription matched the audio recording. To increase the validity of data analysis, two researchers analyzed the data and ensured that the codes were unified. An independent analysis of two researchers decreases the possibility of partiality and increases the interpretative basis of the research. With the thematic analysis, we demonstrated that data analysis has been conducted in a precise, consistent, and exhaustive manner through recording, systematizing, and disclosing the methods of analysis with enough detail [ 37 ]. Also, we used traditional tools: colored pens, paper, and sticky notes for ensuring rigor [ 38 ]. Authors checked the participants to ensure relevant evaluation [ 39 ].
Data collection
The group interview took place in September 2019 at the end of the education module and was guided by a moderator and a semi-structured questionnaire. There was also an administrator who recorded the discussions. The research participants attended a two-day education module, Clinical skills of mentors , as part of the Strengthening BiH Project. The purpose of the module was to inform and educate nurse educators about active learning methods and assessment of students of Nursing: Mind Mapping, Debriefing, Peyton’s Four-Step Approach methodology and the OSCE stations. We presented the purpose of the research and topics before conducting the group interview. The average time of the group interview was 90 min. Discussions were recorded upon obtaining a written permission by the participants. To ensure anonymity we added randomly selected letters to the interviewers.
Data analysis
For qualitative data, the method of thematic content analysis was employed. All recordings were transcribed verbatim and the texts were read several times. After coding units were identified, coding was conducted and categories and key topics were defined. Each participant in the group interview was ascribed a corresponding code. The nominal identity of a transcription was lost while the traceability of content was ensured. Authors state that a thematic analysis is a widely used qualitative analytical method that offers an accessible and theoretically adjustable approach to the analysis of qualitative data [ 40 ].
Based on an analysis of the text, 47 codes were designed alongside 14 umbrella categories. The obtained categories fall into four final topics: (1) a positive effect on the development of students’ critical thinking skills (2) a positive effect of learning methods on the development of students’ critical thinking skills (3) providing a safe learning environment (4) implementation of active learning methods (Table 1 ).
Table 2 presents topics that are substantiated by representative quotes, their effects on the education of students of nursing, the obstacles and consequences that nurse educators have observed, and suggestions regarding improvements based on the presented topics and statements.
1. A positive effect on the development of students’ communication skills
Participants in the group interview believed that various active methods have a positive effect on the development of Nursing students’ communication skills, and on achieving professional competencies in communication. They emphasize the importance of feedback exchanged between a student and a nurse educator that should be given at a time when a student is still thinking about their work and there is still time to improve the process itself. They think that feedback has an impact on the active role of a student and on achievement of the set goals. The research participants believe that showing nursing interventions several times during the learning process has positive effects on students’ memorizing skills and results in less errors when providing health care to patients.
2. The effect of learning methods on the development of critical thinking
In their statements, the participants of the group interview most often stated that using various innovative methods in a simulation setting encourages critical thinking skills of nursing students, impacts the development of students’ self-confidence and motivates them to work and study. Active participation and critical thinking lead students to successful problem solving. Participants believe that teaching by means of actively solving problems results in students’ reflecting and encourages them to show and say what they know. The participants emphasize that using certain methods of learning also depends on external resources.
3. Ensuring a safe learning environment
The participants of the group interview all thought that methods such as the Peyton’s Four-Step Approach method, the OSCE stations and Debriefing contribute to a safe clinical environment since students revise their knowledge and skills several times in simulated conditions and in this way strengthen their knowledge. They believe that preparing students to perform safe nursing intervention is connected to safe and quality patient health care in a clinical setting.
4. Implementation of active learning methods
The nurse educators included in the research found the presented methods highly suitable for use in the education process of Nursing students, but emphasized that a suitable venue should be provided, and that teachers or clinical mentors should be suitably prepared. They think that nurse educators neither have enough pedagogical and andragogical experiences and skills, nor knowledge on active learning methods.
With qualitative research, we obtained the views and opinions of nurse educators from some nursing faculties and clinical settings in BiH on the effects of active learning methods on students of nursing. Participants in the group interview believed that various active methods have a positive effect on the development of Nursing students’ communication skills, and on achieving professional competencies in communication. They emphasized the importance of feedback exchanged between a student and a nurse educator. Other research [ 41 , 42 , 43 ] also emphasizes the importance of communication skills, giving feedback and providing quality in nursing care. In our study the participants of the conducted research thought that active learning methods contribute to a more effective learning of nursing interventions, provide an active approach to learning about nursing interventions and enable a more confident performance of nursing interventions in a clinical setting with a patient, and provide a safe environment either for the patient or for the student.
Participants believe that the use of innovative methods in a simulation environment encourages students’ critical thinking, motivation, development of self-confidence and problem-based learning. Christianson Krista [ 44 ] puts great importance on the connection between emotional intelligence and critical thinking in nursing education. A study [ 45 ] demonstrated that critical thinking education improves problem-solving skills. A good relationship between a nurse educator and a student brings positive results in students’ education and motivates them for work in a clinical setting [ 46 ]. In addition, a teacher’s professional knowledge and their organizational and communication skills also have an effect on successful learning [ 47 ]. Baksi et al. [ 48 ] researched the effects that clinical preparatory education provided before the first clinical experience had on anxiety.
The opinions of the participants regarding the Debriefing method mostly refer to the importance of feedback. In researching debriefing practices in interprofessional simulation with students from the socio-material perspective, the findings have shown how debriefing intertwines with, and is shaped by social and material relationships. Two patterns of enacting debriefing were identified. First, debriefing as an algorithm was enacted as a protocol-based, closed inquiry approach and secondly, laissez-faire debriefing was enacted as a collegial conversation with an open inquiry approach that has a loose structure [ 49 ].
Nursing educators believe that active pedagogical methods of learning might help students to optimize the development of their critical thinking skills. Therefore, we believe that Peyton’s Four-Step Approach method, Mind Mapping and Debriefing should be included as a tool for successful learning of students and preparation for working directly with patients, which has already been pointed out by previous research conducted by Janicas and Narchi [ 24 ] and Francis and O’Brien [ 3 ].
The use of Mind Mapping helps students to understand their thinking process, obtain basic knowledge that they will upgrade with in-depth professional knowledge [ 18 ], and encourages them to learn independently, be independent and think critically [ 50 ]. While students were developing mind maps, they were also exploring the critical thinking concept by reflecting on how they make patient care decisions in a clinical setting [ 22 ]. The reflection resulted in the students being better able to describe their critical thinking process and demonstrate the concept graphically. Mind Mapping may be used to illustrate the pathways that encourage reflection on patient care [ 51 ].
The participants of our research believe that the methods that were presented and demonstrated with examples contribute to a safe clinical setting. Clark [ 25 ] also emphasizes that one of the more challenging tasks of faculties of health sciences is to educate students with competencies that will secure safe and effective nursing and patient care. In the research, nurse educators believe that active methods are very useful in the education process of Nursing students, but emphasize that an appropriate location should be provided and that nurse educators should be suitably trained. They also believe that nurse educators must have pedagogical and andragogical knowledge, so that they can implement active and quality teaching methods in the pedagogical process. The challenges in the training of nursing educators are in the transition from traditional education to simulated learning environment [ 52 ]. Addressing nurse educator challenges and empowering them with the means, opportunity and skills to utilize student-centered teaching and learning strategies may contribute to the development of undergraduate student nurses’ clinical reasoning skills. Raising awareness of the challenges that nurse educators experience in implementing student-centered facilitation of learning can assist in developing the strategies to ensure nurse educators become more student-centered in their teaching [ 53 ].
Based on the conducted research, we propose an implementation of active teaching methods in the educational process of nursing students. Recommendations relate to regular monitoring of learning objectives, evaluation, updating teaching methods and the transition from traditional forms of learning to innovative forms.
Limitations and Strengths
Nurse educators that had previously been included in the training on active teaching methods in Nursing were included in the research. An advantage of the research is that we have obtained the views and opinions of nurse educators regarding the usefulness and effectiveness of the presented methods in the undergraduate study program of Nursing immediately after the conducted theoretical and practical training. An important limitation is also the local context of nursing development in BiH. The convenient sampling does not always allow us to select the best representatives related to the research question. It is likely that the members included in the group are more motivated for improvements in nursing education than other nurses at faculties and clinical settings.
Further research should focus on two areas. Firstly, it should be researched how often active learning methods are used in the education process and secondly, the opinions of students on how active learning methods impact the understanding and learning of nursing intervention could be obtained. The limitation of the research is the time span of the education on active teaching methods and the selection of guiding questions, since we are aware that the selection of questions might partially impact the answers given by the participants. It may be supposed that a different selection of guiding questions might result in different opinions of nurse educators.
The results of the qualitative research were used to present the meaning and understanding of implementing active learning methods in undergraduate study programs of Nursing. Based on the conducted research we believe that nurse educators lack pedagogical and andragogical knowledge as well as knowledge of active learning methods. The use of active learning methods by nurse educators improves communication skills and develop students’ critical thinking skills. The final results of implementing active learning methods are in the acquired learning outcomes, nursing interventions that are performed optimally, development of competent professionals, boosting self-confidence, improvement of communication and critical thinking skills, as well as the self-initiative and readiness to work with patients in a clinical setting. Cutting edge and active learning methods are important for ensuring the quality of a study process and in the teaching of students of Nursing. We also wish to encourage study programs where the presented learning methods would be used in the study process, so that students will become active participants who can use their knowledge in providing safe patient care as a result of these active methods of teaching and learning.
We considered ethical principles of ensuring the voluntary nature of participating in the research, protecting the identity of individuals, confidentiality, privacy and respecting the truth. Research was carried out in accordance with the Helsinki-Tokyo Declaration [ 54 ], the Code of Ethics for Nurses and Nurse Assistants of Slovenia [ 55 ] and the ethical guidelines of the Social Research Ethics Guidance [ 56 , 57 ]. We did not apply for the approval by the National Medical Ethics Committee as the National Medical Ethics Committee only makes decisions concerning experimental research and non-experimental research conducted on patients and vulnerable groups in the population (patients, the elderly, children, disabled adults). Nurse educators do not form part of vulnerable groups and our questions were not considered to belong to the group of vulnerable questions. The study is exempt from ethical approval according national legislation (European Commission: Accession countries - legislation related to research ethics Slovenia).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Bosnia and Herzegovina
Objective Structured Clinical Examination
Avdić M, Jović D, Dropić E, Van Malderen, Schwendimann R. Formal education of medical nurses in Bosnia and Herzegovina. Nursing Journal. 2014;1:25–27.
Google Scholar
Strengthening Nursing in Bosnia and Hercegovina Project, n. d. http://www.fondacijafami.org/Sestrinstvo_pdf_/Project%20Leaflet.pdf . Accessed 15 Jan 2020.
Francis G, O’Brien M. Teaching clinical skills in pre-registration nurse education: value and methods. Br J Nurs. 2019;28:452–6.
Article Google Scholar
Awad SA, Mohamed MHN. Effectiveness of Peyton’s Four-Step Approach on nursing students’ performance in skill-lab training. J Nurs Educ Pract. 2019;5:1–5.
Jović D, Avdić M, Katić-Vrdoljak I. Assessment of the needs for additional training for clinical skills mentors at the faculties with nursing studies in BiH. In: Pesjak K, Pivač S, editors. Inter-professional integration at different levels of healthcare: trends, needs and challenges. 11th International Scientific Conference, Bled, Slovenia, June 7th, 2018. Jesenice: Angela Boškin Faculty of Health Care; 2018. p. 83 – 8.
Jović D, Avdić M, Marković N, Katić-Vrdoljak I. Training scheme for clinical skills mentors in Bosnia and Herzegovina. In: Pesjak K, Mlakar S, editors. Responsibilities of health policy-makers and managers for the retention and development of nurses and other healthcare professionals – 2020: International year of the nurse and the midwife. 13th International Scientific Conference, Jesenice, Slovenia, September 24th, 2020. Jesenice: Angela Boškin Faculty of Health Care; 2020. p. 174-8.
Parikh ND. Effectiveness of teaching through mind mapping technique. Int J Indian Psychol. 2016;3:148–56.
Alexander BJ, Lindow LE, Schock MD. Measuring the impact of cooperative learning exercises on student perception of peerto - peer learning: a case study. J Physican Assist Educ. 2008;3:18–25.
Bristol T, Hagler D, McMillian-Bohler J, Wermers R, Hatch D, Oermann MH. Nurse educators’ use of lecture and active learning. Teach Learn Nurs. 2019;14:94–96.
Waldeck JN, Weimer M. Sound decision making about the lecture’s role in the college classroom. Commun Educ. 2017; doi: https://doi.org/10.1080/03634523.2016.1275721 .
Benner P, Sutphen M, Leonard V, Day L. Educating nurses: a call for radical transformation. San Francisco: Jossey-Bass; 2010.
Smrekar M, Ledinski Fičko S, Hošnjak AM, Ilić B. Use of the objective structured clinical examination in undergraduate nursing education. Croat Nurs J. 2017;1:91–102.
Hashim R, Qamar K, Khan MA, Rehman S. Role of skill laboratory training in medical education: students’ perspective. J Coll Physicians Surg Pak. 2016;3:195–8.
Nikendei C, Huber J, Stiepak J, Huhn D, Lauter J, Herzog W, et al. Modification of Peyton’s Four-Step Approach for small group teaching – a descriptive study. BMC Med Educ. 2014;14:1–8.
Ahmed FR, Morsi SR, Mostafa HM. Effect of Peyton’s Four Step Approach on skill acquisition, self-confidence and self - satisfaction among critical care nursing students. IOSR-JNHS. 2018;6:38–47.
Krauter M, Weyrich P, Schultz JH, Buss SJ, Nikendei C, Junger J, et al. Effects of Peyton’s Four-Step Approach on objective performance measures in technical skills training: a controlled trial. Teach Learn Med. 2011;3:244–50.
Kernan WD, Basch CH, Carodett V. Using mind mapping to indentify reserach topics: a llesson for teaching research methods. Pedagogy Health Promot. 2017; doi: https://doi.org/10.1177/2373379917719729 .
Buran A, Filyukov A. Mind mapping tehnique in language learning. Procedia Soc Behav Sci. 2015;206:215–8.
Noonan M. Mind maps: enhancing midwifery education. Nurse Educ Today. 2013;8:847–52.
D’Antoni AV, Zipp GP, Olson VG, Cahill TF. Does the mind map learning strategy facilitate information retrieval and critical thinking in medical students? BMC Med Educ. 2010; doi: https://doi.org/10.1186/1472-6920-10-61 .
Article PubMed PubMed Central Google Scholar
Vilela VV, Pereira Barbosa LC, Miranda Vilela AL, Santos Neto LL. The use of mind maps as support in medical education. J Contemp Med Edu. 2013;4:199–206.
Rosciano A. The effectiveness of mind mapping as an active learning strategy among associate degree nursing students. Teach Learn Nurs. 2015;2:93–9.
Karnjuš I, Križmarić M, Zazula D. Importance of debriefing in high-fidelity simulations. Slov Med J. 2014;3:246–54.
Vieira Janicas RCS, Zanon Narchi N. Evaluation of nursing students’ learning using realistic scenarios with and without debriefing. Rev Lat Am Enfermagem. 2019;27:e3187.
Clark CA. Evaluating nurse practitioner students through objective structured clinical examination. Nurs Educ Perspect. 2015;1:53–4.
Hermansyah D, Witansa R. Influence of use of mind mapping method by teachers on teaching preparation in basic school in subject of materials teaching eyes lesson science natural science (IPA). Journal Elementary Educ. 2017;1:37–52.
Lloyd D, Boyd B, Den Exter K. Mind mapping as an interactive tool for engaging complex geographical issuess. New Zealand Geographer Society. 2010; doi: https://doi.org/10.1111/j.1745-7939.2010.01185.x .
Zipp GP, Maher C, D’Antoni AV. Mind mapping: teaching and learning strategy for physical therapy curricula. J Phys Ther Educ. 2015;1:43–8.
Luo J. Teaching mode of thinking development learning based on mind mapping in the course of health fitness education. iJET. 2019;8:192–205.
Green J, Thorogood N. Qualitative methods for health research. London, New Delhi: Sage Publications; 2004.
European Union. Directive 2005/36/EC of the European Parliament and of the Council. 2005. http://eur-lex.europa.eu/LexUriServ/LexUriServ.do? uri = OJ:L:2005:255:0022:0142:en:PDF. Accessed 17 Jul 2013.
European Union. Directive 2013/55/EU of the European Parlament of the Council. 2013. https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ: L:2013:354:0132:0170:en:PDF. Accessed 9 Jan 2016.
Skela-Savič B. Smernice za izobraževanje v zdravstveni negi na študijskem programu prve stopnje Zdravstvene nege (VS). Obzor Zdrav Neg. 2015;4:320–33.
Clarke A. Focus group interviews in health-care research. Prof Nurs. 1999;14:395–7.
CAS Google Scholar
Bolderston A. Conducting a research interview. J Med Imaging Radiat Sci. 2012;43:66–76.
Polgar S, Thomas SA. Introduction to research in the health sciences. 4th ed. Oxford: Churchill Livingstone: 2000.
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16:1–13.
Maher C, Hadfield M, Hutchings M, de Eyto A. Ensuring rigor in qualitative data analysis: a design research approach to coding combining NVivo with traditional material methods. Int J Qual Methods. 2018; doi: https://doi.org/10.1177/1609406918786362 .
Guba EG, Lincoln YS. Effective evaluation: improving the usefulness of evaluation results through responsive and naturalistic approaches. San Francisco: Jossey-Bass; 1981.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Hardavella G, Aamli-Gaagnat A, Saad N, Rousalova I, Sreter KB. How to give and receive feedback effectively. Breathe. 2017; doi: https://doi.org/10.1183/20734735.009917 .
Ratna H. The importance of effective communication in healthcare practice. Harvard Public Health Review. 2019;23.
Bodys-Cupak I, Łatka J, Ziarko E, Majda A, Zalewska-Puchała J. Medical simulation with simulated patients in the education of Polish nursing students - pilot study. Polish Nurs. 2020;3:166–73.
Christianson KL. Emotional intelligence and critical thinking in nursing students: integrative review of literature. Nurse Educ. 2020;6:E62-E65.
Kanbay Y, Okanlı A. The effect of critical thinking education on nursing students’ problem-solving skills. Contemp Nurse. 2017;3:313–21.
Haakma I, Janssen M, Minnaert A. Understanding the relationship between teacher behavior and motivation in students with acquired deafblindness. Am Ann Deaf. 2016;161:314–26.
Al Naqbi S. The use of mind mapping to develop writing skills in UAE schools. Education, Business and Society: Contemporary Middle Eastern Issues. 2011;2:120–33.
Baksi A, Gumus F, Zengin L. Effectiveness of the preparatory clinical education on nursing students anxiety: a randomized controlled trial. Int J Caring Sci. 2017;2:1003–12.
Nyström S, Dahlberg J, Edelbring S, Hult H, Dahlgren MA. Debriefing practices in interprofessional simulation with students: a sociomaterial perspective. BMC Med Educ. 2016; doi: https://doi.org/10.1186/s12909-016-0666-5 .
Kalyanasundaram M, Abraham SB, Ramachandran D, Jayaseelan JB, Singh Z, Purty AJ. Effectiveness of mind mapping technique in information retrieval among medical college students in Puducherry – apilot study. Indian J Community Med. 2017;19:19–23.
Picton C. Mind maps: reflecting on nature. Emerg Nurse. 2009; doi: https://doi.org/10.7748/en.17.2.3.s1 .
Article PubMed Google Scholar
Lillekroken D. A privilege but also a challenge.“ Nurse educators’ perceptions about teaching fundamental care in a simulated learning environment: A qualitative study. J Clin Nurs. 2020;11/12: 2011–22.
van Wyngaarden A, Leech R, Coetzee I. Challenges nurse educators experience with development of student nurses’ clinical reasoning skills. Nurse Educ Pract. 2019; doi: https://doi.org/10.1016/j.nepr.2019.102623 .
World Medical Association. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ 2013. Accessed 12 Feb 2020.
Kodeks etike v zdravstveni negi in oskrbi Slovenije. 2014. http://www.kme-nmec.si/files/2018/03/Kodeks-etike-v-zdravstveni-negi-in-oskrbi-Slovenije-marec-2014.pdf . Accessed 12 Feb 2020.
Social Resarch Association Research Ethics Guidance. 2003. ethical guidelines 2003.pdf (the-sra.org.uk). Accessed 12 May 2019.
Social Resarch Association Research Ethics Guidance. 2021. https://the-sra.org.uk/common/Uploaded%20files/Resources/SRA%20Research%20Ethics%20guidance%202021.pdf . Accessed 14 Jun 2021.
Download references
Acknowledgements
We would like to thank the Strengthening Nursing in BiH Project for inviting us to participate in the provision of training as a part of the education module: Clinical skills of mentors that enabled us to conduct the research among the training participants after completing the training. We would also like to thank all the participants of the research, who shared their opinions and views about the presented issue.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Angela Boškin Faculty of Health Care, Spodnji Plavž 3, SI-4270, Jesenice, Slovenia
Sanela Pivač, Brigita Skela-Savič & Sedina Kalender-Smajlović
Faculty of Medicine, Department of Health Care, University of Banja Luka, Banja Luka, Bosnia and Herzegovina
Duška Jović
Public Institution Health Centre of Sarajevo Canton, Sarajevo, Bosnia and Herzegovina
Mediha Avdić
You can also search for this author in PubMed Google Scholar
Contributions
SP contributed to the conception and design of the study, definition of sample, theoretical introduction and discussion, acquisition of data, analysis and interpretation of data. BSS contributed to the design of the study, theoretical introduction, methods, final reading of article. DJ contributed to the theoretical introduction and discussion and acquisition of data. MA contributed to the theoretical introduction and discussion and acquisition of data. SKS contributed to the theoretical introduction, analysis and interpretation of data discussion and conclusions. All authors drafted the manuscript and approved of the final version of the manuscript.
Corresponding author
Correspondence to Sanela Pivač .
Ethics declarations
Ethics approval and consent to participate.
In order to conduct the research, we received a written consent from all the research participants. We ensured the anonymity of all the research participants. Informed consent was obtained. The participants received information about different aspects of the study; their rights on voluntary participation and withdrawal from the study at any time as well as their privacy and confidentiality rights were explained to them. Permission to conduct the study was obtained from the Senate Committee for Science, Research and Development at the Angela Boškin Faculty of Health Care in August 2019. We obtained the consent from the Fami Foundation for improving Health Care and Social Welfare.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pivač, S., Skela-Savič, B., Jović, D. et al. Implementation of active learning methods by nurse educators in undergraduate nursing students’ programs – a group interview. BMC Nurs 20 , 173 (2021). https://doi.org/10.1186/s12912-021-00688-y
Download citation
Received : 27 May 2021
Accepted : 28 August 2021
Published : 18 September 2021
DOI : https://doi.org/10.1186/s12912-021-00688-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nursing education
- Teaching tools
- Critical thinking
- Communication skills
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 16 March 2024
Clinical virtual simulation: predictors of user acceptance in nursing education
- José Miguel Padilha 2 nAff1 ,
- Patrício Costa 3 , 4 , 5 ,
- Paulino Sousa 6 &
- Ana Ferreira 7
BMC Medical Education volume 24 , Article number: 299 ( 2024 ) Cite this article
27 Accesses
Metrics details
Using virtual patients integrated in simulators expands students’ training opportunities in healthcare. However, little is known about the usability perceived by students and the factors/determinants that predict the acceptance and use of clinical virtual simulation in nursing education.
To identify the factors/determinants that predict the acceptance and use of clinical virtual simulation in learning in nursing education.
Observational, cross-sectional, analytical study of the use of clinical virtual simulation in nursing to answer the research question: What factors/determinants predict the acceptance and use of a clinical virtual simulator in nursing education? We used a non-probabilistic sampling, more specifically a convenience sample of nursing degree students. The data were collected through a questionnaire adapted from the Technology Acceptance Model 3. In technology and education, the Technology Acceptance Model is a theoretical model that predicts the acceptance of the use of technology by users.
The sample comprised 619 nursing students, who revealed mean values of perceived usefulness (M = 5.34; SD = 1.19), ease of use (M = 4.74; SD = 1.07), and intention to use the CVS (M = 5.21; SD = 1.18), in a Likert scale of seven points (1—the worst and 7 the best possible opinion).
This study validated the use of Technology Acceptance Model 3 adapted and tested the related hypotheses, showing that the model explains 62% of perceived utility, 32% of ease of use, and 54% of intention to use the clinical virtual simulation in nursing by nursing students. The adequacy of the model was tested by analysis of the direct effects of the relationships between the internal constructs (PU-BI, β = 0.11, p = 0.012; PEOU-BI, β = -0.11, p = 0.002) and the direct relations between some of the constructs internal to the Technology Acceptance Model 3 and the external determinants Relevance for learning and Enjoyability.
In the proposed model, the external constructs that best predicted perceived usefulness, ease of use, and behaviour intention to use the clinical virtual simulation in nursing were Relevance for learning and Enjoyability.
Conclusions
These study results allowed us to identify relevance for learning and enjoyability as the main factors/determinants that predict the acceptance and use of clinical virtual simulation in learning in nursing.
Peer Review reports
Introduction
The rapid transformation of society in recent decades and the technical and scientific advancements in health sciences continually challenge higher education institutions (HEIs) to innovate, develop, and implement new pedagogical methodologies that guarantee up-to-date and quality training. Translating knowledge into clinical practice has become one of the main challenges of the first decades of the twenty-first century in research and higher education in health [ 1 , 2 ]. The higher education institutions have been systematically confronted with the difficulty of teaching central and structuring concepts of clinical practice and difficulty in translating these concepts into clinical practice [ 1 , 2 ]. Since the 1950s, multiple pedagogical strategies have been developed and implemented, such as Problem-Based Learning. These strategies intend to help students develop cognitive, instrumental, and attitudinal skills (Knowledge, Skills, Attitudes), among others, as structuring elements to ensure the quality and safety of their clinical practice. Quality and safety in clinical practice are associated with intrinsic and extrinsic factors for healthcare professionals. Of the intrinsic factors, clinical decision-making skills stand out. The development of clinical decision-making skills in healthcare students is one of the biggest challenges posed to higher education institutions teachers [ 3 ]. This becomes more evident in pre-graduate training with students without clinical experience. In addition, from a student's point of view, this is also one of the main challenges faced. Learning in the healthcare field implicates the need to ensure the quality and safety of the decision in each action, usually linked to fear of making mistakes, causing harm to the patient and, consequently, likely to negatively impact students’ mental health [ 4 , 5 , 6 , 7 ]. Thus, it is crucial to develop, implement and evaluate strategies that enable or recreate clinical environments and clinical decision scenarios before tutored or autonomous clinical practice. These environments must recreate spaces of high realism and fidelity creating friendly learning environments and recreating emotionally safe but simultaneously challenging spaces where students can build their learning [ 8 ].
The educational strategies traditionally used in health have almost reached their highest potential, thus stimulating innovation through new andragogical strategies that support the interaction of those involved in learning in enhancing active learning and capturing the intrinsic motivation of students, directing them to the translation of knowledge, enabling more meaningful learning, and leading to greater perception of effectiveness and less likelihood of clinical error [ 3 , 8 ].
In the last decades, simulation in health has emerged as a pedagogical strategy whose evidence demonstrates improved knowledge retention, instrumental, relational and communication skills, leadership and teamwork skills, and the transference of competencies [ 9 , 10 , 11 ].
- Clinical virtual simulation
Currently, the technological development in information and communication technologies allows to recreate patients and clinical conditions in virtual learning environments. These virtual patients are computer programs that simulate real-life clinical scenarios in which students act as health professionals, collecting the clinical history, performing the physical examination, defining the diagnosis, the intervention to be implemented, and evaluating the outcome of the clinical decision. Virtual simulation is defined as a type of simulation that places the student at the centre of decision-making, motor and/or communication skills [ 12 ].
The use of virtual patients in a virtual healthcare environment to train clinical reasoning and/or clinical decision-making skills has been defined as clinical virtual simulation (CVS) [ 13 , 14 ]. Using virtual patients in education effectively improves knowledge, critical thinking, clinical reasoning, instrumental skills, self-efficacy perception, learning satisfaction, interaction and feedback, teamwork, learning experience, and realism of simulation spaces, making them emotionally safer [ 13 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 ].
The increased use of clinical virtual simulation in recent years in health education was boosted during and after the COVID-19 pandemic. Despite the recognition achieved during these pandemic years, little is known about the factors that influence the acceptance by students of the use of clinical virtual simulation.
In 2016, the Nursing School of Porto began developing clinical virtual scenarios in Nursing to be integrated into the clinical virtual simulator Body Interact® (BY).
The use of clinical virtual simulation in the Nursing Degree as an andragogical strategy began in 2018–2019. Since then, studies have been conducted on usability [ 13 , 25 ], knowledge retention, satisfaction and learning perception [ 14 ], the impact on learning in small groups, and the perception of curricular integration [ 26 ].
However, further investigation is needed regarding the factors that promote the adoption and use of clinical virtual simulation by students. The use of clinical virtual simulation as an integrated pedagogical strategy in a health degree implies the reorganization of the curricular plans and the introduction of andragogical strategies directed to enhancing active learning and capturing the intrinsic motivation of the student to learn [ 8 ].
The technology acceptance model
In technology and education, the Technology Acceptance Model (TAM) is a theoretical model that predicts the acceptance of the use of technology by users [ 27 ]. This model was developed by Davis F.D. (1989) [ 28 ], to which were added the determinants of perceived utility by Davis & Venkatesh (2000) [ 29 ] and the determinants of ease of use by Venkatesh V. (2000) [ 30 ]. More recently, Venkatesh V. & Bala H. (2008) developed an integrated Technology Acceptance Model 3 (TAM3) including a structure of the individual determinants for the adoption and use of technology.
Based on the TAM3 [ 31 ], this study sought to identify the factors/determinants that predict the use of clinical virtual simulation in nursing education.
Methodology
An observational, cross-sectional, analytical study of the use of clinical virtual simulation was carried out to answer the research question: What factors/determinants predict the acceptance and use of a clinical virtual simulator in nursing education? (Table 1 ).
Selection of participants
All students of the 2nd, 3rd, and 4th year of the Nursing Degree in the Nursing School of Porto (ESEP) ( n = 870) were invited to participate in this study.
Considering all items related to TAM, with a count of 62 items, and applying the rule of thumb suggested by Nunnally (1978) [ 32 ] of 10 cases per variable, the recommended sample size would be 620 participants.
Following a non-probabilistic sampling methodology, a convenience sample of nursing students was selected, who voluntarily agreed to participate, and following the inclusion/exclusion criteria:
Inclusion criteria: ESEP degree students who completed attendance, with or without success, of the curricular unit Body Responses to Disease 1 (RCD 1) in the academic years 2019–2020, 2020–2021, and 2021–2022.
Exclusion criteria: ESEP degree students who have not attended the curricular unit Body Responses to Disease 1 in the academic years 2019–2020, 2020–2021, and 2021–2022, and students who obtained accreditation to the curricular unit.
In our study, the actual sample size is n = 619 participants. It's important to note that we do not conduct a unified analysis for all 62 items. Therefore, our sample size is similar to the calculated requirement, providing a robust foundation for the statistical analyses employed in our study.
Ethical considerations
The ESEP’s ethics committee granted authorisation for the study 697/2022 and informed consent was obtained from all participants.
Data collection
Data were collected through a questionnaire adapted from the Technology Acceptance Model 3 [ 31 , 33 ].
The variables under study are defined in Tables 2 and 3 .
For the translation and validation into European Portuguese of the Technology Acceptance Model 3, authorization was granted from the authors and the following steps were carried out [ 33 , 34 ]:
Stage I – Initial translation
Translation 1 from English into Portuguese performed by a professional Portuguese native translator (without knowledge of the TAM3);
Two translations by Portuguese native speakers, one trained in the field of Computer Sciences (without knowledge of the TAM3) (Translation 2) and one healthcare professional with experience using the TAM3 and clinical virtual simulation (Translation 3), both proficient in English.
Stage II—Synthesis of translations Translation 1, 2 and 3
Production of the Translation final version 1 (Researcher, two native Portuguese speakers, one from the health area with experience in the use of clinical virtual simulation and the TAM3 and another from the area of Computer Sciences—different from the participants in stage I);
Stage III—Back-translation by two English native speakers (without medical background).
Stage IV—Analysis by an expert group with experience in the use of the TAM3 and virtual simulation in nursing education
Semantic equivalence (adapted to the clinical virtual simulation);
Ideological equivalence;
Experiential equity;
Conceptual equivalence.
Stage V—Pre-test of the pre-final version with a group of 10 students who were not included in the study sample.
Final version—The authors waived submission of the version for evaluation and approval.
Data were collected between May and July 2022.
Data analysis
In the initial phase, frequencies and descriptive statistics were extracted from all the collected variables. This approach allowed the analysis of the distribution of variables, evaluating the sensitivity of items (used to evaluate latent constructs) and detecting potential atypical values (outliers). Then, the Shapiro–Wilk test was used to assess the normality of the distribution of variables, and values of asymmetry and kurtosis were used to assess the degree of separation of variables from normal distribution. The main psychometric properties of the different dimensions of the TAM3 were studied. Different validity criteria (criterion and construct validity) were applied considering best practices [ 35 ] and the evaluation of their internal consistency. To evaluate the constructs internal to the TAM3 and external (individual determinants), exploratory factor analysis (EFA) was performed to define the factors associated with the constructs of the TAM3. Subsequently, confirmatory factor analysis (CFA) was employed to verify whether the items of each scale saturated the identified factors. Path analysis was used to determine the main predictors (and relevant interactions between predictors) of the intention to use clinical virtual simulation in learning, the main dependent variable to model. This analysis included other variables besides its immediate predictors, such as the perceived usefulness and perceived ease of use. Different mediation models were also developed to test whether some of the explored variables inhibited the relationship between the most relevant variables of the TAM3.
The data related to the global score variables of utilization (GS) and system utilization (SU) were extracted from the Learning Management System (LMS) of the clinical virtual simulation. The global score variable refers to the average overall evaluation obtained by the student in clinical virtual simulation utilization regarding his/her clinical decision-making skills, measured in percentage of success. The system utilization variable (SU) refers to the total number of clinical scenarios the student completed in the clinical virtual simulation.
Statistical analysis was performed using JASP, Jamovi, IBM SPSS Amos v.26, and IBM SPSS Statistics v. 26. The results are reported following the APA standards, presenting the magnitude measurements of the Cohen d effect (0.2 low; 0.5 medium, and 0.8 high) and considering of P < 0.05 as significant. In the confirmatory factor analysis, the criteria applied to evaluate the adjustment of the model were the χ2 value and its p-value, ideally nonsignificant, the CFI > 0.95, GFI > 0.90 and RMSEA > 0.03 and < 0.08 [ 36 ]. In the analysis of the convergent validity of the items internal to the TAM3, the reliability value of the construct (CR) > 0.8, the mean extracted variance (AVE) > 0.5 [ 36 ], and factor loads in inter-correlation items lower than the square root of the AVE for each construct were the adopted criteria [ 37 ].
A total of 619 Nursing students participated in this study, being 85.50% ( n = 531) female, 35.1% ( n = 218) 2nd-year students; 36.2% ( n = 225) 3rd-year students; and 28.7% ( n = 178) 4th-year students. Table 4 presents the descriptive statistics of the sample, and Table 5 the correlation matrix of age, course marks, number of completed scenarios and mean global evaluation score.
Analysis of the acceptance of the use of CVS by the TAM3
Descriptive analysis of the items, followed by the exploratory factor analysis (EFA), confirmatory factor analysis (CFA), and trajectories analysis, were performed sequentially to investigate the acceptance of the use of the CVS and to identify the factors that determine the acceptance and use of the clinical virtual simulation in nursing education, as presented below.
Descriptive analysis of the items of the TAM3
The descriptive results of the Technology Acceptance Model 3 items, organised according to the constructs internal to the TAM and the individual determinants (constructs external to the TAM).
Exploratory factor analysis of the TAM
After the descriptive analysis of the data, the internal constructs associated with the Technology Acceptance Model 3 (PU-perceived usefulness; PEOU-perceived ease of use and BI-Behaviour intention to use) were analysed. Firstly, the EFA, using the Axis Factoring Main method, the Oblimin rotation method and the Kaiser Normalization criterion (KMO = 0.894, and Bartlett’s sphericity test < 0.001) were applied to analyse whether the items presented adequate factor loadings in each construct of the Technology Acceptance Model 3. The EFA allowed to identify three factors associated with the internal constructs of the Technology Acceptance Model 3 that explain 74.6% of the total variance of the data and present an adequate internal consistency (Table 6 ).
Then, EFA was performed with the items of individual determinants of the TAM3 (e.g., CSE-Self-efficacy in the use of CVS; PEC-Perception of external control; CPLAY-Perceived playfulness in the use of CVS; CANX-Anxiety with the use of CVS; ENJ-Enjoyability associated with the use of CVS) to analyse whether the items revealed adequate factor loadings in each individual determinants of the TAM3. In the EFA, the principal axis factoring method was used with the Oblimin rotation, and the Kaiser Normalization criterion for factor extraction. To analyse the adequacy of the data to perform the EFA, the Kaiser–Meyer–Olkin test (KMO) was performed considering a value greater than 0.8 as meritorious [ 38 ] and the Bartlett’s Sphericity test p < 0.05 to test the relationship between the variables (KMO = 0.879; Bartlett’s sphericity test < 0.001). The EFA allowed to identify ten factors that explained 59.4% of the total variance of the data. However, items OUT_2_TAM34; CANX_1_TAM13; CPLAY_4_TAM47; PEC_4_TAM12; SN_3_TAM22; SN_4_TAM23; CPLAY_4_TAM47; PEC_4_TAM47; PEC_4_TAM12; SN_TAM23; SN_4_TAM3; SN_TA3; SN_2_TA3; SN_TAM3; SN_TAM3; SN_TAM3; SN_TAM3; SN_TAM3; SN_TAM3; SN_TAM33; SN_2_TAM3; SN_TAM3; SN_TAM3; SN_TAM3; SN_TAM_TAM3; SN_TAM3; SN_TAM33; SN_TAM3; SN_TAM3 presented factor loadings < 0.3 [ 36 ] or cross factor loadings in more than one factor, so they were excluded from the analysis. We performed a second EFA excluding the problem items described (KMO = 0.867; Bartlett’s sphericity test < 0.001). This analysis allowed to identify eight factors that explain 68.64% of the variance of the data. However, we verified that items PEC_2_TAM10, PEC_3_TAM11, and PEC_1_TAM9 had factor loadings < 0.3 or cross-factor loadings in more than one factor, so they were excluded from the analysis. Excluding these items, we performed a new EFA (KMO = 0.856; Bartlett’s Sphericity test < 0.001) that identified 7 factors, explaining 63.1% of the total variance of the data and presenting adequate internal consistency (Table 7 ).
Confirmatory factor analysis of the TAM
Once the factorial structure of the Technology Acceptance Model 3 was defined for this study, a confirmatory factor analysis (CFA) was performed to validate the constructs internal to the Technology Acceptance Model 3 (Perceived usefulness, Perceived ease of use, and Behaviour intention to use), although ideally, this analysis requires a new sample. The results revealed acceptable adequacy of the model (Fig. 1 ) [(χ2(41) = 178, P < 0.001, CFI = 0.976, PCFI = 0.727, GFI = 0.948; PGFI = 0.589, RMSEA = 0.075; p (rmsea 0.05) < 0.001)]. Table 8 presents the results of the construct’s validity.
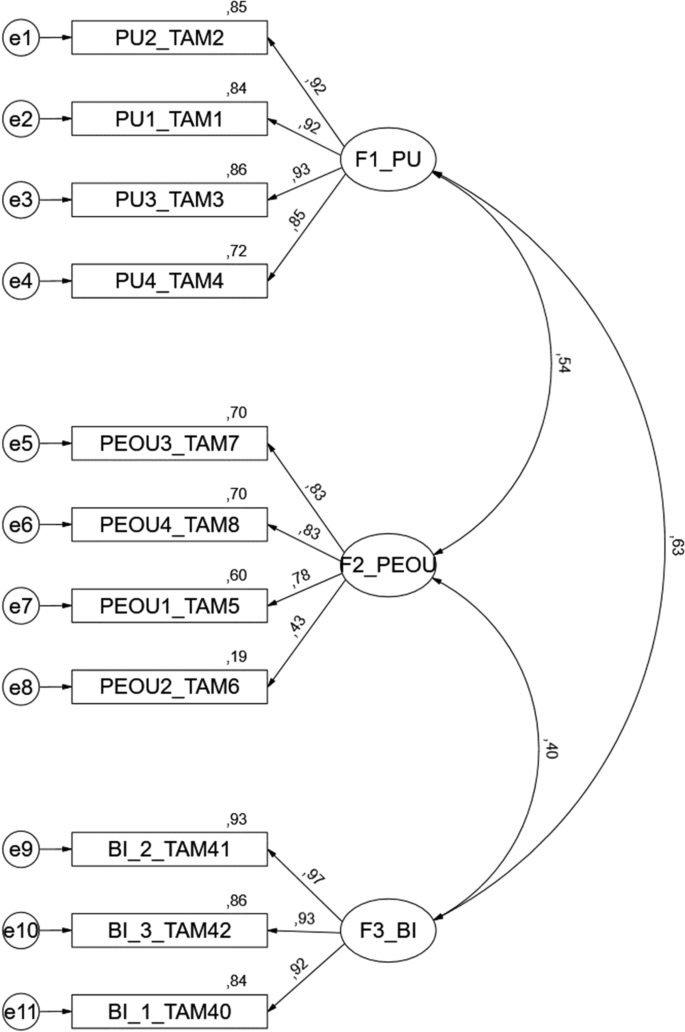
CFA model of factors internal to the TAM3. Footnote: F1-PU-Perceived usefulness; F2-PEOU-Perceived ease of use; F3-BI-Behaviour intention to use
The analysis of Table 9 shows the appropriateness of convergent and discriminant validity of the proposed model (Fig. 1 ). CFA was performed to validate the constructs associated with the determinants external to the Technology Acceptance Model 3 (REL-Relevance for learning; CANX-Anxiety with the use of CVS; CSE-Self-efficacy in the use of CVS; VOL-Voluntariness; PEC-Perception of external control; SN-Subjective Norm; CPLAY-Perceived playfulness in the use of CVS; ENJ-Enjoyability associated with the use of CVS) (Fig. 2 ). The results showed an acceptable fit to the model [(χ2(275) = 621, P < 0.001, CFI = 0.949, PCFI = 0.803, GFI = 0.888; PGFI = 0.695, RMSEA = 0.057; p (rmsea 0.05) = 0.025)]. Table 10 shows the construct validity results, with all items, except CSE_4_TAM55, presenting factorial loads greater than 0.5, revealing an acceptable convergent validity [ 36 ].
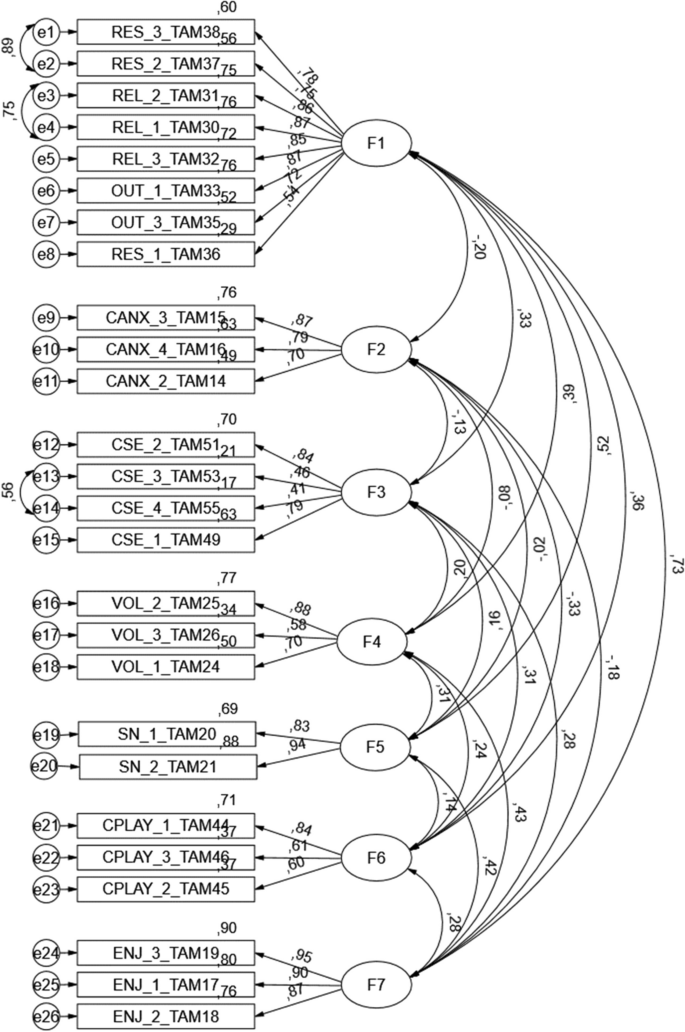
CFA model of the individual determinants of TAM 3. Footnote: F1-REL-Relevance to learning; F2—CANX—Anxiety with the use of CVS; F3—CSE—Self-efficacy in the use of CVS; F4—VOL—Voluntariness; F5—SN—Subjective Norm; F6—CPLAY—Perceived Playfulness in the use of CVS; F7—ENJ—Enjoyability associated with the use of CVS
The errors of the items with higher modification index values were correlated to improve the adjustment of the model. More specifically, a correlation was established between the following items: RES_3_TAM38 and RES_2_TAM37; REL_2_TAM31 and REL_1_TAM30; CSE_3_TAM53, and CSE_3_TAM55. This decision was based on the content similarity presented by the correlated items.
The convergent validity of the individual determinant items of the TAM3, a Construct Reliability (CR) revealed a value greater than 0.73, an Average Extracted Variance (AVE) greater than 0.42 [ 36 ], and factorial loadings in the inter-item correlation lower than the square root of the AVE for each construct [ 38 ], highlighted bold in Table 11 above the diagonal. The global analysis indicates the appropriateness of convergent and discriminant validity of the proposed model.
Trajectory analysis
In the proposed model, the items’ global average score of evaluation of the use of the virtual simulator (GS) and those related to the use of clinical virtual simulation (SU) were not considered (Table 12 ), given the high number of missing values (higher than 30%) that negatively influenced data quality and weakened the proposed model. The high number of missing values is justified by the participation in this sample of 4th-year students who attended the curricular unit Body Responses to Disease 1 in 2019–2020, an academic year in which it was not possible to extract the variables per student from the LMS.
Trajectory analysis was used to analyse the adequacy of the TAM3 adapted to assess the acceptance of the use of clinical virtual simulation. Table 13 summarises the tested hypotheses. Figure 3 represents the standardised constructs coefficients of the model and coefficients of determination ( R 2 ) associated with the modelling of the dependent variables. The model presents values of [(χ 2 (5) = 7.22, p = 0.205, CFI = 0.999, PCFI = 0.111, GFI = 0.998; PGFI = 0.091, RMSEA = 0.027; p (rmsea 0.05) = 0.789)]. In Fig. 3 , the proposed model explains a high variance of perceived usefulness ( R 2 = 62%), intention to use the CVS ( R 2 = 54%), and a lower variance of ease of use ( R 2 = 32%).
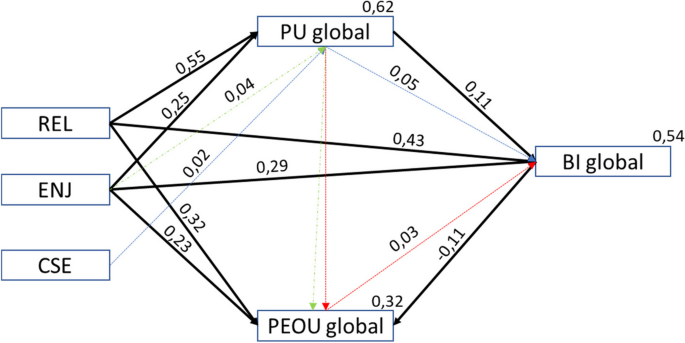
Model proposed for the acceptance of the technology for CVS (TAM3CVS_MP). Legend: REL-Relevance for learning; CSE-Self-efficacy in the use of CVS; ENJ-Enjoyability associated with the use of CVS; Black lines in Bold—direct effects; Dashed lines (blue/green and red)—indirect effects
Table 13 shows that the defined hypotheses related to the internal constructs and the individual determinants of the TAM3 regarding the acceptance of the clinical virtual simulation, the perceived usefulness (PU), the perceived ease of use (PEOU) and the behaviour intention to use (BI)], are influenced by Relevance for learning (REL) [REL → PU ( β = 0.55; P < 0.001), REL → PEOU ( β = 0.32; P < 0.001), REL → BI ( β = 0.43; P < 0.001)], and Enjoyability (ENJ) [ENJ → PU ( β = 0.25; P < 0.001), ENJ → PEOU ( β = 0.23; P < 0.001), ENJ → BI ( β = 0.29; P < 0.001)]. The remaining hypotheses were not supported in this study.
Table 14 shows the standardised indirect effects of the Model proposed for the acceptance of the technology for CVS (TAM3CVS_MP).
The participants showed mean values of perceived usefulness (M = 5.34; SD = 1.19), ease of use (M = 4.74; SD = 1.07), and behaviour intention to use the clinical virtual simulation (M = 5.21; SD = 1.18), indicating the acceptance of the use of clinical virtual simulation in nursing education.
This study validated the use of the Technology Acceptance Model 3 adapted to clinical virtual simulation and tested the related hypotheses, showing that the model explains 62% of perceived usefulness, 32% of ease of use, and 54% of behaviour intention to use the clinical virtual simulation by nursing students. The adequacy of the model was tested by analysing the direct effects of the relationships between the internal constructs (PU → BI, β = 0.11, P = 0.012; PEOU → BI, β = -0.11, P = 0.002) and direct relations between some of the constructs internal to the TAM and the external determinants, Relevance for learning and Enjoyability. Also, the adequacy of the proposed model was determined by analysing the indirect effects of self-efficacy in the use of clinical virtual simulation (CES) on BI ( P = 0.05) through PU ( P = 0.02) and the indirect effect on Enjoyability (ENJ) on PU through PEOU ( P = 0.044) and the indirect effect of PU on BI through PEOU ( P = 0.026).
In sum, regarding the technology acceptance model for clinical virtual simulation, the internal constructs that predicted the intention to use were perceived usefulness and perceived ease of use. However, perceived ease of use emerges as new its inverse relationship with the behaviour intention to use. This fact finds no parallel in the evidence [ 33 , 39 , 40 , 41 , 42 , 43 ]. This data points out that the responses expressed by the students are not related to the ease of use inherent to technology but rather to the cognitive performance necessary for the resolution of clinical scenarios and the training of clinical decision-making skills. Thus, the greater the perception of ease of use in a perspective of greater competence in the clinical decision-making process, the lower the intention to use the clinical virtual simulation. These data also reveals the need for clinical scenarios to present an increasing level of complexity according to the development of clinical decision-making skills.
In the proposed model, Relevance for learning (REL) and Enjoyability (ENJ) were the external constructs that best predicted perceived usefulness, ease of use, and behaviour intention to use clinical virtual simulation. This is in line with some of the findings of a meta-analysis by Rosli M.S et al. (2022) [ 43 ], the study of the adequacy of the Technology Acceptance Model 3 to virtual reality by Jiang, M et al. [ 39 ], and the study on the acceptance of computer games as an educational strategy, where Relevance for learning was also identified as one of the best predictors of perceived usefulness and/or ease of use by Lemay, D. J et al. [ 41 ].
The decision on the behaviour intention to use the clinical virtual simulation should consider three indirect effects identified:
The self-efficacy in the use of the clinical virtual simulation (CVS) indirectly predicts the behaviour intention to use the CVS through the moderation of perceived usefulness. This emphasises the need to optimise the support to students with less perceived self-efficacy in the use of CVS;
Enjoyability predicts ease of use of CVS through moderation of perceived usefulness. This fact points to the perception of enjoyability having a positive influence on the perceived usefulness, which positively influences the ease of use of the CVS. Also, this demonstrates that the increased Enjoyability associated with use can help overcome some of the complexity perceived by the student in the use of CVS;
The perceived usefulness predicts the behaviour intention to use CVS through moderation of perceived ease of use. These data point out that a greater utility perceived by the student in the use of CVS helps overcome some of the complexity perceived in the use of CVS in clinical reasoning training.
The analysis of the descriptive data associated with each construct internal to the TAM3 and the individual determinants showed average scores ranging between 4.14–5.59, except for Anxiety related to the use of the CVS, with an average score of 1.5, indicating its low perception by the students. The average self-efficacy score of the use of CVS (M = 6.72) is explained by the fact that it is evaluated on a 10-point Guttman scale. The lowest average score observed is for the subjective norm, indicating that it is not the influence of other people, particularly teachers, that determined the use of CVS by students. Regarding the voluntary use of CVS, data should be interpreted with caution since items TAM25 (M = 4.71) and TAM26 (M = 4.34) revealed a low perception of obligation perceived by the student to use the CVS, while item TAM24 (M = 5.24) showed a higher value associated to the voluntary use of the CVS. Regarding the ease of use, item TAM6 (M = 4.06) revealed that the use of CVS did not require much effort, as opposed to item TAM7 (M = 5.10), expressing the ease of use.
These are innovative results as they highlight the positive influence that the relevance attributed to learning and development of clinical reasoning and clinical decision-making skills (Learning Relevance) have on the perception of ease of use, perceived usefulness in the use of CVS, and the effective use of CVS. These results are associated with the relevance attributed by the student who views the use of CVS as linked to the triggering of emotions such as enjoyability, a fact previously determined as a variable to adjust the use of technology by Venkatesh V. & Bala H. (2008) [ 31 ] but still little explored by Kim, S et al. [ 44 ]. This study shows that the use of CVS, ease of use, and usefulness are influenced by the positive representation that the student has of the contribution to their training as a future nurse. Also, these study results demonstrate that the use of CVS creates a playful context that helps students learn actively in a friendly environment, bringing aspects of gamification that help them set goals, get scores, and compare results between students [ 44 , 45 ] while simultaneously anticipating clinical challenges. Using game elements added to the CVS contributes to developing intrinsic motivation [ 46 ] and satisfaction with the learning process [ 8 ].
The use of CVS promotes students’ active learning and the capture of their intrinsic motivation through facilitated access to pedagogical resources according to the pacing and learning preferences of the students. This learning environment promotes autonomy, the development of effectiveness and belonging to a learning community, an environment in which the teacher is a facilitator of the learning process, and the student learns while having fun [ 46 , 47 , 48 ]. It can be argued that the motivation under analysis can be extrinsic [ 46 ] because it uses a perception of locus of internal causality associated with an integrated regulation process by anticipating the results that students may achieve, a fact represented by the construct Relevance for learning (REL). However, the construct Enjoyability clarifies the existence of intrinsic motivation based on interest and student satisfaction with the learning process using the CVS [ 46 ]. Thus, this study showed that a personal determinant of the student (REL) and an adjustment determinant (ENJ) are central to the use of CVS in nursing education.
Currently, the acceptance and adoption of CVS in Nursing education, in this context, goes beyond external variables to the student that may determine the adoption of CVS, for example, the influence of teachers and significant people or individual determinants related only to characteristics of CVS, for example, the effectiveness in the use of CVS, anxiety associated with the use of CVS, and playfulness. This study revealed that the current characteristics of pre-graduation students, who are digital natives [ 49 ], lead to features related to the use of technology that may be overcome by the nature of the learning outcomes anticipated by students.
In sum, this study produced interesting outcomes for nursing education in this context, affirming that the use of CVS in learning is directly determined by students’ perceived relevance and enjoyability. This positively influences the usefulness and perceived ease of use and consequently the behaviour intention to use the CVS. Perceived Self-efficacy indirectly predicted the behaviour intention to use CVS through moderation by perceived usefulness.
The results of this study require careful interpretation because they only represent a single context of nursing degree education and were implemented in one of the curriculum units of the syllabus. Notwithstanding, this study presents data that can support educators in the health field in making decisions or developing new studies, overcoming some of the limitations of this study.
Study limitations
The main limitations of this study were the use of the same sample of students to perform the EFA and CFA.
Another identified limitation was not having included the construct of the attitude referred to in other studies. This option was based on the expectation of having data related to the behaviour from the evaluation and use of the CVS. Also, the lack of data for the entire sample regarding the Global Scores of use and the number of completed scenarios per student conditioned the potential of the presented model. Thus, using this model in samples with these available data is recommended. This limitation stems from the fact that CVS is still little used as an andragogical strategy in health education.
This study provided noteworthy contributions to propose a technology acceptance model for clinical virtual simulation (TAM3CVS_MP), identifying the factors determining the acceptance and use of clinical virtual simulation by nursing students.
The results showed the potential of clinical virtual simulation as a pedagogical strategy to capture students' intrinsic motivation to develop active and optimised learning while potentiating their skills.
Integrating clinical virtual simulation as an andragogical strategy in nursing education curriculums needs to rely on higher education institutions and teachers, investment in training, technology and time for reflection, discussion, and analysis. However, this study provides information that can support the decision and shape the implementation strategy.
Furthermore, this study evidences the importance of teachers’ and institutional decision-makers’ attention to students' perception of relevance for learning, enjoyability, and perceived self-efficacy associated with the use of clinical virtual simulation during conceptualisation, design, and implementation processes.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author but restrictions apply to the availability of these data, which were used under license from the Nursing School of Porto (Portugal) for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission from Nursing School of Porto (Portugal).

Abbreviations
Average extracted variance
Behaviour intention to use
Anxiety with the use of CVS
Confirmatory factor analysis
Playfulness in the use of CVS
Construct reliability
Self-efficacy in the use of CVS
European credit transfer and accumulation system
Exploratory factor analysis
Enjoyability associated with the use of CVS
Nursing School of Porto
Global score
Higher education institutions
Maiser-Meyer-Olkin test
Learning management system
Objective usability
Evaluation result
Perception of external control
Perceived ease of use
Perceived usefulness;
Body responses to disease 1 course
Relevance for learning
Learning relevance
Subjective norm
- Technology acceptance model
Voluntariness
Wensing M. Grol R. Knowledge translation in health: how implementation science could contribute more. BMC Med, 2019;8(17). https://doi.org/10.1186/s12916-019-1322-9 .
Légaré F. Zhang P. Barriers and facilitators - Strategies for identification and measurement. (J. T. Sharon E. Straus, Ed.) Knowledge translation in health care: moving from evidence to practice. 2013
Berman NB, et al. The Role for Virtual Patients in the Future of Medical Education. Acad Med. 2016;91(9):1217–22. https://doi.org/10.1097/ACM.0000000000001146 .
Article PubMed Google Scholar
Ruud N. et. al. Comparing mental distress and help-seeking among first-year medical students in Norway: results of two cross-sectional surveys 20 years apart. 2020;10. doi: https://doi.org/10.1136/bmjopen-2020-036968 .
Mao Y. et al. A systematic review of depression and anxiety in medical students in China. 2019;19. https://doi.org/10.1186/s12909-019-1744-2 .
Moreira S.J. et. al.Anxiety, Depression and Academic Performance: A Study Amongst Portuguese Medical Students Versus Non-Medical Students. Acta Med Port, 2018 ;28(31(9)), pp. 454–462. doi: https://doi.org/10.20344/amp.9996 .
Karaca A, et al. Relationship between mental health of nursing students and coping, self-esteem and social support. Nurse Educ Today. 2019;76:44–50. https://doi.org/10.1016/j.nedt.2019.01.029 .
Article CAS PubMed Google Scholar
Padilha, J. M., Rosa, J. L., & Cunha, D. J. Gamification in Healthcare Education: Demystifying a Trend. Em B. Oscar, V. Amorim, & A. C. Moreira, Handbook of Research on the Influence and Effectiveness of Gamification in Education. IGI Global. 2022. doi: https://doi.org/10.4018/978-1-6684-4287-6.ch003 .
Shin S et al.. Effectiveness of patient simulation in nursing education: Meta-analysis. 2015;35(1), pp. 176–182. Doi. https://doi.org/10.1016/j.nedt.2014.09.009 .
Vlachopoulos D. Makri A. The effect of games and simulations on higher education: a systematic literature review. Int J Educ Technol High Educ, 2017;14(22). https://doi.org/10.1186/s41239-017-0062-1 .
Moslehi S, Masoumi G, Barghi-Shirazi F. Benefits of simulation-based education in hospital emergency departments: A systematic review. J Educ Health Promot. 2022. https://doi.org/10.4103/jehp.jehp_558_21 .
Article PubMed PubMed Central Google Scholar
-Lioce L. (Ed.) et al. Healthcare Simulation Dictionary - Seconde edition. 2020.doi: https://doi.org/10.23970/simulationv2 .
Padilha JM, et al. Clinical Virtual Simulation in Nursing Education. Clin Simul Nurs. 2018. https://doi.org/10.1016/j.ecns.2017.09.005 .
Article Google Scholar
Padilha JM, et al. Clinical Virtual Simulation in Nursing Education: Randomized Controlled Trial. J Med Internet Res. 2019. https://doi.org/10.2196/11529 .
Pence, P. L. Student satisfaction and self-confidence in learning with virtual simulations. Teaching andLearninginNursing, 2022;31–35. doi:doi.org/ https://doi.org/10.1016/j.teln.2021.07.008 .
Plackett, R., Kassianos, A. P., Mylan, S., Kambouri, M., Raine, R., & Sheringham, J. The effectiveness of using virtual patient educational tools to improve medical students’ clinical reasoning skills: a systematic review. BMC Medical Education, 2022;1–18. doi: https://doi.org/10.1186/s12909-022-03410-x .
Sim JJ, Rusli KD, Seah B, Levett-Jones T, Lau Y, Liaw SY. Virtual Simulation to Enhance Clinical Reasoning in Nursing: A Systematic Review and Meta-analysis. Clin Simul Nurs. 2022;69:26–39. https://doi.org/10.1016/j.ecns.2022.05.006 .
Brown K.M. et al. Integrating Virtual Simulation into Nursing Simulation Roadmap. Clinical Simulation in Nursing, 2021; pp. 1-9. https://doi.org/10.1016/j.ecns.2021.08.002 .
Dale-Tam J. et. al. Creating Psychological Safety During a Virtual Simulation session. Clinical Simulation in Nursing, 2021; pp. 14–17. doi: https://doi.org/10.1016/j.ecns.2021.01.017 .
Foronda C.L. et. al. Virtual simulation in nursing education: a systematic review spanning 1996 to 2018. Simulation in Healthcare 2020;(15), pp. 46–54. doi: https://doi.org/10.1097/SIH.0000000000000411 .
Fogg N, et al. Using virtual simulation to develop clinical judgment in undergraduate nursing students. Clin Simul Nurs. 2020;48:55–8. https://doi.org/10.1016/j.ecns.2020.08.010 .
Kyaw B.M. et. al. Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J Med Internet Res, 2019; 21(1). doi: https://doi.org/10.2196/12959 .
Kononowicz A. et. al. Virtual Patient Simulations in Health Professions Education: Systematic Review and Meta-Analysis by Digital Helath Education Collaboration. J Med Internet Res, 2019; 21(7). doi: https://doi.org/10.2196/14676 .
Baumann-Birkbeck L. et. al. Appraising the role of the virtual patient for therapeutics health education. Curr Pharm Teach Learn, 2017;9(5), pp. 934–944. doi:doi: https://doi.org/10.1016/j.cptl.2017.05.012 . Epub
Padilha JM, et al. Clinical Virtual Simulation as Lifelong Learning Strategy—Nurse’s Verdict. Clin Simul Nurs. 2020. https://doi.org/10.1016/j.ecns.2020.06.012 .
Mestre A, Muster M, El Adib AR, Egilsdottir HÖ, Byermoen KR, Padilha J, M.,… Marreiros, A. The impact of small group virtual patient simulator training on perceptions of individual learning process and curricular integration: a multicentre cohort study of nursing and medical students. BMC Med Educ. 2022. https://doi.org/10.1186/s12909-022-03426-3 .
Granić A, Marangunić N. Technology acceptance model in educational context: A systematic literature review. Br J Edu Technol. 2019;50(5):2572–93. https://doi.org/10.1111/bjet.12864 .
Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of infrmation technology. MIS Q. 1989;19:319–40.
Venkatesh V. Davis FD. A theoretical extension of the technology acceptance model: four longitudinal field studies. Manag Sci. 2000;46:186–204.
Venkatesh V. Determinants of perceived ease of use: integrating perceived behavioral control, computer anxiety and enjoyment into technology acceptance model. Inf Syst Res. 2000;342–65.
Venkatesh V. Bala H. Technology Acceptance Model 3. 2008;39(2), pp. 273–315. doi: https://doi.org/10.1111/j.1540-5915.2008.00192.x .
Nunnally JC. Psychometric theory. 2nd ed. New York: McGraw-Hill; 1978.
Google Scholar
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the Process of Cross-Cultural Adaptation of Self-Report Measures. Spine. 2000;25(24):3186–91.
Boateng et. al.Boateng GO, Neilands TB, Frongillo EA, Melgar-QuiñoBest Practices for Developing and Validating Scales for Health, Social, and Behavioral Research: A Primer. Front Public Health, 2018; 6(49). doi: https://doi.org/10.3389/fpubh.2018.00149 .
Hair JF Jr, Black WC, Babin BJ, Anderson RE. Multivariate data analysis (7. th. New York: Pearson; 2010.
Fornell C, Larcker DF, (Feb de,. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J Mark Res. 1981;18(1):39–50.
Kaiser, H. F. An index of factorial simplicity. Psychometrika, 1974; 31–36. doi: https://doi.org/10.1007/BF02291575 .
Fussell SG, Truong D. Using virtual reality for dynamic learning: an extended technology acceptance model. Virtual Reality. 2022;26:249–67. https://doi.org/10.1007/s10055-021-00554-x .
Jiang, M. Y.-C., Jong, M. S.-Y., Lau, W. W.-f., Meng, Y.-l., Chai, C.-S., & Chen, M. Validating the General Extended Technology Acceptance Model for E-Learning: Evidence From an Online English as a Foreign Language Course Amid COVID-19. Front. Psychol., 2021;12. doi: https://doi.org/10.3389/fpsyg.2021.671615 .
Huang Y-M. Exploring students’ acceptance of educational computer games from the perspective of learning strategy. Australas J Educ Technol. 2019;35(3):132–49. https://doi.org/10.14742/ajet.3330 .
Lemay DJ, Morin MM, Bazelais P, Doleck T, (July de,. Modeling students’ perceptions of. Clin Simul Nurs. 2018;20:28–37. https://doi.org/10.1016/j.ecns.2018.04.004 .
Abdullah F, Ward R. Developing a General Extended Technology Acceptance Model for E-Learning (GETAMEL) by analysing commonly used external factors. Comput Hum Behav. 2016;56:238–56. https://doi.org/10.1016/j.chb.2015.11.036 .
Rosli, M. S., Saleh, N. S., Ali, A., Bakar, S. A., & Tahir, L. M. A Systematic Review of the Technology Acceptance Model for the Sustainability of Higher Education during the COVID-19Pandemic and Identified Research Gaps. Sustainability, 2022; 14. doi: https://doi.org/10.3390/su141811389 .
Kim, S., Song, K., Lockee, B., & Burton. Gamification in Learning and education - Enjoy Learning Like Gaming. Springer International Publishing AG. 2018. doi: https://doi.org/10.1007/978-3-319-47283-6 .
-van Gaalen, A., Brouwer, J., Schönrock-Adema, J., Bouwkamp-Timmer, T., Jaarsma, A., & Georgiadis, J. (May de,. Gamification of health professions education: a systematic review. Adv Health Sci Educ Theory Pract. 2021;12:683–711. https://doi.org/10.1007/s10459-020-10000-3 .
Ryan, R. M., & Deci, E. L. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. American Psychologist, 2000.pp. 68–78. doi:10.1037110003–066X.55.1.68
Kusurkark RA, Croiset G, Ten Cate TJ. Twelve tips to stimulate intrinsic motivation in students through autonomy-supportive classroom teaching derived from self-determination theory. Med Teach. 2011. https://doi.org/10.3109/0142159X.2011.599896 .
Ten Cate, O. T., Kusurkar, R. A., & Williams, G. C. How self-determination theory can assist our understanding of the teaching and learningprocesses in medical education. AMEE Guide No. 59. Medical Teacher, 2011;33(12), pp. 961–973. doi: https://doi.org/10.3109/0142159X.2011.595435 .
Prensky, M. Digital Natives, Digital Immigrants Part 1. 2001; 9(5), pp. 1–6. doi: https://doi.org/10.1108/10748120110424816 .
Download references
Acknowledgements
The authors wish to acknowledge the contribution of the professional translator Maria do Amparo Alves on the editing of this article.
None declared.
Author information
José Miguel Padilha
Present address: Nursing School of Porto, CINTESIS@RISE, Porto, Portugal
Authors and Affiliations
Faculty of Medicine, University of Porto, Porto, Portugal
Life and Health Sciences Research Institute (ICVS), School of Medicine, University of Minho, Braga, Portugal
Patrício Costa
ICVS/3B’s - PT Government Associate Laboratory, Braga/Guimarães, Portugal
Faculty of Psychology and Education Sciences, University of Porto, Porto, Portugal
Nursing School of Porto, CINTESIS@RISE, Porto, Portugal
Paulino Sousa
CINTESIS@RISE, FMUP-MEDCIDS, Porto, Portugal
Ana Ferreira
You can also search for this author in PubMed Google Scholar
Contributions
All authors conceived the study. JMP collected, prepared, and analysed the data with PC. All authors confirm that they had full access to all the data in the study, take responsibility for the integrity of the data and the accuracy of the analysis, and accept responsibility to submit the paper for publication. JMP drafted the initial and final versions of the manuscript. All authors critically revised the early and final versions of the manuscript.
Corresponding author
Correspondence to José Miguel Padilha .
Ethics declarations
Ethics approval and consent to participate.
The Nursing School of Porto ethics committee granted authorisation for the study 697/2022 and informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Descriptive analysis of the TAM item.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Padilha, J.M., Costa, P., Sousa, P. et al. Clinical virtual simulation: predictors of user acceptance in nursing education. BMC Med Educ 24 , 299 (2024). https://doi.org/10.1186/s12909-024-05154-2
Download citation
Received : 12 October 2023
Accepted : 09 February 2024
Published : 16 March 2024
DOI : https://doi.org/10.1186/s12909-024-05154-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Virtual patients
- Nursing education
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

The experiences of nurse educators in implementing evidence-based practice in teaching and learning
Gloria n. mthiyane.
1 Department of Health Studies, University of South Africa, South Africa
Debbie S. Habedi
Nurse educators have a vital role to mentor student nurses in relation to developing evidence-based practice (EBP) skills, accessing research products and participating in research projects. This requires more innovative teaching approaches that promote active participation, creativity and critical thinking in students such as online teaching and learning, accessing electronic resources, video conferencing and research-based teaching and learning.
To determine the nurse educators’ experiences in implementing EBP in teaching and learning, and to describe the importance and benefits of EBP teaching and learning to the nursing profession, especially for nurse educators and student nurses.
Two chosen campuses from Umgungundlovu Health District under the KwaZulu-Natal College of Nursing (KZNCN) and offering a 4-year R425 training programme.
Qualitative research design and methods were followed in conducting the study. A non-probability purposive sampling technique was used to access the sample of 12 nurse educators. Data were collected using semi-structured interviews, the interview guide, and the digital voice recorder.
Data were analysed manually, following a content thematic approach and two themes emerged as challenges experienced by nurse educators with the implementation of EBP in teaching and learning and benefits and value of EBP in teaching and learning. Findings revealed that, although most of the nurse educators are supportive and displayed a positive attitude towards implementing EBP in teaching and learning, the level of knowledge and skills was questionable. This was coupled with a lack of motivation and commitment towards research.
Conclusions
Evidence-based practice has an essential potential role to play through incorporating more practice-based evidence of nurse educators in teaching and learning implementation. The nurse educators should use EBP to ensure that student nurses receive high-quality nursing education.
Introduction
Evidenced-based practice (EBP) is described by Melnyk et al. ( 2012 :410) as a problem-solving approach to clinical decision-making in health care. Evidence-based practice integrates the best evidence from well-designed studies with the clinicians’ expertise, including internal evidence from patient assessments and practice data, and patients’ preferences and values. Melnyk et al. ( 2012 :410) further revealed that implementation of EBP leads to a higher quality of care, improved patient outcomes, and decreased health care costs.
Evidence-based practice teaching and learning has become an important function for nursing education. Research is used as an instrument in developing new teaching and learning strategies. Nurse educators are guided by evidence-based practice in teaching and on research reports. Evidence-based practice in learning is also based on research, meaning that students learn by using research findings. Research-based teaching and learning encourages and stimulates critical thinking for students (Felicilda-Reynaldo & Utley 2015 :91).
Although EBP is known to improve health care quality, decreasing costs and empowering nurses, the challenge is the way in which it ensures successful implementation by the nurses (Levin et al. 2011 :21). The implementation of successful EBP education serves the function of developing practitioners who value EBP and have the knowledge and skills to implement such practice (Lehane et al. 2017 :8).
Nurse educators play a key role in creation of opportunities for implementing EBP and in facilitating the implementation process. The question now is how to foster implementation of EBP. The most important factor that is likely to help nurses and nurse educators to adopt EBP is the provision of adequate training in EBP (Heikkila et al. 2017 :3). The importance of embedding EBP in nurse education programmes cannot be underestimated if EBP and its positive patient outcomes are to be realised in health care settings. According to Felicilda-Reynaldo and Utley ( 2015 :93), one nurse educator noted that ‘nurse graduates will be prepared to facilitate a transformation of the health care system culture by implementing practice review and revision consistent with evidence-based nursing (EBN) research’. The above-mentioned statement highlights the importance of incorporating EBP throughout the curriculum to prepare students for future success in using EBP in their professional nursing practice (Felicilda-Reynaldo & Utley 2015 :93). Mackey and Bassendowski ( 2016 :54) indicated that utilising nursing best practice guidelines, reviewing and implementing applicable research evidence, and taking advantage of technological advances are ways in which nursing can move forward as a well-informed discipline.
Malik, McKenna and Griffiths ( 2015 a:158) in Australia reported that integrating EBP into undergraduate nursing education and preparing future nurses to embrace EBP into clinical practice becomes crucial in today’s complex and evolving health care environment. The study further implies that the role that EBP plays in the practical lives of student nurses will depend on the degree to which it is promoted by academics; the extent to which it is incorporated in course objectives, content and assessments; and its application within the clinical setting (Malik et al. 2015 a:158). In this way, nurses’ willingness to carry out research projects, as well as to utilise the research findings effectively in practice is enhanced.
Traditional teaching methods and learning styles still dominate in nursing education and these strategies do not encourage critical thinking among the nursing students; therefore, these methods will not prepare student nurses to make sound clinical judgements in practice (Subhan 2014 :35). With the nursing profession experiencing many changes on contemporary issues, nursing students need to be prepared for these challenges. Using EBP as one of the teaching and learning strategies will qualify student nurses to become excellent critical thinkers and solve problems in the clinical area. However, EBP remains a relatively new concept to nursing, and there is limited literature available addressing the incorporation of EBP into nursing curricula, especially at the undergraduate level (Malik et al. 2015 a:158). In South Africa, there is a dearth of literature in the implementation of EBP in nursing education.
To determine the experiences of nurse educators in implementing EBP in teaching and learning, and to describe the importance and benefits of EBP in teaching and learning in the nursing profession, especially for nurse educators and student nurses.
- What are the experiences of nurse educators regarding implementation of EBP in teaching and learning?
- What recommendations may be made for nurse educators to implement EBP in teaching and learning?
Design and methods
A qualitative, explorative, descriptive research design, using non-probability purposive sampling, focusing on understanding the social settings, facilitating the exploration of relationships and human experience within the research setting was followed. It also enabled face-to-face, personal contact in data collection (Moule & Goodman 2014 :175). Participants selected and interviewed were individuals who were more knowledgeable about the phenomenon and qualified enough to answer the question at hand.
The total target population was 62 nurse educators in June 2017.The sample comprised 12 nurse educators in possession of a nursing education qualification, registered by South African Nursing Council (SANC) as nurse educators and employed by the KwaZulu-Natal Department of Health. The focus of the study was on nurse educators involved in classroom teaching at the two chosen campuses from Umgungundlovu Health District under the KwaZulu-Natal College of Nursing (KZNCN) and offering a 4-year R425 training programme.
Sampling method
The sampling process followed the non-probability method using a purposive sampling technique to select the participants. This type of sampling assisted the researcher to select those homogeneous participants who knew most about the phenomenon under study (Brink, Van der Walt & Van Rensburg 2012 :139). All nurse educators who met the inclusion criteria were requested to volunteer for participation in the study. Clinical nurse educators were excluded from the study. The sample size was 12 participants and was based on collecting detailed data to address the research questions, objectives, and the purpose of the study.
Data collection
Data were collected in June 2017 using semi-structured interviews, interview guide and the digital voice recorder. To ensure anonymity, code numbers were allocated to each participant. The researcher kept all collected and private information shared safely locked and/or encrypted in the researchers’ computer for 5 years. Participants were informed of the presence of the research assistant during the interview process and all participants granted the researcher permission to record interviews.
Semi-structured individual interviews were conducted using the self-developed interview guide and digital voice recorder as data-collection instruments. The interview guide was developed in English based on the research purpose, research objectives, research questions and literature review. It comprised predetermined open-ended questions to get in-depth information about participants’ experiences and was pre-tested before conducting the main study to determine the feasibility of the instrument. All interviews were captured on the digital voice recorder with the help of the research assistant who had training in doing qualitative interviews prior to data collection.
Data analysis
Data were analysed manually following a content thematic analysis approach which involved a thorough review of all recorded information that the researcher obtained during data collection (Brink et al. 2012 :194). The researcher listened to recorded interviews repeatedly. All recorded data were transcribed into written format. Transcriptions were read thoroughly and repeatedly; common themes and categories of information were identified and grouped together. Electronic files for each theme were created and labelled, allowing for ease of access and management of data. Discussion and interpretation of the findings commenced thereafter.
Trustworthiness
Strategies employed to ensure the quality of data included the following measures of trustworthiness as suggested by Lincoln and Guba’s framework (Polit & Beck 2017 :560).
Credibility : Data were collected through face-to-face interviews, directly from the participants using a digital voice recorder and they were given a chance to confirm data before the final written report. Participants were provided with the opportunity to review the researchers’ interpretation of data.
Transferability : Sufficient description and interpretation of data was supported by the relevant literature so that it can be easily transferrable and applicable to other settings.
To ensure dependability , the researcher ensured that data collected remained stable over a period of time; meaning that information related to data collected would remain unchanged over time. Therefore, data were collected using the digital voice recorder with a memory card and all other information were properly stored and kept safely.
The use of actual quotations from the participants in the discussion of the report supports the confirmability of data.
Ethical considerations
Ethics approval certificate (reference number HSHDC/537/2016) was obtained from the Research Ethics Committee of the Department of Health Studies, University of South Africa (UNISA). Permission to conduct the study was granted by the KwaZulu-Natal Department of Health, KwaZulu-Natal College of Nursing, and both principals of the colleges. Participants were informed about the study and that their participation was voluntary and they were advised of their rights to withdraw at any time. All participants signed informed consent forms, their responses were kept confidential and anonymous and their identities were not divulged or disclosed during reporting of the findings.
Biographical data of the participants
Participants were from three race groups: African, Indian and Coloured. 1 They were all women. Their years of experience ranged between 5 and 30 years, occupying the ranks of junior nurse educator, senior nurse educator and Head of Department. The highest qualifications were a Bachelor’s, Honour’s or Master’s degree in Health and Nursing Science Studies as indicated in Table 1 .
Demographic information of the sample.
Themes, categories and findings
The following themes and categories emerged during data analysis and are summarised in Table 2 .
Themes and categories.
EBP, evidence-based practice.
Theme 1: Challenges with implementation of evidence-based practice in teaching and learning
The findings revealed that nurse educators are experiencing certain challenges with the implementation of EBP in teaching and learning. They include time constraints, lack of and poor access to relevant resources, the use of traditional teaching approaches which are still dominant, nurse educators’ lack of or poor knowledge and skills, and the quality of nursing students. Emmanuel et al. ( 2011 :22) in their study on developing EBP among student nurses in the United Kingdom identified similar challenges that prevented the nurses from successfully using EBP, which included poor access to facilities and information, lack of experience and little confidence in using computers.
Schoonees, Rohwer and Young ( 2017 :11) reported that the challenges experienced by lecturers at a sub-Saharan African academic institution were a lack of time by the programme to dedicate to evidence-based health care, lack of evidence related to a specific field, lack of student motivation and the students’ schooling background.
Category 1.1: Time constraints
This study indicated that, for the nurse educators to successfully implement EBP in teaching and learning, more time is required in the library to search for information, for reading the literature, and for preparation and presentation of the content. This applied to both the nurse educators and student nurses. This statement is supported in the study conducted by Emmanuel et al. ( 2011 :22), which indicated that the use of EBP by the professionals requires accessing and integrating a number of different resources which could be time consuming. Lack of time was also mentioned as a major barrier when trying to access and review any of the evidence (Emmanuel et al. 2011 :22).
Nurse educators indicated that time is not allocated or distributed fairly between library, theory and practice. The prescribed time in the curriculum does not provide sufficient time for students to visit the library to search for information. The location of the library also contributed to time limits, neither campus under study having a library on site. On one campus, the library is 8 km away from the campus. At the other campus, the library is within the hospital premises and not on the campus. These are both medical libraries, which means that they are accessed by all hospital staff. The following statements were reported by the participants with regard to time allocation, prescribed time, and preparation time:
‘Yes, yes, the students have library, the problem that we encounter when they are in block is that they do not have enough time to go to the library because the libraries are not situated in the facilities, like colleges they must go out and find information that is our challenge for now.’ (Participant 1, Junior, 40 years old) ‘So, you find that even the time that is allocated for library the moment they walk out to go to the library, you find that library is in use full of doctors then that is a challenge and you find that now when they come back they are somehow late for classes so that is a challenge.’ (Participant 2, Junior, 42 years old) ‘Maybe we can move from what we have already, because you know generally there is allocated time for clinical exposure, allocated time for theory. Maybe we can look at both these components and also allocate time for self-directed learning so that it comes in as part of the curriculum, like a prescribed kind of thing, like for example saying that the students must have so many assignments, must have so much library time.’ (Participant 3, Senior, 50 years old)
A study conducted by Malik et al. ( 2015 b:50) on nurse educators and clinical nurse coaches and specialists regarding their perceived knowledge, skills, attitudes and contextual factors affecting EBP, revealed that insufficient time prevented appraisal of literature on a regular basis and the searching of research reports. There is no time to find and read research articles. Again, in circumstances where shortages of staff exist, allowing staff adequate time to complete the requisite reading to update their clinical or EBP knowledge or to attend continuing nursing education is not always possible (Boswell & Cannon 2017 :20).
Category 1.2: Lack of and poor access to relevant resources
It is clear that for the nurse educators to implement EBP in teaching and learning, special resources must be available and accessible to both nurse educators and student nurses for successful implementation. Evidence is available in various forms, such as books, videos, journals, and articles. Access to evidence comes through the libraries, computer laboratories with Internet access and mobile technology.
Participants responded this way when asked about their resources:
‘For instance, if you look at the in-house, what you need to make your teaching learning process smarter, is sometimes not available.’ (Participant 11, Senior, 48 years old) ‘It could be available but you cannot access it easily.’ (Participant 8, Junior, 53 years old) ‘No not easily especially with the IT, we are limited for resources; I would have to go to the library to use it.’ (Participant 10, Senior, 59 years old) ‘Eh I don’t think especially with our college, I do not think that we do not, I mean we have enough resources, like for instance we need to have enough resources, the most recent textbooks you know, even the library should make sure that it is well equipped with most recent textbooks, we have the computers so that they have access to the internet which is the problem that we are experiencing that we don’t have with our campus.’ (Participant 4, HOD, 56 years old)
Hussein and Hussein ( 2014 :870) agree with the statements above in their study conducted in Egypt. Nursing education must be committed to the principles of EBP and critical thinking. Such education must provide resources and create a supportive environment for the implementation of EBP in teaching and learning. The fundamentals of teaching student nurses must be based on the best available evidence to recognise and deliver high-quality patient care (Emmanuel et al. 2011 :21).
Insufficient financial resources as well as journals, reports and computers for making EBP a reality in theoretical and clinical teaching could affect negatively the nurse educators’ ability to access evidence from various sources. It has been discovered that when nurses are provided with the necessary tools such as smart phones and computers inter alia, they are much more likely to access relevant information and best practice guidelines (Mackey & Bassendowski 2016 :53).
Category 1.3: Current teaching approaches
The study revealed that, currently, traditional teaching approaches are still dominant in nursing education. The participants identified the following current teaching strategies used for teaching and learning: facilitation, group discussion, simulation, assignments, role play, case study, clinical debates, lecture, self-activities, demonstrations, peer group teaching, problem-solving, group presentations, games, case-based research, videos, reflective journals, portfolio of evidence, and learning package. Most of these approaches lead to technical skills mastery but they do not stimulate the development of critical-thinking skills, as one participant stated that:
‘They promote psychomotor skills; the students get technical skills to do the procedures and more.’ (Participant 9, HOD, 59 years old)
Felicilda-Reynaldo and Utley ( 2015 :94) recommended a change in educational technology for nurse academics, which include the teaching approaches that facilitate critical thinking and provide opportunities for practising evidence-based patient care. The study by Leufer and Clearly-Holdforth ( 2015 :6) mentions that the continuous assessment element of the module comprising an EBP project and the lectures must provide ongoing support to student nurses throughout the research module as they develop their project. Tailored teaching and assessment methods must be implemented within the academy to foster a culture of EBP at undergraduate level and beyond (Leufer & Clearly-Holdforth 2015 :7). Teaching of student nurses must be based on the best available evidence to recognise and deliver high-quality patient care (Emmanuel et al. 2011 :21).
Category 1.4: Lack of knowledge and skills by nurse educators
Other challenges experienced by nurse educators on EBP implementation in teaching and learning were expressed by some of the participants as lack of confidence, lack of motivation, and lack of relevant knowledge and skills about EBP teaching. The following quotes were stated:
‘I think educators need to know how to use EBP research, I think that research for educators is something very important. I am not really completely involved with research, I think they got to understand research, they got to practice research and then, we can bring it to the students.’ (Participant 8, Junior, 53 years old) ‘Maybe the in-service or the education of the staff themselves, the information that they have regarding what problem-based practice or research is all about. They need to be in serviced as well.’ (Participant 10, Senior, 59 years old) ‘The first challenges will be the lack of motivation if they have not been motivated that’s a challenge, because there need to be like more workshops on evidence-based and the importance of using evidence-based, which is the challenge at the present moment because it is not everybody that is well tuned with evidence-based that is the challenge.’ (Participant 4, HOD, 56 years old) ‘Research is very good, it is good and as much as this off the topic you know we hate research, nurses hate research but I think they should be encouraged so we have more EBP and you know encourage the students.’ (Participant 6, Senior, 56 years old)
Although various studies indicate that nurse educators have a positive attitude towards EBP, it has been reported that a positive attitude is increased with advanced educational level, higher academic ranking, years of experience, and a teaching and research role (Hussein & Hussein 2013 :609). Therefore, findings suggest that continuing education for nurse educators on the EBP process is necessary to enhance their knowledge and skills in acquiring appropriate research and analytic skills relevant to their teaching specialties (Hussein & Hussein 2013 :617).
In an Australian study on integration of EBP into the curriculum, Malik et al. ( 2015 a:158) mention that there is lack of clarity on EBP content and process. Clarity is frequently blurred with research processes and outcomes, which often results in continuation of traditional nursing research courses in the hope of preparing EBP practitioners. Leufer and Clearly-Holdforth ( 2015 :11) state that if optimal patient outcomes are to be maximised, practitioners’ skills and knowledge base must be fostered and enhanced through ongoing education, training and support.
Category 1.5: Student characteristics
Nurse educators had a challenge with students’ attitude and perceptions towards EBP, and their lack of computer skills. According to participants, students appear to have preconceived ideas about research in general. These perceptions are negative and overwhelming for students. A negative attitude develops among the student nurses, because students do not understand the importance of EBP. Nurse educators felt that students’ lack of confidence, motivation, and commitment to perform and use research contributed to misperception and their resultant negative attitude. The nursing programme R425 is perceived as being full, overwhelming, with competing priorities of research, clinical, and theoretical workloads.
‘Students feel that it is an added responsibility.’ (Participant 7, Junior, 49 years old) ‘Students that we are teaching, they look at this research as a monster.’ (Participant 12, Senior, 60 years old) ‘So, the experience that I am coming across when I teach is that these students they do not like it.’ (Participant 12, Senior, 60 years old) ‘These students, they think that no eh eh we are overloading them.’ (Participant 5, Junior, 50 years old) ‘Yah there are challenges because at times the learners are lazy, they do not want to do work.’ (Participant 11, Senior, 48 years old)
Students’ attitudes and perceptions can influence EBP learning either positively or negatively. Should students’ roles be clearly defined early during training, so that they understand the importance of EBP, a positive attitude develops within them. According to Malik et al. ( 2015 a:158), the role that is played by EBP in the practical lives of nursing students depends on the degree to which it is promoted by academics, the extent to which it is incorporated into course objectives, content and assessments; and its application to clinical practice.
In a study by Hickman, Kelly and Phillips ( 2014 :603) on exploring ways to optimise the uptake of EBP to undergraduate nurses, findings indicated that students were initially hesitant and reluctant towards the subject of research. However, as they advanced with the subject their perceptions and beliefs changed to understanding the relevance of the research subject and its importance in improving patient outcomes.
Students’ lack of computer skills is another challenge that nurse educators encountered. Students are fully dependent on them for these skills and more time is needed to orientate students on how to use the computers. The use of EBP requires searching of information from the Internet. To accomplish this one must be able to use computers to search for information. These are the quotes from participants:
‘When you ask students for instance, initially we had challenges with them not knowing, because you find that at school they never did anything that has to do with computers, like any classes and now when they come here they have to sit in front of the computer, they do not even know what the mouse is, you know.’ (Participant 3, Senior, 50 years old) ‘So, I would love to see in the initial stage of training, this newly employed student nurses to have a basic course in computer literacy so that when we send them to fish information or explore they have the skills on how to like do internet surfing, go through the specific web, SANC web and etc., so that we are offload with them relying on us with computer skills.’ (Participant 9, HOD, 59 years old)
Increasing competence in information literacy is the foundation for EBP; this provides nurses with the skills to be literate consumers of information in an electronic environment (Emanuel et al. 2011 :22). According to Emmanuel et al. ( 2011 :23), advances in IT have had a radical impact on health care delivery and nurse education. The use of sophisticated equipment and electronic assessment care packages requires nurses to be competent in IT skills.
For students to be ready for EBP learning, they need to have good basic computer skills and to develop the right attitude towards learning using EBP. Their learning styles must support the inculcation of EBP. Fostering a culture of EBP in student nurses is essential to delivering effective health care (Leufer & Clearly-Holdforth 2007 :4) and it is also important that student nurses be equipped with EBP knowledge and skills to encourage evidence-informed decision-making after graduation (Schoonees et al. 2017 :1). Students should have the right attitude for functioning as independent health care providers (Young et al. 2015 :354). Nursing education institutions (NEIs) have a responsibility to provide support to student nurses in the development of relevant IT skills. This calls for services of the librarian to provide skills to student nurses in searching electronic databases for evidence. Clinical librarians in health services have to promote information literacy in the workplace. Health-related degree programmes need to adopt and incorporate EBP methods into their curricula to prepare practitioners in training for their future professional roles and responsibilities (Spring & McCuskey 2010 :249).
The recommendations that were made by the participants concerning student nurses were about creating good networking between the clinical practitioners and nurse educators to support the student nurses, providing students with basic computer skills so that they can work independently, and introducing a reward system as motivation for student nurses who are doing well.
Theme 2: Benefits and value of evidence-based practice in teaching and learning
Although some studies indicated that the main barrier to EBP is lack of value for EBP (Melnyk et al. 2012 :415), this study revealed that participants also believed that integration of EBP in teaching and learning as the best way to follow. It showed ways in which EBP teaching and learning could benefit the nurse educator, the nursing education discipline, student nurses, patients, and the employer or institution. Evidence-based practice is associated with critical-thinking skills which must be developed among the student nurses, and lifelong learning for nurses, to expand their knowledge and quality of care related to patient and health care facilities (Felicilda-Reynaldo & Utley 2015 :91-92). The following categories of information offer the benefits that come with implementation of EBP in teaching and learning.
Category 2.1: Keeping up to date with current information
Participants believed that EBP empowers and enriches the nurse educators and student nurses with up-to-date information, thus keeping their knowledge current. They also believe that EBP is based on researched international studies, and grounded on expert knowledge. These remarks were made by participants:
‘I think it is the best way to do your teaching and learning because you have evidence to base your information on.’ (Participant 1, Junior, 40 years old) ‘The other thing, you will find that you do not have to waste more time trying to give information to the students because everything is there.’ (Participant 1, Junior, 40 years old) ‘Again, that are not going to be having people that would be having something that is outdated, again when we actually engage in that we also update ourselves as lecturers.’ (Participant 12, Senior, 60 years old)
Nurse educators displayed a positive attitude and appeared to be very supportive of EBP teaching and learning. Reinforcing this statement, Mehrdad et al. ( 2012 :507) reported that nurses’ knowledge and attitude towards EBP contribute to its implementation in health care. Therefore, nurse educators and nursing students need to keep up to date with current evidence for use in practice. Current practices relied on by senior nurses and nurse educators are frequently based on personal experience, tradition, intuition, and organisational policies or protocols, rather than on evidence (Malik et al. 2015 b:47).
There is a belief that the use of up-to-date scientific findings will improve the quality of care for patients and fill the gap between research, theory, and practice (Mehrdad et al. 2012 :509). It is important that nurses use evidence to ensure their practice is up to date and based upon the best available research (Hickman et al. 2014 :604). Malik et al. ( 2015 a:159) emphasise that the health professionals are required to be using up-to-date knowledge and evidence to guide their decisions, hence improving patient care. In order for nursing education to keep up with the changes in nursing and health care, such professionals should be immersed in EBP (Felicilda-Reynaldo & Utley 2015 :92).
Category 2.2: Preparing student nurses to engage in evidence-based practice
According to the nurse educators, student nurses lack interest in research. However, once they become involved with research activities, the tendency is for students gradually to develop more interest and a concomitantly positive attitude towards research. Equally, increased motivation and eagerness to learn is noticed. The following statement was reported:
‘But when they come back from the library with those articles you could see that they are now developing interest you know, they are developing interest, they seem to understand it is like now there is that curtain that has fallen away so they can see now the light in this research.’ (Participant 6, Senior, 56 years old)
Hickman et al. ( 2014 :603) agree that developing the EBP capabilities of the emerging nursing workforce is essential in improving patient outcomes, promoting organisational efficiencies and creating a satisfying work environment. Engaging students in applying evidence into professional practice is a critical role of nursing faculties. This results in student nurses gaining confidence in the use of research and EBP to inform decision-making. Hickman et al. ( 2014 :603-604) further reveal that students demonstrated the ability to identify, criticise, and translate research to practice owing to the increased understanding. Students also understood the difference between research and EBP and how one informs the other. Therefore, teaching concepts of EBP to student nurses to enable them to recognise and deliver high-quality care that is evidence-based is a key outcome of all nurse education programmes (Leufer & Clearly-Holdforth 2015 :4).
Category 2.3: Improvement to quality care for patients
Evidence-based practice allows for individualised care, improvement in quality care leading to quick recovery of patients and shortened period of hospitalisation which saves money for patients. Participants stated the following:
‘Research helps in the improvement in the quality of care and in how quick the patient recovers or how long he stays ill in the ward.’ (Participant 3, Senior, 50 years old) ‘I think the benefits, the benefits are, because EBP is more patient centered I think and therefore it is beneficial and also sometimes it becomes meaningful, you can even individualize the care to the patient based on that EBP and the outcome of that so I think it is beneficial in that way but eh those are the benefits I think and also improvement, improvement in patient care.’ (Participant 8, Junior, 53 years old)
When patient care is informed by sound evidence, it results in better and more affordable care towards people and the community. Nursing evolved from a series of dictated tasks to a holistic care approach which requires evidence that is developed into guidelines. These guidelines support nurses to promote individualised care (Emmanuel et al. 2011 :22).
Evidence-based practice is a patient-centred approach as it influences patient care and minimises the theory-practice gap with nursing (Mackey & Bassendowski 2016 :53). The main aim of EBP is to optimise outcomes for patients and clients by selecting interventions that have the greatest chance of success (Leufer & Clearly-Holdforth 2015 :4).
Category 2.4: Reducing health care delivery cost
The use of EBP leads to improvement in the quality of care, thus reducing patient stay in hospital. Although quality is sometimes expensive, it comes with positive implications for health care facilities, for example, when patients receive quality care, their recovery is quicker and the numbers of days spent in hospital are reduced, resulting in reduction of patient-care costs. Therefore, the employer and institutions benefit positively from the use of EBP because of the end result, which is improvement in the patient outcomes. One participant reported that:
‘You know I feel like with EBP teaching and learning, it will be more important to use more in the clinical area.’ (Participant 10, Senior, 59 years old)
For the health institutions to provide effective services, their functioning, planning, policies, and guidelines are informed by researched evidence. The following statements were reported:
‘I think EBP will be an excellent way to have proficient and efficient nurses in the ward.’ (Participant 5, Junior, 50 years old) ‘You get in improvement, quality improvement in nursing care and you find that with research, research helps in the improvement in the quality of care and in how quick the patient recovers or how long he stays ill in the ward.’ (Participant 4, HOD, 56 years old)
Reducing health care costs requires that nursing and health care services be based on best current available evidence. Improved cost-effectiveness of the health institutions allows the administrators the ability to negotiate for better sponsorship and incentives from health care funders and insurers (Levin et al. 2011 :22).
Evidence-based practice teaching and learning is not explicitly implemented. The current curriculum (R425) does not have any specific guidelines for EBP teaching and learning; it only requires that research processes and steps to conduct research projects be taught to student nurses. For KZNCN, the research module is taught at third-year level, and it is covered under the Community Nursing Science component. The learner study guide only requires the nursing students to conduct and present a mini research project. There is no mention of EBP skills or competencies that must be acquired or achieved.
The researchers concluded that the information generated as experiences of nurse educators is not directly linked to EBP in teaching and learning: it was more about teaching and learning of research in general. Nevertheless, EBP depends for its success on researched information. Research is conducted to develop evidence that may be used for EBP. The utilisation of researched evidence in practice is known as EBP. It is never easy to separate research from EBP because one complements the other. However, it remains the responsibility of the NEIs to encourage student nurses to promote and deliver EBP from the onset of training; therefore, the principles of EBP should be introduced to students as part of pre-registration education (Emmanuel et al. 2011 :21).
Lack of resources was one of the challenges mentioned by most of the nurse educators, mainly the physical resources like lack of or poor access to computers and libraries. Non-availability of Internet access, current books, journals, and articles also contributed to poor access to relevant evidence needed for successful implementation of EBP teaching and learning.
From the list of teaching strategies identified by nurse educators, it was clear that traditional teaching strategies are still dominant in nursing education. Such strategies do not promote or stimulate critical-thinking skills and EBP competencies to student nurses. A teaching method is understood to be a particular technique a teacher uses to help learners gain the knowledge which they need and to achieve a desired outcome. A desired outcome in this context is the development of critical thinking, problem-solving and good decision-making skills for student nurses, which can be achieved by the use of EBP in teaching and learning as one of the innovative teaching strategies.
Though it transpired that most nurse educators were supportive and had a positive attitude towards the implementation of EBP in teaching and learning, their level of knowledge and skills was questionable; there was uncertainty in understanding the use of EBP in teaching and learning; and a lack of motivation and commitment towards research was evident. Malik et al. ( 2015 b:46), in a tertiary health care facility in Victoria, Australia, investigated the perceptions of nurse educators on factors promoting EBP and perceived barriers to facilitating EBP in a clinical setting before developing an educational programme. The findings revealed that nurse educators had positive attitudes towards EBP implementation. However, they demonstrated a lack of knowledge and skills in appraising and incorporating evidence into practice. Nurse educators cannot be expected to teach what is not known to them, therefore; they must be equipped with knowledge and skills so that they can teach EBP to produce professional nurses who are competent in evidence-based care (Melnyk et al. 2012 :416).
Limitations
It may not be possible to generalise the findings to all nurse educators because the study was limited to nurse educators who work in the public institutions under Umgungundlovu Health District, and who only provide R425 comprehensive 4-year programmes at two campuses. Therefore, findings cannot be generalised to private institutions like universities, other districts, provinces or even nationally and for other nursing programmes.
Recommendations
The current curriculum (R174) should be reviewed and restructured to allow for early introduction of EBP principles at the onset of training. In addition, online and telematics studies together with the use of mobile technologies should be included in the curriculum.
Relevant adequate resources should be made available and accessible to nurse educators and nursing students. Access to sufficient clinical facilities that are appropriate for the achievement of the outcomes of the programme should also be considered.
Nurse educators should be supported through in-service training, workshops and affiliation to journal clubs to improve their knowledge and skills regarding EBP competencies.
The findings revealed both the challenges and benefits that come with the use of EBP in teaching and learning skills for the nursing education discipline, thus paving the way for the implementation of the suggested recommendations. Evidence-based practice has an essential potential role to play through incorporating more practice-based evidence of nurse educators in teaching and learning implementation. Therefore, nurse educators should use EBP to ensure that student nurses receive high-quality nursing education.
Acknowledgements
Thanks to Dr D.K.S. Habedi for her assistance and supervision in writing this article. I am also thankful to the participants for their willingness to contribute in the study.
Competing interests
The authors declare that there are no competing interests with regard to the writing of this article.
Authors’ contributions
G.N.M. is the author of the article and conducted the research. D.S.K.H. provided guidance and assisted with the writing of the manuscript.
How to cite this article: Mthiyane, G.N. & Habedi, D.S., 2018, ‘The experiences of nurse educators in implementing evidence-based practice in teaching and learning’, Health SA Gesondheid 23(0), a1177. https://doi.org/10.4102/hsag.v23i0.1177
1 The author understands and acknowledges the sensitivity of the terms used and prefers to use as classified according to the Republic of South Africa’s Government Application Form for Employment in order to avoid misinterpretation of the study results.
- Boswell C. & Cannon S., 2017, Introduction to nursing research , 4th edn., Jones & Bartlett Learning, TX. [ Google Scholar ]
- Brink H., Van der Walt C. & Van Rensburg G., 2012, Fundamentals of research methodology for healthcare professionals , 3rd edn., Juta & Company Ltd, Cape Town. [ Google Scholar ]
- Emmanuel V., Day K., Diegnan L. & Pryce-Miller M., 2011, ‘ Developing evidence-based practice among students ’, Nursing Times 107 ( 49/50 ), 21–23. [ PubMed ] [ Google Scholar ]
- Felicilda-Reynaldo R.D. & Utley R., 2015, ‘ Reflections of evidence-based practice in nurse educators teaching philosophy statements ’, Nursing Education Perspectives 36 ( 2 ), 89–94. 10.5480/13-1176 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Heikkila J., Hopia H., Hasselberg J., Tiittanen H. & Biaghorzina Z., 2017, ‘ A cross sectional study of nurses’ and nurse educators’ perceptions of evidence-based practice in Kazakhstan ’, Annals of Nursing Research and Practice 2 ( 1 ), 1016. [ Google Scholar ]
- Hickman D.L., Kelly H. & Phillips J.l., 2014, ‘ EVITEACH: A study exploring ways to optimize the uptake of EBP to undergraduate nurses ’, Nurse Education in Practice 14 , 598–604. 10.1016/j.nepr.2014.05.013 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hussein A.H.M. & Hussein R.G., 2013, ‘ The attitudes and barriers towards evidence-based practice among nurse educators ’, Journal of American Science 9 , ( 12 ), 609–618. [ Google Scholar ]
- Hussein A.H.M. & Hussein R.G., 2014, ‘ Nursing educators’ knowledge, skills in evidence-based practice and their critical thinking skills. Self-report study ’, Journal of Education and Practice 5 ( 27 ), 860–894. [ Google Scholar ]
- Lehane E., Leahy Warren L., O’Riodan C., Savage E., Drennan J., O’Tauthaigh C. et al., 2017, Research on teaching of evidence-based practice in Ireland to healthcare professionals and healthcare students , Report prepared for the Department of Health, Clinical Effectiveness Unit, viewed n.d., from http/[email protected] .
- Leufer T. & Clearly-Holdforth J., 2015, ‘ Advancing evidence-based practice through nurse education ’, Care 1 ( 1 ), viewed 10 May 2018, from http//www.researchgate.net/publication/266370377 . [ Google Scholar ]
- Leufer T. & Clearly-Holdforth J., 2007, ‘ Essential elements in developing evidence-based Practice ’, Nursing Standard 23 ( 2 ), 42–46. 10.7748/ns2008.09.23.2.c6670 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levin R.F., Fineout-Overholt E., Menlyk B.M., Barnes M. & Vetter M.J., 2011, ‘ Fostering evidence-based practice to improve nurse and cost outcomes in a community health setting: A pilot test of the advancing research and clinical practice through close collaboration model ’, Nursing Administration Quarterly 35 ( 1 ), 21–33. https://doi.org/10.1097NAQ.0b13e31820320ff [ PubMed ] [ Google Scholar ]
- Mackey A. & Bassendowski S., 2016, ‘ The history of evidence-based practice in nursing education and practice ’, Journal of Professional Nursing 33 ( 1 ), 51–55. 10.1016/j.profnurs.2016.05.009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Malik G., McKenna L. & Griffiths D., 2015a, ‘ An analysis of evidence-based practice curriculum integration in Australian undergraduate nursing programs ’, GSTF Journal of Nursing and Health Care 3 ( 1 ), 158–164. 10.5176/2345-718X-3.1.104 [ CrossRef ] [ Google Scholar ]
- Malik G., McKenna L. & Plummer V., 2015b, ‘ Perceived knowledge, skills, attitudes and contextual factors affecting evidence-based practice among nurse educators, clinical coaches and nurse specialists ’, International Journal of Nursing 21 ( 2 ), 46–57. [ PubMed ] [ Google Scholar ]
- Mehrdad N., Joolaee S., Joolaee A.,& Bahrani N., 2012, ‘ Nursing faculties’ knowledge and attitude on evidence-based practice ’, Iranian Journal of Nursing Midwifery Research 17 ( 7 ), 506–511. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Melnyk B.M., Fineout-Overholt E., Gallagher-Ford L. & Kaplan L., 2012, ‘ The state of evidence-based practice in US nurses: Clinical implications for nurse leaders and educators ’, JONA 2 ( 9 ), 410–417. [ PubMed ] [ Google Scholar ]
- Moule P. & Goodman M., 2014 Nursing research: An introduction , 2nd edn., Sage, Los Angeles, CA. [ Google Scholar ]
- Mthiyane G.N., 2018, ‘ The experiences of nurse educators in implementing evidence-based practice in teaching and learning ’, Masters dissertation, University of South Africa, Pretoria. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Polit D.F. & Beck C.T., 2017, Nursing research: Generating and assessing evidence for nursing practice , 10th edn., Wolters Kluwer, Lippincott Williams & Wilkins, Philadelphia, PA. [ Google Scholar ]
- Schoonees A., Rohwer A. & Young T., 2017, ‘ Evaluating evidence-based health care teaching and learning in the undergraduate human nutrition; occupational therapy; physiotherapy; and speech, language and hearing therapy programs at a sub-Saharan African academic institution ’, PLoS One 12 ( 2 ), 0172199 10.137/journal.pone.0172199 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Spring H. & McCluskey C., 2010, ‘ Learning and teaching in action ’, Health Libraries Group Health Information and Libraries Journal 27 , 249–252. 10.1111/j.1471-1842.2010.00894.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Subhan M.S., 2014, Current pedagogic strategies being used by educators at KwaZulu-Natal College of Nursing campuses across varied subjects and their views regarding innovation methodology , viewed 10 May 2018, from ir.dut.ac.za/bitstream/handle/10321/1262/Subhan_2014.pdf?Sequence=1
- Young T., Rohwer A., Volmink J. & Clarke M., 2015, ‘ Perspectives of undergraduate module convenors at South African academic institution on medical student training in evidence-based health care: A qualitative study ’, South African Family Practice 57 ( 6 ), 354–360. 10.1080/20786190.2015.1090689 [ CrossRef ] [ Google Scholar ]

COMMENTS
The Essentials documents published by the American Association of Colleges of Nursing (AACN) have guided curricular development across baccalaureate and higher degree programs since the mid-1980s (AACN, 2019a).In response to shifts within healthcare delivery, AACN began revisions to the Essentials documents in 2018. Since that time, collaboration between academe and practice has resulted in a ...
The Future of Nursing Education: Reimagined is a special issue of the journal Nursing Education Perspectives that explores how nursing education can adapt to the changing needs and challenges of the health care system. The issue features articles on topics such as curriculum transformation, diversity and inclusion, interprofessional education, simulation, technology, and innovation. The issue ...
Leaders in nursing education have initiated efforts to appraise the state of the academy and find approaches to lessen the transition gap, such as competency-based education. ... H. H. (2018). Using technologies in nursing research education: A mixed methods case study. Computers, Informatics, Nursing, 36(6), 293-304. doi: 10.1097/CIN ...
Throughout the coming decade, it will be essential for nursing education to evolve rapidly in order to prepare nurses who can meet the challenges articulated in this report with respect to addressing social determinants of health (SDOH), improving population health, and promoting health equity. Nurses will need to be educated to care for a population that is both aging, with declining mental ...
Nursing Education Perspectives is the official research journal of the National League for Nursing. Lean more about the journal and subscribe today! ... Nursing Education Perspectives. 44(6):380-381, November/December 2023. Abstract. Favorite; PDF. Permissions Buy ...
Introduction. Clinical education of undergraduate nurses remains an integral part of the nursing curriculum and forms the foundation for bridging the theory-practice gap (Wells & McLoughlin 2014).Therefore, the nursing curriculum needs to be aligned to the clinical setting to ensure that graduates are equipped to face the challenges of complex and dynamic healthcare delivery system (Bvumbwe 2016).
This was a qualitative study aimed to explaining the nursing students' views and experiences concerning the problems and limitations of the current nursing education system. The students described the teaching methods as traditional and teacher-centered, inevitably resulting in minimal student participation.
Simulation-based experiences encompass a variety of teaching and learning methodologies. The INACSL Standards Committee (2016b) defines a simulation-based experience as, "A broad array of structured activities that represent actual or potential situations in education, practice, and research" (p.S45). The most significant research in the role and outcomes of simulation in prelicensure ...
A New Era. Oermann, Marilyn H. PhD, RN, ANEF, FAAN. Author Affiliation: Editor-in-Chief, Nurse Educator, and Thelma M. Ingles Professor of Nursing, Duke University School of Nursing, Durham, North Carolina. The author declares no conflicts of interest. Correspondence: Dr Oermann, Duke University School of Nursing, DUMC 3322, 307 Trent Drive ...
Background Modern and active learning methods form an important part in the education of Nursing students. They encourage the development of communication and critical thinking skills, and ensure the safe health care of patients. Our aim was to obtain naturalistic data from nurse educators regarding want the use and effects of implementing active learning methods (Peyton's Four-Step Approach ...
A Paradigm Shift for the Nursing Education Model: A Scoping Review. Mary Jo Stanley, PhD, RN, CNE and. Kathleen Hall, PhD, APRN, GNP-BC, AGPCNP-BC. Vol. 63, No. 3 pp 141-147March 01, 2024. Purchase Save for later. Journal of Nursing Education 2024 Electronic Only $171.00. Journal of Nursing Education 2024 Print & Electronic $222.00.
Nurse Education Today is the leading international journal providing a forum for the publication of high quality original research, review and debate in the discussion of nursing, midwifery and interprofessional health care education, publishing papers which contribute to the advancement of educational theory and pedagogy that support the evidence-based practice for educationalists worldwide.
Nursing skill teaching is an important part of basic nursing course. In the teaching course structure of basic nursing for undergraduate nursing students, the proportion of class hours accounts for 50% to 60%. 6 The traditional nursing skill teaching method is "demonstration-practice-guidance," which focuses on nursing students to master the skill operation through imitation of the ...
Regarding human subjects' review for studies involving students, faculty, or academic administrators, the majority of journals (n = 32, 86.5%) always required a review by an IRB or other ethics committee for research studies, and 17 (45.9%) required the same for educational quality improvement projects (Table 2).One respondent offered that a review by the IRB or other ethics committee was ...
A literature search completed in the Cumulative Index to Nursing and Allied Health Literature and PubMed/MEDLINE, using the search terms of nursing education or curriculum development and implementation science, yielded 165 results. The majority of articles focused on using educational strategies to implement evidence-based interventions in ...
The Journal of Nursing Education is a monthly, peer-reviewed journal publishing original articles and new ideas for nurse educators in various types and levels of nursing programs for over 60 years. The Journal enhances the teaching-learning process, promotes curriculum development, and stimulates creative innovation and research in nursing education.
RESULTS: The 2 main categories, 7 subcategories, and 19 sub-sub categories extracted from interviews. The two categories were "challenges of clinical education in nursing with four subcategories: fear, insufficient readiness of student, incompetency of clinical educators, unpleasant atmosphere of clinical environment," and "strategies for improving clinical education of nursing with ...
Background Using virtual patients integrated in simulators expands students' training opportunities in healthcare. However, little is known about the usability perceived by students and the factors/determinants that predict the acceptance and use of clinical virtual simulation in nursing education. Objectives To identify the factors/determinants that predict the acceptance and use of ...
Nursing Education Perspectives is the official research journal of the National League for Nursing. Lean more about the journal and subscribe today! ... A Dynamic Relationship Between Theory and Research in Nursing Education. Patterson, Barbara J. Nursing Education Perspectives. 42(6):337-338, November/December 2021. ...
Nursing Outlook. Impact factor: 2.540 (source - journal website) Overview: Nursing Outlook is the official journal of both the American Academy of Nursing and the Council for the Advancement of Nursing Science. It publishes peer-reviewed articles and reports that focus on " current issues and trends in nursing practice, education and research
This article focuses on the unique needs and concerns of nursing educators and nursing students in the face of the COVID-19 pandemic. Drawing from firsthand experience as nurse educators leading clinical courses in a post-licensure nursing program, we consider some of the early lessons as we face this health crisis.
Evidence-based practice in nursing involves providing holistic, quality care based on the most up-to-date research and knowledge rather than traditional methods, advice from colleagues, or personal beliefs. Nurses can expand their knowledge and improve their clinical practice experience by collecting, processing, and implementing research findings.
Journal of Research in Nursing publishes quality research papers on healthcare issues that inform nurses and other healthcare professionals globally through linking policy, research and development initiatives to clinical and academic excellence. View full journal description. This journal is a member of the Committee on Publication Ethics (COPE).
Introduction. One of the essential requirements of healthcare systems to meet the broad needs of patients is the employment of well-qualified nurses [].In this respect, one of the important responsibilities of nursing education systems is providing high-quality education to nursing students and preparing competent nurses so that they can provide patients with safe and high-quality care in the ...
Earning a degree is almost always worthwhile, research shows, but some majors pay off more than others.
Evidence-based practice teaching and learning has become an important function for nursing education. Research is used as an instrument in developing new teaching and learning strategies. Nurse educators are guided by evidence-based practice in teaching and on research reports. ... Moule P. & Goodman M., 2014 Nursing research: An introduction ...