- Previous Article
- Next Article

Assessment and Data Collection
Diagnosis and problem identification, planning and intervention, case presentation, case study: a patient with type 1 diabetes who transitions to insulin pump therapy by working with an advanced practice dietitian.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Claudia Shwide-Slavin; Case Study: A Patient With Type 1 Diabetes Who Transitions to Insulin Pump Therapy by Working With an Advanced Practice Dietitian. Diabetes Spectr 1 January 2003; 16 (1): 37–40. https://doi.org/10.2337/diaspect.16.1.37
Download citation file:
- Ris (Zotero)
- Reference Manager
Registered dietitians (RDs) who have earned the Board Certified–Advanced Diabetes Manager (BC-ADM) credential hold a master’s or doctorate degree in a clinically relevant area and have at least 500 hours of recent experience helping with the clinical management of people with diabetes. 1 They work in both inpatient and outpatient settings, including diabetes or endocrine-based specialty clinics, primary care offices, hospitals, and private practices. Advanced practice dietitians provide all components of diabetes care, including advanced assessment (medical history and physical examination), diagnosis, medical management, education, counseling, and overall case management.
The role of RDs in case and disease management was explored in a recent article 2 that included interviews with three dietitians who work as case managers or disease managers. All three reported experiencing challenges in practice and noted that the meaning of “case management” varies from one health care setting to another. This is also true for RD, BC-ADMs. Advanced practice dietitians specializing in diabetes require case management expertise that stresses communication skills, knowing the limits of your own discipline, knowing how to interact with other health care professionals, and knowing when to seek the expertise of other members of the diabetes care team.
Clinical practice includes assessment and data collection, diagnosis and problem identification, planning, and intervention. In many cases, diabetes educators who are dietitians and those who are nurses are cross-trained to perform the same roles. The first one to meet with a client handles that client’s assessment, and cases are discussed and interventions planned at weekly team meetings.
For advanced practice dietitians, the first session with a client often involves a complete physical assessment, not just a nutrition history. This includes a comprehensive medical history of all body systems. The diabetes-focused physical examination, just as performed by clinicians from other disciplines, includes height and weight measurement, body mass index (BMI) calculation, examination of injection sites, assessment of injection technique, and foot assessment.
Assessment also includes reviewing which medications the client is taking, evaluating their effectiveness and side effects, and determining the need for adjustment based on lifestyle, dietary intake, and blood glucose goals.
When carbohydrate counting is added to therapy, dietitians calculate carbohydrate-to-insulin ratios and teach clients how to use carbohydrate counting instead of a sliding-scale approach to insulin. Medications are adjusted based on clients’ lifestyles until blood glucose goals are achieved.
The therapeutic problem solving, regimen management, case management, and self-management training performed by advanced practice dietitians exceeds the traditional role of most dietetics professionals. 3
A role delineation study for clinical nurse specialists, nurse practitioners, RDs, and registered pharmacists, 4 conducted in 2000 by the American Nurses Credentialing Center, reported equal findings among all four groups for the skills used to identify pathophysiology, analyze diagnostic tests, and list problems. Assessment for medical nutrition therapy typically includes evaluation of food intake, metabolic status, lifestyle, and readiness to change. For people with diabetes, monitoring glucose and measuring hemoglobin A 1c (A1C), lipids, blood pressure, and renal status are essential to evaluating nutrition-related outcomes.
The U.S. Air Force health care system conducted a pilot test giving RDs clinical privileges and evaluating their clinical judgment in patient nutritional care. A protocol was approved, and dietitians were allowed to order and interpret selected outpatient laboratory tests independently. The higher-level clinical judgments and laboratory privileges were linked to additional certifications. 5
The Diabetes Prevention Program (DPP) also provided a unique opportunity for dietitians to demonstrate advance practice roles. 6 Dietitians served as lifestyle coaches, contacting participants at least once a month to address intervention goals. As case managers, they interviewed potential volunteers, assessed past experience with weight loss, and scheduled quarterly outcome assessments and weekly reviews of each participant’s progress at team meetings. Within the DPP’s central management, dietitians served as program coordinators and served on national study committees related to participant recruitment and retention, quality control, the use of protocols, and lifestyle advisory groups. 7
Dietitians now play key roles in translating DPP findings and serving as community advocates to reduce the incidence of obesity and the health care burden of type 2 diabetes. This includes serving in a consultative role to other health care team members on issues regarding weight loss and risk factor reduction.
Advanced practice RDs offer comprehensive diabetes patient care services, including identifying patient goals and expected outcomes, selecting nonpharmacological and pharmacological treatments, and developing integrated plans of care. Problems discussed with patients range from acute and chronic diabetes complications to comorbid conditions, other conditions, preventive interventions, and self-management education. Advanced practice RDs also review patients’ health care resources and order laboratory tests if information is not available from referral sources. They provide supportive counseling and referral to specialists, as needed. And, they provide a full report of their findings and any regimen changes and recommendations they make to referring clinicians after each visit.
These activities and responsibilities go beyond the scope and standards of practice for the RDs and for RD, CDEs. 8 They will be included in the scope of practice document for RD, BC-ADMs that is now being developed by the Diabetes Care and Education Practice Group of The American Dietetic Association.
The following case study illustrates the clinical role of advanced practice dietitians in the field of diabetes.
B.C. is a 51-year-old white man who was diagnosed with type 1 diabetes 21 years ago. He believes that his diabetes has been fairly well controlled during the past 20 years and that his insulin needs have increased. He was recently remarried, and his wife is now helping him care for his diabetes.
His endocrinologist referred him to the RD for an urgent visit because 4 days ago he had a hypoglycemic event requiring treatment in the emergency room (ER). He has come to see the dietitian because his doctor and his wife insisted that he do so.
B.C. has had chronic problems with asymptomatic hypoglycemia. His last doctor’s visit was 3–4 weeks ago, when areas of hypertrophy were found. His endocrinologist asked him to change his injection sites from his thigh to his abdomen after the ER incident.
He does not think he needs any diabetes education but would like help in losing 10 lb. His body mass index is 25 kg/m 2 .
His medications include pravastatin (Pravacol), 10 mg daily; NPH insulin, 34 units in the morning and 13 units at bedtime; and regular insulin at breakfast and dinner following a sliding-scale algorithm. He also takes lispro (Humalog) insulin as needed to correct high blood glucose.
Before his ER visit, B.C. monitored his blood glucose only minimally, testing fasting and sometimes before dinner but not keeping records. Since his severe hypoglycemia 4 days ago, he has begun checking his blood glucose four times a day, before meals and bedtime.
Lab Results
B.C.’s most recent laboratory testing results were as follows:
A1C: 8.3% (normal 4.2–5.9%)
Lipid panel
• Total cholesterol: 207 mg/dl (normal: 100–200 mg/dl)
• HDL cholesterol: 46 mg/dl (normal: 35–65 mg/dl)
• LDL cholesterol: 132 mg/dl (normal: <100 mg/dl)
• Triglycerides: 144 mg/dl (normal: <150 mg/dl)
Creatinine: 0.9 mg/dl (normal: 0.5–1.4 mg/dl)
Microalbumin: 4 μg (normal: 0–29 μg)
At his initial visit with the RD for crisis management of asymptomatic hypoglycemia, she examined his injection sites and asked if he had made the changes recommended by his clinician. She reviewed his injection technique, diet history, incidence of hypoglycemia, and hypoglycemia treatment methods. She discussed with B.C. ways to reduce his risks of hypoglycemia, including food choices, insulin timing, and absorption variations at different injection sites.
The RD reinforced his clinician’s instruction to avoid old injection sites and added a new recommendation to lower insulin doses because of improved absorption at the new sites.
B.C. was now checking his blood glucose and recording results in a handheld electronic device in a form that could be downloaded, e-mailed, or faxed, but he was not recording his food choices. The dietitian asked him to keep food records and started his carbohydrate-counting education. A follow-up visit was scheduled for 1 week later.
At the second visit, B.C.’s mid-afternoon blood glucose was <70 mg/dl. He did not respond to treatment with 15 g carbohydrate from 4 oz. of regular soda. His blood glucose continued to drop, measuring 47 mg/dl 15 minutes later. He drank another 8 oz. of soda, and his blood glucose increased to 63 mg/dl 1 hour later. He then drank another 8 oz. of soda and ate a sandwich before leaving the dietitian’s office. He called in 1 hour later to report that his blood glucose was finally up to 96 mg/dl.
B.C.’s records showed a pattern of mid-afternoon hypoglycemia. He was willing to add a shot of lispro at lunch to his regimen, so the RD recommended reducing his morning NPH to prevent lows later in the day.
The RD also calculated insulin and carbohydrate ratios for blood glucose correction and meal-related insulin coverage using the “1500 rule” and the “500 rule.”
The 1500 rule is a commonly accepted formula for estimating the drop in a person’s blood glucose per unit of fast-acting insulin. This value is referred to as an “insulin sensitivity factor” (ISF) or “correction factor.” To use the 1500 rule, first determine the total daily dose (TDD) of all rapid- and long-acting insulin. Then divide 1500 by the TDD to find the ISF (the number of mg/dl that 1 unit of rapid-acting insulin will lower the blood glucose level). B.C.’s average TDD was 41 units. Therefore, his estimated ISF was 37 mg/dl per 1 unit of insulin. The RD rounded this up to 40 mg/dl to be prudent, given his history of hypoglycemia.
The 500 rule is a formula for calculating the insulin-to-carbohydrate ratio. To use the 500 rule, divide 500 by the TDD. For B.C., the insulin-to-carbohydrate ratio was calculated at 1:12 (1 unit of insulin to cover every 12 g of carbohydrate), but again this was rounded up to 1:14 for safety. Later, his carbohydrate ratio was adjusted down to 1:10 based on blood glucose monitoring results before and 2 hours after meals.
The RD taught B.C. how to use the insulin-to-carbohydrate ratio instead of his sliding scale to adjust his insulin and asked him to try to follow the new recommendations. With his endocrinologist’s approval, she reduced his NPH doses to 34 units and added a shot of lispro at lunchtime, the dose to be based on the amount of carbohydrate in the meal and his before-meal blood glucose level.
The RD asked B.C. to return in 1 week for evaluation and review of his new regimen. However, 3 days later, he returned after having had another severe episode of hypoglycemia.
In the course of these early visits, a good rapport developed between B.C. and the dietitian. B.C. learned that his judgment on how hypo- and hyperglycemia felt was often inaccurate and led him to make insulin adjustments that contributed to his hypoglycemia problems. By improving B.C.’s understanding of insulin doses and blood glucose responses, the RD hoped to help him become more skilled at making insulin dose adjustments. For the time being, however, he was still at risk for asymptomatic hypoglycemia. He had recently filled a prescription for glucagon, but the RD needed to review and encourage its proper use. She also provided literature to support his wife in case she needed to administer glucagon for him.
At this third visit, the RD reduced B.C.’s morning NPH dose to 22 units because of his rapid drop in blood glucose between noon and 1:00 p.m. This reduction finally eliminated his mid-afternoon lows.
B.C. had started using carbohydrate counting to make his decisions about lunchtime insulin doses. He liked carbohydrate counting because it gave him a more viable reason for testing his blood glucose frequently. Over the years, B.C.’s glycemia had become increasingly difficult to control. He had stopped checking his blood glucose because he felt unable to improve the situation once he had the information. In the early 1990s, his endocrinologist had started him self-adjusting insulin doses using the exchange system, but he found that he was always “chasing his blood sugars.” Carbohydrate counting changed everything. He now knew what to do to improve his blood glucose levels, and that made him feel more in charge of his diabetes.
Still, although carbohydrate counting led to more frequent testing and better blood glucose control than his old sliding scale, it was not perfect. At home, he had mastered this technique, but he ate many of his meals in restaurants, where carbohydrate counting was more challenging.
B.C. found it difficult to carry different types of insulin. This and his lifestyle suggested the need to change his multiple daily injections from regular to lispro insulin. He continued checking his blood glucose before and 2 hours after meals. His insulin-to-carbohydrate ratio of 1:10 g and his ISF of 1:40 mg/dl allowed him to stay within his goal of no more than a 30-mg/dl increase in blood glucose 2 hours after meals. He continued to be asymptomatic of hypoglycemia, but lows occurred less frequently. The new goal of therapy was to recover his hypoglycemia symptoms at a more normal level of about 70 mg/dl. He was scheduled for another visit 2 weeks later.
Between visits to the RD, BC-ADM, his clinician identified problems with the timing of his long-acting insulin peak, resulting in early nocturnal lows. Based on the clinician’s clinical experience of lente demonstrating a slightly smoother peak, she changed B.C.’s long-acting insulin unit-for-unit from NPH to lente.
At B.C.’s next visit, he and the RD reviewed his insulin doses of 22 units of lente in the morning and 11 units of lente at night. His TDD including premeal lispro now averaged 49 units. His average blood glucose levels were 130 mg/dl fasting, 100 mg/dl mid-afternoon, 127 mg/dl before dinner, and 200 mg/dl at bedtime.
The bedtime levels were higher because of late meals, the fat content of restaurant meals, his meat food choices, and his inexperience at counting carbohydrates for prepared foods. The dietitian suggested mixing regular and lispro insulin to try and get the average bedtime blood glucose level to 140 mg/dl. Mixing his calculated dose to be one-third regular and two-third lispro would provide coverage lasting a little longer than that of just lispro to cover higher-fat foods that took longer to digest. At the same time, the dietitian encouraged B.C. to choose lower-fat foods to help reduce his LDL cholesterol and assist with weight loss. B.C. now had an incentive to keep accurate food records to help evaluate his accuracy at calculating insulin doses.
B.C. and the RD also reviewed his decisions for treating lows. At his first meeting, B.C. ate anything and everything when he experienced hypoglycemia, which often resulted in blood glucose levels >400 mg/dl. Now, he was appropriately using 15–30 g of quick-acting glucose—usually 4–8 oz. of orange juice. He based this amount on his blood glucose level, expecting about a 40-mg/dl rise over 30 minutes from 10 g of carbohydrate. He checked his glucose level before treating when possible and always checked 15–30 minutes after treating to evaluate the results. Once his glucose reached 80 mg/dl or above, he either ate a meal or ate 15 g of carbohydrate per hour to prevent a recurrence of hypoglycemia until his next meal.
In completing her assessment during the next few meetings with B.C., the RD identified a problem with erectile dysfunction. She notifed his clinician and referred him to a urologist. Eventually, the urologist diagnosed reduced blood flow and started B.C. on sildenafil (Viagra).
B.C. wanted to resume exercise to help his weight loss efforts. Because exercise improves insulin sensitivity and can acutely lower blood glucose, the dietitian taught B.C. how to reduce his insulin doses by 25–50% for planned physical activity to further reduce his risks of hypoglycemia. He learned to carry his blood glucose meter, fluids, and carbohydrate foods during and after exercise. His pre-exercise blood glucose goal was set at 150 mg/dl. The dietitian instructed B.C. to test his blood glucose again after exercise and to eat carbohydrate foods if it was <100 mg/dl.
She also gave instructions for unplanned exercise. He would require additional carbohydrate depending on his blood glucose level before exercise, his previous experience with similar exercise, and the timing of the exercise. Education follow-ups were scheduled with the dietitian for 1 month later and every 3 months thereafter.
At his next annual eye exam, B.C. discovered that he had background retinopathy. He also reported feeling that his daily injection regimen had become too complicated. Still feeling limited in his ability to control his diabetes and looking for an alternative to insulin injections, he wanted to discuss continuous subcutaneous insulin infusion therapy (insulin pump therapy).
He, his endocrinologist, and his dietitian discussed the pros and cons of pump therapy and how it might affect his current situation. They reviewed available insulin pumps and sets and agreed on which ones would best meet his needs. The equipment was ordered, and a training session was scheduled with the dietitian (a certified pump trainer) in 1 month.
B.C. started using an insulin pump 2 years after his first visit with the dietitian. His insulin-to-carbohydrate ratio was adjusted for his new therapy regimen, and a new ISF was calculated to help him reduce high blood glucose levels. His endocrinologist set basal insulin rates at 0.3 units/hour to start at midnight and 0.5 units/hour to start at 3:00 a.m. This more natural delivery of insulin based on B.C.’s body rhythms and lifestyle further improved his diabetes control.
One week after starting pump therapy, B.C. called the dietitian to report large urine ketones and a blood glucose level of 317 mg/dl. His endocrinologist had changed his basal rates, but he wanted to meet with the dietitian to review his sites, set insertion, troubleshooting skills, and related issues. Working together, they eventually discovered that problems with his pump sites required using a bent-needle set to resolve absorption issues.
B.C’s relationship with his endocrinologist and dietitian was seamless. He met with the dietitian when his clinician was unavailable or when he needed more time to work through problems.
B.C. has met with the RD 15 times over 3 years. Eventually, he recovered symptoms of hypoglycemia when his blood glucose levels were 70 mg/dl. After 6 months of education meetings, his lab values had reached target ranges. Most recently, his LDL cholesterol was <100 mg/dl, his A1C results were <7%, his hypoglycemia symptoms were maintained at a blood glucose level of 70 mg/dl, and his blood glucose had been stabilized using the square-wave and dual-wave features on his insulin pump.
B.C. learned how to achieve recommended goals and to self-manage his diabetes with the help of his care team: endocrinologist, cardiologist, ophthalmologist, podiatrist, urologist, and advanced practice dietitian.
Advanced practice dietitians in diabetes work in many settings and see clients referred from many different types of medical professionals. They may see clients either before or after their appointments with other members of the health care team, depending on appointment availability and their need for nutrition therapy and diabetes education. Referring clinicians rely on their evaluations and findings. When necessary, clinician approval can be obtained for immediate interventions, enhancing the timeliness of care.
Why would an RD want to obtain the skills and certification necessary to earn the BC-ADM credential? The answer, as illustrated in the case study above, lies in their routine use of two sets of skills and performance of two roles: patient education and clinical management.
Dietitians who specialize in diabetes often find that their role expands beyond provider of nutrition counseling. As part of a multidisciplinary team, they become increasingly involved with patient care. As they move patients toward self-management of their disease, they necessarily participate actively in assessment and diagnosis of patients; planning, implementation, and coordination of their diabetes care regimens; and monitoring and evaluation of their treatment options and strategies. They find that their daily professional activities go beyond diabetes education, crossing over into identifying problems, providing or coordinating clinical care, adjusting therapy, and referring to other medical professionals. They often work independently, providing consultation both to people with diabetes and to other diabetes care team members.
The BC-ADM credential acknowledges this professional autonomy while promoting team collaboration and thus improving the quality of care for people with diabetes. The new certification formally recognizes advanced practice dietitians as they move beyond their traditional roles and into clinical problem solving and case management.
Claudia Shwide-Slavin, MS, RD, BC-ADM, CDE, is a private practice dietitian in New York, N.Y.
Note of disclosure: Ms. Shwide-Slavin has received honoraria for speaking engagements from Medtronic Minimed, which manufactures insulin pumps, and Eli Lilly and Co., which manufactures insulin products for the treatment of diabetes.
Email alerts
- Advanced Practice Care: Advanced Practice Care in Diabetes: Epilogue
- Advanced Practice Care: Advanced Practice Care in Diabetes: Preface
- Online ISSN 1944-7353
- Print ISSN 1040-9165
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Arch Clin Cases
- v.8(3); 2021

An atypical presentation of type 1 diabetes
Brandon w. knopp.
1 Charles E. Schmidt College of Medicine, Florida Atlantic University, Boca Raton, FL, USA
Parvathi Perumareddi
2 Department of Integrated Medical Science, Charles E. Schmidt College of Medicine, Florida Atlantic University, Boca Raton, FL, USA
Type 1 and type 2 diabetes have been described historically as occurring in distinct patient populations; however, atypical demographics are becoming more frequent as the prevalence of diabetes increases, crossing boundaries of ages. Some of these cases can be challenging to diagnose clinically as the patient symptomatology and progression can differ from the standard features of type 1 and 2 diabetes. Our case is an example of a patient whose type 1 diabetes presented atypically with characteristics often associated with type 2 diabetes. Patient presentations such as this are uncommon, with our patient having presented with the “textbook” characteristics of type 2 diabetes. When first diagnosed with diabetes mellitus type 2, the patient was 60 years old, had a BMI around 30 and experienced a gradual onset of symptoms over the course of several months. At the age of 64, the patient tested positive for GAD65 autoantibodies following a year of declining glycemic control and was re-evaluated and classified as a type 1 diabetes patient. Subsequent insulin injections resolved his diabetes-related complications which included polyuria, weakness and weight loss and improved his glycemic control. This case provides an example of an unusual clinical presentation of type 1 diabetes and serves to raise awareness for atypical presentations of diabetes to improve accurate classifications at earlier stages.
Introduction
Diabetes mellitus is a metabolic disease characterized by insulin deficiency and/or insulin resistance. Type 1 diabetes results from the autoimmune destruction of pancreatic β cells and is typically found in younger patients while type 2 diabetes occurs due to insulin resistance and is most often found in middle aged to older adults. Each type has been associated with a distinct patient population, however, there are reports of cases with atypical demographics characterized by a crossover in age, weight and other factors [ 1 , 2 ].
These rare cases are difficult to identify clinically and may require antibody testing to confirm the diagnosis. The incidence of atypical presentations of diabetes mellitus is unknown, however, with the rise in diabetes cases over the past several decades and an expected increase of 54% between 2015 and 2030 [ 3 ], a concomitant increase in atypical cases can be reasonably expected.
Case report
This case describes a 64-year-old Caucasian male who was referred for evaluation and treatment of diabetes mellitus which was first diagnosed at the age of 60. At the age of 60 he presented with minimal clinical signs of diabetes mellitus, including mild fatigue, and was diagnosed with type 2 diabetes due to hyperglycemia and elevated HbA1c. He was treated as a type 2 diabetes patient for four years before being placed on insulin at the age of 64 following a significant deterioration in glycemic control. He had no known risk factors for diabetes mellitus and was screened with self-monitoring of blood glucose (SMBG). His past medical history was significant for elevated thyroid stimulating hormone (TSH), but otherwise no significant abnormalities.
Clinical Progression
On 10/28/2020, the patient presented with a multi-day history of polyuria and weakness with deterioration since his previous visit on 7/3/20. Following a weight loss of 5.4 kg during the previous several days, the patient weighed 84.4 kg with a BMI of 29.1. He rarely checked his blood glucose but measured a value of almost 500 mg/dL at home during this time and a value of close to 400 mg/dL in office. On a physical exam, the patient did not appear weak or ill and reported no changes in vision or neurologic symptoms. He reported consistency in taking metformin and glimepiride, with sertraline being added a few months prior. Because of the significant hyperglycemia and concerns of potential diabetic ketoacidosis, he was injected with 20 units of insulin degludec, given 5 units of insulin lispro with instructions for later use and asked to drink 5 cups of water while in office. ( Note : treatments vary among providers)
At his follow up on 11/5/2020, he improved with no significant incidences of hyperglycemia, though he experienced blood sugar spikes after breakfast. Along with dietary interventions to mitigate post-breakfast spikes, Insulin degludec increased to 23 units daily and 5 units of insulin lispro with meals. Metformin and Glimepiride were discontinued.
During his visit on 3/29/2021, the patient stated his diabetes was not well-controlled and had variable glucose ranges with hypoglycemia typically occurring before dinnertime. He had a temperature of 36.4 o C, weight of 90.7 kg, height of 171.5 cm and BMI of 30.86. The physical exam findings were normal with no foot ulcers or other visible abnormalities. He also had an intact sensory exam. The patient had a recent c-peptide of 0.5 ng/mL on 12/24/2020 and an HbA1c of 7.4% (normal 4.2–5.7%).
During his visit on 5/17/2021, the patient stated his diabetes was well-controlled. He used an insulin pump and continuous glucose monitoring (CGM) sensor between 5/4/2021 and 5/17/2021. Between those dates, his blood glucose was 88% in range with no significant hypoglycemia since beginning insulin pump use. He gained 3.6 kg since 3/29/2021 with no new development of diabetes-related symptoms. Table 1 presents the most important laboratory parameters.
Select laboratory results
Diagnosis and outcome
The patient tested positive for a concentration of 16 IU/mL of GAD 65 autoantibodies on 3/29/2021, indicating a diagnosis of type 1 diabetes. Likewise, he tested positive for Thyroid Peroxidase antibodies (TPO) at 499 IU/mL, confirming his diagnosis of autoimmune thyroid disease, Hashimoto thyroiditis in this case.
As indicated on Table 2 , the patient’s HbA1c levels rose from 9.1% to 13.5% in about 9 months before being treated with insulin in November 2020. While taking insulin in the form of insulin lispro and insulin degludec, his HbA1c levels dropped from 13.5% to 7.4% in under 4 months. Based on the continuous glucose monitoring (CGM) values between 5/4/21 and 5/17/21, the Glucose Management Indicator (GMI) predicted an HbA1c of 6.4% just 7 months after the first insulin injection. Likewise, his glycemic control improved with a blood glucose 88% in range with no significant lows as of 5/17/21.
HbA1c level evolution
Discussions
Type 1 and 2 diabetes have clinically distinct pathophysiologic etiologies. These discrete pathologies lead to unique presentations for each type and are useful in informing clinical diagnostic practices as well as treatment regimens. The clinical determination of type 1 vs. 2 diabetes is made with consideration of factors including the patient’s age, body composition, symptom progression and clinical presentation. Type 1 diabetes typically manifests in young patients, often before the age of 14, who frequently appear thin and have a sudden onset of symptoms, with diabetic ketoacidosis presenting as the first sign of disease in many cases. Type 2 diabetes, on the other hand, often develops around the age of 45 or later and is associated with obesity and metabolic syndrome and usually has a gradual onset.
As both types of diabetes generally have distinct etiologies, diagnosis can often be made based on patient demographics. However, atypical cases can exist in contravention of diagnostic norms. The case detailed above discusses one such patient whose clinical characteristics and progression matched closely with the criteria for type 2 diabetes, even though his pathophysiology pointed to type 1 diabetes. While his initial diagnosis of type 2 diabetes was made based on his clinical characteristics, antibody tests significant for glutamic acid decarboxylase 65 autoantibody (GAD 65 ) confirmed his diagnosis with type 1 diabetes [ 3 ]. While rare, similar atypical cases of diabetes have been reported [ 1 , 2 ]. With the increasing number of diabetes cases expected in the coming years [ 4 ], unusual cases such as the case presented above may become more common. To ensure timely and accurate diagnosis and management of patients with atypical cases of diabetes, we seek to raise awareness of cases which do not adhere to presentational or diagnostic norms.
Key Messages
- It is known that atypical cases of diabetes exist and can complicate the diagnosis of diabetes mellitus.
- This manuscript provides evidence that atypical cases can present with symptoms typically associated with another type of diabetes.
- The case described is an example of a type 1 diabetes patient presenting with several classic features of type 2 diabetes.
Conflicts of interest
There are no personal, financial, or other conflicts of interest to disclose.
Consent for publication
Written informed consent from the patient has been taken and is available for review by Editor in chief of the journal.
- Patient Care & Health Information
- Diseases & Conditions
- Type 1 diabetes
What is type 1 diabetes? A Mayo Clinic expert explains
Learn more about type 1 diabetes from endocrinologist Yogish Kudva, M.B.B.S.
I'm Dr. Yogish C. Kudva an endocrinologist at Mayo Clinic. In this video, we'll cover the basics of type 1 diabetes. What is it? Who gets it? The symptoms, diagnosis, and treatment. Whether you're looking for answers for yourself or someone you love. We are here to give you the best information available. Type 1 diabetes is a chronic condition that affects the insulin making cells of the pancreas. It's estimated that about 1.25 million Americans live with it. People with type 1 diabetes don't make enough insulin. An important hormone produced by the pancreas. Insulin allows your cells to store sugar or glucose and fat and produce energy. Unfortunately, there is no known cure. But treatment can prevent complications and also improve everyday life for patients with type 1 diabetes. Lots of people with type 1 diabetes live a full life. And the more we learn and develop treatment for the disorder, the better the outcome.
We don't know what exactly causes type 1 diabetes. We believe that it is an auto-immune disorder where the body mistakenly destroys insulin producing cells in the pancreas. Typically, the pancreas secretes insulin into the bloodstream. The insulin circulates, letting sugar enter your cells. This sugar or glucose, is the main source of energy for cells in the brain, muscle cells, and other tissues. However, once most insulin producing cells are destroyed, the pancreas can't produce enough insulin, meaning the glucose can't enter the cells, resulting in an excess of blood sugar floating in the bloodstream. This can cause life-threatening complications. And this condition is called diabetic ketoacidosis. Although we don't know what causes it, we do know certain factors can contribute to the onset of type 1 diabetes. Family history. Anyone with a parent or sibling with type 1 diabetes has a slightly increased risk of developing it. Genetics. The presence of certain genes can also indicate an increased risk. Geography. Type 1 diabetes becomes more common as you travel away from the equator. Age, although it can occur at any age there are two noticeable peaks. The first occurs in children between four and seven years of age and the second is between 10 and 14 years old.
Signs and symptoms of type 1 diabetes can appear rather suddenly, especially in children. They may include increased thirst, frequent urination, bed wetting in children who previously didn't wet the bed. Extreme hunger, unintended weight loss, fatigue and weakness, blurred vision, irritability, and other mood changes. If you or your child are experiencing any of these symptoms, you should talk to your doctor.
The best way to determine if you have type 1 diabetes is a blood test. There are different methods such as an A1C test, a random blood sugar test, or a fasting blood sugar test. They are all effective and your doctor can help determine what's appropriate for you. If you are diagnosed with diabetes, your doctor may order additional tests to check for antibodies that are common in type 1 diabetes in the test called C-peptide, which measures the amount of insulin produced when checked simultaneously with a fasting glucose. These tests can help distinguish between type 1 and type 2 diabetes when a diagnosis is uncertain.
If you have been diagnosed with type 1 diabetes, you may be wondering what treatment looks like. It could mean taking insulin, counting carbohydrates, fat protein, and monitoring your glucose frequently, eating healthy foods, and exercising regularly to maintain a healthy weight. Generally, those with type 1 diabetes will need lifelong insulin therapy. There are many different types of insulin and more are being developed that are more efficient. And what you may take may change. Again, your doctor will help you navigate what's right for you. A significant advance in treatment from the last several years has been the development and availability of continuous glucose monitoring and insulin pumps that automatically adjust insulin working with the continuous glucose monitor. This type of treatment is the best treatment at this time for type 1 diabetes. This is an exciting time for patients and for physicians that are keen to develop, prescribe such therapies. Surgery is another option. A successful pancreas transplant can erase the need for additional insulin. However, transplants aren't always available, not successful and the procedure can pose serious risks. Sometimes it may outweigh the dangers of diabetes itself. So transplants are often reserved for those with very difficult to manage conditions. A successful transplant can bring life transforming results. However, surgery is always a serious endeavor and requires ample research and concentration from you, your family, and your medical team.
The fact that we don't know what causes type 1 diabetes can be alarming. The fact that we don't have a cure for it even more so. But with the right doctor, medical team and treatment, type 1 diabetes can be managed. So those who live with it can get on living. If you would like to learn even more about type 1 diabetes, watch our other related videos or visit mayoclinic.org. We wish you well.
Type 1 diabetes, once known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition. In this condition, the pancreas makes little or no insulin. Insulin is a hormone the body uses to allow sugar (glucose) to enter cells to produce energy.
Different factors, such as genetics and some viruses, may cause type 1 diabetes. Although type 1 diabetes usually appears during childhood or adolescence, it can develop in adults.
Even after a lot of research, type 1 diabetes has no cure. Treatment is directed toward managing the amount of sugar in the blood using insulin, diet and lifestyle to prevent complications.
Products & Services
- A Book: The Essential Diabetes Book
Type 1 diabetes symptoms can appear suddenly and may include:
- Feeling more thirsty than usual
- Urinating a lot
- Bed-wetting in children who have never wet the bed during the night
- Feeling very hungry
- Losing weight without trying
- Feeling irritable or having other mood changes
- Feeling tired and weak
- Having blurry vision
When to see a doctor
Talk to your health care provider if you notice any of the above symptoms in you or your child.
The exact cause of type 1 diabetes is unknown. Usually, the body's own immune system — which normally fights harmful bacteria and viruses — destroys the insulin-producing (islet) cells in the pancreas. Other possible causes include:
- Exposure to viruses and other environmental factors
The role of insulin
Once a large number of islet cells are destroyed, the body will produce little or no insulin. Insulin is a hormone that comes from a gland behind and below the stomach (pancreas).
- The pancreas puts insulin into the bloodstream.
- Insulin travels through the body, allowing sugar to enter the cells.
- Insulin lowers the amount of sugar in the bloodstream.
- As the blood sugar level drops, the pancreas puts less insulin into the bloodstream.
The role of glucose
Glucose — a sugar — is a main source of energy for the cells that make up muscles and other tissues.
- Glucose comes from two major sources: food and the liver.
- Sugar is absorbed into the bloodstream, where it enters cells with the help of insulin.
- The liver stores glucose in the form of glycogen.
- When glucose levels are low, such as when you haven't eaten in a while, the liver breaks down the stored glycogen into glucose. This keeps glucose levels within a typical range.
In type 1 diabetes, there's no insulin to let glucose into the cells. Because of this, sugar builds up in the bloodstream. This can cause life-threatening complications.
Risk factors
Some factors that can raise your risk for type 1 diabetes include:
- Family history. Anyone with a parent or sibling with type 1 diabetes has a slightly higher risk of developing the condition.
- Genetics. Having certain genes increases the risk of developing type 1 diabetes.
- Geography. The number of people who have type 1 diabetes tends to be higher as you travel away from the equator.
- Age. Type 1 diabetes can appear at any age, but it appears at two noticeable peaks. The first peak occurs in children between 4 and 7 years old. The second is in children between 10 and 14 years old.
Complications
Over time, type 1 diabetes complications can affect major organs in the body. These organs include the heart, blood vessels, nerves, eyes and kidneys. Having a normal blood sugar level can lower the risk of many complications.
Diabetes complications can lead to disabilities or even threaten your life.
- Heart and blood vessel disease. Diabetes increases the risk of some problems with the heart and blood vessels. These include coronary artery disease with chest pain (angina), heart attack, stroke, narrowing of the arteries (atherosclerosis) and high blood pressure.
Nerve damage (neuropathy). Too much sugar in the blood can injure the walls of the tiny blood vessels (capillaries) that feed the nerves. This is especially true in the legs. This can cause tingling, numbness, burning or pain. This usually begins at the tips of the toes or fingers and spreads upward. Poorly controlled blood sugar could cause you to lose all sense of feeling in the affected limbs over time.
Damage to the nerves that affect the digestive system can cause problems with nausea, vomiting, diarrhea or constipation. For men, erectile dysfunction may be an issue.
- Kidney damage (nephropathy). The kidneys have millions of tiny blood vessels that keep waste from entering the blood. Diabetes can damage this system. Severe damage can lead to kidney failure or end-stage kidney disease that can't be reversed. End-stage kidney disease needs to be treated with mechanical filtering of the kidneys (dialysis) or a kidney transplant.
- Eye damage. Diabetes can damage the blood vessels in the retina (part of the eye that senses light) (diabetic retinopathy). This could cause blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
- Foot damage. Nerve damage in the feet or poor blood flow to the feet increases the risk of some foot complications. Left untreated, cuts and blisters can become serious infections. These infections may need to be treated with toe, foot or leg removal (amputation).
- Skin and mouth conditions. Diabetes may leave you more prone to infections of the skin and mouth. These include bacterial and fungal infections. Gum disease and dry mouth also are more likely.
- Pregnancy complications. High blood sugar levels can be dangerous for both the parent and the baby. The risk of miscarriage, stillbirth and birth defects increases when diabetes isn't well-controlled. For the parent, diabetes increases the risk of diabetic ketoacidosis, diabetic eye problems (retinopathy), pregnancy-induced high blood pressure and preeclampsia.
There's no known way to prevent type 1 diabetes. But researchers are working on preventing the disease or further damage of the islet cells in people who are newly diagnosed.
Ask your provider if you might be eligible for one of these clinical trials. It is important to carefully weigh the risks and benefits of any treatment available in a trial.
- Summary of revisions: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-Srev.
- Papadakis MA, et al., eds. Diabetes mellitus. In: Current Medical Diagnosis & Treatment 2022. 61st ed. McGraw Hill; 2022. https://accessmedicine.mhmedical.com. Accessed May 4, 2022.
- What is diabetes? National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes. Accessed May 4, 2022.
- Levitsky LL, et al. Epidemiology, presentation, and diagnosis of type 1 diabetes mellitus in children and adolescents. https://www.uptodate.com/contents/search. Accessed May 4, 2022.
- Diabetes mellitus (DM). Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetes-mellitus-dm. Accessed May 4, 2022.
- AskMayoExpert. Type 1 diabetes mellitus. Mayo Clinic; 2021.
- Robertson RP. Pancreas and islet transplantation in diabetes mellitus. https://www.uptodate.com/contents/search. Accessed May 4, 2022.
- Levitsky LL, et al. Management of type 1 diabetes mellitus in children during illness, procedures, school, or travel. https://www.uptodate.com/contents/search. Accessed May 4, 2022.
- Hyperglycemia (high blood glucose). American Diabetes Association. https://www.diabetes.org/healthy-living/medication-treatments/blood-glucose-testing-and-control/hyperglycemia. Accessed May 4, 2022.
- Diabetes and DKA (ketoacidosis). American Diabetes Association. https://www.diabetes.org/diabetes/dka-ketoacidosis-ketones. Accessed May 4, 2022.
- Insulin resistance & prediabetes. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance. Accessed May 4, 2022.
- Blood sugar and insulin at work. American Diabetes Association. https://www.diabetes.org/tools-support/diabetes-prevention/high-blood-sugar. Accessed May 4, 2022.
- Inzucchi SE, et al. Glycemic control and vascular complications in type 1 diabetes. https://www.uptodate.com/contents/search. Accessed May 4, 2022.
- Diabetes and oral health. American Diabetes Association. https://www.diabetes.org/diabetes/keeping-your-mouth-healthy. Accessed May 4, 2022.
- Drug treatment of diabetes mellitus. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/drug-treatment-of-diabetes-mellitus. Accessed May 4, 2022.
- Weinstock DK, et al. Management of blood glucose in adults with type 1 diabetes mellitus. https://www.uptodate.com/contents/search. Accessed May 7, 2022.
- FDA proves first automated insulin delivery device for type 1 diabetes. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-approves-first-automated-insulin-delivery-device-type-1-diabetes. Accessed May 4, 2022.
- Boughton CK, et al. Advances in artificial pancreas systems. Science Translational Medicine. 2019; doi:10.1126/scitranslmed.aaw4949.
- Hypoglycemia (low blood sugar). American Diabetes Association. https://www.diabetes.org/healthy-living/medication-treatments/blood-glucose-testing-and-control/hypoglycemia. Accessed May 4, 2022.
- Diabetes in the workplace and the ADA. U.S. Equal Opportunity Employment Commission. https://www.eeoc.gov/laws/guidance/diabetes-workplace-and-ada. Accessed May 4, 2022.
- Cardiovascular disease and risk management: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S010.
- Diabetes technology. Standards of Medical Care in Diabetes — 2022. 2022; doi:10.2337/dc22-S007.
- FDA authorizes a second artificial pancreas system. JDRF. https://www.jdrf.org/blog/2019/12/13/jdrf-reports-fda-authorizes-second-artificial-pancreas-system/. Accessed May 4, 2022.
- Classification and diagnosis of diabetes: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S002.
- Retinopathy, neuropathy, and foot care: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S012.
- Glycemic targets: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S012.
- Pharmacologic approaches to glycemic treatment: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S009.
- Facilitating behavior change and well-being to improve health outcomes: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S005.
- Centers for Disease Control and Prevention. Use of hepatitis B vaccination for adults with diabetes mellitus: Recommendations of the Advisory Committee on Immunization Practices (ACIP). Morbidity and Mortality Weekly Report. 2011;60:1709.
- Management of diabetes in pregnancy: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S015.
- Older adults: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S013.
- FDA approves first-of-its-kind automated insulin delivery and monitoring system for use in young pediatric patients. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-approves-first-its-kind-automated-insulin-delivery-and-monitoring-system-use-young-pediatric#:~:text=Today, the U.S. Food and,by individuals aged 2 to. Accessed May 8, 2022.
- What you need to know: Getting a COVID-19 vaccine. American Diabetes Association. https://www.diabetes.org/coronavirus-covid-19/vaccination-guide. Accessed June 1, 2022.
News from Mayo Clinic
- Driven by family, fueled by hope: Mayo Clinic researcher fights against Type 1 diabetes Aug. 06, 2023, 11:00 a.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities

Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Presentation to primary care during the prodrome of type 1 diabetes in childhood: A case-control study using record data linkage
Affiliations.
- 1 Centre for Trials Research, College of Biomedical & Life Sciences, Cardiff University, Cardiff, UK.
- 2 Division of Population Medicine, School of Medicine, Cardiff University, Cardiff, UK.
- 3 SAIL Databank, School of Medicine, Swansea University, Swansea, UK.
- PMID: 30737875
- DOI: 10.1111/pedi.12829
Objective: To evaluate primary care presentations during the prodrome (12 months prior to onset type-1 diabetes (T1D), with or without diabetic ketoacidosis [DKA]), to identify opportunities for earlier diagnosis.
Methods: This was a case-control study, linking 16 years of data from children (≤15 years) registered at diagnosis of T1D, and routinely collected primary care records in Wales (United Kingdom). Controls (without T1D) were matched on a 3:1 ratio. Conditional logistic regression modeling was used to compare characteristics occurring in cases (children with T1D) and controls; and cases that presented with/without DKA.
Results: A total of 1345 children with T1D (19% DKA) and 4035 controls were identified. During the 12 months prior to diagnosis, cases were 6.5 times more likely to have at least one primary care contact (P < 0.001). One to 30 days prior to diagnosis, contacts relating to blood tests, fungal conditions, respiratory tract infections (RTIs), urinary conditions, vomiting, and weight were independently associated with T1D, as were contacts relating to blood tests, between 91 and 180 days prior to diagnosis. Children with a contact up to a month prior to diagnosis, relating to RTIs, antibiotic prescriptions, and vomiting, were more likely to present in DKA, as were boys (P = 0.047).
Conclusion: There are opportunities in primary care for an earlier diagnosis of T1D in childhood. These data could be used to create a predictive diagnostic tool, as a potential aid for primary care health professionals, to prevent presentation in DKA.
Keywords: childhood; diabetic ketoacidosis; primary care data linkage; prodrome; type 1 diabetes mellitus.
© 2019 The Authors. Pediatric Diabetes published by John Wiley & Sons Ltd.
Publication types
- Research Support, Non-U.S. Gov't
- Age Factors
- Case-Control Studies
- Child, Preschool
- Diabetes Mellitus, Type 1 / diagnosis
- Diabetes Mellitus, Type 1 / epidemiology*
- Diabetes Mellitus, Type 1 / therapy
- Early Diagnosis
- Early Medical Intervention / statistics & numerical data
- Electronic Health Records / statistics & numerical data
- Information Storage and Retrieval
- Office Visits / statistics & numerical data*
- Pediatrics / statistics & numerical data
- Prediabetic State / diagnosis
- Prediabetic State / epidemiology*
- Prediabetic State / therapy
- Primary Health Care / statistics & numerical data*
- Prodromal Symptoms*
- United Kingdom / epidemiology
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
- Katherine Kupfer
- Mackenzie Morris
- Elizabeth Mount
- Chelsea Taylor
- Brittney Wex
Our rationale for choosing this condition:
Throughout our clinical experiences, previous careers, and personal lives, diabetes has been prevalent. As practitioners, we will continue to see this condition often and have to recognize/treat it in our patients. In light of this, we wanted to have a good understanding of Type 1 diabetes, its presentation, and its treatment.
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Diabetes Overview
Healthy Living with Diabetes
- Español
On this page:
How can I plan what to eat or drink when I have diabetes?
How can physical activity help manage my diabetes, what can i do to reach or maintain a healthy weight, should i quit smoking, how can i take care of my mental health, clinical trials for healthy living with diabetes.
Healthy living is a way to manage diabetes . To have a healthy lifestyle, take steps now to plan healthy meals and snacks, do physical activities, get enough sleep, and quit smoking or using tobacco products.
Healthy living may help keep your body’s blood pressure , cholesterol , and blood glucose level, also called blood sugar level, in the range your primary health care professional recommends. Your primary health care professional may be a doctor, a physician assistant, or a nurse practitioner. Healthy living may also help prevent or delay health problems from diabetes that can affect your heart, kidneys, eyes, brain, and other parts of your body.
Making lifestyle changes can be hard, but starting with small changes and building from there may benefit your health. You may want to get help from family, loved ones, friends, and other trusted people in your community. You can also get information from your health care professionals.
What you choose to eat, how much you eat, and when you eat are parts of a meal plan. Having healthy foods and drinks can help keep your blood glucose, blood pressure, and cholesterol levels in the ranges your health care professional recommends. If you have overweight or obesity, a healthy meal plan—along with regular physical activity, getting enough sleep, and other healthy behaviors—may help you reach and maintain a healthy weight. In some cases, health care professionals may also recommend diabetes medicines that may help you lose weight, or weight-loss surgery, also called metabolic and bariatric surgery.
Choose healthy foods and drinks
There is no right or wrong way to choose healthy foods and drinks that may help manage your diabetes. Healthy meal plans for people who have diabetes may include
- dairy or plant-based dairy products
- nonstarchy vegetables
- protein foods
- whole grains
Try to choose foods that include nutrients such as vitamins, calcium , fiber , and healthy fats . Also try to choose drinks with little or no added sugar , such as tap or bottled water, low-fat or non-fat milk, and unsweetened tea, coffee, or sparkling water.
Try to plan meals and snacks that have fewer
- foods high in saturated fat
- foods high in sodium, a mineral found in salt
- sugary foods , such as cookies and cakes, and sweet drinks, such as soda, juice, flavored coffee, and sports drinks
Your body turns carbohydrates , or carbs, from food into glucose, which can raise your blood glucose level. Some fruits, beans, and starchy vegetables—such as potatoes and corn—have more carbs than other foods. Keep carbs in mind when planning your meals.
You should also limit how much alcohol you drink. If you take insulin or certain diabetes medicines , drinking alcohol can make your blood glucose level drop too low, which is called hypoglycemia . If you do drink alcohol, be sure to eat food when you drink and remember to check your blood glucose level after drinking. Talk with your health care team about your alcohol-drinking habits.

Find the best times to eat or drink
Talk with your health care professional or health care team about when you should eat or drink. The best time to have meals and snacks may depend on
- what medicines you take for diabetes
- what your level of physical activity or your work schedule is
- whether you have other health conditions or diseases
Ask your health care team if you should eat before, during, or after physical activity. Some diabetes medicines, such as sulfonylureas or insulin, may make your blood glucose level drop too low during exercise or if you skip or delay a meal.
Plan how much to eat or drink
You may worry that having diabetes means giving up foods and drinks you enjoy. The good news is you can still have your favorite foods and drinks, but you might need to have them in smaller portions or enjoy them less often.
For people who have diabetes, carb counting and the plate method are two common ways to plan how much to eat or drink. Talk with your health care professional or health care team to find a method that works for you.
Carb counting
Carbohydrate counting , or carb counting, means planning and keeping track of the amount of carbs you eat and drink in each meal or snack. Not all people with diabetes need to count carbs. However, if you take insulin, counting carbs can help you know how much insulin to take.
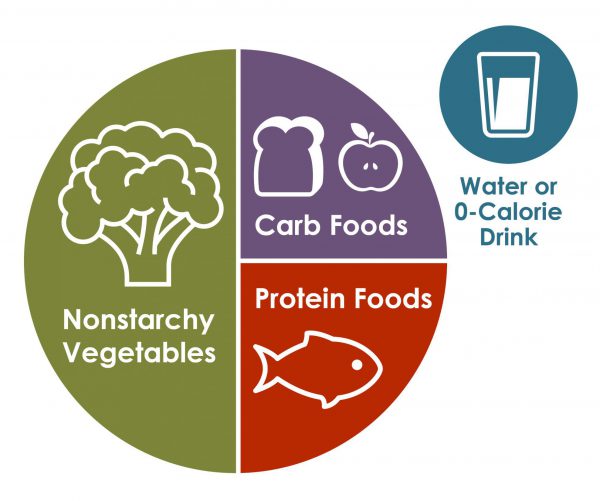
Plate method
The plate method helps you control portion sizes without counting and measuring. This method divides a 9-inch plate into the following three sections to help you choose the types and amounts of foods to eat for each meal.
- Nonstarchy vegetables—such as leafy greens, peppers, carrots, or green beans—should make up half of your plate.
- Carb foods that are high in fiber—such as brown rice, whole grains, beans, or fruits—should make up one-quarter of your plate.
- Protein foods—such as lean meats, fish, dairy, or tofu or other soy products—should make up one quarter of your plate.
If you are not taking insulin, you may not need to count carbs when using the plate method.
Work with your health care team to create a meal plan that works for you. You may want to have a diabetes educator or a registered dietitian on your team. A registered dietitian can provide medical nutrition therapy , which includes counseling to help you create and follow a meal plan. Your health care team may be able to recommend other resources, such as a healthy lifestyle coach, to help you with making changes. Ask your health care team or your insurance company if your benefits include medical nutrition therapy or other diabetes care resources.
Talk with your health care professional before taking dietary supplements
There is no clear proof that specific foods, herbs, spices, or dietary supplements —such as vitamins or minerals—can help manage diabetes. Your health care professional may ask you to take vitamins or minerals if you can’t get enough from foods. Talk with your health care professional before you take any supplements, because some may cause side effects or affect how well your diabetes medicines work.
Research shows that regular physical activity helps people manage their diabetes and stay healthy. Benefits of physical activity may include
- lower blood glucose, blood pressure, and cholesterol levels
- better heart health
- healthier weight
- better mood and sleep
- better balance and memory
Talk with your health care professional before starting a new physical activity or changing how much physical activity you do. They may suggest types of activities based on your ability, schedule, meal plan, interests, and diabetes medicines. Your health care professional may also tell you the best times of day to be active or what to do if your blood glucose level goes out of the range recommended for you.

Do different types of physical activity
People with diabetes can be active, even if they take insulin or use technology such as insulin pumps .
Try to do different kinds of activities . While being more active may have more health benefits, any physical activity is better than none. Start slowly with activities you enjoy. You may be able to change your level of effort and try other activities over time. Having a friend or family member join you may help you stick to your routine.
The physical activities you do may need to be different if you are age 65 or older , are pregnant , or have a disability or health condition . Physical activities may also need to be different for children and teens . Ask your health care professional or health care team about activities that are safe for you.
Aerobic activities
Aerobic activities make you breathe harder and make your heart beat faster. You can try walking, dancing, wheelchair rolling, or swimming. Most adults should try to get at least 150 minutes of moderate-intensity physical activity each week. Aim to do 30 minutes a day on most days of the week. You don’t have to do all 30 minutes at one time. You can break up physical activity into small amounts during your day and still get the benefit. 1
Strength training or resistance training
Strength training or resistance training may make your muscles and bones stronger. You can try lifting weights or doing other exercises such as wall pushups or arm raises. Try to do this kind of training two times a week. 1
Balance and stretching activities
Balance and stretching activities may help you move better and have stronger muscles and bones. You may want to try standing on one leg or stretching your legs when sitting on the floor. Try to do these kinds of activities two or three times a week. 1
Some activities that need balance may be unsafe for people with nerve damage or vision problems caused by diabetes. Ask your health care professional or health care team about activities that are safe for you.

Stay safe during physical activity
Staying safe during physical activity is important. Here are some tips to keep in mind.
Drink liquids
Drinking liquids helps prevent dehydration , or the loss of too much water in your body. Drinking water is a way to stay hydrated. Sports drinks often have a lot of sugar and calories , and you don’t need them for most moderate physical activities.
Avoid low blood glucose
Check your blood glucose level before, during, and right after physical activity. Physical activity often lowers the level of glucose in your blood. Low blood glucose levels may last for hours or days after physical activity. You are most likely to have low blood glucose if you take insulin or some other diabetes medicines, such as sulfonylureas.
Ask your health care professional if you should take less insulin or eat carbs before, during, or after physical activity. Low blood glucose can be a serious medical emergency that must be treated right away. Take steps to protect yourself. You can learn how to treat low blood glucose , let other people know what to do if you need help, and use a medical alert bracelet.
Avoid high blood glucose and ketoacidosis
Taking less insulin before physical activity may help prevent low blood glucose, but it may also make you more likely to have high blood glucose. If your body does not have enough insulin, it can’t use glucose as a source of energy and will use fat instead. When your body uses fat for energy, your body makes chemicals called ketones .
High levels of ketones in your blood can lead to a condition called diabetic ketoacidosis (DKA) . DKA is a medical emergency that should be treated right away. DKA is most common in people with type 1 diabetes . Occasionally, DKA may affect people with type 2 diabetes who have lost their ability to produce insulin. Ask your health care professional how much insulin you should take before physical activity, whether you need to test your urine for ketones, and what level of ketones is dangerous for you.
Take care of your feet
People with diabetes may have problems with their feet because high blood glucose levels can damage blood vessels and nerves. To help prevent foot problems, wear comfortable and supportive shoes and take care of your feet before, during, and after physical activity.

If you have diabetes, managing your weight may bring you several health benefits. Ask your health care professional or health care team if you are at a healthy weight or if you should try to lose weight.
If you are an adult with overweight or obesity, work with your health care team to create a weight-loss plan. Losing 5% to 7% of your current weight may help you prevent or improve some health problems and manage your blood glucose, cholesterol, and blood pressure levels. 2 If you are worried about your child’s weight and they have diabetes, talk with their health care professional before your child starts a new weight-loss plan.
You may be able to reach and maintain a healthy weight by
- following a healthy meal plan
- consuming fewer calories
- being physically active
- getting 7 to 8 hours of sleep each night 3
If you have type 2 diabetes, your health care professional may recommend diabetes medicines that may help you lose weight.
Online tools such as the Body Weight Planner may help you create eating and physical activity plans. You may want to talk with your health care professional about other options for managing your weight, including joining a weight-loss program that can provide helpful information, support, and behavioral or lifestyle counseling. These options may have a cost, so make sure to check the details of the programs.
Your health care professional may recommend weight-loss surgery if you aren’t able to reach a healthy weight with meal planning, physical activity, and taking diabetes medicines that help with weight loss.
If you are pregnant , trying to lose weight may not be healthy. However, you should ask your health care professional whether it makes sense to monitor or limit your weight gain during pregnancy.
Both diabetes and smoking —including using tobacco products and e-cigarettes—cause your blood vessels to narrow. Both diabetes and smoking increase your risk of having a heart attack or stroke , nerve damage , kidney disease , eye disease , or amputation . Secondhand smoke can also affect the health of your family or others who live with you.
If you smoke or use other tobacco products, stop. Ask for help . You don’t have to do it alone.
Feeling stressed, sad, or angry can be common for people with diabetes. Managing diabetes or learning to cope with new information about your health can be hard. People with chronic illnesses such as diabetes may develop anxiety or other mental health conditions .
Learn healthy ways to lower your stress , and ask for help from your health care team or a mental health professional. While it may be uncomfortable to talk about your feelings, finding a health care professional whom you trust and want to talk with may help you
- lower your feelings of stress, depression, or anxiety
- manage problems sleeping or remembering things
- see how diabetes affects your family, school, work, or financial situation
Ask your health care team for mental health resources for people with diabetes.
Sleeping too much or too little may raise your blood glucose levels. Your sleep habits may also affect your mental health and vice versa. People with diabetes and overweight or obesity can also have other health conditions that affect sleep, such as sleep apnea , which can raise your blood pressure and risk of heart disease.

NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for healthy living with diabetes?
Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of healthy living for people with diabetes, such as
- how changing when you eat may affect body weight and metabolism
- how less access to healthy foods may affect diabetes management, other health problems, and risk of dying
- whether low-carbohydrate meal plans can help lower blood glucose levels
- which diabetes medicines are more likely to help people lose weight
Find out if clinical trials are right for you .
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for healthy living with diabetes are looking for participants?
You can view a filtered list of clinical studies on healthy living with diabetes that are federally funded, open, and recruiting at www.ClinicalTrials.gov . You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe for you. Always talk with your primary health care professional before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank: Elizabeth M. Venditti, Ph.D., University of Pittsburgh School of Medicine.

IMAGES
VIDEO
COMMENTS
Registered dietitians (RDs) who have earned the Board Certified-Advanced Diabetes Manager (BC-ADM) credential hold a master's or doctorate degree in a clinically relevant area and have at least 500 hours of recent experience helping with the clinical management of people with diabetes.1 They work in both inpatient and outpatient settings, including diabetes or endocrine-based specialty ...
PRESENTATION OF CASE. Dr. Max C. Petersen (Medicine): A 34-year-old woman was evaluated in the diabetes clinic of this hospital for hyperglycemia. Eleven years before this presentation, the blood glucose level was 126 mg per deciliter (7.0 mmol per liter) on routine laboratory evaluation, which was performed as part of an annual well visit.
CASE PRESENTATION. A previously healthy 35‐month‐old girl was brought to the emergency room of the Namazi hospital, Shiraz, Iran, due to reduced level of consciousness. ... First presentation of diabetes mellitus type 1 with severe hyperosmolar hyperglycemic state in a 35‐month‐old girl. Clin Case Rep. 2021; 9:e04984. 10.1002/ccr3.4984 ...
A 59-year-old woman with type 1 diabetes and a 2-year history of cognitive decline presented with obtundation. There was diffuse, symmetric hypointensity in the brain on T2-weighted images and abno...
Type 1 Diabetes Mellitus Clinical Presentation. Updated: Dec 13, 2023 Author: Romesh Khardori, MD, PhD, FACP; ... In either case, recovery to baseline visual acuity can take up to a month, and some patients are almost completely unable to read small print or do close work during this period. ... Noor N, Gallagher MP, Alonso GT. Type 1 Diabetes ...
Describe the physiologic consequences of diabetes mellitus. Outline the importance of maintaining glycemic control in reducing the risk of diabetic complications. Detail specific clinical applications of insulin therapy to achieve both basal and meal-related glycemic control. Manage a patient's glycemic status by continuously refining the ...
Type 1 diabetes mellitus (T1D) is an autoimmune disease that leads to the destruction of insulin-producing pancreatic beta cells. There is heterogeneity in the metabolic, genetic, and immunogenetic characteristics of T1D and age-related differences, requiring a personalized approach for each individual. Loss of insulin secretion can occur quickly or gradually.
Type 1 diabetes mellitus is a chronic metabolic disease resulting from autoimmune destruction of pancreatic beta cells. More than half the cases of type 1 diabetes are diagnosed in adulthood; 62% ...
Pathophysiology and Clinical Presentation. Pathophysiology: Type 1 Diabetes Mellitus is a syndrome characterized by hyperglycemia and insulin deficiency resulting from the loss of beta cells in pancreatic islets (Mapes & Faulds, 2014). Nonimmune (type 1B diabetes), occurs secondary to other diseases and is much less common than autoimmune (type ...
Rationale: Fulminant type 1 diabetes mellitus (FT1DM) is a new subtype of type 1 diabetes mellitus that was first proposed by the Japanese scholar Imagawa in 2000. In the 2 patient cases described in this study, gastrointestinal symptoms were the first symptoms reported, and the initial blood glucose levels were very high.
LADA is a form of autoimmune type 1 diabetes in which the immune system gradually attacks the insulin-producing beta cells of the pancreas, sometimes resulting in a temporary remission from the need for insulin. , , The gradual attack on the beta cells leads to a slower decline in insulin production compared with the more typical presentation ...
A case report: First presentation of diabetes mellitus type 1 with severe hyperosmolar hyperglycemic state in a 35-month-old girl Clin Case Rep. 2021 Nov 6;9(11):e04984. doi: 10.1002/ccr3.4984. ... Clinical Case Reports published by John Wiley & Sons Ltd. Publication types
Patient Presentation and History. Chief Complaint: the patient's wife is bringing the patient in after a fall at their home. Presentation: J.S. a 50-year-old African American male who presents with his wife after he fell at home. After the fall, he told his wife "I will be fine, I think my vision just needs checked.".
American Diabetes Association (ADA) guidelines Oral Glucose Tolerance Test (OGTT) 1.75 g/kg (max 75 g) of glucola after overnight fast. Venous blood glucose at zero (0) and two (2) hours Normal results for OGTT. Fasting blood glucose <100 mg/dl. Two hour post challenge <140 mg/dl Abnormal OGTT.
Our case is an example of a patient whose type 1 diabetes presented atypically with characteristics often associated with type 2 diabetes. Patient presentations such as this are uncommon, with our patient having presented with the "textbook" characteristics of type 2 diabetes. When first diagnosed with diabetes mellitus type 2, the patient ...
Type 1 diabetes, once known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition. In this condition, the pancreas makes little or no insulin. Insulin is a hormone the body uses to allow sugar (glucose) to enter cells to produce energy. Different factors, such as genetics and some viruses, may cause type 1 diabetes.
If a diagnosis is delayed, untreated Type 1 diabetes can be life-threatening due to a complication called diabetes-related ketoacidosis (DKA). Seek emergency medical care if you or your child are experiencing any combination of the following symptoms: Fruity-smelling breath. Nausea and vomiting.
Objective: To evaluate primary care presentations during the prodrome (12 months prior to onset type-1 diabetes (T1D), with or without diabetic ketoacidosis [DKA]), to identify opportunities for earlier diagnosis. Methods: This was a case-control study, linking 16 years of data from children (≤15 years) registered at diagnosis of T1D, and routinely collected primary care records in Wales ...
Throughout our clinical experiences, previous careers, and personal lives, diabetes has been prevalent. As practitioners, we will continue to see this condition often and have to recognize/treat it in our patients. In light of this, we wanted to have a good understanding of Type 1 diabetes, its presentation, and its treatment.
Nevertheless, it can present in younger adults and teenagers as the first presentation of diabetes mellitus type 2 (T2DM). 1 HHS is diagnosed by the following criteria: plasma glucose more than 600 mg/dl, venous pH > 7.25, serum bicarbonate >15 mmol/L, small amount of ketonuria or its absence, effective serum osmolality >320 mOsm/kg, and ...
This presentation is a general summary that explains certain aspects of the Medicare Program, but is not a legal document. ... - Case report/case series, cross-sectional, case-control ... Level 2 hypoglycemia more common in type 1 than in type 2 diabetes. Time in range. more common for CLS than for pump or CGM ;
Apr 3, 2017 •. 321 likes • 227,610 views. education4227. Diabetes mellitus. Health & Medicine. 1 of 72. Case study on Diabetes Mellitus - Download as a PDF or view online for free.
Healthy living is a way to manage diabetes. To have a healthy lifestyle, take steps now to plan healthy meals and snacks, do physical activities, get enough sleep, and quit smoking or using tobacco products. Healthy living may help keep your body's blood pressure, cholesterol, and blood glucose level, also called blood sugar level, in the ...