- Patient Care & Health Information
- Diseases & Conditions
- Schizophrenia
Schizophrenia is a serious mental disorder in which people interpret reality abnormally. Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behavior that impairs daily functioning, and can be disabling.
People with schizophrenia require lifelong treatment. Early treatment may help get symptoms under control before serious complications develop and may help improve the long-term outlook.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Schizophrenia involves a range of problems with thinking (cognition), behavior and emotions. Signs and symptoms may vary, but usually involve delusions, hallucinations or disorganized speech, and reflect an impaired ability to function. Symptoms may include:
- Delusions. These are false beliefs that are not based in reality. For example, you think that you're being harmed or harassed; certain gestures or comments are directed at you; you have exceptional ability or fame; another person is in love with you; or a major catastrophe is about to occur. Delusions occur in most people with schizophrenia.
- Hallucinations. These usually involve seeing or hearing things that don't exist. Yet for the person with schizophrenia, they have the full force and impact of a normal experience. Hallucinations can be in any of the senses, but hearing voices is the most common hallucination.
- Disorganized thinking (speech). Disorganized thinking is inferred from disorganized speech. Effective communication can be impaired, and answers to questions may be partially or completely unrelated. Rarely, speech may include putting together meaningless words that can't be understood, sometimes known as word salad.
- Extremely disorganized or abnormal motor behavior. This may show in a number of ways, from childlike silliness to unpredictable agitation. Behavior isn't focused on a goal, so it's hard to do tasks. Behavior can include resistance to instructions, inappropriate or bizarre posture, a complete lack of response, or useless and excessive movement.
- Negative symptoms. This refers to reduced or lack of ability to function normally. For example, the person may neglect personal hygiene or appear to lack emotion (doesn't make eye contact, doesn't change facial expressions or speaks in a monotone). Also, the person may lose interest in everyday activities, socially withdraw or lack the ability to experience pleasure.
Symptoms can vary in type and severity over time, with periods of worsening and remission of symptoms. Some symptoms may always be present.
In men, schizophrenia symptoms typically start in the early to mid-20s. In women, symptoms typically begin in the late 20s. It's uncommon for children to be diagnosed with schizophrenia and rare for those older than age 45.
Symptoms in teenagers
Schizophrenia symptoms in teenagers are similar to those in adults, but the condition may be more difficult to recognize. This may be in part because some of the early symptoms of schizophrenia in teenagers are common for typical development during teen years, such as:
- Withdrawal from friends and family
- A drop in performance at school
- Trouble sleeping
- Irritability or depressed mood
- Lack of motivation
Also, recreational substance use, such as marijuana, methamphetamines or LSD, can sometimes cause similar signs and symptoms.
Compared with schizophrenia symptoms in adults, teens may be:
- Less likely to have delusions
- More likely to have visual hallucinations
When to see a doctor
People with schizophrenia often lack awareness that their difficulties stem from a mental disorder that requires medical attention. So it often falls to family or friends to get them help.
Helping someone who may have schizophrenia
If you think someone you know may have symptoms of schizophrenia, talk to him or her about your concerns. Although you can't force someone to seek professional help, you can offer encouragement and support and help your loved one find a qualified doctor or mental health professional.
If your loved one poses a danger to self or others or can't provide his or her own food, clothing, or shelter, you may need to call 911 or other emergency responders for help so that your loved one can be evaluated by a mental health professional.
In some cases, emergency hospitalization may be needed. Laws on involuntary commitment for mental health treatment vary by state. You can contact community mental health agencies or police departments in your area for details.
Suicidal thoughts and behavior
Suicidal thoughts and behavior are common among people with schizophrenia. If you have a loved one who is in danger of attempting suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
It's not known what causes schizophrenia, but researchers believe that a combination of genetics, brain chemistry and environment contributes to development of the disorder.
Problems with certain naturally occurring brain chemicals, including neurotransmitters called dopamine and glutamate, may contribute to schizophrenia. Neuroimaging studies show differences in the brain structure and central nervous system of people with schizophrenia. While researchers aren't certain about the significance of these changes, they indicate that schizophrenia is a brain disease.
Risk factors
Although the precise cause of schizophrenia isn't known, certain factors seem to increase the risk of developing or triggering schizophrenia, including:
- Having a family history of schizophrenia
- Some pregnancy and birth complications, such as malnutrition or exposure to toxins or viruses that may impact brain development
- Taking mind-altering (psychoactive or psychotropic) drugs during teen years and young adulthood
Complications
Left untreated, schizophrenia can result in severe problems that affect every area of life. Complications that schizophrenia may cause or be associated with include:
- Suicide, suicide attempts and thoughts of suicide
- Anxiety disorders and obsessive-compulsive disorder (OCD)
- Abuse of alcohol or other drugs, including nicotine
- Inability to work or attend school
- Financial problems and homelessness
- Social isolation
- Health and medical problems
- Being victimized
- Aggressive behavior, although it's uncommon
There's no sure way to prevent schizophrenia, but sticking with the treatment plan can help prevent relapses or worsening of symptoms. In addition, researchers hope that learning more about risk factors for schizophrenia may lead to earlier diagnosis and treatment.
- Schizophrenia. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. American Psychiatric Association; 2013. https://dsm.psychiatryonline.org. Accessed Sept. 5, 2019.
- AskMayoExpert. Schizophrenia (adult). Mayo Clinic; 2018.
- Valton V, et al. Comprehensive review: Computational modeling of schizophrenia. Neuroscience and Biobehavioral Reviews. 2017; doi:10.1016/j.neubiorev.2017.08.022.
- Fisher DJ, et al. The neurophysiology of schizophrenia: Current update and future directions. International Journal of Psychophysiology. 2019; doi:10.1016/j.ijpsycho.2019.08.005.
- Schizophrenia. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/schizophrenia/index.shtml. Accessed Sept. 5, 2019.
- Schizophrenia. National Alliance on Mental Illness. https://www.nami.org/learn-more/mental-health-conditions/schizophrenia. Accessed Sept. 5, 2019.
- What is schizophrenia? American Psychiatric Association. https://www.psychiatry.org/patients-families/schizophrenia/what-is-schizophrenia. Accessed Sept. 5, 2019.
- Schizophrenia. Merck Manual Professional Version. https://www.merckmanuals.com/professional/psychiatric-disorders/schizophrenia-and-related-disorders/schizophrenia. Accessed Sept. 5, 2019.
- How to cope when a loved one has a serious mental illness. American Psychological Association. https://www.apa.org/helpcenter/serious-mental-illness. Accessed Sept. 5, 2019.
- Supporting a friend or family member with mental health problems. MentalHealth.gov. https://www.mentalhealth.gov/talk/friends-family-members. Accessed Sept. 5, 2019.
- For people with mental health problems. MentalHealth.gov. https://www.mentalhealth.gov/talk/people-mental-health-problems. Accessed Sept. 5, 2019.
- Roberts LW, ed. Schizophrenia spectrum and other psychotic disorders. In: The American Psychiatric Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Publishing; 2019.
- Schak KM (expert opinion). Mayo Clinic. Dec. 11, 2019.
- Leung, JG (expert opinion). Mayo Clinic. Dec. 10, 2019.
Associated Procedures
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
This topic discusses clinical manifestations, diagnosis, and course of schizophrenia. The epidemiology and pathogenesis of schizophrenia in adults and children, and their treatment are discussed separately.
● (See "Psychosis in adults: Epidemiology, clinical manifestations, and diagnostic evaluation" .)
● (See "Schizophrenia in adults: Epidemiology and pathogenesis" .)
● (See "Depression in schizophrenia" .)
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- Winter 2024 | VOL. 22, NO. 1 Reproductive Psychiatry: Postpartum Depression is Only the Tip of the Iceberg CURRENT ISSUE pp.1-142
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Schizophrenia: An Overview
- Tahir Rahman , M.D. , and
- John Lauriello , M.D.
Search for more papers by this author
Few changes were made to the diagnostic criteria for schizophrenia in DSM-5 . Schizophrenia is a chronic mental illness with positive symptoms (delusions, hallucinations, disorganized speech and behavior), negative symptoms, and cognitive impairment. Discoveries in genetics, neuroimaging, and immune function continue to advance understanding of the etiologies for this elusive disease. The authors reviewed the current literature to give an overview. The topics include historical foundations, epidemiology, suicide risk, genomewide association studies, twin studies, neuroimaging, ventricular size, complement component 4 mediated synapse elimination, major histocompatibility complex markers, and associations seen in obstetrical complications, nutritional issues, prodromal and attenuated states, cannabis use, childhood trauma, immigration, and traumatic brain injury. Also reviewed are expressed emotions of caregivers and recidivism, conditions comorbid with obsessive-compulsive disorder, mood disorders, substance use, and finally some legal and ethical issues. These important developments in elucidating the disease mechanism will likely allow for the development of future novel treatment strategies.
A homeless man arrives at the emergency room, reporting that his brother is a space alien who is trying to take over the world. The man claims to hear voices and feel the presence of aliens in his body that are controlling his thoughts and actions. Such bizarre presentations are often seen among psychotic patients diagnosed as having schizophrenia. Physicians beginning to practice psychiatry are often drawn to the field after seeing patients with dramatic psychotic symptoms and soon learn that the illness is quite complex. Schizophrenia is a chronic psychiatric illness characterized by positive symptoms (delusions, hallucinations, and grossly disorganized speech and behavior), negative symptoms (apathy, social isolation, and diminished affect), and cognitive impairment ( 1 ). Any combination of these symptoms can lead to marked disruption in behavior and significant negative effects on functioning and an increased risk for the development of many comorbid health problems, suicide risk, and substance use disorders. Despite advances in epidemiology, genetics, and neuroimaging, psychiatrists still rely on a comprehensive history, physical exam, and laboratory studies to diagnose schizophrenia. The exact etiologic factors remain elusive. It is by definition a diagnosis made after the exclusion of other possible conditions such as a mood disorder, substance abuse, or certain medical conditions. We begin by discussing historical foundations of this illness, and DSM-5 criteria, and we review the epidemiologic, genetic, and neuroanatomical markers seen in this disease.
Historical Foundations
In 1911, the Swiss psychiatrist Eugene Blueler chose the Greek roots “schizo” (split) and “phrene” (mind) to describe the disorganized thinking of people with schizophrenia. Arnold Pick had noted in 1891 both psychotic and cognitive deficits among those with this disorder and called it “dementia praecox.” More notably, Emil Kraepelin in 1893 differentiated the episodic nature of psychosis seen in manic-depression from dementia praecox ( 2 ). Kurt Schneider tried to distinguish various forms of psychotic symptoms that he thought had special value in distinguishing schizophrenia from psychosis resulting from other disorders. These are known as Schneider's “first-rank” symptoms. They include passivity experiences, such as bizarre delusions of being controlled by an external force, thought insertion or withdrawal, and thought broadcasting. He used the German term gedankenlautwerden to describe the auditory hallucinations in schizophrenia as voices that are heard aloud. These voices could comment on an individual’s thoughts or behavior. The individual could also hear third-person conversations with other hallucinated voices talking to each other ( 3 ). Blueler, Kraepelin, Schneider, and other pioneers of psychiatry based schizophrenia’s classification on the observation that many psychotic symptoms tend to occur together. Despite such elegant descriptions, extensive diagnostic evaluations and follow-up have shown that there are no specific psychotic symptoms that are pathognomonic for schizophrenia. Schizophrenia was also traditionally subclassified into disorganized, catatonic, paranoid, residual, or undifferentiated types. These subtypes have not been shown to be reliable or predictive of outcome of the disorder and were eliminated in DSM-5 ( 4 ). The box on this page highlights the DSM-5 criteria for schizophrenia. If the full criteria are met but the duration of illness is less than six months, the diagnosis of schizophreniform disorder should be diagnosed.
DSM-5 CRITERIA FOR SCHIZOPHRENIA a
For a significant portion of the time since the onset of the disturbance, level of functioning in one or more major areas, such as work, interpersonal relations, or self-care, is markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, there is failure to achieve expected level of interpersonal, academic, or occupational functioning).
Continuous signs of the disturbance persist for at least 6 months. This 6-month period must include at least 1 month of symptoms (or less if successfully treated) that meet Criterion A (i.e., active-phase symptoms) and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or by two or more symptoms listed in Criterion A present in an attenuated form (e.g., odd beliefs, unusual perceptual experiences).
Schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out because either 1) no major depressive or manic episodes have occurred concurrently with the active-phase symptoms, or 2) if mood episodes have occurred during active-phase symptoms, they have been present for a minority of the total duration of the active and residual periods of the illness.
The disturbance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition.
If there is a history of autism spectrum disorder or a communication disorder of childhood onset, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations, in addition to the other required symptoms of schizophrenia, are also present for at least 1 month (or less if successfully treated).
Specify if:
The following course specifiers are only to be used after a 1-year duration of the disorder and if they are not in contradiction to the diagnostic course criteria.
Specify current severity:
_________________
a Reprinted from the Diagnostic and Statistical Manual of Mental Disorders , 5th ed. Washington, DC, American Psychiatric Association, 2013. Copyright © 2013, American Psychiatric Association. Used with permission.
Psychosis is generally defined as a break in reality testing either by abnormal sensory experiences, such as hallucinations, or by holding fixed false beliefs (delusions) that are not accepted by most people. Impairment is also commonly seen in thought and speech patterns. An individual with schizophrenia may develop disorganized speech that makes maintaining discourse during an interview difficult (formal thought disorder) ( 5 ). A few minor changes were made to the diagnostic criteria for schizophrenia from DSM-IV to DSM-5 . Five cardinal symptoms (delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms) are all still recognized in criterion A. However, two of the first three (delusions, hallucinations, and disorganized speech) are now required to make the diagnosis. The concept of bizarre hallucinations or commenting voices was given more credence in earlier diagnostic criteria, but the phenomena are no longer given special consideration (as Schneider believed they should) in DSM-5 ( 6 ).
Despite these changes in diagnostic criteria, it is imperative for clinicians to screen patients for the cardinal signs of psychosis and to clinically elicit the classical symptoms of the disorder. This often requires a careful mental status examination and the collection of external sources of information such as records and interviews of family members ( 1 , 7 ).
Epidemiology
The prevalence of schizophrenia is around 1% (0.3% to 0.7%) worldwide ( 1 , 8 ). The incidence is about 1.5 per 10,000 individuals. The male:female ratio is 1.4:1. The increased risk among men has been of interest to researchers. Some have suggested that this may result from higher drug use among men or a possible protective effect from contraceptive use among women ( 8 , 9 ). On the basis of a large genomewide association study, the genetic basis of schizophrenia is similar among males and females. Females are often diagnosed later than males, and males typically have a worse outcome ( 1 , 10 ). About 20% of patients with schizophrenia attempt suicide. There is a 5%−6% lifetime prevalence rate of completed suicide, making this a life-threatening disorder. However, most individuals with schizophrenia die of natural causes and have a mortality rate that is two to three times greater than the rest of the population. The disease often strikes patients in the prime of their young adult life. The adult incidence curve increases until it reaches its highest point in the mid-20s, then declines. A second, much smaller peak of increased incidence of schizophrenia is seen in the 40s, which is more common in females ( 1 , 11 ).
Individuals with schizophrenia are much more vulnerable to becoming homeless than are people with no mental illness. Some of the highest rates of schizophrenia are found in the chronically homeless population. A large public mental health system study found that 15% were homeless at the time of at least one service encounter in a one-year period. Male gender, African American ethnicity, presence of substance use disorder, and a lack of Medicaid insurance were associated with homelessness of patients diagnosed as having schizophrenia. Patients often develop a complex array of social, medical, psychiatric, and financial issues. High levels of general medical comorbidities are commonly found among patients with schizophrenia and add a tremendous burden to the health care needs and cost in this population. Earlier diagnosis and treatment may be of great importance to prevent a declining health and psychosocial course ( 10 , 12 , 13 ).
Genetic Studies
Schizophrenia is often thought to be a number of disorders sharing a similar presentation ( 1 , 14 ). This is because no specific gene or environmental factor explains the etiology for all of the affected individuals ( 15 ). Genetic research has not revealed a robust understanding of the etiology of schizophrenia. Instead, genomewide association studies (GWAS) have revealed only a few weak-effect associations, which account for only a small part of the genetic risk. A complex interplay of genes and environment is likely responsible for the similar presentations of schizophrenia. The total heritable risk for schizophrenia is 70%−80% ( 14 – 16 ). A large number of statistical analyses are needed to estimate the genetic and environmental aspects of variance. Estimates are sometimes obtained with large data sample sets from individuals with a close genetic relationship—such as twins and siblings—rather than from more distantly related individuals. It has been determined that the monozygotic twin concordance rate is 40%−50% and that the dizygotic twin concordance rate is 10%−15%. Offspring of the unaffected monozygotic twin are at increased risk of schizophrenia, and there is a high incidence of disease among adopted children whose biological mothers have a diagnosis of schizophrenia ( 15 ). The following are some genes that have been of interest to schizophrenia researchers: catechol O -methyltransferase (COMT), DAO/G30, DISC 1, DTNB 1, GABRB2, NRG 1, and ZNF804A. Rare deletions at 15q13 and 22q11 (DiGeorge syndrome) regions may also predispose individuals to schizophrenia ( 15 – 17 ). There is genetic support for the existence of common DNA variants (single nucleotide polymorphisms) that influence risk of both bipolar disorder and schizophrenia, differing from Kraeplin’s model, which assumes that these are two very separate entities ( 17 ).
GWASs have a greater power to detect weak associations to common variants. In 2014, the largest molecular genetic study of schizophrenia ever conducted was published by the schizophrenia genetics consortium. In this landmark schizophrenia GWAS, 108 conservatively defined loci met genomewide significance ( 18 ). Associations found that were relevant to hypotheses of the etiology and treatment of schizophrenia included DRD2 (the target of antipsychotic drugs) and multiple genes (e.g., GRM3, GRIN2A, SRR, GRIA1) involved in glutamatergic neurotransmission and synaptic plasticity. Epidemiological studies have also long hinted at a role for immune dysregulation involving the MHC in schizophrenia; the findings also provided genetic support for this hypothesis.
Another large multisite study was recently conducted to characterize 12 neurophysiological and neurocognitive endophenotypic measures in schizophrenia. Several genes of potential interest were identified: HTR6 on chromosome 1p36 (emotion recognition), ZNF804A on 2q32 (sensorimotor dexterity), ATXN7 on 3p14 (the antisaccade task), DAT on 5p15 (prepulse inhibition), GRIN2B on 12p12 (face memory), and YWHAE on 17p13 (multivariate cognitive phenotype) ( 19 ). Many of the candidate genes are involved in neurotransmission, synaptic plasticity, and brain development. Genetic markers involving the MHC along chromosome 6 are of great interest ( 20 ). The complement activation cascade is normally integral to the immune system’s ability to eliminate pathogens. However, excessive complement, particularly component 4 mediated synapse elimination, may play a role in the development of schizophrenia. In the brain, microglia are phagocyte immune cells that express complement receptors. Inappropriate or intense synaptic pruning may be explained by this aberrant immunological function ( 21 , 22 ). Advanced paternal age has also been linked to schizophrenia, possibly implicating de novo mutations in paternal germ cells. One study found that the odds of schizophrenia occurring among offspring of fathers 45 years old or older were 2.8 times as great as among offspring of fathers ages 20–24 years ( 23 ). However, in a large meta-analysis, increased genetic risk from the mother was thought to explain the association between advanced paternal age and psychosis and argued against the de novo mutation hypothesis. Instead, assortative mating may contribute to the observed association between advanced paternal age and maternal schizophrenia ( 24 ).
Gestational, Nutritional, and Immune System Factors
A host of environmental factors are also implicated in the development of schizophrenia. These include maternal factors such as immigration, perinatal factors (infections, inflammation, obstetrical complications, maternal stress, and fetal hypoxia), and winter births ( 25 – 27 ). Evidence of vascular involvement, including enlarged retinal venule calibers, are possibly related to genes regulated by hypoxia, altered cerebral blood flow, and mitochondrial dysfunction ( 26 ). Higher winter birth rates may be associated with gestational infections such as influenza or vitamin D deficiency. Famines leading to malnutrition during neurodevelopment are also implicated in schizophrenia ( 26 , 27 ). Folate deficiency in particular has been identified as a risk factor for schizophrenia in epidemiologic and gene-association studies. Low serum folate levels are correlated with negative symptoms of patients with schizophrenia. Elevated concentrations of homocysteine in the third trimester of maternal serum was correlated with a twofold risk of schizophrenia for the offspring. The low functioning 677C>T (222Ala>Val) variant in the methylenetetrahydrofolate reductase gene is overrepresented among patients with schizophrenia. Misvariants in three other genes that regulate 1-carbon metabolism—folate hydrolase 1 (FOLH1), methionine synthase (MTR), and COMT—are correlated with negative, but not positive, symptoms in schizophrenia. On the basis of preliminary trials, folate plus vitamin B12 supplementation may improve negative symptoms of schizophrenia for such genetically susceptible individuals ( 28 ).
Cytokines are signaling molecules of the immune system that exert effects in the periphery and the brain. They are produced by both immune and nonimmune cells and exert their effects by binding specific cytokine receptors on a variety of target cells. There is evidence of an increased prevalence of aberrant cytokine levels among patients with schizophrenia. Infection may induce maternal immune activation, which subsequently leads to a cytokine-mediated inflammatory response in the fetus. The timing of the insult to the developing fetus may also play an important role. Associations between schizophrenia and second-trimester influenza, rubella, respiratory infection, polio, measles, and varicella-zoster have been implicated ( 29 ). Toxoplasma gondii (a protozoan) infection of pregnant women may cause congenital deafness, retinal damage, seizures, and mental retardation. In addition, serum antibodies to Toxoplasma gondii were also found to be a risk factor for the development of schizophrenia ( 30 ). The following are some cytokines and inflammatory pathways that have been studied and found to be potentially associated with schizophrenia: tumor necrosis factor (TNF) and interleukin 1 (IL-1), IL-6, and IL-8 ( 31 , 32 ). Aside from their effects on neurotransmission, particularly dopamine, antipsychotics may additionally have a balancing effect on immune responses, perhaps accounting for the delayed response seen in many cases ( 33 ). For instance, antipsychotic treatment has been found to modulate plasma levels of soluble IL-2 receptors and to reduce the plasma levels of IL-1β and interferon-γ (IFN-γ) ( 33 , 34 ). Anti-inflammatory effects of aspirin, N -acetylcysteine, and estrogens have also been found to be beneficial in treating schizophrenia ( 35 ). In a recent meta-analysis, some cytokines (IL-1β, IL-6, and transforming growth factor-β [TGF-β]) were hypothesized to be state markers for acute exacerbations, whereas others (IL-12, IFN-γ, TNF-α, and soluble IL-2 receptor) may be trait markers ( 36 ).
Brain Injury, Traumatic Events, Cannabis, and Immigration
Environmental insults, such as traumatic brain injury, childhood traumatic events, and cannabis use, are also implicated in schizophrenia ( 25 , 37 ). Compared with native-born populations, immigrant populations, particularly those that face discrimination, have a considerable risk of schizophrenia. However, the exact mechanism of the environmental contribution to this risk remains poorly understood ( 38 ). Traumatic histories are common among patients with schizophrenia, and childhood traumatic events are associated with the development of schizophrenia. Patients diagnosed as having comorbid schizophrenia and posttraumatic stress disorder have worse symptoms, higher rates of suicidal thoughts, and more frequent hospitalizations ( 39 ).
Neurotransmitters and Receptors
In 1975, Seeman et al. discovered that haloperidol bound to dopamine sites with higher potency than did other neurotransmitters. These sites were named antipsychotic/dopamine receptors (now called D2 receptors). The research team further delineated antipsychotics by a rank order of potencies that were directly related to the mean daily antipsychotic dose taken by patients. They found that a minimum occupancy (65%) of D2 receptors was needed for antipsychotic benefit ( 40 ). The “dopamine hypothesis” was thus born and has long been used to describe the underlying pathophysiology of schizophrenia. However, mounting research implicates the dysregulation of other pathways such as glutamatergic, opioid, GABA-ergic, serotonergic, cholinergic, and possibly other systems ( 41 ).
The N -methyl- d -aspartate (NMDA) receptor is a glutamatergic receptor that has been of great interest to schizophrenia researchers, particularly with regard to recently discovered receptor subunits. NMDA receptors may be involved in brain overactivity caused by withdrawal of sedatives such as alcohol, resulting in agitation and seizures. The NMDA antagonists phencyclidine and ketamine induce a psychosis among healthy individuals that can mimic schizophrenia ( 42 , 43 ). In addition, neuroimaging studies using magnetic resonance spectroscopy have linked GABA and NMDA receptors to abnormal brain connectivity of individuals with schizophrenia ( 44 ). Reduced NMDA receptor activity can lead to sensory deficits, generalized cognitive deficits, impaired learning and memory, thought disorder, negative symptoms, positive symptoms, gating deficits, executive dysfunction, and dopamine dysregulation ( 45 ). NMDA receptor sites have now been identified with sophisticated three-dimensional crystallographic studies. These subunits may help lead to new discoveries, because endogenous ligands or pharmacological substances are known to modulate NMDA receptor activity in a subunit selective fashion ( 46 ). GABA-ergic inhibitory function is also of great interest for novel drug development ( 47 ).
Neuroimaging
Expanding data in neuroimaging has found evidence that individuals with schizophrenia have enlarged ventricles and cortical tissue loss of about 5% of brain volume ( 48 ). Some affected structures include the hippocampus, superior temporal cortex, and the prefrontal cortex. Functional MRI studies have found evidence of hyperactivity in the hippocampus and the dorsal lateral prefrontal cortex, leading some researchers to believe that a loss of inhibitory neuron function may be responsible for some of the symptoms in schizophrenia. A combination of structural and functional imaging strategies is currently being investigated to look for patterns of brain connectivity, particularly around the time when clinically high-risk individuals transition into full-blown psychosis ( 49 ). Progressive brain changes over time have been associated with a poorer prognosis. Some studies also suggest that antipsychotic medications have a subtle but measurable influence on brain tissue loss over time ( 50 ).
Prodromal State and Synaptic Pruning
Approximately 80%−90% of patients with schizophrenia have a “prodrome” lasting up to one year, characterized by “attenuated” psychotic symptoms that appear to be on a continuum with softer forms of psychotic symptoms such as delusions and hallucinations. These symptoms may include unusual, odd, or overvalued beliefs, guardedness, or auditory hallucinations. Schizophrenia is thought to derive primarily from deficits in dendritic spines that arise during development, thus posing another challenge to researchers ( 51 ).
From embryonic development to about the age of two years, new neurons and synapses are formed rapidly. This results in far more neurons and synapses than are needed. Synaptic pruning is the process by which these extra synapses are eliminated, thereby increasing the efficiency of the neural network. The entire process continues up until approximately 10 years of age, by which time nearly 50% of the synapses present at two years of age have been eliminated. The pattern and timeline of pruning may differ in various regions of the brain ( 51 ). This process of “editing” of brain connections—in which excess material is discarded—is a mechanism that remains elusive. The cytokine and microglial mediated synaptic pruning and dendritic retraction provide a hypothesis for the disease mechanism seen in the brains of individuals with schizophrenia ( 52 ).
Illness Course
Adolescent or young adult patients often present with the prodrome of symptoms described above in which patients function below their baseline level prior to meeting the full criteria for schizophrenia. This time period is also sometimes referred to as an “at-risk mental state.” It can be challenging to differentiate this from a mood disorder, substance abuse, attentional disorders, or maladaptive personality features ( 25 , 53 ). There are also studies revealing overlaps between autism spectrum disorders and schizophrenia. Childhood-onset schizophrenia is a rare subtype. Genomewide copy number variation studies have identified rare mutations that are strong risk factors for both autism spectrum disorders and schizophrenia. Nevertheless, early intervention is considered vital in reducing adverse outcomes ( 25 , 54 ).
Expressed Emotions and Recidivism
Numerous studies have demonstrated that high levels of expressed emotions (EE) in families of patients with schizophrenia are associated with relapses. Researchers since the 1950s have found that EE is an important environmental stressor that can worsen psychopathology and can often contribute to recidivism. For example, families or caregivers may use a negative tone of voice to convey their feelings of hostility (anger, criticism, rejection, irritability, ignorance, etc.), which ultimately can lead to patient decompensation. Case management interventions such as psychoeducation, improved communication skills, and healthy coping strategies, along with medication adherence, can be effective strategies in reducing high EE and decreasing recidivism ( 55 , 56 ).
Prognostic Considerations
Because the disease is variable, schizophrenia researchers over the past several decades have been examining prognostic indicators. In general, prognostic outcomes are considered better for females and with higher premorbid levels of social adjustment (e.g., being married, higher education levels, occupational status), rapid as opposed to slow onset of psychotic symptoms, positive as opposed to negative symptoms, and having a family environment with low EE scores. Indicators for higher risk of relapse are a genetic history of schizophrenia, a baseline schizoid personality disorder, earlier age of onset, higher levels of negative symptoms, and longer inpatient treatment ( 57 ). Religious, spiritual, artistic, and cultural issues are often pertinent to explore in interactions with patients, and psychiatrists and other clinicians should make efforts to use a person-centered approach during rapport building and treatment. However, aggressively challenging delusions is not generally effective and may agitate or create mistrust among patients with psychosis ( 58 ). Occasionally, patients can incorporate caregivers into their delusional system and thus pose a serious challenge to treatment.
Patients with schizophrenia have a lower overall life expectancy in comparison with that of the general population. This is likely due to a lack of overall quality of health and behavioral issues such as high blood pressure, diabetes, cancer, poor diet, lack of exercise, and cardiopulmonary diseases. Half of all patients with schizophrenia smoke cigarettes, a major contributor to comorbid health problems ( 59 ).
Comorbidity Issues
Teasing apart schizophrenia symptoms from those of other comorbid disorders can be difficult. Multiple studies worldwide have found that depression, anxiety, and substance abuse are found more often among patients with schizophrenia than in the general population ( 60 , 61 ). It is difficult to know whether these problems are part of the syndrome of schizophrenia or a result of having the illness. For example, if a young patient is also abusing substances, a first episode of psychosis can present a challenging clinical problem. One study suggested that 44% of such patients turned out to have had a drug-induced psychosis and that 56% of patients later developed schizophrenia as their primary diagnosis ( 61 , 62 ). Adolescents with a polymorphism (Val 158 Met) of the COMT gene may be especially vulnerable to developing schizophrenia after cannabis abuse ( 62 ).
Obsessive-compulsive disorder (OCD) also has been found at an increased rate (up to 12.5-fold) in schizophrenia. Conversely, there is a 3.77-fold increased risk of schizophrenia among patients with OCD. For some patients, depression and OCD are part of a prodrome for schizophrenia ( 61 , 63 ).
Legal and Ethical Issues
Contrary to popular belief, the proportion of violent crimes committed by people diagnosed with a severe mental illness is small. Despite portrayals in mass media, strangers are at a lower risk of being violently attacked by someone who has a severe mental disorder than by someone who is mentally healthy ( 64 ). However, the presence of substance abuse, treatment nonadherence, and persecutory delusions are associated with a greater risk of violence. Family members and friends are at the highest risk of being victimized by a violent patient who has a severe mental illness ( 64 , 65 ). The presence of psychosis from a severe mental illness is a common basis for the insanity defense used in criminal law in most states and in the federal jurisdiction of the United States. Forensic psychiatrists often reconstruct the accused individual’s lifelong history to determine whether a severe mental illness such as schizophrenia or some other condition, including malingering (faking), is present ( 66 ).
Patients with schizophrenia may become severely disabled by their symptoms. Examples include an inability to care for themselves (e.g., maintaining proper sustenance, shelter, or medical care) or a risk of harming themselves or others. The legal system is often involved to advocate for treatment and is balanced against the patient’s individual freedom and autonomy. For example, a guardian or surrogate decision maker may be legally appointed to make financial or medical decisions on the patient’s behalf. It may also become necessary for patients to be held involuntarily (civilly committed) for a period in an inpatient treatment facility or residential care facility. Medications may be forced on patients in some jurisdictions, usually on the basis of imminent harm criteria such as risk of harm to self or others. The use of injectable medications may become useful in the treatment of nonadherent patients. Obtaining consent for treatment can be challenging with patients who lack insight into their illness. Information should be titrated gradually to ethically treat the patient while revealing important potential harmful side effect issues as the patient regains the capacity to understand them ( 66 – 68 ). Patients with severe mental illnesses, including schizophrenia, have long been the subject of oppression, imprisonment, and even genocide under the Nazi regime. It is therefore critically important for psychiatry to maintain proper ethical codes of conduct with respect to the research and treatment of its most vulnerable populations ( 69 ).
Conclusions
Schizophrenia is a complex and chronic disorder with profound effects on patients, families, and communities. There is no unifying single feature of schizophrenia; psychiatrists have long hypothesized that schizophrenia is a multifactorial disease (or diseases) of the brain, which has in common similar symptoms and effects on functioning. Important advances in genetics, immune function, neuroanatomical markers, and neurodevelopment have increased our understanding of the underlying pathophysiology associated with the illness. In the coming years, we hope that further elucidating the pharmacogenetics, immunological aspects, and neurodevelopmental aspects of schizophrenia will allow for the discovery of novel treatments targeted to individual patients, ideally very early in the course of the illness.
Dr. Lauriello reports that he has served as an advisory member for an educational project that received an unrestricted educational grant from Janssen and Alkermes Pharmaceutical companies, served on a speakers bureau for Otsuka Pharmaceuticals, and received grant or research funding for a clinical trial site supported by Otsuka through Florida Atlantic University. Dr. Rahman reports no financial relationships with commercial interests.
1 American Psychiatric Association : Diagnostic and Statistical Manual of Mental Disorders , 5th ed. Arlington, VA, American Psychiatric Association, 2013 Crossref , Google Scholar
2 Andreasen NC, Carpenter WT Jr : Diagnosis and classification of schizophrenia . Schizophr Bull 1993 ; 19:199–214 Crossref , Google Scholar
3 Schneider K : Clinical Psychopathology (English translation by B A Hamilton) . New York, Grune & Stratton, 1959 Google Scholar
4 Tandon R, Gaebel W, Barch DM, et al. : Definition and description of schizophrenia in the DSM-5 . Schizophr Res 2013 ; 150:3–10 Crossref , Google Scholar
5 Andreasen NC : Thought, language, and communication disorders: I. Clinical assessment, definition of terms, and evaluation of their reliability . Arch Gen Psychiatry 1979 ; 36:1315–1321 Crossref , Google Scholar
6 Heckers S, Barch DM, Bustillo J, et al. : Structure of the psychotic disorders classification in DSM-5 . Schizophr Res 2013 ; 150:11–14 Crossref , Google Scholar
7 Keefe RS, Poe M, Walker TM, et al. : The Schizophrenia Cognition Rating Scale: an interview-based assessment and its relationship to cognition, real-world functioning, and functional capacity . Am J Psychiatry 2006 ; 163:426–432 Crossref , Google Scholar
8 Regier DA, Boyd JH, Burke JD Jr, et al. : One-month prevalence of mental disorders in the United States: based on five Epidemiologic Catchment Area sites . Arch Gen Psychiatry 1988 ; 45:977–986 Crossref , Google Scholar
9 Aleman A, Kahn RS, Selten JP : Sex differences in the risk of schizophrenia: evidence from meta-analysis . Arch Gen Psychiatry 2003 ; 60:565–571 Crossref , Google Scholar
10 Clemmensen L, Vernal DL, Steinhausen HC : A systematic review of the long-term outcome of early onset schizophrenia . BMC Psychiatry 2012 ; 12:150 Crossref , Google Scholar
11 Popovic D, Benabarre A, Crespo JM, et al. : Risk factors for suicide in schizophrenia: systematic review and clinical recommendations . Acta Psychiatr Scand 2014 ; 130:418–426 Crossref , Google Scholar
12 Foster A, Gable J, Buckley J : Homelessness in schizophrenia . Psychiatr Clin North Am 2012 ; 35:717–734 Crossref , Google Scholar
13 Folsom DP, Hawthorne W, Lindamer L, et al. : Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system . Am J Psychiatry 2005 ; 162:370–376 Crossref , Google Scholar
14 Schizophrenia Psychiatric Genome-Wide Association Study (GWAS) Consortium : Genome-wide association study identifies five new schizophrenia loci . Nat Genet 2011 ; 43:969–976 Crossref , Google Scholar
15 Gejman PV, Sanders AR, Duan J : The role of genetics in the etiology of schizophrenia . Psychiatr Clin North Am 2010 ; 33:35–66 Crossref , Google Scholar
16 Farrell MS, Werge T, Sklar P, et al. : Evaluating historical candidate genes for schizophrenia . Mol Psychiatry 2015 ; 20:555–562 Crossref , Google Scholar
17 Pearlson GD : Etiologic, phenomenologic, and endophenotypic overlap of schizophrenia and bipolar disorder . Annu Rev Clin Psychol 2015 ; 11:251–281 Crossref , Google Scholar
18 Ripke S, Neale BM, Corvin A, et al. : Biological insights from 108 schizophrenia-associated genetic loci . Nature 2014 ; 511(7510):421 Crossref , Google Scholar
19 Greenwood TA, Swerdlow NR, Gur RE, et al. : Genome-wide linkage analyses of 12 endophenotypes for schizophrenia from the Consortium on the Genetics of Schizophrenia . Am J Psychiatry 2013 ; 170:521–532 Crossref , Google Scholar
20 Sinkus ML, Adams CE, Logel J, et al. : Expression of immune genes on chromosome 6p21.3-22.1 in schizophrenia . Brain Behav Immun 2013 ; 32:51–62 Crossref , Google Scholar
21 Sekar A, Bialas AR, de Rivera H, et al. : Schizophrenia Working Group of the Psychiatric Genomics Consortium : Schizophrenia risk from complex variation of complement component 4 . Nature 2016 ; 530:177–183 Crossref , Google Scholar
22 Whalley K : Psychiatric disorders: linking genetic risk to pruning . Nat Rev Neurosci 2016 ; 17:199 Crossref , Google Scholar
23 Jaffe AE, Eaton WW, Straub RE, et al. : Paternal age, de novo mutations and schizophrenia . Mol Psychiatry 2014 ; 19:274–275 Crossref , Google Scholar
24 Miller B, Erick M, Jouko M, et al. : Meta-analysis of paternal age and schizophrenia risk in male versus female offspring . Schizophr Bull 2011 ; 37:1039–1047. Crossref , Google Scholar
25 Laurens KR, Luo L, Matheson SL, et al. : Common or distinct pathways to psychosis? A systematic review of evidence from prospective studies for developmental risk factors and antecedents of the schizophrenia spectrum disorders and affective psychoses . BMC Psychiatry 2015 ; 15:205 Crossref , Google Scholar
26 Meier MH, Shalev I, Moffitt TE, et al. : Microvascular abnormality in schizophrenia as shown by retinal imaging . Am J Psychiatry 2013 ; 170:1451–1459 Crossref , Google Scholar
27 Hoek HW, Brown AS, Susser E : The Dutch famine and schizophrenia spectrum disorders . Soc Psychiatry Psychiatr Epidemiol 1998 ; 33:373–379 Crossref , Google Scholar
28 Roffman JL, Lamberti JS, Achtyes E, et al. : Randomized multicenter investigation of folate plus vitamin B12 supplementation in schizophrenia . JAMA Psychiatry 2013 ; 70:481–489 Crossref , Google Scholar
29 Ashdown H, Dumont Y, Ng M, et al. : The role of cytokines in mediating effects of prenatal infection on the fetus: implications for schizophrenia . Mol Psychiatry 2006 ; 11:47–55 Crossref , Google Scholar
30 Torrey EF, Bartko JJ, Lun ZR, et al. : Antibodies to Toxoplasma gondii in patients with schizophrenia: a meta-analysis . Schizophr Bull 2007 ; 33:729–736 Crossref , Google Scholar
31 Pandey GN, Ren X, Rizavi HS, et al. : Proinflammatory cytokines and their membrane-bound receptors are altered in the lymphocytes of schizophrenia patients . Schizophr Res 2015 ; 164:193–198 Crossref , Google Scholar
32 Nielsen PR, Agerbo E, Skogstrand K, et al. : Neonatal levels of inflammatory markers and later risk of schizophrenia . Biol Psychiatry 2015 ; 77:548–555 Crossref , Google Scholar
33 Haring L, Koido K, Vasar V, et al. : Antipsychotic treatment reduces psychotic symptoms and markers of low-grade inflammation in first episode psychosis patients, but increases their body mass index . Schizophr Res 2015 ; 169:22–29 Crossref , Google Scholar
34 Tourjman V, Kouassi É, Koué MÈ, et al. : Antipsychotics’ effects on blood levels of cytokines in schizophrenia: a meta-analysis . Schizophr Res 2013 ; 151:43–47 Crossref , Google Scholar
35 Bumb JM, Enning F, Leweke FM : Drug repurposing and emerging adjunctive treatments for schizophrenia . Expert Opin Pharmacother 2015 ; 16:1049–1067 Crossref , Google Scholar
36 Miller BJ, Buckley P, Seabolt W, et al. : Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects . Biol Psychiatry 2011 ; 70:663–671 Crossref , Google Scholar
37 Rabner J, Gottlieb S, Lazdowsky L, et al. : Psychosis following traumatic brain injury and cannabis use in late adolescence: a case series . Am J Addict 2016 ; 25:92–93 Crossref , Google Scholar
38 Cantor-Graae E, Selten JP : Schizophrenia and migration: a meta-analysis and review . Am J Psychiatry 2005 ; 162:12–24 Crossref , Google Scholar
39 Strauss JL, Calhoun PS, Marx CE, et al. : Comorbid posttraumatic stress disorder is associated with suicidality in male veterans with schizophrenia or schizoaffective disorder . Schizophr Res 2006 ; 84:165–169 Crossref , Google Scholar
40 Madras BK : History of the discovery of the antipsychotic dopamine D2 receptor: a basis for the dopamine hypothesis of schizophrenia . J Hist Neurosci 2013 ; 22:62–78 Crossref , Google Scholar
41 Deng C, Dean B : Mapping the pathophysiology of schizophrenia: interactions between multiple cellular pathways . Front Cell Neurosci 2013 ; 7:238 Crossref , Google Scholar
42 Correll CU, Kane JM : Schizophrenia: mechanism of action of current and novel treatments . J Clin Psychiatry 2014 ; 75:347–348 Crossref , Google Scholar
43 Jentsch JD, Roth RH : The neuropsychopharmacology of phencyclidine: from NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia . Neuropsychopharmacology 1999 ; 20:201–225 Crossref , Google Scholar
44 McGlashan TH, Hoffman RE : Schizophrenia as a disorder of developmentally reduced synaptic connectivity . Arch Gen Psychiatry 2000 ; 57:637–648 Crossref , Google Scholar
45 Coyle JT, Tsai G, Goff D : Converging evidence of NMDA receptor hypofunction in the pathophysiology of schizophrenia . Ann N Y Acad Sci 2003 ; 1003:318–327 Crossref , Google Scholar
46 Paoletti P, Bellone C, Zhou Q : NMDA receptor subunit diversity: impact on receptor properties, synaptic plasticity and disease . Nat Rev Neurosci 2013 ; 14:383–400 Crossref , Google Scholar
47 Cohen SM, Tsien RW, Goff DC, et al. : The impact of NMDA receptor hypofunction on GABAergic neurons in the pathophysiology of schizophrenia . Schizophr Res 2015 ; 167:98–107 Crossref , Google Scholar
48 Shenton ME, Dickey CC, Frumin M, et al. : A review of MRI findings in schizophrenia . Schizophr Res 2001 ; 49:1–52 Crossref , Google Scholar
49 Kerns JG, Lauriello J : Can structural neuroimaging be used to define phenotypes and course of schizophrenia? Psychiatr Clin North Am 2012 ; 35:633–644 Crossref , Google Scholar
50 Andreasen NC, Liu D, Ziebell S, et al. : Relapse duration, treatment intensity, and brain tissue loss in schizophrenia: a prospective longitudinal MRI study . Am J Psychiatry 2013 ; 170:609–615 Crossref , Google Scholar
51 Cannon TD : How schizophrenia develops: cognitive and brain mechanisms underlying onset of psychosis . Trends Cogn Sci 2015 ; 19:744–756 Crossref , Google Scholar
52 Santos E, Noggle CA: Encyclopedia of Child Behavior and Development. New York, Springer, 2011, pp 1464–1465 Google Scholar
53 Maibing CF, Pedersen CB, Benros ME, et al. : Risk of schizophrenia increases after all child and adolescent psychiatric disorders: a nationwide study . Schizophr Bull 2015 ; 41:963–970. Crossref , Google Scholar
54 Vorstman JA, Burbach JP: Autism and schizophrenia: genetic and phenotypic relationships; in Comprehensive Guide to Autism. Edited by Patel VB, Preedy VR, Martin CR. New York, Springer, 2014, pp 1645–1662 Google Scholar
55 Cechnicki A, Bielańska A, Hanuszkiewicz I, et al. : The predictive validity of expressed emotions (EE) in schizophrenia. A 20-year prospective study . J Psychiatr Res 2013 ; 47:208–214 Crossref , Google Scholar
56 Macmillan JF, Crow TJ, Johnson AL, et al. : Expressed emotion and relapse in first episodes of schizophrenia . Br J Psychiatry 1987 ; 151:320–323 Crossref , Google Scholar
57 Juola P, Miettunen J, Veijola J, et al. : Predictors of short- and long-term clinical outcome in schizophrenic psychosis—the Northern Finland 1966 Birth Cohort study . Eur Psychiatry 2013 ; 28:263–268 Crossref , Google Scholar
58 Ryan ME, Melzer T : Delusions in schizophrenia: where are we and where do we need to go? Int J School Cogn Psychol 2014 ; 1:115 Google Scholar
59 Laursen TM, Munk-Olsen T, Vestergaard M : Life expectancy and cardiovascular mortality in persons with schizophrenia . Curr Opin Psychiatry 2012 ; 25:83–88 Crossref , Google Scholar
60 Tsai J, Rosenheck RA : Psychiatric comorbidity among adults with schizophrenia: a latent class analysis . Psychiatry Res 2013 ; 210:16–20 Crossref , Google Scholar
61 Buckley PF, Miller BJ, Lehrer DS, et al. : Psychiatric comorbidities and schizophrenia . Schizophr Bull 2009 ; 35:383–402 Crossref , Google Scholar
62 Estrada G, Fatjó-Vilas M, Muñoz MJ, et al. : Cannabis use and age at onset of psychosis: further evidence of interaction with COMT Val158Met polymorphism . Acta Psychiatr Scand 2011 ; 123:485–492 Crossref , Google Scholar
63 Tibbo P, Kroetsch M, Chue P, et al. : Obsessive-compulsive disorder in schizophrenia . J Psychiatr Res 2000 ; 34:139–146 Crossref , Google Scholar
64 Angermeyer MC : Schizophrenia and violence . Acta Psychiatr Scand Suppl 2000 ; 102(s407):63–67 Crossref , Google Scholar
65 Scott CL, Resnick PJ : Violence risk assessment in persons with mental illness . Aggress Violent Behav 2006 ; 11:598–611 Crossref , Google Scholar
66 Resnick PJ : The detection of malingered psychosis . Psychiatr Clin North Am 1999 ; 22:159–172 Crossref , Google Scholar
67 Appelbaum PS, Grisso T : Assessing patients’ capacities to consent to treatment . N Engl J Med 1988 ; 319:1635–1638 Crossref , Google Scholar
68 Appelbaum PS, Grisso T : The MacArthur Treatment Competence Study: I. Mental illness and competence to consent to treatment . Law Hum Behav 1995 ; 19:105–126 Crossref , Google Scholar
69 Torrey EF, Yolken RH : Psychiatric genocide: Nazi attempts to eradicate schizophrenia . Schizophr Bull 2010 ; 36:26–32. Crossref , Google Scholar
- Techniques for Measurement of Serotonin: Implications in Neuropsychiatric Disorders and Advances in Absolute Value Recording Methods 29 November 2023 | ACS Chemical Neuroscience, Vol. 14, No. 24
- Transferosome-Based Intranasal Drug Delivery Systems for the Management of Schizophrenia: a Futuristic Approach 15 December 2023 | BioNanoScience, Vol. 15
- Evaluation of psychometric properties of a leaflet developed for schizophrenia 17 May 2023 | International Journal of Social Psychiatry, Vol. 69, No. 7
- Association Between Childhood Exposure to Pet Cats and Later Diagnosis of Schizophrenia: A Case-Control Study in Saudi Arabia Cureus, Vol. 36
- Adult abuse and poor prognosis in Taiwan, 2000–2015: a cohort study 6 December 2022 | BMC Public Health, Vol. 22, No. 1
- The differential associations of positive and negative symptoms with suicidality Schizophrenia Research, Vol. 248
- A Literature Review on the Efficacy of Injectable Neuroleptics in the Treatment of Schizophrenia 8 August 2022 | Undergraduate Research in Natural and Clinical Science and Technology (URNCST) Journal, Vol. 6, No. 8
- Effectiveness of sensory modulation for people with schizophrenia: A multisite quantitative prospective cohort study 19 April 2022 | Australian Occupational Therapy Journal, Vol. 69, No. 4
- New Paradigms of Old Psychedelics in Schizophrenia 23 May 2022 | Pharmaceuticals, Vol. 15, No. 5
- Study on Executive Function of Schizophrenia Patients Advances in Psychology, Vol. 12, No. 09
- Incidence of Orthostatic Hypotension in Schizophrenic Patients Using Antipsychotics at Sambang Lihum Mental Health Hospital, South Kalimantan 30 August 2021 | Borneo Journal of Pharmacy, Vol. 4, No. 3
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
- Early Signs
What Are the Different Types of Schizophrenia?
Subtypes No Longer Used in Diagnosis
Why the DSM-5 Eliminated Schizophrenia Types
Dsm-5 criteria for schizophrenia, paranoid schizophrenia, disorganized (hebephrenic) schizophrenia, residual schizophrenia, catatonic schizophrenia, undifferentiated schizophrenia, schizophrenia spectrum disorders.
- Next in Schizophrenia Guide Early Signs and Symptoms of Schizophrenia
Schizophrenia is no longer diagnosed with subtypes. It’s considered a chronic mental health condition that exists on a spectrum. Schizophrenia interferes with a person's perception of reality. People with schizophrenia face emotional difficulties and trouble thinking rationally and clearly. They also have challenges in their relationships with others.
This article will discuss the former schizophrenia subtypes, including why they are no longer used for diagnosis, though can be helpful for providers who treat people living with schizophrenia.
Verywell / Cindy Chung
Until the most recent version of the Diagnostic and Statistical Manual of Mental Disorders ( DSM-5 ) was published in 2013, schizophrenia was officially recognized as having five distinct subtypes:
- Disorganized/ hebephrenic
- Undifferentiated
However, mental health experts said that the symptoms of each subtype were not reliable or consistently valid and got in the way of making a diagnosis . Therefore, the American Psychiatric Association (APA) removed schizophrenia subtypes from the DSM-5.
Although they are no longer used for diagnosis, some mental health providers find schizophrenia subtypes can be helpful when they're deciding on the best treatment for someone with the condition.
The symptoms of the schizophrenia subtypes overlap with those of other mental health conditions. To be diagnosed with schizophrenia, a person must meet the criteria outlined in the DSM-5.
A person must have two or more of the following symptoms for at least one month (or less if they have been treated), and at least one symptom must be delusions, hallucinations, or disorganized speech:
- Positive symptoms (those abnormally present): Hallucinations, such as hearing voices or seeing things that do not exist; paranoia; and exaggerated or distorted perceptions, beliefs, and behaviors
- Negative symptoms (those abnormally absent): A loss of or a decrease in the ability to initiate plans, speak, express emotion, or find pleasure
- Disorganized symptoms: Confused and disordered thinking and speech, trouble with logical thinking, and sometimes bizarre behavior or abnormal movements
Continuous signs of the disturbance must be present for at least six months. Within that time, at least one month must include the above symptoms (or less if the person has been successfully treated).
A person may also have periods of prodromal or residual symptoms.
- A prodrome is the period of early, mild symptoms before a full-on episode.
- Residual schizophrenia is the phase after a person has had an episode where the symptoms are not totally resolved but are not as intense as they were during the episode. Usually, they only have negative symptoms of schizophrenia or very mild positive symptoms.
During prodromal or residual periods, a person may only have negative symptoms or could have two or more symptoms listed above in an attenuated form—that is, odd beliefs or unusual perceptual experiences.
A person must also show a decreased level of functioning in daily life, such as doing self-care, managing their relationships, or working. During this phase, people may start to withdraw socially, lose interest in their usual activities, or struggle with personal hygiene.
Schizoaffective disorder and depressive or bipolar disorder with psychotic features have to be ruled out before a diagnosis of schizophrenia can be made.
This schizophrenia subtype is the one that often comes to mind when people think of schizophrenia. It is also the type that is most often depicted in the media and popular culture.
Fixed, false beliefs that conflict with reality ( delusions ) are a hallmark of paranoid schizophrenia. Hallucinations, particularly hearing voices (auditory hallucinations), are also common.
Paranoid schizophrenia primarily involves the onset of traits, feelings, or behaviors that were not there before—referred to as positive symptoms.
Positive symptoms of schizophrenia include the following:
- Preoccupation with one or more delusions
- Auditory hallucinations
In paranoid schizophrenia, the following symptoms are not typically present (or if they are, they are not prominent):
- Disorganized speech
- Disorganized or catatonic behavior
- Flat or inappropriate affect
Symptoms Can Come and Go
The symptoms of schizophrenia may not be experienced all at once. A person living with the illness may experience different symptoms at different times.
Disorganized schizophrenia is also called hebephrenic schizophrenia. This subtype of schizophrenia is characterized by symptoms that interrupt a person's thinking and communication (disorganized symptoms).
People with this schizophrenia subtype may have the following symptoms:
- Disorganized behavior
Here are some common challenges that people with hebephrenic schizophrenia may face:
- Difficulty with routine tasks like personal hygiene and self-care
- Reacting emotionally in ways that are incongruous or inappropriate to the situation
- Trouble with communication
- Misusing words or placing them in the wrong order
- Difficulty thinking clearly and responding appropriately
- Speaking in neologisms (the use of nonsense words or making up words)
- Moving quickly between thoughts without logical connections
- Forgetting or misplacing items
- Pacing or walking in circles
- Difficulty understanding everyday things
- Giving unrelated answers to questions
- Repeating phrases or words
- Trouble with completing tasks or meeting goals
- Challenges with impulse control
- Failing to make eye contact
- Showing childlike behaviors
- Withdrawing socially
Residual schizophrenia is not the same as the residual phase of schizophrenia. The residual phase of schizophrenia is a period when a person's symptoms are not as intense. However, they may still have negative symptoms—for example, a previous trait or behavior stops, or there's a lack of a trait or behavior that would normally be present.
A person with residual schizophrenia does not currently have prominent delusions, hallucinations, disorganized speech, or highly disorganized or catatonic behavior. Instead, they have negative symptoms and/or two or more diagnostic symptoms of schizophrenia in a milder form (such as odd beliefs or unusual perceptual experiences).
Symptoms of residual schizophrenia can include:
- Blunted affect (e.g., trouble expressing emotions, diminished facial expressions or expressive gestures)
- Odd beliefs
- Unusual perceptions
- Social withdrawal
Other Conditions
People with schizophrenia can also have other mental health disorders at the same time (co-occurring or co-morbid conditions), including depression and substance use disorders.
A person with catatonic schizophrenia meets the criteria for a diagnosis of schizophrenia and also has symptoms of catatonia . Catatonia involves excessive movement (excited catatonia) or decreased movement (retarded catatonia) that affects both speech and behavior.
Catatonic schizophrenia symptoms may include the following:
- Catalepsy (muscular rigidity, lack of response to external stimuli)
- Waxy flexibility (limbs remain for an unusually long time in the position they are placed by another)
- Stupor (unresponsiveness to most stimuli)
- Excessive motor activity (apparently purposeless activity not influenced by external stimuli)
- Extreme negativism (apparently motiveless resistance to all instructions or maintenance of a rigid posture against attempts to be moved)
- Mutism (lack of speech)
- Posturing (voluntary assumption of inappropriate or bizarre postures)
- Stereotyped movements (involuntary, repetitive physical movements such as rocking)
- Prominent grimacing (distorting the face in an expression, usually of pain, disgust, or disapproval)
- Echolalia (repeating what others say)
- Echopraxia (imitating the movements of others)
A person with undifferentiated schizophrenia has symptoms that fit a diagnosis of schizophrenia but do not completely fit with the paranoid type, catatonic type, or disorganized type.
There are no specific symptoms that indicate undifferentiated schizophrenia. Instead, a person shows many symptoms that do not meet the full criteria for a particular subtype.
The symptoms of undifferentiated schizophrenia may include:
- Hallucinations
- Exaggerated or distorted perceptions, beliefs, and behaviors
- Unusual or disorganized speech
- Neglect of personal hygiene
- Social withdrawal
- Excessive sleeping or a lack of sleep
- Difficulty making plans
- Problems with emotions and emotional expression
- Trouble with logical thinking
- Bizarre behavior
- Abnormal movements
Childhood Schizophrenia
Childhood schizophrenia is not a subtype of schizophrenia. This term refers to the age of onset of schizophrenia, not a separate diagnosis.
There are other disorders on the schizophrenia spectrum, along with schizophrenia. The conditions are listed in the DSM-5-TR as “schizophrenia spectrum and other psychotic disorders.”
Schizophrenia spectrum disorders include:
- Schizoaffective disorder
- Delusional disorder
- Brief psychotic disorder
- Schizophreniform disorder
Schizoaffective Disorder
Schizoaffective disorder has features of schizophrenia and features of a mood disorder, either major depressive disorder or bipolar disorder .
Symptoms of schizoaffective disorder fall into the following three categories:
Delusional Disorder
Delusional disorder is a form of psychosis in which a person has fixed, false beliefs. For example, a person with delusion disorder may believe a celebrity is in love with them, that someone is spying on them or "out to get them," or that they have a great talent or importance. They may also hold other beliefs that are outside the realm of reality.
Brief Psychotic Disorder
Brief psychotic disorder is an episode of psychotic behavior with a sudden onset that lasts less than a month. After the episode, the person goes into complete remission. However, it is possible to have another psychotic episode in the future.
A brief psychotic episode is characterized by the sudden onset of delusions, hallucinations, and disorganized speech. The symptoms are are often triggered by stress and only last a few days. For example, a person who witnesses a traumatic event may have hallucinations or delusions temporarily in response to the severe stress of what they experienced.
Schizophreniform Disorder
With schizophreniform disorder, a person has symptoms of schizophrenia that last less than six months.
Schizotypal Personality Disorder
Schizotypal personality disorder involves having odd beliefs, perceptions, and behaviors. A person with schizotypical personality disorder can be suspicious or paranoid of others and often has limited relationships.
Paranoid, disorganized/hebephrenic, residual, catatonic, and undifferentiated schizophrenia are no longer diagnoses in the DSM-5.
However, since the subtypes can show the different ways that schizophrenia spectrum disorders can be experienced, some providers find it useful to talk about them when they're working with patients.
Today, schizophrenia is considered a spectrum disorder that includes schizoaffective disorder, delusional disorder, brief psychotic disorder, schizophreniform disorder, and schizoaffective disorder.
American Psychiatric Association. What is schizophrenia? ,
Administration SA and MHS. Table 3. 22, DSM-IV to DSM-5 schizophrenia comparison .
Substance Abuse and Mental Health Services Administration. Table 3.22, DSM-IV to DSM-5 Schizophrenia Comparison . [Internet] Rockville (MD) (US); 2016 Jun.
Mental Health UK. Types of schizophrenia .
NIMH. Schizophrenia .
Schennach R, Riedel M, Obermeier M, et al. What are residual symptoms in schizophrenia spectrum disorder? Clinical description and 1-year persistence within a naturalistic trial. Eur Arch Psychiatry Clin Neurosci . 2015;265(2):107-116. doi:10.1007/s00406-014-0528-2
Khokhar JY, Dwiel LL, Henricks AM, Doucette WT, Green AI. The link between schizophrenia and substance use disorder: A unifying hypothesis . Schizophr Res . 2018;194:78-85. doi:10.1016/j.schres.2017.04.016
Castle, DJ, Buckley, PF, & Upthegrove, R. Schizophrenia and psychiatric comorbidities: Recognition and management . (2021). Oxford University Press.
Rasmussen SA, Mazurek MF, Rosebush PI. Catatonia: Our current understanding of its diagnosis, treatment and pathophysiology . World J Psychiatry . 2016;6(4):391-398. Published 2016 Dec 22. doi:10.5498/wjp.v6.i4.391
Kendhari J, Shankar R, Young-Walker L. A review of childhood-onset schizophrenia . Focus (Am Psychiatr Publ) . 2016;14(3):328-332. doi:10.1176/appi.focus.20160007
APA. DSM-5-TR fact sheets .
APA. Schizoaffective disorder .
APA. Delusional disorder .
APA. Brief psychotic disorder .
APA. Schizophreniform disorder .
APA. Schizotypal personality disorder .
By Heather Jones Heather M. Jones is a freelance writer with a strong focus on health, parenting, disability, and feminism.

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Schizophrenia
Schizophrenia is a mental disorder characterized by disruptions in thought processes, perceptions, emotional responsiveness, and social interactions. Although the course of schizophrenia varies among individuals, schizophrenia is typically persistent and can be both severe and disabling.
Symptoms of schizophrenia include psychotic symptoms such as hallucinations, delusions, and thought disorder (unusual ways of thinking), as well as reduced expression of emotions, reduced motivation to accomplish goals, difficulty in social relationships, motor impairment, and cognitive impairment. Although symptoms typically start in late adolescence or early adulthood, schizophrenia is often viewed from a developmental perspective. Cognitive impairment and unusual behaviors sometimes appear in childhood, and persistent presence of multiple symptoms represent a later stage of the disorder. This pattern may reflect disruptions in brain development as well as environmental factors such as prenatal or early life stress. This perspective fuels the hope that early interventions will improve the course of schizophrenia which is often severely disabling when left untreated.
Additional information can be found on the NIMH Health Topics page on Schizophrenia .
Age-Of-Onset for Schizophrenia
Schizophrenia is typically diagnosed in the late teens years to early thirties, and tends to emerge earlier in males (late adolescence – early twenties) than females (early twenties – early thirties). 1,2 More subtle changes in cognition and social relationships may precede the actual diagnosis, often by years.
Prevalence of Schizophrenia
Precise prevalence estimates of schizophrenia are difficult to obtain due to clinical and methodological factors such as the complexity of schizophrenia diagnosis, its overlap with other disorders, and varying methods for determining diagnoses. Given these complexities, schizophrenia and other psychotic disorders are often combined in prevalence estimation studies. A summary of currently available data is presented here.
- Across studies that use household-based survey samples, clinical diagnostic interviews, and medical records, estimates of the prevalence of schizophrenia and related psychotic disorders in the U.S. range between 0.25% and 0.64%. 3,4,5
- Estimates of the international prevalence of schizophrenia among non-institutionalized persons is 0.33% to 0.75%. 6,7
Burden of Schizophrenia
Despite its relatively low prevalence, schizophrenia is associated with significant health, social, and economic concerns.
- Schizophrenia is one of the top 15 leading causes of disability worldwide. 8
- The estimated average potential life lost for individuals with schizophrenia in the U.S. is 28.5 years. 10
- Co-occurring medical conditions, such as heart disease, liver disease, and diabetes, contribute to the higher premature mortality rate among individuals with schizophrenia. 10 Possible reasons for this excess early mortality are increased rates of these medical conditions and under-detection and under-treatment of them. 13
- An estimated 4.9% of people with schizophrenia die by suicide, a rate that is far greater than the general population, with the highest risk in the early stages of illness. 9
- Approximately half of individuals with schizophrenia have co-occurring mental and/or behavioral health disorders. 14
- Financial costs associated with schizophrenia are disproportionately high relative to other chronic mental and physical health conditions, reflecting both “direct” costs of health care as well as “indirect” costs of lost productivity, criminal justice involvement, social service needs, and other factors beyond health care. 5
Data Sources
- McGrath J, Saha S, Chant D, Welham J. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30:67-76. PMID: 18480098
- Hollis C, Rapoport J (2008). Child and Adolescent Schizophrenia. In D Weinberger, P Harrison (Eds.). Schizophrenia (3rd ed., pp. 24-46). London: Blackwell.
- Kessler RC, Birnbaum H, Demler O, Falloon IR, Gagnon E, Guyer M, Howes MJ, Kendler KS, Shi L, Walters E, Wu EQ. The prevalence and correlates of nonaffective psychosis in the National Comorbidity Survey Replication (NCS-R). Biol Psychiatry. 2005 Oct 15;58(8):668-76. PMID: 16023620
- Wu EQ, Shi L, Birnbaum H, Hudson T, Kessler R. Annual prevalence of diagnosed schizophrenia in the USA: a claims data analysis approach. Psychol Med. 2006 Nov;36(11):1535-40. PMID: 16907994
- Desai, PR, Lawson, KA, Barner, JC, Rascati, KL. Estimating the direct and indirect costs for community-dwelling patients with schizophrenia. Journal of Pharmaceutical Health Services Research, 2013 Jul;4(4):187-194. doi/10.1111/jphs.12027/epdf
- Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005 May;2(5):e141. PMID: 15916472
- Moreno-Küstner B, Martín C, Pastor L. Prevalence of psychotic disorders and its association with methodological issues. A systematic review and meta-analyses. PLoS One. 2018;13(4):e0195687. PMID: 29649252
- Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017 Sep 16;390(10100):1211-1259. PMID: 28919117
- Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry. 2005 Mar;62(3):247-53. PMID: 15753237
- Olfson M, Gerhard T, Huang C, Crystal S, Stroup TS. Premature Mortality Among Adults With Schizophrenia in the United States. JAMA Psychiatry. 2015 Dec;72(12):1172-81. PMID: 26509694
- Schoenbaum M, Sutherland JM, Chappel A, Azrin S, Goldstein AB, Rupp A, Heinssen RK. Twelve-Month Health Care Use and Mortality in Commercially Insured Young People With Incident Psychosis in the United States. Schizophr Bull. 2017 Oct 21;43(6):1262-1272. PMID: 28398566
- Simon GE, Stewart C, Yarborough BJ, Lynch F, Coleman KJ, Beck A, Operskalski BH, Penfold RB, Hunkeler EM. Mortality Rates After the First Diagnosis of Psychotic Disorder in Adolescents and Young Adults. JAMA Psychiatry. 2018 Mar 1;75(3):254-260. PMID: 29387876
- Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014;10:425-48. PMID: 24313570
- Tsai J, Rosenheck RA. Psychiatric comorbidity among adults with schizophrenia: a latent class analysis. Psychiatry Res. 2013 Nov 30;210(1):16-20. PMID: 23726869
Statistical Methods and Measurement Caveats
The prevalence rate of schizophrenia and related psychotic disorders is difficult to estimate using typical household survey methods alone. Accurate assessment of schizophrenia is best achieved using clinicians trained in the diagnosis of mental illnesses. The U.S. prevalence studies cited here were selected based on their use of U.S. population samples and use of methods that involved clinical diagnosis, either via clinical reappraisal (validation) studies or clinical record studies. 3,4,5
Individuals with schizophrenia and other psychotic disorders may be under-counted in prevalence estimation studies. These individuals may be under-represented in household surveys because they may reside in prisons, other institutions, or may lack a permanent address. Similarly, some people with schizophrenia and other psychotic disorders may not be fully reflected in medical records data because they may not have a documented diagnosis, and/or may receive little or no health care.
Information on statistical methods and measurement caveats can be found in the papers cited on this page and listed in the reference section. Below we provide additional background information for large datasets used in two studies cited on this page. 3,5
National Comorbidity Survey Replication (NCS-R)
- The NCS-R is a nationally representative, face-to-face, household survey conducted between February 2001 and April 2003 with a response rate of 70.9%. DSM-IV mental disorders were assessed using a modified version of the fully structured World Health Organization Composite International Diagnostic Interview (WMH-CIDI), a fully structured lay-administered diagnostic interview that generates both International Classification of Diseases, 10th Revision, and DSM-IV diagnoses. The DSM-IV criteria were used here. Participants for the main interview totaled 9,282 English-speaking, non-institutionalized, civilian respondents. Non-affective psychosis was assessed in a subsample of 2,322 respondents. 3 The Sheehan Disability Scales (SDS) assessed disability in work role performance, household maintenance, social life, and intimate relationships on 0-10 scales. The NCS-R was led by Harvard University.
- Survey non-response: In 2001-2002, non-response was 29.1% of primary respondents and 19.6% of secondary respondents. Reasons for non-response to interviewing include: refusal to participate (7.3% of primary, 6.3% of secondary); respondent was reluctant – too busy but did not refuse (17.7% of primary, 11.6% of secondary); circumstantial, such as intellectual developmental disability or overseas work assignment (2.0% of primary, 1.7% of secondary); and, household units that were never contacted (2.0%).
- For more information, see PMID: 15297905 .
Medical Expenditure Panel Survey (MEPS)
- The MEPS collect data from community-dwelling people in the U.S. It does not include patients living in group homes, supported living arrangements, prisons, and institutions. In addition, homeless people and undocumented immigrants are excluded. These groups may have a higher prevalence of schizophrenia. MEPS survey responses were obtained from a single respondent for all the members of the family, therefore some recall bias may be associated with the responses.
- Patients for the schizophrenia study were selected based on ICD-9 codes only. Due to the stigma associated with the condition, physicians are known to give patients an interim non-schizophrenia diagnosis when uncertain about schizophrenia until it can be confirmed. To capture patients who may be given an interim non-schizophrenia diagnosis, researchers used the ICD-9 code for non-organic psychoses in addition to that for schizophrenic disorder in their study. 5 MEPS collects information about conditions through patient interviews and some miscoding may occur as the household participants describe their conditions during the interviews and the coders record the ICD-9 codes for the diagnosis.
- For more information, see doi/10.1111/jphs.12027/epdf and the MEPS Survey Background Page .

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

8.1: Clinical Presentation
- Last updated
- Save as PDF
- Page ID 65362

- Alexis Bridley and Lee W. Daffin Jr.
- Washington State University
Section Learning Objectives
- Identify and describe the five symptoms of schizophrenia spectrum disorders.
- Describe how schizophrenia presents itself.
- Describe how schizophreniform disorder presents itself.
- Describe how brief psychotic disorder presents itself.
- Describe how schizoaffective disorder presents itself.
- Describe how delusional disorder presents itself.
- Be able to distinguish the five disorders from one another.
\(\PageIndex{1}\): Symptoms of Schizophrenia Spectrum Disorders
Individuals diagnosed with a schizophrenia spectrum disorder experience psychosis, which is defined as a loss of contact with reality and is manifested by delusions and/or hallucinations. These episodes of psychosis can make it difficult for individuals to perceive and respond to environmental stimuli, which can cause significant disturbances in everyday functioning. While there are a number of symptoms displayed in schizophrenia spectrum disorders, presentation of symptoms varies greatly among individuals, as there are rarely two cases similar in presentation, triggers, course, or responsiveness to treatment (APA, 2013). We will now turn our attention to the five major symptoms associated with these disorders: delusions, hallucinations, disorganized speech, disorganized behavior, and negative symptoms.
\(\PageIndex{1.1}\): Delusions
Delusions are defined as “fixed beliefs that are not amenable to change in light of conflicting evidence” (APA, 2013, pp. 87). This means that despite evidence contradicting one’s thoughts, the individual is unable to distinguish them from reality. There are a variety of delusions that can present in many different ways:
- Delusions of grandeur – beliefs they have exceptional abilities, wealth, or fame; the belief they are God or other religious saviors
- Delusions of persecution – beliefs they are going to be harmed, harassed, plotted or discriminated against by either an individual or an institution
- Delusions of reference – beliefs that specific gestures, comments, or even larger environmental cues (e.g., an ad in the newspaper, a terrorist attack) are directed at them
- Delusions of control – beliefs that their thoughts/feelings/actions are controlled by others
- Delusions of thought broadcasting – beliefs that one’s thoughts are transparent and everyone knows what they are thinking
- Delusions of thought withdrawal – belief that one’s thoughts have been removed by another source
The most common delusion is delusions of persecution (APA, 2013). It is believed that the presentation of the delusion is largely related to the social, emotional, educational, and cultural background of the individual (Arango & Carpenter, 2010). For example, an individual with schizophrenia who comes from a highly religious family is more likely to experience religious delusions (e.g., delusions of grandeur) than another type of delusion.
\(\PageIndex{1.2}\): Hallucinations
Hallucinations can occur in any of the five senses including as hearing (auditory hallucinations), seeing (visual hallucinations), smelling (olfactory hallucinations), touching (tactile hallucinations), or tasting (gustatory hallucinations). Additionally, they can occur in a single modality or present across a combination of modalities (i.e. experiencing both auditory and visual hallucinations). For the most part, individuals recognize that their hallucinations are not real and attempt to engage in normal behavior while simultaneously combating ongoing hallucinations.
According to various research studies, nearly half of all people with schizophrenia report auditory hallucinations, 15% report visual hallucinations, and 5% report tactile hallucinations (DeLeon, Cuesta, & Peralta, 1993). Among the most common types of auditory hallucinations are voices talking to the individual or various voices talking to one another. Generally, these hallucinations are not attributable to any one person that the individual knows. However, they are usually clear, objective, and definite (Arango & Carpenter, 2010). Additionally, the auditory hallucinations can be pleasurable, providing comfort to the individuals; however, in other individuals, the auditory hallucinations can be unsettling as they produce commands or have malicious intent.
\(\PageIndex{1.3}\): Disorganized Speech
Among the most common cognitive impairments displayed in individuals with schizophrenia are disorganized speech, communication, and thoughts. More specifically, thoughts and speech patterns may appear to be circumstantial or tangential . For example, individuals with circumstantial speech may give unnecessary details in response to a question before they finally produce the desired response. While the question is eventually answered by individuals with circumstantial speech, those with tangential speech never reach the point or answer the question. Another common cognitive symptom is speech retardation where the individual may take a long period of time before answering a question. Derailment , or the illogical connection in a chain of thoughts, is another common type of disorganized thinking. The most severe form of disorganized speech is incoherence or word salad which is where speech is completely incomprehensible and meaningful sentences are not produced.
These type of distorted thought patterns are often related to concrete thinking. That is, the individual is focused on one aspect of a concept or thing, and neglects all other aspects. This type of thinking makes treatment difficult as individuals lack insight into their illness and symptoms (APA, 2013).
\(\PageIndex{1.4}\): Disorganized Behavior
Psychomotor symptoms can also be observed in individuals with schizophrenia spectrum disorders. These behaviors may manifest as awkward movements or even ritualistic/repetitive behaviors. They are often unpredictable and overwhelming, severely impacting the ability to perform daily activities (APA, 2013). Catatonic behavior , or the decrease or even lack of reactivity to the environment, is among the most commonly seen disorganized motor behavior in schizophrenia spectrum disorders. These catatonic behaviors include:
- Negativism – resistance to instruction
- Mutism – complete lack of verbal responses
- Stupor – complete lack of motor responses
- Rigidity – maintaining a rigid or upright posture while resisting efforts to be moved
- Posturing – holding odd, awkward postures for long periods of time
On the opposite side of the spectrum is catatonic excitement, where the individual experiences a hyperactivity of motor behavior. This can include echolalia (mimicking the speech of others) and echopraxia (mimicking the movement of others) but may also simply be manifested through excessive and/or purposeless motor behaviors.
\(\PageIndex{1.5}\): Negative Symptoms
Up until this point, all the schizophrenia symptoms can be categorized as positive symptoms or symptoms that involve the presence of something that should not be there (e.g., hallucinations and delusions) or disorganized symptoms (disorganized speech and behavior). The final symptom included in the diagnostic criteria of several of the schizophrenia spectrum disorders is negative symptoms , which are defined as the inability, or decreased ability, to initiate actions, speech, express emotion, or to feel pleasure (Barch, 2013). Negative symptoms are typically present before positive symptoms and often remain once positive symptoms remit. They account for much of the morbidity in schizophrenia but not as prominent in the other spectrum disorders (indeed, as you will see, they are not included as a symptom in some of these other disorders). Because of their prevalence through the course of the schizophrenia, they are also more indicative of prognosis, with more negative symptoms suggestive of a poorer prognosis. The poorer prognosis may be explained by the lack of effect that traditional antipsychotic medications have in addressing negative symptoms (Kirkpatrick, Fenton, Carpenter, & Marder, 2006).
There are five main types of negative symptoms seen in individuals with schizophrenia:
- Affective flattening – reduction in emotional expression (i.e., a reduced display of emotional expression)
- Alogia – poverty of speech or speech content
- Anhedonia – decreased ability to experience pleasure
- Asociality – lack of interest in social relationships
- Avolition – lack of motivation of goal-directed behavior
\(\PageIndex{2}\): Types of Schizophrenia Spectrum Disorders
\(\pageindex{2.1}\): schizophrenia.
As stated above, the hallmark symptoms of schizophrenia include the presence of at least two of the following symptoms for at least one month: delusions, hallucinations, disorganized speech, disorganized/abnormal behavior, negative symptoms. These symptoms must create significant impairment in the individual’s ability to engage in normal daily functioning such as work, school, relationships with others, or self-care. It should be noted that presentation of schizophrenia varies greatly among individuals, as it is a heterogeneous clinical syndrome (APA, 2013).
While the presence of active phase symptoms must persist for a minimum of one month to meet criteria for a schizophrenia diagnosis, the total duration of symptoms must persist for at least six months before a diagnosis of schizophrenia can be made. This six month period can comprise a combination of active, prodromal, and residual phase symptoms. Active phase symptoms represent the “full-blown” symptoms previously described. Prodromal symptoms are “subthreshold” symptoms that precede the active phase of the disorder and residual symptoms are subthreshold symptoms that follow the active phase. These prodromal and residual symptoms are milder forms of symptoms that do not cause significant impairment in functioning, with the exception of negative symptoms (Lieberman et al., 2001). Due to the severity of psychotic symptoms, mood disorder symptoms are also common among individuals with schizophrenia; however, to diagnose schizophrenia either there must be no mood symptoms or if mood symptoms have occurred they must be present for only a minority of the total duration of the illness. The latter helps to distinguish schizophrenia from a mood disorder with psychotic features for which psychotic symptoms are limited to the context of the mood episodes and do not extend beyond those episodes.
\(\PageIndex{2.2}\): Schizophreniform Disorder
Schizophreniform disorder is similar to schizophrenia with the exception of the length of presentation of symptoms and the requirement for impairment in functioning. As described above, a diagnosis of schizophrenia requires impairment in functioning and a six-month minimum duration of symptoms. In contrast, impairment in functioning is not required to diagnose schizophreniform disorder. While many individuals with schizophreniform disorder do display impaired functioning, it is not essential for diagnosis. Moreover, symptoms must last at least one month but less than six-months do diagnose schizophreniform disorder. In this way, the duration of schizophreniform disorder is considered an “intermediate” disorder between schizophrenia and brief psychotic disorder (which we will consider next).
Approximately two-thirds of individuals who are initially diagnosed with schizophreniform disorder will have symptoms that last longer than six months, at which time their diagnosis is changed to schizophrenia (APA, 2013). The other one-third will recover within the six month time period and schizophreniform disorder will be their final diagnosis.
Finally, as with schizophrenia, any major mood episodes that are present concurrently with the psychotic features must only be present for a small period of time, otherwise, a diagnosis of schizoaffective disorder may be more appropriate.
\(\PageIndex{2.3}\): Brief Psychotic Disorder
A diagnosis of brief psychotic disorder requires one or more of the following symptoms: delusions, hallucinations, disorganized speech, disorganized behavior. Moreover at least one of these symptoms must be delusions, hallucinations, or disorganized speech. Notice that negative symptoms are not included in this list. Also notice that while schizophrenia and schizophreniform disorder require a minimum of two symptoms, only one is required for a diagnosis of brief psychotic disorder. To diagnose brief psychotic disorder symptom(s) must be present for at least one day but less than one month (recall: one month is the minimum duration of symptoms required to diagnose schizophreniform disorder). After one-month individuals return to their full premorbid level of functioning. Also, while there is typically very severe impairment in functioning associated with brief psychotic disorder it is not required for a diagnosis.
\(\PageIndex{2.4}\): Schizoaffective Disorder
Schizoaffective disorder is characterized by two or more of the symptoms of schizophrenia (delusions, hallucinations, disorganized speech, disorganized behavior, negative symptoms) and a concurrent uninterrupted period of a major mood episode—either a depressive or manic episode. Those who experience only depressive episodes are diagnosed with the depressive type of schizoaffective disorder while those who experience manic episodes (with or without depressive episodes) are diagnosed with the bipolar type of schizoaffective disorder. It should be noted that because a loss of interest in pleasurable activities is a common symptom of schizophrenia, to meet criteria for a depressive episode within schizoaffective disorder, the individual must present with a pervasive depressed mood (not just anhedonia). While schizophrenia and schizophreniform disorder do not have a significant mood component, schizoaffective disorder requires the presence of a depressive or manic episode for the majority, if not the total duration of the disorder. While psychotic symptoms are sometimes present in depressive episodes, they often remit once the depressive episode is resolved. For individuals with schizoaffective disorder, psychotic symptoms should continue for at least two weeks in the absence of a major mood disorder (APA, 2013). This is the key distinguishing feature between schizoaffective disorder and major depressive disorder with psychotic features.
\(\PageIndex{2.5}\): Delusional Disorder
As suggestive of its title, delusional disorder requires the presence of at least one delusion that lasts for at least one month in duration. It is important to note that any other symptom of schizophrenia (i.e., hallucinations, disorganized behavior, disorganized speech, negative symptoms) rules out a diagnosis of delusional disorder. Therefore the only symptom that can be present is delusions. Unlike most other schizophrenia-related disorders, daily functioning is not overtly impacted in individuals with delusional disorder. Additionally, if symptoms of depressive or manic episodes present during delusions, they are typically brief in duration compared to the duration of the delusions.
The DSM 5 (APA, 2013) has identified several subtypes of delusional disorder in efforts to better categorize the symptoms of the individual’s disorder. When making a diagnosis of delusional disorder, one of the following specifiers is included.
- Erotomanic delusion – the individual reports a delusion of another person being in love with them. Generally speaking, the individual whom the convictions are about are of higher status such as a celebrity.
- Grandiose delusion – involves the conviction of having a great talent or insight. Occasionally, individuals will report they have made an important discovery that benefits the general public. Grandiose delusions may also take on a religious affiliation, as some people believe they are prophets or even God, himself.
- Jealous delusion – revolves around the conviction that one’s spouse or partner is/has been unfaithful. While many individuals may have this suspicion at some point in their relationship, a jealous delusion is much more extensive and generally based on incorrect inferences that lack evidence.
- Persecutory delusion – involves beliefs that they are being conspired against, spied on, followed, poisoned or drugged, maliciously maligned, harassed, or obstructed in pursuit of their long-term goals (APA, 2013). Of all subtypes of delusional disorder, those experiencing persecutory delusions are the most at risk of becoming aggressive or hostile, likely due to the persecutory nature of their distorted beliefs.
- Somatic delusion – involves delusions regarding bodily functions or sensations. While these delusions can vary significantly, the most common beliefs are that the individual emits a foul odor despite attempts to rectify their smell; there is an infestation of insects on the skin; or that they have an internal parasite (APA, 2013).
- Mixed delusions – there are several themes of delusions (e.g., jealous and persecutory)
- Unspecified delusion – these are delusions that don’t fit into one of the categories above (e.g., referential delusions without a persecutory or grandiose nature to them).
- Bizarre delusion – delusions that are clearly not plausible and do not stem from ordinary experience (e.g., the delusion that one is an alien/vampire hybrid).
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Dtsch Arztebl Int
- v.117(24); 2020 Jun
Schizophrenia
Alkomiet hasan.
1 Department of Psychiatry, Psychotherapy, and Psychosomatics, Faculty of Medicine, University of Augsburg, District Hospital Augsburg, Augsburg
2 Department of Psychiatry and Psychotherapy, LMU Medical Center, Munich

Peter Falkai
Isabell lehmann.
3 LVR Institute for Health Care Research, Cologne
Wolfgang Gaebel
4 Department of Psychiatry and Psychotherapy, LVR Hospital Düsseldorf, Faculty of Medicine, University of Düsseldorf
The lifetime prevalence of schizophrenia is 1%. Schizophrenia is among the most severe mental illnesses and gives rise to the highest treatment costs per patient of any disease. It is characterized by frequent relapses, marked impairment of quality of life, and reduced social and work participation.
The group entrusted with the creation of the German clinical practice guideline was chosen to be representative and pluralistic in its composition. It carried out a systematic review of the relevant literature up to March 2018 and identified a total of 13 389 publications, five source guidelines, three other relevant German clinical practice guidelines, and four reference guidelines.
As the available antipsychotic drugs do not differ to any great extent in efficacy, it is recommended that acute antipsychotic drug therapy should be side-effect-driven, with a number needed to treat (NNT) of 5 to 8. The choice of treatment should take motor, metabolic, sexual, cardiac, and hematopoietic considerations into account. Ongoing antipsychotic treatment is recommended to prevent relapses (NNT: 3) and should be re-evaluated on a regular basis in every case. It is also recommended, with recommendation grades ranging from strong to intermediate, that disorder- and manifestation-driven forms of psychotherapy and psychosocial therapy, such as cognitive behavioral therapy for positive or negative manifestations (effect sizes ranging from d = 0.372 to d = 0.437) or psycho-education to prevent relapses (NNT: 9), should be used in combination with antipsychotic drug treatment. Further aspects include rehabilitation, the management of special treatment situations, care coordination, and quality management. A large body of evidence is available to provide a basis for guideline recommendations, particularly in the areas of pharmacotherapy and cognitive behavioral therapy.
The evidence-based diagnosis and treatment of persons with schizophrenia should be carried out in a multiprofessional process, with close involvement of the affected persons and the people closest to them.
Schizophrenia is one of the most severe mental illnesses. It has a point prevalence of 4.6 per 1000 inhabitants, a lifetime prevalence of around 1%, and the median reported incidence is 15 cases per 100 000 inhabitants (see [1] for details). Approximately two thirds of newly arising cases of schizophrenia occur before 45 years of age, i.e., in young to middle-aged adults. With regard to the clinical presentation, schizophrenia is characterized by a heterogeneous phenotype and a variable course, so one should really speak of a group of diseases, “the schizophrenias.” However, in accordance with the criteria for diagnosis and classification we used the singular “schizophrenia” for the guidelines. The disease is characterized by psychopathological disorders of perception, ego functions, affectivity, energy, and psychomotor function and by events that occur at particular junctures in the disease course ( 1 ). The latter is inter- and intraindividually variable: there may be one single episode, recurring episodes with no symptoms at all in between, relapses of increasing severity, or continuous illness with no periodic absence of symptoms. Although self-limiting episodes of schizophrenia are known to occur, the majority of episodes require multiprofessional treatment. The diagnosis is made in operationalized manner according to ICD-10 criteria. It is not only very important to differentiate schizophrenia from other mental illnesses; somatic diseases must also be considered as comorbidites or as causes for secondary psychoses.
One important factor that has, so far, received little attention is the very high mortality rate. Studies show that schizophrenia reduces life expectancy by anything from 10 to 25 years ( 2 , 3 ). There are many reasons for the elevated mortality: increased suicidality (especially in the early years of illness), the occurrence of somatic diseases, underdiagnosis of somatic diseases, deficient self-care, and inadequate psychiatric/psychotherapeutic treatment, as well as aspects of treatment-associated adverse effects ( 1 , 4 , 5 ). Around 10% of persons in whom schizophrenia is diagnosed for the first time attempt suicide in the 12 months following diagnosis, and one can conclude, depending on the individual survey, that 5 to 15% of persons with a schizophrenia spectrum disorder kill themselves ( 6 – 12 ). An example of the underdiagnosis of somatic comorbidities is provided by a Swedish cohort study of 6 097 838 adults (including 8277 with schizophrenia): In both women (hazard ratio 3.33, 95% confidence interval [2.73; 4.05]) and men (2.20 [1.83; 2.65]) with schizophrenia, death due to ischemic heart disease occurred more frequently than in the rest of the population. Furthermore, the likelihood of timely diagnosis was significantly lower in those with schizophrenia (26.3% versus 43.7%). The figures for cancer disease were similar ( 13 ). Other clinically relevant characteristics that are associated with schizophrenia and are often interrelated are marked stigmatization; associations with previous trauma and experience of violence (the mean proportion of persons with schizophrenia who fulfill the criteria for post-traumatic stress disorder [PTSD] is as high as 30% [14]); a high prevalence of comorbid substance dependency (principally tobacco (prevalence up to 80% [15]), alcohol, and cannabis (mean prevalences ˜25% [16]); high rates of unemployment and homelessness (˜12% of homeless persons have a psychotic disease [17]); and reduced social participation.
The new German clinical practice guidelines
The clinical practice guidelines on schizophrenia published in 2019 represent a comprehensive revision and expansion of the two previous versions from 1998 and 2006. Each of these earlier documents was conceived, developed, and published as patient-centered, evidence-based, and consensus-based guidelines in accordance with the rules and standards of the Association of the Scientific Medical Societies in Germany (AWMF) ( 1 ).
The guideline revision was undertaken by a committee of persons representative of the intended users, divided into a steering group, an extended steering group, a consensus group, and an additional expert group ( ebox 1 ). For the purpose of revision the subject matter was divided into modules, each dealt with by a dedicated working group in a multistage process (see [18]):
Professional societies, interest groups, and persons involved in the revision of the guideline
Project management
Prof. Dr. Wolfgang Gaebel (lead)
Prof. Dr. Alkomiet Hasan
Prof. Dr. Peter Falkai
Project organization and coordination, methods
Dr. Isabell Lehmann
Other members of steering group
Prof. Dr. Birgit Janssen
Prof. Dr. Thomas Wobrock
Prof. Dr. Jürgen Zielasek
Extended steering group
Prof. Dr. Thomas Becker
Prof. Dr. Andreas Bechdolf
Prof. Dr. Stefan Klingberg
Prof. Dr. Hans Joachim Salize
Prof. Dr. Rainer Richter (to May 2015), Dr. Nikolaus Melcop (from June 2016), Bundespsychotherapeutenkammer
Prof. Dr. Stefan Wilm, Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin e. V.
Prof. Dr. Tania Lincoln, Deutsche Gesellschaft für Psychologie e. V
Dr. Sabine Köhler, Berufsverband Deutscher Psychiater e. V.
Dr. Christian Raida, Berufsverband Deutscher Nervenärzte e. V
Ruth Fricke, Bundesverband Psychiatrie Erfahrener e. V.
Gudrun Schliebener (to August 2017), Karl-Heinz Möhrmann (from September 2017), Bundesverband der Angehörigen psychisch Kranker e. V.
Prof. Dr. Benno Schimmelmann (to May 2016), Prof. Dr. Christoph Correll (from June 2016), Deutsche Gesellschaft für Kinder- und Jugendpsychiatrie, Psychosomatik und Psychotherapie
Consensus group
Officer of association/organization (deputy)
Arbeitsgemeinschaft für Neuropsychopharmakologie und Pharmakotherapie e. V.: Prof. Dr. Helge Frieling (PD Dr. Michael Kluge)
Arzneimittelkommission der deutschen Ärzteschaft: Prof. Dr. Christopher Baethge (Prof. Dr. Tom Bschor)
Berufsverband der Kinder- und Jugendärzte e. V.: Dr. Karin Geitmann
Berufsverband deutscher Nervenärzte: Dr. Christian Raida (Dr. Roland Urban)
Berufsverband deutscher Psychologinnen u. Psychologen e. V.: Inge Neiser (Heinrich Betram)
Berufsverband deutscher Psychiater e. V.: Dr. Sabine Köhler (Dr. Christian Vogel)
Berufsverband für Kinder- und Jugendpsychiatrie, Psychosomatik und Psychotherapie in Deutschland e. V.: Dr. Reinhard Martens
Bundesarbeitsgemeinschaft für Rehabilitation e. V.: Dr. Michael Schubert (to December 2017), Dr. Theresia Widera (from January 2018)
Bundesdirektorenkonferenz: Prof. Dr. Manfred Wolfersdorf (to July 2017), Prof. Dr. Euphrosyne Gouzoulis-Mayfrank (from August 2017) (Prof. Dr. Thomas Pollmächer, Dr. Sylvia Claus (from March 2018)
Bundesfachverband Leitender Krankenpflegepersonen in der Psychiatrie: Heinz Lepper (Stephan Bögershausen)
Bundespsychotherapeutenkammer: Prof. Rainer Richter (to May 2015), Dr. Nikolaus Melcop (from June 2016) (Dr. Tina Wessels)
Bundesverband der Angehörigen Psychisch Kranker e. V.: Gudrun Schliebener (to August 2017), Karl-Heinz Möhrmann (from September 2017) (Wiebke Schubert)
Bundesverband der Berufsbetreuer/innen e. V.: Iris Peymann (Thorsten Becker)
Bundesverband der Vertragspsychotherapeuten e. V.: Hans Ramm (Dr. Christian Willnow to August 2017, Benedikt Waldherr from October 2017)
Bundesarbeitsgemeinschaft Künstlerische Therapien: Eva Maas (to August 2017) (Silke Ratzeburg)
Bundesinitiative Ambulante Psychiatrische Pflege e. V.: Alfred Karsten (Günter Meyer)
Dachverband Deutschsprachiger Psychosen Psychotherapie e. V.: Prof. Dr. Dorothea von Haebler (Dr. Günther Lempa)
Deutsche Fachgesellschaft für Psychiatrische Pflege: Prof. Dr. Michael Schulz (Bruno Hemkendrais)
Dachverband Gemeindepsychiatrie e. V.: Petra Godel-Ehrhardt
Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin e. V.: Prof. Dr. Stefan Wilm (Prof. Dr. Erika Baum, Martin Beyer)
Deutsche Gesellschaft für Gerontopsychiatrie und -psychotherapie e. V.: Prof. Dr. Tillmann Supprian (Dr. Beate Baumgarte)
Deutsche Gesellschaft für Kinder- und Jugendmedizin e. V.: Dr. Burkhardt Lawrenz
Deutsche Gesellschaft für Kinder- und Jugendpsychiatrie, Psychosomatik und Psychotherapie e. V.: Prof. Dr. Gerd Schulte-Körne (to August 2017), Prof. Dr. Christoph Correll (from September 2017) (Prof. Dr. Christian Fleischhaker)
Deutsche Gesellschaft für Neuropsychologie e. V.: Prof. Dr. Cornelia Exner (Dr. Steffen Aschenbrenner from September 2017)
Deutsche Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde: Prof. Dr. Wolfgang Maier (Prof. Dr. Peter Falkai, Prof. Dr. Wolfgang Gaebel)
Deutsche Gesellschaft für Psychoanalyse, Psychotherapie, Psychosomatik und Tiefenpsychologie e. V.: Dr. Christian Maier (to March 2016), Prof. Dr. Christiane Montag (from April 2016) (Dr. Ingrid Rothe-Kirchberger)
Deutsche Gesellschaft für Psychologie e. V.: Prof. Dr. Tania Lincoln (Prof. Dr. Stefan Klingberg)
Deutsche Gesellschaft für Psychoedukation e. V.: Prof. Dr. Josef Bäuml (Dr. Gabriele Pitschel-Walz)
Deutsche Musiktherapeutische Gesellschaft e. V: Beatrix Evers-Grewe
Deutsche PsychotherapeutenVereinigung e. V.: Dr. Cornelia Rabe-Menssen (Mechtild Lahme)
Deutsche Gesellschaft für Soziale Psychiatrie e. V.: Clemens Firnenburg (to August 2017), Prof. Dr. Uwe Gonther (from November 2017) (Ute Merkel to October 2017, PD Dr. Jann Schlimme from November 2017)
Deutsche Gesellschaft für Systemische Therapie und Familientherapie e. V.: Dr. Ulrike Borst (Dr. Volkmar Aderhold)
Deutsche Gesellschaft für Verhaltenstherapie e. V.: Rudi Merod (Prof. Dr. Tania Lincoln)
Deutscher Verband der Ergotherapeuten e. V.: Marina Knuth
Deutscher Verband für Physiotherapie e. V.: Eckhardt Böhle (Angelika Heck-Darabi)
Deutsche Vereinigung für Soziale Arbeit im Gesundheitswesen e. V.: Claudia Welk (Elisabeth Helmich from June 2017)
Kompetenznetz Schizophrenie: Prof. Dr. Wolfgang Wölwer
Expert group
Prof. Dr. Thomas Becker, Prof. Dr. med. Stefan Leucht
Prof. Dr. Andreas Bechdolf, Prof. Dr. Wolfgang Maier
Prof. Dr. Peter Falkai, Prof. Dr. Eva Meisenzahl
Prof. Dr. Wolfgang Gaebel, Prof. Dr. Andreas Meyer-Lindenberg
Prof. Dr. Hermann-Josef Gertz, Prof. Dr. Hans-Jürgen Möller
Prof. Dr. Gerhard Gründer, Prof. Dr. Dipl.-Psych. Wulf Rössler
Prof. Dr. Stefan Klingberg, Prof. Dr. Hans Joachim Salize
PD Dr. Markus Kösters, Prof. Dr. Wolfgang Wölwer
Prof. Dr. Martin Lambert
Expert group (pediatric psychiatry and psychotherapy)
Prof. Dr. Christoph Correll, Prof. Dr. Benno Schimmelmann
Prof. Dr. Frauke Schultze-Lutter, Dr. Reinhard Martens
Prof. Dr. Stefanie J. Schmidt
Support staff
Dr. Andrea Hinsche-Böckenholt, Anja Dorothée Streb, M.A.
- Formulation and agreement of clinical issues within the guidelines group
- Identification and methodological evaluation of existing guidelines on schizophrenia (for the purpose of guideline adaptation)
- Systematic search of the literature with regard to questions not adequately answered by guideline adaptation (start date: 3 March 2016, last research: 1 March 2018)
- Systematic selection and evaluation of the evidence
- Formulation of recommendations and suggestions for recommendation grades by the module working groups and the steering group according to the PICO (patient population, intervention, comparison, outcome) scheme ( 19 )
- Adoption of the recommendations and structured consensus building (consensus conferences and written Delphi process)
- Internal and external reviewing and adoption of the guidelines
Only guidelines of high methodological quality on relevant topics were used as sources ( 20 – 24 ). Domain 3 (Methodological Rigour of Development) of the German Instrument for Methodological Guideline Appraisal (DELBI) was used for assessment. Gradations of evidence and wordings of recommendations from these source guidelines were adapted for use in the revised guidelines. Further sources of recommendations on dependency-specific topics were two AWMF clinical practice guidelines ( 15 , 25 ). An overview of the guidelines from Germany and other countries that were used, together with related AWMF guidelines, can be found in eTable 1 . Moreover, for some of the guideline recommendations systematic de novo research was carried out ( efigure 1 ), while for other recommendations not based on evidence clinical consensus points were compiled.

Flow chart of systematic literature survey.
The diagram summarizes the entire literature survey. The individual searches and the search terms used can be found in the guideline report ( 18 ) (this flow chart does not form part of the guidelines).
*These German clinical practice guidelines were not assessed with the DELBI instrument, because they were previously published, valid guidelines.
Updated content in the revised guidelines
The modular structure of the guidelines is intended to enable future revision on the lines of the “living guidelines” principle. Box 1 summarizes the most important changes in the revised clinical practice guidelines, described in more detail below.
What are the most important changes in the revised guidelines?
- Recommendations for the entire life span: While the previous version of the guidelines focused on the age range 18 to 65, the new guidelines contain key recommendations for children and adolescents and for the elderly (> 65 years).
- Somatic illness: New recommendations were developed to include somatic illness in differential diagnosis (detection of rare somatic causes of secondary schizophrenia). Special attention was paid to the detection and treatment of somatic comorbidity and to reduction of the high morbidity and mortality.
- Adverse effect–guided antipsychotic treatment: In view of the often only small differences in effect among various antipsychotics, most of the recommendations do not prioritize particular substances. Risks and benefits need to be weighed in each case. Thus, emphasis was placed on individualized antipsychotic therapy at the lowest possible dosage, paying attention to adverse effects.
- Antipsychotic prevention of relapse: The necessity of continuous antipsychotic prophylaxis was emphasized. In contrast to the previous guidelines, the duration of antipsychotic treatment to prevent relapses is not specified—this should be determined individually on the basis of various factors, e.g., the severity of the index episode, the stability of the patient’s social network, and the comorbidities present, and should be regularly reevaluated.
- Pharmacological treatment resistance: The necessity of excluding pseudo-treatment resistance was stressed. In the presence of pharmacological treatment resistance, the importance of the antipsychotic agent clozapine was accentuated. Clozapine should be used before offering a treatment with a combination of antipsychotics.
- Psychotherapy: It was emphasized that every person with schizophrenia should be offered cognitive behavioral therapy (CBT)—the therapy content and dosage (at least 16 h, preferably more than 25 h) were specified. Further procedures accorded the highest recommendation grade are psychoeducation, social competence training, cognitive remediation, and work with relatives.
- Psychosocial treatment: The importance of this type of treatment (e.g., artistic therapy, body therapy, ergotherapy) as a further therapeutic pillar was reinforced, but overall the recommendation grades are lower than those for psychotherapeutic procedures.
- Special treatment conditions: This module contains recommendations on the diagnosis and treatment of catatonia, depression and suicidality, post-traumatic stress disorder, and substance consumption disorders (alcohol, tobacco, cannabis). Further elements are sex-specific aspects, pregnancy and the breastfeeding period, and the new section on the at-risk stage.
Diagnosis and differential diagnosis
As stated above, schizophrenia is diagnosed according to the operationalized criteria of ICD-10 ( efigure 2 ). However, the guidelines give a glimpse of the changes that can be anticipated in ICD-11. One particular innovation is the possibility of describing the course of the illness on the basis of symptom domains (positive symptoms, negative symptoms, cognitive disorders, psychomotor disorders, and affective disorders) ( 26 ). Much more importance is attached in the revised guidelines to aspects of organic differential diagnosis: recommendations were agreed with the intention of on the one hand detecting rare organic causes of schizophrenia (e.g., autoimmune encephalitis) in timely fashion, and on the other hand diagnosing the frequently occurring somatic comorbidities and integrating them into the overall treatment plan. eBox 2 presents the accompanying somatic disorders most commonly found in persons with schizophrenia, with the data expressed in terms of prevalence rates, incidence rates, or odds ratios.

Algorithms for psychopathological and somatic differential diagnosis (derived from, but not forming part of, the new German clinical practice guidelines)
General treatment principles
Modern psychiatric/psychotherapeutic treatment of persons with schizophrenia should always be multiprofessional, and all those involved in the treatment should maintain an empathetic, appreciative attitude. According to the guidelines, the “general goal of treatment [is] a person broadly free of symptoms of illness who is capable of living in a self-determined manner, has been informed about the therapeutic options, and is in the position to weigh up the risks and benefits thereof” ( 1 ). To achieve this, the elements of pharmacotherapy, psychotherapy, and psychosocial treatments should be offered in terms of an overall treatment plan with the close involvement of the person with schizophrenia together with their relatives or other reference persons. According to the evidence and consensus opinion, antipsychotic drug treatment alone is generally insufficient, as is renunciation of antipsychotic pharmacotherapy. Other forms of treatment, such as the use of antidepressants or neurostimulation procedures (e.g., electroconvulsive therapy), are reserved for particular indications (e.g., depressive syndromes or clozapine resistance).
Treatment with antipsychotics
Antipsychotics are highly effective with regard to the goals relevant to the disease (e.g., reduction of psychotic symptoms, prevention of relapse). For example, the largest meta-analysis with the highest quality methods shows a number needed to treat (NNT) of 3 for 1-year prevention of relapse (relapse rate 27% with antipsychotic treatment, 64% with placebo) ( 27 ). In respect of the therapeutic response in terms of reduction of psychotic experiences, another large-scale and high-quality meta-analysis shows an NNT of 5 or 8 for a minimal or good response (51%/23% with antipsychotic treatment, 30%/14% with placebo) ( 28 ). One basic innovation in the new German clinical practice guidelines is the emphasis on adverse effect–guided selection of the antipsychotic substances—abolishing the general prioritization of a specific substance group. Based on an adaptation of a NICE guideline ( 20 ) and on a meta-analysis ( 29 ), the following definition was formulated: “We recommend offering antipsychotics at a dose that is within the range recommended by the respective international consensuses and is as low as possible and as high as necessary (lowest possible dose)”. A low dose should be chosen particularly in patients suffering their first episode of schizophrenia, who are more vulnerable to adverse effects and overall respond better to low dosages. It is important that treatment to reduce psychotic symptoms be offered in the form of antipsychotic monotherapy. The recommendation of monotherapy is justified especially on grounds of better tractability and a lower risk of adverse effects and drug interactions. Moreover, nearly all of the source studies and meta-analyses investigated antipsychotics given as monotherapy.
For the first time, and uniquely worldwide, clinical consensus point (CCP) recommendations on the discontinuation of antipsychotic medication were agreed. This should not be defined as the primary course of action, however, because of the low recommendation grade (“may be considered”) compared with administration of antipsychotics to prevent relapse (“we recommend”). Nevertheless, suggestions, recommendations, and strategies are now in place for dealing with the routinely expressed request from both patients and their relatives for antipsychotic medication to be stopped. It is important, in clinical practice, to state that treatment does not end with discontinuation of the medication. On the contrary, regular, coordinated outpatient psychiatric and/or psychotherapeutic follow-up visits should continue for at least 2 years, with two goals: ( 1 ) early detection of signs and symptoms of an impending relapse (e.g., sleep disorders, a brief psychotic episode, depressive symptoms, inner unrest); ( 2 ) implementation of interventions to help manage stress or structure daily activities. It is vital for treatment to continue beyond supervised discontinuation of drug intake.
In contrast to the guideline recommendation of monotherapy, however, in clinical practice the use of polypharmacy is growing, particularly later in the disease course ( 30 ). This discrepancy between clinical practice and evidence was addressed as follows: According to the revised guidelines, a combination of two antipsychotics should be given (recommendation grade CCP) only after the failure of three previous attempts at antipsychotic treatment of adequate dosage and duration—including a course of clozapine—as monotherapy (recommendation 43, recommendation grade A, and recommendation 46, recommendation grade A). The addition of a second antipsychotic or an antidepressant for the temporary treatment of unrest, sleep disorders, elevated prolactin concentration, or depressive symptoms is considered separately in the guidelines—this special situation does not fall under the described recommendation to offer monotherapy, but when any additional substance is given, one must bear in mind the possible increase in adverse effects and monitor the patient accordingly. The Table and eTable 2 summarize the meta-analyses cited in the guidelines and list the corresponding recommendations. The Figure shows a treatment algorithm, derived from relevant recommendations, which focuses on antipsychotic treatment.
BPRS, Brief Psychiatric Rating Scale; LoE, level of evidence; NNT, number needed to treat; PANSS, Positive and Negative Syndrome Scale; RR, relative risk

Treatment algorithm derived from the revised German clinical practice guidelines (focus on pharmacology): Here the guidelines’ essential treatment recommendations are summarized; for clinical application, however, it is vital to consult the long version of the guidelines and the detailed recommendations therein (this algorithm does not form part of the clinical practice guidelines).
ADR, adverse drug reaction; TDM, therapeutic drug monitoring; TMS, transcranial magnetic stimulation
Psychotherapy and psychosocial treatments
The revised clinical practice guidelines place far more emphasis on psychotherapy. Combination of treatment with an antipsychotic substance and cognitive behavioral therapy (CBT) is recommended for all persons with schizophrenia (effect size for positive symptoms: d = 0.372; for negative symptoms: d = 0.437). CBT should be offered (recommendation grade A). If CBT begins while the patient is in the hospital, it should be continued on an outpatient basis after discharge; the duration of treatment should be ≥ 16 sessions, and for optimization of treatment effects and in cases with more complex treatment goals ≥ 25 sessions should be offered (recommendation grade B). The inpatient and outpatient psychotherapeutic care available for persons with schizophrenia in Germany is clearly inadequate, although it remains unclear whether the previously very low rates of psychotherapy in this population have been increased by the extension of the indication to all phases of the disease by the Federal Joint Committee (G-BA) in 2014 (art. 26 para. 2 no. 4 of the G-BA’s Psychotherapy Guidelines) ( 1 ). Other psychotherapeutic procedures with recommendation grade A are psychoeducation (NNT = 9 in prevention of relapse), family interventions, cognitive remediation (a cognitive training and education process), and social competence training. The various procedures should be offered individually, depending on the indications in each case. eTable 3 shows the matrix of psychotherapeutic and psychosocial treatment procedures that can be offered depending on the indications and individual preferences. New in the revised guidelines is the recommendation (grade B) that CBT also be offered to those who reject antipsychotic drug treatment.
CBT, cognitive behavioral therapy; FEP, first-episode psychosis; GA, guideline adaptation; LoE, level of evidence; n.d., no data; REC, relapse
A: recommendation grade A; B: recommendation grade B, 0: recommendation grade 0
The superscripts after LoE show the evidence grade according to SIGN
Management of adverse drug reactions
A large number of preparation-specific adverse drug reactions may be caused by antipsychotics, and these potential side effects must always be borne in mind when prescribing this type of medication. Accordingly, the clinical practice guidelines focus on adverse event–guided prescription of antipsychotic drugs. The following groups of adverse events must be particularly closely respected and monitored:
- Motor reactions
- Metabolic reactions
- Sexual dysfunction/prolactin-associated reactions
- Cardiac reactions
- Disorders of the hematopoietic system.
Specifically for metabolic reactions, the guidelines group approved new evidence-based recommendations in terms of a stepwise procedure for detection and treatment. eBox 3 defines a general stepwise process for the recognition and treatment of adverse events, while eTable 4 presents concrete recommendations for the detection and treatment of metabolic syndrome, a very common occurrence in persons with schizophrenia. eTable 5 shows the follow-up visits as defined by the guidelines group for persons receiving antipsychotic treatment, and eTable 6 lists the preparation-specific adverse events.
Detection and management of adverse drug reactions (modified from [1])
This table from the new German clinical practice guidelines ( 1 ) was compiled on the basis of ( e49 , e50 ) and adapted in an expert consensus process. It should be noted that these are general recommendations. The scope of investigation can be adapted to the risk, oriented on the data in the product information sheet, so that the dose can be increased or decreased in the individual patient. The crucial factors in risk-based adaptation are: comorbidities, accumulation of risk factors, combination treatments, dose escalation, age, and occurrence of organ-specific symptoms. Particularly in a steady-state situation with unchanged risk and medication profiles, the interval between follow-up visits can be increased, taking account of the relevant product information. The recommended diagnostic procedures in persons with a first episode are presented in module 2 of the long version of the new German clinical practice guidelines on schizophrenia.
X: Necessary number of routine follow-up visits. If a single visit in month 1 is recommended, the measurement can take place between week 3 and week 6—the investigation in the first month relates to the usual time to full dosage of an antipsychotic. X = number of follow-up visits in period concerned (e.g., X = one investigation in given month; XXXX = four investigations in given month).
* 1 NB: The SGAs olanzapine, quetiapine and zotepine are, with regard to chemical structure, also tricyclics.
* 2 Supplemented if needed by 24-h blood sugar profile or glucose tolerance test, especially with clozapine and olanzapine
* 3 In steady-state unremarkable constellations, visits annually or even less frequently may suffice.
* 4 Absolute values of >440 ms (men) or >450 ms (women) and medication-induced increases >60 ms are a cause for concern. With a QTc time >480–520 ms or an increase in QTc time >60 ms, the original antipsychotic should be discontinued and a new antipsychotic started.
* 5 Toxic-allergic myocarditis has been described with clozapine; therefore, those taking clozapine should undergo ECG monitoring at shorter intervals and, if thought advisable, have cardiac echocardiography on the occurrence of cardiac symptoms and fever or after 14 days’ treatment.
* 6 On new administration of clozapine: carry out ECG and determine levels of CRP and troponin I, or alternatively measure T value, blood pressure, pulse, and temperature, before starting clozapine; then measure CRP, troponin I, and T value weekly for 4 weeks and blood pressure, pulse, and temperature every 2 days for 4 weeks.
* 7 In the presence of pre-existing or new cardiac symptoms or a significant prolongation of QTc time, cardiological examination is necessary; this will also establish at what intervals ECG needs to be carried out in the longer term.
* 8 More frequent follow-up is advisable for all patients >60 years, and this may also be thought necessary in the presence of cardiac risk factors; more frequent ECG monitoring is recommended with ziprasidone, perazine, fluspirilene, and high-potency butyrophenones, as well as in the event of QTc time prolongation and in combination treatment involving any other substances that may prolong the QTc time.
* 9 With sertindole, ECG (preferably in the morning) is recommended before commencement of treatment, after steady state has been achieved (3 weeks) or at a dose of 16 mg, after 3 months, and subsequently at 3-month intervals, before and after every dose increase during maintenance treatment, and after initiation or dose increase of any accompanying medication that could lead to an elevation of the sertindole concentration.
* 10 EEG before the initiation of clozapine treatment. EEG should be one of the first diagnostic procedures in the presence of signs of an organic process (see module 2). EEG monitoring during the disease course if there are clinical signs of a seizure. More frequent EEG also in the presence of pre-existing cerebral insult, elevated susceptibility to seizures, and, if deemed necessary, before and during antipsychotic treatment if very high dosages (combinations) are being used, as well as unexplained changes in state of consciousness (differential diagnosis: non-convulsive status).
* 11 Measurements of waist size are recommended in addition to calculation of BMI; additionally, monthly weight checks by the patient him-/herself.
* 12 Only blood sugar and HbA 1C, in the case of abnormal findings and (* 2 ) consider treatment and monthly follow-up; in presence of metabolic syndrome, monthly blood sugar measurements and (* 2 ).
* 13 Occurrence of dyspnea or unexplained exhaustion during antipsychotic treatment should be investigated with cardiac ultrasound. This is particularly important for treatment with dibenzodiazepines, dibenzothiazepines, or thienobenzodiazepines.
* 14 The NICE guidelines ( 20 ) recommend determination of prolactin before commencement of antipsychotic treatment. During the disease course, prolactin should be determined if the corresponding symptoms occur.
Adverse effects of antipsychotics (reproduced in full from the revised clinical practice guidelines ( 1 ). The table was compiled on the basis of the CINP Schizophrenia Guidelines and the references contained therein ( e51 ) and on the previous AWMF guidelines on schizophrenia ( 39 ); adaptation took place in an expert consensus process based on product information sheets and recently published meta-analyses ( 28 , 32 ). Gaps in the data were filled using the product information sheets and the standard reference for psychopharmacology in Germany ( e49 ). The data on pneumonia were extracted from a meta-analysis ( e34 ). Unexpected adverse effects may occur with widespread use of the preparations, so pharmacovigilance (see eTable 5 ) is mandatory.
*Lurasidone is approved for the treatment of schizophrenia in Germany, but prescriptions for it cannot be charged to the National Association of Statutory Health Insurance Funds.
0 = None, (+) = sporadic or no significant difference from placebo, + = rare, ++ = occasional, +++ = frequent, ? = data insufficient for estimation of frequency. Please note that these are not systematically compiled quantitative estimates of incidence, but rather qualitative estimates based on clinical experience, taking account of the sources mentioned above. MNS, Malignant neuroleptic syndrome
Problems in coordination of care
In practice, various problems may arise in coordination among caregivers. These can affect the transition from inpatient care to the post-hospital setting (day clinic, outpatient clinic, specialist medical care in the community), coordination in the area of outpatient care (specialist-centered treatment, psychotherapists, primary-care physicians, other parties), or the challenge of hospital admission in an acute phase of illness characterized by decreased or lacking insight. The new module 5 (coordination of care) is dedicated to these and other aspects of optimized organization of patient care. For example, one recommendation (grade CCP) is that whenever treatment by a multiprofessional team is required or intensification of psychopharmacological, psychotherapeutic, or psychosocial measures becomes necessary, it should be considered whether transfer to a specialized and multiprofessional psychiatric hospital outpatient service ( Psychiatrische Institutsambulanz, PIA), or to a community care network in which more complex treatment programs are available if needed, might be beneficial ( 1 ). In another recommendation (CCP, strong consensus) the guidelines group defined indications for hospital admission. Inpatient treatment should be offered to all patients who would benefit from the diagnostic and therapeutic resources available in the hospital setting or from the special protection offered by the hospital in the case of acute danger to themselves or others. This would include, for example:
- Treatment resistance
- Acute suicidality
- States of severe delusion or anxiety
- Lack of proper nutrition or self-care
- Marked apathy or adynamia
- Domestic circumstances hindering remission and recovery
- Treatment of complicating comorbidities
- Complex treatment situations
- Unexplained somatic comorbidities
- Severe adverse drug reactions
- Other problems not amenable to outpatient care.
This incomplete list makes it clear that in patients who present acute danger to themselves or others, or lack insight, one must consider hospitalization under the terms of the Care Act and the laws of the federal state concerned. It also becomes apparent that the guidelines group has defined factors such as the lack of options for care, but most importantly somatic and mental comorbidities, as indications for admission to the hospital. These latter points routinely lead to discussions with the medical service of the health insurance providers in Germany (MDK) on whether hospital beds are being utilized unnecessarily.
The revised German clinical practice guidelines on schizophrenia contain recommendations on both the diagnostic work-up and the pharmacological, psychotherapeutic, and psychosocial treatment of persons with schizophrenia over their entire life span. To conform with the guidelines, the treatment of persons with schizophrenia must be multiprofessional with a basic attitude of empathy, respect, and appreciation on the part of the caregivers. The aim is to render those affected able to enjoy “full and equal enjoyment of all human rights and fundamental freedoms” (article 1, UN CRPD).
Findings of selected meta-analyses published after the end of the literature survey
A dose–response meta-analysis of 68 studies calculated the so-called 95% effective dose (the level at which no additional effect can be anticipated from raising the dose) for the acute treatment of psychotic symptoms based on recent data for all relevant antipsychotic drugs: for example, amisulpride 537 mg/day, aripiprazole 11.5 mg/day, olanzapine 15.2 mg, haloperidol 6.3 mg/day ( 31 ). A new network meta-analysis of 402 randomized controlled trials (RCT) with 53 463 participants expanded the findings of the network meta-analysis used for the clinical practice guidelines ( 32 ) with regard to the differences among antipsychotics in terms of efficacy and tolerability. Six years after the first meta-analysis of this kind, the new publication confirmed that the differences in the efficacy of an antipsychotic preparation are far smaller than the differences in its adverse effect profile ( 33 ). As for the drug safety of antipsychotics, a meta-analysis (596 RCT with 108 747 participants) investigated the endpoint of short-term mortality, i.e., death in the period from 1 day to >13 weeks. For persons with schizophrenia, treatment with an antipsychotic drug showed no higher mortality than placebo (odds ratio 0.69, 95% confidence interval [0.35; 1.35]), while elevated mortality was found in persons with dementia and in elderly participants ( 34 ). Further new meta-analyses have shown, even with close scrutiny of the methods, a beneficial effect of add-on cognitive behavioral therapy on positive symptoms (SMD = -0.29; [-0.55; -0.03]) ( 35 ) and low variability of treatment response to antipsychotics compared with placebo (variation coefficient = 0.86, p <0.001) ( 36 ), and have also confirmed that especially olanzapine and clozapine can induce considerable weight gain ( 33 , 37 ). According to the latest data, aripiprazole, brexpiprazole, cariprazine, haloperidol, lurasidone, and ziprasidone have more favorable metabolic profiles than other antipsychotic ( 33 , 37 ).
Key Messages
- Schizophrenia is one of the most severe mental illnesses and does huge personal, social, and functional damage not only to the person affected but also to their relatives or reference persons.
- Pharmacological, psychotherapeutic, and psychosocial treatments should be offered at all times. Timely detection of somatic comorbidities reduces the general morbidity and mortality.
- In all phases of the disease, smooth cooperation between the person affected, their relatives, and other reference persons and the multiprofessional treatment team is the key to successful treatment.
- Antipsychotics have the most comprehensive evidence for effective reduction of the symptom burden and for prevention of relapse. Cognitive behavioral therapy is the most widely investigated non-pharmacological procedure and should always be offered together with medication.
- Despite their poorer foundation in evidence, other psychotherapeutic and psychosocial treatment procedures, together with elements such as peer-to-peer support, trialog, and outreach, form an important part of the modern treatment of persons with schizophrenia.
Relevant somatic comorbidities (derived from [1] and expanded)
The following somatic disorders occur at statistically significantly higher rates in persons with schizophrenia than in the healthy comparison population ( 3 , 4 , e22 – e29 ). The figures in parentheses are prevalence rates, incidences, or odds ratios (OR) from meta-analyses or cohort studies. It should be noted that most of these publications were not population studies, hardly any data from the German healthcare system are available, and that many of the studies were carried out in inpatients. Therefore, the data on prevalences, risk, and incidences are somewhat uncertain.
Cardiovascular and metabolic diseases
- Obesity (OR = 4.43; 95% confidence interval [2.52; 7.82]) ( e30 )
- Arterial hypertension (OR = 1.36 [1.21; 1.53]) ( e30 )
- Diabetes mellitus type 2 with resulting diseases (10.75% [7.44; 14.5]) ( e31 )
- Hyperlipidemia (41.1% [36.5; 45.7]) ( e32 )
- Cerebrovascular disease (OR = 1.63 [1.19; 2.24]) ( e22 )
- Coronary heart disease (11.8% [7.1; 19.0]) ( e22 )
- Metabolic syndrome (33.4% [30.8; 36]) ( e28 )
Lung diseases
- Chronic obstructive pulmonary disease (COPD) (OR = 1.57 [1.44; 1.72]) ( e33 )
- Lung infections (incidence 1.12 [1.07; 1.18] cases per 100 person years) ( e34 )
Cancers (RR = 0.90 [0.81; 0.99])* 1 ( e29 )
- Gastrointestinal tract
- Hematopoietic system
- Other sites (e.g.,bladder)
Other diseases
- HIV (prevalence 1.9% [0.8; 4.8]) ( e35 )
- Hepatitis B (prevalence 2.7% [1.8; 3.9]) ( e35 )
- Hepatitis C (prevalence 4.9% [3.0; 7.9]) ( e35 )
- Obstructive sleep apnea syndrome (prevalence 15.4% [5.3%; 37.1%]) ( e36 )
- Epilepsy (prevalence of psychotic disorders in epilepsy 5.6% [4.8%; 6.4%]) ( e37 )
- Poor dental hygiene/caries (mean difference 7.66 [3.27; 12.27]) ( e38 )
- Gastrointestinal ulcers (incidence rate 1.27 [1.06; 1.52]) ( e39 )* 3
* 1 The findings for cancer are not clear. A meta-analysis shows a reduced relative risk (RR = 0.90 [0.81; 0.99]) for cancers in general in persons with schizophrenia ( e29 ). Owing to the generally decreased life-expactancy, neoplasms of advanced age are found less frequently in persons with schizophrenia than in the general population (survival bias), while neoplasms (lung cancer) connected with substance use (e.g., tobacco or alcohol) occur more frequently.
* 2 Prevalence figures for Europe
* 3 Not a meta-analysis; population-based study from Taiwan
Acknowledgments
Translated from the original German by David Roseveare
Clinical practice guidelines in the Deutsches Ärzteblatt, as in numerous other specialist journals, are not subject to a peer review procedure, since such guidelines represent texts that have already been evaluated, discussed, and broadly agreed upon multiple times by experts (peers).
We thank all the individuals and groups whose long-term, continuous, and constructive commitment made it possible to draw up this guideline. Thanks are due to the German Association for Psychiatry, Psychotherapy and Psychosomatics for its substantive, structural and financial support of the entire guideline process, without which revision of the guideline could not have been achieved.
We are particularly grateful to Prof. Kopp (AWMF-Institute for Medical Knowledge Management) for her balanced moderation and advice during the entire guideline development process.
Conflict of interest statement
Prof. Hasan has received consultancy honoraria from Lundbeck, Otsuka, Janssen, and Roche as well as speaker’s fees from Desitin, Lundbeck, Otsuka and Janssen. He is the editor of the WFSBP guideline on schizophrenia. He is a member of an IFCN guideline group on rTMS treatment of neurological and mental illnesses.
Prof. Falkai has received consultancy honoraria from Janssen, Richter Pharma, Servier, and Sage as well as speaker’s fees from Otsuka, Lundbeck, Janssen, and Richter Pharma.
Prof. Gaebel is a member of the Lundbeck International Neuroscience Foundation (LINF).
Dr. Lehmann states that no conflict of interest exists.
Schizophrenia – Neurobiology and Aetiology
This presentation covers aetiology of Schizophrenia.
A working knowledge of the normal structure and function of the nervous system is key to understanding psychiatric disorders like schizophrenia. This slide deck presents an introduction to neuroanatomy, the key components of neurosynaptic transmission, neurotransmitters and the pathophysiology of schizophrenia. Last, it includes a discussion of some underlying causes of schizophrenia, such as genetic and environmental factors.
This slide deck has been developed in collaboration with the former Lundbeck International Neuroscience Foundation.
Index for slide deck
Neurobiology and aetiology, introduction to neuroanatomy, organisation of the nervous system.
To understand psychiatric disorders, it is important to have a working understanding of the normal structure and function of the nervous system. The central nervous system (CNS; brain, spinal cord) and peripheral nervous system (PNS) are made up of neurones and glial cell…
The neurone constitutes the functional unit of the nervous system; there are over 100 billion neurones in the brain. [Purves et al., 2008; Martin, 2003; Kandel et al., 2000] Each neurone has the ability to interact with and influence many other cells, which creates a syste…
Anatomical regions of the brain
The brain is divided into four anatomical regions: the diencephalon, brainstem, cerebrum, and cerebellum, as described on the slide. [Kandel et al., 2000; Tortora & Derrickson, 2009]
References: Kandel ER, Schwartz JH, Jessell TM (eds). Principles of Neural Science. 4th e…
The cerebral cortex is the main functional unit of the cerebrum. [Tortora & Derrickson, 2009] The three main functional areas of the cerebral cortex are: [Tortora & Derrickson, 2009; Prise & Wilson, 2003]
- motor areas that control voluntary movement (primary, secondary, an…
Lobes of the brain
The brain can be thought of as comprising five ‘lobes’ – the four lobes of the cerebral cortex and a fifth lobe, the insula, deep within the brain, as shown on the slide. [Martin, 2003; Tortora & Derrickson, 2009; Price & Wilson, 2003] The lobes of the cerebral cortex are …
Neurosynaptic transmission
Neurotransmission.
Information moves through the nervous system via two integrated forms of communication – electrical neurotransmission and chemical neurotransmission, as shown on the slide. [Kandel et al., 2000] An action potential is generated at the origin of the axon following sufficien…
The synapse
Neurones do not physically touch one another; two neurones are separated by a gap, known as a synaptic cleft. [Kandel et al., 2000] Because neurones do not touch, and an action potential cannot ‘jump’ across a synaptic cleft, the signal must be converted to a chemical sign…
Process of chemical neurotransmission
The idea that neurotransmission occurs at synapses and is mediated by chemicals was, at first, a contentious issue. [Purves et al., 2008] It was in the first half of the 1900s that experiments proved chemical neurotransmission occurred. [Purves et al., 2008] The process is …
Related content
Professor Christoph Correll discusses the complexities of bipolar disorder, shedding light on the real-world challenges in treatment, the critical role of clinicians, and the necessity of patient-centric approaches in psychiatry.
Bipolar disorder is a chronic and highly debilitating mental disorder characterized by recurrent mood episodes. A major challenge is its heterogeneous clinical presentation with diverse comorbidities and symptomatology.

To study intra-disease variability in cognitive function, researchers employ data-driven clustering methods to differentiate patients with widespread cognitive abnormalities from patients who are cognitively intact.
-300x169.jpg)
Permissions
Permissions for creative use of the resources from neurotorium.
Permission is granted to download images, slides and videos and use them in your own presentations, provided that copyright notices and the Neurotorium logo are not hidden or removed. For use in publications and on websites, proper attribution must be provided together with a link to Neurotorium.org
Your slides will download now. Do you want to get our latest information?
Sign up to our newsletter and receive news in your inbox. We send newsletters every 1-2 months.
You have been subscribed to our newsletter!
Share or print.
Share content with anyone.
Save to workspace
Select language.
We have detected that you are from “France”. You have the option of switching the language to French, if you would prefer that?.
This site uses cookies
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.
Sign up for our newsletter
Fill in you information below and stay up to date with the latest content on Neurotorium.
We publish newsletters every 2-3 months, keeping you up to date with the latest content on the website. You will receive a welcome e-mail immediately after you sign up for our newsletter. If you do not receive an e-mail, please check your spam folder. Contact support at [email protected] if you require help.
Welcome back
Please enter your details below.

Educational Presentations
I mpact of the covid-19 pandemic on psychosis .
The implications of the COVID-19 pandemic will have pervasive effects on schizophrenia and psychosis research and clinical services worldwide. In this webinar, four presenters share research on the impact of the COVID-19 pandemic on psychosis.
Presented By
Gemma Modinos Institute of Psychiatry, Psychology & Neuroscience, King's College London | United Kingdom Chair and Moderator
James MacCabe Institute of Psychiatry, Psychology and Neuroscience, King’s College London | United Kingdom Clozapine Treatment and Risk of COVID-19 Emily A. Troyer University of California San Diego Department of Psychiatry Hong Laboratory | United States Potential Impact of COVID-19 on Psychosis Risk and Symptomatology
SIRS 2019 Meeting Presentations

Kristen Brennand: Modeling The Impact Of Rare And Common Variants In Schizophrenia Using Stem Cells
Deanna Kelly: Schizophrenia And Gluten New Target And Precision Medicine
Steven Leifman: Awards And Keynote Speaker Judge Steven Leifman
Anthony Morrison: Cognitive Behavior Therapy For People With Psychosis
Sohee Park: Schizophrenia In The Flesh, The Case For Behavioral Sciences In The Age Of Big Data
Jessica Turner: International Collaborative Efforts In The Enigma Schizophrenia Working Group
SIRS 2018 Meeting Presentations
William Carpenter: The Near Future for Schizophrenia (Psychosis) Research
Guusje Collin: Abnormal Modular Organization of the Functional Connectome Predicts Conversion to Psychosis in Clinical High-Risk Youth
Vanessa Cropley: Increased Complement Factors C3 and C4 in Schizophrenia and the Early Stages of Psychosis: Implications for Clinical Symptomatology and Cortical Thickness
John Cryan: The Gut Microbiome: A Key Regulator of Neurodevelopment and Behaviour
Melanie Föcking: Proteomic Analysis of Blood-Based Samples From the Optimise (OPtimization of Treatment and Management of Schizophrenia in Europe) Study Point Towards Complement Pathway Protein Changes
John Gilmore: Early Brain and Cognitive Development in Children at Risk for Schizophrenia
Anthony Grace: Stress-Induced Amygdala Hyperactivity Leads to Interneuron Loss and Schizophrenia-Like Pathology in a Developmental Disruption Model of Schizophrenia
Margaret Hahn: Olanzapine Impairs Central Insulin Action: Effects on Body Fuel Preference in Rats
Viktoria Johansson: Cerebrospinal Fluid Findings in Twins with Psychotic Symptoms – Novel Findings and Future Prospects
Kenneth Koblan: SEP-363856, a Candidate Antipsychotic and Antidepressant Compound With a Novel Non-D2 Mechanism of Action
Martin K. Rimvall: Psychotic Experiences are Associated With Health Anxiety and Functional Somatic Symptoms in Pre-Adolescence
André Schmidt: Disorganized Gyrification Network Properties During the Transition to Psychosis
Sara Tomiello: A Computational Trial-By-Trial EEG Analysis of Hierarchical Precision-Weighted Prediction Errors
Daniel Umbricht: Using Imaging and Behavioral Methods Probing Reward Functions as Tools for Decision Making in a Proof-Of-Mechanism Study of the PDE10 Inhibitor RG7203 in Patients With Schizophrenia and Negative Symptoms
Thomas Weickert: ICAM-1 is Increased in Brain and Peripheral Levels of Soluble ICAM-1 is Related to Cognitive Deficits in Schizophrenia
Dom's Story
Imagine being a child inflicted with hallucinations and delusions so frightening that you cannot differentiate between our world and a living nightmare. Welcome to Dom's world. Dom was diagnosed with Childhood Schizophrenia at age 10. This is Dom's Story.
Latest Articles
Executive Office 5034-A Thoroughbred Lane, Brentwood, TN 37027 USA Phone: 001.615.324.2370 E-mail: [email protected]
Privacy Policy Terms of Use
SIRS Twitter Feed
- Search Menu
- Advance articles
- Editor's Choice
- Supplements
- Submission Site
- Author Guidelines
- Open Access
- About Schizophrenia Bulletin
- About the University of Maryland School of Medicine
- About the Maryland Psychiatric Research Center
- About the NIH Public Access Policy
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- Introduction
- Conclusions
- Acknowledgments
Subgroups of Clinical High Risk for Psychosis Based on Baseline Antipsychotic Exposure: Clinical and Outcome Comparisons Across a 2-Year Follow-up Period
- Article contents
- Figures & tables
- Supplementary Data
Lorenzo Pelizza, Alessandro Di Lisi, Emanuela Leuci, Emanuela Quattrone, Silvia Azzali, Simona Pupo, Giuseppina Paulillo, Pietro Pellegrini, Marco Menchetti, Subgroups of Clinical High Risk for Psychosis Based on Baseline Antipsychotic Exposure: Clinical and Outcome Comparisons Across a 2-Year Follow-up Period, Schizophrenia Bulletin , 2024;, sbae029, https://doi.org/10.1093/schbul/sbae029
- Permissions Icon Permissions
Antipsychotic (AP) prescription in clinical high risk for psychosis (CHR-P) subjects remains a divisive issue. Although official guidelines currently discourage AP treatment in CHR-P, it is common in clinical practice, especially for psychosis prevention. The aim of this study was to investigate whether baseline AP need (especially in high-dose) indexes a CHR-P subgroup with poorer prognosis and differs from AP-naïve subjects in terms of sociodemographic, clinical, and outcome parameters across a 2-year follow-up.
CHR-P participants were treated within an “Early Intervention in Psychosis” program and completed the Positive and Negative Syndrome Scale (PANSS) and the Global Assessment of Functioning (GAF) scale both at baseline and every 12 months. Individuals with baseline AP prescription were included in the high-dose or low-dose CHR-P-AP+ subgroup. The others were grouped as AP-naïve. Cox regression analyses and mixed-design ANOVA were performed.
180 CHR-P individuals were enrolled (32 high-dose, 60 low-dose, and 88 AP-naïve). Compared to AP-naive, CHR-P AP+ subgroups showed older age and more severe clinical presentation. High-dose subgroup also had grater functioning decline at entry and poorer functional recovery at follow-up. No inter-group differences in psychosis transition and symptomatic remission were found. Significant improvement in clinical outcomes were found over time in all subgroups. Baseline AP prescription was specifically associated with a more relevant improvement in PANSS total score, and in negative and disorganized symptoms.
Our results suggest that baseline AP need is an important prognostic parameter in CHR-P and should be considered in risk/benefit calculators.
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations

- Online ISSN 1745-1701
- Print ISSN 0586-7614
- Copyright © 2024 Maryland Psychiatric Research Center and Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Case Report
- Open access
- Published: 29 March 2024
Clinical experiences of guided tapering of antipsychotics for patients with schizophrenia– a case series
- Sofie Norlin Mølgaard ORCID: orcid.org/0009-0008-6268-925X 1 ,
- Mette Ødegaard Nielsen ORCID: orcid.org/0000-0002-0780-7099 1 ,
- Kickan Roed ORCID: orcid.org/0000-0002-2926-6983 2 &
- Jimmi Nielsen ORCID: orcid.org/0000-0002-9868-7028 1
BMC Psychiatry volume 24 , Article number: 240 ( 2024 ) Cite this article
Metrics details
80% of patients value information on treatment options as an important part of recovery, further patients with a history of psychotic episodes feel excluded from decision making about their antipsychotic treatment, and on top of that, mental health staff is prone to be reluctant to support shared decision making and medication tapering for patients with schizophrenia. This case series aims to demonstrate the tapering of antipsychotic medication and how guided tapering affects the patient’s feeling of autonomy and psychiatric rehabilitation.
Case presentation
We present six patients diagnosed with schizophrenia (International Classification of Mental and Behavioral Disorders– 10th Edition codes F20.0–5, F20.7–9) who underwent professionally guided tapering in our clinic. The clinic aims to guide the patients to identify the lowest possible dose of antipsychotic medication in a safe setting to minimise the risk of severe relapse. Two patients completely discontinued their antipsychotic medication, two suffered a relapse during tapering, one chose to stop the tapering at a low dose, and one patient with treatment resistant schizophrenia, which is still tapering down.
Conclusions
Reducing the antipsychotic dose increased emotional awareness in some patients ( n = 4) helping them to develop better strategies to handle stress and increased feelings of recovery. Patients felt a greater sense of autonomy and empowerment during the tapering process, even when discontinuation was not possible. Increased awareness in patients and early intervention during relapse may prevent severe relapse.
Impact and implications
Some patients with schizophrenia might be over medicated, leading to unwanted side effects and the wish to reduce their medication. The patients in our study illustrate how guided tapering of antipsychotic medication done jointly with the patient can lead to improved emotional awareness and the development of effective symptom management strategies. This may in turn lead to a greater sense of empowerment and identity and give life more meaning, supporting the experience of personal recovery.
Peer Review reports
Antipsychotic medication remains a cornerstone in the management of psychotic symptoms [ 1 , 2 ]. With one in three patients possibly experiencing persistent symptoms despite antipsychotic treatment [ 3 ], the beneficial effect of long-term antipsychotic maintenance treatment for people with schizophrenia has been questioned [ 4 , 5 ]. Qualitative research shows that people with schizophrenia often have the desire to reduce or discontinue their antipsychotic medication [ 6 , 7 ]. Medication non-adherence among patients with schizophrenia is 41–49%, [ 8 ] and 47% of patients suffering from first-episode-schizophrenia will discontinue their antipsychotic medication within the first year of medication [ 9 ] despite sudden discontinuation possibly leading to exacerbation of symptoms, relapse, rehospitalisation, functional decline, and increased risk of death [ 10 ].
During recent years, an increased number of studies have focused on antipsychotic dose reduction [ 11 , 12 , 13 , 14 , 15 ] and deprescribing guidelines have also been published [ 16 , 17 ].
This has led to a slight shift in recommendations and clinical guidelines towards dose reduction or possibly discontinuation [ 18 ], however, discontinuation is still increasing the risk of clinical worsening significantly [ 19 ].
Although research shows that 80% of patients believe that having information about treatment options is a crucial aspect of recovery [ 20 ], individuals with a history of psychotic episodes often feel excluded from decision making about their antipsychotic treatment [ 7 ]. Moreover, mental health staff may be reluctant to support shared decision making and the tapering of medication for patients with schizophrenia [ 21 ]. Shared decision making, which is defined as two people, in this case a psychiatrist and a patient, sharing information to build consensus about the preferred treatment before agreeing on a treatment plan, [ 22 ] has been associated with the alleviation of symptoms, improved self-esteem, increased satisfaction with medical care, better treatment adherence, and lower rates of hospitalisation [ 23 ].
Currently, randomised controlled trials investigating the effect of antipsychotic medications largely focus on relapse prevention [ 24 ] but fail to incorporate outcomes that reflect personal recovery [ 25 ], which according to the CHIME framework comprises the five components its name stands for: connection to peers, hope, identity, meaning of life, and empowerment [ 26 ]. To our knowledge, there are no studies that describe how guided tapering unfolds in clinical practice. The case series presents how structured and closely monitored tapering can affect various life domains and how providers of psychiatric rehabilitation can support the decision to reduce medication with the least risk of relapse. Our discussion of the potential benefits and difficulties of tapering reflects that the patients in our study were diverse and had different outcomes.
Keywords: schizophrenia, antipsychotic medication, dose reduction, tapering, recovery, relapse.
In 2018, the health authorities in Denmark and the Capital Region of Denmark supported the establishment of a specialised outpatient clinic to meet the wishes of patients who wanted to taper their medication. The clinic offers guided tapering of antipsychotic medication for patients 18–64 years of age diagnosed with schizophrenia using International Classification of Mental and Behavioral Disorders– 10th Edition (ICD-10) codes F20.0–5, F20.7–9 [ 27 ] and works with patients to identify the lowest suitable dose of medication in a safe and professionally guided setting to minimise the risk of severe relapse.
Patients can be enrolled regardless of initial symptom load and level of function but to ensure the safe tapering of medication, patients must adhere to their medication and individual tapering schedule, as well as be available to speak by telephone weekly and to attend monthly appointments at the clinic. Further, we have a few exclusion criteria: Psychiatric hospitalization during the last 6 months, substance abuse to a degree which affect the possibility of participating in the regular assessments, and acutely increased risk of suicide or violence evaluated. In addition, the patient may be excluded if, following a comprehensive interview, the psychiatrist conclude that tapering is not recommended due to safety issue.
During the monthly visits, experienced and trained healthcare professionals evaluate symptoms based on the semi-structured interview using; the Positive and Negative Syndrome Scale (PANSS) [ 28 ]. We aim to reduce the antipsychotic dose monthly by 10%, and once half of the initial dose is reached, the dose is reduced monthly by approximately 5% until further reduction is no longer possible. Under the guidance of the staff, the patient decides whether to reduce the dose or not based on a thorough evaluation of their symptoms. When the patient decides to stop the tapering, or reach discontinuation, the patient is observed for additional 6 months. Although various models are available to ensure shared decision making [ 29 ], we do not adhere to any specific shared decision-making model.
Our unit’s staff strives to listen and comprehend the perspective and life circumstances of patients, while also connecting their experiences to past events and incorporating insights from other patients and scientific research. We are currently collecting data for a qualitative study on how our patients experience our approach during the tapering process.
The prescribing clinician collected data and case quotations at the monthly visits. The cases were meticulously selected to represent a broad range of tapering.
Patient presentation
Patient A is a 29-year-old male diagnosed with paranoid schizophrenia (ICD–10 code F20.0) at age 20 who has experienced anxiety and tics in stressful situations since age 10. His positive symptoms comprised vague evil thoughts that he did not see as his own, inner dialogue interpreted as internal hallucinations, self-referential thoughts, and the delusion of being persecuted. In addition to experiencing sleep disturbances and avolition, he was described with blunted affect. For several years he received long-acting injectable (LAI) aripiprazole and presented with no psychotic symptoms but continually had severe negative symptoms, e.g., a lack of energy, anhedonia, and avolition.
Patient A was enrolled in our clinic at his request because he had increasingly experienced a lack of energy and motivation over the past five years. At enrolment he had no psychotic symptoms but was severely affected by negative symptoms. He did not work or study but was living independently.
Patient A received LAI aripiprazole 400 mg/month and had a PANSS score of 70, dominated by negative symptoms with a score of 26. He followed the algorithm for dose reduction and did not experience any change in psychotic symptoms. After 10 months, he stated, “ I feel like I may have been stuck in a repetitive narrative of my symptoms. While answering your questions, it occurred to me that there are very few symptoms left. ” After 12 months the medication was discontinued after the last aripiprazole injection of 80 mg, and after an additional 6 months of observation, Patient A stated that his emotional life had returned since he could feel joy and sadness again (PANSS 38, P = 7, N = 11, G = 20).
During the observation period subsequent to discontinuing the medication, some of his tics reoccurred, e.g., clicking his tongue up to 20 times a minute, but he was not affected to a level that required treatment. He worked therapeutically to give his life more structure, especially by keeping a regular diurnal rhythm. At the final clinic visit, Patient A explained that he had been approved for an early retirement pension but that he volunteered at a computer repair shop twice a week and that his social life had expanded. He has currently been without medicine for 12 months and still does not have any psychotic symptoms.
Patient B is a 41-year-old man who was referred for tapering after > 10 years of treatment with aripiprazole. At the age of 28, he was diagnosed with depression and treated with citalopram 30 mg/day and aripiprazole 5 mg/day due to ruminating and racing thoughts. During the following two years, he suffered a severe loss of function, affective flattening, anhedonia, avolition, self-neglect, and social withdrawal, and only partial symptomatic improvement was observed. Patient B was enrolled in a specialised assertive early intervention program [ 30 ] with close contact for five years, during which time his diagnosis was changed from depression to unspecified schizophrenia (ICD–10 code F20.9) due to hypnogogic hallucinations.
The aripiprazole dose was increased to 30 mg/day and then switched to LAI aripiprazole 400 mg/month. Side effects continued, including increased sleep duration and a 13 kg weight gain. A general practitioner (GP) treated patient B for four years to help manage symptoms and reduced the dose to 300 mg/month, whereupon the patient was referred to further tapering at our clinic.
Patient B wanted to taper off medication because he did not feel sick and was in doubt about why he still received medication. In addition to feeling exceedingly tired and sleeping around 14 h a night, he found it impossible to lose weight while on medication. When enrolled in the tapering program, patient B’s PANSS total score was 66, with a negative symptom score of 20 and a general symptom score of 36. He followed the tapering plan, and his last aripiprazole injection of 80 mg was given 10 months after enrolment. His PANSS rating declined to 52 ( P = 9, N = 20, G = 23), mainly due to changes in general symptoms and he now slept only 9–10 h/night. He experienced that, “ the bell jar around him was removed ” and that he suddenly “ had to deal with his emotional life again ”, which worsened his tendency to ruminate about discussions with friends when going to sleep. To specifically address this issue, he was taught strategies in a focused therapeutic relationship before being discharged from the clinic. Patient B has now been without antipsychotic medication for 14 months and has no psychotic symptoms but has type 2 diabetes and hypertension. He regularly works out at a fitness center but continues to struggle with how to manage his emotional life and ruminating before he goes to sleep.
Patient C is a 35-year-old woman who was hospitalised at the age of 22 with visual and external auditory hallucinations with mixed second- and third-person perspective. She was diagnosed with paranoid schizophrenia (ICD–10 code F20.0) and treated with quetiapine 1600 mg/day, which was later changed to aripiprazole 30 mg/day and quetiapine 100 mg/day. After being stable for three years on LAI aripiprazole 400 mg/month, she resumed her education but experienced increased symptoms in terms of thought broadcasting, anxiety, and social isolation and had to interrupt her studies. The symptoms improved after adding quetiapine 200 mg/day, and after being stable for a period, quetiapine was changed to a pro re nata prescription, and aripiprazole was switched to an oral prescription, allowing her to resume her studies.
Patient C entered our clinic on her own initiative after being stable on aripiprazole 20 mg/day for one year. She was still hearing what she considered a good and supportive voice for the last 13 years, and she wanted to find out how well she could do with little or no medicine. Her PANSS baseline score was 40, with a positive symptom score of 10 resulting from a score of four at P3 (hallucinations). In the first week of tapering she said she was more emotional but that diminished before the next dose reduction. After six months, she was on a dose of aripiprazole 5 mg/day, which she chose to continue with even though she was about to move and had to terminate her treatment at the clinic. This decision was made after thorough consideration and discussion with the staff. Patient C explained that she was now “ more in touch with her feelings and her surroundings ” and her boyfriend said that she was also “ more emotionally available ”. Patient C appreciated having close contact with the staff while reducing her dose because it made her feel safer during the process. At this point, Patient C’s dose of aripiprazole 5 mg/day has been stable for four years. She is married and gave birth two years ago without her condition deteriorating. Patient C asserts that the dose reduction made her much more self-confident and “ in charge of her own life ”. She describes how being more in touch with her feelings makes it possible for her to have her own opinion, to judge what is good or bad for her, and that this has made her contact with reality stronger. She still hears a supportive voice in her head but it does not disturb her, and she no longer drifts into a psychotic reality. Her GP suggested stopping her medication completely, but she does not dare to do this without working closely with mental healthcare staff based on how safe and secure she felt while tapering her medication at the clinic.
Patient D was enrolled in the clinic at age 26 because he wanted to discontinue his antipsychotic medication. He was 18 years old when diagnosed with paranoid schizophrenia (ICD–10 code F20.0), and his positive symptoms included auditory hallucinations of second- and third-person perspectives, thought broadcasting, and persecutory delusions. At the time of enrolment, he did not have any symptoms of psychosis and had a total PANSS score of 34. He worked 32 h a week as a peer support worker and lived with his girlfriend. Patient D wished to discontinue the antipsychotic treatment mainly because he believed he had learned to cope with the symptoms through his recovery gains.
At enrolment, Patient D received aripiprazole 10 mg/day, which was reduced to aripiprazole 7.5 mg/day (P aripiprazole < 300 nmol/L, ref: 300–1700 nmol/L) during the first month. Patient D revealed that he had not been taking his medication regularly. To improve adherence, he agreed to switch to LAI aripiprazole 200 mg/month, which was tapered down to 120 mg/month over the next four months. Patient D started experiencing auditory and visual hallucinations, racing thoughts, and depressive delusions about being a hypocrite, his PANSS total score increased from 34 to 40. We practiced watchful waiting, i.e., we did not increase the antipsychotic dose unless symptoms increased, while Patient D went on sick leave.
At his next appointment at the clinic, we suggested adjusting the dose to LAI aripiprazole 300 mg/month. Patient D agreed that this was necessary, even though he was disheartened that he was unable to discontinue the medication, “ I thought I could do without. I tell the patients every day at work that to achieve recovery they need to fill their lives with meaningful things, but this shows that I just need to take the medication, nothing else matters ”.
The symptoms improved with the increased dose. After eight weeks, he was working 32 h a week again and had a PANSS total score of 31, which was lower than when he was enrolled at the clinic. Patient D told us that he felt he was “ functioning on a better level ” than when he began tapering. When we asked about his opinion on tapering, he replied: “ I think the time in the clinic has been good. I’m sad that I couldn’t do without medication, but now I know medication is important for me ”. He still receives and feels stable on LAI aripiprazole 300 mg/month.
Patient E is a 59-year-old woman who was diagnosed with paranoid schizophrenia (ICD–10 code F20.0) at the age of 27, presenting with persecutory delusions, auditory and visual hallucinations, sadness, and anxiety. She was enrolled in the clinic because she wanted to discontinue her medication since she questioned her need for antipsychotic treatment and whether her diagnosis was correct.
At the time of enrolment, Patient E had a PANSS total score of 59, her suspicion was easily aroused, she had trouble planning, and experienced anxiety. She lived on her own, had an adult daughter, and was working 11 h a week in a supermarket.
Patient E described her previous experience with treatment in the mental health services, “ I was hospitalised in Spain on a vacation, and they just injected me with medication. I don’t know which one. I was so scared, and now I don’t remember anything. ”
Patient E received LAI aripiprazole 200 mg/5th week at enrolment. We changed the dose to 160 mg/month, and Patient E began psychotherapy. After two months, her PANSS total score had increased to 62, mainly due to a five-point increase in the positive symptoms score, where P6 (suspiciousness) had increased by three points. She described her brain as stressed; she felt like she was being watched and was afraid of other people. Because of the minor increase in symptoms, we arranged an additional visit after 14 days and refrained from further dose reduction.
At the additional visit, she had a PANSS total score of 56 and told us that everything had cleared up but a week later she called and said that she needed additional medication. Patient E felt destabilised by intrusive thoughts about the time she got sick, a sense of derealisation, increased persecutory delusions, and a feeling of somebody speaking to her. As a result, we added aripiprazole 5 mg/day. At the next visit to the clinic, the PANSS total score had increased to 67 and the aripiprazole dose was increased to 300 mg/month plus 5 mg/day. She was nonetheless hospitalised in an open ward for 11 days without further changes in the medication. One month later, she started working again, and two months later she was stable, with a PANSS score of 48.
She concluded: “ Now I know that I need the medication and that I have a mental disorder. The relapse was very difficult, but it’s over now .” Even so, she asked for a further dose reduction the next month because she believed that the medication was causing pain in her legs. She still receives LAI aripiprazole and individual therapy with a psychodynamic focus to support her understanding of her symptoms related to her previous life experiences.
Patient F, a 30-year-old male diagnosed with paranoid schizophrenia (ICD–10 code F20.0) at the age of 20, was hospitalised after a sudden psychotic breakdown, after which he described delusions of self-reference and surveillance. Initially, he received an eight-week treatment of aripiprazole 20 mg/day, but due to lack of effect this was changed to risperidone 6 mg/day. The delusions disappeared gradually, and his positive symptom load was described as in remission after two years. Patient F experienced side effects such as weight gain (30 kg), increased sleep, apathy, akathisia, hyperprolactinemia, and sexual dysfunction. At his initiative, he discontinued the medication abruptly. Four months later, Patient F was hospitalised because he had covered his windows with oil, tomatoes, and flour to protect himself due to his delusions. Treatment with risperidone was resumed with some effect, but he refused treatment with long-acting antipsychotics. After a few months, Patient F discontinued the medical treatment and refused to have any contact with the mental health services. One year later, he was hospitalised after believing that he had clairvoyant and telepathic abilities. He initially received olanzapine 40 mg/day for two weeks, then zuclopenthixol 40 mg/day for six weeks, and after that, sertindole 24 mg/day for five months, all with insufficient effect. Subsequently, he received clozapine 600 mg/day (P-clozapine 2802 nmol/L, ref: 300-2000nmol/L) without any further improvement, which was augmented with amisulpride 400 mg/day. Since this did not change that he believed that he had clairvoyant abilities, he received 18 electroconvulsive therapy treatments, also without any effect. After being hospitalised for 20 months, Patient F was discharged to his apartment but with daily visits to ensure continuous medication adherence in the form of clozapine 425 mg/day and amisulpride 250 mg/day. During the following three years, he was stable, while clozapine was gradually reduced to 175 mg/day before he was referred for further dose reduction at our clinic.
Patient F wished to discontinue clozapine as he disagreed with the diagnosis and experienced side effects in terms of weight gain (body mass index of 33), newly diagnosed diabetes, and constantly feeling tired. He lived a quiet and socially isolated life, mainly filled with telepathic contacts, and he was still convinced that he had clairvoyant and telekinetic abilities. His initial PANSS total score was 85, with a positive symptom score of 27. After 16 months of enrolment at the clinic, his clozapine had been reduced to 12.5 mg/day without any increase in symptoms or decrease in level of function. Patient F has felt a slight improvement in that he experiences less emotional indifference, with a decrease in PANSS negative score from 26 to 22. Patient F still visits the clinic and aims to stop clozapine within the next four months, after which the plan is to follow him for six months on a stable dose of amisulpride 250 mg/day.
Discussion and conclusions
The benefits of tapering antipsychotic medication are under debate [ 31 ], but many patients request it, despite critics’ contention that it puts patients at unnecessary risk of relapse [ 32 , 33 ]. However, determining whether the current antipsychotic dose is still needed can only be ascertained by reducing the dose, and, as most side effects are dose dependent, treatment with the lowest effective dose is of crucial importance [ 34 ].
Our case series illustrates how diverse tapering, and its outcomes can be while also demonstrating how an increased feeling of autonomy during tapering may lead to an increased feeling of rehabilitation and recovery, despite the outcome. For example, Patient A and Patient B were able to discontinue antipsychotic medication completely with no worsening of positive symptoms but an improvement in negative symptoms and quality of life. Both patients have now been out of antipsychotic medication for more than a year with no signs of worsening, which is considered a favourable predictor [ 35 , 36 ], but as schizophrenia is seen upon as a life long condition the risk of relapsing after 12 months is still present. Many patients wish to reduce their dose or quit their medications entirely due to side effects, but this was only partly the case for Patient A and Patient B. When their antipsychotic medication was reduced and finally stopped, both patients experienced significantly more energy, initiative, pleasure, and emotional fluctuation. Although their files described them as “dominated by negative symptoms”, they appeared to be somewhat secondary to the medical treatment. Discriminating between primary and secondary negative symptoms can be almost impossible, but dose reduction can help to identify the negative symptoms medication causes. Patient A and Patient B increased their level of function and had a greater feeling of personal recovery in terms of hope, identity, the meaning of life, and empowerment [ 26 ]. Another important observation regarding the cases, especially Patient B, is that the level of symptoms led to long-lasting treatment with antipsychotic medication. Patient B’s files indicated that his medical treatment was initiated due to rumination and provided no evidence that he had suffered from delusions, hallucinations, or severe thought disorders. When guidelines recommend continuous antipsychotic treatment for all patients with schizophrenia, it categorises all patients as being at high risk for a severe psychotic episode. We argue that Patient B illustrates that this may not always be the case, underlining the importance of examining the individual patient’s history and evaluating the pros and cons of continuous treatment in collaboration with the patient to reach consensus.
Patient C, who had a similar outcome, decided to stay on 5 mg of aripiprazole with no signs of worsening. Although Patient C did not discontinue the antipsychotic drug completely, she experienced the benefits of the dose reduction and appreciated the tapering. Her decision to stop tapering her medications was partly due to moving to another part of Denmark, which required her to terminate treatment at our clinic. Patient C’s GP had suggested that she stop her antipsychotic treatment multiple times over the past years, but Patient C was aware that discontinuing the final dosage might worsen her symptoms and affect her overall level of functioning. As a result, she preferred to work with specialists to minimise any risks, which emphasises the importance of providing a safe and professional environment for tapering and shows that she felt that professional guidance in a specialised clinic decreased her risk of relapse. Consequently, although patients with no symptoms and no recurring symptoms during tapering seem to be the most suitable group for tapering, many other patients may benefit from a tapering trial.
Both Patient D and Patient E experienced relapses, the appearance of symptoms indicating that antipsychotic treatment was required. For Patient D, this led to psychologically accepting his psychiatric condition and the need for antipsychotic treatment. For Patient E, the impact on her perception of the necessity of medication may not be permanent. We are currently exploring whether a therapeutic relationship with a psychodynamic focus may be helpful to Patient E’s rehabilitation and lead to an increased feeling of personal recovery.
Patient F involved treatment-resistant schizophrenia; the various treatment strategies tried resulted in increased side effects rather than reduced psychotic symptoms. Often treatment is initiated during a worsening of symptoms, but disease fluctuations make evaluating the response difficult. In accordance with our experiences with this patient group, a Finnish study showed that olanzapine, combined with clozapine treatment, could be tapered with no worsening in symptoms [ 37 ]. Gradual tapering of antipsychotic drugs is not only relevant for patients with no symptoms but should also be considered for patients with treatment-resistant schizophrenia, where antipsychotic medication may not be efficient. In addition, treatment with clozapine may be associated with several troublesome side effects [ 38 ]. Today, only few existing guidelines address this issue [ 39 , 40 ].
Several patents in our clinic describe increased emotional awareness or emotional fluctuation during dose reduction. Although we did not monitor the emotional awareness using a rating scale, this is in line with recent findings [ 41 ]. This restoration of emotional reactivity during dose reduction can be a temporary state patients need to go through, but it can also be a warning sign of relapse. Frequent clinical assessment, psychoeducation and therapeutic support may be needed, and it is our experience that sometimes the patients want to resume antipsychotic treatment or increase the dose, even though no psychotic symptoms have occurred. Although tapering is associated with an increased risk of relapse [ 32 ], this case series shows that intensive follow-up can be used to identify relapse at an early stage before it becomes more severe and devastating. Before inclusion in the tapering program, we thoroughly inform patients that tapering is associated with an increased risk of relapse, which is a concern that most patients share with us. However, the desire to reduce their medications exceeds the fear of relapse and, through common agreement, we ensure a therapeutic alliance where patients recount being heard and understood.
Our tapering program is one example of how to reduce medication with the least risk of relapse. Our findings show that taking advantage of specialised mental health services with close contact during gradual tapering may reduce the risk of severe relapse, at least compared to patients who independently initiated abrupt discontinuation. While we have not encountered suicide attempts, violent actions, or other serious complications so far, it is crucial to remember that tapering down antipsychotics carries a risk and must be approached with the utmost precaution.
Regardless of the outcome of tapering, patients regularly visiting the clinic were often grateful for the opportunity to have their antipsychotic medication reduced and to be involved in decisions about their medical treatment, which created a greater feeling of autonomy. We are in the process of collecting data for a qualitative study on how our patients experience our approach during the tapering process. Likewise, well-designed future qualitative studies are required, to shed further light on the benefits of using specialised mental health services with close contact during tapering.
This case series has various limitations, but one in particular must be acknowledged. The cases presented were deliberately chosen from a pool of more than 100 patients from two tapering trials. The presented cases were chosen to achieve a diverse sample and to illustrate some of the various ways in which tapering can occur but are not necessarily quantitatively representative. (The full data and results will be published in the following years) Consequently, the results are not generalisable to all patients suffering from schizophrenia.
Research on antipsychotic tapering remains sparse, and additional quantitative and qualitative data are warranted. Some of the patients in our cases who reduced their antipsychotic dose increased their emotional awareness and seemed to develop better strategies for handling stress, which may have led to an increased feeling of empowerment, identity, and meaning in life. Future research may resolve whether this feeling of personal recovery is a factor that improves tapering outcomes. Notably, some of the patients in our clinic were increasingly open to antipsychotic treatment during stressful periods, indicating that treating schizophrenia more in terms of episodes is warranted.
The diagnoses of schizophrenia cover a heterogeneous group of patients, making it crucial to take an individualised approach to meet the specific treatment requirements of each patient. Also, antipsychotic associated benefits and sideeffects should be carefully and regularly evaluated with the patient. If guided tapering of antipsychotics is considered, the possible risk of relapse and consequences of this should also be discussed.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
International Classification of Mental and Behavioral Disorders– 10th Edition
The Positive and Negative Syndrome Scale
Long-acting injectable
General practitioner
Jibson MD, Waltham M, Marder S, UpToDAte. 2022. Second-generation antipsychotic medications: Pharmacology, administration, and side effects. Available from: https://www.uptodate.com/contents/second-generation-antipsychotic-medications-pharmacology-administration-and-side-effects .
Schneider-Thoma J, Chalkou K, Dörries C, Bighelli I, Ceraso A, Huhn M, et al. Comparative efficacy and tolerability of 32 oral and long-acting injectable antipsychotics for the maintenance treatment of adults with schizophrenia: a systematic review and network meta-analysis. Lancet. 2022;399(10327):824–36.
Article CAS PubMed Google Scholar
Potkin SG, Kane JM, Correll CU, Lindenmayer JP, Agid O, Marder SR, et al. The neurobiology of treatment-resistant schizophrenia: paths to antipsychotic resistance and a roadmap for future research. NPJ Schizophr. 2020;6(1):1.
Article PubMed PubMed Central Google Scholar
Harrow M, Jobe TH, Faull RN. Do all schizophrenia patients need antipsychotic treatment continuously throughout their lifetime? A 20-year longitudinal study. Psychol Med. 2012;42(10):2145–55.
Murray RM, Quattrone D, Natesan S, van Os J, Nordentoft M, Howes O, et al. Should psychiatrists be more cautious about the long-term prophylactic use of antipsychotics? Br J Psychiatry. 2016;209(5):361–5.
Article PubMed Google Scholar
Morant N, Azam K, Johnson S, Moncrieff J. The least worst option: user experiences of antipsychotic medication and lack of involvement in medication decisions in a UK community sample. J Ment Health. 2018;27(4):322–8.
Haugom EW, Stensrud B, Beston G, Ruud T, Landheim AS. Experiences of shared decision making among patients with psychotic disorders in Norway: a qualitative study. BMC Psychiatry. 2022;22(1):192.
Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892–909.
Cheng Z, Yuan Y, Han X, Yang L, Zeng X, Yang F, et al. Rates and predictors of one-year antipsychotic treatment discontinuation in first-episode schizophrenia: results from an open-label, randomized, real world clinical trial. Psychiatry Res. 2019;273:631–40.
Haddad P, Brain C, Scott J. Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Relat Outcome Meas. 2014;43.
Moncrieff J, Crellin N, Stansfeld J, Cooper R, Marston L, Freemantle N, et al. Antipsychotic dose reduction and discontinuation versus maintenance treatment in people with schizophrenia and other recurrent psychotic disorders in England (the RADAR trial): an open, parallel-group, randomised controlled trial. Lancet Psychiatry. 2023;10(11):848–59.
Liu CC, Hsieh MH, Chien YL, Liu CM, Lin YT, Hwang TJ, et al. Guided antipsychotic reduction to reach minimum effective dose (GARMED) in patients with remitted psychosis: a 2-year randomized controlled trial with a naturalistic cohort. Psychol Med. 2023;53(15):7078–86.
Wunderink L, Nienhuis FJ, Sytema S, Slooff CJ, Knegtering R, Wiersma D. Guided discontinuation versus maintenance treatment in remitted first-episode psychosis: relapse rates and functional outcome. J Clin Psychiatry. 2007;68(5):654–61.
Wunderink L, Nieboer RM, Wiersma D, Sytema S, Nienhuis FJ. Recovery in remitted first-episode psychosis at 7 years of follow-up of an early dose reduction/discontinuation or maintenance treatment strategy: long-term follow-up of a 2-year randomized clinical trial. JAMA Psychiatry. 2013;70(9):913–20.
Begemann MJH, Thompson IA, Veling W, Gangadin SS, Geraets CNW, Van ’T, Hag E, et al. To continue or not to continue? Antipsychotic medication maintenance versus dose-reduction/discontinuation in first episode psychosis: HAMLETT, a pragmatic multicenter single-blind randomized controlled trial. Trials. 2020;21(1):147.
Gupta S, Cahill JD, Miller R. Deprescribing antipsychotics: a guide for clinicians. BJPsych Adv. 2018;24(5):295–302.
Article Google Scholar
Horowitz MA, Jauhar S, Natesan S, Murray RM, Taylor D. A method for tapering antipsychotic treatment that May minimize the risk of Relapse. Schizophr Bull. 2021;47(4):1116–29.
Shimomura Y, Kikuchi Y, Suzuki T, Uchida H, Mimura M, Takeuchi H. Antipsychotic treatment in the maintenance phase of schizophrenia: an updated systematic review of the guidelines and algorithms. Schizophr Res. 2020;215:8–16.
Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379(9831):2063–71.
Law H, Morrison AP. Recovery in psychosis: a Delphi study with experts by experience. Schizophr Bull. 2014;40(6):1347–55.
Roed K. Mental Health staffs’ perspectives on tapering of antipsychotic medication: a focus group study. Qual Health Res. 2023.
Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997;44(5):681–92.
Alguera-Lara V, Dowsey MM, Ride J, Kinder S, Castle D. Shared decision making in mental health: the importance for current clinical practice. Australasian Psychiatry. 2017;25(6):578–82.
Ostuzzi G, Vita G, Bertolini F, Tedeschi F, De Luca B, Gastaldon C, et al. Continuing, reducing, switching, or stopping antipsychotics in individuals with schizophrenia-spectrum disorders who are clinically stable: a systematic review and network meta-analysis. Lancet Psychiatry. 2022;9(8):614–24.
Zipursky RB, Agid O. Recovery, not progressive deterioration, should be the expectation in schizophrenia. World Psychiatry. 2015;14(1):94–6.
Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry. 2011;199(6):445–52.
World health Organization. ICD-10 The international Classification of Mental and Behavioural Disorders [Internet]. 1992. Available from: https://icd.who.int/browse10/2019/en .
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–76.
Stacey D, Légaré F, Pouliot S, Kryworuchko J, Dunn S. Shared decision making models to inform an interprofessional perspective on decision making: a theory analysis. Patient Educ Couns. 2010;80(2):164–72.
Secher RG, Hjorthøj CR, Austin SF, Thorup A, Jeppesen P, Mors O, et al. Ten-year follow-up of the OPUS specialized early intervention trial for patients with a first episode of psychosis. Schizophr Bull. 2015;41(3):617–26.
Potla S, Al Qabandi Y, Nandula SA, Boddepalli CS, Gutlapalli SD, Lavu VK, et al. A systematic review of the need for Guideline recommendations; slow tapering vs. maintenance dose in long-term antipsychotic treatment: 2022. Cureus. 2023;15(2):e34746.
PubMed PubMed Central Google Scholar
Højlund M, Kemp AF, Haddad PM, Neill JC, Correll CU. Standard versus reduced dose of antipsychotics for relapse prevention in multi-episode schizophrenia: a systematic review and meta-analysis of randomised controlled trials. Lancet Psychiatry. 2021;8(6):471–86.
Correll CU, Rubio JM, Kane JM. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry. 2018;17(2):149–60.
Leucht S, Bauer S, Siafis S, Hamza T, Wu H, Schneider-Thoma J, et al. Examination of dosing of Antipsychotic Drugs for Relapse Prevention in patients with stable Schizophrenia: a Meta-analysis. JAMA Psychiatry. 2021;78(11):1238–48.
Thompson A, Winsper C, Marwaha S, Haynes J, Alvarez-Jimenez M, Hetrick S, et al. Maintenance antipsychotic treatment versus discontinuation strategies following remission from first episode psychosis: systematic review. BJPsych Open. 2018;4(4):215–25.
Chen EYH, Hui CLM, Lam MML, Chiu CPY, Law CW, Chung DWS et al. Maintenance treatment with quetiapine versus discontinuation after one year of treatment in patients with remitted first episode psychosis: Randomised controlled trial. BMJ (Online). 2010;341(7770).
Repo-Tiihonen E, Hallikainen T, Kivistö P, Tiihonen J. Antipsychotic polypharmacy in Clozapine Resistant Schizophrenia: a randomized controlled trial of tapering antipsychotic co-treatment. Ment Illn. 2012;4(1):e1.
Dong S, Schneider-Thoma J, Bighelli I, Siafis S, Wang D, Burschinski A et al. A network meta-analysis of efficacy, acceptability, and tolerability of antipsychotics in treatment-resistant schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2023.
Baandrup L, Østrup Rasmussen J, Klokker L, Austin S, Bjørnshave T, Fuglsang Bliksted V, et al. Treatment of adult patients with schizophrenia and complex mental health needs - a national clinical guideline. Nord J Psychiatry. 2016;70(3):231–40.
Correll CU, Martin A, Patel C, Benson C, Goulding R, Kern-Sliwa J, et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. Schizophrenia (Heidelberg Germany). 2022;8(1):5.
PubMed Google Scholar
Morant N, Long M, Jayacodi S, Cooper R, Akther-Robertson J, Stansfeld J, et al. Experiences of reduction and discontinuation of antipsychotics: a qualitative investigation within the RADAR trial. EClinicalMedicine. 2023;64:102135.
Download references
Acknowledgements
Not applicable.
No funding to declare.
Open access funding provided by Copenhagen University
Author information
Authors and affiliations.
Mental Health Center Glostrup, Copenhagen University Hospital, Unit for complicated schizophrenia, Glostrup, Denmark
Sofie Norlin Mølgaard, Mette Ødegaard Nielsen & Jimmi Nielsen
Mental Health Centre Glostrup, Copenhagen University Hospital– Mental Health Services CPH, Centre for Applied Research in Mental Health Care, Glostrup, Denmark
Kickan Roed
You can also search for this author in PubMed Google Scholar
Contributions
S.N.M and M.Ø.N., wrote the manuscript and designed the paper, with J.N. K.R. M.Ø.N and J.N have substantively revised it. All authors have approved the submitted version, and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Correspondence to Sofie Norlin Mølgaard .
Ethics declarations
Ethics approval and consent to participate.
Our study was conducted in accordance with the Declaration of Helsinki and approved by the Capital Region of Denmark’s ethics committee and the Danish Data Protection Agency (H-21047524).
Consent for publication
All participants provided written informed consent for publication of identifiable information/ images in open access journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mølgaard, S.N., Nielsen, M.Ø., Roed, K. et al. Clinical experiences of guided tapering of antipsychotics for patients with schizophrenia– a case series. BMC Psychiatry 24 , 240 (2024). https://doi.org/10.1186/s12888-024-05699-y
Download citation
Received : 15 January 2024
Accepted : 19 March 2024
Published : 29 March 2024
DOI : https://doi.org/10.1186/s12888-024-05699-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Schizophrenia
- Antipsychotic medication
- Dose reduction
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- The Student Experience
- Financial Aid
- Degree Finder
- Undergraduate Arts & Sciences
- Departments and Programs
- Research, Scholarship & Creativity
- Centers & Institutes
- Geisel School of Medicine
- Guarini School of Graduate & Advanced Studies
- Thayer School of Engineering
- Tuck School of Business
Campus Life
- Diversity & Inclusion
- Athletics & Recreation
- Student Groups & Activities
- Residential Life
Psychological and Brain Sciences
Department of psychological and brain sciences.
- [email protected] Contact & Department Info Mail
- Undergraduate
- Major & Minor FAQs
- Honors FAQs
- Major and Minor Checklists
- Transfer and AP Credit
- Introductory
- Intermediate
- Independent Research
- Course Syllabi (ID login required)
- Request Form
- Winter 2025
- Spring 2025
- Research Areas
- Coursework and Curriculum
- Mentoring Toolkit
- Current Graduate Students
- Admissions FAQs
- Recent Dissertations
- Recent Research Findings
- Undergraduate Research
- Post-Doctoral Opportunities
- Participate in Experiments
- 2021 Honors Student Thesis Presentations (ID Login Required)
- 2022 Honors Student Thesis Presentations (ID Login Required)
- 2023 Honors Student Thesis Presentations (ID login required)
- Suggestions
- For Current PBS Community (ID Login Required)
- News & Events
Search form
If faces appear distorted, you could have this condition, posted on march 22, 2024 by amy olson.
Research presents a unique case of a patient with prosopometamorphopsia.
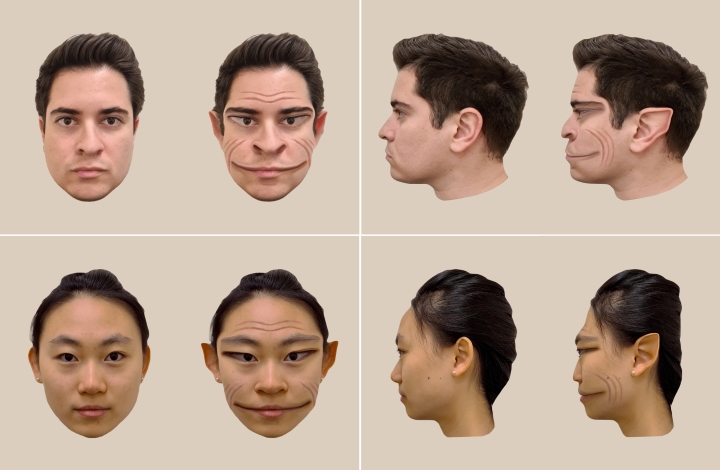
Imagine if every time you saw a face, it appeared distorted. For those who have a very rare condition known as prosopometamorphopsia, which causes facial features to appear distorted, that is reality.
As the website on what is known as PMO explains, “‘Prosopo’ comes from the Greek word for face ‘prosopon’ while ‘metamorphopsia’ refers to perceptual distortions.” The distortions can affect the shape, size, color, and position of facial features, and PMO can last for days, weeks, or even years.
A new Dartmouth study published in the “Clinical Pictures” section of The Lancet reports on a unique case of a patient with PMO. The research is among the first to provide realistic visualizations of how a patient experienced facial distortions.
The patient, a 58-year-old male with PMO, sees faces without any distortions when viewed on a screen and on paper but sees distorted faces that appear “demonic” when viewed in-person. The case is especially rare because he does not see distortions of faces across all contexts.
For the study, the researchers took a photograph of a person’s face. Then, they showed the patient the photograph on a computer screen while he looked at the real face of the same person. The researchers obtained real-time feedback from the patient on how the face on the screen and the real face in front of him differed, as they modified the photograph using computer software to match the distortions perceived by the patient.
Through the process, we were able to visualize the patient’s real-time perception of the face distortions.
“In other studies of the condition, patients with PMO are unable to assess how accurately a visualization of their distortions represents what they see because the visualization itself also depicts a face, so the patients will perceive distortions on it too,” says lead author Antônio Mello , Guarini, a PhD student in the Department of Psychological and Brain Sciences .
In contrast, this patient doesn’t see distortions on a screen. This means that the researchers were able to modify the face in the photograph, and the patient could accurately compare how similar his perception of the real face was to the manipulated photograph. “Through the process, we were able to visualize the patient’s real-time perception of the face distortions,” says Mello.
In their research with other PMO cases, the co-authors state that some of their PMO participants have seen health professionals who wanted to help, but diagnosed them with another health condition, not PMO.
“We’ve heard from multiple people with PMO that they have been diagnosed by psychiatrists as having schizophrenia and put on anti-psychotics, when their condition is a problem with the visual system,” says senior author Brad Duchaine , a professor of psychological and brain sciences and principal investigator of the Social Perception Lab at Dartmouth.

“And it’s not uncommon for people who have PMO to not tell others about their problem with face perception because they fear others will think the distortions are a sign of a psychiatric disorder,” says Duchaine. “It’s a problem that people often don’t understand.”
Through their paper, the researchers hope to increase public awareness of what PMO is .
Daniel Stehr at Dartmouth and Professor of Neurology Krzysztof Bujarski at the Geisel School of Medicine also contributed to the study.
- Reviva Pharmaceuticals Holdings-stock
- News for Reviva Pharmaceuticals Holdings Reviva Pharmaceuticals Holdings
Reviva to Present RECOVER Phase 3 Clinical Trial Data for Brilaroxazine in Schizophrenia at the SIRS 2024 Annual Meeting
CUPERTINO, Calif., March 28, 2024 (GLOBE NEWSWIRE) -- Reviva Pharmaceuticals Holdings, Inc. (NASDAQ: RVPH) (“Reviva” or the “Company”), a late-stage pharmaceutical company developing therapies that seek to address unmet medical needs in the areas of central nervous system (CNS), inflammatory and cardiometabolic diseases, today announced that Laxminarayan Bhat, Ph.D., Founder, President, and CEO of Reviva will be presenting at the 2024 Schizophrenia International Research Society (SIRS) Annual Meeting, to be held April 3-7, 2024, in Florence, Italy.
Details for the Oral and poster presentations can be found below:
Presentation Title: Brilaroxazine Phase 3 Recover Trial in Acute Schizophrenia Supports Efficacy, Safety, and Effects on Neuroinflammation Oral Presentation Date and Time: Thursday, April 4, 2024 at 10:25 – 10:45 AM CET Poster Presentation Date and Time: Thursday, April 4, 2024 at 12:00 – 2:00 PM CET Poster Number: T291 Presenter: Laxminarayan Bhat, Reviva Pharmaceuticals Location: Florence, Italy
About Brilaroxazine Brilaroxazine is an in-house discovered new chemical entity with potent affinity and selectivity against key serotonin and dopamine receptors implicated in schizophrenia and its comorbid symptoms. Positive topline data from the global Phase 3 RECOVER-1 trial in schizophrenia demonstrated the trial successfully met all primary and secondary endpoints with statistically significant and clinically meaningful reductions across all major symptom domains at week 4 with 50 mg of brilaroxazine vs. placebo with a generally well-tolerated side effect profile comparable to placebo and discontinuation rates lower than placebo. Positive data from a clinical drug-drug interaction (DDI) study investigating the potential effect of CYP3A4 enzyme on brilaroxazine in healthy subjects supports no clinically significant interaction when combined with a CYP3A4 inhibitor. Reviva believes that a full battery of regulatory compliant toxicology and safety pharmacology studies has been completed for brilaroxazine. Reviva intends to develop brilaroxazine for other neuropsychiatric indications including bipolar disorder, major depressive disorder (MDD) and attention-deficit/hyperactivity disorder (ADHD).
Additionally, brilaroxazine has shown promising nonclinical activity for inflammatory diseases psoriasis, pulmonary arterial hypertension (PAH) and idiopathic pulmonary fibrosis (IPF) with mitigation of fibrosis and inflammation in translational animal models. Brilaroxazine has already received Orphan Drug Designation by the U.S. FDA for the treatment of PAH and IPF conditions.
To learn more about the clinical and preclinical data available for brilaroxazine, please visit https://revivapharma.com/publications/. About Reviva Reviva is a late-stage biopharmaceutical company that discovers, develops, and seeks to commercialize next-generation therapeutics for diseases representing unmet medical needs and burdens to society, patients, and their families. Reviva’s current pipeline focuses on central nervous system (CNS), inflammatory and cardiometabolic diseases. Reviva’s pipeline currently includes two drug candidates, brilaroxazine (RP5063) and RP1208. Both are new chemical entities discovered in-house. Reviva has been granted composition of matter patents for both brilaroxazine and RP1208 in the United States, Europe, and several other countries.
Forward-Looking Statements This press release contains certain forward-looking statements within the meaning of Section 27A of the Securities Act of 1933 and Section 21E of the Securities Exchange Act of 1934 and the Private Securities Litigation Reform Act, as amended, including those relating to the Company’s 1-year open label extension (OLE) trial evaluating the long-term safety and tolerability for brilaroxazine in schizophrenia, the registrational Phase 3 RECOVER-2 trial, the Company’s expectations regarding the anticipated clinical profile of its product candidates, including statements regarding anticipated efficacy or safety profile, and those relating to the Company’s expectations, intentions or beliefs regarding matters including product development, clinical and regulatory timelines and expenses, planned or additional studies, planned or intended regulatory submissions, market opportunity, ability to raise sufficient funding, competitive position, possible or assumed future results of operations, business strategies, potential opportunities for development including partnerships, growth or expansion opportunities and other statements that are predictive in nature. These forward-looking statements are based on current expectations, estimates, forecasts and projections about the industry and markets in which we operate and management’s current beliefs and assumptions.
These statements may be identified by the use of forward-looking expressions, including, but not limited to, “expect,” “anticipate,” “intend,” “plan,” “believe,” “estimate,” “potential, “predict,” “project,” “should,” “would” and similar expressions and the negatives of those terms. These statements relate to future events or our financial performance and involve known and unknown risks, uncertainties, and other factors which may cause actual results, performance or achievements to be materially different from any future results, performance or achievements expressed or implied by the forward-looking statements. Such factors include those set forth in the Company’s most recent Annual Report on Form 10-K for the fiscal year ended December 31, 2022, and the Company’s other filings from time to time with the Securities and Exchange Commission. Prospective investors are cautioned not to place undue reliance on such forward-looking statements, which speak only as of the date of this press release. The Company undertakes no obligation to publicly update any forward-looking statement, whether as a result of new information, future events or otherwise.
Corporate Contact: Reviva Pharmaceuticals Holdings, Inc. Laxminarayan Bhat, PhD www.revivapharma.com
Investor Relations Contact: LifeSci Advisors, LLC Bruce Mackle [email protected]
Media Contact: Kristin Politi [email protected] (646) 876-4783

Reviva Pharmaceuticals Holdings News MORE
Related stocks.

VIDEO
COMMENTS
The symptoms of schizophrenia may be divided into the following 4 domains: Positive symptoms - Psychotic symptoms, such as hallucinations, which are usually auditory; delusions; and disorganized speech and behavior. Negative symptoms - A decrease in emotional range, poverty of speech, and loss of interests and drive; the person with ...
Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behavior that impairs daily functioning, and can be disabling. People with schizophrenia require lifelong treatment. Early treatment may help get symptoms under control before serious complications develop and may help improve the ...
Schizophrenia symptoms can differ from person to person, but they generally fall into three main categories: psychotic, negative, and cognitive. Psychotic symptoms include changes in the way a person thinks, acts, and experiences the world. People with psychotic symptoms may lose a shared sense of reality with others and experience the world in ...
At least one of these must be (1), (2), or (3): Delusions. Hallucinations. Disorganized speech (e.g., frequent derailment or incoherence). Grossly disorganized or catatonic behavior. Negative symptoms (i.e., diminished emotional expression or avolition). Decreased functioning 2.6 months of symptoms with 1 month meeting criterion A. 3.Not ...
INTRODUCTION. Schizophrenia is a psychiatric disorder involving chronic or recurrent psychosis. It is commonly associated with impairments in social and occupational functioning [].It is among the most disabling and economically catastrophic medical disorders, ranked by the World Health Organization as one of the top 10 illnesses contributing to the global burden of disease [].
Schizophrenia is a serious mental disorder that affects how a person thinks, feels, and behaves. It can cause delusions, hallucinations, and other cognitive and emotional problems. This webpage provides a comprehensive overview of the diagnosis, risk factors, etiology, and treatment of schizophrenia, based on the latest scientific evidence. It is a valuable resource for anyone who wants to ...
Schizophrenia is a psychiatric condition that has severe effects on your physical and mental well-being. It disrupts how your brain works, interfering with things like your thoughts, memory, senses and behaviors. As a result, you may struggle in many parts of your day-to-day life. Untreated schizophrenia often disrupts your relationships ...
Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves. People with schizophrenia may seem as though they have lost touch with reality, which can be distressing for them and for their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but ...
Clinical presentation, signs, and symptoms . Schizophrenia is a major psychiatric illness featuring psychotic symptoms and often social and occupational decline. Lifetime risk is 1·2%, and modestly more frequent in men. Onset is typically in early adult life (later in women than in men).
Schizophrenia is frequently associated with significant distress and impairment in personal, family, social, educational, occupational, and other important areas of life. People with schizophrenia are 2 to 3 times more likely to die early than the general population (3). This is often due to physical illnesses, such as cardiovascular, metabolic ...
Schizophrenia changes how you think, feel, and act. It might affect you differently from someone else. The symptoms can come and go, too. No one has all of them all of the time. They usually start ...
Challenges at Work. 12 /17. People with schizophrenia often have trouble finding or keeping a job. This is partly because the disease affects thinking, concentration, and communication. But it ...
Schizophrenia is a chronic mental illness with positive symptoms (delusions, hallucinations, disorganized speech and behavior), negative symptoms, and cognitive impairment. Discoveries in genetics, neuroimaging, and immune function continue to advance understanding of the etiologies for this elusive disease. ... Such bizarre presentations are ...
CLINICAL PRESENTATION. Schizophrenia is the most common functional psychotic disorder, and (as noted previously) individuals with the disorder can present with a variety of manifestations. Contrary to portrayals of the illness in the media, schizophrenia does not involve a "split personality." Rather, it is a chronic psychotic disorder that ...
Posturing (voluntary assumption of inappropriate or bizarre postures) Stereotyped movements (involuntary, repetitive physical movements such as rocking) Prominent grimacing (distorting the face in an expression, usually of pain, disgust, or disapproval) Echolalia (repeating what others say)
Schizophrenia is a mental disorder characterized by disruptions in thought processes, perceptions, emotional responsiveness, and social interactions. Although the course of schizophrenia varies among individuals, schizophrenia is typically persistent and can be both severe and disabling. Symptoms of schizophrenia include psychotic symptoms such ...
Schizophrenia is a progressive and recurring disease characterized by multiple psychotic relapses. This slide deck covers the course, natural history and prognosis of schizophrenia. Other slides discuss the key components of non-adherence in patients with schizophrenia, highlighting the value of a support system.
For unknown reasons, catatonic presentations of schizophrenia have become uncommon, especially in high-income countries; 23. nevertheless, being seen in just under 10% of cases, their frequency is still appreciable. 24. Originally considered characteristic of schizophrenia, catatonia is now also recognised in patients with major
8.1.2.2 8.1. 2.2: Schizophreniform Disorder. Schizophreniform disorder is similar to schizophrenia with the exception of the length of presentation of symptoms and the requirement for impairment in functioning. As described above, a diagnosis of schizophrenia requires impairment in functioning and a six-month minimum duration of symptoms.
Schizophrenia is one of the most severe mental illnesses. It has a point prevalence of 4.6 per 1000 inhabitants, a lifetime prevalence of around 1%, and the median reported incidence is 15 cases per 100 000 inhabitants (see [1] for details). ... With regard to the clinical presentation, schizophrenia is characterized by a heterogeneous ...
This presentation covers aetiology of Schizophrenia. A working knowledge of the normal structure and function of the nervous system is key to understanding psychiatric disorders like schizophrenia. This slide deck presents an introduction to neuroanatomy, the key components of neurosynaptic transmission, neurotransmitters and the ...
Educational Presentations I mpact of the COVID-19 Pandemic on Psychosis The implications of the COVID-19 pandemic will have pervasive effects on schizophrenia and psychosis research and clinical services worldwide. In this webinar, four presenters share research on the impact of the COVID-19 pandemic on psychosis.
180 CHR-P individuals were enrolled (32 high-dose, 60 low-dose, and 88 AP-naïve). Compared to AP-naive, CHR-P AP+ subgroups showed older age and more severe clinical presentation. High-dose subgroup also had grater functioning decline at entry and poorer functional recovery at follow-up.
Antipsychotic medication remains a cornerstone in the management of psychotic symptoms [1, 2].With one in three patients possibly experiencing persistent symptoms despite antipsychotic treatment [], the beneficial effect of long-term antipsychotic maintenance treatment for people with schizophrenia has been questioned [4, 5].Qualitative research shows that people with schizophrenia often have ...
"We've heard from multiple people with PMO that they have been diagnosed by psychiatrists as having schizophrenia and put on anti-psychotics, when their condition is a problem with the visual system," says senior author Brad Duchaine, a professor of psychological and brain sciences and principal investigator of the Social Perception Lab ...
Presentation Title: Brilaroxazine Phase 3 Recover Trial in Acute Schizophrenia Supports Efficacy, Safety, and Effects on Neuroinflammation. Oral Presentation Date and Time: Thursday, April 4, 2024 ...
Presentation Title: Brilaroxazine Phase 3 Recover Trial in Acute Schizophrenia Supports Efficacy, Safety, and Effects on Neuroinflammation Oral Presentation Date and Time: Thursday, April 4, 2024 ...