Screening for cervical cancer: a systematic review and meta-analysis
Affiliation.
- 1 McMaster Evidence Review and Synthesis Centre-MERSC, 1280 Main Street West, DTC-322, Hamilton, ON L8S 4K1, Canada. [email protected]
- PMID: 23706117
- PMCID: PMC3681632
- DOI: 10.1186/2046-4053-2-35
Background: The systematic review on which this paper is based provided evidence for the Canadian Task Force on Preventive Health Care to update their guideline regarding screening for cervical cancer. In this article we highlight three questions covered in the full review that pertain to the effectiveness of screening for reducing cervical cancer mortality and incidence as well as optimal timing and frequency of screening.
Methods: We searched MEDLINE, Embase and Cochrane Central from 1995 to 2012 for relevant randomized controlled trials and observational studies with comparison groups. Eligible studies included women aged 15 to 70 years who were screened using conventional cytology, liquid-based cytology or human papillomavirus DNA tests. Relevance screening, data extraction, risk of bias analyses and quality assessments were performed in duplicate. We conducted a meta-analysis using a random-effects model on the one body of evidence that could be pooled.
Results: From the 15,145 screened citations, 27 papers (24 studies) were included; five older studies located in a United States Preventive Services Task Force review were also included. A randomized controlled trial in India showed even a single lifetime screening test significantly decreased the risk of mortality from and incidence of advanced cervical cancer compared to no screening (mortality: risk ratio 0.65, 95% confidence interval 0.47, 0.90; incidence: relative risk 0.56, 95% confidence interval 0.42, 0.75). Cytology screening was shown to be beneficial in a cohort study that found testing significantly reduced the risk of being diagnosed with invasive cervical cancer compared to no screening (risk ratio 0.38; 95% confidence interval 0.23, 0.63). Pooled evidence from a dozen case-control studies also indicated a significant protective effect of cytology screening (odds ratio 0.35; 95% confidence interval 0.30, 0.41). This review found no conclusive evidence for establishing optimal ages to start and stop cervical screening, or to determine how often to screen; however the available data suggests substantial protective effects for screening women 30 years and older and for intervals of up to five years.
Conclusions: The available evidence supports the conclusion that cervical screening does offer protective benefits and is associated with a reduction in the incidence of invasive cervical cancer and cervical cancer mortality.

Publication types
- Meta-Analysis
- Research Support, Non-U.S. Gov't
- Systematic Review
- Mass Screening*
- Uterine Cervical Neoplasms / diagnosis*
- Uterine Cervical Neoplasms / mortality
- Uterine Cervical Neoplasms / prevention & control
- Uterine Cervical Neoplasms / virology
- Vaginal Smears*
Grants and funding
- Canadian Institutes of Health Research/Canada
- Open access
- Published: 20 February 2024
Barriers to cervical cancer screening in Africa: a systematic review
- Fennie Mantula 1 , 3 ,
- Yoesrie Toefy 2 &
- Vikash Sewram 1 , 2
BMC Public Health volume 24 , Article number: 525 ( 2024 ) Cite this article
1062 Accesses
1 Citations
7 Altmetric
Metrics details
Introduction
Africa has one of the highest burdens of cervical cancer in the world. The unacceptably high incidence and mortality rates could be reduced through implementing a comprehensive approach to its prevention and control that includes screening, which however, is low in most low-and-middle-income countries. Hence, this systematic review aims at exploring factors that prevent women from utilising cervical cancer screening services in the region.
A mixed method systematic review was conducted. A search was performed on PubMed (Medline), EMBASE, CINAHL (EBSCOHOST) and Scopus databases for articles published until May 2019 without time, language or study design limits. Two reviewers critically appraised the included studies independently using the standard quality assessment criteria for evaluating primary research papers. Results of the quantitative and mixed methods studies were transformed into qualitative data and synthesised using thematic analysis.
From a potential 2 365 studies, 24 from 11 countries met the eligibility criteria and were selected; eight qualitative, 13 quantitative, and three that used the mixed-method approach. The primary barriers were identified as poor access to screening services, lack of awareness and knowledge on cervical cancer and screening, and socio-cultural influences. Service providers perceived lack of skills, screening equipment and supplies, and staff shortages as the major barriers to the provision of screening services.
Barriers to cervical cancer screening in Africa are multifaceted and require a holistic approach that will address them concurrently at the health system, individual, interpersonal, community and structural levels. Political will complimented by stakeholder involvement is required in the development and implementation of strategies that will ensure acceptability, availability, accessibility, and affordability of screening to minimise barriers in accessing the service.
Peer Review reports
Cervical cancer is the fourth most common cancer among women worldwide with an estimated 604,127 new cases and 341,831 deaths reported in 2020 [ 1 ], up from 528,000 new cases and 266,000 deaths reported in 2012 [ 2 ]. The bulk of the global burden rests with Africa, Latin America, the Caribbean and Asia where approximately 90% of deaths occur [ 3 ]. With an estimated population of 372.2 million women aged 15 years and older who are at risk of developing cervical cancer in Africa, 119, 284 women are diagnosed with cervical cancer while 81,687 die from the disease every year [ 4 ]. Compared to other regions in the world, Africa has higher cervical cancer incidence and mortality rates [ 1 , 3 , 5 ]. Cervical cancer screening can reduce the incidence of the disease by 70–80% if targeted appropriately [ 6 , 7 ]. However, in many parts of Africa, the disease is often not identified until it reaches advanced stages that are associated with poor outcomes [ 8 ]. This has been attributed to lack of comprehensive cervical cancer screening programmes in most countries [ 5 ]. Cervical cancer is the most preventable cancer due to its slow progression and early identifiable precancerous lesions which can be treated before they progress to cancer [ 9 ] hence, women need not die from cervical cancer.
Primary studies have been conducted over the past decades to identify barriers to the uptake of cervical cancer screening in various African countries. Although limited, systematic reviews have also been done to look into challenges which women encounter in accessing cervical cancer screening services in Sub-Saharan Africa [ 10 , 11 ]. Despite the recommendations that have been made for overcoming the existing barriers, evidence suggests that cervical cancer incidence rates continue to increase in Africa while declining in many developed countries [ 1 ]. A richer understanding of the reasons for the underutilisation of cervical cancer screening programmes in Africa requires further exploration. This review therefore aimed at identifying the unique contextual circumstances that prevent women from accessing cervical cancer screening in many parts of Africa. Guided by the Socio-ecological framework adopted from Kaufman and colleagues [ 12 ], our systematic review extends the knowledge already available from earlier conducted studies. Findings should guide restructuring of cervical cancer screening policies and guidelines for implementation of proactive context specific interventions that should address the structural, health system, societal, socio-economic and cultural factors at a broader level to overcome screening barriers. This could improve the uptake of screening and subsequently reduce the high cervical cancer morbidity and mortality rates in Africa. Gaps for future research will also be identified.
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines [ 13 ].
Search strategy
We subjectively and iteratively developed a comprehensive set of search terms. In the first instance, we checked PubMed (Medline) to identify controlled vocabulary Medical Subject Headings (MeSH) terms related to cervical cancer, and additionally identified key text words based on our knowledge of the field. This yielded three key concepts; cervical cancer, screening (irrespective of screening method), and Africa. The term ‘barrier’ was not used because the concept can be described in many different ways, and we did not want to risk missing some relevant papers. Medline search terms for other electronic databases were modified to conform to their search functions. PubMed (Medline), Embase (OVID), CINAHL (EBSCOHOST) and Scopus electronic bibliographic databases were searched for articles published until May 2019 without language and study design limits. The "related citations" search key in PubMed was further used to identify similar papers. Reference lists of potentially relevant articles were checked manually for additional citations. A detailed search strategy with terminology specific to each database is included (Supplementary File 1 ).
Study selection
This systematic review included studies on individual, interpersonal, community, health system and structural factors that prevented women from cervical cancer screening attendance in most African countries. The selection criteria were based on original quantitative and qualitative studies that reported barriers from the perspectives of women and health providers. Studies on women with a confirmed cervical cancer diagnosis were not included in the systematic review. Grey literature and conference abstracts without full articles were also excluded. Although these could have been useful sources containing relatively new information on the research area, it is generally premised that non-peer-reviewed articles are less scientifically rigorous than those that are peer reviewed and published [ 14 ].
Our systematic review is grounded on the socio-ecological framework by Kaufman and colleagues which describes the interplay between multiple levels of influence on individual behaviour for the promotion of health [ 12 ]. The model suggests that a health outcome is determined by individual, interpersonal, institutional, community and public policy factors [ 15 ]. In this study “Barrier” refers to any factor that prevents women from accessing cervical cancer screening from any level of the socio-ecological framework and classified into five areas as follows:
Individual level barriers : These are factors at the micro-level that include personal perceptions, knowledge, beliefs and emotions.
Interpersonal barriers : These arise from influences from spouse, family and other social networks.
Community level barriers : These are a result of influences at higher levels which include traditional and cultural norms, religious beliefs and stigma.
Health system related barriers : These are factors within the health system that relate to resources and service delivery.
Structural barriers : These are factors related to policy issues and other macro-contextual factors that affect a woman’s health seeking behaviours directly.
Mendeley reference manager was used to save and view titles and abstracts of all articles retrieved from the electronic databases, and to detect duplicates. Two independent reviewers (FM and VS) screened the 2 365 titles and abstracts of studies obtained through database searches. Two additional articles were identified from references after reading the full text articles ( n = 2 367). Screening of articles excluded duplicates ( n = 65), studies not relevant to the title ( n = 2 248), and abstracts of poster and conference presentations whose full articles were not obtained ( n = 13). The remaining 41 articles were reviewed in full text with 17 studies further eliminated for not meeting the inclusion criteria. The screening process resulted in the selection of 24 articles which met the eligibility criteria. Disagreements on inclusion of certain articles were resolved through discussion to reach a consensus [ 16 ]. The selection process is shown in Fig. 1 .
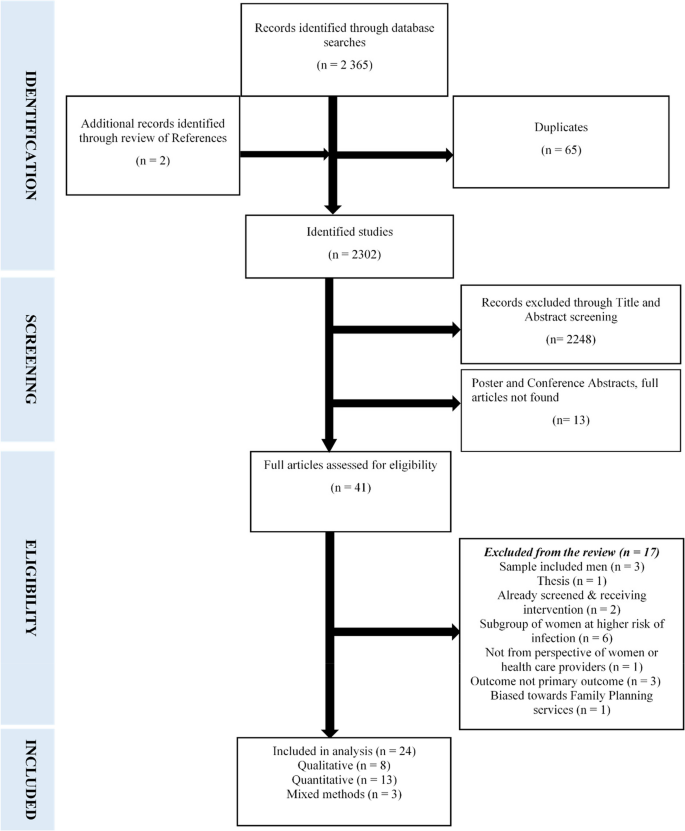
Prisma flow diagram of included studies
Assessment of methodological quality
The quality of each study was evaluated by two independent reviewers (FM and VS) using the standard quality assessment criteria for evaluating primary research papers adapted from Kmet and colleagues [ 17 ]. A checklist specific to each research method required the reviewer to select either; “yes” or “no” to questions focusing on the methodological aspects of each article. This tool was appropriate for assessing the quality of the overall body of evidence given in the heterogeneous literature and helped to gauge the quality of each individual study against set standards. Qualitative studies were evaluated using the following criteria: question or objective clearly described, study design evident and appropriate, context for the study clear, connection to a theoretical framework or wider body of knowledge, sampling strategy described, relevant and justified, data collection methods clearly described and systematic, data analysis clearly described and systematic, and conclusion supported by results [ 17 ]. Quantitative studies were assessed for the following aspects: question or objective sufficiently described, study design evident and appropriate, method of subject selection described and appropriate, subject characteristics sufficiently described, sample size appropriate, analytic methods described, justified and appropriate, results reported in sufficient detail, and conclusions supported by the results [ 17 ]. The quality of studies which used the mixed methods approach was rated under the dominant method that was discussed first in that particular study.
To further determine the overall risk of bias and the quality of evidence, each reviewed article was given a quality of low, medium or high to inform the decision making. Each quality component was rated 0 to 2 based on the reviewer’s subjective assessment, with a possible least score of 0, and a maximum score of 16. A sum score of the quality components gave the overall quality rating of each article. A score of 0–8 was rated as low, 9–12 as medium and 13–16 as high. For a study to be included, it had to attain a minimum rating of medium. All the included studies fulfilled this requirement. The quality assessment for the qualitative studies is presented in Table 1 .
Table 2 presents the quality assessment for the quantitative studies.
Data extraction and synthesis
A data extraction sheet was developed using the following predetermined data fields: first author, country and year of publication, title, research and data collection methods, sampling technique and sample size, and barriers identified for cervical cancer screening. One reviewer extracted the data (FM) while the second (VS) cross checked the extracted data for accuracy. Informed by the variation in the research methodologies between included studies and the multifaceted dimensions of screening barriers given, results of the quantitative and mixed methods studies were transformed into qualitative data and synthesised using thematic analysis. [ 16 ]. Data were summarised in descriptive form. A profile of all the studies included in the review highlighting the major screening barriers identified is given in Table 3 .
Study characteristics
The key characteristics and findings of the 24 included articles are summarised in Table 3 . The studies were published between 2005 and 2019. Eight were conducted in Nigeria, three in Kenya, two each in Uganda, Ethiopia, Malawi and Zimbabwe and one each in South Africa, Burkina Faso, Tanzania, Ghana and Botswana. Eight (33.3%) studies were qualitative, thirteen (54.2%) quantitative and three (12.5%) used the mixed method approach. Sixteen (66.7%) studies evaluated barriers to cervical cancer screening from the perspective of women who are the recipients of screening and six (25%) from the perspective of health service providers. Two (8.3%) evaluated the barriers from the perspective of both women and health service providers.
Qualitative studies
Purposive sampling was used in the majority of qualitative studies (6/8, 75%). For data collection, two studies each used In-depth interviews (25%) and FGDs (25%) respectively. The remaining four each used KIIs (12.5%), interviews (12.5%), a combination of FGDs and KIIs (12.5%) and a combination of interviews and field notes (12.5) respectively.
Quantitative studies
Of the 13 quantitative studies, 5 (38.5%) used convenience sampling. Multi-stage random sampling was used in 4 (30.8%), purposive sampling in 3 (23%) and systematic sampling in 1 (7.7%) study. Interviewer administered questionnaires were used for data collection in 8 (61.5%) studies and self-administered questionnaires in four (30.8%). One (7.7%) study used both self and interviewer-administered questionnaires depending on whether the participant could read and write. The sample size of the studies ranged from 100 to 3 712 participants.
Mixed methods studies
All three studies which employed both the qualitative and quantitative approaches used the interviewer-administered questionnaire for the collection of quantitative data. For the qualitative component, in-depth interviews and FGDs were each used in two studies, respectively. The third study used document analysis, FGDs, in-depth interviews and narratives from two women with a diagnosis of cervical cancer and one who had hysterectomy done. Findings from the narratives were not used in this systematic review as they were obtained from participants who did not meet the eligibility criteria for inclusion.
Barriers to cervical cancer screening
Overall, 28 screening barriers were identified from the perspectives of service recipients, and 10 from the perspectives of service providers. Mostly cited by women were; inaccessibility of screening services, lack of awareness and knowledge on cervical cancer and screening benefits, and financial and socio-cultural constraints. Service providers perceived lack of training necessary to conduct screening, lack of equipment and supplies, staff shortages and gender and age of the health practitioner as major barriers to screening provision. Thematic analysis based on the socio-ecological framework which grounded the review yielded five a priori themes namely: health-system related, individual level, interpersonal, community related, and structural barriers. All the themes were not country-centric and could be transferrable between geographical settings in the region.
Health system related barriers to cervical cancer screening
Inaccessibility of screening services.
Lack of access to screening services was identified as the key barrier to screening. Women maintained that screening services were not available at their local health facilities [ 23 , 26 , 27 , 30 , 32 , 35 , 38 , 41 ]. The long distances they had to travel to reach the nearest screening sites usually located at tertiary levels of health care, were a deterrent to screening [ 18 , 21 , 26 , 29 , 30 , 35 , 37 , 38 ]. This also has financial implications in terms of transport costs and lost time. Screening facilities’ operational times not amenable with women's schedules also posed a challenge and limited their chances of screening [ 38 ]. Those who had physical access to screening facilities found it difficult to navigate their way to the right place as information and directions were in most cases not readily available [ 25 ].
Service providers concurred that health facilities that provide screening were few [ 22 ] and far away from communities [ 23 ]. This resulted in women having to travel long distances to get screened, while not all facilities offered the service on a daily basis [ 20 ]. Transport to get to screening centers was also a challenge [ 22 ]. Access to screening is thus affected by unavailability of local screening facilities, transport constraints and screening operating times which are not user-sensitive.
Limited funding for cervical cancer programmes
Lack of a dedicated budget for cervical cancer programmes was highlighted as a barrier as it resulted in insufficient resources required to provide screening [ 40 ]. This included space for the provision of efficient screening services, [ 20 , 36 ] and technical support to monitor the programme and provide guidance to service providers [ 20 , 40 ]. Follow-up of patients who required further management also posed a challenge for health personnel, thus defeating the whole purpose of screening [ 26 , 31 ].
Lack of skilled providers
Service providers maintained that shortage of personnel is a major hindrance to the uptake of screening considering that staff well equipped in the provision of the service is in short supply [ 20 , 23 , 36 , 40 ]. Consequently the available trained personnel are not able to meet the demand [ 20 , 26 , 36 ]. This is also attributable to the high staff turnover among the trained cadres, [ 40 ] and lack of training opportunities for the available nurses and doctors [ 31 ]. Furthermore, trained providers are assigned to areas not related to screening, thus negatively affecting the availability of screening services [ 20 , 40 ]. At some health facilities, the same personnel who provided screening were also responsible for rendering other maternal and child health services, which increases the workload and reduces their motivation [ 20 ]. Accordingly, the time within which screening sites are operational is limited due to the multiplicity of tasks skilled staff have to perform.
Lack of equipment and supplies
A general shortage of equipment and screening consumables was identified by service providers as a barrier to screening [ 20 , 23 , 30 , 31 , 36 , 40 ]. Facilities often run out of supplies and cryotherapy is sometimes not provided due to broken down equipment which cannot be repaired for lack of funds [ 20 ].
Negative attitudes of service providers
Four studies; three [ 23 , 27 , 38 ] from the perspective of women and one [ 40 ] from the perspective of service providers highlighted negative attitudes of health personnel as an important reason for women's failure to seek screening. Women report that health workers are uncooperative and hostile to them. Such inappropriate behaviour leaves them with no option but to consult traditional healers for health care [ 23 ]. When women request screening, health workers allege to be too busy, and if the service is provided, no explanation related to the procedure is given [ 27 ]. Consistent with this, service providers argue that due to poor motivation, they lack commitment to efficiently provide the service. Such behaviours deprive women access to the screening services which they require [ 40 ].
Individual level barriers to cervical cancer screening
Lack of access to screening information.
Women generally lack awareness of cervical cancer as a disease of public health concern [ 18 , 29 ]. Those who may have heard about the disease have no full knowledge of its risk factors, prevention, and signs and symptoms [ 23 , 25 , 26 , 27 , 32 , 33 , 35 , 41 ]. In concurrence, service providers attribute the low screening uptake to women's low levels of awareness about cervical cancer [ 20 , 22 , 40 ]. This consequently does not give women the motivation to seek screening. Moreover, women often have inadequate [ 36 ] and inaccurate [ 22 ] knowledge on cervical cancer and screening [ 23 , 24 , 25 , 29 , 32 , 33 , 37 ]. Regrettably, some women lack information on the existence of screening programmes even where such services are available locally [ 26 ], are not aware of the location of screening sites [ 18 , 23 , 28 , 29 , 30 , 33 , 35 , 41 ], the appropriate age for screening [ 38 , 41 ], and the need and benefits of screening [ 26 , 27 ]. This dearth of information is partly due to poor information dissemination by health workers as indicated by both service recipients [ 18 , 33 , 41 ] and service providers including private practitioners [ 19 ], and absence of relevant health educational programmes [ 35 ]. In addition, service providers have highlighted that health professionals especially at the lower levels of care lack adequate knowledge on cervical cancer and its prevention and control and are therefore not able to give women up to date screening related information [ 22 ].
Financial constraints
Lack of financial resources was reported as a common obstacle to participation in cervical cancer screening. The cost of the test was considered as expensive by some women [ 23 , 27 , 28 , 35 ] and service providers [ 19 , 22 , 31 ]. This is partly linked to the hidden costs associated with screening since the service is offered for free in most public health facilities. The indirect costs include high transport charges to screening sites [ 21 , 23 , 25 , 27 , 30 ], time lost on travel, [ 21 , 25 ] long waiting times before screening [ 25 , 30 , 36 ] which could have been used productively, and lack of money to pay for treatment should the screen test yield a positive result [ 22 ].
Attitude of indifference to screening
The perception that screening is unnecessary [ 28 ] and not important [ 18 ] was noted as an impediment to screening. Women see no benefit in early detection measures as they believe that one would not be cured anyway, and still die of cancer [ 27 ]. Women also suggested that they had never thought about screening [ 28 ] and therefore were not ready for the test [ 30 ], or had no interest in getting screened [ 32 ]. These negative attitudes could be emanating from their lack of symptoms [ 26 , 28 , 34 , 37 , 41 ] which instils a notion of good health and therefore finding no reason to get screened. Women also believed they were not at risk for cervical cancer [ 18 , 25 , 33 , 39 ], while some were not aware of their being at risk for the disease [ 29 ] and therefore felt no need for screening.
Fear of procedure and outcome
Fear of pain during the procedure was identified as a screening deterrent [ 23 , 24 , 35 , 38 ]. Women receive negative information from friends [ 27 ], or have themselves had bad screening experiences and therefore avoid repeat screens [ 23 ]. Service providers also reported that women are not comfortable with pelvic examinations and fear that insertion of the speculum causes pain, hence will not participate in screening [ 22 , 36 ]. For some women, fear of the possibility of receiving a positive result was a barrier [ 18 , 21 , 23 , 24 , 25 , 29 , 35 , 37 , 38 ]. Finding bliss in ignorance was associated with; fear of being left by spouse if known to have cervical cancer as that was thought to interfere with sexual relations [ 23 ], fatalistic view of cervical cancer, therefore finding it better not to know [ 18 , 21 , 24 , 29 , 37 ], fear of disclosure of results which may result in stigmatisation [ 24 ], fear of the side effects of treatment [ 35 ] and worry which may lead to an early death [ 38 ]. Women also expressed fear of contracting other diseases from the screening equipment and finding out their Human immunodeficiency virus (HIV) status if cervical cancer screening was linked to HIV screening [ 23 ].
Interpersonal barriers to cervical cancer screening
Lack of spousal support.
Spousal or male partner support was found to be an important factor in the practice of screening because of the patriarchal nature of the African society. Husbands were revealed to have an influence on the decision for screening [ 38 ]. Women require their husbands’ permission to get screened for financial and cultural reasons [ 24 ] and since some men do not understand the importance of screening [ 26 ], they refuse to give their consent [ 35 ]. Women get accused of being promiscuous if they express their wish to screen because of the association of cervical cancer with a sexually transmitted virus [ 27 ]. Men can thus be a hindrance to screening. Service providers confirmed men’s lack of emotional and financial support for screening [ 22 ] expressed by women [ 26 , 27 , 35 , 38 ]. Lack of male support for screening also creates barriers to treatment adherence if the woman has a positive result [ 20 ].
Misconceptions about cervical cancer
Negative connotations linked to cervical cancer and screening within women’s social circles has been identified as a big barrier to screening. The misconception that cervical cancer is associated with promiscuity deters women from screening as they do not want to be labelled as being promiscuous [ 38 ]. Additionally, women are misinformed and made to believe that use of the speculum during the test enlarges the vagina [ 20 ], that the uterus is pulled out for examination and reinserted after screening [ 20 , 25 ], and that they may not be able to have children after screening. Subsequently, they get discouraged from utilising the service. Women’s screening behaviour is thus often subject to the influence of family and friends.
Community-related barriers to cervical cancer screening
Family responsibilities.
Six studies revealed that women lacked time to attend screening due to family responsibilities. As household managers whom society expects to place the wellbeing of the family before their own, women have many competing priorities related to family survival which deprive them of time for screening [ 18 , 26 ]. They are too busy with household chores to go to health facilities for preventive health services [ 25 , 27 , 30 ] relative to curative care. Some have no household help and find it hard to leave their tasks unattended since the time it takes to complete the screening processes is long [ 27 , 38 ].
Socio-cultural and religious beliefs
It is very difficult to clearly distinguish between cultural and religious considerations as these two are intricately related. The same factors reported by some women as religious were reported as cultural by others. Consequently, socio-cultural and religious beliefs and gender and age of service provider cannot be discussed independently of each other.
Some women consider participation in cervical cancer screening as inappropriate and against their cultural and religious beliefs [ 35 ]. African women are generally conservative and suffer embarrassment at lying on their backs with their legs open [ 22 , 26 ] and exposing their private parts for examination [ 22 , 27 , 35 ], especially if it is a male providing the service [ 21 ]. Exposure of genitals is viewed as a violation of women’s privacy [ 37 ]. The cultural and religious norms which some women value discourage them from exposing their intimate body parts to other people other than their husbands, unless if there are compelling reasons [ 24 ]. Modesty, embarrassment and religious beliefs are thus significant barriers to the utilisation of screening services.
Gender and age of the service provider were seen to pose a cultural barrier to participation in cervical cancer screening programmes. Women feel ashamed, shy, embarrassed, anxious and uncomfortable if males provide the service [ 23 , 24 , 26 , 27 ]. Service providers echoed that gender of the provider interfered with screening programmes as women do not like their private parts exposed to male practitioners particularly if they have no gynaecological problems [ 19 , 20 , 22 , 36 ]. Furthermore, older women are not willing to be screened by younger male health workers who they consider as their sons [ 19 , 20 , 22 , 23 , 26 ]. This is attributed to cultural norms. The same sentiments in relation to gender and age of service provider are obtaining in the private sector [ 19 ].
Social stigma associated with cervical cancer and screening
One study revealed that women decline cervical cancer screening because of the stigma associated with having cervical cancer [ 21 ]. They avoid going to screening sites because people may think they have the disease and suffer societal rejection. Stigma related to misconceptions was again mentioned by service providers as one of the perceived patient factors that inhibit screening uptake [ 36 ].
Structural barriers
Over and above the health system, individual, interpersonal and community related barriers to screening, clear comprehensive cervical cancer management policies and guidelines to guide cervical cancer screening and systematic cervical cancer screening programmes are not readily available in the region [ 26 , 30 , 40 ]. Efforts to prevent cervical cancer are therefore haphazard, and this has a negative impact on screening [ 26 ]. Where available, the policies are weak and characterised by a lack of political will and backing by governments. Inadequate funding of the programme results in poor availability of all resources necessary for screening due to the low priority which cervical cancer screening is given within the health system [ 40 ].
Suggested strategies for addressing barriers to cervical cancer screening
Women and health service providers mutually suggest that; increasing access to cervical cancer screening within communities by addressing transport challenges [ 23 ], creating and raising awareness on screening through community mobilisation and sensitisation [ 20 , 23 , 26 ], assigning female staff to conduct screening [ 23 ], availing more skilled staff and supplies for the screening programme, and a collaborative approach at crafting policies that accord screening priority like other maternal and child health programmes [ 35 ], would improve the uptake of screening.
This systematic review synthesised findings of the key barriers to the uptake of cervical cancer screening from 24 studies conducted in 11 African countries. The barriers were presented from the viewpoint of service recipients and providers. Our analysis across the included studies indicate lack of information on the importance of screening and poor access to screening services as the most predominant barriers to cervical cancer screening in the region. Concordance of themes was demonstrated between qualitative and quantitative studies, and between women and service providers’ perspectives. Triangulation of findings was thus achieved [ 42 ].
Based on the findings of this review, factors that negatively impact cervical cancer screening in Africa are multidimensional and although common between countries, vary in magnitude from one setting to another. At the level of the health system, restricted access to screening in particular; lack of local health facilities that provide screening services, and prohibitive distances and cost to screening sites were shown to be the biggest challenges in the uptake of screening. The findings compare well with other studies conducted among indigenous populations worldwide [ 7 ], in Sub-Saharan Africa [ 10 ], in the Pacific [ 43 ] and in other middle and upper- middle income countries such as Turkey, Thailand, Jamaica and China which also report poor access to screening services due to various structural and health system related factors[ 44 ].
Most reviewed studies have advanced relatively similar recommendations for addressing the barriers to cervical cancer screening at different time periods yet, the uptake of screening has only slightly improved overtime. Our study attributes this to the fragmented tackling of the socio-ecological framework linked barriers independently of each other, and postulates that responding to challenges at only one level of the framework has the effect of increasing the barriers at a different ignored level. For example; increasing awareness and knowledge on screening among women has the likelihood of increasing the demand for the service. However, if screening facilities are not concurrently increased, the challenge will shift from the demand to the supply side. Our review further hypothesises that even if all other barriers could be addressed, screening incidence would still remain low if screening facilities are not universally rolled out to communities. Evidenced to this is the effective screening programmes in high-income countries that have resulted in low cervical cancer incidence [ 45 ]. Access to services is central to screening uptake in view of the fact that women cannot engage in cervical cancer screening if there are no services to deliver it [ 43 ]. This therefore requires the development of context specific innovative policies and strategies, or the modification of existing ones to make the service readily accessible to all women who need it.
One long term solution which has been recommended in previous studies but has not been universally applied is the inclusion of cervical cancer prevention and control into the nurses’ pre-service training curriculum [ 43 , 46 ]. Our study further recommends that the cervical cancer component be examinable both theoretically and practically to ensure nurses would have acquired the necessary skills upon completion of their training. This is because nurses constitute the most authoritative source of health information especially for women [ 47 ] and are available at all levels of health care. To address the associated financial constraints which have been raised as prohibitive to this recommendation, the training could make use of the already existing resources since all teaching hospitals are likely to have screening units. Screening coverage would consequently be ensured at all levels of health care given the availability of other necessary resources, which may however not be readily available in all settings in the short term. However, women would still benefit from receiving accurate information on cervical cancer prevention and control to enable them to seek screening services where available,
The World Health Organization has also provided guidelines on the attainment of universal screening coverage, its scalability and sustainability [ 48 ], which African countries need to modify and implement. Furthermore, the World Health Organization states that the success of the drive to eliminate cervical cancer depends on political will and country-led action investments [ 49 ]. This is particularly required in African countries for the economic support of cervical cancer screening programmes and development or more effective implementation of country-centric policies and guidelines for screening. Nevertheless, individual and interpersonal factors within the socio-ecological model still need to be addressed given that some low resource countries in Africa with a strong political will still report low screening rates [ 50 ]. Considering alternative screening delivery models like mobile clinics is another viable option that has proved to be effective in other low resource settings [ 46 ]. This should be strengthened or implemented in settings that have not introduced it.
Lack of awareness and knowledge about cervical cancer and screening was commonly reported in this review although not identified as the primary barrier to screening, contrary to findings from previously conducted reviews [ 9 , 10 , 43 , 44 , 51 , 52 ]. This variance could be a result of on-going awareness campaigns and improved education of women about the disease and its prevention, which could be an indication that knowledge about cervical cancer and screening is progressively improving. The limited knowledge that women have on cervical cancer and screening has been linked to failure by health professionals to educate their communities appropriately. A number of studies conducted in similar settings have reported similar findings [ 9 , 11 , 43 ]. Effective health education is likely to improve women’s knowledge about the disease and enhance the uptake of screening [ 15 , 33 ]. Facilitation of intrinsic motivation through establishing systems for continuing knowledge and skills training of health professionals in cervical cancer prevention could help in the scale up of screening coverage to address this gap. More opportunities for the education of communities including men need to be explored in a culturally competent manner using affordable and available resources. Community Health Workers for example, possess authority and influence and are respected in their communities. Such authoritative sources of cultural knowledge could be harnessed and trained to complement the efforts of health professionals in disseminating knowledge on cervical cancer screening. A clearer understanding and increased knowledge among women could dispel myths and misconceptions about cervical cancer and screening and could result in an increased demand for the service. For women to participate in screening, they need to have knowledge of the disease and how it is screened [ 43 ]. As stated by some women; “it is not possible to use what they don’t know about” [ 18 ].
Our review identified that at the interpersonal and community levels of the socio-ecological model, women are essentially constrained from screening by cultural and religious factors. This finding is consistent with other studies which confirm that women need to seek approval and funding from their spouses or partners to enable them to access cervical cancer screening [ 15 ]. Such approval is at times denied for varying reasons [ 11 , 44 , 52 , 53 ]. Moreover, women may also be discreet in discussing reproductive health issues with their spouses for cultural reasons [ 46 ], while husbands are not expected to be involved in talking about women’s health issues [ 11 , 54 ]. Male involvement in reproductive health services needs further support to enhance women's attendance for screening.
The provision of screening services by males has been seen to discourage women, particularly the older ones, from seeking screening. Findings of this review are congruent with evidence from other studies [ 15 , 53 , 55 , 56 ]. For some cultures, it is taboo foe females to expose their nudity to males other than their sexual partners and is contradictory to their and values [ 10 ]. On the contrary, some studies conducted among minority groups in Canada revealed that women felt uncomfortable discussing or undertaking the screening test irrespective of the sex of the service provider [ 9 ]. The differences in findings could be related to cultural beliefs.
However, despite the religious taboos and social stigmas associated with screening, women still respect health providers’ opinions and recommendations [ 9 ]. This reiterates the critical role health workers have in educating women on cervical cancer and screening at every interaction with women for enhanced utilisation of screening services. Evidently, there is a need to change some socio-cultural beliefs if uptake of screening is to increase. This however is a challenging task since women’s understanding of issues is grounded on religious and cultural traditions and makes promotion of screening difficult to address in isolation to those traditions [ 52 ]. Accordingly, a simple educational intervention is unlikely to achieve the desired result. Rather than targeting just the women with cervical cancer screening messages, educational interventions should target all levels of the socio-ecological framework and be extended to include families, communities and traditional/religious leaders who could serve as change agents in support of promotive and preventive health programmes that include cervical cancer screening.
Limitations
Although the search strategy was tailored for studies on barriers to cervical cancer screening conducted in Africa, this was not achievable as no articles were retrieved from North and Central African countries. Screening barriers unique to these countries were therefore not explored. Evidence suggests that cervical cancer is uncommon in Northern Africa [ 3 ] which could be the reason for lack of research in that area. Nevertheless, findings of this review exclude an important segment of the study population which could be having unique barriers to cervical cancer screening. In addition, grey literature which could have provided useful insights for the review was excluded. Despite these limitations, the overall findings were consistent across the studies and can be extrapolated to similar geographical settings in Africa.
Conclusions
In this systematic review, we thematically explored the factors that prevent women from seeking cervical cancer screening services in Africa. Barriers to screening were found to be multi-dimensional spanning all levels of the socio-ecological framework. Poor access to screening facilities, lack of comprehensive knowledge on cervical cancer and screening, and socio-cultural influences were found to be the key factors that contribute to the sub-optimal uptake of cervical cancer screening among women in African countries. From the view of health personnel, trained service providers were insufficient to meet the demand for screening. Similarly, screening equipment is not adequate for the delivery of a comprehensive service.
While women could have the essential knowledge on cervical cancer and get the motivation for screening, geographical, social and financial inaccessibility of the service could prevent them from screening. Conversely, women with full understanding of screening benefits and easy access to screening may still fail to utilise the service if they find it unacceptable due to intrapersonal and community influences related to religion and culture, and health system factors. Our study elucidates the criticality of tackling the barriers to screening at all levels of the socio-ecological model in a structured manner that would prevent increasing barriers at another level in the process.
Success at achieving a high uptake of screening should therefore focus on concurrently addressing all screening barriers at the individual, interpersonal, community, health systems and structural levels and apply the primary health care model which supports the availability, accessibility, acceptability and affordability of services with full community involvement. Application of this holistic approach could provide solutions that are responsive to communities and health services’ needs. There is also a need for dedicated cervical cancer programmes budgets to make available all the required resources for screening. Our review provides insights into the need for long-term strategies to reduce screening barriers at all levels of the socio-ecological model based on the needs of the community for achieving and sustaining high screening rates. Further research is required to investigate the feasibility and cost effectiveness of this multifaceted approach.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre L, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Article PubMed Google Scholar
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide : Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86.
Article CAS PubMed Google Scholar
Vaccarella S, Laversanne M, Ferlay J, Bray F. Cervical cancer in Africa, Latin America and the Caribbean and Asia: Regional inequalities and changing trends. Int J Cancer. 2017;141(10):1997–2001.
Bruni L, Albero G, Serrano B, Mena M, Go’mez D, Munoz J, Bosch FX, de Sanjose S. ICO/ IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Africa. Summary Report 17 June 2019. [cited 2020 Feb 13]. Available from: https://hpvcentre.net/statistics/reports/XFX.pdf .
Akinyemiju TF, Mcdonald JA, Lantz PM. Health care access dimensions and cervical cancer screening in South Africa : analysis of the world health survey. BMC Public Health. 2015;15:382.
Article PubMed PubMed Central Google Scholar
Victor Manuel VH. Screening and Prevention of Cervical Cancer in the World. Journal of Gynaecological Research and Obstetrics. 2017;3(3):86–92.
Article Google Scholar
Kolahdooz F, Jang SL, Corriveau A, Gotay C, Johnston N, Sharma S. Knowledge, attitudes, and behaviours towards cancer screening in indigenous populations : a systematic review. Lancet Oncology. 2014;15:e504–16.
World Health Organization. Cervical cancer common amongst African women. 2020. [cited 2021 Feb 15]. Available from: https://www.afro.who.int/news/cervical-cancer-common-amongst-african-women .
Ferdous M, Lee S, Goopy S, Yang H, Rumana N, Abedin T, et al. Barriers to cervical cancer screening faced by immigrant women in Canada: a systematic scoping review. BMC Women’s Health. 2018;18(1):165.
McFarland DM, Gueldner SM, Mogobe KD. Integrated Review of Barriers to Cervical Cancer Screening in Sub-Saharan Africa. J Nurs Scholarsh. 2016;48(5):490–8.
Lim JNW, Ojo AA. Barriers to utilisation of cervical cancer screening in Sub Sahara Africa: a systematic review. Eur J Cancer Care (Engl). 2017;26(1). https://doi.org/10.1111/ecc.12444 .
Kaufman MR, Cornish F, Zimmerman RS, Johnson BT. Health Behavior Change Models for HIV Prevention and AIDS Care : Practical Recommendations for a Multi-Level Approach. J Acquir Immune Defic Syndr. 2014;66:250–8.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. https://doi.org/10.1136/bmj.b2700 .
Scherer R, Saldanha I. How should systematic reviewers handle conference abstracts? A view from the trenches. Syst Rev. 2019;8(1):4–9.
Binka C, Nyarko SH, Awusabo-Asare K, Doku DT. Barriers to the Uptake of Cervical Cancer Screening and Treatment among Rural Women in Ghana. Biomed Res Int. 2019;2019:6320938. https://doi.org/10.1155/2019/6320938 .
Musa J, Achenbach CJ, O’Dwyer LC, Evans CT, McHugh M, Hou L, et al. Effect of cervical cancer education and provider recommendation for screening on screening rates : A systematic review and meta-analysis. PLoS OneS ONE. 2017;12(9):e0183924.
Kmet LM, Lee RC, Cook LS. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Edmonton: Alberta Heritage Foundation for Medical Research (AHFMR). AHFMR - HTA Initiative #13. 2004.
Ndikom CM, Ofi BA. Awareness, perception and factors affecting utilization of cervical cancer screening services among women in Ibadan, Nigeria: a qualitative study. Reprod health. 2012;9:11.
Mookeng MJ, Mavundla TR, McFarland DM. Barriers to cervical cancer screening within private medical practices in Soshanguve, South Africa. Africa Journal of Nursing & Midwifery. 2010;12(1):27–38.
Google Scholar
Munthali AC, Ngwira BM, Taulo F. Exploring barriers to the delivery of cervical cancer screening and early treatment services in Malawi : some views from service providers. Patient Prefer Adherence. 2015;9:501–8.
Oketch SY, Kwena Z, Choi Y, Adewumi K, Moghadassi M, Bukusi EA, et al. Perspectives of women participating in a cervical cancer screening campaign with community-based HPV self-sampling in rural western Kenya: a qualitative study. BMC Womens Health. 2019;19(1):75.
Mwaka AD, Wabinga HR, Mayanja-Kizza H. Mind the gaps: a qualitative study of perceptions of healthcare professionals on challenges and proposed remedies for cervical cancer help-seeking in post conflict northern Uganda. BMC Fam Pract. 2013;14:193.
Ndejjo R, Mukama T, Kiguli J, Musoke D. Knowledge, facilitators and barriers to cervical cancer screening among women in Uganda: A qualitative study. BMJ Open. 2017;7:e016282.
Modibbo FI, Dareng E, Bamisaye P, Jedy-Agba E, Adewole A, Oyeneyin L, et al. Qualitative study of barriers to cervical cancer screening among Nigerian women. BMJ Open. 2016;
Fort VK, Makin MS, Siegler AJ, Ault K, Rochat R. Barriers to cervical cancer screening in Mulanje, Malawi : a qualitative study. Patient Prefer Adherence. 2011;5:125–31.
Mangoma JF, Chirenje MZ, Chimbari MJ, Chandiwana SK. An assessment of rural women’s knowledge, constraints and perceptions on cervical cancer screening: the case of two districts in Zimbabwe. Afr J Reprod Health. 2006;10(1):91–103.
Ngugi CW, Boga H, Muigai AWT, Wanzala P, Mbithi JN. Factors Affecting Uptake of Cervical Cancer Early Detection Measures Among Women in Thika. Kenya Health Care for Women International. 2012;33(7):595–613.
Nwankwo KC, Aniebue UU, Aguwa EN, Anarado AN, Agunwah E. Knowledge attitudes and practices of cervical cancer screening among urban and rural Nigerian women : a call for education and mass screening. European Journal of Cancer CareJournal of Cancer Care. 2011;20:362–7.
Article CAS Google Scholar
Compaore S, Ouedraogo C, Koanda S, Haynatzki G, Chamberlain R, Soliman A. Barriers to Cervical Cancer Screening in Burkina Faso: Needs for Patient and Professional Education. J Cancer Educ. 2016;31(4):760–6.
Tarwireyi F. Perceptions and barriers to cervical cancer screening in a rural district of Mutoko, Mashonaland East Province. Zimbabwe Cent Afr J Med. 2005;51(11/12):120–2.
CAS PubMed Google Scholar
Kress CM, Sharling L, Owen-Smith AA, Desalegn D, Blumberg HM, Goedken J. Knowledge, attitudes, and practices regarding cervical cancer and screening among Ethiopian health care workers. Int J Womens Health. 2015;7:765–72.
PubMed PubMed Central Google Scholar
Abiodun OA, Fatungase OK, Olu-Abiodun OO, Idowu-Ajiboye BA, Awosile JO. An assessment of women’s awareness and knowledge about cervical cancer and screening and the barriers to cervical screening in Ogun State, Nigeria. Journal of Dental and Medical Sciences. 2013;10(3):52–8.
Okunowo A, Daramola E, Soibi-Harry A, Ezenwankwo F, Kuku J, Okunade K, et al. Women’s knowledge of cervical cancer and uptake of Pap smear testing and the factors influencing it in a Nigerian tertiary hospital. Journal of Cancer Research and Practice. 2018;5:105–11.
Perng P, Perng W, Ngoma T, Kahesa C, Mwaiselange J, Merajver SD, et al. Promoters of and barriers to cervical cancer screening in a rural setting in Tanzania. Int J Gynaecol Obstet. 2013;123(3):221–5.
Ebu NI, Mupepi SC, Siakwa MP, Sampselle CM. Knowledge, practice, and barriers toward cervical cancer screening in Elmina, Southern Ghana. International Journal of Women’s Health. 2015;7:31–9.
PubMed Google Scholar
Rosser JI, Hamisi S, Njoroge B, Huchko MJ. Barriers to Cervical Cancer Screening in Rural Kenya: Perspectives from a Provider Survey. J Community Health. 2015;40(4):756–61.
Chigbu CO, Aniebue U. Why Southeastern Nigerian Women Who Are Aware of Cervical Cancer Screening Do Not Go for Cervical Cancer Screening. Int J Gynecol Cancer. 2011;21(7):1282–6.
Titiloye MA, Womitenren YT, Arulogun OS. Barriers to utilization of cervical cancer screening services among women of reproductive age in Ondo, Southwest Nigeria. Afr J Biomed Res. 2017;20(3):229–35.
Ibekwe CM, Hoque ME, Ntuli-Ngcobo B. Perceived barriers of cervical cancer screening among women attending Mahalapye district hospital, Botswana. Arch Clin Microbiol. 2011;2(1).
Abiodun O, Olu-abiodun O, Ode I, State O. The understanding and perception of service providers about the community- based cervical screening in Nigeria Volume. Annals of Tropical Medicine & Public Health. 2014;6(6):637–43.
Getachew S, Getachew E, Gizaw M, Ayele W, Addissle A, Kantelhardt EJ. Cervical cancer screening knowledge and barriers among women in Addis Ababa, Ethiopia. PLos ONE. 2019;14(5):e0216522.
Heale R, Forbes D. Understanding triangulation in research. Evidence-based Nursing Evid Based Nurs. 2013;16(4):98.
Elia CR, Devine S. Barriers and enablers for cervical cancer screening in the Pacific : A systematic review of the literature. Pacific Journal of Reproductive Health. 2018;1(7):371–82.
Devarapalli P, Labani S, Nagarjuna N, Panchal P. Barriers affecting uptake of cervical cancer screening in low and middle income countries : A systematic review. Indian J Cancer. 2018;55(55):318–26.
Dykens JA, Smith JS, Demment M, Marshall E, Schuh T, Peters K, et al. Evaluating the implementation of cervical cancer screening programs in low-resource settings globally: a systematized review. Cancer Causes Control. 2020;31(5):417–29.
Mutyaba T, Faxelid E, Mirembe F, Weiderpass E. Influences on uptake of reproductive health services in Nsangi community of Uganda and their implications for cervical cancer screening. Reprod Health. 2007;4:4.
Ifemelumma CC, Anikwe CC, Okorochukwu BC, et al. Cervical Cancer Screening: Assessment of Perception and Utilization of Services among Health Workers in Low Resource Setting. Int J Reprod Med. 2019. https://doi.org/10.1155/2019/6505482 .
World Health Organization. Comprehensive Cervical Cancer Control: A guide to essential practice. Second Edition. 2014.
Global strategy to accelerate the elimination of cervical cancer as a public health problem. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
Binagwaho A, Ngabo F, Wagner CM, Mugeni C, Gatera M, Nutt CT, et al. Integration of comprehensive women’s health programmes into health systems: cervical cancer prevention, care and control in Rwanda. Bull World Health Organ. 2013;91(9):697–703.
Islam RM, Billah B, Hossain MN, Oldroyd J. Barriers to Cervical Cancer and Breast Cancer Screening Uptake in Low-Income and Middle-Income Countries : A Systematic Review. Asian Pac J Cancer Prev. 2017;18(7):1751–63.
Anderson de Cuevas RM, Saini P, Roberts D, Beaver K, Chandrashekar M, Jain A, et al. A systematic review of barriers and enablers to South Asian women ’ s attendance for asymptomatic screening of breast and cervical cancers in emigrant countries. BMJ Open. 2018;8:e020892.
Lunsford NB, Ragan K, Lee Smith J, Saraiya M, Aketch M. Environmental and Psychosocial Barriers to and Benefits of Cervical Cancer Screening in Kenya. Oncologist. 2017;22:173–81.
Njoku A, Ngome E. Challenges faced by older women in Botswana in accessing services that address sexual and reproductive health, and family planning needs. South African Family Practice. 2013;55(3):281–8.
Onyenwenyi AOC, Mchunu GG. Barriers to cervical cancer screening uptake among rural women in South West Nigeria: A qualitative study. South African Journal of Obstetrics and Gynaecology. 2018;24(1):22–6.
Williams M, Kuffour G, Ekuadzi E, Yeboah M, ElDuah M, Tuffour P. Assessment of psychological barriers to cervical cancer screening among women in Kumasi, Ghana using a mixed methods approach. Afr Health Sci. 2013;13(4):1054–61.
Article CAS PubMed PubMed Central Google Scholar
Download references
Acknowledgements
This article is a component of a dissertation titled " Barriers to cervical cancer screening in Gwanda district, Zimbabwe: A mixed method analysis'' which is in the Stellenbosch University repository for dissertations. Available at: https://scholar.sun.ac.za/handle/10019.1/125887?show=full
This study is not supported by any funding body.
Author information
Authors and affiliations.
African Cancer Institute, Stellenbosch University, P.O Box 241, Cape Town, 8000, South Africa
Fennie Mantula & Vikash Sewram
Division of Health Systems and Public Health, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, P.O Box 241, Cape Town, 8000, South Africa
Yoesrie Toefy & Vikash Sewram
Department of Nursing and Midwifery, Faculty of Medicine, National University of Science and Technology, P.O. Box A.C. 939, Ascot, Bulawayo, Zimbabwe
Fennie Mantula
You can also search for this author in PubMed Google Scholar
Contributions
FM conceptualised the study, developed the review protocol, screened retrieved articles, extracted and analysed the data, and wrote the first draft of the manuscript.
VS supervised the study, screened retrieved articles, validated the data analysis and critically reviewed and made revisions to the manuscript.
YT supervised the study and critically reviewed and made revisions to the manuscript.
All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Fennie Mantula or Vikash Sewram .
Ethics declarations
Ethics approval and consent to particpate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mantula, F., Toefy, Y. & Sewram, V. Barriers to cervical cancer screening in Africa: a systematic review. BMC Public Health 24 , 525 (2024). https://doi.org/10.1186/s12889-024-17842-1
Download citation
Received : 14 September 2023
Accepted : 22 January 2024
Published : 20 February 2024
DOI : https://doi.org/10.1186/s12889-024-17842-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cervical cancer
- Cervical cancer screening
- Systematic review
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Cervical cancer articles within Nature Reviews Clinical Oncology
Research Highlight | 02 April 2024
Pembrolizumab plus chemoradiotherapy effective in locally advanced cervical cancer
- Peter Sidaway
Research Highlight | 06 March 2024
Non-inferiority of simple versus radical hysterectomy in low-risk cervical cancer
- Diana Romero
Research Highlight | 18 December 2023
Neoadjuvant chemoimmunotherapy is effective in locally advanced cervical cancer
Research Highlight | 25 February 2022
Benefit with cemiplimab in cervical cancer
Research Highlight | 06 October 2021
Pembrolizumab tunes up chemotherapy in cervical cancer
Research Highlight | 29 January 2021
SCRT for early stage cervical cancer
- David Killock
In Brief | 20 December 2018
TIL infusions effective in HPV-associated cancers
Research Highlight | 21 November 2018
Less invasive is not always better
News & Views | 11 April 2017
Novel molecular subtypes of cervical cancer — potential clinical consequences
The Cancer Genome Atlas Research Network recently published the most comprehensive, multi-omic molecular characterization of cervical cancers performed to date. The data reveal novel disease subtypes, and provide new insights into the aetiology and pathogenesis of cervical cancer. Importantly, the information obtained has potentially major clinical implications.
- Chris J. L. M. Meijer
- & Renske D. M. Steenbergen
Research Highlight | 13 October 2015
Therapeutic HPV vaccine holds promise
Opinion | 01 September 2015
HPV-FASTER: broadening the scope for prevention of HPV-related cancer
Human papillomavirus (HPV)-screening technologies and HPV vaccination are revolutionizing the management of cancers related to this virus, in particular, cervical neoplasms. At present, however, the effectiveness of these modalities is not optimal, owing to the limited scope of HPV-vaccination and cervical screening programmes. In this Perspectives, an international panel of experts describes for the first time a new campaign, termed 'HPV-FASTER', which aims to broaden the use of HPV vaccination coupled with HPV testing to women aged up to 30 years, and in some settings up to 50 years, with the aim of accelerating the reduction in the incidence of HPV infections and cervical cancer. The authors describe the evidence supporting this approach and details on how it might be implemented, discuss the opportunities—particularly in low-resource settings—and challenges associated with the strategy, and highlight key research gaps that need to be addressed in future studies.
- F. Xavier Bosch
- , Claudia Robles
- & Jack Cuzick
In Brief | 23 June 2015
Less than three doses of HPV-16/18 prevents HPV infection
News & Views | 02 June 2015
Squamocolumnar junction ablation—tying up loose ends?
Despite the commercialization of HPV vaccines, cervical cancer remains a major cause of death, especially in developing countries. Recent data implicate a discrete population of cells within the cervical squamocolumnar junction in the pathogenesis of cervical precancerous lesions, indicating that ablation of these cells might reduce the rate of cervical cancer in high-risk populations.
- Michael Herfs
- & Christopher P. Crum
News & Views | 24 February 2015
New standard of care—HPV testing for cervical cancer screening
High-risk human papillomavirus (hrHPV) types cause cervical cancer. Hence, a negative hrHPV test provides excellent reassurance against cervical precancer and cancer, superior to a negative cervical smear (Papanicolaou or Pap) test. Screening first for hrHPV might improve the accuracy and positive predictive value of secondary Pap testing in hrHPV-positive women, and thus guide decisions on what care is needed.
- Philip E. Castle
Research Highlight | 17 February 2015
Survival benefit and quality of life
- Lisa Hutchinson
Research Highlight | 09 December 2014
From ENA 2014
News & Views | 08 April 2014
Further delineating bevacizumab's response spectrum
The use of antiangiogenic drugs, such as bevacizumab, represents an appealing intervention against cancer. However, not all malignancies are equally responsive to such treatment. Recent trials demonstrate the efficacy of this drug for advanced-stage cervical cancer and, despite limitations, bevacizumab provides an important clinical respite for most patients with progressive glioblastoma.
- David A. Reardon
- & Patrick Y. Wen
Year in Review | 21 January 2014
Screening comes of age and treatment progress continues
In 2013, studies confirmed that HPV infection of target cells predisposes to cervical (pre)cancer. In developed countries, HPV screening revealed superior protection than cytology screening. In India, visual inspection of the cervix after acetic acid application significantly reduced cervical cancer mortality after 12 years. Improved survival for women with advanced disease was observed after adjuvant bevacizumab.
- & Peter J. F. Snijders
In Brief | 30 July 2013

Declining use of brachytherapy for cervical cancer in USA
Research Highlight | 18 June 2013
Advances in cervical cancer screening and treatment
- Rebecca Kirk
Review Article | 04 June 2013
Clinical trials of human papillomavirus vaccines and beyond
Highly efficacious vaccines are available to protect against persistent human papillomavirus (HPV) infection and, therefore, the associated neoplasias (most notably cervical cancer). This Review article discusses the two approved vaccines in terms of their structure, mode of action, efficacy, cross-reactivity with non-vaccine HPV types, safety and use in vaccination programmes.
- Matti Lehtinen
- & Joakim Dillner
News & Views | 11 September 2012
Cervical cancer—should we abandon cytology for screening?
Convincing data have shown that human papillomavirus (HPV)-DNA testing predicts the development of high-grade cervical cancer better than cytology. However, for HPV-positive women, triage with cytology testing should be performed before colposcopy. The question on how to proceed if the cytology test in HPV-positive women is negative remains unclear.
- & Johannes Berkhof
News & Views | 14 February 2012
More evidence supporting human papillomavirus testing
Clinical trials have consistently demonstrated the superior sensitivity of human papillomavirus (HPV) testing compared with cytology (Pap) testing for identifying women at risk of cervical cancer. Rijkaart et al . have now shown that adding HPV testing to routine cervical cancer screening can further reduce the risk of cervical cancer compared to Pap testing alone.
Research Highlight | 06 September 2011
Cisplatin more effective when given less often
News & Views | 31 May 2011
New treatment paradigm for locally advanced cervical cancer?
Despite the improved progression-free survival and overall survival demonstrated by cisplatin–gemcitabine chemoradiation in a phase III randomized trial in patients with stage IIB to IVA cervical cancer, the acute and chronic toxic effects urge caution before embracing this as a new treatment paradigm.
- Peter G. Rose
News & Views | 01 July 2010
HPV testing for cervical cancer: the good, the bad, and the ugly
A randomized, controlled trial has shown human papillomavirus (HPV) DNA testing with and without liquid-based cytology to be more sensitive but less specific than conventional Papanicolaou smears for detection of precancerous lesions of the cervix. The lead-time advantage of early detection of precancerous lesions by HPV DNA testing resulted in cervical cancer reduction; however, an increased detection of possibly regressive precancerous lesions could result in unnecessary treatment, especially in women aged 25–34 years.
News & Views | 01 February 2010
Cisplatin combinations in cervical cancer—which is best?
We reviewed the results of the Gynecological Oncology Group 204 (GOG-204) randomized phase III trial, which investigated four cisplatin combination chemotherapy regimens for the treatment of patients with recurrent or metastatic cervical carcinoma. As the overall survival was similar between all arms, treatment recommendations need to be tailored based on toxic effects.
- David O. Holtz
- & Charles J. Dunton
Research Highlight | 01 January 2010
IL-12 polymorphism linked to cervical cancer risk
- Vessela Vassileva
Browse broader subjects
- Gynaecological cancer
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
SYSTEMATIC REVIEW article
Recent status and trends of nanotechnology in cervical cancer: a systematic review and bibliometric analysis.
A correction has been applied to this article in:
Corrigendum: Recent status and trends of nanotechnology in cervical cancer: a systematic review and bibliometric analysis
- Read correction

- 1 School of Clinical Medicine, Chengdu Medical College, Chengdu, China
- 2 Department of Pathology, The Second Affiliated Hospital of Chengdu Medical College, China National Nuclear Corporation 416 Hospital, Chengdu, Sichuan, China
- 3 Development and Regeneration Key Laboratory of Sichuan Province, Department of Neurobiology, Chengdu Medical College, Chengdu, China
- 4 Department of Pathology and Pathophysiology, Chengdu Medical College, Chengdu, China
Background: Cervical cancer is currently the second leading cause of cancer death among women from developing countries ( 1 ). However, there is a lack of effective treatment methods, and the existing treatments often result in significant adverse reactions and high chances of recurrence, which ultimately impact the prognosis of patients. As a result, the application of nanotechnology, specifically nanoparticle-based approaches, in the diagnosis and treatment of cervical cancer has gained significant attention. This study aims to examine the current research status and future development trends of nanotechnology in relation to cervical cancer using a bibliometric perspective.
Methods: A bibliometric analysis was performed to gather relevant research papers from the Web of Science database. VOSviewer and CiteSpace were utilized to conduct quantitative analysis and identify hot topics in the field, focusing on countries, institutions, journals, authors, and keywords.
Result: A total of 997 eligible literature were retrieved. From January 1, 2014 to September 20, 2023, the overall number of publications showed an upward trend. The paper mainly comes from China (n=414). The main institution is the Chinese Academy of Sciences (n=62), and 60% of the top 10 institutions in the number of documents issued are from China. First authors Ma, Rong (n=12) and Alifu, Nuernisha (n=12). The journal with the highest publication volume is ACS Applied Materials&INTERFACES (n=35), and the journal with the highest citation frequency is BIOMATERIALS (n=508). “Nanoparticles (n=295)”, “cervical cancer (n=248)”, and “drug delivery (n=218)” are the top three most frequently occurring keywords. In recent years, photothermal therapy and indocyanine green have become research hotspots.
Conclusion: The application of nanotechnology in the field of cervical cancer has garnered considerable attention. Nanoparticles-based methods for diagnosis, administration, and treatment have proven to be instrumental in enhancing the sensitivity of cervical cancer detection, improving the accuracy and efficiency of administration, and reducing drug toxicity. Enhancing treatment efficacy and improving patient prognosis have emerged as current research priorities and future directions.
1 Introduction
Globally, cervical cancer is the fourth most common type of cancer among women and the second leading cause of cancer-related deaths among women from developing countries ( 1 , 2 ). The majority of cervical cancers are caused by human papillomavirus (HPV), a virus similar to the human immunodeficiency virus. HPV poses the highest risk for cervical cancer and can only be managed through a limited number of highly invasive methods ( 2 , 3 ). While chemotherapy and surgery have been proven highly effective in treating early-stage cervical cancer, surgery is still the preferred option due to potential damage to the female reproductive system caused by chemotherapy. Chemotherapy remains effective for those with more advanced conditions ( 4 , 5 ). However, incomplete surgical resection, adverse reactions to chemotherapeutic agents, and cellular resistance to multiple drugs can lead to unsatisfactory long-term results. Additionally, the complex nature of tumor cells and the harsh tumor microenvironment make them resistant to treatment and metastasis, posing a significant obstacle to the possibility of recurrent cervical cancer. This could be due to remaining tumor cells or metastatic tumor cells ( 6 , 7 ). Therefore, there is an urgent need for a more effective method to diagnose early-stage cervical carcinogenesis, improve the efficacy of drug action, reduce adverse effects, and enhance the quality of prognosis.
In comparison to other diagnostic modalities, various nanoparticle-based measurements in nanotechnology have demonstrated improved selectivity and sensitivity, as well as provided support for obtaining information that traditional measurements cannot. By leveraging the exceptional optical and electrical properties of nanomaterials, such as gold nanoparticles, along with their significantly larger surface area, they can be integrated with various types of sensors, including electrochemical sensors and DNA biosensors, to effectively detect biomarkers. This approach successfully addresses the limitations of traditional sensors, such as low conductivity, low sensitivity, and high cost ( 8 – 11 ). This enables early detection of tumor onset and timely intervention, ultimately aiming to enhance patient survival. Nanoparticles can also be utilized to monitor disease progression in patients, facilitating the formulation of more precise treatment strategies ( 12 ). Depending on the characteristics of the tumor microenvironment, such as hypoxia and acidity, nanoparticles can be designed to respond effectively in various environments, thereby enhancing treatment outcomes. By modifying the properties of nanoparticles, they can facilitate the uptake of drugs into the tumor tissue of the uterine cervix, increase their concentration in tumor tissue, and improve treatment efficacy. In addition, nanoparticles can be used as efficient carriers for drug delivery due to their good biocompatibility, permeability, and retention. Utilizing nanoparticles as delivery systems for anticancer agents can enhance drug efficacy, reduce dosing and treatment frequency, and potentially minimize the toxicity of antitumor drugs to the human body ( 13 ). With the deepening of research on nanotechnology, researchers have also designed some progressively stimuli-responsive drug delivery systems based on this foundation, which can enhance drug delivery more effectively ( 14 ). Furthermore, certain nanoparticles can be employed as specific markers targeting cancer cells ( 15 ). For example, using exosomes isolated from the tumors of cervical cancer patients as nanocarriers to transport drugs can robustly target the target cells ( 16 ). The development of nanotechnology has significantly enhanced various aspects of medicine, particularly in the field of cancer diagnosis and treatment, where improved diagnostic methods and novel drug delivery systems hold great promise ( 17 ). The combination of nanotechnology and cervical cancer research may yield unexpected advancements in the future.
Currently, there is no research analyzing the application of nanotechnology in cervical cancer using the bibliometrics approach. Bibliometrics involves analyzing published information, such as books, journal articles, and data sets, along with their associated metadata like abstracts, keywords, and citations. It also includes using statistical information to describe the relationship between published works. Tools like VOSviewer and CiteSpace can be used to visualize and analyze academic literature in this research field ( 18 ). By employing bibliometrics, we can gain a better understanding of existing research, identify current areas of interest, and predict future trends in nanotechnology for cervical cancer. The objective of this study is to conduct a comprehensive analysis of the trends of nanotechnology in cervical cancer from various angles using bibliometric tools. This analysis will identify the prominent countries, journals, institutions, and authors that have contributed to this field. Additionally, the study will focus on analyzing and discussing the current research areas of interest and potential future research directions. The findings will be beneficial for researchers seeking to gain a deeper understanding of this field or for those who are new to it.
2 Materials and methods
2.1 data source and collection.
The Web Science Core Collection (WoSCC) is a widely used bibliometric analysis database that contains over 10,000 high-quality journals and comprehensive citation records ( 19 ). Additionally, WoSCC has been found to have more accurate document type labeling compared to other databases ( 20 , 21 ).
Figure 1 illustrates the workflow for this study. In September 2023, we conducted a search for original research articles related to nanotechnology for cervical cancer that were published between January 1, 2014, and September 20, 2023. To ensure inclusivity and eliminate irrelevant articles, we designed a search strategy that involved the following steps: 1) Using keywords such as ‘cervical cancer’ and ‘nanotechnology’; 2) Including various synonyms for these keywords, including specific names of nanomaterials and nanoparticles; 3) Excluding papers that were not original research; 4) Limiting the search to English publications only; 5) Focusing on the data categories of ‘articles’ and ‘reviews’. After applying these criteria, we evaluated the title and abstract of each article to determine its relevance to the topic. In cases where the literature was inconclusive, two researchers read the full text and conducted a more detailed evaluation to ensure accurate results. Subsequently, we identified pertinent articles and extracted primary data on nations/regions, institutions, authors, journals, and key terms. For the specific search formula used in this article, please refer to Supplementary Materials 1 .
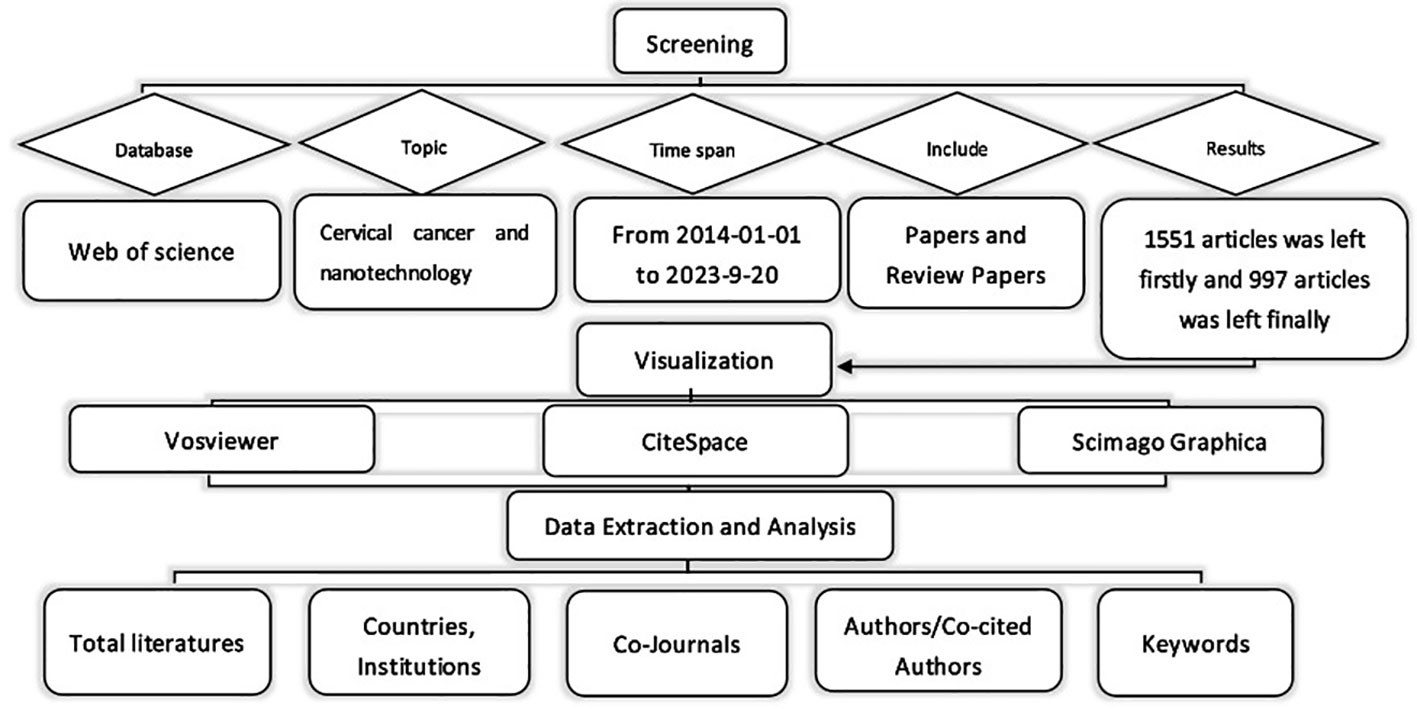
Figure 1 Flow chart of literature selection.
2.2 Data analysis and visualization
The collected literature was analyzed using CiteSpace, which provided insights into authors, countries, institutions, journals, and keywords. To visualize keyword co-occurrence, VOSviewer was employed, representing authors or keywords as nodes with varying sizes based on their frequency. The strength of connections was depicted by line thickness, while node colors indicated different clusters or periods. The Scimago Graphica tool was utilized to visualize the overall distribution of publications.
3.1 Annual publications and trends
To some extent, the number of publications can represent the heat and development of the field in a given time. From January 1, 2014 to September 20, 2023, WOS received a total of 997 publications on nanotechnology in cervical cancer research, including 941 articles and 56 reviews. Figure 2 shows the worldwide trend in number of publications per year and total number of publications for research in cervical cancer for the period January 2014 to September 2023. Each year of the decade, the number of articles published was close to 100, with occasional declines in the intervening years, with an average annual growth rate of 2.39%.
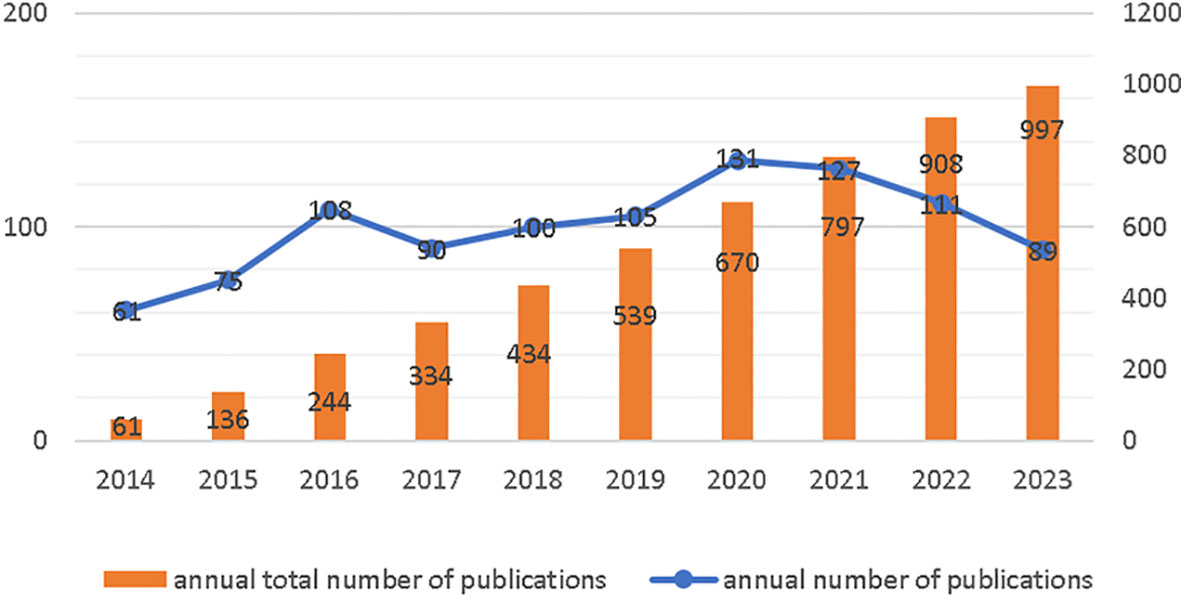
Figure 2 Annual Publications and Trends.
3.2 Contributions of authors
There were 5566 authors included in the study, with the Table 1 showing the top ten authors and co-citations. Ma, Rong (n=12) and Alifu, Nuernisha (n=12) had the highest number of articles published, followed by Yan, Ting (n=11), Alimu, Gulinigaer (n=11). The CiteSpace was used to show the referencing relationships between different authors ( Supplementary Material Figure 1A ). Nodal sizes represent the number of papers, and rows represent connections between authors. Co-citation means that two or more authors are cited simultaneously in one or more articles, and that these two or more authors form a co-citation relationship. Overall, 27787 authors were cited at least once (data obtained from VOSviewer). WANG Y (n=73) is the most cited author of the network built by CiteSpace, LIU Y is the author with the highest centrality (0.18), ranking fifth in terms of publication volume and considerable output (The network of co-cited author relationships can be found in the Supplementary Material Figure 1B ).
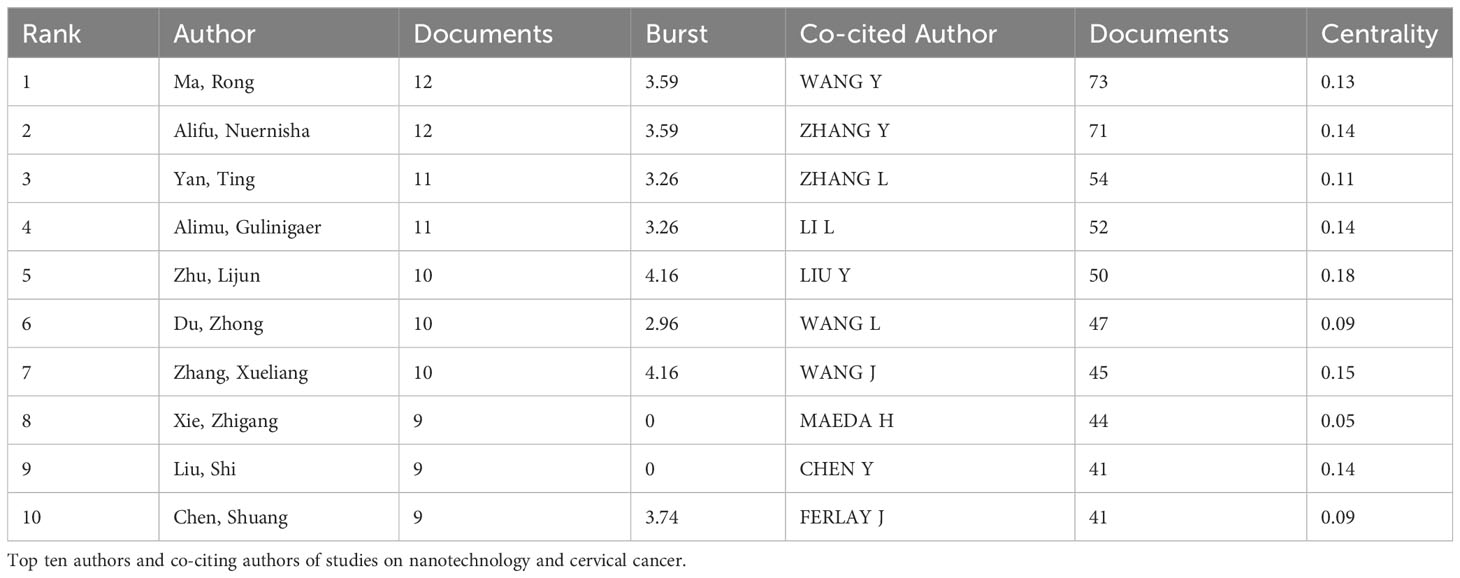
Table 1 Contributions of authors.
3.3 Contributions of countries or regions
Research on nanotechnology/nanomaterials in cervical cancer has been conducted in 164 countries/regions over the last decade. On the country distribution map ( Figure 3A , the darker the color of the country, the more publications there are.), the top three countries/regions are China (n = 414,41.52%), India (n = 208, 20.86%) and the United States (n = 93, 9.32%) on the basis of the number of publications. The cooperation between many countries can be seen in Figure 3B , with the cooperation between China and India being the most evident. We then conducted a more in-depth analysis of high productivity countries in the field, and publications from the top 10 countries are shown in Table 2 and Figure 3C . China was the country with the most publications, the United States had the highest average number of citations with a total of 33.13 citations. The degree of centrality is an assessment of the importance of the nodes in the network, primarily used to measure the value of nodes’ bridge functions across the network structure. The purple circles outside each node in Figure 3C represent the centrality of each country. Among the top 10 countries in the world, the United States has the highest betweenness centrality of 0.34, followed by China (0.25). Although Spain (0.23) did not have a large number of publications, their central values are high. Which shows that they play an essential role in international co-operation. The size of the circle in the visualization diagram built by CiteSpace represents the number of papers published, the thick line indicates cooperation between countries/regions and the width of the purple node ring represents the size of the central value.
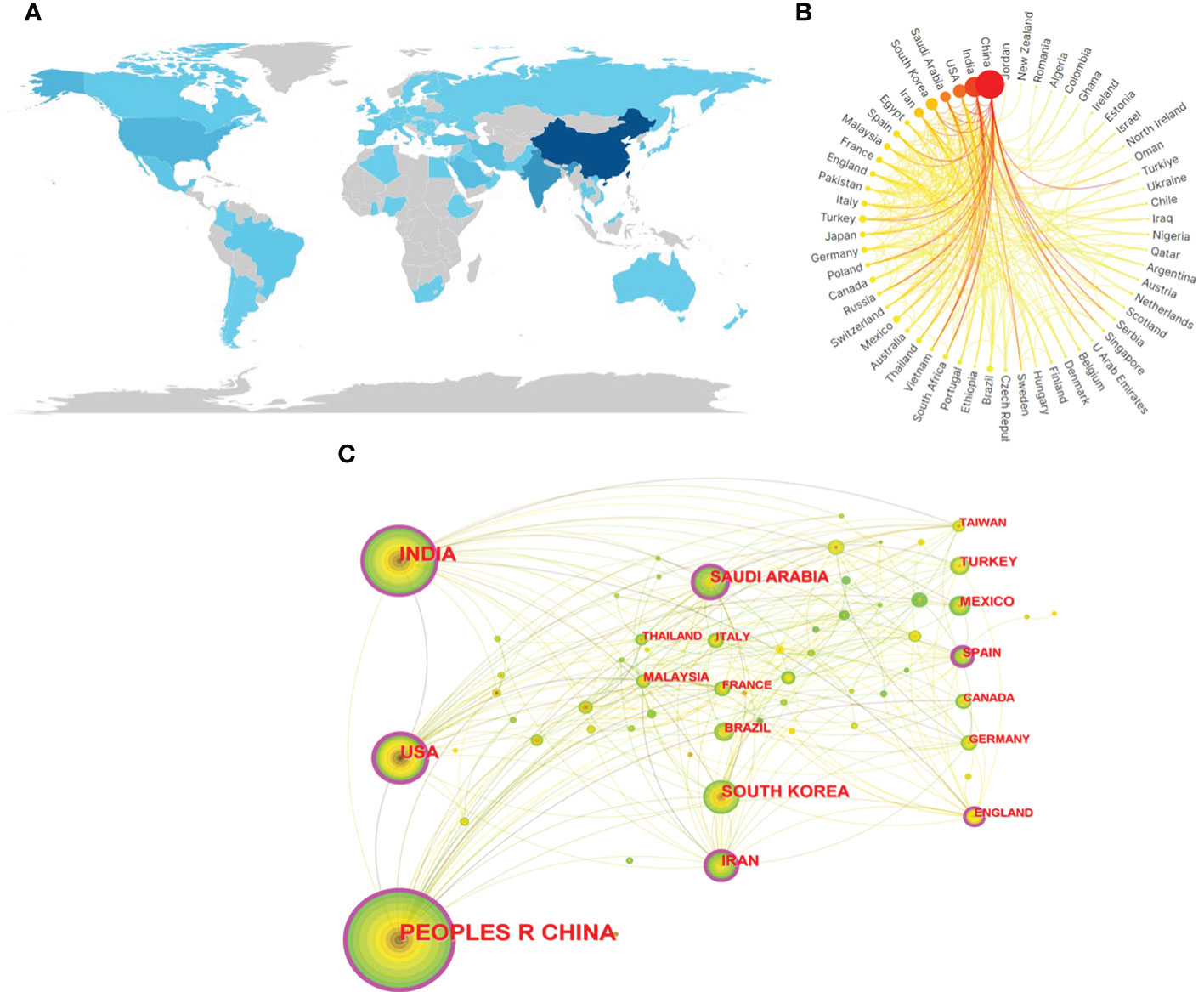
Figure 3 (A) Geographical distribution map based on the total publications of different countries/regions. (B) The international collaborations’ visualization map of countries/regions. (C) The countries/regions’ citation network visualization map was generated by using Citespace. The size of the circle in the visualization diagram built by citespace represents the number of papers published,and the thickness of the purple ring of the node represents the size of the center value.
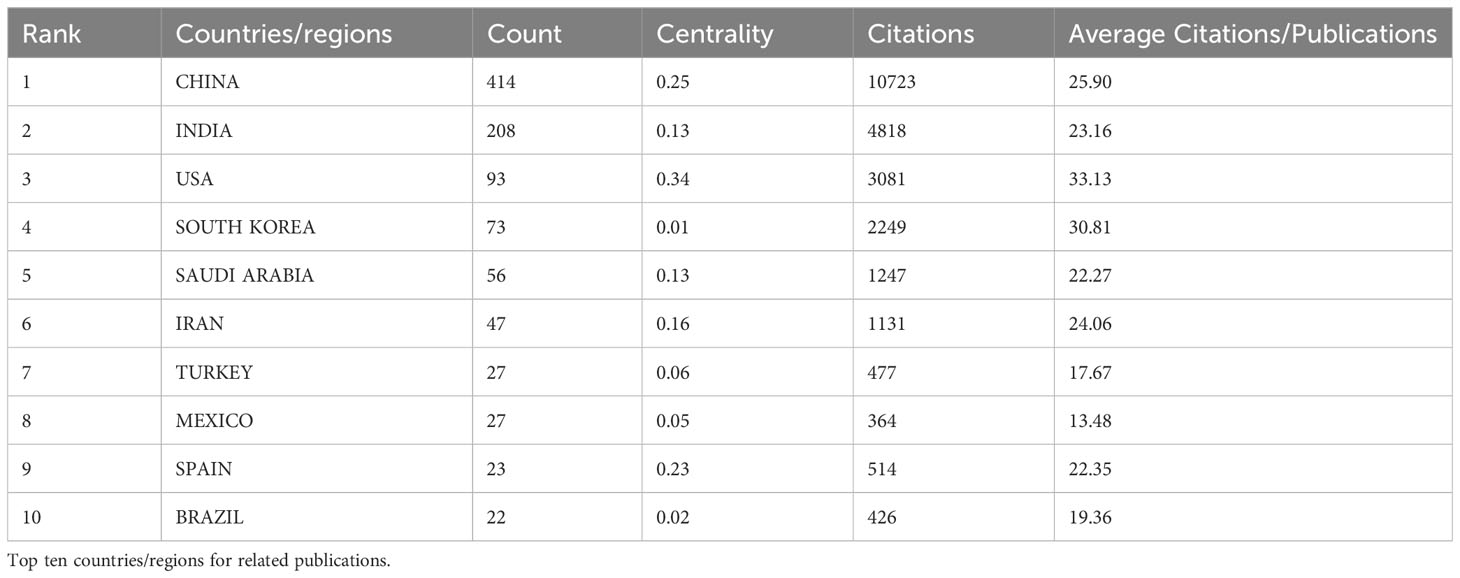
Table 2 Contributions of countries/regions.
3.4 Contributions of institutions
Articles/comments received from the WOS are from 3229 different institutions. On the basis of the number of publications, Table 3 comprises the top ten production agencies. It is not hard to see from table that six institutions are from China, with two institutions from India, one from Saudi Arabia and one from France. The United States has the highest number of citations and the third-highest number of publications, but none of the top ten publications are from it. The Chinese Academy of Sciences(n=62) has the largest number of publications and Indian Institute of Technology System (IIT System) has the highest centrality (0.2). The size of the circle in the visual map of CiteSpace ( Supplementary Material Figure 2 ) represents the number of articles published by each institution, each row represents the collaboration between the two institutes, and the purple circle represents the node with a higher centrality, the higher the number, the greater the centrality. The top 10 universities published 239 articles, or 23.97% of the total, greatly promoted the development of fields related to the subject.
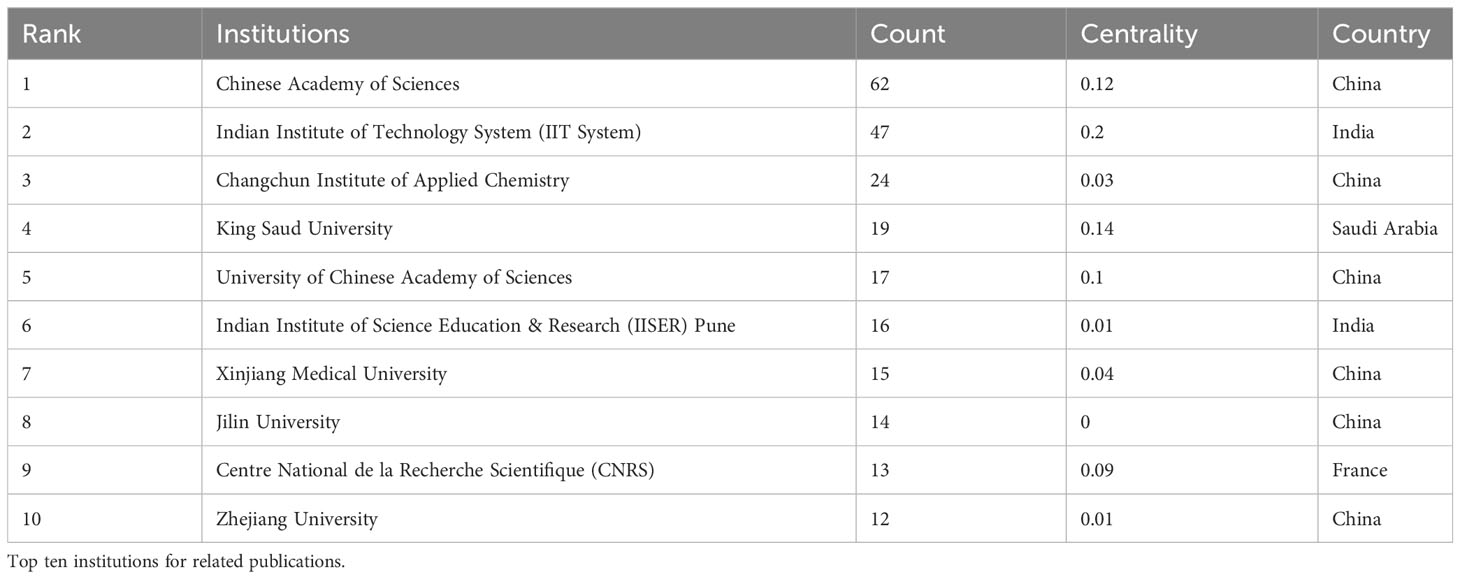
Table 3 Contributions of institutions.
3.5 Analysis of journals/co-cited journals
332 journals have published papers on nanotechnology and hepatic cancer, of which ACS APPLIED MATERIALS & INTERFACES (n = 35, IF 2022 = 9.5) ranks first and JOURNAL OF MATERIALS CHEMISTRY B (n =34, IF 2022 = 7) ranked second. RSC ADVANCES (n = 32, IF 2022 = 3.9) ranked third. Of the top ten journals, 30% (3/10) are from Netherlands and 30% (3/10) are from the England. JOURNAL OF CONTROLLED RELEASE (n = 18, IF 2022 = 10.8) was the journal with the largest impact factor. The details are shown in Table 4A .
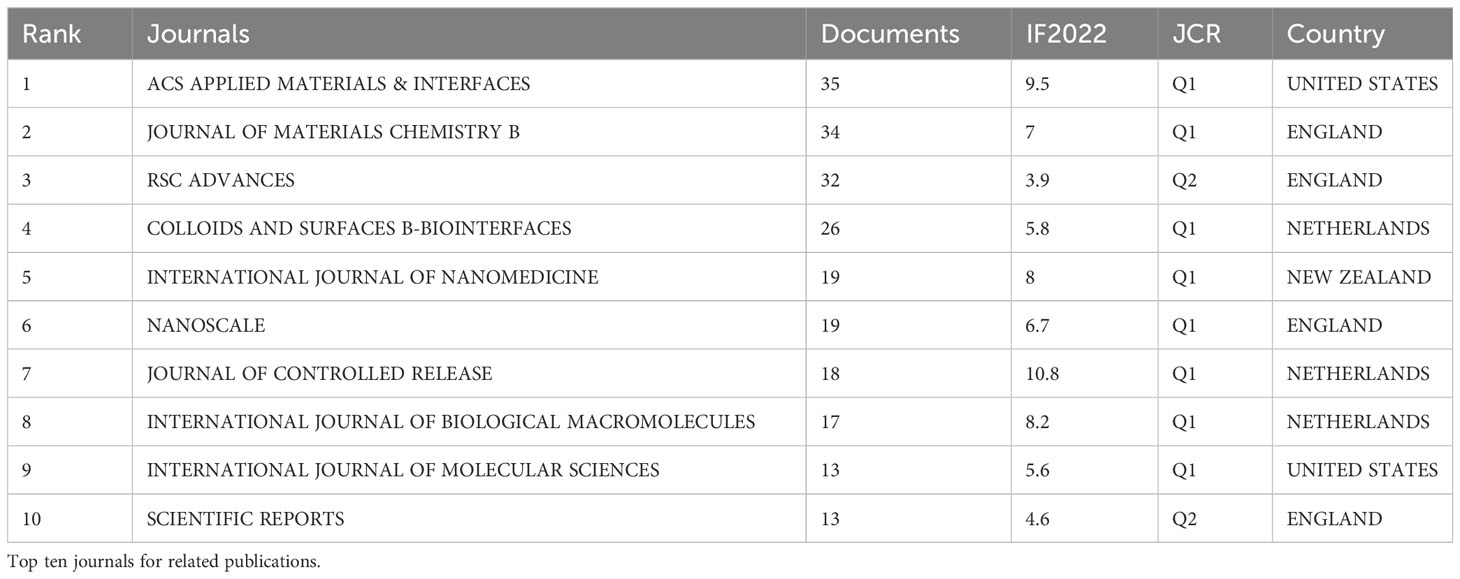
Table 4A Journal analysis.
Among the co-cited journals, BIOMATERIALS (n = 508, IF 2022 = 14) ranked first, ACS NANO (n = 440, IF 2022 = 17.1) ranked second. J CONTROL RELEASE (n = 419, IF 2022 = 3.9) was ranked third but had the largest centrality. The details are shown in Table 4B .
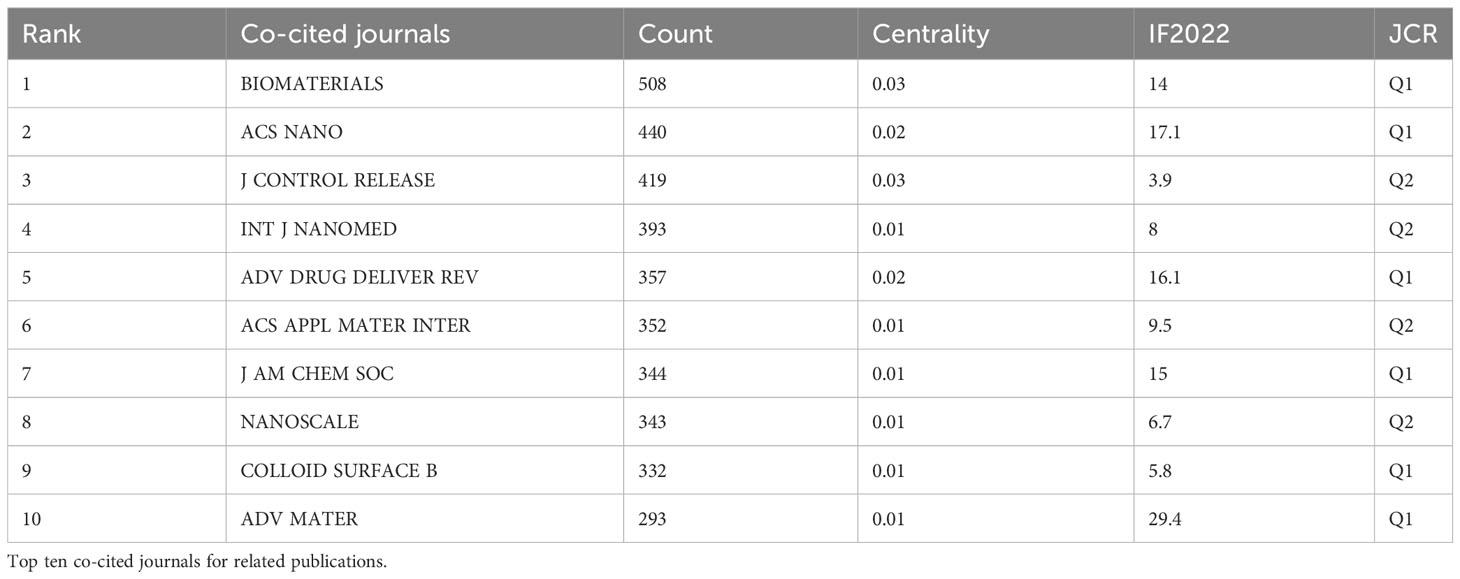
Table 4B Journal analysis.
3.6 Analysis of keywords
Keywords condense the heart and essence of the paper, and through analysis of the co-occurrence of keywords can reveal the research hotspot of a certain scientific field. For example, in a visual network constructed using CiteSpace ( Figure 4A ), the larger the circular node, the greater the number of keywords, and the more representative the hotspot. The nodal line indicates the strength of the association, and the thicker the nodal line, the stronger the connection between them. The highest frequency was observed in nanoparticles (n=295), followed by cervical cancer (n=248) and drug-delivery (n=218) as detailed in Supplementary Material Table 1 .
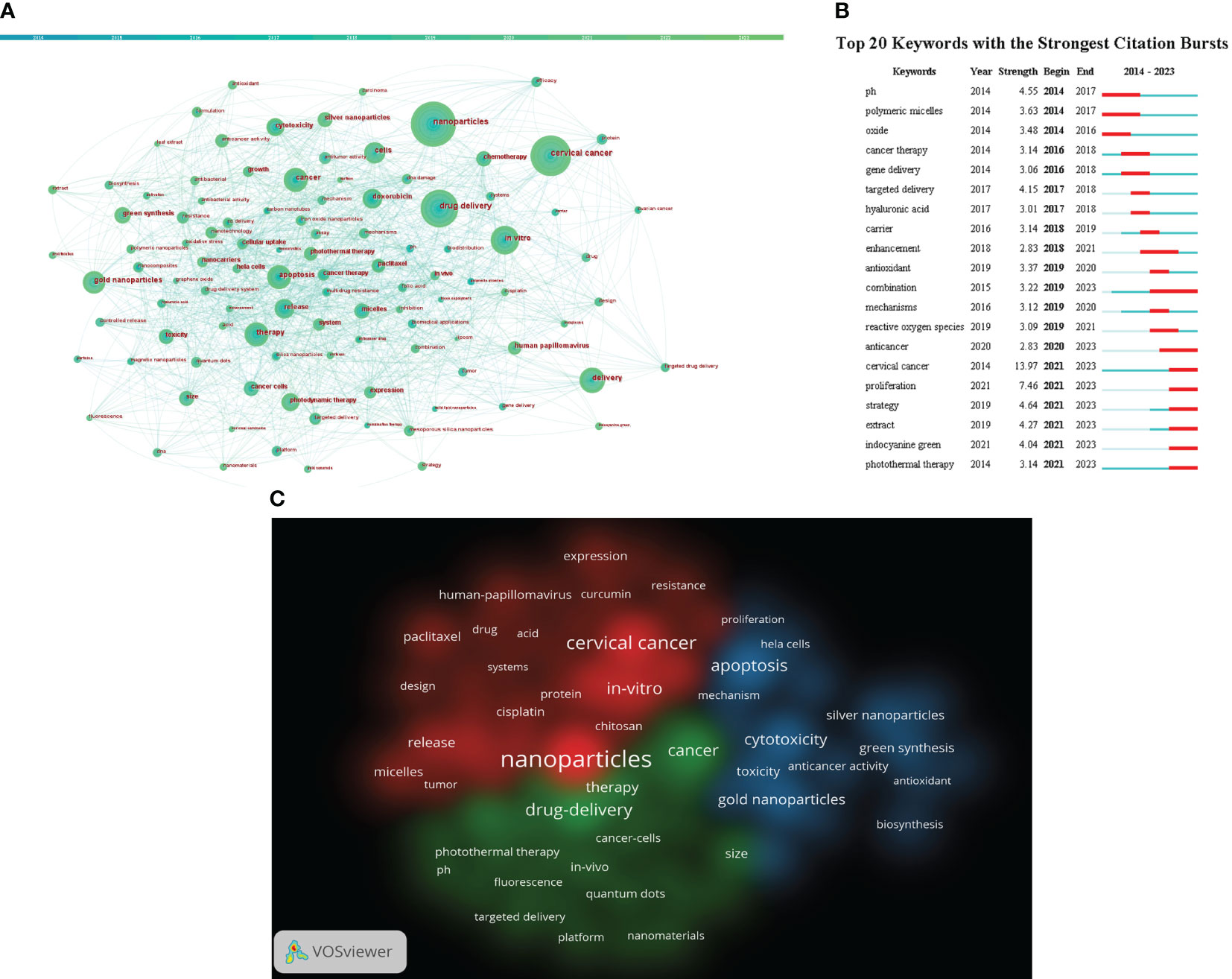
Figure 4 (A) Citespace visualization map of keywords. (B) CiteSpace visualization map of the top 20 keywords for the strongest citation bursts from January 2014 to September 2023 (C) VOSviewer visualization map of Cluster view of keywords. Different colors indicate different clusters. (Source: https://www.vosviewer.com/ ).
The shortest outbreak duration based on the keyword outbreak map is 3 years, citing the top 25 keywords with the highest outbreak intensity (Details can be found in Figure 4B ). From Figure 4B , keywords such as “oxide (2014–2016)”, “polymeric micelles (2014-1017)” and “gene delivery (2016-2018)” have been given more attention in the past. “extract (2021-2023)”, “indocyanine green (2021-2023)” and “photothermal therapy (2021-2023)” have received widespread attention recently. It may be a new direction for future research.
We used VOSviewer to create a view of the keyword co-occurrence network for 4250 documents and select 82 keywords that have a frequency greater than or equal to 20 for visualization (Details can be found in Figure 4C ). Each of the three colors in the picture represents a different cluster, referred to as a research topic. In addition, in the figure, we find that the identified keywords are divided into three clusters: red, green and blue. Red indicates clustering keywords related to drug, including nanoparticles, in-vitro, cisplatin, paclitaxel, etc. The keywords of the green group are primarily bound up with the drug-delivery, including photothermal therapy, fluorescence, targeted delivery, etc. The blue areas are mainly related to cytotoxicity, including gold nanoparticles,silver nanoparticles, green synthesis and so on.
4 Discussion
4.1 general information.
The number of annual publications and the total number of publications are both increasing, indicating a growing interest in the application of nanotechnology in cervical cancer research. The involvement of researchers in this field is also on the rise.
In terms of the number of articles published, China, India, and the United States ranked in the top three, suggesting their overall strength in this area. Among the major publishers, six out of the top ten are from China. The institutions with the highest number of published articles are CAS, Indian Institute of Technology System, and Changchun Institute of Applied Chemistry. However, global cooperation among institutions in this field remains uncommon. Future studies will explore the benefits of strengthening international cooperation between countries and institutions for the continued development of the field.
The majority of nanotechnology and cervical cancer-related journals are published in ACS APPLIED MATERIALS & INTERFACES, JOURNAL OF MATERIALS CHEMISTRY B, and RSC ADVANCES, with impact factors of 9.5, 7, and 3.9, respectively. BIOMATERIALS, ACS NANO, and J CONTROL RELEASE are the three most cited journals. These high-quality journals provide significant support for research in the field and indicate that biological/applied materials are not only the current hotspot but also the future development trend.
Out of the 23,556 researchers, Ma, Rong and Alifu, Nuernisha have published the most articles, followed by Yan, Ting and Alimu, Gulinigaer. Which shows that they are leading researchers in their current field.
4.2 Research hotspots
By analyzing the frequency of occurrence of keywords, it can reflect the hotspot of research and the trend of nanotechnology development in the application of cervical cancers. From the keyword analysis, it can be seen that the combination of nanoparticles and cervical cancer is a hot topic in current research.
4.2.1 Nanoparticles in the field of cervical cancer
The increasing number of cervical cancer cases among women highlights the need to improve diagnostic methods and determine the stage of the disease. Nanotechnology has emerged as a promising field, allowing the utilization of nanomaterials in various diagnostic procedures. This utilization is driven by the unique physical characteristics of nanomaterials, which enhance the precision of diagnosis and the effectiveness of treatment. Therefore, the application of nanotechnology in the diagnosis and treatment of cervical cancer in women holds great potential to significantly improve the efficiency and accuracy of detection and therapy, providing valuable time for subsequent treatment.
4.2.1.1 Role of nanotechnology in HPV virus detection
Based on empirical evidence, it has been established that high-risk variants of HPV exhibit a strong correlation with the onset of cervical cancer, as approximately 96% of cervical cancer cases are associated with these variants ( 22 ). Consequently, the precise identification of the HPV virus plays a pivotal role in both the prevention and early diagnosis of cervical cancer. Traditional methods for detecting HPV infection encompass the Pap test, visual inspection with acetic acid, and HPV serologic testing; however, these methods are hindered by their considerable expenses and limited specificity, thereby necessitating further enhancements ( 23 ). In this particular context, the utilization of nanomaterials’ exceptional properties holds promise for the development of diverse biosensors and electrosensors. These advanced sensors have the potential to enable rapid, accurate, and convenient detection of the HPV virus. Furthermore, they can enhance the sensitivity of detection by accurately identifying specific DNA and mRNA within the HPV virus. Gold nanoparticles are frequently employed in diverse sensor applications owing to their distinctive physicochemical properties, facile synthesis, surface functionalization, capabilities, and the ability to tune their optical properties based on size and shape ( 24 ); Moreover, graphene emerges as a highly efficient sensing technique for rapid detection through integration, with its functional groups demonstrating exceptional reliability in capturing molecules and analyzing their interactions with specific targets ( 25 ). Researchers have made significant progress in developing sensors using nanomaterials for HPV virus detection. One such example is the electrochemical DNA-biosensor developed by Pegah Mahmoodir et al. This biosensor utilizes the unique properties of the GO honeycomb structure, including high surface area, high electrical conductivity, and high chemical stability. Additionally, the incorporation of gold nanoparticles (AuNPs) enhances the electrical conductivity and creates immobilized channels for DNA on the electrode surface. The experiments conducted with this biosensor have demonstrated reliable results ( 26 ). In addition to genetic detection of HPV viruses, nanomaterials can also be used to detect HPV-associated proteins. Nanoparticles such as AuNPs have plasmon resonance (LSPR) properties, which allow them to be ionized under laser irradiation. This ionization generates characteristic mass reporter ions, making AuNPs suitable as mass labels for signal amplification. Additionally, by coupling antibodies to the nanoparticles, specific antigens can be targeted and marker proteins can be detected ( 27 ). Toby Siu-Chung Tam et al. utilized the property of AuNPs to develop an antibody-coupled AuNPs mass tag for the detection of HPV18E7 protein, enabling early cervical cancer diagnosis ( 28 ). Currently, the focus of nanomaterial application lies primarily on AuNPs, but there are still numerous other nanomaterials that require further study. Moreover, the combination of nanomaterials with other nanomaterials or molecules results in multifunctional nanoparticle couplings. These couplings possess both the physicochemical properties of the nanoparticles themselves and the functions of the couplings, thereby significantly enhancing the accuracy of nanoparticle diagnosis. This area of research remains a prominent and active field. With the continuous advancements in nanotechnology, there is immense potential to utilize various high-performance nanomaterials for the detection of HPV virus and the diagnosis of cervical cancer.
4.2.1.2 The role of nanotechnology in the detection of tumor markers for cervical cancer
Tumor markers are molecules that indicate the presence or prognosis of malignant tumors and can be used for the early diagnosis of tumorigenesis and recurrence, as well as to determine tumor prognosis and treatment efficacy ( 29 ). Currently, the application of nanotechnology in the detection of tumor markers is mainly to combine various types of nanoparticles with sensors and use their unique physicochemical properties to improve the accuracy of detection. Common tumor markers for cervical cancer include squamous cell carcinoma antigen (SCCA) and carcinoembryonic antigen (CEA), as well as other characteristic proteins and genes. SCCA is a glycoprotein that shows significantly elevated levels in patients with cervical cancer. It is considered as one of the suitable biomarkers for the detection of cervical cancer ( 30 ). Therefore, it is crucial to identify and quantify the critical level of SCCA for effective detection and treatment of cervical cancer. In addition the serum concentration of SCCA correlates with tumor stage, treatment outcome, recurrence and survival in patients with squamous cell cervical cancer ( 31 ). Therefore, an effective detection method is of particular importance in identifying and quantifying the severity of gynecological tumors. Xinmei Liu et al. utilized the high sensitivity of gold nanoparticles coupled to analyte molecules to detect and quantify SCCA levels ( 32 ). This method has demonstrated exceptional sensitivity in experiments and significantly aided in the detection of cervical cancer. Additionally, the abnormal methylation of genes in the promoter regions of tumor suppressor genes can impede DNA transcription, which is a critical process in tumors ( 33 ). Thus, methylation of genes may also be a biomarker for cervical cancer detection. Jin Huang et al. exploited the property that the transition of AuNPs from the dispersed to the aggregated state can lead to the discoloration of colloidal solutions. They employed this characteristic to develop a novel colorimetric detection method for identifying methylation of the PAX1 gene in cervical scrapings. This was achieved by combining sulfhydryl-labeled primers with AuNPs ( 34 ). Through a clinical trial of 42 patients with cervical cancer, the study found that the percentage of normal median methylation rate detected was 33.11%, while the percentage of CIN1 type median methylation rate detected was 45.14%. Additionally, the percentage of CIN2 type median methylation rate was 74.64%, the percentage of CIN3 type median methylation rate was 67.81%, and the percentage of SCC series median methylation rate was 82.64%. These results indicate a positive correlation between the methylation status and frequency of PAX1 with the severity of cervical cancer. Moreover, the researchers suggest that this simple, fast, and inexpensive colorimetric test has the potential to enhance the efficiency of early cervical cancer screening when compared to traditional detection methods. Furthermore, nanoparticles exhibit promising potential in fluorescence imaging of cervical cancer. This is attributed to their exellent absorption and fluorescence characteristics in the near-infrared region. Consequently, further research in this area is highly recommended ( 35 ). Based on the properties of different types of nanomaterials, including electrical conductivity, optical properties, magnetic or plasma properties, the combination of nano ions with traditional detection methods offers a new approach to enhance detection sensitivity and reduce costs in the diagnosis of cervical cancer. As nanotechnology continues to advance utilization of nanomaterials for detecting cervical cancer is expected to become more widespread. These nanomaterials are anticipated to outperform traditional detection methods in terms of sensitivity and reliability, while also mitigating operational challenges and minimizing the influence of the body environment on diagnostic outcomes. We could believe that this has the potential to revolutionize cervical tumors diagnosis.
4.2.1.3 Nanoparticles in photodynamic therapy
Nowadays, photodynamic therapy (PDT) has emerged as a groundbreaking treatment for cervical cancer in women. In contrast to conventional therapies like surgery, radiotherapy, and chemotherapy, which are associated with drawbacks such as extensive wounds, severe side effects, and drug resistance, PDT offers a minimally invasive approach that is resistant to multidrug resistance. This is due to its utilization of a clinical procedure that minimizes invasiveness, as well as a distinct toxicity mechanism targeting cancer cells, which sets it apart from chemotherapy ( 36 , 37 ). The cytotoxic effect of PDT on cancer cells primarily relies on the accumulation of photosensitizers (PS) in target tissues. When these PS are exposed to light of specific wavelengths matching their absorption spectrum, they transition from the ground state to an unstable excited state. This process generates singlet oxygen species, which further produce other reactive oxygen species (ROS). These ROS oxidize critical components within cancer cells, leading to an acute cellular stress response and ultimately resulting in cell death ( 38 ). Designing a reliable PS is crucial for the efficacy of PDT. Nanoparticles offer several advantages, including enhanced light absorption, higher photostability, and better biocompatibility. These properties assist in stabilizing and absorbing light, while minimizing side effects on the human body. Moreover, nanoparticles possess passive targeting capabilities, allowing them to accumulate intensively in tumor tissues through the enhanced permeability and retention (EPR) effects, thereby enhancing the effectiveness of the treatment ( 39 ). In order to enhance the targeting of tumors and improve the precision of treatment while minimizing damage to normal human cells, researchers have focused on targeting the tumor environment and various markers of cervical cancer. One approach is to load specific moieties onto specific nanoparticles, which has shown promising results ( 40 , 41 ). Such as taking advantage of the elevated expression of molecular proteins, such as the CD44 receptor, in the tumor microenvironment, researchers utilized hyaluronic acid (HA) coupled with chloro e44 (Ce6) to create Ce6-coupled HA nanophotosensitizers. These nanophotosensitizers were specifically designed to target HeLa human cervical cancer cells by binding to the CD44 receptor ( 42 ). In addition, in a clinical trial conducted by Antonio Carlos Figueiredo Vendette et al., 12 patients were treated with PDT, and 11 of them achieved the desired results. Among the 11 patients, two received 2 treatments while the rest received only one treatment. Importantly, none of these patients experienced any cytotoxicity, indicating that the combination of nanotechnology and PDT holds promise as a safe treatment for cervical cancer. However, it should be noted that 11 of the patients in this trial had CIN type 1, while only 1 had CIN type 2. Therefore, further investigation is needed to explore the effectiveness of PDT in treating highly differentiated cervical cancer ( 43 ). However, there are still a number of problems in the practical application of PDT in the clinic: firstly, PDT is currently mainly applied to superficial tumors in the human body, with limited effect on deep tumors where light transmission is blocked; secondly, the photosensitization of the patient’s skin after undergoing PDT is susceptible to side-effects; and lastly, due to the hydrophobicity of PS and the oxygen-dependence of PDT, the potential of PDT for the treatment of cervical cancer is currently limited ( 44 – 47 ). After all, with the continuous advancement of nanotechnology, incorporating nanoparticles into PS may help overcome these challenges faced by PDT in clinical settings.
4.2.2 Nanotechnology in the drug delivery of cervical cancer
The mechanism of nanotechnology in drug delivery for cervical cancer treatment involves the preparation of nanoscale drug carriers. These carriers encapsulate anticancer drugs and deliver them accurately to cervical cancer tumor cells through targeted delivery and release. By altering the surface properties and structure of nanodrug carriers, they can achieve targeted delivery and better interact with cancer cells. Once the nanodrug carrier reaches cancer cells, it gradually releases the drug into the tumor cells through its own special structure or drug release mechanism. This targeted and controlled release method improves drug efficacy, reduces side effects, and minimizes drug resistance during treatment. The application of nanotechnology offers more precise and effective drug delivery methods for the treatment of cervical cancer.
By altering the size, shape, and surface properties of drug carriers, nanotechnology has the potential to enhance the precision of drug delivery ( 48 , 49 ). Chemotherapy is currently the primary treatment for tumors, but its efficiency is hampered by low solubility and lack of selectivity, which can increase toxicity to normal cells. Therefore, there is a need to focus on studying excellent carriers or developing new treatment strategies to address these issues and improve the effectiveness of chemotherapy ( 39 , 50 ). To overcome the limitations of chemotherapeutic agents, various synergistic therapeutic systems have been developed based on the characteristics of the tumor microenvironment. One such system is a targeted redox-sensitive micellar system (DOX/FCH) composed of ferrocene (Fc) and hyaluronic acid (HA), which enables the delivery of doxorubicin (DOX) for synergistic chemotherapy and chemodynamic therapy (CDT). The high affinity between HA and the CD44 receptor, which is highly expressed in human cervical cancer (HeLa) cells, allows DOX/FCH to accurately target the tumor site. The appropriate particle size facilitates the absorption of micelles by cells. Under a reducing environment that mimics the intracellular conditions of tumor cells, disulfide bonds are depolymerized, leading to approximately 50% release of DOX from DOX/FCH within 2 hours. The good biocompatibility of FCH in 3T3 cells and its evident cytotoxicity in HeLa cells suggest that FCH holds great potential as a nanocarrier. In addition, the cytotoxicity of DOX/FCH confirms the synergistic effect of CDT and DOX chemotherapy with FCH. Hence, DOX/FCH shows promising prospects for enhancing the efficacy of combination chemotherapy and CDT ( 51 ).
Nanotechnology has the potential to safeguard medications from the effects of the external environment and enhance their durability. For instance, in a specific research study, nanoparticles were used to encase the chemotherapy medication cisplatin, effectively preventing premature decomposition and metabolism within the body. This prolonged the drug’s duration of action and improved its therapeutic efficacy ( 52 ). Small molecule induced DNA hydrogels with encapsulation and release properties are also effective in maintaining drug properties. DNA, a natural biopolymer, can assemble polyA tail DNA motif into hydrogel using small molecule cyanuric acid. Researchers have conducted experiments on the encapsulation of various substances, including a small chemotherapy drug, a fluorescent molecule, two proteins, and several nanoparticle formulations. The results demonstrated the release of doxorubicin, small fluorescent molecules, and fluorescent labeled antibodies ( 53 ).
Nanotechnology can also enhance the permeability of drugs, allowing them to traverse blood-tissue or tumor tissue barriers and access cervical cancer lesions. In a particular study, doxorubicin, a chemotherapy medication, exhibited improved permeability in cervical cancer lesions, leading to a significant enhancement in its anti-tumor efficacy ( 54 ). Due to the enhanced permeation and retention effects, stereocomplex micelles can selectively accumulate at the tumor site. In this study, a reliable drug delivery mechanism was created by combining enantiomeric 4-armed poly (ethylene glycol)–poly (D-lactide) and poly (ethylene glycol)–poly (L-lactide), aiming to regulate drug release and enhance tumor cell absorption for effective treatment of cervical carcinoma. The DOX-loaded micelles, including poly (D-lactide)-based micelle (PDM/DOX), poly (L-lactide)-based micelle (PLM/DOX), and stereocomplex micelle (SCM/DOX), all had sizes around 100 nm, which is suitable for the augmented permeability and retention (EPR) phenomenon. The effectiveness of DOX-loaded micelles, particularly SCM/DOX, in inhibiting tumors was confirmed in the U14 cervical carcinoma mouse model. The groups treated with DOX-loaded micelles, especially the SCM/DOX group, showed a significant increase in tumor cell death and necrosis. Moreover, these DOX-infused micelles demonstrated a remarkable reduction in DOX’s systemic toxic effects. Therefore, SCM shows potential as an effective drug delivery mechanism for future treatments of cervical carcinoma ( 55 ).
Nanotechnology can be used to transport medications more efficiently to cervical cancer lesions, reducing the accumulation of drugs in healthy tissues and minimizing their adverse effects. For example, in a specific study, researchers utilized nanotechnology to encapsulate the chemotherapy medication doxorubicin within lipid nanoparticles, which helped mitigate the drug’s harmful effects on healthy tissues such as the liver ( 56 ). Moreover, novel epirubicin-loaded nanoformulations were prepared from doxorubicin, which has a higher biocompatible therapeutic index ( 57 ). Cancer-specific drug delivery not only prevents adverse effects but also enhances drug accumulation in tumors. Therefore, surface modification of targeted selenium nanoparticles (SeNPs) with folic acid (FA) is an effective strategy for cancer treatment. FA-SeNPs nanoparticles are created by modifying SeNPs with folic acid, which binds to receptors overexpressed on the surface of cancer cells, including human cervical cancer HeLa cells, resulting in a tumor-targeting delivery vehicle. Subsequently, the anticancer drug DOX is loaded onto the surface of FA-SeNPs to improve its anti-tumor efficacy in the treatment of human cervical cancer ( 58 ).
Moreover, nanotechnology has the potential to create a combination of multiple drugs. Fytas et al. (Year) synthesized novel 1-(2-aryl-2-adamantyl)piperazine derivatives and evaluated their antitumor properties against HeLa cervical cancer in vitro ( 59 ). Chen et al. (Year) investigated the improvement of cancer treatment through the use of an acid-reactive cytotoxic peptide-doxorubicin compound ( 60 ). Nanotechnology has the potential to unite multiple drug carriers, enabling the implementation of multidrug combination therapy, which enhances therapeutic effectiveness and reduces tumor resistance to individual medications.
In the past time, although researchers have done many experiments on nanoparticles in drug delivery, the efficiency of translating research results into clinical applications is still low ( 61 ). Most of the applications of nanomedicines in cervical cancer are still in the laboratory stage. Therefore, it is becoming increasingly important to translate effective nanoparticle delivery methods from the experimental stage to clinical applications.
In conclusion, nanotechnology has the potential to enhance drug targeting, improve drug stability, increase drug permeability, and reduce drug side effects in the treatment of cervical cancer. This technology could offer a novel approach to treating cervical cancer.
4.3 Future trend
The prominence graph of a keyword shows how long a certain keyword stays popular. The prominence graph allows us to obtain the possible trend in the future. From the Figure 4B , we can learn that photothermal therapy, Indocyanine Green, etc may be a new direction for future research.
4.3.1 Photothermal therapy
Despite radiotherapy being the primary treatment for cervical cancer, its potential side effects can significantly impact the outlook for patients. Recently, there has been a growing focus on near-infrared laser-induced photothermal therapy due to its advantageous biological safety characteristics ( 62 ). This therapy involves using light of a specific wavelengthto heat a photothermal agent, effectively killing tumor cells. Figure 5 demonstrates how nanoparticles are internalized in cells and convert light energy into heat, leading to the death of cancer cells. Photothermal therapy not only eliminates local tumor cells and minimizes damage to normal tissue cells, but also avoids the development of drug resistance, making it more effective than traditional radiotherapy. Nanotechnology advancements have enabled various nanomaterials to enhance the effectiveness of photothermal therapy and reduce its adverse effects through superior light absorption, conversion capacity, and biocompatibility. Moreover, certain nanomaterials can serve as both photothermal converters and innovative radiosensitizers, integrating radiotherapy and improving patient prognosis by enhancing photoelectric absorption efficiency and electron presence ( 63 , 64 ). Apart from serving as photothermal converting agents for photothermal therapy, nanoparticles of appropriate size can effectively guide drugs or photothermal agents to the desired tumor site due to their increased permeability and retention effect ( 65 ). This nanomaterial-based transport approach has the potential to significantly enhance treatment precision and effectiveness, while minimizing harm to healthy tissue cells. In addition to passive targeting, magnetic targeting may emerge as a promising technique in clinical applications ( 66 ). Magnetic targeting technology relies on external conditions to enhance the accumulation of nanoparticles in the body, without altering the internal conditions, and has the capability to effectively eliminate tumor tissues ( 67 ). Currently, most experiments in this field are limited to in vitro cellular experiments or in vivo experiments in mice, with limited clinical data. However, nanoparticles have demonstrated promising results in both in vitro and ex vivo experiments. The application of nanotechnology in clinical photothermal therapy requires further investigation. Despite the recognition of nanoparticles’ potential in photothermal therapy, there is still much room for exploration. In the future, the focus may shift towards discovering nanomaterials that are safer, more precise, and more efficient, while also increasing the sensitivity of tumor cells to radiotherapy.
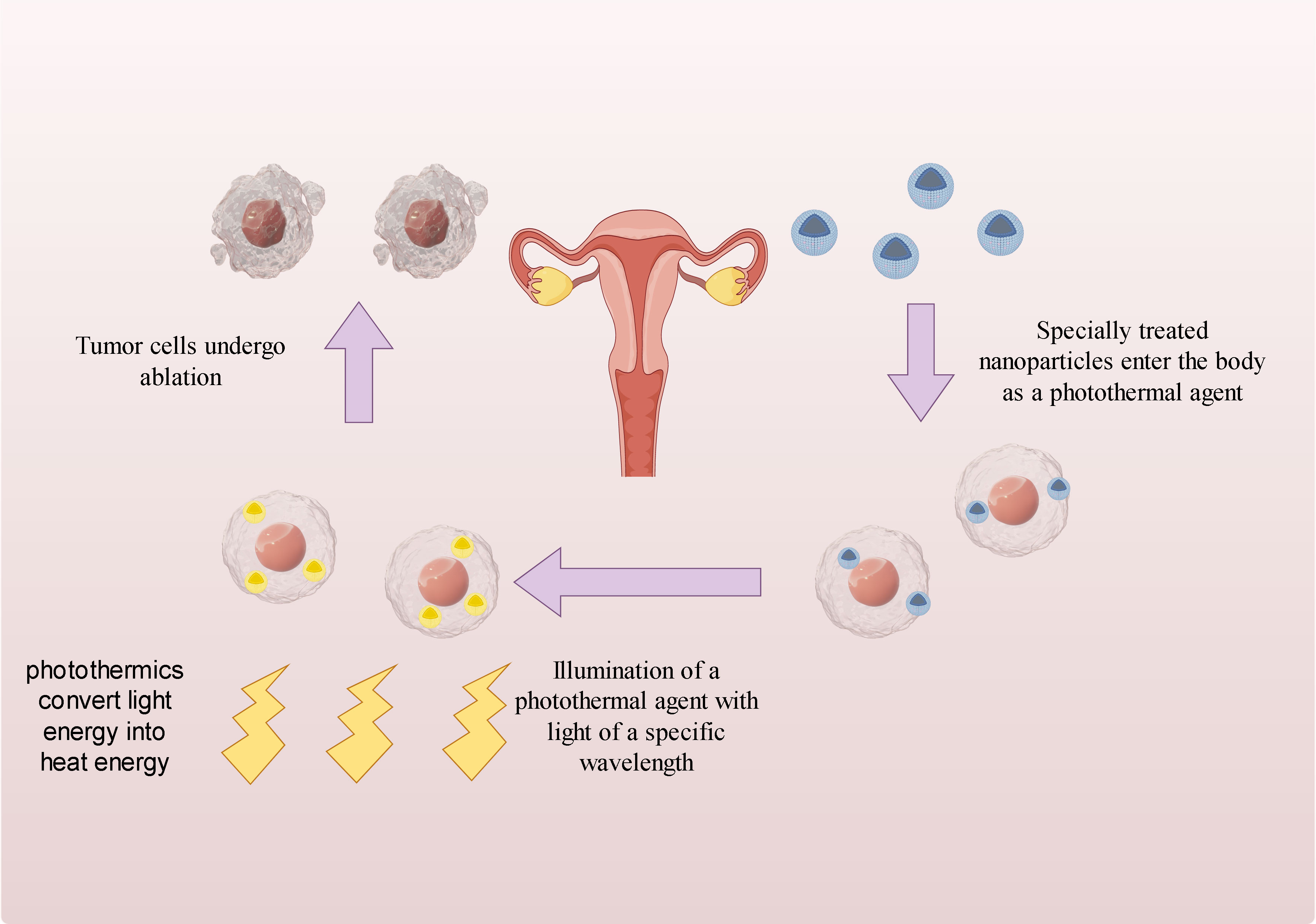
Figure 5 Mechanism of action of photothermal therapy.
4.3.2 Indocyanine green
Indocyanine Green (ICG) is a fluorescent dye commonly used in clinical practice and has been studied for the treatment of cervical cancer in recent years. Its application mechanism can be divided into two aspects:
4.3.2.1 Photothermal therapy
ICG exhibits good photosensitive properties and can absorb specific wavelength laser light sources. When exposed to a laser light source, ICG undergoes a photothermal effect, resulting in an increase in local temperature and causing thermal damage to cervical cancer cells. This therapy can induce tumor cell apoptosis, necrosis, and inhibit tumor growth.
For instance, researchers have explored the use of ICG-loaded lipid nanoparticles to induce intracellular thermal damage for effective treatment of cervical cancer ( 68 ). Additionally, polydopamine encapsulated novel indocyanine green therapeutic diagnostic nanoparticles have shown promise in enhancing the photothermal therapy of cervical cancer Hela cells ( 69 – 71 ). The use of nanomaterials with high photothermal conversion efficiency and excellent biocompatibility can significantly improve the overall photothermal conversion efficiency and increase the accumulation of photoacoustic agents in tumors ( 72 ).
4.3.2.2 Fluorescence guided surgery
ICG exhibits strong fluorescence characteristics and can emit fluorescence under near-infrared spectroscopy. It is a near-infrared fluorescent dye that is biocompatible. When excited by external light with a wavelength of 750-800 nm, it emits longer wavelength near-infrared light, appearing green under fluorescence laparoscopy. In cervical cancer surgery, doctors can intravenously inject ICG into patients, taking advantage of its accumulation in tumor tissue to emit strong fluorescence signals under near-infrared spectroscopy. Fluorescence guided surgery can then be used by doctors to locate and remove tumors, enhancing the accuracy and thoroughness of the procedure. According to Figure 6 , it can be observed that ICG-loaded nanoparticles accumulate in tumor cells after entering the body through blood vessels. Subsequently, when these tumor cells are exposed to infrared light, they exhibit a green fluorescence in the laparoscope.
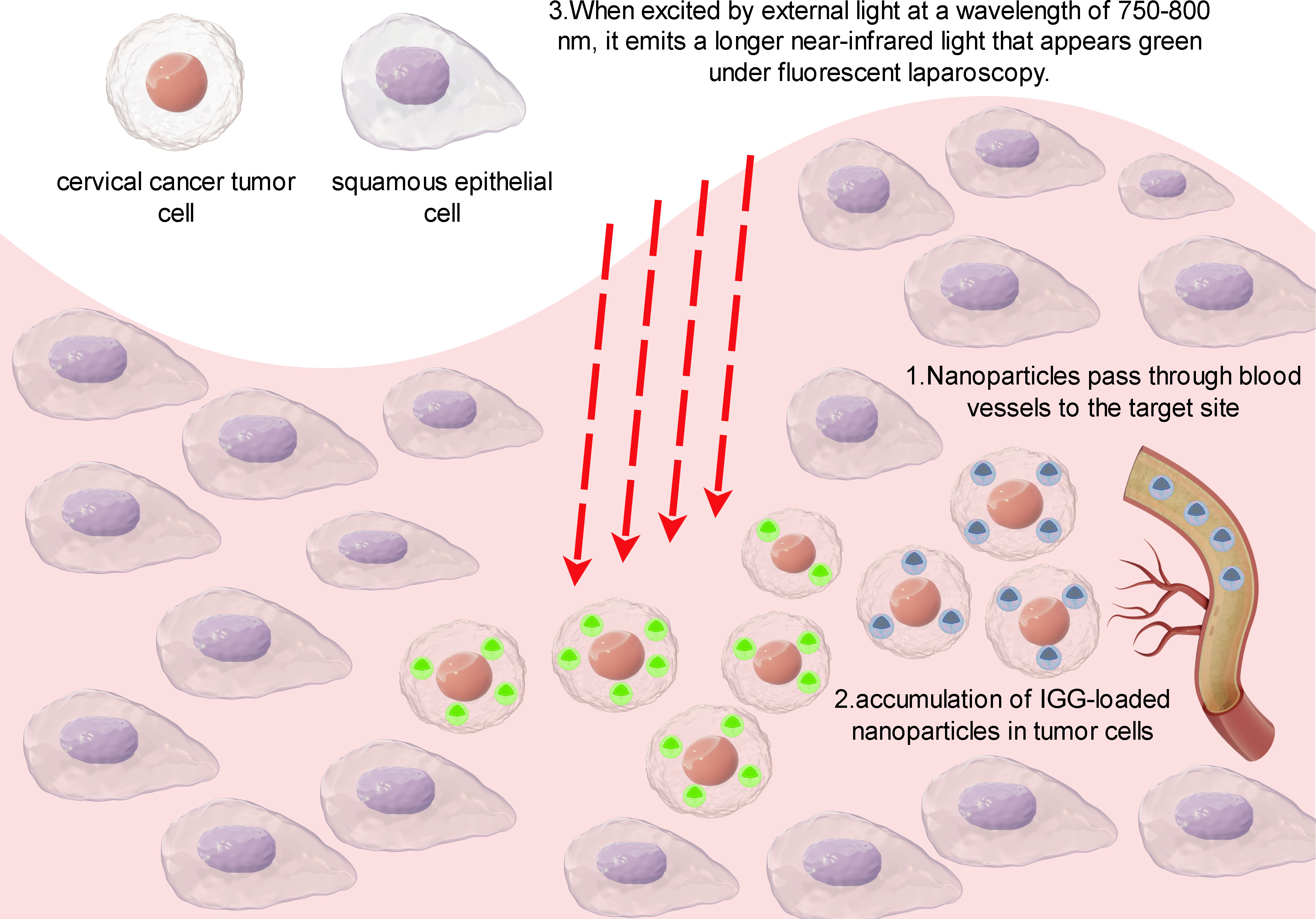
Figure 6 Principles of IGG-guided fluorescence imaging.
For instance, ICG dye can be utilized for sentinel lymph node (SLN) mapping in cervical cancer. SLN mapping is a viable surgical strategy that determines the necessity for radical lymph node dissection. It is based on the concept that SLN serves as the initial site of lymph node metastasis. If SLN is unaffected, it is theoretically assumed that the lymph nodes behind SLN should also be negative. The postoperative pathological confirmation rate of lymph node metastasis in most cervical cancer patients is approximately 24.16% ( 73 ). Therefore, pelvic lymph node dissection would not benefit them. The purpose of SLN biopsy is to avoid over-treatment by performing complete pelvic lymph node dissection on negative lymph nodes. This approach helps prevent complications associated with radical lymphadenectomy ( 74 ).
Combining indocyanine green (ICG) with nanoparticles can improve imaging localization. The use of ICG loaded with hyaluronic acid conjugated lactide-co-glycolide nanoparticles (HINPs) can enhance the target specificity of cervical cancer tumors. In vivo studies have demonstrated that HINPs enable near-infrared fluorescence imaging in cervical cancer cell lines. The efficiency of HINPs in delivering in vivo and the efficiency of free ICG in cervical cancer tumors were compared. Overall, HINPs have the potential to enhance NIR fluorescence image-guided surgery by assisting in the visualization of CD44-positive cervical cancer ( 75 ).
ICG imaging of lymph nodes is non-specific and cannot accurately distinguish between metastatic lymph nodes and inflammatory lymph nodes, resulting in a high false positive rate for tumor metastasis imaging. Additionally, ICG has inherent limitations such as poor water stability and low penetration depth, which affect its imaging performance. Furthermore, the lack of reactive groups in ICG makes it challenging to chemically synthesize it with other agents, such as targeting peptides. To overcome these limitations, active targeting using tumor-targeting ligands, such as targeting peptides, can be achieved by modifying the surface of nanoparticles. In this regard, the combination of the tumor metastasis-targeting peptide TMTP1 and ICG-loaded poly (ethylene glycol)-poly(lactide-co-glycolide acid) (PEG-PLGA) micelles was used to achieve active targeting. PEG-PLGA is a promising biodegradable polymer known for its biocompatibility, biodegradability, and sustained drug release properties, which contribute to more accurate imaging ( 76 ).
In summary, ICG can play a role in cervical cancer through two mechanisms: photothermal therapy and fluorescence guided surgery. Photothermal therapy utilizes the photosensitive properties of ICG to generate thermal effects and kill tumor cells through light irradiation. Fluorescence guided surgery utilizes the fluorescence characteristics of ICG to help doctors accurately locate and remove tumors during surgery, improving surgical effectiveness.
4.4 Limitation
The literature in our study may not be comprehensive. Firstly, our study focused only on WOOSC data and excluded data from other major search engines such as PubMed, EMBASE, and OVERE. Additionally, there is a language bias as we only retrieved articles published in English. Therefore, the articles found may not fully represent the body of research related to nanotechnology and cervical cancer. Secondly, high-quality papers published recently might not have received adequate attention due to low citation rates. These findings highlight the importance of regularly updating research. Although publications beyond September 20th, 2023 were excluded due to insufficient information, this review includes the majority of articles published between 2014 and 2023 in the field of cervical cancer and nanotechnology. Therefore, new data is unlikely to significantly impact the final results.
5 Conclusions
After conducting a comprehensive analysis using various scientometric instruments, we have successfully characterized the nanotechnology literature in the field of cervical cancer. Additionally, we have reviewed the current trends in nanotechnology development in cervical cancer-related fields and identified the current research hotspots. Moreover, we have analyzed the potential future directions for research in this area. The continuous growth of literature in this field signifies its increasing global importance, with China emerging as the leading publisher in this domain. The current research hotspots revolve around ‘nanoparticles’, ‘cervical cancer’, and ‘drug delivery’, while the future research trend may involve the integration of nanotechnology with ‘photothermal therapy’ and ‘indocyanine green’. It is evident that further research is required to fully explore the potential applications of nanotechnology in cervical cancer. The findings of these studies can provide valuable insights for new researchers in this field and contribute to the advancement of cervical cancer therapy.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
XS: Writing – original draft. XL: Writing – original draft. ZT: Writing – review & editing. LZ: Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Sichuan Provincial Medical Research Project Program (No. S19044); Chengdu Medical College Foundation Grant (No. CYZ18-14); the National College Student Innovation and Entrepreneurship Training Program Project (202213705036); Sichuan Provincial College Student Innovation and Entrepreneurship Training Program Project (S202313705089); the Development and Regeneration Key Laboratory of Sichuan Province(NoSYS13-006).
Acknowledgments
The authors are grateful to the reviewers for their thorough review of the manuscript, which allowed them to improve on the first draft.
Conflict of interest
Author ZT was employed by the company China National Nuclear Corporation 416 Hospital.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2024.1327851/full#supplementary-material
Supplementary Figure 1 | (A) Author co-authorship analysis carried on CiteSpace. (B) Analysis of co-cited authors carried on CiteSpace.
Supplementary Figure 2 | The collaboration network of institutions visualization map.
1. Giannella L, Di Giuseppe J, Delli Carpini G, Grelloni C, Fichera M, Sartini G, et al. Hpv-negative adenocarcinomas of the uterine cervix: from molecular characterization to clinical implications. Int J Mol Sci (2022) 23:15022. doi: 10.3390/ijms232315022
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Zafar A, Alruwaili NK, Imam SS, Alharbi KS, Afzal M, Alotaibi NH, et al. Novel nanotechnology approaches for diagnosis and therapy of breast, ovarian and cervical cancer in female: A review. J Drug Delivery Sci Technol (2021) 61:102198. doi: 10.1016/j.jddst.2020.102198
CrossRef Full Text | Google Scholar
3. Hegde YM, Theivendren P, Srinivas G, Palanivel M, Shanmugam N, Kunjiappan S, et al. A recent advancement in nanotechnology approaches for the treatment of cervical cancer. Anticancer Agents Med Chem (2023) 23:37–59. doi: 10.2174/1871520622666220513160706
4. Lee S-J, Yang A, Wu T-C, Hung C-F. Immunotherapy for human papillomavirus-associated disease and cervical cancer: review of clinical and translational research. J Gynecologic Oncol (2016) 27. doi: 10.3802/jgo.2016.27.e51
5. Rob L, Robova H, Chmel R, Komar M, Halaska M, Skapa P. Surgical options in early cervical cancer. Int J Hyperthermia (2012) 28:489–500. doi: 10.3109/02656736.2012.675116
6. Zhang H, Chen J. Current status and future directions of cancer immunotherapy. J Cancer (2018) 9:1773–81. doi: 10.7150/jca.24577
7. Maney V, Singh M. The synergism of platinum-gold bimetallic nanoconjugates enhances 5-fluorouracil delivery in vitro. Pharmaceutics (2019) 11. doi: 10.3390/pharmaceutics11090439
8. Jiang M, Liao J, Liu C, Liu J, Chen P, Zhou J, et al. Metal-organic frameworks/metal nanoparticles as smart nanosensing interfaces for electrochemical sensors applications: A mini-review. Front Bioeng Biotechnol (2023) 11:1251713. doi: 10.3389/fbioe.2023.1251713
9. Mei Y, Lin X, He C, Zeng W, Luo Y, Liu C, et al. Recent progresses in electrochemical DNA biosensors for sars-cov-2 detection. Front Bioeng Biotechnol (2022) 10:952510. doi: 10.3389/fbioe.2022.952510
10. Mei Y, He C, Zeng W, Luo Y, Liu C, Yang M, et al. Electrochemical biosensors for foodborne pathogens detection based on carbon nanomaterials: recent advances and challenges. Food Bioprocess Technol (2022) 15:498–513. doi: 10.1007/s11947-022-02759-7
11. Huang Q, Lin X, Chen D, Tong Q-X. Carbon dots/Α-fe2o3-fe3o4 nanocomposite: efficient synthesis and application as a novel electrochemical aptasensor for the ultrasensitive determination of aflatoxin B1. Food Chem (2022) 373:131415. doi: 10.1016/j.foodchem.2021.131415
12. Wang M, Peng P, Chen Z, Deng X. Nanoparticle delivery of active traditional chinese medicine ingredients: A new strategy for the treatment of liver cancer. Curr Pharm Biotechnol (2023) 24:1630–44. doi: 10.2174/1389201024666230313151316
13. Anwanwan D, Singh SK, Singh S, Saikam V, Singh R. Challenges in liver cancer and possible treatment approaches. Biochim Biophys Acta Rev Cancer (2020) 1873:188314. doi: 10.1016/j.bbcan.2019.188314
14. Yi X, Zeng W, Wang C, Chen Y, Zheng L, Zhu X, et al. A step-by-step multiple stimuli-responsive metal-phenolic network prodrug nanoparticles for chemotherapy. Nano Res (2022) 15:1205–12. doi: 10.1007/s12274-021-3626-2
15. Bakrania A, Zheng G, Bhat M. Nanomedicine in hepatocellular carcinoma: A new frontier in targeted cancer treatment. Pharmaceutics (2021) 14. doi: 10.3390/pharmaceutics14010041
16. Yang Y, Ren S, Huang W, Dong J, Guo J, Zhao J, et al. Camptothecin delivery via tumor-derived exosome for radiosensitization by cell cycle regulation on patient-derived xenograft mice. Front Bioeng Biotechnol (2022) 10:876641. doi: 10.3389/fbioe.2022.876641
17. Sykes PD, Neoptolemos JP, Costello E, Halloran CM. Nanotechnology advances in upper gastrointestinal, liver and pancreatic cancer. Expert Rev Gastroenterol Hepatol (2012) 6:343–56. doi: 10.1586/egh.12.13
18. Chen C, Song M. Visualizing a field of research: A methodology of systematic scientometric reviews. PloS One (2019) 14:e0223994. doi: 10.1371/journal.pone.0223994
19. Liu Y, Xu Y, Cheng X, Lin Y, Jiang S, Yu H, et al. Research trends and most influential clinical studies on anti-pd1/pdl1 immunotherapy for cancers: A bibliometric analysis. Front Immunol (2022) 13:862084. doi: 10.3389/fimmu.2022.862084
20. Yi F, Yang P, Sheng H. Tracing the scientific outputs in the field of ebola research based on publications in the web of science. BMC Res Notes (2016) 9:221. doi: 10.1186/s13104-016-2026-2
21. Ding X, Yang Z. Knowledge mapping of platform research: A visual analysis using vosviewer and citespace. Electronic Commerce Res (2022) 22:787–809. doi: 10.1007/s10660-020-09410-7
22. Rasouli E, Shahnavaz Z, Basirun WJ, Rezayi M, Avan A, Ghayour-Mobarhan M, et al. Advancements in electrochemical DNA sensor for detection of human papilloma virus - a review. Analytical Biochem (2018) 556:136–44. doi: 10.1016/j.ab.2018.07.002
23. Shah SS, Senapati S, Klacsmann F, Miller DL, Johnson JJ, Chang HC, et al. Current technologies and recent developments for screening of hpv-associated cervical and oropharyngeal cancers. Cancers (Basel) (2016) 8. doi: 10.3390/cancers8090085
24. Chinchulkar SA, Patra P, Dehariya D, Appidi T, Rengan AK. 22 - Gold Nanoparticle–Based Biosensing Applications and Fundamentals of Sensor Technology: Principles and Novel Designs. In: Barhoum A, Altintas Z, editors. Fundamentals of Sensor Technology Sawston, Cambridge: Woodhead Publishing (2023). p. 669–723. doi: 10.1016/B978-0-323-88431-0.00014-4
25. Foo ME, Gopinath SCB. Feasibility of graphene in biomedical applications. BioMed Pharmacother (2017) 94:354–61. doi: 10.1016/j.biopha.2017.07.122
26. Mahmoodi P, Rezayi M, Rasouli E, Avan A, Gholami M, Ghayour Mobarhan M, et al. Early-stage cervical cancer diagnosis based on an ultra-sensitive electrochemical DNA nanobiosensor for hpv-18 detection in real samples. J Nanobiotechnology (2020) 18:11. doi: 10.1186/s12951-020-0577-9
27. Cheng YH, Cheung YF, Siu-Chung Tam T, Lok CN, Sun H, Ng KM. Plasmonic metal nanoparticles as efficient mass tags for ion signal amplification and ultrasensitive detection of protein markers. Anal Chim Acta (2019) 1055:1–6. doi: 10.1016/j.aca.2018.12.057
28. Tam TS-C, Cheng Y-H, Lok C-N, Au-Yeung HY, Ni W-X, Wei X-L, et al. Surface optimization of gold nanoparticle mass tags for the sensitive detection of protein biomarkers via immuno-capture li-ms. Analyst (2020) 145:6237–42. doi: 10.1039/D0AN01121E
29. Sikaroodi M, Galachiantz Y, Baranova A. Tumor markers: the potential of “Omics” approach. Curr Mol Med (2010) 10:249–57. doi: 10.2174/156652410790963277
30. Wang H, Lakshmipriya T, Chen Y, Gopinath SCB. Squamous cell carcinoma biomarker sensing on a strontium oxide-modified interdigitated electrode surface for the diagnosis of cervical cancer. BioMed Res Int (2019) 2019:2807123. doi: 10.1155/2019/2807123
31. Wu D, Guo A, Guo Z, Xie L, Wei Q, Du B. Simultaneous electrochemical detection of cervical cancer markers using reduced graphene oxide-tetraethylene pentamine as electrode materials and distinguishable redox probes as labels. Biosensors Bioelectronics (2014) 54:634–9. doi: 10.1016/j.bios.2013.11.042
32. Liu X, Yang X, Shao J, Hong Y, Gopinath SCB, Chen Y, et al. Coordination of nanoconjugation with an antigen/antibody for efficient detection of gynecological tumors. J Analytical Methods Chem (2020) 2020:6528572. doi: 10.1155/2020/6528572
33. Chela-Flores J, Migoni RL. Cg methylation in DNA transcription. Int J Theor Phys (1990) 29:853–62. doi: 10.1007/BF00675102
34. Huang J, Liou YL, Kang YN, Tan ZR, Peng MJ, Zhou HH. Real-time colorimetric detection of DNA methylation of the pax1 gene in cervical scrapings for cervical cancer screening with thiol-labeled pcr primers and gold nanoparticles. Int J Nanomedicine (2016) 11:5335–47. doi: 10.2147/ijn.S116288
35. Zhu L, Yan T, Alimu G, Zhang L, Ma R, Alifu N, et al. Liposome-loaded targeted theranostic fluorescent nano-probes for diagnosis and treatment of cervix carcinoma. J Biomed Nanotechnology (2022) 18:1289–301. doi: 10.1166/jbn.2022.3332
36. Cao W, Zeng X, Liu G, Li Z, Zeng X, Wang L, et al. Porphine functionalized nanoparticles of star-shaped poly(Ε-caprolactone)-B-D-Α-tocopheryl polyethylene glycol 1000 succinate biodegradable copolymer for chemophotodynamic therapy on cervical cancer. Acta Biomater (2015) 26:145–58. doi: 10.1016/j.actbio.2015.08.016
37. Lee S-R, Kim Y-J. Hydrophilic chlorin E6-poly(Amidoamine) dendrimer nanoconjugates for enhanced photodynamic therapy. Nanomaterials (2018) 8. doi: 10.3390/nano8060445
38. Deni E, Zamarrón A, Bonaccorsi P, Carmen Carreño M, Juarranz Á, Puntoriero F, et al. Glucose-functionalized amino-opes as biocompatible photosensitizers in pdt. Eur J Medicinal Chem (2016) 111:58–71. doi: 10.1016/j.ejmech.2016.01.041
39. Maeda H, Nakamura H, Fang J. The epr effect for macromolecular drug delivery to solid tumors: improvement of tumor uptake, lowering of systemic toxicity, and distinct tumor imaging in vivo. Adv Drug Delivery Rev (2013) 65:71–9. doi: 10.1016/j.addr.2012.10.002
40. Steichen SD, Caldorera-Moore M, Peppas NA. A review of current nanoparticle and targeting moieties for the delivery of cancer therapeutics. Eur J Pharm Sci (2013) 48:416–27. doi: 10.1016/j.ejps.2012.12.006
41. Bazak R, Houri M, El Achy S, Kamel S, Refaat T. Cancer active targeting by nanoparticles: A comprehensive review of literature. J Cancer Res Clin Oncol (2015) 141:769–84. doi: 10.1007/s00432-014-1767-3
42. Yoon J, Kim H, Jeong Y-IL, Yang HS. Cd44 receptor-mediated/reactive oxygen species-sensitive delivery of nanophotosensitizers against cervical cancer cells. Int J Mol Sci (2022) 23. doi: 10.3390/ijms23073594
43. Vendette ACF, Piva HL, Muehlmann LA, de Souza DA, Tedesco AC, Azevedo RB. Clinical treatment of intra-epithelia cervical neoplasia with photodynamic therapy. Int J Hyperthermia (2020) 37:50–8. doi: 10.1080/02656736.2020.1804077
44. Garland MJ, Cassidy CM, Woolfson D, Donnelly RF. Designing photosensitizers for photodynamic therapy: strategies, challenges and promising developments. Future Med Chem (2009) 1:667–91. doi: 10.4155/fmc.09.55
45. Huang Z, Xu H, Meyers AD, Musani AI, Wang L, Tagg R, et al. Photodynamic therapy for treatment of solid tumors–potential and technical challenges. Technol Cancer Res Treat (2008) 7:309–20. doi: 10.1177/153303460800700405
46. Kwon N, Kim H, Li X, Yoon J. Supramolecular agents for combination of photodynamic therapy and other treatments. Chem Sci (2021) 12:7248–68. doi: 10.1039/D1SC01125A
47. Li X, Lee S, Yoon J. Supramolecular photosensitizers rejuvenate photodynamic therapy. Chem Soc Rev (2018) 47:1174–88. doi: 10.1039/C7CS00594F
48. Khanna N, Chatterji T, Singh S, Pandey S. Application of stimuli responsive nanocomposites in drug delivery and theranostics to counter cancer proliferation and drug resistance. J Drug Delivery Sci Technol (2023) 88:104958. doi: 10.1016/j.jddst.2023.104958
49. Li B, Xia X, Chen J, Xia D, Xu R, Zou X, et al. Paclitaxel-loaded lignin particle encapsulated into electrospun pva/pvp composite nanofiber for effective cervical cancer cell inhibition. Nanotechnology (2021) 32:015101. doi: 10.1088/1361-6528/abb55a
50. Pourmadadi M, Ghaemi A, Shamsabadipour A, Rajabzadeh-Khosroshahi M, Shaghaghi M, Rahdar A, et al. Nanoparticles loaded with daunorubicin as an advanced tool for cancer therapy. Eur J Medicinal Chem (2023) 258:115547. doi: 10.1016/j.ejmech.2023.115547
51. Yang F, Wei P, Yang M, Chen W, Zhao B, Li W, et al. Redox-sensitive hyaluronic acid-ferrocene micelles delivering doxorubicin for enhanced tumor treatment by synergistic chemo/chemodynamic therepay. J Drug Delivery Sci Technol (2022) 77:103851. doi: 10.1016/j.jddst.2022.103851
52. Kousar K, Naseer F, Abduh MS, Kakar S, Gul R, Anjum S, et al. Green synthesis of hyaluronic acid coated, thiolated chitosan nanoparticles for cd44 targeted delivery and sustained release of cisplatin in cervical carcinoma. Front Pharmacol (2022) 13:1073004. doi: 10.3389/fphar.2022.1073004
53. He M, Nandu N, Uyar TB, Royzen M, Yigit MV. Small molecule-induced DNA hydrogel with encapsulation and release properties. Chem Commun (Camb) (2020) 56:7313–6. doi: 10.1039/d0cc03439h
54. Gabizon AA, Patil Y, La-Beck NM. New insights and evolving role of pegylated liposomal doxorubicin in cancer therapy. Drug Resist Update (2016) 29:90–106. doi: 10.1016/j.drup.2016.10.003
55. Niu K, Yao Y, Xiu M, Guo C, Ge Y, Wang J. Controlled drug delivery by polylactide stereocomplex micelle for cervical cancer chemotherapy. Front Pharmacol (2018) 9:930. doi: 10.3389/fphar.2018.00930
56. Gheibihayat SM, Jaafari MR, Hatamipour M, Sahebkar A. Improvement of the pharmacokinetic characteristics of liposomal doxorubicin using cd47 biomimickry. J Pharm Pharmacol (2021) 73:169–77. doi: 10.1093/jpp/rgaa005
57. Pourmadadi M, Ostovar S, Ruiz-Pulido G, Hassan D, Souri M, Manicum A-LE, et al. Novel epirubicin-loaded nanoformulations: advancements in polymeric nanocarriers for efficient targeted cellular and subcellular anticancer drug delivery. Inorganic Chem Commun (2023) 155:110999. doi: 10.1016/j.inoche.2023.110999
58. Xia Y, Xu T, Zhao M, Hua L, Chen Y, Wang C, et al. Delivery of doxorubicin for human cervical carcinoma targeting therapy by folic acid-modified selenium nanoparticles. Int J Mol Sci (2018) 19. doi: 10.3390/ijms19113582
59. Fytas C, Zoidis G, Tsotinis A, Fytas G, Khan MA, Akhtar S, et al. Novel 1-(2-aryl-2-adamantyl)Piperazine derivatives with antiproliferative activity. Eur J Medicinal Chem (2015) 93:281–90. doi: 10.1016/j.ejmech.2015.02.021
60. Chen L, Chen G, Yang Z, Wang H, Liu N, Liu Y, et al. Enhanced cancer treatment by an acid-sensitive cytotoxic peptide-doxorubicin conjugate. J Drug Delivery Sci Technol (2020) 60:102048. doi: 10.1016/j.jddst.2020.102048
61. Kalaydina R-V, Bajwa K, Qorri B, DeCarlo A, Szewczuk MR. Recent advances in “smart” delivery systems for extended drug release in cancer therapy. Int J Nanomed (2018) 13:4727–45. doi: 10.2147/ijn.S168053
62. Cole JR, Mirin NA, Knight MW, Goodrich GP, Halas NJ. Photothermal efficiencies of nanoshells and nanorods for clinical therapeutic applications. J Phys Chem C (2009) 113:12090–4. doi: 10.1021/jp9003592
63. Huang X, El-Sayed IH, Qian W, El-Sayed MA. Cancer cell imaging and photothermal therapy in the near-infrared region by using gold nanorods. J Am Chem Soc (2006) 128:2115–20. doi: 10.1021/ja057254a
64. Hainfeld JF, Dilmanian FA, Slatkin DN, Smilowitz HM. Radiotherapy enhancement with gold nanoparticles. J Pharm Pharmacol (2010) 60:977–85. doi: 10.1211/jpp.60.8.0005
65. Lucarini M, Franchi P, Pedulli GF, Pengo P, Scrimin P, Pasquato L. Epr study of dialkyl nitroxides as probes to investigate the exchange of solutes between the ligand shell of monolayers of protected gold nanoparticles and aqueous solutions. J Am Chem Soc (2004) 126:9326–9. doi: 10.1021/ja048554f
66. McBain SC, Yiu HH, Dobson J. Magnetic nanoparticles for gene and drug delivery. Int J Nanomedicine (2008) 3:169–80. doi: 10.2147/ijn.s1608
67. Hu R, Zheng M, Wu J, Li C, Shen D, Yang D, et al. Core-shell magnetic gold nanoparticles for magnetic field-enhanced radio-photothermal therapy in cervical cancer. Nanomaterials (2017) 7:111. doi: 10.3390/nano7050111
68. Yan Q-Q, Li B-L. Cinnamaldehyde and indocyanine green loaded lipid nanoparticles induced intracellular oxidative/thermal stress damage for effective cervical cancer therapy. Micro Nano Lett (2022) 17:175–80. doi: 10.1049/mna2.12120
69. Fan HM, Yan T, Chen S, Du Z, Alimu G, Zhu LJ, et al. Polydopamine encapsulated new indocyanine green theranostic nanoparticles for enhanced photothermal therapy in cervical cancer hela cells. Front Bioeng Biotechnol (2022) 10:984166. doi: 10.3389/fbioe.2022.984166
70. Yan T, Alimu G, Zhu LJ, Fan HM, Zhang LX, Du Z, et al. Ppix/ir-820 dual-modal therapeutic agents for enhanced pdt/ptt synergistic therapy in cervical cancer. ACS Omega (2022) 7:44643–56. doi: 10.1021/acsomega.2c02977
71. Ma R, Alifu N, Du Z, Chen S, Heng YQ, Wang J, et al. Indocyanine green-based theranostic nanoplatform for nir fluorescence image-guided chemo/photothermal therapy of cervical cancer. Int J Nanomed (2021) 16:4847–61. doi: 10.2147/ijn.S318678
72. Cheng L, Wang C, Feng L, Yang K, Liu Z. Functional nanomaterials for phototherapies of cancer. Chem Rev (2014) 114:10869–939. doi: 10.1021/cr400532z
73. Fuchs J, Hamann MF, Schulenburg F, Knüpfer S, Osmonov D, Lützen U, et al. [Sentinel lymph node biopsy for penile carcinoma : assessment of reliability]. Urologe A (2013) 52:1447–50. doi: 10.1007/s00120-013-3166-9
74. Lu Y, Wei JY, Yao DS, Pan ZM, Yao Y. Application of carbon nanoparticles in laparoscopic sentinel lymph node detection in patients with early-stage cervical cancer. PloS One (2017) 12:e0183834. doi: 10.1371/journal.pone.0183834
75. Choi S, Lee SH, Park S, Park SH, Park C, Key J. Indocyanine green-loaded plga nanoparticles conjugated with hyaluronic acid improve target specificity in cervical cancer tumors. Yonsei Med J (2021) 62:1042–51. doi: 10.3349/ymj.2021.62.11.1042
76. Wei R, Jiang G, Lv M, Tan S, Wang X, Zhou Y, et al. Tmtp1-modified indocyanine green-loaded polymeric micelles for targeted imaging of cervical cancer and metastasis sentinel lymph node in vivo . Theranostics (2019) 9:7325–44. doi: 10.7150/thno.35346
Keywords: nanotechnology, cervical cancer, bibliometrics, nanoparticles, drug deliver
Citation: Song X, Li X, Tan Z and Zhang L (2024) Recent status and trends of nanotechnology in cervical cancer: a systematic review and bibliometric analysis. Front. Oncol. 14:1327851. doi: 10.3389/fonc.2024.1327851
Received: 25 October 2023; Accepted: 31 January 2024; Published: 20 February 2024.
Reviewed by:
Copyright © 2024 Song, Li, Tan and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhiwei Tan, [email protected] ; Lushun Zhang, [email protected]
† These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Editorial Team
- Exclusive Interviews
- In the News
- Partners & Affiliates
- Advertise With Us
- हिन्दी
- français
- Español
- 中文

- Login Register
- Consult Online Doctor
- Take Telemedicine course
- Health Centers
- Health Tools
- Health info by Speciality
- Know Your Body
- Health and Wellness
- Web Stories
- Health Tips
- Nutrition Facts
- Lifestyle & Wellness
- Beauty Tips
- Diet & Nutrition
- Home Remedies
- Obesity & Weight Loss
- Complementary Medicine
- Special Reports
- Press Releases
- Health Guide
- Health articles
- Health Quiz
- Health Facts
- Travel Health
- Screening Tests
- Medicine and Movies
- Symptom Articles
- Diabetes Tools
- Pediatric Calculators
- Men's Health
- Women's Health
- Height Weight Tools
- Cardiac Tools
- Pharma Tools
- Wellness Interactive Tools
- Drug Information
- Drugs by Condition
- Drug Price List - Brand Names
- Drug Interaction with Food
- Drug Price List - Generic Names
- Drugs - Side Effects
- Drug Videos
- Drug Database
- Doctor Directory
- Diagnostic Lab Directory
- Hospital Directory
- Chemist Directory
- Surgical Suppliers
- Pharma Directory
- Emergency Services
- PG Education
- Family Medicine
- Other Resources
- Medical Aphorism
- Health Acts in India
- Health Quotations
- Medical Conference
- Amazing Body Facts
- Health poll
- Medical Education
- Distance Education
- Cervical Cancer
- << Adenocarcinoma
- Leukocytosis >>
Post a Comment
Comments should be on the topic and should not be abusive. The editorial team reserves the right to review and moderate the comments posted on the site.
Notify me when reply is posted
I agree to the terms and conditions
Post Comment
its so beneficial

CME Lessons
- A Diagnostic approach to Proteinuria
- A Focused approach to Anemia
- Abdominal Pain
- Abdominal pain in women
- Abnormal Vaginal Bleeding
- Acid Peptic Disease
- Acute evaluation and management of ischemic stroke-1
- Acute Respiratory infections in Children
- Acute sinusitis
- Adult immunizations
- Ambulatory Management of Burns
- An Introduction to Biomedical Ethics
- Anorectal Examination
- Approach to Breast Lumps
- Approach to the Somatizing Patient
- Approach to Vaginitis
- Cannot Miss Diagnosis
- Childhood Epilepsy
- Cholelithiasis
- Common Bed Side Procedures
- Conjunctivitis
- Constipation in Children
- Dermatologic
- Diagnosis and Management of Alcohol Problems
- Diarrhea in Children
- Emergency Thora Centesis
- Endometriosis
- Evaluation of headache
- Febrile Seizures
- Fever in Children
- Head Ache in Children
- Heamorrhoids
- Immunization in Children
- Incision and Drainage of abscess
- Infective Endocarditis
- Intraosseous Fluid Infusion
- Introduction to Dermatology
- Laboratory Evaluation of the patient with jaundice
- Leukocytosis
- Low Back Pain
- Management of Heart Failure
- Managing Pshychiatric disorders in Primary Care
- Meningitis in Children
- Obstructed Femoral Hernia
- Overview of the risk factors for cardiovascular disease
- Perforated Peptic Ulcer
- Pericardio Centesis
- Premenstrual syndrome
- Preoperative medical evaluation of the healthy patient
- Pressure Ulcers
- Primary Dysmenorrhea
- Recurrent Abdominal Pain
- School Problems and the Family Physician
- Skin Infections
- Somatoform Disorders
- The Crying Infant Pleural Effusion
- Tuberculosis in Children
- Urinary Incontinence in Women
- Urinary tract infection
- Urinary Tract Infection in the Paediatric Patient
- Alendronate
- Amitriptyline
- Diphenhydramine
- Epinephrine
- Ferrous Sulphate
- Glibenclamide
- Hydroxyzine
- Octreotide Acetate
- Pioglitazone Hydrochlorid
- Propranolol
- Rosiglitazone Maleate
- Silver sulfadiazine
- Sumatriptan
- Valproic Acid
- Spironolactone
What's New on Medindia

Medindia Newsletters
Subscribe to our Free Newsletters!
Terms & Conditions and Privacy Policy.
Stay Connected
This site uses cookies to deliver our services.
By using our site, you acknowledge that you have read and understand our Cookie Policy , Privacy Policy , and our Terms of Use
Cervical Cancer Research
For some people with early-stage cervical cancer, a surgical procedure called a simple hysterectomy may be a safe and effective alternative to treatment with a radical hysterectomy, results from the SHAPE trial show.
It may be worthwhile for some individuals between ages 65 and 69 to get tested for HPV, findings from a Danish study suggest. Specifically, the testing may help prevent cervical cancer among those who haven’t had cervical cancer screening for at least 5 years.
One dose of the HPV vaccine was highly effective in protecting young women against infection from high-risk HPV types, a study in Kenya found. A single dose would make HPV vaccines more accessible worldwide, reducing cervical cancer’s global burden.
The rates of timely cervical cancer screening fell between 2005 and 2019, researchers found, and disparities existed among groups of women. The most common reason for not receiving timely screening was lack of knowledge about screening or not knowing they needed screening.
Fewer women with early-stage cervical cancer are having minimally invasive surgery, including robotic, as part of their treatment, a new study shows. The shift toward more open surgeries follows the release of results from the LACC trial in 2018.
Widespread HPV vaccine use dramatically reduces the number of women who will develop cervical cancer, according to a study of nearly 1.7 million women. Among girls vaccinated before age 17, the vaccine reduced cervical cancer incidence by 90%.
Updated cervical cancer screening guidelines from the American Cancer Society recommend HPV testing as the preferred approach. NCI’s Dr. Nicolas Wentzensen explains the changes and how they compare with other cervical cancer screening recommendations.
In a new study, an automated dual-stain method using artificial intelligence improved the accuracy and efficiency of cervical cancer screening compared with the current standard for follow-up of women who test positive with primary HPV screening.
More than a decade after vaccination, women who had received a single dose of the HPV vaccine continued to be protected against infection with the two cancer-causing HPV types targeted by the vaccine, an NCI-funded clinical trial shows.
Women with cervical or uterine cancer who received radiation to the pelvic region reported side effects much more often using an online reporting system called PRO-CTCAE than they did during conversations with their clinicians, a new study shows.
A research team from NIH and Global Good has developed a computer algorithm that can analyze digital images of the cervix and identify precancerous changes that require medical attention. The AI approach could be valuable in low-resource settings.
A new test can help to improve the clinical management of women who screen positive for HPV infection during routine cervical cancer screening, an NCI-led study has shown.
FDA has approved pembrolizumab (Keytruda) for some women with advanced cervical cancer and some patients with primary mediastinal large B-cell lymphoma (PMBCL), a rare type of non-Hodgkin lymphoma.
By comparing the genomes of women infected with a high-risk type of human papillomavirus (HPV), researchers have found that a precise DNA sequence of a viral gene is associated with cervical cancer.
Investigators with The Cancer Genome Atlas (TCGA) Research Network have identified novel genomic and molecular characteristics of cervical cancer that will aid in subclassification of the disease and may help target therapies that are most appropriate for each patient.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Cervical cancer.
Josephine R. Fowler ; Elizabeth V. Maani ; Charles J. Dunton ; David P. Gasalberti ; Brian W. Jack .
Affiliations
Last Update: November 12, 2023 .
- Continuing Education Activity
Cervical cancer, the fourth most common cancer among women worldwide, is caused almost entirely by human papillomavirus (HPV). High-risk types of HPV can lead to cervical intraepithelial lesions which, over time, can progress to cervical cancer. In the United States and other developed countries, most screening and early detection efforts involve HPV testing and Papanicolaou (Pap) smears. HPV testing identifies exposure to both low- and high-risk types of HPV, whereas Pap smears identify abnormal cytology.
Cervical cancer is a largely preventable disease. Primary prevention and screening are the most effective modalities for decreasing the healthcare burden and mortality attributable to cervical cancer. Since 2006, HPV vaccination has been available to prevent cervical cancer. Interprofessional team members must educate young female patients (ideally, prior to initiating sexual activity) and their families about this highly effective vaccine. This activity details primary prevention strategies, screening guidelines, diagnostic evaluations, current staging, and specific treatment modalities for invasive cervical cancer.
- Identify the risk factors, signs, and symptoms of cervical cancer, including the role of high-risk HPV types in its development.
- Apply evidence-based treatment modalities for precancerous cervical lesions, and assess the indications, techniques, potential complications, and follow-up care associated with these interventions.
- Select appropriate treatment modalities for invasive cervical cancer based on patient characteristics, staging, and available options, including surgery, radiation, and chemotherapy.
- Collaborate with the interprofessional team to increase HPV vaccination initiatives and to ensure coordinated and comprehensive care for patients diagnosed with cervical cancer.
- Introduction
Cervical cancer continues to rank among the top gynecologic cancers worldwide. According to current data, it is ranked 14th among all cancers and is the 4th most common cancer among women worldwide. [1] Cervical cancer intervention focuses on primary and secondary prevention. [2] Primary prevention and screening are the best methods to decrease the burden of cervical cancer and mortality.
In the United States and other developed countries, most screening and diagnostic efforts are directed toward the early identification of high-risk human papillomavirus (HPV) lesions through HPV testing and Papanicolaou (Pap) smears. Although HPV testing is not recommended in women younger than 30 years, low-risk younger women should begin screening with Pap tests at age 21 and continue until age 65, per the United States Preventive Services Task Force (USPSTF) recommendations. Newer recommendations offer 3- to 5-year intervals between screenings based on a patient's prior results and the use of Pap and HPV cotesting. [3] [4]
Like many diseases and cancers, disparities exist in screening, early diagnosis, and timely treatment rates. Screening rates are lower in low socioeconomic and low-resource areas with racial, ethnic, and age variations. Studies show women with obesity and chronic disease may have lower cervical and breast cancer screening rates. A study of ethnic minority women in the United Kingdom reports several barriers to screening, including lack of awareness, fear, embarrassment, shame, and low perceived risk. [5] Another study reviewing the barriers for Haitian women revealed socioeconomic barriers, language barriers, and a limited understanding of health and disease. [6] In the United States, cervical cancer mortality is disproportionately higher in black women.
As cervical cancer is a sexually transmitted infection (STI), it is preventable, and the global incidence can be reduced through targeted education, screening, and intervention. Since 2006, vaccination has been available for the prevention of cervical cancer. Vaccination can improve cancer death rates in populations with higher mortality rates and in developing countries where resources may not be available for routine screening.
Current literature reports that HPV is found in most sexually active people at some point during their lifetime. There are more than 130 types of known HPV, with 20 HPV types identified as cancer-related. HPV exposure rates are only known in women since men are not screened outside of research protocols. HPV types 16 and 18 are the most common HPV types identified in invasive cervical cancer. Population-based HPV prevalence studies show the greatest prevalence of high-risk HPV occurs in adults younger than 25 years, and cervical cancer deaths peak in middle-aged women between 40 and 50 years. Studies have shown that HPV-related cervical disease in women younger than 25 years is largely self-limiting. However, those with coinfection of multiple HPV types may be less likely to have spontaneous clearance and, thus, progress to cancer.
HPV is transmitted by skin-to-skin contact, including during sexual intercourse, hand-to-genital contact, and oral sex. Risk factors for HPV and cervical cancer include young age at sexual initiation, multiple sexual partners, high parity, smoking, herpes simplex, HIV, coinfection with other genital infections, and oral contraceptive use. [7] [8]
- Epidemiology
Persistent HPV infection causes more than 99% of all cervical cancers. Every year, there are more than 500,000 new cases of cervical cancer and approximately 250,000 deaths due to cervical cancer worldwide. Eighty percent of cases occur in developing countries. [9] In the United States, about 4000 women die yearly from cervical cancer. Blacks, Hispanics, and women in low-resource areas have more disparity in evidenced-based care and a significantly higher mortality rate. [10] [11] Mortality is higher among women not screened in the past 5 years and those without consistent follow-up after identifying a precancerous cervical lesion. Trends show that women with the highest-mortality risk may be less likely to receive HPV vaccination.
- Pathophysiology
More than 75% of cervical cancer cases are due to high-risk HPV types 16 and 18. [12] Other HPV types also can cause malignancy. Some low-risk HPV types, specifically types 6 and 11, cause condylomata acuminate, commonly referred to as anogenital warts. Although there are more than half a million cases of HPV identified annually, most are low-grade infections and will spontaneously resolve within 2 years. The progression of high-grade lesions and cancer is seen in the presence of other carcinogenic risk factors, as previously described.
Within HPV DNA, the oncoproteins E6 and E7 interfere with the critical host cell cycle; specifically, E6 interferes with suppressive tumor protein p53, whereas E7 interferes with retinoblastoma protein (pRB). Additionally, the E5 protein may play a role in immune evasion. These are significant factors in HPV-related neoplasia, including primary vagina cancer. [13] Oxidative stress and microRNAs are believed to play a role in cervical carcinogenesis. Future research to elucidate the proposed interplay is needed. [12] [14]
- Histopathology
Squamous cell carcinoma and adenocarcinoma are the most common histological subtypes of cervical cancer, with squamous cell carcinoma being vastly more frequent. Adenocarcinoma constitutes approximately 5% of invasive cervical cancers worldwide, although this percentage is increasing in some countries. [15] Both subtypes result from precursor lesions, cervical intraepithelial neoplasia (CIN), or carcinoma in situ (CIS). Squamous CIS and adenocarcinoma in situ (AIS) are the most immediate precursors to invasive cervical cancer. Adenocarcinoma of the cervix should be carefully distinguished from endometrial adenocarcinoma with immunohistochemistry and HPV in situ hybridization. [16]
Most malignancies arise from the sqamocolumnar junction of the cervix. Microscopically, anastomosing irregular nests or single tumor cells with stromal inflammation or desmoplasia are present. Lymphovascular invasion (LVI) may also be present. Grading is predicated on nuclear pleomorphism, nucleoli size, mitotic activity, and necrosis, and does not correlate with prognosis. [17]
- History and Physical
Patients with cervical cancer are usually asymptomatic during the early stages. A complete medical history must include a sexual history, including the patient's age at first sexual encounter. Sexual history also includes questions about postcoital bleeding and pain during intercourse. Questions about previous STIs, including HPV and HIV, the number of lifetime sexual partners, tobacco use, and prior vaccination against HPV are all vitally important. [18] Women should also be asked about menstrual patterns, abnormal bleeding, persistent vaginal discharges, irritations, and known cervical lesions. [19]
The physical exam must include a complete evaluation of the external and internal genitalia. Positive exam findings in women with cervical cancer might include a friable cervix, visible cervical lesions, erosions, masses, bleeding with the examination, and fixed adnexa. [20] Many patients will have no positive findings on physical examination. Screening by Pap and/or HPV testing is essential in the workup and diagnosis of patients with cervical cancer and its precursor lesions.
According to the United States Preventative Services Task Force (USPTF), Pap screening is recommended beginning at age 21; at age 30, HPV testing starts in conjunction with Pap smear cytology. Screening is recommended every 3 years for women with continued negative screening results and those at low risk for cervical cancer. For women older than 30 years, cytology can be done every 5 years with HPV testing. One Level A recommendation for women with low-risk status and consistently negative screenings is discontinuing cervical cytology and HPV testing at age 65. Women who have had a total abdominal hysterectomy, including removal of the cervix for benign disease, do not require subsequent screening. [4]
Colposcopy is the diagnostic procedure of choice for evaluating abnormal cytology and/or persistent high-risk HPV infection. The American Society for Colposcopy and Cervical Pathology (ASCCP) has issued guidance on procedural indications, and their recommended algorithms are considered standard of care. Multiple colposcopic-guided biopsies and endocervical sampling are often indicated, except during pregnancy. [21] Abnormal colposcopic findings may include acetowhite color change with the application of acetic acid, rich vascularity, atypical vessels, mosaicism, and punctation (see Image. Invasive Cervical Cancer).
Patients diagnosed with invasive disease require a comprehensive staging workup. The International Federation of Gynecology and Obstetrics (FIGO) staging system employs several methods to stage a patient's disease. Classically, staging was based on the local extent of the tumor, which could be determined with a combination of pelvic examination, cystoscopy, proctoscopy, chest x-ray, intravenous pyrography, and basic labs. More recently, advanced imaging modalities such as MRI and PET scans have been utilized for staging. A pelvic MRI is excellent for detecting local tumor extension and can also be used for monitoring tumor response. PET scans are more sensitive than CT scans for detecting nodal and visceral metastases. This is critical as nodal disease can significantly influence prognosis. [22]
- Treatment / Management
Precancerous lesions are managed conservatively for women younger than 25 years. Most positive findings in women younger than 25 years are low-risk cervical dysplasia and will resolve spontaneously. Colposcopy evaluates persistent, abnormal cytology or lesions suspected to be moderate or high risk. These are managed according to findings.
Low-risk lesions may be observed and reevaluated more frequently, and high-risk lesions are treated based on size, depth, and location. Cryotherapy or excision is performed to manage precancerous lesions limited in size and depth. Conization, laser, or loop electrosurgical excision procedure (LEEP) are used to manage lesions that include the endocervical canal and are more extensive. LEEP may provide better visualization of the squamocolumnar junction and provide the benefit of less bleeding in the outpatient setting. [23]
If invasive cancer is diagnosed, the next step in management is staging to determine further treatment. Staging is based on findings and results from reported signs and symptoms, examination, tissue pathology, and imaging. Grading is based on the size and depth of the cancer and signs of spread to other organs. Treatment of early-stage disease is typically surgical resection, ranging from a conization to a modified radical hysterectomy. However, women with high-risk pathology postresection may require adjuvant treatment with chemotherapy and radiation. Conization or trachelectomy may be an option for women with early-stage disease who desire future fertility. For patients with more advanced disease, concurrent chemoradiation is the standard of care.
- Differential Diagnosis
Evaluating visible cervical lesions for invasive cancer is essential. However, as discussed above, most cervical cancer is asymptomatic and will not present with an overt mass in the early stages. Other possible causes of cervical lesions and/or abnormal bleeding include STIs, cervical polyps or fibroids, and endometriosis. Diagnosis may require further evaluation of symptoms and testing to determine whether the disease is cervical cancer. A diagnostic biopsy is needed to finalize the diagnosis.
Other pathology-determined conditions in the differential diagnosis include carcinosarcoma, epithelioid trophoblastic tumor, placental site nodule, immature squamous metaplasia, and metastatic disease from a noncervical primary tumor. Rarely, a routine Pap smear may identify metastatic cancer on the uterine cervix. [24]
- Surgical Oncology
Surgical resection is offered to patients with early-stage disease confined to the cervix; it can range from relatively noninvasive procedures such as cervical conization to more extensive operations such as radical hysterectomy. Although surgery is the preferred treatment modality for early-stage cervical cancer, it is especially important in younger patients for whom preservation of ovarian function and/or fertility is desired. Surgery is also indicated in select patients with recurrent disease.
Types of Surgery
Cervical conization
Cervical conization is typically indicated in patients with CIS or stage IA1 invasive cervical cancer. Using a scalpel or laser, a cold knife cone (CKC) removes the cervical transformation zone and a portion of the cervix with at least a 3-mm margin. Pathologic evaluation of the margins and assessment of the presence or absence of lymphovascular invasion (LVI) are critical. If a positive margin or LVI is present, reexcision or more invasive surgical treatment may be required.
If no LVI exists on the specimen, lymph node involvement is exceedingly rare, so nodal evaluation is unnecessary. Patients without any adverse pathologic findings may be observed. Recurrence rates are typically <10%, but patients must be followed closely with periodic colposcopy and cytology. Five-year survival rates exceed 95%. Complications include hemorrhage, infection, cervical incompetence, cervical stenosis, and infertility. The complication rate ranges from 2% to 12%. [25] [26]
Radical trachelectomy
Patients who are not candidates for conization due to adverse pathological features or more advanced disease but who desire future fertility are candidates for a radical trachelectomy. The procedure consists of removing most of the cervix, resecting the parametria, and mobilizing the ureters, bladder, and rectum. A 5-mm section of the cervix is preserved for the placement of a cerclage, allowing for future pregnancy. Due to the increased risk of nodal involvement, a lymph node evaluation with a sentinel node biopsy or pelvic lymphadenectomy typically accompanies a radical trachelectomy.
Adverse pathologic features such as positive margins, parametria involvement, lymph node involvement, or meeting Sedlis criteria would necessitate adjuvant treatment with radiotherapy with or without chemotherapy. A vaginal approach or laparotomy can be used, but there are insufficient data on minimally invasive techniques. The 5-year recurrence rate is approximately 5%, and the overall survival rate is 97%. The pregnancy rate postprocedure is 24%, with a live birth occurring in 75% of patients. [27] Complications include cervical suture problems, dysmenorrhea, isthmic stenosis, and vaginal discharge.
Extrafascial hysterectomy
Extrafascial hysterectomy, also known as a Type A radical hysterectomy, has a narrow range of clinical indications. [28] Typically, this surgery is offered to patients with stage IA1 disease who are not interested in future fertility; it involves the removal of the entire cervix and uterus. As ovarian removal is optional, ovarian function can be preserved. The parametria are not resected, and a vaginal approach or laparotomy may be utilized. Lymph node evaluations are not usually performed unless adverse pathologic features are discovered postoperatively. Patients with adverse pathologic features may require a complete parametrectomy or external beam radiotherapy with or without chemotherapy.
Radical hysterectomy
A radical hysterectomy may be considered in almost all early-stage cervical cancer cases when fertility preservation is not desired. The older Piver-Rutledge-Smith classification has been replaced by the Querleu–Morrow system, which simplifies the classification process based solely on the extent of lateral parametria resection. Four types of radical hysterectomy are described (Types A through D). Type A includes a minimal parametrial resection. In contrast, Type D completely resects the paracervical region to the pelvic sidewall. The most commonly performed radical hysterectomies fall in the Type B and C categories, which differ in the transection of the paracervical region at the level of the ureters or internal iliac vessels, respectively. [29]
Minimally invasive approaches have been shown to provide inferior oncologic outcomes compared with more established open approaches in terms of disease-free survival (91% vs 97%) and overall survival (93% vs 99%), with most patients having stage IB1 disease. [30] Complications include bleeding, infection, venous thromboembolism, pulmonary embolus, small bowel obstruction, vesicovaginal fistula, hydronephrosis, ureteral injury, urinary stress incontinence, and lower extremity edema.
Laparoscopic radical hysterectomy
Although this procedure offers a quicker recovery for the patient, it has been largely abandoned due to poor oncologic outcomes and increased recurrence compared with open surgery. The mechanism for this difference is unknown, but 2 large independent studies have confirmed this finding. [31] [32] [33]
Lymph node evaluation
Detecting lymph node involvement is essential, as it yields important prognostic information and guides therapeutic decision-making. The risk of nodal involvement should guide the decision to evaluate the lymph nodes and is a function of the disease stage (see Table. Pelvic Nodal Risk by Stage). Para-aortic (PA) nodal risk typically carries one-half the pelvic nodal risk by stage. Although pelvic lymphadenectomies are considered the gold standard, sentinel node biopsies may also be pursued for select early stage I cervical cancer. Generally, sentinel node biopsies are safe and effective. They have been investigated in stage IA1 to stage IIA1 patients with a sensitivity of 92%, a negative predictive value of 98%, less lymphatic morbidity, and no differences in recurrence-free survival. [34] [35] The sentinel node biopsy approach continues to be investigated in large-scale international trials called SENTICOL III ( NCT03386734 ).
Table. Pelvic Nodal Risk by Stage
Pelvic exenteration
Pelvic exenteration is the most radical surgical procedure for cervical cancer. Indications are confined to patients with central pelvic recurrence after radiotherapy or patients with stage IVA disease who cannot receive radiotherapy. Classically, a total pelvic exenteration includes the removal of the uterus, fallopian tubes, ovaries, vagina, bladder, urethra, and rectum. Reconstruction consists of an ileal conduit, or continent diversion, for the urinary system and an end colostomy for the GI system. Continent diversions include the Indiana and Miami pouch techniques. [36] [37]
Total exenteration is generally performed for cervical cancer. Variations of this technique include anterior and posterior exenteration, which spare the rectum or the bladder, respectively. Exenteration can be further classified into supralevator and infralevator, depending on whether the urogenital diaphragm and levator muscles are removed. It is important to ensure that the central tumor can be completely resected and there is no metastatic disease. Minimally invasive pelvic exenteration has been described in the literature, although further evaluation of this technique is warranted. [38] [39]
A neovagina can be formed with a myocutaneuous flap or split-thickness skin graft with an omental J-flap. The posterior supralevator exenteration approach allows for the possibility of maintaining not only urinary function but fecal continence if a colonic anastomosis can be formed. The 5-year survival rate for patients treated with exenteration ranges from 40% to 50% in the recurrent setting. [40] At 3 and 5 years, local recurrence rates are 84% and 75%, respectively. [41] Survival is not impacted by the type of exenteration performed. [42] Mortality from the operation has fallen dramatically over the last 70 years to less than 5%, but surgical morbidity is over 50%. [41] Early complications include infection, abscess formation, thromboembolism, fistulas, urinary leakage, peritonitis, stoma necrosis, flap necrosis, and stump dehiscence. Late complications include stoma stenosis, incontinence, hydronephrosis, stone formation, chronic pain, and abdominal wall hernia.
Cervical Cancer in Pregnancy
Although cervical cancer is one of the most common malignancies diagnosed in pregnancy, it poses unique staging and treatment challenges in pregnant patients. A maternal-fetal medicine specialist should evaluate patients to discuss fetal risks and potential pregnancy loss. Women must weigh the risk of delaying treatment until after delivery versus proceeding immediately with treatment.
The determination of gestational age is crucial. Minimum fetal viability is approximately 24 weeks gestation, but there is a significant risk of neonatal death or long-term disability in those who survive. Disability-free survival at 25 years increases substantially with advancing gestational age, with 4% of infants born at 22 weeks versus 78% for those born at 28 weeks gestation. In contrast, full-term infants have a disability-free survival of 97%. [43]
While the radiation delivered during a PET or CT scan remains far below the threshold for the development of congenital malformations and pregnancy loss, ionizing radiation in imaging studies should be kept to a minimum in this population. [44] Other imaging modalities, such as ultrasound and MRI, are preferred when appropriate to determine local tumor extent and distant metastatic involvement. However, MRI and ultrasound have a low sensitivity for small nodal metastases. Consequently, more invasive staging techniques may need to be employed.
In patients with a high risk of nodal metastasis, laparoscopic pelvic lymphadenectomy may be performed to establish the disease stage. [45] The safety of this procedure has only been studied in limited case series, but it can be performed in any trimester (although earlier in the pregnancy is preferred). These techniques may still be employed when advanced imaging is unavailable or contraindicated. In addition, the FIGO staging system continues to allow the use of proctosigmoidoscopy and cystoscopy for local staging of cervical cancer.
Treatment strategies must be individualized and discussed in a multidisciplinary fashion with medical oncologists, radiation oncologists, obstetrician/gynecologists, maternal-fetal medicine specialists, and gynecologic oncologists. Generally, patients with pregnancies at gestational ages under 22 weeks and stage IA1 disease can be treated with conization, but this carries a 15% risk of significant bleeding and spontaneous abortion. Patients with pregnancies at gestational ages above 22 weeks may be able to delay treatment until after delivery if they have early-stage disease. Patients with more advanced disease (>IB1) may receive platinum-based neoadjuvant chemotherapy (cisplatin/paclitaxel) until delivery, followed by a cesarean radical hysterectomy. Limited data suggest this is a safe regimen for both mother and fetus. [46] Small series indicate approximately a 75% tumor response rate, with 15% of patients experiencing a local recurrence. The risk of fetal toxicity with these regimens is unknown, but complications may include respiratory distress syndrome, malformations, and childhood malignancies. [46] International guidelines for treatment and fetal preservation have been published. [47]
Immediate treatment is recommended for patients with documented lymph node metastasis, disease progression, or pregnancy termination. If the patient opts to terminate the pregnancy before treatment, definitive treatment recommendations are identical to those of a nonpregnant patient.
- Radiation Oncology
Radiotherapy remains a crucial component in the treatment of cervical cancer. Randomized evidence from the 1990s and early 2000s has established radiotherapy in almost every facet of treatment; it may be utilized as a definitive or adjuvant treatment with or without platinum-based chemotherapy.
Definitive Radiotherapy
Early-stage cervical cancer
Radiotherapy may be utilized as the sole treatment modality in early-stage cervical cancer (stages IA1 to IIA1). External beam radiotherapy (EBRT) with a brachytherapy (BT) boost has less morbidity and equivalent 5- and 20-year overall survival rates (83% and 75%, respectively) compared with radical hysterectomy. [48] [49] Some centers may perform an adjuvant hysterectomy for bulky tumors after chemoradiation therapy. However, most guidelines do not recommend this due to significant complication rates. Recent data suggest that survival rates after chemoradiation therapy and adjuvant hysterectomy are suboptimal. [50]
Advanced cervical cancer
Locally aggressive and/or node-positive diseases are typically treated with definitive concurrent platinum-based chemoradiotherapy followed by a BT boost. The addition of chemotherapy to definitive radiotherapy has resulted in considerable improvement in overall survival compared with radiotherapy alone, with an 8-year overall survival of 67% versus 41%. Improvements in local recurrence and distant metastasis have also been noted. [51]
Postoperative radiotherapy
Radiotherapy with or without chemotherapy is recommended in the postoperative setting when specific pathologic findings are present. These findings are thought to represent an increased risk of recurrence.
Conventionally, the Sedlis criteria guided the use of adjuvant radiotherapy without chemotherapy in postradical hysterectomy patients with at least 2 of the following 3 features: tumor size greater than 4 cm, LVI, or more than one-third stromal invasion. [52] These criteria were meant to identify patients with at least a 30% risk of relapse at 3 years. [53] Patients who met these criteria and were treated with pelvic radiotherapy were noted to have improved progression-free survival (78% vs 65%) and local recurrence (21% vs 14%). [52] More recently, there have been concerns that these criteria may overlook women who might benefit from adjuvant radiotherapy due to such a high threshold. A nomogram incorporating the original Sedlis criteria and tumor histology has been developed to provide a more linear and continuous risk assessment rather than a simple threshold. [53]
Classically, the addition of chemotherapy to radiotherapy was guided by the Peters trial, which randomized patients with positive nodes, involved parametria, or positive surgical margins to radiotherapy alone or radiotherapy with concurrent platinum-based chemotherapy. The addition of chemotherapy resulted in a 10% improvement in overall survival at 4 years and almost a 20% improvement in progression-free survival over the same time frame. [54] More contemporary studies such as the STARS trial have sought to expand the use of chemotherapy in the adjuvant setting in patients meeting either the original Sedlis or Peters criteria. [55]
Delivery Techniques
The 2 major delivery methods include ERBT, directed at the primary tumor and pelvic lymphatics, and BT, in which a sealed radiation source is placed in close proximity to the tumor.
EBRT techniques include 3-dimensional conformal radiation therapy (3D-CRT) or intensity-modulated radiotherapy (IMRT). Intact cervical cancer patients’ plans can be employed. A reduction in gastrointestinal and hematological adverse effects has been documented with IMRT in both adjuvant and definitive settings. [56] [57]
ERBT simulation
Patients undergoing EBRT can be placed in the supine position. Accounting for cervical motion is essential when using IMRT. This is accomplished by taking 2 separate scans of patients, first with a full bladder followed by an empty bladder. Prone positioning may also be accomplished using a belly board; however, if there are large daily fraction shifts, IMRT may not be reproducible. Prone positioning may allow for a reduction in the small bowel dose when using IMRT. [58]
ERBT target delineation
Traditionally, pelvic fields were drawn on 2-D x-rays consisting of anterior-posterior (AP)/posterior-anterior (PA) and opposed lateral fields comprising the 4-field box. The superior edge of the field was the bottom of L4 and inferiorly drawn to the bottom of the obturator foramen (or at least 3 cm below the lowest extent of disease). The lateral fields have the same superior/inferior borders, with the anterior border being the anterior pubic symphysis and the posterior border being the sacral hollow, including S2.
More precise delineation of the gross disease and elective volumes can be accomplished in the era of CT-based planning, PET/CT fusions, and IMRT. A gross tumor volume (GTV) consists of gross disease seen on a CT, PET, and physical examination. An internal target volume (ITV) accounts for variation in bladder filling and can also be employed, but this requires the patient to have 2 CT simulations (empty and full bladder). The clinical tumor volume (CTV) 1 expansion includes the entire cervix and uterus (if intact). Planning target volume (PTV) 1 on primary disease is typically 1.5 cm. The CTV2 includes the parametrial tissue, paravaginal tissues, and at least one-half of the upper vagina. If there is vaginal involvement, consideration should be given to covering the entire vagina. This PTV2 expansion should be 1.0 cm. The elective nodal volumes in the CTV3 should include obturator nodes, external iliac nodes, internal iliac nodes, and presacral nodes. If there is lower vaginal involvement, consideration should be given to coverage of the inguinal nodes. PTV expansion on the elective nodes is typically 0.7 cm.
Coverage of the PA nodes may be necessary in cases with evidence of disease in the nodal chain, or in cases in which the patient has a positive pelvic node and will not receive systemic therapy. In those instances, the superior boundary would become the T12/L1 interspace, with the nodal strip ending at the top of the pelvic field L5/S1. [59] [60]
ERBT dosing and dose constraints
The standard whole pelvic dose is 45 to 50.4 Gy, specifically 1.8 to 2.0 Gy per fraction. Any gross nodal disease may be boosted to 60 Gy if possible, given that organs-at-risk (OAR) constraints are not exceeded.
EBRT has dramatically improved with the adoption of IMRT, reducing acute toxicity while maintaining oncologic outcomes. Typical OAR include the rectum, bladder, bowel, femoral heads, and bone marrow. Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC) dose constraints can be an excellent guide. Typically, with EBRT, doses of 45 to 50 Gy alone will not lead to significant rates of acute bladder or bowel toxicity. [57]
If BT is planned, minimizing these doses during the external beam phase of treatment will allow higher doses to be delivered during the boost phase of treatment. Bone marrow suppression resulting in grades 3 to 4 neutropenia has been demonstrably lower (8.6% vs 27.1%) with image-guided radiotherapy and IMRT. [56] The most common constraints are for bone marrow in the pelvis. [56] [57] [61]
BT can be used alone in early-stage cervical cancer or as a boost after EBRT in more advanced disease (stages IB2 to IVA), as it allows for highly conformal dose delivery to the tumor while minimizing exposure to normal tissues. The dose delivery is controlled by adjusting the dwell times within the delivery device. High dose-rate (HDR) BT (>12 Gy/hr) is the most commonly used technique; however, it requires a radioactive source, usually iridium-192.
Typically, BT is started after the external beam portion of the treatment or interdigitated with EBRT in the last week of treatment. EBRT and BT should not be administered on the same day. Total treatment time (EBRT and BT) should not exceed 8 weeks. Excessive treatment times can result in a 1% per day decline in local control and overall survival.
Before undergoing BT, a review of the patient’s history, physical exam, pathology, and imaging should be conducted. A complete blood count and metabolic panel should be obtained within a week of the procedure. Metabolic derangements should be investigated and corrected before the procedure. Patients with an absolute neutrophil count (ANC) less than 500 mm should not undergo the procedure until their count has recovered. A review of medications, especially anticoagulants, should be completed, and a prothrombin time/international normalized ratio result should be obtained. Careful consideration should be given to holding anticoagulant medications before the procedure. Inpatients confined to bed should be given thromboprophylaxis and sequential compression devices. Bowel preparation should also be reviewed with the patient before the procedure.
BT applicators
There are several applicators that may be used in various clinical scenarios. The ring and tandem is the most common device for intact cervical cancer. The tandem is placed in the cervical canal while the ring is placed inside the vaginal fornices. Tandem and ovoids are utilized similarly but are preferred in patients with a barrel-shaped cervix. Interstitial applicators such as the Syed template can be used in patients with extensive parametria involvement, pelvic sidewall involvement, lower vaginal involvement, or vaginal cuff recurrence. Tandem and cylinder applicators can be used in cases of vaginal stenosis, inability to place a ring or ovoid, or lower vaginal involvement less than 5 mm thick. Modifications to the tandem and ring or vaginal cylinder can also be made to accommodate interstitial needles. [62] [63]
Patient discomfort experienced during the procedure can lead to suboptimal placement of the applicator, longer procedure times, and distress for the patient. An anesthetic is typically required to help optimize patient comfort and procedure mechanics. The types of anesthesia administered vary but may include general anesthesia, spinal anesthesia, epidural anesthesia, intravenous conscious sedation, and oral pain medication.
Placement of an intracavitary applicator for an intact cervix
The patient is placed in the dorsal lithotomy position in stirrups. After adequate sterile preparation of the area, a Foley catheter is inserted, and the balloon is inflated with dilute contrast to allow for detection with CT scan. A speculum is inserted to visualize the cervix, and a uterine sound is used to determine the length of the cavity. This will aid in determining the length and angle of the tandem. A Smit sleeve is occasionally used to maintain the patency of the cervical os but, if not available, serial dilations may be required. Once this is complete, the tandem is inserted, followed by the ring or ovoid. Fiducial markers may also be placed during the procedure to outline the extent of the disease or the opening of the cervical os so it is visible on CT scan. These applicators can be locked so their relative positions do not change.
Displacement of the bladder and rectum is critical to reduce the excess dose and limit toxicity. The packing material can consist of gauze soaked in a radiopaque solution. Applicators fitted with inflatable balloons or separate rectal blades are also available. Anterior packing displaces the bladder, whereas posterior packing displaces the rectum. It is essential to ensure no packing is placed in front of the ring or ovoids, as this will significantly reduce the intended dose.
Once complete, the patient will undergo a CT simulation for 3-D BT planning. Three-dimensional CT-based planning has been shown to have improved overall survival (65% vs 74%) and lower rates of grades 3 to 4 toxicity (23% vs 3%) compared with 2-D planning. [64] A 1- to 5-mm slice thickness is recommended. [62] [63] More recently, MRI-guided BT has been incorporated into planning for improved tissue delineation, best seen on the T2-weighted fat-suppressed sequences (T2–fast-spin echo) imaging. [65]
Paraxial and para-coronal images should be obtained concerning the cervix-uteri and sagittal images. [66] These images can also allow for the assessment of chemoradiation response. Technically, low- and high-intensity magnetic field MRI machines can be used. Patients can be given glucagon before MRI to reduce bowel motion. A pelvic coil is recommended to increase the signal-to-noise ratio. Ideally, a 3-mm slice thickness should be obtained, which helps improve the detection of parametrial involvement, but a slice thickness of less than 5mm is acceptable. The disadvantages of this approach are the increased costs, longer procedure times, and the need for strict compatibility of the materials utilized.
Proper applicator placement should be confirmed with plain radiography or more advanced imaging such as a CT scan or MRI. Adequate placement includes the tandem bisecting the ring/ovoids on AP and lateral imaging, the tandem being one-third to one-half the distance between the sacral promontory and the pubic symphysis, the tip of the tandem being below the sacral promontory, no packing located superior to the ring/ovoids, and no inferior displacement of the ring/ovoids relative to the flange.
With HDR BT, a remote afterloading technology allows a small iridium source attached to the end of a cable to be robotically driven through multiple channels, stopping at predetermined points (dwell positions) for varying lengths of time. [67] A Cochrane review failed to show differences between HDR and low dose-rate (LDR) intracavitary brachytherapy (ICBT). Oncologic outcomes included overall survival, disease-free survival, and recurrence-free survival, as well as local control rate, recurrence, and metastasis. There was no difference in treatment-related complications. Regardless, this review recommends HDR ICBT for all clinical stages of cervix cancer due to the advantages of HDR ICBT, including accuracy of the source, applicator positioning, outpatient treatment, and patient convenience. [68]
BT target delineation
As part of 3-D–based planning, contouring the targets is essential. The Groupe Européen de Curiethérapie and the European Society for Radiotherapy and Oncology (GEC-ESTRO) have established standardized terminology regarding target delineation. [66] The high-risk clinical target volume (HR-CTV) consists of the entire cervix and all gross disease at the beginning of BT treatment; the intermediate-risk clinical target volume (IR-CTV) incorporates the HR-CTV and gross disease before any treatment; and the low-risk clinical target volume (LR-CTV), which includes the IR-CTV as well as the entire uterus, upper vagina, entire parametria, and spaces between the bladder and rectum. [69] Normal OAR should be contoured, including the bladder, rectum, sigmoid colon, and vagina.
BT dose and dose constraints
Ensuring adequate dose to the target is critical and has been shown to lead to improved local control and survival. Dose and fractionation schemes may vary by institutional preference, but they must result in a total equivalent dose in 2 Gy fractions (EQD2) of 85 Gy or higher, assuming 45 Gy was initially delivered to the pelvis. There are several calculators to determine EQD2. One of these, colloquially known as the “Vienna Spreadsheet,” was used by the Effects of a Multifaceted Intervention on Blood Pressure Actions in the Primary Care Environment (EMBRACE) trial group; it provides EQD2 calculations to the target structures and OAR. The most common dose fractionation schemes include 4 x 7 Gy, 5 x 6 Gy, and 6 x 5 Gy, with an EQD2 of approximately 90.1, 88.6, and 83.7 Gy, respectively.
For 3D-based planning, the critical dosimetric parameter is the D90 greater than or equal to 90%. The goal is for 90% of the HR-CTV to be covered by at least 90% of the prescription dose. The EQD2 should be calculated to ensure the total dose received is approximately 85 Gy or higher, although there are instances in which it is acceptable for the EQD2 to be slightly lower. In patients with a complete response before BT or partial response with less than 4 cm in residual disease, an EQD2 above 80 Gy may be used, whereas for those patients with more than 4 cm residual disease, an EQD2 greater than 85 Gy is recommended. [62] [63]
Despite the transition to 3D-based volumetric planning and the continued evolution of BT treatment, 2-D dosimetric reporting systems persist and should be understood. Point A, where the uterine artery crosses the ureter, is located 2 cm up the tandem and 2 cm lateral to the tandem and was originally part of the Manchester system. This point was traditionally where the prescription dose was prescribed, but more recently has become a starting point where dose coverage can be further manipulated in 3-D to ensure coverage of the HR-CTV. Point B, also part of the original Manchester system, is located 2 cm up the tandem and 5 cm from the patient’s midline. This location represents the pelvic side wall lymphatics and typically receives one-third of the prescription dose. It has fallen out of favor and is no longer reported. The isodose lines for typical tandem and ring/ovoid implant should appear pear-shaped. In addition, the International Commission on Radiation Units and Measurements (ICRU 38) specified a bladder and rectal point. The bladder point is located posterior to the Foley balloon that has been pulled down to the neck of the bladder. The rectal point is 5 mm posterior to the vaginal wall.
Doses to OAR must also be carefully documented. Again, it is the cumulative dose of EQD2 that is critical. The dosimetric parameter D2 cc, which represents the highest dose received by 2 ccs of tissue, is commonly used for evaluating a BT plan. The American Brachytherapy Society (ABS) guidelines allow for the D2 cc of the bladder to receive 90 Gy or less EQD2, whereas the D2 cc of the rectum and sigmoid should be 75 Gy or less EQD2. However, recent data suggest that late rectal morbidity may be substantially lower even using a D2 cc of 65 Gy or less. [70]
Radiation Therapy Complications
Long-term toxicity is a concern with any patient receiving radiation therapy. Bowel, rectal, and urinary complications are the most frequent. There does not appear to be a difference in the frequency or severity of complications with respect to age. The greatest risk of late sequelae typically occurs within 3 years of treatment.
Radiation proctitis can result in tenesmus and intermittent bleeding with bowel movements. Postradiation proctitis typically occurs 3 months after treatment at the earliest but may take years to develop. Treatments can include mesalamine or steroid-based suppositories to relieve pain and stop bleeding. Randomized trials have suggested that mesalamine may be slightly more efficacious than steroid-based suppositories. [71] Other treatments can include a 4% formaldehyde application to control rectal bleeding. In refractory cases, argon plasma laser coagulation may be performed on the offending vessels.
Radiation cystitis can lead to dysuria, urinary frequency, and, in some cases, hematuria. This complication can occur acutely within 2 to 3 weeks of starting radiotherapy and up to 3 years posttreatment.
For acute cystitis, a urinary tract infection must be ruled out; therefore, a urinalysis is an appropriate first step in the diagnosis. A short course of phenazopyridine can be prescribed for dysuria relief, although the urine color change may be alarming for some patients. Patients should be made aware of this change before starting the medication. Urinary frequency can be treated with anticholinergic drugs such as oxybutynin or mirabegron, although caution is advised in elderly patients.
Chronic cystitis has an incidence of 5% to 10%. [72] These patients are more likely to experience hematuria in addition to frequency and dysuria. The severity can range from mild to severe and life-threatening. Mildly symptomatic patients may be managed conservatively. Any antiplatelet or anticoagulation medications the patient takes should be reviewed, and the necessity questioned. A cystoscopy with clot evacuation and irrigation is necessary in more severe cases. During a cystoscopy, formalin instillation can be used to manage intractable hematuria. In refractory cases, hyperbaric oxygen therapy has been utilized and shown to relieve and control bleeding in 92% of patients; however, recurrences may occur. [73] Barotrauma is a risk associated with this procedure.
Secondary malignancy
Radiation-induced cancers tend to appear several decades after treatment. The overall risk of secondary malignancy is increased with pelvic radiotherapy compared to those treated with surgery alone. Women younger than 50 years had a 40-year cumulative risk of 22% versus 16% for those older than 50 years. [74] Secondary cancers tend to be confined to the rectum, bladder, lungs, and genitals. Other retrospective studies have shown an increase in leukemia risk, which peaks around 5 to 10 years after treatment. [75] Limiting normal organ doses may help to reduce the risk.
Ovarian failure
Radiation-induced ovarian failure typically occurs within 6 to 12 months after radiation. Minimum doses for ovarian failure are inversely related to age ranging from 20.3 Gy at birth to 14.3 Gy at the age of 30 years. [76] The doses used for cervical cancer can easily precipitate ovarian failure. Premenopausal patients have several options for preserving ovarian function, namely definitive surgery or ovarian transposition. Laparoscopic ovarian transposition allows the ovaries to be placed outside the radiation field, usually 3 cm away. This procedure is also useful for fertility preservation. The functional preservation rate is approximately 80%. Ovarian cryopreservation is another option. Exogenous hormonal supplementation with estrogen should be considered to prevent osteoporosis and osteopenia and to maintain libido.
Vaginal stenosis
Vaginal stenosis and vaginal canal shortening can develop over months to years after treatment. Stenosis can make it difficult for intercourse and gynecological exams. Consistent use of a vaginal dilator is typically recommended; however, compliance is highly variable. Sexual dysfunction is quite common, ranging from a lack of desire for sexual activity to a lack of adequate vaginal lubrication.
Bone fracture
Pelvic radiotherapy can increase the risk of pelvic fractures, with most fractures occurring at dose levels of 45 to 63 Gy. Bone health is another concern in patients who undergo radiation to the pelvis. Approximately 10% of patients radiated for cervical cancer experience a pelvic fracture. The most common fracture site is the sacrum, most occurring within 2 years after treatment. Bone mineral density scans and appropriate intervention to maintain bone health may help to reduce this risk.
Uterine perforation
Uterine perforation is a complication related to BT applicator insertion and results in excessive doses to normal tissues, poor target coverage, bleeding, and infection. Rates of perforation range from 2% to 18%. [77] [78] [79] Management is controversial, ranging from postponement of BT to allow for healing to outright abandonment of the procedure. However, treatment delays are known to adversely affect patient outcomes. The risk of vascular and organ injury is low when a blunt instrument causes perforation. Stable patients without signs of infection may be discharged and observed. Prophylactic antibiotics may be prescribed. Signs of hemodynamic instability and infection warrant more aggressive approaches with IV fluids, antibiotics, and surgical exploration.
- Medical Oncology
Definitive Therapy
The Radiation Therapy Oncology Group (RTOG) trials established the utility of platinum-based chemotherapy regimens. Compared with radiotherapy alone, there are consistent overall survival, disease-free survival, and local control advantages. [51] It is postulated that chemotherapy acts as a radiosensitizer. The most common agent used is weekly cisplatin. Single-agent platinum-based regimens have the best progression-free survival and overall survival compared to non-platinum-based regimens and a better toxicity profile than combinations of platinum-based regimens such as cisplatin/5-FU/hydroxyurea. [80] Carboplatin may also be used in patients who cannot tolerate cisplatin. Some practices continue to use a combination of cisplatin/5-FU. This regimen is delivered concurrently with radiotherapy.
Adjuvant Therapy Chemoradiotherapy may be added after surgical resection should the patient have high-risk features. Overall survival and progression-free survival benefits have been demonstrated with the addition of chemotherapy to radiotherapy in certain high-risk postoperative patients. [54]
The use of adjuvant chemotherapy after definitive chemoradiation continues to be investigated in clinical trials. The results have been mixed. Adding adjuvant carboplatin/taxol to chemoradiation for locally advanced cervical cancer resulted in higher rates of grades 3 to 5 toxicity and no difference in overall survival or progression-free survival. Another trial using concurrent and adjuvant cisplatin/gemcitabine demonstrated improved 3-year progression-free survival but markedly higher rates of grades 3 to 4 toxicity and hospitalizations. [81] RTOG 0724 is an ongoing trial investigating the use of adjuvant cisplatin/paclitaxel after definitive chemoradiation in high-risk postoperative patients ( NCT00980954 ).
Recurrence and Metastasis
In recurrent and metastatic disease settings, patients who are not candidates for exenterative surgery or radiotherapy may receive systemic therapy alone. Many patients have previously received single-agent cisplatin-based therapy; therefore, multidrug regimens are typically used. Cisplatin/paclitaxel has been shown to improve progression-free survival in patients with recurrent cervical cancer but yields no difference in median overall survival. [82] Although other drug combinations such as cisplatin/topotecan, cisplatin/gemcitabine, and cisplatin/vinorelbine are potential options, the Gynecologic Oncology Group (GOG) has suggested that these regimens are not superior to cisplatin/paclitaxel (protocol 204). [83] Incorporating biological agents such as vascular endothelial growth factor receptor antagonists like bevacizumab into standard chemotherapeutic regimens has improved overall survival. [84] Immunotherapy with PD-1 inhibition has also been incorporated into chemotherapeutic regimens. Single-agent pembrolizumab has an objective response rate of 12% to 14% in patients with recurrent or metastatic cervical cancer. [85] Keynote-826, a randomized, double-blinded phase 3 study, demonstrated the addition of pembrolizumab to multidrug chemotherapy improved overall and progression-free survival. [86] Follow-up subgroup analysis confirmed this finding in a Japanese population. [87]
- Complications
The most commonly used platinum-based drugs are cisplatin and carboplatin. Common adverse effects include neutropenia, thrombocytopenia, anemia, febrile neutropenia, nephrotoxicity, neurotoxicity, and infection. Although cisplatin is the drug of choice, carboplatin can be used in patients who may not tolerate cisplatin, particularly if they already have underlying renal disease. Carboplatin is thought to have lower efficacy than cisplatin; however, prospective data suggest noninferiority in effectiveness and a statistically significant lower incidence of febrile and nonfebrile neutropenia and creatinine elevation. [88]
Bevacizumab carries the risk of hypertension, hemorrhage, thromboembolic events, renal injury, and ovarian failure in premenopausal women. Pembrolizumab is known for precipitating autoimmune phenomena such as pneumonitis, colitis, hepatitis, nephritis, and endocrinopathies.
The International Federation of Gynecology and Obstetrics (FIGO) staging system was updated in 2018 and remains the dominant staging methodology. The 8th edition of the American Joint Committee on Cancer (AJCC) Staging Manual also has a tumor-node-metastasis classification system in which the tumor stages correspond with the FIGO stages; however, it is not regularly used.
FIGO Staging
Classically, FIGO staging would rely on clinical examination, cystoscopy, proctoscopy, hysteroscopy, urography, and plain film x-ray. These relatively basic tests were utilized so developing countries with fewer healthcare resources could adequately stage patients. More recently, advanced imaging techniques such as MRI and PET scans have become part of the staging workup. MRI is preferred for establishing the tumor stage, given superior tissue delineation compared with CT scan with contrast. [89] [90]
Stage I
- The disease is strictly confined to the cervix, with the A/B designation indicating the depth of invasion (≤5 or >5 mm).
Stage II
- The disease invades beyond the uterus but has not extended into the lower vagina.
- This stage also has an A/B designation based on involvement of the parametria.
Stage III
- The disease has extended to the lower one-third of the vagina (IIIA) or to the pelvic side wall and/or hydronephrosis (IIIB).
Classically, nodal disease did not influence the FIGO staging system; however, it has been shown that nodal disease is one of the most important prognostic indicators for reduced 5-year overall survival. [91] As a result, new stages (IIIC1 and IIIC2) were added to reflect the involvement of pelvic or PA nodes, respectively.
Stage IVA
- The disease is locally aggressive, involving adjacent organs such as the bladder or rectum.
Stage IVB
- The disease has spread to other solid distant organs; this stage can also be indicative of nonregional nodal disease.
Multiple factors contribute to differences in patient outcomes. Potential prognostic factors for cervical cancer patients include disease stage, number of retrieved lymph nodes, use of a uterine manipulator in laparoscopic treatment, age, race, ethnicity, general health before diagnosis, and access to evidence-based care. These prognostic factors highlight opportunities to enhance care and improve overall mortality.
When diagnosed early, the 5-year relative survival rate for cervical cancer is approximately 92%. About 44% of cervical cancer patients are diagnosed at an early stage. Inconsistent screening is an independent risk factor for late diagnosis. [92] A higher stage at presentation decreases survival and increases the chance of recurrence. The 5-year relative survival rate drops to 60% when cervical cancer is diagnosed after it has spread locally or spread to regional lymph nodes. With distant metastasis at diagnosis, the 5-year relative survival rate is 19%.
Studies show certain surgical factors affect survival. It is believed that the number of retrieved lymph nodes corresponds to the thoroughness of surgical treatment. Research indicates that a higher retrieved lymph node count has a statistically significant positive effect on progression-free survival. For women having laparoscopic surgery, the use of a uterine manipulator is associated with a better prognosis. [93]
Survival rates also differ based on race. The 5-year relative survival rate is 67% for women of all races. Black women tend to have the highest mortality and lowest survival rate, with a 5-year relative survival rate of approximately 56%. [11] [94]
Patient age at diagnosis also contributes to differences in prognosis and survival, independent of disease stage and histology. Older age is associated with lower survival rates. Patients younger than 50 years, aged 50 to 64 years, and 65 years and older have relative 5-year survival rates of 77%, 61%, and 46%, respectively. Studies indicate older women are a high-risk subset, often receive suboptimal treatment, and die more frequently. Even with BT alone, older women with cervical cancer obtain significant survival benefits. [95]
Complications of advanced disease and associated treatments are similar to other cancers. These late complications may include renal failure, hydronephrosis, pain, lymphedema, bleeding disorders, and fistulas (see Image. Secondary Lymphedema). [96]
- Deterrence and Patient Education
Traditional and innovative patient education methods can increase overall awareness of cervical cancer and the need for prevention and early screening. [97] [98] Literature shows that healthcare professionals may not consistently recommend or discuss HPV vaccination with all target patients. Some women and parents of young daughters may also have reservations about vaccinations that prevent them from being vaccinated. Additional medical education for clinicians serving high-risk populations may increase awareness, prevention, and screening of those patients at risk for the highest mortality. [99]
Although a patient may prefer counseling directly from the healthcare professional, additional community outreach efforts are necessary. Culturally sensitive information, appropriate language to reach lower health literacy populations, and targeted efforts to reach women not yet sexually active are needed to expand patient awareness and education and to initiate screening beyond the clinical setting. [100] [101]
- Pearls and Other Issues
Primary prevention of cervical cancer involves HPV vaccination to prevent cervical cancer. The estimated effectiveness of HPV vaccination is 90%. [102] A quadrivalent vaccine that prevents cervical cancer and genital warts caused by low-risk HPV types is widely available in the United States. The recommended and approved age for vaccination is 9 to 45 years for both females and males. Vaccination can significantly impact cervical cancer mortality in women in low-resource areas and those in high-risk racial and ethnic groups. A vaccine covering only HPV-16 and -18 is no longer marketed in the United States. However, its use may continue in areas outside the United States.
- Enhancing Healthcare Team Outcomes
The interprofessional team can provide public health education and multidisciplinary care to improve cervical cancer awareness, prevention, screening, and management. [103] [104] [105] Primary care clinicians performing cervical cancer screening, colposcopies, and LEEP procedures, must have ongoing dialogues with gynecologists about findings of suspicious cervical lesions, management, and treatment. Appropriate protocols and guidelines across healthcare systems can improve outcomes by optimizing treatment and follow-up. Developing a culturally sensitive system directed at increasing patient-centered education will require the input of diverse healthcare professionals and staff with multilingual skills and cross-cultural competency.
The interprofessional team can optimize the treatment of patients with cervical cancer through communication and coordination of care. Primary care physicians, gynecologists, gynecologic oncologists, radiation oncologists, and advanced practice practitioners provide diagnoses and care plans. Specialty care, ambulatory care, and oncology nurses should work with the team to coordinate care, support patient education, and provide feedback to the rest of the team. Pharmacists should evaluate vaccinations and medications, recognize drug-to-drug interactions, provide patient education, and monitor compliance. Together, the team can improve outcomes for patients with cervical cancer.
- Review Questions
- Access free multiple choice questions on this topic.
- Access free CME on this topic.
- Comment on this article.
Invasive Cervical Cancer. Colposcopic view of the cervix in a patient with invasive cervical cancer. Centers for Disease Control and Prevention (CDC)
Secondary Lymphedema. Lymphedema related to cervical cancer treatment. Contributed by Molly Nettles, OTR/L, CLT-LANA
Disclosure: Josephine Fowler declares no relevant financial relationships with ineligible companies.
Disclosure: Elizabeth Maani declares no relevant financial relationships with ineligible companies.
Disclosure: Charles Dunton declares no relevant financial relationships with ineligible companies.
Disclosure: David Gasalberti declares no relevant financial relationships with ineligible companies.
Disclosure: Brian Jack declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Fowler JR, Maani EV, Dunton CJ, et al. Cervical Cancer. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Cervical Cancer (Nursing). [StatPearls. 2024] Cervical Cancer (Nursing). Fowler JR, Maani EV, Dunton CJ, Gasalberti DP, Jack BW, Miller JL. StatPearls. 2024 Jan
- Atypical Squamous Cells of Undetermined Significance. [StatPearls. 2024] Atypical Squamous Cells of Undetermined Significance. Ndifon CO, Al-Eyd G. StatPearls. 2024 Jan
- Review Screening for Cervical Cancer With High-Risk Human Papillomavirus Testing: A Systematic Evidence Review for the U.S. Preventive Services Task Force [ 2018] Review Screening for Cervical Cancer With High-Risk Human Papillomavirus Testing: A Systematic Evidence Review for the U.S. Preventive Services Task Force Melnikow J, Henderson JT, Burda BU, Senger CA, Durbin S, Soulsby MA. 2018 Aug
- Anal dysplasia screening: an evidence-based analysis. [Ont Health Technol Assess Ser....] Anal dysplasia screening: an evidence-based analysis. Medical Advisory Secretariat. Ont Health Technol Assess Ser. 2007; 7(4):1-43. Epub 2007 Jun 1.
- Review Screening for Cervical Cancer: A Decision Analysis for the U.S. Preventive Services Task Force [ 2011] Review Screening for Cervical Cancer: A Decision Analysis for the U.S. Preventive Services Task Force Kulasingam SL, Havrilesky L, Ghebre R, Myers ER. 2011 May
Recent Activity
- Cervical Cancer - StatPearls Cervical Cancer - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Cervical Cancer Screening: Review of Issues Essay
Introduction.
Cervical cancer continues to be a significant health problem in the United States. According to the latest statistics by the Centers for Disease Control and Prevention (2022), the US has approximately 13,000 new cases of this cancer annually, and about 4,000 of the diagnosed women die from cervical cancer. Although new screening methods were introduced in the last decades, and women were provided with additional tests, screening rates remain low (Bedell et al., 2020). Therefore, the question of how Advance Practice Nurses can aid patients in undergoing screening arises. Nurses should introduce such initiatives as self-completed test kits that can be used at home for human papillomavirus screening and patient navigation to create a supportive environment for cervical cancer screening.
Describing Quantitative Research
Quantitative research includes studies that approach scientific inquiries with quantifiable measures. In such studies, data is collected for calculations that help answer the research question. For example, one may find a correlation between an independent and dependent variable to see how two or more elements are interconnected (Sürücü & Maslakçi, 2020). Furthermore, quantitative research may help compare group behavior depending on the intervention to which they are exposed (Vu, 2021). Regression and change are also possible investigation goals in this branch of scientific research. Some types of quantitative studies include descriptive, correlational, quasi-experimental, experimental, and more.
To explore the issue of cervical cancer screening, one may look at different types of qualitative research. The problem reviewed is the need to increase cancer screening rates with the help of nurse intervention. Therefore, one needs to look at studies that compare the effectiveness of nursing interventions and usual care regarding screening programs. An experimental study that divides the participants into two or more groups is a type of quantitative research that can support the thesis and provide more information on effective intervention types. Moreover, meta-analyses and systematic reviews of nursing interventions can provide a solid base for further research.
Appraisal Tools, Studies, and Matrix
Two studies were chosen for the appraisal and analysis to support the topic of cervical cancer screening. The first one is a meta-analysis performed by Nelson et al. (2020) – the researchers aim to investigate the impact of patient navigation on cancer screening rates among underserved populations. As seen in Appendices A and B, the study shows a high level of quality, producing consistent results. This review was selected as it contains studies on cervical cancer, and its focus on screening rate improvement aligns with the topic of interest.
The second article under examination is a randomized controlled study. In the clinical research by Winer et al. (2019), the authors test whether mailing a test kit to patients is more effective than simple reminders to get screened for cervical cancer. Similar to the previous study, Appendices A and B demonstrate the high quality of available evidence. The research was chosen for this review due to its interest in additional measures for improving screening rates and a choice of nursing intervention.
Article Discussion
To understand the selection of sources and appraise their quality, one has to discuss them in more detail. First, in the meta-analysis, Nelson et al. (2020) aim to analyze the outcomes of patient navigation on the participants’ cancer screening rates. Breast, colorectal, and cervical cancer are considered in the study, and patient navigation is defined as “services that improve engagement in healthcare by providing personal guidance through the healthcare system” (Nelson et al., 2020, p. 3028). The research design is a meta-analysis that considers quantitative studies. The investigators introduce a new way of appraising the results by adapting them into one measurement. As a result, the article’s methodology synthesizes evidence and calculates the risk ratio.
The data collection process is described in the article in detail. It is noted that the authors gathered sources from such databases as Ovid® MEDLINE®, PsycINFO®, and SocINDEX (Nelson et al. (2020). The inclusion criteria included randomized controlled trials and observational studies with control and intervention groups. Furthermore, the reviewed sources had to consider vulnerable populations, be relevant to US health and practice, and present clear results of screening rates (Nelson et al. (2020). As a result, the data was collected from 37 articles, including 29 randomized controlled trials and eight observational studies. The validity of the data in the papers and their analysis was checked by comparing the selected studies’ results (Vu, 2021). Articles show consistently high significance, but additional research is necessary due to the variance in rates (Nelson et al. (2020). The instrument’s reliability is based on its transparency and consistency, which is supported by the author’s detailed discussion of its operation.
The results of the meta-analysis show that the screening rates for all types of cancer were positively influenced by patient navigation. While studies analyzing cervical cancer were limited in number, the consistency of the results for the available sources and the outcomes for other types of cancer demonstrate the overall effectiveness of this approach (Vu, 2021). These findings have significant implications for practice as they support the idea of additional measures for engaging patients in cancer screening. The study emphasizes the value of individual approaches to patients and communication’s role in improving patients’ preparedness for regular screening. Based on the factors above, the study’s evidence quality level and the findings’ ratings are high, and the meta-analysis can be marked as IA.
The second source presents similarly high-quality results while testing another method of screening rates’ improvement. In a randomized controlled trial, Winer et al. (2019) analyze whether patients are more likely to undergo hospital cervical cancer screening if they receive home test kits for human papillomavirus (HPV). To complete the study, the researchers identified eligible participants using electronic health records and separated them into control and intervention groups. The inclusion criteria are women between 30 and 64 years old who did not have a hysterectomy and had a clinician within the selected system. The control group receives usual care, including yearly reminders to undergo screening and frequent messages from the clinic. For the treatment group, these activities are supplemented by mailing patients a self-sampling kit that tests for HPV (Winer et al., 2019). Then, the screening rate is compared in the next six months after the initiative.
The data collection process in the second study relied on electronic health records. Two major outcomes were considered: diagnosed and treated precancerous conditions, and other measures included increased test uptake and abnormal results (Winer et al., 2019). As a result of investigating health records, it was determined that the difference between control and intervention groups was significant, with the self-testing kits raising the screening uptake by almost 10% (Winer et al., 2019). These results have high validity due to standardized statistical calculations and electronic records use (Vu, 2021). The implication of this study is the effectiveness of reaching out to patients with opportunities for self-testing instead of calling. The quality of data and the transparent explanations of each step allow one to grade this study as IA on the quality scale.
Applicability to Practice and Future Research
The discussed studies can significantly impact practice and positively influence its quality. Based on the six domains presented by the AHRQ (2022), the findings can enhance safety, effectiveness, and focus on patient-centered care. First, the articles demonstrate ways to improve screening rates and better diagnosing for patients to prevent and treat cancer – a severe condition that endangers the lives of many people. Thus, the conclusions and recommendations support the aim of patient safety. Second, the effectiveness of care is improved by engaging patients in screening and providing timely care. The higher rate of timely diagnoses is a result of both studies, showing the positive impact of the considered interventions. Finally, as the research finds ways to solve a problem in patient outreach, especially among underserved populations, it is consistent with the patient-centered approach to care. The recommendations to communicate with patients and provide them with easy methods of pretesting should be implemented in practice to deliver better care.
Cervical cancer is a significant problem that poses risks to population health. Timely screening remains an issue, especially among women with health disparities. The selected studies offer several options for reaching out to patients to provide them with testing recommendations or tests to engage them in cancer detection and treatment. The articles present reliable evidence of the approaches’ effectiveness and demonstrate that patient-centered and effective care is possible with nursing interventions.
Agency for Healthcare Research and Quality [AHRQ]. (2022). Six domains of healthcare quality . Web.
Bedell, S. L., Goldstein, L. S., Goldstein, A. R., & Goldstein, A. T. (2020). Cervical cancer screening: Past, present, and future . Sexual Medicine Reviews , 8 (1), 28-37. Web.
Centers for Disease Control and Prevention. (2022). Cervical cancer: Statistics . Web.
Nelson, H. D., Cantor, A., Wagner, J., Jungbauer, R., Fu, R., Kondo, K., Stillman, L., & Quiñones, A. (2020). Effectiveness of patient navigation to increase cancer screening in populations adversely affected by health disparities: A meta-analysis . Journal of General Internal Medicine , 35 , 3026-3035. Web.
Sürücü, L., & Maslakçi, A. (2020). Validity and reliability in quantitative research . Business & Management Studies: An International Journal , 8 (3), 2694-2726. Web.
Vu, T. T. N. (2021). Understanding validity and reliability from qualitative and quantitative research traditions . VNU Journal of Foreign Studies , 37 (3). Web.
Winer, R. L., Lin, J., Tiro, J. A., Miglioretti, D. L., Beatty, T., Gao, H., Kimbel, K., Thayer, C., & Buist, D. S. (2019). Effect of mailed human papillomavirus test kits vs usual care reminders on cervical cancer screening uptake, precancer detection, and treatment: A randomized clinical trial . JAMA Network Open , 2 (11), e1914729-e1914729. Web.
Individual Evidence Summary Tool
Research evidence appraisal tool – source 1.
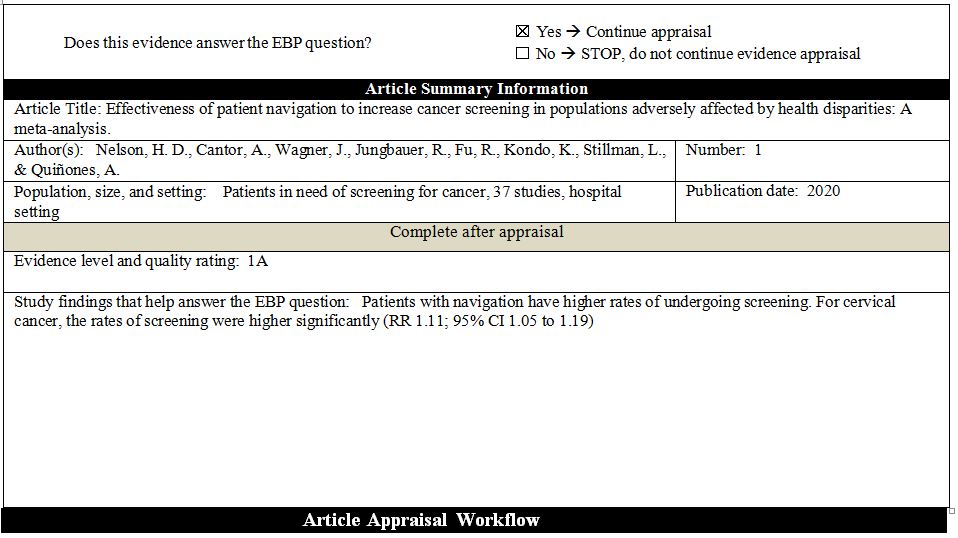
Research Evidence Appraisal Tool – Source 2
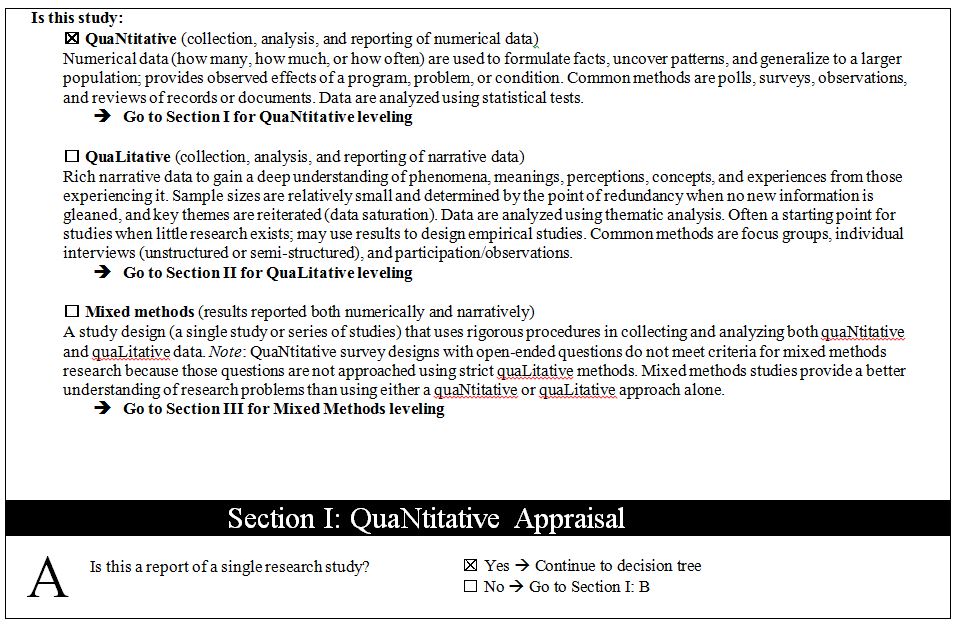
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 19). Cervical Cancer Screening: Review of Issues. https://ivypanda.com/essays/cervical-cancer-screening-review-of-issues/
"Cervical Cancer Screening: Review of Issues." IvyPanda , 19 Feb. 2024, ivypanda.com/essays/cervical-cancer-screening-review-of-issues/.
IvyPanda . (2024) 'Cervical Cancer Screening: Review of Issues'. 19 February.
IvyPanda . 2024. "Cervical Cancer Screening: Review of Issues." February 19, 2024. https://ivypanda.com/essays/cervical-cancer-screening-review-of-issues/.
1. IvyPanda . "Cervical Cancer Screening: Review of Issues." February 19, 2024. https://ivypanda.com/essays/cervical-cancer-screening-review-of-issues/.
Bibliography
IvyPanda . "Cervical Cancer Screening: Review of Issues." February 19, 2024. https://ivypanda.com/essays/cervical-cancer-screening-review-of-issues/.
- The History of Cervical Cancer: Treatment and Care
- Cervical Cancer, Its Nature and Symptoms
- Cervical Cancer: Causes and Treatment
- Cervical Cancer Prevention and Treatment Plan
- Human Papillomavirus Infection and Cervical Cancer
- Effective Solutions to the Prevention of Cervical Cancer
- Cervical Cancer and Women’s Health
- Community-Based Health Education on Cervical Cancer
- Cervical Cancer: Medical Imaging and Radiotherapy
- Cervical Cancer and Risk Factors
- Osteosarcoma: Innovative Treatment Strategies
- Breast Cancer and Its Population Burden
- Neurobiology of Disease: Article Summary
- Pap Smear and Cervical Cancer: Oncology Nursing
- Colorectal Cancer Screening Methodology

IMAGES
VIDEO
COMMENTS
In conclusion, although cervical cancer threatens female health, it could be the first cancer that would be eliminated by human beings with comprehensive preventive and control strategy. ... According to the WHO and International Agency for Research on Cancer (IARC) estimates, the year 2008 saw 529,000 new cases of cervical cancer globally. In ...
Globally, cervical cancer is the fourth most common female cancer after breast, colorectal, and lung cancer and accounts for 600 000 new cases and 340 000 deaths annually [ 1, 3, 4 ]. Importantly, approximately 83% of all new cervical cancer cases and 88% of all deaths occur in LMICs [ 3, 4 ]. Indeed, cervical cancer is the leading cause of ...
Globally, 570 000 cases of Cervical Cancer and 311000 deaths from the disease occurred in 2018. Cervical Cancer is the fourth most common cancer in women, ranking after breast cancer (2.1 million cases), colorectal cancer (0.8 million) and lung cancer (0.7 million). 1 It is the 2nd most leading cause of female cancer among women aged 15-44 years in India.
Cancer of the cervix is predominantly caused by persistent Human Papilloma Virus (HPV) infections. Out of 200 identified HPV types, 12 have been designated as carcinogenic by the International Agency for Research on Cancer, with HPV-16 accounting for 50% and HPV-18 accounting for 10% of cervical cancer cases, respectively. 1 Infection with one of these two strains of HPV accounts for a 435 ...
India. Abstract. Cervical cancer develops in a woman's cervix (the entrance to the uterus from the vagina). Almost all cervical cancer cases (99%) are linke d to infection with high-risk human ...
Cancer is an international interdisciplinary journal publishing articles on the latest clinical cancer research findings, spanning ... Up-to-date cervical cancer screening was lower in rural CHCs than urban CHCs (38.2% vs 43.0% during 2014-2019), and this difference increased during the pandemic (43.5% vs 49.0%). ... Conclusions. Rural ...
Background: The systematic review on which this paper is based provided evidence for the Canadian Task Force on Preventive Health Care to update their guideline regarding screening for cervical cancer. In this article we highlight three questions covered in the full review that pertain to the effectiveness of screening for reducing cervical cancer mortality and incidence as well as optimal ...
To address this, a systematic literature review was conducted using the PubMed database, focusing on research articles published between January 2020 and April 2023. The search strategy involved combining the term "cervical cancer" with "prevention" and "vaccination.". Priority was given to controlled, randomized studies and ...
Cervical cancer is the fourth most common cancer among women worldwide with an estimated 604,127 new cases and 341,831 deaths reported in 2020 [], up from 528,000 new cases and 266,000 deaths reported in 2012 [].The bulk of the global burden rests with Africa, Latin America, the Caribbean and Asia where approximately 90% of deaths occur [].With an estimated population of 372.2 million women ...
Clinical trials have consistently demonstrated the superior sensitivity of human papillomavirus (HPV) testing compared with cytology (Pap) testing for identifying women at risk of cervical cancer ...
Cervical cancer, the fourth most common cancer world-wide [1] with 80% of the cases occurring in low-income countries is a global concern [2]. Paradoxically, cervical cancer is a potentially preventable disease, yet it affects millions of women across the world [2]. In Zimbabwe, at least 2270 new cases of cervical cancer are diagnosed
Introduction. Carcinoma of the cervix (CC) is the fourth most commonly diagnosed cancer among women with an annual new registered case of 569,847 and 311,365 deaths worldwide (1, 2).Human papillomaviruses (HPV) have been shown to be one of the most common pathogens transmitted through sexual contact in the cervix, and chronic infections of the cervix with high-risk human papillomavirus is ...
In 2020, the American Cancer Society (ACS) released updated guidelines for cervical cancer screening. The main changes to current practices were to initiate screening at age 25 years instead of age 21 years and to screen using primary human papillomavirus (HPV) testing rather than cytology alone or in combination with HPV testing.
Conclusion: The application of nanotechnology in the field of cervical cancer has garnered considerable attention. Nanoparticles-based methods for diagnosis, administration, and treatment have proven to be instrumental in enhancing the sensitivity of cervical cancer detection, improving the accuracy and efficiency of administration, and ...
Conclusion. Tremendous strides have been made in reducing the rate of cervical cancer. However, women continue to be afflicted by a disease that is potentially preventable and curable. The women ...
Find research articles on cervical cancer, which may include news stories, clinical trials, blog posts, and descriptions of active studies. ... The rates of timely cervical cancer screening fell between 2005 and 2019, researchers found, and disparities existed among groups of women. The most common reason for not receiving timely screening was ...
Cervical cancer continues to rank among the top gynecologic cancers worldwide. According to current data, it is ranked 14th among all cancers and is the 4th most common cancer among women worldwide.[1] Cervical cancer intervention focuses on primary and secondary prevention.[2] Primary prevention and screening are the best methods to decrease the burden of cervical cancer and mortality.
Research Evidence Appraisal Tool - Source 2. This essay, "Cervical Cancer Screening: Review of Issues" is published exclusively on IvyPanda's free essay examples database. You can use it for research and reference purposes to write your own paper. However, you must cite it accordingly . Donate a paper.