- Newsletters

Site search
- Israel-Hamas war
- Home Planet
- 2024 election
- Supreme Court
- Relationships
- Homelessness
- All explainers
- Future Perfect
Filed under:
Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
Share this story
- Share this on Facebook
- Share this on Twitter
- Share this on Reddit
- Share All sharing options
Share All sharing options for: Read these 12 moving essays about life during coronavirus
/cdn.vox-cdn.com/uploads/chorus_image/image/66606035/1207638131.jpg.0.jpg)
The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
Will you support Vox today?
We believe that everyone deserves to understand the world that they live in. That kind of knowledge helps create better citizens, neighbors, friends, parents, and stewards of this planet. Producing deeply researched, explanatory journalism takes resources. You can support this mission by making a financial gift to Vox today. Will you join us?
We accept credit card, Apple Pay, and Google Pay. You can also contribute via
Next Up In Culture
Sign up for the newsletter today, explained.
Understand the world with a daily explainer plus the most compelling stories of the day.
Thanks for signing up!
Check your inbox for a welcome email.
Oops. Something went wrong. Please enter a valid email and try again.

Ukraine aid and a potential TikTok ban: What’s in the House’s new $95 billion bill

The Supreme Court doesn’t seem eager to get involved with homelessness policy
Drake vs. everyone, explained

On Earth Day, Vox Releases Home Planet, A Project Highlighting the Personal Dimensions of Climate Change in our Daily Lives

Do you need to worry about “forever chemicals”?

Donald Trump already won the only Supreme Court fight that mattered

What We’ve Learned About So-Called ‘Lockdowns’ and the COVID-19 Pandemic
By Lori Robertson
Posted on March 8, 2022
SciCheck Digest
Plenty of peer-reviewed studies have found government restrictions early in the pandemic, such as business closures and physical distancing measures, reduced COVID-19 cases and/or mortality, compared with what would have happened without those measures. But conservative news outlets and commentators have seized on a much-criticized, unpublished working paper that concluded “lockdowns” had only a small impact on mortality as definitive evidence the restrictions don’t work.
Multiple lines of evidence back the use of face masks to protect against the coronavirus, although some uncertainty remains as to how effective mask interventions are in preventing spread in the community.
Lab tests, for example, show that certain masks and N95 respirators can partially block exhaled respiratory droplets or aerosols, which are thought to be the primary ways the virus spreads.
Observational studies, while limited, have generally found mask-wearing to be associated with a reduced risk of contracting the virus or fewer COVID-19 cases in a community.
A few randomized controlled trials have found that providing free masks and encouraging people to wear them results in a small to moderate reduction in transmission, although these results have not always been statistically significant.
Masks should not be viewed as foolproof, as no mask is thought to offer complete protection to the wearer or to others. The Centers for Disease Control and Prevention recommends that people wear the most protective mask that fits well and can be worn consistently. Loosely woven cloth masks are the least protective. Layered, tightly woven cloth masks offer more protection, while well-fitting surgical masks and KN95 respirators provide even more protection and N95 respirators are the most protective.
Link to this
In the early months of the COVID-19 pandemic in 2020, as the virus spread around the globe, many countries implemented restrictions on movement and social gatherings in an effort to flatten the curve — or reduce sharp spikes in caseloads to avoid overwhelming health care facilities. Without vaccines or evidence-based treatments, these non-pharmaceutical interventions, or NPIs, were the only public health measures available for months to combat the pandemic.

There have been a lot of studies assessing whether and to what extent so-called “lockdowns” and various NPIs have been effective, and plenty of research that has concluded these measures can limit transmission, or reduce cases and deaths. For instance, a study published in Nature in June 2020 found that “major non-pharmaceutical interventions—and lockdowns in particular—have had a large effect on reducing transmission” in 11 European countries. It estimated what would have happened if the transmission of the virus hadn’t been reduced, finding that 3.1 million deaths “have been averted owing to interventions since the beginning of the epidemic.” The estimate doesn’t account for behavior changes or the impact of overwhelmed health systems.
In May 2020, the same journal published a study that estimated the number of cases in mainland China would have been “67-fold higher” by the end of February 2020 without a combination of non-pharmaceutical interventions.
But one working paper posted online in January — and not peer-reviewed — has gotten a lot of attention in conservative circles for its conclusion that “lockdowns have had little to no effect on COVID-19 mortality.” The paper, which is an analysis of other studies, has been touted as a “Johns Hopkins University study,” but it’s not a product of the university’s Bloomberg School of Public Health, whose vice dean — among other public health experts — has criticized the paper.
“The working paper is not a peer-reviewed scientific study,” Dr. Joshua Sharfstein, vice dean of the Johns Hopkins Bloomberg School of Public Health, said in a Feb. 8 statement sent to us in an email. “To reach their conclusion that ‘lockdowns’ had a small effect on mortality, the authors redefined the term ‘lockdown’ and disregarded many peer-reviewed studies. The working paper did not include new data, and serious questions have already been raised about its methodology.”
Sharfstein said that early on “when so little was known about COVID-19, stay-at-home policies kept the virus from infecting people and saved many lives. Thankfully, these policies are no longer needed, as a result of vaccines, masks, testing, and other tools that protect against life-threatening COVID-19 infections.”
The authors of the working paper are economists: Steve H. Hanke , a senior fellow at the libertarian Cato Institute and founder and co-director of the Johns Hopkins Institute for Applied Economics, Global Health, and the Study of Business Enterprise; Jonas Herby , a special adviser at the Center for Political Studies in Copenhagen, Denmark; and Lars Jonung , a professor emeritus at Sweden’s Lund University.
Fox News published a Feb. 4 story questioning why other mainstream media outlets hadn’t written stories about the working paper, saying there had been “a full-on media blackout,” and “Fox & Friends” co-host Brian Kilmeade asked in a Facebook post , “Will some people get an apology after this?” On Feb. 21, former Republican vice presidential nominee Sarah Palin posted a video to Facebook highlighting the working paper and asking if lockdowns were about “power,” not “safety.”
But the non-peer-reviewed paper isn’t the definitive or final word on lockdowns, and the attention it has received has, in turn, sparked criticism of the paper’s analysis.
Criticisms of the Working Paper
The working paper was a literature review and meta-analysis , meaning it searched the available scientific literature and identified studies that met certain criteria, and then combined similar studies statistically to reach a conclusion. It identified 24 papers, published or posted as of early July 2021, that met its criteria for the meta-analysis — 17 of which were peer-reviewed. Among the criticisms: The paper excluded many relevant studies, broadly defined “lockdown,” and overwhelmingly based one of its headline figures on a study whose conclusions it rejected. That study also didn’t estimate the delayed effect of government restrictions on death rates a few weeks later, according to experts we consulted. Instead, it only assessed the effect of current death rates on current policies.

Excluded research. One of the criticisms is that the working paper excluded a lot of relevant research. The paper said it considered “difference-in-difference” studies, which would compare outcomes in areas or populations that were subject to a restriction with those that were not, and limited its analysis to the impact on mortality. The paper excluded studies that use modeling on mortality, that compare before and after a “lockdown” and that consider the timing of restrictions. Gideon Meyerowitz-Katz , an epidemiologist working on his Ph.D. at the University of Wollongong in Australia, said in a long Twitter thread: “Many of the most robust papers on the impact of lockdowns are, by definition, excluded.”
He called the working paper “a very weak review that doesn’t really show much, if anything.” It excluded “modelled counterfactuals,” which would compare what happened with what would have happened without the intervention. “Because this is the most common method used in infectious disease assessments, this has the practical impact of excluding most epidemiological research from the review,” Meyerowitz-Katz said.
Hanke told us: “Models are fine if they are based on empirical observations,” meaning from experience, “rather than assumptions. In those circumstances, models are able to reliably forecast the real world. But the models used during the pandemic have been inaccurate, as they, for the most part, have not been based on empirical observations but assumptions,” he said in an email. “A prime example of modelers gone astray is the Imperial College London study of March 16, 2020.”
That March 2020 report , early in the pandemic, estimated that 2.2 million lives would be lost in the U.S. in “the (unlikely) absence of any control measures or spontaneous changes in individual behaviour.” As we’ve written before , it wasn’t intended to be a practical estimate, as doing absolutely nothing was, in the author’s words, “unlikely.”
One of the authors of that report has been critical of Hanke’s working paper. Neil Ferguson, director of the MRC Centre for Global Infectious Disease Analysis, Jameel Institute, Imperial College London, said in a statement that the working paper “does not significantly advance our understanding of the relative effectiveness of the plethora of public health measures adopted by different countries to limit COVID-19 transmission.”
Ferguson said that NPIs “are intended to reduce contact rates between individuals in a population, so their primary impact, if effective, is on transmission rates. Impacts on hospitalisation and mortality are delayed, in some cases by several weeks. In addition, such measures were generally introduced (or intensified) during periods where governments saw rapidly growing hospitalisations and deaths. Hence mortality immediately following the introduction of lockdowns is generally substantially higher than before. Neither is lockdown a single event as some of the studies feeding into this meta-analysis assume; the duration of the intervention needs to be accounted for when assessing its impact.”
Ferguson said because NPIs affect transmission rates, “the appropriate outcome measures to consider are growth rates (of cases or deaths) over time, with appropriate time lags – not total cases or deaths.”
Definition of “lockdown.” The working paper also had a very broad definition of “lockdown”: “Lockdowns are defined as the imposition of at least one compulsory, non-pharmaceutical intervention (NPI),” it said. “NPIs are any government mandate that directly restrict peoples’ possibilities, such as policies that limit internal movement, close schools and businesses, and ban international travel.”
The paper did not examine the impact of voluntary behavior or recommendations, as opposed to mandates. “Our definition does not include governmental recommendations, governmental information campaigns, access to mass testing, voluntary social distancing, etc., but do include mandated interventions such as closing schools or businesses, mandated face masks etc.”
The paper then divided the 24 studies it considered into three groups: studies using a stringency index for restrictions, studies on shelter-in-place orders and those looking at specific NPIs. The last category included 11 studies on various measures, including face mask policies and limits on gatherings.
Stringency index studies. The authors examined seven studies on the impact of more severe restrictions, calculating from those studies that, compared with a policy of recommendations, “lockdowns in Europe and the United States only reduced COVID-19 mortality by 0.2% on average” — the figure that conservatives have cited . But six of the seven studies concluded that lockdown policies helped reduce mortality, and the 0.2% figure is overwhelmingly based on one study that mistakenly estimated the wrong effect, according to economists we consulted.
The studies in this group used the Oxford COVID-19 Government Response Tracker , which looked at government responses worldwide to the pandemic and created a stringency index, measuring how strict the measures were over time. The index is from 0 to 100, with 100 being the most stringent restrictions. For instance, the OxCGRT heat map shows that many countries around the world had stringency levels above 70 in April 2020.
The working paper calculates mortality impact estimates for each of the seven studies aiming to show the effect of the average mandated restrictions in Europe and the United States early in the pandemic compared with a policy of only recommendations. The paper then calculates a weighted average, giving more weight to studies that said their findings were more precise. Nearly all of the weight — 91.8% — goes to one study, even though the working paper rejects the conclusions of that study.
That study — coauthored by Carolyn Chisadza , a senior lecturer in economics at the University of Pretoria, and published on March 10, 2021, in the journal Sustainability — looked at a sample of countries between March and September 2020 and concluded: “Less stringent interventions increase the number of deaths, whereas more severe responses to the pandemic can lower fatalities.”
The working paper claims the researchers’ conclusion is incorrect — but it uses the study’s estimates, saying the figures show an increase in mortality due to “lockdowns.”
Chisadza told us in an email that the study showed: “Stricter lockdowns will reduce the rate of deaths than would have occurred without lockdown or too lenient of restrictions.” But Hanke said the data from Chisadza and her colleagues only show that “stricter lockdowns will reduce mortality” relative to “the worst possible lockdown,” meaning a more lenient lockdown that, under the study, was associated with the highest rate of deaths.
We reached out to a third party about this disagreement. Victor Chernozhukov , a professor in the Massachusetts Institute of Technology’s Department of Economics and the Statistics and Data Science Center, along with Professor Hiroyuki Kasahara and Associate Professor Paul Schrimpf , both with the Vancouver School of Economics at the University of British Columbia — the authors of another study that was included in the working paper — looked at the Chisadza study and provided FactCheck.org with a peer review of it . They found the Chisadza study only measured the correlation between current death growth rates and current policies. It did not show the lagged effect of more stringent policies, implemented three weeks prior, on current death growth rates, which is what one would want to look at to evaluate the effectiveness of “lockdowns.”
In an email and in a phone interview, Chernozhukov told us the Chisadza study made an “honest mistake.” He said the working paper is “deeply flawed” partly because it relies heavily on a study that “estimates the wrong effect very precisely.”
In their review, Chernozhukov, Kasahara and Schrimpf write that the Chisadza et al. study “should be interpreted as saying that the countries currently experiencing high death rates (or death growth rates) are more likely to implement more stringent current policy. That is the only conclusion we can draw from [the study], because the current policy can not possibly influence the current deaths,” given the several weeks of delay between new infections and deaths.
The effect that should be examined for the meta-analysis is “the effect of the previous (e.g., 3 week lagged) policy stringency index on the current death growth rates.”
Chernozhukov, Kasahara and Schrimpf conducted a “quick reanalysis of similar data” to the Chisadza study, finding results that “suggest that more stringent policies in the past predict lower death growth rates.” Chernozhukov said much more analysis would be needed to further characterize this effect, but that it is “actually quite substantial.”
If the Chisadza study were removed from the working paper, according to one of the paper’s footnotes, the result would be a weighted average reduction in mortality of 3.5%, which Hanke said doesn’t change the “overall conclusions.” He said it “simply demonstrates the obvious fact that the conclusions contained in our meta-analysis are robust.”
But experts have pointed out other issues with the meta-analysis. Chernozhukov also said the paper “excluded a whole bunch of studies,” including synthetic control method studies, which evaluate treatment effects. He also questioned the utility of looking at a policy index that considers the U.S. as a whole, lumping all the states together. He said the meta-analysis is “not credible at all.”
Among the other six stringency index studies included in the meta-analysis, only one concluded that its findings suggested “lockdowns” had zero effect on mortality. In a review of 24 European countries’ weekly mortality rates for the first six months of 2017-2020, the study, published in CESifo Economic Studies , found “no clear association between lockdown policies and mortality development.” The author and Herby , one of the authors of the working paper, have written for the American Institute for Economic Research , which facilitated the controversial Great Barrington Declaration , an October 2020 statement advocating those at low risk of dying from COVID-19 “live their lives normally to build up immunity to the virus through natural infection,” while those at “highest risk” are protected.
The other studies found lockdown policies helped COVID-19 health outcomes. For instance, a CDC study published in the agency’s Morbidity and Mortality Weekly Report in January 2021, on the experience of 37 European countries from Jan. 23 to June 30, 2020, concluded that “countries that implemented more stringent mitigation policies earlier in their outbreak response tended to report fewer COVID-19 deaths through the end of June 2020. These countries might have saved several thousand lives relative to countries that implemented similar policies, but later.”
A working paper from Harvard University’s Center for International Development , which looked at 152 countries from the beginning of the pandemic until Dec. 31, 2020, found that “lockdowns tend to significantly reduce the spread of the virus and the number of related deaths.” But the effect fades over time, so lengthy (after four months) or second-phase “lockdowns” don’t have the same impact.
A study published in World Medical & Health Policy in November 2020 — that looked at whether 24 European countries responded quickly enough — found that the fluctuating containment measures, from country to country and over time, “prohibited a clear association with the mortality rate.” But it said “the implementation speed of these containment measures in response to the coronavirus had a strong effect on the successful mitigation of fatalities.”
Many studies found restrictions worked. Meyerowitz-Katz noted that the working paper authors disagreed with the conclusions of other studies included in the review, pointing to one included in the group of shelter-in-place orders. Meyerowitz-Katz said that study “found that significant restrictions were effective, but is included in this review as estimating a 13.1% INCREASE in fatalities.”
That study, by Yale School of Management researchers, published by The Review of Financial Studies in June 2021 , developed “a time-series database” on several types of restrictions for every U.S. county from March to December 2020. The authors concluded: “We find strong evidence consistent with the idea that employee mask policies, mask mandates for the general population, restaurant and bar closures, gym closures, and high-risk business closures reduce future fatality growth. Other business restrictions, such as second-round closures of low- to medium-risk businesses and personal care/spa services, did not generate consistent evidence of lowered fatality growth and may have been counterproductive.” The authors said the study’s “findings lie somewhere in the middle of the existing results on how NPIs influenced the spread of COVID-19.”
In terms of hard figures on fatality reductions, the study said the estimates suggest a county with a mandatory mask policy would see 15.3% fewer new deaths per 10,000 residents on average six weeks later, compared with a county without a mandatory mask policy. The impact for restaurant closures would be a decrease of 36.4%. But the estimates suggest other measures, including limits on gatherings of 100 people or more, appeared to increase deaths. The authors said one possible explanation of such effects could be that the public is substituting other activities that actually increase transmission of the virus — such as hosting weddings with 99 people in attendance, just under the 100-person limitation.
Another study in the shelter-in-place group is the study by Chernozhukov, Kasahara and Schrimpf, published in the Journal of Econometrics in January 2021 . It looked at the policies in U.S. states and found that “nationally mandating face masks for employees early in the pandemic … could have led to as much as 19 to 47 percent less deaths nationally by the end of May, which roughly translates into 19 to 47 thousand saved lives.” It found cases would have been 6% to 63% higher without stay-at-home orders and found “considerable uncertainty” over the impact of closing schools. It also found “substantial declines in growth rates are attributable to private behavioral response, but policies played an important role as well.”
The working paper considered 13 studies that evaluated stay-in-place orders, either alone or in combination with other NPIs. The estimated effect on total fatalities for each study calculated by the authors varied quite widely, from a decrease of 40.8% to an increase of 13.1% (the study above mentioned by Meyerowitz-Katz). The authors then combined the studies into a weighted average showing a 2.9% decrease in mortality from these studies on shelter-in-place orders.
Sizable impact from some NPIs. The working paper actually found a sizable decrease in deaths related to closing nonessential businesses: a 10.6% weighted average reduction in mortality. The authors said this “is likely to be related to the closure of bars.” It also calculated a 21.2% weighted average reduction in deaths due to mask requirements, but notes “this conclusion is based on only two studies.”
As with the shelter-in-place group, the calculated effects in the specific NPIs group varied widely – from a 50% reduction in mortality due to business closures to a 36% increase due to border closures. The paper said “differences in the choice of NPIs and in the number of NPIs make it challenging to create an overview of the results.”
“The review itself does refer to other papers that reported that the lockdowns had a significant impact in preventing deaths,” Dr. Lee Riley , chair of the Division of Infectious Disease and Vaccinology at the University of California, Berkeley School of Public Health, told us when we asked for his thoughts on the working paper. “The pandemic has now been occurring long enough that it’s not surprising to begin to see many more reports that now contradict each other. As we all know, the US and Europe went through several periods when they relaxed their lockdowns, which was followed by a resurgence of the cases.”
Riley said that “many of the studies that this review included may suffer from the classic ‘chicken-or-egg’ bias. Whenever there was an increase in cases of deaths, lockdowns got instituted so it’s not surprising that some of the studies showed no impact of the lockdowns. If there was no surge of cases or deaths, most places in the US did not impose restrictions.”
Meyerowitz-Katz noted on Twitter that “the impact of ‘lockdowns’ is very hard to assess, if for no other reason than we have no good definition of ‘lockdown’ in the first place. … In most cases, it seems the authors have taken estimates for stay-at-home orders as their practical definition of ‘lockdown’ (this is pretty common) And honestly, I’d agree that the evidence for marginal benefit from stay-at-home orders once you’ve already implemented dozens of restrictions is probably quite weak.”
But, “if we consider ‘lockdown’ to be any compulsory restriction at all, the reality is that virtually all research shows a (short-term) mortality benefit from at least some restrictions.”
Additional Studies
We’ve already mentioned two studies beyond those in the working paper: the Nature June 2020 study by Imperial College London researchers that estimated interventions in 11 countries in Europe in the first few months of the pandemic reduced transmission and averted 3.1 million deaths; and the Nature May 2020 study that estimated cases in mainland China would have been 67-fold greater without several NPIs by the end of February.
There are many more that aimed to evaluate the effectiveness of various mitigation strategies, not included in the working paper’s analysis.
- A 2020 unpublished observational study — cited in the working paper as the basis for the Oxford stringency index but not included in the analysis — found that more stringent restrictions implemented more quickly led to fewer deaths. “A lower degree of government stringency and slower response times were associated with more deaths from COVID-19. These findings highlight the importance of non-pharmaceutical responses to COVID-19 as more robust testing, treatment, and vaccination measures are developed.” In considering nine NPIs, the authors said the average daily growth rates in deaths were affected by each additional stringency index point and each day that a country delayed reaching an index of 40 on the stringency scale. “These daily differences in growth rates lead to large cumulative differences in total deaths. For example, a week delay in enacting policy measures to [a stringency index of 40] would lead to 1.7 times as many deaths overall,” they wrote.
- A more up-to-date study by many of the same authors, posted July 9, 2021, by the journal Plos One, looked at data for 186 countries from Jan. 1, 2020, to March 11, 2021, a period over which 10 countries experienced three waves of the pandemic. In the first wave in those countries, 10 additional points on the stringency index — in other words more stringent restrictions — “resulted in lower average daily deaths by 21 percentage points” and by 28 percentage points in the third wave. “Moreover, interaction effects show that government policies were effective in reducing deaths in all waves in all groups of countries,” the authors said.
- A Dec. 15, 2020, study in Science used data from 41 countries to model which NPIs were most effective at reducing transmission. “Limiting gatherings to fewer than 10 people, closing high-exposure businesses, and closing schools and universities were each more effective than stay-at-home orders, which were of modest effect in slowing transmission,” the authors said. “When these interventions were already in place, issuing a stay-at-home order had only a small additional effect. These results indicate that, by using effective interventions, some countries could control the epidemic while avoiding stay-at-home orders.” The study, like many others, looked at the impact on the reproduction number of SARS-CoV-2, or the average number of people each person with COVID-19 infects at a given time. It notes that a reduction in this number would affect COVID-19 mortality, and that the impact of NPIs can depend on other factors, including when and for how long they are implemented, and how much the public adhered to them.
- A study in Nature Human Behaviour on Nov. 16, 2020 , considered the impact on the reproduction number of COVID-19 by 6,068 NPIs in 79 territories, finding that a combination of less intrusive measures could be as effective as a national lockdown. “The most effective NPIs include curfews, lockdowns and closing and restricting places where people gather in smaller or large numbers for an extended period of time. This includes small gathering cancellations (closures of shops, restaurants, gatherings of 50 persons or fewer, mandatory home working and so on) and closure of educational institutions.” The authors said this doesn’t mean an early national lockdown isn’t effective in reducing transmission but that “a suitable combination (sequence and time of implementation) of a smaller package of such measures can substitute for a full lockdown in terms of effectiveness, while reducing adverse impacts on society, the economy, the humanitarian response system and the environment.” They found that “risk-communication strategies” were highly effective, meaning government education and communication efforts that would encourage voluntary behavior. “Surprisingly, communicating on the importance of social distancing has been only marginally less effective than imposing distancing measures by law.”
- Another study in Nature in June 2020 looked at 1,700 NPIs in six countries, including the United States. “We estimate that across these 6 countries, interventions prevented or delayed on the order of 61 million confirmed cases, corresponding to averting approximately 495 million total infections,” the authors concluded. “Without these policies employed, we would have lived through a very different April and May” in 2020, Solomon Hsiang, the lead researcher and director of the Global Policy Laboratory at the University of California at Berkeley, told reporters . The study didn’t estimate how many lives were saved, but Hsiang said the benefits of the lockdown are in a sense invisible because they reflect “infections that never occurred and deaths that did not happen.”
- A more recently published study in Nature Communications in October , by U.K. and European researchers, found that closures of businesses and educational institutions, as well as gathering bans, reduced transmission during the second wave of COVID-19 in Europe — but by less than in the first wave. “This difference is likely due to organisational safety measures and individual protective behaviours—such as distancing—which made various areas of public life safer and thereby reduced the effect of closing them,” the authors said. The 17 NPIs considered by the study led to median reductions in the reproduction number of 77% to 82% in the first wave and 66% in the second wave.
- A February 2021 study in Chaos: An Interdisciplinary Journal of Nonlinear Science estimated large reductions in infections (by 72%) and deaths (by 76%) in New York City in 2020, based on numerical experiments in a model. “Among all the NPIs, social distancing for the entire population and protection for the elderly in public facilities is the most effective control measure in reducing severe infections and deceased cases. School closure policy may not work as effectively as one might expect in terms of reducing the number of deceased cases,” the authors said.
Near the end of his lengthy Twitter thread on the working paper, Meyerowitz-Katz said he agrees that “a lot of people originally underestimated the impact of voluntary behaviour change on COVID-19 death rates – it’s probably not wrong to argue that lockdowns weren’t as effective as we initially thought.” He pointed to the Nature Communications study mentioned above, showing less of an impact from NPIs in a second wave of COVID-19 and positing individual safety behaviors were playing more of a role in that second wave.
“HOWEVER, this runs both ways,” Meyerowitz-Katz said. “[I]t is also quite likely that lockdowns did not have the NEGATIVE impact most people propose, because some behaviour changes were voluntary!”
He and others examined whether lockdowns were more harmful than the pandemic itself in a 2021 commentary piece in BMJ Global Health . They concluded that “government interventions, even more restrictive ones such as stay-at-home orders, are beneficial in some circumstances and unlikely to be causing harms more extreme than the pandemic itself.” Analyzing excess mortality suggested that “ lockdowns are not associated with large numbers of deaths in places that avoided large COVID-19 epidemics,” such as Australia and New Zealand, they wrote.
Editor’s note: SciCheck’s COVID-19/Vaccination Project is made possible by a grant from the Robert Wood Johnson Foundation. The foundation has no control over FactCheck.org’s editorial decisions, and the views expressed in our articles do not necessarily reflect the views of the foundation. The goal of the project is to increase exposure to accurate information about COVID-19 and vaccines, while decreasing the impact of misinformation.
Herby, Jonas et al. “ A Literature Review and Meta-Analysis of the Effects of Lockdowns on COVID-19 Mortality .” Studies in Applied Economics, Institute for Applied Economics, Global Health, and the Study of Business Enterprise, Johns Hopkins University. posted Jan 2022.
World Health Organization. “ Coronavirus disease (COVID-19): Herd immunity, lockdowns and COVID-19 .” 31 Dec 2020.
Flaxman, Seth et al. “ Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe .” Nature. 584 (2020).
Lai, Shengjie et al. “ Effect of non-pharmaceutical interventions to contain COVID-19 in China .” Nature. 585 (2020).
Sharfstein, Joshua, vice dean of the Johns Hopkins Bloomberg School of Public Health. Statement emailed to FactCheck.org. 8 Feb 2022.
Best, Paul. “ Lockdowns only reduced COVID-19 death rate by .2%, study finds: ‘Lockdowns should be rejected out of hand .'” Fox News. 1 Feb 2022.
Meyerowitz-Katz, Gideon. @GidMK. “ This paper has been doing the rounds, claiming that lockdown was useless (the source of the 0.2% effect of lockdown claim). Dozens of people have asked my opinion of it, so here we go: In my opinion, it is a very weak review that doesn’t really show much, if anything 1/n .” Twitter.com. 4 Feb 2022.
Hanke, Steve H., founder and co-director of the Johns Hopkins Institute for Applied Economics, Global Health, and the Study of Business Enterprise. Email interview with FactCheck.org. 18 Feb 2022.
Ferguson, Neil, director of the MRC Centre for Global Infectious Disease Analysis, Jameel Institute, Imperial College London. Statement posted by Science Media Centre . 3 Feb 2022.
Oxford COVID-19 Government Response Tracker . Blavatnik School of Government, University of Oxford. https://covidtracker.bsg.ox.ac.uk/. website accessed 20 Feb 2022.
Chisadza, Carolyn, senior lecturer in economics at the University of Pretoria. Email interview with FactCheck.org. 15 Feb 2022.
Clance, Matthew, associate professor in the Department of Economics at the University of Pretoria. Email interview with FactCheck.org. 16 Feb 2022.
Our World in Data. Cumulative confirmed COVID-19 deaths . website accessed 22 Feb 2022.
Bjornskov, Christian. “ Did Lockdown Work? An Economist’s Cross-Country Comparison .” CESifo Economic Studies. 67.3 (2021).
Fuller, James A. et al. “ Mitigation Policies and COVID-19–Associated Mortality — 37 European Countries, January 23–June 30, 2020 .” Morbidity and Mortality Weekly Report. 70.2 (2021).
Goldstein, P. et al. “ Lockdown Fatigue: The Diminishing Effects of Quarantines on the Spread of COVID-19 .” Harvard University Center for International Development. 2021.
Stockenhuber, Reinhold. “ Did We Respond Quickly Enough? How Policy-Implementation Speed in Response to COVID-19 Affects the Number of Fatal Cases in Europe .” World Medical & Health Policy. 12.4 (2020).
Riley, Lee, chair of the Division of Infectious Disease and Vaccinology at the University of California, Berkeley School of Public Health. Email interview with FactCheck.org. 14 Feb 2022.
Spiegel, Matthew and Heather Tookes. “ Business Restrictions and COVID-19 Fatalities .” The Review of Financial Studies. 34.11 (2021).
Chernozhukov, Victor et al. “ Causal impact of masks, policies, behavior on early covid-19 pandemic in the U.S. ” Journal of Econometrics. 220. 1 (2021).
Hale, Thomas et al. “ Global Assessment of the Relationship between Government Response Measures and COVID-19 Deaths .” medrxiv.org. 6 Jul 2020.
Hale, Thomas et al. “ Government responses and COVID-19 deaths: Global evidence across multiple pandemic waves .” Plos One. 9 Jul 2021.
Brauner, Jan M. et al. “ Inferring the effectiveness of government interventions against COVID-19 .” Science. 371.6531 (2020).
Haug, Mils et al. “ Ranking the effectiveness of worldwide COVID-19 government interventions .” Nature Human Behaviour. 4 (2020).
Sharma, Mrinank et al. “ Understanding the effectiveness of government interventions against the resurgence of COVID-19 in Europe .” Nature Communications. 12 (2021).
Yang, Jiannan et al. “ The impact of non-pharmaceutical interventions on the prevention and control of COVID-19 in New York City .” Chaos: An Interdisciplinary Journal of Nonlinear Science. 31.2 (2021).
Achenbach, Joel and Laura Meckler. “ Shutdowns prevented 60 million coronavirus infections in the U.S., study finds .” Washington Post. 8 Jun 2020.
Hsiang, Solomon et al. “ The effect of large-scale anti-contagion policies on the COVID-19 pandemic .” Nature. 584 (2020).
Chernozhukov, Victor et al. “ Comments on the ‘John Hopkins’ Meta Study (Herby et al., 2022) and Chisadza et al. (2021) .” Provided to FactCheck.org. 4 Mar 2022.
Chernozhukov, Victor, professor, Massachusetts Institute of Technology Department of Economics and the Statistics and Data Science Center. Phone interview with FactCheck.org. 8 Mar 2022.
ORIGINAL RESEARCH article
How did the covid-19 lockdown affect children and adolescent's well-being: spanish parents, children, and adolescents respond.

- 1 ISGlobal, Hospital Clínic—Universitat de Barcelona, Barcelona, Spain
- 2 Institut de Recerca Sant Joan de Déu, University of Barcelona, Barcelona, Spain
- 3 Universitat Politècnica de Catalunya, BarcelonaTech, Barcelona, Spain
- 4 B2SLab, Departament d'Enginyeria de Sistemes, Automàtica i Informàtica Industrial, Universitat Politècnica de Catalunya, Barcelona, Spain
- 5 Centro de Investigação em Saúde de Manhiça, Maputo, Mozambique
- 6 Networking Biomedical Research Centre in the Subject Area of Bioengineering, Biomaterials and Nanomedicine (CIBER-BBN), Madrid, Spain
- 7 Institut de Recerca Sant Joan de Déu, Barcelona, Spain
- 8 Pediatric Intensive Care Unit, Hospital Sant Joan de Déu, University of Barcelona, Barcelona, Spain
- 9 Consorcio de Investigación Biomédica en Red de Epidemiología y Salud Pública, Madrid, Spain
- 10 Department of Medicine, Universitat Internacional de Catalunya, Barcelona, Spain
- 11 Molecular Microbiology Department, Hospital Sant Joan de Deu, Esplugues, Barcelona, Spain
- 12 BCNatal Fetal Medicine Research Center (Hospital Clínic and Hospital Sant Joan de Déu), University of Barcelona, Barcelona, Spain
- 13 Institut d'Investigacions Biomèdiques August Pi i Sunyer, Barcelona, Spain
- 14 Child and Adolescent Psychiatry and Psychology Department, Hospital Sant Joan de Déu, Barcelona, Spain
- 15 Pediatrics Department, Hospital Sant Joan de Déu, Universitat de Barcelona, Barcelona, Spain
- 16 ICREA, Catalan Institution for Research and Advanced Studies, Barcelona, Spain
Background: During the COVID-19 pandemic, lockdown strategies have been widely used to contain SARS-CoV-2 virus spread. Children and adolescents are especially vulnerable to suffering psychological effects as result of such measures. In Spain, children were enforced to a strict home lockdown for 42 days during the first wave. Here, we studied the effects of lockdown in children and adolescents through an online questionnaire.
Methods: A cross-sectional study was conducted in Spain using an open online survey from July (after the lockdown resulting from the first pandemic wave) to November 2020 (second wave). We included families with children under 16 years-old living in Spain. Parents answered a survey regarding the lockdown effects on their children and were instructed to invite their children from 7 to 16 years-old (mandatory scholar age in Spain) to respond a specific set of questions. Answers were collected through an application programming interface system, and data analysis was performed using R.
Results: We included 1,957 families who completed the questionnaires, covering a total of 3,347 children. The specific children's questionnaire was completed by 167 kids (7–11 years-old), and 100 adolescents (12–16 years-old). Children, in general, showed high resilience and capability to adapt to new situations. Sleeping problems were reported in more than half of the children (54%) and adolescents (59%), and these were strongly associated with less time doing sports and spending more than 5 h per day using electronic devices. Parents perceived their children to gain weight (41%), be more irritable and anxious (63%) and sadder (46%). Parents and children differed significantly when evaluating children's sleeping disturbances.
Conclusions: Enforced lockdown measures and isolation can have a negative impact on children and adolescent's mental health and well-being. In future waves of the current pandemic, or in the light of potential epidemics of new emerging infections, lockdown measures targeting children, and adolescents should be reconsidered taking into account their infectiousness potential and their age-specific needs, especially to facilitate physical activity and to limit time spent on electronic devices.
Nearly 80–90% of school-age youth could not physically attend school in more than 160 countries during the first wave of the coronavirus disease 2019 (COVID-19) pandemic ( 1 , 2 ). In Spain, one of the first measures implemented when cases started increasing was to close all schools and impose a strict home confinement. During the first period of the lockdown (March 14th–April 27th of 2020), referred as “strict lockdown” hereinafter, only essential activities were allowed, and children were compelled to stay home except for emergency situations. From April 28th to June 21st, children were progressively allowed to leave the household in a very controlled manner and for a limited period (i.e., 1 h per day with no close interactions), during what became referred as the “relaxed lockdown.” Schools remained closed and pupils attended online lectures whenever possible. Children did not return to face-to-face learning until September 2020. Home confinement measures due to the COVID-19 pandemic, which were particularly stringent for children, may have had deleterious effects on the physical and mental health of this particularly vulnerable age group ( 3 , 4 ). Herein, we aimed to understand the perceived impact of lockdown measures on the mental health and well-being of minors, as reported by parents, but also adolescents and children themselves. We focused on risk perception and attitudes toward lockdown, perceptions of schooling, emotional responses, changes in biorhythms, psychical activity, sleep and eating attitudes, and screen time.
Study Design
We performed a cross-sectional study using convenience sampling through an online survey, launched in July 2020 and available until November 2020. The study was promoted via social media and the landing page of the Kids Corona Project. The questionnaire (see Supplementary Material ) was created by a team of pediatricians at Hospital Sant Joan de Déu of Barcelona, Spain, and was available in Spanish or Catalan (the two official languages in Catalonia). Questions specifically referred to the strict lockdown but also enquired about feelings/perceptions at the moment of survey completion (which was after the lockdown). To avoid collecting disturbances present before lockdown, we asked about “new problems detected during lockdown.” Most questions had yes/no as possible answers, but some asked respondents to choose between few closed answers or grade a perception on a scale from 0 (minimum) to 10 (maximum). Families living in Spain with children under 16 years of age were invited to participate and to answer questions regarding COVID-19 and the physical, mental health and wellbeing of children during lockdown. Parents answered the survey regarding their children (0–16 years). Those children old enough to read and answer the questionnaire themselves, and who were in the age group for which there is mandatory schooling (>6–<16 years of age), were invited to answer the survey. Children aged 7–11 years were instructed to do it with caregivers' support, and adolescents over 11 years old were instructed to do it on their own.
Data Collection
The answers to these surveys were collected through an API system using a custom code written in Python ( 5 ). Selection criteria for household enrollment were (i) accepted informed consent, (ii) respondent aged 18 years old or more, (iii) one or more children under 16 years old, and (iv) declared a valid Spanish postal code. Additionally, children and adolescents' answers were considered if both parents and the participating minor provided assent.
Statistical Analysis
The analysis was performed using R language ( 6 ). The significance level for the statistical tests was α = 0.05; Bonferroni correction was applied when using multiple tests. Chi-squared test was applied to tabulated counts of categorical data ( p -values are estimated using Monte Carlo method in the case of small cell counts). Mann–Whitney test is applied to numerical answers; the reported p -value results from the corresponding one-sided test.
Ethical Considerations
The study was conducted in accordance with the protocol and the Declaration of Helsinki (current version Fortaleza, Brazil, October 2013), and following the relevant legal requirements (Law 14/2007 of July 3, 2007, on Biomedical Research). The study protocol, informed consent forms and data collection tools were approved by the Ethics Committee for clinical research of the Hospital Sant Joan de Déu, Barcelona, Spain (C.I. PIC-123-20), prior to study initiation.
Demographics
A total of 2,054 families answered the survey, of which 1,957 met the study inclusion criteria. The included surveys covered a total of 3,347 children: 1,463 aged 0–6 years, 1,284 aged 7–11 years, and 600 adolescents aged 12–15 years. All parents answered a questionnaire, one for each daughter or son, independently. Additionally, 13% of the older children (167 answers) and 17% of the adolescents (100 answers) completed the questionnaire specifically addressed to their respective age group. In 57% of the households there was at least 1 adult working in a highly COVID-19 exposed environment (e.g., health centers, hospitals, or old people's retirement homes). The main participants sociodemographic characteristics are presented in Table 1 .
Table 1 . Characteristics of the 1,957 families included in the study.
Risk Perception and Transmission Knowledge
At the time of survey completion, 6% of the households reported at least one family member having been affected or currently infected by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (microbiologically confirmed infection), and 12% reported at least one suspected case. The majority (84%) of families knew someone infected and 20% knew someone close who had died of COVID-19. Among families with either a suspected or microbiologically confirmed infection, 47% considered a 5–15 year-old child to have been the index case, 22% a 0–4 year-old, 12% a >16 year-old, and 19% reported a simultaneous infection among more than one household member (of varying ages). Median time to subsequent secondary cases was 6.5 days (interquartile range [IQR]: 3–10). When a case was confirmed or suspected at home, measures adopted varied widely between families: 42% followed a strict lockdown of the family, 21% a strict lockdown of the affected person, 16% used a facemask at home, 19% ensured an exclusive use of the sleeping room and bathroom, 19% restricted the use of common spaces, and 39% did not follow any of the aforementioned measures. Regarding parents' opinion about children's role in the pandemic, 42% perceived them to be at high risk of getting infected by SARS-CoV-2, 50% thought strict lockdown measures for children were necessary, 60% considered that children should have had permission to go outside in a controlled way since the first day, and 65% found re-opening of schools was appropriate (98% of them suggested to do it with safety measures in place). During strict lockdown, 88% of children never set foot on the street, while during relaxed lockdown the majority (54%) spent time outdoors at least 3–6 days a week for <1 h/day. Masks were worn by 95% of older children and adolescents and by almost half of the children below 6 years of age, even if this was not mandatory in Spain.
Coping With Confinement
The overall rate of good coping with confinement (rated on a 0–10 scale) was generally very positive. Parents scored their children an 8 [IQR: 6–9] both during strict and relaxed lockdown. Older children scored themselves a 7 [IQR: 5–10] and an 8 [IQR: 6–10], and adolescents scored themselves a 7 [IQR: 6–9] and an 8.5 [IQR: 7–10], during strict and relaxed lockdown, respectively ( Figure 1 ). When asking if they would accept another strict lockdown if necessary due to a hypothetical worsening of the pandemic, 73% of parents, 81% of older children, and 83% of adolescents would accept it. Of note, we found no differences in these answers between children living with a confirmed/suspected case of SARS-CoV-2 and those living without it. One in every five families had an episode of a child needing healthcare attention during strict lockdown (58% febrile episodes, 4% acute mental health problems).
Figure 1 . Overall coping with strict and relaxed lockdown according to parents and to children and adolescents.
Biorhythms (Physical Activity, Alimentary Patterns, and Sleeping Disturbances)
According to parents' perception, during strict lockdown 90% of older children and 81% of adolescents practiced less sports than usual ( Figure 2 ), and 64% of older children and 39% adolescents did not do any kind of sports. On the other hand, during relaxed lockdown, 65% of children and adolescents used the allowed time outdoors to do some kind of sport. When asking parents about weight and eating disturbances, 10% perceived in their children to lose weight and 41% to gain weight. Additionally, 17% reported new eating problems not present before lockdown such as eating less, more and/or in different periodicity than usual, being picky with food, and eating due to anxiety or boredom.
Figure 2 . Time spent doing sports according to parents and to children and adolescents. According to parents' perception, during strict lockdown 90% of older children and 81% of adolescents practiced less sports than usual, similarly as children themselves reported when asked.
Parents reported sleeping problems during the strict lockdown in 54% of young children, 57% of older children and 59% of adolescents. The most common problem among all age groups was hard time falling asleep. Interestingly, when children and adolescents answered, they reported more sleeping disturbances than their parents ( p = 0.000004 and p = 0.009). In older children, higher self-perception was observed for awakening in the middle of the night (Parents Answering [PA]: 18%, Children Answering [CA]: 33%), sleeping more than usual (PA: 14%, CA: 32%), having a hard time falling asleep (PA: 40%, CA: 48%), and having nightmares (PA: 12%, CA: 28%). Similarly, increased self-perception in adolescents was observed for awakening in the middle of the night (PA: 6%, CA: 22%), sleeping more than usual (PA: 21%, CA: 35%), having a hard time falling asleep (PA: 34%, CA: 46%), and having nightmares (PA: 4%, CA: 11%; Figure 3 ).
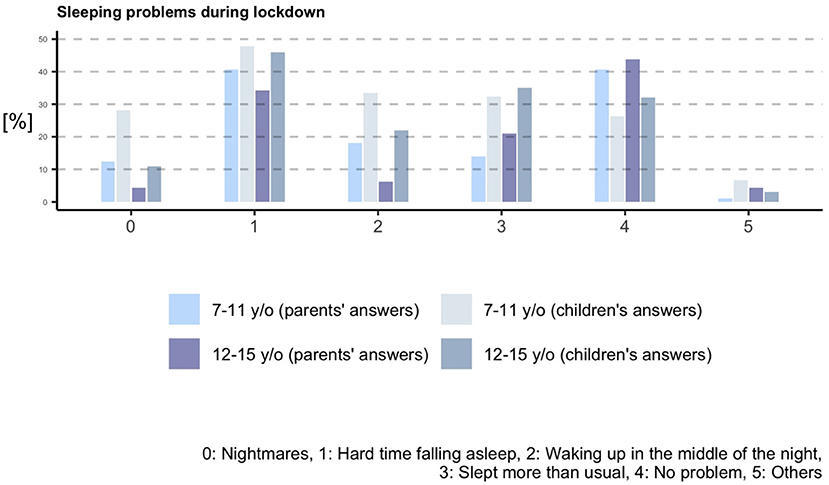
Figure 3 . Sleeping problems during lockdown according to parents and to children and adolescents.
Emotional Distress
When we asked parents about emotional distress signs observed in their children, 63% reported to have witnessed them to be more anxious than usual, 63% to be more irritable, 46% to be sadder, and 34% to have other emotional alterations. More than half of older children reported themselves to be more anxious (62%), irritable (55%), and sadder (52%), with median intensities from 4 to 5 out of 10 during strict lockdown. In adolescents, these feelings were reported in 49, 46, and 41% individuals, respectively, with median intensities from 3 to 5 out of 10 during strict lockdown.
Electronic Devices and Social Media
Parents reported that at least one type of electronic device (i.e., smartphone, television or online audiovisual content, videogames, or social media) was used more than usual during strict lockdown in 77% of younger children, 93% of older children, and 95% of adolescents. The most widely used device was television together with online audiovisual content, with 75% of younger children, 85% of older children, and 82% of adolescents using it more often than before the lockdown. Playing videogames also increased in 65% of older children and 62% of adolescents. In addition, adolescents also increased use of their smartphone (68%) and social media (61%). The use time of electronic devices increased with age, being 1–3 h/day the predominant option among all children and 3–5 h/day the predominant option among adolescents. Higher use of social media increased during lockdown in comparison with the usual utilization before lockdown, and was self-reported by 28% of older children and 52% of adolescents. These results are summarized in Table 2 .
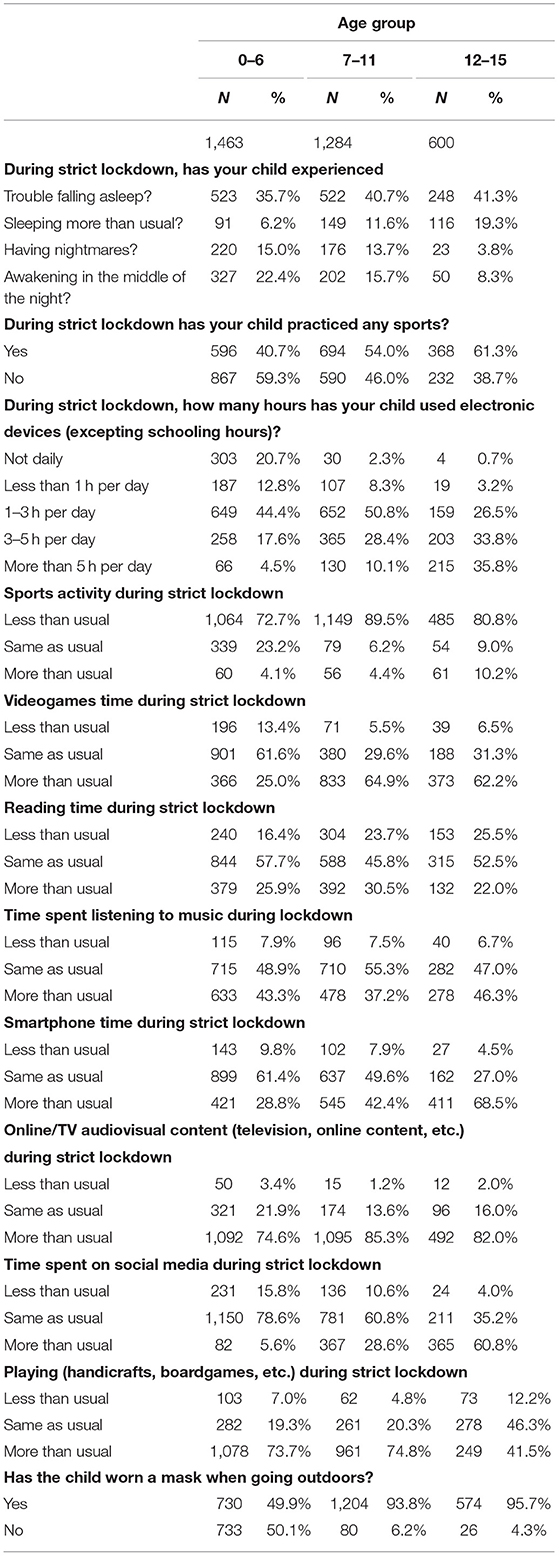
Table 2 . Answers about sleeping troubles, sports, and electronic devices use reported by parents for each child, distributed by age groups.
Parents scored satisfaction with remote schooling in a 0–10 scale, with a median of 6 [IQR: 4–9] for younger children, and with a median of 7 [IQR: 5–8] for older children. Children themselves scored it with a median of 7 [IQR: 5–8]. The most common score was 10 among the three groups. Both parents of adolescents and teenagers themselves scored schooling satisfaction with a median of 7 [IQR: 5–9], but in this group the mode score was 10 for parents and 8 for the students. When children were asked if they were satisfied with school activities, 26% of children and 35% of adolescents were not. Importantly, 81% of children reported to feel comfortable with schools re-opening compared to a 65% of adolescents, and 52% of the latter thought it was necessary.
Comparisons and Inference
In all age groups, we found higher number of reported sleeping problems (either by parents or by children) among those knowing someone who died of COVID-19 compared to those who did not. Older children who reported to have felt fear or anxiety about going out reported a higher incidence of sleeping disturbances than the ones who did not feel that way (56 vs. 39.3%, p = 0.047). In general, sleeping problems were less likely to happen among children who did sport during lockdown vs. the ones who did not (49.15 vs. 41.67%), especially regarding having trouble falling asleep and sleeping more than usual. Doing sport activities as usual seems to be mildly protective against sleeping problems when compared to spending less time than usual ( p = 0.04). Spending more than 5 h per day looking at screens was a risk factor for some of the sleeping disturbances in teenagers, when compared to 1–3 h of daily use ( p = 0.00087).
Regarding the reported feelings by children and adolescents, the score on irritability was significantly lower among kids (5 [IQR: 2–7] vs. 6 [IQR: 3–8], p = 0.0062) and adolescents (4 [IQR: 1–6] vs. 6 [IQR: 3–7], p = 0.015) who did sport as compared to those who did not. In addition, less physical activity than usual was also found to be associated with an increased feeling of sadness in adolescents, as compared to spending more time than usual doing sport ( p = 0.01). The increased use of social networks above usual levels was found to be associated with increased anxiety levels in teenager reported answers ( p = 0.0077). Among adolescents, being unsatisfied with academic training during lockdown was found to be associated with anxiety ( p = 0.04), and fear of going out in the street was associated with increased perceived sadness ( p = 0.00017).
Here, we described how COVID-19 lockdown has affected children and adolescents' well-being using a set of online questionnaires targeting families in Catalonia and Spain, which reported the status of 3,347 children.
We found that, at the onset of the pandemic, parental perception of children's risk of infection and transmission were generally high, probably supported by the containment measures applied in many countries, which included schools' closure. In other studies, the greatest risk perception has been found in women with lower education who have children in their care ( 7 ). However, recent research suggests that children are less ( 8 ) or equally ( 9 ) likely to become infected than adults when exposed to a case and, when infected, children's symptoms are usually milder ( 9 , 10 ). Interestingly, despite the high-risk initial perception, the majority of parents would have preferred their children to be allowed to spend time outdoors during the entire lockdown period and strongly supported the re-opening of schools with prevention measures in place. It has been recently demonstrated that children's role in SARS-CoV-2 transmission is likely to be weaker than for other age groups during school re-opening due to the prevention tools adopted and children compliance with them ( 11 ).
Parents reported children to cope with confinement reasonably well, according to a previous study where parents reported a more engagement than disengagement-oriented coping strategy in Spanish children during lockdown ( 12 ). Parents, but especially children and adolescents, reported to cope better during the relaxed lockdown compared to the strict lockdown. The change in lockdown measures was positively rated and the allowed time outdoors was mostly used for sports activities. Actually, it has been shown that children missed outdoor exercise during strict lockdown ( 13 ), and that having an outdoor exit in the house (e.g., garden, terrace) contributed to lower levels of psychological and behavioral symptomatology ( 14 ). Indeed, we showed physical and sports activities were highly decreased during lockdown in most children and adolescents as previously reported ( 13 – 16 ), and 39% of children and adolescent did not do sport at all. In addition, 41% of parents reported their children to have suffered weight increases, probably as a result of the reduced physical activity and the reduction of fruit and vegetable consumption ( 15 ).
We found sleeping disturbances during lockdown were reported for the majority of children and adolescents, in accordance with previous studies ( 14 – 17 ). Importantly, we observed that children and adolescents self-reported more sleeping disturbances than what was reported by their parents. Given many of these disturbances are probably not easily observed by caregivers (i.e., nightmares, awakening in the night) unless children are directly asked, interviewing children and adolescents about their well-being should be included in this type of studies, and children's participation in surveys should be further promoted. Despite clear instructions to parents to encourage their children and adolescents to respond a questionnaire, we obtained low participation of children and adolescents in our survey. Eventhough, we still reached a total of 267, allowing making valuable conclusions about their self-reported well-being.
On the other hand, knowing someone who died from COVID-19 was associated with sleeping disturbances, as well as the statement “being afraid or anxious about going outside.” Accordingly, it has been shown that children who knew someone who had suffered from COVID-19 at home or whose parent was directly involved in the pandemic, presented higher anxiety scores ( 18 ). Of note, anxiety and irritability were reported for the majority of children and adolescents, being the youngest the most affected. Similar results have been recently described ( 14 , 17 , 19 , 20 ) and underline the need to consider how we communicate information to children and help them manage this information. Furthermore, it has been shown that anxiety and depressive symptoms and other negative outcomes were more likely in children whose parents reported higher levels of stress, depression or were unemployed ( 18 , 20 – 23 ), and that those were often more important among the youngest ones ( 20 ). Thus, supporting parents' mental health and providing them with accurate information, strategies and support to cope with lockdown is essential to protect their children's mental health ( 24 , 25 ).
We also found that sleeping disturbances were associated with doing less sports than usual, which supports allowing outdoor activity and sports during lockdown periods to protect children's mental health and well-being. Actually, it has been shown a significantly different sleeping time between strict and relaxed confinement ( 15 ). Of note, children who could go outside during COVID-19 restrictions, as well as children whose parents were less stressed, were more likely to meet the physical activity suggested by WHO guidelines ( 24 ), which in turn resulted in reduced psychosocial difficulties ( 16 ). The increase in anxiety, irritability, sadness and changes in biorhythms are adaptive symptoms to stressful situations, and although the expectation is that they will slowly improve when the pandemic restrictions are eased, it is possible that a number of these children and adolescents develop a more serious mental health problem.
In accordance with recent studies, we also found a dramatic increase in electronic devices' usage in all age groups ( 14 , 15 , 23 , 26 ), which has been shown to pose a risk on mental health regardless of the pandemic. The use of Internet has undoubtedly facilitated to some extent the continuity of social and schooling activity during lockdown, especially during strict lockdown. However, deprivation of sports and outdoors activities in favor of screen time consumption might be a damaging trade-off. We found an association between spending more time in electronic devices (>5 h per day) and sleeping disturbances, as well as with reported irritability, sadness and anxiety. In line with our findings, frequent social media exposure has been shown to be positively associated with anxiety ( 26 ). Interestingly, lower screen exposure was observed for the relaxed lockdown period ( 15 ).
Interestingly, and despite having endured the strictest lockdown, most children and adolescents reported acceptance to go back to a strict lockdown if this was required due to the epidemiological situation, reflecting their high resilience and capability to adapt to new situations. The reported acceptance of prevention measures was very high, and even though the use of facemask was not among the most popular measures according to parents, older children and adolescents reported to wear it when spending time outdoors. Of note, the use of facemask is not mandatory in Spain under 6 years of age; however, its use was reported for half of this young children's age group. Despite the possible social desirability bias, the use of facemasks is certainly extended among children. Indeed, a recent study in Spain found that risk perception and age groups with the highest self-perceived risk of disease (51–64 years of age) were also those who went most often outside their homes ( 27 , 28 ). This differs markedly from our results among children, who scrupulously followed the rules and would do so again. Furthermore, children whose parents were more resilient and adopted prevention and safety measures presented fewer negative responses during lockdown ( 12 ), pointing to the impact of adults adhering to prevention measures not only in terms of viral spread, but also in children's safety perception and emotional well-being.
A major strength of our study is the large number of families who answered the survey, largely superior to previous studies carried out in Spain and capturing information about 3,347 children. Another major strength is the collection of questionnaires directly from children and adolescents, which is not often included in similar studies. On the other hand, since our study is based on questionnaires answered by parents and their children after the lockdown periods studied, it could be affected by a recall bias and social desirability bias. However, the surveys performed to Spanish children and adolescents during the strict lockdown showed similar emotional and behavioral alterations ( 21 , 24 , 29 ). Another limitation is the timespan during which the questionnaires could be completed, which included few months and the beginning of the second COVID-19 wave in Spain, something that could have affected the responses. On the other hand, using online surveys based on volunteer participation probably resulted in a biased population, where underrepresentation of families with less-resources (which might lack a smartphone or computer, and/or lack access to the internet) is certainly present. This could have influenced the answers obtained, such as satisfaction with remote schooling, which was relatively good in our study. In addition, since our online survey did not include sensitive personal data, we could not exclude data from repetition of study participants. However, families were asked to answer the survey only once and data analysis suggests these instructions have been generally followed, given we found no repetition of descriptive family data among participants. Finally, since this is a cross-sectional study, we cannot infer cause-effect relationships. However, our associations could be further explored in future studies to determine if a cause-effect relationship exists. Although longitudinal assessments of the lockdown effects in children are needed, our results point out the importance of considering mental health and well-being protection during lockdown measures implementation to control COVID-19 outbreaks.
In summary, our study showed a negative impact of strict lockdown in the mental health and well-being of children and adolescents but also showed their high resilience and capability to adapt to new situations. Lockdown measures should consider their age-specific needs in future waves of the pandemic and in similar potential emergencies, facilitating physical activity and limiting time spent on electronic devices. Maintaining schools open or, at least, ensuring children can spend a minimum time outdoors, can help address these priorities.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The study protocol, informed consent forms, and data collection tools were approved by the Ethics Committee for Clinical Research of the Hospital Sant Joan de Déu, Barcelona, Spain (C.I. PIC-123-20), prior to study initiation. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
QB, JG-G, SAj, BB, NB, RV, PM-M, and SAr: conceptualization and methodology. QB, AC-S, BN, and JG-A: survey preparation and software development. JG-A, JF, and AP-L: data collection, curation, data analysis, and statistics. SAj: writing-original draft. BB, NB, RV, PM-M, SAj, and JG-A: writing-review and editing. JG-G and QB: funding acquisition and project administration. All authors contributed to the article and approved the submitted version.
This study was supported by Banco Santander and Stavros Niarchos Foundation, through KIDS corona platform. This study has been partially funded by Stavros Niarchos Foundation (SNF), Banco Santander and other private donors of Kidscorona. ISGlobal receives support from the Spanish Ministry of Science and Innovation through the Centro de Excelencia Severo Ochoa 2019–2023 Program (CEX2018-000806-S), and support from the Generalitat de Catalunya through the CERCA Program. This work was supported by the Spanish Ministry of Economy and Competitiveness ( www.mineco.gob.es ) TEC2014-60337-R, DPI2017-89827-R, Networking Biomedical Research Center in the subject area of Bioengineering, Biomaterials, and Nanomedicine (CIBER-BBN), initiatives of Instituto de Investigación Carlos III (ISCIII), and Share4Rare project (Grant Agreement 780262). B2SLab is certified as 2017 SGR 952. BB is a Beatriu de Pinós postdoctoral fellow granted by the Government of Catalonia's Secretariat for Universities and Research, and by Marie Sklodowska-Curie Actions COFUND Programme (BP3, 801370). NB was supported by an FPU predoctoral fellowship from the Spanish Ministry of Universities (FPU18/04260). JF acknowledges the support from the Serra Húnter program.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We acknowledge all participants for their acceptance and collaboration in this research.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.746052/full#supplementary-material
Abbreviations
CA, Children answering; COVID-19, Coronavirus disease 2019; IQR, Interquartile range; PA, Parents answering; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
1. Masonbrink AR, Hurley E. Advocating for children during the COVID-19 school closures. Pediatrics. (2020) 146:e20201440. doi: 10.1542/peds.2020-1440
PubMed Abstract | CrossRef Full Text | Google Scholar
2. UNESCO. Education: From Disruption to Recovery . (2020). Available online at: https://en.unesco.org/covid19/educationresponse (accessed June 10, 2021).
3. Liu JJ, Bao Y, Huang X, Shi J, Lu L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc Health. (2020) 4:347–9. doi: 10.1016/S2352-4642(20)30096-1
4. Imran N, Zeshan M, Pervaiz Z. Mental health considerations for children & adolescents in COVID-19 Pandemic. Pak J Med Sci. mayo de. (2020) 36:S67–S72. doi: 10.12669/pjms.36.COVID19-S4.2759
5. Van Rossum G, Drake FL. Python 3 Reference Manual . Scotts Valley, CA: CreateSpace (2009).
Google Scholar
6. R Core Team. R: A Language and Environment for Statistical Computing . Vienna: R Foundation for Statistical Computing (2020). Available online at: http://www.R-project.org/
7. Pérez-Fuentes M del C, Herrera-Peco I, Jurado M del MM, Oropesa NF, Gázquez Linares JJ. Predictors of threat from COVID-19: a cross-sectional study in the Spanish Population. J Clin Med. (2021) 10:692. doi: 10.3390/jcm10040692
8. Dattner I, Goldberg Y, Katriel G, Yaari R, Gal N, Miron Y, et al. The role of children in the spread of COVID-19: using household data from Bnei Brak, Israel, to estimate the relative susceptibility and infectivity of children. PLoS Comput Biol. (2021) 17:e1008559. doi: 10.1371/journal.pcbi.1008559
9. Brotons P, Launes C, Buetas E, Fumado V, Henares D, Sevilla MF de, et al. Susceptibility to SARS-COV-2 infection among children an adults: a seroprevalence study of family households in the Barcelona metropolitan region, Spain. Clin Infect Dis. (2021) 72:e970–e7. doi: 10.1093/cid/ciaa1721
10. Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Carducci FIC, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. (2020) 4:653–61. doi: 10.1016/S2352-4642(20)30177-2
11. Jordan I, de Sevilla MF, Fumado V, Bassat Q, Bonet-Carne E, Fortuny C, et al. Transmission of SARS-CoV-2 infection among children in summer schools applying stringent control measures in Barcelona, Spain. Clin Infect Dis. (2021) ciab227. doi: 10.1093/cid/ciab227
12. Domínguez-Álvarez B, López-Romero L, Isdahl-Troye A, Gómez-Fraguela JA, Romero E. Children coping, contextual risk and their interplay during the COVID-19 pandemic: aSpanish Case. Front Psychol. (2020) 11:577763. doi: 10.3389/fpsyg.2020.577763
13. Mondragon NI, Sancho NB, Santamaria MD, Munitis AE. Struggling to breathe: a qualitative study of children's wellbeing during lockdown in Spain. Psychol Health. (2021) 36:179–94. doi: 10.1080/08870446.2020.1804570
14. Francisco R, Pedro M, Delvecchio E, Espada JP, Morales A, Mazzeschi C, et al. Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Front Psychiatry. (2020) 11:570164. doi: 10.3389/fpsyt.2020.570164
PubMed Abstract | CrossRef Full Text
15. López-Bueno R, López-Sánchez GF, Casajús JA, Calatayud J, Gil-Salmerón A, Grabovac I, et al. Health-related behaviors among school-aged children and adolescents during the Spanish Covid-19 confinement. Front Pediatr. (2020) 8:573. doi: 10.3389/fped.2020.00573
16. Alonso-Martínez AM, Ramírez-Vélez R, García-Alonso Y, Izquierdo M, García-Hermoso A. Physical activity, sedentary behavior, sleep and self-regulation in Spanish preschoolers during the COVID-19 lockdown. Int J Environ Res Public Health. (2021) 18:693. doi: 10.3390/ijerph18020693
17. Lavigne-Cerván R, Costa-López B, Juárez-Ruiz de Mier R, Real-Fernández M, Sánchez-Muñoz de León M, Navarro-Soria I. Consequences of COVID-19 confinement on anxiety, sleep and executive functions of children and adolescents in Spain. Front Psychol. (2021) 12:565516. doi: 10.3389/fpsyg.2021.565516
18. Garcia-Adasme SI, Cárdenas-Rebollo JM, Jimenez-Perianes A, Lalinde M, Jimeno S, Ventura PS, et al. Pediatric home confinement due to COVID-19: Somatic and anxiety spectrum consequences. J Clin Nurs. (2021) 30:3238–48. doi: 10.1111/jocn.15829
19. Pizarro-Ruiz JP, Ordóñez-Camblor N. Effects of Covid-19 confinement on the mental health of children and adolescents in Spain. Sci Rep . (2021) 11:11713. doi: 10.1038/s41598-021-91299-9
20. Via E, Estrada-Prat X, Tor J, Virgili C, Fàbrega M, Duran L, et al. COVID-19 Pandemic: Increased risk for psychopathology in children and adolescents? In Review. (2020). Avaliable online at: https://www.researchsquare.com/article/rs-104507/v1 (accessed November 11, 2020).
21. Orgilés M, Espada JP, Delvecchio E, Francisco R, Mazzeschi C, Pedro M, et al. Anxiety and depressive symptoms in children and adolescents during COVID-19 pandemic: a transcultural approach. Psicothema. (2021) 33:125–30. doi: 10.7334/psicothema2020.287
22. Romero E, López-Romero L, Domínguez-Álvarez B, Villar P, Gómez-Fraguela JA. Testing the effects of COVID-19 confinement in Spanish Children: the role of parents' distress, emotional problems and specific parenting. Int J Environ Res Public Health. (2020) 17:6975. doi: 10.3390/ijerph17196975
23. Lopez-Serrano J, Díaz-Bóveda R, González-Vallespí L, Santamarina-Pérez P, Bretones-Rodríguez A, Calvo R, et al. Psychological impact during COVID-19 lockdown in children and adolescents with previous mental health disorders. Rev Psiquiatr Salud Ment. (2021). doi: 10.1016/j.rpsm.2021.04.002
24. Okely AD, Kariippanon KE, Guan H, Taylor EK, Suesse T, Cross PL, et al. Global effect of COVID-19 pandemic on physical activity, sedentary behaviour and sleep among 3- to 5-year-old children: a longitudinal study of 14 countries. BMC Public Health. (2021) 21:940. doi: 10.1186/s12889-021-10852-3
25. Orgilés M, Morales A, Delvecchio E, Francisco R, Mazzeschi C, Pedro M, et al. Coping behaviors and psychological disturbances in youth affected by the COVID-19 health crisis. Front Psychol. (2021) 12:565657. doi: 10.3389/fpsyg.2021.565657
26. Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. (2020) 15:e0231924. doi: 10.1371/journal.pone.0231924
27. Jacques-Aviñó C, López-Jiménez T, Medina-Perucha L, de Bont J, Gonçalves AQ, Duarte-Salles T, et al. Gender-based approach on the social impact and mental health in Spain during COVID-19 lockdown: a cross-sectional study. BMJ Open. (2020) 10:e044617. doi: 10.1136/bmjopen-2020-044617
28. Jacques-Aviñó C, López-Jiménez T, Medina-Perucha L, Rodríguez Giralt I, Gonçalves AQ, de Bont J, et al. Policy Brief: El Impacto Psicosocial del Confinamiento Domiciliario por la Pandemia de la COVID-19 en España IDIAP JordiGol. Avaliable online at: https://www.idiapjgol.org/index.php/es/actualidad/noticias/1307-salut-mental-confinament-2
29. Orgilés M, Morales A, Delvecchio E, Mazzeschi C, Espada JP. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. Front Psychol. (2020) 11:579038. doi: 10.3389/fpsyg.2020.579038
Keywords: COVID-19, lockdown, children, adolescent, mental health, well-being
Citation: Ajanovic S, Garrido-Aguirre J, Baro B, Balanza N, Varo R, Millat-Martínez P, Arias S, Fonollosa J, Perera-Lluna A, Jordan I, Muñoz-Almagro C, Bonet-Carne E, Crosas-Soler A, Via E, Nafria B, García-García JJ and Bassat Q (2021) How Did the COVID-19 Lockdown Affect Children and Adolescent's Well-Being: Spanish Parents, Children, and Adolescents Respond. Front. Public Health 9:746052. doi: 10.3389/fpubh.2021.746052
Received: 23 July 2021; Accepted: 05 November 2021; Published: 25 November 2021.
Reviewed by:
Copyright © 2021 Ajanovic, Garrido-Aguirre, Baro, Balanza, Varo, Millat-Martínez, Arias, Fonollosa, Perera-Lluna, Jordan, Muñoz-Almagro, Bonet-Carne, Crosas-Soler, Via, Nafria, García-García and Bassat. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Quique Bassat, quique.bassat@isglobal.org
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Open access
- Published: 08 February 2021
Impacts of the Covid-19 lockdown and relevant vulnerabilities on capability well-being, mental health and social support: an Austrian survey study
- Judit Simon 1 , 2 ,
- Timea M. Helter 1 ,
- Ross G. White 3 ,
- Catharina van der Boor 3 &
- Agata Łaszewska 1
BMC Public Health volume 21 , Article number: 314 ( 2021 ) Cite this article
87k Accesses
86 Citations
112 Altmetric
Metrics details
Impacts of the Covid-19 pandemic and its public health measures go beyond physical and mental health and incorporate wider well-being impacts in terms of what people are free to do or be. We explored the impacts of the Covid-19 lockdown and relevant vulnerabilities on capability well-being, mental health and social support in Austria.
Adult Austrian residents ( n = 560) provided responses to a cross-sectional online survey about their experiences during Covid-19 lockdown (15 March-15 April 2020). Instruments measuring capabilities (OxCAP-MH), depression and anxiety (HADS), social support (MSPSS) and mental well-being (WHO-5) were used in association with six pre-defined vulnerabilities using multivariable linear regression.
31% of the participants reported low mental well-being and only 30% of those with a history of mental health treatment received treatment during lockdown. Past mental health treatment had a significant negative effect across all outcome measures with an associated capability well-being score reduction of − 6.54 (95%CI, − 9.26, − 3.82). Direct Covid-19 experience and being ‘at risk’ due to age and/or physical health conditions were also associated with significant capability deprivations. When adjusted for vulnerabilities, significant capability reductions were observed in association with increased levels of depression (− 1.77) and anxiety (− 1.50), and significantly higher capability levels (+ 3.75) were associated with higher levels of social support. Compared to the cohort average, individual capability impacts varied between − 9% for those reporting past mental health treatment and + 5% for those reporting one score higher on the social support scale.
Conclusions
Our study is the first to assess the capability limiting aspects of lockdown and relevant vulnerabilities alongside their impacts on mental health and social support. The negative capability well-being, mental health and social support impacts of the Covid-19 lockdown were strongest for people with a history of mental health treatment. Future public health policies concerning lockdowns should pay special attention to improve social support levels in order to increase public resilience.
Peer Review reports
Introduction
The recently discovered coronavirus, known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread globally within a span of a few months since December 2019 [ 1 ]. The Covid-19 disease caused by the virus was declared as a pandemic by the World Health Organisation (WHO) on 11 March 2020. Initial evidence suggested that the infection has a high effective reproduction rate with older populations and those with underlying health conditions being at high risk of severe disease and death, thereby forcing numerous countries into temporary lockdowns to limit the spread of the disease. Consequently, the Covid-19 pandemic went from a direct health emergency to a systemic crisis affecting people’s lives in multiple ways [ 2 ]. Covid-19 impacts have been unprecedented because of its evolution from a health shock to a global economic and social crisis [ 2 ].
Substantial evidence from the past studies of the impacts of Severe Acute Respiratory Syndrome, Middle East Respiratory Syndrome, and Ebola epidemics on the suffering individuals and the healthcare providers showed substantial neuropsychiatric linkage [ 3 ]. There is an increasing amount of research related to the impacts Covid-19 on people’s mental health and well-being [ 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 ]. Beside the direct health impact, public health emergencies may also affect individuals and communities through isolation, stigma, job insecurity, or inadequate resources for medical response [ 15 ]. These effects generate a range of emotional reactions, and can be particularly prevalent among those individuals who contract the disease, or those who are at increased risk due to their age or pre-existing medical conditions [ 15 ]. Evidence from previous pandemics shows that individuals who contracted the disease experienced fear, anxiety, emotional distress, and post-trauma stress symptoms [ 3 ]. The mental health/well-being impacts of the Covid-19 pandemic have been shown to be even more significant for those who are prone to psychological problems [ 6 ].
Impacts of the Covid19 pandemic and its public health measures go beyond physical and mental health and incorporate wider well-being impacts in terms of what people are free to do or be. Due to these complexities, the assessment of personal consequences related to well-being is challenging and may be best addressed within the conceptual framework of the capability approach introduced by Amartya Sen in the early 1980s [ 23 ]. The core focus of the capability approach is on what individuals are able to be and do in their lives, in other words, what they are capable of [ 23 ]. The capability approach provides a richer evaluative space beyond health and proposes that well-being is determined by people’s freedom to engage in forms of being and doing that are of intrinsic value to the person [ 23 ]. Beside the recently proposed use of the capability framework in the understanding of policy challenges [ 24 ], this freedom aspect can be interpreted in the narrower mental health context as both the actual capabilities of a person, for instance, good mental health, and the processes that enable them, for instance, legal regulations [ 25 ]. Not only has the Covid-19 pandemic had a profound psychological impact, but it also affects personal freedoms to engage in behaviours that are consistent with subjectively held values beyond health, for instance, visiting loved ones, engaging in recreational activities, spending time outdoors. Despite these important links, the connection between pandemics and individual capabilities have not yet been researched.
In Europe, Austria stood out as a nation that adopted aggressive and early strategies and thereby saw a smaller proportion of deaths from Covid-19 compared to some other European countries [ 26 ]. The first Covid-19 case in Austria was reported on 25 February 2020 [ 27 ]. The Austrian government issued general laws to contain the epidemic by restricting social contacts and imposing strict lockdown measures from 16 March onwards [ 27 ] most of which have been lifted gradually since 15 April.
Early studies assessing the Covid-19 pandemic, and related public health measures, impacts found significant impact on the mental health of the Austrian population. The studies found that symptoms of moderate to severe anxiety and depression have tripled in Austria, and 8–13% of the population showed severe depression and 6–11% severe anxiety symptoms [ 28 , 29 ].
The capability approach embodies a range of interlinking concepts and several studies have indicated that capability outcomes are strongly associated with mental health and social outcomes [ 30 , 31 , 32 , 33 , 34 ]. However, despite the increasing number of studies exploring the Covid-19 impact on mental health/well-being, information is still missing on the broader capability impact of the pandemic. Hence, this study aimed to explore the impact the Covid-19 lockdown period on people’s capabilities in association with mental health/well-being and social support, especially in the case of specific vulnerable groups in Austria. Covid-19 lockdown vulnerable groups were pre-defined as: (i) being categorised as ‘at risk’ group based on age and/or pre-existing physical health conditions; (ii) self-reported mental health treatment prior to the coronavirus pandemic; (iii) direct exposure to Covid-19 (having symptoms or being tested positive); (iv) indirect exposure to Covid-19 through a family member/friend; (v) having employment status impacted by the lockdown; or (vi) being categorised as critical worker.
Study participants
Participants were recruited using convenience sampling, i.e. the study sample consisted of people who responded to our survey advert. The advert was distributed via multiple channels including social media platforms (including Facebook, Twitter, WhatsApp) and emails targeting a wide range of individuals and organisations (universities, non-profit organisation such as Red Cross, and local governments) throughout Austria. In order to be able to participate in the study, respondents had to be older than 18 years, have sufficient German knowledge, and be residents in Austria at the time of the Covid-19 outbreak.
Study design and data collection
Cross-sectional data were collected via an online survey in May/June 2020, with all questions, including standardised outcome instruments, referring to the one-month lockdown period in Austria between 15 March and 15 April 2020.
The survey was developed in the SoSci online survey platform (Version 2), which is a publicly available tool and is free of charge for academic research [ 35 ]. The weblink of the survey was included in an advert, along with a QR code, that was circulated via social media platforms (including Facebook, Twitter, WhatsApp, etc.) and emails targeting a wide range of individuals and organisations throughout Austria.
Respondents who provided sociodemographic and Covid-19-related information and completed at least one standardised outcome instrument were considered for analysis. Those participants who discontinued the survey before fully completing at least one standardised outcome instrument were excluded from the analyses. The current analysis is based on the questions that were completed as part of the survey as outlined in the supplementary file (Supplementary file 1 ).
Survey and instruments
The online survey consisted of the participant information and consent forms followed by a section on sociodemographics. Subsequent sections assessed people’s perceptions about the Covid-19 pandemic and the public health measures in place during the lockdown in Austria in response to the outbreak. The final part of the questionnaire consisted of four self-reported standardised and validated outcome instruments, which were used to assess capability well-being (OxCAP-MH), depression and anxiety levels (HADS), social support (MSPSS) and mental well-being (WHO-5) similar to a parallel linked survey in the UK [ 36 ]. The outcome instruments were adapted to the online survey including the adaptation of their introductory text reflecting the period of interest, i.e. the one-month lockdown period in Austria between 15 March and 15 April 2020.
The Oxford CAPabilities questionnaire-Mental Health (OxCAP-MH) instrument was developed by Simon et al. in 2013 [ 37 ]. It is specifically designed to capture different well-being dimensions within the capability framework in the area of mental health across 16 items. The OxCAP-MH is scored on a 0–100 scale, with higher scores indicating better capabilities. The OxCAP-MH has shown good psychometric properties including internal consistency (Cronbach’s alpha between 0.79 and 0.85), test-retest reliability (intra class correlation coefficient 0.80), construct validity and responsiveness in both English and German populations [ 33 , 34 ]. The German version of the OxCAP-MH [ 38 ] was obtained from the authors for the study.
The Hospital Anxiety and Depression Scale (HADS) was developed by Zigmond and Snaith in 1983 [ 39 ]. The questionnaire is divided into Anxiety (HADS-A) and Depression (HADS-D) subscales both containing seven items scored on a four-point scale from zero (not present) to three (considerable). Both the HADS-A and HADS-D subscales are scored from 0 to 21, with higher scores indicating higher anxiety or depression levels. Normal, borderline and abnormal anxiety/depression scores are defined as 0–7, 8–10 and 11–21, respectively [ 39 ]. The HADS was found to perform well in assessing the presence and severity of anxiety disorders and depression in both somatic and psychiatric cases, also beyond the hospital setting, including the primary care patients and general population (mean sensitivity 0.90 and mean specificity 0.78 for a cut-off score of 8+ for HADS-A; and mean sensitivity 0.83 and mean specificity 0.79 for a cut-off score of 8+ for HADS-D) [ 40 ]. Cronbach’s alpha coefficient of internal consistency reported in several studies varied from 0.68 to 0.93 for HADS-A and from 0.67 to 0.90 for HADS-D [ 40 ]. The German translation of HADS was obtained from Hogrefe Publishing Group.
The Multidimensional Scale of Perceived Social Support (MSPSS) is a self-reported measure of subjectively assessed social support developed by Zimet et al. in 1988 [ 41 ]. The questionnaire can be divided into three subscales, each addressing a different source of support: Family, Friends, and Significant Other. Low, moderate and high support are defined as < 3, 3–5 and > 5, respectively [ 41 ]. The instrument has good internal consistency (Cronbach’s alpha 0.88) and test-retest reliability (0.85) [ 41 ]. An official German translation of MSPSS was obtained from the developer of the original English version.
The World Health Organisation-Five Well-being Index (WHO-5) is a short self-reported measure of current mental well-being introduced in 1998 by the WHO Regional Office in Europe [ 42 ]. Respondents are asked to rate how well each of the five statements about positive well-being applied to them in the given period from 5 (all of the time) to 0 (none of the time). The WHO-5 is scored 0–25, with higher scores representing higher well-being [ 43 ]. The WHO-5 has been used in multiple studies across countries and disease areas [ 43 ]. A review of 213 articles using the WHO-5 as an outcome measure confirmed that the instrument has satisfactory construct validity, responsiveness and it can be used as a screening tool for depression [ 43 ]. The German translation of the WHO-5 is available in the public domain without registration.
Definition of vulnerabilities
In the current study, six hypothesised associations between increased levels of mental health symptoms and decreased levels of well-being were tested according to pre-defined vulnerabilities identified as relevant to Covid-19: 1) “At risk” group; 2) Past mental health treatment; 3) Direct Covid-19 experience; 4) Indirect Covid-19 experience; 5) Employment status affected by Covid-19; and 6) Critical worker. Individuals were defined as ‘at risk’ if they were aged 65 years or over and/or had a self-reported underlying physical health condition including diabetes, heart/cardiovascular disease, stroke/cerebrovascular disease, lung disease, liver disease, or cancer. Participants who reported mental health service use prior to the period of interest were categorised as ‘having past mental health treatment’. Participants with ‘direct Covid-19 experience’ were those who tested positive for Covid-19 or experienced Covid-19 symptoms, but were not tested. ‘Indirect Covid-19 experience’ was defined as having a friend and/or family member infected or knowing someone who died of Covid-19. Participants with ‘employment status affected’ were those who reported losing their job due to the pandemic or being sent to short-time working (German ‘Kurzarbeit’). Finally, participants who reported having a job categorised by the government as critical worker, e.g. healthcare staff, police officer or food supply worker, were defined as ‘critical workers’.
Statistical analysis
Anonymous data were extracted from the online survey and checked for logical inconsistencies. Characteristics of the study cohort in comparison to the general Austrian population were presented.
Correlations between the different outcome measures were explored using Pearson’s correlations and interpreted as small < 0.3, moderate 0.3–0.49, or large ≥0.50 [ 44 ]. In order to explore the impacts of the Covid-19 lockdown and relevant pre-defined vulnerabilities on capabilities, mental health/well-being and social support, multivariable linear regression analyses were conducted using the OxCAP-MH, HADS-D, HADS-A, MSPSS and WHO-5 scores as dependent variables and six binary variables that defined vulnerable groups as independent variables. Analyses were adjusted for age, gender, having children, education level and initial employment status.
The potential impact of current depression, anxiety and social support on capabilities was investigated separately in a multivariable regression with OxCAP-MH capability score as the dependent variable and HADS-D, HADS-A, MSPSS scores as independent variables, adjusted for sociodemographic characteristics (age, gender, having children, education level and initial employment status) and the six relevant vulnerabilities as described above. Significance level of p < 0.05 was considered in all analyses. Analyses were conducted on complete cases in STATA v.15.1 [ 45 ].
Participant characteristics
Of the 848 persons who accessed the survey, 560 respondents (74.1% female, mean age M = 40.22 years, SD = 11.60) completed it and were included in the analyses (Fig. 1 ). The average time needed to complete the survey was 17 min.
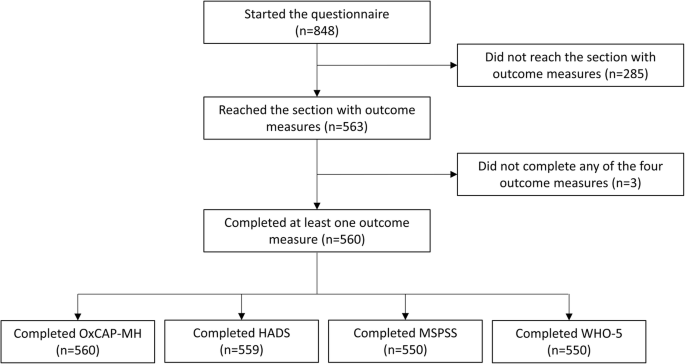
Survey flowchart
The majority of participants were Austrian citizens (87%) and employed at the beginning of the Covid-19 lockdown (73%). More than half of the survey participants (56%) had children, 52% were married or had a registered partnership. Data relating to the sociodemographic characteristics of the sample compared to official Austrian population statistics, with respect to age, gender, distribution of population across federal states [ 46 ], migration background [ 47 ], education level [ 48 ], and employment status [ 49 ], are shown in Table 1 .
Vulnerabilities
A total of 13% of the respondents ( N = 72) were categorised as belonging to the ‘at risk’ group based on age and/or co-existing physical health conditions. While 17% of the participants ( N = 97) reported that they received treatment for mental disorders before the period of interest, only 6% of the participants ( N = 34) reported receiving mental health treatment during the pandemic. Overall, only 30% of those with a mental health service use history ( N = 29) reported receiving treatment also during the lockdown.
A total of 1% of participants ( N = 7) had been diagnosed with Covid-19, another 6% ( N = 32) of the participants experienced Covid-19-like symptoms without being tested, and 20% of the respondents ( N = 110) had indirect Covid-19 experience through an infected friend and/or family member, or knew someone who died of Covid-19. Employment status was affected for 15% ( N = 84) of participants (job terminated: 3%, N = 15; short-term work: 12%, N = 69), and 38% of the respondents ( N = 214) reported having a job categorised as ‘critical worker’ (Table 1 ).
The level of missing values for the standardised outcome instruments was low with a maximum of ten observations missing (1.8%) for MSPSS and WHO-5. The mean OxCAP-MH score was 74.10 ( SD = 12.30). The mean WHO-5 score was 15.10 ( SD = 4.80) with 31% ( N = 174) of the respondents reporting a score below 13 indicating low mental well-being [ 42 ]. The mean scores on HADS-A and HADS-D subscales were 6.26 ( SD = 4.19) and 4.72 ( SD = 4.09), respectively, indicating that respondents on average reported higher levels of anxiety than depression symptoms. A total of 74% of participants ( N = 416) reached the threshold of > 5 for high social support on the MPSS scale. Average scores for the MSPSS subscales were 5.41 for family support, 5.53 for support from friends and 5.96 for support from significant others.
Correlations between capability well-being, mental health/well-being and social support outcomes
Capability well-being (OxCAP-MH) was significantly strongly/moderately associated with all other outcome measures, the strongest correlation being with depression (HADS-D: r (557) = −.64, p < .01; HADS-A: r (557) = −.56, p < .01; WHO-5: r (448) = .58, p < .01; MSPSS: r (448) = .42, p < .01). In terms of social support, capabilities and depression had the same strength of correlations, but of opposite directions. (Table 2 ).
Outcome associations with different types of vulnerability
Outcome associations with different types of vulnerabilities adjusted for sociodemographics are shown in Table 3 . Past mental health treatment had a significant negative effect across all outcome measures with an associated capability well-being score reduction of − 6.54 ( b = − 6.54, t (502) = − 4.73, p < .01), while direct Covid-19 experience had the second most detrimental impact with an associated capability well-being score reduction of − 4.58 ( b = − 4.58, t (502) = − 2.27, p = 0.02). Capabilities were similarly negatively affected also for those who belonged to the category ‘at risk’ ( b = − 4.45, t (502) = − 2.70, p < .01). These correspond to capability deprivations of − 9% and − 6%, respectively, when compared to the average capability level of the study cohort.
Having employment status affected by the pandemic produced consistently lower capability and mental well-being scores as well as higher depression and anxiety scores, but these associations did not reach statistical significance. We did not observe any significant impacts for the category ‘critical worker’ either.
Associations between capability well-being and current depression, anxiety and social support levels
Additional associations between current levels of depression and anxiety as well as social support with capability well-being were investigated in a separate multivariable regression analysis adjusted for all vulnerabilities and sociodemographics (Table 4 ). Current levels of depression and anxiety separately showed a capability score reduction of − 1.77 ( b = − 1.77, t (500) = − 16.89, p < .01) and − 1.50 ( b = − 1.50, t (500) = − 13.52, p < .01), respectively, per one point difference in the relevant HADS scores. Social support on the other hand proved to be a major capability resilience factor. One point score improvement on the MSPSS scale was associated with an improvement of + 3.75 ( b = 3.75, t (491) = 9.60, p < .01) in the capability scores.
This is the first study to assess the impact of the Covid-19 lockdown and relevant vulnerabilities on capabilities well-being, mental health and social support and their associations as observed in Austria.
Our findings that Covid-19 direct experience is associated with intensified anxiety symptoms, lower mental well-being and lower capabilities are in line with other recent studies exploring the impact of the Covid-19 pandemic on mental health and well-being in Austria [ 28 , 29 , 50 , 51 , 52 ]. Our study showed that participants who reported mental health treatment before the Covid-19 pandemic reported worse outcomes on all measures, including the OxCAP-MH, HADS-D, HADS-A, MSPSS and WHO-5. However, only the OxCAP-MH capability questionnaire showed a significant negative impact for participants categorised as belonging to the ‘at risk’ group. It should be noted that it is likely that the Covid-19 lockdown restrictions accentuated levels of distress experienced by those with existing physical health conditions. This association has not been captured by any other outcome measure, suggesting an increased sensitivity of the OxCAP-MH in comparison to the other scales used in this study and confirming the advantage of its broader measurement scope when assessing the well-being impact of a pandemic and related public health measures. The study also confirmed that the capability approach, which provides an indication of people’s freedom to engage in forms of being and doing that are of intrinsic value to the person, has direct relevance to situations/policies that inherently limit personal freedoms, i.e. public health emergencies.
The vulnerabilities referred to in this study as ‘employment status affected’ by Covid-19 or being a ‘critical worker’ were not significantly associated with any of the outcomes. Besides the issue of sample size, this may also reflect the Austrian government’s employment support policy implemented in the early stages of the pandemic including the introduction of the short-term working scheme to help retain jobs [ 53 , 54 ].
When considering the average capability well-being score observed in our cohort, the relative impact of different vulnerabilities and other factors on capability levels were estimated between − 9% for those reporting past mental health treatment vs. + 5% for reporting one score higher on the social support scale. In future analyses, the outcome scores obtained in this study could also be compared to scores observed in studies prior to the Covid-19 pandemic to further asses the overall impact of this public health emergency and lockdown on the well-being of the Austrian population. Previous studies using the WHO-5 instrument found that 26–27% of the Austrian sample reported scores corresponding to low mental well-being [ 55 , 56 ]. This is lower than the 31% of respondents who were identified as having low mental well-being (WHO-5 score below 13) in our study. Furthermore, 19% of the participants in this study had borderline and 16% ‘abnormal’ anxiety levels according to HADS-A scoring system, somewhat higher than the levels reported in earlier Austrian studies [ 57 , 58 , 59 , 60 ]. These results seem to be confirmative of the expected negative impacts of the Covid-19 pandemic, including those of the lockdown, on mental well-being including increased levels of anxiety and stress. Previous studies using the MSPSS scale in Austrian populations reported comparable scores, indicating relatively high social support [ 61 , 62 ].
In addition to providing an indication of the Covid-19 and lockdown impacts on vulnerable groups, this study also highlighted the interactions between capability well-being levels and current mental health that indicate a strong negative impact of current depression and anxiety. On the other hand, social support was shown as a major capability resilience factor. Future (public health) policies should take the strong associations between capabilities and current mental health and social support levels directly into consideration to minimise the negative long-term health, social and economic issues related to future public health emergencies.
Furthermore, our results suggest that amongst all investigated vulnerabilities, people with past mental health treatment represent the most vulnerable group. A recent study from Austria found that the number of people treated with psychotherapy during lockdown (personal, phone or virtual contacts) decreased by one-third [ 63 ]. In our study, the proportion of people receiving mental health treatment during lockdown in comparison to the period before the pandemic was 6% vs. 17%, respectively. We found evidence of the continuation of treatment between the two periods for only 30% of those participants who received mental health treatment prior to the pandemic. Even under the most conservative assumptions, these results suggest a substantial level of under-utilisation of mental health services (due to whatever causes) during the lockdown period. For future strategic healthcare planning during next waves of the pandemic, policy makers and health and social care providers need to be aware of the exceptional vulnerability of this group and efforts should be focused on maintaining continuity in mental health service provision. Digital e-health treatment options provide potential solution to assure this continuity of treatment whilst simultaneously protecting the health of the service-users and professionals [ 64 , 65 ].
The results of this research also have major implications for government departments, social care services and community-based support initiatives in planning how best to support the population during future pandemics, and in terms of the special attention needed for those with pre-existing mental health service use. Findings also provide crucial evidence for policy makers and members of the public by indicating how important and protective social support networks can be in mitigating the mental health and (capability) well-being impacts of public health emergencies through increased resilience. The latter finding goes beyond the health sector with relevant implications also for the education sector when considering decisions about university openings and necessary support networks for students. Future research should explore whether the observed impacts on capabilities, mental health and social support levels remain, worsen or diminish (via adjustment) as the pandemic continues and how they develop in the long-term after the public health situation is resolved.
Furthermore, strategies that can help to alleviate the negative impacts of the Covid-19 lockdown in the Austrian population should be identified. Priority should be given to assuring the continuity of mental health services, as well as identifying new cases of mental disorders, mental distress and anxiety that might arise due to lockdowns. This will require the capacity of mental health support services to be increased, policy initiatives to be communicated in a clear and transparent way so that anxiety is reduced among the population, and the introduction of work arrangements that allow for home-schooling for both parents (reducing the burden posed on mothers) that prevent loss of household income [ 66 ]. Moreover, governments should implement economic measures and reinforce essential health, social and education services to identify population needs, reduce inequalities in health and protect most vulnerable citizens including people with pre-existing conditions, elderly, migrant population, children and those with lower socio-economic status [ 67 ].
The main limitation of our study is that the participants completed the survey retrospectively about 1 month after the lockdown (mid-May 2020). This time-lag may have introduced some recall bias considering the self-reported outcome measures. Since data were collected at the time when the number of new Covid-19 cases were relatively low and the Austrian epidemic curve has flattened, we assume that the presented estimates are more conservative and optimistic than if the survey questions would have been completed directly during the lockdown. Moreover, since the analysis is based on one measurement point, the study allows no causal conclusions. Our study is also prone to limitations of online survey; results are based fully on self-reporting with the potential to reporting bias [ 68 ] and some groups (females, younger ages, higher educated), were over-represented in the survey sample compared to the general population [ 69 , 70 ]. The survey on the other hand achieved satisfactory representation in terms of more than half of the Austrian provinces, migration background and employment status.
This research contributes to the understanding of the impact that pandemics and nationwide responses to pandemics can have on mental health and broader capability well-beings in light of their major policy relevance. Furthermore, the study confirms that the OxCAP-MH capability measure is a valid and relevant tool to understand the impacts of the Covid-19 pandemic and related public health measures, which due to the negative externalities of any infectious disease inherently limit individual freedoms to some extent. Future research is planned to compare cultural aspects of lockdown experiences across countries and explore long-term mental health/well-being impacts from the perspective of the capability approach.
Availability of data and materials
The datasets generated during the current study and the study protocol have been released in a scientific data repository and can be accessed under the link: https://doi.org/10.5281/zenodo.4271534 .
Abbreviations
The Hospital Anxiety and Depression Scale
The Multidimensional Scale of Perceived Social Support
The Oxford CAPabilities questionnaire-Mental Health
World Health Organisation
The World Health Organisation-Five Well-being Index
WHO. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/ . Accessed 30 Oct 2020.
UNDP. COVID-19 and human development: Assessing the crisis, envisioning the recovery. http://hdr.undp.org/en/hdp-covid . Accessed 30 Oct 2020.
Shah K, Kamrai D, Mekala H, Mann B, Desai K, Patel RS. Focus on mental health during the coronavirus (COVID-19) pandemic: applying Learnings from the past outbreaks. Cureus. 2020;12(3):e7405. https://doi.org/10.7759/cureus.7405 .
Article PubMed PubMed Central Google Scholar
Caqueo-Urízar A, Urzúa A, Aragón-Caqueo D, Charles CH, El-Khatib Z, Otu A, et al. Mental health and the COVID-19 pandemic in Chile. Psychol Trauma. 2020;12(5):521–3. https://doi.org/10.1037/tra0000753 .
Article PubMed Google Scholar
Chen S, Bonanno GA. Psychological adjustment during the global outbreak of COVID-19: a resilience perspective. Psychol Trauma. 2020;12(S1):S51–S4. https://doi.org/10.1037/tra0000685 .
Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM. 2020;113(5):311–2. https://doi.org/10.1093/qjmed/hcaa110 .
Article CAS PubMed Google Scholar
Dong L, Bouey J. Public mental health crisis during COVID-19 pandemic, China. Emerg Infect Dis. 2020;26(7):1616–8. https://doi.org/10.3201/eid2607.200407 .
Article CAS PubMed PubMed Central Google Scholar
Javed B, Sarwer A, Soto EB, Mashwani ZU. The coronavirus (COVID-19) pandemic's impact on mental health. Int J Health Plann Manag. 2020;35:993–6. https://doi.org/10.1002/hpm.3008 .
Article Google Scholar
Kavčič T, Avsec A, Zager KG. Psychological functioning of Slovene adults during the COVID-19 pandemic: does resilience matter? Psychiatr Q. 2020:1–10. https://doi.org/10.1007/s11126-020-09789-4 .
Khoury B, El-Khoury J, Ammar J. Psychological needs and response during the COVID-19 pandemic in Lebanon. Psychol Trauma. 2020;12(5):497–8. https://doi.org/10.1037/tra0000757 .
Koushik NS. A population mental health perspective on the impact of COVID-19. Psychol Trauma. 2020;12(5):529–30. https://doi.org/10.1037/tra0000737 .
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 .
Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218–1239.e3. https://doi.org/10.1016/j.jaac.2020.05.009 .
Mancini AD. Heterogeneous mental health consequences of COVID-19: costs and benefits. Psychol Trauma. 2020;12(S1):S15–S6. https://doi.org/10.1037/tra0000894 .
Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383(6):510–2. https://doi.org/10.1056/NEJMp2008017 .
Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F, et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiatry. 2020;11:790. https://doi.org/10.3389/fpsyt.2020.00790 .
Seghi F, Barbini B, Franchini L, Colombo C. The challenge of mental health during Covid-19 outbreak: experience from metropolitan area of Milan. Eur Arch Psychiatry Clin Neurosci. 2020:1–2. https://doi.org/10.1007/s00406-020-01154-7 .
Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020;113(8):531–7. https://doi.org/10.1093/qjmed/hcaa201 .
Article CAS PubMed Central Google Scholar
Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;133(11):707–12. https://doi.org/10.1093/qjmed/hcaa202 .
Article CAS Google Scholar
Talevi D, Socci V, Carai M, Carnaghi G, Faleri S, Trebbi E, et al. Mental health outcomes of the CoViD-19 pandemic. Riv Psichiatr. 2020;55(3):137–44. https://doi.org/10.1708/3382.33569 .
Tang F, Liang J, Zhang H, Kelifa MM, He Q, Wang P. COVID-19 related depression and anxiety among quarantined respondents. Psychol Health. 2020:1–15. https://doi.org/10.1080/08870446.2020.1782410 .
Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–20. https://doi.org/10.1177/0020764020915212 .
Sen A. Commodities and capabilities: OUP catalogue; 1999.
Google Scholar
Sen A. Capability and well-being. In: Nusbaum M, Sen A, editors. The Quality of Life: Oxford: Clarendon Press; 1993. p. 30–53.
Anand P, Ferrer B, Gao Q, Nogales R, Unterhalter E. COVID-19 as a capability crisis: using the capability framework to understand policy challenges. J Human Dev Capabil. 2020:293–9. https://doi.org/10.1080/19452829.2020.1789079 .
Gibney E. Whose coronavirus strategy worked best? Scientists hunt most effective policies. Nature. 2020;581(7806):15–6. https://doi.org/10.1038/d41586-020-01248-1 .
Moshammer H, Poteser M, Lemmerer K, Wallner P, Hutter HP. Time course of COVID-19 cases in Austria. Int J Environ Res Public Health. 2020;17(9):3270. https://doi.org/10.3390/ijerph17093270 .
Pieh C, Budimir S, Probst T. Mental health during COVID-19 lockdown: a comparison of Austria and the UK. SSRN. https://doi.org/10.2139/ssrn.3592372 .
Traunmüller C, Stefitz R, Gaisbachgrabner K, Schwerdtfeger A. Psychological correlates of COVID-19 pandemic in the Austrian population. BMC Public Health. 2020;20:1395. https://doi.org/10.1186/s12889-020-09489-5 .
Brunner R. Why do people with mental distress have poor social outcomes? Four lessons from the capabilities approach. Soc Sci Med. 2017;191:160–7.
Mitchell PM, Al-Janabi H, Byford S, Kuyken W, Richardson J, Iezzi A, et al. Assessing the validity of the ICECAP-A capability measure for adults with depression. BMC Psychiatry. 2017;17(1):46. https://doi.org/10.1186/s12888-017-1211-8 .
Hackert MQN, van Exel J, Brouwer WBF. Does the ICECAP-O cover the physical, mental and social functioning of older people in the UK? Qual Life Res. 2019;28(3):761–70. https://doi.org/10.1007/s11136-018-2042-x .
Łaszewska A, Schwab M, Leutner E, Oberrauter M, Spiel G, Simon J. Measuring broader wellbeing in mental health services: validity of the German language OxCAP-MH capability instrument. Qual Life Res. 2019;28(8):2311–23. https://doi.org/10.1007/s11136-019-02187-9 .
Vergunst F, Jenkinson C, Burns T, Anand P, Gray A, Rugkåsa J, et al. Psychometric validation of a multi-dimensional capability instrument for outcome measurement in mental health research (OxCAP-MH). Health Qual Life Outcomes. 2017;15(1):250. https://doi.org/10.1186/s12955-017-0825-3 .
Leiner DJ. SoSci Survey (Version 3.1.06). 2019. https://www.soscisurvey.de .
White RG, Van Der Boor C. Impact of the COVID-19 pandemic and initial period of lockdown on the mental health and well-being of adults in the UK. B J Psych Open. 2020;6(5):e90. https://doi.org/10.1192/bjo.2020.79 .
Simon J, Anand P, Gray A, Rugkåsa J, Yeeles K, Burns T. Operationalising the capability approach for outcome measurement in mental health research. Soc Sci Med. 2013;98:187–96. https://doi.org/10.1016/j.socscimed.2013.09.019 .
Simon J, Łaszewska A, Leutner E, Spiel G, Churchman D, Mayer S. Cultural and linguistic transferability of the multi-dimensional OxCAP-MH capability instrument for outcome measurement in mental health: the German language version. BMC Psychiatry. 2018;18(1):173. https://doi.org/10.1186/s12888-018-1762-3 .
Snaith RP, Zigmond AS. The hospital anxiety and depression scale. Br Med J. 1986;292(6516):344. https://doi.org/10.1136/bmj.292.6516.344 .
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. https://doi.org/10.1016/s0022-3999(01)00296-3 .
Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52(1):30–41. https://doi.org/10.1207/s15327752jpa5201_2 .
WHO. Wellbeing Measures in Primary Health Care/The Depcare Project. Copenhagen: Report on a WHO Meeting; 1998. https://www.euro.who.int/__data/assets/pdf_file/0016/130750/E60246.pdf Accessed 30 Oct 2020
Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 well-being index: a systematic review of the literature. Psychother Psychosom. 2015;84(3):167–76. https://doi.org/10.1159/000376585 .
Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Erbaum Press; 1988.
StataCorp. Stata Statistical Software: Release 15. College Station: TX: StataCorp LLC; 2017.
Statistik Austria. Bevölkerung am 1.1.2019 nach Alter und Bundesland. 2019. http://www.statistik.at/web_de/statistiken/menschen_und_gesellschaft/bevoelkerung/bevoelkerungsstruktur/bevoelkerung_nach_alter_geschlecht/023470.html . Accessed 30 Oct 2020.
Statistik Austria. Bevölkerung 2017 nach detaillierter Staatsangehörigkeit, Geschlecht und Bundesland. 2017. http://www.statistik.at/web_de/statistiken/menschen_und_gesellschaft/bevoelkerung/volkszaehlungen_registerzaehlungen_abgestimmte_erwerbsstatistik/bevoelkerung_nach_demographischen_merkmalen/index.html . Accessed 30 Oct 2020.
Statistik Austria. Bildungsstand der Bevölkerung ab 15 Jahren 2017 nach Altersgruppen und Geschlecht. 2017. http://www.statistik.at/web_de/statistiken/menschen_und_gesellschaft/bildung/bildungsstand_der_bevoelkerung/121189.html . Accessed 30 Oct 2020.
Statistik Austria. Austria: Data. Figures Facts http://www.statistik.at/wcm/idc/idcplg?IdcService=GET_NATIVE_FILE&dDocName=029252 . Accessed 30 Oct 2020.
Braun M, Niederkronenthaler T, Till B. SARS CoV-2: Mental Health in Österreich Ausgewählte Ergebnisse zur ersten Befragungswelle, 23.04.-05.05.2020: Unit Suizidforschung und Mental Health Promotion, Abteilung für Sozial- und Präventivmedizin, Zentrum für Public Health, Medizinische Universität Wien; 2020.
Nitschke JP, Forbes P, Ali N, Cutler J, Apps MAJ, Lockwood P, Lamm C. Resilience during uncertainty? Greater social connectedness during COVID-19 lockdown is associated with reduced distress and fatigue. Br J Health Psychol. 2020. https://doi.org/10.1111/bjhp.12485 .
Stieger S, Lewetz D, Swami V. Psychological well-being under conditions of lockdown: an experience sampling study in Austria during the COVID-19 pandemic. PsyArXiv Preprints. 2020. https://doi.org/10.31234/osf.io/qjhfp .
Hofer H, Titelbach G, Fink M. Die österreichische Arbeitsmarktpolitik vor dem Hintergrund der Covid-19-Krise. Vienna: Institute for Advanced Studies; 2020. https://irihs.ihs.ac.at/id/eprint/5388/7/ihs-report-2020-hofer-titelbach-fink-oesterreich-arbeitsmarktpolitik-covid-19.pdf . Accessed 30 Oct 2020
Müller M. The start of the Austrian response to the COVID-19 crisis: a personal account. Wien Klin Wochenschr. 2020;132(13–14):353–5. https://doi.org/10.1007/s00508-020-01693-y .
de Wit L, Jelsma JG, van Poppel MN, Bogaerts A, Simmons D, Desoye G, et al. Physical activity, depressed mood and pregnancy worries in European obese pregnant women: results from the DALI study. BMC Pregnancy Childbirth. 2015;15:158.
Loder AKF, Schwerdtfeger AR, van Poppel MNM. Perceived greenness at home and at university are independently associated with mental health. BMC Public Health. 2020;20(1):802. https://doi.org/10.1186/s12889-020-8412-7 .
Cenik F, Keilani M, Hasenöhrl T, Huber D, Stuhlpfarrer B, Pataraia A, et al. Relevant parameters for recommendations of physical activity in patients suffering from multiple myeloma: a pilot study. Wien Klin Wochenschr. 2020;132:124–31. https://doi.org/10.1007/s00508-019-01582-z .
Clever K, Schepper F, Pletschko T, Herschbach P, Christiansen H, Martini J. Psychometric properties of the fear of progression questionnaire for parents of children with cancer (FoP-Q-SF/PR). J Psychosom Res. 2018;107:7–13. https://doi.org/10.1016/j.jpsychores.2018.01.008 .
Herrmann C, Snaith RP BU. Hospital anxiety and depression scale–deutsche version (HADS-D). Verlag Hans Huber: Ein Fragebogen zur Erfassung von Angst und Depressivität; 1995.
Sipötz J, Friedrich O, Höfer S, Benzer W, Chatsakos T, Gaul G, et al. Health related quality of life and mental distress after PCI: restoring a state of equilibrium. Health Qual Life Outcomes. 2013;11:144. https://doi.org/10.1186/1477-7525-11-144 .
Greimel E, Kato Y, Müller-Gartner M, Salchinger B, Roth R, Freidl W. Internal and external resources as determinants of health and quality of life. PLoS One. 2016;11(5):e0153232. https://doi.org/10.1371/journal.pone.0153232 .
Mautner E, Ashida C, Greimel E, Lang U, Kolman C, Alton D, et al. Are there differences in the health outcomes of mothers in Europe and East-Asia? A cross-cultural health survey. Biomed Res Int. 2014;856543. https://doi.org/10.1155/2014/856543 .
Probst T, Stippl P, Pieh C. Changes in provision of psychotherapy in the early weeks of the COVID-19 lockdown in Austria. Int J Environ Res Public Health. 2020;17(11):3815. https://doi.org/10.3390/ijerph17113815 .
Tullio V, Perrone G, Bilotta C, Lanzarone A, Argo A. Psychological support and psychotherapy via digital devices in Covid-19 emergency time: some critical issues. Med Leg J. 2020;88(2):73–6. https://doi.org/10.1177/0025817220926942 .
Van Daele T, Karekla M, Kassianos AP, Compare A, Haddouk L, Salgado J, et al. Recommendations for policy and practice of telepsychotherapy and e-mental health in Europe and beyond. J Psychother Integr. 2020;30(2):160–73. https://doi.org/10.1037/int0000218 .
Prajapati N, Łaszewska A, Franco D, Ericson R, Leroy S, Lindert J, et al. What are the COVID-19 Lockdown-induced illnesses and why should European public health systems be investigating their epidemiology, treatment, and prevention? The Association of Schools of Public Health in the European Region. 2020. https://www.aspher.org/download/531/aspher-lockdown-induced-illnesses.pdf . Accessed 21 Dec 2020.
Middleton J, Lopes H, Michelson K, Reid J. Planning for a second wave pandemic of COVID-19 and planning for winter. A statement from the Association of Schools of Public Health in the European region. Int J Public Health. 2020;65:1525–7. https://doi.org/10.1007/s00038-020-01455-7 .
Devaux M, Sassi F. Social disparities in hazardous alcohol use: self-report bias may lead to incorrect estimates. Eur J Pub Health. 2016;26(1):129–34. https://doi.org/10.1093/eurpub/ckv190 .
Mulder J, de Bruijne M. Willingness of Online Respondents to Participate in Alternative Modes of Data Collection. Survey Practice. 2019;12(1). https://doi.org/10.29115/SP-2019-0001 .
Yetter G, Capaccioli K. Differences in responses to web and paper surveys among school professionals. Behav Res Methods. 2010;42(1):266–72.
Download references
Acknowledgements
We would like to say thank you to all survey participants and to colleagues at the Department of Health Economics for piloting the survey.
The study received no funding.
Author information
Authors and affiliations.
Department of Health Economics, Center for Public Health, Medical University of Vienna, Kinderspitalgasse 15, 1090, Vienna, Austria
Judit Simon, Timea M. Helter & Agata Łaszewska
Department of Psychiatry, University of Oxford, Warneford Hospital, Oxford, OX3 7JX, UK
Judit Simon
Primary Care and Mental Health, Institute of Population Health, University of Liverpool, School of Psychology, Brownlow Hill, Liverpool, L69 3GB, UK
Ross G. White & Catharina van der Boor
You can also search for this author in PubMed Google Scholar
Contributions
JS, RW and CV conceived the study idea, and developed the conceptual framework and methods of the research. JS provided the resources to this study. TH and AL executed the survey and conducted the analysis supervised by JS. JS, TH and AL wrote the manuscript which was reviewed by all. All authors provided critical feedback and helped shape the research, analysis and manuscript. All authors approved the final manuscript.
Corresponding author
Correspondence to Judit Simon .
Ethics declarations
Ethics approval and consent to participate.
The study and experimental protocols were approved by the Ethics Committee of the Medical University of Vienna on 26 May 2020 (EK Nr: 1529/2020). Informed consent was obtained from all individual participants included in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Commission of the Medical University of Vienna (EK 1529/2020) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
JS has led the development of the OxCAP-MH measure. The remaining authors declare that they have no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Simon, J., Helter, T.M., White, R.G. et al. Impacts of the Covid-19 lockdown and relevant vulnerabilities on capability well-being, mental health and social support: an Austrian survey study. BMC Public Health 21 , 314 (2021). https://doi.org/10.1186/s12889-021-10351-5
Download citation
Received : 09 November 2020
Accepted : 11 January 2021
Published : 08 February 2021
DOI : https://doi.org/10.1186/s12889-021-10351-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Capabilities
- Mental health
- Vulnerability
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Epidemiological and economic effects of lockdown
- Download the full paper
- Download the online appendix
- Download the data and programs
Subscribe to the Economic Studies Bulletin
Alexander d. arnon , alexander d. arnon penn wharton budget model john a. ricco , and john a. ricco penn wharton budget model kent a. smetters kent a. smetters the wharton school discussants: alessandra fogli alessandra fogli federal reserve bank of minneapolis.
September 23, 2020
This paper is part of the fall 2020 edition of the Brookings Papers on Economic Activity , the leading conference series and journal in economics for timely, cutting-edge research about real-world policy issues. Research findings are presented in a clear and accessible style to maximize their impact on economic understanding and policymaking. The editors are Brookings Nonresident Senior Fellow and Northwestern University Professor of Economics Janice Eberly and Brookings Nonresident Senior Fellow and Harvard University Professor of Economics James Stock . Read summaries of all the papers from the journal here.
Orders encouraging people to leave their homes for only their most essential needs during the early months of the COVID-19 pandemic reduced deaths at a lower economic cost than mandatory business shutdowns, suggests a paper discussed at the Brookings Papers on Economic Activity (BPEA) conference on September 24.
The paper’s authors—Alex Arnon, John Ricco, and Kent Smetters of the University of Pennsylvania—created an integrated framework that evaluated the health and economic effects of “non-pharmaceutical interventions” by state and local governments at the county level. They focused on three major interventions—stay-at-home orders, nonessential business closures, and school closures.
They used different types of cell phone data to estimate the effect of interventions on people’s contacts with people they did not live with. They then looked at COVID-19 deaths and estimated changes in employment at the county level, relying a range of nontraditional data, including from mobile devices, web searches, and business payrolls.
Interventions “that target individual behavior (such as stay-at-home orders) were more effective at reducing [virus] transmission at lower economic cost than those that target businesses (shutdowns),” the authors conclude in Epidemiological and economic effects of lockdown . School closures fell between stay-at-home orders and business closures in terms of the tradeoff between job losses and social distancing gains, they write.
The authors also find that state and local government interventions explain only nine percent of the reduction in social contacts through the second week of April. Voluntary social distancing explains most of the reduction. But, importantly, they estimate that the modest additional reduction in social contacts achieved by government interventions prevented about 33,000 deaths through May 31 (U.S. virus deaths at that point totaled nearly 115,000).
“It appears policy played a role in changing people’s behavior,” Smetters said in an interview with Brookings. “People took it much more seriously because there was a policy.”
At the same time, the authors estimate that non-pharmaceutical interventions reduced employment by about three million, nearly 15 percent of the total decline from the start of the pandemic through the end of May.
The paper also suggests that jurisdictions that imposed stay-at-home orders swiftly, as the virus was first spreading, were better able to avoid harsher business shutdowns later.
“If you impose a stay-at-home order at the first sign of an occurrence … the tradeoff will probably be better than if you wait until things get worse and then … close everything all at once,” Arnon said.
One of the paper’s objectives, the authors write, is “to provide useful insights to policymakers managing the current and any future infectious disease outbreaks.” But, they caution, “no analysis … can answer the question of whether the economic costs of a particular intervention are worth it” without explicitly considering the value of the years of life saved and other potential health benefits gained. “We hope that our analysis serves as a key part of helping to make that determination.”
David Skidmore authored the summary language for this paper.
Arnon , Alex ander D. , John Ricco, and Kent A. Smetters . 2020. “ Epidemiological and Economic Effects of Lockdown . ” Brookings Papers on Economic Activity , Fall, 61-108.
CONFLICT OF INTEREST DISCLOSURE
The authors did not receive financial support from any firm or person for this article or from any firm or person with a financial or political interest in this paper. They are currently not officers, directors, or board members of any organization with an interest in this paper.
Discussants
Economic Studies
Brookings Papers on Economic Activity
Constanze Stelzenmüller
April 22, 2024
Nicol Turner Lee, Dominique Duval-Diop
Molly E. Reynolds, Fred Dews
Lockdown has led to positive change for some people. Here's why

70% of participants reported having experienced at least one positive effect of the COVID-19 lockdown.
.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Lynn Williams

.chakra .wef-9dduvl{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-9dduvl{font-size:1.125rem;}} Explore and monitor how .chakra .wef-15eoq1r{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;color:#F7DB5E;}@media screen and (min-width:56.5rem){.chakra .wef-15eoq1r{font-size:1.125rem;}} SDG 03: Good Health and Well-Being is affecting economies, industries and global issues


.chakra .wef-1nk5u5d{margin-top:16px;margin-bottom:16px;line-height:1.388;color:#2846F8;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-1nk5u5d{font-size:1.125rem;}} Get involved with our crowdsourced digital platform to deliver impact at scale
Stay up to date:, sdg 03: good health and well-being.
- Studies show some people are reporting positive changes in lockdown, with 83% having more time to do enjoyable things and 65% spending more time in outdoors.
- It is believed that additional time and the removal of daily demands during lockdown may be improving quality of life for some people.
- Unfortunately, groups such as older adults and those living on their own may be less able to benefit.
- Half of the participants who reported positive changes were able to keep these going once restrictions were eased, which bodes well for their post-pandemic lives.
National lockdowns have been the most profound and significant public health interventions within living memory. They have been difficult socially and economically, and have negatively affected people’s health in many different ways .
But for some people lockdowns have provided an unexpected opportunity to make positive changes to their lives, running counter to prevailing narratives of disrupted daily lives, health inequalities and damaged mental health .
Have you read?
In lockdown britain, 'mancunian motivator' brings fun and fitness to neighbours, fitness apps grew by nearly 50% during the first half of 2020, study finds, covid-19 lets us see the world through a different lens.
In May 2020, my colleagues and I surveyed over 3,000 people in Scotland to find out what positive changes people had made in their lives during the lockdown period. We also wanted to find out who had made these positive changes, to see if there were particular groups that were more able to do this than others.
In the survey, we assessed the positive changes that people had experienced across a number of different aspects of their lives since the start of lockdown. There were questions about whether people had experienced positive changes in relationships with family and friends and in the wider community. We also asked about beneficial changes in people’s behaviour relating to their health, including physical activity and sleep.

More than half the people we surveyed reported these changes for the better: being more appreciative of things usually taken for granted (reported by 83% of participants), having more time to do enjoyable things (by 67%), spending more time in nature or outdoors (by 65%), paying more attention to personal health (by 62%), doing more physical activity (by 54%) and spending more time with a partner or spouse (by 53%).
An Australian study (still in preprint, meaning its findings are yet to be reviewed by other scientists) also sought to find out similar information. In a survey of over 1,000 people, it found that 70% of participants reported having experienced at least one positive effect of the pandemic. Three main positive effects noted in this survey were: having the opportunity to spend more time with family, having greater flexibility in working arrangements and appreciating having a less busy life.
The important role of time was highlighted across both studies. Lockdown has removed many of life’s routines and demands – and for some people this has afforded them more time to spend on activities they enjoyed and valued. Noticing that how we spend time has changed – and thinking about what we can do with any additional time that we have – may be an important first step in making positive changes to our lives during lockdown.
People also noted being more appreciative of things previously taken for granted and the slower pace of life that lockdown has brought. For many people, this may have enabled them to step back and reflect on their lives, their futures and what is important to them in a way that they would not otherwise have the opportunity to do, without the demands of daily commutes or social commitments.
Positive changes not universal
Turning to who experienced the positive changes, our study revealed that the groups with higher levels of positive change were women, younger people, people who were married or living with their partner, those who were employed and those reporting better health. These findings suggest that while some groups were able to take advantage of lockdown as an unexpected opportunity to make positive changes in their lives, others – such as older adults and those living on their own – were not.
We were also interested in finding out what would happen to the positive changes that people had made once restrictions started lifting. Would they be able to keep them up? In a separate paper , based on the same group of participants, we examined the changes that people had made to their physical activity, sitting and sleep during the first national lockdown period and whether they had maintained these two months later, once restrictions had been eased.
The good news was that half of the participants who reported positive changes in their behaviours during lockdown were able to keep these going once restrictions were eased. Some were even able to improve them further. So, while we are currently experiencing another period of national lockdown in the UK, it’s reassuring to know that some positives could emerge.
However, we should keep in mind that winter, the new strains of the virus circulating and being over a year into the pandemic will all give this lockdown a different feel to last spring’s, and that this might have an influence on what positive changes people are able to make and sustain. But as we think ahead to the post-pandemic recovery phase, the lesson from our research is that there are definitely some changes people will want to keep.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
The Agenda .chakra .wef-n7bacu{margin-top:16px;margin-bottom:16px;line-height:1.388;font-weight:400;} Weekly
A weekly update of the most important issues driving the global agenda
.chakra .wef-1dtnjt5{display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;} More on Health and Healthcare Systems .chakra .wef-17xejub{-webkit-flex:1;-ms-flex:1;flex:1;justify-self:stretch;-webkit-align-self:stretch;-ms-flex-item-align:stretch;align-self:stretch;} .chakra .wef-nr1rr4{display:-webkit-inline-box;display:-webkit-inline-flex;display:-ms-inline-flexbox;display:inline-flex;white-space:normal;vertical-align:middle;text-transform:uppercase;font-size:0.75rem;border-radius:0.25rem;font-weight:700;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;line-height:1.2;-webkit-letter-spacing:1.25px;-moz-letter-spacing:1.25px;-ms-letter-spacing:1.25px;letter-spacing:1.25px;background:none;padding:0px;color:#B3B3B3;-webkit-box-decoration-break:clone;box-decoration-break:clone;-webkit-box-decoration-break:clone;}@media screen and (min-width:37.5rem){.chakra .wef-nr1rr4{font-size:0.875rem;}}@media screen and (min-width:56.5rem){.chakra .wef-nr1rr4{font-size:1rem;}} See all

This Earth Day we consider the impact of climate change on human health
Shyam Bishen and Annika Green
April 22, 2024

Scientists have invented a method to break down 'forever chemicals' in our drinking water. Here’s how
Johnny Wood
April 17, 2024

Young people are becoming unhappier, a new report finds

Promoting healthy habit formation is key to improving public health. Here's why
Adrian Gore
April 15, 2024

What's 'biophilic design' and how can it benefit neurodivergent people?
Fatemeh Aminpour, Ilan Katz and Jennifer Skattebol

Why stemming the rise of antibiotic resistance will be an historic achievement
Carel du Marchie Sarvaas
April 11, 2024
- Share full article
Advertisement
Supported by
Guest essay
Teenagers Are Struggling, and It’s Not Just Lockdown

By Emily Esfahani Smith
Ms. Esfahani Smith is a doctoral student in clinical psychology and the author of “The Power of Meaning.” At the beginning of the pandemic, she wrote about how a key to surviving the mental-health trials of isolation is to look for meaning rather than happiness.
When schools shut down last spring, Carson Roubison, a charter school student in Phoenix, was initially relieved. There were some difficulties in those early days at home — when classes went online, Carson and his parents , both public-school teachers, had to share the sole family computer. But Carson’s stress levels fell as school became less demanding during the transition to distance learning.
“I wasn’t aware of the giant impact the pandemic would have,” he said, “so I was excited, to be honest, to have some time off school.”
But things changed in the fall. The academic load went back to prepandemic levels, even though learning was still remote. Carson, a senior, struggled to stay motivated. His mental health suffered. He hoped to attend community college the following fall, but grew increasingly “terrified” that the education he’d received in high school over the past year would leave him unprepared.
“I’m afraid I’m going to get to community college,” he said, “and be held to the same standards as past students, and fail. That’s the biggest source of my anxiety.”
Carson’s story is not unique. The pandemic has taken a toll on the mental health of millions. But adolescents have been hit especially hard. According to a national poll conducted in January by the University of Michigan’s C.S. Mott Children’s Hospital, 46 percent of parents say their teenagers ’ mental health has worsened during the pandemic. More alarmingly, a report by the Centers for Disease Control and Prevention found that the proportion of 12- to 17-year-olds visiting emergency rooms for mental health reasons rose 31 percent for most of 2020 compared with 2019. And this is all on top of an already existing mental health crisis among young people.
While many experts believe that the reason adolescents are struggling today is that they’re away from friends and school, a closer look at the research reveals a more complicated picture. According to psychologists who study adolescent resilience, one of the biggest threats to the well-being of today’s teenagers is not social isolation but something else — the pressure to achieve, which has intensified over the past year.
Psychologists define resilience as the ability to adapt well to stress. For decades, they have studied why some kids are more resilient in adversity than others. Suniya Luthar , emerita professor of psychology at Columbia’s Teachers College and a leading resilience researcher, believes the pandemic is a “natural experiment” that can help answer that question: When you expose adolescents to an event that changes their lives significantly, how do they cope?
Dr. Luthar began her career studying resilience among urban youth living in poverty in Connecticut in the 1990s. At the urging of one of her students at Yale, where she was teaching, she also started studying teenagers living in middle- and upper-middle-class suburbs like Westport, Conn., where many of the parents are high-achieving professionals who emphasize the value of status and achievement to their children.
Comparing these students with the poor, urban adolescents, she was shocked to discover that the suburban children were doing worse on drug and alcohol abuse. They also had higher rates of anxiety and depression as compared with national norms. Researchers knew that social conditions were important determinants of resilience, but they hadn’t known that living in success-oriented cultures was a risk factor.
In the years since, Dr. Luthar and her colleagues at Authentic Connections , a research group that works to foster resilience in school communities, have studied tens of thousands of teenagers attending “high-achieving schools,” which she defines as public and private institutions where students on average score in the top third on standardized tests. The students in these samples come from a variety of racial, regional and socioeconomic backgrounds. In one group of students Dr. Luthar studied, for example, one-third were members of ethnic and racial minorities and one-quarter came from homes where at least one parent did not attend college.
But regardless of these differences, many of them were struggling in the same way. In a paper published in 2020 in the academic journal American Psychologist, Dr. Luthar and her colleagues — the psychological researchers Nina Kumar and Nicole Zillmer — reviewed three decades’ worth of research findings showing that adolescents at high-achieving schools suffer from symptoms of clinical depression and anxiety at rates three to seven times higher than national norms for children their age.
What’s driving their misery, the research shows, is the pressure to excel in multiple academic and extracurricular pursuits. The National Academies of Sciences, Engineering, and Medicine and the Robert Wood Johnson Foundation suggest children living in an achievement-oriented culture are at risk for adjustment problems, like those facing more predictable forms of adversity, such as poverty and trauma.
The pandemic offered a rare reprieve for students — at first. Since 2019, Dr. Luthar and her colleagues have surveyed thousands of adolescents each year at public and private schools across the nation. Replicating findings of earlier research, these students reported suffering from anxiety and depression at higher rates than national norms before the pandemic. But when schools closed last spring, something unexpected happened — the well-being of these students actually improved . As classes and exams were canceled, grading moved to pass/fail and extracurricular activity ceased, they reported lower levels of stress, anxiety and depression compared with 2019.
But these improvements were short-lived. Dr. Luthar and her colleagues found that beginning in the fall of 2020, as schoolwork ramped back up, the mental health of adolescents returned to prepandemic levels or worse. According to research that will be published in Social Policy Report, a quarterly publication of the Society for Research in Child Development, the strongest predictor of depression among these students was perceived parental criticism and unreachable standards.
“Even though I’m trying my best, it never really goes the way I wished,” a student Dr. Luthar studied wrote, “and my mother adds stress because she is always saying that I NEED to have a 90 or higher averages in all my classes.”
Other research supports these findings. In a nationally representative study conducted by NBC News and Challenge Success, a nonprofit affiliated with Stanford’s education school, researchers studied over 10,000 high school students in the fall of 2020. Comparing the experience of these students with about 65,000 adolescents surveyed between 2018 and February 2020, these researchers, too, found that many students reported feeling more stressed about school during the fall of 2020 than before the pandemic. A chief cause of their stress: the pressure to achieve.
Nearly half of all students reported that the pressure to do well in school had increased since 2019, and over half said their school-related stress over all had risen. Grades, workload, time management, lack of sleep and college fears were the most commonly cited sources of stress. These findings held across socioeconomically diverse schools. At underresourced schools, students were more likely to report being stressed about family finances, according to Denise Pope, a founder of Challenge Success, but the top stressors were still grades, assessments and college.
“My school is giving too much work,” a 10th grader in this study wrote, “even though times are tough for everyone. At first, this was just a break from school, but now all I feel is stress, anxiety and pain.”
Parents appear to play a big role in this phenomenon. Fifty-seven percent of students said that their parents’ expectations for their performance stayed the same during the pandemic, while 34 percent said their expectations increased. The stereotype of the adolescent aloof from parental influence doesn’t seem to apply to these students, who report feeling more stressed about family pressure than peer pressure.
When Dr. Pope asks parents to define success, they inevitably say that they want their children to be happy and healthy, have loving relationships and give back to society. But when she asks children how they define success, many describe a narrow path: getting good grades, going to college and securing a high-paying job.
Dr. Pope believes the gap is due in part to how parents praise their kids. Many parents reward their children when they perform well, which sends a signal to the kids that the approval and love of their parents depends on how much they’re achieving. So inevitably, if they believe they are falling short of their parents’ expectations, their sense of worth and well-being suffers.
Larger cultural forces are also pushing students to define success narrowly. As inequality rises and two major recessions in the past decade have left millions out of work, many students may feel compelled to climb the ladder to ensure their economic security as adults. College admissions at top-tiered schools has become more selective over the same period of time, leaving students competing harder for fewer spots — only to receive an education that will likely leave them or their parents in debt for many years to come.
If we want more-resilient kids coming out of the pandemic, then we need to heed a lesson of this past year — that the pressure to achieve is crushing the spirits of many young people and should be dialed back. Parents can play a vital role here. They can help ease their children’s anxiety by reminding them that where they attend college will not make or break them — and that getting Bs does not equal failure.
They can encourage them to prioritize their health and well-being by getting enough sleep and making time for play and leisure. And above all, they can teach their children that loss is an inevitable part of life by speaking to them about the grief of the past year. This doesn’t mean parents should necessarily lower their standards. But they might emphasize different benchmarks for achievement, like those they themselves claim to most value for their children — happiness, health and love.
If you are having thoughts of suicide, call the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK). You can find a list of additional resources at SpeakingOfSuicide.com/resources .
Emily Esfahani Smith is the author of “ The Power of Meaning: Finding Fulfillment in a World Obsessed With Happiness .”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow The New York Times Opinion section on Facebook , Twitter (@NYTopinion) and Instagram .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 07 March 2024
The impact of COVID-19 lockdowns on mental health patient populations in the United States
- Ibtihal Ferwana 1 &
- Lav R. Varshney ORCID: orcid.org/0000-0003-2798-5308 1
Scientific Reports volume 14 , Article number: 5689 ( 2024 ) Cite this article
1531 Accesses
19 Altmetric
Metrics details
- Health care economics
- Health policy
During the start of the COVID-19 pandemic in 2020, lockdowns and movement restrictions were thought to negatively impact population mental health, since depression and anxiety symptoms were frequently reported. This study investigates the effect of COVID-19 mitigation measures on mental health across the United States, at county and state levels using difference-in-differences analysis. It examines the effect on mental health facility usage and the prevalence of mental illnesses, drawing on large-scale medical claims data for mental health patients joined with publicly available state- and county-specific COVID-19 cases and lockdown information. For consistency, the main focus is on two types of social distancing policies, stay-at-home and school closure orders. Results show that lockdown has significantly and causally increased the usage of mental health facilities in regions with lockdowns in comparison to regions without such lockdowns. Particularly, resource usage increased by 18% in regions with a lockdown compared to 1% decline in regions without a lockdown. Also, female populations have been exposed to a larger lockdown effect on their mental health. Diagnosis of panic disorders and reaction to severe stress significantly increased by the lockdown. Mental health was more sensitive to lockdowns than to the presence of the pandemic itself. The effects of the lockdown increased over an extended time to the end of December 2020.
Similar content being viewed by others
Multivariable modelling of factors associated with criminal convictions among people experiencing homelessness and serious mental illness: a multi-year study
Milad Parpouchi, Akm Moniruzzaman, … Julian M. Somers
COVID-19 restrictions and age-specific mental health—U.S. probability-based panel evidence
Elvira Sojli, Wing Wah Tham, … Michael McAleer

COVID-19 non-pharmaceutical interventions: data annotation for rapidly changing local policy information
Benjamin Hurt, Oishee Bintey Hoque, … Madhav Marathe
Introduction
As the COVID-19 pandemic began, confirmed cases rose, and mandated policy responses were enacted, mental health concerns started to be alarming 1 , 2 , 3 . The deterioration of mental health was observed during the first few months of the COVID-19 pandemic, March–June 2020 4 , 5 , especially among women and college students 6 , 7 , 8 . Further, people with preexisting psychiatric disorders 9 , 10 and people that encountered COVID-19 itself 4 developed more mental health issues during the pandemic.
In the early stage of the COVID-19 pandemic, people voluntarily stayed at home and limited their trips for weeks before public policy interventions were imposed 11 . Subsequently, social distancing policies were issued globally as a form of non-pharmaceutical intervention, including limiting people’s gatherings, closing schools, and fully restricting movements by lockdown orders (also called stay-at-home or shelter-in-place orders) 12 , so as to contain virus spread in light of the increasing number of COVID-19 cases and fatalities.
Given that various intertwined events took place during the COVID-19 pandemic, the cause of mental health deterioration is not clear. One possible explanation is the increased severity of COVID-19 which led to increased anxiety, worry, and depression 13 . Another explanation is that policy responses to the pandemic, particularly the lockdown orders, contributed to worsening mental health.
Previous studies observing the decline in mental health have faced a challenge in determining possible causes or selecting direct measures. For example, Refs. 14 , 15 found that depression and anxiety symptoms almost quadrupled from 2019 to June 2020, but could not infer causality given the study design. Other studies found that reduced physical activity resulting from restricted mobility led to higher rates of depression during the pandemic, but could not establish causality since they lacked pre-COVID-19 data 10 , 16 , 17 . Two other important studies by Refs. 18 , 19 used Google search data and found that the timing of lockdown policies has been significantly associated with searches of terms related to worry , sadness , and boredom revealing negative feelings. A recent study established causality of the effect of lockdown restrictions on worsening mental health using a clinical mental health questionnaire in Europe 20 . Although these studies considered pre-COVID-19 trends and have established causality on the lockdown orders, they lacked measures that reflect the rising need for mental health treatment and lacked a large representative population.
Examining the use of mental health resources and the prevalence of mental illnesses would further help in measuring the actual cost of COVID-19 lockdowns on mental health and inform mental health treatment resource planning for future lockdowns. Mental disorders have been more economically costly than any other disease, in which mental disorders were the leading segment of healthcare spending in the United States 21 , with the potential cause of a global economic burden 22 . Mental health has been related to social capital on individual and community levels 23 , 24 . Indeed, good social capital plays a role in promoting healthier public behaviors, especially during COVID-19 25 . The risk of mental health degradation goes beyond to impact the advantage of social capital in the face of viral diseases. Given these consequences of poor mental health on health care systems 26 , it has been essential to mitigate additional mental degradation and avoid potential future economic and social costs.
In this work, we consider measures that reflect the actual seeking of mental health services covering a large fraction of the United States population. To the best of our knowledge, there is no large-scale study that has investigated the effect of lockdown on the usage of mental health resources across the country. We empirically estimate the causal effect of COVID-19 social distancing policies on mental health across counties and states in the United States by comparing the differences in changes between locked and non-locked down regions using a large-scale medical claims dataset that covers most hospitals in the country. Specifically, we are interested to know whether the increase in mental health patients can be explained by COVID-19 lockdowns. Causal inference gives us the tools to uncover causal relationships rather than correlational relationships 27 , in order to understand the impact of COVID-19 policies on mental health.
We use the daily number of patients who visit mental health facilities as a measure for the usage of mental health resources, and we consider emergency department (ED) visits for mental health issues as a proxy for the development of new mental diseases, here, so severe that treatment could not be avoided. We consider ED visits to reflect the utilization of hospital resources under the shortage of medical staff. During COVID-19 there were patients with acute conditions reaching ED in which they have not been in regular outpatient visits 28 . Also, given the shortage in in-patient beds during the pandemic, mental health patients were admitted to ED instead 29 . Therefore, ED visits were of interest to indicate unmet mental health needs. The usage of mental health resources can further trigger analysis of economic costs borne by health care systems and the country as a whole. Mental health ED treatment visits might further reflect the mental health cost on an individual level.
Our results show that extended lockdown measures significantly increase the usage of mental health resources and ED visits. In particular, mental health resource usage in regions with lockdown orders has significantly increased compared to regions without a lockdown. The effect size of lockdowns was not only positive and significant but was also increasing till the end of December 2020. Our results further imply that mental health is more sensitive to policy interventions rather than the evolution of the pandemic itself.
The University of Illinois Urbana-Champaign Institutional Review Board declared this work to be exempt from review. The University of Illinois Urbana-Champaign Institutional Review Board waived the need for informed consent for the current study. All methods were carried out in accordance with relevant guidelines and regulations.
We used three sets of data to conduct our study: mental health claims data including emergency department (ED) claims, COVID-19 cases data, and lockdown dates data.
The mental health data is a large de-identified medical claims corpus provided by Change Healthcare for years 2019 and 2020. Change Healthcare serves 1 million providers covering 5500 hospitals with 220 million patients (which is roughly two-thirds of the US population) and represents over 50% of private insurance claims across the United States. It covers 51 states/territories and a total of 3141 counties (and equivalent jurisdictions like parishes). The data set includes millions of claims per month from the private insurance marketplace, and some Medicare Advantage programs and Medicaid programs using private insurance carriers, excluding Medicare and Medicaid indemnity claims, which is a limitation in the dataset coverage.
Given that different age and gender groups were affected differently during the pandemic 6 , 7 , 8 , we consider a variety of population subgroups in our analysis. Specifically, we consider subgroups of different age, gender, and mental health conditions. Not only do we look at the total mental health claims, but we also select specific mental health conditions, such as anxiety disorders, major depressive disorder, bipolar disorder. Our selected mental health conditions have been also been examined by others 30 during the COVID-19 pandemic. More details on the used clinical codes of mental health records are found in Supplementary Appendix Table 1 . We show summary statistics of the data and its subset representing gender, age, and mental disorders in Table 1 .
For COVID-19 cases, we considered state-level and county-level cases reported in the United States taken from the New York Times database 31 from the first case date in late January 2020 to December 31, 2020, covering 3218 counties in 51 states/territories. Given that reported cases depend on the testing results, thus, the data is limited by the fact that there was a widespread shortage of available tests in different regions at different times. The undercounts of COVID-19 cases used in this study would only weaken the effect we present, and so fixing the data would only strengthen the resultant effect.
For lockdown data, we used the data from the COVIDVis project URL: https://covidvis.berkeley.edu/ led by the University of California Berkeley to track policy interventions on state and county levels, in which they depended on government pandemic responses to construct the dataset. We considered the dates of two order types, shelter-in-place and K-12 school closure at state and county levels. The earliest and latest shelter-in-place orders were on March 14 and April 7, 2020, covering 2598 counties in 43 states. The earliest K-12 school closure was on March 10 and the latest was on April 28, 2020, covering 2465 counties in 39 states. The data is comprehensive, in which states and counties that do not appear in the dataset are considered without officially imposed lockdown. We focus on the impact of the initial shutdowns to avoid complications related to re-opening and repeated closures. Given that in some regions people tend to voluntarily isolate themselves at home and limit their trips before official lockdown orders 11 , therefore, lockdown dates might be limited to reflect the actual social distancing behavior across regions during the pandemic. However, lockdown dates would better reflect the beginning of persistent social distancing behaviors for a larger population group, which is useful to our study, unlike voluntary behaviors.
Difference-in-differences analysis
To estimate the effects of COVID-19 mitigation policies on mental health patients at county and state levels, we conducted a difference-in-differences (DID) analysis, which allows for inferring causality based on parallel trends assumption. For DID analysis we considered daily mental health patients’ visits from the date of September 1, 2019, till December 31, 2020, to observe the prolonged effects since mental health disorders may appear sometime after a trauma 32 . We aim to have balanced periods for pre- and post-lockdown interventions, and this is achievable with this selected range of dates. We used two outcomes, weighted and raw numbers of daily patient visits, weighted outcomes are normalized by the region population.
Our approach leveraged the variation of policy-mandated dates in different counties or states with 8 states that did not declare an official lockdown. Accordingly, we constructed both treated and control groups to implement the analysis. We estimated the following regression as our main equation:
where \(Y_{cd}\) is the outcome in a given region c (county or state) on a date d , \(policy_{jcd}\) indicates whether a policy j has been mandated for a region c on a date d , \(\beta _j\) is the DID interaction coefficient, representing the effect of introducing policy j , and \(\delta _c\) and \(\delta _{d}\) are fixed effects for region and date respectively. The region fixed-effect is included to adjust for time-invariant (independent of time) unobserved regional characteristics that might affect the outcome. For example, each county/state has its local health care system, social capital index, age profile, and socioeconomic status that the fixed effect controls for. Further, the date fixed effect \(\delta _{d}\) is included to adjust for factors that vary over time, such as COVID-19 rates or social behavioral change.
Control by the evolution of COVID-19 cases
Even though DID avoids the bias encountered in time-invariant factors, the bias of time-varying confounders may still be present 33 . Therefore, we consider the COVID-19 confirmed cases \(x_{cd}\) as a main confounder factor in counties or states and we control for it. We follow 34 to use a time-varying adjusted (TVA) model, based on the assumption that the confounding variable affects both treated and untreated groups regardless of policy intervention. We measured the interaction of time and the confounding \(x_{cd}\) covariate at county- and state-levels
Therefore, to mitigate the effect of potential confounders, e.g. socio-economic status and COVID-19 growth, we use several techniques from econometrics 35 . Specifically, we use the fixed effects \(\delta _c\) and \(\delta _d\) in ( 1 ) to adjust for time-invariant confounders related to location and time. Additionally, we use TVA 34 to adjust for time-varying confounders such as COVID-19 growth.
Event-study model
DID models rely on the assumption of parallel pre-treatment trends to exist in both treated and untreated groups. Hence, in the absence of a policy, treated counties or states would evolve similarly as untreated counties or states. To assess equal pre-policy trends, we designed an event-study type model 36 . We calculated k periods before policy implementation and used an event-study coefficient to indicate whether an outcome in specific date d and county/state c is within k periods before the policy implementation 18 , 37 . We estimated the following regression model:
where \(policy_{hsd}^k\) , a dummy variable, equals 1 if policy h took place k periods before the mandate, and zero otherwise. Period k is calculated in months, \(k=\{- 6, - 5, - 4, - 2, - 1, 0\}\) months, and the month of the policy implementation ( \(k=0\) ) is considered as the omitted category. Here, \(\beta _h^k\) is the event-study coefficient and we included all control variables as defined in ( 1 ).
Descriptive analysis
Before we delve into the causal DID inference, we report some statistics to describe the data of mental health patients. Among 16.7 million mental health patients in the United States, the mean age was 38.7 years and 56% were female. As seen in Fig. 1 , the distribution of mental health patients in states and counties shifted between 2019 and 2020. The total increase is 22% of all mental health patients of any mental health disorder as seen in Table 2 in the Supplementary Appendix.
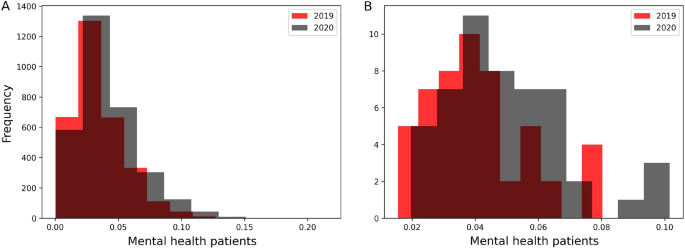
Distributions of mental health patients weighted by regions’ populations in years of 2019 and 2020 in counties ( A ) and states ( B ). The total population increase is 22% in 2020.
Figure 2 shows the increasing trend of the number of mental health daily patients’ visits, though it decreased between March and April 2020, during lockdown mandates.
An obvious increase was during June 2020, which can be attributed to telemedicine options or relaxed lockdown measures.
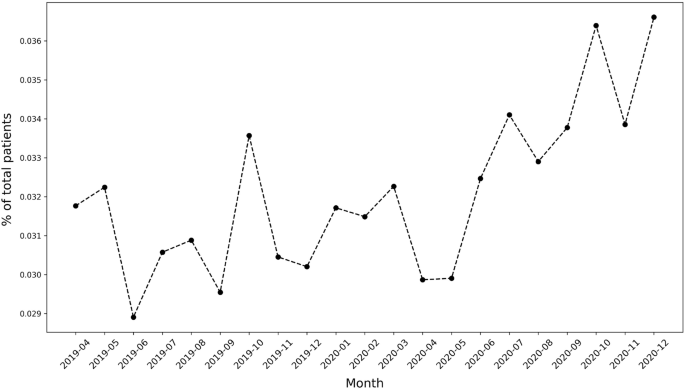
Mental health patients over time.
Parallel trend assumption
To apply DID, first, we validate the pre-policy parallel trends assumption. We tested the equality of pre-policy trends for counties and states using ( 3 ). We plot the event-study coefficients for 6 months before policy implementation from the models of stay-at-home and school-closure orders and the corresponding 95 % confidence intervals. Figure 1 (in Supplementary Appendix) shows that the event-study coefficients are generally non-significant, therefore we cannot reject the null hypothesis of parallel trends. Accordingly, the key assumption of parallel trends of DID is satisfied for both counties and states.
Correlation to COVID-19
Given the possibility that COVID-19 increasing cases act as a confounding factor to the increasing mental health burden, we adjusted our main DID regression to COVID-19 cases using the TVA model in ( 2 ). First, we validate that a correlation exists between mental health visits number and COVID-19 increasing cases. Figure 3 shows that a significant correlation between COVID-19 and mental health patients populations (R \(^2\) = 0.77, p-value < 2 \(\times 10^{-16}\) ) with an increase of 0.043 mental health visits for each new COVID-19 confirmed case. Adjusting for the COVID-19 cases acts as a proxy for adjusting for the pandemic effect itself.
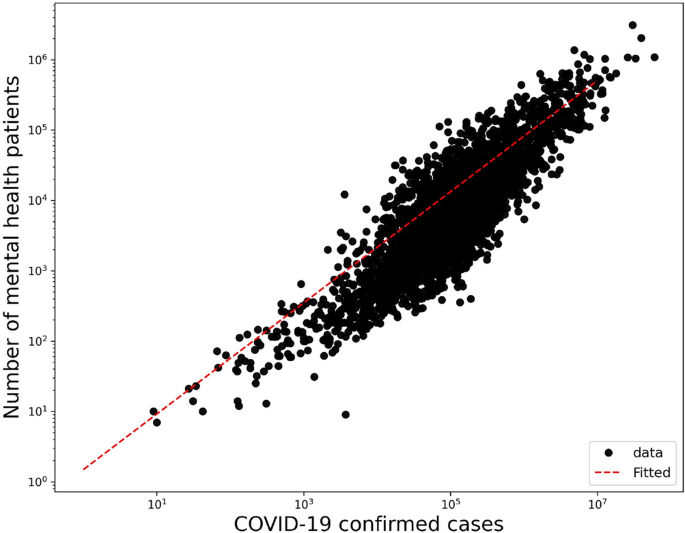
Correlation of mental health daily visits and COVID-19 confirmed cases in a log-log plot with an increase of 0.043 mental health visits for each confirmed COVID-19 case in counties (R \(^2\) = 0.77, p-value < \(2 \times 10^{-16}\) ).
Effects on the usage of mental health resources
We consider daily visits of mental health patients for the causal DID inference model from September 1, 2019, to December 31, 2020. Figure 4 shows the monthly average mental health visits in counties with stay-at-home orders and without. In general, there is an increase in monthly visits in months after COVID-19 lockdowns in regions with enacted lockdowns. There is also a clear similar trend of visits between regions with and without lockdowns. This pre-COVID-19 trend has been validated in the previously mentioned event study. Figure 2 (in Supplementary Appendix) shows the monthly average visits in counties with and without school closure orders. Similarly, Figs. 3 and 4 (in Supplementary Appendix) show the average monthly visits at the state level.
We further investigate the causality relationship between daily visits and lockdown measures. In Tables 2 and 3 we summarize the estimated effects of COVID-19 lockdown measures on the weighted outcomes for counties and states respectively for different population groups with the adjusted results after controlling for COVID-19 cases. Tables 5 and 6 (in Supplementary Appendix) summarize the raw outcomes. Along with regression estimates, we include significance measures of p-value, 95% confidence intervals of standard errors, and R-squared ( \(R^2\) ). We will further discuss results for each population group in both counties and states in the following sections.
Tables 11 and 12 (in Supplementary Appendix) summarize the estimated effects of Eq. ( 1 ) at different periods of time k where k = {1, 5, 9}-months after lockdowns, to show the dynamic effect of stay-at-home and school closures in counties and states respectively.
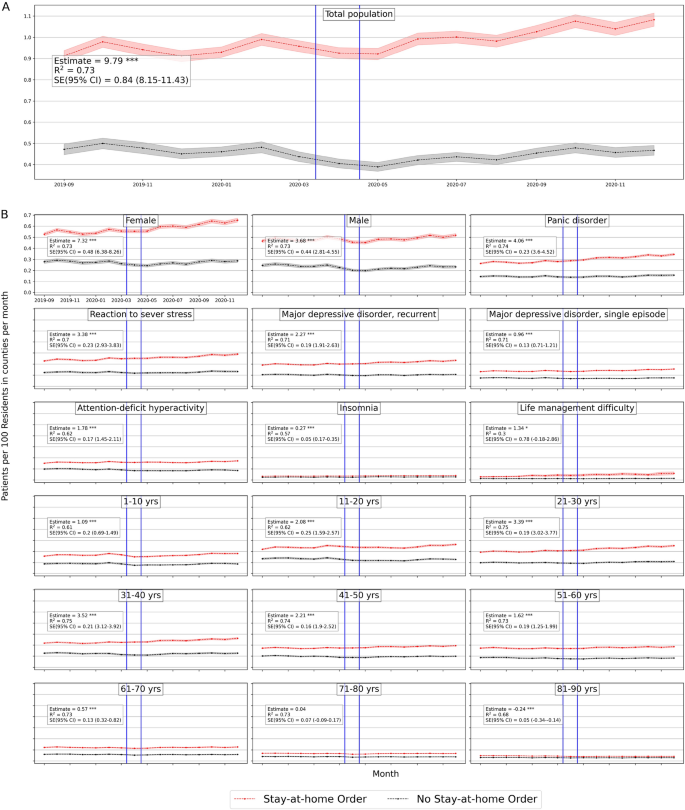
Average number of mental health patients over time (September 2019–December 2020) in counties with stay-at-home orders and without. Vertical lines show the first stay-at-home order on 3/14/2020 and last on 4/07/2020 across United States. Difference-in-differences estimates are included for each population. (Detailed average percentage changes are listed in Table 3 ). \(***p < 0.01\) , \(**p < 0.05\) , \(*p < 0.1\) .
Effects on total population
We consider the overall mental health population including all mental health disorders with clinical codes defined in Supplementary Table 1 . Based on Table 2 there is a significant positive effect of stay-at-home order across counties on the weighted population of mental health patients’ daily visits, with a mean difference of 1 in 10,000 daily patient visits between counties with stay-at-home orders and counties without. On average, mental health patients increased by 18.7% but declined by 1% in counties without lockdown (Fig. 4 ). Adjusting for COVID-19 confounding effect preserves the positive effect significant on the mental health population with a similar effect size. School closure has also a significant, but a lower effect on the mental health patient population (estimated mean difference = 8.8 in 100,000 population), with a percentage increase of 17% and 16% in counties with closed schools and without respectively (Table 3 in Supplementary Appendix), with significant similar size effect while adjusted for COVID-19 cases.
Similar results are found at the state level, Table 3 shows that the effect of stay-at-home order is positively significant for total mental health patients (difference estimate is 8.8 and 8.6 when adjusted in 10 \(^5\) population) with 22% increase by December 2020 as compared to less than 2% increase in states without lockdown (Table 4 in Supplementary Appendix). However, school closures have no significant effect at the state level.
We further investigate whether the effect on mental health differs if we shorten the period of observation after lockdown interventions. We applied our main regression model ( 1 ) on outcomes after a 1-month of lockdown (maximum mid-May) and 5-month of lockdown (maximum mid-August) for each region. The sizes of the lockdown effects are positive and significant at different times. Also, they keep increasing from the first month after the lockdown date until the end of the year 2020, for both stay-at-home orders and school closures in counties (Table 11 in Supplementary Appendix) and states (Table 12 in Supplementary Appendix).
We further examined the sensitivity of our DID results by sequentially adding controls to the baseline DID model. Table 7 in the Supplementary Appendix shows results are robust and neither COVID-19 growth nor the social capital index contributed to the effect of lockdowns on mental health populations.
Gender effects
In counties, the estimated effects of stay-at-home orders on both women and men are 6.8 (6.6 when adjusted) and 5.7 (5.7 when adjusted) respectively (Table 2 ). Female patients’ daily visits increased by 24% in counties with stay-at-home orders in comparison with 3% in counties without (Table 3 in Supplementary Appendix). Male patients declined by 5% in counties without stay-at-home orders. Whereas the estimated effects of school closures are negative for females (mean difference = − 1.67, and − 3.89 when adjusted) and significant when adjusted. While for men, school closure effects were significantly positive (mean difference = 4.5 and 3.4 when adjusted) (Table 2 ). This implies that women have been affected more by stay-at-home orders than by school closures across counties.
Similarly in states, the estimated mean difference for women is 5.1 (5.6 when adjusted) and for men is 3.8 (4.1 when adjusted) in 10 \(^5\) population (Table 3 ). Female patients’ daily visits increased by 29% and 6% in states with stay-at-home orders and without respectively, while male patients’ daily visits decreased in states without stay-at-home lockdown (Table 4 in Supplementary Appendix). School closure did not show significant effects on women or men at the state level.
Even at an early stage of the COVID-19 lockdown, mental health visits for female and male patients were larger than in non-locked regions, which they were increasing significantly throughout the year 2020 in counties and states (Tables 11 , 12 in Supplementary Appendix)
Diagnosis effects
We selected the top five mental disorders (e.g. panic disorder ) that peaked in 2020, and other disorders of interest ( insomnia and life management difficulty ) to investigate the effect of lockdowns on patient populations for specific diagnosis. We provide the definition of each considered mental condition in Table 1 in Supplementary Appendix.
In counties, all disorders were positively and significantly affected by stay-at-home orders and by school closures with lower effect sizes. Patients diagnosed with panic disorder (ICD-10: F41) had the largest difference among other mental illnesses and increased in both county groups (31.8% vs 8.88%) with an estimated effect of 3.3 (3.2 when adjusted in 10 \(^5\) population). Patients with attention-deficit hyperactivity disorder (ICD-10: F90) decreased in counties without stay-at-home orders by − 13.6% with an estimated effect of 3.2 (3.1 when adjusted) in 10 \(^5\) population.
Unlikely, patients with insomnia , with a significant estimated effect of \(-\,0.053\) in 10 \(^5\) population when adjusted, increased more in counties without school closures by 24% compared to 17% in counties with closures, which implies that insomnia was more in counties without school closures. Patients diagnosed with life management difficulty disorder increased more in counties without school closures as well by 127.85% compared with 94.64% with closures, and the estimated effect is − 0.6 (in 10 \(^5\) population) when adjusted (Tables 2 , 3 in Supplementary Appendix).
Similarly, at the state level, panic disorder (ICD-10: F41) increased by 38.4% in states with stay-at-home orders (Table 4 in Supplementary Appendix) and had the largest difference effect size with a mean difference of 2 in 10 \(^{5}\) population, similarly when adjusted (Table 3 ). Daily visits of patients with life management difficulty increased more in states without a school closure by 161.49% compared to 123.36% in states with closures with a significant estimated effect of \(-\,0.2\) (in 10 \(^{5}\) population) similarly when adjusted.
Over time, the effect of stay-at-home order kept increasing significantly for all selected mental disorders across counties (Table 11 in Supplementary Appendix) and states (Table 12 in Supplementary Appendix). While school closure effect is significantly increasing for most diagnoses except for life management difficulty diagnosis where the effect kept declining.
Age effects
At the county level, all age groups, both lockdowns have positive significant effects on the mental health patients’ daily visits. Based on Table 2 , the two largest significant differences were for adults between 31 and 40 years old and adults between 21 and 30 years old. Adults in their thirties increased by 20.47% in counties with stay-at-home orders but declined by − 0.1% in counties without, with a mean difference of 3.2 (in 10 \(^5\) population, similarly when adjusted). Adults in their twenties increased more in counties with stay-at-home orders by 30.01% compared to 11% in counties without, with an estimated effect of 1.5 (in 10 \(^5\) population, similarly when adjusted). Daily visits of young patients under 11 and adolescent patients under 21 are lower in counties without stay-at-home orders with significant positive effects of stay-at-home lockdown (Table 2 ).
Similarly, school closures affected patients in their thirties but with lower mean differences of 1.9 in 10 \(^5\) population (not significant when adjusted) (Table 3 ). They increased by 18.75 vs. 18.62 in regions with and without closures respectively. While daily visits of teenagers and adolescent (11 to 20) patients increased more in counties with school closures by 27.16%, compared to 19.17% in counties without closures, with estimated effect 2.2 in 10 \(^5\) population (not significant when adjusted) (Fig. 2 in Supplementary Appendix).
Similar observations are found at the state-level based on Table 3 . For most age groups both stay-at-home and school closure orders show significant positive effects, with the largest effect size for people in their thirties. Mental health patients who are in their thirties increased by 28% and 1% in states with stay-at-home orders and without respectively. Similarly, patients in their twenties increased by 40% and 15% in states with stay-at-home order and without respectively (Table 4 in Supplementary Appendix).
The effect sizes of both lockdowns on most age groups kept increasing significantly throughout the year of 2020. Children less than 11 years old had the largest change of estimation size, which indicates a greater effect on children appeared later on in counties with stay-at-home orders (Table 11 in Supplementary Appendix).
Effects on urgent treatment-seeking
We consider daily emergency department (ED) visits to reflect the emergent need to seek a mental health facility during the COVID-19 pandemic such that the condition is so severe to avoid treatment. The ED visits are defined according to the codes in Table 1 in Supplementary Appendix.
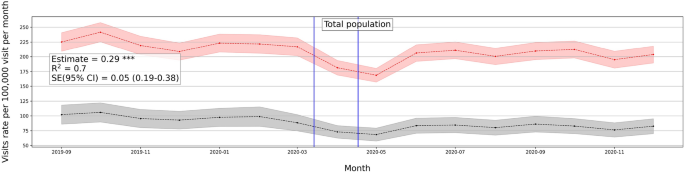
Average number of mental health ED visits over time (September 2019–December 2020) in counties with stay-at-home orders and without. Vertical lines show the first stay-at-home order on 3/14/2020 and last on 4/07/2020 across United States. Difference-in-differences estimates are included for each population. \(***p < 0.01\) , \(**p < 0.05\) , \(*p < 0.1\) .
ED visits decreased at the beginning of the pandemic, with a further finding that only patients with serious medical conditions were seeking care in ED 38 . One reason is that some patients were more willing to self-treat a variety of medical conditions than risk being exposed to COVID-19 in emergency rooms 39 . Given the role played by the ED during the first few months of the pandemic, it is linked with acute conditions for which patients could not avoid treatment
ED visits show a similar increasing positive trend in response to the lockdown measures (see Fig. 5 ). We also investigated ED visits outcomes on different population groups and the trend is consistent (Fig. 5 in Supplementary Appendix).
The effect of stay-at-home order on the overall ED visits is positive and significant with a magnitude of 0.29 weighted by population on state-level, and 0.32 when adjusted to the pandemic factor. Similarly, the effect of school closure is positive and significant with a value of 0.12 weighted by state population, same when adjusted (see Table 9 in Supplementary Appendix). Women and men groups show similar effect sizes with regard to ED visits, with an effect size of 0.2 for both groups even with adjusting for the pandemic factor. Similarly for psychiatric diagnosis, the effects are positive and significant with the largest effect size on panic disorder patients with a magnitude of 0.1 and 0.09 when adjusted. Age groups also show a similar trend of increasing daily ED visits with the largest effect size on the 21–30 age group of 0.07 and 0.05 when adjusted. Younger group ages did not show a significant effect on daily ED visits (Table 9 in Supplementary Appendix). Similar results appear for the school closures and county-level outcomes (Table 8 in Supplementary Appendix).
Robustness check
Given the differences in regions with respect to the number of hospitals, facilities, and patients, we conducted robustness checks of our main analysis to show that dropping multiple states does not change the estimates and that our results are not driven by specific regions. We dropped New York and Ohio states which were two states with the largest patient volume relative to population, and we apply our DID regression model to the weighted outcomes in states. The estimates remained robust, significant, and positive (Table 4 ). We also added all 2019 samples to expand the control group and the pre-intervention period. The relationship inferred from our analysis stayed significant and positive with this expansion.
We also conducted a similar check for ED analysis and found a similar observation of consistent robustness (Table 10 in Supplementary Appendix).
Early in March 2020, non-pharmaceutical interventions, such as social distancing policies, were imposed around the world to contain the spread of COVID-19 and proved to reduce the number of COVID-19 cases and fatalities 3 , 40 , 41 . Mitigation policies come with both costs and benefits, which may be further analyzed to help determine the optimal time to release or stop a policy intervention 42 . Prior research showed significant mental health degradation associated with the COVID-19 pandemic 6 , 7 , 18 , 19 , however, no research investigated the causal relation between COVID-19 mitigation policies and the usage of mental health resources. Yet the effects on the usage of mental health resources can further reflect the economic and health costs brought by the pandemic interventions. In our study, using large-scale medical claims data, we estimated the effects of lockdowns on the usage of mental health facilities and the prevalence of mental health issues at the state- and county levels in the United States.
Our findings demonstrate a statistically significant causal effect of lockdown measures (stay-at-home and school closure orders) on the usage of mental health facilities represented by an increasing number of issued medical claims for mental health appointments during COVID-19 pandemic. Also, ED visits were statistically significant and positive in locked-down regions which reflects the increase in emergent mental help-seeking due to the COVID-19 lockdowns. Results further emphasize the cost brought by extra months of lockdowns, in which effect sizes keep increasing through the end of 2020 in both mental health visits and ED visits. Some sub-population groups were exposed to a larger deterioration effect than other groups, such as women and adolescent groups.
Some mental health conditions were of particular interest to investigate during the COVID-19 lockdown. For example, sleep disturbance have been widely observed 43 specifically being a large concern in Italy 44 and China 45 during COVID-19 lockdown. Our results showed a similar observation, in which insomnia visits increased in counties with lockdowns. Similarly, burnout has been observed among health providers 46 and some working parents 47 during lockdown measures. Life-management difficulty disorder reflects burn-out and mental health issues in the workplace. Although this is not classified as a medical condition, but rather as an occupational phenomenon 48 , it is certainly a public health challenge 49 . Our results show that life management difficulty disorder, including burnout, increased with lockdowns at the state-level.
There have been several observations on the relation of school closures with increased mental health risks. Specifically, it was observed that some children were more likely to suffer from attention-deficit hyperactivity disorder (ADHD) symptoms during the COVID-19 pandemic 50 . This further confirms our findings of increased ADHD visits with school closures.
Our findings were observed at two granularity levels, county and state levels, with very similar trends of observations of increasing daily patient visits to mental health facilities. This further strengthens the established relationship of the effect of lockdowns on the mental health population with controlled possible sources of confoundedness. We also note our results stay the same when controlling for the evolution of the pandemic. This adds to the validity and robustness of the effects of lockdown measures on mental health despite the presence of the pandemic. It also implies that mental health is more sensitive to policy measures rather than to the evolution of the pandemic.
Given the various intertwined events and causes during the COVID-19 pandemic, our analysis is limited by several factors. First, it is important to point out that the adoption of lockdowns across states did not happen at random. Differences in shutdown orders’ timings and adoption across regions were associated with the differences in COVID-19 confirmed cases and fatality rates across those regions 51 , 52 and the differences in their health systems capacity 53 . Also, there exist other political, economical, and institutional factors that affect the adoption of COVID-19 measures and their strictness level across countries 54 . Even though the lockdown timing may be affected by regional factors related to the virus, such as the number of cases or institutional factors, however, there is no reason to believe that lockdown timing was affected by the prevalence of mental health in regions. Given that, we have also encountered regional fixed effects in our model to adjust for regional differences. Second, though mental illnesses have a negative economic impact 55 , the opposite is true as well, in which economic disadvantage may lead to a greater mental illness 56 . During COVID-19, there have been negative consequences on individuals in different industry sectors who were more likely to lose their jobs due to the lockdown measures 57 with significant employment loss in occupations that require interpersonal contact 58 . Therefore, the loss of employment due to shutdowns may have a confounding effect on increased mental health issues.
In addition, the medical claims used in this study do not cover Medicare and Medicaid health insurance programs which creates a limitation on our data. Medicare covers most aged and disabled populations across the US, while Medicare covers a wider range of populations including low-income beneficiaries covering 30% of US population 59 . This limitation would impact the representativeness of results since our data misses some population groups in the US. We also note that our medical claims dataset does not provide demographics information such as race and ethnicity. This limitation restricts our analysis to only age and gender demographics information.
Despite the mentioned limitations, our results provide important policy implications from economic and social impacts. There is a notable mental health cost brought by non-pharmaceutical interventions, especially interventions that are extended to longer duration. Our results suggest that there should be considerations to the mental health cost through ensuring mental health treatment capacity.
Furthermore, we showed that number of patients’ daily visits had dropped right after lockdowns and then progressively increased in June and July 2020, supporting the findings of Refs. 60 , 61 . This suggests that people with mental health afflictions did not have the ability to seek immediate care during restrictive lockdowns. Findings suggest that policy interventions should be accompanied by strategies that facilitate mental health treatment reachability despite restrictive lockdowns, in order to avoid the exacerbated effect of delayed treatment.
Data availability
There is a Research Data Access and Services Agreement between Change Healthcare Operations, LLC and the Board of Trustees of the University of Illinois, through which data access was granted. This work is exempt from review, as per the University of Illinois Urbana-Champaign institutional review board process. Medical claims data analyzed during the current study are not publicly available because it is under the agreement between Change Healthcare, LLC and the University of Illinois Urbana-Champaign. The NYTimes data analyzed during the current study is available in the NYTiems repository, https://github.com/nytimes/covid-19-data . The COVID-19 data analyzed during the current study is available in the COVIDVis repository, https://github.com/covidvis/covid19-vis/tree/master/data .
Thunström, L., Newbold, S. C., Finnoff, D., Ashworth, M. & Shogren, J. F. The benefits and costs of using social distancing to flatten the curve for COVID-19. J. Benefit-Cost Anal. 11 , 179–195. https://doi.org/10.1017/bca.2020.12 (2020).
Article Google Scholar
Anderson, R. M., Heesterbeek, H., Klinkenberg, D. & Hollingsworth, T. D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? The Lancet 395 , 931–934. https://doi.org/10.1016/S0140-6736(20)30567-5 (2020).
Article CAS Google Scholar
Fowler, J. H., Hill, S. J., Levin, R. & Obradovich, N. The effect of stay-at-home orders on COVID-19 cases and fatalities in the United States. MedRxiv 1 , 628. https://doi.org/10.1101/2020.04.13.20063628 (2020).
Pfefferbaum, B. & North, C. S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 383 , 510–512. https://doi.org/10.1056/NEJMp2008017 (2020).
Article CAS PubMed Google Scholar
File, T. & Marlay, M. Living Alone has More Impact on Mental Health of Young Adults than Older Adults (United States Census Bureau, 2021).
Google Scholar
Elmer, T., Mepham, K. & Stadtfeld, C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE 15 , e0236337. https://doi.org/10.1371/journal.pone.0236337 (2020).
Article CAS PubMed PubMed Central Google Scholar
Adams-Prassl, A., Boneva, T., Golin, M. & Rauh, C. The Impact of the Coronavirus Lockdown on Mental Health: Evidence from the US. Cambridge Working Papers in Economics 2037 (University of Cambridge, 2020).
Wathelet, M. et al. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw. Open 3 , e2025591. https://doi.org/10.1001/jamanetworkopen.2020.25591 (2020).
Article PubMed PubMed Central Google Scholar
Zhu, Y. et al. The risk and prevention of novel coronavirus pneumonia infections among inpatients in psychiatric hospitals. Neurosci. Bull. 36 , 299–302. https://doi.org/10.1007/s12264-020-00476-9 (2020).
Melamed, O. C. et al. Physical health among people with serious mental illness in the face of COVID-19: Concerns and mitigation strategies. Gen. Hosp. Psychiatry 66 , 30–33. https://doi.org/10.1016/j.genhosppsych.2020.06.013 (2020).
Lee, M. et al. Human mobility trends during the early stage of the COVID-19 pandemic in the United States. PLoS ONE 15 , 1–15. https://doi.org/10.1371/journal.pone.0241468 (2020).
Musinguzi, G. & Asamoah, B. O. The science of social distancing and total lock down: Does it work? Whom does it benefit? Electron. J. Gen. Med. 17 , 230. https://doi.org/10.29333/ejgm/7895 (2020).
Le, K. & Nguyen, M. The psychological burden of the covid-19 pandemic severity. Econom. Hum. Biol. 41 , 100979 (2021).
Czeisler, M. É. et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report 32 (Centers for Disease Control and Prevention, 2020).
Abbott, A. COVID’s mental-health toll: How scientists are tracking a surge in depression. Nature 590 , 194–195. https://doi.org/10.1038/d41586-021-00175-z (2021).
Article CAS PubMed ADS Google Scholar
Giuntella, O., Hyde, K., Saccardo, S. & Sadoff, S. Lifestyle and mental health disruptions during COVID-19. Proc. Natl. Acad. Sci. U.S.A. 118 , e2016632118. https://doi.org/10.1073/pnas.2016632118 (2021).
Devaraj, S. & Patel, P. C. Change in psychological distress in response to changes in reduced mobility during the early 2020 COVID-19 pandemic: Evidence of modest effects from the US. Soc. Sci. Med. 270 , 113615. https://doi.org/10.1016/j.socscimed.2020.113615 (2021).
Article PubMed Google Scholar
Farkhad, B. F. & Albarracín, D. Insights on the implications of COVID-19 mitigation measures for mental health. Econom. Hum. Biol. 40 , 100963. https://doi.org/10.1016/j.ehb.2020.100963 (2021).
Brodeur, A., Clark, A. E., Fleched, S. & Powdthavee, N. COVID-19, lockdowns and well-being: Evidence from Google Trends. J. Public Econ. 193 , 104346. https://doi.org/10.1016/j.jpubeco.2020.104346 (2021).
Serrano-Alarcón, M., Kentikelenis, A., Mckee, M. & Stuckler, D. Impact of covid-19 lockdowns on mental health: Evidence from a quasi-natural experiment in England and Scotland. Health Econ. 31 , 284–296 (2022).
Roehrig, C. Mental disorders top the list of the most costly conditions in the United States: \$201 billion. Health Aff. 35 , 1130–1135. https://doi.org/10.1377/hlthaff.2015.1659 (2016).
Bloom, D. et al. The Global Economic Burden of Noncommunicable Diseases. Geneva. Tech. Rep (World Economic Forum, 2011).
McKenzie, K. W. S. & Whitley, R. Social capital and mental health. Br. J. Psychiatry 181 , 280–283 (2002).
Berkman, L. F. & Syme, S. L. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. Am. J. Epidemiol. 109 , 186–204 (1979).
Ferwana, I. & Varshney, L. R. Social capital dimensions are differentially associated with COVID-19 vaccinations, masks, and physical distancing. PLoS ONE 16 , e0260818 (2021).
Simon, N. M., Saxe, G. N. & Marmar, C. R. Mental health disorders related to COVID-19-related deaths. JAMA 324 , 1493–1494 (2020).
Ross, L. & Bassett, D. Causation in neuroscience: Keeping mechanism meaningful. Nat. Rev. Neurosci. 1 , 81–90 (2024).
Bommersbach, T. J., McKean, A. J., Olfson, M. & Rhee, T. G. National trends in mental health-related emergency department visits among youth, 2011–2020. JAMA 329 , 1469–1477 (2023).
Kuehn, B. M. Clinician shortage exacerbates pandemic-fueled “mental health crisis’’. JAMA 327 , 2179–2181 (2022).
Cantor, J. H., McBain, R. K., Ho, P. C., Bravata, D. M. & Whaley, C. Telehealth and in-person mental health service utilization and spending, 2019 to 2022. JAMA Health Forum 4 , e232645. https://doi.org/10.1001/jamahealthforum.2023.2645 (2023).
Times, T. N. Y. Coronavirus (Covid-19) Data in the United States. Dataset (2021).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet 395 , 912–920. https://doi.org/10.1016/S0140-6736(20)30460-8 (2020).
Keele, L. J., Small, D. S., Hsu, J. Y. & Fogarty, C. B. Patterns of effects and sensitivity analysis for differences-in-differences. http://arxiv.org/abs/1901.01869 (2019).
Zeldow, B. & Hatfield, L. A. Confounding and regression adjustment in difference-in-differences studies. Health Serv. Res. 56 , 932–941 (2021).
Angrist, J. D. & Pischke, J.-S. Mostly Harmless Econometrics: An Empiricist’s Companion (Princeton University Press, 2008).
Book Google Scholar
Goodman-Bacon, A. & Marcus, J. Using difference-in-differences to identify causal effects of COVID-19 policies. Survey Res. Methods 14 , 153–158. https://doi.org/10.18148/srm/2020.v14i2.7723 (2020).
Rambachan, A. & Roth, J. An Honest Approach to Parallel Trends. Unpublished (2020).
Hartnett, K. P. et al. Impact of the covid-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. Morb. Mortal. Wkly. Rep. 23 , 699–704 (2020).
Kocher, K. E. & Macy, M. L. Emergency department patients in the early months of the coronavirus disease 2019 (covid-19) pandemic-what have we learned? JAMA Health Forum 6 , e200705 (2020).
Friedson, A. I., McNichols, D., Sabia, J. J. & Dave, D. Did California’s Shelter-in-Place Order Work? Early Coronavirus-Related Public Health Effects. Working Paper 26992 (National Bureau of Economic Research, 2020).
Cucinotta, D. WHO declares COVID-19 a pandemic. Acta Bio-med. 91 , 157–160. https://doi.org/10.23750/abm.v91i1.9397 (2020).
Layard, R. et al. When to Release the Lockdown? A Wellbeing Framework for Analysing Costs and Benefits IZA. Discussion Papers 13186 (Institute of Labor Economics, 2020).
Gupta, R. et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J. Psychiatry 62 , 370–378. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_523_20 (2020).
Gualano, M. R., Lo Moro, G., Voglino, G., Bert, F. & Siliquini, R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int. J. Environ. Res. Public Health 17 , 4779. https://doi.org/10.3390/ijerph17134779 (2020).
Xiao, H., Zhang, Y., Kong, D., Li, S. & Yang, N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 26 , 1–8. https://doi.org/10.12659/MSM.923549 (2020).
Joshi, G. & Sharma, G. Burnout: A risk factor amongst mental health professionals during COVID-19. Asian J. Psychiatry 54 , 102300 (2020).
Aguiar, J. et al. Parental burnout and the COVID-19 pandemic: How Portuguese parents experienced lockdown measures. Fam. Relat. 70 , 927–938 (2021).
Murthy, V. H. Confronting health worker burnout and well-being. N. Engl. J. Med. 387 , 577–579 (2022).
Bailhache, M., Monnier, M. & Moulin, F. E. A. Emotional and attention-deficit/hyperactivity disorder symptoms of preterm vs full-term children during covid-19 pandemic restrictions. Pediatr. Res. 92 , 1749–1756 (2022).
Huang, X. et al. The impact of lockdown timing on COVID-19 transmission across US counties. EClinicalMedicine 38 , 101035 (2021).
Loewenthal, G. et al. COVID-19 pandemic-related lockdown: Response time is more important than its strictness. EMBO Mol. Med. 12 , e13171. https://doi.org/10.15252/emmm.202013171 (2020).
Gutkowski, V. A. Lockdown Responses to COVID-19. Tech. Rep. (Federal Reserve Bank of St. Louis, 2021).
Ferraresi, M., Kotsogiannis, C., Rizzod, L. & Secomandi, R. The ‘Great Lockdown’ and its determinants. Econ. Lett. 197 , 109628. https://doi.org/10.1016/j.econlet.2020.109628 (2020).
JoAnn, P., Dooley, D. & Huh, J. Income volatility and psychological depression. Am. J. Community Psychol. 43 , 57–70. https://doi.org/10.1007/s10464-008-9219-3 (2009).
Knapp, M. & Wong, G. Economics and mental health: The current scenario. World Psychiatry 19 , 3–14 (2020).
Fana, M., Pérez, S. T. & Fernández-Macías, E. Employment impact of Covid-19 crisis: From short term effects to long terms prospects. J. Ind. Bus. Econom. 47 , 391–410. https://doi.org/10.1007/s40812-020-00168-5 (2020).
Montenovo, L. et al. Determinants of Disparities in COVID-19 Job Losses NBER. Working Paper 27132 (National Bureau of Economic Research, 2021).
Klees, B. S. & Curtis, C. A. Brief Summaries of Medicare & Medicaid. Summary Report (Centers for Medicare & Medicaid Services, Department of Health and Human Services, 2020).
Trinkl, J. & Muñoz del Río, A. Effect of COVID-19 Pandemic on Visit Patterns for Anxiety and Depression (2020).
Patel, S. Y. et al. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern. Med. 181 , 388–391. https://doi.org/10.1001/jamainternmed.2020.5928 (2020).
Article PubMed Central Google Scholar
Download references
Acknowledgements
The authors thank the Change Healthcare team, Craig Midgett, Mina Atia, Andrew Harris, Anil Konda, Tim Suther, and Jaideep Kulkarni for facilitating our access to medical claims data and for their help in large-scale analysis.
Author information
Authors and affiliations.
Coordinated Science Laboratory, University of Illinois Urbana-Champaign, Urbana, IL, 61801, USA
Ibtihal Ferwana & Lav R. Varshney
You can also search for this author in PubMed Google Scholar
Contributions
IF was responsible for data curation, formal analysis, writing an original draft, and reviewing. LV was responsible for conceptualization, funding acquisition, methodology, reviewing, and editing.
Corresponding author
Correspondence to Ibtihal Ferwana .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Ferwana, I., Varshney, L.R. The impact of COVID-19 lockdowns on mental health patient populations in the United States. Sci Rep 14 , 5689 (2024). https://doi.org/10.1038/s41598-024-55879-9
Download citation
Received : 14 April 2023
Accepted : 27 February 2024
Published : 07 March 2024
DOI : https://doi.org/10.1038/s41598-024-55879-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Do economic effects of the anti-COVID-19 lockdowns in different regions interact through supply chains?
Roles Conceptualization, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Graduate School of Information Science, University of Hyogo, Kobe, Hyogo, Japan
Roles Methodology, Validation, Writing – original draft
Affiliation RIKEN Center for Computational Science, Kobe, Hyogo, Japan
Roles Conceptualization, Methodology, Writing – original draft, Writing – review & editing
Affiliation Graduate School of Economics, Waseda University, Tokyo, Japan
- Hiroyasu Inoue,
- Yohsuke Murase,
- Yasuyuki Todo

- Published: July 30, 2021
- https://doi.org/10.1371/journal.pone.0255031
- Reader Comments
To prevent the spread of COVID-19, many cities, states, and countries have ‘locked down’, restricting economic activities in non-essential sectors. Such lockdowns have substantially shrunk production in most countries. This study examines how the economic effects of lockdowns in different regions interact through supply chains, which are a network of firms for production, by simulating an agent-based model of production using supply-chain data for 1.6 million firms in Japan. We further investigate how the complex network structure affects the interactions between lockdown regions, emphasising the role of upstreamness and loops by decomposing supply-chain flows into potential and circular flow components. We find that a region’s upstreamness, intensity of loops, and supplier substitutability in supply chains with other regions largely determine the economic effect of the lockdown in the region. In particular, when a region lifts its lockdown, its economic recovery substantially varies depending on whether it lifts the lockdown alone or together with another region closely linked through supply chains. These results indicate that the economic effect produced by exogenous shocks in a region can affect other regions and therefore this study proposes the need for inter-region policy coordination to reduce economic loss due to lockdowns.
Citation: Inoue H, Murase Y, Todo Y (2021) Do economic effects of the anti-COVID-19 lockdowns in different regions interact through supply chains? PLoS ONE 16(7): e0255031. https://doi.org/10.1371/journal.pone.0255031
Editor: Ashkan Memari, Sunway University, MALAYSIA
Received: November 1, 2020; Accepted: July 8, 2021; Published: July 30, 2021
Copyright: © 2021 Inoue et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data for supply chain network are based on a survey done by Tokyo Shoko Research (TSR), one of the leading credit research agencies in Tokyo, supplied to us through the Research Institute of Economy, Trade and Industry (RIETI). The data are not in the public domain but are commercially available from Tokyo Shoko Research, Ltd., http://www.tsr-net.co.jp/ , [email protected] . The authors had no special access privileges to the data.
Funding: H.I., 18K04615, Japan Society for the Promotion of Science, https://www.jsps.go.jp/english/index.html , The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Y.T, 18H03642, Japan Society for the Promotion of Science, https://www.jsps.go.jp/english/index.html , The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
1 Introduction
COVID-19, a novel coronavirus (SARS-CoV-2) disease, has been spreading worldwide. To prevent its spread, many cities, regions, and countries were or have been under lockdown, suppressing economic activities. On 18 April 2020, 158 countries out of 181 implemented measures that required temporary closure or work-from-home for some sectors in some or all cities. Although some countries later lifted their lockdowns, 95 countries remained under lockdown on 30 July 2020 [ 1 ].
Closing workplaces shrinks the economic output of regions under lockdown. The negative economic effect of a lockdown in one region may diffuse through supply chains, i.e., supplier-client relationships of firms, and to other regions that are not necessarily in a lockdown. When a firm is closed due to a lockdown strategy, its client firms located elsewhere would suffer decreased production due to the lack of supply of intermediate goods and services. Suppliers of the closed firms would also see reduced production because of a shortage of demand.
Many studies have empirically confirmed the propagation of economic shocks through supply chains, particularly shocks originating from natural disasters [ 2 – 7 ]. Some examine the diffusion of the effect of lockdowns because of COVID-19 on production across regions and countries and estimate the total effect using input–output (IO) linkages at the country-sector level [ 8 – 11 ] and supply chains at the firm level [ 12 ].
Several studies focusing on natural disasters [ 5 , 6 ] examine how the network structure of supply chains affects the propagation of shocks. They find that scale-free property, non-substitutability of suppliers, and loops are major drivers of such propagation. However, the role of the network structure has not been fully examined in the context of the propagation of the lockdown effect. This issue should be of great interest from the perspective of network science for the following two reasons.
First, the literature on network interventions has investigated the types of individuals or groups in a network, such as those with high centrality, who should be targeted to promote (prevent) the diffusion of positive (negative) behaviours and outcomes [ 13 , 14 ]. Similarly, we are interested in how the economic effect of imposing and lifting a lockdown in one region, an example of a network intervention, diffuses to other regions. Compared to existing research, this study is novel in many respects. For example, we consider interventions in a network of firms and their economic outcomes, while previous studies focus on the health behaviours and outcomes in human networks [ 15 ], with a few exceptions that examine economic outcomes in human networks [ 16 ]. In addition, because a lockdown is usually imposed in a city, state, or country, the scale of interventions is large. Firms targeted by such interventions are exogenously determined by geography, and thus we should assess the network characteristics of exogenously grouped nodes, rather than the endogenously connected ones identified by network centrality [ 13 , 17 ] or community detection algorithms [ 18 ].
Second, at any point during the spread of COVID-19, some regions imposed a lockdown, while others remained open. Therefore, when we evaluate the lockdown strategy of a region, the interactions between the strategies of different regions need to be considered. In other words, the economic effect of a lockdown in a region depends on whether other regions connected to it through supply chains are similarly locked down. For example, Sweden did not impose a strict lockdown, unlike other European countries. However, it still expects a 4.5% reduction in gross domestic product (GDP) in 2020, a decline comparable to that in neighbouring countries that did impose a lockdown, possibly because of its close economic ties with its neighbours [ 19 ]. Motivated by the Swedish experience, this study examines the network structure between regions—an aspect that is usually ignored in the literature on network interventions—and discusses the need for policy coordination among regions depending on their network characteristics. Some studies call for inter-regional and international policy coordination in the presence of spillover effects in the context of health, environment, and macroeconomics [ 20 , 21 ], but they do not explicitly incorporate the network structure.
The present study fills the above gaps in research on network interventions and regional interactions. We conduct a simulation analysis by applying actual supply-chain data of 1.6 million firms and their experiences of the lockdowns in Japan to an agent-based model of production. Specifically, we analyse the network characteristics of a prefecture in Japan that led to greater economic recovery by lifting its lockdown when all other prefectures remained locked down. In addition, to further highlight the interactions between regions, our simulation investigates how the characteristics of the supply-chain links between two prefectures affect their economic recovery when they simultaneously lift their lockdowns. One novelty of our study is to decompose supply-chain flows into potential and loop flow components and test the role of upstreamness (potential) in supply chains and intra- and inter-prefectural loops in diffusion.
The data used in this study are taken from the Company Information Database and Company Linkage Database compiled by Tokyo Shoko Research (TSR), one of the largest credit research companies in Japan. The former database includes information about the attributes of each firm, including the location, industry, sales, and number of employees, and the latter includes the major customers and suppliers of each firm. Due to availability, we use the data on firm attributes and supply chains from 2016. The number of firms in the data is 1,668,567 and the number of supply-chain links is 5,943,073. Hence, our data identify the major supply chains of most firms in Japan, although they lack information about supply-chain links with foreign entities. Because the transaction value of each supply-chain tie is not available in the data, we estimate sales from a supplier to each of its customers and consumers using the total sales of the supplier and the 2015 Input-Output (IO) Tables for Japan [ 22 ]. In this estimation process, we drop firms without any sales information. Accordingly, the number of firms in our final analysis is 966,627 and the number of links is 3,544,343. Although the firms in the TSR data are classified into 1,460 industries according to the Japan Standard Industrial Classification [ 23 ], we simplify this into the 187 industries classified in the IO tables. S1 Appendix provides details on the data construction process.
In the supply-chain data described above, the degree, or the number of links, of firms follows a power-law distribution [ 5 ], as often found in the literature [ 24 ]. The average path length between firms, or the number of steps between them through supply chains, is 4.8, indicating a small-world network. Using the same dataset, previous studies [ 5 , 25 ] find that 46–48% of firms are included in the giant strongly connected component (GSCC), in which all firms are indirectly connected to each other through supply chains. The large size of the GSCC clearly shows that the network has a significant number of cycles unlike the common image of a layered or tree-like supply-chain structure.
Agent-based models that incorporate the interactions of agents through networks have been widely used in the social sciences [ 26 – 28 ]. Following the literature, we employ the dynamic agent-based model of Inoue and Todo [ 5 , 6 ], an extension of Hallegatte’s [ 29 ] model, which assumes that supply chains are at the firm level. In the model, each firm utilises the inputs purchased from other firms to produce an output and sells it to other firms and consumers. Firms in the same industry are assumed to produce the same output. Supply chains are predetermined, and do not change over time in the following two respects. First, each firm utilises a firm-specific set of input varieties and does not change the input set over time. Second, each firm is linked with fixed suppliers and customers and cannot be linked with any new firm over time, even after a supply-chain disruption. Accordingly, our analysis focuses on short-term changes in production. Furthermore, we assume that each firm keeps inventories of each input at a level randomly determined from the Poisson distribution. Following Inoue and Todo [ 5 ], in which parameter values are calibrated from the case of the Great East Japan earthquake, we assume that firms aim to keep inventories for 10 days of production on average (see S2 Appendix for the details).
When a restriction is imposed on a firm’s production, both its upstream and downstream of the firm are affected. On the one hand, the firm’s demand for parts and components from its suppliers immediately declines, and thus suppliers have to shrink their production. Because demand for the products of suppliers’ suppliers also declines, the negative effect of the restriction propagates upstream. On the other hand, the supply of products from the directly restricted firm to its customer firms declines. Therefore, one way for customer firms to maintain the current level of production is to use their inventories of inputs. Alternatively, customers can procure inputs from other suppliers in the same industry that were already connected before the restriction, provided these suppliers have additional production capacity. If the inventories and inputs from substitute suppliers are insufficient, customers have to shrink their production because of a shortage of inputs. Accordingly, the effect of the restriction propagates downstream through supply chains. Such downstream propagation is likely to be slower than upstream propagation because of the inventory buffer and input substitution.
3.2 Lockdowns in Japan
In Japan, lockdown strategies were implemented at the prefecture level under the state of emergency [ 30 ] first declared on 7 April, 2020 in seven prefectures with a large number of confirmed COVID-19 cases. Because populated regions tended to be affected more and earlier, these seven prefectures are industrial clusters in Japan, including Tokyo, Osaka, Fukuoka, and their neighbouring prefectures. The state of emergency was expanded to all 47 prefectures on 16 April. The state of emergency was lifted for 39 prefectures on 14 May and for an additional three on 21 May; it was lifted for the remaining five prefectures on 25 May. (The summary of the timeline of the lockdowns in different prefectures can be found in Fig A.3 of [ 31 ]).
Although the national government declared a state of emergency, the extent to which the restrictions were imposed was determined by each prefecture’s government. Therefore, the level of lockdown in each prefecture may have varied. Although all prefectures were in the state of emergency from 16 April to 14 May, prefectures with larger numbers of confirmed COVID-19 cases, such as the seven prefectures in which a state of emergency was first declared, requested more stringent restrictions than others. The national or prefectural government can only request closing workplaces, staying at home, and social distancing rather than enforcing these actions through legal enforcement or punishment. However, strong social pressure in Japan led people and businesses to voluntarily restrict their activities to a large extent. As a result, production activities including those in sectors not officially restricted shrunk substantially (Mainichi Newspaper, 27 May 2020).
3.3 Simulation procedure
3.3.1 replication of the actual effect..
In our simulation analysis, we first confirm whether our model and data can replicate the actual reduction in production caused by the lockdown in Japan during this state of emergency. Because we cannot observe the extent to which each firm reduces its production capacity by obeying government requests, the rate of reduction in production capacity for each sector assumed in our simulation analysis depends on its characteristics. As the reduction rate, particularly during the lockdowns in Japan is not available, we follow the literature that defines the reduction rate in general settings. Specifically, the rate of reduction in a sector is the product of the level of reduction determined by the degree of exposure to the virus given by [ 9 ] and the share of workers who cannot work from home given by [ 8 ]. For example, in lifeline/essential sectors such as utilities, health, and transport, the rate of reduction is assumed to be zero; in other words, the production capacity in these sectors does not change during a lockdown. In sectors in which it is assumed that exposure to the virus is low (50%) and 13.4% of workers can work from home, such as the agriculture and fishery sectors, the rate of reduction is 43.3% (= 0.5 × (1 − 0.134)). Sectors with ordinary exposure (100%) and 47.5% of workers were working from home, such as the retail and wholesale sectors, show a reduction in production capacity by 52.5% (= 1 × (1 − 0.475)). See S1 Table for the rate of reduction of each sector.
After the lockdown in a prefecture is lifted, all the firms in that prefecture immediately return to their pre-lockdown production capacity. Moreover, we assume that inventories do not decay over time: inventories stocked before the lockdown can be fully utilised after the lockdown is lifted. The results given below are an averaged of over 30 Monte Carlo runs.
3.3.2 Interactions among regions.
After checking the accuracy of our simulation model, we examine how changing the restriction level of the lockdown in a region affects production in another region. For this purpose, we experiment with different sets of sector-specific rates of reduction in production capacity by multiplying the benchmark rates of reduction defined above by a multiplier such as 0.4 or 0.8. For example, when the benchmark rate of reduction in a sector is 52.5%, as in the case of the iron and other metal product sectors, and the multiplier is 0.4, we alternatively assume a rate of reduction of 21.0%.
Moreover, we assume that the rates of reduction can vary among prefectures, because each prefecture can determine its own level of restrictions under the state of emergency (Section 3.2). In practice, the restrictions requested by the prefectural governments were tougher and people were more obedient to the requests in the seven prefectures in which the state of emergency was first declared because of the larger COVID-19 caseloads than in other prefectures. Accordingly, we run the same simulation assuming different rates of reduction for the two types of prefectures, defined as more and less restricted groups, to investigate how different rates of reduction in one group affect production in the other.
3.3.3 Lifting lockdown in only one region.
In practice, some prefectures lifted their lockdowns earlier than others (Section 3.2). Although this may have led to the recovery of value added production, or gross regional product (GRP), the extent of such a recovery should have been affected by the links between firms in the prefecture and others still under lockdown. To highlight this network effect, we simulate what would happen to the GRP of a prefecture if it lifted its lockdown while all others were still imposing lockdowns. Next, we investigate what network characteristics of each prefecture determine the recovery from lockdown, measured by the ratio of the increase in the GRP of the prefecture by lifting its lockdown to the reduction in its GRP because of the lockdown of all prefectures.
In particular, we focus on four types of network characteristics. First, when a prefecture is more isolated from others in the supply-chain network, the effect of others’ lockdowns should be smaller. We measure the level of isolation using the number of links within the prefecture relative to the total degree of firms (total number of links from and to firms) in the prefecture.
Second, an alternative and more interesting measure of isolation is the intensity of loops in supply chains. Although supply chains usually flow from suppliers of materials to those of parts and components and then to assemblers, some suppliers use final products such as machinery and computers as inputs. This results in many complex loops in supply chains [ 32 ], in which negative shocks circulate and can become aggravated [ 5 ]. Such loops in a network are found to generate instability in the system dynamics literature [ 33 ] and more recently in the context of supply chains [ 34 ]. In the case of lifting the lockdown in only one prefecture, the loops within that prefecture may magnify its recovery because of the circulation of positive effects in the loops.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Each dot indicates a firm. Firms with a higher Helmholtz–Hodge (HH) potential are located more upward in both panels. In the left panel, the grey lines illustrate the potential flows computed from the HHD. The red and blue node colours represent higher and lower HH potentials, respectively. The right panel shows loop flows computed from HHD, while the different colours represent different cycles.
https://doi.org/10.1371/journal.pone.0255031.g001
Third, we pay attention to the upstreamness of firms in supply chains. Theoretically, upstream firms are affected by supply-chain disruptions through a lack of demand, whereas downstream firms are affected through a lack of supply. However, the effect of upstream and downstream links can differ in size. A recent sectoral analysis [ 36 ] finds that the profits of more upstream sectors in global value chains are substantially lower than those of more downstream sectors, implying that negative economic shocks propagate upstream more than downstream. To clarify the possible effect of upstreamness, we define the upstream position of each firm i in supply chains by its Helmholtz–Hodge (HH) potential, φ i computed from the HHD. In other words, the hierarchical position of a firm can be consistently defined by focusing on gradient flows, in other words, all flows less loop flows. The HH potential is higher when the firm is located in a more upstream position. In practice, it is generally higher for firms in the mining, manufacturing, and information and communication sectors, while lower for those in the wholesale, retail, finance, healthcare, and accommodation and food service sectors [ 32 ]. We average the HH potential over the firms in each prefecture to measure the upstreamness of the prefecture in supply chains. The visualization on the map can be found in Fig B.2 of [ 31 ].
Our measure of upstreamness based on the HH potential, is conceptually similar to the upstreamness measures developed and widely used in the literature on international trade [ 37 – 41 ] in that both measure the hierarchical position in supply chains. However, a clear difference between the two types of measures is that ours is based on firm-level data while others are based on sector-level IO tables. Therefore, our measure can incorporate firm-level heterogeneity within the same sector that is ignored in others. In addition, our measure is defined by gradient flows in supply chains that are constructed by eliminating loop flows from all flows. Although many loops at the firm level are found in supply chains, even within the industry [ 32 ], upstream measures based on IO tables do not incorporate such loops. For these reasons, we will rely on our upstreamness measures at the firm level, and not on existing measures at the sector level.
Finally, even when the supply of parts and components from other prefectures is shut down because of their lockdowns, the negative effect can be mitigated if suppliers can be replaced by those in the prefecture lifting its lockdown. Existing studies [ 2 , 5 ] have found that input substitutability can largely mitigate the propagation of negative economic shocks through supply chains. By assumption, suppliers of firms in prefecture a that are in other prefectures currently under lockdown can be replaced by suppliers in prefecture a that are in the same industry and already connected. To measure the degree of supplier substitutability for prefecture a , we divide the number of the latter suppliers by the number of the former.
3.3.4 Lifting lockdowns in two regions simultaneously.
S2 Appendix describes how to calculate Pot ab , Pot ba , and Loop ab using a simple example.
Finally, when suppliers of firms in prefecture a are located outside prefectures a and b and thus are locked down, they can be replaced by suppliers in the same industry in prefecture b that are already connected with firms in prefecture a . To measure the degree of this supplier substitutability, we divide the total number of the latter suppliers by the total number of the former. See S2 Appendix for the details.
4.1 Simulation of the effect of the actual lockdown
In Fig 2 , the blue lines indicate the results of the 30 Monte Carlo runs conducted to estimate the effect of the actual lockdown in Japan given the sector-specific rates of reduction in production capacity assumed in the literature [ 9 , 36 ] and shown in S1 Table . The horizontal axis indicates the number of days since the declaration of the state of emergency (7 April) and the vertical axis represents the total value added production, or GDP, of Japan on each day. See Section 3.2 for the sequence of the state of emergency across the country. Averaged over the 30 runs, the estimated loss in GDP is 35.0 trillion yen (3,280 billion U.S. dollars), or 6.60% of yearly GDP.
The blue and green lines indicate the simulation results given the sector-specific rates of reduction in production capacity assumed in the literature [ 9 , 36 ] and shown in S1 Table and the 26.7% of those rates to calibrate the actual production dynamics, respectively. Each line represents the daily GDP from one Monte Carlo run. The red segments indicate the daily GDP estimated from pre-lockdown GDP and the post-lockdown monthly Indices of All Industry Activity (IAIA) for April and May.
https://doi.org/10.1371/journal.pone.0255031.g002
Without relying on our model and simulation, we also estimate the changes in daily GDP from pre-lockdown GDP and the post-lockdown monthly Indices of All Industry Activity (IAIA) [ 42 ]. The average daily GDP in April and May estimated from the IAIA is indicated by the red lines in Fig 2 (see S3 Appendix for the detailed procedures). The total loss of GDP estimated by the IAIA, or the pink area in Fig 2 , is 7.52 trillion yen (1.44% of yearly GDP), 21.5% of the estimate from our simulations. Our simulation thus overestimates the loss of GDP from the lockdown, possibly because the assumed rates of reduction in production capacity due to the lockdown taken from the literature [ 8 , 9 ] are larger than the actual rates in Japan. Therefore, we experiment with different rates of reduction in production capacity by multiplying the benchmark rates by a weight to calibrate changes in production. We find that a weight of 26.7% results in a close fit between our estimates and those from the IAIA, and indicate the results using green lines in Fig 2 .
In either case (blue or green lines), the production loss rises during the lockdown. For example, the value added declined monotonically from days 9 to 37, when all prefectures were in a state of emergency, assuming a fixed rate of reduction in production capacity throughout the period. This is because the economic contraction in different regions interacted with each other through supply chains, and thus worsened over time. This worsening trend in GDP is consistent with GDP estimated using the IAIA.
Another notable finding from the simulation is that prefectures that were not locked down were heavily affected by those under lockdowns. The visualization on the map can be found in Fig 3 of [ 31 ]. In addition, a video presents a temporal and geographical visualisation of this. See S3 Appendix .
Moreover, because of the network effect, the earlier lifting of the lockdown in some prefectures does not result in a full recovery of production in these prefectures. Notably, when the lockdown was lifted in 39 prefectures on day 37 (14 May), the simulated GDP show a sharp recovery but drops again substantially a few days after the recovery. This drop occurred because the lockdown remained active in eight prefectures including the top two industrial clusters in Japan, greater Tokyo and greater Osaka. Although economic activities returned to normal in these 39 prefectures, their production did not recover monotonically but rather declined again because the major industrial clusters linked with them were still locked down. This finding points to the interactions of the economic effect of lockdown between regions through firm-level supply chains.
4.2 Interactions between lockdowns in different regions
Next, we experiment with simulations assuming different levels of restrictions, or different sets of multipliers for the sector-specific benchmark rates of reduction in production capacity, between the more and less restricted groups (Section 3.3). The more restricted group comprises the seven prefectures with a large number of COVID-19 cases, whereas the less restricted group includes the other 40 prefectures. The left, middle, and right panels of Fig 3 indicate the loss in GDP for different multipliers for the more restricted group when fixing the multiplier for the less restricted group at 0%, 50%, and 100%, respectively. Here, 100% corresponds to the rates of reduction shown in S1 Table and used in the previous subsection and 0% implies no restriction. In each bar, the blue and red portions indicate the loss of value added in the more and less restricted groups, respectively.
A restriction level is defined by a multiplier for the sector-specific benchmark rates of reduction in production capacity. For example, the left bar presents the result assuming a multiplier of 0% (i.e., no restriction) for the less restricted group and 20% for the more restricted group. The red and blue portions of each bar show the loss of value added in the less and more restricted groups, respectively, as a percentage of GDP.
https://doi.org/10.1371/journal.pone.0255031.g003
As shown, the total loss of GDP increases in the levels of restrictions in both groups. For example, the total production loss is 4.18% of GDP when the multiplier is 50% for both groups (the left bar in the middle panel), while it is larger, or 9.39%, when the multiplier is 100% for both (the right panel). More interestingly, the left panel shows that while the group with fewer restrictions imposes no restrictions, its value added decreases more (i.e., the red portion in Fig 3 increases) as the group with more restrictions imposes more restrictions. When the level of restrictions in the group with more restrictions is the highest (i.e., the multiplier is 100%), the loss in value added in the group with fewer restrictions without any lockdown is large: 18.6 trillion yen, or 3.51% of its pre-lockdown value added. These results clearly indicate that even when prefectures are not locked down, their economies can be damaged because of the propagation of the effect of the lockdowns in other prefectures through supply chains.
4.3 Effect of lifting the lockdown in one region
We further examine, how the recovery of a prefecture where lockdown is lifted is determined by its network characteristics, when only one prefecture lifts its lockdown and others remain locked down. We define the recovery rate of each prefecture as the ratio of the total gain of its value added or gross regional production (GRP) from lifting the lockdown to its total loss from the lockdown of all the prefectures for two weeks. The visualization of the recovery rate can be found in Fig 5 of [ 31 ]. See S6 Fig for the bar plot of the recovery rate of each prefecture.
One notable finding is that the prefectures that recover the most, including Hokkaido, Shimane, and Okinawa, which are remote from industrial hubs in terms of both geography and supply chains, suggesting the effect of network characteristics on economic recovery by lifting a lockdown. The name and location of each prefecture can be found in Fig A.2 of [ 31 ].
We further examine the correlation between the recovery rate and network measures explained in Section 3.3 (i.e. those for isolation, loops, upstreamness, and supplier substitution) and test the significance of the correlation using ordinary least squares (OLS) estimations. Fig 4 illustrates the correlation between the recovery rate and network measures. To control for the effect of the prefecture’s economic size on its recovery ( Fig 4(f) ), we include GRP in logs in all the OLS estimations and exclude the effect of GRP from the recovery rate in Fig 4 . The number of links of each prefecture could also be controlled for; however, because its correlation coefficient with GRP is 0.965 ( S3 Table ), we do not use the total links in our regressions to avoid multicollinearity. S4 Table presents the OLS results.
The vertical axis indicates the recovery rate, defined as the ratio of the increase in the GRP of a prefecture by lifting its own lockdown to its decrease because of the lockdown of all prefectures. Except for panel (f), the effect of GRP is excluded from the recovery rate. The horizontal axis indicates the share of the links within the prefecture to its all links in (a), the share of the loop flows within the prefecture to its total flows in (b), the share of the links to other prefectures to all links in (c), the standardised potential flows in (d), the share of substitutable suppliers to all suppliers outside the prefecture in (e), and GRP in logs in panel (f). The orange line in each panel specifies the fitted value from a linear regression that controls for the effect of GRP. The blue, black, and red dots show prefectures whose GRP is among the top 10, bottom 10, and others, respectively.
https://doi.org/10.1371/journal.pone.0255031.g004
In panels (a) and (b) of Fig 4 , the supply-chain links and loops within the prefecture are found to be positively correlated with the recovery rate. These results suggest that when a prefecture is more isolated in the network and has more loops within it, the positive effect of lifting a lockdown circulates in the loops, which can mitigate the propagation of the negative effects of other prefectures’ lockdowns. By contrast, the outward links to other prefectures and the HH potential of the prefecture are negatively and significantly correlated with the recovery rate (panels (c) and (d)). These findings imply that prefectures with more upstream firms in supply chains tend to recover less from lifting their own lockdowns. Panel (e) indicates that the recovery rate is higher when more suppliers in other prefectures under lockdown can be replaced by those in the prefecture lifting its lockdown.
4.4 Effect of lifting the lockdowns in two regions simultaneously
Finally, we simulate the effect on the production of prefecture a if it lifted its lockdown together with prefecture b . We compare the recovery in prefecture a ’s GRP by lifting its lockdown together with prefecture b and that by lifting its lockdown alone, and compute the relative recovery measure, as shown in S7 Fig . Using a regression framework as above, we investigate how the relative recovery measure of prefecture a is affected by the network relationships between prefectures a and b . Fig 5 illustrates the correlation between selected key variables and the relative recovery. In the regression analysis, we always control for the GRP of prefecture b , its squares, and the number of links between prefectures a and b that may affect the relative recovery ( Fig 5(e) and 5(f) ). Following this, we exclude these effects from the relative recovery in panels (a)–(d) in the figure. S6 Table presents the results of the OLS estimations.
The vertical axis indicates the relative recovery of prefecture a , defined as the ratio of the increase in the GRP of prefecture a by lifting its lockdown together with prefecture b to its increase by lifting its lockdown alone. The effect of the GRP of b and total links between the two are excluded from the relative recovery measure. The variable in the horizontal axis is given by Eqs 3 and 4 in panels (a) and (b), respectively, Eq 5 in (c), the share of substitutable suppliers in b for those in a among a ’s locked-down suppliers in (d), the number of links between prefectures a and b in (e) and the GRP of b in logs in (f). The orange line in each panel signifies the fitted value from a linear regression that controls for the effect of the GRP of b and total number of links between a and b in (a)–(d). The blue, black, and red dots show the pairs of prefectures a and b for which the GRP of b is among the top 10, bottom 10, and others, respectively.
https://doi.org/10.1371/journal.pone.0255031.g005
Panels (a) and (b) of Fig 5 show that even after controlling for the effect of economic size and number of links between the two prefectures, the ratio of potential flows from prefecture a to b and from b to a to the total flows of a is positively correlated with the relative recovery. S8 Fig shows a similarly positive correlation for the number of links between the two, rather than potential flows, and the relative recovery. These results suggest that the recovery from lifting a lockdown is greater when two prefectures closely linked through their supply chains, regardless of the direction, lift their lockdowns together. Further, we find that prefecture a recovers more when prefectures a and b are linked through more circular flows (panel (c)), confirming that the positive impacts of lifting a lockdown can circulate and be strengthened in inter-regional supply-chain loops. Panel (d) indicates that if prefecture a ’s suppliers in other prefectures are in lockdown but can be replaced by suppliers in prefecture b easily, prefecture a ’s recovery is higher when the two prefectures lift their lockdowns together. Although the correlation between the relative recovery measure and network variables seems to be largely driven by the observations for which the GRP of prefecture b is large (depicted by the blue dots in Fig 5 ), we find that the positive correlation still exists without these observations ( S9 Fig ).
5 Discussion and conclusion
Our simulation analysis reveals that the economic effects of lockdowns in different regions interact with each other through supply chains. Our results and their implications can be summarised as follows.
First, when a firm is locked down, its suppliers and customer firms are affected because of a lack of demand and supply, respectively. Therefore, a region’s production can improve more if prefectures lift their lockdowns together when they are closely linked through supply chains in either direction ( Fig 5(a) and 5(b) ). In addition to the total number of links between the two regions, the intensity of such links compared with those with others is also important.
Second, when the firms in a region are in more upstream positions in the whole network or are predominantly suppliers of simple parts, the production of the region does not recover substantially by lifting its lockdown alone ( Fig 4(d) ). Although the negative economic effect of a lockdown can propagate downstream and upstream, firms can mitigate downstream propagation easily by using inventory or by replacing suppliers who are under lockdown. The difference between the downstream and upstream effects of lockdown is aggravated as the effect propagates further through supply chains. This finding is in line with the literature [ 36 , 43 ] that also finds the upstream accumulation of negative effects on profits and assets. In practice, our result implies that a region with many small- and medium-sized suppliers of simple materials and parts should be cautious about whether it lifts its lockdown, which may not result in a large economic benefit but could still promote the spread of COVID-19.
Third, the production of a region can recover more by lifting its lockdown when it is more isolated in the network or embodies more supply-chain loops within the region ( Fig 4(a) and 4(b) ). Similarly, the production of the two regions can recover more by lifting their lockdowns together when their inter-regional links have more loops ( Fig 5(c) ). These results imply that the positive economic effect of lifting a lockdown circulates and is intensified in loops, consistent with those in [ 5 ]. Supply-chain loops exist between two regions when the final goods produced are used as inputs by suppliers, while suppliers provide parts and components to final-good producers and the loop stretches across two regions. The importance of loops in the diffusion of the economic effects in networks is not fully recognised, either in academic literature or in policymaking.
Finally, the recovery of a region from its lockdown is greater when suppliers who are still under lockdown can be replaced by those within the region or in other regions without a lockdown in place (Figs 4(e) and 5(f) ). The role of the substitutability of suppliers in mitigating the propagation effect through supply chains has been empirically found in the literature [ 2 , 5 – 7 ]. In practice, this finding suggests two management strategies for regional governments and firms. To minimise the economic loss from lockdown, a region should develop a full set of industries to allow for the possibility of the substitution of any industry. Alternatively, the firms in a region should be linked with geographically diverse suppliers so that suppliers in a region under lockdown can be replaced by those in other regions without a lockdown.
All these results point to the need for policy coordination among regions when regional governments impose or lift a lockdown. Although this study uses the inter-firm supply chains within a country and considers the economic effect of prefecture-level lockdowns, our results can be applied to examine the effect of country-level lockdowns propagating through international supply chains. For example, many suppliers of German firms are located in Eastern Europe and many suppliers of US firms are in Mexico. Our results thus suggest that the economic gains of Eastern Europe and Mexico from lifting their lockdowns are minimal if Germany and the United States, respectively, remain under lockdown. In addition, our framework can be applied to the case of other infectious diseases, and it is likely to suggest a need for the inter-regional and international coordination of lockdown strategies to prevent the spread of infection.
Since our model does not incorporate how lockdown strategies affect the spread of COVID-19, and because it is unclear how human and economic loss should be balanced to maximise social welfare, we cannot explicitly conclude in which cases a lockdown should be imposed or lifted. However, our analysis points to the importance of coordination between lockdown strategies among regions and countries that consider their economic effect in addition to their health effect.
Supporting information
S1 appendix. data..
https://doi.org/10.1371/journal.pone.0255031.s001
S2 Appendix. Methods.
https://doi.org/10.1371/journal.pone.0255031.s002
S3 Appendix. Results.
https://doi.org/10.1371/journal.pone.0255031.s003
S1 Fig. An example of the HHD and loop and potential flow measures of prefectures.
The left panel shows the supply chains of the six firms in the two prefectures. The right top and bottom panels present the potential flows and loop flows, respectively obtained from the HHD.
https://doi.org/10.1371/journal.pone.0255031.s004
S2 Fig. An example of the substitutability measure for two regions.
The bottom shows the equation. A i is the total number of suppliers outside prefectures a and b . The lowest two suppliers are applicable. A supplier in prefecture b belongs to the same industry as the upper firm of the outside suppliers, whereas the lower firm of the outside suppliers is not substitutable. Hence, A i = 2 and B i = 1.
https://doi.org/10.1371/journal.pone.0255031.s005
S3 Fig. Loss in value added as a percentage of total GDP, assuming different restriction levels for a lockdown of 14 days, between the groups with fewer and greater restrictions.
A restriction level is defined by a multiplier for the sector-specific benchmark rates of reduction in production capacity. The red and blue parts of each bar show the loss of value added in the less and more restricted groups, respectively, as a percentage of GDP.
https://doi.org/10.1371/journal.pone.0255031.s006
S4 Fig. Loss in value added as a percentage of total GDP, assuming different restriction levels for a lockdown of 30 days, between the groups with fewer and greater restrictions.
A restriction level is defined by a multiplier for the sector-specific benchmark rates of reduction in production capacity. The red and blue parts of each bar show the loss of value added in the less and more restricted groups, respectively as a percentage of GDP.
https://doi.org/10.1371/journal.pone.0255031.s007
S5 Fig. The ratio of the improvement in GDP by lifting the lockdown in each prefecture.
The improvement is defined as the ratio of the increase in the national GDP by each prefecture lifting its lockdown to the decrease in GDP by all prefectures’ lockdowns. The horizontal axis indicates the JIS codes of the prefectures. The yellow, dark green, and light green bars show the ratio of the improvement when lockdowns persist for 14, 30, and 60 days, respectively.
https://doi.org/10.1371/journal.pone.0255031.s008
S6 Fig. Recovery rate in GRP by lifting the lockdown in each prefecture.
The recovery rate is defined as the ratio of the increase in the GRP of each prefecture by lifting its lockdown to the decrease in its GRP by all prefectures’ lockdowns. The horizontal axis indicates the JIS codes of the prefectures. The yellow, dark green, and light green bars show the recovery rate when lockdowns persist for 14, 30, and 60 days, respectively.
https://doi.org/10.1371/journal.pone.0255031.s009
S7 Fig. Relative recovery from lifting the lockdown together to the recovery from lifting the lockdown alone.
The relative recovery measure is defined as the ratio of the increase in the GRP of prefecture a when it lifts its lockdown together with prefecture b to its increase when prefecture a lifts its lockdown alone. The horizontal axis shows the JIS code of prefecture a . The colour of each dot indicates whether the GRP of prefecture b is among the top 10 (blue), the bottom 10 (black), or others (red).
https://doi.org/10.1371/journal.pone.0255031.s010
S8 Fig. Correlation between the relative recovery and selected network measures.
The vertical axis indicates the relative recovery of prefecture a , defined as the ratio of the increase in the GRP of prefecture a by lifting its lockdown together with prefecture b to its increase by lifting its lockdown alone. The effect of the GRP of b and total links between the two are excluded from the relative recovery measure. The variable in the horizontal axis is given by Eqs 1 and 2 in panels (a) and (b), respectively. The orange line in each panel signifies the fitted value from a linear regression that controls for the effect of the GRP of b and total number of links between a and b . The blue, black, and red dots indicate the pairs of prefectures a and b for which the GRP of b is among the top 10, bottom 10, and others, respectively.
https://doi.org/10.1371/journal.pone.0255031.s011
S9 Fig. Correlation between the relative recovery and selected network measures.
See the caption of Fig 5 and S8 Fig . for the definitions of the variables used here. The green line in each panel signifies the fitted value from a linear regression that controls for the effect of the GRP of b and total number of links between a and b in (a)–(g). The black and red dots indicate the pairs of prefectures a and b for which the GRP of b is among the bottom 10 and between 11 and 37, respectively.
https://doi.org/10.1371/journal.pone.0255031.s012
S10 Fig. Correlation between the recovery rate and selected network measures.
See the caption of Fig 4 for the definitions of the variables used here. The orange line in each panel specifies the fitted value from a linear regression that controls for the effect of GRP in (b)–(f). The blue, black, and red dots indicate the prefectures whose GRP is among the top 10, the bottom 10, or others, respectively.
https://doi.org/10.1371/journal.pone.0255031.s013
S11 Fig. Correlation between the relative recovery and selected network measures.
See the caption of Fig 5 for the definitions of the variables used here. The red line in each panel signifies the fitted value from a linear regression that controls for the effect of the GRP of b and total number of links between a and b in (a)–(g). The blue, black, and red dots indicate the pairs of prefectures a and b for which the GRP of b is among the top 10, the bottom 10, or others, respectively.
https://doi.org/10.1371/journal.pone.0255031.s014
S1 Table. Sector-specific rates of reduction in production capacity.
Sectors are classified by the JSIC [ 23 ] at the two-digit level, except for industries 560, 561, and 569 for which we use three-digit codes to reflect the actual circumstances. The sector names are abbreviated. S1 Table lists the sector descriptions and abbreviations.
https://doi.org/10.1371/journal.pone.0255031.s015
S2 Table. Sector classifications and abbreviations.
https://doi.org/10.1371/journal.pone.0255031.s016
S3 Table. Correlation matrix of the variables used in Section 4.3.
The definitions of the variables are as follows. RecRatio: the recovery rate defined as the ratio of the increase in the GRP of each prefecture by lifting its lockdown to the decrease in its GRP by all prefectures’ lockdowns. GRP: gross regional product (log). Links: the degree (log). InLink: the share of links within the prefecture to all its links. InLoop: the share of loop flows within the prefecture to all its flows. OutLink: the share of outward inter-prefectural links to all the links of the prefecture. Potential: the average HH potential of the firms in the prefecture. Sub: the share of substitutable suppliers to all suppliers of the prefecture located outside the prefecture.
https://doi.org/10.1371/journal.pone.0255031.s017
S4 Table. Regression results for Section 4.3.
The dependent variable is the recovery rate. See the caption of Table S3 Table for the definitions of the independent variables. Standard errors are in parentheses. *** p<0.01, ** p<0.05, * p<0.1.
https://doi.org/10.1371/journal.pone.0255031.s018
S5 Table. Correlation matrix of the variables used in Section 4.4.
The definitions of the variables are as follows. Recov a : the relative recovery of prefecture a defined as the ratio of the increase in the GRP of prefecture a by lifting its lockdown together with prefecture b to its increase by lifting its lockdown alone. Link ab : the share of links from a to b to all links from a . Link ba : the share of links from b to a to all links from a . Pot ab : the share of potential flows from b to a to the total links of a . Pot ba : the share of potential flows from a to b to the total links of a . Sub ab : the share of suppliers substitutable by those in b to a ’s suppliers outside a and b . Sub ba : the share of suppliers substitutable by those in a to b ’s suppliers outside a and b . Loop ab : the share of loop flows between a and b to the total flows between the two. Bi ab : the number of inter-prefecture links between a and b in logs. GRP j : GRP of b in logs.
https://doi.org/10.1371/journal.pone.0255031.s019
S6 Table. Regression results for Section 4.4.
The dependent variable is the relative recovery measure. See the caption of Table S5 Table for the definitions of the independent variables. Standard errors are in parentheses. *** p<0.01, ** p<0.05, * p<0.1.
https://doi.org/10.1371/journal.pone.0255031.s020
Acknowledgments
This study used the computational resources of the supercomputer Fugaku (the evaluation environment in the trial phase) provided by the RIKEN Center for Computational Science. OACIS [ 44 ] and CARAVAN [ 45 ] were used for the simulations in this study. This study was conducted as part of a project entitled ‘Research on relationships between economic and social networks and globalization’ undertaken at the Research Institute of Economy, Trade, and Industry (RIETI). We thank Yoshi Fujiwara for advise on the Helmholtz–Hodge decomposition (HHD) computation.
- 1. Thomas Hale, Sam Webster, Anna Petherick, Toby Phillips, and Beatriz Kira. Oxford COVID-19 government response tracker. https://www.bsg.ox.ac.uk/research/research-projects/coronavirus-government-response-tracker , 2020.
- View Article
- Google Scholar
- 4. Vasco M Carvalho, Makoto Nirei, Yukiko U Saito, and Alireza Tahbaz-Salehi. Supply chain disruptions: Evidence from the Great East Japan earthquake. Technical Report No. 17-5, Columbia Business School Research Paper, 2016.
- 7. Yuzuka Kashiwagi, Yasuyuki Todo, and Petr Matous. International propagation of economic shocks through global supply chains. Technical Report E1810, WINPEC Working Paper, 2018.
- 8. Barthélémy Bonadio, Zhen Huo, Andrei A Levchenko, and Nitya Pandalai-Nayar. Global supply chains in the pandemic. NBER Working Paper Series No. 27224, National Bureau of Economic Research, 2020.
- 10. Fergal McCann and Samantha Myers. Covid-19 and the transmission of shocks through domestic supply chains. Financial Stability Notes No. 2020-3, Central Bank of Ireland, 2020.
- 11. Warwick J McKibbin and Roshen Fernando. The global macroeconomic impacts of COVID-19: Seven scenarios. Technical Report 19/2020, CAMA Working Paper, 2020.
- PubMed/NCBI
- 17. Garry Robins and Philippa Pattison. Interdependencies and social processes: Dependence graphs and generalized dependence structures. In Peter J Carrington, John Scott, and Stanley Wasserman, editors, Models and methods in social network analysis , volume 28, book section 10, pages 192–214. Cambridge University Press, Cambridge, 2005.
- 19. Peter S. Goodman. Sweden has become the world’s cautionary tale, July 2020.
- 22. Ministry of Internal Affairs and Communications, the Cabinet Office, the Financial Services Agency, the Ministry of Finance, the Ministry of Education, Culture, Sports, Science and Technology, the Ministry of Health, Labour and Welfare, the Ministry of Agriculture, Forestry and Fisheries, the Ministry of Economy, Trade and Industry, the Ministry of Land, Infrastructure, Transport and Tourism, and the Ministry of Environment, Japan. 2015 Input-Output tables for Japan. https://www.soumu.go.jp/english/dgpp_ss/data/io/index.htm , 2015.
- 23. Ministry of International Affairs and Communications. Japan Standard Industrial Classification (Revision 13) , 2013 (accessed June 1, 2020).
- 24. Barabási Albert-László. Network science . Cambridge University Press, 2016.
- 26. Axtell Robert, Blair Bruce, Bowles Samuel, DeVany Art, DeBevoise Malcolm, Durlauf Steven, et al. Generative Social Science: Studies in Agent-based Computational Modeling . Princeton University Press, Princeton, 2006.
- 30. The Prime Minister of Japan and His Cabinet. Government responses on the coronavirus disease 2019. http://japan.kantei.go.jp/ongoingtopics/_00013.html , 2020.
- 31. Hiroyasu Inoue, Yohsuke Murase, and Todo Yasuyuki. Do economic effects of the “anti-covid-19” lockdowns in different regions interact through supply chains? SSRN 3692937, Social Science Research Network, 2021.
- 36. Nicole Branger, René Marian Flacke, and Steffen Windmueller. Industry returns in global value chains: The role of upstreamness and downstreamness. SSRN 3476690, Social Science Research Network, 2019.
- 40. Thibault Fally. Production staging: measurement and facts, 2012.
- 41. Thibault Fally and Russell Hillberry. A coasian model of international production chains, 2017.
- 42. Ministry of Economy, Trade, and Industry. Indices of all industry production. https://www.meti.go.jp/english/statistics/tyo/zenkatu/index.html , 2020.
- 43. Jiangtao Fu, Petr Matous, and Yasuyuki Todo. Trade credit in global supply chains. RIETI Discussion Paper Series 18-E-049, Research Institute of Economy, Trade and Industry, 2018.
- 44. Yohsuke Murase, Takeshi Uchitane, and Nobuyasu Ito. An open-source job management framework for parameter-space exploration: Oacis. In Journal of Physics: Conference Series , volume 921, page 012001, 2017.
- 45. Yohsuke Murase, Hiroyasu Matsushima, Itsuki Noda, and Tomio Kamada. Caravan: a framework for comprehensive simulations on massive parallel machines. In International Workshop on Massively Multiagent Systems , pages 130–143. Springer, 2018.

IMAGES
VIDEO
COMMENTS
Purpose of the present study. In the present study, we took advantage of a growing evidence base using more sophisticated methodologies. When experimental randomized trials are neither feasible nor ethical, both longitudinal within-person designs (with at least one data collection point before and one during the lockdown) and natural experiments involving a control group provide a ...
Amidst the rapid global spread of Covid-19, many governments enforced country-wide lockdowns, with likely severe well-being consequences. In this regard, South Africa is an extreme case suffering from low levels of well-being, but at the same time enforcing very strict lockdown regulations. In this study, we analyse the causal effect of a lockdown and consequently, the determinants of ...
Based on these inclusion criteria we included 22 articles. Three independent authors participated in study selection and all authors reached a consensus on the studies to be included. Being a narrative review, we did not attempt computation of effect sizes or do a risk of bias assessment for included papers.
The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good ...
In considering the use of antidepressants among children and adolescents to deal with the mental distress of lockdown, the risks and benefits should be carefully weighed . There are multiple possible ways to limit the health-based deleterious effects of lockdowns among children and adolescents. Parents need to limit the screen hours for children.
The psychological effects of loneliness are a health risk comparable with risk obesity or smoking. Anxiety and depression have spiked since lockdown orders went into effect.
of noticeable effects on COVID-19 mortality. While this meta-analysis concludes that lockdowns have had little to no public health effects, they have imposed enormous economic and social costs where they have been adopted. In consequence, lockdown policies are ill-founded and should be rejected as a pandemic policy instrument. Acknowledgements
COVID-19 is a viral disease caused by the novel SARS CoV-2 virus, a single-stranded enveloped positive-sense RNA virus 1 that emanated from Wuhan-China and has spread across all major cities and countries the world over. 2 The virus gained attention after clusters of pneumonia of unknown aetiology were reported in Wuhan, the Hubei province of China, on the 31st of December 2019. 3 The global ...
The widespread effects of the COVID-19 pandemic that emerged in 2019-2020 have drastically increased health, social and economic inequalities 1,2.For more than 900 million learners around the ...
The implications of the coronavirus disease (COVID-19) lockdown measurements and social isolation in children and their parents are still unknown. The aims of this study were to examine the impact of COVID-19 lockdown on emotional state, feelings and lifestyle of children and their parents, to explore the association between parental characteristics and child well-being and to examine whether ...
It identified 24 papers, published or posted as of early July 2021, that met its criteria for the meta-analysis — 17 of which were peer-reviewed. ... (the source of the 0.2% effect of lockdown ...
Here, we studied the effects of lockdown in children and adolescents through an online questionnaire. Methods: A cross-sectional study was conducted in Spain using an open online survey from July (after the lockdown resulting from the first pandemic wave) to November 2020 (second wave). We included families with children under 16 years-old ...
Meanwhile, COVID-19's impact was inequitable: Deaths were concentrated among the elderly and minorities working in essential jobs, groups who up to the pandemic had been reporting better mental ...
Impacts of the Covid-19 pandemic and its public health measures go beyond physical and mental health and incorporate wider well-being impacts in terms of what people are free to do or be. We explored the impacts of the Covid-19 lockdown and relevant vulnerabilities on capability well-being, mental health and social support in Austria. Adult Austrian residents (n = 560) provided responses to a ...
Epidemiological and economic effects of lockdown. This paper is part of the fall 2020 edition of the Brookings Papers on Economic Activity, the leading conference series and journal in economics ...
Lynn Williams. Studies show some people are reporting positive changes in lockdown, with 83% having more time to do enjoyable things and 65% spending more time in outdoors. It is believed that additional time and the removal of daily demands during lockdown may be improving quality of life for some people. Unfortunately, groups such as older ...
The pandemic has taken a toll on the mental health of millions. But adolescents have been hit especially hard. According to a national poll conducted in January by the University of Michigan's C ...
The effects of the lockdown increased over an extended time to the end of December 2020. Scientific Reports - The impact of COVID-19 lockdowns on mental health patient populations in the United States
We used segmented regression to investigate the effects of lockdown timing on cumulative COVID-19 incidence across the US. We found a critical time point after which delays in lockdown are associated with a rapid spread of COVID-19 in that community. This critical time point occurred approximately 7 days prior to communities reporting at least ...
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
Therefore, the spatial analysis of lockdown effects should take into account the factor of the distance between countries, particularly considering that air pollutants and contagious diseases are highly mobile. Consequently, a country imposing lockdown measures can produce impacts on the economy, environment, and public health of its ...
To prevent the spread of COVID-19, many cities, states, and countries have 'locked down', restricting economic activities in non-essential sectors. Such lockdowns have substantially shrunk production in most countries. This study examines how the economic effects of lockdowns in different regions interact through supply chains, which are a network of firms for production, by simulating an ...