- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games

Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
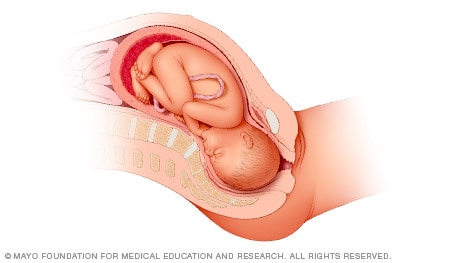
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
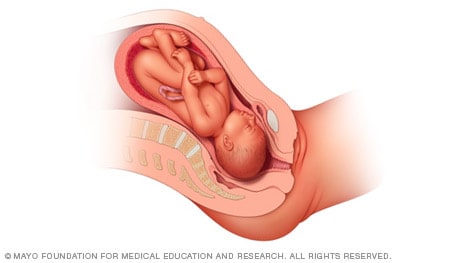
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
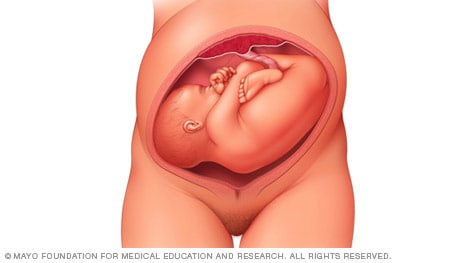
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
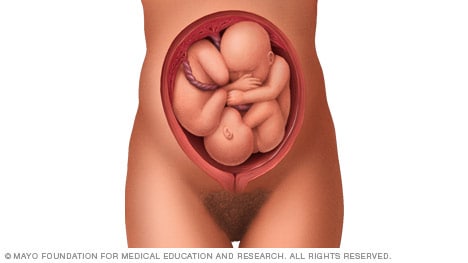
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

How your twins’ fetal positions affect labor and delivery

What happens to your baby right after birth

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.
Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.
Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.
If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.
- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.
Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.
Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death
Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
- Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
- Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History
Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Original Author(s): Minesh Mistry Last updated: 12th November 2018 Revisions: 7
- 1 Introduction
- 2 Preparation
- 3 General Inspection
- 4 Abdominal Inspection
- 5.1 Fundal Height
- 5.3 Presentation
- 5.4 Liquor Volume
- 5.5 Engagement
- 6 Fetal Auscultation
- 7 Completing the Examination
The obstetric examination is a type of abdominal examination performed in pregnancy.
It is unique in the fact that the clinician is simultaneously trying to assess the health of two individuals – the mother and the fetus.
In this article, we shall look at how to perform an obstetric examination in an OSCE-style setting.
Introduction
- Introduce yourself to the patient
- Wash your hands
- Explain to the patient what the examination involves and why it is necessary
- Obtain verbal consent
Preparation
- In the UK, this is performed at the booking appointment, and is not routinely recommended at subsequent visits
- Patient should have an empty bladder
- Cover above and below where appropriate
- Ask the patient to lie in the supine position with the head of the bed raised to 15 degrees
- Prepare your equipment: measuring tape, pinnard stethoscope or doppler transducer, ultrasound gel
General Inspection
- General wellbeing – at ease or distressed by physical pain.
- Hands – palpate the radial pulse.
- Head and neck – melasma, conjunctival pallor, jaundice, oedema.
- Legs and feet – calf swelling, oedema and varicose veins.
Abdominal Inspection
In the obstetric examination, inspect the abdomen for:
- Distension compatible with pregnancy
- Fetal movement (>24 weeks)
- Surgical scars – previous Caesarean section, laproscopic port scars
- Skin changes indicative of pregnancy – linea nigra (dark vertical line from umbilicus to the pubis), striae gravidarum (‘stretch marks’), striae albicans (old, silvery-white striae)
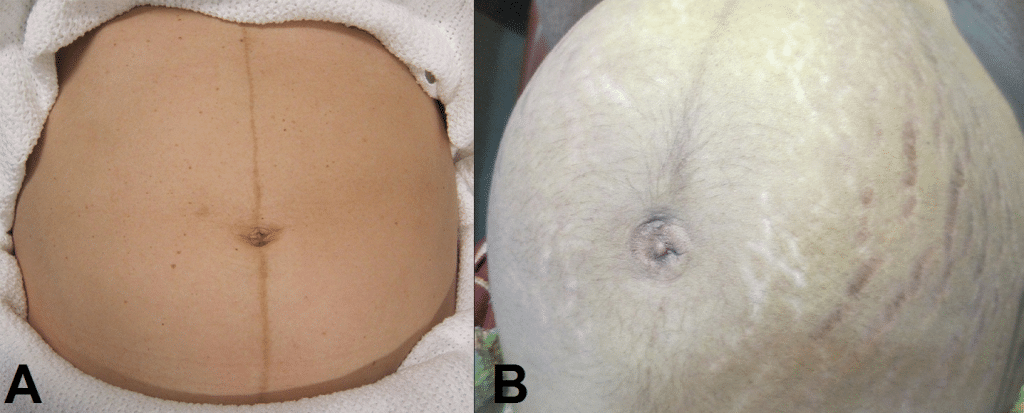
Fig 1 – Skin changes in pregnancy. A) Linea nigra. B) Striae gravidarum and albicans.
Ask the patient to comment on any tenderness and observe her facial and verbal responses throughout. Note any guarding.
Fundal Height
- Use the medial edge of the left hand to press down at the xiphisternum, working downwards to locate the fundus.
- Measure from here to the pubic symphysis in both cm and inches. Turn the measuring tape so that the numbers face the abdomen (to avoid bias in your measurements).
- Uterus should be palpable after 12 weeks, near the umbilicus at 20 weeks and near the xiphisternum at 36 weeks (these measurements are often slightly different if the woman is tall or short).
- The distance should be similar to gestational age in weeks (+/- 2 cm).
- Facing the patient’s head, place hands on either side of the top of the uterus and gently apply pressure
- Move the hands and palpate down the abdomen
- One side will feel fuller and firmer – this is the back. Fetal limbs may be palpable on the opposing side
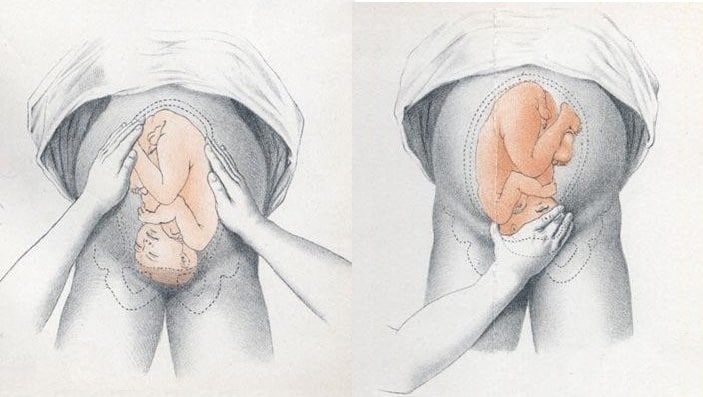
Fig 2 – Assessing fetal lie and presentation.
Presentation
- Palpate the lower uterus (below the umbilicus) to find the presenting part.
- Firm and round signifies cephalic, soft and/or non-round suggests breech. If breech presentation is suspected, the fetal head can be often be palpated in the upper uterus.
- Ballot head by pushing it gently from one side to the other.
Liquor Volume
- Palpate and ballot fluid to approximate volume to determine if there is oligohydraminos/polyhydramnios
- When assessing the lie, only feeling fetal parts on deep palpation suggests large amounts of fluid
- Fetal engagement refers to whether the presenting part has entered the bony pelvis
- Note how much of the head is palpable – if the entire head is palpable, the fetus is unengaged.
- Engagement is measured in 1/5s
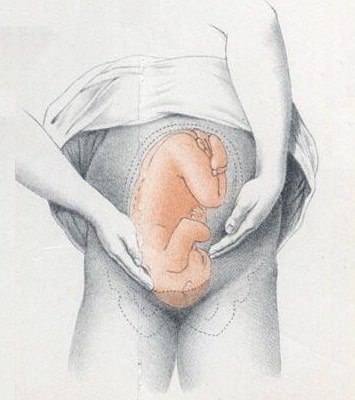
Fig 3 – Assessing fetal engagement.
Fetal Auscultation
- Hand-held Doppler machine >16 weeks (trying before this gestation often leads to anxiety if the heart cannot be auscultated).
- Pinard stethoscope over the anterior shoulder >28 weeks
- Feel the mother’s pulse at the same time
- Should be 110-160bpm (>24 weeks)
Completing the Examination
- Palpate the ankles for oedema and test for hyperreflexia (pre-eclampsia)
- Thank the patient and allow them to dress in private
- Summarise findings
- Blood pressure
- Urine dipstick
- Hands - palpate the radial pulse.
- Skin changes indicative of pregnancy - linea nigra (dark vertical line from umbilicus to the pubis), striae gravidarum ('stretch marks'), striae albicans (old, silvery-white striae)
- One side will feel fuller and firmer - this is the back. Fetal limbs may be palpable on the opposing side
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
- Management of breech presentation
Evidence review M
NICE Guideline, No. 201
National Guideline Alliance (UK) .
- Copyright and Permissions
Review question
What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy?
Introduction
Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman’s and the baby’s health. The aim of this review is to determine the most effective way of managing a breech presentation in late pregnancy.
Summary of the protocol
Please see Table 1 for a summary of the Population, Intervention, Comparison and Outcome (PICO) characteristics of this review.
Summary of the protocol (PICO table).
For further details see the review protocol in appendix A .
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual 2014 . Methods specific to this review question are described in the review protocol in appendix A .
Declarations of interest were recorded according to NICE’s conflicts of interest policy .
Clinical evidence
Included studies.
Thirty-six randomised controlled trials (RCTs) were identified for this review.
The included studies are summarised in Table 2 .
Three studies reported on external cephalic version (ECV) versus no intervention ( Dafallah 2004 , Hofmeyr 1983 , Rita 2011 ). One study reported on a 4-arm trial comparing acupuncture, sweeping of fetal membranes, acupuncture plus sweeping, and no intervention ( Andersen 2013 ). Two studies reported on postural management versus no intervention ( Chenia 1987 , Smith 1999 ).
Seven studies reported on ECV plus anaesthesia ( Chalifoux 2017 , Dugoff 1999 , Khaw 2015 , Mancuso 2000 , Schorr 1997 , Sullivan 2009 , Weiniger 2010 ). Of these studies, 1 study compared ECV plus anaesthesia to ECV plus other dosages of the same anaesthetic ( Chalifoux 2017 ); 4 studies compared ECV plus anaesthesia to ECV only ( Dugoff 1999 , Mancuso 2000 , Schorr 1997 , Weiniger 2010 ); and 2 studies compared ECV plus anaesthesia to ECV plus a different anaesthetic ( Khaw 2015 , Sullivan 2009 ).
Ten studies reported ECV plus a β2 receptor agonist ( Brocks 1984 , Fernandez 1997 , Hindawi 2005 , Impey 2005 , Mahomed 1991 , Marquette 1996 , Nor Azlin 2005 , Robertson 1987 , Van Dorsten 1981 , Vani 2009 ). Of these studies, 5 studies compared ECV plus a β2 receptor agonist to ECV plus placebo ( Fernandez 1997 , Impey 2005 , Marquette 1996 , Nor Azlin 2005 , Vani 2009 ); 1 study compared ECV plus a β2 receptor agonist to ECV alone ( Robertson 1987 ); and 4 studies compared ECV plus a β2 receptor agonist to no intervention ( Brocks 1984 , Hindawi 2005 , Mahomed 1991 , Van Dorsten 1981 ).
One study reported on ECV plus Ca 2+ channel blocker versus ECV plus placebo ( Kok 2008 ). Two studies reported on ECV plus β2 receptor agonist versus ECV plus Ca 2+ channel blocker ( Collaris 2009 , Mohamed Ismail 2008 ). Four studies reported on ECV plus a µ-receptor agonist ( Burgos 2016 , Liu 2016 , Munoz 2014 , Wang 2017 ), of which 3 compared against ECV plus placebo ( Liu 2016 , Munoz 2014 , Wang 2017 ) and 1 compared to ECV plus nitrous oxide ( Burgos 2016 ).
Four studies reported on ECV plus nitroglycerin ( Bujold 2003a , Bujold 2003b , El-Sayed 2004 , Hilton 2009 ), of which 2 compared it to ECV plus β2 receptor agonist ( Bujold 2003b , El-Sayed 2004 ) and compared it to ECV plus placebo ( Bujold 2003a , Hilton 2009 ). One study compared ECV plus amnioinfusion versus ECV alone ( Diguisto 2018 ) and 1 study compared ECV plus talcum powder to ECV plus gel ( Vallikkannu 2014 ).
One study was conducted in Australia ( Smith 1999 ); 4 studies in Canada ( Bujold 2003a , Bujold 2003b , Hilton 2009 , Marquette 1996 ); 2 studies in China ( Liu 2016 , Wang 2017 ); 2 studies in Denmark ( Andersen 2013 , Brocks 1984 ); 1 study in France ( Diguisto 2018 ); 1 study in Hong Kong ( Khaw 2015 ); 1 study in India ( Rita 2011 ); 1 study in Israel ( Weiniger 2010 ); 1 study in Jordan ( Hindawi 2005 ); 5 studies in Malaysia ( Collaris 2009 , Mohamed Ismail 2008 , Nor Azlin 2005 , Vallikkannu 2014 , Vani 2009 ); 1 study in South Africa ( Hofmeyr 1983 ); 2 studies in Spain ( Burgos 2016 , Munoz 2014 ); 1 study in Sudan ( Dafallah 2004 ); 1 study in The Netherlands ( Kok 2008 ); 2 studies in the UK ( Impey 2005 , Chenia 1987 ); 9 studies in US ( Chalifoux 2017 , Dugoff 1999 , El-Sayed 2004 , Fernandez 1997 , Mancuso 2000 , Robertson 1987 , Schorr 1997 , Sullivan 2009 , Van Dorsten 1981 ); and 1 study in Zimbabwe ( Mahomed 1991 ).
The majority of studies were 2-arm trials, but there was one 3-arm trial ( Khaw 2015 ) and two 4-arm trials ( Andersen 2013 , Chalifoux 2017 ). All studies were conducted in a hospital or an outpatient ward connected to a hospital.
See the literature search strategy in appendix B and study selection flow chart in appendix C .
Excluded studies
Studies not included in this review with reasons for their exclusions are provided in appendix K .
Summary of clinical studies included in the evidence review
Summaries of the studies that were included in this review are presented in Table 2 .
Summary of included studies.
See the full evidence tables in appendix D and the forest plots in appendix E .
Quality assessment of clinical outcomes included in the evidence review
See the evidence profiles in appendix F .
Economic evidence
A systematic review of the economic literature was conducted but no economic studies were identified which were applicable to this review question.
A single economic search was undertaken for all topics included in the scope of this guideline. See supplementary material 2 for details.
Economic studies not included in this review are listed, and reasons for their exclusion are provided in appendix K .
Summary of studies included in the economic evidence review
No economic studies were identified which were applicable to this review question.
Economic model
No economic modelling was undertaken for this review because the committee agreed that other topics were higher priorities for economic evaluation.
Evidence statements
Clinical evidence statements, comparison 1. complementary therapy versus control (no intervention), critical outcomes, cephalic presentation in labour.
No evidence was identified to inform this outcome.
Method of birth
Caesarean section.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.74 (95% CI 0.38 to 1.43).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 1.29 (95% CI 0.73 to 2.29).
Admission to SCBU/NICU
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.19 (95% CI 0.02 to 1.62).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.40 (0.08 to 2.01).
Fetal death after 36 +0 weeks gestation
Infant death up to 4 weeks chronological age, important outcomes, apgar score <7 at 5 minutes.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.32 (95% CI 0.01 to 7.78).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.33 (0.01 to 8.09).
Birth before 39 +0 weeks of gestation
Comparison 2. complementary therapy versus other treatment.
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.64 (95% CI 0.34 to 1.22).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.57 (95% CI 0.30 to 1.07).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 1.13 (95% CI 0.66 to 1.94).
- Very low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.33 (95% CI 0.03 to 3.12).
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.48 (95% CI 0.04 to 5.22).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.69 (95% CI 0.12 to 4.02).
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 3. ECV versus no ECV
- Moderate quality evidence from 2 RCTs (N=680) showed that there is clinically important difference favouring ECV over no ECV on cephalic presentation in labour in pregnant women with breech presentation: RR 1.83 (95% CI 1.53 to 2.18).
Cephalic vaginal birth
- Very low quality evidence from 3 RCTs (N=740) showed that there is a clinically important difference favouring ECV over no ECV on cephalic vaginal birth in pregnant women with breech presentation: RR 1.67 (95% CI 1.20 to 2.31).
Breech vaginal birth
- Very low quality evidence from 2 RCTs (N=680) showed that there is no clinically important difference between ECV and no ECV on breech vaginal birth in pregnant women with breech presentation: RR 0.29 (95% CI 0.03 to 2.84).
- Very low quality evidence from 3 RCTs (N=740) showed that there is no clinically important difference between ECV and no ECV on the number of caesarean sections in pregnant women with breech presentation: RR 0.52 (95% CI 0.23 to 1.20).
- Very low quality evidence from 1 RCT (N=60) showed that there is no clinically important difference between ECV and no ECV on admission to SCBU//NICU in pregnant women with breech presentation: RR 0.50 (95% CI 0.14 to 1.82).
- Very low evidence from 3 RCTs (N=740) showed that there is no statistically significant difference between ECV and no ECV on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: Peto OR 0.29 (95% CI 0.05 to 1.73) p=0.18.
- Very low quality evidence from 2 RCTs (N=120) showed that there is no clinically important difference between ECV and no ECV on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.28 (95% CI 0.04 to 1.70).
Comparison 4. ECV + Amnioinfusion versus ECV only
- Very low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.74 (95% CI 0.74 to 4.12).
- Low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.95 (95% CI 0.75 to 1.19).
Comparison 5. ECV + Anaesthesia versus ECV only
- Very low quality evidence from 2 RCTs (N=210) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.16 (95% CI 0.56 to 2.41).
- Very low quality evidence from 5 RCTs (N=435) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.16 (95% CI 0.77 to 1.74).
- Very low quality evidence from 1 RCT (N=108) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on breech vaginal birth in pregnant women with breech presentation: RR 0.33 (95% CI 0.04 to 3.10).
- Very low quality evidence from 3 RCTs (N=263) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.76 (95% CI 0.42 to 1.38).
- Moderate quality evidence from 1 RCT (N=69) showed that there is a clinically important difference favouring ECV plus anaesthesia over ECV alone on admission to SCBU/NICU in pregnant women with breech presentation: MD −1.80 (95% CI −2.53 to −1.07).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 6. ECV + Anaesthesia versus ECV + Anaesthesia
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.13 (95% CI 0.73 to 1.74).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 0.05mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.69 (95% CI 0.37 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.19 (95% CI 0.79 to 1.79).
- Low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.92 (95% CI 0.68 to 1.24).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.08 (95% CI 0.78 to 1.50).
- Very low evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.70 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.17 (95% CI 0.86 to 1.61).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.03 (95% CI 0.77 to 1.37).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.88 (95% CI 0.64 to 1.20).
Comparison 7. ECV + β2 agonist versus Control (no intervention)
- Moderate quality evidence from 2 RCTs (N=256) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on cephalic presentation in labour in pregnant women with breech presentation: RR 4.83 (95% CI 3.27 to 7.11).
- Very low quality evidence from 3 RCTs (N=265) showed that there no clinically important difference between ECV plus β2 agonist and control (no intervention) on cephalic vaginal birth in pregnant women with breech presentation: RR 2.03 (95% CI 0.22 to 19.01).
- Very low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on breech vaginal birth in pregnant women with breech presentation: RR 0.38 (95% CI 0.20 to 0.69).
- Low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.53 (95% CI 0.41 to 0.67).
- Very low quality evidence from 1 RCT (N=48) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RD 0.00 (95% CI −0.08 to 0.08).
- Very low quality evidence from 3 RCTs (N=208) showed that there is no statistically significant difference between ECV plus β2 agonist and control (no intervention) on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD −0.01 (95% CI −0.03 to 0.01) p=0.66.
- Very low quality evidence from 2 RCTs (N=208) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.80 (95% CI 0.31 to 2.10).
Comparison 8. ECV + β2 agonist versus ECV only
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on cephalic vaginal birth in pregnant women with breech presentation: RR 1.32 (95% CI 0.67 to 2.62).
- Very low quality evidence from 1 RCT (N=58) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on breech vaginal birth in pregnant women with breech presentation: RR 0.75 (95% CI 0.22 to 2.50).
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 0.79 (95% CI 0.27 to 2.28).
- Very low quality evidence from 1 RCT (N=114) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.00 (95% CI 0.21 to 4.75).
Comparison 9. ECV + β2 agonist versus ECV + Placebo
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.54 (95% CI 0.24 to 9.76).
- Very low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 1.27 (95% CI 0.41 to 3.89).
- Very low quality evidence from 2 RCTs (N=227) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on breech vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.33 to 2.97).
- Low quality evidence from 4 RCTs (N=532) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.81 (95% CI 0.72 to 0.92)
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.78 (95% CI 0.17 to 3.63).
- Very low quality evidence from 1 RCT (N=124) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 10. ECV + Ca 2+ channel blocker versus ECV + Placebo
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.87 to 1.48).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.90 (95% CI 0.73 to 1.12).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 1.11 (95% CI 0.88 to 1.40).
- High quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: MD −0.20 (95% CI −0.70 to 0.30).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no statistically significant difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.01 to 0.01) p=1.00.
- Low quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.52 (95% 0.05 to 5.02).
Comparison 11. ECV + Ca2+ channel blocker versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=90) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on cephalic presentation in labour in pregnant women with breech presentation: RR 0.62 (95% CI 0.39 to 0.98).
- Very low quality evidence from 2 RCTs (N=126) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 1.26 (95% CI 0.55 to 2.89).
- Very low quality evidence from 2 RCTs (N=132) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on the number of caesarean sections in pregnant women with breech presentation: RR 1.42 (95% CI 1.06 to 1.91).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on admission to SCBU/NICU in pregnant women with breech presentation: Peto OR 0.53 (95% CI 0.05 to 5.22).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 12. ECV + µ-receptor agonist versus ECV only
- High quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.80 to 1.24).
- Low quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 1.00 (95% CI 0.42 to 2.40).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 13. ECV + µ-receptor agonist versus ECV + Placebo
Cephalic vaginal birth after successful ecv.
- High quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on cephalic vaginal birth after successful ECV in pregnant women with breech presentation: RR 1.00 (95% CI 0.86 to 1.17).
Caesarean section after successful ECV
- Low quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after successful ECV in pregnant women with breech presentation: RR 0.97 (95% CI 0.33 to 2.84).
Breech vaginal birth after unsuccessful ECV
- High quality evidence from 3 RCTs (N=186) showed that there is a clinically important difference favouring ECV plus µ-receptor agonist over ECV plus placebo on breech vaginal birth after unsuccessful ECV in pregnant women with breech presentation: RR 0.10 (95% CI 0.02 to 0.53).
Caesarean section after unsuccessful ECV
- Moderate quality evidence from 3 RCTs (N=186) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after unsuccessful ECV in pregnant women with breech presentation: RR 1.19 (95% CI 1.09 to 1.31).
- Low quality evidence from 1 RCT (N=137) showed that there is no statistically significant difference between ECV plus µ-receptor agonist and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03) p=1.00.
Comparison 14. ECV + µ-receptor agonist versus ECV + Anaesthesia
- Moderate quality evidence from 1 RCT (N=92) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on cephalic vaginal birth in pregnant women with breech presentation: RR 1.04 (95% CI 0.84 to 1.29).
- Very low quality evidence from 2 RCTs (N=212) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on the number of caesarean sections in pregnant women with breech presentation: RR 0.90 (95% CI 0.61 to 1.34).
- Very low quality evidence from 1 RCT (N=129) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on admission to SCBU/NICU in pregnant women with breech presentation: RR 2.30 (95% CI 0.21 to 24.74).
- Low quality evidence from 2 RCTs (N=255) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 15. ECV + Nitric oxide donor versus ECV + Placebo
- Very low quality evidence from 3 RCTs (N=224) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.59 to 2.16).
- Low quality evidence from 1 RCT (N=99) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.78 (95% CI 0.49 to 1.22).
- Low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.83 (95% CI 0.68 to 1.01).
Comparison 16. ECV + Nitric oxide donor versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=74) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus nitric oxide donor on cephalic presentation in labour in pregnant women with breech presentation: RR 0.56 (95% CI 0.29 to 1.09).
- Very low quality evidence from 2 RCTs (N=97) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 0.98 (95% CI 0.47 to 2.05).
- Very low quality evidence from 1 RCT (N=59) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on the number of caesarean sections in pregnant women with breech presentation: RR 1.07 (95% CI 0.73 to 1.57).
Comparison 17. ECV + Talcum powder versus ECV + Gel
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic presentation in labour in pregnant women with breech presentation: RR 1.02 (95% CI 0.68 to 1.53).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic vaginal birth in pregnant women with breech presentation: RR 1.08 (95% CI 0.67 to 1.74).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.67 to 1.33).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.96 (95% CI 0.38 to 10.19).
Comparison 18. Postural management versus No postural management
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic presentation in labour in pregnant women with breech presentation: RR 1.26 (95% CI 0.70 to 2.30).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic vaginal birth in pregnant women with breech presentation: RR 1.11 (95% CI 0.59 to 2.07).
Breech vaginal delivery
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on breech vaginal delivery in pregnant women with breech presentation: RR 1.15 (95% CI 0.67 to 1.99).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on the number of caesarean sections in pregnant women with breech presentation: RR 0.69 (95% CI 0.31 to 1.52).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.24 (95% CI 0.03 to 2.03).
Comparison 19. Postural management + ECV versus ECV only
- Moderate quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 1.05 (95% CI 0.80 to 1.38).
- Low quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.13 (95% CI 0.00 to 6.55).
Economic evidence statements
No economic evidence was identified which was applicable to this review question.
The committee’s discussion of the evidence
Interpreting the evidence, the outcomes that matter most.
Provision of antenatal care is important for the health and wellbeing of both mother and baby with the aim of avoiding adverse pregnancy outcomes and enhancing maternal satisfaction and wellbeing. Breech presentation in labour may be associated with adverse outcomes for the fetus, which has contributed to an increased likelihood of caesarean birth. The committee therefore agreed that cephalic presentation in labour and method of birth were critical outcomes for the woman, and admission to SCBU/NICU, fetal death after 36 +0 weeks gestation, and infant death up to 4 weeks chronological age were critical outcomes for the baby. Apgar score <7 at 5 minutes and birth before 39 +0 weeks of gestation were important outcomes for the baby.
The quality of the evidence
The quality of the evidence for interventions for managing a longitudinal lie fetal malpresentation (that is breech presentation) in late pregnancy ranged from very low to high, with most of the evidence being of a very low or low quality.
This was predominately due to serious overall risk of bias in some outcomes; imprecision around the effect estimate in some outcomes; indirect population in some outcomes; and the presence of serious heterogeneity in some outcomes, which was unresolved by subgroup analysis. The majority of included studies had a small sample size, which contributed to imprecision around the effect estimate.
No evidence was identified to inform the outcomes of infant death up to 4 weeks chronological age and birth before 39 +0 weeks of gestation.
There was no publication bias identified in the evidence. However, the committee noted the influence pharmacological developers may have in these trials as funders, and took this into account in their decision making.
Benefits and harms
The committee discussed that in the case of breech presentation, a discussion with the woman about the different options and their potential benefits, harms and implications is needed to ensure an informed decision. The committee discussed that some women may prefer a breech vaginal birth or choose an elective caesarean birth, and that her preferences should be supported, in line with shared decision making.
The committee discussed that external cephalic version is standard practice for managing breech presentation in uncomplicated singleton pregnancies at or after 36+0 weeks. The committee discussed that there could be variation in the success rates of ECV based on the experience of the healthcare professional providing the ECV. There was some evidence supporting the use of ECV for managing a breech presentation in late pregnancy. The evidence showed ECV had a clinically important benefit in terms of cephalic presentations in labour and cephalic vaginal deliveries, when compared to no intervention. The committee noted that the evidence suggested that ECV was not harmful to the baby, although the effect estimate was imprecise relating to the relative rarity of the fetal death as an outcome.
Cephalic (head-down) vaginal birth is preferred by many women and the evidence suggests that external cephalic version is an effective way to achieve this. The evidence suggested ECV increased the chance for a cephalic vaginal birth and the committee agreed that it was important to explain this to the woman during her consultation.
The committee discussed the optimum timing for ECV. Timing of ECV must take into account the likelihood of the baby turning naturally before a woman commences labour and the possibility of the baby turning back to a breech presentation after ECV if it is done too early. The committee noted that in their experience, current practice was to perform ECV at 37 gestational weeks. The majority of the evidence demonstrating a benefit of ECV in this review involved ECV performed around 37 gestational weeks, although the review did not look for studies directly comparing different timings of ECV and their relative success rates.
The evidence in this review excluded women with previous complicated pregnancies, such as those with previous caesarean section or uterine surgery. The committee discussed that a previous caesarean section indicates a complicated pregnancy and that this population of women are not the focus of this guideline, which concentrates on women with uncomplicated pregnancies.
The committee’s recommendations align with other NICE guidance and cross references to the NICE guideline on caesarean birth and the section on breech presenting in labour in the NICE guideline on intrapartum care for women with existing medical conditions or obstetric complications and their babies were made.
ECV combined with pharmacological agents
There were some small studies comparing a variety of pharmacological agents (including β2 agonists, Ca 2+ channel blockers, µ-receptor agonists and nitric oxide donors) given alongside ECV. Overall the evidence typically showed no clinically important benefit of adding any pharmacological agent to ECV except in comparisons with a control arm with no ECV where it was not possible to isolate the effect of the ECV versus the pharmacological agent. The evidence tended toward benefit most for β2 agonists and µ-receptor agonists however there was no consistent or high quality evidence of benefit even for these agents. The committee agreed that although these pharmacological agents are used in practice, there was insufficient evidence to make a recommendation supporting or refuting their use or on which pharmacological agent should be used.
The committee discussed that the evidence suggesting µ-receptor agonist, remifentanil, had a clinically important benefit in terms reducing breech vaginal births after unsuccessful ECV was biologically implausible. The committee noted that this pharmacological agent has strong sedative effects, depending on the dosage, and therefore studies comparing it to a placebo had possible design flaws as it would be obvious to all parties whether placebo or active drug had been received. The committee discussed that the risks associated with using remifentanil such as respiratory depression, likely outweigh any potential added benefit it may have on managing breech presentation.
There was some evidence comparing different anaesthetics together with ECV. Although there was little consistent evidence of benefit overall, one small study of low quality showed a combination of 2% lidocaine and epinephrine via epidural catheter (anaesthesia) with ECV showed a clinically important benefit in terms of cephalic presentations in labour and the method of birth. The committee discussed the evidence and agreed the use of anaesthesia via epidural catheter during ECV was uncommon practice in the UK and could be expensive, overall they agreed the strength of the evidence available was insufficient to support a change in practice.

Postural management
There was limited evidence on postural management as an intervention for managing breech presentation in late pregnancy, which showed no difference in effectiveness. Postural management was defined as ‘knee-chest position for 15 minutes, 3 times a day’. The committee agreed that in their experience women valued trying interventions at home first which might make postural management an attractive option for some women, however, there was no evidence that postural management was beneficial. The committee also noted that in their experience postural management can cause notable discomfort so it is not an intervention without disadvantages.
Cost effectiveness and resource use
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question.
The committee’s recommendations to offer external cephalic version reinforces current practice. The committee noted that, compared to no intervention, external cephalic version results in clinically important benefits and that there would also be overall downstream cost savings from lower adverse events. It was therefore the committee’s view that offering external cephalic version is cost effective and would not entail any resource impact.
Andersen 2013
Brocks 1984
Bujold 2003
Burgos 2016
Chalifoux 2017
Chenia 1987
Collaris 2009
Dafallah 2004
Diguisto 2018
Dugoff 1999
El-Sayed 2004
Fernandez 1997
Hindawi 2005
Hilton 2009
Hofmeyr 1983
Mahomed 1991
Mancuso 2000
Marquette 1996
Mohamed Ismail 2008
NorAzlin 2005
Robertson 1987
Schorr 1997
Sullivan 2009
VanDorsten 1981
Vallikkannu 2014
Weiniger 2010
Appendix A. Review protocols
Review protocol for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 260K)
Appendix B. Literature search strategies
Literature search strategies for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 281K)
Appendix C. Clinical evidence study selection
Clinical study selection for: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 113K)
Appendix D. Clinical evidence tables
Clinical evidence tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.2M)
Appendix E. Forest plots
Forest plots for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 678K)
Appendix F. GRADE tables
GRADE tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.0M)
Appendix G. Economic evidence study selection
Economic evidence study selection for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix h. economic evidence tables, economic evidence tables for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix i. economic evidence profiles, economic evidence profiles for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix j. economic analysis, economic evidence analysis for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No economic analysis was conducted for this review question.
Appendix K. Excluded studies
Excluded clinical and economic studies for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, clinical studies, table 24 excluded studies.
View in own window
Economic studies
No economic evidence was identified for this review.
Appendix L. Research recommendations
Research recommendations for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No research recommendations were made for this review question.
Evidence reviews underpinning recommendation 1.2.38
These evidence reviews were developed by the National Guideline Alliance, which is a part of the Royal College of Obstetricians and Gynaecologists
Disclaimer : The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government , Scottish Government , and Northern Ireland Executive . All NICE guidance is subject to regular review and may be updated or withdrawn.
- Cite this Page National Guideline Alliance (UK). Management of breech presentation: Antenatal care: Evidence review M. London: National Institute for Health and Care Excellence (NICE); 2021 Aug. (NICE Guideline, No. 201.)
- PDF version of this title (2.2M)
In this Page
Other titles in this collection.
- NICE Evidence Reviews Collection
Related NICE guidance and evidence
- NICE Guideline 201: Antenatal care
Supplemental NICE documents
- Supplement 1: Methods (PDF)
- Supplement 2: Health economics (PDF)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Identification of breech presentation: Antenatal care: Evidence review L [ 2021] Review Identification of breech presentation: Antenatal care: Evidence review L National Guideline Alliance (UK). 2021 Aug
- Vaginal delivery of breech presentation. [J Obstet Gynaecol Can. 2009] Vaginal delivery of breech presentation. Kotaska A, Menticoglou S, Gagnon R, MATERNAL FETAL MEDICINE COMMITTEE. J Obstet Gynaecol Can. 2009 Jun; 31(6):557-566.
- Review Cephalic version by moxibustion for breech presentation. [Cochrane Database Syst Rev. 2005] Review Cephalic version by moxibustion for breech presentation. Coyle ME, Smith CA, Peat B. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD003928. Epub 2005 Apr 18.
- [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. [Gynecol Obstet Fertil Senol. 2...] [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. Riethmuller D, Ramanah R, Mottet N. Gynecol Obstet Fertil Senol. 2018 Dec; 46(12):937-947. Epub 2018 Oct 28.
- Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. [J Obstet Gynaecol Br Emp. 1961] Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. BAINBRIDGE MN, NIXON WC, SMYTH CN. J Obstet Gynaecol Br Emp. 1961 Oct; 68:748-54.
Recent Activity
- Management of breech presentation Management of breech presentation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.
Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.
Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death
Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Malpresentation
8-minute read
If you feel your waters break and you have been told that your baby is not in a head-first position, seek medical help immediately .
- Malpresentation is when your baby is not facing head-first down the birth canal as birth approaches.
- The most common type of malpresentation is breech — when your baby’s bottom or feet are facing downwards.
- A procedure called external cephalic version can sometimes turn a breech baby into a head-first position at 36 weeks.
- Most babies with malpresentation are born by caesarean, but you may be able to have a vaginal birth if your baby is breech.
- There is a serious risk of cord prolapse if your waters break and your baby is not head-first.
What are presentation and malpresentation?
‘Presentation’ describes how your baby is facing down the birth canal. The ‘presenting part’ is the part of your baby’s body that is against the cervix .
The ideal presentation is head-first, with the crown (top) of the baby’s head against the cervix, with the chin tucked into the baby’s chest. This is called ‘vertex presentation’.
If your baby is in any other position, it’s called ‘malpresentation’. Malpresentation can mean your baby’s face, brow, buttocks, foot, back, shoulder, arms or legs or the umbilical cord are against the cervix.
It’s safest for your baby’s head to come out first. If any other body part goes down the birth canal first, the risks to you and your baby may be higher. Malpresentation increases the chance that you will have a more complex vaginal birth or a caesarean.
If my baby is not head-first, what position could they be in?
Malpresentation is caused by your baby’s position (‘lie’). There are different types of malpresentation.
Breech presentation
This is when your baby is lying with their bottom or feet facing down. Sometimes one foot may enter the birth canal first (called a ‘footling presentation’).
Breech presentation is the most common type of malpresentation.
Face presentation
This is when your baby is head-first but stretching their neck, with their face against the cervix.
Transverse lie
This is when your baby is lying sideways. Their back, shoulders, arms or legs may be the first to enter the birth canal.
Oblique lie
This is when your baby is lying diagonally. No particular part of their body is against the cervix.
Unstable lie
This is when your baby continually changes their position after 36 weeks of pregnancy.
Cord presentation
This is when the umbilical cord is against the cervix, between your baby and the birth canal. It can happen in any situation where your baby’s presenting part is not sitting snugly in your pelvis. It can become an emergency if it leads to cord prolapse (when the cord is born before your baby, potentially reducing placental blood flow to your baby).
What is malposition?
If your baby is lying head-first, the best position for labour is when their face is towards your back.
If your baby is facing the front of your body (posterior position) or facing your side (transverse position) this is called malposition. Transverse position is not the same as transverse lie. A transverse position means your labour may take a bit longer and you might feel more pain in your back. Often your baby will move into a better position before or during labour.
Why might my baby be in the wrong position?
Malpresentation may be caused by:
- a low-lying placenta
- too much or too little amniotic fluid
- many previous pregnancies, making the muscles of the uterus less stable
- carrying twins or more
Often no cause is found.
Is it likely that my baby will be in the wrong position?
Many babies are in a breech position during pregnancy. They usually turn head-first as pregnancy progresses, and more than 9 in 10 babies in Australia have a vertex presentation (ideal presentation, head-first) at birth.
You are more likely to have a malpresentation if:
- this is your first baby
- you are over 40 years old
- you've had a previous breech baby
- you go into labour prematurely
How is malpresentation diagnosed?
Malpresentation is normally diagnosed when your doctor or midwife examines you, from 36 weeks of pregnancy. If it’s not clear, it can be confirmed with an ultrasound.
Can my baby’s position be changed?
If you are 36 weeks pregnant , it may be possible to gently turn your baby into a head-first position. This is done by an obstetrician using a technique called external cephalic version (ECV).
Some people try different postures or acupuncture to correct malpresentation, but there isn’t reliable evidence that either of these work.
Will I need a caesarean if my baby has a malpresentation?
Most babies with a malpresentation close to birth are born by caesarean . You may be able to have a vaginal birth with a breech baby, but you will need to go to a hospital that can offer you and your baby specialised care.
If your baby is breech, an elective (planned) caesarean is safer for your baby than a vaginal birth in the short term. However, in the longer term their health will be similar, on average, regardless of how they were born.
A vaginal birth is safer for you than an elective caesarean. However, about 4 in 10 people planning a vaginal breech birth end up needing an emergency caesarean . If this happens to you, the risk of complications will be higher.
Your doctor can talk to you about your options. Whether it’s safe for you to try a vaginal birth will depend on many factors. These include how big your baby is, the position of your baby, the structure of your pelvis and whether you’ve had a caesarean in the past.
What are the risks if I have my baby when it’s not head-first?
If your waters break when your baby is not head-first, there is a risk of cord prolapse. This is an emergency.
Vaginal breech birth
Risks to your baby can include:
- Erb’s palsy
- fractures, dislocations or other injuries
- bleeding in your baby’s brain
- low Apgar scores
- their head getting stuck – this is an emergency
Risks to you include:
- blood loss or blood clots
- infection in the wound
- problems with the anaesthetic
- damage to other organs nearby, such as your bladder
- a higher chance of problems in future pregnancies
- a longer recovery time than after a vaginal birth
Risks to your baby include:
- trouble with breathing — this is temporary
- getting a small cut during the surgery
Will I have a malpresentation in my future pregnancies?
If you had a malpresentation in one pregnancy, you have a higher chance of it happening again, but it won’t necessarily happen in future pregnancies. If you’re worried, it may help to talk to your doctor or midwife so they can explain what happened.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: July 2022
Related pages
Labour complications.
- Interventions during labour
- Giving birth - stages of labour
Breech pregnancy
Search our site for.
- Caesarean Section
- Foetal Version
Need more information?
Top results
When a baby is positioned bottom-down late in pregnancy, this is called the breech position. Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website

Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

Presentation and position of baby through pregnancy and at birth
Presentation and position refer to where your baby’s head and body is in relation to your birth canal. Learn why it’s important for labour and birth.
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
- MSD careers
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.
Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.
Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death
Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

Pregnant Workers Fairness Act Final Regulations Released
The Equal Employment Opportunity Commission (EEOC) released the text of the final regulations and interpretative guidance implementing the Pregnant Workers Fairness Act (PWFA) on April 15, 2024. The final regulations are expected to be formally published in the April 19, 2024, Federal Register and will be effective 60 days later.
The EEOC received more than 100,000 public comments, including comments from Jackson Lewis, in response to the Commission’s notice of the proposed regulations issued on Aug. 11, 2023 . Although largely unchanged from the proposed regulations, the final regulations provide important clarifications and insights into how the EEOC will enforce the law. Discussed below are some key points employers need to know about the final regulations.
Key PWFA Requirements
The PWFA, which went into effect on June 27, 2023, requires employers with at least 15 employees and other covered entities to provide reasonable accommodations to a qualified employee’s or applicant’s known limitations related to, affected by, or arising out of pregnancy, childbirth, or related medical conditions, unless the accommodation will cause undue hardship on the operation of the employer’s business.
Qualified Employee
Under the PWFA, an employee has two ways to establish they are a “qualified employee”:
- Like under the Americans With Disabilities Act (ADA), “an employee or applicant who, with or without reasonable accommodation, can perform the essential functions of the employment position” is qualified.
- If an employee (or applicant) cannot perform all essential job functions even with reasonable accommodation, the employee can be qualified for accommodations under the PWFA if: (a) the inability to perform an essential job function is for a temporary period; (b) the essential job function(s) could be performed in the near future; and (c) the inability to perform the essential function(s) can be reasonably accommodated. The Act, however, does not define “temporary” or “in the near future.” Several commentors raised concerns about the EEOC’s definition of these terms in the proposed regulations.
Like the proposed regulations, the final regulations state that “temporary” means “lasting for a limited time, not permanent, and may extend beyond ‘in the near future.’” Unlike the proposed regulations, however, the final regulations state that assessing whether all essential job functions can be performed in the near future depends on the circumstances:
- For a current pregnancy, “in the near future” is generally defined as 40 weeks from the start of the temporary suspension of an essential function.
- For conditions other than a current pregnancy, “in the near future” is not defined as any particular length of time. However, the preamble to the final regulations explains that an employee who needs indefinite leave cannot perform essential job functions “in the near future.”
The final regulations explain that employers should consider whether an employee will be able to perform the essential functions “in the near future” each time an employee asks for an accommodation that requires suspension of an essential job function.
Ultimately, whether an employee is “qualified” involves a fact-sensitive evaluation whether the temporary suspension of essential job functions can be reasonably accommodated by the employer. This is significantly different from the ADA reasonable accommodation obligation and may involve, as the final regulations state, removing essential job functions and other arrangements including, but not limited to, requiring the employee perform the remaining job functions and other functions assigned by the employer, temporarily transferring the employee to another job or assigning the employee to light or modified duty, or allowing the employee to participate in an employer’s light or modified duty program.
Accommodations Only Required for Individual With Limitation
The EEOC explains that the regulations do not require employers to provide accommodations to an employee when an employee’s partner, spouse, or family member — not the employee themselves — has a physical or mental condition related to, affected by, or arising out of pregnancy, childbirth, or related medical conditions. For clarity, the EEOC revised the final regulations’ definition of “limited” to state the limitation must be the specific employee.
Known Limitations
Employers are only obligated under the PWFA to accommodate an individual’s “known limitation.”
A “limitation” is defined as a “physical or mental condition related to, affected by, or arising out of pregnancy, childbirth, or related medical conditions, of the specific employee in question.” The condition may be “modest, minor, and/or episodic, and does not need to meet the definition of “disability” under the ADA.
It becomes “known” to the employer when the employee or the employee’s representative has communicated the limitation to the employer. An employee’s representative may include a family member, friend, healthcare provider, union representative, or other representative.
The limitation may be communicated to a supervisor, a manager, someone who has supervisory authority for the employee or who regularly directs the employee’s tasks (or the equivalent in the case of an applicant), human resources personnel, or other appropriate official or by following the steps in the employer’s policy to request an accommodation.
This communication need not be in any specific format and may also be oral.
Pregnancy, Childbirth, Related Medical Conditions
Although the EEOC acknowledged receiving many comments on the scope of the proposed definition of “pregnancy, childbirth or related medical conditions,” it made no substantive changes to the definition in the final regulations.
“Pregnancy” and “childbirth” are still defined as including current pregnancy, past pregnancy, potential or intended pregnancy (which can include infertility, fertility treatments and the use of contraception), labor, and childbirth (including vaginal and cesarean delivery).
The term “related medical conditions” continues to be defined as conditions that are “related to, are affected by, or arise out of pregnancy or childbirth.” The regulations provide the following non-exhaustive list of examples: termination of pregnancy, including by miscarriage, stillbirth, or abortion; lactation and conditions related to lactation; menstruation; postpartum depression, anxiety or psychosis; vaginal bleeding; preeclampsia; pelvic prolapse; preterm labor; ectopic pregnancy; gestational diabetes; cesarean or perineal wound infection; maternal cardiometabolic disease; endometriosis; changes in hormone levels; and many other conditions.
The final regulations also reference related medical conditions that are not unique to pregnancy or childbirth, such as chronic migraine headaches, nausea or vomiting, high blood pressure, incontinence, carpal tunnel syndrome, and many other medical conditions. These conditions are covered by the PWFA only if the condition relates to pregnancy or childbirth or are exacerbated by pregnancy or childbirth, although the ADA or other civil rights statutes may apply.
Documentation
The final PWFA regulations continue to provide for a “reasonableness” standard in evaluating the circumstances under which an employer may request documentation from an employee. The final regulations, however, modify the definition of “reasonable documentation.” An employer may only request the “minimum documentation” necessary to confirm the employee has a physical or mental condition related to, affected by, or arising out of pregnancy, childbirth, or related medical conditions (a limitation) and describe the adjustment or change at work due to the limitation.
In addition to stating when an employer can ask for documentation, the PWFA regulations add a paragraph regarding an employee’s self-confirmation of their pregnancy status. It provides that an employer must accept as sufficient an employee’s self-confirmation when: (1) the pregnancy is obvious; or (2) an employee seeks one of the “predictable assessment” accommodation requests set forth in the regulations (discussed below).
The final PWFA regulations make clear the circumstances where it is not reasonable to seek supporting documentation. These circumstances include when: (1) the limitation and adjustment or change needed is obvious and the employee provides self-confirmation; (2) the employer has sufficient information to determine whether the employee has a qualifying limitation and needs an adjustment or change due to the limitation; (3) when the employee is pregnant a “predictable assessment”; (4) the reasonable accommodation relates to a time and/or place to pump or to nurse during work hours, and the employee provides self-confirmation; or (5) the requested accommodation is available to employees without known limitations under the PWFA pursuant to a policy or practice without submitting supporting documentation.
Importantly, the same prohibitions on disability-related inquiries and medical examinations as well as the protection of medical information enforced under the ADA apply with equal force to documentation collected under the PWFA. Employers should ensure they continue to limit inquiries to only those that are job-related and consistent with business necessity. Employers should also treat all documentation relating to a PWFA accommodation request like they treat ADA documentation — maintain it confidentially and separate from an employee’s personnel file.
Reasonable Accommodations
The PFWA requires employers to provide reasonable accommodations, which the final regulations define to be generally consistently with the ADA except for temporarily excusing or eliminating the performance of an essential job function. Otherwise, the rule provides that a reasonable accommodation is a modification or adjustment that is “reasonable on its face, i.e., ordinarily or in the run of cases” if it appears to be “feasible” or “plausible.” An accommodation also must be effective in meeting the qualified employee’s needs to remove a work-related barrier and provide an employee with equal employment opportunity to benefit from all privileges of employment.
The final regulations include examples of requests that may be reasonable. These include schedule changes due to morning sickness or to treat medical issues following delivery, adjustments to accommodate restrictions for lifting or requests for light duty, time and/or space to pump or nurse during work hours, or time off to recover from childbirth.
Lactation Accommodations
The EEOC’s final regulations require reasonable accommodation for lactation beyond what may be required under the Providing Urgent Maternal Protection for Nursing Mothers Act (PUMP Act). The PUMP Act generally requires reasonable break time and space shielded from view and free from intrusion for a nursing mother to express breast milk. The final PWFA regulations provide a non-exhaustive list of examples of accommodations relating to lactation, including space for pumping that is in reasonable proximity to a sink, running water, and refrigeration for storing milk.
The final regulations add nursing during working hours (as distinct from pumping) to the list of potentially reasonable accommodations. In the comments explaining this addition, the EEOC cautioned that accommodations for nursing mothers during work hours address situations where the employee and child are in close proximity in the normal course of business, such as where the employee works from home or where the employer offers on-site daycare. The EEOC stated this is not intended to create a right to proximity to nurse because of an employee’s preference.
Predictable Assessments
Like the proposed regulations, the final regulations recognize four “predictable assessments” that will not impose an undue hardship in “virtually all cases”:
- Allowing an employee to carry or keep water near to enable them to drink;
- Permitting an employee to take additional restroom breaks as needed;
- Allowing an employee whose work requires standing to sit and whose work requires sitting to stand as needed; and
- Allowing an employee to take breaks to eat and drink as needed.
Despite stating the predictable assessments above will not “in virtually all cases” impose an undue hardship, the EEOC clarified this does not mean such requests are reasonable per se. The EEOC recognized that in certain industries, these predictable assessments may cause an undue hardship. Accordingly, employers may still conduct an individualized assessment of a predictable assessment accommodation request. However, the final regulations make clear that any such individualized assessment should be particularly simple and straightforward.
Many individuals and organizations that submitted comments on the proposed regulations suggested the addition of other types of predictable assessment accommodations, including dress code modifications, minor workstation modifications, proximity to a restroom, permitting eating and drinking at a workstation, rest breaks, and personal protective equipment. Although noting agreement with the commenters and stating that employers should be able to provide such requests with “little difficulty,” the EEOC declined to expand the list of predictable assessments beyond the four originally listed that in “virtually all cases” will be considered reasonable and will not pose an undue hardship. In response to comments objecting to predictable assessments based on different challenges by industry, the EEOC guidance recognizes that an employer in certain industries may assert an accommodation request otherwise deemed to be a predictable assessment causes the employer an undue hardship and may deny the request.
Undue Hardship
The EEOC adopted the same standard for undue hardship in the final regulations as was in the proposed regulations. When an employee can perform all their essential job functions, the EEOC stated that undue hardship has the same meaning as under the ADA and generally means significant difficulty or expense for the employer’s operation. If an employee cannot perform all essential functions and the accommodation is temporary suspension of an essential job function, the employer needs to consider the ADA definition of undue hardship and the following relevant factors: (1) the length of time the employee or applicant will be unable to perform the essential function(s); (2) whether there is work for the employee to accomplish by allowing the employee to perform all the other functions of the job, transferring the employee to a different position, or otherwise; (3) the nature of the essential function, including its frequency; (4) whether the covered entity has temporarily suspended the performance of essential job functions for other employees in similar positions; (5) whether there are other employees, temporary employees, or third parties who can perform or be temporarily hired to perform the essential function(s); and (6) whether the essential function(s) can be postponed or remain unperformed for any length of time and for how long.
EEOC Interpretative Guidance
The EEOC’s final regulations include an appendix entitled “Appendix A to Part 1636—Interpretative Guidance on the Pregnant Workers Fairness Act” (Interpretative Guidance). The Interpretative Guidance, which becomes part of the final regulations, has the same force and effect as the final regulations.
The Interpretative Guidance addresses the major provisions of the PWFA and its regulations and explains the main concepts pertaining to an employer’s legal requirements under the PWFA to make reasonable accommodations for known limitations (physical or mental conditions related to, affected by, or arising out of pregnancy, childbirth, or related medical conditions). It represents the EEOC’s interpretation of the PWFA and, as stated in comments to the final regulations, the EEOC will be guided by the Interpretive Guidance when enforcing the PWFA. The Interpretative Guidance includes many examples and other practical guidance illustrating common workplace scenarios and how the PWFA applies.
Remedies, Enforcement
The final regulations’ remedies and enforcement are the same as proposed. Remedies under the PWFA mirror those under Title VII of the Civil Rights Act and include injunctive and other equitable relief, compensatory and punitive damages, and attorney’s fees. Employers that demonstrate good faith efforts to work with employees to identify and make reasonable accommodations have an affirmative defense to money damages.
PWFA’s Relationship to Other Federal, State, Local Laws
The final regulations provide that the PWFA does not invalidate or limit the powers, remedies, or procedures available under any federal, state, or local law that provides greater or equal protection for individuals affected by pregnancy, childbirth, or related medical conditions. About 40 states and cities have laws protecting employees and applicants from discrimination due to pregnancy, childbirth, and related medical conditions. Accordingly, employers should evaluate whether state and/or local law may provide greater rights and obligations than the PWFA. To the extent such laws provide greater obligations, the PWFA final regulations require employers to comply with both the PWFA and analogous state and local law.
Jackson Lewis invites you to a complimentary webinar on the PWFA final regulations on May 10 at 1:00 p.m. ET.
If you have any questions about the PWFA, the implications of the final regulations for your organization, or the many state and local laws, please contact a Jackson Lewis attorney.
© 2024 Jackson Lewis P.C. This material is provided for informational purposes only. It is not intended to constitute legal advice nor does it create a client-lawyer relationship between Jackson Lewis and any recipient. Recipients should consult with counsel before taking any actions based on the information contained within this material. This material may be considered attorney advertising in some jurisdictions. Prior results do not guarantee a similar outcome.
Focused on labor and employment law since 1958, Jackson Lewis P.C.'s 950+ attorneys located in major cities nationwide consistently identify and respond to new ways workplace law intersects business. We help employers develop proactive strategies, strong policies and business-oriented solutions to cultivate high-functioning workforces that are engaged, stable and diverse, and share our clients' goals to emphasize inclusivity and respect for the contribution of every employee. For more information, visit https://www.jacksonlewis.com .
Related services
Practice Advice and Counsel
Practice Disability, Leave and Health Management
Issue Disability, Leave and Health Management > Pregnant Workers Fairness Act and PUMP for Nursing Mothers Act
- Anti-Abortion Movement
- Women’s History
- Film & TV
- Gender Violence
- #50YearsofMs

More Than A Magazine, A Movement

- Justice & Law
The Lie at the Heart of the Latest Supreme Court Abortion Case
‘life of the mother’ exceptions are nothing more than a politically expedient lie designed to distract from the violence inherent in the maintenance of abortion bans..

Idaho will attempt to defend its extreme abortion ban at the Supreme Court this Wednesday . Like many other abortion bans in the United States, the Idaho law contains a so-called life exception, which purports to allow an abortion when “necessary to prevent the death” of the pregnant person. But do these exceptions actually preserve the lives of patients in practice? As Mayron Hollis , Amanda Zurawski , the family of Yeniifer Alvarez-Estrada Glick, and countless other women can attest, the answer is no. And the truth is, they’re not designed to.
No matter how they’re drafted and redrafted, abortion bans rest on the denial of the fundamental human right to reproductive autonomy. So-called life exceptions are designed to make abortion bans seem more politically palatable by allegedly allowing for abortions in “extreme” circumstances. But their political function is revealed by their unworkability: The exceptions are medically incoherent and designed in ways that are not possible to implement.
Thanks to a deadly combination of factors—including the wording of so-called life exceptions and a climate of fear in medical settings generated by abortion bans— life-threatening denials of care are inevitable.
For abortion rights opponents, this is a feature, not a bug. The goal is not to save lives but to drive the number of abortions (and abortion providers) down to zero, no matter the cost to the lives, health, dignity and autonomy of pregnant people. These life exceptions merely mask the quieter devastation all abortion bans cause: the stripping away of people’s bodily autonomy and their ability to make the best decision for themselves and their families in order to pursue their dreams and life projects .
The incoherence of life exceptions is well-established. Many lack definitions of what constitutes a life-threatening condition, recite lists of qualifying conditions that omit significant complications, or contain definitions that do not correspond to specific medical conditions.
Risks to life also emerge on a sliding scale, and the lack of clarity in law means patients are forced to wait—often bleeding and risking sepsis, organ damage or sudden death—until the threats to their life are deemed severe enough to permit abortion.
This is what happened to Anya Cook , a Florida woman who was sent home from the emergency room after being diagnosed with a life-threatening pregnancy complication. The next day, she lost roughly half the blood in her body during the process of a harrowing miscarriage.
How Abortion Bans Hinder Providers
Cases like these are not outliers. Abortion bans have led hospitals to fundamentally alter how they provide care, implementing new policies to minimize legal risks to clinicians and hospitals rather than medical risks to patients, according to a recent report from Physicians for Human Rights.
And yet, attempts to clarify these “life exceptions” have also proven ineffective. In Texas, the state medical board punted on offering further guidance to doctors to help them determine what would qualify as a life-threatening condition, saying, “We can only do so much” to clarify the terms of the law.
The goal is not to save lives but to drive the number of abortions (and abortion providers) down to zero, no matter the cost to the lives, health, dignity and autonomy of pregnant people
The chief victims of abortion bans are pregnant people. But the impact on clinicians and medical systems renders life exceptions even more ineffective. Unclear criminal laws, aggressive statements from law enforcement officials, and penalties up to life in prison make clinicians hesitant to provide life-saving care even in clear cases. The consequences for making an assessment that a state attorney general disagrees with about the necessity of care could be years of prosecution and threats to their medical license, even if they’re ultimately acquitted.
Clinicians in some states are also contending with privately enforced abortion prohibitions. These so-called bounty laws empower private individuals—sometimes limited to relatives of the pregnant woman, sometimes including strangers—to sue health providers who perform abortions. Because suits can be brought by bystanders who may have no understanding of the medical and legal contexts (but who are financially incentivized to push the boundaries of these laws), providers face the prospect of continuously defending themselves from frivolous or malicious lawsuits whenever they provide abortions or related care.
As a result, providers will predictably be less likely to provide any abortion care ever, even under life-threatening circumstances, and marginally less likely in each case to be willing to provide care.
All of this has driven clinicians out of practicing in entire states or regions—leaving patients in those regions who experience pregnancy complications without access to providers who have the skills to help them.
One doctor trained in specialized miscarriage and abortion care reported being forced out of her home state because she couldn’t bear to keep denying care and feared prosecution for the care she did provide.
This experience is echoed in other states, where clinicians report feeling “like there’s a target on [their] back[s].” In Idaho, a recent report showed that the state has lost 22 percent of its OB-GYNs since Roe v. Wade was overturned.
Ultimately, abortion bans put the health and human rights of pregnant people at risk, which can’t be eliminated by creating medically incoherent lists of exceptions. According to the World Health Organization (WHO), such an environment is created by all criminal abortion restrictions—not just extreme bans. For this reason, the WHO recommends the full decriminalization of abortion care and that it be made available at the request of the pregnant person.
The WHO guidelines recognize a fundamental reality: Pregnant people are not safe unless abortion is protected and fulfilled as a human right (as we argue in our amicus brief to the Supreme Court in the Idaho case). “Life of the mother” exceptions are nothing more than a politically expedient lie designed to distract from the violence inherent in the maintenance of abortion bans.
Abortion ban exceptions don’t protect lives—robust, effective access to abortion does.
Abortion Ranks Among Top Issues for Young Women Voters
Arizona Republicans Are Divided Over Abortion. For Progressives, This Is a Political Opportunity.
Anti-Abortion Extremists Are Diverting Tax Dollars to Crisis Pregnancy Centers
U.S. democracy is at a dangerous inflection point—from the demise of abortion rights, to a lack of pay equity and parental leave, to skyrocketing maternal mortality, and attacks on trans health. Left unchecked, these crises will lead to wider gaps in political participation and representation. For 50 years, Ms . has been forging feminist journalism—reporting, rebelling and truth-telling from the front-lines, championing the Equal Rights Amendment, and centering the stories of those most impacted. With all that’s at stake for equality, we are redoubling our commitment for the next 50 years. In turn, we need your help, Support Ms . today with a donation—any amount that is meaningful to you . For as little as $5 each month , you’ll receive the print magazine along with our e-newsletters, action alerts, and invitations to Ms . Studios events and podcasts . We are grateful for your loyalty and ferocity .
About Tess Graham

You May Also Like:

A Comedian in the War on Abortion: The Ms. Q&A with Lizz Winstead and Ruth Leitman

The Arizona Supreme Court Winds Back the Clock to 1864: ‘The Eyes of the World Are Watching’

PBS, ‘Frontline' Lead as Peabody Awards Announces 2024 Nominations for Documentary, News, Public Service and Radio/Podcast
PBS landed 11 nominations, by far the most of any outlet, as Peabody Awards Board of Jurors announced this year's 41 nominees across its documentary, news, public service and radio/podcast categories. The pubcaster's Peabody noms include "20 Days in Mariupol," which recently won the Oscar for best documentary feature film.
"20 Days in Mariupol" is a production of "Frontline" and the Associated Press. Among PBS series, "Frontline" landed five noms, the most of any program, while "Independent Lens" received three.
Also scoring multiple nominations was the combination of HBO and Max, which received four - including one for the doc "All the Beauty and the Bloodshed," which HBO Documentary Films produced with Neon and Participant. That's notable in light of last week's news that Participant Media is shutting its operations.
This year's Peabody Award nominees are selected from stories and projects that were released in broadcast or steaming media in 2023 and chosen via unanimous vote by 32 jurors (made up of media industry professionals, media scholars, critics and journalists). This year's entries numbered more than 1,100 projects across television, podcasts/radio and the web in entertainment, news, documentary, arts, children's/youth, public service and multimedia programming.
"From exposing injustice to capturing the struggles and triumphs of inspirational figures across the world, these extraordinary nominees demonstrate the power and beauty of compelling storytelling," said Peabody exec director Jeffrey Jones in a statement. "Within an increasingly diverse and constantly evolving media ecosystem, Peabody believes these nominees deserve special recognition for crafting bold stories that continue to inspire us, but also challenge us to do better."
Additional nominations in categories including entertainment, arts, children's/youth and interactive & immersive will be announced on Thursday, April 25, with winners revealed on May 9.
The 84th annual Peabody Awards will celebrate those winners with a ceremony at the Beverly Wilshire Hotel on Sunday, June 9. This reps the Peabody Award's return to an in-person event for the first time since 2019, and also its first time in L.A. - having previously been held in New York (and virtually over the past four years during the pandemic and Hollywood strikes). Peabody is based at the University of Georgia's Grady College of Journalism and Mass Communication.
Variety serves as media partner for the awards ceremony, which will be produced by Bob Bain Productions.
The Peabody Award nominees for documentary, news, public service and radio/podcast, listed by category and in alphabetical order (network/platform in parentheses) are:
DOCUMENTAR Y
"20 Days in Mariupol" (PBS)
"A team of Ukrainian journalists are trapped in the besieged city of Mariupol as they endeavor to continue their work documenting atrocities of the Russian invasion. As the only international reporters remaining in the city while Russian forces close in, they capture what will become some of the most defining images of the war-dying children, mass graves, the bombing of a maternity hospital, and more."
Frontline, The Associated Press
"All That Breathes" (HBO | Max)
"Two brothers devote their lives to the quixotic effort of protecting the black kite, a majestic bird of prey essential to the ecosystem of New Delhi that has been falling from the sky at alarming rates. Amid environmental toxicity and social unrest, the ‘kite brothers' spend day and night caring for the creatures in their makeshift avian basement hospital."
HBO Documentary Films in association with Submarine Deluxe and Sideshow; a Kiterabbit Films and Rise Films production in collaboration with HHMI Tangled Bank Studios
"All the Beauty and the Bloodshed" (HBO | Max)
"This film documents the life of artist Nan Goldin and her activism against the Sackler family, whose Purdue Pharma aggressively marketed its OxyContin painkiller-a substance largely responsible for America's opioid crisis. Goldin, who herself was once addicted to the drug, has led creative protests in an effort to stop major museums from taking Sackler donations and naming galleries after the family."
HBO Documentary Films presents a Participant and Neon presentation
"Bobi Wine: The People's President" (National Geographic)
"National Geographic documents Uganda's 2021 presidential election, in which music star, activist, and opposition leader Bobi Wine rallies his people in a dangerous fight for freedom from President Yoweri Museveni's oppressive 35-year regime."
Southern Films / Ventureland / National Geographic Documentary Films
"The Eternal Memory" (Paramount+)
"Augusto and Paulina, a couple who have been together for 25 years, face down Augusto's recent Alzheimer's disease diagnosis, wondering when the moment will come that he no longer recognizes her."
Micromundo, Fabula, MTV Documentary Films
"Eternal Spring" [Vice (US) / CBC (Canada) / ARTE (France & Germany) / BBC Storyville (UK)]
This animated documentary written, directed, and co-produced by Jason Loftus is based on the animation of Chinese artist Daxiong and centers the Falun Gong's 2002 hijacking of broadcast TV stations in Changchun, and China's continued repression of ethnic and religious minority groups.
Lofty Sky Entertainment Inc.
"Independent Lens: Hidden Letters" (PBS)
"Directors Violet Du Feng and Zhao Qing reveal how modern women in China are working to maintain the tradition of Nüshu, a secret calligraphy language used to communicate during a time when many women were kept from literacy."
Fish and Bear Pictures LLC, Ten Thousand Images, ITVS, ZDF/ARTE, Bird Street Productions LLC, InMaat Productions, EST Media Holdings Inc., Nika Media, Chicken & Egg Pictures
"Independent Lens: The Picture Taker" (PBS)
"PBS' Independent Lens recognizes the complicated life of Ernest Withers, a Civil Rights photographer and FBI informant. Withers' nearly 2 million images provided an important record of Black history, but his legacy was marred by decades of secret FBI service revealed after his death."
Picture Taker, LLC, Realization Pictures, ITVS, and BPM, in association with K2 Pictures and Ark Media
"Independent Lens: Sam Now" (PBS)
"A boy helps his half-brother search for his missing mother in this coming-of-age documentary about generational trauma, following Sam Harkness from age 11 to 36 as his middle-class Seattle family is heartbroken and bewildered after his mother suddenly leaves them."
HA/HA Films, 2R Productions, ITVS
"Murder in Boston: Roots, Rampage & Reckoning" (HBO | Max)
"HBO's series traces the complex history of race-based hostilities in Boston, explored against the backdrop of the 1989 case of Charles Stuart, whose frantic 911 call reporting that he and his wife, a white couple, had been shot by a Black man would ignite a firestorm."
HBO Documentary Films in association with The Boston Globe presents A Little Room Films Production
"POV: While We Watched" (PBS)
"This timely depiction of a newsroom in crisis follows Indian journalist Ravish Kumar for two years as he battles a barrage of fake news, falling ratings, and the resulting cutbacks while struggling to maintain fact-based analyses."
Britdoc Films, American Documentary | POV
"Still: A Michael J. Fox Movie" (Apple TV+)
"This film follows the life of beloved actor and activist Michael J. Fox, detailing his personal and professional triumphs and barriers in light of a Parkinson's disease diagnosis, and what happens when an optimist faces down an incurable disease."
Concordia Studio in association with Apple
"The Stroll" (HBO | Max)
"‘The Stroll" tells the history of New York's Meatpacking District from the point of view of transgender sex workers who lived and worked there, recounting the violence, policing, and gentrification that eventually led to a movement for trans rights."
HBO Documentary Films
"To Kill a Tiger" (TVO, Knowledge Network)
"Ranjit, a farmer in India, demands justice for his 13-year-old daughter, the victim of a brutal gang rape. His decision to support his daughter is virtually unheard of, and his journey unprecedented."
Notice Pictures Inc., National Film Board of Canada
"ABC News Studios Impact x Nightline: On The Brink" (Hulu)
"ABC anchor Diane Sawyer and senior congressional correspondent Rachel Scott report on the harrowing stories resulting from new healthcare restrictions on pregnant women, with severe penalties threatening physicians and women facing life-threatening delays."
"Against All Enemies" (NBC 5 / KXAS-TV Dallas-Fort Worth)
"NBC 5 in North Texas investigates a group with ties to the Oath Keepers, a far-right anti-government movement that is recruiting and training Texas police to enforce its beliefs instead of established laws, claiming that sheriffs are more powerful than the FBI and the president."
NBC 5 / KXAS-TV Dallas-Fort Worth
"Clarence and Ginni Thomas: Politics, Power and the Supreme Court" (PBS)
"Controversy has swirled around U.S. Supreme Court justice Clarence Thomas and his political activist wife, Ginni. ‘Frontline' traces the couple's rise to power in a narrative that intersects with the history of race and conservatism in America."
Frontline/PBS
"Hate Comes to Main Street" (WTVF-TV, NewsChannel 5)
"As a bizarre political campaign unfolded in a small Tennessee town, WTVF's chief investigative reporter Phil Williams was unflinching in exposing the lies of a Christian nationalist, anti-LBGTQ mayoral candidate, even in the face of threats from white supremacists. Williams' committed coverage resulted in record voter turnout and a resounding defeat for the controversial candidate and her far-right allies."
WTVF-TV, NewsChannel 5
"Inside the Iranian Uprising" (PBS)
"In this documentary, ‘Frontline' uses protestor footage to take viewers inside the uprising in Iran after the death of a young woman who was in police custody, accused of breaking the Islamic regime's strict, gendered dress code. More than 500 Iranians were killed in the ensuing crackdown, including 72 children, and these citizen videos provide unique documentation of the events, given press restrictions in the country."
"It's Bisan from Gaza and I'm Still Alive" (Al Jazeera Media Network)
"Independent journalist Bisan Owda reports from her own social media account as she leaves her home in Gaza City and is repeatedly displaced during the Israeli bombing of Gaza Strip. In collaboration with AJ+, Bisan provides a critical, on-the-ground perspective in a place that has been difficult for international journalists to access."
"Nowhere To Turn" (Tegna/KARE-TV/KARE11.com)
"Minnesota's KARE-TV begins with a local case that leads to a nationwide investigation of widespread sexual assault perpetrated by private contractors who are charged with transporting inmates over long distances."
KARE-TV, KUSA-TV, WHAS-TV
"Shadow Men: Inside Wagner, Russia's Secret War Company" (wsj.com)
"This 40-minute documentary film goes behind the scenes of the Wagner Group, a nefarious organization led by Yevgeny Prigozhin-a mercenary, oligarch, and onetime associate of Russian President Vladimir Putin-who has since rebelled against the leader and died in a plane crash."
The Wall Street Journal
"The Sixth" (WANF-TV, CBS)
"This Atlanta News First series documents Georgia's failure to represent defendants who can't afford lawyers, and the ways they languish in various states of imprisonment without a speedy trial, including a man who has spent ten years in jail without getting his day in court."
Atlanta News First
"War in the Holy Land" (PBS NewsHour)
"PBS News' one-hour primetime special aired one week after the October 7th Hamas attacks, helping viewers make sense of the devastation, the Palestinian group responsible, the intelligence failures of Israel and its allies, and the history of the region's tensions."
PBS NewsHour, PBS News
"The Wrong Man" (KFOR)
"Twenty years ago, an imprisoned man, Glynn Simmons, sent a letter to Oklahoma's News 4 explaining that he had been wrongfully convicted. For two decades, the station's Ali Meyer investigated, and now, finally, Simmons has been exonerated."
PUBLIC SERVICE
"911: Hanging on the Line" (KNTV)
"After a stabbed Oakland, California, police officer almost died because his own 911 calls failed to connect to an operator, the NBC Bay Area Investigative Unit uncovered a deeply broken city, state, and federal 911 system. Their persistent coverage led to state action and, ultimately, Oakland investing millions of dollars into its 911 center."
NBC Bay Area
"After Uvalde: Guns, Grief & Texas Politics" (PBS)
"A year after the Uvalde school shooting, Frontline, Futuro Investigates, and The Texas Tribune teamed up to document one community's trauma amid the ongoing fight over assault rifles. Journalist Maria Hinojosa examines the police response, Uvalde's history of struggle, and its efforts to heal."
Frontline/PBS, Futuro Investigates, The Texas Tribune
"America and the Taliban" (PBS)
"Frontline's three-part documentary looks into how the United States lost the war in Afghanistan, who is responsible, and what the human cost has ultimately been, using decades of on-the-ground reporting as well as interviews with U.S. and Taliban officials."
"America's Dangerous Trucks" (PBS)
"Deadly traffic accidents involving large trucks have surged over the past decade. In an unforgettable hourlong documentary, ‘Frontline' and ProPublica examine a particularly harrowing type of truck accident-'underride crashes'-and why they keep happening despite a relatively inexpensive solution."
Frontline/PBS , ProPublica
"The Post Roe Baby Boom: Inside Mississippi's Maternal Health Crisis" (USA Today streaming channels)
"Thousands more babies are expected to be born each year in Mississippi after the state's restrictive abortion ban was passed in the wake of the overturning of Roe v. Wade. This USA Today film takes viewers to the Mississippi Delta to document how these pregnancies are playing out, particularly for women in rural areas where the maternal healthcare system was already pushed to its brink."
USA Today and The Tennessean
RADIO/PODCAST
"The Big Dig" (GBH News)
"Boston Public Radio station WGBH takes on the humdrum subject of infrastructure and makes it riveting by going deep on Boston's large-scale "Big Dig" project, a highway tunneling effort that became infamous for its ballooning price and ever-lengthening timeline, though in the end delivering on its promises."
GBH News and PRX
"Borrowed and Banned" (Brooklyn Public Library)
"Over a ten-episode podcast series, the Brooklyn Public Library traces the war against books in America by talking to those who are most affected by it-students, librarians, and teachers whose livelihoods are threatened when they resist, and writers whose books are embattled."
Brooklyn Public Library
"How the Far Right is Making Voting Fraud Easier" (NPR)
"The ERIC system is one of the best tools states have to catch voter fraud. In a months-long reporting project, NPR uncovered the conservative movement working to sabotage the system, despite the Republican Party's claims that it is dedicated to catching and rooting out voting improprieties."
"The COVID Tracking Project" (PRX)
"The COVID Tracking Project, a massive volunteer effort to document tests, hospitalizations, and deaths in an effort to show where the virus was, and who was dying, became a de facto source of data amid the chaos of COVID-19. The series addresses the crucial concerns the United States faces about why the nation had to rely on volunteerism, rather than federal and state public health institutions, to receive critical COVID data during the worst public health crisis in a century."
Reveal from The Center for Investigative Reporting and PRX, and ACKO Productions
"The Empty Grave of Comrade Bishop" (Podcast platforms)
"A two-year investigation by The Washington Post uncovers new details in a long-running international mystery: When Maurice Bishop, the revolutionary leader of Grenada, was executed in 1983 alongside seven others, where did their remains go? Through more than 100 interviews and archival research, this podcast examines the evidence, including the role played by the U.S. government."
The Washington Post
"Post Reports: Surviving to graduation" (Podcast platforms)
"Post Reports' three-part series chronicles a year inside Huguenot High School in Richmond, Virginia, a school that experienced several shootings and deaths to learn how the fallout is affecting students and teachers and what educators are doing to prevent future tragedies. But while the reporters were embedded at the school, a student was shot and killed behind the baseball fields, making this a real-time look at the ripple effects of gun violence."
"Prison Town" (Spotify)
"In the midst of a federal investigation into civil rights violations in Georgia's prisons, this podcast uses one prison in South Georgia as a case study, tracing murders on the outside back to inmates on the inside. With hitmen for hire, prison riots, a multimillion-dollar contraband circle, and a warden that has been charged with corruption, the episodes illuminate many of the complex problems that plague our criminal justice system."
The Macon Newsroom and The Georgia Virtue
"The Retrievals" (Serial Productions and The New York Times)
"Serial Productions and The New York Times tell the story of how dozens of women seeking to get pregnant at a Yale fertility clinic endured excruciating-and, it turns out, unnecessary-pain during the egg retrieval process. The real story behind their pain touches on the intersection of the fentanyl epidemic in America, women's health issues, and the ways female patients are routinely gaslit."
Serial Productions and The New York Times
"The Uncertain Hour: Season 6 (The Welfare-to-Work Industrial Complex)" (Marketplace/American Public Media)
"Many Americans have long believed that welfare recipients must get a job-or be preparing for one-to receive government assistance. This Marketplace production delves into the lucrative business that surrounds welfare-to-work policies, and the ways those businesses work to keep recipients dependent on their services."
Marketplace
"Unreformed: the Story of the Alabama Industrial School for Negro Children" (iHeart Podcasts)
"‘Unreformed' tells the story of how the state-run Alabama Industrial School for Negro Children derailed the lives of thousands of Black children in the mid-20th century and what happened when five girls escaped in 1968. Listeners hear of physical and sexual abuse, unlivable facilities and grueling labor in the fields surrounding the school, which led many former students to call it a ‘slave camp.'"
School of Humans
"You Didn't See Nothin" (Podcast platforms)
"Formerly incarcerated journalist Yohance Lacour revisits the 1997 hate crime on the South Side of Chicago that inspired him to enter the world of investigative journalism before his own ten-year prison sentence. He looks at the ways the crime shaped his own life and reinterprets its implications through a current-day lens."
Invisible Institute and USG Audio
More from Variety
- PBS Stand-Up Comedy Documentary Series 'Roots of Comedy with Jesus Trejo' Set to Stream for Free in May (EXCLUSIVE)
- Quinta Brunson, Damon Lindelof Among First Guests on New Peabody Awards Podcast 'We Disrupt this Broadcast'


IMAGES
VIDEO
COMMENTS
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant person's spine) and with the face and body angled to one side and the neck flexed. Variations in fetal presentations include face, brow, breech, and shoulder.
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse. Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position. Abnormal fetal lie, presentation, or position may occur with. Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). ... If your baby stays in a transverse lie until the end of your pregnancy, it can ...
Abnormal Fetal Lie. If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation. ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen. It has an approximate success rate of 50% in primiparous women and 60% in multiparous women.
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
During routine prenatal care, clinicians assess fetal lie and presentation with physical examination in the late third trimester. Ultrasonography can also be done. If breech presentation is detected, external cephalic version can sometimes move the fetus to vertex presentation before labor, usually at 37 or 38 weeks.
This is called cephalic or occiput anterior presentation. Most fetuses settle into this position by the 36th week of pregnancy. Other fetal positions, like breech presentation, make a vaginal delivery more challenging. ... Fetal lie describes how the fetus's spine lines up with its birth parent's spine. Ideally, they line up vertically ...
Transverse lie occurs frequently in early pregnancy, when it is of no consequence. At 16 weeks gestation, about half of all pregnancies will be transverse lie. This number steadily falls as pregnancy advances and the incidence of transverse lie by the 28th week is well below 10%. ... A compound presentation may be resolvable if the fetus can be ...
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position.
The concepts of breech presentation, unstable lie, malpresentations, and malposition have not changed for many years but the diagnostic tools and management options change periodically as new management techniques are developed and the evidence for their use improves. ... Early in pregnancy the position, presentation, and lie of a fetus are ...
The term presentation refers to that part of the fetus presenting to the lower pole of the uterus. It can more precisely be defined by the presenting part, i.e., that part of the presentation that lies in close proximity to the internal os of the cervix. Thus the usual presentation is cephalic, and the presenting part is the vertex or occiput.
Lie. Facing the patient's head, place hands on either side of the top of the uterus and gently apply pressure. Move the hands and palpate down the abdomen. One side will feel fuller and firmer - this is the back. Fetal limbs may be palpable on the opposing side. Fig 2 - Assessing fetal lie and presentation.
To our knowledge this study is the most detailed and comprehensive study of fetal lie/presentation throughout pregnancy. The study was based on a large sample size; however, there was great variation in the sample sizes across all analyzed GA from 269 at 18 weeks to more than 10 times this number of observations. The calculated mathematical ...
The quality of the evidence for interventions for managing a longitudinal lie fetal malpresentation (that is breech presentation) in late pregnancy ranged from very low to high, with most of the evidence being of a very low or low quality. ... Cost-effectiveness of external cephalic version for term breech presentation, BMC Pregnancy and ...
The Trusted Provider of Medical Information since 1899
Reviewed/Revised Jan 2024. Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery, or cesarean delivery.
The relative incidence of differing fetopelvic relations varies with diagnostic and clinical approaches to care. Among longitudinal lies, about 1 in 25 fetuses are not cephalic but breech at the onset of labor. 1 Of the differing lies a fetus may assume, about 1 in 100 is transverse or oblique, also referred to as nonaxial. As pregnancy proceeds to term, most fetuses assume a longitudinal lie ...
Malpresentation is caused by your baby's position ('lie'). There are different types of malpresentation. Breech presentation. This is when your baby is lying with their bottom or feet facing down. Sometimes one foot may enter the birth canal first (called a 'footling presentation'). Breech presentation is the most common type of ...
Fetal Presentation, Position, and Lie (Including Breech Presentation) - Learn about the causes, symptoms, diagnosis & treatment from the MSD Manuals - Medical Consumer Version. ... During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front.
A normal fetal lie is an ideal position for labor and baby delivery in which the baby is head-down with the chin tucked into its chest. The back of the head is positioned so that it is ready to enter the pelvis. The fetus faces the mother's back, called cephalic presentation, and the babies mostly settle in this position by 32 to 36 weeks of ...
During routine prenatal care, clinicians assess fetal lie and presentation with physical examination in the late third trimester. Ultrasonography can also be done. If breech presentation is detected, external cephalic version can sometimes move the fetus to vertex presentation before labor, usually at 37 or 38 weeks.
High-Risk Pregnancy: Management Options - April 2024. Introduction. The concepts of breech presentation, unstable lie, malpresentations, and malposition have not changed for many years but the diagnostic tools and management options change periodically as new management techniques are developed and the evidence for their use improves.
Pregnancy complications, such as gestational diabetes or preeclampsia, may be linked to an elevated risk of death even decades after giving birth, according to a new study. The study, published ...
The Equal Employment Opportunity Commission (EEOC) released the text of the final regulations and interpretative guidance implementing the Pregnant Workers Fairness Act (PWFA) on April 15, 2024. The final regulations are expected to be formally published in the April 19, 2024, Federal Register and will be effective 60 days later.
'Life of the mother' exceptions are nothing more than a politically expedient lie designed to distract from the violence inherent in the maintenance of abortion bans. Pro-abortion rights demonstrators rally in Scottsdale, Ariz., on April 15, 2024, after the top court in Arizona ruled a 160-year-old near-total ban on abortion is enforceable.
PBS landed 11 nominations, by far the most of any outlet, as Peabody Awards Board of Jurors announced this year's 41 nominees across its documentary, news, public service and radio/podcast categories.